User login
Dupilumab Earns FDA Priority Review for Add-On COPD Care
The Food and Drug Administration (FDA) has accepted an application for Priority Review for dupilumab as an add-on therapy for adults with uncontrolled chronic obstructive pulmonary disease (COPD), according to a press release from manufacturer Regeneron.
If approved, dupilumab would be the only biologic option for COPD and the first new treatment option in approximately 10 years, according to the company.
Dupilumab works by blocking signaling by the interleukin (IL) 4 and IL-13 pathways, and Regeneron’s development program focuses on a population of COPD patients who also have type 2 inflammation.
The supplemental Biologics License Application was based on data from a pair of clinical trials in the company’s phase 3 COPD clinical research program.
In the studies, known as BOREAS and NOTUS, adults with uncontrolled COPD and type 2 inflammation who were current or former smokers were randomized to 300 mg of subcutaneous dupilumab or placebo once every 2 weeks. Type 2 inflammation was defined as blood eosinophil counts of at least 300 cells per microliter.
All patients received standard-of-care therapy. The primary endpoint of reduced annualized moderate or severe acute COPD exacerbations was 30% and 34% greater in the dupilumab groups in the two studies, respectively, compared with the placebo groups, and the significant differences in improvement persisted at 52 weeks.
Safety data were similar to previous studies of dupilumab for its approved indications. The most common adverse events seen in 5% or more of dupilumab patients compared with placebo patients across the two studies included back pain, COVID-19, diarrhea, headache, and nasopharyngitis.
Priority Review status is granted to applications for approval for therapies that may offer significant improvements, although the therapies are still in clinical development. The target action date for the FDA decision is June 27, 2024, and regulatory submissions for dupilumab for COPD are under consideration in China and Europe in addition to the United States, according to the company.
A version of this article appeared on Medscape.com.
The Food and Drug Administration (FDA) has accepted an application for Priority Review for dupilumab as an add-on therapy for adults with uncontrolled chronic obstructive pulmonary disease (COPD), according to a press release from manufacturer Regeneron.
If approved, dupilumab would be the only biologic option for COPD and the first new treatment option in approximately 10 years, according to the company.
Dupilumab works by blocking signaling by the interleukin (IL) 4 and IL-13 pathways, and Regeneron’s development program focuses on a population of COPD patients who also have type 2 inflammation.
The supplemental Biologics License Application was based on data from a pair of clinical trials in the company’s phase 3 COPD clinical research program.
In the studies, known as BOREAS and NOTUS, adults with uncontrolled COPD and type 2 inflammation who were current or former smokers were randomized to 300 mg of subcutaneous dupilumab or placebo once every 2 weeks. Type 2 inflammation was defined as blood eosinophil counts of at least 300 cells per microliter.
All patients received standard-of-care therapy. The primary endpoint of reduced annualized moderate or severe acute COPD exacerbations was 30% and 34% greater in the dupilumab groups in the two studies, respectively, compared with the placebo groups, and the significant differences in improvement persisted at 52 weeks.
Safety data were similar to previous studies of dupilumab for its approved indications. The most common adverse events seen in 5% or more of dupilumab patients compared with placebo patients across the two studies included back pain, COVID-19, diarrhea, headache, and nasopharyngitis.
Priority Review status is granted to applications for approval for therapies that may offer significant improvements, although the therapies are still in clinical development. The target action date for the FDA decision is June 27, 2024, and regulatory submissions for dupilumab for COPD are under consideration in China and Europe in addition to the United States, according to the company.
A version of this article appeared on Medscape.com.
The Food and Drug Administration (FDA) has accepted an application for Priority Review for dupilumab as an add-on therapy for adults with uncontrolled chronic obstructive pulmonary disease (COPD), according to a press release from manufacturer Regeneron.
If approved, dupilumab would be the only biologic option for COPD and the first new treatment option in approximately 10 years, according to the company.
Dupilumab works by blocking signaling by the interleukin (IL) 4 and IL-13 pathways, and Regeneron’s development program focuses on a population of COPD patients who also have type 2 inflammation.
The supplemental Biologics License Application was based on data from a pair of clinical trials in the company’s phase 3 COPD clinical research program.
In the studies, known as BOREAS and NOTUS, adults with uncontrolled COPD and type 2 inflammation who were current or former smokers were randomized to 300 mg of subcutaneous dupilumab or placebo once every 2 weeks. Type 2 inflammation was defined as blood eosinophil counts of at least 300 cells per microliter.
All patients received standard-of-care therapy. The primary endpoint of reduced annualized moderate or severe acute COPD exacerbations was 30% and 34% greater in the dupilumab groups in the two studies, respectively, compared with the placebo groups, and the significant differences in improvement persisted at 52 weeks.
Safety data were similar to previous studies of dupilumab for its approved indications. The most common adverse events seen in 5% or more of dupilumab patients compared with placebo patients across the two studies included back pain, COVID-19, diarrhea, headache, and nasopharyngitis.
Priority Review status is granted to applications for approval for therapies that may offer significant improvements, although the therapies are still in clinical development. The target action date for the FDA decision is June 27, 2024, and regulatory submissions for dupilumab for COPD are under consideration in China and Europe in addition to the United States, according to the company.
A version of this article appeared on Medscape.com.
FDA Clears Medical Grade Over-the-Counter Pulse Oximeter
The MightySat Medical, an over-the-counter medical fingertip pulse oximeter, has received clearance from the US Food and Drug Administration (FDA) for use without a prescription, according to a press release from manufacturer Masimo.
The device is the first medical fingertip pulse oximeter available directly to consumers without a prescription that includes the same technology used by many hospitals, according to the company.
According to the FDA, home pulse oximeters are currently generally of two classes: hospital-grade prescription devices which have been vetted for accuracy through clinical trials, and over-the-counter devices which are sold direct to consumers but often estimate oxygen saturation. FDA communication on pulse oximeter accuracy states "OTC oximeters that are sold as either general wellness or sporting/aviation products are not intended for medical purposes, so they do not undergo FDA review."
Pulse oximeter use is important for patients diagnosed with breathing problems or lung diseases such as asthma, chronic obstructive pulmonary disease, pulmonary fibrosis, lung cancer, flu, pneumonia, or COVID-19 to collect accurate data on arterial blood oxygen saturation that they can share with their healthcare providers, according to the company. Patients with cardiac conditions, including pulmonary hypertension and heart failure may also benefit from pulse oximeter monitoring.
However, challenges of pulse oximeter use include measuring accuracy when patients are moving, measuring patients with poor circulation, and measuring patients with cool, thick, or darker skin. The MightySat Medical is designed to provide reliable measures of oxygen saturation and pulse rate across all patient groups, the manufacturers wrote in the press release.
Asked for additional comment, Diego J. Maselli, MD, FCCP, Professor and Chief in the division of Pulmonary Diseases and Critical Care at UT Health at San Antonio, noted, "Over the past decades, there has been an increased interest in home monitoring of medical conditions, particulrly with the development of more portable and accessible technology."
"This was heightended by the COVID-19 pandemic where telemedicine was frequently required as a means of delivering care," Dr. Maselli continued. "One of the important characteristics to monitor was the oxgen saturation in patients that had an active COVID-19 infection as it would dictate management and was part of the protocol for monitoring the clinical course of infection. Because of this need, many companies developed portable pulse oximeters for home use. This resulted in widespread use of pulse oximeters at home and other places outside clinic or hospital."
Other over-the-counter pulse oximeters that are not cleared by the FDA may create confusion among patients about the accuracy of their measurements, according to the company.
Dr. Maselli also commented that pulse oximeters' value can vary. "Unfortunately, these devices vary in quality and reliability and patients may not be fully aware of this. Most recently, the FDA approved a hospital-grade pulse oximeter that requires no prescription. This device may provide a more accurate reading in a wide range of clinical situations outside the healthcare setting. Patients should be aware that there are different grades of pulse oximeter before selecting one for home use. In addition, patients should work closely with their providers to better select the monitoring modaility that best fits their clinical situation," he said.
MightySat Medical is indicated for individuals aged 18 years and older who are well or poorly perfused under no motion conditions and is not intended as a diagnostic or screening tool for lung disease, according to the release. Treatment decisions based on data from the device should be made only in consultation with a healthcare provider, the company said. Dr. Maselli serves as a member of the CHEST Physician editorial board.
The FDA’s website offers further guidance related to at-home pulse oximeter use, with recommendations and limitations, as well as information on initiatives to ensure accurate and equitable pulse oximetry for all patients.
A version of this article appeared on Medscape.com.
The MightySat Medical, an over-the-counter medical fingertip pulse oximeter, has received clearance from the US Food and Drug Administration (FDA) for use without a prescription, according to a press release from manufacturer Masimo.
The device is the first medical fingertip pulse oximeter available directly to consumers without a prescription that includes the same technology used by many hospitals, according to the company.
According to the FDA, home pulse oximeters are currently generally of two classes: hospital-grade prescription devices which have been vetted for accuracy through clinical trials, and over-the-counter devices which are sold direct to consumers but often estimate oxygen saturation. FDA communication on pulse oximeter accuracy states "OTC oximeters that are sold as either general wellness or sporting/aviation products are not intended for medical purposes, so they do not undergo FDA review."
Pulse oximeter use is important for patients diagnosed with breathing problems or lung diseases such as asthma, chronic obstructive pulmonary disease, pulmonary fibrosis, lung cancer, flu, pneumonia, or COVID-19 to collect accurate data on arterial blood oxygen saturation that they can share with their healthcare providers, according to the company. Patients with cardiac conditions, including pulmonary hypertension and heart failure may also benefit from pulse oximeter monitoring.
However, challenges of pulse oximeter use include measuring accuracy when patients are moving, measuring patients with poor circulation, and measuring patients with cool, thick, or darker skin. The MightySat Medical is designed to provide reliable measures of oxygen saturation and pulse rate across all patient groups, the manufacturers wrote in the press release.
Asked for additional comment, Diego J. Maselli, MD, FCCP, Professor and Chief in the division of Pulmonary Diseases and Critical Care at UT Health at San Antonio, noted, "Over the past decades, there has been an increased interest in home monitoring of medical conditions, particulrly with the development of more portable and accessible technology."
"This was heightended by the COVID-19 pandemic where telemedicine was frequently required as a means of delivering care," Dr. Maselli continued. "One of the important characteristics to monitor was the oxgen saturation in patients that had an active COVID-19 infection as it would dictate management and was part of the protocol for monitoring the clinical course of infection. Because of this need, many companies developed portable pulse oximeters for home use. This resulted in widespread use of pulse oximeters at home and other places outside clinic or hospital."
Other over-the-counter pulse oximeters that are not cleared by the FDA may create confusion among patients about the accuracy of their measurements, according to the company.
Dr. Maselli also commented that pulse oximeters' value can vary. "Unfortunately, these devices vary in quality and reliability and patients may not be fully aware of this. Most recently, the FDA approved a hospital-grade pulse oximeter that requires no prescription. This device may provide a more accurate reading in a wide range of clinical situations outside the healthcare setting. Patients should be aware that there are different grades of pulse oximeter before selecting one for home use. In addition, patients should work closely with their providers to better select the monitoring modaility that best fits their clinical situation," he said.
MightySat Medical is indicated for individuals aged 18 years and older who are well or poorly perfused under no motion conditions and is not intended as a diagnostic or screening tool for lung disease, according to the release. Treatment decisions based on data from the device should be made only in consultation with a healthcare provider, the company said. Dr. Maselli serves as a member of the CHEST Physician editorial board.
The FDA’s website offers further guidance related to at-home pulse oximeter use, with recommendations and limitations, as well as information on initiatives to ensure accurate and equitable pulse oximetry for all patients.
A version of this article appeared on Medscape.com.
The MightySat Medical, an over-the-counter medical fingertip pulse oximeter, has received clearance from the US Food and Drug Administration (FDA) for use without a prescription, according to a press release from manufacturer Masimo.
The device is the first medical fingertip pulse oximeter available directly to consumers without a prescription that includes the same technology used by many hospitals, according to the company.
According to the FDA, home pulse oximeters are currently generally of two classes: hospital-grade prescription devices which have been vetted for accuracy through clinical trials, and over-the-counter devices which are sold direct to consumers but often estimate oxygen saturation. FDA communication on pulse oximeter accuracy states "OTC oximeters that are sold as either general wellness or sporting/aviation products are not intended for medical purposes, so they do not undergo FDA review."
Pulse oximeter use is important for patients diagnosed with breathing problems or lung diseases such as asthma, chronic obstructive pulmonary disease, pulmonary fibrosis, lung cancer, flu, pneumonia, or COVID-19 to collect accurate data on arterial blood oxygen saturation that they can share with their healthcare providers, according to the company. Patients with cardiac conditions, including pulmonary hypertension and heart failure may also benefit from pulse oximeter monitoring.
However, challenges of pulse oximeter use include measuring accuracy when patients are moving, measuring patients with poor circulation, and measuring patients with cool, thick, or darker skin. The MightySat Medical is designed to provide reliable measures of oxygen saturation and pulse rate across all patient groups, the manufacturers wrote in the press release.
Asked for additional comment, Diego J. Maselli, MD, FCCP, Professor and Chief in the division of Pulmonary Diseases and Critical Care at UT Health at San Antonio, noted, "Over the past decades, there has been an increased interest in home monitoring of medical conditions, particulrly with the development of more portable and accessible technology."
"This was heightended by the COVID-19 pandemic where telemedicine was frequently required as a means of delivering care," Dr. Maselli continued. "One of the important characteristics to monitor was the oxgen saturation in patients that had an active COVID-19 infection as it would dictate management and was part of the protocol for monitoring the clinical course of infection. Because of this need, many companies developed portable pulse oximeters for home use. This resulted in widespread use of pulse oximeters at home and other places outside clinic or hospital."
