User login
2016 Update on abnormal uterine bleeding
How abnormal uterine bleeding (AUB) is managed has a significant impact on health care. In the United States, almost one-third of all gynecologic visits are related to AUB, with estimated annual direct costs of up to $1.55 billion and indirect costs as high as $36 billion.1 Not surprisingly, office-based procedures for AUB are being emphasized. While in the short term it is more cost efficient to perform surgery in the office rather than in the operating room, questions have arisen regarding the long-term efficacy and durability of in-office procedures. Insurers are undoubtedly raising these questions as well.
Notably, some ObGyns are early adopters of office-based surgery while others tend to adopt in-office procedures more slowly. As the literature for such procedures for AUB matures to provide more data on efficacy and acceptability, we will have a greater evidence base for understanding which procedures are more appropriate for the office. And while practice shifts sometimes occur due to cost-containment initiatives, some shifts are patient driven. Studies that address these driving variables, as well as efficacy considerations, are helpful. As we counsel women about procedures for AUB, the relative advantages and disadvantages of available treatment settings likely will become a greater part of that discussion so that they can make an informed decision.
In this Update, we discuss the results of 3 studies that examined various procedures and settings for AUB management:
- outpatient vs inpatient polypectomy
- hysteroscopic morcellation of polyps and myomas in an office vs ambulatory surgical center
- comparative costs of endometrial ablation and hysterectomy.
Outpatient vs inpatient polypectomy: Similar success rates in the short term
Cooper NA, Clark TJ, Middleton L, et al; OPT Trial Collaborative Group. Outpatient versus inpatient uterine polyp treatment for abnormal uterine bleeding: randomised controlled non-inferiority study. BMJ. 2015;350:h1398. doi:10.1136/bmj.h1398.
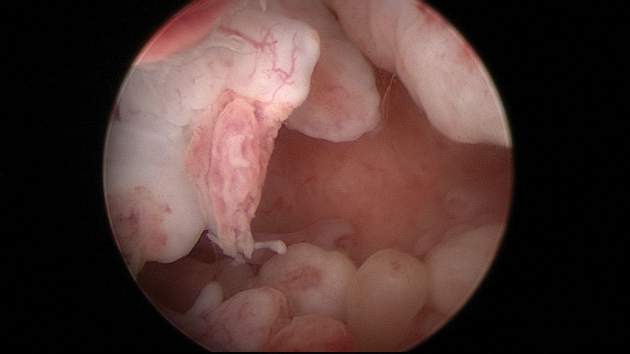
A collaborative group in the United Kingdom studied the common problem of endometrial polyps. Their objective was to evaluate whether outpatient polypectomy was as effective and well accepted as polypectomy performed in the operating room (OR).
Patients with a hysteroscopically diagnosed polyp were randomly assigned to hysteroscopic polyp removal in either a hysteroscopy clinic or an OR; polyp removal was performed using miniature mechanical or electrosurgical instruments. The primary outcome was successful treatment, determined by the participants’ assessment of their bleeding at 6 months.
Overall, 73% of women (166 of 228) in the clinic group and 80% (168 of 211) in the OR group reported a successful response to surgery at 6 months, with treatment effects being maintained at 12 and 24 months. A “see and treat” approach—that is, treatment carried out at the same time as diagnosis—was possible in 72% of women (174 of 242).
Partial or failed polyp removal occurred in 46 of 242 women (19%) in the clinic group, mostly because of pain issues, and in 18 of 233 women (7%) in the OR group (relative risk, 2.5; 95% confidence interval, 1.5−4.1; P<.001). Four uterine perforations (2% of patients) occurred in the OR group.
Mean pain scores were higher in the clinic group, and treatment was unacceptable for 2% of the women in each group.
The results of this trial show that clinic polypectomy has some limitations, but the outpatient procedure was deemed noninferior to polypectomy performed in the OR for the successful alleviation of uterine bleeding associated with uterine polyps.
What this EVIDENCE means for practice
Office-based polypectomy allowed a “see and treat” model in 72% of cases. Office polypectomy had similar successful therapeutic responses as inpatient polypectomy; however, over a 2-year follow-up period, women treated in the office were twice as likely to undergo at least 1 further polyp removal and were 1.6 times more likely to have further gynecologic surgery.
In-office hysteroscopic morcellation of polyps and myomas improves health-related quality of life
Rubino RJ, Lukes AS. Twelve-month outcomes for patients undergoing hysteroscopic morcellation of uterine polyps and myomas in an office or ambulatory surgical center. J Minim Invasive Gynecol. 2015;22(2):285–290.
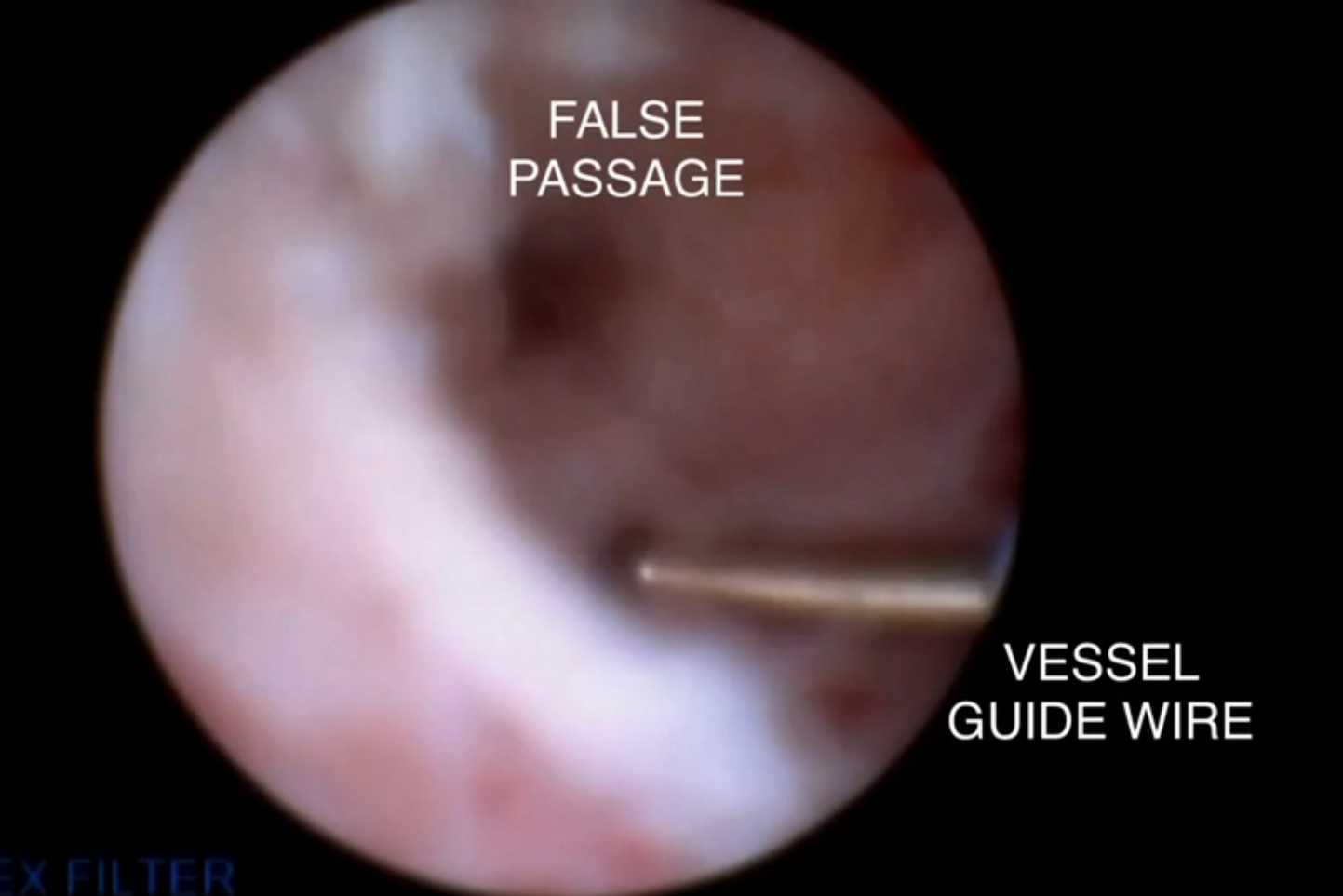
Is it feasible to morcellate fibroids, as well as polyps, in the clinic? Rubino and colleagues investigated this question in a randomized, prospective clinical trial. They examined the efficacy of hysteroscopic removal of polyps and myomas on health-related quality of life and symptom severity at 1-year postprocedure. Women aged 18 to 55 years, with hysteroscopic and saline-infusion sonogram–assessed polyps and/or type 0 or I myomas (1.5−3.0 cm), were enrolled from 9 US clinical sites. Some patient populations were excluded, such as women with a long narcotic abuse history, current intrauterine device (IUD), type II submucous myomas, and type I fundal myomas.
A total of 118 pathologies were removed in 74 patients. Forty-two women were treated in the office setting; 32 were treated in the OR setting. Among the 118 pathologies removed, 53 were removed in the office (28 myomas and 25 polyps), and 55 were removed in the OR (14 myomas and 41 polyps).
The percentage of patients who reported being satisfied or highly satisfied was higher in the OR cohort (96.5%) compared with the office cohort (83.3%), although this difference was not statistically significant (P = .06). The percentage of patients who had 100% of their pathology removed was significantly higher in those with polyps compared with patients with myomas (96.0% vs 63.6%, respectively; P<.01).
These findings indicate that there were several cases in which the majority of a myoma was removed but a small residual portion remained. This disparity was especially pronounced in the office setting, where 96% of polyps were completely removed, compared with 52% of fibroids. There was no statistically significant difference in health-related quality of life between patients with complete removal and those with residual pathology, and there was no difference in satisfaction rates between patients who were treated in the office and those treated in the OR.
What this EVIDENCE means for practice
In general, office-based hysteroscopic myomectomy and polypectomy using morcellation for small- to medium-size lesions was associated with low rates of adverse events, high physician acceptance, and significant durable health-related quality-of-life improvements for up to 12 months post‑ procedure. Partial removal of myomas did not seem to be a significant factor in patients’ perceived outcomes.
Endometrial ablation for AUB costs less, has fewer complications at 1 year than hysterectomy
Miller JD, Lenhart GM, Bonafede MM, Lukes AS, Laughlin-Tommaso SK. Cost-effectiveness of global endometrial ablation vs hysterectomy for treatment of abnormal uterine bleeding: US commercial and Medicaid payer perspectives. Popul Health Manag. 2015;18(5):373–382.
Endometrial ablation often is performed in the office for AUB management. Miller and colleagues suggested that cost-effectiveness modeling studies of endometrial ablation for AUB treatment from a US perspective are lacking. They therefore designed a study to model the cost-effectiveness of endometrial ablation versus hysterectomy for treatment of AUB from both commercial and Medicaid payer perspectives.
They developed a decision-tree, state-transition (semi-Markov) model to simulate 2 hypothetical patient cohorts of women with AUB: one treated with endometrial ablation and the other with hysterectomy. Twenty-one health states were included in the model of intervention with endometrial ablation or hysterectomy; these comprised postablation reintervention with secondary ablation, tranexamic acid, or a levonorgestrel-containing IUD due to AUB, use of adjunctive pharmacotherapy following ablation, and a small probability of death from hysterectomy or actuarial death from all other causes.
The 1-year direct costs of endometrial ablation were $7,352 and $6,306 in the commercial payer and Medicaid payer perspectives, respectively; these were about half the costs of hysterectomy. The cost differential between the 2 treatments narrowed over time but, even at 5 years, endometrial ablation costs were still one-third less than hysterectomy costs.
In the first year, 35.6% of patients who had a hysterectomy and only 17.1% of patients undergoing ablation had complications. Short-term results were similar under the Medicaid perspective. By 5 years intervention/reintervention, however, complications of endometrial ablation were higher than those for hysterectomy by about 1.6%.
Over a 5-year time frame, direct costs of endometrial ablation were lower than those of hysterectomy from both the commercial payer and Medicaid perspectives. In the commercial payer analysis, the indirect costs of endometrial ablation were also lower than for hysterectomy, with 38.5 workdays lost for endometrial ablation compared with 55.3 days lost for hysterectomy, resulting in indirect costs of $8,976 versus $13,087.
What this EVIDENCE means for practice
Costs and cost-effectiveness of endometrial ablation from a US perspective are understudied. This model estimates a financial advantage for endometrial ablation over hysterectomy from both the commercial payer and Medicaid payer perspectives. Over a variety of time frames, endometrial ablation may save costs while reducing treatment complications and lost workdays. From the patient perspective, this model suggests better quality of life in the short term after endometrial ablation. It will be interesting to see whether longer term impacts show this model to be predictive.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Reference
- Liu Z, Doan QV, Blumenthal P, Dubois RW. A systematic review evaluating health-related quality of life, work impairment, and healthcare costs and utilization in abnormal uterine bleeding. Value Health. 2007;10(3):183–194.
How abnormal uterine bleeding (AUB) is managed has a significant impact on health care. In the United States, almost one-third of all gynecologic visits are related to AUB, with estimated annual direct costs of up to $1.55 billion and indirect costs as high as $36 billion.1 Not surprisingly, office-based procedures for AUB are being emphasized. While in the short term it is more cost efficient to perform surgery in the office rather than in the operating room, questions have arisen regarding the long-term efficacy and durability of in-office procedures. Insurers are undoubtedly raising these questions as well.
Notably, some ObGyns are early adopters of office-based surgery while others tend to adopt in-office procedures more slowly. As the literature for such procedures for AUB matures to provide more data on efficacy and acceptability, we will have a greater evidence base for understanding which procedures are more appropriate for the office. And while practice shifts sometimes occur due to cost-containment initiatives, some shifts are patient driven. Studies that address these driving variables, as well as efficacy considerations, are helpful. As we counsel women about procedures for AUB, the relative advantages and disadvantages of available treatment settings likely will become a greater part of that discussion so that they can make an informed decision.
In this Update, we discuss the results of 3 studies that examined various procedures and settings for AUB management:
- outpatient vs inpatient polypectomy
- hysteroscopic morcellation of polyps and myomas in an office vs ambulatory surgical center
- comparative costs of endometrial ablation and hysterectomy.
Outpatient vs inpatient polypectomy: Similar success rates in the short term
Cooper NA, Clark TJ, Middleton L, et al; OPT Trial Collaborative Group. Outpatient versus inpatient uterine polyp treatment for abnormal uterine bleeding: randomised controlled non-inferiority study. BMJ. 2015;350:h1398. doi:10.1136/bmj.h1398.
A collaborative group in the United Kingdom studied the common problem of endometrial polyps. Their objective was to evaluate whether outpatient polypectomy was as effective and well accepted as polypectomy performed in the operating room (OR).
Patients with a hysteroscopically diagnosed polyp were randomly assigned to hysteroscopic polyp removal in either a hysteroscopy clinic or an OR; polyp removal was performed using miniature mechanical or electrosurgical instruments. The primary outcome was successful treatment, determined by the participants’ assessment of their bleeding at 6 months.
Overall, 73% of women (166 of 228) in the clinic group and 80% (168 of 211) in the OR group reported a successful response to surgery at 6 months, with treatment effects being maintained at 12 and 24 months. A “see and treat” approach—that is, treatment carried out at the same time as diagnosis—was possible in 72% of women (174 of 242).
Partial or failed polyp removal occurred in 46 of 242 women (19%) in the clinic group, mostly because of pain issues, and in 18 of 233 women (7%) in the OR group (relative risk, 2.5; 95% confidence interval, 1.5−4.1; P<.001). Four uterine perforations (2% of patients) occurred in the OR group.
Mean pain scores were higher in the clinic group, and treatment was unacceptable for 2% of the women in each group.
The results of this trial show that clinic polypectomy has some limitations, but the outpatient procedure was deemed noninferior to polypectomy performed in the OR for the successful alleviation of uterine bleeding associated with uterine polyps.
What this EVIDENCE means for practice
Office-based polypectomy allowed a “see and treat” model in 72% of cases. Office polypectomy had similar successful therapeutic responses as inpatient polypectomy; however, over a 2-year follow-up period, women treated in the office were twice as likely to undergo at least 1 further polyp removal and were 1.6 times more likely to have further gynecologic surgery.
In-office hysteroscopic morcellation of polyps and myomas improves health-related quality of life
Rubino RJ, Lukes AS. Twelve-month outcomes for patients undergoing hysteroscopic morcellation of uterine polyps and myomas in an office or ambulatory surgical center. J Minim Invasive Gynecol. 2015;22(2):285–290.
Is it feasible to morcellate fibroids, as well as polyps, in the clinic? Rubino and colleagues investigated this question in a randomized, prospective clinical trial. They examined the efficacy of hysteroscopic removal of polyps and myomas on health-related quality of life and symptom severity at 1-year postprocedure. Women aged 18 to 55 years, with hysteroscopic and saline-infusion sonogram–assessed polyps and/or type 0 or I myomas (1.5−3.0 cm), were enrolled from 9 US clinical sites. Some patient populations were excluded, such as women with a long narcotic abuse history, current intrauterine device (IUD), type II submucous myomas, and type I fundal myomas.
A total of 118 pathologies were removed in 74 patients. Forty-two women were treated in the office setting; 32 were treated in the OR setting. Among the 118 pathologies removed, 53 were removed in the office (28 myomas and 25 polyps), and 55 were removed in the OR (14 myomas and 41 polyps).
The percentage of patients who reported being satisfied or highly satisfied was higher in the OR cohort (96.5%) compared with the office cohort (83.3%), although this difference was not statistically significant (P = .06). The percentage of patients who had 100% of their pathology removed was significantly higher in those with polyps compared with patients with myomas (96.0% vs 63.6%, respectively; P<.01).
These findings indicate that there were several cases in which the majority of a myoma was removed but a small residual portion remained. This disparity was especially pronounced in the office setting, where 96% of polyps were completely removed, compared with 52% of fibroids. There was no statistically significant difference in health-related quality of life between patients with complete removal and those with residual pathology, and there was no difference in satisfaction rates between patients who were treated in the office and those treated in the OR.
What this EVIDENCE means for practice
In general, office-based hysteroscopic myomectomy and polypectomy using morcellation for small- to medium-size lesions was associated with low rates of adverse events, high physician acceptance, and significant durable health-related quality-of-life improvements for up to 12 months post‑ procedure. Partial removal of myomas did not seem to be a significant factor in patients’ perceived outcomes.
Endometrial ablation for AUB costs less, has fewer complications at 1 year than hysterectomy
Miller JD, Lenhart GM, Bonafede MM, Lukes AS, Laughlin-Tommaso SK. Cost-effectiveness of global endometrial ablation vs hysterectomy for treatment of abnormal uterine bleeding: US commercial and Medicaid payer perspectives. Popul Health Manag. 2015;18(5):373–382.
Endometrial ablation often is performed in the office for AUB management. Miller and colleagues suggested that cost-effectiveness modeling studies of endometrial ablation for AUB treatment from a US perspective are lacking. They therefore designed a study to model the cost-effectiveness of endometrial ablation versus hysterectomy for treatment of AUB from both commercial and Medicaid payer perspectives.
They developed a decision-tree, state-transition (semi-Markov) model to simulate 2 hypothetical patient cohorts of women with AUB: one treated with endometrial ablation and the other with hysterectomy. Twenty-one health states were included in the model of intervention with endometrial ablation or hysterectomy; these comprised postablation reintervention with secondary ablation, tranexamic acid, or a levonorgestrel-containing IUD due to AUB, use of adjunctive pharmacotherapy following ablation, and a small probability of death from hysterectomy or actuarial death from all other causes.
