User login
Helping families understand internalized racism
Ms. Jones brings her 15-year-old daughter, Angela, to the resident clinic. Angela is becoming increasingly anxious, withdrawn, and difficult to manage. As part of the initial interview, the resident, Dr. Sota, asks about the sociocultural background of the family. Ms. Jones is African American and recently began a relationship with a white man. Her daughter, Angela, is biracial; her biological father is white and has moved out of state with little ongoing contact with Angela and her mother.
At interview, Angela expresses a lot of anger at her mother, her biological father, and her new “stepfather.” Ms. Jones says: “I do not want Angela growing up as an ‘angry black woman.’ ” When asked for an explanation, she stated that she doesn’t want her daughter to be stereotyped, to be perceived as an angry black person. “She needs to fit in with our new life. She has lots of opportunities if only she would take them.”
Dr. Sota recognizes that Angela’s struggle, and perhaps also the struggle of Ms. Jones, has a component of internalized racism. How should Dr. Sota proceed? Dr. Sota puts herself in Angela’s shoes: How does Angela see herself? Angela has light brown skin, and
The term internalized racism (IR) first appeared in the 1980s. IR was compared to the oppression of black people in the 1800s: “The slavery that captures the mind and incarcerates the motivation, perception, aspiration, and identity in a web of anti-self images, generating a personal and collective self destruction, is more cruel than the shackles on the wrists and ankles.”1 According to Susanne Lipsky,2 IR “in African Americans manifests as internalizing stereotypes, mistrusting the self and other Blacks, and narrows one’s view of authentic Black culture.”
IR refers to the internalization and acceptance of the dominant white culture’s actions and beliefs, while rejecting one’s own cultural background. There is a long history of negative cultural representations of African Americans in popular American culture, and IR has a detrimental impact on the emotional well-being of African Americans.3
IR is associated with poorer metabolic health4 and psychological distress, depression and anxiety,5-8 and decreased self-esteem.9 However, protective processes can reduce one’s response to risk and can be developed through the psychotherapeutic relationship.
Interventions at an individual, family, or community levels
Angela: Tell me about yourself: What type of person are you? How do you identify? How do you feel about yourself/your appearance/your language?
Tell me about your friends/family? What interests do you have?
“Tell me more” questions can reveal conflicted feelings, etc., even if Angela does not answer. A good therapist can talk about IR; even if Angela does not bring it up, it is important for the therapist to find language suitable for the age of the patient.
Dr. Sota has some luck with Angela, who nods her head but says little. Dr. Sota then turns to Ms. Jones and asks whether she can answer these questions, too, and rephrases the questions for an adult. Interviewing parents in the presence of their children gives Dr. Sota and Angela an idea of what is permitted to talk about in the family.
A therapist can also note other permissions in the family: How do Angela and her mother use language? Do they claim or reject words and phrases such as “angry black woman” and choose, instead, to use language to “fit in” with the dominant white culture?
Dr. Sota notices that Ms. Jones presents herself as keen to fit in with her new future husband’s life. She wants Angela to do likewise. Dr. Sota notices that Angela vacillates between wanting to claim her black identity and having to navigate what that means in this family (not a good thing) – and wanting to assimilate into white culture. Her peers fall into two separate groups: a set of black friends and a set of white friends. Her mother prefers that she see her white friends, mistrusting her black friends.
Dr. Sota’s supervisor suggests that she introduce IR more forcefully because this seems to be a major course of conflict for Angela and encourage a frank discussion between mother and daughter. Dr. Sota starts the next session in the following way: “I noticed last week that the way you each identify yourselves is quite different. Ms. Jones, you want Angela to ‘fit in’ and perhaps just embrace white culture, whereas Angela, perhaps you vacillate between a white identity and a black identity?”
The following questions can help Dr. Sota elicit IR:
- What information about yourself would you like others to know – about your heritage, country of origin, family, class background, and so on?
- What makes you proud about being a member of this group, and what do you love about other members of this group?
- What has been hard about being a member of this group, and what don’t you like about others in this group?
- What were your early life experiences with people in this group? How were you treated? How did you feel about others in your group when you were young?
At a community level, family workshops support positive cultural identities that strengthen family functioning and reducing behavioral health risks. In a study of 575 urban American Indian (AI) families from diverse tribal backgrounds, the AI families who participated in such a workshop had significant increases in their ethnic identity, improved sense of spirituality, and a more positive cultural identification. The workshops provided culturally adaptive parenting interventions.10
IR is a serious determinant of both physical and mental health. Assessment of IR can be done using rating scales, such as the Nadanolitization Scale11 or the Internalized Racial Oppression Scale.12 IR also can also be assessed using a more formalized interview guide, such as the DSM-5 Cultural Formulation Interview (CFI).13 This 16-question interview guide helps behavioral health providers better understand the way service users and their social networks (e.g., families, friends) understand what is happening to them and why, as well as the barriers they experience, such as racism, discrimination, stigma, and financial stressors.
Individuals’ cultures and experiences have a profound impact on their understanding of their symptoms and their engagement in care. The American Psychiatric Association considers it to be part of mental health providers’ duty of care to engage all individuals in culturally relevant conversations about their past experiences and care expectations. More relevant, I submit that you cannot treat someone without having made this inquiry. A cultural assessment improves understanding but also shifts power relationships between providers and patients. The DSM-5 CFI and training guides are widely available and provide additional information for those who want to improve their cultural literacy.
Conclusion
Internalized racism is the component of racism that is the most difficult to discern. Psychiatrists and mental health professionals are uniquely poised to address IR, and any subsequent internal conflict and identity difficulties. Each program, office, and clinic can easily find the resources to do this through the APA. If you would like help providing education, contact me at alisonheru@gmail.com.
References
1. Akbar N. J Black Studies. 1984. doi: 10.11771002193478401400401.
2. Lipsky S. Internalized Racism. Seattle: Rational Island Publishers, 1987.
3. Williams DR and Mohammed SA. Am Behav Sci. 2013 May 8. doi: 10.1177/00027642134873340.
4. DeLilly CR and Flaskerud JH. Issues Ment Health Nurs. 2012 Nov;33(11):804-11.
5. Molina KM and James D. Group Process Intergroup Relat. 2016 Jul;19(4):439-61.
6. Szymanski D and Obiri O. Couns Psychologist. 2011;39(3):438-62.
7. Carter RT et al. J Multicul Couns Dev. 2017 Oct 5;45(4):232-59.
8. Mouzon DM and McLean JS. Ethn Health. 2017 Feb;22(1):36-48.
9. Szymanski DM and Gupta A. J Couns Psychol. 2009;56(1):110-18.
10. Kulis SS et al. Cultural Diversity and Ethnic Minority Psychol. 2019. doi: 10.1037/cpd000315.
11. Taylor J and Grundy C. “Measuring black internalization of white stereotypes about African Americans: The Nadanolization Scale.” In: Jones RL, ed. Handbook of Tests and Measurements of Black Populations. Hampton, Va.: Cobb & Henry, 1996.
12. Bailey T-K M et al. J Couns Psychol. 2011 Oct;58(4):481-93.
13. American Psychiatric Association. Cultural Formulation Interview. DSM-5. American Psychiatric Association Publishing: Arlington, Va. 2013.
Various aspects about the case described above have been changed to protect the clinician’s and patients’ identities. Thanks to the following individuals for their contributions to this article: Suzanne Huberty, MD, and Shiona Heru, JD.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (Routledge, 2013). She has no conflicts of interest to disclose.
Ms. Jones brings her 15-year-old daughter, Angela, to the resident clinic. Angela is becoming increasingly anxious, withdrawn, and difficult to manage. As part of the initial interview, the resident, Dr. Sota, asks about the sociocultural background of the family. Ms. Jones is African American and recently began a relationship with a white man. Her daughter, Angela, is biracial; her biological father is white and has moved out of state with little ongoing contact with Angela and her mother.
At interview, Angela expresses a lot of anger at her mother, her biological father, and her new “stepfather.” Ms. Jones says: “I do not want Angela growing up as an ‘angry black woman.’ ” When asked for an explanation, she stated that she doesn’t want her daughter to be stereotyped, to be perceived as an angry black person. “She needs to fit in with our new life. She has lots of opportunities if only she would take them.”
Dr. Sota recognizes that Angela’s struggle, and perhaps also the struggle of Ms. Jones, has a component of internalized racism. How should Dr. Sota proceed? Dr. Sota puts herself in Angela’s shoes: How does Angela see herself? Angela has light brown skin, and
The term internalized racism (IR) first appeared in the 1980s. IR was compared to the oppression of black people in the 1800s: “The slavery that captures the mind and incarcerates the motivation, perception, aspiration, and identity in a web of anti-self images, generating a personal and collective self destruction, is more cruel than the shackles on the wrists and ankles.”1 According to Susanne Lipsky,2 IR “in African Americans manifests as internalizing stereotypes, mistrusting the self and other Blacks, and narrows one’s view of authentic Black culture.”
IR refers to the internalization and acceptance of the dominant white culture’s actions and beliefs, while rejecting one’s own cultural background. There is a long history of negative cultural representations of African Americans in popular American culture, and IR has a detrimental impact on the emotional well-being of African Americans.3
IR is associated with poorer metabolic health4 and psychological distress, depression and anxiety,5-8 and decreased self-esteem.9 However, protective processes can reduce one’s response to risk and can be developed through the psychotherapeutic relationship.
Interventions at an individual, family, or community levels
Angela: Tell me about yourself: What type of person are you? How do you identify? How do you feel about yourself/your appearance/your language?
Tell me about your friends/family? What interests do you have?
“Tell me more” questions can reveal conflicted feelings, etc., even if Angela does not answer. A good therapist can talk about IR; even if Angela does not bring it up, it is important for the therapist to find language suitable for the age of the patient.
Dr. Sota has some luck with Angela, who nods her head but says little. Dr. Sota then turns to Ms. Jones and asks whether she can answer these questions, too, and rephrases the questions for an adult. Interviewing parents in the presence of their children gives Dr. Sota and Angela an idea of what is permitted to talk about in the family.
A therapist can also note other permissions in the family: How do Angela and her mother use language? Do they claim or reject words and phrases such as “angry black woman” and choose, instead, to use language to “fit in” with the dominant white culture?
Dr. Sota notices that Ms. Jones presents herself as keen to fit in with her new future husband’s life. She wants Angela to do likewise. Dr. Sota notices that Angela vacillates between wanting to claim her black identity and having to navigate what that means in this family (not a good thing) – and wanting to assimilate into white culture. Her peers fall into two separate groups: a set of black friends and a set of white friends. Her mother prefers that she see her white friends, mistrusting her black friends.
Dr. Sota’s supervisor suggests that she introduce IR more forcefully because this seems to be a major course of conflict for Angela and encourage a frank discussion between mother and daughter. Dr. Sota starts the next session in the following way: “I noticed last week that the way you each identify yourselves is quite different. Ms. Jones, you want Angela to ‘fit in’ and perhaps just embrace white culture, whereas Angela, perhaps you vacillate between a white identity and a black identity?”
The following questions can help Dr. Sota elicit IR:
- What information about yourself would you like others to know – about your heritage, country of origin, family, class background, and so on?
- What makes you proud about being a member of this group, and what do you love about other members of this group?
- What has been hard about being a member of this group, and what don’t you like about others in this group?
- What were your early life experiences with people in this group? How were you treated? How did you feel about others in your group when you were young?
At a community level, family workshops support positive cultural identities that strengthen family functioning and reducing behavioral health risks. In a study of 575 urban American Indian (AI) families from diverse tribal backgrounds, the AI families who participated in such a workshop had significant increases in their ethnic identity, improved sense of spirituality, and a more positive cultural identification. The workshops provided culturally adaptive parenting interventions.10
IR is a serious determinant of both physical and mental health. Assessment of IR can be done using rating scales, such as the Nadanolitization Scale11 or the Internalized Racial Oppression Scale.12 IR also can also be assessed using a more formalized interview guide, such as the DSM-5 Cultural Formulation Interview (CFI).13 This 16-question interview guide helps behavioral health providers better understand the way service users and their social networks (e.g., families, friends) understand what is happening to them and why, as well as the barriers they experience, such as racism, discrimination, stigma, and financial stressors.
Individuals’ cultures and experiences have a profound impact on their understanding of their symptoms and their engagement in care. The American Psychiatric Association considers it to be part of mental health providers’ duty of care to engage all individuals in culturally relevant conversations about their past experiences and care expectations. More relevant, I submit that you cannot treat someone without having made this inquiry. A cultural assessment improves understanding but also shifts power relationships between providers and patients. The DSM-5 CFI and training guides are widely available and provide additional information for those who want to improve their cultural literacy.
Conclusion
Internalized racism is the component of racism that is the most difficult to discern. Psychiatrists and mental health professionals are uniquely poised to address IR, and any subsequent internal conflict and identity difficulties. Each program, office, and clinic can easily find the resources to do this through the APA. If you would like help providing education, contact me at alisonheru@gmail.com.
References
1. Akbar N. J Black Studies. 1984. doi: 10.11771002193478401400401.
2. Lipsky S. Internalized Racism. Seattle: Rational Island Publishers, 1987.
3. Williams DR and Mohammed SA. Am Behav Sci. 2013 May 8. doi: 10.1177/00027642134873340.
4. DeLilly CR and Flaskerud JH. Issues Ment Health Nurs. 2012 Nov;33(11):804-11.
5. Molina KM and James D. Group Process Intergroup Relat. 2016 Jul;19(4):439-61.
6. Szymanski D and Obiri O. Couns Psychologist. 2011;39(3):438-62.
7. Carter RT et al. J Multicul Couns Dev. 2017 Oct 5;45(4):232-59.
8. Mouzon DM and McLean JS. Ethn Health. 2017 Feb;22(1):36-48.
9. Szymanski DM and Gupta A. J Couns Psychol. 2009;56(1):110-18.
10. Kulis SS et al. Cultural Diversity and Ethnic Minority Psychol. 2019. doi: 10.1037/cpd000315.
11. Taylor J and Grundy C. “Measuring black internalization of white stereotypes about African Americans: The Nadanolization Scale.” In: Jones RL, ed. Handbook of Tests and Measurements of Black Populations. Hampton, Va.: Cobb & Henry, 1996.
12. Bailey T-K M et al. J Couns Psychol. 2011 Oct;58(4):481-93.
13. American Psychiatric Association. Cultural Formulation Interview. DSM-5. American Psychiatric Association Publishing: Arlington, Va. 2013.
Various aspects about the case described above have been changed to protect the clinician’s and patients’ identities. Thanks to the following individuals for their contributions to this article: Suzanne Huberty, MD, and Shiona Heru, JD.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (Routledge, 2013). She has no conflicts of interest to disclose.
Ms. Jones brings her 15-year-old daughter, Angela, to the resident clinic. Angela is becoming increasingly anxious, withdrawn, and difficult to manage. As part of the initial interview, the resident, Dr. Sota, asks about the sociocultural background of the family. Ms. Jones is African American and recently began a relationship with a white man. Her daughter, Angela, is biracial; her biological father is white and has moved out of state with little ongoing contact with Angela and her mother.
At interview, Angela expresses a lot of anger at her mother, her biological father, and her new “stepfather.” Ms. Jones says: “I do not want Angela growing up as an ‘angry black woman.’ ” When asked for an explanation, she stated that she doesn’t want her daughter to be stereotyped, to be perceived as an angry black person. “She needs to fit in with our new life. She has lots of opportunities if only she would take them.”
Dr. Sota recognizes that Angela’s struggle, and perhaps also the struggle of Ms. Jones, has a component of internalized racism. How should Dr. Sota proceed? Dr. Sota puts herself in Angela’s shoes: How does Angela see herself? Angela has light brown skin, and
The term internalized racism (IR) first appeared in the 1980s. IR was compared to the oppression of black people in the 1800s: “The slavery that captures the mind and incarcerates the motivation, perception, aspiration, and identity in a web of anti-self images, generating a personal and collective self destruction, is more cruel than the shackles on the wrists and ankles.”1 According to Susanne Lipsky,2 IR “in African Americans manifests as internalizing stereotypes, mistrusting the self and other Blacks, and narrows one’s view of authentic Black culture.”
IR refers to the internalization and acceptance of the dominant white culture’s actions and beliefs, while rejecting one’s own cultural background. There is a long history of negative cultural representations of African Americans in popular American culture, and IR has a detrimental impact on the emotional well-being of African Americans.3
IR is associated with poorer metabolic health4 and psychological distress, depression and anxiety,5-8 and decreased self-esteem.9 However, protective processes can reduce one’s response to risk and can be developed through the psychotherapeutic relationship.
Interventions at an individual, family, or community levels
Angela: Tell me about yourself: What type of person are you? How do you identify? How do you feel about yourself/your appearance/your language?
Tell me about your friends/family? What interests do you have?
“Tell me more” questions can reveal conflicted feelings, etc., even if Angela does not answer. A good therapist can talk about IR; even if Angela does not bring it up, it is important for the therapist to find language suitable for the age of the patient.
Dr. Sota has some luck with Angela, who nods her head but says little. Dr. Sota then turns to Ms. Jones and asks whether she can answer these questions, too, and rephrases the questions for an adult. Interviewing parents in the presence of their children gives Dr. Sota and Angela an idea of what is permitted to talk about in the family.
A therapist can also note other permissions in the family: How do Angela and her mother use language? Do they claim or reject words and phrases such as “angry black woman” and choose, instead, to use language to “fit in” with the dominant white culture?
Dr. Sota notices that Ms. Jones presents herself as keen to fit in with her new future husband’s life. She wants Angela to do likewise. Dr. Sota notices that Angela vacillates between wanting to claim her black identity and having to navigate what that means in this family (not a good thing) – and wanting to assimilate into white culture. Her peers fall into two separate groups: a set of black friends and a set of white friends. Her mother prefers that she see her white friends, mistrusting her black friends.
Dr. Sota’s supervisor suggests that she introduce IR more forcefully because this seems to be a major course of conflict for Angela and encourage a frank discussion between mother and daughter. Dr. Sota starts the next session in the following way: “I noticed last week that the way you each identify yourselves is quite different. Ms. Jones, you want Angela to ‘fit in’ and perhaps just embrace white culture, whereas Angela, perhaps you vacillate between a white identity and a black identity?”
The following questions can help Dr. Sota elicit IR:
- What information about yourself would you like others to know – about your heritage, country of origin, family, class background, and so on?
- What makes you proud about being a member of this group, and what do you love about other members of this group?
- What has been hard about being a member of this group, and what don’t you like about others in this group?
- What were your early life experiences with people in this group? How were you treated? How did you feel about others in your group when you were young?
At a community level, family workshops support positive cultural identities that strengthen family functioning and reducing behavioral health risks. In a study of 575 urban American Indian (AI) families from diverse tribal backgrounds, the AI families who participated in such a workshop had significant increases in their ethnic identity, improved sense of spirituality, and a more positive cultural identification. The workshops provided culturally adaptive parenting interventions.10
IR is a serious determinant of both physical and mental health. Assessment of IR can be done using rating scales, such as the Nadanolitization Scale11 or the Internalized Racial Oppression Scale.12 IR also can also be assessed using a more formalized interview guide, such as the DSM-5 Cultural Formulation Interview (CFI).13 This 16-question interview guide helps behavioral health providers better understand the way service users and their social networks (e.g., families, friends) understand what is happening to them and why, as well as the barriers they experience, such as racism, discrimination, stigma, and financial stressors.
Individuals’ cultures and experiences have a profound impact on their understanding of their symptoms and their engagement in care. The American Psychiatric Association considers it to be part of mental health providers’ duty of care to engage all individuals in culturally relevant conversations about their past experiences and care expectations. More relevant, I submit that you cannot treat someone without having made this inquiry. A cultural assessment improves understanding but also shifts power relationships between providers and patients. The DSM-5 CFI and training guides are widely available and provide additional information for those who want to improve their cultural literacy.
Conclusion
Internalized racism is the component of racism that is the most difficult to discern. Psychiatrists and mental health professionals are uniquely poised to address IR, and any subsequent internal conflict and identity difficulties. Each program, office, and clinic can easily find the resources to do this through the APA. If you would like help providing education, contact me at alisonheru@gmail.com.
References
1. Akbar N. J Black Studies. 1984. doi: 10.11771002193478401400401.
2. Lipsky S. Internalized Racism. Seattle: Rational Island Publishers, 1987.
3. Williams DR and Mohammed SA. Am Behav Sci. 2013 May 8. doi: 10.1177/00027642134873340.
4. DeLilly CR and Flaskerud JH. Issues Ment Health Nurs. 2012 Nov;33(11):804-11.
5. Molina KM and James D. Group Process Intergroup Relat. 2016 Jul;19(4):439-61.
6. Szymanski D and Obiri O. Couns Psychologist. 2011;39(3):438-62.
7. Carter RT et al. J Multicul Couns Dev. 2017 Oct 5;45(4):232-59.
8. Mouzon DM and McLean JS. Ethn Health. 2017 Feb;22(1):36-48.
9. Szymanski DM and Gupta A. J Couns Psychol. 2009;56(1):110-18.
10. Kulis SS et al. Cultural Diversity and Ethnic Minority Psychol. 2019. doi: 10.1037/cpd000315.
11. Taylor J and Grundy C. “Measuring black internalization of white stereotypes about African Americans: The Nadanolization Scale.” In: Jones RL, ed. Handbook of Tests and Measurements of Black Populations. Hampton, Va.: Cobb & Henry, 1996.
12. Bailey T-K M et al. J Couns Psychol. 2011 Oct;58(4):481-93.
13. American Psychiatric Association. Cultural Formulation Interview. DSM-5. American Psychiatric Association Publishing: Arlington, Va. 2013.
Various aspects about the case described above have been changed to protect the clinician’s and patients’ identities. Thanks to the following individuals for their contributions to this article: Suzanne Huberty, MD, and Shiona Heru, JD.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (Routledge, 2013). She has no conflicts of interest to disclose.
Calculations of an academic hospitalist
The term “academic hospitalist” has come to mean more than a mere affiliation to an academic medical center (AMC). Academic hospitalists perform various clinical roles like staffing house staff teams, covering nonteaching services, critical care services, procedure teams, night services, medical consultation, and comanagement services.
Over the last decade, academic hospitalists have successfully managed many nonclinical roles in areas like research, medical unit leadership, faculty development, faculty affairs, quality, safety, informatics, utilization review, clinical documentation, throughput, group management, hospital administration, and educational leadership. The role of an academic hospital is as clear as a chocolate martini these days. Here we present some recent trends in academic hospital medicine.
Compensation
From SHM’s State of Hospital Medicine report (SoHM)2014 to 2018 data, the median compensation for U.S. academic hospitalists has risen by an average of 5.15% every year, although increases vary by rank.1 From 2016 to 2018, clinical instructors saw the most significant growth, 11.23% per year, suggesting a need to remain competitive for junior hospitalists. Compensation also varies by geographic area, with the Southern region reporting the highest compensation. Over the last decade, academic hospitalists received, on average, a 28%-35% lower salary, compared with community hospitalists.
Patient population and census
Lower patient encounters and compensation of the academic hospitalists poses the chicken or the egg dilemma. In the 2018 SoHM report, academic hospitalists had an average of 17% fewer encounters. Of note, AMC patients tend to have higher complexity, as measured by the Case Mix Index (CMI – the average diagnosis-related group weight of a hospital).2 A higher CMI is a surrogate marker for the diagnostic diversity, clinical complexity, and resource needs of the patient population in the hospital.
Productivity and financial metrics
The financial bottom line is a critical aspect, and as a report in the Journal of Hospital Medicine described, all health care executives look at business metrics while making decisions.3 Below are some significant academic and community comparisons from SoHM 2018.
- Collections, encounters, and wRVUs (work relative value units) were highly correlated. All of them were lower for academic hospitalists, corroborating the fact that they see a smaller number of patients. Clinical full-time equivalents (cFTE) is a vernacular of how much of the faculty time is devoted to clinical activities. The academic data from SoHM achieves the same target, as it is standardized to 100% billable clinical activity, so the fact that many academic hospitalists do not work a full-time clinical schedule is not a factor in their lower production.
- Charges had a smaller gap likely because of sicker patients in AMCs. The higher acuity difference can also explain 12% higher wRVU/encounter for academic hospitalists.
- The wRVU/encounter ratio can indicate a few patterns: high acuity of patients in AMCs, higher levels of evaluation and management documentation, or both. As the encounters and charges have the same percentage differences, we would place our bets on the former.
- Compensation per encounter and compensation per wRVU showed that academic hospitalists do get a slight advantage.
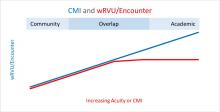
CMI and wRVUs
Although the SoHM does not capture information on patient acuity or CMI, we speculate that the relationship between CMI and wRVUs may be more or less linear at lower levels of acuity. However, once level III E/M billing is achieved (assuming there is no critical care provided), wRVUs/encounter plateau, even as acuity continues to increase. This plateau effect may be seen more often in high-acuity AMC settings than in community hospitals.
So, in our opinion, compensation models based solely on wRVU production would not do justice for hospitalists in AMC settings since these models would fail to capture the extra work involved with very-high-acuity patients. SoHM 2018 shows the financial support per wRVU for AMC is $45.81, and for the community is $41.28, an 11% difference. We think the higher financial support per wRVU for academic practices may be related to the lost wRVU potential of caring for very-high-acuity patients.
Conclusion
In an academic setting, hospitalists are reforming the field of hospital medicine and defining the ways we could deliver care. They are the pillars of collaboration, education, research, innovation, quality, and safety. It would be increasingly crucial for academic hospitalist leaders to use comparative metrics from SoHM to advocate for their group. The bottom line can be explained by the title of the qualitative study in JHM referenced above: “Collaboration, not calculation.”3
Dr. Chadha is division chief for the division of hospital medicine at the University of Kentucky Healthcare, Lexington. He actively leads efforts of recruiting, scheduling, practice analysis, and operation of the group. He is a first-time member of the practice analysis committee. Ms. Dede is division administrator for the division of hospital medicine at the University of Kentucky Healthcare. She prepares and manages budgets, liaisons with the downstream revenue teams, and contributes to the building of academic compensation models. She is serving in the practice administrators committee for the second year and is currently vice chair of the Executive Council for the Practice Administrators special interest group.
References
1. State of Hospital Medicine Report. https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/
2. Deloitte Center for Health Solutions. Academic Medical Centers: Joining forces with community providers for broad benefits and positive outcomes. 2015. https://www2.deloitte.com/us/en/pages/life-sciences-and-health-care/articles/academic-medical-centers-consolidation.html
3. White AA et al. Collaboration, not calculation: A qualitative study of how hospital executives value hospital medicine groups. J Hosp Med. 2019;14(10):662‐7.
The term “academic hospitalist” has come to mean more than a mere affiliation to an academic medical center (AMC). Academic hospitalists perform various clinical roles like staffing house staff teams, covering nonteaching services, critical care services, procedure teams, night services, medical consultation, and comanagement services.
Over the last decade, academic hospitalists have successfully managed many nonclinical roles in areas like research, medical unit leadership, faculty development, faculty affairs, quality, safety, informatics, utilization review, clinical documentation, throughput, group management, hospital administration, and educational leadership. The role of an academic hospital is as clear as a chocolate martini these days. Here we present some recent trends in academic hospital medicine.
Compensation
From SHM’s State of Hospital Medicine report (SoHM)2014 to 2018 data, the median compensation for U.S. academic hospitalists has risen by an average of 5.15% every year, although increases vary by rank.1 From 2016 to 2018, clinical instructors saw the most significant growth, 11.23% per year, suggesting a need to remain competitive for junior hospitalists. Compensation also varies by geographic area, with the Southern region reporting the highest compensation. Over the last decade, academic hospitalists received, on average, a 28%-35% lower salary, compared with community hospitalists.
Patient population and census
Lower patient encounters and compensation of the academic hospitalists poses the chicken or the egg dilemma. In the 2018 SoHM report, academic hospitalists had an average of 17% fewer encounters. Of note, AMC patients tend to have higher complexity, as measured by the Case Mix Index (CMI – the average diagnosis-related group weight of a hospital).2 A higher CMI is a surrogate marker for the diagnostic diversity, clinical complexity, and resource needs of the patient population in the hospital.
