User login
IQ and concussion recovery
Pediatric concussion is one of those rare phenomena in which we may be witnessing its emergence and clarification in a generation. When I was serving as the game doctor for our local high school football team in the 1970s, I and many other physicians had a very simplistic view of concussion. If the patient never lost conscious and had a reasonably intact short-term memory, we didn’t seriously entertain concussion as a diagnosis. “What’s the score and who is the president?” Were my favorite screening questions.
Obviously, we were underdiagnosing and mismanaging concussion. In part thanks to some high-profile athletes who suffered multiple concussions and eventually chronic traumatic encephalopathy (CTE) physicians began to realize that they should be looking more closely at children who sustained a head injury. The diagnostic criteria were expanded to include any injury that even temporarily effected brain function.
With the new appreciation for the risk of multiple concussions, the focus broadened to include the question of when is it safe for the athlete to return to competition. What signs or symptoms can the patient offer us so we can be sure his or her brain is sufficiently recovered? Here we stepped off into a deep abyss of ignorance. Fortunately, it became obvious fairly quickly that imaging studies weren’t going to help us, as they were invariably normal or at least didn’t tell us anything that wasn’t obvious on a physical exam.
If the patient had a headache, complained of dizziness, or manifested amnesia, monitoring the patient was fairly straightforward. But, in the absence of symptoms and no obvious way to determine the pace of recovery of an organ we couldn’t visualize, clinicians were pulling criteria and time tables out of thin air. Guessing that the concussed brain was in some ways like a torn muscle or overstretched tendon, “brain rest” was often suggested. So no TV, no reading, and certainly none of the cerebral challenging activity of school. Fortunately, we don’t hear much about the notion of brain rest anymore and there is at least one study that suggests that patients kept home from school recover more slowly.
But . Sometimes they describe headache or dizziness but often they complain of a vague mental unwellness. “Brain fog,” a term that has emerged in the wake of the COVID pandemic, might be an apt descriptor. Management of these slow recoverers has been a challenge.
However, two recent articles in the journal Pediatrics may provide some clarity and offer guidance in their management. In a study coming from the psychology department at Georgia State University, researchers reported that they have been able to find “no evidence of clinical meaningful differences in IQ after pediatric concussion.” In their words there is “strong evidence against reduced intelligence in the first few weeks to month after pediatric concussion.”
While their findings may simply toss the IQ onto the pile of worthless measures of healing, a companion commentary by Talin Babikian, PhD, a psychologist at the Semel Institute for Neuroscience and Human Behavior at UCLA, provides a more nuanced interpretation. He writes that if we are looking for an explanation when a patient’s recovery is taking longer than we might expect we need to look beyond some structural damage. Maybe the patient has a previously undiagnosed premorbid condition effecting his or her intellectual, cognitive, or learning abilities. Could the stall in improvement be the result of other symptoms? Here fatigue and sleep deprivation may be the culprits. Could some underlying emotional factor such as anxiety or depression be the problem? For example, I have seen patients whose fear of re-injury has prevented their return to full function. And, finally, the patient may be avoiding a “nonpreferred or challenging situation” unrelated to the injury.
In other words, the concussion may simply be the most obvious rip in a fabric that was already frayed and under stress. This kind of broad holistic (a word I usually like to avoid) thinking may be what is lacking as we struggle to understand other mysterious and chronic conditions such as Lyme disease and chronic fatigue syndrome.
While these two papers help provide some clarity in the management of pediatric concussion, what they fail to address is the bigger question of the relationship between head injury and CTE. The answers to that conundrum are enshrouded in a mix of politics and publicity that I doubt will clear in the near future.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Pediatric concussion is one of those rare phenomena in which we may be witnessing its emergence and clarification in a generation. When I was serving as the game doctor for our local high school football team in the 1970s, I and many other physicians had a very simplistic view of concussion. If the patient never lost conscious and had a reasonably intact short-term memory, we didn’t seriously entertain concussion as a diagnosis. “What’s the score and who is the president?” Were my favorite screening questions.
Obviously, we were underdiagnosing and mismanaging concussion. In part thanks to some high-profile athletes who suffered multiple concussions and eventually chronic traumatic encephalopathy (CTE) physicians began to realize that they should be looking more closely at children who sustained a head injury. The diagnostic criteria were expanded to include any injury that even temporarily effected brain function.
With the new appreciation for the risk of multiple concussions, the focus broadened to include the question of when is it safe for the athlete to return to competition. What signs or symptoms can the patient offer us so we can be sure his or her brain is sufficiently recovered? Here we stepped off into a deep abyss of ignorance. Fortunately, it became obvious fairly quickly that imaging studies weren’t going to help us, as they were invariably normal or at least didn’t tell us anything that wasn’t obvious on a physical exam.
If the patient had a headache, complained of dizziness, or manifested amnesia, monitoring the patient was fairly straightforward. But, in the absence of symptoms and no obvious way to determine the pace of recovery of an organ we couldn’t visualize, clinicians were pulling criteria and time tables out of thin air. Guessing that the concussed brain was in some ways like a torn muscle or overstretched tendon, “brain rest” was often suggested. So no TV, no reading, and certainly none of the cerebral challenging activity of school. Fortunately, we don’t hear much about the notion of brain rest anymore and there is at least one study that suggests that patients kept home from school recover more slowly.
But . Sometimes they describe headache or dizziness but often they complain of a vague mental unwellness. “Brain fog,” a term that has emerged in the wake of the COVID pandemic, might be an apt descriptor. Management of these slow recoverers has been a challenge.
However, two recent articles in the journal Pediatrics may provide some clarity and offer guidance in their management. In a study coming from the psychology department at Georgia State University, researchers reported that they have been able to find “no evidence of clinical meaningful differences in IQ after pediatric concussion.” In their words there is “strong evidence against reduced intelligence in the first few weeks to month after pediatric concussion.”
While their findings may simply toss the IQ onto the pile of worthless measures of healing, a companion commentary by Talin Babikian, PhD, a psychologist at the Semel Institute for Neuroscience and Human Behavior at UCLA, provides a more nuanced interpretation. He writes that if we are looking for an explanation when a patient’s recovery is taking longer than we might expect we need to look beyond some structural damage. Maybe the patient has a previously undiagnosed premorbid condition effecting his or her intellectual, cognitive, or learning abilities. Could the stall in improvement be the result of other symptoms? Here fatigue and sleep deprivation may be the culprits. Could some underlying emotional factor such as anxiety or depression be the problem? For example, I have seen patients whose fear of re-injury has prevented their return to full function. And, finally, the patient may be avoiding a “nonpreferred or challenging situation” unrelated to the injury.
In other words, the concussion may simply be the most obvious rip in a fabric that was already frayed and under stress. This kind of broad holistic (a word I usually like to avoid) thinking may be what is lacking as we struggle to understand other mysterious and chronic conditions such as Lyme disease and chronic fatigue syndrome.
While these two papers help provide some clarity in the management of pediatric concussion, what they fail to address is the bigger question of the relationship between head injury and CTE. The answers to that conundrum are enshrouded in a mix of politics and publicity that I doubt will clear in the near future.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Pediatric concussion is one of those rare phenomena in which we may be witnessing its emergence and clarification in a generation. When I was serving as the game doctor for our local high school football team in the 1970s, I and many other physicians had a very simplistic view of concussion. If the patient never lost conscious and had a reasonably intact short-term memory, we didn’t seriously entertain concussion as a diagnosis. “What’s the score and who is the president?” Were my favorite screening questions.
Obviously, we were underdiagnosing and mismanaging concussion. In part thanks to some high-profile athletes who suffered multiple concussions and eventually chronic traumatic encephalopathy (CTE) physicians began to realize that they should be looking more closely at children who sustained a head injury. The diagnostic criteria were expanded to include any injury that even temporarily effected brain function.
With the new appreciation for the risk of multiple concussions, the focus broadened to include the question of when is it safe for the athlete to return to competition. What signs or symptoms can the patient offer us so we can be sure his or her brain is sufficiently recovered? Here we stepped off into a deep abyss of ignorance. Fortunately, it became obvious fairly quickly that imaging studies weren’t going to help us, as they were invariably normal or at least didn’t tell us anything that wasn’t obvious on a physical exam.
If the patient had a headache, complained of dizziness, or manifested amnesia, monitoring the patient was fairly straightforward. But, in the absence of symptoms and no obvious way to determine the pace of recovery of an organ we couldn’t visualize, clinicians were pulling criteria and time tables out of thin air. Guessing that the concussed brain was in some ways like a torn muscle or overstretched tendon, “brain rest” was often suggested. So no TV, no reading, and certainly none of the cerebral challenging activity of school. Fortunately, we don’t hear much about the notion of brain rest anymore and there is at least one study that suggests that patients kept home from school recover more slowly.
But . Sometimes they describe headache or dizziness but often they complain of a vague mental unwellness. “Brain fog,” a term that has emerged in the wake of the COVID pandemic, might be an apt descriptor. Management of these slow recoverers has been a challenge.
However, two recent articles in the journal Pediatrics may provide some clarity and offer guidance in their management. In a study coming from the psychology department at Georgia State University, researchers reported that they have been able to find “no evidence of clinical meaningful differences in IQ after pediatric concussion.” In their words there is “strong evidence against reduced intelligence in the first few weeks to month after pediatric concussion.”
While their findings may simply toss the IQ onto the pile of worthless measures of healing, a companion commentary by Talin Babikian, PhD, a psychologist at the Semel Institute for Neuroscience and Human Behavior at UCLA, provides a more nuanced interpretation. He writes that if we are looking for an explanation when a patient’s recovery is taking longer than we might expect we need to look beyond some structural damage. Maybe the patient has a previously undiagnosed premorbid condition effecting his or her intellectual, cognitive, or learning abilities. Could the stall in improvement be the result of other symptoms? Here fatigue and sleep deprivation may be the culprits. Could some underlying emotional factor such as anxiety or depression be the problem? For example, I have seen patients whose fear of re-injury has prevented their return to full function. And, finally, the patient may be avoiding a “nonpreferred or challenging situation” unrelated to the injury.
In other words, the concussion may simply be the most obvious rip in a fabric that was already frayed and under stress. This kind of broad holistic (a word I usually like to avoid) thinking may be what is lacking as we struggle to understand other mysterious and chronic conditions such as Lyme disease and chronic fatigue syndrome.
While these two papers help provide some clarity in the management of pediatric concussion, what they fail to address is the bigger question of the relationship between head injury and CTE. The answers to that conundrum are enshrouded in a mix of politics and publicity that I doubt will clear in the near future.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
‘Decapitated’ boy saved by surgery team
This transcript has been edited for clarity.
F. Perry Wilson, MD, MSCE: I am joined today by Dr. Ohad Einav. He’s a staff surgeon in orthopedics at Hadassah Medical Center in Jerusalem. He’s with me to talk about an absolutely incredible surgical case, something that is terrifying to most non–orthopedic surgeons and I imagine is fairly scary for spine surgeons like him as well. But what we don’t have is information about how this works from a medical perspective. So, first of all, Dr. Einav, thank you for taking time to speak with me today.
Ohad Einav, MD: Thank you for having me.
Dr. Wilson: Can you tell us about Suleiman Hassan and what happened to him before he came into your care?
Dr. Einav: Hassan is a 12-year-old child who was riding his bicycle on the West Bank, about 40 minutes from here. Unfortunately, he was involved in a motor vehicle accident and he suffered injuries to his abdomen and cervical spine. He was transported to our service by helicopter from the scene of the accident.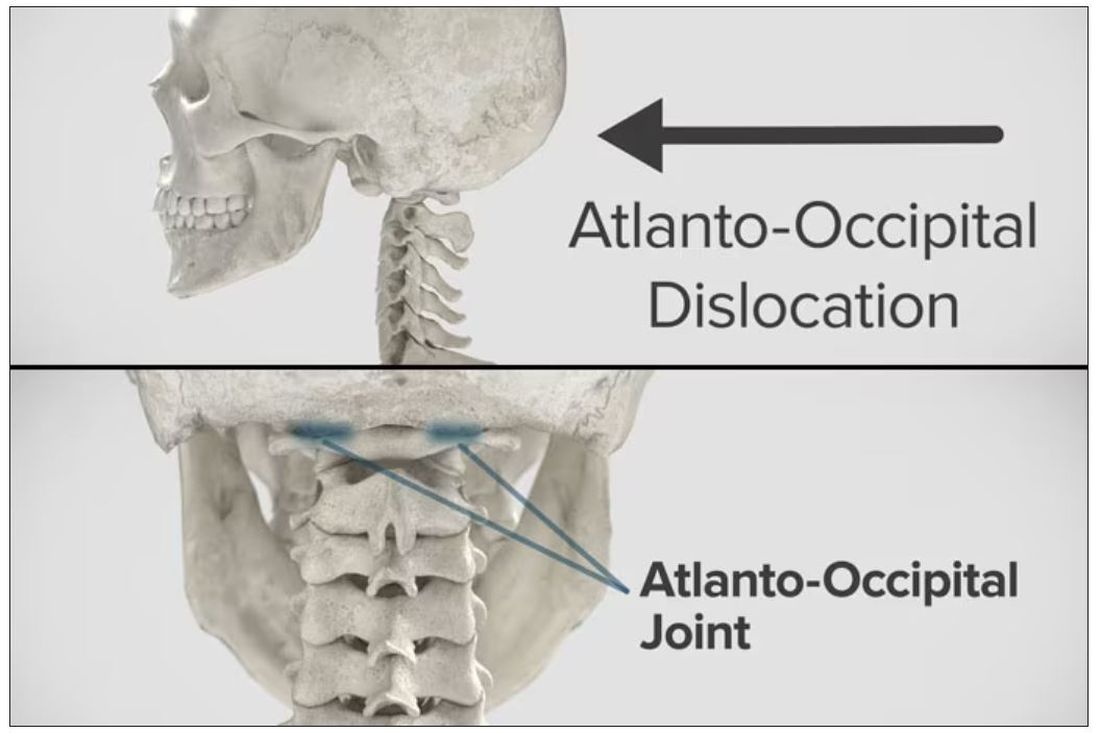
Dr. Wilson: “Injury to the cervical spine” might be something of an understatement. He had what’s called atlanto-occipital dislocation, colloquially often referred to as internal decapitation. Can you tell us what that means? It sounds terrifying.
Dr. Einav: It’s an injury to the ligaments between the occiput and the upper cervical spine, with or without bony fracture. The atlanto-occipital joint is formed by the superior articular facet of the atlas and the occipital condyle, stabilized by an articular capsule between the head and neck, and is supported by various ligaments around it that stabilize the joint and allow joint movements, including flexion, extension, and some rotation in the lower levels.
Dr. Wilson: This joint has several degrees of freedom, which means it needs a lot of support. With this type of injury, where essentially you have severing of the ligaments, is it usually survivable? How dangerous is this?
Dr. Einav: The mortality rate is 50%-60%, depending on the primary impact, the injury, transportation later on, and then the surgery and surgical management.
Dr. Wilson: Tell us a bit about this patient’s status when he came to your medical center. I assume he was in bad shape.
Dr. Einav: Hassan arrived at our medical center with a Glasgow Coma Scale score of 15. He was fully conscious. He was hemodynamically stable except for a bad laceration on his abdomen. He had a Philadelphia collar around his neck. He was transported by chopper because the paramedics suspected that he had a cervical spine injury and decided to bring him to a Level 1 trauma center.
He was monitored and we treated him according to the ATLS [advanced trauma life support] protocol. He didn’t have any gross sensory deficits, but he was a little confused about the whole situation and the accident. Therefore, we could do a general examination but we couldn’t rely on that regarding any sensory deficit that he may or may not have. We decided as a team that it would be better to slow down and control the situation. We decided not to operate on him immediately. We basically stabilized him and made sure that he didn’t have any traumatic internal organ damage. Later on we took him to the OR and performed surgery.
Dr. Wilson: It’s amazing that he had intact motor function, considering the extent of his injury. The spinal cord was spared somewhat during the injury. There must have been a moment when you realized that this kid, who was conscious and could move all four extremities, had a very severe neck injury. Was that due to a CT scan or physical exam? And what was your feeling when you saw that he had atlanto-occipital dislocation?
Dr. Einav: As a surgeon, you have a gut feeling in regard to the general examination of the patient. But I never rely on gut feelings. On the CT, I understood exactly what he had, what we needed to do, and the time frame.
Dr. Wilson: You’ve done these types of surgeries before, right? Obviously, no one has done a lot of them because this isn’t very common. But you knew what to do. Did you have a plan? Where does your experience come into play in a situation like this?
Dr. Einav: I graduated from the spine program of Toronto University, where I did a fellowship in trauma of the spine and complex spine surgery. I had very good teachers, and during my fellowship I treated a few cases in older patients that were similar but not the same. Therefore, I knew exactly what needed to be done.
Dr. Wilson: For those of us who aren’t surgeons, take us into the OR with you. This is obviously an incredibly delicate procedure. You are high up in the spinal cord at the base of the brain. The slightest mistake could have devastating consequences. What are the key elements of this procedure? What can go wrong here? What is the number-one thing you have to look out for when you’re trying to fix an internal decapitation?
Dr. Einav: The key element in surgeries of the cervical spine – trauma and complex spine surgery – is planning. I never go to the OR without knowing what I’m going to do. I have a few plans – plan A, plan B, plan C – in case something fails. So, I definitely know what the next step will be. I always think about the surgery a few hours before, if I have time to prepare.
The second thing that is very important is teamwork. The team needs to be coordinated. Everybody needs to know what their job is. With these types of injuries, it’s not the time for rookies. If you are new, please stand back and let the more experienced people do that job. I’m talking about surgeons, nurses, anesthesiologists – everyone.
Another important thing in planning is choosing the right hardware. For example, in this case we had a problem because most of the hardware is designed for adults, and we had to improvise because there isn’t a lot of hardware on the market for the pediatric population. The adult plates and screws are too big, so we had to improvise.
Dr. Wilson: Tell us more about that. How do you improvise spinal hardware for a 12-year-old?
Dr. Einav: In this case, I chose to use hardware from one of the companies that works with us.
You can see in this model the area of the injury, and the area that we worked on. To perform the surgery, I had to use some plates and rods from a different company. This company’s (NuVasive) hardware has a small attachment to the skull, which was helpful for affixing the skull to the cervical spine, instead of using a big plate that would sit at the base of the skull and would not be very good for him. Most of the hardware is made for adults and not for kids.
Dr. Wilson: Will that hardware preserve the motor function of his neck? Will he be able to turn his head and extend and flex it?
Dr. Einav: The injury leads to instability and destruction of both articulations between the head and neck. Therefore, those articulations won’t be able to function the same way in the future. There is a decrease of something like 50% of the flexion and extension of Hassan’s cervical spine. Therefore, I decided that in this case there would be no chance of saving Hassan’s motor function unless we performed a fusion between the head and the neck, and therefore I decided that this would be the best procedure with the best survival rate. So, in the future, he will have some diminished flexion, extension, and rotation of his head.
Dr. Wilson: How long did his surgery take?
Dr. Einav: To be honest, I don’t remember. But I can tell you that it took us time. It was very challenging to coordinate with everyone. The most problematic part of the surgery to perform is what we call “flip-over.”
The anesthesiologist intubated the patient when he was supine, and later on, we flipped him prone to operate on the spine. This maneuver can actually lead to injury by itself, and injury at this level is fatal. So, we took our time and got Hassan into the OR. The anesthesiologist did a great job with the GlideScope – inserting the endotracheal tube. Later on, we neuromonitored him. Basically, we connected Hassan’s peripheral nerves to a computer and monitored his motor function. Gently we flipped him over, and after that we saw a little change in his motor function, so we had to modify his position so we could preserve his motor function. We then started the procedure, which took a few hours. I don’t know exactly how many.
Dr. Wilson: That just speaks to how delicate this is for everything from the intubation, where typically you’re manipulating the head, to the repositioning. Clearly this requires a lot of teamwork.
What happened after the operation? How is he doing?
Dr. Einav: After the operation, Hassan had a great recovery. He’s doing well. He doesn’t have any motor or sensory deficits. He’s able to ambulate without any aid. He had no signs of infection, which can happen after a car accident, neither from his abdominal wound nor from the occipital cervical surgery. He feels well. We saw him in the clinic. We removed his collar. We monitored him at the clinic. He looked amazing.
Dr. Wilson: That’s incredible. Are there long-term risks for him that you need to be looking out for?
Dr. Einav: Yes, and that’s the reason that we are monitoring him post surgery. While he was in the hospital, we monitored his motor and sensory functions, as well as his wound healing. Later on, in the clinic, for a few weeks after surgery we monitored for any failure of the hardware and bone graft. We check for healing of the bone graft and bone substitutes we put in to heal those bones.
