User login
The wave of the future
Longtime CEO bids farewell to SHM
Changing times
After more than 20 years, my leadership role as CEO at the Society of Hospital Medicine (SHM) has ended with the transition to Dr. Eric Howell as the new SHM CEO on July 1, 2020. Looking back, I think we can all be proud of how we have helped to shape the specialty of hospital medicine over these two decades and of how strong SHM has become to support our new specialty.
In 2000, few people knew what a hospitalist was (or more importantly what we could become) and the specialty of hospital medicine had not even been named yet. Today the reputation of SHM is firmly established and the specialty has been defined by a unique curriculum through the Core Competencies in Hospital Medicine for both adult and pediatric patients, and by several textbooks in hospital medicine. There are divisions or departments of hospital medicine at many hospitals and academic medical centers. We even managed to convince the American Board of Internal Medicine, the American Board of Family Medicine, and the American Board of Medical Specialties to create a credential of Focused Practice in Hospital Medicine as the first-ever certification not tied to specific fellowship training.
To recognize the contributions of our members, SHM has established Awards of Excellence and the Fellow and Senior Fellow in Hospital Medicine (FHM and SFHM) designations. We have gone from a small national association in Philadelphia to create 68 active chapters and more than 20 Special Interest Groups. In my time at SHM I have attended more than 75-chapter meetings and met with thousands of hospitalists in 46 states. We now have over 20,000 members at SHM, making us the fastest growing medical specialty ever.
When I started at the National Association of Inpatient Physicians (NAIP) our only meeting was an annual CME meeting for about 150-200 people. We now hold a national meeting every year for more than 4,000 attendees that is the “Center of the Universe for Hospital Medicine.” Understanding that we needed to educate the people who will lead change in our health care system, we developed from scratch a set of Leadership Academies that has already educated more than 2,500 hospitalist leaders. To train the educators in quality improvement in medical education we developed our Quality and Safety Educator Academy (QSEA) programs, and to promote career development of academic hospitalists we created our Academic Hospitalist Academy.
SHM is the leader in adult in-practice learning, specifically designed for hospitalists. SHM members have access to a state-of-the-art comprehensive hospitalist-based online education system as well as board review and maintenance of certification (MOC) review tools in our SPARK program, specifically for hospital medicine.
In the area of quality improvement, most medical societies convene a panel of experts, develop guidelines, publish them, and hope that change will occur. SHM has been much more proactive, creating the Center for Quality Improvement that has raised more than $10 million and developed Quality Improvement programs in more than 400 hospitals over the years, winning the prestigious Eisenberg Award along the way.
When I started at NAIP in 2000, our only communication tools were a 4-page newsletter and an email listserv. Along the way we have developed a broadly read newsmagazine (The Hospitalist), a well-recognized peer reviewed journal (Journal of Hospital Medicine), a robust website, and a significant social media presence.
From the very early days we knew that our specialty would not be totally successful by only facing inward. Change was coming to our health care system and hospitalists were going to be right in the middle. Despite our young age and limited resources, we have always hit above our weight class in advocacy. We actively participated in the development of the Affordable Care Act (Obamacare), making suggestions in payment reform, expanding the workforce with visa reform, and expanding the team of clinicians. Along the way SHM members rose to run the Centers for Medicare & Medicaid Services (CMS) and the Food and Drug Administration (FDA), and serve as U.S. Surgeon General.
Today in these troubled times, SHM continues to be a positive voice in promoting the use of PPE, the need for increased COVID-19 testing, and the recognition of our nation’s 60,000 hospitalists as essential frontline workers in the COVID-19 pandemic. With its longstanding role in promoting diversity and overcoming social injustice, SHM has had a positive national voice during the protests over police brutality.
We have proved to be a good partner with many other organizations and consistently were invited to partner in coalitions with the ED physicians (ACEP), the critical care docs (SCCM), the hospitals (AHA), the house of medicine (AMA), other internists (ACP), surgeons (ACS), and pediatricians (AAP), and so many other much more established societies, because we could be an active, flexible, and knowledgeable partner for more than 20 years.
Today, SHM and hospital medicine are clearly recognized as a force in the rapidly evolving health care system. With this comes not only influence but also responsibility, and I am certain the SHM Board, membership, and staff are ready for this challenge. The economic toll of our current pandemic will see colleges and other major companies and institutions go out of business and leave the landscape. SHM has a deep foundation and a well of strength to call on and will survive and thrive into the future.
SHM has been a good fit for me professionally and personally. Many of my skills and strengths have served SHM in our “early” years. I am very proud of what we have been able to accomplish TOGETHER. In the end it is the people I have been fortunate enough to meet and work with throughout these past 20 years that will stay with me, many of whom are lifelong friends. My mother, even today at 93, has always asked me to leave anything I do better off than when I came in the door. As I look back at my time helping to shape and lead SHM, I am sure I have answered my mother’s challenge and more.
I look forward to seeing many of you at a future SHM meeting and reveling in the way that hospitalists will actively play an important role in shaping our health care system in the future.
Dr. Wellikson is retiring as CEO of SHM.
Live long and prosper
Back in 2000, I was extremely fortunate to land my dream job as a hospitalist at Johns Hopkins Bayview in Baltimore. That dream exceeded my wildest aspirations. During my 20-year career as faculty in the Johns Hopkins School of Medicine I grew our tiny, 4 physician hospitalist group at Johns Hopkins Bayview into a multihospital program, complete with more than 150 physicians. That exceedingly rewarding work helped to shape the field of hospital medicine nationally and provided the foundation for my promotion to professor of medicine at Johns Hopkins in 2016.
Most professionals are lucky if they find one inspiring institution; I have found two. SHM has been my professional home since I became a hospitalist in 2000, and in that time I have dedicated as much creative energy to SHM as I have at Johns Hopkins.
Even at this time when the medical profession, and the entire world, has been rocked by the coronavirus, the fundamentals that have made SHM so successful will serve us well through the effects of this pandemic and beyond. It takes a skilled leader to nurture a professional society through the growth from only a few hundred members to thousands upon thousands, and at the same time crafting the profession into one of quality and high impact. These past 22 years Dr. Larry Wellikson, our retiring CEO, has skillfully accomplished just that by building lasting programs and people.
As you might imagine, my approach will work to add onto the legacy that Larry has left us. Yes, we will have to adapt SHM to the realities of the near future: virtual meetings, in-person events (yes, those will return one day) with appropriate social distancing until the coronavirus has faded, modified chapter meetings, and more. Someday the world will find a new normal, and SHM will evolve to meet the needs of our members and the patients we serve.
Through this pandemic and beyond, my vision – in partnership with the Board of Directors – will be to:
- Continue the work to enhance member engagement. We are primarily a membership organization, after all.
- Maintain our profession’s leadership role in the care continuum, particularly acute care.
- Be a deliberate sponsor of diversity and inclusion. I believe social justice is a moral imperative, and good business.
- Invest in teams: Chapters, special interest groups, and committees are key to success.
- Be financially prudent, so that this organization can serve its members through the best of times and those most challenging times.
Back in 2000 I joined my dream society, the Society of Hospital Medicine. That society exceeded my wildest aspirations. During my 20-year membership I started an SHM Chapter, was a leader in the Leadership Academies, joined the Board of Directors, participated in Annual Conferences, and helped lead the SHM Center for Quality Improvement. That exceedingly rewarding partnership helped shape the field of hospital medicine nationally and provided the foundation for my next role at SHM. I am excited and grateful to be the CEO of SHM.
I’ll end with something I use every day – “Eric Howell’s Core Values”:
- Make the world a better place.
- Invest in people.
- Be ethical and transparent.
- Do what you love.
- Try to use Star Trek references whenever possible. (Okay, this last one is not really a core value, but maybe a character trait?) At least the Vulcan greeting is appropriate for our times: Live long and prosper.
Dr. Howell is the new CEO for SHM as of July 1, 2020.
Longtime CEO bids farewell to SHM
Longtime CEO bids farewell to SHM
Changing times
After more than 20 years, my leadership role as CEO at the Society of Hospital Medicine (SHM) has ended with the transition to Dr. Eric Howell as the new SHM CEO on July 1, 2020. Looking back, I think we can all be proud of how we have helped to shape the specialty of hospital medicine over these two decades and of how strong SHM has become to support our new specialty.
In 2000, few people knew what a hospitalist was (or more importantly what we could become) and the specialty of hospital medicine had not even been named yet. Today the reputation of SHM is firmly established and the specialty has been defined by a unique curriculum through the Core Competencies in Hospital Medicine for both adult and pediatric patients, and by several textbooks in hospital medicine. There are divisions or departments of hospital medicine at many hospitals and academic medical centers. We even managed to convince the American Board of Internal Medicine, the American Board of Family Medicine, and the American Board of Medical Specialties to create a credential of Focused Practice in Hospital Medicine as the first-ever certification not tied to specific fellowship training.
To recognize the contributions of our members, SHM has established Awards of Excellence and the Fellow and Senior Fellow in Hospital Medicine (FHM and SFHM) designations. We have gone from a small national association in Philadelphia to create 68 active chapters and more than 20 Special Interest Groups. In my time at SHM I have attended more than 75-chapter meetings and met with thousands of hospitalists in 46 states. We now have over 20,000 members at SHM, making us the fastest growing medical specialty ever.
When I started at the National Association of Inpatient Physicians (NAIP) our only meeting was an annual CME meeting for about 150-200 people. We now hold a national meeting every year for more than 4,000 attendees that is the “Center of the Universe for Hospital Medicine.” Understanding that we needed to educate the people who will lead change in our health care system, we developed from scratch a set of Leadership Academies that has already educated more than 2,500 hospitalist leaders. To train the educators in quality improvement in medical education we developed our Quality and Safety Educator Academy (QSEA) programs, and to promote career development of academic hospitalists we created our Academic Hospitalist Academy.
SHM is the leader in adult in-practice learning, specifically designed for hospitalists. SHM members have access to a state-of-the-art comprehensive hospitalist-based online education system as well as board review and maintenance of certification (MOC) review tools in our SPARK program, specifically for hospital medicine.
In the area of quality improvement, most medical societies convene a panel of experts, develop guidelines, publish them, and hope that change will occur. SHM has been much more proactive, creating the Center for Quality Improvement that has raised more than $10 million and developed Quality Improvement programs in more than 400 hospitals over the years, winning the prestigious Eisenberg Award along the way.
When I started at NAIP in 2000, our only communication tools were a 4-page newsletter and an email listserv. Along the way we have developed a broadly read newsmagazine (The Hospitalist), a well-recognized peer reviewed journal (Journal of Hospital Medicine), a robust website, and a significant social media presence.
From the very early days we knew that our specialty would not be totally successful by only facing inward. Change was coming to our health care system and hospitalists were going to be right in the middle. Despite our young age and limited resources, we have always hit above our weight class in advocacy. We actively participated in the development of the Affordable Care Act (Obamacare), making suggestions in payment reform, expanding the workforce with visa reform, and expanding the team of clinicians. Along the way SHM members rose to run the Centers for Medicare & Medicaid Services (CMS) and the Food and Drug Administration (FDA), and serve as U.S. Surgeon General.
Today in these troubled times, SHM continues to be a positive voice in promoting the use of PPE, the need for increased COVID-19 testing, and the recognition of our nation’s 60,000 hospitalists as essential frontline workers in the COVID-19 pandemic. With its longstanding role in promoting diversity and overcoming social injustice, SHM has had a positive national voice during the protests over police brutality.
We have proved to be a good partner with many other organizations and consistently were invited to partner in coalitions with the ED physicians (ACEP), the critical care docs (SCCM), the hospitals (AHA), the house of medicine (AMA), other internists (ACP), surgeons (ACS), and pediatricians (AAP), and so many other much more established societies, because we could be an active, flexible, and knowledgeable partner for more than 20 years.
Today, SHM and hospital medicine are clearly recognized as a force in the rapidly evolving health care system. With this comes not only influence but also responsibility, and I am certain the SHM Board, membership, and staff are ready for this challenge. The economic toll of our current pandemic will see colleges and other major companies and institutions go out of business and leave the landscape. SHM has a deep foundation and a well of strength to call on and will survive and thrive into the future.
SHM has been a good fit for me professionally and personally. Many of my skills and strengths have served SHM in our “early” years. I am very proud of what we have been able to accomplish TOGETHER. In the end it is the people I have been fortunate enough to meet and work with throughout these past 20 years that will stay with me, many of whom are lifelong friends. My mother, even today at 93, has always asked me to leave anything I do better off than when I came in the door. As I look back at my time helping to shape and lead SHM, I am sure I have answered my mother’s challenge and more.
I look forward to seeing many of you at a future SHM meeting and reveling in the way that hospitalists will actively play an important role in shaping our health care system in the future.
Dr. Wellikson is retiring as CEO of SHM.