Other over-the-counter pulse oximeters that are not cleared by the FDA may create confusion among patients about the accuracy of their measurements, according to the company.
Dr. Maselli also commented that pulse oximeters' value can vary. "Unfortunately, these devices vary in quality and reliability and patients may not be fully aware of this. Most recently, the FDA approved a hospital-grade pulse oximeter that requires no prescription. This device may provide a more accurate reading in a wide range of clinical situations outside the healthcare setting. Patients should be aware that there are different grades of pulse oximeter before selecting one for home use. In addition, patients should work closely with their providers to better select the monitoring modaility that best fits their clinical situation," he said.
MightySat Medical is indicated for individuals aged 18 years and older who are well or poorly perfused under no motion conditions and is not intended as a diagnostic or screening tool for lung disease, according to the release. Treatment decisions based on data from the device should be made only in consultation with a healthcare provider, the company said. Dr. Maselli serves as a member of the CHEST Physician editorial board.
The FDA’s website offers further guidance related to at-home pulse oximeter use, with recommendations and limitations, as well as information on initiatives to ensure accurate and equitable pulse oximetry for all patients.
A version of this article appeared on Medscape.com.
Female Reproductive Factors Could Predict COPD Risk
TOPLINE:
Several female reproductive factors across the life cycle were significantly associated with increased COPD risk, including age at menarche, number of children, infertility, pregnancy outcomes, and age at menopause.
METHODOLOGY:
- The researchers reviewed data from women in the International Collaboration for a Life Course Approach to Reproductive Health and Chronic Disease Events (InterLACE) consortium, which includes 27 observational studies involving more than 850,000 women in 12 countries.
- The current study included 283,070 women, 3.8% of whom developed COPD over a median of 11 years.
- The researchers examined the association between COPD and age at menarche, number of children, infertility, miscarriage, stillbirth, and age at natural menopause.
TAKEAWAY:
- Higher risk of COPD was significantly associated with menarche at age 11 years or younger (hazard ratio [HR], 1.17), and at 16 years and older (HR, 1.24), as well as having three or more children.
- Higher risk of COPD was significantly associated with a history of infertility, and with miscarriage, or stillbirth compared with no miscarriages or stillbirths; the risk increased with the number of miscarriages or stillbirths (HR, 1.36 for ≥ 3 miscarriages and 1.67 for ≥ 2 stillbirths).
- COPD risk was significantly increased with earlier age at the time of natural menopause (HR, 1.69 for those aged < 40 years and 1.42 for those aged 40-44 years compared with those aged 50-51 years).
IN PRACTICE:
“Further research is needed to understand the mechanisms linking multiple female reproductive histories and COPD,” which could include autoimmune components and social/environmental factors, the researchers wrote.
SOURCE:
The lead author on the study was Chen Liang, MD, of the University of Queensland, Australia. The study was published online in BMJ Thorax).
LIMITATIONS:
Study limitations included volunteer bias, underreporting of COPD, potential confounders such as childhood respiratory infections and smoking history, and the inability to assess the effects of medications including contraceptives and hormone replacement therapy on COPD.
DISCLOSURES:
The InterLACE project is supported by the Australian National Health and Medical Research Council and Centres of Research Excellence. Corresponding author Gita D. Mishra disclosed support from the Australian National Health and Medical Research Council Leadership Fellowship.
A version of this article appeared on Medscape.com.
TOPLINE:
Several female reproductive factors across the life cycle were significantly associated with increased COPD risk, including age at menarche, number of children, infertility, pregnancy outcomes, and age at menopause.
METHODOLOGY:
- The researchers reviewed data from women in the International Collaboration for a Life Course Approach to Reproductive Health and Chronic Disease Events (InterLACE) consortium, which includes 27 observational studies involving more than 850,000 women in 12 countries.
- The current study included 283,070 women, 3.8% of whom developed COPD over a median of 11 years.
- The researchers examined the association between COPD and age at menarche, number of children, infertility, miscarriage, stillbirth, and age at natural menopause.
TAKEAWAY:
- Higher risk of COPD was significantly associated with menarche at age 11 years or younger (hazard ratio [HR], 1.17), and at 16 years and older (HR, 1.24), as well as having three or more children.
- Higher risk of COPD was significantly associated with a history of infertility, and with miscarriage, or stillbirth compared with no miscarriages or stillbirths; the risk increased with the number of miscarriages or stillbirths (HR, 1.36 for ≥ 3 miscarriages and 1.67 for ≥ 2 stillbirths).
- COPD risk was significantly increased with earlier age at the time of natural menopause (HR, 1.69 for those aged < 40 years and 1.42 for those aged 40-44 years compared with those aged 50-51 years).
IN PRACTICE:
“Further research is needed to understand the mechanisms linking multiple female reproductive histories and COPD,” which could include autoimmune components and social/environmental factors, the researchers wrote.
SOURCE:
The lead author on the study was Chen Liang, MD, of the University of Queensland, Australia. The study was published online in BMJ Thorax).
LIMITATIONS:
Study limitations included volunteer bias, underreporting of COPD, potential confounders such as childhood respiratory infections and smoking history, and the inability to assess the effects of medications including contraceptives and hormone replacement therapy on COPD.
DISCLOSURES:
The InterLACE project is supported by the Australian National Health and Medical Research Council and Centres of Research Excellence. Corresponding author Gita D. Mishra disclosed support from the Australian National Health and Medical Research Council Leadership Fellowship.
A version of this article appeared on Medscape.com.
TOPLINE:
Several female reproductive factors across the life cycle were significantly associated with increased COPD risk, including age at menarche, number of children, infertility, pregnancy outcomes, and age at menopause.
METHODOLOGY:
- The researchers reviewed data from women in the International Collaboration for a Life Course Approach to Reproductive Health and Chronic Disease Events (InterLACE) consortium, which includes 27 observational studies involving more than 850,000 women in 12 countries.
- The current study included 283,070 women, 3.8% of whom developed COPD over a median of 11 years.
- The researchers examined the association between COPD and age at menarche, number of children, infertility, miscarriage, stillbirth, and age at natural menopause.
TAKEAWAY:
- Higher risk of COPD was significantly associated with menarche at age 11 years or younger (hazard ratio [HR], 1.17), and at 16 years and older (HR, 1.24), as well as having three or more children.
- Higher risk of COPD was significantly associated with a history of infertility, and with miscarriage, or stillbirth compared with no miscarriages or stillbirths; the risk increased with the number of miscarriages or stillbirths (HR, 1.36 for ≥ 3 miscarriages and 1.67 for ≥ 2 stillbirths).
- COPD risk was significantly increased with earlier age at the time of natural menopause (HR, 1.69 for those aged < 40 years and 1.42 for those aged 40-44 years compared with those aged 50-51 years).
IN PRACTICE:
“Further research is needed to understand the mechanisms linking multiple female reproductive histories and COPD,” which could include autoimmune components and social/environmental factors, the researchers wrote.
SOURCE:
The lead author on the study was Chen Liang, MD, of the University of Queensland, Australia. The study was published online in BMJ Thorax).
LIMITATIONS:
Study limitations included volunteer bias, underreporting of COPD, potential confounders such as childhood respiratory infections and smoking history, and the inability to assess the effects of medications including contraceptives and hormone replacement therapy on COPD.
DISCLOSURES:
The InterLACE project is supported by the Australian National Health and Medical Research Council and Centres of Research Excellence. Corresponding author Gita D. Mishra disclosed support from the Australian National Health and Medical Research Council Leadership Fellowship.
A version of this article appeared on Medscape.com.
Postinfectious Cough: Are Treatments Ever Warranted?
Lingering postinfectious cough has been a concern across Canada this winter. , according to an overview published on February 12 in the Canadian Medical Association Journal
“It’s something a lot of patients are worried about: That lingering cough after a common cold or flu,” lead author Kevin Liang, MD, of the Department of Family Medicine at The University of British Columbia in Vancouver, British Columbia, Canada, told this news organization. He added that some studies show that as much as a quarter of adult patients have this complaint.
Dr. Liang and his colleagues emphasized that the diagnosis of postinfectious cough is one of exclusion. It relies on the absence of concerning physical examination findings and other “subacute cough mimics” such as asthma, chronic obstructive pulmonary disease (COPD), gastroesophageal reflux disease, or use of angiotensin-converting enzyme inhibitors.
“Pertussis should be considered in patients with a paroxysmal cough, post-tussive vomiting, and inspiratory whoop,” they added. Coughs that persist beyond 8 weeks warrant further workup such as a pulmonary function test to rule out asthma or COPD. Coughs accompanied by hemoptysis, systemic symptoms, dysphagia, excessive dyspnea, or hoarseness also warrant further workup, they added. And patients with a history of smoking or recurrent pneumonia should be followed more closely.
In the absence of red flags, Dr. Liang and coauthors advised that there is no evidence supporting pharmacologic treatment, “which is associated with harms,” such as medication adverse effects, cost, strain on the medical supply chain, and the fact that pressurized metered-dose inhalers emit powerful greenhouse gases. “A lot of patients come in looking for solutions, but really, all the evidence says the over-the-counter cough syrup just doesn’t work. Or I see clinicians prescribing inhalers or different medication that can cost hundreds of dollars, and their efficacy, at least from the literature, shows that there’s really no improvement. Time and patience are the two keys to solving this,” Dr. Liang told this news organization.
Moreover, there is a distinct absence of guidelines on this topic. The College of Family Physicians of Canada’s recent literature review cited limited data supporting a trial of inhaled corticosteroids, a bronchodilator such as ipratropium-salbutamol, or an intranasal steroid if postnasal drip is suspected. However, “there’s a high risk of bias in the study they cite from using the short-acting bronchodilators, and what it ultimately says is that in most cases, this is self-resolving by around the 20-day mark,” said Dr. Liang. “Our advice is just to err on the side of caution and just provide that information piece to the patient.”
‘Significant Nuance’
Imran Satia, MD, assistant professor of respirology at McMaster University in Hamilton, Ontario, Canada, agreed that “most people who get a viral or bacterial upper or lower respiratory tract infection will get better with time, and there is very little evidence that giving steroids, antibiotics, or cough suppressants is better than waiting it out.” There is “significant nuance” in how to manage this situation, however.
“In some patients with underlying lung disease like asthma or COPD, increasing the frequency of regular inhaled steroids, bronchodilators, oral steroids, antibiotics, and chest imaging with breathing tests may be clinically warranted, and many physicians will do this,” he told this news organization. “In some patients with refractory chronic cough, there is no underlying identifiable disease, despite completing the necessary investigations. Or coughing persists despite trials of treatment for lung diseases, nasal diseases, and stomach reflux disease. This is commonly described as cough hypersensitivity syndrome, for which therapies targeting the neuronal pathways that control coughing are needed.”
Physicians should occasionally consider trying a temporary course of a short-acting bronchodilator inhaler, said Nicholas Vozoris, MD, assistant professor and clinician investigator in respirology at the University of Toronto, Toronto, Ontario, Canada. “I think that would be a reasonable first step in a case of really bad postinfectious cough,” he told this news organization. “But in general, drug treatments are not indicated.”
Environmental Concerns
Yet some things should raise clinicians’ suspicion of more complex issues.
“A pattern of recurrent colds or bronchitis with protracted coughing afterward raises strong suspicion for asthma, which can present as repeated, prolonged respiratory exacerbations,” he said. “Unless asthma is treated with appropriate inhaler therapy on a regular basis, it will unlikely come under control.”
Dr. Vozoris added that the environmental concerns over the use of metered dose inhalers (MDIs) are minimal compared with the other sources of pollution and the risks for undertreatment. “The authors are overplaying the environmental impact of MDI, in my opinion,” he said. “Physicians already have to deal with the challenging issue of suboptimal patient adherence to inhalers, and I fear that such comments may further drive that up. Furthermore, there is also an environmental footprint with not using inhalers, as patients can then experience suboptimally controlled lung disease as a result — and then present to the ER and get admitted to hospital for exacerbations of disease, where more resources and medications are used up.”
“In addition, in patients who are immunocompromised, protracted coughing after what was thought to be a cold may be associated with an “atypical” respiratory infection, such as tuberculosis, that will require special medical treatment,” Dr. Vozoris concluded.
No funding for the review of postinfectious cough was reported. Dr. Liang and Dr. Vozoris disclosed no competing interests. Dr. Satia reported receiving funding from the ERS Respire 3 Fellowship Award, BMA James Trust Award, North-West Lung Centre Charity (Manchester), NIHR CRF Manchester, Merck MSD, AstraZeneca, and GSK. Dr. Satia also has received consulting fees from Merck MSD, Genentech, and Respiplus; as well as speaker fees from AstraZeneca, GSK, Merck MSD, Sanofi-Regeneron. Satia has served on the following task force committees: Chronic Cough (ERS), Asthma Diagnosis and Management (ERS), NEUROCOUGH (ERS CRC), and the CTS Chronic Cough working group.
A version of this article appeared on Medscape.com.
Lingering postinfectious cough has been a concern across Canada this winter. , according to an overview published on February 12 in the Canadian Medical Association Journal
“It’s something a lot of patients are worried about: That lingering cough after a common cold or flu,” lead author Kevin Liang, MD, of the Department of Family Medicine at The University of British Columbia in Vancouver, British Columbia, Canada, told this news organization. He added that some studies show that as much as a quarter of adult patients have this complaint.
