User login
Focus groups seek transgender experience with HIV prevention
A pair of focus groups explored the experience of transgender patients with HIV prevention, finding many were discouraged by experiences of care that was not culturally competent and affirming.
The findings, including other important themes, were published in Pediatrics.
The pair of online asynchronous focus groups, conducted by Holly B. Fontenot, PhD, RN/NP, of the Fenway Institute in Boston, and colleagues, sought input from 30 transgender participants from across the United States. Eleven were aged 13-18 years, and 19 were aged 18-24 years, with an average age of 19. Most (70%) were white, and the remainder were African American (7%), Asian American (3%), multiracial (17%), and other (3%); 10% identified as Hispanic. Participants were given multiple options for reporting gender identity; 27% reported identifying as transgender males, 17% reported identifying as transgender females, and the rest identified with other terms, including 27% using one or more terms.
The quantitative analysis found four common themes, which the study explored in depth: “barriers to self-efficacy in sexual decision making; safety concerns, fear, and other challenges in forming romantic and/or sexual relationships; need for support and education; and desire for affirmative and culturally competent experiences and interactions.”
Based on their findings, the authors suggested ways of improving transgender youth experiences:
- Increasing provider knowledge and skills in providing affirming care through transgender health education programs.
- Addressing the barriers, such as stigma and lack of accessibility.
- Expanding sexual health education to be more inclusive regarding gender identities, sexual orientations, and definitions of sex.
Providers also need to include information on sexually transmitted infection and HIV prevention, including “discussion of safer sexual behaviors, negotiation and consent, sexual and physical assault, condoms, lubrication, STI and HIV testing, human papillomavirus vaccination, and PrEP [preexposure prophylaxis]” the authors emphasized.
Dr. Fontenot and associates determined that this study’s findings were consistent with what’s known about adult transgender patients, but this study provides more context regarding transgender youth experiences.
“It is important to elicit transgender youth experiences and perspectives related to HIV risk and preventive services,” they concluded. “This study provided a greater understanding of barriers to and facilitators of youth obtaining HIV preventive services and sexual health education.”
Limitations of the study included that non–English speaking participants were excluded, and that participants were predominantly white, non-Hispanic, and assigned female sex at birth.
This study was funded by the Centers for Disease Control and Prevention and NORC at The University of Chicago. The authors had no relevant financial disclosures.
SOURCE: Fontenot HB et al., Pediatrics. 2020. doi: 10.1542/peds.2019-2204.
A pair of focus groups explored the experience of transgender patients with HIV prevention, finding many were discouraged by experiences of care that was not culturally competent and affirming.
The findings, including other important themes, were published in Pediatrics.
The pair of online asynchronous focus groups, conducted by Holly B. Fontenot, PhD, RN/NP, of the Fenway Institute in Boston, and colleagues, sought input from 30 transgender participants from across the United States. Eleven were aged 13-18 years, and 19 were aged 18-24 years, with an average age of 19. Most (70%) were white, and the remainder were African American (7%), Asian American (3%), multiracial (17%), and other (3%); 10% identified as Hispanic. Participants were given multiple options for reporting gender identity; 27% reported identifying as transgender males, 17% reported identifying as transgender females, and the rest identified with other terms, including 27% using one or more terms.
The quantitative analysis found four common themes, which the study explored in depth: “barriers to self-efficacy in sexual decision making; safety concerns, fear, and other challenges in forming romantic and/or sexual relationships; need for support and education; and desire for affirmative and culturally competent experiences and interactions.”
Based on their findings, the authors suggested ways of improving transgender youth experiences:
- Increasing provider knowledge and skills in providing affirming care through transgender health education programs.
- Addressing the barriers, such as stigma and lack of accessibility.
- Expanding sexual health education to be more inclusive regarding gender identities, sexual orientations, and definitions of sex.
Providers also need to include information on sexually transmitted infection and HIV prevention, including “discussion of safer sexual behaviors, negotiation and consent, sexual and physical assault, condoms, lubrication, STI and HIV testing, human papillomavirus vaccination, and PrEP [preexposure prophylaxis]” the authors emphasized.
Dr. Fontenot and associates determined that this study’s findings were consistent with what’s known about adult transgender patients, but this study provides more context regarding transgender youth experiences.
“It is important to elicit transgender youth experiences and perspectives related to HIV risk and preventive services,” they concluded. “This study provided a greater understanding of barriers to and facilitators of youth obtaining HIV preventive services and sexual health education.”
Limitations of the study included that non–English speaking participants were excluded, and that participants were predominantly white, non-Hispanic, and assigned female sex at birth.
This study was funded by the Centers for Disease Control and Prevention and NORC at The University of Chicago. The authors had no relevant financial disclosures.
SOURCE: Fontenot HB et al., Pediatrics. 2020. doi: 10.1542/peds.2019-2204.
A pair of focus groups explored the experience of transgender patients with HIV prevention, finding many were discouraged by experiences of care that was not culturally competent and affirming.
The findings, including other important themes, were published in Pediatrics.
The pair of online asynchronous focus groups, conducted by Holly B. Fontenot, PhD, RN/NP, of the Fenway Institute in Boston, and colleagues, sought input from 30 transgender participants from across the United States. Eleven were aged 13-18 years, and 19 were aged 18-24 years, with an average age of 19. Most (70%) were white, and the remainder were African American (7%), Asian American (3%), multiracial (17%), and other (3%); 10% identified as Hispanic. Participants were given multiple options for reporting gender identity; 27% reported identifying as transgender males, 17% reported identifying as transgender females, and the rest identified with other terms, including 27% using one or more terms.
The quantitative analysis found four common themes, which the study explored in depth: “barriers to self-efficacy in sexual decision making; safety concerns, fear, and other challenges in forming romantic and/or sexual relationships; need for support and education; and desire for affirmative and culturally competent experiences and interactions.”
Based on their findings, the authors suggested ways of improving transgender youth experiences:
- Increasing provider knowledge and skills in providing affirming care through transgender health education programs.
- Addressing the barriers, such as stigma and lack of accessibility.
- Expanding sexual health education to be more inclusive regarding gender identities, sexual orientations, and definitions of sex.
Providers also need to include information on sexually transmitted infection and HIV prevention, including “discussion of safer sexual behaviors, negotiation and consent, sexual and physical assault, condoms, lubrication, STI and HIV testing, human papillomavirus vaccination, and PrEP [preexposure prophylaxis]” the authors emphasized.
Dr. Fontenot and associates determined that this study’s findings were consistent with what’s known about adult transgender patients, but this study provides more context regarding transgender youth experiences.
“It is important to elicit transgender youth experiences and perspectives related to HIV risk and preventive services,” they concluded. “This study provided a greater understanding of barriers to and facilitators of youth obtaining HIV preventive services and sexual health education.”
Limitations of the study included that non–English speaking participants were excluded, and that participants were predominantly white, non-Hispanic, and assigned female sex at birth.
This study was funded by the Centers for Disease Control and Prevention and NORC at The University of Chicago. The authors had no relevant financial disclosures.
SOURCE: Fontenot HB et al., Pediatrics. 2020. doi: 10.1542/peds.2019-2204.
FROM PEDIATRICS
Cervical pessary didn’t prevent preterm birth in selected women
GRAPEVINE, TEX. – or a composite measure of adverse neonatal outcomes, according to a randomized, open-label study.
“The Arabin pessary should not be used to prevent preterm birth in women with twin pregnancy,” Jane E. Norman, MD, dean of health sciences at the University of Bristol (England), said at the Pregnancy Meeting.
“Preterm birth is very common in twin pregnancy” and leads to “excess neonatal mortality amongst twins,” Dr. Norman said at the meeting, which is sponsored by the Society for Maternal-Fetal Medicine. “Preventing preterm birth is important for both singletons and twins, but it could have even more benefits in twins.”
Emerging evidence has suggested that the Arabin cervical pessary may be useful for the prevention of preterm birth in women with singleton pregnancy and a short cervix. In twin pregnancy, data are more limited.
The ProTwin study randomized 813 women with twin pregnancy to a cervical pessary or standard care. Although the pessary had no impact on preterm birth overall, among women with cervical length of less than 38 mm, those who received a pessary were less likely to have preterm birth. The sample size was small, however, and the average length of the cervix in ProTwin differed from that in a previous U.K. study, Dr. Norman said.
Inspired by the study, Dr. Norman and coinvestigators conducted STOPPIT-2, a multicenter, open-label, randomized, controlled trial to further study whether a certain cervical length threshold was associated with benefit of a cervical pessary in preventing preterm birth. The trial included women with twin pregnancy who had a cervical length ultrasound between 18 and 20 weeks and 6 days of gestation. Women with a cervical length of 35 mm or less were eligible for randomization. Patients received an Arabin pessary plus standard care or standard care alone.
The primary obstetric outcome was spontaneous onset of labor leading to delivery before 34 weeks and 6 days of gestation. The primary neonatal outcome was a composite of outcomes – stillbirth, neonatal death, periventricular leukomalacia, respiratory morbidity, intraventricular hemorrhage, necrotizing enterocolitis, or sepsis – measured up to 28 days after the expected date of delivery.
The investigators randomized 503 women in all, including 250 to the pessary and 253 to standard care. Both groups had similar baseline characteristics, Dr. Norman said. The average age was about 33 years, and the average cervical length was about 29 mm. A total of 20% had monochorionic diamniotic pregnancies, and 80% had dichorionic pregnancies. The researchers excluded women with monochorionic monoamniotic pregnancies. In the pessary group, 16 patients declined the intervention, and 4 were unable to have the pessary inserted.
Spontaneous preterm birth occurred in 18% of patients in the Arabin pessary group, compared with 21% in the standard treatment group. The adjusted odds ratio, 0.87, was not statistically significant. In subgroups of patients with monochorionic pregnancy, cervical length less than 28 mm, or cervical length less than 25 mm, there was no significant benefit.
The composite measure of adverse neonatal outcomes also did not significantly differ between the groups. None of the individual components indicated benefit of the pessary either, Dr. Norman said.
In subgroup analyses, odds ratios for adverse neonatal outcomes were “tending towards harm for the Arabin pessary group ... although clearly none of them conferring statistical significance,” she said. Among women with cervical length less than 28 mm, a primary neonatal outcome – at least one of the adverse outcomes – occurred in 23% of patients in the Arabin pessary group, compared with 20% of patients in the standard care group.
Approximately two-thirds of patients found pessary insertion painless or slightly uncomfortable, whereas about 10% described the experience of device fitting as very uncomfortable, and about 1% described it as the worse pain imaginable.
“Since we started STOPPIT-2, in addition to ProTwin, another three studies have been published on the efficacy of the Arabin pessary in twins,” said Dr. Norman. Combined data show no significant effect of the pessary on preventing preterm birth in twin pregnancy. Still, the meta-analysis does not rule out the possibility that there could subgroups of patients who may benefit from the intervention, Dr. Norman said.
STOPPIT-2 was funded by the National Institute for Health Research (NIHR) in the United Kingdom. Dr. Norman chaired the UK National Institute for Health and Care Excellence guidelines on preterm labor and birth in 2015. In addition, Dr. Norman was a member of a GlaxoSmithKline data safety and monitoring group for a trial of a preterm birth prevention agent, has consulted for Dilafor, and has received research grants for preterm birth prevention from the U.K. Medical Research Council, NIHR, and Tommy’s: Together, for every baby charity.
SOURCE: Norman JE et al. Am J Obstet Gynecol. 2020 Jan;222(1):S756. Abstract LB 1.
GRAPEVINE, TEX. – or a composite measure of adverse neonatal outcomes, according to a randomized, open-label study.
“The Arabin pessary should not be used to prevent preterm birth in women with twin pregnancy,” Jane E. Norman, MD, dean of health sciences at the University of Bristol (England), said at the Pregnancy Meeting.
“Preterm birth is very common in twin pregnancy” and leads to “excess neonatal mortality amongst twins,” Dr. Norman said at the meeting, which is sponsored by the Society for Maternal-Fetal Medicine. “Preventing preterm birth is important for both singletons and twins, but it could have even more benefits in twins.”
Emerging evidence has suggested that the Arabin cervical pessary may be useful for the prevention of preterm birth in women with singleton pregnancy and a short cervix. In twin pregnancy, data are more limited.
The ProTwin study randomized 813 women with twin pregnancy to a cervical pessary or standard care. Although the pessary had no impact on preterm birth overall, among women with cervical length of less than 38 mm, those who received a pessary were less likely to have preterm birth. The sample size was small, however, and the average length of the cervix in ProTwin differed from that in a previous U.K. study, Dr. Norman said.
Inspired by the study, Dr. Norman and coinvestigators conducted STOPPIT-2, a multicenter, open-label, randomized, controlled trial to further study whether a certain cervical length threshold was associated with benefit of a cervical pessary in preventing preterm birth. The trial included women with twin pregnancy who had a cervical length ultrasound between 18 and 20 weeks and 6 days of gestation. Women with a cervical length of 35 mm or less were eligible for randomization. Patients received an Arabin pessary plus standard care or standard care alone.
The primary obstetric outcome was spontaneous onset of labor leading to delivery before 34 weeks and 6 days of gestation. The primary neonatal outcome was a composite of outcomes – stillbirth, neonatal death, periventricular leukomalacia, respiratory morbidity, intraventricular hemorrhage, necrotizing enterocolitis, or sepsis – measured up to 28 days after the expected date of delivery.
The investigators randomized 503 women in all, including 250 to the pessary and 253 to standard care. Both groups had similar baseline characteristics, Dr. Norman said. The average age was about 33 years, and the average cervical length was about 29 mm. A total of 20% had monochorionic diamniotic pregnancies, and 80% had dichorionic pregnancies. The researchers excluded women with monochorionic monoamniotic pregnancies. In the pessary group, 16 patients declined the intervention, and 4 were unable to have the pessary inserted.
Spontaneous preterm birth occurred in 18% of patients in the Arabin pessary group, compared with 21% in the standard treatment group. The adjusted odds ratio, 0.87, was not statistically significant. In subgroups of patients with monochorionic pregnancy, cervical length less than 28 mm, or cervical length less than 25 mm, there was no significant benefit.
The composite measure of adverse neonatal outcomes also did not significantly differ between the groups. None of the individual components indicated benefit of the pessary either, Dr. Norman said.
In subgroup analyses, odds ratios for adverse neonatal outcomes were “tending towards harm for the Arabin pessary group ... although clearly none of them conferring statistical significance,” she said. Among women with cervical length less than 28 mm, a primary neonatal outcome – at least one of the adverse outcomes – occurred in 23% of patients in the Arabin pessary group, compared with 20% of patients in the standard care group.
Approximately two-thirds of patients found pessary insertion painless or slightly uncomfortable, whereas about 10% described the experience of device fitting as very uncomfortable, and about 1% described it as the worse pain imaginable.
