User login
New UTI Guideline Offers Treatment Clarity, Reveals Gaps in Knowledge
New recommendations from the WikiGuidelines Group offer strategies for the prevention, diagnosis, and management of urinary tract infections (UTIs) in children and adults.
While the guideline covers a range of clinical topics, including prophylaxis and antimicrobial stewardship, many key clinical questions remain unanswered because of a lack of high-quality evidence, according to lead author Zachary Nelson, PharmD, MPH, of HealthPartners and Park Nicollet Health Services, St. Louis Park, Minnesota, and colleagues.
“This guideline fills a critical gap by providing pragmatic, broadly applicable recommendations tailored for generalist care and systems-based practice,” Nelson and colleagues wrote in JAMA Network Open. “Our guidance is rooted in the best available evidence and is designed for clinicians from various backgrounds and healthcare environments. It emphasizes a patient-centered approach to the diagnosis, prevention, and treatment of UTIs and related genitourinary infections.”
The guideline panelists, including 54 experts from 12 countries, developed the document in accordance with Standards for Quality Improvement Reporting Excellence and the WikiGuidelines charter. The latter requires that “clear recommendations” are based on data from at least two concordant randomized clinical trials (RCTs), or one RCT plus one concordant prospective observational study.
This approach allowed the panel to provide clear recommendations for 6 out of 37 unique questions, while 3 other questions were partially answered. In other words, 75% of the questions lacked sufficient evidence for answers.
“These guidelines are important because they illuminate the clinical data and lack of data we have for approaching diagnosis and treatment of this common infection that leads to a wide array of morbidity and sometimes mortality, as well as significant cost burden to the healthcare system,” said coauthor Sarah Kurz, MD, clinical assistant professor of internal medicine at Michigan Medicine, Ann Arbor, in a written comment.
Jessica Hammett, MD, a urologist at Emory Healthcare, Atlanta, Georgia, who was not an author of the study, suggested that the guideline is additionally impactful because of the panel’s geographic diversity.
“It is an international collaboration that takes into account regional and international practice patterns and differences,” Hammett said in a written comment.
The key guideline recommendations are briefly summarized below.
Preventive Strategies for UTI
The guideline endorses cranberry products as preventive for UTI-prone women, children, and post-intervention patients, though data are insufficient to recommend them for older adults, those with bladder issues, or pregnant women.
Topical estrogen is recommended for postmenopausal women with recurrent UTIs, as it helps restore the vaginal microbiome with minimal systemic absorption. It may also benefit patients with breast cancer when nonhormonal alternatives fail.
For those with intact bladder anatomy, methenamine hippurate is suggested as a noninferior alternative to low-dose antibiotics for preventing recurrent UTIs.
“These findings confirm the best practice of starting postmenopausal women on vaginal estrogen to prevent UTIs, which is a treatment option that should be implemented more commonly,” Hammett said. “Interestingly as compared to the AUA guidelines, this paper recommends the use of cranberry supplementation and methenamine as antibiotic alternatives for preventing UTIs.”
Empirical Treatment Recommendations
According to the guideline, empirical treatment for UTIs should focus on antimicrobials with high urinary tract concentration and local pathogen efficacy.
Nitrofurantoin is recommended for uncomplicated cystitis, while trimethoprim/sulfamethoxazole (TMP/SMX) and first-generation cephalosporins are advised for pyelonephritis.
For intravenous therapy, ceftriaxone is preferred unless there are risk factors for multidrug resistance.
Recommended treatment durations include 5 days for nitrofurantoin, 3 days for TMP/SMX and fluoroquinolones, and a single dose for fosfomycin in acute cystitis cases. For acute pyelonephritis, fluoroquinolones are advised for 5-7 days, with dose-optimized beta-lactams for 7 days. Gram-negative bacteremia from urinary sources warrants a 7-day course.
Stewardship and Clinical Management
The guideline emphasizes antimicrobial stewardship, with support for antibiotic de-escalation and oral regimens where feasible, to reduce adverse effects and hospital stays. Although evidence is limited, the authors suggest thorough allergy assessment and selective reporting of susceptibility results to enhance antibiotic selection.
While data were insufficient to make clear recommendations about the treatment of asymptomatic bacteriuria, Nelson and colleagues suggested that this practice “risks side effects without benefit” while threatening antimicrobial sustainability.
Hammett agreed, noting that “[this] serves as an important reminder not to treat asymptomatic bacteriuria, as it increases side effects and bacterial resistance without any improvement as compared to placebo.”
Special Considerations for Urologic Procedures
Finally, patients undergoing urologic procedures, routine cystoscopy, and urodynamic studies generally do not require prophylactic antibiotics, according to the guideline. Single-dose antibiotic prophylaxis is recommended for low-risk nephrolithotomy patients, though high-risk individuals, such as those who are pregnant or post kidney transplant, may require extended prophylaxis.
Kurz suggested that the guideline consolidates and supports the foundation of evidence driving common practices.
“I don’t think these guidelines offer any strikingly new strategies, which is unsurprising, as they were created after a deep dive into existing literature,” Kurz said. “But more importantly, what I think they do is to highlight where and what the evidence is for many of the clinical strategies that are commonly employed. For example, in terms of prevention, it is common for primary care physicians, urologists, and infectious diseases doctors to recommend cranberry and hydration and to use methenamine. These guidelines highlight that there is sufficient quality and quantity of evidence to support these interventions.”
She also noted how the guidelines emphasize the need for symptoms to make a UTI diagnosis and advise against routine testing of asymptomatic individuals.
“Despite this not being new information, typical clinical practice is often out of step here, and this [guideline] reemphasizes the important factors when considering UTI diagnosis,” Kurz said.
Finally, she expressed frustration for the numerous knowledge gaps remaining in this area, which may be traced back to barriers ranging from the semantic to the more systemic.
“Some of the difficulty is lack of clear definitions and precise terminology regarding UTIs,” Kurz said, noting the unclear distinction between complicated and uncomplicated UTIs. “I would also argue that UTIs are a disease that predominantly affects women, and like many other diseases where this is the case, [they] tend to be less studied. Hopefully, this guideline’s spotlight on all that we do not know can inspire high-quality research to address these gaps, leading to optimal patient care along with decreased burden on the system as a whole in terms of cost and antimicrobial resistance.”
The study was funded by Merck. The WikiGuidelines Group that established this guideline is entirely voluntary and unpaid; the group intends to establish a nonprofit organization to support the development of other guidelines using this novel methodology and eventually intends to trademark the name WikiGuidelines. The authors disclosed relationships with Pfizer, Eumedica, GSK, and others.
A version of this article first appeared on Medscape.com.
New recommendations from the WikiGuidelines Group offer strategies for the prevention, diagnosis, and management of urinary tract infections (UTIs) in children and adults.
While the guideline covers a range of clinical topics, including prophylaxis and antimicrobial stewardship, many key clinical questions remain unanswered because of a lack of high-quality evidence, according to lead author Zachary Nelson, PharmD, MPH, of HealthPartners and Park Nicollet Health Services, St. Louis Park, Minnesota, and colleagues.
“This guideline fills a critical gap by providing pragmatic, broadly applicable recommendations tailored for generalist care and systems-based practice,” Nelson and colleagues wrote in JAMA Network Open. “Our guidance is rooted in the best available evidence and is designed for clinicians from various backgrounds and healthcare environments. It emphasizes a patient-centered approach to the diagnosis, prevention, and treatment of UTIs and related genitourinary infections.”
The guideline panelists, including 54 experts from 12 countries, developed the document in accordance with Standards for Quality Improvement Reporting Excellence and the WikiGuidelines charter. The latter requires that “clear recommendations” are based on data from at least two concordant randomized clinical trials (RCTs), or one RCT plus one concordant prospective observational study.
This approach allowed the panel to provide clear recommendations for 6 out of 37 unique questions, while 3 other questions were partially answered. In other words, 75% of the questions lacked sufficient evidence for answers.
“These guidelines are important because they illuminate the clinical data and lack of data we have for approaching diagnosis and treatment of this common infection that leads to a wide array of morbidity and sometimes mortality, as well as significant cost burden to the healthcare system,” said coauthor Sarah Kurz, MD, clinical assistant professor of internal medicine at Michigan Medicine, Ann Arbor, in a written comment.
Jessica Hammett, MD, a urologist at Emory Healthcare, Atlanta, Georgia, who was not an author of the study, suggested that the guideline is additionally impactful because of the panel’s geographic diversity.
“It is an international collaboration that takes into account regional and international practice patterns and differences,” Hammett said in a written comment.
The key guideline recommendations are briefly summarized below.
Preventive Strategies for UTI
The guideline endorses cranberry products as preventive for UTI-prone women, children, and post-intervention patients, though data are insufficient to recommend them for older adults, those with bladder issues, or pregnant women.
Topical estrogen is recommended for postmenopausal women with recurrent UTIs, as it helps restore the vaginal microbiome with minimal systemic absorption. It may also benefit patients with breast cancer when nonhormonal alternatives fail.
For those with intact bladder anatomy, methenamine hippurate is suggested as a noninferior alternative to low-dose antibiotics for preventing recurrent UTIs.
“These findings confirm the best practice of starting postmenopausal women on vaginal estrogen to prevent UTIs, which is a treatment option that should be implemented more commonly,” Hammett said. “Interestingly as compared to the AUA guidelines, this paper recommends the use of cranberry supplementation and methenamine as antibiotic alternatives for preventing UTIs.”
Empirical Treatment Recommendations
According to the guideline, empirical treatment for UTIs should focus on antimicrobials with high urinary tract concentration and local pathogen efficacy.
Nitrofurantoin is recommended for uncomplicated cystitis, while trimethoprim/sulfamethoxazole (TMP/SMX) and first-generation cephalosporins are advised for pyelonephritis.
For intravenous therapy, ceftriaxone is preferred unless there are risk factors for multidrug resistance.
Recommended treatment durations include 5 days for nitrofurantoin, 3 days for TMP/SMX and fluoroquinolones, and a single dose for fosfomycin in acute cystitis cases. For acute pyelonephritis, fluoroquinolones are advised for 5-7 days, with dose-optimized beta-lactams for 7 days. Gram-negative bacteremia from urinary sources warrants a 7-day course.
Stewardship and Clinical Management
The guideline emphasizes antimicrobial stewardship, with support for antibiotic de-escalation and oral regimens where feasible, to reduce adverse effects and hospital stays. Although evidence is limited, the authors suggest thorough allergy assessment and selective reporting of susceptibility results to enhance antibiotic selection.
While data were insufficient to make clear recommendations about the treatment of asymptomatic bacteriuria, Nelson and colleagues suggested that this practice “risks side effects without benefit” while threatening antimicrobial sustainability.
Hammett agreed, noting that “[this] serves as an important reminder not to treat asymptomatic bacteriuria, as it increases side effects and bacterial resistance without any improvement as compared to placebo.”
Special Considerations for Urologic Procedures
Finally, patients undergoing urologic procedures, routine cystoscopy, and urodynamic studies generally do not require prophylactic antibiotics, according to the guideline. Single-dose antibiotic prophylaxis is recommended for low-risk nephrolithotomy patients, though high-risk individuals, such as those who are pregnant or post kidney transplant, may require extended prophylaxis.
Kurz suggested that the guideline consolidates and supports the foundation of evidence driving common practices.
“I don’t think these guidelines offer any strikingly new strategies, which is unsurprising, as they were created after a deep dive into existing literature,” Kurz said. “But more importantly, what I think they do is to highlight where and what the evidence is for many of the clinical strategies that are commonly employed. For example, in terms of prevention, it is common for primary care physicians, urologists, and infectious diseases doctors to recommend cranberry and hydration and to use methenamine. These guidelines highlight that there is sufficient quality and quantity of evidence to support these interventions.”
She also noted how the guidelines emphasize the need for symptoms to make a UTI diagnosis and advise against routine testing of asymptomatic individuals.
“Despite this not being new information, typical clinical practice is often out of step here, and this [guideline] reemphasizes the important factors when considering UTI diagnosis,” Kurz said.
Finally, she expressed frustration for the numerous knowledge gaps remaining in this area, which may be traced back to barriers ranging from the semantic to the more systemic.
“Some of the difficulty is lack of clear definitions and precise terminology regarding UTIs,” Kurz said, noting the unclear distinction between complicated and uncomplicated UTIs. “I would also argue that UTIs are a disease that predominantly affects women, and like many other diseases where this is the case, [they] tend to be less studied. Hopefully, this guideline’s spotlight on all that we do not know can inspire high-quality research to address these gaps, leading to optimal patient care along with decreased burden on the system as a whole in terms of cost and antimicrobial resistance.”
The study was funded by Merck. The WikiGuidelines Group that established this guideline is entirely voluntary and unpaid; the group intends to establish a nonprofit organization to support the development of other guidelines using this novel methodology and eventually intends to trademark the name WikiGuidelines. The authors disclosed relationships with Pfizer, Eumedica, GSK, and others.
A version of this article first appeared on Medscape.com.
New recommendations from the WikiGuidelines Group offer strategies for the prevention, diagnosis, and management of urinary tract infections (UTIs) in children and adults.
While the guideline covers a range of clinical topics, including prophylaxis and antimicrobial stewardship, many key clinical questions remain unanswered because of a lack of high-quality evidence, according to lead author Zachary Nelson, PharmD, MPH, of HealthPartners and Park Nicollet Health Services, St. Louis Park, Minnesota, and colleagues.
“This guideline fills a critical gap by providing pragmatic, broadly applicable recommendations tailored for generalist care and systems-based practice,” Nelson and colleagues wrote in JAMA Network Open. “Our guidance is rooted in the best available evidence and is designed for clinicians from various backgrounds and healthcare environments. It emphasizes a patient-centered approach to the diagnosis, prevention, and treatment of UTIs and related genitourinary infections.”
The guideline panelists, including 54 experts from 12 countries, developed the document in accordance with Standards for Quality Improvement Reporting Excellence and the WikiGuidelines charter. The latter requires that “clear recommendations” are based on data from at least two concordant randomized clinical trials (RCTs), or one RCT plus one concordant prospective observational study.
This approach allowed the panel to provide clear recommendations for 6 out of 37 unique questions, while 3 other questions were partially answered. In other words, 75% of the questions lacked sufficient evidence for answers.
“These guidelines are important because they illuminate the clinical data and lack of data we have for approaching diagnosis and treatment of this common infection that leads to a wide array of morbidity and sometimes mortality, as well as significant cost burden to the healthcare system,” said coauthor Sarah Kurz, MD, clinical assistant professor of internal medicine at Michigan Medicine, Ann Arbor, in a written comment.
Jessica Hammett, MD, a urologist at Emory Healthcare, Atlanta, Georgia, who was not an author of the study, suggested that the guideline is additionally impactful because of the panel’s geographic diversity.
“It is an international collaboration that takes into account regional and international practice patterns and differences,” Hammett said in a written comment.
The key guideline recommendations are briefly summarized below.
Preventive Strategies for UTI
The guideline endorses cranberry products as preventive for UTI-prone women, children, and post-intervention patients, though data are insufficient to recommend them for older adults, those with bladder issues, or pregnant women.
Topical estrogen is recommended for postmenopausal women with recurrent UTIs, as it helps restore the vaginal microbiome with minimal systemic absorption. It may also benefit patients with breast cancer when nonhormonal alternatives fail.
For those with intact bladder anatomy, methenamine hippurate is suggested as a noninferior alternative to low-dose antibiotics for preventing recurrent UTIs.
“These findings confirm the best practice of starting postmenopausal women on vaginal estrogen to prevent UTIs, which is a treatment option that should be implemented more commonly,” Hammett said. “Interestingly as compared to the AUA guidelines, this paper recommends the use of cranberry supplementation and methenamine as antibiotic alternatives for preventing UTIs.”
Empirical Treatment Recommendations
According to the guideline, empirical treatment for UTIs should focus on antimicrobials with high urinary tract concentration and local pathogen efficacy.
Nitrofurantoin is recommended for uncomplicated cystitis, while trimethoprim/sulfamethoxazole (TMP/SMX) and first-generation cephalosporins are advised for pyelonephritis.
For intravenous therapy, ceftriaxone is preferred unless there are risk factors for multidrug resistance.
Recommended treatment durations include 5 days for nitrofurantoin, 3 days for TMP/SMX and fluoroquinolones, and a single dose for fosfomycin in acute cystitis cases. For acute pyelonephritis, fluoroquinolones are advised for 5-7 days, with dose-optimized beta-lactams for 7 days. Gram-negative bacteremia from urinary sources warrants a 7-day course.
Stewardship and Clinical Management
The guideline emphasizes antimicrobial stewardship, with support for antibiotic de-escalation and oral regimens where feasible, to reduce adverse effects and hospital stays. Although evidence is limited, the authors suggest thorough allergy assessment and selective reporting of susceptibility results to enhance antibiotic selection.
While data were insufficient to make clear recommendations about the treatment of asymptomatic bacteriuria, Nelson and colleagues suggested that this practice “risks side effects without benefit” while threatening antimicrobial sustainability.
Hammett agreed, noting that “[this] serves as an important reminder not to treat asymptomatic bacteriuria, as it increases side effects and bacterial resistance without any improvement as compared to placebo.”
Special Considerations for Urologic Procedures
Finally, patients undergoing urologic procedures, routine cystoscopy, and urodynamic studies generally do not require prophylactic antibiotics, according to the guideline. Single-dose antibiotic prophylaxis is recommended for low-risk nephrolithotomy patients, though high-risk individuals, such as those who are pregnant or post kidney transplant, may require extended prophylaxis.
Kurz suggested that the guideline consolidates and supports the foundation of evidence driving common practices.
“I don’t think these guidelines offer any strikingly new strategies, which is unsurprising, as they were created after a deep dive into existing literature,” Kurz said. “But more importantly, what I think they do is to highlight where and what the evidence is for many of the clinical strategies that are commonly employed. For example, in terms of prevention, it is common for primary care physicians, urologists, and infectious diseases doctors to recommend cranberry and hydration and to use methenamine. These guidelines highlight that there is sufficient quality and quantity of evidence to support these interventions.”
She also noted how the guidelines emphasize the need for symptoms to make a UTI diagnosis and advise against routine testing of asymptomatic individuals.
“Despite this not being new information, typical clinical practice is often out of step here, and this [guideline] reemphasizes the important factors when considering UTI diagnosis,” Kurz said.
Finally, she expressed frustration for the numerous knowledge gaps remaining in this area, which may be traced back to barriers ranging from the semantic to the more systemic.
“Some of the difficulty is lack of clear definitions and precise terminology regarding UTIs,” Kurz said, noting the unclear distinction between complicated and uncomplicated UTIs. “I would also argue that UTIs are a disease that predominantly affects women, and like many other diseases where this is the case, [they] tend to be less studied. Hopefully, this guideline’s spotlight on all that we do not know can inspire high-quality research to address these gaps, leading to optimal patient care along with decreased burden on the system as a whole in terms of cost and antimicrobial resistance.”
The study was funded by Merck. The WikiGuidelines Group that established this guideline is entirely voluntary and unpaid; the group intends to establish a nonprofit organization to support the development of other guidelines using this novel methodology and eventually intends to trademark the name WikiGuidelines. The authors disclosed relationships with Pfizer, Eumedica, GSK, and others.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Is Acute Kidney Injury Really a Single Disease?
The search for a better biomarker than creatine for acute kidney injury (AKI) has been “long and elusive.” However, could researchers be on the right path now?
“The thinking is moving away from trying to find one biomarker that can be used for different types of kidney injury to a recognition that AKI is not just a single disease that a patient has or doesn’t have,” Rob D. Nerenz, PhD, an associate professor in the Department of Pathology and Laboratory Medicine at the Medical College of Wisconsin, Milwaukee, told this news organization. “It’s lots of different diseases that all affect the kidney in different ways.”
AKI is actually a “loose collection” of hepatorenal, cardiorenal, nephrotoxic, and sepsis-associated syndromes, as well as acute interstitial nephritis (AIN), he said. “So the question is not: ‘Is AKI present — yes or no?’ It’s: ‘What kind of AKI is present, and how do I treat it?’ ”
‘Mediocre Markers’
AKI affects about 10%-30% of hospitalized patients, according to Nerenz. It’s associated with an increased risk for adverse outcomes, including post-AKI chronic kidney disease and a mortality rate of approximately 24%.
Currently, AKI is defined by a rapid increase in serum creatinine, a decrease in urine output, or both.
“Those are mediocre markers,” Nerenz said, as serum creatinine is not very sensitive to acute change, and the increase is often detected after the therapeutic window of intervention has passed. In addition, “it only tells us that the kidneys are unhappy; it doesn’t say anything about the cause.”
Urine output is limited as a marker because many conditions affect it. “If you’re dehydrated, urine output is going to decrease,” he said. “And in some forms of AKI, urine output actually goes up.”
What’s needed, he said, is a more sensitive biomarker that’s detectable within a shorter timeframe of 2-6 hours following injury.
“Right now, we’re looking at 48 hours before a change becomes apparent, and that’s just too long. Plus, it should be kidney specific. One of the major limitations of the biomarkers that have been evaluated to this point is that, yes, they’re released by the kidney, but they’re also released by other tissue types within the body, and that hinders their effectiveness as a marker.”
Neutrophil Gelatinase-Associated Lipocalin (NGAL)
Although research on better biomarkers is ongoing, “there’s also a recognition that some of the protein markers that have been around for a while, if used appropriately, can provide value,” Nerenz said. These include, among others, NGAL.
NGAL works well in pediatric patients without other comorbidities, but it has been less useful in adult patients because it is also released by other cell types. However, recent research suggests it shows promise in patients with both cirrhosis and AKI.
There are three main causes of AKI in cirrhosis, Nerenz explained. The first is prerenal and can be primarily addressed through rehydration.
“When these patients come in, clinicians won’t do anything right away other than provide fluids. If creatinine improves over the 48-hour period of fluid replenishment, then the patient is sent home because there really isn’t extensive damage to the kidneys.”
If improvement isn’t seen after those 48 hours, then it could be one of two things: Hepatorenal syndrome or acute tubular necrosis. Patients with hepatorenal syndrome are candidates for terlipressin, which the Food and Drug Administration (FDA) approved for this indication in 2022 after it displayed notable efficacy in a double-blind study.
“You don’t want to give terlipressin to just anybody because if the issue is not a diminished blood supply to the kidney, it’s not going to help, and comes with some serious side effects, such as respiratory failure,” Nerenz explained. “Having a biomarker that can distinguish between hepatorenal syndrome and acute tubular necrosis really helps clinicians confidently identify which patients are good candidates for this drug. Right now, we’re flying blind to a certain extent, basically using clinical intuition.”
Currently, the determination of NGAL is FDA cleared only for pediatric use. One way hospitals have dealt with that is by making the test in their own labs, using appropriate reagents, validation, and so forth. These tests are then safe for use in adults but haven’t gone through the FDA approval process.
However, the FDA’s recent announcement stating that the agency should oversee lab-developed tests has made this situation unclear, Nerenz said.
“At this point, we don’t know if there’s still an opportunity to take the NGAL test (or any other cleared biomarker) and validate it for use in a different patient population. Many hospital labs simply don’t have the resources to take these tests through the whole FDA approval process.”
A New Biomarker for AIN?
Meanwhile, research is also moving forward on a better biomarker for AIN, which is also under the AKI umbrella.
