User login
Pap testing much less likely in women without regular provider
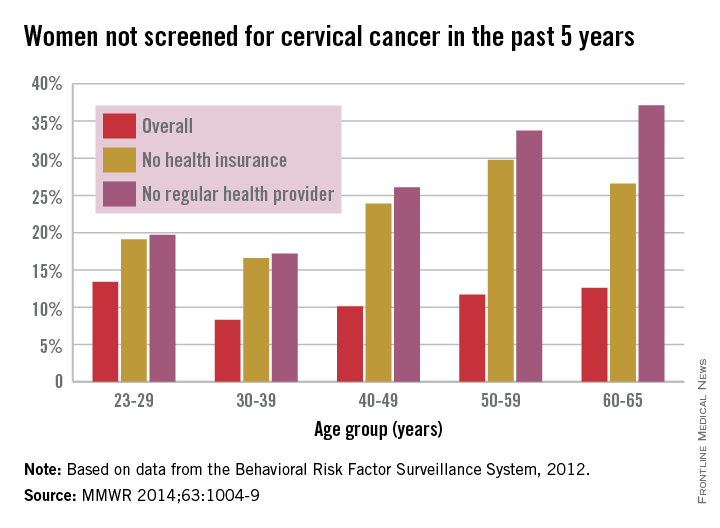
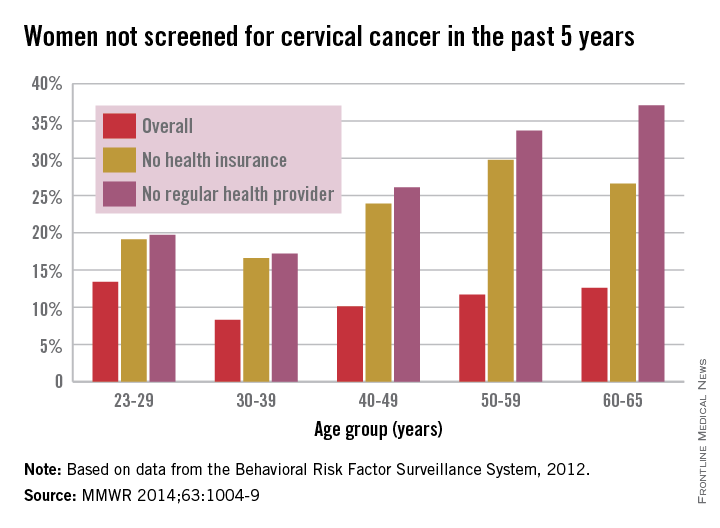
Adult women with no regular health care provider or no health insurance were much less likely to have been screened for cervical cancer in the past 5 years, a study from the Centers for Disease Control and Prevention showed.
In 2012, an estimated 11.4% of U.S. women aged 21-65 years had not had a Pap test to screen for cervical cancer in the past 5 years, compared with 25.5% of women without a regular health care provider and 23.1% of those without insurance, the CDC reported (MMWR 2014;63:1004-9).
By age group, women aged 30-39 years had the lowest overall rate, with only 8.3% not receiving screening in the past 5 years, as well as the lowest rates for those who did not have health insurance or a health care provider, at 16.6% and 17.2%, respectively. In 2012, women aged 23-29 years had the highest overall rate at 13.4%, women aged 50-59 years had the highest rate for no insurance at 29.8%, and women aged 60-65 years had the highest rate for no health care provider at 37.1%.
By ethnicity, black women had the lowest overall 5-year nonscreening rate at 9.2%, although Hispanics had the lowest rate for women without health insurance or a health care provider, at 16.7% and 18.4%, respectively. At 19.7%, Asian/Pacific Islanders had the highest overall rate, as well as the highest rate for women without health insurance at 32.5% and women without a regular health care provider at 40.8%, according to data from the Behavioral Risk Factor Surveillance System.
From 2007 to 2011, a total of 62,150 cervical cancer cases were reported in the United States, and in 2011, the incidence rate was 7.5 per 100,000 people, with the rate falling an average of 1.9% a year over that 5-year period. For the same time period, there were 19,969 deaths, with the overall U.S. death rate at 2.3 per 100,000 people in 2011, with a slight average decrease per year but not enough to be statistically significant, the CDC noted.
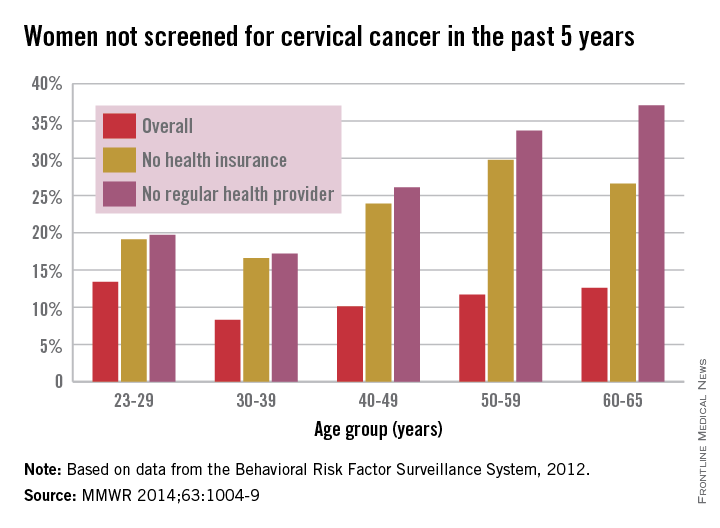
Adult women with no regular health care provider or no health insurance were much less likely to have been screened for cervical cancer in the past 5 years, a study from the Centers for Disease Control and Prevention showed.
In 2012, an estimated 11.4% of U.S. women aged 21-65 years had not had a Pap test to screen for cervical cancer in the past 5 years, compared with 25.5% of women without a regular health care provider and 23.1% of those without insurance, the CDC reported (MMWR 2014;63:1004-9).
By age group, women aged 30-39 years had the lowest overall rate, with only 8.3% not receiving screening in the past 5 years, as well as the lowest rates for those who did not have health insurance or a health care provider, at 16.6% and 17.2%, respectively. In 2012, women aged 23-29 years had the highest overall rate at 13.4%, women aged 50-59 years had the highest rate for no insurance at 29.8%, and women aged 60-65 years had the highest rate for no health care provider at 37.1%.
By ethnicity, black women had the lowest overall 5-year nonscreening rate at 9.2%, although Hispanics had the lowest rate for women without health insurance or a health care provider, at 16.7% and 18.4%, respectively. At 19.7%, Asian/Pacific Islanders had the highest overall rate, as well as the highest rate for women without health insurance at 32.5% and women without a regular health care provider at 40.8%, according to data from the Behavioral Risk Factor Surveillance System.
From 2007 to 2011, a total of 62,150 cervical cancer cases were reported in the United States, and in 2011, the incidence rate was 7.5 per 100,000 people, with the rate falling an average of 1.9% a year over that 5-year period. For the same time period, there were 19,969 deaths, with the overall U.S. death rate at 2.3 per 100,000 people in 2011, with a slight average decrease per year but not enough to be statistically significant, the CDC noted.
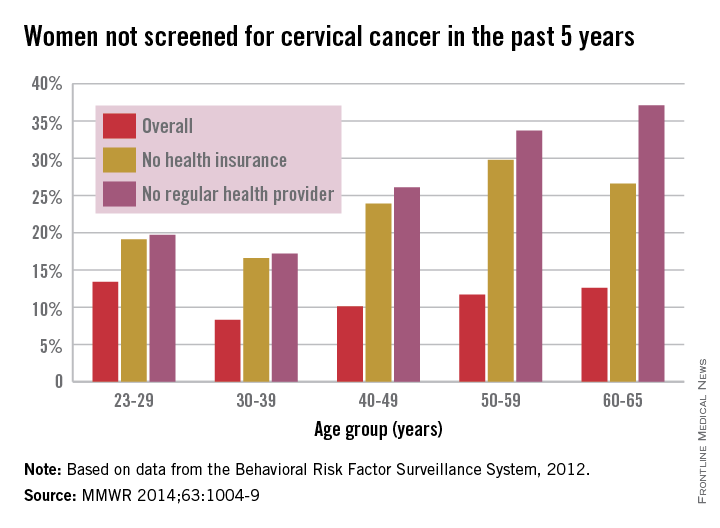
Adult women with no regular health care provider or no health insurance were much less likely to have been screened for cervical cancer in the past 5 years, a study from the Centers for Disease Control and Prevention showed.
In 2012, an estimated 11.4% of U.S. women aged 21-65 years had not had a Pap test to screen for cervical cancer in the past 5 years, compared with 25.5% of women without a regular health care provider and 23.1% of those without insurance, the CDC reported (MMWR 2014;63:1004-9).
By age group, women aged 30-39 years had the lowest overall rate, with only 8.3% not receiving screening in the past 5 years, as well as the lowest rates for those who did not have health insurance or a health care provider, at 16.6% and 17.2%, respectively. In 2012, women aged 23-29 years had the highest overall rate at 13.4%, women aged 50-59 years had the highest rate for no insurance at 29.8%, and women aged 60-65 years had the highest rate for no health care provider at 37.1%.
By ethnicity, black women had the lowest overall 5-year nonscreening rate at 9.2%, although Hispanics had the lowest rate for women without health insurance or a health care provider, at 16.7% and 18.4%, respectively. At 19.7%, Asian/Pacific Islanders had the highest overall rate, as well as the highest rate for women without health insurance at 32.5% and women without a regular health care provider at 40.8%, according to data from the Behavioral Risk Factor Surveillance System.
From 2007 to 2011, a total of 62,150 cervical cancer cases were reported in the United States, and in 2011, the incidence rate was 7.5 per 100,000 people, with the rate falling an average of 1.9% a year over that 5-year period. For the same time period, there were 19,969 deaths, with the overall U.S. death rate at 2.3 per 100,000 people in 2011, with a slight average decrease per year but not enough to be statistically significant, the CDC noted.
FROM MORBIDITY AND MORTALITY WEEKLY REPORT
Salpingectomy associated with reduced ovarian cancer risk
MELBOURNE – Surgical removal of the fallopian tubes could be a viable option for reducing the risk of ovarian cancer in high-risk women, a speaker said at the biennial meeting of the International Gynecologic Cancer Society.
Dr. Henrik Falconer, head of gynecologic oncology at the Karolinska Institute, Stockholm, said there is an emerging hypothesis that ovarian cancer arises primarily in the fallopian tubes, not in the ovaries, although this is difficult to prove.
Researchers therefore conducted a retrospective, population-based cohort study of women who had previously undergone sterilization; salpingectomy; hysterectomy and bilateral salpingo-oophorectomy; or hysterectomy for a benign indication between 1972 and 2010 in Sweden.