“Since we started STOPPIT-2, in addition to ProTwin, another three studies have been published on the efficacy of the Arabin pessary in twins,” said Dr. Norman. Combined data show no significant effect of the pessary on preventing preterm birth in twin pregnancy. Still, the meta-analysis does not rule out the possibility that there could subgroups of patients who may benefit from the intervention, Dr. Norman said.
STOPPIT-2 was funded by the National Institute for Health Research (NIHR) in the United Kingdom. Dr. Norman chaired the UK National Institute for Health and Care Excellence guidelines on preterm labor and birth in 2015. In addition, Dr. Norman was a member of a GlaxoSmithKline data safety and monitoring group for a trial of a preterm birth prevention agent, has consulted for Dilafor, and has received research grants for preterm birth prevention from the U.K. Medical Research Council, NIHR, and Tommy’s: Together, for every baby charity.
SOURCE: Norman JE et al. Am J Obstet Gynecol. 2020 Jan;222(1):S756. Abstract LB 1.
GRAPEVINE, TEX. – or a composite measure of adverse neonatal outcomes, according to a randomized, open-label study.
“The Arabin pessary should not be used to prevent preterm birth in women with twin pregnancy,” Jane E. Norman, MD, dean of health sciences at the University of Bristol (England), said at the Pregnancy Meeting.
“Preterm birth is very common in twin pregnancy” and leads to “excess neonatal mortality amongst twins,” Dr. Norman said at the meeting, which is sponsored by the Society for Maternal-Fetal Medicine. “Preventing preterm birth is important for both singletons and twins, but it could have even more benefits in twins.”
Emerging evidence has suggested that the Arabin cervical pessary may be useful for the prevention of preterm birth in women with singleton pregnancy and a short cervix. In twin pregnancy, data are more limited.
The ProTwin study randomized 813 women with twin pregnancy to a cervical pessary or standard care. Although the pessary had no impact on preterm birth overall, among women with cervical length of less than 38 mm, those who received a pessary were less likely to have preterm birth. The sample size was small, however, and the average length of the cervix in ProTwin differed from that in a previous U.K. study, Dr. Norman said.
Inspired by the study, Dr. Norman and coinvestigators conducted STOPPIT-2, a multicenter, open-label, randomized, controlled trial to further study whether a certain cervical length threshold was associated with benefit of a cervical pessary in preventing preterm birth. The trial included women with twin pregnancy who had a cervical length ultrasound between 18 and 20 weeks and 6 days of gestation. Women with a cervical length of 35 mm or less were eligible for randomization. Patients received an Arabin pessary plus standard care or standard care alone.
The primary obstetric outcome was spontaneous onset of labor leading to delivery before 34 weeks and 6 days of gestation. The primary neonatal outcome was a composite of outcomes – stillbirth, neonatal death, periventricular leukomalacia, respiratory morbidity, intraventricular hemorrhage, necrotizing enterocolitis, or sepsis – measured up to 28 days after the expected date of delivery.
The investigators randomized 503 women in all, including 250 to the pessary and 253 to standard care. Both groups had similar baseline characteristics, Dr. Norman said. The average age was about 33 years, and the average cervical length was about 29 mm. A total of 20% had monochorionic diamniotic pregnancies, and 80% had dichorionic pregnancies. The researchers excluded women with monochorionic monoamniotic pregnancies. In the pessary group, 16 patients declined the intervention, and 4 were unable to have the pessary inserted.
Spontaneous preterm birth occurred in 18% of patients in the Arabin pessary group, compared with 21% in the standard treatment group. The adjusted odds ratio, 0.87, was not statistically significant. In subgroups of patients with monochorionic pregnancy, cervical length less than 28 mm, or cervical length less than 25 mm, there was no significant benefit.
The composite measure of adverse neonatal outcomes also did not significantly differ between the groups. None of the individual components indicated benefit of the pessary either, Dr. Norman said.
In subgroup analyses, odds ratios for adverse neonatal outcomes were “tending towards harm for the Arabin pessary group ... although clearly none of them conferring statistical significance,” she said. Among women with cervical length less than 28 mm, a primary neonatal outcome – at least one of the adverse outcomes – occurred in 23% of patients in the Arabin pessary group, compared with 20% of patients in the standard care group.
Approximately two-thirds of patients found pessary insertion painless or slightly uncomfortable, whereas about 10% described the experience of device fitting as very uncomfortable, and about 1% described it as the worse pain imaginable.
“Since we started STOPPIT-2, in addition to ProTwin, another three studies have been published on the efficacy of the Arabin pessary in twins,” said Dr. Norman. Combined data show no significant effect of the pessary on preventing preterm birth in twin pregnancy. Still, the meta-analysis does not rule out the possibility that there could subgroups of patients who may benefit from the intervention, Dr. Norman said.
STOPPIT-2 was funded by the National Institute for Health Research (NIHR) in the United Kingdom. Dr. Norman chaired the UK National Institute for Health and Care Excellence guidelines on preterm labor and birth in 2015. In addition, Dr. Norman was a member of a GlaxoSmithKline data safety and monitoring group for a trial of a preterm birth prevention agent, has consulted for Dilafor, and has received research grants for preterm birth prevention from the U.K. Medical Research Council, NIHR, and Tommy’s: Together, for every baby charity.
SOURCE: Norman JE et al. Am J Obstet Gynecol. 2020 Jan;222(1):S756. Abstract LB 1.
REPORTING FROM THE PREGNANCY MEETING
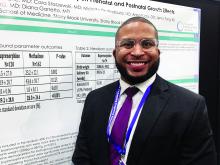
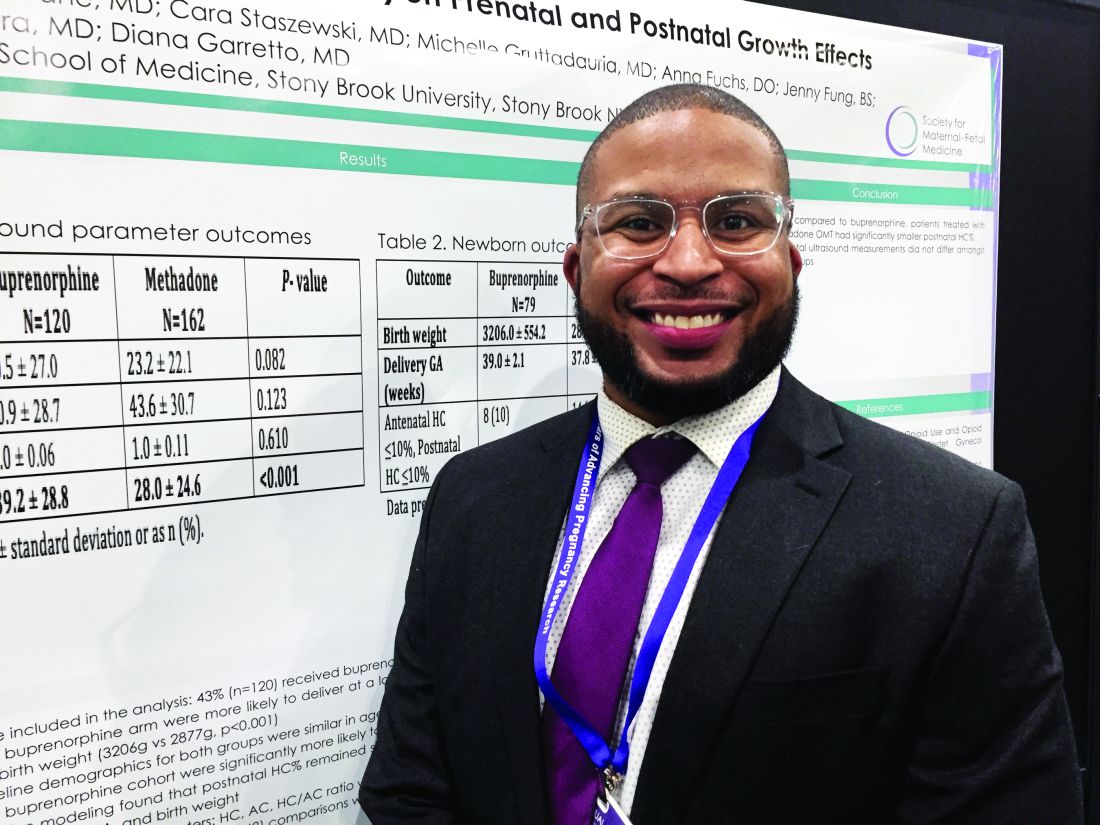
Maternal methadone opioid maintenance therapy may be tied to smaller postnatal head circumference
GRAPEVINE, TEX. – compared with opioid maintenance therapy with buprenorphine, according to a study presented at the Pregnancy Meeting.
Antenatal ultrasound measurements do not differ by treatment, however, the researchers said. A separate study suggests that serial ultrasound examinations of fetal brain and biometry measurements may not be helpful in patients who receive these medications for opioid use disorder.
To examine the effects of methadone and buprenorphine opioid maintenance therapy on prenatal and postnatal growth parameters, Jay Davis, MD, a maternal-fetal medicine fellow at Stony Brook University in New York, and coinvestigators conducted a retrospective cohort study using medical records from an academic center during 2007-2017. They included women with singleton pregnancies receiving opioid maintenance therapy with methadone or buprenorphine. They compared head circumference percentile, abdominal circumference percentile, head circumference/abdominal circumference ratio, and postnatal head circumference percentile between the two groups. The investigators analyzed the data using the Wilcoxon–Mann–Whitney test, chi-square test, and logistic regression.
The researchers studied 282 cases, including 120 patients who received buprenorphine and 162 who received methadone. Patients who received buprenorphine delivered at a later average gestational age (39 weeks vs. 37.8 weeks) and had newborns with greater average birth weights (3,206 g vs. 2,877 g). Compared with patients who received methadone, patients who received buprenorphine were significantly more likely to have a larger postnatal head circumference percentile (39 vs. 30), Dr. Davis and colleagues reported. This difference remained significant after controlling for race, prescriber, gestational age at delivery, and birth weight.
In a separate study presented at the meeting sponsored by the Society for Maternal-Fetal Medicine, Jose M. Perez Yordan, MD, of the University of New Mexico, Albuquerque, and colleagues examined effects of medications for opioid use disorder on fetal brain and body measurements.
They found that maternal medications for opioid use disorder do not have a clinically significant effect on fetal brain and body measurements, compared with controls. “No consistent pattern of decreased fetal growth was identified, since the body measurement affected did not persist with serial ultrasounds,” they said. “Serial ultrasound examinations do not appear to be helpful in patients” who take medications of opioid use disorder, with or without alcohol coexposure, unless other risk factors are present.
To evaluate the effects of medications of opioid use disorder and alcohol coexposure on fetal brain and biometric measurements at the second- and third-trimester ultrasound measurements, the investigators are conducting a prospective study known as ENRICH-1. The study includes healthy controls, patients taking medications of opioid use disorder (that is, buprenorphine or methadone), and patients taking medications of opioid use disorder with alcohol coexposure.
Ultrasound measurements from the second and third trimesters evaluated biparietal diameter, femur length, frontal lobe width and length, front-thalamic distance, and caval-calvarial distance. Univariate and multivariate analyses assessed differences in measurements adjusting for gestational age and other factors.
The present analysis included data from 171 participants, including 56 healthy controls, 75 patients taking medications of opioid use disorder, and 40 patients taking medications of opioid use disorder with alcohol coexposure. There was no consistent pattern of decreased fetal growth. Affected measurements did not persist over time.
The study presented by Dr. Perez Yordan was supported by a National Institute on Alcohol Abuse and Alcoholism grant. The remaining investigators in both studies had no relevant financial disclosures.
SOURCE: Perez Yordan JM et al. Am J Obstet Gynecol. 2020 Jan;222(1):S110, Abstract 149; Davis J et al. Am J Obstet Gynecol. 2020 Jan;222(1):S430, Abstract 678.
GRAPEVINE, TEX. – compared with opioid maintenance therapy with buprenorphine, according to a study presented at the Pregnancy Meeting.
Antenatal ultrasound measurements do not differ by treatment, however, the researchers said. A separate study suggests that serial ultrasound examinations of fetal brain and biometry measurements may not be helpful in patients who receive these medications for opioid use disorder.
To examine the effects of methadone and buprenorphine opioid maintenance therapy on prenatal and postnatal growth parameters, Jay Davis, MD, a maternal-fetal medicine fellow at Stony Brook University in New York, and coinvestigators conducted a retrospective cohort study using medical records from an academic center during 2007-2017. They included women with singleton pregnancies receiving opioid maintenance therapy with methadone or buprenorphine. They compared head circumference percentile, abdominal circumference percentile, head circumference/abdominal circumference ratio, and postnatal head circumference percentile between the two groups. The investigators analyzed the data using the Wilcoxon–Mann–Whitney test, chi-square test, and logistic regression.
The researchers studied 282 cases, including 120 patients who received buprenorphine and 162 who received methadone. Patients who received buprenorphine delivered at a later average gestational age (39 weeks vs. 37.8 weeks) and had newborns with greater average birth weights (3,206 g vs. 2,877 g). Compared with patients who received methadone, patients who received buprenorphine were significantly more likely to have a larger postnatal head circumference percentile (39 vs. 30), Dr. Davis and colleagues reported. This difference remained significant after controlling for race, prescriber, gestational age at delivery, and birth weight.
In a separate study presented at the meeting sponsored by the Society for Maternal-Fetal Medicine, Jose M. Perez Yordan, MD, of the University of New Mexico, Albuquerque, and colleagues examined effects of medications for opioid use disorder on fetal brain and body measurements.
They found that maternal medications for opioid use disorder do not have a clinically significant effect on fetal brain and body measurements, compared with controls. “No consistent pattern of decreased fetal growth was identified, since the body measurement affected did not persist with serial ultrasounds,” they said. “Serial ultrasound examinations do not appear to be helpful in patients” who take medications of opioid use disorder, with or without alcohol coexposure, unless other risk factors are present.
To evaluate the effects of medications of opioid use disorder and alcohol coexposure on fetal brain and biometric measurements at the second- and third-trimester ultrasound measurements, the investigators are conducting a prospective study known as ENRICH-1. The study includes healthy controls, patients taking medications of opioid use disorder (that is, buprenorphine or methadone), and patients taking medications of opioid use disorder with alcohol coexposure.
Ultrasound measurements from the second and third trimesters evaluated biparietal diameter, femur length, frontal lobe width and length, front-thalamic distance, and caval-calvarial distance. Univariate and multivariate analyses assessed differences in measurements adjusting for gestational age and other factors.
The present analysis included data from 171 participants, including 56 healthy controls, 75 patients taking medications of opioid use disorder, and 40 patients taking medications of opioid use disorder with alcohol coexposure. There was no consistent pattern of decreased fetal growth. Affected measurements did not persist over time.