The 1-year direct costs of endometrial ablation were $7,352 and $6,306 in the commercial payer and Medicaid payer perspectives, respectively; these were about half the costs of hysterectomy. The cost differential between the 2 treatments narrowed over time but, even at 5 years, endometrial ablation costs were still one-third less than hysterectomy costs.
In the first year, 35.6% of patients who had a hysterectomy and only 17.1% of patients undergoing ablation had complications. Short-term results were similar under the Medicaid perspective. By 5 years intervention/reintervention, however, complications of endometrial ablation were higher than those for hysterectomy by about 1.6%.
Over a 5-year time frame, direct costs of endometrial ablation were lower than those of hysterectomy from both the commercial payer and Medicaid perspectives. In the commercial payer analysis, the indirect costs of endometrial ablation were also lower than for hysterectomy, with 38.5 workdays lost for endometrial ablation compared with 55.3 days lost for hysterectomy, resulting in indirect costs of $8,976 versus $13,087.
What this EVIDENCE means for practice
Costs and cost-effectiveness of endometrial ablation from a US perspective are understudied. This model estimates a financial advantage for endometrial ablation over hysterectomy from both the commercial payer and Medicaid payer perspectives. Over a variety of time frames, endometrial ablation may save costs while reducing treatment complications and lost workdays. From the patient perspective, this model suggests better quality of life in the short term after endometrial ablation. It will be interesting to see whether longer term impacts show this model to be predictive.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
How abnormal uterine bleeding (AUB) is managed has a significant impact on health care. In the United States, almost one-third of all gynecologic visits are related to AUB, with estimated annual direct costs of up to $1.55 billion and indirect costs as high as $36 billion.1 Not surprisingly, office-based procedures for AUB are being emphasized. While in the short term it is more cost efficient to perform surgery in the office rather than in the operating room, questions have arisen regarding the long-term efficacy and durability of in-office procedures. Insurers are undoubtedly raising these questions as well.
Notably, some ObGyns are early adopters of office-based surgery while others tend to adopt in-office procedures more slowly. As the literature for such procedures for AUB matures to provide more data on efficacy and acceptability, we will have a greater evidence base for understanding which procedures are more appropriate for the office. And while practice shifts sometimes occur due to cost-containment initiatives, some shifts are patient driven. Studies that address these driving variables, as well as efficacy considerations, are helpful. As we counsel women about procedures for AUB, the relative advantages and disadvantages of available treatment settings likely will become a greater part of that discussion so that they can make an informed decision.
In this Update, we discuss the results of 3 studies that examined various procedures and settings for AUB management:
- outpatient vs inpatient polypectomy
- hysteroscopic morcellation of polyps and myomas in an office vs ambulatory surgical center
- comparative costs of endometrial ablation and hysterectomy.
Outpatient vs inpatient polypectomy: Similar success rates in the short term
Cooper NA, Clark TJ, Middleton L, et al; OPT Trial Collaborative Group. Outpatient versus inpatient uterine polyp treatment for abnormal uterine bleeding: randomised controlled non-inferiority study. BMJ. 2015;350:h1398. doi:10.1136/bmj.h1398.
A collaborative group in the United Kingdom studied the common problem of endometrial polyps. Their objective was to evaluate whether outpatient polypectomy was as effective and well accepted as polypectomy performed in the operating room (OR).
Patients with a hysteroscopically diagnosed polyp were randomly assigned to hysteroscopic polyp removal in either a hysteroscopy clinic or an OR; polyp removal was performed using miniature mechanical or electrosurgical instruments. The primary outcome was successful treatment, determined by the participants’ assessment of their bleeding at 6 months.
Overall, 73% of women (166 of 228) in the clinic group and 80% (168 of 211) in the OR group reported a successful response to surgery at 6 months, with treatment effects being maintained at 12 and 24 months. A “see and treat” approach—that is, treatment carried out at the same time as diagnosis—was possible in 72% of women (174 of 242).
Partial or failed polyp removal occurred in 46 of 242 women (19%) in the clinic group, mostly because of pain issues, and in 18 of 233 women (7%) in the OR group (relative risk, 2.5; 95% confidence interval, 1.5−4.1; P<.001). Four uterine perforations (2% of patients) occurred in the OR group.
Mean pain scores were higher in the clinic group, and treatment was unacceptable for 2% of the women in each group.
The results of this trial show that clinic polypectomy has some limitations, but the outpatient procedure was deemed noninferior to polypectomy performed in the OR for the successful alleviation of uterine bleeding associated with uterine polyps.
What this EVIDENCE means for practice
Office-based polypectomy allowed a “see and treat” model in 72% of cases. Office polypectomy had similar successful therapeutic responses as inpatient polypectomy; however, over a 2-year follow-up period, women treated in the office were twice as likely to undergo at least 1 further polyp removal and were 1.6 times more likely to have further gynecologic surgery.
In-office hysteroscopic morcellation of polyps and myomas improves health-related quality of life
Rubino RJ, Lukes AS. Twelve-month outcomes for patients undergoing hysteroscopic morcellation of uterine polyps and myomas in an office or ambulatory surgical center. J Minim Invasive Gynecol. 2015;22(2):285–290.
Is it feasible to morcellate fibroids, as well as polyps, in the clinic? Rubino and colleagues investigated this question in a randomized, prospective clinical trial. They examined the efficacy of hysteroscopic removal of polyps and myomas on health-related quality of life and symptom severity at 1-year postprocedure. Women aged 18 to 55 years, with hysteroscopic and saline-infusion sonogram–assessed polyps and/or type 0 or I myomas (1.5−3.0 cm), were enrolled from 9 US clinical sites. Some patient populations were excluded, such as women with a long narcotic abuse history, current intrauterine device (IUD), type II submucous myomas, and type I fundal myomas.
A total of 118 pathologies were removed in 74 patients. Forty-two women were treated in the office setting; 32 were treated in the OR setting. Among the 118 pathologies removed, 53 were removed in the office (28 myomas and 25 polyps), and 55 were removed in the OR (14 myomas and 41 polyps).
The percentage of patients who reported being satisfied or highly satisfied was higher in the OR cohort (96.5%) compared with the office cohort (83.3%), although this difference was not statistically significant (P = .06). The percentage of patients who had 100% of their pathology removed was significantly higher in those with polyps compared with patients with myomas (96.0% vs 63.6%, respectively; P<.01).
These findings indicate that there were several cases in which the majority of a myoma was removed but a small residual portion remained. This disparity was especially pronounced in the office setting, where 96% of polyps were completely removed, compared with 52% of fibroids. There was no statistically significant difference in health-related quality of life between patients with complete removal and those with residual pathology, and there was no difference in satisfaction rates between patients who were treated in the office and those treated in the OR.
What this EVIDENCE means for practice
In general, office-based hysteroscopic myomectomy and polypectomy using morcellation for small- to medium-size lesions was associated with low rates of adverse events, high physician acceptance, and significant durable health-related quality-of-life improvements for up to 12 months post‑ procedure. Partial removal of myomas did not seem to be a significant factor in patients’ perceived outcomes.
Endometrial ablation for AUB costs less, has fewer complications at 1 year than hysterectomy
Miller JD, Lenhart GM, Bonafede MM, Lukes AS, Laughlin-Tommaso SK. Cost-effectiveness of global endometrial ablation vs hysterectomy for treatment of abnormal uterine bleeding: US commercial and Medicaid payer perspectives. Popul Health Manag. 2015;18(5):373–382.
Endometrial ablation often is performed in the office for AUB management. Miller and colleagues suggested that cost-effectiveness modeling studies of endometrial ablation for AUB treatment from a US perspective are lacking. They therefore designed a study to model the cost-effectiveness of endometrial ablation versus hysterectomy for treatment of AUB from both commercial and Medicaid payer perspectives.
They developed a decision-tree, state-transition (semi-Markov) model to simulate 2 hypothetical patient cohorts of women with AUB: one treated with endometrial ablation and the other with hysterectomy. Twenty-one health states were included in the model of intervention with endometrial ablation or hysterectomy; these comprised postablation reintervention with secondary ablation, tranexamic acid, or a levonorgestrel-containing IUD due to AUB, use of adjunctive pharmacotherapy following ablation, and a small probability of death from hysterectomy or actuarial death from all other causes.
The 1-year direct costs of endometrial ablation were $7,352 and $6,306 in the commercial payer and Medicaid payer perspectives, respectively; these were about half the costs of hysterectomy. The cost differential between the 2 treatments narrowed over time but, even at 5 years, endometrial ablation costs were still one-third less than hysterectomy costs.
In the first year, 35.6% of patients who had a hysterectomy and only 17.1% of patients undergoing ablation had complications. Short-term results were similar under the Medicaid perspective. By 5 years intervention/reintervention, however, complications of endometrial ablation were higher than those for hysterectomy by about 1.6%.
Over a 5-year time frame, direct costs of endometrial ablation were lower than those of hysterectomy from both the commercial payer and Medicaid perspectives. In the commercial payer analysis, the indirect costs of endometrial ablation were also lower than for hysterectomy, with 38.5 workdays lost for endometrial ablation compared with 55.3 days lost for hysterectomy, resulting in indirect costs of $8,976 versus $13,087.
What this EVIDENCE means for practice
Costs and cost-effectiveness of endometrial ablation from a US perspective are understudied. This model estimates a financial advantage for endometrial ablation over hysterectomy from both the commercial payer and Medicaid payer perspectives. Over a variety of time frames, endometrial ablation may save costs while reducing treatment complications and lost workdays. From the patient perspective, this model suggests better quality of life in the short term after endometrial ablation. It will be interesting to see whether longer term impacts show this model to be predictive.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Reference
- Liu Z, Doan QV, Blumenthal P, Dubois RW. A systematic review evaluating health-related quality of life, work impairment, and healthcare costs and utilization in abnormal uterine bleeding. Value Health. 2007;10(3):183–194.
Reference
- Liu Z, Doan QV, Blumenthal P, Dubois RW. A systematic review evaluating health-related quality of life, work impairment, and healthcare costs and utilization in abnormal uterine bleeding. Value Health. 2007;10(3):183–194.
IN THIS ARTICLE
- Polypectomy in the clinic vs OR
- In-office polyp, fibroid morcellation
- Cost-effectiveness of endometrial ablation
Antibiotic-resistant infections remain a persistent threat
One in every seven infections in acute care hospitals related to catheters and surgeries was caused by antibiotic-resistant bacteria. In long-term acute care hospitals, that number increased to one in four.
Those are key findings from a study published March 3 in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report that is the first to combine national data on antibiotic-resistant (AR) bacteria threats with progress on health care–associated infections (HAIs).
“Antibiotic resistance threatens to return us to a time when a simple infection could kill,” CDC Director Thomas Frieden said during a March 3 telebriefing. “The more people who get infected with resistant bacteria, the more people who suffer complications, the more who, tragically, may die from preventable infections. On any given day about one in 25 hospitalized patients has at least one health care–associated infection that they didn’t come in with. No one should get sick when they’re trying to get well.”
For the study, researchers led by Dr. Clifford McDonald of the CDC’s Division of Healthcare Quality Promotion, collected data on specific infections that were reported to the National Healthcare Safety Network in 2014 by approximately 4,000 short-term acute care hospitals, 501 long-term acute care hospitals, and 1,135 inpatient rehabilitation facilities in all 50 states (MMWR. 2016 Mar 3. doi: 10.15585/mmwr.mm6509e1er). Next, they determined the proportions of AR pathogens and HAIs caused by any of six resistant bacteria highlighted by the CDC in 2013 as urgent or serious threats: CRE (carbapenem-resistant Enterobacteriaceae), MRSA (methicillin-resistant Staphylococcus aureus), ESBL-producing Enterobacteriaceae (extended-spectrum beta-lactamases), VRE (vancomycin-resistant enterococci), multidrug-resistant pseudomonas, and multidrug-resistant Acinetobacter.
The researchers found that, compared with historical data from 5-8 years earlier, central line–associated bloodstream infections decreased by 50% and surgical site infections (SSIs) by 17% in 2014.
“There is encouraging news here,” Dr. Frieden said. “Doctors, nurses, hospitals, health care systems and other partners have made progress preventing some health care–associated infections.” However, the study found that one in six remaining central line-associated bloodstream infections were caused by urgent or serious antibiotic-resistant bacteria, while one in seven remaining surgical site infections were caused by urgent or serious antibiotic-resistant bacteria.
While catheter-associated urinary tract infections appear unchanged from baseline, there have been recent decreases, according to the study. In addition, C. difficile infections in hospitals decreased 8% between 2011 and 2014.
Dr. McDonald and his associates determined that in 2014, one in seven infections in acute care hospitals related to catheters and surgeries was caused by one of the six antibiotic-resistance threat bacteria, “which is deeply concerning,” Dr. Frieden said. That number increased to one in four infections in long-term acute care hospitals, a proportion that he characterized as “chilling.”
The CDC recommends three strategies that doctors, nurses, and other health care providers should take with every patient, to prevent HAIs and stop the spread of antibiotic resistance:
• Prevent the spread of bacteria between patients. Dr. Peter Pronovost, who participated in the telebriefing, said that he and his associates at Johns Hopkins University in Baltimore “do this by practicing good hand hygiene techniques by wearing sterile equipment when inserting lines.”
• Prevent surgery-related infections and/or placement of a catheter. “Check catheters frequently and remove them when you no longer need them,” advised Dr. Pronovost, director of the Armstrong Institute for Patient Safety and Quality at Johns Hopkins. “Ask if you actually need them before you even place them.”
• Improve antibiotic use through stewardship. This means using “the right antibiotics for the right duration,” Dr. Pronovost said. “Antibiotics could be lifesaving and are necessary for critically ill patients, especially those with septic shock. But these antibiotics need to be adjusted based on lab results and new information about the organisms that are causing these infections. Forty-eight hours after antibiotics are initiated, take a ‘time out.’ Perform a brief but focused assessment to determine if antibiotic therapy is still needed, or if it should be refined. A common mistake we make is to continue vancomycin when there is no presence of MRSA. We often tell our staff at Johns Hopkins, ‘if it doesn’t grow, let it go.’ ”
Dr. Frieden concluded his remarks by noting that physicians and other clinicians on the front lines “need support of their facility leadership,” to prevent HAIs. “Health care facilities, CEOs, and administrators are a major part of the solution. It’s important that they make a priority of infection prevention, sepsis prevention, and antibiotic stewardship. Know your facility’s data and target prevention efforts to ensure improvements in patient safety.”
One in every seven infections in acute care hospitals related to catheters and surgeries was caused by antibiotic-resistant bacteria. In long-term acute care hospitals, that number increased to one in four.
Those are key findings from a study published March 3 in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report that is the first to combine national data on antibiotic-resistant (AR) bacteria threats with progress on health care–associated infections (HAIs).
“Antibiotic resistance threatens to return us to a time when a simple infection could kill,” CDC Director Thomas Frieden said during a March 3 telebriefing. “The more people who get infected with resistant bacteria, the more people who suffer complications, the more who, tragically, may die from preventable infections. On any given day about one in 25 hospitalized patients has at least one health care–associated infection that they didn’t come in with. No one should get sick when they’re trying to get well.”
For the study, researchers led by Dr. Clifford McDonald of the CDC’s Division of Healthcare Quality Promotion, collected data on specific infections that were reported to the National Healthcare Safety Network in 2014 by approximately 4,000 short-term acute care hospitals, 501 long-term acute care hospitals, and 1,135 inpatient rehabilitation facilities in all 50 states (MMWR. 2016 Mar 3. doi: 10.15585/mmwr.mm6509e1er). Next, they determined the proportions of AR pathogens and HAIs caused by any of six resistant bacteria highlighted by the CDC in 2013 as urgent or serious threats: CRE (carbapenem-resistant Enterobacteriaceae), MRSA (methicillin-resistant Staphylococcus aureus), ESBL-producing Enterobacteriaceae (extended-spectrum beta-lactamases), VRE (vancomycin-resistant enterococci), multidrug-resistant pseudomonas, and multidrug-resistant Acinetobacter.
The researchers found that, compared with historical data from 5-8 years earlier, central line–associated bloodstream infections decreased by 50% and surgical site infections (SSIs) by 17% in 2014.
“There is encouraging news here,” Dr. Frieden said. “Doctors, nurses, hospitals, health care systems and other partners have made progress preventing some health care–associated infections.” However, the study found that one in six remaining central line-associated bloodstream infections were caused by urgent or serious antibiotic-resistant bacteria, while one in seven remaining surgical site infections were caused by urgent or serious antibiotic-resistant bacteria.
While catheter-associated urinary tract infections appear unchanged from baseline, there have been recent decreases, according to the study. In addition, C. difficile infections in hospitals decreased 8% between 2011 and 2014.
Dr. McDonald and his associates determined that in 2014, one in seven infections in acute care hospitals related to catheters and surgeries was caused by one of the six antibiotic-resistance threat bacteria, “which is deeply concerning,” Dr. Frieden said. That number increased to one in four infections in long-term acute care hospitals, a proportion that he characterized as “chilling.”
The CDC recommends three strategies that doctors, nurses, and other health care providers should take with every patient, to prevent HAIs and stop the spread of antibiotic resistance:
• Prevent the spread of bacteria between patients. Dr. Peter Pronovost, who participated in the telebriefing, said that he and his associates at Johns Hopkins University in Baltimore “do this by practicing good hand hygiene techniques by wearing sterile equipment when inserting lines.”
• Prevent surgery-related infections and/or placement of a catheter. “Check catheters frequently and remove them when you no longer need them,” advised Dr. Pronovost, director of the Armstrong Institute for Patient Safety and Quality at Johns Hopkins. “Ask if you actually need them before you even place them.”
• Improve antibiotic use through stewardship. This means using “the right antibiotics for the right duration,” Dr. Pronovost said. “Antibiotics could be lifesaving and are necessary for critically ill patients, especially those with septic shock. But these antibiotics need to be adjusted based on lab results and new information about the organisms that are causing these infections. Forty-eight hours after antibiotics are initiated, take a ‘time out.’ Perform a brief but focused assessment to determine if antibiotic therapy is still needed, or if it should be refined. A common mistake we make is to continue vancomycin when there is no presence of MRSA. We often tell our staff at Johns Hopkins, ‘if it doesn’t grow, let it go.’ ”
Dr. Frieden concluded his remarks by noting that physicians and other clinicians on the front lines “need support of their facility leadership,” to prevent HAIs. “Health care facilities, CEOs, and administrators are a major part of the solution. It’s important that they make a priority of infection prevention, sepsis prevention, and antibiotic stewardship. Know your facility’s data and target prevention efforts to ensure improvements in patient safety.”
One in every seven infections in acute care hospitals related to catheters and surgeries was caused by antibiotic-resistant bacteria. In long-term acute care hospitals, that number increased to one in four.
Those are key findings from a study published March 3 in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report that is the first to combine national data on antibiotic-resistant (AR) bacteria threats with progress on health care–associated infections (HAIs).
“Antibiotic resistance threatens to return us to a time when a simple infection could kill,” CDC Director Thomas Frieden said during a March 3 telebriefing. “The more people who get infected with resistant bacteria, the more people who suffer complications, the more who, tragically, may die from preventable infections. On any given day about one in 25 hospitalized patients has at least one health care–associated infection that they didn’t come in with. No one should get sick when they’re trying to get well.”
