User login
Skip lymphadenectomy if SLN mapping finds low-grade endometrial cancer
SAN DIEGO – Lymphadenectomy is unnecessary if sentinel lymph node mapping successfully stages low-grade endometrial cancer, according to researchers from Johns Hopkins University in Baltimore.
Lymphadenectomy guided by frozen section remains common in the United States. But the Johns Hopkins research team found that using sentinel lymph node (SLN) mapping and biopsy instead cuts the rate of lymphadenectomy by 76%, without reducing the detection of lymphatic metastases.
It’s an important finding for cancer patients likely to survive their diagnosis. “We see low-grade patients in the clinic” who’ve had unnecessary lymphadenectomies, “and they are in terrible shape,” said investigator Dr. Abdulrahman Sinno, a gynecologic oncology fellow at Johns Hopkins. Up to half “have horrible side effects,” including crippling lymphedema and pain.
SLN mapping is “an alternative that gives us the information we need for nodal assessment without putting patients at risk. You’ll know if patients have metastases or not. If they fail to map, you do a frozen section, and if you have high-risk features, a lymphadenectomy only on [the side] that didn’t map,” Dr. Sinno said at the annual meeting of the Society of Gynecologic Oncology.
For the past several years, physicians at Johns Hopkins has been doing both SLN mapping for low-grade endometrial cancer as well as frozen sections to decide the need for lymphadenectomy. Using both approaches allowed the investigators to review how patients would have fared if they had gotten only one.
“[We could] safely study the utility of SLN mapping while maintaining the historical standard of using frozen sections to direct the need for lymphadenectomy,” Dr. Sinno said.
SLN mapping outperformed frozen section. Among 114 women, most with grade 1 disease but some with grade 2 or complex atypical hyperplasia, 8 had lymph node metastases. Mapping identified every one, five by standard hematoxylin-eosin staining, and three by ultrastaging. Frozen-section guided lymphadenectomy missed three.
Eighty four (37%) of the 224 hemi-pelvises in the study had lymphadenectomies based on worrisome frozen-section findings. If SLN mapping had been relied on to make the call, lymphadenectomies would have been performed in 20 (9%), a statistically significant difference (P = 0.004).
“Strategies that rely exclusively on uterine frozen section result in significant overtreatment. In the absence of a therapeutic benefit to lymphadenectomy, we believe” this is “unjustifiable when an alternative exists.” At Johns Hopkins these days, “if you map, you’re done,” Dr. Sinno said.
Almost two-thirds of the women had grade 1 endometrial cancer on preoperative histopathology, and about the same number on final pathology. Bilateral SLN mapping was successful in 71 cases (62%) and unilateral mapping in 27 cases (24%). At least one SLN was detected in 98 women (86%).
There were six recurrences after a median follow-up of 15 months. Four were in women who had full pelvic and periaortic lymphadenectomies that were negative. There was also a port site recurrence and a recurrence in an outlying patient with advanced disease. Overall, “recurrence was independent of whether sentinel nodes were applied,” Dr. Sinno said.
Women in the study were a median of 60 years old, with a median body mass index of 33.3 kg/m2.
Dr. Sinno reported having no relevant financial disclosures.
SAN DIEGO – Lymphadenectomy is unnecessary if sentinel lymph node mapping successfully stages low-grade endometrial cancer, according to researchers from Johns Hopkins University in Baltimore.
Lymphadenectomy guided by frozen section remains common in the United States. But the Johns Hopkins research team found that using sentinel lymph node (SLN) mapping and biopsy instead cuts the rate of lymphadenectomy by 76%, without reducing the detection of lymphatic metastases.
It’s an important finding for cancer patients likely to survive their diagnosis. “We see low-grade patients in the clinic” who’ve had unnecessary lymphadenectomies, “and they are in terrible shape,” said investigator Dr. Abdulrahman Sinno, a gynecologic oncology fellow at Johns Hopkins. Up to half “have horrible side effects,” including crippling lymphedema and pain.
SLN mapping is “an alternative that gives us the information we need for nodal assessment without putting patients at risk. You’ll know if patients have metastases or not. If they fail to map, you do a frozen section, and if you have high-risk features, a lymphadenectomy only on [the side] that didn’t map,” Dr. Sinno said at the annual meeting of the Society of Gynecologic Oncology.
For the past several years, physicians at Johns Hopkins has been doing both SLN mapping for low-grade endometrial cancer as well as frozen sections to decide the need for lymphadenectomy. Using both approaches allowed the investigators to review how patients would have fared if they had gotten only one.
“[We could] safely study the utility of SLN mapping while maintaining the historical standard of using frozen sections to direct the need for lymphadenectomy,” Dr. Sinno said.
SLN mapping outperformed frozen section. Among 114 women, most with grade 1 disease but some with grade 2 or complex atypical hyperplasia, 8 had lymph node metastases. Mapping identified every one, five by standard hematoxylin-eosin staining, and three by ultrastaging. Frozen-section guided lymphadenectomy missed three.
Eighty four (37%) of the 224 hemi-pelvises in the study had lymphadenectomies based on worrisome frozen-section findings. If SLN mapping had been relied on to make the call, lymphadenectomies would have been performed in 20 (9%), a statistically significant difference (P = 0.004).
“Strategies that rely exclusively on uterine frozen section result in significant overtreatment. In the absence of a therapeutic benefit to lymphadenectomy, we believe” this is “unjustifiable when an alternative exists.” At Johns Hopkins these days, “if you map, you’re done,” Dr. Sinno said.
Almost two-thirds of the women had grade 1 endometrial cancer on preoperative histopathology, and about the same number on final pathology. Bilateral SLN mapping was successful in 71 cases (62%) and unilateral mapping in 27 cases (24%). At least one SLN was detected in 98 women (86%).
There were six recurrences after a median follow-up of 15 months. Four were in women who had full pelvic and periaortic lymphadenectomies that were negative. There was also a port site recurrence and a recurrence in an outlying patient with advanced disease. Overall, “recurrence was independent of whether sentinel nodes were applied,” Dr. Sinno said.
Women in the study were a median of 60 years old, with a median body mass index of 33.3 kg/m2.
Dr. Sinno reported having no relevant financial disclosures.
SAN DIEGO – Lymphadenectomy is unnecessary if sentinel lymph node mapping successfully stages low-grade endometrial cancer, according to researchers from Johns Hopkins University in Baltimore.
Lymphadenectomy guided by frozen section remains common in the United States. But the Johns Hopkins research team found that using sentinel lymph node (SLN) mapping and biopsy instead cuts the rate of lymphadenectomy by 76%, without reducing the detection of lymphatic metastases.
It’s an important finding for cancer patients likely to survive their diagnosis. “We see low-grade patients in the clinic” who’ve had unnecessary lymphadenectomies, “and they are in terrible shape,” said investigator Dr. Abdulrahman Sinno, a gynecologic oncology fellow at Johns Hopkins. Up to half “have horrible side effects,” including crippling lymphedema and pain.
SLN mapping is “an alternative that gives us the information we need for nodal assessment without putting patients at risk. You’ll know if patients have metastases or not. If they fail to map, you do a frozen section, and if you have high-risk features, a lymphadenectomy only on [the side] that didn’t map,” Dr. Sinno said at the annual meeting of the Society of Gynecologic Oncology.
For the past several years, physicians at Johns Hopkins has been doing both SLN mapping for low-grade endometrial cancer as well as frozen sections to decide the need for lymphadenectomy. Using both approaches allowed the investigators to review how patients would have fared if they had gotten only one.
“[We could] safely study the utility of SLN mapping while maintaining the historical standard of using frozen sections to direct the need for lymphadenectomy,” Dr. Sinno said.
SLN mapping outperformed frozen section. Among 114 women, most with grade 1 disease but some with grade 2 or complex atypical hyperplasia, 8 had lymph node metastases. Mapping identified every one, five by standard hematoxylin-eosin staining, and three by ultrastaging. Frozen-section guided lymphadenectomy missed three.
Eighty four (37%) of the 224 hemi-pelvises in the study had lymphadenectomies based on worrisome frozen-section findings. If SLN mapping had been relied on to make the call, lymphadenectomies would have been performed in 20 (9%), a statistically significant difference (P = 0.004).
“Strategies that rely exclusively on uterine frozen section result in significant overtreatment. In the absence of a therapeutic benefit to lymphadenectomy, we believe” this is “unjustifiable when an alternative exists.” At Johns Hopkins these days, “if you map, you’re done,” Dr. Sinno said.
Almost two-thirds of the women had grade 1 endometrial cancer on preoperative histopathology, and about the same number on final pathology. Bilateral SLN mapping was successful in 71 cases (62%) and unilateral mapping in 27 cases (24%). At least one SLN was detected in 98 women (86%).
There were six recurrences after a median follow-up of 15 months. Four were in women who had full pelvic and periaortic lymphadenectomies that were negative. There was also a port site recurrence and a recurrence in an outlying patient with advanced disease. Overall, “recurrence was independent of whether sentinel nodes were applied,” Dr. Sinno said.
Women in the study were a median of 60 years old, with a median body mass index of 33.3 kg/m2.
Dr. Sinno reported having no relevant financial disclosures.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: Successful sentinel lymph node mapping gives all the information needed for nodal assessment.
Major finding: Sentinel lymph node mapping identified all eight nodal metastases; frozen-section guided lymphadenectomy missed three.
Data source: A review of 114 cases at Johns Hopkins University.
Disclosures: Dr. Sinno reported having no relevant financial disclosures.
Endometriosis linked to higher CHD risk
Endometriosis is associated with a significantly increased risk of coronary heart disease, at least in part because of one of its principal treatments – hysterectomy/oophorectomy, according to a new analysis of the Nurses’ Health Study II.
In what the researchers described as the first large prospective study to examine this possible association, the link between endometriosis and coronary heart disease (CHD) was mediated by patient age.
Women with endometriosis had a higher incidence of CHD than those without the gynecologic disorder until they reached their late 50s; after that, the two populations had similar CHD rates, wrote Fan Mu, Sc.D., of the department of epidemiology, Harvard T. H. Chan School of Public Health in Boston, and her associates (Circ Cardiovasc Qual Outcomes. 2016 Mar 29. doi: 10.1161/circoutcomes.115.002224).
“This association may have important clinical and public health implications among women in their early 40s to early 50s,” the researchers wrote. “It is possible that the observed increased risk associated with surgical menopause from hysterectomy/oophorectomy among women with endometriosis started to diminish with age partially because nearly every woman had reached menopause by the age of 55 years.”
The researchers chose to study this topic because endometriosis has been linked to chronic systemic inflammation, oxidative stress, and adverse lipid profiles, factors that also play key roles in the pathogenesis of atherosclerotic CHD. They assessed the incidence of myocardial infarction, angina, and the combined outcome of coronary artery bypass graft (CABG)/angioplasty/stenting using data from the Nurses’ Health Study II, a prospective cohort study involving 116,430 women, aged 25-42 years at baseline in 1989, who were followed for approximately 20 years.
A total of 5,296 of the study participants had laparoscopically confirmed endometriosis at baseline, and another 6,607 developed the disorder during follow-up. There were 1,438 incident cases of CHD during follow-up.
Compared with women who didn’t have endometriosis, those who did showed increased relative risks for myocardial infarction (1.63), angiographically confirmed angina (2.07), CABG/angioplasty/stent (1.49), and combined CHD (1.73). The results remained statistically significant after the researchers adjusted for potential confounders.
About 42% of this association was statistically accounted for by the greater frequency of hysterectomy/oophorectomy among women who had endometriosis and the earlier age of these surgeries among women with endometriosis. Women who underwent the surgery had an absolute incidence of CHD of 139 per 100,000 person-years, compared with an incidence of 60 per 100,000 person-years among the women who didn’t have hysterectomy/oophorectomy.
“Physicians need to consider the potential long-term impact that the surgeries may cause and weigh the risks and benefits of the treatment in dialogue with patients, particularly with respect to endometriosis where pain recurrence risk remains,” the researchers wrote. “Although oophorectomy confers obvious prevention for ovarian cancer, with which endometriosis has been associated, CHD is the leading cause of mortality and morbidity in women in the United States and United Kingdom.”
The study was supported by the National Institutes of Health. The researchers reported having no relevant financial disclosures.
Endometriosis is associated with a significantly increased risk of coronary heart disease, at least in part because of one of its principal treatments – hysterectomy/oophorectomy, according to a new analysis of the Nurses’ Health Study II.
In what the researchers described as the first large prospective study to examine this possible association, the link between endometriosis and coronary heart disease (CHD) was mediated by patient age.
Women with endometriosis had a higher incidence of CHD than those without the gynecologic disorder until they reached their late 50s; after that, the two populations had similar CHD rates, wrote Fan Mu, Sc.D., of the department of epidemiology, Harvard T. H. Chan School of Public Health in Boston, and her associates (Circ Cardiovasc Qual Outcomes. 2016 Mar 29. doi: 10.1161/circoutcomes.115.002224).
“This association may have important clinical and public health implications among women in their early 40s to early 50s,” the researchers wrote. “It is possible that the observed increased risk associated with surgical menopause from hysterectomy/oophorectomy among women with endometriosis started to diminish with age partially because nearly every woman had reached menopause by the age of 55 years.”
The researchers chose to study this topic because endometriosis has been linked to chronic systemic inflammation, oxidative stress, and adverse lipid profiles, factors that also play key roles in the pathogenesis of atherosclerotic CHD. They assessed the incidence of myocardial infarction, angina, and the combined outcome of coronary artery bypass graft (CABG)/angioplasty/stenting using data from the Nurses’ Health Study II, a prospective cohort study involving 116,430 women, aged 25-42 years at baseline in 1989, who were followed for approximately 20 years.
A total of 5,296 of the study participants had laparoscopically confirmed endometriosis at baseline, and another 6,607 developed the disorder during follow-up. There were 1,438 incident cases of CHD during follow-up.
Compared with women who didn’t have endometriosis, those who did showed increased relative risks for myocardial infarction (1.63), angiographically confirmed angina (2.07), CABG/angioplasty/stent (1.49), and combined CHD (1.73). The results remained statistically significant after the researchers adjusted for potential confounders.
About 42% of this association was statistically accounted for by the greater frequency of hysterectomy/oophorectomy among women who had endometriosis and the earlier age of these surgeries among women with endometriosis. Women who underwent the surgery had an absolute incidence of CHD of 139 per 100,000 person-years, compared with an incidence of 60 per 100,000 person-years among the women who didn’t have hysterectomy/oophorectomy.
“Physicians need to consider the potential long-term impact that the surgeries may cause and weigh the risks and benefits of the treatment in dialogue with patients, particularly with respect to endometriosis where pain recurrence risk remains,” the researchers wrote. “Although oophorectomy confers obvious prevention for ovarian cancer, with which endometriosis has been associated, CHD is the leading cause of mortality and morbidity in women in the United States and United Kingdom.”
The study was supported by the National Institutes of Health. The researchers reported having no relevant financial disclosures.
Endometriosis is associated with a significantly increased risk of coronary heart disease, at least in part because of one of its principal treatments – hysterectomy/oophorectomy, according to a new analysis of the Nurses’ Health Study II.
In what the researchers described as the first large prospective study to examine this possible association, the link between endometriosis and coronary heart disease (CHD) was mediated by patient age.
Women with endometriosis had a higher incidence of CHD than those without the gynecologic disorder until they reached their late 50s; after that, the two populations had similar CHD rates, wrote Fan Mu, Sc.D., of the department of epidemiology, Harvard T. H. Chan School of Public Health in Boston, and her associates (Circ Cardiovasc Qual Outcomes. 2016 Mar 29. doi: 10.1161/circoutcomes.115.002224).
“This association may have important clinical and public health implications among women in their early 40s to early 50s,” the researchers wrote. “It is possible that the observed increased risk associated with surgical menopause from hysterectomy/oophorectomy among women with endometriosis started to diminish with age partially because nearly every woman had reached menopause by the age of 55 years.”
The researchers chose to study this topic because endometriosis has been linked to chronic systemic inflammation, oxidative stress, and adverse lipid profiles, factors that also play key roles in the pathogenesis of atherosclerotic CHD. They assessed the incidence of myocardial infarction, angina, and the combined outcome of coronary artery bypass graft (CABG)/angioplasty/stenting using data from the Nurses’ Health Study II, a prospective cohort study involving 116,430 women, aged 25-42 years at baseline in 1989, who were followed for approximately 20 years.
A total of 5,296 of the study participants had laparoscopically confirmed endometriosis at baseline, and another 6,607 developed the disorder during follow-up. There were 1,438 incident cases of CHD during follow-up.
Compared with women who didn’t have endometriosis, those who did showed increased relative risks for myocardial infarction (1.63), angiographically confirmed angina (2.07), CABG/angioplasty/stent (1.49), and combined CHD (1.73). The results remained statistically significant after the researchers adjusted for potential confounders.
About 42% of this association was statistically accounted for by the greater frequency of hysterectomy/oophorectomy among women who had endometriosis and the earlier age of these surgeries among women with endometriosis. Women who underwent the surgery had an absolute incidence of CHD of 139 per 100,000 person-years, compared with an incidence of 60 per 100,000 person-years among the women who didn’t have hysterectomy/oophorectomy.
“Physicians need to consider the potential long-term impact that the surgeries may cause and weigh the risks and benefits of the treatment in dialogue with patients, particularly with respect to endometriosis where pain recurrence risk remains,” the researchers wrote. “Although oophorectomy confers obvious prevention for ovarian cancer, with which endometriosis has been associated, CHD is the leading cause of mortality and morbidity in women in the United States and United Kingdom.”
The study was supported by the National Institutes of Health. The researchers reported having no relevant financial disclosures.
FROM CIRCULATION: CARDIOVASCULAR QUALITY AND OUTCOMES
Key clinical point: Endometriosis is associated with a significantly increased risk of coronary heart disease.
Major finding: Women with endometriosis showed increased relative risks for MI (1.63), angiographically confirmed angina (2.07), CABG/angioplasty/stent (1.49), and combined CHD (1.73).
Data source: A secondary analysis of data from the Nurses’ Health Study II, a prospective cohort study involving 116,430 women followed for 20 years.
Disclosures: The study was supported by the National Institutes of Health. The researchers reported having no relevant financial disclosures.
Malpractice claims for small bowel obstruction costly, frequent for general surgeons
MONTREAL – When surgeons are sued and lose or settle in cases relating to management of small bowel obstruction, the payout is often costly, according a study involving a close examination of 158 such cases.
The odds of a positive outcome aren’t great. “When looking at award payouts, close to half of cases resulted in a verdict with monetary compensation for the patient,” said Dr. Asad Choudhry, a postdoctoral fellow in the department of trauma, critical care, and surgery at the Mayo Clinic, Rochester, Minn.
Dr. Choudhry, presenting his findings at the annual meeting of the Central Surgical Association, said that general surgeons are the third most likely specialty to be sued, coming only after neurosurgeons and cardiothoracic surgeons. In a given year, about 15% of all general surgeons will be sued, with almost a third of those suits resulting in a payment to the plaintiff. By age 65 years, said Dr. Choudhry, 99% of physicians in higher-risk specialties will face a malpractice claim, compared with 75% of those in lower-risk specialties.
Overall, one-third of malpractice payments come from suits that allege diagnostic error; 24% of suits allege malpractice in surgery. “Small bowel obstruction accounts for 12% to 16% of surgical admissions, with 300,000 operations performed each year,” he said.
Dr. Choudhry and his colleagues searched the Westlaw database using key search terms to identify U.S. malpractice cases that involved small bowel obstruction (SBO), focusing only on cases in which management of SBO was the primary reason for the suit. Cases from 1982 to 2015 were included.
Looking more closely at the 158 cases that resulted from the search, Dr. Choudhry examined variables that included patient demographics, the alleged reason for the malpractice, the settlement or verdict, and the amount paid out, adjusted to 2015 dollars.
In this sample of SBO cases, 139 patients were adults and 19 were children. The median age was 45 years. Over half of the patients in the group died (94/158, 60%), although neither age nor patient death were factors significantly associated with verdict outcome or award amount, he said.
