User login
Product Update: FUJIFILM; Freemie, Preventeza, and C-Panty
NEW VISUALIZATION SYSTEMS FROM FUJIFILM
FUJIFILM New Development, USA, has introduced 2 visualization systems for minimally invasive surgery. Using proprietary technology, the Ultra-Slim Video Laparoscope System (EL-580FN) delivers enhanced image resolution, color fidelity, and display quality, says FUJIFILM. The product features include “Chip on the Tip” high-definition digital imaging processing, less fogging, autoclave sterilization reprocessing, and a low profile, lightweight ergonomic handle. The 3.8-mm-diameter distal end was designed to improve workflow, reduce physician fatigue, and potentially reduce the size of incisions. The accompanying Digital Video Processor System is used for endoscopic procedures with automatic light control, an anti-blur function for motion images, and digital zoom.
FUJIFILM reports that the Full High Definition Surgical Visualization System is designed for a wide variety of surgical applications and offers edge enhancement, automatic gain control, dynamic contrast function, selective color enhancement, smoke reduction, and grid removal features. It includes a portfolio of rigid scopes, cameras, and video processing systems.
FOR MORE INFORMATION, VISIT: http://www.fujifilmusa.com
FREEMIE BREAST MILK COLLECTION SYSTEM
Freemie® offers a hands-free breast-milk collection system with the Freemie Liberty Mobile Hands Free Breast Pump System and Next Generation Freemie Closed System Collection Cups.
The concealable pump has a rechargeable battery and hospital-power suction for single or double pumping. Programmable memory buttons allow the mother to preset or adjust speed and suction functions. Tubing lengths can be changed so that the pump can be placed on a desk, worn with a detachable belt clip, or carried in a bag.
Freemie says the cups are lower-profile and more compact than other pump system cups, and when placed on the breast under the mother’s bra, can be easily removed so that milk can be transferred to storage. Each cup, with a 25 mm or 28 mm funnel and valve, holds 8 oz of milk.
FOR MORE INFORMATION, VISIT: http://www.freemie.com
PREVENTEZA: EMERGENCY CONTRACEPTIVE
Combe, Inc, the maker of Vagisil®, has launched Preventeza™ (levonorgestrel tablet, 1.5 mg), an emergency contraceptive for the prevention of pregnancy if unprotected sex or failed birth control occurs.
Available online or over-the-counter as a single tablet, Preventeza is a proven option to help women prevent pregnancy before it starts by using a higher dose of levonorgestrel than most birth control pills. It must be used within 72 hours of unprotected intercourse, and is not intended to be used as regular birth control. Combe says that Preventeza works mainly by stopping the release of an egg from the ovary and may also prevent fertilization of an egg or prevent a fertilized egg from implanting in the uterus. Combe also says that levonorgestrel 1.5 mg will not work if the woman is already pregnant and will not affect an existing pregnancy.
FOR MORE INFORMATION, VISIT: https://www.vagisil.com/products/preventeza-emergency-contraceptive
UPSPRING’S C-PANTY FOR POSTCESAREAN RECOVERY
UpSpring® says that its patented C-Panty® undergarment provides medical-grade compression and speeds recovery after cesarean delivery. C-Panty helps to reduce swelling and discomfort, supports weakened muscles, and reduces the incision bulge without hooks, straps, or Velcro that might irritate the incision area.
C-Panty’s medical-grade silicone panel suppresses the formation of excess or improperly formed collagen, which can contribute to scarring, says UpSpring. The silicone may help reduce itchiness, and can lessen the chance of infection at the incision area. The silicone is durable, washable, and integrated into the panty, eliminating the need for scar gel or scar gel pads.
The C-Panty can be worn immediately after birth and for up to 12 months. If worn when the incision is not healed, the silicone panel should be covered with a panty liner or pad. Once the incision has healed, the covering can be discontinued.
FOR MORE INFORMATION, VISIT: https://www.upspringbaby.com/cpanty
NEW VISUALIZATION SYSTEMS FROM FUJIFILM
FUJIFILM New Development, USA, has introduced 2 visualization systems for minimally invasive surgery. Using proprietary technology, the Ultra-Slim Video Laparoscope System (EL-580FN) delivers enhanced image resolution, color fidelity, and display quality, says FUJIFILM. The product features include “Chip on the Tip” high-definition digital imaging processing, less fogging, autoclave sterilization reprocessing, and a low profile, lightweight ergonomic handle. The 3.8-mm-diameter distal end was designed to improve workflow, reduce physician fatigue, and potentially reduce the size of incisions. The accompanying Digital Video Processor System is used for endoscopic procedures with automatic light control, an anti-blur function for motion images, and digital zoom.
FUJIFILM reports that the Full High Definition Surgical Visualization System is designed for a wide variety of surgical applications and offers edge enhancement, automatic gain control, dynamic contrast function, selective color enhancement, smoke reduction, and grid removal features. It includes a portfolio of rigid scopes, cameras, and video processing systems.
FOR MORE INFORMATION, VISIT: http://www.fujifilmusa.com
FREEMIE BREAST MILK COLLECTION SYSTEM
Freemie® offers a hands-free breast-milk collection system with the Freemie Liberty Mobile Hands Free Breast Pump System and Next Generation Freemie Closed System Collection Cups.
The concealable pump has a rechargeable battery and hospital-power suction for single or double pumping. Programmable memory buttons allow the mother to preset or adjust speed and suction functions. Tubing lengths can be changed so that the pump can be placed on a desk, worn with a detachable belt clip, or carried in a bag.
Freemie says the cups are lower-profile and more compact than other pump system cups, and when placed on the breast under the mother’s bra, can be easily removed so that milk can be transferred to storage. Each cup, with a 25 mm or 28 mm funnel and valve, holds 8 oz of milk.
FOR MORE INFORMATION, VISIT: http://www.freemie.com
PREVENTEZA: EMERGENCY CONTRACEPTIVE
Combe, Inc, the maker of Vagisil®, has launched Preventeza™ (levonorgestrel tablet, 1.5 mg), an emergency contraceptive for the prevention of pregnancy if unprotected sex or failed birth control occurs.
Available online or over-the-counter as a single tablet, Preventeza is a proven option to help women prevent pregnancy before it starts by using a higher dose of levonorgestrel than most birth control pills. It must be used within 72 hours of unprotected intercourse, and is not intended to be used as regular birth control. Combe says that Preventeza works mainly by stopping the release of an egg from the ovary and may also prevent fertilization of an egg or prevent a fertilized egg from implanting in the uterus. Combe also says that levonorgestrel 1.5 mg will not work if the woman is already pregnant and will not affect an existing pregnancy.
FOR MORE INFORMATION, VISIT: https://www.vagisil.com/products/preventeza-emergency-contraceptive
UPSPRING’S C-PANTY FOR POSTCESAREAN RECOVERY
UpSpring® says that its patented C-Panty® undergarment provides medical-grade compression and speeds recovery after cesarean delivery. C-Panty helps to reduce swelling and discomfort, supports weakened muscles, and reduces the incision bulge without hooks, straps, or Velcro that might irritate the incision area.
C-Panty’s medical-grade silicone panel suppresses the formation of excess or improperly formed collagen, which can contribute to scarring, says UpSpring. The silicone may help reduce itchiness, and can lessen the chance of infection at the incision area. The silicone is durable, washable, and integrated into the panty, eliminating the need for scar gel or scar gel pads.
The C-Panty can be worn immediately after birth and for up to 12 months. If worn when the incision is not healed, the silicone panel should be covered with a panty liner or pad. Once the incision has healed, the covering can be discontinued.
FOR MORE INFORMATION, VISIT: https://www.upspringbaby.com/cpanty
NEW VISUALIZATION SYSTEMS FROM FUJIFILM
FUJIFILM New Development, USA, has introduced 2 visualization systems for minimally invasive surgery. Using proprietary technology, the Ultra-Slim Video Laparoscope System (EL-580FN) delivers enhanced image resolution, color fidelity, and display quality, says FUJIFILM. The product features include “Chip on the Tip” high-definition digital imaging processing, less fogging, autoclave sterilization reprocessing, and a low profile, lightweight ergonomic handle. The 3.8-mm-diameter distal end was designed to improve workflow, reduce physician fatigue, and potentially reduce the size of incisions. The accompanying Digital Video Processor System is used for endoscopic procedures with automatic light control, an anti-blur function for motion images, and digital zoom.
FUJIFILM reports that the Full High Definition Surgical Visualization System is designed for a wide variety of surgical applications and offers edge enhancement, automatic gain control, dynamic contrast function, selective color enhancement, smoke reduction, and grid removal features. It includes a portfolio of rigid scopes, cameras, and video processing systems.
FOR MORE INFORMATION, VISIT: http://www.fujifilmusa.com
FREEMIE BREAST MILK COLLECTION SYSTEM
Freemie® offers a hands-free breast-milk collection system with the Freemie Liberty Mobile Hands Free Breast Pump System and Next Generation Freemie Closed System Collection Cups.
The concealable pump has a rechargeable battery and hospital-power suction for single or double pumping. Programmable memory buttons allow the mother to preset or adjust speed and suction functions. Tubing lengths can be changed so that the pump can be placed on a desk, worn with a detachable belt clip, or carried in a bag.
Freemie says the cups are lower-profile and more compact than other pump system cups, and when placed on the breast under the mother’s bra, can be easily removed so that milk can be transferred to storage. Each cup, with a 25 mm or 28 mm funnel and valve, holds 8 oz of milk.
FOR MORE INFORMATION, VISIT: http://www.freemie.com
PREVENTEZA: EMERGENCY CONTRACEPTIVE
Combe, Inc, the maker of Vagisil®, has launched Preventeza™ (levonorgestrel tablet, 1.5 mg), an emergency contraceptive for the prevention of pregnancy if unprotected sex or failed birth control occurs.
Available online or over-the-counter as a single tablet, Preventeza is a proven option to help women prevent pregnancy before it starts by using a higher dose of levonorgestrel than most birth control pills. It must be used within 72 hours of unprotected intercourse, and is not intended to be used as regular birth control. Combe says that Preventeza works mainly by stopping the release of an egg from the ovary and may also prevent fertilization of an egg or prevent a fertilized egg from implanting in the uterus. Combe also says that levonorgestrel 1.5 mg will not work if the woman is already pregnant and will not affect an existing pregnancy.
FOR MORE INFORMATION, VISIT: https://www.vagisil.com/products/preventeza-emergency-contraceptive
UPSPRING’S C-PANTY FOR POSTCESAREAN RECOVERY
UpSpring® says that its patented C-Panty® undergarment provides medical-grade compression and speeds recovery after cesarean delivery. C-Panty helps to reduce swelling and discomfort, supports weakened muscles, and reduces the incision bulge without hooks, straps, or Velcro that might irritate the incision area.
C-Panty’s medical-grade silicone panel suppresses the formation of excess or improperly formed collagen, which can contribute to scarring, says UpSpring. The silicone may help reduce itchiness, and can lessen the chance of infection at the incision area. The silicone is durable, washable, and integrated into the panty, eliminating the need for scar gel or scar gel pads.
The C-Panty can be worn immediately after birth and for up to 12 months. If worn when the incision is not healed, the silicone panel should be covered with a panty liner or pad. Once the incision has healed, the covering can be discontinued.
FOR MORE INFORMATION, VISIT: https://www.upspringbaby.com/cpanty
Hospital safety program curbs surgical site infections
The Agency for Healthcare Research and Quality (AHRQ) designed the program to reduce surgical site infections (SSIs), which are harmful to patients and expensive for the health care system, wrote Della M. Lin, MD, of Johns Hopkins University, Baltimore, and the department of surgery at the University of Hawaii, Honolulu, and her colleagues.
In a study published in the Journal of the American College of Surgeons, the researchers reviewed data from a statewide intervention conducted at 15 hospitals in Hawaii from January 2013 to June 2015. The intervention included the Comprehensive Unit-based Safety Program and individualized interventions for each hospital to help reduce SSIs. The primary outcome was the number of colorectal SSIs. A secondary outcome of hospital safety culture was assessed using the AHRQ Hospital Survey on Patient Safety Culture. The participating hospitals ranged from a 25-bed critical-access hospital to a 533-bed academic medical center.
Overall, the colorectal SSI rate decreased significantly (from 12% to 5%) from the first quarter of 2013 to the second quarter of 2015, with a significant linear decrease over the study period. The rate of superficial SSIs decreased significantly, falling from 8% to 3%. However, the rate of deep SSIs was not significantly different before and after the intervention program (2% vs. 0%), nor was the organ space SSI rate (3% vs. 2%). The standardized infection ratio decreased from 1.83 to 0.92.