The study presented by Dr. Perez Yordan was supported by a National Institute on Alcohol Abuse and Alcoholism grant. The remaining investigators in both studies had no relevant financial disclosures.
SOURCE: Perez Yordan JM et al. Am J Obstet Gynecol. 2020 Jan;222(1):S110, Abstract 149; Davis J et al. Am J Obstet Gynecol. 2020 Jan;222(1):S430, Abstract 678.
GRAPEVINE, TEX. – compared with opioid maintenance therapy with buprenorphine, according to a study presented at the Pregnancy Meeting.
Antenatal ultrasound measurements do not differ by treatment, however, the researchers said. A separate study suggests that serial ultrasound examinations of fetal brain and biometry measurements may not be helpful in patients who receive these medications for opioid use disorder.
To examine the effects of methadone and buprenorphine opioid maintenance therapy on prenatal and postnatal growth parameters, Jay Davis, MD, a maternal-fetal medicine fellow at Stony Brook University in New York, and coinvestigators conducted a retrospective cohort study using medical records from an academic center during 2007-2017. They included women with singleton pregnancies receiving opioid maintenance therapy with methadone or buprenorphine. They compared head circumference percentile, abdominal circumference percentile, head circumference/abdominal circumference ratio, and postnatal head circumference percentile between the two groups. The investigators analyzed the data using the Wilcoxon–Mann–Whitney test, chi-square test, and logistic regression.
The researchers studied 282 cases, including 120 patients who received buprenorphine and 162 who received methadone. Patients who received buprenorphine delivered at a later average gestational age (39 weeks vs. 37.8 weeks) and had newborns with greater average birth weights (3,206 g vs. 2,877 g). Compared with patients who received methadone, patients who received buprenorphine were significantly more likely to have a larger postnatal head circumference percentile (39 vs. 30), Dr. Davis and colleagues reported. This difference remained significant after controlling for race, prescriber, gestational age at delivery, and birth weight.
In a separate study presented at the meeting sponsored by the Society for Maternal-Fetal Medicine, Jose M. Perez Yordan, MD, of the University of New Mexico, Albuquerque, and colleagues examined effects of medications for opioid use disorder on fetal brain and body measurements.
They found that maternal medications for opioid use disorder do not have a clinically significant effect on fetal brain and body measurements, compared with controls. “No consistent pattern of decreased fetal growth was identified, since the body measurement affected did not persist with serial ultrasounds,” they said. “Serial ultrasound examinations do not appear to be helpful in patients” who take medications of opioid use disorder, with or without alcohol coexposure, unless other risk factors are present.
To evaluate the effects of medications of opioid use disorder and alcohol coexposure on fetal brain and biometric measurements at the second- and third-trimester ultrasound measurements, the investigators are conducting a prospective study known as ENRICH-1. The study includes healthy controls, patients taking medications of opioid use disorder (that is, buprenorphine or methadone), and patients taking medications of opioid use disorder with alcohol coexposure.
Ultrasound measurements from the second and third trimesters evaluated biparietal diameter, femur length, frontal lobe width and length, front-thalamic distance, and caval-calvarial distance. Univariate and multivariate analyses assessed differences in measurements adjusting for gestational age and other factors.
The present analysis included data from 171 participants, including 56 healthy controls, 75 patients taking medications of opioid use disorder, and 40 patients taking medications of opioid use disorder with alcohol coexposure. There was no consistent pattern of decreased fetal growth. Affected measurements did not persist over time.
The study presented by Dr. Perez Yordan was supported by a National Institute on Alcohol Abuse and Alcoholism grant. The remaining investigators in both studies had no relevant financial disclosures.
SOURCE: Perez Yordan JM et al. Am J Obstet Gynecol. 2020 Jan;222(1):S110, Abstract 149; Davis J et al. Am J Obstet Gynecol. 2020 Jan;222(1):S430, Abstract 678.
REPORTING FROM THE PREGNANCY MEETING
CVH in pregnant women: Ample room for improvement
Cardiovascular disease is both common and chronic, and it remains the leading cause of death in women. Because it is a life-long condition, cardiovascular disease must be managed over the entire lifespan. In recognition of the important role of obstetricians and gynecologists in monitoring women’s health, the American Heart Association/American College of Obstetricians and Gynecologists 2018 guidelines1 promoted the use of “Life’s Simple 7”2 for assessing cardiovascular health (CVH) in women.
These seven metrics include diet, physical activity, smoking status, body mass index (BMI), blood pressure, total cholesterol, and fasting blood glucose levels. They have been shown to predict positive health outcomes in nonpregnant adults. However, until now, CVH had not been assessed in pregnant women.
Perak et al. recently performed the first cross-sectional study of the prevalence of CVH metrics in pregnant women using the AHA definition.3 Using data from the National Health and Nutrition Examination Surveys (NHANES), they used the Life’s Simple 7 metrics to assess CVH in 1,117 pregnant and 8,200 nonpregnant women in the United States aged 20-44 years. Each of the Life’s Simple 7 metrics was scored 0, 1, or 2 points, corresponding to a rating of poor, intermediate, or ideal, respectively. Thus, the total CVH score ranged from 0-14 points, with total scores of 0-7 indicating low CVH, 8-11 indicating moderate CVH, and 12-14 indicating high CVH.
which was even worse than in nonpregnant women, of whom only 13% were scored as having ideal CVH. Ideal scores were observed for 0.1% of pregnant women for diet, 27% for physical activity, 39% for cholesterol levels, 51% for BMI, 78% for smoking, 90% for blood pressure, and 92% for fasting blood glucose. Physical activity and cholesterol levels appeared to be the major drivers of the lower CVH scores in pregnant women.
Although further studies are warranted to determine the relevance of CVH during pregnancy to outcomes for both mother and offspring, the study by Perak et al. is an important step toward the development of pregnancy-specific guidelines and definitions for CVH metrics. These are stated goals of the AHA/ACOG that will help promote CVH in women across their lifespans, but which have not been possible due to scant data.
Emerging data suggest that cumulative lifetime exposure is a significant factor in cardiovascular disease outcomes; therefore, earlier intervention would have a more significant impact. Just as gestational diabetes is a predictor of future type 2 diabetes, CVH earlier in a woman’s life predicts cardiovascular disease later in life.4-7 The best data in this regard come from genetic and other studies of hyperlipidemia, which suggest that lowering lipid levels before symptoms develop may prevent cardiovascular disease. In contrast, treatment of patients with clinically manifest disease neither offers a cure nor prevents the occurrence of most cardiovascular events.
It is a particularly salient point in this regard that there currently are no guidelines on treatment of hypercholesterolemia during pregnancy. Notably, the study by Perak et al. suggested that cholesterol levels may have a significant impact on CVH in pregnant women. There also is emerging data supporting the importance of controlling blood pressure across the lifespan,7,8 including during pregnancy.9
For many women, their ob.gyn. is their primary care physician, and pregnancy is often the first time that a woman will have a substantial interaction with the health care system. The AHA/ACOG advisory panel described pregnancy as a “physiological stress test” for women that offers the opportunity to identify those at increased risk of cardiovascular disease.1
As pregnancy is a time when women particularly are motivated to improve their health,10 it also presents a valuable opportunity for physicians, including ob.gyns., to make a lifelong impact on the CVH of their patients through early identification, education, and intervention.
Dr. Charles Hong is the Melvin Sharoky, MD, Professor of Medicine and director of cardiovascular research in the department of medicine at the University of Maryland School of Medicine. Dr. E. Albert Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland School of Medicine as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Neither physician had any relevant financial disclosures. Contact him at obnews@mdedge.com.
References
1. Circulation. 2018;137:e843–e852.
2. Circulation. 2010 Jan 20;121(4):586–613.
3. J Am Heart Assoc. 2020 Feb 17;9:e015123.
4. J Am Coll Cardiol. 2018 Sep 4;72(10):1141-56.
5. N Engl J Med. 2016 Dec 1;375:2144-53.
6. Nat Rev Cardiol. 2011 Nov 1;8(12):721-5.
7. J Am Coll Cardiol. 2019 Jul 23;74(3):330-41.
8. Circulation. 2020 Mar 2:141:725-7.
9. Circulation. 2013 Feb 12;127(6):681-90.
10. Nutrients. 2018 Aug 8. doi: 10.3390/nu10081032.
Cardiovascular disease is both common and chronic, and it remains the leading cause of death in women. Because it is a life-long condition, cardiovascular disease must be managed over the entire lifespan. In recognition of the important role of obstetricians and gynecologists in monitoring women’s health, the American Heart Association/American College of Obstetricians and Gynecologists 2018 guidelines1 promoted the use of “Life’s Simple 7”2 for assessing cardiovascular health (CVH) in women.
These seven metrics include diet, physical activity, smoking status, body mass index (BMI), blood pressure, total cholesterol, and fasting blood glucose levels. They have been shown to predict positive health outcomes in nonpregnant adults. However, until now, CVH had not been assessed in pregnant women.
Perak et al. recently performed the first cross-sectional study of the prevalence of CVH metrics in pregnant women using the AHA definition.3 Using data from the National Health and Nutrition Examination Surveys (NHANES), they used the Life’s Simple 7 metrics to assess CVH in 1,117 pregnant and 8,200 nonpregnant women in the United States aged 20-44 years. Each of the Life’s Simple 7 metrics was scored 0, 1, or 2 points, corresponding to a rating of poor, intermediate, or ideal, respectively. Thus, the total CVH score ranged from 0-14 points, with total scores of 0-7 indicating low CVH, 8-11 indicating moderate CVH, and 12-14 indicating high CVH.
which was even worse than in nonpregnant women, of whom only 13% were scored as having ideal CVH. Ideal scores were observed for 0.1% of pregnant women for diet, 27% for physical activity, 39% for cholesterol levels, 51% for BMI, 78% for smoking, 90% for blood pressure, and 92% for fasting blood glucose. Physical activity and cholesterol levels appeared to be the major drivers of the lower CVH scores in pregnant women.
Although further studies are warranted to determine the relevance of CVH during pregnancy to outcomes for both mother and offspring, the study by Perak et al. is an important step toward the development of pregnancy-specific guidelines and definitions for CVH metrics. These are stated goals of the AHA/ACOG that will help promote CVH in women across their lifespans, but which have not been possible due to scant data.
Emerging data suggest that cumulative lifetime exposure is a significant factor in cardiovascular disease outcomes; therefore, earlier intervention would have a more significant impact. Just as gestational diabetes is a predictor of future type 2 diabetes, CVH earlier in a woman’s life predicts cardiovascular disease later in life.4-7 The best data in this regard come from genetic and other studies of hyperlipidemia, which suggest that lowering lipid levels before symptoms develop may prevent cardiovascular disease. In contrast, treatment of patients with clinically manifest disease neither offers a cure nor prevents the occurrence of most cardiovascular events.
It is a particularly salient point in this regard that there currently are no guidelines on treatment of hypercholesterolemia during pregnancy. Notably, the study by Perak et al. suggested that cholesterol levels may have a significant impact on CVH in pregnant women. There also is emerging data supporting the importance of controlling blood pressure across the lifespan,7,8 including during pregnancy.9
For many women, their ob.gyn. is their primary care physician, and pregnancy is often the first time that a woman will have a substantial interaction with the health care system. The AHA/ACOG advisory panel described pregnancy as a “physiological stress test” for women that offers the opportunity to identify those at increased risk of cardiovascular disease.1
As pregnancy is a time when women particularly are motivated to improve their health,10 it also presents a valuable opportunity for physicians, including ob.gyns., to make a lifelong impact on the CVH of their patients through early identification, education, and intervention.
Dr. Charles Hong is the Melvin Sharoky, MD, Professor of Medicine and director of cardiovascular research in the department of medicine at the University of Maryland School of Medicine. Dr. E. Albert Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland School of Medicine as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Neither physician had any relevant financial disclosures. Contact him at obnews@mdedge.com.
References
1. Circulation. 2018;137:e843–e852.
2. Circulation. 2010 Jan 20;121(4):586–613.
3. J Am Heart Assoc. 2020 Feb 17;9:e015123.
4. J Am Coll Cardiol. 2018 Sep 4;72(10):1141-56.
5. N Engl J Med. 2016 Dec 1;375:2144-53.
6. Nat Rev Cardiol. 2011 Nov 1;8(12):721-5.
7. J Am Coll Cardiol. 2019 Jul 23;74(3):330-41.
8. Circulation. 2020 Mar 2:141:725-7.
9. Circulation. 2013 Feb 12;127(6):681-90.
10. Nutrients. 2018 Aug 8. doi: 10.3390/nu10081032.
Cardiovascular disease is both common and chronic, and it remains the leading cause of death in women. Because it is a life-long condition, cardiovascular disease must be managed over the entire lifespan. In recognition of the important role of obstetricians and gynecologists in monitoring women’s health, the American Heart Association/American College of Obstetricians and Gynecologists 2018 guidelines1 promoted the use of “Life’s Simple 7”2 for assessing cardiovascular health (CVH) in women.
These seven metrics include diet, physical activity, smoking status, body mass index (BMI), blood pressure, total cholesterol, and fasting blood glucose levels. They have been shown to predict positive health outcomes in nonpregnant adults. However, until now, CVH had not been assessed in pregnant women.
Perak et al. recently performed the first cross-sectional study of the prevalence of CVH metrics in pregnant women using the AHA definition.3 Using data from the National Health and Nutrition Examination Surveys (NHANES), they used the Life’s Simple 7 metrics to assess CVH in 1,117 pregnant and 8,200 nonpregnant women in the United States aged 20-44 years. Each of the Life’s Simple 7 metrics was scored 0, 1, or 2 points, corresponding to a rating of poor, intermediate, or ideal, respectively. Thus, the total CVH score ranged from 0-14 points, with total scores of 0-7 indicating low CVH, 8-11 indicating moderate CVH, and 12-14 indicating high CVH.
which was even worse than in nonpregnant women, of whom only 13% were scored as having ideal CVH. Ideal scores were observed for 0.1% of pregnant women for diet, 27% for physical activity, 39% for cholesterol levels, 51% for BMI, 78% for smoking, 90% for blood pressure, and 92% for fasting blood glucose. Physical activity and cholesterol levels appeared to be the major drivers of the lower CVH scores in pregnant women.
Although further studies are warranted to determine the relevance of CVH during pregnancy to outcomes for both mother and offspring, the study by Perak et al. is an important step toward the development of pregnancy-specific guidelines and definitions for CVH metrics. These are stated goals of the AHA/ACOG that will help promote CVH in women across their lifespans, but which have not been possible due to scant data.
