User login
Active Comparator Trial Designs Used to Promote Development of Innovative New Medications
Spending on medications is expected to grow from $344 billion in 2018 to $420 billion in 2023, largely driven by the introduction of new branded drugs.1 These costs place substantial financial burden on patients, with nearly 30% of patients not taking their prescriptions as directed because of costs. Although many new medications have transformed how we care for patients, others may not offer meaningful benefit over existing less-costly alternatives that are supported by declining effect sizes of conventional placebo-controlled trials.2 Most medications are approved based on placebo-controlled trial data that does not include an arm comparing the new drug to standard of care, leaving clinicians and patients unable to make meaningful comparisons when deciding on the most appropriate or cost-effective treatment. We consider ways in which clinicians, patients, payers, and regulators could compel more meaningful trials from industry.
Although we often look to the US Food and Drug Administration (FDA) to ensure rigorous and appropriate testing of new medications, the primary mission of the FDA is to ensure efficacy and safety. As a result, pharmaceutical companies seeking approval in the United States have little incentive to go beyond providing the minimal level of evidence required: placebo-controlled randomized trials. Although these trials provide important data on whether a treatment works and its associated risks, they do not provide data on comparative effectiveness. When relevant inexpensive medications are already on the market for the same indication, these placebo-controlled trials provide inadequate evidence to guide clinical decision-making. This issue is particularly relevant in dermatology given how easily topical medications can be combined or reformulated to pursue additional market exclusivity. The addition of an active comparator arm represents an important opportunity to improve the value of these studies.
In the pivotal trials of clindamycin phosphate 1.2%–benzoyl peroxide 2.5% gel for the treatment of acne, the experimental group was not only compared to vehicle but also the active comparator arms of clindamycin alone and benzoyl peroxide alone. The mean percentage change in total lesions was 47.9% with clindamycin phosphate 1.2%–benzoyl peroxide 2.5% gel, 41.6% with the active comparator arm of benzoyl peroxide alone, 40.4% with the active comparator arm of clindamycin alone, and 26.2% for vehicle.3 With these data in mind, clinicians and patients can decide whether the additional benefit of this new product over benzoyl peroxide alone is worth the increased cost.
In contrast, the trials of dapsone gel 7.5% for the treatment of acne did not include an active comparator. The mean percentage change in total lesions was 48.9% for dapsone gel and 43.2% for vehicle.4 Given these data, it is possible that dapsone gel may be no more effective, or possibly less effective, than alternatives such as benzoyl peroxide or other topical antibiotics. Nevertheless, dapsone annual sales were more than $200 million in 2016,5 suggesting that effectively marketed new products can achieve high sales even without convincing evidence of their value compared to standard of care. Although dapsone may be a useful treatment, we cannot effectively make patient-centered clinical decisions given the lack of an active comparator trial design.
This issue is not limited to acne. Phase 3 trials of halobetasol propionate foam 0.05% for psoriasis and crisaborole for atopic dermatitis also did not include an active comparator arm.6,7 Given that topical steroids—and calcineurin inhibitors for atopic dermatitis—are mainstays of treatment for each condition, it is difficult to determine whether these new treatments offer meaningful advantages over existing options and how to incorporate them into our management strategies.
Unfortunately, expensive new medications that are adopted without convincing evidence of their benefit above standard of care can put patients at risk for financial toxicity, either directly through higher out-of-pocket costs or indirectly through higher premiums. Given the impact of rising medication costs on clinicians, patients, and payers, we propose several approaches these stakeholders could adopt to encourage the use of active comparator trial designs.
Clinicians and patients can encourage these trials by remaining skeptical of new treatments that were only compared to vehicle or placebo. Because new medications often are more expensive, clinicians and patients could avoid using these treatments without evidence of either increased efficacy or improved safety and tolerability. In addition, health care institutions should consider reducing pharmaceutical representatives’ access to clinicians to encourage treatment decisions based on the published literature and comparative effectiveness data rather than marketing.
Payers, such as Medicare, also could play a role by requiring active comparator trials for coverage of new medications, particularly when there are already other effective treatments available or other medications in the same class. Payers also could give preferred coverage tier or step therapy status to medications that demonstrate value over existing options.
Although regulatory approaches to increase use of active comparator designs may be more politically challenging to introduce, these options would be more administratively robust. The FDA or a novel regulatory body could require that new treatments demonstrate value in addition to safety and efficacy. This approach would be similar to the role of The National Institute for Health and Care Excellence in the United Kingdom or the recommendations of the European Medicines Agency. Such a group also could provide independent adjudication to ensure appropriate selection of a relevant active comparator. Another approach would be to give extended market exclusivity to medications that are approved based on trials including an additional active comparator arm, an approach used by the European Medicines Agency.
Any approach that encourages increased use of active comparator trials is not without potential downsides. It will be important to avoid unintended consequences of reduced research for rare diseases with smaller markets that may not be able to support the increased cost of these trials. As a result, it would be reasonable to forgo active comparator designs for mediations indicated for rare and orphan diseases or for medications with novel mechanisms of action.
Another argument against including an active comparator arm is that it may stifle innovation by driving up the cost of conducting trials; however, if a product is so marginally innovative that it cannot demonstrate superior safety or efficacy to an existing product, such a new treatment may not be worth the increased cost. In addition, patients provide a notable contribution by participating in these trials, and it is important to ensure that their efforts result in the highest-quality data possible. Furthermore, given the adverse physical and psychosocial impact of a wide variety of dermatologic diseases, the inclusion of an active comparator arm reduces the likelihood that patients will receive placebo, which will make these trials more ethical when effective treatments are available.8 By raising the bar, we can encourage pharmaceutical companies to pursue novel approaches that are more likely to have a revolutionary impact rather than minor modifications or formulations that offer little to no benefit at substantially increased cost.
Although some recent clinical trials in dermatology have included active comparators, many new medications continue to be introduced without any evidence of how they compare to existing standards of care. Until clinicians, patients, payers, and regulators demand that pharmaceutical companies conduct the necessary trials to not only demonstrate whether a treatment is effective and safe but also how it provides value, there will be continued introduction of marginal innovations rather than revolutionary treatments that improve patients’ lives. The next time a new medication is approved, as clinicians, patients, and payers, we must ask ourselves, is this treatment worth it?
- Aitken M, Kleinrock M. Medicine Use and Spending in the U.S.: A Review of 2018 and Outlook to 2023. IQVIA Institute for Human Data Science. https://www.iqvia.com/insights/the-iqvia-institute/reports/medicine-use-and-spending-in-the-us-a-review-of-2018-and-outlook-to-2023. Published May 9, 2019. Accessed August 15, 2020.
- Olfson M, Marcus SC. Decline in placebo-controlled trial results suggests new directions for comparative effectiveness research. Health Aff Proj Hope. 2019;32:1116-1125.
- Thiboutot D, Zaenglein A, Weiss J, et al. An aqueous gel fixed combination of clindamycin phosphate 1.2% and benzoyl peroxide 2.5% for the once-daily treatment of moderate to severe acne vulgaris: assessment of efficacy and safety in 2813 patients. J Am Acad Dermatol. 2008;59:792-800.
- Eichenfield LF, Lain T, Frankel EH, et al. Efficacy and safety of once-daily dapsone gel, 7.5% for treatment of adolescents and adults with acne vulgaris: second of two identically designed, large, multicenter, randomized, vehicle-controlled trials. J Drugs Dermatol. 2016;15:962-969.
- Allergan. 2017 Form 10-K. https://www.abbvie.com/content/dam/abbvie-dotcom/uploads/PDFs/allergan/allergan-annual-report-form-10K-123117.pdf. Accessed August 19, 2020.
- Paller AS, Tom WL, Lebwohl MG, et al. Efficacy and safety of crisaborole ointment, a novel, nonsteroidal phosphodiesterase 4 (PDE4) inhibitor for the topical treatment of atopic dermatitis (AD) in children and adults. J Am Acad Dermatol. 2016;75:494-503.e6.
- Bhatia N, Stein Gold L, Kircik LH, et al. Two multicenter, randomized, double-blind, parallel group comparison studies of a novel foam formulation of halobetasol propionate, 0.05% vs its vehicle in adult subjects with plaque psoriasis. J Drugs Dermatol. 2019;18:790-796.
- Temple R, Ellenberg SS. Placebo-controlled trials and active-control trials in the evaluation of new treatments. part 1: ethical and scientific issues. Ann Intern Med. 2000;133:455-463.
Spending on medications is expected to grow from $344 billion in 2018 to $420 billion in 2023, largely driven by the introduction of new branded drugs.1 These costs place substantial financial burden on patients, with nearly 30% of patients not taking their prescriptions as directed because of costs. Although many new medications have transformed how we care for patients, others may not offer meaningful benefit over existing less-costly alternatives that are supported by declining effect sizes of conventional placebo-controlled trials.2 Most medications are approved based on placebo-controlled trial data that does not include an arm comparing the new drug to standard of care, leaving clinicians and patients unable to make meaningful comparisons when deciding on the most appropriate or cost-effective treatment. We consider ways in which clinicians, patients, payers, and regulators could compel more meaningful trials from industry.
Although we often look to the US Food and Drug Administration (FDA) to ensure rigorous and appropriate testing of new medications, the primary mission of the FDA is to ensure efficacy and safety. As a result, pharmaceutical companies seeking approval in the United States have little incentive to go beyond providing the minimal level of evidence required: placebo-controlled randomized trials. Although these trials provide important data on whether a treatment works and its associated risks, they do not provide data on comparative effectiveness. When relevant inexpensive medications are already on the market for the same indication, these placebo-controlled trials provide inadequate evidence to guide clinical decision-making. This issue is particularly relevant in dermatology given how easily topical medications can be combined or reformulated to pursue additional market exclusivity. The addition of an active comparator arm represents an important opportunity to improve the value of these studies.
In the pivotal trials of clindamycin phosphate 1.2%–benzoyl peroxide 2.5% gel for the treatment of acne, the experimental group was not only compared to vehicle but also the active comparator arms of clindamycin alone and benzoyl peroxide alone. The mean percentage change in total lesions was 47.9% with clindamycin phosphate 1.2%–benzoyl peroxide 2.5% gel, 41.6% with the active comparator arm of benzoyl peroxide alone, 40.4% with the active comparator arm of clindamycin alone, and 26.2% for vehicle.3 With these data in mind, clinicians and patients can decide whether the additional benefit of this new product over benzoyl peroxide alone is worth the increased cost.
In contrast, the trials of dapsone gel 7.5% for the treatment of acne did not include an active comparator. The mean percentage change in total lesions was 48.9% for dapsone gel and 43.2% for vehicle.4 Given these data, it is possible that dapsone gel may be no more effective, or possibly less effective, than alternatives such as benzoyl peroxide or other topical antibiotics. Nevertheless, dapsone annual sales were more than $200 million in 2016,5 suggesting that effectively marketed new products can achieve high sales even without convincing evidence of their value compared to standard of care. Although dapsone may be a useful treatment, we cannot effectively make patient-centered clinical decisions given the lack of an active comparator trial design.
This issue is not limited to acne. Phase 3 trials of halobetasol propionate foam 0.05% for psoriasis and crisaborole for atopic dermatitis also did not include an active comparator arm.6,7 Given that topical steroids—and calcineurin inhibitors for atopic dermatitis—are mainstays of treatment for each condition, it is difficult to determine whether these new treatments offer meaningful advantages over existing options and how to incorporate them into our management strategies.
Unfortunately, expensive new medications that are adopted without convincing evidence of their benefit above standard of care can put patients at risk for financial toxicity, either directly through higher out-of-pocket costs or indirectly through higher premiums. Given the impact of rising medication costs on clinicians, patients, and payers, we propose several approaches these stakeholders could adopt to encourage the use of active comparator trial designs.
Clinicians and patients can encourage these trials by remaining skeptical of new treatments that were only compared to vehicle or placebo. Because new medications often are more expensive, clinicians and patients could avoid using these treatments without evidence of either increased efficacy or improved safety and tolerability. In addition, health care institutions should consider reducing pharmaceutical representatives’ access to clinicians to encourage treatment decisions based on the published literature and comparative effectiveness data rather than marketing.
Payers, such as Medicare, also could play a role by requiring active comparator trials for coverage of new medications, particularly when there are already other effective treatments available or other medications in the same class. Payers also could give preferred coverage tier or step therapy status to medications that demonstrate value over existing options.
Although regulatory approaches to increase use of active comparator designs may be more politically challenging to introduce, these options would be more administratively robust. The FDA or a novel regulatory body could require that new treatments demonstrate value in addition to safety and efficacy. This approach would be similar to the role of The National Institute for Health and Care Excellence in the United Kingdom or the recommendations of the European Medicines Agency. Such a group also could provide independent adjudication to ensure appropriate selection of a relevant active comparator. Another approach would be to give extended market exclusivity to medications that are approved based on trials including an additional active comparator arm, an approach used by the European Medicines Agency.
Any approach that encourages increased use of active comparator trials is not without potential downsides. It will be important to avoid unintended consequences of reduced research for rare diseases with smaller markets that may not be able to support the increased cost of these trials. As a result, it would be reasonable to forgo active comparator designs for mediations indicated for rare and orphan diseases or for medications with novel mechanisms of action.
Another argument against including an active comparator arm is that it may stifle innovation by driving up the cost of conducting trials; however, if a product is so marginally innovative that it cannot demonstrate superior safety or efficacy to an existing product, such a new treatment may not be worth the increased cost. In addition, patients provide a notable contribution by participating in these trials, and it is important to ensure that their efforts result in the highest-quality data possible. Furthermore, given the adverse physical and psychosocial impact of a wide variety of dermatologic diseases, the inclusion of an active comparator arm reduces the likelihood that patients will receive placebo, which will make these trials more ethical when effective treatments are available.8 By raising the bar, we can encourage pharmaceutical companies to pursue novel approaches that are more likely to have a revolutionary impact rather than minor modifications or formulations that offer little to no benefit at substantially increased cost.
Although some recent clinical trials in dermatology have included active comparators, many new medications continue to be introduced without any evidence of how they compare to existing standards of care. Until clinicians, patients, payers, and regulators demand that pharmaceutical companies conduct the necessary trials to not only demonstrate whether a treatment is effective and safe but also how it provides value, there will be continued introduction of marginal innovations rather than revolutionary treatments that improve patients’ lives. The next time a new medication is approved, as clinicians, patients, and payers, we must ask ourselves, is this treatment worth it?
Spending on medications is expected to grow from $344 billion in 2018 to $420 billion in 2023, largely driven by the introduction of new branded drugs.1 These costs place substantial financial burden on patients, with nearly 30% of patients not taking their prescriptions as directed because of costs. Although many new medications have transformed how we care for patients, others may not offer meaningful benefit over existing less-costly alternatives that are supported by declining effect sizes of conventional placebo-controlled trials.2 Most medications are approved based on placebo-controlled trial data that does not include an arm comparing the new drug to standard of care, leaving clinicians and patients unable to make meaningful comparisons when deciding on the most appropriate or cost-effective treatment. We consider ways in which clinicians, patients, payers, and regulators could compel more meaningful trials from industry.
Although we often look to the US Food and Drug Administration (FDA) to ensure rigorous and appropriate testing of new medications, the primary mission of the FDA is to ensure efficacy and safety. As a result, pharmaceutical companies seeking approval in the United States have little incentive to go beyond providing the minimal level of evidence required: placebo-controlled randomized trials. Although these trials provide important data on whether a treatment works and its associated risks, they do not provide data on comparative effectiveness. When relevant inexpensive medications are already on the market for the same indication, these placebo-controlled trials provide inadequate evidence to guide clinical decision-making. This issue is particularly relevant in dermatology given how easily topical medications can be combined or reformulated to pursue additional market exclusivity. The addition of an active comparator arm represents an important opportunity to improve the value of these studies.
In the pivotal trials of clindamycin phosphate 1.2%–benzoyl peroxide 2.5% gel for the treatment of acne, the experimental group was not only compared to vehicle but also the active comparator arms of clindamycin alone and benzoyl peroxide alone. The mean percentage change in total lesions was 47.9% with clindamycin phosphate 1.2%–benzoyl peroxide 2.5% gel, 41.6% with the active comparator arm of benzoyl peroxide alone, 40.4% with the active comparator arm of clindamycin alone, and 26.2% for vehicle.3 With these data in mind, clinicians and patients can decide whether the additional benefit of this new product over benzoyl peroxide alone is worth the increased cost.
In contrast, the trials of dapsone gel 7.5% for the treatment of acne did not include an active comparator. The mean percentage change in total lesions was 48.9% for dapsone gel and 43.2% for vehicle.4 Given these data, it is possible that dapsone gel may be no more effective, or possibly less effective, than alternatives such as benzoyl peroxide or other topical antibiotics. Nevertheless, dapsone annual sales were more than $200 million in 2016,5 suggesting that effectively marketed new products can achieve high sales even without convincing evidence of their value compared to standard of care. Although dapsone may be a useful treatment, we cannot effectively make patient-centered clinical decisions given the lack of an active comparator trial design.
This issue is not limited to acne. Phase 3 trials of halobetasol propionate foam 0.05% for psoriasis and crisaborole for atopic dermatitis also did not include an active comparator arm.6,7 Given that topical steroids—and calcineurin inhibitors for atopic dermatitis—are mainstays of treatment for each condition, it is difficult to determine whether these new treatments offer meaningful advantages over existing options and how to incorporate them into our management strategies.
Unfortunately, expensive new medications that are adopted without convincing evidence of their benefit above standard of care can put patients at risk for financial toxicity, either directly through higher out-of-pocket costs or indirectly through higher premiums. Given the impact of rising medication costs on clinicians, patients, and payers, we propose several approaches these stakeholders could adopt to encourage the use of active comparator trial designs.
Clinicians and patients can encourage these trials by remaining skeptical of new treatments that were only compared to vehicle or placebo. Because new medications often are more expensive, clinicians and patients could avoid using these treatments without evidence of either increased efficacy or improved safety and tolerability. In addition, health care institutions should consider reducing pharmaceutical representatives’ access to clinicians to encourage treatment decisions based on the published literature and comparative effectiveness data rather than marketing.
Payers, such as Medicare, also could play a role by requiring active comparator trials for coverage of new medications, particularly when there are already other effective treatments available or other medications in the same class. Payers also could give preferred coverage tier or step therapy status to medications that demonstrate value over existing options.
Although regulatory approaches to increase use of active comparator designs may be more politically challenging to introduce, these options would be more administratively robust. The FDA or a novel regulatory body could require that new treatments demonstrate value in addition to safety and efficacy. This approach would be similar to the role of The National Institute for Health and Care Excellence in the United Kingdom or the recommendations of the European Medicines Agency. Such a group also could provide independent adjudication to ensure appropriate selection of a relevant active comparator. Another approach would be to give extended market exclusivity to medications that are approved based on trials including an additional active comparator arm, an approach used by the European Medicines Agency.
Any approach that encourages increased use of active comparator trials is not without potential downsides. It will be important to avoid unintended consequences of reduced research for rare diseases with smaller markets that may not be able to support the increased cost of these trials. As a result, it would be reasonable to forgo active comparator designs for mediations indicated for rare and orphan diseases or for medications with novel mechanisms of action.
Another argument against including an active comparator arm is that it may stifle innovation by driving up the cost of conducting trials; however, if a product is so marginally innovative that it cannot demonstrate superior safety or efficacy to an existing product, such a new treatment may not be worth the increased cost. In addition, patients provide a notable contribution by participating in these trials, and it is important to ensure that their efforts result in the highest-quality data possible. Furthermore, given the adverse physical and psychosocial impact of a wide variety of dermatologic diseases, the inclusion of an active comparator arm reduces the likelihood that patients will receive placebo, which will make these trials more ethical when effective treatments are available.8 By raising the bar, we can encourage pharmaceutical companies to pursue novel approaches that are more likely to have a revolutionary impact rather than minor modifications or formulations that offer little to no benefit at substantially increased cost.
Although some recent clinical trials in dermatology have included active comparators, many new medications continue to be introduced without any evidence of how they compare to existing standards of care. Until clinicians, patients, payers, and regulators demand that pharmaceutical companies conduct the necessary trials to not only demonstrate whether a treatment is effective and safe but also how it provides value, there will be continued introduction of marginal innovations rather than revolutionary treatments that improve patients’ lives. The next time a new medication is approved, as clinicians, patients, and payers, we must ask ourselves, is this treatment worth it?
- Aitken M, Kleinrock M. Medicine Use and Spending in the U.S.: A Review of 2018 and Outlook to 2023. IQVIA Institute for Human Data Science. https://www.iqvia.com/insights/the-iqvia-institute/reports/medicine-use-and-spending-in-the-us-a-review-of-2018-and-outlook-to-2023. Published May 9, 2019. Accessed August 15, 2020.
- Olfson M, Marcus SC. Decline in placebo-controlled trial results suggests new directions for comparative effectiveness research. Health Aff Proj Hope. 2019;32:1116-1125.
- Thiboutot D, Zaenglein A, Weiss J, et al. An aqueous gel fixed combination of clindamycin phosphate 1.2% and benzoyl peroxide 2.5% for the once-daily treatment of moderate to severe acne vulgaris: assessment of efficacy and safety in 2813 patients. J Am Acad Dermatol. 2008;59:792-800.
- Eichenfield LF, Lain T, Frankel EH, et al. Efficacy and safety of once-daily dapsone gel, 7.5% for treatment of adolescents and adults with acne vulgaris: second of two identically designed, large, multicenter, randomized, vehicle-controlled trials. J Drugs Dermatol. 2016;15:962-969.
- Allergan. 2017 Form 10-K. https://www.abbvie.com/content/dam/abbvie-dotcom/uploads/PDFs/allergan/allergan-annual-report-form-10K-123117.pdf. Accessed August 19, 2020.
- Paller AS, Tom WL, Lebwohl MG, et al. Efficacy and safety of crisaborole ointment, a novel, nonsteroidal phosphodiesterase 4 (PDE4) inhibitor for the topical treatment of atopic dermatitis (AD) in children and adults. J Am Acad Dermatol. 2016;75:494-503.e6.