The culture of safety in the hospitals improved, but more modestly, in 10 of 12 areas that were measured over the study period.
The overall perception of patient safety improved from 49% to 53%, teamwork across different units improved from 49% to 54%, management and support for patient safety improved from 53% to 60%, and nonpunitive response to errors improved from 36% to 40%.
In addition, communication and openness improved from 50% to 53%, frequency of reported events improved from 51% to 60%, feedback and communication about errors improved from 52% to 59%, organizational learning and continuous improvement increased from 59% to 70%, teamwork within units improved from 68% to 75%, and expectations and actions by supervisors and managers to promote safety improved from 58% to 64%. Staff responses reflect agreement on improvement in the areas of issues of communication, feedback mechanisms, and teamwork, but the change in culture was not on the order of the SSI change.
The most common interventions to reduce SSIs were the use of reliable chlorhexidine wash or wipe before surgery/surgical prep; appropriate use of antibiotics with respect to selection, dosage, and timing; standardized postsurgical debriefing; and differentiating clean/dirty/clean in the use of anastomosis trays and closing trays.
One bundle component, the implementation of the standard operating room debrief, was found to be of particular value to participants. The investigators noted that debrief questions such as “What went well?” and “What needs to be improved?” had “encouraged new processes of thinking beyond first-order problem solving. The debrief challenge embraced by the teams emphasized that ‘bundles’ did not consist of only technical interventions [e.g. clean/dirty trays, chlorhexidine gluconate wipes in preop], but embedded culture interventions—new processes for problem solving.”
The study findings were limited by several factors, such as the use of public SSI data that were not audited for accuracy and the inability to monitor the reliability of the implementation of the various interventions, the researchers said. In addition, “In this current study, there was a change in SSI rates and a change in safety culture, but correlations between the two were negligible or weak for most domains of safety culture,” they noted. The question of sustainability of the SSI improvement without the concomitant staff support of culture change was not addressed by the investigators.
However, the results suggest that a 62% decrease is robust, and that for some hospitals with a low volume of colorectal cases, “teams could attend to iteratively reduce surgical harm beyond SSI,” the researchers wrote.
The study was supported in part by the AHRQ. Dr. Lin disclosed serving as a board member and as a paid independent contractor to the Hawaii Medical Service Association. Her coauthors had no financial conflicts to disclose.
SOURCE: Lin DM et al. J Am Coll Surg. 2018 May 18. doi: 10.1016/j.jamcollsurg.2018.04.031.
The Agency for Healthcare Research and Quality (AHRQ) designed the program to reduce surgical site infections (SSIs), which are harmful to patients and expensive for the health care system, wrote Della M. Lin, MD, of Johns Hopkins University, Baltimore, and the department of surgery at the University of Hawaii, Honolulu, and her colleagues.
In a study published in the Journal of the American College of Surgeons, the researchers reviewed data from a statewide intervention conducted at 15 hospitals in Hawaii from January 2013 to June 2015. The intervention included the Comprehensive Unit-based Safety Program and individualized interventions for each hospital to help reduce SSIs. The primary outcome was the number of colorectal SSIs. A secondary outcome of hospital safety culture was assessed using the AHRQ Hospital Survey on Patient Safety Culture. The participating hospitals ranged from a 25-bed critical-access hospital to a 533-bed academic medical center.
Overall, the colorectal SSI rate decreased significantly (from 12% to 5%) from the first quarter of 2013 to the second quarter of 2015, with a significant linear decrease over the study period. The rate of superficial SSIs decreased significantly, falling from 8% to 3%. However, the rate of deep SSIs was not significantly different before and after the intervention program (2% vs. 0%), nor was the organ space SSI rate (3% vs. 2%). The standardized infection ratio decreased from 1.83 to 0.92.
The culture of safety in the hospitals improved, but more modestly, in 10 of 12 areas that were measured over the study period.
The overall perception of patient safety improved from 49% to 53%, teamwork across different units improved from 49% to 54%, management and support for patient safety improved from 53% to 60%, and nonpunitive response to errors improved from 36% to 40%.
In addition, communication and openness improved from 50% to 53%, frequency of reported events improved from 51% to 60%, feedback and communication about errors improved from 52% to 59%, organizational learning and continuous improvement increased from 59% to 70%, teamwork within units improved from 68% to 75%, and expectations and actions by supervisors and managers to promote safety improved from 58% to 64%. Staff responses reflect agreement on improvement in the areas of issues of communication, feedback mechanisms, and teamwork, but the change in culture was not on the order of the SSI change.
The most common interventions to reduce SSIs were the use of reliable chlorhexidine wash or wipe before surgery/surgical prep; appropriate use of antibiotics with respect to selection, dosage, and timing; standardized postsurgical debriefing; and differentiating clean/dirty/clean in the use of anastomosis trays and closing trays.
One bundle component, the implementation of the standard operating room debrief, was found to be of particular value to participants. The investigators noted that debrief questions such as “What went well?” and “What needs to be improved?” had “encouraged new processes of thinking beyond first-order problem solving. The debrief challenge embraced by the teams emphasized that ‘bundles’ did not consist of only technical interventions [e.g. clean/dirty trays, chlorhexidine gluconate wipes in preop], but embedded culture interventions—new processes for problem solving.”
The study findings were limited by several factors, such as the use of public SSI data that were not audited for accuracy and the inability to monitor the reliability of the implementation of the various interventions, the researchers said. In addition, “In this current study, there was a change in SSI rates and a change in safety culture, but correlations between the two were negligible or weak for most domains of safety culture,” they noted. The question of sustainability of the SSI improvement without the concomitant staff support of culture change was not addressed by the investigators.
However, the results suggest that a 62% decrease is robust, and that for some hospitals with a low volume of colorectal cases, “teams could attend to iteratively reduce surgical harm beyond SSI,” the researchers wrote.
The study was supported in part by the AHRQ. Dr. Lin disclosed serving as a board member and as a paid independent contractor to the Hawaii Medical Service Association. Her coauthors had no financial conflicts to disclose.
SOURCE: Lin DM et al. J Am Coll Surg. 2018 May 18. doi: 10.1016/j.jamcollsurg.2018.04.031.
The Agency for Healthcare Research and Quality (AHRQ) designed the program to reduce surgical site infections (SSIs), which are harmful to patients and expensive for the health care system, wrote Della M. Lin, MD, of Johns Hopkins University, Baltimore, and the department of surgery at the University of Hawaii, Honolulu, and her colleagues.
In a study published in the Journal of the American College of Surgeons, the researchers reviewed data from a statewide intervention conducted at 15 hospitals in Hawaii from January 2013 to June 2015. The intervention included the Comprehensive Unit-based Safety Program and individualized interventions for each hospital to help reduce SSIs. The primary outcome was the number of colorectal SSIs. A secondary outcome of hospital safety culture was assessed using the AHRQ Hospital Survey on Patient Safety Culture. The participating hospitals ranged from a 25-bed critical-access hospital to a 533-bed academic medical center.
Overall, the colorectal SSI rate decreased significantly (from 12% to 5%) from the first quarter of 2013 to the second quarter of 2015, with a significant linear decrease over the study period. The rate of superficial SSIs decreased significantly, falling from 8% to 3%. However, the rate of deep SSIs was not significantly different before and after the intervention program (2% vs. 0%), nor was the organ space SSI rate (3% vs. 2%). The standardized infection ratio decreased from 1.83 to 0.92.
The culture of safety in the hospitals improved, but more modestly, in 10 of 12 areas that were measured over the study period.
The overall perception of patient safety improved from 49% to 53%, teamwork across different units improved from 49% to 54%, management and support for patient safety improved from 53% to 60%, and nonpunitive response to errors improved from 36% to 40%.
In addition, communication and openness improved from 50% to 53%, frequency of reported events improved from 51% to 60%, feedback and communication about errors improved from 52% to 59%, organizational learning and continuous improvement increased from 59% to 70%, teamwork within units improved from 68% to 75%, and expectations and actions by supervisors and managers to promote safety improved from 58% to 64%. Staff responses reflect agreement on improvement in the areas of issues of communication, feedback mechanisms, and teamwork, but the change in culture was not on the order of the SSI change.
The most common interventions to reduce SSIs were the use of reliable chlorhexidine wash or wipe before surgery/surgical prep; appropriate use of antibiotics with respect to selection, dosage, and timing; standardized postsurgical debriefing; and differentiating clean/dirty/clean in the use of anastomosis trays and closing trays.
One bundle component, the implementation of the standard operating room debrief, was found to be of particular value to participants. The investigators noted that debrief questions such as “What went well?” and “What needs to be improved?” had “encouraged new processes of thinking beyond first-order problem solving. The debrief challenge embraced by the teams emphasized that ‘bundles’ did not consist of only technical interventions [e.g. clean/dirty trays, chlorhexidine gluconate wipes in preop], but embedded culture interventions—new processes for problem solving.”
The study findings were limited by several factors, such as the use of public SSI data that were not audited for accuracy and the inability to monitor the reliability of the implementation of the various interventions, the researchers said. In addition, “In this current study, there was a change in SSI rates and a change in safety culture, but correlations between the two were negligible or weak for most domains of safety culture,” they noted. The question of sustainability of the SSI improvement without the concomitant staff support of culture change was not addressed by the investigators.
However, the results suggest that a 62% decrease is robust, and that for some hospitals with a low volume of colorectal cases, “teams could attend to iteratively reduce surgical harm beyond SSI,” the researchers wrote.
The study was supported in part by the AHRQ. Dr. Lin disclosed serving as a board member and as a paid independent contractor to the Hawaii Medical Service Association. Her coauthors had no financial conflicts to disclose.
SOURCE: Lin DM et al. J Am Coll Surg. 2018 May 18. doi: 10.1016/j.jamcollsurg.2018.04.031.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Key clinical point: Hospital participation in an Agency for Healthcare Research and Quality safety program improved safety culture and reduced surgical site infections.
Major finding: Surgical site infections among colorectal surgery patients decreased by 61.7% after the intervention.
Study details: The data come from a cohort study of 15 hospitals in Hawaii from January 2013 to June 2015.
Disclosures: The study was supported in part by the AHRQ. Dr. Lin disclosed serving as a board member and as a paid independent contractor to the Hawaii Medical Service Association. Her coauthors had no financial conflicts to disclose.
Source: Lin DM et al. J Am Coll Surg. 2018 May 18. doi: 10.1016/j.jamcollsurg.2018.04.031.
Postop delirium management proposed as hospital performance measure
A study suggests that outcome measures, and assessment of hospital performance.
Lead author Julia R. Berian, MD, of the University of Chicago Medical Center and her colleagues wrote, “Postoperative delirium has been associated with mortality, morbidity, prolonged length of stay, and increased costs of care. Furthermore, postoperative delirium may be associated with long-term cognitive and functional decline. However, postoperative delirium has not been incorporated as an outcome measure into major surgical quality registries. Approximately one-third of hospitalized delirium is believed to be preventable, making postoperative delirium an ideal target for surgical quality improvement efforts,” Dr. Berian and her colleagues reported in the Annals of Surgery.
The Geriatric Surgery Pilot data abstractors were instructed to assign postoperative delirium if the medical record words indicating an acute confusional stat such a mental status change, confusion, disorientation, agitation, delirium, and inappropriate behavior. Data were collected from the period 2 hours after surgery to exclude effects of the pharmacologic agents of anesthesia. Delirium status was ascertained as a binary outcome (Yes/No).
Postoperative delirium was observed in 2,427 patients for an average, unadjusted rate of 12.0%. Investigators identified 20 risk factors markedly associated with delirium. The strongest predictors included preoperative cognitive impairment, preoperative use of mobility aid, surrogate consent form, ASA class 4 or greater, age 80 years and older, preoperative sepsis, and fall history within 1 year. Patients with delirium generally were older than patients without delirium were and accounted for a greater proportion of emergency cases. Postoperative hospital length of stay was about 4 days longer on average for patients with delirium, compared with those without delirium.
By specialty, the highest rates of postoperative delirium occurred following cardiothoracic (13.7%), orthopedic (13.0%), and general surgeries (13.0%). Study authors found varied associated risk for postoperative delirium within each surgical specialty. For example, in general surgery, the risk for postoperative delirium with partial mastectomy was low, compared with a mid-level risk in the repair of a recurrent, incarcerated, or strangulated inguinal hernia and a high-level risk in Whipple operations.
The model developed to measure delirium management success in 30 hospitals found that adjusted delirium rates ranged from 3.2% to 27.5%, with eight poor- and five excellent-performing outliers. Authors noted that their model demonstrated good calibration and discrimination. Examination of changes in the Bayesian Information Criteria indicates that as few as 10-12 variables may suffice in building a parsimonious model with “an excellent fit.”
