User login
For MD-IQ use only
From Our President
Society for Vascular Surgery President Michel S. Makaroun, MD, will reflect on his presidency during the 2019 Presidential Address, on Friday, June 14, from 11:15 a.m. to 12:15 p.m. President-Elect Kim Hodgson, MD, will introduce Dr. Makaroun, beginning at 11 a.m.
Dr. Makaroun is professor of surgery and clinical translational science at the University of Pittsburgh. He is the chair of vascular surgery and codirector of the University of Pittsburgh Medical Center Heart and Vascular Institute.
His address, “I am in Favor of Progress ... It is Change I Do Not Like,” will take place in Ballroom A/B.
Society for Vascular Surgery President Michel S. Makaroun, MD, will reflect on his presidency during the 2019 Presidential Address, on Friday, June 14, from 11:15 a.m. to 12:15 p.m. President-Elect Kim Hodgson, MD, will introduce Dr. Makaroun, beginning at 11 a.m.
Dr. Makaroun is professor of surgery and clinical translational science at the University of Pittsburgh. He is the chair of vascular surgery and codirector of the University of Pittsburgh Medical Center Heart and Vascular Institute.
His address, “I am in Favor of Progress ... It is Change I Do Not Like,” will take place in Ballroom A/B.
Society for Vascular Surgery President Michel S. Makaroun, MD, will reflect on his presidency during the 2019 Presidential Address, on Friday, June 14, from 11:15 a.m. to 12:15 p.m. President-Elect Kim Hodgson, MD, will introduce Dr. Makaroun, beginning at 11 a.m.
Dr. Makaroun is professor of surgery and clinical translational science at the University of Pittsburgh. He is the chair of vascular surgery and codirector of the University of Pittsburgh Medical Center Heart and Vascular Institute.
His address, “I am in Favor of Progress ... It is Change I Do Not Like,” will take place in Ballroom A/B.
Mentoring during fellowship to improve career fit, decrease burnout, and optimize career satisfaction among young gastroenterologists
Introduction
Burnout in physicians has received significant attention within the past several years, particularly among trainees and early-career physicians. The subspecialties of gastroenterology and hepatology are not immune to burnout, with multiple studies indicating that early career gastroenterologists may be disproportionately affected, compared with their more-established counterparts.1-4 Although the drivers of depersonalization, emotional exhaustion, and a reduced sense of personal accomplishment among trainees and early-career gastroenterologists are not fully understood, maximizing career fit during the transition from fellowship into the first posttraining position has been promoted as a potential method to decrease burnout in this population.4,5
While most trainees enter gastroenterology fellowships with a set of predefined career goals, mentorship during fellowship can provide critical guidance along with exposure to new areas and career tracks that were not previously considered. In a survey of gastroenterology and transplant hepatology fellows, 94% of participants with a mentor reported that the mentor significantly influenced their career decision.6 Effective mentoring also has been identified as one possible method to decrease burnout among trainees.7,8
Formal mentoring in gastroenterology fellowship programs might decrease burnout through effectively identifying risk factors such as work hour violations or a lack of social support. Additionally, when fellows are being prepared for transition to their first positions as attending gastroenterologists, there is a critical opportunity to improve career fit and decrease burnout rates among early-career gastroenterologists. Making the correct choice of subsequent career path after fellowship might be a source of stress, but this should allow early-career gastroenterologists to maximize the time spent doing those activities they feel are the most rewarding. A formal mentoring system and an accessible career mentor can be invaluable in allowing the mentee to identify and select that position.
Career fit
The concept of career fit has been described as the ability of individuals to focus their effort on the aspect or aspects of their work that they find most meaningful.5 Multiple specialties have recognized the importance of career fit and the need to choose appropriately when selecting a position and career path upon completing fellowship. In one evaluation of faculty members from the department of medicine at a large academic medical center, those individuals who spent less than 20% of their time working on the activity that they found most meaningful were significantly more likely to demonstrate burnout.5
In a relatively short time period, gastroenterology fellows are required to gather multiple new skill sets, including functioning as a consultant, performing endoscopic procedures, and potentially gaining formal training in clinical, basic, or translational research methods. During this same period, an intense phase of self-assessment should begin, with one critical aim of training being to identify those factors most likely to lead to a long, satisfying career. The growth that occurs during fellowship may allow for the identification of a career track that is likely to be the most rewarding, such as a career as a clinical investigator, clinician educator, or in clinical practice. Importantly, the trainee must decide which career track will most likely lead to self-fulfillment, even if the chosen path does not align with a mentor or advisor. Additionally, self-assessment also may aid in the identification of a niche that an individual finds most intellectually stimulating, which may lead to an area of research or clinical expertise.
While the demonstrated relationship between career fit and burnout is only an association without demonstrated causation, this does merit further consideration. For the first time in most trainees’ careers, the position after fellowship represents an opportunity to choose a job as opposed to going through a “match” process. Therefore, the trainee must strongly consider the factors that will ultimately lead to career satisfaction. If a large disconnect is present between self-identified career goals and the actual tasks required within daily workflow, this may lead to burnout relatively early in a career. Perhaps more importantly, if an individual did not perform adequate self-reflection when choosing a career path or did not receive effective guidance from career mentors, this also might lead to decreased career satisfaction, poor career fit, and an increased risk for burnout as an early-career gastroenterologist.
The mentor’s role
Although a structured career mentoring program is in place within many gastroenterology training programs, other fellowships encourage the mentee to select from a pool of potential mentors. In many cases, trainees and early career gastroenterologists will benefit from building a mentorship team, including career mentor or mentors, research mentors, and other advisors.9
While the mentor-mentee relationship can be an extremely rewarding experience for both parties, the effective mentor must meet a high standard. Several qualities have been identified that will maximize the benefit of the mentor-mentee relationship for the trainee, including the mentor taking a selfless approach to the relationship, working to assist the mentee in choosing a career path that will be the most rewarding, and then aiding the mentee in making helpful connections to promote growth along that chosen path.9 A good mentors should inspire a mentees, but also should be willing to provide honest and at times critical feedback to ensure that mentees maximizes their potential and ultimately assume the appropriate career trajectory. Unbiased mentorship, as well as continued reevaluations of strengths, weaknesses, and career goals by the mentor and mentee, will ultimately offer an opportunity to ensure the best combination of career fit,5 work-life balance,10 and satisfaction with career choice.11
The mentor-mentee relationship after training is complete
Once a trainee has completed gastroenterology fellowship, another stressful transition to the role of an attending physician commences. It is critical that early-career gastroenterologists not only have confidence in the guidance that their mentor has provided to ensure appropriate career fit in their new role but also maintain these critical mentor-mentee relationships during this transition. A good mentor does not disappear because one phase of training is complete. The need for effective mentoring at the junior faculty level also is well recognized,12 and early-career gastroenterologists should continue to rely on established mentoring relationships when new decision points are encountered.
Depending on the career track of an early-career gastroenterologist, formal mentoring also may be offered in the new role as a junior faculty member.12 Additionally, external mentoring can exist within foundations or other subspecialty groups. One example of extramural mentoring is the Career Connection Program offered through the Crohn’s & Colitis Foundation’s Rising Educators Academics and Clinicians Helping IBD (REACH-IBD) platform. In this program, early-career gastroenterologists are selected and paired with national opinion leaders for one-on-one mentoring relationships. Such a program offers further opportunities for career growth, establishing connections within a smaller subspecialty of gastroenterology, and maximizing career fit.
Conclusion
In an era where the toll of burnout and other influences on early-career gastroenterologists are increasingly being recognized, the importance of career fit during the transition into the role of an attending should not be underestimated. In conjunction with appropriate self-reflection, unbiased and critical mentorship during fellowship can promote significant growth among trainees and allow for the ultimate selection of a career track or career path that will promote happiness, work-life balance, and long-term success as defined by the mentee.
Edward L. Barnes, MD, MPH, is with the Multidisciplinary Center for Inflammatory Bowel Diseases and the Center for Gastrointestinal Biology and Disease in the division of gastroenterology and hepatology at the University of North Carolina at Chapel Hill. Dr. Barnes reports no relevant disclosures.
References
1. Keswani RN et al. Am J Gastroenterol. 2011;106(10):1734-40.
2. Burke C et al. Am J Gastroenterol. 2017;112:S593-4.
3. DeCross AJ. AGA Perspectives. 2017.
4. Barnes EL et al. Dig Dis Sci. 2019;64(2):302-6.
5. Shanafelt TD et al. Arch Intern Med. 2009;169(10):990-5.
6. Ordway SM et al. Hepatol Commun. 2017;1(4):347-53.
7. Janko MR, Smeds MR. J Vasc Surg. 2019;69(4):1233-42.
8. Eckleberry-Hunt J et al. Acad Med. 2009;84(2):269-77.
9. Lieberman D. Gastroenterology. 2016;151(1):17-9.
10. Shanafelt TD et al. Mayo Clin Proc. 2015;90(12):1600-13.
11. Shanafelt TD et al. Ann Surg. 2009;250(3):463-71.
12. Shaheen NJ, Sandler RS. Gastroenterology. 2018;155(5):1293-7.
Introduction
Burnout in physicians has received significant attention within the past several years, particularly among trainees and early-career physicians. The subspecialties of gastroenterology and hepatology are not immune to burnout, with multiple studies indicating that early career gastroenterologists may be disproportionately affected, compared with their more-established counterparts.1-4 Although the drivers of depersonalization, emotional exhaustion, and a reduced sense of personal accomplishment among trainees and early-career gastroenterologists are not fully understood, maximizing career fit during the transition from fellowship into the first posttraining position has been promoted as a potential method to decrease burnout in this population.4,5
While most trainees enter gastroenterology fellowships with a set of predefined career goals, mentorship during fellowship can provide critical guidance along with exposure to new areas and career tracks that were not previously considered. In a survey of gastroenterology and transplant hepatology fellows, 94% of participants with a mentor reported that the mentor significantly influenced their career decision.6 Effective mentoring also has been identified as one possible method to decrease burnout among trainees.7,8
Formal mentoring in gastroenterology fellowship programs might decrease burnout through effectively identifying risk factors such as work hour violations or a lack of social support. Additionally, when fellows are being prepared for transition to their first positions as attending gastroenterologists, there is a critical opportunity to improve career fit and decrease burnout rates among early-career gastroenterologists. Making the correct choice of subsequent career path after fellowship might be a source of stress, but this should allow early-career gastroenterologists to maximize the time spent doing those activities they feel are the most rewarding. A formal mentoring system and an accessible career mentor can be invaluable in allowing the mentee to identify and select that position.
Career fit
The concept of career fit has been described as the ability of individuals to focus their effort on the aspect or aspects of their work that they find most meaningful.5 Multiple specialties have recognized the importance of career fit and the need to choose appropriately when selecting a position and career path upon completing fellowship. In one evaluation of faculty members from the department of medicine at a large academic medical center, those individuals who spent less than 20% of their time working on the activity that they found most meaningful were significantly more likely to demonstrate burnout.5
In a relatively short time period, gastroenterology fellows are required to gather multiple new skill sets, including functioning as a consultant, performing endoscopic procedures, and potentially gaining formal training in clinical, basic, or translational research methods. During this same period, an intense phase of self-assessment should begin, with one critical aim of training being to identify those factors most likely to lead to a long, satisfying career. The growth that occurs during fellowship may allow for the identification of a career track that is likely to be the most rewarding, such as a career as a clinical investigator, clinician educator, or in clinical practice. Importantly, the trainee must decide which career track will most likely lead to self-fulfillment, even if the chosen path does not align with a mentor or advisor. Additionally, self-assessment also may aid in the identification of a niche that an individual finds most intellectually stimulating, which may lead to an area of research or clinical expertise.
While the demonstrated relationship between career fit and burnout is only an association without demonstrated causation, this does merit further consideration. For the first time in most trainees’ careers, the position after fellowship represents an opportunity to choose a job as opposed to going through a “match” process. Therefore, the trainee must strongly consider the factors that will ultimately lead to career satisfaction. If a large disconnect is present between self-identified career goals and the actual tasks required within daily workflow, this may lead to burnout relatively early in a career. Perhaps more importantly, if an individual did not perform adequate self-reflection when choosing a career path or did not receive effective guidance from career mentors, this also might lead to decreased career satisfaction, poor career fit, and an increased risk for burnout as an early-career gastroenterologist.
The mentor’s role
Although a structured career mentoring program is in place within many gastroenterology training programs, other fellowships encourage the mentee to select from a pool of potential mentors. In many cases, trainees and early career gastroenterologists will benefit from building a mentorship team, including career mentor or mentors, research mentors, and other advisors.9
While the mentor-mentee relationship can be an extremely rewarding experience for both parties, the effective mentor must meet a high standard. Several qualities have been identified that will maximize the benefit of the mentor-mentee relationship for the trainee, including the mentor taking a selfless approach to the relationship, working to assist the mentee in choosing a career path that will be the most rewarding, and then aiding the mentee in making helpful connections to promote growth along that chosen path.9 A good mentors should inspire a mentees, but also should be willing to provide honest and at times critical feedback to ensure that mentees maximizes their potential and ultimately assume the appropriate career trajectory. Unbiased mentorship, as well as continued reevaluations of strengths, weaknesses, and career goals by the mentor and mentee, will ultimately offer an opportunity to ensure the best combination of career fit,5 work-life balance,10 and satisfaction with career choice.11
The mentor-mentee relationship after training is complete
Once a trainee has completed gastroenterology fellowship, another stressful transition to the role of an attending physician commences. It is critical that early-career gastroenterologists not only have confidence in the guidance that their mentor has provided to ensure appropriate career fit in their new role but also maintain these critical mentor-mentee relationships during this transition. A good mentor does not disappear because one phase of training is complete. The need for effective mentoring at the junior faculty level also is well recognized,12 and early-career gastroenterologists should continue to rely on established mentoring relationships when new decision points are encountered.
Depending on the career track of an early-career gastroenterologist, formal mentoring also may be offered in the new role as a junior faculty member.12 Additionally, external mentoring can exist within foundations or other subspecialty groups. One example of extramural mentoring is the Career Connection Program offered through the Crohn’s & Colitis Foundation’s Rising Educators Academics and Clinicians Helping IBD (REACH-IBD) platform. In this program, early-career gastroenterologists are selected and paired with national opinion leaders for one-on-one mentoring relationships. Such a program offers further opportunities for career growth, establishing connections within a smaller subspecialty of gastroenterology, and maximizing career fit.
Conclusion
In an era where the toll of burnout and other influences on early-career gastroenterologists are increasingly being recognized, the importance of career fit during the transition into the role of an attending should not be underestimated. In conjunction with appropriate self-reflection, unbiased and critical mentorship during fellowship can promote significant growth among trainees and allow for the ultimate selection of a career track or career path that will promote happiness, work-life balance, and long-term success as defined by the mentee.
Edward L. Barnes, MD, MPH, is with the Multidisciplinary Center for Inflammatory Bowel Diseases and the Center for Gastrointestinal Biology and Disease in the division of gastroenterology and hepatology at the University of North Carolina at Chapel Hill. Dr. Barnes reports no relevant disclosures.
References
1. Keswani RN et al. Am J Gastroenterol. 2011;106(10):1734-40.
2. Burke C et al. Am J Gastroenterol. 2017;112:S593-4.
3. DeCross AJ. AGA Perspectives. 2017.
4. Barnes EL et al. Dig Dis Sci. 2019;64(2):302-6.
5. Shanafelt TD et al. Arch Intern Med. 2009;169(10):990-5.
6. Ordway SM et al. Hepatol Commun. 2017;1(4):347-53.
7. Janko MR, Smeds MR. J Vasc Surg. 2019;69(4):1233-42.
8. Eckleberry-Hunt J et al. Acad Med. 2009;84(2):269-77.
9. Lieberman D. Gastroenterology. 2016;151(1):17-9.
10. Shanafelt TD et al. Mayo Clin Proc. 2015;90(12):1600-13.
11. Shanafelt TD et al. Ann Surg. 2009;250(3):463-71.
12. Shaheen NJ, Sandler RS. Gastroenterology. 2018;155(5):1293-7.
Introduction
Burnout in physicians has received significant attention within the past several years, particularly among trainees and early-career physicians. The subspecialties of gastroenterology and hepatology are not immune to burnout, with multiple studies indicating that early career gastroenterologists may be disproportionately affected, compared with their more-established counterparts.1-4 Although the drivers of depersonalization, emotional exhaustion, and a reduced sense of personal accomplishment among trainees and early-career gastroenterologists are not fully understood, maximizing career fit during the transition from fellowship into the first posttraining position has been promoted as a potential method to decrease burnout in this population.4,5
While most trainees enter gastroenterology fellowships with a set of predefined career goals, mentorship during fellowship can provide critical guidance along with exposure to new areas and career tracks that were not previously considered. In a survey of gastroenterology and transplant hepatology fellows, 94% of participants with a mentor reported that the mentor significantly influenced their career decision.6 Effective mentoring also has been identified as one possible method to decrease burnout among trainees.7,8
Formal mentoring in gastroenterology fellowship programs might decrease burnout through effectively identifying risk factors such as work hour violations or a lack of social support. Additionally, when fellows are being prepared for transition to their first positions as attending gastroenterologists, there is a critical opportunity to improve career fit and decrease burnout rates among early-career gastroenterologists. Making the correct choice of subsequent career path after fellowship might be a source of stress, but this should allow early-career gastroenterologists to maximize the time spent doing those activities they feel are the most rewarding. A formal mentoring system and an accessible career mentor can be invaluable in allowing the mentee to identify and select that position.
Career fit
The concept of career fit has been described as the ability of individuals to focus their effort on the aspect or aspects of their work that they find most meaningful.5 Multiple specialties have recognized the importance of career fit and the need to choose appropriately when selecting a position and career path upon completing fellowship. In one evaluation of faculty members from the department of medicine at a large academic medical center, those individuals who spent less than 20% of their time working on the activity that they found most meaningful were significantly more likely to demonstrate burnout.5
In a relatively short time period, gastroenterology fellows are required to gather multiple new skill sets, including functioning as a consultant, performing endoscopic procedures, and potentially gaining formal training in clinical, basic, or translational research methods. During this same period, an intense phase of self-assessment should begin, with one critical aim of training being to identify those factors most likely to lead to a long, satisfying career. The growth that occurs during fellowship may allow for the identification of a career track that is likely to be the most rewarding, such as a career as a clinical investigator, clinician educator, or in clinical practice. Importantly, the trainee must decide which career track will most likely lead to self-fulfillment, even if the chosen path does not align with a mentor or advisor. Additionally, self-assessment also may aid in the identification of a niche that an individual finds most intellectually stimulating, which may lead to an area of research or clinical expertise.
While the demonstrated relationship between career fit and burnout is only an association without demonstrated causation, this does merit further consideration. For the first time in most trainees’ careers, the position after fellowship represents an opportunity to choose a job as opposed to going through a “match” process. Therefore, the trainee must strongly consider the factors that will ultimately lead to career satisfaction. If a large disconnect is present between self-identified career goals and the actual tasks required within daily workflow, this may lead to burnout relatively early in a career. Perhaps more importantly, if an individual did not perform adequate self-reflection when choosing a career path or did not receive effective guidance from career mentors, this also might lead to decreased career satisfaction, poor career fit, and an increased risk for burnout as an early-career gastroenterologist.
The mentor’s role
Although a structured career mentoring program is in place within many gastroenterology training programs, other fellowships encourage the mentee to select from a pool of potential mentors. In many cases, trainees and early career gastroenterologists will benefit from building a mentorship team, including career mentor or mentors, research mentors, and other advisors.9
While the mentor-mentee relationship can be an extremely rewarding experience for both parties, the effective mentor must meet a high standard. Several qualities have been identified that will maximize the benefit of the mentor-mentee relationship for the trainee, including the mentor taking a selfless approach to the relationship, working to assist the mentee in choosing a career path that will be the most rewarding, and then aiding the mentee in making helpful connections to promote growth along that chosen path.9 A good mentors should inspire a mentees, but also should be willing to provide honest and at times critical feedback to ensure that mentees maximizes their potential and ultimately assume the appropriate career trajectory. Unbiased mentorship, as well as continued reevaluations of strengths, weaknesses, and career goals by the mentor and mentee, will ultimately offer an opportunity to ensure the best combination of career fit,5 work-life balance,10 and satisfaction with career choice.11
The mentor-mentee relationship after training is complete
Once a trainee has completed gastroenterology fellowship, another stressful transition to the role of an attending physician commences. It is critical that early-career gastroenterologists not only have confidence in the guidance that their mentor has provided to ensure appropriate career fit in their new role but also maintain these critical mentor-mentee relationships during this transition. A good mentor does not disappear because one phase of training is complete. The need for effective mentoring at the junior faculty level also is well recognized,12 and early-career gastroenterologists should continue to rely on established mentoring relationships when new decision points are encountered.
