User login
Enhancing Opportunities for Physical Activity Among Long-Term Care Residents: A Narrative Review
From the Geriatric Education and Research in Aging Sciences (GERAS) Centre for Aging Research, McMaster University, Hamilton, ON.
Abstract
- Objective. To summarize the literature on improving opportunities for physical activity for residents in long-term care (LTC).
- Method. Narrative review of the literature.
- Results. Residents in LTC spend much of their time in sedentary activities such as sitting or lying in bed. Physical activity is important to help decrease the negative effects of sedentary time, such as poor mood and increased risk of death, and to improve physical function. This review identifies several strategies for promoting physical activity for LTC residents: incorporating simple strategies into daily activities, participating in group activities (eg, exercise, dance, or music therapy), using motivational strategies to encourage staff to promote activity, leveraging the physical environment, reducing physical and chemical restraints, and using innovative solutions such as robots or interactive technology.
- Conclusion. While the quality of evidence to date is limited, preliminary work suggests that the strategies identified in this article could be included as part of a multifactorial approach to increasing physical activity in LTC.
Keywords: long-term care; nursing homes; physical activity; sedentary; mobility.
The United Nations estimates that between 2013 and 2050 the population aged 60 years or older will double.1 Furthermore, the fastest growth rate will be seen in older adults over the age of 80 years.1 With this demographic shift, a growing number of older adults will require supportive housing, such as long-term care (LTC). Indeed, it is projected that the number of older adults requiring LTC will double by 2036.2
Residents in LTC are often medically complex and experience multimorbidity, cognitive impairment, and functional decline,3 making it difficult for them to engage in physical activity. LTC residents spend approximately 75% of their waking time in sedentary activities (eg, sitting, lying down, watching TV), which amounts to more than 12 hours per day.4-6 Residents with cognitive impairment are even more sedentary, spending as little as 1 minute per day in moderate physical activity and approximately 87% of their time in sedentary activities.7 Additionally, a high prevalence of use of psychotropic drugs and physical restraints contributes to high levels of physical inactivity for residents in LTC.8 Increased time spent in sedentary activities has been associated with adverse health outcomes, such as incidence of cardiovascular disease and type 2 diabetes, and mortality.9-11 Moreover, bed and chair rest are associated with muscle disuse, which can lead to functional impairment.12,13
Given the large amount of time LTC residents spend in sedentary activities and the negative consequences this has on their health, it is essential to find opportunities to engage residents in physical activity throughout the day. This article summarizes evidence about increasing opportunities for physical activity for LTC residents. Physical activity is defined as “any bodily movement produced by skeletal muscles that results in energy expenditure,” while exercise, which is a subset of physical activity, is purposefully planned, structured, and repetitive and has a goal of maintaining or improving physical fitness.14 Previous work has described exercise among LTC residents in detail,8,15,16 and thus exercise is not addressed here. Also, as a narrative review, this article provides an overview of available interventions to improve physical activity for LTC residents and does not provide comments on efficacy or an exhaustive list of potential interventions. Rather, it provides a starting point for LTC homes to consider when providing opportunities to improve physical activity for their residents.
Guidelines for Increasing Physical Activity
There are currently no published evidence-based guidelines for increasing physical activity and reducing sedentary time for residents of LTC homes. However, an international task force of experts in geriatrics, exercise, and LTC research convened in 2015 and made recommendations on this matter.8 They emphasize the importance of considering the needs of residents, family members, health care professionals, LTC staff, and policy-makers when designing strategies to promote movement in LTC.8 This will ensure that the strategies to promote movement will be realistic and sustainable. Additionally, the task force identified motivation and pleasure as key to engaging residents in physical activities, and recommended that interests and preferences should be used to guide the selection of activities.8 The following sections describe example strategies to improve physical activity for residents in LTC that LTC homes can use to help facilitate movement for their residents.
Strategies for Promoting Physical Activity
Leveraging Daily Activities
One approach to promoting physical activity in LTC homes is to systematically use simple strategies embedded within routine care to engage residents in movement.8 Function-focused, or restorative care,17 is a philosophy of care that promotes increasing physical activity and maintaining functional abilities based on the resident’s abilities. Examples include walking with residents to the dining room rather than pushing them in a wheelchair where appropriate, inviting residents to events that require them to leave their room, improving independent wheelchair propulsion for residents who cannot walk, and increasing opportunities for sit-to-stand activities where possible. These activities are scaled to the resident’s underlying physical and cognitive capabilities. A systematic review of function-focused care revealed that it can help maintain functional skills for residents in LTC, and there is no significant risk associated with implementation.18 In a study by Slaughter et al19 that examined the effectiveness of techniques to encourage mobility by residents’ usual caregivers, health care aides prompted residents to perform the sit-to-stand activity 4 times per day, with the number of repetitions individualized based on resident ability, fatigue, and motivation. Residents who completed the sit-to-stand activity had smaller declines in mobility and functional outcomes (ie, less decline on the Functional Independence Measure).19 This study included residents with Alzheimer’s disease and dementia who could transfer independently or with the assistance of one person,20 indicating that this type of intervention is feasible and appropriate for residents with cognitive impairment.
Group Activities
Group activities in LTC homes are another way of engaging residents in physical activity in a motivating and pleasant setting that also encourages social engagement among residents and LTC staff. Group exercise classes can be effective for improving mood and functional outcomes. For example, a systematic review of dance classes in LTC homes revealed an improvement in problematic behaviors, mood, cognition, communication, and socialization.21 Most studies included participants with dementia, and no adverse events were reported, supporting the feasibility and safety of implementing group dance activities for residents with cognitive impairment. Group exercise is the most common delivery method for exercise within LTC homes22 and has been demonstrated to have small positive effects on activities of daily living (ADL; ie, improvement in ADL independence equivalent to 1.3 points on the Barthel Index).23 Other group activities, such as music therapy, have demonstrated improvements in depressive symptoms, emotional well-being, and anxiety for LTC residents with dementia.24 Group activities also provide the opportunity for movement as residents leave their rooms, walk to a new location (if able), and return to their rooms when the activity is complete.
Barriers to Physical Activity and Strategies to Overcome Them
Caregiver-related Factors
LTC staff have limited time to spend promoting physical activity since residents often have complex health care needs and staffing levels are often constrained.25 Indeed, having lower staffing levels has been associated with lower levels of physical activity for residents.26,27 LTC staff have identified a lack of time to walk with residents28,29 and having other tasks to do (eg, clean) as barriers to promoting movement.28,29 However, asking residents to help staff with small household chores, such as folding laundry or clearing dishes, was a facilitator to promoting movement.30 Activating residents by helping them transfer to a wheelchair for independent mobilization around the home or by assisting them to walk where appropriate were also facilitators.30,31 Leveraging facilitators will help staff who have limited time to help residents engage in more physical activity.
Motivation of LTC staff can also be a barrier to encouraging physical activity for residents in LTC. Fear that increasing physical activity will cause adverse events like falls, illness, or exacerbation of symptoms often decreases motivation for staff to facilitate physical activity.32,33 Another potential barrier is the conceptualization of the role of nursing in LTC as protecting residents from harm by encouraging them to engage in “risk-free” activities like staying in bed.34-39 Strategies to increase staff motivation to engage LTC residents in physical activity that have been shown to be effective are verbal prompts, modelling behaviors, goal setting, and home champions to promote function-focused care.17,33,40-43
The Physical Environment
Aspects of the physical environment of LTC homes may facilitate or limit residents’ ability to be physically active. A 2017 systematic review examined elements of the physical environment that acted as barriers and facilitators to physical activity for older adults living in LTC.30 The authors found that the person-environment fit, security, accessibility, and comfort were key components of the physical environment that were associated with residents’ physical activity levels.30 First, an appropriate fit between the residents’ abilities and the demands of the environment was related to improved activity as measured by actigraphy.44 For example, having long hallways between residents’ rooms and common spaces discourages residents who can only walk short distances from walking to these locations. However, residents were more active in larger-scaled LTC homes with shorter distances between different areas (eg, resident rooms and dining rooms).45 Clearly, there must be enough space to encourage walking between areas, but not so much space that walking is not feasible. Residents participating in a focus group identified accessibility and comfort features as being facilitators for walking in the corridor, such as wide corridors, sturdy handrails, carpet, chairs placed at short intervals for seated breaks, windows to look out, plants, and accessible activity rooms and restrooms.45,46 On the other hand, limited things to see and do indoors and outdoors, along with restricted walking areas, were identified as barriers to corridor walking by residents.46
One method for optimizing LTC home architecture to promote movement is to provide therapeutic outdoor spaces, such as gardens. Indeed, therapeutic gardens have been studied as a nonpharmacological method of engaging LTC residents with dementia and have been shown to benefit mood, pain, and fall prevention.47 Secure therapeutic gardens or outdoor spaces provide opportunities for various activities to increase movement, including gardening, animal care, and walking.48 However, there is a higher propensity for residents who use walkers or wheelchairs to slide off paths or become stuck in mud or mulch.49 Residents with physical limitations may require additional supervision in garden spaces, and as such spaces should be designed with improved safety in mind (eg, barriers between paths and places where mud could accumulate). The number of available indoor (eg, a physical therapy gym) and outdoor (eg, gardens) spaces was also found to be positively related to residents’ physical activity levels.50 However, these relationships were mediated by the number of activity programs available in the LTC homes.50 Therefore, having staff available to facilitate activities is also important for promoting physical activity.
Chemical and Physical Restraints
Physical and chemical restraints (eg, antipsychotics and sedatives) are sometimes used to manage the behavioral and psychological symptoms of dementia,51,52 which many residents in LTC experience.3 Though there has been an emphasis in North America to decrease their use, physical and chemical restraints are still used in LTC.53 Physical restraint use is associated with a higher risk of functional and cognitive decline.53,54 Residents who are both physically and chemically restrained through antipsychotic use are at even higher risk for these declines.54 Thus, to improve opportunities for movement in LTC, physical restraint use should be minimized. The risks and benefits of using psychotropic medications that often decrease residents’ physical activity levels must be evaluated individually, and other nonpharmacological strategies should be used to manage the behavioral and psychological symptoms of dementia. These could include functional analysis-based interventions (ie, individualized interventions aimed at identifying unmet needs, causes, antecedents, and consequences of the behavior),55 music therapy,55 or other interventions described above.
Emerging Innovative Interventions
Robots are an emerging nonpharmacological intervention for improving the behavioral and psychological symptoms of dementia and facilitating physical activity in LTC. Robotic animal interventions, where LTC residents interact with robotic animals in an individual or group setting, have been shown to reduce negative behaviors and increase positive mood.56 Additionally, robots are being used in rehabilitation to provide exercise post-stroke57 and could easily be transitioned to do similar tasks in LTC. Robotic interventions are attractive for the LTC sector as they could help relieve the workload demands on an often overloaded sector, and, in the case of pet therapy, surmount regulations for bringing live animals into a LTC home. Though studies examining the use of robots in LTC have mainly focused on the effect of pet therapy on reducing behavioral symptoms, the use of robots to promote physical activity and exercise in LTC is a natural progression for the work that has been done in inpatient rehabilitation.57 On a similar note, an interactive technology (similar to a Kinect system) used to promote 30-minute, twice-weekly physical activity sessions has demonstrated improvements in physical function (Short Physical Performance Battery [SPPB]) for pre-disabled (SPPB of 6 to 9) residents in LTC without dementia.58 The role of technology to promote physical activity in LTC is an emerging area of interest, and future innovations in this area will continue to help facilitate movement.
Quality of Evidence
Most studies aimed at improving physical activity for LTC residents to date are small, have nonrandomized designs, and have limited generalizability and evidence to support the efficacy of the interventions. For example, most studies included in systematic reviews for function-focused care, dance, group exercise, and music therapy are small, observational, or quasi-experimental studies with methodological issues resulting in bias.18,21,23,24 Likewise, the evidence surrounding nonpharmacological interventions for reducing behavioral and psychological symptoms of dementia is of very low to moderate quality.55 Innovative interventions, such as robotics and interactive technology, to promote physical activity in LTC are in their infancy. There are no data syntheses available to date to summarize the available literature on this topic, and conclusions rely on small, nonrandomized designs or extrapolations of results from similar sectors (eg, inpatient rehabilitation). Thus, the studies described in this review can be used as preliminary evidence to support the implementation of interventions to improve physical activity, but discretion should be used when interpreting the efficacy of these interventions.
Discussion
This review identifies several strategies for promoting physical activity for LTC residents, including incorporating simple strategies into daily activities, participating in group activities (eg, exercise, dance, or music therapy), using motivational strategies to encourage staff to promote activity, leveraging the physical environment, reducing physical and chemical restraints, and using innovation solutions like robots or interactive technology. While the quality of evidence to date is limited, preliminary work suggests that strategies identified in this paper could be included as part of a multifactorial approach to increasing physical activity in LTC.
The current evidence does not suggest that any one strategy is more effective at improving physical activity, and it is likely that LTC homes will need to employ a combination of strategies to help residents move more. Additionally, residents’ preferences, goals, and capabilities should always be considered when designing an individualized physical activity plan. For example, if a resident does not like to be outdoors or gardening but enjoys dancing and music, then their physical activity plan should include group dance class and music therapy rather than gardening. LTC homes will need to have a menu of opportunities for movement that residents can choose from so that activities are pleasant and motivating, and therefore more likely to be completed.
Many of the interventions described in this review are safe and feasible to implement with residents who have physical or cognitive impairments. Function-focused care is scaled to the residents’ capabilities and did not increase the risk of falling, though LTC staff require the skills to scale physical activities appropriately.18 Likewise, group dance activities and music therapy were tested with residents with dementia, with no adverse events reported.21,24 However, more work is needed to determine the feasibility of implementing emerging methods, such as robotics and interactive technology, for increasing physical activity for residents with physical and cognitive impairments. Most studies to date have included mobile residents or those with minimal cognitive impairment. Similarly, outdoor garden spaces may be less safe for residents who use walkers or wheelchairs if there is an opportunity for them to slip off paths or get stuck in mud or mulch. LTC homes implementing any of these interventions should evaluate the benefits and risks of each intervention, the resources available within the home to support them (eg, trained staff), and the target residents’ physical and cognitive capabilities.
While increasing physical activity is important, structured exercise is needed to see gains in components of physical fitness such as strength, aerobic capacity, and balance. Indeed, one major consideration highlighted by the aforementioned task force is that every resident who does not have contraindications must also have a personalized multicomponent exercise program as part of their care plan.8 The task force recommends moderate- to high-intensity strength, aerobic, and balance exercises 2 times per week for 35 to 45 minutes per session.8 There is an interrelationship between physical activity and structured exercise: structured exercise programs can certainly be part of a physical activity plan, but physical activity can include more than structured exercise. Physical activity also includes any activity that involves movement, such as walking in gardens or between home areas, or physically participating more in personal care activities (eg, assisting with bathing or dressing).14 Both structured exercise and physical activity are important for LTC residents. Structured exercise provides an opportunity to improve strength and cardiovascular fitness, which aim to decrease the negative effects of sarcopenia and cardiovascular disease, such as disability and death.59,60 However, structured exercise should not be done daily for the same muscle groups.8 Rather, it is recommended for LTC residents to engage in structured exercise 2 times per week.8 Increasing physical activity is a daily goal, as daily physical activity decreases sedentary time, which has negative consequences such as decreased mood61 and increased mortality.62 LTC homes should incorporate strategies to both increase daily physical activity and promote individualized, structured exercise programs.
Conclusion
Residents in LTC spend much of their time in sedentary activities such as sitting or lying in bed. Physical activity is important to help decrease the negative effects of sedentary time, like poor mood and increased risk of death, and to improve physical function. This review describes several strategies to promote physical activity within LTC homes, such as leveraging daily activities and the physical environment, providing group activities, reducing physical and chemical restraint use, and using innovative technology such as robots. LTC homes can use the information in this review to plan strategies to promote physical activity.
Corresponding author: Caitlin McArthur, MScPT, PhD, Hamilton Health Sciences, St. Peter’s Hospital, 88 Maplewood Avenue, Hamilton, ON L8M 1W9; mcarthurc@hhsc.ca.
Financial disclosures: None.
1. United Nations Department of Economic and Social Affairs Population Division. World Population Ageing 2013. New York, NY: United Nations; 2013.
2. Pickard L, Comas-Herrera A, Costa-Font J, et al. Modelling an entitlement to long-term care services for older people in Europe: projections for long-term care expenditure to 2050. J Eur Soc Policy. 2007;17:33-48.
3. Hirdes JP, Mitchell L, Maxwell CJ, White N. Beyond the “iron lungs of gerontology”: Using evidence to shape the future of nursing homes in Canada. Can J Aging. 2011;30:371-390.
4. Chin A Paw MJM, van Poppel MNM, van Mechelen W. Effects of resistance and functional-skills training on habitual activity and constipation among older adults living in long-term care facilities: a randomized controlled trial. BMC Geriatr. 2006;6:9.
5. Ikezoe T, Asakawa Y, Shima H, Kishibuchi K, Ichihashi N. Daytime physical activity patterns and physical fitness in institutionalized elderly women: an exploratory study. Arch Gerontol Geriatr. 2013;57:221-225.
6. Keogh JW, Senior H, Beller EM, Henwood T. Prevalence and risk factors for low habitual walking speed in nursing home residents: an observational study. Arch Phys Med Rehabil. 2015;96:1993-1999.
7. Marmeleira J, Ferreira S, Raimundo A. Physical activity and physical fitness of nursing home residents with cognitive impairment: A pilot study. Exp Gerontol. 2017;100:63-69.
8. de Souto Barreto P, Morley JE, Chodzko-Zajko W, et al. Recommendations on physical activity and exercise for older adults living in long-term care facilities: a taskforce report. J Am Med Dir Assoc. 2016;17:381-392.
9. van der Ploeg HP, Chey T, Korda RJ, et al. Sitting time and all-cause mortality risk in 222 497 Australian adults. Arch Intern Med. 2012;172:494-500.
10. Chau JY, Grunseit AC, Chey T, et al. Daily sitting time and all-cause mortality: a meta-analysis. PLoS One. 2013;8:e80000.
11. Grøntved A, Hu FB. Television viewing and risk of type 2 diabetes, cardiovascular disease, and all-cause mortality: a meta-analysis. JAMA. 2011;305:2448-2455.
12. Senior HE, Henwood TR, Beller EM, et al. Prevalence and risk factors of sarcopenia among adults living in nursing homes. Maturitas. 2015;82:418-423.
13. Wall BT, Dirks ML, van Loon LJC. Skeletal muscle atrophy during short-term disuse: implications for age-related sarcopenia. Ageing Res Rev. 2013;12:898-906.
14. Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100:126-131.
15. McArthur C, Giangregorio LM. Improving strength and balance for long-term care residents at risk for falling: Suggestions for practice. J Clin Outcomes Manag. 2018;25:28-38.
16. Crocker T, Forster A, Young J, et al. Physical rehabilitation for older people in long-term care. Cochrane Database Syst Rev. 2013;2:CD004294.
17. Resnick B, Galik E, Boltz M, Pretzer-Aboff IE. Implementing Restorative Care Nursing in All Settings. 2nd ed. New York, NY: Spring Publishing Company; 2011.
18. Resnick B, Galik E, Boltz M. Function focused care approaches: literature review of progress and future possibilities. J Am Med Dir Assoc. 2013;14:313-318.
19. Slaughter SE, Estabrooks CA, Jones CA, Wagg AS. Mobility of Vulnerable Elders (MOVE): study protocol to evaluate the implementation and outcomes of a mobility intervention in long-term care facilities. BMC Geriatr. 2011;11:84.
20. Slaughter SE, Wagg AS, Jones CA, et al. Mobility of Vulnerable Elders study: effect of the sit-to-stand activity on mobility, function, and quality of life. J Am Med Dir Assoc. 2015;16(2):138-143.
21. Guzmán-García A, Hughes JC, James IA, Rochester L. Dancing as a psychosocial intervention in care homes: a systematic review of the literature. Int J Geriatr Psychiatry. 2013;28:914-924.
22. McArthur C, Gibbs JC, Patel R, et al. A scoping review of physical rehabilitation in long-term care: interventions, outcomes, tools. Can J Aging/La Rev Can du Vieil. 2017;36:435-452.
23. Crocker T, Young J, Forster A, et al. The effect of physical rehabilitation on activities of daily living in older residents of long-term care facilities: Systematic review with meta-analysis. Age Ageing. 2013;42:682-688.
24. van der Steen JT, Smaling HJ, van der Wouden JC, et al. Music-based therapeutic interventions for people with dementia. Cochrane Database Syst Rev. 2018;7:CD003477.
25. Froggatt K, Davies S, Meyer J. Understanding Care Homes, A Research and Development Perspective. London: Jessica Kingsley Publishers; 2009.
26. Shore BA, Lerman DC, Smith RG, et al. Direct assessment of quality of care in a geriatric nursing home. J Appl Behav Anal. 1995;28:435-448.
27. Bates-Jensen BM, Schnelle JF, Alessi CA, et al. The effects of staffing on in-bed times of nursing home residents. J Am Geriatr Soc. 2004;52:931-938.
28. Ericson-Lidman E, Renström A-S, Åhlin J, Strandberg G. Relatives’ perceptions of residents’ life in a municipal care facility for older people with a focus on quality of life and care environment. Int J Older People Nurs. 2015;10:160-169.
29. Häggström E, Kihlgren A, Kihlgren M, Sörlie V. Relatives’ struggle for an improved and more just care for older people in community care. J Clin Nurs. 2007;16:1749-1757.
30. Douma JG, Volkers KM, Engels G, et al. Setting-related influences on physical inactivity of older adults in residential care settings: a review. BMC Geriatr. 2017;17:97.
31. Zegelin A. ’Tied down’- the process of becoming bedridden through gradual local confinement. J Clin Nurs. 2008;17:2294-2301.
32. Resnick B, Galik E, Gruber-Baldini AL, Zimmerman S. Falls and fall-related injuries associated with function-focused care. Clin Nurs Res. 2012;21:43-63.
33. Pretzer-Aboff I, Galik E. Feasibility and impact of a function focused care intervention for Parkinson’s disease in the community. Nursing Res. 2011;60:276-283.
34. Leditschke IA, Green M, Irvine J, et al. What are the barriers to mobilizing intensive care patients? Cardiopulm Phys Ther J. 2012;23:26-29.
35. Mittmann N, Seung SJ, Pisterzi LF, et al. Nursing workload associated with hospital patient care. Dis Manag Heal Outcomes. 2008;16:53-61.
36. Dykes PC, Carroll DL, Hurley AC, et al. Why do patients in acute care hospitals fall? Can falls be prevented? J Nurs Adm. 2009;39:299-304.
37. Brownie S, Nancarrow S. Effects of person-centered care on residents and staff in aged-care facilities: a systematic review. Clin Interv Aging. 2013;8:1-10.
38. Wakefield BJ, Holman JE. Functional trajectories associated with hospitalization in older adults. West J Nurs Res. 2007;29:161-177.
39. Boltz M, Resnick B, Capezuti E, Shuluk J. Activity restriction vs. self-direction: hospitalised older adults’ response to fear of falling. Int J Older People Nurs. 2014;9:44-53.
40. Resnick B, Galik E, Gruber-Baldini A, Zimmerman S. Testing the effect of function-focused care in assisted living. J Am Geriatr Soc. 2011;59:2233-2240.