Productivity and financial metrics
The financial bottom line is a critical aspect, and as a report in the Journal of Hospital Medicine described, all health care executives look at business metrics while making decisions.3 Below are some significant academic and community comparisons from SoHM 2018.
- Collections, encounters, and wRVUs (work relative value units) were highly correlated. All of them were lower for academic hospitalists, corroborating the fact that they see a smaller number of patients. Clinical full-time equivalents (cFTE) is a vernacular of how much of the faculty time is devoted to clinical activities. The academic data from SoHM achieves the same target, as it is standardized to 100% billable clinical activity, so the fact that many academic hospitalists do not work a full-time clinical schedule is not a factor in their lower production.
- Charges had a smaller gap likely because of sicker patients in AMCs. The higher acuity difference can also explain 12% higher wRVU/encounter for academic hospitalists.
- The wRVU/encounter ratio can indicate a few patterns: high acuity of patients in AMCs, higher levels of evaluation and management documentation, or both. As the encounters and charges have the same percentage differences, we would place our bets on the former.
- Compensation per encounter and compensation per wRVU showed that academic hospitalists do get a slight advantage.
CMI and wRVUs
Although the SoHM does not capture information on patient acuity or CMI, we speculate that the relationship between CMI and wRVUs may be more or less linear at lower levels of acuity. However, once level III E/M billing is achieved (assuming there is no critical care provided), wRVUs/encounter plateau, even as acuity continues to increase. This plateau effect may be seen more often in high-acuity AMC settings than in community hospitals.
So, in our opinion, compensation models based solely on wRVU production would not do justice for hospitalists in AMC settings since these models would fail to capture the extra work involved with very-high-acuity patients. SoHM 2018 shows the financial support per wRVU for AMC is $45.81, and for the community is $41.28, an 11% difference. We think the higher financial support per wRVU for academic practices may be related to the lost wRVU potential of caring for very-high-acuity patients.
Conclusion
In an academic setting, hospitalists are reforming the field of hospital medicine and defining the ways we could deliver care. They are the pillars of collaboration, education, research, innovation, quality, and safety. It would be increasingly crucial for academic hospitalist leaders to use comparative metrics from SoHM to advocate for their group. The bottom line can be explained by the title of the qualitative study in JHM referenced above: “Collaboration, not calculation.”3
Dr. Chadha is division chief for the division of hospital medicine at the University of Kentucky Healthcare, Lexington. He actively leads efforts of recruiting, scheduling, practice analysis, and operation of the group. He is a first-time member of the practice analysis committee. Ms. Dede is division administrator for the division of hospital medicine at the University of Kentucky Healthcare. She prepares and manages budgets, liaisons with the downstream revenue teams, and contributes to the building of academic compensation models. She is serving in the practice administrators committee for the second year and is currently vice chair of the Executive Council for the Practice Administrators special interest group.
References
1. State of Hospital Medicine Report. https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/
2. Deloitte Center for Health Solutions. Academic Medical Centers: Joining forces with community providers for broad benefits and positive outcomes. 2015. https://www2.deloitte.com/us/en/pages/life-sciences-and-health-care/articles/academic-medical-centers-consolidation.html
3. White AA et al. Collaboration, not calculation: A qualitative study of how hospital executives value hospital medicine groups. J Hosp Med. 2019;14(10):662‐7.
The term “academic hospitalist” has come to mean more than a mere affiliation to an academic medical center (AMC). Academic hospitalists perform various clinical roles like staffing house staff teams, covering nonteaching services, critical care services, procedure teams, night services, medical consultation, and comanagement services.
Over the last decade, academic hospitalists have successfully managed many nonclinical roles in areas like research, medical unit leadership, faculty development, faculty affairs, quality, safety, informatics, utilization review, clinical documentation, throughput, group management, hospital administration, and educational leadership. The role of an academic hospital is as clear as a chocolate martini these days. Here we present some recent trends in academic hospital medicine.
Compensation
From SHM’s State of Hospital Medicine report (SoHM)2014 to 2018 data, the median compensation for U.S. academic hospitalists has risen by an average of 5.15% every year, although increases vary by rank.1 From 2016 to 2018, clinical instructors saw the most significant growth, 11.23% per year, suggesting a need to remain competitive for junior hospitalists. Compensation also varies by geographic area, with the Southern region reporting the highest compensation. Over the last decade, academic hospitalists received, on average, a 28%-35% lower salary, compared with community hospitalists.
Patient population and census
Lower patient encounters and compensation of the academic hospitalists poses the chicken or the egg dilemma. In the 2018 SoHM report, academic hospitalists had an average of 17% fewer encounters. Of note, AMC patients tend to have higher complexity, as measured by the Case Mix Index (CMI – the average diagnosis-related group weight of a hospital).2 A higher CMI is a surrogate marker for the diagnostic diversity, clinical complexity, and resource needs of the patient population in the hospital.
Productivity and financial metrics
The financial bottom line is a critical aspect, and as a report in the Journal of Hospital Medicine described, all health care executives look at business metrics while making decisions.3 Below are some significant academic and community comparisons from SoHM 2018.
- Collections, encounters, and wRVUs (work relative value units) were highly correlated. All of them were lower for academic hospitalists, corroborating the fact that they see a smaller number of patients. Clinical full-time equivalents (cFTE) is a vernacular of how much of the faculty time is devoted to clinical activities. The academic data from SoHM achieves the same target, as it is standardized to 100% billable clinical activity, so the fact that many academic hospitalists do not work a full-time clinical schedule is not a factor in their lower production.
- Charges had a smaller gap likely because of sicker patients in AMCs. The higher acuity difference can also explain 12% higher wRVU/encounter for academic hospitalists.
- The wRVU/encounter ratio can indicate a few patterns: high acuity of patients in AMCs, higher levels of evaluation and management documentation, or both. As the encounters and charges have the same percentage differences, we would place our bets on the former.
- Compensation per encounter and compensation per wRVU showed that academic hospitalists do get a slight advantage.
CMI and wRVUs
Although the SoHM does not capture information on patient acuity or CMI, we speculate that the relationship between CMI and wRVUs may be more or less linear at lower levels of acuity. However, once level III E/M billing is achieved (assuming there is no critical care provided), wRVUs/encounter plateau, even as acuity continues to increase. This plateau effect may be seen more often in high-acuity AMC settings than in community hospitals.
So, in our opinion, compensation models based solely on wRVU production would not do justice for hospitalists in AMC settings since these models would fail to capture the extra work involved with very-high-acuity patients. SoHM 2018 shows the financial support per wRVU for AMC is $45.81, and for the community is $41.28, an 11% difference. We think the higher financial support per wRVU for academic practices may be related to the lost wRVU potential of caring for very-high-acuity patients.
Conclusion
In an academic setting, hospitalists are reforming the field of hospital medicine and defining the ways we could deliver care. They are the pillars of collaboration, education, research, innovation, quality, and safety. It would be increasingly crucial for academic hospitalist leaders to use comparative metrics from SoHM to advocate for their group. The bottom line can be explained by the title of the qualitative study in JHM referenced above: “Collaboration, not calculation.”3
Dr. Chadha is division chief for the division of hospital medicine at the University of Kentucky Healthcare, Lexington. He actively leads efforts of recruiting, scheduling, practice analysis, and operation of the group. He is a first-time member of the practice analysis committee. Ms. Dede is division administrator for the division of hospital medicine at the University of Kentucky Healthcare. She prepares and manages budgets, liaisons with the downstream revenue teams, and contributes to the building of academic compensation models. She is serving in the practice administrators committee for the second year and is currently vice chair of the Executive Council for the Practice Administrators special interest group.
References
1. State of Hospital Medicine Report. https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/
2. Deloitte Center for Health Solutions. Academic Medical Centers: Joining forces with community providers for broad benefits and positive outcomes. 2015. https://www2.deloitte.com/us/en/pages/life-sciences-and-health-care/articles/academic-medical-centers-consolidation.html
3. White AA et al. Collaboration, not calculation: A qualitative study of how hospital executives value hospital medicine groups. J Hosp Med. 2019;14(10):662‐7.
As a black psychiatrist, she is ‘exhausted’ and ‘furious’
I didn’t have any doctors in my family. The only doctor I knew was my pediatrician. At 6 years old – and this gives you a glimpse into my personality – I told my parents I did not think he was a good doctor. I said, “When I grow up to be a doctor, I’m going to be a better doctor than him.” Fast forward to 7th grade, when I saw an orthopedic surgeon for my scoliosis. He was phenomenal. He listened. He explained to me all of the science and medicine and his rationale for decisions. I thought, “That is the kind of doctor I want to be.”
I went to medical school at Penn and didn’t think psychiatry was a medical specialty. I thought it was just Freud and laying on couches. I thought, “Where’s the science, where’s the physiology, where’s the genetics?” I was headed toward surgery.
Then, I rotated with an incredible psychiatrist. I saw behavior was biological, chemical, electrical, and physiological. I realize, looking back, that I had an interest because there is mental illness in my family. And there is so much stigma against psychiatric illnesses and addiction. It’s shocking how badly our patients get treated in the general medicine construct. So, I thought, “This field has science, the human body, activism, and marginalized patients? This is for me!”
I went to Howard University, which was the most freeing time of my life. There was no code-switching, no working hard to be a “presentable” Black person. When I started interviewing for medical schools, I was told by someone I interviewed with at one school that I should straighten my hair if I wanted to get accepted. I marked that school off my list. I decided right then that I would rather not go to medical school than straighten my hair to get into medical school. I went to Penn; they accepted me without my hair straight.
Penn Med was majorly White. There were six of us who were Black in a class of about 150 people. There was this feeling like “we let you in” even though every single one of us who was there was clearly at the top of the game to have been able to get there. I loved Penn Med. My class was amazing. I became the first Black president of medical student government there and I won a lot of awards.
When I was finishing up, my dean at the time, who was a White woman, said, “I’m so proud of you. You came in a piece of coal and look how we shined you up. “What do you say? I have a smart mouth, so I said, “I was already shiny when I got here.” She said, “See, that’s part of your problem, you don’t know how to take a compliment.” That was 2002, and I still remember every word of that conversation.
I was on the psychiatry unit rounding as a medical student and introduced myself to a patient. He said, “What’s your name?” And I thought, here it comes. I said, “Nzinga Ajabu,” my name at the time. He said “Nzinga? You probably have a spear in your closet.” When I tell these stories to White people, they’re always shocked. When I tell these stories to Black people, they say, “Yeah, that sounds about right.”
You can talk to Black medical students, Black interns, Black residents. When patients say something racist to you, nobody speaks up for you, nobody. It should be the attending that professionally approaches the patient and says something, anything. But they just laugh uncomfortably, they let it pass, they pretend they didn’t hear it. Meanwhile, you are fuming, and injured, and have to maintain your professionalism. It happens all the time. When people say, “Oh, you don’t look like a doctor,” I know what that means, but someone else may not even notice it’s an insult. When they do notice an insult, they don’t have the language or the courage to address it. And it’s not always a patient leveling racial insults. It very often is the attending, the fellow, the resident, or another medical student.
These things happen to me less now because I’m in a position of power. I’d say most insults that come my way now are overwhelmingly unintentional. I call people out on it 95% of the time. The other 5% of the time, I’m either exhausted, or I’m in some power structure where I decide it’s too risky. And those are the days – when I decide it’s too risky for me to speak up – when I come home exhausted. Because there will always be a power dynamic, as long as I’m alive, where you can’t speak up because you’re a Black woman, and that just wears me out.
Ultimately, I opted out of academic medicine because I thought it was too constraining, that I wouldn’t be able to raise my voice and do the activism I needed to do. – I’m able to advocate for people who are marginalized by medicine and, in treating addiction, advocate for people who are marginalized by psychiatry, which is marginalized by medicine.
A bias people have is that when you talk about Black people, they think you are talking about poor people. When we talk about police brutality, or being pulled over by the police, or dying in childbirth, our colleagues don’t think that’s happening to us. They think that’s happening to “those” Black people. Regardless of my socioeconomic status, I still have a higher chance of dying in childbirth or dying from COVID.
COVID had already turned my work up to 100 – we had staff losing loved ones and coming down with fevers themselves. And I had just launched my podcast. Then they killed Breonna Taylor, Ahmaud Arbery, Amy Cooper called the cops on Christian Cooper, and they killed George Floyd. This is how it happens. Bam. Bam. Bam.
The series of killings turned up my work at Physicians for Criminal Justice Reform, but it also turned up my work as a mother. My boys are 13 and 14. I personally can’t watch some of the videos because I see my own sons. I was already tired. Now I’m exhausted, I’m furious and I’m desperate to protect my kids. They have this on their backs already. Both of them have already had to deal with overt racism – they’ve had this burden since they were 5 years old, if not younger. I have to teach them to fight this war. Should that be how it is?
Nzinga Harrison, MD, 43, is a psychiatrist and the cofounder and chief medical officer of Eleanor Health, a network of physician clinics that treats people affected by addiction in North Carolina and New Jersey. She is also a cofounder of Physicians for Criminal Justice Reform. and host of the new podcast In Recovery. Harrison was raised in Indianapolis, went to college at Howard University and received her MD from the Perelman School of Medicine at the University of Pennsylvania in 2002. Her mother was an elementary school teacher. Her father, an electrical engineer, was commander of the local Black Panther Militia. Both supported her love of math and science and brought her with them to picket lines and marches.
This article first appeared on Medscape.com.
I didn’t have any doctors in my family. The only doctor I knew was my pediatrician. At 6 years old – and this gives you a glimpse into my personality – I told my parents I did not think he was a good doctor. I said, “When I grow up to be a doctor, I’m going to be a better doctor than him.” Fast forward to 7th grade, when I saw an orthopedic surgeon for my scoliosis. He was phenomenal. He listened. He explained to me all of the science and medicine and his rationale for decisions. I thought, “That is the kind of doctor I want to be.”
I went to medical school at Penn and didn’t think psychiatry was a medical specialty. I thought it was just Freud and laying on couches. I thought, “Where’s the science, where’s the physiology, where’s the genetics?” I was headed toward surgery.
Then, I rotated with an incredible psychiatrist. I saw behavior was biological, chemical, electrical, and physiological. I realize, looking back, that I had an interest because there is mental illness in my family. And there is so much stigma against psychiatric illnesses and addiction. It’s shocking how badly our patients get treated in the general medicine construct. So, I thought, “This field has science, the human body, activism, and marginalized patients? This is for me!”
I went to Howard University, which was the most freeing time of my life. There was no code-switching, no working hard to be a “presentable” Black person. When I started interviewing for medical schools, I was told by someone I interviewed with at one school that I should straighten my hair if I wanted to get accepted. I marked that school off my list. I decided right then that I would rather not go to medical school than straighten my hair to get into medical school. I went to Penn; they accepted me without my hair straight.
Penn Med was majorly White. There were six of us who were Black in a class of about 150 people. There was this feeling like “we let you in” even though every single one of us who was there was clearly at the top of the game to have been able to get there. I loved Penn Med. My class was amazing. I became the first Black president of medical student government there and I won a lot of awards.
When I was finishing up, my dean at the time, who was a White woman, said, “I’m so proud of you. You came in a piece of coal and look how we shined you up. “What do you say? I have a smart mouth, so I said, “I was already shiny when I got here.” She said, “See, that’s part of your problem, you don’t know how to take a compliment.” That was 2002, and I still remember every word of that conversation.
I was on the psychiatry unit rounding as a medical student and introduced myself to a patient. He said, “What’s your name?” And I thought, here it comes. I said, “Nzinga Ajabu,” my name at the time. He said “Nzinga? You probably have a spear in your closet.” When I tell these stories to White people, they’re always shocked. When I tell these stories to Black people, they say, “Yeah, that sounds about right.”
You can talk to Black medical students, Black interns, Black residents. When patients say something racist to you, nobody speaks up for you, nobody. It should be the attending that professionally approaches the patient and says something, anything. But they just laugh uncomfortably, they let it pass, they pretend they didn’t hear it. Meanwhile, you are fuming, and injured, and have to maintain your professionalism. It happens all the time. When people say, “Oh, you don’t look like a doctor,” I know what that means, but someone else may not even notice it’s an insult. When they do notice an insult, they don’t have the language or the courage to address it. And it’s not always a patient leveling racial insults. It very often is the attending, the fellow, the resident, or another medical student.
These things happen to me less now because I’m in a position of power. I’d say most insults that come my way now are overwhelmingly unintentional. I call people out on it 95% of the time. The other 5% of the time, I’m either exhausted, or I’m in some power structure where I decide it’s too risky. And those are the days – when I decide it’s too risky for me to speak up – when I come home exhausted. Because there will always be a power dynamic, as long as I’m alive, where you can’t speak up because you’re a Black woman, and that just wears me out.
Ultimately, I opted out of academic medicine because I thought it was too constraining, that I wouldn’t be able to raise my voice and do the activism I needed to do. – I’m able to advocate for people who are marginalized by medicine and, in treating addiction, advocate for people who are marginalized by psychiatry, which is marginalized by medicine.
A bias people have is that when you talk about Black people, they think you are talking about poor people. When we talk about police brutality, or being pulled over by the police, or dying in childbirth, our colleagues don’t think that’s happening to us. They think that’s happening to “those” Black people. Regardless of my socioeconomic status, I still have a higher chance of dying in childbirth or dying from COVID.
COVID had already turned my work up to 100 – we had staff losing loved ones and coming down with fevers themselves. And I had just launched my podcast. Then they killed Breonna Taylor, Ahmaud Arbery, Amy Cooper called the cops on Christian Cooper, and they killed George Floyd. This is how it happens. Bam. Bam. Bam.
The series of killings turned up my work at Physicians for Criminal Justice Reform, but it also turned up my work as a mother. My boys are 13 and 14. I personally can’t watch some of the videos because I see my own sons. I was already tired. Now I’m exhausted, I’m furious and I’m desperate to protect my kids. They have this on their backs already. Both of them have already had to deal with overt racism – they’ve had this burden since they were 5 years old, if not younger. I have to teach them to fight this war. Should that be how it is?
Nzinga Harrison, MD, 43, is a psychiatrist and the cofounder and chief medical officer of Eleanor Health, a network of physician clinics that treats people affected by addiction in North Carolina and New Jersey. She is also a cofounder of Physicians for Criminal Justice Reform. and host of the new podcast In Recovery. Harrison was raised in Indianapolis, went to college at Howard University and received her MD from the Perelman School of Medicine at the University of Pennsylvania in 2002. Her mother was an elementary school teacher. Her father, an electrical engineer, was commander of the local Black Panther Militia. Both supported her love of math and science and brought her with them to picket lines and marches.
This article first appeared on Medscape.com.
I didn’t have any doctors in my family. The only doctor I knew was my pediatrician. At 6 years old – and this gives you a glimpse into my personality – I told my parents I did not think he was a good doctor. I said, “When I grow up to be a doctor, I’m going to be a better doctor than him.” Fast forward to 7th grade, when I saw an orthopedic surgeon for my scoliosis. He was phenomenal. He listened. He explained to me all of the science and medicine and his rationale for decisions. I thought, “That is the kind of doctor I want to be.”
I went to medical school at Penn and didn’t think psychiatry was a medical specialty. I thought it was just Freud and laying on couches. I thought, “Where’s the science, where’s the physiology, where’s the genetics?” I was headed toward surgery.
Then, I rotated with an incredible psychiatrist. I saw behavior was biological, chemical, electrical, and physiological. I realize, looking back, that I had an interest because there is mental illness in my family. And there is so much stigma against psychiatric illnesses and addiction. It’s shocking how badly our patients get treated in the general medicine construct. So, I thought, “This field has science, the human body, activism, and marginalized patients? This is for me!”
I went to Howard University, which was the most freeing time of my life. There was no code-switching, no working hard to be a “presentable” Black person. When I started interviewing for medical schools, I was told by someone I interviewed with at one school that I should straighten my hair if I wanted to get accepted. I marked that school off my list. I decided right then that I would rather not go to medical school than straighten my hair to get into medical school. I went to Penn; they accepted me without my hair straight.
Penn Med was majorly White. There were six of us who were Black in a class of about 150 people. There was this feeling like “we let you in” even though every single one of us who was there was clearly at the top of the game to have been able to get there. I loved Penn Med. My class was amazing. I became the first Black president of medical student government there and I won a lot of awards.
When I was finishing up, my dean at the time, who was a White woman, said, “I’m so proud of you. You came in a piece of coal and look how we shined you up. “What do you say? I have a smart mouth, so I said, “I was already shiny when I got here.” She said, “See, that’s part of your problem, you don’t know how to take a compliment.” That was 2002, and I still remember every word of that conversation.
I was on the psychiatry unit rounding as a medical student and introduced myself to a patient. He said, “What’s your name?” And I thought, here it comes. I said, “Nzinga Ajabu,” my name at the time. He said “Nzinga? You probably have a spear in your closet.” When I tell these stories to White people, they’re always shocked. When I tell these stories to Black people, they say, “Yeah, that sounds about right.”
You can talk to Black medical students, Black interns, Black residents. When patients say something racist to you, nobody speaks up for you, nobody. It should be the attending that professionally approaches the patient and says something, anything. But they just laugh uncomfortably, they let it pass, they pretend they didn’t hear it. Meanwhile, you are fuming, and injured, and have to maintain your professionalism. It happens all the time. When people say, “Oh, you don’t look like a doctor,” I know what that means, but someone else may not even notice it’s an insult. When they do notice an insult, they don’t have the language or the courage to address it. And it’s not always a patient leveling racial insults. It very often is the attending, the fellow, the resident, or another medical student.
These things happen to me less now because I’m in a position of power. I’d say most insults that come my way now are overwhelmingly unintentional. I call people out on it 95% of the time. The other 5% of the time, I’m either exhausted, or I’m in some power structure where I decide it’s too risky. And those are the days – when I decide it’s too risky for me to speak up – when I come home exhausted. Because there will always be a power dynamic, as long as I’m alive, where you can’t speak up because you’re a Black woman, and that just wears me out.
Ultimately, I opted out of academic medicine because I thought it was too constraining, that I wouldn’t be able to raise my voice and do the activism I needed to do. – I’m able to advocate for people who are marginalized by medicine and, in treating addiction, advocate for people who are marginalized by psychiatry, which is marginalized by medicine.
A bias people have is that when you talk about Black people, they think you are talking about poor people. When we talk about police brutality, or being pulled over by the police, or dying in childbirth, our colleagues don’t think that’s happening to us. They think that’s happening to “those” Black people. Regardless of my socioeconomic status, I still have a higher chance of dying in childbirth or dying from COVID.
COVID had already turned my work up to 100 – we had staff losing loved ones and coming down with fevers themselves. And I had just launched my podcast. Then they killed Breonna Taylor, Ahmaud Arbery, Amy Cooper called the cops on Christian Cooper, and they killed George Floyd. This is how it happens. Bam. Bam. Bam.
The series of killings turned up my work at Physicians for Criminal Justice Reform, but it also turned up my work as a mother. My boys are 13 and 14. I personally can’t watch some of the videos because I see my own sons. I was already tired. Now I’m exhausted, I’m furious and I’m desperate to protect my kids. They have this on their backs already. Both of them have already had to deal with overt racism – they’ve had this burden since they were 5 years old, if not younger. I have to teach them to fight this war. Should that be how it is?
Nzinga Harrison, MD, 43, is a psychiatrist and the cofounder and chief medical officer of Eleanor Health, a network of physician clinics that treats people affected by addiction in North Carolina and New Jersey. She is also a cofounder of Physicians for Criminal Justice Reform. and host of the new podcast In Recovery. Harrison was raised in Indianapolis, went to college at Howard University and received her MD from the Perelman School of Medicine at the University of Pennsylvania in 2002. Her mother was an elementary school teacher. Her father, an electrical engineer, was commander of the local Black Panther Militia. Both supported her love of math and science and brought her with them to picket lines and marches.
This article first appeared on Medscape.com.
Medication-assisted treatment in corrections: A life-saving intervention
Opioid overdose deaths in the United States have more than tripled in recent years, from 6.1 deaths per 100,000 individuals in 1999 to 20.7 per 100,000 individuals in 2018.1 Although the availability of medication-assisted treatment (MAT) has expanded over the past decade, this lifesaving treatment remains largely inaccessible to some of the most vulnerable members of our communities: opioid users facing reentry after incarceration.
Just as abstinence in the community brings a loss of tolerance to opioids, individuals who are incarcerated lose tolerance as well. Clinicians who treat patients with opioid use disorders (OUD) are accustomed to warning patients about the risk of returning to prior levels of use too quickly. Harm reduction strategies include using slowly, using with friends, and having naloxone on hand to prevent unintended overdose.
The risks of opioid use are magnified for those facing reentry; incarceration contributes to a loss of employment, social supports, and connection to care. Those changes can create an exceptionally stressful reentry period – one that places individuals at an acutely high risk of relapse and overdose. Within the first 2 years of release, an individual with a history of incarceration has a risk of death 3.5 times higher than that of someone in the general population. Within the first 2 weeks, those recently incarcerated are 129 times more likely to overdose on opioids and 12.7 times more likely to die than members of the general population.2
Treatment with MAT dramatically reduces deaths during this crucial period. In England, large national studies have shown a similar 75% decrease in all-cause mortality within the first 4 weeks of release among individuals with OUD.4 In California, the counties with the highest overdose death rates are consistently those with fewer opioid treatment programs, which suggests that access to treatment is necessary to prolong the lives of those suffering from OUD.5 In-custody overdose deaths are quite rare, and access to MAT during incarceration has decreased in-custody deaths by 74%.6
Decreased opioid overdose deaths is not the only outcome of MAT. Pharmacotherapy for OUD also has been shown to increase treatment retention,7 reduce reincarceration,8 prevent communicable infections,9 and decrease use of other illicit substances.10 The provision of MAT also has been shown to be cost effective.11
Despite those benefits, as of 2017, only 30 out of 5,100 jails and prisons in the United States provided treatment with methadone or buprenorphine.12 When individuals on maintenance therapy are incarcerated, most correctional facilities force them to taper and discontinue those medications. This practice can cause distressing withdrawal symptoms and actively increase the risk of death for these individuals.
Concerns related to the provision of MAT, and specifically buprenorphine, in the correctional health setting often are related to diversion. Although safe administration of opioid full and partial agonists is a priority, recent literature has suggested that buprenorphine is not a medication frequently used for euphoric properties. In fact, the literature suggests that individuals using illicit buprenorphine primarily do so to treat withdrawal symptoms and that illicit use diminishes with access to formal treatment.13,14
Another concern is that pharmacotherapy for OUD should not be used without adjunctive psychotherapies and social supports. While dual pharmacotherapy and psychotherapy is ideal, the American Society for Addiction Medicine 2020 National Practice Guidelines for the treatment of OUD state: “a patient’s decision to decline psychosocial treatment or the absence of available psychosocial treatment should not preclude or delay pharmacotherapy, with appropriate medication management.”15 Just as some patients wish to engage in mutual help or psychotherapeutic modalities only, some patients wish to engage only in psychopharmacologic interventions. Declaring one modality of treatment better, or worse, or more worthwhile is not borne out by the literature and often places clinicians’ preferences over the preferences of patients.
Individuals who suffer from substance use disorders are at high risk of incarceration, relapse, and overdose death. These patients also suffer from stigmatization from peers and health care workers alike, making the process of engaging in care incredibly burdensome. Because of the disease of addiction, many of our patients cannot envision a healthy future: a future with the potential for intimate relationships, meaningful community engagement, and a rich inner life. The provision of MAT is lifesaving and improves the chances of a successful reentry – an intuitive first step in a long, but worthwhile, journey.
References
1. Hedegaard H et al; National Center for Health Statistics. Drug overdose deaths in the United States, 1999–2018. NCHS Data Brief, 2020 Jan, No. 356.