For the study, researchers led by Dr. Clifford McDonald of the CDC’s Division of Healthcare Quality Promotion, collected data on specific infections that were reported to the National Healthcare Safety Network in 2014 by approximately 4,000 short-term acute care hospitals, 501 long-term acute care hospitals, and 1,135 inpatient rehabilitation facilities in all 50 states (MMWR. 2016 Mar 3. doi: 10.15585/mmwr.mm6509e1er). Next, they determined the proportions of AR pathogens and HAIs caused by any of six resistant bacteria highlighted by the CDC in 2013 as urgent or serious threats: CRE (carbapenem-resistant Enterobacteriaceae), MRSA (methicillin-resistant Staphylococcus aureus), ESBL-producing Enterobacteriaceae (extended-spectrum beta-lactamases), VRE (vancomycin-resistant enterococci), multidrug-resistant pseudomonas, and multidrug-resistant Acinetobacter.
The researchers found that, compared with historical data from 5-8 years earlier, central line–associated bloodstream infections decreased by 50% and surgical site infections (SSIs) by 17% in 2014.
“There is encouraging news here,” Dr. Frieden said. “Doctors, nurses, hospitals, health care systems and other partners have made progress preventing some health care–associated infections.” However, the study found that one in six remaining central line-associated bloodstream infections were caused by urgent or serious antibiotic-resistant bacteria, while one in seven remaining surgical site infections were caused by urgent or serious antibiotic-resistant bacteria.
While catheter-associated urinary tract infections appear unchanged from baseline, there have been recent decreases, according to the study. In addition, C. difficile infections in hospitals decreased 8% between 2011 and 2014.
Dr. McDonald and his associates determined that in 2014, one in seven infections in acute care hospitals related to catheters and surgeries was caused by one of the six antibiotic-resistance threat bacteria, “which is deeply concerning,” Dr. Frieden said. That number increased to one in four infections in long-term acute care hospitals, a proportion that he characterized as “chilling.”
The CDC recommends three strategies that doctors, nurses, and other health care providers should take with every patient, to prevent HAIs and stop the spread of antibiotic resistance:
• Prevent the spread of bacteria between patients. Dr. Peter Pronovost, who participated in the telebriefing, said that he and his associates at Johns Hopkins University in Baltimore “do this by practicing good hand hygiene techniques by wearing sterile equipment when inserting lines.”
• Prevent surgery-related infections and/or placement of a catheter. “Check catheters frequently and remove them when you no longer need them,” advised Dr. Pronovost, director of the Armstrong Institute for Patient Safety and Quality at Johns Hopkins. “Ask if you actually need them before you even place them.”
• Improve antibiotic use through stewardship. This means using “the right antibiotics for the right duration,” Dr. Pronovost said. “Antibiotics could be lifesaving and are necessary for critically ill patients, especially those with septic shock. But these antibiotics need to be adjusted based on lab results and new information about the organisms that are causing these infections. Forty-eight hours after antibiotics are initiated, take a ‘time out.’ Perform a brief but focused assessment to determine if antibiotic therapy is still needed, or if it should be refined. A common mistake we make is to continue vancomycin when there is no presence of MRSA. We often tell our staff at Johns Hopkins, ‘if it doesn’t grow, let it go.’ ”
Dr. Frieden concluded his remarks by noting that physicians and other clinicians on the front lines “need support of their facility leadership,” to prevent HAIs. “Health care facilities, CEOs, and administrators are a major part of the solution. It’s important that they make a priority of infection prevention, sepsis prevention, and antibiotic stewardship. Know your facility’s data and target prevention efforts to ensure improvements in patient safety.”
FROM MMWR
Chronic pain among surgeons needs to be addressed
Within the community of surgeons, chronic pain is a four-letter word, spoken about in hushed tones – if it’s spoken about at all, that is – and rarely ever discussed as something that urgently needs to be addressed.
But surgeons are susceptible to the same chronic conditions as are the patients they treat. In addition to the fatigue associated with conducting long, grueling surgical operations, surgeons can experience repetitive motion injury from using laparoscopic tools for minimally invasive procedures – injuries that can, if left untreated, lead to long-term consequences.
“There have been a few studies on this, but I think we’re just scratching the surface,” explained Dr. Adrian Park, chair of surgery at the Anne Arundel Medical Center in Annapolis, Md. Dr. Park was the lead author of a 2010 study that identified chronic pain among surgeons as a serious and underreported issue within medicine.
That study, which evaluated 317 surgeons using a 23-question survey, found that 86.9% of surgeons experience “physical symptoms or discomfort,” with the most significant indicator of such symptoms being a high case load. Subsequent studies from Europe and eastern Asia also found rates of 80% or higher among surgeons in those regions of the world.
With so pervasive a problem, however, the relative paucity of data and conversation among medical professionals is alarming. “As a surgeon leader, I can tell you surgeons complain about a lot of stuff, but one of the things they tend not to complain about is themselves and their own health and well-being,” said Dr. Park.
The reasons for that, Dr. Park explained, are plentiful. Most surgeons simply don’t find it acceptable to speak up about any pain they’re experiencing, while “some may have felt it was a sign of weakness to report these injuries, some may have felt it would affect their referral base and their work,” according to Dr. Park.
To that end, Dr. Mario Cerame is well aware of what a seemingly innocuous, relatively small chronic pain can do to a surgeon. A surgeon in North Carolina, Dr. Cerame began to experience symptoms of repetitive motion injury about 2 years ago, symptoms which he says “crept up on me.”
It began as simply numbness at the tips of his fingers, affecting the way he held laparoscopic tools during surgery and other, more menial, daily tasks. Initially suspecting it was carpel tunnel syndrome, Dr. Cerame brushed it off, until the numbness spread to three whole fingers and, eventually, his entire hand. His physician explained what was happening, instructing him that if he didn’t undergo orthopedic surgery immediately, he ran the risk of becoming quadriplegic.
“I got the diagnosis on Thursday, and had the operation on Tuesday,” said Dr. Cerame, explaining that the diagnosis was spinal stenosis. Two areas of his spinal column were pinching inward, causing the slow but steady paralysis he was experiencing. With physical therapy, Dr. Cerame could have some function back within 2 years of the operation – so far, it’s been just over 16 months. The point of the operation, however, was to prevent further damage and paralysis, not necessarily to restore Dr. Cerame’s motor function to 100%.
Dr. Cerame’s story, however, isn’t what usually happens. Because surgeons generally keep things to themselves, they have to find other ways of coping with chronic pain. Some choose noninvasive options: massages, physical therapy, and so on. Other do choose to go under the knife, but such surgeries don’t provide a permanent solution to the problem. With laparoscopic tools becoming increasingly ergonomic, and monitors allowing surgeons not to keep their heads bent at an angle for hours on end during surgery, things are improving – but more can be done.
“I’ve published an awful lot of papers, but the thing that struck me about [the 2010] paper is the response I got,” said Dr. Parks. “Surgeons, literally from around the country, would call me saying ‘I used to be able to do this operation, I no longer can do that,’ or ‘this used to be what my case list looked like, I can no longer do this, you can use me as an example.’ People came forward.”
Then there’s the darker side of coping with chronic pain: substance abuse. Tight-lipped surgeons who won’t talk about pain certainly won’t talk openly about using painkillers or narcotics to ease their muscle aches or joint stiffness, but with physicians having relatively easy access to such products, could substance abuse among surgeons be a problem?
“When livelihoods are at stake, I think folks will take opportunities to stay in the game,” admitted Dr. Parks, adding that “it’s not something that folks advertise, but in anonymous surveys [surgeons] respond amazingly to stuff like this.”
The bottom line, according to both Dr. Parks and Dr. Cerame, is for surgeons not to keep quiet about these issues if they ever do experience them. Asking for help and getting things checked right away is better, not only for a surgeon, but for his family and patients, too. While Dr. Cerame has gone back to work, he is unable to handle the case load he once had and isn’t sure if he’ll ever be able to.
“Surgeons and physicians in general have a tendency to get so consumed with other people’s health that they don’t focus on their own health issues,” said Dr. Cerame. “It took me almost 8 months from the time I had symptoms to actually get it checked out [because] I thought it would go away, [so] if you find something that’s not kosher or you feel something that isn’t normal, take care of it.”
The other side of this, Dr. Parks elaborated, is the overload of mental stress, leading to surgeon burnout. “There’s really a growing literature on surgeon burnout, and it is not a trifling issue; in studies from North American, Australasia, Europe, Great Britain, the rate of burnout among surgeons averages about 35%, and again, surgeons are very reluctant to talk about this sort of thing.”
Dr. Park and Dr. Cerame did not have any relevant financial disclosures.
Dr. Park and Dr. Cerame deserve credit for bringing to light an issue that has rarely been discussed, but is of great importance to all surgeons and particularly to vascular surgeons: occupational health hazards. In addition to the general problems pointed out by Dr. Park, vascular surgeons face special hazards.
Aside from the long hours, little sleep, and the stresses of taking care of sick patients who may not do well despite our best efforts, vascular surgeons should be aware of special risks they face. These risks are associated both with open vascular and endovascular procedures. It is crucial that even young vascular surgeons maintain an awareness of these risks so they can be prevented or at least minimized – and treated promptly if symptoms develop.
 |
Dr. Frank J. Veith |
The open operations that vascular surgeons are called upon to perform, particularly for advanced disease, are often time consuming and intense. They may require bending or working with the head or back flexed for long periods. A difficult redo leg bypass is one such example. Spinal disk problems are common in both the cervical and lumbosacral areas in vascular surgeons who perform these lengthy arterial operations.
Vascular surgeons with busy endovascular practices face even greater occupational risks.
Endovascular surgeons are exposed daily to radiation, none of which is totally safe. Increased risks of cancer and cataracts are the most prominent risks, and there are marked differences in individual susceptibility to these dangers. Accordingly every effort must be made throughout a vascular surgeon’s career to minimize this exposure, both by emphasizing radiation safety, taking every possible protective measure, and being constantly aware of the hazards.
One of the protective measures is the wearing of lead gowns. Heavier lead aprons are more protective and should be used. It is not surprising, however, that all interventionalists who use lead protective gear for long hours also face an increased risk of cervical and lumbosacral disk problems, which can require treatment or even end their careers. Devices that limit the weight of these aprons and place the operator further from the radiation source are being developed and should be explored by all those who use radiation imaging in their daily practice.
All vascular surgeons should take the study by these researchers seriously and heed its warnings.
Dr. Frank J. Veith is professor of surgery at New York University Medical Center and Case Western Reserve University, and the William J. von Liebig Chair in Vascular Surgery at the Cleveland Clinic Foundation. He is also an associate medical editor of Vascular Specialist.
Dr. Park and Dr. Cerame deserve credit for bringing to light an issue that has rarely been discussed, but is of great importance to all surgeons and particularly to vascular surgeons: occupational health hazards. In addition to the general problems pointed out by Dr. Park, vascular surgeons face special hazards.
Aside from the long hours, little sleep, and the stresses of taking care of sick patients who may not do well despite our best efforts, vascular surgeons should be aware of special risks they face. These risks are associated both with open vascular and endovascular procedures. It is crucial that even young vascular surgeons maintain an awareness of these risks so they can be prevented or at least minimized – and treated promptly if symptoms develop.
 |
Dr. Frank J. Veith |
The open operations that vascular surgeons are called upon to perform, particularly for advanced disease, are often time consuming and intense. They may require bending or working with the head or back flexed for long periods. A difficult redo leg bypass is one such example. Spinal disk problems are common in both the cervical and lumbosacral areas in vascular surgeons who perform these lengthy arterial operations.
Vascular surgeons with busy endovascular practices face even greater occupational risks.
Endovascular surgeons are exposed daily to radiation, none of which is totally safe. Increased risks of cancer and cataracts are the most prominent risks, and there are marked differences in individual susceptibility to these dangers. Accordingly every effort must be made throughout a vascular surgeon’s career to minimize this exposure, both by emphasizing radiation safety, taking every possible protective measure, and being constantly aware of the hazards.
One of the protective measures is the wearing of lead gowns. Heavier lead aprons are more protective and should be used. It is not surprising, however, that all interventionalists who use lead protective gear for long hours also face an increased risk of cervical and lumbosacral disk problems, which can require treatment or even end their careers. Devices that limit the weight of these aprons and place the operator further from the radiation source are being developed and should be explored by all those who use radiation imaging in their daily practice.
All vascular surgeons should take the study by these researchers seriously and heed its warnings.
Dr. Frank J. Veith is professor of surgery at New York University Medical Center and Case Western Reserve University, and the William J. von Liebig Chair in Vascular Surgery at the Cleveland Clinic Foundation. He is also an associate medical editor of Vascular Specialist.
Dr. Park and Dr. Cerame deserve credit for bringing to light an issue that has rarely been discussed, but is of great importance to all surgeons and particularly to vascular surgeons: occupational health hazards. In addition to the general problems pointed out by Dr. Park, vascular surgeons face special hazards.
Aside from the long hours, little sleep, and the stresses of taking care of sick patients who may not do well despite our best efforts, vascular surgeons should be aware of special risks they face. These risks are associated both with open vascular and endovascular procedures. It is crucial that even young vascular surgeons maintain an awareness of these risks so they can be prevented or at least minimized – and treated promptly if symptoms develop.
 |
Dr. Frank J. Veith |
The open operations that vascular surgeons are called upon to perform, particularly for advanced disease, are often time consuming and intense. They may require bending or working with the head or back flexed for long periods. A difficult redo leg bypass is one such example. Spinal disk problems are common in both the cervical and lumbosacral areas in vascular surgeons who perform these lengthy arterial operations.
Vascular surgeons with busy endovascular practices face even greater occupational risks.
Endovascular surgeons are exposed daily to radiation, none of which is totally safe. Increased risks of cancer and cataracts are the most prominent risks, and there are marked differences in individual susceptibility to these dangers. Accordingly every effort must be made throughout a vascular surgeon’s career to minimize this exposure, both by emphasizing radiation safety, taking every possible protective measure, and being constantly aware of the hazards.
One of the protective measures is the wearing of lead gowns. Heavier lead aprons are more protective and should be used. It is not surprising, however, that all interventionalists who use lead protective gear for long hours also face an increased risk of cervical and lumbosacral disk problems, which can require treatment or even end their careers. Devices that limit the weight of these aprons and place the operator further from the radiation source are being developed and should be explored by all those who use radiation imaging in their daily practice.
All vascular surgeons should take the study by these researchers seriously and heed its warnings.
Dr. Frank J. Veith is professor of surgery at New York University Medical Center and Case Western Reserve University, and the William J. von Liebig Chair in Vascular Surgery at the Cleveland Clinic Foundation. He is also an associate medical editor of Vascular Specialist.
Within the community of surgeons, chronic pain is a four-letter word, spoken about in hushed tones – if it’s spoken about at all, that is – and rarely ever discussed as something that urgently needs to be addressed.
But surgeons are susceptible to the same chronic conditions as are the patients they treat. In addition to the fatigue associated with conducting long, grueling surgical operations, surgeons can experience repetitive motion injury from using laparoscopic tools for minimally invasive procedures – injuries that can, if left untreated, lead to long-term consequences.
“There have been a few studies on this, but I think we’re just scratching the surface,” explained Dr. Adrian Park, chair of surgery at the Anne Arundel Medical Center in Annapolis, Md. Dr. Park was the lead author of a 2010 study that identified chronic pain among surgeons as a serious and underreported issue within medicine.
That study, which evaluated 317 surgeons using a 23-question survey, found that 86.9% of surgeons experience “physical symptoms or discomfort,” with the most significant indicator of such symptoms being a high case load. Subsequent studies from Europe and eastern Asia also found rates of 80% or higher among surgeons in those regions of the world.
With so pervasive a problem, however, the relative paucity of data and conversation among medical professionals is alarming. “As a surgeon leader, I can tell you surgeons complain about a lot of stuff, but one of the things they tend not to complain about is themselves and their own health and well-being,” said Dr. Park.
The reasons for that, Dr. Park explained, are plentiful. Most surgeons simply don’t find it acceptable to speak up about any pain they’re experiencing, while “some may have felt it was a sign of weakness to report these injuries, some may have felt it would affect their referral base and their work,” according to Dr. Park.
To that end, Dr. Mario Cerame is well aware of what a seemingly innocuous, relatively small chronic pain can do to a surgeon. A surgeon in North Carolina, Dr. Cerame began to experience symptoms of repetitive motion injury about 2 years ago, symptoms which he says “crept up on me.”
It began as simply numbness at the tips of his fingers, affecting the way he held laparoscopic tools during surgery and other, more menial, daily tasks. Initially suspecting it was carpel tunnel syndrome, Dr. Cerame brushed it off, until the numbness spread to three whole fingers and, eventually, his entire hand. His physician explained what was happening, instructing him that if he didn’t undergo orthopedic surgery immediately, he ran the risk of becoming quadriplegic.
“I got the diagnosis on Thursday, and had the operation on Tuesday,” said Dr. Cerame, explaining that the diagnosis was spinal stenosis. Two areas of his spinal column were pinching inward, causing the slow but steady paralysis he was experiencing. With physical therapy, Dr. Cerame could have some function back within 2 years of the operation – so far, it’s been just over 16 months. The point of the operation, however, was to prevent further damage and paralysis, not necessarily to restore Dr. Cerame’s motor function to 100%.
Dr. Cerame’s story, however, isn’t what usually happens. Because surgeons generally keep things to themselves, they have to find other ways of coping with chronic pain. Some choose noninvasive options: massages, physical therapy, and so on. Other do choose to go under the knife, but such surgeries don’t provide a permanent solution to the problem. With laparoscopic tools becoming increasingly ergonomic, and monitors allowing surgeons not to keep their heads bent at an angle for hours on end during surgery, things are improving – but more can be done.
“I’ve published an awful lot of papers, but the thing that struck me about [the 2010] paper is the response I got,” said Dr. Parks. “Surgeons, literally from around the country, would call me saying ‘I used to be able to do this operation, I no longer can do that,’ or ‘this used to be what my case list looked like, I can no longer do this, you can use me as an example.’ People came forward.”
Then there’s the darker side of coping with chronic pain: substance abuse. Tight-lipped surgeons who won’t talk about pain certainly won’t talk openly about using painkillers or narcotics to ease their muscle aches or joint stiffness, but with physicians having relatively easy access to such products, could substance abuse among surgeons be a problem?
“When livelihoods are at stake, I think folks will take opportunities to stay in the game,” admitted Dr. Parks, adding that “it’s not something that folks advertise, but in anonymous surveys [surgeons] respond amazingly to stuff like this.”
The bottom line, according to both Dr. Parks and Dr. Cerame, is for surgeons not to keep quiet about these issues if they ever do experience them. Asking for help and getting things checked right away is better, not only for a surgeon, but for his family and patients, too. While Dr. Cerame has gone back to work, he is unable to handle the case load he once had and isn’t sure if he’ll ever be able to.
“Surgeons and physicians in general have a tendency to get so consumed with other people’s health that they don’t focus on their own health issues,” said Dr. Cerame. “It took me almost 8 months from the time I had symptoms to actually get it checked out [because] I thought it would go away, [so] if you find something that’s not kosher or you feel something that isn’t normal, take care of it.”
The other side of this, Dr. Parks elaborated, is the overload of mental stress, leading to surgeon burnout. “There’s really a growing literature on surgeon burnout, and it is not a trifling issue; in studies from North American, Australasia, Europe, Great Britain, the rate of burnout among surgeons averages about 35%, and again, surgeons are very reluctant to talk about this sort of thing.”
Dr. Park and Dr. Cerame did not have any relevant financial disclosures.
Within the community of surgeons, chronic pain is a four-letter word, spoken about in hushed tones – if it’s spoken about at all, that is – and rarely ever discussed as something that urgently needs to be addressed.