The decade-over-decade growth in the number of suits was striking, increasing 188% during the 1994-2004 period from the previous decade and another 87% from 2005 to 2015.
In a lawsuit involving a SBO, the defendant is more likely to be a general surgeon than to belong to any other specialty. General surgeons were the defendant in 37% of cases, followed by internists in 24% and emergency physicians in 11%.
Dr. Choudhry and his associates conceptually grouped the reasons for the suits into preoperative, intraoperative, and postoperative care. Among the reasons for litigation, by far the most common was untimely intervention in managing of the SBO, a preoperative care component. This was the primary allegation in over 100 of the 158 cases; the next most common reason for bringing suit was incomplete or incorrect surgical procedure, deemed an intraoperative problem and seen in fewer than 20 of the suits.
Almost half of the cases resulted either in a verdict in favor of the plaintiff (n = 37, 23%) or a settlement (n = 36, 23%). When verdicts were returned against the defendant physician, payout amounts varied widely. The smallest amount paid was $29,575 and the largest was over $12 million. Payment amounts were larger with a verdict in favor of the plaintiff, at a median $1,438,800, compared with the median of $1,043,100 received by the plaintiff in a settlement.
Dr. Choudhry noted that early intervention may improve mortality from SBO in some patient groups. “Small bowel obstruction protocols which identify patients at high risk for adverse outcomes and ensure timely management may lessen the chance of litigation,” he said.
Dr. Choudhry acknowledged that the Westlaw database included just a limited amount of medical information. Various tort reform initiatives may have had a confounding effect on award size. It’s possible that using malpractice insurance data could provide more detailed medical information, he said.
Dr. Choudhry reported no relevant disclosures.
On Twitter @karioakes
MONTREAL – When surgeons are sued and lose or settle in cases relating to management of small bowel obstruction, the payout is often costly, according a study involving a close examination of 158 such cases.
The odds of a positive outcome aren’t great. “When looking at award payouts, close to half of cases resulted in a verdict with monetary compensation for the patient,” said Dr. Asad Choudhry, a postdoctoral fellow in the department of trauma, critical care, and surgery at the Mayo Clinic, Rochester, Minn.
Dr. Choudhry, presenting his findings at the annual meeting of the Central Surgical Association, said that general surgeons are the third most likely specialty to be sued, coming only after neurosurgeons and cardiothoracic surgeons. In a given year, about 15% of all general surgeons will be sued, with almost a third of those suits resulting in a payment to the plaintiff. By age 65 years, said Dr. Choudhry, 99% of physicians in higher-risk specialties will face a malpractice claim, compared with 75% of those in lower-risk specialties.
Overall, one-third of malpractice payments come from suits that allege diagnostic error; 24% of suits allege malpractice in surgery. “Small bowel obstruction accounts for 12% to 16% of surgical admissions, with 300,000 operations performed each year,” he said.
Dr. Choudhry and his colleagues searched the Westlaw database using key search terms to identify U.S. malpractice cases that involved small bowel obstruction (SBO), focusing only on cases in which management of SBO was the primary reason for the suit. Cases from 1982 to 2015 were included.
Looking more closely at the 158 cases that resulted from the search, Dr. Choudhry examined variables that included patient demographics, the alleged reason for the malpractice, the settlement or verdict, and the amount paid out, adjusted to 2015 dollars.
In this sample of SBO cases, 139 patients were adults and 19 were children. The median age was 45 years. Over half of the patients in the group died (94/158, 60%), although neither age nor patient death were factors significantly associated with verdict outcome or award amount, he said.
The decade-over-decade growth in the number of suits was striking, increasing 188% during the 1994-2004 period from the previous decade and another 87% from 2005 to 2015.
In a lawsuit involving a SBO, the defendant is more likely to be a general surgeon than to belong to any other specialty. General surgeons were the defendant in 37% of cases, followed by internists in 24% and emergency physicians in 11%.
Dr. Choudhry and his associates conceptually grouped the reasons for the suits into preoperative, intraoperative, and postoperative care. Among the reasons for litigation, by far the most common was untimely intervention in managing of the SBO, a preoperative care component. This was the primary allegation in over 100 of the 158 cases; the next most common reason for bringing suit was incomplete or incorrect surgical procedure, deemed an intraoperative problem and seen in fewer than 20 of the suits.
Almost half of the cases resulted either in a verdict in favor of the plaintiff (n = 37, 23%) or a settlement (n = 36, 23%). When verdicts were returned against the defendant physician, payout amounts varied widely. The smallest amount paid was $29,575 and the largest was over $12 million. Payment amounts were larger with a verdict in favor of the plaintiff, at a median $1,438,800, compared with the median of $1,043,100 received by the plaintiff in a settlement.
Dr. Choudhry noted that early intervention may improve mortality from SBO in some patient groups. “Small bowel obstruction protocols which identify patients at high risk for adverse outcomes and ensure timely management may lessen the chance of litigation,” he said.
Dr. Choudhry acknowledged that the Westlaw database included just a limited amount of medical information. Various tort reform initiatives may have had a confounding effect on award size. It’s possible that using malpractice insurance data could provide more detailed medical information, he said.
Dr. Choudhry reported no relevant disclosures.
On Twitter @karioakes
MONTREAL – When surgeons are sued and lose or settle in cases relating to management of small bowel obstruction, the payout is often costly, according a study involving a close examination of 158 such cases.
The odds of a positive outcome aren’t great. “When looking at award payouts, close to half of cases resulted in a verdict with monetary compensation for the patient,” said Dr. Asad Choudhry, a postdoctoral fellow in the department of trauma, critical care, and surgery at the Mayo Clinic, Rochester, Minn.
Dr. Choudhry, presenting his findings at the annual meeting of the Central Surgical Association, said that general surgeons are the third most likely specialty to be sued, coming only after neurosurgeons and cardiothoracic surgeons. In a given year, about 15% of all general surgeons will be sued, with almost a third of those suits resulting in a payment to the plaintiff. By age 65 years, said Dr. Choudhry, 99% of physicians in higher-risk specialties will face a malpractice claim, compared with 75% of those in lower-risk specialties.
Overall, one-third of malpractice payments come from suits that allege diagnostic error; 24% of suits allege malpractice in surgery. “Small bowel obstruction accounts for 12% to 16% of surgical admissions, with 300,000 operations performed each year,” he said.
Dr. Choudhry and his colleagues searched the Westlaw database using key search terms to identify U.S. malpractice cases that involved small bowel obstruction (SBO), focusing only on cases in which management of SBO was the primary reason for the suit. Cases from 1982 to 2015 were included.
Looking more closely at the 158 cases that resulted from the search, Dr. Choudhry examined variables that included patient demographics, the alleged reason for the malpractice, the settlement or verdict, and the amount paid out, adjusted to 2015 dollars.
In this sample of SBO cases, 139 patients were adults and 19 were children. The median age was 45 years. Over half of the patients in the group died (94/158, 60%), although neither age nor patient death were factors significantly associated with verdict outcome or award amount, he said.
The decade-over-decade growth in the number of suits was striking, increasing 188% during the 1994-2004 period from the previous decade and another 87% from 2005 to 2015.
In a lawsuit involving a SBO, the defendant is more likely to be a general surgeon than to belong to any other specialty. General surgeons were the defendant in 37% of cases, followed by internists in 24% and emergency physicians in 11%.
Dr. Choudhry and his associates conceptually grouped the reasons for the suits into preoperative, intraoperative, and postoperative care. Among the reasons for litigation, by far the most common was untimely intervention in managing of the SBO, a preoperative care component. This was the primary allegation in over 100 of the 158 cases; the next most common reason for bringing suit was incomplete or incorrect surgical procedure, deemed an intraoperative problem and seen in fewer than 20 of the suits.
Almost half of the cases resulted either in a verdict in favor of the plaintiff (n = 37, 23%) or a settlement (n = 36, 23%). When verdicts were returned against the defendant physician, payout amounts varied widely. The smallest amount paid was $29,575 and the largest was over $12 million. Payment amounts were larger with a verdict in favor of the plaintiff, at a median $1,438,800, compared with the median of $1,043,100 received by the plaintiff in a settlement.
Dr. Choudhry noted that early intervention may improve mortality from SBO in some patient groups. “Small bowel obstruction protocols which identify patients at high risk for adverse outcomes and ensure timely management may lessen the chance of litigation,” he said.
Dr. Choudhry acknowledged that the Westlaw database included just a limited amount of medical information. Various tort reform initiatives may have had a confounding effect on award size. It’s possible that using malpractice insurance data could provide more detailed medical information, he said.
Dr. Choudhry reported no relevant disclosures.
On Twitter @karioakes
AT THE ANNUAL MEETING OF THE CENTRAL SURGICAL ASSOCIATION
Key clinical point: Almost half of surgical small bowel obstruction lawsuits involved a payout of a median $1.1 million.
Major finding: About 15% of general surgeons are sued annually, and SBO is a common diagnosis in these suits.
Data source: Review of the Westlaw database that identified 158 lawsuits involving general surgeons and small bowel obstruction from 1982 to 2015.
Disclosures: The study authors reported no relevant disclosures.
Small bowel surgery for the benign gynecologist

For more videos from the Society of Gynecologic Surgeons, click here
Visit the Society of Gynecologic Surgeons online: sgsonline.org

For more videos from the Society of Gynecologic Surgeons, click here
Visit the Society of Gynecologic Surgeons online: sgsonline.org

For more videos from the Society of Gynecologic Surgeons, click here
Visit the Society of Gynecologic Surgeons online: sgsonline.org
This video is brought to you by ![]()
ACOG releases new Choosing Wisely list
Prenatal ultrasounds for nonmedical purposes and routine use of robotic assisted laparoscopic surgery for benign gynecologic disease are among the interventions physicians and patients should question, according to the American College of Obstetricians and Gynecologists.
The organization produced the list of five interventions to be questioned as part of the ABIM (American Board of Internal Medicine) Foundation’s Choosing Wisely initiative, which “aims to promote conversations between clinicians and patients by helping patients choose care that is supported by evidence, not duplicative of other tests or procedures already received, free from harm, and truly necessary,” according to the Choosing Wisely website.
ACOG released its first Choosing Wisely list in 2003, advising clinicians to avoid elective labor inductions before 39 weeks as well as annual pap tests in women aged 30-65.
“These are good topics to bring up in discussion with patients,” said Dr. Gerardo Bustillo, an ob.gyn. at Orange Coast Memorial Medical Center in Fountain Valley, Calif. “Patients may ask for inappropriate interventions such as early induction of labor, and these recommendations will equip physicians and other healthcare providers in explaining the dangers of certain interventions.”
The five new items include:
1. Avoid using robotic assisted laparoscopic surgery for benign gynecologic disease when it is feasible to use a conventional laparoscopic or vaginal approach.
ACOG states that comparable perioperative outcomes, intraoperative complications, length of hospital stay, and rate of conversion to open surgery result from both robotic-assisted and conventional laparoscopic surgeries but that robotic-assisted techniques cost more and can take longer. But Dr. Bustillo questioned this item’s addition to the list in light of new evidence that “robotic-assisted hysterectomies resulted in fewer postoperative complications than conventional laparoscopic and vaginal hysterectomies, when performed by high-volume robotic gynecologic surgeons,” he said.
The patients undergoing robotic-assisted hysterectomy, he added, experienced the same or decreased intraoperative and postoperative complications compared with those undergoing conventional techniques despite being more complex patients. They were older with higher rates of adhesive disease, large uteri, and morbid obesity.
2. Don’t perform prenatal ultrasounds for nonmedical purposes, for example, solely to create keepsake videos or photographs.
Keepsake imaging is not an approved use of a medical device by the Food and Drug Administration and is also discouraged by the American Institute of Ultrasound in Medicine. These “comfort ultrasounds” are often performed by the request of the patient and are done without true medical indications,” said Dr. Sherry Ross, an ob.gyn. at Providence Saint John’s Health Center in Santa Monica, Calif.
“Not only are these types of ultrasounds excessive, but they are costly as well,” she said. “Counseling the pregnant woman is the best way to reduce unnecessary ultrasounds, especially those performed at the local mall.”
3. Don’t routinely transfuse stable, asymptomatic hospitalized patients with a hemoglobin level greater than 7-8 grams.
“Arbitrary hemoglobin or hematocrit thresholds should not be used as the only criterion for transfusions of packed red blood cells,” ACOG advises. The potential risks of transfusion make this item the most important of the additions, according to Dr. Bustillo. “These risks include infection with certain pathogens, allergic and immune transfusion reactions, volume overload, hyperkalemia, and iron overload,” he said.
4. Don’t perform pelvic ultrasound in average risk women to screen for ovarian cancer.
With an age-adjusted incidence of just 13 ovarian cancer cases per 100,000 women annually, the positive predictive value is low for screening for ovarian cancer, leading to a high rate of false positives, ACOG notes.
“The tools that are currently available for screening women who are high risk include transvaginal pelvic ultrasound and CA 125 blood tests done every 6 months to 1 year along with pelvic examinations,” Dr. Ross said. “Those at high risk include those with a family history or who test positive for BRCA1 and 2 mutations and Ashkenazi women with a single family member with breast cancer before age 50 or with ovarian cancer.” Without a family history or other risk factors, a CA 125 or pelvic ultrasound in asymptomatic women does not reduce deaths, she added.
5. Don’t routinely recommend activity restriction or bed rest during pregnancy for any indication.
Historically, physicians have recommended bed rest for a range of pregnancy conditions, including multiple gestation, intrauterine growth restriction, preterm labor, premature rupture of membranes, vaginal bleeding, and hypertensive disorders in pregnancy, ACOG notes. “The negative financial and psychosocial implications of putting women on activity restriction, specifically bed rest, are well documented,” said Dr. Anthony C. Sciscione, director of Maternal-Fetal Medicine at Christiana Care Health System and program director for Christiana Care’s ob.gyn. residency program in Wilmington, Del. “However, no study has demonstrated a benefit to activity restriction during pregnancy for any diagnosis.”
The only clinical benefit resulting from bed rest has been a modest decrease in blood pressure that does not translate to improved outcomes, Dr. Sciscione said. Additional risks of activity restriction include an increase in maternal anxiety and depression, significant financial impact on the family, physical deconditioning, bone loss, and a potential increase in blood clots. Being active in pregnancy, however, is linked to a decrease in preterm birth, he added.
The 2013 list
Among the previous five items included in the 2013 list are not scheduling elective, nonmedically indicated inductions of labor or cesarean deliveries before 39 weeks 0 days of gestational age and not scheduling elective, non-medically indicated labor inductions between 39 weeks 0 days and 41 weeks 0 days unless the cervix is favorable.
ACOG also recommended that asymptomatic women of average risk do not receive screenings for ovarian cancer, that patients with mild dysplasia for less than 2 years do not receive treatment, and that women aged 30-65 years do not receive routine annual cervical cytology screenings.
Prenatal ultrasounds for nonmedical purposes and routine use of robotic assisted laparoscopic surgery for benign gynecologic disease are among the interventions physicians and patients should question, according to the American College of Obstetricians and Gynecologists.
The organization produced the list of five interventions to be questioned as part of the ABIM (American Board of Internal Medicine) Foundation’s Choosing Wisely initiative, which “aims to promote conversations between clinicians and patients by helping patients choose care that is supported by evidence, not duplicative of other tests or procedures already received, free from harm, and truly necessary,” according to the Choosing Wisely website.
ACOG released its first Choosing Wisely list in 2003, advising clinicians to avoid elective labor inductions before 39 weeks as well as annual pap tests in women aged 30-65.
“These are good topics to bring up in discussion with patients,” said Dr. Gerardo Bustillo, an ob.gyn. at Orange Coast Memorial Medical Center in Fountain Valley, Calif. “Patients may ask for inappropriate interventions such as early induction of labor, and these recommendations will equip physicians and other healthcare providers in explaining the dangers of certain interventions.”
The five new items include:
1. Avoid using robotic assisted laparoscopic surgery for benign gynecologic disease when it is feasible to use a conventional laparoscopic or vaginal approach.
ACOG states that comparable perioperative outcomes, intraoperative complications, length of hospital stay, and rate of conversion to open surgery result from both robotic-assisted and conventional laparoscopic surgeries but that robotic-assisted techniques cost more and can take longer. But Dr. Bustillo questioned this item’s addition to the list in light of new evidence that “robotic-assisted hysterectomies resulted in fewer postoperative complications than conventional laparoscopic and vaginal hysterectomies, when performed by high-volume robotic gynecologic surgeons,” he said.
The patients undergoing robotic-assisted hysterectomy, he added, experienced the same or decreased intraoperative and postoperative complications compared with those undergoing conventional techniques despite being more complex patients. They were older with higher rates of adhesive disease, large uteri, and morbid obesity.
2. Don’t perform prenatal ultrasounds for nonmedical purposes, for example, solely to create keepsake videos or photographs.
Keepsake imaging is not an approved use of a medical device by the Food and Drug Administration and is also discouraged by the American Institute of Ultrasound in Medicine. These “comfort ultrasounds” are often performed by the request of the patient and are done without true medical indications,” said Dr. Sherry Ross, an ob.gyn. at Providence Saint John’s Health Center in Santa Monica, Calif.
“Not only are these types of ultrasounds excessive, but they are costly as well,” she said. “Counseling the pregnant woman is the best way to reduce unnecessary ultrasounds, especially those performed at the local mall.”
3. Don’t routinely transfuse stable, asymptomatic hospitalized patients with a hemoglobin level greater than 7-8 grams.
“Arbitrary hemoglobin or hematocrit thresholds should not be used as the only criterion for transfusions of packed red blood cells,” ACOG advises. The potential risks of transfusion make this item the most important of the additions, according to Dr. Bustillo. “These risks include infection with certain pathogens, allergic and immune transfusion reactions, volume overload, hyperkalemia, and iron overload,” he said.
4. Don’t perform pelvic ultrasound in average risk women to screen for ovarian cancer.
With an age-adjusted incidence of just 13 ovarian cancer cases per 100,000 women annually, the positive predictive value is low for screening for ovarian cancer, leading to a high rate of false positives, ACOG notes.
“The tools that are currently available for screening women who are high risk include transvaginal pelvic ultrasound and CA 125 blood tests done every 6 months to 1 year along with pelvic examinations,” Dr. Ross said. “Those at high risk include those with a family history or who test positive for BRCA1 and 2 mutations and Ashkenazi women with a single family member with breast cancer before age 50 or with ovarian cancer.” Without a family history or other risk factors, a CA 125 or pelvic ultrasound in asymptomatic women does not reduce deaths, she added.
5. Don’t routinely recommend activity restriction or bed rest during pregnancy for any indication.
Historically, physicians have recommended bed rest for a range of pregnancy conditions, including multiple gestation, intrauterine growth restriction, preterm labor, premature rupture of membranes, vaginal bleeding, and hypertensive disorders in pregnancy, ACOG notes. “The negative financial and psychosocial implications of putting women on activity restriction, specifically bed rest, are well documented,” said Dr. Anthony C. Sciscione, director of Maternal-Fetal Medicine at Christiana Care Health System and program director for Christiana Care’s ob.gyn. residency program in Wilmington, Del. “However, no study has demonstrated a benefit to activity restriction during pregnancy for any diagnosis.”
The only clinical benefit resulting from bed rest has been a modest decrease in blood pressure that does not translate to improved outcomes, Dr. Sciscione said. Additional risks of activity restriction include an increase in maternal anxiety and depression, significant financial impact on the family, physical deconditioning, bone loss, and a potential increase in blood clots. Being active in pregnancy, however, is linked to a decrease in preterm birth, he added.
The 2013 list
Among the previous five items included in the 2013 list are not scheduling elective, nonmedically indicated inductions of labor or cesarean deliveries before 39 weeks 0 days of gestational age and not scheduling elective, non-medically indicated labor inductions between 39 weeks 0 days and 41 weeks 0 days unless the cervix is favorable.