They found that women who had undergone unilateral salpingectomy had a 28% lower risk of ovarian cancer, while those who had undergone bilateral salpingectomy had a 65% lower risk, compared with the general population.
Women who underwent hysterectomy with removal of fallopian tubes and ovaries had the lowest overall risk of ovarian cancer (hazard ratio, 0.06; 95% confidence interval, 0.03-0.12), while those who had hysterectomy alone had a 22% reduction in risk.
Dr. Falconer said a case could be made for proactive removal of the fallopian tubes in women carrying the BRCA mutation, which might then enable a delay in removal of their ovaries.
“Today, we counsel the patients and advise them to take away the tubes and the ovaries, sometimes at 40-45, after they have completed their family planning,” Dr. Falconer said in an interview.
“I think now we could take away the tubes instead earlier, to have risk reduction while they wait to have their ovaries removed, perhaps in their 50s or 60s then, or maybe never.”
This would avoid the morbidity associated with oophorectomy, such as cardiovascular disease and Alzheimer’s disease, Dr. Falconer said, and could not only reduce the risk of cancer but also improve the quality of life in this population of relatively young women.
He also suggested that prophylactic salpingectomy might even be considered in women undergoing sterilization, even if they weren’t necessarily at high risk of ovarian cancer.
The study included data from more than 5 million women, with over 250,000 women exposed to some form of surgery and more than 30,000 cases of ovarian cancer.
One audience member raised concerns about the use of prophylactic salpingectomy in an otherwise healthy population, suggesting that the procedure was not without its risks and could have unintended consequences because of the loss of blood supply to the ovaries.
The study did not control for oral contraceptive use or histological subtypes.
Dr. Falconer declared support from Intuitive Surgical. There were no other conflicts of interest declared.
MELBOURNE – Surgical removal of the fallopian tubes could be a viable option for reducing the risk of ovarian cancer in high-risk women, a speaker said at the biennial meeting of the International Gynecologic Cancer Society.
Dr. Henrik Falconer, head of gynecologic oncology at the Karolinska Institute, Stockholm, said there is an emerging hypothesis that ovarian cancer arises primarily in the fallopian tubes, not in the ovaries, although this is difficult to prove.
Researchers therefore conducted a retrospective, population-based cohort study of women who had previously undergone sterilization; salpingectomy; hysterectomy and bilateral salpingo-oophorectomy; or hysterectomy for a benign indication between 1972 and 2010 in Sweden.
They found that women who had undergone unilateral salpingectomy had a 28% lower risk of ovarian cancer, while those who had undergone bilateral salpingectomy had a 65% lower risk, compared with the general population.
Women who underwent hysterectomy with removal of fallopian tubes and ovaries had the lowest overall risk of ovarian cancer (hazard ratio, 0.06; 95% confidence interval, 0.03-0.12), while those who had hysterectomy alone had a 22% reduction in risk.
Dr. Falconer said a case could be made for proactive removal of the fallopian tubes in women carrying the BRCA mutation, which might then enable a delay in removal of their ovaries.
“Today, we counsel the patients and advise them to take away the tubes and the ovaries, sometimes at 40-45, after they have completed their family planning,” Dr. Falconer said in an interview.
“I think now we could take away the tubes instead earlier, to have risk reduction while they wait to have their ovaries removed, perhaps in their 50s or 60s then, or maybe never.”
This would avoid the morbidity associated with oophorectomy, such as cardiovascular disease and Alzheimer’s disease, Dr. Falconer said, and could not only reduce the risk of cancer but also improve the quality of life in this population of relatively young women.
He also suggested that prophylactic salpingectomy might even be considered in women undergoing sterilization, even if they weren’t necessarily at high risk of ovarian cancer.
The study included data from more than 5 million women, with over 250,000 women exposed to some form of surgery and more than 30,000 cases of ovarian cancer.
One audience member raised concerns about the use of prophylactic salpingectomy in an otherwise healthy population, suggesting that the procedure was not without its risks and could have unintended consequences because of the loss of blood supply to the ovaries.
The study did not control for oral contraceptive use or histological subtypes.
Dr. Falconer declared support from Intuitive Surgical. There were no other conflicts of interest declared.
MELBOURNE – Surgical removal of the fallopian tubes could be a viable option for reducing the risk of ovarian cancer in high-risk women, a speaker said at the biennial meeting of the International Gynecologic Cancer Society.
Dr. Henrik Falconer, head of gynecologic oncology at the Karolinska Institute, Stockholm, said there is an emerging hypothesis that ovarian cancer arises primarily in the fallopian tubes, not in the ovaries, although this is difficult to prove.
Researchers therefore conducted a retrospective, population-based cohort study of women who had previously undergone sterilization; salpingectomy; hysterectomy and bilateral salpingo-oophorectomy; or hysterectomy for a benign indication between 1972 and 2010 in Sweden.
They found that women who had undergone unilateral salpingectomy had a 28% lower risk of ovarian cancer, while those who had undergone bilateral salpingectomy had a 65% lower risk, compared with the general population.
Women who underwent hysterectomy with removal of fallopian tubes and ovaries had the lowest overall risk of ovarian cancer (hazard ratio, 0.06; 95% confidence interval, 0.03-0.12), while those who had hysterectomy alone had a 22% reduction in risk.
Dr. Falconer said a case could be made for proactive removal of the fallopian tubes in women carrying the BRCA mutation, which might then enable a delay in removal of their ovaries.
“Today, we counsel the patients and advise them to take away the tubes and the ovaries, sometimes at 40-45, after they have completed their family planning,” Dr. Falconer said in an interview.
“I think now we could take away the tubes instead earlier, to have risk reduction while they wait to have their ovaries removed, perhaps in their 50s or 60s then, or maybe never.”
This would avoid the morbidity associated with oophorectomy, such as cardiovascular disease and Alzheimer’s disease, Dr. Falconer said, and could not only reduce the risk of cancer but also improve the quality of life in this population of relatively young women.
He also suggested that prophylactic salpingectomy might even be considered in women undergoing sterilization, even if they weren’t necessarily at high risk of ovarian cancer.
The study included data from more than 5 million women, with over 250,000 women exposed to some form of surgery and more than 30,000 cases of ovarian cancer.
One audience member raised concerns about the use of prophylactic salpingectomy in an otherwise healthy population, suggesting that the procedure was not without its risks and could have unintended consequences because of the loss of blood supply to the ovaries.
The study did not control for oral contraceptive use or histological subtypes.
Dr. Falconer declared support from Intuitive Surgical. There were no other conflicts of interest declared.
AT IGCS 2014
Key clinical point: Salpingectomy is associated with a significant reduction in the risk of ovarian cancer, even in women who do not have their ovaries removed.
Major finding: Bilateral salpingectomy is associated with a 65% reduction in the risk of ovarian cancer, compared with the general population.
Data source: Retrospective, population-based cohort study.
Disclosures: Dr. Falconer declared support from Intuitive Surgical. There were no other conflicts of interest declared.
No recurrence of cervical cancer seen with simple trachelectomy
MELBOURNE – Simple trachelectomy can achieve fertility-sparing outcomes similar to those obtained from radical trachelectomy in women with early-stage cervical cancer without any increased risk of recurrence, according to a poster presented at the biennial meeting of the International Gynecologic Cancer Society.
A retrospective cohort study of 25 patients who underwent a simple vaginal trachelectomy to remove the cervix after a diagnosis of cervical cancer found that 6 of the 10 patients who declared an intention to conceive were successful in doing so.
“The radical trachelectomy procedures [resulted in] a pregnancy rate between 70% and 80%, so we think the simple trachelectomy will do quite well,” said lead author Dr. Shamitha Kathurusinghe, an obstetrics/gynecology trainee at Royal Women’s Hospital, Melbourne.“We had 10 people with the intention to conceive, and we had 10 pregnancies in 6 patients, and our intention to conceive was about 50%,” she said in an interview.
While the majority of patients in the study sought assisted reproductive technologies, some also conceived naturally.
All pregnancies were treated as high risk, and all patients delivered via cesarean section. Two pregnancies were achieved via a surrogate; there was one first-trimester miscarriage; one ectopic pregnancy; and one second-trimester miscarriage, but the cause was unknown.”
Researchers found no incidence of cancer recurrence during the median 54-month follow-up period, among a group of patients which included 7 with stage IA1 disease, 5 with stage IA2, 11 with stage IB1 disease, and 2 with stage IB2 disease.
The study group included 7 cases of squamous cell carcinoma, 10 adenocarcinomas, 4 adenosquamous tumors, 2 adenosarcomas, and 2 neuroendocrine tumors. In all, 48% of patients were nulliparous prior to the procedure.
Dr. Kathurusinghe said surgical treatments for cervical cancer seemed to be shifting away from more radical toward more conservative approaches.
“What we’ve noticed over time is that the gold standard management is a radical hysterectomy, but we’ve gone back from that and said, maybe we can get away without that, let’s do a radical trachelectomy,” Dr. Kathurusinghe said.
“Now we’re slowly going back and saying we can be a little bit less radical and leave a bit more behind.”
While the study included women with stage IB2 tumors, Dr. Kathurusinghe said the general advice would be to use the more conservative procedure up to stage IB1 tumors only.
“Every patient should be considered on an individual basis by a specialist that’s in that area. Sit down with the patient and decide, does this patient need radical therapy? Is this woman still of a childbearing age, [who] would want to preserve their fertility; and can this be an option for that patient?”
Researchers also found that 15 patients actually had no residual disease on the final histopathology, echoing similar findings from an earlier study.
There were no conflicts of interest declared.
MELBOURNE – Simple trachelectomy can achieve fertility-sparing outcomes similar to those obtained from radical trachelectomy in women with early-stage cervical cancer without any increased risk of recurrence, according to a poster presented at the biennial meeting of the International Gynecologic Cancer Society.
A retrospective cohort study of 25 patients who underwent a simple vaginal trachelectomy to remove the cervix after a diagnosis of cervical cancer found that 6 of the 10 patients who declared an intention to conceive were successful in doing so.
“The radical trachelectomy procedures [resulted in] a pregnancy rate between 70% and 80%, so we think the simple trachelectomy will do quite well,” said lead author Dr. Shamitha Kathurusinghe, an obstetrics/gynecology trainee at Royal Women’s Hospital, Melbourne.“We had 10 people with the intention to conceive, and we had 10 pregnancies in 6 patients, and our intention to conceive was about 50%,” she said in an interview.
While the majority of patients in the study sought assisted reproductive technologies, some also conceived naturally.