2. Binswanger IA et al. N Engl J Med. 2007;356:157-65.
3. Green TC et al. JAMA Psychiatry. 2018;75(4):405-7.
4. Marsden J et al. Addiction. 2017;112(8):1408-18.
5. Joshi V and Urada D. State Targeted Response to the Opioid Crisis: California Strategic Plan. 2017 Aug 30.
6. Larney S et al. BMJ Open. 2014. doi: 10.1136/bmjopen-2013-004666.
7. Rich JD et al. Lancet. 2015;386(9991):350-9.
8. Deck D et al. J Addict Dis. 2009. 28(2):89-102.
9. MacArthur GJ et al. BMJ. 2012. doi: 10.1136/bmj.e5945.
10. Tsui J et al. J Subst Abuse Treat. 2019. 109:80-5.
11. Gisev N et al. Addiction. 2015 Dec;110(12):1975-84.
12. National Mental Health and Substance Use Policy Laboratory. “Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings.” HHS Publication No. PEP19-MATUSECJS. Rockville, Md.: Substance Abuse and Mental Health Services Administration, 2019.
13. Bazazi AR et al. J Addict Med. 2011;5(3):175-80.
14. Schuman-Olivier Z. et al. J Subst Abuse Treat. 2010 Jul;39(1):41-50.
15. Crotty K et al. J Addict Med. 2020;14(2)99-112.
Dr. Barnes is chief resident at San Mateo County Behavioral Health and Recovery Services in California. He disclosed no relevant financial relationships. Dr. Lenane is resident* at San Mateo County Behavioral Health and Recovery Services. He disclosed no relevant financial relationships. The opinions shared in this article represent the viewpoints of the authors and are not necessarily representative of the viewpoints or policies of their academic program or employer.
*This article was updated 7/9/2020.
Opioid overdose deaths in the United States have more than tripled in recent years, from 6.1 deaths per 100,000 individuals in 1999 to 20.7 per 100,000 individuals in 2018.1 Although the availability of medication-assisted treatment (MAT) has expanded over the past decade, this lifesaving treatment remains largely inaccessible to some of the most vulnerable members of our communities: opioid users facing reentry after incarceration.
Just as abstinence in the community brings a loss of tolerance to opioids, individuals who are incarcerated lose tolerance as well. Clinicians who treat patients with opioid use disorders (OUD) are accustomed to warning patients about the risk of returning to prior levels of use too quickly. Harm reduction strategies include using slowly, using with friends, and having naloxone on hand to prevent unintended overdose.
The risks of opioid use are magnified for those facing reentry; incarceration contributes to a loss of employment, social supports, and connection to care. Those changes can create an exceptionally stressful reentry period – one that places individuals at an acutely high risk of relapse and overdose. Within the first 2 years of release, an individual with a history of incarceration has a risk of death 3.5 times higher than that of someone in the general population. Within the first 2 weeks, those recently incarcerated are 129 times more likely to overdose on opioids and 12.7 times more likely to die than members of the general population.2
Treatment with MAT dramatically reduces deaths during this crucial period. In England, large national studies have shown a similar 75% decrease in all-cause mortality within the first 4 weeks of release among individuals with OUD.4 In California, the counties with the highest overdose death rates are consistently those with fewer opioid treatment programs, which suggests that access to treatment is necessary to prolong the lives of those suffering from OUD.5 In-custody overdose deaths are quite rare, and access to MAT during incarceration has decreased in-custody deaths by 74%.6
Decreased opioid overdose deaths is not the only outcome of MAT. Pharmacotherapy for OUD also has been shown to increase treatment retention,7 reduce reincarceration,8 prevent communicable infections,9 and decrease use of other illicit substances.10 The provision of MAT also has been shown to be cost effective.11
Despite those benefits, as of 2017, only 30 out of 5,100 jails and prisons in the United States provided treatment with methadone or buprenorphine.12 When individuals on maintenance therapy are incarcerated, most correctional facilities force them to taper and discontinue those medications. This practice can cause distressing withdrawal symptoms and actively increase the risk of death for these individuals.
Concerns related to the provision of MAT, and specifically buprenorphine, in the correctional health setting often are related to diversion. Although safe administration of opioid full and partial agonists is a priority, recent literature has suggested that buprenorphine is not a medication frequently used for euphoric properties. In fact, the literature suggests that individuals using illicit buprenorphine primarily do so to treat withdrawal symptoms and that illicit use diminishes with access to formal treatment.13,14
Another concern is that pharmacotherapy for OUD should not be used without adjunctive psychotherapies and social supports. While dual pharmacotherapy and psychotherapy is ideal, the American Society for Addiction Medicine 2020 National Practice Guidelines for the treatment of OUD state: “a patient’s decision to decline psychosocial treatment or the absence of available psychosocial treatment should not preclude or delay pharmacotherapy, with appropriate medication management.”15 Just as some patients wish to engage in mutual help or psychotherapeutic modalities only, some patients wish to engage only in psychopharmacologic interventions. Declaring one modality of treatment better, or worse, or more worthwhile is not borne out by the literature and often places clinicians’ preferences over the preferences of patients.
Individuals who suffer from substance use disorders are at high risk of incarceration, relapse, and overdose death. These patients also suffer from stigmatization from peers and health care workers alike, making the process of engaging in care incredibly burdensome. Because of the disease of addiction, many of our patients cannot envision a healthy future: a future with the potential for intimate relationships, meaningful community engagement, and a rich inner life. The provision of MAT is lifesaving and improves the chances of a successful reentry – an intuitive first step in a long, but worthwhile, journey.
References
1. Hedegaard H et al; National Center for Health Statistics. Drug overdose deaths in the United States, 1999–2018. NCHS Data Brief, 2020 Jan, No. 356.
2. Binswanger IA et al. N Engl J Med. 2007;356:157-65.
3. Green TC et al. JAMA Psychiatry. 2018;75(4):405-7.
4. Marsden J et al. Addiction. 2017;112(8):1408-18.
5. Joshi V and Urada D. State Targeted Response to the Opioid Crisis: California Strategic Plan. 2017 Aug 30.
6. Larney S et al. BMJ Open. 2014. doi: 10.1136/bmjopen-2013-004666.
7. Rich JD et al. Lancet. 2015;386(9991):350-9.
8. Deck D et al. J Addict Dis. 2009. 28(2):89-102.
9. MacArthur GJ et al. BMJ. 2012. doi: 10.1136/bmj.e5945.
10. Tsui J et al. J Subst Abuse Treat. 2019. 109:80-5.
11. Gisev N et al. Addiction. 2015 Dec;110(12):1975-84.
12. National Mental Health and Substance Use Policy Laboratory. “Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings.” HHS Publication No. PEP19-MATUSECJS. Rockville, Md.: Substance Abuse and Mental Health Services Administration, 2019.
13. Bazazi AR et al. J Addict Med. 2011;5(3):175-80.
14. Schuman-Olivier Z. et al. J Subst Abuse Treat. 2010 Jul;39(1):41-50.
15. Crotty K et al. J Addict Med. 2020;14(2)99-112.
Dr. Barnes is chief resident at San Mateo County Behavioral Health and Recovery Services in California. He disclosed no relevant financial relationships. Dr. Lenane is resident* at San Mateo County Behavioral Health and Recovery Services. He disclosed no relevant financial relationships. The opinions shared in this article represent the viewpoints of the authors and are not necessarily representative of the viewpoints or policies of their academic program or employer.
*This article was updated 7/9/2020.
Opioid overdose deaths in the United States have more than tripled in recent years, from 6.1 deaths per 100,000 individuals in 1999 to 20.7 per 100,000 individuals in 2018.1 Although the availability of medication-assisted treatment (MAT) has expanded over the past decade, this lifesaving treatment remains largely inaccessible to some of the most vulnerable members of our communities: opioid users facing reentry after incarceration.
Just as abstinence in the community brings a loss of tolerance to opioids, individuals who are incarcerated lose tolerance as well. Clinicians who treat patients with opioid use disorders (OUD) are accustomed to warning patients about the risk of returning to prior levels of use too quickly. Harm reduction strategies include using slowly, using with friends, and having naloxone on hand to prevent unintended overdose.
The risks of opioid use are magnified for those facing reentry; incarceration contributes to a loss of employment, social supports, and connection to care. Those changes can create an exceptionally stressful reentry period – one that places individuals at an acutely high risk of relapse and overdose. Within the first 2 years of release, an individual with a history of incarceration has a risk of death 3.5 times higher than that of someone in the general population. Within the first 2 weeks, those recently incarcerated are 129 times more likely to overdose on opioids and 12.7 times more likely to die than members of the general population.2
Treatment with MAT dramatically reduces deaths during this crucial period. In England, large national studies have shown a similar 75% decrease in all-cause mortality within the first 4 weeks of release among individuals with OUD.4 In California, the counties with the highest overdose death rates are consistently those with fewer opioid treatment programs, which suggests that access to treatment is necessary to prolong the lives of those suffering from OUD.5 In-custody overdose deaths are quite rare, and access to MAT during incarceration has decreased in-custody deaths by 74%.6
Decreased opioid overdose deaths is not the only outcome of MAT. Pharmacotherapy for OUD also has been shown to increase treatment retention,7 reduce reincarceration,8 prevent communicable infections,9 and decrease use of other illicit substances.10 The provision of MAT also has been shown to be cost effective.11
Despite those benefits, as of 2017, only 30 out of 5,100 jails and prisons in the United States provided treatment with methadone or buprenorphine.12 When individuals on maintenance therapy are incarcerated, most correctional facilities force them to taper and discontinue those medications. This practice can cause distressing withdrawal symptoms and actively increase the risk of death for these individuals.
Concerns related to the provision of MAT, and specifically buprenorphine, in the correctional health setting often are related to diversion. Although safe administration of opioid full and partial agonists is a priority, recent literature has suggested that buprenorphine is not a medication frequently used for euphoric properties. In fact, the literature suggests that individuals using illicit buprenorphine primarily do so to treat withdrawal symptoms and that illicit use diminishes with access to formal treatment.13,14
Another concern is that pharmacotherapy for OUD should not be used without adjunctive psychotherapies and social supports. While dual pharmacotherapy and psychotherapy is ideal, the American Society for Addiction Medicine 2020 National Practice Guidelines for the treatment of OUD state: “a patient’s decision to decline psychosocial treatment or the absence of available psychosocial treatment should not preclude or delay pharmacotherapy, with appropriate medication management.”15 Just as some patients wish to engage in mutual help or psychotherapeutic modalities only, some patients wish to engage only in psychopharmacologic interventions. Declaring one modality of treatment better, or worse, or more worthwhile is not borne out by the literature and often places clinicians’ preferences over the preferences of patients.
Individuals who suffer from substance use disorders are at high risk of incarceration, relapse, and overdose death. These patients also suffer from stigmatization from peers and health care workers alike, making the process of engaging in care incredibly burdensome. Because of the disease of addiction, many of our patients cannot envision a healthy future: a future with the potential for intimate relationships, meaningful community engagement, and a rich inner life. The provision of MAT is lifesaving and improves the chances of a successful reentry – an intuitive first step in a long, but worthwhile, journey.
References
1. Hedegaard H et al; National Center for Health Statistics. Drug overdose deaths in the United States, 1999–2018. NCHS Data Brief, 2020 Jan, No. 356.
2. Binswanger IA et al. N Engl J Med. 2007;356:157-65.
3. Green TC et al. JAMA Psychiatry. 2018;75(4):405-7.
4. Marsden J et al. Addiction. 2017;112(8):1408-18.
5. Joshi V and Urada D. State Targeted Response to the Opioid Crisis: California Strategic Plan. 2017 Aug 30.
6. Larney S et al. BMJ Open. 2014. doi: 10.1136/bmjopen-2013-004666.
7. Rich JD et al. Lancet. 2015;386(9991):350-9.
8. Deck D et al. J Addict Dis. 2009. 28(2):89-102.
9. MacArthur GJ et al. BMJ. 2012. doi: 10.1136/bmj.e5945.
10. Tsui J et al. J Subst Abuse Treat. 2019. 109:80-5.
11. Gisev N et al. Addiction. 2015 Dec;110(12):1975-84.
12. National Mental Health and Substance Use Policy Laboratory. “Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings.” HHS Publication No. PEP19-MATUSECJS. Rockville, Md.: Substance Abuse and Mental Health Services Administration, 2019.
13. Bazazi AR et al. J Addict Med. 2011;5(3):175-80.
14. Schuman-Olivier Z. et al. J Subst Abuse Treat. 2010 Jul;39(1):41-50.
15. Crotty K et al. J Addict Med. 2020;14(2)99-112.
Dr. Barnes is chief resident at San Mateo County Behavioral Health and Recovery Services in California. He disclosed no relevant financial relationships. Dr. Lenane is resident* at San Mateo County Behavioral Health and Recovery Services. He disclosed no relevant financial relationships. The opinions shared in this article represent the viewpoints of the authors and are not necessarily representative of the viewpoints or policies of their academic program or employer.
*This article was updated 7/9/2020.
International medical graduates facing challenges amid COVID-19
International medical graduates (IMGs) constitute more than 24% of the total percentage of active physicians, 30% of active psychiatrists, and 33% of psychiatry residents in the United States.1 IMGs serve in various medical specialties and provide medical care to socioeconomically disadvantaged patients in underserved communities.2 Evidence suggests that patient outcomes among elderly patients admitted in U.S. hospitals for those treated by IMGs were on par with outcomes of U.S. graduates. Moreover, patients who were treated by IMGs had a lower mortality rates.3
IMGs trained in the United States make considerable contributions to psychiatry and have been very successful as educators, researchers, and leaders. Over the last 3 decades, for example, three American Psychiatric Association (APA) presidents and one past president of the American Academy of Child and Adolescent Psychiatry were IMGs. Many of them also hold department chair positions at many academic institutions.4,5
In short, IMGs are an important part of the U.S. health care system – particularly in psychiatry.
In addition to participating in psychiatry residency programs, IMG physicians are heavily represented in subspecialties, including geriatric psychiatry (45%), addiction psychiatry (42%), child and adolescent psychiatry (36%), psychosomatic medicine (32%), and forensic psychiatry (25%).6 IMG trainees face multiple challenges that begin as they transition to psychiatry residency in the United States, including understanding the American health care system, electronic medical records and documentation, and evidence-based medicine. In addition, they need to adapt to cultural changes, and work on language barriers, communication skills, and social isolation.7,8 Training programs account for these challenges and proactively take essential steps to facilitate the transition of IMGs into the U.S. system.9,10
As training programs prepare for the new academic year starting from July 2020 and continue to provide educational experiences to current trainees, the COVID-19 pandemic has brought additional challenges for the training programs. The gravity of the novel coronavirus pandemic continues to deepen, causing immense fear and uncertainty globally. An APA poll of more than 1,000 adults conducted early in the pandemic showed that about 40% of Americans were anxious about becoming seriously ill or dying with COVID-19. Nearly half of the respondents (48%) were anxious about the possibility of getting COVID-19, and even more (62%) were anxious about the possibility of their loved ones getting infected by this virus. Also, one-third of Americans reported a serious impact on their mental health.
Furthermore, the ailing economy and increasing unemployment are raising financial concerns for individuals and families. This pandemic also has had an impact on our patients’ sleep hygiene, relationships with their loved ones, and consumption of alcohol or other drugs/substances.11 Deteriorating mental health raises concerns about increased suicide risk as a secondary consequence.12
Physicians and other frontline teams who are taking care of these patients and their families continue to provide unexcelled, compassionate care in these unprecedented times. Selfless care continues despite awareness of the high probability of getting exposed to the virus and spreading it further to family members. Physicians involved in direct patient care for COVID-19 patients are at high risk for demoralization, burnout, depression, and anxiety.13
Struggles experienced by IMGs
On the personal front, IMGs often struggle with multiple stressors, such as lack of social support, ethnic-minority prejudice, and the need to understand financial structures such as mortgages in the new countries even after extended periods of residence.14 This virus has killed many health care professionals, including physicians around the world. There was a report of suicide by an emergency medicine physician who was treating patients with COVID-19 and ended up contracting the virus. That news was devastating and overwhelming for everyone, especially health care clinicians. It also adds to the stress and worries of IMGs who are still on nonimmigrant visas.
Bigger concerns exist if there is a demise of a nonimmigrant IMG and the implications of that loss for dependent families – who might face deportation. Even for those who were recently granted permanent residency status, worries about limited support systems and financial hardships to their families can be stressors.
Also, a large number of IMGs represent the geographical area where the pandemic began. Fortunately, the World Health Organization has taken a firm stance against possible discrimination by calling for global solidarity in these times. Furthermore, the WHO has emphasized the importance of referring to the disease caused by SARS-CoV-2 as “COVID-19” only – and not by the name of a particular country or city.15 Despite those official positions, people continue to express racially discriminatory opinions related to the virus, and those comments are not only disturbing to IMGs, they also are demoralizing.
Travel restrictions
In addition to the worries that IMGs might have about their own health and that of their families residing with them, the well-being of their extended families, including their aging parents back in their countries of origin, is unsettling as well. It is even more unnerving during the pandemic because the Centers for Disease Control and Prevention and the State Department advised avoiding all international travel at this time. Under these circumstances, IMGs are concerned about travel to their countries of origin in the event of a family emergency and the quarantine protocols in place, at both the country of origin and at residences.
Immigration issues
The U.S. administration temporarily suspended all immigration for 60 days, starting from April 2020. Recently, an executive order was signed suspending entry in the country on several visas, including the J-1 and the H1-B. Those are two categories that allow physicians to train and work in the United States.
IMGs in the United States reside and practice here under different types of immigrant and nonimmigrant visas (J-1, H1-B). This year, the Match results coincided with the timeline of those new immigration restrictions. Many IMGs are currently in the process of renewing their H1-B visas. They are worried because their visas will expire in the coming months. During the pandemic, U.S. Citizenship and Immigration Services suspended routine visa services and premium processing for visa renewals. This halt led to a delay in visa processing for graduating residents in June and practicing physicians seeking visa renewal. Those delays add to personal stress, and furthermore, distract these immigrant physicians from fighting this pandemic.
Another complication is that rules for J-1 visa holders have changed so that trainees must return to their countries of origin for at least 2 years after completing their training. If they decide to continue practicing medicine in the United States, they need a specific type of J-1 waiver and must gain a pathway to be a lawful permanent resident (Green Card). Many IMGs who are on waiver positions might not be able to treat patients ailing from COVID-19 to the full extent because waivers restrict them to practicing only in certain identified health systems.
IMGs who are coming from a country such India have to wait for more than 11 years after completing their accredited training to get permanent residency because of backlog for the permanent residency process.16 While waiting for a Green Card, they must continue to work on an H1-B visa, which requires periodic renewal.
Potential impact on training
Non-U.S. citizen IMGs accounted for 13% of the total of first-year positions in the 2020 Match. They will start medical training in residency programs in the United States in the coming months. The numbers for psychiatry residency matches are higher; about 16% of total first-year positions are filled by non-U.S. IMGs.17 At this time, when they should be celebrating their successful Match after many years of hard work and persistence, there is increased anxiety. They wonder whether they will be able to enter the United States to begin their training program on time. Their concerns are multifold, but the main concern is related to uncertainties around getting visas on time. With the recent executive order in place, physicians only working actively with COVID-19 patients will be able to enter the country on visas. As mental health concerns continue to rise during these times, incoming residents might not be able to start training if they are out of the country.
Furthermore, because of travel/air restrictions, there are worries about whether physicians will be able to get flights to the United States, given the lockdown in many countries around the world. Conversely, IMGs who will be graduating from residency and fellowship programs this summer and have accepted new positions also are dealing with similar uncertainty. Their new jobs will require visa processing, and the current scenario provides limited insight, so far, about whether they will be able to start their respective jobs or whether they will have to return to their home countries until their visa processing is completed.
The American Medical Association has advised the Secretary of State and acting Secretary of Homeland Security to expedite physician workforce expansion in an effort to meet the growing need for health care services during this pandemic.18 It is encouraging that, recently, the State Department declared that visa processing will continue for medical professionals and that cases would be expedited for those who meet the criteria. However, the requirement for in-person interviews remains for individuals who are seeking a U.S. visa outside the country.
As residency programs are trying their best to continue to provide educational experiences to trainees during this phase, if psychiatry residents are placed on quarantine because of either getting exposed or contracting the illness, there is a possibility that they might need to extend their training. This would bring another challenge for IMGs, requiring them to extend their visas to complete their training. Future J-1 waiver jobs could be compromised.
Investment in physician wellness critical
Psychiatrists, along with other health care workers, are front-line soldiers in the fight against COVID-19. All physicians are at high risk for demoralization, burnout, depression, anxiety, and suicide. It is of utmost importance that we invest immediately in physicians’ wellness. As noted, significant numbers of psychiatrists are IMGs who are dealing with additional challenges while responding to the pandemic. There are certain challenges for IMGs, such as the well-being of their extended families in other countries, and travel bans put in place because of the pandemic. Those issues are not easy to resolve. However, addressing visa issues and providing support to their families in the event that something happens to physicians during the pandemic would be reassuring and would help alleviate additional stress. Those kinds of actions also would allow immigrant physicians to focus on clinical work and to improve their overall well-being. Given the health risks and numerous other insecurities that go along with living amid a pandemic, IMGs should not have the additional pressure of visa uncertainty.
Public health crises such as COVID-19 are associated with increased rates of anxiety,19 depression,20 illicit substance use,21 and an increased rate of suicide.22 Patients with serious mental illness might be among the hardest hit both physically and mentally during the pandemic.23 Even in the absence of a pandemic, there is already a shortage of psychiatrists at the national level, and it is expected that this shortage will grow in the future. Rural and underserved areas are expected to experience the physician deficit more acutely.24
The pandemic is likely to resolve gradually and unpredictably – and might recur along the way over the next 1-2 years. However, the psychiatrist shortage will escalate more, as the mental health needs in the United States increase further in coming months. We need psychiatrists now more than ever, and it will be crucial that prospective residents, graduating residents, and fellows are able to come on board to join the American health care system promptly. In addition to national-level interventions, residency programs, potential employers, and communities must be aware of and do whatever they can to address the challenges faced by IMGs during these times.
Dr. Raman Baweja is affiliated with the department of psychiatry and behavioral health at Penn State University, Hershey. He has no conflicts of interest. Dr. Verma is affiliated with Rogers Behavioral Health in Kenosha County, Wis., and the department of psychiatry and behavioral health at Rosalind Franklin University of Medicine and Science in North Chicago. She has no conflicts of interest. Dr. Ritika Baweja is affiliated with the department of psychiatry and behavioral health at Penn State. Dr. Ritika Baweja is the spouse of Dr. Raman Baweja. Dr. Adam is affiliated with the department of psychiatry at the University of Missouri, Columbia.
References
1. American Psychiatric Association. Navigating psychiatry residency in the United States. A Guide for IMG Physicians.
2. Berg S. 5 IMG physicians who speak up for patients and fellow doctors. American Medical Association. 2019 Oct 22.
3. Tsugawa Y et al. BMJ. 2017 Feb 3;256. doi: 10.1136/bmj.j273.
4. Gogineni RR et al. Child Adolesc Psychiatr Clin N Am. 2010 Oct 1;19(4):833-53.
5. Majeed MH et al. Academic Psychiatry. 2017 Dec 1;41(6):849-51.
6. Brotherton SE and Etzel SI. JAMA. 2018 Sep 11;320(10):1051-70.
7. Sockalingam S et al. Acad Psychiatry. 2012 Jul 1;36(4):277-81.
8. Singareddy R et al. Acad Psychiatry. 2008 Jul-Aug;32(4):343-4.
9. Kramer MN. Acad Psychiatry. 2005 Jul-Aug;29(3):322-4.
10. Rao NR and Kotapati VP. Pathways for success in academic medicine for an international medical graduate: Challenges and opportunities. In “Roberts Academic Medicine Handbook” 2020. Springer:163-70.
11. American Psychiatric Association. New poll: COVID-19 impacting mental well-being: Americans feeling anxious, especially for loved ones; older adults are less anxious. 2020 Mar 25.
12. Reger MA et al. JAMA Psychiatry. 2020 Apr 10. doi: 10.1001/jamapsychiatry.2020.1060.
13. Lai J et al. JAMA Netw Open. 2020 Mar 23;3(3):e203976-e203976. doi: 10.1001/jamanetworkopen.2020.3976.
14. Kalra G et al. Acad Psychiatry. 2012 Jul;36(4):323-9.
15. WHO best practices for the naming of new human infectious diseases. World Health Organization. 2015.
16. U.S. Department of State. Bureau of Consular Affairs. Visa Bulletin for March 2020.
17. National Resident Matching Program® (NRMP®). Thousands of medical students and graduates celebrate NRMP Match results.
18. American Medical Association. AMA: U.S. should open visas to international physicians amid COVID-19. AMA press release. 2020 Mar 25.
19. McKay D et al. J Anxiety Disord. 2020 Jun;73:02233. doi: 10.1016/j.janxdis.2020.102233.
20. Tang W et al. J Affect Disord. 2020 May 13;274:1-7.
21. Collins F et al. NIH Director’s Blog. NIH.gov. 2020 Apr 21.
22. Reger M et al. JAMA Psychiatry. 2020 Apr 10. doi: 10.1001/jamapsychiatry.2020.1060.
23. Druss BG. JAMA Psychiatry. 2020 Apr 3. doi: 10.1001/jamapsychiatry.2020.0894.
24. American Association of Medical Colleges. “The complexities of physician supply and demand: Projections from 2018-2033.” 2020 Jun.
International medical graduates (IMGs) constitute more than 24% of the total percentage of active physicians, 30% of active psychiatrists, and 33% of psychiatry residents in the United States.1 IMGs serve in various medical specialties and provide medical care to socioeconomically disadvantaged patients in underserved communities.2 Evidence suggests that patient outcomes among elderly patients admitted in U.S. hospitals for those treated by IMGs were on par with outcomes of U.S. graduates. Moreover, patients who were treated by IMGs had a lower mortality rates.3
IMGs trained in the United States make considerable contributions to psychiatry and have been very successful as educators, researchers, and leaders. Over the last 3 decades, for example, three American Psychiatric Association (APA) presidents and one past president of the American Academy of Child and Adolescent Psychiatry were IMGs. Many of them also hold department chair positions at many academic institutions.4,5
In short, IMGs are an important part of the U.S. health care system – particularly in psychiatry.
In addition to participating in psychiatry residency programs, IMG physicians are heavily represented in subspecialties, including geriatric psychiatry (45%), addiction psychiatry (42%), child and adolescent psychiatry (36%), psychosomatic medicine (32%), and forensic psychiatry (25%).6 IMG trainees face multiple challenges that begin as they transition to psychiatry residency in the United States, including understanding the American health care system, electronic medical records and documentation, and evidence-based medicine. In addition, they need to adapt to cultural changes, and work on language barriers, communication skills, and social isolation.7,8 Training programs account for these challenges and proactively take essential steps to facilitate the transition of IMGs into the U.S. system.9,10
As training programs prepare for the new academic year starting from July 2020 and continue to provide educational experiences to current trainees, the COVID-19 pandemic has brought additional challenges for the training programs. The gravity of the novel coronavirus pandemic continues to deepen, causing immense fear and uncertainty globally. An APA poll of more than 1,000 adults conducted early in the pandemic showed that about 40% of Americans were anxious about becoming seriously ill or dying with COVID-19. Nearly half of the respondents (48%) were anxious about the possibility of getting COVID-19, and even more (62%) were anxious about the possibility of their loved ones getting infected by this virus. Also, one-third of Americans reported a serious impact on their mental health.
Furthermore, the ailing economy and increasing unemployment are raising financial concerns for individuals and families. This pandemic also has had an impact on our patients’ sleep hygiene, relationships with their loved ones, and consumption of alcohol or other drugs/substances.11 Deteriorating mental health raises concerns about increased suicide risk as a secondary consequence.12
Physicians and other frontline teams who are taking care of these patients and their families continue to provide unexcelled, compassionate care in these unprecedented times. Selfless care continues despite awareness of the high probability of getting exposed to the virus and spreading it further to family members. Physicians involved in direct patient care for COVID-19 patients are at high risk for demoralization, burnout, depression, and anxiety.13
Struggles experienced by IMGs
On the personal front, IMGs often struggle with multiple stressors, such as lack of social support, ethnic-minority prejudice, and the need to understand financial structures such as mortgages in the new countries even after extended periods of residence.14 This virus has killed many health care professionals, including physicians around the world. There was a report of suicide by an emergency medicine physician who was treating patients with COVID-19 and ended up contracting the virus. That news was devastating and overwhelming for everyone, especially health care clinicians. It also adds to the stress and worries of IMGs who are still on nonimmigrant visas.