ACOG also recommended that asymptomatic women of average risk do not receive screenings for ovarian cancer, that patients with mild dysplasia for less than 2 years do not receive treatment, and that women aged 30-65 years do not receive routine annual cervical cytology screenings.
Prenatal ultrasounds for nonmedical purposes and routine use of robotic assisted laparoscopic surgery for benign gynecologic disease are among the interventions physicians and patients should question, according to the American College of Obstetricians and Gynecologists.
The organization produced the list of five interventions to be questioned as part of the ABIM (American Board of Internal Medicine) Foundation’s Choosing Wisely initiative, which “aims to promote conversations between clinicians and patients by helping patients choose care that is supported by evidence, not duplicative of other tests or procedures already received, free from harm, and truly necessary,” according to the Choosing Wisely website.
ACOG released its first Choosing Wisely list in 2003, advising clinicians to avoid elective labor inductions before 39 weeks as well as annual pap tests in women aged 30-65.
“These are good topics to bring up in discussion with patients,” said Dr. Gerardo Bustillo, an ob.gyn. at Orange Coast Memorial Medical Center in Fountain Valley, Calif. “Patients may ask for inappropriate interventions such as early induction of labor, and these recommendations will equip physicians and other healthcare providers in explaining the dangers of certain interventions.”
The five new items include:
1. Avoid using robotic assisted laparoscopic surgery for benign gynecologic disease when it is feasible to use a conventional laparoscopic or vaginal approach.
ACOG states that comparable perioperative outcomes, intraoperative complications, length of hospital stay, and rate of conversion to open surgery result from both robotic-assisted and conventional laparoscopic surgeries but that robotic-assisted techniques cost more and can take longer. But Dr. Bustillo questioned this item’s addition to the list in light of new evidence that “robotic-assisted hysterectomies resulted in fewer postoperative complications than conventional laparoscopic and vaginal hysterectomies, when performed by high-volume robotic gynecologic surgeons,” he said.
The patients undergoing robotic-assisted hysterectomy, he added, experienced the same or decreased intraoperative and postoperative complications compared with those undergoing conventional techniques despite being more complex patients. They were older with higher rates of adhesive disease, large uteri, and morbid obesity.
2. Don’t perform prenatal ultrasounds for nonmedical purposes, for example, solely to create keepsake videos or photographs.
Keepsake imaging is not an approved use of a medical device by the Food and Drug Administration and is also discouraged by the American Institute of Ultrasound in Medicine. These “comfort ultrasounds” are often performed by the request of the patient and are done without true medical indications,” said Dr. Sherry Ross, an ob.gyn. at Providence Saint John’s Health Center in Santa Monica, Calif.
“Not only are these types of ultrasounds excessive, but they are costly as well,” she said. “Counseling the pregnant woman is the best way to reduce unnecessary ultrasounds, especially those performed at the local mall.”
3. Don’t routinely transfuse stable, asymptomatic hospitalized patients with a hemoglobin level greater than 7-8 grams.
“Arbitrary hemoglobin or hematocrit thresholds should not be used as the only criterion for transfusions of packed red blood cells,” ACOG advises. The potential risks of transfusion make this item the most important of the additions, according to Dr. Bustillo. “These risks include infection with certain pathogens, allergic and immune transfusion reactions, volume overload, hyperkalemia, and iron overload,” he said.
4. Don’t perform pelvic ultrasound in average risk women to screen for ovarian cancer.
With an age-adjusted incidence of just 13 ovarian cancer cases per 100,000 women annually, the positive predictive value is low for screening for ovarian cancer, leading to a high rate of false positives, ACOG notes.
“The tools that are currently available for screening women who are high risk include transvaginal pelvic ultrasound and CA 125 blood tests done every 6 months to 1 year along with pelvic examinations,” Dr. Ross said. “Those at high risk include those with a family history or who test positive for BRCA1 and 2 mutations and Ashkenazi women with a single family member with breast cancer before age 50 or with ovarian cancer.” Without a family history or other risk factors, a CA 125 or pelvic ultrasound in asymptomatic women does not reduce deaths, she added.
5. Don’t routinely recommend activity restriction or bed rest during pregnancy for any indication.
Historically, physicians have recommended bed rest for a range of pregnancy conditions, including multiple gestation, intrauterine growth restriction, preterm labor, premature rupture of membranes, vaginal bleeding, and hypertensive disorders in pregnancy, ACOG notes. “The negative financial and psychosocial implications of putting women on activity restriction, specifically bed rest, are well documented,” said Dr. Anthony C. Sciscione, director of Maternal-Fetal Medicine at Christiana Care Health System and program director for Christiana Care’s ob.gyn. residency program in Wilmington, Del. “However, no study has demonstrated a benefit to activity restriction during pregnancy for any diagnosis.”
The only clinical benefit resulting from bed rest has been a modest decrease in blood pressure that does not translate to improved outcomes, Dr. Sciscione said. Additional risks of activity restriction include an increase in maternal anxiety and depression, significant financial impact on the family, physical deconditioning, bone loss, and a potential increase in blood clots. Being active in pregnancy, however, is linked to a decrease in preterm birth, he added.
The 2013 list
Among the previous five items included in the 2013 list are not scheduling elective, nonmedically indicated inductions of labor or cesarean deliveries before 39 weeks 0 days of gestational age and not scheduling elective, non-medically indicated labor inductions between 39 weeks 0 days and 41 weeks 0 days unless the cervix is favorable.
ACOG also recommended that asymptomatic women of average risk do not receive screenings for ovarian cancer, that patients with mild dysplasia for less than 2 years do not receive treatment, and that women aged 30-65 years do not receive routine annual cervical cytology screenings.
Flu vaccination found safe in surgical patients
Immunizing surgical patients against seasonal influenza before they are discharged from the hospital appears safe and is a sound strategy for expanding vaccine coverage, especially among people at high risk, according to a report published online March 14 in Annals of Internal Medicine.
All health care contacts, including hospitalizations, are considered excellent opportunities for influenza vaccination, and current recommendations advise that eligible inpatients receive the immunization before discharge. However, surgical patients don’t often get the flu vaccine before they leave the hospital, likely because of concerns that potential adverse effects like fever and myalgia could be falsely attributed to surgical complications. This would lead to unnecessary patient evaluations and could interfere with postsurgical care, said Sara Y. Tartof, Ph.D., and her associates in the department of research and evaluation, Kaiser Permanente Southern California, Pasadena.
“Although this concern is understandable, few clinical data support it,” they noted.
“To provide clinical evidence that would either substantiate or refute” these concerns about perioperative flu vaccination, the investigators analyzed data in the electronic health records for 81,647 surgeries. All the study participants were deemed eligible for flu vaccination. They were socioeconomically and ethnically diverse, ranged in age from 6 months to 106 years, and underwent surgery at 14 hospitals during three consecutive flu seasons. Operations included general, cardiac, eye, dermatologic, ENT, neurologic, ob.gyn., oral/maxillofacial, orthopedic, plastic, podiatric, urologic, and vascular procedures.
Patients received a flu vaccine in 6,420 hospital stays for surgery – only 15% of 42,777 eligible hospitalizations – usually on the day of discharge. (The remaining 38,870 patients either had been vaccinated before hospital admission or were vaccinated more than a week after discharge and were not included in further analyses.)
Compared with eligible patients who didn’t receive a flu vaccine during hospitalization for surgery, those who did showed no increased risk for subsequent inpatient visits, ED visits, or clinical work-ups for infection. Patients who received the flu vaccine before discharge showed a minimally increased risk for outpatient visits during the week following hospitalization, but this was considered unlikely “to translate into substantial clinical impact,” especially when balanced against the benefit of immunization, Dr. Tartof and her associates said (Ann Intern Med. 2016 Mar 14. doi: 10.7326/M15-1667).
Giving the flu vaccine during a surgical hospitalization “is an opportunity to protect a high-risk population,” because surgery patients tend to be of an age, and to have comorbid conditions, that raise their risk for flu complications. In addition, previous research has reported that 39%-46% of adults hospitalized for influenza-related disease in a given year had been hospitalized during the preceding autumn, indicating that recent hospitalization also raises the risk for flu complications, the investigators said.
“Our data support the rationale for increasing vaccination rates among surgical inpatients,” they said.
This study was funded by the U.S. Centers for Disease Control and Prevention through the Vaccine Safety Datalink program. Dr. Tartof reported receiving grants from Merck outside of this work; two of her associates reported receiving grants from Novartis and GlaxoSmithKline outside of this work.
Immunizing surgical patients against seasonal influenza before they are discharged from the hospital appears safe and is a sound strategy for expanding vaccine coverage, especially among people at high risk, according to a report published online March 14 in Annals of Internal Medicine.
All health care contacts, including hospitalizations, are considered excellent opportunities for influenza vaccination, and current recommendations advise that eligible inpatients receive the immunization before discharge. However, surgical patients don’t often get the flu vaccine before they leave the hospital, likely because of concerns that potential adverse effects like fever and myalgia could be falsely attributed to surgical complications. This would lead to unnecessary patient evaluations and could interfere with postsurgical care, said Sara Y. Tartof, Ph.D., and her associates in the department of research and evaluation, Kaiser Permanente Southern California, Pasadena.
“Although this concern is understandable, few clinical data support it,” they noted.
“To provide clinical evidence that would either substantiate or refute” these concerns about perioperative flu vaccination, the investigators analyzed data in the electronic health records for 81,647 surgeries. All the study participants were deemed eligible for flu vaccination. They were socioeconomically and ethnically diverse, ranged in age from 6 months to 106 years, and underwent surgery at 14 hospitals during three consecutive flu seasons. Operations included general, cardiac, eye, dermatologic, ENT, neurologic, ob.gyn., oral/maxillofacial, orthopedic, plastic, podiatric, urologic, and vascular procedures.
Patients received a flu vaccine in 6,420 hospital stays for surgery – only 15% of 42,777 eligible hospitalizations – usually on the day of discharge. (The remaining 38,870 patients either had been vaccinated before hospital admission or were vaccinated more than a week after discharge and were not included in further analyses.)
Compared with eligible patients who didn’t receive a flu vaccine during hospitalization for surgery, those who did showed no increased risk for subsequent inpatient visits, ED visits, or clinical work-ups for infection. Patients who received the flu vaccine before discharge showed a minimally increased risk for outpatient visits during the week following hospitalization, but this was considered unlikely “to translate into substantial clinical impact,” especially when balanced against the benefit of immunization, Dr. Tartof and her associates said (Ann Intern Med. 2016 Mar 14. doi: 10.7326/M15-1667).
Giving the flu vaccine during a surgical hospitalization “is an opportunity to protect a high-risk population,” because surgery patients tend to be of an age, and to have comorbid conditions, that raise their risk for flu complications. In addition, previous research has reported that 39%-46% of adults hospitalized for influenza-related disease in a given year had been hospitalized during the preceding autumn, indicating that recent hospitalization also raises the risk for flu complications, the investigators said.
“Our data support the rationale for increasing vaccination rates among surgical inpatients,” they said.
This study was funded by the U.S. Centers for Disease Control and Prevention through the Vaccine Safety Datalink program. Dr. Tartof reported receiving grants from Merck outside of this work; two of her associates reported receiving grants from Novartis and GlaxoSmithKline outside of this work.
Immunizing surgical patients against seasonal influenza before they are discharged from the hospital appears safe and is a sound strategy for expanding vaccine coverage, especially among people at high risk, according to a report published online March 14 in Annals of Internal Medicine.
All health care contacts, including hospitalizations, are considered excellent opportunities for influenza vaccination, and current recommendations advise that eligible inpatients receive the immunization before discharge. However, surgical patients don’t often get the flu vaccine before they leave the hospital, likely because of concerns that potential adverse effects like fever and myalgia could be falsely attributed to surgical complications. This would lead to unnecessary patient evaluations and could interfere with postsurgical care, said Sara Y. Tartof, Ph.D., and her associates in the department of research and evaluation, Kaiser Permanente Southern California, Pasadena.
“Although this concern is understandable, few clinical data support it,” they noted.
“To provide clinical evidence that would either substantiate or refute” these concerns about perioperative flu vaccination, the investigators analyzed data in the electronic health records for 81,647 surgeries. All the study participants were deemed eligible for flu vaccination. They were socioeconomically and ethnically diverse, ranged in age from 6 months to 106 years, and underwent surgery at 14 hospitals during three consecutive flu seasons. Operations included general, cardiac, eye, dermatologic, ENT, neurologic, ob.gyn., oral/maxillofacial, orthopedic, plastic, podiatric, urologic, and vascular procedures.
Patients received a flu vaccine in 6,420 hospital stays for surgery – only 15% of 42,777 eligible hospitalizations – usually on the day of discharge. (The remaining 38,870 patients either had been vaccinated before hospital admission or were vaccinated more than a week after discharge and were not included in further analyses.)
Compared with eligible patients who didn’t receive a flu vaccine during hospitalization for surgery, those who did showed no increased risk for subsequent inpatient visits, ED visits, or clinical work-ups for infection. Patients who received the flu vaccine before discharge showed a minimally increased risk for outpatient visits during the week following hospitalization, but this was considered unlikely “to translate into substantial clinical impact,” especially when balanced against the benefit of immunization, Dr. Tartof and her associates said (Ann Intern Med. 2016 Mar 14. doi: 10.7326/M15-1667).
Giving the flu vaccine during a surgical hospitalization “is an opportunity to protect a high-risk population,” because surgery patients tend to be of an age, and to have comorbid conditions, that raise their risk for flu complications. In addition, previous research has reported that 39%-46% of adults hospitalized for influenza-related disease in a given year had been hospitalized during the preceding autumn, indicating that recent hospitalization also raises the risk for flu complications, the investigators said.
“Our data support the rationale for increasing vaccination rates among surgical inpatients,” they said.
This study was funded by the U.S. Centers for Disease Control and Prevention through the Vaccine Safety Datalink program. Dr. Tartof reported receiving grants from Merck outside of this work; two of her associates reported receiving grants from Novartis and GlaxoSmithKline outside of this work.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point: Immunizing surgical patients against seasonal influenza before they leave the hospital appears safe.
Major finding: Patients received a flu vaccine in only 6,420 hospital stays for surgery, comprising only 15% of the patient hospitalizations that were eligible.
Data source: A retrospective cohort study involving 81,647 surgeries at 14 California hospitals during three consecutive flu seasons.
Disclosures: This study was funded by the U.S. Centers for Disease Control and Prevention through the Vaccine Safety Datalink program. Dr. Tartof reported receiving grants from Merck outside of this work; two of her associates reported receiving grants from Novartis and GlaxoSmithKline outside of this work.
Enlarged uterus helps predict morcellation in vaginal hysterectomy
Women undergoing vaginal hysterectomy are more likely to receive cold-knife morcellation if they have an enlarged uterus, leiomyoma, or no prolapse, according to new research.
Electromechanical morcellation, a technique used during laparoscopic hysterectomy to cut the uterus into small pieces for removal, has come under heavy scrutiny in recent years due to risk of disseminating undiagnosed uterine cancers. However, morcellation can also be performed manually during a vaginal hysterectomy. While current recommendations stress caution for all types of morcellation, the risks and prognostic factors for cold-knife morcellation are poorly understood.
In a retrospective cohort study, Dr. Megan Wasson, of the Mayo Clinic Arizona in Phoenix, and her colleagues examined a cohort of 743 women who underwent hysterectomy with either intact uterine removal (383 women) or with cold-knife morcellation (360 women).
Dr. Wasson and her colleagues found that women were significantly more likely to undergo morcellation, compared with intact uterine removal if they had larger uterine weight (adjusted odds ratio, 7.25; P less than .001), lack of prolapse (aOR, 3.87; P less than .001), or the presence of leiomyoma (aOR, 2.77, P = .035).
Women with prior vaginal delivery were significantly less likely to receive morcellation (aOR, 0.79, P = .005).
Younger age, lower parity, and nonwhite race were also associated with a higher likelihood of undergoing morcellation (Obstet Gynecol. 2016;127:752–7).
“This study identified prognostic factors associated with an increased likelihood of morcellation required at the time of vaginal hysterectomy,” Dr. Wasson and her colleagues wrote, stressing that higher uterine weight was the strongest predictor. “The ability to preoperatively predict uterine weight and size is essential for surgical planning given that a large uterus is most predictive of needing morcellation at the time of vaginal hysterectomy.”
The findings, they wrote, may help clinicians identify those patients who need additional counseling about the potential risks of morcellation, as well as patients who may need to avoid vaginal hysterectomy to negate the risks of morcellation.
The investigators identified limitations to their study, including that the majority of the women (88%) were white, and that candidates for vaginal hysterectomy were carefully chosen by expert surgeons, leading to likely selection bias.
The investigators reported having no financial disclosures.
Women undergoing vaginal hysterectomy are more likely to receive cold-knife morcellation if they have an enlarged uterus, leiomyoma, or no prolapse, according to new research.
Electromechanical morcellation, a technique used during laparoscopic hysterectomy to cut the uterus into small pieces for removal, has come under heavy scrutiny in recent years due to risk of disseminating undiagnosed uterine cancers. However, morcellation can also be performed manually during a vaginal hysterectomy. While current recommendations stress caution for all types of morcellation, the risks and prognostic factors for cold-knife morcellation are poorly understood.
In a retrospective cohort study, Dr. Megan Wasson, of the Mayo Clinic Arizona in Phoenix, and her colleagues examined a cohort of 743 women who underwent hysterectomy with either intact uterine removal (383 women) or with cold-knife morcellation (360 women).
Dr. Wasson and her colleagues found that women were significantly more likely to undergo morcellation, compared with intact uterine removal if they had larger uterine weight (adjusted odds ratio, 7.25; P less than .001), lack of prolapse (aOR, 3.87; P less than .001), or the presence of leiomyoma (aOR, 2.77, P = .035).
Women with prior vaginal delivery were significantly less likely to receive morcellation (aOR, 0.79, P = .005).
Younger age, lower parity, and nonwhite race were also associated with a higher likelihood of undergoing morcellation (Obstet Gynecol. 2016;127:752–7).
“This study identified prognostic factors associated with an increased likelihood of morcellation required at the time of vaginal hysterectomy,” Dr. Wasson and her colleagues wrote, stressing that higher uterine weight was the strongest predictor. “The ability to preoperatively predict uterine weight and size is essential for surgical planning given that a large uterus is most predictive of needing morcellation at the time of vaginal hysterectomy.”
The findings, they wrote, may help clinicians identify those patients who need additional counseling about the potential risks of morcellation, as well as patients who may need to avoid vaginal hysterectomy to negate the risks of morcellation.
The investigators identified limitations to their study, including that the majority of the women (88%) were white, and that candidates for vaginal hysterectomy were carefully chosen by expert surgeons, leading to likely selection bias.
The investigators reported having no financial disclosures.
Women undergoing vaginal hysterectomy are more likely to receive cold-knife morcellation if they have an enlarged uterus, leiomyoma, or no prolapse, according to new research.
Electromechanical morcellation, a technique used during laparoscopic hysterectomy to cut the uterus into small pieces for removal, has come under heavy scrutiny in recent years due to risk of disseminating undiagnosed uterine cancers. However, morcellation can also be performed manually during a vaginal hysterectomy. While current recommendations stress caution for all types of morcellation, the risks and prognostic factors for cold-knife morcellation are poorly understood.
In a retrospective cohort study, Dr. Megan Wasson, of the Mayo Clinic Arizona in Phoenix, and her colleagues examined a cohort of 743 women who underwent hysterectomy with either intact uterine removal (383 women) or with cold-knife morcellation (360 women).
Dr. Wasson and her colleagues found that women were significantly more likely to undergo morcellation, compared with intact uterine removal if they had larger uterine weight (adjusted odds ratio, 7.25; P less than .001), lack of prolapse (aOR, 3.87; P less than .001), or the presence of leiomyoma (aOR, 2.77, P = .035).
Women with prior vaginal delivery were significantly less likely to receive morcellation (aOR, 0.79, P = .005).
Younger age, lower parity, and nonwhite race were also associated with a higher likelihood of undergoing morcellation (Obstet Gynecol. 2016;127:752–7).