Dr. Wilson: He will grow, right? He’s only 12, so he still has some years of growth in him. Is he going to need more surgery or any kind of hardware upgrade?
Dr. Einav: I hope not. In my surgeries, I never rely on the hardware for long durations. If I decide to do, for example, fusion, I rely on the hardware for a certain amount of time. And then I plan that the biology will do the work. If I plan for fusion, I put bone grafts in the preferred area for a fusion. Then if the hardware fails, I wouldn’t need to take out the hardware, and there would be no change in the condition of the patient.
Dr. Wilson: What an incredible story. It’s clear that you and your team kept your cool despite a very high-acuity situation with a ton of risk. What a tremendous outcome that this boy is not only alive but fully functional. So, congratulations to you and your team. That was very strong work.
Dr. Einav: Thank you very much. I would like to thank our team. We have to remember that the surgeon is not standing alone in the war. Hassan’s story is a success story of a very big group of people from various backgrounds and religions. They work day and night to help people and save lives. To the paramedics, the physiologists, the traumatologists, the pediatricians, the nurses, the physiotherapists, and obviously the surgeons, a big thank you. His story is our success story.
Dr. Wilson: It’s inspiring to see so many people come together to do what we all are here for, which is to fight against suffering, disease, and death. Thank you for keeping up that fight. And thank you for joining me here.
Dr. Einav: Thank you very much.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
F. Perry Wilson, MD, MSCE: I am joined today by Dr. Ohad Einav. He’s a staff surgeon in orthopedics at Hadassah Medical Center in Jerusalem. He’s with me to talk about an absolutely incredible surgical case, something that is terrifying to most non–orthopedic surgeons and I imagine is fairly scary for spine surgeons like him as well. But what we don’t have is information about how this works from a medical perspective. So, first of all, Dr. Einav, thank you for taking time to speak with me today.
Ohad Einav, MD: Thank you for having me.
Dr. Wilson: Can you tell us about Suleiman Hassan and what happened to him before he came into your care?
Dr. Einav: Hassan is a 12-year-old child who was riding his bicycle on the West Bank, about 40 minutes from here. Unfortunately, he was involved in a motor vehicle accident and he suffered injuries to his abdomen and cervical spine. He was transported to our service by helicopter from the scene of the accident.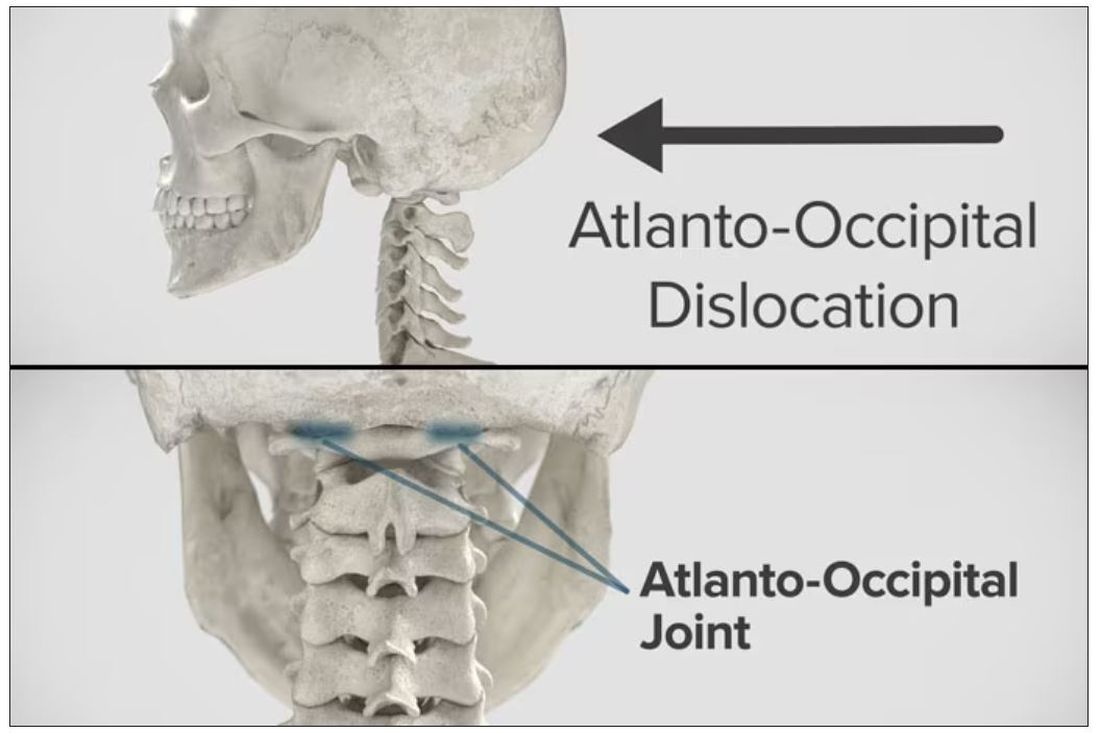
Dr. Wilson: “Injury to the cervical spine” might be something of an understatement. He had what’s called atlanto-occipital dislocation, colloquially often referred to as internal decapitation. Can you tell us what that means? It sounds terrifying.
Dr. Einav: It’s an injury to the ligaments between the occiput and the upper cervical spine, with or without bony fracture. The atlanto-occipital joint is formed by the superior articular facet of the atlas and the occipital condyle, stabilized by an articular capsule between the head and neck, and is supported by various ligaments around it that stabilize the joint and allow joint movements, including flexion, extension, and some rotation in the lower levels.
Dr. Wilson: This joint has several degrees of freedom, which means it needs a lot of support. With this type of injury, where essentially you have severing of the ligaments, is it usually survivable? How dangerous is this?
Dr. Einav: The mortality rate is 50%-60%, depending on the primary impact, the injury, transportation later on, and then the surgery and surgical management.
Dr. Wilson: Tell us a bit about this patient’s status when he came to your medical center. I assume he was in bad shape.
Dr. Einav: Hassan arrived at our medical center with a Glasgow Coma Scale score of 15. He was fully conscious. He was hemodynamically stable except for a bad laceration on his abdomen. He had a Philadelphia collar around his neck. He was transported by chopper because the paramedics suspected that he had a cervical spine injury and decided to bring him to a Level 1 trauma center.
He was monitored and we treated him according to the ATLS [advanced trauma life support] protocol. He didn’t have any gross sensory deficits, but he was a little confused about the whole situation and the accident. Therefore, we could do a general examination but we couldn’t rely on that regarding any sensory deficit that he may or may not have. We decided as a team that it would be better to slow down and control the situation. We decided not to operate on him immediately. We basically stabilized him and made sure that he didn’t have any traumatic internal organ damage. Later on we took him to the OR and performed surgery.
Dr. Wilson: It’s amazing that he had intact motor function, considering the extent of his injury. The spinal cord was spared somewhat during the injury. There must have been a moment when you realized that this kid, who was conscious and could move all four extremities, had a very severe neck injury. Was that due to a CT scan or physical exam? And what was your feeling when you saw that he had atlanto-occipital dislocation?
Dr. Einav: As a surgeon, you have a gut feeling in regard to the general examination of the patient. But I never rely on gut feelings. On the CT, I understood exactly what he had, what we needed to do, and the time frame.
Dr. Wilson: You’ve done these types of surgeries before, right? Obviously, no one has done a lot of them because this isn’t very common. But you knew what to do. Did you have a plan? Where does your experience come into play in a situation like this?
Dr. Einav: I graduated from the spine program of Toronto University, where I did a fellowship in trauma of the spine and complex spine surgery. I had very good teachers, and during my fellowship I treated a few cases in older patients that were similar but not the same. Therefore, I knew exactly what needed to be done.
Dr. Wilson: For those of us who aren’t surgeons, take us into the OR with you. This is obviously an incredibly delicate procedure. You are high up in the spinal cord at the base of the brain. The slightest mistake could have devastating consequences. What are the key elements of this procedure? What can go wrong here? What is the number-one thing you have to look out for when you’re trying to fix an internal decapitation?
Dr. Einav: The key element in surgeries of the cervical spine – trauma and complex spine surgery – is planning. I never go to the OR without knowing what I’m going to do. I have a few plans – plan A, plan B, plan C – in case something fails. So, I definitely know what the next step will be. I always think about the surgery a few hours before, if I have time to prepare.
The second thing that is very important is teamwork. The team needs to be coordinated. Everybody needs to know what their job is. With these types of injuries, it’s not the time for rookies. If you are new, please stand back and let the more experienced people do that job. I’m talking about surgeons, nurses, anesthesiologists – everyone.
Another important thing in planning is choosing the right hardware. For example, in this case we had a problem because most of the hardware is designed for adults, and we had to improvise because there isn’t a lot of hardware on the market for the pediatric population. The adult plates and screws are too big, so we had to improvise.
Dr. Wilson: Tell us more about that. How do you improvise spinal hardware for a 12-year-old?
Dr. Einav: In this case, I chose to use hardware from one of the companies that works with us.
You can see in this model the area of the injury, and the area that we worked on. To perform the surgery, I had to use some plates and rods from a different company. This company’s (NuVasive) hardware has a small attachment to the skull, which was helpful for affixing the skull to the cervical spine, instead of using a big plate that would sit at the base of the skull and would not be very good for him. Most of the hardware is made for adults and not for kids.
Dr. Wilson: Will that hardware preserve the motor function of his neck? Will he be able to turn his head and extend and flex it?
Dr. Einav: The injury leads to instability and destruction of both articulations between the head and neck. Therefore, those articulations won’t be able to function the same way in the future. There is a decrease of something like 50% of the flexion and extension of Hassan’s cervical spine. Therefore, I decided that in this case there would be no chance of saving Hassan’s motor function unless we performed a fusion between the head and the neck, and therefore I decided that this would be the best procedure with the best survival rate. So, in the future, he will have some diminished flexion, extension, and rotation of his head.
Dr. Wilson: How long did his surgery take?
Dr. Einav: To be honest, I don’t remember. But I can tell you that it took us time. It was very challenging to coordinate with everyone. The most problematic part of the surgery to perform is what we call “flip-over.”
The anesthesiologist intubated the patient when he was supine, and later on, we flipped him prone to operate on the spine. This maneuver can actually lead to injury by itself, and injury at this level is fatal. So, we took our time and got Hassan into the OR. The anesthesiologist did a great job with the GlideScope – inserting the endotracheal tube. Later on, we neuromonitored him. Basically, we connected Hassan’s peripheral nerves to a computer and monitored his motor function. Gently we flipped him over, and after that we saw a little change in his motor function, so we had to modify his position so we could preserve his motor function. We then started the procedure, which took a few hours. I don’t know exactly how many.
Dr. Wilson: That just speaks to how delicate this is for everything from the intubation, where typically you’re manipulating the head, to the repositioning. Clearly this requires a lot of teamwork.
What happened after the operation? How is he doing?
Dr. Einav: After the operation, Hassan had a great recovery. He’s doing well. He doesn’t have any motor or sensory deficits. He’s able to ambulate without any aid. He had no signs of infection, which can happen after a car accident, neither from his abdominal wound nor from the occipital cervical surgery. He feels well. We saw him in the clinic. We removed his collar. We monitored him at the clinic. He looked amazing.
Dr. Wilson: That’s incredible. Are there long-term risks for him that you need to be looking out for?
Dr. Einav: Yes, and that’s the reason that we are monitoring him post surgery. While he was in the hospital, we monitored his motor and sensory functions, as well as his wound healing. Later on, in the clinic, for a few weeks after surgery we monitored for any failure of the hardware and bone graft. We check for healing of the bone graft and bone substitutes we put in to heal those bones.
Dr. Wilson: He will grow, right? He’s only 12, so he still has some years of growth in him. Is he going to need more surgery or any kind of hardware upgrade?
Dr. Einav: I hope not. In my surgeries, I never rely on the hardware for long durations. If I decide to do, for example, fusion, I rely on the hardware for a certain amount of time. And then I plan that the biology will do the work. If I plan for fusion, I put bone grafts in the preferred area for a fusion. Then if the hardware fails, I wouldn’t need to take out the hardware, and there would be no change in the condition of the patient.
Dr. Wilson: What an incredible story. It’s clear that you and your team kept your cool despite a very high-acuity situation with a ton of risk. What a tremendous outcome that this boy is not only alive but fully functional. So, congratulations to you and your team. That was very strong work.
Dr. Einav: Thank you very much. I would like to thank our team. We have to remember that the surgeon is not standing alone in the war. Hassan’s story is a success story of a very big group of people from various backgrounds and religions. They work day and night to help people and save lives. To the paramedics, the physiologists, the traumatologists, the pediatricians, the nurses, the physiotherapists, and obviously the surgeons, a big thank you. His story is our success story.
Dr. Wilson: It’s inspiring to see so many people come together to do what we all are here for, which is to fight against suffering, disease, and death. Thank you for keeping up that fight. And thank you for joining me here.
Dr. Einav: Thank you very much.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
F. Perry Wilson, MD, MSCE: I am joined today by Dr. Ohad Einav. He’s a staff surgeon in orthopedics at Hadassah Medical Center in Jerusalem. He’s with me to talk about an absolutely incredible surgical case, something that is terrifying to most non–orthopedic surgeons and I imagine is fairly scary for spine surgeons like him as well. But what we don’t have is information about how this works from a medical perspective. So, first of all, Dr. Einav, thank you for taking time to speak with me today.
Ohad Einav, MD: Thank you for having me.
Dr. Wilson: Can you tell us about Suleiman Hassan and what happened to him before he came into your care?
Dr. Einav: Hassan is a 12-year-old child who was riding his bicycle on the West Bank, about 40 minutes from here. Unfortunately, he was involved in a motor vehicle accident and he suffered injuries to his abdomen and cervical spine. He was transported to our service by helicopter from the scene of the accident.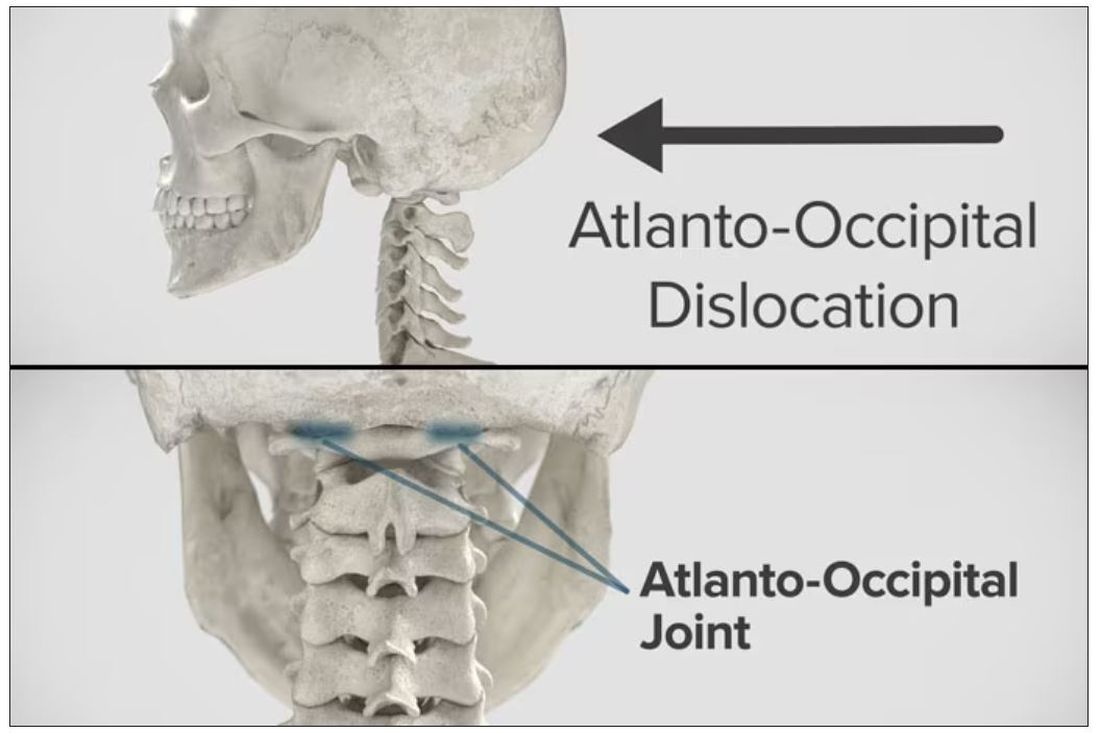
Dr. Wilson: “Injury to the cervical spine” might be something of an understatement. He had what’s called atlanto-occipital dislocation, colloquially often referred to as internal decapitation. Can you tell us what that means? It sounds terrifying.
Dr. Einav: It’s an injury to the ligaments between the occiput and the upper cervical spine, with or without bony fracture. The atlanto-occipital joint is formed by the superior articular facet of the atlas and the occipital condyle, stabilized by an articular capsule between the head and neck, and is supported by various ligaments around it that stabilize the joint and allow joint movements, including flexion, extension, and some rotation in the lower levels.
Dr. Wilson: This joint has several degrees of freedom, which means it needs a lot of support. With this type of injury, where essentially you have severing of the ligaments, is it usually survivable? How dangerous is this?
Dr. Einav: The mortality rate is 50%-60%, depending on the primary impact, the injury, transportation later on, and then the surgery and surgical management.
Dr. Wilson: Tell us a bit about this patient’s status when he came to your medical center. I assume he was in bad shape.
Dr. Einav: Hassan arrived at our medical center with a Glasgow Coma Scale score of 15. He was fully conscious. He was hemodynamically stable except for a bad laceration on his abdomen. He had a Philadelphia collar around his neck. He was transported by chopper because the paramedics suspected that he had a cervical spine injury and decided to bring him to a Level 1 trauma center.
He was monitored and we treated him according to the ATLS [advanced trauma life support] protocol. He didn’t have any gross sensory deficits, but he was a little confused about the whole situation and the accident. Therefore, we could do a general examination but we couldn’t rely on that regarding any sensory deficit that he may or may not have. We decided as a team that it would be better to slow down and control the situation. We decided not to operate on him immediately. We basically stabilized him and made sure that he didn’t have any traumatic internal organ damage. Later on we took him to the OR and performed surgery.
Dr. Wilson: It’s amazing that he had intact motor function, considering the extent of his injury. The spinal cord was spared somewhat during the injury. There must have been a moment when you realized that this kid, who was conscious and could move all four extremities, had a very severe neck injury. Was that due to a CT scan or physical exam? And what was your feeling when you saw that he had atlanto-occipital dislocation?
Dr. Einav: As a surgeon, you have a gut feeling in regard to the general examination of the patient. But I never rely on gut feelings. On the CT, I understood exactly what he had, what we needed to do, and the time frame.
Dr. Wilson: You’ve done these types of surgeries before, right? Obviously, no one has done a lot of them because this isn’t very common. But you knew what to do. Did you have a plan? Where does your experience come into play in a situation like this?
Dr. Einav: I graduated from the spine program of Toronto University, where I did a fellowship in trauma of the spine and complex spine surgery. I had very good teachers, and during my fellowship I treated a few cases in older patients that were similar but not the same. Therefore, I knew exactly what needed to be done.
Dr. Wilson: For those of us who aren’t surgeons, take us into the OR with you. This is obviously an incredibly delicate procedure. You are high up in the spinal cord at the base of the brain. The slightest mistake could have devastating consequences. What are the key elements of this procedure? What can go wrong here? What is the number-one thing you have to look out for when you’re trying to fix an internal decapitation?
Dr. Einav: The key element in surgeries of the cervical spine – trauma and complex spine surgery – is planning. I never go to the OR without knowing what I’m going to do. I have a few plans – plan A, plan B, plan C – in case something fails. So, I definitely know what the next step will be. I always think about the surgery a few hours before, if I have time to prepare.
The second thing that is very important is teamwork. The team needs to be coordinated. Everybody needs to know what their job is. With these types of injuries, it’s not the time for rookies. If you are new, please stand back and let the more experienced people do that job. I’m talking about surgeons, nurses, anesthesiologists – everyone.
Another important thing in planning is choosing the right hardware. For example, in this case we had a problem because most of the hardware is designed for adults, and we had to improvise because there isn’t a lot of hardware on the market for the pediatric population. The adult plates and screws are too big, so we had to improvise.
Dr. Wilson: Tell us more about that. How do you improvise spinal hardware for a 12-year-old?
Dr. Einav: In this case, I chose to use hardware from one of the companies that works with us.