Bigger concerns exist if there is a demise of a nonimmigrant IMG and the implications of that loss for dependent families – who might face deportation. Even for those who were recently granted permanent residency status, worries about limited support systems and financial hardships to their families can be stressors.
Also, a large number of IMGs represent the geographical area where the pandemic began. Fortunately, the World Health Organization has taken a firm stance against possible discrimination by calling for global solidarity in these times. Furthermore, the WHO has emphasized the importance of referring to the disease caused by SARS-CoV-2 as “COVID-19” only – and not by the name of a particular country or city.15 Despite those official positions, people continue to express racially discriminatory opinions related to the virus, and those comments are not only disturbing to IMGs, they also are demoralizing.
Travel restrictions
In addition to the worries that IMGs might have about their own health and that of their families residing with them, the well-being of their extended families, including their aging parents back in their countries of origin, is unsettling as well. It is even more unnerving during the pandemic because the Centers for Disease Control and Prevention and the State Department advised avoiding all international travel at this time. Under these circumstances, IMGs are concerned about travel to their countries of origin in the event of a family emergency and the quarantine protocols in place, at both the country of origin and at residences.
Immigration issues
The U.S. administration temporarily suspended all immigration for 60 days, starting from April 2020. Recently, an executive order was signed suspending entry in the country on several visas, including the J-1 and the H1-B. Those are two categories that allow physicians to train and work in the United States.
IMGs in the United States reside and practice here under different types of immigrant and nonimmigrant visas (J-1, H1-B). This year, the Match results coincided with the timeline of those new immigration restrictions. Many IMGs are currently in the process of renewing their H1-B visas. They are worried because their visas will expire in the coming months. During the pandemic, U.S. Citizenship and Immigration Services suspended routine visa services and premium processing for visa renewals. This halt led to a delay in visa processing for graduating residents in June and practicing physicians seeking visa renewal. Those delays add to personal stress, and furthermore, distract these immigrant physicians from fighting this pandemic.
Another complication is that rules for J-1 visa holders have changed so that trainees must return to their countries of origin for at least 2 years after completing their training. If they decide to continue practicing medicine in the United States, they need a specific type of J-1 waiver and must gain a pathway to be a lawful permanent resident (Green Card). Many IMGs who are on waiver positions might not be able to treat patients ailing from COVID-19 to the full extent because waivers restrict them to practicing only in certain identified health systems.
IMGs who are coming from a country such India have to wait for more than 11 years after completing their accredited training to get permanent residency because of backlog for the permanent residency process.16 While waiting for a Green Card, they must continue to work on an H1-B visa, which requires periodic renewal.
Potential impact on training
Non-U.S. citizen IMGs accounted for 13% of the total of first-year positions in the 2020 Match. They will start medical training in residency programs in the United States in the coming months. The numbers for psychiatry residency matches are higher; about 16% of total first-year positions are filled by non-U.S. IMGs.17 At this time, when they should be celebrating their successful Match after many years of hard work and persistence, there is increased anxiety. They wonder whether they will be able to enter the United States to begin their training program on time. Their concerns are multifold, but the main concern is related to uncertainties around getting visas on time. With the recent executive order in place, physicians only working actively with COVID-19 patients will be able to enter the country on visas. As mental health concerns continue to rise during these times, incoming residents might not be able to start training if they are out of the country.
Furthermore, because of travel/air restrictions, there are worries about whether physicians will be able to get flights to the United States, given the lockdown in many countries around the world. Conversely, IMGs who will be graduating from residency and fellowship programs this summer and have accepted new positions also are dealing with similar uncertainty. Their new jobs will require visa processing, and the current scenario provides limited insight, so far, about whether they will be able to start their respective jobs or whether they will have to return to their home countries until their visa processing is completed.
The American Medical Association has advised the Secretary of State and acting Secretary of Homeland Security to expedite physician workforce expansion in an effort to meet the growing need for health care services during this pandemic.18 It is encouraging that, recently, the State Department declared that visa processing will continue for medical professionals and that cases would be expedited for those who meet the criteria. However, the requirement for in-person interviews remains for individuals who are seeking a U.S. visa outside the country.
As residency programs are trying their best to continue to provide educational experiences to trainees during this phase, if psychiatry residents are placed on quarantine because of either getting exposed or contracting the illness, there is a possibility that they might need to extend their training. This would bring another challenge for IMGs, requiring them to extend their visas to complete their training. Future J-1 waiver jobs could be compromised.
Investment in physician wellness critical
Psychiatrists, along with other health care workers, are front-line soldiers in the fight against COVID-19. All physicians are at high risk for demoralization, burnout, depression, anxiety, and suicide. It is of utmost importance that we invest immediately in physicians’ wellness. As noted, significant numbers of psychiatrists are IMGs who are dealing with additional challenges while responding to the pandemic. There are certain challenges for IMGs, such as the well-being of their extended families in other countries, and travel bans put in place because of the pandemic. Those issues are not easy to resolve. However, addressing visa issues and providing support to their families in the event that something happens to physicians during the pandemic would be reassuring and would help alleviate additional stress. Those kinds of actions also would allow immigrant physicians to focus on clinical work and to improve their overall well-being. Given the health risks and numerous other insecurities that go along with living amid a pandemic, IMGs should not have the additional pressure of visa uncertainty.
Public health crises such as COVID-19 are associated with increased rates of anxiety,19 depression,20 illicit substance use,21 and an increased rate of suicide.22 Patients with serious mental illness might be among the hardest hit both physically and mentally during the pandemic.23 Even in the absence of a pandemic, there is already a shortage of psychiatrists at the national level, and it is expected that this shortage will grow in the future. Rural and underserved areas are expected to experience the physician deficit more acutely.24
The pandemic is likely to resolve gradually and unpredictably – and might recur along the way over the next 1-2 years. However, the psychiatrist shortage will escalate more, as the mental health needs in the United States increase further in coming months. We need psychiatrists now more than ever, and it will be crucial that prospective residents, graduating residents, and fellows are able to come on board to join the American health care system promptly. In addition to national-level interventions, residency programs, potential employers, and communities must be aware of and do whatever they can to address the challenges faced by IMGs during these times.
Dr. Raman Baweja is affiliated with the department of psychiatry and behavioral health at Penn State University, Hershey. He has no conflicts of interest. Dr. Verma is affiliated with Rogers Behavioral Health in Kenosha County, Wis., and the department of psychiatry and behavioral health at Rosalind Franklin University of Medicine and Science in North Chicago. She has no conflicts of interest. Dr. Ritika Baweja is affiliated with the department of psychiatry and behavioral health at Penn State. Dr. Ritika Baweja is the spouse of Dr. Raman Baweja. Dr. Adam is affiliated with the department of psychiatry at the University of Missouri, Columbia.
References
1. American Psychiatric Association. Navigating psychiatry residency in the United States. A Guide for IMG Physicians.
2. Berg S. 5 IMG physicians who speak up for patients and fellow doctors. American Medical Association. 2019 Oct 22.
3. Tsugawa Y et al. BMJ. 2017 Feb 3;256. doi: 10.1136/bmj.j273.
4. Gogineni RR et al. Child Adolesc Psychiatr Clin N Am. 2010 Oct 1;19(4):833-53.
5. Majeed MH et al. Academic Psychiatry. 2017 Dec 1;41(6):849-51.
6. Brotherton SE and Etzel SI. JAMA. 2018 Sep 11;320(10):1051-70.
7. Sockalingam S et al. Acad Psychiatry. 2012 Jul 1;36(4):277-81.
8. Singareddy R et al. Acad Psychiatry. 2008 Jul-Aug;32(4):343-4.
9. Kramer MN. Acad Psychiatry. 2005 Jul-Aug;29(3):322-4.
10. Rao NR and Kotapati VP. Pathways for success in academic medicine for an international medical graduate: Challenges and opportunities. In “Roberts Academic Medicine Handbook” 2020. Springer:163-70.
11. American Psychiatric Association. New poll: COVID-19 impacting mental well-being: Americans feeling anxious, especially for loved ones; older adults are less anxious. 2020 Mar 25.
12. Reger MA et al. JAMA Psychiatry. 2020 Apr 10. doi: 10.1001/jamapsychiatry.2020.1060.
13. Lai J et al. JAMA Netw Open. 2020 Mar 23;3(3):e203976-e203976. doi: 10.1001/jamanetworkopen.2020.3976.
14. Kalra G et al. Acad Psychiatry. 2012 Jul;36(4):323-9.
15. WHO best practices for the naming of new human infectious diseases. World Health Organization. 2015.
16. U.S. Department of State. Bureau of Consular Affairs. Visa Bulletin for March 2020.
17. National Resident Matching Program® (NRMP®). Thousands of medical students and graduates celebrate NRMP Match results.
18. American Medical Association. AMA: U.S. should open visas to international physicians amid COVID-19. AMA press release. 2020 Mar 25.
19. McKay D et al. J Anxiety Disord. 2020 Jun;73:02233. doi: 10.1016/j.janxdis.2020.102233.
20. Tang W et al. J Affect Disord. 2020 May 13;274:1-7.
21. Collins F et al. NIH Director’s Blog. NIH.gov. 2020 Apr 21.
22. Reger M et al. JAMA Psychiatry. 2020 Apr 10. doi: 10.1001/jamapsychiatry.2020.1060.
23. Druss BG. JAMA Psychiatry. 2020 Apr 3. doi: 10.1001/jamapsychiatry.2020.0894.
24. American Association of Medical Colleges. “The complexities of physician supply and demand: Projections from 2018-2033.” 2020 Jun.
International medical graduates (IMGs) constitute more than 24% of the total percentage of active physicians, 30% of active psychiatrists, and 33% of psychiatry residents in the United States.1 IMGs serve in various medical specialties and provide medical care to socioeconomically disadvantaged patients in underserved communities.2 Evidence suggests that patient outcomes among elderly patients admitted in U.S. hospitals for those treated by IMGs were on par with outcomes of U.S. graduates. Moreover, patients who were treated by IMGs had a lower mortality rates.3
IMGs trained in the United States make considerable contributions to psychiatry and have been very successful as educators, researchers, and leaders. Over the last 3 decades, for example, three American Psychiatric Association (APA) presidents and one past president of the American Academy of Child and Adolescent Psychiatry were IMGs. Many of them also hold department chair positions at many academic institutions.4,5
In short, IMGs are an important part of the U.S. health care system – particularly in psychiatry.
In addition to participating in psychiatry residency programs, IMG physicians are heavily represented in subspecialties, including geriatric psychiatry (45%), addiction psychiatry (42%), child and adolescent psychiatry (36%), psychosomatic medicine (32%), and forensic psychiatry (25%).6 IMG trainees face multiple challenges that begin as they transition to psychiatry residency in the United States, including understanding the American health care system, electronic medical records and documentation, and evidence-based medicine. In addition, they need to adapt to cultural changes, and work on language barriers, communication skills, and social isolation.7,8 Training programs account for these challenges and proactively take essential steps to facilitate the transition of IMGs into the U.S. system.9,10
As training programs prepare for the new academic year starting from July 2020 and continue to provide educational experiences to current trainees, the COVID-19 pandemic has brought additional challenges for the training programs. The gravity of the novel coronavirus pandemic continues to deepen, causing immense fear and uncertainty globally. An APA poll of more than 1,000 adults conducted early in the pandemic showed that about 40% of Americans were anxious about becoming seriously ill or dying with COVID-19. Nearly half of the respondents (48%) were anxious about the possibility of getting COVID-19, and even more (62%) were anxious about the possibility of their loved ones getting infected by this virus. Also, one-third of Americans reported a serious impact on their mental health.
Furthermore, the ailing economy and increasing unemployment are raising financial concerns for individuals and families. This pandemic also has had an impact on our patients’ sleep hygiene, relationships with their loved ones, and consumption of alcohol or other drugs/substances.11 Deteriorating mental health raises concerns about increased suicide risk as a secondary consequence.12
Physicians and other frontline teams who are taking care of these patients and their families continue to provide unexcelled, compassionate care in these unprecedented times. Selfless care continues despite awareness of the high probability of getting exposed to the virus and spreading it further to family members. Physicians involved in direct patient care for COVID-19 patients are at high risk for demoralization, burnout, depression, and anxiety.13
Struggles experienced by IMGs
On the personal front, IMGs often struggle with multiple stressors, such as lack of social support, ethnic-minority prejudice, and the need to understand financial structures such as mortgages in the new countries even after extended periods of residence.14 This virus has killed many health care professionals, including physicians around the world. There was a report of suicide by an emergency medicine physician who was treating patients with COVID-19 and ended up contracting the virus. That news was devastating and overwhelming for everyone, especially health care clinicians. It also adds to the stress and worries of IMGs who are still on nonimmigrant visas.
Bigger concerns exist if there is a demise of a nonimmigrant IMG and the implications of that loss for dependent families – who might face deportation. Even for those who were recently granted permanent residency status, worries about limited support systems and financial hardships to their families can be stressors.
Also, a large number of IMGs represent the geographical area where the pandemic began. Fortunately, the World Health Organization has taken a firm stance against possible discrimination by calling for global solidarity in these times. Furthermore, the WHO has emphasized the importance of referring to the disease caused by SARS-CoV-2 as “COVID-19” only – and not by the name of a particular country or city.15 Despite those official positions, people continue to express racially discriminatory opinions related to the virus, and those comments are not only disturbing to IMGs, they also are demoralizing.
Travel restrictions
In addition to the worries that IMGs might have about their own health and that of their families residing with them, the well-being of their extended families, including their aging parents back in their countries of origin, is unsettling as well. It is even more unnerving during the pandemic because the Centers for Disease Control and Prevention and the State Department advised avoiding all international travel at this time. Under these circumstances, IMGs are concerned about travel to their countries of origin in the event of a family emergency and the quarantine protocols in place, at both the country of origin and at residences.
Immigration issues
The U.S. administration temporarily suspended all immigration for 60 days, starting from April 2020. Recently, an executive order was signed suspending entry in the country on several visas, including the J-1 and the H1-B. Those are two categories that allow physicians to train and work in the United States.
IMGs in the United States reside and practice here under different types of immigrant and nonimmigrant visas (J-1, H1-B). This year, the Match results coincided with the timeline of those new immigration restrictions. Many IMGs are currently in the process of renewing their H1-B visas. They are worried because their visas will expire in the coming months. During the pandemic, U.S. Citizenship and Immigration Services suspended routine visa services and premium processing for visa renewals. This halt led to a delay in visa processing for graduating residents in June and practicing physicians seeking visa renewal. Those delays add to personal stress, and furthermore, distract these immigrant physicians from fighting this pandemic.
Another complication is that rules for J-1 visa holders have changed so that trainees must return to their countries of origin for at least 2 years after completing their training. If they decide to continue practicing medicine in the United States, they need a specific type of J-1 waiver and must gain a pathway to be a lawful permanent resident (Green Card). Many IMGs who are on waiver positions might not be able to treat patients ailing from COVID-19 to the full extent because waivers restrict them to practicing only in certain identified health systems.
IMGs who are coming from a country such India have to wait for more than 11 years after completing their accredited training to get permanent residency because of backlog for the permanent residency process.16 While waiting for a Green Card, they must continue to work on an H1-B visa, which requires periodic renewal.
Potential impact on training
Non-U.S. citizen IMGs accounted for 13% of the total of first-year positions in the 2020 Match. They will start medical training in residency programs in the United States in the coming months. The numbers for psychiatry residency matches are higher; about 16% of total first-year positions are filled by non-U.S. IMGs.17 At this time, when they should be celebrating their successful Match after many years of hard work and persistence, there is increased anxiety. They wonder whether they will be able to enter the United States to begin their training program on time. Their concerns are multifold, but the main concern is related to uncertainties around getting visas on time. With the recent executive order in place, physicians only working actively with COVID-19 patients will be able to enter the country on visas. As mental health concerns continue to rise during these times, incoming residents might not be able to start training if they are out of the country.
Furthermore, because of travel/air restrictions, there are worries about whether physicians will be able to get flights to the United States, given the lockdown in many countries around the world. Conversely, IMGs who will be graduating from residency and fellowship programs this summer and have accepted new positions also are dealing with similar uncertainty. Their new jobs will require visa processing, and the current scenario provides limited insight, so far, about whether they will be able to start their respective jobs or whether they will have to return to their home countries until their visa processing is completed.
The American Medical Association has advised the Secretary of State and acting Secretary of Homeland Security to expedite physician workforce expansion in an effort to meet the growing need for health care services during this pandemic.18 It is encouraging that, recently, the State Department declared that visa processing will continue for medical professionals and that cases would be expedited for those who meet the criteria. However, the requirement for in-person interviews remains for individuals who are seeking a U.S. visa outside the country.
As residency programs are trying their best to continue to provide educational experiences to trainees during this phase, if psychiatry residents are placed on quarantine because of either getting exposed or contracting the illness, there is a possibility that they might need to extend their training. This would bring another challenge for IMGs, requiring them to extend their visas to complete their training. Future J-1 waiver jobs could be compromised.
Investment in physician wellness critical
Psychiatrists, along with other health care workers, are front-line soldiers in the fight against COVID-19. All physicians are at high risk for demoralization, burnout, depression, anxiety, and suicide. It is of utmost importance that we invest immediately in physicians’ wellness. As noted, significant numbers of psychiatrists are IMGs who are dealing with additional challenges while responding to the pandemic. There are certain challenges for IMGs, such as the well-being of their extended families in other countries, and travel bans put in place because of the pandemic. Those issues are not easy to resolve. However, addressing visa issues and providing support to their families in the event that something happens to physicians during the pandemic would be reassuring and would help alleviate additional stress. Those kinds of actions also would allow immigrant physicians to focus on clinical work and to improve their overall well-being. Given the health risks and numerous other insecurities that go along with living amid a pandemic, IMGs should not have the additional pressure of visa uncertainty.
Public health crises such as COVID-19 are associated with increased rates of anxiety,19 depression,20 illicit substance use,21 and an increased rate of suicide.22 Patients with serious mental illness might be among the hardest hit both physically and mentally during the pandemic.23 Even in the absence of a pandemic, there is already a shortage of psychiatrists at the national level, and it is expected that this shortage will grow in the future. Rural and underserved areas are expected to experience the physician deficit more acutely.24
The pandemic is likely to resolve gradually and unpredictably – and might recur along the way over the next 1-2 years. However, the psychiatrist shortage will escalate more, as the mental health needs in the United States increase further in coming months. We need psychiatrists now more than ever, and it will be crucial that prospective residents, graduating residents, and fellows are able to come on board to join the American health care system promptly. In addition to national-level interventions, residency programs, potential employers, and communities must be aware of and do whatever they can to address the challenges faced by IMGs during these times.
Dr. Raman Baweja is affiliated with the department of psychiatry and behavioral health at Penn State University, Hershey. He has no conflicts of interest. Dr. Verma is affiliated with Rogers Behavioral Health in Kenosha County, Wis., and the department of psychiatry and behavioral health at Rosalind Franklin University of Medicine and Science in North Chicago. She has no conflicts of interest. Dr. Ritika Baweja is affiliated with the department of psychiatry and behavioral health at Penn State. Dr. Ritika Baweja is the spouse of Dr. Raman Baweja. Dr. Adam is affiliated with the department of psychiatry at the University of Missouri, Columbia.
References
1. American Psychiatric Association. Navigating psychiatry residency in the United States. A Guide for IMG Physicians.
2. Berg S. 5 IMG physicians who speak up for patients and fellow doctors. American Medical Association. 2019 Oct 22.
3. Tsugawa Y et al. BMJ. 2017 Feb 3;256. doi: 10.1136/bmj.j273.
4. Gogineni RR et al. Child Adolesc Psychiatr Clin N Am. 2010 Oct 1;19(4):833-53.
5. Majeed MH et al. Academic Psychiatry. 2017 Dec 1;41(6):849-51.
6. Brotherton SE and Etzel SI. JAMA. 2018 Sep 11;320(10):1051-70.
7. Sockalingam S et al. Acad Psychiatry. 2012 Jul 1;36(4):277-81.
8. Singareddy R et al. Acad Psychiatry. 2008 Jul-Aug;32(4):343-4.
9. Kramer MN. Acad Psychiatry. 2005 Jul-Aug;29(3):322-4.
10. Rao NR and Kotapati VP. Pathways for success in academic medicine for an international medical graduate: Challenges and opportunities. In “Roberts Academic Medicine Handbook” 2020. Springer:163-70.
11. American Psychiatric Association. New poll: COVID-19 impacting mental well-being: Americans feeling anxious, especially for loved ones; older adults are less anxious. 2020 Mar 25.
12. Reger MA et al. JAMA Psychiatry. 2020 Apr 10. doi: 10.1001/jamapsychiatry.2020.1060.
13. Lai J et al. JAMA Netw Open. 2020 Mar 23;3(3):e203976-e203976. doi: 10.1001/jamanetworkopen.2020.3976.
14. Kalra G et al. Acad Psychiatry. 2012 Jul;36(4):323-9.
15. WHO best practices for the naming of new human infectious diseases. World Health Organization. 2015.
16. U.S. Department of State. Bureau of Consular Affairs. Visa Bulletin for March 2020.
17. National Resident Matching Program® (NRMP®). Thousands of medical students and graduates celebrate NRMP Match results.
18. American Medical Association. AMA: U.S. should open visas to international physicians amid COVID-19. AMA press release. 2020 Mar 25.
19. McKay D et al. J Anxiety Disord. 2020 Jun;73:02233. doi: 10.1016/j.janxdis.2020.102233.
20. Tang W et al. J Affect Disord. 2020 May 13;274:1-7.
21. Collins F et al. NIH Director’s Blog. NIH.gov. 2020 Apr 21.
22. Reger M et al. JAMA Psychiatry. 2020 Apr 10. doi: 10.1001/jamapsychiatry.2020.1060.
23. Druss BG. JAMA Psychiatry. 2020 Apr 3. doi: 10.1001/jamapsychiatry.2020.0894.
24. American Association of Medical Colleges. “The complexities of physician supply and demand: Projections from 2018-2033.” 2020 Jun.
‘Doc, can I get a mask exemption?’
As more jurisdictions mandate facial coverings in public, questions have arisen about whether it’s safe for everyone – including those with lung disease – to wear masks.
To address these issues, Medscape spoke with the chief medical officer of the American Lung Association, Dr. Albert Rizzo.
The CDC recommendations on mask wearing say, “Cloth face coverings should not be placed on young children under age 2, anyone who has trouble breathing, or is unconscious, incapacitated, or otherwise unable to remove the mask without assistance.” Does this language suggest that there indeed is a subset of the adult population with lung disease who shouldn’t wear masks?
It makes sense to say that if it makes you uncomfortable to wear a mask because it affects your breathing, you should think twice about getting in a situation where you would have to wear a mask.
I’ve told many of my high-risk patients, “The best way to avoid getting COVID-19 is to stay home and stay away from sick people, especially if you feel that you are not going to be able to wear a mask or facial covering of some sort.”
The reason that some people have trouble with a mask is that they haven’t tried the right style of mask – by that I mean how tightly it fits and the material it’s made out of. Sometimes it really is just that people with lung disease don’t like to have anything covering their faces. Many of these patients feel better where there is air blowing across their faces – they will have a fan blowing even in the middle of winter because they feel more comfortable.
I won’t say it’s all in their heads, but sometimes it’s a matter of desensitizing themselves to wearing a mask. I liken it to people who have sleep apnea. We often have to desensitize them to wearing a mask for sleeping. We tell them to put it on while they are watching TV — don’t hook it up to anything yet, just get used to having something on your face.
I’ve told my patients the same thing about masks for COVID-19. Put on the mask, see how it feels. If you become uncomfortable breathing with it on, take it off, but maybe you can handle it for a half hour or 45 minutes. Find out how much time you have for a trip to the grocery store based on how comfortable you are wearing it at home.
It’s a matter of training the patient, giving them options of how to get comfortable with it, and then making them realize that they have to weigh the benefits and risks of wearing the mask and feeling out of breath versus going out in public and being potentially exposed to coronavirus. And the bottom line is, anybody who is wearing a mask and starts to feel uncomfortable, they can take the mask off.
You mentioned different types of masks. Is there a type of mask that is typically more breathable that clinicians can recommend to patients with lung disease?
First, I remind patients who think they will have trouble breathing with a mask on that they are choosing a mask not so much to protect themselves – that would take an N95 mask to filter out the virus. The mask is worn so that when they cough or drink or speak, they aren’t sending respiratory droplets out into the environment. Even when we speak, respiratory droplets can easily go out as far as 6 feet, or further with coughing or sneezing. With facial coverings, we try to keep those respiratory droplets from getting out and infecting others.
So when choosing a mask, you don’t have to worry as much about a tight-fitting mask. I recommend a loose-fitting mask that covers the nose and mouth and isn’t going to fall off but isn’t so tight around the ears and neck to make them feel uncomfortable. Even though it doesn’t really protect the wearer, it is cutting down on the ability to breathe in droplets – maybe not microscopic particles, but it’s better than nothing.
Is a face shield a reasonable alternative for someone who feels they can’t breathe with a mask on?
Yes. I’m surprised that face shields don’t get more attention. I’ve tried them out, and they are actually more comfortable than masks. They do impede the spilling out of droplets into the public, but they are not as close fitting to the face as a mask. If you want to protect others, the face shield should be adequate. It is not as good at preventing you from breathing in viral particles.
Some people have claimed that wearing a mask makes them hyperventilate and feel like they are going to pass out, or the mask causes them to become hypoxic. Are these valid concerns?
We get two questions about masks from patients who feel that they are short of breath or are worried about wearing a mask. One is whether their oxygen level is dropping. It’s usually not that. It’s usually because they feel that the mask is an impediment to getting air in. Their oxygen levels are stable.
The other question is whether the mask causes CO2 retention. For the mask to trap enough exhaled CO2 and for us to breathe enough of that CO2 back in to raise our CO2 level, it has to be a pretty tight-fitting mask. With the type of masks we are suggesting that people wear, that’s very unlikely to occur.
What can clinicians do to reassure patients with some type of lung disease that they can safely wear masks?
There are a few things they can do right in the office. Have them put the mask on for a few minutes and make sure they feel comfortable with it. With an oximeter, patients can see that their oxygen levels don’t change when they are breathing through the mask for a period of time.
You can’t really measure CO2 retention that easily, but most patients with chronic obstructive pulmonary disease or pulmonary fibrosis don’t have an elevated CO2 at baseline. A little more education is helpful in those situations. In most cases, they aren’t going to retain enough CO2 to have problems wearing a mask.
Only a small percentage of patients with lung disease are CO2 retainers, and many of those patients are being seen by pulmonary specialists. Those are the patients you might want to be more cautious with, to make sure they aren’t wearing anything that is tight fitting or that makes them work harder to breathe. It’s not that the mask is causing CO2 retention, but the increased work of breathing may make it harder to exhale the CO2.
Does a mask interfere with supplemental oxygen in any way?
Supplemental oxygen is typically supplied through a nasal cannula, so 100% oxygen is still getting to the nasal passages and entrained down into the airway, so it shouldn’t be a problem.
Some of the resistance to wearing masks has come from people with asthma. Is it safe for patients with asthma to wear masks, or should these patients be exempt from wearing masks?
In general, the breathing of people with mild asthma, both young and old, should not be impeded by the wearing of facial coverings. The concerns about oxygen and carbon dioxide among patients with more severe lung disease should not play a role in asthma.
Since younger adults with COVID-19 seem to have fewer or no symptoms and may actually be carrying the virus unknowingly, this should be the main population who should wear masks to prevent transmission to others.
Exemptions for mask wearing for mild asthma should be discouraged and dealt with on a case-by-case basis if there is a particular concern for that individual.
How do you respond if a patient asks you for a formal medical exemption to wearing a mask?
We’ve been asked to do a lot of letter writing for patients around going back to work, as well as the issue of wearing masks. The discussion usually revolves around trying to avoid going somewhere where you would have to wear a mask if it makes you feel uncomfortable.