All pregnancies were treated as high risk, and all patients delivered via cesarean section. Two pregnancies were achieved via a surrogate; there was one first-trimester miscarriage; one ectopic pregnancy; and one second-trimester miscarriage, but the cause was unknown.”
Researchers found no incidence of cancer recurrence during the median 54-month follow-up period, among a group of patients which included 7 with stage IA1 disease, 5 with stage IA2, 11 with stage IB1 disease, and 2 with stage IB2 disease.
The study group included 7 cases of squamous cell carcinoma, 10 adenocarcinomas, 4 adenosquamous tumors, 2 adenosarcomas, and 2 neuroendocrine tumors. In all, 48% of patients were nulliparous prior to the procedure.
Dr. Kathurusinghe said surgical treatments for cervical cancer seemed to be shifting away from more radical toward more conservative approaches.
“What we’ve noticed over time is that the gold standard management is a radical hysterectomy, but we’ve gone back from that and said, maybe we can get away without that, let’s do a radical trachelectomy,” Dr. Kathurusinghe said.
“Now we’re slowly going back and saying we can be a little bit less radical and leave a bit more behind.”
While the study included women with stage IB2 tumors, Dr. Kathurusinghe said the general advice would be to use the more conservative procedure up to stage IB1 tumors only.
“Every patient should be considered on an individual basis by a specialist that’s in that area. Sit down with the patient and decide, does this patient need radical therapy? Is this woman still of a childbearing age, [who] would want to preserve their fertility; and can this be an option for that patient?”
Researchers also found that 15 patients actually had no residual disease on the final histopathology, echoing similar findings from an earlier study.
There were no conflicts of interest declared.
MELBOURNE – Simple trachelectomy can achieve fertility-sparing outcomes similar to those obtained from radical trachelectomy in women with early-stage cervical cancer without any increased risk of recurrence, according to a poster presented at the biennial meeting of the International Gynecologic Cancer Society.
A retrospective cohort study of 25 patients who underwent a simple vaginal trachelectomy to remove the cervix after a diagnosis of cervical cancer found that 6 of the 10 patients who declared an intention to conceive were successful in doing so.
“The radical trachelectomy procedures [resulted in] a pregnancy rate between 70% and 80%, so we think the simple trachelectomy will do quite well,” said lead author Dr. Shamitha Kathurusinghe, an obstetrics/gynecology trainee at Royal Women’s Hospital, Melbourne.“We had 10 people with the intention to conceive, and we had 10 pregnancies in 6 patients, and our intention to conceive was about 50%,” she said in an interview.
While the majority of patients in the study sought assisted reproductive technologies, some also conceived naturally.
All pregnancies were treated as high risk, and all patients delivered via cesarean section. Two pregnancies were achieved via a surrogate; there was one first-trimester miscarriage; one ectopic pregnancy; and one second-trimester miscarriage, but the cause was unknown.”
Researchers found no incidence of cancer recurrence during the median 54-month follow-up period, among a group of patients which included 7 with stage IA1 disease, 5 with stage IA2, 11 with stage IB1 disease, and 2 with stage IB2 disease.
The study group included 7 cases of squamous cell carcinoma, 10 adenocarcinomas, 4 adenosquamous tumors, 2 adenosarcomas, and 2 neuroendocrine tumors. In all, 48% of patients were nulliparous prior to the procedure.
Dr. Kathurusinghe said surgical treatments for cervical cancer seemed to be shifting away from more radical toward more conservative approaches.
“What we’ve noticed over time is that the gold standard management is a radical hysterectomy, but we’ve gone back from that and said, maybe we can get away without that, let’s do a radical trachelectomy,” Dr. Kathurusinghe said.
“Now we’re slowly going back and saying we can be a little bit less radical and leave a bit more behind.”
While the study included women with stage IB2 tumors, Dr. Kathurusinghe said the general advice would be to use the more conservative procedure up to stage IB1 tumors only.
“Every patient should be considered on an individual basis by a specialist that’s in that area. Sit down with the patient and decide, does this patient need radical therapy? Is this woman still of a childbearing age, [who] would want to preserve their fertility; and can this be an option for that patient?”
Researchers also found that 15 patients actually had no residual disease on the final histopathology, echoing similar findings from an earlier study.
There were no conflicts of interest declared.
AT IGCS 2014
Key clinical point: Simple trachelectomy can achieve fertility-sparing outcomes similar to outcomes obtained from radical trachelectomy, with no increase in recurrence of cervical cancer.
Major finding: Half of women undergoing simple trachelectomy were able to conceive, and without cancer recurrence.
Data source: Retrospective cohort study of 25 patients undergoing simple vaginal trachelectomy for cervical cancer.
Disclosures: There were no conflicts of interest declared.
HPV vaccine rates perpetuate racial and geographic cancer disparities
SAN ANTONIO – Girls who live in states with higher rates of cervical cancer incidence and mortality are less likely to receive the human papilloma virus vaccine, researchers reported at a meeting on disparities in cancer health care held by the American Association for Cancer Research.
Additionally, girls living in states with a higher proportion of black residents and a lower proportion of high-income residents were less likely to receive the full three-dose course of human papilloma virus (HPV) vaccine. Immunization with the HPV vaccine can help prevent several types of cancers including cervical, anal, vaginal, and vulvar cancers. The researchers analyzed state data primarily from 2012 on vaccination rates, cancer rates, demographics, and use of healthcare.
A health care provider’s recommendation was the biggest influence on whether a teen received the vaccine, said Jennifer L. Moss, a doctoral student at the University of North Carolina Gillings School of Global Public Health, who led the research. Ms. Moss said the research team hopes the findings will encourage clinicians in states with higher rates of cancer linked to HPV to recommend vaccination to adolescents at every visit.
Teens who have more contact with the health care system are also more likely to receive the full three doses of vaccine, the researchers found. As a result, the researchers also suggest improving access to preventive health care for adolescents in states with higher rates of HPV-related cancers.
SAN ANTONIO – Girls who live in states with higher rates of cervical cancer incidence and mortality are less likely to receive the human papilloma virus vaccine, researchers reported at a meeting on disparities in cancer health care held by the American Association for Cancer Research.
Additionally, girls living in states with a higher proportion of black residents and a lower proportion of high-income residents were less likely to receive the full three-dose course of human papilloma virus (HPV) vaccine. Immunization with the HPV vaccine can help prevent several types of cancers including cervical, anal, vaginal, and vulvar cancers. The researchers analyzed state data primarily from 2012 on vaccination rates, cancer rates, demographics, and use of healthcare.
A health care provider’s recommendation was the biggest influence on whether a teen received the vaccine, said Jennifer L. Moss, a doctoral student at the University of North Carolina Gillings School of Global Public Health, who led the research. Ms. Moss said the research team hopes the findings will encourage clinicians in states with higher rates of cancer linked to HPV to recommend vaccination to adolescents at every visit.
Teens who have more contact with the health care system are also more likely to receive the full three doses of vaccine, the researchers found. As a result, the researchers also suggest improving access to preventive health care for adolescents in states with higher rates of HPV-related cancers.
SAN ANTONIO – Girls who live in states with higher rates of cervical cancer incidence and mortality are less likely to receive the human papilloma virus vaccine, researchers reported at a meeting on disparities in cancer health care held by the American Association for Cancer Research.
Additionally, girls living in states with a higher proportion of black residents and a lower proportion of high-income residents were less likely to receive the full three-dose course of human papilloma virus (HPV) vaccine. Immunization with the HPV vaccine can help prevent several types of cancers including cervical, anal, vaginal, and vulvar cancers. The researchers analyzed state data primarily from 2012 on vaccination rates, cancer rates, demographics, and use of healthcare.
A health care provider’s recommendation was the biggest influence on whether a teen received the vaccine, said Jennifer L. Moss, a doctoral student at the University of North Carolina Gillings School of Global Public Health, who led the research. Ms. Moss said the research team hopes the findings will encourage clinicians in states with higher rates of cancer linked to HPV to recommend vaccination to adolescents at every visit.
Teens who have more contact with the health care system are also more likely to receive the full three doses of vaccine, the researchers found. As a result, the researchers also suggest improving access to preventive health care for adolescents in states with higher rates of HPV-related cancers.
FROM AN AACR MEETING
Vigorous exercise better in PCOS
HONOLULU – An hour of vigorous exercise per week decreased the risk for metabolic syndrome in women with polycystic ovary syndrome by 22%, a retrospective study of 326 women found.
Moderate-intensity exercise for at least 150 minutes per week also was beneficial, compared with inactivity, but vigorous exercise produced added benefits in risk for metabolic syndrome, body mass index (BMI), cholesterol levels, glucose tolerance, and insulin resistance, Dr. Eleni A. Greenwood said at the annual meeting of the American Society for Reproductive Medicine.
The results point to “the power of sweat” when recommending exercise to women with polycystic ovary syndrome (PCOS), she said.
The observational study of women seen at a single PCOS clinic in 2006-2013 compared three groups: those who reported exercising vigorously for at least 75 minutes per week; those who reported moderate-intensity exercise for at least 150 minutes per week but not vigorous exercise, or “inactive” women who reported neither of these activity levels, which are recommended by the U.S. Department of Health & Human Services.
Patients reported activity on the self-administered International Physical Activity Questionnaire, which defines vigorous exercise as hard physical effort that makes you breathe much harder than normal and moderate-intensity exercise as moderate physical effort that makes you breathe somewhat harder than normal. They were evaluated systematically for evidence of metabolic dysfunction.
Among the 56% of women who reported activity that met HHS recommendations, 83% reported vigorous activity and 17% reported moderate activity. The other 44% were classified as inactive.
The proportion of women with metabolic syndrome was lowest in the vigorous activity group (33%), higher in the moderate activity group (36%), and highest in the inactive group (47%), reported Dr. Greenwood of the University of California, San Francisco, and her associates.
Doing 60 minutes of vigorous exercise per week decreased the odds of metabolic syndrome by 22% after adjusting for the influence of age, BMI, and total volume of exercise as measured by metabolic equivalents, she said.
There was a significant trend toward lower BMI with more intense activity. The mean BMI was 27 kg/m2 in the vigorous activity group, 30 kg/m2 in the moderate activity group, and 31 kg/m2 in the inactive group, she said. The mean HDL cholesterol level was significantly higher in the vigorous exercise group (56 mg/dL), compared with the moderate exercise group (46 mg/dL) or the inactive group (51 mg/dL).
Measures of glucose tolerance using the 2-hour oral glucose tolerance test trended significantly better in the vigorous exercise group – a mean of 93 mg/dL with vigorous exercise, 104 mg/dL with moderate exercise, or 106 mg/dL in the inactive group. Fasting glucose measurements did not differ significantly between groups.