Depending on the career track of an early-career gastroenterologist, formal mentoring also may be offered in the new role as a junior faculty member.12 Additionally, external mentoring can exist within foundations or other subspecialty groups. One example of extramural mentoring is the Career Connection Program offered through the Crohn’s & Colitis Foundation’s Rising Educators Academics and Clinicians Helping IBD (REACH-IBD) platform. In this program, early-career gastroenterologists are selected and paired with national opinion leaders for one-on-one mentoring relationships. Such a program offers further opportunities for career growth, establishing connections within a smaller subspecialty of gastroenterology, and maximizing career fit.
Conclusion
In an era where the toll of burnout and other influences on early-career gastroenterologists are increasingly being recognized, the importance of career fit during the transition into the role of an attending should not be underestimated. In conjunction with appropriate self-reflection, unbiased and critical mentorship during fellowship can promote significant growth among trainees and allow for the ultimate selection of a career track or career path that will promote happiness, work-life balance, and long-term success as defined by the mentee.
Edward L. Barnes, MD, MPH, is with the Multidisciplinary Center for Inflammatory Bowel Diseases and the Center for Gastrointestinal Biology and Disease in the division of gastroenterology and hepatology at the University of North Carolina at Chapel Hill. Dr. Barnes reports no relevant disclosures.
References
1. Keswani RN et al. Am J Gastroenterol. 2011;106(10):1734-40.
2. Burke C et al. Am J Gastroenterol. 2017;112:S593-4.
3. DeCross AJ. AGA Perspectives. 2017.
4. Barnes EL et al. Dig Dis Sci. 2019;64(2):302-6.
5. Shanafelt TD et al. Arch Intern Med. 2009;169(10):990-5.
6. Ordway SM et al. Hepatol Commun. 2017;1(4):347-53.
7. Janko MR, Smeds MR. J Vasc Surg. 2019;69(4):1233-42.
8. Eckleberry-Hunt J et al. Acad Med. 2009;84(2):269-77.
9. Lieberman D. Gastroenterology. 2016;151(1):17-9.
10. Shanafelt TD et al. Mayo Clin Proc. 2015;90(12):1600-13.
11. Shanafelt TD et al. Ann Surg. 2009;250(3):463-71.
12. Shaheen NJ, Sandler RS. Gastroenterology. 2018;155(5):1293-7.
Focus on science, not format
How JHM is improving the author experience
“No hassle” new manuscript submission process
Many authors have experienced the frustration of formatting a manuscript for submission to a medical journal. The process is time consuming and each journal has different requirements. This means that if you decide to submit your manuscript to one journal and later decide that another journal is a better fit, you may spend an hour (or several hours) reformatting to meet the new journal’s unique requirements.
To allow authors to spend more time on what matters to them, we’re pleased to introduce our “No Hassle” process for initial original research and brief report manuscript submissions to the Journal of Hospital Medicine. Our goal is to eliminate unnecessary and burdensome steps in the manuscript submission process. Thus, we have relaxed formatting requirements for initial manuscript submissions. Any conventional and readable manuscript format and reference style is acceptable.
Tables and figures can be embedded in the main document file or uploaded individually, depending on your preference. Funding and disclosures should be included on the title page but there is no need to submit completed disclosure or copyright forms unless we request a manuscript revision.
Timely decisions
We have all experienced the agony of waiting months on end for a journal to make a decision about our manuscript. The review process itself can take many months (or even longer). Furthermore, a manuscript may not be published for many more months (or even longer) following acceptance. At the Journal of Hospital Medicine, we commit to making timely decisions and publishing your accepted manuscript as fast as we can.
We currently reject approximately half of all original research and brief report manuscript submissions without formal peer review. We do this for two reasons. First, we want to ensure that we’re not overburdening our peer reviewers so we only ask them to review manuscripts that we are seriously considering for publication. Second, we want to ensure that we’re being respectful of our authors’ time. If we are unlikely to publish a manuscript based on lower priority scores assigned by me, as editor-in-chief, or other journal editors, we don’t want to subject your manuscript to a lengthy peer review, but would rather return the manuscript to you quickly for timely submission elsewhere.
Here are data that support our timely decision making:
- 1.3 days = our average time from manuscript submission to rejection without formal peer review (median, less than one day).
- 23 days = our average time from manuscript submission to first decision for manuscripts sent for peer review.
We also are working to improve our time to publication. Our goal is to publish accepted manuscripts within 120 days from initial submission to publication, and within 60 days from acceptance to publication.
Dissemination
Finally, little public knowledge is gleaned from medical research unless the study is published and widely read. The Journal of Hospital Medicine is at the leading edge of helping authors disseminate their work to a broader audience. Of course, we produce press releases and distribute those to many media outlets in partnership with the Society of Hospital Medicine. We also leverage social media to promote your article through tweets, visual abstracts, and, more recently, comics or graphic medicine abstracts. Some articles are even discussed on #JHMChat, our twitter-based journal club. This work is led by our exceptional Digital Media Editors, Dr. Vineet Arora (@FutureDocs), Dr. Charlie Wray (@WrayCharles), and Dr. Grace Farris (@gracefarris).
In summary, we are committed to making the Journal of Hospital Medicine even more author friendly. To that end, we’re making it easy for authors to submit their work, making timely disposition decisions, and facilitating dissemination of the work we publish.
Dr. Shah is chief metrics officer and director of the division of hospital medicine at Cincinnati Children’s Hospital Medical Center. He is the current editor-in-chief of the Journal of Hospital Medicine.
How JHM is improving the author experience
How JHM is improving the author experience
“No hassle” new manuscript submission process
Many authors have experienced the frustration of formatting a manuscript for submission to a medical journal. The process is time consuming and each journal has different requirements. This means that if you decide to submit your manuscript to one journal and later decide that another journal is a better fit, you may spend an hour (or several hours) reformatting to meet the new journal’s unique requirements.
To allow authors to spend more time on what matters to them, we’re pleased to introduce our “No Hassle” process for initial original research and brief report manuscript submissions to the Journal of Hospital Medicine. Our goal is to eliminate unnecessary and burdensome steps in the manuscript submission process. Thus, we have relaxed formatting requirements for initial manuscript submissions. Any conventional and readable manuscript format and reference style is acceptable.
Tables and figures can be embedded in the main document file or uploaded individually, depending on your preference. Funding and disclosures should be included on the title page but there is no need to submit completed disclosure or copyright forms unless we request a manuscript revision.
Timely decisions
We have all experienced the agony of waiting months on end for a journal to make a decision about our manuscript. The review process itself can take many months (or even longer). Furthermore, a manuscript may not be published for many more months (or even longer) following acceptance. At the Journal of Hospital Medicine, we commit to making timely decisions and publishing your accepted manuscript as fast as we can.
We currently reject approximately half of all original research and brief report manuscript submissions without formal peer review. We do this for two reasons. First, we want to ensure that we’re not overburdening our peer reviewers so we only ask them to review manuscripts that we are seriously considering for publication. Second, we want to ensure that we’re being respectful of our authors’ time. If we are unlikely to publish a manuscript based on lower priority scores assigned by me, as editor-in-chief, or other journal editors, we don’t want to subject your manuscript to a lengthy peer review, but would rather return the manuscript to you quickly for timely submission elsewhere.
Here are data that support our timely decision making:
- 1.3 days = our average time from manuscript submission to rejection without formal peer review (median, less than one day).
- 23 days = our average time from manuscript submission to first decision for manuscripts sent for peer review.
We also are working to improve our time to publication. Our goal is to publish accepted manuscripts within 120 days from initial submission to publication, and within 60 days from acceptance to publication.
Dissemination
Finally, little public knowledge is gleaned from medical research unless the study is published and widely read. The Journal of Hospital Medicine is at the leading edge of helping authors disseminate their work to a broader audience. Of course, we produce press releases and distribute those to many media outlets in partnership with the Society of Hospital Medicine. We also leverage social media to promote your article through tweets, visual abstracts, and, more recently, comics or graphic medicine abstracts. Some articles are even discussed on #JHMChat, our twitter-based journal club. This work is led by our exceptional Digital Media Editors, Dr. Vineet Arora (@FutureDocs), Dr. Charlie Wray (@WrayCharles), and Dr. Grace Farris (@gracefarris).
In summary, we are committed to making the Journal of Hospital Medicine even more author friendly. To that end, we’re making it easy for authors to submit their work, making timely disposition decisions, and facilitating dissemination of the work we publish.
Dr. Shah is chief metrics officer and director of the division of hospital medicine at Cincinnati Children’s Hospital Medical Center. He is the current editor-in-chief of the Journal of Hospital Medicine.
“No hassle” new manuscript submission process
Many authors have experienced the frustration of formatting a manuscript for submission to a medical journal. The process is time consuming and each journal has different requirements. This means that if you decide to submit your manuscript to one journal and later decide that another journal is a better fit, you may spend an hour (or several hours) reformatting to meet the new journal’s unique requirements.
To allow authors to spend more time on what matters to them, we’re pleased to introduce our “No Hassle” process for initial original research and brief report manuscript submissions to the Journal of Hospital Medicine. Our goal is to eliminate unnecessary and burdensome steps in the manuscript submission process. Thus, we have relaxed formatting requirements for initial manuscript submissions. Any conventional and readable manuscript format and reference style is acceptable.
Tables and figures can be embedded in the main document file or uploaded individually, depending on your preference. Funding and disclosures should be included on the title page but there is no need to submit completed disclosure or copyright forms unless we request a manuscript revision.
Timely decisions
We have all experienced the agony of waiting months on end for a journal to make a decision about our manuscript. The review process itself can take many months (or even longer). Furthermore, a manuscript may not be published for many more months (or even longer) following acceptance. At the Journal of Hospital Medicine, we commit to making timely decisions and publishing your accepted manuscript as fast as we can.
We currently reject approximately half of all original research and brief report manuscript submissions without formal peer review. We do this for two reasons. First, we want to ensure that we’re not overburdening our peer reviewers so we only ask them to review manuscripts that we are seriously considering for publication. Second, we want to ensure that we’re being respectful of our authors’ time. If we are unlikely to publish a manuscript based on lower priority scores assigned by me, as editor-in-chief, or other journal editors, we don’t want to subject your manuscript to a lengthy peer review, but would rather return the manuscript to you quickly for timely submission elsewhere.
Here are data that support our timely decision making:
- 1.3 days = our average time from manuscript submission to rejection without formal peer review (median, less than one day).
- 23 days = our average time from manuscript submission to first decision for manuscripts sent for peer review.
We also are working to improve our time to publication. Our goal is to publish accepted manuscripts within 120 days from initial submission to publication, and within 60 days from acceptance to publication.
Dissemination
Finally, little public knowledge is gleaned from medical research unless the study is published and widely read. The Journal of Hospital Medicine is at the leading edge of helping authors disseminate their work to a broader audience. Of course, we produce press releases and distribute those to many media outlets in partnership with the Society of Hospital Medicine. We also leverage social media to promote your article through tweets, visual abstracts, and, more recently, comics or graphic medicine abstracts. Some articles are even discussed on #JHMChat, our twitter-based journal club. This work is led by our exceptional Digital Media Editors, Dr. Vineet Arora (@FutureDocs), Dr. Charlie Wray (@WrayCharles), and Dr. Grace Farris (@gracefarris).
In summary, we are committed to making the Journal of Hospital Medicine even more author friendly. To that end, we’re making it easy for authors to submit their work, making timely disposition decisions, and facilitating dissemination of the work we publish.
Dr. Shah is chief metrics officer and director of the division of hospital medicine at Cincinnati Children’s Hospital Medical Center. He is the current editor-in-chief of the Journal of Hospital Medicine.
AGA News
AGA journals select new editorial fellows
Congrats to the six GIs selected for this competitive program.
The AGA journals – Gastroenterology, Clinical Gastroenterology and Hepatology (CGH), and Cellular and Molecular Gastroenterology and Hepatology (CMGH) – are pleased to announce their 2019-2020 editorial fellows.
Gastroenterology
Feng Su, MD
University of Washington, Seattle
Victoria Weis, PhD
Wake Forest University, Winston-Salem, N.C.
CGH
Austin Chiang, MD, MPH
Jefferson Medical College, Philadelphia, Penn.
Jennifer Kolb, MD
University of Colorado at Denver, Aurora
CMGH
Cambrian Liu, PhD
The Saban Research Institute, Children’s Hospital Los Angeles, Calif.
Tirthadipa Pradhan-Sundd, PhD
University of Pittsburgh, Penn.
The editorial fellows will be mentored on their respective journals’ editorial processes, including peer review and the publication process from manuscript submission to acceptance. They will participate in discussions and conferences with the boards of editors and work closely with the AGA editorial staff. Additionally, the fellows will participate in AGA’s new reviewer education program and will also be offered the opportunity to contribute content to their respective journals. The newly expanded program builds on the success of the previous 2 years when Gastroenterology had an editorial fellow.
The journals’ board of editors and editorial staff congratulate the fellows and are excited to work with them over the next year.
Get to know this rock star IBS researcher and mom
AGA Research Foundation pilot awards are an invaluable tool for investigators – they provide seed funding to explore promising new lines of research and generate preliminary data for larger grants. So, when Meenakshi Rao, MD, PhD, received the 2016 AGA–Takeda Pharmaceuticals International Research Scholar Award in Neurogastroenterology, she was able to double down on a project to identify why men and women with irritable bowel syndrome (IBS), the most common but least understood of all digestive disorders, report different symptoms and respond differently to treatment. Based on her recent accomplishments, we’re excited for you to get to know Dr. Rao, assistant professor of pediatrics at Harvard Medical School, Boston, and our AGA Research Foundation researcher of the month.
The Rao lab AGA-funded project focused on building upon Dr. Rao’s previous findings, which showed that disrupting nerves in the bowel had vastly different effects on males and females. These surprising results led Dr. Rao to explore whether sex hormones, such as testosterone and estrogen, might regulate how well things move through the bowel. Dr. Rao believes that identifying the underlying causes for sex differences in bowel function could lead to more effective and personalized treatments for patients with IBS. You can read the specifics of Dr. Rao’s research in the October 2017 issue of Gastroenterology and the October 2018 issue of Journal of Neuroscience.
IBS symptoms in women more typically involve constipation while young men with IBS more commonly report diarrhea. Over time, as men age, however, they tend to experience more constipation, Dr. Rao said. “Sex hormones might be signaling directly to the nerves in our gut and playing a role in these sex differences,” Dr. Rao said. “It might mean we can’t think of this as one disorder. IBS in a male may be different than IBS in a female, and that could change how we approach diagnosis and treatment.”
The AGA grant laid the groundwork for Dr. Rao’s findings, which led to a new understanding of how different types of cells in the gut nervous system regulate bowel functions – and how this regulation is different in males and females. The AGA grant helped Dr. Rao secure funding from the National Institutes of Health to launch new projects focused on how disruption of the gut nervous system causes disease.
Dr. Rao received the AGA award in 2015, when her son, Avinash, was aged 2 years. She acknowledged the delicate balancing act of raising a family and advancing her research.
“A lot of things were happening at once,” she said. “As a young parent, having the support of this award and having a technician (made possible by the award) made a big difference.”
Her son, now 5 years old, is growing up in a science-centric household because Dr. Rao’s husband is also a scientist. Not surprisingly, Dr. Rao says, her son is becoming a budding scientist.
“He talks about experiments all the time,” she says. “He even articulated to me the other day why we work on mice to learn how to help people. I never taught him that. I was floored.”
Five new GI technologies to know
The AGA Tech Summit Shark Tank is our annual reminder that the field of GI is ripe for innovation. Continue reading for an overview of the five new technologies pitched to our panel of sharks.
The smart toilet seat. A toilet seat developed by Toi Labs, called TrueLoo, is equipped with lighting and cameras that capture images of bowel movements and urination for subsequent analysis. The company describes TrueLoo as a low-cost disease-screening tool that has major potential for early detection of conditions ranging from dehydration to gastrointestinal cancer.
AI to aid screening endoscopy. A new tool called Ultivision, being developed by the startup Docbot, was described as a strategy to employ artificial intelligence (AI) to aid endoscopists in screening for dysplasia in either screening colonoscopy or in surveillance of Barrett’s esophagus. The tool integrates with existing endoscopic tools. As tissue is visualized, the AI is programmed to highlight suspected dysplasia with a colored box to alert the endoscopist.
Obesity phenotyping tool. The Pheno Test, developed by Phenomix Sciences, applies “multi-omics” to a blood-based test to separate patients with obesity into four phenotypes: hungry brain (satiation signal is impaired), hungry gut (signals to eat are upregulated), emotional hunger (psychological reasons drive eating behavior), and slow metabolism (failure to burn fat at normal rates). With this knowledge, treatment can be tailored appropriately leading to better outcomes.
Capsule diagnostic tool. The Atmo Gas Capsule from Atmo Biosciences is an ingestible capsule that measures gases at the source, which can accelerate the diagnosis of diseases such as IBS and inflammatory bowel disease (IBD). According to the company, this technique is highly accurate and offers an alternative to more invasive and expensive diagnostic tools.
Winner: “all-in-one” IBD app. Our Shark Tank winner by both popular vote from AGA Tech Summit attendees and the six-member Shark Tank panel was Oshi Health, selected for its IBD app. The app allows patients to track symptoms, a first step in understanding personalized flare pattern, as well as find resources to learn about their disease and communicate with other patients about their experiences. In a future iteration, information gathered by the app will be made available to physicians to provide current information about disease status to better individualize therapy.
2020 Crohn’s & Colitis Congress now open for registration
Join the Crohn’s & Colitis Foundation and AGA next January in Austin, Tex., for the premier conference on IBD.
The Crohn’s & Colitis Congress combines the strengths of the nation’s leading IBD patient organization, the Crohn’s & Colitis Foundation, and the premier GI professional organization, AGA, to bring together IBD professionals, across all disciplines, to transform IBD care.
The 2020 Congress Committee Chair David T. Rubin, MD, AGAF, University of Chicago, and Cochair Uma Mahadevan, MD, AGAF, University of California, San Francisco, lead a faculty that includes thought leaders in the fields of GI, research investigation, surgery, pediatrics, advanced practice, IBD nursing, diet and nutrition, mental health, radiology, and pathology.
The congress’s agenda includes main sessions that will emphasize case studies and panel discussions. There will also be parallel sessions on basic and translational science for senior and junior investigators. In addition, opening breakout sessions, taking place Jan. 23, will be available for selection free of charge.
Attendees of the 2020 congress will be able to meet with IBD leaders, discover different perspectives, leave with practical information they can immediately implement to take care of their next IBD patient and hear what’s on the horizon in potential treatment.
There will also be plenty of social events and plenty of time to build a strong network, including a Friday night Welcome Reception that should not be missed.
In addition, the 2020 congress is taking place in Austin, Tex. The capital of Texas and the Live Music Capital of the World, Austin is famous for its inspiring and enticing entertainment, culture, cuisine, and outdoor settings. Make a week of it and enjoy all Austin has to offer.
Early-bird registration ends Sept. 18. General abstract submissions for basic, translational, and clinical research begin Aug. 28 and end Oct. 23. To learn more and register, visit www.crohnscolitiscongress.org.
AGA welcomes new president, Hashem B. El-Serag, MD, MPH, AGAF
Hashem B. El-Serag, MD, MPH, AGAF, began his term as the 114th president of the AGA Institute at Digestive Disease Week® (DDW 2019).
Dr. El-Serag is former editor in chief of Clinical Gastroenterology and Hepatology. He currently serves as chair of the department of medicine at Baylor College of Medicine, Houston, following a decade leading and expanding Baylor’s gastroenterology and hepatology section. He is one of the few academic gastroenterologists serving as a chair of a department of medicine in the United States.