I do not recommend automatically exempting individuals from wearing masks, even many of my pulmonary patients. There needs to be an understanding by the patient regarding the purpose of the mask and the overall advice to stay out of situations where social distancing is not being practiced. If you can take the time to discuss options as mentioned above – mask styles, desensitization, etc – the patient usually understands and will try wearing a mask.
On a case-by-case basis, some individuals may need to be exempted, but I feel this is a small number. I prefer my high-risk (older, chronic disease, etc) patients do everything they can to avoid infection – handwashing, mask wearing, and socially distancing.
They should also realize that even with a note, it is not going to help if they are in the middle of the grocery store and someone confronts them about not wearing a mask. It may help as they enter a store that says “masks required” and they can show it to someone monitoring the door. But I’m not really sure in what situations having that note is going to be helpful if confrontations occur.
Patients are also asking how safe is it for them to go back to work and be out in public. I tell them, nothing is going to be 100% safe. Until we have an effective vaccine, we are all going to have to weigh the potential risks of going to an area where social distancing isn’t maintained, people aren’t wearing face masks, and you can’t wash your hands as much as you’d like to. That’s going to be a struggle for all of us to get back out into situations where people interact socially.
Albert A. Rizzo, MD, is chief medical officer for the American Lung Association, chief of the Section of Pulmonary and Critical Care Medicine at the Christiana Care Health System in Newark, Delaware, and a member of Christiana Care Pulmonary Associates. He is board certified in internal medicine, pulmonary medicine, critical care medicine, and sleep medicine and is a clinical assistant professor of medicine at Thomas Jefferson University Medical School, Philadelphia.
This article first appeared on Medscape.com.
As more jurisdictions mandate facial coverings in public, questions have arisen about whether it’s safe for everyone – including those with lung disease – to wear masks.
To address these issues, Medscape spoke with the chief medical officer of the American Lung Association, Dr. Albert Rizzo.
The CDC recommendations on mask wearing say, “Cloth face coverings should not be placed on young children under age 2, anyone who has trouble breathing, or is unconscious, incapacitated, or otherwise unable to remove the mask without assistance.” Does this language suggest that there indeed is a subset of the adult population with lung disease who shouldn’t wear masks?
It makes sense to say that if it makes you uncomfortable to wear a mask because it affects your breathing, you should think twice about getting in a situation where you would have to wear a mask.
I’ve told many of my high-risk patients, “The best way to avoid getting COVID-19 is to stay home and stay away from sick people, especially if you feel that you are not going to be able to wear a mask or facial covering of some sort.”
The reason that some people have trouble with a mask is that they haven’t tried the right style of mask – by that I mean how tightly it fits and the material it’s made out of. Sometimes it really is just that people with lung disease don’t like to have anything covering their faces. Many of these patients feel better where there is air blowing across their faces – they will have a fan blowing even in the middle of winter because they feel more comfortable.
I won’t say it’s all in their heads, but sometimes it’s a matter of desensitizing themselves to wearing a mask. I liken it to people who have sleep apnea. We often have to desensitize them to wearing a mask for sleeping. We tell them to put it on while they are watching TV — don’t hook it up to anything yet, just get used to having something on your face.
I’ve told my patients the same thing about masks for COVID-19. Put on the mask, see how it feels. If you become uncomfortable breathing with it on, take it off, but maybe you can handle it for a half hour or 45 minutes. Find out how much time you have for a trip to the grocery store based on how comfortable you are wearing it at home.
It’s a matter of training the patient, giving them options of how to get comfortable with it, and then making them realize that they have to weigh the benefits and risks of wearing the mask and feeling out of breath versus going out in public and being potentially exposed to coronavirus. And the bottom line is, anybody who is wearing a mask and starts to feel uncomfortable, they can take the mask off.
You mentioned different types of masks. Is there a type of mask that is typically more breathable that clinicians can recommend to patients with lung disease?
First, I remind patients who think they will have trouble breathing with a mask on that they are choosing a mask not so much to protect themselves – that would take an N95 mask to filter out the virus. The mask is worn so that when they cough or drink or speak, they aren’t sending respiratory droplets out into the environment. Even when we speak, respiratory droplets can easily go out as far as 6 feet, or further with coughing or sneezing. With facial coverings, we try to keep those respiratory droplets from getting out and infecting others.
So when choosing a mask, you don’t have to worry as much about a tight-fitting mask. I recommend a loose-fitting mask that covers the nose and mouth and isn’t going to fall off but isn’t so tight around the ears and neck to make them feel uncomfortable. Even though it doesn’t really protect the wearer, it is cutting down on the ability to breathe in droplets – maybe not microscopic particles, but it’s better than nothing.
Is a face shield a reasonable alternative for someone who feels they can’t breathe with a mask on?
Yes. I’m surprised that face shields don’t get more attention. I’ve tried them out, and they are actually more comfortable than masks. They do impede the spilling out of droplets into the public, but they are not as close fitting to the face as a mask. If you want to protect others, the face shield should be adequate. It is not as good at preventing you from breathing in viral particles.
Some people have claimed that wearing a mask makes them hyperventilate and feel like they are going to pass out, or the mask causes them to become hypoxic. Are these valid concerns?
We get two questions about masks from patients who feel that they are short of breath or are worried about wearing a mask. One is whether their oxygen level is dropping. It’s usually not that. It’s usually because they feel that the mask is an impediment to getting air in. Their oxygen levels are stable.
The other question is whether the mask causes CO2 retention. For the mask to trap enough exhaled CO2 and for us to breathe enough of that CO2 back in to raise our CO2 level, it has to be a pretty tight-fitting mask. With the type of masks we are suggesting that people wear, that’s very unlikely to occur.
What can clinicians do to reassure patients with some type of lung disease that they can safely wear masks?
There are a few things they can do right in the office. Have them put the mask on for a few minutes and make sure they feel comfortable with it. With an oximeter, patients can see that their oxygen levels don’t change when they are breathing through the mask for a period of time.
You can’t really measure CO2 retention that easily, but most patients with chronic obstructive pulmonary disease or pulmonary fibrosis don’t have an elevated CO2 at baseline. A little more education is helpful in those situations. In most cases, they aren’t going to retain enough CO2 to have problems wearing a mask.
Only a small percentage of patients with lung disease are CO2 retainers, and many of those patients are being seen by pulmonary specialists. Those are the patients you might want to be more cautious with, to make sure they aren’t wearing anything that is tight fitting or that makes them work harder to breathe. It’s not that the mask is causing CO2 retention, but the increased work of breathing may make it harder to exhale the CO2.
Does a mask interfere with supplemental oxygen in any way?
Supplemental oxygen is typically supplied through a nasal cannula, so 100% oxygen is still getting to the nasal passages and entrained down into the airway, so it shouldn’t be a problem.
Some of the resistance to wearing masks has come from people with asthma. Is it safe for patients with asthma to wear masks, or should these patients be exempt from wearing masks?
In general, the breathing of people with mild asthma, both young and old, should not be impeded by the wearing of facial coverings. The concerns about oxygen and carbon dioxide among patients with more severe lung disease should not play a role in asthma.
Since younger adults with COVID-19 seem to have fewer or no symptoms and may actually be carrying the virus unknowingly, this should be the main population who should wear masks to prevent transmission to others.
Exemptions for mask wearing for mild asthma should be discouraged and dealt with on a case-by-case basis if there is a particular concern for that individual.
How do you respond if a patient asks you for a formal medical exemption to wearing a mask?
We’ve been asked to do a lot of letter writing for patients around going back to work, as well as the issue of wearing masks. The discussion usually revolves around trying to avoid going somewhere where you would have to wear a mask if it makes you feel uncomfortable.
I do not recommend automatically exempting individuals from wearing masks, even many of my pulmonary patients. There needs to be an understanding by the patient regarding the purpose of the mask and the overall advice to stay out of situations where social distancing is not being practiced. If you can take the time to discuss options as mentioned above – mask styles, desensitization, etc – the patient usually understands and will try wearing a mask.
On a case-by-case basis, some individuals may need to be exempted, but I feel this is a small number. I prefer my high-risk (older, chronic disease, etc) patients do everything they can to avoid infection – handwashing, mask wearing, and socially distancing.
They should also realize that even with a note, it is not going to help if they are in the middle of the grocery store and someone confronts them about not wearing a mask. It may help as they enter a store that says “masks required” and they can show it to someone monitoring the door. But I’m not really sure in what situations having that note is going to be helpful if confrontations occur.
Patients are also asking how safe is it for them to go back to work and be out in public. I tell them, nothing is going to be 100% safe. Until we have an effective vaccine, we are all going to have to weigh the potential risks of going to an area where social distancing isn’t maintained, people aren’t wearing face masks, and you can’t wash your hands as much as you’d like to. That’s going to be a struggle for all of us to get back out into situations where people interact socially.
Albert A. Rizzo, MD, is chief medical officer for the American Lung Association, chief of the Section of Pulmonary and Critical Care Medicine at the Christiana Care Health System in Newark, Delaware, and a member of Christiana Care Pulmonary Associates. He is board certified in internal medicine, pulmonary medicine, critical care medicine, and sleep medicine and is a clinical assistant professor of medicine at Thomas Jefferson University Medical School, Philadelphia.
This article first appeared on Medscape.com.
As more jurisdictions mandate facial coverings in public, questions have arisen about whether it’s safe for everyone – including those with lung disease – to wear masks.
To address these issues, Medscape spoke with the chief medical officer of the American Lung Association, Dr. Albert Rizzo.
The CDC recommendations on mask wearing say, “Cloth face coverings should not be placed on young children under age 2, anyone who has trouble breathing, or is unconscious, incapacitated, or otherwise unable to remove the mask without assistance.” Does this language suggest that there indeed is a subset of the adult population with lung disease who shouldn’t wear masks?
It makes sense to say that if it makes you uncomfortable to wear a mask because it affects your breathing, you should think twice about getting in a situation where you would have to wear a mask.
I’ve told many of my high-risk patients, “The best way to avoid getting COVID-19 is to stay home and stay away from sick people, especially if you feel that you are not going to be able to wear a mask or facial covering of some sort.”
The reason that some people have trouble with a mask is that they haven’t tried the right style of mask – by that I mean how tightly it fits and the material it’s made out of. Sometimes it really is just that people with lung disease don’t like to have anything covering their faces. Many of these patients feel better where there is air blowing across their faces – they will have a fan blowing even in the middle of winter because they feel more comfortable.
I won’t say it’s all in their heads, but sometimes it’s a matter of desensitizing themselves to wearing a mask. I liken it to people who have sleep apnea. We often have to desensitize them to wearing a mask for sleeping. We tell them to put it on while they are watching TV — don’t hook it up to anything yet, just get used to having something on your face.
I’ve told my patients the same thing about masks for COVID-19. Put on the mask, see how it feels. If you become uncomfortable breathing with it on, take it off, but maybe you can handle it for a half hour or 45 minutes. Find out how much time you have for a trip to the grocery store based on how comfortable you are wearing it at home.
It’s a matter of training the patient, giving them options of how to get comfortable with it, and then making them realize that they have to weigh the benefits and risks of wearing the mask and feeling out of breath versus going out in public and being potentially exposed to coronavirus. And the bottom line is, anybody who is wearing a mask and starts to feel uncomfortable, they can take the mask off.
You mentioned different types of masks. Is there a type of mask that is typically more breathable that clinicians can recommend to patients with lung disease?
First, I remind patients who think they will have trouble breathing with a mask on that they are choosing a mask not so much to protect themselves – that would take an N95 mask to filter out the virus. The mask is worn so that when they cough or drink or speak, they aren’t sending respiratory droplets out into the environment. Even when we speak, respiratory droplets can easily go out as far as 6 feet, or further with coughing or sneezing. With facial coverings, we try to keep those respiratory droplets from getting out and infecting others.
So when choosing a mask, you don’t have to worry as much about a tight-fitting mask. I recommend a loose-fitting mask that covers the nose and mouth and isn’t going to fall off but isn’t so tight around the ears and neck to make them feel uncomfortable. Even though it doesn’t really protect the wearer, it is cutting down on the ability to breathe in droplets – maybe not microscopic particles, but it’s better than nothing.
Is a face shield a reasonable alternative for someone who feels they can’t breathe with a mask on?
Yes. I’m surprised that face shields don’t get more attention. I’ve tried them out, and they are actually more comfortable than masks. They do impede the spilling out of droplets into the public, but they are not as close fitting to the face as a mask. If you want to protect others, the face shield should be adequate. It is not as good at preventing you from breathing in viral particles.
Some people have claimed that wearing a mask makes them hyperventilate and feel like they are going to pass out, or the mask causes them to become hypoxic. Are these valid concerns?
We get two questions about masks from patients who feel that they are short of breath or are worried about wearing a mask. One is whether their oxygen level is dropping. It’s usually not that. It’s usually because they feel that the mask is an impediment to getting air in. Their oxygen levels are stable.
The other question is whether the mask causes CO2 retention. For the mask to trap enough exhaled CO2 and for us to breathe enough of that CO2 back in to raise our CO2 level, it has to be a pretty tight-fitting mask. With the type of masks we are suggesting that people wear, that’s very unlikely to occur.
What can clinicians do to reassure patients with some type of lung disease that they can safely wear masks?
There are a few things they can do right in the office. Have them put the mask on for a few minutes and make sure they feel comfortable with it. With an oximeter, patients can see that their oxygen levels don’t change when they are breathing through the mask for a period of time.
You can’t really measure CO2 retention that easily, but most patients with chronic obstructive pulmonary disease or pulmonary fibrosis don’t have an elevated CO2 at baseline. A little more education is helpful in those situations. In most cases, they aren’t going to retain enough CO2 to have problems wearing a mask.
Only a small percentage of patients with lung disease are CO2 retainers, and many of those patients are being seen by pulmonary specialists. Those are the patients you might want to be more cautious with, to make sure they aren’t wearing anything that is tight fitting or that makes them work harder to breathe. It’s not that the mask is causing CO2 retention, but the increased work of breathing may make it harder to exhale the CO2.
Does a mask interfere with supplemental oxygen in any way?
Supplemental oxygen is typically supplied through a nasal cannula, so 100% oxygen is still getting to the nasal passages and entrained down into the airway, so it shouldn’t be a problem.
Some of the resistance to wearing masks has come from people with asthma. Is it safe for patients with asthma to wear masks, or should these patients be exempt from wearing masks?
In general, the breathing of people with mild asthma, both young and old, should not be impeded by the wearing of facial coverings. The concerns about oxygen and carbon dioxide among patients with more severe lung disease should not play a role in asthma.
Since younger adults with COVID-19 seem to have fewer or no symptoms and may actually be carrying the virus unknowingly, this should be the main population who should wear masks to prevent transmission to others.
Exemptions for mask wearing for mild asthma should be discouraged and dealt with on a case-by-case basis if there is a particular concern for that individual.
How do you respond if a patient asks you for a formal medical exemption to wearing a mask?
We’ve been asked to do a lot of letter writing for patients around going back to work, as well as the issue of wearing masks. The discussion usually revolves around trying to avoid going somewhere where you would have to wear a mask if it makes you feel uncomfortable.
I do not recommend automatically exempting individuals from wearing masks, even many of my pulmonary patients. There needs to be an understanding by the patient regarding the purpose of the mask and the overall advice to stay out of situations where social distancing is not being practiced. If you can take the time to discuss options as mentioned above – mask styles, desensitization, etc – the patient usually understands and will try wearing a mask.
On a case-by-case basis, some individuals may need to be exempted, but I feel this is a small number. I prefer my high-risk (older, chronic disease, etc) patients do everything they can to avoid infection – handwashing, mask wearing, and socially distancing.
They should also realize that even with a note, it is not going to help if they are in the middle of the grocery store and someone confronts them about not wearing a mask. It may help as they enter a store that says “masks required” and they can show it to someone monitoring the door. But I’m not really sure in what situations having that note is going to be helpful if confrontations occur.
Patients are also asking how safe is it for them to go back to work and be out in public. I tell them, nothing is going to be 100% safe. Until we have an effective vaccine, we are all going to have to weigh the potential risks of going to an area where social distancing isn’t maintained, people aren’t wearing face masks, and you can’t wash your hands as much as you’d like to. That’s going to be a struggle for all of us to get back out into situations where people interact socially.
Albert A. Rizzo, MD, is chief medical officer for the American Lung Association, chief of the Section of Pulmonary and Critical Care Medicine at the Christiana Care Health System in Newark, Delaware, and a member of Christiana Care Pulmonary Associates. He is board certified in internal medicine, pulmonary medicine, critical care medicine, and sleep medicine and is a clinical assistant professor of medicine at Thomas Jefferson University Medical School, Philadelphia.
This article first appeared on Medscape.com.
Meditations in an emergency: Talking through pandemic anxiety with a pioneer of mind-body medicine
Andrew N. Wilner, MD: Welcome to Medscape. I’m Dr Andrew Wilner. Today I have a special guest, Dr James Gordon, founder and executive director of the Center for Mind-Body Medicine. Welcome, Dr Gordon.
James S. Gordon, MD: Thank you very much. It’s good to be with you.
Dr. Wilner: Thanks for joining us. We are recording this in late May 2020, in the midst of the coronavirus pandemic. Millions of people have been infected. Hundreds of thousands have died. Millions have lost their jobs. I think it’s fair to say that people are under a greater degree of stress than they’re normally accustomed to. Would you agree with that?
Dr. Gordon: I think it’s more than fair to say that everybody in the United States, and actually pretty much everyone in the world, is under extreme stress. And that compounds any stresses that they’ve experienced before in their lives. Everyone is affected.
Dr. Wilner: The mind-body medicine concept is one that you’ve pursued for decades. Tell us a little bit about the Center for Mind-Body Medicine and how that’s led to the program that you have to help us deal with the coronavirus.
Dr. Gordon: I started the Center for Mind-Body Medicine about 30 years ago. I’d been a researcher at the National Institute of Mental Health for a number of years, in private practice, and a professor at Georgetown Medical School. But I wanted to really focus on how to change and enrich medicine by making self-care, self-awareness, and group support central to all healthcare.
Western medicine is enormously powerful in certain situations, such as physical trauma, high levels of infection, congenital anomalies. But we’re not so good at working with chronic physical or psychological problems. Those are much more complex.
We’ve been discovering that what is going to make the long-term difference in conditions like type 2 diabetes, pain syndromes, hypertension, depression, and anxiety are those approaches that we can learn to do for ourselves. These are changes we can make in how we deal with stress, eat, exercise, relate to other people, and whether we find meaning and purpose in our lives.
by wars, climate-related disasters, the opioid epidemic, chronic poverty, historical trauma. We do a lot of work with indigenous people here in North America. We’ve worked in a number of communities where school shootings have traumatized everyone.
What we’ve learned over these past 25 years, and what interested me professionally as well as personally over the past 50 years, is what we’re now bringing out on an even larger scale. The kind of approaches that we’ve developed, studied, and published research on are exactly what everyone needs to include and incorporate in their daily life, as well as in their medical and health care, from now on.
Dr. Wilner: Do you have a program that’s specifically for health care providers?
Dr. Gordon: Yes. The Center for Mind-Body Medicine is primarily an educational organization rather than a service organization. Since the beginning, I’ve been focused on training health professionals. My first passion was for training physicians – I’m a physician, so there’s a feeling of fellowship there – but also health care workers and mental health professionals of every kind.
We teach health professionals a whole system, a comprehensive program of techniques of self-awareness and self-care. We teach them so that they can practice on themselves and study the underlying science, so they can then teach what they’ve learned to the patients or clients they work with. They integrate it into what they’re already doing, regardless of their specialty. At times we also offer some of the same kinds of mind-body skills groups that are the fundamental part of our training as a stand-alone intervention. You can’t really teach other people how to take care of themselves unless you’re also doing it yourself. Otherwise, it’s just a theory.
Dr. Wilner: As a neurologist, I’m interested in the mind-body system. You are a psychiatrist and understand that it’s a lot more difficult to objectify certain things. What is stress? What is happiness? What is sadness? It’s very hard to measure. You can have scales, but it requires insight on the part of the individual. So I think it’s certainly an ambitious project.
Dr. Gordon: You’re absolutely right. It requires insight. And one of the shortcomings of our medical education is that it doesn’t encourage us to look inside ourselves enough. There’s so much focus on objectivity and on data, that we’ve lost some of the subjective art of medicine.
My experience with myself, as well as with the thousands of people we’ve trained here in the United States and around the world and the many hundreds of thousands with whom they’ve worked, is that all of us have a greater capacity to understand and help ourselves than we ordinarily think or than most of us learn about in our medical education.
This work is saying to people to take a little bit of time and relax a little in order to allow yourself to come into a meditative state. And I don’t mean anything fancy by that. Meditation is just being relaxed. Moment-to-moment awareness doesn’t have to do with any particular religion or spiritual practice. It’s part of all of them. If you can get into that state, then you can begin to say, “Oh, that’s what’s going on with me. That’s why my pain is worse.”
For example, you often wonder in people with peripheral neuropathy why it becomes worse or better at certain points. I would encourage neurologists and other physicians to ask your patients, “Why do you think it’s worse?” They may say, “I don’t know, doc; that’s why I’m here.” But I would ask them to take a couple of minutes to let me know. They could think it has something to do with the fact that they had a big fight with their wife that morning, they don’t want to go to work, or whatever it is. This is part of the lost art that we need to bring back into medicine for ourselves and especially for our patients.
Dr. Wilner: Can you give me an example of some of the exercises you’d do in a class?
Dr. Gordon: All of the exercises and our entire program that we teach at the Center for Mind-Body Medicine is in this new book of mine, “The Transformation: Discovering Wholeness and Healing After Trauma.” It’s really the distillation of not just the past 25 or 30 years, but really 50 years of work.
The techniques are all pretty simple and, as we say, evidence based. There is evidence that shows how they work on us physiologically, as well as psychologically. And they’re all pretty easy to teach to anyone.
Myself and about 60 or 70 of our faculty at the Center for Mind-Body Medicine are currently leading online groups. Then several hundred of the other people we’ve trained are also leading these groups. We’re still counting it up, but we probably have between 700 and 1,000 groups going around the world, led by our faculty and by people we’ve trained.
We teach a different technique every week in these online groups. Last week, after getting people energized and focused, we did a written dialogue with an emotion. You put down the initial of your name – in my case, “J” for Jim – and create a dialogue with an emotion, such as sadness. I would write it as fast as I can.
I would say, “OK, Sadness. Why are you here? What are you doing? I don’t enjoy having you around.” And Sadness writes back to me, “But you need me.” And J says, “What do you mean I need you?” And Sadness says, “Well, your brother died 7 weeks ago, didn’t he?” And I say, “Yes, he did.” And Sadness says, “Aren’t you sad?” I say, “Yes. I’m terribly sad and grieving all the time. But I wasn’t thinking about him at this moment.” And Sadness says, “But he’s there with you all the time and that sadness is in you.” And I say, “You mean it’s in me even here, now, as I’m talking with Andrew in this interview?” And Sadness says, “Yes. You can talk about your work. But in between the words, as you take a breath, don’t you feel it in your chest?” That’s the way the dialogue goes.
Dr. Wilner: What about specifically with the coronavirus? Fear is certainly an emotion. Nobody wants to get sick and die. Nobody wants to bring this disease home to their family. People are reluctant to even go outside and you can’t shake someone’s hand. Are there precedents for this?
Dr. Gordon: There are precedents, but only relatively small groups were affected before by, for example, severe acute respiratory syndrome or H1N1, at least in the United States. But we haven’t seen a global pandemic like this since 1918. None of us was around then – or I certainly wasn’t around. So for most everyone, not only has it not happened before, but we’ve never been so globally aware of everything that’s going on and how different groups are reacting.
I’ve been reading Daniel Defoe’s book, “A Journal of the Plague Year.” It’s really very interesting. It’s about the bubonic plague in 1665 London, although he wrote it in the 1720s. Some of the same things were going on then: the enormous fear, the isolation; rich people being able to escape, poor people having nowhere to go; conspiracy theories of one kind or another, about where the plague came from or blaming a group of people for it; magical thinking that it’s just going to go away. All of those things that happened several hundred years ago are going on now.
And we’re all simultaneously aware of all those things. There’s not only the fear, which should be universal because it’s a reasonable response to this situation, but also the terrible confusion about what to do. The President is saying one thing, governors something else; Anthony Fauci is saying something else, and Deborah Birx is saying something a little bit different. There’s this tremendous confusion that overlays the fear, and I think everybody is more or less feeling these things.
So yes, a dialogue with fear is a good thing to do because it can be clarifying. What we need here is a sense of, what is it that makes sense for me to do? What precautions should I take? What precautions shouldn’t I take?
I have a 17-year-old son who lives with his mom in California. He and I were on the phone the other day. He’s a basketball player and very serious about it. He said, “I don’t want to put my life on hold.” And my response was, “If you go outside too soon, your life may be on hold for a hell of a lot longer than if you stay inside because, if you get sick, it’s serious. But you also need to start looking at the evidence and asking yourself the right questions because I can’t be there all the time and neither can your mom.”
Everybody really needs to use these kinds of tools to help themselves. The tools we teach are extremely good at bringing us back into a state of psychological and physiological balance — slow, deep breathing being a very basic one. Because it’s only in that state that we’re going to be able to make the most intelligent decisions about what to do. It’s only in that state that we’re going to be able to really look our fear in the face and find out what we should be afraid of and what we shouldn’t be afraid of.
It’s a process that’s very much integrated. We’re talking now about how to deal with the emotions. But the first part of what we do in our groups and our online trainings and webinars is teach people to just take a few deep breaths. Just take a few deep breaths in through the nose, out through the mouth, with your belly soft and relaxed. You can keep breathing this way while talking. That’s the antidote to the fight-or-flight response. We all learn about fight-or-flight in first-year physiology. We need to deal with it. We need to bring ourselves into balance. That’s the way we’re going to make the wisest decisions for ourselves and be best able to help our patients.
Dr. Wilner: As you mentioned, part of modern culture is that we now have access to all of this information worldwide. There’s a continual stream of newsfeeds, people flipping on their phones, receiving constant updates, 24/7. That’s a new phenomenon. Does that steal from us the time we had before for just breathing and synthesizing data as opposed to just acquiring it all the time?
Dr. Gordon: You’re absolutely right. It does and it’s a challenge. It can’t steal from us unless we’re letting our emotional, psychological, and physiological pockets be picked!
What we need to do is to make it our priority to come into balance. I don’t watch news all day long – a little tiny bit in the morning and in the evening, just to get a sense of what’s happening. That’s enough. And I think everybody needs to take a step back, ask if this is really what they want to be doing, and to come into balance.
The other thing that’s really important is physical activity, especially during this time. In addition to using slow, deep breathing to come into balance, physical exercise and movement of any kind is extremely good as an antidote to fight-or-flight and that shut-down, freeze-up response that we get into when we feel completely overwhelmed.
We’ve got to take it into our own hands. The media just want to sell us things. Let’s face it: They’re not here for our good. Our job as physicians and health care professionals is to really reinforce for people not only what we can do for them but what they can do for themselves.
Dr. Wilner: I’m certainly interested in learning more about mind-body medicine. For those who feel the same, where do you recommend they go to learn more?
Dr. Gordon: We have a website, cmbm.org, which features a number of webinars. I do a free webinar there every week. We have mind-body skills groups that meet once a week for 8 weeks. There are six physicians in my group and all kinds of health professionals in other groups. We have a training program that we’re bringing online. We’ve trained well over 6,000 people around the world and would love to train more. You can read about that on the website.
We’re starting to do more and more consulting with health care organizations. We’re working with the largest division of Veterans Affairs, which is in Florida, as well as in south Georgia and the Caribbean. We’re working with a large health system in Indiana and others elsewhere. In addition, we’re working with groups of physicians and mental health professionals, helping them to integrate what we have to offer into what they’re already doing.
That’s our job – to help you do your job.
Dr. Wilner: Dr Gordon, I feel more relaxed just speaking with you. Thank you for talking with me and sharing your experiences with Medscape. I look forward to learning more.
Dr. Gordon: Thank you. My pleasure.
A version of this article originally appeared on Medscape.com.
Andrew N. Wilner, MD: Welcome to Medscape. I’m Dr Andrew Wilner. Today I have a special guest, Dr James Gordon, founder and executive director of the Center for Mind-Body Medicine. Welcome, Dr Gordon.