But surgeons are susceptible to the same chronic conditions as are the patients they treat. In addition to the fatigue associated with conducting long, grueling surgical operations, surgeons can experience repetitive motion injury from using laparoscopic tools for minimally invasive procedures – injuries that can, if left untreated, lead to long-term consequences.
“There have been a few studies on this, but I think we’re just scratching the surface,” explained Dr. Adrian Park, chair of surgery at the Anne Arundel Medical Center in Annapolis, Md. Dr. Park was the lead author of a 2010 study that identified chronic pain among surgeons as a serious and underreported issue within medicine.
That study, which evaluated 317 surgeons using a 23-question survey, found that 86.9% of surgeons experience “physical symptoms or discomfort,” with the most significant indicator of such symptoms being a high case load. Subsequent studies from Europe and eastern Asia also found rates of 80% or higher among surgeons in those regions of the world.
With so pervasive a problem, however, the relative paucity of data and conversation among medical professionals is alarming. “As a surgeon leader, I can tell you surgeons complain about a lot of stuff, but one of the things they tend not to complain about is themselves and their own health and well-being,” said Dr. Park.
The reasons for that, Dr. Park explained, are plentiful. Most surgeons simply don’t find it acceptable to speak up about any pain they’re experiencing, while “some may have felt it was a sign of weakness to report these injuries, some may have felt it would affect their referral base and their work,” according to Dr. Park.
To that end, Dr. Mario Cerame is well aware of what a seemingly innocuous, relatively small chronic pain can do to a surgeon. A surgeon in North Carolina, Dr. Cerame began to experience symptoms of repetitive motion injury about 2 years ago, symptoms which he says “crept up on me.”
It began as simply numbness at the tips of his fingers, affecting the way he held laparoscopic tools during surgery and other, more menial, daily tasks. Initially suspecting it was carpel tunnel syndrome, Dr. Cerame brushed it off, until the numbness spread to three whole fingers and, eventually, his entire hand. His physician explained what was happening, instructing him that if he didn’t undergo orthopedic surgery immediately, he ran the risk of becoming quadriplegic.
“I got the diagnosis on Thursday, and had the operation on Tuesday,” said Dr. Cerame, explaining that the diagnosis was spinal stenosis. Two areas of his spinal column were pinching inward, causing the slow but steady paralysis he was experiencing. With physical therapy, Dr. Cerame could have some function back within 2 years of the operation – so far, it’s been just over 16 months. The point of the operation, however, was to prevent further damage and paralysis, not necessarily to restore Dr. Cerame’s motor function to 100%.
Dr. Cerame’s story, however, isn’t what usually happens. Because surgeons generally keep things to themselves, they have to find other ways of coping with chronic pain. Some choose noninvasive options: massages, physical therapy, and so on. Other do choose to go under the knife, but such surgeries don’t provide a permanent solution to the problem. With laparoscopic tools becoming increasingly ergonomic, and monitors allowing surgeons not to keep their heads bent at an angle for hours on end during surgery, things are improving – but more can be done.
“I’ve published an awful lot of papers, but the thing that struck me about [the 2010] paper is the response I got,” said Dr. Parks. “Surgeons, literally from around the country, would call me saying ‘I used to be able to do this operation, I no longer can do that,’ or ‘this used to be what my case list looked like, I can no longer do this, you can use me as an example.’ People came forward.”
Then there’s the darker side of coping with chronic pain: substance abuse. Tight-lipped surgeons who won’t talk about pain certainly won’t talk openly about using painkillers or narcotics to ease their muscle aches or joint stiffness, but with physicians having relatively easy access to such products, could substance abuse among surgeons be a problem?
“When livelihoods are at stake, I think folks will take opportunities to stay in the game,” admitted Dr. Parks, adding that “it’s not something that folks advertise, but in anonymous surveys [surgeons] respond amazingly to stuff like this.”
The bottom line, according to both Dr. Parks and Dr. Cerame, is for surgeons not to keep quiet about these issues if they ever do experience them. Asking for help and getting things checked right away is better, not only for a surgeon, but for his family and patients, too. While Dr. Cerame has gone back to work, he is unable to handle the case load he once had and isn’t sure if he’ll ever be able to.
“Surgeons and physicians in general have a tendency to get so consumed with other people’s health that they don’t focus on their own health issues,” said Dr. Cerame. “It took me almost 8 months from the time I had symptoms to actually get it checked out [because] I thought it would go away, [so] if you find something that’s not kosher or you feel something that isn’t normal, take care of it.”
The other side of this, Dr. Parks elaborated, is the overload of mental stress, leading to surgeon burnout. “There’s really a growing literature on surgeon burnout, and it is not a trifling issue; in studies from North American, Australasia, Europe, Great Britain, the rate of burnout among surgeons averages about 35%, and again, surgeons are very reluctant to talk about this sort of thing.”
Dr. Park and Dr. Cerame did not have any relevant financial disclosures.
Adding azithromycin cuts postcesarean maternal infections
ATLANTA – Preincisional azithromycin reduced postcesarean maternal infections by half, and significantly cut postpartum trips to the hospital.
Given in tandem with standard prophylactic antibiotics, broad-spectrum intravenous azithromycin was highly effective, with a number needed to treat of 17 to prevent one postsurgical infection, and 43 to prevent one case of endometritis, Dr. Alan Tita reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
“We also saw fewer maternal adverse events, and the protocol was safe for the newborn,” said Dr. Tita, a professor of obstetrics and gynecology at the University of Alabama, Birmingham.
The Study of Effectiveness and Safety of Azithromycin-Based Extended-Spectrum Prophylaxis to Prevent Post Cesarean Infection (C/SOAP) trial enrolled 2,013 women at 14 sites. All patients had singleton pregnancies of at least 24 weeks’ gestation. Patients had a cesarean after at least 4 hours of active labor or 4 hours after rupture of membranes.
All women received standard narrow-spectrum antibiotic prophylaxis with either cefazolin or clindamycin. They were randomized to either preincisional intravenous azithromycin 500 mg or saline placebo. The study had a pragmatic design, so skin disinfection was performed according to each facility’s standard protocol.
The primary outcome was a composite of endometritis, wound infection, abscess, pelvic septic thrombophlebitis, pyelonephritis, pneumonia, and meningitis. Secondary outcomes were maternal fever, unscheduled visits to health care providers (including hospital readmissions and emergency department visits), and death.
The neonatal outcome was a composite of death; primary or suspected sepsis; and serious neonatal morbidities, including respiratory distress syndrome, necrotizing enterocolitis, periventricular leukomalacia, intraventricular hemorrhage of grade 3 or higher, and bronchopulmonary dysplasia.
There were no baseline differences in the indication for cesarean or type of skin and uterine incision, Dr. Tita said. Most patients (88%) received their study drug before the incision.
The rate of the primary composite outcome was reduced by half in women who had azithromycin added to their cephalosporin prophylaxis (6% vs. 12%; relative risk, 0.49). Wound infection was cut by 65% (2.4% vs. 6.6%; RR, 0.35).
Azithromycin significantly improved the secondary maternal outcomes over placebo, including fever (5% vs. 8.2%; RR, 0.61), and readmissions or unscheduled visits (8.2% vs. 12.4%; RR, 0.66). The addition of azithromycin was associated with a significant decrease in the rate of severe maternal adverse events (1.5% vs. 2.9%).
Study site, obesity, and the type of skin prep did not significantly affect any of these outcomes, Dr. Tita noted.
The addition of azithromycin was safe for neonates. The composite neonatal safety outcome occurred in 14.3% of the treated group and 13.6% of the placebo group – not a significant difference. There were no differences in suspected or confirmed sepsis (11.8% vs. 12.5%), serious neonatal morbidities (4.4% vs. 3.4%), or NICU admission (16.8% vs. 17%), Dr. Tita reported.
There were no deaths in either mothers or infants. There were 11 maternal allergic reactions, five admissions to intensive care, and five suspected cardiac events.
When asked whether even brief systemic exposure to azithromycin could alter the fetal microbiome, Dr. Tita said he shares that concern but the answer is still unknown.
“We have collected additional information and specimens and we will be looking at these to try and answer this. We also hope to get funding to do a long-term evaluation of these kids. I will say that we collected adverse event data on them for 3 months and we did not see anything concerning, but I agree more needs to be done,” he said. “Having said that, azithromycin is something we already use quite a lot in obstetrics, and overall it has been shown to be safe for the newborn.”
The study was sponsored by the National Institute of Child Health and Human Development. Dr. Tita reported having no financial disclosures.
ATLANTA – Preincisional azithromycin reduced postcesarean maternal infections by half, and significantly cut postpartum trips to the hospital.
Given in tandem with standard prophylactic antibiotics, broad-spectrum intravenous azithromycin was highly effective, with a number needed to treat of 17 to prevent one postsurgical infection, and 43 to prevent one case of endometritis, Dr. Alan Tita reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
“We also saw fewer maternal adverse events, and the protocol was safe for the newborn,” said Dr. Tita, a professor of obstetrics and gynecology at the University of Alabama, Birmingham.
The Study of Effectiveness and Safety of Azithromycin-Based Extended-Spectrum Prophylaxis to Prevent Post Cesarean Infection (C/SOAP) trial enrolled 2,013 women at 14 sites. All patients had singleton pregnancies of at least 24 weeks’ gestation. Patients had a cesarean after at least 4 hours of active labor or 4 hours after rupture of membranes.
All women received standard narrow-spectrum antibiotic prophylaxis with either cefazolin or clindamycin. They were randomized to either preincisional intravenous azithromycin 500 mg or saline placebo. The study had a pragmatic design, so skin disinfection was performed according to each facility’s standard protocol.
The primary outcome was a composite of endometritis, wound infection, abscess, pelvic septic thrombophlebitis, pyelonephritis, pneumonia, and meningitis. Secondary outcomes were maternal fever, unscheduled visits to health care providers (including hospital readmissions and emergency department visits), and death.
The neonatal outcome was a composite of death; primary or suspected sepsis; and serious neonatal morbidities, including respiratory distress syndrome, necrotizing enterocolitis, periventricular leukomalacia, intraventricular hemorrhage of grade 3 or higher, and bronchopulmonary dysplasia.
There were no baseline differences in the indication for cesarean or type of skin and uterine incision, Dr. Tita said. Most patients (88%) received their study drug before the incision.
The rate of the primary composite outcome was reduced by half in women who had azithromycin added to their cephalosporin prophylaxis (6% vs. 12%; relative risk, 0.49). Wound infection was cut by 65% (2.4% vs. 6.6%; RR, 0.35).
Azithromycin significantly improved the secondary maternal outcomes over placebo, including fever (5% vs. 8.2%; RR, 0.61), and readmissions or unscheduled visits (8.2% vs. 12.4%; RR, 0.66). The addition of azithromycin was associated with a significant decrease in the rate of severe maternal adverse events (1.5% vs. 2.9%).
Study site, obesity, and the type of skin prep did not significantly affect any of these outcomes, Dr. Tita noted.
The addition of azithromycin was safe for neonates. The composite neonatal safety outcome occurred in 14.3% of the treated group and 13.6% of the placebo group – not a significant difference. There were no differences in suspected or confirmed sepsis (11.8% vs. 12.5%), serious neonatal morbidities (4.4% vs. 3.4%), or NICU admission (16.8% vs. 17%), Dr. Tita reported.
There were no deaths in either mothers or infants. There were 11 maternal allergic reactions, five admissions to intensive care, and five suspected cardiac events.
When asked whether even brief systemic exposure to azithromycin could alter the fetal microbiome, Dr. Tita said he shares that concern but the answer is still unknown.
“We have collected additional information and specimens and we will be looking at these to try and answer this. We also hope to get funding to do a long-term evaluation of these kids. I will say that we collected adverse event data on them for 3 months and we did not see anything concerning, but I agree more needs to be done,” he said. “Having said that, azithromycin is something we already use quite a lot in obstetrics, and overall it has been shown to be safe for the newborn.”
The study was sponsored by the National Institute of Child Health and Human Development. Dr. Tita reported having no financial disclosures.
ATLANTA – Preincisional azithromycin reduced postcesarean maternal infections by half, and significantly cut postpartum trips to the hospital.
Given in tandem with standard prophylactic antibiotics, broad-spectrum intravenous azithromycin was highly effective, with a number needed to treat of 17 to prevent one postsurgical infection, and 43 to prevent one case of endometritis, Dr. Alan Tita reported at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
“We also saw fewer maternal adverse events, and the protocol was safe for the newborn,” said Dr. Tita, a professor of obstetrics and gynecology at the University of Alabama, Birmingham.
The Study of Effectiveness and Safety of Azithromycin-Based Extended-Spectrum Prophylaxis to Prevent Post Cesarean Infection (C/SOAP) trial enrolled 2,013 women at 14 sites. All patients had singleton pregnancies of at least 24 weeks’ gestation. Patients had a cesarean after at least 4 hours of active labor or 4 hours after rupture of membranes.
All women received standard narrow-spectrum antibiotic prophylaxis with either cefazolin or clindamycin. They were randomized to either preincisional intravenous azithromycin 500 mg or saline placebo. The study had a pragmatic design, so skin disinfection was performed according to each facility’s standard protocol.
The primary outcome was a composite of endometritis, wound infection, abscess, pelvic septic thrombophlebitis, pyelonephritis, pneumonia, and meningitis. Secondary outcomes were maternal fever, unscheduled visits to health care providers (including hospital readmissions and emergency department visits), and death.
The neonatal outcome was a composite of death; primary or suspected sepsis; and serious neonatal morbidities, including respiratory distress syndrome, necrotizing enterocolitis, periventricular leukomalacia, intraventricular hemorrhage of grade 3 or higher, and bronchopulmonary dysplasia.
There were no baseline differences in the indication for cesarean or type of skin and uterine incision, Dr. Tita said. Most patients (88%) received their study drug before the incision.
The rate of the primary composite outcome was reduced by half in women who had azithromycin added to their cephalosporin prophylaxis (6% vs. 12%; relative risk, 0.49). Wound infection was cut by 65% (2.4% vs. 6.6%; RR, 0.35).
Azithromycin significantly improved the secondary maternal outcomes over placebo, including fever (5% vs. 8.2%; RR, 0.61), and readmissions or unscheduled visits (8.2% vs. 12.4%; RR, 0.66). The addition of azithromycin was associated with a significant decrease in the rate of severe maternal adverse events (1.5% vs. 2.9%).
Study site, obesity, and the type of skin prep did not significantly affect any of these outcomes, Dr. Tita noted.
The addition of azithromycin was safe for neonates. The composite neonatal safety outcome occurred in 14.3% of the treated group and 13.6% of the placebo group – not a significant difference. There were no differences in suspected or confirmed sepsis (11.8% vs. 12.5%), serious neonatal morbidities (4.4% vs. 3.4%), or NICU admission (16.8% vs. 17%), Dr. Tita reported.
There were no deaths in either mothers or infants. There were 11 maternal allergic reactions, five admissions to intensive care, and five suspected cardiac events.
When asked whether even brief systemic exposure to azithromycin could alter the fetal microbiome, Dr. Tita said he shares that concern but the answer is still unknown.
“We have collected additional information and specimens and we will be looking at these to try and answer this. We also hope to get funding to do a long-term evaluation of these kids. I will say that we collected adverse event data on them for 3 months and we did not see anything concerning, but I agree more needs to be done,” he said. “Having said that, azithromycin is something we already use quite a lot in obstetrics, and overall it has been shown to be safe for the newborn.”
The study was sponsored by the National Institute of Child Health and Human Development. Dr. Tita reported having no financial disclosures.
AT THE PREGNANCY MEETING
Key clinical point: Prophylactic azithromycin added to standard antibiotics decreased maternal infections after cesarean.
Major finding: The number needed to treat to prevent one postsurgical infection was 17.
Data source: The randomized, placebo-controlled trial comprised 2,013 women.
Disclosures: The study was sponsored by the National Institute of Child Health and Human Development. Dr. Tita reported having no financial disclosures.
MRI assessment of pulmonary vein stenosis predicts outcomes
A retrospective analysis of children who underwent pulmonary vein stenosis repair with preoperative computed tomography and magnetic resonance imaging from 1990 to 2012 showed that smaller upstream or downstream total cross-sectional area indexed (TCSAi) for body surface area led to poorer survival.
The study of 31 patients at a single institution also indicated that early survival seemed especially poor for patients with a greater number of stenotic veins and upstream pulmonary vein (PV) involvement. The study was published in the March issue of the Journal of Thoracic and Cardiovascular Surgery.
Dr. Mauro Lo Rito and his colleagues at The Hospital for Sick Children, Toronto, retrospectively assessed the 31 patients out of 145 who underwent surgical repair who had had preoperative CT and MRI imaging. Complete sutureless repair was done in 18 (58%), single-side sutureless repair in 12 (39%), and pericardial patch reconstruction in 1 (3%). The mean follow-up was 4.3 years; the median patient age at time of operation was 226 days. Stenosis was bilateral in 45% of patients and unilateral in 55 (J Thorac Cardiovasc Surg. 2016;151:657-66).
In-hospital mortality was 9.7%, with an overall survival of 75%, 69%, and 64% at 1, 3, and 5 years, respectively. Univariate analysis showed that a younger age at operation, lower body surface area, smaller upstream TCSAi, and greater number of PV with stenosis/occlusion were associated with an increased risk of death.
Multivariate analysis showed that smaller upstream TCSAi for body surface area (P = .030) and greater number of stenotic PVs (P = .007) were associated with poor early (less than 1 year) survival. There was a nonsignificant tendency for smaller downstream TCSAi to be associated with poor late survival (greater than 1 year). None of the different PV morphologies were found to influence survival, according to Dr. Lo Rito and his colleagues.
Among the 28 hospital survivors, restenosis occurred in 10 patients, 7 of whom did not undergo further surgery (3 of these were alive at last follow-up and 4 died secondary to disease progression). Of the 3 patients who underwent subsequent intervention, 2 were alive at last follow-up.
“Risk stratification for patients with PV stenosis is currently challenging because of the variability in the anatomic configuration and the unknown relationship between these anatomic variants and survival. Our study demonstrates that by using cross-sectional areas, pulmonary vein cross-sectional area indexed to body surface area (PVCSAi) and TCSAi and tabulating the number of stenotic PVs, we can identify high-risk subsets of patients with high predicted mortality.” Dr. Lo Rito and his colleagues stated.
“The upstream total cross-sectional area and the number of stenotic PVs influence early survival and can be used to guide counseling. Smaller downstream cross-sectional area influences late survival, and those patients should be monitored with close follow-up. This methodology could aid in risk stratification for future clinical trials of pharmacologic agents designed to target upstream pulmonary vasculopathy,” the investigators concluded.
The authors reported that they had no conflicts of interest.
A webcast of the original presentation of these results at the 95th American Association for Thoracic Surgery Annual Meeting is available online (http://webcast.aats.org/2015/Video/Tuesday/04-28-15_6A_1615_Lo_Rito.mp4).
“The Toronto group has contributed significantly to our knowledge and management of pulmonary vein stenosis during the past decade. This article by Dr. Lo Rito and coworkers continues that contribution by reinforcing the values of MRI in imaging PVs before intervention and providing a valuable “hint” that preoperative PV size measurements are related to outcome,” Dr. William M. DeCampli wrote in his invited commentary (J Thorac Cardiovasc Surg. 2016;1510:667-8).