Study authors noted that screening for postoperative delirium in older adults is likely in the best interests of patients. However, they also mentioned that such screening may identify cases of postoperative delirium that were previously unrecognized, resulting in higher rates. In addition, the inclusion of only ACS NSQIP hospitals and the voluntary participation may mean a biased dataset. No one delirium prevention intervention was implemented across the hospitals and so the study doesn’t indicate why some hospitals are more successful than are others. Chart-based identification of patients who have delirium needs further study to assess validity.
Authors concluded that one solution may be to “standardize and consistently employ delirium screening in high-risk patients across hospitals, as has been advocated by a coalition of interdisciplinary experts in geriatric care.”
This project is funded in part by a grant from the John A. Hartford Foundation. The authors declare no conflict of interests.
SOURCE: Berlan JR et al. Ann Surg. 2017 July 24. doi: 10.1097/SLA.0000000000002436
A study suggests that outcome measures, and assessment of hospital performance.
Lead author Julia R. Berian, MD, of the University of Chicago Medical Center and her colleagues wrote, “Postoperative delirium has been associated with mortality, morbidity, prolonged length of stay, and increased costs of care. Furthermore, postoperative delirium may be associated with long-term cognitive and functional decline. However, postoperative delirium has not been incorporated as an outcome measure into major surgical quality registries. Approximately one-third of hospitalized delirium is believed to be preventable, making postoperative delirium an ideal target for surgical quality improvement efforts,” Dr. Berian and her colleagues reported in the Annals of Surgery.
The Geriatric Surgery Pilot data abstractors were instructed to assign postoperative delirium if the medical record words indicating an acute confusional stat such a mental status change, confusion, disorientation, agitation, delirium, and inappropriate behavior. Data were collected from the period 2 hours after surgery to exclude effects of the pharmacologic agents of anesthesia. Delirium status was ascertained as a binary outcome (Yes/No).
Postoperative delirium was observed in 2,427 patients for an average, unadjusted rate of 12.0%. Investigators identified 20 risk factors markedly associated with delirium. The strongest predictors included preoperative cognitive impairment, preoperative use of mobility aid, surrogate consent form, ASA class 4 or greater, age 80 years and older, preoperative sepsis, and fall history within 1 year. Patients with delirium generally were older than patients without delirium were and accounted for a greater proportion of emergency cases. Postoperative hospital length of stay was about 4 days longer on average for patients with delirium, compared with those without delirium.
By specialty, the highest rates of postoperative delirium occurred following cardiothoracic (13.7%), orthopedic (13.0%), and general surgeries (13.0%). Study authors found varied associated risk for postoperative delirium within each surgical specialty. For example, in general surgery, the risk for postoperative delirium with partial mastectomy was low, compared with a mid-level risk in the repair of a recurrent, incarcerated, or strangulated inguinal hernia and a high-level risk in Whipple operations.
The model developed to measure delirium management success in 30 hospitals found that adjusted delirium rates ranged from 3.2% to 27.5%, with eight poor- and five excellent-performing outliers. Authors noted that their model demonstrated good calibration and discrimination. Examination of changes in the Bayesian Information Criteria indicates that as few as 10-12 variables may suffice in building a parsimonious model with “an excellent fit.”
Study authors noted that screening for postoperative delirium in older adults is likely in the best interests of patients. However, they also mentioned that such screening may identify cases of postoperative delirium that were previously unrecognized, resulting in higher rates. In addition, the inclusion of only ACS NSQIP hospitals and the voluntary participation may mean a biased dataset. No one delirium prevention intervention was implemented across the hospitals and so the study doesn’t indicate why some hospitals are more successful than are others. Chart-based identification of patients who have delirium needs further study to assess validity.
Authors concluded that one solution may be to “standardize and consistently employ delirium screening in high-risk patients across hospitals, as has been advocated by a coalition of interdisciplinary experts in geriatric care.”
This project is funded in part by a grant from the John A. Hartford Foundation. The authors declare no conflict of interests.
SOURCE: Berlan JR et al. Ann Surg. 2017 July 24. doi: 10.1097/SLA.0000000000002436
A study suggests that outcome measures, and assessment of hospital performance.
Lead author Julia R. Berian, MD, of the University of Chicago Medical Center and her colleagues wrote, “Postoperative delirium has been associated with mortality, morbidity, prolonged length of stay, and increased costs of care. Furthermore, postoperative delirium may be associated with long-term cognitive and functional decline. However, postoperative delirium has not been incorporated as an outcome measure into major surgical quality registries. Approximately one-third of hospitalized delirium is believed to be preventable, making postoperative delirium an ideal target for surgical quality improvement efforts,” Dr. Berian and her colleagues reported in the Annals of Surgery.
The Geriatric Surgery Pilot data abstractors were instructed to assign postoperative delirium if the medical record words indicating an acute confusional stat such a mental status change, confusion, disorientation, agitation, delirium, and inappropriate behavior. Data were collected from the period 2 hours after surgery to exclude effects of the pharmacologic agents of anesthesia. Delirium status was ascertained as a binary outcome (Yes/No).
Postoperative delirium was observed in 2,427 patients for an average, unadjusted rate of 12.0%. Investigators identified 20 risk factors markedly associated with delirium. The strongest predictors included preoperative cognitive impairment, preoperative use of mobility aid, surrogate consent form, ASA class 4 or greater, age 80 years and older, preoperative sepsis, and fall history within 1 year. Patients with delirium generally were older than patients without delirium were and accounted for a greater proportion of emergency cases. Postoperative hospital length of stay was about 4 days longer on average for patients with delirium, compared with those without delirium.
By specialty, the highest rates of postoperative delirium occurred following cardiothoracic (13.7%), orthopedic (13.0%), and general surgeries (13.0%). Study authors found varied associated risk for postoperative delirium within each surgical specialty. For example, in general surgery, the risk for postoperative delirium with partial mastectomy was low, compared with a mid-level risk in the repair of a recurrent, incarcerated, or strangulated inguinal hernia and a high-level risk in Whipple operations.
The model developed to measure delirium management success in 30 hospitals found that adjusted delirium rates ranged from 3.2% to 27.5%, with eight poor- and five excellent-performing outliers. Authors noted that their model demonstrated good calibration and discrimination. Examination of changes in the Bayesian Information Criteria indicates that as few as 10-12 variables may suffice in building a parsimonious model with “an excellent fit.”
Study authors noted that screening for postoperative delirium in older adults is likely in the best interests of patients. However, they also mentioned that such screening may identify cases of postoperative delirium that were previously unrecognized, resulting in higher rates. In addition, the inclusion of only ACS NSQIP hospitals and the voluntary participation may mean a biased dataset. No one delirium prevention intervention was implemented across the hospitals and so the study doesn’t indicate why some hospitals are more successful than are others. Chart-based identification of patients who have delirium needs further study to assess validity.
Authors concluded that one solution may be to “standardize and consistently employ delirium screening in high-risk patients across hospitals, as has been advocated by a coalition of interdisciplinary experts in geriatric care.”
This project is funded in part by a grant from the John A. Hartford Foundation. The authors declare no conflict of interests.
SOURCE: Berlan JR et al. Ann Surg. 2017 July 24. doi: 10.1097/SLA.0000000000002436
FROM ANNALS OF SURGERY
Key clinical point: Through predictive modeling, the study identified 20 risk factors markedly associated with delirium that can be used to identify high-risk patients.
Major finding: Among the 2,427 patients who experienced delirium, 35% had preoperative cognitive impairment, 30 % had a surrogate sign the consent form, and 32% experienced serious postoperative complications or death.
Study details: An analysis of 2,427 elderly patients at 30 hospitals through data from the ACS NSQIP Geriatric Surgery Pilot Project.
Disclosures: This project is funded in part by a grant from the John A. Hartford Foundation. The authors declare no conflict of interests.
Source: Berian JR et al. Ann Surg. 2017Jul 24. doi: 10.1097/SLA.0000000000002436
Ureteral reimplantation for injuries not easily managed with stenting
The risk of lower urinary tract injury (bladder or ureters) at the time of benign gynecologic surgery is estimated to be between 0.3% and 4%. The majority are bladder injuries, with ureteral injuries occurring in 0.3%-1.8% of hysterectomies. While urologic procedures account for the majority of iatrogenic ureteral injuries, gynecologic surgery is the second leading cause, followed by general surgery and colorectal surgery.
With respect to hysterectomy in particular, the risk of ureteral injury is less than 1%. In a large prospective cohort of women undergoing hysterectomy for benign indications in 53 hospitals in Finland, rates of ureteral injury varied based on the route of hysterectomy, with laparoscopic and abdominal routes having an injury rate of 0.3% and the vaginal route having an injury rate of 0.04% (Human Reprod. 2011;26[7]:1741-51). The risk generally is higher with procedures for endometriosis, large fibroids, cancer, or pelvic organ prolapse.
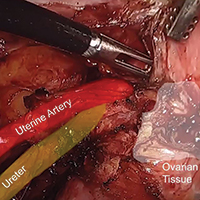
During hysterectomy and with gynecologic surgery overall, ureteral injuries occur most commonly at three locations: at the level of the infundibulopelvic ligament and ovarian vessels, at the level of the uterine artery, and near the vaginal cuff. Identification and knowledge of the course of the ureter at these three locations is essential in preventing ureteral injury during pelvic surgery.

SOURCE: DR. MUELLER AND DR. KENTON
Perioperative ureteral stenting has been proposed as a method of preventing iatrogenic injury by allowing surgeons to more easily identify the ureters during surgery. Available reports suggest, however, that the actual risk of injury is not decreased and may even be increased by placing prophylactic ureteral stents, and most surgeons have moved away from this practice. The use of lighted ureteral stents during complex laparoscopic endometriosis resections may be helpful.
Many health care systems recommend intraoperative cystoscopy with bladder and ureteral survey to evaluate the integrity of the lower urinary tract at the time of all hysterectomies. A recent study of nearly 3,000 women undergoing benign hysterectomies at the University of Michigan, Ann Arbor, showed a significant decrease in the rate of delayed diagnosis of urinary tract injuries with implementation of a universal cystoscopy policy. While the rate of lower urinary tract injury was fairly consistent before and after implementation of the policy (2.6% and 1.8%, respectively), the rate of delayed detection of a lower urinary tract injury decreased from 0.7% before the policy to 0.1% after implementation (Obstet Gynecol. 2016;127[2]:369-75). The study also showed that hospital costs nearly doubled with a delayed detection of a lower urinary tract injury.
Unfortunately, even a normal postoperative cystoscopy does not ensure there is no lower urinary tract injury, especially considering that thermal injuries resulting from the use of energy devices typically do not present until 7-14 days after surgery. Overall, however, ureteral injury detection rates with universal cystoscopy approach 97% (Obstet Gynecol. 2009;113:6-10).
Identifying injuries
Intraoperative recognition and repair always is preferred, and when ureteral injuries are discovered or suspected in the operating room, cystoscopy and retrograde pyelography is the most helpful imaging tool. Contrast dye is injected during cystoscopy directly into the renal collecting system through the ureteral orifices; with fluoroscopy, the surgeon can visualize the integrity of the ureter from the bladder to the renal pelvis to diagnosis a ureteral injury, including ureteral transection, kinking, or ligation caused by a suture or sealing device.
If retrograde pyelography shows a transection or injury from a crushing clamp or sealing device, we recommend ureteroureteral anastomosis or urethral neocystostomy depending on the extent and location of the injury. If the ureter just appears kinked, sometime simply releasing the cuff sutures or uterosacral ligament sutures will resolve the obstruction. If there is extravasation of contrast suggesting a partial tear, placing a double-J ureteral stent for 6-8 weeks is frequently sufficient.
Patients with delayed iatrogenic ureteral injuries present with symptoms that often are nonspecific and that include abdominal or flank pain, fever, nausea, vomiting, back pain, and leukocytosis.
We recommend that patients with a history of surgery and symptoms suggestive of a ureteral injury be initially evaluated with CT urography that images the renal collecting system both as contrast dye is instilled and again several minutes later as it has progressed through the entire urinary tract. Alternatively, if CT urography is unavailable, a retrograde pyelogram can be performed as an emergency procedure to determine the location of renal injury.
Surgical management
Delayed ureteral injuries resulting in partial ureteral obstruction or extravasation of urine into the pelvis can sometimes be managed conservatively though placement of an internalized double J stent. The stent can be placed in a retrograde fashion via cystoscopy by a
We typically manage delayed ureteral injuries that are not amenable to, or do not heal with, ureteral stenting with ureteroneocystotomy, or ureteral reimplantation, into the bladder. This technique is effective for distal ureteral injuries that result in obstruction or fistula and are in close proximity to the bladder (most iatrogenic gynecologic injuries). We perform ureteroneocystotomy via an open, robotic, or laparoscopic route of access depending on the circumstance.