You can see in this model the area of the injury, and the area that we worked on. To perform the surgery, I had to use some plates and rods from a different company. This company’s (NuVasive) hardware has a small attachment to the skull, which was helpful for affixing the skull to the cervical spine, instead of using a big plate that would sit at the base of the skull and would not be very good for him. Most of the hardware is made for adults and not for kids.
Dr. Wilson: Will that hardware preserve the motor function of his neck? Will he be able to turn his head and extend and flex it?
Dr. Einav: The injury leads to instability and destruction of both articulations between the head and neck. Therefore, those articulations won’t be able to function the same way in the future. There is a decrease of something like 50% of the flexion and extension of Hassan’s cervical spine. Therefore, I decided that in this case there would be no chance of saving Hassan’s motor function unless we performed a fusion between the head and the neck, and therefore I decided that this would be the best procedure with the best survival rate. So, in the future, he will have some diminished flexion, extension, and rotation of his head.
Dr. Wilson: How long did his surgery take?
Dr. Einav: To be honest, I don’t remember. But I can tell you that it took us time. It was very challenging to coordinate with everyone. The most problematic part of the surgery to perform is what we call “flip-over.”
The anesthesiologist intubated the patient when he was supine, and later on, we flipped him prone to operate on the spine. This maneuver can actually lead to injury by itself, and injury at this level is fatal. So, we took our time and got Hassan into the OR. The anesthesiologist did a great job with the GlideScope – inserting the endotracheal tube. Later on, we neuromonitored him. Basically, we connected Hassan’s peripheral nerves to a computer and monitored his motor function. Gently we flipped him over, and after that we saw a little change in his motor function, so we had to modify his position so we could preserve his motor function. We then started the procedure, which took a few hours. I don’t know exactly how many.
Dr. Wilson: That just speaks to how delicate this is for everything from the intubation, where typically you’re manipulating the head, to the repositioning. Clearly this requires a lot of teamwork.
What happened after the operation? How is he doing?
Dr. Einav: After the operation, Hassan had a great recovery. He’s doing well. He doesn’t have any motor or sensory deficits. He’s able to ambulate without any aid. He had no signs of infection, which can happen after a car accident, neither from his abdominal wound nor from the occipital cervical surgery. He feels well. We saw him in the clinic. We removed his collar. We monitored him at the clinic. He looked amazing.
Dr. Wilson: That’s incredible. Are there long-term risks for him that you need to be looking out for?
Dr. Einav: Yes, and that’s the reason that we are monitoring him post surgery. While he was in the hospital, we monitored his motor and sensory functions, as well as his wound healing. Later on, in the clinic, for a few weeks after surgery we monitored for any failure of the hardware and bone graft. We check for healing of the bone graft and bone substitutes we put in to heal those bones.
Dr. Wilson: He will grow, right? He’s only 12, so he still has some years of growth in him. Is he going to need more surgery or any kind of hardware upgrade?
Dr. Einav: I hope not. In my surgeries, I never rely on the hardware for long durations. If I decide to do, for example, fusion, I rely on the hardware for a certain amount of time. And then I plan that the biology will do the work. If I plan for fusion, I put bone grafts in the preferred area for a fusion. Then if the hardware fails, I wouldn’t need to take out the hardware, and there would be no change in the condition of the patient.
Dr. Wilson: What an incredible story. It’s clear that you and your team kept your cool despite a very high-acuity situation with a ton of risk. What a tremendous outcome that this boy is not only alive but fully functional. So, congratulations to you and your team. That was very strong work.
Dr. Einav: Thank you very much. I would like to thank our team. We have to remember that the surgeon is not standing alone in the war. Hassan’s story is a success story of a very big group of people from various backgrounds and religions. They work day and night to help people and save lives. To the paramedics, the physiologists, the traumatologists, the pediatricians, the nurses, the physiotherapists, and obviously the surgeons, a big thank you. His story is our success story.
Dr. Wilson: It’s inspiring to see so many people come together to do what we all are here for, which is to fight against suffering, disease, and death. Thank you for keeping up that fight. And thank you for joining me here.
Dr. Einav: Thank you very much.
A version of this article first appeared on Medscape.com.
New guideline for managing toothache in children
Nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, or both medications together can effectively manage a child’s toothache as a stopgap until definitive treatment is available, according to a new guideline.
The guideline, published in the September issue of the Journal of the American Dental Association, does not recommend opioids for a toothache or after tooth extraction in this population.
Opioid prescriptions for children entail risk for hospitalization and death. Yet, some dentists continued to prescribe contraindicated opioids to young children after a Food and Drug Administration warning in 2017 about the use of tramadol and codeine in this population, the guideline notes.
Opioid prescribing to children also continued after the American Academy of Pediatric Dentistry in 2018 recommended acetaminophen and NSAIDs as first-line medications for pain management and said that the use of opioids should be “rare.”
Although the new guidance, which also covers pain management after tooth extraction, is geared toward general dentists, it could help emergency clinicians and primary care providers manage children’s pain when definitive treatment is not immediately available, the authors noted.
Definitive treatment could include pulpectomy, nonsurgical root canal, incision for drainage of an abscess, or tooth extraction.
If definitive care in 2-3 days is not possible, parents should let the health care team know, the guideline says.
“These pharmacologic strategies will alleviate dental pain temporarily until a referral for definitive dental treatment is in place,” the authors wrote.
The American Dental Association (ADA) endorsed the new guideline, which was developed by researchers with the ADA Science & Research Institute, the University of Pittsburgh School of Dental Medicine, and the Center for Integrative Global Oral Health at the University of Pennsylvania School of Dental Medicine in Philadelphia.
The guideline recommends ibuprofen and, for children older than 2 years, naproxen as NSAID options. The use of naproxen in children younger than 12 years for this purpose is off label, they noted.
The guideline suggests doses of acetaminophen and NSAIDs on the basis of age and weight that may differ from those on medication packaging.
“When acetaminophen or NSAIDs are administered as directed, the risk of harm to children from either medication is low,” the guideline states.
“While prescribing opioids to children has become less frequent overall, this guideline ensures that both dentists and parents have evidence-based recommendations to determine the most appropriate treatment for dental pain,” senior guideline author Paul Moore, DMD, PhD, MPH, professor emeritus at the University of Pittsburgh’s School of Dental Medicine, said in a news release from the ADA. “Parents and caregivers can take comfort that widely available medications that have no abuse potential, such as acetaminophen or ibuprofen, are safe and effective for helping their children find relief from short-term dental pain.”
A 2018 review by Dr. Moore and coauthors found that NSAIDs, with or without acetaminophen, were effective and minimized adverse events, relative to opioids, for acute dental pain across ages.
The new recommendations for children will “allow for better treatment of this kind of pain” and “will help prevent unnecessary prescribing of medications with abuse potential, including opioids,” Patrizia Cavazzoni, MD, director of the FDA Center for Drug Evaluation and Research, said in the news release.
The report stems from a 3-year, $1.5 million grant awarded by the FDA in 2020 to the University of Pittsburgh and the ADA Science & Research Institute to develop a clinical practice guideline for the management of acute pain in dentistry in children, adolescents, and adults. The recommendations for adolescents and adults are still in development.
The report was supported by an FDA grant, and the guideline authors received technical and methodologic support from the agency. Some authors disclosed ties to pharmaceutical companies.
A version of this article appeared on Medscape.com.
Nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, or both medications together can effectively manage a child’s toothache as a stopgap until definitive treatment is available, according to a new guideline.
The guideline, published in the September issue of the Journal of the American Dental Association, does not recommend opioids for a toothache or after tooth extraction in this population.
Opioid prescriptions for children entail risk for hospitalization and death. Yet, some dentists continued to prescribe contraindicated opioids to young children after a Food and Drug Administration warning in 2017 about the use of tramadol and codeine in this population, the guideline notes.
Opioid prescribing to children also continued after the American Academy of Pediatric Dentistry in 2018 recommended acetaminophen and NSAIDs as first-line medications for pain management and said that the use of opioids should be “rare.”
Although the new guidance, which also covers pain management after tooth extraction, is geared toward general dentists, it could help emergency clinicians and primary care providers manage children’s pain when definitive treatment is not immediately available, the authors noted.
Definitive treatment could include pulpectomy, nonsurgical root canal, incision for drainage of an abscess, or tooth extraction.
If definitive care in 2-3 days is not possible, parents should let the health care team know, the guideline says.
“These pharmacologic strategies will alleviate dental pain temporarily until a referral for definitive dental treatment is in place,” the authors wrote.
The American Dental Association (ADA) endorsed the new guideline, which was developed by researchers with the ADA Science & Research Institute, the University of Pittsburgh School of Dental Medicine, and the Center for Integrative Global Oral Health at the University of Pennsylvania School of Dental Medicine in Philadelphia.
The guideline recommends ibuprofen and, for children older than 2 years, naproxen as NSAID options. The use of naproxen in children younger than 12 years for this purpose is off label, they noted.
The guideline suggests doses of acetaminophen and NSAIDs on the basis of age and weight that may differ from those on medication packaging.
“When acetaminophen or NSAIDs are administered as directed, the risk of harm to children from either medication is low,” the guideline states.
“While prescribing opioids to children has become less frequent overall, this guideline ensures that both dentists and parents have evidence-based recommendations to determine the most appropriate treatment for dental pain,” senior guideline author Paul Moore, DMD, PhD, MPH, professor emeritus at the University of Pittsburgh’s School of Dental Medicine, said in a news release from the ADA. “Parents and caregivers can take comfort that widely available medications that have no abuse potential, such as acetaminophen or ibuprofen, are safe and effective for helping their children find relief from short-term dental pain.”
A 2018 review by Dr. Moore and coauthors found that NSAIDs, with or without acetaminophen, were effective and minimized adverse events, relative to opioids, for acute dental pain across ages.
The new recommendations for children will “allow for better treatment of this kind of pain” and “will help prevent unnecessary prescribing of medications with abuse potential, including opioids,” Patrizia Cavazzoni, MD, director of the FDA Center for Drug Evaluation and Research, said in the news release.
The report stems from a 3-year, $1.5 million grant awarded by the FDA in 2020 to the University of Pittsburgh and the ADA Science & Research Institute to develop a clinical practice guideline for the management of acute pain in dentistry in children, adolescents, and adults. The recommendations for adolescents and adults are still in development.
The report was supported by an FDA grant, and the guideline authors received technical and methodologic support from the agency. Some authors disclosed ties to pharmaceutical companies.
A version of this article appeared on Medscape.com.
Nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, or both medications together can effectively manage a child’s toothache as a stopgap until definitive treatment is available, according to a new guideline.
The guideline, published in the September issue of the Journal of the American Dental Association, does not recommend opioids for a toothache or after tooth extraction in this population.
Opioid prescriptions for children entail risk for hospitalization and death. Yet, some dentists continued to prescribe contraindicated opioids to young children after a Food and Drug Administration warning in 2017 about the use of tramadol and codeine in this population, the guideline notes.
Opioid prescribing to children also continued after the American Academy of Pediatric Dentistry in 2018 recommended acetaminophen and NSAIDs as first-line medications for pain management and said that the use of opioids should be “rare.”
Although the new guidance, which also covers pain management after tooth extraction, is geared toward general dentists, it could help emergency clinicians and primary care providers manage children’s pain when definitive treatment is not immediately available, the authors noted.
Definitive treatment could include pulpectomy, nonsurgical root canal, incision for drainage of an abscess, or tooth extraction.
If definitive care in 2-3 days is not possible, parents should let the health care team know, the guideline says.
“These pharmacologic strategies will alleviate dental pain temporarily until a referral for definitive dental treatment is in place,” the authors wrote.
The American Dental Association (ADA) endorsed the new guideline, which was developed by researchers with the ADA Science & Research Institute, the University of Pittsburgh School of Dental Medicine, and the Center for Integrative Global Oral Health at the University of Pennsylvania School of Dental Medicine in Philadelphia.
The guideline recommends ibuprofen and, for children older than 2 years, naproxen as NSAID options. The use of naproxen in children younger than 12 years for this purpose is off label, they noted.
The guideline suggests doses of acetaminophen and NSAIDs on the basis of age and weight that may differ from those on medication packaging.
“When acetaminophen or NSAIDs are administered as directed, the risk of harm to children from either medication is low,” the guideline states.
“While prescribing opioids to children has become less frequent overall, this guideline ensures that both dentists and parents have evidence-based recommendations to determine the most appropriate treatment for dental pain,” senior guideline author Paul Moore, DMD, PhD, MPH, professor emeritus at the University of Pittsburgh’s School of Dental Medicine, said in a news release from the ADA. “Parents and caregivers can take comfort that widely available medications that have no abuse potential, such as acetaminophen or ibuprofen, are safe and effective for helping their children find relief from short-term dental pain.”
A 2018 review by Dr. Moore and coauthors found that NSAIDs, with or without acetaminophen, were effective and minimized adverse events, relative to opioids, for acute dental pain across ages.
The new recommendations for children will “allow for better treatment of this kind of pain” and “will help prevent unnecessary prescribing of medications with abuse potential, including opioids,” Patrizia Cavazzoni, MD, director of the FDA Center for Drug Evaluation and Research, said in the news release.
The report stems from a 3-year, $1.5 million grant awarded by the FDA in 2020 to the University of Pittsburgh and the ADA Science & Research Institute to develop a clinical practice guideline for the management of acute pain in dentistry in children, adolescents, and adults. The recommendations for adolescents and adults are still in development.
The report was supported by an FDA grant, and the guideline authors received technical and methodologic support from the agency. Some authors disclosed ties to pharmaceutical companies.
A version of this article appeared on Medscape.com.
Innovations in pediatric chronic pain management
At the new Walnut Creek Clinic in the East Bay of the San Francisco Bay area, kids get a “Comfort Promise.”
The clinic extends the work of the Stad Center for Pediatric Pain, Palliative & Integrative Medicine beyond the locations in University of California San Francisco Benioff Children’s Hospitals in San Francisco and Oakland.
At Walnut Creek, clinical acupuncturists, massage therapists, and specialists in hypnosis complement advanced medical care with integrative techniques.
The “Comfort Promise” program, which is being rolled out at that clinic and other UCSF pediatric clinics through the end of 2024, is the clinicians’ pledge to do everything in their power to make tests, infusions, and vaccinations “practically pain free.”
Needle sticks, for example, can be a common source of pain and anxiety for kids. Techniques to minimize pain vary by age. Among the ways the clinicians minimize needle pain for a child 6- to 12-years-old are:
- Giving the child control options to pick which arm; and watch the injection, pause it, or stop it with a communication sign.
- Introducing memory shaping by asking the child about the experience afterward and presenting it in a positive way by praising the acts of sitting still, breathing deeply, or being brave.
- Using distractors such as asking the child to hold a favorite item from home, storytelling, coloring, singing, or using breathing exercises.
Stefan Friedrichsdorf, MD, chief of the UCSF division of pediatric pain, palliative & integrative medicine, said in a statement: “For kids with chronic pain, complex pain medications can cause more harm than benefit. Our goal is to combine exercise and physical therapy with integrative medicine and skills-based psychotherapy to help them become pain free in their everyday life.”
Bundling appointments for early impact
At Lurie Children’s Hospital of Chicago, the chronic pain treatment program bundles visits with experts in several disciplines, include social workers, psychologists, and physical therapists, in addition to the medical team, so that patients can complete a first round of visits with multiple specialists in a short period, as opposed to several months.
Natalie Weatherred, APRN-NP, CPNP-PC, a pediatric nurse practitioner in anesthesiology and the pain clinic coordinator, said in an interview that the up-front visits involve between four and eight follow-up sessions in a short period with everybody in the multidisciplinary team “to really help jump-start their pain treatment.”
She pointed out that many families come from distant parts of the state or beyond so the bundled appointments are also important for easing burden on families.
Sarah Duggan, APRN-NP, CPNP-PC, also a pediatric nurse practitioner in anesthesiology at Lurie’s, pointed out that patients at their clinic often have other chronic conditions as well, such as such as postural orthostatic tachycardia syndrome so the care integration is particularly important.
“We can get them the appropriate care that they need and the resources they need, much sooner than we would have been able to do 5 or 10 years ago,” Ms. Duggan said.
Virtual reality distraction instead of sedation
Henry Huang, MD, anesthesiologist and pain physician at Texas Children’s Hospital, Houston, said a special team there collaborates with the Chariot Program at Stanford (Calif.) University and incorporates virtual reality to distract children from pain and anxiety and harness their imaginations during induction for anesthesia, intravenous placement, and vaccinations.
“At our institution we’ve been recruiting patients to do a proof of concept to do virtual reality distraction for pain procedures, such as nerve blocks or steroid injections,” Dr. Huang said.
Traditionally, kids would have received oral or intravenous sedation to help them cope with the fear and pain.
“We’ve been successful in several cases without relying on any sedation,” he said. “The next target is to expand that to the chronic pain population.”
The distraction techniques are promising for a wide range of ages, he said, and the programming is tailored to the child’s ability to interact with the technology.
He said he is also part of a group promoting use of ultrasound instead of x-rays to guide injections to the spine and chest to reduce children’s exposure to radiation. His group is helping teach these methods to other clinicians nationally.
Dr. Huang said the most important development in chronic pediatric pain has been the growth of rehab centers that include the medical team, and practitioners from psychology as well as occupational and physical therapy.
“More and more hospitals are recognizing the importance of these pain rehab centers,” he said.
The problem, Dr. Huang said, is that these programs have always been resource intensive and involve highly specialized clinicians. The cost and the limited number of specialists make it difficult for widespread rollout.
“That’s always been the challenge from the pediatric pain world,” he said.
Recognizing the complexity of kids’ chronic pain
Angela Garcia, MD, a consulting physician for pediatric rehabilitation medicine at UPMC Children’s Hospital of Pittsburgh said
Techniques such as biofeedback and acupuncture are becoming more mainstream in pediatric chronic care, she said.
At the UPMC clinic, children and their families talk with a care team about their values and what they want to accomplish in managing the child’s pain. They ask what the pain is preventing the child from doing.
“Their goals really are our goals,” she said.
She said she also refers almost all patients to one of the center’s pain psychologists.
“Pain is biopsychosocial,” she said. “We want to make sure we’re addressing how to cope with pain.”
Dr. Garcia said she hopes nutritional therapy is one of the next approaches the clinic will incorporate, particularly surrounding how dietary changes can reduce inflammation “and heal the body from the inside out.”
She said the hospital is also looking at developing an inpatient pain program for kids whose functioning has changed so drastically that they need more intensive therapies.
Whatever the treatment approach, she said, addressing the pain early is critical.
“There is an increased risk of a child with chronic pain becoming an adult with chronic pain,” Dr. Garcia pointed out, “and that can lead to a decrease in the ability to participate in society.”
Ms. Weatherred, Ms. Duggan, Dr. Huang, and Dr. Garcia reported no relevant financial relationships.
At the new Walnut Creek Clinic in the East Bay of the San Francisco Bay area, kids get a “Comfort Promise.”
The clinic extends the work of the Stad Center for Pediatric Pain, Palliative & Integrative Medicine beyond the locations in University of California San Francisco Benioff Children’s Hospitals in San Francisco and Oakland.
At Walnut Creek, clinical acupuncturists, massage therapists, and specialists in hypnosis complement advanced medical care with integrative techniques.
The “Comfort Promise” program, which is being rolled out at that clinic and other UCSF pediatric clinics through the end of 2024, is the clinicians’ pledge to do everything in their power to make tests, infusions, and vaccinations “practically pain free.”
Needle sticks, for example, can be a common source of pain and anxiety for kids. Techniques to minimize pain vary by age. Among the ways the clinicians minimize needle pain for a child 6- to 12-years-old are:
- Giving the child control options to pick which arm; and watch the injection, pause it, or stop it with a communication sign.
- Introducing memory shaping by asking the child about the experience afterward and presenting it in a positive way by praising the acts of sitting still, breathing deeply, or being brave.
- Using distractors such as asking the child to hold a favorite item from home, storytelling, coloring, singing, or using breathing exercises.
Stefan Friedrichsdorf, MD, chief of the UCSF division of pediatric pain, palliative & integrative medicine, said in a statement: “For kids with chronic pain, complex pain medications can cause more harm than benefit. Our goal is to combine exercise and physical therapy with integrative medicine and skills-based psychotherapy to help them become pain free in their everyday life.”
Bundling appointments for early impact
At Lurie Children’s Hospital of Chicago, the chronic pain treatment program bundles visits with experts in several disciplines, include social workers, psychologists, and physical therapists, in addition to the medical team, so that patients can complete a first round of visits with multiple specialists in a short period, as opposed to several months.