41. Galik EM, Resnick B, Gruber-Baldini A, et al. Pilot testing of the restorative care intervention for the cognitively impaired. J Am Med Dir Assoc. 2008;9:516-522.
42. Resnick B, Galik E, Gruber-Baldini AL, Zimmerman S. Implementing a restorative care philosophy of care in assisted living: pilot testing of Res-Care-AL. J Am Acad Nurse Pract. 2009;21:123-133.
43. Resnick B, Gruber-Baldini AL, Zimmerman S, et al. Nursing home resident outcomes from the Res-Care intervention. J Am Geriatr Soc. 2009;57:1156-1165.
44. Pomeroy SH, Scherer Y, Runkawatt V, et al. Person-environment fit and functioning among older adults in a long-term care setting. Geriatr Nurs. 2011;32:368-378.
45. Moos RH, David TG, Lemke S, Postle E. Coping with an intra-institutional relocation: changes in resident and staff behavior patterns. Gerontologist. 1984;24:495-502.
46. Lu Z, Rodiek SD, Shepley MM, Duffy M. Influences of physical environment on corridor walking among assisted living residents. J Appl Gerontol. 2011;30:463-484.
47. Detweiler MB, Sharma T, Detweiler JG, et al. What is the evidence to support the use of therapeutic gardens for the elderly? Psychiatry Investig. 2012;9:100.
48. Blake M, Mitchell G. Horticultural therapy in dementia care: a literature review. Nurs Stand. 2016;30:41-47.
49. Detweiler MB, Murphy PF, Myers LC, Kim KY. Does a wander garden influence inappropriate behaviors in dementia residents? Am J Alzheimers Dis Other Demen. 2008;23:31-45.
50. Joseph A, Zimring C, Harris-Kojetin L, Kiefer K. Presence and visibility of outdoor and indoor physical activity features and participation in physical activity among older adults in retirement communities. J Hous Elderly. 2006;19:141-165.
51. Feng Z, Hirdes JP, Smith TF, et al. Use of physical restraints and antipsychotic medications in nursing homes: a cross-national study. Int J Geriatr Psychiatry. 2009;24:1110-1118.
52. Herrmann N. Recommendations for the management of behavioral and psychological symptoms of dementia. Can J Neurol Sci. 2001;28 Suppl 1:S96-107.
53. Freeman S, Spirgiene L, Martin-Khan M, Hirdes JP. Relationship between restraint use, engagement in social activity, and decline in cognitive status among residents newly admitted to long-term care facilities. Geriatr Gerontol Int. 2017;17:246-255.
54. Foebel AD, Onder G, Finne-Soveri H, et al. Physical restraint and antipsychotic medication use among nursing home residents with dementia. J Am Med Dir Assoc. 2016;17:184.e9-184.e14.
55. Dyer SM, Harrison SL, Laver K, Whitehead C, Crotty M. An overview of systematic reviews of pharmacological and non-pharmacological interventions for the treatment of behavioral and psychological symptoms of dementia. Int Psychogeriatr. 2018;30:295-309.
56. Robinson H, MacDonald B, Kerse N, Broadbent E. The psychosocial effects of a companion robot: a randomized controlled trial. J Am Med Dir Assoc. 2013;14:661-667.
57. Lo K, Stephenson M, Lockwood C. Effectiveness of robotic assisted rehabilitation for mobility and functional ability in adult stroke patients. JBI Database System Rev Implement Rep. 2017;15:3049-3091.
58. Valiani V, Lauzé M, Martel D, et al. A new adaptive home-based exercise technology among older adults living in nursing home: a pilot study on feasibility, acceptability and physical performance. J Nutr Health Aging. 2017;21:819-824.
59. Locquet M, Beaudart C, Hajaoui M, et al. Three-year adverse health consequences of sarcopenia in community-dwelling older adults according to 5 diagnosis definitions. J Am Med Dir Assoc. 2019;20:43-46.e2.
60. Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, et al. Exercise and physical activity for older adults. Med Sci Sports Exerc. 2009;41:1510-1530.
61. Park S-Y, Lee K, Um YJ, Paek S, Ryou IS. Association between physical activity and depressive mood among Korean adults with chronic diseases. Korean J Fam Med. 2018;39:185-190.
62. Loprinzi PD. Light-intensity physical activity and all-cause mortality. Am J Health Promot. 2017;31:340-342.
From the Geriatric Education and Research in Aging Sciences (GERAS) Centre for Aging Research, McMaster University, Hamilton, ON.
Abstract
- Objective. To summarize the literature on improving opportunities for physical activity for residents in long-term care (LTC).
- Method. Narrative review of the literature.
- Results. Residents in LTC spend much of their time in sedentary activities such as sitting or lying in bed. Physical activity is important to help decrease the negative effects of sedentary time, such as poor mood and increased risk of death, and to improve physical function. This review identifies several strategies for promoting physical activity for LTC residents: incorporating simple strategies into daily activities, participating in group activities (eg, exercise, dance, or music therapy), using motivational strategies to encourage staff to promote activity, leveraging the physical environment, reducing physical and chemical restraints, and using innovative solutions such as robots or interactive technology.
- Conclusion. While the quality of evidence to date is limited, preliminary work suggests that the strategies identified in this article could be included as part of a multifactorial approach to increasing physical activity in LTC.
Keywords: long-term care; nursing homes; physical activity; sedentary; mobility.
The United Nations estimates that between 2013 and 2050 the population aged 60 years or older will double.1 Furthermore, the fastest growth rate will be seen in older adults over the age of 80 years.1 With this demographic shift, a growing number of older adults will require supportive housing, such as long-term care (LTC). Indeed, it is projected that the number of older adults requiring LTC will double by 2036.2
Residents in LTC are often medically complex and experience multimorbidity, cognitive impairment, and functional decline,3 making it difficult for them to engage in physical activity. LTC residents spend approximately 75% of their waking time in sedentary activities (eg, sitting, lying down, watching TV), which amounts to more than 12 hours per day.4-6 Residents with cognitive impairment are even more sedentary, spending as little as 1 minute per day in moderate physical activity and approximately 87% of their time in sedentary activities.7 Additionally, a high prevalence of use of psychotropic drugs and physical restraints contributes to high levels of physical inactivity for residents in LTC.8 Increased time spent in sedentary activities has been associated with adverse health outcomes, such as incidence of cardiovascular disease and type 2 diabetes, and mortality.9-11 Moreover, bed and chair rest are associated with muscle disuse, which can lead to functional impairment.12,13
Given the large amount of time LTC residents spend in sedentary activities and the negative consequences this has on their health, it is essential to find opportunities to engage residents in physical activity throughout the day. This article summarizes evidence about increasing opportunities for physical activity for LTC residents. Physical activity is defined as “any bodily movement produced by skeletal muscles that results in energy expenditure,” while exercise, which is a subset of physical activity, is purposefully planned, structured, and repetitive and has a goal of maintaining or improving physical fitness.14 Previous work has described exercise among LTC residents in detail,8,15,16 and thus exercise is not addressed here. Also, as a narrative review, this article provides an overview of available interventions to improve physical activity for LTC residents and does not provide comments on efficacy or an exhaustive list of potential interventions. Rather, it provides a starting point for LTC homes to consider when providing opportunities to improve physical activity for their residents.
Guidelines for Increasing Physical Activity
There are currently no published evidence-based guidelines for increasing physical activity and reducing sedentary time for residents of LTC homes. However, an international task force of experts in geriatrics, exercise, and LTC research convened in 2015 and made recommendations on this matter.8 They emphasize the importance of considering the needs of residents, family members, health care professionals, LTC staff, and policy-makers when designing strategies to promote movement in LTC.8 This will ensure that the strategies to promote movement will be realistic and sustainable. Additionally, the task force identified motivation and pleasure as key to engaging residents in physical activities, and recommended that interests and preferences should be used to guide the selection of activities.8 The following sections describe example strategies to improve physical activity for residents in LTC that LTC homes can use to help facilitate movement for their residents.
Strategies for Promoting Physical Activity
Leveraging Daily Activities
One approach to promoting physical activity in LTC homes is to systematically use simple strategies embedded within routine care to engage residents in movement.8 Function-focused, or restorative care,17 is a philosophy of care that promotes increasing physical activity and maintaining functional abilities based on the resident’s abilities. Examples include walking with residents to the dining room rather than pushing them in a wheelchair where appropriate, inviting residents to events that require them to leave their room, improving independent wheelchair propulsion for residents who cannot walk, and increasing opportunities for sit-to-stand activities where possible. These activities are scaled to the resident’s underlying physical and cognitive capabilities. A systematic review of function-focused care revealed that it can help maintain functional skills for residents in LTC, and there is no significant risk associated with implementation.18 In a study by Slaughter et al19 that examined the effectiveness of techniques to encourage mobility by residents’ usual caregivers, health care aides prompted residents to perform the sit-to-stand activity 4 times per day, with the number of repetitions individualized based on resident ability, fatigue, and motivation. Residents who completed the sit-to-stand activity had smaller declines in mobility and functional outcomes (ie, less decline on the Functional Independence Measure).19 This study included residents with Alzheimer’s disease and dementia who could transfer independently or with the assistance of one person,20 indicating that this type of intervention is feasible and appropriate for residents with cognitive impairment.
Group Activities
Group activities in LTC homes are another way of engaging residents in physical activity in a motivating and pleasant setting that also encourages social engagement among residents and LTC staff. Group exercise classes can be effective for improving mood and functional outcomes. For example, a systematic review of dance classes in LTC homes revealed an improvement in problematic behaviors, mood, cognition, communication, and socialization.21 Most studies included participants with dementia, and no adverse events were reported, supporting the feasibility and safety of implementing group dance activities for residents with cognitive impairment. Group exercise is the most common delivery method for exercise within LTC homes22 and has been demonstrated to have small positive effects on activities of daily living (ADL; ie, improvement in ADL independence equivalent to 1.3 points on the Barthel Index).23 Other group activities, such as music therapy, have demonstrated improvements in depressive symptoms, emotional well-being, and anxiety for LTC residents with dementia.24 Group activities also provide the opportunity for movement as residents leave their rooms, walk to a new location (if able), and return to their rooms when the activity is complete.
Barriers to Physical Activity and Strategies to Overcome Them
Caregiver-related Factors
LTC staff have limited time to spend promoting physical activity since residents often have complex health care needs and staffing levels are often constrained.25 Indeed, having lower staffing levels has been associated with lower levels of physical activity for residents.26,27 LTC staff have identified a lack of time to walk with residents28,29 and having other tasks to do (eg, clean) as barriers to promoting movement.28,29 However, asking residents to help staff with small household chores, such as folding laundry or clearing dishes, was a facilitator to promoting movement.30 Activating residents by helping them transfer to a wheelchair for independent mobilization around the home or by assisting them to walk where appropriate were also facilitators.30,31 Leveraging facilitators will help staff who have limited time to help residents engage in more physical activity.
Motivation of LTC staff can also be a barrier to encouraging physical activity for residents in LTC. Fear that increasing physical activity will cause adverse events like falls, illness, or exacerbation of symptoms often decreases motivation for staff to facilitate physical activity.32,33 Another potential barrier is the conceptualization of the role of nursing in LTC as protecting residents from harm by encouraging them to engage in “risk-free” activities like staying in bed.34-39 Strategies to increase staff motivation to engage LTC residents in physical activity that have been shown to be effective are verbal prompts, modelling behaviors, goal setting, and home champions to promote function-focused care.17,33,40-43
The Physical Environment
Aspects of the physical environment of LTC homes may facilitate or limit residents’ ability to be physically active. A 2017 systematic review examined elements of the physical environment that acted as barriers and facilitators to physical activity for older adults living in LTC.30 The authors found that the person-environment fit, security, accessibility, and comfort were key components of the physical environment that were associated with residents’ physical activity levels.30 First, an appropriate fit between the residents’ abilities and the demands of the environment was related to improved activity as measured by actigraphy.44 For example, having long hallways between residents’ rooms and common spaces discourages residents who can only walk short distances from walking to these locations. However, residents were more active in larger-scaled LTC homes with shorter distances between different areas (eg, resident rooms and dining rooms).45 Clearly, there must be enough space to encourage walking between areas, but not so much space that walking is not feasible. Residents participating in a focus group identified accessibility and comfort features as being facilitators for walking in the corridor, such as wide corridors, sturdy handrails, carpet, chairs placed at short intervals for seated breaks, windows to look out, plants, and accessible activity rooms and restrooms.45,46 On the other hand, limited things to see and do indoors and outdoors, along with restricted walking areas, were identified as barriers to corridor walking by residents.46
One method for optimizing LTC home architecture to promote movement is to provide therapeutic outdoor spaces, such as gardens. Indeed, therapeutic gardens have been studied as a nonpharmacological method of engaging LTC residents with dementia and have been shown to benefit mood, pain, and fall prevention.47 Secure therapeutic gardens or outdoor spaces provide opportunities for various activities to increase movement, including gardening, animal care, and walking.48 However, there is a higher propensity for residents who use walkers or wheelchairs to slide off paths or become stuck in mud or mulch.49 Residents with physical limitations may require additional supervision in garden spaces, and as such spaces should be designed with improved safety in mind (eg, barriers between paths and places where mud could accumulate). The number of available indoor (eg, a physical therapy gym) and outdoor (eg, gardens) spaces was also found to be positively related to residents’ physical activity levels.50 However, these relationships were mediated by the number of activity programs available in the LTC homes.50 Therefore, having staff available to facilitate activities is also important for promoting physical activity.
Chemical and Physical Restraints
Physical and chemical restraints (eg, antipsychotics and sedatives) are sometimes used to manage the behavioral and psychological symptoms of dementia,51,52 which many residents in LTC experience.3 Though there has been an emphasis in North America to decrease their use, physical and chemical restraints are still used in LTC.53 Physical restraint use is associated with a higher risk of functional and cognitive decline.53,54 Residents who are both physically and chemically restrained through antipsychotic use are at even higher risk for these declines.54 Thus, to improve opportunities for movement in LTC, physical restraint use should be minimized. The risks and benefits of using psychotropic medications that often decrease residents’ physical activity levels must be evaluated individually, and other nonpharmacological strategies should be used to manage the behavioral and psychological symptoms of dementia. These could include functional analysis-based interventions (ie, individualized interventions aimed at identifying unmet needs, causes, antecedents, and consequences of the behavior),55 music therapy,55 or other interventions described above.
Emerging Innovative Interventions
Robots are an emerging nonpharmacological intervention for improving the behavioral and psychological symptoms of dementia and facilitating physical activity in LTC. Robotic animal interventions, where LTC residents interact with robotic animals in an individual or group setting, have been shown to reduce negative behaviors and increase positive mood.56 Additionally, robots are being used in rehabilitation to provide exercise post-stroke57 and could easily be transitioned to do similar tasks in LTC. Robotic interventions are attractive for the LTC sector as they could help relieve the workload demands on an often overloaded sector, and, in the case of pet therapy, surmount regulations for bringing live animals into a LTC home. Though studies examining the use of robots in LTC have mainly focused on the effect of pet therapy on reducing behavioral symptoms, the use of robots to promote physical activity and exercise in LTC is a natural progression for the work that has been done in inpatient rehabilitation.57 On a similar note, an interactive technology (similar to a Kinect system) used to promote 30-minute, twice-weekly physical activity sessions has demonstrated improvements in physical function (Short Physical Performance Battery [SPPB]) for pre-disabled (SPPB of 6 to 9) residents in LTC without dementia.58 The role of technology to promote physical activity in LTC is an emerging area of interest, and future innovations in this area will continue to help facilitate movement.
Quality of Evidence
Most studies aimed at improving physical activity for LTC residents to date are small, have nonrandomized designs, and have limited generalizability and evidence to support the efficacy of the interventions. For example, most studies included in systematic reviews for function-focused care, dance, group exercise, and music therapy are small, observational, or quasi-experimental studies with methodological issues resulting in bias.18,21,23,24 Likewise, the evidence surrounding nonpharmacological interventions for reducing behavioral and psychological symptoms of dementia is of very low to moderate quality.55 Innovative interventions, such as robotics and interactive technology, to promote physical activity in LTC are in their infancy. There are no data syntheses available to date to summarize the available literature on this topic, and conclusions rely on small, nonrandomized designs or extrapolations of results from similar sectors (eg, inpatient rehabilitation). Thus, the studies described in this review can be used as preliminary evidence to support the implementation of interventions to improve physical activity, but discretion should be used when interpreting the efficacy of these interventions.
Discussion
This review identifies several strategies for promoting physical activity for LTC residents, including incorporating simple strategies into daily activities, participating in group activities (eg, exercise, dance, or music therapy), using motivational strategies to encourage staff to promote activity, leveraging the physical environment, reducing physical and chemical restraints, and using innovation solutions like robots or interactive technology. While the quality of evidence to date is limited, preliminary work suggests that strategies identified in this paper could be included as part of a multifactorial approach to increasing physical activity in LTC.
The current evidence does not suggest that any one strategy is more effective at improving physical activity, and it is likely that LTC homes will need to employ a combination of strategies to help residents move more. Additionally, residents’ preferences, goals, and capabilities should always be considered when designing an individualized physical activity plan. For example, if a resident does not like to be outdoors or gardening but enjoys dancing and music, then their physical activity plan should include group dance class and music therapy rather than gardening. LTC homes will need to have a menu of opportunities for movement that residents can choose from so that activities are pleasant and motivating, and therefore more likely to be completed.
Many of the interventions described in this review are safe and feasible to implement with residents who have physical or cognitive impairments. Function-focused care is scaled to the residents’ capabilities and did not increase the risk of falling, though LTC staff require the skills to scale physical activities appropriately.18 Likewise, group dance activities and music therapy were tested with residents with dementia, with no adverse events reported.21,24 However, more work is needed to determine the feasibility of implementing emerging methods, such as robotics and interactive technology, for increasing physical activity for residents with physical and cognitive impairments. Most studies to date have included mobile residents or those with minimal cognitive impairment. Similarly, outdoor garden spaces may be less safe for residents who use walkers or wheelchairs if there is an opportunity for them to slip off paths or get stuck in mud or mulch. LTC homes implementing any of these interventions should evaluate the benefits and risks of each intervention, the resources available within the home to support them (eg, trained staff), and the target residents’ physical and cognitive capabilities.
While increasing physical activity is important, structured exercise is needed to see gains in components of physical fitness such as strength, aerobic capacity, and balance. Indeed, one major consideration highlighted by the aforementioned task force is that every resident who does not have contraindications must also have a personalized multicomponent exercise program as part of their care plan.8 The task force recommends moderate- to high-intensity strength, aerobic, and balance exercises 2 times per week for 35 to 45 minutes per session.8 There is an interrelationship between physical activity and structured exercise: structured exercise programs can certainly be part of a physical activity plan, but physical activity can include more than structured exercise. Physical activity also includes any activity that involves movement, such as walking in gardens or between home areas, or physically participating more in personal care activities (eg, assisting with bathing or dressing).14 Both structured exercise and physical activity are important for LTC residents. Structured exercise provides an opportunity to improve strength and cardiovascular fitness, which aim to decrease the negative effects of sarcopenia and cardiovascular disease, such as disability and death.59,60 However, structured exercise should not be done daily for the same muscle groups.8 Rather, it is recommended for LTC residents to engage in structured exercise 2 times per week.8 Increasing physical activity is a daily goal, as daily physical activity decreases sedentary time, which has negative consequences such as decreased mood61 and increased mortality.62 LTC homes should incorporate strategies to both increase daily physical activity and promote individualized, structured exercise programs.
Conclusion
Residents in LTC spend much of their time in sedentary activities such as sitting or lying in bed. Physical activity is important to help decrease the negative effects of sedentary time, like poor mood and increased risk of death, and to improve physical function. This review describes several strategies to promote physical activity within LTC homes, such as leveraging daily activities and the physical environment, providing group activities, reducing physical and chemical restraint use, and using innovative technology such as robots. LTC homes can use the information in this review to plan strategies to promote physical activity.
Corresponding author: Caitlin McArthur, MScPT, PhD, Hamilton Health Sciences, St. Peter’s Hospital, 88 Maplewood Avenue, Hamilton, ON L8M 1W9; mcarthurc@hhsc.ca.
Financial disclosures: None.
From the Geriatric Education and Research in Aging Sciences (GERAS) Centre for Aging Research, McMaster University, Hamilton, ON.
Abstract
- Objective. To summarize the literature on improving opportunities for physical activity for residents in long-term care (LTC).
- Method. Narrative review of the literature.
- Results. Residents in LTC spend much of their time in sedentary activities such as sitting or lying in bed. Physical activity is important to help decrease the negative effects of sedentary time, such as poor mood and increased risk of death, and to improve physical function. This review identifies several strategies for promoting physical activity for LTC residents: incorporating simple strategies into daily activities, participating in group activities (eg, exercise, dance, or music therapy), using motivational strategies to encourage staff to promote activity, leveraging the physical environment, reducing physical and chemical restraints, and using innovative solutions such as robots or interactive technology.
- Conclusion. While the quality of evidence to date is limited, preliminary work suggests that the strategies identified in this article could be included as part of a multifactorial approach to increasing physical activity in LTC.
Keywords: long-term care; nursing homes; physical activity; sedentary; mobility.
The United Nations estimates that between 2013 and 2050 the population aged 60 years or older will double.1 Furthermore, the fastest growth rate will be seen in older adults over the age of 80 years.1 With this demographic shift, a growing number of older adults will require supportive housing, such as long-term care (LTC). Indeed, it is projected that the number of older adults requiring LTC will double by 2036.2
Residents in LTC are often medically complex and experience multimorbidity, cognitive impairment, and functional decline,3 making it difficult for them to engage in physical activity. LTC residents spend approximately 75% of their waking time in sedentary activities (eg, sitting, lying down, watching TV), which amounts to more than 12 hours per day.4-6 Residents with cognitive impairment are even more sedentary, spending as little as 1 minute per day in moderate physical activity and approximately 87% of their time in sedentary activities.7 Additionally, a high prevalence of use of psychotropic drugs and physical restraints contributes to high levels of physical inactivity for residents in LTC.8 Increased time spent in sedentary activities has been associated with adverse health outcomes, such as incidence of cardiovascular disease and type 2 diabetes, and mortality.9-11 Moreover, bed and chair rest are associated with muscle disuse, which can lead to functional impairment.12,13
Given the large amount of time LTC residents spend in sedentary activities and the negative consequences this has on their health, it is essential to find opportunities to engage residents in physical activity throughout the day. This article summarizes evidence about increasing opportunities for physical activity for LTC residents. Physical activity is defined as “any bodily movement produced by skeletal muscles that results in energy expenditure,” while exercise, which is a subset of physical activity, is purposefully planned, structured, and repetitive and has a goal of maintaining or improving physical fitness.14 Previous work has described exercise among LTC residents in detail,8,15,16 and thus exercise is not addressed here. Also, as a narrative review, this article provides an overview of available interventions to improve physical activity for LTC residents and does not provide comments on efficacy or an exhaustive list of potential interventions. Rather, it provides a starting point for LTC homes to consider when providing opportunities to improve physical activity for their residents.