Originally Palestinian, Dr. El-Serag became a U.S. citizen in the early 2000s after medical school in Libya. He completed his training at community hospitals in the United States. His path from Benghazi to Baylor is described in the May issue of Gastroenterology by Baylor colleague Dr. Fasiha Kanwal.
“I firmly believe that the success I achieved in the United States would not have been possible anywhere else in the world, and it is as much a testament to the accepting society and medical system as to whatever intrinsic ability or skill I have,” noted Dr. El-Serag.
The major focus of Dr. El-Serag’s scholarly work is the epidemiology and clinical outcomes of hepatocellular carcinoma. Much of the modern literature on this topic includes his more than 100 publications. Since 2014, Dr. El-Serag has been named by Thomson Reuter as among the top 1% of clinical scientists.
Dr. El-Serag “is an innovative scientist, a compassionate physician, and a gifted educator. He is a relentless advocate of science and training, with an astute political sense — all key to influencing and shaping policy,” said Dr. Kanwal.
Dr. El-Serag’s term as AGA president concludes May 2020. Follow him on twitter at @SeragHashem.
AGA journals select new editorial fellows
Congrats to the six GIs selected for this competitive program.
The AGA journals – Gastroenterology, Clinical Gastroenterology and Hepatology (CGH), and Cellular and Molecular Gastroenterology and Hepatology (CMGH) – are pleased to announce their 2019-2020 editorial fellows.
Gastroenterology
Feng Su, MD
University of Washington, Seattle
Victoria Weis, PhD
Wake Forest University, Winston-Salem, N.C.
CGH
Austin Chiang, MD, MPH
Jefferson Medical College, Philadelphia, Penn.
Jennifer Kolb, MD
University of Colorado at Denver, Aurora
CMGH
Cambrian Liu, PhD
The Saban Research Institute, Children’s Hospital Los Angeles, Calif.
Tirthadipa Pradhan-Sundd, PhD
University of Pittsburgh, Penn.
The editorial fellows will be mentored on their respective journals’ editorial processes, including peer review and the publication process from manuscript submission to acceptance. They will participate in discussions and conferences with the boards of editors and work closely with the AGA editorial staff. Additionally, the fellows will participate in AGA’s new reviewer education program and will also be offered the opportunity to contribute content to their respective journals. The newly expanded program builds on the success of the previous 2 years when Gastroenterology had an editorial fellow.
The journals’ board of editors and editorial staff congratulate the fellows and are excited to work with them over the next year.
Get to know this rock star IBS researcher and mom
AGA Research Foundation pilot awards are an invaluable tool for investigators – they provide seed funding to explore promising new lines of research and generate preliminary data for larger grants. So, when Meenakshi Rao, MD, PhD, received the 2016 AGA–Takeda Pharmaceuticals International Research Scholar Award in Neurogastroenterology, she was able to double down on a project to identify why men and women with irritable bowel syndrome (IBS), the most common but least understood of all digestive disorders, report different symptoms and respond differently to treatment. Based on her recent accomplishments, we’re excited for you to get to know Dr. Rao, assistant professor of pediatrics at Harvard Medical School, Boston, and our AGA Research Foundation researcher of the month.
The Rao lab AGA-funded project focused on building upon Dr. Rao’s previous findings, which showed that disrupting nerves in the bowel had vastly different effects on males and females. These surprising results led Dr. Rao to explore whether sex hormones, such as testosterone and estrogen, might regulate how well things move through the bowel. Dr. Rao believes that identifying the underlying causes for sex differences in bowel function could lead to more effective and personalized treatments for patients with IBS. You can read the specifics of Dr. Rao’s research in the October 2017 issue of Gastroenterology and the October 2018 issue of Journal of Neuroscience.
IBS symptoms in women more typically involve constipation while young men with IBS more commonly report diarrhea. Over time, as men age, however, they tend to experience more constipation, Dr. Rao said. “Sex hormones might be signaling directly to the nerves in our gut and playing a role in these sex differences,” Dr. Rao said. “It might mean we can’t think of this as one disorder. IBS in a male may be different than IBS in a female, and that could change how we approach diagnosis and treatment.”
The AGA grant laid the groundwork for Dr. Rao’s findings, which led to a new understanding of how different types of cells in the gut nervous system regulate bowel functions – and how this regulation is different in males and females. The AGA grant helped Dr. Rao secure funding from the National Institutes of Health to launch new projects focused on how disruption of the gut nervous system causes disease.
Dr. Rao received the AGA award in 2015, when her son, Avinash, was aged 2 years. She acknowledged the delicate balancing act of raising a family and advancing her research.
“A lot of things were happening at once,” she said. “As a young parent, having the support of this award and having a technician (made possible by the award) made a big difference.”
Her son, now 5 years old, is growing up in a science-centric household because Dr. Rao’s husband is also a scientist. Not surprisingly, Dr. Rao says, her son is becoming a budding scientist.
“He talks about experiments all the time,” she says. “He even articulated to me the other day why we work on mice to learn how to help people. I never taught him that. I was floored.”
Five new GI technologies to know
The AGA Tech Summit Shark Tank is our annual reminder that the field of GI is ripe for innovation. Continue reading for an overview of the five new technologies pitched to our panel of sharks.
The smart toilet seat. A toilet seat developed by Toi Labs, called TrueLoo, is equipped with lighting and cameras that capture images of bowel movements and urination for subsequent analysis. The company describes TrueLoo as a low-cost disease-screening tool that has major potential for early detection of conditions ranging from dehydration to gastrointestinal cancer.
AI to aid screening endoscopy. A new tool called Ultivision, being developed by the startup Docbot, was described as a strategy to employ artificial intelligence (AI) to aid endoscopists in screening for dysplasia in either screening colonoscopy or in surveillance of Barrett’s esophagus. The tool integrates with existing endoscopic tools. As tissue is visualized, the AI is programmed to highlight suspected dysplasia with a colored box to alert the endoscopist.
Obesity phenotyping tool. The Pheno Test, developed by Phenomix Sciences, applies “multi-omics” to a blood-based test to separate patients with obesity into four phenotypes: hungry brain (satiation signal is impaired), hungry gut (signals to eat are upregulated), emotional hunger (psychological reasons drive eating behavior), and slow metabolism (failure to burn fat at normal rates). With this knowledge, treatment can be tailored appropriately leading to better outcomes.
Capsule diagnostic tool. The Atmo Gas Capsule from Atmo Biosciences is an ingestible capsule that measures gases at the source, which can accelerate the diagnosis of diseases such as IBS and inflammatory bowel disease (IBD). According to the company, this technique is highly accurate and offers an alternative to more invasive and expensive diagnostic tools.
Winner: “all-in-one” IBD app. Our Shark Tank winner by both popular vote from AGA Tech Summit attendees and the six-member Shark Tank panel was Oshi Health, selected for its IBD app. The app allows patients to track symptoms, a first step in understanding personalized flare pattern, as well as find resources to learn about their disease and communicate with other patients about their experiences. In a future iteration, information gathered by the app will be made available to physicians to provide current information about disease status to better individualize therapy.
2020 Crohn’s & Colitis Congress now open for registration
Join the Crohn’s & Colitis Foundation and AGA next January in Austin, Tex., for the premier conference on IBD.
The Crohn’s & Colitis Congress combines the strengths of the nation’s leading IBD patient organization, the Crohn’s & Colitis Foundation, and the premier GI professional organization, AGA, to bring together IBD professionals, across all disciplines, to transform IBD care.
The 2020 Congress Committee Chair David T. Rubin, MD, AGAF, University of Chicago, and Cochair Uma Mahadevan, MD, AGAF, University of California, San Francisco, lead a faculty that includes thought leaders in the fields of GI, research investigation, surgery, pediatrics, advanced practice, IBD nursing, diet and nutrition, mental health, radiology, and pathology.
The congress’s agenda includes main sessions that will emphasize case studies and panel discussions. There will also be parallel sessions on basic and translational science for senior and junior investigators. In addition, opening breakout sessions, taking place Jan. 23, will be available for selection free of charge.
Attendees of the 2020 congress will be able to meet with IBD leaders, discover different perspectives, leave with practical information they can immediately implement to take care of their next IBD patient and hear what’s on the horizon in potential treatment.
There will also be plenty of social events and plenty of time to build a strong network, including a Friday night Welcome Reception that should not be missed.
In addition, the 2020 congress is taking place in Austin, Tex. The capital of Texas and the Live Music Capital of the World, Austin is famous for its inspiring and enticing entertainment, culture, cuisine, and outdoor settings. Make a week of it and enjoy all Austin has to offer.
Early-bird registration ends Sept. 18. General abstract submissions for basic, translational, and clinical research begin Aug. 28 and end Oct. 23. To learn more and register, visit www.crohnscolitiscongress.org.
AGA welcomes new president, Hashem B. El-Serag, MD, MPH, AGAF
Hashem B. El-Serag, MD, MPH, AGAF, began his term as the 114th president of the AGA Institute at Digestive Disease Week® (DDW 2019).
Dr. El-Serag is former editor in chief of Clinical Gastroenterology and Hepatology. He currently serves as chair of the department of medicine at Baylor College of Medicine, Houston, following a decade leading and expanding Baylor’s gastroenterology and hepatology section. He is one of the few academic gastroenterologists serving as a chair of a department of medicine in the United States.
Originally Palestinian, Dr. El-Serag became a U.S. citizen in the early 2000s after medical school in Libya. He completed his training at community hospitals in the United States. His path from Benghazi to Baylor is described in the May issue of Gastroenterology by Baylor colleague Dr. Fasiha Kanwal.
“I firmly believe that the success I achieved in the United States would not have been possible anywhere else in the world, and it is as much a testament to the accepting society and medical system as to whatever intrinsic ability or skill I have,” noted Dr. El-Serag.
The major focus of Dr. El-Serag’s scholarly work is the epidemiology and clinical outcomes of hepatocellular carcinoma. Much of the modern literature on this topic includes his more than 100 publications. Since 2014, Dr. El-Serag has been named by Thomson Reuter as among the top 1% of clinical scientists.
Dr. El-Serag “is an innovative scientist, a compassionate physician, and a gifted educator. He is a relentless advocate of science and training, with an astute political sense — all key to influencing and shaping policy,” said Dr. Kanwal.
Dr. El-Serag’s term as AGA president concludes May 2020. Follow him on twitter at @SeragHashem.
AGA journals select new editorial fellows
Congrats to the six GIs selected for this competitive program.
The AGA journals – Gastroenterology, Clinical Gastroenterology and Hepatology (CGH), and Cellular and Molecular Gastroenterology and Hepatology (CMGH) – are pleased to announce their 2019-2020 editorial fellows.
Gastroenterology
Feng Su, MD
University of Washington, Seattle
Victoria Weis, PhD
Wake Forest University, Winston-Salem, N.C.
CGH
Austin Chiang, MD, MPH
Jefferson Medical College, Philadelphia, Penn.
Jennifer Kolb, MD
University of Colorado at Denver, Aurora
CMGH
Cambrian Liu, PhD
The Saban Research Institute, Children’s Hospital Los Angeles, Calif.
Tirthadipa Pradhan-Sundd, PhD
University of Pittsburgh, Penn.
The editorial fellows will be mentored on their respective journals’ editorial processes, including peer review and the publication process from manuscript submission to acceptance. They will participate in discussions and conferences with the boards of editors and work closely with the AGA editorial staff. Additionally, the fellows will participate in AGA’s new reviewer education program and will also be offered the opportunity to contribute content to their respective journals. The newly expanded program builds on the success of the previous 2 years when Gastroenterology had an editorial fellow.
The journals’ board of editors and editorial staff congratulate the fellows and are excited to work with them over the next year.
Get to know this rock star IBS researcher and mom
AGA Research Foundation pilot awards are an invaluable tool for investigators – they provide seed funding to explore promising new lines of research and generate preliminary data for larger grants. So, when Meenakshi Rao, MD, PhD, received the 2016 AGA–Takeda Pharmaceuticals International Research Scholar Award in Neurogastroenterology, she was able to double down on a project to identify why men and women with irritable bowel syndrome (IBS), the most common but least understood of all digestive disorders, report different symptoms and respond differently to treatment. Based on her recent accomplishments, we’re excited for you to get to know Dr. Rao, assistant professor of pediatrics at Harvard Medical School, Boston, and our AGA Research Foundation researcher of the month.
The Rao lab AGA-funded project focused on building upon Dr. Rao’s previous findings, which showed that disrupting nerves in the bowel had vastly different effects on males and females. These surprising results led Dr. Rao to explore whether sex hormones, such as testosterone and estrogen, might regulate how well things move through the bowel. Dr. Rao believes that identifying the underlying causes for sex differences in bowel function could lead to more effective and personalized treatments for patients with IBS. You can read the specifics of Dr. Rao’s research in the October 2017 issue of Gastroenterology and the October 2018 issue of Journal of Neuroscience.
IBS symptoms in women more typically involve constipation while young men with IBS more commonly report diarrhea. Over time, as men age, however, they tend to experience more constipation, Dr. Rao said. “Sex hormones might be signaling directly to the nerves in our gut and playing a role in these sex differences,” Dr. Rao said. “It might mean we can’t think of this as one disorder. IBS in a male may be different than IBS in a female, and that could change how we approach diagnosis and treatment.”
The AGA grant laid the groundwork for Dr. Rao’s findings, which led to a new understanding of how different types of cells in the gut nervous system regulate bowel functions – and how this regulation is different in males and females. The AGA grant helped Dr. Rao secure funding from the National Institutes of Health to launch new projects focused on how disruption of the gut nervous system causes disease.
Dr. Rao received the AGA award in 2015, when her son, Avinash, was aged 2 years. She acknowledged the delicate balancing act of raising a family and advancing her research.
“A lot of things were happening at once,” she said. “As a young parent, having the support of this award and having a technician (made possible by the award) made a big difference.”
Her son, now 5 years old, is growing up in a science-centric household because Dr. Rao’s husband is also a scientist. Not surprisingly, Dr. Rao says, her son is becoming a budding scientist.
“He talks about experiments all the time,” she says. “He even articulated to me the other day why we work on mice to learn how to help people. I never taught him that. I was floored.”
Five new GI technologies to know
The AGA Tech Summit Shark Tank is our annual reminder that the field of GI is ripe for innovation. Continue reading for an overview of the five new technologies pitched to our panel of sharks.
The smart toilet seat. A toilet seat developed by Toi Labs, called TrueLoo, is equipped with lighting and cameras that capture images of bowel movements and urination for subsequent analysis. The company describes TrueLoo as a low-cost disease-screening tool that has major potential for early detection of conditions ranging from dehydration to gastrointestinal cancer.
AI to aid screening endoscopy. A new tool called Ultivision, being developed by the startup Docbot, was described as a strategy to employ artificial intelligence (AI) to aid endoscopists in screening for dysplasia in either screening colonoscopy or in surveillance of Barrett’s esophagus. The tool integrates with existing endoscopic tools. As tissue is visualized, the AI is programmed to highlight suspected dysplasia with a colored box to alert the endoscopist.
Obesity phenotyping tool. The Pheno Test, developed by Phenomix Sciences, applies “multi-omics” to a blood-based test to separate patients with obesity into four phenotypes: hungry brain (satiation signal is impaired), hungry gut (signals to eat are upregulated), emotional hunger (psychological reasons drive eating behavior), and slow metabolism (failure to burn fat at normal rates). With this knowledge, treatment can be tailored appropriately leading to better outcomes.
Capsule diagnostic tool. The Atmo Gas Capsule from Atmo Biosciences is an ingestible capsule that measures gases at the source, which can accelerate the diagnosis of diseases such as IBS and inflammatory bowel disease (IBD). According to the company, this technique is highly accurate and offers an alternative to more invasive and expensive diagnostic tools.
Winner: “all-in-one” IBD app. Our Shark Tank winner by both popular vote from AGA Tech Summit attendees and the six-member Shark Tank panel was Oshi Health, selected for its IBD app. The app allows patients to track symptoms, a first step in understanding personalized flare pattern, as well as find resources to learn about their disease and communicate with other patients about their experiences. In a future iteration, information gathered by the app will be made available to physicians to provide current information about disease status to better individualize therapy.
2020 Crohn’s & Colitis Congress now open for registration
Join the Crohn’s & Colitis Foundation and AGA next January in Austin, Tex., for the premier conference on IBD.
The Crohn’s & Colitis Congress combines the strengths of the nation’s leading IBD patient organization, the Crohn’s & Colitis Foundation, and the premier GI professional organization, AGA, to bring together IBD professionals, across all disciplines, to transform IBD care.
The 2020 Congress Committee Chair David T. Rubin, MD, AGAF, University of Chicago, and Cochair Uma Mahadevan, MD, AGAF, University of California, San Francisco, lead a faculty that includes thought leaders in the fields of GI, research investigation, surgery, pediatrics, advanced practice, IBD nursing, diet and nutrition, mental health, radiology, and pathology.
The congress’s agenda includes main sessions that will emphasize case studies and panel discussions. There will also be parallel sessions on basic and translational science for senior and junior investigators. In addition, opening breakout sessions, taking place Jan. 23, will be available for selection free of charge.
Attendees of the 2020 congress will be able to meet with IBD leaders, discover different perspectives, leave with practical information they can immediately implement to take care of their next IBD patient and hear what’s on the horizon in potential treatment.
There will also be plenty of social events and plenty of time to build a strong network, including a Friday night Welcome Reception that should not be missed.
In addition, the 2020 congress is taking place in Austin, Tex. The capital of Texas and the Live Music Capital of the World, Austin is famous for its inspiring and enticing entertainment, culture, cuisine, and outdoor settings. Make a week of it and enjoy all Austin has to offer.
Early-bird registration ends Sept. 18. General abstract submissions for basic, translational, and clinical research begin Aug. 28 and end Oct. 23. To learn more and register, visit www.crohnscolitiscongress.org.
AGA welcomes new president, Hashem B. El-Serag, MD, MPH, AGAF
Hashem B. El-Serag, MD, MPH, AGAF, began his term as the 114th president of the AGA Institute at Digestive Disease Week® (DDW 2019).
Dr. El-Serag is former editor in chief of Clinical Gastroenterology and Hepatology. He currently serves as chair of the department of medicine at Baylor College of Medicine, Houston, following a decade leading and expanding Baylor’s gastroenterology and hepatology section. He is one of the few academic gastroenterologists serving as a chair of a department of medicine in the United States.
Originally Palestinian, Dr. El-Serag became a U.S. citizen in the early 2000s after medical school in Libya. He completed his training at community hospitals in the United States. His path from Benghazi to Baylor is described in the May issue of Gastroenterology by Baylor colleague Dr. Fasiha Kanwal.
“I firmly believe that the success I achieved in the United States would not have been possible anywhere else in the world, and it is as much a testament to the accepting society and medical system as to whatever intrinsic ability or skill I have,” noted Dr. El-Serag.
The major focus of Dr. El-Serag’s scholarly work is the epidemiology and clinical outcomes of hepatocellular carcinoma. Much of the modern literature on this topic includes his more than 100 publications. Since 2014, Dr. El-Serag has been named by Thomson Reuter as among the top 1% of clinical scientists.
Dr. El-Serag “is an innovative scientist, a compassionate physician, and a gifted educator. He is a relentless advocate of science and training, with an astute political sense — all key to influencing and shaping policy,” said Dr. Kanwal.
Dr. El-Serag’s term as AGA president concludes May 2020. Follow him on twitter at @SeragHashem.
Calendar
For more information about upcoming events and award deadlines, please visit http://agau.gastro.org and http://www.gastro.org/research-funding.
UPCOMING EVENTS
Aug. 9-10, 2019
2019 Freston Conference: Food at the Intersection of Gut Health and Disease
GI clinicians and allied health professionals are increasingly focused on how nutrients influence GI physiology and how diet can promote sound gut health. In response to this growing body of knowledge, the 2019 James W. Freston Conference — Food at the Intersection of Gut Health and Disease, Aug. 9-10, 2019, in Chicago — will examine how nutrition management therapies can combat GI disorders such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and celiac disease and how diet supports improvement across the care continuum.