“It’s important to diagnose AIN because it has a very specific treatment,” Dennis G. Moledina, MD, PhD, Yale School of Medicine in New Haven, Connecticut, told this news organization.
“AIN is caused by a bunch of different medications, such as proton pump inhibitors, cancer drugs, nonsteroidal anti-inflammatory drugs, and antibiotics, so when someone has this condition, you have to stop potentially life-saving medications and give unnecessary and potentially toxic immunosuppressive drugs, like prednisone,” he said. “If you get the diagnosis wrong, you’re stopping vital drugs and giving immunosuppression for no reason. And if you miss the diagnosis, AIN can lead to permanent chronic kidney disease.”
“Right now, the only way to diagnose AIN is to do a kidney biopsy, which is risky because it can often lead to significant bleeding,” he said. “Some people can’t undergo a biopsy because they’re on medications that increase the risk of bleeding, and they can’t be stopped.”
Furthermore, he noted, “the longer a patient takes a drug that’s causing AIN without getting a diagnosis, the less the chances of recovery because the longer you let this kidney inflammation go on, the more fibrosis and permanent damage develops. So it is important to diagnose it as early as possible, and that’s again why we have a real need for a noninvasive biomarker that can be tested rapidly.”
Moledina and colleagues have been working on identifying a suitable biomarker for close to 10 years, the latest example of which is their 2023 study validating urinary CXCL9 as just such a marker.
“We’re most excited about CXCL9 because it’s already used to diagnose some other diseases in plasma,” Moledina said. “We think that we can convince labs to test it in urine.”
In an accompanying editorial, Mark Canney, PhD, and colleagues at the University of Ottawa and The Ottawa Hospital in Ontario, Canada, wrote that the CXCL9 study findings “are exciting because they provide a road map of where diagnostics can get to for this common, yet poorly identified and treated, cause of kidney damage. The need for a different approach can be readily identified from the fact that clinicians’ gestalt for diagnosing AIN was almost tantamount to tossing a coin (AUC, 0.57). CXCL9 alone outperformed not only the clinician’s prebiopsy suspicion but also an existing diagnostic model and other candidate biomarkers both in the discovery and external validation cohorts.”
Like NGAL, CXCL9 will have to go through the FDA approval process before it can be used for AIN. Therefore, it may be a few years before it can become routinely available, Moledina said.
Nevertheless, Nerenz added, “I think the next steps for AKI are probably continuing on this path of context-dependent, selective biomarker use. I anticipate that we’ll see ongoing development in this space, just expanding to a wider variety of clinical scenarios.”
Nerenz declared receiving research funding from Abbott Labs for evaluation of an AKI biomarker. Moledina is a co-inventor on a pending patent, “Methods and Systems for Diagnosis of Acute Interstitial Nephritis”; a cofounder of the diagnostics company Predict AIN; and a consultant for Biohaven.
A version of this article first appeared on Medscape.com.
The search for a better biomarker than creatine for acute kidney injury (AKI) has been “long and elusive.” However, could researchers be on the right path now?
“The thinking is moving away from trying to find one biomarker that can be used for different types of kidney injury to a recognition that AKI is not just a single disease that a patient has or doesn’t have,” Rob D. Nerenz, PhD, an associate professor in the Department of Pathology and Laboratory Medicine at the Medical College of Wisconsin, Milwaukee, told this news organization. “It’s lots of different diseases that all affect the kidney in different ways.”
AKI is actually a “loose collection” of hepatorenal, cardiorenal, nephrotoxic, and sepsis-associated syndromes, as well as acute interstitial nephritis (AIN), he said. “So the question is not: ‘Is AKI present — yes or no?’ It’s: ‘What kind of AKI is present, and how do I treat it?’ ”
‘Mediocre Markers’
AKI affects about 10%-30% of hospitalized patients, according to Nerenz. It’s associated with an increased risk for adverse outcomes, including post-AKI chronic kidney disease and a mortality rate of approximately 24%.
Currently, AKI is defined by a rapid increase in serum creatinine, a decrease in urine output, or both.
“Those are mediocre markers,” Nerenz said, as serum creatinine is not very sensitive to acute change, and the increase is often detected after the therapeutic window of intervention has passed. In addition, “it only tells us that the kidneys are unhappy; it doesn’t say anything about the cause.”
Urine output is limited as a marker because many conditions affect it. “If you’re dehydrated, urine output is going to decrease,” he said. “And in some forms of AKI, urine output actually goes up.”
What’s needed, he said, is a more sensitive biomarker that’s detectable within a shorter timeframe of 2-6 hours following injury.
“Right now, we’re looking at 48 hours before a change becomes apparent, and that’s just too long. Plus, it should be kidney specific. One of the major limitations of the biomarkers that have been evaluated to this point is that, yes, they’re released by the kidney, but they’re also released by other tissue types within the body, and that hinders their effectiveness as a marker.”
Neutrophil Gelatinase-Associated Lipocalin (NGAL)
Although research on better biomarkers is ongoing, “there’s also a recognition that some of the protein markers that have been around for a while, if used appropriately, can provide value,” Nerenz said. These include, among others, NGAL.
NGAL works well in pediatric patients without other comorbidities, but it has been less useful in adult patients because it is also released by other cell types. However, recent research suggests it shows promise in patients with both cirrhosis and AKI.
There are three main causes of AKI in cirrhosis, Nerenz explained. The first is prerenal and can be primarily addressed through rehydration.
“When these patients come in, clinicians won’t do anything right away other than provide fluids. If creatinine improves over the 48-hour period of fluid replenishment, then the patient is sent home because there really isn’t extensive damage to the kidneys.”
If improvement isn’t seen after those 48 hours, then it could be one of two things: Hepatorenal syndrome or acute tubular necrosis. Patients with hepatorenal syndrome are candidates for terlipressin, which the Food and Drug Administration (FDA) approved for this indication in 2022 after it displayed notable efficacy in a double-blind study.
“You don’t want to give terlipressin to just anybody because if the issue is not a diminished blood supply to the kidney, it’s not going to help, and comes with some serious side effects, such as respiratory failure,” Nerenz explained. “Having a biomarker that can distinguish between hepatorenal syndrome and acute tubular necrosis really helps clinicians confidently identify which patients are good candidates for this drug. Right now, we’re flying blind to a certain extent, basically using clinical intuition.”
Currently, the determination of NGAL is FDA cleared only for pediatric use. One way hospitals have dealt with that is by making the test in their own labs, using appropriate reagents, validation, and so forth. These tests are then safe for use in adults but haven’t gone through the FDA approval process.
However, the FDA’s recent announcement stating that the agency should oversee lab-developed tests has made this situation unclear, Nerenz said.
“At this point, we don’t know if there’s still an opportunity to take the NGAL test (or any other cleared biomarker) and validate it for use in a different patient population. Many hospital labs simply don’t have the resources to take these tests through the whole FDA approval process.”
A New Biomarker for AIN?
Meanwhile, research is also moving forward on a better biomarker for AIN, which is also under the AKI umbrella.
“It’s important to diagnose AIN because it has a very specific treatment,” Dennis G. Moledina, MD, PhD, Yale School of Medicine in New Haven, Connecticut, told this news organization.
“AIN is caused by a bunch of different medications, such as proton pump inhibitors, cancer drugs, nonsteroidal anti-inflammatory drugs, and antibiotics, so when someone has this condition, you have to stop potentially life-saving medications and give unnecessary and potentially toxic immunosuppressive drugs, like prednisone,” he said. “If you get the diagnosis wrong, you’re stopping vital drugs and giving immunosuppression for no reason. And if you miss the diagnosis, AIN can lead to permanent chronic kidney disease.”
“Right now, the only way to diagnose AIN is to do a kidney biopsy, which is risky because it can often lead to significant bleeding,” he said. “Some people can’t undergo a biopsy because they’re on medications that increase the risk of bleeding, and they can’t be stopped.”
Furthermore, he noted, “the longer a patient takes a drug that’s causing AIN without getting a diagnosis, the less the chances of recovery because the longer you let this kidney inflammation go on, the more fibrosis and permanent damage develops. So it is important to diagnose it as early as possible, and that’s again why we have a real need for a noninvasive biomarker that can be tested rapidly.”
Moledina and colleagues have been working on identifying a suitable biomarker for close to 10 years, the latest example of which is their 2023 study validating urinary CXCL9 as just such a marker.
“We’re most excited about CXCL9 because it’s already used to diagnose some other diseases in plasma,” Moledina said. “We think that we can convince labs to test it in urine.”
In an accompanying editorial, Mark Canney, PhD, and colleagues at the University of Ottawa and The Ottawa Hospital in Ontario, Canada, wrote that the CXCL9 study findings “are exciting because they provide a road map of where diagnostics can get to for this common, yet poorly identified and treated, cause of kidney damage. The need for a different approach can be readily identified from the fact that clinicians’ gestalt for diagnosing AIN was almost tantamount to tossing a coin (AUC, 0.57). CXCL9 alone outperformed not only the clinician’s prebiopsy suspicion but also an existing diagnostic model and other candidate biomarkers both in the discovery and external validation cohorts.”
Like NGAL, CXCL9 will have to go through the FDA approval process before it can be used for AIN. Therefore, it may be a few years before it can become routinely available, Moledina said.
Nevertheless, Nerenz added, “I think the next steps for AKI are probably continuing on this path of context-dependent, selective biomarker use. I anticipate that we’ll see ongoing development in this space, just expanding to a wider variety of clinical scenarios.”
Nerenz declared receiving research funding from Abbott Labs for evaluation of an AKI biomarker. Moledina is a co-inventor on a pending patent, “Methods and Systems for Diagnosis of Acute Interstitial Nephritis”; a cofounder of the diagnostics company Predict AIN; and a consultant for Biohaven.
A version of this article first appeared on Medscape.com.
The search for a better biomarker than creatine for acute kidney injury (AKI) has been “long and elusive.” However, could researchers be on the right path now?
“The thinking is moving away from trying to find one biomarker that can be used for different types of kidney injury to a recognition that AKI is not just a single disease that a patient has or doesn’t have,” Rob D. Nerenz, PhD, an associate professor in the Department of Pathology and Laboratory Medicine at the Medical College of Wisconsin, Milwaukee, told this news organization. “It’s lots of different diseases that all affect the kidney in different ways.”
AKI is actually a “loose collection” of hepatorenal, cardiorenal, nephrotoxic, and sepsis-associated syndromes, as well as acute interstitial nephritis (AIN), he said. “So the question is not: ‘Is AKI present — yes or no?’ It’s: ‘What kind of AKI is present, and how do I treat it?’ ”
‘Mediocre Markers’
AKI affects about 10%-30% of hospitalized patients, according to Nerenz. It’s associated with an increased risk for adverse outcomes, including post-AKI chronic kidney disease and a mortality rate of approximately 24%.
Currently, AKI is defined by a rapid increase in serum creatinine, a decrease in urine output, or both.
“Those are mediocre markers,” Nerenz said, as serum creatinine is not very sensitive to acute change, and the increase is often detected after the therapeutic window of intervention has passed. In addition, “it only tells us that the kidneys are unhappy; it doesn’t say anything about the cause.”
Urine output is limited as a marker because many conditions affect it. “If you’re dehydrated, urine output is going to decrease,” he said. “And in some forms of AKI, urine output actually goes up.”
What’s needed, he said, is a more sensitive biomarker that’s detectable within a shorter timeframe of 2-6 hours following injury.
“Right now, we’re looking at 48 hours before a change becomes apparent, and that’s just too long. Plus, it should be kidney specific. One of the major limitations of the biomarkers that have been evaluated to this point is that, yes, they’re released by the kidney, but they’re also released by other tissue types within the body, and that hinders their effectiveness as a marker.”
Neutrophil Gelatinase-Associated Lipocalin (NGAL)
Although research on better biomarkers is ongoing, “there’s also a recognition that some of the protein markers that have been around for a while, if used appropriately, can provide value,” Nerenz said. These include, among others, NGAL.
NGAL works well in pediatric patients without other comorbidities, but it has been less useful in adult patients because it is also released by other cell types. However, recent research suggests it shows promise in patients with both cirrhosis and AKI.
There are three main causes of AKI in cirrhosis, Nerenz explained. The first is prerenal and can be primarily addressed through rehydration.
“When these patients come in, clinicians won’t do anything right away other than provide fluids. If creatinine improves over the 48-hour period of fluid replenishment, then the patient is sent home because there really isn’t extensive damage to the kidneys.”
If improvement isn’t seen after those 48 hours, then it could be one of two things: Hepatorenal syndrome or acute tubular necrosis. Patients with hepatorenal syndrome are candidates for terlipressin, which the Food and Drug Administration (FDA) approved for this indication in 2022 after it displayed notable efficacy in a double-blind study.
“You don’t want to give terlipressin to just anybody because if the issue is not a diminished blood supply to the kidney, it’s not going to help, and comes with some serious side effects, such as respiratory failure,” Nerenz explained. “Having a biomarker that can distinguish between hepatorenal syndrome and acute tubular necrosis really helps clinicians confidently identify which patients are good candidates for this drug. Right now, we’re flying blind to a certain extent, basically using clinical intuition.”
Currently, the determination of NGAL is FDA cleared only for pediatric use. One way hospitals have dealt with that is by making the test in their own labs, using appropriate reagents, validation, and so forth. These tests are then safe for use in adults but haven’t gone through the FDA approval process.
However, the FDA’s recent announcement stating that the agency should oversee lab-developed tests has made this situation unclear, Nerenz said.
“At this point, we don’t know if there’s still an opportunity to take the NGAL test (or any other cleared biomarker) and validate it for use in a different patient population. Many hospital labs simply don’t have the resources to take these tests through the whole FDA approval process.”
A New Biomarker for AIN?
Meanwhile, research is also moving forward on a better biomarker for AIN, which is also under the AKI umbrella.
“It’s important to diagnose AIN because it has a very specific treatment,” Dennis G. Moledina, MD, PhD, Yale School of Medicine in New Haven, Connecticut, told this news organization.
“AIN is caused by a bunch of different medications, such as proton pump inhibitors, cancer drugs, nonsteroidal anti-inflammatory drugs, and antibiotics, so when someone has this condition, you have to stop potentially life-saving medications and give unnecessary and potentially toxic immunosuppressive drugs, like prednisone,” he said. “If you get the diagnosis wrong, you’re stopping vital drugs and giving immunosuppression for no reason. And if you miss the diagnosis, AIN can lead to permanent chronic kidney disease.”
“Right now, the only way to diagnose AIN is to do a kidney biopsy, which is risky because it can often lead to significant bleeding,” he said. “Some people can’t undergo a biopsy because they’re on medications that increase the risk of bleeding, and they can’t be stopped.”
Furthermore, he noted, “the longer a patient takes a drug that’s causing AIN without getting a diagnosis, the less the chances of recovery because the longer you let this kidney inflammation go on, the more fibrosis and permanent damage develops. So it is important to diagnose it as early as possible, and that’s again why we have a real need for a noninvasive biomarker that can be tested rapidly.”
Moledina and colleagues have been working on identifying a suitable biomarker for close to 10 years, the latest example of which is their 2023 study validating urinary CXCL9 as just such a marker.
“We’re most excited about CXCL9 because it’s already used to diagnose some other diseases in plasma,” Moledina said. “We think that we can convince labs to test it in urine.”
In an accompanying editorial, Mark Canney, PhD, and colleagues at the University of Ottawa and The Ottawa Hospital in Ontario, Canada, wrote that the CXCL9 study findings “are exciting because they provide a road map of where diagnostics can get to for this common, yet poorly identified and treated, cause of kidney damage. The need for a different approach can be readily identified from the fact that clinicians’ gestalt for diagnosing AIN was almost tantamount to tossing a coin (AUC, 0.57). CXCL9 alone outperformed not only the clinician’s prebiopsy suspicion but also an existing diagnostic model and other candidate biomarkers both in the discovery and external validation cohorts.”
Like NGAL, CXCL9 will have to go through the FDA approval process before it can be used for AIN. Therefore, it may be a few years before it can become routinely available, Moledina said.
Nevertheless, Nerenz added, “I think the next steps for AKI are probably continuing on this path of context-dependent, selective biomarker use. I anticipate that we’ll see ongoing development in this space, just expanding to a wider variety of clinical scenarios.”
Nerenz declared receiving research funding from Abbott Labs for evaluation of an AKI biomarker. Moledina is a co-inventor on a pending patent, “Methods and Systems for Diagnosis of Acute Interstitial Nephritis”; a cofounder of the diagnostics company Predict AIN; and a consultant for Biohaven.
A version of this article first appeared on Medscape.com.
Plastic Pollution’s Next Victim: The Human Urinary Tract
Although a 2019 World Health Organization (WHO) report concluded that microplastics in drinking water posed no risk to human health, accumulating evidence is beginning to challenge these findings.
Since plastics became widely used in the mid-20th century, they have evolved from a novel substance to an essential component in countless applications, with global production reaching 368 million tons in 2019 and expected to double by 2039. The production and degradation of plastics involve physical, chemical, and biological processes, leading to the formation of tiny fragments known as microplastics (MPs) and nanoplastics (NPs), which accumulate in the environment. Beyond the well-documented environmental harms of MPs and NPs, growing evidence of their presence within the human body raises concerns about their potential to trigger various harmful biological processes. Their detection in the urinary tract and their potential links to kidney and bladder diseases, as shown in animal studies, are particularly alarming.
Impacts Becoming Apparent
As the impact of plastic pollution becomes increasingly apparent, the need for standardized international definitions of MPs and NPs is pressing. Government publications reveal notable discrepancies between organizations in defining these fragmented plastics. The lack of consensus among regulatory bodies highlights the challenges in mitigating the environmental and health impacts of MPs and NPs. The International Organization for Standardization offers the most precise classification, defining MPs as solid, insoluble plastic particles ranging from 1 µm to 1 mm and NPs as particles smaller than 1 µm.
The intrusion of MPs and NPs into the human body, whether through inhalation, ingestion, or skin exposure (via wounds, hair follicles, or sweat glands), has been linked to harmful biological effects, including inflammation, alterations in cellular metabolism, physical cellular damage, and reduced cell viability.
Urinary Tract Plastics
The detection of MPs and NPs in the human urinary tract, combined with limited understanding of their effects, is a growing concern. An exploratory study published earlier this year aimed to systematically summarize the existing literature regarding the presence of MPs and NPs in the urinary tract and their potential consequences, guided by these research questions:
- What are the characteristics of the plastics detected in the human urinary tract?
- How are MPs and NPs defined in the current literature?
- What methodologies are used to explore the presence and effects of MPs and NPs?
- What are the pathophysiologic consequences of the presence of MPs and NPs in the human urinary tract?
For this study, the “urinary tract” included the kidneys, bladder, ureter, urethra, and urine. By focusing on the urinary tract, the study aimed to consolidate current understanding of MPs and NPs, raise awareness of this emerging issue, and lay the groundwork for further research that could contribute to public health policies and clinical practice guidelines.
The researchers conducted a scoping literature review following the recommendations of the JBI [formerly known as the Joanna Briggs Institute). They systematically searched five databases — PubMed, Scopus, CINAHL, Web of Science, and Embase — as well as gray literature sources.
Concerning Study Results
Eighteen articles were identified. The authors represent seven countries: Pakistan (n = 1), the Netherlands (n = 1), the US (n = 1), Taiwan (n = 1), Germany (n = 3), China (n = 5), and Italy (n = 6). Among these studies, six investigated and characterized the presence of MPs and NPs in the human urinary tract. MPs and NPs were detected in urine samples (n = 5), kidney cancer samples (n = 2), and bladder cancer samples (n = 1).
Additionally, 12 studies examined the effects of MPs and NPs on human urinary tract cell lines. Their findings suggest that MPs and NPs have cytotoxic effects, increase inflammation, reduce cell viability, and alter mitogen-activated protein kinase signaling pathways.
Raman spectroscopy was the primary method used to detect and characterize MPs and NPs in human samples (five out of six studies; 83%). Alternatively, pyrolysis-gas chromatography-mass spectrometry combined with direct laser infrared spectroscopy was used in one study.
Further Research Needed
This exploratory study underscores the urgent need for further research and policy development to address the challenges posed by microplastic contamination. It highlights the rapidly emerging threat of human urinary tract contamination by microplastics, questioning the WHO’s claim that microplastics pose no public health risk. The documented cytotoxic effects of microplastics, and their ability to induce inflammation, reduce cell viability, and disrupt signaling pathways, raise significant public health concerns related to bladder cancer, chronic kidney disease, chronic urinary infections, and incontinence.
Bernard-Alex Gauzere, retired physician formerly with the national health system in France (intensive care unit, tropical medicine), has disclosed no relevant financial relationships.
This story was translated from JIM using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Although a 2019 World Health Organization (WHO) report concluded that microplastics in drinking water posed no risk to human health, accumulating evidence is beginning to challenge these findings.
Since plastics became widely used in the mid-20th century, they have evolved from a novel substance to an essential component in countless applications, with global production reaching 368 million tons in 2019 and expected to double by 2039. The production and degradation of plastics involve physical, chemical, and biological processes, leading to the formation of tiny fragments known as microplastics (MPs) and nanoplastics (NPs), which accumulate in the environment. Beyond the well-documented environmental harms of MPs and NPs, growing evidence of their presence within the human body raises concerns about their potential to trigger various harmful biological processes. Their detection in the urinary tract and their potential links to kidney and bladder diseases, as shown in animal studies, are particularly alarming.
Impacts Becoming Apparent
As the impact of plastic pollution becomes increasingly apparent, the need for standardized international definitions of MPs and NPs is pressing. Government publications reveal notable discrepancies between organizations in defining these fragmented plastics. The lack of consensus among regulatory bodies highlights the challenges in mitigating the environmental and health impacts of MPs and NPs. The International Organization for Standardization offers the most precise classification, defining MPs as solid, insoluble plastic particles ranging from 1 µm to 1 mm and NPs as particles smaller than 1 µm.
The intrusion of MPs and NPs into the human body, whether through inhalation, ingestion, or skin exposure (via wounds, hair follicles, or sweat glands), has been linked to harmful biological effects, including inflammation, alterations in cellular metabolism, physical cellular damage, and reduced cell viability.
Urinary Tract Plastics
The detection of MPs and NPs in the human urinary tract, combined with limited understanding of their effects, is a growing concern. An exploratory study published earlier this year aimed to systematically summarize the existing literature regarding the presence of MPs and NPs in the urinary tract and their potential consequences, guided by these research questions:
- What are the characteristics of the plastics detected in the human urinary tract?
- How are MPs and NPs defined in the current literature?
- What methodologies are used to explore the presence and effects of MPs and NPs?
- What are the pathophysiologic consequences of the presence of MPs and NPs in the human urinary tract?
For this study, the “urinary tract” included the kidneys, bladder, ureter, urethra, and urine. By focusing on the urinary tract, the study aimed to consolidate current understanding of MPs and NPs, raise awareness of this emerging issue, and lay the groundwork for further research that could contribute to public health policies and clinical practice guidelines.
The researchers conducted a scoping literature review following the recommendations of the JBI [formerly known as the Joanna Briggs Institute). They systematically searched five databases — PubMed, Scopus, CINAHL, Web of Science, and Embase — as well as gray literature sources.
Concerning Study Results
Eighteen articles were identified. The authors represent seven countries: Pakistan (n = 1), the Netherlands (n = 1), the US (n = 1), Taiwan (n = 1), Germany (n = 3), China (n = 5), and Italy (n = 6). Among these studies, six investigated and characterized the presence of MPs and NPs in the human urinary tract. MPs and NPs were detected in urine samples (n = 5), kidney cancer samples (n = 2), and bladder cancer samples (n = 1).