“This study identified prognostic factors associated with an increased likelihood of morcellation required at the time of vaginal hysterectomy,” Dr. Wasson and her colleagues wrote, stressing that higher uterine weight was the strongest predictor. “The ability to preoperatively predict uterine weight and size is essential for surgical planning given that a large uterus is most predictive of needing morcellation at the time of vaginal hysterectomy.”
The findings, they wrote, may help clinicians identify those patients who need additional counseling about the potential risks of morcellation, as well as patients who may need to avoid vaginal hysterectomy to negate the risks of morcellation.
The investigators identified limitations to their study, including that the majority of the women (88%) were white, and that candidates for vaginal hysterectomy were carefully chosen by expert surgeons, leading to likely selection bias.
The investigators reported having no financial disclosures.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point: Women with a larger-than-normal uterus are likelier to undergo cold-knife morcellation versus intact uterine removal during a vaginal hysterectomy.
Major finding: Larger-than-normal uterine weight was associated with increased odds of morcellation (aOR, 7.25; P less than .001).
Data source: A retrospective cohort study of 743 women selected for vaginal hysterectomy.
Disclosures: The investigators reported having no financial disclosures.
14-Year-Old Boy With Mild Antecedent Neck Pain in Setting of Acute Trauma: A Rare Case of Benign Fibrous Histiocytoma of the Spine
Benign fibrous histiocytoma (BFH) is a rare, well-recognized, primary skeletal tumor accounting for approximately 1% of all benign bone tumors. Spinal involvement is exceedingly rare with only 11 cases reported in the literature.1,2 We present a case of BFH located in the cervical spine of a pediatric patient that was successfully treated with curretage through an anterior surgical approach, along with a review of the literature and appropriate management concerning BFH of the spine.
Case Report
A 14-year-old boy was tackled while playing football and noticed immediate neck pain and subjective paresthesia in the upper extremities. Examination revealed a nontender spine (cervical, thoracic, lumbar) and normal strength and range of motion in all extremities. Sensation was diffusely intact, long tract signs were absent, and gait was normal. On questioning, the patient endorsed mild antecedent neck pain but denied prior history of any trauma. Neck pain did not radiate and was slightly worsened by activity but was mostly intermittent and random. As the neck pain was very mild and was not interfering with daily activities, the patient had not sought care before presenting to the emergency department. He had no pertinent past medical or surgical history.
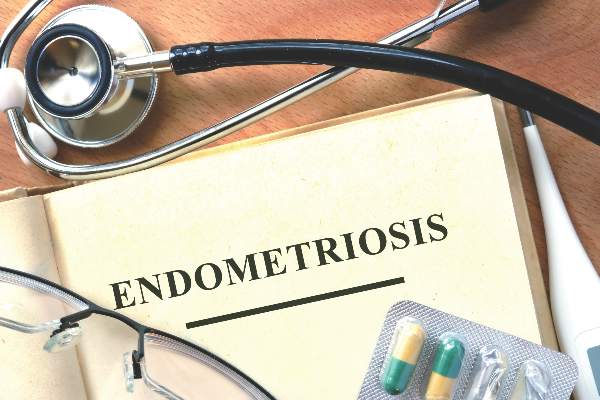
The patient presented with a computed tomography (CT) scan of his head and cervical spine and a magnetic resonance imaging (MRI) scan of the cervical spine. A magnetic resonance angiography (MRA) scan of the neck was ordered after his arrival.
Axial and sagittal CT (Figures 1A, 1B) showed a 1×1.2-cm discrete, expansile, lytic, radiolucent mass extending anterior from the left C2 vertebral body. The mass appeared to abut the left vertebral artery foramen. The cortical bone surrounding the lesion was thin but uniform. Sagittal and axial T1-weighted MRI (Figures 2A, 2B) showed the discrete, expansile, homogenous lesion with the same intensity as normal bone marrow. Sagittal and axial T2-weighted MRI (Figures 2C, 2D) showed a discrete, expansile, homogenous lesion with primarily high signal intensity. Sagittal short tau inversion recovery (STIR) MRI (Figure 2E) again showed the lesion with primarily low intensity. Given the close proximity of the lesion to the vertebral foramen, MRA was ordered; it showed the lesion was not interfering with the vertebral artery (Figure 2F).
The tumor’s location, in the left anterior aspect of the C2 vertebral body, was not conducive to percutaneous biopsy for establishing tissue diagnosis, so the decision was made to surgically excise the lesion. A left-sided anterior incision was made 2 fingerbreadths inferior to the jaw line in a neck crease. A head and neck surgeon assisted with dissection. Dissection was carried down through the skin, subcutaneous tissue, and platysma on to the anterior part of the spine medial to the carotid sheath. Superior thyroid nerve and vessels and superior laryngeal nerve were identified and preserved. Fluoroscopy confirmed correct location at C2. The tumor was easily visualized, and the outer shell broke easily with palpation. Gentle curettage was necessary when removing the tumor off the vertebral artery. A portion of the specimen was sent during surgery for frozen section, which showed infrequent mitotic figures and no other findings concerning for malignancy. No instability was created after curettage and excision of the tumor, so no grafting or instrumentation was necessary.
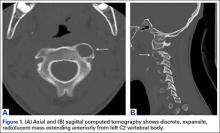
Grossly, the tumor was pale tan and firm. Histologic examination with hematoxylin-eosin staining revealed a bland spindle-cell neoplasm that focally involved bone. A storiform pattern was present. The cells had scant cytoplasm and oval to elongate nuclei with tapered ends. Significant nuclear pleomorphism was not seen. The stroma was loose, with focal myxoid change. Benign multinucleated giant cells were present. Mitotic activity was infrequent (Figures 3A–3D). Two attending pathologists reviewed the case material and the frozen and formalin-fixed specimens independently and concurred with the diagnosis of BFH. In addition, the case was reviewed at the surgical pathology consensus conference; the reviewers agreed on BFH, and additional studies were deemed unnecessary.
Given the patient’s complete clinical picture, the differential diagnosis included nonossifying fibroma (NOF), eosinophilic granuloma (EG), BFH, fibrous dysplasia, giant cell tumor (GCT), aneurysmal bone cyst (ABC), and osteoblastoma (OB).
Discussion
BFH is an extremely rare bone lesion, accounting for only 1% of all surgically managed bone tumors; not counting the present case, only 11 spine cases have been reported in the literature.1,2 BFH of the spine traditionally causes nonspecific, poorly localized pain. The Table lists the reported cases of spinal BFH and their presenting symptoms, location, and treatment. BFH usually occurs in young adults, but the age range is 5 to 75 years.2-4 Mean age of the 12 patients with spinal BFH in the literature (including ours) is 25 years.1 In addition, spinal BFH appears to have no predilection for sex.
Skeletal BFH presents as a discrete, well-defined, osteolytic lesion with sharp borders and potentially a sclerotic rim.4-6 Cortical expansion and even cortical disruption with invasion into adjacent tissue have occurred in flat bones.7 Histologically, BFHs contain spindle cells, multinucleated giant cells, and foam cells in storiform pattern.6
BFH shares many of its radiologic and histologic characteristics and clinical symptoms with other benign bone lesions (the tumors listed above). Therefore, accurate diagnosis of BFH requires appropriate correlation of clinical, radiographic, and histologic data.2,3,8 Below is a comparison of BFH with related bone lesions.
Spinal BFH causes a nonspecific, poorly localized pain similar to that of EG, ABC, GCT, and OB.3,9 NOF and fibrous dysplasia generally do not cause pain, unless these lesions are discovered secondary to a pathologic fracture.8,10,11 Our patient had minor antecedent neck pain, which was brought to light by his football accident. ABC and OB are more locally aggressive than BFH and can cause neurologic symptoms by mass effect and spinal cord or nerve root compression.1,8 In this case and in the 6 other cases of BFH of the cervical spine, there were no neurologic changes.4,10
Of the tumors mentioned, NOF and EG almost always occur in children. However, NOF usually occurs in the metaphyseal region of long bones, and EG is usually accompanied by systemic symptoms, such as lymphadenopathy, hepatomegaly, and increased inflammatory markers.1,8 Fibrous dysplasia usually presents in childhood but does not become symptomatic until adulthood. GCTs and OB predominantly occur in adulthood.12,13 Our patient’s age and lack of other systemic symptoms supported the diagnosis of BFH.
Appearance on MRI is reported less with BFH than with other tumors, but heterogenous signal intensity similar to that of skeletal muscle on T1-weighted images and high signal intensity on T2-weighted images is typically reported.8,14 NOF and fibrous dysplasia do not disrupt the bony cortex unless a pathologic fracture has occurred.4 GCTs are more aggressive lytic lesions with more aggressive radiologic features. GCTs generally cause cortical expansion/attenuation, and lack a sclerotic rim. GCTs also have a heterogenous appearance on MRI and give a low to intermediate signal on both T1- and T2-weighted images.12,15 The appearance of EG is similar to that of BFH as an osteolytic lesion with a sclerotic rim, though EGs typically break through the cortex and acquire a “punched-out” look.1,8 ABC typically is described as an expansile osteolytic lesion with a “soap-bubble” appearance on radiographs; periosteal elevation and cortical attenuation can also be visualized. MRI shows the typical multilobular appearance of the lesion with fluid levels.13
OB appears as a radiolucent lesion, with or without calcifications, surrounded by a thin margin of reactive bone.14,16 A distinguishing characteristic of OB was thought to be intense radioisotope uptake on bone scintigraphy, but recently a bony BFH demonstrated intense uptake.17 OBs typically demonstrate nonspecific MRI results similar to those of BFH: low to intermediate signal on T1-weighted images and intermediate to high signal on T2-weighted images.13 In our patient’s case, the radiographic appearance and lack of specific radiographic findings consistent with the other tumors supported the diagnosis of BFH.
Histologically, BFHs contain spindle cells, multinucleated giant cells, and foam cells in a storiform pattern6 which was demonstrated in our patient’s case. In addition, significant nuclear pleomorphism, mitotic activity, and necrosis were absent—a difference between BFH and malignant fibrous histiocytoma.4,15 The microscopic characteristics of BFH readily differentiate it from OB, ABC, EG, and GCT, but not from NOF on microscopic appearance alone. Clinical and radiographic findings must be consistent, as mentioned.7,18
Complete surgical excision is the reported treatment for BFH. Prognosis after resection or curettage is usually good, and recurrences have been rare.1,2 Depending on the intraspinous location of BFH, stabilization after resection or curettage may be necessary to prevent residual instability. Three of the 11 reported cases of spinal BFH required stabilization by anterior fusion or posterior pedicle screw fixation after resection.1,2 The other 8 cases underwent excision alone or excision and grafting. All 11 patients were disease-free at a mean follow-up of 3.5 years.1 In nonspinal BFH, however, both local recurrence and lung metastasis have been reported.2,5,9,19 Clarke and colleagues9 reported local recurrences in 3 of 8 cases. These recurrences involved BFH in long bones of the leg, which had been treated with curettage and grafting. There has been no reliable report of a malignant change in BFH.2,9 The only case of lung metastasis, reported by Unni and Dahlin6 in their study of 10 cases, occurred 2 years after local recurrence in the distal femur.Our patient was doing well at most recent follow-up, 6 months after surgery. He had no pain and had returned to normal activities. Although there are no reported cases of spinal BFH recurrence, we will follow this patient with imaging on an annual basis. His case is of particular interest to orthopedic surgeons because they encounter benign bone lesions every day, and many of these lesions are in difficult anatomical locations. Knowing the characteristics, differential diagnoses, and appropriate diagnostic workups for benign bone lesions is important for optimal and timely patient care.
1. Demiralp B, Kose O, Oguz E, Sanal T, Ozcan A, Sehirlioglu A. Benign fibrous histiocytoma of the lumbar vertebrae. Skeletal Radiol. 2009;38(2):187-191.
2. Kuruvath S, O’Donovan DG, Aspoas AR, David KM. Benign fibrous histiocytoma of the thoracic spine: case report and review of the literature. J Neurosurg Spine. 2006;4(3):260-264.
3. Ceroni D, Dayer R, De Coulon G, Kaelin A. Benign fibrous histiocytoma of bone in a paediatric population: a report of 6 cases. Musculoskelet Surg. 2011;95(2):107-114.
4. Dorfman HD, Czerniak B. Bone Tumors. St. Louis, MO: Mosby; 1998.
5. Grohs JG, Nicolakis M, Kainberger F, Lang S, Kotz R. Benign fibrous histiocytoma of bone: a report of ten cases and review of literature. Wien Klin Wochenschr. 2002;114(1-2):56-63.
6. Unni KK, Dahlin DC. Dahlin’s Bone Tumors. 5th ed. Philadelphia, PA: Lippincott-Raven; 1996.
7. Balasubramanian C, Rajaraman G, Singh CS, Baliga DK. Benign fibrous histiocytoma of the sacrum—diagnostic difficulties facing this rare bone tumor. Pediatr Neurosurg. 2005;41(5):253-257.
8. van Giffen NH, van Rhijn LW, van Ooij A, et al. Benign fibrous histiocytoma of the posterior arch of C1 in a 6-year old boy: a case report. Spine. 2003;28(18):E359-E363.
9. Clarke BE, Xipell JM, Thomas DP. Benign fibrous histiocytoma of bone. Am J Surg Pathol. 1985;9(11):806-815.
10. Peicha G, Siebert FJ, Bratschitsch G, Fankhauser F, Grechenig W. Pathologic odontoid fracture and benign fibrous histiocytoma of bone. Eur Spine J. 1999;8(2):161-163.
11. Unni KK, Inwards CY, Bridge JA, Kindblom LG, Wold LE. Tumors of the Bones and Joints (AFIP Atlas of Tumor Pathology Series IV). Annapolis Junction, MD: American Registry of Pathology Press; 2005.
12. Dee R. Principles of Orthopaedic Practice. 2nd ed. New York, NY: McGraw-Hill; 1997.
13. Murphey M, Andrews C, Flemming D, Temple HT, Smith WS, Smirniotopoulos JG. Primary tumors of the spine: radiologic–pathologic correlation. Radiographics. 1996;16(5):1131-1158.
14. Hamada T, Ito H, Araki Y, Fujii K, Inoue M, Ishida O. Benign fibrous histiocytoma of the femur: review of three cases. Skeletal Radiol. 1996;25(1):25-29.
15. Mirra JM, Picci P, Gold RH. Bone Tumors: Clinical, Radiologic, and Pathologic Correlations. Vol 1. Philadelphia, PA: Lea & Febiger; 1989.
16. Theodorou DJ, Theodorou SJ, Sartoris DJ. An imaging overview of primary tumors of the spine: part 1. Benign tumors. Clin Imaging. 2008;32(3):196-203.
17. Li X, Meng Z, Li D, Tan J, Song X. Benign fibrous histiocytoma of a rib. Clin Nucl Med. 2014;39(9): 837-841.
18. Roessner A, Immenkamp M, Weidner A, Hobik HP, Grundmann E. Benign fibrous histiocytoma of bone. Light- and electron-microscopic observations. J Cancer Res Clin Oncol. 1981;101(2):191-202.
19. Destouet JM, Kyriakos M, Gilula LA. Fibrous histiocytoma (fibroxanthoma) of a cervical vertebra. A report with a review of the literature. Skeletal Radiol. 1980;5(4):241-246.
20. Hoeffel JC, Bomand-Ferrand F, Tachet F, Lascombes P, Czorny A, Bernard C. So-called benign fibrous histiocytoma: report of a case. J Pediatr Surg. 1992;27(5):672-674.
Benign fibrous histiocytoma (BFH) is a rare, well-recognized, primary skeletal tumor accounting for approximately 1% of all benign bone tumors. Spinal involvement is exceedingly rare with only 11 cases reported in the literature.1,2 We present a case of BFH located in the cervical spine of a pediatric patient that was successfully treated with curretage through an anterior surgical approach, along with a review of the literature and appropriate management concerning BFH of the spine.
Case Report
A 14-year-old boy was tackled while playing football and noticed immediate neck pain and subjective paresthesia in the upper extremities. Examination revealed a nontender spine (cervical, thoracic, lumbar) and normal strength and range of motion in all extremities. Sensation was diffusely intact, long tract signs were absent, and gait was normal. On questioning, the patient endorsed mild antecedent neck pain but denied prior history of any trauma. Neck pain did not radiate and was slightly worsened by activity but was mostly intermittent and random. As the neck pain was very mild and was not interfering with daily activities, the patient had not sought care before presenting to the emergency department. He had no pertinent past medical or surgical history.
The patient presented with a computed tomography (CT) scan of his head and cervical spine and a magnetic resonance imaging (MRI) scan of the cervical spine. A magnetic resonance angiography (MRA) scan of the neck was ordered after his arrival.
Axial and sagittal CT (Figures 1A, 1B) showed a 1×1.2-cm discrete, expansile, lytic, radiolucent mass extending anterior from the left C2 vertebral body. The mass appeared to abut the left vertebral artery foramen. The cortical bone surrounding the lesion was thin but uniform. Sagittal and axial T1-weighted MRI (Figures 2A, 2B) showed the discrete, expansile, homogenous lesion with the same intensity as normal bone marrow. Sagittal and axial T2-weighted MRI (Figures 2C, 2D) showed a discrete, expansile, homogenous lesion with primarily high signal intensity. Sagittal short tau inversion recovery (STIR) MRI (Figure 2E) again showed the lesion with primarily low intensity. Given the close proximity of the lesion to the vertebral foramen, MRA was ordered; it showed the lesion was not interfering with the vertebral artery (Figure 2F).
The tumor’s location, in the left anterior aspect of the C2 vertebral body, was not conducive to percutaneous biopsy for establishing tissue diagnosis, so the decision was made to surgically excise the lesion. A left-sided anterior incision was made 2 fingerbreadths inferior to the jaw line in a neck crease. A head and neck surgeon assisted with dissection. Dissection was carried down through the skin, subcutaneous tissue, and platysma on to the anterior part of the spine medial to the carotid sheath. Superior thyroid nerve and vessels and superior laryngeal nerve were identified and preserved. Fluoroscopy confirmed correct location at C2. The tumor was easily visualized, and the outer shell broke easily with palpation. Gentle curettage was necessary when removing the tumor off the vertebral artery. A portion of the specimen was sent during surgery for frozen section, which showed infrequent mitotic figures and no other findings concerning for malignancy. No instability was created after curettage and excision of the tumor, so no grafting or instrumentation was necessary.
Grossly, the tumor was pale tan and firm. Histologic examination with hematoxylin-eosin staining revealed a bland spindle-cell neoplasm that focally involved bone. A storiform pattern was present. The cells had scant cytoplasm and oval to elongate nuclei with tapered ends. Significant nuclear pleomorphism was not seen. The stroma was loose, with focal myxoid change. Benign multinucleated giant cells were present. Mitotic activity was infrequent (Figures 3A–3D). Two attending pathologists reviewed the case material and the frozen and formalin-fixed specimens independently and concurred with the diagnosis of BFH. In addition, the case was reviewed at the surgical pathology consensus conference; the reviewers agreed on BFH, and additional studies were deemed unnecessary.
Given the patient’s complete clinical picture, the differential diagnosis included nonossifying fibroma (NOF), eosinophilic granuloma (EG), BFH, fibrous dysplasia, giant cell tumor (GCT), aneurysmal bone cyst (ABC), and osteoblastoma (OB).
Discussion
BFH is an extremely rare bone lesion, accounting for only 1% of all surgically managed bone tumors; not counting the present case, only 11 spine cases have been reported in the literature.1,2 BFH of the spine traditionally causes nonspecific, poorly localized pain. The Table lists the reported cases of spinal BFH and their presenting symptoms, location, and treatment. BFH usually occurs in young adults, but the age range is 5 to 75 years.2-4 Mean age of the 12 patients with spinal BFH in the literature (including ours) is 25 years.1 In addition, spinal BFH appears to have no predilection for sex.