Dr. Liang and his colleagues emphasized that the diagnosis of postinfectious cough is one of exclusion. It relies on the absence of concerning physical examination findings and other “subacute cough mimics” such as asthma, chronic obstructive pulmonary disease (COPD), gastroesophageal reflux disease, or use of angiotensin-converting enzyme inhibitors.
“Pertussis should be considered in patients with a paroxysmal cough, post-tussive vomiting, and inspiratory whoop,” they added. Coughs that persist beyond 8 weeks warrant further workup such as a pulmonary function test to rule out asthma or COPD. Coughs accompanied by hemoptysis, systemic symptoms, dysphagia, excessive dyspnea, or hoarseness also warrant further workup, they added. And patients with a history of smoking or recurrent pneumonia should be followed more closely.
In the absence of red flags, Dr. Liang and coauthors advised that there is no evidence supporting pharmacologic treatment, “which is associated with harms,” such as medication adverse effects, cost, strain on the medical supply chain, and the fact that pressurized metered-dose inhalers emit powerful greenhouse gases. “A lot of patients come in looking for solutions, but really, all the evidence says the over-the-counter cough syrup just doesn’t work. Or I see clinicians prescribing inhalers or different medication that can cost hundreds of dollars, and their efficacy, at least from the literature, shows that there’s really no improvement. Time and patience are the two keys to solving this,” Dr. Liang told this news organization.
Moreover, there is a distinct absence of guidelines on this topic. The College of Family Physicians of Canada’s recent literature review cited limited data supporting a trial of inhaled corticosteroids, a bronchodilator such as ipratropium-salbutamol, or an intranasal steroid if postnasal drip is suspected. However, “there’s a high risk of bias in the study they cite from using the short-acting bronchodilators, and what it ultimately says is that in most cases, this is self-resolving by around the 20-day mark,” said Dr. Liang. “Our advice is just to err on the side of caution and just provide that information piece to the patient.”
‘Significant Nuance’
Imran Satia, MD, assistant professor of respirology at McMaster University in Hamilton, Ontario, Canada, agreed that “most people who get a viral or bacterial upper or lower respiratory tract infection will get better with time, and there is very little evidence that giving steroids, antibiotics, or cough suppressants is better than waiting it out.” There is “significant nuance” in how to manage this situation, however.
“In some patients with underlying lung disease like asthma or COPD, increasing the frequency of regular inhaled steroids, bronchodilators, oral steroids, antibiotics, and chest imaging with breathing tests may be clinically warranted, and many physicians will do this,” he told this news organization. “In some patients with refractory chronic cough, there is no underlying identifiable disease, despite completing the necessary investigations. Or coughing persists despite trials of treatment for lung diseases, nasal diseases, and stomach reflux disease. This is commonly described as cough hypersensitivity syndrome, for which therapies targeting the neuronal pathways that control coughing are needed.”
Physicians should occasionally consider trying a temporary course of a short-acting bronchodilator inhaler, said Nicholas Vozoris, MD, assistant professor and clinician investigator in respirology at the University of Toronto, Toronto, Ontario, Canada. “I think that would be a reasonable first step in a case of really bad postinfectious cough,” he told this news organization. “But in general, drug treatments are not indicated.”
Environmental Concerns
Yet some things should raise clinicians’ suspicion of more complex issues.
“A pattern of recurrent colds or bronchitis with protracted coughing afterward raises strong suspicion for asthma, which can present as repeated, prolonged respiratory exacerbations,” he said. “Unless asthma is treated with appropriate inhaler therapy on a regular basis, it will unlikely come under control.”
Dr. Vozoris added that the environmental concerns over the use of metered dose inhalers (MDIs) are minimal compared with the other sources of pollution and the risks for undertreatment. “The authors are overplaying the environmental impact of MDI, in my opinion,” he said. “Physicians already have to deal with the challenging issue of suboptimal patient adherence to inhalers, and I fear that such comments may further drive that up. Furthermore, there is also an environmental footprint with not using inhalers, as patients can then experience suboptimally controlled lung disease as a result — and then present to the ER and get admitted to hospital for exacerbations of disease, where more resources and medications are used up.”
“In addition, in patients who are immunocompromised, protracted coughing after what was thought to be a cold may be associated with an “atypical” respiratory infection, such as tuberculosis, that will require special medical treatment,” Dr. Vozoris concluded.
No funding for the review of postinfectious cough was reported. Dr. Liang and Dr. Vozoris disclosed no competing interests. Dr. Satia reported receiving funding from the ERS Respire 3 Fellowship Award, BMA James Trust Award, North-West Lung Centre Charity (Manchester), NIHR CRF Manchester, Merck MSD, AstraZeneca, and GSK. Dr. Satia also has received consulting fees from Merck MSD, Genentech, and Respiplus; as well as speaker fees from AstraZeneca, GSK, Merck MSD, Sanofi-Regeneron. Satia has served on the following task force committees: Chronic Cough (ERS), Asthma Diagnosis and Management (ERS), NEUROCOUGH (ERS CRC), and the CTS Chronic Cough working group.
A version of this article appeared on Medscape.com.
Lingering postinfectious cough has been a concern across Canada this winter. , according to an overview published on February 12 in the Canadian Medical Association Journal
“It’s something a lot of patients are worried about: That lingering cough after a common cold or flu,” lead author Kevin Liang, MD, of the Department of Family Medicine at The University of British Columbia in Vancouver, British Columbia, Canada, told this news organization. He added that some studies show that as much as a quarter of adult patients have this complaint.
Dr. Liang and his colleagues emphasized that the diagnosis of postinfectious cough is one of exclusion. It relies on the absence of concerning physical examination findings and other “subacute cough mimics” such as asthma, chronic obstructive pulmonary disease (COPD), gastroesophageal reflux disease, or use of angiotensin-converting enzyme inhibitors.
“Pertussis should be considered in patients with a paroxysmal cough, post-tussive vomiting, and inspiratory whoop,” they added. Coughs that persist beyond 8 weeks warrant further workup such as a pulmonary function test to rule out asthma or COPD. Coughs accompanied by hemoptysis, systemic symptoms, dysphagia, excessive dyspnea, or hoarseness also warrant further workup, they added. And patients with a history of smoking or recurrent pneumonia should be followed more closely.
In the absence of red flags, Dr. Liang and coauthors advised that there is no evidence supporting pharmacologic treatment, “which is associated with harms,” such as medication adverse effects, cost, strain on the medical supply chain, and the fact that pressurized metered-dose inhalers emit powerful greenhouse gases. “A lot of patients come in looking for solutions, but really, all the evidence says the over-the-counter cough syrup just doesn’t work. Or I see clinicians prescribing inhalers or different medication that can cost hundreds of dollars, and their efficacy, at least from the literature, shows that there’s really no improvement. Time and patience are the two keys to solving this,” Dr. Liang told this news organization.
Moreover, there is a distinct absence of guidelines on this topic. The College of Family Physicians of Canada’s recent literature review cited limited data supporting a trial of inhaled corticosteroids, a bronchodilator such as ipratropium-salbutamol, or an intranasal steroid if postnasal drip is suspected. However, “there’s a high risk of bias in the study they cite from using the short-acting bronchodilators, and what it ultimately says is that in most cases, this is self-resolving by around the 20-day mark,” said Dr. Liang. “Our advice is just to err on the side of caution and just provide that information piece to the patient.”
‘Significant Nuance’
Imran Satia, MD, assistant professor of respirology at McMaster University in Hamilton, Ontario, Canada, agreed that “most people who get a viral or bacterial upper or lower respiratory tract infection will get better with time, and there is very little evidence that giving steroids, antibiotics, or cough suppressants is better than waiting it out.” There is “significant nuance” in how to manage this situation, however.
“In some patients with underlying lung disease like asthma or COPD, increasing the frequency of regular inhaled steroids, bronchodilators, oral steroids, antibiotics, and chest imaging with breathing tests may be clinically warranted, and many physicians will do this,” he told this news organization. “In some patients with refractory chronic cough, there is no underlying identifiable disease, despite completing the necessary investigations. Or coughing persists despite trials of treatment for lung diseases, nasal diseases, and stomach reflux disease. This is commonly described as cough hypersensitivity syndrome, for which therapies targeting the neuronal pathways that control coughing are needed.”
Physicians should occasionally consider trying a temporary course of a short-acting bronchodilator inhaler, said Nicholas Vozoris, MD, assistant professor and clinician investigator in respirology at the University of Toronto, Toronto, Ontario, Canada. “I think that would be a reasonable first step in a case of really bad postinfectious cough,” he told this news organization. “But in general, drug treatments are not indicated.”
Environmental Concerns
Yet some things should raise clinicians’ suspicion of more complex issues.
“A pattern of recurrent colds or bronchitis with protracted coughing afterward raises strong suspicion for asthma, which can present as repeated, prolonged respiratory exacerbations,” he said. “Unless asthma is treated with appropriate inhaler therapy on a regular basis, it will unlikely come under control.”
Dr. Vozoris added that the environmental concerns over the use of metered dose inhalers (MDIs) are minimal compared with the other sources of pollution and the risks for undertreatment. “The authors are overplaying the environmental impact of MDI, in my opinion,” he said. “Physicians already have to deal with the challenging issue of suboptimal patient adherence to inhalers, and I fear that such comments may further drive that up. Furthermore, there is also an environmental footprint with not using inhalers, as patients can then experience suboptimally controlled lung disease as a result — and then present to the ER and get admitted to hospital for exacerbations of disease, where more resources and medications are used up.”
“In addition, in patients who are immunocompromised, protracted coughing after what was thought to be a cold may be associated with an “atypical” respiratory infection, such as tuberculosis, that will require special medical treatment,” Dr. Vozoris concluded.
No funding for the review of postinfectious cough was reported. Dr. Liang and Dr. Vozoris disclosed no competing interests. Dr. Satia reported receiving funding from the ERS Respire 3 Fellowship Award, BMA James Trust Award, North-West Lung Centre Charity (Manchester), NIHR CRF Manchester, Merck MSD, AstraZeneca, and GSK. Dr. Satia also has received consulting fees from Merck MSD, Genentech, and Respiplus; as well as speaker fees from AstraZeneca, GSK, Merck MSD, Sanofi-Regeneron. Satia has served on the following task force committees: Chronic Cough (ERS), Asthma Diagnosis and Management (ERS), NEUROCOUGH (ERS CRC), and the CTS Chronic Cough working group.
A version of this article appeared on Medscape.com.
FROM THE CANADIAN MEDICAL ASSOCIATION JOURNAL
Obesity and lung disease in the era of GLP-1 agonists
Now is the time for pulmonary clinicians to become comfortable counseling patients about and treating obesity. By 2030, half of the US population will have obesity, a quarter of which will be severe (Ward et al. NEJM. 2019;2440-2450).
Many pulmonary diseases, including asthma, COPD, and interstitial pulmonary fibrosis (IPF) are linked to and made worse by obesity with increased exacerbations, patient-reported decreased quality of life, and resistance to therapy (Ray et al. Am Rev Respir Dis. 1983;501-6). Asthma is even recognized as an obesity-related comorbid condition by both the American Society Metabolic and Bariatric Surgery (ASMBS) and the American Association of Clinical Endocrinologists (AACE) when considering indications for early or more aggressive treatment of obesity (Eisenberg et al. Obesity Surg. 2023;3-14) (Garvey et al. Endocr Pract. 2016;1-203).
Obesity has multiple negative effects on pulmonary function due to the physical forces of extra weight on the lungs and inflammation related to adipose tissue (see Figure 1) (Zerah et al. Chest. 1993;1470-6).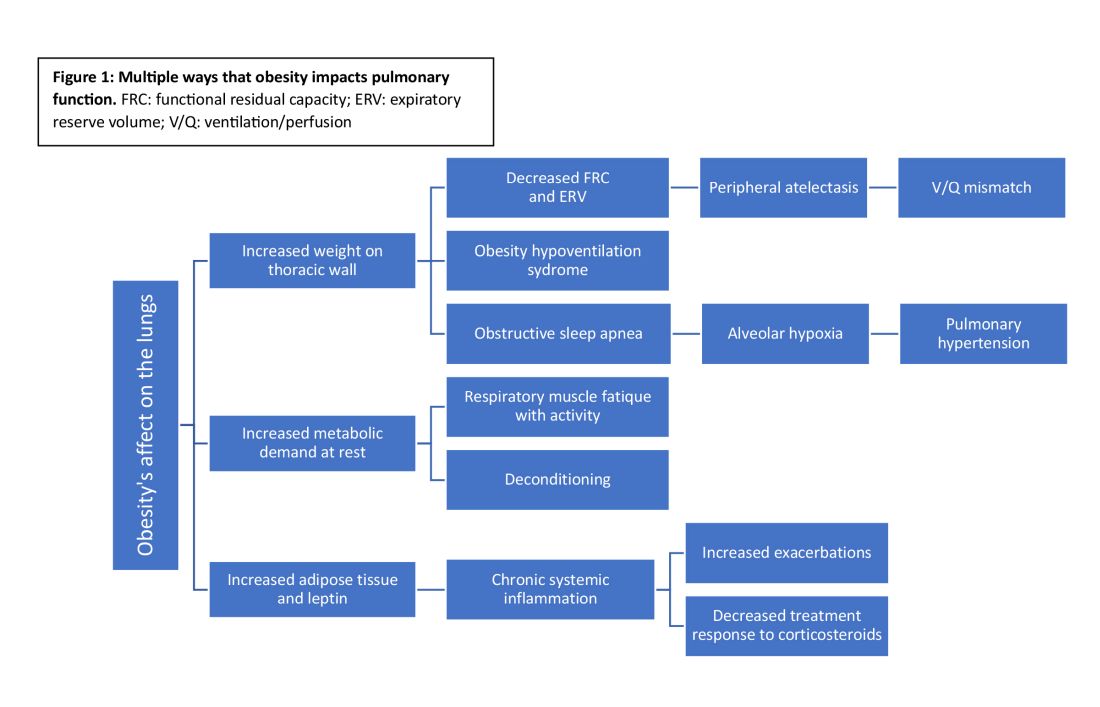
Obesity-related respiratory changes include reduced lung compliance, functional residual capacity (FRC), and expiratory reserve volume (ERV). These changes lead to peripheral atelectasis and V/Q mismatch and increased metabolic demands placed on the respiratory system (Parameswaran et al. Can Respir J. 2006;203-10). The increased weight supported by the thoracic cage alters the equilibrium between the chest wall and lung tissue decreasing FRC and ERV. This reduces lung compliance and increases stiffness by promoting areas of atelectasis and increased alveolar surface tension (Dixon et al. Expert Rev Respir Med. 2018;755-67).