- Bhatia N, Stein Gold L, Kircik LH, et al. Two multicenter, randomized, double-blind, parallel group comparison studies of a novel foam formulation of halobetasol propionate, 0.05% vs its vehicle in adult subjects with plaque psoriasis. J Drugs Dermatol. 2019;18:790-796.
- Temple R, Ellenberg SS. Placebo-controlled trials and active-control trials in the evaluation of new treatments. part 1: ethical and scientific issues. Ann Intern Med. 2000;133:455-463.
- Aitken M, Kleinrock M. Medicine Use and Spending in the U.S.: A Review of 2018 and Outlook to 2023. IQVIA Institute for Human Data Science. https://www.iqvia.com/insights/the-iqvia-institute/reports/medicine-use-and-spending-in-the-us-a-review-of-2018-and-outlook-to-2023. Published May 9, 2019. Accessed August 15, 2020.
- Olfson M, Marcus SC. Decline in placebo-controlled trial results suggests new directions for comparative effectiveness research. Health Aff Proj Hope. 2019;32:1116-1125.
- Thiboutot D, Zaenglein A, Weiss J, et al. An aqueous gel fixed combination of clindamycin phosphate 1.2% and benzoyl peroxide 2.5% for the once-daily treatment of moderate to severe acne vulgaris: assessment of efficacy and safety in 2813 patients. J Am Acad Dermatol. 2008;59:792-800.
- Eichenfield LF, Lain T, Frankel EH, et al. Efficacy and safety of once-daily dapsone gel, 7.5% for treatment of adolescents and adults with acne vulgaris: second of two identically designed, large, multicenter, randomized, vehicle-controlled trials. J Drugs Dermatol. 2016;15:962-969.
- Allergan. 2017 Form 10-K. https://www.abbvie.com/content/dam/abbvie-dotcom/uploads/PDFs/allergan/allergan-annual-report-form-10K-123117.pdf. Accessed August 19, 2020.
- Paller AS, Tom WL, Lebwohl MG, et al. Efficacy and safety of crisaborole ointment, a novel, nonsteroidal phosphodiesterase 4 (PDE4) inhibitor for the topical treatment of atopic dermatitis (AD) in children and adults. J Am Acad Dermatol. 2016;75:494-503.e6.
- Bhatia N, Stein Gold L, Kircik LH, et al. Two multicenter, randomized, double-blind, parallel group comparison studies of a novel foam formulation of halobetasol propionate, 0.05% vs its vehicle in adult subjects with plaque psoriasis. J Drugs Dermatol. 2019;18:790-796.
- Temple R, Ellenberg SS. Placebo-controlled trials and active-control trials in the evaluation of new treatments. part 1: ethical and scientific issues. Ann Intern Med. 2000;133:455-463.
Practice Points
- When evaluating a new treatment, it is important to consider not only whether it is effective but also whether it provides additional value compared to existing treatment options.
- Encouraging active comparator trials will provide clinicians and patients with important data to guide decision-making regarding the most appropriate treatment options.
Review finds evidence for beta-blockers for some rosacea symptoms
, while at the same time underscoring the paucity of evidence supporting their use, investigators reported.
“The evidence was highest for carvedilol and propranolol, two nonselective beta-blockers,” wrote the authors of the review, Jade G.M. Logger, MD, of the department of dermatology, Radboud University Medical Center in Nijmegen, the Netherlands, and coauthors. Their review is in the Journal of the American Academy of Dermatology.
The systematic review included a case control study of 53,927 patients and an equal number of controls that evaluated beta-blockers in general, but the remaining studies and case reports included only 106 patients in total. The largest was a prospective cohort study of propranolol in 63 patients. Other studies included a 15-patient randomized clinical trial of nadolol published 31 years ago and three single-patient case reports.
The studies included patients with a history of failed therapies; only a small number of beta-blockers were evaluated. Outcomes reported in the studies varied widely, which ruled out doing a meta-analysis. “Erythema and flushing were assessed by using a wide spectrum of mostly subjective clinical and patient-based scores, and method standardization was often missing,” the researchers stated.
“Most studies showed improved erythema and flushing after initiation of oral beta-blockers,” Dr. Logger and colleagues wrote. Treatment of facial erythema and flushing remains a clinical challenge despite approved therapies, for which poor response and reactivation are common. “Diminishing erythema and flushing in rosacea is challenging because it hardly responds to conventional anti-inflammatory treatment,” they noted.
“The study adds no new evidence to support the use of beta-blockers,” Diane M. Thiboutot, MD, professor of dermatology at Penn State University, Hershey, said in an interview. “As the authors point out, the nine studies reviewed were of low quality with a variety of outcome measures that precluded generation of a meta-analysis, which would have represented new information.”
Dr. Thiboutot is lead author of a 2019 update of management options for rosacea published by the National Rosacea Society Expert Committee last year.. Beta blockers are among the drugs that are sometimes prescribed off label to help rosacea-associated flushing, along with nonsteroidal anti-inflammatory drugs, antihistamines, and clonidine, according to the update.
Dr. Logger and coauthors noted that beta-blockers come with risks, and can aggravate asthma and psoriasis and are contraindicated in patients with heart failure, cardiogenic shock, and other cardiovascular diseases, along with hyperactive airway and Raynaud’s disease. “It is important to monitor patients for adverse effects, especially blood pressure and heart rate,” they stated. Carvedilol and propranolol may have more antioxidant and anti-inflammatory properties than other nonselective beta-blockers that may curtail rosacea manifestations, they wrote.
They called for large, prospective clinical trials to more accurately assess the efficacy of beta-blockers in rosacea patients. “Researchers should further focus on the determination of the optimal dosage, treatment duration, and long-term therapeutic effects for adequate treatment of erythema and flushing in rosacea,” they said.
Getting those trials is challenging, Dr. Thiboutot said. “Objective and even subjective measurement of transient and persistent facial erythema is extremely challenging, particularly in the setting of a prospective clinical trial.” The trials would have to control for a number of variables, including room conditions, patient diet, and timing of medication, and large trials require multiple sites,” which could add to the variability of the data,” she said in the interview. Funding such trials would be difficult because adding an indication for rosacea-related symptoms would have limited commercial potential, she added.
Nonetheless, the studies would be welcome, Dr. Thiboutot said. “If standardized outcome measures for facial erythema were to be developed, a study would be more feasible.”
Dr. Logger disclosed financial relationships with Galderma, AbbVie, Novartis, Janssen, and LEO Pharma; one author disclosed conducting clinical trials for AbbVie and Novartis; the third author disclosed relationships with Galderma, Cutanea Life Sciences, AbbVie, Novartis, and Janssen, with fees paid to his institution. Dr. Thiboutot disclosed a financial relationship with Galderma.
SOURCE: Logger JGM et al. J Am Acad Dermatol. 2020 Oct;83(4):1088-97.
, while at the same time underscoring the paucity of evidence supporting their use, investigators reported.
“The evidence was highest for carvedilol and propranolol, two nonselective beta-blockers,” wrote the authors of the review, Jade G.M. Logger, MD, of the department of dermatology, Radboud University Medical Center in Nijmegen, the Netherlands, and coauthors. Their review is in the Journal of the American Academy of Dermatology.
The systematic review included a case control study of 53,927 patients and an equal number of controls that evaluated beta-blockers in general, but the remaining studies and case reports included only 106 patients in total. The largest was a prospective cohort study of propranolol in 63 patients. Other studies included a 15-patient randomized clinical trial of nadolol published 31 years ago and three single-patient case reports.
The studies included patients with a history of failed therapies; only a small number of beta-blockers were evaluated. Outcomes reported in the studies varied widely, which ruled out doing a meta-analysis. “Erythema and flushing were assessed by using a wide spectrum of mostly subjective clinical and patient-based scores, and method standardization was often missing,” the researchers stated.
“Most studies showed improved erythema and flushing after initiation of oral beta-blockers,” Dr. Logger and colleagues wrote. Treatment of facial erythema and flushing remains a clinical challenge despite approved therapies, for which poor response and reactivation are common. “Diminishing erythema and flushing in rosacea is challenging because it hardly responds to conventional anti-inflammatory treatment,” they noted.
“The study adds no new evidence to support the use of beta-blockers,” Diane M. Thiboutot, MD, professor of dermatology at Penn State University, Hershey, said in an interview. “As the authors point out, the nine studies reviewed were of low quality with a variety of outcome measures that precluded generation of a meta-analysis, which would have represented new information.”
Dr. Thiboutot is lead author of a 2019 update of management options for rosacea published by the National Rosacea Society Expert Committee last year.. Beta blockers are among the drugs that are sometimes prescribed off label to help rosacea-associated flushing, along with nonsteroidal anti-inflammatory drugs, antihistamines, and clonidine, according to the update.
Dr. Logger and coauthors noted that beta-blockers come with risks, and can aggravate asthma and psoriasis and are contraindicated in patients with heart failure, cardiogenic shock, and other cardiovascular diseases, along with hyperactive airway and Raynaud’s disease. “It is important to monitor patients for adverse effects, especially blood pressure and heart rate,” they stated. Carvedilol and propranolol may have more antioxidant and anti-inflammatory properties than other nonselective beta-blockers that may curtail rosacea manifestations, they wrote.
They called for large, prospective clinical trials to more accurately assess the efficacy of beta-blockers in rosacea patients. “Researchers should further focus on the determination of the optimal dosage, treatment duration, and long-term therapeutic effects for adequate treatment of erythema and flushing in rosacea,” they said.
Getting those trials is challenging, Dr. Thiboutot said. “Objective and even subjective measurement of transient and persistent facial erythema is extremely challenging, particularly in the setting of a prospective clinical trial.” The trials would have to control for a number of variables, including room conditions, patient diet, and timing of medication, and large trials require multiple sites,” which could add to the variability of the data,” she said in the interview. Funding such trials would be difficult because adding an indication for rosacea-related symptoms would have limited commercial potential, she added.
Nonetheless, the studies would be welcome, Dr. Thiboutot said. “If standardized outcome measures for facial erythema were to be developed, a study would be more feasible.”
Dr. Logger disclosed financial relationships with Galderma, AbbVie, Novartis, Janssen, and LEO Pharma; one author disclosed conducting clinical trials for AbbVie and Novartis; the third author disclosed relationships with Galderma, Cutanea Life Sciences, AbbVie, Novartis, and Janssen, with fees paid to his institution. Dr. Thiboutot disclosed a financial relationship with Galderma.
SOURCE: Logger JGM et al. J Am Acad Dermatol. 2020 Oct;83(4):1088-97.
, while at the same time underscoring the paucity of evidence supporting their use, investigators reported.
“The evidence was highest for carvedilol and propranolol, two nonselective beta-blockers,” wrote the authors of the review, Jade G.M. Logger, MD, of the department of dermatology, Radboud University Medical Center in Nijmegen, the Netherlands, and coauthors. Their review is in the Journal of the American Academy of Dermatology.
The systematic review included a case control study of 53,927 patients and an equal number of controls that evaluated beta-blockers in general, but the remaining studies and case reports included only 106 patients in total. The largest was a prospective cohort study of propranolol in 63 patients. Other studies included a 15-patient randomized clinical trial of nadolol published 31 years ago and three single-patient case reports.
The studies included patients with a history of failed therapies; only a small number of beta-blockers were evaluated. Outcomes reported in the studies varied widely, which ruled out doing a meta-analysis. “Erythema and flushing were assessed by using a wide spectrum of mostly subjective clinical and patient-based scores, and method standardization was often missing,” the researchers stated.
“Most studies showed improved erythema and flushing after initiation of oral beta-blockers,” Dr. Logger and colleagues wrote. Treatment of facial erythema and flushing remains a clinical challenge despite approved therapies, for which poor response and reactivation are common. “Diminishing erythema and flushing in rosacea is challenging because it hardly responds to conventional anti-inflammatory treatment,” they noted.
“The study adds no new evidence to support the use of beta-blockers,” Diane M. Thiboutot, MD, professor of dermatology at Penn State University, Hershey, said in an interview. “As the authors point out, the nine studies reviewed were of low quality with a variety of outcome measures that precluded generation of a meta-analysis, which would have represented new information.”
Dr. Thiboutot is lead author of a 2019 update of management options for rosacea published by the National Rosacea Society Expert Committee last year.. Beta blockers are among the drugs that are sometimes prescribed off label to help rosacea-associated flushing, along with nonsteroidal anti-inflammatory drugs, antihistamines, and clonidine, according to the update.
Dr. Logger and coauthors noted that beta-blockers come with risks, and can aggravate asthma and psoriasis and are contraindicated in patients with heart failure, cardiogenic shock, and other cardiovascular diseases, along with hyperactive airway and Raynaud’s disease. “It is important to monitor patients for adverse effects, especially blood pressure and heart rate,” they stated. Carvedilol and propranolol may have more antioxidant and anti-inflammatory properties than other nonselective beta-blockers that may curtail rosacea manifestations, they wrote.
They called for large, prospective clinical trials to more accurately assess the efficacy of beta-blockers in rosacea patients. “Researchers should further focus on the determination of the optimal dosage, treatment duration, and long-term therapeutic effects for adequate treatment of erythema and flushing in rosacea,” they said.
Getting those trials is challenging, Dr. Thiboutot said. “Objective and even subjective measurement of transient and persistent facial erythema is extremely challenging, particularly in the setting of a prospective clinical trial.” The trials would have to control for a number of variables, including room conditions, patient diet, and timing of medication, and large trials require multiple sites,” which could add to the variability of the data,” she said in the interview. Funding such trials would be difficult because adding an indication for rosacea-related symptoms would have limited commercial potential, she added.
Nonetheless, the studies would be welcome, Dr. Thiboutot said. “If standardized outcome measures for facial erythema were to be developed, a study would be more feasible.”
Dr. Logger disclosed financial relationships with Galderma, AbbVie, Novartis, Janssen, and LEO Pharma; one author disclosed conducting clinical trials for AbbVie and Novartis; the third author disclosed relationships with Galderma, Cutanea Life Sciences, AbbVie, Novartis, and Janssen, with fees paid to his institution. Dr. Thiboutot disclosed a financial relationship with Galderma.
SOURCE: Logger JGM et al. J Am Acad Dermatol. 2020 Oct;83(4):1088-97.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Severe Phymatous Rosacea of the Nose, Cheeks, and Chin Treated With Hydrosurgery
Phymatous rosacea is a rare and severe form of rosacea that manifests as disfiguring soft-tissue hypertrophy and hyperplasia as well as fibrosis of the sebaceous glands. 1 Treatments for phymatous rosacea include pharmacotherapeutic and surgical modalities; most cases are treated surgically. Surgical modalities vary, ranging from cryosurgery to conventional excision, and consensus guidelines for surgical management do not exist because data are largely limited to case reports and small case series. 2 The Versajet II Hydrosurgery System (Smith-Nephew) is a high-pressure, pulsatile lavage system that has been used for phymatous rosacea and then only for rosacea of the nose (rhinophyma). We present the case of a patient with phymatous rosacea of the nose, cheeks, and chin who was successfully treated with the Versajet II Hydrosurgery System beyond just the nose region.
Case Report
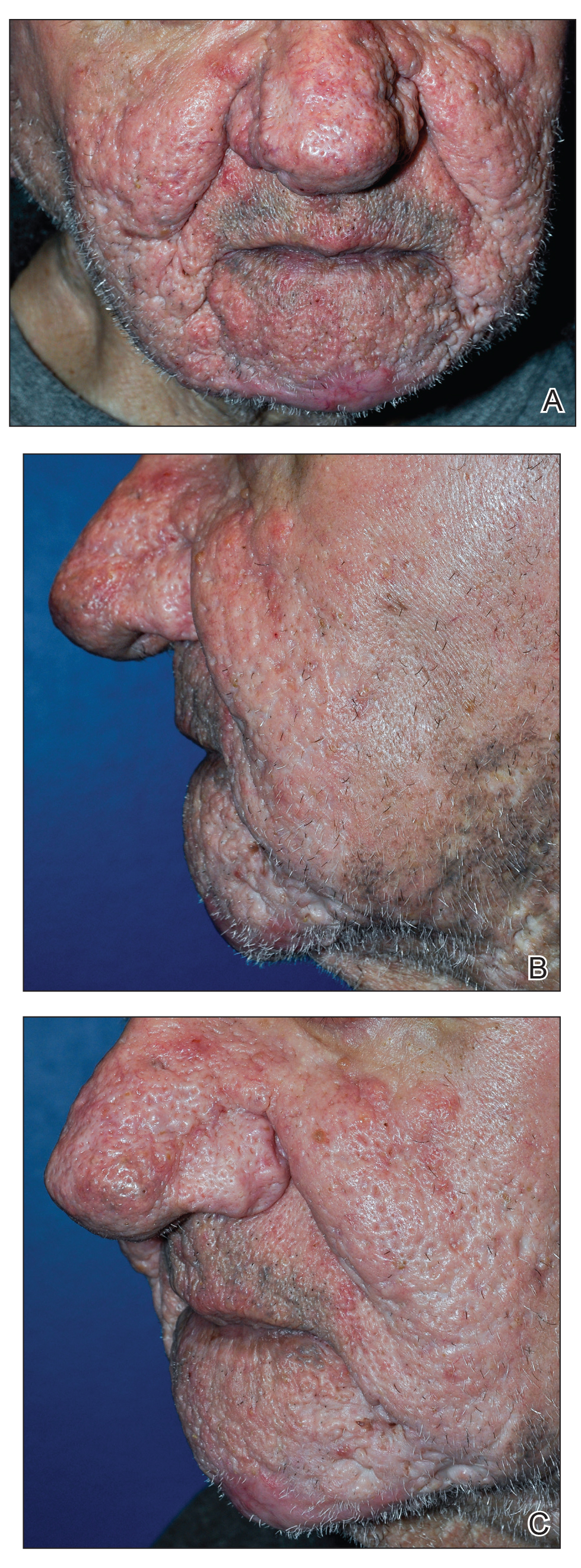
A 75-year-old man presented to the dermatology clinic for evaluation of severe phymatous rosacea of the nose, cheeks, and chin that had been present for several years. Examination revealed verruciform, thickened, erythematous skin of the nose, cheeks, and chin; marked blue-gray hyperpigmentation on the neck and hands; generalized facial redness; and cystic and depressed scars (Figure 1). The patient had been treated with topical metronidazole without response, and isotretinoin worsened the symptoms. He also was taking minocycline but stopped it at our request because of concern that the drug was causing the blue-gray hyperpigmentation. The patient was referred to plastic surgery and tangential excision was recommended. Fractional ablative laser therapy was considered but deferred because the patient wanted quicker results.

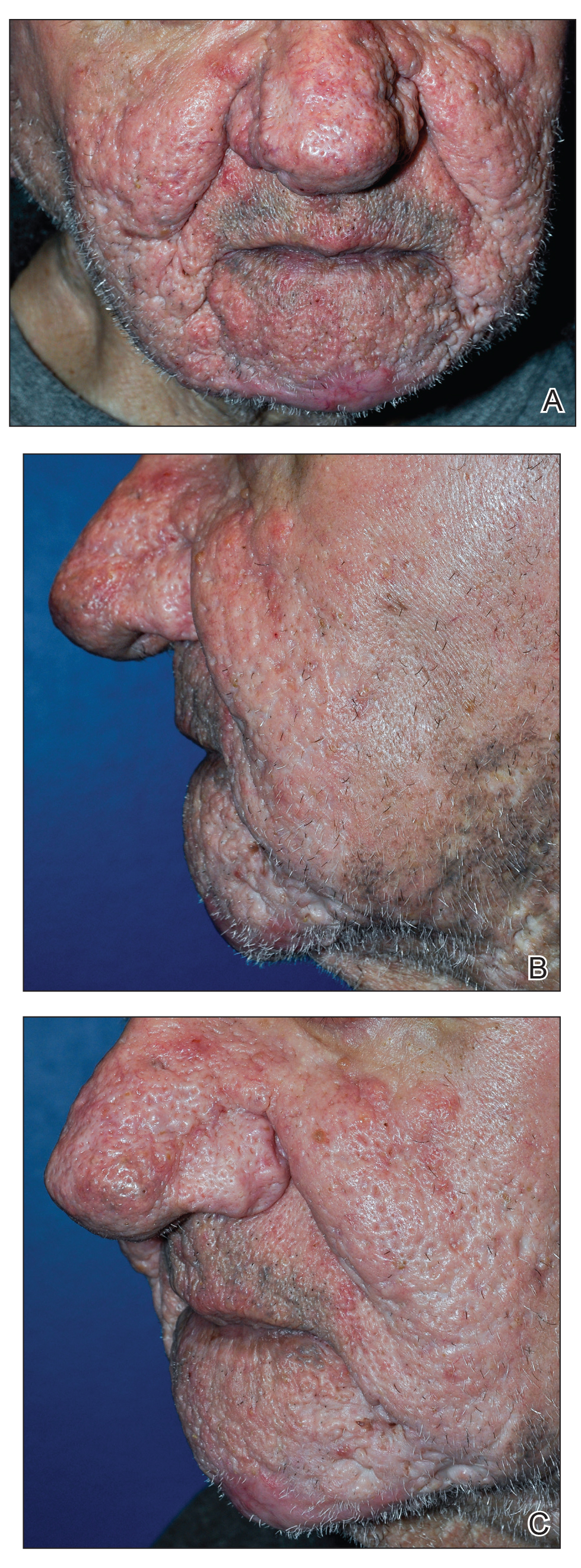
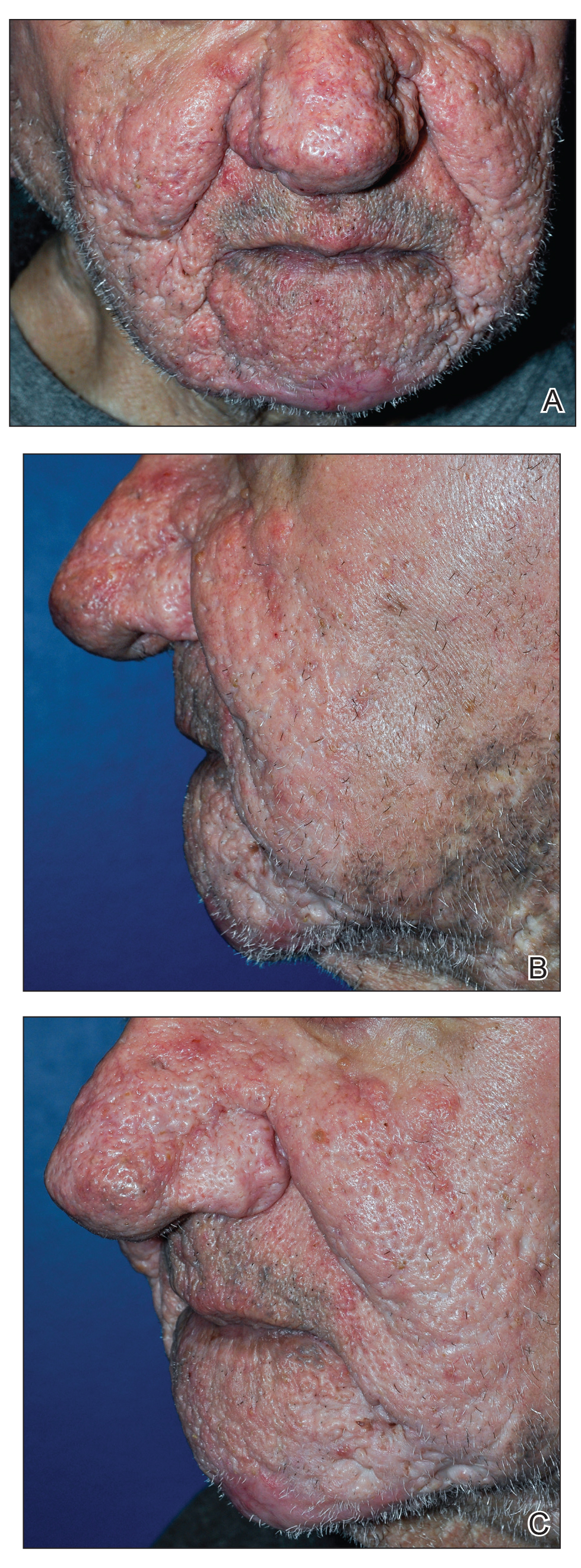
The patient received tangential excision of the phymatous areas of the chin, bilateral cheeks, and nose with the Versajet II Hydrosurgery System until a pleasing contour was noted. At 1-month follow-up, the patient had an excellent contour of the nose, cheeks, and chin (Figure 2).