Additionally, 12 studies examined the effects of MPs and NPs on human urinary tract cell lines. Their findings suggest that MPs and NPs have cytotoxic effects, increase inflammation, reduce cell viability, and alter mitogen-activated protein kinase signaling pathways.
Raman spectroscopy was the primary method used to detect and characterize MPs and NPs in human samples (five out of six studies; 83%). Alternatively, pyrolysis-gas chromatography-mass spectrometry combined with direct laser infrared spectroscopy was used in one study.
Further Research Needed
This exploratory study underscores the urgent need for further research and policy development to address the challenges posed by microplastic contamination. It highlights the rapidly emerging threat of human urinary tract contamination by microplastics, questioning the WHO’s claim that microplastics pose no public health risk. The documented cytotoxic effects of microplastics, and their ability to induce inflammation, reduce cell viability, and disrupt signaling pathways, raise significant public health concerns related to bladder cancer, chronic kidney disease, chronic urinary infections, and incontinence.
Bernard-Alex Gauzere, retired physician formerly with the national health system in France (intensive care unit, tropical medicine), has disclosed no relevant financial relationships.
This story was translated from JIM using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Although a 2019 World Health Organization (WHO) report concluded that microplastics in drinking water posed no risk to human health, accumulating evidence is beginning to challenge these findings.
Since plastics became widely used in the mid-20th century, they have evolved from a novel substance to an essential component in countless applications, with global production reaching 368 million tons in 2019 and expected to double by 2039. The production and degradation of plastics involve physical, chemical, and biological processes, leading to the formation of tiny fragments known as microplastics (MPs) and nanoplastics (NPs), which accumulate in the environment. Beyond the well-documented environmental harms of MPs and NPs, growing evidence of their presence within the human body raises concerns about their potential to trigger various harmful biological processes. Their detection in the urinary tract and their potential links to kidney and bladder diseases, as shown in animal studies, are particularly alarming.
Impacts Becoming Apparent
As the impact of plastic pollution becomes increasingly apparent, the need for standardized international definitions of MPs and NPs is pressing. Government publications reveal notable discrepancies between organizations in defining these fragmented plastics. The lack of consensus among regulatory bodies highlights the challenges in mitigating the environmental and health impacts of MPs and NPs. The International Organization for Standardization offers the most precise classification, defining MPs as solid, insoluble plastic particles ranging from 1 µm to 1 mm and NPs as particles smaller than 1 µm.
The intrusion of MPs and NPs into the human body, whether through inhalation, ingestion, or skin exposure (via wounds, hair follicles, or sweat glands), has been linked to harmful biological effects, including inflammation, alterations in cellular metabolism, physical cellular damage, and reduced cell viability.
Urinary Tract Plastics
The detection of MPs and NPs in the human urinary tract, combined with limited understanding of their effects, is a growing concern. An exploratory study published earlier this year aimed to systematically summarize the existing literature regarding the presence of MPs and NPs in the urinary tract and their potential consequences, guided by these research questions:
- What are the characteristics of the plastics detected in the human urinary tract?
- How are MPs and NPs defined in the current literature?
- What methodologies are used to explore the presence and effects of MPs and NPs?
- What are the pathophysiologic consequences of the presence of MPs and NPs in the human urinary tract?
For this study, the “urinary tract” included the kidneys, bladder, ureter, urethra, and urine. By focusing on the urinary tract, the study aimed to consolidate current understanding of MPs and NPs, raise awareness of this emerging issue, and lay the groundwork for further research that could contribute to public health policies and clinical practice guidelines.
The researchers conducted a scoping literature review following the recommendations of the JBI [formerly known as the Joanna Briggs Institute). They systematically searched five databases — PubMed, Scopus, CINAHL, Web of Science, and Embase — as well as gray literature sources.
Concerning Study Results
Eighteen articles were identified. The authors represent seven countries: Pakistan (n = 1), the Netherlands (n = 1), the US (n = 1), Taiwan (n = 1), Germany (n = 3), China (n = 5), and Italy (n = 6). Among these studies, six investigated and characterized the presence of MPs and NPs in the human urinary tract. MPs and NPs were detected in urine samples (n = 5), kidney cancer samples (n = 2), and bladder cancer samples (n = 1).
Additionally, 12 studies examined the effects of MPs and NPs on human urinary tract cell lines. Their findings suggest that MPs and NPs have cytotoxic effects, increase inflammation, reduce cell viability, and alter mitogen-activated protein kinase signaling pathways.
Raman spectroscopy was the primary method used to detect and characterize MPs and NPs in human samples (five out of six studies; 83%). Alternatively, pyrolysis-gas chromatography-mass spectrometry combined with direct laser infrared spectroscopy was used in one study.
Further Research Needed
This exploratory study underscores the urgent need for further research and policy development to address the challenges posed by microplastic contamination. It highlights the rapidly emerging threat of human urinary tract contamination by microplastics, questioning the WHO’s claim that microplastics pose no public health risk. The documented cytotoxic effects of microplastics, and their ability to induce inflammation, reduce cell viability, and disrupt signaling pathways, raise significant public health concerns related to bladder cancer, chronic kidney disease, chronic urinary infections, and incontinence.
Bernard-Alex Gauzere, retired physician formerly with the national health system in France (intensive care unit, tropical medicine), has disclosed no relevant financial relationships.
This story was translated from JIM using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Evaluating Use of Empagliflozin for Diabetes Management in Veterans With Chronic Kidney Disease
More than 37 million Americans have diabetes mellitus (DM), and approximately 90% have type 2 DM (T2DM), including about 25% of veterans.1,2 The current guidelines suggest that therapy depends on a patient's comorbidities, management needs, and patient-centered treatment factors.3 About 1 in 3 adults with DM have chronic kidney disease (CKD), defined as the presence of kidney damage or an estimated glomerular filtration rate (eGFR) < 60 mL/min per 1.73 m2, persisting for ≥ 3 months.4
Sodium-glucose cotransporter-2 (SGLT-2) inhibitors are a class of antihyperglycemic agents acting on the SGLT-2 proteins expressed in the renal proximal convoluted tubules. They exert their effects by preventing the reabsorption of filtered glucose from the tubular lumen. There are 4 SGLT-2 inhibitors approved by the US Food and Drug Administration: canagliflozin, dapagliflozin, empagliflozin, and ertugliflozin. Empagliflozin is currently the preferred SGLT-2 inhibitor on the US Department of Veterans Affairs (VA) formulary.
According to the American Diabetes Association guidelines, empagliflozin is considered when an individual has or is at risk for atherosclerotic cardiovascular disease, heart failure, and CKD.3 SGLT-2 inhibitors are a favorable option due to their low risk for hypoglycemia while also promoting weight loss. The EMPEROR-Reduced trial demonstrated that, in addition to benefits for patients with heart failure, empagliflozin also slowed the progressive decline in kidney function in those with and without DM.5 The purpose of this study was to evaluate the effectiveness of empagliflozin on hemoglobin A1c (HbA1c) levels in patients with CKD at the Hershel “Woody” Williams VA Medical Center (HWWVAMC) in Huntington, West Virginia, along with other laboratory test markers.
Methods
The Marshall University Institutional Review Board #1 (Medical) and the HWWVAMC institutional review board and research and development committee each reviewed and approved this study. A retrospective chart review was conducted on patients diagnosed with T2DM and stage 3 CKD who were prescribed empagliflozin for DM management between January 1, 2015, and October 1, 2022, yielding 1771 patients. Data were obtained through the VHA Corporate Data Warehouse (CDW) and stored on the VA Informatics and Computing Infrastructure (VINCI) research server.
Patients were included if they were aged 18 to 89 years, prescribed empagliflozin by a VA clinician for the treatment of T2DM, had an eGFR between 30 and 59 mL/min/1.73 m2, and had an initial HbA1c between 7% and 10%. Using further random sampling, patients were either excluded or divided into, those with stage 3a CKD and those with stage 3b CKD. The primary endpoint of this study was the change in HbA1c levels in patients with stage 3b CKD (eGFR 30-44 mL/min/1.73 m2) compared with stage 3a (eGFR 45-59 mL/min/1.73 m2) after 12 months. The secondary endpoints included effects on renal function, weight, blood pressure, incidence of adverse drug events, and cardiovascular events. Of the excluded, 38 had HbA1c < 7%, 30 had HbA1c ≥ 10%, 21 did not have data at 1-year mark, 15 had the medication discontinued due to decline in renal function, 14 discontinued their medication without documented reason, 10 discontinued their medication due to adverse drug reactions (ADRs), 12 had eGFR > 60 mL/ min/1.73 m2, 9 died within 1 year of initiation, 4 had eGFR < 30 mL/min/1.73 m2, 1 had no baseline eGFR, and 1 was the spouse of a veteran.
Statistical Analysis
All statistical analyses were performed using STATA v.15. We used t tests to examine changes within each group, along with paired t tests to compare the 2 groups. Two-sample t tests were used to analyze the continuous data at both the primary and secondary endpoints.
Results
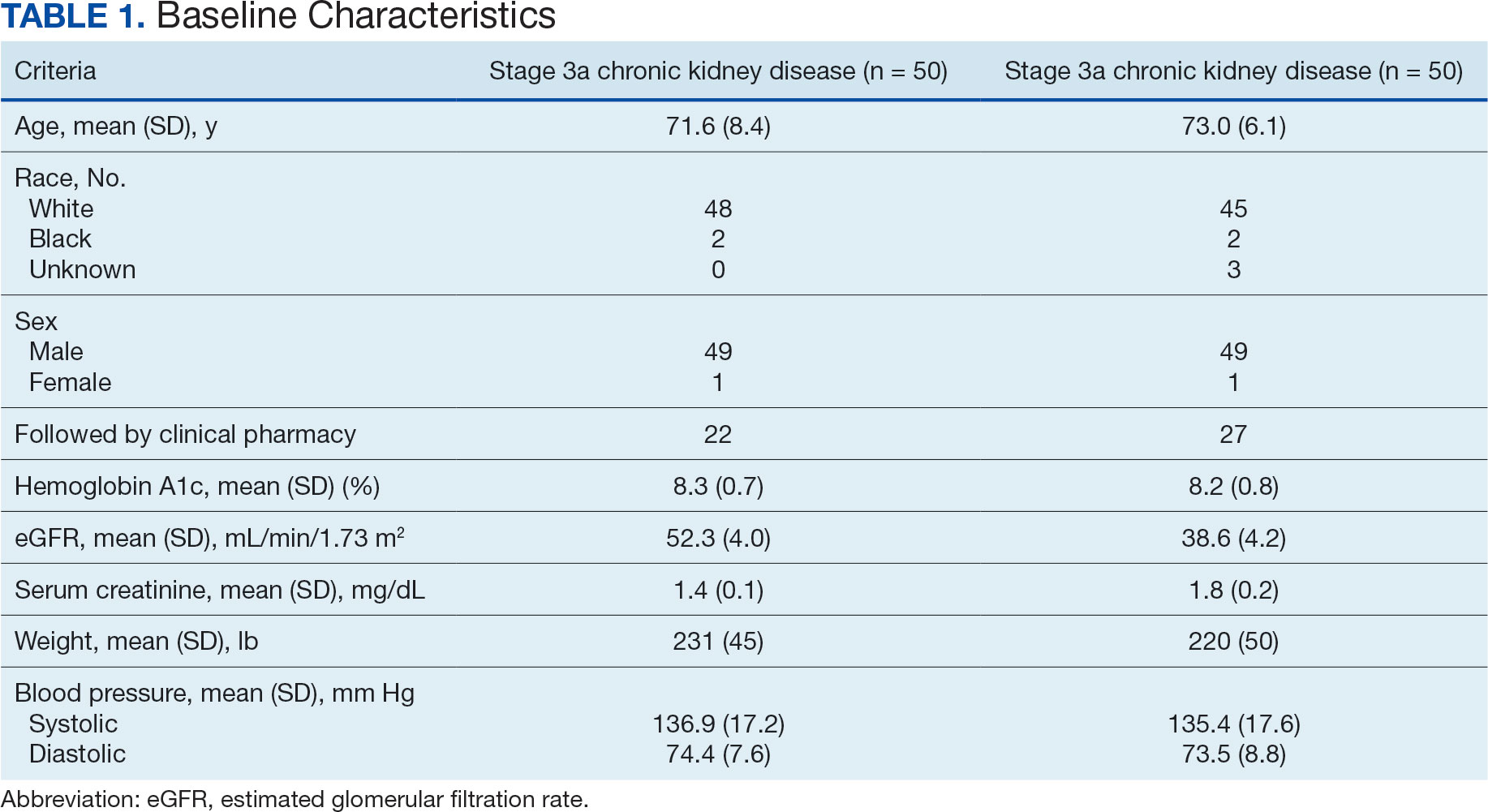
Of the 1771 patients included in the initial data set, a randomized sample of 255 charts were reviewed, 155 were excluded, and 100 were included. Fifty patients, had stage 3a CKD and 50 had stage 3b CKD. Baseline demographics were similar between the stage 3a and 3b groups (Table 1). Both groups were predominantly White and male, with mean age > 70 years.
The primary endpoint was the differences in HbA1c levels over time and between groups for patients with stage 3a and stage 3b CKD 1 year after initiation of empagliflozin. The starting doses of empagliflozin were either 12.5 mg or 25.0 mg. For both groups, the changes in HbA1c levels were statistically significant (Table 2). HbA1c levels dropped 0.65% for the stage 3a group and 0.48% for the 3b group. When compared to one another, the results were not statistically significant (P = .51).
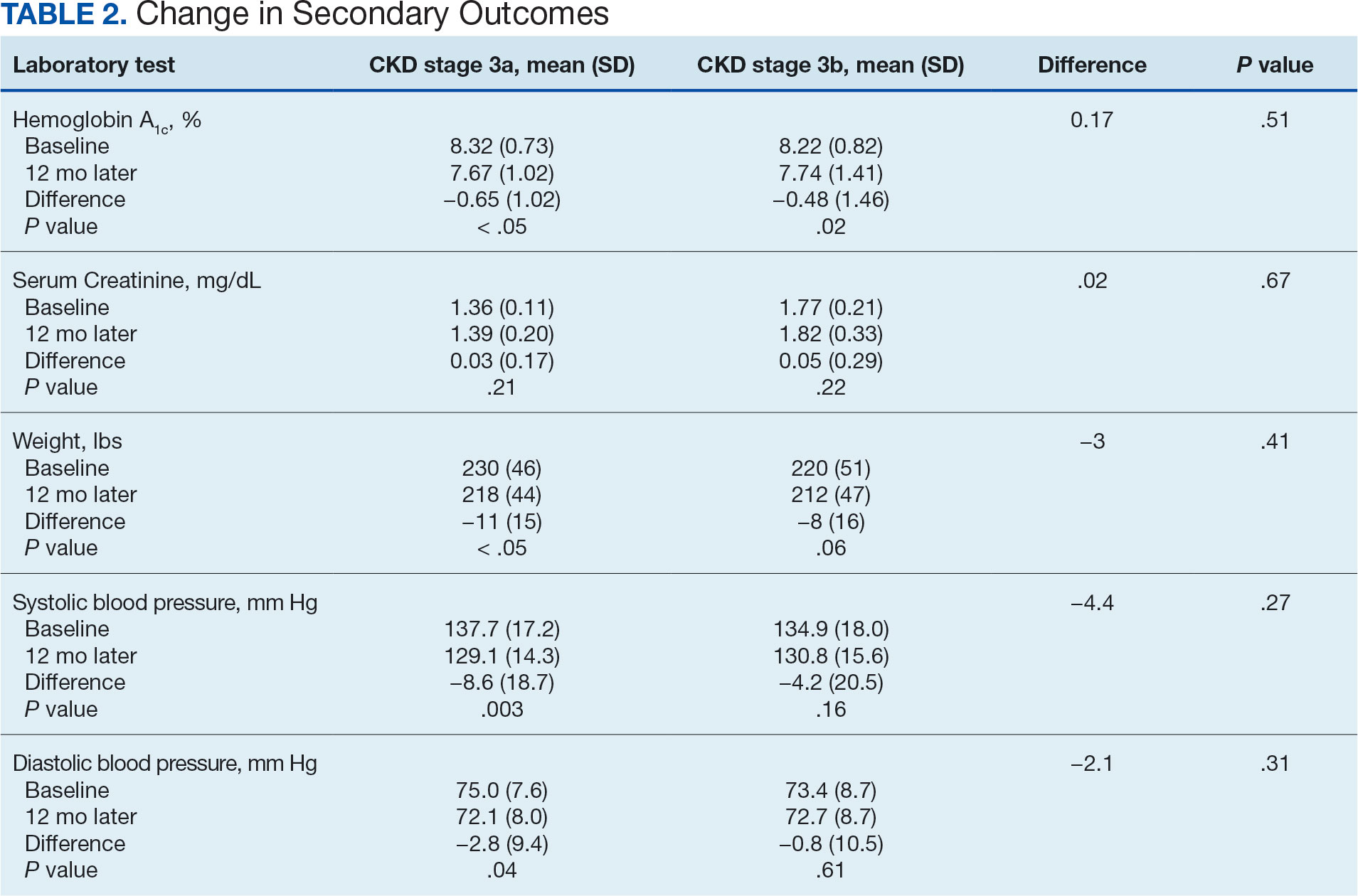
Secondary Endpoint
There was no statistically significant difference in serum creatinine levels within each group between baselines and 1 year later for the stage 3a (P = .21) and stage 3b (P = .22) groups, or when compared to each other (P = .67). There were statistically significant changes in weight for patients in the stage 3a group (P < .05), but not for stage 3b group (P = .06) or when compared to each other (P = .41). A statistically significant change in systolic blood pressure was observed for the stage 3a group (P = .003), but not the stage 3b group (P = .16) or when compared to each other (P = .27). There were statistically significant changes in diastolic blood pressure within the stage 3a group (P = .04), but not within the stage 3b group (P = .61) or when compared to each other (P = .31).
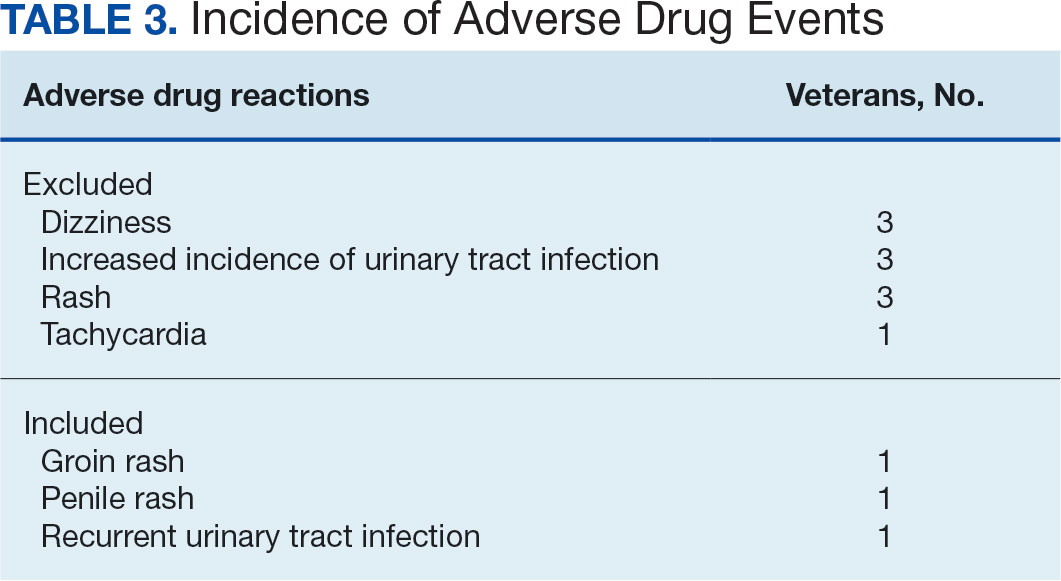
Ten patients discontinued empagliflozin before the 1-year mark due to ADRs, including dizziness, increased incidence of urinary tract infections, rash, and tachycardia (Table 3). Additionally, 3 ADRs resulted in the empagliflozin discontinuation after 1 year (Table 3).
Discussion
This study showed a statistically significant change in HbA1c levels for patients with stage 3a and stage 3b CKD. With eGFR levels in these 2 groups > 30 mL/min/1.73 m2, patients were able to achieve glycemic benefits. There were no significant changes to the serum creatinine levels. Both groups saw statistically significant changes in weight loss within their own group; however, there were no statistically significant changes when compared to each other. With both systolic and diastolic blood pressure, the stage 3a group had statistically significant changes.
The EMPA-REG BP study demonstrated that empagliflozin was associated with significant and clinically meaningful reductions in blood pressure and HbA1c levels compared with placebo and was well tolerated in patients with T2DM and hypertension.6,7,8
Limitations
This study had a retrospective study design, which resulted in missing information for many patients and higher rates of exclusion. The population was predominantly older, White, and male and may not reflect other populations. The starting doses of empagliflozin varied between the groups. The VA employs tablet splitting for some patients, and the available doses were either 10.0 mg, 12.5 mg, or 25.0 mg. Some prescribers start veterans at lower doses and gradually increase to the higher dose of 25.0 mg, adding to the variability in starting doses.
Patients with eGFR < 30 mL/min/1.73 m2 make it difficult to determine any potential benefit in this population. The EMPA-KIDNEY trial demonstrated that the benefits of empagliflozin treatment were consistent among patients with or without DM and regardless of eGFR at randomization.9 Furthermore, many veterans had an initial HbA1c levels outside the inclusion criteria range, which was a factor in the smaller sample size.
Conclusions
While the reduction in HbA1c levels was less in patients with stage 3b CKD compared to patients stage 3a CKD, all patients experienced a benefit. The overall incidence of ADRs was low in the study population, showing empagliflozin as a favorable choice for those with T2DM and CKD. Based on the findings of this study, empagliflozin is a potentially beneficial option for reducing HbA1c levels in patients with CKD.