Our preferred route of access is minimally invasive with the da Vinci robot. A camera port is placed at the umbilicus, two robotic ports are placed on the patient’s left side at the level of the umbilicus, and one is placed on the patient’s right side at the level of the umbilicus with an additional assistant port on the right side. It is helpful if each port is at least 8 cm apart. If obstruction or transection is suspected to be more proximal, the ports may have been shifted above the umbilicus to optimally mobilize the ureter.
First, the ureter is identified and dissected. Regardless of the site of injury, which is usually identifiable with inflammation and scar tissue, it is always easiest to identify the ureter at the bifurcation of the common iliac vessels. The isolated ureter is inspected proximally and above the area of injury, and we find it helpful to place a vessel loop around the ureter for easy manipulation and counter traction. Care must be taken not to disturb the adventitia and blood supply. We do not transect the ureter until we’re ready to reimplant it in the bladder.
To mobilize the bladder and prepare for a tension-free anastomosis, an adequate retropubic dissection is performed, starting with an incision in the anterior abdominal wall peritoneum and taking it down to the level of the pubic bone and into the retropubic space. It is important to be mindful of the location of the obturator neurovascular bundle when performing this dissection.
Achieving a tension-free and water-tight anastomosis of the ureter to the bladder is critical. The bladder should be mobilized such that it reaches to above the injured portion of the ureter. The bladder is retrograde filled with approximately 300 mL and a reimplantation site of the posterior bladder is identified. When there is concern about tension, a psoas hitch suture can be placed to keep the bladder in a superior position with reduced tension. Because of high rates of the congenital absence of the psoas tendon minor, we advocate direct visualization of the genitofemoral nerve by incising the peritoneum; this will avoid nerve entrapment.
Once the bladder is mobilized and the ureter isolated, we perform an intentional cystotomy in the posterior lateral aspect of the bladder. The ureter, which is on the vessel loop, must be transected proximal to the site of injury. To facilitate this, we spatulate the ureter, making a vertical incision of often about 5 mm in length to increase our surface area for anastomosis. Placement of a suture at the apex of the spatulated ureter helps us maintain orientation.
Anastomosis of the ureter and bladder is achieved in a mucosa-to-mucosa fashion using a series of interrupted monofilament fine absorbable sutures; we use a 3-0 monocryl suture. The most posterior anastomotic sutures are placed first to allow for optimal visualization, and prior to completing the anastomosis, a guide wire is placed through the open ureter and a double-J stent is introduced into the renal pelvis. The wire is then removed and the distal end of the stent coiled in the bladder. This stent will protect the ureter for about 6 weeks while it heals. The anastomosis is then completed on the anterior aspect, with a watertight closure ensured.
Postoperatively, we routinely perform an x-ray to ensure proper placement of the stent in the reimplanted ureter. To determine correct stent placement, the last rib is identified at T12 vertebrae. The renal pelvis is located at the level of the L2-L3 with the left being slightly higher than the right. A Foley catheter is maintained in the bladder for approximately 2 weeks, and the stent is maintained for approximately 6 weeks. Both the catheter and the stent can be removed in the office with cystoscopic guidance.
Imaging at 4-6 weeks after removal of the stent is performed to rule out development of an obstruction or a stricture. In patients who did not have a dilated ureter and renal collecting system prior to reimplantation, a renal ultrasound is sufficient to identify hydroureter/hydronephrosis or a urinoma. Many patients with a markedly dilated renal-collecting system prior to ureteral reimplantation will have persistent hydroureter/hydronephrosis (similar to a latex balloon that does not return to its original size after it is blown up) after reimplantation. A Lasix renal scan is a better imaging modality in these patients because it can differentiate a ureter that is dilated from one that is dilated and obstructed.
It is important to note that prompt ureteroneocystotomy is feasible only when the delayed ureteral injury presents within approximately 7 days of surgery. If the patient presents more than a week after surgery, inflammation is so significant that conservative management is necessary with reevaluation for reimplantation in another 6 weeks. Decompression of the system prior to reimplantation can be achieved through either stent placement or placement of a percutaneous nephrostomy tube. We prefer the latter because it reduces inflammation around the ureter that may make subsequent dissection and surgery more difficult.
Dr. Kenton is chief of urogynecology, Northwestern University, Chicago, and Dr. Mueller also is in the division of female pelvic medicine and reconstructive surgery–urogynecology at Northwestern. Dr. Kenton discloses grant funding from Boston Scientific.
The risk of lower urinary tract injury (bladder or ureters) at the time of benign gynecologic surgery is estimated to be between 0.3% and 4%. The majority are bladder injuries, with ureteral injuries occurring in 0.3%-1.8% of hysterectomies. While urologic procedures account for the majority of iatrogenic ureteral injuries, gynecologic surgery is the second leading cause, followed by general surgery and colorectal surgery.
With respect to hysterectomy in particular, the risk of ureteral injury is less than 1%. In a large prospective cohort of women undergoing hysterectomy for benign indications in 53 hospitals in Finland, rates of ureteral injury varied based on the route of hysterectomy, with laparoscopic and abdominal routes having an injury rate of 0.3% and the vaginal route having an injury rate of 0.04% (Human Reprod. 2011;26[7]:1741-51). The risk generally is higher with procedures for endometriosis, large fibroids, cancer, or pelvic organ prolapse.
During hysterectomy and with gynecologic surgery overall, ureteral injuries occur most commonly at three locations: at the level of the infundibulopelvic ligament and ovarian vessels, at the level of the uterine artery, and near the vaginal cuff. Identification and knowledge of the course of the ureter at these three locations is essential in preventing ureteral injury during pelvic surgery.

SOURCE: DR. MUELLER AND DR. KENTON
Perioperative ureteral stenting has been proposed as a method of preventing iatrogenic injury by allowing surgeons to more easily identify the ureters during surgery. Available reports suggest, however, that the actual risk of injury is not decreased and may even be increased by placing prophylactic ureteral stents, and most surgeons have moved away from this practice. The use of lighted ureteral stents during complex laparoscopic endometriosis resections may be helpful.
Many health care systems recommend intraoperative cystoscopy with bladder and ureteral survey to evaluate the integrity of the lower urinary tract at the time of all hysterectomies. A recent study of nearly 3,000 women undergoing benign hysterectomies at the University of Michigan, Ann Arbor, showed a significant decrease in the rate of delayed diagnosis of urinary tract injuries with implementation of a universal cystoscopy policy. While the rate of lower urinary tract injury was fairly consistent before and after implementation of the policy (2.6% and 1.8%, respectively), the rate of delayed detection of a lower urinary tract injury decreased from 0.7% before the policy to 0.1% after implementation (Obstet Gynecol. 2016;127[2]:369-75). The study also showed that hospital costs nearly doubled with a delayed detection of a lower urinary tract injury.
Unfortunately, even a normal postoperative cystoscopy does not ensure there is no lower urinary tract injury, especially considering that thermal injuries resulting from the use of energy devices typically do not present until 7-14 days after surgery. Overall, however, ureteral injury detection rates with universal cystoscopy approach 97% (Obstet Gynecol. 2009;113:6-10).
Identifying injuries
Intraoperative recognition and repair always is preferred, and when ureteral injuries are discovered or suspected in the operating room, cystoscopy and retrograde pyelography is the most helpful imaging tool. Contrast dye is injected during cystoscopy directly into the renal collecting system through the ureteral orifices; with fluoroscopy, the surgeon can visualize the integrity of the ureter from the bladder to the renal pelvis to diagnosis a ureteral injury, including ureteral transection, kinking, or ligation caused by a suture or sealing device.
If retrograde pyelography shows a transection or injury from a crushing clamp or sealing device, we recommend ureteroureteral anastomosis or urethral neocystostomy depending on the extent and location of the injury. If the ureter just appears kinked, sometime simply releasing the cuff sutures or uterosacral ligament sutures will resolve the obstruction. If there is extravasation of contrast suggesting a partial tear, placing a double-J ureteral stent for 6-8 weeks is frequently sufficient.
Patients with delayed iatrogenic ureteral injuries present with symptoms that often are nonspecific and that include abdominal or flank pain, fever, nausea, vomiting, back pain, and leukocytosis.
We recommend that patients with a history of surgery and symptoms suggestive of a ureteral injury be initially evaluated with CT urography that images the renal collecting system both as contrast dye is instilled and again several minutes later as it has progressed through the entire urinary tract. Alternatively, if CT urography is unavailable, a retrograde pyelogram can be performed as an emergency procedure to determine the location of renal injury.
Surgical management
Delayed ureteral injuries resulting in partial ureteral obstruction or extravasation of urine into the pelvis can sometimes be managed conservatively though placement of an internalized double J stent. The stent can be placed in a retrograde fashion via cystoscopy by a
We typically manage delayed ureteral injuries that are not amenable to, or do not heal with, ureteral stenting with ureteroneocystotomy, or ureteral reimplantation, into the bladder. This technique is effective for distal ureteral injuries that result in obstruction or fistula and are in close proximity to the bladder (most iatrogenic gynecologic injuries). We perform ureteroneocystotomy via an open, robotic, or laparoscopic route of access depending on the circumstance.
Our preferred route of access is minimally invasive with the da Vinci robot. A camera port is placed at the umbilicus, two robotic ports are placed on the patient’s left side at the level of the umbilicus, and one is placed on the patient’s right side at the level of the umbilicus with an additional assistant port on the right side. It is helpful if each port is at least 8 cm apart. If obstruction or transection is suspected to be more proximal, the ports may have been shifted above the umbilicus to optimally mobilize the ureter.
First, the ureter is identified and dissected. Regardless of the site of injury, which is usually identifiable with inflammation and scar tissue, it is always easiest to identify the ureter at the bifurcation of the common iliac vessels. The isolated ureter is inspected proximally and above the area of injury, and we find it helpful to place a vessel loop around the ureter for easy manipulation and counter traction. Care must be taken not to disturb the adventitia and blood supply. We do not transect the ureter until we’re ready to reimplant it in the bladder.
To mobilize the bladder and prepare for a tension-free anastomosis, an adequate retropubic dissection is performed, starting with an incision in the anterior abdominal wall peritoneum and taking it down to the level of the pubic bone and into the retropubic space. It is important to be mindful of the location of the obturator neurovascular bundle when performing this dissection.
Achieving a tension-free and water-tight anastomosis of the ureter to the bladder is critical. The bladder should be mobilized such that it reaches to above the injured portion of the ureter. The bladder is retrograde filled with approximately 300 mL and a reimplantation site of the posterior bladder is identified. When there is concern about tension, a psoas hitch suture can be placed to keep the bladder in a superior position with reduced tension. Because of high rates of the congenital absence of the psoas tendon minor, we advocate direct visualization of the genitofemoral nerve by incising the peritoneum; this will avoid nerve entrapment.
Once the bladder is mobilized and the ureter isolated, we perform an intentional cystotomy in the posterior lateral aspect of the bladder. The ureter, which is on the vessel loop, must be transected proximal to the site of injury. To facilitate this, we spatulate the ureter, making a vertical incision of often about 5 mm in length to increase our surface area for anastomosis. Placement of a suture at the apex of the spatulated ureter helps us maintain orientation.
Anastomosis of the ureter and bladder is achieved in a mucosa-to-mucosa fashion using a series of interrupted monofilament fine absorbable sutures; we use a 3-0 monocryl suture. The most posterior anastomotic sutures are placed first to allow for optimal visualization, and prior to completing the anastomosis, a guide wire is placed through the open ureter and a double-J stent is introduced into the renal pelvis. The wire is then removed and the distal end of the stent coiled in the bladder. This stent will protect the ureter for about 6 weeks while it heals. The anastomosis is then completed on the anterior aspect, with a watertight closure ensured.
Postoperatively, we routinely perform an x-ray to ensure proper placement of the stent in the reimplanted ureter. To determine correct stent placement, the last rib is identified at T12 vertebrae. The renal pelvis is located at the level of the L2-L3 with the left being slightly higher than the right. A Foley catheter is maintained in the bladder for approximately 2 weeks, and the stent is maintained for approximately 6 weeks. Both the catheter and the stent can be removed in the office with cystoscopic guidance.
Imaging at 4-6 weeks after removal of the stent is performed to rule out development of an obstruction or a stricture. In patients who did not have a dilated ureter and renal collecting system prior to reimplantation, a renal ultrasound is sufficient to identify hydroureter/hydronephrosis or a urinoma. Many patients with a markedly dilated renal-collecting system prior to ureteral reimplantation will have persistent hydroureter/hydronephrosis (similar to a latex balloon that does not return to its original size after it is blown up) after reimplantation. A Lasix renal scan is a better imaging modality in these patients because it can differentiate a ureter that is dilated from one that is dilated and obstructed.