Comment
Phymatous rosacea is a rare disfiguring disease that most commonly presents on the nose but also can affect the chin, cheeks, eyelids, ears, and forehead. Incidence is greater in individuals of Scottish descent and in men due to the influence of androgens. The etiology of the condition is unknown.1
Aside from clinical findings of hyperplastic and fibrotic sebaceous glands in conjunction with enlargement of the affected facial areas, histopathologic findings of phymatous rosacea vary but typically include hypertrophy of subcutaneous tissue, enlarged sebaceous ducts filled with keratin and sebum, atrophy of the dermis, and abnormal vascular development in the form of telangiectases.
Phymatous rosacea adversely affects patients’ physical, mental, and social well-being. Left untreated, it can cause nasal obstruction and recurrent bacterial infections. Furthermore, because of the potential extent of facial deformity, phymatous rosacea can be highly stigmatizing.3 Nonmelanoma skin cancers have been reported within phymatous skin, but evidence of an association between the 2 diseases remains inconclusive.4 Excised tissue from our patient was not submitted to pathology for analysis.
Given the far-reaching physical and psychological consequences of phymatous rosacea, treatment is critical but, regrettably, challenging. Although medical and surgical interventions exist, surgery is the most common practice. Oral isotretinoin may help, but many cases are recalcitrant, as was the disease in our patient. Therefore, procedural remedies often are sought, including scalpel excision, cryosurgery, argon laser, CO2 laser, dermabrasion, and electrocautery.2
Our patient underwent Versajet II Hydrosurgery System treatment of the phymatous rosacea on the nose, cheeks, and chin. Versajet is not yet commonly used to treat phymatous rosacea, likely due to the upfront cost of obtaining a new device, lack of physician familiarity, and few reports of its use for phymatous skin. A search of PubMed, EMBASE, and the Web of Science using the terms Rosacea AND (Versajet OR Hydrosurgery) yielded only 6 cases of rosacea treated by hydrosurgery; all were limited to rhinophyma and reported excellent cosmetic and functional results.5-10 Our case was unique in that hydrosurgery was used to treat phymatous rosacea beyond the nose.
Hydrosurgery has many advantages in the treatment of phymatous rosacea and other conditions in which surgical debridement is necessary, such as burns and wounds. A randomized clinical trial demonstrated that hydrosurgery is more cost-effective than conventional excision because of decreased operative time and intraoperative blood loss, fewer debridement procedures, and fewer postoperative complications.11
Rennekampff et al12 showed that Versajet debridement is superior to conventional surgery in contouring facial and acral sites and has a lower probability of infection. They proposed that by running a highly pressurized constant stream of saline across the device, Versajet clears blood and debris from the surgical site during excision.12 Hydrosurgical debridement also has been shown to reduce Staphylococcus aureus inoculate levels from in vitro–contaminated equine models significantly more than conventional debridement methods (P<.05).13
Versajet surgery appears to be well tolerated, with side effects comparable to those of classic surgical excision. A randomized controlled trial in burn patients in which treatment with Versajet was compared to traditional debridement found no significant difference in postoperative pain, healing time, and contracture rate.13
Overall, tangential excision of our patient’s phymatous rosacea using the Versajet II Hydrosurgery System yielded excellent contouring. However, due to the paucity of literature on the subject, it is difficult to discern the optimal treatment modality. Therefore, more research—ideally randomized trials—should be pursued to examine the comparative effectiveness of different interventions for phymatous rosacea.
- Curnier A, Choudhary S. Rhinophyma: dispelling the myths. Plast Reconstr Surg. 2004;114:351-354.
- Sadick H, Goepel B, Bersch C, et al. Rhinophyma: diagnosis and treatment options for a disfiguring tumor of the nose. Ann Plast Surg. 2008;61:114-120.
- Dirschka T, Micali G, Papadopoulos L, et al. Perceptions on the psychological impact of facial erythema associated with rosacea: results of international survey. Dermatol Ther (Heidelb). 2015;5:117-127.
- Lazzeri D, Colizzi L, Licata G, et al. Malignancies within rhinophyma: report of three new cases and review of the literature. Aesthetic Plast Surg. 2012;36:396-405.
- Dunne JA, Saleh DB, Rawlins JM. Management of rhinophyma with Versajet™ and ReCell®. Br J Oral Maxillofac Surg. 2013;51:e282-e284.
- Yildiz K, Kayan BR, Dulgeroglu T, et al. Treatment of rhinophyma with the Versajet™ Hydrosurgery System and autologous cell suspension (ReCELL®): a case report. J Cosmet Laser Ther. 2018;20:114-116.
- Nicolas J, Garmi R, Labbé D, et al. The role of Versajet in the surgical treatment of rhinophyma. case report. Ann Chir Plast Esthet. 2009;54:78-81.
- Novati FC, Franchi A, Roggio T, et al. Treatment of a double-giant rhinophyma with electrocautery and Versajet Hydrosurgery System. Ann Ital Chir. 2015;86. pii: S2239253X15023269.
- Taghizadeh R, Mackay SP, Gilbert PM. Treatment of rhinophyma with the Versajet Hydrosurgery System. J Plast Reconstr Aesthet Surg. 2008;61:330-333.
- Wong WL, Wong She R, Mathy JA. Rhinophyma treatment using Versajet Hydrosurgery. ANZ J Surg. 2017;87:E331-E332.
- Liu J, Ko JH, Secretov E, et al. Comparing the hydrosurgery system to conventional debridement techniques for the treatment of delayed healing wounds: a prospective, randomised clinical trial to investigate clinical efficacy and cost-effectiveness. Int Wound J. 2015;12:456-461.
- Rennekampff H-O, Schaller H-E, Wisser D, et al. Debridement of burn wounds with a water jet surgical tool. Burns. 2006;32:64-69.
- Skarlina EM, Wilmink JM, Fall N, et al. Effectiveness of conventional and hydrosurgical debridement methods in reducing Staphylococcus aureus inoculation of equine muscle in vitro. Equine Vet J. 2015;47:218-222.
Phymatous rosacea is a rare and severe form of rosacea that manifests as disfiguring soft-tissue hypertrophy and hyperplasia as well as fibrosis of the sebaceous glands. 1 Treatments for phymatous rosacea include pharmacotherapeutic and surgical modalities; most cases are treated surgically. Surgical modalities vary, ranging from cryosurgery to conventional excision, and consensus guidelines for surgical management do not exist because data are largely limited to case reports and small case series. 2 The Versajet II Hydrosurgery System (Smith-Nephew) is a high-pressure, pulsatile lavage system that has been used for phymatous rosacea and then only for rosacea of the nose (rhinophyma). We present the case of a patient with phymatous rosacea of the nose, cheeks, and chin who was successfully treated with the Versajet II Hydrosurgery System beyond just the nose region.
Case Report
A 75-year-old man presented to the dermatology clinic for evaluation of severe phymatous rosacea of the nose, cheeks, and chin that had been present for several years. Examination revealed verruciform, thickened, erythematous skin of the nose, cheeks, and chin; marked blue-gray hyperpigmentation on the neck and hands; generalized facial redness; and cystic and depressed scars (Figure 1). The patient had been treated with topical metronidazole without response, and isotretinoin worsened the symptoms. He also was taking minocycline but stopped it at our request because of concern that the drug was causing the blue-gray hyperpigmentation. The patient was referred to plastic surgery and tangential excision was recommended. Fractional ablative laser therapy was considered but deferred because the patient wanted quicker results.

The patient received tangential excision of the phymatous areas of the chin, bilateral cheeks, and nose with the Versajet II Hydrosurgery System until a pleasing contour was noted. At 1-month follow-up, the patient had an excellent contour of the nose, cheeks, and chin (Figure 2).
Comment
Phymatous rosacea is a rare disfiguring disease that most commonly presents on the nose but also can affect the chin, cheeks, eyelids, ears, and forehead. Incidence is greater in individuals of Scottish descent and in men due to the influence of androgens. The etiology of the condition is unknown.1
Aside from clinical findings of hyperplastic and fibrotic sebaceous glands in conjunction with enlargement of the affected facial areas, histopathologic findings of phymatous rosacea vary but typically include hypertrophy of subcutaneous tissue, enlarged sebaceous ducts filled with keratin and sebum, atrophy of the dermis, and abnormal vascular development in the form of telangiectases.
Phymatous rosacea adversely affects patients’ physical, mental, and social well-being. Left untreated, it can cause nasal obstruction and recurrent bacterial infections. Furthermore, because of the potential extent of facial deformity, phymatous rosacea can be highly stigmatizing.3 Nonmelanoma skin cancers have been reported within phymatous skin, but evidence of an association between the 2 diseases remains inconclusive.4 Excised tissue from our patient was not submitted to pathology for analysis.
Given the far-reaching physical and psychological consequences of phymatous rosacea, treatment is critical but, regrettably, challenging. Although medical and surgical interventions exist, surgery is the most common practice. Oral isotretinoin may help, but many cases are recalcitrant, as was the disease in our patient. Therefore, procedural remedies often are sought, including scalpel excision, cryosurgery, argon laser, CO2 laser, dermabrasion, and electrocautery.2
Our patient underwent Versajet II Hydrosurgery System treatment of the phymatous rosacea on the nose, cheeks, and chin. Versajet is not yet commonly used to treat phymatous rosacea, likely due to the upfront cost of obtaining a new device, lack of physician familiarity, and few reports of its use for phymatous skin. A search of PubMed, EMBASE, and the Web of Science using the terms Rosacea AND (Versajet OR Hydrosurgery) yielded only 6 cases of rosacea treated by hydrosurgery; all were limited to rhinophyma and reported excellent cosmetic and functional results.5-10 Our case was unique in that hydrosurgery was used to treat phymatous rosacea beyond the nose.
Hydrosurgery has many advantages in the treatment of phymatous rosacea and other conditions in which surgical debridement is necessary, such as burns and wounds. A randomized clinical trial demonstrated that hydrosurgery is more cost-effective than conventional excision because of decreased operative time and intraoperative blood loss, fewer debridement procedures, and fewer postoperative complications.11
Rennekampff et al12 showed that Versajet debridement is superior to conventional surgery in contouring facial and acral sites and has a lower probability of infection. They proposed that by running a highly pressurized constant stream of saline across the device, Versajet clears blood and debris from the surgical site during excision.12 Hydrosurgical debridement also has been shown to reduce Staphylococcus aureus inoculate levels from in vitro–contaminated equine models significantly more than conventional debridement methods (P<.05).13
Versajet surgery appears to be well tolerated, with side effects comparable to those of classic surgical excision. A randomized controlled trial in burn patients in which treatment with Versajet was compared to traditional debridement found no significant difference in postoperative pain, healing time, and contracture rate.13
Overall, tangential excision of our patient’s phymatous rosacea using the Versajet II Hydrosurgery System yielded excellent contouring. However, due to the paucity of literature on the subject, it is difficult to discern the optimal treatment modality. Therefore, more research—ideally randomized trials—should be pursued to examine the comparative effectiveness of different interventions for phymatous rosacea.
Phymatous rosacea is a rare and severe form of rosacea that manifests as disfiguring soft-tissue hypertrophy and hyperplasia as well as fibrosis of the sebaceous glands. 1 Treatments for phymatous rosacea include pharmacotherapeutic and surgical modalities; most cases are treated surgically. Surgical modalities vary, ranging from cryosurgery to conventional excision, and consensus guidelines for surgical management do not exist because data are largely limited to case reports and small case series. 2 The Versajet II Hydrosurgery System (Smith-Nephew) is a high-pressure, pulsatile lavage system that has been used for phymatous rosacea and then only for rosacea of the nose (rhinophyma). We present the case of a patient with phymatous rosacea of the nose, cheeks, and chin who was successfully treated with the Versajet II Hydrosurgery System beyond just the nose region.
Case Report
A 75-year-old man presented to the dermatology clinic for evaluation of severe phymatous rosacea of the nose, cheeks, and chin that had been present for several years. Examination revealed verruciform, thickened, erythematous skin of the nose, cheeks, and chin; marked blue-gray hyperpigmentation on the neck and hands; generalized facial redness; and cystic and depressed scars (Figure 1). The patient had been treated with topical metronidazole without response, and isotretinoin worsened the symptoms. He also was taking minocycline but stopped it at our request because of concern that the drug was causing the blue-gray hyperpigmentation. The patient was referred to plastic surgery and tangential excision was recommended. Fractional ablative laser therapy was considered but deferred because the patient wanted quicker results.

The patient received tangential excision of the phymatous areas of the chin, bilateral cheeks, and nose with the Versajet II Hydrosurgery System until a pleasing contour was noted. At 1-month follow-up, the patient had an excellent contour of the nose, cheeks, and chin (Figure 2).
Comment
Phymatous rosacea is a rare disfiguring disease that most commonly presents on the nose but also can affect the chin, cheeks, eyelids, ears, and forehead. Incidence is greater in individuals of Scottish descent and in men due to the influence of androgens. The etiology of the condition is unknown.1
Aside from clinical findings of hyperplastic and fibrotic sebaceous glands in conjunction with enlargement of the affected facial areas, histopathologic findings of phymatous rosacea vary but typically include hypertrophy of subcutaneous tissue, enlarged sebaceous ducts filled with keratin and sebum, atrophy of the dermis, and abnormal vascular development in the form of telangiectases.
Phymatous rosacea adversely affects patients’ physical, mental, and social well-being. Left untreated, it can cause nasal obstruction and recurrent bacterial infections. Furthermore, because of the potential extent of facial deformity, phymatous rosacea can be highly stigmatizing.3 Nonmelanoma skin cancers have been reported within phymatous skin, but evidence of an association between the 2 diseases remains inconclusive.4 Excised tissue from our patient was not submitted to pathology for analysis.
Given the far-reaching physical and psychological consequences of phymatous rosacea, treatment is critical but, regrettably, challenging. Although medical and surgical interventions exist, surgery is the most common practice. Oral isotretinoin may help, but many cases are recalcitrant, as was the disease in our patient. Therefore, procedural remedies often are sought, including scalpel excision, cryosurgery, argon laser, CO2 laser, dermabrasion, and electrocautery.2
Our patient underwent Versajet II Hydrosurgery System treatment of the phymatous rosacea on the nose, cheeks, and chin. Versajet is not yet commonly used to treat phymatous rosacea, likely due to the upfront cost of obtaining a new device, lack of physician familiarity, and few reports of its use for phymatous skin. A search of PubMed, EMBASE, and the Web of Science using the terms Rosacea AND (Versajet OR Hydrosurgery) yielded only 6 cases of rosacea treated by hydrosurgery; all were limited to rhinophyma and reported excellent cosmetic and functional results.5-10 Our case was unique in that hydrosurgery was used to treat phymatous rosacea beyond the nose.
Hydrosurgery has many advantages in the treatment of phymatous rosacea and other conditions in which surgical debridement is necessary, such as burns and wounds. A randomized clinical trial demonstrated that hydrosurgery is more cost-effective than conventional excision because of decreased operative time and intraoperative blood loss, fewer debridement procedures, and fewer postoperative complications.11
Rennekampff et al12 showed that Versajet debridement is superior to conventional surgery in contouring facial and acral sites and has a lower probability of infection. They proposed that by running a highly pressurized constant stream of saline across the device, Versajet clears blood and debris from the surgical site during excision.12 Hydrosurgical debridement also has been shown to reduce Staphylococcus aureus inoculate levels from in vitro–contaminated equine models significantly more than conventional debridement methods (P<.05).13
Versajet surgery appears to be well tolerated, with side effects comparable to those of classic surgical excision. A randomized controlled trial in burn patients in which treatment with Versajet was compared to traditional debridement found no significant difference in postoperative pain, healing time, and contracture rate.13
Overall, tangential excision of our patient’s phymatous rosacea using the Versajet II Hydrosurgery System yielded excellent contouring. However, due to the paucity of literature on the subject, it is difficult to discern the optimal treatment modality. Therefore, more research—ideally randomized trials—should be pursued to examine the comparative effectiveness of different interventions for phymatous rosacea.
- Curnier A, Choudhary S. Rhinophyma: dispelling the myths. Plast Reconstr Surg. 2004;114:351-354.
- Sadick H, Goepel B, Bersch C, et al. Rhinophyma: diagnosis and treatment options for a disfiguring tumor of the nose. Ann Plast Surg. 2008;61:114-120.
- Dirschka T, Micali G, Papadopoulos L, et al. Perceptions on the psychological impact of facial erythema associated with rosacea: results of international survey. Dermatol Ther (Heidelb). 2015;5:117-127.
- Lazzeri D, Colizzi L, Licata G, et al. Malignancies within rhinophyma: report of three new cases and review of the literature. Aesthetic Plast Surg. 2012;36:396-405.
- Dunne JA, Saleh DB, Rawlins JM. Management of rhinophyma with Versajet™ and ReCell®. Br J Oral Maxillofac Surg. 2013;51:e282-e284.
- Yildiz K, Kayan BR, Dulgeroglu T, et al. Treatment of rhinophyma with the Versajet™ Hydrosurgery System and autologous cell suspension (ReCELL®): a case report. J Cosmet Laser Ther. 2018;20:114-116.
- Nicolas J, Garmi R, Labbé D, et al. The role of Versajet in the surgical treatment of rhinophyma. case report. Ann Chir Plast Esthet. 2009;54:78-81.
- Novati FC, Franchi A, Roggio T, et al. Treatment of a double-giant rhinophyma with electrocautery and Versajet Hydrosurgery System. Ann Ital Chir. 2015;86. pii: S2239253X15023269.
- Taghizadeh R, Mackay SP, Gilbert PM. Treatment of rhinophyma with the Versajet Hydrosurgery System. J Plast Reconstr Aesthet Surg. 2008;61:330-333.
- Wong WL, Wong She R, Mathy JA. Rhinophyma treatment using Versajet Hydrosurgery. ANZ J Surg. 2017;87:E331-E332.
- Liu J, Ko JH, Secretov E, et al. Comparing the hydrosurgery system to conventional debridement techniques for the treatment of delayed healing wounds: a prospective, randomised clinical trial to investigate clinical efficacy and cost-effectiveness. Int Wound J. 2015;12:456-461.
- Rennekampff H-O, Schaller H-E, Wisser D, et al. Debridement of burn wounds with a water jet surgical tool. Burns. 2006;32:64-69.
- Skarlina EM, Wilmink JM, Fall N, et al. Effectiveness of conventional and hydrosurgical debridement methods in reducing Staphylococcus aureus inoculation of equine muscle in vitro. Equine Vet J. 2015;47:218-222.
- Curnier A, Choudhary S. Rhinophyma: dispelling the myths. Plast Reconstr Surg. 2004;114:351-354.
- Sadick H, Goepel B, Bersch C, et al. Rhinophyma: diagnosis and treatment options for a disfiguring tumor of the nose. Ann Plast Surg. 2008;61:114-120.
- Dirschka T, Micali G, Papadopoulos L, et al. Perceptions on the psychological impact of facial erythema associated with rosacea: results of international survey. Dermatol Ther (Heidelb). 2015;5:117-127.
- Lazzeri D, Colizzi L, Licata G, et al. Malignancies within rhinophyma: report of three new cases and review of the literature. Aesthetic Plast Surg. 2012;36:396-405.