Significant trends toward better measures of insulin resistance were seen with more vigorous activity. Fasting insulin levels were 6.9 mU/L in the vigorous exercise group, 9.8 mU/L with moderate exercise, and 11 mU/L in the inactive group. Scores on the homeostatic model assessment of estimated insulin resistance were 1.5 in the vigorous exercise group, 2.2 in the moderate exercise group, and 2.4 in the inactive group.
Significant trends toward smaller waist circumference and rate of acanthosis nigricans were seen with more vigorous activity. The mean waist circumference was 33 inches in the vigorous exercise group and 35 inches in the other two groups. In the vigorous exercise group, 24% had acanthosis nigricans, compared with 30% in the moderate exercise group and 40% in the inactive group.
The mean age in each group was 28 years.
“Vigorous activity is associated with additional benefits, compared to moderate activity,” Dr. Greenwood said. “Women with PCOS should strive to meet HHS guidelines through vigorous physical activity.”
She reported having no financial disclosures. Her associates reported associations with Nora Therapeutics, Ferring Pharmaceuticals, and Ziva Medical.
On Twitter @sherryboschert
HONOLULU – An hour of vigorous exercise per week decreased the risk for metabolic syndrome in women with polycystic ovary syndrome by 22%, a retrospective study of 326 women found.
Moderate-intensity exercise for at least 150 minutes per week also was beneficial, compared with inactivity, but vigorous exercise produced added benefits in risk for metabolic syndrome, body mass index (BMI), cholesterol levels, glucose tolerance, and insulin resistance, Dr. Eleni A. Greenwood said at the annual meeting of the American Society for Reproductive Medicine.
The results point to “the power of sweat” when recommending exercise to women with polycystic ovary syndrome (PCOS), she said.
The observational study of women seen at a single PCOS clinic in 2006-2013 compared three groups: those who reported exercising vigorously for at least 75 minutes per week; those who reported moderate-intensity exercise for at least 150 minutes per week but not vigorous exercise, or “inactive” women who reported neither of these activity levels, which are recommended by the U.S. Department of Health & Human Services.
Patients reported activity on the self-administered International Physical Activity Questionnaire, which defines vigorous exercise as hard physical effort that makes you breathe much harder than normal and moderate-intensity exercise as moderate physical effort that makes you breathe somewhat harder than normal. They were evaluated systematically for evidence of metabolic dysfunction.
Among the 56% of women who reported activity that met HHS recommendations, 83% reported vigorous activity and 17% reported moderate activity. The other 44% were classified as inactive.
The proportion of women with metabolic syndrome was lowest in the vigorous activity group (33%), higher in the moderate activity group (36%), and highest in the inactive group (47%), reported Dr. Greenwood of the University of California, San Francisco, and her associates.
Doing 60 minutes of vigorous exercise per week decreased the odds of metabolic syndrome by 22% after adjusting for the influence of age, BMI, and total volume of exercise as measured by metabolic equivalents, she said.
There was a significant trend toward lower BMI with more intense activity. The mean BMI was 27 kg/m2 in the vigorous activity group, 30 kg/m2 in the moderate activity group, and 31 kg/m2 in the inactive group, she said. The mean HDL cholesterol level was significantly higher in the vigorous exercise group (56 mg/dL), compared with the moderate exercise group (46 mg/dL) or the inactive group (51 mg/dL).
Measures of glucose tolerance using the 2-hour oral glucose tolerance test trended significantly better in the vigorous exercise group – a mean of 93 mg/dL with vigorous exercise, 104 mg/dL with moderate exercise, or 106 mg/dL in the inactive group. Fasting glucose measurements did not differ significantly between groups.
Significant trends toward better measures of insulin resistance were seen with more vigorous activity. Fasting insulin levels were 6.9 mU/L in the vigorous exercise group, 9.8 mU/L with moderate exercise, and 11 mU/L in the inactive group. Scores on the homeostatic model assessment of estimated insulin resistance were 1.5 in the vigorous exercise group, 2.2 in the moderate exercise group, and 2.4 in the inactive group.
Significant trends toward smaller waist circumference and rate of acanthosis nigricans were seen with more vigorous activity. The mean waist circumference was 33 inches in the vigorous exercise group and 35 inches in the other two groups. In the vigorous exercise group, 24% had acanthosis nigricans, compared with 30% in the moderate exercise group and 40% in the inactive group.
The mean age in each group was 28 years.
“Vigorous activity is associated with additional benefits, compared to moderate activity,” Dr. Greenwood said. “Women with PCOS should strive to meet HHS guidelines through vigorous physical activity.”
She reported having no financial disclosures. Her associates reported associations with Nora Therapeutics, Ferring Pharmaceuticals, and Ziva Medical.
On Twitter @sherryboschert
HONOLULU – An hour of vigorous exercise per week decreased the risk for metabolic syndrome in women with polycystic ovary syndrome by 22%, a retrospective study of 326 women found.
Moderate-intensity exercise for at least 150 minutes per week also was beneficial, compared with inactivity, but vigorous exercise produced added benefits in risk for metabolic syndrome, body mass index (BMI), cholesterol levels, glucose tolerance, and insulin resistance, Dr. Eleni A. Greenwood said at the annual meeting of the American Society for Reproductive Medicine.
The results point to “the power of sweat” when recommending exercise to women with polycystic ovary syndrome (PCOS), she said.
The observational study of women seen at a single PCOS clinic in 2006-2013 compared three groups: those who reported exercising vigorously for at least 75 minutes per week; those who reported moderate-intensity exercise for at least 150 minutes per week but not vigorous exercise, or “inactive” women who reported neither of these activity levels, which are recommended by the U.S. Department of Health & Human Services.
Patients reported activity on the self-administered International Physical Activity Questionnaire, which defines vigorous exercise as hard physical effort that makes you breathe much harder than normal and moderate-intensity exercise as moderate physical effort that makes you breathe somewhat harder than normal. They were evaluated systematically for evidence of metabolic dysfunction.
Among the 56% of women who reported activity that met HHS recommendations, 83% reported vigorous activity and 17% reported moderate activity. The other 44% were classified as inactive.
The proportion of women with metabolic syndrome was lowest in the vigorous activity group (33%), higher in the moderate activity group (36%), and highest in the inactive group (47%), reported Dr. Greenwood of the University of California, San Francisco, and her associates.
Doing 60 minutes of vigorous exercise per week decreased the odds of metabolic syndrome by 22% after adjusting for the influence of age, BMI, and total volume of exercise as measured by metabolic equivalents, she said.
There was a significant trend toward lower BMI with more intense activity. The mean BMI was 27 kg/m2 in the vigorous activity group, 30 kg/m2 in the moderate activity group, and 31 kg/m2 in the inactive group, she said. The mean HDL cholesterol level was significantly higher in the vigorous exercise group (56 mg/dL), compared with the moderate exercise group (46 mg/dL) or the inactive group (51 mg/dL).
Measures of glucose tolerance using the 2-hour oral glucose tolerance test trended significantly better in the vigorous exercise group – a mean of 93 mg/dL with vigorous exercise, 104 mg/dL with moderate exercise, or 106 mg/dL in the inactive group. Fasting glucose measurements did not differ significantly between groups.
Significant trends toward better measures of insulin resistance were seen with more vigorous activity. Fasting insulin levels were 6.9 mU/L in the vigorous exercise group, 9.8 mU/L with moderate exercise, and 11 mU/L in the inactive group. Scores on the homeostatic model assessment of estimated insulin resistance were 1.5 in the vigorous exercise group, 2.2 in the moderate exercise group, and 2.4 in the inactive group.
Significant trends toward smaller waist circumference and rate of acanthosis nigricans were seen with more vigorous activity. The mean waist circumference was 33 inches in the vigorous exercise group and 35 inches in the other two groups. In the vigorous exercise group, 24% had acanthosis nigricans, compared with 30% in the moderate exercise group and 40% in the inactive group.
The mean age in each group was 28 years.
“Vigorous activity is associated with additional benefits, compared to moderate activity,” Dr. Greenwood said. “Women with PCOS should strive to meet HHS guidelines through vigorous physical activity.”
She reported having no financial disclosures. Her associates reported associations with Nora Therapeutics, Ferring Pharmaceuticals, and Ziva Medical.
On Twitter @sherryboschert
AT 2014 ASRM
Key clinical point: Tell patients with PCOS that vigorous exercise is better than moderate exercise.
Major finding: Metabolic syndrome was present in 33% with vigorous exercise, 36% with moderate exercise, and 47% with inactivity.
Data source: An analysis of clinical data and questionnaire results from 326 women with PCOS.
Disclosures: Dr. Greenwood reported having no financial disclosures. Her associates reported associations with Nora Therapeutics, Ferring Pharmaceuticals, and Ziva Medical.
Racial, geographic, insurance disparities in endometrial cancer outcomes
MELBOURNE – Residents of the mountain region of the United States are significantly less likely to receive postoperative treatment for advanced endometrial cancer, compared with residents of the Northeast or Midwest, according to an oral presentation made at the biennial meeting of the International Gynecologic Cancer Society.
Retrospective analysis of data from 228,511 patients registered in the National Cancer Data Base – 15.5% of whom were stage III or IV – showed that women living in the mountain region and the Midwest were also significantly more likely to be diagnosed with advanced stage disease than those living in the South (hazard ratio 1.29 and 1.27 respectively, P < .0001)
Researchers also found having Medicaid insurance significantly increased the likelihood of being diagnosed with stage III-IV endometrial cancer (HR 1.51, P < .0001) and decreased overall survival, compared with individuals with private insurance or in managed care (HR 0.85).
“The aim of this study was to estimate the contribution of race and ethnicity, socioeconomic factors such as education and income, as well as place of residence on eventual cancer outcome,” said Dr. Sean Dowdy, professor and chair of gynecologic surgery at the Mayo Clinic.
“Specifically we looked at three questions: one was the factors that are associated with advanced stage at diagnosis, stage III-IV; whether patients received postsurgical treatment when they had advanced disease; and also their overall survival,” Dr. Dowdy told the conference.
While the study initially found that African American women were significantly more likely to be diagnosed with advanced disease than white women, this difference was no longer statistically significant after adjusting for other factors, such as the fourfold higher incidence of serous cancer in African American women.
African American women also had a reduced overall survival, compared with white women, although the study did not find any significant impact of race on treatment rates or the likelihood of being treated at a high-volume facility.
“I expected African Americans to have worse access, and to be diagnosed with advanced-stage disease, and I thought that that would be the reason for their reduced survival, but we actually didn’t see that,” Dr. Dowdy said in an interview.
“The other possibility is, there is something unique about African Americans, about their tumors or about their host response, so maybe their immunological response or something like that may impact their survival.”