Chicago, Illinois
Aug. 9–11, 2019
2019 Principles of GI for the NP and PA
The Principles of Gastroenterology for the Nurse Practitioner and Physician Assistant (NPPA) is the medical industry’s premiere course guiding and enabling nurse practitioners and physician assistants with the intricacies of identifying, treating, and managing GI disorders. Designed and taught by expert clinicians and advanced practice providers, NPPA provides the latest insights, knowledge, and research on how to improve GI patient care. Attendees will leave with stronger diagnostic and therapeutic skills, a more robust professional network, and an enhanced value for their practices.
Chicago, Illinois
Sept. 18-19, 2019; Oct. 9-10. 2019
Two-Day, In-Depth Coding Seminar by McVey Associates, Inc.
Become a certified GI coder with a two-day, in-depth training course provided by McVey Associates, Inc.
Atlanta, GA (9/18-19); Las Vegas, NV (10/9-10)
Oct. 4, 2019
2019 AGA Partners in Value
Join GI trailblazers and leaders from AGA and DHPA to network and discuss strategies that will help your practice succeed in the changing business of health care. Leave equipped to make better decisions for the future.
Chicago, Illinois
May 2-5, 2020
Digestive Disease Week® (DDW)
Digestive Disease Week® (DDW) is the world’s leading educational forum for academicians, clinicians, researchers, students, and trainees working in gastroenterology, hepatology, GI endoscopy, gastrointestinal surgery, and related fields. Whether you work in patient care, research, education, or administration, the DDW program offers something for you. Abstract submissions will be due on Dec. 1, and registration will open in January 2020.
Chicago, Illinois
AWARDS APPLICATION DEADLINES
AGA-Elsevier Pilot Research Award
This award provides $30,000 for 1 year to a recipient at any career stage performing research in gastroenterology- or hepatology-related areas.
Application Deadline: Sept. 4, 2019
AGA-Allergan Foundation Pilot Research Award in Inflammatory Bowel Disease
This award provides $30,000 for 1 year to an investigator at any career stage researching the pathophysiology and/or treatment of inflammatory bowel disease (IBD).
Application Deadline: Sept. 4, 2019
AGA-Allergan Foundation Pilot Research Award in Nonalcoholic Fatty Liver Disease
This award provides $30,000 for 1 year to an investigator at any career stage researching the pathophysiology and/or treatment of nonalcoholic fatty liver disease (NAFLD).
Application Deadline: Sept. 4, 2019
AGA-Pfizer Pilot Research Award in Inflammatory Bowel Disease
This award provides $30,000 for 1 year to recipients at any career stage researching new directions focused on improving the diagnosis and treatment of inflammatory bowel disease.
Application Deadline: Sept. 4, 2019
AGA-Rome Foundation Functional GI and Motility Disorders Pilot Research Award
This award provides $30,000 for 1 year to a recipient at any career stage performing clinical or translational research pertaining to functional GI and motility disorders.
Application Deadline: Sept. 4, 2019
AGA Research Scholar Award (RSA)
This award provides $100,000 per year for 3 years (total $300,000) to early career faculty (i.e., investigator, instructor, research associate or equivalent) working toward an independent career in digestive disease research.
Application Deadline: Nov. 13, 2019
AGA-Gastric Cancer Foundation Ben Feinstein Memorial Research Scholar Award in Gastric Cancer
This award provides $100,000 per year for 3 years (total $300,000) to early career faculty (i.e., investigator, instructor, research associate or equivalent) working toward an independent career in gastric cancer research. Research involving precancerous lesions will be considered if relevance to gastric cancer is explicitly outlined.
Application Deadline: Nov. 13, 2019
AGA-Takeda Pharmaceuticals Research Scholar Award in Inflammatory Bowel Disease
This award provides $100,000 per year for 3 years (total $300,000) to a young investigator, instructor, research associate or equivalent working toward an independent career in inflammatory bowel disease research.
Application Deadline: Nov. 13, 2019
AGA Fellow Abstract Award
This $500 travel award supports recipients who are MD, PhD or equivalent fellows giving abstract-based oral or poster presentations at Digestive Disease Week® (DDW). The top-scoring abstract will be designated the Fellow Abstract of the Year and receive a $1,000 award.
Application Deadline: Feb. 26, 2020
AGA Student Abstract Award
This $500 travel award supports recipients who are graduate students, medical students, or medical residents (residents up to postgraduate year three) giving abstract-based oral or poster presentations at Digestive Disease Week® (DDW).
Application Deadline: Feb. 26, 2020
AGA-Moti L. & Kamla Rustgi International Travel Awards
This $750 travel award supports recipients who are young (i.e., 35 years of age or younger at the time of DDW) basic, translational, or clinical investigators residing outside North America to support travel and related expenses to attend Digestive Disease Week® (DDW).
Application Deadline: Feb. 26, 2020
For more information about upcoming events and award deadlines, please visit http://agau.gastro.org and http://www.gastro.org/research-funding.
UPCOMING EVENTS
Aug. 9-10, 2019
2019 Freston Conference: Food at the Intersection of Gut Health and Disease
GI clinicians and allied health professionals are increasingly focused on how nutrients influence GI physiology and how diet can promote sound gut health. In response to this growing body of knowledge, the 2019 James W. Freston Conference — Food at the Intersection of Gut Health and Disease, Aug. 9-10, 2019, in Chicago — will examine how nutrition management therapies can combat GI disorders such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and celiac disease and how diet supports improvement across the care continuum.
Chicago, Illinois
Aug. 9–11, 2019
2019 Principles of GI for the NP and PA
The Principles of Gastroenterology for the Nurse Practitioner and Physician Assistant (NPPA) is the medical industry’s premiere course guiding and enabling nurse practitioners and physician assistants with the intricacies of identifying, treating, and managing GI disorders. Designed and taught by expert clinicians and advanced practice providers, NPPA provides the latest insights, knowledge, and research on how to improve GI patient care. Attendees will leave with stronger diagnostic and therapeutic skills, a more robust professional network, and an enhanced value for their practices.
Chicago, Illinois
Sept. 18-19, 2019; Oct. 9-10. 2019
Two-Day, In-Depth Coding Seminar by McVey Associates, Inc.
Become a certified GI coder with a two-day, in-depth training course provided by McVey Associates, Inc.
Atlanta, GA (9/18-19); Las Vegas, NV (10/9-10)
Oct. 4, 2019
2019 AGA Partners in Value
Join GI trailblazers and leaders from AGA and DHPA to network and discuss strategies that will help your practice succeed in the changing business of health care. Leave equipped to make better decisions for the future.
Chicago, Illinois
May 2-5, 2020
Digestive Disease Week® (DDW)
Digestive Disease Week® (DDW) is the world’s leading educational forum for academicians, clinicians, researchers, students, and trainees working in gastroenterology, hepatology, GI endoscopy, gastrointestinal surgery, and related fields. Whether you work in patient care, research, education, or administration, the DDW program offers something for you. Abstract submissions will be due on Dec. 1, and registration will open in January 2020.
Chicago, Illinois
AWARDS APPLICATION DEADLINES
AGA-Elsevier Pilot Research Award
This award provides $30,000 for 1 year to a recipient at any career stage performing research in gastroenterology- or hepatology-related areas.
Application Deadline: Sept. 4, 2019
AGA-Allergan Foundation Pilot Research Award in Inflammatory Bowel Disease
This award provides $30,000 for 1 year to an investigator at any career stage researching the pathophysiology and/or treatment of inflammatory bowel disease (IBD).
Application Deadline: Sept. 4, 2019
AGA-Allergan Foundation Pilot Research Award in Nonalcoholic Fatty Liver Disease
This award provides $30,000 for 1 year to an investigator at any career stage researching the pathophysiology and/or treatment of nonalcoholic fatty liver disease (NAFLD).
Application Deadline: Sept. 4, 2019
AGA-Pfizer Pilot Research Award in Inflammatory Bowel Disease
This award provides $30,000 for 1 year to recipients at any career stage researching new directions focused on improving the diagnosis and treatment of inflammatory bowel disease.
Application Deadline: Sept. 4, 2019
AGA-Rome Foundation Functional GI and Motility Disorders Pilot Research Award
This award provides $30,000 for 1 year to a recipient at any career stage performing clinical or translational research pertaining to functional GI and motility disorders.
Application Deadline: Sept. 4, 2019
AGA Research Scholar Award (RSA)
This award provides $100,000 per year for 3 years (total $300,000) to early career faculty (i.e., investigator, instructor, research associate or equivalent) working toward an independent career in digestive disease research.
Application Deadline: Nov. 13, 2019
AGA-Gastric Cancer Foundation Ben Feinstein Memorial Research Scholar Award in Gastric Cancer
This award provides $100,000 per year for 3 years (total $300,000) to early career faculty (i.e., investigator, instructor, research associate or equivalent) working toward an independent career in gastric cancer research. Research involving precancerous lesions will be considered if relevance to gastric cancer is explicitly outlined.
Application Deadline: Nov. 13, 2019
AGA-Takeda Pharmaceuticals Research Scholar Award in Inflammatory Bowel Disease
This award provides $100,000 per year for 3 years (total $300,000) to a young investigator, instructor, research associate or equivalent working toward an independent career in inflammatory bowel disease research.
Application Deadline: Nov. 13, 2019
AGA Fellow Abstract Award
This $500 travel award supports recipients who are MD, PhD or equivalent fellows giving abstract-based oral or poster presentations at Digestive Disease Week® (DDW). The top-scoring abstract will be designated the Fellow Abstract of the Year and receive a $1,000 award.
Application Deadline: Feb. 26, 2020
AGA Student Abstract Award
This $500 travel award supports recipients who are graduate students, medical students, or medical residents (residents up to postgraduate year three) giving abstract-based oral or poster presentations at Digestive Disease Week® (DDW).
Application Deadline: Feb. 26, 2020
AGA-Moti L. & Kamla Rustgi International Travel Awards
This $750 travel award supports recipients who are young (i.e., 35 years of age or younger at the time of DDW) basic, translational, or clinical investigators residing outside North America to support travel and related expenses to attend Digestive Disease Week® (DDW).
Application Deadline: Feb. 26, 2020
For more information about upcoming events and award deadlines, please visit http://agau.gastro.org and http://www.gastro.org/research-funding.
UPCOMING EVENTS
Aug. 9-10, 2019
2019 Freston Conference: Food at the Intersection of Gut Health and Disease
GI clinicians and allied health professionals are increasingly focused on how nutrients influence GI physiology and how diet can promote sound gut health. In response to this growing body of knowledge, the 2019 James W. Freston Conference — Food at the Intersection of Gut Health and Disease, Aug. 9-10, 2019, in Chicago — will examine how nutrition management therapies can combat GI disorders such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and celiac disease and how diet supports improvement across the care continuum.
Chicago, Illinois
Aug. 9–11, 2019
2019 Principles of GI for the NP and PA
The Principles of Gastroenterology for the Nurse Practitioner and Physician Assistant (NPPA) is the medical industry’s premiere course guiding and enabling nurse practitioners and physician assistants with the intricacies of identifying, treating, and managing GI disorders. Designed and taught by expert clinicians and advanced practice providers, NPPA provides the latest insights, knowledge, and research on how to improve GI patient care. Attendees will leave with stronger diagnostic and therapeutic skills, a more robust professional network, and an enhanced value for their practices.
Chicago, Illinois
Sept. 18-19, 2019; Oct. 9-10. 2019
Two-Day, In-Depth Coding Seminar by McVey Associates, Inc.
Become a certified GI coder with a two-day, in-depth training course provided by McVey Associates, Inc.
Atlanta, GA (9/18-19); Las Vegas, NV (10/9-10)
Oct. 4, 2019
2019 AGA Partners in Value
Join GI trailblazers and leaders from AGA and DHPA to network and discuss strategies that will help your practice succeed in the changing business of health care. Leave equipped to make better decisions for the future.
Chicago, Illinois
May 2-5, 2020
Digestive Disease Week® (DDW)
Digestive Disease Week® (DDW) is the world’s leading educational forum for academicians, clinicians, researchers, students, and trainees working in gastroenterology, hepatology, GI endoscopy, gastrointestinal surgery, and related fields. Whether you work in patient care, research, education, or administration, the DDW program offers something for you. Abstract submissions will be due on Dec. 1, and registration will open in January 2020.
Chicago, Illinois
AWARDS APPLICATION DEADLINES
AGA-Elsevier Pilot Research Award
This award provides $30,000 for 1 year to a recipient at any career stage performing research in gastroenterology- or hepatology-related areas.
Application Deadline: Sept. 4, 2019
AGA-Allergan Foundation Pilot Research Award in Inflammatory Bowel Disease
This award provides $30,000 for 1 year to an investigator at any career stage researching the pathophysiology and/or treatment of inflammatory bowel disease (IBD).
Application Deadline: Sept. 4, 2019
AGA-Allergan Foundation Pilot Research Award in Nonalcoholic Fatty Liver Disease
This award provides $30,000 for 1 year to an investigator at any career stage researching the pathophysiology and/or treatment of nonalcoholic fatty liver disease (NAFLD).
Application Deadline: Sept. 4, 2019
AGA-Pfizer Pilot Research Award in Inflammatory Bowel Disease
This award provides $30,000 for 1 year to recipients at any career stage researching new directions focused on improving the diagnosis and treatment of inflammatory bowel disease.
Application Deadline: Sept. 4, 2019
AGA-Rome Foundation Functional GI and Motility Disorders Pilot Research Award
This award provides $30,000 for 1 year to a recipient at any career stage performing clinical or translational research pertaining to functional GI and motility disorders.
Application Deadline: Sept. 4, 2019
AGA Research Scholar Award (RSA)
This award provides $100,000 per year for 3 years (total $300,000) to early career faculty (i.e., investigator, instructor, research associate or equivalent) working toward an independent career in digestive disease research.
Application Deadline: Nov. 13, 2019
AGA-Gastric Cancer Foundation Ben Feinstein Memorial Research Scholar Award in Gastric Cancer
This award provides $100,000 per year for 3 years (total $300,000) to early career faculty (i.e., investigator, instructor, research associate or equivalent) working toward an independent career in gastric cancer research. Research involving precancerous lesions will be considered if relevance to gastric cancer is explicitly outlined.
Application Deadline: Nov. 13, 2019
AGA-Takeda Pharmaceuticals Research Scholar Award in Inflammatory Bowel Disease
This award provides $100,000 per year for 3 years (total $300,000) to a young investigator, instructor, research associate or equivalent working toward an independent career in inflammatory bowel disease research.
Application Deadline: Nov. 13, 2019
AGA Fellow Abstract Award
This $500 travel award supports recipients who are MD, PhD or equivalent fellows giving abstract-based oral or poster presentations at Digestive Disease Week® (DDW). The top-scoring abstract will be designated the Fellow Abstract of the Year and receive a $1,000 award.
Application Deadline: Feb. 26, 2020
AGA Student Abstract Award
This $500 travel award supports recipients who are graduate students, medical students, or medical residents (residents up to postgraduate year three) giving abstract-based oral or poster presentations at Digestive Disease Week® (DDW).
Application Deadline: Feb. 26, 2020
AGA-Moti L. & Kamla Rustgi International Travel Awards
This $750 travel award supports recipients who are young (i.e., 35 years of age or younger at the time of DDW) basic, translational, or clinical investigators residing outside North America to support travel and related expenses to attend Digestive Disease Week® (DDW).
Application Deadline: Feb. 26, 2020
August 2019 – ICYMI
Gastroenterology
Promoting leadership by women in gastroenterology: Lessons learned and future directions. Pascua M et al. 2019 May;156(6):1548-52. doi. org/10.1053/j.gastro.2019.03.012.
How to incorporate esophageal manometry teaching in your fellowship program. Kraft C et al. 2019 June;156(8):2120-3. doi. org/10.1053/j.gastro.2019.04.024.
How to incorporate bariatric training into your fellowship program. Jirapinyo P et al. 2019 July;157(1):9-13. doi. org/10.1053/j.gastro.2019.05.034.
Clin Gastroenterol Hepatol.
Preparing for large-scale disruptions in health care delivery: Nursing strikes and beyond. Allen JI et al. 2019 July;17(8):1424-7. doi. org/10.1016/j.cgh.2019.02.001.
Optimal management of malignant polyps, from endoscopic assessment and resection to decisions about surgery. Rex DK et al. 2019 July;17(8):1428-37. doi. org/10.1016/j.cgh.2018.09.040.
Bowel cleansing strategies after suboptimal bowel preparation. Sharara AI et al. 2019 June;17(7):1239-41. doi. org/10.1016/j.cgh.2018.12.042.
Holding gastroenterologists accountable for colonoscopy through MACRA episode–based cost measure. Siddique SM et al. 2019 May;17(6):1015-8. doi. org/10.1016/j.cgh.2019.01.009.
Endoscopic mucosal resection vs endoscopic submucosal dissection for Barrett’s esophagus and colorectal neoplasia. Yang D et al. May;17(6):1019-28. doi. org/10.1016/j.cgh.2018.09.030.
Metal biliary stents in benign disease. Haseeb A et al. 2019 May;17(6):1029-32. doi. org/10.1016/j.cgh.2018.12.010.
Cell Mol Gastroenterol Hepatol.
Rigor, reproducibility, and responsibility: A quantum of solace. Turner JR. 2019;7(4):869-71. doi. org/10.1016/j.jcmgh.2019.03.006.
Gastroenterology
Promoting leadership by women in gastroenterology: Lessons learned and future directions. Pascua M et al. 2019 May;156(6):1548-52. doi. org/10.1053/j.gastro.2019.03.012.
How to incorporate esophageal manometry teaching in your fellowship program. Kraft C et al. 2019 June;156(8):2120-3. doi. org/10.1053/j.gastro.2019.04.024.
How to incorporate bariatric training into your fellowship program. Jirapinyo P et al. 2019 July;157(1):9-13. doi. org/10.1053/j.gastro.2019.05.034.
Clin Gastroenterol Hepatol.
Preparing for large-scale disruptions in health care delivery: Nursing strikes and beyond. Allen JI et al. 2019 July;17(8):1424-7. doi. org/10.1016/j.cgh.2019.02.001.
Optimal management of malignant polyps, from endoscopic assessment and resection to decisions about surgery. Rex DK et al. 2019 July;17(8):1428-37. doi. org/10.1016/j.cgh.2018.09.040.
Bowel cleansing strategies after suboptimal bowel preparation. Sharara AI et al. 2019 June;17(7):1239-41. doi. org/10.1016/j.cgh.2018.12.042.
Holding gastroenterologists accountable for colonoscopy through MACRA episode–based cost measure. Siddique SM et al. 2019 May;17(6):1015-8. doi. org/10.1016/j.cgh.2019.01.009.
Endoscopic mucosal resection vs endoscopic submucosal dissection for Barrett’s esophagus and colorectal neoplasia. Yang D et al. May;17(6):1019-28. doi. org/10.1016/j.cgh.2018.09.030.
Metal biliary stents in benign disease. Haseeb A et al. 2019 May;17(6):1029-32. doi. org/10.1016/j.cgh.2018.12.010.
Cell Mol Gastroenterol Hepatol.
Rigor, reproducibility, and responsibility: A quantum of solace. Turner JR. 2019;7(4):869-71. doi. org/10.1016/j.jcmgh.2019.03.006.
Gastroenterology
Promoting leadership by women in gastroenterology: Lessons learned and future directions. Pascua M et al. 2019 May;156(6):1548-52. doi. org/10.1053/j.gastro.2019.03.012.
How to incorporate esophageal manometry teaching in your fellowship program. Kraft C et al. 2019 June;156(8):2120-3. doi. org/10.1053/j.gastro.2019.04.024.
How to incorporate bariatric training into your fellowship program. Jirapinyo P et al. 2019 July;157(1):9-13. doi. org/10.1053/j.gastro.2019.05.034.
Clin Gastroenterol Hepatol.
Preparing for large-scale disruptions in health care delivery: Nursing strikes and beyond. Allen JI et al. 2019 July;17(8):1424-7. doi. org/10.1016/j.cgh.2019.02.001.
Optimal management of malignant polyps, from endoscopic assessment and resection to decisions about surgery. Rex DK et al. 2019 July;17(8):1428-37. doi. org/10.1016/j.cgh.2018.09.040.