“The task of definitively demonstrating this relationship is daunting for any single institution, however, because 1) PVS is relatively rare, 2) MRI and computed tomography are relatively recently used diagnostic modalities, and 3) MRI is not easily used in an important subset of the cohort, small infants.” This limited the study to a small number of covariates,” noted Dr. DeCampli, and prevented the researchers from taking into account a myriad of additional covariates commonly associated with survival in complex congenital heart disease.
 |
Dr. William M. DeCampli |
Such covariates included in a sufficiently large model could significantly alter the observed odds ratios otherwise calculated for the included variables in this study, he added, citing a study of PVS by Boston Children’s Hospital (J Thorac Cardiovasc Surg. 2015;150:911-7), which found a different set of covariates associated with death; in that case, age younger than 6 months at operation, weight less than 3 kg at operation, and lesser preoperative right ventricular systolic pressure.
“The challenges in studying PVS encountered by these two high-volume, research-oriented programs leads us to suggest that PVS should be studied in a different way. Perhaps it is time to consider a multi-institutional, mixed or inception cohort registry for PVS. The spring 2015 Society of Thoracic Surgeons Congenital Heart Database report lists 506 cases of PVS repair as the primary procedure between January 2011 and December 2014. If a study were to enroll just one-third of these subjects it would accrue more than 40 subjects per year. Five years hence with an anticipated 50-80 events (deaths), it would be possible to carry out more robust risk-hazard analyses,” Dr. DeCampli suggested.
Dr. DeCampli is a congenital heart surgeon at the department of clinical sciences, University of Central Florida, and the Heart Center at Arnold Palmer Hospital for Children, both in Orlando. He reported having no conflicts.
“The Toronto group has contributed significantly to our knowledge and management of pulmonary vein stenosis during the past decade. This article by Dr. Lo Rito and coworkers continues that contribution by reinforcing the values of MRI in imaging PVs before intervention and providing a valuable “hint” that preoperative PV size measurements are related to outcome,” Dr. William M. DeCampli wrote in his invited commentary (J Thorac Cardiovasc Surg. 2016;1510:667-8).
“The task of definitively demonstrating this relationship is daunting for any single institution, however, because 1) PVS is relatively rare, 2) MRI and computed tomography are relatively recently used diagnostic modalities, and 3) MRI is not easily used in an important subset of the cohort, small infants.” This limited the study to a small number of covariates,” noted Dr. DeCampli, and prevented the researchers from taking into account a myriad of additional covariates commonly associated with survival in complex congenital heart disease.
 |
Dr. William M. DeCampli |
Such covariates included in a sufficiently large model could significantly alter the observed odds ratios otherwise calculated for the included variables in this study, he added, citing a study of PVS by Boston Children’s Hospital (J Thorac Cardiovasc Surg. 2015;150:911-7), which found a different set of covariates associated with death; in that case, age younger than 6 months at operation, weight less than 3 kg at operation, and lesser preoperative right ventricular systolic pressure.
“The challenges in studying PVS encountered by these two high-volume, research-oriented programs leads us to suggest that PVS should be studied in a different way. Perhaps it is time to consider a multi-institutional, mixed or inception cohort registry for PVS. The spring 2015 Society of Thoracic Surgeons Congenital Heart Database report lists 506 cases of PVS repair as the primary procedure between January 2011 and December 2014. If a study were to enroll just one-third of these subjects it would accrue more than 40 subjects per year. Five years hence with an anticipated 50-80 events (deaths), it would be possible to carry out more robust risk-hazard analyses,” Dr. DeCampli suggested.
Dr. DeCampli is a congenital heart surgeon at the department of clinical sciences, University of Central Florida, and the Heart Center at Arnold Palmer Hospital for Children, both in Orlando. He reported having no conflicts.
“The Toronto group has contributed significantly to our knowledge and management of pulmonary vein stenosis during the past decade. This article by Dr. Lo Rito and coworkers continues that contribution by reinforcing the values of MRI in imaging PVs before intervention and providing a valuable “hint” that preoperative PV size measurements are related to outcome,” Dr. William M. DeCampli wrote in his invited commentary (J Thorac Cardiovasc Surg. 2016;1510:667-8).
“The task of definitively demonstrating this relationship is daunting for any single institution, however, because 1) PVS is relatively rare, 2) MRI and computed tomography are relatively recently used diagnostic modalities, and 3) MRI is not easily used in an important subset of the cohort, small infants.” This limited the study to a small number of covariates,” noted Dr. DeCampli, and prevented the researchers from taking into account a myriad of additional covariates commonly associated with survival in complex congenital heart disease.
 |
Dr. William M. DeCampli |
Such covariates included in a sufficiently large model could significantly alter the observed odds ratios otherwise calculated for the included variables in this study, he added, citing a study of PVS by Boston Children’s Hospital (J Thorac Cardiovasc Surg. 2015;150:911-7), which found a different set of covariates associated with death; in that case, age younger than 6 months at operation, weight less than 3 kg at operation, and lesser preoperative right ventricular systolic pressure.
“The challenges in studying PVS encountered by these two high-volume, research-oriented programs leads us to suggest that PVS should be studied in a different way. Perhaps it is time to consider a multi-institutional, mixed or inception cohort registry for PVS. The spring 2015 Society of Thoracic Surgeons Congenital Heart Database report lists 506 cases of PVS repair as the primary procedure between January 2011 and December 2014. If a study were to enroll just one-third of these subjects it would accrue more than 40 subjects per year. Five years hence with an anticipated 50-80 events (deaths), it would be possible to carry out more robust risk-hazard analyses,” Dr. DeCampli suggested.
Dr. DeCampli is a congenital heart surgeon at the department of clinical sciences, University of Central Florida, and the Heart Center at Arnold Palmer Hospital for Children, both in Orlando. He reported having no conflicts.
A retrospective analysis of children who underwent pulmonary vein stenosis repair with preoperative computed tomography and magnetic resonance imaging from 1990 to 2012 showed that smaller upstream or downstream total cross-sectional area indexed (TCSAi) for body surface area led to poorer survival.
The study of 31 patients at a single institution also indicated that early survival seemed especially poor for patients with a greater number of stenotic veins and upstream pulmonary vein (PV) involvement. The study was published in the March issue of the Journal of Thoracic and Cardiovascular Surgery.
Dr. Mauro Lo Rito and his colleagues at The Hospital for Sick Children, Toronto, retrospectively assessed the 31 patients out of 145 who underwent surgical repair who had had preoperative CT and MRI imaging. Complete sutureless repair was done in 18 (58%), single-side sutureless repair in 12 (39%), and pericardial patch reconstruction in 1 (3%). The mean follow-up was 4.3 years; the median patient age at time of operation was 226 days. Stenosis was bilateral in 45% of patients and unilateral in 55 (J Thorac Cardiovasc Surg. 2016;151:657-66).
In-hospital mortality was 9.7%, with an overall survival of 75%, 69%, and 64% at 1, 3, and 5 years, respectively. Univariate analysis showed that a younger age at operation, lower body surface area, smaller upstream TCSAi, and greater number of PV with stenosis/occlusion were associated with an increased risk of death.
Multivariate analysis showed that smaller upstream TCSAi for body surface area (P = .030) and greater number of stenotic PVs (P = .007) were associated with poor early (less than 1 year) survival. There was a nonsignificant tendency for smaller downstream TCSAi to be associated with poor late survival (greater than 1 year). None of the different PV morphologies were found to influence survival, according to Dr. Lo Rito and his colleagues.
Among the 28 hospital survivors, restenosis occurred in 10 patients, 7 of whom did not undergo further surgery (3 of these were alive at last follow-up and 4 died secondary to disease progression). Of the 3 patients who underwent subsequent intervention, 2 were alive at last follow-up.
“Risk stratification for patients with PV stenosis is currently challenging because of the variability in the anatomic configuration and the unknown relationship between these anatomic variants and survival. Our study demonstrates that by using cross-sectional areas, pulmonary vein cross-sectional area indexed to body surface area (PVCSAi) and TCSAi and tabulating the number of stenotic PVs, we can identify high-risk subsets of patients with high predicted mortality.” Dr. Lo Rito and his colleagues stated.
“The upstream total cross-sectional area and the number of stenotic PVs influence early survival and can be used to guide counseling. Smaller downstream cross-sectional area influences late survival, and those patients should be monitored with close follow-up. This methodology could aid in risk stratification for future clinical trials of pharmacologic agents designed to target upstream pulmonary vasculopathy,” the investigators concluded.
The authors reported that they had no conflicts of interest.
A webcast of the original presentation of these results at the 95th American Association for Thoracic Surgery Annual Meeting is available online (http://webcast.aats.org/2015/Video/Tuesday/04-28-15_6A_1615_Lo_Rito.mp4).
A retrospective analysis of children who underwent pulmonary vein stenosis repair with preoperative computed tomography and magnetic resonance imaging from 1990 to 2012 showed that smaller upstream or downstream total cross-sectional area indexed (TCSAi) for body surface area led to poorer survival.
The study of 31 patients at a single institution also indicated that early survival seemed especially poor for patients with a greater number of stenotic veins and upstream pulmonary vein (PV) involvement. The study was published in the March issue of the Journal of Thoracic and Cardiovascular Surgery.
Dr. Mauro Lo Rito and his colleagues at The Hospital for Sick Children, Toronto, retrospectively assessed the 31 patients out of 145 who underwent surgical repair who had had preoperative CT and MRI imaging. Complete sutureless repair was done in 18 (58%), single-side sutureless repair in 12 (39%), and pericardial patch reconstruction in 1 (3%). The mean follow-up was 4.3 years; the median patient age at time of operation was 226 days. Stenosis was bilateral in 45% of patients and unilateral in 55 (J Thorac Cardiovasc Surg. 2016;151:657-66).
In-hospital mortality was 9.7%, with an overall survival of 75%, 69%, and 64% at 1, 3, and 5 years, respectively. Univariate analysis showed that a younger age at operation, lower body surface area, smaller upstream TCSAi, and greater number of PV with stenosis/occlusion were associated with an increased risk of death.
Multivariate analysis showed that smaller upstream TCSAi for body surface area (P = .030) and greater number of stenotic PVs (P = .007) were associated with poor early (less than 1 year) survival. There was a nonsignificant tendency for smaller downstream TCSAi to be associated with poor late survival (greater than 1 year). None of the different PV morphologies were found to influence survival, according to Dr. Lo Rito and his colleagues.
Among the 28 hospital survivors, restenosis occurred in 10 patients, 7 of whom did not undergo further surgery (3 of these were alive at last follow-up and 4 died secondary to disease progression). Of the 3 patients who underwent subsequent intervention, 2 were alive at last follow-up.
“Risk stratification for patients with PV stenosis is currently challenging because of the variability in the anatomic configuration and the unknown relationship between these anatomic variants and survival. Our study demonstrates that by using cross-sectional areas, pulmonary vein cross-sectional area indexed to body surface area (PVCSAi) and TCSAi and tabulating the number of stenotic PVs, we can identify high-risk subsets of patients with high predicted mortality.” Dr. Lo Rito and his colleagues stated.
“The upstream total cross-sectional area and the number of stenotic PVs influence early survival and can be used to guide counseling. Smaller downstream cross-sectional area influences late survival, and those patients should be monitored with close follow-up. This methodology could aid in risk stratification for future clinical trials of pharmacologic agents designed to target upstream pulmonary vasculopathy,” the investigators concluded.
The authors reported that they had no conflicts of interest.
A webcast of the original presentation of these results at the 95th American Association for Thoracic Surgery Annual Meeting is available online (http://webcast.aats.org/2015/Video/Tuesday/04-28-15_6A_1615_Lo_Rito.mp4).
FROM JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Survival after pulmonary vein stenosis repair was adversely affected by smaller upstream cross-sectional area indexed to body surface area.
Major finding: Smaller upstream total cross-sectional area indexed for body surface area (P = .30) and greater number of stenotic pulmonary veins (P = .007) were associated with increased early risk of death.
Data source: Researchers reviewed the outcomes of 31/145 patients who underwent surgical repair of pulmonary stenosis who had preoperative computed tomography and magnetic resonance imaging between 1990 and 2012.
Disclosures: The authors reported that they had no conflicts of interest.
Study finds lower-than-expected rate of occult uterine sarcoma
The risk of finding occult uterine sarcoma during hysterectomy for benign indications was lower than expected in a single-center retrospective cohort study, at 0.089%, or 1 in 1,124 hysterectomies, according to a recent analysis.
This is markedly lower than the estimated risks in previous studies, which ranged from 1 in 204 to 1 in 667 procedures for women with presumed myomas. The American College of Obstetricians and Gynecologists estimated the risk to be 1 in 500 hysterectomies, and the Food and Drug Administration pegged it at 1 in 352 based on a pooled analysis of nine studies of women undergoing hysterectomy or myomectomy for presumed myomas. The last estimate in particular has been criticized as inaccurate because of concerns about the quality of data and methodologic flaws of the nine studies, reported Dr. Kimberly A. Kho of the University of Texas Southwestern Medical Center, Dallas, and her associates (Obstet. Gynecol. 2016;127:468-73.).
The investigators analyzed information in a database for all 10,119 hysterectomies performed for benign indications at their medical center during a 14-year period, and correlated it with data concerning all cases of uterine sarcoma in their center’s tumor registry. A total of 59.4% of these procedures used an abdominal approach, 21.6% were laparoscopic or robot assisted, and 18.9% used a vaginal approach. The most common indications were leiomyomata (37%), abnormal uterine bleeding (28%), and pelvic organ prolapse (11%).
Nine women were found to have an occult uterine sarcoma, including five leiomyosarcomas, two endometrial stromal sarcomas, and two uterine adenocarcinomas.
“All patients had received up-to-date cervical cancer screening and, in the majority of cases, women had received preoperative evaluation with either endometrial sampling or imaging, which did not suggest malignancy. Of the suggested risk factors for sarcoma, it is notable that none of the women we identified were postmenopausal, exposed to pelvic radiation or tamoxifen, nor had a family history of cancer,” the researchers wrote.
Only one patient underwent manual morcellation of a large, bulky uterus before her sarcoma was discovered during total abdominal hysterectomy. The abdominal cavity was then thoroughly explored, and no suspicious lesions were found. This patient later received chemotherapy and had no evidence of disease 3 years later.
The study findings may be helpful for surgical planning and for counseling patients about management options. “It is important to stress that although low, the risk of encountering an occult sarcoma exists. Hence, ongoing efforts to identify potentially safer methods for tissue extraction are essential, as are efforts to improve preoperative identification of malignancies,” the researchers noted.
The study was supported by the University of Texas Southwestern Medical Center. Dr. Kho reported ties to Actamax Surgical Materials and Applied Medical; one of her associates reported ties to AstraZeneca and Genentech.
The risk of finding occult uterine sarcoma during hysterectomy for benign indications was lower than expected in a single-center retrospective cohort study, at 0.089%, or 1 in 1,124 hysterectomies, according to a recent analysis.
This is markedly lower than the estimated risks in previous studies, which ranged from 1 in 204 to 1 in 667 procedures for women with presumed myomas. The American College of Obstetricians and Gynecologists estimated the risk to be 1 in 500 hysterectomies, and the Food and Drug Administration pegged it at 1 in 352 based on a pooled analysis of nine studies of women undergoing hysterectomy or myomectomy for presumed myomas. The last estimate in particular has been criticized as inaccurate because of concerns about the quality of data and methodologic flaws of the nine studies, reported Dr. Kimberly A. Kho of the University of Texas Southwestern Medical Center, Dallas, and her associates (Obstet. Gynecol. 2016;127:468-73.).
The investigators analyzed information in a database for all 10,119 hysterectomies performed for benign indications at their medical center during a 14-year period, and correlated it with data concerning all cases of uterine sarcoma in their center’s tumor registry. A total of 59.4% of these procedures used an abdominal approach, 21.6% were laparoscopic or robot assisted, and 18.9% used a vaginal approach. The most common indications were leiomyomata (37%), abnormal uterine bleeding (28%), and pelvic organ prolapse (11%).
Nine women were found to have an occult uterine sarcoma, including five leiomyosarcomas, two endometrial stromal sarcomas, and two uterine adenocarcinomas.
“All patients had received up-to-date cervical cancer screening and, in the majority of cases, women had received preoperative evaluation with either endometrial sampling or imaging, which did not suggest malignancy. Of the suggested risk factors for sarcoma, it is notable that none of the women we identified were postmenopausal, exposed to pelvic radiation or tamoxifen, nor had a family history of cancer,” the researchers wrote.
Only one patient underwent manual morcellation of a large, bulky uterus before her sarcoma was discovered during total abdominal hysterectomy. The abdominal cavity was then thoroughly explored, and no suspicious lesions were found. This patient later received chemotherapy and had no evidence of disease 3 years later.
The study findings may be helpful for surgical planning and for counseling patients about management options. “It is important to stress that although low, the risk of encountering an occult sarcoma exists. Hence, ongoing efforts to identify potentially safer methods for tissue extraction are essential, as are efforts to improve preoperative identification of malignancies,” the researchers noted.
The study was supported by the University of Texas Southwestern Medical Center. Dr. Kho reported ties to Actamax Surgical Materials and Applied Medical; one of her associates reported ties to AstraZeneca and Genentech.
The risk of finding occult uterine sarcoma during hysterectomy for benign indications was lower than expected in a single-center retrospective cohort study, at 0.089%, or 1 in 1,124 hysterectomies, according to a recent analysis.
This is markedly lower than the estimated risks in previous studies, which ranged from 1 in 204 to 1 in 667 procedures for women with presumed myomas. The American College of Obstetricians and Gynecologists estimated the risk to be 1 in 500 hysterectomies, and the Food and Drug Administration pegged it at 1 in 352 based on a pooled analysis of nine studies of women undergoing hysterectomy or myomectomy for presumed myomas. The last estimate in particular has been criticized as inaccurate because of concerns about the quality of data and methodologic flaws of the nine studies, reported Dr. Kimberly A. Kho of the University of Texas Southwestern Medical Center, Dallas, and her associates (Obstet. Gynecol. 2016;127:468-73.).
The investigators analyzed information in a database for all 10,119 hysterectomies performed for benign indications at their medical center during a 14-year period, and correlated it with data concerning all cases of uterine sarcoma in their center’s tumor registry. A total of 59.4% of these procedures used an abdominal approach, 21.6% were laparoscopic or robot assisted, and 18.9% used a vaginal approach. The most common indications were leiomyomata (37%), abnormal uterine bleeding (28%), and pelvic organ prolapse (11%).
Nine women were found to have an occult uterine sarcoma, including five leiomyosarcomas, two endometrial stromal sarcomas, and two uterine adenocarcinomas.
“All patients had received up-to-date cervical cancer screening and, in the majority of cases, women had received preoperative evaluation with either endometrial sampling or imaging, which did not suggest malignancy. Of the suggested risk factors for sarcoma, it is notable that none of the women we identified were postmenopausal, exposed to pelvic radiation or tamoxifen, nor had a family history of cancer,” the researchers wrote.
Only one patient underwent manual morcellation of a large, bulky uterus before her sarcoma was discovered during total abdominal hysterectomy. The abdominal cavity was then thoroughly explored, and no suspicious lesions were found. This patient later received chemotherapy and had no evidence of disease 3 years later.
The study findings may be helpful for surgical planning and for counseling patients about management options. “It is important to stress that although low, the risk of encountering an occult sarcoma exists. Hence, ongoing efforts to identify potentially safer methods for tissue extraction are essential, as are efforts to improve preoperative identification of malignancies,” the researchers noted.
The study was supported by the University of Texas Southwestern Medical Center. Dr. Kho reported ties to Actamax Surgical Materials and Applied Medical; one of her associates reported ties to AstraZeneca and Genentech.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point: The rate of occult uterine sarcoma in women undergoing hysterectomy for benign indications was lower than expected at 0.089%.