It is important to note that prompt ureteroneocystotomy is feasible only when the delayed ureteral injury presents within approximately 7 days of surgery. If the patient presents more than a week after surgery, inflammation is so significant that conservative management is necessary with reevaluation for reimplantation in another 6 weeks. Decompression of the system prior to reimplantation can be achieved through either stent placement or placement of a percutaneous nephrostomy tube. We prefer the latter because it reduces inflammation around the ureter that may make subsequent dissection and surgery more difficult.
Dr. Kenton is chief of urogynecology, Northwestern University, Chicago, and Dr. Mueller also is in the division of female pelvic medicine and reconstructive surgery–urogynecology at Northwestern. Dr. Kenton discloses grant funding from Boston Scientific.
The risk of lower urinary tract injury (bladder or ureters) at the time of benign gynecologic surgery is estimated to be between 0.3% and 4%. The majority are bladder injuries, with ureteral injuries occurring in 0.3%-1.8% of hysterectomies. While urologic procedures account for the majority of iatrogenic ureteral injuries, gynecologic surgery is the second leading cause, followed by general surgery and colorectal surgery.
With respect to hysterectomy in particular, the risk of ureteral injury is less than 1%. In a large prospective cohort of women undergoing hysterectomy for benign indications in 53 hospitals in Finland, rates of ureteral injury varied based on the route of hysterectomy, with laparoscopic and abdominal routes having an injury rate of 0.3% and the vaginal route having an injury rate of 0.04% (Human Reprod. 2011;26[7]:1741-51). The risk generally is higher with procedures for endometriosis, large fibroids, cancer, or pelvic organ prolapse.
During hysterectomy and with gynecologic surgery overall, ureteral injuries occur most commonly at three locations: at the level of the infundibulopelvic ligament and ovarian vessels, at the level of the uterine artery, and near the vaginal cuff. Identification and knowledge of the course of the ureter at these three locations is essential in preventing ureteral injury during pelvic surgery.

SOURCE: DR. MUELLER AND DR. KENTON
Perioperative ureteral stenting has been proposed as a method of preventing iatrogenic injury by allowing surgeons to more easily identify the ureters during surgery. Available reports suggest, however, that the actual risk of injury is not decreased and may even be increased by placing prophylactic ureteral stents, and most surgeons have moved away from this practice. The use of lighted ureteral stents during complex laparoscopic endometriosis resections may be helpful.
Many health care systems recommend intraoperative cystoscopy with bladder and ureteral survey to evaluate the integrity of the lower urinary tract at the time of all hysterectomies. A recent study of nearly 3,000 women undergoing benign hysterectomies at the University of Michigan, Ann Arbor, showed a significant decrease in the rate of delayed diagnosis of urinary tract injuries with implementation of a universal cystoscopy policy. While the rate of lower urinary tract injury was fairly consistent before and after implementation of the policy (2.6% and 1.8%, respectively), the rate of delayed detection of a lower urinary tract injury decreased from 0.7% before the policy to 0.1% after implementation (Obstet Gynecol. 2016;127[2]:369-75). The study also showed that hospital costs nearly doubled with a delayed detection of a lower urinary tract injury.
Unfortunately, even a normal postoperative cystoscopy does not ensure there is no lower urinary tract injury, especially considering that thermal injuries resulting from the use of energy devices typically do not present until 7-14 days after surgery. Overall, however, ureteral injury detection rates with universal cystoscopy approach 97% (Obstet Gynecol. 2009;113:6-10).
Identifying injuries
Intraoperative recognition and repair always is preferred, and when ureteral injuries are discovered or suspected in the operating room, cystoscopy and retrograde pyelography is the most helpful imaging tool. Contrast dye is injected during cystoscopy directly into the renal collecting system through the ureteral orifices; with fluoroscopy, the surgeon can visualize the integrity of the ureter from the bladder to the renal pelvis to diagnosis a ureteral injury, including ureteral transection, kinking, or ligation caused by a suture or sealing device.
If retrograde pyelography shows a transection or injury from a crushing clamp or sealing device, we recommend ureteroureteral anastomosis or urethral neocystostomy depending on the extent and location of the injury. If the ureter just appears kinked, sometime simply releasing the cuff sutures or uterosacral ligament sutures will resolve the obstruction. If there is extravasation of contrast suggesting a partial tear, placing a double-J ureteral stent for 6-8 weeks is frequently sufficient.
Patients with delayed iatrogenic ureteral injuries present with symptoms that often are nonspecific and that include abdominal or flank pain, fever, nausea, vomiting, back pain, and leukocytosis.
We recommend that patients with a history of surgery and symptoms suggestive of a ureteral injury be initially evaluated with CT urography that images the renal collecting system both as contrast dye is instilled and again several minutes later as it has progressed through the entire urinary tract. Alternatively, if CT urography is unavailable, a retrograde pyelogram can be performed as an emergency procedure to determine the location of renal injury.
Surgical management
Delayed ureteral injuries resulting in partial ureteral obstruction or extravasation of urine into the pelvis can sometimes be managed conservatively though placement of an internalized double J stent. The stent can be placed in a retrograde fashion via cystoscopy by a
We typically manage delayed ureteral injuries that are not amenable to, or do not heal with, ureteral stenting with ureteroneocystotomy, or ureteral reimplantation, into the bladder. This technique is effective for distal ureteral injuries that result in obstruction or fistula and are in close proximity to the bladder (most iatrogenic gynecologic injuries). We perform ureteroneocystotomy via an open, robotic, or laparoscopic route of access depending on the circumstance.
Our preferred route of access is minimally invasive with the da Vinci robot. A camera port is placed at the umbilicus, two robotic ports are placed on the patient’s left side at the level of the umbilicus, and one is placed on the patient’s right side at the level of the umbilicus with an additional assistant port on the right side. It is helpful if each port is at least 8 cm apart. If obstruction or transection is suspected to be more proximal, the ports may have been shifted above the umbilicus to optimally mobilize the ureter.
First, the ureter is identified and dissected. Regardless of the site of injury, which is usually identifiable with inflammation and scar tissue, it is always easiest to identify the ureter at the bifurcation of the common iliac vessels. The isolated ureter is inspected proximally and above the area of injury, and we find it helpful to place a vessel loop around the ureter for easy manipulation and counter traction. Care must be taken not to disturb the adventitia and blood supply. We do not transect the ureter until we’re ready to reimplant it in the bladder.
To mobilize the bladder and prepare for a tension-free anastomosis, an adequate retropubic dissection is performed, starting with an incision in the anterior abdominal wall peritoneum and taking it down to the level of the pubic bone and into the retropubic space. It is important to be mindful of the location of the obturator neurovascular bundle when performing this dissection.
Achieving a tension-free and water-tight anastomosis of the ureter to the bladder is critical. The bladder should be mobilized such that it reaches to above the injured portion of the ureter. The bladder is retrograde filled with approximately 300 mL and a reimplantation site of the posterior bladder is identified. When there is concern about tension, a psoas hitch suture can be placed to keep the bladder in a superior position with reduced tension. Because of high rates of the congenital absence of the psoas tendon minor, we advocate direct visualization of the genitofemoral nerve by incising the peritoneum; this will avoid nerve entrapment.
Once the bladder is mobilized and the ureter isolated, we perform an intentional cystotomy in the posterior lateral aspect of the bladder. The ureter, which is on the vessel loop, must be transected proximal to the site of injury. To facilitate this, we spatulate the ureter, making a vertical incision of often about 5 mm in length to increase our surface area for anastomosis. Placement of a suture at the apex of the spatulated ureter helps us maintain orientation.
Anastomosis of the ureter and bladder is achieved in a mucosa-to-mucosa fashion using a series of interrupted monofilament fine absorbable sutures; we use a 3-0 monocryl suture. The most posterior anastomotic sutures are placed first to allow for optimal visualization, and prior to completing the anastomosis, a guide wire is placed through the open ureter and a double-J stent is introduced into the renal pelvis. The wire is then removed and the distal end of the stent coiled in the bladder. This stent will protect the ureter for about 6 weeks while it heals. The anastomosis is then completed on the anterior aspect, with a watertight closure ensured.
Postoperatively, we routinely perform an x-ray to ensure proper placement of the stent in the reimplanted ureter. To determine correct stent placement, the last rib is identified at T12 vertebrae. The renal pelvis is located at the level of the L2-L3 with the left being slightly higher than the right. A Foley catheter is maintained in the bladder for approximately 2 weeks, and the stent is maintained for approximately 6 weeks. Both the catheter and the stent can be removed in the office with cystoscopic guidance.
Imaging at 4-6 weeks after removal of the stent is performed to rule out development of an obstruction or a stricture. In patients who did not have a dilated ureter and renal collecting system prior to reimplantation, a renal ultrasound is sufficient to identify hydroureter/hydronephrosis or a urinoma. Many patients with a markedly dilated renal-collecting system prior to ureteral reimplantation will have persistent hydroureter/hydronephrosis (similar to a latex balloon that does not return to its original size after it is blown up) after reimplantation. A Lasix renal scan is a better imaging modality in these patients because it can differentiate a ureter that is dilated from one that is dilated and obstructed.
It is important to note that prompt ureteroneocystotomy is feasible only when the delayed ureteral injury presents within approximately 7 days of surgery. If the patient presents more than a week after surgery, inflammation is so significant that conservative management is necessary with reevaluation for reimplantation in another 6 weeks. Decompression of the system prior to reimplantation can be achieved through either stent placement or placement of a percutaneous nephrostomy tube. We prefer the latter because it reduces inflammation around the ureter that may make subsequent dissection and surgery more difficult.
Dr. Kenton is chief of urogynecology, Northwestern University, Chicago, and Dr. Mueller also is in the division of female pelvic medicine and reconstructive surgery–urogynecology at Northwestern. Dr. Kenton discloses grant funding from Boston Scientific.
The diagnosis and treatment of ureteral injury
A gynecologic surgeon learns very early in his/her career to respect the ureter. Whether from the procedure being performed (endometriosis surgery, hysterectomy, myomectomy for ligamentous fibroids, salpingo-oophorectomy, excision of ovarian remnants, adhesiolysis), blood loss that obscures visualization and must be controlled, or use of energy for cutting, desiccation, and coagulation leading to potential lateral tissue damage, ureteral injury is a well-known complication. Even normal anatomic variations may put some women at greater risk; according to Hurd et al. (Am J Obstet Gynecol. 2001;184:336-9). In a small subset of women, the distance between the cervix and the ureter may be less than 0.5 cm.
As a practicing minimally invasive gynecologic surgeon for the past 30 years, and an early adapter to laparoscopic hysterectomy, I remember quite well the recommendation to always dissect out ureters at time of the procedure. At present, most will agree that selective dissection is safe and thus, more desirable, as bleeding, damage secondary to desiccation, and ureter devascularization with subsequent necrosis are all increased with ureterolysis.
I agree with Dr. Kenton and Dr. Mueller that ureteral stenting has not been shown to significantly decrease ureteral injury rates. Often times, with loss of peristalsis secondary to stent placement, locating the ureter may be even more difficult. Recent advances using lighted stents or indocyanine green, which fluoresces in response to near-infrared laser and can be injected into the ureter via the ureteral catheter tip, are still in the feasibility phase of evaluation and can be costly.
As most urogenital fistulae are secondary to unrecognized injuries at time of surgery, and due to the fact that intraoperative recognition of the injury allows for primary repair, thus, decreasing the rate of secondary surgery and the associated increased morbidity, I recommend cystoscopy to check for ureteral jets (ureteral efflux) be performed when there is concern regarding ureter compromise.
Currently, I utilize a 70° cystoscope to visualize the ureters. While in the past, I have used intravenous indigo carmine, methylene blue, or fluorescein sodium, I currently use Pyridium (phenazopyridine) 200 mg taken by mouth 1 hour prior to the procedure.
Unfortunately, ureteral jetting still may be noted despite partial ligation, laceration, or desiccation of the ureter.
If ureteral injury is not recognized at time of surgery, it can lead to various postoperative symptoms. If there is a ureteral defect, the patient may note profuse wound leakage, increased abdominal fluid, or a urinoma, ileus, fever, peritonitis, or hematuria. With ureteral obstruction, flank or abdominal pain or anuria can be noted; while, with fistula formation, the patient will likely present with urinary incontinence or watery vaginal discharge.
Dr. Miller is a minimally invasive gynecologic surgeon in Naperville, Ill., and a past president of the AAGL.