Natalie Weatherred, APRN-NP, CPNP-PC, a pediatric nurse practitioner in anesthesiology and the pain clinic coordinator, said in an interview that the up-front visits involve between four and eight follow-up sessions in a short period with everybody in the multidisciplinary team “to really help jump-start their pain treatment.”
She pointed out that many families come from distant parts of the state or beyond so the bundled appointments are also important for easing burden on families.
Sarah Duggan, APRN-NP, CPNP-PC, also a pediatric nurse practitioner in anesthesiology at Lurie’s, pointed out that patients at their clinic often have other chronic conditions as well, such as such as postural orthostatic tachycardia syndrome so the care integration is particularly important.
“We can get them the appropriate care that they need and the resources they need, much sooner than we would have been able to do 5 or 10 years ago,” Ms. Duggan said.
Virtual reality distraction instead of sedation
Henry Huang, MD, anesthesiologist and pain physician at Texas Children’s Hospital, Houston, said a special team there collaborates with the Chariot Program at Stanford (Calif.) University and incorporates virtual reality to distract children from pain and anxiety and harness their imaginations during induction for anesthesia, intravenous placement, and vaccinations.
“At our institution we’ve been recruiting patients to do a proof of concept to do virtual reality distraction for pain procedures, such as nerve blocks or steroid injections,” Dr. Huang said.
Traditionally, kids would have received oral or intravenous sedation to help them cope with the fear and pain.
“We’ve been successful in several cases without relying on any sedation,” he said. “The next target is to expand that to the chronic pain population.”
The distraction techniques are promising for a wide range of ages, he said, and the programming is tailored to the child’s ability to interact with the technology.
He said he is also part of a group promoting use of ultrasound instead of x-rays to guide injections to the spine and chest to reduce children’s exposure to radiation. His group is helping teach these methods to other clinicians nationally.
Dr. Huang said the most important development in chronic pediatric pain has been the growth of rehab centers that include the medical team, and practitioners from psychology as well as occupational and physical therapy.
“More and more hospitals are recognizing the importance of these pain rehab centers,” he said.
The problem, Dr. Huang said, is that these programs have always been resource intensive and involve highly specialized clinicians. The cost and the limited number of specialists make it difficult for widespread rollout.
“That’s always been the challenge from the pediatric pain world,” he said.
Recognizing the complexity of kids’ chronic pain
Angela Garcia, MD, a consulting physician for pediatric rehabilitation medicine at UPMC Children’s Hospital of Pittsburgh said
Techniques such as biofeedback and acupuncture are becoming more mainstream in pediatric chronic care, she said.
At the UPMC clinic, children and their families talk with a care team about their values and what they want to accomplish in managing the child’s pain. They ask what the pain is preventing the child from doing.
“Their goals really are our goals,” she said.
She said she also refers almost all patients to one of the center’s pain psychologists.
“Pain is biopsychosocial,” she said. “We want to make sure we’re addressing how to cope with pain.”
Dr. Garcia said she hopes nutritional therapy is one of the next approaches the clinic will incorporate, particularly surrounding how dietary changes can reduce inflammation “and heal the body from the inside out.”
She said the hospital is also looking at developing an inpatient pain program for kids whose functioning has changed so drastically that they need more intensive therapies.
Whatever the treatment approach, she said, addressing the pain early is critical.
“There is an increased risk of a child with chronic pain becoming an adult with chronic pain,” Dr. Garcia pointed out, “and that can lead to a decrease in the ability to participate in society.”
Ms. Weatherred, Ms. Duggan, Dr. Huang, and Dr. Garcia reported no relevant financial relationships.
At the new Walnut Creek Clinic in the East Bay of the San Francisco Bay area, kids get a “Comfort Promise.”
The clinic extends the work of the Stad Center for Pediatric Pain, Palliative & Integrative Medicine beyond the locations in University of California San Francisco Benioff Children’s Hospitals in San Francisco and Oakland.
At Walnut Creek, clinical acupuncturists, massage therapists, and specialists in hypnosis complement advanced medical care with integrative techniques.
The “Comfort Promise” program, which is being rolled out at that clinic and other UCSF pediatric clinics through the end of 2024, is the clinicians’ pledge to do everything in their power to make tests, infusions, and vaccinations “practically pain free.”
Needle sticks, for example, can be a common source of pain and anxiety for kids. Techniques to minimize pain vary by age. Among the ways the clinicians minimize needle pain for a child 6- to 12-years-old are:
- Giving the child control options to pick which arm; and watch the injection, pause it, or stop it with a communication sign.
- Introducing memory shaping by asking the child about the experience afterward and presenting it in a positive way by praising the acts of sitting still, breathing deeply, or being brave.
- Using distractors such as asking the child to hold a favorite item from home, storytelling, coloring, singing, or using breathing exercises.
Stefan Friedrichsdorf, MD, chief of the UCSF division of pediatric pain, palliative & integrative medicine, said in a statement: “For kids with chronic pain, complex pain medications can cause more harm than benefit. Our goal is to combine exercise and physical therapy with integrative medicine and skills-based psychotherapy to help them become pain free in their everyday life.”
Bundling appointments for early impact
At Lurie Children’s Hospital of Chicago, the chronic pain treatment program bundles visits with experts in several disciplines, include social workers, psychologists, and physical therapists, in addition to the medical team, so that patients can complete a first round of visits with multiple specialists in a short period, as opposed to several months.
Natalie Weatherred, APRN-NP, CPNP-PC, a pediatric nurse practitioner in anesthesiology and the pain clinic coordinator, said in an interview that the up-front visits involve between four and eight follow-up sessions in a short period with everybody in the multidisciplinary team “to really help jump-start their pain treatment.”
She pointed out that many families come from distant parts of the state or beyond so the bundled appointments are also important for easing burden on families.
Sarah Duggan, APRN-NP, CPNP-PC, also a pediatric nurse practitioner in anesthesiology at Lurie’s, pointed out that patients at their clinic often have other chronic conditions as well, such as such as postural orthostatic tachycardia syndrome so the care integration is particularly important.
“We can get them the appropriate care that they need and the resources they need, much sooner than we would have been able to do 5 or 10 years ago,” Ms. Duggan said.
Virtual reality distraction instead of sedation
Henry Huang, MD, anesthesiologist and pain physician at Texas Children’s Hospital, Houston, said a special team there collaborates with the Chariot Program at Stanford (Calif.) University and incorporates virtual reality to distract children from pain and anxiety and harness their imaginations during induction for anesthesia, intravenous placement, and vaccinations.
“At our institution we’ve been recruiting patients to do a proof of concept to do virtual reality distraction for pain procedures, such as nerve blocks or steroid injections,” Dr. Huang said.
Traditionally, kids would have received oral or intravenous sedation to help them cope with the fear and pain.
“We’ve been successful in several cases without relying on any sedation,” he said. “The next target is to expand that to the chronic pain population.”
The distraction techniques are promising for a wide range of ages, he said, and the programming is tailored to the child’s ability to interact with the technology.
He said he is also part of a group promoting use of ultrasound instead of x-rays to guide injections to the spine and chest to reduce children’s exposure to radiation. His group is helping teach these methods to other clinicians nationally.
Dr. Huang said the most important development in chronic pediatric pain has been the growth of rehab centers that include the medical team, and practitioners from psychology as well as occupational and physical therapy.
“More and more hospitals are recognizing the importance of these pain rehab centers,” he said.
The problem, Dr. Huang said, is that these programs have always been resource intensive and involve highly specialized clinicians. The cost and the limited number of specialists make it difficult for widespread rollout.
“That’s always been the challenge from the pediatric pain world,” he said.
Recognizing the complexity of kids’ chronic pain
Angela Garcia, MD, a consulting physician for pediatric rehabilitation medicine at UPMC Children’s Hospital of Pittsburgh said
Techniques such as biofeedback and acupuncture are becoming more mainstream in pediatric chronic care, she said.
At the UPMC clinic, children and their families talk with a care team about their values and what they want to accomplish in managing the child’s pain. They ask what the pain is preventing the child from doing.
“Their goals really are our goals,” she said.
She said she also refers almost all patients to one of the center’s pain psychologists.
“Pain is biopsychosocial,” she said. “We want to make sure we’re addressing how to cope with pain.”
Dr. Garcia said she hopes nutritional therapy is one of the next approaches the clinic will incorporate, particularly surrounding how dietary changes can reduce inflammation “and heal the body from the inside out.”
She said the hospital is also looking at developing an inpatient pain program for kids whose functioning has changed so drastically that they need more intensive therapies.
Whatever the treatment approach, she said, addressing the pain early is critical.
“There is an increased risk of a child with chronic pain becoming an adult with chronic pain,” Dr. Garcia pointed out, “and that can lead to a decrease in the ability to participate in society.”
Ms. Weatherred, Ms. Duggan, Dr. Huang, and Dr. Garcia reported no relevant financial relationships.
Pain mismanagement by the numbers
Despite my best efforts to cultivate acquaintances across a broader age group, my social circle still has the somewhat musty odor of septuagenarians. We try to talk about things beyond the weather and grandchildren but pain scenarios surface with unfortunate frequency. Arthritic joints ache, body parts wear out or become diseased and have to be removed or replaced. That stuff can hurt.
There are two pain-related themes that seem to crop up more frequently than you might expect. The first is the unfortunate side effects of opioid medication – most often gastric distress and vomiting, then of course there’s constipation. They seem so common that a good many of my acquaintances just plain refuse to take opioids when they have been prescribed postoperatively because of their vivid memories of the consequences or horror stories friends have told.
The second theme is the general annoyance with the damn “Please rate your pain from one to ten” request issued by every well-intentioned nurse. Do you mean the pain I am having right now, this second, or last night, or the average over the last day and a half? Or should I be comparing it with when I gave birth 70 years ago, or when I stubbed my toe getting out of the shower last week? And then what are you going to do with my guesstimated number?
It may surprise some of you that 40 years ago there wasn’t a pain scale fetish. But a few observant health care professionals realized that many of our patients were suffering because we weren’t adequately managing their pain. In postoperative situations this was slowing recovery and effecting outcomes. Like good pseudoscientists, they realized that we should first quantify the pain and the notion that no pain should go unrated came into being. Nor should pain go untreated, which is too frequently interpreted as meaning unmedicated.
For example a systematic review of 61 studies of juvenile idiopathic arthritis (JIA) published in the journal Pediatric Rheumatology found that there was positive relationship between pain and a child’s belief that pain causes harm, disability, and lack of control. Not surprisingly, stress was also associated with pain intensity.
It is a long paper and touches on numerous other associations of varying degrees of strength between parental, social, and other external factors. But, in general, they were not as consistent as those related to a child’s beliefs.
Before, or at least at the same time, we treat a patient’s pain, we should learn more about that patient – his or her concerns, beliefs, and stressors. You and I may have exactly the same hernia operation, but if you have a better understanding of why you are going to feel uncomfortable after the surgery, and understand that not every pain is the result of a complication, I suspect you are more likely to complain of less pain.
The recent JIA study doesn’t claim to suggest therapeutic methods. However, one wonders what the result would be if we could somehow alter a patient’s belief system so that he or she no longer sees pain as always harmful, nor does the patient see himself or herself as powerless to do anything about the pain. To do this experiment we must follow up our robotic request to “rate your pain” with a dialogue in which we learn more about the patient. Which means probing believes, fears, and stressors.
You can tell me this exercise would be unrealistic and time consuming. But I bet in the long run it will save time. Even if it doesn’t it is the better way to manage pain.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Despite my best efforts to cultivate acquaintances across a broader age group, my social circle still has the somewhat musty odor of septuagenarians. We try to talk about things beyond the weather and grandchildren but pain scenarios surface with unfortunate frequency. Arthritic joints ache, body parts wear out or become diseased and have to be removed or replaced. That stuff can hurt.
There are two pain-related themes that seem to crop up more frequently than you might expect. The first is the unfortunate side effects of opioid medication – most often gastric distress and vomiting, then of course there’s constipation. They seem so common that a good many of my acquaintances just plain refuse to take opioids when they have been prescribed postoperatively because of their vivid memories of the consequences or horror stories friends have told.
The second theme is the general annoyance with the damn “Please rate your pain from one to ten” request issued by every well-intentioned nurse. Do you mean the pain I am having right now, this second, or last night, or the average over the last day and a half? Or should I be comparing it with when I gave birth 70 years ago, or when I stubbed my toe getting out of the shower last week? And then what are you going to do with my guesstimated number?
It may surprise some of you that 40 years ago there wasn’t a pain scale fetish. But a few observant health care professionals realized that many of our patients were suffering because we weren’t adequately managing their pain. In postoperative situations this was slowing recovery and effecting outcomes. Like good pseudoscientists, they realized that we should first quantify the pain and the notion that no pain should go unrated came into being. Nor should pain go untreated, which is too frequently interpreted as meaning unmedicated.
For example a systematic review of 61 studies of juvenile idiopathic arthritis (JIA) published in the journal Pediatric Rheumatology found that there was positive relationship between pain and a child’s belief that pain causes harm, disability, and lack of control. Not surprisingly, stress was also associated with pain intensity.
It is a long paper and touches on numerous other associations of varying degrees of strength between parental, social, and other external factors. But, in general, they were not as consistent as those related to a child’s beliefs.
Before, or at least at the same time, we treat a patient’s pain, we should learn more about that patient – his or her concerns, beliefs, and stressors. You and I may have exactly the same hernia operation, but if you have a better understanding of why you are going to feel uncomfortable after the surgery, and understand that not every pain is the result of a complication, I suspect you are more likely to complain of less pain.
The recent JIA study doesn’t claim to suggest therapeutic methods. However, one wonders what the result would be if we could somehow alter a patient’s belief system so that he or she no longer sees pain as always harmful, nor does the patient see himself or herself as powerless to do anything about the pain. To do this experiment we must follow up our robotic request to “rate your pain” with a dialogue in which we learn more about the patient. Which means probing believes, fears, and stressors.
You can tell me this exercise would be unrealistic and time consuming. But I bet in the long run it will save time. Even if it doesn’t it is the better way to manage pain.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Despite my best efforts to cultivate acquaintances across a broader age group, my social circle still has the somewhat musty odor of septuagenarians. We try to talk about things beyond the weather and grandchildren but pain scenarios surface with unfortunate frequency. Arthritic joints ache, body parts wear out or become diseased and have to be removed or replaced. That stuff can hurt.
There are two pain-related themes that seem to crop up more frequently than you might expect. The first is the unfortunate side effects of opioid medication – most often gastric distress and vomiting, then of course there’s constipation. They seem so common that a good many of my acquaintances just plain refuse to take opioids when they have been prescribed postoperatively because of their vivid memories of the consequences or horror stories friends have told.
The second theme is the general annoyance with the damn “Please rate your pain from one to ten” request issued by every well-intentioned nurse. Do you mean the pain I am having right now, this second, or last night, or the average over the last day and a half? Or should I be comparing it with when I gave birth 70 years ago, or when I stubbed my toe getting out of the shower last week? And then what are you going to do with my guesstimated number?
It may surprise some of you that 40 years ago there wasn’t a pain scale fetish. But a few observant health care professionals realized that many of our patients were suffering because we weren’t adequately managing their pain. In postoperative situations this was slowing recovery and effecting outcomes. Like good pseudoscientists, they realized that we should first quantify the pain and the notion that no pain should go unrated came into being. Nor should pain go untreated, which is too frequently interpreted as meaning unmedicated.
For example a systematic review of 61 studies of juvenile idiopathic arthritis (JIA) published in the journal Pediatric Rheumatology found that there was positive relationship between pain and a child’s belief that pain causes harm, disability, and lack of control. Not surprisingly, stress was also associated with pain intensity.
It is a long paper and touches on numerous other associations of varying degrees of strength between parental, social, and other external factors. But, in general, they were not as consistent as those related to a child’s beliefs.
Before, or at least at the same time, we treat a patient’s pain, we should learn more about that patient – his or her concerns, beliefs, and stressors. You and I may have exactly the same hernia operation, but if you have a better understanding of why you are going to feel uncomfortable after the surgery, and understand that not every pain is the result of a complication, I suspect you are more likely to complain of less pain.
The recent JIA study doesn’t claim to suggest therapeutic methods. However, one wonders what the result would be if we could somehow alter a patient’s belief system so that he or she no longer sees pain as always harmful, nor does the patient see himself or herself as powerless to do anything about the pain. To do this experiment we must follow up our robotic request to “rate your pain” with a dialogue in which we learn more about the patient. Which means probing believes, fears, and stressors.
You can tell me this exercise would be unrealistic and time consuming. But I bet in the long run it will save time. Even if it doesn’t it is the better way to manage pain.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Dangerous grandparents
Many decades ago I wrote a book I brazenly titled: “The Good Grandmother Handbook.” I had been a parent for a scant 7 or 8 years but based on my experiences in the office I felt I had accumulated enough wisdom to suggest to women in their fifth to seventh decades how they might conduct themselves around their grandchildren. Luckily, the book never got further than several hundred pages of crudely typed manuscript. This was before word processing programs had settled into the home computer industry, which was still in its infancy.
But I continue find the subject of grandparents interesting. Now, with grandchildren of my own (the oldest has just graduated from high school) and scores of peers knee deep in their own grandparenting adventures, I hope that my perspective now has a bit less of a holier-than-thou aroma.
My most recent muse-prodding event came when I stumbled across an article about the epidemiology of unintentional pediatric firearm fatalities. Looking at 10 years of data from the National Violent Death Reporting System, the investigators found that in 80% of the cases the firearm owner was a relative of the victim; in slightly more than 60% of the cases the event occurred in the victim’s home.
The data set was not granular enough to define the exact relationship between the child and relative who owned the gun. I suspect that most often the relative was a parent or an uncle or aunt. However, viewed through my septuagenarian prism, this paper prompted me to wonder in how many of these fatalities the firearm owner was a grandparent.
I have only anecdotal observations, but I can easily recall situations here in Maine in which a child has been injured by his or her grandfather’s gun. The data from the study show that pediatric fatalities are bimodal, with the majority occurring in the 1- to 5-year age group and a second peak in adolescence. The grandparent-involved cases I can recall were in the younger demographic.
Unfortunately, firearms aren’t the only threat that other grandparents and I pose to the health and safety of our grandchildren. I can remember before the development of, and the widespread use of, tamper-proof pill bottles, “grandma’s purse” overdoses were an unfortunately common occurrence.
More recently, at least here in Maine, we have been hearing more about motorized vehicle–related injuries and fatalities – grandparents backing over their grandchildren in the driveway or, more often, grandfathers (usually) taking their young grandchildren for rides on their snowmobiles, ATVs, lawn tractors, (fill in the blank). Whenever one of these events occurs, my mind quickly jumps beyond the tragic loss of life to imagining what terrible and long-lasting emotional chaos these incidents have spawned in those families.
During the pandemic, many parents and grandparents became aware of the threat that viral-spewing young children pose to the older and more vulnerable generation. On the other hand, many parents have been told that having a grandparent around can present a risk to the health and safety of their grandchildren. It can be a touchy subject in families, and grandparents may bristle at “being treated like a child” when they are reminded that children aren’t small adults and that their own behavior may be setting a bad example or putting their grandchildren at risk.
My generation had to learn how to buckle infants and toddlers into car seats because it was something that wasn’t done for our children. Fortunately, most new grandparents now already have those buckle-and-click skills and mindset. But,
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Many decades ago I wrote a book I brazenly titled: “The Good Grandmother Handbook.” I had been a parent for a scant 7 or 8 years but based on my experiences in the office I felt I had accumulated enough wisdom to suggest to women in their fifth to seventh decades how they might conduct themselves around their grandchildren. Luckily, the book never got further than several hundred pages of crudely typed manuscript. This was before word processing programs had settled into the home computer industry, which was still in its infancy.
But I continue find the subject of grandparents interesting. Now, with grandchildren of my own (the oldest has just graduated from high school) and scores of peers knee deep in their own grandparenting adventures, I hope that my perspective now has a bit less of a holier-than-thou aroma.
My most recent muse-prodding event came when I stumbled across an article about the epidemiology of unintentional pediatric firearm fatalities. Looking at 10 years of data from the National Violent Death Reporting System, the investigators found that in 80% of the cases the firearm owner was a relative of the victim; in slightly more than 60% of the cases the event occurred in the victim’s home.
The data set was not granular enough to define the exact relationship between the child and relative who owned the gun. I suspect that most often the relative was a parent or an uncle or aunt. However, viewed through my septuagenarian prism, this paper prompted me to wonder in how many of these fatalities the firearm owner was a grandparent.