Major finding: A total of 9 out of 10,119 women were found to have an occult uterine sarcoma, including five leiomyosarcomas, two endometrial stromal sarcomas, and two uterine adenocarcinomas.
Data source: A retrospective single-center cohort study involving 10,119 hysterectomies performed during a 14-year period.
Disclosures: The study was supported by the University of Texas Southwestern Medical Center. Dr. Kho reported ties to Actamax Surgical Materials and Applied Medical; one of her associates reported ties to AstraZeneca and Genentech.
A novel approach to overcoming cervical stenosis and false passages

For more videos from the Society of Gynecologic Surgeons, click here
Visit the Society of Gynecologic Surgeons online: sgsonline.org

For more videos from the Society of Gynecologic Surgeons, click here
Visit the Society of Gynecologic Surgeons online: sgsonline.org

For more videos from the Society of Gynecologic Surgeons, click here
Visit the Society of Gynecologic Surgeons online: sgsonline.org
This video is brought to you by ![]()
STS: Valved conduit shows right ventricular outflow durability
PHOENIX – A prosthetic conduit that contains a porcine valve showed excellent intermediate-term durability for repairing the right ventricular outflow tract in 100 teenagers and young adults at a single U.S. center.
“The Carpentier-Edwards xenograft for right ventricular outflow tract [RVOT] reconstruction provides excellent freedom from reoperation and valve dysfunction, as well as sustained improvement in right-ventricular chamber size at intermediate-term follow-up,” Dr. Heidi B. Schubmehl said at the Society of Thoracic Surgeons annual meeting.
Dr. Schubmehl reported a 92% rate of freedom from valve dysfunction with follow-up out to about 10 years, and significant reductions in right ventricular size at follow-up, compared with baseline, as measured by both echocardiography and by MRI.
The Carpentier-Edwards porcine valve and conduit “seemed to hold up better than a lot of other [prosthetic] valves,” said Dr. George M. Alfieris, director of pediatric cardiac surgery at the University of Rochester (N.Y.), and senior author for the study. In addition to the valve’s durability over approximately the first 10 years following placement, the results also showed the positive impact the valve had on right ventricular size, an important result of the repair’s efficacy, Dr. Alfieris said.
“It’s a mistake to allow the right ventricle to be under high pressure or to reach a large volume. We now focus on preserving the right ventricle,” he said in an interview. “I’ve become very concerned about preventing right ventricular dilation and preserving right ventricular function.”
Dr. Alfieris noted that his prior experience using other types of valves in the pulmonary valve and RVOT position showed those valves “did great for the first 10 years and then failed. What’s different in this series is that after 10 years, we have not seen the same dysfunction as with the prior generation of valves. I will be very interested to see what happens to them” as follow-up continues beyond 10 years. He also expressed dismay that recently the company that had been marketing the valve and conduit used in the current study, the Carpentier-Edwards, stopped selling them. He expects that as his supply of conduits runs out he’ll have to start using a different commercial valve and conduit that he believes will not perform as well or create his own conduits with a porcine valve from a different supplier.
The series of 100 patients comprised individuals aged 17 or older who received a pulmonary artery and had RVOT reconstruction at the University of Rochester during 2000-2010, Dr. Schubmehl reported. The series included 78 patients with a history of tetralogy of Fallot, 8 patients born with transposition of their great arteries, 8 patients with truncus arteriosus, and 6 patients with other congenital heart diseases. Their median age at the time they received the RVOT conduit was 24 years, 59% were men, and 99 had undergone a prior sternotomy. At the time they received the conduit, 55 had pulmonary valve insufficiency, 30 had valve stenosis, and 15 had both. Follow-up occurred an average of 7 years after conduit placement.
Two recipients died: One death occurred perioperatively in a 41-year old who had a massive cerebrovascular event, and the second death was in a 39-year old who died 2.6 years after conduit placement from respiratory failure. Two additional patients required a reintervention during follow-up, said Dr. Schubmehl, a general surgeon at the University of Rochester. One reintervention occurred after 11 years to treat endocarditis, and the second after 11 years to perform balloon valvuloplasty because of valve stenosis.
The results reported by Dr. Schubmehl for echocardiography examinations showed that the patients had a statistically significant reduction in their RVOT pressure gradient from baseline to 1-year follow-up that was sustained through their intermediate-term follow-up. Seventy-seven patients had pulmonary valve insufficiency at baseline that resolved in all patients at 1-year follow-up and remained resolved in all but one patient at extended follow-up. Nineteen patients underwent additional imaging with MRI at an average follow-up of 7 years, and these findings confirmed the echo results.
On Twitter @mitchelzoler
The intermediate-term results reported by Dr. Schubmehl using a Carpentier-Edwards conduit in the right-ventricular outflow tract are clearly better than what we have seen using other types of valves and conduits in this position. If the valve and conduit they used persists with similar performance beyond 10 years, it would be a very good option. However, what typically happens is that replacement valves look good for about 10 years and then start to fail, often with a steep failure curve. I suspect that during the next 10 years of follow-up many more of the valves they placed will start to fail. The 10- to 20-year follow-up period is critical for demonstrating long-term durability of this valve and conduit.
 |
Dr. James Jaggers |
One additional potential advantage of the Carpentier-Edwards prosthesis is that the valve it contains is larger than the usual valve placed in the right ventricular outflow tract (RVOT). Failed valves increasingly are replaced by a transcatheter approach that puts a new valve inside the old, failed valve. As patients who received these replacement valves continue to survive we anticipate their need over time for a series of valve-in-valve procedures. The larger the valve at the outset, the more feasible it will be to have multiple episodes of valve-in-valve replacement.
At one time, we regarded early surgical repair of a tetralogy of Fallot defect as curative. We now know that as children with a repaired tetralogy of Fallot grow into teens and adults they require additional repairs, most often replacement of their RVOTs. This has made pulmonary valve replacement the most common surgery for adult survivors of congenital heart disease. The numbers of teen or adult patients who require a new RVOT will steadily increase as more of these children survive.
Dr. James Jaggers, professor of surgery at the University of Colorado and chief of cardiothoracic surgery at Children’s Hospital Colorado in Denver, made these comments in an interview. He had no disclosures.
The intermediate-term results reported by Dr. Schubmehl using a Carpentier-Edwards conduit in the right-ventricular outflow tract are clearly better than what we have seen using other types of valves and conduits in this position. If the valve and conduit they used persists with similar performance beyond 10 years, it would be a very good option. However, what typically happens is that replacement valves look good for about 10 years and then start to fail, often with a steep failure curve. I suspect that during the next 10 years of follow-up many more of the valves they placed will start to fail. The 10- to 20-year follow-up period is critical for demonstrating long-term durability of this valve and conduit.
 |
Dr. James Jaggers |
One additional potential advantage of the Carpentier-Edwards prosthesis is that the valve it contains is larger than the usual valve placed in the right ventricular outflow tract (RVOT). Failed valves increasingly are replaced by a transcatheter approach that puts a new valve inside the old, failed valve. As patients who received these replacement valves continue to survive we anticipate their need over time for a series of valve-in-valve procedures. The larger the valve at the outset, the more feasible it will be to have multiple episodes of valve-in-valve replacement.
At one time, we regarded early surgical repair of a tetralogy of Fallot defect as curative. We now know that as children with a repaired tetralogy of Fallot grow into teens and adults they require additional repairs, most often replacement of their RVOTs. This has made pulmonary valve replacement the most common surgery for adult survivors of congenital heart disease. The numbers of teen or adult patients who require a new RVOT will steadily increase as more of these children survive.
Dr. James Jaggers, professor of surgery at the University of Colorado and chief of cardiothoracic surgery at Children’s Hospital Colorado in Denver, made these comments in an interview. He had no disclosures.
The intermediate-term results reported by Dr. Schubmehl using a Carpentier-Edwards conduit in the right-ventricular outflow tract are clearly better than what we have seen using other types of valves and conduits in this position. If the valve and conduit they used persists with similar performance beyond 10 years, it would be a very good option. However, what typically happens is that replacement valves look good for about 10 years and then start to fail, often with a steep failure curve. I suspect that during the next 10 years of follow-up many more of the valves they placed will start to fail. The 10- to 20-year follow-up period is critical for demonstrating long-term durability of this valve and conduit.
 |
Dr. James Jaggers |
One additional potential advantage of the Carpentier-Edwards prosthesis is that the valve it contains is larger than the usual valve placed in the right ventricular outflow tract (RVOT). Failed valves increasingly are replaced by a transcatheter approach that puts a new valve inside the old, failed valve. As patients who received these replacement valves continue to survive we anticipate their need over time for a series of valve-in-valve procedures. The larger the valve at the outset, the more feasible it will be to have multiple episodes of valve-in-valve replacement.
At one time, we regarded early surgical repair of a tetralogy of Fallot defect as curative. We now know that as children with a repaired tetralogy of Fallot grow into teens and adults they require additional repairs, most often replacement of their RVOTs. This has made pulmonary valve replacement the most common surgery for adult survivors of congenital heart disease. The numbers of teen or adult patients who require a new RVOT will steadily increase as more of these children survive.
Dr. James Jaggers, professor of surgery at the University of Colorado and chief of cardiothoracic surgery at Children’s Hospital Colorado in Denver, made these comments in an interview. He had no disclosures.
PHOENIX – A prosthetic conduit that contains a porcine valve showed excellent intermediate-term durability for repairing the right ventricular outflow tract in 100 teenagers and young adults at a single U.S. center.
“The Carpentier-Edwards xenograft for right ventricular outflow tract [RVOT] reconstruction provides excellent freedom from reoperation and valve dysfunction, as well as sustained improvement in right-ventricular chamber size at intermediate-term follow-up,” Dr. Heidi B. Schubmehl said at the Society of Thoracic Surgeons annual meeting.
Dr. Schubmehl reported a 92% rate of freedom from valve dysfunction with follow-up out to about 10 years, and significant reductions in right ventricular size at follow-up, compared with baseline, as measured by both echocardiography and by MRI.
The Carpentier-Edwards porcine valve and conduit “seemed to hold up better than a lot of other [prosthetic] valves,” said Dr. George M. Alfieris, director of pediatric cardiac surgery at the University of Rochester (N.Y.), and senior author for the study. In addition to the valve’s durability over approximately the first 10 years following placement, the results also showed the positive impact the valve had on right ventricular size, an important result of the repair’s efficacy, Dr. Alfieris said.
“It’s a mistake to allow the right ventricle to be under high pressure or to reach a large volume. We now focus on preserving the right ventricle,” he said in an interview. “I’ve become very concerned about preventing right ventricular dilation and preserving right ventricular function.”
Dr. Alfieris noted that his prior experience using other types of valves in the pulmonary valve and RVOT position showed those valves “did great for the first 10 years and then failed. What’s different in this series is that after 10 years, we have not seen the same dysfunction as with the prior generation of valves. I will be very interested to see what happens to them” as follow-up continues beyond 10 years. He also expressed dismay that recently the company that had been marketing the valve and conduit used in the current study, the Carpentier-Edwards, stopped selling them. He expects that as his supply of conduits runs out he’ll have to start using a different commercial valve and conduit that he believes will not perform as well or create his own conduits with a porcine valve from a different supplier.
The series of 100 patients comprised individuals aged 17 or older who received a pulmonary artery and had RVOT reconstruction at the University of Rochester during 2000-2010, Dr. Schubmehl reported. The series included 78 patients with a history of tetralogy of Fallot, 8 patients born with transposition of their great arteries, 8 patients with truncus arteriosus, and 6 patients with other congenital heart diseases. Their median age at the time they received the RVOT conduit was 24 years, 59% were men, and 99 had undergone a prior sternotomy. At the time they received the conduit, 55 had pulmonary valve insufficiency, 30 had valve stenosis, and 15 had both. Follow-up occurred an average of 7 years after conduit placement.
Two recipients died: One death occurred perioperatively in a 41-year old who had a massive cerebrovascular event, and the second death was in a 39-year old who died 2.6 years after conduit placement from respiratory failure. Two additional patients required a reintervention during follow-up, said Dr. Schubmehl, a general surgeon at the University of Rochester. One reintervention occurred after 11 years to treat endocarditis, and the second after 11 years to perform balloon valvuloplasty because of valve stenosis.
The results reported by Dr. Schubmehl for echocardiography examinations showed that the patients had a statistically significant reduction in their RVOT pressure gradient from baseline to 1-year follow-up that was sustained through their intermediate-term follow-up. Seventy-seven patients had pulmonary valve insufficiency at baseline that resolved in all patients at 1-year follow-up and remained resolved in all but one patient at extended follow-up. Nineteen patients underwent additional imaging with MRI at an average follow-up of 7 years, and these findings confirmed the echo results.
On Twitter @mitchelzoler
PHOENIX – A prosthetic conduit that contains a porcine valve showed excellent intermediate-term durability for repairing the right ventricular outflow tract in 100 teenagers and young adults at a single U.S. center.
“The Carpentier-Edwards xenograft for right ventricular outflow tract [RVOT] reconstruction provides excellent freedom from reoperation and valve dysfunction, as well as sustained improvement in right-ventricular chamber size at intermediate-term follow-up,” Dr. Heidi B. Schubmehl said at the Society of Thoracic Surgeons annual meeting.
Dr. Schubmehl reported a 92% rate of freedom from valve dysfunction with follow-up out to about 10 years, and significant reductions in right ventricular size at follow-up, compared with baseline, as measured by both echocardiography and by MRI.
The Carpentier-Edwards porcine valve and conduit “seemed to hold up better than a lot of other [prosthetic] valves,” said Dr. George M. Alfieris, director of pediatric cardiac surgery at the University of Rochester (N.Y.), and senior author for the study. In addition to the valve’s durability over approximately the first 10 years following placement, the results also showed the positive impact the valve had on right ventricular size, an important result of the repair’s efficacy, Dr. Alfieris said.
“It’s a mistake to allow the right ventricle to be under high pressure or to reach a large volume. We now focus on preserving the right ventricle,” he said in an interview. “I’ve become very concerned about preventing right ventricular dilation and preserving right ventricular function.”
Dr. Alfieris noted that his prior experience using other types of valves in the pulmonary valve and RVOT position showed those valves “did great for the first 10 years and then failed. What’s different in this series is that after 10 years, we have not seen the same dysfunction as with the prior generation of valves. I will be very interested to see what happens to them” as follow-up continues beyond 10 years. He also expressed dismay that recently the company that had been marketing the valve and conduit used in the current study, the Carpentier-Edwards, stopped selling them. He expects that as his supply of conduits runs out he’ll have to start using a different commercial valve and conduit that he believes will not perform as well or create his own conduits with a porcine valve from a different supplier.
The series of 100 patients comprised individuals aged 17 or older who received a pulmonary artery and had RVOT reconstruction at the University of Rochester during 2000-2010, Dr. Schubmehl reported. The series included 78 patients with a history of tetralogy of Fallot, 8 patients born with transposition of their great arteries, 8 patients with truncus arteriosus, and 6 patients with other congenital heart diseases. Their median age at the time they received the RVOT conduit was 24 years, 59% were men, and 99 had undergone a prior sternotomy. At the time they received the conduit, 55 had pulmonary valve insufficiency, 30 had valve stenosis, and 15 had both. Follow-up occurred an average of 7 years after conduit placement.
Two recipients died: One death occurred perioperatively in a 41-year old who had a massive cerebrovascular event, and the second death was in a 39-year old who died 2.6 years after conduit placement from respiratory failure. Two additional patients required a reintervention during follow-up, said Dr. Schubmehl, a general surgeon at the University of Rochester. One reintervention occurred after 11 years to treat endocarditis, and the second after 11 years to perform balloon valvuloplasty because of valve stenosis.
The results reported by Dr. Schubmehl for echocardiography examinations showed that the patients had a statistically significant reduction in their RVOT pressure gradient from baseline to 1-year follow-up that was sustained through their intermediate-term follow-up. Seventy-seven patients had pulmonary valve insufficiency at baseline that resolved in all patients at 1-year follow-up and remained resolved in all but one patient at extended follow-up. Nineteen patients underwent additional imaging with MRI at an average follow-up of 7 years, and these findings confirmed the echo results.
On Twitter @mitchelzoler
AT THE STS ANNUAL MEETING
Key clinical point: A prosthetic conduit with a porcine valve showed excellent durability for congenital heart defect repairs at intermediate-term follow-up.
Major finding: After an average 7-year follow-up, the replacement valve and conduit had a 92% rate of freedom from valve dysfunction.
Data source: Single-center series of 100 patients.
Disclosures: Dr. Schubmehl and Dr. Alfieris had no disclosures.
Limited benefits with mesh versus tissue repair for prolapse
There is limited evidence in favor of permanent transvaginal mesh or grafts over native tissue repair for vaginal prolapse, according to a systematic review of 37 randomized controlled trials.
Researchers reviewed trials involving 4,023 women comparing transvaginal grafts with traditional native tissue repair for vaginal prolapse. They found that permanent mesh repair was associated with a 34% lower likelihood of awareness of prolapse at 1-3 years after the procedure (risk ratio, 0.66) and a 60% lower likelihood of recurrent prolapse on examination (RR, 0.40), compared with native tissue repair, according to a paper published online Feb. 9 (Cochrane Database Syst Rev. doi: 10.1002/14651858.CD012079).
Women who underwent permanent mesh repair also had 47% lower rates of repeat surgery for prolapse than those who had native tissue repair (RR, 0.53), although neither approach achieved a significant difference in rates of repeat surgery for continence.
Overall, more than twice as many women in the mesh group needed repeat surgery for a combined outcome of prolapse, stress incontinence, or mesh exposure (RR, 2.40).
“This suggests that if 5% of women require repeat surgery after native tissue repair, between 7% and 18% in the permanent mesh group will do so,” wrote Dr. Christopher Maher of the Royal Brisbane and Women’s Hospital, Australia, and his coauthors.
However permanent mesh was also associated with 39% higher rates of de novo stress incontinence (RR, 1.39) and nearly a four-fold greater risk of bladder injury (RR, 3.92), compared with native tissue repair. There were no differences between the groups in rates of de novo dyspareunia and the researchers could not determine the impact on quality of life due to very low-quality evidence.
The researchers also examined the relative impact of absorbable mesh, compared with native tissue repair and, while the evidence for the effectiveness of either at 2 years was found to be of very low quality, the risk of recurrent prolapse on examination was 29% lower with the absorbable mesh group, compared with native tissue repair.
Similarly, studies comparing biological graft with native tissue repair were of low quality and found no evidence of a significant difference in the impact on the risk of recurrent prolapse or repeat surgery for prolapse.
Given the higher rates of repeat surgery for prolapse, stress urinary incontinence, mesh exposure, as well as higher rates of bladder injury at surgery and de novo stress incontinence, the review authors commented that the risk-benefit profile of transvaginal mesh suggested it had limited utility in primary surgery.
“While it is possible that in women with higher risk of recurrence the benefits may outweigh the risks, there is currently no evidence to support this position,” the authors wrote.
Overall, the quality of study evidence ranged from very low to moderate, with the main limitations being poor reporting of study methods, inconsistency, and imprecision.
“In 2011, many transvaginal permanent meshes were voluntarily withdrawn from the market, and the newer, lightweight transvaginal permanent meshes still available have not been evaluated within a randomized controlled trial,” the authors wrote. “In the meantime, these newer transvaginal meshes should be utilised under the discretion of the ethics committee.”
Dr. Maher reported involvement in two trials of pelvic prolapse. There were no other conflicts of interest reported.
There is limited evidence in favor of permanent transvaginal mesh or grafts over native tissue repair for vaginal prolapse, according to a systematic review of 37 randomized controlled trials.