Guidelines for Increasing Physical Activity
There are currently no published evidence-based guidelines for increasing physical activity and reducing sedentary time for residents of LTC homes. However, an international task force of experts in geriatrics, exercise, and LTC research convened in 2015 and made recommendations on this matter.8 They emphasize the importance of considering the needs of residents, family members, health care professionals, LTC staff, and policy-makers when designing strategies to promote movement in LTC.8 This will ensure that the strategies to promote movement will be realistic and sustainable. Additionally, the task force identified motivation and pleasure as key to engaging residents in physical activities, and recommended that interests and preferences should be used to guide the selection of activities.8 The following sections describe example strategies to improve physical activity for residents in LTC that LTC homes can use to help facilitate movement for their residents.
Strategies for Promoting Physical Activity
Leveraging Daily Activities
One approach to promoting physical activity in LTC homes is to systematically use simple strategies embedded within routine care to engage residents in movement.8 Function-focused, or restorative care,17 is a philosophy of care that promotes increasing physical activity and maintaining functional abilities based on the resident’s abilities. Examples include walking with residents to the dining room rather than pushing them in a wheelchair where appropriate, inviting residents to events that require them to leave their room, improving independent wheelchair propulsion for residents who cannot walk, and increasing opportunities for sit-to-stand activities where possible. These activities are scaled to the resident’s underlying physical and cognitive capabilities. A systematic review of function-focused care revealed that it can help maintain functional skills for residents in LTC, and there is no significant risk associated with implementation.18 In a study by Slaughter et al19 that examined the effectiveness of techniques to encourage mobility by residents’ usual caregivers, health care aides prompted residents to perform the sit-to-stand activity 4 times per day, with the number of repetitions individualized based on resident ability, fatigue, and motivation. Residents who completed the sit-to-stand activity had smaller declines in mobility and functional outcomes (ie, less decline on the Functional Independence Measure).19 This study included residents with Alzheimer’s disease and dementia who could transfer independently or with the assistance of one person,20 indicating that this type of intervention is feasible and appropriate for residents with cognitive impairment.
Group Activities
Group activities in LTC homes are another way of engaging residents in physical activity in a motivating and pleasant setting that also encourages social engagement among residents and LTC staff. Group exercise classes can be effective for improving mood and functional outcomes. For example, a systematic review of dance classes in LTC homes revealed an improvement in problematic behaviors, mood, cognition, communication, and socialization.21 Most studies included participants with dementia, and no adverse events were reported, supporting the feasibility and safety of implementing group dance activities for residents with cognitive impairment. Group exercise is the most common delivery method for exercise within LTC homes22 and has been demonstrated to have small positive effects on activities of daily living (ADL; ie, improvement in ADL independence equivalent to 1.3 points on the Barthel Index).23 Other group activities, such as music therapy, have demonstrated improvements in depressive symptoms, emotional well-being, and anxiety for LTC residents with dementia.24 Group activities also provide the opportunity for movement as residents leave their rooms, walk to a new location (if able), and return to their rooms when the activity is complete.
Barriers to Physical Activity and Strategies to Overcome Them
Caregiver-related Factors
LTC staff have limited time to spend promoting physical activity since residents often have complex health care needs and staffing levels are often constrained.25 Indeed, having lower staffing levels has been associated with lower levels of physical activity for residents.26,27 LTC staff have identified a lack of time to walk with residents28,29 and having other tasks to do (eg, clean) as barriers to promoting movement.28,29 However, asking residents to help staff with small household chores, such as folding laundry or clearing dishes, was a facilitator to promoting movement.30 Activating residents by helping them transfer to a wheelchair for independent mobilization around the home or by assisting them to walk where appropriate were also facilitators.30,31 Leveraging facilitators will help staff who have limited time to help residents engage in more physical activity.
Motivation of LTC staff can also be a barrier to encouraging physical activity for residents in LTC. Fear that increasing physical activity will cause adverse events like falls, illness, or exacerbation of symptoms often decreases motivation for staff to facilitate physical activity.32,33 Another potential barrier is the conceptualization of the role of nursing in LTC as protecting residents from harm by encouraging them to engage in “risk-free” activities like staying in bed.34-39 Strategies to increase staff motivation to engage LTC residents in physical activity that have been shown to be effective are verbal prompts, modelling behaviors, goal setting, and home champions to promote function-focused care.17,33,40-43
The Physical Environment
Aspects of the physical environment of LTC homes may facilitate or limit residents’ ability to be physically active. A 2017 systematic review examined elements of the physical environment that acted as barriers and facilitators to physical activity for older adults living in LTC.30 The authors found that the person-environment fit, security, accessibility, and comfort were key components of the physical environment that were associated with residents’ physical activity levels.30 First, an appropriate fit between the residents’ abilities and the demands of the environment was related to improved activity as measured by actigraphy.44 For example, having long hallways between residents’ rooms and common spaces discourages residents who can only walk short distances from walking to these locations. However, residents were more active in larger-scaled LTC homes with shorter distances between different areas (eg, resident rooms and dining rooms).45 Clearly, there must be enough space to encourage walking between areas, but not so much space that walking is not feasible. Residents participating in a focus group identified accessibility and comfort features as being facilitators for walking in the corridor, such as wide corridors, sturdy handrails, carpet, chairs placed at short intervals for seated breaks, windows to look out, plants, and accessible activity rooms and restrooms.45,46 On the other hand, limited things to see and do indoors and outdoors, along with restricted walking areas, were identified as barriers to corridor walking by residents.46
One method for optimizing LTC home architecture to promote movement is to provide therapeutic outdoor spaces, such as gardens. Indeed, therapeutic gardens have been studied as a nonpharmacological method of engaging LTC residents with dementia and have been shown to benefit mood, pain, and fall prevention.47 Secure therapeutic gardens or outdoor spaces provide opportunities for various activities to increase movement, including gardening, animal care, and walking.48 However, there is a higher propensity for residents who use walkers or wheelchairs to slide off paths or become stuck in mud or mulch.49 Residents with physical limitations may require additional supervision in garden spaces, and as such spaces should be designed with improved safety in mind (eg, barriers between paths and places where mud could accumulate). The number of available indoor (eg, a physical therapy gym) and outdoor (eg, gardens) spaces was also found to be positively related to residents’ physical activity levels.50 However, these relationships were mediated by the number of activity programs available in the LTC homes.50 Therefore, having staff available to facilitate activities is also important for promoting physical activity.
Chemical and Physical Restraints
Physical and chemical restraints (eg, antipsychotics and sedatives) are sometimes used to manage the behavioral and psychological symptoms of dementia,51,52 which many residents in LTC experience.3 Though there has been an emphasis in North America to decrease their use, physical and chemical restraints are still used in LTC.53 Physical restraint use is associated with a higher risk of functional and cognitive decline.53,54 Residents who are both physically and chemically restrained through antipsychotic use are at even higher risk for these declines.54 Thus, to improve opportunities for movement in LTC, physical restraint use should be minimized. The risks and benefits of using psychotropic medications that often decrease residents’ physical activity levels must be evaluated individually, and other nonpharmacological strategies should be used to manage the behavioral and psychological symptoms of dementia. These could include functional analysis-based interventions (ie, individualized interventions aimed at identifying unmet needs, causes, antecedents, and consequences of the behavior),55 music therapy,55 or other interventions described above.
Emerging Innovative Interventions
Robots are an emerging nonpharmacological intervention for improving the behavioral and psychological symptoms of dementia and facilitating physical activity in LTC. Robotic animal interventions, where LTC residents interact with robotic animals in an individual or group setting, have been shown to reduce negative behaviors and increase positive mood.56 Additionally, robots are being used in rehabilitation to provide exercise post-stroke57 and could easily be transitioned to do similar tasks in LTC. Robotic interventions are attractive for the LTC sector as they could help relieve the workload demands on an often overloaded sector, and, in the case of pet therapy, surmount regulations for bringing live animals into a LTC home. Though studies examining the use of robots in LTC have mainly focused on the effect of pet therapy on reducing behavioral symptoms, the use of robots to promote physical activity and exercise in LTC is a natural progression for the work that has been done in inpatient rehabilitation.57 On a similar note, an interactive technology (similar to a Kinect system) used to promote 30-minute, twice-weekly physical activity sessions has demonstrated improvements in physical function (Short Physical Performance Battery [SPPB]) for pre-disabled (SPPB of 6 to 9) residents in LTC without dementia.58 The role of technology to promote physical activity in LTC is an emerging area of interest, and future innovations in this area will continue to help facilitate movement.
Quality of Evidence
Most studies aimed at improving physical activity for LTC residents to date are small, have nonrandomized designs, and have limited generalizability and evidence to support the efficacy of the interventions. For example, most studies included in systematic reviews for function-focused care, dance, group exercise, and music therapy are small, observational, or quasi-experimental studies with methodological issues resulting in bias.18,21,23,24 Likewise, the evidence surrounding nonpharmacological interventions for reducing behavioral and psychological symptoms of dementia is of very low to moderate quality.55 Innovative interventions, such as robotics and interactive technology, to promote physical activity in LTC are in their infancy. There are no data syntheses available to date to summarize the available literature on this topic, and conclusions rely on small, nonrandomized designs or extrapolations of results from similar sectors (eg, inpatient rehabilitation). Thus, the studies described in this review can be used as preliminary evidence to support the implementation of interventions to improve physical activity, but discretion should be used when interpreting the efficacy of these interventions.
Discussion
This review identifies several strategies for promoting physical activity for LTC residents, including incorporating simple strategies into daily activities, participating in group activities (eg, exercise, dance, or music therapy), using motivational strategies to encourage staff to promote activity, leveraging the physical environment, reducing physical and chemical restraints, and using innovation solutions like robots or interactive technology. While the quality of evidence to date is limited, preliminary work suggests that strategies identified in this paper could be included as part of a multifactorial approach to increasing physical activity in LTC.
The current evidence does not suggest that any one strategy is more effective at improving physical activity, and it is likely that LTC homes will need to employ a combination of strategies to help residents move more. Additionally, residents’ preferences, goals, and capabilities should always be considered when designing an individualized physical activity plan. For example, if a resident does not like to be outdoors or gardening but enjoys dancing and music, then their physical activity plan should include group dance class and music therapy rather than gardening. LTC homes will need to have a menu of opportunities for movement that residents can choose from so that activities are pleasant and motivating, and therefore more likely to be completed.
Many of the interventions described in this review are safe and feasible to implement with residents who have physical or cognitive impairments. Function-focused care is scaled to the residents’ capabilities and did not increase the risk of falling, though LTC staff require the skills to scale physical activities appropriately.18 Likewise, group dance activities and music therapy were tested with residents with dementia, with no adverse events reported.21,24 However, more work is needed to determine the feasibility of implementing emerging methods, such as robotics and interactive technology, for increasing physical activity for residents with physical and cognitive impairments. Most studies to date have included mobile residents or those with minimal cognitive impairment. Similarly, outdoor garden spaces may be less safe for residents who use walkers or wheelchairs if there is an opportunity for them to slip off paths or get stuck in mud or mulch. LTC homes implementing any of these interventions should evaluate the benefits and risks of each intervention, the resources available within the home to support them (eg, trained staff), and the target residents’ physical and cognitive capabilities.
While increasing physical activity is important, structured exercise is needed to see gains in components of physical fitness such as strength, aerobic capacity, and balance. Indeed, one major consideration highlighted by the aforementioned task force is that every resident who does not have contraindications must also have a personalized multicomponent exercise program as part of their care plan.8 The task force recommends moderate- to high-intensity strength, aerobic, and balance exercises 2 times per week for 35 to 45 minutes per session.8 There is an interrelationship between physical activity and structured exercise: structured exercise programs can certainly be part of a physical activity plan, but physical activity can include more than structured exercise. Physical activity also includes any activity that involves movement, such as walking in gardens or between home areas, or physically participating more in personal care activities (eg, assisting with bathing or dressing).14 Both structured exercise and physical activity are important for LTC residents. Structured exercise provides an opportunity to improve strength and cardiovascular fitness, which aim to decrease the negative effects of sarcopenia and cardiovascular disease, such as disability and death.59,60 However, structured exercise should not be done daily for the same muscle groups.8 Rather, it is recommended for LTC residents to engage in structured exercise 2 times per week.8 Increasing physical activity is a daily goal, as daily physical activity decreases sedentary time, which has negative consequences such as decreased mood61 and increased mortality.62 LTC homes should incorporate strategies to both increase daily physical activity and promote individualized, structured exercise programs.
Conclusion
Residents in LTC spend much of their time in sedentary activities such as sitting or lying in bed. Physical activity is important to help decrease the negative effects of sedentary time, like poor mood and increased risk of death, and to improve physical function. This review describes several strategies to promote physical activity within LTC homes, such as leveraging daily activities and the physical environment, providing group activities, reducing physical and chemical restraint use, and using innovative technology such as robots. LTC homes can use the information in this review to plan strategies to promote physical activity.
Corresponding author: Caitlin McArthur, MScPT, PhD, Hamilton Health Sciences, St. Peter’s Hospital, 88 Maplewood Avenue, Hamilton, ON L8M 1W9; mcarthurc@hhsc.ca.
Financial disclosures: None.
1. United Nations Department of Economic and Social Affairs Population Division. World Population Ageing 2013. New York, NY: United Nations; 2013.
2. Pickard L, Comas-Herrera A, Costa-Font J, et al. Modelling an entitlement to long-term care services for older people in Europe: projections for long-term care expenditure to 2050. J Eur Soc Policy. 2007;17:33-48.
3. Hirdes JP, Mitchell L, Maxwell CJ, White N. Beyond the “iron lungs of gerontology”: Using evidence to shape the future of nursing homes in Canada. Can J Aging. 2011;30:371-390.
4. Chin A Paw MJM, van Poppel MNM, van Mechelen W. Effects of resistance and functional-skills training on habitual activity and constipation among older adults living in long-term care facilities: a randomized controlled trial. BMC Geriatr. 2006;6:9.
5. Ikezoe T, Asakawa Y, Shima H, Kishibuchi K, Ichihashi N. Daytime physical activity patterns and physical fitness in institutionalized elderly women: an exploratory study. Arch Gerontol Geriatr. 2013;57:221-225.
6. Keogh JW, Senior H, Beller EM, Henwood T. Prevalence and risk factors for low habitual walking speed in nursing home residents: an observational study. Arch Phys Med Rehabil. 2015;96:1993-1999.
7. Marmeleira J, Ferreira S, Raimundo A. Physical activity and physical fitness of nursing home residents with cognitive impairment: A pilot study. Exp Gerontol. 2017;100:63-69.
8. de Souto Barreto P, Morley JE, Chodzko-Zajko W, et al. Recommendations on physical activity and exercise for older adults living in long-term care facilities: a taskforce report. J Am Med Dir Assoc. 2016;17:381-392.
9. van der Ploeg HP, Chey T, Korda RJ, et al. Sitting time and all-cause mortality risk in 222 497 Australian adults. Arch Intern Med. 2012;172:494-500.
10. Chau JY, Grunseit AC, Chey T, et al. Daily sitting time and all-cause mortality: a meta-analysis. PLoS One. 2013;8:e80000.
11. Grøntved A, Hu FB. Television viewing and risk of type 2 diabetes, cardiovascular disease, and all-cause mortality: a meta-analysis. JAMA. 2011;305:2448-2455.
12. Senior HE, Henwood TR, Beller EM, et al. Prevalence and risk factors of sarcopenia among adults living in nursing homes. Maturitas. 2015;82:418-423.
13. Wall BT, Dirks ML, van Loon LJC. Skeletal muscle atrophy during short-term disuse: implications for age-related sarcopenia. Ageing Res Rev. 2013;12:898-906.
14. Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100:126-131.
15. McArthur C, Giangregorio LM. Improving strength and balance for long-term care residents at risk for falling: Suggestions for practice. J Clin Outcomes Manag. 2018;25:28-38.
16. Crocker T, Forster A, Young J, et al. Physical rehabilitation for older people in long-term care. Cochrane Database Syst Rev. 2013;2:CD004294.
17. Resnick B, Galik E, Boltz M, Pretzer-Aboff IE. Implementing Restorative Care Nursing in All Settings. 2nd ed. New York, NY: Spring Publishing Company; 2011.
18. Resnick B, Galik E, Boltz M. Function focused care approaches: literature review of progress and future possibilities. J Am Med Dir Assoc. 2013;14:313-318.
19. Slaughter SE, Estabrooks CA, Jones CA, Wagg AS. Mobility of Vulnerable Elders (MOVE): study protocol to evaluate the implementation and outcomes of a mobility intervention in long-term care facilities. BMC Geriatr. 2011;11:84.
20. Slaughter SE, Wagg AS, Jones CA, et al. Mobility of Vulnerable Elders study: effect of the sit-to-stand activity on mobility, function, and quality of life. J Am Med Dir Assoc. 2015;16(2):138-143.
21. Guzmán-García A, Hughes JC, James IA, Rochester L. Dancing as a psychosocial intervention in care homes: a systematic review of the literature. Int J Geriatr Psychiatry. 2013;28:914-924.
22. McArthur C, Gibbs JC, Patel R, et al. A scoping review of physical rehabilitation in long-term care: interventions, outcomes, tools. Can J Aging/La Rev Can du Vieil. 2017;36:435-452.
23. Crocker T, Young J, Forster A, et al. The effect of physical rehabilitation on activities of daily living in older residents of long-term care facilities: Systematic review with meta-analysis. Age Ageing. 2013;42:682-688.
24. van der Steen JT, Smaling HJ, van der Wouden JC, et al. Music-based therapeutic interventions for people with dementia. Cochrane Database Syst Rev. 2018;7:CD003477.
25. Froggatt K, Davies S, Meyer J. Understanding Care Homes, A Research and Development Perspective. London: Jessica Kingsley Publishers; 2009.
26. Shore BA, Lerman DC, Smith RG, et al. Direct assessment of quality of care in a geriatric nursing home. J Appl Behav Anal. 1995;28:435-448.
27. Bates-Jensen BM, Schnelle JF, Alessi CA, et al. The effects of staffing on in-bed times of nursing home residents. J Am Geriatr Soc. 2004;52:931-938.
28. Ericson-Lidman E, Renström A-S, Åhlin J, Strandberg G. Relatives’ perceptions of residents’ life in a municipal care facility for older people with a focus on quality of life and care environment. Int J Older People Nurs. 2015;10:160-169.
29. Häggström E, Kihlgren A, Kihlgren M, Sörlie V. Relatives’ struggle for an improved and more just care for older people in community care. J Clin Nurs. 2007;16:1749-1757.
30. Douma JG, Volkers KM, Engels G, et al. Setting-related influences on physical inactivity of older adults in residential care settings: a review. BMC Geriatr. 2017;17:97.
31. Zegelin A. ’Tied down’- the process of becoming bedridden through gradual local confinement. J Clin Nurs. 2008;17:2294-2301.
32. Resnick B, Galik E, Gruber-Baldini AL, Zimmerman S. Falls and fall-related injuries associated with function-focused care. Clin Nurs Res. 2012;21:43-63.
33. Pretzer-Aboff I, Galik E. Feasibility and impact of a function focused care intervention for Parkinson’s disease in the community. Nursing Res. 2011;60:276-283.
34. Leditschke IA, Green M, Irvine J, et al. What are the barriers to mobilizing intensive care patients? Cardiopulm Phys Ther J. 2012;23:26-29.
35. Mittmann N, Seung SJ, Pisterzi LF, et al. Nursing workload associated with hospital patient care. Dis Manag Heal Outcomes. 2008;16:53-61.
36. Dykes PC, Carroll DL, Hurley AC, et al. Why do patients in acute care hospitals fall? Can falls be prevented? J Nurs Adm. 2009;39:299-304.
37. Brownie S, Nancarrow S. Effects of person-centered care on residents and staff in aged-care facilities: a systematic review. Clin Interv Aging. 2013;8:1-10.
38. Wakefield BJ, Holman JE. Functional trajectories associated with hospitalization in older adults. West J Nurs Res. 2007;29:161-177.
39. Boltz M, Resnick B, Capezuti E, Shuluk J. Activity restriction vs. self-direction: hospitalised older adults’ response to fear of falling. Int J Older People Nurs. 2014;9:44-53.
40. Resnick B, Galik E, Gruber-Baldini A, Zimmerman S. Testing the effect of function-focused care in assisted living. J Am Geriatr Soc. 2011;59:2233-2240.
41. Galik EM, Resnick B, Gruber-Baldini A, et al. Pilot testing of the restorative care intervention for the cognitively impaired. J Am Med Dir Assoc. 2008;9:516-522.
42. Resnick B, Galik E, Gruber-Baldini AL, Zimmerman S. Implementing a restorative care philosophy of care in assisted living: pilot testing of Res-Care-AL. J Am Acad Nurse Pract. 2009;21:123-133.
43. Resnick B, Gruber-Baldini AL, Zimmerman S, et al. Nursing home resident outcomes from the Res-Care intervention. J Am Geriatr Soc. 2009;57:1156-1165.
44. Pomeroy SH, Scherer Y, Runkawatt V, et al. Person-environment fit and functioning among older adults in a long-term care setting. Geriatr Nurs. 2011;32:368-378.
45. Moos RH, David TG, Lemke S, Postle E. Coping with an intra-institutional relocation: changes in resident and staff behavior patterns. Gerontologist. 1984;24:495-502.
46. Lu Z, Rodiek SD, Shepley MM, Duffy M. Influences of physical environment on corridor walking among assisted living residents. J Appl Gerontol. 2011;30:463-484.
47. Detweiler MB, Sharma T, Detweiler JG, et al. What is the evidence to support the use of therapeutic gardens for the elderly? Psychiatry Investig. 2012;9:100.
48. Blake M, Mitchell G. Horticultural therapy in dementia care: a literature review. Nurs Stand. 2016;30:41-47.
49. Detweiler MB, Murphy PF, Myers LC, Kim KY. Does a wander garden influence inappropriate behaviors in dementia residents? Am J Alzheimers Dis Other Demen. 2008;23:31-45.
50. Joseph A, Zimring C, Harris-Kojetin L, Kiefer K. Presence and visibility of outdoor and indoor physical activity features and participation in physical activity among older adults in retirement communities. J Hous Elderly. 2006;19:141-165.
51. Feng Z, Hirdes JP, Smith TF, et al. Use of physical restraints and antipsychotic medications in nursing homes: a cross-national study. Int J Geriatr Psychiatry. 2009;24:1110-1118.
52. Herrmann N. Recommendations for the management of behavioral and psychological symptoms of dementia. Can J Neurol Sci. 2001;28 Suppl 1:S96-107.
53. Freeman S, Spirgiene L, Martin-Khan M, Hirdes JP. Relationship between restraint use, engagement in social activity, and decline in cognitive status among residents newly admitted to long-term care facilities. Geriatr Gerontol Int. 2017;17:246-255.
54. Foebel AD, Onder G, Finne-Soveri H, et al. Physical restraint and antipsychotic medication use among nursing home residents with dementia. J Am Med Dir Assoc. 2016;17:184.e9-184.e14.
55. Dyer SM, Harrison SL, Laver K, Whitehead C, Crotty M. An overview of systematic reviews of pharmacological and non-pharmacological interventions for the treatment of behavioral and psychological symptoms of dementia. Int Psychogeriatr. 2018;30:295-309.