Emerging data suggest that cumulative lifetime exposure is a significant factor in cardiovascular disease outcomes; therefore, earlier intervention would have a more significant impact. Just as gestational diabetes is a predictor of future type 2 diabetes, CVH earlier in a woman’s life predicts cardiovascular disease later in life.4-7 The best data in this regard come from genetic and other studies of hyperlipidemia, which suggest that lowering lipid levels before symptoms develop may prevent cardiovascular disease. In contrast, treatment of patients with clinically manifest disease neither offers a cure nor prevents the occurrence of most cardiovascular events.
It is a particularly salient point in this regard that there currently are no guidelines on treatment of hypercholesterolemia during pregnancy. Notably, the study by Perak et al. suggested that cholesterol levels may have a significant impact on CVH in pregnant women. There also is emerging data supporting the importance of controlling blood pressure across the lifespan,7,8 including during pregnancy.9
For many women, their ob.gyn. is their primary care physician, and pregnancy is often the first time that a woman will have a substantial interaction with the health care system. The AHA/ACOG advisory panel described pregnancy as a “physiological stress test” for women that offers the opportunity to identify those at increased risk of cardiovascular disease.1
As pregnancy is a time when women particularly are motivated to improve their health,10 it also presents a valuable opportunity for physicians, including ob.gyns., to make a lifelong impact on the CVH of their patients through early identification, education, and intervention.
Dr. Charles Hong is the Melvin Sharoky, MD, Professor of Medicine and director of cardiovascular research in the department of medicine at the University of Maryland School of Medicine. Dr. E. Albert Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland School of Medicine as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Neither physician had any relevant financial disclosures. Contact him at obnews@mdedge.com.
References
1. Circulation. 2018;137:e843–e852.
2. Circulation. 2010 Jan 20;121(4):586–613.
3. J Am Heart Assoc. 2020 Feb 17;9:e015123.
4. J Am Coll Cardiol. 2018 Sep 4;72(10):1141-56.
5. N Engl J Med. 2016 Dec 1;375:2144-53.
6. Nat Rev Cardiol. 2011 Nov 1;8(12):721-5.
7. J Am Coll Cardiol. 2019 Jul 23;74(3):330-41.
8. Circulation. 2020 Mar 2:141:725-7.
9. Circulation. 2013 Feb 12;127(6):681-90.
10. Nutrients. 2018 Aug 8. doi: 10.3390/nu10081032.
Responsible use of breast cancer screening
In this edition of “Applying research to practice,” I examine a study suggesting that annual screening mammography does not reduce the risk of death from breast cancer in women aged 75 years and older. I also highlight a related editorial noting that we should optimize treatment as well as screening for breast cancer.
Regular screening mammography in women aged 50-69 years prevents 21.3 breast cancer deaths among 10,000 women over a 10-year time period (Ann Intern Med. 2016 Feb 16;164[4]:244-55). However, in the published screening trials, few participants were older than 70 years of age.
More than half of women above age 74 receive annual mammograms (Health, United States, 2018. www.cdc.gov/nchs/data/hus/hus18.pdf). And more than a third of breast cancer deaths occur in women aged 70 years or older (CA Cancer J Clin. 2016 Mar-Apr;66[2]:96-114).
Do older women benefit from annual mammography to the same extent as younger women? Is there a point at which benefit ends?
To answer these questions, Xabier García-Albéniz, MD, PhD, of Harvard Medical School in Boston, and colleagues studied 1,058,013 women enrolled in Medicare during 2000-2008 (Ann Intern Med. 2020 Feb 25. doi: 10.7326/M18-1199).
The researchers examined data on patients aged 70-84 years who had a life expectancy of at least 10 years, at least one recent mammogram, and no history of breast cancer. The team emulated a prospective trial by examining deaths over an 8-year period for women aged 70 years and older who either continued or stopped screening mammography. The researchers conducted separate analyses for women aged 70-74 years and those aged 75-84 years.
Diagnoses of breast cancer were, not surprisingly, higher in the continued-screening group, but there were no major reductions in breast cancer–related deaths.
Among women aged 70-74 years, the estimated 8-year risk for breast cancer death was reduced for women who continued screening versus those who stopped it by one death per 1,000 women (hazard ratio, 0.78). Among women aged 75-84 years, the 8-year risk reduction was 0.07 deaths per 1,000 women (HR, 1.00).
The authors concluded that continuing mammographic screening past age 75 years resulted in no material difference in cancer-specific mortality over an 8-year time period, in comparison with stopping regular screening examinations.
Considering treatment as well as screening
For a variety of reasons (ethical, economic, methodologic), it is unreasonable to expect a randomized, clinical trial examining the value of mammography in older women. An informative alternative would be a well-designed, large-scale, population-based, observational study that takes into consideration potentially confounding variables of the binary strategies of continuing screening versus stopping it.
Although the 8-year risk of breast cancer in older women is not low among screened women – 5.5% in women aged 70-74 years and 5.8% in women aged 75-84 years – and mammography remains an effective screening tool, the effect of screening on breast cancer mortality appears to decline as women age.
In the editorial that accompanies the study by Dr. García-Albéniz and colleagues, Otis Brawley, MD, of Johns Hopkins University, Baltimore, highlighted the role of inadequate, ineffective, inconvenient, or poorly tolerated treatment in older women (Ann Intern Med. 2020 Feb 25. doi: 10.7326/M20-0429).
Dr. Brawley illustrated that focusing too much on screening diverts attention from the major driver of cancer mortality in older women: suboptimal treatment. That certainly has been the case for the dramatic impact of improved lung cancer treatment on mortality, despite a statistically significant impact of screening on lung cancer mortality as well.
As with lung cancer screening, Dr. Brawley describes the goal of defining “personalized screening recommendations” in breast cancer, or screening that is targeted to the highest-risk women and those who stand a high chance of benefiting from treatment if they are diagnosed with breast cancer.
As our population ages and health care expenditures continue to rise, there can be little disagreement that responsible use of cancer diagnostics will be as vital as judicious application of treatment.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations.
In this edition of “Applying research to practice,” I examine a study suggesting that annual screening mammography does not reduce the risk of death from breast cancer in women aged 75 years and older. I also highlight a related editorial noting that we should optimize treatment as well as screening for breast cancer.
Regular screening mammography in women aged 50-69 years prevents 21.3 breast cancer deaths among 10,000 women over a 10-year time period (Ann Intern Med. 2016 Feb 16;164[4]:244-55). However, in the published screening trials, few participants were older than 70 years of age.
More than half of women above age 74 receive annual mammograms (Health, United States, 2018. www.cdc.gov/nchs/data/hus/hus18.pdf). And more than a third of breast cancer deaths occur in women aged 70 years or older (CA Cancer J Clin. 2016 Mar-Apr;66[2]:96-114).
Do older women benefit from annual mammography to the same extent as younger women? Is there a point at which benefit ends?
To answer these questions, Xabier García-Albéniz, MD, PhD, of Harvard Medical School in Boston, and colleagues studied 1,058,013 women enrolled in Medicare during 2000-2008 (Ann Intern Med. 2020 Feb 25. doi: 10.7326/M18-1199).
The researchers examined data on patients aged 70-84 years who had a life expectancy of at least 10 years, at least one recent mammogram, and no history of breast cancer. The team emulated a prospective trial by examining deaths over an 8-year period for women aged 70 years and older who either continued or stopped screening mammography. The researchers conducted separate analyses for women aged 70-74 years and those aged 75-84 years.
Diagnoses of breast cancer were, not surprisingly, higher in the continued-screening group, but there were no major reductions in breast cancer–related deaths.
Among women aged 70-74 years, the estimated 8-year risk for breast cancer death was reduced for women who continued screening versus those who stopped it by one death per 1,000 women (hazard ratio, 0.78). Among women aged 75-84 years, the 8-year risk reduction was 0.07 deaths per 1,000 women (HR, 1.00).
The authors concluded that continuing mammographic screening past age 75 years resulted in no material difference in cancer-specific mortality over an 8-year time period, in comparison with stopping regular screening examinations.
Considering treatment as well as screening
For a variety of reasons (ethical, economic, methodologic), it is unreasonable to expect a randomized, clinical trial examining the value of mammography in older women. An informative alternative would be a well-designed, large-scale, population-based, observational study that takes into consideration potentially confounding variables of the binary strategies of continuing screening versus stopping it.
Although the 8-year risk of breast cancer in older women is not low among screened women – 5.5% in women aged 70-74 years and 5.8% in women aged 75-84 years – and mammography remains an effective screening tool, the effect of screening on breast cancer mortality appears to decline as women age.
In the editorial that accompanies the study by Dr. García-Albéniz and colleagues, Otis Brawley, MD, of Johns Hopkins University, Baltimore, highlighted the role of inadequate, ineffective, inconvenient, or poorly tolerated treatment in older women (Ann Intern Med. 2020 Feb 25. doi: 10.7326/M20-0429).
Dr. Brawley illustrated that focusing too much on screening diverts attention from the major driver of cancer mortality in older women: suboptimal treatment. That certainly has been the case for the dramatic impact of improved lung cancer treatment on mortality, despite a statistically significant impact of screening on lung cancer mortality as well.
As with lung cancer screening, Dr. Brawley describes the goal of defining “personalized screening recommendations” in breast cancer, or screening that is targeted to the highest-risk women and those who stand a high chance of benefiting from treatment if they are diagnosed with breast cancer.
As our population ages and health care expenditures continue to rise, there can be little disagreement that responsible use of cancer diagnostics will be as vital as judicious application of treatment.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations.
In this edition of “Applying research to practice,” I examine a study suggesting that annual screening mammography does not reduce the risk of death from breast cancer in women aged 75 years and older. I also highlight a related editorial noting that we should optimize treatment as well as screening for breast cancer.
Regular screening mammography in women aged 50-69 years prevents 21.3 breast cancer deaths among 10,000 women over a 10-year time period (Ann Intern Med. 2016 Feb 16;164[4]:244-55). However, in the published screening trials, few participants were older than 70 years of age.
More than half of women above age 74 receive annual mammograms (Health, United States, 2018. www.cdc.gov/nchs/data/hus/hus18.pdf). And more than a third of breast cancer deaths occur in women aged 70 years or older (CA Cancer J Clin. 2016 Mar-Apr;66[2]:96-114).
Do older women benefit from annual mammography to the same extent as younger women? Is there a point at which benefit ends?
To answer these questions, Xabier García-Albéniz, MD, PhD, of Harvard Medical School in Boston, and colleagues studied 1,058,013 women enrolled in Medicare during 2000-2008 (Ann Intern Med. 2020 Feb 25. doi: 10.7326/M18-1199).
The researchers examined data on patients aged 70-84 years who had a life expectancy of at least 10 years, at least one recent mammogram, and no history of breast cancer. The team emulated a prospective trial by examining deaths over an 8-year period for women aged 70 years and older who either continued or stopped screening mammography. The researchers conducted separate analyses for women aged 70-74 years and those aged 75-84 years.
Diagnoses of breast cancer were, not surprisingly, higher in the continued-screening group, but there were no major reductions in breast cancer–related deaths.
Among women aged 70-74 years, the estimated 8-year risk for breast cancer death was reduced for women who continued screening versus those who stopped it by one death per 1,000 women (hazard ratio, 0.78). Among women aged 75-84 years, the 8-year risk reduction was 0.07 deaths per 1,000 women (HR, 1.00).
The authors concluded that continuing mammographic screening past age 75 years resulted in no material difference in cancer-specific mortality over an 8-year time period, in comparison with stopping regular screening examinations.
Considering treatment as well as screening
For a variety of reasons (ethical, economic, methodologic), it is unreasonable to expect a randomized, clinical trial examining the value of mammography in older women. An informative alternative would be a well-designed, large-scale, population-based, observational study that takes into consideration potentially confounding variables of the binary strategies of continuing screening versus stopping it.
Although the 8-year risk of breast cancer in older women is not low among screened women – 5.5% in women aged 70-74 years and 5.8% in women aged 75-84 years – and mammography remains an effective screening tool, the effect of screening on breast cancer mortality appears to decline as women age.
In the editorial that accompanies the study by Dr. García-Albéniz and colleagues, Otis Brawley, MD, of Johns Hopkins University, Baltimore, highlighted the role of inadequate, ineffective, inconvenient, or poorly tolerated treatment in older women (Ann Intern Med. 2020 Feb 25. doi: 10.7326/M20-0429).
Dr. Brawley illustrated that focusing too much on screening diverts attention from the major driver of cancer mortality in older women: suboptimal treatment. That certainly has been the case for the dramatic impact of improved lung cancer treatment on mortality, despite a statistically significant impact of screening on lung cancer mortality as well.
As with lung cancer screening, Dr. Brawley describes the goal of defining “personalized screening recommendations” in breast cancer, or screening that is targeted to the highest-risk women and those who stand a high chance of benefiting from treatment if they are diagnosed with breast cancer.
As our population ages and health care expenditures continue to rise, there can be little disagreement that responsible use of cancer diagnostics will be as vital as judicious application of treatment.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations.
HPV vaccine-chemo combo prolongs cervical cancer survival
Longer survival was observed in women who had a stronger immune response to an investigational human papillomavirus (HPV) vaccine while treated with standard chemotherapy for advanced, metastatic, or recurrent cervical cancer.
The results, from a phase 1/2 study, showed that women with a vaccine-induced immune response higher than the median had a median overall survival of 16.8 months, compared with a median overall survival of 11.2 months for women with an immune response lower than the median (hazard ratio, 0.491; P = .012).
Cornelis “Kees” Melief, MD, chief scientific officer of ISA Pharmaceuticals in Leiden, the Netherlands, and colleagues reported these findings in Science Translational Medicine.
The researchers previously evaluated the HPV16 vaccine, ISA101, in combination with carboplatin and paclitaxel in a pilot study. Results showed that carboplatin and paclitaxel reduced abnormally high numbers of immunosuppressive myeloid cells, which allowed for “much stronger” ISA101-induced tumor immunity.
To investigate further, the researchers tested the chemotherapy-ISA101 combination in a phase 1/2 study (NCT02128126) of 79 women with advanced, metastatic, or recurrent HPV16-positive cervical cancer.
The patients received the vaccine 2 weeks after starting the second, third, and fourth cycles of chemotherapy. They received various doses of the vaccine (20, 40, 100, or 300 mcg) with or without pegylated type 1 interferon (1 mcg/kg body weight).
“ISA101 was generally safe and well tolerated in that its safety profile was not different from chemotherapy alone,” Dr. Melief and colleagues wrote.
Chemotherapy-associated adverse events occurred in 98.9% of patients, with more than 80% of patients reporting adverse events possibly related to the vaccine or interferon-alpha. However, less than 16% of patients withdrew from the study because of an adverse event.
Of the 72 patients evaluable for efficacy, 43% experienced tumor regression, and 43% had stable disease. The researchers observed regression of the target lesion in 29 of 59 patients with a measurable target lesion.