- Centers for Disease Control and Prevention. Type 2 diabetes. Updated May 25, 2024. Accessed September 27, 2024. https://www.cdc.gov/diabetes/about/about-type-2-diabetes.html?CDC_AAref_Val
- US Department of Veterans Affairs, VA research on diabetes. Updated September 2019. Accessed September 27, 2024. https://www.research.va.gov/pubs/docs/va_factsheets/Diabetes.pdf
- American Diabetes Association. Standards of Medical Care in Diabetes-2022 Abridged for Primary Care Providers. Clin Diabetes. 2022;40(1):10-38. doi:10.2337/cd22-as01
- Centers for Disease Control and Prevention. Diabetes, chronic kidney disease. Updated May 15, 2024. Accessed September 27, 2024. https://www.cdc.gov/diabetes/diabetes-complications/diabetes-and-chronic-kidney-disease.html
- Packer M, Anker SD, Butler J, et al. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. N Engl J Med. 2020;383(15):1413-1424. doi:10.1056/NEJMoa2022190
- Tikkanen I, Narko K, Zeller C, et al. Empagliflozin reduces blood pressure in patients with type 2 diabetes and hypertension. Diabetes Care. 2015;38(3):420-428. doi:10.2337/dc14-1096
- Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117-2128. doi:10.1056/NEJMoa1504720
- Chilton R, Tikkanen I, Cannon CP, et al. Effects of empagliflozin on blood pressure and markers of arterial stiffness and vascular resistance in patients with type 2 diabetes. Diabetes Obes Metab. 2015;17(12):1180-1193. doi:10.1111/dom.12572
- The EMPA-KIDNEY Collaborative Group, Herrington WG, Staplin N, et al. Empagliflozin in Patients with Chronic Kidney Disease. N Engl J Med. 2023;388(2):117-127. doi:10.1056/NEJMoa2204233
More than 37 million Americans have diabetes mellitus (DM), and approximately 90% have type 2 DM (T2DM), including about 25% of veterans.1,2 The current guidelines suggest that therapy depends on a patient's comorbidities, management needs, and patient-centered treatment factors.3 About 1 in 3 adults with DM have chronic kidney disease (CKD), defined as the presence of kidney damage or an estimated glomerular filtration rate (eGFR) < 60 mL/min per 1.73 m2, persisting for ≥ 3 months.4
Sodium-glucose cotransporter-2 (SGLT-2) inhibitors are a class of antihyperglycemic agents acting on the SGLT-2 proteins expressed in the renal proximal convoluted tubules. They exert their effects by preventing the reabsorption of filtered glucose from the tubular lumen. There are 4 SGLT-2 inhibitors approved by the US Food and Drug Administration: canagliflozin, dapagliflozin, empagliflozin, and ertugliflozin. Empagliflozin is currently the preferred SGLT-2 inhibitor on the US Department of Veterans Affairs (VA) formulary.
According to the American Diabetes Association guidelines, empagliflozin is considered when an individual has or is at risk for atherosclerotic cardiovascular disease, heart failure, and CKD.3 SGLT-2 inhibitors are a favorable option due to their low risk for hypoglycemia while also promoting weight loss. The EMPEROR-Reduced trial demonstrated that, in addition to benefits for patients with heart failure, empagliflozin also slowed the progressive decline in kidney function in those with and without DM.5 The purpose of this study was to evaluate the effectiveness of empagliflozin on hemoglobin A1c (HbA1c) levels in patients with CKD at the Hershel “Woody” Williams VA Medical Center (HWWVAMC) in Huntington, West Virginia, along with other laboratory test markers.
Methods
The Marshall University Institutional Review Board #1 (Medical) and the HWWVAMC institutional review board and research and development committee each reviewed and approved this study. A retrospective chart review was conducted on patients diagnosed with T2DM and stage 3 CKD who were prescribed empagliflozin for DM management between January 1, 2015, and October 1, 2022, yielding 1771 patients. Data were obtained through the VHA Corporate Data Warehouse (CDW) and stored on the VA Informatics and Computing Infrastructure (VINCI) research server.
Patients were included if they were aged 18 to 89 years, prescribed empagliflozin by a VA clinician for the treatment of T2DM, had an eGFR between 30 and 59 mL/min/1.73 m2, and had an initial HbA1c between 7% and 10%. Using further random sampling, patients were either excluded or divided into, those with stage 3a CKD and those with stage 3b CKD. The primary endpoint of this study was the change in HbA1c levels in patients with stage 3b CKD (eGFR 30-44 mL/min/1.73 m2) compared with stage 3a (eGFR 45-59 mL/min/1.73 m2) after 12 months. The secondary endpoints included effects on renal function, weight, blood pressure, incidence of adverse drug events, and cardiovascular events. Of the excluded, 38 had HbA1c < 7%, 30 had HbA1c ≥ 10%, 21 did not have data at 1-year mark, 15 had the medication discontinued due to decline in renal function, 14 discontinued their medication without documented reason, 10 discontinued their medication due to adverse drug reactions (ADRs), 12 had eGFR > 60 mL/ min/1.73 m2, 9 died within 1 year of initiation, 4 had eGFR < 30 mL/min/1.73 m2, 1 had no baseline eGFR, and 1 was the spouse of a veteran.
Statistical Analysis
All statistical analyses were performed using STATA v.15. We used t tests to examine changes within each group, along with paired t tests to compare the 2 groups. Two-sample t tests were used to analyze the continuous data at both the primary and secondary endpoints.
Results
Of the 1771 patients included in the initial data set, a randomized sample of 255 charts were reviewed, 155 were excluded, and 100 were included. Fifty patients, had stage 3a CKD and 50 had stage 3b CKD. Baseline demographics were similar between the stage 3a and 3b groups (Table 1). Both groups were predominantly White and male, with mean age > 70 years.
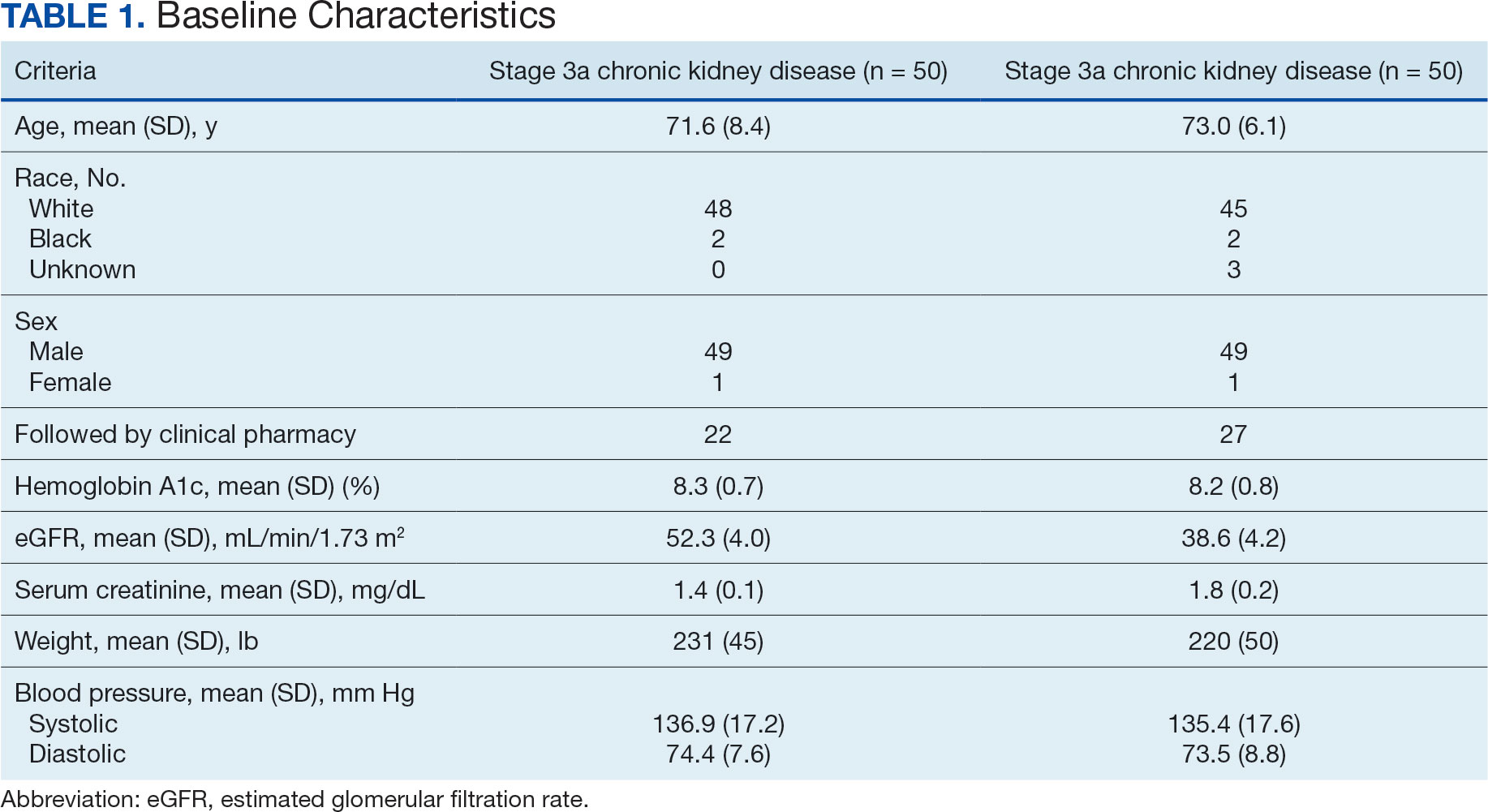
The primary endpoint was the differences in HbA1c levels over time and between groups for patients with stage 3a and stage 3b CKD 1 year after initiation of empagliflozin. The starting doses of empagliflozin were either 12.5 mg or 25.0 mg. For both groups, the changes in HbA1c levels were statistically significant (Table 2). HbA1c levels dropped 0.65% for the stage 3a group and 0.48% for the 3b group. When compared to one another, the results were not statistically significant (P = .51).
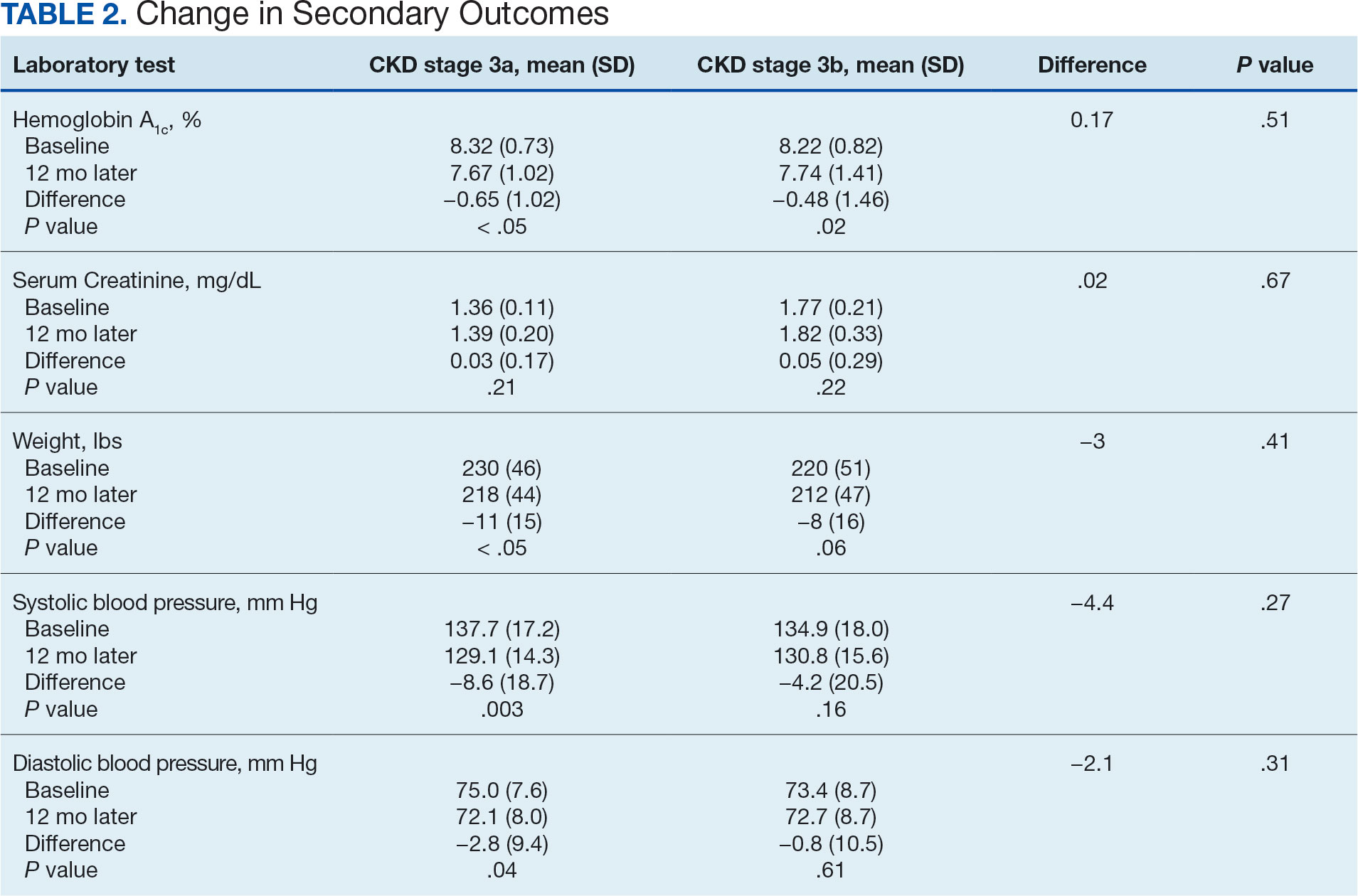
Secondary Endpoint
There was no statistically significant difference in serum creatinine levels within each group between baselines and 1 year later for the stage 3a (P = .21) and stage 3b (P = .22) groups, or when compared to each other (P = .67). There were statistically significant changes in weight for patients in the stage 3a group (P < .05), but not for stage 3b group (P = .06) or when compared to each other (P = .41). A statistically significant change in systolic blood pressure was observed for the stage 3a group (P = .003), but not the stage 3b group (P = .16) or when compared to each other (P = .27). There were statistically significant changes in diastolic blood pressure within the stage 3a group (P = .04), but not within the stage 3b group (P = .61) or when compared to each other (P = .31).
Ten patients discontinued empagliflozin before the 1-year mark due to ADRs, including dizziness, increased incidence of urinary tract infections, rash, and tachycardia (Table 3). Additionally, 3 ADRs resulted in the empagliflozin discontinuation after 1 year (Table 3).
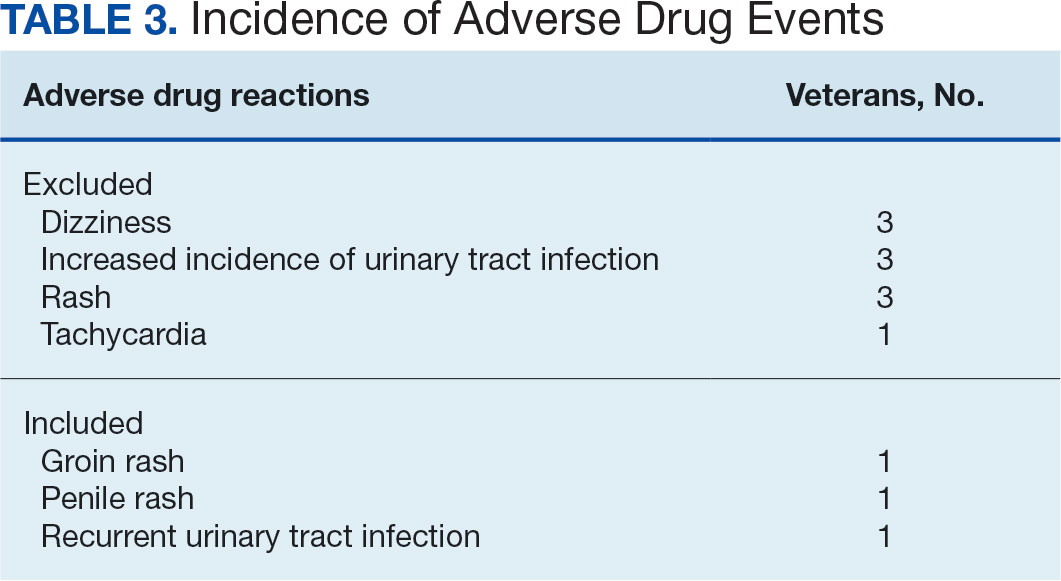
Discussion
This study showed a statistically significant change in HbA1c levels for patients with stage 3a and stage 3b CKD. With eGFR levels in these 2 groups > 30 mL/min/1.73 m2, patients were able to achieve glycemic benefits. There were no significant changes to the serum creatinine levels. Both groups saw statistically significant changes in weight loss within their own group; however, there were no statistically significant changes when compared to each other. With both systolic and diastolic blood pressure, the stage 3a group had statistically significant changes.
The EMPA-REG BP study demonstrated that empagliflozin was associated with significant and clinically meaningful reductions in blood pressure and HbA1c levels compared with placebo and was well tolerated in patients with T2DM and hypertension.6,7,8
Limitations
This study had a retrospective study design, which resulted in missing information for many patients and higher rates of exclusion. The population was predominantly older, White, and male and may not reflect other populations. The starting doses of empagliflozin varied between the groups. The VA employs tablet splitting for some patients, and the available doses were either 10.0 mg, 12.5 mg, or 25.0 mg. Some prescribers start veterans at lower doses and gradually increase to the higher dose of 25.0 mg, adding to the variability in starting doses.
Patients with eGFR < 30 mL/min/1.73 m2 make it difficult to determine any potential benefit in this population. The EMPA-KIDNEY trial demonstrated that the benefits of empagliflozin treatment were consistent among patients with or without DM and regardless of eGFR at randomization.9 Furthermore, many veterans had an initial HbA1c levels outside the inclusion criteria range, which was a factor in the smaller sample size.
Conclusions
While the reduction in HbA1c levels was less in patients with stage 3b CKD compared to patients stage 3a CKD, all patients experienced a benefit. The overall incidence of ADRs was low in the study population, showing empagliflozin as a favorable choice for those with T2DM and CKD. Based on the findings of this study, empagliflozin is a potentially beneficial option for reducing HbA1c levels in patients with CKD.
More than 37 million Americans have diabetes mellitus (DM), and approximately 90% have type 2 DM (T2DM), including about 25% of veterans.1,2 The current guidelines suggest that therapy depends on a patient's comorbidities, management needs, and patient-centered treatment factors.3 About 1 in 3 adults with DM have chronic kidney disease (CKD), defined as the presence of kidney damage or an estimated glomerular filtration rate (eGFR) < 60 mL/min per 1.73 m2, persisting for ≥ 3 months.4
Sodium-glucose cotransporter-2 (SGLT-2) inhibitors are a class of antihyperglycemic agents acting on the SGLT-2 proteins expressed in the renal proximal convoluted tubules. They exert their effects by preventing the reabsorption of filtered glucose from the tubular lumen. There are 4 SGLT-2 inhibitors approved by the US Food and Drug Administration: canagliflozin, dapagliflozin, empagliflozin, and ertugliflozin. Empagliflozin is currently the preferred SGLT-2 inhibitor on the US Department of Veterans Affairs (VA) formulary.
According to the American Diabetes Association guidelines, empagliflozin is considered when an individual has or is at risk for atherosclerotic cardiovascular disease, heart failure, and CKD.3 SGLT-2 inhibitors are a favorable option due to their low risk for hypoglycemia while also promoting weight loss. The EMPEROR-Reduced trial demonstrated that, in addition to benefits for patients with heart failure, empagliflozin also slowed the progressive decline in kidney function in those with and without DM.5 The purpose of this study was to evaluate the effectiveness of empagliflozin on hemoglobin A1c (HbA1c) levels in patients with CKD at the Hershel “Woody” Williams VA Medical Center (HWWVAMC) in Huntington, West Virginia, along with other laboratory test markers.
Methods
The Marshall University Institutional Review Board #1 (Medical) and the HWWVAMC institutional review board and research and development committee each reviewed and approved this study. A retrospective chart review was conducted on patients diagnosed with T2DM and stage 3 CKD who were prescribed empagliflozin for DM management between January 1, 2015, and October 1, 2022, yielding 1771 patients. Data were obtained through the VHA Corporate Data Warehouse (CDW) and stored on the VA Informatics and Computing Infrastructure (VINCI) research server.
Patients were included if they were aged 18 to 89 years, prescribed empagliflozin by a VA clinician for the treatment of T2DM, had an eGFR between 30 and 59 mL/min/1.73 m2, and had an initial HbA1c between 7% and 10%. Using further random sampling, patients were either excluded or divided into, those with stage 3a CKD and those with stage 3b CKD. The primary endpoint of this study was the change in HbA1c levels in patients with stage 3b CKD (eGFR 30-44 mL/min/1.73 m2) compared with stage 3a (eGFR 45-59 mL/min/1.73 m2) after 12 months. The secondary endpoints included effects on renal function, weight, blood pressure, incidence of adverse drug events, and cardiovascular events. Of the excluded, 38 had HbA1c < 7%, 30 had HbA1c ≥ 10%, 21 did not have data at 1-year mark, 15 had the medication discontinued due to decline in renal function, 14 discontinued their medication without documented reason, 10 discontinued their medication due to adverse drug reactions (ADRs), 12 had eGFR > 60 mL/ min/1.73 m2, 9 died within 1 year of initiation, 4 had eGFR < 30 mL/min/1.73 m2, 1 had no baseline eGFR, and 1 was the spouse of a veteran.
Statistical Analysis
All statistical analyses were performed using STATA v.15. We used t tests to examine changes within each group, along with paired t tests to compare the 2 groups. Two-sample t tests were used to analyze the continuous data at both the primary and secondary endpoints.
Results
Of the 1771 patients included in the initial data set, a randomized sample of 255 charts were reviewed, 155 were excluded, and 100 were included. Fifty patients, had stage 3a CKD and 50 had stage 3b CKD. Baseline demographics were similar between the stage 3a and 3b groups (Table 1). Both groups were predominantly White and male, with mean age > 70 years.
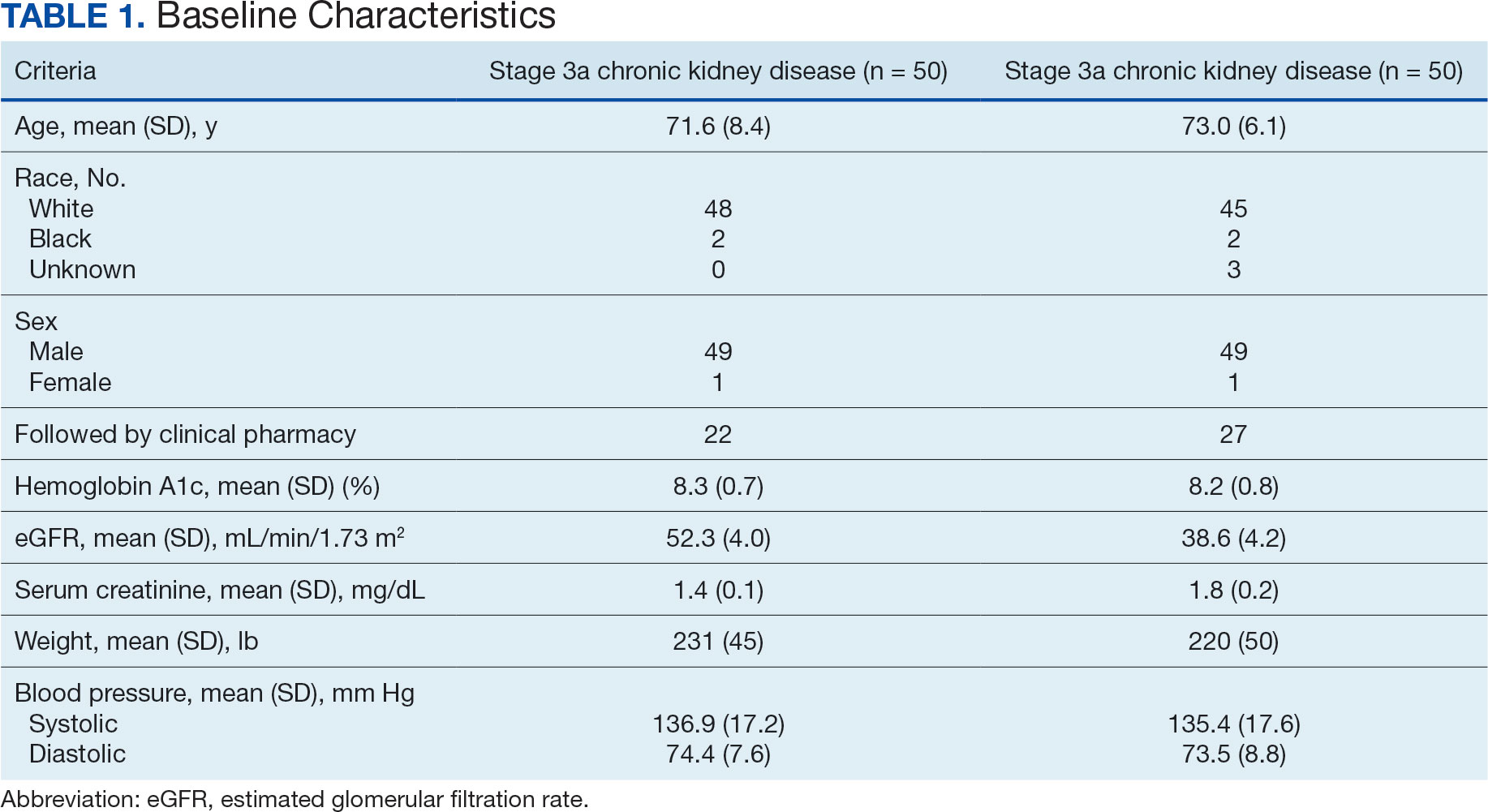
The primary endpoint was the differences in HbA1c levels over time and between groups for patients with stage 3a and stage 3b CKD 1 year after initiation of empagliflozin. The starting doses of empagliflozin were either 12.5 mg or 25.0 mg. For both groups, the changes in HbA1c levels were statistically significant (Table 2). HbA1c levels dropped 0.65% for the stage 3a group and 0.48% for the 3b group. When compared to one another, the results were not statistically significant (P = .51).