Live long and prosper
Back in 2000, I was extremely fortunate to land my dream job as a hospitalist at Johns Hopkins Bayview in Baltimore. That dream exceeded my wildest aspirations. During my 20-year career as faculty in the Johns Hopkins School of Medicine I grew our tiny, 4 physician hospitalist group at Johns Hopkins Bayview into a multihospital program, complete with more than 150 physicians. That exceedingly rewarding work helped to shape the field of hospital medicine nationally and provided the foundation for my promotion to professor of medicine at Johns Hopkins in 2016.
Most professionals are lucky if they find one inspiring institution; I have found two. SHM has been my professional home since I became a hospitalist in 2000, and in that time I have dedicated as much creative energy to SHM as I have at Johns Hopkins.
Even at this time when the medical profession, and the entire world, has been rocked by the coronavirus, the fundamentals that have made SHM so successful will serve us well through the effects of this pandemic and beyond. It takes a skilled leader to nurture a professional society through the growth from only a few hundred members to thousands upon thousands, and at the same time crafting the profession into one of quality and high impact. These past 22 years Dr. Larry Wellikson, our retiring CEO, has skillfully accomplished just that by building lasting programs and people.
As you might imagine, my approach will work to add onto the legacy that Larry has left us. Yes, we will have to adapt SHM to the realities of the near future: virtual meetings, in-person events (yes, those will return one day) with appropriate social distancing until the coronavirus has faded, modified chapter meetings, and more. Someday the world will find a new normal, and SHM will evolve to meet the needs of our members and the patients we serve.
Through this pandemic and beyond, my vision – in partnership with the Board of Directors – will be to:
- Continue the work to enhance member engagement. We are primarily a membership organization, after all.
- Maintain our profession’s leadership role in the care continuum, particularly acute care.
- Be a deliberate sponsor of diversity and inclusion. I believe social justice is a moral imperative, and good business.
- Invest in teams: Chapters, special interest groups, and committees are key to success.
- Be financially prudent, so that this organization can serve its members through the best of times and those most challenging times.
Back in 2000 I joined my dream society, the Society of Hospital Medicine. That society exceeded my wildest aspirations. During my 20-year membership I started an SHM Chapter, was a leader in the Leadership Academies, joined the Board of Directors, participated in Annual Conferences, and helped lead the SHM Center for Quality Improvement. That exceedingly rewarding partnership helped shape the field of hospital medicine nationally and provided the foundation for my next role at SHM. I am excited and grateful to be the CEO of SHM.
I’ll end with something I use every day – “Eric Howell’s Core Values”:
- Make the world a better place.
- Invest in people.
- Be ethical and transparent.
- Do what you love.
- Try to use Star Trek references whenever possible. (Okay, this last one is not really a core value, but maybe a character trait?) At least the Vulcan greeting is appropriate for our times: Live long and prosper.
Dr. Howell is the new CEO for SHM as of July 1, 2020.
Changing times
After more than 20 years, my leadership role as CEO at the Society of Hospital Medicine (SHM) has ended with the transition to Dr. Eric Howell as the new SHM CEO on July 1, 2020. Looking back, I think we can all be proud of how we have helped to shape the specialty of hospital medicine over these two decades and of how strong SHM has become to support our new specialty.
In 2000, few people knew what a hospitalist was (or more importantly what we could become) and the specialty of hospital medicine had not even been named yet. Today the reputation of SHM is firmly established and the specialty has been defined by a unique curriculum through the Core Competencies in Hospital Medicine for both adult and pediatric patients, and by several textbooks in hospital medicine. There are divisions or departments of hospital medicine at many hospitals and academic medical centers. We even managed to convince the American Board of Internal Medicine, the American Board of Family Medicine, and the American Board of Medical Specialties to create a credential of Focused Practice in Hospital Medicine as the first-ever certification not tied to specific fellowship training.
To recognize the contributions of our members, SHM has established Awards of Excellence and the Fellow and Senior Fellow in Hospital Medicine (FHM and SFHM) designations. We have gone from a small national association in Philadelphia to create 68 active chapters and more than 20 Special Interest Groups. In my time at SHM I have attended more than 75-chapter meetings and met with thousands of hospitalists in 46 states. We now have over 20,000 members at SHM, making us the fastest growing medical specialty ever.
When I started at the National Association of Inpatient Physicians (NAIP) our only meeting was an annual CME meeting for about 150-200 people. We now hold a national meeting every year for more than 4,000 attendees that is the “Center of the Universe for Hospital Medicine.” Understanding that we needed to educate the people who will lead change in our health care system, we developed from scratch a set of Leadership Academies that has already educated more than 2,500 hospitalist leaders. To train the educators in quality improvement in medical education we developed our Quality and Safety Educator Academy (QSEA) programs, and to promote career development of academic hospitalists we created our Academic Hospitalist Academy.
SHM is the leader in adult in-practice learning, specifically designed for hospitalists. SHM members have access to a state-of-the-art comprehensive hospitalist-based online education system as well as board review and maintenance of certification (MOC) review tools in our SPARK program, specifically for hospital medicine.
In the area of quality improvement, most medical societies convene a panel of experts, develop guidelines, publish them, and hope that change will occur. SHM has been much more proactive, creating the Center for Quality Improvement that has raised more than $10 million and developed Quality Improvement programs in more than 400 hospitals over the years, winning the prestigious Eisenberg Award along the way.
When I started at NAIP in 2000, our only communication tools were a 4-page newsletter and an email listserv. Along the way we have developed a broadly read newsmagazine (The Hospitalist), a well-recognized peer reviewed journal (Journal of Hospital Medicine), a robust website, and a significant social media presence.
From the very early days we knew that our specialty would not be totally successful by only facing inward. Change was coming to our health care system and hospitalists were going to be right in the middle. Despite our young age and limited resources, we have always hit above our weight class in advocacy. We actively participated in the development of the Affordable Care Act (Obamacare), making suggestions in payment reform, expanding the workforce with visa reform, and expanding the team of clinicians. Along the way SHM members rose to run the Centers for Medicare & Medicaid Services (CMS) and the Food and Drug Administration (FDA), and serve as U.S. Surgeon General.
Today in these troubled times, SHM continues to be a positive voice in promoting the use of PPE, the need for increased COVID-19 testing, and the recognition of our nation’s 60,000 hospitalists as essential frontline workers in the COVID-19 pandemic. With its longstanding role in promoting diversity and overcoming social injustice, SHM has had a positive national voice during the protests over police brutality.
We have proved to be a good partner with many other organizations and consistently were invited to partner in coalitions with the ED physicians (ACEP), the critical care docs (SCCM), the hospitals (AHA), the house of medicine (AMA), other internists (ACP), surgeons (ACS), and pediatricians (AAP), and so many other much more established societies, because we could be an active, flexible, and knowledgeable partner for more than 20 years.
Today, SHM and hospital medicine are clearly recognized as a force in the rapidly evolving health care system. With this comes not only influence but also responsibility, and I am certain the SHM Board, membership, and staff are ready for this challenge. The economic toll of our current pandemic will see colleges and other major companies and institutions go out of business and leave the landscape. SHM has a deep foundation and a well of strength to call on and will survive and thrive into the future.
SHM has been a good fit for me professionally and personally. Many of my skills and strengths have served SHM in our “early” years. I am very proud of what we have been able to accomplish TOGETHER. In the end it is the people I have been fortunate enough to meet and work with throughout these past 20 years that will stay with me, many of whom are lifelong friends. My mother, even today at 93, has always asked me to leave anything I do better off than when I came in the door. As I look back at my time helping to shape and lead SHM, I am sure I have answered my mother’s challenge and more.
I look forward to seeing many of you at a future SHM meeting and reveling in the way that hospitalists will actively play an important role in shaping our health care system in the future.
Dr. Wellikson is retiring as CEO of SHM.
Live long and prosper
Back in 2000, I was extremely fortunate to land my dream job as a hospitalist at Johns Hopkins Bayview in Baltimore. That dream exceeded my wildest aspirations. During my 20-year career as faculty in the Johns Hopkins School of Medicine I grew our tiny, 4 physician hospitalist group at Johns Hopkins Bayview into a multihospital program, complete with more than 150 physicians. That exceedingly rewarding work helped to shape the field of hospital medicine nationally and provided the foundation for my promotion to professor of medicine at Johns Hopkins in 2016.
Most professionals are lucky if they find one inspiring institution; I have found two. SHM has been my professional home since I became a hospitalist in 2000, and in that time I have dedicated as much creative energy to SHM as I have at Johns Hopkins.
Even at this time when the medical profession, and the entire world, has been rocked by the coronavirus, the fundamentals that have made SHM so successful will serve us well through the effects of this pandemic and beyond. It takes a skilled leader to nurture a professional society through the growth from only a few hundred members to thousands upon thousands, and at the same time crafting the profession into one of quality and high impact. These past 22 years Dr. Larry Wellikson, our retiring CEO, has skillfully accomplished just that by building lasting programs and people.
As you might imagine, my approach will work to add onto the legacy that Larry has left us. Yes, we will have to adapt SHM to the realities of the near future: virtual meetings, in-person events (yes, those will return one day) with appropriate social distancing until the coronavirus has faded, modified chapter meetings, and more. Someday the world will find a new normal, and SHM will evolve to meet the needs of our members and the patients we serve.
Through this pandemic and beyond, my vision – in partnership with the Board of Directors – will be to:
- Continue the work to enhance member engagement. We are primarily a membership organization, after all.
- Maintain our profession’s leadership role in the care continuum, particularly acute care.
- Be a deliberate sponsor of diversity and inclusion. I believe social justice is a moral imperative, and good business.
- Invest in teams: Chapters, special interest groups, and committees are key to success.
- Be financially prudent, so that this organization can serve its members through the best of times and those most challenging times.
Back in 2000 I joined my dream society, the Society of Hospital Medicine. That society exceeded my wildest aspirations. During my 20-year membership I started an SHM Chapter, was a leader in the Leadership Academies, joined the Board of Directors, participated in Annual Conferences, and helped lead the SHM Center for Quality Improvement. That exceedingly rewarding partnership helped shape the field of hospital medicine nationally and provided the foundation for my next role at SHM. I am excited and grateful to be the CEO of SHM.
I’ll end with something I use every day – “Eric Howell’s Core Values”:
- Make the world a better place.
- Invest in people.
- Be ethical and transparent.
- Do what you love.
- Try to use Star Trek references whenever possible. (Okay, this last one is not really a core value, but maybe a character trait?) At least the Vulcan greeting is appropriate for our times: Live long and prosper.
Dr. Howell is the new CEO for SHM as of July 1, 2020.
Manage the pandemic with a multidisciplinary coalition
Implement a 6-P framework
The ongoing COVID-19 pandemic, arguably the biggest public health and economic catastrophe of modern times, elevated multiple deficiencies in public health infrastructures across the world, such as a slow or delayed response to suppress and mitigate the virus, an inadequately prepared and protected health care and public health workforce, and decentralized, siloed efforts.1 COVID-19 further highlighted the vulnerabilities of the health care, public health, and economic sectors.2,3 Irrespective of how robust health care systems may have been initially, rapidly spreading and deadly infectious diseases like COVID-19 can quickly derail the system, bringing the workforce and the patients they serve to a breaking point.
Hospital systems in the United States are not only at the crux of the current pandemic but are also well positioned to lead the response to the pandemic. Hospital administrators oversee nearly 33% of national health expenditure that amounts to the hospital-based care in the United States. Additionally, they may have an impact on nearly 30% of the expenditure that is related to physicians, prescriptions, and other facilities.4
The two primary goals underlying our proposed framework to target COVID-19 are based on the World Health Organization recommendations and lessons learned from countries such as South Korea that have successfully implemented these recommendations.5
1. Flatten the curve. According to the WHO and the Centers for Disease Control and Prevention, flattening the curve means that we must do everything that will help us to slow down the rate of infection, so the number of cases do not exceed the capacity of health systems.
2. Establish a standardized, interdisciplinary approach to flattening the curve. Pandemics can have major adverse consequences beyond health outcomes (e.g., economy) that can impact adherence to advisories and introduce multiple unintended consequences (e.g., deferred chronic care, unemployment). Managing the current pandemic and thoughtful consideration of and action regarding its ripple effects is heavily dependent on a standardized, interdisciplinary approach that is monitored, implemented, and evaluated well.
To achieve these two goals, we recommend establishing an interdisciplinary coalition representing multiple sectors. Our 6-P framework described below is intended to guide hospital administrators, to build the coalition, and to achieve these goals.
Structure of the pandemic coalition
A successful coalition invites a collaborative partnership involving senior members of respective disciplines, who would provide valuable, complementary perspectives in the coalition. We recommend hospital administrators take a lead in the formation of such a coalition. While we present the stakeholders and their roles below based on their intended influence and impact on the overall outcome of COVID-19, the basic guiding principles behind our 6-P framework remain true for any large-scale population health intervention.