- Dunne JA, Saleh DB, Rawlins JM. Management of rhinophyma with Versajet™ and ReCell®. Br J Oral Maxillofac Surg. 2013;51:e282-e284.
- Yildiz K, Kayan BR, Dulgeroglu T, et al. Treatment of rhinophyma with the Versajet™ Hydrosurgery System and autologous cell suspension (ReCELL®): a case report. J Cosmet Laser Ther. 2018;20:114-116.
- Nicolas J, Garmi R, Labbé D, et al. The role of Versajet in the surgical treatment of rhinophyma. case report. Ann Chir Plast Esthet. 2009;54:78-81.
- Novati FC, Franchi A, Roggio T, et al. Treatment of a double-giant rhinophyma with electrocautery and Versajet Hydrosurgery System. Ann Ital Chir. 2015;86. pii: S2239253X15023269.
- Taghizadeh R, Mackay SP, Gilbert PM. Treatment of rhinophyma with the Versajet Hydrosurgery System. J Plast Reconstr Aesthet Surg. 2008;61:330-333.
- Wong WL, Wong She R, Mathy JA. Rhinophyma treatment using Versajet Hydrosurgery. ANZ J Surg. 2017;87:E331-E332.
- Liu J, Ko JH, Secretov E, et al. Comparing the hydrosurgery system to conventional debridement techniques for the treatment of delayed healing wounds: a prospective, randomised clinical trial to investigate clinical efficacy and cost-effectiveness. Int Wound J. 2015;12:456-461.
- Rennekampff H-O, Schaller H-E, Wisser D, et al. Debridement of burn wounds with a water jet surgical tool. Burns. 2006;32:64-69.
- Skarlina EM, Wilmink JM, Fall N, et al. Effectiveness of conventional and hydrosurgical debridement methods in reducing Staphylococcus aureus inoculation of equine muscle in vitro. Equine Vet J. 2015;47:218-222.
Practice Points
- Phymatous rosacea is a rare disfiguring disease that most commonly affects men and can have considerable effects on a patient’s physical, mental, and social well-being.
- Treatment of phymatous rosacea usually is surgical; however, no consensus guidelines exist for best surgical management.
- The Versajet II Hydrosurgery System can be useful and effective for the treatment of phymatous rosacea, not only on the nose but elsewhere on the face.
Today’s top news highlights: Remdesivir data dive, FDA approves contraceptive gel
:
Remdesivir trial data published
Weeks after topline remdesivir data appeared in the press, investigators published their full experience using the drug to treat COVID-19 patients. The study, published in the New England Journal of Medicine, showed the drug reduced recovery time from 15 to 11 days, compared with placebo. Patients receiving oxygen seemed to fare best from treatment with remdesivir. “There is clear and consistent evidence of clinically significant benefit for those hospitalized on oxygen but not yet requiring mechanical ventilation,” Daniel Kaul, MD, a professor of infectious diseases at the University of Michigan, Ann Arbor, said after seeing the published results. “Surprisingly, early dosing as measured from time to onset of symptoms did not seem to make a difference.” READ MORE.
FDA approves contraceptive gel
The Food and Drug Administration approved Phexxi (lactic acid, citric acid, and potassium bitartrate) vaginal gel to prevent pregnancy in women of reproductive potential. It’s the first nonhormonal, on-demand, vaginal pH regulator contraceptive designed to maintain vaginal pH within the range of 3.5-4.5. READ MORE.
COVID-19 lessons from one cancer center
Physicians at Levine Cancer Institute in Charlotte, N.C., largely have been able to keep hematologic oncology patients on their treatment regimens and continue to care for inpatients during the early months of the COVID-19 pandemic. How have they kept the situation managable? Strict infection control, liberal testing, and a proactive plan to defer and temporarily replace infusion care when medically appropriate were all part of the strategy. “My impression is that the incidence has been low partly because our patients, especially those with hematologic malignancies including those on active chemotherapy, were already getting warned to be cautious, even before the coronavirus, using distancing, masking, and meticulous hand hygiene,” said Peter Voorhees, MD, professor of medicine and director of Medical Operations and Outreach Services in Levine Cancer Institute’s Department of Hematologic Oncology and Blood Disorders. READ MORE.
Convalescent plasma: Hope or hype?
There are currently more than two dozen trials of convalescent plasma in the United States and elsewhere but most are single-arm trials to determine if one infusion can decrease the need for intubation or help patients on a ventilator to improve. Others researchers are investigating whether convalescent plasma might be used before severe disease sets in. Meanwhile, about 2,200 hospitals are participating in an expanded access program being led by the Mayo Clinic nationwide. The National Institutes of Health recently said that “there are insufficient clinical data to recommend either for or against” its use for COVID-19. READ MORE.
New rosacea treatment guidelines
Patients with rosacea should receive treatments based on their phenotype and specific symptoms, rather than being assigned into distinct subtype categories, according to updated guidance published in the Journal of the American Academy of Dermatology. The update comes from the National Rosacea Society Expert Committee and is based on a review of the evidence. Patients “shouldn’t be classified as having a certain subtype of rosacea” since “many patients have features that overlap more than one subtype,” said Diane Thiboutot, MD, lead author of the update and a professor of dermatology and associate dean of clinical and translational research education at Penn State University, Hershey. READ MORE.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
:
Remdesivir trial data published
Weeks after topline remdesivir data appeared in the press, investigators published their full experience using the drug to treat COVID-19 patients. The study, published in the New England Journal of Medicine, showed the drug reduced recovery time from 15 to 11 days, compared with placebo. Patients receiving oxygen seemed to fare best from treatment with remdesivir. “There is clear and consistent evidence of clinically significant benefit for those hospitalized on oxygen but not yet requiring mechanical ventilation,” Daniel Kaul, MD, a professor of infectious diseases at the University of Michigan, Ann Arbor, said after seeing the published results. “Surprisingly, early dosing as measured from time to onset of symptoms did not seem to make a difference.” READ MORE.
FDA approves contraceptive gel
The Food and Drug Administration approved Phexxi (lactic acid, citric acid, and potassium bitartrate) vaginal gel to prevent pregnancy in women of reproductive potential. It’s the first nonhormonal, on-demand, vaginal pH regulator contraceptive designed to maintain vaginal pH within the range of 3.5-4.5. READ MORE.
COVID-19 lessons from one cancer center
Physicians at Levine Cancer Institute in Charlotte, N.C., largely have been able to keep hematologic oncology patients on their treatment regimens and continue to care for inpatients during the early months of the COVID-19 pandemic. How have they kept the situation managable? Strict infection control, liberal testing, and a proactive plan to defer and temporarily replace infusion care when medically appropriate were all part of the strategy. “My impression is that the incidence has been low partly because our patients, especially those with hematologic malignancies including those on active chemotherapy, were already getting warned to be cautious, even before the coronavirus, using distancing, masking, and meticulous hand hygiene,” said Peter Voorhees, MD, professor of medicine and director of Medical Operations and Outreach Services in Levine Cancer Institute’s Department of Hematologic Oncology and Blood Disorders. READ MORE.
Convalescent plasma: Hope or hype?
There are currently more than two dozen trials of convalescent plasma in the United States and elsewhere but most are single-arm trials to determine if one infusion can decrease the need for intubation or help patients on a ventilator to improve. Others researchers are investigating whether convalescent plasma might be used before severe disease sets in. Meanwhile, about 2,200 hospitals are participating in an expanded access program being led by the Mayo Clinic nationwide. The National Institutes of Health recently said that “there are insufficient clinical data to recommend either for or against” its use for COVID-19. READ MORE.
New rosacea treatment guidelines
Patients with rosacea should receive treatments based on their phenotype and specific symptoms, rather than being assigned into distinct subtype categories, according to updated guidance published in the Journal of the American Academy of Dermatology. The update comes from the National Rosacea Society Expert Committee and is based on a review of the evidence. Patients “shouldn’t be classified as having a certain subtype of rosacea” since “many patients have features that overlap more than one subtype,” said Diane Thiboutot, MD, lead author of the update and a professor of dermatology and associate dean of clinical and translational research education at Penn State University, Hershey. READ MORE.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
:
Remdesivir trial data published
Weeks after topline remdesivir data appeared in the press, investigators published their full experience using the drug to treat COVID-19 patients. The study, published in the New England Journal of Medicine, showed the drug reduced recovery time from 15 to 11 days, compared with placebo. Patients receiving oxygen seemed to fare best from treatment with remdesivir. “There is clear and consistent evidence of clinically significant benefit for those hospitalized on oxygen but not yet requiring mechanical ventilation,” Daniel Kaul, MD, a professor of infectious diseases at the University of Michigan, Ann Arbor, said after seeing the published results. “Surprisingly, early dosing as measured from time to onset of symptoms did not seem to make a difference.” READ MORE.
FDA approves contraceptive gel
The Food and Drug Administration approved Phexxi (lactic acid, citric acid, and potassium bitartrate) vaginal gel to prevent pregnancy in women of reproductive potential. It’s the first nonhormonal, on-demand, vaginal pH regulator contraceptive designed to maintain vaginal pH within the range of 3.5-4.5. READ MORE.
COVID-19 lessons from one cancer center
Physicians at Levine Cancer Institute in Charlotte, N.C., largely have been able to keep hematologic oncology patients on their treatment regimens and continue to care for inpatients during the early months of the COVID-19 pandemic. How have they kept the situation managable? Strict infection control, liberal testing, and a proactive plan to defer and temporarily replace infusion care when medically appropriate were all part of the strategy. “My impression is that the incidence has been low partly because our patients, especially those with hematologic malignancies including those on active chemotherapy, were already getting warned to be cautious, even before the coronavirus, using distancing, masking, and meticulous hand hygiene,” said Peter Voorhees, MD, professor of medicine and director of Medical Operations and Outreach Services in Levine Cancer Institute’s Department of Hematologic Oncology and Blood Disorders. READ MORE.
Convalescent plasma: Hope or hype?
There are currently more than two dozen trials of convalescent plasma in the United States and elsewhere but most are single-arm trials to determine if one infusion can decrease the need for intubation or help patients on a ventilator to improve. Others researchers are investigating whether convalescent plasma might be used before severe disease sets in. Meanwhile, about 2,200 hospitals are participating in an expanded access program being led by the Mayo Clinic nationwide. The National Institutes of Health recently said that “there are insufficient clinical data to recommend either for or against” its use for COVID-19. READ MORE.
New rosacea treatment guidelines
Patients with rosacea should receive treatments based on their phenotype and specific symptoms, rather than being assigned into distinct subtype categories, according to updated guidance published in the Journal of the American Academy of Dermatology. The update comes from the National Rosacea Society Expert Committee and is based on a review of the evidence. Patients “shouldn’t be classified as having a certain subtype of rosacea” since “many patients have features that overlap more than one subtype,” said Diane Thiboutot, MD, lead author of the update and a professor of dermatology and associate dean of clinical and translational research education at Penn State University, Hershey. READ MORE.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
New rosacea clinical management guidelines focus on symptomatology
, as was previously practiced, according to an update on options for managing rosacea published in the Journal of the American Academy of Dermatology.
The update, by the National Rosacea Society Expert Committee, is based on a review of the evidence, and is a follow-up to the classification system for rosacea that was updated in 2017, which recommended classification of rosacea based on phenotype (Am Acad Dermatol. 2018;78:148-155).
The key take-away is “that patients shouldn’t be classified as having a certain subtype of rosacea” since “many patients have features that overlap more than one subtype,” lead author of the management update, Diane Thiboutot, MD, professor of dermatology and associate dean of clinical and translational research education at Penn State University, Hershey, said in an interview.
“There is an opportunity for physicians to recognize that the symptom complex of rosacea differs widely and treatments should be selected to address the symptoms experienced by the patient, particularly with regard to ocular rosacea,” she said.
Until there were updated guidelines on rosacea classification, published in 2018, relying primarily on diagnostic subtypes “tended to limit consideration of the full range of potential signs and symptoms as well as the frequent simultaneous occurrence of more than one subtype or the potential progression from one subtype to another,” Dr. Thiboutot and coauthors wrote in the management update (J Am Acad Dermatol 2020;82:1501-10).
“The more we learn, the more complex rosacea becomes,” she said in the interview. “The clinical manifestations of rosacea are so varied, ranging from skin erythema, eye findings, papules and pustules to rhinophyma, [that] it calls into question, if all of these are actually one disease (rosacea) or if they represent localized reaction patterns to a multitude of stimuli that vary among individuals.”
Etiology and impact
Dr. Thiboutot and colleagues summarized the management options and recommendations from a committee of 27 experts who assessed the data on rosacea therapies using the updated standard classification system. They also highlighted the suspected systemic nature of rosacea etiology and its psychosocial impact on those with the condition.
“Recent studies have found an association between rosacea and increased risk of a growing number of systemic disorders, including cardiovascular, gastrointestinal, neurologic, and autoimmune diseases as well as certain types of cancer,” the authors wrote. “These findings further elevate the clinical significance of rosacea as growing evidence of its potential link with systemic inflammation is increasingly understood.”
Dr. Thiboutot said that research has implicated both the innate and adaptive immune systems and the neuromuscular system in rosacea’s underpinnings.
“Many of the triggers associated with clinical exacerbation of rosacea are known to activate the immune system and/or the neurovasculature, such as demodex, sunlight, alcohol, and changes in temperature,” she said, adding that therapies targeting the neurovascular effects of rosacea are particularly needed.
More than 50% of patients with rosacea have ocular manifestations, with symptoms such as “dryness, burning and stinging, light sensitivity, blurred vision, and foreign body sensation,” the authors reported.
Diagnosis and management
Without definitive laboratory tests, it’s essential that the clinical diagnosis takes into account not only the physical examination findings, but also patient history, the authors stressed, since “some features may not be visually evident or present at the time of the patient’s visit.”
The authors also recommend taking into account patients’ perception and response to their appearance and its effects on their emotional, social, and professional lives when selecting interventions.
“Rosacea’s unsightly and conspicuous appearance often has significant emotional ramifications, potentially resulting in depression or anxiety, and frequently interferes with social and occupational interactions,” the authors wrote. “It may also be advisable to remind patients that normalization of skin tone and color is the goal rather than complete eradication of facial coloration, which can leave the face with a sallow appearance.”
Therapy will often require multiple agents, such as topical and oral agents for inflammatory papules/pustules of rosacea. If insufficient, adjunctive therapy with oral antibiotics or retinoids may be options, though the latter requires prevention of pregnancy during treatment. The authors also discussed pharmacological treatments for facial erythema and flushing, with all these drugs organized in tables according to symptoms and their levels of evidence and effectiveness.
Despite limited clinical evidence, the authors noted success with two types of laser therapy – pulsed-dye and potassium titanyl phosphate – for telangiectasia and erythema. They also noted the option of intense pulsed light for flushing, ocular symptoms, and meibomian gland dysfunction, and of ablative lasers for rhinophymatous nose. But they highlighted the importance of being cautious when using these therapies on darker skin.
In their discussion of ocular rosacea, the authors described the various manifestations and the two “mainstays” of treatment: “eyelash hygiene and oral [omega-3] supplementation, followed by topical azithromycin or calcineurin inhibitors.” In addition to pharmacological and light therapy options, attention to environmental contributors and conscientious skin care regimens can benefit patients with rosacea as well.
“Clinicians may advise patients to keep a daily diary of lifestyle and environmental factors that appear to affect their rosacea to help identify and avoid their personal triggers,” the authors wrote. “The most common factors are sun exposure, emotional stress, hot weather, wind, heavy exercise, alcohol consumption, hot baths, cold weather, spicy foods, humidity, indoor heat, certain skin-care products, heated beverages, certain medications, medical conditions, certain fruits, marinated meats, certain vegetables, and dairy products.”
The paper also emphasizes the importance of gentle skin care given the highly sensitive and easily irritated skin of patients with rosacea. Sunscreen use, particularly with mineral sunscreens that provide physical barriers and reflect ultraviolet light, should be a key aspect of patients’ skin care, and clinicians should advise patients to seek out gentle, nonirritating cleansers.
Funding was provided by the National Rosacea Society, which receives funding from patients and corporations that include Aclaris Therapeutics, Allergan, Bayer, Cutanea Life Sciences, and Galderma Laboratories. Dr. Thiboutot consults for Galderma. Six of the other nine coauthors have financial links to industry through advisory boards, consulting, or research funding.
SOURCE: Thiboutot D et al. J Am Acad Dermatol. 2020;82:1501-10.
, as was previously practiced, according to an update on options for managing rosacea published in the Journal of the American Academy of Dermatology.
The update, by the National Rosacea Society Expert Committee, is based on a review of the evidence, and is a follow-up to the classification system for rosacea that was updated in 2017, which recommended classification of rosacea based on phenotype (Am Acad Dermatol. 2018;78:148-155).
The key take-away is “that patients shouldn’t be classified as having a certain subtype of rosacea” since “many patients have features that overlap more than one subtype,” lead author of the management update, Diane Thiboutot, MD, professor of dermatology and associate dean of clinical and translational research education at Penn State University, Hershey, said in an interview.
“There is an opportunity for physicians to recognize that the symptom complex of rosacea differs widely and treatments should be selected to address the symptoms experienced by the patient, particularly with regard to ocular rosacea,” she said.
Until there were updated guidelines on rosacea classification, published in 2018, relying primarily on diagnostic subtypes “tended to limit consideration of the full range of potential signs and symptoms as well as the frequent simultaneous occurrence of more than one subtype or the potential progression from one subtype to another,” Dr. Thiboutot and coauthors wrote in the management update (J Am Acad Dermatol 2020;82:1501-10).
“The more we learn, the more complex rosacea becomes,” she said in the interview. “The clinical manifestations of rosacea are so varied, ranging from skin erythema, eye findings, papules and pustules to rhinophyma, [that] it calls into question, if all of these are actually one disease (rosacea) or if they represent localized reaction patterns to a multitude of stimuli that vary among individuals.”
Etiology and impact
Dr. Thiboutot and colleagues summarized the management options and recommendations from a committee of 27 experts who assessed the data on rosacea therapies using the updated standard classification system. They also highlighted the suspected systemic nature of rosacea etiology and its psychosocial impact on those with the condition.
“Recent studies have found an association between rosacea and increased risk of a growing number of systemic disorders, including cardiovascular, gastrointestinal, neurologic, and autoimmune diseases as well as certain types of cancer,” the authors wrote. “These findings further elevate the clinical significance of rosacea as growing evidence of its potential link with systemic inflammation is increasingly understood.”
Dr. Thiboutot said that research has implicated both the innate and adaptive immune systems and the neuromuscular system in rosacea’s underpinnings.
“Many of the triggers associated with clinical exacerbation of rosacea are known to activate the immune system and/or the neurovasculature, such as demodex, sunlight, alcohol, and changes in temperature,” she said, adding that therapies targeting the neurovascular effects of rosacea are particularly needed.
More than 50% of patients with rosacea have ocular manifestations, with symptoms such as “dryness, burning and stinging, light sensitivity, blurred vision, and foreign body sensation,” the authors reported.
Diagnosis and management
Without definitive laboratory tests, it’s essential that the clinical diagnosis takes into account not only the physical examination findings, but also patient history, the authors stressed, since “some features may not be visually evident or present at the time of the patient’s visit.”
The authors also recommend taking into account patients’ perception and response to their appearance and its effects on their emotional, social, and professional lives when selecting interventions.
“Rosacea’s unsightly and conspicuous appearance often has significant emotional ramifications, potentially resulting in depression or anxiety, and frequently interferes with social and occupational interactions,” the authors wrote. “It may also be advisable to remind patients that normalization of skin tone and color is the goal rather than complete eradication of facial coloration, which can leave the face with a sallow appearance.”
Therapy will often require multiple agents, such as topical and oral agents for inflammatory papules/pustules of rosacea. If insufficient, adjunctive therapy with oral antibiotics or retinoids may be options, though the latter requires prevention of pregnancy during treatment. The authors also discussed pharmacological treatments for facial erythema and flushing, with all these drugs organized in tables according to symptoms and their levels of evidence and effectiveness.
Despite limited clinical evidence, the authors noted success with two types of laser therapy – pulsed-dye and potassium titanyl phosphate – for telangiectasia and erythema. They also noted the option of intense pulsed light for flushing, ocular symptoms, and meibomian gland dysfunction, and of ablative lasers for rhinophymatous nose. But they highlighted the importance of being cautious when using these therapies on darker skin.
In their discussion of ocular rosacea, the authors described the various manifestations and the two “mainstays” of treatment: “eyelash hygiene and oral [omega-3] supplementation, followed by topical azithromycin or calcineurin inhibitors.” In addition to pharmacological and light therapy options, attention to environmental contributors and conscientious skin care regimens can benefit patients with rosacea as well.
“Clinicians may advise patients to keep a daily diary of lifestyle and environmental factors that appear to affect their rosacea to help identify and avoid their personal triggers,” the authors wrote. “The most common factors are sun exposure, emotional stress, hot weather, wind, heavy exercise, alcohol consumption, hot baths, cold weather, spicy foods, humidity, indoor heat, certain skin-care products, heated beverages, certain medications, medical conditions, certain fruits, marinated meats, certain vegetables, and dairy products.”
The paper also emphasizes the importance of gentle skin care given the highly sensitive and easily irritated skin of patients with rosacea. Sunscreen use, particularly with mineral sunscreens that provide physical barriers and reflect ultraviolet light, should be a key aspect of patients’ skin care, and clinicians should advise patients to seek out gentle, nonirritating cleansers.
Funding was provided by the National Rosacea Society, which receives funding from patients and corporations that include Aclaris Therapeutics, Allergan, Bayer, Cutanea Life Sciences, and Galderma Laboratories. Dr. Thiboutot consults for Galderma. Six of the other nine coauthors have financial links to industry through advisory boards, consulting, or research funding.
SOURCE: Thiboutot D et al. J Am Acad Dermatol. 2020;82:1501-10.
, as was previously practiced, according to an update on options for managing rosacea published in the Journal of the American Academy of Dermatology.