James S. Gordon, MD: Thank you very much. It’s good to be with you.
Dr. Wilner: Thanks for joining us. We are recording this in late May 2020, in the midst of the coronavirus pandemic. Millions of people have been infected. Hundreds of thousands have died. Millions have lost their jobs. I think it’s fair to say that people are under a greater degree of stress than they’re normally accustomed to. Would you agree with that?
Dr. Gordon: I think it’s more than fair to say that everybody in the United States, and actually pretty much everyone in the world, is under extreme stress. And that compounds any stresses that they’ve experienced before in their lives. Everyone is affected.
Dr. Wilner: The mind-body medicine concept is one that you’ve pursued for decades. Tell us a little bit about the Center for Mind-Body Medicine and how that’s led to the program that you have to help us deal with the coronavirus.
Dr. Gordon: I started the Center for Mind-Body Medicine about 30 years ago. I’d been a researcher at the National Institute of Mental Health for a number of years, in private practice, and a professor at Georgetown Medical School. But I wanted to really focus on how to change and enrich medicine by making self-care, self-awareness, and group support central to all healthcare.
Western medicine is enormously powerful in certain situations, such as physical trauma, high levels of infection, congenital anomalies. But we’re not so good at working with chronic physical or psychological problems. Those are much more complex.
We’ve been discovering that what is going to make the long-term difference in conditions like type 2 diabetes, pain syndromes, hypertension, depression, and anxiety are those approaches that we can learn to do for ourselves. These are changes we can make in how we deal with stress, eat, exercise, relate to other people, and whether we find meaning and purpose in our lives.
by wars, climate-related disasters, the opioid epidemic, chronic poverty, historical trauma. We do a lot of work with indigenous people here in North America. We’ve worked in a number of communities where school shootings have traumatized everyone.
What we’ve learned over these past 25 years, and what interested me professionally as well as personally over the past 50 years, is what we’re now bringing out on an even larger scale. The kind of approaches that we’ve developed, studied, and published research on are exactly what everyone needs to include and incorporate in their daily life, as well as in their medical and health care, from now on.
Dr. Wilner: Do you have a program that’s specifically for health care providers?
Dr. Gordon: Yes. The Center for Mind-Body Medicine is primarily an educational organization rather than a service organization. Since the beginning, I’ve been focused on training health professionals. My first passion was for training physicians – I’m a physician, so there’s a feeling of fellowship there – but also health care workers and mental health professionals of every kind.
We teach health professionals a whole system, a comprehensive program of techniques of self-awareness and self-care. We teach them so that they can practice on themselves and study the underlying science, so they can then teach what they’ve learned to the patients or clients they work with. They integrate it into what they’re already doing, regardless of their specialty. At times we also offer some of the same kinds of mind-body skills groups that are the fundamental part of our training as a stand-alone intervention. You can’t really teach other people how to take care of themselves unless you’re also doing it yourself. Otherwise, it’s just a theory.
Dr. Wilner: As a neurologist, I’m interested in the mind-body system. You are a psychiatrist and understand that it’s a lot more difficult to objectify certain things. What is stress? What is happiness? What is sadness? It’s very hard to measure. You can have scales, but it requires insight on the part of the individual. So I think it’s certainly an ambitious project.
Dr. Gordon: You’re absolutely right. It requires insight. And one of the shortcomings of our medical education is that it doesn’t encourage us to look inside ourselves enough. There’s so much focus on objectivity and on data, that we’ve lost some of the subjective art of medicine.
My experience with myself, as well as with the thousands of people we’ve trained here in the United States and around the world and the many hundreds of thousands with whom they’ve worked, is that all of us have a greater capacity to understand and help ourselves than we ordinarily think or than most of us learn about in our medical education.
This work is saying to people to take a little bit of time and relax a little in order to allow yourself to come into a meditative state. And I don’t mean anything fancy by that. Meditation is just being relaxed. Moment-to-moment awareness doesn’t have to do with any particular religion or spiritual practice. It’s part of all of them. If you can get into that state, then you can begin to say, “Oh, that’s what’s going on with me. That’s why my pain is worse.”
For example, you often wonder in people with peripheral neuropathy why it becomes worse or better at certain points. I would encourage neurologists and other physicians to ask your patients, “Why do you think it’s worse?” They may say, “I don’t know, doc; that’s why I’m here.” But I would ask them to take a couple of minutes to let me know. They could think it has something to do with the fact that they had a big fight with their wife that morning, they don’t want to go to work, or whatever it is. This is part of the lost art that we need to bring back into medicine for ourselves and especially for our patients.
Dr. Wilner: Can you give me an example of some of the exercises you’d do in a class?
Dr. Gordon: All of the exercises and our entire program that we teach at the Center for Mind-Body Medicine is in this new book of mine, “The Transformation: Discovering Wholeness and Healing After Trauma.” It’s really the distillation of not just the past 25 or 30 years, but really 50 years of work.
The techniques are all pretty simple and, as we say, evidence based. There is evidence that shows how they work on us physiologically, as well as psychologically. And they’re all pretty easy to teach to anyone.
Myself and about 60 or 70 of our faculty at the Center for Mind-Body Medicine are currently leading online groups. Then several hundred of the other people we’ve trained are also leading these groups. We’re still counting it up, but we probably have between 700 and 1,000 groups going around the world, led by our faculty and by people we’ve trained.
We teach a different technique every week in these online groups. Last week, after getting people energized and focused, we did a written dialogue with an emotion. You put down the initial of your name – in my case, “J” for Jim – and create a dialogue with an emotion, such as sadness. I would write it as fast as I can.
I would say, “OK, Sadness. Why are you here? What are you doing? I don’t enjoy having you around.” And Sadness writes back to me, “But you need me.” And J says, “What do you mean I need you?” And Sadness says, “Well, your brother died 7 weeks ago, didn’t he?” And I say, “Yes, he did.” And Sadness says, “Aren’t you sad?” I say, “Yes. I’m terribly sad and grieving all the time. But I wasn’t thinking about him at this moment.” And Sadness says, “But he’s there with you all the time and that sadness is in you.” And I say, “You mean it’s in me even here, now, as I’m talking with Andrew in this interview?” And Sadness says, “Yes. You can talk about your work. But in between the words, as you take a breath, don’t you feel it in your chest?” That’s the way the dialogue goes.
Dr. Wilner: What about specifically with the coronavirus? Fear is certainly an emotion. Nobody wants to get sick and die. Nobody wants to bring this disease home to their family. People are reluctant to even go outside and you can’t shake someone’s hand. Are there precedents for this?
Dr. Gordon: There are precedents, but only relatively small groups were affected before by, for example, severe acute respiratory syndrome or H1N1, at least in the United States. But we haven’t seen a global pandemic like this since 1918. None of us was around then – or I certainly wasn’t around. So for most everyone, not only has it not happened before, but we’ve never been so globally aware of everything that’s going on and how different groups are reacting.
I’ve been reading Daniel Defoe’s book, “A Journal of the Plague Year.” It’s really very interesting. It’s about the bubonic plague in 1665 London, although he wrote it in the 1720s. Some of the same things were going on then: the enormous fear, the isolation; rich people being able to escape, poor people having nowhere to go; conspiracy theories of one kind or another, about where the plague came from or blaming a group of people for it; magical thinking that it’s just going to go away. All of those things that happened several hundred years ago are going on now.
And we’re all simultaneously aware of all those things. There’s not only the fear, which should be universal because it’s a reasonable response to this situation, but also the terrible confusion about what to do. The President is saying one thing, governors something else; Anthony Fauci is saying something else, and Deborah Birx is saying something a little bit different. There’s this tremendous confusion that overlays the fear, and I think everybody is more or less feeling these things.
So yes, a dialogue with fear is a good thing to do because it can be clarifying. What we need here is a sense of, what is it that makes sense for me to do? What precautions should I take? What precautions shouldn’t I take?
I have a 17-year-old son who lives with his mom in California. He and I were on the phone the other day. He’s a basketball player and very serious about it. He said, “I don’t want to put my life on hold.” And my response was, “If you go outside too soon, your life may be on hold for a hell of a lot longer than if you stay inside because, if you get sick, it’s serious. But you also need to start looking at the evidence and asking yourself the right questions because I can’t be there all the time and neither can your mom.”
Everybody really needs to use these kinds of tools to help themselves. The tools we teach are extremely good at bringing us back into a state of psychological and physiological balance — slow, deep breathing being a very basic one. Because it’s only in that state that we’re going to be able to make the most intelligent decisions about what to do. It’s only in that state that we’re going to be able to really look our fear in the face and find out what we should be afraid of and what we shouldn’t be afraid of.
It’s a process that’s very much integrated. We’re talking now about how to deal with the emotions. But the first part of what we do in our groups and our online trainings and webinars is teach people to just take a few deep breaths. Just take a few deep breaths in through the nose, out through the mouth, with your belly soft and relaxed. You can keep breathing this way while talking. That’s the antidote to the fight-or-flight response. We all learn about fight-or-flight in first-year physiology. We need to deal with it. We need to bring ourselves into balance. That’s the way we’re going to make the wisest decisions for ourselves and be best able to help our patients.
Dr. Wilner: As you mentioned, part of modern culture is that we now have access to all of this information worldwide. There’s a continual stream of newsfeeds, people flipping on their phones, receiving constant updates, 24/7. That’s a new phenomenon. Does that steal from us the time we had before for just breathing and synthesizing data as opposed to just acquiring it all the time?
Dr. Gordon: You’re absolutely right. It does and it’s a challenge. It can’t steal from us unless we’re letting our emotional, psychological, and physiological pockets be picked!
What we need to do is to make it our priority to come into balance. I don’t watch news all day long – a little tiny bit in the morning and in the evening, just to get a sense of what’s happening. That’s enough. And I think everybody needs to take a step back, ask if this is really what they want to be doing, and to come into balance.
The other thing that’s really important is physical activity, especially during this time. In addition to using slow, deep breathing to come into balance, physical exercise and movement of any kind is extremely good as an antidote to fight-or-flight and that shut-down, freeze-up response that we get into when we feel completely overwhelmed.
We’ve got to take it into our own hands. The media just want to sell us things. Let’s face it: They’re not here for our good. Our job as physicians and health care professionals is to really reinforce for people not only what we can do for them but what they can do for themselves.
Dr. Wilner: I’m certainly interested in learning more about mind-body medicine. For those who feel the same, where do you recommend they go to learn more?
Dr. Gordon: We have a website, cmbm.org, which features a number of webinars. I do a free webinar there every week. We have mind-body skills groups that meet once a week for 8 weeks. There are six physicians in my group and all kinds of health professionals in other groups. We have a training program that we’re bringing online. We’ve trained well over 6,000 people around the world and would love to train more. You can read about that on the website.
We’re starting to do more and more consulting with health care organizations. We’re working with the largest division of Veterans Affairs, which is in Florida, as well as in south Georgia and the Caribbean. We’re working with a large health system in Indiana and others elsewhere. In addition, we’re working with groups of physicians and mental health professionals, helping them to integrate what we have to offer into what they’re already doing.
That’s our job – to help you do your job.
Dr. Wilner: Dr Gordon, I feel more relaxed just speaking with you. Thank you for talking with me and sharing your experiences with Medscape. I look forward to learning more.
Dr. Gordon: Thank you. My pleasure.
A version of this article originally appeared on Medscape.com.
Andrew N. Wilner, MD: Welcome to Medscape. I’m Dr Andrew Wilner. Today I have a special guest, Dr James Gordon, founder and executive director of the Center for Mind-Body Medicine. Welcome, Dr Gordon.
James S. Gordon, MD: Thank you very much. It’s good to be with you.
Dr. Wilner: Thanks for joining us. We are recording this in late May 2020, in the midst of the coronavirus pandemic. Millions of people have been infected. Hundreds of thousands have died. Millions have lost their jobs. I think it’s fair to say that people are under a greater degree of stress than they’re normally accustomed to. Would you agree with that?
Dr. Gordon: I think it’s more than fair to say that everybody in the United States, and actually pretty much everyone in the world, is under extreme stress. And that compounds any stresses that they’ve experienced before in their lives. Everyone is affected.
Dr. Wilner: The mind-body medicine concept is one that you’ve pursued for decades. Tell us a little bit about the Center for Mind-Body Medicine and how that’s led to the program that you have to help us deal with the coronavirus.
Dr. Gordon: I started the Center for Mind-Body Medicine about 30 years ago. I’d been a researcher at the National Institute of Mental Health for a number of years, in private practice, and a professor at Georgetown Medical School. But I wanted to really focus on how to change and enrich medicine by making self-care, self-awareness, and group support central to all healthcare.
Western medicine is enormously powerful in certain situations, such as physical trauma, high levels of infection, congenital anomalies. But we’re not so good at working with chronic physical or psychological problems. Those are much more complex.
We’ve been discovering that what is going to make the long-term difference in conditions like type 2 diabetes, pain syndromes, hypertension, depression, and anxiety are those approaches that we can learn to do for ourselves. These are changes we can make in how we deal with stress, eat, exercise, relate to other people, and whether we find meaning and purpose in our lives.
by wars, climate-related disasters, the opioid epidemic, chronic poverty, historical trauma. We do a lot of work with indigenous people here in North America. We’ve worked in a number of communities where school shootings have traumatized everyone.
What we’ve learned over these past 25 years, and what interested me professionally as well as personally over the past 50 years, is what we’re now bringing out on an even larger scale. The kind of approaches that we’ve developed, studied, and published research on are exactly what everyone needs to include and incorporate in their daily life, as well as in their medical and health care, from now on.
Dr. Wilner: Do you have a program that’s specifically for health care providers?
Dr. Gordon: Yes. The Center for Mind-Body Medicine is primarily an educational organization rather than a service organization. Since the beginning, I’ve been focused on training health professionals. My first passion was for training physicians – I’m a physician, so there’s a feeling of fellowship there – but also health care workers and mental health professionals of every kind.
We teach health professionals a whole system, a comprehensive program of techniques of self-awareness and self-care. We teach them so that they can practice on themselves and study the underlying science, so they can then teach what they’ve learned to the patients or clients they work with. They integrate it into what they’re already doing, regardless of their specialty. At times we also offer some of the same kinds of mind-body skills groups that are the fundamental part of our training as a stand-alone intervention. You can’t really teach other people how to take care of themselves unless you’re also doing it yourself. Otherwise, it’s just a theory.
Dr. Wilner: As a neurologist, I’m interested in the mind-body system. You are a psychiatrist and understand that it’s a lot more difficult to objectify certain things. What is stress? What is happiness? What is sadness? It’s very hard to measure. You can have scales, but it requires insight on the part of the individual. So I think it’s certainly an ambitious project.
Dr. Gordon: You’re absolutely right. It requires insight. And one of the shortcomings of our medical education is that it doesn’t encourage us to look inside ourselves enough. There’s so much focus on objectivity and on data, that we’ve lost some of the subjective art of medicine.
My experience with myself, as well as with the thousands of people we’ve trained here in the United States and around the world and the many hundreds of thousands with whom they’ve worked, is that all of us have a greater capacity to understand and help ourselves than we ordinarily think or than most of us learn about in our medical education.
This work is saying to people to take a little bit of time and relax a little in order to allow yourself to come into a meditative state. And I don’t mean anything fancy by that. Meditation is just being relaxed. Moment-to-moment awareness doesn’t have to do with any particular religion or spiritual practice. It’s part of all of them. If you can get into that state, then you can begin to say, “Oh, that’s what’s going on with me. That’s why my pain is worse.”
For example, you often wonder in people with peripheral neuropathy why it becomes worse or better at certain points. I would encourage neurologists and other physicians to ask your patients, “Why do you think it’s worse?” They may say, “I don’t know, doc; that’s why I’m here.” But I would ask them to take a couple of minutes to let me know. They could think it has something to do with the fact that they had a big fight with their wife that morning, they don’t want to go to work, or whatever it is. This is part of the lost art that we need to bring back into medicine for ourselves and especially for our patients.
Dr. Wilner: Can you give me an example of some of the exercises you’d do in a class?
Dr. Gordon: All of the exercises and our entire program that we teach at the Center for Mind-Body Medicine is in this new book of mine, “The Transformation: Discovering Wholeness and Healing After Trauma.” It’s really the distillation of not just the past 25 or 30 years, but really 50 years of work.
The techniques are all pretty simple and, as we say, evidence based. There is evidence that shows how they work on us physiologically, as well as psychologically. And they’re all pretty easy to teach to anyone.
Myself and about 60 or 70 of our faculty at the Center for Mind-Body Medicine are currently leading online groups. Then several hundred of the other people we’ve trained are also leading these groups. We’re still counting it up, but we probably have between 700 and 1,000 groups going around the world, led by our faculty and by people we’ve trained.
We teach a different technique every week in these online groups. Last week, after getting people energized and focused, we did a written dialogue with an emotion. You put down the initial of your name – in my case, “J” for Jim – and create a dialogue with an emotion, such as sadness. I would write it as fast as I can.
I would say, “OK, Sadness. Why are you here? What are you doing? I don’t enjoy having you around.” And Sadness writes back to me, “But you need me.” And J says, “What do you mean I need you?” And Sadness says, “Well, your brother died 7 weeks ago, didn’t he?” And I say, “Yes, he did.” And Sadness says, “Aren’t you sad?” I say, “Yes. I’m terribly sad and grieving all the time. But I wasn’t thinking about him at this moment.” And Sadness says, “But he’s there with you all the time and that sadness is in you.” And I say, “You mean it’s in me even here, now, as I’m talking with Andrew in this interview?” And Sadness says, “Yes. You can talk about your work. But in between the words, as you take a breath, don’t you feel it in your chest?” That’s the way the dialogue goes.
Dr. Wilner: What about specifically with the coronavirus? Fear is certainly an emotion. Nobody wants to get sick and die. Nobody wants to bring this disease home to their family. People are reluctant to even go outside and you can’t shake someone’s hand. Are there precedents for this?
Dr. Gordon: There are precedents, but only relatively small groups were affected before by, for example, severe acute respiratory syndrome or H1N1, at least in the United States. But we haven’t seen a global pandemic like this since 1918. None of us was around then – or I certainly wasn’t around. So for most everyone, not only has it not happened before, but we’ve never been so globally aware of everything that’s going on and how different groups are reacting.
I’ve been reading Daniel Defoe’s book, “A Journal of the Plague Year.” It’s really very interesting. It’s about the bubonic plague in 1665 London, although he wrote it in the 1720s. Some of the same things were going on then: the enormous fear, the isolation; rich people being able to escape, poor people having nowhere to go; conspiracy theories of one kind or another, about where the plague came from or blaming a group of people for it; magical thinking that it’s just going to go away. All of those things that happened several hundred years ago are going on now.
And we’re all simultaneously aware of all those things. There’s not only the fear, which should be universal because it’s a reasonable response to this situation, but also the terrible confusion about what to do. The President is saying one thing, governors something else; Anthony Fauci is saying something else, and Deborah Birx is saying something a little bit different. There’s this tremendous confusion that overlays the fear, and I think everybody is more or less feeling these things.
So yes, a dialogue with fear is a good thing to do because it can be clarifying. What we need here is a sense of, what is it that makes sense for me to do? What precautions should I take? What precautions shouldn’t I take?
I have a 17-year-old son who lives with his mom in California. He and I were on the phone the other day. He’s a basketball player and very serious about it. He said, “I don’t want to put my life on hold.” And my response was, “If you go outside too soon, your life may be on hold for a hell of a lot longer than if you stay inside because, if you get sick, it’s serious. But you also need to start looking at the evidence and asking yourself the right questions because I can’t be there all the time and neither can your mom.”
Everybody really needs to use these kinds of tools to help themselves. The tools we teach are extremely good at bringing us back into a state of psychological and physiological balance — slow, deep breathing being a very basic one. Because it’s only in that state that we’re going to be able to make the most intelligent decisions about what to do. It’s only in that state that we’re going to be able to really look our fear in the face and find out what we should be afraid of and what we shouldn’t be afraid of.
It’s a process that’s very much integrated. We’re talking now about how to deal with the emotions. But the first part of what we do in our groups and our online trainings and webinars is teach people to just take a few deep breaths. Just take a few deep breaths in through the nose, out through the mouth, with your belly soft and relaxed. You can keep breathing this way while talking. That’s the antidote to the fight-or-flight response. We all learn about fight-or-flight in first-year physiology. We need to deal with it. We need to bring ourselves into balance. That’s the way we’re going to make the wisest decisions for ourselves and be best able to help our patients.
Dr. Wilner: As you mentioned, part of modern culture is that we now have access to all of this information worldwide. There’s a continual stream of newsfeeds, people flipping on their phones, receiving constant updates, 24/7. That’s a new phenomenon. Does that steal from us the time we had before for just breathing and synthesizing data as opposed to just acquiring it all the time?
Dr. Gordon: You’re absolutely right. It does and it’s a challenge. It can’t steal from us unless we’re letting our emotional, psychological, and physiological pockets be picked!
What we need to do is to make it our priority to come into balance. I don’t watch news all day long – a little tiny bit in the morning and in the evening, just to get a sense of what’s happening. That’s enough. And I think everybody needs to take a step back, ask if this is really what they want to be doing, and to come into balance.
The other thing that’s really important is physical activity, especially during this time. In addition to using slow, deep breathing to come into balance, physical exercise and movement of any kind is extremely good as an antidote to fight-or-flight and that shut-down, freeze-up response that we get into when we feel completely overwhelmed.
We’ve got to take it into our own hands. The media just want to sell us things. Let’s face it: They’re not here for our good. Our job as physicians and health care professionals is to really reinforce for people not only what we can do for them but what they can do for themselves.
Dr. Wilner: I’m certainly interested in learning more about mind-body medicine. For those who feel the same, where do you recommend they go to learn more?
Dr. Gordon: We have a website, cmbm.org, which features a number of webinars. I do a free webinar there every week. We have mind-body skills groups that meet once a week for 8 weeks. There are six physicians in my group and all kinds of health professionals in other groups. We have a training program that we’re bringing online. We’ve trained well over 6,000 people around the world and would love to train more. You can read about that on the website.
We’re starting to do more and more consulting with health care organizations. We’re working with the largest division of Veterans Affairs, which is in Florida, as well as in south Georgia and the Caribbean. We’re working with a large health system in Indiana and others elsewhere. In addition, we’re working with groups of physicians and mental health professionals, helping them to integrate what we have to offer into what they’re already doing.
That’s our job – to help you do your job.
Dr. Wilner: Dr Gordon, I feel more relaxed just speaking with you. Thank you for talking with me and sharing your experiences with Medscape. I look forward to learning more.
Dr. Gordon: Thank you. My pleasure.
A version of this article originally appeared on Medscape.com.
‘I can’t breathe’: Health inequity and state-sanctioned violence
One might immediately think of the deaths of Eric Garner, George Floyd, or even the fictional character Radio Raheem from Spike Lee’s critically acclaimed film, “Do the Right Thing,” when they hear the words “I can’t breathe.” These words are a cry for help. The deaths of these unarmed black men is devastating and has led to a state of rage, palpable pain, and protest across the world.
However, in this moment, I am talking about the health inequity exposed by the COVID-19 pandemic. Whether it be acute respiratory distress syndrome (ARDS) secondary to severe COVID-19, or the subsequent hypercoagulable state of COVID-19 that leads to venous thromboembolism, many black people in this country are left breathless. Many black patients who had no employee-based health insurance also had no primary care physician to order a SARS-CoV2 PCR lab test for them. Many of these patients have preexisting conditions, such as asthma from living in redlined communities affected by environmental racism. Many grew up in food deserts, where no fresh-produce store was interested enough to set up shop in their neighborhoods. They have been eating fast food since early childhood, as a fast-food burger is still cheaper than a salad. The result is obesity, an epidemic that can lead to diabetes mellitus, hypertension that can lead to coronary artery disease, stroke, and end-stage renal disease.
Earlier in my career, I once had a colleague gleefully tell me that all black people drank Kool-Aid while in discussion of the effects of high-sugar diets in our patients; this colleague was sure I would agree. Not all black people drink Kool-Aid. Secondary to my fear of the backlash that can come from the discomfort of “white fragility” that Robin DiAngelo describes in her New York Times bestseller by the same name, ”White Fragility: Why It’s So Hard for White People to Talk About Racism,” I refrained from expressing my own hurt, and I did not offer explicit correction. I, instead, took a serious pause. That pause, which lasted only minutes, seemed to last 400 years. It was a brief reflection of the 400 years of systemic racism seeping into everyday life. This included the circumstances that would lead to the health inequities that result in the health disparities from which many black patients suffer. It is that same systemic racism that could create two America’s in which my colleague might not have to know the historic context in which that question could be hurtful. I retorted with modified shock and a chuckle so that I could muster up enough strength to repeat what was said and leave it open for reflection. The goal was for my colleague to realize the obvious implicit bias that lingered, despite intention. The chuckle was also to cover my pain.
Whether we know it or not, we all carry some form of implicit bias, regardless of race, class, gender, ethnicity, sexual preference, or socioeconomic status. In this case, it is the same implicit bias that causes physicians to ignore some black patients when they have said that they are in pain. A groundbreaking April 2016 article in Proceedings of the National Academy of Sciences, “Racial Bias in Pain Assessment and Treatment Recommendations, and False Beliefs about Biological Differences Between Blacks and Whites” (doi: 10.1073/pnas.1516047113), revealed that racial disparities in pain assessment and treatment recommendations can be directly connected to the racial bias of the provider. It could be possible that this phenomenon has affected black patients who have walked into clinics and emergency departments and said, “I’m short of breath. I think that I might have coronavirus and need to be tested.” It may be that same implicit bias that has cut the air supply to a patient encounter. Instead of inquiring further, the patient might be met with minimum questions while their provider obtains their history and physical. Assumptions and blame on behavior and lack of personal responsibility secretly replace questions that could have been asked. Differentials between exacerbations and other etiologies are not explored. Could that patient have been sent home without a SARS-CoV2 polymerase chain reaction test? Well, what if the tests were in short supply? Sometimes they may have been sent home without a chest x-ray. In most cases, there are no funds to send them home with a pulse oximeter.
The act of assuming a person’s story that we consider to be one dimensional is always dangerous – and even more so during this pandemic. That person we can relate to – secondary to a cool pop culture moment, a TikTok song, or a negative stereotype – is not one dimensional. That assumption and that stereotype can make room for implicit bias. That same implicit bias is the knee on a neck of any marginalized patient. Implicit bias is the choke hold that slowly removes the light and life from a person who has a story, who has a family, and who has been an essential worker who can’t work from home. That person is telling us that they can’t breathe, but sometimes the only things seen are comorbidities through a misinformed or biased lens that suggest an assumed lack of personal responsibility. In a May 2020 New England Journal of Medicine perspective, “Racial health disparities and Covid-19” (doi: 10.1056/NEJMp2012910), Merlin Chowkwanyun, PhD, MPH, and Adolph L. Reed Jr., PhD, caution us against creating race-based explanations for presumed behavioral patterns.
Systemic racism has created the myth that the playing field has been leveled since the end of enslavement. It hasn’t. That black man, woman, or nonbinary person is telling you “I can’t breathe. I’m tired. I’m short of breath ... I have a cough ... I’m feeling weak these days, Doc.” However, implicit bias is still that knee that won’t let up. It has not let up. Communities with lower-income black and Hispanic patients have already seen local hospitals and frontline workers fight to save their lives while losing their own to COVID-19. We all witnessed the battle for scarce resources and PPE [personal protective equipment]. In contrast, some wealthy neighborhoods have occupants who most likely have access to a primary care physician and more testing centers.
As we reexamine ourselves and look at these cases of police brutality against unarmed black men, women, and children with the appropriate shame and outrage, let us reflect upon the privileges that we enjoy. Let us find our voice as we speak up for black lives. Let us look deeply into the history of medicine as it relates to black patients by reading “Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present” by Harriet A. Washington. Let us examine that painful legacy, which, while having moments of good intention, still carries the stain of indifference, racism, neglect, and even experimentation without informed consent.
Why should we do these things? Because some of our black patients have also yelled or whispered, “I can’t breathe,” and we were not always listening either.
Dr. Ajala is a hospitalist and associate site director for education at Grady Memorial Hospital in Atlanta. She is a member of the executive council for SHM’s Care for Vulnerable Populations special interest group.