Bowel cleansing strategies after suboptimal bowel preparation. Sharara AI et al. 2019 June;17(7):1239-41. doi. org/10.1016/j.cgh.2018.12.042.
Holding gastroenterologists accountable for colonoscopy through MACRA episode–based cost measure. Siddique SM et al. 2019 May;17(6):1015-8. doi. org/10.1016/j.cgh.2019.01.009.
Endoscopic mucosal resection vs endoscopic submucosal dissection for Barrett’s esophagus and colorectal neoplasia. Yang D et al. May;17(6):1019-28. doi. org/10.1016/j.cgh.2018.09.030.
Metal biliary stents in benign disease. Haseeb A et al. 2019 May;17(6):1029-32. doi. org/10.1016/j.cgh.2018.12.010.
Cell Mol Gastroenterol Hepatol.
Rigor, reproducibility, and responsibility: A quantum of solace. Turner JR. 2019;7(4):869-71. doi. org/10.1016/j.jcmgh.2019.03.006.
June 2019 - Question 2
Q2. Correct Answer: C
Rationale
This patient has a main duct IPMN, which has a high potential for malignant transformation and should be resected if possible. Resection is also indicated for branch-duct IPMN's, which are symptomatic (e.g. pancreatitis), associated with obstructive jaundice or main duct involvement, have a solid component within the cyst, or have concerning features on EUS-FNA.
Reference
1. Elta GH, et al, ACG Clinical Guideline: Diagnosis and Management of Pancreatic Cysts. Am J Gastroenterol. 2018;113:464-79.
ginews@gastro.org
Q2. Correct Answer: C
Rationale
This patient has a main duct IPMN, which has a high potential for malignant transformation and should be resected if possible. Resection is also indicated for branch-duct IPMN's, which are symptomatic (e.g. pancreatitis), associated with obstructive jaundice or main duct involvement, have a solid component within the cyst, or have concerning features on EUS-FNA.
Reference
1. Elta GH, et al, ACG Clinical Guideline: Diagnosis and Management of Pancreatic Cysts. Am J Gastroenterol. 2018;113:464-79.
ginews@gastro.org
Q2. Correct Answer: C
Rationale
This patient has a main duct IPMN, which has a high potential for malignant transformation and should be resected if possible. Resection is also indicated for branch-duct IPMN's, which are symptomatic (e.g. pancreatitis), associated with obstructive jaundice or main duct involvement, have a solid component within the cyst, or have concerning features on EUS-FNA.
Reference
1. Elta GH, et al, ACG Clinical Guideline: Diagnosis and Management of Pancreatic Cysts. Am J Gastroenterol. 2018;113:464-79.
ginews@gastro.org
Q2. A 64-year-old male with a recent history of acute pancreatitis has a dilated main pancreatic duct with prominent side branch lesions seen on CT scan. Endoscopic evaluation reveals mucus extruding from a dilated ampulla.
June 2019 - Question 1
Q1. Correct Answer: D
Rationale
The severe reflux may be due to the hiatal hernia and worsened by the obesity. This patient has medically complicated obesity and thus bariatric surgery is an option. A gastric bypass in this situation offers the best anti-reflux procedure for this patient. A fundoplication in the setting of obesity has a higher rate of recurrence of symptoms (Answers A, B). While a gastric sleeve is an option for the obesity, a gastric sleeve (Answer E) may cause de novo reflux or worsen pre-existing symptoms. Magnetic sphincter augmentation (Answer C) has demonstrated promising results in patients with a BMI less than 35 and hiatal hernia less than 3 cm. Data are not available for patients with higher BMIs.
References
1. Abdelrahman T, Latif A, Chan DS, et al. Outcomes after laparoscopic anti-reflux surgery related to obesity: A systematic review and meta-analysis. Int J Surg. 2018 Mar;51:76-82.
2. Stenard F, Iannelli A. Laparoscopic sleeve gastrectomy and gastroesophageal reflux. World J Gastroenterol. 2015 Sep 28;21(36):10348-57.
Q1. Correct Answer: D
Rationale
The severe reflux may be due to the hiatal hernia and worsened by the obesity. This patient has medically complicated obesity and thus bariatric surgery is an option. A gastric bypass in this situation offers the best anti-reflux procedure for this patient. A fundoplication in the setting of obesity has a higher rate of recurrence of symptoms (Answers A, B). While a gastric sleeve is an option for the obesity, a gastric sleeve (Answer E) may cause de novo reflux or worsen pre-existing symptoms. Magnetic sphincter augmentation (Answer C) has demonstrated promising results in patients with a BMI less than 35 and hiatal hernia less than 3 cm. Data are not available for patients with higher BMIs.
References
1. Abdelrahman T, Latif A, Chan DS, et al. Outcomes after laparoscopic anti-reflux surgery related to obesity: A systematic review and meta-analysis. Int J Surg. 2018 Mar;51:76-82.
2. Stenard F, Iannelli A. Laparoscopic sleeve gastrectomy and gastroesophageal reflux. World J Gastroenterol. 2015 Sep 28;21(36):10348-57.
Q1. Correct Answer: D
Rationale
The severe reflux may be due to the hiatal hernia and worsened by the obesity. This patient has medically complicated obesity and thus bariatric surgery is an option. A gastric bypass in this situation offers the best anti-reflux procedure for this patient. A fundoplication in the setting of obesity has a higher rate of recurrence of symptoms (Answers A, B). While a gastric sleeve is an option for the obesity, a gastric sleeve (Answer E) may cause de novo reflux or worsen pre-existing symptoms. Magnetic sphincter augmentation (Answer C) has demonstrated promising results in patients with a BMI less than 35 and hiatal hernia less than 3 cm. Data are not available for patients with higher BMIs.
References
1. Abdelrahman T, Latif A, Chan DS, et al. Outcomes after laparoscopic anti-reflux surgery related to obesity: A systematic review and meta-analysis. Int J Surg. 2018 Mar;51:76-82.
2. Stenard F, Iannelli A. Laparoscopic sleeve gastrectomy and gastroesophageal reflux. World J Gastroenterol. 2015 Sep 28;21(36):10348-57.
Q1. A 56-year-old female with a BMI of 42 (kg/m2), diabetes, and hyperlipidemia presents with a 5-cm hiatal hernia. She has symptoms of heartburn during the day and significant nocturnal regurgitation such that she is sleeping in a recliner at night.
Evolving Sex and Gender in Electronic Health Records
Providing consistent and high-quality services to gender diverse patients is a top priority for health care systems, including the Veterans Health Administration (VHA).1 Over the past decade, awareness of transgender and gender nonconforming (TGNC) people in the US has increased. Gender identity refers to a person’s inner sense of where that person belongs on a continuum of masculine to androgynous to feminine traits. This identity range can additionally include nonbinary identifications, such as “gender fluid” or “genderqueer.” A goal of patient-centered care is for health care providers (HCPs) to refer to TGNC individuals, like their cisgender counterparts, according to their gender identity. Gender identity for TGNC individuals may be different from their birth sex. Birth sex, commonly referred to as “sex assigned at birth,” is the biologic and physiologic characteristics that are reflected on a person’s original birth certificate and described as male or female.
Background
In the electronic health record (EHR), birth sex is an important, structured variable that is used to facilitate effective patient care that is efficient, equitable, and patient-centered. Birth sex in an EHR often is used to cue automatic timely generation of health screens (eg, pap smears, prostate exams) and calculation of medication dosages and laboratory test ranges by adjusting for a person’s typical hormonal history and anatomy.
Gender identity fields are independently helpful to include in the EHR, because clinicians can use this information to ensure proper pronoun use and avoid misgendering a patient. Additionally, the gender identity field informs HCPs who may conduct more frequent or different health screenings to evaluate specific health risks that are more prevalent in gender minority (ie, lesbian, gay, bisexual) patients.2,3
EHRs rely on structured data elements to standardize data about patients for clinical care, quality improvement, data sharing, and patient safety.4,5 However, health care organizations are grappling with how to incorporate gender identity and birth sex information into EHRs.3 A 2011 Veterans Health Administration (VHA) directive required staff and providers to address and provide care to veterans based on their gender identity. Like other health systems, VHA had 1 demographic data field in the EHR to indicate birth sex, with no field for gender identity. A HCP could enter gender identity information into a progress note, but this addition might not be noticed by other HCPs. Consequently, staff and providers had no effective way of knowing a veteran’s gender identity from the EHR, which contributed to misgendering TGNC veterans.
With the singular demographic field of sex representing both birth sex and gender identity, some TGNC veterans chose to change their birth sex information to align with their gender identity. This change assured TGNC veterans that staff and providers would not misgender them because the birth sex field is easily observed and would allow providers to use respectful, gender-consistent pronouns when speaking with them. However, changing the birth sex field can misalign natal sex–based clinical reminders, medication dosages, and laboratory test values, which created potential patient safety risks. Thus, birth sex created potential hazards to quality and safety when used as a marker even with other variables—such as current anatomy, height, and weight—for health screenings, medication dosing, and other medical decisions.
In this article, we: (1) outline several patient safety issues that can arise with the birth sex field serving as an indicator for both birth sex and gender identity; (2) present case examples that illustrate the benefits of self-identified gender identity (SIGI) in an EHR; (3) describe the process of work-group development of patient-provider communication tools to improve patient safety; and (4) provide a brief overview of resources rolled out as a part of SIGI. This report serves as a guide for other federal organizations that wish to increase affirmative care and safe practices for transgender consumers. We will provide an overview of the tasks leading up to SIGI implementation, deliverables from the project, and lessons learned.
Veterans Affairs SIGI EHR Field
In 2016, the US Department of Veterans Affairs (VA) began implementing a SIGI demographic field across all EHRs, requiring administrative staff to ask enrolled and new veterans their gender identity (full implementation of SIGI has not yet occurred and will occur when a later EHR upgrade displays SIGI in the EHR). The initiation of SIGI did not change any information in the birth sex field, meaning that some veterans continue to have birth sex field information that results in problematic automatic medical reminders and dosing values. Consequently, the National Center for Patient Safety (NCPS) noted that this discrepancy may be a pertinent patient safety issue. The NCPS and Lesbian, Gay Bisexual, and Transgender (LGBT) Health national program offices worked to provide documentation to TGNC veterans to inform them of the clinical health care implications of having their birth sex demographic field reflect gender identity that is inconsistent with their natal sex (ie, original birth certificate record of sex).
Patient Safety Issues
Conversations between transgender patients and their HCPs about transition goals, necessary medical tests, and laboratory ranges based on their current anatomy and physiology can improve patient safety and satisfaction with medical care. Prior to the availability of the SIGI field, VA facilities varied in their documentation of gender identity in the patient chart. LGBT veteran care coordinators discussed diverse suggestions that ranged from informally documenting SIGI in each progress note to using flags to draw attention to use certain sections of local EHRs. These suggestions, though well intentioned, were not adequate for documenting gender identity at the national level because of regional variations in EHR customization options. Furthermore, the use of flags for drawing clinical attention to gender identity posed a potential for stigma toward patients, given that flags are typically reserved for behavioral or other risk concerns.
Several problems can emerge when HCPs are not equipped with accurate information about patient birth sex and SIGI. For instance, TGNC patients lack a way of being known from clinic to clinic by proper pronouns or self-labels. Providers may misgender veterans, which is a negative experience for TGNC veterans linked with increased barriers to care and decreased frequency of health care visits.4 Moreover, the quality and personalization of care across clinic locations in the facility’s system is variable without a consistent method of documenting birth sex and SIGI. For example, in clinics where the veteran is well known (eg, primary care), staff may be more affirming of the veteran’s gender identity than those in specialty care clinics that lack prior patient contact.
Furthermore, depending on hormone and surgical interventions, some health screenings may be irrelevant for TGNC patients. To determine appropriate health screens and assess potential risks associated with hormone therapy, providers must have access to current information regarding a patient’s physiologic anatomy.6 Health screenings and laboratory results in sophisticated EHRs (ie, EHRs that might autodetermine normative values) may populate incorrect treatment recommendations, such as sex-based medication dosages. Furthermore, laboratory test results could be incorrectly paired with a different assumed hormonal history, potentially putting the patient at risk.
Case Examples
An important element of EHRs facilitating the goal of patient-centered care is that patients have their EHR validate their sense of self, and their providers can use names and pronouns that correspond to the patient’s SIGI. Some patients have spent a great amount of effort altering their name and sex in legal records and may want their birth sex field to conform to their gender identity. To that end, patients may seek to alter their birth sex information so that it is congruent with how they see themselves to affirm their identity, despite patient safety risks. Several scenarios below demonstrate the potential costs and benefits to patients altering birth sex and SIGI in the EHR.
Case 1 Presentation
A young transman is working with his therapist on engaging in self-validating behaviors. This veteran has met with his PCP and informed the provider of his decision to alter the birth sex field in his EHR from female to male.
Ideally, the patient would begin to have regular conversations with his HCPs about his birth sex and gender identity, so that medical professionals can provide relevant screenings and affirm the patient’s gender identity while acknowledging his right to list his birth sex as he chooses. However, particular attention will need to be paid to assuring that natal sex–based health screenings (eg, pap smears, mammograms) are conducted on an appropriate schedule and that the veteran continues to discuss his current anatomy with providers.
Case 2 Presentation
A veteran has a male birth sex, identifies as a transwoman, and uses nongendered plural pronouns “they/them/theirs.” The word “they,” used as a singular pronoun may feel uncomfortable to some providers, but it validates the veteran’s sense of self and helps them feel welcome in the treatment environment. This patient communicated proactively with their HCPs about their transition goals and current hormone use.
They opted to have their birth sex field continue to indicate “male” because they, after a discussion with their PCP, are aware of the health implications of receiving an incorrect dose for their diabetes medication. They understand that having open communication and receiving input from their HCPs is part of good health care.
Case 3 Presentation
A patient with a sexual development disorder (intersex condition) identifies as a man (indicated as “male” in the SIGI field) and had his birth sex field changed to match his gender identity. He now seeks to change his birth sex field back to female, as he has complicated health considerations due to breast cancer.
The veteran thinks it is important that providers know about his intersex condition so that his breast cancer care is as seamless as possible. In particular, although this veteran is comfortable talking about his intersex condition and his identity with his PCP and oncologist, he wants to ensure that all people involved in his care (eg, pharmacists, radiologists) use the correct values in interpreting his medical data. Providers will need to use the female birth sex field for interpreting his medical data but use male pronouns when interacting with the veteran and documenting his care.
These case examples illustrate the need for HCPs to have patient-affirming education and appropriate clinical tools available when speaking to patients about birth sex, SIGI, and the implications of changing birth sex in the EHR. Moreover, these cases highlight that patient health needs may vary over time, due to factors such as perceived costs/benefits of a change in the sex field of the EHR as well as patient comfort with providers.
Current Status of SIGI and EHR
Although having separate fields for birth sex and SIGI in the EHR is ideal, the VHA does not yet have a fully functional SIGI field, and several TGNC veterans have changed their birth sex field to align with their gender identity. Roughly 9,700 patients have diagnostic codes related to transgender care in the VHA, meaning thousands of current patients would potentially benefit from SIGI implementation (John Blosnich, written communication, March 2018). A possible action that the VHA could take with the goal of enhancing patient safety would be to revert the birth sex field of patients who had previously changed the field back to the patient’s original birth sex. However, if this alteration to the EHR were done without the patient’s consent, numerous additional problems would result—including invalidating a veteran’s wishes—potentially driving patients away from receiving health care.
Moreover, in the absence of updated SIGI information (which only the veteran can provide), making a change in the EHR would perpetuate the misgendering of TGNC veterans who have already sought an administrative fix for this problem. Thus, the agency decided to engage patients in a discussion about their decision to keep the birth sex field consistent with their original birth certificate. In cases in which the field had been changed previously, the recommendation is for HCPs to gain patient consent to change the birth sex field back to what was on their original birth certificate. Thus, decisions about what should be listed in the EHR are made by the veteran using an informed decision-making model.
Patient Safety Education Workgroup
To begin the process of disentangling birth sex and SIGI fields in the EHR, 2 work groups were created: a technical work group (coding the patches for SIGI implementation) and a SIGI patient safety education work group. The patient safety education work group was committed to promoting affirmative VA policies that require validation of the gender identity of all veterans and pursuing best practices through clinical guidelines to promote effective, efficient, equitable, and safe veteran care. The patient safety education work group included representatives from all 3 branches of the VA (VHA, Veterans Benefits Administration, and National Cemetery Administration), including clinical media, patient safety, information technology, and education specialists. The group developed trainings for administrative staff about the appropriate ways to ask birth sex and SIGI questions, and how to record veteran-driven responses.
SIGI Fact Sheet
The patient safety education work group examined clinical literature and developed tools for staff and veterans to facilitate effective discussions about the importance and utility of documenting both birth sex and SIGI in the EHR. The patient safety education work group along with media and educational experts created basic key term definition documents to address the importance, purpose, and use of the SIGI field. The patient safety education work group developed 2 documents to facilitate communication between patients and providers.
A 1-page veteran-facing fact sheet was developed that described the differences between birth sex and SIGI fields and how these fields are used in the VA EHR system (Figure 1). In addition, a 1-page HCP-facing fact sheet was designed to inform HCPs that patients may have changed their birth sex in their EHR or might still wish to change their birth sex field, and to inform HCPs of the importance of patient-centered, gender-affirmative care (Figure 2). An additional goal of both documents was to educate veterans and HCPs on how the EHR automatically calculates laboratory results and screening notifications based on birth sex.
Review Process
As part of reviewing and finalizing the SIGI patient fact sheet, the patient safety education work group previewed the document’s content with veterans who provided feedback on drafts to improve comprehension, patient-centered care, and clinical accuracy. For instance, several patients commented that the document should address many gender identities, including intersex identities. As noted in one of the case presentations earlier, individuals who identify as intersex may have changed their birth sex to be consistent with their gender and might benefit from being informed about the EHR’s autocalculation feature. The patient safety education work group adjusted the SIGI patient fact sheet to include individuals who identify as intersex and instructed them to have a conversation with their HCP regarding potential birth sex changes in the EHR.
Much of the veteran feedback to the patient safety education work group reflected veteran concerns, more broadly, about implementation of SIGI. Many veterans were interested in how federal policy changes might affect their benefits package or clinical care within the VA. The SIGI patient fact sheet was a tool for communicating that Department of Defense (DoD) policies, specifically, do not have a bearing on VA care for LGBT veterans. Therefore, SIGI information does not affect service connection or benefits eligibility and is not shared with the DoD. Veterans found this information helpful to see reflected in the SIGI patient fact sheet.
The patient safety education work group also shared the SIGI provider fact sheet with VHA providers before finalizing the content. PCPs gave feedback to improve the specification of patient safety concerns and appropriate readership language. The patient safety education work group adjusted the SIGI provider fact sheet to be inclusive of relevant literature and an e-consultation link for assisting HCPs who are unsure how to proceed with a patient.
Implementation
The patient safety education work group also developed several materials to provide information about the birth sex and SIGI fields in the EHR. Because the SIGI demographic field is new and collected by clerical staff, training was necessary to explain the difference between birth sex and SIGI before implementation in the EHR. The training sessions educated staff about the difference between birth sex and SIGI, how to ask and respond to questions respectfully, and how to update these fields in the EHR. These trainings included a 20-minute video demonstrating best practices for asking about SIGI, a frequently asked questions document responding to 7 common questions about the new fields, and a quick reference guide for administrative staff to have handy at their desks.
Dissemination of the SIGI patient and provider fact sheets is planned to occur, ideally, several weeks before implementation of the new patches updating the EHR fields in spring 2020. Building on existing resources, the patient safety education work group plans to disseminate the patient fact sheets via e-mail lists for the national mental health facility leaders as well as through e-mail lists for VA PCPs, nursing and clerical staff, privacy officers, facility LGBT veteran care coordinators, VISN leads, transgender e-consultation, the Office of Connected Care, the LGBT external homepage for the VA, and the training website for VA employees. The goal is to target potential points of contact for veterans who may have already changed their birth sex and might benefit medically from altering birth sex to be consistent with their original birth certificate.