I have only anecdotal observations, but I can easily recall situations here in Maine in which a child has been injured by his or her grandfather’s gun. The data from the study show that pediatric fatalities are bimodal, with the majority occurring in the 1- to 5-year age group and a second peak in adolescence. The grandparent-involved cases I can recall were in the younger demographic.
Unfortunately, firearms aren’t the only threat that other grandparents and I pose to the health and safety of our grandchildren. I can remember before the development of, and the widespread use of, tamper-proof pill bottles, “grandma’s purse” overdoses were an unfortunately common occurrence.
More recently, at least here in Maine, we have been hearing more about motorized vehicle–related injuries and fatalities – grandparents backing over their grandchildren in the driveway or, more often, grandfathers (usually) taking their young grandchildren for rides on their snowmobiles, ATVs, lawn tractors, (fill in the blank). Whenever one of these events occurs, my mind quickly jumps beyond the tragic loss of life to imagining what terrible and long-lasting emotional chaos these incidents have spawned in those families.
During the pandemic, many parents and grandparents became aware of the threat that viral-spewing young children pose to the older and more vulnerable generation. On the other hand, many parents have been told that having a grandparent around can present a risk to the health and safety of their grandchildren. It can be a touchy subject in families, and grandparents may bristle at “being treated like a child” when they are reminded that children aren’t small adults and that their own behavior may be setting a bad example or putting their grandchildren at risk.
My generation had to learn how to buckle infants and toddlers into car seats because it was something that wasn’t done for our children. Fortunately, most new grandparents now already have those buckle-and-click skills and mindset. But,
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Many decades ago I wrote a book I brazenly titled: “The Good Grandmother Handbook.” I had been a parent for a scant 7 or 8 years but based on my experiences in the office I felt I had accumulated enough wisdom to suggest to women in their fifth to seventh decades how they might conduct themselves around their grandchildren. Luckily, the book never got further than several hundred pages of crudely typed manuscript. This was before word processing programs had settled into the home computer industry, which was still in its infancy.
But I continue find the subject of grandparents interesting. Now, with grandchildren of my own (the oldest has just graduated from high school) and scores of peers knee deep in their own grandparenting adventures, I hope that my perspective now has a bit less of a holier-than-thou aroma.
My most recent muse-prodding event came when I stumbled across an article about the epidemiology of unintentional pediatric firearm fatalities. Looking at 10 years of data from the National Violent Death Reporting System, the investigators found that in 80% of the cases the firearm owner was a relative of the victim; in slightly more than 60% of the cases the event occurred in the victim’s home.
The data set was not granular enough to define the exact relationship between the child and relative who owned the gun. I suspect that most often the relative was a parent or an uncle or aunt. However, viewed through my septuagenarian prism, this paper prompted me to wonder in how many of these fatalities the firearm owner was a grandparent.
I have only anecdotal observations, but I can easily recall situations here in Maine in which a child has been injured by his or her grandfather’s gun. The data from the study show that pediatric fatalities are bimodal, with the majority occurring in the 1- to 5-year age group and a second peak in adolescence. The grandparent-involved cases I can recall were in the younger demographic.
Unfortunately, firearms aren’t the only threat that other grandparents and I pose to the health and safety of our grandchildren. I can remember before the development of, and the widespread use of, tamper-proof pill bottles, “grandma’s purse” overdoses were an unfortunately common occurrence.
More recently, at least here in Maine, we have been hearing more about motorized vehicle–related injuries and fatalities – grandparents backing over their grandchildren in the driveway or, more often, grandfathers (usually) taking their young grandchildren for rides on their snowmobiles, ATVs, lawn tractors, (fill in the blank). Whenever one of these events occurs, my mind quickly jumps beyond the tragic loss of life to imagining what terrible and long-lasting emotional chaos these incidents have spawned in those families.
During the pandemic, many parents and grandparents became aware of the threat that viral-spewing young children pose to the older and more vulnerable generation. On the other hand, many parents have been told that having a grandparent around can present a risk to the health and safety of their grandchildren. It can be a touchy subject in families, and grandparents may bristle at “being treated like a child” when they are reminded that children aren’t small adults and that their own behavior may be setting a bad example or putting their grandchildren at risk.
My generation had to learn how to buckle infants and toddlers into car seats because it was something that wasn’t done for our children. Fortunately, most new grandparents now already have those buckle-and-click skills and mindset. But,
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
AAP statement on child pedestrian safety: Educate families, advocate for walkable communities
The policy statement recommends that pediatricians advocate for environmental and urban planning that aims for no pedestrian fatalities or serious injuries, according to authors Sadiqa A. I. Kendi, MD, MPH, CPST; and Brian D. Johnston, MD, MPH, and colleagues.
While pedestrian fatalities have declined over the last 3 decades, child pedestrian fatalities have increased by 11% since 2013, the AAP Council on Injury, Violence, and Poison Prevention noted. Many of these fatalities occur in rural areas, during 6 to 9 p.m., mid-block rather than at intersections, and among adolescents aged 10-19 years, according to statistics from the National Highway Traffic Safety Administration.
“The reminder to ‘Look both ways before you cross the street,’ is good advice, but just part of the equation,” Dr. Kendi stated in a press release. “Research tells us that an even more effective way to consistently improve safety is when communities take intentional steps to create pedestrian-safe environments. We live in a busy, distracted world, and when local leaders create walkable spaces, they also enhance the appeal and vibrance of their communities.”
Advocating for safer communities
The AAP’s policy statement recommends that pediatricians advocate for legislation at the federal, state, and local level that supports a “Complete Streets” policy of including all forms of transportation and people on the roadways as well as incorporates a “Vision Zero” policy of reducing traffic fatalities and injuries. Other recommendations include supporting legislation that reduces speeds in urban areas, and the use of photo speed limit enforcement in areas such as school zones.
The AAP also highlighted the need for the adoption of new safety technology such as pedestrian detection systems, automatic braking in vehicles, and the consideration of child pedestrians with the development of new technologies such as autonomous vehicles.
“Drivers may not see small children when backing up their vehicles in a driveway or lot,” Dr. Kendi said. “Newer and self-driving vehicles are increasingly equipped with safety features and technology to detect pedestrians and avoid crashes, but they’re often more likely to detect adults and may not be able to account for the less predictable movements of a small child.”
In addition, the AAP’s policy statement recommends that pediatricians participate in community advocacy for safer and healthier pedestrian environments, community-level Vision Zero interventions, development of safe routes to school, alternative nonmotorized transportation methods to reduce vehicular traffic, the development of pedestrian infrastructure in communities, 20-mph zones in residential and commercial areas, research into pedestrian education, and surveillance systems that could identify locations where pedestrian injury is a high risk.
Educating families on pedestrian safety
There is also an opportunity to engage in anticipatory guidance with children and their parents, according to the policy statement. The AAP recommends pediatricians counsel families on the complexity of the traffic environment, remind parents that children may not be visible to drivers, and that driveways and unfenced yards are considered unsafe play areas. Adults should be with children aged younger than 10 years and teach young children the importance of pedestrian safety based on the child’s developmental level, the AAP said. When children are older, they can be more independent, but should still use “protected routes with signalized crossings in low-traffic environments,” they noted.
For parents of children with limited mobility or another disability, extra time may be needed to help children safely navigate a pedestrian environment, the AAP explained. “This might include selection of routes with low barriers to mobility, interventions to increase pedestrian visibility, instruction on use of audible pedestrian signals, and white-cane skills for children with visual impairment,” they noted.
All children should be educated on the risk of distracted walking, whether through texting, talking on the phone, or listening to music.
“We know that active transportation, like walking or biking, is good for kids and it’s good for the environment,” Brian D. Johnston, MD, MPH, coauthor of the report, said in a press release. “As children grow older, they will be able to be more independent. Each of us can help keep children safe by paying attention to the people around us and by promoting safer environments that benefit all of us.”
‘Pediatricians always find a way to reach their patients’
In an interview, Christina Johns, MD, MEd, pediatric emergency doctor and senior medical adviser at PM Pediatric Care, said that implementing this policy statement “requires a multilayered approach” that includes funding infrastructure and city planning, policy changes, family education, and other stakeholders and “will require support and buy-in at all levels.”
“While challenging to implement, the return in potential lives saved and additional health benefits of increased mobility for children (decreasing obesity burden, for example) cannot be overstated,” Dr. Johns said. “It will be helpful to create a checklist of the recommended counseling points that can be added to health records to keep this topic top of mind and document that it has been discussed at well visits.”
Emma Sartin, PhD, MPH, a research scientist at the Center for Injury Research and Prevention at Children’s Hospital of Philadelphia, said environmental risks will still be present regardless of whether a child is a safe pedestrian. “Adults and children need to balance practical safe mobility behavior with being present and aware in the current moment; as a pedestrian, without the protection of active and passive safety systems in motor vehicles, staying vigilant is critical to safety,” she said. Many pedestrian injuries and fatalities come from marginalized racial and ethnic groups, and those with neurodivergent statuses, Dr. Sartin explained, who “get licensed later than their peers, which may make being a pedestrian or using other modes of transportation (such as cycling) necessary.”
“These groups also often have higher rates of crash injuries and fatalities when they are inside of vehicles,” she said. “We need to be better at supporting safe mobility across different transportation options – driving, walking, cycling, and public transit – for all children and adults.”
Pediatricians excel at using anticipatory guidance to counsel families, and the refinements in the latest AAP policy statement on child pedestrian safety are something pediatricians can focus on at well visits, Dr. Johns said. Specific age groups will require pediatricians to adjust their conversation based on the child’s development as well as the family’s questions and concerns, she noted.
Dorothy Novick, MD, a pediatrician at Children’s Hospital of Philadelphia, said guidance to families will change as a child grows and develops, starting with teaching young children to hold hands when crossing the street, and not to play near driveways and roads.
“As children grow older, I remind families what I myself was surprised to learn as a new parent – that most children don’t develop the depth perception, judgment, and motor skills they need to cross the street safely by themselves until they’re at least 10 years old,” she explained. “Of course, with teens we place enormous emphasis on avoiding distractions, such as texting and watching videos while walking. One message remains the same for all parents, no matter the child’s age – the importance of modeling safe pedestrian behavior.
“Even during busy annual checkups, pediatricians always find a way to reach their patients and families about topics important to child health and wellness, so I have confidence that my colleagues and I will execute this mission,” Dr. Johns said. “The time required for advocacy and lobbying can be challenging however, and so having advocacy groups like the AAP is key to creating agency for pediatricians to have a voice in their communities and the legislature.
“Children cannot speak or advocate for themselves when it comes to funding, development of social programs or safety policy, or infrastructure planning and building, so it’s up to pediatricians to have a loud and unified voice to make sure that we watch out for their safety and incorporate their unique needs into their surroundings as much as possible,” she added.
The AAP reports that it has not accepted commercial involvement in developing the policy statement, and all authors have resolved potential conflicts of interest through a process approved by the AAP board of directors. Dr. Johns, Dr. Novick, and Dr. Sartin report no relevant financial disclosures.
The policy statement recommends that pediatricians advocate for environmental and urban planning that aims for no pedestrian fatalities or serious injuries, according to authors Sadiqa A. I. Kendi, MD, MPH, CPST; and Brian D. Johnston, MD, MPH, and colleagues.
While pedestrian fatalities have declined over the last 3 decades, child pedestrian fatalities have increased by 11% since 2013, the AAP Council on Injury, Violence, and Poison Prevention noted. Many of these fatalities occur in rural areas, during 6 to 9 p.m., mid-block rather than at intersections, and among adolescents aged 10-19 years, according to statistics from the National Highway Traffic Safety Administration.
“The reminder to ‘Look both ways before you cross the street,’ is good advice, but just part of the equation,” Dr. Kendi stated in a press release. “Research tells us that an even more effective way to consistently improve safety is when communities take intentional steps to create pedestrian-safe environments. We live in a busy, distracted world, and when local leaders create walkable spaces, they also enhance the appeal and vibrance of their communities.”
Advocating for safer communities
The AAP’s policy statement recommends that pediatricians advocate for legislation at the federal, state, and local level that supports a “Complete Streets” policy of including all forms of transportation and people on the roadways as well as incorporates a “Vision Zero” policy of reducing traffic fatalities and injuries. Other recommendations include supporting legislation that reduces speeds in urban areas, and the use of photo speed limit enforcement in areas such as school zones.
The AAP also highlighted the need for the adoption of new safety technology such as pedestrian detection systems, automatic braking in vehicles, and the consideration of child pedestrians with the development of new technologies such as autonomous vehicles.
“Drivers may not see small children when backing up their vehicles in a driveway or lot,” Dr. Kendi said. “Newer and self-driving vehicles are increasingly equipped with safety features and technology to detect pedestrians and avoid crashes, but they’re often more likely to detect adults and may not be able to account for the less predictable movements of a small child.”
In addition, the AAP’s policy statement recommends that pediatricians participate in community advocacy for safer and healthier pedestrian environments, community-level Vision Zero interventions, development of safe routes to school, alternative nonmotorized transportation methods to reduce vehicular traffic, the development of pedestrian infrastructure in communities, 20-mph zones in residential and commercial areas, research into pedestrian education, and surveillance systems that could identify locations where pedestrian injury is a high risk.
Educating families on pedestrian safety
There is also an opportunity to engage in anticipatory guidance with children and their parents, according to the policy statement. The AAP recommends pediatricians counsel families on the complexity of the traffic environment, remind parents that children may not be visible to drivers, and that driveways and unfenced yards are considered unsafe play areas. Adults should be with children aged younger than 10 years and teach young children the importance of pedestrian safety based on the child’s developmental level, the AAP said. When children are older, they can be more independent, but should still use “protected routes with signalized crossings in low-traffic environments,” they noted.
For parents of children with limited mobility or another disability, extra time may be needed to help children safely navigate a pedestrian environment, the AAP explained. “This might include selection of routes with low barriers to mobility, interventions to increase pedestrian visibility, instruction on use of audible pedestrian signals, and white-cane skills for children with visual impairment,” they noted.
All children should be educated on the risk of distracted walking, whether through texting, talking on the phone, or listening to music.
“We know that active transportation, like walking or biking, is good for kids and it’s good for the environment,” Brian D. Johnston, MD, MPH, coauthor of the report, said in a press release. “As children grow older, they will be able to be more independent. Each of us can help keep children safe by paying attention to the people around us and by promoting safer environments that benefit all of us.”
‘Pediatricians always find a way to reach their patients’
In an interview, Christina Johns, MD, MEd, pediatric emergency doctor and senior medical adviser at PM Pediatric Care, said that implementing this policy statement “requires a multilayered approach” that includes funding infrastructure and city planning, policy changes, family education, and other stakeholders and “will require support and buy-in at all levels.”
“While challenging to implement, the return in potential lives saved and additional health benefits of increased mobility for children (decreasing obesity burden, for example) cannot be overstated,” Dr. Johns said. “It will be helpful to create a checklist of the recommended counseling points that can be added to health records to keep this topic top of mind and document that it has been discussed at well visits.”
Emma Sartin, PhD, MPH, a research scientist at the Center for Injury Research and Prevention at Children’s Hospital of Philadelphia, said environmental risks will still be present regardless of whether a child is a safe pedestrian. “Adults and children need to balance practical safe mobility behavior with being present and aware in the current moment; as a pedestrian, without the protection of active and passive safety systems in motor vehicles, staying vigilant is critical to safety,” she said. Many pedestrian injuries and fatalities come from marginalized racial and ethnic groups, and those with neurodivergent statuses, Dr. Sartin explained, who “get licensed later than their peers, which may make being a pedestrian or using other modes of transportation (such as cycling) necessary.”
“These groups also often have higher rates of crash injuries and fatalities when they are inside of vehicles,” she said. “We need to be better at supporting safe mobility across different transportation options – driving, walking, cycling, and public transit – for all children and adults.”
Pediatricians excel at using anticipatory guidance to counsel families, and the refinements in the latest AAP policy statement on child pedestrian safety are something pediatricians can focus on at well visits, Dr. Johns said. Specific age groups will require pediatricians to adjust their conversation based on the child’s development as well as the family’s questions and concerns, she noted.
Dorothy Novick, MD, a pediatrician at Children’s Hospital of Philadelphia, said guidance to families will change as a child grows and develops, starting with teaching young children to hold hands when crossing the street, and not to play near driveways and roads.
“As children grow older, I remind families what I myself was surprised to learn as a new parent – that most children don’t develop the depth perception, judgment, and motor skills they need to cross the street safely by themselves until they’re at least 10 years old,” she explained. “Of course, with teens we place enormous emphasis on avoiding distractions, such as texting and watching videos while walking. One message remains the same for all parents, no matter the child’s age – the importance of modeling safe pedestrian behavior.
“Even during busy annual checkups, pediatricians always find a way to reach their patients and families about topics important to child health and wellness, so I have confidence that my colleagues and I will execute this mission,” Dr. Johns said. “The time required for advocacy and lobbying can be challenging however, and so having advocacy groups like the AAP is key to creating agency for pediatricians to have a voice in their communities and the legislature.
“Children cannot speak or advocate for themselves when it comes to funding, development of social programs or safety policy, or infrastructure planning and building, so it’s up to pediatricians to have a loud and unified voice to make sure that we watch out for their safety and incorporate their unique needs into their surroundings as much as possible,” she added.
The AAP reports that it has not accepted commercial involvement in developing the policy statement, and all authors have resolved potential conflicts of interest through a process approved by the AAP board of directors. Dr. Johns, Dr. Novick, and Dr. Sartin report no relevant financial disclosures.
The policy statement recommends that pediatricians advocate for environmental and urban planning that aims for no pedestrian fatalities or serious injuries, according to authors Sadiqa A. I. Kendi, MD, MPH, CPST; and Brian D. Johnston, MD, MPH, and colleagues.
While pedestrian fatalities have declined over the last 3 decades, child pedestrian fatalities have increased by 11% since 2013, the AAP Council on Injury, Violence, and Poison Prevention noted. Many of these fatalities occur in rural areas, during 6 to 9 p.m., mid-block rather than at intersections, and among adolescents aged 10-19 years, according to statistics from the National Highway Traffic Safety Administration.
“The reminder to ‘Look both ways before you cross the street,’ is good advice, but just part of the equation,” Dr. Kendi stated in a press release. “Research tells us that an even more effective way to consistently improve safety is when communities take intentional steps to create pedestrian-safe environments. We live in a busy, distracted world, and when local leaders create walkable spaces, they also enhance the appeal and vibrance of their communities.”
Advocating for safer communities
The AAP’s policy statement recommends that pediatricians advocate for legislation at the federal, state, and local level that supports a “Complete Streets” policy of including all forms of transportation and people on the roadways as well as incorporates a “Vision Zero” policy of reducing traffic fatalities and injuries. Other recommendations include supporting legislation that reduces speeds in urban areas, and the use of photo speed limit enforcement in areas such as school zones.
The AAP also highlighted the need for the adoption of new safety technology such as pedestrian detection systems, automatic braking in vehicles, and the consideration of child pedestrians with the development of new technologies such as autonomous vehicles.
“Drivers may not see small children when backing up their vehicles in a driveway or lot,” Dr. Kendi said. “Newer and self-driving vehicles are increasingly equipped with safety features and technology to detect pedestrians and avoid crashes, but they’re often more likely to detect adults and may not be able to account for the less predictable movements of a small child.”
In addition, the AAP’s policy statement recommends that pediatricians participate in community advocacy for safer and healthier pedestrian environments, community-level Vision Zero interventions, development of safe routes to school, alternative nonmotorized transportation methods to reduce vehicular traffic, the development of pedestrian infrastructure in communities, 20-mph zones in residential and commercial areas, research into pedestrian education, and surveillance systems that could identify locations where pedestrian injury is a high risk.
Educating families on pedestrian safety
There is also an opportunity to engage in anticipatory guidance with children and their parents, according to the policy statement. The AAP recommends pediatricians counsel families on the complexity of the traffic environment, remind parents that children may not be visible to drivers, and that driveways and unfenced yards are considered unsafe play areas. Adults should be with children aged younger than 10 years and teach young children the importance of pedestrian safety based on the child’s developmental level, the AAP said. When children are older, they can be more independent, but should still use “protected routes with signalized crossings in low-traffic environments,” they noted.
For parents of children with limited mobility or another disability, extra time may be needed to help children safely navigate a pedestrian environment, the AAP explained. “This might include selection of routes with low barriers to mobility, interventions to increase pedestrian visibility, instruction on use of audible pedestrian signals, and white-cane skills for children with visual impairment,” they noted.
All children should be educated on the risk of distracted walking, whether through texting, talking on the phone, or listening to music.