Another biomechanical cost of obesity on respiratory function is the increased consumption of oxygen to sustain ventilation at rest (Koenig SM, Am J Med Sci. 2001;249-79). This can lead to early respiratory muscle fatigue when respiratory rate and tidal volume increase with activity. Patients with obesity are more likely to develop obstructive sleep apnea and obesity hypoventilation syndrome. The resulting alveolar hypoxemia is thought to contribute to the increase in pulmonary hypertension observed in patients with obesity (Shah et al. Breathe. 2023;19[1]). In addition to the biomechanical consequences of obesity, increased adipose tissue can lead to chronic, systemic inflammation that can exacerbate or unmask underlying respiratory disease. Increased leptin and downregulation of adiponectin have been shown to increase systemic cytokine production (Ray et al. Am Rev Respir Dis. 1983;501-6). This inflammatory process contributes to increased airway resistance and an altered response to corticosteroids (inhaled or systemic) in obese patients treated for bronchial hyperresponsiveness. This perhaps reflects the Th2-low phenotype seen in patients with obesity and metabolic syndrome-related asthma (Shah et al. Breathe. 2023;19[1]) (Kanwar et al. Cureus. 2022 Oct 28. doi: 10.7759/cureus.30812).
Multiple studies have demonstrated weight loss through lifestyle changes, medical therapy, and obesity surgery result benefits pulmonary disease (Forno et al. PloS One. 2019;14[4]) (Ardila-Gatas et al. Surg Endosc. 2019;1952-8). Benefits include decreased exacerbation frequency, improved functional testing, and improved patient-reported quality of life. Pulmonary clinicians should be empowered to address obesity as a comorbid condition and treat with appropriate referrals for obesity surgery and initiation of medications when indicated.
GLP-1 receptor agonists
In the past year, glucagon-like peptide receptor agonists (GLP-1RAs) have garnered attention in the medical literature and popular news outlets. GLP-1RAs, including semaglutide, liraglutide, and tirzepatide, are currently FDA approved for the treatment of obesity in patients with a body mass index (BMI) greater than or equal to 30 or a BMI greater than or equal to 27 in the setting of an obesity-related comorbidity, including asthma.
This class of medications acts by increasing the physiologic insulin response to a glucose load, delaying gastric emptying, and reducing production of glucagon. In a phase III study, semaglutide resulted in greater than 15% weight reduction from baseline (Wadden et al. JAMA. 2021;1403-13). In clinical trials, these medications have not only resulted in significant, sustained weight loss but also improved lipid profiles, decreased A1c, and reduced major cardiovascular events (Lincoff et al. N Engl J Med. 2023;389[23]:2221-32) (Verma et al. Circulation. 2018;138[25]:2884-94).
GLP-1RAs and lung disease
GLP-1RAs are associated with ranges of weight loss that lead to symptom improvement. Beyond the anticipated benefits for pulmonary health, there is interest in whether GLP-1RAs may improve specific lung diseases. GLP-1 receptors are found throughout the body (eg, gastrointestinal tract, kidneys, and heart) with the largest proportion located in the lungs (Wu AY and Peebles RS. Expert Rev Clin Immunol. 2021;1053-7). In addition to their known effect on insulin response, GLP-1RAs are hypothesized to reduce proinflammatory cytokine signaling and alter surfactant production potentially improving both airway resistance and lung compliance (Kanwar et al. Cureus. 2022 Oct 28. doi: 10.7759/cureus.30812). Animal models suggest an antifibrotic effect with delay in the endothelial-mesenchymal transition. If further substantiated, this could impact both acute and chronic lung injury.
Early clinical studies of GLP-1RAs in patients with respiratory diseases have demonstrated improved symptoms and pulmonary function (Kanwar et al. Cureus. 2022 Oct 28. doi: 10.7759/cureus.30812). Even modest weight loss (2.5 kg in a year) with GLP-1RAs leads to improved symptoms and a reduction in asthma exacerbations. Other asthma literature shows GLP-1RAs improve symptoms and reduce exacerbations independent of changes in weight, supporting the hypothesis that the benefit of GLP-1RAs may be more than biomechanical improvement from weight loss alone (Foer et al. Am J Respir Crit Care Med. 2021;831-40).
GLP-1RAs reduce the proinflammatory cytokine signaling in both TH2-high and TH2-low asthma phenotypes and alter surfactant production, airway resistance, and perhaps even pulmonary vascular resistance (Altintas Dogan et al. Int J Chron Obstruct Pulmon Dis. 2022,405-14). GATA-3 is an ongoing clinical trial examining whether GLP-1RAs reduce airway inflammation via direct effects on of the respiratory tract (NCT05254314).
Drugs developed to treat one condition are often found to impact others during validation studies or postmarketing observation. Some examples are aspirin, sildenafil, minoxidil, hydroxychloroquine, and SGLT-2 inhibitors. Will GLP-1RAs be the latest medication to affect a broad array of physiologic process and end up improving not just metabolic but also lung health?
Now is the time for pulmonary clinicians to become comfortable counseling patients about and treating obesity. By 2030, half of the US population will have obesity, a quarter of which will be severe (Ward et al. NEJM. 2019;2440-2450).
Many pulmonary diseases, including asthma, COPD, and interstitial pulmonary fibrosis (IPF) are linked to and made worse by obesity with increased exacerbations, patient-reported decreased quality of life, and resistance to therapy (Ray et al. Am Rev Respir Dis. 1983;501-6). Asthma is even recognized as an obesity-related comorbid condition by both the American Society Metabolic and Bariatric Surgery (ASMBS) and the American Association of Clinical Endocrinologists (AACE) when considering indications for early or more aggressive treatment of obesity (Eisenberg et al. Obesity Surg. 2023;3-14) (Garvey et al. Endocr Pract. 2016;1-203).
Obesity has multiple negative effects on pulmonary function due to the physical forces of extra weight on the lungs and inflammation related to adipose tissue (see Figure 1) (Zerah et al. Chest. 1993;1470-6).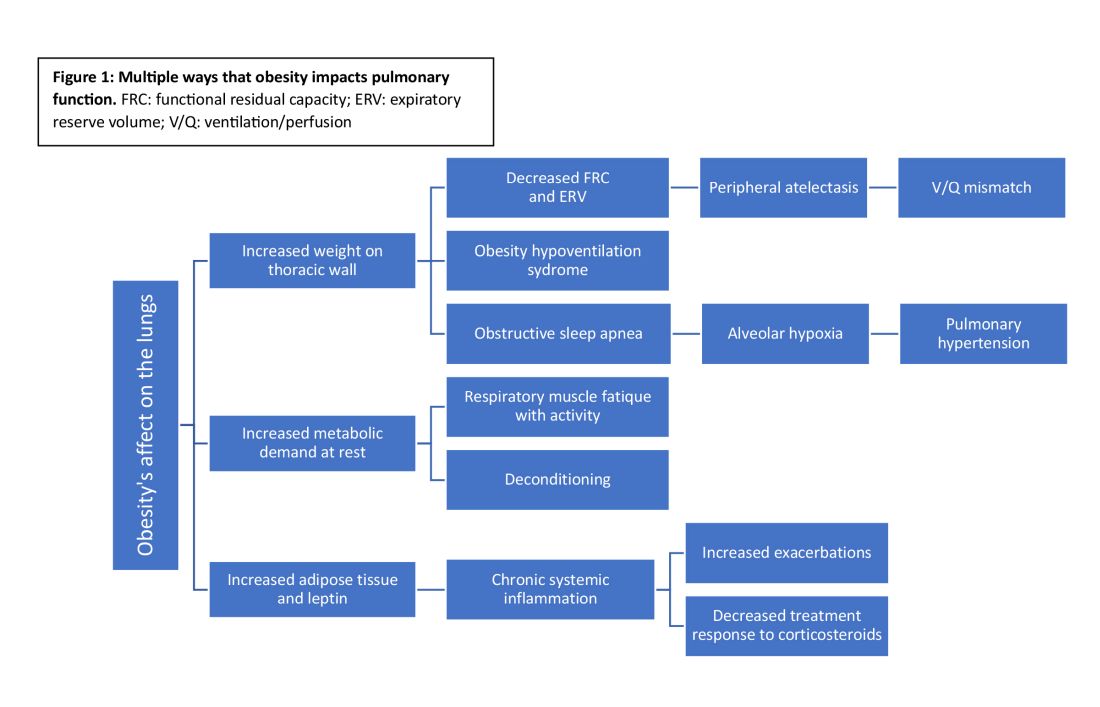
Obesity-related respiratory changes include reduced lung compliance, functional residual capacity (FRC), and expiratory reserve volume (ERV). These changes lead to peripheral atelectasis and V/Q mismatch and increased metabolic demands placed on the respiratory system (Parameswaran et al. Can Respir J. 2006;203-10). The increased weight supported by the thoracic cage alters the equilibrium between the chest wall and lung tissue decreasing FRC and ERV. This reduces lung compliance and increases stiffness by promoting areas of atelectasis and increased alveolar surface tension (Dixon et al. Expert Rev Respir Med. 2018;755-67).
Another biomechanical cost of obesity on respiratory function is the increased consumption of oxygen to sustain ventilation at rest (Koenig SM, Am J Med Sci. 2001;249-79). This can lead to early respiratory muscle fatigue when respiratory rate and tidal volume increase with activity. Patients with obesity are more likely to develop obstructive sleep apnea and obesity hypoventilation syndrome. The resulting alveolar hypoxemia is thought to contribute to the increase in pulmonary hypertension observed in patients with obesity (Shah et al. Breathe. 2023;19[1]). In addition to the biomechanical consequences of obesity, increased adipose tissue can lead to chronic, systemic inflammation that can exacerbate or unmask underlying respiratory disease. Increased leptin and downregulation of adiponectin have been shown to increase systemic cytokine production (Ray et al. Am Rev Respir Dis. 1983;501-6). This inflammatory process contributes to increased airway resistance and an altered response to corticosteroids (inhaled or systemic) in obese patients treated for bronchial hyperresponsiveness. This perhaps reflects the Th2-low phenotype seen in patients with obesity and metabolic syndrome-related asthma (Shah et al. Breathe. 2023;19[1]) (Kanwar et al. Cureus. 2022 Oct 28. doi: 10.7759/cureus.30812).
Multiple studies have demonstrated weight loss through lifestyle changes, medical therapy, and obesity surgery result benefits pulmonary disease (Forno et al. PloS One. 2019;14[4]) (Ardila-Gatas et al. Surg Endosc. 2019;1952-8). Benefits include decreased exacerbation frequency, improved functional testing, and improved patient-reported quality of life. Pulmonary clinicians should be empowered to address obesity as a comorbid condition and treat with appropriate referrals for obesity surgery and initiation of medications when indicated.
GLP-1 receptor agonists
In the past year, glucagon-like peptide receptor agonists (GLP-1RAs) have garnered attention in the medical literature and popular news outlets. GLP-1RAs, including semaglutide, liraglutide, and tirzepatide, are currently FDA approved for the treatment of obesity in patients with a body mass index (BMI) greater than or equal to 30 or a BMI greater than or equal to 27 in the setting of an obesity-related comorbidity, including asthma.
This class of medications acts by increasing the physiologic insulin response to a glucose load, delaying gastric emptying, and reducing production of glucagon. In a phase III study, semaglutide resulted in greater than 15% weight reduction from baseline (Wadden et al. JAMA. 2021;1403-13). In clinical trials, these medications have not only resulted in significant, sustained weight loss but also improved lipid profiles, decreased A1c, and reduced major cardiovascular events (Lincoff et al. N Engl J Med. 2023;389[23]:2221-32) (Verma et al. Circulation. 2018;138[25]:2884-94).
GLP-1RAs and lung disease
GLP-1RAs are associated with ranges of weight loss that lead to symptom improvement. Beyond the anticipated benefits for pulmonary health, there is interest in whether GLP-1RAs may improve specific lung diseases. GLP-1 receptors are found throughout the body (eg, gastrointestinal tract, kidneys, and heart) with the largest proportion located in the lungs (Wu AY and Peebles RS. Expert Rev Clin Immunol. 2021;1053-7). In addition to their known effect on insulin response, GLP-1RAs are hypothesized to reduce proinflammatory cytokine signaling and alter surfactant production potentially improving both airway resistance and lung compliance (Kanwar et al. Cureus. 2022 Oct 28. doi: 10.7759/cureus.30812). Animal models suggest an antifibrotic effect with delay in the endothelial-mesenchymal transition. If further substantiated, this could impact both acute and chronic lung injury.