Although several models for staging the transmission of COVID-19 are available, we adopted a four-stage model followed by the Indian Council for Medical Research.6 Irrespective of the origin of the infection, we believe that the four-stage model can cultivate situational awareness that can help guide the strategic design and systematic implementation of interventions.
Our 6-P framework integrates the four-stage model of COVID-19 transmission to identify action items for each stakeholder group and appropriate strategies selected based on the stages targeted.

1. Policy makers: Policy makers at all levels are critical in establishing policies, orders, and advisories, as well as dedicating resources and infrastructure, to enhance adherence to recommendations and guidelines at the community and population levels.7 They can assist hospitals in workforce expansion across county/state/discipline lines (e.g., accelerate the licensing and credentialing process, authorize graduate medical trainees, nurse practitioners, and other allied health professionals). Policy revisions for data sharing, privacy, communication, liability, and telehealth expansion.82. Providers: The health of the health care workforce itself is at risk because of their frontline services. Their buy-in will be crucial in both the formulation and implementation of evidence- and practice-based guidelines.9 Rapid adoption of telehealth for care continuum, policy revisions for elective procedures, visitor restriction, surge, resurge planning, capacity expansion, effective population health management, and working with employee unions, professional staff organizations are few, but very important action items that need to be implemented.
3. Public health authorities: Representation of public health authorities will be crucial in standardizing data collection, management, and reporting; providing up-to-date guidelines and advisories; developing, implementing, and evaluating short- and long-term public health interventions; and preparing and helping communities throughout the course of the pandemic. They also play a key role in identifying and reducing barriers related to the expansion of testing and contact tracing efforts.
4. Payers: In the United States, the Centers for Medicare & Medicaid Services oversees primary federally funded programs and serves as a point of reference for the American health care system. Having representation from all payer sources is crucial for achieving uniformity and standardization of the care process during the pandemic, with particular priority given to individuals and families who may have recently lost their health insurance because of job loss from COVID-19–related business furloughs, layoffs, and closures. Customer outreach initiatives, revision of patients’ out of pocket responsibilities, rapid claim settlement and denial management services, expansion of telehealth, elimination of prior authorization barriers, rapid credentialing of providers, data sharing, and assisting hospital systems in chronic disease management are examples of time-sensitive initiatives that are vital for population health management.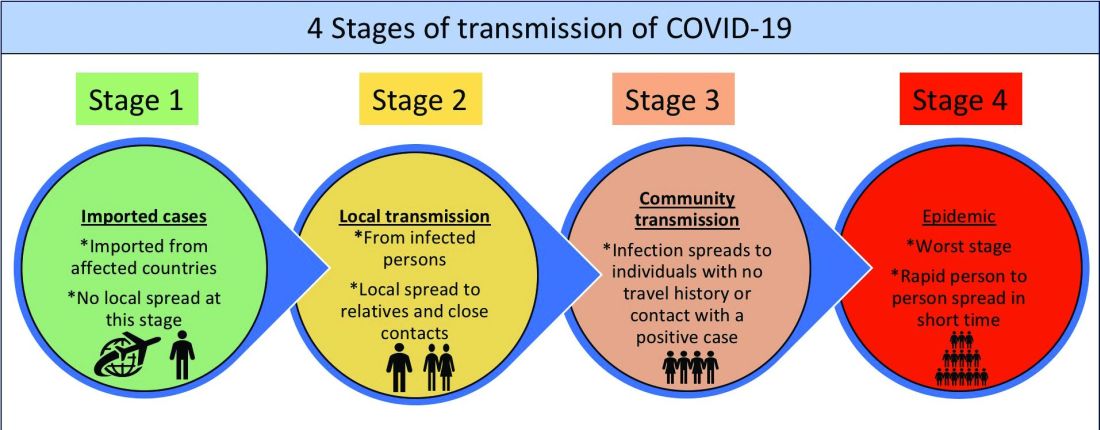
5. Partners: Establishing partnerships with pharma, health IT, labs, device industries, and other ancillary services is important to facilitate rapid innovation, production, and supply of essential medical devices and resources. These partners directly influence the outcomes of the pandemic and long-term health of the society through expansion of testing capability, contact tracing, leveraging technology for expanding access to COVID-19 and non–COVID-19 care, home monitoring of cases, innovation of treatment and prevention, and data sharing. Partners should consider options such as flexible medication delivery, electronic prescription services, and use of drones in supply chain to deliver test kits, test samples, medication, and blood products.
6. People/patients: Lastly and perhaps most critically, the trust, buy-in, and needs of the overall population are needed to enhance adherence to guidelines and recommendations. Many millions more than those who test positive for COVID-19 have and will continue to experience the crippling adverse economic, social, physical, and mental health effects of stay-at-home advisories, business and school closures, and physical distancing orders. Members of each community need to be heard in voicing their concerns and priorities and providing input on public health interventions to enhance acceptance and adherence (e.g., wear mask/face coverings in public, engage in physical distancing, etc.). Special attention should be given to managing chronic or existing medical problems and seek care when needed (e.g., avoid delaying of medical care).
An interdisciplinary and multipronged approach is necessary to address a complex, widespread, disruptive, and deadly pandemic such as COVID-19. The suggested activities put forth in our table are by no means exhaustive, nor do we expect all coalitions to be able to carry them all out. Our intention is that the 6-P framework encourages cross-sector collaboration to facilitate the design, implementation, evaluation, and scalability of preventive and intervention efforts based on the menu of items we have provided. Each coalition may determine which strategies they are able to prioritize and when within the context of specific national, regional, and local advisories, resulting in a tailored approach for each community or region that is thus better positioned for success.
Dr. Lingisetty is a hospitalist and physician executive at Baptist Health System, Little Rock, Ark. He is cofounder/president of SHM’s Arkansas chapter. Dr. Wang is assistant professor in the department of community health sciences at Boston University and adjunct assistant professor of health policy and management at the Harvard School of Public Health. Dr. Palabindala is the medical director, utilization management and physician advisory services, at the University of Mississippi Medical Center, Jackson. He is an associate professor of medicine and academic hospitalist at the University of Mississippi.
References
1. Powles J, Comim F. Public health infrastructure and knowledge, in Smith R et al. “Global Public Goods for Health.” Oxford: Oxford University Press, 2003.
2. Lombardi P, Petroni G. Virus outbreak pushes Italy’s health care system to the brink. Wall Street Journal. 2020 Mar 12. https://www.wsj.com/articles/virus-outbreak-pushes-italys-healthcare-system-to-the-brink-11583968769
3. Davies, R. How coronavirus is affecting the global economy. The Guardian. 2020 Feb 5. https://www.theguardian.com/world/2020/feb/05/coronavirus-global-economy
4. National Center for Health Statistics. FastStats. 2017. https://www.cdc.gov/nchs/fastats/health-expenditures.htm.
5. World Health Organization. Country & Technical Guidance–Coronavirus disease (COVID-19). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance
6. Indian Council of Medical Research. Stages of transmission of COVID-19. https://main.icmr.nic.in/content/covid-19
7. Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19) – Prevention & treatment. 2020 Apr 24. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html
8. Ostriker R. Cutbacks for some doctors and nurses as they battle on the front line. Boston Globe. 2020 Mar 27. https://www.bostonglobe.com/2020/03/27/metro/coronavirus-rages-doctors-hit-with-cuts-compensation/
9. Centers for Medicare & Medicaid Services. News alert. 2020 Mar 26. https://www.cms.gov/newsroom/press-releases/cms-news-alert-march-26-2020
Implement a 6-P framework
Implement a 6-P framework
The ongoing COVID-19 pandemic, arguably the biggest public health and economic catastrophe of modern times, elevated multiple deficiencies in public health infrastructures across the world, such as a slow or delayed response to suppress and mitigate the virus, an inadequately prepared and protected health care and public health workforce, and decentralized, siloed efforts.1 COVID-19 further highlighted the vulnerabilities of the health care, public health, and economic sectors.2,3 Irrespective of how robust health care systems may have been initially, rapidly spreading and deadly infectious diseases like COVID-19 can quickly derail the system, bringing the workforce and the patients they serve to a breaking point.
Hospital systems in the United States are not only at the crux of the current pandemic but are also well positioned to lead the response to the pandemic. Hospital administrators oversee nearly 33% of national health expenditure that amounts to the hospital-based care in the United States. Additionally, they may have an impact on nearly 30% of the expenditure that is related to physicians, prescriptions, and other facilities.4
The two primary goals underlying our proposed framework to target COVID-19 are based on the World Health Organization recommendations and lessons learned from countries such as South Korea that have successfully implemented these recommendations.5
1. Flatten the curve. According to the WHO and the Centers for Disease Control and Prevention, flattening the curve means that we must do everything that will help us to slow down the rate of infection, so the number of cases do not exceed the capacity of health systems.
2. Establish a standardized, interdisciplinary approach to flattening the curve. Pandemics can have major adverse consequences beyond health outcomes (e.g., economy) that can impact adherence to advisories and introduce multiple unintended consequences (e.g., deferred chronic care, unemployment). Managing the current pandemic and thoughtful consideration of and action regarding its ripple effects is heavily dependent on a standardized, interdisciplinary approach that is monitored, implemented, and evaluated well.
To achieve these two goals, we recommend establishing an interdisciplinary coalition representing multiple sectors. Our 6-P framework described below is intended to guide hospital administrators, to build the coalition, and to achieve these goals.
Structure of the pandemic coalition
A successful coalition invites a collaborative partnership involving senior members of respective disciplines, who would provide valuable, complementary perspectives in the coalition. We recommend hospital administrators take a lead in the formation of such a coalition. While we present the stakeholders and their roles below based on their intended influence and impact on the overall outcome of COVID-19, the basic guiding principles behind our 6-P framework remain true for any large-scale population health intervention.
Although several models for staging the transmission of COVID-19 are available, we adopted a four-stage model followed by the Indian Council for Medical Research.6 Irrespective of the origin of the infection, we believe that the four-stage model can cultivate situational awareness that can help guide the strategic design and systematic implementation of interventions.
Our 6-P framework integrates the four-stage model of COVID-19 transmission to identify action items for each stakeholder group and appropriate strategies selected based on the stages targeted.

1. Policy makers: Policy makers at all levels are critical in establishing policies, orders, and advisories, as well as dedicating resources and infrastructure, to enhance adherence to recommendations and guidelines at the community and population levels.7 They can assist hospitals in workforce expansion across county/state/discipline lines (e.g., accelerate the licensing and credentialing process, authorize graduate medical trainees, nurse practitioners, and other allied health professionals). Policy revisions for data sharing, privacy, communication, liability, and telehealth expansion.82. Providers: The health of the health care workforce itself is at risk because of their frontline services. Their buy-in will be crucial in both the formulation and implementation of evidence- and practice-based guidelines.9 Rapid adoption of telehealth for care continuum, policy revisions for elective procedures, visitor restriction, surge, resurge planning, capacity expansion, effective population health management, and working with employee unions, professional staff organizations are few, but very important action items that need to be implemented.
3. Public health authorities: Representation of public health authorities will be crucial in standardizing data collection, management, and reporting; providing up-to-date guidelines and advisories; developing, implementing, and evaluating short- and long-term public health interventions; and preparing and helping communities throughout the course of the pandemic. They also play a key role in identifying and reducing barriers related to the expansion of testing and contact tracing efforts.
4. Payers: In the United States, the Centers for Medicare & Medicaid Services oversees primary federally funded programs and serves as a point of reference for the American health care system. Having representation from all payer sources is crucial for achieving uniformity and standardization of the care process during the pandemic, with particular priority given to individuals and families who may have recently lost their health insurance because of job loss from COVID-19–related business furloughs, layoffs, and closures. Customer outreach initiatives, revision of patients’ out of pocket responsibilities, rapid claim settlement and denial management services, expansion of telehealth, elimination of prior authorization barriers, rapid credentialing of providers, data sharing, and assisting hospital systems in chronic disease management are examples of time-sensitive initiatives that are vital for population health management.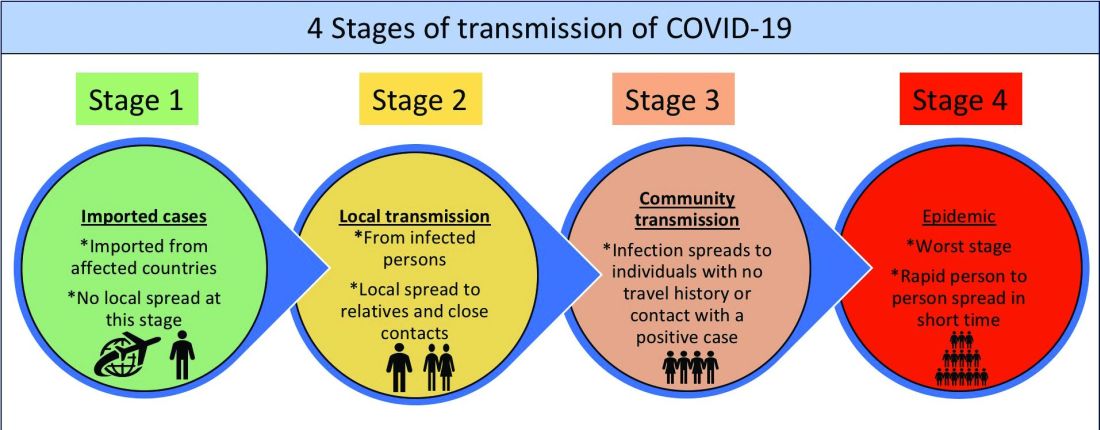
5. Partners: Establishing partnerships with pharma, health IT, labs, device industries, and other ancillary services is important to facilitate rapid innovation, production, and supply of essential medical devices and resources. These partners directly influence the outcomes of the pandemic and long-term health of the society through expansion of testing capability, contact tracing, leveraging technology for expanding access to COVID-19 and non–COVID-19 care, home monitoring of cases, innovation of treatment and prevention, and data sharing. Partners should consider options such as flexible medication delivery, electronic prescription services, and use of drones in supply chain to deliver test kits, test samples, medication, and blood products.