The study also observed reduced survival among patients treated at low-volume facilities – although this represented a relatively small number of patients – and noted a twofold increase in reduced survival among patients aged over 80 years.
“In the age category, it’s not surprising that patients were less likely to be treated, but it’s surprising the magnitude of this, so patients that were 90 years were ten times less likely to be treated than patients who were in their 50s,” Dr. Dowdy told the audience.
Commenting on the negative impact of Medicaid and Medicare insurance, Dr. Dowdy pointed out that the study predated the introduction of the Affordable Care Act, and it was too early to tell what impact that might have on the outcomes for those patients without private insurance.
However he also called for more research into the racial disparities in overall survival.
“If the problem is access, then we need to put money into education, and we need to maybe change the system so that it’s more accessible,” Dr. Dowdy said.
“If it’s a biology thing then we need to figure out what that is and figure out whether there are specific treatments that we should be using in these patients.”
The study was supported by the Mayo Clinic, and there were no conflicts of interest declared.
MELBOURNE – Residents of the mountain region of the United States are significantly less likely to receive postoperative treatment for advanced endometrial cancer, compared with residents of the Northeast or Midwest, according to an oral presentation made at the biennial meeting of the International Gynecologic Cancer Society.
Retrospective analysis of data from 228,511 patients registered in the National Cancer Data Base – 15.5% of whom were stage III or IV – showed that women living in the mountain region and the Midwest were also significantly more likely to be diagnosed with advanced stage disease than those living in the South (hazard ratio 1.29 and 1.27 respectively, P < .0001)
Researchers also found having Medicaid insurance significantly increased the likelihood of being diagnosed with stage III-IV endometrial cancer (HR 1.51, P < .0001) and decreased overall survival, compared with individuals with private insurance or in managed care (HR 0.85).
“The aim of this study was to estimate the contribution of race and ethnicity, socioeconomic factors such as education and income, as well as place of residence on eventual cancer outcome,” said Dr. Sean Dowdy, professor and chair of gynecologic surgery at the Mayo Clinic.
“Specifically we looked at three questions: one was the factors that are associated with advanced stage at diagnosis, stage III-IV; whether patients received postsurgical treatment when they had advanced disease; and also their overall survival,” Dr. Dowdy told the conference.
While the study initially found that African American women were significantly more likely to be diagnosed with advanced disease than white women, this difference was no longer statistically significant after adjusting for other factors, such as the fourfold higher incidence of serous cancer in African American women.
African American women also had a reduced overall survival, compared with white women, although the study did not find any significant impact of race on treatment rates or the likelihood of being treated at a high-volume facility.
“I expected African Americans to have worse access, and to be diagnosed with advanced-stage disease, and I thought that that would be the reason for their reduced survival, but we actually didn’t see that,” Dr. Dowdy said in an interview.
“The other possibility is, there is something unique about African Americans, about their tumors or about their host response, so maybe their immunological response or something like that may impact their survival.”
The study also observed reduced survival among patients treated at low-volume facilities – although this represented a relatively small number of patients – and noted a twofold increase in reduced survival among patients aged over 80 years.
“In the age category, it’s not surprising that patients were less likely to be treated, but it’s surprising the magnitude of this, so patients that were 90 years were ten times less likely to be treated than patients who were in their 50s,” Dr. Dowdy told the audience.
Commenting on the negative impact of Medicaid and Medicare insurance, Dr. Dowdy pointed out that the study predated the introduction of the Affordable Care Act, and it was too early to tell what impact that might have on the outcomes for those patients without private insurance.
However he also called for more research into the racial disparities in overall survival.
“If the problem is access, then we need to put money into education, and we need to maybe change the system so that it’s more accessible,” Dr. Dowdy said.
“If it’s a biology thing then we need to figure out what that is and figure out whether there are specific treatments that we should be using in these patients.”
The study was supported by the Mayo Clinic, and there were no conflicts of interest declared.
MELBOURNE – Residents of the mountain region of the United States are significantly less likely to receive postoperative treatment for advanced endometrial cancer, compared with residents of the Northeast or Midwest, according to an oral presentation made at the biennial meeting of the International Gynecologic Cancer Society.
Retrospective analysis of data from 228,511 patients registered in the National Cancer Data Base – 15.5% of whom were stage III or IV – showed that women living in the mountain region and the Midwest were also significantly more likely to be diagnosed with advanced stage disease than those living in the South (hazard ratio 1.29 and 1.27 respectively, P < .0001)
Researchers also found having Medicaid insurance significantly increased the likelihood of being diagnosed with stage III-IV endometrial cancer (HR 1.51, P < .0001) and decreased overall survival, compared with individuals with private insurance or in managed care (HR 0.85).
“The aim of this study was to estimate the contribution of race and ethnicity, socioeconomic factors such as education and income, as well as place of residence on eventual cancer outcome,” said Dr. Sean Dowdy, professor and chair of gynecologic surgery at the Mayo Clinic.
“Specifically we looked at three questions: one was the factors that are associated with advanced stage at diagnosis, stage III-IV; whether patients received postsurgical treatment when they had advanced disease; and also their overall survival,” Dr. Dowdy told the conference.
While the study initially found that African American women were significantly more likely to be diagnosed with advanced disease than white women, this difference was no longer statistically significant after adjusting for other factors, such as the fourfold higher incidence of serous cancer in African American women.
African American women also had a reduced overall survival, compared with white women, although the study did not find any significant impact of race on treatment rates or the likelihood of being treated at a high-volume facility.
“I expected African Americans to have worse access, and to be diagnosed with advanced-stage disease, and I thought that that would be the reason for their reduced survival, but we actually didn’t see that,” Dr. Dowdy said in an interview.
“The other possibility is, there is something unique about African Americans, about their tumors or about their host response, so maybe their immunological response or something like that may impact their survival.”
The study also observed reduced survival among patients treated at low-volume facilities – although this represented a relatively small number of patients – and noted a twofold increase in reduced survival among patients aged over 80 years.
“In the age category, it’s not surprising that patients were less likely to be treated, but it’s surprising the magnitude of this, so patients that were 90 years were ten times less likely to be treated than patients who were in their 50s,” Dr. Dowdy told the audience.
Commenting on the negative impact of Medicaid and Medicare insurance, Dr. Dowdy pointed out that the study predated the introduction of the Affordable Care Act, and it was too early to tell what impact that might have on the outcomes for those patients without private insurance.
However he also called for more research into the racial disparities in overall survival.
“If the problem is access, then we need to put money into education, and we need to maybe change the system so that it’s more accessible,” Dr. Dowdy said.
“If it’s a biology thing then we need to figure out what that is and figure out whether there are specific treatments that we should be using in these patients.”
The study was supported by the Mayo Clinic, and there were no conflicts of interest declared.
AT IGCS 2014
Key clinical point: Geographic location and insurance status have a significant impact on stage at diagnosis, rates of postoperative treatment, and overall survival among women with endometrial cancer.
Major finding: Women with Medicaid insurance have a 51% increase in the likelihood of being diagnosed with stage III-IV endometrial cancer, compared with the privately insured.
Data source: Retrospective analysis of data from 228,511 patients registered in the National Cancer Database.
Disclosures: The study was supported by the Mayo Clinic. There were no conflicts of interest declared.
Vulvar pruritus in young girls usually due to toilet hygiene
NEWPORT BEACH, CALIF. – All it takes to clear up vulvar pruritus in most young girls prior to puberty is a little reminder about proper toilet habits, according to Dr. Bethanee J. Schlosser.
“There are a whole slew of conditions that cause itching of the genitals in young girls, but the most common is poor hygiene,” explained Dr. Schlosser of the departments of dermatology and obstetrics and gynecology at Northwestern University in Chicago.
Afraid they might miss out on something, children often rush bathroom visits and don’t take the time to wipe properly. Itching and redness soon follow. Gentle guidance is mostly all that’s needed to clear the problem. Loose-fitting cotton underwear helps, too, along with quickly changing soiled underpants, avoiding wet wipes, and taking baths to make sure the genitalia are adequately rinsed, Dr. Schlosser said at the Skin Disease Education Foundation’s Women’s & Pediatric Dermatology Seminar.
Simple as those steps are, they can be overlooked in the clinic. One study found that young girls are sometimes misdiagnosed with candidiasis, and treated with topical antifungals for years, even though yeast infections – the most common cause of vulvovaginal pruritus in adult women – are estrogen dependent, and so far less likely before puberty (Australas. J. Dermatol. 2010;51:118-23). After hygiene issues, lichen sclerosus is perhaps the next most common cause of vulvar pruritus in young girls, and tends to present with more urinary problems and bleeding than in adults, and more GI complaints, especially constipation. It’s “the most common inflammatory vulvar dermatosis that we see, with the possible exception of contact dermatitis,” Dr. Schlosser wrote (Arch. Dermatol. 2004;140:702-6). As in adult women, the first-line treatment is once-daily clobetasol propionate ointment 0.05% for several weeks, followed by maintenance therapy. Dr. Schlosser said she used to switch patients to a less potent topical steroid, but “then I had a couple patients get confused about which tube they were supposed to use at home, so now I taper the frequency of their clobetasol ointment” to once or twice a week instead of switching them to a less potent topical steroid. It’s easier for them, but as with any topical steroid, “you need to continue ongoing monitoring for cutaneous atrophy,” she said.
In general, pelvic exams in pediatric patients “require special consideration. These are not 5-minute visits. You have to take the time to make yourself available. Educate patients and parents about what’s going to happen,” and use the child’s own terms for her genitals, asking parents beforehand what they are, so that the child understands what she’s hearing, Dr. Schlosser said.
“When I see young girls,” mom is in the room and “I only have gauze, gloves, and maybe a Q-tip [swab] here and there. I often” begin by asking the child if it’s okay to look at her scalp, face, and hands, then “gradually work my way down. I think that gives patients some sense of comfort and control,” she said.
Dr. Schlosser said she prefers the frog-leg position, with very young girls in their mothers’ laps. The literature sometimes advocates the prone knee-to-chest position, but “I find it makes people feel very vulnerable. They can’t see you, and they have no idea of what’s going on. I don’t advocate it,” she said.
Dr. Schlosser said she has no relevant financial disclosures.
SDEF and this news organization are owned by Frontline Medical Communications.
NEWPORT BEACH, CALIF. – All it takes to clear up vulvar pruritus in most young girls prior to puberty is a little reminder about proper toilet habits, according to Dr. Bethanee J. Schlosser.
“There are a whole slew of conditions that cause itching of the genitals in young girls, but the most common is poor hygiene,” explained Dr. Schlosser of the departments of dermatology and obstetrics and gynecology at Northwestern University in Chicago.