Early clinical studies of GLP-1RAs in patients with respiratory diseases have demonstrated improved symptoms and pulmonary function (Kanwar et al. Cureus. 2022 Oct 28. doi: 10.7759/cureus.30812). Even modest weight loss (2.5 kg in a year) with GLP-1RAs leads to improved symptoms and a reduction in asthma exacerbations. Other asthma literature shows GLP-1RAs improve symptoms and reduce exacerbations independent of changes in weight, supporting the hypothesis that the benefit of GLP-1RAs may be more than biomechanical improvement from weight loss alone (Foer et al. Am J Respir Crit Care Med. 2021;831-40).
GLP-1RAs reduce the proinflammatory cytokine signaling in both TH2-high and TH2-low asthma phenotypes and alter surfactant production, airway resistance, and perhaps even pulmonary vascular resistance (Altintas Dogan et al. Int J Chron Obstruct Pulmon Dis. 2022,405-14). GATA-3 is an ongoing clinical trial examining whether GLP-1RAs reduce airway inflammation via direct effects on of the respiratory tract (NCT05254314).
Drugs developed to treat one condition are often found to impact others during validation studies or postmarketing observation. Some examples are aspirin, sildenafil, minoxidil, hydroxychloroquine, and SGLT-2 inhibitors. Will GLP-1RAs be the latest medication to affect a broad array of physiologic process and end up improving not just metabolic but also lung health?
Now is the time for pulmonary clinicians to become comfortable counseling patients about and treating obesity. By 2030, half of the US population will have obesity, a quarter of which will be severe (Ward et al. NEJM. 2019;2440-2450).
Many pulmonary diseases, including asthma, COPD, and interstitial pulmonary fibrosis (IPF) are linked to and made worse by obesity with increased exacerbations, patient-reported decreased quality of life, and resistance to therapy (Ray et al. Am Rev Respir Dis. 1983;501-6). Asthma is even recognized as an obesity-related comorbid condition by both the American Society Metabolic and Bariatric Surgery (ASMBS) and the American Association of Clinical Endocrinologists (AACE) when considering indications for early or more aggressive treatment of obesity (Eisenberg et al. Obesity Surg. 2023;3-14) (Garvey et al. Endocr Pract. 2016;1-203).
Obesity has multiple negative effects on pulmonary function due to the physical forces of extra weight on the lungs and inflammation related to adipose tissue (see Figure 1) (Zerah et al. Chest. 1993;1470-6).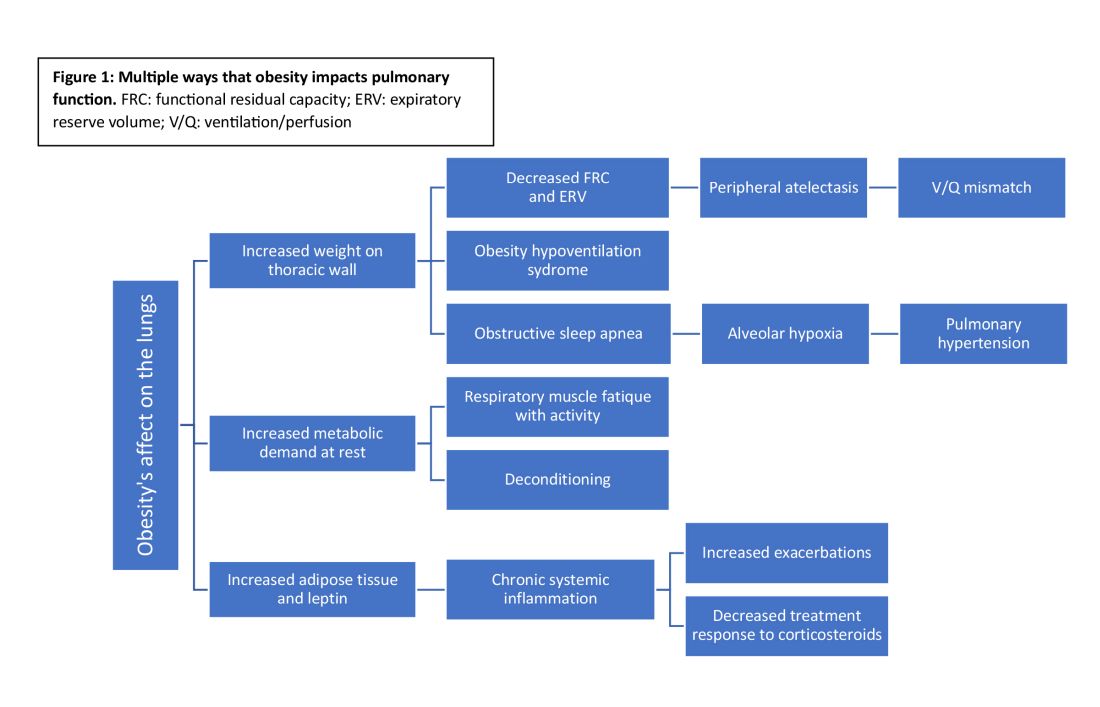
Obesity-related respiratory changes include reduced lung compliance, functional residual capacity (FRC), and expiratory reserve volume (ERV). These changes lead to peripheral atelectasis and V/Q mismatch and increased metabolic demands placed on the respiratory system (Parameswaran et al. Can Respir J. 2006;203-10). The increased weight supported by the thoracic cage alters the equilibrium between the chest wall and lung tissue decreasing FRC and ERV. This reduces lung compliance and increases stiffness by promoting areas of atelectasis and increased alveolar surface tension (Dixon et al. Expert Rev Respir Med. 2018;755-67).
Another biomechanical cost of obesity on respiratory function is the increased consumption of oxygen to sustain ventilation at rest (Koenig SM, Am J Med Sci. 2001;249-79). This can lead to early respiratory muscle fatigue when respiratory rate and tidal volume increase with activity. Patients with obesity are more likely to develop obstructive sleep apnea and obesity hypoventilation syndrome. The resulting alveolar hypoxemia is thought to contribute to the increase in pulmonary hypertension observed in patients with obesity (Shah et al. Breathe. 2023;19[1]). In addition to the biomechanical consequences of obesity, increased adipose tissue can lead to chronic, systemic inflammation that can exacerbate or unmask underlying respiratory disease. Increased leptin and downregulation of adiponectin have been shown to increase systemic cytokine production (Ray et al. Am Rev Respir Dis. 1983;501-6). This inflammatory process contributes to increased airway resistance and an altered response to corticosteroids (inhaled or systemic) in obese patients treated for bronchial hyperresponsiveness. This perhaps reflects the Th2-low phenotype seen in patients with obesity and metabolic syndrome-related asthma (Shah et al. Breathe. 2023;19[1]) (Kanwar et al. Cureus. 2022 Oct 28. doi: 10.7759/cureus.30812).
Multiple studies have demonstrated weight loss through lifestyle changes, medical therapy, and obesity surgery result benefits pulmonary disease (Forno et al. PloS One. 2019;14[4]) (Ardila-Gatas et al. Surg Endosc. 2019;1952-8). Benefits include decreased exacerbation frequency, improved functional testing, and improved patient-reported quality of life. Pulmonary clinicians should be empowered to address obesity as a comorbid condition and treat with appropriate referrals for obesity surgery and initiation of medications when indicated.
GLP-1 receptor agonists
In the past year, glucagon-like peptide receptor agonists (GLP-1RAs) have garnered attention in the medical literature and popular news outlets. GLP-1RAs, including semaglutide, liraglutide, and tirzepatide, are currently FDA approved for the treatment of obesity in patients with a body mass index (BMI) greater than or equal to 30 or a BMI greater than or equal to 27 in the setting of an obesity-related comorbidity, including asthma.
This class of medications acts by increasing the physiologic insulin response to a glucose load, delaying gastric emptying, and reducing production of glucagon. In a phase III study, semaglutide resulted in greater than 15% weight reduction from baseline (Wadden et al. JAMA. 2021;1403-13). In clinical trials, these medications have not only resulted in significant, sustained weight loss but also improved lipid profiles, decreased A1c, and reduced major cardiovascular events (Lincoff et al. N Engl J Med. 2023;389[23]:2221-32) (Verma et al. Circulation. 2018;138[25]:2884-94).
GLP-1RAs and lung disease
GLP-1RAs are associated with ranges of weight loss that lead to symptom improvement. Beyond the anticipated benefits for pulmonary health, there is interest in whether GLP-1RAs may improve specific lung diseases. GLP-1 receptors are found throughout the body (eg, gastrointestinal tract, kidneys, and heart) with the largest proportion located in the lungs (Wu AY and Peebles RS. Expert Rev Clin Immunol. 2021;1053-7). In addition to their known effect on insulin response, GLP-1RAs are hypothesized to reduce proinflammatory cytokine signaling and alter surfactant production potentially improving both airway resistance and lung compliance (Kanwar et al. Cureus. 2022 Oct 28. doi: 10.7759/cureus.30812). Animal models suggest an antifibrotic effect with delay in the endothelial-mesenchymal transition. If further substantiated, this could impact both acute and chronic lung injury.
Early clinical studies of GLP-1RAs in patients with respiratory diseases have demonstrated improved symptoms and pulmonary function (Kanwar et al. Cureus. 2022 Oct 28. doi: 10.7759/cureus.30812). Even modest weight loss (2.5 kg in a year) with GLP-1RAs leads to improved symptoms and a reduction in asthma exacerbations. Other asthma literature shows GLP-1RAs improve symptoms and reduce exacerbations independent of changes in weight, supporting the hypothesis that the benefit of GLP-1RAs may be more than biomechanical improvement from weight loss alone (Foer et al. Am J Respir Crit Care Med. 2021;831-40).
GLP-1RAs reduce the proinflammatory cytokine signaling in both TH2-high and TH2-low asthma phenotypes and alter surfactant production, airway resistance, and perhaps even pulmonary vascular resistance (Altintas Dogan et al. Int J Chron Obstruct Pulmon Dis. 2022,405-14). GATA-3 is an ongoing clinical trial examining whether GLP-1RAs reduce airway inflammation via direct effects on of the respiratory tract (NCT05254314).
Drugs developed to treat one condition are often found to impact others during validation studies or postmarketing observation. Some examples are aspirin, sildenafil, minoxidil, hydroxychloroquine, and SGLT-2 inhibitors. Will GLP-1RAs be the latest medication to affect a broad array of physiologic process and end up improving not just metabolic but also lung health?
Bivalent COVID Vaccine Protected Children, Adolescents
Children and adolescents ages 5-17 who received a bivalent COVID-19 mRNA vaccine were less likely to become infected with SARS-CoV-2 compared with those who were unvaccinated or received only the monovalent COVID-19 vaccine, according to new data published February 6 in JAMA.
“All eligible children and adolescents should remain up to date with recommended COVID-19 vaccinations,” wrote the authors, led by Leora R. Feldstein, PhD, with the US Centers for Disease Control and Prevention (CDC) in Atlanta.
By the end of 2023, at least 911 youths ages 5-17 had died from COVID-related causes.
Researchers found that compared with participants who did not receive the COVID-19 vaccine or got monovalent-only doses 180 days or more before, the adjusted vaccine effectiveness of a bivalent COVID-19 vaccine dose against SARS-CoV-2 infection was 51.3% (95% confidence interval [CI], 23.6%-71.9%) 7-60 days after vaccination. Relative effectiveness was 62.4% (95% CI, 38.5%-81.1%) 61-150 days after vaccination. The researchers said the confidence intervals were wide because of the small sample size.
The information can help inform public health strategies, the authors noted, especially as new variants emerge.
Bivalent Dose Recommended in Fall of 2022
Bivalent mRNA COVID vaccines were recommended in the United States for children and adolescents ages 12 years or older on Sept. 1, 2022, and for children ages 5-11 on Oct. 12, 2022, when Omicron BA.4/5 types were the predominant circulating variant.
The study included 2,959 participants who completed periodic surveys (answering questions on demographics, household details, chronic medical conditions, and COVID-19 symptoms) and submitted weekly self-collected nasal swabs (whether or not they had symptoms). Those in the study submitted additional nasal swabs if they developed any symptoms.
Median adherence to weekly upper respiratory specimen swabbing was high throughout the study period at 93.8%.
Data from Sept. 4, 2022, to Jan. 31, 2023, were combined from three prospective US cohort studies at six sites. In addition to the surveys, researchers used information from state immunization information systems and electronic medical records.
Most of the Infected Were Unvaccinated or Had Monovalent Vax
Of the 426 participants (14.4% of the combined cohorts) infected with SARS-CoV-2, 383 (89.9%) were either unvaccinated or received monovalent vaccine doses only.
Calculations were adjusted for age, sex, race, ethnicity, health conditions, prior SARS-CoV-2 infections, geographic location, proportion of circulating variants by site, and local virus prevalence.
Participants living in Oregon, for example, had the highest uptake of bivalent COVID-19 vaccine (56.2%), whereas those in Texas had the lowest (2.4%). Participants reporting Hispanic ethnicity had lower bivalent uptake (17.1%) compared with non-Hispanic participants of all races (27.1%).
Of the 2,207 participants who did not receive a bivalent dose, 24.2% were unvaccinated and 1,672 (75.8%) received at least 1 monovalent dose.
The researchers said they saw no sign of waning effectiveness 61-150 days (the limit for this analysis) after receipt of the bivalent COVID-19 vaccine.
They wrote that continuation of the cohorts will allow study of waning patterns, which could help inform vaccine recommendations.
Among the limitations of the study are that testing methods and the COVID-19 symptoms surveyed varied among the three cohorts, so there may be some differences in defining infection or symptomatic COVID. In addition, the researchers were not able to account for the social vulnerability index and immunocompromised status, which could have affected vaccine uptake and risk of SARS-CoV-2 infection.