6. People/patients: Lastly and perhaps most critically, the trust, buy-in, and needs of the overall population are needed to enhance adherence to guidelines and recommendations. Many millions more than those who test positive for COVID-19 have and will continue to experience the crippling adverse economic, social, physical, and mental health effects of stay-at-home advisories, business and school closures, and physical distancing orders. Members of each community need to be heard in voicing their concerns and priorities and providing input on public health interventions to enhance acceptance and adherence (e.g., wear mask/face coverings in public, engage in physical distancing, etc.). Special attention should be given to managing chronic or existing medical problems and seek care when needed (e.g., avoid delaying of medical care).
An interdisciplinary and multipronged approach is necessary to address a complex, widespread, disruptive, and deadly pandemic such as COVID-19. The suggested activities put forth in our table are by no means exhaustive, nor do we expect all coalitions to be able to carry them all out. Our intention is that the 6-P framework encourages cross-sector collaboration to facilitate the design, implementation, evaluation, and scalability of preventive and intervention efforts based on the menu of items we have provided. Each coalition may determine which strategies they are able to prioritize and when within the context of specific national, regional, and local advisories, resulting in a tailored approach for each community or region that is thus better positioned for success.
Dr. Lingisetty is a hospitalist and physician executive at Baptist Health System, Little Rock, Ark. He is cofounder/president of SHM’s Arkansas chapter. Dr. Wang is assistant professor in the department of community health sciences at Boston University and adjunct assistant professor of health policy and management at the Harvard School of Public Health. Dr. Palabindala is the medical director, utilization management and physician advisory services, at the University of Mississippi Medical Center, Jackson. He is an associate professor of medicine and academic hospitalist at the University of Mississippi.
References
1. Powles J, Comim F. Public health infrastructure and knowledge, in Smith R et al. “Global Public Goods for Health.” Oxford: Oxford University Press, 2003.
2. Lombardi P, Petroni G. Virus outbreak pushes Italy’s health care system to the brink. Wall Street Journal. 2020 Mar 12. https://www.wsj.com/articles/virus-outbreak-pushes-italys-healthcare-system-to-the-brink-11583968769
3. Davies, R. How coronavirus is affecting the global economy. The Guardian. 2020 Feb 5. https://www.theguardian.com/world/2020/feb/05/coronavirus-global-economy
4. National Center for Health Statistics. FastStats. 2017. https://www.cdc.gov/nchs/fastats/health-expenditures.htm.
5. World Health Organization. Country & Technical Guidance–Coronavirus disease (COVID-19). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance
6. Indian Council of Medical Research. Stages of transmission of COVID-19. https://main.icmr.nic.in/content/covid-19
7. Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19) – Prevention & treatment. 2020 Apr 24. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html
8. Ostriker R. Cutbacks for some doctors and nurses as they battle on the front line. Boston Globe. 2020 Mar 27. https://www.bostonglobe.com/2020/03/27/metro/coronavirus-rages-doctors-hit-with-cuts-compensation/
9. Centers for Medicare & Medicaid Services. News alert. 2020 Mar 26. https://www.cms.gov/newsroom/press-releases/cms-news-alert-march-26-2020
The ongoing COVID-19 pandemic, arguably the biggest public health and economic catastrophe of modern times, elevated multiple deficiencies in public health infrastructures across the world, such as a slow or delayed response to suppress and mitigate the virus, an inadequately prepared and protected health care and public health workforce, and decentralized, siloed efforts.1 COVID-19 further highlighted the vulnerabilities of the health care, public health, and economic sectors.2,3 Irrespective of how robust health care systems may have been initially, rapidly spreading and deadly infectious diseases like COVID-19 can quickly derail the system, bringing the workforce and the patients they serve to a breaking point.
Hospital systems in the United States are not only at the crux of the current pandemic but are also well positioned to lead the response to the pandemic. Hospital administrators oversee nearly 33% of national health expenditure that amounts to the hospital-based care in the United States. Additionally, they may have an impact on nearly 30% of the expenditure that is related to physicians, prescriptions, and other facilities.4
The two primary goals underlying our proposed framework to target COVID-19 are based on the World Health Organization recommendations and lessons learned from countries such as South Korea that have successfully implemented these recommendations.5
1. Flatten the curve. According to the WHO and the Centers for Disease Control and Prevention, flattening the curve means that we must do everything that will help us to slow down the rate of infection, so the number of cases do not exceed the capacity of health systems.
2. Establish a standardized, interdisciplinary approach to flattening the curve. Pandemics can have major adverse consequences beyond health outcomes (e.g., economy) that can impact adherence to advisories and introduce multiple unintended consequences (e.g., deferred chronic care, unemployment). Managing the current pandemic and thoughtful consideration of and action regarding its ripple effects is heavily dependent on a standardized, interdisciplinary approach that is monitored, implemented, and evaluated well.
To achieve these two goals, we recommend establishing an interdisciplinary coalition representing multiple sectors. Our 6-P framework described below is intended to guide hospital administrators, to build the coalition, and to achieve these goals.
Structure of the pandemic coalition
A successful coalition invites a collaborative partnership involving senior members of respective disciplines, who would provide valuable, complementary perspectives in the coalition. We recommend hospital administrators take a lead in the formation of such a coalition. While we present the stakeholders and their roles below based on their intended influence and impact on the overall outcome of COVID-19, the basic guiding principles behind our 6-P framework remain true for any large-scale population health intervention.
Although several models for staging the transmission of COVID-19 are available, we adopted a four-stage model followed by the Indian Council for Medical Research.6 Irrespective of the origin of the infection, we believe that the four-stage model can cultivate situational awareness that can help guide the strategic design and systematic implementation of interventions.
Our 6-P framework integrates the four-stage model of COVID-19 transmission to identify action items for each stakeholder group and appropriate strategies selected based on the stages targeted.

1. Policy makers: Policy makers at all levels are critical in establishing policies, orders, and advisories, as well as dedicating resources and infrastructure, to enhance adherence to recommendations and guidelines at the community and population levels.7 They can assist hospitals in workforce expansion across county/state/discipline lines (e.g., accelerate the licensing and credentialing process, authorize graduate medical trainees, nurse practitioners, and other allied health professionals). Policy revisions for data sharing, privacy, communication, liability, and telehealth expansion.82. Providers: The health of the health care workforce itself is at risk because of their frontline services. Their buy-in will be crucial in both the formulation and implementation of evidence- and practice-based guidelines.9 Rapid adoption of telehealth for care continuum, policy revisions for elective procedures, visitor restriction, surge, resurge planning, capacity expansion, effective population health management, and working with employee unions, professional staff organizations are few, but very important action items that need to be implemented.
3. Public health authorities: Representation of public health authorities will be crucial in standardizing data collection, management, and reporting; providing up-to-date guidelines and advisories; developing, implementing, and evaluating short- and long-term public health interventions; and preparing and helping communities throughout the course of the pandemic. They also play a key role in identifying and reducing barriers related to the expansion of testing and contact tracing efforts.
4. Payers: In the United States, the Centers for Medicare & Medicaid Services oversees primary federally funded programs and serves as a point of reference for the American health care system. Having representation from all payer sources is crucial for achieving uniformity and standardization of the care process during the pandemic, with particular priority given to individuals and families who may have recently lost their health insurance because of job loss from COVID-19–related business furloughs, layoffs, and closures. Customer outreach initiatives, revision of patients’ out of pocket responsibilities, rapid claim settlement and denial management services, expansion of telehealth, elimination of prior authorization barriers, rapid credentialing of providers, data sharing, and assisting hospital systems in chronic disease management are examples of time-sensitive initiatives that are vital for population health management.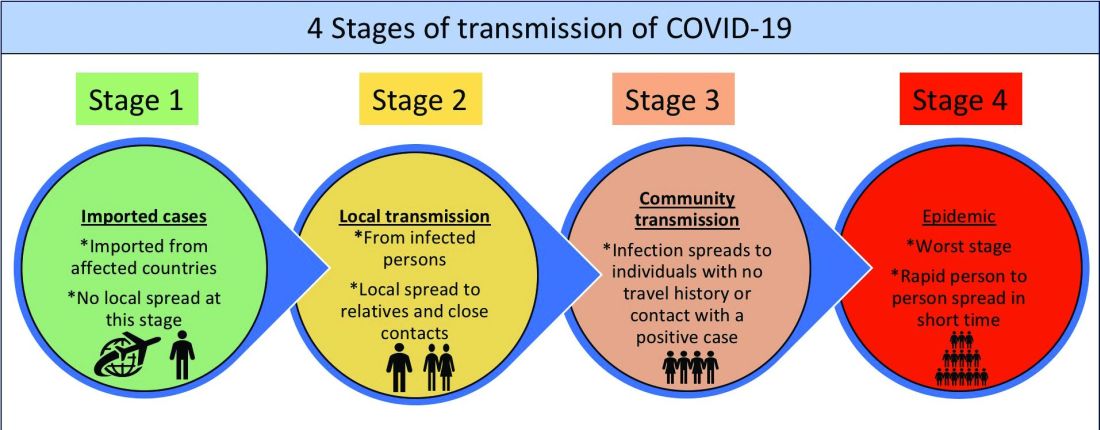
5. Partners: Establishing partnerships with pharma, health IT, labs, device industries, and other ancillary services is important to facilitate rapid innovation, production, and supply of essential medical devices and resources. These partners directly influence the outcomes of the pandemic and long-term health of the society through expansion of testing capability, contact tracing, leveraging technology for expanding access to COVID-19 and non–COVID-19 care, home monitoring of cases, innovation of treatment and prevention, and data sharing. Partners should consider options such as flexible medication delivery, electronic prescription services, and use of drones in supply chain to deliver test kits, test samples, medication, and blood products.
6. People/patients: Lastly and perhaps most critically, the trust, buy-in, and needs of the overall population are needed to enhance adherence to guidelines and recommendations. Many millions more than those who test positive for COVID-19 have and will continue to experience the crippling adverse economic, social, physical, and mental health effects of stay-at-home advisories, business and school closures, and physical distancing orders. Members of each community need to be heard in voicing their concerns and priorities and providing input on public health interventions to enhance acceptance and adherence (e.g., wear mask/face coverings in public, engage in physical distancing, etc.). Special attention should be given to managing chronic or existing medical problems and seek care when needed (e.g., avoid delaying of medical care).
An interdisciplinary and multipronged approach is necessary to address a complex, widespread, disruptive, and deadly pandemic such as COVID-19. The suggested activities put forth in our table are by no means exhaustive, nor do we expect all coalitions to be able to carry them all out. Our intention is that the 6-P framework encourages cross-sector collaboration to facilitate the design, implementation, evaluation, and scalability of preventive and intervention efforts based on the menu of items we have provided. Each coalition may determine which strategies they are able to prioritize and when within the context of specific national, regional, and local advisories, resulting in a tailored approach for each community or region that is thus better positioned for success.
Dr. Lingisetty is a hospitalist and physician executive at Baptist Health System, Little Rock, Ark. He is cofounder/president of SHM’s Arkansas chapter. Dr. Wang is assistant professor in the department of community health sciences at Boston University and adjunct assistant professor of health policy and management at the Harvard School of Public Health. Dr. Palabindala is the medical director, utilization management and physician advisory services, at the University of Mississippi Medical Center, Jackson. He is an associate professor of medicine and academic hospitalist at the University of Mississippi.
References
1. Powles J, Comim F. Public health infrastructure and knowledge, in Smith R et al. “Global Public Goods for Health.” Oxford: Oxford University Press, 2003.