A gynecologic surgeon learns very early in his/her career to respect the ureter. Whether from the procedure being performed (endometriosis surgery, hysterectomy, myomectomy for ligamentous fibroids, salpingo-oophorectomy, excision of ovarian remnants, adhesiolysis), blood loss that obscures visualization and must be controlled, or use of energy for cutting, desiccation, and coagulation leading to potential lateral tissue damage, ureteral injury is a well-known complication. Even normal anatomic variations may put some women at greater risk; according to Hurd et al. (Am J Obstet Gynecol. 2001;184:336-9). In a small subset of women, the distance between the cervix and the ureter may be less than 0.5 cm.
As a practicing minimally invasive gynecologic surgeon for the past 30 years, and an early adapter to laparoscopic hysterectomy, I remember quite well the recommendation to always dissect out ureters at time of the procedure. At present, most will agree that selective dissection is safe and thus, more desirable, as bleeding, damage secondary to desiccation, and ureter devascularization with subsequent necrosis are all increased with ureterolysis.
I agree with Dr. Kenton and Dr. Mueller that ureteral stenting has not been shown to significantly decrease ureteral injury rates. Often times, with loss of peristalsis secondary to stent placement, locating the ureter may be even more difficult. Recent advances using lighted stents or indocyanine green, which fluoresces in response to near-infrared laser and can be injected into the ureter via the ureteral catheter tip, are still in the feasibility phase of evaluation and can be costly.
As most urogenital fistulae are secondary to unrecognized injuries at time of surgery, and due to the fact that intraoperative recognition of the injury allows for primary repair, thus, decreasing the rate of secondary surgery and the associated increased morbidity, I recommend cystoscopy to check for ureteral jets (ureteral efflux) be performed when there is concern regarding ureter compromise.
Currently, I utilize a 70° cystoscope to visualize the ureters. While in the past, I have used intravenous indigo carmine, methylene blue, or fluorescein sodium, I currently use Pyridium (phenazopyridine) 200 mg taken by mouth 1 hour prior to the procedure.
Unfortunately, ureteral jetting still may be noted despite partial ligation, laceration, or desiccation of the ureter.
If ureteral injury is not recognized at time of surgery, it can lead to various postoperative symptoms. If there is a ureteral defect, the patient may note profuse wound leakage, increased abdominal fluid, or a urinoma, ileus, fever, peritonitis, or hematuria. With ureteral obstruction, flank or abdominal pain or anuria can be noted; while, with fistula formation, the patient will likely present with urinary incontinence or watery vaginal discharge.
Dr. Miller is a minimally invasive gynecologic surgeon in Naperville, Ill., and a past president of the AAGL.
A gynecologic surgeon learns very early in his/her career to respect the ureter. Whether from the procedure being performed (endometriosis surgery, hysterectomy, myomectomy for ligamentous fibroids, salpingo-oophorectomy, excision of ovarian remnants, adhesiolysis), blood loss that obscures visualization and must be controlled, or use of energy for cutting, desiccation, and coagulation leading to potential lateral tissue damage, ureteral injury is a well-known complication. Even normal anatomic variations may put some women at greater risk; according to Hurd et al. (Am J Obstet Gynecol. 2001;184:336-9). In a small subset of women, the distance between the cervix and the ureter may be less than 0.5 cm.
As a practicing minimally invasive gynecologic surgeon for the past 30 years, and an early adapter to laparoscopic hysterectomy, I remember quite well the recommendation to always dissect out ureters at time of the procedure. At present, most will agree that selective dissection is safe and thus, more desirable, as bleeding, damage secondary to desiccation, and ureter devascularization with subsequent necrosis are all increased with ureterolysis.
I agree with Dr. Kenton and Dr. Mueller that ureteral stenting has not been shown to significantly decrease ureteral injury rates. Often times, with loss of peristalsis secondary to stent placement, locating the ureter may be even more difficult. Recent advances using lighted stents or indocyanine green, which fluoresces in response to near-infrared laser and can be injected into the ureter via the ureteral catheter tip, are still in the feasibility phase of evaluation and can be costly.
As most urogenital fistulae are secondary to unrecognized injuries at time of surgery, and due to the fact that intraoperative recognition of the injury allows for primary repair, thus, decreasing the rate of secondary surgery and the associated increased morbidity, I recommend cystoscopy to check for ureteral jets (ureteral efflux) be performed when there is concern regarding ureter compromise.
Currently, I utilize a 70° cystoscope to visualize the ureters. While in the past, I have used intravenous indigo carmine, methylene blue, or fluorescein sodium, I currently use Pyridium (phenazopyridine) 200 mg taken by mouth 1 hour prior to the procedure.
Unfortunately, ureteral jetting still may be noted despite partial ligation, laceration, or desiccation of the ureter.
If ureteral injury is not recognized at time of surgery, it can lead to various postoperative symptoms. If there is a ureteral defect, the patient may note profuse wound leakage, increased abdominal fluid, or a urinoma, ileus, fever, peritonitis, or hematuria. With ureteral obstruction, flank or abdominal pain or anuria can be noted; while, with fistula formation, the patient will likely present with urinary incontinence or watery vaginal discharge.
Dr. Miller is a minimally invasive gynecologic surgeon in Naperville, Ill., and a past president of the AAGL.
Prevention of ovarian remnant syndrome: Adnexal adhesiolysis from the pelvic sidewall

Visit the Society of Gynecologic Surgeons online: sgsonline.org
Additional videos from SGS are available here, including these recent offerings:

Visit the Society of Gynecologic Surgeons online: sgsonline.org
Additional videos from SGS are available here, including these recent offerings:

Visit the Society of Gynecologic Surgeons online: sgsonline.org
Additional videos from SGS are available here, including these recent offerings:
This video is brought to you by
In abdominal myomectomy, cell salvage may reduce transfusions
ORLANDO – Cell salvage may help reduce the need for allogeneic blood transfusion in patients undergoing abdominal myomectomy, according to findings from a retrospective cohort study.
Of 138 women who underwent abdominal myomectomy, 52 had no cell salvage and 86 had cell salvage ordered. Of those who had cell salvage ordered, 60 had salvage fully set up and 26 had salvage on standby; 46 of the 60 with full set-up had autologous blood returned, and of those, 14 required subsequent allogeneic transfusion of more than 20 U of blood, Julian A. Gingold, MD, reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
Notable differences between those who did and those who did not have cell salvage ordered included the number of patients with fibroids weighing more than 250 g (52% vs. 13%) and with five or more total fibroids (83% vs. 56%), he said.
“And interestingly, reproductive surgeons were less likely (than general surgeons) to order cell salvage,” he said.
Surgery was performed by a reproductive surgeon in 25% of cases in the cell salvage group vs. in 67% of cases in the non–cell salvage group.
The finding of comparable allogeneic transfusion requirement between the two groups despite differences in blood loss and “arguably less complex surgeries [in those] without cell salvage” was striking, Dr. Gingold said.
“If you take these 86 patients who had cell salvage intraoperatively, 14 of them ultimately required donor blood, and that amounted to 23 units, giving kind of a lower limit for the potential benefit of cell salvage in this patient cohort,” he said.
Abdominal myomectomy often has a high rate of blood loss, with about a 10%-20% rate of transfusion. While the technique of cell salvage is widely used in other fields, it hasn’t been fully investigated in the context of gynecologic surgery, he said, explaining the rationale for the study.
Subjects included were women aged 18-60 years who underwent abdominal myomectomy for benign indications at the Cleveland Clinic during 2011-2016. Those with current malignancy or with surgery performed by a gynecologic oncologist were excluded.
The non–cell salvage and cell salvage groups were comparable with respect to age, body mass index, ethnicity, and preoperative and postoperative hemoglobin.
Dr. Gingold noted that “prospective study with randomization will be required to better define the role of cell salvage in abdominal myomectomies.”
During a question and answer session following his presentation, Charles Ascher-Walsh, MD, of Mount Sinai Health System, N.Y. noted that the transfusion rates and blood loss were high in the study, and that solid data support the use of tourniquets for patients undergoing abdominal myomectomy, with studies showing only a 1%-2% transfusion rate with continuous tourniquet use. Dr. Gingold said the use of tourniquets in the study was low and was dictated by surgeon preference. He agreed that tourniquet use is “certainly an option that should be adjunctive,” and that it would be useful to look at the outcomes in the cases with and without tourniquet use.
Dr. Gingold reported having no disclosures.
SOURCE: Gingold J et al. SGS 2018 Oral Poster 18.
ORLANDO – Cell salvage may help reduce the need for allogeneic blood transfusion in patients undergoing abdominal myomectomy, according to findings from a retrospective cohort study.
Of 138 women who underwent abdominal myomectomy, 52 had no cell salvage and 86 had cell salvage ordered. Of those who had cell salvage ordered, 60 had salvage fully set up and 26 had salvage on standby; 46 of the 60 with full set-up had autologous blood returned, and of those, 14 required subsequent allogeneic transfusion of more than 20 U of blood, Julian A. Gingold, MD, reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
Notable differences between those who did and those who did not have cell salvage ordered included the number of patients with fibroids weighing more than 250 g (52% vs. 13%) and with five or more total fibroids (83% vs. 56%), he said.
“And interestingly, reproductive surgeons were less likely (than general surgeons) to order cell salvage,” he said.
Surgery was performed by a reproductive surgeon in 25% of cases in the cell salvage group vs. in 67% of cases in the non–cell salvage group.
The finding of comparable allogeneic transfusion requirement between the two groups despite differences in blood loss and “arguably less complex surgeries [in those] without cell salvage” was striking, Dr. Gingold said.
“If you take these 86 patients who had cell salvage intraoperatively, 14 of them ultimately required donor blood, and that amounted to 23 units, giving kind of a lower limit for the potential benefit of cell salvage in this patient cohort,” he said.
Abdominal myomectomy often has a high rate of blood loss, with about a 10%-20% rate of transfusion. While the technique of cell salvage is widely used in other fields, it hasn’t been fully investigated in the context of gynecologic surgery, he said, explaining the rationale for the study.
Subjects included were women aged 18-60 years who underwent abdominal myomectomy for benign indications at the Cleveland Clinic during 2011-2016. Those with current malignancy or with surgery performed by a gynecologic oncologist were excluded.
The non–cell salvage and cell salvage groups were comparable with respect to age, body mass index, ethnicity, and preoperative and postoperative hemoglobin.
Dr. Gingold noted that “prospective study with randomization will be required to better define the role of cell salvage in abdominal myomectomies.”
During a question and answer session following his presentation, Charles Ascher-Walsh, MD, of Mount Sinai Health System, N.Y. noted that the transfusion rates and blood loss were high in the study, and that solid data support the use of tourniquets for patients undergoing abdominal myomectomy, with studies showing only a 1%-2% transfusion rate with continuous tourniquet use. Dr. Gingold said the use of tourniquets in the study was low and was dictated by surgeon preference. He agreed that tourniquet use is “certainly an option that should be adjunctive,” and that it would be useful to look at the outcomes in the cases with and without tourniquet use.
Dr. Gingold reported having no disclosures.
SOURCE: Gingold J et al. SGS 2018 Oral Poster 18.
ORLANDO – Cell salvage may help reduce the need for allogeneic blood transfusion in patients undergoing abdominal myomectomy, according to findings from a retrospective cohort study.
Of 138 women who underwent abdominal myomectomy, 52 had no cell salvage and 86 had cell salvage ordered. Of those who had cell salvage ordered, 60 had salvage fully set up and 26 had salvage on standby; 46 of the 60 with full set-up had autologous blood returned, and of those, 14 required subsequent allogeneic transfusion of more than 20 U of blood, Julian A. Gingold, MD, reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
Notable differences between those who did and those who did not have cell salvage ordered included the number of patients with fibroids weighing more than 250 g (52% vs. 13%) and with five or more total fibroids (83% vs. 56%), he said.
“And interestingly, reproductive surgeons were less likely (than general surgeons) to order cell salvage,” he said.
Surgery was performed by a reproductive surgeon in 25% of cases in the cell salvage group vs. in 67% of cases in the non–cell salvage group.
The finding of comparable allogeneic transfusion requirement between the two groups despite differences in blood loss and “arguably less complex surgeries [in those] without cell salvage” was striking, Dr. Gingold said.
“If you take these 86 patients who had cell salvage intraoperatively, 14 of them ultimately required donor blood, and that amounted to 23 units, giving kind of a lower limit for the potential benefit of cell salvage in this patient cohort,” he said.
Abdominal myomectomy often has a high rate of blood loss, with about a 10%-20% rate of transfusion. While the technique of cell salvage is widely used in other fields, it hasn’t been fully investigated in the context of gynecologic surgery, he said, explaining the rationale for the study.