“We know that active transportation, like walking or biking, is good for kids and it’s good for the environment,” Brian D. Johnston, MD, MPH, coauthor of the report, said in a press release. “As children grow older, they will be able to be more independent. Each of us can help keep children safe by paying attention to the people around us and by promoting safer environments that benefit all of us.”
‘Pediatricians always find a way to reach their patients’
In an interview, Christina Johns, MD, MEd, pediatric emergency doctor and senior medical adviser at PM Pediatric Care, said that implementing this policy statement “requires a multilayered approach” that includes funding infrastructure and city planning, policy changes, family education, and other stakeholders and “will require support and buy-in at all levels.”
“While challenging to implement, the return in potential lives saved and additional health benefits of increased mobility for children (decreasing obesity burden, for example) cannot be overstated,” Dr. Johns said. “It will be helpful to create a checklist of the recommended counseling points that can be added to health records to keep this topic top of mind and document that it has been discussed at well visits.”
Emma Sartin, PhD, MPH, a research scientist at the Center for Injury Research and Prevention at Children’s Hospital of Philadelphia, said environmental risks will still be present regardless of whether a child is a safe pedestrian. “Adults and children need to balance practical safe mobility behavior with being present and aware in the current moment; as a pedestrian, without the protection of active and passive safety systems in motor vehicles, staying vigilant is critical to safety,” she said. Many pedestrian injuries and fatalities come from marginalized racial and ethnic groups, and those with neurodivergent statuses, Dr. Sartin explained, who “get licensed later than their peers, which may make being a pedestrian or using other modes of transportation (such as cycling) necessary.”
“These groups also often have higher rates of crash injuries and fatalities when they are inside of vehicles,” she said. “We need to be better at supporting safe mobility across different transportation options – driving, walking, cycling, and public transit – for all children and adults.”
Pediatricians excel at using anticipatory guidance to counsel families, and the refinements in the latest AAP policy statement on child pedestrian safety are something pediatricians can focus on at well visits, Dr. Johns said. Specific age groups will require pediatricians to adjust their conversation based on the child’s development as well as the family’s questions and concerns, she noted.
Dorothy Novick, MD, a pediatrician at Children’s Hospital of Philadelphia, said guidance to families will change as a child grows and develops, starting with teaching young children to hold hands when crossing the street, and not to play near driveways and roads.
“As children grow older, I remind families what I myself was surprised to learn as a new parent – that most children don’t develop the depth perception, judgment, and motor skills they need to cross the street safely by themselves until they’re at least 10 years old,” she explained. “Of course, with teens we place enormous emphasis on avoiding distractions, such as texting and watching videos while walking. One message remains the same for all parents, no matter the child’s age – the importance of modeling safe pedestrian behavior.
“Even during busy annual checkups, pediatricians always find a way to reach their patients and families about topics important to child health and wellness, so I have confidence that my colleagues and I will execute this mission,” Dr. Johns said. “The time required for advocacy and lobbying can be challenging however, and so having advocacy groups like the AAP is key to creating agency for pediatricians to have a voice in their communities and the legislature.
“Children cannot speak or advocate for themselves when it comes to funding, development of social programs or safety policy, or infrastructure planning and building, so it’s up to pediatricians to have a loud and unified voice to make sure that we watch out for their safety and incorporate their unique needs into their surroundings as much as possible,” she added.
The AAP reports that it has not accepted commercial involvement in developing the policy statement, and all authors have resolved potential conflicts of interest through a process approved by the AAP board of directors. Dr. Johns, Dr. Novick, and Dr. Sartin report no relevant financial disclosures.
FROM PEDIATRICS
Addressing the new mortality: Counseling on lethal means
Although I have worked with depressed patients for many years, I have come to realize that
Firearms are now the leading cause of death for U.S. children and youth aged 1-24 years, an increase of 29.5% from 2019 to 2020. Among all youth firearm deaths, homicides (58%), suicides (37%), unintentional shootings (2%), and legal intervention (1%) were causes. These horrific numbers do not even include almost 400,000 child ED visits from 2010 to 2019 for nonfatal firearm injuries that were unintentional (39.4%), assault-related (37.7%), or self-harm (1.7%).
Accidental injury from firearms is greater when the weapon is a handgun or pistol as these are small enough to be fired by a 2-year-old, more likely to be stored loaded with ammunition as “self-protection,” and less likely to be in a gun storage case.
While an overall decline in gun ownership has occurred in homes with children ages 1-5, the proportion of weapons that are handguns has actually increased, posing higher danger to the family itself. We can’t assume hiding a weapon is ever enough as children often know the location of guns and their keys or lock codes.
Many Americans fear for their safety, have doubts about policing as protective, and strongly assert the need to protect themselves. While asking about guns in the home is universally recommended, these beliefs need to be taken into account in the discussion. It is also important to speak with the firearm owner, most often the father. We might ask, “Do you feel that you need a firearm in your home to feel safe?” as a way to nonjudgmentally acknowledge their beliefs. Because women are more likely to be killed by their spouses than by all other types of assailants combined, we can ask, “What dangers worry you the most?” and “Do you feel safe in your current and any past relationships?” If their answer is worrisome, the discussion must first turn to dealing with the family situation. If the perceived threat is outside the family, we can inform families that having a gun in evidence in the home greatly increases the risk of being hurt by an assailant as well as risk for child injury and death. We might ask, “Can you think of any other ways to protect your home (for example, alarm system, outdoor lighting, dog, or pepper spray)?”
If parents insist on keeping a gun, we can strongly and directly recommend that all firearms be stored locked, unloaded, and with ammunition locked and stored separately. We can provide information on such locking and storage options. Programs in which information on devices to disable the gun were provided – such as cables to pass through the chamber or trigger locks – have shown big increases in safe gun storage. It may be worth saying/posting information on the Child Access Prevention (CAP) laws, enacted by many states, making adults owning firearms that are not stored safely unloaded legally responsible for any resulting injuries or deaths. Such laws have reduced injuries of both children and adults by 30%-40%, unintentional gun deaths by 23%, and gun suicides by 11% (for 14- to 17-year-olds).
If the reason for owning a gun is for hunting, the owner is more likely to have had firearm safety training and use a long gun. Long guns are more difficult for a child. Discussing safe hunting gun storage is still worth recommending, as is removing any handguns they may own as these are most dangerous.
Removing or securing firearms is important for everyone’s safety but it is an essential and perhaps more difficult topic of discussion when a child is at risk for suicide or harming others. We need to consider some crucial facts about completed suicide, now the leading cause of death in children and adolescents and largely from guns. Most suicide attempts occur within 10 minutes of having a wave of suicidal thoughts. These waves of thoughts may be acted upon immediately when lethal means are available, with guns by far the most likely to result in death. It is therefore critical to assess access and counsel about lethal means in every family with a child reporting thoughts of killing themselves or others, or a history of violence or substance use. Even without imminent risk of self-harm, we can start a discussion about securing lethal means by saying, “It’s like wearing a seatbelt; you don’t expect a car crash, but if one happens, wearing a safety belt can greatly reduce injury. Guns are the most frequent cause of dying, so let’s make a plan to reduce access to those.”
Creating a written plan to deal with waves of suicidal thoughts is the basis of a Safety Plan. We can accurately remind families and youth that “When someone is struggling like this, sometimes suicidal feelings can show up and get worse fast. There are steps I routinely recommend to make things safer at home.”
It is important to assess the presence of guns in the primary home and other places the child spends time even if we have asked in the past, as things change. If firearms are present, even if locked up appropriately, when a child is having suicidal thoughts we can say, “What some gun owners in your situation do is store weapons elsewhere temporarily with someone they trust, at a self-storage unit, gun or pawn shop, or police department. I’d like to talk over storage options like that with you.” If the child themself owns the firearm, they need to agree with a removal or lock up plan for giving up their access.
If the gun owner is unwilling to remove firearms, even temporarily, we can ask them to lock them up separately from ammunition, a move that alone reduces danger a lot, and ensure the child has no access to the keys or combination. Better yet, we can ask, “Would you be willing to ask someone who doesn’t live in your home to hold the keys or to change the combination temporarily or at least store the ammunition?” They could also remove from the home a critical component of the gun so that it can’t fire, such as the slide or firing pin. If even those steps are not accepted, we can ask, “What other options would you be willing to consider to increase your child’s safety, at least until s/he is doing better?”
Whatever plan we negotiate with the family, as for any health behavior change strategy, it is more likely to be implemented if we summarize the specifics, write them down, and set a time-frame for carrying it out. We might say, “Let’s review who’s doing what and when: Dad will take the guns to his uncle’s house tomorrow and meanwhile, he will put them in the gun safe.” A follow-up call or contact soon, a key part of management of suicidal ideation, also signals how strongly we care about these safety measures and has been shown to increase implementation. We might call to say, “I wanted to check in and see how [you/your child] is doing and also ask how the plan is going that we talked about for gun storage.”
Discussions about firearms can spark strong emotions, especially if the family suspects political motivations. The Florida law prohibiting health care providers from discussing guns with patients was overturned but the thinking remains and may give us pause before having these important conversations. First of all, we need to stay calm and be prepared with key facts. The “sandwich” method is a useful approach to reduce resistance: start with something you can agree on (such as “What we hear on the news can make us all scared about safety”); then add the facts we want to convey (such as “You are actually less likely to get hurt in a break-in if you do not have a gun”); then conclude with a positive (such as “I can see that you are giving a lot of thought to how to keep your family safe”). Families generally trust our intentions and knowledge and appreciate rather than resent safety counseling when it is given in a nonjudgmental manner. Because we are protectors of child health, firearm safety must be an essential part of our anticipatory guidance.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at pdnews@mdedge.com.
*Wording suggestions adapted from https://www.hsph.harvard.edu/means-matter/recommendations/clinicians.
Although I have worked with depressed patients for many years, I have come to realize that
Firearms are now the leading cause of death for U.S. children and youth aged 1-24 years, an increase of 29.5% from 2019 to 2020. Among all youth firearm deaths, homicides (58%), suicides (37%), unintentional shootings (2%), and legal intervention (1%) were causes. These horrific numbers do not even include almost 400,000 child ED visits from 2010 to 2019 for nonfatal firearm injuries that were unintentional (39.4%), assault-related (37.7%), or self-harm (1.7%).
Accidental injury from firearms is greater when the weapon is a handgun or pistol as these are small enough to be fired by a 2-year-old, more likely to be stored loaded with ammunition as “self-protection,” and less likely to be in a gun storage case.
While an overall decline in gun ownership has occurred in homes with children ages 1-5, the proportion of weapons that are handguns has actually increased, posing higher danger to the family itself. We can’t assume hiding a weapon is ever enough as children often know the location of guns and their keys or lock codes.
Many Americans fear for their safety, have doubts about policing as protective, and strongly assert the need to protect themselves. While asking about guns in the home is universally recommended, these beliefs need to be taken into account in the discussion. It is also important to speak with the firearm owner, most often the father. We might ask, “Do you feel that you need a firearm in your home to feel safe?” as a way to nonjudgmentally acknowledge their beliefs. Because women are more likely to be killed by their spouses than by all other types of assailants combined, we can ask, “What dangers worry you the most?” and “Do you feel safe in your current and any past relationships?” If their answer is worrisome, the discussion must first turn to dealing with the family situation. If the perceived threat is outside the family, we can inform families that having a gun in evidence in the home greatly increases the risk of being hurt by an assailant as well as risk for child injury and death. We might ask, “Can you think of any other ways to protect your home (for example, alarm system, outdoor lighting, dog, or pepper spray)?”
If parents insist on keeping a gun, we can strongly and directly recommend that all firearms be stored locked, unloaded, and with ammunition locked and stored separately. We can provide information on such locking and storage options. Programs in which information on devices to disable the gun were provided – such as cables to pass through the chamber or trigger locks – have shown big increases in safe gun storage. It may be worth saying/posting information on the Child Access Prevention (CAP) laws, enacted by many states, making adults owning firearms that are not stored safely unloaded legally responsible for any resulting injuries or deaths. Such laws have reduced injuries of both children and adults by 30%-40%, unintentional gun deaths by 23%, and gun suicides by 11% (for 14- to 17-year-olds).
If the reason for owning a gun is for hunting, the owner is more likely to have had firearm safety training and use a long gun. Long guns are more difficult for a child. Discussing safe hunting gun storage is still worth recommending, as is removing any handguns they may own as these are most dangerous.
Removing or securing firearms is important for everyone’s safety but it is an essential and perhaps more difficult topic of discussion when a child is at risk for suicide or harming others. We need to consider some crucial facts about completed suicide, now the leading cause of death in children and adolescents and largely from guns. Most suicide attempts occur within 10 minutes of having a wave of suicidal thoughts. These waves of thoughts may be acted upon immediately when lethal means are available, with guns by far the most likely to result in death. It is therefore critical to assess access and counsel about lethal means in every family with a child reporting thoughts of killing themselves or others, or a history of violence or substance use. Even without imminent risk of self-harm, we can start a discussion about securing lethal means by saying, “It’s like wearing a seatbelt; you don’t expect a car crash, but if one happens, wearing a safety belt can greatly reduce injury. Guns are the most frequent cause of dying, so let’s make a plan to reduce access to those.”
Creating a written plan to deal with waves of suicidal thoughts is the basis of a Safety Plan. We can accurately remind families and youth that “When someone is struggling like this, sometimes suicidal feelings can show up and get worse fast. There are steps I routinely recommend to make things safer at home.”
It is important to assess the presence of guns in the primary home and other places the child spends time even if we have asked in the past, as things change. If firearms are present, even if locked up appropriately, when a child is having suicidal thoughts we can say, “What some gun owners in your situation do is store weapons elsewhere temporarily with someone they trust, at a self-storage unit, gun or pawn shop, or police department. I’d like to talk over storage options like that with you.” If the child themself owns the firearm, they need to agree with a removal or lock up plan for giving up their access.
If the gun owner is unwilling to remove firearms, even temporarily, we can ask them to lock them up separately from ammunition, a move that alone reduces danger a lot, and ensure the child has no access to the keys or combination. Better yet, we can ask, “Would you be willing to ask someone who doesn’t live in your home to hold the keys or to change the combination temporarily or at least store the ammunition?” They could also remove from the home a critical component of the gun so that it can’t fire, such as the slide or firing pin. If even those steps are not accepted, we can ask, “What other options would you be willing to consider to increase your child’s safety, at least until s/he is doing better?”
Whatever plan we negotiate with the family, as for any health behavior change strategy, it is more likely to be implemented if we summarize the specifics, write them down, and set a time-frame for carrying it out. We might say, “Let’s review who’s doing what and when: Dad will take the guns to his uncle’s house tomorrow and meanwhile, he will put them in the gun safe.” A follow-up call or contact soon, a key part of management of suicidal ideation, also signals how strongly we care about these safety measures and has been shown to increase implementation. We might call to say, “I wanted to check in and see how [you/your child] is doing and also ask how the plan is going that we talked about for gun storage.”
Discussions about firearms can spark strong emotions, especially if the family suspects political motivations. The Florida law prohibiting health care providers from discussing guns with patients was overturned but the thinking remains and may give us pause before having these important conversations. First of all, we need to stay calm and be prepared with key facts. The “sandwich” method is a useful approach to reduce resistance: start with something you can agree on (such as “What we hear on the news can make us all scared about safety”); then add the facts we want to convey (such as “You are actually less likely to get hurt in a break-in if you do not have a gun”); then conclude with a positive (such as “I can see that you are giving a lot of thought to how to keep your family safe”). Families generally trust our intentions and knowledge and appreciate rather than resent safety counseling when it is given in a nonjudgmental manner. Because we are protectors of child health, firearm safety must be an essential part of our anticipatory guidance.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at pdnews@mdedge.com.
*Wording suggestions adapted from https://www.hsph.harvard.edu/means-matter/recommendations/clinicians.
Although I have worked with depressed patients for many years, I have come to realize that
Firearms are now the leading cause of death for U.S. children and youth aged 1-24 years, an increase of 29.5% from 2019 to 2020. Among all youth firearm deaths, homicides (58%), suicides (37%), unintentional shootings (2%), and legal intervention (1%) were causes. These horrific numbers do not even include almost 400,000 child ED visits from 2010 to 2019 for nonfatal firearm injuries that were unintentional (39.4%), assault-related (37.7%), or self-harm (1.7%).
Accidental injury from firearms is greater when the weapon is a handgun or pistol as these are small enough to be fired by a 2-year-old, more likely to be stored loaded with ammunition as “self-protection,” and less likely to be in a gun storage case.
While an overall decline in gun ownership has occurred in homes with children ages 1-5, the proportion of weapons that are handguns has actually increased, posing higher danger to the family itself. We can’t assume hiding a weapon is ever enough as children often know the location of guns and their keys or lock codes.
Many Americans fear for their safety, have doubts about policing as protective, and strongly assert the need to protect themselves. While asking about guns in the home is universally recommended, these beliefs need to be taken into account in the discussion. It is also important to speak with the firearm owner, most often the father. We might ask, “Do you feel that you need a firearm in your home to feel safe?” as a way to nonjudgmentally acknowledge their beliefs. Because women are more likely to be killed by their spouses than by all other types of assailants combined, we can ask, “What dangers worry you the most?” and “Do you feel safe in your current and any past relationships?” If their answer is worrisome, the discussion must first turn to dealing with the family situation. If the perceived threat is outside the family, we can inform families that having a gun in evidence in the home greatly increases the risk of being hurt by an assailant as well as risk for child injury and death. We might ask, “Can you think of any other ways to protect your home (for example, alarm system, outdoor lighting, dog, or pepper spray)?”
If parents insist on keeping a gun, we can strongly and directly recommend that all firearms be stored locked, unloaded, and with ammunition locked and stored separately. We can provide information on such locking and storage options. Programs in which information on devices to disable the gun were provided – such as cables to pass through the chamber or trigger locks – have shown big increases in safe gun storage. It may be worth saying/posting information on the Child Access Prevention (CAP) laws, enacted by many states, making adults owning firearms that are not stored safely unloaded legally responsible for any resulting injuries or deaths. Such laws have reduced injuries of both children and adults by 30%-40%, unintentional gun deaths by 23%, and gun suicides by 11% (for 14- to 17-year-olds).
If the reason for owning a gun is for hunting, the owner is more likely to have had firearm safety training and use a long gun. Long guns are more difficult for a child. Discussing safe hunting gun storage is still worth recommending, as is removing any handguns they may own as these are most dangerous.
Removing or securing firearms is important for everyone’s safety but it is an essential and perhaps more difficult topic of discussion when a child is at risk for suicide or harming others. We need to consider some crucial facts about completed suicide, now the leading cause of death in children and adolescents and largely from guns. Most suicide attempts occur within 10 minutes of having a wave of suicidal thoughts. These waves of thoughts may be acted upon immediately when lethal means are available, with guns by far the most likely to result in death. It is therefore critical to assess access and counsel about lethal means in every family with a child reporting thoughts of killing themselves or others, or a history of violence or substance use. Even without imminent risk of self-harm, we can start a discussion about securing lethal means by saying, “It’s like wearing a seatbelt; you don’t expect a car crash, but if one happens, wearing a safety belt can greatly reduce injury. Guns are the most frequent cause of dying, so let’s make a plan to reduce access to those.”
Creating a written plan to deal with waves of suicidal thoughts is the basis of a Safety Plan. We can accurately remind families and youth that “When someone is struggling like this, sometimes suicidal feelings can show up and get worse fast. There are steps I routinely recommend to make things safer at home.”
It is important to assess the presence of guns in the primary home and other places the child spends time even if we have asked in the past, as things change. If firearms are present, even if locked up appropriately, when a child is having suicidal thoughts we can say, “What some gun owners in your situation do is store weapons elsewhere temporarily with someone they trust, at a self-storage unit, gun or pawn shop, or police department. I’d like to talk over storage options like that with you.” If the child themself owns the firearm, they need to agree with a removal or lock up plan for giving up their access.
If the gun owner is unwilling to remove firearms, even temporarily, we can ask them to lock them up separately from ammunition, a move that alone reduces danger a lot, and ensure the child has no access to the keys or combination. Better yet, we can ask, “Would you be willing to ask someone who doesn’t live in your home to hold the keys or to change the combination temporarily or at least store the ammunition?” They could also remove from the home a critical component of the gun so that it can’t fire, such as the slide or firing pin. If even those steps are not accepted, we can ask, “What other options would you be willing to consider to increase your child’s safety, at least until s/he is doing better?”