The team noted that, since all patients received chemotherapy, it is “difficult to interpret short-term clinical outcomes as being due to chemotherapy alone or to the combination,” although they noted that the use of interferon-alpha did not seem to provide any additional benefit.
“Eleven of 14 patients still alive at the end of the study displayed a strong vaccine-induced response and included 9 patients with FIGO stage IVa/IVb cancer who had a mean OS [overall survival] of 3 years,” the researchers noted.
Considering that patients with higher vaccine-induced immune responses lived longer, the researchers concluded that “chemoimmunotherapy can be exploited to the benefit of patients with advanced cancer based on a defined mode of action.”
This trial was funded by ISA Pharmaceuticals and a Dutch Cancer Society grant. Investigators disclosed relationships with ISA Pharmaceuticals and other companies.
SOURCE: Melief CJM et al. Sci Transl Med. 2020;12:eaaz8235.
Longer survival was observed in women who had a stronger immune response to an investigational human papillomavirus (HPV) vaccine while treated with standard chemotherapy for advanced, metastatic, or recurrent cervical cancer.
The results, from a phase 1/2 study, showed that women with a vaccine-induced immune response higher than the median had a median overall survival of 16.8 months, compared with a median overall survival of 11.2 months for women with an immune response lower than the median (hazard ratio, 0.491; P = .012).
Cornelis “Kees” Melief, MD, chief scientific officer of ISA Pharmaceuticals in Leiden, the Netherlands, and colleagues reported these findings in Science Translational Medicine.
The researchers previously evaluated the HPV16 vaccine, ISA101, in combination with carboplatin and paclitaxel in a pilot study. Results showed that carboplatin and paclitaxel reduced abnormally high numbers of immunosuppressive myeloid cells, which allowed for “much stronger” ISA101-induced tumor immunity.
To investigate further, the researchers tested the chemotherapy-ISA101 combination in a phase 1/2 study (NCT02128126) of 79 women with advanced, metastatic, or recurrent HPV16-positive cervical cancer.
The patients received the vaccine 2 weeks after starting the second, third, and fourth cycles of chemotherapy. They received various doses of the vaccine (20, 40, 100, or 300 mcg) with or without pegylated type 1 interferon (1 mcg/kg body weight).
“ISA101 was generally safe and well tolerated in that its safety profile was not different from chemotherapy alone,” Dr. Melief and colleagues wrote.
Chemotherapy-associated adverse events occurred in 98.9% of patients, with more than 80% of patients reporting adverse events possibly related to the vaccine or interferon-alpha. However, less than 16% of patients withdrew from the study because of an adverse event.
Of the 72 patients evaluable for efficacy, 43% experienced tumor regression, and 43% had stable disease. The researchers observed regression of the target lesion in 29 of 59 patients with a measurable target lesion.
The team noted that, since all patients received chemotherapy, it is “difficult to interpret short-term clinical outcomes as being due to chemotherapy alone or to the combination,” although they noted that the use of interferon-alpha did not seem to provide any additional benefit.
“Eleven of 14 patients still alive at the end of the study displayed a strong vaccine-induced response and included 9 patients with FIGO stage IVa/IVb cancer who had a mean OS [overall survival] of 3 years,” the researchers noted.
Considering that patients with higher vaccine-induced immune responses lived longer, the researchers concluded that “chemoimmunotherapy can be exploited to the benefit of patients with advanced cancer based on a defined mode of action.”
This trial was funded by ISA Pharmaceuticals and a Dutch Cancer Society grant. Investigators disclosed relationships with ISA Pharmaceuticals and other companies.
SOURCE: Melief CJM et al. Sci Transl Med. 2020;12:eaaz8235.
Longer survival was observed in women who had a stronger immune response to an investigational human papillomavirus (HPV) vaccine while treated with standard chemotherapy for advanced, metastatic, or recurrent cervical cancer.
The results, from a phase 1/2 study, showed that women with a vaccine-induced immune response higher than the median had a median overall survival of 16.8 months, compared with a median overall survival of 11.2 months for women with an immune response lower than the median (hazard ratio, 0.491; P = .012).
Cornelis “Kees” Melief, MD, chief scientific officer of ISA Pharmaceuticals in Leiden, the Netherlands, and colleagues reported these findings in Science Translational Medicine.
The researchers previously evaluated the HPV16 vaccine, ISA101, in combination with carboplatin and paclitaxel in a pilot study. Results showed that carboplatin and paclitaxel reduced abnormally high numbers of immunosuppressive myeloid cells, which allowed for “much stronger” ISA101-induced tumor immunity.
To investigate further, the researchers tested the chemotherapy-ISA101 combination in a phase 1/2 study (NCT02128126) of 79 women with advanced, metastatic, or recurrent HPV16-positive cervical cancer.
The patients received the vaccine 2 weeks after starting the second, third, and fourth cycles of chemotherapy. They received various doses of the vaccine (20, 40, 100, or 300 mcg) with or without pegylated type 1 interferon (1 mcg/kg body weight).
“ISA101 was generally safe and well tolerated in that its safety profile was not different from chemotherapy alone,” Dr. Melief and colleagues wrote.
Chemotherapy-associated adverse events occurred in 98.9% of patients, with more than 80% of patients reporting adverse events possibly related to the vaccine or interferon-alpha. However, less than 16% of patients withdrew from the study because of an adverse event.
Of the 72 patients evaluable for efficacy, 43% experienced tumor regression, and 43% had stable disease. The researchers observed regression of the target lesion in 29 of 59 patients with a measurable target lesion.
The team noted that, since all patients received chemotherapy, it is “difficult to interpret short-term clinical outcomes as being due to chemotherapy alone or to the combination,” although they noted that the use of interferon-alpha did not seem to provide any additional benefit.
“Eleven of 14 patients still alive at the end of the study displayed a strong vaccine-induced response and included 9 patients with FIGO stage IVa/IVb cancer who had a mean OS [overall survival] of 3 years,” the researchers noted.
Considering that patients with higher vaccine-induced immune responses lived longer, the researchers concluded that “chemoimmunotherapy can be exploited to the benefit of patients with advanced cancer based on a defined mode of action.”
This trial was funded by ISA Pharmaceuticals and a Dutch Cancer Society grant. Investigators disclosed relationships with ISA Pharmaceuticals and other companies.
SOURCE: Melief CJM et al. Sci Transl Med. 2020;12:eaaz8235.
FROM SCIENCE TRANSLATIONAL MEDICINE
Key clinical point: There may be an overall survival benefit of combining human papillomavirus vaccination with standard-of-care chemotherapy for cervical cancer.
Major finding: The median overall survival was 16.8 months for patients with immune responses to the vaccine that were higher than the median and 11.2 months for patients with immune responses lower than the median (hazard ratio, 0.491; P = .012).
Study details: A phase 1/2 study of 77 women with HPV16-positive advanced, metastatic, or recurrent cervical cancer.
Disclosures: The study was funded by ISA Pharmaceuticals and a Dutch Cancer Society grant. Investigators disclosed relationships with ISA Pharmaceuticals and other companies.
Source: Melief CJM et al. Sci Transl Med. 2020;12:eaaz8235.
Prospective algorithm favors vaginal hysterectomy
based on data from a prospective study of 365 patients.
“Total vaginal hysterectomy is the most cost-effective route, with a low complication rate, and, therefore, should be performed when feasible,” wrote Jennifer J. Schmitt, DO, of the Mayo Clinic, Rochester, Minn., and colleagues.
However, algorithms to support the decision to choose vaginal hysterectomy are not widely used, they said.
To assess the optimal surgical route for hysterectomy, the researchers devised a prospective algorithm and decision tree based on history of laparotomy, uterine size, and vaginal access. The results of their study were published in Obstetrics & Gynecology.
The study population included 365 women aged 18 years and older who underwent hysterectomies between Nov. 24, 2015, and Dec. 31, 2017, at a single center. A total of 202 patients (55%) met criteria for a total vaginal hysterectomy using the algorithm, and 57 (15.6%) were assigned to have an examination under anesthesia followed by total vaginal hysterectomy, for a total of 259 expected vaginal hysterectomies. Ultimately, 211 (81.5%) of the patients identified as being the best candidates for having a vaginal hysterectomy underwent the procedure. Almost all of the procedures – 99.1% – were completed successfully.
The algorithm predicted that 52 patients were expected to have an examination under anesthesia followed by a robot-assisted total laparoscopic hysterectomy and 54 were expected to have an abdominal, robotic, or laparoscopic hysterectomy. A total of 46 procedures (44 robotic, when vaginal was expected and 2 abdominal, when vaginal was expected) deviated to a more invasive route than prescribed by the algorithm, and 7 procedures deviated from the algorithm-predicted robotic or abdominal procedure to total vaginal hysterectomy.
Approximately 95% of the patients were discharged within 24 hours of surgery. These patients included 7 who had vaginal surgery when a more invasive method was predicted and did not experience intraoperative complications or Accordion grade 3 complications.
“Prospective algorithm use predicts that 55.3% of all hysterectomies were expected to have an a priori total vaginal hysterectomy, which is higher than the actual total vaginal hysterectomy rate of 11.5% reported previously,” the researchers noted, and they added that vaginal hysterectomy would be associated with cost savings of $657,524 if the total hysterectomy rate was 55% instead of 11%.
The study findings were limited by several factors including an expertise bias at the center where the study was conducted, as well as the small number of patients with algorithm deviations or poor outcomes, and the lack of a control group, the researchers noted. However, the results support the use of the algorithm “in combination with educating gynecologic surgeons about the feasibility of vaginal surgery,” they said.
“Prospective use of this algorithm nationally may increase the rate of total vaginal hysterectomy and decrease health care delivery costs,” they concluded.
“The American College of Obstetricians and Gynecologists continues to recommend vaginal hysterectomy as the approach of choice whenever feasible, and although clinical evidence and societal endorsements support vaginal hysterectomy as a superior high-value modality, the rate of vaginal hysterectomy in the United States has continued to decline,” Arnold P. Advincula, MD, of Columbia University Medical Center, New York, wrote in an accompanying editorial.
Many variables beyond clinical will determine the optimal hysterectomy route, Dr. Advincula said.
“Although historical evidence demonstrates that vaginal hysterectomy is associated with better outcomes when compared with other approaches, a multitude of studies now exist that challenge this notion. Given the financial implications and overall costs of care with surgical complications and 30-day readmissions, experienced high-volume surgeons using all available routes have shown robotics to be the best surgical approach in terms of fewer postoperative complications and lowest 30-day readmission rates,” he noted. However, “one should not split hairs and subtly pit one minimally invasive option against another, but instead should work toward the goal of minimizing laparotomy, which is still performed at a high rate,” Dr. Advincula emphasized.
The study was supported in part by the National Center for Advancing Translational Science. Dr. Schmitt had no financial conflicts to disclose. Dr. Advincula disclosed serving as a consultant for AbbVie, Baxter, ConMed, Eximis Surgical, Intuitive Surgical, and Titan Medical, and performing consultancy work and receiving royalties from Cooper Surgical.
SOURCES: Schmitt JJ et al. Obstet Gynecol. 2020;135:761-9. doi: 10.1097/AOG.0000000000003725; Advincula A. Obstet Gynecol. 2020;135:759-60. doi: doi: 10.1097/AOG.0000000000003814.
based on data from a prospective study of 365 patients.
“Total vaginal hysterectomy is the most cost-effective route, with a low complication rate, and, therefore, should be performed when feasible,” wrote Jennifer J. Schmitt, DO, of the Mayo Clinic, Rochester, Minn., and colleagues.
However, algorithms to support the decision to choose vaginal hysterectomy are not widely used, they said.
To assess the optimal surgical route for hysterectomy, the researchers devised a prospective algorithm and decision tree based on history of laparotomy, uterine size, and vaginal access. The results of their study were published in Obstetrics & Gynecology.
The study population included 365 women aged 18 years and older who underwent hysterectomies between Nov. 24, 2015, and Dec. 31, 2017, at a single center. A total of 202 patients (55%) met criteria for a total vaginal hysterectomy using the algorithm, and 57 (15.6%) were assigned to have an examination under anesthesia followed by total vaginal hysterectomy, for a total of 259 expected vaginal hysterectomies. Ultimately, 211 (81.5%) of the patients identified as being the best candidates for having a vaginal hysterectomy underwent the procedure. Almost all of the procedures – 99.1% – were completed successfully.
The algorithm predicted that 52 patients were expected to have an examination under anesthesia followed by a robot-assisted total laparoscopic hysterectomy and 54 were expected to have an abdominal, robotic, or laparoscopic hysterectomy. A total of 46 procedures (44 robotic, when vaginal was expected and 2 abdominal, when vaginal was expected) deviated to a more invasive route than prescribed by the algorithm, and 7 procedures deviated from the algorithm-predicted robotic or abdominal procedure to total vaginal hysterectomy.
Approximately 95% of the patients were discharged within 24 hours of surgery. These patients included 7 who had vaginal surgery when a more invasive method was predicted and did not experience intraoperative complications or Accordion grade 3 complications.
“Prospective algorithm use predicts that 55.3% of all hysterectomies were expected to have an a priori total vaginal hysterectomy, which is higher than the actual total vaginal hysterectomy rate of 11.5% reported previously,” the researchers noted, and they added that vaginal hysterectomy would be associated with cost savings of $657,524 if the total hysterectomy rate was 55% instead of 11%.
The study findings were limited by several factors including an expertise bias at the center where the study was conducted, as well as the small number of patients with algorithm deviations or poor outcomes, and the lack of a control group, the researchers noted. However, the results support the use of the algorithm “in combination with educating gynecologic surgeons about the feasibility of vaginal surgery,” they said.
“Prospective use of this algorithm nationally may increase the rate of total vaginal hysterectomy and decrease health care delivery costs,” they concluded.
“The American College of Obstetricians and Gynecologists continues to recommend vaginal hysterectomy as the approach of choice whenever feasible, and although clinical evidence and societal endorsements support vaginal hysterectomy as a superior high-value modality, the rate of vaginal hysterectomy in the United States has continued to decline,” Arnold P. Advincula, MD, of Columbia University Medical Center, New York, wrote in an accompanying editorial.
Many variables beyond clinical will determine the optimal hysterectomy route, Dr. Advincula said.
“Although historical evidence demonstrates that vaginal hysterectomy is associated with better outcomes when compared with other approaches, a multitude of studies now exist that challenge this notion. Given the financial implications and overall costs of care with surgical complications and 30-day readmissions, experienced high-volume surgeons using all available routes have shown robotics to be the best surgical approach in terms of fewer postoperative complications and lowest 30-day readmission rates,” he noted. However, “one should not split hairs and subtly pit one minimally invasive option against another, but instead should work toward the goal of minimizing laparotomy, which is still performed at a high rate,” Dr. Advincula emphasized.