One might immediately think of the deaths of Eric Garner, George Floyd, or even the fictional character Radio Raheem from Spike Lee’s critically acclaimed film, “Do the Right Thing,” when they hear the words “I can’t breathe.” These words are a cry for help. The deaths of these unarmed black men is devastating and has led to a state of rage, palpable pain, and protest across the world.
However, in this moment, I am talking about the health inequity exposed by the COVID-19 pandemic. Whether it be acute respiratory distress syndrome (ARDS) secondary to severe COVID-19, or the subsequent hypercoagulable state of COVID-19 that leads to venous thromboembolism, many black people in this country are left breathless. Many black patients who had no employee-based health insurance also had no primary care physician to order a SARS-CoV2 PCR lab test for them. Many of these patients have preexisting conditions, such as asthma from living in redlined communities affected by environmental racism. Many grew up in food deserts, where no fresh-produce store was interested enough to set up shop in their neighborhoods. They have been eating fast food since early childhood, as a fast-food burger is still cheaper than a salad. The result is obesity, an epidemic that can lead to diabetes mellitus, hypertension that can lead to coronary artery disease, stroke, and end-stage renal disease.
Earlier in my career, I once had a colleague gleefully tell me that all black people drank Kool-Aid while in discussion of the effects of high-sugar diets in our patients; this colleague was sure I would agree. Not all black people drink Kool-Aid. Secondary to my fear of the backlash that can come from the discomfort of “white fragility” that Robin DiAngelo describes in her New York Times bestseller by the same name, ”White Fragility: Why It’s So Hard for White People to Talk About Racism,” I refrained from expressing my own hurt, and I did not offer explicit correction. I, instead, took a serious pause. That pause, which lasted only minutes, seemed to last 400 years. It was a brief reflection of the 400 years of systemic racism seeping into everyday life. This included the circumstances that would lead to the health inequities that result in the health disparities from which many black patients suffer. It is that same systemic racism that could create two America’s in which my colleague might not have to know the historic context in which that question could be hurtful. I retorted with modified shock and a chuckle so that I could muster up enough strength to repeat what was said and leave it open for reflection. The goal was for my colleague to realize the obvious implicit bias that lingered, despite intention. The chuckle was also to cover my pain.
Whether we know it or not, we all carry some form of implicit bias, regardless of race, class, gender, ethnicity, sexual preference, or socioeconomic status. In this case, it is the same implicit bias that causes physicians to ignore some black patients when they have said that they are in pain. A groundbreaking April 2016 article in Proceedings of the National Academy of Sciences, “Racial Bias in Pain Assessment and Treatment Recommendations, and False Beliefs about Biological Differences Between Blacks and Whites” (doi: 10.1073/pnas.1516047113), revealed that racial disparities in pain assessment and treatment recommendations can be directly connected to the racial bias of the provider. It could be possible that this phenomenon has affected black patients who have walked into clinics and emergency departments and said, “I’m short of breath. I think that I might have coronavirus and need to be tested.” It may be that same implicit bias that has cut the air supply to a patient encounter. Instead of inquiring further, the patient might be met with minimum questions while their provider obtains their history and physical. Assumptions and blame on behavior and lack of personal responsibility secretly replace questions that could have been asked. Differentials between exacerbations and other etiologies are not explored. Could that patient have been sent home without a SARS-CoV2 polymerase chain reaction test? Well, what if the tests were in short supply? Sometimes they may have been sent home without a chest x-ray. In most cases, there are no funds to send them home with a pulse oximeter.
The act of assuming a person’s story that we consider to be one dimensional is always dangerous – and even more so during this pandemic. That person we can relate to – secondary to a cool pop culture moment, a TikTok song, or a negative stereotype – is not one dimensional. That assumption and that stereotype can make room for implicit bias. That same implicit bias is the knee on a neck of any marginalized patient. Implicit bias is the choke hold that slowly removes the light and life from a person who has a story, who has a family, and who has been an essential worker who can’t work from home. That person is telling us that they can’t breathe, but sometimes the only things seen are comorbidities through a misinformed or biased lens that suggest an assumed lack of personal responsibility. In a May 2020 New England Journal of Medicine perspective, “Racial health disparities and Covid-19” (doi: 10.1056/NEJMp2012910), Merlin Chowkwanyun, PhD, MPH, and Adolph L. Reed Jr., PhD, caution us against creating race-based explanations for presumed behavioral patterns.
Systemic racism has created the myth that the playing field has been leveled since the end of enslavement. It hasn’t. That black man, woman, or nonbinary person is telling you “I can’t breathe. I’m tired. I’m short of breath ... I have a cough ... I’m feeling weak these days, Doc.” However, implicit bias is still that knee that won’t let up. It has not let up. Communities with lower-income black and Hispanic patients have already seen local hospitals and frontline workers fight to save their lives while losing their own to COVID-19. We all witnessed the battle for scarce resources and PPE [personal protective equipment]. In contrast, some wealthy neighborhoods have occupants who most likely have access to a primary care physician and more testing centers.
As we reexamine ourselves and look at these cases of police brutality against unarmed black men, women, and children with the appropriate shame and outrage, let us reflect upon the privileges that we enjoy. Let us find our voice as we speak up for black lives. Let us look deeply into the history of medicine as it relates to black patients by reading “Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present” by Harriet A. Washington. Let us examine that painful legacy, which, while having moments of good intention, still carries the stain of indifference, racism, neglect, and even experimentation without informed consent.
Why should we do these things? Because some of our black patients have also yelled or whispered, “I can’t breathe,” and we were not always listening either.
Dr. Ajala is a hospitalist and associate site director for education at Grady Memorial Hospital in Atlanta. She is a member of the executive council for SHM’s Care for Vulnerable Populations special interest group.
One might immediately think of the deaths of Eric Garner, George Floyd, or even the fictional character Radio Raheem from Spike Lee’s critically acclaimed film, “Do the Right Thing,” when they hear the words “I can’t breathe.” These words are a cry for help. The deaths of these unarmed black men is devastating and has led to a state of rage, palpable pain, and protest across the world.
However, in this moment, I am talking about the health inequity exposed by the COVID-19 pandemic. Whether it be acute respiratory distress syndrome (ARDS) secondary to severe COVID-19, or the subsequent hypercoagulable state of COVID-19 that leads to venous thromboembolism, many black people in this country are left breathless. Many black patients who had no employee-based health insurance also had no primary care physician to order a SARS-CoV2 PCR lab test for them. Many of these patients have preexisting conditions, such as asthma from living in redlined communities affected by environmental racism. Many grew up in food deserts, where no fresh-produce store was interested enough to set up shop in their neighborhoods. They have been eating fast food since early childhood, as a fast-food burger is still cheaper than a salad. The result is obesity, an epidemic that can lead to diabetes mellitus, hypertension that can lead to coronary artery disease, stroke, and end-stage renal disease.
Earlier in my career, I once had a colleague gleefully tell me that all black people drank Kool-Aid while in discussion of the effects of high-sugar diets in our patients; this colleague was sure I would agree. Not all black people drink Kool-Aid. Secondary to my fear of the backlash that can come from the discomfort of “white fragility” that Robin DiAngelo describes in her New York Times bestseller by the same name, ”White Fragility: Why It’s So Hard for White People to Talk About Racism,” I refrained from expressing my own hurt, and I did not offer explicit correction. I, instead, took a serious pause. That pause, which lasted only minutes, seemed to last 400 years. It was a brief reflection of the 400 years of systemic racism seeping into everyday life. This included the circumstances that would lead to the health inequities that result in the health disparities from which many black patients suffer. It is that same systemic racism that could create two America’s in which my colleague might not have to know the historic context in which that question could be hurtful. I retorted with modified shock and a chuckle so that I could muster up enough strength to repeat what was said and leave it open for reflection. The goal was for my colleague to realize the obvious implicit bias that lingered, despite intention. The chuckle was also to cover my pain.
Whether we know it or not, we all carry some form of implicit bias, regardless of race, class, gender, ethnicity, sexual preference, or socioeconomic status. In this case, it is the same implicit bias that causes physicians to ignore some black patients when they have said that they are in pain. A groundbreaking April 2016 article in Proceedings of the National Academy of Sciences, “Racial Bias in Pain Assessment and Treatment Recommendations, and False Beliefs about Biological Differences Between Blacks and Whites” (doi: 10.1073/pnas.1516047113), revealed that racial disparities in pain assessment and treatment recommendations can be directly connected to the racial bias of the provider. It could be possible that this phenomenon has affected black patients who have walked into clinics and emergency departments and said, “I’m short of breath. I think that I might have coronavirus and need to be tested.” It may be that same implicit bias that has cut the air supply to a patient encounter. Instead of inquiring further, the patient might be met with minimum questions while their provider obtains their history and physical. Assumptions and blame on behavior and lack of personal responsibility secretly replace questions that could have been asked. Differentials between exacerbations and other etiologies are not explored. Could that patient have been sent home without a SARS-CoV2 polymerase chain reaction test? Well, what if the tests were in short supply? Sometimes they may have been sent home without a chest x-ray. In most cases, there are no funds to send them home with a pulse oximeter.
The act of assuming a person’s story that we consider to be one dimensional is always dangerous – and even more so during this pandemic. That person we can relate to – secondary to a cool pop culture moment, a TikTok song, or a negative stereotype – is not one dimensional. That assumption and that stereotype can make room for implicit bias. That same implicit bias is the knee on a neck of any marginalized patient. Implicit bias is the choke hold that slowly removes the light and life from a person who has a story, who has a family, and who has been an essential worker who can’t work from home. That person is telling us that they can’t breathe, but sometimes the only things seen are comorbidities through a misinformed or biased lens that suggest an assumed lack of personal responsibility. In a May 2020 New England Journal of Medicine perspective, “Racial health disparities and Covid-19” (doi: 10.1056/NEJMp2012910), Merlin Chowkwanyun, PhD, MPH, and Adolph L. Reed Jr., PhD, caution us against creating race-based explanations for presumed behavioral patterns.
Systemic racism has created the myth that the playing field has been leveled since the end of enslavement. It hasn’t. That black man, woman, or nonbinary person is telling you “I can’t breathe. I’m tired. I’m short of breath ... I have a cough ... I’m feeling weak these days, Doc.” However, implicit bias is still that knee that won’t let up. It has not let up. Communities with lower-income black and Hispanic patients have already seen local hospitals and frontline workers fight to save their lives while losing their own to COVID-19. We all witnessed the battle for scarce resources and PPE [personal protective equipment]. In contrast, some wealthy neighborhoods have occupants who most likely have access to a primary care physician and more testing centers.
As we reexamine ourselves and look at these cases of police brutality against unarmed black men, women, and children with the appropriate shame and outrage, let us reflect upon the privileges that we enjoy. Let us find our voice as we speak up for black lives. Let us look deeply into the history of medicine as it relates to black patients by reading “Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present” by Harriet A. Washington. Let us examine that painful legacy, which, while having moments of good intention, still carries the stain of indifference, racism, neglect, and even experimentation without informed consent.
Why should we do these things? Because some of our black patients have also yelled or whispered, “I can’t breathe,” and we were not always listening either.
Dr. Ajala is a hospitalist and associate site director for education at Grady Memorial Hospital in Atlanta. She is a member of the executive council for SHM’s Care for Vulnerable Populations special interest group.
COVID-19: Haiti is vulnerable, but the international community can help
Doctors Without Borders, other groups urged to mobilize
Do you want to know what keeps us up at night? As 4th-year medical students born, raised, and living in Haiti, we worry about the impact of COVID-19 on our patients.
The pandemic has shaken the world, and Haiti is no exception.
It has taken several months for the disease to spread, and it began with two confirmed cases, one from France and the other from Belgium, on March 19.1 Much of the spread of COVID-19 in Haiti has been tied to workers returning from the Dominican Republic. As of June 29, Haiti had 5,975 confirmed cases and 105 deaths.2 Of course, those numbers sound minuscule, compared with those in the United States, where the number of deaths from COVID-19 surpassed 100,000 several weeks ago. But the population of Haiti is 30 times smaller than that of the United States, and Haiti is the poorest country in the Western Hemisphere. We have watched in horror as the virus has ravaged marginalized groups in the United States and worry that it will do the same in our own country.
Just as the Haitian Ministry of Health worked with various groups to reach the 1-year free of cholera mark in Haiti, groups such as Doctors Without Borders must mobilize to rein in COVID-19.
Community transmission rapid
After the first two cases were confirmed, a state of health emergency was immediately declared. Haitian President Jovenel Moïse and other government officials called for the implementation of several measures aimed at limiting the spread of COVID-19.
Schools, universities, clinical training programs, vocational centers, factories, airports, and ports, except for the transport of goods, were all ordered to close until further notice. Gatherings of larger than 10 people were banned. A curfew from 8 p.m. EST time to 5 a.m. EST was imposed. Measures such as those encouraged by U.S. Centers for Disease Control and Prevention, such as hand washing, physical distancing, and staying at home were also encouraged by the Haitian Ministry of Health. Mask wearing in public places was deemed mandatory.
The latest testing data show that community spread has been occurring among the Haitian population at a rapid rate. According to Jean William Pape, MD, Haiti’s top infectious diseases expert and founder of GHESKIO, an iconic infectious disease center that cares for people with HIV-AIDS and tuberculosis, a COVID-19 simulation from Cornell University in New York shows that about 35% of the Haitian population will be infected by the end of August 2020. A simulation by the University of Oxford (England) paints an even more dire picture. That simulation shows that 86% of the population could be infected, More than 9,000 additional hospital beds would be needed, and 20,000 people would be likely to die from COVID-19, Dr. Pape said in an interview with Haiti’s Nouvelliste newspaper.3
Medical response
We know that there is a global shortage of health care workers,4 and Haiti is no exception. According to a 2018 report from the Haitian Ministry of Health, the country has 11,775 health care professionals, including about 3,354 medical doctors, to care for more than 11 million people. That translates to about 23.4 physicians per 100,000.5
The pandemic has led some members of this already anemic health care workforce to stay home because of a lack of personal protective equipment. Others, because of reduced hospital or clinic budgets, have been furloughed, making the COVID-19 national health emergency even harder to manage.
But a severe health care shortage is not the only challenge facing Haiti. It spends about $131 U.S. per capita, which makes Haiti one of most vulnerable among low- and middle-income countries in the world. As a poor country,7 its health care infrastructure is among the most inadequate and weakest. Prior to COVID-19, medical advocacy groups already had started movements and strikes demanding that the government improve the health care system. The country’s precarious health care infrastructure includes a lack of hospital beds, and basic medical supplies and equipment, such as oxygen and ventilators.8 The emergence of COVID-19 has only exacerbated the situation.
Clinical training programs have been suspended, many doctors and nurses are on quarantine, and some hospitals and clinics are closing. We have witnessed makeshift voodoo clinics built by Haitian voodoo leaders to receive, hospitalize, and treat COVID-19 patients through rituals and herbal remedies. In some areas of the country, residents have protested against the opening of several COVID-19 treatment and management centers.
Unique cultural challenges
Public health officials around the world are facing challenges persuading citizens to engage in behaviors that could protect them from the virus.
Just as in America, where many people opt to not wear face coverings9,10 despite the public health risks, deep distrust of the Haitian government has undermined the messages of President Moïse and public healthofficials about the role of masks in limiting the spread of COVID.We see large numbers of unmasked people on the streets in the informal markets every day. Crammed tap-taps and overloaded motorcycles are moving everywhere. This also could be tied to cultural attitudes about COVID that persist among some Haitians.For example, many people with signs and symptoms of COVID-19 are afraid of going to the hospital to get tested and receive care, and resort to going to the voodoo clinics. Along with rituals, voodoo priests have been serving up teas with ingredients, including moringa, eucalyptus, ginger, and honey to those seeking COVID-19 care in the centers. The voodoo priests claim that the teas they serve strengthen the immune system.
In addition, it is difficult for poor people who live in small quarters with several other people to adhere to physical distancing.11
Stigma and violence
Other barriers in the fight against COVID-19 in Haiti are stigma and violence. If widespread testing were available, some Haitians would opt not to do so – despite clear signs and symptoms of the infection. Some people who would get tested if they could are afraid to do so because of fears tied to being attacked by neighbors.
When Haitian University professor Bellamy Nelson and his girlfriend returned to Haiti from the United States in March and began experiencing some pain and fever, he experienced attacks from neighbors, he said in an interview. He said neighbors threatened to burn down his house. When an ambulance arrived at his house to transport him to a hospital, it had to drive through back roads to avoid people armed with rocks, fire, and machetes, he told us. No hospital wanted to admit him. Eventually, Professor Nelson self-quarantined at home, he said.
In another incident, a national ambulance center in Gonaïves, a town toward the northern region of Haiti, reportedly was vandalized, because COVID-19 equipment and supplies used to treat people had been stored there. Hospital Bernard Mevs, along with many other hospitals, was forced by the area’s residents to suspend the plan to open a center for COVID-19 management. Threats to burn down the hospitals caused the leaders of the hospitals to back down and give up a plan to build a 20-bed COVID-19 response center.
Maternal health
Another concern we have about the pandemic is the risk it could be to pregnant women. On average, 94,000 deaths occur annually in Haiti. Out of this number, maternal mortality accounts for 1,000. In 2017, for every 100,000 live births for women of reproductive age from 15 to 49 years old, 480 women died. In contrast, in the Dominican Republic, 95 women died per 100,000 that same year. In the United States, 19 died, and in Norway, no more than 2 died that year.12
Some of the primary factors contributing to the crisis are limited accessibility, inadequate health care facilities, and an inadequate number of trained health care practitioners; low percentages of skilled attendants at deliveries and of prenatal and postnatal visits; and high numbers of high-risk deliveries in nonqualified health facilities.
During the COVID-19 national health emergency, with most hospitals reducing their health care personnel either because of budget-related reasons or because they are on quarantine, this maternal-fetal health crisis has escalated.
One of the biggest hospitals in Jacmel, a town in the southern region of Haiti, has stopped its prenatal care program. In Delmas, the city with the highest incidence and prevalence of COVID-19, Hôpital Universitaire de la Paix has reduced this program to 50% of its capacity and gynecologic care has been completely suspended. Hôpital St. Luc, one of the first hospitals in the western region of Haiti to open its doors to care for COVID-19 patients, has recently shut down the entire maternal-fetal department.
So, access to prenatal and postnatal care, including the ability to deliver babies in health care institutions, is significantly reduced because of COVID-19. This leaves thousands of already vulnerable pregnant women at risk and having to deliver domestically with little to no health care professional assistance. We worry that, in light of the data, more women and babies will die because of the COVID-19 pandemic.
A call to action
Despite these conditions, there are reasons for hope. Various groups, both from the international community and locally have mobilized to respond to the pandemic.
International health care organizations such as Doctors Without Borders and Partners in Health, and local groups such as GHESKIO, the St. Luke Foundation for Haiti, and others have been collaborating with the Haitian Ministry of Health to devise and strategic plans and deploy valuable resources with the common goal of saving lives from COVID-19.
GHESKIO, for example, under Dr. Pape’s leadership, currently has one of the three COVID-19 testing centers in the country. It also has two COVID-19 treatment centers in full operation, in Port-au-Prince, the capital city, managing and treating 520 patients with confirmed COVID-19. GHESKIO, which has been in the front lines of previous major infectious disease outbreaks,13 has trained about 200 clinicians from both public and private health care institutions to care for COVID-19 patients.
Doctors Without Borders has been investing in efforts to support the Ministry of Health by converting and renovating its Burn Center in Drouillard, a small section of the city of Cité Soleil, one of the country’s biggest slums. In May, as part of its COVID-19 response, it launched a 20-bed capacity center that can accommodate up to 45 beds to care for patients who have tested positive for COVID-19.
Partners in Health, the Boston-based nonprofit health care organization cofounded in 1987 by American anthropologist and infectious disease specialist, Paul Farmer, MD, and the largest nonprofit health care provider in Haiti, also joined the Ministry of Health through its national and public health efforts to tackle COVID-19 in Haiti. Partners in Health, through its sister organization, Zanmi Lasante, has pioneered the movement of diagnosing and treating people with HIV-AIDS and TB. Since the late 1990s, its efforts against both infectious diseases have helped 15,000 HIV-positive patients begin and remain on treatment. And every year, 1,500 TB patients have started treatment on the path to a cure.
Early in the pandemic in Haiti, Partners in Health, through its state-of-the-art 300-bed university hospital (Hôpital Universitaire de Mirebalais de Mirebalais), was the first to open a COVID-19 center with a 20-bed capacity and has been caring for COVID-19 patients since then. In June, Partners in Health supported and inaugurated the renovation of the internal medicine department at one of its affiliated community hospitals, Hôpital Saint-Nicolas de Saint Marc. That department will have a 24-bed capacity that can extend up to 36 beds to manage and treat COVID-19 patients.
In total, currently, 26 COVID-19 centers with a capacity of 1,011 beds are available to serve, manage, and treat Haitian patients affected with COVID-19. But are those efforts enough? No.
Haiti, as a weak state even before COVID-19, continues to need funding from the international community so it can strengthen its health care infrastructure to be effective and strong in fighting against COVID-19.
In addition, we would like to see preventive initiatives implemented on the local level. Our family has taken on a role that, we think, could help conquer COVID-19 if others followed suit on a large scale.
As part of our contribution in tackling COVID-19, the two of us have launched a small-scale community experiment. We have educated our family in Delmas about COVID-19 and subsequently launched an awareness campaign in the community. We dispatched small groups that go door to door in the community to educate neighbors about the disease in an effort to help them understand that COVID-19 is real and it is normal for people that feel they may have the disease to seek medical care. This approach helps suppress the transmission of the virus. This pilot project could be reproduced in several other communities. It is easy to operate, rapid, effective, and cost-free. The community has been very receptive to and grateful for our efforts.
Like other countries across the world, Haiti was not ready for COVID-19. But we are confident that, with help from the international community, organizations such as GHESKIO,14 and with due diligence on the local level, we are strong and resilient enough to beat COVID. We must act together – quickly.
References
1. Sénat JD. Coronavirus: 2 cas confirmés en Haïti, Jovenel Moïse décrète l’état d’ur-gence sanitaire. 2020 Le Nouvelliste.
2. Haitian Ministry of Health.
3. “Entre appel a la solidarite et de sombres previsions, le Dr William Pape fait le point.” Le Nouvelliste.
4. Darzi A and Evans T. Lancet. 2016 Nov-Dec 26. 388;10060:2576-7.
5. Rapport Statistique 2018. 2019 Republic of Haiti.
6. Sentlinger K. “Water Crisis in Haiti.” The Water Project.
7. The World Bank in Haiti. worldbank.org.
8. Cenat JM. Travel Med Infect Dis. 2020 Mar 28. doi: 10.1016/jtmaid.2020.101684.
9. Block D. “Why some Americans resist wearing face masks.” voanews.com. 2020 May 31.
10. Panceski B and Douglas J. “Masks could help stop coronavirus. So why are they still controversial?” wsj.com. Updated 29 Jun 2020.
11. Bojarski S. “Social distancing: A luxury Haiti’s poor cannot afford. The Haitian Times. 2020 Apr.
12. World Health Organization, UNICEF, World Bank Group, and the U.N. Population Division. Maternal mortality ratio, Haiti.
13. Feliciano I and Kargbo C. “As COVID cases surge, Haiti’s Dr. Pape is on the front line again.” PBS NewsHour Weekend. 2020 Jun 13.
14. Liautaud B and Deschamps MM. New Engl J Med. 2020 Jun 16.
Mr. Dorcela is a senior medical student at Faculté des Sciences de la Santé Université Quisqueya in Port-au-Prince, Haiti. He also is a medical intern at Unité de Médecine Familiale Hôpital Saint Nicolas in Saint-Marc. Mr. Dorcela has no disclosures. Mr. St. Jean, who is Mr. Dorcela’s brother, is also a senior medical student at Faculté des Sciences de la Santé Université Quisqueya in Port-au-Prince. He has no disclosures.
Doctors Without Borders, other groups urged to mobilize
Doctors Without Borders, other groups urged to mobilize
Do you want to know what keeps us up at night? As 4th-year medical students born, raised, and living in Haiti, we worry about the impact of COVID-19 on our patients.
The pandemic has shaken the world, and Haiti is no exception.
It has taken several months for the disease to spread, and it began with two confirmed cases, one from France and the other from Belgium, on March 19.1 Much of the spread of COVID-19 in Haiti has been tied to workers returning from the Dominican Republic. As of June 29, Haiti had 5,975 confirmed cases and 105 deaths.2 Of course, those numbers sound minuscule, compared with those in the United States, where the number of deaths from COVID-19 surpassed 100,000 several weeks ago. But the population of Haiti is 30 times smaller than that of the United States, and Haiti is the poorest country in the Western Hemisphere. We have watched in horror as the virus has ravaged marginalized groups in the United States and worry that it will do the same in our own country.
Just as the Haitian Ministry of Health worked with various groups to reach the 1-year free of cholera mark in Haiti, groups such as Doctors Without Borders must mobilize to rein in COVID-19.
Community transmission rapid
After the first two cases were confirmed, a state of health emergency was immediately declared. Haitian President Jovenel Moïse and other government officials called for the implementation of several measures aimed at limiting the spread of COVID-19.
Schools, universities, clinical training programs, vocational centers, factories, airports, and ports, except for the transport of goods, were all ordered to close until further notice. Gatherings of larger than 10 people were banned. A curfew from 8 p.m. EST time to 5 a.m. EST was imposed. Measures such as those encouraged by U.S. Centers for Disease Control and Prevention, such as hand washing, physical distancing, and staying at home were also encouraged by the Haitian Ministry of Health. Mask wearing in public places was deemed mandatory.
The latest testing data show that community spread has been occurring among the Haitian population at a rapid rate. According to Jean William Pape, MD, Haiti’s top infectious diseases expert and founder of GHESKIO, an iconic infectious disease center that cares for people with HIV-AIDS and tuberculosis, a COVID-19 simulation from Cornell University in New York shows that about 35% of the Haitian population will be infected by the end of August 2020. A simulation by the University of Oxford (England) paints an even more dire picture. That simulation shows that 86% of the population could be infected, More than 9,000 additional hospital beds would be needed, and 20,000 people would be likely to die from COVID-19, Dr. Pape said in an interview with Haiti’s Nouvelliste newspaper.3
Medical response
We know that there is a global shortage of health care workers,4 and Haiti is no exception. According to a 2018 report from the Haitian Ministry of Health, the country has 11,775 health care professionals, including about 3,354 medical doctors, to care for more than 11 million people. That translates to about 23.4 physicians per 100,000.5
The pandemic has led some members of this already anemic health care workforce to stay home because of a lack of personal protective equipment. Others, because of reduced hospital or clinic budgets, have been furloughed, making the COVID-19 national health emergency even harder to manage.
But a severe health care shortage is not the only challenge facing Haiti. It spends about $131 U.S. per capita, which makes Haiti one of most vulnerable among low- and middle-income countries in the world. As a poor country,7 its health care infrastructure is among the most inadequate and weakest. Prior to COVID-19, medical advocacy groups already had started movements and strikes demanding that the government improve the health care system. The country’s precarious health care infrastructure includes a lack of hospital beds, and basic medical supplies and equipment, such as oxygen and ventilators.8 The emergence of COVID-19 has only exacerbated the situation.
Clinical training programs have been suspended, many doctors and nurses are on quarantine, and some hospitals and clinics are closing. We have witnessed makeshift voodoo clinics built by Haitian voodoo leaders to receive, hospitalize, and treat COVID-19 patients through rituals and herbal remedies. In some areas of the country, residents have protested against the opening of several COVID-19 treatment and management centers.
Unique cultural challenges
Public health officials around the world are facing challenges persuading citizens to engage in behaviors that could protect them from the virus.