56. Robinson H, MacDonald B, Kerse N, Broadbent E. The psychosocial effects of a companion robot: a randomized controlled trial. J Am Med Dir Assoc. 2013;14:661-667.
57. Lo K, Stephenson M, Lockwood C. Effectiveness of robotic assisted rehabilitation for mobility and functional ability in adult stroke patients. JBI Database System Rev Implement Rep. 2017;15:3049-3091.
58. Valiani V, Lauzé M, Martel D, et al. A new adaptive home-based exercise technology among older adults living in nursing home: a pilot study on feasibility, acceptability and physical performance. J Nutr Health Aging. 2017;21:819-824.
59. Locquet M, Beaudart C, Hajaoui M, et al. Three-year adverse health consequences of sarcopenia in community-dwelling older adults according to 5 diagnosis definitions. J Am Med Dir Assoc. 2019;20:43-46.e2.
60. Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, et al. Exercise and physical activity for older adults. Med Sci Sports Exerc. 2009;41:1510-1530.
61. Park S-Y, Lee K, Um YJ, Paek S, Ryou IS. Association between physical activity and depressive mood among Korean adults with chronic diseases. Korean J Fam Med. 2018;39:185-190.
62. Loprinzi PD. Light-intensity physical activity and all-cause mortality. Am J Health Promot. 2017;31:340-342.
1. United Nations Department of Economic and Social Affairs Population Division. World Population Ageing 2013. New York, NY: United Nations; 2013.
2. Pickard L, Comas-Herrera A, Costa-Font J, et al. Modelling an entitlement to long-term care services for older people in Europe: projections for long-term care expenditure to 2050. J Eur Soc Policy. 2007;17:33-48.
3. Hirdes JP, Mitchell L, Maxwell CJ, White N. Beyond the “iron lungs of gerontology”: Using evidence to shape the future of nursing homes in Canada. Can J Aging. 2011;30:371-390.
4. Chin A Paw MJM, van Poppel MNM, van Mechelen W. Effects of resistance and functional-skills training on habitual activity and constipation among older adults living in long-term care facilities: a randomized controlled trial. BMC Geriatr. 2006;6:9.
5. Ikezoe T, Asakawa Y, Shima H, Kishibuchi K, Ichihashi N. Daytime physical activity patterns and physical fitness in institutionalized elderly women: an exploratory study. Arch Gerontol Geriatr. 2013;57:221-225.
6. Keogh JW, Senior H, Beller EM, Henwood T. Prevalence and risk factors for low habitual walking speed in nursing home residents: an observational study. Arch Phys Med Rehabil. 2015;96:1993-1999.
7. Marmeleira J, Ferreira S, Raimundo A. Physical activity and physical fitness of nursing home residents with cognitive impairment: A pilot study. Exp Gerontol. 2017;100:63-69.
8. de Souto Barreto P, Morley JE, Chodzko-Zajko W, et al. Recommendations on physical activity and exercise for older adults living in long-term care facilities: a taskforce report. J Am Med Dir Assoc. 2016;17:381-392.
9. van der Ploeg HP, Chey T, Korda RJ, et al. Sitting time and all-cause mortality risk in 222 497 Australian adults. Arch Intern Med. 2012;172:494-500.
10. Chau JY, Grunseit AC, Chey T, et al. Daily sitting time and all-cause mortality: a meta-analysis. PLoS One. 2013;8:e80000.
11. Grøntved A, Hu FB. Television viewing and risk of type 2 diabetes, cardiovascular disease, and all-cause mortality: a meta-analysis. JAMA. 2011;305:2448-2455.
12. Senior HE, Henwood TR, Beller EM, et al. Prevalence and risk factors of sarcopenia among adults living in nursing homes. Maturitas. 2015;82:418-423.
13. Wall BT, Dirks ML, van Loon LJC. Skeletal muscle atrophy during short-term disuse: implications for age-related sarcopenia. Ageing Res Rev. 2013;12:898-906.
14. Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100:126-131.
15. McArthur C, Giangregorio LM. Improving strength and balance for long-term care residents at risk for falling: Suggestions for practice. J Clin Outcomes Manag. 2018;25:28-38.
16. Crocker T, Forster A, Young J, et al. Physical rehabilitation for older people in long-term care. Cochrane Database Syst Rev. 2013;2:CD004294.
17. Resnick B, Galik E, Boltz M, Pretzer-Aboff IE. Implementing Restorative Care Nursing in All Settings. 2nd ed. New York, NY: Spring Publishing Company; 2011.
18. Resnick B, Galik E, Boltz M. Function focused care approaches: literature review of progress and future possibilities. J Am Med Dir Assoc. 2013;14:313-318.
19. Slaughter SE, Estabrooks CA, Jones CA, Wagg AS. Mobility of Vulnerable Elders (MOVE): study protocol to evaluate the implementation and outcomes of a mobility intervention in long-term care facilities. BMC Geriatr. 2011;11:84.
20. Slaughter SE, Wagg AS, Jones CA, et al. Mobility of Vulnerable Elders study: effect of the sit-to-stand activity on mobility, function, and quality of life. J Am Med Dir Assoc. 2015;16(2):138-143.
21. Guzmán-García A, Hughes JC, James IA, Rochester L. Dancing as a psychosocial intervention in care homes: a systematic review of the literature. Int J Geriatr Psychiatry. 2013;28:914-924.
22. McArthur C, Gibbs JC, Patel R, et al. A scoping review of physical rehabilitation in long-term care: interventions, outcomes, tools. Can J Aging/La Rev Can du Vieil. 2017;36:435-452.
23. Crocker T, Young J, Forster A, et al. The effect of physical rehabilitation on activities of daily living in older residents of long-term care facilities: Systematic review with meta-analysis. Age Ageing. 2013;42:682-688.
24. van der Steen JT, Smaling HJ, van der Wouden JC, et al. Music-based therapeutic interventions for people with dementia. Cochrane Database Syst Rev. 2018;7:CD003477.
25. Froggatt K, Davies S, Meyer J. Understanding Care Homes, A Research and Development Perspective. London: Jessica Kingsley Publishers; 2009.
26. Shore BA, Lerman DC, Smith RG, et al. Direct assessment of quality of care in a geriatric nursing home. J Appl Behav Anal. 1995;28:435-448.
27. Bates-Jensen BM, Schnelle JF, Alessi CA, et al. The effects of staffing on in-bed times of nursing home residents. J Am Geriatr Soc. 2004;52:931-938.
28. Ericson-Lidman E, Renström A-S, Åhlin J, Strandberg G. Relatives’ perceptions of residents’ life in a municipal care facility for older people with a focus on quality of life and care environment. Int J Older People Nurs. 2015;10:160-169.
29. Häggström E, Kihlgren A, Kihlgren M, Sörlie V. Relatives’ struggle for an improved and more just care for older people in community care. J Clin Nurs. 2007;16:1749-1757.
30. Douma JG, Volkers KM, Engels G, et al. Setting-related influences on physical inactivity of older adults in residential care settings: a review. BMC Geriatr. 2017;17:97.
31. Zegelin A. ’Tied down’- the process of becoming bedridden through gradual local confinement. J Clin Nurs. 2008;17:2294-2301.
32. Resnick B, Galik E, Gruber-Baldini AL, Zimmerman S. Falls and fall-related injuries associated with function-focused care. Clin Nurs Res. 2012;21:43-63.
33. Pretzer-Aboff I, Galik E. Feasibility and impact of a function focused care intervention for Parkinson’s disease in the community. Nursing Res. 2011;60:276-283.
34. Leditschke IA, Green M, Irvine J, et al. What are the barriers to mobilizing intensive care patients? Cardiopulm Phys Ther J. 2012;23:26-29.
35. Mittmann N, Seung SJ, Pisterzi LF, et al. Nursing workload associated with hospital patient care. Dis Manag Heal Outcomes. 2008;16:53-61.
36. Dykes PC, Carroll DL, Hurley AC, et al. Why do patients in acute care hospitals fall? Can falls be prevented? J Nurs Adm. 2009;39:299-304.
37. Brownie S, Nancarrow S. Effects of person-centered care on residents and staff in aged-care facilities: a systematic review. Clin Interv Aging. 2013;8:1-10.
38. Wakefield BJ, Holman JE. Functional trajectories associated with hospitalization in older adults. West J Nurs Res. 2007;29:161-177.
39. Boltz M, Resnick B, Capezuti E, Shuluk J. Activity restriction vs. self-direction: hospitalised older adults’ response to fear of falling. Int J Older People Nurs. 2014;9:44-53.
40. Resnick B, Galik E, Gruber-Baldini A, Zimmerman S. Testing the effect of function-focused care in assisted living. J Am Geriatr Soc. 2011;59:2233-2240.
41. Galik EM, Resnick B, Gruber-Baldini A, et al. Pilot testing of the restorative care intervention for the cognitively impaired. J Am Med Dir Assoc. 2008;9:516-522.
42. Resnick B, Galik E, Gruber-Baldini AL, Zimmerman S. Implementing a restorative care philosophy of care in assisted living: pilot testing of Res-Care-AL. J Am Acad Nurse Pract. 2009;21:123-133.
43. Resnick B, Gruber-Baldini AL, Zimmerman S, et al. Nursing home resident outcomes from the Res-Care intervention. J Am Geriatr Soc. 2009;57:1156-1165.
44. Pomeroy SH, Scherer Y, Runkawatt V, et al. Person-environment fit and functioning among older adults in a long-term care setting. Geriatr Nurs. 2011;32:368-378.
45. Moos RH, David TG, Lemke S, Postle E. Coping with an intra-institutional relocation: changes in resident and staff behavior patterns. Gerontologist. 1984;24:495-502.
46. Lu Z, Rodiek SD, Shepley MM, Duffy M. Influences of physical environment on corridor walking among assisted living residents. J Appl Gerontol. 2011;30:463-484.
47. Detweiler MB, Sharma T, Detweiler JG, et al. What is the evidence to support the use of therapeutic gardens for the elderly? Psychiatry Investig. 2012;9:100.
48. Blake M, Mitchell G. Horticultural therapy in dementia care: a literature review. Nurs Stand. 2016;30:41-47.
49. Detweiler MB, Murphy PF, Myers LC, Kim KY. Does a wander garden influence inappropriate behaviors in dementia residents? Am J Alzheimers Dis Other Demen. 2008;23:31-45.
50. Joseph A, Zimring C, Harris-Kojetin L, Kiefer K. Presence and visibility of outdoor and indoor physical activity features and participation in physical activity among older adults in retirement communities. J Hous Elderly. 2006;19:141-165.
51. Feng Z, Hirdes JP, Smith TF, et al. Use of physical restraints and antipsychotic medications in nursing homes: a cross-national study. Int J Geriatr Psychiatry. 2009;24:1110-1118.
52. Herrmann N. Recommendations for the management of behavioral and psychological symptoms of dementia. Can J Neurol Sci. 2001;28 Suppl 1:S96-107.
53. Freeman S, Spirgiene L, Martin-Khan M, Hirdes JP. Relationship between restraint use, engagement in social activity, and decline in cognitive status among residents newly admitted to long-term care facilities. Geriatr Gerontol Int. 2017;17:246-255.
54. Foebel AD, Onder G, Finne-Soveri H, et al. Physical restraint and antipsychotic medication use among nursing home residents with dementia. J Am Med Dir Assoc. 2016;17:184.e9-184.e14.
55. Dyer SM, Harrison SL, Laver K, Whitehead C, Crotty M. An overview of systematic reviews of pharmacological and non-pharmacological interventions for the treatment of behavioral and psychological symptoms of dementia. Int Psychogeriatr. 2018;30:295-309.
56. Robinson H, MacDonald B, Kerse N, Broadbent E. The psychosocial effects of a companion robot: a randomized controlled trial. J Am Med Dir Assoc. 2013;14:661-667.
57. Lo K, Stephenson M, Lockwood C. Effectiveness of robotic assisted rehabilitation for mobility and functional ability in adult stroke patients. JBI Database System Rev Implement Rep. 2017;15:3049-3091.
58. Valiani V, Lauzé M, Martel D, et al. A new adaptive home-based exercise technology among older adults living in nursing home: a pilot study on feasibility, acceptability and physical performance. J Nutr Health Aging. 2017;21:819-824.
59. Locquet M, Beaudart C, Hajaoui M, et al. Three-year adverse health consequences of sarcopenia in community-dwelling older adults according to 5 diagnosis definitions. J Am Med Dir Assoc. 2019;20:43-46.e2.
60. Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, et al. Exercise and physical activity for older adults. Med Sci Sports Exerc. 2009;41:1510-1530.
61. Park S-Y, Lee K, Um YJ, Paek S, Ryou IS. Association between physical activity and depressive mood among Korean adults with chronic diseases. Korean J Fam Med. 2018;39:185-190.
62. Loprinzi PD. Light-intensity physical activity and all-cause mortality. Am J Health Promot. 2017;31:340-342.
Multicomponent Exercise Program Can Reverse Hospitalization-Associated Functional Decline in Elderly Patients
Study Overview
Objective. To assess the effects of an individualized, multicomponent exercise intervention on the functional status of very elderly patients who were acutely hospitalized compared with those who received usual care.
Design. A single-center, single-blind randomized clinical trial comparing elderly (≥ 75 years old) hospitalized patients who received in-hospital exercise (ie, individualized low-intensity resistance, balance, and walking exercises) versus control (ie, usual care that included physical rehabilitation if needed) interventions. The exercise intervention was adapted from the multicomponent physical exercise program Vivifrail and was supervised and conducted by a fitness specialist in 2 daily (1 morning and 1 evening) sessions lasting 20 minutes for 5 to 7 consecutive days. The morning session consisted of supervised and individualized progressive resistance, balance, and walking exercises. The evening session consisted of functional unsupervised exercises including light weights, extension and flexion of knee and hip, and walking.
Setting and participants. The study was conducted in an acute care unit in a tertiary public hospital in Navarra, Spain, between 1 February 2015 and 30 August 2017. A total of 370 elderly patients undergoing acute care hospitalization were enrolled in the study and randomly assigned to receive in-hospital exercise or control intervention. Inclusion criteria were: age ≥ 75 years, Barthel Index score ≥ 60, and ambulatory with or without assistance.
Main outcome measures. The primary outcome was change in functional capacity from baseline (beginning of exercise or control intervention) to hospital discharge as assessed by the Barthel Index of independence and the Short Physical Performance Battery (SPPB). Secondary outcomes were changes in cognitive capacity (Mini-Mental State Examination [MMSE]) and mood status (Yesavage Geriatric Depression Scale [GDS]), quality of life (QoL; EuroQol-5D), handgrip strength (dominant hand), incident delirium (Confusion Assessment Method), length of stay (LOS), falls during hospitalization, transfer after discharge, and readmission rate and mortality at 3 months after discharge. Intention-to-treat analysis was conducted.
Main results. Of the 370 patients included in the study’s analyses, 209 (56.5%) were women, mean age was 87.3 ± 4.9 years (range, 75-101 years; 130 [35.1%] nonagenarians). The median LOS was 8 days in both groups (interquartile range [IQR], 4 and 4 days, respectively). The median duration of the intervention was 5 days (IQR, 0 days), with 5 ± 1 morning and 4 ± 1 evening sessions in the exercise group. Adherence to the exercise intervention was high (95.8% for morning sessions; 83.4% for evening sessions), and no adverse effects were observed with the intervention.
The in-hospital exercise intervention program yielded significant benefits over usual care in functional outcomes in elderly patients. The exercise group had an increased change in measures of functional capacity compared to the usual care group (ie, Barthel Index, 6.9 points; 95% confidence interval [CI], 4.4-9.5; SPPB score, 2.2 points; 95% CI, 1.7-2.6). Furthermore, acute hospitalization led to an impairment in functional capacity from baseline to discharge in the Barthel Index (−5.0 points; 95% CI, −6.8 to −3.2) in the usual care group. In contrast, exercise intervention reversed this decline and improved functional outcomes as assessed by Barthel Index (1.9 points; 95% CI, 0.2-3.7) and SPPB score (2.4 points; 95% CI, 2.1-2.7).
The beneficial effects of the in-hospital exercise intervention extended to secondary end points indicative of cognitive capacity (MMSE, 1.8 points; 95% CI, 1.3-2.3), mood status (GDS, −2.0 points; 95% CI, −2.5 to −1.6), QoL (EuroQol-5D, 13.2 points; 95% CI, 8.2-18.2), and handgrip strength (2.3 kg; 95% CI, 1.8-2.8) compared to those who received usual care. In contrast, no differences were observed between groups that received exercise intervention and usual care in incident delirium, LOS, falls during hospitalization, transfer after discharge, and 3-month hospital readmission rate and mortality.
Conclusion. An individualized, multicomponent physical exercise program that includes low-intensity resistance, balance, and walking exercises performed during the course of hospitalization (average of 5 days) can reverse functional decline associated with acute hospitalization in very elderly patients. Furthermore, this in-hospital exercise intervention is safe and has a high adherence rate, and thus represents an opportunity to improve quality of care in this vulnerable population.
Commentary
Frail elderly patients are highly susceptible to adverse outcomes of acute hospitalization, including functional decline, disability, nursing home placement, rehospitalization, and mortality.1 Mobility limitation, a major hazard of hospitalization, has been associated with poorer functional recovery and increased vulnerability to these major adverse events after hospital discharge.2-4 Interdisciplinary care models delivered during hospitalization (eg, Geriatric Evaluation Unit, Acute Care for Elders) that emphasize functional independence and provide protocols for exercise and rehabilitation have demonstrated reduced hospital LOS, discharge to nursing home, and mortality, and improved functional status in elderly patients.5-7 Despite this evidence, significant gaps in knowledge exist in understanding whether early implementation of an individualized, multicomponent exercise training program can benefit the oldest old patients who are acutely hospitalized.
This study reported by Martinez-Velilla and colleagues provides an important and timely investigation in examining the effects of an individualized, multicomponent (ie, low-intensity resistance, balance, and walking) in-hospital exercise intervention on functional outcomes of hospitalized octogenarians and nonagenarians. The authors reported that such an intervention, administered 2 sessions per day for 5 to 7 consecutive days, can be safely implemented and reverse functional decline (ie, improvement in Barthel Index and SPPB score over course of hospital stay) typically associated with acute hospitalization in these vulnerable individuals. These findings are particularly significant given the paucity of randomized controlled trials evaluating the impact of exercise intervention in preserving functional capacity of geriatric patients in the setting of acute hospitalization. While much more research is needed to facilitate future development of a consensus opinion in this regard, results from this study provide the rationale that implementation of an individualized multicomponent exercise program is feasible and safe and may attenuate functional decline in hospitalized older patients. Finally, the beneficial effects of in-hospital exercise intervention may extend to cognitive capacity, mood status, and QoL—domains that are essential to optimizing patient-centered care in the frailest elderly patients.
The study was well conceived with a number of strengths, including its randomized clinical trial design. In addition, the trial patients were advanced in age (35.1% were nonagenarians), which is particularly important because this is a vulnerable population that is frequently excluded from participation in trials of exercise interventions and because the evidence-base for physical activity guidelines is suboptimal. Moreover, the authors demonstrated that an individualized multicomponent exercise program could be successfully implemented in elderly patients in an acute setting via daily exercise sessions. This test of feasibility is significant in that clinical trials in exercise intervention in geriatrics are commonly performed in nonacute settings in the community, long-term care facilities, or subacute care. The major limitation in this study centers on the generalizability of its findings. It was noted that some patients were not assessed for changes from baseline to discharge on the Barthel Index (6.1%) and SPPB (2.3%) because of their poor condition. The exclusion of the most debilitated patients limits the application of the study’s key findings to the frailest elderly patients, who are most likely to require acute hospital care.
Applications for Clinical Pract
Functional decline is an exceedingly common adverse outcome associated with hospitalization in older patients. While more evidence is needed, early implementation of an individualized, multicomponent exercise regimen during hospitalization may help to prevent functional decline in vulnerable elderly patients.
—Fred Ko, MD, MS
1. Goldwater DS, Dharmarajan K, McEwan BS, Krumholz HM. Is posthospital syndrome a result of hospitalization-induced allostatic overload? J Hosp Med. 2018;13(5).doi:10.12788/jhm.2986.
2. Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med. 1993;118:219-223.
3. Minnick AF, Mion LC, Johnson ME, et al. Prevalence and variation of physical restraint use in acute care settings in the US. J Nurs Scholarsh. 2007;39:30-37.
4. Zisberg A, Shadmi E, Sinoff G et al. Low mobility during hospitalization and functional decline in older adults. J Am Geriatr Soc. 2011;59:266-273.
5. Rubenstein LZ, et al. Effectiveness of a geriatric evaluation unit. A randomized clinical trial. N Engl J Med. 1984;311:1664-1670.
6. Landefeld CS, Palmer RM, Kresevic DM, et al. A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995;332:1338-1344.
7. de Morton NA, Keating JL, Jeffs K. Exercise for acutely hospitalised older medical patients. Cochrane Database Syst Rev. 2007;CD005955.
Study Overview
Objective. To assess the effects of an individualized, multicomponent exercise intervention on the functional status of very elderly patients who were acutely hospitalized compared with those who received usual care.
Design. A single-center, single-blind randomized clinical trial comparing elderly (≥ 75 years old) hospitalized patients who received in-hospital exercise (ie, individualized low-intensity resistance, balance, and walking exercises) versus control (ie, usual care that included physical rehabilitation if needed) interventions. The exercise intervention was adapted from the multicomponent physical exercise program Vivifrail and was supervised and conducted by a fitness specialist in 2 daily (1 morning and 1 evening) sessions lasting 20 minutes for 5 to 7 consecutive days. The morning session consisted of supervised and individualized progressive resistance, balance, and walking exercises. The evening session consisted of functional unsupervised exercises including light weights, extension and flexion of knee and hip, and walking.
Setting and participants. The study was conducted in an acute care unit in a tertiary public hospital in Navarra, Spain, between 1 February 2015 and 30 August 2017. A total of 370 elderly patients undergoing acute care hospitalization were enrolled in the study and randomly assigned to receive in-hospital exercise or control intervention. Inclusion criteria were: age ≥ 75 years, Barthel Index score ≥ 60, and ambulatory with or without assistance.
Main outcome measures. The primary outcome was change in functional capacity from baseline (beginning of exercise or control intervention) to hospital discharge as assessed by the Barthel Index of independence and the Short Physical Performance Battery (SPPB). Secondary outcomes were changes in cognitive capacity (Mini-Mental State Examination [MMSE]) and mood status (Yesavage Geriatric Depression Scale [GDS]), quality of life (QoL; EuroQol-5D), handgrip strength (dominant hand), incident delirium (Confusion Assessment Method), length of stay (LOS), falls during hospitalization, transfer after discharge, and readmission rate and mortality at 3 months after discharge. Intention-to-treat analysis was conducted.
Main results. Of the 370 patients included in the study’s analyses, 209 (56.5%) were women, mean age was 87.3 ± 4.9 years (range, 75-101 years; 130 [35.1%] nonagenarians). The median LOS was 8 days in both groups (interquartile range [IQR], 4 and 4 days, respectively). The median duration of the intervention was 5 days (IQR, 0 days), with 5 ± 1 morning and 4 ± 1 evening sessions in the exercise group. Adherence to the exercise intervention was high (95.8% for morning sessions; 83.4% for evening sessions), and no adverse effects were observed with the intervention.