Afraid they might miss out on something, children often rush bathroom visits and don’t take the time to wipe properly. Itching and redness soon follow. Gentle guidance is mostly all that’s needed to clear the problem. Loose-fitting cotton underwear helps, too, along with quickly changing soiled underpants, avoiding wet wipes, and taking baths to make sure the genitalia are adequately rinsed, Dr. Schlosser said at the Skin Disease Education Foundation’s Women’s & Pediatric Dermatology Seminar.
Simple as those steps are, they can be overlooked in the clinic. One study found that young girls are sometimes misdiagnosed with candidiasis, and treated with topical antifungals for years, even though yeast infections – the most common cause of vulvovaginal pruritus in adult women – are estrogen dependent, and so far less likely before puberty (Australas. J. Dermatol. 2010;51:118-23). After hygiene issues, lichen sclerosus is perhaps the next most common cause of vulvar pruritus in young girls, and tends to present with more urinary problems and bleeding than in adults, and more GI complaints, especially constipation. It’s “the most common inflammatory vulvar dermatosis that we see, with the possible exception of contact dermatitis,” Dr. Schlosser wrote (Arch. Dermatol. 2004;140:702-6). As in adult women, the first-line treatment is once-daily clobetasol propionate ointment 0.05% for several weeks, followed by maintenance therapy. Dr. Schlosser said she used to switch patients to a less potent topical steroid, but “then I had a couple patients get confused about which tube they were supposed to use at home, so now I taper the frequency of their clobetasol ointment” to once or twice a week instead of switching them to a less potent topical steroid. It’s easier for them, but as with any topical steroid, “you need to continue ongoing monitoring for cutaneous atrophy,” she said.
In general, pelvic exams in pediatric patients “require special consideration. These are not 5-minute visits. You have to take the time to make yourself available. Educate patients and parents about what’s going to happen,” and use the child’s own terms for her genitals, asking parents beforehand what they are, so that the child understands what she’s hearing, Dr. Schlosser said.
“When I see young girls,” mom is in the room and “I only have gauze, gloves, and maybe a Q-tip [swab] here and there. I often” begin by asking the child if it’s okay to look at her scalp, face, and hands, then “gradually work my way down. I think that gives patients some sense of comfort and control,” she said.
Dr. Schlosser said she prefers the frog-leg position, with very young girls in their mothers’ laps. The literature sometimes advocates the prone knee-to-chest position, but “I find it makes people feel very vulnerable. They can’t see you, and they have no idea of what’s going on. I don’t advocate it,” she said.
Dr. Schlosser said she has no relevant financial disclosures.
SDEF and this news organization are owned by Frontline Medical Communications.
NEWPORT BEACH, CALIF. – All it takes to clear up vulvar pruritus in most young girls prior to puberty is a little reminder about proper toilet habits, according to Dr. Bethanee J. Schlosser.
“There are a whole slew of conditions that cause itching of the genitals in young girls, but the most common is poor hygiene,” explained Dr. Schlosser of the departments of dermatology and obstetrics and gynecology at Northwestern University in Chicago.
Afraid they might miss out on something, children often rush bathroom visits and don’t take the time to wipe properly. Itching and redness soon follow. Gentle guidance is mostly all that’s needed to clear the problem. Loose-fitting cotton underwear helps, too, along with quickly changing soiled underpants, avoiding wet wipes, and taking baths to make sure the genitalia are adequately rinsed, Dr. Schlosser said at the Skin Disease Education Foundation’s Women’s & Pediatric Dermatology Seminar.
Simple as those steps are, they can be overlooked in the clinic. One study found that young girls are sometimes misdiagnosed with candidiasis, and treated with topical antifungals for years, even though yeast infections – the most common cause of vulvovaginal pruritus in adult women – are estrogen dependent, and so far less likely before puberty (Australas. J. Dermatol. 2010;51:118-23). After hygiene issues, lichen sclerosus is perhaps the next most common cause of vulvar pruritus in young girls, and tends to present with more urinary problems and bleeding than in adults, and more GI complaints, especially constipation. It’s “the most common inflammatory vulvar dermatosis that we see, with the possible exception of contact dermatitis,” Dr. Schlosser wrote (Arch. Dermatol. 2004;140:702-6). As in adult women, the first-line treatment is once-daily clobetasol propionate ointment 0.05% for several weeks, followed by maintenance therapy. Dr. Schlosser said she used to switch patients to a less potent topical steroid, but “then I had a couple patients get confused about which tube they were supposed to use at home, so now I taper the frequency of their clobetasol ointment” to once or twice a week instead of switching them to a less potent topical steroid. It’s easier for them, but as with any topical steroid, “you need to continue ongoing monitoring for cutaneous atrophy,” she said.
In general, pelvic exams in pediatric patients “require special consideration. These are not 5-minute visits. You have to take the time to make yourself available. Educate patients and parents about what’s going to happen,” and use the child’s own terms for her genitals, asking parents beforehand what they are, so that the child understands what she’s hearing, Dr. Schlosser said.
“When I see young girls,” mom is in the room and “I only have gauze, gloves, and maybe a Q-tip [swab] here and there. I often” begin by asking the child if it’s okay to look at her scalp, face, and hands, then “gradually work my way down. I think that gives patients some sense of comfort and control,” she said.
Dr. Schlosser said she prefers the frog-leg position, with very young girls in their mothers’ laps. The literature sometimes advocates the prone knee-to-chest position, but “I find it makes people feel very vulnerable. They can’t see you, and they have no idea of what’s going on. I don’t advocate it,” she said.
Dr. Schlosser said she has no relevant financial disclosures.
SDEF and this news organization are owned by Frontline Medical Communications.
AT THE SDEF WOMEN’S & PEDIATRIC DERMATOLOGY SEMINAR
Diet, exercise boost ovulation in PCOS
HONOLULU – Preconception diet and exercise, by themselves or in combination with oral contraceptives, improved ovulation rates, compared with birth control pills alone, in a randomized study of 149 women with polycystic ovary syndrome.
The study randomized women with polycystic ovary syndrome (PCOS) who wanted to conceive to 16 weeks of either oral contraceptive pills; lifestyle modification consisting of increased physical activity, brief behavior modification lessons, a weight-loss medication, and caloric restriction using meal replacements; or a combination of both lifestyle interventions and oral contraceptives. All subjects then received four monitored cycles of ovulation induction with clomiphene.
Ovulation rates in the lifestyle intervention group and the combination therapy group were significantly higher (60% and 67%, respectively) than in the oral contraceptives group (46%), Dr. Richard S. Legro and his associates reported in a prize-winning presentation at the 2014 annual meeting of the American Society for Reproductive Medicine.
“Looking at the relative rate of ovulation, there was a 30%-50% improved rate of ovulation if the patient had undergone a preconception lifestyle modification,” compared with oral contraceptives alone, said Dr. Legro, professor of ob.gyn. at Pennsylvania State University in Hershey.
There was a trend toward higher live birth rates in the lifestyle intervention group (26%) and the oral contraceptives group (12%, P = .05), with the live birth rate in the combination group nearing that of the lifestyle intervention group (24%).
Investigators stopped the study before enrolling its goal of 248 women after the two groups with lifestyle intervention separated from the oral contraceptives group and an interim analysis concluded that further data would be unlikely to show a significant difference in results between the two groups employing lifestyle interventions.
Women in the combination therapy group lost 6.5% of body weight on average, compared with a 6.2% loss in the lifestyle interventions group and a 1% loss on oral contraceptives. The weight loss goal was 7% of body weight.
Dr. Legro said he was surprised by marked exacerbation of glucose intolerance in women on oral contraceptives that was ameliorated by lifestyle interventions. After the 16 weeks of preinduction treatment, changes in oral glucose tolerance test areas under the curve showed significant differences between the oral contraceptives group (a mean increase of 24 mg/dL/hour) and the lifestyle modifications group (a decrease of 1 mg/dL per hour) or the combination therapy group (a decrease of 17 mg/dL/hour).
The oral contraceptives group also showed trends toward increased blood pressure and fasting glucose levels plus a significant increase in triglyceride levels. The risk for developing metabolic syndrome during the 16 weeks of treatment more than doubled in the oral contraceptives group, compared with a statistically nonsignificant 20% increased risk in the lifestyle interventions group and a nonsignificant 30% decrease in risk in the combination therapy group, he reported.
The continuous oral contraceptive was ethinyl estradiol 10 mcg/norethindrone acetate 1 mg under the brand name LoEstrin 1/20.
The lifestyle modifications involved meal replacements for all three meals per day using fresh vegetables and fruit for a 500 kcal/day deficit. The goal for physical activity was 150 minutes per week, and the monthly behavioral modification lessons were adapted from the Diabetes Prevention Program. Participants with a body mass index of at least 30 received 5-15 mg/day of the antiobesity drug sibutramine until it was removed from the market, after which obese participants received 60 mg of orlistat with meals.
“Is it worth doing all this?” Dr. Legro asked. To answer that question, he and his associates conducted a post-hoc analysis comparing the results from the lifestyle modifications or combination therapy groups with results from the Pregnancy in Polycystic Ovary Syndrome II (PPCOS II) study of clomiphene citrate or letrozole for ovulation induction without any pretreatment.
Cumulative ovulation rates were 40%-50% higher in the current study’s groups that included lifestyle interventions than in the PPCOS II study’s clomiphene group. The likelihood of a live birth more than doubled in the current study’s groups that included lifestyle interventions, compared with the PPCOS II clomiphene group.
The lifestyle interventions treatment “is very reproducible. It’s simple. It’s safe, and it’s well tolerated,” he said. “Oral contraceptive pills pretreatment likely offers little benefit versus immediate treatment with ovulation induction.”
One serious adverse event in the current study occurred in the oral contraceptive group, an episode of menorrhagia that sent the patient to an emergency department.
Concurrent lifestyle modification should be recommended for overweight or obese women with PCOS who are taking oral contraceptives, whether or not they are seeking fertility treatment, Dr. Legro said.
The National Institutes of Health funded the study. Dr. Legro reported financial associations with AstraZeneca, Euroscreen, Takeda Pharmaceuticals, and Ferring Pharmaceuticals. One of his associates reported financial associations with BAROnova and EnteroMedics.
On Twitter @sherryboschert
These findings emphasize the importance of lifestyle intervention in women with PCOS who are trying to have children. This reasonably large study found that diet and exercise offer advantages to women with PCOS, not only in reversing some of the metabolic effects of PCOS, but also in higher ovulation rates and trends toward improved pregnancy rates.
 |
Bradley J. Van Voorhis |
It’s also noteworthy that simply putting women on birth control pills alone had some negative effects on glucose metabolism and the risk for metabolic syndrome. So, the other significant message is that it’s probably not wise to simply place women with PCOS on oral contraceptives alone, and oral contraceptive therapy should be done in conjunction with lifestyle interventions.