The update, by the National Rosacea Society Expert Committee, is based on a review of the evidence, and is a follow-up to the classification system for rosacea that was updated in 2017, which recommended classification of rosacea based on phenotype (Am Acad Dermatol. 2018;78:148-155).
The key take-away is “that patients shouldn’t be classified as having a certain subtype of rosacea” since “many patients have features that overlap more than one subtype,” lead author of the management update, Diane Thiboutot, MD, professor of dermatology and associate dean of clinical and translational research education at Penn State University, Hershey, said in an interview.
“There is an opportunity for physicians to recognize that the symptom complex of rosacea differs widely and treatments should be selected to address the symptoms experienced by the patient, particularly with regard to ocular rosacea,” she said.
Until there were updated guidelines on rosacea classification, published in 2018, relying primarily on diagnostic subtypes “tended to limit consideration of the full range of potential signs and symptoms as well as the frequent simultaneous occurrence of more than one subtype or the potential progression from one subtype to another,” Dr. Thiboutot and coauthors wrote in the management update (J Am Acad Dermatol 2020;82:1501-10).
“The more we learn, the more complex rosacea becomes,” she said in the interview. “The clinical manifestations of rosacea are so varied, ranging from skin erythema, eye findings, papules and pustules to rhinophyma, [that] it calls into question, if all of these are actually one disease (rosacea) or if they represent localized reaction patterns to a multitude of stimuli that vary among individuals.”
Etiology and impact
Dr. Thiboutot and colleagues summarized the management options and recommendations from a committee of 27 experts who assessed the data on rosacea therapies using the updated standard classification system. They also highlighted the suspected systemic nature of rosacea etiology and its psychosocial impact on those with the condition.
“Recent studies have found an association between rosacea and increased risk of a growing number of systemic disorders, including cardiovascular, gastrointestinal, neurologic, and autoimmune diseases as well as certain types of cancer,” the authors wrote. “These findings further elevate the clinical significance of rosacea as growing evidence of its potential link with systemic inflammation is increasingly understood.”
Dr. Thiboutot said that research has implicated both the innate and adaptive immune systems and the neuromuscular system in rosacea’s underpinnings.
“Many of the triggers associated with clinical exacerbation of rosacea are known to activate the immune system and/or the neurovasculature, such as demodex, sunlight, alcohol, and changes in temperature,” she said, adding that therapies targeting the neurovascular effects of rosacea are particularly needed.
More than 50% of patients with rosacea have ocular manifestations, with symptoms such as “dryness, burning and stinging, light sensitivity, blurred vision, and foreign body sensation,” the authors reported.
Diagnosis and management
Without definitive laboratory tests, it’s essential that the clinical diagnosis takes into account not only the physical examination findings, but also patient history, the authors stressed, since “some features may not be visually evident or present at the time of the patient’s visit.”
The authors also recommend taking into account patients’ perception and response to their appearance and its effects on their emotional, social, and professional lives when selecting interventions.
“Rosacea’s unsightly and conspicuous appearance often has significant emotional ramifications, potentially resulting in depression or anxiety, and frequently interferes with social and occupational interactions,” the authors wrote. “It may also be advisable to remind patients that normalization of skin tone and color is the goal rather than complete eradication of facial coloration, which can leave the face with a sallow appearance.”
Therapy will often require multiple agents, such as topical and oral agents for inflammatory papules/pustules of rosacea. If insufficient, adjunctive therapy with oral antibiotics or retinoids may be options, though the latter requires prevention of pregnancy during treatment. The authors also discussed pharmacological treatments for facial erythema and flushing, with all these drugs organized in tables according to symptoms and their levels of evidence and effectiveness.
Despite limited clinical evidence, the authors noted success with two types of laser therapy – pulsed-dye and potassium titanyl phosphate – for telangiectasia and erythema. They also noted the option of intense pulsed light for flushing, ocular symptoms, and meibomian gland dysfunction, and of ablative lasers for rhinophymatous nose. But they highlighted the importance of being cautious when using these therapies on darker skin.
In their discussion of ocular rosacea, the authors described the various manifestations and the two “mainstays” of treatment: “eyelash hygiene and oral [omega-3] supplementation, followed by topical azithromycin or calcineurin inhibitors.” In addition to pharmacological and light therapy options, attention to environmental contributors and conscientious skin care regimens can benefit patients with rosacea as well.
“Clinicians may advise patients to keep a daily diary of lifestyle and environmental factors that appear to affect their rosacea to help identify and avoid their personal triggers,” the authors wrote. “The most common factors are sun exposure, emotional stress, hot weather, wind, heavy exercise, alcohol consumption, hot baths, cold weather, spicy foods, humidity, indoor heat, certain skin-care products, heated beverages, certain medications, medical conditions, certain fruits, marinated meats, certain vegetables, and dairy products.”
The paper also emphasizes the importance of gentle skin care given the highly sensitive and easily irritated skin of patients with rosacea. Sunscreen use, particularly with mineral sunscreens that provide physical barriers and reflect ultraviolet light, should be a key aspect of patients’ skin care, and clinicians should advise patients to seek out gentle, nonirritating cleansers.
Funding was provided by the National Rosacea Society, which receives funding from patients and corporations that include Aclaris Therapeutics, Allergan, Bayer, Cutanea Life Sciences, and Galderma Laboratories. Dr. Thiboutot consults for Galderma. Six of the other nine coauthors have financial links to industry through advisory boards, consulting, or research funding.
SOURCE: Thiboutot D et al. J Am Acad Dermatol. 2020;82:1501-10.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Energy-based therapy plus oxymetazoline proves safe for rosacea
according to results from a phase 4 study.
“The current study was designed to evaluate the safety and tolerability of oxymetazoline when used as an adjunctive treatment with energy‐based therapy for patients with moderate to severe facial erythema associated with rosacea,” wrote Emil A. Tanghetti, MD, of the Center for Dermatology and Laser Surgery in Sacramento, and coauthors. The findings were published in Lasers in Surgery and Medicine.
The open-label, interventional study included 46 patients with rosacea, with moderate to severe facial erythema. Study participants received treatment with one of four energy-based devices: pulsed‐dye laser Vbeam Perfecta (PDL-Vbeam), pulsed‐dye laser Cynergy (PDL-Cynergy), intense pulsed-light therapy (IPL), or potassium titanyl phosphate laser (KTP laser), in combination with adjunctive oxymetazoline hydrochloride cream (1%).
On days 3-27 and 31-56, oxymetazoline, an alpha1A adrenoceptor agonist was applied once daily, while energy-based therapy was provided on day 1 and day 29.
The primary safety endpoints were the incidence of treatment‐emergent adverse events (TEAEs) and serious adverse events; the exploratory efficacy endpoint was the change in clinician erythema assessment (CEA) score from start of therapy measured over a 6-hour period post treatment.
Among 43 evaluable patients (who completed the study), CEA score was improved in 39 (90.7%) patients 6 hours post treatment on day 56 and in 30 (68.2%) patients pretreatment.
On day 31, of the 43 evaluable patients, “one‐grade or greater improvement was observed” in 26 (60.5%) patients before application of oxymetazoline, and in 38 (88.4%) of patients 6 hours post treatment, they wrote.
Overall, patient satisfaction increased over the course of the study, with 28 (65.1%) of patients reporting they were satisfied or very satisfied with the treatment on day 56.
Among 46 patients who received at least one treatment, 5 (10.9%) patients had one or more TEAEs (KTP laser, n = 1; PDL-Vbeam, n = 4), and 4 patients had one or more treatment‐related TEAEs (PDL-Vbeam, n = 4); All TEAEs were considered mild or moderate. “Three (6.5%) patients experienced TEAEs related to oxymetazoline; all led to study discontinuation,” the researchers reported.
The researchers acknowledged that a key limitation of the study was the use of multiple energy-based devices, delivered by different providers, which could have caused inconsistency in the results.
“Prospective clinical studies assessing the long‐term safety and efficacy of combined treatment with oxymetazoline and energy‐based therapies are needed,” they concluded.
The manuscript was funded by oxymetazoline manufacturer Aclaris Therapeutics. Several authors disclosed being an investigator, consultant, and/or laser manufacturers. One author was an employee of Aclaris at the time of the study.
SOURCE: Tanghetti EA et al. Lasers Surg Med. 2020 May 6. doi: 10.1002/lsm.23253.
according to results from a phase 4 study.
“The current study was designed to evaluate the safety and tolerability of oxymetazoline when used as an adjunctive treatment with energy‐based therapy for patients with moderate to severe facial erythema associated with rosacea,” wrote Emil A. Tanghetti, MD, of the Center for Dermatology and Laser Surgery in Sacramento, and coauthors. The findings were published in Lasers in Surgery and Medicine.
The open-label, interventional study included 46 patients with rosacea, with moderate to severe facial erythema. Study participants received treatment with one of four energy-based devices: pulsed‐dye laser Vbeam Perfecta (PDL-Vbeam), pulsed‐dye laser Cynergy (PDL-Cynergy), intense pulsed-light therapy (IPL), or potassium titanyl phosphate laser (KTP laser), in combination with adjunctive oxymetazoline hydrochloride cream (1%).
On days 3-27 and 31-56, oxymetazoline, an alpha1A adrenoceptor agonist was applied once daily, while energy-based therapy was provided on day 1 and day 29.
The primary safety endpoints were the incidence of treatment‐emergent adverse events (TEAEs) and serious adverse events; the exploratory efficacy endpoint was the change in clinician erythema assessment (CEA) score from start of therapy measured over a 6-hour period post treatment.
Among 43 evaluable patients (who completed the study), CEA score was improved in 39 (90.7%) patients 6 hours post treatment on day 56 and in 30 (68.2%) patients pretreatment.
On day 31, of the 43 evaluable patients, “one‐grade or greater improvement was observed” in 26 (60.5%) patients before application of oxymetazoline, and in 38 (88.4%) of patients 6 hours post treatment, they wrote.
Overall, patient satisfaction increased over the course of the study, with 28 (65.1%) of patients reporting they were satisfied or very satisfied with the treatment on day 56.
Among 46 patients who received at least one treatment, 5 (10.9%) patients had one or more TEAEs (KTP laser, n = 1; PDL-Vbeam, n = 4), and 4 patients had one or more treatment‐related TEAEs (PDL-Vbeam, n = 4); All TEAEs were considered mild or moderate. “Three (6.5%) patients experienced TEAEs related to oxymetazoline; all led to study discontinuation,” the researchers reported.
The researchers acknowledged that a key limitation of the study was the use of multiple energy-based devices, delivered by different providers, which could have caused inconsistency in the results.
“Prospective clinical studies assessing the long‐term safety and efficacy of combined treatment with oxymetazoline and energy‐based therapies are needed,” they concluded.
The manuscript was funded by oxymetazoline manufacturer Aclaris Therapeutics. Several authors disclosed being an investigator, consultant, and/or laser manufacturers. One author was an employee of Aclaris at the time of the study.
SOURCE: Tanghetti EA et al. Lasers Surg Med. 2020 May 6. doi: 10.1002/lsm.23253.
according to results from a phase 4 study.
“The current study was designed to evaluate the safety and tolerability of oxymetazoline when used as an adjunctive treatment with energy‐based therapy for patients with moderate to severe facial erythema associated with rosacea,” wrote Emil A. Tanghetti, MD, of the Center for Dermatology and Laser Surgery in Sacramento, and coauthors. The findings were published in Lasers in Surgery and Medicine.
The open-label, interventional study included 46 patients with rosacea, with moderate to severe facial erythema. Study participants received treatment with one of four energy-based devices: pulsed‐dye laser Vbeam Perfecta (PDL-Vbeam), pulsed‐dye laser Cynergy (PDL-Cynergy), intense pulsed-light therapy (IPL), or potassium titanyl phosphate laser (KTP laser), in combination with adjunctive oxymetazoline hydrochloride cream (1%).
On days 3-27 and 31-56, oxymetazoline, an alpha1A adrenoceptor agonist was applied once daily, while energy-based therapy was provided on day 1 and day 29.
The primary safety endpoints were the incidence of treatment‐emergent adverse events (TEAEs) and serious adverse events; the exploratory efficacy endpoint was the change in clinician erythema assessment (CEA) score from start of therapy measured over a 6-hour period post treatment.
Among 43 evaluable patients (who completed the study), CEA score was improved in 39 (90.7%) patients 6 hours post treatment on day 56 and in 30 (68.2%) patients pretreatment.
On day 31, of the 43 evaluable patients, “one‐grade or greater improvement was observed” in 26 (60.5%) patients before application of oxymetazoline, and in 38 (88.4%) of patients 6 hours post treatment, they wrote.
Overall, patient satisfaction increased over the course of the study, with 28 (65.1%) of patients reporting they were satisfied or very satisfied with the treatment on day 56.
Among 46 patients who received at least one treatment, 5 (10.9%) patients had one or more TEAEs (KTP laser, n = 1; PDL-Vbeam, n = 4), and 4 patients had one or more treatment‐related TEAEs (PDL-Vbeam, n = 4); All TEAEs were considered mild or moderate. “Three (6.5%) patients experienced TEAEs related to oxymetazoline; all led to study discontinuation,” the researchers reported.
The researchers acknowledged that a key limitation of the study was the use of multiple energy-based devices, delivered by different providers, which could have caused inconsistency in the results.
“Prospective clinical studies assessing the long‐term safety and efficacy of combined treatment with oxymetazoline and energy‐based therapies are needed,” they concluded.
The manuscript was funded by oxymetazoline manufacturer Aclaris Therapeutics. Several authors disclosed being an investigator, consultant, and/or laser manufacturers. One author was an employee of Aclaris at the time of the study.
SOURCE: Tanghetti EA et al. Lasers Surg Med. 2020 May 6. doi: 10.1002/lsm.23253.
FROM LASERS IN SURGERY AND MEDICINE
Studies add clarity to link between rosacea and Demodex, coffee
LAHAINA, HAWAII – Recent data on the roles of caffeinated coffee and two types of Demodex species play in rosacea were discussed by Linda Stein Gold, MD, at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
When considering rosacea triggers, the role of coffee has been difficult to determine, according to Dr. Stein Gold, director of dermatology research at the Henry Ford Health System in Detroit.
“We know that caffeine can vasoconstrict, it also has anti-inflammatory properties so ... that might help rosacea,” while the heat from a hot cup of coffee may cause vasodilation “and make rosacea worse,” she noted.
But a recent study of data from the Nurses’ Health Study II that evaluated intake of coffee, tea, soda, and chocolate every 4 years in over 82,000 women shed some light on the role coffee may play (JAMA Dermatol. 2018 Dec 1;154[12]:1394-1400). There were almost 5,000 cases of physician-diagnosed rosacea in the cohort. When the investigators looked at caffeinated coffee consumption, she said.
Those who consumed four or more servings of caffeinated coffee a day had a significantly lower risk of rosacea, compared with those who consumed one or fewer servings per month (hazard ratio, 0.77; 95% confidence interval, 0.69-0.87; P less than .001).
But there was no significant association with decaffeinated coffee or with edibles that contained caffeine such as tea, soda, and chocolate, “so something about caffeinated coffee seems to be protective for the development of rosacea,” Dr. Stein Gold said.
Demodex mites
A few years ago, “we really didn’t think much of Demodex, but now we know Demodex tends to be a key player” in people with rosacea, Dr. Stein Gold said.
In adults, the colonization rate of Demodex ranges from 70% to 100%, but the skin of people with rosacea have a particularly high density of Demodex: About 35%-50% of patients with rosacea have an increased Demodex load above 5 mites per cm2, as measured with a standard skin surface biopsy, she noted. The density of Demodex in the skin of patients with rosacea has been measured at sixfold higher, compared with age-matched controls.
There also are two different Demodex species: Demodex folliculorum, which are longer, and Demodex brevis, which are short, and there is evidence that each “may cause an individual reaction,” Dr. Stein Gold said.
She referred to a study that found a difference in the Demodex population in patients with highly inflammatory disease with a high level of Demodex, mild rosacea patients who did not have a lot of Demodex, and people with no rosacea (Dermatol Reports. 2019 Jan 23;11[1]:7675).
“Those people who had really severe, inflammatory rosacea had Demodex folliculorum,” and the patients with the more mild disease or those with clear skin had Demodex brevis, she said, so “different species of Demodex might cause a different inflammatory reaction within individual rosacea patients.”
Dr. Stein Gold reported that she has served as a consultant, investigator, or speaker for Galderma, Dermira, Foamix Pharmaceuticals, Valeant (now Bausch Health), Allergan, Actavis, and Roche.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
LAHAINA, HAWAII – Recent data on the roles of caffeinated coffee and two types of Demodex species play in rosacea were discussed by Linda Stein Gold, MD, at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
When considering rosacea triggers, the role of coffee has been difficult to determine, according to Dr. Stein Gold, director of dermatology research at the Henry Ford Health System in Detroit.
“We know that caffeine can vasoconstrict, it also has anti-inflammatory properties so ... that might help rosacea,” while the heat from a hot cup of coffee may cause vasodilation “and make rosacea worse,” she noted.
But a recent study of data from the Nurses’ Health Study II that evaluated intake of coffee, tea, soda, and chocolate every 4 years in over 82,000 women shed some light on the role coffee may play (JAMA Dermatol. 2018 Dec 1;154[12]:1394-1400). There were almost 5,000 cases of physician-diagnosed rosacea in the cohort. When the investigators looked at caffeinated coffee consumption, she said.
Those who consumed four or more servings of caffeinated coffee a day had a significantly lower risk of rosacea, compared with those who consumed one or fewer servings per month (hazard ratio, 0.77; 95% confidence interval, 0.69-0.87; P less than .001).
But there was no significant association with decaffeinated coffee or with edibles that contained caffeine such as tea, soda, and chocolate, “so something about caffeinated coffee seems to be protective for the development of rosacea,” Dr. Stein Gold said.
Demodex mites
A few years ago, “we really didn’t think much of Demodex, but now we know Demodex tends to be a key player” in people with rosacea, Dr. Stein Gold said.
In adults, the colonization rate of Demodex ranges from 70% to 100%, but the skin of people with rosacea have a particularly high density of Demodex: About 35%-50% of patients with rosacea have an increased Demodex load above 5 mites per cm2, as measured with a standard skin surface biopsy, she noted. The density of Demodex in the skin of patients with rosacea has been measured at sixfold higher, compared with age-matched controls.
There also are two different Demodex species: Demodex folliculorum, which are longer, and Demodex brevis, which are short, and there is evidence that each “may cause an individual reaction,” Dr. Stein Gold said.
She referred to a study that found a difference in the Demodex population in patients with highly inflammatory disease with a high level of Demodex, mild rosacea patients who did not have a lot of Demodex, and people with no rosacea (Dermatol Reports. 2019 Jan 23;11[1]:7675).
“Those people who had really severe, inflammatory rosacea had Demodex folliculorum,” and the patients with the more mild disease or those with clear skin had Demodex brevis, she said, so “different species of Demodex might cause a different inflammatory reaction within individual rosacea patients.”
Dr. Stein Gold reported that she has served as a consultant, investigator, or speaker for Galderma, Dermira, Foamix Pharmaceuticals, Valeant (now Bausch Health), Allergan, Actavis, and Roche.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
LAHAINA, HAWAII – Recent data on the roles of caffeinated coffee and two types of Demodex species play in rosacea were discussed by Linda Stein Gold, MD, at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
When considering rosacea triggers, the role of coffee has been difficult to determine, according to Dr. Stein Gold, director of dermatology research at the Henry Ford Health System in Detroit.
“We know that caffeine can vasoconstrict, it also has anti-inflammatory properties so ... that might help rosacea,” while the heat from a hot cup of coffee may cause vasodilation “and make rosacea worse,” she noted.
But a recent study of data from the Nurses’ Health Study II that evaluated intake of coffee, tea, soda, and chocolate every 4 years in over 82,000 women shed some light on the role coffee may play (JAMA Dermatol. 2018 Dec 1;154[12]:1394-1400). There were almost 5,000 cases of physician-diagnosed rosacea in the cohort. When the investigators looked at caffeinated coffee consumption, she said.
Those who consumed four or more servings of caffeinated coffee a day had a significantly lower risk of rosacea, compared with those who consumed one or fewer servings per month (hazard ratio, 0.77; 95% confidence interval, 0.69-0.87; P less than .001).
But there was no significant association with decaffeinated coffee or with edibles that contained caffeine such as tea, soda, and chocolate, “so something about caffeinated coffee seems to be protective for the development of rosacea,” Dr. Stein Gold said.
Demodex mites
A few years ago, “we really didn’t think much of Demodex, but now we know Demodex tends to be a key player” in people with rosacea, Dr. Stein Gold said.
In adults, the colonization rate of Demodex ranges from 70% to 100%, but the skin of people with rosacea have a particularly high density of Demodex: About 35%-50% of patients with rosacea have an increased Demodex load above 5 mites per cm2, as measured with a standard skin surface biopsy, she noted. The density of Demodex in the skin of patients with rosacea has been measured at sixfold higher, compared with age-matched controls.
There also are two different Demodex species: Demodex folliculorum, which are longer, and Demodex brevis, which are short, and there is evidence that each “may cause an individual reaction,” Dr. Stein Gold said.
She referred to a study that found a difference in the Demodex population in patients with highly inflammatory disease with a high level of Demodex, mild rosacea patients who did not have a lot of Demodex, and people with no rosacea (Dermatol Reports. 2019 Jan 23;11[1]:7675).
“Those people who had really severe, inflammatory rosacea had Demodex folliculorum,” and the patients with the more mild disease or those with clear skin had Demodex brevis, she said, so “different species of Demodex might cause a different inflammatory reaction within individual rosacea patients.”
Dr. Stein Gold reported that she has served as a consultant, investigator, or speaker for Galderma, Dermira, Foamix Pharmaceuticals, Valeant (now Bausch Health), Allergan, Actavis, and Roche.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM SDEF HAWAII DERMATOLOGY SEMINAR
Data back botulinum toxin for facial flushing, androgenetic alopecia
LAHAINA, HAWAII – The list of Mark Rubin, MD, said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
There are data to support these uses, and there are data associating botulinum toxin treatment with improvement in depression, which suggest the effect may not be necessarily be related to improvement in appearance, said Dr. Rubin, who is in private practice in Beverly Hills, Calif., and is associate professor of dermatology at the University of California, San Diego.