Skeletal BFH presents as a discrete, well-defined, osteolytic lesion with sharp borders and potentially a sclerotic rim.4-6 Cortical expansion and even cortical disruption with invasion into adjacent tissue have occurred in flat bones.7 Histologically, BFHs contain spindle cells, multinucleated giant cells, and foam cells in storiform pattern.6
BFH shares many of its radiologic and histologic characteristics and clinical symptoms with other benign bone lesions (the tumors listed above). Therefore, accurate diagnosis of BFH requires appropriate correlation of clinical, radiographic, and histologic data.2,3,8 Below is a comparison of BFH with related bone lesions.
Spinal BFH causes a nonspecific, poorly localized pain similar to that of EG, ABC, GCT, and OB.3,9 NOF and fibrous dysplasia generally do not cause pain, unless these lesions are discovered secondary to a pathologic fracture.8,10,11 Our patient had minor antecedent neck pain, which was brought to light by his football accident. ABC and OB are more locally aggressive than BFH and can cause neurologic symptoms by mass effect and spinal cord or nerve root compression.1,8 In this case and in the 6 other cases of BFH of the cervical spine, there were no neurologic changes.4,10
Of the tumors mentioned, NOF and EG almost always occur in children. However, NOF usually occurs in the metaphyseal region of long bones, and EG is usually accompanied by systemic symptoms, such as lymphadenopathy, hepatomegaly, and increased inflammatory markers.1,8 Fibrous dysplasia usually presents in childhood but does not become symptomatic until adulthood. GCTs and OB predominantly occur in adulthood.12,13 Our patient’s age and lack of other systemic symptoms supported the diagnosis of BFH.
Appearance on MRI is reported less with BFH than with other tumors, but heterogenous signal intensity similar to that of skeletal muscle on T1-weighted images and high signal intensity on T2-weighted images is typically reported.8,14 NOF and fibrous dysplasia do not disrupt the bony cortex unless a pathologic fracture has occurred.4 GCTs are more aggressive lytic lesions with more aggressive radiologic features. GCTs generally cause cortical expansion/attenuation, and lack a sclerotic rim. GCTs also have a heterogenous appearance on MRI and give a low to intermediate signal on both T1- and T2-weighted images.12,15 The appearance of EG is similar to that of BFH as an osteolytic lesion with a sclerotic rim, though EGs typically break through the cortex and acquire a “punched-out” look.1,8 ABC typically is described as an expansile osteolytic lesion with a “soap-bubble” appearance on radiographs; periosteal elevation and cortical attenuation can also be visualized. MRI shows the typical multilobular appearance of the lesion with fluid levels.13
OB appears as a radiolucent lesion, with or without calcifications, surrounded by a thin margin of reactive bone.14,16 A distinguishing characteristic of OB was thought to be intense radioisotope uptake on bone scintigraphy, but recently a bony BFH demonstrated intense uptake.17 OBs typically demonstrate nonspecific MRI results similar to those of BFH: low to intermediate signal on T1-weighted images and intermediate to high signal on T2-weighted images.13 In our patient’s case, the radiographic appearance and lack of specific radiographic findings consistent with the other tumors supported the diagnosis of BFH.
Histologically, BFHs contain spindle cells, multinucleated giant cells, and foam cells in a storiform pattern6 which was demonstrated in our patient’s case. In addition, significant nuclear pleomorphism, mitotic activity, and necrosis were absent—a difference between BFH and malignant fibrous histiocytoma.4,15 The microscopic characteristics of BFH readily differentiate it from OB, ABC, EG, and GCT, but not from NOF on microscopic appearance alone. Clinical and radiographic findings must be consistent, as mentioned.7,18
Complete surgical excision is the reported treatment for BFH. Prognosis after resection or curettage is usually good, and recurrences have been rare.1,2 Depending on the intraspinous location of BFH, stabilization after resection or curettage may be necessary to prevent residual instability. Three of the 11 reported cases of spinal BFH required stabilization by anterior fusion or posterior pedicle screw fixation after resection.1,2 The other 8 cases underwent excision alone or excision and grafting. All 11 patients were disease-free at a mean follow-up of 3.5 years.1 In nonspinal BFH, however, both local recurrence and lung metastasis have been reported.2,5,9,19 Clarke and colleagues9 reported local recurrences in 3 of 8 cases. These recurrences involved BFH in long bones of the leg, which had been treated with curettage and grafting. There has been no reliable report of a malignant change in BFH.2,9 The only case of lung metastasis, reported by Unni and Dahlin6 in their study of 10 cases, occurred 2 years after local recurrence in the distal femur.Our patient was doing well at most recent follow-up, 6 months after surgery. He had no pain and had returned to normal activities. Although there are no reported cases of spinal BFH recurrence, we will follow this patient with imaging on an annual basis. His case is of particular interest to orthopedic surgeons because they encounter benign bone lesions every day, and many of these lesions are in difficult anatomical locations. Knowing the characteristics, differential diagnoses, and appropriate diagnostic workups for benign bone lesions is important for optimal and timely patient care.
Benign fibrous histiocytoma (BFH) is a rare, well-recognized, primary skeletal tumor accounting for approximately 1% of all benign bone tumors. Spinal involvement is exceedingly rare with only 11 cases reported in the literature.1,2 We present a case of BFH located in the cervical spine of a pediatric patient that was successfully treated with curretage through an anterior surgical approach, along with a review of the literature and appropriate management concerning BFH of the spine.
Case Report
A 14-year-old boy was tackled while playing football and noticed immediate neck pain and subjective paresthesia in the upper extremities. Examination revealed a nontender spine (cervical, thoracic, lumbar) and normal strength and range of motion in all extremities. Sensation was diffusely intact, long tract signs were absent, and gait was normal. On questioning, the patient endorsed mild antecedent neck pain but denied prior history of any trauma. Neck pain did not radiate and was slightly worsened by activity but was mostly intermittent and random. As the neck pain was very mild and was not interfering with daily activities, the patient had not sought care before presenting to the emergency department. He had no pertinent past medical or surgical history.
The patient presented with a computed tomography (CT) scan of his head and cervical spine and a magnetic resonance imaging (MRI) scan of the cervical spine. A magnetic resonance angiography (MRA) scan of the neck was ordered after his arrival.
Axial and sagittal CT (Figures 1A, 1B) showed a 1×1.2-cm discrete, expansile, lytic, radiolucent mass extending anterior from the left C2 vertebral body. The mass appeared to abut the left vertebral artery foramen. The cortical bone surrounding the lesion was thin but uniform. Sagittal and axial T1-weighted MRI (Figures 2A, 2B) showed the discrete, expansile, homogenous lesion with the same intensity as normal bone marrow. Sagittal and axial T2-weighted MRI (Figures 2C, 2D) showed a discrete, expansile, homogenous lesion with primarily high signal intensity. Sagittal short tau inversion recovery (STIR) MRI (Figure 2E) again showed the lesion with primarily low intensity. Given the close proximity of the lesion to the vertebral foramen, MRA was ordered; it showed the lesion was not interfering with the vertebral artery (Figure 2F).
The tumor’s location, in the left anterior aspect of the C2 vertebral body, was not conducive to percutaneous biopsy for establishing tissue diagnosis, so the decision was made to surgically excise the lesion. A left-sided anterior incision was made 2 fingerbreadths inferior to the jaw line in a neck crease. A head and neck surgeon assisted with dissection. Dissection was carried down through the skin, subcutaneous tissue, and platysma on to the anterior part of the spine medial to the carotid sheath. Superior thyroid nerve and vessels and superior laryngeal nerve were identified and preserved. Fluoroscopy confirmed correct location at C2. The tumor was easily visualized, and the outer shell broke easily with palpation. Gentle curettage was necessary when removing the tumor off the vertebral artery. A portion of the specimen was sent during surgery for frozen section, which showed infrequent mitotic figures and no other findings concerning for malignancy. No instability was created after curettage and excision of the tumor, so no grafting or instrumentation was necessary.
Grossly, the tumor was pale tan and firm. Histologic examination with hematoxylin-eosin staining revealed a bland spindle-cell neoplasm that focally involved bone. A storiform pattern was present. The cells had scant cytoplasm and oval to elongate nuclei with tapered ends. Significant nuclear pleomorphism was not seen. The stroma was loose, with focal myxoid change. Benign multinucleated giant cells were present. Mitotic activity was infrequent (Figures 3A–3D). Two attending pathologists reviewed the case material and the frozen and formalin-fixed specimens independently and concurred with the diagnosis of BFH. In addition, the case was reviewed at the surgical pathology consensus conference; the reviewers agreed on BFH, and additional studies were deemed unnecessary.
Given the patient’s complete clinical picture, the differential diagnosis included nonossifying fibroma (NOF), eosinophilic granuloma (EG), BFH, fibrous dysplasia, giant cell tumor (GCT), aneurysmal bone cyst (ABC), and osteoblastoma (OB).
Discussion
BFH is an extremely rare bone lesion, accounting for only 1% of all surgically managed bone tumors; not counting the present case, only 11 spine cases have been reported in the literature.1,2 BFH of the spine traditionally causes nonspecific, poorly localized pain. The Table lists the reported cases of spinal BFH and their presenting symptoms, location, and treatment. BFH usually occurs in young adults, but the age range is 5 to 75 years.2-4 Mean age of the 12 patients with spinal BFH in the literature (including ours) is 25 years.1 In addition, spinal BFH appears to have no predilection for sex.
Skeletal BFH presents as a discrete, well-defined, osteolytic lesion with sharp borders and potentially a sclerotic rim.4-6 Cortical expansion and even cortical disruption with invasion into adjacent tissue have occurred in flat bones.7 Histologically, BFHs contain spindle cells, multinucleated giant cells, and foam cells in storiform pattern.6
BFH shares many of its radiologic and histologic characteristics and clinical symptoms with other benign bone lesions (the tumors listed above). Therefore, accurate diagnosis of BFH requires appropriate correlation of clinical, radiographic, and histologic data.2,3,8 Below is a comparison of BFH with related bone lesions.
Spinal BFH causes a nonspecific, poorly localized pain similar to that of EG, ABC, GCT, and OB.3,9 NOF and fibrous dysplasia generally do not cause pain, unless these lesions are discovered secondary to a pathologic fracture.8,10,11 Our patient had minor antecedent neck pain, which was brought to light by his football accident. ABC and OB are more locally aggressive than BFH and can cause neurologic symptoms by mass effect and spinal cord or nerve root compression.1,8 In this case and in the 6 other cases of BFH of the cervical spine, there were no neurologic changes.4,10
Of the tumors mentioned, NOF and EG almost always occur in children. However, NOF usually occurs in the metaphyseal region of long bones, and EG is usually accompanied by systemic symptoms, such as lymphadenopathy, hepatomegaly, and increased inflammatory markers.1,8 Fibrous dysplasia usually presents in childhood but does not become symptomatic until adulthood. GCTs and OB predominantly occur in adulthood.12,13 Our patient’s age and lack of other systemic symptoms supported the diagnosis of BFH.
Appearance on MRI is reported less with BFH than with other tumors, but heterogenous signal intensity similar to that of skeletal muscle on T1-weighted images and high signal intensity on T2-weighted images is typically reported.8,14 NOF and fibrous dysplasia do not disrupt the bony cortex unless a pathologic fracture has occurred.4 GCTs are more aggressive lytic lesions with more aggressive radiologic features. GCTs generally cause cortical expansion/attenuation, and lack a sclerotic rim. GCTs also have a heterogenous appearance on MRI and give a low to intermediate signal on both T1- and T2-weighted images.12,15 The appearance of EG is similar to that of BFH as an osteolytic lesion with a sclerotic rim, though EGs typically break through the cortex and acquire a “punched-out” look.1,8 ABC typically is described as an expansile osteolytic lesion with a “soap-bubble” appearance on radiographs; periosteal elevation and cortical attenuation can also be visualized. MRI shows the typical multilobular appearance of the lesion with fluid levels.13
OB appears as a radiolucent lesion, with or without calcifications, surrounded by a thin margin of reactive bone.14,16 A distinguishing characteristic of OB was thought to be intense radioisotope uptake on bone scintigraphy, but recently a bony BFH demonstrated intense uptake.17 OBs typically demonstrate nonspecific MRI results similar to those of BFH: low to intermediate signal on T1-weighted images and intermediate to high signal on T2-weighted images.13 In our patient’s case, the radiographic appearance and lack of specific radiographic findings consistent with the other tumors supported the diagnosis of BFH.
Histologically, BFHs contain spindle cells, multinucleated giant cells, and foam cells in a storiform pattern6 which was demonstrated in our patient’s case. In addition, significant nuclear pleomorphism, mitotic activity, and necrosis were absent—a difference between BFH and malignant fibrous histiocytoma.4,15 The microscopic characteristics of BFH readily differentiate it from OB, ABC, EG, and GCT, but not from NOF on microscopic appearance alone. Clinical and radiographic findings must be consistent, as mentioned.7,18
Complete surgical excision is the reported treatment for BFH. Prognosis after resection or curettage is usually good, and recurrences have been rare.1,2 Depending on the intraspinous location of BFH, stabilization after resection or curettage may be necessary to prevent residual instability. Three of the 11 reported cases of spinal BFH required stabilization by anterior fusion or posterior pedicle screw fixation after resection.1,2 The other 8 cases underwent excision alone or excision and grafting. All 11 patients were disease-free at a mean follow-up of 3.5 years.1 In nonspinal BFH, however, both local recurrence and lung metastasis have been reported.2,5,9,19 Clarke and colleagues9 reported local recurrences in 3 of 8 cases. These recurrences involved BFH in long bones of the leg, which had been treated with curettage and grafting. There has been no reliable report of a malignant change in BFH.2,9 The only case of lung metastasis, reported by Unni and Dahlin6 in their study of 10 cases, occurred 2 years after local recurrence in the distal femur.Our patient was doing well at most recent follow-up, 6 months after surgery. He had no pain and had returned to normal activities. Although there are no reported cases of spinal BFH recurrence, we will follow this patient with imaging on an annual basis. His case is of particular interest to orthopedic surgeons because they encounter benign bone lesions every day, and many of these lesions are in difficult anatomical locations. Knowing the characteristics, differential diagnoses, and appropriate diagnostic workups for benign bone lesions is important for optimal and timely patient care.
1. Demiralp B, Kose O, Oguz E, Sanal T, Ozcan A, Sehirlioglu A. Benign fibrous histiocytoma of the lumbar vertebrae. Skeletal Radiol. 2009;38(2):187-191.
2. Kuruvath S, O’Donovan DG, Aspoas AR, David KM. Benign fibrous histiocytoma of the thoracic spine: case report and review of the literature. J Neurosurg Spine. 2006;4(3):260-264.
3. Ceroni D, Dayer R, De Coulon G, Kaelin A. Benign fibrous histiocytoma of bone in a paediatric population: a report of 6 cases. Musculoskelet Surg. 2011;95(2):107-114.
4. Dorfman HD, Czerniak B. Bone Tumors. St. Louis, MO: Mosby; 1998.
5. Grohs JG, Nicolakis M, Kainberger F, Lang S, Kotz R. Benign fibrous histiocytoma of bone: a report of ten cases and review of literature. Wien Klin Wochenschr. 2002;114(1-2):56-63.
6. Unni KK, Dahlin DC. Dahlin’s Bone Tumors. 5th ed. Philadelphia, PA: Lippincott-Raven; 1996.
7. Balasubramanian C, Rajaraman G, Singh CS, Baliga DK. Benign fibrous histiocytoma of the sacrum—diagnostic difficulties facing this rare bone tumor. Pediatr Neurosurg. 2005;41(5):253-257.
8. van Giffen NH, van Rhijn LW, van Ooij A, et al. Benign fibrous histiocytoma of the posterior arch of C1 in a 6-year old boy: a case report. Spine. 2003;28(18):E359-E363.
9. Clarke BE, Xipell JM, Thomas DP. Benign fibrous histiocytoma of bone. Am J Surg Pathol. 1985;9(11):806-815.
10. Peicha G, Siebert FJ, Bratschitsch G, Fankhauser F, Grechenig W. Pathologic odontoid fracture and benign fibrous histiocytoma of bone. Eur Spine J. 1999;8(2):161-163.
11. Unni KK, Inwards CY, Bridge JA, Kindblom LG, Wold LE. Tumors of the Bones and Joints (AFIP Atlas of Tumor Pathology Series IV). Annapolis Junction, MD: American Registry of Pathology Press; 2005.
12. Dee R. Principles of Orthopaedic Practice. 2nd ed. New York, NY: McGraw-Hill; 1997.
13. Murphey M, Andrews C, Flemming D, Temple HT, Smith WS, Smirniotopoulos JG. Primary tumors of the spine: radiologic–pathologic correlation. Radiographics. 1996;16(5):1131-1158.
14. Hamada T, Ito H, Araki Y, Fujii K, Inoue M, Ishida O. Benign fibrous histiocytoma of the femur: review of three cases. Skeletal Radiol. 1996;25(1):25-29.
15. Mirra JM, Picci P, Gold RH. Bone Tumors: Clinical, Radiologic, and Pathologic Correlations. Vol 1. Philadelphia, PA: Lea & Febiger; 1989.
16. Theodorou DJ, Theodorou SJ, Sartoris DJ. An imaging overview of primary tumors of the spine: part 1. Benign tumors. Clin Imaging. 2008;32(3):196-203.
17. Li X, Meng Z, Li D, Tan J, Song X. Benign fibrous histiocytoma of a rib. Clin Nucl Med. 2014;39(9): 837-841.
18. Roessner A, Immenkamp M, Weidner A, Hobik HP, Grundmann E. Benign fibrous histiocytoma of bone. Light- and electron-microscopic observations. J Cancer Res Clin Oncol. 1981;101(2):191-202.
19. Destouet JM, Kyriakos M, Gilula LA. Fibrous histiocytoma (fibroxanthoma) of a cervical vertebra. A report with a review of the literature. Skeletal Radiol. 1980;5(4):241-246.
20. Hoeffel JC, Bomand-Ferrand F, Tachet F, Lascombes P, Czorny A, Bernard C. So-called benign fibrous histiocytoma: report of a case. J Pediatr Surg. 1992;27(5):672-674.
1. Demiralp B, Kose O, Oguz E, Sanal T, Ozcan A, Sehirlioglu A. Benign fibrous histiocytoma of the lumbar vertebrae. Skeletal Radiol. 2009;38(2):187-191.
2. Kuruvath S, O’Donovan DG, Aspoas AR, David KM. Benign fibrous histiocytoma of the thoracic spine: case report and review of the literature. J Neurosurg Spine. 2006;4(3):260-264.
3. Ceroni D, Dayer R, De Coulon G, Kaelin A. Benign fibrous histiocytoma of bone in a paediatric population: a report of 6 cases. Musculoskelet Surg. 2011;95(2):107-114.
4. Dorfman HD, Czerniak B. Bone Tumors. St. Louis, MO: Mosby; 1998.
5. Grohs JG, Nicolakis M, Kainberger F, Lang S, Kotz R. Benign fibrous histiocytoma of bone: a report of ten cases and review of literature. Wien Klin Wochenschr. 2002;114(1-2):56-63.
6. Unni KK, Dahlin DC. Dahlin’s Bone Tumors. 5th ed. Philadelphia, PA: Lippincott-Raven; 1996.
7. Balasubramanian C, Rajaraman G, Singh CS, Baliga DK. Benign fibrous histiocytoma of the sacrum—diagnostic difficulties facing this rare bone tumor. Pediatr Neurosurg. 2005;41(5):253-257.
8. van Giffen NH, van Rhijn LW, van Ooij A, et al. Benign fibrous histiocytoma of the posterior arch of C1 in a 6-year old boy: a case report. Spine. 2003;28(18):E359-E363.
9. Clarke BE, Xipell JM, Thomas DP. Benign fibrous histiocytoma of bone. Am J Surg Pathol. 1985;9(11):806-815.
10. Peicha G, Siebert FJ, Bratschitsch G, Fankhauser F, Grechenig W. Pathologic odontoid fracture and benign fibrous histiocytoma of bone. Eur Spine J. 1999;8(2):161-163.