The study was supported in part by the National Center for Advancing Translational Science. Dr. Schmitt had no financial conflicts to disclose. Dr. Advincula disclosed serving as a consultant for AbbVie, Baxter, ConMed, Eximis Surgical, Intuitive Surgical, and Titan Medical, and performing consultancy work and receiving royalties from Cooper Surgical.
SOURCES: Schmitt JJ et al. Obstet Gynecol. 2020;135:761-9. doi: 10.1097/AOG.0000000000003725; Advincula A. Obstet Gynecol. 2020;135:759-60. doi: doi: 10.1097/AOG.0000000000003814.
based on data from a prospective study of 365 patients.
“Total vaginal hysterectomy is the most cost-effective route, with a low complication rate, and, therefore, should be performed when feasible,” wrote Jennifer J. Schmitt, DO, of the Mayo Clinic, Rochester, Minn., and colleagues.
However, algorithms to support the decision to choose vaginal hysterectomy are not widely used, they said.
To assess the optimal surgical route for hysterectomy, the researchers devised a prospective algorithm and decision tree based on history of laparotomy, uterine size, and vaginal access. The results of their study were published in Obstetrics & Gynecology.
The study population included 365 women aged 18 years and older who underwent hysterectomies between Nov. 24, 2015, and Dec. 31, 2017, at a single center. A total of 202 patients (55%) met criteria for a total vaginal hysterectomy using the algorithm, and 57 (15.6%) were assigned to have an examination under anesthesia followed by total vaginal hysterectomy, for a total of 259 expected vaginal hysterectomies. Ultimately, 211 (81.5%) of the patients identified as being the best candidates for having a vaginal hysterectomy underwent the procedure. Almost all of the procedures – 99.1% – were completed successfully.
The algorithm predicted that 52 patients were expected to have an examination under anesthesia followed by a robot-assisted total laparoscopic hysterectomy and 54 were expected to have an abdominal, robotic, or laparoscopic hysterectomy. A total of 46 procedures (44 robotic, when vaginal was expected and 2 abdominal, when vaginal was expected) deviated to a more invasive route than prescribed by the algorithm, and 7 procedures deviated from the algorithm-predicted robotic or abdominal procedure to total vaginal hysterectomy.
Approximately 95% of the patients were discharged within 24 hours of surgery. These patients included 7 who had vaginal surgery when a more invasive method was predicted and did not experience intraoperative complications or Accordion grade 3 complications.
“Prospective algorithm use predicts that 55.3% of all hysterectomies were expected to have an a priori total vaginal hysterectomy, which is higher than the actual total vaginal hysterectomy rate of 11.5% reported previously,” the researchers noted, and they added that vaginal hysterectomy would be associated with cost savings of $657,524 if the total hysterectomy rate was 55% instead of 11%.
The study findings were limited by several factors including an expertise bias at the center where the study was conducted, as well as the small number of patients with algorithm deviations or poor outcomes, and the lack of a control group, the researchers noted. However, the results support the use of the algorithm “in combination with educating gynecologic surgeons about the feasibility of vaginal surgery,” they said.
“Prospective use of this algorithm nationally may increase the rate of total vaginal hysterectomy and decrease health care delivery costs,” they concluded.
“The American College of Obstetricians and Gynecologists continues to recommend vaginal hysterectomy as the approach of choice whenever feasible, and although clinical evidence and societal endorsements support vaginal hysterectomy as a superior high-value modality, the rate of vaginal hysterectomy in the United States has continued to decline,” Arnold P. Advincula, MD, of Columbia University Medical Center, New York, wrote in an accompanying editorial.
Many variables beyond clinical will determine the optimal hysterectomy route, Dr. Advincula said.
“Although historical evidence demonstrates that vaginal hysterectomy is associated with better outcomes when compared with other approaches, a multitude of studies now exist that challenge this notion. Given the financial implications and overall costs of care with surgical complications and 30-day readmissions, experienced high-volume surgeons using all available routes have shown robotics to be the best surgical approach in terms of fewer postoperative complications and lowest 30-day readmission rates,” he noted. However, “one should not split hairs and subtly pit one minimally invasive option against another, but instead should work toward the goal of minimizing laparotomy, which is still performed at a high rate,” Dr. Advincula emphasized.
The study was supported in part by the National Center for Advancing Translational Science. Dr. Schmitt had no financial conflicts to disclose. Dr. Advincula disclosed serving as a consultant for AbbVie, Baxter, ConMed, Eximis Surgical, Intuitive Surgical, and Titan Medical, and performing consultancy work and receiving royalties from Cooper Surgical.
SOURCES: Schmitt JJ et al. Obstet Gynecol. 2020;135:761-9. doi: 10.1097/AOG.0000000000003725; Advincula A. Obstet Gynecol. 2020;135:759-60. doi: doi: 10.1097/AOG.0000000000003814.
FROM OBSTETRICS & GYNECOLOGY
Nearly half of STI events go without HIV testing
according to Danielle Petsis, MPH, of the Children’s Hospital of Philadelphia, and associates.
In a study published in Pediatrics, the investigators conducted a retrospective analysis of 1,816 acute STI events from 1,313 patients aged 13-24 years admitted between July 2014 and Dec. 2017 at two urban health care clinics. The most common STIs in the analysis were Chlamydia, gonorrhea, trichomoniasis, and syphilis; the mean age at diagnosis was 17 years, 71% of episodes occurred in females, and 97% occurred in African American patients.
Of the 1,816 events, HIV testing was completed within 90 days of the STI diagnosis for only 55%; there was 1 confirmed HIV diagnosis among the completed tests. When HIV testing did occur, in 38% of cases it was completed concurrently with STI testing or HIV testing was performed in 35% of the 872 follow-up cases. Of the 815 events where HIV testing was not performed, 27% had a test ordered by the provider but not completed by the patient; the patient leaving the laboratory before the test could be performed was the most common reason for test noncompletion (67%), followed by not showing up at all (18%) and errors in the medical record or laboratory (5%); the remaining patients gave as reasons for test noncompletion: declining an HIV test, a closed lab, or no reason.
Logistic regression showed that participants who were female and those with a previous history of STIs had significantly lower adjusted odds of HIV test completion, compared with males and those with no previous history of STIs, respectively, the investigators said. In addition, having insurance and having a family planning visit were associated with decreased odds of HIV testing, compared with not having insurance or a family planning visit.
“As we enter the fourth decade of the HIV epidemic, it remains clear that missed opportunities for diagnosis have the potential to delay HIV diagnosis and linkage to antiretroviral therapy or PrEP and prevention services, thus increasing the population risk of HIV transmission. Our data underscore the need for improved HIV testing education for providers of all levels of training and the need for public health agencies to clearly communicate the need for testing at the time of STI infection to reduce the number of missed opportunities for testing,” Ms. Petsis and colleagues concluded.
The study was supported by the National Institutes of Mental Health and the Children’s Hospital of Philadelphia Research Institute K-Readiness Award. One coauthor reported receiving funding from Bayer Healthcare, the Templeton Foundation, the National Institutes of Health, and Janssen Biotech. She also serves on expert advisory boards for Mylan Pharmaceuticals and Merck. The other authors have no relevant financial disclosures.
SOURCE: Wood S et al. Pediatrics. 2020 Mar 16. doi: 10.1542/peds.2019-2265.
according to Danielle Petsis, MPH, of the Children’s Hospital of Philadelphia, and associates.
In a study published in Pediatrics, the investigators conducted a retrospective analysis of 1,816 acute STI events from 1,313 patients aged 13-24 years admitted between July 2014 and Dec. 2017 at two urban health care clinics. The most common STIs in the analysis were Chlamydia, gonorrhea, trichomoniasis, and syphilis; the mean age at diagnosis was 17 years, 71% of episodes occurred in females, and 97% occurred in African American patients.
Of the 1,816 events, HIV testing was completed within 90 days of the STI diagnosis for only 55%; there was 1 confirmed HIV diagnosis among the completed tests. When HIV testing did occur, in 38% of cases it was completed concurrently with STI testing or HIV testing was performed in 35% of the 872 follow-up cases. Of the 815 events where HIV testing was not performed, 27% had a test ordered by the provider but not completed by the patient; the patient leaving the laboratory before the test could be performed was the most common reason for test noncompletion (67%), followed by not showing up at all (18%) and errors in the medical record or laboratory (5%); the remaining patients gave as reasons for test noncompletion: declining an HIV test, a closed lab, or no reason.
Logistic regression showed that participants who were female and those with a previous history of STIs had significantly lower adjusted odds of HIV test completion, compared with males and those with no previous history of STIs, respectively, the investigators said. In addition, having insurance and having a family planning visit were associated with decreased odds of HIV testing, compared with not having insurance or a family planning visit.
“As we enter the fourth decade of the HIV epidemic, it remains clear that missed opportunities for diagnosis have the potential to delay HIV diagnosis and linkage to antiretroviral therapy or PrEP and prevention services, thus increasing the population risk of HIV transmission. Our data underscore the need for improved HIV testing education for providers of all levels of training and the need for public health agencies to clearly communicate the need for testing at the time of STI infection to reduce the number of missed opportunities for testing,” Ms. Petsis and colleagues concluded.
The study was supported by the National Institutes of Mental Health and the Children’s Hospital of Philadelphia Research Institute K-Readiness Award. One coauthor reported receiving funding from Bayer Healthcare, the Templeton Foundation, the National Institutes of Health, and Janssen Biotech. She also serves on expert advisory boards for Mylan Pharmaceuticals and Merck. The other authors have no relevant financial disclosures.
SOURCE: Wood S et al. Pediatrics. 2020 Mar 16. doi: 10.1542/peds.2019-2265.
according to Danielle Petsis, MPH, of the Children’s Hospital of Philadelphia, and associates.
In a study published in Pediatrics, the investigators conducted a retrospective analysis of 1,816 acute STI events from 1,313 patients aged 13-24 years admitted between July 2014 and Dec. 2017 at two urban health care clinics. The most common STIs in the analysis were Chlamydia, gonorrhea, trichomoniasis, and syphilis; the mean age at diagnosis was 17 years, 71% of episodes occurred in females, and 97% occurred in African American patients.
Of the 1,816 events, HIV testing was completed within 90 days of the STI diagnosis for only 55%; there was 1 confirmed HIV diagnosis among the completed tests. When HIV testing did occur, in 38% of cases it was completed concurrently with STI testing or HIV testing was performed in 35% of the 872 follow-up cases. Of the 815 events where HIV testing was not performed, 27% had a test ordered by the provider but not completed by the patient; the patient leaving the laboratory before the test could be performed was the most common reason for test noncompletion (67%), followed by not showing up at all (18%) and errors in the medical record or laboratory (5%); the remaining patients gave as reasons for test noncompletion: declining an HIV test, a closed lab, or no reason.
Logistic regression showed that participants who were female and those with a previous history of STIs had significantly lower adjusted odds of HIV test completion, compared with males and those with no previous history of STIs, respectively, the investigators said. In addition, having insurance and having a family planning visit were associated with decreased odds of HIV testing, compared with not having insurance or a family planning visit.
“As we enter the fourth decade of the HIV epidemic, it remains clear that missed opportunities for diagnosis have the potential to delay HIV diagnosis and linkage to antiretroviral therapy or PrEP and prevention services, thus increasing the population risk of HIV transmission. Our data underscore the need for improved HIV testing education for providers of all levels of training and the need for public health agencies to clearly communicate the need for testing at the time of STI infection to reduce the number of missed opportunities for testing,” Ms. Petsis and colleagues concluded.
The study was supported by the National Institutes of Mental Health and the Children’s Hospital of Philadelphia Research Institute K-Readiness Award. One coauthor reported receiving funding from Bayer Healthcare, the Templeton Foundation, the National Institutes of Health, and Janssen Biotech. She also serves on expert advisory boards for Mylan Pharmaceuticals and Merck. The other authors have no relevant financial disclosures.
SOURCE: Wood S et al. Pediatrics. 2020 Mar 16. doi: 10.1542/peds.2019-2265.
FROM PEDIATRICS
CV health in pregnancy improves outcomes for mother and infant
PHOENIX – according to results from a multinational cohort study.
“Over the past 10 years, cardiovascular health [CVH] has been characterized across most of the life course and is associated with a variety of health outcomes, but CVH as a whole has not been well studied during pregnancy,” Amanda M. Perak, MD, said at the Epidemiology and Prevention/Lifestyle and Cardiometabolic Health meeting.
In an effort to examine the associations of maternal gestational CVH with adverse maternal and newborn outcomes, Dr. Perak of the departments of pediatrics and preventive medicine at Northwestern University and Lurie Children’s Hospital, both in Chicago, and colleagues drew from the Hyperglycemia and Adverse Pregnancy Outcome (HAPO) Study, which examined pregnant women at a target of 28 weeks’ gestation and assessed the associations of glycemia with pregnancy outcomes. The researchers analyzed data from an ancillary study of 2,230 mother-child dyads to characterize clinical gestational CVH with use of five metrics: body mass index, blood pressure, cholesterol, glucose, and smoking. The study excluded women with prepregnancy diabetes, preterm births, and cases of fetal death/major malformations.
Each maternal CVH metric was classified as ideal, intermediate, or poor according to modified definitions based on pregnancy guidelines. “For lipids, it’s known that levels change substantially during pregnancy, but there are no pregnancy guidelines,” Dr. Perak said. “We and others have also shown that higher triglycerides in pregnancy are associated with adverse pregnancy outcomes. We selected thresholds of less than 250 mg/dL for ideal and at least 500 mg/dL for poor, based on triglyceride distribution and clinical relevance.”
Total CVH was scored by assigning 2 points for ideal, 1 for intermediate, and 0 for each poor metric, for a total possible 10 points, with 10 being most favorable. They also created four CVH categories, ranging from all ideal to two or more poor metrics. Maternal adverse pregnancy outcomes included preeclampsia and unplanned primary cesarean section. Newborn adverse pregnancy outcomes included birth weight above the 90th percentile and a cord blood insulin sensitivity index lower than the 10th percentile.
The researchers used logistic and multinomial logistic regression of pregnancy outcomes on maternal gestational CVH in two adjusted models. Secondarily, they examined associations of individual CVH metrics with outcomes, with adjustment for the other metrics.
The cohort comprised mother-child dyads from nine field centers in six countries: the United States (25%), Barbados (23%), United Kingdom (21%), China (18%), Thailand (7%), and Canada (7%). The mothers’ mean age was 30 years, and the mean gestational age was 28 weeks. The mean gestational CVH score was 8.8 out of 10. Nearly half of mothers (42%) had ideal metrics, while 4% had two or more poor metrics. Delivery occurred at a mean of 39.8 weeks, and adverse pregnancy outcomes occurred in 4.7%-17.9% of pregnancies.