Facial flushing: Very few people use botulinum toxin for facial flushing, but Dr. Rubin, who is among those who do not, described the data as “impressive.” Several trials, he noted, have found that very small doses can significantly reduce the amount of facial erythema, including an average 45% reduction after 60 days in one trial of 24 women (Acta Med Iran. 2016 Jul;54[7]:454-7).
In another study of 25 patients with facial erythema related to rosacea who were treated with 14-45 units intradermally to the nasal tip, bridge, and alae, there were statistically significant improvements in erythema 1, 2, and 3 months after treatment among the 15 with complete data (Dermatol Surg. 2015 Jan;41 Suppl 1:S9-16).
“If you’re using very small doses and they’re intradermal, there really is minimal risk you’re going to have a problem by inadvertently affecting musculature” in these patients, Dr. Rubin commented.
In another study of 9 patients with rosacea, treatment with incobotulinumtoxinA was associated with a significant reduction in erythema, papules, pustules, and telangiectasias, up to 15 weeks, compared with saline. The treatment patients also experienced less burning and stinging that did those who received saline (J Drugs Dermatol. 2017 Jun 1;16[6]:549-54.)
Menopausal hot flashes: Dr. Rubin described one study of 60 patients with severe hot flashes that compared saline with botulinum toxin, injected in 40 sites (2 units per site), including the neck, hairline, scalp, and chest. At 60 days’ follow-up, those treated with botulinum toxin had a significant reduction in sweating and in the number and severity of hot flashes; these women also had improved mood in terms of depression and irritability (Dermatol Surg. 2011 Nov;37[11]:1579-83).
Androgenetic alopecia: In a 60-week study of 50 men with androgenetic alopecia (Hamilton ratings of II-IV), 150 units of botulinum toxin A was injected into the scalp muscles (temporalis, frontalis, periauricular, and occipital), and repeated 6 months later (Plast Reconstr Surg. 2010 Nov;126[5]:246e-8e). Among the 40 patients who completed the trial, 75% had a response, and from baseline to 48 weeks, there was an 18% increase in mean hair counts in a 2 cm area, and a“profound” 39% reduction in hair loss (as measured by hair counts on the pillow in the morning), Dr. Rubin noted.
“Presumably, this is because if you’re relaxing the scalp muscles you’re getting increased blood flow into the scalp,” including increased oxygenation, which decreases the conversion of testosterone to dihydrotestosterone and increases the conversion of testosterone to estradiol, he said.
In another study, 8 of 10 patients with androgenic alopecia has “good to excellent” results 24 weeks after botulinum toxin injections with 5 units per site at 30 sites. Referring to the increasing popularity of platelet-rich plasma (PRP) injections for male pattern alopecia, Dr. Rubin said that in his opinion “PRP certainly doesn’t do any better” than botulinum toxin for male pattern alopecia and is a much more involved injection, “so this is definitely something worth considering if you have more people coming into your practice thinking about injections for male pattern alopecia.”
Pore size and sebum production: A 2019 review of published studies of botulinum toxin A looking at the effect on sebum and pore size, Dr. Rubin said, found that most studies “suggest it does actually reduce pore size and sebum production” (J Cosmet Dermatol. 2019 Apr;18[2]:451-7).
This can be considered an option for those patients concerned about pore size, who are not satisfied with results of retinoid or laser treatment, he commented. This approach may not have an effect in all patients, so he advised first treating a small trial area, and photographing patients to record their level of improvement. “It’s rarely profound, but it’s additive, it’s one more thing you can do.”
Depression: These data include a study of 30 patients with major depression, half who received one onabotulinumtoxinA injection in the glabellar area as adjunctive treatment of depression. After 6 weeks, those who were treated had an average of 47% reduction in depression scores on the Hamilton Depression Rating Scale, compared with an average 9% reduction among those on placebo (J Psychiatr Res. 2012 May;46[5]:574-81). Two recent studies have had similar results, according to Dr. Rubin.
Results of another study, he said, raise the question of whether patients are less depressed because they are pleased with the cosmetic effects or if there is another explanation (J Am Acad Dermatol. 2016 Jan;74[1]:171-3.e1). The study, which included 59 patients with depression treated in the glabellar areas with botulinum toxin injections, found no association between severity of the furrows and degree of depression or between the degree of furrow correction and degree of relief from depression after treatment. “So the patients who had the most improvement were not necessarily the ones who were the least depressed afterwards,” he said.
These data imply that something else may be occurring that is not necessarily muscle related, he said.
Dr. Rubin said he had no relevant disclosures. SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
LAHAINA, HAWAII – The list of Mark Rubin, MD, said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
There are data to support these uses, and there are data associating botulinum toxin treatment with improvement in depression, which suggest the effect may not be necessarily be related to improvement in appearance, said Dr. Rubin, who is in private practice in Beverly Hills, Calif., and is associate professor of dermatology at the University of California, San Diego.
Facial flushing: Very few people use botulinum toxin for facial flushing, but Dr. Rubin, who is among those who do not, described the data as “impressive.” Several trials, he noted, have found that very small doses can significantly reduce the amount of facial erythema, including an average 45% reduction after 60 days in one trial of 24 women (Acta Med Iran. 2016 Jul;54[7]:454-7).
In another study of 25 patients with facial erythema related to rosacea who were treated with 14-45 units intradermally to the nasal tip, bridge, and alae, there were statistically significant improvements in erythema 1, 2, and 3 months after treatment among the 15 with complete data (Dermatol Surg. 2015 Jan;41 Suppl 1:S9-16).
“If you’re using very small doses and they’re intradermal, there really is minimal risk you’re going to have a problem by inadvertently affecting musculature” in these patients, Dr. Rubin commented.
In another study of 9 patients with rosacea, treatment with incobotulinumtoxinA was associated with a significant reduction in erythema, papules, pustules, and telangiectasias, up to 15 weeks, compared with saline. The treatment patients also experienced less burning and stinging that did those who received saline (J Drugs Dermatol. 2017 Jun 1;16[6]:549-54.)
Menopausal hot flashes: Dr. Rubin described one study of 60 patients with severe hot flashes that compared saline with botulinum toxin, injected in 40 sites (2 units per site), including the neck, hairline, scalp, and chest. At 60 days’ follow-up, those treated with botulinum toxin had a significant reduction in sweating and in the number and severity of hot flashes; these women also had improved mood in terms of depression and irritability (Dermatol Surg. 2011 Nov;37[11]:1579-83).
Androgenetic alopecia: In a 60-week study of 50 men with androgenetic alopecia (Hamilton ratings of II-IV), 150 units of botulinum toxin A was injected into the scalp muscles (temporalis, frontalis, periauricular, and occipital), and repeated 6 months later (Plast Reconstr Surg. 2010 Nov;126[5]:246e-8e). Among the 40 patients who completed the trial, 75% had a response, and from baseline to 48 weeks, there was an 18% increase in mean hair counts in a 2 cm area, and a“profound” 39% reduction in hair loss (as measured by hair counts on the pillow in the morning), Dr. Rubin noted.
“Presumably, this is because if you’re relaxing the scalp muscles you’re getting increased blood flow into the scalp,” including increased oxygenation, which decreases the conversion of testosterone to dihydrotestosterone and increases the conversion of testosterone to estradiol, he said.
In another study, 8 of 10 patients with androgenic alopecia has “good to excellent” results 24 weeks after botulinum toxin injections with 5 units per site at 30 sites. Referring to the increasing popularity of platelet-rich plasma (PRP) injections for male pattern alopecia, Dr. Rubin said that in his opinion “PRP certainly doesn’t do any better” than botulinum toxin for male pattern alopecia and is a much more involved injection, “so this is definitely something worth considering if you have more people coming into your practice thinking about injections for male pattern alopecia.”
Pore size and sebum production: A 2019 review of published studies of botulinum toxin A looking at the effect on sebum and pore size, Dr. Rubin said, found that most studies “suggest it does actually reduce pore size and sebum production” (J Cosmet Dermatol. 2019 Apr;18[2]:451-7).
This can be considered an option for those patients concerned about pore size, who are not satisfied with results of retinoid or laser treatment, he commented. This approach may not have an effect in all patients, so he advised first treating a small trial area, and photographing patients to record their level of improvement. “It’s rarely profound, but it’s additive, it’s one more thing you can do.”
Depression: These data include a study of 30 patients with major depression, half who received one onabotulinumtoxinA injection in the glabellar area as adjunctive treatment of depression. After 6 weeks, those who were treated had an average of 47% reduction in depression scores on the Hamilton Depression Rating Scale, compared with an average 9% reduction among those on placebo (J Psychiatr Res. 2012 May;46[5]:574-81). Two recent studies have had similar results, according to Dr. Rubin.
Results of another study, he said, raise the question of whether patients are less depressed because they are pleased with the cosmetic effects or if there is another explanation (J Am Acad Dermatol. 2016 Jan;74[1]:171-3.e1). The study, which included 59 patients with depression treated in the glabellar areas with botulinum toxin injections, found no association between severity of the furrows and degree of depression or between the degree of furrow correction and degree of relief from depression after treatment. “So the patients who had the most improvement were not necessarily the ones who were the least depressed afterwards,” he said.
These data imply that something else may be occurring that is not necessarily muscle related, he said.
Dr. Rubin said he had no relevant disclosures. SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
LAHAINA, HAWAII – The list of Mark Rubin, MD, said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
There are data to support these uses, and there are data associating botulinum toxin treatment with improvement in depression, which suggest the effect may not be necessarily be related to improvement in appearance, said Dr. Rubin, who is in private practice in Beverly Hills, Calif., and is associate professor of dermatology at the University of California, San Diego.
Facial flushing: Very few people use botulinum toxin for facial flushing, but Dr. Rubin, who is among those who do not, described the data as “impressive.” Several trials, he noted, have found that very small doses can significantly reduce the amount of facial erythema, including an average 45% reduction after 60 days in one trial of 24 women (Acta Med Iran. 2016 Jul;54[7]:454-7).
In another study of 25 patients with facial erythema related to rosacea who were treated with 14-45 units intradermally to the nasal tip, bridge, and alae, there were statistically significant improvements in erythema 1, 2, and 3 months after treatment among the 15 with complete data (Dermatol Surg. 2015 Jan;41 Suppl 1:S9-16).
“If you’re using very small doses and they’re intradermal, there really is minimal risk you’re going to have a problem by inadvertently affecting musculature” in these patients, Dr. Rubin commented.
In another study of 9 patients with rosacea, treatment with incobotulinumtoxinA was associated with a significant reduction in erythema, papules, pustules, and telangiectasias, up to 15 weeks, compared with saline. The treatment patients also experienced less burning and stinging that did those who received saline (J Drugs Dermatol. 2017 Jun 1;16[6]:549-54.)
Menopausal hot flashes: Dr. Rubin described one study of 60 patients with severe hot flashes that compared saline with botulinum toxin, injected in 40 sites (2 units per site), including the neck, hairline, scalp, and chest. At 60 days’ follow-up, those treated with botulinum toxin had a significant reduction in sweating and in the number and severity of hot flashes; these women also had improved mood in terms of depression and irritability (Dermatol Surg. 2011 Nov;37[11]:1579-83).
Androgenetic alopecia: In a 60-week study of 50 men with androgenetic alopecia (Hamilton ratings of II-IV), 150 units of botulinum toxin A was injected into the scalp muscles (temporalis, frontalis, periauricular, and occipital), and repeated 6 months later (Plast Reconstr Surg. 2010 Nov;126[5]:246e-8e). Among the 40 patients who completed the trial, 75% had a response, and from baseline to 48 weeks, there was an 18% increase in mean hair counts in a 2 cm area, and a“profound” 39% reduction in hair loss (as measured by hair counts on the pillow in the morning), Dr. Rubin noted.
“Presumably, this is because if you’re relaxing the scalp muscles you’re getting increased blood flow into the scalp,” including increased oxygenation, which decreases the conversion of testosterone to dihydrotestosterone and increases the conversion of testosterone to estradiol, he said.
In another study, 8 of 10 patients with androgenic alopecia has “good to excellent” results 24 weeks after botulinum toxin injections with 5 units per site at 30 sites. Referring to the increasing popularity of platelet-rich plasma (PRP) injections for male pattern alopecia, Dr. Rubin said that in his opinion “PRP certainly doesn’t do any better” than botulinum toxin for male pattern alopecia and is a much more involved injection, “so this is definitely something worth considering if you have more people coming into your practice thinking about injections for male pattern alopecia.”
Pore size and sebum production: A 2019 review of published studies of botulinum toxin A looking at the effect on sebum and pore size, Dr. Rubin said, found that most studies “suggest it does actually reduce pore size and sebum production” (J Cosmet Dermatol. 2019 Apr;18[2]:451-7).
This can be considered an option for those patients concerned about pore size, who are not satisfied with results of retinoid or laser treatment, he commented. This approach may not have an effect in all patients, so he advised first treating a small trial area, and photographing patients to record their level of improvement. “It’s rarely profound, but it’s additive, it’s one more thing you can do.”
Depression: These data include a study of 30 patients with major depression, half who received one onabotulinumtoxinA injection in the glabellar area as adjunctive treatment of depression. After 6 weeks, those who were treated had an average of 47% reduction in depression scores on the Hamilton Depression Rating Scale, compared with an average 9% reduction among those on placebo (J Psychiatr Res. 2012 May;46[5]:574-81). Two recent studies have had similar results, according to Dr. Rubin.
Results of another study, he said, raise the question of whether patients are less depressed because they are pleased with the cosmetic effects or if there is another explanation (J Am Acad Dermatol. 2016 Jan;74[1]:171-3.e1). The study, which included 59 patients with depression treated in the glabellar areas with botulinum toxin injections, found no association between severity of the furrows and degree of depression or between the degree of furrow correction and degree of relief from depression after treatment. “So the patients who had the most improvement were not necessarily the ones who were the least depressed afterwards,” he said.
These data imply that something else may be occurring that is not necessarily muscle related, he said.
Dr. Rubin said he had no relevant disclosures. SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM SDEF HAWAII DERMATOLOGY SEMINAR
Rosacea: Target treatment to pathogenic pathway
LAHAINA, HAWAII – The pathophysiology of rosacea is complicated, which is why “we try to target our treatments to various areas in this pathogenic pathway” to achieve optimal results, according to Linda Stein Gold, MD, director of dermatology research at the Henry Ford Health System in Detroit.
For example, in a patient with papules and pustules, a topical or oral anti-inflammatory agent is needed “to calm that down.” If background erythema is present, separate from papules and pustules, use a topical alpha-adrenergic agonist, she advised. For telangiectasias, consider a device-based treatment, and for a phyma, a surgical approach, she recommended at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
For the background erythema of rosacea, which she described as “that pink face that’s always there,” the two alpha-adrenergic receptor agonists available, brimonidine gel 0.33%, approved by the Food and Drug Administration in 2013, and oxymetazoline cream 1%, approved in 2017, both work on the neurovascular junction, but on different receptors.
Brimonidine “kicks in very, very rapidly,” with a significant decrease in background erythema evident within 30 minutes and improvements that last over a 12-hour day, she said. It is effective over a year, but in longterm and postmarketing studies, about 20% of patients experienced exacerbation of erythema, with two peaks of redness. “One occurs at 3-6 hours,” and the other peak occurs when the drug is wearing off later in the day, Dr. Stein Gold said.
A study that sought to identify factors that might make patients more prone to this adverse effect found that “less is better” regarding brimonidine application, with an optimal application of one to three pea-sized dollops on the face, not five as instructed in the package insert. In addition, patients with more than five flushing episodes a week, particularly women, “tend to have more labile disease and [are] more likely to get that rebound erythema,” the study found.
Oxymetazoline 1% in a cream formulation has a “slightly more gentle onset of action and a more gentle offset of action,” without exacerbation of erythema and has been shown to have sustained efficacy over 52 weeks. In a yearlong safety study, there were “no new red flags and we weren’t seeing that redness at hours 3 to 6, or even when you take the patient off the drug,” she noted.
Dr. Stein Gold reported that she has served as a consultant, investigator, or speaker for Galderma, Dermira, Foamix Pharmaceuticals, Valeant, Allergan, Actavis, and Roche.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
LAHAINA, HAWAII – The pathophysiology of rosacea is complicated, which is why “we try to target our treatments to various areas in this pathogenic pathway” to achieve optimal results, according to Linda Stein Gold, MD, director of dermatology research at the Henry Ford Health System in Detroit.
For example, in a patient with papules and pustules, a topical or oral anti-inflammatory agent is needed “to calm that down.” If background erythema is present, separate from papules and pustules, use a topical alpha-adrenergic agonist, she advised. For telangiectasias, consider a device-based treatment, and for a phyma, a surgical approach, she recommended at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
For the background erythema of rosacea, which she described as “that pink face that’s always there,” the two alpha-adrenergic receptor agonists available, brimonidine gel 0.33%, approved by the Food and Drug Administration in 2013, and oxymetazoline cream 1%, approved in 2017, both work on the neurovascular junction, but on different receptors.
Brimonidine “kicks in very, very rapidly,” with a significant decrease in background erythema evident within 30 minutes and improvements that last over a 12-hour day, she said. It is effective over a year, but in longterm and postmarketing studies, about 20% of patients experienced exacerbation of erythema, with two peaks of redness. “One occurs at 3-6 hours,” and the other peak occurs when the drug is wearing off later in the day, Dr. Stein Gold said.
A study that sought to identify factors that might make patients more prone to this adverse effect found that “less is better” regarding brimonidine application, with an optimal application of one to three pea-sized dollops on the face, not five as instructed in the package insert. In addition, patients with more than five flushing episodes a week, particularly women, “tend to have more labile disease and [are] more likely to get that rebound erythema,” the study found.
Oxymetazoline 1% in a cream formulation has a “slightly more gentle onset of action and a more gentle offset of action,” without exacerbation of erythema and has been shown to have sustained efficacy over 52 weeks. In a yearlong safety study, there were “no new red flags and we weren’t seeing that redness at hours 3 to 6, or even when you take the patient off the drug,” she noted.
Dr. Stein Gold reported that she has served as a consultant, investigator, or speaker for Galderma, Dermira, Foamix Pharmaceuticals, Valeant, Allergan, Actavis, and Roche.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
LAHAINA, HAWAII – The pathophysiology of rosacea is complicated, which is why “we try to target our treatments to various areas in this pathogenic pathway” to achieve optimal results, according to Linda Stein Gold, MD, director of dermatology research at the Henry Ford Health System in Detroit.
For example, in a patient with papules and pustules, a topical or oral anti-inflammatory agent is needed “to calm that down.” If background erythema is present, separate from papules and pustules, use a topical alpha-adrenergic agonist, she advised. For telangiectasias, consider a device-based treatment, and for a phyma, a surgical approach, she recommended at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
For the background erythema of rosacea, which she described as “that pink face that’s always there,” the two alpha-adrenergic receptor agonists available, brimonidine gel 0.33%, approved by the Food and Drug Administration in 2013, and oxymetazoline cream 1%, approved in 2017, both work on the neurovascular junction, but on different receptors.
Brimonidine “kicks in very, very rapidly,” with a significant decrease in background erythema evident within 30 minutes and improvements that last over a 12-hour day, she said. It is effective over a year, but in longterm and postmarketing studies, about 20% of patients experienced exacerbation of erythema, with two peaks of redness. “One occurs at 3-6 hours,” and the other peak occurs when the drug is wearing off later in the day, Dr. Stein Gold said.
A study that sought to identify factors that might make patients more prone to this adverse effect found that “less is better” regarding brimonidine application, with an optimal application of one to three pea-sized dollops on the face, not five as instructed in the package insert. In addition, patients with more than five flushing episodes a week, particularly women, “tend to have more labile disease and [are] more likely to get that rebound erythema,” the study found.
Oxymetazoline 1% in a cream formulation has a “slightly more gentle onset of action and a more gentle offset of action,” without exacerbation of erythema and has been shown to have sustained efficacy over 52 weeks. In a yearlong safety study, there were “no new red flags and we weren’t seeing that redness at hours 3 to 6, or even when you take the patient off the drug,” she noted.