Just as in America, where many people opt to not wear face coverings9,10 despite the public health risks, deep distrust of the Haitian government has undermined the messages of President Moïse and public healthofficials about the role of masks in limiting the spread of COVID.We see large numbers of unmasked people on the streets in the informal markets every day. Crammed tap-taps and overloaded motorcycles are moving everywhere. This also could be tied to cultural attitudes about COVID that persist among some Haitians.For example, many people with signs and symptoms of COVID-19 are afraid of going to the hospital to get tested and receive care, and resort to going to the voodoo clinics. Along with rituals, voodoo priests have been serving up teas with ingredients, including moringa, eucalyptus, ginger, and honey to those seeking COVID-19 care in the centers. The voodoo priests claim that the teas they serve strengthen the immune system.
In addition, it is difficult for poor people who live in small quarters with several other people to adhere to physical distancing.11
Stigma and violence
Other barriers in the fight against COVID-19 in Haiti are stigma and violence. If widespread testing were available, some Haitians would opt not to do so – despite clear signs and symptoms of the infection. Some people who would get tested if they could are afraid to do so because of fears tied to being attacked by neighbors.
When Haitian University professor Bellamy Nelson and his girlfriend returned to Haiti from the United States in March and began experiencing some pain and fever, he experienced attacks from neighbors, he said in an interview. He said neighbors threatened to burn down his house. When an ambulance arrived at his house to transport him to a hospital, it had to drive through back roads to avoid people armed with rocks, fire, and machetes, he told us. No hospital wanted to admit him. Eventually, Professor Nelson self-quarantined at home, he said.
In another incident, a national ambulance center in Gonaïves, a town toward the northern region of Haiti, reportedly was vandalized, because COVID-19 equipment and supplies used to treat people had been stored there. Hospital Bernard Mevs, along with many other hospitals, was forced by the area’s residents to suspend the plan to open a center for COVID-19 management. Threats to burn down the hospitals caused the leaders of the hospitals to back down and give up a plan to build a 20-bed COVID-19 response center.
Maternal health
Another concern we have about the pandemic is the risk it could be to pregnant women. On average, 94,000 deaths occur annually in Haiti. Out of this number, maternal mortality accounts for 1,000. In 2017, for every 100,000 live births for women of reproductive age from 15 to 49 years old, 480 women died. In contrast, in the Dominican Republic, 95 women died per 100,000 that same year. In the United States, 19 died, and in Norway, no more than 2 died that year.12
Some of the primary factors contributing to the crisis are limited accessibility, inadequate health care facilities, and an inadequate number of trained health care practitioners; low percentages of skilled attendants at deliveries and of prenatal and postnatal visits; and high numbers of high-risk deliveries in nonqualified health facilities.
During the COVID-19 national health emergency, with most hospitals reducing their health care personnel either because of budget-related reasons or because they are on quarantine, this maternal-fetal health crisis has escalated.
One of the biggest hospitals in Jacmel, a town in the southern region of Haiti, has stopped its prenatal care program. In Delmas, the city with the highest incidence and prevalence of COVID-19, Hôpital Universitaire de la Paix has reduced this program to 50% of its capacity and gynecologic care has been completely suspended. Hôpital St. Luc, one of the first hospitals in the western region of Haiti to open its doors to care for COVID-19 patients, has recently shut down the entire maternal-fetal department.
So, access to prenatal and postnatal care, including the ability to deliver babies in health care institutions, is significantly reduced because of COVID-19. This leaves thousands of already vulnerable pregnant women at risk and having to deliver domestically with little to no health care professional assistance. We worry that, in light of the data, more women and babies will die because of the COVID-19 pandemic.
A call to action
Despite these conditions, there are reasons for hope. Various groups, both from the international community and locally have mobilized to respond to the pandemic.
International health care organizations such as Doctors Without Borders and Partners in Health, and local groups such as GHESKIO, the St. Luke Foundation for Haiti, and others have been collaborating with the Haitian Ministry of Health to devise and strategic plans and deploy valuable resources with the common goal of saving lives from COVID-19.
GHESKIO, for example, under Dr. Pape’s leadership, currently has one of the three COVID-19 testing centers in the country. It also has two COVID-19 treatment centers in full operation, in Port-au-Prince, the capital city, managing and treating 520 patients with confirmed COVID-19. GHESKIO, which has been in the front lines of previous major infectious disease outbreaks,13 has trained about 200 clinicians from both public and private health care institutions to care for COVID-19 patients.
Doctors Without Borders has been investing in efforts to support the Ministry of Health by converting and renovating its Burn Center in Drouillard, a small section of the city of Cité Soleil, one of the country’s biggest slums. In May, as part of its COVID-19 response, it launched a 20-bed capacity center that can accommodate up to 45 beds to care for patients who have tested positive for COVID-19.
Partners in Health, the Boston-based nonprofit health care organization cofounded in 1987 by American anthropologist and infectious disease specialist, Paul Farmer, MD, and the largest nonprofit health care provider in Haiti, also joined the Ministry of Health through its national and public health efforts to tackle COVID-19 in Haiti. Partners in Health, through its sister organization, Zanmi Lasante, has pioneered the movement of diagnosing and treating people with HIV-AIDS and TB. Since the late 1990s, its efforts against both infectious diseases have helped 15,000 HIV-positive patients begin and remain on treatment. And every year, 1,500 TB patients have started treatment on the path to a cure.
Early in the pandemic in Haiti, Partners in Health, through its state-of-the-art 300-bed university hospital (Hôpital Universitaire de Mirebalais de Mirebalais), was the first to open a COVID-19 center with a 20-bed capacity and has been caring for COVID-19 patients since then. In June, Partners in Health supported and inaugurated the renovation of the internal medicine department at one of its affiliated community hospitals, Hôpital Saint-Nicolas de Saint Marc. That department will have a 24-bed capacity that can extend up to 36 beds to manage and treat COVID-19 patients.
In total, currently, 26 COVID-19 centers with a capacity of 1,011 beds are available to serve, manage, and treat Haitian patients affected with COVID-19. But are those efforts enough? No.
Haiti, as a weak state even before COVID-19, continues to need funding from the international community so it can strengthen its health care infrastructure to be effective and strong in fighting against COVID-19.
In addition, we would like to see preventive initiatives implemented on the local level. Our family has taken on a role that, we think, could help conquer COVID-19 if others followed suit on a large scale.
As part of our contribution in tackling COVID-19, the two of us have launched a small-scale community experiment. We have educated our family in Delmas about COVID-19 and subsequently launched an awareness campaign in the community. We dispatched small groups that go door to door in the community to educate neighbors about the disease in an effort to help them understand that COVID-19 is real and it is normal for people that feel they may have the disease to seek medical care. This approach helps suppress the transmission of the virus. This pilot project could be reproduced in several other communities. It is easy to operate, rapid, effective, and cost-free. The community has been very receptive to and grateful for our efforts.
Like other countries across the world, Haiti was not ready for COVID-19. But we are confident that, with help from the international community, organizations such as GHESKIO,14 and with due diligence on the local level, we are strong and resilient enough to beat COVID. We must act together – quickly.
References
1. Sénat JD. Coronavirus: 2 cas confirmés en Haïti, Jovenel Moïse décrète l’état d’ur-gence sanitaire. 2020 Le Nouvelliste.
2. Haitian Ministry of Health.
3. “Entre appel a la solidarite et de sombres previsions, le Dr William Pape fait le point.” Le Nouvelliste.
4. Darzi A and Evans T. Lancet. 2016 Nov-Dec 26. 388;10060:2576-7.
5. Rapport Statistique 2018. 2019 Republic of Haiti.
6. Sentlinger K. “Water Crisis in Haiti.” The Water Project.
7. The World Bank in Haiti. worldbank.org.
8. Cenat JM. Travel Med Infect Dis. 2020 Mar 28. doi: 10.1016/jtmaid.2020.101684.
9. Block D. “Why some Americans resist wearing face masks.” voanews.com. 2020 May 31.
10. Panceski B and Douglas J. “Masks could help stop coronavirus. So why are they still controversial?” wsj.com. Updated 29 Jun 2020.
11. Bojarski S. “Social distancing: A luxury Haiti’s poor cannot afford. The Haitian Times. 2020 Apr.
12. World Health Organization, UNICEF, World Bank Group, and the U.N. Population Division. Maternal mortality ratio, Haiti.
13. Feliciano I and Kargbo C. “As COVID cases surge, Haiti’s Dr. Pape is on the front line again.” PBS NewsHour Weekend. 2020 Jun 13.
14. Liautaud B and Deschamps MM. New Engl J Med. 2020 Jun 16.
Mr. Dorcela is a senior medical student at Faculté des Sciences de la Santé Université Quisqueya in Port-au-Prince, Haiti. He also is a medical intern at Unité de Médecine Familiale Hôpital Saint Nicolas in Saint-Marc. Mr. Dorcela has no disclosures. Mr. St. Jean, who is Mr. Dorcela’s brother, is also a senior medical student at Faculté des Sciences de la Santé Université Quisqueya in Port-au-Prince. He has no disclosures.
Do you want to know what keeps us up at night? As 4th-year medical students born, raised, and living in Haiti, we worry about the impact of COVID-19 on our patients.
The pandemic has shaken the world, and Haiti is no exception.
It has taken several months for the disease to spread, and it began with two confirmed cases, one from France and the other from Belgium, on March 19.1 Much of the spread of COVID-19 in Haiti has been tied to workers returning from the Dominican Republic. As of June 29, Haiti had 5,975 confirmed cases and 105 deaths.2 Of course, those numbers sound minuscule, compared with those in the United States, where the number of deaths from COVID-19 surpassed 100,000 several weeks ago. But the population of Haiti is 30 times smaller than that of the United States, and Haiti is the poorest country in the Western Hemisphere. We have watched in horror as the virus has ravaged marginalized groups in the United States and worry that it will do the same in our own country.
Just as the Haitian Ministry of Health worked with various groups to reach the 1-year free of cholera mark in Haiti, groups such as Doctors Without Borders must mobilize to rein in COVID-19.
Community transmission rapid
After the first two cases were confirmed, a state of health emergency was immediately declared. Haitian President Jovenel Moïse and other government officials called for the implementation of several measures aimed at limiting the spread of COVID-19.
Schools, universities, clinical training programs, vocational centers, factories, airports, and ports, except for the transport of goods, were all ordered to close until further notice. Gatherings of larger than 10 people were banned. A curfew from 8 p.m. EST time to 5 a.m. EST was imposed. Measures such as those encouraged by U.S. Centers for Disease Control and Prevention, such as hand washing, physical distancing, and staying at home were also encouraged by the Haitian Ministry of Health. Mask wearing in public places was deemed mandatory.
The latest testing data show that community spread has been occurring among the Haitian population at a rapid rate. According to Jean William Pape, MD, Haiti’s top infectious diseases expert and founder of GHESKIO, an iconic infectious disease center that cares for people with HIV-AIDS and tuberculosis, a COVID-19 simulation from Cornell University in New York shows that about 35% of the Haitian population will be infected by the end of August 2020. A simulation by the University of Oxford (England) paints an even more dire picture. That simulation shows that 86% of the population could be infected, More than 9,000 additional hospital beds would be needed, and 20,000 people would be likely to die from COVID-19, Dr. Pape said in an interview with Haiti’s Nouvelliste newspaper.3
Medical response
We know that there is a global shortage of health care workers,4 and Haiti is no exception. According to a 2018 report from the Haitian Ministry of Health, the country has 11,775 health care professionals, including about 3,354 medical doctors, to care for more than 11 million people. That translates to about 23.4 physicians per 100,000.5
The pandemic has led some members of this already anemic health care workforce to stay home because of a lack of personal protective equipment. Others, because of reduced hospital or clinic budgets, have been furloughed, making the COVID-19 national health emergency even harder to manage.
But a severe health care shortage is not the only challenge facing Haiti. It spends about $131 U.S. per capita, which makes Haiti one of most vulnerable among low- and middle-income countries in the world. As a poor country,7 its health care infrastructure is among the most inadequate and weakest. Prior to COVID-19, medical advocacy groups already had started movements and strikes demanding that the government improve the health care system. The country’s precarious health care infrastructure includes a lack of hospital beds, and basic medical supplies and equipment, such as oxygen and ventilators.8 The emergence of COVID-19 has only exacerbated the situation.
Clinical training programs have been suspended, many doctors and nurses are on quarantine, and some hospitals and clinics are closing. We have witnessed makeshift voodoo clinics built by Haitian voodoo leaders to receive, hospitalize, and treat COVID-19 patients through rituals and herbal remedies. In some areas of the country, residents have protested against the opening of several COVID-19 treatment and management centers.
Unique cultural challenges
Public health officials around the world are facing challenges persuading citizens to engage in behaviors that could protect them from the virus.
Just as in America, where many people opt to not wear face coverings9,10 despite the public health risks, deep distrust of the Haitian government has undermined the messages of President Moïse and public healthofficials about the role of masks in limiting the spread of COVID.We see large numbers of unmasked people on the streets in the informal markets every day. Crammed tap-taps and overloaded motorcycles are moving everywhere. This also could be tied to cultural attitudes about COVID that persist among some Haitians.For example, many people with signs and symptoms of COVID-19 are afraid of going to the hospital to get tested and receive care, and resort to going to the voodoo clinics. Along with rituals, voodoo priests have been serving up teas with ingredients, including moringa, eucalyptus, ginger, and honey to those seeking COVID-19 care in the centers. The voodoo priests claim that the teas they serve strengthen the immune system.
In addition, it is difficult for poor people who live in small quarters with several other people to adhere to physical distancing.11
Stigma and violence
Other barriers in the fight against COVID-19 in Haiti are stigma and violence. If widespread testing were available, some Haitians would opt not to do so – despite clear signs and symptoms of the infection. Some people who would get tested if they could are afraid to do so because of fears tied to being attacked by neighbors.
When Haitian University professor Bellamy Nelson and his girlfriend returned to Haiti from the United States in March and began experiencing some pain and fever, he experienced attacks from neighbors, he said in an interview. He said neighbors threatened to burn down his house. When an ambulance arrived at his house to transport him to a hospital, it had to drive through back roads to avoid people armed with rocks, fire, and machetes, he told us. No hospital wanted to admit him. Eventually, Professor Nelson self-quarantined at home, he said.
In another incident, a national ambulance center in Gonaïves, a town toward the northern region of Haiti, reportedly was vandalized, because COVID-19 equipment and supplies used to treat people had been stored there. Hospital Bernard Mevs, along with many other hospitals, was forced by the area’s residents to suspend the plan to open a center for COVID-19 management. Threats to burn down the hospitals caused the leaders of the hospitals to back down and give up a plan to build a 20-bed COVID-19 response center.
Maternal health
Another concern we have about the pandemic is the risk it could be to pregnant women. On average, 94,000 deaths occur annually in Haiti. Out of this number, maternal mortality accounts for 1,000. In 2017, for every 100,000 live births for women of reproductive age from 15 to 49 years old, 480 women died. In contrast, in the Dominican Republic, 95 women died per 100,000 that same year. In the United States, 19 died, and in Norway, no more than 2 died that year.12
Some of the primary factors contributing to the crisis are limited accessibility, inadequate health care facilities, and an inadequate number of trained health care practitioners; low percentages of skilled attendants at deliveries and of prenatal and postnatal visits; and high numbers of high-risk deliveries in nonqualified health facilities.
During the COVID-19 national health emergency, with most hospitals reducing their health care personnel either because of budget-related reasons or because they are on quarantine, this maternal-fetal health crisis has escalated.
One of the biggest hospitals in Jacmel, a town in the southern region of Haiti, has stopped its prenatal care program. In Delmas, the city with the highest incidence and prevalence of COVID-19, Hôpital Universitaire de la Paix has reduced this program to 50% of its capacity and gynecologic care has been completely suspended. Hôpital St. Luc, one of the first hospitals in the western region of Haiti to open its doors to care for COVID-19 patients, has recently shut down the entire maternal-fetal department.
So, access to prenatal and postnatal care, including the ability to deliver babies in health care institutions, is significantly reduced because of COVID-19. This leaves thousands of already vulnerable pregnant women at risk and having to deliver domestically with little to no health care professional assistance. We worry that, in light of the data, more women and babies will die because of the COVID-19 pandemic.
A call to action
Despite these conditions, there are reasons for hope. Various groups, both from the international community and locally have mobilized to respond to the pandemic.
International health care organizations such as Doctors Without Borders and Partners in Health, and local groups such as GHESKIO, the St. Luke Foundation for Haiti, and others have been collaborating with the Haitian Ministry of Health to devise and strategic plans and deploy valuable resources with the common goal of saving lives from COVID-19.
GHESKIO, for example, under Dr. Pape’s leadership, currently has one of the three COVID-19 testing centers in the country. It also has two COVID-19 treatment centers in full operation, in Port-au-Prince, the capital city, managing and treating 520 patients with confirmed COVID-19. GHESKIO, which has been in the front lines of previous major infectious disease outbreaks,13 has trained about 200 clinicians from both public and private health care institutions to care for COVID-19 patients.
Doctors Without Borders has been investing in efforts to support the Ministry of Health by converting and renovating its Burn Center in Drouillard, a small section of the city of Cité Soleil, one of the country’s biggest slums. In May, as part of its COVID-19 response, it launched a 20-bed capacity center that can accommodate up to 45 beds to care for patients who have tested positive for COVID-19.
Partners in Health, the Boston-based nonprofit health care organization cofounded in 1987 by American anthropologist and infectious disease specialist, Paul Farmer, MD, and the largest nonprofit health care provider in Haiti, also joined the Ministry of Health through its national and public health efforts to tackle COVID-19 in Haiti. Partners in Health, through its sister organization, Zanmi Lasante, has pioneered the movement of diagnosing and treating people with HIV-AIDS and TB. Since the late 1990s, its efforts against both infectious diseases have helped 15,000 HIV-positive patients begin and remain on treatment. And every year, 1,500 TB patients have started treatment on the path to a cure.
Early in the pandemic in Haiti, Partners in Health, through its state-of-the-art 300-bed university hospital (Hôpital Universitaire de Mirebalais de Mirebalais), was the first to open a COVID-19 center with a 20-bed capacity and has been caring for COVID-19 patients since then. In June, Partners in Health supported and inaugurated the renovation of the internal medicine department at one of its affiliated community hospitals, Hôpital Saint-Nicolas de Saint Marc. That department will have a 24-bed capacity that can extend up to 36 beds to manage and treat COVID-19 patients.
In total, currently, 26 COVID-19 centers with a capacity of 1,011 beds are available to serve, manage, and treat Haitian patients affected with COVID-19. But are those efforts enough? No.
Haiti, as a weak state even before COVID-19, continues to need funding from the international community so it can strengthen its health care infrastructure to be effective and strong in fighting against COVID-19.
In addition, we would like to see preventive initiatives implemented on the local level. Our family has taken on a role that, we think, could help conquer COVID-19 if others followed suit on a large scale.
As part of our contribution in tackling COVID-19, the two of us have launched a small-scale community experiment. We have educated our family in Delmas about COVID-19 and subsequently launched an awareness campaign in the community. We dispatched small groups that go door to door in the community to educate neighbors about the disease in an effort to help them understand that COVID-19 is real and it is normal for people that feel they may have the disease to seek medical care. This approach helps suppress the transmission of the virus. This pilot project could be reproduced in several other communities. It is easy to operate, rapid, effective, and cost-free. The community has been very receptive to and grateful for our efforts.
Like other countries across the world, Haiti was not ready for COVID-19. But we are confident that, with help from the international community, organizations such as GHESKIO,14 and with due diligence on the local level, we are strong and resilient enough to beat COVID. We must act together – quickly.
References
1. Sénat JD. Coronavirus: 2 cas confirmés en Haïti, Jovenel Moïse décrète l’état d’ur-gence sanitaire. 2020 Le Nouvelliste.
2. Haitian Ministry of Health.
3. “Entre appel a la solidarite et de sombres previsions, le Dr William Pape fait le point.” Le Nouvelliste.
4. Darzi A and Evans T. Lancet. 2016 Nov-Dec 26. 388;10060:2576-7.
5. Rapport Statistique 2018. 2019 Republic of Haiti.
6. Sentlinger K. “Water Crisis in Haiti.” The Water Project.
7. The World Bank in Haiti. worldbank.org.
8. Cenat JM. Travel Med Infect Dis. 2020 Mar 28. doi: 10.1016/jtmaid.2020.101684.
9. Block D. “Why some Americans resist wearing face masks.” voanews.com. 2020 May 31.
10. Panceski B and Douglas J. “Masks could help stop coronavirus. So why are they still controversial?” wsj.com. Updated 29 Jun 2020.
11. Bojarski S. “Social distancing: A luxury Haiti’s poor cannot afford. The Haitian Times. 2020 Apr.
12. World Health Organization, UNICEF, World Bank Group, and the U.N. Population Division. Maternal mortality ratio, Haiti.
13. Feliciano I and Kargbo C. “As COVID cases surge, Haiti’s Dr. Pape is on the front line again.” PBS NewsHour Weekend. 2020 Jun 13.
14. Liautaud B and Deschamps MM. New Engl J Med. 2020 Jun 16.
Mr. Dorcela is a senior medical student at Faculté des Sciences de la Santé Université Quisqueya in Port-au-Prince, Haiti. He also is a medical intern at Unité de Médecine Familiale Hôpital Saint Nicolas in Saint-Marc. Mr. Dorcela has no disclosures. Mr. St. Jean, who is Mr. Dorcela’s brother, is also a senior medical student at Faculté des Sciences de la Santé Université Quisqueya in Port-au-Prince. He has no disclosures.
Letter from the Board of Editors: Call to action (again)
This editorial is the first to be published in GI & Hepatology News since the murder of George Floyd in Minneapolis. The corner of 38th and Chicago is 9 miles from my home in Bloomington, Minn. This corner became the epicenter of protests that have spread around the nation and world. Early on, protests were accompanied by widespread riots, looting, and destruction. In the ensuing weeks, this corner has become a memorial for Mr. Floyd and a place where people now go to reflect, pray, pay tribute, and pledge to work for change.
A coalition of willing businesses has formed in the area around 38th and Chicago. The largest employer in the area is Allina Health (I sit on the Governing Board of Allina Health). Our flagship hospital is 8 blocks from the site of George Floyd’s memorial. We will be a change leader by committing funds for local rebuilding, ensuring use of construction firms that promote minority workers (as was done when the Viking’s stadium was built), examining our investment portfolio with racial equity as one guiding principle, increasing our focus on barriers to access, enhancing equity education of our workforce, and working with city and state leaders to promote police reform.
As the Editor in Chief of the official newspaper of the AGA, I invited our board of editors to stand united in our condemnation of the racial injustices that led to the protests we now see. We each agree with the message from the combined Governing Boards of our GI societies (published June 2, 2020) stating “As health care providers, we have dedicated our lives to caring for our fellow human beings. Therefore, we are compelled to speak out against any treatment that results in unacceptable disparities that marginalize the vulnerable among us.”
Our responsibility as editors is to guide the content we deliver, ensuring its relevancy to our readers. In this light, we commit to delivering content that highlights racial injustices and health disparities for all people, as we seek to understand the many factors that result in barriers to health. We will emphasize content that leads to impactful change and will highlight progress we make as a specialty. We hope our collective work will help ensure that George Floyd’s memory, and the memories of all such victims, become a catalyst for permanent cultural change.
Editor in Chief, GI & Hepatology News
John I. Allen, MD, MBA, AGAF
Editor in Chief, The New Gastroenterologist
Vijaya L. Rao, MD
Associate Editors
Megan A. Adams, MD, JD, MSc
Ziad Gellad, MD, MPH, AGAF
Kim L. Isaacs, MD, PhD, AGAF
Charles J. Kahi, MD, MS, AGAF
Gyanprakash A. Ketwaroo, MD, MSc
Larry R. Kosinski, MD, MBA, AGAF
Sonia S. Kupfer, MD
Wajahat Mehal, MD, PhD
This editorial is the first to be published in GI & Hepatology News since the murder of George Floyd in Minneapolis. The corner of 38th and Chicago is 9 miles from my home in Bloomington, Minn. This corner became the epicenter of protests that have spread around the nation and world. Early on, protests were accompanied by widespread riots, looting, and destruction. In the ensuing weeks, this corner has become a memorial for Mr. Floyd and a place where people now go to reflect, pray, pay tribute, and pledge to work for change.
A coalition of willing businesses has formed in the area around 38th and Chicago. The largest employer in the area is Allina Health (I sit on the Governing Board of Allina Health). Our flagship hospital is 8 blocks from the site of George Floyd’s memorial. We will be a change leader by committing funds for local rebuilding, ensuring use of construction firms that promote minority workers (as was done when the Viking’s stadium was built), examining our investment portfolio with racial equity as one guiding principle, increasing our focus on barriers to access, enhancing equity education of our workforce, and working with city and state leaders to promote police reform.
As the Editor in Chief of the official newspaper of the AGA, I invited our board of editors to stand united in our condemnation of the racial injustices that led to the protests we now see. We each agree with the message from the combined Governing Boards of our GI societies (published June 2, 2020) stating “As health care providers, we have dedicated our lives to caring for our fellow human beings. Therefore, we are compelled to speak out against any treatment that results in unacceptable disparities that marginalize the vulnerable among us.”
Our responsibility as editors is to guide the content we deliver, ensuring its relevancy to our readers. In this light, we commit to delivering content that highlights racial injustices and health disparities for all people, as we seek to understand the many factors that result in barriers to health. We will emphasize content that leads to impactful change and will highlight progress we make as a specialty. We hope our collective work will help ensure that George Floyd’s memory, and the memories of all such victims, become a catalyst for permanent cultural change.
Editor in Chief, GI & Hepatology News
John I. Allen, MD, MBA, AGAF
Editor in Chief, The New Gastroenterologist
Vijaya L. Rao, MD
Associate Editors
Megan A. Adams, MD, JD, MSc
Ziad Gellad, MD, MPH, AGAF
Kim L. Isaacs, MD, PhD, AGAF
Charles J. Kahi, MD, MS, AGAF
Gyanprakash A. Ketwaroo, MD, MSc
Larry R. Kosinski, MD, MBA, AGAF
Sonia S. Kupfer, MD
Wajahat Mehal, MD, PhD
This editorial is the first to be published in GI & Hepatology News since the murder of George Floyd in Minneapolis. The corner of 38th and Chicago is 9 miles from my home in Bloomington, Minn. This corner became the epicenter of protests that have spread around the nation and world. Early on, protests were accompanied by widespread riots, looting, and destruction. In the ensuing weeks, this corner has become a memorial for Mr. Floyd and a place where people now go to reflect, pray, pay tribute, and pledge to work for change.
A coalition of willing businesses has formed in the area around 38th and Chicago. The largest employer in the area is Allina Health (I sit on the Governing Board of Allina Health). Our flagship hospital is 8 blocks from the site of George Floyd’s memorial. We will be a change leader by committing funds for local rebuilding, ensuring use of construction firms that promote minority workers (as was done when the Viking’s stadium was built), examining our investment portfolio with racial equity as one guiding principle, increasing our focus on barriers to access, enhancing equity education of our workforce, and working with city and state leaders to promote police reform.
As the Editor in Chief of the official newspaper of the AGA, I invited our board of editors to stand united in our condemnation of the racial injustices that led to the protests we now see. We each agree with the message from the combined Governing Boards of our GI societies (published June 2, 2020) stating “As health care providers, we have dedicated our lives to caring for our fellow human beings. Therefore, we are compelled to speak out against any treatment that results in unacceptable disparities that marginalize the vulnerable among us.”
Our responsibility as editors is to guide the content we deliver, ensuring its relevancy to our readers. In this light, we commit to delivering content that highlights racial injustices and health disparities for all people, as we seek to understand the many factors that result in barriers to health. We will emphasize content that leads to impactful change and will highlight progress we make as a specialty. We hope our collective work will help ensure that George Floyd’s memory, and the memories of all such victims, become a catalyst for permanent cultural change.
Editor in Chief, GI & Hepatology News
John I. Allen, MD, MBA, AGAF
Editor in Chief, The New Gastroenterologist
Vijaya L. Rao, MD
Associate Editors
Megan A. Adams, MD, JD, MSc
Ziad Gellad, MD, MPH, AGAF
Kim L. Isaacs, MD, PhD, AGAF
Charles J. Kahi, MD, MS, AGAF
Gyanprakash A. Ketwaroo, MD, MSc
Larry R. Kosinski, MD, MBA, AGAF
Sonia S. Kupfer, MD
Wajahat Mehal, MD, PhD