Researchers reviewed trials involving 4,023 women comparing transvaginal grafts with traditional native tissue repair for vaginal prolapse. They found that permanent mesh repair was associated with a 34% lower likelihood of awareness of prolapse at 1-3 years after the procedure (risk ratio, 0.66) and a 60% lower likelihood of recurrent prolapse on examination (RR, 0.40), compared with native tissue repair, according to a paper published online Feb. 9 (Cochrane Database Syst Rev. doi: 10.1002/14651858.CD012079).
Women who underwent permanent mesh repair also had 47% lower rates of repeat surgery for prolapse than those who had native tissue repair (RR, 0.53), although neither approach achieved a significant difference in rates of repeat surgery for continence.
Overall, more than twice as many women in the mesh group needed repeat surgery for a combined outcome of prolapse, stress incontinence, or mesh exposure (RR, 2.40).
“This suggests that if 5% of women require repeat surgery after native tissue repair, between 7% and 18% in the permanent mesh group will do so,” wrote Dr. Christopher Maher of the Royal Brisbane and Women’s Hospital, Australia, and his coauthors.
However permanent mesh was also associated with 39% higher rates of de novo stress incontinence (RR, 1.39) and nearly a four-fold greater risk of bladder injury (RR, 3.92), compared with native tissue repair. There were no differences between the groups in rates of de novo dyspareunia and the researchers could not determine the impact on quality of life due to very low-quality evidence.
The researchers also examined the relative impact of absorbable mesh, compared with native tissue repair and, while the evidence for the effectiveness of either at 2 years was found to be of very low quality, the risk of recurrent prolapse on examination was 29% lower with the absorbable mesh group, compared with native tissue repair.
Similarly, studies comparing biological graft with native tissue repair were of low quality and found no evidence of a significant difference in the impact on the risk of recurrent prolapse or repeat surgery for prolapse.
Given the higher rates of repeat surgery for prolapse, stress urinary incontinence, mesh exposure, as well as higher rates of bladder injury at surgery and de novo stress incontinence, the review authors commented that the risk-benefit profile of transvaginal mesh suggested it had limited utility in primary surgery.
“While it is possible that in women with higher risk of recurrence the benefits may outweigh the risks, there is currently no evidence to support this position,” the authors wrote.
Overall, the quality of study evidence ranged from very low to moderate, with the main limitations being poor reporting of study methods, inconsistency, and imprecision.
“In 2011, many transvaginal permanent meshes were voluntarily withdrawn from the market, and the newer, lightweight transvaginal permanent meshes still available have not been evaluated within a randomized controlled trial,” the authors wrote. “In the meantime, these newer transvaginal meshes should be utilised under the discretion of the ethics committee.”
Dr. Maher reported involvement in two trials of pelvic prolapse. There were no other conflicts of interest reported.
There is limited evidence in favor of permanent transvaginal mesh or grafts over native tissue repair for vaginal prolapse, according to a systematic review of 37 randomized controlled trials.
Researchers reviewed trials involving 4,023 women comparing transvaginal grafts with traditional native tissue repair for vaginal prolapse. They found that permanent mesh repair was associated with a 34% lower likelihood of awareness of prolapse at 1-3 years after the procedure (risk ratio, 0.66) and a 60% lower likelihood of recurrent prolapse on examination (RR, 0.40), compared with native tissue repair, according to a paper published online Feb. 9 (Cochrane Database Syst Rev. doi: 10.1002/14651858.CD012079).
Women who underwent permanent mesh repair also had 47% lower rates of repeat surgery for prolapse than those who had native tissue repair (RR, 0.53), although neither approach achieved a significant difference in rates of repeat surgery for continence.
Overall, more than twice as many women in the mesh group needed repeat surgery for a combined outcome of prolapse, stress incontinence, or mesh exposure (RR, 2.40).
“This suggests that if 5% of women require repeat surgery after native tissue repair, between 7% and 18% in the permanent mesh group will do so,” wrote Dr. Christopher Maher of the Royal Brisbane and Women’s Hospital, Australia, and his coauthors.
However permanent mesh was also associated with 39% higher rates of de novo stress incontinence (RR, 1.39) and nearly a four-fold greater risk of bladder injury (RR, 3.92), compared with native tissue repair. There were no differences between the groups in rates of de novo dyspareunia and the researchers could not determine the impact on quality of life due to very low-quality evidence.
The researchers also examined the relative impact of absorbable mesh, compared with native tissue repair and, while the evidence for the effectiveness of either at 2 years was found to be of very low quality, the risk of recurrent prolapse on examination was 29% lower with the absorbable mesh group, compared with native tissue repair.
Similarly, studies comparing biological graft with native tissue repair were of low quality and found no evidence of a significant difference in the impact on the risk of recurrent prolapse or repeat surgery for prolapse.
Given the higher rates of repeat surgery for prolapse, stress urinary incontinence, mesh exposure, as well as higher rates of bladder injury at surgery and de novo stress incontinence, the review authors commented that the risk-benefit profile of transvaginal mesh suggested it had limited utility in primary surgery.
“While it is possible that in women with higher risk of recurrence the benefits may outweigh the risks, there is currently no evidence to support this position,” the authors wrote.
Overall, the quality of study evidence ranged from very low to moderate, with the main limitations being poor reporting of study methods, inconsistency, and imprecision.
“In 2011, many transvaginal permanent meshes were voluntarily withdrawn from the market, and the newer, lightweight transvaginal permanent meshes still available have not been evaluated within a randomized controlled trial,” the authors wrote. “In the meantime, these newer transvaginal meshes should be utilised under the discretion of the ethics committee.”
Dr. Maher reported involvement in two trials of pelvic prolapse. There were no other conflicts of interest reported.
FROM THE COCHRANE DATABASE OF SYSTEMATIC REVIEWS
Key clinical point: Permanent mesh offers some advantages over native tissue repair for vaginal prolapse but with a greater risk of repeat surgery and incontinence.
Major finding: Permanent mesh repair is associated with a 34% lower likelihood of awareness of prolapse at 1-3 years after the procedure, compared with native tissue repair.
Data source: Review of 37 randomized controlled trials in 4,023 women with vaginal prolapse.
Disclosures: Dr. Maher reported involvement in two trials of pelvic prolapse. There were no other conflicts of interest reported.
The Daily Safety Brief in a Safety Net Hospital: Development and Outcomes
From the MetroHealth Medical Center, Cleveland, OH.
Abstract
- Objective: To describe the process for the creation and development of the Daily Safety Brief (DSB) in our safety net hospital.
- Methods: We developed the DSB, a daily interdepartmental briefing intended to increase the safety of patients, employees, and visitors by improving communication and situational awareness. Situational awareness involves gathering the right information, analyzing it, and making predictions and projections based on the analysis. Reporting issues while they are small oftentimes makes them easier to manage. The average call length with 25 departments reporting is just 9.5 minutes.
- Results: Survey results reveal an overall average improvement in awareness among DSB participants about hospital safety issues. Average days to issue resolution is currently 2.3 days, with open issues tracked and reported on daily.
- Conclusion: The DSB has improved real-time communication and awareness about safety issues in our organization.
As health care organizations strive to ensure a culture of safety for patients and staff, they must also be able to demonstrate reliability in that culture. The concept of highly reliable organizations originated in aviation and military fields due to the high-stakes environment and need for rapid and effective communication across departments. High reliability in health care organizations is described by the Joint Commission as consistent excellence in quality and safety for every patient, every time [1].
Highly reliable organizations put systems in place that makes them resilient with methods that lead to consistent accomplishment of goals and strategies to avoid potentially catastrophic errors [2]. An integral component to success in all high reliability organizations is a method of “Plan-of-the-Day” meetings to keep staff apprised of critical updates throughout the health system impacting care delivery [3]. Leaders at MetroHealth Medical Center believed that a daily safety briefing would help support the hospital’s journey to high reliability. We developed the Daily Safety Brief (DSB), a daily interdepartmental briefing intended to increase the safety of patients, employees, and visitors by improving communication and situational awareness. Situational awareness involves gathering the right information, analyzing it, and making predictions and projections based on the analysis [4]. Reporting issues while they are small oftentimes makes them easier to manage. This article will describe the development and implementation of the DSB in our hospital.
Setting
MetroHealth Medical Center is an academic medical center in Cleveland, OH, affiliated with Case Western Reserve University. Metrohealth is a public safety net hospital with 731 licensed beds and a total of 1,160,773 patient visits in 2014, with 27,933 inpatient stays and 106,000 emergency department (ED) visits. The staff includes 507 physicians, 374 resident physicians, and 1222 nurses.
Program Development
As Metrohealth was contemplating the DSB, a group of senior leaders, including the chief medical officer, visited the Cincinnati Children’s Hospital, which had a DSB process in place. Following that visit, a larger group of physicians and administrators from intake points, procedural areas, and ancillary departments were invited to listen in live to Cincinnati’s DSB. This turned out to be a pivotal step in gaining buy-in. The initial concerns from participants were that this would be another scheduled meeting in an already busy day. What we learned from listening in was that the DSB was conducted in a manner that was succinct and professional. Issues were identified without accusations or unrelated agendas. Following the call, participants discussed how impressed they were and clearly saw the value of the information that was shared. They began to brainstorm about what they could report that would be relevant to the audience.
It was determined that a leader and 2 facilitators would be assigned to each call. The role of the DSB leader is to trigger individual department report outs and to ensure follow-up on unresolved safety issues from the previous DSB. Leaders are recruited by senior leadership and need to be familiar with the effects that issues can have across the health care system. Leaders need to be able to ask pertinent questions, have the credibility to raise concerns, and have access to senior administration when they need to bypass usual administrative channels.
The role of the facilitators, who are all members of the Center for Quality, is to connect to the conference bridge line, to keep the DSB leader on task, and to record all departmental data and pertinent details of the DSB. The facilitators maintain the daily DSB document, which outlines the order in which departments are called to report and identifies for the leader any open items identified in the previous day’s DSB.
The Daily Safety Brief
Rollout
The DSB began 3 days per week on Monday, Wednesday and Friday at 0830. The time was moved to 0800 since participants found the later time difficult as it fell in the middle of an hour, potentially conflicting with other meetings and preparation for the daily bed huddle. We recognized that many meetings began right at the start of the DSB. The CEO requested that all 0800 meetings begin with a call in to listen to the DSB. After 2 months, the frequency was increased to 5 days per week, Monday through Friday. The hospital trialed a weekend DSB, however, feedback from participants found this extremely difficult to attend due to leaner weekend staffing models and found that information shared was not impactful. In particular, items were identified on the weekend daily safety briefs but the staff needed to resolve those items were generally not available until Monday.
Refinements
Coaching occurred to help people be more succinct in sharing information that would impact other areas. Information that was relevant only internally to their department was streamlined. The participants were counseled to identify items that had potential impact on other departments or where other departments had resources that might improve operations.
After a year, participating departments requested the addition of the logistics and construction departments to the DSB. The addition of the logistics department offered the opportunity for clinical departments to communicate what equipment was needed to start the day and created the opportunity for logistics to close the feedback loop by giving an estimate on expected time of arrival of equipment. The addition of the construction department helped communicate issues that may impact the organization, and helps to coordinate care to minimally impact patients and operations.
Examples of Safety Improvements
The DSB keeps the departmental leadership aware of problems developing in all areas of the hospital. Upcoming safety risks are identified early so that plans can be put in place to ameliorate them. The expectation of the DSB leader is that a problem that isn’t readily solved during the DSB must be taken to senior administration for resolution. As an example, an issue involving delays in the purchase of a required neonatal ventilator was taken directly to the CEO by the DSB leader, resulting in completion of the purchase within days. Importantly, the requirement to report at the DSB leads to a preoccupation with risk and reporting and leads to transparency among interdependent departments.
Another issue effectively addressed by the DSB was when we received notification of a required mandatory power shutdown for an extended period of time. The local power company informed our facilities management department director that they discovered issues requiring urgent replacement of the transformer within 2 weeks. Facilities management reported this in the morning DSB. The DSB leader requested all stakeholders to stay on the call following completion of the DSB, and plans were set in motion to plan for the shutdown of power. The team agreed to conference call again at noon the same day to continue planning, and the affected building was prepared for the shutdown by the following day.
Another benefit of the DSB is illustrated by our inpatient psychiatry unit, which reports an acuity measure each day on a scale of 1 to 10. The MetroHealth Police Department utilizes the report to adjust their rounding schedule, with increased presence on days with high acuity, which has led to an improvement in morale among psychiatry unit staff.
Challenges and Solutions
Since these reports are available to a wide audience in the organization, it is important to assure the reporters that no repercussions will ensue from any information that they provide. Senior leadership was enlisted to communicate with their departments that no repercussions would occur from reporting. As an example, some managers reported to the DSB development team privately that their supervisors were concerned about reporting of staff shortages on the DSB. As the shortages had patient care implications and affected other clinical departments, the DSB development team met with the involved supervisors to address the need for open reporting. In fact, repeated reporting of shortages in one support department on the DSB resulted in that issue being taken to high levels of administration leading to an increase in their staffing levels.
Scheduling can be a challenge for DSB participants. Holding the DSB at 0800 has led some departments to delegate the reporting or information gathering. For the individual reporting departments, creating a reporting workflow was a challenge. The departments needed to ensure that their DSB report was ready to go by 0800. This timeline forced departments to improve their own interdepartmental communication structure. An unexpected benefit of this requirement is that some departments have created a morning huddle to share information, which has reportedly improved communication and morale. The ambulatory network created a separate shared database for clinics to post concerns meeting DSB reporting criteria. One designated staff member would access this collective information when preparing for the DSB report. While most departments have a senior manager providing their report, this is not a requirement. In many departments, that reporter varies from day to day, although consistently it is someone with some administrative or leadership role in the department.
Conference call technology presented the solution to the problem of acquiring a meeting space for a large group. The DSB is broadcast from one physical location, where the facilitators and leader convene. While this conference room is open to anyone who wants to attend in person, most departments choose to participate through the conference line. The DSB conference call is open to anyone in the organization to access. Typically 35 to 40 phones are accessing the line each DSB. Challenges included callers not muting their phones, creating distracting background noise, and callers placing their phones on hold, which prompted the hospital hold message to play continuously. Multiple repeated reminders via email and at the start of the DSB has rectified this issue for the most part, with occasional reminders made when the issue recurs.
Data Management
Initially, an Excel file was created with columns for each reporting department as well as each item they were asked to report on. This “running” file became cumbersome. Retrieving information on past issues was not automated. Therefore, we enlisted the help of a data analyst to create an Access database. When it was complete, this new database allowed us to save information by individual dates, query number of days to issue resolution, and create reports noting unresolved issues for the leader to reference. Many data points can be queried in the access database. Real-time reports are available at all times and updated with every data entry. The database is able to identify departments not on the daily call and trend information, ie, how many listeners were on the DSB, number of falls, forensic patients in house, number of patients awaiting admission from the ED, number of ambulatory visits scheduled each day, equipment needed, number of cardiac arrest calls, and number of neonatal resuscitations.
At the conclusion of the call, the DSB report is completed and posted to a shared website on the hospital intranet for the entire hospital to access and read. Feedback from participant indicated that they found it cumbersome to access this. The communications department was enlisted to enable easy access and staff can now access the DSB report from the front page of the hospital intranet.
Outcomes
Since initiation of our DSB, we have tracked the average number of minutes spent on each call. When calls began, the average time on the call was 12.4 minutes. With the evolution of the DSB and coaching managers in various departments, the average time on the call is now 9.5 minutes in 2015, despite additional reporting departments joining the DSB.
Summary
The DSB has become an important tool in creating and moving towards a culture of safety and high reliability within the MetroHealth System. Over time, processes have become organized and engrained in all departments. This format has allowed issues to be brought forward timely where immediate attention can be given to achieve resolution in a nonthreatening manner, improving transparency. The fluidity of the DSB allows it to be enhanced and modified as improvements and opportunities are identified in the organization. The DSB has provided opportunities to create situational awareness which allows a look forward to prevention and creates a proactive environment. The results of these efforts has made MetroHealth a safer place for patients, visitors, and employees.
Corresponding author: Anne M. Aulisio, MSN, aaulisio@metrohealth.org.
Financial disclosures: None.
1. Joint Commission Center for Transforming Healthcare. Available at www.centerfortransforminghealthcare.org.
2. Gamble M. 5 traits of high reliability organizations: how to hardwire each in your organization. Becker’s Hospital Review 29 Apr 2013. Accessed at www.beckershospitalreview.com/hospital-management-administration/5-traits-of-high-reliability-organizations-how-to-hardwire-each-in-your-organization.html.
3. Stockmeier C, Clapper C. Daily check-in for safety: from best practice to common practice. Patient Safety Qual Healthcare 2011:23. Accessed at psqh.com/daily-check-in-for-safety-from-best-practice-to-common-practice.
4. Creating situational awareness: a systems approach. In: Institute of Medicine (US) Forum on Medical and Public Health Preparedness for Catastrophic Events. Medical surge capacity: workshop summary. Washington, DC: National Academies Press; 2010. Accessed at www.ncbi.nlm.nih.gov/books/NBK32859/.
5. TeamSTEPPS. Available at www.ahrq.gov/professionals/education/curriculum-tools/teamstepps/index.html.
From the MetroHealth Medical Center, Cleveland, OH.
Abstract
- Objective: To describe the process for the creation and development of the Daily Safety Brief (DSB) in our safety net hospital.
- Methods: We developed the DSB, a daily interdepartmental briefing intended to increase the safety of patients, employees, and visitors by improving communication and situational awareness. Situational awareness involves gathering the right information, analyzing it, and making predictions and projections based on the analysis. Reporting issues while they are small oftentimes makes them easier to manage. The average call length with 25 departments reporting is just 9.5 minutes.
- Results: Survey results reveal an overall average improvement in awareness among DSB participants about hospital safety issues. Average days to issue resolution is currently 2.3 days, with open issues tracked and reported on daily.
- Conclusion: The DSB has improved real-time communication and awareness about safety issues in our organization.
As health care organizations strive to ensure a culture of safety for patients and staff, they must also be able to demonstrate reliability in that culture. The concept of highly reliable organizations originated in aviation and military fields due to the high-stakes environment and need for rapid and effective communication across departments. High reliability in health care organizations is described by the Joint Commission as consistent excellence in quality and safety for every patient, every time [1].
Highly reliable organizations put systems in place that makes them resilient with methods that lead to consistent accomplishment of goals and strategies to avoid potentially catastrophic errors [2]. An integral component to success in all high reliability organizations is a method of “Plan-of-the-Day” meetings to keep staff apprised of critical updates throughout the health system impacting care delivery [3]. Leaders at MetroHealth Medical Center believed that a daily safety briefing would help support the hospital’s journey to high reliability. We developed the Daily Safety Brief (DSB), a daily interdepartmental briefing intended to increase the safety of patients, employees, and visitors by improving communication and situational awareness. Situational awareness involves gathering the right information, analyzing it, and making predictions and projections based on the analysis [4]. Reporting issues while they are small oftentimes makes them easier to manage. This article will describe the development and implementation of the DSB in our hospital.
Setting
MetroHealth Medical Center is an academic medical center in Cleveland, OH, affiliated with Case Western Reserve University. Metrohealth is a public safety net hospital with 731 licensed beds and a total of 1,160,773 patient visits in 2014, with 27,933 inpatient stays and 106,000 emergency department (ED) visits. The staff includes 507 physicians, 374 resident physicians, and 1222 nurses.