The findings are practice changing in that they’ll motivate me to always counsel patients with PCOS who are starting oral contraceptives on the potential for adverse effects and the need for dietary control and weight loss. It was surprising to me, the effect of a relatively short course of birth control pills on glucose metabolism and metabolic syndrome.
Dr. Bradley Van Voorhis, professor of medicine and director of the division of reproductive endocrinology and infertility at the University of Iowa, Iowa City, made these comments in an interview. He reported having no financial disclosures.
These findings emphasize the importance of lifestyle intervention in women with PCOS who are trying to have children. This reasonably large study found that diet and exercise offer advantages to women with PCOS, not only in reversing some of the metabolic effects of PCOS, but also in higher ovulation rates and trends toward improved pregnancy rates.
 |
Bradley J. Van Voorhis |
It’s also noteworthy that simply putting women on birth control pills alone had some negative effects on glucose metabolism and the risk for metabolic syndrome. So, the other significant message is that it’s probably not wise to simply place women with PCOS on oral contraceptives alone, and oral contraceptive therapy should be done in conjunction with lifestyle interventions.
The findings are practice changing in that they’ll motivate me to always counsel patients with PCOS who are starting oral contraceptives on the potential for adverse effects and the need for dietary control and weight loss. It was surprising to me, the effect of a relatively short course of birth control pills on glucose metabolism and metabolic syndrome.
Dr. Bradley Van Voorhis, professor of medicine and director of the division of reproductive endocrinology and infertility at the University of Iowa, Iowa City, made these comments in an interview. He reported having no financial disclosures.
These findings emphasize the importance of lifestyle intervention in women with PCOS who are trying to have children. This reasonably large study found that diet and exercise offer advantages to women with PCOS, not only in reversing some of the metabolic effects of PCOS, but also in higher ovulation rates and trends toward improved pregnancy rates.
 |
Bradley J. Van Voorhis |
It’s also noteworthy that simply putting women on birth control pills alone had some negative effects on glucose metabolism and the risk for metabolic syndrome. So, the other significant message is that it’s probably not wise to simply place women with PCOS on oral contraceptives alone, and oral contraceptive therapy should be done in conjunction with lifestyle interventions.
The findings are practice changing in that they’ll motivate me to always counsel patients with PCOS who are starting oral contraceptives on the potential for adverse effects and the need for dietary control and weight loss. It was surprising to me, the effect of a relatively short course of birth control pills on glucose metabolism and metabolic syndrome.
Dr. Bradley Van Voorhis, professor of medicine and director of the division of reproductive endocrinology and infertility at the University of Iowa, Iowa City, made these comments in an interview. He reported having no financial disclosures.
HONOLULU – Preconception diet and exercise, by themselves or in combination with oral contraceptives, improved ovulation rates, compared with birth control pills alone, in a randomized study of 149 women with polycystic ovary syndrome.
The study randomized women with polycystic ovary syndrome (PCOS) who wanted to conceive to 16 weeks of either oral contraceptive pills; lifestyle modification consisting of increased physical activity, brief behavior modification lessons, a weight-loss medication, and caloric restriction using meal replacements; or a combination of both lifestyle interventions and oral contraceptives. All subjects then received four monitored cycles of ovulation induction with clomiphene.
Ovulation rates in the lifestyle intervention group and the combination therapy group were significantly higher (60% and 67%, respectively) than in the oral contraceptives group (46%), Dr. Richard S. Legro and his associates reported in a prize-winning presentation at the 2014 annual meeting of the American Society for Reproductive Medicine.
“Looking at the relative rate of ovulation, there was a 30%-50% improved rate of ovulation if the patient had undergone a preconception lifestyle modification,” compared with oral contraceptives alone, said Dr. Legro, professor of ob.gyn. at Pennsylvania State University in Hershey.
There was a trend toward higher live birth rates in the lifestyle intervention group (26%) and the oral contraceptives group (12%, P = .05), with the live birth rate in the combination group nearing that of the lifestyle intervention group (24%).
Investigators stopped the study before enrolling its goal of 248 women after the two groups with lifestyle intervention separated from the oral contraceptives group and an interim analysis concluded that further data would be unlikely to show a significant difference in results between the two groups employing lifestyle interventions.
Women in the combination therapy group lost 6.5% of body weight on average, compared with a 6.2% loss in the lifestyle interventions group and a 1% loss on oral contraceptives. The weight loss goal was 7% of body weight.
Dr. Legro said he was surprised by marked exacerbation of glucose intolerance in women on oral contraceptives that was ameliorated by lifestyle interventions. After the 16 weeks of preinduction treatment, changes in oral glucose tolerance test areas under the curve showed significant differences between the oral contraceptives group (a mean increase of 24 mg/dL/hour) and the lifestyle modifications group (a decrease of 1 mg/dL per hour) or the combination therapy group (a decrease of 17 mg/dL/hour).
The oral contraceptives group also showed trends toward increased blood pressure and fasting glucose levels plus a significant increase in triglyceride levels. The risk for developing metabolic syndrome during the 16 weeks of treatment more than doubled in the oral contraceptives group, compared with a statistically nonsignificant 20% increased risk in the lifestyle interventions group and a nonsignificant 30% decrease in risk in the combination therapy group, he reported.
The continuous oral contraceptive was ethinyl estradiol 10 mcg/norethindrone acetate 1 mg under the brand name LoEstrin 1/20.
The lifestyle modifications involved meal replacements for all three meals per day using fresh vegetables and fruit for a 500 kcal/day deficit. The goal for physical activity was 150 minutes per week, and the monthly behavioral modification lessons were adapted from the Diabetes Prevention Program. Participants with a body mass index of at least 30 received 5-15 mg/day of the antiobesity drug sibutramine until it was removed from the market, after which obese participants received 60 mg of orlistat with meals.
“Is it worth doing all this?” Dr. Legro asked. To answer that question, he and his associates conducted a post-hoc analysis comparing the results from the lifestyle modifications or combination therapy groups with results from the Pregnancy in Polycystic Ovary Syndrome II (PPCOS II) study of clomiphene citrate or letrozole for ovulation induction without any pretreatment.
Cumulative ovulation rates were 40%-50% higher in the current study’s groups that included lifestyle interventions than in the PPCOS II study’s clomiphene group. The likelihood of a live birth more than doubled in the current study’s groups that included lifestyle interventions, compared with the PPCOS II clomiphene group.
The lifestyle interventions treatment “is very reproducible. It’s simple. It’s safe, and it’s well tolerated,” he said. “Oral contraceptive pills pretreatment likely offers little benefit versus immediate treatment with ovulation induction.”
One serious adverse event in the current study occurred in the oral contraceptive group, an episode of menorrhagia that sent the patient to an emergency department.
Concurrent lifestyle modification should be recommended for overweight or obese women with PCOS who are taking oral contraceptives, whether or not they are seeking fertility treatment, Dr. Legro said.
The National Institutes of Health funded the study. Dr. Legro reported financial associations with AstraZeneca, Euroscreen, Takeda Pharmaceuticals, and Ferring Pharmaceuticals. One of his associates reported financial associations with BAROnova and EnteroMedics.
On Twitter @sherryboschert
HONOLULU – Preconception diet and exercise, by themselves or in combination with oral contraceptives, improved ovulation rates, compared with birth control pills alone, in a randomized study of 149 women with polycystic ovary syndrome.
The study randomized women with polycystic ovary syndrome (PCOS) who wanted to conceive to 16 weeks of either oral contraceptive pills; lifestyle modification consisting of increased physical activity, brief behavior modification lessons, a weight-loss medication, and caloric restriction using meal replacements; or a combination of both lifestyle interventions and oral contraceptives. All subjects then received four monitored cycles of ovulation induction with clomiphene.
Ovulation rates in the lifestyle intervention group and the combination therapy group were significantly higher (60% and 67%, respectively) than in the oral contraceptives group (46%), Dr. Richard S. Legro and his associates reported in a prize-winning presentation at the 2014 annual meeting of the American Society for Reproductive Medicine.
“Looking at the relative rate of ovulation, there was a 30%-50% improved rate of ovulation if the patient had undergone a preconception lifestyle modification,” compared with oral contraceptives alone, said Dr. Legro, professor of ob.gyn. at Pennsylvania State University in Hershey.
There was a trend toward higher live birth rates in the lifestyle intervention group (26%) and the oral contraceptives group (12%, P = .05), with the live birth rate in the combination group nearing that of the lifestyle intervention group (24%).
Investigators stopped the study before enrolling its goal of 248 women after the two groups with lifestyle intervention separated from the oral contraceptives group and an interim analysis concluded that further data would be unlikely to show a significant difference in results between the two groups employing lifestyle interventions.
Women in the combination therapy group lost 6.5% of body weight on average, compared with a 6.2% loss in the lifestyle interventions group and a 1% loss on oral contraceptives. The weight loss goal was 7% of body weight.
Dr. Legro said he was surprised by marked exacerbation of glucose intolerance in women on oral contraceptives that was ameliorated by lifestyle interventions. After the 16 weeks of preinduction treatment, changes in oral glucose tolerance test areas under the curve showed significant differences between the oral contraceptives group (a mean increase of 24 mg/dL/hour) and the lifestyle modifications group (a decrease of 1 mg/dL per hour) or the combination therapy group (a decrease of 17 mg/dL/hour).
The oral contraceptives group also showed trends toward increased blood pressure and fasting glucose levels plus a significant increase in triglyceride levels. The risk for developing metabolic syndrome during the 16 weeks of treatment more than doubled in the oral contraceptives group, compared with a statistically nonsignificant 20% increased risk in the lifestyle interventions group and a nonsignificant 30% decrease in risk in the combination therapy group, he reported.
The continuous oral contraceptive was ethinyl estradiol 10 mcg/norethindrone acetate 1 mg under the brand name LoEstrin 1/20.
The lifestyle modifications involved meal replacements for all three meals per day using fresh vegetables and fruit for a 500 kcal/day deficit. The goal for physical activity was 150 minutes per week, and the monthly behavioral modification lessons were adapted from the Diabetes Prevention Program. Participants with a body mass index of at least 30 received 5-15 mg/day of the antiobesity drug sibutramine until it was removed from the market, after which obese participants received 60 mg of orlistat with meals.
“Is it worth doing all this?” Dr. Legro asked. To answer that question, he and his associates conducted a post-hoc analysis comparing the results from the lifestyle modifications or combination therapy groups with results from the Pregnancy in Polycystic Ovary Syndrome II (PPCOS II) study of clomiphene citrate or letrozole for ovulation induction without any pretreatment.