This study was supported by the National Center for Immunization and Respiratory Diseases, US Centers for Disease Control and Prevention, and by the National Institute of Allergy and Infectious Diseases. Coauthor Dr. Caban-Martinez reported grants from the Florida Firefighter Cancer Initiative and the Florida Department of Health. Coauthors Dr. Chu, Dr. Englund, Dr. Martin, and Dr. Monto reported receiving personal fees or grants from multiple pharmaceutical companies. Dr. Hegmann reported being the editor of the American College of Occupational and Environmental Medicine practice guidelines. Coauthor Dr. Gaglani reported serving as cochair of the infectious diseases and immunization committee and the respiratory syncytial virus task force lead for the Texas Pediatric Society and the Texas Chapter of the American Academy of Pediatrics. No other disclosures were reported.
Children and adolescents ages 5-17 who received a bivalent COVID-19 mRNA vaccine were less likely to become infected with SARS-CoV-2 compared with those who were unvaccinated or received only the monovalent COVID-19 vaccine, according to new data published February 6 in JAMA.
“All eligible children and adolescents should remain up to date with recommended COVID-19 vaccinations,” wrote the authors, led by Leora R. Feldstein, PhD, with the US Centers for Disease Control and Prevention (CDC) in Atlanta.
By the end of 2023, at least 911 youths ages 5-17 had died from COVID-related causes.
Researchers found that compared with participants who did not receive the COVID-19 vaccine or got monovalent-only doses 180 days or more before, the adjusted vaccine effectiveness of a bivalent COVID-19 vaccine dose against SARS-CoV-2 infection was 51.3% (95% confidence interval [CI], 23.6%-71.9%) 7-60 days after vaccination. Relative effectiveness was 62.4% (95% CI, 38.5%-81.1%) 61-150 days after vaccination. The researchers said the confidence intervals were wide because of the small sample size.
The information can help inform public health strategies, the authors noted, especially as new variants emerge.
Bivalent Dose Recommended in Fall of 2022
Bivalent mRNA COVID vaccines were recommended in the United States for children and adolescents ages 12 years or older on Sept. 1, 2022, and for children ages 5-11 on Oct. 12, 2022, when Omicron BA.4/5 types were the predominant circulating variant.
The study included 2,959 participants who completed periodic surveys (answering questions on demographics, household details, chronic medical conditions, and COVID-19 symptoms) and submitted weekly self-collected nasal swabs (whether or not they had symptoms). Those in the study submitted additional nasal swabs if they developed any symptoms.
Median adherence to weekly upper respiratory specimen swabbing was high throughout the study period at 93.8%.
Data from Sept. 4, 2022, to Jan. 31, 2023, were combined from three prospective US cohort studies at six sites. In addition to the surveys, researchers used information from state immunization information systems and electronic medical records.
Most of the Infected Were Unvaccinated or Had Monovalent Vax
Of the 426 participants (14.4% of the combined cohorts) infected with SARS-CoV-2, 383 (89.9%) were either unvaccinated or received monovalent vaccine doses only.
Calculations were adjusted for age, sex, race, ethnicity, health conditions, prior SARS-CoV-2 infections, geographic location, proportion of circulating variants by site, and local virus prevalence.
Participants living in Oregon, for example, had the highest uptake of bivalent COVID-19 vaccine (56.2%), whereas those in Texas had the lowest (2.4%). Participants reporting Hispanic ethnicity had lower bivalent uptake (17.1%) compared with non-Hispanic participants of all races (27.1%).
Of the 2,207 participants who did not receive a bivalent dose, 24.2% were unvaccinated and 1,672 (75.8%) received at least 1 monovalent dose.
The researchers said they saw no sign of waning effectiveness 61-150 days (the limit for this analysis) after receipt of the bivalent COVID-19 vaccine.
They wrote that continuation of the cohorts will allow study of waning patterns, which could help inform vaccine recommendations.
Among the limitations of the study are that testing methods and the COVID-19 symptoms surveyed varied among the three cohorts, so there may be some differences in defining infection or symptomatic COVID. In addition, the researchers were not able to account for the social vulnerability index and immunocompromised status, which could have affected vaccine uptake and risk of SARS-CoV-2 infection.
This study was supported by the National Center for Immunization and Respiratory Diseases, US Centers for Disease Control and Prevention, and by the National Institute of Allergy and Infectious Diseases. Coauthor Dr. Caban-Martinez reported grants from the Florida Firefighter Cancer Initiative and the Florida Department of Health. Coauthors Dr. Chu, Dr. Englund, Dr. Martin, and Dr. Monto reported receiving personal fees or grants from multiple pharmaceutical companies. Dr. Hegmann reported being the editor of the American College of Occupational and Environmental Medicine practice guidelines. Coauthor Dr. Gaglani reported serving as cochair of the infectious diseases and immunization committee and the respiratory syncytial virus task force lead for the Texas Pediatric Society and the Texas Chapter of the American Academy of Pediatrics. No other disclosures were reported.
Children and adolescents ages 5-17 who received a bivalent COVID-19 mRNA vaccine were less likely to become infected with SARS-CoV-2 compared with those who were unvaccinated or received only the monovalent COVID-19 vaccine, according to new data published February 6 in JAMA.
“All eligible children and adolescents should remain up to date with recommended COVID-19 vaccinations,” wrote the authors, led by Leora R. Feldstein, PhD, with the US Centers for Disease Control and Prevention (CDC) in Atlanta.
By the end of 2023, at least 911 youths ages 5-17 had died from COVID-related causes.
Researchers found that compared with participants who did not receive the COVID-19 vaccine or got monovalent-only doses 180 days or more before, the adjusted vaccine effectiveness of a bivalent COVID-19 vaccine dose against SARS-CoV-2 infection was 51.3% (95% confidence interval [CI], 23.6%-71.9%) 7-60 days after vaccination. Relative effectiveness was 62.4% (95% CI, 38.5%-81.1%) 61-150 days after vaccination. The researchers said the confidence intervals were wide because of the small sample size.
The information can help inform public health strategies, the authors noted, especially as new variants emerge.
Bivalent Dose Recommended in Fall of 2022
Bivalent mRNA COVID vaccines were recommended in the United States for children and adolescents ages 12 years or older on Sept. 1, 2022, and for children ages 5-11 on Oct. 12, 2022, when Omicron BA.4/5 types were the predominant circulating variant.
The study included 2,959 participants who completed periodic surveys (answering questions on demographics, household details, chronic medical conditions, and COVID-19 symptoms) and submitted weekly self-collected nasal swabs (whether or not they had symptoms). Those in the study submitted additional nasal swabs if they developed any symptoms.
Median adherence to weekly upper respiratory specimen swabbing was high throughout the study period at 93.8%.
Data from Sept. 4, 2022, to Jan. 31, 2023, were combined from three prospective US cohort studies at six sites. In addition to the surveys, researchers used information from state immunization information systems and electronic medical records.
Most of the Infected Were Unvaccinated or Had Monovalent Vax
Of the 426 participants (14.4% of the combined cohorts) infected with SARS-CoV-2, 383 (89.9%) were either unvaccinated or received monovalent vaccine doses only.
Calculations were adjusted for age, sex, race, ethnicity, health conditions, prior SARS-CoV-2 infections, geographic location, proportion of circulating variants by site, and local virus prevalence.
Participants living in Oregon, for example, had the highest uptake of bivalent COVID-19 vaccine (56.2%), whereas those in Texas had the lowest (2.4%). Participants reporting Hispanic ethnicity had lower bivalent uptake (17.1%) compared with non-Hispanic participants of all races (27.1%).
Of the 2,207 participants who did not receive a bivalent dose, 24.2% were unvaccinated and 1,672 (75.8%) received at least 1 monovalent dose.
The researchers said they saw no sign of waning effectiveness 61-150 days (the limit for this analysis) after receipt of the bivalent COVID-19 vaccine.
They wrote that continuation of the cohorts will allow study of waning patterns, which could help inform vaccine recommendations.
Among the limitations of the study are that testing methods and the COVID-19 symptoms surveyed varied among the three cohorts, so there may be some differences in defining infection or symptomatic COVID. In addition, the researchers were not able to account for the social vulnerability index and immunocompromised status, which could have affected vaccine uptake and risk of SARS-CoV-2 infection.
This study was supported by the National Center for Immunization and Respiratory Diseases, US Centers for Disease Control and Prevention, and by the National Institute of Allergy and Infectious Diseases. Coauthor Dr. Caban-Martinez reported grants from the Florida Firefighter Cancer Initiative and the Florida Department of Health. Coauthors Dr. Chu, Dr. Englund, Dr. Martin, and Dr. Monto reported receiving personal fees or grants from multiple pharmaceutical companies. Dr. Hegmann reported being the editor of the American College of Occupational and Environmental Medicine practice guidelines. Coauthor Dr. Gaglani reported serving as cochair of the infectious diseases and immunization committee and the respiratory syncytial virus task force lead for the Texas Pediatric Society and the Texas Chapter of the American Academy of Pediatrics. No other disclosures were reported.
FROM JAMA
Gabapentinoids Increase Exacerbation in COPD
TOPLINE:
Gabapentinoid use significantly increased the risk for exacerbations in adults with chronic obstructive pulmonary disease (COPD).
METHODOLOGY:
- Previous research has prompted warnings from North American and European health agencies of severe exacerbations associated with gabapentinoid use by patients with COPD.
- The researchers compared data from patients with COPD in Canadian databases between 1994 and 2015 who were new to gabapentinoids and matched them to patients who did not use gabapentinoids.
- The primary outcome was exacerbation of COPD that required hospitalization in a propensity score-matched study.
TAKEAWAY:
- The study population included 356 epilepsy patients, 9411 neuropathic pain patients, and 3737 patients with other chronic pain.
- Use of gabapentinoids was significantly associated with an overall increased risk for severe COPD exacerbation (hazard ratio, 1.49) compared with nonuse.
- Gabapentinoid use was associated with a significantly increased COPD exacerbation risk for each group of users compared with nonusers, with hazard ratios of 1.58, 1.35, and 1.49 for epilepsy, neuropathic pain, and other chronic pain, respectively.
IN PRACTICE:
“This study supports the warnings from regulatory agencies and highlights the importance of considering this potential risk when prescribing gabapentin and pregabalin to patients with COPD,” the researchers wrote.
SOURCE:
The lead author on the study was Alvi A. Rahman, MSc, of Jewish General Hospital, Montreal. The study was published online on January 16, 2024, in Annals of Internal Medicine.
LIMITATIONS:
A lack of data on smoking status and other residual confounding factors limited the study findings.
DISCLOSURES:
The study was supported by the Canadian Institutes of Health Research and the Canadian Lung Association. Mr. Rahman had no financial conflicts to disclose, but some coauthors disclosed consulting and advisory relationships with various companies, including Merck, Pfizer, Seqirus, Boehringer-Ingelheim, and Novartis outside of the current work.
A version of this article appeared on Medscape.com.
TOPLINE:
Gabapentinoid use significantly increased the risk for exacerbations in adults with chronic obstructive pulmonary disease (COPD).
METHODOLOGY:
- Previous research has prompted warnings from North American and European health agencies of severe exacerbations associated with gabapentinoid use by patients with COPD.
- The researchers compared data from patients with COPD in Canadian databases between 1994 and 2015 who were new to gabapentinoids and matched them to patients who did not use gabapentinoids.
- The primary outcome was exacerbation of COPD that required hospitalization in a propensity score-matched study.
TAKEAWAY:
- The study population included 356 epilepsy patients, 9411 neuropathic pain patients, and 3737 patients with other chronic pain.
- Use of gabapentinoids was significantly associated with an overall increased risk for severe COPD exacerbation (hazard ratio, 1.49) compared with nonuse.
- Gabapentinoid use was associated with a significantly increased COPD exacerbation risk for each group of users compared with nonusers, with hazard ratios of 1.58, 1.35, and 1.49 for epilepsy, neuropathic pain, and other chronic pain, respectively.
IN PRACTICE:
“This study supports the warnings from regulatory agencies and highlights the importance of considering this potential risk when prescribing gabapentin and pregabalin to patients with COPD,” the researchers wrote.
SOURCE:
The lead author on the study was Alvi A. Rahman, MSc, of Jewish General Hospital, Montreal. The study was published online on January 16, 2024, in Annals of Internal Medicine.
LIMITATIONS:
A lack of data on smoking status and other residual confounding factors limited the study findings.
DISCLOSURES:
The study was supported by the Canadian Institutes of Health Research and the Canadian Lung Association. Mr. Rahman had no financial conflicts to disclose, but some coauthors disclosed consulting and advisory relationships with various companies, including Merck, Pfizer, Seqirus, Boehringer-Ingelheim, and Novartis outside of the current work.
A version of this article appeared on Medscape.com.
TOPLINE:
Gabapentinoid use significantly increased the risk for exacerbations in adults with chronic obstructive pulmonary disease (COPD).
METHODOLOGY:
- Previous research has prompted warnings from North American and European health agencies of severe exacerbations associated with gabapentinoid use by patients with COPD.
- The researchers compared data from patients with COPD in Canadian databases between 1994 and 2015 who were new to gabapentinoids and matched them to patients who did not use gabapentinoids.
- The primary outcome was exacerbation of COPD that required hospitalization in a propensity score-matched study.
TAKEAWAY:
- The study population included 356 epilepsy patients, 9411 neuropathic pain patients, and 3737 patients with other chronic pain.
- Use of gabapentinoids was significantly associated with an overall increased risk for severe COPD exacerbation (hazard ratio, 1.49) compared with nonuse.
- Gabapentinoid use was associated with a significantly increased COPD exacerbation risk for each group of users compared with nonusers, with hazard ratios of 1.58, 1.35, and 1.49 for epilepsy, neuropathic pain, and other chronic pain, respectively.