Subjects included were women aged 18-60 years who underwent abdominal myomectomy for benign indications at the Cleveland Clinic during 2011-2016. Those with current malignancy or with surgery performed by a gynecologic oncologist were excluded.
The non–cell salvage and cell salvage groups were comparable with respect to age, body mass index, ethnicity, and preoperative and postoperative hemoglobin.
Dr. Gingold noted that “prospective study with randomization will be required to better define the role of cell salvage in abdominal myomectomies.”
During a question and answer session following his presentation, Charles Ascher-Walsh, MD, of Mount Sinai Health System, N.Y. noted that the transfusion rates and blood loss were high in the study, and that solid data support the use of tourniquets for patients undergoing abdominal myomectomy, with studies showing only a 1%-2% transfusion rate with continuous tourniquet use. Dr. Gingold said the use of tourniquets in the study was low and was dictated by surgeon preference. He agreed that tourniquet use is “certainly an option that should be adjunctive,” and that it would be useful to look at the outcomes in the cases with and without tourniquet use.
Dr. Gingold reported having no disclosures.
SOURCE: Gingold J et al. SGS 2018 Oral Poster 18.
REPORTING FROM SGS 2018
Key clinical point: Cell salvage may help reduce the need for allogeneic blood transfusion in patients undergoing abdominal myomectomy.
Major finding: Transfusion rates were similar (23% and 17%) despite greater blood loss in the cell salvage group.
Study details: A retrospective review of 138 patients’ charts.
Disclosures: Dr. Gingold reported having no disclosures.
Source: Gingold J et al. SGS 2018 Oral poster 18.
FDA approves Doptelet for liver disease patients undergoing procedures
Doptelet (avatrombopag) is the first drug to be approved by the Food and Drug Administration for thrombocytopenia in adults with chronic liver disease who are scheduled to undergo a medical or dental procedure, the FDA announced in a statement.
“Patients with chronic liver disease who have low platelet counts and require a procedure are at increased risk of bleeding,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research. “Doptelet was demonstrated to safely increase the platelet count. This drug may decrease or eliminate the need for platelet transfusions, which are associated with risk of infection and other adverse reactions.”
The safety and efficacy of two different doses of Doptelet administered orally over 5 days, as compared with placebo, was studied in the ADAPT trials (ADAPT-1 and ADAPT-2) involving 435 patients with chronic liver disease and severe thrombocytopenia who were scheduled to undergo a procedure that would typically require platelet transfusion. At both dose levels of Doptelet, a higher proportion of patients had increased platelet counts and did not require platelet transfusion or any rescue therapy on the day of the procedure and up to 7 days following the procedure as compared with those treated with placebo.
The most common side effects reported by clinical trial participants who received Doptelet were fever, stomach (abdominal) pain, nausea, headache, fatigue and edema in the hands or feet. People with chronic liver disease and people with certain blood clotting conditions may have an increased risk of developing blood clots when taking Doptelet, the FDA said in a press release announcing the approval.
The FDA granted the Doptelet approval to AkaRx.
Doptelet (avatrombopag) is the first drug to be approved by the Food and Drug Administration for thrombocytopenia in adults with chronic liver disease who are scheduled to undergo a medical or dental procedure, the FDA announced in a statement.
“Patients with chronic liver disease who have low platelet counts and require a procedure are at increased risk of bleeding,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research. “Doptelet was demonstrated to safely increase the platelet count. This drug may decrease or eliminate the need for platelet transfusions, which are associated with risk of infection and other adverse reactions.”
The safety and efficacy of two different doses of Doptelet administered orally over 5 days, as compared with placebo, was studied in the ADAPT trials (ADAPT-1 and ADAPT-2) involving 435 patients with chronic liver disease and severe thrombocytopenia who were scheduled to undergo a procedure that would typically require platelet transfusion. At both dose levels of Doptelet, a higher proportion of patients had increased platelet counts and did not require platelet transfusion or any rescue therapy on the day of the procedure and up to 7 days following the procedure as compared with those treated with placebo.
The most common side effects reported by clinical trial participants who received Doptelet were fever, stomach (abdominal) pain, nausea, headache, fatigue and edema in the hands or feet. People with chronic liver disease and people with certain blood clotting conditions may have an increased risk of developing blood clots when taking Doptelet, the FDA said in a press release announcing the approval.
The FDA granted the Doptelet approval to AkaRx.
Doptelet (avatrombopag) is the first drug to be approved by the Food and Drug Administration for thrombocytopenia in adults with chronic liver disease who are scheduled to undergo a medical or dental procedure, the FDA announced in a statement.
“Patients with chronic liver disease who have low platelet counts and require a procedure are at increased risk of bleeding,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research. “Doptelet was demonstrated to safely increase the platelet count. This drug may decrease or eliminate the need for platelet transfusions, which are associated with risk of infection and other adverse reactions.”
The safety and efficacy of two different doses of Doptelet administered orally over 5 days, as compared with placebo, was studied in the ADAPT trials (ADAPT-1 and ADAPT-2) involving 435 patients with chronic liver disease and severe thrombocytopenia who were scheduled to undergo a procedure that would typically require platelet transfusion. At both dose levels of Doptelet, a higher proportion of patients had increased platelet counts and did not require platelet transfusion or any rescue therapy on the day of the procedure and up to 7 days following the procedure as compared with those treated with placebo.
The most common side effects reported by clinical trial participants who received Doptelet were fever, stomach (abdominal) pain, nausea, headache, fatigue and edema in the hands or feet. People with chronic liver disease and people with certain blood clotting conditions may have an increased risk of developing blood clots when taking Doptelet, the FDA said in a press release announcing the approval.
The FDA granted the Doptelet approval to AkaRx.
Complete MUS mesh removal not linked to incontinence
SAN FRANCISCO – Stress urinary incontinence (SUI) following removal of a mid-urethral sling (MUS) mesh is not necessarily associated with increased risk of postsurgical urinary incontinence, according to a retrospective study at a high-volume, tertiary medical center.
Follow-up procedures occurred more often in women with preoperative urodynamic SUI and less often in women who were stress continent.
Among women who were stress continent, obesity and postmenopausal status were linked to postsurgical SUI. There was no association between postsurgical SUI and the extent of mesh excision or prior revisions.
The study grew out of observations that SUI occurred less often than expected.
“There’s an increasing recognition of complications related to synthetic MUS,” said Janine Oliver, MD, who presented the study at the annual meeting of the American Urological Association. “As mesh removal procedures were being performed, we assumed that the majority of patients, if not all, would be incontinent afterward, since we were removing the sling that was put in to fix stress incontinence in most cases.”
In a patient who would benefit from a complete mesh removal, “the fear that it may lead to a higher risk of urinary incontinence is not a good justification to not do it,” Dr. Oliver said. She did note, however, that the procedures were done by specialists, so findings may not be applicable to general practitioners.
The study was performed while Dr. Oliver was a fellow at the University of California, Los Angeles. She is now with the division of urology at the University of Colorado, Anschutz, in Aurora.
Dr. Oliver and her colleagues analyzed data from 233 patients who underwent MUS excision at UCLA for MUS-related complications during 2013-2015, and who had at least 3 months of follow-up. The average patient age was 55.4 years; an average of 5.4 years passed between the placement and excision of MUS. The mean body mass index was 28.9, and mean follow-up was 23.5 months.
A total of 84% of patients underwent a total excision; 45% of MUS were retropubic, 35% were transobturator, 10% were single incision, and 10% were multiple incision.
Nearly half (49%) of patients required a second procedure for SUI, such as bulking agent injection, bladder neck suspension, or repeat sling procedure.
In the entire cohort, multivariate analyses found significant associations between heightened risk of postoperative SUI and increasing time to MUS excision (odds ratio, 1.16; 95% confidence interval, 1.03-1.30), total MUS excision (OR, 4.14; 95% CI, 1.38-12.37), and preoperative urodynamic SUI (OR, 4.66; 95% CI, 2.13-10.19).
Of 51 patients who had preoperative urodynamic SUI, 39 (76%) ultimately underwent another surgery. Although increased time to MUS excision and total mesh removal were associated with urinary incontinence in this group in univariate analyses, they were no longer significant following a multivariate analysis.
Of 140 patients with a negative preoperative urodynamic testing for SUI, 59 (42%) went on to have another SUI procedure. After multivariate analysis, the only risk factors for urinary incontinence were obesity (OR, 4.74; 95% CI, 1.73-13.02) and postmenopausal status (OR, 3.78; 95% CI, 1.16-12.33).
“I think there’s a lot of fear, even among urologists and specialists who see these problems, that complete mesh removal is associated with a higher risk of complications and a higher risk of incontinence,” said Dr. Oliver. “These data would suggest that, in certain subgroups, that’s not true. The risks factors that we identified in a multivariate analysis were being obese and being postmenopausal, but not complete mesh removal.”
The study received no external funding. Dr. Oliver reported having no financial conflicts of interest.
SOURCE: Oliver J et al. AUA Annual Meeting. Abstract PD05-10.
SAN FRANCISCO – Stress urinary incontinence (SUI) following removal of a mid-urethral sling (MUS) mesh is not necessarily associated with increased risk of postsurgical urinary incontinence, according to a retrospective study at a high-volume, tertiary medical center.
Follow-up procedures occurred more often in women with preoperative urodynamic SUI and less often in women who were stress continent.
Among women who were stress continent, obesity and postmenopausal status were linked to postsurgical SUI. There was no association between postsurgical SUI and the extent of mesh excision or prior revisions.
The study grew out of observations that SUI occurred less often than expected.
“There’s an increasing recognition of complications related to synthetic MUS,” said Janine Oliver, MD, who presented the study at the annual meeting of the American Urological Association. “As mesh removal procedures were being performed, we assumed that the majority of patients, if not all, would be incontinent afterward, since we were removing the sling that was put in to fix stress incontinence in most cases.”
In a patient who would benefit from a complete mesh removal, “the fear that it may lead to a higher risk of urinary incontinence is not a good justification to not do it,” Dr. Oliver said. She did note, however, that the procedures were done by specialists, so findings may not be applicable to general practitioners.
The study was performed while Dr. Oliver was a fellow at the University of California, Los Angeles. She is now with the division of urology at the University of Colorado, Anschutz, in Aurora.
Dr. Oliver and her colleagues analyzed data from 233 patients who underwent MUS excision at UCLA for MUS-related complications during 2013-2015, and who had at least 3 months of follow-up. The average patient age was 55.4 years; an average of 5.4 years passed between the placement and excision of MUS. The mean body mass index was 28.9, and mean follow-up was 23.5 months.
A total of 84% of patients underwent a total excision; 45% of MUS were retropubic, 35% were transobturator, 10% were single incision, and 10% were multiple incision.
Nearly half (49%) of patients required a second procedure for SUI, such as bulking agent injection, bladder neck suspension, or repeat sling procedure.
In the entire cohort, multivariate analyses found significant associations between heightened risk of postoperative SUI and increasing time to MUS excision (odds ratio, 1.16; 95% confidence interval, 1.03-1.30), total MUS excision (OR, 4.14; 95% CI, 1.38-12.37), and preoperative urodynamic SUI (OR, 4.66; 95% CI, 2.13-10.19).
Of 51 patients who had preoperative urodynamic SUI, 39 (76%) ultimately underwent another surgery. Although increased time to MUS excision and total mesh removal were associated with urinary incontinence in this group in univariate analyses, they were no longer significant following a multivariate analysis.
Of 140 patients with a negative preoperative urodynamic testing for SUI, 59 (42%) went on to have another SUI procedure. After multivariate analysis, the only risk factors for urinary incontinence were obesity (OR, 4.74; 95% CI, 1.73-13.02) and postmenopausal status (OR, 3.78; 95% CI, 1.16-12.33).
“I think there’s a lot of fear, even among urologists and specialists who see these problems, that complete mesh removal is associated with a higher risk of complications and a higher risk of incontinence,” said Dr. Oliver. “These data would suggest that, in certain subgroups, that’s not true. The risks factors that we identified in a multivariate analysis were being obese and being postmenopausal, but not complete mesh removal.”
The study received no external funding. Dr. Oliver reported having no financial conflicts of interest.
SOURCE: Oliver J et al. AUA Annual Meeting. Abstract PD05-10.
SAN FRANCISCO – Stress urinary incontinence (SUI) following removal of a mid-urethral sling (MUS) mesh is not necessarily associated with increased risk of postsurgical urinary incontinence, according to a retrospective study at a high-volume, tertiary medical center.
Follow-up procedures occurred more often in women with preoperative urodynamic SUI and less often in women who were stress continent.
Among women who were stress continent, obesity and postmenopausal status were linked to postsurgical SUI. There was no association between postsurgical SUI and the extent of mesh excision or prior revisions.