Dr. Stein Gold reported that she has served as a consultant, investigator, or speaker for Galderma, Dermira, Foamix Pharmaceuticals, Valeant, Allergan, Actavis, and Roche.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
REPORTING FROM SDEF HAWAII DERMATOLOGY SEMINAR
Effect of In-Office Samples on Dermatologists’ Prescribing Habits: A Retrospective Review
Over the years, there has been growing concern about the relationship between physicians and pharmaceutical companies. Many studies have demonstrated that pharmaceutical interactions and incentives can influence physicians’ prescribing habits.1-3 As a result, many academic centers have adopted policies that attempt to limit the pharmaceutical industry’s influence on faculty and in-training physicians. Although these policies can vary greatly, they generally limit access of pharmaceutical representatives to providers and restrict pharmaceutical samples.4,5 This policy shift has even been reported in private practice.6
At the heart of the matter is the question: What really influences physicians to write a prescription for a particular medication? Is it cost, efficacy, or representatives pushing a product? Prior studies illustrate that generic medications are equivalent to their brand-name counterparts. In fact, current regulations require no more than 5% to 7% difference in bioequivalence.7-9 Although most generic medications are bioequivalent, it may not be universal.10
Garrison and Levin11 distributed a survey to US-based prescribers in family practice, psychiatry, and internal medicine and found that prescribers deemed patient response and success as the highest priority when determining which drugs to prescribe. In contrast, drug representatives and free samples only slightly contributed.11 Considering the minimum duration for efficacy of a medication such as an antidepressant vs a topical steroid, this pattern may differ with samples in dermatologic settings. Interestingly, another survey concluded that samples were associated with “sticky” prescribing habits, noting that physicians would prescribe a brand-name medication after using a sample, despite increased cost to the patient.12 Further, it has been suggested that recipients of free samples may experience increased costs in the long run, which contrasts a stated goal of affordability to patients.12,13
Physician interaction with pharmaceutical companies begins as early as medical school,14 with physicians reporting interactions as often as 4 times each month.14-18 Interactions can include meetings with pharmaceutical representatives, sponsored meals, gifts, continuing medical education sponsorship, funding for travel, pharmaceutical representative speakers, research funding, and drug samples.3
A 2014 study reported that prescribing habits are influenced by the free drug samples provided by nongeneric pharmaceutical companies.19 Nationally, the number of brand-name and branded generic medications constitute 79% of prescriptions, yet together they only comprise 17% of medications prescribed at an academic medical clinic that does not provide samples. The number of medications with samples being prescribed by dermatologists increased by 15% over 9 years, which may correlate with the wider availability of medication samples, more specifically an increase in branded generic samples.19 This potential interaction is the reason why institutions question the current influence of pharmaceutical companies. Samples may appear convenient, allowing a patient to test the medication prior to committing; however, with brand-name samples being provided to the physician, he/she may become more inclined to prescribe the branded medication.12,15,19-22 Because brand-name medications are more expensive than generic medications, this practice can increase the cost of health care.13 One study found that over 1 year, the overuse of nongeneric medications led to a loss of potential savings throughout 49 states, equating to $229 million just through Medicaid; interestingly, it was noted that in some states, a maximum reimbursement is set by Medicaid, regardless of whether the generic or branded medication is dispensed. The authors also noted variability in the potential savings by state, which may be a function of the state-by-state maximum reimbursements for certain medications.23 Another study on oral combination medications estimated Medicare spending on branded drugs relative to the cost if generic combinations had been purchased instead. This study examined branded medications for which the active components were available as over-the-counter (OTC), generic, or same-class generic, and the authors estimated that $925 million could have been saved in 2016 by purchasing a generic substitute.24 The overuse of nongeneric medications when generic alternatives are available becomes an issue that not only financially impacts patients but all taxpayers. However, this pattern may differ if limited only to dermatologic medications, which was not the focus of the prior studies.
To limit conflicts of interest in interactions with the pharmaceutical, medical device, and biotechnology industries, the University of South Florida (USF) Morsani College of Medicine (COM)(Tampa, Florida) implemented its own set of regulations that eliminated in-office pharmaceutical samples, in addition to other restrictions. This study aimed to investigate if there was a change in the prescribing habits of academic dermatologists after their medical school implemented these new policies.
We hypothesized that the number of brand-name drugs prescribed by physicians in the Department of Dermatology & Cutaneous Surgery would change following USF Morsani COM pharmaceutical policy changes. We sought to determine how physician prescribing practices within the Department of Dermatology & Cutaneous Surgery changed following USF Morsani COM pharmaceutical policy changes.
Methods
Data Collection
A retrospective review of medical records was conducted to investigate the effect of the USF Morsani COM pharmaceutical policy changes on physician prescribing practices within the Department of Dermatology & Cutaneous Surgery. Medical records of patients seen for common dermatology diagnoses before (January 1, 2010, to May 30, 2010) and after (August 1, 2011, to December 31, 2011) the pharmaceutical policy changes were reviewed, and all medications prescribed were recorded. Data were collected from medical records within the USF Health electronic medical record system and included visits with each of the department’s 3 attending dermatologists. The diagnoses included in the study—acne vulgaris, atopic dermatitis, onychomycosis, psoriasis, and rosacea—were chosen because in-office samples were available. Prescribing data from the first 100 consecutive medical records were collected from each time period, and a medical record was included only if it contained at least 1 of the following diagnoses: acne vulgaris, atopic dermatitis, onychomycosis, psoriasis, or rosacea. The assessment and plan of each progress note were reviewed, and the exact medication name and associated diagnosis were recorded for each prescription. Subsequently, each medication was reviewed and placed in 1 of 3 categories: brand name, generic, and OTC. The total number of prescriptions for each diagnosis (per visit/note); the specific number of brand, generic, and OTC medications prescribed (per visit/note); and the percentage of brand, generic, and OTC medications prescribed (per visit/note and per diagnosis in total) were calculated. To ensure only intended medications were included, each medication recorded in the medical record note was cross-referenced with the prescribed medication in the electronic medical record. The primary objective of this study was to capture the prescribing physician’s intent as proxied by the pattern of prescription. Thus, changes made in prescriptions after the initial plan—whether insurance related or otherwise—were not relevant to this investigation.
The data were collected to compare the percentage of brand vs generic or OTC prescriptions per diagnosis to see if there was a difference in the prescribing habits before and after the pharmaceutical policy changes. Of note, several other pieces of data were collected from each medical record, including age, race, class of insurance (ie, Medicare, Medicaid, private health maintenance organization, private preferred provider organization), subtype diagnoses, and whether the prescription was new or a refill. The information gathered from the written record on the assessment and plan was verified using prescriptions ordered in the Allscripts electronic record, and any difference was noted. No identifying information that could be used to easily identify study participants was recorded.
Differences in prescribing habits across diagnoses before and after the policy changes were ascertained using a Fisher exact test and were further assessed using a mixed effects ordinal logistic regression model that accounted for within-provider clustering and baseline patient characteristics. An ordinal model was chosen to recognize differences in average cost among brand-name, generic, and OTC medications.
Results
In total, 200 medical records were collected. For the period analyzed before the policy change, 252 brand-name medications were prescribed compared to 231 prescribed for the period analyzed after the policy changes. There was insufficient evidence of an overall difference in brand-name medications prescribed before and after the policy changes (P=.145; Fisher exact test)(Table 1). There also was insufficient evidence of an overall difference in generic prescriptions, which totaled 153 before and 134 after the policy changes (P=.872; Fisher exact test)(Table 2). Over-the-counter prescriptions totaled 49 before and 69 after the policy changes. There was insufficient evidence of an overall difference before and after the policy changes for OTC medications (P=.192; Fisher exact test)(Table 3).
Comment
Although some medical institutions are diligently working to limit the potential influence pharmaceutical companies have on physician prescribing habits,4,5,25 the effect on physician prescribing habits is only now being established.15 Prior studies12,19,21 have found evidence that medication samples may lead to overuse of brand-name medications, but these findings do not hold true for the USF dermatologists included in this study, perhaps due to the difference in pharmaceutical company interactions or physicians maintaining prior prescription habits that were unrelated to the policy. Although this study focused on policy changes for in-office samples, prior studies either included other forms of interaction21 or did not include samples.22
Pharmaceutical samples allow patients to try a medication before committing to a long-term course of treatment with a particular medication, which has utility for physicians and patients. Although brand-name prescriptions may cost more, a trial period may assist the patient in deciding whether the medication is worth purchasing. Furthermore, physicians may feel more comfortable prescribing a medication once the individual patient has demonstrated a benefit from the sample, which may be particularly true in a specialty such as dermatology in which many branded topical medications contain a different vehicle than generic formulations, resulting in notable variations in active medication delivery and efficacy. Given the higher cost of branded topical medications, proving efficacy in patients through samples can provide a useful tool to the physician to determine the need for a branded formulation.
The benefits described are subjective but should not be disregarded. Although Hurley et al19 found that the number of brand-name medications prescribed increases as more samples are given out, our study demonstrated that after eliminating medication samples, there was no significant difference in the percentage of brand-name medications prescribed compared to generic and OTC medications.
Physician education concerning the price of each brand-name medication prescribed in office may be one method of reducing the amount of such prescriptions. Physicians generally are uninformed of the cost of the medications being prescribed26 and may not recognize the financial burden one medication may have compared to its alternative. However, educating physicians will empower them to make the conscious decision to prefer or not prefer a brand-name medication. With some generic medications shown to have a difference in bioequivalence compared to their brand-name counterparts, a physician may find more success prescribing the brand-name medications, regardless of pharmaceutical company influence, which is an alternative solution to policy changes that eliminate samples entirely. Although this study found insufficient evidence that removing samples decreases brand-name medication prescriptions, it is imperative that solutions are established to reduce the country’s increasing burden of medical costs.
Possible shortfalls of this study include the short period of time between which prepolicy data and postpolicy data were collected. It is possible that providers did not have enough time to adjust their prescribing habits or that providers would not have changed a prescribing pattern or preference simply because of a policy change. Future studies could allow a time period greater than 2 years to compare prepolicy and postpolicy prescribing habits, or a future study might make comparisons of prescriber patterns at different institutions that have different policies. Another possible shortfall is that providers and patients were limited to those at the Department of Dermatology & Cutaneous Surgery at the USF Morsani COM. Although this study has found insufficient evidence of a difference in prescribing habits, it may be beneficial to conduct a larger study that encompasses multiple academic institutions with similar policy changes. Most importantly, this study only investigated the influence of in-office pharmaceutical samples on prescribing patterns. This study did not look at the many other ways in which providers may be influenced by pharmaceutical companies, which likely is a significant confounding variable in this study. Continued additional studies that specifically examine other methods through which providers may be influenced would be helpful in further examining the many ways in which physician prescription habits are influenced.
Conclusion
Changes in pharmaceutical policy in 2011 at USF Morsani COM specifically banned in-office samples. The totality of evidence in this study shows modest observational evidence of a change in the postpolicy odds relative to prepolicy odds, but the data also are compatible with no change between prescribing habits before and after the policy changes. Further study is needed to fully understand this relationship.
- Sondergaard J, Vach K, Kragstrup J, et al. Impact of pharmaceutical representative visits on GPs’ drug preferences. Fam Pract. 2009;26:204-209.
- Jelinek GA, Neate SL. The influence of the pharmaceutical industry in medicine. J Law Med. 2009;17:216-223.
- Wazana A. Physicians and the pharmaceutical industry: is a gift ever just a gift? JAMA. 2000;283:373-380.
- Coleman DL. Establishing policies for the relationship between industry and clinicians: lessons learned from two academic health centers. Acad Med. 2008;83:882-887.
- Coleman DL, Kazdin AE, Miller LA, et al. Guidelines for interactions between clinical faculty and the pharmaceutical industry: one medical school’s approach. Acad Med. 2006;81:154-160.
- Evans D, Hartung DM, Beasley D, et al. Breaking up is hard to do: lessons learned from a pharma-free practice transformation. J Am Board Fam Med. 2013;26:332-338.
- Davit BM, Nwakama PE, Buehler GJ, et al. Comparing generic and innovator drugs: a review of 12 years of bioequivalence data from the United States Food and Drug Administration. Ann Pharmacother. 2009;43:1583-1597.
- Kesselheim AS, Misono AS, Lee JL, et al. Clinical equivalence of generic and brand-name drugs used in cardiovascular disease: a systematic review and meta-analysis. JAMA. 2008;300:2514-2526.
- McCormack J, Chmelicek JT. Generic versus brand name: the other drug war. Can Fam Physician. 2014;60:911.
- Borgheini G. The bioequivalence and therapeutic efficacy of generic versus brand-name psychoactive drugs. Clin Ther. 2003;25:1578-1592.
- Garrison GD, Levin GM. Factors affecting prescribing of the newer antidepressants. Ann Pharmacother. 2000;34:10-14.
- Rafique S, Sarwar W, Rashid A, et al. Influence of free drug samples on prescribing by physicians: a cross sectional survey. J Pak Med Assoc. 2017;67:465-467.
- Alexander GC, Zhang J, Basu A. Characteristics of patients receiving pharmaceutical samples and association between sample receipt and out-of-pocket prescription costs. Med Care. 2008;46:394-402.
- Hodges B. Interactions with the pharmaceutical industry: experiences and attitudes of psychiatry residents, interns and clerks. CMAJ. 1995;153:553-559.
- Brotzman GL, Mark DH. The effect on resident attitudes of regulatory policies regarding pharmaceutical representative activities. J Gen Intern Med. 1993;8:130-134.
- Keim SM, Sanders AB, Witzke DB, et al. Beliefs and practices of emergency medicine faculty and residents regarding professional interactions with the biomedical industry. Ann Emerg Med. 1993;22:1576-1581.
- Thomson AN, Craig BJ, Barham PM. Attitudes of general practitioners in New Zealand to pharmaceutical representatives. Br J Gen Pract. 1994;44:220-223.
- Ziegler MG, Lew P, Singer BC. The accuracy of drug information from pharmaceutical sales representatives. JAMA. 1995;273:1296-1298.
- Hurley MP, Stafford RS, Lane AT. Characterizing the relationship between free drug samples and prescription patterns for acne vulgaris and rosacea. JAMA Dermatol. 2014;150:487-493.
- Lexchin J. Interactions between physicians and the pharmaceutical industry: what does the literature say? CMAJ. 1993;149:1401-1407.
- Lieb K, Scheurich A. Contact between doctors and the pharmaceutical industry, their perceptions, and the effects on prescribing habits. PLoS One. 2014;9:e110130.
- Spurling GK, Mansfield PR, Montgomery BD, et al. Information from pharmaceutical companies and the quality, quantity, and cost of physicians’ prescribing: a systematic review. PLoS Med. 2010;7:e1000352.
- Fischer MA, Avorn J. Economic consequences of underuse of generic drugs: evidence from Medicaid and implications for prescription drug benefit plans. Health Serv Res. 2003;38:1051-1064.
- Sacks CA, Lee CC, Kesselheim AS, et al. Medicare spending on brand-name combination medications vs their generic constituents. JAMA. 2018;320:650-656.
- Brennan TA, Rothman DJ, Blank L, et al. Health industry practices that create conflicts of interest: a policy proposal for academic medical centers. JAMA. 2006;295:429-433.
- Allan GM, Lexchin J, Wiebe N. Physician awareness of drug cost: a systematic review. PLoS Med. 2007;4:e283.
Over the years, there has been growing concern about the relationship between physicians and pharmaceutical companies. Many studies have demonstrated that pharmaceutical interactions and incentives can influence physicians’ prescribing habits.1-3 As a result, many academic centers have adopted policies that attempt to limit the pharmaceutical industry’s influence on faculty and in-training physicians. Although these policies can vary greatly, they generally limit access of pharmaceutical representatives to providers and restrict pharmaceutical samples.4,5 This policy shift has even been reported in private practice.6
At the heart of the matter is the question: What really influences physicians to write a prescription for a particular medication? Is it cost, efficacy, or representatives pushing a product? Prior studies illustrate that generic medications are equivalent to their brand-name counterparts. In fact, current regulations require no more than 5% to 7% difference in bioequivalence.7-9 Although most generic medications are bioequivalent, it may not be universal.10
Garrison and Levin11 distributed a survey to US-based prescribers in family practice, psychiatry, and internal medicine and found that prescribers deemed patient response and success as the highest priority when determining which drugs to prescribe. In contrast, drug representatives and free samples only slightly contributed.11 Considering the minimum duration for efficacy of a medication such as an antidepressant vs a topical steroid, this pattern may differ with samples in dermatologic settings. Interestingly, another survey concluded that samples were associated with “sticky” prescribing habits, noting that physicians would prescribe a brand-name medication after using a sample, despite increased cost to the patient.12 Further, it has been suggested that recipients of free samples may experience increased costs in the long run, which contrasts a stated goal of affordability to patients.12,13
Physician interaction with pharmaceutical companies begins as early as medical school,14 with physicians reporting interactions as often as 4 times each month.14-18 Interactions can include meetings with pharmaceutical representatives, sponsored meals, gifts, continuing medical education sponsorship, funding for travel, pharmaceutical representative speakers, research funding, and drug samples.3
A 2014 study reported that prescribing habits are influenced by the free drug samples provided by nongeneric pharmaceutical companies.19 Nationally, the number of brand-name and branded generic medications constitute 79% of prescriptions, yet together they only comprise 17% of medications prescribed at an academic medical clinic that does not provide samples. The number of medications with samples being prescribed by dermatologists increased by 15% over 9 years, which may correlate with the wider availability of medication samples, more specifically an increase in branded generic samples.19 This potential interaction is the reason why institutions question the current influence of pharmaceutical companies. Samples may appear convenient, allowing a patient to test the medication prior to committing; however, with brand-name samples being provided to the physician, he/she may become more inclined to prescribe the branded medication.12,15,19-22 Because brand-name medications are more expensive than generic medications, this practice can increase the cost of health care.13 One study found that over 1 year, the overuse of nongeneric medications led to a loss of potential savings throughout 49 states, equating to $229 million just through Medicaid; interestingly, it was noted that in some states, a maximum reimbursement is set by Medicaid, regardless of whether the generic or branded medication is dispensed. The authors also noted variability in the potential savings by state, which may be a function of the state-by-state maximum reimbursements for certain medications.23 Another study on oral combination medications estimated Medicare spending on branded drugs relative to the cost if generic combinations had been purchased instead. This study examined branded medications for which the active components were available as over-the-counter (OTC), generic, or same-class generic, and the authors estimated that $925 million could have been saved in 2016 by purchasing a generic substitute.24 The overuse of nongeneric medications when generic alternatives are available becomes an issue that not only financially impacts patients but all taxpayers. However, this pattern may differ if limited only to dermatologic medications, which was not the focus of the prior studies.
To limit conflicts of interest in interactions with the pharmaceutical, medical device, and biotechnology industries, the University of South Florida (USF) Morsani College of Medicine (COM)(Tampa, Florida) implemented its own set of regulations that eliminated in-office pharmaceutical samples, in addition to other restrictions. This study aimed to investigate if there was a change in the prescribing habits of academic dermatologists after their medical school implemented these new policies.
We hypothesized that the number of brand-name drugs prescribed by physicians in the Department of Dermatology & Cutaneous Surgery would change following USF Morsani COM pharmaceutical policy changes. We sought to determine how physician prescribing practices within the Department of Dermatology & Cutaneous Surgery changed following USF Morsani COM pharmaceutical policy changes.
Methods
Data Collection
A retrospective review of medical records was conducted to investigate the effect of the USF Morsani COM pharmaceutical policy changes on physician prescribing practices within the Department of Dermatology & Cutaneous Surgery. Medical records of patients seen for common dermatology diagnoses before (January 1, 2010, to May 30, 2010) and after (August 1, 2011, to December 31, 2011) the pharmaceutical policy changes were reviewed, and all medications prescribed were recorded. Data were collected from medical records within the USF Health electronic medical record system and included visits with each of the department’s 3 attending dermatologists. The diagnoses included in the study—acne vulgaris, atopic dermatitis, onychomycosis, psoriasis, and rosacea—were chosen because in-office samples were available. Prescribing data from the first 100 consecutive medical records were collected from each time period, and a medical record was included only if it contained at least 1 of the following diagnoses: acne vulgaris, atopic dermatitis, onychomycosis, psoriasis, or rosacea. The assessment and plan of each progress note were reviewed, and the exact medication name and associated diagnosis were recorded for each prescription. Subsequently, each medication was reviewed and placed in 1 of 3 categories: brand name, generic, and OTC. The total number of prescriptions for each diagnosis (per visit/note); the specific number of brand, generic, and OTC medications prescribed (per visit/note); and the percentage of brand, generic, and OTC medications prescribed (per visit/note and per diagnosis in total) were calculated. To ensure only intended medications were included, each medication recorded in the medical record note was cross-referenced with the prescribed medication in the electronic medical record. The primary objective of this study was to capture the prescribing physician’s intent as proxied by the pattern of prescription. Thus, changes made in prescriptions after the initial plan—whether insurance related or otherwise—were not relevant to this investigation.
The data were collected to compare the percentage of brand vs generic or OTC prescriptions per diagnosis to see if there was a difference in the prescribing habits before and after the pharmaceutical policy changes. Of note, several other pieces of data were collected from each medical record, including age, race, class of insurance (ie, Medicare, Medicaid, private health maintenance organization, private preferred provider organization), subtype diagnoses, and whether the prescription was new or a refill. The information gathered from the written record on the assessment and plan was verified using prescriptions ordered in the Allscripts electronic record, and any difference was noted. No identifying information that could be used to easily identify study participants was recorded.
Differences in prescribing habits across diagnoses before and after the policy changes were ascertained using a Fisher exact test and were further assessed using a mixed effects ordinal logistic regression model that accounted for within-provider clustering and baseline patient characteristics. An ordinal model was chosen to recognize differences in average cost among brand-name, generic, and OTC medications.
Results
In total, 200 medical records were collected. For the period analyzed before the policy change, 252 brand-name medications were prescribed compared to 231 prescribed for the period analyzed after the policy changes. There was insufficient evidence of an overall difference in brand-name medications prescribed before and after the policy changes (P=.145; Fisher exact test)(Table 1). There also was insufficient evidence of an overall difference in generic prescriptions, which totaled 153 before and 134 after the policy changes (P=.872; Fisher exact test)(Table 2). Over-the-counter prescriptions totaled 49 before and 69 after the policy changes. There was insufficient evidence of an overall difference before and after the policy changes for OTC medications (P=.192; Fisher exact test)(Table 3).
Comment
Although some medical institutions are diligently working to limit the potential influence pharmaceutical companies have on physician prescribing habits,4,5,25 the effect on physician prescribing habits is only now being established.15 Prior studies12,19,21 have found evidence that medication samples may lead to overuse of brand-name medications, but these findings do not hold true for the USF dermatologists included in this study, perhaps due to the difference in pharmaceutical company interactions or physicians maintaining prior prescription habits that were unrelated to the policy. Although this study focused on policy changes for in-office samples, prior studies either included other forms of interaction21 or did not include samples.22
Pharmaceutical samples allow patients to try a medication before committing to a long-term course of treatment with a particular medication, which has utility for physicians and patients. Although brand-name prescriptions may cost more, a trial period may assist the patient in deciding whether the medication is worth purchasing. Furthermore, physicians may feel more comfortable prescribing a medication once the individual patient has demonstrated a benefit from the sample, which may be particularly true in a specialty such as dermatology in which many branded topical medications contain a different vehicle than generic formulations, resulting in notable variations in active medication delivery and efficacy. Given the higher cost of branded topical medications, proving efficacy in patients through samples can provide a useful tool to the physician to determine the need for a branded formulation.