11. Unni KK, Inwards CY, Bridge JA, Kindblom LG, Wold LE. Tumors of the Bones and Joints (AFIP Atlas of Tumor Pathology Series IV). Annapolis Junction, MD: American Registry of Pathology Press; 2005.
12. Dee R. Principles of Orthopaedic Practice. 2nd ed. New York, NY: McGraw-Hill; 1997.
13. Murphey M, Andrews C, Flemming D, Temple HT, Smith WS, Smirniotopoulos JG. Primary tumors of the spine: radiologic–pathologic correlation. Radiographics. 1996;16(5):1131-1158.
14. Hamada T, Ito H, Araki Y, Fujii K, Inoue M, Ishida O. Benign fibrous histiocytoma of the femur: review of three cases. Skeletal Radiol. 1996;25(1):25-29.
15. Mirra JM, Picci P, Gold RH. Bone Tumors: Clinical, Radiologic, and Pathologic Correlations. Vol 1. Philadelphia, PA: Lea & Febiger; 1989.
16. Theodorou DJ, Theodorou SJ, Sartoris DJ. An imaging overview of primary tumors of the spine: part 1. Benign tumors. Clin Imaging. 2008;32(3):196-203.
17. Li X, Meng Z, Li D, Tan J, Song X. Benign fibrous histiocytoma of a rib. Clin Nucl Med. 2014;39(9): 837-841.
18. Roessner A, Immenkamp M, Weidner A, Hobik HP, Grundmann E. Benign fibrous histiocytoma of bone. Light- and electron-microscopic observations. J Cancer Res Clin Oncol. 1981;101(2):191-202.
19. Destouet JM, Kyriakos M, Gilula LA. Fibrous histiocytoma (fibroxanthoma) of a cervical vertebra. A report with a review of the literature. Skeletal Radiol. 1980;5(4):241-246.
20. Hoeffel JC, Bomand-Ferrand F, Tachet F, Lascombes P, Czorny A, Bernard C. So-called benign fibrous histiocytoma: report of a case. J Pediatr Surg. 1992;27(5):672-674.
First U.S. uterus transplant raises questions about ethics, cost
The recipient of the first uterus transplant performed in the United States is recovering well and looking forward to the next phase of the research project: pregnancy, according to the team of Cleveland Clinic surgeons who performed the groundbreaking Feb. 24 transplant.
“I’m pleased to report to you that our patient is doing very well,” lead surgeon Dr. Andreas G. Tzakis said during a press conference on March 7.
The transplant recipient, known only as “Lindsey” to protect her privacy, is a 26-year-old woman with uterine factor infertility (UFI). She was selected from among more than 250 applicants to undergo the 9-hour procedure involving transplantation of a uterus from a deceased organ donor of reproductive age. She is the first of 10 women set to undergo the procedure as part of the Cleveland Clinic study.
“Lindsey” made an appearance at the press conference and expressed, first and foremost, her “immense gratitude” to the donor’s family.
“They have provided me with a gift that I will never be able to repay,” she said in an emotional statement in which she shared about learning at age 16 that she would never be able to have children.
“From that moment on I prayed that God would allow me the opportunity to experience pregnancy, and here we are today at the beginning of that journey,” she said.
Lindsey will undergo a year of anti-rejection treatment prior to undergoing in vitro fertilization; her eggs were previously fertilized using her husband’s sperm, and the embryos are in cryogenic storage, according to Dr. Rebecca Flyckt, another member of the surgical team.
The embryos will be transferred one by one until the goal of a healthy pregnancy and healthy baby delivered by cesarean section is achieved, Dr. Flyckt said.
After one or two successful pregnancies and births, the uterus will be removed. Although substantial evidence suggests that anti-rejection medications are relatively safe in pregnancy, minimizing and ultimately eliminating the need for them is advisable, thus uterus transplants, at least under the Cleveland Clinic research protocol, are meant to be temporary.
Uterus transplants are performed to enable patients – who have either lost their uterus to disease or who were born without a uterus or a functioning uterus – to experience pregnancy and childbirth.
Prior to the Cleveland Clinic transplant, nine had been performed successfully with healthy outcomes (the first post-transplant baby was born healthy in 2014). All were performed at the University of Gothenburg in Sweden. Dr. Tzakis traveled there to work with surgeons prior to performing the procedure at the Cleveland Clinic, where he is the Transplant Center program director.
Ethical issues
Addressing the bioethical issues surrounding uterine transplant was an important part of this project, according to team member Dr. Ruth Farrell, a bioethicist and ob.gyn. surgeon at the Cleveland Clinic.
“Despite the name uterine transplant, the focus of this procedure is not on the uterus. It’s on women and children and families,” she said, adding that to understand the ethical issues of uterine transplant, it’s important to consider the perspectives of women with UFI.
“For instance, women born without a uterus have a medical condition that affects every aspect of their lives, from the time they are diagnosed in adolescence, to when they are adults looking for relationships and trying to decide if and how to have a family,” she said, adding that “these women face the real possibility of never having children.”
But this advance in reproductive medicine and science also requires a close look at how the potential risks and benefits of uterine transplant weigh against existing options of adoption and surrogacy. While there are many successful stories involving surrogacy and adoption, these options are not available to all women because of “legal, cultural, religious, and other very personal reasons,” Dr. Farrell said.
“Our research on uterine transplant, we hope, may give women another option which may work better for them and their families,” she said, also noting that while living donor transplants have been performed, these come with some risk, thus deceased donors are being used for the current study.
Insurance coverage
As for the feasibility of uterine transplant, many questions remain to be answered, according to Dr. Tommaso Falcone, chair of the department of obstetrics and gynecology at the Cleveland Clinic, who said that the procedures done as part of the current study will be paid for by an institutional grant.
While the American Society for Reproductive Medicine contends that infertility is a disease worthy of insurance coverage, that is “outside of our hands,” he said.
Indeed, while this first uterine transplant in the United States is a “huge and exciting breakthrough,” and while “the folks at Cleveland Clinic should be congratulated,” the possibility of this procedure ever being covered by insurance and being available to women outside of the research protocol is questionable, especially given the available alternatives, such as gestational carriers and surrogacy, Dr. David A. Forstein, a reproductive endocrinologist at the University of South Carolina, Greenville, said in an interview.
In a patient-centered model, this “tremendous, wonderful gift from science” would give patients – like the 1 in 5,000 women in the United States who are born without a uterus – a very viable alternative, but the question is whether having one’s own children is a right, and whether extensive financial resources should be committed to helping women achieve that, he said.
Dr. Charles E. Miller, a reproductive endocrinologist in Chicago, and head of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital in Park Ridge, Ill., agreed that this transplant is to be celebrated.
“It’s a big moment, to say the least,” he said in an interview.
But Dr. Miller also questioned the feasibility of the procedure and whether society will “look favorably upon donation,” given the availability of alternatives for which there is now great success.
“I salute the pioneering effort,” he said, “But at the end of the day, can society take on this burden of a procedure performed not to sustain life, but to help create life? That’s a tough one.”
The recipient of the first uterus transplant performed in the United States is recovering well and looking forward to the next phase of the research project: pregnancy, according to the team of Cleveland Clinic surgeons who performed the groundbreaking Feb. 24 transplant.
“I’m pleased to report to you that our patient is doing very well,” lead surgeon Dr. Andreas G. Tzakis said during a press conference on March 7.
The transplant recipient, known only as “Lindsey” to protect her privacy, is a 26-year-old woman with uterine factor infertility (UFI). She was selected from among more than 250 applicants to undergo the 9-hour procedure involving transplantation of a uterus from a deceased organ donor of reproductive age. She is the first of 10 women set to undergo the procedure as part of the Cleveland Clinic study.
“Lindsey” made an appearance at the press conference and expressed, first and foremost, her “immense gratitude” to the donor’s family.
“They have provided me with a gift that I will never be able to repay,” she said in an emotional statement in which she shared about learning at age 16 that she would never be able to have children.
“From that moment on I prayed that God would allow me the opportunity to experience pregnancy, and here we are today at the beginning of that journey,” she said.
Lindsey will undergo a year of anti-rejection treatment prior to undergoing in vitro fertilization; her eggs were previously fertilized using her husband’s sperm, and the embryos are in cryogenic storage, according to Dr. Rebecca Flyckt, another member of the surgical team.
The embryos will be transferred one by one until the goal of a healthy pregnancy and healthy baby delivered by cesarean section is achieved, Dr. Flyckt said.
After one or two successful pregnancies and births, the uterus will be removed. Although substantial evidence suggests that anti-rejection medications are relatively safe in pregnancy, minimizing and ultimately eliminating the need for them is advisable, thus uterus transplants, at least under the Cleveland Clinic research protocol, are meant to be temporary.
Uterus transplants are performed to enable patients – who have either lost their uterus to disease or who were born without a uterus or a functioning uterus – to experience pregnancy and childbirth.
Prior to the Cleveland Clinic transplant, nine had been performed successfully with healthy outcomes (the first post-transplant baby was born healthy in 2014). All were performed at the University of Gothenburg in Sweden. Dr. Tzakis traveled there to work with surgeons prior to performing the procedure at the Cleveland Clinic, where he is the Transplant Center program director.
Ethical issues
Addressing the bioethical issues surrounding uterine transplant was an important part of this project, according to team member Dr. Ruth Farrell, a bioethicist and ob.gyn. surgeon at the Cleveland Clinic.
“Despite the name uterine transplant, the focus of this procedure is not on the uterus. It’s on women and children and families,” she said, adding that to understand the ethical issues of uterine transplant, it’s important to consider the perspectives of women with UFI.
“For instance, women born without a uterus have a medical condition that affects every aspect of their lives, from the time they are diagnosed in adolescence, to when they are adults looking for relationships and trying to decide if and how to have a family,” she said, adding that “these women face the real possibility of never having children.”
But this advance in reproductive medicine and science also requires a close look at how the potential risks and benefits of uterine transplant weigh against existing options of adoption and surrogacy. While there are many successful stories involving surrogacy and adoption, these options are not available to all women because of “legal, cultural, religious, and other very personal reasons,” Dr. Farrell said.
“Our research on uterine transplant, we hope, may give women another option which may work better for them and their families,” she said, also noting that while living donor transplants have been performed, these come with some risk, thus deceased donors are being used for the current study.
Insurance coverage
As for the feasibility of uterine transplant, many questions remain to be answered, according to Dr. Tommaso Falcone, chair of the department of obstetrics and gynecology at the Cleveland Clinic, who said that the procedures done as part of the current study will be paid for by an institutional grant.
While the American Society for Reproductive Medicine contends that infertility is a disease worthy of insurance coverage, that is “outside of our hands,” he said.
Indeed, while this first uterine transplant in the United States is a “huge and exciting breakthrough,” and while “the folks at Cleveland Clinic should be congratulated,” the possibility of this procedure ever being covered by insurance and being available to women outside of the research protocol is questionable, especially given the available alternatives, such as gestational carriers and surrogacy, Dr. David A. Forstein, a reproductive endocrinologist at the University of South Carolina, Greenville, said in an interview.
In a patient-centered model, this “tremendous, wonderful gift from science” would give patients – like the 1 in 5,000 women in the United States who are born without a uterus – a very viable alternative, but the question is whether having one’s own children is a right, and whether extensive financial resources should be committed to helping women achieve that, he said.
Dr. Charles E. Miller, a reproductive endocrinologist in Chicago, and head of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital in Park Ridge, Ill., agreed that this transplant is to be celebrated.
“It’s a big moment, to say the least,” he said in an interview.
But Dr. Miller also questioned the feasibility of the procedure and whether society will “look favorably upon donation,” given the availability of alternatives for which there is now great success.
“I salute the pioneering effort,” he said, “But at the end of the day, can society take on this burden of a procedure performed not to sustain life, but to help create life? That’s a tough one.”
The recipient of the first uterus transplant performed in the United States is recovering well and looking forward to the next phase of the research project: pregnancy, according to the team of Cleveland Clinic surgeons who performed the groundbreaking Feb. 24 transplant.
“I’m pleased to report to you that our patient is doing very well,” lead surgeon Dr. Andreas G. Tzakis said during a press conference on March 7.
The transplant recipient, known only as “Lindsey” to protect her privacy, is a 26-year-old woman with uterine factor infertility (UFI). She was selected from among more than 250 applicants to undergo the 9-hour procedure involving transplantation of a uterus from a deceased organ donor of reproductive age. She is the first of 10 women set to undergo the procedure as part of the Cleveland Clinic study.
“Lindsey” made an appearance at the press conference and expressed, first and foremost, her “immense gratitude” to the donor’s family.
“They have provided me with a gift that I will never be able to repay,” she said in an emotional statement in which she shared about learning at age 16 that she would never be able to have children.
“From that moment on I prayed that God would allow me the opportunity to experience pregnancy, and here we are today at the beginning of that journey,” she said.
Lindsey will undergo a year of anti-rejection treatment prior to undergoing in vitro fertilization; her eggs were previously fertilized using her husband’s sperm, and the embryos are in cryogenic storage, according to Dr. Rebecca Flyckt, another member of the surgical team.
The embryos will be transferred one by one until the goal of a healthy pregnancy and healthy baby delivered by cesarean section is achieved, Dr. Flyckt said.
After one or two successful pregnancies and births, the uterus will be removed. Although substantial evidence suggests that anti-rejection medications are relatively safe in pregnancy, minimizing and ultimately eliminating the need for them is advisable, thus uterus transplants, at least under the Cleveland Clinic research protocol, are meant to be temporary.
Uterus transplants are performed to enable patients – who have either lost their uterus to disease or who were born without a uterus or a functioning uterus – to experience pregnancy and childbirth.
Prior to the Cleveland Clinic transplant, nine had been performed successfully with healthy outcomes (the first post-transplant baby was born healthy in 2014). All were performed at the University of Gothenburg in Sweden. Dr. Tzakis traveled there to work with surgeons prior to performing the procedure at the Cleveland Clinic, where he is the Transplant Center program director.
Ethical issues
Addressing the bioethical issues surrounding uterine transplant was an important part of this project, according to team member Dr. Ruth Farrell, a bioethicist and ob.gyn. surgeon at the Cleveland Clinic.
“Despite the name uterine transplant, the focus of this procedure is not on the uterus. It’s on women and children and families,” she said, adding that to understand the ethical issues of uterine transplant, it’s important to consider the perspectives of women with UFI.
“For instance, women born without a uterus have a medical condition that affects every aspect of their lives, from the time they are diagnosed in adolescence, to when they are adults looking for relationships and trying to decide if and how to have a family,” she said, adding that “these women face the real possibility of never having children.”
But this advance in reproductive medicine and science also requires a close look at how the potential risks and benefits of uterine transplant weigh against existing options of adoption and surrogacy. While there are many successful stories involving surrogacy and adoption, these options are not available to all women because of “legal, cultural, religious, and other very personal reasons,” Dr. Farrell said.
“Our research on uterine transplant, we hope, may give women another option which may work better for them and their families,” she said, also noting that while living donor transplants have been performed, these come with some risk, thus deceased donors are being used for the current study.
Insurance coverage
As for the feasibility of uterine transplant, many questions remain to be answered, according to Dr. Tommaso Falcone, chair of the department of obstetrics and gynecology at the Cleveland Clinic, who said that the procedures done as part of the current study will be paid for by an institutional grant.
While the American Society for Reproductive Medicine contends that infertility is a disease worthy of insurance coverage, that is “outside of our hands,” he said.
Indeed, while this first uterine transplant in the United States is a “huge and exciting breakthrough,” and while “the folks at Cleveland Clinic should be congratulated,” the possibility of this procedure ever being covered by insurance and being available to women outside of the research protocol is questionable, especially given the available alternatives, such as gestational carriers and surrogacy, Dr. David A. Forstein, a reproductive endocrinologist at the University of South Carolina, Greenville, said in an interview.
In a patient-centered model, this “tremendous, wonderful gift from science” would give patients – like the 1 in 5,000 women in the United States who are born without a uterus – a very viable alternative, but the question is whether having one’s own children is a right, and whether extensive financial resources should be committed to helping women achieve that, he said.
Dr. Charles E. Miller, a reproductive endocrinologist in Chicago, and head of minimally invasive gynecologic surgery at Advocate Lutheran General Hospital in Park Ridge, Ill., agreed that this transplant is to be celebrated.
“It’s a big moment, to say the least,” he said in an interview.
But Dr. Miller also questioned the feasibility of the procedure and whether society will “look favorably upon donation,” given the availability of alternatives for which there is now great success.
“I salute the pioneering effort,” he said, “But at the end of the day, can society take on this burden of a procedure performed not to sustain life, but to help create life? That’s a tough one.”
Applying a Quality Improvement Framework to Operating Room Efficiency in an Academic-Practice Partnership
From the Case Western Reserve University School of Medicine, Cleveland, OH.
Abstract
- Objective: To improve operating room (OR) scheduling efficiency at a large academic institution through the use of an academic-practice partnership and quality improvement (QI) methods.
- Methods: The OR administrative team at a large academic hospital partnered with students in a graduate level QI course to apply QI tools to the problem of OR efficiency.
- Results: The team found wide variation in the way that surgeries were scheduled and other factors that contributed to inefficient OR utilization. A plan-do-study-act (PDSA) cycle was applied to the problem of discrepancy in surgeons’ interpretation of case length, resulting in poor case length accuracy. Our intervention, adding time on the schedule for cases, did not show consistent improvement in case length accuracy.
- Conclusion: Although our intervention did not lead to sustained improvements in OR scheduling efficiency, our project demonstrates how QI tools can be taught and applied in an academic course to address a management problem. Further research is needed to study the impact of student teams on health care improvement.
Operating rooms are one of the most costly departments of a hospital. At University Hospitals Case Medical Center (UHCMC), as at many hospitals, operating room utilization is a key area of focus for both operating room (OR) and hospital administrators. Efficient use of the OR is an important aspect of a hospital’s finances and patient-centeredness.
UHCMC uses block scheduling, a common OR scheduling design. Each surgical department is allotted a certain number of blocks (hours of reserved OR time) that they are responsible for filling with surgical cases and that the hospital is responsible for staffing. Block utilization rate is a metric commonly used to measure OR efficiency. It divides the time that the OR is in use by the total block time allocated to the department (while accounting for room turnaround time). An industry benchmark is 75% block utilization [1], which was adopted as an internal target at UHCMC. Achieving this metric is necessary because the hospital (rather than each individual surgical department) is responsible for ensuring that the appropriate amount of non-surgeon staff (eg, anesthesiologists, nurses, scrub techs, and facilities staff) is available. Poor utilization rates indicate that the staff and equipment are inefficiently used, which can impact the hospital’s financial well-being [2]. Block utilization is the result of a complex system, making it challenging to improve. Many people are involved in scheduling, and a large degree of inherent uncertainty exists in the system.
At UHCMC, block utilization rates by department ranged from 52% to 80%, with an overall utilization of 64% from February to July 2014. Given this wide variation, higher level management staff in the OR initiated a project in which OR administrators partnered with students in a graduate level QI course in an effort to improve overall block utilization. They believed that improving block utilization rate would improve the effectiveness, patient-centeredness, and efficiency of care, health care delivery goals described by the Institute of Medicine [3].
Methods
Setting
The OR at UHCMC contains 4 operating suites that serve over 25,000 patients per year and train over 900 residents each year. Nearly 250 surgeons in 23 departments use the OR. The OR schedule at our institution is coordinated by block scheduling, as described above. If a surgical department cannot fill the block, they must release the time to central scheduling for re-allocation of the time to another department.
Application of QI Process
This QI project was an academic-practice collaboration between UHCMC and a graduate level course at Case Western Reserve University called The Continual Improvement of Healthcare: an Interdisciplinary Course [4]. Faculty course instructors solicit applications of QI projects from departments at UHCMC. The project team consisted of 4 students (from medicine, social work, public health, and bioethics), 2 administrative staff from UHCMC, and a QI coach who is on the faculty at Case Western. Guidance was provided by 2 faculty facilitators. The students attended 15 weekly class sessions, 4 meetings with the project team, numerous data gathering sessions with other hospital staff, and held a handful of outside-class student team meetings. An early class session was devoted to team skills and the Seven-Step meeting process [5]. Each classroom session consisted of structured group activities to practice the tools of the QI process.