The SIGI provider fact sheet will be disseminated using internal e-mails, announcements on routine LGBT veteran care coordinator calls, weekly Ask LGBT Health teleconferences, and announcements at LGBT health training events both internally and externally. Several dissemination tools have already ensured that VA employees are aware of the SIGI field in the EHR. Leadership throughout the VA will be encouraged to share SIGI trainings with clerical staff. Additionally, broad-based e-mails summarizing changes to the EHR will be provided concurrent to the SIGI patch implementation to VA staff as well as links to the resources and training materials.
Challenges
One difficulty in the development process for both SIGI fact sheets was addressing the issue of patient safety for veterans who may be at different points in their gender transition process. It was challenging for the patient safety education work group to not sound alarmist in discussing the safety implications of birth sex changes in the EHR, as this is just one factor in clinical decision making. The goal was to educate veterans from a patient safety perspective about the implications of having a state-of-the-art, automated EHR. However, text can be perceived differently by different people, which is why the patient safety education work group asked veterans to preview the patient document and clinical providers to preview the provider document.
Both work groups encountered technologic challenges, including a delay in the implementation of the SIGI field due to a systemwide delay of EHR updates. Although it released training and educational materials to the VHA, the patient safety education work group understood that at some point in the future, VA programmers will update the EHR to change the information clerks and HCPs can see in the EHR. Coordination of the fact sheet release alongside information technology has been an important part of the SIGI rollout process.
Conclusion
HCPs have a complex role in providing treatment to TGNC patients in the VHA: They must affirm a patient’s gender identity through how they address them, while openly communicating the health risks inherent in having their birth sex field be incongruent with the sex recorded on their original birth certificate. Accomplishing these tasks simultaneously is difficult without invalidating the veteran’s identity or right to choose their EHR demographic birth sex label. Furthermore, patients may ask HCPs to write letters of support for either medical or surgical intervention or other documentation changes (eg, changes to a patient’s legal name, passport changes, or a safe passage letter for TGNC patients). Navigating the dialectic of safety and validation requires strong rapport, trust, and effective communication in the patient-provider relationship and great empathy by the provider.
A future task for the SIGI patient safety education work group is to continue to communicate with the technical work group and providers in the field about how demographic fields in the EHR are utilized to enable future EHR changes. This hurdle is not easy because EHR updates change the infrastructure through which demographic content is delivered and incorporated into a patient’s treatment. The VA HCPs are tasked with thoroughly examining the results that automated systems produce to ensure safe and accurate medical services are always provided to all patients. An integral part of patient-centered care is balancing any computer-guided recommendations with an understanding that actual patient needs may differ due to presence/absence of anatomy and other factors (eg, weight, current medications).
From a systems perspective, a benefit of adding the SIGI demographic field is systemic improvement in calculating the number of transgender veterans under VA care and evaluating health outcomes for this population. SIGI is particularly important for signaling gender pronouns for veterans, regardless of whether they are receiving care for a gender-related diagnosis. In terms of scope, the SIGI project potentially will apply to > 9 million enrolled veterans and nearly 400,000 VA employees.
Improvements could be made in the SIGI field of the new EHR, such as expanding the options for self-labels. Additionally, a text field could be used to enhance the quality of personalization provided to veterans self-identifying in the EHR, including pronoun specification. Moreover, adding new fields such as “preferred name” could improve the health care experience of not only TGNC veterans but all veterans who use something other than their full legal name (eg, a nickname). It will be good practice to notify providers and staff of a veteran’s requested name and pronouns when the patient checks in at an electronic kiosk so that all staff immediately know how to address the patient. The VHA can continue to adjust the options for the SIGI field once the new EHR system is operational. Ideally, this new EHR will display birth sex and SIGI to clinicians or clerks engaged in patient interactions.
Technology will continue to automate medical care, meaning that HCPs must be vigilant about how computer programming and the accuracy of prepopulated information affect patient care. The concerns discussed in this report relating to patient safety are relatively absent in the medical literature, even though substantial health risks exist to patients who have birth sex listed incorrectly for any reason.6,7 Additionally, administrative burden can be reduced if patients who do not need certain screenings based on their current anatomy are not contacted for unnecessary screenings. Future EHR systems might incorporate anatomical considerations from an inventory to assist in automating patient care in safe and accessible ways.
1. Institute of Medicine Committee on Quality of Health Care. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001. https://www.ncbi.nlm.nih.gov/books/NBK222274. Accessed April 10, 2019.
2. Cahill SR, Baker K, Deutsch MB, Keatley J, Makadon HJ. Inclusion of sexual orientation and gender identity in stage 3 meaningful use guidelines: a huge step forward for LGBT health. LGBT Health. 2016;3(2):100-102.
3. Cahill SR, Makadon HJ. Sexual orientation and gender identity data collection update: U.S. government takes steps to promote sexual orientation and gender identity data collection through meaningful use guidelines. LGBT Health. 2014;1(3):157-160.
4. Fridsma D. EHR interoperability: the structured data capture initiative. https://www.healthit.gov/buzz-blog/electronic-health-and-medical-records/ehr-interoperabiity-structured-data-capture-initiative. Published January 31, 2013. Accessed April 10, 2019.
5. Muray T, Berberian L. The importance of structured data elements in EHRs. Computerworld website. https://www.computerworld.com/article/2470987/healthcare-it/the-importance-of-structured-data-elements-in-ehrs.html. Published March 31, 2011. Accessed April 10, 2019.
6. Deutsch MB, Green J, Keatley J, Mayer G, Hastings J, Hall AM; World Professional Association for Transgender Health EMR Working Group. Electronic medical records and the transgender patient: recommendations from the World Professional Association for Transgender Health EMR Working Group.
7. Deutsch MB, Keatley J, Sevelius J, Shade SB. Collection of gender identity data using electronic medical records: survey of current end-user practices. J Assoc Nurses AIDS Care. 2014;25(6):657-663.
Providing consistent and high-quality services to gender diverse patients is a top priority for health care systems, including the Veterans Health Administration (VHA).1 Over the past decade, awareness of transgender and gender nonconforming (TGNC) people in the US has increased. Gender identity refers to a person’s inner sense of where that person belongs on a continuum of masculine to androgynous to feminine traits. This identity range can additionally include nonbinary identifications, such as “gender fluid” or “genderqueer.” A goal of patient-centered care is for health care providers (HCPs) to refer to TGNC individuals, like their cisgender counterparts, according to their gender identity. Gender identity for TGNC individuals may be different from their birth sex. Birth sex, commonly referred to as “sex assigned at birth,” is the biologic and physiologic characteristics that are reflected on a person’s original birth certificate and described as male or female.
Background
In the electronic health record (EHR), birth sex is an important, structured variable that is used to facilitate effective patient care that is efficient, equitable, and patient-centered. Birth sex in an EHR often is used to cue automatic timely generation of health screens (eg, pap smears, prostate exams) and calculation of medication dosages and laboratory test ranges by adjusting for a person’s typical hormonal history and anatomy.
Gender identity fields are independently helpful to include in the EHR, because clinicians can use this information to ensure proper pronoun use and avoid misgendering a patient. Additionally, the gender identity field informs HCPs who may conduct more frequent or different health screenings to evaluate specific health risks that are more prevalent in gender minority (ie, lesbian, gay, bisexual) patients.2,3
EHRs rely on structured data elements to standardize data about patients for clinical care, quality improvement, data sharing, and patient safety.4,5 However, health care organizations are grappling with how to incorporate gender identity and birth sex information into EHRs.3 A 2011 Veterans Health Administration (VHA) directive required staff and providers to address and provide care to veterans based on their gender identity. Like other health systems, VHA had 1 demographic data field in the EHR to indicate birth sex, with no field for gender identity. A HCP could enter gender identity information into a progress note, but this addition might not be noticed by other HCPs. Consequently, staff and providers had no effective way of knowing a veteran’s gender identity from the EHR, which contributed to misgendering TGNC veterans.
With the singular demographic field of sex representing both birth sex and gender identity, some TGNC veterans chose to change their birth sex information to align with their gender identity. This change assured TGNC veterans that staff and providers would not misgender them because the birth sex field is easily observed and would allow providers to use respectful, gender-consistent pronouns when speaking with them. However, changing the birth sex field can misalign natal sex–based clinical reminders, medication dosages, and laboratory test values, which created potential patient safety risks. Thus, birth sex created potential hazards to quality and safety when used as a marker even with other variables—such as current anatomy, height, and weight—for health screenings, medication dosing, and other medical decisions.
In this article, we: (1) outline several patient safety issues that can arise with the birth sex field serving as an indicator for both birth sex and gender identity; (2) present case examples that illustrate the benefits of self-identified gender identity (SIGI) in an EHR; (3) describe the process of work-group development of patient-provider communication tools to improve patient safety; and (4) provide a brief overview of resources rolled out as a part of SIGI. This report serves as a guide for other federal organizations that wish to increase affirmative care and safe practices for transgender consumers. We will provide an overview of the tasks leading up to SIGI implementation, deliverables from the project, and lessons learned.
Veterans Affairs SIGI EHR Field
In 2016, the US Department of Veterans Affairs (VA) began implementing a SIGI demographic field across all EHRs, requiring administrative staff to ask enrolled and new veterans their gender identity (full implementation of SIGI has not yet occurred and will occur when a later EHR upgrade displays SIGI in the EHR). The initiation of SIGI did not change any information in the birth sex field, meaning that some veterans continue to have birth sex field information that results in problematic automatic medical reminders and dosing values. Consequently, the National Center for Patient Safety (NCPS) noted that this discrepancy may be a pertinent patient safety issue. The NCPS and Lesbian, Gay Bisexual, and Transgender (LGBT) Health national program offices worked to provide documentation to TGNC veterans to inform them of the clinical health care implications of having their birth sex demographic field reflect gender identity that is inconsistent with their natal sex (ie, original birth certificate record of sex).
Patient Safety Issues
Conversations between transgender patients and their HCPs about transition goals, necessary medical tests, and laboratory ranges based on their current anatomy and physiology can improve patient safety and satisfaction with medical care. Prior to the availability of the SIGI field, VA facilities varied in their documentation of gender identity in the patient chart. LGBT veteran care coordinators discussed diverse suggestions that ranged from informally documenting SIGI in each progress note to using flags to draw attention to use certain sections of local EHRs. These suggestions, though well intentioned, were not adequate for documenting gender identity at the national level because of regional variations in EHR customization options. Furthermore, the use of flags for drawing clinical attention to gender identity posed a potential for stigma toward patients, given that flags are typically reserved for behavioral or other risk concerns.
Several problems can emerge when HCPs are not equipped with accurate information about patient birth sex and SIGI. For instance, TGNC patients lack a way of being known from clinic to clinic by proper pronouns or self-labels. Providers may misgender veterans, which is a negative experience for TGNC veterans linked with increased barriers to care and decreased frequency of health care visits.4 Moreover, the quality and personalization of care across clinic locations in the facility’s system is variable without a consistent method of documenting birth sex and SIGI. For example, in clinics where the veteran is well known (eg, primary care), staff may be more affirming of the veteran’s gender identity than those in specialty care clinics that lack prior patient contact.
Furthermore, depending on hormone and surgical interventions, some health screenings may be irrelevant for TGNC patients. To determine appropriate health screens and assess potential risks associated with hormone therapy, providers must have access to current information regarding a patient’s physiologic anatomy.6 Health screenings and laboratory results in sophisticated EHRs (ie, EHRs that might autodetermine normative values) may populate incorrect treatment recommendations, such as sex-based medication dosages. Furthermore, laboratory test results could be incorrectly paired with a different assumed hormonal history, potentially putting the patient at risk.
Case Examples
An important element of EHRs facilitating the goal of patient-centered care is that patients have their EHR validate their sense of self, and their providers can use names and pronouns that correspond to the patient’s SIGI. Some patients have spent a great amount of effort altering their name and sex in legal records and may want their birth sex field to conform to their gender identity. To that end, patients may seek to alter their birth sex information so that it is congruent with how they see themselves to affirm their identity, despite patient safety risks. Several scenarios below demonstrate the potential costs and benefits to patients altering birth sex and SIGI in the EHR.
Case 1 Presentation
A young transman is working with his therapist on engaging in self-validating behaviors. This veteran has met with his PCP and informed the provider of his decision to alter the birth sex field in his EHR from female to male.
Ideally, the patient would begin to have regular conversations with his HCPs about his birth sex and gender identity, so that medical professionals can provide relevant screenings and affirm the patient’s gender identity while acknowledging his right to list his birth sex as he chooses. However, particular attention will need to be paid to assuring that natal sex–based health screenings (eg, pap smears, mammograms) are conducted on an appropriate schedule and that the veteran continues to discuss his current anatomy with providers.
Case 2 Presentation
A veteran has a male birth sex, identifies as a transwoman, and uses nongendered plural pronouns “they/them/theirs.” The word “they,” used as a singular pronoun may feel uncomfortable to some providers, but it validates the veteran’s sense of self and helps them feel welcome in the treatment environment. This patient communicated proactively with their HCPs about their transition goals and current hormone use.
They opted to have their birth sex field continue to indicate “male” because they, after a discussion with their PCP, are aware of the health implications of receiving an incorrect dose for their diabetes medication. They understand that having open communication and receiving input from their HCPs is part of good health care.
Case 3 Presentation
A patient with a sexual development disorder (intersex condition) identifies as a man (indicated as “male” in the SIGI field) and had his birth sex field changed to match his gender identity. He now seeks to change his birth sex field back to female, as he has complicated health considerations due to breast cancer.
The veteran thinks it is important that providers know about his intersex condition so that his breast cancer care is as seamless as possible. In particular, although this veteran is comfortable talking about his intersex condition and his identity with his PCP and oncologist, he wants to ensure that all people involved in his care (eg, pharmacists, radiologists) use the correct values in interpreting his medical data. Providers will need to use the female birth sex field for interpreting his medical data but use male pronouns when interacting with the veteran and documenting his care.
These case examples illustrate the need for HCPs to have patient-affirming education and appropriate clinical tools available when speaking to patients about birth sex, SIGI, and the implications of changing birth sex in the EHR. Moreover, these cases highlight that patient health needs may vary over time, due to factors such as perceived costs/benefits of a change in the sex field of the EHR as well as patient comfort with providers.
Current Status of SIGI and EHR
Although having separate fields for birth sex and SIGI in the EHR is ideal, the VHA does not yet have a fully functional SIGI field, and several TGNC veterans have changed their birth sex field to align with their gender identity. Roughly 9,700 patients have diagnostic codes related to transgender care in the VHA, meaning thousands of current patients would potentially benefit from SIGI implementation (John Blosnich, written communication, March 2018). A possible action that the VHA could take with the goal of enhancing patient safety would be to revert the birth sex field of patients who had previously changed the field back to the patient’s original birth sex. However, if this alteration to the EHR were done without the patient’s consent, numerous additional problems would result—including invalidating a veteran’s wishes—potentially driving patients away from receiving health care.
Moreover, in the absence of updated SIGI information (which only the veteran can provide), making a change in the EHR would perpetuate the misgendering of TGNC veterans who have already sought an administrative fix for this problem. Thus, the agency decided to engage patients in a discussion about their decision to keep the birth sex field consistent with their original birth certificate. In cases in which the field had been changed previously, the recommendation is for HCPs to gain patient consent to change the birth sex field back to what was on their original birth certificate. Thus, decisions about what should be listed in the EHR are made by the veteran using an informed decision-making model.
Patient Safety Education Workgroup
To begin the process of disentangling birth sex and SIGI fields in the EHR, 2 work groups were created: a technical work group (coding the patches for SIGI implementation) and a SIGI patient safety education work group. The patient safety education work group was committed to promoting affirmative VA policies that require validation of the gender identity of all veterans and pursuing best practices through clinical guidelines to promote effective, efficient, equitable, and safe veteran care. The patient safety education work group included representatives from all 3 branches of the VA (VHA, Veterans Benefits Administration, and National Cemetery Administration), including clinical media, patient safety, information technology, and education specialists. The group developed trainings for administrative staff about the appropriate ways to ask birth sex and SIGI questions, and how to record veteran-driven responses.
SIGI Fact Sheet
The patient safety education work group examined clinical literature and developed tools for staff and veterans to facilitate effective discussions about the importance and utility of documenting both birth sex and SIGI in the EHR. The patient safety education work group along with media and educational experts created basic key term definition documents to address the importance, purpose, and use of the SIGI field. The patient safety education work group developed 2 documents to facilitate communication between patients and providers.
A 1-page veteran-facing fact sheet was developed that described the differences between birth sex and SIGI fields and how these fields are used in the VA EHR system (Figure 1). In addition, a 1-page HCP-facing fact sheet was designed to inform HCPs that patients may have changed their birth sex in their EHR or might still wish to change their birth sex field, and to inform HCPs of the importance of patient-centered, gender-affirmative care (Figure 2). An additional goal of both documents was to educate veterans and HCPs on how the EHR automatically calculates laboratory results and screening notifications based on birth sex.
Review Process
As part of reviewing and finalizing the SIGI patient fact sheet, the patient safety education work group previewed the document’s content with veterans who provided feedback on drafts to improve comprehension, patient-centered care, and clinical accuracy. For instance, several patients commented that the document should address many gender identities, including intersex identities. As noted in one of the case presentations earlier, individuals who identify as intersex may have changed their birth sex to be consistent with their gender and might benefit from being informed about the EHR’s autocalculation feature. The patient safety education work group adjusted the SIGI patient fact sheet to include individuals who identify as intersex and instructed them to have a conversation with their HCP regarding potential birth sex changes in the EHR.
Much of the veteran feedback to the patient safety education work group reflected veteran concerns, more broadly, about implementation of SIGI. Many veterans were interested in how federal policy changes might affect their benefits package or clinical care within the VA. The SIGI patient fact sheet was a tool for communicating that Department of Defense (DoD) policies, specifically, do not have a bearing on VA care for LGBT veterans. Therefore, SIGI information does not affect service connection or benefits eligibility and is not shared with the DoD. Veterans found this information helpful to see reflected in the SIGI patient fact sheet.
The patient safety education work group also shared the SIGI provider fact sheet with VHA providers before finalizing the content. PCPs gave feedback to improve the specification of patient safety concerns and appropriate readership language. The patient safety education work group adjusted the SIGI provider fact sheet to be inclusive of relevant literature and an e-consultation link for assisting HCPs who are unsure how to proceed with a patient.
Implementation
The patient safety education work group also developed several materials to provide information about the birth sex and SIGI fields in the EHR. Because the SIGI demographic field is new and collected by clerical staff, training was necessary to explain the difference between birth sex and SIGI before implementation in the EHR. The training sessions educated staff about the difference between birth sex and SIGI, how to ask and respond to questions respectfully, and how to update these fields in the EHR. These trainings included a 20-minute video demonstrating best practices for asking about SIGI, a frequently asked questions document responding to 7 common questions about the new fields, and a quick reference guide for administrative staff to have handy at their desks.
Dissemination of the SIGI patient and provider fact sheets is planned to occur, ideally, several weeks before implementation of the new patches updating the EHR fields in spring 2020. Building on existing resources, the patient safety education work group plans to disseminate the patient fact sheets via e-mail lists for the national mental health facility leaders as well as through e-mail lists for VA PCPs, nursing and clerical staff, privacy officers, facility LGBT veteran care coordinators, VISN leads, transgender e-consultation, the Office of Connected Care, the LGBT external homepage for the VA, and the training website for VA employees. The goal is to target potential points of contact for veterans who may have already changed their birth sex and might benefit medically from altering birth sex to be consistent with their original birth certificate.
The SIGI provider fact sheet will be disseminated using internal e-mails, announcements on routine LGBT veteran care coordinator calls, weekly Ask LGBT Health teleconferences, and announcements at LGBT health training events both internally and externally. Several dissemination tools have already ensured that VA employees are aware of the SIGI field in the EHR. Leadership throughout the VA will be encouraged to share SIGI trainings with clerical staff. Additionally, broad-based e-mails summarizing changes to the EHR will be provided concurrent to the SIGI patch implementation to VA staff as well as links to the resources and training materials.
Challenges
One difficulty in the development process for both SIGI fact sheets was addressing the issue of patient safety for veterans who may be at different points in their gender transition process. It was challenging for the patient safety education work group to not sound alarmist in discussing the safety implications of birth sex changes in the EHR, as this is just one factor in clinical decision making. The goal was to educate veterans from a patient safety perspective about the implications of having a state-of-the-art, automated EHR. However, text can be perceived differently by different people, which is why the patient safety education work group asked veterans to preview the patient document and clinical providers to preview the provider document.