2. Lombardi P, Petroni G. Virus outbreak pushes Italy’s health care system to the brink. Wall Street Journal. 2020 Mar 12. https://www.wsj.com/articles/virus-outbreak-pushes-italys-healthcare-system-to-the-brink-11583968769
3. Davies, R. How coronavirus is affecting the global economy. The Guardian. 2020 Feb 5. https://www.theguardian.com/world/2020/feb/05/coronavirus-global-economy
4. National Center for Health Statistics. FastStats. 2017. https://www.cdc.gov/nchs/fastats/health-expenditures.htm.
5. World Health Organization. Country & Technical Guidance–Coronavirus disease (COVID-19). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance
6. Indian Council of Medical Research. Stages of transmission of COVID-19. https://main.icmr.nic.in/content/covid-19
7. Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19) – Prevention & treatment. 2020 Apr 24. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html
8. Ostriker R. Cutbacks for some doctors and nurses as they battle on the front line. Boston Globe. 2020 Mar 27. https://www.bostonglobe.com/2020/03/27/metro/coronavirus-rages-doctors-hit-with-cuts-compensation/
9. Centers for Medicare & Medicaid Services. News alert. 2020 Mar 26. https://www.cms.gov/newsroom/press-releases/cms-news-alert-march-26-2020
Two pandemics
This column is adapted from Dr. Eleryan’s speech at the George Washington University dermatology residency program’s virtual graduation ceremony on June 12.
I’ve been reflecting on my entire residency and the last 2 weeks have stood out the most. I have to admit that I’ve been angry, and so are numerous others who look like me. However, after conversations with a few important people in my life, I’ve realized that people care and are open to listening and changing if I give them the opportunity to see through my lens. I don’t want my legacy to be one of anger, but to be one of change, one of activism, one of heroism, and one of taking a stand in the midst of adversity.
So thank you to everyone who has played a part in my residency and is here to celebrate as I transition to the next step in my career.
But I must pause for a moment to say “I can’t breathe.” I can’t breathe because while I sit here in a place of honor for my accomplishments, I can’t forget that I’m standing in the gap for all of the black men and women who will never have the opportunity to experience a moment like this.
I can’t breathe because George Floyd, Breonna Taylor, Ahmaud Arbery, Tony McDade, Trayvon Martin, Philando Castile, Sandra Bland, Eric Garner, Tamir Rice, Mike Brown, Emmett Till, and so many others will never get to experience a celebratory occasion such as this because of their senseless executions as a likely result of racial bias.
As a black person in “the land of the free,” I have to live with the fact that my life may be taken for simply taking a stroll through a park, jogging through a neighborhood, driving down the street, walking back home from the store, or even sitting in my own home!
As a black physician, I must contend with the very notion that my privilege as a physician does not shield me from discrimination and bias. I recognize that my race walks into the room before I ever do. I know that many of my patients will question my abilities or my title – thinking I am the receptionist, food services worker, or even part of the janitorial staff – simply because of the color of my skin. And what’s even more disturbing is that some of my colleagues will confuse me with another black woman whom I look nothing like or challenge my intelligence and abilities and how I got my position.
All of this boils down to racism – pure and simple. Black people in this country don’t have the privilege of ignoring this truth. We know that this world is not colorblind; neither is anyone in it. We know that this is entrenched racism that for generations has created racial disparities in health care, education, housing, employment, and law enforcement. We weren’t born into a fragile or vulnerable state, yet we were born into a system of dis-enfranchisement, dis-investment, dis-crimination, dis-advantage, and dis-respect.
As physicians, we must recognize and acknowledge the lived experiences that walk through the door with our black patients. And we must understand that black patients walk around with the effects of trauma and toxic stress from just being black in America. That trauma and stress show up in very real ways that contribute to black people experiencing the brunt of chronic diseases and poorer health outcomes. There is no better example than the current COVID-19 pandemic. We are in the midst of a global pandemic from a virus that does not discriminate based on race, but black people are almost three times as likely to be hospitalized as are white people with COVID-19 . And why is that? Because of the “comorbidity” of racism that black people in this country live with. It is not a mere coincidence that the black population is overrepresented in essential jobs and black people are more likely to work in health care than are white people – all positions that increase the risk of infection and death from the virus. So, if we call COVID-19 a pandemic, racism most certainly has been a pandemic that this country has refused to acknowledge, treat, and vaccinate for centuries. We cannot ignore that both have tragically affected black people.
So as Pastor Reginald Sharpe Jr. in Chicago recently said, we’re dealing with two pandemics: One has no vaccination and one has no explanation; one can physiologically take your breath away because it affects the respiratory system, while the second can also take your breath away. Just ask Eric Garner and George Floyd.
As physicians, we must recognize that the mechanisms that tragically resulted in the deaths of George Floyd, Breonna Taylor, Ahmaud Arbery, and so many other black men and women are the same mechanisms that are harming and killing black people in our health care system. It’s not acceptable for institutions that built themselves on black and brown bodies to offer condolences, but to continue to do nothing about the racism that still runs rampant within. It’s not acceptable to do nothing. It’s important to note: Racist systems do not perpetuate themselves – the individuals operating within them do.
Martin Luther King Jr. once said, “He who passively accepts evil is as much involved in it as he who helps to perpetuate it. He who accepts evil without protesting against it is really cooperating with it.” Being well-intentioned, good-hearted, sad, or disheartened is not enough. We won’t be able to tear down the systems and institutions that have been a breeding ground for racism until outrage is met by action, not just from black people and people of color, but also by the white majority.
As physicians it’s time for us to look at how our health care institution – an institution instrumental in the victimization of black people – is affecting the health and well-being of our black patients. (For example, increased maternal mortality among black women.)
Are they being seen and heard? Are they receiving culturally relevant and sensitive care? Are their needs and concerns receiving the same amount of time and attention as other patients? It’s time to understand that, for many black patients, the health care system is another place of injustice that has not proved itself to be trustworthy or inclusive of black culture.
As physicians, we must affirm that the lives and health of black and brown people matter to us, that we see the racism they experience, and that we will use our platform as physicians to eliminate racism not just in the hospitals but in the world our patients live in.
So while I didn’t choose the body that I was born into, I fully embrace it and the challenges that come with it. I’m not here to make people feel comfortable, I’m here to continue the work of my ancestors, accomplish the dreams that they fought and lost their lives for, and most importantly, I’m here to continue the fight against the systems that work to prevent other marginalized persons from getting to where I am and even further.
The author James Baldwin once wrote, “Not everything that is faced can be changed, but nothing can be changed until it is faced.” So, I urge you to be loudly antiracist in every space that you hold. I urge you to educate yourselves about racism and white supremacy and privilege and how it permeates our health care system. I urge you to stand beside black people rather than in front of them. Use your privilege to amplify underheard voices and to challenge the biases of your peers, friends, and family members. Use your platform as physicians to advocate for a more just and equitable health care system.
So let me repeat ... we as physicians have the responsibility to eliminate racial bias in the practice of medicine and recognize racism as a threat to the health and well-being of black people and other people of color.
How do we do this? We are beyond lengthy dialogue and “Black History Month” talks. Now is the time for action. Taking action includes the following:
1. Medical academic institutions committing to having a diverse and inclusive faculty. We know it is critical and vital to the recruitment, success, and matriculation of medical students and residents of color to see faculty, particularly senior level faculty in their specialty, who look like them and can serve as mentors. Every year, these institutions need to set a goal that they will take additional steps to have at least one-third of their faculty be black and another third persons of color. In addition, senior faculty positions – those setting curricula, selecting incoming students and residents – must include at least one-third from underrepresented backgrounds (black, Hispanic, Native American/Indigenous).
2. Hospital administration has to resemble the communities in which the hospital serves. Unfortunately, all too often, we know this is not the case, and as a result, decisions that affect the care of black and brown people are often to their detriment because they perpetuate the racism within the existing system. In order to dismantle racism in the hospital system, hospital administrations must consist of diverse individuals. Therefore, hospitals need to commit to hiring and promoting black and brown staff to ensure one-third of its senior leaderships consists of individuals from underrepresented backgrounds.
3. Improving the pipeline that matriculates black and brown students into medical school and residency programs. Lack of access to mentors within the medical field, lack of funding for travel to/from interviews, and lack of knowledge of the overall application process are a few barriers faced by students of color seeking to enter into the medical field. In addition to current scholarship opportunities, medical schools need to allocate funds to connect underrepresented minority students with a range of lived experiences (not just those from impoverished backgrounds but also those from middle class backgrounds who face difficulty gaining acceptance into medical school and residency programs), such as connecting them with mentors by opening opportunities for them to shadow professionals at a conference, travel to residency interviews with most, if not all, expenses covered up front, and have access to local programs that expose them to physicians in several specialties.
These are just a few examples of the active steps we can take to dismantle racism and reconcile the effects of it in the medical field. So if I may borrow from other movements, “Time’s Up” for silence regarding the existence of racism and white supremacy, and now it’s time to truly show that “We are all in this together.”
It is not just my duty but yours also – to ensure that we never have to hear another black man, woman, or child say “I can’t breathe” at the hands of injustice.
Dr. Eleryan (@skinclusionMD) is a social justice activist and was co-chief resident in dermatology (2019-2020) at George Washington University, Washington, DC, and is an Alpha Omega Alpha inductee (2020). She will be a micrographic surgery and dermatologic oncology fellow at the University of California, Los Angeles, in July 2020.
This column is adapted from Dr. Eleryan’s speech at the George Washington University dermatology residency program’s virtual graduation ceremony on June 12.
I’ve been reflecting on my entire residency and the last 2 weeks have stood out the most. I have to admit that I’ve been angry, and so are numerous others who look like me. However, after conversations with a few important people in my life, I’ve realized that people care and are open to listening and changing if I give them the opportunity to see through my lens. I don’t want my legacy to be one of anger, but to be one of change, one of activism, one of heroism, and one of taking a stand in the midst of adversity.
So thank you to everyone who has played a part in my residency and is here to celebrate as I transition to the next step in my career.
But I must pause for a moment to say “I can’t breathe.” I can’t breathe because while I sit here in a place of honor for my accomplishments, I can’t forget that I’m standing in the gap for all of the black men and women who will never have the opportunity to experience a moment like this.
I can’t breathe because George Floyd, Breonna Taylor, Ahmaud Arbery, Tony McDade, Trayvon Martin, Philando Castile, Sandra Bland, Eric Garner, Tamir Rice, Mike Brown, Emmett Till, and so many others will never get to experience a celebratory occasion such as this because of their senseless executions as a likely result of racial bias.
As a black person in “the land of the free,” I have to live with the fact that my life may be taken for simply taking a stroll through a park, jogging through a neighborhood, driving down the street, walking back home from the store, or even sitting in my own home!
As a black physician, I must contend with the very notion that my privilege as a physician does not shield me from discrimination and bias. I recognize that my race walks into the room before I ever do. I know that many of my patients will question my abilities or my title – thinking I am the receptionist, food services worker, or even part of the janitorial staff – simply because of the color of my skin. And what’s even more disturbing is that some of my colleagues will confuse me with another black woman whom I look nothing like or challenge my intelligence and abilities and how I got my position.
All of this boils down to racism – pure and simple. Black people in this country don’t have the privilege of ignoring this truth. We know that this world is not colorblind; neither is anyone in it. We know that this is entrenched racism that for generations has created racial disparities in health care, education, housing, employment, and law enforcement. We weren’t born into a fragile or vulnerable state, yet we were born into a system of dis-enfranchisement, dis-investment, dis-crimination, dis-advantage, and dis-respect.
As physicians, we must recognize and acknowledge the lived experiences that walk through the door with our black patients. And we must understand that black patients walk around with the effects of trauma and toxic stress from just being black in America. That trauma and stress show up in very real ways that contribute to black people experiencing the brunt of chronic diseases and poorer health outcomes. There is no better example than the current COVID-19 pandemic. We are in the midst of a global pandemic from a virus that does not discriminate based on race, but black people are almost three times as likely to be hospitalized as are white people with COVID-19 . And why is that? Because of the “comorbidity” of racism that black people in this country live with. It is not a mere coincidence that the black population is overrepresented in essential jobs and black people are more likely to work in health care than are white people – all positions that increase the risk of infection and death from the virus. So, if we call COVID-19 a pandemic, racism most certainly has been a pandemic that this country has refused to acknowledge, treat, and vaccinate for centuries. We cannot ignore that both have tragically affected black people.
So as Pastor Reginald Sharpe Jr. in Chicago recently said, we’re dealing with two pandemics: One has no vaccination and one has no explanation; one can physiologically take your breath away because it affects the respiratory system, while the second can also take your breath away. Just ask Eric Garner and George Floyd.