The in-hospital exercise intervention program yielded significant benefits over usual care in functional outcomes in elderly patients. The exercise group had an increased change in measures of functional capacity compared to the usual care group (ie, Barthel Index, 6.9 points; 95% confidence interval [CI], 4.4-9.5; SPPB score, 2.2 points; 95% CI, 1.7-2.6). Furthermore, acute hospitalization led to an impairment in functional capacity from baseline to discharge in the Barthel Index (−5.0 points; 95% CI, −6.8 to −3.2) in the usual care group. In contrast, exercise intervention reversed this decline and improved functional outcomes as assessed by Barthel Index (1.9 points; 95% CI, 0.2-3.7) and SPPB score (2.4 points; 95% CI, 2.1-2.7).
The beneficial effects of the in-hospital exercise intervention extended to secondary end points indicative of cognitive capacity (MMSE, 1.8 points; 95% CI, 1.3-2.3), mood status (GDS, −2.0 points; 95% CI, −2.5 to −1.6), QoL (EuroQol-5D, 13.2 points; 95% CI, 8.2-18.2), and handgrip strength (2.3 kg; 95% CI, 1.8-2.8) compared to those who received usual care. In contrast, no differences were observed between groups that received exercise intervention and usual care in incident delirium, LOS, falls during hospitalization, transfer after discharge, and 3-month hospital readmission rate and mortality.
Conclusion. An individualized, multicomponent physical exercise program that includes low-intensity resistance, balance, and walking exercises performed during the course of hospitalization (average of 5 days) can reverse functional decline associated with acute hospitalization in very elderly patients. Furthermore, this in-hospital exercise intervention is safe and has a high adherence rate, and thus represents an opportunity to improve quality of care in this vulnerable population.
Commentary
Frail elderly patients are highly susceptible to adverse outcomes of acute hospitalization, including functional decline, disability, nursing home placement, rehospitalization, and mortality.1 Mobility limitation, a major hazard of hospitalization, has been associated with poorer functional recovery and increased vulnerability to these major adverse events after hospital discharge.2-4 Interdisciplinary care models delivered during hospitalization (eg, Geriatric Evaluation Unit, Acute Care for Elders) that emphasize functional independence and provide protocols for exercise and rehabilitation have demonstrated reduced hospital LOS, discharge to nursing home, and mortality, and improved functional status in elderly patients.5-7 Despite this evidence, significant gaps in knowledge exist in understanding whether early implementation of an individualized, multicomponent exercise training program can benefit the oldest old patients who are acutely hospitalized.
This study reported by Martinez-Velilla and colleagues provides an important and timely investigation in examining the effects of an individualized, multicomponent (ie, low-intensity resistance, balance, and walking) in-hospital exercise intervention on functional outcomes of hospitalized octogenarians and nonagenarians. The authors reported that such an intervention, administered 2 sessions per day for 5 to 7 consecutive days, can be safely implemented and reverse functional decline (ie, improvement in Barthel Index and SPPB score over course of hospital stay) typically associated with acute hospitalization in these vulnerable individuals. These findings are particularly significant given the paucity of randomized controlled trials evaluating the impact of exercise intervention in preserving functional capacity of geriatric patients in the setting of acute hospitalization. While much more research is needed to facilitate future development of a consensus opinion in this regard, results from this study provide the rationale that implementation of an individualized multicomponent exercise program is feasible and safe and may attenuate functional decline in hospitalized older patients. Finally, the beneficial effects of in-hospital exercise intervention may extend to cognitive capacity, mood status, and QoL—domains that are essential to optimizing patient-centered care in the frailest elderly patients.
The study was well conceived with a number of strengths, including its randomized clinical trial design. In addition, the trial patients were advanced in age (35.1% were nonagenarians), which is particularly important because this is a vulnerable population that is frequently excluded from participation in trials of exercise interventions and because the evidence-base for physical activity guidelines is suboptimal. Moreover, the authors demonstrated that an individualized multicomponent exercise program could be successfully implemented in elderly patients in an acute setting via daily exercise sessions. This test of feasibility is significant in that clinical trials in exercise intervention in geriatrics are commonly performed in nonacute settings in the community, long-term care facilities, or subacute care. The major limitation in this study centers on the generalizability of its findings. It was noted that some patients were not assessed for changes from baseline to discharge on the Barthel Index (6.1%) and SPPB (2.3%) because of their poor condition. The exclusion of the most debilitated patients limits the application of the study’s key findings to the frailest elderly patients, who are most likely to require acute hospital care.
Applications for Clinical Pract
Functional decline is an exceedingly common adverse outcome associated with hospitalization in older patients. While more evidence is needed, early implementation of an individualized, multicomponent exercise regimen during hospitalization may help to prevent functional decline in vulnerable elderly patients.
—Fred Ko, MD, MS
Study Overview
Objective. To assess the effects of an individualized, multicomponent exercise intervention on the functional status of very elderly patients who were acutely hospitalized compared with those who received usual care.
Design. A single-center, single-blind randomized clinical trial comparing elderly (≥ 75 years old) hospitalized patients who received in-hospital exercise (ie, individualized low-intensity resistance, balance, and walking exercises) versus control (ie, usual care that included physical rehabilitation if needed) interventions. The exercise intervention was adapted from the multicomponent physical exercise program Vivifrail and was supervised and conducted by a fitness specialist in 2 daily (1 morning and 1 evening) sessions lasting 20 minutes for 5 to 7 consecutive days. The morning session consisted of supervised and individualized progressive resistance, balance, and walking exercises. The evening session consisted of functional unsupervised exercises including light weights, extension and flexion of knee and hip, and walking.
Setting and participants. The study was conducted in an acute care unit in a tertiary public hospital in Navarra, Spain, between 1 February 2015 and 30 August 2017. A total of 370 elderly patients undergoing acute care hospitalization were enrolled in the study and randomly assigned to receive in-hospital exercise or control intervention. Inclusion criteria were: age ≥ 75 years, Barthel Index score ≥ 60, and ambulatory with or without assistance.
Main outcome measures. The primary outcome was change in functional capacity from baseline (beginning of exercise or control intervention) to hospital discharge as assessed by the Barthel Index of independence and the Short Physical Performance Battery (SPPB). Secondary outcomes were changes in cognitive capacity (Mini-Mental State Examination [MMSE]) and mood status (Yesavage Geriatric Depression Scale [GDS]), quality of life (QoL; EuroQol-5D), handgrip strength (dominant hand), incident delirium (Confusion Assessment Method), length of stay (LOS), falls during hospitalization, transfer after discharge, and readmission rate and mortality at 3 months after discharge. Intention-to-treat analysis was conducted.
Main results. Of the 370 patients included in the study’s analyses, 209 (56.5%) were women, mean age was 87.3 ± 4.9 years (range, 75-101 years; 130 [35.1%] nonagenarians). The median LOS was 8 days in both groups (interquartile range [IQR], 4 and 4 days, respectively). The median duration of the intervention was 5 days (IQR, 0 days), with 5 ± 1 morning and 4 ± 1 evening sessions in the exercise group. Adherence to the exercise intervention was high (95.8% for morning sessions; 83.4% for evening sessions), and no adverse effects were observed with the intervention.
The in-hospital exercise intervention program yielded significant benefits over usual care in functional outcomes in elderly patients. The exercise group had an increased change in measures of functional capacity compared to the usual care group (ie, Barthel Index, 6.9 points; 95% confidence interval [CI], 4.4-9.5; SPPB score, 2.2 points; 95% CI, 1.7-2.6). Furthermore, acute hospitalization led to an impairment in functional capacity from baseline to discharge in the Barthel Index (−5.0 points; 95% CI, −6.8 to −3.2) in the usual care group. In contrast, exercise intervention reversed this decline and improved functional outcomes as assessed by Barthel Index (1.9 points; 95% CI, 0.2-3.7) and SPPB score (2.4 points; 95% CI, 2.1-2.7).
The beneficial effects of the in-hospital exercise intervention extended to secondary end points indicative of cognitive capacity (MMSE, 1.8 points; 95% CI, 1.3-2.3), mood status (GDS, −2.0 points; 95% CI, −2.5 to −1.6), QoL (EuroQol-5D, 13.2 points; 95% CI, 8.2-18.2), and handgrip strength (2.3 kg; 95% CI, 1.8-2.8) compared to those who received usual care. In contrast, no differences were observed between groups that received exercise intervention and usual care in incident delirium, LOS, falls during hospitalization, transfer after discharge, and 3-month hospital readmission rate and mortality.
Conclusion. An individualized, multicomponent physical exercise program that includes low-intensity resistance, balance, and walking exercises performed during the course of hospitalization (average of 5 days) can reverse functional decline associated with acute hospitalization in very elderly patients. Furthermore, this in-hospital exercise intervention is safe and has a high adherence rate, and thus represents an opportunity to improve quality of care in this vulnerable population.
Commentary
Frail elderly patients are highly susceptible to adverse outcomes of acute hospitalization, including functional decline, disability, nursing home placement, rehospitalization, and mortality.1 Mobility limitation, a major hazard of hospitalization, has been associated with poorer functional recovery and increased vulnerability to these major adverse events after hospital discharge.2-4 Interdisciplinary care models delivered during hospitalization (eg, Geriatric Evaluation Unit, Acute Care for Elders) that emphasize functional independence and provide protocols for exercise and rehabilitation have demonstrated reduced hospital LOS, discharge to nursing home, and mortality, and improved functional status in elderly patients.5-7 Despite this evidence, significant gaps in knowledge exist in understanding whether early implementation of an individualized, multicomponent exercise training program can benefit the oldest old patients who are acutely hospitalized.
This study reported by Martinez-Velilla and colleagues provides an important and timely investigation in examining the effects of an individualized, multicomponent (ie, low-intensity resistance, balance, and walking) in-hospital exercise intervention on functional outcomes of hospitalized octogenarians and nonagenarians. The authors reported that such an intervention, administered 2 sessions per day for 5 to 7 consecutive days, can be safely implemented and reverse functional decline (ie, improvement in Barthel Index and SPPB score over course of hospital stay) typically associated with acute hospitalization in these vulnerable individuals. These findings are particularly significant given the paucity of randomized controlled trials evaluating the impact of exercise intervention in preserving functional capacity of geriatric patients in the setting of acute hospitalization. While much more research is needed to facilitate future development of a consensus opinion in this regard, results from this study provide the rationale that implementation of an individualized multicomponent exercise program is feasible and safe and may attenuate functional decline in hospitalized older patients. Finally, the beneficial effects of in-hospital exercise intervention may extend to cognitive capacity, mood status, and QoL—domains that are essential to optimizing patient-centered care in the frailest elderly patients.
The study was well conceived with a number of strengths, including its randomized clinical trial design. In addition, the trial patients were advanced in age (35.1% were nonagenarians), which is particularly important because this is a vulnerable population that is frequently excluded from participation in trials of exercise interventions and because the evidence-base for physical activity guidelines is suboptimal. Moreover, the authors demonstrated that an individualized multicomponent exercise program could be successfully implemented in elderly patients in an acute setting via daily exercise sessions. This test of feasibility is significant in that clinical trials in exercise intervention in geriatrics are commonly performed in nonacute settings in the community, long-term care facilities, or subacute care. The major limitation in this study centers on the generalizability of its findings. It was noted that some patients were not assessed for changes from baseline to discharge on the Barthel Index (6.1%) and SPPB (2.3%) because of their poor condition. The exclusion of the most debilitated patients limits the application of the study’s key findings to the frailest elderly patients, who are most likely to require acute hospital care.
Applications for Clinical Pract
Functional decline is an exceedingly common adverse outcome associated with hospitalization in older patients. While more evidence is needed, early implementation of an individualized, multicomponent exercise regimen during hospitalization may help to prevent functional decline in vulnerable elderly patients.
—Fred Ko, MD, MS
1. Goldwater DS, Dharmarajan K, McEwan BS, Krumholz HM. Is posthospital syndrome a result of hospitalization-induced allostatic overload? J Hosp Med. 2018;13(5).doi:10.12788/jhm.2986.
2. Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med. 1993;118:219-223.
3. Minnick AF, Mion LC, Johnson ME, et al. Prevalence and variation of physical restraint use in acute care settings in the US. J Nurs Scholarsh. 2007;39:30-37.
4. Zisberg A, Shadmi E, Sinoff G et al. Low mobility during hospitalization and functional decline in older adults. J Am Geriatr Soc. 2011;59:266-273.
5. Rubenstein LZ, et al. Effectiveness of a geriatric evaluation unit. A randomized clinical trial. N Engl J Med. 1984;311:1664-1670.
6. Landefeld CS, Palmer RM, Kresevic DM, et al. A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995;332:1338-1344.
7. de Morton NA, Keating JL, Jeffs K. Exercise for acutely hospitalised older medical patients. Cochrane Database Syst Rev. 2007;CD005955.
1. Goldwater DS, Dharmarajan K, McEwan BS, Krumholz HM. Is posthospital syndrome a result of hospitalization-induced allostatic overload? J Hosp Med. 2018;13(5).doi:10.12788/jhm.2986.
2. Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med. 1993;118:219-223.
3. Minnick AF, Mion LC, Johnson ME, et al. Prevalence and variation of physical restraint use in acute care settings in the US. J Nurs Scholarsh. 2007;39:30-37.
4. Zisberg A, Shadmi E, Sinoff G et al. Low mobility during hospitalization and functional decline in older adults. J Am Geriatr Soc. 2011;59:266-273.
5. Rubenstein LZ, et al. Effectiveness of a geriatric evaluation unit. A randomized clinical trial. N Engl J Med. 1984;311:1664-1670.
6. Landefeld CS, Palmer RM, Kresevic DM, et al. A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995;332:1338-1344.
7. de Morton NA, Keating JL, Jeffs K. Exercise for acutely hospitalised older medical patients. Cochrane Database Syst Rev. 2007;CD005955.
Simple screening for risk of falling in elderly can guide prevention
NEW ORLEANS – , according to an update on this field at the annual meeting at the Endocrine Society.
“The risk of falling in older adults is very high, but risk can be evaluated, and there are effective strategies for risk reduction,” reported Kenton R. Kaufman, PhD, codirector of the Biomechanics and Motion Analysis Laboratory at the Mayo Clinic, Rochester, Minn.
There is not much debate that aging individuals are at an increased risk of falls, but Dr. Kaufman presented his own set of data to reinforce this point. In a longitudinal study of 125 individuals over the age of 65 years who were followed for a year at his institution, 59% had at least one fall even though all were healthy and functional when enrolled.
“It was more common to fall in summer than in winter, and most occurred on a level surface,” said Dr. Kaufman citing data from a study published 2 years ago (Arch Gerontol Geriatr. 2017;73:240-7). About half of the falls occurred at home.
Only 20%-30% of falls lead to moderate to severe injuries, but this is enough to make fall prevention an appropriate and important focus of public health initiatives to reduce morbidity and lower health costs, according to Dr. Kaufman, citing data suggesting that the medical costs total in the billions of dollars.
As a result of a substantial body of research in this area, there are now multiple clinical tests, such as grip strength, the functional reach test, and the 5-minute walk, that provide some degree of predictive value for identifying elderly individuals at risk for falls.
In addition, simple questionnaires that measure the fear of falling, such as the Activities-Specific Balance Confidence Scale (ABC test), and the Falls Efficacy Scale, also identify individuals at higher risk of falling. According to Dr. Kaufman, the predictive value of these questionnaires stems from the fact that those with more fears are more likely to fall.
Dr. Kaufman advised using these simple measures alone or in combination to screen aging patients for risk of failing. Although he singled out grip strength and the ABC test as the clinical test and the questionnaire he is most likely to employ, he believes others are also reasonable. When performed by primary care physicians, although not specialists, evaluating patients for risk of falling is Medicare-reimbursable, according to Dr. Kaufman.
There are two components to effective prophylaxis. One is improving muscle strength. The other is improving neuromuscular response, which means moving quickly enough to compensate when one’s center of gravity is disturbed. According to Dr. Kaufman, who cited two randomized trials, exercise to restore muscle strength can by itself reduce the risk of falling by 10%-20%.
Neuromuscular training is more intensive and not widely available but very effective. This involves training patients to improve their reaction time in the event of an impending fall. This approach, called postural perturbation training, employs a harness to prevent injury.
“The elderly can lose their facility for rapid recovery but this can be relearned,” said Dr. Kaufman, who cited another two randomized trials with this approach that reduced falls by 45% and 55%.
Postural perturbation training, although used to train amputees to gain comfort ambulating on artificial limbs, has so far had limited use in the elderly, but Dr. Kaufman said it might have utility in selected individuals, and he noted that there is at least one commercial device now being marketed.
Many elderly patients will not be candidates for training to reduce falls due to frailty or comorbid conditions that prevent exercise, but Dr. Kaufman encouraged clinicians to evaluate risk of falls in aging individuals who are active because there are strategies to reduce risk, and falls are a major source of morbidity and mortality.
Even for those who are not suitable for risk reduction strategies, testing for risk of falls has the ancillary benefit of raising awareness, according to Dr. Kaufman.
Dr. Kaufman reported no relevant financial relationships to disclose.
NEW ORLEANS – , according to an update on this field at the annual meeting at the Endocrine Society.
“The risk of falling in older adults is very high, but risk can be evaluated, and there are effective strategies for risk reduction,” reported Kenton R. Kaufman, PhD, codirector of the Biomechanics and Motion Analysis Laboratory at the Mayo Clinic, Rochester, Minn.
There is not much debate that aging individuals are at an increased risk of falls, but Dr. Kaufman presented his own set of data to reinforce this point. In a longitudinal study of 125 individuals over the age of 65 years who were followed for a year at his institution, 59% had at least one fall even though all were healthy and functional when enrolled.
“It was more common to fall in summer than in winter, and most occurred on a level surface,” said Dr. Kaufman citing data from a study published 2 years ago (Arch Gerontol Geriatr. 2017;73:240-7). About half of the falls occurred at home.
Only 20%-30% of falls lead to moderate to severe injuries, but this is enough to make fall prevention an appropriate and important focus of public health initiatives to reduce morbidity and lower health costs, according to Dr. Kaufman, citing data suggesting that the medical costs total in the billions of dollars.
As a result of a substantial body of research in this area, there are now multiple clinical tests, such as grip strength, the functional reach test, and the 5-minute walk, that provide some degree of predictive value for identifying elderly individuals at risk for falls.
In addition, simple questionnaires that measure the fear of falling, such as the Activities-Specific Balance Confidence Scale (ABC test), and the Falls Efficacy Scale, also identify individuals at higher risk of falling. According to Dr. Kaufman, the predictive value of these questionnaires stems from the fact that those with more fears are more likely to fall.
Dr. Kaufman advised using these simple measures alone or in combination to screen aging patients for risk of failing. Although he singled out grip strength and the ABC test as the clinical test and the questionnaire he is most likely to employ, he believes others are also reasonable. When performed by primary care physicians, although not specialists, evaluating patients for risk of falling is Medicare-reimbursable, according to Dr. Kaufman.
There are two components to effective prophylaxis. One is improving muscle strength. The other is improving neuromuscular response, which means moving quickly enough to compensate when one’s center of gravity is disturbed. According to Dr. Kaufman, who cited two randomized trials, exercise to restore muscle strength can by itself reduce the risk of falling by 10%-20%.
Neuromuscular training is more intensive and not widely available but very effective. This involves training patients to improve their reaction time in the event of an impending fall. This approach, called postural perturbation training, employs a harness to prevent injury.
“The elderly can lose their facility for rapid recovery but this can be relearned,” said Dr. Kaufman, who cited another two randomized trials with this approach that reduced falls by 45% and 55%.
Postural perturbation training, although used to train amputees to gain comfort ambulating on artificial limbs, has so far had limited use in the elderly, but Dr. Kaufman said it might have utility in selected individuals, and he noted that there is at least one commercial device now being marketed.
Many elderly patients will not be candidates for training to reduce falls due to frailty or comorbid conditions that prevent exercise, but Dr. Kaufman encouraged clinicians to evaluate risk of falls in aging individuals who are active because there are strategies to reduce risk, and falls are a major source of morbidity and mortality.
Even for those who are not suitable for risk reduction strategies, testing for risk of falls has the ancillary benefit of raising awareness, according to Dr. Kaufman.
Dr. Kaufman reported no relevant financial relationships to disclose.
NEW ORLEANS – , according to an update on this field at the annual meeting at the Endocrine Society.
“The risk of falling in older adults is very high, but risk can be evaluated, and there are effective strategies for risk reduction,” reported Kenton R. Kaufman, PhD, codirector of the Biomechanics and Motion Analysis Laboratory at the Mayo Clinic, Rochester, Minn.
There is not much debate that aging individuals are at an increased risk of falls, but Dr. Kaufman presented his own set of data to reinforce this point. In a longitudinal study of 125 individuals over the age of 65 years who were followed for a year at his institution, 59% had at least one fall even though all were healthy and functional when enrolled.
“It was more common to fall in summer than in winter, and most occurred on a level surface,” said Dr. Kaufman citing data from a study published 2 years ago (Arch Gerontol Geriatr. 2017;73:240-7). About half of the falls occurred at home.
Only 20%-30% of falls lead to moderate to severe injuries, but this is enough to make fall prevention an appropriate and important focus of public health initiatives to reduce morbidity and lower health costs, according to Dr. Kaufman, citing data suggesting that the medical costs total in the billions of dollars.
As a result of a substantial body of research in this area, there are now multiple clinical tests, such as grip strength, the functional reach test, and the 5-minute walk, that provide some degree of predictive value for identifying elderly individuals at risk for falls.
In addition, simple questionnaires that measure the fear of falling, such as the Activities-Specific Balance Confidence Scale (ABC test), and the Falls Efficacy Scale, also identify individuals at higher risk of falling. According to Dr. Kaufman, the predictive value of these questionnaires stems from the fact that those with more fears are more likely to fall.
Dr. Kaufman advised using these simple measures alone or in combination to screen aging patients for risk of failing. Although he singled out grip strength and the ABC test as the clinical test and the questionnaire he is most likely to employ, he believes others are also reasonable. When performed by primary care physicians, although not specialists, evaluating patients for risk of falling is Medicare-reimbursable, according to Dr. Kaufman.
There are two components to effective prophylaxis. One is improving muscle strength. The other is improving neuromuscular response, which means moving quickly enough to compensate when one’s center of gravity is disturbed. According to Dr. Kaufman, who cited two randomized trials, exercise to restore muscle strength can by itself reduce the risk of falling by 10%-20%.
Neuromuscular training is more intensive and not widely available but very effective. This involves training patients to improve their reaction time in the event of an impending fall. This approach, called postural perturbation training, employs a harness to prevent injury.
“The elderly can lose their facility for rapid recovery but this can be relearned,” said Dr. Kaufman, who cited another two randomized trials with this approach that reduced falls by 45% and 55%.
Postural perturbation training, although used to train amputees to gain comfort ambulating on artificial limbs, has so far had limited use in the elderly, but Dr. Kaufman said it might have utility in selected individuals, and he noted that there is at least one commercial device now being marketed.
Many elderly patients will not be candidates for training to reduce falls due to frailty or comorbid conditions that prevent exercise, but Dr. Kaufman encouraged clinicians to evaluate risk of falls in aging individuals who are active because there are strategies to reduce risk, and falls are a major source of morbidity and mortality.