Tool 1: Global Aim
The team first established a global aim: to improve the OR block utilization rate at UHCMC. This aim was based on the initial project proposal from UHCMC. The global aim explains the reason that the project team was established, and frames all future work [7].
Tool 2: Industry Assessment
Based on the global aim, the student team performed an industry assessment in order to understand strategies for improving block utilization rate in use at other institutions. Peer-reviewed journal articles and case reports were reviewed and the student team was able to contact a team at another institution working on similar issues.
Overall, 2 broad categories of interventions to improve block utilization were identified. Some institutions addressed the way time in the OR was scheduled. They made improvements to how block time was allotted, timing of cases, and dealing with add-on cases [8]. Others focused on using time in the OR more efficiently by addressing room turnover, delays including waiting for surgeons, and waiting for hospital beds [9]. Because the specific case mix of each hospital is so distinct, hospitals that successfully made changes all used a variety of interventions [10–12]. After the industry assessment, the student team realized that there would be a large number of possible approaches to the problem of block utilization, and a better understanding of the actual process of scheduling at UHCMC was necessary to find an area of focus.
Tool 3: Process Map
As the project team began to address the global aim of improving OR block utilization at UHCMC, they needed to have a thorough understanding of how OR time was allotted and used. To do this, the student team created a process map by interviewing process stakeholders, including the OR managers and department schedulers in orthopedics, general surgery, and urology, as suggested by the OR managers. The perspective of these staff were critical to understanding the process of operating room scheduling.
Through the creation of the process map, the project team found that there was wide variation in the process and structure for scheduling surgeries. Some departments used one central scheduler while others used individual secretaries for each surgeon. Some surgeons maintained control over changing their schedule, while others did not. Further, the project team learned that the metric of block utilization rate was of varying importance to people working on the ground.
Tool 4: Fishbone Diagram
After understanding the process, the project team considered all of the factors that
Tool 5: Specific Aim
Though the global aim was to improve block utilization, the project team needed to chose a specific aim that met S.M.A.R.T criteria: Specific, Measureable, Achievable, Results-focused, and Time-bound [7]. After considering multiple potential areas of initial focus, the OR staff suggested focusing on the issue of case length accuracy. In qualitative interviews, the student team had found that the surgery request forms ask for “case length,” and the schedulers were not sure how the surgeons defined it. When the OR is booked for an operation, the amount of time blocked out is the time from when the patient is brought into the operating room to the time that the patient leaves the room, or WIWO (Wheels In Wheels Out). This WIWO time includes anesthesia induction and preparations for surgery such as positioning. Some surgeons think about case length as only the time that the patient is operated on, or CTC (Cut to Close). Thus, the surgeon may be requesting less time than is really necessary for the case if he or she is only thinking about CTC time. The student team created a survey and found that 2 urology surgeons considered case length to be WIWO, and 4 considered case length to mean CTC.
Tools 6 and 7: PDSA Cycle and Control Charts
The Plan-Do-Study-Act cycle is an iterative plan of action for designing and testing a specific change [7]. This part of the QI cycle involved implementing and testing a change to address our specific aim. As the first cycle of change, the team requested that the scheduler add 15 minutes to the surgeons’ requested case time over 1 week. Of the urologists scheduled that week, one had used CTC and the other had not completed the student team’s survey. In order to study the change, the project team used control charts for the 2 surgeons whose case times were adapted. Prior to the intervention, the surgeons averaged at least 20 minutes over their scheduled time, with wide variation. Surgeons were infrequently completing cases at or below their requested case time. Most of the inaccuracy came from going long. The team used control charts to understand the impact of the change. The control charts showed that after the change in scheduling time, the 2 surgeons still went over their allotted case time, but to a lesser degree.
After gaining new information, the next step in the PDSA cycle is to determine the next test of change. The student team recommended sharing these data with the surgeons to consider next steps in improving block utilization, though time constraints of the semester limited continued involvement of the student team in the next PDSA cycle.
Discussion
Through the application of QI tools, new insight was gained about OR efficiency and potential improvements. The student team talked to numerous staff involved in scheduling and each discussion increased understanding of the issues that lead to OR inefficiency. The process map and fishbone diagram provided a visual expression of how small issues could impact the overall OR system. Application of QI tools also led the team to the discovery that surgeons may be interpreting case length in disparate ways, contributing to problems with scheduling.
Though the intervention did not have significant impact over 1 week, more time for subsequent PDSA cycles may have resulted in clinical improvements. Despite the limitations, the student team uncovered an important aspect of the block scheduling process, providing valuable information and insight for the department around this scheduling issue. The student team’s work was shared between multiple surgical departments, and the QI work in the department is ongoing.
Implications for Health Care Institutions
Nontraditional Projects Can Work
The issue of OR utilization is perhaps not a “traditional” QI project given the macro nature of the problem. Once it was broken down into discrete processes, problems such as OR turnover, scheduling redundancies, and others look much more like traditional QI projects. It may be beneficial to institutions to broaden the scope of QI to problems that may, at first glance, seem out of the realm of process mapping, fishbone diagramming, and SMART aims. QI tools can turn management problems into projects that can be tackled by small teams, creating an culture of change in an organization [13].
Benefits of Student Teams
There are clear benefits to the institution working with students. Our hospital-based team members found it beneficial to have independent observers review the process and recommend improvements. Students were able to challenge the status quo and point out inefficiencies that have remained due to institutional complacency and lack of resources. The hospital employees were impressed and surprised that the students found the misunderstanding about case length, and noted that it suggests that there may be other places where there are miscommunications between various people involved in OR scheduling. The students’ energy and time was supported by the QI expertise of the course instructors, and the practical knowledge of the hospital-based team members. Similar benefits have been noted by others utilizing collaborative QI educational models [14,15].
Benefits for Students
For the students on the team, the opportunity to apply QI concepts to the real world was a unique learning opportunity. First, the project was truly interdisciplinary. The students were from varied fields and they worked with schedulers, surgeons, and office managers providing the students with insight into the meaning and perspectives of interprofessional collaboration. The students appreciated the complexity and tensions of the OR staff who were working to balance the schedules of nurses, anesthesiologists, and other OR support staff. Additionally, interdisciplinary collaboration in health care is of increasing importance in everyday practice [16,17]. A strong understanding of collaboration across professions will be a cornerstone of the students’ credentials as they move into the workforce.
There is also value in adding real work experience to academics. The students were able to appreciate not only the concepts of QI but the actual challenges of implementing QI methodology in an institution where people had varying levels of buy-in. Quality improvement is about more than sitting at a whiteboard coming up with charts—it is about enacting actual change and understanding specific real-world situations. The hospital collaboration allowed the students to gain experience that is impossible to replicate in the classroom.
Limitations and Barriers
As noted in other academic-practice collaborations, the limitation of completing the project in one semester presents a barrier to collaboration; the working world does not operate on an academic timeline [14]. Students were limited to only testing one cycle of change. This part of the semester was disappointing as the students would have liked to implement multiple PDSA cycles. The OR managers faced barriers as well; they invested time in educating students who would soon move on, and would have to repeat the process with a new group of students. The department has continued on with this work, but losing the students who they oriented was not ideal.
The course instructors were flexible in allowing the project team to spend the majority of time breaking down the problem of OR block utilization into testable changes, which was the bulk of our work. However, the skill that the team was able to dedicate the least amount time to, testing and implementing change, is useful for the students to learn and beneficial for the organization. Moving forward, allowing teams to build on the previous semester’s work, and even implementing a student handoff, might be tried.
Future Directions
Although our intervention did not lead to sustained improvements in OR scheduling efficiency, our project demonstrates how QI tools can be taught and applied in an academic course to address a management problem. Research to specifically understand institutional benefits of academic-practice collaborations would be helpful in recruiting partners and furthering best practices for participants in these partnerships. Research is also needed to understand the impact of QI collaborative models such as the one described in this paper on improving interprofessional teamwork and communication skills, as called for by health care professional educators [16].
Corresponding author: Danielle O’Rourke-Suchoff, BA, Case Western Reserve University School of Medicine, Office of Student Affairs, 10900 Euclid Ave., Cleveland, OH 44106, dko@case.edu.
Financial disclosures: none.
1. The right strategies can help increase OR utilization. OR Manager 2013;29:21–2.
2. Jackson RL. The business of surgery. Managing the OR as a profit center requires more than just IT. It requires a profit-making mindset, too. Health Manage Technol 2002;23:20–2.
3. Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. Washington (DC): National Academy Press; 2001.
4. Hand R, Dolansky MA, Hanahan E, Tinsley N. Quality comes alive: an interdisciplinary student team’s quality improvement experience in learning by doing—health care education case study. Qual Approaches Higher Educ 2014;5:26–32.
5. Scholtes PR, Joiner BL, Streibel BJ. The team handbook. Oriel; 2003.
6. Institute for Healthcare Improvement. Open School. 2015. Accessed 13 Apr 2015 at www.ihi.org/education/ihiopenschool/Pages/default.aspx.
7. Ogrinc GS, Headrick LA, Moore SM, et al. Fundamentals of health care improvement: A guide to improving your patients’ care. 2nd ed. Oakbrook Terrace, IL: Joint Commission Resources and the Institute for Healthcare Improvement; 2012.
8. Managing patient flow: Smoothing OR schedule can ease capacity crunches, researchers say. OR Manager 2003;19:1,9–10.
9. Harders M, Malangoni MA, Weight S, Sidhu T. Improving operating room efficiency through process redesign. Surgery 2006;140:509–16.
10. Paynter J, Horne W, Sizemore R. Realizing revenue opportunities in the operating room. 2015. Accessed 13 Apr 2015 at www.ihi.org/resources/Pages/ImprovementStories/RealizingRevenueOpportunitiesintheOperatingRoom.aspx.
11. Cima RR, Brown MJ, Hebl JR, et al. Use of Lean and Six Sigma methodology to improve operating room efficiency in a high-volume tertiary-care academic medical center. J Am Coll Surg 2011;213:83–92.
12. Day R, Garfinkel R, Thompson S. Integrated block sharing: a win–win strategy for hospitals and surgeons. Manufact Serv Op Manage 2012;14:567–83.
13. Pardini-Kiely K, Greenlee E, Hopkins J, et al. Improving and Sustaining core measure performance through effective accountability of clinical microsystems in an academic medical center. Jt Comm J Qual Improv Pt Safety 2010;36:387–98.
14. Hall LW, Headrick LA, Cox KR, et al. Linking health professional learners and health care workers on action-based improvement teams. Qual Manag Health Care 2009;18:194–201.
15. Ogrinc GS, Nierenberg DW, Batalden PB. Building experiential learning about quality improvement into a medical school curriculum: The Dartmouth Experience. Health Aff 2011;30:716–22.
16. Interprofessional Education Collaborative Expert Panel. Core competencies for interprofessional collaborative practice. Washington, DC: Interprofessional Education Collaborative; 2011.
17. World Health Organization. Framework for action on inerprofessional education and collaborative practice. Geneva: World Health Organization; 2010.
From the Case Western Reserve University School of Medicine, Cleveland, OH.
Abstract
- Objective: To improve operating room (OR) scheduling efficiency at a large academic institution through the use of an academic-practice partnership and quality improvement (QI) methods.
- Methods: The OR administrative team at a large academic hospital partnered with students in a graduate level QI course to apply QI tools to the problem of OR efficiency.
- Results: The team found wide variation in the way that surgeries were scheduled and other factors that contributed to inefficient OR utilization. A plan-do-study-act (PDSA) cycle was applied to the problem of discrepancy in surgeons’ interpretation of case length, resulting in poor case length accuracy. Our intervention, adding time on the schedule for cases, did not show consistent improvement in case length accuracy.
- Conclusion: Although our intervention did not lead to sustained improvements in OR scheduling efficiency, our project demonstrates how QI tools can be taught and applied in an academic course to address a management problem. Further research is needed to study the impact of student teams on health care improvement.
Operating rooms are one of the most costly departments of a hospital. At University Hospitals Case Medical Center (UHCMC), as at many hospitals, operating room utilization is a key area of focus for both operating room (OR) and hospital administrators. Efficient use of the OR is an important aspect of a hospital’s finances and patient-centeredness.
UHCMC uses block scheduling, a common OR scheduling design. Each surgical department is allotted a certain number of blocks (hours of reserved OR time) that they are responsible for filling with surgical cases and that the hospital is responsible for staffing. Block utilization rate is a metric commonly used to measure OR efficiency. It divides the time that the OR is in use by the total block time allocated to the department (while accounting for room turnaround time). An industry benchmark is 75% block utilization [1], which was adopted as an internal target at UHCMC. Achieving this metric is necessary because the hospital (rather than each individual surgical department) is responsible for ensuring that the appropriate amount of non-surgeon staff (eg, anesthesiologists, nurses, scrub techs, and facilities staff) is available. Poor utilization rates indicate that the staff and equipment are inefficiently used, which can impact the hospital’s financial well-being [2]. Block utilization is the result of a complex system, making it challenging to improve. Many people are involved in scheduling, and a large degree of inherent uncertainty exists in the system.
At UHCMC, block utilization rates by department ranged from 52% to 80%, with an overall utilization of 64% from February to July 2014. Given this wide variation, higher level management staff in the OR initiated a project in which OR administrators partnered with students in a graduate level QI course in an effort to improve overall block utilization. They believed that improving block utilization rate would improve the effectiveness, patient-centeredness, and efficiency of care, health care delivery goals described by the Institute of Medicine [3].
Methods
Setting
The OR at UHCMC contains 4 operating suites that serve over 25,000 patients per year and train over 900 residents each year. Nearly 250 surgeons in 23 departments use the OR. The OR schedule at our institution is coordinated by block scheduling, as described above. If a surgical department cannot fill the block, they must release the time to central scheduling for re-allocation of the time to another department.
Application of QI Process
This QI project was an academic-practice collaboration between UHCMC and a graduate level course at Case Western Reserve University called The Continual Improvement of Healthcare: an Interdisciplinary Course [4]. Faculty course instructors solicit applications of QI projects from departments at UHCMC. The project team consisted of 4 students (from medicine, social work, public health, and bioethics), 2 administrative staff from UHCMC, and a QI coach who is on the faculty at Case Western. Guidance was provided by 2 faculty facilitators. The students attended 15 weekly class sessions, 4 meetings with the project team, numerous data gathering sessions with other hospital staff, and held a handful of outside-class student team meetings. An early class session was devoted to team skills and the Seven-Step meeting process [5]. Each classroom session consisted of structured group activities to practice the tools of the QI process.
Tool 1: Global Aim
The team first established a global aim: to improve the OR block utilization rate at UHCMC. This aim was based on the initial project proposal from UHCMC. The global aim explains the reason that the project team was established, and frames all future work [7].
Tool 2: Industry Assessment
Based on the global aim, the student team performed an industry assessment in order to understand strategies for improving block utilization rate in use at other institutions. Peer-reviewed journal articles and case reports were reviewed and the student team was able to contact a team at another institution working on similar issues.
Overall, 2 broad categories of interventions to improve block utilization were identified. Some institutions addressed the way time in the OR was scheduled. They made improvements to how block time was allotted, timing of cases, and dealing with add-on cases [8]. Others focused on using time in the OR more efficiently by addressing room turnover, delays including waiting for surgeons, and waiting for hospital beds [9]. Because the specific case mix of each hospital is so distinct, hospitals that successfully made changes all used a variety of interventions [10–12]. After the industry assessment, the student team realized that there would be a large number of possible approaches to the problem of block utilization, and a better understanding of the actual process of scheduling at UHCMC was necessary to find an area of focus.
Tool 3: Process Map
As the project team began to address the global aim of improving OR block utilization at UHCMC, they needed to have a thorough understanding of how OR time was allotted and used. To do this, the student team created a process map by interviewing process stakeholders, including the OR managers and department schedulers in orthopedics, general surgery, and urology, as suggested by the OR managers. The perspective of these staff were critical to understanding the process of operating room scheduling.
Through the creation of the process map, the project team found that there was wide variation in the process and structure for scheduling surgeries. Some departments used one central scheduler while others used individual secretaries for each surgeon. Some surgeons maintained control over changing their schedule, while others did not. Further, the project team learned that the metric of block utilization rate was of varying importance to people working on the ground.
Tool 4: Fishbone Diagram
After understanding the process, the project team considered all of the factors that
Tool 5: Specific Aim
Though the global aim was to improve block utilization, the project team needed to chose a specific aim that met S.M.A.R.T criteria: Specific, Measureable, Achievable, Results-focused, and Time-bound [7]. After considering multiple potential areas of initial focus, the OR staff suggested focusing on the issue of case length accuracy. In qualitative interviews, the student team had found that the surgery request forms ask for “case length,” and the schedulers were not sure how the surgeons defined it. When the OR is booked for an operation, the amount of time blocked out is the time from when the patient is brought into the operating room to the time that the patient leaves the room, or WIWO (Wheels In Wheels Out). This WIWO time includes anesthesia induction and preparations for surgery such as positioning. Some surgeons think about case length as only the time that the patient is operated on, or CTC (Cut to Close). Thus, the surgeon may be requesting less time than is really necessary for the case if he or she is only thinking about CTC time. The student team created a survey and found that 2 urology surgeons considered case length to be WIWO, and 4 considered case length to mean CTC.
Tools 6 and 7: PDSA Cycle and Control Charts
The Plan-Do-Study-Act cycle is an iterative plan of action for designing and testing a specific change [7]. This part of the QI cycle involved implementing and testing a change to address our specific aim. As the first cycle of change, the team requested that the scheduler add 15 minutes to the surgeons’ requested case time over 1 week. Of the urologists scheduled that week, one had used CTC and the other had not completed the student team’s survey. In order to study the change, the project team used control charts for the 2 surgeons whose case times were adapted. Prior to the intervention, the surgeons averaged at least 20 minutes over their scheduled time, with wide variation. Surgeons were infrequently completing cases at or below their requested case time. Most of the inaccuracy came from going long. The team used control charts to understand the impact of the change. The control charts showed that after the change in scheduling time, the 2 surgeons still went over their allotted case time, but to a lesser degree.
After gaining new information, the next step in the PDSA cycle is to determine the next test of change. The student team recommended sharing these data with the surgeons to consider next steps in improving block utilization, though time constraints of the semester limited continued involvement of the student team in the next PDSA cycle.
Discussion
Through the application of QI tools, new insight was gained about OR efficiency and potential improvements. The student team talked to numerous staff involved in scheduling and each discussion increased understanding of the issues that lead to OR inefficiency. The process map and fishbone diagram provided a visual expression of how small issues could impact the overall OR system. Application of QI tools also led the team to the discovery that surgeons may be interpreting case length in disparate ways, contributing to problems with scheduling.
Though the intervention did not have significant impact over 1 week, more time for subsequent PDSA cycles may have resulted in clinical improvements. Despite the limitations, the student team uncovered an important aspect of the block scheduling process, providing valuable information and insight for the department around this scheduling issue. The student team’s work was shared between multiple surgical departments, and the QI work in the department is ongoing.
Implications for Health Care Institutions
Nontraditional Projects Can Work
The issue of OR utilization is perhaps not a “traditional” QI project given the macro nature of the problem. Once it was broken down into discrete processes, problems such as OR turnover, scheduling redundancies, and others look much more like traditional QI projects. It may be beneficial to institutions to broaden the scope of QI to problems that may, at first glance, seem out of the realm of process mapping, fishbone diagramming, and SMART aims. QI tools can turn management problems into projects that can be tackled by small teams, creating an culture of change in an organization [13].