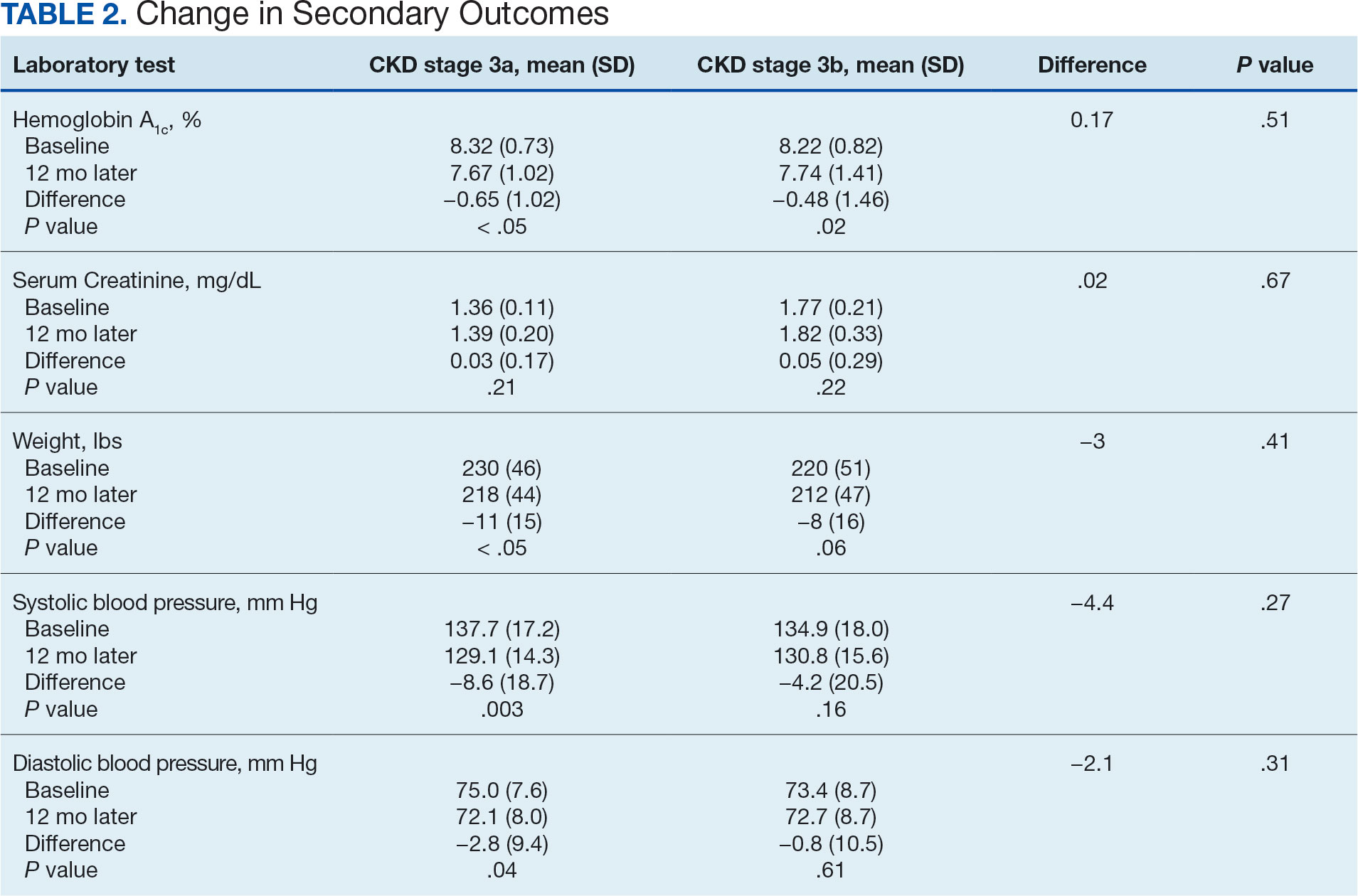
Secondary Endpoint
There was no statistically significant difference in serum creatinine levels within each group between baselines and 1 year later for the stage 3a (P = .21) and stage 3b (P = .22) groups, or when compared to each other (P = .67). There were statistically significant changes in weight for patients in the stage 3a group (P < .05), but not for stage 3b group (P = .06) or when compared to each other (P = .41). A statistically significant change in systolic blood pressure was observed for the stage 3a group (P = .003), but not the stage 3b group (P = .16) or when compared to each other (P = .27). There were statistically significant changes in diastolic blood pressure within the stage 3a group (P = .04), but not within the stage 3b group (P = .61) or when compared to each other (P = .31).
Ten patients discontinued empagliflozin before the 1-year mark due to ADRs, including dizziness, increased incidence of urinary tract infections, rash, and tachycardia (Table 3). Additionally, 3 ADRs resulted in the empagliflozin discontinuation after 1 year (Table 3).
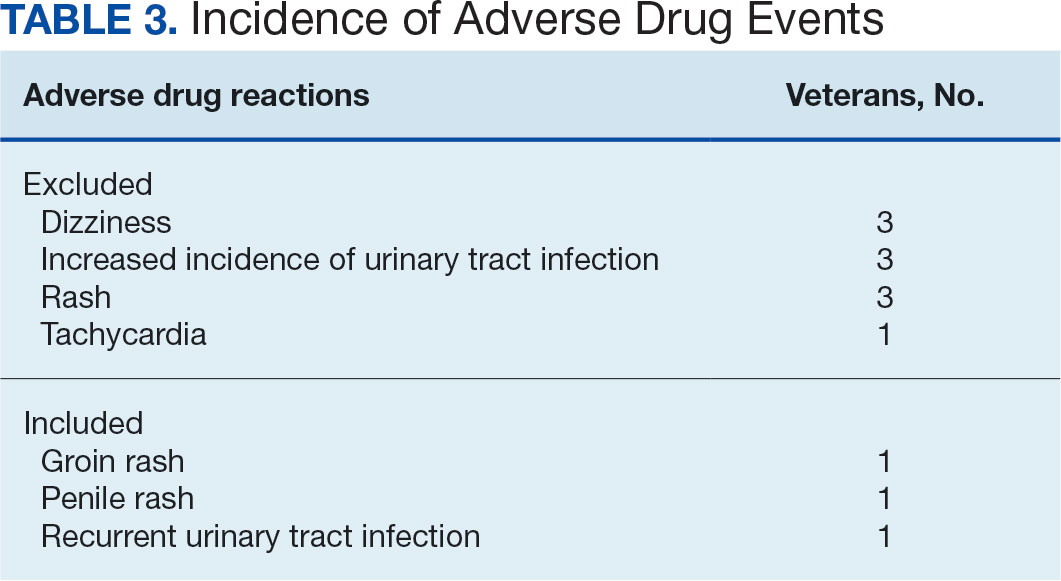
Discussion
This study showed a statistically significant change in HbA1c levels for patients with stage 3a and stage 3b CKD. With eGFR levels in these 2 groups > 30 mL/min/1.73 m2, patients were able to achieve glycemic benefits. There were no significant changes to the serum creatinine levels. Both groups saw statistically significant changes in weight loss within their own group; however, there were no statistically significant changes when compared to each other. With both systolic and diastolic blood pressure, the stage 3a group had statistically significant changes.
The EMPA-REG BP study demonstrated that empagliflozin was associated with significant and clinically meaningful reductions in blood pressure and HbA1c levels compared with placebo and was well tolerated in patients with T2DM and hypertension.6,7,8
Limitations
This study had a retrospective study design, which resulted in missing information for many patients and higher rates of exclusion. The population was predominantly older, White, and male and may not reflect other populations. The starting doses of empagliflozin varied between the groups. The VA employs tablet splitting for some patients, and the available doses were either 10.0 mg, 12.5 mg, or 25.0 mg. Some prescribers start veterans at lower doses and gradually increase to the higher dose of 25.0 mg, adding to the variability in starting doses.
Patients with eGFR < 30 mL/min/1.73 m2 make it difficult to determine any potential benefit in this population. The EMPA-KIDNEY trial demonstrated that the benefits of empagliflozin treatment were consistent among patients with or without DM and regardless of eGFR at randomization.9 Furthermore, many veterans had an initial HbA1c levels outside the inclusion criteria range, which was a factor in the smaller sample size.
Conclusions
While the reduction in HbA1c levels was less in patients with stage 3b CKD compared to patients stage 3a CKD, all patients experienced a benefit. The overall incidence of ADRs was low in the study population, showing empagliflozin as a favorable choice for those with T2DM and CKD. Based on the findings of this study, empagliflozin is a potentially beneficial option for reducing HbA1c levels in patients with CKD.
- Centers for Disease Control and Prevention. Type 2 diabetes. Updated May 25, 2024. Accessed September 27, 2024. https://www.cdc.gov/diabetes/about/about-type-2-diabetes.html?CDC_AAref_Val
- US Department of Veterans Affairs, VA research on diabetes. Updated September 2019. Accessed September 27, 2024. https://www.research.va.gov/pubs/docs/va_factsheets/Diabetes.pdf
- American Diabetes Association. Standards of Medical Care in Diabetes-2022 Abridged for Primary Care Providers. Clin Diabetes. 2022;40(1):10-38. doi:10.2337/cd22-as01
- Centers for Disease Control and Prevention. Diabetes, chronic kidney disease. Updated May 15, 2024. Accessed September 27, 2024. https://www.cdc.gov/diabetes/diabetes-complications/diabetes-and-chronic-kidney-disease.html
- Packer M, Anker SD, Butler J, et al. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. N Engl J Med. 2020;383(15):1413-1424. doi:10.1056/NEJMoa2022190
- Tikkanen I, Narko K, Zeller C, et al. Empagliflozin reduces blood pressure in patients with type 2 diabetes and hypertension. Diabetes Care. 2015;38(3):420-428. doi:10.2337/dc14-1096
- Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117-2128. doi:10.1056/NEJMoa1504720
- Chilton R, Tikkanen I, Cannon CP, et al. Effects of empagliflozin on blood pressure and markers of arterial stiffness and vascular resistance in patients with type 2 diabetes. Diabetes Obes Metab. 2015;17(12):1180-1193. doi:10.1111/dom.12572
- The EMPA-KIDNEY Collaborative Group, Herrington WG, Staplin N, et al. Empagliflozin in Patients with Chronic Kidney Disease. N Engl J Med. 2023;388(2):117-127. doi:10.1056/NEJMoa2204233
- Centers for Disease Control and Prevention. Type 2 diabetes. Updated May 25, 2024. Accessed September 27, 2024. https://www.cdc.gov/diabetes/about/about-type-2-diabetes.html?CDC_AAref_Val
- US Department of Veterans Affairs, VA research on diabetes. Updated September 2019. Accessed September 27, 2024. https://www.research.va.gov/pubs/docs/va_factsheets/Diabetes.pdf
- American Diabetes Association. Standards of Medical Care in Diabetes-2022 Abridged for Primary Care Providers. Clin Diabetes. 2022;40(1):10-38. doi:10.2337/cd22-as01
- Centers for Disease Control and Prevention. Diabetes, chronic kidney disease. Updated May 15, 2024. Accessed September 27, 2024. https://www.cdc.gov/diabetes/diabetes-complications/diabetes-and-chronic-kidney-disease.html
- Packer M, Anker SD, Butler J, et al. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. N Engl J Med. 2020;383(15):1413-1424. doi:10.1056/NEJMoa2022190
- Tikkanen I, Narko K, Zeller C, et al. Empagliflozin reduces blood pressure in patients with type 2 diabetes and hypertension. Diabetes Care. 2015;38(3):420-428. doi:10.2337/dc14-1096
- Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117-2128. doi:10.1056/NEJMoa1504720
- Chilton R, Tikkanen I, Cannon CP, et al. Effects of empagliflozin on blood pressure and markers of arterial stiffness and vascular resistance in patients with type 2 diabetes. Diabetes Obes Metab. 2015;17(12):1180-1193. doi:10.1111/dom.12572
- The EMPA-KIDNEY Collaborative Group, Herrington WG, Staplin N, et al. Empagliflozin in Patients with Chronic Kidney Disease. N Engl J Med. 2023;388(2):117-127. doi:10.1056/NEJMoa2204233
Help Your Patients Reap the Benefits of Plant-Based Diets
Research pooled from nearly 100 studies has indicated that people who adhere to a vegan diet (ie, completely devoid of animal products) or a vegetarian diet (ie, devoid of meat, but may include dairy and eggs) are able to ward off some chronic diseases, such as cardiovascular disease, optimize glycemic control, and decrease their risk for cancer compared with those who consume omnivorous diets.
Vegan and vegetarian diets, or flexitarian diets — which are less reliant on animal protein than the standard US diet but do not completely exclude meat, fish, eggs, or dairy — may promote homeostasis and decrease inflammation by providing more fiber, antioxidants, and unsaturated fatty acids than the typical Western diet.
Inflammation and Obesity
Adipose tissue is a major producer of pro-inflammatory cytokines like interleukin (IL)-6, whose presence then triggers a rush of acute-phase reactants such as C-reactive protein (CRP) by the liver. This process develops into chronic low-grade inflammation that can increase a person’s chances of developing diabetes, cardiovascular disease, kidney disease, metabolic syndrome, and related complications.
Adopting a plant-based diet can improve markers of chronic low-grade inflammation that can lead to chronic disease and worsen existent chronic disease. A meta-analysis of 29 studies encompassing nearly 2700 participants found that initiation of a plant-based diet showed significant improvement in CRP, IL-6, and soluble intercellular adhesion molecule 1.
If we want to prevent these inflammatory disease states and their complications, the obvious response is to counsel patients to avoid excessive weight gain or to lose weight if obesity is their baseline. This can be tough for some patients, but it is nonetheless an important step in chronic disease prevention and management.
Plant-Based Diet for Type 2 Diabetes
According to a review of nine studies of patients living with type 2 diabetes who adhered to a plant-based diet, all but one found that this approach led to significantly lower A1c values than those seen in control groups. Six of the included studies reported that participants were able to decrease or discontinue medications for the management of diabetes. Researchers across all included studies also noted a decrease in total cholesterol, low-density lipoprotein cholesterol, and triglycerides, as well as increased weight loss in participants in each intervention group.
Such improvements are probably the result of the increase in fiber intake that occurs with a plant-based diet. A high-fiber diet is known to promote improved glucose and lipid metabolism as well as weight loss.
It is also worth noting that participants in the intervention groups also experienced improvements in depression and less chronic pain than did those in the control groups.
Plant-Based Diet for Chronic Kidney Disease (CKD)
Although the use of a plant-based diet in the prevention of CKD is well documented, adopting such diets for the treatment of CKD may intimidate both patients and practitioners owing to the high potassium and phosphorus content of many fruits and vegetables.
However, research indicates that the bioavailability of both potassium and phosphorus is lower in plant-based, whole foods than in preservatives and the highly processed food items that incorporate them. This makes a plant-based diet more viable than previously thought.
Diets rich in vegetables, whole grains, nuts, and legumes have been shown to decrease dietary acid load, both preventing and treating metabolic acidosis. Such diets have also been shown to decrease blood pressure and the risk for a decline in estimated glomerular filtration rate. This type of diet would also prioritize the unsaturated fatty acids and fiber-rich proteins such as avocados, beans, and nuts shown to improve dyslipidemia, which may occur alongside CKD.
Realistic Options for Patients on Medical Diets
There is one question that I always seem to get from when recommending a plant-based diet: “These patients already have so many restrictions. Why would you add more?” And my answer is also always the same: I don’t.
I rarely, if ever, recommend completely cutting out any food item or food group. Instead, I ask the patient to increase their intake of plant-based foods and only limit highly processed foods and fatty meats. By shifting a patient’s focus to beans; nuts; and low-carbohydrate, high-fiber fruits and vegetables, I am often opening up a whole new world of possibilities.
Instead of a sandwich with low-sodium turkey and cheese on white bread with a side of unsalted pretzels, I recommend a caprese salad with blueberries and almonds or a Southwest salad with black beans, corn, and avocado. I don’t encourage my patients to skip the foods that they love, but instead to only think about all the delicious plant-based options that will provide them with more than just calories.
Meat, dairy, seafood, and eggs can certainly be a part of a healthy diet, but what if our chronically ill patients, especially those with diabetes, had more options than just grilled chicken and green beans for every meal? What if we focus on decreasing dietary restrictions, incorporating a variety of nourishing foods, and educating our patients, instead of on portion control and moderation?
This is how I choose to incorporate plant-based diets into my practice to treat and prevent these chronic inflammatory conditions and promote sustainable, realistic change in my clients’ health.
Brandy Winfree Root, a renal dietitian in private practice in Mary Esther, Florida, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Research pooled from nearly 100 studies has indicated that people who adhere to a vegan diet (ie, completely devoid of animal products) or a vegetarian diet (ie, devoid of meat, but may include dairy and eggs) are able to ward off some chronic diseases, such as cardiovascular disease, optimize glycemic control, and decrease their risk for cancer compared with those who consume omnivorous diets.
Vegan and vegetarian diets, or flexitarian diets — which are less reliant on animal protein than the standard US diet but do not completely exclude meat, fish, eggs, or dairy — may promote homeostasis and decrease inflammation by providing more fiber, antioxidants, and unsaturated fatty acids than the typical Western diet.
Inflammation and Obesity
Adipose tissue is a major producer of pro-inflammatory cytokines like interleukin (IL)-6, whose presence then triggers a rush of acute-phase reactants such as C-reactive protein (CRP) by the liver. This process develops into chronic low-grade inflammation that can increase a person’s chances of developing diabetes, cardiovascular disease, kidney disease, metabolic syndrome, and related complications.
Adopting a plant-based diet can improve markers of chronic low-grade inflammation that can lead to chronic disease and worsen existent chronic disease. A meta-analysis of 29 studies encompassing nearly 2700 participants found that initiation of a plant-based diet showed significant improvement in CRP, IL-6, and soluble intercellular adhesion molecule 1.
If we want to prevent these inflammatory disease states and their complications, the obvious response is to counsel patients to avoid excessive weight gain or to lose weight if obesity is their baseline. This can be tough for some patients, but it is nonetheless an important step in chronic disease prevention and management.
Plant-Based Diet for Type 2 Diabetes
According to a review of nine studies of patients living with type 2 diabetes who adhered to a plant-based diet, all but one found that this approach led to significantly lower A1c values than those seen in control groups. Six of the included studies reported that participants were able to decrease or discontinue medications for the management of diabetes. Researchers across all included studies also noted a decrease in total cholesterol, low-density lipoprotein cholesterol, and triglycerides, as well as increased weight loss in participants in each intervention group.
Such improvements are probably the result of the increase in fiber intake that occurs with a plant-based diet. A high-fiber diet is known to promote improved glucose and lipid metabolism as well as weight loss.
It is also worth noting that participants in the intervention groups also experienced improvements in depression and less chronic pain than did those in the control groups.
Plant-Based Diet for Chronic Kidney Disease (CKD)
Although the use of a plant-based diet in the prevention of CKD is well documented, adopting such diets for the treatment of CKD may intimidate both patients and practitioners owing to the high potassium and phosphorus content of many fruits and vegetables.
However, research indicates that the bioavailability of both potassium and phosphorus is lower in plant-based, whole foods than in preservatives and the highly processed food items that incorporate them. This makes a plant-based diet more viable than previously thought.
Diets rich in vegetables, whole grains, nuts, and legumes have been shown to decrease dietary acid load, both preventing and treating metabolic acidosis. Such diets have also been shown to decrease blood pressure and the risk for a decline in estimated glomerular filtration rate. This type of diet would also prioritize the unsaturated fatty acids and fiber-rich proteins such as avocados, beans, and nuts shown to improve dyslipidemia, which may occur alongside CKD.
Realistic Options for Patients on Medical Diets
There is one question that I always seem to get from when recommending a plant-based diet: “These patients already have so many restrictions. Why would you add more?” And my answer is also always the same: I don’t.
I rarely, if ever, recommend completely cutting out any food item or food group. Instead, I ask the patient to increase their intake of plant-based foods and only limit highly processed foods and fatty meats. By shifting a patient’s focus to beans; nuts; and low-carbohydrate, high-fiber fruits and vegetables, I am often opening up a whole new world of possibilities.
Instead of a sandwich with low-sodium turkey and cheese on white bread with a side of unsalted pretzels, I recommend a caprese salad with blueberries and almonds or a Southwest salad with black beans, corn, and avocado. I don’t encourage my patients to skip the foods that they love, but instead to only think about all the delicious plant-based options that will provide them with more than just calories.
Meat, dairy, seafood, and eggs can certainly be a part of a healthy diet, but what if our chronically ill patients, especially those with diabetes, had more options than just grilled chicken and green beans for every meal? What if we focus on decreasing dietary restrictions, incorporating a variety of nourishing foods, and educating our patients, instead of on portion control and moderation?
This is how I choose to incorporate plant-based diets into my practice to treat and prevent these chronic inflammatory conditions and promote sustainable, realistic change in my clients’ health.
Brandy Winfree Root, a renal dietitian in private practice in Mary Esther, Florida, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Research pooled from nearly 100 studies has indicated that people who adhere to a vegan diet (ie, completely devoid of animal products) or a vegetarian diet (ie, devoid of meat, but may include dairy and eggs) are able to ward off some chronic diseases, such as cardiovascular disease, optimize glycemic control, and decrease their risk for cancer compared with those who consume omnivorous diets.
Vegan and vegetarian diets, or flexitarian diets — which are less reliant on animal protein than the standard US diet but do not completely exclude meat, fish, eggs, or dairy — may promote homeostasis and decrease inflammation by providing more fiber, antioxidants, and unsaturated fatty acids than the typical Western diet.