Even for those who are not suitable for risk reduction strategies, testing for risk of falls has the ancillary benefit of raising awareness, according to Dr. Kaufman.
Dr. Kaufman reported no relevant financial relationships to disclose.
REPORTING FROM ENDO 2019
BP control slowed brain damage in elderly hypertensives
NEW ORLEANS – Hypertensive elderly patients treated to maintain an ambulatory systolic blood pressure of 130 mm Hg had significantly slower progression of white matter lesions in their brains than did control hypertensive patients maintained at an ambulatory systolic pressure of about 145 mm Hg during 3 years of follow-up in a randomized, single-center study with 199 patients.
The results also showed similar rates of death, syncope episodes, and falls in the intensively and less rigorously treated subgroups, and the patients treated to a systolic of 130 mm Hg also had significantly fewer nonfatal cardiovascular disease events, further documenting the safety and efficacy in elderly patients of a more aggressive blood pressure goal like the one promoted in current guidelines from the American College of Cardiology and American Heart Association, William B. White, MD, said at the annual meeting of the American College of Cardiology.
The study’s findings also showed that in one measure of cognitive function, the serial reaction time task, the patients treated to a systolic pressure of 130 mm Hg had an average 23 millisecond improvement in their reaction time from baseline to their 3-year follow-up, while patients in the control group treated to a systolic pressure of 145 mm Hg had a 33 millisecond increase in their average reaction time during follow-up. This 56 millisecond between-group difference from baseline in average change in reaction time over 3 years was both statistically significant and represents a clinically meaningful difference for a measure of both processing speed and executive function, said Dr. White, professor of medicine at the University of Connecticut in Farmington. However, the participants also underwent assessment by five other clinical measures of cognitive function and in none of the other five tests did more intensive blood pressure control link with an improvement, compared with the results in control patients.
The study had two primary endpoints. One was progression of white matter hyperintensity on brain MR images, which is a measure of neuron necrosis in the brain, and this analysis showed that the growth of white matter occurred at a 40% reduced rate among 99 patients treated to an average ambulatory systolic blood pressure of 130 mm Hg, compared with the average progression among 100 controls treated to an average ambulatory systolic of 145 mm Hg. The second measure was improvement during 3 years, compared with controls, in any of six different measures of mobility, including gait speed. The results showed no significant differences between the treatment arms in any of these measures. The average progression of white matter disease among control patients after 3 years was of a magnitude that would trigger concern in a neurologist who saw these scans, said Dr. White. The researchers could already begin to see a between-group difference in the accumulation of white matter hyperintensity on the MR scans of patients at 18 months in the study, he added.
During his presentation, Dr. White suggested that the absence of discerned improvements in mobility from more aggressive blood pressure control despite the observed slowed progression of white matter disease may have resulted from the study’s relatively brief follow-up.
The INFINITY (Intensive versus Standard Ambulatory Blood Pressure Lowering to Prevent Functional Decline in the Elderly) study enrolled hypertensive patients at least 75 years old who already showed visible evidence of white matter hypertrophy on their brain MR scan at baseline but also had normal mobility and mental function (their baseline score on the mini mental state examination had to be within the normal range, with an average score of 28 among enrolled patients), and they had no history of any chronic neurological condition (Am Heart J. 2013 Mar;165[3]:258-65). The median age of enrolled patients was 80 years. They had an average of 15 years of education, indicating a study cohort with a high level of education and function, Dr. White noted. The inclusion and exclusion criteria led to a study population that was substantially older but without as much comorbidity as patients enrolled in the SPRINT MIND study (JAMA. 2019 Jan 28;321[6]:553-61), he said. The study exclusively used 24-hour ambulatory monitoring for baseline and follow-up blood pressure measurements.
The participating clinicians successfully maintained patients in each of the treatment groups at close to their goal systolic blood pressures. At 18 months, the actual average systolic pressures among patients in the two study groups were 132 mm Hg and 146 mm Hg, and at 36 months their pressures averaged 131 mm Hg and 146 mm Hg for 163 patients who remained in the study out to 36-months. Maintenance of the lower pressure generally required treatment with one additional antihypertensive medication, compared with the control patients’ treatment, Dr. White said.
The rates of total falls and falls causing injury were virtually identical in the two treatment groups. The incidence of nonfatal cardiovascular disease events over 3 years, including MI, strokes, and cardiovascular disease hospitalizations, was 4 cases in the intensively-treated patients and 17 among those treated to a higher systolic pressure, a statistically significant and unexpected difference, Dr. White reported.
This is another dataset showing that blood pressure reduction in elderly people with hypertension is safe and extremely important. Clinicians today often exclude elderly patients from aggressive blood pressure control because of an unrealized fear of causing hypotension and falls. These new data add to what’s already been reported in support of the American College of Cardiology and American Heart Association blood pressure treatment target of less than 130/80 mm Hg for noninstitutionalized, ambulatory, community-dwelling adults who are aged at least 65 years (Hypertension. 2018 June;71[6]:e13-e115). Many clinicians continue to have concerns about what this guideline says about treating older patients. These new findings support the idea that blood pressure can safely be treated to the level the guideline recommends while producing signals of beneficial changes in brain health and in cognitive function.
Providers worry a lot about the potential for harm from treatment. These findings add to the data that say clinicians can safely follow the blood pressure management guideline to benefit even very old patients.
Eileen Handberg, PhD , is a research professor of medicine and director of the Cardiovascular Clinical Trials Program at the University of Florida in Gainesville. She had no relevant disclosures. She made these comments in an interview.
This is another dataset showing that blood pressure reduction in elderly people with hypertension is safe and extremely important. Clinicians today often exclude elderly patients from aggressive blood pressure control because of an unrealized fear of causing hypotension and falls. These new data add to what’s already been reported in support of the American College of Cardiology and American Heart Association blood pressure treatment target of less than 130/80 mm Hg for noninstitutionalized, ambulatory, community-dwelling adults who are aged at least 65 years (Hypertension. 2018 June;71[6]:e13-e115). Many clinicians continue to have concerns about what this guideline says about treating older patients. These new findings support the idea that blood pressure can safely be treated to the level the guideline recommends while producing signals of beneficial changes in brain health and in cognitive function.
Providers worry a lot about the potential for harm from treatment. These findings add to the data that say clinicians can safely follow the blood pressure management guideline to benefit even very old patients.
Eileen Handberg, PhD , is a research professor of medicine and director of the Cardiovascular Clinical Trials Program at the University of Florida in Gainesville. She had no relevant disclosures. She made these comments in an interview.
This is another dataset showing that blood pressure reduction in elderly people with hypertension is safe and extremely important. Clinicians today often exclude elderly patients from aggressive blood pressure control because of an unrealized fear of causing hypotension and falls. These new data add to what’s already been reported in support of the American College of Cardiology and American Heart Association blood pressure treatment target of less than 130/80 mm Hg for noninstitutionalized, ambulatory, community-dwelling adults who are aged at least 65 years (Hypertension. 2018 June;71[6]:e13-e115). Many clinicians continue to have concerns about what this guideline says about treating older patients. These new findings support the idea that blood pressure can safely be treated to the level the guideline recommends while producing signals of beneficial changes in brain health and in cognitive function.
Providers worry a lot about the potential for harm from treatment. These findings add to the data that say clinicians can safely follow the blood pressure management guideline to benefit even very old patients.
Eileen Handberg, PhD , is a research professor of medicine and director of the Cardiovascular Clinical Trials Program at the University of Florida in Gainesville. She had no relevant disclosures. She made these comments in an interview.
NEW ORLEANS – Hypertensive elderly patients treated to maintain an ambulatory systolic blood pressure of 130 mm Hg had significantly slower progression of white matter lesions in their brains than did control hypertensive patients maintained at an ambulatory systolic pressure of about 145 mm Hg during 3 years of follow-up in a randomized, single-center study with 199 patients.
The results also showed similar rates of death, syncope episodes, and falls in the intensively and less rigorously treated subgroups, and the patients treated to a systolic of 130 mm Hg also had significantly fewer nonfatal cardiovascular disease events, further documenting the safety and efficacy in elderly patients of a more aggressive blood pressure goal like the one promoted in current guidelines from the American College of Cardiology and American Heart Association, William B. White, MD, said at the annual meeting of the American College of Cardiology.
The study’s findings also showed that in one measure of cognitive function, the serial reaction time task, the patients treated to a systolic pressure of 130 mm Hg had an average 23 millisecond improvement in their reaction time from baseline to their 3-year follow-up, while patients in the control group treated to a systolic pressure of 145 mm Hg had a 33 millisecond increase in their average reaction time during follow-up. This 56 millisecond between-group difference from baseline in average change in reaction time over 3 years was both statistically significant and represents a clinically meaningful difference for a measure of both processing speed and executive function, said Dr. White, professor of medicine at the University of Connecticut in Farmington. However, the participants also underwent assessment by five other clinical measures of cognitive function and in none of the other five tests did more intensive blood pressure control link with an improvement, compared with the results in control patients.
The study had two primary endpoints. One was progression of white matter hyperintensity on brain MR images, which is a measure of neuron necrosis in the brain, and this analysis showed that the growth of white matter occurred at a 40% reduced rate among 99 patients treated to an average ambulatory systolic blood pressure of 130 mm Hg, compared with the average progression among 100 controls treated to an average ambulatory systolic of 145 mm Hg. The second measure was improvement during 3 years, compared with controls, in any of six different measures of mobility, including gait speed. The results showed no significant differences between the treatment arms in any of these measures. The average progression of white matter disease among control patients after 3 years was of a magnitude that would trigger concern in a neurologist who saw these scans, said Dr. White. The researchers could already begin to see a between-group difference in the accumulation of white matter hyperintensity on the MR scans of patients at 18 months in the study, he added.
During his presentation, Dr. White suggested that the absence of discerned improvements in mobility from more aggressive blood pressure control despite the observed slowed progression of white matter disease may have resulted from the study’s relatively brief follow-up.
The INFINITY (Intensive versus Standard Ambulatory Blood Pressure Lowering to Prevent Functional Decline in the Elderly) study enrolled hypertensive patients at least 75 years old who already showed visible evidence of white matter hypertrophy on their brain MR scan at baseline but also had normal mobility and mental function (their baseline score on the mini mental state examination had to be within the normal range, with an average score of 28 among enrolled patients), and they had no history of any chronic neurological condition (Am Heart J. 2013 Mar;165[3]:258-65). The median age of enrolled patients was 80 years. They had an average of 15 years of education, indicating a study cohort with a high level of education and function, Dr. White noted. The inclusion and exclusion criteria led to a study population that was substantially older but without as much comorbidity as patients enrolled in the SPRINT MIND study (JAMA. 2019 Jan 28;321[6]:553-61), he said. The study exclusively used 24-hour ambulatory monitoring for baseline and follow-up blood pressure measurements.
The participating clinicians successfully maintained patients in each of the treatment groups at close to their goal systolic blood pressures. At 18 months, the actual average systolic pressures among patients in the two study groups were 132 mm Hg and 146 mm Hg, and at 36 months their pressures averaged 131 mm Hg and 146 mm Hg for 163 patients who remained in the study out to 36-months. Maintenance of the lower pressure generally required treatment with one additional antihypertensive medication, compared with the control patients’ treatment, Dr. White said.
The rates of total falls and falls causing injury were virtually identical in the two treatment groups. The incidence of nonfatal cardiovascular disease events over 3 years, including MI, strokes, and cardiovascular disease hospitalizations, was 4 cases in the intensively-treated patients and 17 among those treated to a higher systolic pressure, a statistically significant and unexpected difference, Dr. White reported.
NEW ORLEANS – Hypertensive elderly patients treated to maintain an ambulatory systolic blood pressure of 130 mm Hg had significantly slower progression of white matter lesions in their brains than did control hypertensive patients maintained at an ambulatory systolic pressure of about 145 mm Hg during 3 years of follow-up in a randomized, single-center study with 199 patients.
The results also showed similar rates of death, syncope episodes, and falls in the intensively and less rigorously treated subgroups, and the patients treated to a systolic of 130 mm Hg also had significantly fewer nonfatal cardiovascular disease events, further documenting the safety and efficacy in elderly patients of a more aggressive blood pressure goal like the one promoted in current guidelines from the American College of Cardiology and American Heart Association, William B. White, MD, said at the annual meeting of the American College of Cardiology.
The study’s findings also showed that in one measure of cognitive function, the serial reaction time task, the patients treated to a systolic pressure of 130 mm Hg had an average 23 millisecond improvement in their reaction time from baseline to their 3-year follow-up, while patients in the control group treated to a systolic pressure of 145 mm Hg had a 33 millisecond increase in their average reaction time during follow-up. This 56 millisecond between-group difference from baseline in average change in reaction time over 3 years was both statistically significant and represents a clinically meaningful difference for a measure of both processing speed and executive function, said Dr. White, professor of medicine at the University of Connecticut in Farmington. However, the participants also underwent assessment by five other clinical measures of cognitive function and in none of the other five tests did more intensive blood pressure control link with an improvement, compared with the results in control patients.
The study had two primary endpoints. One was progression of white matter hyperintensity on brain MR images, which is a measure of neuron necrosis in the brain, and this analysis showed that the growth of white matter occurred at a 40% reduced rate among 99 patients treated to an average ambulatory systolic blood pressure of 130 mm Hg, compared with the average progression among 100 controls treated to an average ambulatory systolic of 145 mm Hg. The second measure was improvement during 3 years, compared with controls, in any of six different measures of mobility, including gait speed. The results showed no significant differences between the treatment arms in any of these measures. The average progression of white matter disease among control patients after 3 years was of a magnitude that would trigger concern in a neurologist who saw these scans, said Dr. White. The researchers could already begin to see a between-group difference in the accumulation of white matter hyperintensity on the MR scans of patients at 18 months in the study, he added.
During his presentation, Dr. White suggested that the absence of discerned improvements in mobility from more aggressive blood pressure control despite the observed slowed progression of white matter disease may have resulted from the study’s relatively brief follow-up.
The INFINITY (Intensive versus Standard Ambulatory Blood Pressure Lowering to Prevent Functional Decline in the Elderly) study enrolled hypertensive patients at least 75 years old who already showed visible evidence of white matter hypertrophy on their brain MR scan at baseline but also had normal mobility and mental function (their baseline score on the mini mental state examination had to be within the normal range, with an average score of 28 among enrolled patients), and they had no history of any chronic neurological condition (Am Heart J. 2013 Mar;165[3]:258-65). The median age of enrolled patients was 80 years. They had an average of 15 years of education, indicating a study cohort with a high level of education and function, Dr. White noted. The inclusion and exclusion criteria led to a study population that was substantially older but without as much comorbidity as patients enrolled in the SPRINT MIND study (JAMA. 2019 Jan 28;321[6]:553-61), he said. The study exclusively used 24-hour ambulatory monitoring for baseline and follow-up blood pressure measurements.
The participating clinicians successfully maintained patients in each of the treatment groups at close to their goal systolic blood pressures. At 18 months, the actual average systolic pressures among patients in the two study groups were 132 mm Hg and 146 mm Hg, and at 36 months their pressures averaged 131 mm Hg and 146 mm Hg for 163 patients who remained in the study out to 36-months. Maintenance of the lower pressure generally required treatment with one additional antihypertensive medication, compared with the control patients’ treatment, Dr. White said.
The rates of total falls and falls causing injury were virtually identical in the two treatment groups. The incidence of nonfatal cardiovascular disease events over 3 years, including MI, strokes, and cardiovascular disease hospitalizations, was 4 cases in the intensively-treated patients and 17 among those treated to a higher systolic pressure, a statistically significant and unexpected difference, Dr. White reported.
REPORTING FROM ACC 19
Biogen, Eisai discontinue aducanumab Alzheimer’s trials
Biogen and Eisai have announced that they are discontinuing the ENGAGE and EMERGE trials, which were designed to test the efficacy and safety of aducanumab in patients with mild cognitive impairment caused by Alzheimer’s disease and mild Alzheimer’s disease dementia.
The phase 3, multicenter, randomized, double-blind, placebo-controlled, parallel-group trials were canceled not because of safety concerns but because of a futility analysis conducted by an independent data monitoring committee that indicated the drug would not meet the trials’ primary endpoint, which was the slowing of cognitive and functional impairment as measured by changes in Clinical Dementia Rating–Sum of Boxes score, compared with placebo.
In addition to ENGAGE and EMERGE, the phase 2 EVOLVE safety study and the long-term extension of the phase 1b PRIME study have also been canceled. Data from the ENGAGE and EMERGE trials will be presented at future medical meetings.
Aducanumab is a human monoclonal antibody derived from B cells collected from healthy elderly subjects with no cognitive decline or those with unusually slow cognitive decline through Neurimmune’s technology platform called Reverse Translational Medicine. It was granted Fast Track designation by the Food and Drug Administration.
“This disappointing news confirms the complexity of treating Alzheimer’s disease and the need to further advance knowledge in neuroscience. We are incredibly grateful to all the Alzheimer’s disease patients, their families, and the investigators who participated in the trials and contributed greatly to this research,” Michel Vounatsos, CEO at Biogen, said in a press release.
Biogen and Eisai have announced that they are discontinuing the ENGAGE and EMERGE trials, which were designed to test the efficacy and safety of aducanumab in patients with mild cognitive impairment caused by Alzheimer’s disease and mild Alzheimer’s disease dementia.
The phase 3, multicenter, randomized, double-blind, placebo-controlled, parallel-group trials were canceled not because of safety concerns but because of a futility analysis conducted by an independent data monitoring committee that indicated the drug would not meet the trials’ primary endpoint, which was the slowing of cognitive and functional impairment as measured by changes in Clinical Dementia Rating–Sum of Boxes score, compared with placebo.
In addition to ENGAGE and EMERGE, the phase 2 EVOLVE safety study and the long-term extension of the phase 1b PRIME study have also been canceled. Data from the ENGAGE and EMERGE trials will be presented at future medical meetings.
Aducanumab is a human monoclonal antibody derived from B cells collected from healthy elderly subjects with no cognitive decline or those with unusually slow cognitive decline through Neurimmune’s technology platform called Reverse Translational Medicine. It was granted Fast Track designation by the Food and Drug Administration.
“This disappointing news confirms the complexity of treating Alzheimer’s disease and the need to further advance knowledge in neuroscience. We are incredibly grateful to all the Alzheimer’s disease patients, their families, and the investigators who participated in the trials and contributed greatly to this research,” Michel Vounatsos, CEO at Biogen, said in a press release.
Biogen and Eisai have announced that they are discontinuing the ENGAGE and EMERGE trials, which were designed to test the efficacy and safety of aducanumab in patients with mild cognitive impairment caused by Alzheimer’s disease and mild Alzheimer’s disease dementia.
The phase 3, multicenter, randomized, double-blind, placebo-controlled, parallel-group trials were canceled not because of safety concerns but because of a futility analysis conducted by an independent data monitoring committee that indicated the drug would not meet the trials’ primary endpoint, which was the slowing of cognitive and functional impairment as measured by changes in Clinical Dementia Rating–Sum of Boxes score, compared with placebo.
In addition to ENGAGE and EMERGE, the phase 2 EVOLVE safety study and the long-term extension of the phase 1b PRIME study have also been canceled. Data from the ENGAGE and EMERGE trials will be presented at future medical meetings.
Aducanumab is a human monoclonal antibody derived from B cells collected from healthy elderly subjects with no cognitive decline or those with unusually slow cognitive decline through Neurimmune’s technology platform called Reverse Translational Medicine. It was granted Fast Track designation by the Food and Drug Administration.
“This disappointing news confirms the complexity of treating Alzheimer’s disease and the need to further advance knowledge in neuroscience. We are incredibly grateful to all the Alzheimer’s disease patients, their families, and the investigators who participated in the trials and contributed greatly to this research,” Michel Vounatsos, CEO at Biogen, said in a press release.
Light physical activity lowers CVD risk in older women
Even light physical activity can significantly reduce the risks of acquiring coronary heart disease specifically and the broad range of cardiovascular diseases in older women, new data suggests.
A paper published in JAMA Network Open reported the outcome of a prospective cohort study in 5,861 women, with a mean age of 78.5 years, who wore accelerometers for 7 days to measure physical activity.
than those in the lowest quartile of activity, who engaged in less than 3.9 hours per day, after adjusting for factors such as comorbidities, lifestyle, and cardiovascular risk.
Similarly, those in the highest quartile had an 18% lower risk of cardiovascular disease than those in the lowest quartile, after adjusting for potential confounders.
Researchers saw a significant dose-dependent decrease in the risk for incident coronary heart disease and cardiovascular disease with increasing light physical activity, such that each 1-hour increment of activity was associated with a 20% decrease in coronary heart disease risk and 10% decrease in cardiovascular disease risk.
Andrea Z. LaCroix, PhD, from the University of California, San Diego, and her coauthors noted that physical activity guidelines for aerobic activity suggest 75 minutes of vigorous physical activity or 150 minutes of moderate activity each day, but only around 25% of U.S. women aged over 75 years are estimated to meet this requirement.
“These guidelines may have discouraged PA [physical activity] when perceived to be unattainable by large segments of the population,” they wrote.
While the majority of active time in older adults is spent doing light physical activity, little is known about the cardiovascular effects of participating in this level of activity. “A major barrier has been that self-reported questionnaires measuring leisure-time PA do not adequately capture light PA that is acquired throughout the day in activities of daily living,” they wrote.
The study also looked at the impact of moderate to vigorous physical activity, finding a significant 46% reduction between the highest to lowest quartiles of activity in coronary heart disease risk and a 31% reduction in cardiovascular disease risk.
Even after adjusting for the use of lipid-lowering medication, antihypertensive medication or healthy eating scores, the results remained unchanged. The researchers also saw no change when women with angina and heart failure at baseline were excluded or when they excluded cardiovascular events that occurred during the first 6 months of follow-up.
The study was supported by the National Heart, Lung, and Blood Institute; the National Institutes of Health; and the Department of Health & Human Services. Six authors reported receiving funding from the study supporters and other research institutions, and one reported membership on the advisory committee for physical activity guidelines. No other conflicts of interest were reported.
SOURCE: LaCroix AZ et al. JAMA Netw Open. 2019 Mar 15. doi: 10.1001/jamanetworkopen.2019.0419.
Older women do not get enough physical activity, so this finding that light physical activity is associated with improved coronary heart disease and cardiovascular disease outcomes supports the recent scientific report by the 2018 Physical Activity Guidelines Advisory Committee. It is also helpful in extending the evidence about the benefits of physical activity in reducing incident coronary heart disease to older women, as previous studies on this topic showed such benefits in men.
These findings should remind health care professionals, systems, and agencies to promote the 2018 Physical Activity Guidelines for Americans to all patients. Otherwise, the future health and well-being of older women is likely to suffer from the consequences of sedentary behavior and inadequate physical activity.
Gregory W. Heath, DHSc, MPH, is from the department of health and human performance at the University of Tennessee, Chattanooga. These comments are adapted from an accompanying editorial (JAMA Netw Open. 2019 Mar 15. doi: 10.1001/jamanetworkopen.2019.0405). No conflicts of interest were reported.