Benefits of Student Teams
There are clear benefits to the institution working with students. Our hospital-based team members found it beneficial to have independent observers review the process and recommend improvements. Students were able to challenge the status quo and point out inefficiencies that have remained due to institutional complacency and lack of resources. The hospital employees were impressed and surprised that the students found the misunderstanding about case length, and noted that it suggests that there may be other places where there are miscommunications between various people involved in OR scheduling. The students’ energy and time was supported by the QI expertise of the course instructors, and the practical knowledge of the hospital-based team members. Similar benefits have been noted by others utilizing collaborative QI educational models [14,15].
Benefits for Students
For the students on the team, the opportunity to apply QI concepts to the real world was a unique learning opportunity. First, the project was truly interdisciplinary. The students were from varied fields and they worked with schedulers, surgeons, and office managers providing the students with insight into the meaning and perspectives of interprofessional collaboration. The students appreciated the complexity and tensions of the OR staff who were working to balance the schedules of nurses, anesthesiologists, and other OR support staff. Additionally, interdisciplinary collaboration in health care is of increasing importance in everyday practice [16,17]. A strong understanding of collaboration across professions will be a cornerstone of the students’ credentials as they move into the workforce.
There is also value in adding real work experience to academics. The students were able to appreciate not only the concepts of QI but the actual challenges of implementing QI methodology in an institution where people had varying levels of buy-in. Quality improvement is about more than sitting at a whiteboard coming up with charts—it is about enacting actual change and understanding specific real-world situations. The hospital collaboration allowed the students to gain experience that is impossible to replicate in the classroom.
Limitations and Barriers
As noted in other academic-practice collaborations, the limitation of completing the project in one semester presents a barrier to collaboration; the working world does not operate on an academic timeline [14]. Students were limited to only testing one cycle of change. This part of the semester was disappointing as the students would have liked to implement multiple PDSA cycles. The OR managers faced barriers as well; they invested time in educating students who would soon move on, and would have to repeat the process with a new group of students. The department has continued on with this work, but losing the students who they oriented was not ideal.
The course instructors were flexible in allowing the project team to spend the majority of time breaking down the problem of OR block utilization into testable changes, which was the bulk of our work. However, the skill that the team was able to dedicate the least amount time to, testing and implementing change, is useful for the students to learn and beneficial for the organization. Moving forward, allowing teams to build on the previous semester’s work, and even implementing a student handoff, might be tried.
Future Directions
Although our intervention did not lead to sustained improvements in OR scheduling efficiency, our project demonstrates how QI tools can be taught and applied in an academic course to address a management problem. Research to specifically understand institutional benefits of academic-practice collaborations would be helpful in recruiting partners and furthering best practices for participants in these partnerships. Research is also needed to understand the impact of QI collaborative models such as the one described in this paper on improving interprofessional teamwork and communication skills, as called for by health care professional educators [16].
Corresponding author: Danielle O’Rourke-Suchoff, BA, Case Western Reserve University School of Medicine, Office of Student Affairs, 10900 Euclid Ave., Cleveland, OH 44106, dko@case.edu.
Financial disclosures: none.
From the Case Western Reserve University School of Medicine, Cleveland, OH.
Abstract
- Objective: To improve operating room (OR) scheduling efficiency at a large academic institution through the use of an academic-practice partnership and quality improvement (QI) methods.
- Methods: The OR administrative team at a large academic hospital partnered with students in a graduate level QI course to apply QI tools to the problem of OR efficiency.
- Results: The team found wide variation in the way that surgeries were scheduled and other factors that contributed to inefficient OR utilization. A plan-do-study-act (PDSA) cycle was applied to the problem of discrepancy in surgeons’ interpretation of case length, resulting in poor case length accuracy. Our intervention, adding time on the schedule for cases, did not show consistent improvement in case length accuracy.
- Conclusion: Although our intervention did not lead to sustained improvements in OR scheduling efficiency, our project demonstrates how QI tools can be taught and applied in an academic course to address a management problem. Further research is needed to study the impact of student teams on health care improvement.
Operating rooms are one of the most costly departments of a hospital. At University Hospitals Case Medical Center (UHCMC), as at many hospitals, operating room utilization is a key area of focus for both operating room (OR) and hospital administrators. Efficient use of the OR is an important aspect of a hospital’s finances and patient-centeredness.
UHCMC uses block scheduling, a common OR scheduling design. Each surgical department is allotted a certain number of blocks (hours of reserved OR time) that they are responsible for filling with surgical cases and that the hospital is responsible for staffing. Block utilization rate is a metric commonly used to measure OR efficiency. It divides the time that the OR is in use by the total block time allocated to the department (while accounting for room turnaround time). An industry benchmark is 75% block utilization [1], which was adopted as an internal target at UHCMC. Achieving this metric is necessary because the hospital (rather than each individual surgical department) is responsible for ensuring that the appropriate amount of non-surgeon staff (eg, anesthesiologists, nurses, scrub techs, and facilities staff) is available. Poor utilization rates indicate that the staff and equipment are inefficiently used, which can impact the hospital’s financial well-being [2]. Block utilization is the result of a complex system, making it challenging to improve. Many people are involved in scheduling, and a large degree of inherent uncertainty exists in the system.
At UHCMC, block utilization rates by department ranged from 52% to 80%, with an overall utilization of 64% from February to July 2014. Given this wide variation, higher level management staff in the OR initiated a project in which OR administrators partnered with students in a graduate level QI course in an effort to improve overall block utilization. They believed that improving block utilization rate would improve the effectiveness, patient-centeredness, and efficiency of care, health care delivery goals described by the Institute of Medicine [3].
Methods
Setting
The OR at UHCMC contains 4 operating suites that serve over 25,000 patients per year and train over 900 residents each year. Nearly 250 surgeons in 23 departments use the OR. The OR schedule at our institution is coordinated by block scheduling, as described above. If a surgical department cannot fill the block, they must release the time to central scheduling for re-allocation of the time to another department.
Application of QI Process
This QI project was an academic-practice collaboration between UHCMC and a graduate level course at Case Western Reserve University called The Continual Improvement of Healthcare: an Interdisciplinary Course [4]. Faculty course instructors solicit applications of QI projects from departments at UHCMC. The project team consisted of 4 students (from medicine, social work, public health, and bioethics), 2 administrative staff from UHCMC, and a QI coach who is on the faculty at Case Western. Guidance was provided by 2 faculty facilitators. The students attended 15 weekly class sessions, 4 meetings with the project team, numerous data gathering sessions with other hospital staff, and held a handful of outside-class student team meetings. An early class session was devoted to team skills and the Seven-Step meeting process [5]. Each classroom session consisted of structured group activities to practice the tools of the QI process.
Tool 1: Global Aim
The team first established a global aim: to improve the OR block utilization rate at UHCMC. This aim was based on the initial project proposal from UHCMC. The global aim explains the reason that the project team was established, and frames all future work [7].
Tool 2: Industry Assessment
Based on the global aim, the student team performed an industry assessment in order to understand strategies for improving block utilization rate in use at other institutions. Peer-reviewed journal articles and case reports were reviewed and the student team was able to contact a team at another institution working on similar issues.
Overall, 2 broad categories of interventions to improve block utilization were identified. Some institutions addressed the way time in the OR was scheduled. They made improvements to how block time was allotted, timing of cases, and dealing with add-on cases [8]. Others focused on using time in the OR more efficiently by addressing room turnover, delays including waiting for surgeons, and waiting for hospital beds [9]. Because the specific case mix of each hospital is so distinct, hospitals that successfully made changes all used a variety of interventions [10–12]. After the industry assessment, the student team realized that there would be a large number of possible approaches to the problem of block utilization, and a better understanding of the actual process of scheduling at UHCMC was necessary to find an area of focus.
Tool 3: Process Map
As the project team began to address the global aim of improving OR block utilization at UHCMC, they needed to have a thorough understanding of how OR time was allotted and used. To do this, the student team created a process map by interviewing process stakeholders, including the OR managers and department schedulers in orthopedics, general surgery, and urology, as suggested by the OR managers. The perspective of these staff were critical to understanding the process of operating room scheduling.
Through the creation of the process map, the project team found that there was wide variation in the process and structure for scheduling surgeries. Some departments used one central scheduler while others used individual secretaries for each surgeon. Some surgeons maintained control over changing their schedule, while others did not. Further, the project team learned that the metric of block utilization rate was of varying importance to people working on the ground.
Tool 4: Fishbone Diagram
After understanding the process, the project team considered all of the factors that
Tool 5: Specific Aim
Though the global aim was to improve block utilization, the project team needed to chose a specific aim that met S.M.A.R.T criteria: Specific, Measureable, Achievable, Results-focused, and Time-bound [7]. After considering multiple potential areas of initial focus, the OR staff suggested focusing on the issue of case length accuracy. In qualitative interviews, the student team had found that the surgery request forms ask for “case length,” and the schedulers were not sure how the surgeons defined it. When the OR is booked for an operation, the amount of time blocked out is the time from when the patient is brought into the operating room to the time that the patient leaves the room, or WIWO (Wheels In Wheels Out). This WIWO time includes anesthesia induction and preparations for surgery such as positioning. Some surgeons think about case length as only the time that the patient is operated on, or CTC (Cut to Close). Thus, the surgeon may be requesting less time than is really necessary for the case if he or she is only thinking about CTC time. The student team created a survey and found that 2 urology surgeons considered case length to be WIWO, and 4 considered case length to mean CTC.
Tools 6 and 7: PDSA Cycle and Control Charts
The Plan-Do-Study-Act cycle is an iterative plan of action for designing and testing a specific change [7]. This part of the QI cycle involved implementing and testing a change to address our specific aim. As the first cycle of change, the team requested that the scheduler add 15 minutes to the surgeons’ requested case time over 1 week. Of the urologists scheduled that week, one had used CTC and the other had not completed the student team’s survey. In order to study the change, the project team used control charts for the 2 surgeons whose case times were adapted. Prior to the intervention, the surgeons averaged at least 20 minutes over their scheduled time, with wide variation. Surgeons were infrequently completing cases at or below their requested case time. Most of the inaccuracy came from going long. The team used control charts to understand the impact of the change. The control charts showed that after the change in scheduling time, the 2 surgeons still went over their allotted case time, but to a lesser degree.
After gaining new information, the next step in the PDSA cycle is to determine the next test of change. The student team recommended sharing these data with the surgeons to consider next steps in improving block utilization, though time constraints of the semester limited continued involvement of the student team in the next PDSA cycle.
Discussion
Through the application of QI tools, new insight was gained about OR efficiency and potential improvements. The student team talked to numerous staff involved in scheduling and each discussion increased understanding of the issues that lead to OR inefficiency. The process map and fishbone diagram provided a visual expression of how small issues could impact the overall OR system. Application of QI tools also led the team to the discovery that surgeons may be interpreting case length in disparate ways, contributing to problems with scheduling.
Though the intervention did not have significant impact over 1 week, more time for subsequent PDSA cycles may have resulted in clinical improvements. Despite the limitations, the student team uncovered an important aspect of the block scheduling process, providing valuable information and insight for the department around this scheduling issue. The student team’s work was shared between multiple surgical departments, and the QI work in the department is ongoing.
Implications for Health Care Institutions
Nontraditional Projects Can Work
The issue of OR utilization is perhaps not a “traditional” QI project given the macro nature of the problem. Once it was broken down into discrete processes, problems such as OR turnover, scheduling redundancies, and others look much more like traditional QI projects. It may be beneficial to institutions to broaden the scope of QI to problems that may, at first glance, seem out of the realm of process mapping, fishbone diagramming, and SMART aims. QI tools can turn management problems into projects that can be tackled by small teams, creating an culture of change in an organization [13].
Benefits of Student Teams
There are clear benefits to the institution working with students. Our hospital-based team members found it beneficial to have independent observers review the process and recommend improvements. Students were able to challenge the status quo and point out inefficiencies that have remained due to institutional complacency and lack of resources. The hospital employees were impressed and surprised that the students found the misunderstanding about case length, and noted that it suggests that there may be other places where there are miscommunications between various people involved in OR scheduling. The students’ energy and time was supported by the QI expertise of the course instructors, and the practical knowledge of the hospital-based team members. Similar benefits have been noted by others utilizing collaborative QI educational models [14,15].
Benefits for Students
For the students on the team, the opportunity to apply QI concepts to the real world was a unique learning opportunity. First, the project was truly interdisciplinary. The students were from varied fields and they worked with schedulers, surgeons, and office managers providing the students with insight into the meaning and perspectives of interprofessional collaboration. The students appreciated the complexity and tensions of the OR staff who were working to balance the schedules of nurses, anesthesiologists, and other OR support staff. Additionally, interdisciplinary collaboration in health care is of increasing importance in everyday practice [16,17]. A strong understanding of collaboration across professions will be a cornerstone of the students’ credentials as they move into the workforce.
There is also value in adding real work experience to academics. The students were able to appreciate not only the concepts of QI but the actual challenges of implementing QI methodology in an institution where people had varying levels of buy-in. Quality improvement is about more than sitting at a whiteboard coming up with charts—it is about enacting actual change and understanding specific real-world situations. The hospital collaboration allowed the students to gain experience that is impossible to replicate in the classroom.
Limitations and Barriers
As noted in other academic-practice collaborations, the limitation of completing the project in one semester presents a barrier to collaboration; the working world does not operate on an academic timeline [14]. Students were limited to only testing one cycle of change. This part of the semester was disappointing as the students would have liked to implement multiple PDSA cycles. The OR managers faced barriers as well; they invested time in educating students who would soon move on, and would have to repeat the process with a new group of students. The department has continued on with this work, but losing the students who they oriented was not ideal.
The course instructors were flexible in allowing the project team to spend the majority of time breaking down the problem of OR block utilization into testable changes, which was the bulk of our work. However, the skill that the team was able to dedicate the least amount time to, testing and implementing change, is useful for the students to learn and beneficial for the organization. Moving forward, allowing teams to build on the previous semester’s work, and even implementing a student handoff, might be tried.
Future Directions
Although our intervention did not lead to sustained improvements in OR scheduling efficiency, our project demonstrates how QI tools can be taught and applied in an academic course to address a management problem. Research to specifically understand institutional benefits of academic-practice collaborations would be helpful in recruiting partners and furthering best practices for participants in these partnerships. Research is also needed to understand the impact of QI collaborative models such as the one described in this paper on improving interprofessional teamwork and communication skills, as called for by health care professional educators [16].
Corresponding author: Danielle O’Rourke-Suchoff, BA, Case Western Reserve University School of Medicine, Office of Student Affairs, 10900 Euclid Ave., Cleveland, OH 44106, dko@case.edu.
Financial disclosures: none.
1. The right strategies can help increase OR utilization. OR Manager 2013;29:21–2.
2. Jackson RL. The business of surgery. Managing the OR as a profit center requires more than just IT. It requires a profit-making mindset, too. Health Manage Technol 2002;23:20–2.
3. Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. Washington (DC): National Academy Press; 2001.
4. Hand R, Dolansky MA, Hanahan E, Tinsley N. Quality comes alive: an interdisciplinary student team’s quality improvement experience in learning by doing—health care education case study. Qual Approaches Higher Educ 2014;5:26–32.
5. Scholtes PR, Joiner BL, Streibel BJ. The team handbook. Oriel; 2003.
6. Institute for Healthcare Improvement. Open School. 2015. Accessed 13 Apr 2015 at www.ihi.org/education/ihiopenschool/Pages/default.aspx.
7. Ogrinc GS, Headrick LA, Moore SM, et al. Fundamentals of health care improvement: A guide to improving your patients’ care. 2nd ed. Oakbrook Terrace, IL: Joint Commission Resources and the Institute for Healthcare Improvement; 2012.
8. Managing patient flow: Smoothing OR schedule can ease capacity crunches, researchers say. OR Manager 2003;19:1,9–10.
9. Harders M, Malangoni MA, Weight S, Sidhu T. Improving operating room efficiency through process redesign. Surgery 2006;140:509–16.
10. Paynter J, Horne W, Sizemore R. Realizing revenue opportunities in the operating room. 2015. Accessed 13 Apr 2015 at www.ihi.org/resources/Pages/ImprovementStories/RealizingRevenueOpportunitiesintheOperatingRoom.aspx.
11. Cima RR, Brown MJ, Hebl JR, et al. Use of Lean and Six Sigma methodology to improve operating room efficiency in a high-volume tertiary-care academic medical center. J Am Coll Surg 2011;213:83–92.
12. Day R, Garfinkel R, Thompson S. Integrated block sharing: a win–win strategy for hospitals and surgeons. Manufact Serv Op Manage 2012;14:567–83.
13. Pardini-Kiely K, Greenlee E, Hopkins J, et al. Improving and Sustaining core measure performance through effective accountability of clinical microsystems in an academic medical center. Jt Comm J Qual Improv Pt Safety 2010;36:387–98.
14. Hall LW, Headrick LA, Cox KR, et al. Linking health professional learners and health care workers on action-based improvement teams. Qual Manag Health Care 2009;18:194–201.
15. Ogrinc GS, Nierenberg DW, Batalden PB. Building experiential learning about quality improvement into a medical school curriculum: The Dartmouth Experience. Health Aff 2011;30:716–22.
16. Interprofessional Education Collaborative Expert Panel. Core competencies for interprofessional collaborative practice. Washington, DC: Interprofessional Education Collaborative; 2011.
17. World Health Organization. Framework for action on inerprofessional education and collaborative practice. Geneva: World Health Organization; 2010.
1. The right strategies can help increase OR utilization. OR Manager 2013;29:21–2.
2. Jackson RL. The business of surgery. Managing the OR as a profit center requires more than just IT. It requires a profit-making mindset, too. Health Manage Technol 2002;23:20–2.
3. Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. Washington (DC): National Academy Press; 2001.
4. Hand R, Dolansky MA, Hanahan E, Tinsley N. Quality comes alive: an interdisciplinary student team’s quality improvement experience in learning by doing—health care education case study. Qual Approaches Higher Educ 2014;5:26–32.
5. Scholtes PR, Joiner BL, Streibel BJ. The team handbook. Oriel; 2003.
6. Institute for Healthcare Improvement. Open School. 2015. Accessed 13 Apr 2015 at www.ihi.org/education/ihiopenschool/Pages/default.aspx.
7. Ogrinc GS, Headrick LA, Moore SM, et al. Fundamentals of health care improvement: A guide to improving your patients’ care. 2nd ed. Oakbrook Terrace, IL: Joint Commission Resources and the Institute for Healthcare Improvement; 2012.
8. Managing patient flow: Smoothing OR schedule can ease capacity crunches, researchers say. OR Manager 2003;19:1,9–10.
9. Harders M, Malangoni MA, Weight S, Sidhu T. Improving operating room efficiency through process redesign. Surgery 2006;140:509–16.
10. Paynter J, Horne W, Sizemore R. Realizing revenue opportunities in the operating room. 2015. Accessed 13 Apr 2015 at www.ihi.org/resources/Pages/ImprovementStories/RealizingRevenueOpportunitiesintheOperatingRoom.aspx.
11. Cima RR, Brown MJ, Hebl JR, et al. Use of Lean and Six Sigma methodology to improve operating room efficiency in a high-volume tertiary-care academic medical center. J Am Coll Surg 2011;213:83–92.
12. Day R, Garfinkel R, Thompson S. Integrated block sharing: a win–win strategy for hospitals and surgeons. Manufact Serv Op Manage 2012;14:567–83.
13. Pardini-Kiely K, Greenlee E, Hopkins J, et al. Improving and Sustaining core measure performance through effective accountability of clinical microsystems in an academic medical center. Jt Comm J Qual Improv Pt Safety 2010;36:387–98.
14. Hall LW, Headrick LA, Cox KR, et al. Linking health professional learners and health care workers on action-based improvement teams. Qual Manag Health Care 2009;18:194–201.
15. Ogrinc GS, Nierenberg DW, Batalden PB. Building experiential learning about quality improvement into a medical school curriculum: The Dartmouth Experience. Health Aff 2011;30:716–22.
16. Interprofessional Education Collaborative Expert Panel. Core competencies for interprofessional collaborative practice. Washington, DC: Interprofessional Education Collaborative; 2011.
17. World Health Organization. Framework for action on inerprofessional education and collaborative practice. Geneva: World Health Organization; 2010.