Cumulative ovulation rates were 40%-50% higher in the current study’s groups that included lifestyle interventions than in the PPCOS II study’s clomiphene group. The likelihood of a live birth more than doubled in the current study’s groups that included lifestyle interventions, compared with the PPCOS II clomiphene group.
The lifestyle interventions treatment “is very reproducible. It’s simple. It’s safe, and it’s well tolerated,” he said. “Oral contraceptive pills pretreatment likely offers little benefit versus immediate treatment with ovulation induction.”
One serious adverse event in the current study occurred in the oral contraceptive group, an episode of menorrhagia that sent the patient to an emergency department.
Concurrent lifestyle modification should be recommended for overweight or obese women with PCOS who are taking oral contraceptives, whether or not they are seeking fertility treatment, Dr. Legro said.
The National Institutes of Health funded the study. Dr. Legro reported financial associations with AstraZeneca, Euroscreen, Takeda Pharmaceuticals, and Ferring Pharmaceuticals. One of his associates reported financial associations with BAROnova and EnteroMedics.
On Twitter @sherryboschert
AT 2014 ASRM
Key clinical point: Lifestyle interventions improve ovulation and health in women with PCOS.
Major finding: Ovulation rates were 46% on oral contraceptives, 60% with lifestyle interventions, or 67% with both.
Data source: A prematurely terminated, randomized study of 149 women with PCOS desiring children.
Disclosures: The National Institutes of Health funded the study. Dr. Legro reported financial associations with AstraZeneca, Euroscreen, Takeda Pharmaceuticals, and Ferring Pharmaceuticals. One of his associates reported financial associations with BAROnova and EnteroMedics.
CDC: More can be done to prevent cervical cancer fatalities
Close to 8 million women aged 21-65 years were not screened for cervical cancer in the past 5 years even though the disease claims nearly 4,000 lives per year, according to 2012 data, the Centers for Disease Control and Prevention reported.
In its November Vital Signs report, the CDC stated that it is committed to providing Americans with easier and more affordable access to screening and treatment options for human papillomavirus (HPV) and cervical cancer, reiterating that 93% of cervical cancers can be prevented with early screening and HPV vaccination.
“We know that cervical cancer screening works,” Dr. Ileana Arias, CDC deputy principal director, said during a telebriefing on Nov. 5. With new resources and increased awareness, “we can reach and actually go beyond the 2020 Health People Objective,” she said.
The Healthy People objective, a federal program designed to promote healthy living and disease prevention with specific goals, aims to reduce the number of invasive uterine cervical cancer cases from 7.9 per 100,000 females to 7.1 per 100,000 females, while increasing the average female screening percentage from 84.5% to 93.0%.
Dr. Arias explained that the Affordable Care Act will help eliminate some of the “financial barriers” that prevent girls and women from getting screened, which should be done every 3 years, and said that the ACA should cover preventative screening for no cost under most plans. The CDC points to a lack of health insurance as being a leading cause for nonscreening, as one out of every four women without insurance did not get screened in the last 5 years.
Other factors inhibiting more widespread HPV and cervical cancer screening include lack of awareness, knowledge, and transportation in rural and “lower resource” areas of the United States, as well as cultural beliefs. The American South continues to have the highest rates of cervical cancer incidence and death, while overall death rates across the country have remained stagnant from 2007 to 2011, making it difficult for the CDC to reach its 2020 Healthy People Objective.
The CDC recommends that all adolescents receive the HPV vaccine at around 11-12 years of age, although Dr. Arias pointed out that the vaccine could be administered to girls as young as 9 years and women as old as 26. According to CDC statistics, one out of every three girls and one out of every seven boys receive the vaccine.
“We continue to miss opportunities to screen for cervical cancers,” admitted Dr. Arias, calling on primary care providers and community outreach centers to advocate for screenings and make resources available to women and adolescents across the country.
The November Vital Signs report can be found in its entirety on the CDC website.
Close to 8 million women aged 21-65 years were not screened for cervical cancer in the past 5 years even though the disease claims nearly 4,000 lives per year, according to 2012 data, the Centers for Disease Control and Prevention reported.
In its November Vital Signs report, the CDC stated that it is committed to providing Americans with easier and more affordable access to screening and treatment options for human papillomavirus (HPV) and cervical cancer, reiterating that 93% of cervical cancers can be prevented with early screening and HPV vaccination.
“We know that cervical cancer screening works,” Dr. Ileana Arias, CDC deputy principal director, said during a telebriefing on Nov. 5. With new resources and increased awareness, “we can reach and actually go beyond the 2020 Health People Objective,” she said.
The Healthy People objective, a federal program designed to promote healthy living and disease prevention with specific goals, aims to reduce the number of invasive uterine cervical cancer cases from 7.9 per 100,000 females to 7.1 per 100,000 females, while increasing the average female screening percentage from 84.5% to 93.0%.
Dr. Arias explained that the Affordable Care Act will help eliminate some of the “financial barriers” that prevent girls and women from getting screened, which should be done every 3 years, and said that the ACA should cover preventative screening for no cost under most plans. The CDC points to a lack of health insurance as being a leading cause for nonscreening, as one out of every four women without insurance did not get screened in the last 5 years.
Other factors inhibiting more widespread HPV and cervical cancer screening include lack of awareness, knowledge, and transportation in rural and “lower resource” areas of the United States, as well as cultural beliefs. The American South continues to have the highest rates of cervical cancer incidence and death, while overall death rates across the country have remained stagnant from 2007 to 2011, making it difficult for the CDC to reach its 2020 Healthy People Objective.
The CDC recommends that all adolescents receive the HPV vaccine at around 11-12 years of age, although Dr. Arias pointed out that the vaccine could be administered to girls as young as 9 years and women as old as 26. According to CDC statistics, one out of every three girls and one out of every seven boys receive the vaccine.
“We continue to miss opportunities to screen for cervical cancers,” admitted Dr. Arias, calling on primary care providers and community outreach centers to advocate for screenings and make resources available to women and adolescents across the country.
The November Vital Signs report can be found in its entirety on the CDC website.
Close to 8 million women aged 21-65 years were not screened for cervical cancer in the past 5 years even though the disease claims nearly 4,000 lives per year, according to 2012 data, the Centers for Disease Control and Prevention reported.
In its November Vital Signs report, the CDC stated that it is committed to providing Americans with easier and more affordable access to screening and treatment options for human papillomavirus (HPV) and cervical cancer, reiterating that 93% of cervical cancers can be prevented with early screening and HPV vaccination.
“We know that cervical cancer screening works,” Dr. Ileana Arias, CDC deputy principal director, said during a telebriefing on Nov. 5. With new resources and increased awareness, “we can reach and actually go beyond the 2020 Health People Objective,” she said.
The Healthy People objective, a federal program designed to promote healthy living and disease prevention with specific goals, aims to reduce the number of invasive uterine cervical cancer cases from 7.9 per 100,000 females to 7.1 per 100,000 females, while increasing the average female screening percentage from 84.5% to 93.0%.
Dr. Arias explained that the Affordable Care Act will help eliminate some of the “financial barriers” that prevent girls and women from getting screened, which should be done every 3 years, and said that the ACA should cover preventative screening for no cost under most plans. The CDC points to a lack of health insurance as being a leading cause for nonscreening, as one out of every four women without insurance did not get screened in the last 5 years.
Other factors inhibiting more widespread HPV and cervical cancer screening include lack of awareness, knowledge, and transportation in rural and “lower resource” areas of the United States, as well as cultural beliefs. The American South continues to have the highest rates of cervical cancer incidence and death, while overall death rates across the country have remained stagnant from 2007 to 2011, making it difficult for the CDC to reach its 2020 Healthy People Objective.
The CDC recommends that all adolescents receive the HPV vaccine at around 11-12 years of age, although Dr. Arias pointed out that the vaccine could be administered to girls as young as 9 years and women as old as 26. According to CDC statistics, one out of every three girls and one out of every seven boys receive the vaccine.
“We continue to miss opportunities to screen for cervical cancers,” admitted Dr. Arias, calling on primary care providers and community outreach centers to advocate for screenings and make resources available to women and adolescents across the country.
The November Vital Signs report can be found in its entirety on the CDC website.
FROM A CDC TELEBRIEFING
VIDEO: Ovarian function is exciting possible CV risk marker
HONOLULU– A woman’s ovarian “clock” is dissociated from her general health, according to widely accepted thinking – but a new study has suggested the opposite.
That study showed greater cardiovascular risk in women with markers of greater ovarian aging. Dr. Marcelle I. Cedars of the University of California, San Francisco, and her associates presented the results at the annual meeting of the American Society for Reproductive Medicine, where the study won an award.
In a video interview, the society’s vice president, Dr. Owen K. Davis, described the potential significance of the study.
Women with cardiovascular disease tend to get diagnosed later and have worse outcomes, compared with men. If markers of ovarian function can help identify cardiovascular risk earlier in some women, the women may be candidates for more intensive surveillance, said Dr. Davis, professor of ob.gyn. and reproductive medicine at Weill Cornell Medical College, New York.
Dr. Davis reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
HONOLULU– A woman’s ovarian “clock” is dissociated from her general health, according to widely accepted thinking – but a new study has suggested the opposite.
That study showed greater cardiovascular risk in women with markers of greater ovarian aging. Dr. Marcelle I. Cedars of the University of California, San Francisco, and her associates presented the results at the annual meeting of the American Society for Reproductive Medicine, where the study won an award.
In a video interview, the society’s vice president, Dr. Owen K. Davis, described the potential significance of the study.
Women with cardiovascular disease tend to get diagnosed later and have worse outcomes, compared with men. If markers of ovarian function can help identify cardiovascular risk earlier in some women, the women may be candidates for more intensive surveillance, said Dr. Davis, professor of ob.gyn. and reproductive medicine at Weill Cornell Medical College, New York.
Dr. Davis reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
HONOLULU– A woman’s ovarian “clock” is dissociated from her general health, according to widely accepted thinking – but a new study has suggested the opposite.
That study showed greater cardiovascular risk in women with markers of greater ovarian aging. Dr. Marcelle I. Cedars of the University of California, San Francisco, and her associates presented the results at the annual meeting of the American Society for Reproductive Medicine, where the study won an award.
In a video interview, the society’s vice president, Dr. Owen K. Davis, described the potential significance of the study.
Women with cardiovascular disease tend to get diagnosed later and have worse outcomes, compared with men. If markers of ovarian function can help identify cardiovascular risk earlier in some women, the women may be candidates for more intensive surveillance, said Dr. Davis, professor of ob.gyn. and reproductive medicine at Weill Cornell Medical College, New York.
Dr. Davis reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
EXPERT ANALYSIS FROM ASRM 2014