Whatever plan we negotiate with the family, as for any health behavior change strategy, it is more likely to be implemented if we summarize the specifics, write them down, and set a time-frame for carrying it out. We might say, “Let’s review who’s doing what and when: Dad will take the guns to his uncle’s house tomorrow and meanwhile, he will put them in the gun safe.” A follow-up call or contact soon, a key part of management of suicidal ideation, also signals how strongly we care about these safety measures and has been shown to increase implementation. We might call to say, “I wanted to check in and see how [you/your child] is doing and also ask how the plan is going that we talked about for gun storage.”
Discussions about firearms can spark strong emotions, especially if the family suspects political motivations. The Florida law prohibiting health care providers from discussing guns with patients was overturned but the thinking remains and may give us pause before having these important conversations. First of all, we need to stay calm and be prepared with key facts. The “sandwich” method is a useful approach to reduce resistance: start with something you can agree on (such as “What we hear on the news can make us all scared about safety”); then add the facts we want to convey (such as “You are actually less likely to get hurt in a break-in if you do not have a gun”); then conclude with a positive (such as “I can see that you are giving a lot of thought to how to keep your family safe”). Families generally trust our intentions and knowledge and appreciate rather than resent safety counseling when it is given in a nonjudgmental manner. Because we are protectors of child health, firearm safety must be an essential part of our anticipatory guidance.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at pdnews@mdedge.com.
*Wording suggestions adapted from https://www.hsph.harvard.edu/means-matter/recommendations/clinicians.
High school athletes sustaining worse injuries
High school students are injuring themselves more severely even as overall injury rates have declined, according to a new study presented at the annual meeting of the American Academy of Orthopaedic Surgeons.
The study compared injuries from a 4-year period ending in 2019 to data from 2005 and 2006. The overall rate of injuries dropped 9%, from 2.51 injuries per 1,000 athletic games or practices to 2.29 per 1,000; injuries requiring less than 1 week of recovery time fell by 13%. But, the number of head and neck injuries increased by 10%, injuries requiring surgery increased by 1%, and injuries leading to medical disqualification jumped by 11%.
“It’s wonderful that the injury rate is declining,” said Jordan Neoma Pizzarro, a medical student at George Washington University, Washington, who led the study. “But the data does suggest that the injuries that are happening are worse.”
The increases may also reflect increased education and awareness of how to detect concussions and other injuries that need medical attention, said Micah Lissy, MD, MS, an orthopedic surgeon specializing in sports medicine at Michigan State University, East Lansing. Dr. Lissy cautioned against physicians and others taking the data at face value.
“We need to be implementing preventive measures wherever possible, but I think we can also consider that there may be some confounding factors in the data,” Dr. Lissy told this news organization.
Ms. Pizzarro and her team analyzed data collected from athletic trainers at 100 high schools across the country for the ongoing National Health School Sports-Related Injury Surveillance Study.
Athletes participating in sports such as football, soccer, basketball, volleyball, and softball were included in the analysis. Trainers report the number of injuries for every competition and practice, also known as “athletic exposures.”
Boys’ football carried the highest injury rate, with 3.96 injuries per 1,000 AEs, amounting to 44% of all injuries reported. Girls’ soccer and boys’ wrestling followed, with injury rates of 2.65 and 1.56, respectively.
Sprains and strains accounted for 37% of injuries, followed by concussions (21.6%). The head and/or face was the most injured body site, followed by the ankles and/or knees. Most injuries took place during competitions rather than in practices (relative risk, 3.39; 95% confidence interval, 3.28-3.49; P < .05).
Ms. Pizzarro said that an overall increase in intensity, physical contact, and collisions may account for the spike in more severe injuries.
“Kids are encouraged to specialize in one sport early on and stick with it year-round,” she said. “They’re probably becoming more agile and better athletes, but they’re probably also getting more competitive.”
Dr. Lissy, who has worked with high school athletes as a surgeon, physical therapist, athletic trainer, and coach, said that some of the increases in severity of injuries may reflect trends in sports over the past two decades: Student athletes have become stronger and faster and have put on more muscle mass.
“When you have something that’s much larger, moving much faster and with more force, you’re going to have more force when you bump into things,” he said. “This can lead to more significant injuries.”
The study was independently supported. Study authors report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
High school students are injuring themselves more severely even as overall injury rates have declined, according to a new study presented at the annual meeting of the American Academy of Orthopaedic Surgeons.
The study compared injuries from a 4-year period ending in 2019 to data from 2005 and 2006. The overall rate of injuries dropped 9%, from 2.51 injuries per 1,000 athletic games or practices to 2.29 per 1,000; injuries requiring less than 1 week of recovery time fell by 13%. But, the number of head and neck injuries increased by 10%, injuries requiring surgery increased by 1%, and injuries leading to medical disqualification jumped by 11%.
“It’s wonderful that the injury rate is declining,” said Jordan Neoma Pizzarro, a medical student at George Washington University, Washington, who led the study. “But the data does suggest that the injuries that are happening are worse.”
The increases may also reflect increased education and awareness of how to detect concussions and other injuries that need medical attention, said Micah Lissy, MD, MS, an orthopedic surgeon specializing in sports medicine at Michigan State University, East Lansing. Dr. Lissy cautioned against physicians and others taking the data at face value.
“We need to be implementing preventive measures wherever possible, but I think we can also consider that there may be some confounding factors in the data,” Dr. Lissy told this news organization.
Ms. Pizzarro and her team analyzed data collected from athletic trainers at 100 high schools across the country for the ongoing National Health School Sports-Related Injury Surveillance Study.
Athletes participating in sports such as football, soccer, basketball, volleyball, and softball were included in the analysis. Trainers report the number of injuries for every competition and practice, also known as “athletic exposures.”
Boys’ football carried the highest injury rate, with 3.96 injuries per 1,000 AEs, amounting to 44% of all injuries reported. Girls’ soccer and boys’ wrestling followed, with injury rates of 2.65 and 1.56, respectively.
Sprains and strains accounted for 37% of injuries, followed by concussions (21.6%). The head and/or face was the most injured body site, followed by the ankles and/or knees. Most injuries took place during competitions rather than in practices (relative risk, 3.39; 95% confidence interval, 3.28-3.49; P < .05).
Ms. Pizzarro said that an overall increase in intensity, physical contact, and collisions may account for the spike in more severe injuries.
“Kids are encouraged to specialize in one sport early on and stick with it year-round,” she said. “They’re probably becoming more agile and better athletes, but they’re probably also getting more competitive.”
Dr. Lissy, who has worked with high school athletes as a surgeon, physical therapist, athletic trainer, and coach, said that some of the increases in severity of injuries may reflect trends in sports over the past two decades: Student athletes have become stronger and faster and have put on more muscle mass.
“When you have something that’s much larger, moving much faster and with more force, you’re going to have more force when you bump into things,” he said. “This can lead to more significant injuries.”
The study was independently supported. Study authors report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
High school students are injuring themselves more severely even as overall injury rates have declined, according to a new study presented at the annual meeting of the American Academy of Orthopaedic Surgeons.
The study compared injuries from a 4-year period ending in 2019 to data from 2005 and 2006. The overall rate of injuries dropped 9%, from 2.51 injuries per 1,000 athletic games or practices to 2.29 per 1,000; injuries requiring less than 1 week of recovery time fell by 13%. But, the number of head and neck injuries increased by 10%, injuries requiring surgery increased by 1%, and injuries leading to medical disqualification jumped by 11%.
“It’s wonderful that the injury rate is declining,” said Jordan Neoma Pizzarro, a medical student at George Washington University, Washington, who led the study. “But the data does suggest that the injuries that are happening are worse.”
The increases may also reflect increased education and awareness of how to detect concussions and other injuries that need medical attention, said Micah Lissy, MD, MS, an orthopedic surgeon specializing in sports medicine at Michigan State University, East Lansing. Dr. Lissy cautioned against physicians and others taking the data at face value.
“We need to be implementing preventive measures wherever possible, but I think we can also consider that there may be some confounding factors in the data,” Dr. Lissy told this news organization.
Ms. Pizzarro and her team analyzed data collected from athletic trainers at 100 high schools across the country for the ongoing National Health School Sports-Related Injury Surveillance Study.
Athletes participating in sports such as football, soccer, basketball, volleyball, and softball were included in the analysis. Trainers report the number of injuries for every competition and practice, also known as “athletic exposures.”
Boys’ football carried the highest injury rate, with 3.96 injuries per 1,000 AEs, amounting to 44% of all injuries reported. Girls’ soccer and boys’ wrestling followed, with injury rates of 2.65 and 1.56, respectively.
Sprains and strains accounted for 37% of injuries, followed by concussions (21.6%). The head and/or face was the most injured body site, followed by the ankles and/or knees. Most injuries took place during competitions rather than in practices (relative risk, 3.39; 95% confidence interval, 3.28-3.49; P < .05).
Ms. Pizzarro said that an overall increase in intensity, physical contact, and collisions may account for the spike in more severe injuries.
“Kids are encouraged to specialize in one sport early on and stick with it year-round,” she said. “They’re probably becoming more agile and better athletes, but they’re probably also getting more competitive.”
Dr. Lissy, who has worked with high school athletes as a surgeon, physical therapist, athletic trainer, and coach, said that some of the increases in severity of injuries may reflect trends in sports over the past two decades: Student athletes have become stronger and faster and have put on more muscle mass.
“When you have something that’s much larger, moving much faster and with more force, you’re going to have more force when you bump into things,” he said. “This can lead to more significant injuries.”
The study was independently supported. Study authors report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Clinician violence: Virtual reality to the rescue?
This discussion was recorded on Feb. 21, 2023. This transcript has been edited for clarity.
Robert D. Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical adviser for Medscape Emergency Medicine. Welcome, Dr. Salazar. It’s a pleasure to have you join us today.
Gilberto A. Salazar, MD: The pleasure is all mine, Dr. Glatter. Thank you so much for having me.
Dr. Glatter: This is such an important topic, as you can imagine. Workplace violence is affecting so many providers in hospital emergency departments but also throughout other parts of the hospital.
First, can you describe how the virtual reality (VR) program was designed that you developed and what type of situations it simulates?
Dr. Salazar: We worked in conjunction with the University of Texas at Dallas. They help people like me, subject matter experts in health care, to bring ideas to reality. I worked very closely with a group of engineers from their department in designing a module specifically designed to tackle, as you mentioned, one of our biggest threats in workplace violence.
We decided to bring in a series of competencies and proficiencies that we wanted to bring into the virtual reality space. In leveraging the technology and the expertise from UT Dallas, we were able to make that happen.
Dr. Glatter: I think it’s important to understand, in terms of virtual reality, what type of environment the program creates. Can you describe what a provider who puts the goggles on is experiencing? Do they feel anything? Is there technology that enables this?
Dr. Salazar: Yes, absolutely. We were able to bring to reality a series of scenarios very common from what you and I see in the emergency department on a daily basis. We wanted to immerse a learner into that specific environment. We didn’t feel that a module or something on a computer or a slide set could really bring the reality of what it’s like to interact with a patient who may be escalating or may be aggressive.
We are immersing learners into an actual hospital room to our specifications, very similar to exactly where we practice each and every day, and taking the learners through different situations that we designed with various levels of escalation and aggression, and asking the learner to manage that situation as best as they possibly can using the competencies and proficiencies that we taught them.
Dr. Glatter: Haptic feedback is an important part of the program and also the approach and technique that you’re using. Can you describe what haptic feedback means and what people actually feel?
Dr. Salazar: Absolutely. One of the most unfortunate things in my professional career is physical abuse suffered by people like me and you and our colleagues, nursing personnel, technicians, and others, resulting in injury.
We wanted to provide the most realistic experience that we could design. Haptics engage digital senses other than your auditory and your visuals. They really engage your tactile senses. These haptic vests and gloves and technology allow us to provide a third set of sensory stimuli for the learner.
At one of the modules, we have an actual physical assault that takes place, and the learner is actually able to feel in their body the strikes – of course, not painful – but just bringing in those senses and that stimulus, really leaving the learner with an experience that’s going to be long-lasting.
Dr. Glatter: Feeling that stimulus certainly affects your vital signs. Do you monitor a provider’s vital signs, such as their blood pressure and heart rate, as the situation and the threat escalate? That could potentially trigger some issues in people with prior PTSD or people with other mental health issues. Has that ever been considered in the design of your program?
Dr. Salazar: Yes, 100%. The beautiful thing about haptics is that they can be tailored to our specific parameters. The sensory stimulus that’s provided is actually very mild. It feels more like a tap than an actual strike. It just reminds us that when we’re having or experiencing an actual physical attack, we’re really engaging the senses.
We have an emergency physician or an EMT-paramedic on site at all times during the training so that we can monitor our subjects and make sure that they’re comfortable and healthy.
Dr. Glatter: Do they have actual sensors attached to their bodies that are part of your program or distinct in terms of monitoring their vital signs?
Dr. Salazar: It’s completely different. We have two different systems that we are planning on utilizing. Frankly, in the final version of this virtual reality module, we may not even involve the haptics. We’re going to study it and see how our learners behave and how much information they’re able to acquire and retain.
It may be very possible that just the visuals – the auditory and the immersion taking place within the hospital room – may be enough. It’s very possible that, in the next final version of this, we may find that haptics bring in quite a bit of value, and we may incorporate that. If that is the case, then we will, of course, acquire different technology to monitor the patient’s vital signs.
Dr. Glatter: Clearly, when situations escalate in the department, everyone gets more concerned about the patient, but providers are part of this equation, as you allude to.
In 2022, there was a poll by the American College of Emergency Physicians that stated that 85% of emergency physicians reported an increase in violent activity in their ERs in the past 5 years. Nearly two-thirds of nearly 3,000 emergency physicians surveyed reported being assaulted in the past year. This is an important module that we integrate into training providers in terms of these types of tense situations that can result not only in mental anguish but also in physical injury.
Dr. Salazar: One hundred percent. I frankly got tired of seeing my friends and my colleagues suffer both the physical and mental effects of verbal and physical abuse, and I wanted to design a project that was very patient centric while allowing our personnel to really manage these situations a little bit better.
Frankly, we don’t receive great training in this space, and I wanted to rewrite that narrative and make things better for our clinicians out there while remaining patient centric. I wanted to do something about it, and hopefully this dream will become a reality.
Dr. Glatter: Absolutely. There are other data from the Bureau of Labor Statistics stating that health care workers are five times more likely than employees in any other area of work to experience workplace violence. This could, again, range from verbal to physical violence. This is a very important module that you’re developing.
Are there any thoughts to extend this to active-shooter scenarios or any other high-stakes scenarios that you can imagine in the department?
Dr. Salazar: We’re actually working with the same developer that’s helping us with this VR module in developing a mass-casualty incident module so that we can get better training in responding to these very unfortunate high-stakes situations.
Dr. Glatter: In terms of using the module remotely, certainly not requiring resources or having to be in a physical place, can providers in your plan be able to take such a headset home and practice on their own in the sense of being able to deal with a situation? Would this be more reserved for in-department use?
Dr. Salazar: That’s a phenomenal question. I wanted to create the most flexible module that I possibly could. Ideally, a dream scenario is leveraging a simulation center at an academic center and not just do the VR module but also have a brief didactics incorporating a small slide set, some feedback, and some standardized patients. I wanted it to be flexible enough so that folks here in my state, a different state, or even internationally could take advantage of this technology and do it from the comfort of their home.
As you mentioned, this is going to strike some people. It’s going to hit them heavier than others in terms of prior experience as PTSD. For some people, it may be more comfortable to do it in the comfort of their homes. I wanted to create something very flexible and dynamic.
Dr. Glatter: I think that’s ideal. Just one other point. Can you discuss the different levels of competencies involved in this module and how that would be attained?
Dr. Salazar: It’s all evidence based, so we borrowed from literature and the specialties of emergency medicine. We collaborated with psychiatrists within our medical center. We looked at all available literature and methods, proficiencies, competencies, and best practices, and we took all of them together to form something that we think is organized and concise.
We were able to create our own algorithm, but it’s not brand new. We’re just borrowing what we think is the best to create something that the majority of health care personnel are going to be able to relate to and be able to really be proficient at.
This includes things like active listening, bargaining, how to respond, where to put yourself in a situation, and the best possible situation to respond to a scenario, how to prevent things – how to get out of a chokehold, for example. We’re borrowing from several different disciplines and creating something that can be very concise and organized.
Dr. Glatter: Does this program that you’ve developed allow the provider to get feedback in the sense that when they’re in such a danger, their life could be at risk? For example, if they don’t remove themselves in a certain amount of time, this could be lethal.
Dr. Salazar: Yes, 100%. Probably the one thing that differentiates our project from any others is the ability to customize the experience so that a learner who is doing the things that we ask them to do in terms of safety and response is able to get out of a situation successfully within the environment. If they don’t, they get some kind of feedback.
Not to spoil the surprise here, but we’re going to be doing things like looking at decibel meters to see what the volume in the room is doing and how you’re managing the volume and the stimulation within the room. If you are able to maintain the decibel readings at a specific level, you’re going to succeed through the module. If you don’t, we keep the patient escalation going.
Dr. Glatter: There is a debrief built into this type of approach where, in other words, learning points are emphasized – where you could have done better and such.
Dr. Salazar: Yes, absolutely. We are going to be able to get individualized data for each learner so that we can tailor the debrief to their own performance and be able to give them actionable items to work on. It’s a debrief that’s productive and individualized, and folks can walk away with something useful in the end.
Dr. Glatter: Are the data shared or confidential at present?
Dr. Salazar: At this very moment, the data are confidential. We are going to look at how to best use this. We’re hoping to eventually write this up and see how this information can be best used to train personnel.
Eventually, we may see that some of the advice that we’re giving is very common to most folks. Others may require some individualized type of feedback. That said, it remains to be seen, but right now, it’s confidential.
Dr. Glatter: Is this currently being implemented as part of your curriculum for emergency medicine residents?
Dr. Salazar: We’re going to study it first. We’re very excited to include our emergency medicine residents as one of our cohorts that’s going to be undergoing the module, and we’re going to be studying other forms of workplace violence mitigation strategies. We’re really excited about the possibility of this eventually becoming the standard of education for not only our emergency medicine residents, but also health care personnel all over the world.
Dr. Glatter: I’m glad you mentioned that, because obviously nurses, clerks in the department, and anyone who’s working in the department, for that matter, and who interfaces with patients really should undergo such training.
Dr. Salazar: Absolutely. The folks at intake, at check-in, and at kiosks. Do they go through a separate area for screening? You’re absolutely right. There are many folks who interface with patients and all of us are potential victims of workplace violence. We want to give our health care family the best opportunity to succeed in these situations.
Dr. Glatter:: Absolutely. Even EMS providers, being on the front lines and encountering patients in such situations, would benefit, in my opinion.
Dr. Salazar: Yes, absolutely. Behavioral health emergencies and organically induced altered mental status results in injury, both physical and mental, to EMS professionals as well, and there’s good evidence of that. I’ll be very glad to see this type of education make it out to our initial and continuing education efforts for EMS as well.
Dr. Glatter: I want to thank you. This has been very helpful. It’s such an important task that you’ve started to explore, and I look forward to follow-up on this. Again, thank you for your time.
Dr. Salazar: It was my pleasure. Thank you so much for having me.
Dr. Glatter is an attending physician at Lenox Hill Hospital in New York City and assistant professor of emergency medicine at Zucker School of Medicine at Hofstra/Northwell in Hempstead, N.Y. He is an editorial adviser and hosts the Hot Topics in EM series on Medscape. He is also a medical contributor for Forbes. Dr. Salazar is a board-certified emergency physician and associate professor at UT Southwestern Medicine Center in Dallas. He is involved with the UTSW Emergency Medicine Education Program and serves as the medical director to teach both initial and continuing the emergency medicine education for emergency medical technicians and paramedics, which trains most of the Dallas Fire Rescue personnel and the vast majority for EMS providers in the Dallas County. In addition, he serves as an associate chief of service at Parkland’s emergency department, and liaison to surgical services. A version of this article originally appeared on Medscape.com.
This discussion was recorded on Feb. 21, 2023. This transcript has been edited for clarity.
Robert D. Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical adviser for Medscape Emergency Medicine. Welcome, Dr. Salazar. It’s a pleasure to have you join us today.
Gilberto A. Salazar, MD: The pleasure is all mine, Dr. Glatter. Thank you so much for having me.
Dr. Glatter: This is such an important topic, as you can imagine. Workplace violence is affecting so many providers in hospital emergency departments but also throughout other parts of the hospital.
First, can you describe how the virtual reality (VR) program was designed that you developed and what type of situations it simulates?