Older women do not get enough physical activity, so this finding that light physical activity is associated with improved coronary heart disease and cardiovascular disease outcomes supports the recent scientific report by the 2018 Physical Activity Guidelines Advisory Committee. It is also helpful in extending the evidence about the benefits of physical activity in reducing incident coronary heart disease to older women, as previous studies on this topic showed such benefits in men.
These findings should remind health care professionals, systems, and agencies to promote the 2018 Physical Activity Guidelines for Americans to all patients. Otherwise, the future health and well-being of older women is likely to suffer from the consequences of sedentary behavior and inadequate physical activity.
Gregory W. Heath, DHSc, MPH, is from the department of health and human performance at the University of Tennessee, Chattanooga. These comments are adapted from an accompanying editorial (JAMA Netw Open. 2019 Mar 15. doi: 10.1001/jamanetworkopen.2019.0405). No conflicts of interest were reported.
Older women do not get enough physical activity, so this finding that light physical activity is associated with improved coronary heart disease and cardiovascular disease outcomes supports the recent scientific report by the 2018 Physical Activity Guidelines Advisory Committee. It is also helpful in extending the evidence about the benefits of physical activity in reducing incident coronary heart disease to older women, as previous studies on this topic showed such benefits in men.
These findings should remind health care professionals, systems, and agencies to promote the 2018 Physical Activity Guidelines for Americans to all patients. Otherwise, the future health and well-being of older women is likely to suffer from the consequences of sedentary behavior and inadequate physical activity.
Gregory W. Heath, DHSc, MPH, is from the department of health and human performance at the University of Tennessee, Chattanooga. These comments are adapted from an accompanying editorial (JAMA Netw Open. 2019 Mar 15. doi: 10.1001/jamanetworkopen.2019.0405). No conflicts of interest were reported.
Even light physical activity can significantly reduce the risks of acquiring coronary heart disease specifically and the broad range of cardiovascular diseases in older women, new data suggests.
A paper published in JAMA Network Open reported the outcome of a prospective cohort study in 5,861 women, with a mean age of 78.5 years, who wore accelerometers for 7 days to measure physical activity.
than those in the lowest quartile of activity, who engaged in less than 3.9 hours per day, after adjusting for factors such as comorbidities, lifestyle, and cardiovascular risk.
Similarly, those in the highest quartile had an 18% lower risk of cardiovascular disease than those in the lowest quartile, after adjusting for potential confounders.
Researchers saw a significant dose-dependent decrease in the risk for incident coronary heart disease and cardiovascular disease with increasing light physical activity, such that each 1-hour increment of activity was associated with a 20% decrease in coronary heart disease risk and 10% decrease in cardiovascular disease risk.
Andrea Z. LaCroix, PhD, from the University of California, San Diego, and her coauthors noted that physical activity guidelines for aerobic activity suggest 75 minutes of vigorous physical activity or 150 minutes of moderate activity each day, but only around 25% of U.S. women aged over 75 years are estimated to meet this requirement.
“These guidelines may have discouraged PA [physical activity] when perceived to be unattainable by large segments of the population,” they wrote.
While the majority of active time in older adults is spent doing light physical activity, little is known about the cardiovascular effects of participating in this level of activity. “A major barrier has been that self-reported questionnaires measuring leisure-time PA do not adequately capture light PA that is acquired throughout the day in activities of daily living,” they wrote.
The study also looked at the impact of moderate to vigorous physical activity, finding a significant 46% reduction between the highest to lowest quartiles of activity in coronary heart disease risk and a 31% reduction in cardiovascular disease risk.
Even after adjusting for the use of lipid-lowering medication, antihypertensive medication or healthy eating scores, the results remained unchanged. The researchers also saw no change when women with angina and heart failure at baseline were excluded or when they excluded cardiovascular events that occurred during the first 6 months of follow-up.
The study was supported by the National Heart, Lung, and Blood Institute; the National Institutes of Health; and the Department of Health & Human Services. Six authors reported receiving funding from the study supporters and other research institutions, and one reported membership on the advisory committee for physical activity guidelines. No other conflicts of interest were reported.
SOURCE: LaCroix AZ et al. JAMA Netw Open. 2019 Mar 15. doi: 10.1001/jamanetworkopen.2019.0419.
Even light physical activity can significantly reduce the risks of acquiring coronary heart disease specifically and the broad range of cardiovascular diseases in older women, new data suggests.
A paper published in JAMA Network Open reported the outcome of a prospective cohort study in 5,861 women, with a mean age of 78.5 years, who wore accelerometers for 7 days to measure physical activity.
than those in the lowest quartile of activity, who engaged in less than 3.9 hours per day, after adjusting for factors such as comorbidities, lifestyle, and cardiovascular risk.
Similarly, those in the highest quartile had an 18% lower risk of cardiovascular disease than those in the lowest quartile, after adjusting for potential confounders.
Researchers saw a significant dose-dependent decrease in the risk for incident coronary heart disease and cardiovascular disease with increasing light physical activity, such that each 1-hour increment of activity was associated with a 20% decrease in coronary heart disease risk and 10% decrease in cardiovascular disease risk.
Andrea Z. LaCroix, PhD, from the University of California, San Diego, and her coauthors noted that physical activity guidelines for aerobic activity suggest 75 minutes of vigorous physical activity or 150 minutes of moderate activity each day, but only around 25% of U.S. women aged over 75 years are estimated to meet this requirement.
“These guidelines may have discouraged PA [physical activity] when perceived to be unattainable by large segments of the population,” they wrote.
While the majority of active time in older adults is spent doing light physical activity, little is known about the cardiovascular effects of participating in this level of activity. “A major barrier has been that self-reported questionnaires measuring leisure-time PA do not adequately capture light PA that is acquired throughout the day in activities of daily living,” they wrote.
The study also looked at the impact of moderate to vigorous physical activity, finding a significant 46% reduction between the highest to lowest quartiles of activity in coronary heart disease risk and a 31% reduction in cardiovascular disease risk.
Even after adjusting for the use of lipid-lowering medication, antihypertensive medication or healthy eating scores, the results remained unchanged. The researchers also saw no change when women with angina and heart failure at baseline were excluded or when they excluded cardiovascular events that occurred during the first 6 months of follow-up.
The study was supported by the National Heart, Lung, and Blood Institute; the National Institutes of Health; and the Department of Health & Human Services. Six authors reported receiving funding from the study supporters and other research institutions, and one reported membership on the advisory committee for physical activity guidelines. No other conflicts of interest were reported.
SOURCE: LaCroix AZ et al. JAMA Netw Open. 2019 Mar 15. doi: 10.1001/jamanetworkopen.2019.0419.
FROM JAMA NETWORK OPEN
Advance care planning codes not being used
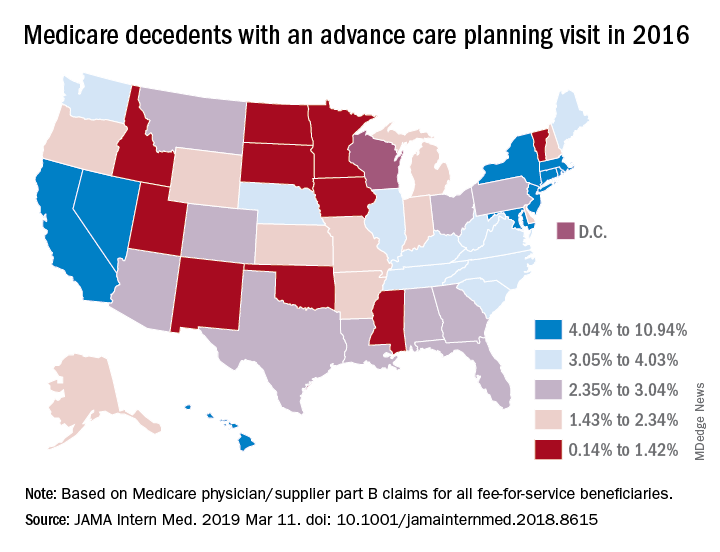
Starting in 2016, the Centers for Medicare & Medicaid Services began paying physicians for advance care planning discussions with the approval of two new codes: 99497 and 99498. The codes pay about $86 for the first 30 minutes of a face-to-face conversation with a patient, family member, and/or surrogate and about $75 for additional sessions. Services can be furnished in both inpatient and ambulatory settings, and payment is not limited to particular physician specialties.
In 2016, health care professionals in New England (Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, and Vermont) billed Medicare 26,522 times for the advance care planning (ACP) codes for a total of 24,536 patients, which represented less than 1% of Medicare beneficiaries in New England at the time, according to Kimberly Pelland, MPH, of Healthcentric Advisors, Providence, R.I., and her colleagues. Most claims were billed in the office, followed by in nursing homes, and in hospitals; 40% of conversations occurred during an annual wellness visit (JAMA Intern Med. 2019 March 11. doi:10.1001/jamainternmed.2018.8107).
Internists billed Medicare the most for ACP claims (65%), followed by family physicians (22%) gerontologists (5%), and oncologist/hematologists (0.3%), according to the analysis based on 2016 Medicare claims data and Census Bureau data. A greater proportion of patients with ACP claims were female, aged 85 years or older, enrolled in hospice, and died in the study year. Patients had higher odds of having an ACP claim if they were older and had lower income, and if they had cancer, heart failure, stroke, chronic kidney disease, or dementia. Male patients who were Asian, black, and Hispanic had lower chances of having an ACP claim.
In a related study, Emmanuelle Belanger, PhD, of Brown University, Providence, R.I., and her colleagues examined national Medicare data from 2016 to the third quarter of 2017. Across the United States, 2% of Medicare patients aged 65 years and older received advance care planning services that were billed under the ACP codes (JAMA Intern Med. 2019 March 11. doi: 10.1001/jamainternmed.2018.8615). Visits billed under the ACP codes increased from 538,275 to 633,214 during the same time period. Claim rates were higher among patients who died within the study period, reaching 3% in 2016 and 6% in 2017. The percentage of decedents with an ACP billed visit varied strongly across states, with states such as North Dakota, South Dakota, and Wyoming having the fewest ACP visits billed and states such as California and Nevada having the most. ACP billed visits increased in all settings in 2017, but primarily in hospitals and nursing homes. Nationally, internists billed the codes most (48%), followed by family physicians (28%).
While the two studies indicate low usage of the ACP codes, many physicians are discussing advance care planning with their patients, said Mary M. Newman, MD, an internist based in Lutherville, Md., and former American College of Physicians adviser to the American Medical Association Relative Scale Value Update Committee (RUC).
“What cannot be captured by tracking under Medicare claims data are those shorter conversations that we have frequently,” Dr. Newman said in an interview. “If we have a short conversation about advance care planning, it gets folded into our evaluation and management visit. It’s not going to be separately billed.”
At the same time, some patients are not ready to discuss end-of-life options and decline the discussions when asked, Dr. Newman said. Particularly for healthier patients, end of life care is not a primary focus, she noted.
“Not everybody’s ready to have an advance care planning [discussion] that lasts 16-45 minutes,” she said. “Many people over age 65 are not ready to deal with advance care planning in their day-to-day lives, and it may not be what they wish to discuss. I offer the option to patients and some say, ‘Yes, I’d love to,’ and others decline or postpone.”
Low usage of the ACP codes may be associated with lack of awareness, uncertainty about appropriate code use, or associated billing that is not part of the standard workflow, Ankita Mehta, MD, of Mount Sinai in New York wrote an editorial accompanying the studies (JAMA Intern Med. 2019 March 11. doi:10.1001/jamainternmed.2018.8105).
“Regardless, the low rates of utilization of ACP codes is alarming and highlights the need to create strategies to integrate ACP discussions into standard practice and build ACP documentation and billing in clinical workflow,” Dr. Mehta said.
Dr. Newman agreed that more education among physicians is needed.
“The amount of education clinicians have received varies tremendously across the geography of the country,” she said. “I think the codes are going to be slowly adopted. The challenge to us is to make sure we’re all better educated on palliative care as people age and get sick and that we are sensitive to our patients explicit and implicit needs for these discussions.”
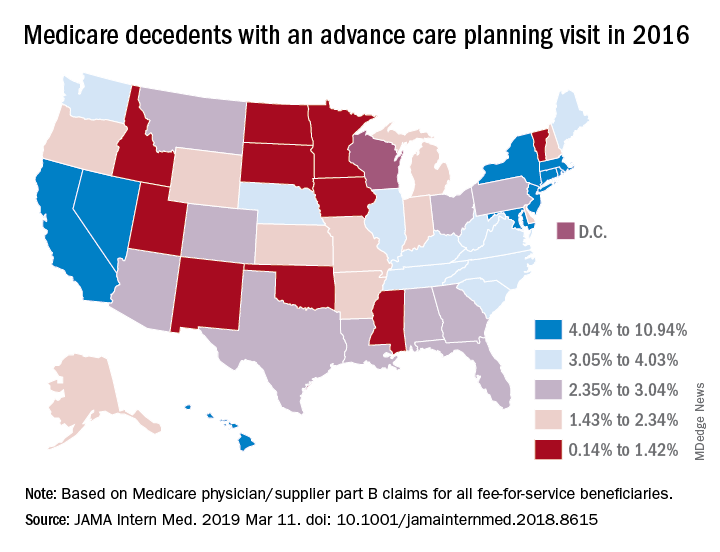
Starting in 2016, the Centers for Medicare & Medicaid Services began paying physicians for advance care planning discussions with the approval of two new codes: 99497 and 99498. The codes pay about $86 for the first 30 minutes of a face-to-face conversation with a patient, family member, and/or surrogate and about $75 for additional sessions. Services can be furnished in both inpatient and ambulatory settings, and payment is not limited to particular physician specialties.
In 2016, health care professionals in New England (Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, and Vermont) billed Medicare 26,522 times for the advance care planning (ACP) codes for a total of 24,536 patients, which represented less than 1% of Medicare beneficiaries in New England at the time, according to Kimberly Pelland, MPH, of Healthcentric Advisors, Providence, R.I., and her colleagues. Most claims were billed in the office, followed by in nursing homes, and in hospitals; 40% of conversations occurred during an annual wellness visit (JAMA Intern Med. 2019 March 11. doi:10.1001/jamainternmed.2018.8107).
Internists billed Medicare the most for ACP claims (65%), followed by family physicians (22%) gerontologists (5%), and oncologist/hematologists (0.3%), according to the analysis based on 2016 Medicare claims data and Census Bureau data. A greater proportion of patients with ACP claims were female, aged 85 years or older, enrolled in hospice, and died in the study year. Patients had higher odds of having an ACP claim if they were older and had lower income, and if they had cancer, heart failure, stroke, chronic kidney disease, or dementia. Male patients who were Asian, black, and Hispanic had lower chances of having an ACP claim.
In a related study, Emmanuelle Belanger, PhD, of Brown University, Providence, R.I., and her colleagues examined national Medicare data from 2016 to the third quarter of 2017. Across the United States, 2% of Medicare patients aged 65 years and older received advance care planning services that were billed under the ACP codes (JAMA Intern Med. 2019 March 11. doi: 10.1001/jamainternmed.2018.8615). Visits billed under the ACP codes increased from 538,275 to 633,214 during the same time period. Claim rates were higher among patients who died within the study period, reaching 3% in 2016 and 6% in 2017. The percentage of decedents with an ACP billed visit varied strongly across states, with states such as North Dakota, South Dakota, and Wyoming having the fewest ACP visits billed and states such as California and Nevada having the most. ACP billed visits increased in all settings in 2017, but primarily in hospitals and nursing homes. Nationally, internists billed the codes most (48%), followed by family physicians (28%).
While the two studies indicate low usage of the ACP codes, many physicians are discussing advance care planning with their patients, said Mary M. Newman, MD, an internist based in Lutherville, Md., and former American College of Physicians adviser to the American Medical Association Relative Scale Value Update Committee (RUC).
“What cannot be captured by tracking under Medicare claims data are those shorter conversations that we have frequently,” Dr. Newman said in an interview. “If we have a short conversation about advance care planning, it gets folded into our evaluation and management visit. It’s not going to be separately billed.”
At the same time, some patients are not ready to discuss end-of-life options and decline the discussions when asked, Dr. Newman said. Particularly for healthier patients, end of life care is not a primary focus, she noted.
“Not everybody’s ready to have an advance care planning [discussion] that lasts 16-45 minutes,” she said. “Many people over age 65 are not ready to deal with advance care planning in their day-to-day lives, and it may not be what they wish to discuss. I offer the option to patients and some say, ‘Yes, I’d love to,’ and others decline or postpone.”
Low usage of the ACP codes may be associated with lack of awareness, uncertainty about appropriate code use, or associated billing that is not part of the standard workflow, Ankita Mehta, MD, of Mount Sinai in New York wrote an editorial accompanying the studies (JAMA Intern Med. 2019 March 11. doi:10.1001/jamainternmed.2018.8105).
“Regardless, the low rates of utilization of ACP codes is alarming and highlights the need to create strategies to integrate ACP discussions into standard practice and build ACP documentation and billing in clinical workflow,” Dr. Mehta said.
Dr. Newman agreed that more education among physicians is needed.
“The amount of education clinicians have received varies tremendously across the geography of the country,” she said. “I think the codes are going to be slowly adopted. The challenge to us is to make sure we’re all better educated on palliative care as people age and get sick and that we are sensitive to our patients explicit and implicit needs for these discussions.”
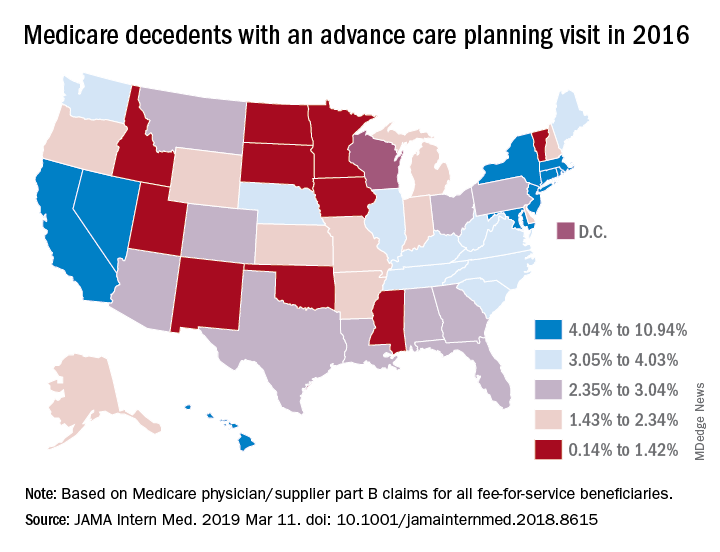
Starting in 2016, the Centers for Medicare & Medicaid Services began paying physicians for advance care planning discussions with the approval of two new codes: 99497 and 99498. The codes pay about $86 for the first 30 minutes of a face-to-face conversation with a patient, family member, and/or surrogate and about $75 for additional sessions. Services can be furnished in both inpatient and ambulatory settings, and payment is not limited to particular physician specialties.
In 2016, health care professionals in New England (Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, and Vermont) billed Medicare 26,522 times for the advance care planning (ACP) codes for a total of 24,536 patients, which represented less than 1% of Medicare beneficiaries in New England at the time, according to Kimberly Pelland, MPH, of Healthcentric Advisors, Providence, R.I., and her colleagues. Most claims were billed in the office, followed by in nursing homes, and in hospitals; 40% of conversations occurred during an annual wellness visit (JAMA Intern Med. 2019 March 11. doi:10.1001/jamainternmed.2018.8107).
Internists billed Medicare the most for ACP claims (65%), followed by family physicians (22%) gerontologists (5%), and oncologist/hematologists (0.3%), according to the analysis based on 2016 Medicare claims data and Census Bureau data. A greater proportion of patients with ACP claims were female, aged 85 years or older, enrolled in hospice, and died in the study year. Patients had higher odds of having an ACP claim if they were older and had lower income, and if they had cancer, heart failure, stroke, chronic kidney disease, or dementia. Male patients who were Asian, black, and Hispanic had lower chances of having an ACP claim.
In a related study, Emmanuelle Belanger, PhD, of Brown University, Providence, R.I., and her colleagues examined national Medicare data from 2016 to the third quarter of 2017. Across the United States, 2% of Medicare patients aged 65 years and older received advance care planning services that were billed under the ACP codes (JAMA Intern Med. 2019 March 11. doi: 10.1001/jamainternmed.2018.8615). Visits billed under the ACP codes increased from 538,275 to 633,214 during the same time period. Claim rates were higher among patients who died within the study period, reaching 3% in 2016 and 6% in 2017. The percentage of decedents with an ACP billed visit varied strongly across states, with states such as North Dakota, South Dakota, and Wyoming having the fewest ACP visits billed and states such as California and Nevada having the most. ACP billed visits increased in all settings in 2017, but primarily in hospitals and nursing homes. Nationally, internists billed the codes most (48%), followed by family physicians (28%).
While the two studies indicate low usage of the ACP codes, many physicians are discussing advance care planning with their patients, said Mary M. Newman, MD, an internist based in Lutherville, Md., and former American College of Physicians adviser to the American Medical Association Relative Scale Value Update Committee (RUC).
“What cannot be captured by tracking under Medicare claims data are those shorter conversations that we have frequently,” Dr. Newman said in an interview. “If we have a short conversation about advance care planning, it gets folded into our evaluation and management visit. It’s not going to be separately billed.”
At the same time, some patients are not ready to discuss end-of-life options and decline the discussions when asked, Dr. Newman said. Particularly for healthier patients, end of life care is not a primary focus, she noted.
“Not everybody’s ready to have an advance care planning [discussion] that lasts 16-45 minutes,” she said. “Many people over age 65 are not ready to deal with advance care planning in their day-to-day lives, and it may not be what they wish to discuss. I offer the option to patients and some say, ‘Yes, I’d love to,’ and others decline or postpone.”
Low usage of the ACP codes may be associated with lack of awareness, uncertainty about appropriate code use, or associated billing that is not part of the standard workflow, Ankita Mehta, MD, of Mount Sinai in New York wrote an editorial accompanying the studies (JAMA Intern Med. 2019 March 11. doi:10.1001/jamainternmed.2018.8105).
“Regardless, the low rates of utilization of ACP codes is alarming and highlights the need to create strategies to integrate ACP discussions into standard practice and build ACP documentation and billing in clinical workflow,” Dr. Mehta said.
Dr. Newman agreed that more education among physicians is needed.
“The amount of education clinicians have received varies tremendously across the geography of the country,” she said. “I think the codes are going to be slowly adopted. The challenge to us is to make sure we’re all better educated on palliative care as people age and get sick and that we are sensitive to our patients explicit and implicit needs for these discussions.”
Hypoglycemia in the elderly: Watch for atypical symptoms
We read with interest the review article by Keber and Fiebert, “Diabetes in the elderly: Matching meds to needs” (J Fam Pract. 2018;67:408-410,412-415). The authors have provided a timely overview of antidiabetes medications for elderly people with type 2 diabetes mellitus (T2DM) and their relative risks for hypoglycemia.
We’d like to add to this important conversation.
Aging, per se, modifies the glycemic thresholds for autonomic symptoms and cognitive impairment; in older nondiabetic men (mean + SD: age 65 ± 3 years), autonomic symptoms and cognitive dysfunction commence at identical glycemic thresholds (3 ± 0.2 mmol/L [54 ± 4 mg/dL]). By contrast, in younger men (age 23 ± 2 years), a significant gap is observed between the glycemic threshold for symptom generation (3.6 mmol/L [65 mg/dL]) and the onset of cognitive dysfunction (2.6 mmol/L [47 mg/dL]).1,2 The simultaneous occurrence of symptoms and cognitive impairment in older people may adversely affect their ability to recognize and treat hypoglycemia promptly.