Inflammation and Obesity
Adipose tissue is a major producer of pro-inflammatory cytokines like interleukin (IL)-6, whose presence then triggers a rush of acute-phase reactants such as C-reactive protein (CRP) by the liver. This process develops into chronic low-grade inflammation that can increase a person’s chances of developing diabetes, cardiovascular disease, kidney disease, metabolic syndrome, and related complications.
Adopting a plant-based diet can improve markers of chronic low-grade inflammation that can lead to chronic disease and worsen existent chronic disease. A meta-analysis of 29 studies encompassing nearly 2700 participants found that initiation of a plant-based diet showed significant improvement in CRP, IL-6, and soluble intercellular adhesion molecule 1.
If we want to prevent these inflammatory disease states and their complications, the obvious response is to counsel patients to avoid excessive weight gain or to lose weight if obesity is their baseline. This can be tough for some patients, but it is nonetheless an important step in chronic disease prevention and management.
Plant-Based Diet for Type 2 Diabetes
According to a review of nine studies of patients living with type 2 diabetes who adhered to a plant-based diet, all but one found that this approach led to significantly lower A1c values than those seen in control groups. Six of the included studies reported that participants were able to decrease or discontinue medications for the management of diabetes. Researchers across all included studies also noted a decrease in total cholesterol, low-density lipoprotein cholesterol, and triglycerides, as well as increased weight loss in participants in each intervention group.
Such improvements are probably the result of the increase in fiber intake that occurs with a plant-based diet. A high-fiber diet is known to promote improved glucose and lipid metabolism as well as weight loss.
It is also worth noting that participants in the intervention groups also experienced improvements in depression and less chronic pain than did those in the control groups.
Plant-Based Diet for Chronic Kidney Disease (CKD)
Although the use of a plant-based diet in the prevention of CKD is well documented, adopting such diets for the treatment of CKD may intimidate both patients and practitioners owing to the high potassium and phosphorus content of many fruits and vegetables.
However, research indicates that the bioavailability of both potassium and phosphorus is lower in plant-based, whole foods than in preservatives and the highly processed food items that incorporate them. This makes a plant-based diet more viable than previously thought.
Diets rich in vegetables, whole grains, nuts, and legumes have been shown to decrease dietary acid load, both preventing and treating metabolic acidosis. Such diets have also been shown to decrease blood pressure and the risk for a decline in estimated glomerular filtration rate. This type of diet would also prioritize the unsaturated fatty acids and fiber-rich proteins such as avocados, beans, and nuts shown to improve dyslipidemia, which may occur alongside CKD.
Realistic Options for Patients on Medical Diets
There is one question that I always seem to get from when recommending a plant-based diet: “These patients already have so many restrictions. Why would you add more?” And my answer is also always the same: I don’t.
I rarely, if ever, recommend completely cutting out any food item or food group. Instead, I ask the patient to increase their intake of plant-based foods and only limit highly processed foods and fatty meats. By shifting a patient’s focus to beans; nuts; and low-carbohydrate, high-fiber fruits and vegetables, I am often opening up a whole new world of possibilities.
Instead of a sandwich with low-sodium turkey and cheese on white bread with a side of unsalted pretzels, I recommend a caprese salad with blueberries and almonds or a Southwest salad with black beans, corn, and avocado. I don’t encourage my patients to skip the foods that they love, but instead to only think about all the delicious plant-based options that will provide them with more than just calories.
Meat, dairy, seafood, and eggs can certainly be a part of a healthy diet, but what if our chronically ill patients, especially those with diabetes, had more options than just grilled chicken and green beans for every meal? What if we focus on decreasing dietary restrictions, incorporating a variety of nourishing foods, and educating our patients, instead of on portion control and moderation?
This is how I choose to incorporate plant-based diets into my practice to treat and prevent these chronic inflammatory conditions and promote sustainable, realistic change in my clients’ health.
Brandy Winfree Root, a renal dietitian in private practice in Mary Esther, Florida, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Low Follow-up of Abnormal Urine Proteinuria Dipstick Tests in Primary Care
Only 1 in 15 urine dipstick tests showing proteinuria in the primary care setting are followed up with albuminuria quantification testing, according to investigators.
These findings expose a broad gap in screening for chronic kidney disease (CKD), which is especially concerning since newer kidney-protecting agents are more effective when prescribed earlier in the disease course, reported lead author Yunwen Xu, PhD, of Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, and colleagues.
“Evidence-based prescription of renin-angiotensin system inhibitors, glucagon-like peptide-1 receptor (GLP-1) agonists, sodium-glucose cotransporter 2 (SGLT2) inhibitors, and nonsteroidal mineralocorticoid receptor antagonists (nsMRAs) relies on the level of albuminuria,” the investigators wrote in Annals of Internal Medicine.
“Although urine albumin-creatinine ratio (ACR) is the most accurate method for quantifying albuminuria, dipstick urinalysis tests are inexpensive and are often used as an initial screening test, with guidelines recommending follow-up ACR testing if the protein dipstick test result is abnormal.”
Despite this guidance, real-world follow-up rates have been unknown, prompting the present study. Real-world data show a low follow-up rate. Dr. Xu and colleagues analyzed data from 1 million patients in 33 health systems who underwent urine dipstick testing in a primary care setting.
Across this population, 13% of patients had proteinuria, but only 6.7% underwent follow-up albuminuria quantification testing within the next year. ACR was the most common method (86%).
Likelihood of follow-up increased slightly with the level of proteinuria detected; however, absolute differences were marginal, with a 3+ result yielding a follow-up rate of just 8%, compared with 7.3% for a 2+ result and 6.3% for a 1+ result. When albuminuria quantification tests were conducted, 1+, 2+, and 3+ dipstick results were associated with albuminuria rates of 36.3%, 53.0%, and 64.9%, respectively.
Patients with diabetes had the highest follow-up rate, at 16.6%, vs 3.8% for those without diabetes.
Reasons for Low Follow-up Unclear
The dataset did not include information about reasons for ordering urinalyses, whether primary care providers knew about the abnormal dipstick tests, or awareness of guideline recommendations.
“I think they know it should be done,” said principal investigator Alexander R. Chang, MD, associate professor in the department of nephrology and population health sciences at Geisinger Health, Danville, Pennsylvania.
He suggested that real-time awareness issues, especially within electronic health record (EHR) systems, could explain the low follow-up rates. Blood test abnormalities are often flagged in red in EHRs, he said in an interview, but urine dipstick results typically remain in plain black and white.
“So, then it sort of requires that extra cognitive step to kind of look at that [result], and say, okay, that is pretty abnormal; I should do something about that,” he said.
Neil S. Skolnik, MD, a primary care physician at Jefferson Health, Abington, Pennsylvania, was surprised by the findings. “If you get a urinalysis and there’s protein, normally you follow up,” Dr. Skolnik said in an interview. “I have a feeling that there’s something we’re not seeing here about what’s going on. It is hard to imagine that in only 1 out of 15 times that proteinuria is identified, is there any follow-up. I really don’t have a good explanation.”
Renee Marie Betancourt, MD, associate professor and vice chair of diversity, equity, and inclusion in the Department of Family Medicine and Community Health at the University of Pennsylvania Perelman School of Medicine, Philadelphia, said it is hard to draw conclusions from the available data, but agreed that low visibility of results could be partially to blame.
“The chart doesn’t tell me [a urine dipstick result] is abnormal,” Dr. Betancourt said in an interview. “The chart just reports it, agnostic of normal or abnormal.”
Beyond issues with visibility, Dr. Betancourt described how primary care physicians are often so flooded with other concerns that a positive dipstick test can become a low priority, particularly among patients with CKD, who typically have other health issues.
“I oftentimes spend the majority of my visit on the patient’s concerns, and sometimes, beyond their concerns, I have concerns, and [a urine dipstick result] might not make it to the top of the list,” she said.
EHR-Based Interventions Might Help Improve Follow-up
Dr. Chang suggested that improved visibility of dipstick results could help, or possibly EHR-integrated clinical decision tools.
Dr. Betancourt and colleagues at Penn Medicine are actively working on such a solution. Their EHR-based intervention is aimed at identifying and managing patients with CKD. The present design, slated for pilot testing at one or two primary care clinics beginning in January 2025, depends upon estimated glomerular filtration rate (eGFR) to flag CKD patients, with ACR testing recommended yearly to predict disease progression.
Although urine dipstick findings are not currently a part of this software pathway, the findings from the present study might influence future strategy.
“I’m going to take this to our collaborators and ask about opportunities to ... encourage providers to be more active with dipsticks,” Dr. Betancourt said.
Newer Medications Are Effective, but Prescribing Challenges Remain
Ideally, CKD screening improvements will unlock a greater goal: prescribing kidney-protecting medications to patients who need them — as soon as they need them.
Here might lie the real knowledge gap among experienced primary care physicians, Dr. Chang suggested. “In the past, there wasn’t quite as much that you could do about having proteinuria,” he said. “But now we have lots more medications ... it’s not just tracking that they have a bad prognostic factor. [Proteinuria is] actually something that we can act upon.”
Who exactly should be prescribing these kidney-protecting medications, however, remains contested, as agents like GLP-1 agonists and SGLT2 inhibitors yield benefits across specialties, including nephrology, cardiology, and endocrinology.
“Everyone’s going to have to work together,” Dr. Chang said. “You can’t really put it all on the [primary care physician] to quarterback everything.”
And, regardless of who throws the ball, a touchdown is not guaranteed.
Dr. Betancourt called out the high cost of these newer drugs and described how some of her patients, already facing multiple health inequities, are left without.
“I have patients who cannot fill these medications because the copay is too high,” she said. “Just last week I received a message from a patient who stopped taking his SGLT2 inhibitor because the cost was too high ... it was over $300 per month.”
This study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health. The authors’ conflicts of interests are available in the original paper. Dr. Skolnik and Dr. Betancourt reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Only 1 in 15 urine dipstick tests showing proteinuria in the primary care setting are followed up with albuminuria quantification testing, according to investigators.
These findings expose a broad gap in screening for chronic kidney disease (CKD), which is especially concerning since newer kidney-protecting agents are more effective when prescribed earlier in the disease course, reported lead author Yunwen Xu, PhD, of Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, and colleagues.
“Evidence-based prescription of renin-angiotensin system inhibitors, glucagon-like peptide-1 receptor (GLP-1) agonists, sodium-glucose cotransporter 2 (SGLT2) inhibitors, and nonsteroidal mineralocorticoid receptor antagonists (nsMRAs) relies on the level of albuminuria,” the investigators wrote in Annals of Internal Medicine.
“Although urine albumin-creatinine ratio (ACR) is the most accurate method for quantifying albuminuria, dipstick urinalysis tests are inexpensive and are often used as an initial screening test, with guidelines recommending follow-up ACR testing if the protein dipstick test result is abnormal.”
Despite this guidance, real-world follow-up rates have been unknown, prompting the present study. Real-world data show a low follow-up rate. Dr. Xu and colleagues analyzed data from 1 million patients in 33 health systems who underwent urine dipstick testing in a primary care setting.
Across this population, 13% of patients had proteinuria, but only 6.7% underwent follow-up albuminuria quantification testing within the next year. ACR was the most common method (86%).
Likelihood of follow-up increased slightly with the level of proteinuria detected; however, absolute differences were marginal, with a 3+ result yielding a follow-up rate of just 8%, compared with 7.3% for a 2+ result and 6.3% for a 1+ result. When albuminuria quantification tests were conducted, 1+, 2+, and 3+ dipstick results were associated with albuminuria rates of 36.3%, 53.0%, and 64.9%, respectively.
Patients with diabetes had the highest follow-up rate, at 16.6%, vs 3.8% for those without diabetes.
Reasons for Low Follow-up Unclear
The dataset did not include information about reasons for ordering urinalyses, whether primary care providers knew about the abnormal dipstick tests, or awareness of guideline recommendations.
“I think they know it should be done,” said principal investigator Alexander R. Chang, MD, associate professor in the department of nephrology and population health sciences at Geisinger Health, Danville, Pennsylvania.
He suggested that real-time awareness issues, especially within electronic health record (EHR) systems, could explain the low follow-up rates. Blood test abnormalities are often flagged in red in EHRs, he said in an interview, but urine dipstick results typically remain in plain black and white.
“So, then it sort of requires that extra cognitive step to kind of look at that [result], and say, okay, that is pretty abnormal; I should do something about that,” he said.
Neil S. Skolnik, MD, a primary care physician at Jefferson Health, Abington, Pennsylvania, was surprised by the findings. “If you get a urinalysis and there’s protein, normally you follow up,” Dr. Skolnik said in an interview. “I have a feeling that there’s something we’re not seeing here about what’s going on. It is hard to imagine that in only 1 out of 15 times that proteinuria is identified, is there any follow-up. I really don’t have a good explanation.”
Renee Marie Betancourt, MD, associate professor and vice chair of diversity, equity, and inclusion in the Department of Family Medicine and Community Health at the University of Pennsylvania Perelman School of Medicine, Philadelphia, said it is hard to draw conclusions from the available data, but agreed that low visibility of results could be partially to blame.
“The chart doesn’t tell me [a urine dipstick result] is abnormal,” Dr. Betancourt said in an interview. “The chart just reports it, agnostic of normal or abnormal.”
Beyond issues with visibility, Dr. Betancourt described how primary care physicians are often so flooded with other concerns that a positive dipstick test can become a low priority, particularly among patients with CKD, who typically have other health issues.
“I oftentimes spend the majority of my visit on the patient’s concerns, and sometimes, beyond their concerns, I have concerns, and [a urine dipstick result] might not make it to the top of the list,” she said.
EHR-Based Interventions Might Help Improve Follow-up
Dr. Chang suggested that improved visibility of dipstick results could help, or possibly EHR-integrated clinical decision tools.
Dr. Betancourt and colleagues at Penn Medicine are actively working on such a solution. Their EHR-based intervention is aimed at identifying and managing patients with CKD. The present design, slated for pilot testing at one or two primary care clinics beginning in January 2025, depends upon estimated glomerular filtration rate (eGFR) to flag CKD patients, with ACR testing recommended yearly to predict disease progression.
Although urine dipstick findings are not currently a part of this software pathway, the findings from the present study might influence future strategy.
“I’m going to take this to our collaborators and ask about opportunities to ... encourage providers to be more active with dipsticks,” Dr. Betancourt said.
Newer Medications Are Effective, but Prescribing Challenges Remain
Ideally, CKD screening improvements will unlock a greater goal: prescribing kidney-protecting medications to patients who need them — as soon as they need them.
Here might lie the real knowledge gap among experienced primary care physicians, Dr. Chang suggested. “In the past, there wasn’t quite as much that you could do about having proteinuria,” he said. “But now we have lots more medications ... it’s not just tracking that they have a bad prognostic factor. [Proteinuria is] actually something that we can act upon.”
Who exactly should be prescribing these kidney-protecting medications, however, remains contested, as agents like GLP-1 agonists and SGLT2 inhibitors yield benefits across specialties, including nephrology, cardiology, and endocrinology.
“Everyone’s going to have to work together,” Dr. Chang said. “You can’t really put it all on the [primary care physician] to quarterback everything.”
And, regardless of who throws the ball, a touchdown is not guaranteed.
Dr. Betancourt called out the high cost of these newer drugs and described how some of her patients, already facing multiple health inequities, are left without.
“I have patients who cannot fill these medications because the copay is too high,” she said. “Just last week I received a message from a patient who stopped taking his SGLT2 inhibitor because the cost was too high ... it was over $300 per month.”
This study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health. The authors’ conflicts of interests are available in the original paper. Dr. Skolnik and Dr. Betancourt reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Only 1 in 15 urine dipstick tests showing proteinuria in the primary care setting are followed up with albuminuria quantification testing, according to investigators.
These findings expose a broad gap in screening for chronic kidney disease (CKD), which is especially concerning since newer kidney-protecting agents are more effective when prescribed earlier in the disease course, reported lead author Yunwen Xu, PhD, of Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, and colleagues.
“Evidence-based prescription of renin-angiotensin system inhibitors, glucagon-like peptide-1 receptor (GLP-1) agonists, sodium-glucose cotransporter 2 (SGLT2) inhibitors, and nonsteroidal mineralocorticoid receptor antagonists (nsMRAs) relies on the level of albuminuria,” the investigators wrote in Annals of Internal Medicine.
“Although urine albumin-creatinine ratio (ACR) is the most accurate method for quantifying albuminuria, dipstick urinalysis tests are inexpensive and are often used as an initial screening test, with guidelines recommending follow-up ACR testing if the protein dipstick test result is abnormal.”
Despite this guidance, real-world follow-up rates have been unknown, prompting the present study. Real-world data show a low follow-up rate. Dr. Xu and colleagues analyzed data from 1 million patients in 33 health systems who underwent urine dipstick testing in a primary care setting.
Across this population, 13% of patients had proteinuria, but only 6.7% underwent follow-up albuminuria quantification testing within the next year. ACR was the most common method (86%).
Likelihood of follow-up increased slightly with the level of proteinuria detected; however, absolute differences were marginal, with a 3+ result yielding a follow-up rate of just 8%, compared with 7.3% for a 2+ result and 6.3% for a 1+ result. When albuminuria quantification tests were conducted, 1+, 2+, and 3+ dipstick results were associated with albuminuria rates of 36.3%, 53.0%, and 64.9%, respectively.
Patients with diabetes had the highest follow-up rate, at 16.6%, vs 3.8% for those without diabetes.
Reasons for Low Follow-up Unclear
The dataset did not include information about reasons for ordering urinalyses, whether primary care providers knew about the abnormal dipstick tests, or awareness of guideline recommendations.
“I think they know it should be done,” said principal investigator Alexander R. Chang, MD, associate professor in the department of nephrology and population health sciences at Geisinger Health, Danville, Pennsylvania.
He suggested that real-time awareness issues, especially within electronic health record (EHR) systems, could explain the low follow-up rates. Blood test abnormalities are often flagged in red in EHRs, he said in an interview, but urine dipstick results typically remain in plain black and white.
“So, then it sort of requires that extra cognitive step to kind of look at that [result], and say, okay, that is pretty abnormal; I should do something about that,” he said.
Neil S. Skolnik, MD, a primary care physician at Jefferson Health, Abington, Pennsylvania, was surprised by the findings. “If you get a urinalysis and there’s protein, normally you follow up,” Dr. Skolnik said in an interview. “I have a feeling that there’s something we’re not seeing here about what’s going on. It is hard to imagine that in only 1 out of 15 times that proteinuria is identified, is there any follow-up. I really don’t have a good explanation.”
Renee Marie Betancourt, MD, associate professor and vice chair of diversity, equity, and inclusion in the Department of Family Medicine and Community Health at the University of Pennsylvania Perelman School of Medicine, Philadelphia, said it is hard to draw conclusions from the available data, but agreed that low visibility of results could be partially to blame.
“The chart doesn’t tell me [a urine dipstick result] is abnormal,” Dr. Betancourt said in an interview. “The chart just reports it, agnostic of normal or abnormal.”
Beyond issues with visibility, Dr. Betancourt described how primary care physicians are often so flooded with other concerns that a positive dipstick test can become a low priority, particularly among patients with CKD, who typically have other health issues.
“I oftentimes spend the majority of my visit on the patient’s concerns, and sometimes, beyond their concerns, I have concerns, and [a urine dipstick result] might not make it to the top of the list,” she said.
EHR-Based Interventions Might Help Improve Follow-up
Dr. Chang suggested that improved visibility of dipstick results could help, or possibly EHR-integrated clinical decision tools.
Dr. Betancourt and colleagues at Penn Medicine are actively working on such a solution. Their EHR-based intervention is aimed at identifying and managing patients with CKD. The present design, slated for pilot testing at one or two primary care clinics beginning in January 2025, depends upon estimated glomerular filtration rate (eGFR) to flag CKD patients, with ACR testing recommended yearly to predict disease progression.
Although urine dipstick findings are not currently a part of this software pathway, the findings from the present study might influence future strategy.
“I’m going to take this to our collaborators and ask about opportunities to ... encourage providers to be more active with dipsticks,” Dr. Betancourt said.
Newer Medications Are Effective, but Prescribing Challenges Remain
Ideally, CKD screening improvements will unlock a greater goal: prescribing kidney-protecting medications to patients who need them — as soon as they need them.
Here might lie the real knowledge gap among experienced primary care physicians, Dr. Chang suggested. “In the past, there wasn’t quite as much that you could do about having proteinuria,” he said. “But now we have lots more medications ... it’s not just tracking that they have a bad prognostic factor. [Proteinuria is] actually something that we can act upon.”
Who exactly should be prescribing these kidney-protecting medications, however, remains contested, as agents like GLP-1 agonists and SGLT2 inhibitors yield benefits across specialties, including nephrology, cardiology, and endocrinology.
“Everyone’s going to have to work together,” Dr. Chang said. “You can’t really put it all on the [primary care physician] to quarterback everything.”
And, regardless of who throws the ball, a touchdown is not guaranteed.
Dr. Betancourt called out the high cost of these newer drugs and described how some of her patients, already facing multiple health inequities, are left without.
“I have patients who cannot fill these medications because the copay is too high,” she said. “Just last week I received a message from a patient who stopped taking his SGLT2 inhibitor because the cost was too high ... it was over $300 per month.”
This study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health. The authors’ conflicts of interests are available in the original paper. Dr. Skolnik and Dr. Betancourt reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF INTERNAL MEDICINE
Diabetic Kidney Disease Therapies Keep on FLOWing
Further data from the FLOW study were presented during the 2024 congress of the European Association for the Study of Diabetes (EASD) in Madrid. The FLOW study was originally presented in May at the European Renal Association’s 2024 congress in Stockholm. It was the first dedicated kidney outcomes trial to examine a GLP-1 receptor agonist.
The FLOW study demonstrated significant kidney, cardiovascular, and mortality benefits with semaglutide 1 mg once weekly in patients with type 2 diabetes and chronic kidney disease (CKD). This study has elevated semaglutide to a new pillar of care for the management of diabetic kidney disease (DKD) alongside RAAS inhibitors, SGLT2 inhibitors, and finerenone.
At first, whether the benefits of semaglutide were independent of baseline SGLT2 inhibitor use was uncertain. The data presented at the EASD congress, however, appeared to confirm the additive benefits of semaglutide, when combined with SGLT2 inhibitor use, in patients with DKD. The authors did acknowledge that study power was limited, given the low use of SGLT2 inhibitors at trial recruitment (no licensed SGLT2 inhibitor was available for CKD at that point), so small, clinically relevant interactions may not have been detected.
So, what are the implications of the FLOW study for primary care?
DKD is a common clinical challenge in primary care; a national diabetes audit in the United Kingdom suggested that over 40% of patients with type 2 diabetes had kidney disease. Moreover, DKD is the most common cause of kidney failure in adults starting renal replacement therapy in the United Kingdom.
Residual renal risk in patients with DKD persists despite optimal use of guideline-directed medical therapy (GDMT) with RAAS inhibitors, SGLT2 inhibitors, and finerenone, as demonstrated in the many landmark kidney outcomes trials over the past 25 years.
So, a new pillar of GDMT is welcome, but I am worried that this widened choice of therapies may worsen therapeutic inertia; baseline use of the newer DKD therapies (specifically SGLT2 inhibitors and finerenone) remains low.