Both work groups encountered technologic challenges, including a delay in the implementation of the SIGI field due to a systemwide delay of EHR updates. Although it released training and educational materials to the VHA, the patient safety education work group understood that at some point in the future, VA programmers will update the EHR to change the information clerks and HCPs can see in the EHR. Coordination of the fact sheet release alongside information technology has been an important part of the SIGI rollout process.
Conclusion
HCPs have a complex role in providing treatment to TGNC patients in the VHA: They must affirm a patient’s gender identity through how they address them, while openly communicating the health risks inherent in having their birth sex field be incongruent with the sex recorded on their original birth certificate. Accomplishing these tasks simultaneously is difficult without invalidating the veteran’s identity or right to choose their EHR demographic birth sex label. Furthermore, patients may ask HCPs to write letters of support for either medical or surgical intervention or other documentation changes (eg, changes to a patient’s legal name, passport changes, or a safe passage letter for TGNC patients). Navigating the dialectic of safety and validation requires strong rapport, trust, and effective communication in the patient-provider relationship and great empathy by the provider.
A future task for the SIGI patient safety education work group is to continue to communicate with the technical work group and providers in the field about how demographic fields in the EHR are utilized to enable future EHR changes. This hurdle is not easy because EHR updates change the infrastructure through which demographic content is delivered and incorporated into a patient’s treatment. The VA HCPs are tasked with thoroughly examining the results that automated systems produce to ensure safe and accurate medical services are always provided to all patients. An integral part of patient-centered care is balancing any computer-guided recommendations with an understanding that actual patient needs may differ due to presence/absence of anatomy and other factors (eg, weight, current medications).
From a systems perspective, a benefit of adding the SIGI demographic field is systemic improvement in calculating the number of transgender veterans under VA care and evaluating health outcomes for this population. SIGI is particularly important for signaling gender pronouns for veterans, regardless of whether they are receiving care for a gender-related diagnosis. In terms of scope, the SIGI project potentially will apply to > 9 million enrolled veterans and nearly 400,000 VA employees.
Improvements could be made in the SIGI field of the new EHR, such as expanding the options for self-labels. Additionally, a text field could be used to enhance the quality of personalization provided to veterans self-identifying in the EHR, including pronoun specification. Moreover, adding new fields such as “preferred name” could improve the health care experience of not only TGNC veterans but all veterans who use something other than their full legal name (eg, a nickname). It will be good practice to notify providers and staff of a veteran’s requested name and pronouns when the patient checks in at an electronic kiosk so that all staff immediately know how to address the patient. The VHA can continue to adjust the options for the SIGI field once the new EHR system is operational. Ideally, this new EHR will display birth sex and SIGI to clinicians or clerks engaged in patient interactions.
Technology will continue to automate medical care, meaning that HCPs must be vigilant about how computer programming and the accuracy of prepopulated information affect patient care. The concerns discussed in this report relating to patient safety are relatively absent in the medical literature, even though substantial health risks exist to patients who have birth sex listed incorrectly for any reason.6,7 Additionally, administrative burden can be reduced if patients who do not need certain screenings based on their current anatomy are not contacted for unnecessary screenings. Future EHR systems might incorporate anatomical considerations from an inventory to assist in automating patient care in safe and accessible ways.
Providing consistent and high-quality services to gender diverse patients is a top priority for health care systems, including the Veterans Health Administration (VHA).1 Over the past decade, awareness of transgender and gender nonconforming (TGNC) people in the US has increased. Gender identity refers to a person’s inner sense of where that person belongs on a continuum of masculine to androgynous to feminine traits. This identity range can additionally include nonbinary identifications, such as “gender fluid” or “genderqueer.” A goal of patient-centered care is for health care providers (HCPs) to refer to TGNC individuals, like their cisgender counterparts, according to their gender identity. Gender identity for TGNC individuals may be different from their birth sex. Birth sex, commonly referred to as “sex assigned at birth,” is the biologic and physiologic characteristics that are reflected on a person’s original birth certificate and described as male or female.
Background
In the electronic health record (EHR), birth sex is an important, structured variable that is used to facilitate effective patient care that is efficient, equitable, and patient-centered. Birth sex in an EHR often is used to cue automatic timely generation of health screens (eg, pap smears, prostate exams) and calculation of medication dosages and laboratory test ranges by adjusting for a person’s typical hormonal history and anatomy.
Gender identity fields are independently helpful to include in the EHR, because clinicians can use this information to ensure proper pronoun use and avoid misgendering a patient. Additionally, the gender identity field informs HCPs who may conduct more frequent or different health screenings to evaluate specific health risks that are more prevalent in gender minority (ie, lesbian, gay, bisexual) patients.2,3
EHRs rely on structured data elements to standardize data about patients for clinical care, quality improvement, data sharing, and patient safety.4,5 However, health care organizations are grappling with how to incorporate gender identity and birth sex information into EHRs.3 A 2011 Veterans Health Administration (VHA) directive required staff and providers to address and provide care to veterans based on their gender identity. Like other health systems, VHA had 1 demographic data field in the EHR to indicate birth sex, with no field for gender identity. A HCP could enter gender identity information into a progress note, but this addition might not be noticed by other HCPs. Consequently, staff and providers had no effective way of knowing a veteran’s gender identity from the EHR, which contributed to misgendering TGNC veterans.
With the singular demographic field of sex representing both birth sex and gender identity, some TGNC veterans chose to change their birth sex information to align with their gender identity. This change assured TGNC veterans that staff and providers would not misgender them because the birth sex field is easily observed and would allow providers to use respectful, gender-consistent pronouns when speaking with them. However, changing the birth sex field can misalign natal sex–based clinical reminders, medication dosages, and laboratory test values, which created potential patient safety risks. Thus, birth sex created potential hazards to quality and safety when used as a marker even with other variables—such as current anatomy, height, and weight—for health screenings, medication dosing, and other medical decisions.
In this article, we: (1) outline several patient safety issues that can arise with the birth sex field serving as an indicator for both birth sex and gender identity; (2) present case examples that illustrate the benefits of self-identified gender identity (SIGI) in an EHR; (3) describe the process of work-group development of patient-provider communication tools to improve patient safety; and (4) provide a brief overview of resources rolled out as a part of SIGI. This report serves as a guide for other federal organizations that wish to increase affirmative care and safe practices for transgender consumers. We will provide an overview of the tasks leading up to SIGI implementation, deliverables from the project, and lessons learned.
Veterans Affairs SIGI EHR Field
In 2016, the US Department of Veterans Affairs (VA) began implementing a SIGI demographic field across all EHRs, requiring administrative staff to ask enrolled and new veterans their gender identity (full implementation of SIGI has not yet occurred and will occur when a later EHR upgrade displays SIGI in the EHR). The initiation of SIGI did not change any information in the birth sex field, meaning that some veterans continue to have birth sex field information that results in problematic automatic medical reminders and dosing values. Consequently, the National Center for Patient Safety (NCPS) noted that this discrepancy may be a pertinent patient safety issue. The NCPS and Lesbian, Gay Bisexual, and Transgender (LGBT) Health national program offices worked to provide documentation to TGNC veterans to inform them of the clinical health care implications of having their birth sex demographic field reflect gender identity that is inconsistent with their natal sex (ie, original birth certificate record of sex).
Patient Safety Issues
Conversations between transgender patients and their HCPs about transition goals, necessary medical tests, and laboratory ranges based on their current anatomy and physiology can improve patient safety and satisfaction with medical care. Prior to the availability of the SIGI field, VA facilities varied in their documentation of gender identity in the patient chart. LGBT veteran care coordinators discussed diverse suggestions that ranged from informally documenting SIGI in each progress note to using flags to draw attention to use certain sections of local EHRs. These suggestions, though well intentioned, were not adequate for documenting gender identity at the national level because of regional variations in EHR customization options. Furthermore, the use of flags for drawing clinical attention to gender identity posed a potential for stigma toward patients, given that flags are typically reserved for behavioral or other risk concerns.
Several problems can emerge when HCPs are not equipped with accurate information about patient birth sex and SIGI. For instance, TGNC patients lack a way of being known from clinic to clinic by proper pronouns or self-labels. Providers may misgender veterans, which is a negative experience for TGNC veterans linked with increased barriers to care and decreased frequency of health care visits.4 Moreover, the quality and personalization of care across clinic locations in the facility’s system is variable without a consistent method of documenting birth sex and SIGI. For example, in clinics where the veteran is well known (eg, primary care), staff may be more affirming of the veteran’s gender identity than those in specialty care clinics that lack prior patient contact.
Furthermore, depending on hormone and surgical interventions, some health screenings may be irrelevant for TGNC patients. To determine appropriate health screens and assess potential risks associated with hormone therapy, providers must have access to current information regarding a patient’s physiologic anatomy.6 Health screenings and laboratory results in sophisticated EHRs (ie, EHRs that might autodetermine normative values) may populate incorrect treatment recommendations, such as sex-based medication dosages. Furthermore, laboratory test results could be incorrectly paired with a different assumed hormonal history, potentially putting the patient at risk.
Case Examples
An important element of EHRs facilitating the goal of patient-centered care is that patients have their EHR validate their sense of self, and their providers can use names and pronouns that correspond to the patient’s SIGI. Some patients have spent a great amount of effort altering their name and sex in legal records and may want their birth sex field to conform to their gender identity. To that end, patients may seek to alter their birth sex information so that it is congruent with how they see themselves to affirm their identity, despite patient safety risks. Several scenarios below demonstrate the potential costs and benefits to patients altering birth sex and SIGI in the EHR.
Case 1 Presentation
A young transman is working with his therapist on engaging in self-validating behaviors. This veteran has met with his PCP and informed the provider of his decision to alter the birth sex field in his EHR from female to male.
Ideally, the patient would begin to have regular conversations with his HCPs about his birth sex and gender identity, so that medical professionals can provide relevant screenings and affirm the patient’s gender identity while acknowledging his right to list his birth sex as he chooses. However, particular attention will need to be paid to assuring that natal sex–based health screenings (eg, pap smears, mammograms) are conducted on an appropriate schedule and that the veteran continues to discuss his current anatomy with providers.
Case 2 Presentation
A veteran has a male birth sex, identifies as a transwoman, and uses nongendered plural pronouns “they/them/theirs.” The word “they,” used as a singular pronoun may feel uncomfortable to some providers, but it validates the veteran’s sense of self and helps them feel welcome in the treatment environment. This patient communicated proactively with their HCPs about their transition goals and current hormone use.
They opted to have their birth sex field continue to indicate “male” because they, after a discussion with their PCP, are aware of the health implications of receiving an incorrect dose for their diabetes medication. They understand that having open communication and receiving input from their HCPs is part of good health care.
Case 3 Presentation
A patient with a sexual development disorder (intersex condition) identifies as a man (indicated as “male” in the SIGI field) and had his birth sex field changed to match his gender identity. He now seeks to change his birth sex field back to female, as he has complicated health considerations due to breast cancer.
The veteran thinks it is important that providers know about his intersex condition so that his breast cancer care is as seamless as possible. In particular, although this veteran is comfortable talking about his intersex condition and his identity with his PCP and oncologist, he wants to ensure that all people involved in his care (eg, pharmacists, radiologists) use the correct values in interpreting his medical data. Providers will need to use the female birth sex field for interpreting his medical data but use male pronouns when interacting with the veteran and documenting his care.
These case examples illustrate the need for HCPs to have patient-affirming education and appropriate clinical tools available when speaking to patients about birth sex, SIGI, and the implications of changing birth sex in the EHR. Moreover, these cases highlight that patient health needs may vary over time, due to factors such as perceived costs/benefits of a change in the sex field of the EHR as well as patient comfort with providers.
Current Status of SIGI and EHR
Although having separate fields for birth sex and SIGI in the EHR is ideal, the VHA does not yet have a fully functional SIGI field, and several TGNC veterans have changed their birth sex field to align with their gender identity. Roughly 9,700 patients have diagnostic codes related to transgender care in the VHA, meaning thousands of current patients would potentially benefit from SIGI implementation (John Blosnich, written communication, March 2018). A possible action that the VHA could take with the goal of enhancing patient safety would be to revert the birth sex field of patients who had previously changed the field back to the patient’s original birth sex. However, if this alteration to the EHR were done without the patient’s consent, numerous additional problems would result—including invalidating a veteran’s wishes—potentially driving patients away from receiving health care.
Moreover, in the absence of updated SIGI information (which only the veteran can provide), making a change in the EHR would perpetuate the misgendering of TGNC veterans who have already sought an administrative fix for this problem. Thus, the agency decided to engage patients in a discussion about their decision to keep the birth sex field consistent with their original birth certificate. In cases in which the field had been changed previously, the recommendation is for HCPs to gain patient consent to change the birth sex field back to what was on their original birth certificate. Thus, decisions about what should be listed in the EHR are made by the veteran using an informed decision-making model.
Patient Safety Education Workgroup
To begin the process of disentangling birth sex and SIGI fields in the EHR, 2 work groups were created: a technical work group (coding the patches for SIGI implementation) and a SIGI patient safety education work group. The patient safety education work group was committed to promoting affirmative VA policies that require validation of the gender identity of all veterans and pursuing best practices through clinical guidelines to promote effective, efficient, equitable, and safe veteran care. The patient safety education work group included representatives from all 3 branches of the VA (VHA, Veterans Benefits Administration, and National Cemetery Administration), including clinical media, patient safety, information technology, and education specialists. The group developed trainings for administrative staff about the appropriate ways to ask birth sex and SIGI questions, and how to record veteran-driven responses.
SIGI Fact Sheet
The patient safety education work group examined clinical literature and developed tools for staff and veterans to facilitate effective discussions about the importance and utility of documenting both birth sex and SIGI in the EHR. The patient safety education work group along with media and educational experts created basic key term definition documents to address the importance, purpose, and use of the SIGI field. The patient safety education work group developed 2 documents to facilitate communication between patients and providers.
A 1-page veteran-facing fact sheet was developed that described the differences between birth sex and SIGI fields and how these fields are used in the VA EHR system (Figure 1). In addition, a 1-page HCP-facing fact sheet was designed to inform HCPs that patients may have changed their birth sex in their EHR or might still wish to change their birth sex field, and to inform HCPs of the importance of patient-centered, gender-affirmative care (Figure 2). An additional goal of both documents was to educate veterans and HCPs on how the EHR automatically calculates laboratory results and screening notifications based on birth sex.
Review Process
As part of reviewing and finalizing the SIGI patient fact sheet, the patient safety education work group previewed the document’s content with veterans who provided feedback on drafts to improve comprehension, patient-centered care, and clinical accuracy. For instance, several patients commented that the document should address many gender identities, including intersex identities. As noted in one of the case presentations earlier, individuals who identify as intersex may have changed their birth sex to be consistent with their gender and might benefit from being informed about the EHR’s autocalculation feature. The patient safety education work group adjusted the SIGI patient fact sheet to include individuals who identify as intersex and instructed them to have a conversation with their HCP regarding potential birth sex changes in the EHR.
Much of the veteran feedback to the patient safety education work group reflected veteran concerns, more broadly, about implementation of SIGI. Many veterans were interested in how federal policy changes might affect their benefits package or clinical care within the VA. The SIGI patient fact sheet was a tool for communicating that Department of Defense (DoD) policies, specifically, do not have a bearing on VA care for LGBT veterans. Therefore, SIGI information does not affect service connection or benefits eligibility and is not shared with the DoD. Veterans found this information helpful to see reflected in the SIGI patient fact sheet.
The patient safety education work group also shared the SIGI provider fact sheet with VHA providers before finalizing the content. PCPs gave feedback to improve the specification of patient safety concerns and appropriate readership language. The patient safety education work group adjusted the SIGI provider fact sheet to be inclusive of relevant literature and an e-consultation link for assisting HCPs who are unsure how to proceed with a patient.
Implementation
The patient safety education work group also developed several materials to provide information about the birth sex and SIGI fields in the EHR. Because the SIGI demographic field is new and collected by clerical staff, training was necessary to explain the difference between birth sex and SIGI before implementation in the EHR. The training sessions educated staff about the difference between birth sex and SIGI, how to ask and respond to questions respectfully, and how to update these fields in the EHR. These trainings included a 20-minute video demonstrating best practices for asking about SIGI, a frequently asked questions document responding to 7 common questions about the new fields, and a quick reference guide for administrative staff to have handy at their desks.
Dissemination of the SIGI patient and provider fact sheets is planned to occur, ideally, several weeks before implementation of the new patches updating the EHR fields in spring 2020. Building on existing resources, the patient safety education work group plans to disseminate the patient fact sheets via e-mail lists for the national mental health facility leaders as well as through e-mail lists for VA PCPs, nursing and clerical staff, privacy officers, facility LGBT veteran care coordinators, VISN leads, transgender e-consultation, the Office of Connected Care, the LGBT external homepage for the VA, and the training website for VA employees. The goal is to target potential points of contact for veterans who may have already changed their birth sex and might benefit medically from altering birth sex to be consistent with their original birth certificate.
The SIGI provider fact sheet will be disseminated using internal e-mails, announcements on routine LGBT veteran care coordinator calls, weekly Ask LGBT Health teleconferences, and announcements at LGBT health training events both internally and externally. Several dissemination tools have already ensured that VA employees are aware of the SIGI field in the EHR. Leadership throughout the VA will be encouraged to share SIGI trainings with clerical staff. Additionally, broad-based e-mails summarizing changes to the EHR will be provided concurrent to the SIGI patch implementation to VA staff as well as links to the resources and training materials.
Challenges
One difficulty in the development process for both SIGI fact sheets was addressing the issue of patient safety for veterans who may be at different points in their gender transition process. It was challenging for the patient safety education work group to not sound alarmist in discussing the safety implications of birth sex changes in the EHR, as this is just one factor in clinical decision making. The goal was to educate veterans from a patient safety perspective about the implications of having a state-of-the-art, automated EHR. However, text can be perceived differently by different people, which is why the patient safety education work group asked veterans to preview the patient document and clinical providers to preview the provider document.
Both work groups encountered technologic challenges, including a delay in the implementation of the SIGI field due to a systemwide delay of EHR updates. Although it released training and educational materials to the VHA, the patient safety education work group understood that at some point in the future, VA programmers will update the EHR to change the information clerks and HCPs can see in the EHR. Coordination of the fact sheet release alongside information technology has been an important part of the SIGI rollout process.
Conclusion
HCPs have a complex role in providing treatment to TGNC patients in the VHA: They must affirm a patient’s gender identity through how they address them, while openly communicating the health risks inherent in having their birth sex field be incongruent with the sex recorded on their original birth certificate. Accomplishing these tasks simultaneously is difficult without invalidating the veteran’s identity or right to choose their EHR demographic birth sex label. Furthermore, patients may ask HCPs to write letters of support for either medical or surgical intervention or other documentation changes (eg, changes to a patient’s legal name, passport changes, or a safe passage letter for TGNC patients). Navigating the dialectic of safety and validation requires strong rapport, trust, and effective communication in the patient-provider relationship and great empathy by the provider.
A future task for the SIGI patient safety education work group is to continue to communicate with the technical work group and providers in the field about how demographic fields in the EHR are utilized to enable future EHR changes. This hurdle is not easy because EHR updates change the infrastructure through which demographic content is delivered and incorporated into a patient’s treatment. The VA HCPs are tasked with thoroughly examining the results that automated systems produce to ensure safe and accurate medical services are always provided to all patients. An integral part of patient-centered care is balancing any computer-guided recommendations with an understanding that actual patient needs may differ due to presence/absence of anatomy and other factors (eg, weight, current medications).
From a systems perspective, a benefit of adding the SIGI demographic field is systemic improvement in calculating the number of transgender veterans under VA care and evaluating health outcomes for this population. SIGI is particularly important for signaling gender pronouns for veterans, regardless of whether they are receiving care for a gender-related diagnosis. In terms of scope, the SIGI project potentially will apply to > 9 million enrolled veterans and nearly 400,000 VA employees.