As physicians, we must recognize that the mechanisms that tragically resulted in the deaths of George Floyd, Breonna Taylor, Ahmaud Arbery, and so many other black men and women are the same mechanisms that are harming and killing black people in our health care system. It’s not acceptable for institutions that built themselves on black and brown bodies to offer condolences, but to continue to do nothing about the racism that still runs rampant within. It’s not acceptable to do nothing. It’s important to note: Racist systems do not perpetuate themselves – the individuals operating within them do.
Martin Luther King Jr. once said, “He who passively accepts evil is as much involved in it as he who helps to perpetuate it. He who accepts evil without protesting against it is really cooperating with it.” Being well-intentioned, good-hearted, sad, or disheartened is not enough. We won’t be able to tear down the systems and institutions that have been a breeding ground for racism until outrage is met by action, not just from black people and people of color, but also by the white majority.
As physicians it’s time for us to look at how our health care institution – an institution instrumental in the victimization of black people – is affecting the health and well-being of our black patients. (For example, increased maternal mortality among black women.)
Are they being seen and heard? Are they receiving culturally relevant and sensitive care? Are their needs and concerns receiving the same amount of time and attention as other patients? It’s time to understand that, for many black patients, the health care system is another place of injustice that has not proved itself to be trustworthy or inclusive of black culture.
As physicians, we must affirm that the lives and health of black and brown people matter to us, that we see the racism they experience, and that we will use our platform as physicians to eliminate racism not just in the hospitals but in the world our patients live in.
So while I didn’t choose the body that I was born into, I fully embrace it and the challenges that come with it. I’m not here to make people feel comfortable, I’m here to continue the work of my ancestors, accomplish the dreams that they fought and lost their lives for, and most importantly, I’m here to continue the fight against the systems that work to prevent other marginalized persons from getting to where I am and even further.
The author James Baldwin once wrote, “Not everything that is faced can be changed, but nothing can be changed until it is faced.” So, I urge you to be loudly antiracist in every space that you hold. I urge you to educate yourselves about racism and white supremacy and privilege and how it permeates our health care system. I urge you to stand beside black people rather than in front of them. Use your privilege to amplify underheard voices and to challenge the biases of your peers, friends, and family members. Use your platform as physicians to advocate for a more just and equitable health care system.
So let me repeat ... we as physicians have the responsibility to eliminate racial bias in the practice of medicine and recognize racism as a threat to the health and well-being of black people and other people of color.
How do we do this? We are beyond lengthy dialogue and “Black History Month” talks. Now is the time for action. Taking action includes the following:
1. Medical academic institutions committing to having a diverse and inclusive faculty. We know it is critical and vital to the recruitment, success, and matriculation of medical students and residents of color to see faculty, particularly senior level faculty in their specialty, who look like them and can serve as mentors. Every year, these institutions need to set a goal that they will take additional steps to have at least one-third of their faculty be black and another third persons of color. In addition, senior faculty positions – those setting curricula, selecting incoming students and residents – must include at least one-third from underrepresented backgrounds (black, Hispanic, Native American/Indigenous).
2. Hospital administration has to resemble the communities in which the hospital serves. Unfortunately, all too often, we know this is not the case, and as a result, decisions that affect the care of black and brown people are often to their detriment because they perpetuate the racism within the existing system. In order to dismantle racism in the hospital system, hospital administrations must consist of diverse individuals. Therefore, hospitals need to commit to hiring and promoting black and brown staff to ensure one-third of its senior leaderships consists of individuals from underrepresented backgrounds.
3. Improving the pipeline that matriculates black and brown students into medical school and residency programs. Lack of access to mentors within the medical field, lack of funding for travel to/from interviews, and lack of knowledge of the overall application process are a few barriers faced by students of color seeking to enter into the medical field. In addition to current scholarship opportunities, medical schools need to allocate funds to connect underrepresented minority students with a range of lived experiences (not just those from impoverished backgrounds but also those from middle class backgrounds who face difficulty gaining acceptance into medical school and residency programs), such as connecting them with mentors by opening opportunities for them to shadow professionals at a conference, travel to residency interviews with most, if not all, expenses covered up front, and have access to local programs that expose them to physicians in several specialties.
These are just a few examples of the active steps we can take to dismantle racism and reconcile the effects of it in the medical field. So if I may borrow from other movements, “Time’s Up” for silence regarding the existence of racism and white supremacy, and now it’s time to truly show that “We are all in this together.”
It is not just my duty but yours also – to ensure that we never have to hear another black man, woman, or child say “I can’t breathe” at the hands of injustice.
Dr. Eleryan (@skinclusionMD) is a social justice activist and was co-chief resident in dermatology (2019-2020) at George Washington University, Washington, DC, and is an Alpha Omega Alpha inductee (2020). She will be a micrographic surgery and dermatologic oncology fellow at the University of California, Los Angeles, in July 2020.
This column is adapted from Dr. Eleryan’s speech at the George Washington University dermatology residency program’s virtual graduation ceremony on June 12.
I’ve been reflecting on my entire residency and the last 2 weeks have stood out the most. I have to admit that I’ve been angry, and so are numerous others who look like me. However, after conversations with a few important people in my life, I’ve realized that people care and are open to listening and changing if I give them the opportunity to see through my lens. I don’t want my legacy to be one of anger, but to be one of change, one of activism, one of heroism, and one of taking a stand in the midst of adversity.
So thank you to everyone who has played a part in my residency and is here to celebrate as I transition to the next step in my career.
But I must pause for a moment to say “I can’t breathe.” I can’t breathe because while I sit here in a place of honor for my accomplishments, I can’t forget that I’m standing in the gap for all of the black men and women who will never have the opportunity to experience a moment like this.
I can’t breathe because George Floyd, Breonna Taylor, Ahmaud Arbery, Tony McDade, Trayvon Martin, Philando Castile, Sandra Bland, Eric Garner, Tamir Rice, Mike Brown, Emmett Till, and so many others will never get to experience a celebratory occasion such as this because of their senseless executions as a likely result of racial bias.
As a black person in “the land of the free,” I have to live with the fact that my life may be taken for simply taking a stroll through a park, jogging through a neighborhood, driving down the street, walking back home from the store, or even sitting in my own home!
As a black physician, I must contend with the very notion that my privilege as a physician does not shield me from discrimination and bias. I recognize that my race walks into the room before I ever do. I know that many of my patients will question my abilities or my title – thinking I am the receptionist, food services worker, or even part of the janitorial staff – simply because of the color of my skin. And what’s even more disturbing is that some of my colleagues will confuse me with another black woman whom I look nothing like or challenge my intelligence and abilities and how I got my position.
All of this boils down to racism – pure and simple. Black people in this country don’t have the privilege of ignoring this truth. We know that this world is not colorblind; neither is anyone in it. We know that this is entrenched racism that for generations has created racial disparities in health care, education, housing, employment, and law enforcement. We weren’t born into a fragile or vulnerable state, yet we were born into a system of dis-enfranchisement, dis-investment, dis-crimination, dis-advantage, and dis-respect.
As physicians, we must recognize and acknowledge the lived experiences that walk through the door with our black patients. And we must understand that black patients walk around with the effects of trauma and toxic stress from just being black in America. That trauma and stress show up in very real ways that contribute to black people experiencing the brunt of chronic diseases and poorer health outcomes. There is no better example than the current COVID-19 pandemic. We are in the midst of a global pandemic from a virus that does not discriminate based on race, but black people are almost three times as likely to be hospitalized as are white people with COVID-19 . And why is that? Because of the “comorbidity” of racism that black people in this country live with. It is not a mere coincidence that the black population is overrepresented in essential jobs and black people are more likely to work in health care than are white people – all positions that increase the risk of infection and death from the virus. So, if we call COVID-19 a pandemic, racism most certainly has been a pandemic that this country has refused to acknowledge, treat, and vaccinate for centuries. We cannot ignore that both have tragically affected black people.
So as Pastor Reginald Sharpe Jr. in Chicago recently said, we’re dealing with two pandemics: One has no vaccination and one has no explanation; one can physiologically take your breath away because it affects the respiratory system, while the second can also take your breath away. Just ask Eric Garner and George Floyd.
As physicians, we must recognize that the mechanisms that tragically resulted in the deaths of George Floyd, Breonna Taylor, Ahmaud Arbery, and so many other black men and women are the same mechanisms that are harming and killing black people in our health care system. It’s not acceptable for institutions that built themselves on black and brown bodies to offer condolences, but to continue to do nothing about the racism that still runs rampant within. It’s not acceptable to do nothing. It’s important to note: Racist systems do not perpetuate themselves – the individuals operating within them do.
Martin Luther King Jr. once said, “He who passively accepts evil is as much involved in it as he who helps to perpetuate it. He who accepts evil without protesting against it is really cooperating with it.” Being well-intentioned, good-hearted, sad, or disheartened is not enough. We won’t be able to tear down the systems and institutions that have been a breeding ground for racism until outrage is met by action, not just from black people and people of color, but also by the white majority.
As physicians it’s time for us to look at how our health care institution – an institution instrumental in the victimization of black people – is affecting the health and well-being of our black patients. (For example, increased maternal mortality among black women.)
Are they being seen and heard? Are they receiving culturally relevant and sensitive care? Are their needs and concerns receiving the same amount of time and attention as other patients? It’s time to understand that, for many black patients, the health care system is another place of injustice that has not proved itself to be trustworthy or inclusive of black culture.
As physicians, we must affirm that the lives and health of black and brown people matter to us, that we see the racism they experience, and that we will use our platform as physicians to eliminate racism not just in the hospitals but in the world our patients live in.
So while I didn’t choose the body that I was born into, I fully embrace it and the challenges that come with it. I’m not here to make people feel comfortable, I’m here to continue the work of my ancestors, accomplish the dreams that they fought and lost their lives for, and most importantly, I’m here to continue the fight against the systems that work to prevent other marginalized persons from getting to where I am and even further.
The author James Baldwin once wrote, “Not everything that is faced can be changed, but nothing can be changed until it is faced.” So, I urge you to be loudly antiracist in every space that you hold. I urge you to educate yourselves about racism and white supremacy and privilege and how it permeates our health care system. I urge you to stand beside black people rather than in front of them. Use your privilege to amplify underheard voices and to challenge the biases of your peers, friends, and family members. Use your platform as physicians to advocate for a more just and equitable health care system.
So let me repeat ... we as physicians have the responsibility to eliminate racial bias in the practice of medicine and recognize racism as a threat to the health and well-being of black people and other people of color.
How do we do this? We are beyond lengthy dialogue and “Black History Month” talks. Now is the time for action. Taking action includes the following:
1. Medical academic institutions committing to having a diverse and inclusive faculty. We know it is critical and vital to the recruitment, success, and matriculation of medical students and residents of color to see faculty, particularly senior level faculty in their specialty, who look like them and can serve as mentors. Every year, these institutions need to set a goal that they will take additional steps to have at least one-third of their faculty be black and another third persons of color. In addition, senior faculty positions – those setting curricula, selecting incoming students and residents – must include at least one-third from underrepresented backgrounds (black, Hispanic, Native American/Indigenous).
2. Hospital administration has to resemble the communities in which the hospital serves. Unfortunately, all too often, we know this is not the case, and as a result, decisions that affect the care of black and brown people are often to their detriment because they perpetuate the racism within the existing system. In order to dismantle racism in the hospital system, hospital administrations must consist of diverse individuals. Therefore, hospitals need to commit to hiring and promoting black and brown staff to ensure one-third of its senior leaderships consists of individuals from underrepresented backgrounds.
3. Improving the pipeline that matriculates black and brown students into medical school and residency programs. Lack of access to mentors within the medical field, lack of funding for travel to/from interviews, and lack of knowledge of the overall application process are a few barriers faced by students of color seeking to enter into the medical field. In addition to current scholarship opportunities, medical schools need to allocate funds to connect underrepresented minority students with a range of lived experiences (not just those from impoverished backgrounds but also those from middle class backgrounds who face difficulty gaining acceptance into medical school and residency programs), such as connecting them with mentors by opening opportunities for them to shadow professionals at a conference, travel to residency interviews with most, if not all, expenses covered up front, and have access to local programs that expose them to physicians in several specialties.
These are just a few examples of the active steps we can take to dismantle racism and reconcile the effects of it in the medical field. So if I may borrow from other movements, “Time’s Up” for silence regarding the existence of racism and white supremacy, and now it’s time to truly show that “We are all in this together.”
It is not just my duty but yours also – to ensure that we never have to hear another black man, woman, or child say “I can’t breathe” at the hands of injustice.
Dr. Eleryan (@skinclusionMD) is a social justice activist and was co-chief resident in dermatology (2019-2020) at George Washington University, Washington, DC, and is an Alpha Omega Alpha inductee (2020). She will be a micrographic surgery and dermatologic oncology fellow at the University of California, Los Angeles, in July 2020.
How racism contributes to the effects of SARS-CoV-2
It’s been about two months since I volunteered in a hospital in Brooklyn, working in an ICU taking care of patients with COVID-19.