In addition, hypoglycemia in older T2DM patients often presents with atypical neurologic symptoms, including incoordination and ataxia, slurring of speech, and visual disturbances, which either are not identified as hypoglycemia or are misdiagnosed as other medical disorders (eg, transient ischemic attack).3 Knowledge about hypoglycemia symptoms is poor, in both elderly people with diabetes and their relatives and caregivers, which compromises the ability to identify hypoglycemia and provide effective treatment.4 Education about the possible presentations of hypoglycemia and its effective treatment is essential for older patients and their relatives.
Jan Brož, MD
Prague, Czech Republic
1. Meneilly GS, Elahi D. Physiological importance of first-phase insulin release in elderly patients with diabetes. Diabetes Care. 1998;21:1326-1329.
2. Matyka K, Evans M, Lomas J, et al. Altered hierarchy of protective responses against severe hypoglycemia in normal aging in healthy men. Diabetes Care. 1997;20:135-141.
3. Jaap AJ, Jones GC, McCrimmon RJ, et al. Perceived symptoms of hypoglycaemia in elderly type 2 diabetic patients treated with insulin. Diabet Med. 1998;15:398-401.
4. Thomson FJ, Masson EA, Leeming JT, et al. Lack of knowledge of symptoms of hypoglycaemia by elderly diabetic patients. Age Ageing. 1991;20:404-406.
We read with interest the review article by Keber and Fiebert, “Diabetes in the elderly: Matching meds to needs” (J Fam Pract. 2018;67:408-410,412-415). The authors have provided a timely overview of antidiabetes medications for elderly people with type 2 diabetes mellitus (T2DM) and their relative risks for hypoglycemia.
We’d like to add to this important conversation.
Aging, per se, modifies the glycemic thresholds for autonomic symptoms and cognitive impairment; in older nondiabetic men (mean + SD: age 65 ± 3 years), autonomic symptoms and cognitive dysfunction commence at identical glycemic thresholds (3 ± 0.2 mmol/L [54 ± 4 mg/dL]). By contrast, in younger men (age 23 ± 2 years), a significant gap is observed between the glycemic threshold for symptom generation (3.6 mmol/L [65 mg/dL]) and the onset of cognitive dysfunction (2.6 mmol/L [47 mg/dL]).1,2 The simultaneous occurrence of symptoms and cognitive impairment in older people may adversely affect their ability to recognize and treat hypoglycemia promptly.
In addition, hypoglycemia in older T2DM patients often presents with atypical neurologic symptoms, including incoordination and ataxia, slurring of speech, and visual disturbances, which either are not identified as hypoglycemia or are misdiagnosed as other medical disorders (eg, transient ischemic attack).3 Knowledge about hypoglycemia symptoms is poor, in both elderly people with diabetes and their relatives and caregivers, which compromises the ability to identify hypoglycemia and provide effective treatment.4 Education about the possible presentations of hypoglycemia and its effective treatment is essential for older patients and their relatives.
Jan Brož, MD
Prague, Czech Republic
We read with interest the review article by Keber and Fiebert, “Diabetes in the elderly: Matching meds to needs” (J Fam Pract. 2018;67:408-410,412-415). The authors have provided a timely overview of antidiabetes medications for elderly people with type 2 diabetes mellitus (T2DM) and their relative risks for hypoglycemia.
We’d like to add to this important conversation.
Aging, per se, modifies the glycemic thresholds for autonomic symptoms and cognitive impairment; in older nondiabetic men (mean + SD: age 65 ± 3 years), autonomic symptoms and cognitive dysfunction commence at identical glycemic thresholds (3 ± 0.2 mmol/L [54 ± 4 mg/dL]). By contrast, in younger men (age 23 ± 2 years), a significant gap is observed between the glycemic threshold for symptom generation (3.6 mmol/L [65 mg/dL]) and the onset of cognitive dysfunction (2.6 mmol/L [47 mg/dL]).1,2 The simultaneous occurrence of symptoms and cognitive impairment in older people may adversely affect their ability to recognize and treat hypoglycemia promptly.
In addition, hypoglycemia in older T2DM patients often presents with atypical neurologic symptoms, including incoordination and ataxia, slurring of speech, and visual disturbances, which either are not identified as hypoglycemia or are misdiagnosed as other medical disorders (eg, transient ischemic attack).3 Knowledge about hypoglycemia symptoms is poor, in both elderly people with diabetes and their relatives and caregivers, which compromises the ability to identify hypoglycemia and provide effective treatment.4 Education about the possible presentations of hypoglycemia and its effective treatment is essential for older patients and their relatives.
Jan Brož, MD
Prague, Czech Republic
1. Meneilly GS, Elahi D. Physiological importance of first-phase insulin release in elderly patients with diabetes. Diabetes Care. 1998;21:1326-1329.
2. Matyka K, Evans M, Lomas J, et al. Altered hierarchy of protective responses against severe hypoglycemia in normal aging in healthy men. Diabetes Care. 1997;20:135-141.
3. Jaap AJ, Jones GC, McCrimmon RJ, et al. Perceived symptoms of hypoglycaemia in elderly type 2 diabetic patients treated with insulin. Diabet Med. 1998;15:398-401.
4. Thomson FJ, Masson EA, Leeming JT, et al. Lack of knowledge of symptoms of hypoglycaemia by elderly diabetic patients. Age Ageing. 1991;20:404-406.
1. Meneilly GS, Elahi D. Physiological importance of first-phase insulin release in elderly patients with diabetes. Diabetes Care. 1998;21:1326-1329.
2. Matyka K, Evans M, Lomas J, et al. Altered hierarchy of protective responses against severe hypoglycemia in normal aging in healthy men. Diabetes Care. 1997;20:135-141.
3. Jaap AJ, Jones GC, McCrimmon RJ, et al. Perceived symptoms of hypoglycaemia in elderly type 2 diabetic patients treated with insulin. Diabet Med. 1998;15:398-401.
4. Thomson FJ, Masson EA, Leeming JT, et al. Lack of knowledge of symptoms of hypoglycaemia by elderly diabetic patients. Age Ageing. 1991;20:404-406.
Boosting Alzheimer’s trial participation via Medicare Advantage ‘memory fitness programs’
Clinical trials represent future hope for patients seeking better care, and there is no disease more in need of better care than Alzheimer’s disease. While death rates among most cancers, as well as heart disease, HIV-related illness, and other categories, have declined in the past decade, there has been no progress for Alzheimer’s disease. Better health and wellness overall may be having a beneficial effect that has produced a reduction in age-adjusted dementia rates, but with the aging of the population there are a greater absolute number of dementia cases than ever before, and that number is expected to continue rising. Finding a disease-modifying therapy seems to be the best hope for changing this dim outlook. Clinical trials intend to do just that but are hampered by patient enrollment rates that remain low. Far fewer eligible patients enroll than are needed, causing studies to take longer to complete, driving up their costs and essentially slowing progress. There is a need to increase patient enrollment, and there has been a variety of efforts intended to address this, not the least of which has been an explosion of media coverage of Alzheimer’s disease.
The Global Alzheimer’s Platform (GAP) Foundation, a nonprofit, self-described patient-centric entity dedicated to reducing the time and cost of Alzheimer’s disease clinical trials, recently announced an initiative to increase participation in Alzheimer’s clinical trials by supporting and collaborating with “memory fitness programs” through select Medicare Advantage plans. At worst, this seems a harmless way to increase attention and hopefully interest in clinical trial participation. At best, this may be a cost-effective way to increase enrollment and even improve dementia care. Dementia is notoriously underdiagnosed, especially by overworked, busy primary care providers who simply lack the time to perform the time-consuming testing that is typically required to diagnose and follow such patients.
There are some caveats to consider. First, memory fitness programs are of dubious benefit. They generally fit the description of being harmless, but there is little compelling evidence that they preserve or improve memory.
Second, enrollment in a clinical trial, for a patient, is not always a winning proposition. To date, there has been little success and in the absence of benefit, any downside – even if simply an inconvenience – is a net negative. Recently at the 2018 Clinical Trials on Alzheimer’s Disease meeting, Merck reported that patients with mild cognitive impairment receiving active treatment in the BACE1 inhibitor verubecestat trial actually declined at a more rapid rate than did those on placebo. While the absolute difference was small, and one could argue whether it was clinically significant or simply a random occurrence, it was a reminder that intervention with an experimental agent is not necessarily benign.
Third, Medicare Advantage plans, while popular in some circles, are not considered advantageous to providers so that the proliferation of inadequate reimbursement will potentially fuel the accelerating number of providers who opt out of insurance plans altogether. This is not necessarily an issue for the GAP Foundation specifically but is nonetheless an issue for anything that promotes MA plans).
Finally, it remains important to help patients and families maintain a positive outlook, especially when we have nothing better to offer. Alzheimer’s disease is not a death sentence for every patient affected. While many have difficult and heartbreaking courses, some have slowly progressive courses with relatively little impairment for an extended period of time. There are also the dementia-phobic, cognitively unimpaired individuals (or who simply have normal age-associated cognitive changes) in whom the continued drumbeat of dementia awareness and memory testing raises their paranoia ever higher. We treat deficits (or try to), but we have to live based on our preserved skills. The challenge clinicians must face with patients and families is how to maximize function while compensating for deficits and making sure that patients and families maintain their hope.
Dr. Caselli is professor of neurology at the Mayo Clinic Arizona in Scottsdale and associate director and clinical core director of the Arizona Alzheimer’s Disease Center.
Clinical trials represent future hope for patients seeking better care, and there is no disease more in need of better care than Alzheimer’s disease. While death rates among most cancers, as well as heart disease, HIV-related illness, and other categories, have declined in the past decade, there has been no progress for Alzheimer’s disease. Better health and wellness overall may be having a beneficial effect that has produced a reduction in age-adjusted dementia rates, but with the aging of the population there are a greater absolute number of dementia cases than ever before, and that number is expected to continue rising. Finding a disease-modifying therapy seems to be the best hope for changing this dim outlook. Clinical trials intend to do just that but are hampered by patient enrollment rates that remain low. Far fewer eligible patients enroll than are needed, causing studies to take longer to complete, driving up their costs and essentially slowing progress. There is a need to increase patient enrollment, and there has been a variety of efforts intended to address this, not the least of which has been an explosion of media coverage of Alzheimer’s disease.
The Global Alzheimer’s Platform (GAP) Foundation, a nonprofit, self-described patient-centric entity dedicated to reducing the time and cost of Alzheimer’s disease clinical trials, recently announced an initiative to increase participation in Alzheimer’s clinical trials by supporting and collaborating with “memory fitness programs” through select Medicare Advantage plans. At worst, this seems a harmless way to increase attention and hopefully interest in clinical trial participation. At best, this may be a cost-effective way to increase enrollment and even improve dementia care. Dementia is notoriously underdiagnosed, especially by overworked, busy primary care providers who simply lack the time to perform the time-consuming testing that is typically required to diagnose and follow such patients.
There are some caveats to consider. First, memory fitness programs are of dubious benefit. They generally fit the description of being harmless, but there is little compelling evidence that they preserve or improve memory.
Second, enrollment in a clinical trial, for a patient, is not always a winning proposition. To date, there has been little success and in the absence of benefit, any downside – even if simply an inconvenience – is a net negative. Recently at the 2018 Clinical Trials on Alzheimer’s Disease meeting, Merck reported that patients with mild cognitive impairment receiving active treatment in the BACE1 inhibitor verubecestat trial actually declined at a more rapid rate than did those on placebo. While the absolute difference was small, and one could argue whether it was clinically significant or simply a random occurrence, it was a reminder that intervention with an experimental agent is not necessarily benign.
Third, Medicare Advantage plans, while popular in some circles, are not considered advantageous to providers so that the proliferation of inadequate reimbursement will potentially fuel the accelerating number of providers who opt out of insurance plans altogether. This is not necessarily an issue for the GAP Foundation specifically but is nonetheless an issue for anything that promotes MA plans).
Finally, it remains important to help patients and families maintain a positive outlook, especially when we have nothing better to offer. Alzheimer’s disease is not a death sentence for every patient affected. While many have difficult and heartbreaking courses, some have slowly progressive courses with relatively little impairment for an extended period of time. There are also the dementia-phobic, cognitively unimpaired individuals (or who simply have normal age-associated cognitive changes) in whom the continued drumbeat of dementia awareness and memory testing raises their paranoia ever higher. We treat deficits (or try to), but we have to live based on our preserved skills. The challenge clinicians must face with patients and families is how to maximize function while compensating for deficits and making sure that patients and families maintain their hope.
Dr. Caselli is professor of neurology at the Mayo Clinic Arizona in Scottsdale and associate director and clinical core director of the Arizona Alzheimer’s Disease Center.
Clinical trials represent future hope for patients seeking better care, and there is no disease more in need of better care than Alzheimer’s disease. While death rates among most cancers, as well as heart disease, HIV-related illness, and other categories, have declined in the past decade, there has been no progress for Alzheimer’s disease. Better health and wellness overall may be having a beneficial effect that has produced a reduction in age-adjusted dementia rates, but with the aging of the population there are a greater absolute number of dementia cases than ever before, and that number is expected to continue rising. Finding a disease-modifying therapy seems to be the best hope for changing this dim outlook. Clinical trials intend to do just that but are hampered by patient enrollment rates that remain low. Far fewer eligible patients enroll than are needed, causing studies to take longer to complete, driving up their costs and essentially slowing progress. There is a need to increase patient enrollment, and there has been a variety of efforts intended to address this, not the least of which has been an explosion of media coverage of Alzheimer’s disease.
The Global Alzheimer’s Platform (GAP) Foundation, a nonprofit, self-described patient-centric entity dedicated to reducing the time and cost of Alzheimer’s disease clinical trials, recently announced an initiative to increase participation in Alzheimer’s clinical trials by supporting and collaborating with “memory fitness programs” through select Medicare Advantage plans. At worst, this seems a harmless way to increase attention and hopefully interest in clinical trial participation. At best, this may be a cost-effective way to increase enrollment and even improve dementia care. Dementia is notoriously underdiagnosed, especially by overworked, busy primary care providers who simply lack the time to perform the time-consuming testing that is typically required to diagnose and follow such patients.
There are some caveats to consider. First, memory fitness programs are of dubious benefit. They generally fit the description of being harmless, but there is little compelling evidence that they preserve or improve memory.
Second, enrollment in a clinical trial, for a patient, is not always a winning proposition. To date, there has been little success and in the absence of benefit, any downside – even if simply an inconvenience – is a net negative. Recently at the 2018 Clinical Trials on Alzheimer’s Disease meeting, Merck reported that patients with mild cognitive impairment receiving active treatment in the BACE1 inhibitor verubecestat trial actually declined at a more rapid rate than did those on placebo. While the absolute difference was small, and one could argue whether it was clinically significant or simply a random occurrence, it was a reminder that intervention with an experimental agent is not necessarily benign.
Third, Medicare Advantage plans, while popular in some circles, are not considered advantageous to providers so that the proliferation of inadequate reimbursement will potentially fuel the accelerating number of providers who opt out of insurance plans altogether. This is not necessarily an issue for the GAP Foundation specifically but is nonetheless an issue for anything that promotes MA plans).
Finally, it remains important to help patients and families maintain a positive outlook, especially when we have nothing better to offer. Alzheimer’s disease is not a death sentence for every patient affected. While many have difficult and heartbreaking courses, some have slowly progressive courses with relatively little impairment for an extended period of time. There are also the dementia-phobic, cognitively unimpaired individuals (or who simply have normal age-associated cognitive changes) in whom the continued drumbeat of dementia awareness and memory testing raises their paranoia ever higher. We treat deficits (or try to), but we have to live based on our preserved skills. The challenge clinicians must face with patients and families is how to maximize function while compensating for deficits and making sure that patients and families maintain their hope.
Dr. Caselli is professor of neurology at the Mayo Clinic Arizona in Scottsdale and associate director and clinical core director of the Arizona Alzheimer’s Disease Center.
Blood-based signature helps predict status of early AD indicator
A recently developed blood-based signature can help predict the status of an early Alzheimer’s disease risk indicator with high accuracy, investigators are reporting.
By analyzing as few as four proteins, the machine learning-derived test can predict the status of cerebrospinal fluid (CSF) amyloid beta1-42 (Abeta1-42), according to Noel G. Faux, PHD, of IBM Australia and the University of Melbourne, and co-investigators.
While shifts in Abeta1-42 may signal the presence of disease long before significant cognitive decline is clinically apparent, collection of CSF is highly invasive and expensive, Faux and investigators said in their report.
By contrast, blood biomarkers could prove to be a useful alternative not only to invasive lumbar punctures, they said, but also to the positron emission tomography (PET) evaluation of Abeta1-42, which is expensive and limited in some regions.
“In conjunction with biomarkers for neocortical amyloid burden, the CSF Abeta1-42biomarkers presented in this work may help yield a cheap, non-invasive tool for both improving clinical trials targeting amyloid and population screening,” Dr. Faux and co-authors said in Scientific Reports.
Dr. Faux and colleagues used a Random Forest approach to build models for CSF Abeta1-42 using blood biomarkers and other variables.
They found that a model incorporating age, APOEe4 carrier status, and a number of plasma protein levels predicted Abeta1-42 normal/abnormalstatus with an AUC, sensitivity and specificity of 0.84, 0.78 and 0.73 respectively.
In a model they said was more suitable for clinical application, they narrowed down the variables to 4 plasma analytes and APOEe4 carrier status, which had an AUC, sensitivity, and specificity of 0.81, 0.81 and 0.64 respectively.
They validated the models on a cohort of individuals in the Alzheimer’s Disease Neuroimaging Initiative (ADNI), a large, longitudinal, multicenter study.
Patients with mild cognitive impairment with predicted abnormal CSF Abeta1-42 levels indeed did transition to a diagnosis of Alzheimer’s disease more quickly than those with predicted normal levels, according to investigators.
That helps provide “strong evidence” that the blood-based model is generalizable, robust, and could help stratify patients based on risk of progressing to Alzheimer’s disease, they said in their report.
Dr. Faux and colleagues declared no conflicts of interest related to the research.
SOURCE: Goudey B, et al. Sci Rep. 2019 Mar 10. doi: 10.1101/190207v3.
A recently developed blood-based signature can help predict the status of an early Alzheimer’s disease risk indicator with high accuracy, investigators are reporting.
By analyzing as few as four proteins, the machine learning-derived test can predict the status of cerebrospinal fluid (CSF) amyloid beta1-42 (Abeta1-42), according to Noel G. Faux, PHD, of IBM Australia and the University of Melbourne, and co-investigators.
While shifts in Abeta1-42 may signal the presence of disease long before significant cognitive decline is clinically apparent, collection of CSF is highly invasive and expensive, Faux and investigators said in their report.
By contrast, blood biomarkers could prove to be a useful alternative not only to invasive lumbar punctures, they said, but also to the positron emission tomography (PET) evaluation of Abeta1-42, which is expensive and limited in some regions.
“In conjunction with biomarkers for neocortical amyloid burden, the CSF Abeta1-42biomarkers presented in this work may help yield a cheap, non-invasive tool for both improving clinical trials targeting amyloid and population screening,” Dr. Faux and co-authors said in Scientific Reports.
Dr. Faux and colleagues used a Random Forest approach to build models for CSF Abeta1-42 using blood biomarkers and other variables.
They found that a model incorporating age, APOEe4 carrier status, and a number of plasma protein levels predicted Abeta1-42 normal/abnormalstatus with an AUC, sensitivity and specificity of 0.84, 0.78 and 0.73 respectively.
In a model they said was more suitable for clinical application, they narrowed down the variables to 4 plasma analytes and APOEe4 carrier status, which had an AUC, sensitivity, and specificity of 0.81, 0.81 and 0.64 respectively.
They validated the models on a cohort of individuals in the Alzheimer’s Disease Neuroimaging Initiative (ADNI), a large, longitudinal, multicenter study.
Patients with mild cognitive impairment with predicted abnormal CSF Abeta1-42 levels indeed did transition to a diagnosis of Alzheimer’s disease more quickly than those with predicted normal levels, according to investigators.
That helps provide “strong evidence” that the blood-based model is generalizable, robust, and could help stratify patients based on risk of progressing to Alzheimer’s disease, they said in their report.
Dr. Faux and colleagues declared no conflicts of interest related to the research.
SOURCE: Goudey B, et al. Sci Rep. 2019 Mar 10. doi: 10.1101/190207v3.
A recently developed blood-based signature can help predict the status of an early Alzheimer’s disease risk indicator with high accuracy, investigators are reporting.
By analyzing as few as four proteins, the machine learning-derived test can predict the status of cerebrospinal fluid (CSF) amyloid beta1-42 (Abeta1-42), according to Noel G. Faux, PHD, of IBM Australia and the University of Melbourne, and co-investigators.
While shifts in Abeta1-42 may signal the presence of disease long before significant cognitive decline is clinically apparent, collection of CSF is highly invasive and expensive, Faux and investigators said in their report.
By contrast, blood biomarkers could prove to be a useful alternative not only to invasive lumbar punctures, they said, but also to the positron emission tomography (PET) evaluation of Abeta1-42, which is expensive and limited in some regions.
“In conjunction with biomarkers for neocortical amyloid burden, the CSF Abeta1-42biomarkers presented in this work may help yield a cheap, non-invasive tool for both improving clinical trials targeting amyloid and population screening,” Dr. Faux and co-authors said in Scientific Reports.
Dr. Faux and colleagues used a Random Forest approach to build models for CSF Abeta1-42 using blood biomarkers and other variables.
They found that a model incorporating age, APOEe4 carrier status, and a number of plasma protein levels predicted Abeta1-42 normal/abnormalstatus with an AUC, sensitivity and specificity of 0.84, 0.78 and 0.73 respectively.
In a model they said was more suitable for clinical application, they narrowed down the variables to 4 plasma analytes and APOEe4 carrier status, which had an AUC, sensitivity, and specificity of 0.81, 0.81 and 0.64 respectively.
They validated the models on a cohort of individuals in the Alzheimer’s Disease Neuroimaging Initiative (ADNI), a large, longitudinal, multicenter study.
Patients with mild cognitive impairment with predicted abnormal CSF Abeta1-42 levels indeed did transition to a diagnosis of Alzheimer’s disease more quickly than those with predicted normal levels, according to investigators.
That helps provide “strong evidence” that the blood-based model is generalizable, robust, and could help stratify patients based on risk of progressing to Alzheimer’s disease, they said in their report.
Dr. Faux and colleagues declared no conflicts of interest related to the research.
SOURCE: Goudey B, et al. Sci Rep. 2019 Mar 10. doi: 10.1101/190207v3.
FROM SCIENTIFIC REPORTS
Key clinical point: A blood-based signature can help predict the status of an early Alzheimer’s disease risk indicator.
Major finding:
Study details: Machine learning analysis of blood biomarkers and other variables in a validation cohort of 198 individuals.
Disclosures: The study authors declared no conflicts of interest.
Source: Goudey B, et al. Sci Rep. 2019 Mar 10. doi: 10.1101/190207v3.