IN PRACTICE:
“This study supports the warnings from regulatory agencies and highlights the importance of considering this potential risk when prescribing gabapentin and pregabalin to patients with COPD,” the researchers wrote.
SOURCE:
The lead author on the study was Alvi A. Rahman, MSc, of Jewish General Hospital, Montreal. The study was published online on January 16, 2024, in Annals of Internal Medicine.
LIMITATIONS:
A lack of data on smoking status and other residual confounding factors limited the study findings.
DISCLOSURES:
The study was supported by the Canadian Institutes of Health Research and the Canadian Lung Association. Mr. Rahman had no financial conflicts to disclose, but some coauthors disclosed consulting and advisory relationships with various companies, including Merck, Pfizer, Seqirus, Boehringer-Ingelheim, and Novartis outside of the current work.
A version of this article appeared on Medscape.com.
Success with Sirolimus in Treating Skin Sarcoidosis Could Spur Studies in Other Organs
Sirolimus may be an effective treatment for patients with persistent cutaneous sarcoidosis.
In a small clinical trial, 7 of 10 patients treated with sirolimus via oral solution had improvements in skin lesions after 4 months, which was sustained for up to 2 years after the study concluded.
The results suggested that mechanistic target of rapamycin (mTOR) inhibition is a potential therapeutic avenue for sarcoidosis, which the authors said should be explored in larger clinical trials.
In the past decade, there has been a growing amount of evidence suggesting mTOR’s role in sarcoidosis. In 2017, researchers showed that activation of mTOR in macrophages could cause progressive sarcoidosis in mice. In additional studies, high levels of mTOR activity were detected in human sarcoidosis granulomas in various organs, including the skin, lung, and heart.
Three case reports also documented using the mTOR inhibitor sirolimus to effectively treat systemic sarcoidosis.
“Although all reports observed improvement of the disease following the treatment, no clinical trial investigating the efficacy and safety of sirolimus in patients with sarcoidosis had been published” prior to this study, wrote senior author Georg Stary, MD, of the Medical University of Vienna and the Research Center for Molecular Medicine of the Austrian Academy of Sciences, Vienna, Austria, and colleagues.
The findings were published in the The Lancet Rheumatology.
For the study, researchers recruited 16 individuals with persistent and glucocorticoid-refractory cutaneous sarcoidosis between September 2019 and June 2021. A total of 14 participants were randomly assigned to the topical phase of the study, whereas two immediately received systemic treatment. All treatment was conducted at Vienna General Hospital.
In the placebo-controlled, double-blinded topical treatment arm, patients received either 0.1% topical sirolimus in Vaseline or Vaseline alone (placebo) twice daily for 2 months. After a 1-month washout period, participants were switched to the alternate treatment arm for an additional 2 months.
Following this topical phase and an additional 1-month washout period, all remaining participants received systemic sirolimus via a 1-mg/mL solution, starting with a 6-mg loading dose and continuing with 2 mg once daily for 4 months. The primary outcome was change in Cutaneous Sarcoidosis Activity and Morphology Index (CSAMI) from baseline, with decrease of more than five points representing a response to treatment.
A total of 10 patients completed the trial.
There was no change in CSAMI in either topical treatment groups. In the systemic group, 70% of patients had clinical improvement in skin lesions, with three responders in this group having complete resolution of skin lesions. The median change in CSAMI was −7.0 points (P = .018).
This improvement persisted for 2 months following study conclusion, with more pronounced improvement from baseline after 2 years of drug-free follow-up (−11.5 points).
There were no serious adverse events reported during the study, but 42% of patients treated with systemic sirolimus reported mild skin reactions, such as acne and eczema. Other related adverse events were hypertriglyceridemia (17%), hyperglycemia (17%), and proteinuria (8%).
Compared with clinical outcomes with tofacitinib and tumor necrosis factor (TNF) inhibitors, “the strength of our study lies in the sustained treatment effect after drug withdrawal among all responders. This prolonged effect has not yet been explored with tofacitinib, whereas with TNF inhibitors disease relapse was seen in more than 50% of patients at 3-8 months,” the authors wrote.
The researchers also analyzed participants’ skin biopsies to gain a better understanding of how mTOR inhibition affected granuloma structures. They found that, at baseline, mTOR activity was significantly lower in the fibroblasts of treatment nonresponders than in responders. They speculated that lower expression of mTOR could make these granuloma-associated cells resistant to systemic sirolimus.
These promising findings combine “clinical response with a molecular analysis,” Avrom Caplan, MD, co-director of the Sarcoidosis Program at NYU Langone in New York City, told this news organization. He was not involved with the research. Adding molecular information to clinical outcome data “helps solidify that [the mTOR] pathway has relevance in the sarcoid granuloma formation.”
The study had a limited sample size — a challenge for many clinical trials of rare diseases, Dr. Caplan said. Larger clinical trials are necessary to explore mTOR inhibition in sarcoidosis, both he and the authors agreed. A larger trial could also include greater heterogeneity of patients, including varied sarcoid presentation and demographics, Dr. Caplan noted. In this study, all but one participants were White individuals, and 63% of participants were female.
Larger studies could also address important questions on ideal length of therapy, dosing, and where this therapy “would fall within the therapeutic step ladder,” Dr. Caplan continued.
Whether mTOR inhibition could be effective at treating individuals with sarcoidosis in other organs beyond the skin is also unknown.
“If the pathogenesis of sarcoid granuloma formation does include mTOR upregulation, which they are showing here…then you could hypothesize that, yes, using this therapy could benefit other organs,” he said. “But that has to be investigated in larger trials.”
The study was funded in part by a Vienna Science and Technology Fund project. Several authors report receiving grants from the Austrian Science Fund and one from the Ann Theodore Foundation Breakthrough Sarcoidosis Initiative. Dr. Caplan reported no relevant financial relationships.
A version of this article appeared on Medscape.com .
Sirolimus may be an effective treatment for patients with persistent cutaneous sarcoidosis.
In a small clinical trial, 7 of 10 patients treated with sirolimus via oral solution had improvements in skin lesions after 4 months, which was sustained for up to 2 years after the study concluded.
The results suggested that mechanistic target of rapamycin (mTOR) inhibition is a potential therapeutic avenue for sarcoidosis, which the authors said should be explored in larger clinical trials.
In the past decade, there has been a growing amount of evidence suggesting mTOR’s role in sarcoidosis. In 2017, researchers showed that activation of mTOR in macrophages could cause progressive sarcoidosis in mice. In additional studies, high levels of mTOR activity were detected in human sarcoidosis granulomas in various organs, including the skin, lung, and heart.
Three case reports also documented using the mTOR inhibitor sirolimus to effectively treat systemic sarcoidosis.
“Although all reports observed improvement of the disease following the treatment, no clinical trial investigating the efficacy and safety of sirolimus in patients with sarcoidosis had been published” prior to this study, wrote senior author Georg Stary, MD, of the Medical University of Vienna and the Research Center for Molecular Medicine of the Austrian Academy of Sciences, Vienna, Austria, and colleagues.
The findings were published in the The Lancet Rheumatology.
For the study, researchers recruited 16 individuals with persistent and glucocorticoid-refractory cutaneous sarcoidosis between September 2019 and June 2021. A total of 14 participants were randomly assigned to the topical phase of the study, whereas two immediately received systemic treatment. All treatment was conducted at Vienna General Hospital.
In the placebo-controlled, double-blinded topical treatment arm, patients received either 0.1% topical sirolimus in Vaseline or Vaseline alone (placebo) twice daily for 2 months. After a 1-month washout period, participants were switched to the alternate treatment arm for an additional 2 months.
Following this topical phase and an additional 1-month washout period, all remaining participants received systemic sirolimus via a 1-mg/mL solution, starting with a 6-mg loading dose and continuing with 2 mg once daily for 4 months. The primary outcome was change in Cutaneous Sarcoidosis Activity and Morphology Index (CSAMI) from baseline, with decrease of more than five points representing a response to treatment.
A total of 10 patients completed the trial.
There was no change in CSAMI in either topical treatment groups. In the systemic group, 70% of patients had clinical improvement in skin lesions, with three responders in this group having complete resolution of skin lesions. The median change in CSAMI was −7.0 points (P = .018).
This improvement persisted for 2 months following study conclusion, with more pronounced improvement from baseline after 2 years of drug-free follow-up (−11.5 points).
There were no serious adverse events reported during the study, but 42% of patients treated with systemic sirolimus reported mild skin reactions, such as acne and eczema. Other related adverse events were hypertriglyceridemia (17%), hyperglycemia (17%), and proteinuria (8%).
Compared with clinical outcomes with tofacitinib and tumor necrosis factor (TNF) inhibitors, “the strength of our study lies in the sustained treatment effect after drug withdrawal among all responders. This prolonged effect has not yet been explored with tofacitinib, whereas with TNF inhibitors disease relapse was seen in more than 50% of patients at 3-8 months,” the authors wrote.
The researchers also analyzed participants’ skin biopsies to gain a better understanding of how mTOR inhibition affected granuloma structures. They found that, at baseline, mTOR activity was significantly lower in the fibroblasts of treatment nonresponders than in responders. They speculated that lower expression of mTOR could make these granuloma-associated cells resistant to systemic sirolimus.
These promising findings combine “clinical response with a molecular analysis,” Avrom Caplan, MD, co-director of the Sarcoidosis Program at NYU Langone in New York City, told this news organization. He was not involved with the research. Adding molecular information to clinical outcome data “helps solidify that [the mTOR] pathway has relevance in the sarcoid granuloma formation.”
The study had a limited sample size — a challenge for many clinical trials of rare diseases, Dr. Caplan said. Larger clinical trials are necessary to explore mTOR inhibition in sarcoidosis, both he and the authors agreed. A larger trial could also include greater heterogeneity of patients, including varied sarcoid presentation and demographics, Dr. Caplan noted. In this study, all but one participants were White individuals, and 63% of participants were female.
Larger studies could also address important questions on ideal length of therapy, dosing, and where this therapy “would fall within the therapeutic step ladder,” Dr. Caplan continued.
Whether mTOR inhibition could be effective at treating individuals with sarcoidosis in other organs beyond the skin is also unknown.
“If the pathogenesis of sarcoid granuloma formation does include mTOR upregulation, which they are showing here…then you could hypothesize that, yes, using this therapy could benefit other organs,” he said. “But that has to be investigated in larger trials.”
The study was funded in part by a Vienna Science and Technology Fund project. Several authors report receiving grants from the Austrian Science Fund and one from the Ann Theodore Foundation Breakthrough Sarcoidosis Initiative. Dr. Caplan reported no relevant financial relationships.
A version of this article appeared on Medscape.com .
Sirolimus may be an effective treatment for patients with persistent cutaneous sarcoidosis.
In a small clinical trial, 7 of 10 patients treated with sirolimus via oral solution had improvements in skin lesions after 4 months, which was sustained for up to 2 years after the study concluded.
The results suggested that mechanistic target of rapamycin (mTOR) inhibition is a potential therapeutic avenue for sarcoidosis, which the authors said should be explored in larger clinical trials.
In the past decade, there has been a growing amount of evidence suggesting mTOR’s role in sarcoidosis. In 2017, researchers showed that activation of mTOR in macrophages could cause progressive sarcoidosis in mice. In additional studies, high levels of mTOR activity were detected in human sarcoidosis granulomas in various organs, including the skin, lung, and heart.
Three case reports also documented using the mTOR inhibitor sirolimus to effectively treat systemic sarcoidosis.
“Although all reports observed improvement of the disease following the treatment, no clinical trial investigating the efficacy and safety of sirolimus in patients with sarcoidosis had been published” prior to this study, wrote senior author Georg Stary, MD, of the Medical University of Vienna and the Research Center for Molecular Medicine of the Austrian Academy of Sciences, Vienna, Austria, and colleagues.
The findings were published in the The Lancet Rheumatology.
For the study, researchers recruited 16 individuals with persistent and glucocorticoid-refractory cutaneous sarcoidosis between September 2019 and June 2021. A total of 14 participants were randomly assigned to the topical phase of the study, whereas two immediately received systemic treatment. All treatment was conducted at Vienna General Hospital.
In the placebo-controlled, double-blinded topical treatment arm, patients received either 0.1% topical sirolimus in Vaseline or Vaseline alone (placebo) twice daily for 2 months. After a 1-month washout period, participants were switched to the alternate treatment arm for an additional 2 months.
Following this topical phase and an additional 1-month washout period, all remaining participants received systemic sirolimus via a 1-mg/mL solution, starting with a 6-mg loading dose and continuing with 2 mg once daily for 4 months. The primary outcome was change in Cutaneous Sarcoidosis Activity and Morphology Index (CSAMI) from baseline, with decrease of more than five points representing a response to treatment.
A total of 10 patients completed the trial.
There was no change in CSAMI in either topical treatment groups. In the systemic group, 70% of patients had clinical improvement in skin lesions, with three responders in this group having complete resolution of skin lesions. The median change in CSAMI was −7.0 points (P = .018).
This improvement persisted for 2 months following study conclusion, with more pronounced improvement from baseline after 2 years of drug-free follow-up (−11.5 points).
There were no serious adverse events reported during the study, but 42% of patients treated with systemic sirolimus reported mild skin reactions, such as acne and eczema. Other related adverse events were hypertriglyceridemia (17%), hyperglycemia (17%), and proteinuria (8%).
Compared with clinical outcomes with tofacitinib and tumor necrosis factor (TNF) inhibitors, “the strength of our study lies in the sustained treatment effect after drug withdrawal among all responders. This prolonged effect has not yet been explored with tofacitinib, whereas with TNF inhibitors disease relapse was seen in more than 50% of patients at 3-8 months,” the authors wrote.