Program Development
As Metrohealth was contemplating the DSB, a group of senior leaders, including the chief medical officer, visited the Cincinnati Children’s Hospital, which had a DSB process in place. Following that visit, a larger group of physicians and administrators from intake points, procedural areas, and ancillary departments were invited to listen in live to Cincinnati’s DSB. This turned out to be a pivotal step in gaining buy-in. The initial concerns from participants were that this would be another scheduled meeting in an already busy day. What we learned from listening in was that the DSB was conducted in a manner that was succinct and professional. Issues were identified without accusations or unrelated agendas. Following the call, participants discussed how impressed they were and clearly saw the value of the information that was shared. They began to brainstorm about what they could report that would be relevant to the audience.
It was determined that a leader and 2 facilitators would be assigned to each call. The role of the DSB leader is to trigger individual department report outs and to ensure follow-up on unresolved safety issues from the previous DSB. Leaders are recruited by senior leadership and need to be familiar with the effects that issues can have across the health care system. Leaders need to be able to ask pertinent questions, have the credibility to raise concerns, and have access to senior administration when they need to bypass usual administrative channels.
The role of the facilitators, who are all members of the Center for Quality, is to connect to the conference bridge line, to keep the DSB leader on task, and to record all departmental data and pertinent details of the DSB. The facilitators maintain the daily DSB document, which outlines the order in which departments are called to report and identifies for the leader any open items identified in the previous day’s DSB.
The Daily Safety Brief
Rollout
The DSB began 3 days per week on Monday, Wednesday and Friday at 0830. The time was moved to 0800 since participants found the later time difficult as it fell in the middle of an hour, potentially conflicting with other meetings and preparation for the daily bed huddle. We recognized that many meetings began right at the start of the DSB. The CEO requested that all 0800 meetings begin with a call in to listen to the DSB. After 2 months, the frequency was increased to 5 days per week, Monday through Friday. The hospital trialed a weekend DSB, however, feedback from participants found this extremely difficult to attend due to leaner weekend staffing models and found that information shared was not impactful. In particular, items were identified on the weekend daily safety briefs but the staff needed to resolve those items were generally not available until Monday.
Refinements
Coaching occurred to help people be more succinct in sharing information that would impact other areas. Information that was relevant only internally to their department was streamlined. The participants were counseled to identify items that had potential impact on other departments or where other departments had resources that might improve operations.
After a year, participating departments requested the addition of the logistics and construction departments to the DSB. The addition of the logistics department offered the opportunity for clinical departments to communicate what equipment was needed to start the day and created the opportunity for logistics to close the feedback loop by giving an estimate on expected time of arrival of equipment. The addition of the construction department helped communicate issues that may impact the organization, and helps to coordinate care to minimally impact patients and operations.
Examples of Safety Improvements
The DSB keeps the departmental leadership aware of problems developing in all areas of the hospital. Upcoming safety risks are identified early so that plans can be put in place to ameliorate them. The expectation of the DSB leader is that a problem that isn’t readily solved during the DSB must be taken to senior administration for resolution. As an example, an issue involving delays in the purchase of a required neonatal ventilator was taken directly to the CEO by the DSB leader, resulting in completion of the purchase within days. Importantly, the requirement to report at the DSB leads to a preoccupation with risk and reporting and leads to transparency among interdependent departments.
Another issue effectively addressed by the DSB was when we received notification of a required mandatory power shutdown for an extended period of time. The local power company informed our facilities management department director that they discovered issues requiring urgent replacement of the transformer within 2 weeks. Facilities management reported this in the morning DSB. The DSB leader requested all stakeholders to stay on the call following completion of the DSB, and plans were set in motion to plan for the shutdown of power. The team agreed to conference call again at noon the same day to continue planning, and the affected building was prepared for the shutdown by the following day.
Another benefit of the DSB is illustrated by our inpatient psychiatry unit, which reports an acuity measure each day on a scale of 1 to 10. The MetroHealth Police Department utilizes the report to adjust their rounding schedule, with increased presence on days with high acuity, which has led to an improvement in morale among psychiatry unit staff.
Challenges and Solutions
Since these reports are available to a wide audience in the organization, it is important to assure the reporters that no repercussions will ensue from any information that they provide. Senior leadership was enlisted to communicate with their departments that no repercussions would occur from reporting. As an example, some managers reported to the DSB development team privately that their supervisors were concerned about reporting of staff shortages on the DSB. As the shortages had patient care implications and affected other clinical departments, the DSB development team met with the involved supervisors to address the need for open reporting. In fact, repeated reporting of shortages in one support department on the DSB resulted in that issue being taken to high levels of administration leading to an increase in their staffing levels.
Scheduling can be a challenge for DSB participants. Holding the DSB at 0800 has led some departments to delegate the reporting or information gathering. For the individual reporting departments, creating a reporting workflow was a challenge. The departments needed to ensure that their DSB report was ready to go by 0800. This timeline forced departments to improve their own interdepartmental communication structure. An unexpected benefit of this requirement is that some departments have created a morning huddle to share information, which has reportedly improved communication and morale. The ambulatory network created a separate shared database for clinics to post concerns meeting DSB reporting criteria. One designated staff member would access this collective information when preparing for the DSB report. While most departments have a senior manager providing their report, this is not a requirement. In many departments, that reporter varies from day to day, although consistently it is someone with some administrative or leadership role in the department.
Conference call technology presented the solution to the problem of acquiring a meeting space for a large group. The DSB is broadcast from one physical location, where the facilitators and leader convene. While this conference room is open to anyone who wants to attend in person, most departments choose to participate through the conference line. The DSB conference call is open to anyone in the organization to access. Typically 35 to 40 phones are accessing the line each DSB. Challenges included callers not muting their phones, creating distracting background noise, and callers placing their phones on hold, which prompted the hospital hold message to play continuously. Multiple repeated reminders via email and at the start of the DSB has rectified this issue for the most part, with occasional reminders made when the issue recurs.
Data Management
Initially, an Excel file was created with columns for each reporting department as well as each item they were asked to report on. This “running” file became cumbersome. Retrieving information on past issues was not automated. Therefore, we enlisted the help of a data analyst to create an Access database. When it was complete, this new database allowed us to save information by individual dates, query number of days to issue resolution, and create reports noting unresolved issues for the leader to reference. Many data points can be queried in the access database. Real-time reports are available at all times and updated with every data entry. The database is able to identify departments not on the daily call and trend information, ie, how many listeners were on the DSB, number of falls, forensic patients in house, number of patients awaiting admission from the ED, number of ambulatory visits scheduled each day, equipment needed, number of cardiac arrest calls, and number of neonatal resuscitations.
At the conclusion of the call, the DSB report is completed and posted to a shared website on the hospital intranet for the entire hospital to access and read. Feedback from participant indicated that they found it cumbersome to access this. The communications department was enlisted to enable easy access and staff can now access the DSB report from the front page of the hospital intranet.
Outcomes
Since initiation of our DSB, we have tracked the average number of minutes spent on each call. When calls began, the average time on the call was 12.4 minutes. With the evolution of the DSB and coaching managers in various departments, the average time on the call is now 9.5 minutes in 2015, despite additional reporting departments joining the DSB.
Summary
The DSB has become an important tool in creating and moving towards a culture of safety and high reliability within the MetroHealth System. Over time, processes have become organized and engrained in all departments. This format has allowed issues to be brought forward timely where immediate attention can be given to achieve resolution in a nonthreatening manner, improving transparency. The fluidity of the DSB allows it to be enhanced and modified as improvements and opportunities are identified in the organization. The DSB has provided opportunities to create situational awareness which allows a look forward to prevention and creates a proactive environment. The results of these efforts has made MetroHealth a safer place for patients, visitors, and employees.
Corresponding author: Anne M. Aulisio, MSN, aaulisio@metrohealth.org.
Financial disclosures: None.
From the MetroHealth Medical Center, Cleveland, OH.
Abstract
- Objective: To describe the process for the creation and development of the Daily Safety Brief (DSB) in our safety net hospital.
- Methods: We developed the DSB, a daily interdepartmental briefing intended to increase the safety of patients, employees, and visitors by improving communication and situational awareness. Situational awareness involves gathering the right information, analyzing it, and making predictions and projections based on the analysis. Reporting issues while they are small oftentimes makes them easier to manage. The average call length with 25 departments reporting is just 9.5 minutes.
- Results: Survey results reveal an overall average improvement in awareness among DSB participants about hospital safety issues. Average days to issue resolution is currently 2.3 days, with open issues tracked and reported on daily.
- Conclusion: The DSB has improved real-time communication and awareness about safety issues in our organization.
As health care organizations strive to ensure a culture of safety for patients and staff, they must also be able to demonstrate reliability in that culture. The concept of highly reliable organizations originated in aviation and military fields due to the high-stakes environment and need for rapid and effective communication across departments. High reliability in health care organizations is described by the Joint Commission as consistent excellence in quality and safety for every patient, every time [1].
Highly reliable organizations put systems in place that makes them resilient with methods that lead to consistent accomplishment of goals and strategies to avoid potentially catastrophic errors [2]. An integral component to success in all high reliability organizations is a method of “Plan-of-the-Day” meetings to keep staff apprised of critical updates throughout the health system impacting care delivery [3]. Leaders at MetroHealth Medical Center believed that a daily safety briefing would help support the hospital’s journey to high reliability. We developed the Daily Safety Brief (DSB), a daily interdepartmental briefing intended to increase the safety of patients, employees, and visitors by improving communication and situational awareness. Situational awareness involves gathering the right information, analyzing it, and making predictions and projections based on the analysis [4]. Reporting issues while they are small oftentimes makes them easier to manage. This article will describe the development and implementation of the DSB in our hospital.
Setting
MetroHealth Medical Center is an academic medical center in Cleveland, OH, affiliated with Case Western Reserve University. Metrohealth is a public safety net hospital with 731 licensed beds and a total of 1,160,773 patient visits in 2014, with 27,933 inpatient stays and 106,000 emergency department (ED) visits. The staff includes 507 physicians, 374 resident physicians, and 1222 nurses.
Program Development
As Metrohealth was contemplating the DSB, a group of senior leaders, including the chief medical officer, visited the Cincinnati Children’s Hospital, which had a DSB process in place. Following that visit, a larger group of physicians and administrators from intake points, procedural areas, and ancillary departments were invited to listen in live to Cincinnati’s DSB. This turned out to be a pivotal step in gaining buy-in. The initial concerns from participants were that this would be another scheduled meeting in an already busy day. What we learned from listening in was that the DSB was conducted in a manner that was succinct and professional. Issues were identified without accusations or unrelated agendas. Following the call, participants discussed how impressed they were and clearly saw the value of the information that was shared. They began to brainstorm about what they could report that would be relevant to the audience.
It was determined that a leader and 2 facilitators would be assigned to each call. The role of the DSB leader is to trigger individual department report outs and to ensure follow-up on unresolved safety issues from the previous DSB. Leaders are recruited by senior leadership and need to be familiar with the effects that issues can have across the health care system. Leaders need to be able to ask pertinent questions, have the credibility to raise concerns, and have access to senior administration when they need to bypass usual administrative channels.
The role of the facilitators, who are all members of the Center for Quality, is to connect to the conference bridge line, to keep the DSB leader on task, and to record all departmental data and pertinent details of the DSB. The facilitators maintain the daily DSB document, which outlines the order in which departments are called to report and identifies for the leader any open items identified in the previous day’s DSB.
The Daily Safety Brief
Rollout
The DSB began 3 days per week on Monday, Wednesday and Friday at 0830. The time was moved to 0800 since participants found the later time difficult as it fell in the middle of an hour, potentially conflicting with other meetings and preparation for the daily bed huddle. We recognized that many meetings began right at the start of the DSB. The CEO requested that all 0800 meetings begin with a call in to listen to the DSB. After 2 months, the frequency was increased to 5 days per week, Monday through Friday. The hospital trialed a weekend DSB, however, feedback from participants found this extremely difficult to attend due to leaner weekend staffing models and found that information shared was not impactful. In particular, items were identified on the weekend daily safety briefs but the staff needed to resolve those items were generally not available until Monday.
Refinements
Coaching occurred to help people be more succinct in sharing information that would impact other areas. Information that was relevant only internally to their department was streamlined. The participants were counseled to identify items that had potential impact on other departments or where other departments had resources that might improve operations.
After a year, participating departments requested the addition of the logistics and construction departments to the DSB. The addition of the logistics department offered the opportunity for clinical departments to communicate what equipment was needed to start the day and created the opportunity for logistics to close the feedback loop by giving an estimate on expected time of arrival of equipment. The addition of the construction department helped communicate issues that may impact the organization, and helps to coordinate care to minimally impact patients and operations.
Examples of Safety Improvements
The DSB keeps the departmental leadership aware of problems developing in all areas of the hospital. Upcoming safety risks are identified early so that plans can be put in place to ameliorate them. The expectation of the DSB leader is that a problem that isn’t readily solved during the DSB must be taken to senior administration for resolution. As an example, an issue involving delays in the purchase of a required neonatal ventilator was taken directly to the CEO by the DSB leader, resulting in completion of the purchase within days. Importantly, the requirement to report at the DSB leads to a preoccupation with risk and reporting and leads to transparency among interdependent departments.
Another issue effectively addressed by the DSB was when we received notification of a required mandatory power shutdown for an extended period of time. The local power company informed our facilities management department director that they discovered issues requiring urgent replacement of the transformer within 2 weeks. Facilities management reported this in the morning DSB. The DSB leader requested all stakeholders to stay on the call following completion of the DSB, and plans were set in motion to plan for the shutdown of power. The team agreed to conference call again at noon the same day to continue planning, and the affected building was prepared for the shutdown by the following day.
Another benefit of the DSB is illustrated by our inpatient psychiatry unit, which reports an acuity measure each day on a scale of 1 to 10. The MetroHealth Police Department utilizes the report to adjust their rounding schedule, with increased presence on days with high acuity, which has led to an improvement in morale among psychiatry unit staff.
Challenges and Solutions
Since these reports are available to a wide audience in the organization, it is important to assure the reporters that no repercussions will ensue from any information that they provide. Senior leadership was enlisted to communicate with their departments that no repercussions would occur from reporting. As an example, some managers reported to the DSB development team privately that their supervisors were concerned about reporting of staff shortages on the DSB. As the shortages had patient care implications and affected other clinical departments, the DSB development team met with the involved supervisors to address the need for open reporting. In fact, repeated reporting of shortages in one support department on the DSB resulted in that issue being taken to high levels of administration leading to an increase in their staffing levels.
Scheduling can be a challenge for DSB participants. Holding the DSB at 0800 has led some departments to delegate the reporting or information gathering. For the individual reporting departments, creating a reporting workflow was a challenge. The departments needed to ensure that their DSB report was ready to go by 0800. This timeline forced departments to improve their own interdepartmental communication structure. An unexpected benefit of this requirement is that some departments have created a morning huddle to share information, which has reportedly improved communication and morale. The ambulatory network created a separate shared database for clinics to post concerns meeting DSB reporting criteria. One designated staff member would access this collective information when preparing for the DSB report. While most departments have a senior manager providing their report, this is not a requirement. In many departments, that reporter varies from day to day, although consistently it is someone with some administrative or leadership role in the department.
Conference call technology presented the solution to the problem of acquiring a meeting space for a large group. The DSB is broadcast from one physical location, where the facilitators and leader convene. While this conference room is open to anyone who wants to attend in person, most departments choose to participate through the conference line. The DSB conference call is open to anyone in the organization to access. Typically 35 to 40 phones are accessing the line each DSB. Challenges included callers not muting their phones, creating distracting background noise, and callers placing their phones on hold, which prompted the hospital hold message to play continuously. Multiple repeated reminders via email and at the start of the DSB has rectified this issue for the most part, with occasional reminders made when the issue recurs.
Data Management
Initially, an Excel file was created with columns for each reporting department as well as each item they were asked to report on. This “running” file became cumbersome. Retrieving information on past issues was not automated. Therefore, we enlisted the help of a data analyst to create an Access database. When it was complete, this new database allowed us to save information by individual dates, query number of days to issue resolution, and create reports noting unresolved issues for the leader to reference. Many data points can be queried in the access database. Real-time reports are available at all times and updated with every data entry. The database is able to identify departments not on the daily call and trend information, ie, how many listeners were on the DSB, number of falls, forensic patients in house, number of patients awaiting admission from the ED, number of ambulatory visits scheduled each day, equipment needed, number of cardiac arrest calls, and number of neonatal resuscitations.
At the conclusion of the call, the DSB report is completed and posted to a shared website on the hospital intranet for the entire hospital to access and read. Feedback from participant indicated that they found it cumbersome to access this. The communications department was enlisted to enable easy access and staff can now access the DSB report from the front page of the hospital intranet.
Outcomes
Since initiation of our DSB, we have tracked the average number of minutes spent on each call. When calls began, the average time on the call was 12.4 minutes. With the evolution of the DSB and coaching managers in various departments, the average time on the call is now 9.5 minutes in 2015, despite additional reporting departments joining the DSB.
Summary
The DSB has become an important tool in creating and moving towards a culture of safety and high reliability within the MetroHealth System. Over time, processes have become organized and engrained in all departments. This format has allowed issues to be brought forward timely where immediate attention can be given to achieve resolution in a nonthreatening manner, improving transparency. The fluidity of the DSB allows it to be enhanced and modified as improvements and opportunities are identified in the organization. The DSB has provided opportunities to create situational awareness which allows a look forward to prevention and creates a proactive environment. The results of these efforts has made MetroHealth a safer place for patients, visitors, and employees.
Corresponding author: Anne M. Aulisio, MSN, aaulisio@metrohealth.org.
Financial disclosures: None.
1. Joint Commission Center for Transforming Healthcare. Available at www.centerfortransforminghealthcare.org.
2. Gamble M. 5 traits of high reliability organizations: how to hardwire each in your organization. Becker’s Hospital Review 29 Apr 2013. Accessed at www.beckershospitalreview.com/hospital-management-administration/5-traits-of-high-reliability-organizations-how-to-hardwire-each-in-your-organization.html.
3. Stockmeier C, Clapper C. Daily check-in for safety: from best practice to common practice. Patient Safety Qual Healthcare 2011:23. Accessed at psqh.com/daily-check-in-for-safety-from-best-practice-to-common-practice.
4. Creating situational awareness: a systems approach. In: Institute of Medicine (US) Forum on Medical and Public Health Preparedness for Catastrophic Events. Medical surge capacity: workshop summary. Washington, DC: National Academies Press; 2010. Accessed at www.ncbi.nlm.nih.gov/books/NBK32859/.
5. TeamSTEPPS. Available at www.ahrq.gov/professionals/education/curriculum-tools/teamstepps/index.html.
1. Joint Commission Center for Transforming Healthcare. Available at www.centerfortransforminghealthcare.org.
2. Gamble M. 5 traits of high reliability organizations: how to hardwire each in your organization. Becker’s Hospital Review 29 Apr 2013. Accessed at www.beckershospitalreview.com/hospital-management-administration/5-traits-of-high-reliability-organizations-how-to-hardwire-each-in-your-organization.html.
3. Stockmeier C, Clapper C. Daily check-in for safety: from best practice to common practice. Patient Safety Qual Healthcare 2011:23. Accessed at psqh.com/daily-check-in-for-safety-from-best-practice-to-common-practice.
4. Creating situational awareness: a systems approach. In: Institute of Medicine (US) Forum on Medical and Public Health Preparedness for Catastrophic Events. Medical surge capacity: workshop summary. Washington, DC: National Academies Press; 2010. Accessed at www.ncbi.nlm.nih.gov/books/NBK32859/.
5. TeamSTEPPS. Available at www.ahrq.gov/professionals/education/curriculum-tools/teamstepps/index.html.