The benefits described are subjective but should not be disregarded. Although Hurley et al19 found that the number of brand-name medications prescribed increases as more samples are given out, our study demonstrated that after eliminating medication samples, there was no significant difference in the percentage of brand-name medications prescribed compared to generic and OTC medications.
Physician education concerning the price of each brand-name medication prescribed in office may be one method of reducing the amount of such prescriptions. Physicians generally are uninformed of the cost of the medications being prescribed26 and may not recognize the financial burden one medication may have compared to its alternative. However, educating physicians will empower them to make the conscious decision to prefer or not prefer a brand-name medication. With some generic medications shown to have a difference in bioequivalence compared to their brand-name counterparts, a physician may find more success prescribing the brand-name medications, regardless of pharmaceutical company influence, which is an alternative solution to policy changes that eliminate samples entirely. Although this study found insufficient evidence that removing samples decreases brand-name medication prescriptions, it is imperative that solutions are established to reduce the country’s increasing burden of medical costs.
Possible shortfalls of this study include the short period of time between which prepolicy data and postpolicy data were collected. It is possible that providers did not have enough time to adjust their prescribing habits or that providers would not have changed a prescribing pattern or preference simply because of a policy change. Future studies could allow a time period greater than 2 years to compare prepolicy and postpolicy prescribing habits, or a future study might make comparisons of prescriber patterns at different institutions that have different policies. Another possible shortfall is that providers and patients were limited to those at the Department of Dermatology & Cutaneous Surgery at the USF Morsani COM. Although this study has found insufficient evidence of a difference in prescribing habits, it may be beneficial to conduct a larger study that encompasses multiple academic institutions with similar policy changes. Most importantly, this study only investigated the influence of in-office pharmaceutical samples on prescribing patterns. This study did not look at the many other ways in which providers may be influenced by pharmaceutical companies, which likely is a significant confounding variable in this study. Continued additional studies that specifically examine other methods through which providers may be influenced would be helpful in further examining the many ways in which physician prescription habits are influenced.
Conclusion
Changes in pharmaceutical policy in 2011 at USF Morsani COM specifically banned in-office samples. The totality of evidence in this study shows modest observational evidence of a change in the postpolicy odds relative to prepolicy odds, but the data also are compatible with no change between prescribing habits before and after the policy changes. Further study is needed to fully understand this relationship.
Over the years, there has been growing concern about the relationship between physicians and pharmaceutical companies. Many studies have demonstrated that pharmaceutical interactions and incentives can influence physicians’ prescribing habits.1-3 As a result, many academic centers have adopted policies that attempt to limit the pharmaceutical industry’s influence on faculty and in-training physicians. Although these policies can vary greatly, they generally limit access of pharmaceutical representatives to providers and restrict pharmaceutical samples.4,5 This policy shift has even been reported in private practice.6
At the heart of the matter is the question: What really influences physicians to write a prescription for a particular medication? Is it cost, efficacy, or representatives pushing a product? Prior studies illustrate that generic medications are equivalent to their brand-name counterparts. In fact, current regulations require no more than 5% to 7% difference in bioequivalence.7-9 Although most generic medications are bioequivalent, it may not be universal.10
Garrison and Levin11 distributed a survey to US-based prescribers in family practice, psychiatry, and internal medicine and found that prescribers deemed patient response and success as the highest priority when determining which drugs to prescribe. In contrast, drug representatives and free samples only slightly contributed.11 Considering the minimum duration for efficacy of a medication such as an antidepressant vs a topical steroid, this pattern may differ with samples in dermatologic settings. Interestingly, another survey concluded that samples were associated with “sticky” prescribing habits, noting that physicians would prescribe a brand-name medication after using a sample, despite increased cost to the patient.12 Further, it has been suggested that recipients of free samples may experience increased costs in the long run, which contrasts a stated goal of affordability to patients.12,13
Physician interaction with pharmaceutical companies begins as early as medical school,14 with physicians reporting interactions as often as 4 times each month.14-18 Interactions can include meetings with pharmaceutical representatives, sponsored meals, gifts, continuing medical education sponsorship, funding for travel, pharmaceutical representative speakers, research funding, and drug samples.3
A 2014 study reported that prescribing habits are influenced by the free drug samples provided by nongeneric pharmaceutical companies.19 Nationally, the number of brand-name and branded generic medications constitute 79% of prescriptions, yet together they only comprise 17% of medications prescribed at an academic medical clinic that does not provide samples. The number of medications with samples being prescribed by dermatologists increased by 15% over 9 years, which may correlate with the wider availability of medication samples, more specifically an increase in branded generic samples.19 This potential interaction is the reason why institutions question the current influence of pharmaceutical companies. Samples may appear convenient, allowing a patient to test the medication prior to committing; however, with brand-name samples being provided to the physician, he/she may become more inclined to prescribe the branded medication.12,15,19-22 Because brand-name medications are more expensive than generic medications, this practice can increase the cost of health care.13 One study found that over 1 year, the overuse of nongeneric medications led to a loss of potential savings throughout 49 states, equating to $229 million just through Medicaid; interestingly, it was noted that in some states, a maximum reimbursement is set by Medicaid, regardless of whether the generic or branded medication is dispensed. The authors also noted variability in the potential savings by state, which may be a function of the state-by-state maximum reimbursements for certain medications.23 Another study on oral combination medications estimated Medicare spending on branded drugs relative to the cost if generic combinations had been purchased instead. This study examined branded medications for which the active components were available as over-the-counter (OTC), generic, or same-class generic, and the authors estimated that $925 million could have been saved in 2016 by purchasing a generic substitute.24 The overuse of nongeneric medications when generic alternatives are available becomes an issue that not only financially impacts patients but all taxpayers. However, this pattern may differ if limited only to dermatologic medications, which was not the focus of the prior studies.
To limit conflicts of interest in interactions with the pharmaceutical, medical device, and biotechnology industries, the University of South Florida (USF) Morsani College of Medicine (COM)(Tampa, Florida) implemented its own set of regulations that eliminated in-office pharmaceutical samples, in addition to other restrictions. This study aimed to investigate if there was a change in the prescribing habits of academic dermatologists after their medical school implemented these new policies.
We hypothesized that the number of brand-name drugs prescribed by physicians in the Department of Dermatology & Cutaneous Surgery would change following USF Morsani COM pharmaceutical policy changes. We sought to determine how physician prescribing practices within the Department of Dermatology & Cutaneous Surgery changed following USF Morsani COM pharmaceutical policy changes.
Methods
Data Collection
A retrospective review of medical records was conducted to investigate the effect of the USF Morsani COM pharmaceutical policy changes on physician prescribing practices within the Department of Dermatology & Cutaneous Surgery. Medical records of patients seen for common dermatology diagnoses before (January 1, 2010, to May 30, 2010) and after (August 1, 2011, to December 31, 2011) the pharmaceutical policy changes were reviewed, and all medications prescribed were recorded. Data were collected from medical records within the USF Health electronic medical record system and included visits with each of the department’s 3 attending dermatologists. The diagnoses included in the study—acne vulgaris, atopic dermatitis, onychomycosis, psoriasis, and rosacea—were chosen because in-office samples were available. Prescribing data from the first 100 consecutive medical records were collected from each time period, and a medical record was included only if it contained at least 1 of the following diagnoses: acne vulgaris, atopic dermatitis, onychomycosis, psoriasis, or rosacea. The assessment and plan of each progress note were reviewed, and the exact medication name and associated diagnosis were recorded for each prescription. Subsequently, each medication was reviewed and placed in 1 of 3 categories: brand name, generic, and OTC. The total number of prescriptions for each diagnosis (per visit/note); the specific number of brand, generic, and OTC medications prescribed (per visit/note); and the percentage of brand, generic, and OTC medications prescribed (per visit/note and per diagnosis in total) were calculated. To ensure only intended medications were included, each medication recorded in the medical record note was cross-referenced with the prescribed medication in the electronic medical record. The primary objective of this study was to capture the prescribing physician’s intent as proxied by the pattern of prescription. Thus, changes made in prescriptions after the initial plan—whether insurance related or otherwise—were not relevant to this investigation.
The data were collected to compare the percentage of brand vs generic or OTC prescriptions per diagnosis to see if there was a difference in the prescribing habits before and after the pharmaceutical policy changes. Of note, several other pieces of data were collected from each medical record, including age, race, class of insurance (ie, Medicare, Medicaid, private health maintenance organization, private preferred provider organization), subtype diagnoses, and whether the prescription was new or a refill. The information gathered from the written record on the assessment and plan was verified using prescriptions ordered in the Allscripts electronic record, and any difference was noted. No identifying information that could be used to easily identify study participants was recorded.
Differences in prescribing habits across diagnoses before and after the policy changes were ascertained using a Fisher exact test and were further assessed using a mixed effects ordinal logistic regression model that accounted for within-provider clustering and baseline patient characteristics. An ordinal model was chosen to recognize differences in average cost among brand-name, generic, and OTC medications.
Results
In total, 200 medical records were collected. For the period analyzed before the policy change, 252 brand-name medications were prescribed compared to 231 prescribed for the period analyzed after the policy changes. There was insufficient evidence of an overall difference in brand-name medications prescribed before and after the policy changes (P=.145; Fisher exact test)(Table 1). There also was insufficient evidence of an overall difference in generic prescriptions, which totaled 153 before and 134 after the policy changes (P=.872; Fisher exact test)(Table 2). Over-the-counter prescriptions totaled 49 before and 69 after the policy changes. There was insufficient evidence of an overall difference before and after the policy changes for OTC medications (P=.192; Fisher exact test)(Table 3).
Comment
Although some medical institutions are diligently working to limit the potential influence pharmaceutical companies have on physician prescribing habits,4,5,25 the effect on physician prescribing habits is only now being established.15 Prior studies12,19,21 have found evidence that medication samples may lead to overuse of brand-name medications, but these findings do not hold true for the USF dermatologists included in this study, perhaps due to the difference in pharmaceutical company interactions or physicians maintaining prior prescription habits that were unrelated to the policy. Although this study focused on policy changes for in-office samples, prior studies either included other forms of interaction21 or did not include samples.22
Pharmaceutical samples allow patients to try a medication before committing to a long-term course of treatment with a particular medication, which has utility for physicians and patients. Although brand-name prescriptions may cost more, a trial period may assist the patient in deciding whether the medication is worth purchasing. Furthermore, physicians may feel more comfortable prescribing a medication once the individual patient has demonstrated a benefit from the sample, which may be particularly true in a specialty such as dermatology in which many branded topical medications contain a different vehicle than generic formulations, resulting in notable variations in active medication delivery and efficacy. Given the higher cost of branded topical medications, proving efficacy in patients through samples can provide a useful tool to the physician to determine the need for a branded formulation.
The benefits described are subjective but should not be disregarded. Although Hurley et al19 found that the number of brand-name medications prescribed increases as more samples are given out, our study demonstrated that after eliminating medication samples, there was no significant difference in the percentage of brand-name medications prescribed compared to generic and OTC medications.
Physician education concerning the price of each brand-name medication prescribed in office may be one method of reducing the amount of such prescriptions. Physicians generally are uninformed of the cost of the medications being prescribed26 and may not recognize the financial burden one medication may have compared to its alternative. However, educating physicians will empower them to make the conscious decision to prefer or not prefer a brand-name medication. With some generic medications shown to have a difference in bioequivalence compared to their brand-name counterparts, a physician may find more success prescribing the brand-name medications, regardless of pharmaceutical company influence, which is an alternative solution to policy changes that eliminate samples entirely. Although this study found insufficient evidence that removing samples decreases brand-name medication prescriptions, it is imperative that solutions are established to reduce the country’s increasing burden of medical costs.
Possible shortfalls of this study include the short period of time between which prepolicy data and postpolicy data were collected. It is possible that providers did not have enough time to adjust their prescribing habits or that providers would not have changed a prescribing pattern or preference simply because of a policy change. Future studies could allow a time period greater than 2 years to compare prepolicy and postpolicy prescribing habits, or a future study might make comparisons of prescriber patterns at different institutions that have different policies. Another possible shortfall is that providers and patients were limited to those at the Department of Dermatology & Cutaneous Surgery at the USF Morsani COM. Although this study has found insufficient evidence of a difference in prescribing habits, it may be beneficial to conduct a larger study that encompasses multiple academic institutions with similar policy changes. Most importantly, this study only investigated the influence of in-office pharmaceutical samples on prescribing patterns. This study did not look at the many other ways in which providers may be influenced by pharmaceutical companies, which likely is a significant confounding variable in this study. Continued additional studies that specifically examine other methods through which providers may be influenced would be helpful in further examining the many ways in which physician prescription habits are influenced.
Conclusion
Changes in pharmaceutical policy in 2011 at USF Morsani COM specifically banned in-office samples. The totality of evidence in this study shows modest observational evidence of a change in the postpolicy odds relative to prepolicy odds, but the data also are compatible with no change between prescribing habits before and after the policy changes. Further study is needed to fully understand this relationship.
- Sondergaard J, Vach K, Kragstrup J, et al. Impact of pharmaceutical representative visits on GPs’ drug preferences. Fam Pract. 2009;26:204-209.
- Jelinek GA, Neate SL. The influence of the pharmaceutical industry in medicine. J Law Med. 2009;17:216-223.
- Wazana A. Physicians and the pharmaceutical industry: is a gift ever just a gift? JAMA. 2000;283:373-380.
- Coleman DL. Establishing policies for the relationship between industry and clinicians: lessons learned from two academic health centers. Acad Med. 2008;83:882-887.
- Coleman DL, Kazdin AE, Miller LA, et al. Guidelines for interactions between clinical faculty and the pharmaceutical industry: one medical school’s approach. Acad Med. 2006;81:154-160.
- Evans D, Hartung DM, Beasley D, et al. Breaking up is hard to do: lessons learned from a pharma-free practice transformation. J Am Board Fam Med. 2013;26:332-338.
- Davit BM, Nwakama PE, Buehler GJ, et al. Comparing generic and innovator drugs: a review of 12 years of bioequivalence data from the United States Food and Drug Administration. Ann Pharmacother. 2009;43:1583-1597.
- Kesselheim AS, Misono AS, Lee JL, et al. Clinical equivalence of generic and brand-name drugs used in cardiovascular disease: a systematic review and meta-analysis. JAMA. 2008;300:2514-2526.
- McCormack J, Chmelicek JT. Generic versus brand name: the other drug war. Can Fam Physician. 2014;60:911.
- Borgheini G. The bioequivalence and therapeutic efficacy of generic versus brand-name psychoactive drugs. Clin Ther. 2003;25:1578-1592.
- Garrison GD, Levin GM. Factors affecting prescribing of the newer antidepressants. Ann Pharmacother. 2000;34:10-14.
- Rafique S, Sarwar W, Rashid A, et al. Influence of free drug samples on prescribing by physicians: a cross sectional survey. J Pak Med Assoc. 2017;67:465-467.
- Alexander GC, Zhang J, Basu A. Characteristics of patients receiving pharmaceutical samples and association between sample receipt and out-of-pocket prescription costs. Med Care. 2008;46:394-402.
- Hodges B. Interactions with the pharmaceutical industry: experiences and attitudes of psychiatry residents, interns and clerks. CMAJ. 1995;153:553-559.
- Brotzman GL, Mark DH. The effect on resident attitudes of regulatory policies regarding pharmaceutical representative activities. J Gen Intern Med. 1993;8:130-134.
- Keim SM, Sanders AB, Witzke DB, et al. Beliefs and practices of emergency medicine faculty and residents regarding professional interactions with the biomedical industry. Ann Emerg Med. 1993;22:1576-1581.
- Thomson AN, Craig BJ, Barham PM. Attitudes of general practitioners in New Zealand to pharmaceutical representatives. Br J Gen Pract. 1994;44:220-223.
- Ziegler MG, Lew P, Singer BC. The accuracy of drug information from pharmaceutical sales representatives. JAMA. 1995;273:1296-1298.
- Hurley MP, Stafford RS, Lane AT. Characterizing the relationship between free drug samples and prescription patterns for acne vulgaris and rosacea. JAMA Dermatol. 2014;150:487-493.
- Lexchin J. Interactions between physicians and the pharmaceutical industry: what does the literature say? CMAJ. 1993;149:1401-1407.
- Lieb K, Scheurich A. Contact between doctors and the pharmaceutical industry, their perceptions, and the effects on prescribing habits. PLoS One. 2014;9:e110130.
- Spurling GK, Mansfield PR, Montgomery BD, et al. Information from pharmaceutical companies and the quality, quantity, and cost of physicians’ prescribing: a systematic review. PLoS Med. 2010;7:e1000352.
- Fischer MA, Avorn J. Economic consequences of underuse of generic drugs: evidence from Medicaid and implications for prescription drug benefit plans. Health Serv Res. 2003;38:1051-1064.
- Sacks CA, Lee CC, Kesselheim AS, et al. Medicare spending on brand-name combination medications vs their generic constituents. JAMA. 2018;320:650-656.
- Brennan TA, Rothman DJ, Blank L, et al. Health industry practices that create conflicts of interest: a policy proposal for academic medical centers. JAMA. 2006;295:429-433.
- Allan GM, Lexchin J, Wiebe N. Physician awareness of drug cost: a systematic review. PLoS Med. 2007;4:e283.
- Sondergaard J, Vach K, Kragstrup J, et al. Impact of pharmaceutical representative visits on GPs’ drug preferences. Fam Pract. 2009;26:204-209.
- Jelinek GA, Neate SL. The influence of the pharmaceutical industry in medicine. J Law Med. 2009;17:216-223.
- Wazana A. Physicians and the pharmaceutical industry: is a gift ever just a gift? JAMA. 2000;283:373-380.
- Coleman DL. Establishing policies for the relationship between industry and clinicians: lessons learned from two academic health centers. Acad Med. 2008;83:882-887.
- Coleman DL, Kazdin AE, Miller LA, et al. Guidelines for interactions between clinical faculty and the pharmaceutical industry: one medical school’s approach. Acad Med. 2006;81:154-160.
- Evans D, Hartung DM, Beasley D, et al. Breaking up is hard to do: lessons learned from a pharma-free practice transformation. J Am Board Fam Med. 2013;26:332-338.
- Davit BM, Nwakama PE, Buehler GJ, et al. Comparing generic and innovator drugs: a review of 12 years of bioequivalence data from the United States Food and Drug Administration. Ann Pharmacother. 2009;43:1583-1597.
- Kesselheim AS, Misono AS, Lee JL, et al. Clinical equivalence of generic and brand-name drugs used in cardiovascular disease: a systematic review and meta-analysis. JAMA. 2008;300:2514-2526.
- McCormack J, Chmelicek JT. Generic versus brand name: the other drug war. Can Fam Physician. 2014;60:911.
- Borgheini G. The bioequivalence and therapeutic efficacy of generic versus brand-name psychoactive drugs. Clin Ther. 2003;25:1578-1592.
- Garrison GD, Levin GM. Factors affecting prescribing of the newer antidepressants. Ann Pharmacother. 2000;34:10-14.
- Rafique S, Sarwar W, Rashid A, et al. Influence of free drug samples on prescribing by physicians: a cross sectional survey. J Pak Med Assoc. 2017;67:465-467.
- Alexander GC, Zhang J, Basu A. Characteristics of patients receiving pharmaceutical samples and association between sample receipt and out-of-pocket prescription costs. Med Care. 2008;46:394-402.
- Hodges B. Interactions with the pharmaceutical industry: experiences and attitudes of psychiatry residents, interns and clerks. CMAJ. 1995;153:553-559.
- Brotzman GL, Mark DH. The effect on resident attitudes of regulatory policies regarding pharmaceutical representative activities. J Gen Intern Med. 1993;8:130-134.
- Keim SM, Sanders AB, Witzke DB, et al. Beliefs and practices of emergency medicine faculty and residents regarding professional interactions with the biomedical industry. Ann Emerg Med. 1993;22:1576-1581.
- Thomson AN, Craig BJ, Barham PM. Attitudes of general practitioners in New Zealand to pharmaceutical representatives. Br J Gen Pract. 1994;44:220-223.
- Ziegler MG, Lew P, Singer BC. The accuracy of drug information from pharmaceutical sales representatives. JAMA. 1995;273:1296-1298.
- Hurley MP, Stafford RS, Lane AT. Characterizing the relationship between free drug samples and prescription patterns for acne vulgaris and rosacea. JAMA Dermatol. 2014;150:487-493.
- Lexchin J. Interactions between physicians and the pharmaceutical industry: what does the literature say? CMAJ. 1993;149:1401-1407.
- Lieb K, Scheurich A. Contact between doctors and the pharmaceutical industry, their perceptions, and the effects on prescribing habits. PLoS One. 2014;9:e110130.
- Spurling GK, Mansfield PR, Montgomery BD, et al. Information from pharmaceutical companies and the quality, quantity, and cost of physicians’ prescribing: a systematic review. PLoS Med. 2010;7:e1000352.
- Fischer MA, Avorn J. Economic consequences of underuse of generic drugs: evidence from Medicaid and implications for prescription drug benefit plans. Health Serv Res. 2003;38:1051-1064.
- Sacks CA, Lee CC, Kesselheim AS, et al. Medicare spending on brand-name combination medications vs their generic constituents. JAMA. 2018;320:650-656.
- Brennan TA, Rothman DJ, Blank L, et al. Health industry practices that create conflicts of interest: a policy proposal for academic medical centers. JAMA. 2006;295:429-433.
- Allan GM, Lexchin J, Wiebe N. Physician awareness of drug cost: a systematic review. PLoS Med. 2007;4:e283.
Practice Points
- There has been growing concern that pharmaceutical interactions and incentives can influence physicians’ prescribing habits.
- Many academic centers have adopted policies that attempt to limit the pharmaceutical industry’s influence on faculty and in-training physicians.
- This study aimed to investigate if there was a change in the prescribing habits of academic dermatologists after the medical school implemented new policies that banned in-office samples.