The study grew out of observations that SUI occurred less often than expected.
“There’s an increasing recognition of complications related to synthetic MUS,” said Janine Oliver, MD, who presented the study at the annual meeting of the American Urological Association. “As mesh removal procedures were being performed, we assumed that the majority of patients, if not all, would be incontinent afterward, since we were removing the sling that was put in to fix stress incontinence in most cases.”
In a patient who would benefit from a complete mesh removal, “the fear that it may lead to a higher risk of urinary incontinence is not a good justification to not do it,” Dr. Oliver said. She did note, however, that the procedures were done by specialists, so findings may not be applicable to general practitioners.
The study was performed while Dr. Oliver was a fellow at the University of California, Los Angeles. She is now with the division of urology at the University of Colorado, Anschutz, in Aurora.
Dr. Oliver and her colleagues analyzed data from 233 patients who underwent MUS excision at UCLA for MUS-related complications during 2013-2015, and who had at least 3 months of follow-up. The average patient age was 55.4 years; an average of 5.4 years passed between the placement and excision of MUS. The mean body mass index was 28.9, and mean follow-up was 23.5 months.
A total of 84% of patients underwent a total excision; 45% of MUS were retropubic, 35% were transobturator, 10% were single incision, and 10% were multiple incision.
Nearly half (49%) of patients required a second procedure for SUI, such as bulking agent injection, bladder neck suspension, or repeat sling procedure.
In the entire cohort, multivariate analyses found significant associations between heightened risk of postoperative SUI and increasing time to MUS excision (odds ratio, 1.16; 95% confidence interval, 1.03-1.30), total MUS excision (OR, 4.14; 95% CI, 1.38-12.37), and preoperative urodynamic SUI (OR, 4.66; 95% CI, 2.13-10.19).
Of 51 patients who had preoperative urodynamic SUI, 39 (76%) ultimately underwent another surgery. Although increased time to MUS excision and total mesh removal were associated with urinary incontinence in this group in univariate analyses, they were no longer significant following a multivariate analysis.
Of 140 patients with a negative preoperative urodynamic testing for SUI, 59 (42%) went on to have another SUI procedure. After multivariate analysis, the only risk factors for urinary incontinence were obesity (OR, 4.74; 95% CI, 1.73-13.02) and postmenopausal status (OR, 3.78; 95% CI, 1.16-12.33).
“I think there’s a lot of fear, even among urologists and specialists who see these problems, that complete mesh removal is associated with a higher risk of complications and a higher risk of incontinence,” said Dr. Oliver. “These data would suggest that, in certain subgroups, that’s not true. The risks factors that we identified in a multivariate analysis were being obese and being postmenopausal, but not complete mesh removal.”
The study received no external funding. Dr. Oliver reported having no financial conflicts of interest.
SOURCE: Oliver J et al. AUA Annual Meeting. Abstract PD05-10.
REPORTING FROM THE AUA ANNUAL MEETING
Key clinical point: There was no association between postsurgical incontinence risk and complete mesh removal.
Major finding: In patients without presurgical urodynamic incontinence, only obesity (OR, 4.74) and postmenopausal status (OR, 3.78) were linked to incontinence risk.
Study details: A retrospective analysis of 233 patients.
Disclosures: The study received no external funding. Dr. Oliver reported having no financial conflicts of interest.
Source: Oliver J et al. AUA Annual Meeting. Abstract PD05-10.
ESBL-B before colorectal surgery ups risk of surgical site infection
MADRID – Patients who are carriers of , despite a standard prophylactic antibiotic regimen.
Surgical site infections (SSIs) occurred in 23% of those who tested positive for the pathogens preoperatively, compared with 10.5% of ESBL-B–negative patients – a significant increased risk of 2.25, Yehuda Carmeli, MD, said at the European Congress of Clinical Microbiology and Infectious Diseases annual congress.
ESBL-B was not the infective pathogen in most infection cases, but being a carrier increased the likelihood of an ESBL-B SSI. ESBL-B was the pathogen in 7.2% of the carriers and 1.6% of the noncarriers. However, investigators are still working to determine if the species present in the wound infection are the same as the ones present at baseline, said Dr. Carmeli of Tel Aviv Medical Center.
All of these results are emerging from the WP4 study, which was carried out in three hospitals in Serbia, Switzerland, and Israel. Designed as a before-and-after trial, it tested the theory that identifying ESBL carriers and targeting presurgical antibiotic prophylaxis could improve their surgical outcomes.
WP4 was one of five studies in the multinational R-GNOSIS project. “Resistance in Gram-Negative Organisms: Studying Intervention Strategies” is a 12-million-euro, 5-year European collaborative research project designed to identify effective interventions for reducing the carriage, infection, and spread of multi-drug resistant Gram-negative bacteria. From 2012 to 2017, WP4 enrolled almost 4,000 adults scheduled to undergo colorectal surgery (excluding appendectomy or minor anorectal procedures).
Several of the studies were reported at ECCMID 2018.
This portion of R-GNOSIS was intended to investigate the relationship between ESBL-B carriage and postoperative surgical site infections among colorectal surgery patients.
The study comprised 3,626 patients who were preoperatively screened for ESBL-B within 2 weeks of colorectal surgery. The ESBL-B carriage rate was 15.3% overall, but ranged from 12% to 20% by site. Of the carriers, 222 were included in this study sample. They were randomly matched with 444 noncarriers.
Anywhere from 2 weeks to 2 days before surgery, all of the patients received a standard prophylactic antibiotic. This was most often an infusion of 1.5 g cefuroxime plus 500 mg metronidazole. Other cephalosporins were allowed at the clinician’s discretion.
Patients were a mean of 62 years old. Nearly half (48%) had cardiovascular disease and about a third had undergone a prior colorectal surgical procedure. Cancer was the surgical indication in about 70%. Other indications were inflammatory bowel disease and diverticular disease.
A multivariate analysis controlled for age, cardiovascular disease, indication for surgery, and whether the procedure included a rectal resection, retention of drain at the surgical site, or stoma. The model also controlled for National Nosocomial Infection Surveillance score, a three-point scale that estimates surgical infection risk. Among this cohort, 48% were at low risk, 43% at moderate risk, and 10% at high risk.
Dr. Carmeli made no financial disclosures.
SOURCE: Carmeli et al, ECCMID 2018, Oral Abstract O1133.
MADRID – Patients who are carriers of , despite a standard prophylactic antibiotic regimen.
Surgical site infections (SSIs) occurred in 23% of those who tested positive for the pathogens preoperatively, compared with 10.5% of ESBL-B–negative patients – a significant increased risk of 2.25, Yehuda Carmeli, MD, said at the European Congress of Clinical Microbiology and Infectious Diseases annual congress.
ESBL-B was not the infective pathogen in most infection cases, but being a carrier increased the likelihood of an ESBL-B SSI. ESBL-B was the pathogen in 7.2% of the carriers and 1.6% of the noncarriers. However, investigators are still working to determine if the species present in the wound infection are the same as the ones present at baseline, said Dr. Carmeli of Tel Aviv Medical Center.
All of these results are emerging from the WP4 study, which was carried out in three hospitals in Serbia, Switzerland, and Israel. Designed as a before-and-after trial, it tested the theory that identifying ESBL carriers and targeting presurgical antibiotic prophylaxis could improve their surgical outcomes.
WP4 was one of five studies in the multinational R-GNOSIS project. “Resistance in Gram-Negative Organisms: Studying Intervention Strategies” is a 12-million-euro, 5-year European collaborative research project designed to identify effective interventions for reducing the carriage, infection, and spread of multi-drug resistant Gram-negative bacteria. From 2012 to 2017, WP4 enrolled almost 4,000 adults scheduled to undergo colorectal surgery (excluding appendectomy or minor anorectal procedures).
Several of the studies were reported at ECCMID 2018.
This portion of R-GNOSIS was intended to investigate the relationship between ESBL-B carriage and postoperative surgical site infections among colorectal surgery patients.
The study comprised 3,626 patients who were preoperatively screened for ESBL-B within 2 weeks of colorectal surgery. The ESBL-B carriage rate was 15.3% overall, but ranged from 12% to 20% by site. Of the carriers, 222 were included in this study sample. They were randomly matched with 444 noncarriers.
Anywhere from 2 weeks to 2 days before surgery, all of the patients received a standard prophylactic antibiotic. This was most often an infusion of 1.5 g cefuroxime plus 500 mg metronidazole. Other cephalosporins were allowed at the clinician’s discretion.
Patients were a mean of 62 years old. Nearly half (48%) had cardiovascular disease and about a third had undergone a prior colorectal surgical procedure. Cancer was the surgical indication in about 70%. Other indications were inflammatory bowel disease and diverticular disease.
A multivariate analysis controlled for age, cardiovascular disease, indication for surgery, and whether the procedure included a rectal resection, retention of drain at the surgical site, or stoma. The model also controlled for National Nosocomial Infection Surveillance score, a three-point scale that estimates surgical infection risk. Among this cohort, 48% were at low risk, 43% at moderate risk, and 10% at high risk.
Dr. Carmeli made no financial disclosures.
SOURCE: Carmeli et al, ECCMID 2018, Oral Abstract O1133.
MADRID – Patients who are carriers of , despite a standard prophylactic antibiotic regimen.
Surgical site infections (SSIs) occurred in 23% of those who tested positive for the pathogens preoperatively, compared with 10.5% of ESBL-B–negative patients – a significant increased risk of 2.25, Yehuda Carmeli, MD, said at the European Congress of Clinical Microbiology and Infectious Diseases annual congress.
ESBL-B was not the infective pathogen in most infection cases, but being a carrier increased the likelihood of an ESBL-B SSI. ESBL-B was the pathogen in 7.2% of the carriers and 1.6% of the noncarriers. However, investigators are still working to determine if the species present in the wound infection are the same as the ones present at baseline, said Dr. Carmeli of Tel Aviv Medical Center.
All of these results are emerging from the WP4 study, which was carried out in three hospitals in Serbia, Switzerland, and Israel. Designed as a before-and-after trial, it tested the theory that identifying ESBL carriers and targeting presurgical antibiotic prophylaxis could improve their surgical outcomes.
WP4 was one of five studies in the multinational R-GNOSIS project. “Resistance in Gram-Negative Organisms: Studying Intervention Strategies” is a 12-million-euro, 5-year European collaborative research project designed to identify effective interventions for reducing the carriage, infection, and spread of multi-drug resistant Gram-negative bacteria. From 2012 to 2017, WP4 enrolled almost 4,000 adults scheduled to undergo colorectal surgery (excluding appendectomy or minor anorectal procedures).
Several of the studies were reported at ECCMID 2018.
This portion of R-GNOSIS was intended to investigate the relationship between ESBL-B carriage and postoperative surgical site infections among colorectal surgery patients.
The study comprised 3,626 patients who were preoperatively screened for ESBL-B within 2 weeks of colorectal surgery. The ESBL-B carriage rate was 15.3% overall, but ranged from 12% to 20% by site. Of the carriers, 222 were included in this study sample. They were randomly matched with 444 noncarriers.
Anywhere from 2 weeks to 2 days before surgery, all of the patients received a standard prophylactic antibiotic. This was most often an infusion of 1.5 g cefuroxime plus 500 mg metronidazole. Other cephalosporins were allowed at the clinician’s discretion.
Patients were a mean of 62 years old. Nearly half (48%) had cardiovascular disease and about a third had undergone a prior colorectal surgical procedure. Cancer was the surgical indication in about 70%. Other indications were inflammatory bowel disease and diverticular disease.
A multivariate analysis controlled for age, cardiovascular disease, indication for surgery, and whether the procedure included a rectal resection, retention of drain at the surgical site, or stoma. The model also controlled for National Nosocomial Infection Surveillance score, a three-point scale that estimates surgical infection risk. Among this cohort, 48% were at low risk, 43% at moderate risk, and 10% at high risk.
Dr. Carmeli made no financial disclosures.
SOURCE: Carmeli et al, ECCMID 2018, Oral Abstract O1133.
REPORTING FROM ECCMID 2018
Key clinical point: ESBL-B colonization increased the risk of surgical site infections after colorectal surgery, despite use of standard preoperative antibiotics.
Major finding: ESBL-B carriage more than doubled the risk of a colorectal surgical site infection by (OR 2.25).
Study details: The prospective study comprised 222 carriers and 444 noncarriers.
Disclosures: The study is part of the R-GNOSIS project, a 12-million-euro, 5-year European collaborative research project designed to identify effective interventions for reducing the carriage, infection, and spread of multi-drug resistant Gram-negative bacteria.
Source: Carmeli Y et al. ECCMID 2018, Oral Abstract O1130.