In the fully adjusted model, which accounted for maternal age, height, alcohol use, gestational age at pregnancy exam, maternal parity, and newborn sex and race/ethnicity, odds ratios per 1-point higher (better) CVH score were 0.61 (95% confidence interval, 0.53-0.70) for preeclampsia, 0.85 (95% CI, 0.76-0.95) for unplanned primary cesarean section (among primiparous mothers), 0.83 (95% CI, 0.77-0.91) for large for gestational age infant, and 0.79 (95% CI, 0.72-0.87) for infant insulin sensitivity index below the 10th percentile. CVH categories were also associated with outcomes. For example, odds ratios for preeclampsia were 4.61 (95% CI, 2.13-11.14) for mothers with one or more intermediate metrics, 7.62 (95% CI, 3.60-18.13) for mothers with one poor metric, and 12.02 (95% CI, 4.70-32.50) for mothers with two or more poor metrics, compared with mothers with all metrics ideal.
“Except for smoking, each CVH metric was independently associated with adverse outcomes,” Dr. Perak said. “However, total CVH was associated with a wider range of outcomes than any single metric. This suggests that CVH provides health insights beyond single risk factors.”
Strengths of the study, she continued, included geographic and racial diversity of participants and high-quality research measurements of CVH. Limitations were that the cohort excluded prepregnancy diabetes and preterm births. “Diet and exercise data were not available, and CVH was measured once at 28 weeks,” she said. “Further study is needed across pregnancy and in other settings, but this study provides the first data on the relevance of gestational CVH for pregnancy outcomes.”
In an interview, Stephen S. Rich, PhD, who directs the Center for Public Health Genomics at the University of Virginia, said that the data “provide strong epidemiologic support to focus on the full range of cardiovascular health. In my view, the primary limitation of the study is that there may be significant differences in how one achieves ideal CHV across a single country, not to mention across the world, particularly in absence of a highly controlled, research environment. It is not clear that the approach used in this study at nine selected sites in six relatively highly developed countries could be translated into primary care – particularly in the U.S. with different regulatory and reimbursement plans and payers. Nonetheless, the evidence suggests a way to reduce adverse outcomes in pregnancy and the area deserves greater research.”
According to Dr. Perak, gestational diabetes is associated with a twofold higher maternal risk for cardiovascular disease (Diabetologia. 2019;62:905-14), while diabetes is also associated with higher offspring risk for CVD (BMJ. 2019;367:16398). However, a paucity of data exists on gestational CVH. In one report, better gestational CVH was associated with less subclinical CVD for the mother 10 years later (J Am Heart Assoc. 2019 Jul 23. doi:10.1161/JAHA.118.011394). In a separate analysis, Dr. Perak and her colleagues found that better gestational CVH was associated with better offspring CVH in childhood. “Unfortunately, we also reported that, among pregnant women in the United States, fewer than 1 in 10 had high CVH,” she said (J Am Heart Assoc. 2020 Feb 17. doi:10.1161/JAHA.119.015123). “However, the relevance of gestational CVH for pregnancy outcomes is unknown, but a it’s key question when considering CVH monitoring in prenatal care.”
Dr. Perak reported having received grant support from the National Heart, Lung, and Blood Institute, the American Heart Association, and Northwestern University. The HAPO Study was supported by NHLBI and the National Institute of Diabetes and Digestive and Kidney Diseases.
The meeting was sponsored by the American Heart Association.
SOURCE: Perak A et al. Epi/Lifestyle 2020, Abstract 33.
PHOENIX – according to results from a multinational cohort study.
“Over the past 10 years, cardiovascular health [CVH] has been characterized across most of the life course and is associated with a variety of health outcomes, but CVH as a whole has not been well studied during pregnancy,” Amanda M. Perak, MD, said at the Epidemiology and Prevention/Lifestyle and Cardiometabolic Health meeting.
In an effort to examine the associations of maternal gestational CVH with adverse maternal and newborn outcomes, Dr. Perak of the departments of pediatrics and preventive medicine at Northwestern University and Lurie Children’s Hospital, both in Chicago, and colleagues drew from the Hyperglycemia and Adverse Pregnancy Outcome (HAPO) Study, which examined pregnant women at a target of 28 weeks’ gestation and assessed the associations of glycemia with pregnancy outcomes. The researchers analyzed data from an ancillary study of 2,230 mother-child dyads to characterize clinical gestational CVH with use of five metrics: body mass index, blood pressure, cholesterol, glucose, and smoking. The study excluded women with prepregnancy diabetes, preterm births, and cases of fetal death/major malformations.
Each maternal CVH metric was classified as ideal, intermediate, or poor according to modified definitions based on pregnancy guidelines. “For lipids, it’s known that levels change substantially during pregnancy, but there are no pregnancy guidelines,” Dr. Perak said. “We and others have also shown that higher triglycerides in pregnancy are associated with adverse pregnancy outcomes. We selected thresholds of less than 250 mg/dL for ideal and at least 500 mg/dL for poor, based on triglyceride distribution and clinical relevance.”
Total CVH was scored by assigning 2 points for ideal, 1 for intermediate, and 0 for each poor metric, for a total possible 10 points, with 10 being most favorable. They also created four CVH categories, ranging from all ideal to two or more poor metrics. Maternal adverse pregnancy outcomes included preeclampsia and unplanned primary cesarean section. Newborn adverse pregnancy outcomes included birth weight above the 90th percentile and a cord blood insulin sensitivity index lower than the 10th percentile.
The researchers used logistic and multinomial logistic regression of pregnancy outcomes on maternal gestational CVH in two adjusted models. Secondarily, they examined associations of individual CVH metrics with outcomes, with adjustment for the other metrics.
The cohort comprised mother-child dyads from nine field centers in six countries: the United States (25%), Barbados (23%), United Kingdom (21%), China (18%), Thailand (7%), and Canada (7%). The mothers’ mean age was 30 years, and the mean gestational age was 28 weeks. The mean gestational CVH score was 8.8 out of 10. Nearly half of mothers (42%) had ideal metrics, while 4% had two or more poor metrics. Delivery occurred at a mean of 39.8 weeks, and adverse pregnancy outcomes occurred in 4.7%-17.9% of pregnancies.
In the fully adjusted model, which accounted for maternal age, height, alcohol use, gestational age at pregnancy exam, maternal parity, and newborn sex and race/ethnicity, odds ratios per 1-point higher (better) CVH score were 0.61 (95% confidence interval, 0.53-0.70) for preeclampsia, 0.85 (95% CI, 0.76-0.95) for unplanned primary cesarean section (among primiparous mothers), 0.83 (95% CI, 0.77-0.91) for large for gestational age infant, and 0.79 (95% CI, 0.72-0.87) for infant insulin sensitivity index below the 10th percentile. CVH categories were also associated with outcomes. For example, odds ratios for preeclampsia were 4.61 (95% CI, 2.13-11.14) for mothers with one or more intermediate metrics, 7.62 (95% CI, 3.60-18.13) for mothers with one poor metric, and 12.02 (95% CI, 4.70-32.50) for mothers with two or more poor metrics, compared with mothers with all metrics ideal.
“Except for smoking, each CVH metric was independently associated with adverse outcomes,” Dr. Perak said. “However, total CVH was associated with a wider range of outcomes than any single metric. This suggests that CVH provides health insights beyond single risk factors.”
Strengths of the study, she continued, included geographic and racial diversity of participants and high-quality research measurements of CVH. Limitations were that the cohort excluded prepregnancy diabetes and preterm births. “Diet and exercise data were not available, and CVH was measured once at 28 weeks,” she said. “Further study is needed across pregnancy and in other settings, but this study provides the first data on the relevance of gestational CVH for pregnancy outcomes.”
In an interview, Stephen S. Rich, PhD, who directs the Center for Public Health Genomics at the University of Virginia, said that the data “provide strong epidemiologic support to focus on the full range of cardiovascular health. In my view, the primary limitation of the study is that there may be significant differences in how one achieves ideal CHV across a single country, not to mention across the world, particularly in absence of a highly controlled, research environment. It is not clear that the approach used in this study at nine selected sites in six relatively highly developed countries could be translated into primary care – particularly in the U.S. with different regulatory and reimbursement plans and payers. Nonetheless, the evidence suggests a way to reduce adverse outcomes in pregnancy and the area deserves greater research.”
According to Dr. Perak, gestational diabetes is associated with a twofold higher maternal risk for cardiovascular disease (Diabetologia. 2019;62:905-14), while diabetes is also associated with higher offspring risk for CVD (BMJ. 2019;367:16398). However, a paucity of data exists on gestational CVH. In one report, better gestational CVH was associated with less subclinical CVD for the mother 10 years later (J Am Heart Assoc. 2019 Jul 23. doi:10.1161/JAHA.118.011394). In a separate analysis, Dr. Perak and her colleagues found that better gestational CVH was associated with better offspring CVH in childhood. “Unfortunately, we also reported that, among pregnant women in the United States, fewer than 1 in 10 had high CVH,” she said (J Am Heart Assoc. 2020 Feb 17. doi:10.1161/JAHA.119.015123). “However, the relevance of gestational CVH for pregnancy outcomes is unknown, but a it’s key question when considering CVH monitoring in prenatal care.”
Dr. Perak reported having received grant support from the National Heart, Lung, and Blood Institute, the American Heart Association, and Northwestern University. The HAPO Study was supported by NHLBI and the National Institute of Diabetes and Digestive and Kidney Diseases.
The meeting was sponsored by the American Heart Association.
SOURCE: Perak A et al. Epi/Lifestyle 2020, Abstract 33.
PHOENIX – according to results from a multinational cohort study.
“Over the past 10 years, cardiovascular health [CVH] has been characterized across most of the life course and is associated with a variety of health outcomes, but CVH as a whole has not been well studied during pregnancy,” Amanda M. Perak, MD, said at the Epidemiology and Prevention/Lifestyle and Cardiometabolic Health meeting.
In an effort to examine the associations of maternal gestational CVH with adverse maternal and newborn outcomes, Dr. Perak of the departments of pediatrics and preventive medicine at Northwestern University and Lurie Children’s Hospital, both in Chicago, and colleagues drew from the Hyperglycemia and Adverse Pregnancy Outcome (HAPO) Study, which examined pregnant women at a target of 28 weeks’ gestation and assessed the associations of glycemia with pregnancy outcomes. The researchers analyzed data from an ancillary study of 2,230 mother-child dyads to characterize clinical gestational CVH with use of five metrics: body mass index, blood pressure, cholesterol, glucose, and smoking. The study excluded women with prepregnancy diabetes, preterm births, and cases of fetal death/major malformations.
Each maternal CVH metric was classified as ideal, intermediate, or poor according to modified definitions based on pregnancy guidelines. “For lipids, it’s known that levels change substantially during pregnancy, but there are no pregnancy guidelines,” Dr. Perak said. “We and others have also shown that higher triglycerides in pregnancy are associated with adverse pregnancy outcomes. We selected thresholds of less than 250 mg/dL for ideal and at least 500 mg/dL for poor, based on triglyceride distribution and clinical relevance.”
Total CVH was scored by assigning 2 points for ideal, 1 for intermediate, and 0 for each poor metric, for a total possible 10 points, with 10 being most favorable. They also created four CVH categories, ranging from all ideal to two or more poor metrics. Maternal adverse pregnancy outcomes included preeclampsia and unplanned primary cesarean section. Newborn adverse pregnancy outcomes included birth weight above the 90th percentile and a cord blood insulin sensitivity index lower than the 10th percentile.
The researchers used logistic and multinomial logistic regression of pregnancy outcomes on maternal gestational CVH in two adjusted models. Secondarily, they examined associations of individual CVH metrics with outcomes, with adjustment for the other metrics.
The cohort comprised mother-child dyads from nine field centers in six countries: the United States (25%), Barbados (23%), United Kingdom (21%), China (18%), Thailand (7%), and Canada (7%). The mothers’ mean age was 30 years, and the mean gestational age was 28 weeks. The mean gestational CVH score was 8.8 out of 10. Nearly half of mothers (42%) had ideal metrics, while 4% had two or more poor metrics. Delivery occurred at a mean of 39.8 weeks, and adverse pregnancy outcomes occurred in 4.7%-17.9% of pregnancies.
In the fully adjusted model, which accounted for maternal age, height, alcohol use, gestational age at pregnancy exam, maternal parity, and newborn sex and race/ethnicity, odds ratios per 1-point higher (better) CVH score were 0.61 (95% confidence interval, 0.53-0.70) for preeclampsia, 0.85 (95% CI, 0.76-0.95) for unplanned primary cesarean section (among primiparous mothers), 0.83 (95% CI, 0.77-0.91) for large for gestational age infant, and 0.79 (95% CI, 0.72-0.87) for infant insulin sensitivity index below the 10th percentile. CVH categories were also associated with outcomes. For example, odds ratios for preeclampsia were 4.61 (95% CI, 2.13-11.14) for mothers with one or more intermediate metrics, 7.62 (95% CI, 3.60-18.13) for mothers with one poor metric, and 12.02 (95% CI, 4.70-32.50) for mothers with two or more poor metrics, compared with mothers with all metrics ideal.
“Except for smoking, each CVH metric was independently associated with adverse outcomes,” Dr. Perak said. “However, total CVH was associated with a wider range of outcomes than any single metric. This suggests that CVH provides health insights beyond single risk factors.”
Strengths of the study, she continued, included geographic and racial diversity of participants and high-quality research measurements of CVH. Limitations were that the cohort excluded prepregnancy diabetes and preterm births. “Diet and exercise data were not available, and CVH was measured once at 28 weeks,” she said. “Further study is needed across pregnancy and in other settings, but this study provides the first data on the relevance of gestational CVH for pregnancy outcomes.”
In an interview, Stephen S. Rich, PhD, who directs the Center for Public Health Genomics at the University of Virginia, said that the data “provide strong epidemiologic support to focus on the full range of cardiovascular health. In my view, the primary limitation of the study is that there may be significant differences in how one achieves ideal CHV across a single country, not to mention across the world, particularly in absence of a highly controlled, research environment. It is not clear that the approach used in this study at nine selected sites in six relatively highly developed countries could be translated into primary care – particularly in the U.S. with different regulatory and reimbursement plans and payers. Nonetheless, the evidence suggests a way to reduce adverse outcomes in pregnancy and the area deserves greater research.”
According to Dr. Perak, gestational diabetes is associated with a twofold higher maternal risk for cardiovascular disease (Diabetologia. 2019;62:905-14), while diabetes is also associated with higher offspring risk for CVD (BMJ. 2019;367:16398). However, a paucity of data exists on gestational CVH. In one report, better gestational CVH was associated with less subclinical CVD for the mother 10 years later (J Am Heart Assoc. 2019 Jul 23. doi:10.1161/JAHA.118.011394). In a separate analysis, Dr. Perak and her colleagues found that better gestational CVH was associated with better offspring CVH in childhood. “Unfortunately, we also reported that, among pregnant women in the United States, fewer than 1 in 10 had high CVH,” she said (J Am Heart Assoc. 2020 Feb 17. doi:10.1161/JAHA.119.015123). “However, the relevance of gestational CVH for pregnancy outcomes is unknown, but a it’s key question when considering CVH monitoring in prenatal care.”