Everyone seems to have forgotten the early days of the pandemic – the time when the ICUs were overrun, we were using FEMA ventilators, and endocrinologists and psychiatrists were acting as intensivists.
Even though things are opening up and people are taking summer vacations in a seemingly amnestic state, having witnessed multiple daily deaths remains a part of my daily consciousness. As I see the case numbers climbing juxtaposed against people being out and about without masks, my anxiety level is rising.
A virus doesn’t discriminate. It can fly through the air, landing on the next available surface. If that virus is SARS-CoV-2 and that surface is a human mucosal membrane, the virus makes itself at home. It orders furniture, buys a fancy mattress and a large high definition TV, hangs art on the walls, and settles in for the long haul. It’s not going anywhere anytime soon.
Even as an equal opportunity virus, what SARS-CoV-2 has done is to hold a mirror up to the healthcare system. It has shown us what was here all along. When people first started noticing that underrepresented minorities were more likely to contract the virus and get sick from it, I heard musings that this was likely because of their preexisting health conditions. For example, commentators on cable news were quick to point out that black people are more likely than other people to have hypertension or diabetes. So doesn’t that explain why they are more affected by this virus?
That certainly is part of the story, but it doesn’t entirely explain the discrepancies we’ve seen. For example, in New York 14% of the population is black, and 25% of those who had a COVID-related death were black patients. Similarly, 19% of the population is Hispanic or Latino, and they made up 26% of COVID-related deaths. On the other hand, 55% of the population in New York is white, and white people account for only 34% of COVID-related deaths.
Working in Brooklyn, I didn’t need to be a keen observer to notice that, out of our entire unit of about 20-25 patients, there was only one patient in a 2-week period who was neither black nor Hispanic.
As others have written, there are other factors at play. I’m not sure how many of those commentators back in March stopped to think about why black patients are more likely to have hypertension and diabetes, but the chronic stress of facing racism on a daily basis surely contributes. Beyond those medical problems, minorities are more likely to live in multigenerational housing, which means that it is harder for them to isolate from others. In addition, their living quarters tend to be further from health care centers and grocery stores, which makes it harder for them to access medical care and healthy food.
As if that weren’t enough to put their health at risk, people of color are also affected by environmental racism . Factories with toxic waste are more likely to be built in or near neighborhoods filled with people of color than in other communities. On top of that, black and Hispanic people are also more likely to be under- or uninsured, meaning they often delay seeking care in order to avoid astronomic healthcare costs.
Black and Hispanic people are also more likely than others to be working in the service industry or other essential services, which means they are less likely to be able to work from home. Consequently, they have to risk more exposures to other people and the virus than do those who have the privilege of working safely from home. They also are less likely to have available paid leave and, therefore, are more likely to work while sick.
With the deck completely stacked against them, underrepresented minorities also face systemic bias and racism when interacting with the health care system. Physicians mistakenly believe black patients experience less pain than other patients, according to some research. Black mothers have significantly worse health care outcomes than do their non-black counterparts, and the infant mortality rate for Black infants is much higher as well.
In my limited time in Brooklyn, taking care of almost exclusively black and Hispanic patients, I saw one physician assistant and one nurse who were black; one nurse practitioner was Hispanic. This mismatch is sadly common. Although 13% of the population of the United States is black, only 5% of physicians in the United States are black. Hispanic people, who make up 18% of the US population, are only 6% of physicians. This undoubtedly contributes to poorer outcomes for underrepresented minority patients who have a hard time finding physicians who look like them and understand them.
So while SARS-CoV-2 may not discriminate, the effects it has on patients depends on all of these other factors. If it flies through the air and lands on the mucosal tract of a person who works from home, has effective health insurance and a primary care physician, and lives in a community with no toxic exposures, that person may be more likely to kick it out before it has a chance to settle in. The reason we have such a huge disparity in outcomes related to COVID-19 by race is that a person meeting that description is less likely to be black or Hispanic. Race is not an independent risk factor; structural racism is.
When I drive by the mall that is now open or the restaurants that are now open with indoor dining, my heart rate quickens just a bit with anxiety. The pandemic fatigue people are experiencing is leading them to act in unsafe ways – gathering with more people, not wearing masks, not keeping a safe distance. I worry about everyone, sure, but I really worry about black and Hispanic people who are most vulnerable as a result of everyone else’s refusal to follow guidelines.
Dr. Salles is a bariatric surgeon and is currently a Scholar in Residence at Stanford (Calif.) University. Find her on Twitter @arghavan_salles.
It’s been about two months since I volunteered in a hospital in Brooklyn, working in an ICU taking care of patients with COVID-19.
Everyone seems to have forgotten the early days of the pandemic – the time when the ICUs were overrun, we were using FEMA ventilators, and endocrinologists and psychiatrists were acting as intensivists.
Even though things are opening up and people are taking summer vacations in a seemingly amnestic state, having witnessed multiple daily deaths remains a part of my daily consciousness. As I see the case numbers climbing juxtaposed against people being out and about without masks, my anxiety level is rising.
A virus doesn’t discriminate. It can fly through the air, landing on the next available surface. If that virus is SARS-CoV-2 and that surface is a human mucosal membrane, the virus makes itself at home. It orders furniture, buys a fancy mattress and a large high definition TV, hangs art on the walls, and settles in for the long haul. It’s not going anywhere anytime soon.
Even as an equal opportunity virus, what SARS-CoV-2 has done is to hold a mirror up to the healthcare system. It has shown us what was here all along. When people first started noticing that underrepresented minorities were more likely to contract the virus and get sick from it, I heard musings that this was likely because of their preexisting health conditions. For example, commentators on cable news were quick to point out that black people are more likely than other people to have hypertension or diabetes. So doesn’t that explain why they are more affected by this virus?
That certainly is part of the story, but it doesn’t entirely explain the discrepancies we’ve seen. For example, in New York 14% of the population is black, and 25% of those who had a COVID-related death were black patients. Similarly, 19% of the population is Hispanic or Latino, and they made up 26% of COVID-related deaths. On the other hand, 55% of the population in New York is white, and white people account for only 34% of COVID-related deaths.
Working in Brooklyn, I didn’t need to be a keen observer to notice that, out of our entire unit of about 20-25 patients, there was only one patient in a 2-week period who was neither black nor Hispanic.
As others have written, there are other factors at play. I’m not sure how many of those commentators back in March stopped to think about why black patients are more likely to have hypertension and diabetes, but the chronic stress of facing racism on a daily basis surely contributes. Beyond those medical problems, minorities are more likely to live in multigenerational housing, which means that it is harder for them to isolate from others. In addition, their living quarters tend to be further from health care centers and grocery stores, which makes it harder for them to access medical care and healthy food.
As if that weren’t enough to put their health at risk, people of color are also affected by environmental racism . Factories with toxic waste are more likely to be built in or near neighborhoods filled with people of color than in other communities. On top of that, black and Hispanic people are also more likely to be under- or uninsured, meaning they often delay seeking care in order to avoid astronomic healthcare costs.
Black and Hispanic people are also more likely than others to be working in the service industry or other essential services, which means they are less likely to be able to work from home. Consequently, they have to risk more exposures to other people and the virus than do those who have the privilege of working safely from home. They also are less likely to have available paid leave and, therefore, are more likely to work while sick.
With the deck completely stacked against them, underrepresented minorities also face systemic bias and racism when interacting with the health care system. Physicians mistakenly believe black patients experience less pain than other patients, according to some research. Black mothers have significantly worse health care outcomes than do their non-black counterparts, and the infant mortality rate for Black infants is much higher as well.
In my limited time in Brooklyn, taking care of almost exclusively black and Hispanic patients, I saw one physician assistant and one nurse who were black; one nurse practitioner was Hispanic. This mismatch is sadly common. Although 13% of the population of the United States is black, only 5% of physicians in the United States are black. Hispanic people, who make up 18% of the US population, are only 6% of physicians. This undoubtedly contributes to poorer outcomes for underrepresented minority patients who have a hard time finding physicians who look like them and understand them.
So while SARS-CoV-2 may not discriminate, the effects it has on patients depends on all of these other factors. If it flies through the air and lands on the mucosal tract of a person who works from home, has effective health insurance and a primary care physician, and lives in a community with no toxic exposures, that person may be more likely to kick it out before it has a chance to settle in. The reason we have such a huge disparity in outcomes related to COVID-19 by race is that a person meeting that description is less likely to be black or Hispanic. Race is not an independent risk factor; structural racism is.
When I drive by the mall that is now open or the restaurants that are now open with indoor dining, my heart rate quickens just a bit with anxiety. The pandemic fatigue people are experiencing is leading them to act in unsafe ways – gathering with more people, not wearing masks, not keeping a safe distance. I worry about everyone, sure, but I really worry about black and Hispanic people who are most vulnerable as a result of everyone else’s refusal to follow guidelines.
Dr. Salles is a bariatric surgeon and is currently a Scholar in Residence at Stanford (Calif.) University. Find her on Twitter @arghavan_salles.
It’s been about two months since I volunteered in a hospital in Brooklyn, working in an ICU taking care of patients with COVID-19.
Everyone seems to have forgotten the early days of the pandemic – the time when the ICUs were overrun, we were using FEMA ventilators, and endocrinologists and psychiatrists were acting as intensivists.
Even though things are opening up and people are taking summer vacations in a seemingly amnestic state, having witnessed multiple daily deaths remains a part of my daily consciousness. As I see the case numbers climbing juxtaposed against people being out and about without masks, my anxiety level is rising.
A virus doesn’t discriminate. It can fly through the air, landing on the next available surface. If that virus is SARS-CoV-2 and that surface is a human mucosal membrane, the virus makes itself at home. It orders furniture, buys a fancy mattress and a large high definition TV, hangs art on the walls, and settles in for the long haul. It’s not going anywhere anytime soon.
Even as an equal opportunity virus, what SARS-CoV-2 has done is to hold a mirror up to the healthcare system. It has shown us what was here all along. When people first started noticing that underrepresented minorities were more likely to contract the virus and get sick from it, I heard musings that this was likely because of their preexisting health conditions. For example, commentators on cable news were quick to point out that black people are more likely than other people to have hypertension or diabetes. So doesn’t that explain why they are more affected by this virus?
That certainly is part of the story, but it doesn’t entirely explain the discrepancies we’ve seen. For example, in New York 14% of the population is black, and 25% of those who had a COVID-related death were black patients. Similarly, 19% of the population is Hispanic or Latino, and they made up 26% of COVID-related deaths. On the other hand, 55% of the population in New York is white, and white people account for only 34% of COVID-related deaths.
Working in Brooklyn, I didn’t need to be a keen observer to notice that, out of our entire unit of about 20-25 patients, there was only one patient in a 2-week period who was neither black nor Hispanic.
As others have written, there are other factors at play. I’m not sure how many of those commentators back in March stopped to think about why black patients are more likely to have hypertension and diabetes, but the chronic stress of facing racism on a daily basis surely contributes. Beyond those medical problems, minorities are more likely to live in multigenerational housing, which means that it is harder for them to isolate from others. In addition, their living quarters tend to be further from health care centers and grocery stores, which makes it harder for them to access medical care and healthy food.
As if that weren’t enough to put their health at risk, people of color are also affected by environmental racism . Factories with toxic waste are more likely to be built in or near neighborhoods filled with people of color than in other communities. On top of that, black and Hispanic people are also more likely to be under- or uninsured, meaning they often delay seeking care in order to avoid astronomic healthcare costs.
Black and Hispanic people are also more likely than others to be working in the service industry or other essential services, which means they are less likely to be able to work from home. Consequently, they have to risk more exposures to other people and the virus than do those who have the privilege of working safely from home. They also are less likely to have available paid leave and, therefore, are more likely to work while sick.
With the deck completely stacked against them, underrepresented minorities also face systemic bias and racism when interacting with the health care system. Physicians mistakenly believe black patients experience less pain than other patients, according to some research. Black mothers have significantly worse health care outcomes than do their non-black counterparts, and the infant mortality rate for Black infants is much higher as well.
In my limited time in Brooklyn, taking care of almost exclusively black and Hispanic patients, I saw one physician assistant and one nurse who were black; one nurse practitioner was Hispanic. This mismatch is sadly common. Although 13% of the population of the United States is black, only 5% of physicians in the United States are black. Hispanic people, who make up 18% of the US population, are only 6% of physicians. This undoubtedly contributes to poorer outcomes for underrepresented minority patients who have a hard time finding physicians who look like them and understand them.
So while SARS-CoV-2 may not discriminate, the effects it has on patients depends on all of these other factors. If it flies through the air and lands on the mucosal tract of a person who works from home, has effective health insurance and a primary care physician, and lives in a community with no toxic exposures, that person may be more likely to kick it out before it has a chance to settle in. The reason we have such a huge disparity in outcomes related to COVID-19 by race is that a person meeting that description is less likely to be black or Hispanic. Race is not an independent risk factor; structural racism is.