Improvements could be made in the SIGI field of the new EHR, such as expanding the options for self-labels. Additionally, a text field could be used to enhance the quality of personalization provided to veterans self-identifying in the EHR, including pronoun specification. Moreover, adding new fields such as “preferred name” could improve the health care experience of not only TGNC veterans but all veterans who use something other than their full legal name (eg, a nickname). It will be good practice to notify providers and staff of a veteran’s requested name and pronouns when the patient checks in at an electronic kiosk so that all staff immediately know how to address the patient. The VHA can continue to adjust the options for the SIGI field once the new EHR system is operational. Ideally, this new EHR will display birth sex and SIGI to clinicians or clerks engaged in patient interactions.
Technology will continue to automate medical care, meaning that HCPs must be vigilant about how computer programming and the accuracy of prepopulated information affect patient care. The concerns discussed in this report relating to patient safety are relatively absent in the medical literature, even though substantial health risks exist to patients who have birth sex listed incorrectly for any reason.6,7 Additionally, administrative burden can be reduced if patients who do not need certain screenings based on their current anatomy are not contacted for unnecessary screenings. Future EHR systems might incorporate anatomical considerations from an inventory to assist in automating patient care in safe and accessible ways.
1. Institute of Medicine Committee on Quality of Health Care. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001. https://www.ncbi.nlm.nih.gov/books/NBK222274. Accessed April 10, 2019.
2. Cahill SR, Baker K, Deutsch MB, Keatley J, Makadon HJ. Inclusion of sexual orientation and gender identity in stage 3 meaningful use guidelines: a huge step forward for LGBT health. LGBT Health. 2016;3(2):100-102.
3. Cahill SR, Makadon HJ. Sexual orientation and gender identity data collection update: U.S. government takes steps to promote sexual orientation and gender identity data collection through meaningful use guidelines. LGBT Health. 2014;1(3):157-160.
4. Fridsma D. EHR interoperability: the structured data capture initiative. https://www.healthit.gov/buzz-blog/electronic-health-and-medical-records/ehr-interoperabiity-structured-data-capture-initiative. Published January 31, 2013. Accessed April 10, 2019.
5. Muray T, Berberian L. The importance of structured data elements in EHRs. Computerworld website. https://www.computerworld.com/article/2470987/healthcare-it/the-importance-of-structured-data-elements-in-ehrs.html. Published March 31, 2011. Accessed April 10, 2019.
6. Deutsch MB, Green J, Keatley J, Mayer G, Hastings J, Hall AM; World Professional Association for Transgender Health EMR Working Group. Electronic medical records and the transgender patient: recommendations from the World Professional Association for Transgender Health EMR Working Group.
7. Deutsch MB, Keatley J, Sevelius J, Shade SB. Collection of gender identity data using electronic medical records: survey of current end-user practices. J Assoc Nurses AIDS Care. 2014;25(6):657-663.
1. Institute of Medicine Committee on Quality of Health Care. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001. https://www.ncbi.nlm.nih.gov/books/NBK222274. Accessed April 10, 2019.
2. Cahill SR, Baker K, Deutsch MB, Keatley J, Makadon HJ. Inclusion of sexual orientation and gender identity in stage 3 meaningful use guidelines: a huge step forward for LGBT health. LGBT Health. 2016;3(2):100-102.
3. Cahill SR, Makadon HJ. Sexual orientation and gender identity data collection update: U.S. government takes steps to promote sexual orientation and gender identity data collection through meaningful use guidelines. LGBT Health. 2014;1(3):157-160.
4. Fridsma D. EHR interoperability: the structured data capture initiative. https://www.healthit.gov/buzz-blog/electronic-health-and-medical-records/ehr-interoperabiity-structured-data-capture-initiative. Published January 31, 2013. Accessed April 10, 2019.
5. Muray T, Berberian L. The importance of structured data elements in EHRs. Computerworld website. https://www.computerworld.com/article/2470987/healthcare-it/the-importance-of-structured-data-elements-in-ehrs.html. Published March 31, 2011. Accessed April 10, 2019.
6. Deutsch MB, Green J, Keatley J, Mayer G, Hastings J, Hall AM; World Professional Association for Transgender Health EMR Working Group. Electronic medical records and the transgender patient: recommendations from the World Professional Association for Transgender Health EMR Working Group.
7. Deutsch MB, Keatley J, Sevelius J, Shade SB. Collection of gender identity data using electronic medical records: survey of current end-user practices. J Assoc Nurses AIDS Care. 2014;25(6):657-663.
Why you should re-credential with Medicare as a hospitalist
CMS needs a better database of hospitalist information
In April 2017, the Centers for Medicare and Medicaid Services implemented the new physician specialty code C6, specifically for hospitalists. There has been a lot of confusion about what this means and some uncertainty about why clinicians should bother to use it.
Some folks thought initially that it was a new CPT code they could use to bill hospitalist services, which might recognize the increased intensity of services hospitalists often provide to their hospitalized patients compared to many traditional internal medicine and family medicine primary care physicians. Others thought it was a code that was added to the HCFA 1500 billing form somewhere to designate that the service was provided by a hospitalist.
Neither is true. The C6 physician specialty code is one of a large number of such codes used by physicians to designate their primary physician specialty when they enroll with Medicare via the PECOS online enrollment system. It describes the unique type of medicine practiced by the enrolling physician and is used by the CMS both for claims processing purposes and for “programmatic” purposes (whatever that means).
It doesn’t change how your claim is processed or how much you get paid. So why bother going through the laborious process of re-credentialing with CMS via PECOS just to change your specialty code? Well, I believe there are several ways in which the C6 specialty code provides value – both to you and to the specialty of hospital medicine.
Reduce concurrent care denials
First, it distinguishes you from a general internal medicine or general family medicine practitioner by recognizing “hospitalist” as a distinct specialty. This can be valuable from a financial perspective because it may reduce the risk that claims for your services might be denied due to “concurrent care” by another provider in the same specialty on the same calendar day.
And it’s not just a general internist or family medicine physician that you might run into concurrent care trouble with. I’ve seen situations where doctors completed critical care or cardiology fellowships but never got around to re-credentialing with Medicare in their new specialty, so their claims still showed up with an “internal medicine” physician specialty code, resulting in denied “concurrent care” claims for either the hospitalist or the specialist.
While Medicare may still see unnecessary overlap between services provided by you and an internal medicine or family physician to the same patient on the same calendar day, you can make a better argument that your services were unique and complementary to (not duplicative of) the services of others if you are credentialed as a hospitalist.
Ensure “apples to apples” comparisons
A second reason to re-credential as a hospitalist is to ensure that when the CMS looks at the services you are providing and the CPT codes you are selecting, it is comparing you to an appropriate peer group for compliance purposes.
The mix of CPT codes reported by hospitalists in the SHM State of Hospital Medicine Survey has historically tilted toward higher-level care than has the mix of CPT codes reported by the CMS for internal medicine or family medicine physicians. But last year when Medicare released the utilization of evaluation and management services by specialty for calendar year 2017, CPT utilization was shown separately for hospitalists for the first time!
The volume of services reported for physicians credentialed as hospitalists was very small relative to the volume of inpatient services provided by internal medicine and family medicine physicians, but the distribution of inpatient admission, subsequent visit, and discharge codes for hospitalists closely mirrored those reported by SHM in its 2018 State of Hospital Medicine Report (see graphic).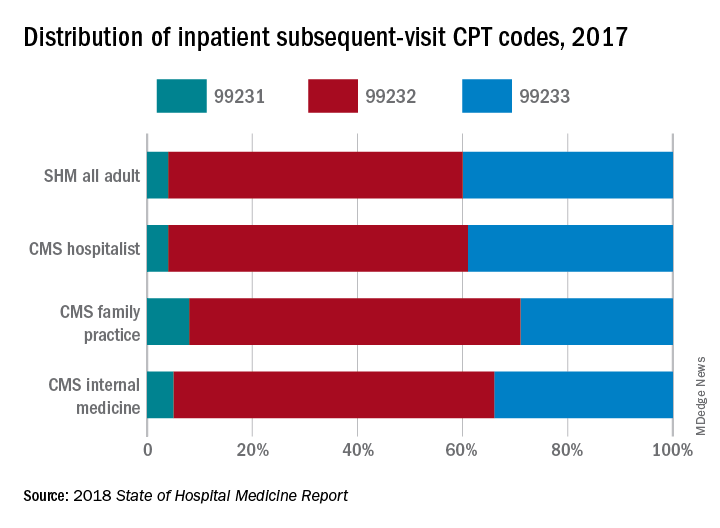
If you’re going to be targeted in a RAC audit for the high proportion of 99233s you bill, you want to be sure the CMS is looking at your performance compared to those who are truly your peers, caring for patients of the same type and complexity.
Improve CMS data used for research purposes
Finally, the ability of academic hospitalists and other health services researchers to utilize Medicare claims data to better understand the care provided by hospitalists and its impact on the overall health care system will be significantly enhanced by a more robust presence of physicians who have identified themselves as hospitalists in the PECOS credentialing system.
We care for the majority of patients in most hospitals these days, yet “hospitalists” billed only 2,009,869 inpatient subsequent visits (CPT codes 99231, 99232, and 99233) in 2017 compared to 25,903,829 billed by internal medicine physicians and 4,678,111 billed by family medicine physicians. And regardless of what you think about using claims data as a proxy for health care services and quality, it’s undeniably the best data set we currently have.
So, let’s work together to build a bigger, better database of hospitalist information at the CMS. I urge you to go to your credentialing folks today and find out how you can work with them to get yourself re-credentialed in PECOS using the C6 “hospitalist” physician specialty.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants, La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Meeting Committees, and helps to coordinate SHM’s bi-annual State of Hospital Medicine Survey. This article appeared originally in SHM's official blog The Hospital Leader. Read more recent posts here.
CMS needs a better database of hospitalist information
CMS needs a better database of hospitalist information
In April 2017, the Centers for Medicare and Medicaid Services implemented the new physician specialty code C6, specifically for hospitalists. There has been a lot of confusion about what this means and some uncertainty about why clinicians should bother to use it.
Some folks thought initially that it was a new CPT code they could use to bill hospitalist services, which might recognize the increased intensity of services hospitalists often provide to their hospitalized patients compared to many traditional internal medicine and family medicine primary care physicians. Others thought it was a code that was added to the HCFA 1500 billing form somewhere to designate that the service was provided by a hospitalist.
Neither is true. The C6 physician specialty code is one of a large number of such codes used by physicians to designate their primary physician specialty when they enroll with Medicare via the PECOS online enrollment system. It describes the unique type of medicine practiced by the enrolling physician and is used by the CMS both for claims processing purposes and for “programmatic” purposes (whatever that means).
It doesn’t change how your claim is processed or how much you get paid. So why bother going through the laborious process of re-credentialing with CMS via PECOS just to change your specialty code? Well, I believe there are several ways in which the C6 specialty code provides value – both to you and to the specialty of hospital medicine.
Reduce concurrent care denials
First, it distinguishes you from a general internal medicine or general family medicine practitioner by recognizing “hospitalist” as a distinct specialty. This can be valuable from a financial perspective because it may reduce the risk that claims for your services might be denied due to “concurrent care” by another provider in the same specialty on the same calendar day.
And it’s not just a general internist or family medicine physician that you might run into concurrent care trouble with. I’ve seen situations where doctors completed critical care or cardiology fellowships but never got around to re-credentialing with Medicare in their new specialty, so their claims still showed up with an “internal medicine” physician specialty code, resulting in denied “concurrent care” claims for either the hospitalist or the specialist.
While Medicare may still see unnecessary overlap between services provided by you and an internal medicine or family physician to the same patient on the same calendar day, you can make a better argument that your services were unique and complementary to (not duplicative of) the services of others if you are credentialed as a hospitalist.
Ensure “apples to apples” comparisons
A second reason to re-credential as a hospitalist is to ensure that when the CMS looks at the services you are providing and the CPT codes you are selecting, it is comparing you to an appropriate peer group for compliance purposes.
The mix of CPT codes reported by hospitalists in the SHM State of Hospital Medicine Survey has historically tilted toward higher-level care than has the mix of CPT codes reported by the CMS for internal medicine or family medicine physicians. But last year when Medicare released the utilization of evaluation and management services by specialty for calendar year 2017, CPT utilization was shown separately for hospitalists for the first time!
The volume of services reported for physicians credentialed as hospitalists was very small relative to the volume of inpatient services provided by internal medicine and family medicine physicians, but the distribution of inpatient admission, subsequent visit, and discharge codes for hospitalists closely mirrored those reported by SHM in its 2018 State of Hospital Medicine Report (see graphic).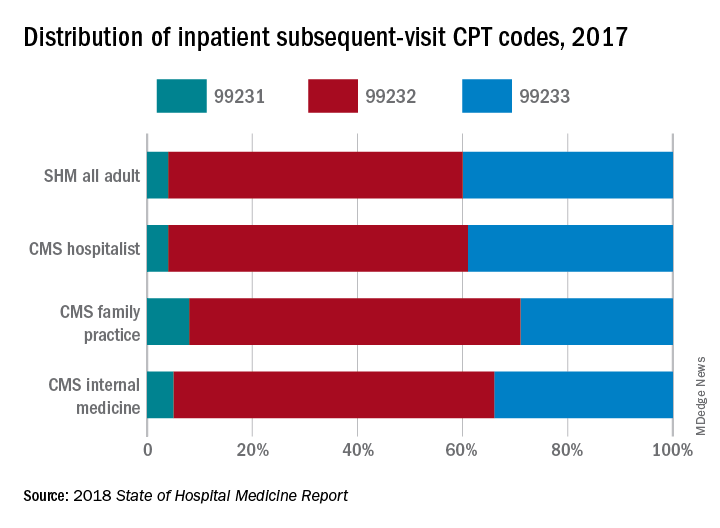
If you’re going to be targeted in a RAC audit for the high proportion of 99233s you bill, you want to be sure the CMS is looking at your performance compared to those who are truly your peers, caring for patients of the same type and complexity.
Improve CMS data used for research purposes
Finally, the ability of academic hospitalists and other health services researchers to utilize Medicare claims data to better understand the care provided by hospitalists and its impact on the overall health care system will be significantly enhanced by a more robust presence of physicians who have identified themselves as hospitalists in the PECOS credentialing system.
We care for the majority of patients in most hospitals these days, yet “hospitalists” billed only 2,009,869 inpatient subsequent visits (CPT codes 99231, 99232, and 99233) in 2017 compared to 25,903,829 billed by internal medicine physicians and 4,678,111 billed by family medicine physicians. And regardless of what you think about using claims data as a proxy for health care services and quality, it’s undeniably the best data set we currently have.
So, let’s work together to build a bigger, better database of hospitalist information at the CMS. I urge you to go to your credentialing folks today and find out how you can work with them to get yourself re-credentialed in PECOS using the C6 “hospitalist” physician specialty.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants, La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Meeting Committees, and helps to coordinate SHM’s bi-annual State of Hospital Medicine Survey. This article appeared originally in SHM's official blog The Hospital Leader. Read more recent posts here.
In April 2017, the Centers for Medicare and Medicaid Services implemented the new physician specialty code C6, specifically for hospitalists. There has been a lot of confusion about what this means and some uncertainty about why clinicians should bother to use it.
Some folks thought initially that it was a new CPT code they could use to bill hospitalist services, which might recognize the increased intensity of services hospitalists often provide to their hospitalized patients compared to many traditional internal medicine and family medicine primary care physicians. Others thought it was a code that was added to the HCFA 1500 billing form somewhere to designate that the service was provided by a hospitalist.
Neither is true. The C6 physician specialty code is one of a large number of such codes used by physicians to designate their primary physician specialty when they enroll with Medicare via the PECOS online enrollment system. It describes the unique type of medicine practiced by the enrolling physician and is used by the CMS both for claims processing purposes and for “programmatic” purposes (whatever that means).
It doesn’t change how your claim is processed or how much you get paid. So why bother going through the laborious process of re-credentialing with CMS via PECOS just to change your specialty code? Well, I believe there are several ways in which the C6 specialty code provides value – both to you and to the specialty of hospital medicine.
Reduce concurrent care denials
First, it distinguishes you from a general internal medicine or general family medicine practitioner by recognizing “hospitalist” as a distinct specialty. This can be valuable from a financial perspective because it may reduce the risk that claims for your services might be denied due to “concurrent care” by another provider in the same specialty on the same calendar day.
And it’s not just a general internist or family medicine physician that you might run into concurrent care trouble with. I’ve seen situations where doctors completed critical care or cardiology fellowships but never got around to re-credentialing with Medicare in their new specialty, so their claims still showed up with an “internal medicine” physician specialty code, resulting in denied “concurrent care” claims for either the hospitalist or the specialist.
While Medicare may still see unnecessary overlap between services provided by you and an internal medicine or family physician to the same patient on the same calendar day, you can make a better argument that your services were unique and complementary to (not duplicative of) the services of others if you are credentialed as a hospitalist.
Ensure “apples to apples” comparisons
A second reason to re-credential as a hospitalist is to ensure that when the CMS looks at the services you are providing and the CPT codes you are selecting, it is comparing you to an appropriate peer group for compliance purposes.
The mix of CPT codes reported by hospitalists in the SHM State of Hospital Medicine Survey has historically tilted toward higher-level care than has the mix of CPT codes reported by the CMS for internal medicine or family medicine physicians. But last year when Medicare released the utilization of evaluation and management services by specialty for calendar year 2017, CPT utilization was shown separately for hospitalists for the first time!
The volume of services reported for physicians credentialed as hospitalists was very small relative to the volume of inpatient services provided by internal medicine and family medicine physicians, but the distribution of inpatient admission, subsequent visit, and discharge codes for hospitalists closely mirrored those reported by SHM in its 2018 State of Hospital Medicine Report (see graphic).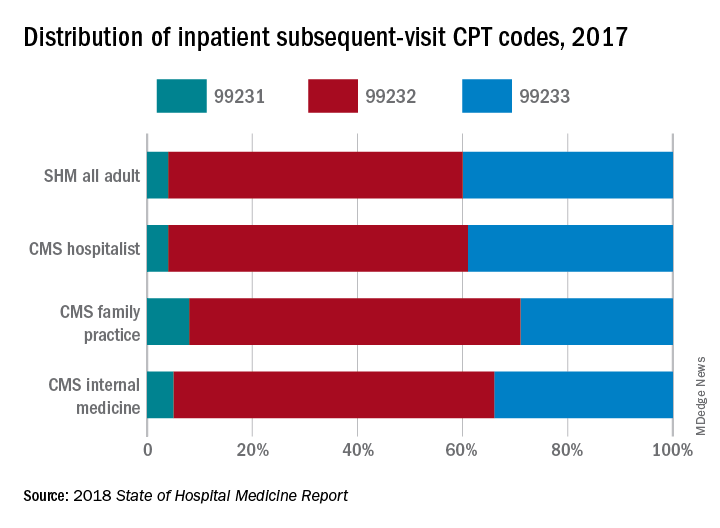
If you’re going to be targeted in a RAC audit for the high proportion of 99233s you bill, you want to be sure the CMS is looking at your performance compared to those who are truly your peers, caring for patients of the same type and complexity.
Improve CMS data used for research purposes
Finally, the ability of academic hospitalists and other health services researchers to utilize Medicare claims data to better understand the care provided by hospitalists and its impact on the overall health care system will be significantly enhanced by a more robust presence of physicians who have identified themselves as hospitalists in the PECOS credentialing system.
We care for the majority of patients in most hospitals these days, yet “hospitalists” billed only 2,009,869 inpatient subsequent visits (CPT codes 99231, 99232, and 99233) in 2017 compared to 25,903,829 billed by internal medicine physicians and 4,678,111 billed by family medicine physicians. And regardless of what you think about using claims data as a proxy for health care services and quality, it’s undeniably the best data set we currently have.
So, let’s work together to build a bigger, better database of hospitalist information at the CMS. I urge you to go to your credentialing folks today and find out how you can work with them to get yourself re-credentialed in PECOS using the C6 “hospitalist” physician specialty.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants, La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Meeting Committees, and helps to coordinate SHM’s bi-annual State of Hospital Medicine Survey. This article appeared originally in SHM's official blog The Hospital Leader. Read more recent posts here.