In addition, during the EASD FLOW session, Katherine Tuttle, MD, executive director for research at Providence Inland Northwest Health Services in Spokane, Washington, presented data from the US CURE-CKD registry study showing that baseline ACE inhibitor/ARB use of about 70% dropped to 50% after just 90 days. Baseline use of SGLT2 inhibitors was only about 6% and dropped to 5% after 90 days.
I suspect that much of this reduction in prescribing of ACE inhibitors/ARBs will have been in response to an acute dip in estimated glomerular filtration rate (eGFR) or hyperkalemia, which has been a perennial challenge with RAAS inhibitor use in primary care. Ongoing education in primary care is required to manage hyperkalemia and reductions in eGFR after RAAS inhibitor initiation to prevent premature cessation of these foundational therapies.
On a positive note, there was no acute dip in eGFR after prescribing semaglutide in DKD. This observation will be reassuring for primary care and hopefully prevent unnecessary cessation of therapy.
Also reassuring was the lack of difference in diabetic retinopathy adverse events between the semaglutide and placebo groups. These events raised concerns about semaglutide following the SUSTAIN-6 CVOT study and have affected attitudes in primary care. But the rapidity and magnitude of improvement in glycemic control with semaglutide was believed to be the underlying issue, rather than semaglutide itself. A similar phenomenon has been observed with insulin. The ongoing FOCUS study is exploring the long-term effects of semaglutide on diabetic retinopathy in patients with type 2 diabetes. This study will hopefully provide a definite answer to this issue.
Another useful message from the FLOW study for primary care is the utility of semaglutide for glucose-lowering in the context of CKD. A1c was 0.81% lower in the semaglutide group compared with the placebo group in participants with eGFRs as low as 25 mL/min/1.73 m2. It is well established that SGLT2 inhibitors have negligible glucose-lowering effects once eGFR drops below 45 mL/min/1.73 m2. Indeed, my usual practice in CKD, if additional glucose-lowering is required once renal protection has been established with an SGLT2 inhibitor, was to add a GLP-1 receptor agonist. It is reassuring to have my clinical practice ratified by the FLOW study.
Semaglutide also helpfully provides an alternative therapeutic option for patients who do not tolerate SGLT2 inhibitors because of, for example, recurrent mycotic genital infections or polyuria, or for those in whom SGLT2 inhibitors are contraindicated, such as patients who have experienced an unprovoked episode of diabetic ketoacidosis. Many of these patients still require cardiovascular and kidney protection, so the FLOW study gives me a viable evidence-based alternative.
As a class, semaglutide and GLP-1 receptor agonists are, of course, not without side effects. Gastrointestinal side effects are the most common, and this finding was echoed in the FLOW study. Gastrointestinal disorders led to permanent treatment discontinuation in 4.5% of the semaglutide group compared with 1.1% of the placebo group. The overall safety profile of semaglutide was favorable, however.
Gastrointestinal side effects can be particularly concerning in the context of CKD because of the possibility of clinical dehydration and acute kidney injury with persistent vomiting or diarrhea. Patient education is particularly important when using GLP-1 receptor agonists in this group of individuals. Reassuringly, there was no imbalance in dehydration and acute kidney injury between trial arms in the FLOW study.
Notably, past studies have suggested that patients with CKD are more likely to experience gastrointestinal side effects with GLP-1 receptor agonists; in these patients, the usual mantra of GLP-1 receptor agonist prescribing is particularly important: Start low, go slow.
Finally, medication adherence is a challenge with multiple pillars of GDMT: These evidence-based disease-modifying therapies work only if our patients take them regularly. My senior partner had a lovely turn of phrase when reviewing patients with multiple long-term conditions; he would always start the consultation by asking individuals which medications they were not taking regularly.
Overall, the FLOW study confirms semaglutide’s position as a new therapeutic pillar for DKD. This treatment will help address the residual renal risk for patients with DKD despite optimal use of GDMT. However, education and support will be required in primary care to prevent worsening therapeutic inertia.
Kevin Fernando, general practitioner partner, North Berwick Health Centre, North Berwick, UK, has disclosed the following relevant financial relationships: Received speaker fees from: Amarin; Amgen; AstraZeneca; Bayer; Boehringer Ingelheim; Dexcom; Daiichi Sankyo; Lilly; Menarini; Novartis; Novo Nordisk; Roche Diagnostics; Embecta; Roche Diabetes Care. Received honoraria for participation in advisory boards from: Amarin; Amgen; AstraZen
A version of this article first appeared on Medscape.com.
Further data from the FLOW study were presented during the 2024 congress of the European Association for the Study of Diabetes (EASD) in Madrid. The FLOW study was originally presented in May at the European Renal Association’s 2024 congress in Stockholm. It was the first dedicated kidney outcomes trial to examine a GLP-1 receptor agonist.
The FLOW study demonstrated significant kidney, cardiovascular, and mortality benefits with semaglutide 1 mg once weekly in patients with type 2 diabetes and chronic kidney disease (CKD). This study has elevated semaglutide to a new pillar of care for the management of diabetic kidney disease (DKD) alongside RAAS inhibitors, SGLT2 inhibitors, and finerenone.
At first, whether the benefits of semaglutide were independent of baseline SGLT2 inhibitor use was uncertain. The data presented at the EASD congress, however, appeared to confirm the additive benefits of semaglutide, when combined with SGLT2 inhibitor use, in patients with DKD. The authors did acknowledge that study power was limited, given the low use of SGLT2 inhibitors at trial recruitment (no licensed SGLT2 inhibitor was available for CKD at that point), so small, clinically relevant interactions may not have been detected.
So, what are the implications of the FLOW study for primary care?
DKD is a common clinical challenge in primary care; a national diabetes audit in the United Kingdom suggested that over 40% of patients with type 2 diabetes had kidney disease. Moreover, DKD is the most common cause of kidney failure in adults starting renal replacement therapy in the United Kingdom.
Residual renal risk in patients with DKD persists despite optimal use of guideline-directed medical therapy (GDMT) with RAAS inhibitors, SGLT2 inhibitors, and finerenone, as demonstrated in the many landmark kidney outcomes trials over the past 25 years.
So, a new pillar of GDMT is welcome, but I am worried that this widened choice of therapies may worsen therapeutic inertia; baseline use of the newer DKD therapies (specifically SGLT2 inhibitors and finerenone) remains low.
In addition, during the EASD FLOW session, Katherine Tuttle, MD, executive director for research at Providence Inland Northwest Health Services in Spokane, Washington, presented data from the US CURE-CKD registry study showing that baseline ACE inhibitor/ARB use of about 70% dropped to 50% after just 90 days. Baseline use of SGLT2 inhibitors was only about 6% and dropped to 5% after 90 days.
I suspect that much of this reduction in prescribing of ACE inhibitors/ARBs will have been in response to an acute dip in estimated glomerular filtration rate (eGFR) or hyperkalemia, which has been a perennial challenge with RAAS inhibitor use in primary care. Ongoing education in primary care is required to manage hyperkalemia and reductions in eGFR after RAAS inhibitor initiation to prevent premature cessation of these foundational therapies.
On a positive note, there was no acute dip in eGFR after prescribing semaglutide in DKD. This observation will be reassuring for primary care and hopefully prevent unnecessary cessation of therapy.
Also reassuring was the lack of difference in diabetic retinopathy adverse events between the semaglutide and placebo groups. These events raised concerns about semaglutide following the SUSTAIN-6 CVOT study and have affected attitudes in primary care. But the rapidity and magnitude of improvement in glycemic control with semaglutide was believed to be the underlying issue, rather than semaglutide itself. A similar phenomenon has been observed with insulin. The ongoing FOCUS study is exploring the long-term effects of semaglutide on diabetic retinopathy in patients with type 2 diabetes. This study will hopefully provide a definite answer to this issue.
Another useful message from the FLOW study for primary care is the utility of semaglutide for glucose-lowering in the context of CKD. A1c was 0.81% lower in the semaglutide group compared with the placebo group in participants with eGFRs as low as 25 mL/min/1.73 m2. It is well established that SGLT2 inhibitors have negligible glucose-lowering effects once eGFR drops below 45 mL/min/1.73 m2. Indeed, my usual practice in CKD, if additional glucose-lowering is required once renal protection has been established with an SGLT2 inhibitor, was to add a GLP-1 receptor agonist. It is reassuring to have my clinical practice ratified by the FLOW study.
Semaglutide also helpfully provides an alternative therapeutic option for patients who do not tolerate SGLT2 inhibitors because of, for example, recurrent mycotic genital infections or polyuria, or for those in whom SGLT2 inhibitors are contraindicated, such as patients who have experienced an unprovoked episode of diabetic ketoacidosis. Many of these patients still require cardiovascular and kidney protection, so the FLOW study gives me a viable evidence-based alternative.
As a class, semaglutide and GLP-1 receptor agonists are, of course, not without side effects. Gastrointestinal side effects are the most common, and this finding was echoed in the FLOW study. Gastrointestinal disorders led to permanent treatment discontinuation in 4.5% of the semaglutide group compared with 1.1% of the placebo group. The overall safety profile of semaglutide was favorable, however.
Gastrointestinal side effects can be particularly concerning in the context of CKD because of the possibility of clinical dehydration and acute kidney injury with persistent vomiting or diarrhea. Patient education is particularly important when using GLP-1 receptor agonists in this group of individuals. Reassuringly, there was no imbalance in dehydration and acute kidney injury between trial arms in the FLOW study.
Notably, past studies have suggested that patients with CKD are more likely to experience gastrointestinal side effects with GLP-1 receptor agonists; in these patients, the usual mantra of GLP-1 receptor agonist prescribing is particularly important: Start low, go slow.
Finally, medication adherence is a challenge with multiple pillars of GDMT: These evidence-based disease-modifying therapies work only if our patients take them regularly. My senior partner had a lovely turn of phrase when reviewing patients with multiple long-term conditions; he would always start the consultation by asking individuals which medications they were not taking regularly.
Overall, the FLOW study confirms semaglutide’s position as a new therapeutic pillar for DKD. This treatment will help address the residual renal risk for patients with DKD despite optimal use of GDMT. However, education and support will be required in primary care to prevent worsening therapeutic inertia.
Kevin Fernando, general practitioner partner, North Berwick Health Centre, North Berwick, UK, has disclosed the following relevant financial relationships: Received speaker fees from: Amarin; Amgen; AstraZeneca; Bayer; Boehringer Ingelheim; Dexcom; Daiichi Sankyo; Lilly; Menarini; Novartis; Novo Nordisk; Roche Diagnostics; Embecta; Roche Diabetes Care. Received honoraria for participation in advisory boards from: Amarin; Amgen; AstraZen
A version of this article first appeared on Medscape.com.
Further data from the FLOW study were presented during the 2024 congress of the European Association for the Study of Diabetes (EASD) in Madrid. The FLOW study was originally presented in May at the European Renal Association’s 2024 congress in Stockholm. It was the first dedicated kidney outcomes trial to examine a GLP-1 receptor agonist.
The FLOW study demonstrated significant kidney, cardiovascular, and mortality benefits with semaglutide 1 mg once weekly in patients with type 2 diabetes and chronic kidney disease (CKD). This study has elevated semaglutide to a new pillar of care for the management of diabetic kidney disease (DKD) alongside RAAS inhibitors, SGLT2 inhibitors, and finerenone.
At first, whether the benefits of semaglutide were independent of baseline SGLT2 inhibitor use was uncertain. The data presented at the EASD congress, however, appeared to confirm the additive benefits of semaglutide, when combined with SGLT2 inhibitor use, in patients with DKD. The authors did acknowledge that study power was limited, given the low use of SGLT2 inhibitors at trial recruitment (no licensed SGLT2 inhibitor was available for CKD at that point), so small, clinically relevant interactions may not have been detected.
So, what are the implications of the FLOW study for primary care?
DKD is a common clinical challenge in primary care; a national diabetes audit in the United Kingdom suggested that over 40% of patients with type 2 diabetes had kidney disease. Moreover, DKD is the most common cause of kidney failure in adults starting renal replacement therapy in the United Kingdom.
Residual renal risk in patients with DKD persists despite optimal use of guideline-directed medical therapy (GDMT) with RAAS inhibitors, SGLT2 inhibitors, and finerenone, as demonstrated in the many landmark kidney outcomes trials over the past 25 years.
So, a new pillar of GDMT is welcome, but I am worried that this widened choice of therapies may worsen therapeutic inertia; baseline use of the newer DKD therapies (specifically SGLT2 inhibitors and finerenone) remains low.
In addition, during the EASD FLOW session, Katherine Tuttle, MD, executive director for research at Providence Inland Northwest Health Services in Spokane, Washington, presented data from the US CURE-CKD registry study showing that baseline ACE inhibitor/ARB use of about 70% dropped to 50% after just 90 days. Baseline use of SGLT2 inhibitors was only about 6% and dropped to 5% after 90 days.
I suspect that much of this reduction in prescribing of ACE inhibitors/ARBs will have been in response to an acute dip in estimated glomerular filtration rate (eGFR) or hyperkalemia, which has been a perennial challenge with RAAS inhibitor use in primary care. Ongoing education in primary care is required to manage hyperkalemia and reductions in eGFR after RAAS inhibitor initiation to prevent premature cessation of these foundational therapies.
On a positive note, there was no acute dip in eGFR after prescribing semaglutide in DKD. This observation will be reassuring for primary care and hopefully prevent unnecessary cessation of therapy.
Also reassuring was the lack of difference in diabetic retinopathy adverse events between the semaglutide and placebo groups. These events raised concerns about semaglutide following the SUSTAIN-6 CVOT study and have affected attitudes in primary care. But the rapidity and magnitude of improvement in glycemic control with semaglutide was believed to be the underlying issue, rather than semaglutide itself. A similar phenomenon has been observed with insulin. The ongoing FOCUS study is exploring the long-term effects of semaglutide on diabetic retinopathy in patients with type 2 diabetes. This study will hopefully provide a definite answer to this issue.
Another useful message from the FLOW study for primary care is the utility of semaglutide for glucose-lowering in the context of CKD. A1c was 0.81% lower in the semaglutide group compared with the placebo group in participants with eGFRs as low as 25 mL/min/1.73 m2. It is well established that SGLT2 inhibitors have negligible glucose-lowering effects once eGFR drops below 45 mL/min/1.73 m2. Indeed, my usual practice in CKD, if additional glucose-lowering is required once renal protection has been established with an SGLT2 inhibitor, was to add a GLP-1 receptor agonist. It is reassuring to have my clinical practice ratified by the FLOW study.
Semaglutide also helpfully provides an alternative therapeutic option for patients who do not tolerate SGLT2 inhibitors because of, for example, recurrent mycotic genital infections or polyuria, or for those in whom SGLT2 inhibitors are contraindicated, such as patients who have experienced an unprovoked episode of diabetic ketoacidosis. Many of these patients still require cardiovascular and kidney protection, so the FLOW study gives me a viable evidence-based alternative.
As a class, semaglutide and GLP-1 receptor agonists are, of course, not without side effects. Gastrointestinal side effects are the most common, and this finding was echoed in the FLOW study. Gastrointestinal disorders led to permanent treatment discontinuation in 4.5% of the semaglutide group compared with 1.1% of the placebo group. The overall safety profile of semaglutide was favorable, however.
Gastrointestinal side effects can be particularly concerning in the context of CKD because of the possibility of clinical dehydration and acute kidney injury with persistent vomiting or diarrhea. Patient education is particularly important when using GLP-1 receptor agonists in this group of individuals. Reassuringly, there was no imbalance in dehydration and acute kidney injury between trial arms in the FLOW study.
Notably, past studies have suggested that patients with CKD are more likely to experience gastrointestinal side effects with GLP-1 receptor agonists; in these patients, the usual mantra of GLP-1 receptor agonist prescribing is particularly important: Start low, go slow.
Finally, medication adherence is a challenge with multiple pillars of GDMT: These evidence-based disease-modifying therapies work only if our patients take them regularly. My senior partner had a lovely turn of phrase when reviewing patients with multiple long-term conditions; he would always start the consultation by asking individuals which medications they were not taking regularly.
Overall, the FLOW study confirms semaglutide’s position as a new therapeutic pillar for DKD. This treatment will help address the residual renal risk for patients with DKD despite optimal use of GDMT. However, education and support will be required in primary care to prevent worsening therapeutic inertia.
Kevin Fernando, general practitioner partner, North Berwick Health Centre, North Berwick, UK, has disclosed the following relevant financial relationships: Received speaker fees from: Amarin; Amgen; AstraZeneca; Bayer; Boehringer Ingelheim; Dexcom; Daiichi Sankyo; Lilly; Menarini; Novartis; Novo Nordisk; Roche Diagnostics; Embecta; Roche Diabetes Care. Received honoraria for participation in advisory boards from: Amarin; Amgen; AstraZen
A version of this article first appeared on Medscape.com.
FROM EASD 2024
Does Screening for CKD Benefit Older Adults?
TOPLINE:
Short-term mortality, hospitalizations, and cardiovascular disease (CVD) events are not significantly different between patients diagnosed with chronic kidney disease (CKD) during routine medical care and those through screening, in a study that found older age, being male, and having a diagnosis of heart failure are associated with an increased risk for mortality in patients with CKD.
METHODOLOGY:
- Researchers conducted a prospective cohort study involving 892 primary care patients aged 60 years or older with CKD from the Oxford Renal Cohort Study in England.
- Participants were categorized into those with existing CKD (n = 257; median age, 75 years), screen-detected CKD (n = 185; median age, roughly 73 years), or temporary reduction in kidney function (n = 450; median age, roughly 73 years).
- The primary outcome was a composite of all-cause mortality, hospitalization, CVD, or end-stage kidney disease.
- The secondary outcomes were the individual components of the composite primary outcome and factors associated with mortality in those with CKD.
TAKEAWAY:
- The composite outcomes were not significantly different between patients with preexisting CKD and kidney disease identified during screening (adjusted hazard ratio [aHR], 0.94; 95% CI, 0.67-1.33).
- Risks for death, hospitalization, CVD, or end-stage kidney disease were not significantly different between the two groups.
- Older age (aHR per year, 1.10; 95% CI, 1.06-1.15), male sex (aHR, 2.31; 95% CI, 1.26-4.24), and heart failure (aHR, 5.18; 95% CI, 2.45-10.97) were associated with higher risks for death.
- No cases of end-stage kidney disease were reported during the study period.
IN PRACTICE:
“Our findings show that the risk of short-term mortality, hospitalization, and CVD is comparable in people diagnosed through screening to those diagnosed routinely in primary care. This suggests that screening older people for CKD may be of value to increase detection and enable disease-modifying treatment to be initiated at an earlier stage,” the study authors wrote.
SOURCE:
The study was led by Anna K. Forbes, MBChB, and José M. Ordóñez-Mena, PhD, of the Nuffield Department of Primary Care Health Sciences at the University of Oxford, England. It was published online in BJGP Open.
LIMITATIONS:
The study had a relatively short follow-up period and a cohort primarily consisting of individuals with early-stage CKD, which may have limited the identification of end-stage cases of the condition. The study population predominantly consisted of White individuals, affecting the generalizability of the results to more diverse populations. Misclassification bias may have occurred due to changes in the kidney function over time.
DISCLOSURES:
The data linkage provided by NHS Digital was supported by funding from the NIHR School of Primary Care Research. Some authors were partly supported by the NIHR Oxford Biomedical Research Centre and NIHR Oxford Thames Valley Applied Research Collaborative. One author reported receiving financial support for attending a conference, while another received consulting fees from various pharmaceutical companies. Another author reported receiving a grant from the Wellcome Trust and payment while working as a presenter for NB Medical and is an unpaid trustee of some charities.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Short-term mortality, hospitalizations, and cardiovascular disease (CVD) events are not significantly different between patients diagnosed with chronic kidney disease (CKD) during routine medical care and those through screening, in a study that found older age, being male, and having a diagnosis of heart failure are associated with an increased risk for mortality in patients with CKD.
METHODOLOGY:
- Researchers conducted a prospective cohort study involving 892 primary care patients aged 60 years or older with CKD from the Oxford Renal Cohort Study in England.
- Participants were categorized into those with existing CKD (n = 257; median age, 75 years), screen-detected CKD (n = 185; median age, roughly 73 years), or temporary reduction in kidney function (n = 450; median age, roughly 73 years).
- The primary outcome was a composite of all-cause mortality, hospitalization, CVD, or end-stage kidney disease.
- The secondary outcomes were the individual components of the composite primary outcome and factors associated with mortality in those with CKD.
TAKEAWAY:
- The composite outcomes were not significantly different between patients with preexisting CKD and kidney disease identified during screening (adjusted hazard ratio [aHR], 0.94; 95% CI, 0.67-1.33).
- Risks for death, hospitalization, CVD, or end-stage kidney disease were not significantly different between the two groups.
- Older age (aHR per year, 1.10; 95% CI, 1.06-1.15), male sex (aHR, 2.31; 95% CI, 1.26-4.24), and heart failure (aHR, 5.18; 95% CI, 2.45-10.97) were associated with higher risks for death.
- No cases of end-stage kidney disease were reported during the study period.
IN PRACTICE:
“Our findings show that the risk of short-term mortality, hospitalization, and CVD is comparable in people diagnosed through screening to those diagnosed routinely in primary care. This suggests that screening older people for CKD may be of value to increase detection and enable disease-modifying treatment to be initiated at an earlier stage,” the study authors wrote.
SOURCE:
The study was led by Anna K. Forbes, MBChB, and José M. Ordóñez-Mena, PhD, of the Nuffield Department of Primary Care Health Sciences at the University of Oxford, England. It was published online in BJGP Open.
LIMITATIONS:
The study had a relatively short follow-up period and a cohort primarily consisting of individuals with early-stage CKD, which may have limited the identification of end-stage cases of the condition. The study population predominantly consisted of White individuals, affecting the generalizability of the results to more diverse populations. Misclassification bias may have occurred due to changes in the kidney function over time.
DISCLOSURES:
The data linkage provided by NHS Digital was supported by funding from the NIHR School of Primary Care Research. Some authors were partly supported by the NIHR Oxford Biomedical Research Centre and NIHR Oxford Thames Valley Applied Research Collaborative. One author reported receiving financial support for attending a conference, while another received consulting fees from various pharmaceutical companies. Another author reported receiving a grant from the Wellcome Trust and payment while working as a presenter for NB Medical and is an unpaid trustee of some charities.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Short-term mortality, hospitalizations, and cardiovascular disease (CVD) events are not significantly different between patients diagnosed with chronic kidney disease (CKD) during routine medical care and those through screening, in a study that found older age, being male, and having a diagnosis of heart failure are associated with an increased risk for mortality in patients with CKD.
METHODOLOGY:
- Researchers conducted a prospective cohort study involving 892 primary care patients aged 60 years or older with CKD from the Oxford Renal Cohort Study in England.
- Participants were categorized into those with existing CKD (n = 257; median age, 75 years), screen-detected CKD (n = 185; median age, roughly 73 years), or temporary reduction in kidney function (n = 450; median age, roughly 73 years).
- The primary outcome was a composite of all-cause mortality, hospitalization, CVD, or end-stage kidney disease.
- The secondary outcomes were the individual components of the composite primary outcome and factors associated with mortality in those with CKD.
TAKEAWAY:
- The composite outcomes were not significantly different between patients with preexisting CKD and kidney disease identified during screening (adjusted hazard ratio [aHR], 0.94; 95% CI, 0.67-1.33).
- Risks for death, hospitalization, CVD, or end-stage kidney disease were not significantly different between the two groups.