The researchers also analyzed participants’ skin biopsies to gain a better understanding of how mTOR inhibition affected granuloma structures. They found that, at baseline, mTOR activity was significantly lower in the fibroblasts of treatment nonresponders than in responders. They speculated that lower expression of mTOR could make these granuloma-associated cells resistant to systemic sirolimus.
These promising findings combine “clinical response with a molecular analysis,” Avrom Caplan, MD, co-director of the Sarcoidosis Program at NYU Langone in New York City, told this news organization. He was not involved with the research. Adding molecular information to clinical outcome data “helps solidify that [the mTOR] pathway has relevance in the sarcoid granuloma formation.”
The study had a limited sample size — a challenge for many clinical trials of rare diseases, Dr. Caplan said. Larger clinical trials are necessary to explore mTOR inhibition in sarcoidosis, both he and the authors agreed. A larger trial could also include greater heterogeneity of patients, including varied sarcoid presentation and demographics, Dr. Caplan noted. In this study, all but one participants were White individuals, and 63% of participants were female.
Larger studies could also address important questions on ideal length of therapy, dosing, and where this therapy “would fall within the therapeutic step ladder,” Dr. Caplan continued.
Whether mTOR inhibition could be effective at treating individuals with sarcoidosis in other organs beyond the skin is also unknown.
“If the pathogenesis of sarcoid granuloma formation does include mTOR upregulation, which they are showing here…then you could hypothesize that, yes, using this therapy could benefit other organs,” he said. “But that has to be investigated in larger trials.”
The study was funded in part by a Vienna Science and Technology Fund project. Several authors report receiving grants from the Austrian Science Fund and one from the Ann Theodore Foundation Breakthrough Sarcoidosis Initiative. Dr. Caplan reported no relevant financial relationships.
A version of this article appeared on Medscape.com .
FROM THE LANCET RHEUMATOLOGY
e-Cigarettes Best Nicotine Gum for Smoking Cessation
UPDATE: On March 29, 2024, the authors of this study published in JAMA Internal Medicine issued a formal retraction of their article. "Unfortunately, we have found significant coding errors that are difficult to rectify," the author wrote. "We also discovered discrepancies in the calculation process that cast doubt on the accuracy and reliability of the reported findings." The CHEST Physician® Editorial Board apologizes for any confusion this may have caused.
TOPLINE:
and as effective as varenicline in achieving sustained abstinence at 6 months, a randomized trial found. Questions about the long-term safety of e-cigarettes remain, however, according to the researchers.
METHODOLOGY:
- The study included 1068 participants in China who were smoking at least 10 cigarettes per day.
- They were randomly assigned to undergo 12 weeks of treatment with a cartridge-based e-cigarette, varenicline, or nicotine chewing gum.
TAKEAWAY:
- At 6 months, the biochemically validated rate of quitting was 15.7% for those who received e-cigarettes, 14.2% for those who received varenicline, and 8.8% for those who chewed nicotine gum.
- At 6 months, 62.8% of participants in the e-cigarette arm were still using the devices, whereas those in the other study arms had not continued their treatments.
- Adverse reactions with e-cigarettes and nicotine chewing gum included irritation of the throat and mouth, which occurred in 7%-8% of participants.
- In the varenicline group, 8.8% experienced nausea.
- No serious adverse events were reported.
IN PRACTICE:
“A moderate approach would be to recommend approved medications as the first step and, if that fails, then inform the patient of the evidence regarding the use of electronic cigarettes as a possible approach, acknowledging all its caveats,” Dorothy K. Hatsukami, PhD, with the University of Minnesota in Minneapolis, and Judith J. Prochaska, PhD, MPH, with Stanford (California) University, wrote in an invited commentary.
SOURCE:
Zhao Liu, PhD, with the China-Japan Friendship Hospital in Beijing, was the corresponding author for the study. The study was published online on January 29, 2024, in JAMA Internal Medicine.
LIMITATIONS:
The trial had an open-label design, so participants’ expectations about their assigned treatment may have influenced the results.
The study did not include participants older than 45 years, so it is unclear how the results apply to older populations.
More studies are needed to see whether continued use of e-cigarettes is beneficial or harmful, the researchers wrote.
Combining forms of nicotine replacement therapy, such as gum plus a patch, may be more effective than a single form, but the trial did not assess a combined approach, the commentary authors noted. The dose of nicotine gum for some participants may have been suboptimal, they added.
DISCLOSURES:
The study was supported by the Scientific Research Project Fund of China-Japan Friendship Hospital. The researchers had no conflict of interest disclosures. Dr. Prochaska disclosed receiving fees from Achieve Life Sciences, OneLeaf, and attorneys who are involved in litigation against tobacco companies.
A version of this article appeared on Medscape.com.
UPDATE: On March 29, 2024, the authors of this study published in JAMA Internal Medicine issued a formal retraction of their article. "Unfortunately, we have found significant coding errors that are difficult to rectify," the author wrote. "We also discovered discrepancies in the calculation process that cast doubt on the accuracy and reliability of the reported findings." The CHEST Physician® Editorial Board apologizes for any confusion this may have caused.
TOPLINE:
and as effective as varenicline in achieving sustained abstinence at 6 months, a randomized trial found. Questions about the long-term safety of e-cigarettes remain, however, according to the researchers.
METHODOLOGY:
- The study included 1068 participants in China who were smoking at least 10 cigarettes per day.
- They were randomly assigned to undergo 12 weeks of treatment with a cartridge-based e-cigarette, varenicline, or nicotine chewing gum.
TAKEAWAY:
- At 6 months, the biochemically validated rate of quitting was 15.7% for those who received e-cigarettes, 14.2% for those who received varenicline, and 8.8% for those who chewed nicotine gum.
- At 6 months, 62.8% of participants in the e-cigarette arm were still using the devices, whereas those in the other study arms had not continued their treatments.
- Adverse reactions with e-cigarettes and nicotine chewing gum included irritation of the throat and mouth, which occurred in 7%-8% of participants.
- In the varenicline group, 8.8% experienced nausea.
- No serious adverse events were reported.
IN PRACTICE:
“A moderate approach would be to recommend approved medications as the first step and, if that fails, then inform the patient of the evidence regarding the use of electronic cigarettes as a possible approach, acknowledging all its caveats,” Dorothy K. Hatsukami, PhD, with the University of Minnesota in Minneapolis, and Judith J. Prochaska, PhD, MPH, with Stanford (California) University, wrote in an invited commentary.
SOURCE:
Zhao Liu, PhD, with the China-Japan Friendship Hospital in Beijing, was the corresponding author for the study. The study was published online on January 29, 2024, in JAMA Internal Medicine.
LIMITATIONS:
The trial had an open-label design, so participants’ expectations about their assigned treatment may have influenced the results.
The study did not include participants older than 45 years, so it is unclear how the results apply to older populations.
More studies are needed to see whether continued use of e-cigarettes is beneficial or harmful, the researchers wrote.
Combining forms of nicotine replacement therapy, such as gum plus a patch, may be more effective than a single form, but the trial did not assess a combined approach, the commentary authors noted. The dose of nicotine gum for some participants may have been suboptimal, they added.
DISCLOSURES:
The study was supported by the Scientific Research Project Fund of China-Japan Friendship Hospital. The researchers had no conflict of interest disclosures. Dr. Prochaska disclosed receiving fees from Achieve Life Sciences, OneLeaf, and attorneys who are involved in litigation against tobacco companies.
A version of this article appeared on Medscape.com.
UPDATE: On March 29, 2024, the authors of this study published in JAMA Internal Medicine issued a formal retraction of their article. "Unfortunately, we have found significant coding errors that are difficult to rectify," the author wrote. "We also discovered discrepancies in the calculation process that cast doubt on the accuracy and reliability of the reported findings." The CHEST Physician® Editorial Board apologizes for any confusion this may have caused.
TOPLINE:
and as effective as varenicline in achieving sustained abstinence at 6 months, a randomized trial found. Questions about the long-term safety of e-cigarettes remain, however, according to the researchers.
METHODOLOGY:
- The study included 1068 participants in China who were smoking at least 10 cigarettes per day.
- They were randomly assigned to undergo 12 weeks of treatment with a cartridge-based e-cigarette, varenicline, or nicotine chewing gum.
TAKEAWAY:
- At 6 months, the biochemically validated rate of quitting was 15.7% for those who received e-cigarettes, 14.2% for those who received varenicline, and 8.8% for those who chewed nicotine gum.
- At 6 months, 62.8% of participants in the e-cigarette arm were still using the devices, whereas those in the other study arms had not continued their treatments.
- Adverse reactions with e-cigarettes and nicotine chewing gum included irritation of the throat and mouth, which occurred in 7%-8% of participants.
- In the varenicline group, 8.8% experienced nausea.
- No serious adverse events were reported.
IN PRACTICE:
“A moderate approach would be to recommend approved medications as the first step and, if that fails, then inform the patient of the evidence regarding the use of electronic cigarettes as a possible approach, acknowledging all its caveats,” Dorothy K. Hatsukami, PhD, with the University of Minnesota in Minneapolis, and Judith J. Prochaska, PhD, MPH, with Stanford (California) University, wrote in an invited commentary.
SOURCE:
Zhao Liu, PhD, with the China-Japan Friendship Hospital in Beijing, was the corresponding author for the study. The study was published online on January 29, 2024, in JAMA Internal Medicine.
LIMITATIONS:
The trial had an open-label design, so participants’ expectations about their assigned treatment may have influenced the results.
The study did not include participants older than 45 years, so it is unclear how the results apply to older populations.
More studies are needed to see whether continued use of e-cigarettes is beneficial or harmful, the researchers wrote.
Combining forms of nicotine replacement therapy, such as gum plus a patch, may be more effective than a single form, but the trial did not assess a combined approach, the commentary authors noted. The dose of nicotine gum for some participants may have been suboptimal, they added.
DISCLOSURES:
The study was supported by the Scientific Research Project Fund of China-Japan Friendship Hospital. The researchers had no conflict of interest disclosures. Dr. Prochaska disclosed receiving fees from Achieve Life Sciences, OneLeaf, and attorneys who are involved in litigation against tobacco companies.
A version of this article appeared on Medscape.com.
Robitussin Cough Syrup Recalled Nationwide Due to Fungus Concerns
The company that makes Robitussin syrups did not specify which microorganisms may be in the products. The recall announcement from the global consumer health products company Haleon stated that the contamination could lead to fungal infections or the presence of fungi or yeasts in a person’s blood. So far, the company has not received any reports of people being sickened by the recalled products.
The recall applies to bottles of Robitussin Honey CF Max Day and Robitussin Honey CF Max Nighttime. Both varieties are for adults. Affected products were sold nationwide and have specific lot numbers printed at the bottom of the back of the bottles. Consumers can view the lot numbers on the FDA’s recall webpage.
People with weakened immune systems have a higher risk of life-threatening health problems due to the cough syrup, the company warned.
“In non-immunocompromised consumers, the population most likely to use the product, life-threatening infections are not likely to occur,” the recall notice from Haleon stated. “However, the occurrence of an infection that may necessitate medical intervention cannot be completely ruled out.”
People who have affected products should stop using them immediately. The company asked that anyone with the products email Haleon at mystory.us@haleon.com, or call the company at 800-245-1040 Monday through Friday from 8 a.m. to 6 p.m. Eastern time.
A version of this article appeared on WebMD.com.
The company that makes Robitussin syrups did not specify which microorganisms may be in the products. The recall announcement from the global consumer health products company Haleon stated that the contamination could lead to fungal infections or the presence of fungi or yeasts in a person’s blood. So far, the company has not received any reports of people being sickened by the recalled products.
The recall applies to bottles of Robitussin Honey CF Max Day and Robitussin Honey CF Max Nighttime. Both varieties are for adults. Affected products were sold nationwide and have specific lot numbers printed at the bottom of the back of the bottles. Consumers can view the lot numbers on the FDA’s recall webpage.
People with weakened immune systems have a higher risk of life-threatening health problems due to the cough syrup, the company warned.
“In non-immunocompromised consumers, the population most likely to use the product, life-threatening infections are not likely to occur,” the recall notice from Haleon stated. “However, the occurrence of an infection that may necessitate medical intervention cannot be completely ruled out.”
People who have affected products should stop using them immediately. The company asked that anyone with the products email Haleon at mystory.us@haleon.com, or call the company at 800-245-1040 Monday through Friday from 8 a.m. to 6 p.m. Eastern time.
A version of this article appeared on WebMD.com.
The company that makes Robitussin syrups did not specify which microorganisms may be in the products. The recall announcement from the global consumer health products company Haleon stated that the contamination could lead to fungal infections or the presence of fungi or yeasts in a person’s blood. So far, the company has not received any reports of people being sickened by the recalled products.
The recall applies to bottles of Robitussin Honey CF Max Day and Robitussin Honey CF Max Nighttime. Both varieties are for adults. Affected products were sold nationwide and have specific lot numbers printed at the bottom of the back of the bottles. Consumers can view the lot numbers on the FDA’s recall webpage.
People with weakened immune systems have a higher risk of life-threatening health problems due to the cough syrup, the company warned.
“In non-immunocompromised consumers, the population most likely to use the product, life-threatening infections are not likely to occur,” the recall notice from Haleon stated. “However, the occurrence of an infection that may necessitate medical intervention cannot be completely ruled out.”
People who have affected products should stop using them immediately. The company asked that anyone with the products email Haleon at mystory.us@haleon.com, or call the company at 800-245-1040 Monday through Friday from 8 a.m. to 6 p.m. Eastern time.
A version of this article appeared on WebMD.com.