Dr. Salazar: We worked in conjunction with the University of Texas at Dallas. They help people like me, subject matter experts in health care, to bring ideas to reality. I worked very closely with a group of engineers from their department in designing a module specifically designed to tackle, as you mentioned, one of our biggest threats in workplace violence.
We decided to bring in a series of competencies and proficiencies that we wanted to bring into the virtual reality space. In leveraging the technology and the expertise from UT Dallas, we were able to make that happen.
Dr. Glatter: I think it’s important to understand, in terms of virtual reality, what type of environment the program creates. Can you describe what a provider who puts the goggles on is experiencing? Do they feel anything? Is there technology that enables this?
Dr. Salazar: Yes, absolutely. We were able to bring to reality a series of scenarios very common from what you and I see in the emergency department on a daily basis. We wanted to immerse a learner into that specific environment. We didn’t feel that a module or something on a computer or a slide set could really bring the reality of what it’s like to interact with a patient who may be escalating or may be aggressive.
We are immersing learners into an actual hospital room to our specifications, very similar to exactly where we practice each and every day, and taking the learners through different situations that we designed with various levels of escalation and aggression, and asking the learner to manage that situation as best as they possibly can using the competencies and proficiencies that we taught them.
Dr. Glatter: Haptic feedback is an important part of the program and also the approach and technique that you’re using. Can you describe what haptic feedback means and what people actually feel?
Dr. Salazar: Absolutely. One of the most unfortunate things in my professional career is physical abuse suffered by people like me and you and our colleagues, nursing personnel, technicians, and others, resulting in injury.
We wanted to provide the most realistic experience that we could design. Haptics engage digital senses other than your auditory and your visuals. They really engage your tactile senses. These haptic vests and gloves and technology allow us to provide a third set of sensory stimuli for the learner.
At one of the modules, we have an actual physical assault that takes place, and the learner is actually able to feel in their body the strikes – of course, not painful – but just bringing in those senses and that stimulus, really leaving the learner with an experience that’s going to be long-lasting.
Dr. Glatter: Feeling that stimulus certainly affects your vital signs. Do you monitor a provider’s vital signs, such as their blood pressure and heart rate, as the situation and the threat escalate? That could potentially trigger some issues in people with prior PTSD or people with other mental health issues. Has that ever been considered in the design of your program?
Dr. Salazar: Yes, 100%. The beautiful thing about haptics is that they can be tailored to our specific parameters. The sensory stimulus that’s provided is actually very mild. It feels more like a tap than an actual strike. It just reminds us that when we’re having or experiencing an actual physical attack, we’re really engaging the senses.
We have an emergency physician or an EMT-paramedic on site at all times during the training so that we can monitor our subjects and make sure that they’re comfortable and healthy.
Dr. Glatter: Do they have actual sensors attached to their bodies that are part of your program or distinct in terms of monitoring their vital signs?
Dr. Salazar: It’s completely different. We have two different systems that we are planning on utilizing. Frankly, in the final version of this virtual reality module, we may not even involve the haptics. We’re going to study it and see how our learners behave and how much information they’re able to acquire and retain.
It may be very possible that just the visuals – the auditory and the immersion taking place within the hospital room – may be enough. It’s very possible that, in the next final version of this, we may find that haptics bring in quite a bit of value, and we may incorporate that. If that is the case, then we will, of course, acquire different technology to monitor the patient’s vital signs.
Dr. Glatter: Clearly, when situations escalate in the department, everyone gets more concerned about the patient, but providers are part of this equation, as you allude to.
In 2022, there was a poll by the American College of Emergency Physicians that stated that 85% of emergency physicians reported an increase in violent activity in their ERs in the past 5 years. Nearly two-thirds of nearly 3,000 emergency physicians surveyed reported being assaulted in the past year. This is an important module that we integrate into training providers in terms of these types of tense situations that can result not only in mental anguish but also in physical injury.
Dr. Salazar: One hundred percent. I frankly got tired of seeing my friends and my colleagues suffer both the physical and mental effects of verbal and physical abuse, and I wanted to design a project that was very patient centric while allowing our personnel to really manage these situations a little bit better.
Frankly, we don’t receive great training in this space, and I wanted to rewrite that narrative and make things better for our clinicians out there while remaining patient centric. I wanted to do something about it, and hopefully this dream will become a reality.
Dr. Glatter: Absolutely. There are other data from the Bureau of Labor Statistics stating that health care workers are five times more likely than employees in any other area of work to experience workplace violence. This could, again, range from verbal to physical violence. This is a very important module that you’re developing.
Are there any thoughts to extend this to active-shooter scenarios or any other high-stakes scenarios that you can imagine in the department?
Dr. Salazar: We’re actually working with the same developer that’s helping us with this VR module in developing a mass-casualty incident module so that we can get better training in responding to these very unfortunate high-stakes situations.
Dr. Glatter: In terms of using the module remotely, certainly not requiring resources or having to be in a physical place, can providers in your plan be able to take such a headset home and practice on their own in the sense of being able to deal with a situation? Would this be more reserved for in-department use?
Dr. Salazar: That’s a phenomenal question. I wanted to create the most flexible module that I possibly could. Ideally, a dream scenario is leveraging a simulation center at an academic center and not just do the VR module but also have a brief didactics incorporating a small slide set, some feedback, and some standardized patients. I wanted it to be flexible enough so that folks here in my state, a different state, or even internationally could take advantage of this technology and do it from the comfort of their home.
As you mentioned, this is going to strike some people. It’s going to hit them heavier than others in terms of prior experience as PTSD. For some people, it may be more comfortable to do it in the comfort of their homes. I wanted to create something very flexible and dynamic.
Dr. Glatter: I think that’s ideal. Just one other point. Can you discuss the different levels of competencies involved in this module and how that would be attained?
Dr. Salazar: It’s all evidence based, so we borrowed from literature and the specialties of emergency medicine. We collaborated with psychiatrists within our medical center. We looked at all available literature and methods, proficiencies, competencies, and best practices, and we took all of them together to form something that we think is organized and concise.
We were able to create our own algorithm, but it’s not brand new. We’re just borrowing what we think is the best to create something that the majority of health care personnel are going to be able to relate to and be able to really be proficient at.
This includes things like active listening, bargaining, how to respond, where to put yourself in a situation, and the best possible situation to respond to a scenario, how to prevent things – how to get out of a chokehold, for example. We’re borrowing from several different disciplines and creating something that can be very concise and organized.
Dr. Glatter: Does this program that you’ve developed allow the provider to get feedback in the sense that when they’re in such a danger, their life could be at risk? For example, if they don’t remove themselves in a certain amount of time, this could be lethal.
Dr. Salazar: Yes, 100%. Probably the one thing that differentiates our project from any others is the ability to customize the experience so that a learner who is doing the things that we ask them to do in terms of safety and response is able to get out of a situation successfully within the environment. If they don’t, they get some kind of feedback.
Not to spoil the surprise here, but we’re going to be doing things like looking at decibel meters to see what the volume in the room is doing and how you’re managing the volume and the stimulation within the room. If you are able to maintain the decibel readings at a specific level, you’re going to succeed through the module. If you don’t, we keep the patient escalation going.
Dr. Glatter: There is a debrief built into this type of approach where, in other words, learning points are emphasized – where you could have done better and such.
Dr. Salazar: Yes, absolutely. We are going to be able to get individualized data for each learner so that we can tailor the debrief to their own performance and be able to give them actionable items to work on. It’s a debrief that’s productive and individualized, and folks can walk away with something useful in the end.
Dr. Glatter: Are the data shared or confidential at present?
Dr. Salazar: At this very moment, the data are confidential. We are going to look at how to best use this. We’re hoping to eventually write this up and see how this information can be best used to train personnel.
Eventually, we may see that some of the advice that we’re giving is very common to most folks. Others may require some individualized type of feedback. That said, it remains to be seen, but right now, it’s confidential.
Dr. Glatter: Is this currently being implemented as part of your curriculum for emergency medicine residents?
Dr. Salazar: We’re going to study it first. We’re very excited to include our emergency medicine residents as one of our cohorts that’s going to be undergoing the module, and we’re going to be studying other forms of workplace violence mitigation strategies. We’re really excited about the possibility of this eventually becoming the standard of education for not only our emergency medicine residents, but also health care personnel all over the world.
Dr. Glatter: I’m glad you mentioned that, because obviously nurses, clerks in the department, and anyone who’s working in the department, for that matter, and who interfaces with patients really should undergo such training.
Dr. Salazar: Absolutely. The folks at intake, at check-in, and at kiosks. Do they go through a separate area for screening? You’re absolutely right. There are many folks who interface with patients and all of us are potential victims of workplace violence. We want to give our health care family the best opportunity to succeed in these situations.
Dr. Glatter:: Absolutely. Even EMS providers, being on the front lines and encountering patients in such situations, would benefit, in my opinion.
Dr. Salazar: Yes, absolutely. Behavioral health emergencies and organically induced altered mental status results in injury, both physical and mental, to EMS professionals as well, and there’s good evidence of that. I’ll be very glad to see this type of education make it out to our initial and continuing education efforts for EMS as well.
Dr. Glatter: I want to thank you. This has been very helpful. It’s such an important task that you’ve started to explore, and I look forward to follow-up on this. Again, thank you for your time.
Dr. Salazar: It was my pleasure. Thank you so much for having me.
Dr. Glatter is an attending physician at Lenox Hill Hospital in New York City and assistant professor of emergency medicine at Zucker School of Medicine at Hofstra/Northwell in Hempstead, N.Y. He is an editorial adviser and hosts the Hot Topics in EM series on Medscape. He is also a medical contributor for Forbes. Dr. Salazar is a board-certified emergency physician and associate professor at UT Southwestern Medicine Center in Dallas. He is involved with the UTSW Emergency Medicine Education Program and serves as the medical director to teach both initial and continuing the emergency medicine education for emergency medical technicians and paramedics, which trains most of the Dallas Fire Rescue personnel and the vast majority for EMS providers in the Dallas County. In addition, he serves as an associate chief of service at Parkland’s emergency department, and liaison to surgical services. A version of this article originally appeared on Medscape.com.
This discussion was recorded on Feb. 21, 2023. This transcript has been edited for clarity.
Robert D. Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical adviser for Medscape Emergency Medicine. Welcome, Dr. Salazar. It’s a pleasure to have you join us today.
Gilberto A. Salazar, MD: The pleasure is all mine, Dr. Glatter. Thank you so much for having me.
Dr. Glatter: This is such an important topic, as you can imagine. Workplace violence is affecting so many providers in hospital emergency departments but also throughout other parts of the hospital.
First, can you describe how the virtual reality (VR) program was designed that you developed and what type of situations it simulates?
Dr. Salazar: We worked in conjunction with the University of Texas at Dallas. They help people like me, subject matter experts in health care, to bring ideas to reality. I worked very closely with a group of engineers from their department in designing a module specifically designed to tackle, as you mentioned, one of our biggest threats in workplace violence.
We decided to bring in a series of competencies and proficiencies that we wanted to bring into the virtual reality space. In leveraging the technology and the expertise from UT Dallas, we were able to make that happen.
Dr. Glatter: I think it’s important to understand, in terms of virtual reality, what type of environment the program creates. Can you describe what a provider who puts the goggles on is experiencing? Do they feel anything? Is there technology that enables this?
Dr. Salazar: Yes, absolutely. We were able to bring to reality a series of scenarios very common from what you and I see in the emergency department on a daily basis. We wanted to immerse a learner into that specific environment. We didn’t feel that a module or something on a computer or a slide set could really bring the reality of what it’s like to interact with a patient who may be escalating or may be aggressive.
We are immersing learners into an actual hospital room to our specifications, very similar to exactly where we practice each and every day, and taking the learners through different situations that we designed with various levels of escalation and aggression, and asking the learner to manage that situation as best as they possibly can using the competencies and proficiencies that we taught them.
Dr. Glatter: Haptic feedback is an important part of the program and also the approach and technique that you’re using. Can you describe what haptic feedback means and what people actually feel?
Dr. Salazar: Absolutely. One of the most unfortunate things in my professional career is physical abuse suffered by people like me and you and our colleagues, nursing personnel, technicians, and others, resulting in injury.
We wanted to provide the most realistic experience that we could design. Haptics engage digital senses other than your auditory and your visuals. They really engage your tactile senses. These haptic vests and gloves and technology allow us to provide a third set of sensory stimuli for the learner.
At one of the modules, we have an actual physical assault that takes place, and the learner is actually able to feel in their body the strikes – of course, not painful – but just bringing in those senses and that stimulus, really leaving the learner with an experience that’s going to be long-lasting.
Dr. Glatter: Feeling that stimulus certainly affects your vital signs. Do you monitor a provider’s vital signs, such as their blood pressure and heart rate, as the situation and the threat escalate? That could potentially trigger some issues in people with prior PTSD or people with other mental health issues. Has that ever been considered in the design of your program?
Dr. Salazar: Yes, 100%. The beautiful thing about haptics is that they can be tailored to our specific parameters. The sensory stimulus that’s provided is actually very mild. It feels more like a tap than an actual strike. It just reminds us that when we’re having or experiencing an actual physical attack, we’re really engaging the senses.
We have an emergency physician or an EMT-paramedic on site at all times during the training so that we can monitor our subjects and make sure that they’re comfortable and healthy.
Dr. Glatter: Do they have actual sensors attached to their bodies that are part of your program or distinct in terms of monitoring their vital signs?
Dr. Salazar: It’s completely different. We have two different systems that we are planning on utilizing. Frankly, in the final version of this virtual reality module, we may not even involve the haptics. We’re going to study it and see how our learners behave and how much information they’re able to acquire and retain.
It may be very possible that just the visuals – the auditory and the immersion taking place within the hospital room – may be enough. It’s very possible that, in the next final version of this, we may find that haptics bring in quite a bit of value, and we may incorporate that. If that is the case, then we will, of course, acquire different technology to monitor the patient’s vital signs.
Dr. Glatter: Clearly, when situations escalate in the department, everyone gets more concerned about the patient, but providers are part of this equation, as you allude to.
In 2022, there was a poll by the American College of Emergency Physicians that stated that 85% of emergency physicians reported an increase in violent activity in their ERs in the past 5 years. Nearly two-thirds of nearly 3,000 emergency physicians surveyed reported being assaulted in the past year. This is an important module that we integrate into training providers in terms of these types of tense situations that can result not only in mental anguish but also in physical injury.
Dr. Salazar: One hundred percent. I frankly got tired of seeing my friends and my colleagues suffer both the physical and mental effects of verbal and physical abuse, and I wanted to design a project that was very patient centric while allowing our personnel to really manage these situations a little bit better.
Frankly, we don’t receive great training in this space, and I wanted to rewrite that narrative and make things better for our clinicians out there while remaining patient centric. I wanted to do something about it, and hopefully this dream will become a reality.
Dr. Glatter: Absolutely. There are other data from the Bureau of Labor Statistics stating that health care workers are five times more likely than employees in any other area of work to experience workplace violence. This could, again, range from verbal to physical violence. This is a very important module that you’re developing.
Are there any thoughts to extend this to active-shooter scenarios or any other high-stakes scenarios that you can imagine in the department?
Dr. Salazar: We’re actually working with the same developer that’s helping us with this VR module in developing a mass-casualty incident module so that we can get better training in responding to these very unfortunate high-stakes situations.
Dr. Glatter: In terms of using the module remotely, certainly not requiring resources or having to be in a physical place, can providers in your plan be able to take such a headset home and practice on their own in the sense of being able to deal with a situation? Would this be more reserved for in-department use?
Dr. Salazar: That’s a phenomenal question. I wanted to create the most flexible module that I possibly could. Ideally, a dream scenario is leveraging a simulation center at an academic center and not just do the VR module but also have a brief didactics incorporating a small slide set, some feedback, and some standardized patients. I wanted it to be flexible enough so that folks here in my state, a different state, or even internationally could take advantage of this technology and do it from the comfort of their home.
As you mentioned, this is going to strike some people. It’s going to hit them heavier than others in terms of prior experience as PTSD. For some people, it may be more comfortable to do it in the comfort of their homes. I wanted to create something very flexible and dynamic.
Dr. Glatter: I think that’s ideal. Just one other point. Can you discuss the different levels of competencies involved in this module and how that would be attained?
Dr. Salazar: It’s all evidence based, so we borrowed from literature and the specialties of emergency medicine. We collaborated with psychiatrists within our medical center. We looked at all available literature and methods, proficiencies, competencies, and best practices, and we took all of them together to form something that we think is organized and concise.
We were able to create our own algorithm, but it’s not brand new. We’re just borrowing what we think is the best to create something that the majority of health care personnel are going to be able to relate to and be able to really be proficient at.
This includes things like active listening, bargaining, how to respond, where to put yourself in a situation, and the best possible situation to respond to a scenario, how to prevent things – how to get out of a chokehold, for example. We’re borrowing from several different disciplines and creating something that can be very concise and organized.
Dr. Glatter: Does this program that you’ve developed allow the provider to get feedback in the sense that when they’re in such a danger, their life could be at risk? For example, if they don’t remove themselves in a certain amount of time, this could be lethal.
Dr. Salazar: Yes, 100%. Probably the one thing that differentiates our project from any others is the ability to customize the experience so that a learner who is doing the things that we ask them to do in terms of safety and response is able to get out of a situation successfully within the environment. If they don’t, they get some kind of feedback.
Not to spoil the surprise here, but we’re going to be doing things like looking at decibel meters to see what the volume in the room is doing and how you’re managing the volume and the stimulation within the room. If you are able to maintain the decibel readings at a specific level, you’re going to succeed through the module. If you don’t, we keep the patient escalation going.
Dr. Glatter: There is a debrief built into this type of approach where, in other words, learning points are emphasized – where you could have done better and such.
Dr. Salazar: Yes, absolutely. We are going to be able to get individualized data for each learner so that we can tailor the debrief to their own performance and be able to give them actionable items to work on. It’s a debrief that’s productive and individualized, and folks can walk away with something useful in the end.
Dr. Glatter: Are the data shared or confidential at present?
Dr. Salazar: At this very moment, the data are confidential. We are going to look at how to best use this. We’re hoping to eventually write this up and see how this information can be best used to train personnel.
Eventually, we may see that some of the advice that we’re giving is very common to most folks. Others may require some individualized type of feedback. That said, it remains to be seen, but right now, it’s confidential.
Dr. Glatter: Is this currently being implemented as part of your curriculum for emergency medicine residents?
Dr. Salazar: We’re going to study it first. We’re very excited to include our emergency medicine residents as one of our cohorts that’s going to be undergoing the module, and we’re going to be studying other forms of workplace violence mitigation strategies. We’re really excited about the possibility of this eventually becoming the standard of education for not only our emergency medicine residents, but also health care personnel all over the world.
Dr. Glatter: I’m glad you mentioned that, because obviously nurses, clerks in the department, and anyone who’s working in the department, for that matter, and who interfaces with patients really should undergo such training.
Dr. Salazar: Absolutely. The folks at intake, at check-in, and at kiosks. Do they go through a separate area for screening? You’re absolutely right. There are many folks who interface with patients and all of us are potential victims of workplace violence. We want to give our health care family the best opportunity to succeed in these situations.
Dr. Glatter:: Absolutely. Even EMS providers, being on the front lines and encountering patients in such situations, would benefit, in my opinion.
Dr. Salazar: Yes, absolutely. Behavioral health emergencies and organically induced altered mental status results in injury, both physical and mental, to EMS professionals as well, and there’s good evidence of that. I’ll be very glad to see this type of education make it out to our initial and continuing education efforts for EMS as well.
Dr. Glatter: I want to thank you. This has been very helpful. It’s such an important task that you’ve started to explore, and I look forward to follow-up on this. Again, thank you for your time.
Dr. Salazar: It was my pleasure. Thank you so much for having me.
Dr. Glatter is an attending physician at Lenox Hill Hospital in New York City and assistant professor of emergency medicine at Zucker School of Medicine at Hofstra/Northwell in Hempstead, N.Y. He is an editorial adviser and hosts the Hot Topics in EM series on Medscape. He is also a medical contributor for Forbes. Dr. Salazar is a board-certified emergency physician and associate professor at UT Southwestern Medicine Center in Dallas. He is involved with the UTSW Emergency Medicine Education Program and serves as the medical director to teach both initial and continuing the emergency medicine education for emergency medical technicians and paramedics, which trains most of the Dallas Fire Rescue personnel and the vast majority for EMS providers in the Dallas County. In addition, he serves as an associate chief of service at Parkland’s emergency department, and liaison to surgical services. A version of this article originally appeared on Medscape.com.