Dr. Perak reported having received grant support from the National Heart, Lung, and Blood Institute, the American Heart Association, and Northwestern University. The HAPO Study was supported by NHLBI and the National Institute of Diabetes and Digestive and Kidney Diseases.
The meeting was sponsored by the American Heart Association.
SOURCE: Perak A et al. Epi/Lifestyle 2020, Abstract 33.
REPORTING FROM EPI/LIFESTYLE 2020
Study supports genetic testing for all breast cancer patients age 65 and younger
Current National Comprehensive Cancer Network (NCCN) criteria may prevent genetic testing in “a substantial proportion” of women who carry germline pathogenic variants in breast cancer predisposition genes, according to investigators.
They found that, by expanding NCCN criteria to include germline genetic testing for all women diagnosed with breast cancer at age 65 or younger, the sensitivity of testing for nine well-established breast cancer predisposition genes would improve from 70% to more than 90%. The sensitivity for detection of BRCA1 and BRCA2 only would improve from 87% to greater than 98%.
Siddhartha Yadav, MD, of the Mayo Clinic, Rochester, Minn., and colleagues reported these findings in the Journal of Clinical Oncology.
“In a large unselected series of women with breast cancer, we demonstrate that expanding the NCCN testing criteria to include all women diagnosed with breast cancer at or before the age of 65 years has the potential to improve the sensitivity of germline genetic testing without the need for evaluation of all women with breast cancer,” Dr. Yadav and colleagues wrote.
Robert Pilarski, who was vice-chair of the panel that drew up the NCCN guidelines, said in an interview that the guideline authors tried to achieve a balance.
“We’ve known that NCCN misses cases and indications, but it comes down to whether the goal is to test all women with mutations or to have criteria that are a cost-effective and reasonable compromise to capture as many patients as possible,” said Mr. Pilarski, a licensed genetic counselor at the Ohio State University Wexner Medical Center in Columbus.
Current NCCN criteria for genetic/familial high-risk assessment for breast, ovarian, and pancreatic cancer recommend testing for individuals with blood relatives who have known or likely pathogenic variants, as well as patients with breast cancer diagnosed at age 45 or younger, patients aged 46-50 years with unknown or limited family history, patients with a second breast cancer diagnosed at any age, patients with triple-negative breast cancer diagnosed at age 60 or younger, and patients with breast cancer diagnosed at any age if they are of Ashkenazi Jewish ancestry.
But as Dr. Yadav and colleagues note, two recent studies (J Clin Oncol. 2019 Feb 20;37[6]:453-60; Ann Surg Oncol. 2018 Oct;25[10]:2925-31) suggested that up to 50% of germline pathogenic variants could be missed if testing were based solely on NCCN criteria.
Based on these findings, the American Society of Breast Surgeons issued a consensus guideline on genetic testing for hereditary breast cancer (Ann Surg Oncol. 2019 Oct;26[10]:3025-31), which states that, “genetic testing should be made available to all patients with a personal history of breast cancer.”
“Without question, if your goal is to identify everyone with a mutation, you’d have to test every cancer patient,” Mr. Pilarski said. “At this point, the ASBrS [American Society of Breast Surgeons] are the only group that have proposed that, and a lot of us feel that’s going too far at this point in time, and so the issue becomes what’s reasonable before that, and I think this paper is a great step forward.”
Cutting through the confusion
To see whether tweaking the existing guidelines could help clarify the issues surrounding genetic testing for breast cancer, Dr. Yadav and colleagues looked at a cohort of patients from the Mayo Clinic Breast Cancer Study. This prospective registry was open to all women evaluated at the Mayo Clinic Rochester for a first diagnosis of invasive breast cancer or ductal carcinoma in situ from May 2000 through May 2016.
The women were evaluated for germline pathogenic variants in nine breast cancer predisposition genes: ATM, BRCA1, BRCA2, CDH1, CHEK2, NF1, PALB2, PTEN, and TP53.
The researchers found that, of the 3,907 women in the sample, 1,872 (47.9%) would have been recommended for testing under the NCCN criteria, but the remaining 2,035 would not.
Women who met NCCN criteria were significantly more likely to carry a pathogenic variant (9% vs. 3.5%, P less than .001). However, 29.9% of women with pathogenic variants in the nine-gene panel and 13.1% of those with pathogenic variants in BRCA1 or BRCA2 did not qualify for testing by NCCN criteria.
The sensitivity of NCCN criteria was 70% for the nine-gene panel and 87% for BRCA 1 and BRCA 2, with a 53% specificity.
But if the criteria were expanded to include all women age 65 years and younger with a breast cancer diagnosis, the sensitivity for the nine-gene panel would increase to 92.1%, and the sensitivity for BRCA1 and BRCA2 only would climb to greater than 98.1%, with a specificity of approximately 22% for each test combination.
The authors acknowledged that they did not assess the cost-effectiveness of the testing criteria.
This study was supported by grants from the National Institutes of Health and the Breast Cancer Research Foundation. Authors disclosed relationships with Grail, bioTheranostics, Myriad Genetics, and other companies. Mr. Pilarski reported no conflicts of interest.
SOURCE: Yadav S et al. J Clin Oncol. 2020 Mar 3. doi: 10.1200/JCO.19.02190
Current National Comprehensive Cancer Network (NCCN) criteria may prevent genetic testing in “a substantial proportion” of women who carry germline pathogenic variants in breast cancer predisposition genes, according to investigators.
They found that, by expanding NCCN criteria to include germline genetic testing for all women diagnosed with breast cancer at age 65 or younger, the sensitivity of testing for nine well-established breast cancer predisposition genes would improve from 70% to more than 90%. The sensitivity for detection of BRCA1 and BRCA2 only would improve from 87% to greater than 98%.
Siddhartha Yadav, MD, of the Mayo Clinic, Rochester, Minn., and colleagues reported these findings in the Journal of Clinical Oncology.
“In a large unselected series of women with breast cancer, we demonstrate that expanding the NCCN testing criteria to include all women diagnosed with breast cancer at or before the age of 65 years has the potential to improve the sensitivity of germline genetic testing without the need for evaluation of all women with breast cancer,” Dr. Yadav and colleagues wrote.
Robert Pilarski, who was vice-chair of the panel that drew up the NCCN guidelines, said in an interview that the guideline authors tried to achieve a balance.
“We’ve known that NCCN misses cases and indications, but it comes down to whether the goal is to test all women with mutations or to have criteria that are a cost-effective and reasonable compromise to capture as many patients as possible,” said Mr. Pilarski, a licensed genetic counselor at the Ohio State University Wexner Medical Center in Columbus.
Current NCCN criteria for genetic/familial high-risk assessment for breast, ovarian, and pancreatic cancer recommend testing for individuals with blood relatives who have known or likely pathogenic variants, as well as patients with breast cancer diagnosed at age 45 or younger, patients aged 46-50 years with unknown or limited family history, patients with a second breast cancer diagnosed at any age, patients with triple-negative breast cancer diagnosed at age 60 or younger, and patients with breast cancer diagnosed at any age if they are of Ashkenazi Jewish ancestry.
But as Dr. Yadav and colleagues note, two recent studies (J Clin Oncol. 2019 Feb 20;37[6]:453-60; Ann Surg Oncol. 2018 Oct;25[10]:2925-31) suggested that up to 50% of germline pathogenic variants could be missed if testing were based solely on NCCN criteria.
Based on these findings, the American Society of Breast Surgeons issued a consensus guideline on genetic testing for hereditary breast cancer (Ann Surg Oncol. 2019 Oct;26[10]:3025-31), which states that, “genetic testing should be made available to all patients with a personal history of breast cancer.”
“Without question, if your goal is to identify everyone with a mutation, you’d have to test every cancer patient,” Mr. Pilarski said. “At this point, the ASBrS [American Society of Breast Surgeons] are the only group that have proposed that, and a lot of us feel that’s going too far at this point in time, and so the issue becomes what’s reasonable before that, and I think this paper is a great step forward.”
Cutting through the confusion
To see whether tweaking the existing guidelines could help clarify the issues surrounding genetic testing for breast cancer, Dr. Yadav and colleagues looked at a cohort of patients from the Mayo Clinic Breast Cancer Study. This prospective registry was open to all women evaluated at the Mayo Clinic Rochester for a first diagnosis of invasive breast cancer or ductal carcinoma in situ from May 2000 through May 2016.
The women were evaluated for germline pathogenic variants in nine breast cancer predisposition genes: ATM, BRCA1, BRCA2, CDH1, CHEK2, NF1, PALB2, PTEN, and TP53.
The researchers found that, of the 3,907 women in the sample, 1,872 (47.9%) would have been recommended for testing under the NCCN criteria, but the remaining 2,035 would not.
Women who met NCCN criteria were significantly more likely to carry a pathogenic variant (9% vs. 3.5%, P less than .001). However, 29.9% of women with pathogenic variants in the nine-gene panel and 13.1% of those with pathogenic variants in BRCA1 or BRCA2 did not qualify for testing by NCCN criteria.
The sensitivity of NCCN criteria was 70% for the nine-gene panel and 87% for BRCA 1 and BRCA 2, with a 53% specificity.
But if the criteria were expanded to include all women age 65 years and younger with a breast cancer diagnosis, the sensitivity for the nine-gene panel would increase to 92.1%, and the sensitivity for BRCA1 and BRCA2 only would climb to greater than 98.1%, with a specificity of approximately 22% for each test combination.
The authors acknowledged that they did not assess the cost-effectiveness of the testing criteria.
This study was supported by grants from the National Institutes of Health and the Breast Cancer Research Foundation. Authors disclosed relationships with Grail, bioTheranostics, Myriad Genetics, and other companies. Mr. Pilarski reported no conflicts of interest.
SOURCE: Yadav S et al. J Clin Oncol. 2020 Mar 3. doi: 10.1200/JCO.19.02190
Current National Comprehensive Cancer Network (NCCN) criteria may prevent genetic testing in “a substantial proportion” of women who carry germline pathogenic variants in breast cancer predisposition genes, according to investigators.
They found that, by expanding NCCN criteria to include germline genetic testing for all women diagnosed with breast cancer at age 65 or younger, the sensitivity of testing for nine well-established breast cancer predisposition genes would improve from 70% to more than 90%. The sensitivity for detection of BRCA1 and BRCA2 only would improve from 87% to greater than 98%.
Siddhartha Yadav, MD, of the Mayo Clinic, Rochester, Minn., and colleagues reported these findings in the Journal of Clinical Oncology.
“In a large unselected series of women with breast cancer, we demonstrate that expanding the NCCN testing criteria to include all women diagnosed with breast cancer at or before the age of 65 years has the potential to improve the sensitivity of germline genetic testing without the need for evaluation of all women with breast cancer,” Dr. Yadav and colleagues wrote.
Robert Pilarski, who was vice-chair of the panel that drew up the NCCN guidelines, said in an interview that the guideline authors tried to achieve a balance.
“We’ve known that NCCN misses cases and indications, but it comes down to whether the goal is to test all women with mutations or to have criteria that are a cost-effective and reasonable compromise to capture as many patients as possible,” said Mr. Pilarski, a licensed genetic counselor at the Ohio State University Wexner Medical Center in Columbus.
Current NCCN criteria for genetic/familial high-risk assessment for breast, ovarian, and pancreatic cancer recommend testing for individuals with blood relatives who have known or likely pathogenic variants, as well as patients with breast cancer diagnosed at age 45 or younger, patients aged 46-50 years with unknown or limited family history, patients with a second breast cancer diagnosed at any age, patients with triple-negative breast cancer diagnosed at age 60 or younger, and patients with breast cancer diagnosed at any age if they are of Ashkenazi Jewish ancestry.
But as Dr. Yadav and colleagues note, two recent studies (J Clin Oncol. 2019 Feb 20;37[6]:453-60; Ann Surg Oncol. 2018 Oct;25[10]:2925-31) suggested that up to 50% of germline pathogenic variants could be missed if testing were based solely on NCCN criteria.
Based on these findings, the American Society of Breast Surgeons issued a consensus guideline on genetic testing for hereditary breast cancer (Ann Surg Oncol. 2019 Oct;26[10]:3025-31), which states that, “genetic testing should be made available to all patients with a personal history of breast cancer.”
“Without question, if your goal is to identify everyone with a mutation, you’d have to test every cancer patient,” Mr. Pilarski said. “At this point, the ASBrS [American Society of Breast Surgeons] are the only group that have proposed that, and a lot of us feel that’s going too far at this point in time, and so the issue becomes what’s reasonable before that, and I think this paper is a great step forward.”
Cutting through the confusion
To see whether tweaking the existing guidelines could help clarify the issues surrounding genetic testing for breast cancer, Dr. Yadav and colleagues looked at a cohort of patients from the Mayo Clinic Breast Cancer Study. This prospective registry was open to all women evaluated at the Mayo Clinic Rochester for a first diagnosis of invasive breast cancer or ductal carcinoma in situ from May 2000 through May 2016.
The women were evaluated for germline pathogenic variants in nine breast cancer predisposition genes: ATM, BRCA1, BRCA2, CDH1, CHEK2, NF1, PALB2, PTEN, and TP53.
The researchers found that, of the 3,907 women in the sample, 1,872 (47.9%) would have been recommended for testing under the NCCN criteria, but the remaining 2,035 would not.
Women who met NCCN criteria were significantly more likely to carry a pathogenic variant (9% vs. 3.5%, P less than .001). However, 29.9% of women with pathogenic variants in the nine-gene panel and 13.1% of those with pathogenic variants in BRCA1 or BRCA2 did not qualify for testing by NCCN criteria.
The sensitivity of NCCN criteria was 70% for the nine-gene panel and 87% for BRCA 1 and BRCA 2, with a 53% specificity.
But if the criteria were expanded to include all women age 65 years and younger with a breast cancer diagnosis, the sensitivity for the nine-gene panel would increase to 92.1%, and the sensitivity for BRCA1 and BRCA2 only would climb to greater than 98.1%, with a specificity of approximately 22% for each test combination.
The authors acknowledged that they did not assess the cost-effectiveness of the testing criteria.
This study was supported by grants from the National Institutes of Health and the Breast Cancer Research Foundation. Authors disclosed relationships with Grail, bioTheranostics, Myriad Genetics, and other companies. Mr. Pilarski reported no conflicts of interest.
SOURCE: Yadav S et al. J Clin Oncol. 2020 Mar 3. doi: 10.1200/JCO.19.02190
FROM THE JOURNAL OF CLINICAL ONCOLOGY