- Older age (aHR per year, 1.10; 95% CI, 1.06-1.15), male sex (aHR, 2.31; 95% CI, 1.26-4.24), and heart failure (aHR, 5.18; 95% CI, 2.45-10.97) were associated with higher risks for death.
- No cases of end-stage kidney disease were reported during the study period.
IN PRACTICE:
“Our findings show that the risk of short-term mortality, hospitalization, and CVD is comparable in people diagnosed through screening to those diagnosed routinely in primary care. This suggests that screening older people for CKD may be of value to increase detection and enable disease-modifying treatment to be initiated at an earlier stage,” the study authors wrote.
SOURCE:
The study was led by Anna K. Forbes, MBChB, and José M. Ordóñez-Mena, PhD, of the Nuffield Department of Primary Care Health Sciences at the University of Oxford, England. It was published online in BJGP Open.
LIMITATIONS:
The study had a relatively short follow-up period and a cohort primarily consisting of individuals with early-stage CKD, which may have limited the identification of end-stage cases of the condition. The study population predominantly consisted of White individuals, affecting the generalizability of the results to more diverse populations. Misclassification bias may have occurred due to changes in the kidney function over time.
DISCLOSURES:
The data linkage provided by NHS Digital was supported by funding from the NIHR School of Primary Care Research. Some authors were partly supported by the NIHR Oxford Biomedical Research Centre and NIHR Oxford Thames Valley Applied Research Collaborative. One author reported receiving financial support for attending a conference, while another received consulting fees from various pharmaceutical companies. Another author reported receiving a grant from the Wellcome Trust and payment while working as a presenter for NB Medical and is an unpaid trustee of some charities.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Benralizumab Now FDA Approved to Treat EGPA Vasculitis
The Food and Drug Administration (FDA) has approved benralizumab (Fasenra) for the treatment of adults with eosinophilic granulomatosis with polyangiitis (EGPA), formerly known as Churg-Strauss syndrome.
The drug is the second approved biologic for the treatment of EGPA. The first, mepolizumab (Nucala), was approved in 2017.
“This disease has a devastating impact on patients and the quality of their life, and they need more treatment options. The approval of another treatment in EGPA is welcome news to the approximately 15,000 patients living in the US with this difficult-to-treat rare disease,” said Joyce Kullman, executive director of the Vasculitis Foundation, in a press release on September 18.
Benralizumab, developed by AstraZeneca, is a monoclonal antibody against the interleukin-5 alpha receptor expressed on eosinophils. The drug was first approved in 2017 as an add-on treatment for patients 12 years and older with severe eosinophilic asthma, and is now approved for use in children aged 6 years and older.
The new indication was based on positive results from a noninferiority trial comparing benralizumab and mepolizumab. For the trial, published in the New England Journal of Medicine earlier in 2024, 140 adults with relapsing or refractory EGPA were randomized to a 30-mg subcutaneous injection of benralizumab or three separate 100-mg mepolizumab injections every 4 weeks for 1 year. At weeks 36 and 48, 59% of patients in the benralizumab group and 56% of patients in the mepolizumab group achieved remission (95% CI, –13 to 18; P = .73 for superiority). From week 42 to 52, 41% of patients who received benralizumab completely stopped taking oral glucocorticoids, compared with 26% of those who received mepolizumab.
“Patients often rely on long-term oral corticosteroids, which can cause serious and lasting side effects. Benralizumab is a much-needed treatment option, with data showing that not only is remission an achievable goal for EGPA patients, but benralizumab can also help patients taper off steroid therapy,” Michael Wechsler, MD, director of The Asthma Institute at National Jewish Health in Denver, Colorado, and the international coordinating investigator for the clinical trial, said in the press release.
Benralizumab is administered via subcutaneous injection. In adults with EGPA, the recommended dosage is 30 mg every 4 weeks for the first three doses, then once every 8 weeks.
The most common adverse reactions include headache and pharyngitis, according to the prescribing information.
Benralizumab is also in development for the treatment of chronic obstructive pulmonary disease, chronic rhinosinusitis with nasal polyps, and hypereosinophilic syndrome.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration (FDA) has approved benralizumab (Fasenra) for the treatment of adults with eosinophilic granulomatosis with polyangiitis (EGPA), formerly known as Churg-Strauss syndrome.
The drug is the second approved biologic for the treatment of EGPA. The first, mepolizumab (Nucala), was approved in 2017.
“This disease has a devastating impact on patients and the quality of their life, and they need more treatment options. The approval of another treatment in EGPA is welcome news to the approximately 15,000 patients living in the US with this difficult-to-treat rare disease,” said Joyce Kullman, executive director of the Vasculitis Foundation, in a press release on September 18.
Benralizumab, developed by AstraZeneca, is a monoclonal antibody against the interleukin-5 alpha receptor expressed on eosinophils. The drug was first approved in 2017 as an add-on treatment for patients 12 years and older with severe eosinophilic asthma, and is now approved for use in children aged 6 years and older.
The new indication was based on positive results from a noninferiority trial comparing benralizumab and mepolizumab. For the trial, published in the New England Journal of Medicine earlier in 2024, 140 adults with relapsing or refractory EGPA were randomized to a 30-mg subcutaneous injection of benralizumab or three separate 100-mg mepolizumab injections every 4 weeks for 1 year. At weeks 36 and 48, 59% of patients in the benralizumab group and 56% of patients in the mepolizumab group achieved remission (95% CI, –13 to 18; P = .73 for superiority). From week 42 to 52, 41% of patients who received benralizumab completely stopped taking oral glucocorticoids, compared with 26% of those who received mepolizumab.
“Patients often rely on long-term oral corticosteroids, which can cause serious and lasting side effects. Benralizumab is a much-needed treatment option, with data showing that not only is remission an achievable goal for EGPA patients, but benralizumab can also help patients taper off steroid therapy,” Michael Wechsler, MD, director of The Asthma Institute at National Jewish Health in Denver, Colorado, and the international coordinating investigator for the clinical trial, said in the press release.
Benralizumab is administered via subcutaneous injection. In adults with EGPA, the recommended dosage is 30 mg every 4 weeks for the first three doses, then once every 8 weeks.
The most common adverse reactions include headache and pharyngitis, according to the prescribing information.
Benralizumab is also in development for the treatment of chronic obstructive pulmonary disease, chronic rhinosinusitis with nasal polyps, and hypereosinophilic syndrome.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration (FDA) has approved benralizumab (Fasenra) for the treatment of adults with eosinophilic granulomatosis with polyangiitis (EGPA), formerly known as Churg-Strauss syndrome.
The drug is the second approved biologic for the treatment of EGPA. The first, mepolizumab (Nucala), was approved in 2017.
“This disease has a devastating impact on patients and the quality of their life, and they need more treatment options. The approval of another treatment in EGPA is welcome news to the approximately 15,000 patients living in the US with this difficult-to-treat rare disease,” said Joyce Kullman, executive director of the Vasculitis Foundation, in a press release on September 18.
Benralizumab, developed by AstraZeneca, is a monoclonal antibody against the interleukin-5 alpha receptor expressed on eosinophils. The drug was first approved in 2017 as an add-on treatment for patients 12 years and older with severe eosinophilic asthma, and is now approved for use in children aged 6 years and older.
The new indication was based on positive results from a noninferiority trial comparing benralizumab and mepolizumab. For the trial, published in the New England Journal of Medicine earlier in 2024, 140 adults with relapsing or refractory EGPA were randomized to a 30-mg subcutaneous injection of benralizumab or three separate 100-mg mepolizumab injections every 4 weeks for 1 year. At weeks 36 and 48, 59% of patients in the benralizumab group and 56% of patients in the mepolizumab group achieved remission (95% CI, –13 to 18; P = .73 for superiority). From week 42 to 52, 41% of patients who received benralizumab completely stopped taking oral glucocorticoids, compared with 26% of those who received mepolizumab.
“Patients often rely on long-term oral corticosteroids, which can cause serious and lasting side effects. Benralizumab is a much-needed treatment option, with data showing that not only is remission an achievable goal for EGPA patients, but benralizumab can also help patients taper off steroid therapy,” Michael Wechsler, MD, director of The Asthma Institute at National Jewish Health in Denver, Colorado, and the international coordinating investigator for the clinical trial, said in the press release.
Benralizumab is administered via subcutaneous injection. In adults with EGPA, the recommended dosage is 30 mg every 4 weeks for the first three doses, then once every 8 weeks.
The most common adverse reactions include headache and pharyngitis, according to the prescribing information.
Benralizumab is also in development for the treatment of chronic obstructive pulmonary disease, chronic rhinosinusitis with nasal polyps, and hypereosinophilic syndrome.
A version of this article first appeared on Medscape.com.
Stones, Bones, Groans, and Moans: Could This Be Primary Hyperparathyroidism?
This transcript has been edited for clarity.
Matthew F. Watto, MD: Welcome back to The Curbsiders. I’m Dr Matthew Frank Watto, here with my great friend and America’s primary care physician, Dr. Paul Nelson Williams.
Paul, we’re going to talk about our primary hyperparathyroidism podcast with Dr. Lindsay Kuo. It’s a topic that I feel much more clear on now.
Now, Paul, in primary care, you see a lot of calcium that is just slightly high. Can we just blame that on thiazide diuretics?
Paul N. Williams, MD: It’s a place to start. As you’re starting to think about the possible etiologies, primary hyperparathyroidism and malignancy are the two that roll right off the tongue, but it is worth going back to the patient’s medication list and making sure you’re not missing something.
Thiazides famously cause hypercalcemia, but in some of the reading I did for this episode, they may just uncover it a little bit early. Patients who are on thiazides who become hypercalcemic seem to go on to develop primary hyperthyroidism anyway. So I don’t think you can solely blame the thiazide.
Another medication that can be causative is lithium. So a good place to look first after you’ve repeated the labs and confirmed hypercalcemia is the patient’s medication list.
Dr. Watto: We’ve talked before about the basic workup for hypercalcemia, and determining whether it’s PTH dependent or PTH independent. On the podcast, we talk more about the full workup, but I wanted to talk about the classic symptoms. Our expert made the point that we don’t see them as much anymore, although we do see kidney stones. People used to present very late in the disease because they weren’t having labs done routinely.
The classic symptoms include osteoporosis and bone tumors. People can get nephrocalcinosis and kidney stones. I hadn’t really thought of it this way because we’re used to diagnosing it early now. Do you feel the same?
Dr. Williams: As labs have started routinely reporting calcium levels, this is more and more often how it’s picked up. The other aspect is that as we are screening for and finding osteoporosis, part of the workup almost always involves getting a parathyroid hormone and a calcium level. We’re seeing these lab abnormalities before we’re seeing symptoms, which is good.
But it also makes things more diagnostically thorny.
Dr. Watto: Dr. Lindsay Kuo made the point that when she sees patients before and after surgery, she’s aware of these nonclassic symptoms — the stones, bones, groans, and the psychiatric overtones that can be anything from fatigue or irritability to dysphoria.
Some people have a generalized weakness that’s very nonspecific. Dr. Kuo said that sometimes these symptoms will disappear after surgery. The patients may just have gotten used to them, or they thought these symptoms were caused by something else, but after surgery they went away.
There are these nonclassic symptoms that are harder to pin down. I was surprised by that.
Dr. Williams: She mentioned polydipsia and polyuria, which have been reported in other studies. It seems like it can be anything. You have to take a good history, but none of those things in and of themselves is an indication for operating unless the patient has the classic renal or bone manifestations.
Dr. Watto: The other thing we talked about is a normal calcium level in a patient with primary hyperparathyroidism, or the finding of a PTH level in the normal range but with a high calcium level that is inappropriate. Can you talk a little bit about those two situations?
Dr. Williams: They’re hard to say but kind of easy to manage because you treat them the same way as someone who has elevated calcium and PTH levels.
The normocalcemic patient is something we might stumble across with osteoporosis screening. Initially the calcium level is elevated, so you repeat it and it’s normal but with an elevated PTH level. You’re like, shoot. Now what?
It turns out that most endocrine surgeons say that the indications for surgery for the classic form of primary hyperparathyroidism apply to these patients as well, and it probably helps with the bone outcomes, which is one of the things they follow most closely. If you have hypercalcemia, you should have a suppressed PTH level, the so-called normohormonal hyperparathyroidism, which is not normal at all. So even if the PTH is in the normal range, it’s still relatively elevated compared with what it should be. That situation is treated in the same way as the classic elevated PTH and elevated calcium levels.
Dr. Watto: If the calcium is abnormal and the PTH is not quite what you’d expect it to be, you can always ask your friendly neighborhood endocrinologist to help you figure out whether the patient really has one of these conditions. You have to make sure that they don’t have a simple secondary cause like a low vitamin D level. In that case, you fix the vitamin D and then recheck the numbers to see if they’ve normalized. But I have found a bunch of these edge cases in which it has been helpful to confer with an endocrinologist, especially before you send someone to a surgeon to take out their parathyroid gland.
This was a really fantastic conversation. If you want to hear the full podcast episode, click here.
Dr. Watto, Clinical Assistant Professor, Department of Medicine, Perelman School of Medicine at University of Pennsylvania; Internist, Department of Medicine, Hospital Medicine Section, Pennsylvania Hospital, Philadelphia, Pennsylvania, has disclosed no relevant financial relationships. Dr. Williams, Associate Professor of Clinical Medicine, Department of General Internal Medicine, Lewis Katz School of Medicine; Staff Physician, Department of General Internal Medicine, Temple Internal Medicine Associates, Philadelphia, Pennsylvania, served as a director, officer, partner, employee, adviser, consultant, or trustee for The Curbsiders, and has received income in an amount equal to or greater than $250 from The Curbsiders.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Matthew F. Watto, MD: Welcome back to The Curbsiders. I’m Dr Matthew Frank Watto, here with my great friend and America’s primary care physician, Dr. Paul Nelson Williams.
Paul, we’re going to talk about our primary hyperparathyroidism podcast with Dr. Lindsay Kuo. It’s a topic that I feel much more clear on now.
Now, Paul, in primary care, you see a lot of calcium that is just slightly high. Can we just blame that on thiazide diuretics?
Paul N. Williams, MD: It’s a place to start. As you’re starting to think about the possible etiologies, primary hyperparathyroidism and malignancy are the two that roll right off the tongue, but it is worth going back to the patient’s medication list and making sure you’re not missing something.
Thiazides famously cause hypercalcemia, but in some of the reading I did for this episode, they may just uncover it a little bit early. Patients who are on thiazides who become hypercalcemic seem to go on to develop primary hyperthyroidism anyway. So I don’t think you can solely blame the thiazide.
Another medication that can be causative is lithium. So a good place to look first after you’ve repeated the labs and confirmed hypercalcemia is the patient’s medication list.
Dr. Watto: We’ve talked before about the basic workup for hypercalcemia, and determining whether it’s PTH dependent or PTH independent. On the podcast, we talk more about the full workup, but I wanted to talk about the classic symptoms. Our expert made the point that we don’t see them as much anymore, although we do see kidney stones. People used to present very late in the disease because they weren’t having labs done routinely.
The classic symptoms include osteoporosis and bone tumors. People can get nephrocalcinosis and kidney stones. I hadn’t really thought of it this way because we’re used to diagnosing it early now. Do you feel the same?
Dr. Williams: As labs have started routinely reporting calcium levels, this is more and more often how it’s picked up. The other aspect is that as we are screening for and finding osteoporosis, part of the workup almost always involves getting a parathyroid hormone and a calcium level. We’re seeing these lab abnormalities before we’re seeing symptoms, which is good.
But it also makes things more diagnostically thorny.
Dr. Watto: Dr. Lindsay Kuo made the point that when she sees patients before and after surgery, she’s aware of these nonclassic symptoms — the stones, bones, groans, and the psychiatric overtones that can be anything from fatigue or irritability to dysphoria.
Some people have a generalized weakness that’s very nonspecific. Dr. Kuo said that sometimes these symptoms will disappear after surgery. The patients may just have gotten used to them, or they thought these symptoms were caused by something else, but after surgery they went away.
There are these nonclassic symptoms that are harder to pin down. I was surprised by that.
Dr. Williams: She mentioned polydipsia and polyuria, which have been reported in other studies. It seems like it can be anything. You have to take a good history, but none of those things in and of themselves is an indication for operating unless the patient has the classic renal or bone manifestations.
Dr. Watto: The other thing we talked about is a normal calcium level in a patient with primary hyperparathyroidism, or the finding of a PTH level in the normal range but with a high calcium level that is inappropriate. Can you talk a little bit about those two situations?
Dr. Williams: They’re hard to say but kind of easy to manage because you treat them the same way as someone who has elevated calcium and PTH levels.
The normocalcemic patient is something we might stumble across with osteoporosis screening. Initially the calcium level is elevated, so you repeat it and it’s normal but with an elevated PTH level. You’re like, shoot. Now what?
It turns out that most endocrine surgeons say that the indications for surgery for the classic form of primary hyperparathyroidism apply to these patients as well, and it probably helps with the bone outcomes, which is one of the things they follow most closely. If you have hypercalcemia, you should have a suppressed PTH level, the so-called normohormonal hyperparathyroidism, which is not normal at all. So even if the PTH is in the normal range, it’s still relatively elevated compared with what it should be. That situation is treated in the same way as the classic elevated PTH and elevated calcium levels.
Dr. Watto: If the calcium is abnormal and the PTH is not quite what you’d expect it to be, you can always ask your friendly neighborhood endocrinologist to help you figure out whether the patient really has one of these conditions. You have to make sure that they don’t have a simple secondary cause like a low vitamin D level. In that case, you fix the vitamin D and then recheck the numbers to see if they’ve normalized. But I have found a bunch of these edge cases in which it has been helpful to confer with an endocrinologist, especially before you send someone to a surgeon to take out their parathyroid gland.
This was a really fantastic conversation. If you want to hear the full podcast episode, click here.
Dr. Watto, Clinical Assistant Professor, Department of Medicine, Perelman School of Medicine at University of Pennsylvania; Internist, Department of Medicine, Hospital Medicine Section, Pennsylvania Hospital, Philadelphia, Pennsylvania, has disclosed no relevant financial relationships. Dr. Williams, Associate Professor of Clinical Medicine, Department of General Internal Medicine, Lewis Katz School of Medicine; Staff Physician, Department of General Internal Medicine, Temple Internal Medicine Associates, Philadelphia, Pennsylvania, served as a director, officer, partner, employee, adviser, consultant, or trustee for The Curbsiders, and has received income in an amount equal to or greater than $250 from The Curbsiders.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Matthew F. Watto, MD: Welcome back to The Curbsiders. I’m Dr Matthew Frank Watto, here with my great friend and America’s primary care physician, Dr. Paul Nelson Williams.
Paul, we’re going to talk about our primary hyperparathyroidism podcast with Dr. Lindsay Kuo. It’s a topic that I feel much more clear on now.
Now, Paul, in primary care, you see a lot of calcium that is just slightly high. Can we just blame that on thiazide diuretics?
Paul N. Williams, MD: It’s a place to start. As you’re starting to think about the possible etiologies, primary hyperparathyroidism and malignancy are the two that roll right off the tongue, but it is worth going back to the patient’s medication list and making sure you’re not missing something.
Thiazides famously cause hypercalcemia, but in some of the reading I did for this episode, they may just uncover it a little bit early. Patients who are on thiazides who become hypercalcemic seem to go on to develop primary hyperthyroidism anyway. So I don’t think you can solely blame the thiazide.
Another medication that can be causative is lithium. So a good place to look first after you’ve repeated the labs and confirmed hypercalcemia is the patient’s medication list.
Dr. Watto: We’ve talked before about the basic workup for hypercalcemia, and determining whether it’s PTH dependent or PTH independent. On the podcast, we talk more about the full workup, but I wanted to talk about the classic symptoms. Our expert made the point that we don’t see them as much anymore, although we do see kidney stones. People used to present very late in the disease because they weren’t having labs done routinely.
The classic symptoms include osteoporosis and bone tumors. People can get nephrocalcinosis and kidney stones. I hadn’t really thought of it this way because we’re used to diagnosing it early now. Do you feel the same?
Dr. Williams: As labs have started routinely reporting calcium levels, this is more and more often how it’s picked up. The other aspect is that as we are screening for and finding osteoporosis, part of the workup almost always involves getting a parathyroid hormone and a calcium level. We’re seeing these lab abnormalities before we’re seeing symptoms, which is good.
But it also makes things more diagnostically thorny.
Dr. Watto: Dr. Lindsay Kuo made the point that when she sees patients before and after surgery, she’s aware of these nonclassic symptoms — the stones, bones, groans, and the psychiatric overtones that can be anything from fatigue or irritability to dysphoria.
Some people have a generalized weakness that’s very nonspecific. Dr. Kuo said that sometimes these symptoms will disappear after surgery. The patients may just have gotten used to them, or they thought these symptoms were caused by something else, but after surgery they went away.
There are these nonclassic symptoms that are harder to pin down. I was surprised by that.
Dr. Williams: She mentioned polydipsia and polyuria, which have been reported in other studies. It seems like it can be anything. You have to take a good history, but none of those things in and of themselves is an indication for operating unless the patient has the classic renal or bone manifestations.
Dr. Watto: The other thing we talked about is a normal calcium level in a patient with primary hyperparathyroidism, or the finding of a PTH level in the normal range but with a high calcium level that is inappropriate. Can you talk a little bit about those two situations?
Dr. Williams: They’re hard to say but kind of easy to manage because you treat them the same way as someone who has elevated calcium and PTH levels.
The normocalcemic patient is something we might stumble across with osteoporosis screening. Initially the calcium level is elevated, so you repeat it and it’s normal but with an elevated PTH level. You’re like, shoot. Now what?
It turns out that most endocrine surgeons say that the indications for surgery for the classic form of primary hyperparathyroidism apply to these patients as well, and it probably helps with the bone outcomes, which is one of the things they follow most closely. If you have hypercalcemia, you should have a suppressed PTH level, the so-called normohormonal hyperparathyroidism, which is not normal at all. So even if the PTH is in the normal range, it’s still relatively elevated compared with what it should be. That situation is treated in the same way as the classic elevated PTH and elevated calcium levels.
Dr. Watto: If the calcium is abnormal and the PTH is not quite what you’d expect it to be, you can always ask your friendly neighborhood endocrinologist to help you figure out whether the patient really has one of these conditions. You have to make sure that they don’t have a simple secondary cause like a low vitamin D level. In that case, you fix the vitamin D and then recheck the numbers to see if they’ve normalized. But I have found a bunch of these edge cases in which it has been helpful to confer with an endocrinologist, especially before you send someone to a surgeon to take out their parathyroid gland.
This was a really fantastic conversation. If you want to hear the full podcast episode, click here.
Dr. Watto, Clinical Assistant Professor, Department of Medicine, Perelman School of Medicine at University of Pennsylvania; Internist, Department of Medicine, Hospital Medicine Section, Pennsylvania Hospital, Philadelphia, Pennsylvania, has disclosed no relevant financial relationships. Dr. Williams, Associate Professor of Clinical Medicine, Department of General Internal Medicine, Lewis Katz School of Medicine; Staff Physician, Department of General Internal Medicine, Temple Internal Medicine Associates, Philadelphia, Pennsylvania, served as a director, officer, partner, employee, adviser, consultant, or trustee for The Curbsiders, and has received income in an amount equal to or greater than $250 from The Curbsiders.
A version of this article first appeared on Medscape.com.