When I drive by the mall that is now open or the restaurants that are now open with indoor dining, my heart rate quickens just a bit with anxiety. The pandemic fatigue people are experiencing is leading them to act in unsafe ways – gathering with more people, not wearing masks, not keeping a safe distance. I worry about everyone, sure, but I really worry about black and Hispanic people who are most vulnerable as a result of everyone else’s refusal to follow guidelines.
Dr. Salles is a bariatric surgeon and is currently a Scholar in Residence at Stanford (Calif.) University. Find her on Twitter @arghavan_salles.
Masks are a public health issue, not a political one
Masks should not be a political issue. It is ridiculous that they’ve become one. The pandemic, and masks, are a public health issue, and we’re in the biggest public health crisis since 1918.
Mounting data show that common mask usage reduces the spread of COVID-19. Yet many people refuse to wear masks on the grounds that it’s a matter of personal freedom.
If it were that simple, I might agree. After all, it’s your health. Like smoking and skydiving, you’re the one taking risks knowingly.
But it’s not just a single person’s health with an infectious disease. Every person with it is a vector for others to catch it, knowingly or not.
The constitution twice mentions the government’s responsibility to maintain “the general welfare,” but many apparently don’t believe it applies to the pandemic.
A large part of this is a glut of pseudo-science circulating out there, buoyed by the Internet, as well as ties to conspiracy theories and thoroughly debunked claims that the masks cause decreased oxygen, strokes, and a host of other unrelated issues. To many doctors, including myself, this is incredibly frustrating. Medicine is a science. We deal in facts, probabilities, and statistics. After spending so many years learning and trying to teach patients what is and isn’t real out there, it’s disheartening, to say the least, when they choose the meandering advice found on a Facebook or Twitter account over our hard-earned knowledge.
Here in Arizona, the governor’s stay-at-home order expired in mid-May. Although not intended as such, many treated it as a declaration of victory over coronavirus, quickly flocking back to restaurants, bars, and other public gathering places. Our case numbers have since skyrocketed. Yet the climbing numbers of cases as people associate more are ignored and belittled by many in the name of freedom.
People have donned the cloak of freedom and the Bill of Rights to take a stand against wearing masks.
In 1942, U-Boats were sinking ships off the east coast in huge numbers, with targeting made easy because they were silhouetted against cities. Black-outs were ordered to help stop this. Would these same people today have stood up then to declare “They’re my lights, and I’m free to keep them on if I want”? Would they have done the same if bombs were raining on New York like they did in London blackouts during the Blitz?
Self preservation is a powerful instinct. Every animal on Earth has it. Yet humans are the only ones that willfully ignore ways to prevent an as-yet untreatable disease.
You’d think, after all these years of civilization, scientific discovery, and research that we’d be better than this.
Dr. Block has a solo neurology practice in Scottsdale, Ariz. He has no relevant disclosures.
Masks should not be a political issue. It is ridiculous that they’ve become one. The pandemic, and masks, are a public health issue, and we’re in the biggest public health crisis since 1918.
Mounting data show that common mask usage reduces the spread of COVID-19. Yet many people refuse to wear masks on the grounds that it’s a matter of personal freedom.
If it were that simple, I might agree. After all, it’s your health. Like smoking and skydiving, you’re the one taking risks knowingly.
But it’s not just a single person’s health with an infectious disease. Every person with it is a vector for others to catch it, knowingly or not.
The constitution twice mentions the government’s responsibility to maintain “the general welfare,” but many apparently don’t believe it applies to the pandemic.
A large part of this is a glut of pseudo-science circulating out there, buoyed by the Internet, as well as ties to conspiracy theories and thoroughly debunked claims that the masks cause decreased oxygen, strokes, and a host of other unrelated issues. To many doctors, including myself, this is incredibly frustrating. Medicine is a science. We deal in facts, probabilities, and statistics. After spending so many years learning and trying to teach patients what is and isn’t real out there, it’s disheartening, to say the least, when they choose the meandering advice found on a Facebook or Twitter account over our hard-earned knowledge.
Here in Arizona, the governor’s stay-at-home order expired in mid-May. Although not intended as such, many treated it as a declaration of victory over coronavirus, quickly flocking back to restaurants, bars, and other public gathering places. Our case numbers have since skyrocketed. Yet the climbing numbers of cases as people associate more are ignored and belittled by many in the name of freedom.
People have donned the cloak of freedom and the Bill of Rights to take a stand against wearing masks.
In 1942, U-Boats were sinking ships off the east coast in huge numbers, with targeting made easy because they were silhouetted against cities. Black-outs were ordered to help stop this. Would these same people today have stood up then to declare “They’re my lights, and I’m free to keep them on if I want”? Would they have done the same if bombs were raining on New York like they did in London blackouts during the Blitz?
Self preservation is a powerful instinct. Every animal on Earth has it. Yet humans are the only ones that willfully ignore ways to prevent an as-yet untreatable disease.
You’d think, after all these years of civilization, scientific discovery, and research that we’d be better than this.
Dr. Block has a solo neurology practice in Scottsdale, Ariz. He has no relevant disclosures.
Masks should not be a political issue. It is ridiculous that they’ve become one. The pandemic, and masks, are a public health issue, and we’re in the biggest public health crisis since 1918.
Mounting data show that common mask usage reduces the spread of COVID-19. Yet many people refuse to wear masks on the grounds that it’s a matter of personal freedom.
If it were that simple, I might agree. After all, it’s your health. Like smoking and skydiving, you’re the one taking risks knowingly.
But it’s not just a single person’s health with an infectious disease. Every person with it is a vector for others to catch it, knowingly or not.
The constitution twice mentions the government’s responsibility to maintain “the general welfare,” but many apparently don’t believe it applies to the pandemic.
A large part of this is a glut of pseudo-science circulating out there, buoyed by the Internet, as well as ties to conspiracy theories and thoroughly debunked claims that the masks cause decreased oxygen, strokes, and a host of other unrelated issues. To many doctors, including myself, this is incredibly frustrating. Medicine is a science. We deal in facts, probabilities, and statistics. After spending so many years learning and trying to teach patients what is and isn’t real out there, it’s disheartening, to say the least, when they choose the meandering advice found on a Facebook or Twitter account over our hard-earned knowledge.
Here in Arizona, the governor’s stay-at-home order expired in mid-May. Although not intended as such, many treated it as a declaration of victory over coronavirus, quickly flocking back to restaurants, bars, and other public gathering places. Our case numbers have since skyrocketed. Yet the climbing numbers of cases as people associate more are ignored and belittled by many in the name of freedom.
People have donned the cloak of freedom and the Bill of Rights to take a stand against wearing masks.
In 1942, U-Boats were sinking ships off the east coast in huge numbers, with targeting made easy because they were silhouetted against cities. Black-outs were ordered to help stop this. Would these same people today have stood up then to declare “They’re my lights, and I’m free to keep them on if I want”? Would they have done the same if bombs were raining on New York like they did in London blackouts during the Blitz?
Self preservation is a powerful instinct. Every animal on Earth has it. Yet humans are the only ones that willfully ignore ways to prevent an as-yet untreatable disease.
You’d think, after all these years of civilization, scientific discovery, and research that we’d be better than this.
Dr. Block has a solo neurology practice in Scottsdale, Ariz. He has no relevant disclosures.
‘Nietzsche was wrong’: Past stressors do not create psychological resilience.
The famous quote from the German philosopher Friedrich Nietzsche, “That which does not kill us makes us stronger,” may not be true after all – at least when it comes to mental health.
Results of a new study show that individuals who have a history of a stressful life events are more likely to develop posttraumatic stress disorder (PTSD) and/or major depressive disorder (MDD) following a major natural disaster than their counterparts who do not have such a history.
The investigation of more than a thousand Chilean residents – all of whom experienced one of the most powerful earthquakes in the country’s history – showed that the odds of developing postdisaster PTSD or MDD increased according to the number of predisaster stressors participants had experienced.
“We’ve learned that Nietzsche was wrong in this case and that the people who have had prior stressful and traumatic histories were more likely to develop PTSD and depression than those with fewer, study investigator Stephen L. Buka, PhD, professor of epidemiology at Brown University, Providence, Rhode Island, said in an interview.
The study was published online June 11 in the British Journal of Psychiatry.
Stress inoculation hypothesis
The so-called stress inoculation hypothesis proposes that individuals who experience manageable stressors may be able to better cope with subsequent stressors, inasmuch as such experience affords them opportunities to practice effective coping skills and develop a sense of mastery over stressors.
, particularly with respect to such common mental health disorders as MDD and PTSD. Although less severe day-to-day stressors may be easier to cope with, major trauma can overwhelm an individual’s coping mechanisms.
Findings from previous research have been mixed. Some studiessuggest that prior stressors can increase the risk of developing later psychiatric disorders. On the other hand, previous research has also shown that exposure to prior trauma alone does not predict subsequent PTSD.
Given these contradictions, the investigators wanted to determine whether a history of prior stressors was associated with psychiatric resilience among individuals who had no psychiatric history of MDD or PTSD.
“Only a small minority of people who have experienced a traumatic event go on to develop PTSD or MDD,” said lead author Cristina Fernandez, PhD, a psychiatric epidemiologist at the PAHO/WHO Collaborating Center for Research on Psychiatric Epidemiology and Mental Health, Brown University, Providence, R.I.
“So most people are resilient and move on without developing these disorders. But what is unique about this minority of individuals that makes them more susceptible to developing these disorders?” she continued. “It’s one of the most significant questions in the PTSD literature,” she added.
The analysis included data from 10 sites in the Chilean cities of Concepción and Talcahuano that had participated in the PREDICT investigation, a prospective cohort study that sought to predict mental health outcomes among primary care patients.
While the PREDICT study was being conducted, in February 2010, a major earthquake struck the coast of central Chile, killing more than 500 people and displacing 800,000. Concepción and Talcahuano experienced the most damage from the earthquake and its subsequent effects, including a tsunami that ravaged Talcahuano.
Dose-dependent effect
At baseline and 1 year after the disaster, all participants completed the Composite International Diagnostic Interview, which assesses for the presence of PTSD and/or MDD. Participants also completed the List of Threatening Experiences, a 12-item questionnaire that measures major stressful life events.
Of 3,000 participants who initially agreed to take part in the trial, 1708 completed both the predisaster assessment in 2003 and the postdisaster assessment in 2011, 1 year after the earthquake and tsunami occurred. After excluding for a variety other criteria, 1,160 individuals were included in the final analysis.
“As it turns out, it was a very natural experiment,” said Dr. Buka. “We had a group of people whose past traumatic experiences we knew about, and then they were all subjected to this terrible earthquake, and then we were able to look forward into time and see who did and didn’t develop PTSD and MDD.”
When the study began in 2003, none of the 1,160 participants had a history of PTSD or MDD. After the 2010 earthquake, 9.1% of the survivors (n = 106) were diagnosed with PTSD, and 14.4% were diagnosed with MDD (n = 167).
Further analyses showed that prior disaster exposure was not a significant predictor of postdisaster PTSD. Nevertheless, for every unit increase in prior nondisaster stressors, the odds of developing postdisaster PTSD increased (odds ratio, 1.21; 95% confidence interval, 1.08-1.37; P = .001).
When categorizing predisaster stressors, the investigators found that individuals who had four or more predisaster stressors had a significantly greater chance of developing postdisaster PTSD than those with no predisaster stressors (OR, 2.77; 95% CI, 1.52 – 5.04).
Similar logistic regression analyses were performed for MDD, with comparable results. Although prior disaster exposure was not a significant predictor of postdisaster MDD, each one-unit increase in prior nondisaster stressors increased the odds of developing postdisaster MDD by 16% (OR, 1.16; 95% CI, 1.06-1.27; P = .001).
Categorization of these stressors revealed that experiencing any number of stressors significantly increased the odds of developing postdisaster MDD in a dose-response fashion.
In other words, every predisaster stressor – even a single one – increased an individual’s risk of developing postdisaster MDD, and each additional stressor further increased the risk.
Predisaster stressors
Interestingly, the study also showed that the risk of developing both PTSD and MDD was particularly high among those who had experienced multiple predisaster stressors, such as serious illness or injury, death of a loved one, divorce, unemployment, financial struggles, legal troubles, or the loss of a valuable possession.
These findings, the researchers note, demonstrate that a history of stressors increases what they called “stress sensitization,” which may make individuals more vulnerable to the negative effects of subsequent stressors rather than more resilient.
As such, individuals who have experienced several stressors over the course of a lifetime are at higher risk of developing a psychiatric disorder.
This was the case with PTSD, in which exposure to at least four previous manageable stressors was associated with greater odds of developing postdisaster PTSD. For MDD, on the other hand, there was a distinct dose-response relationship between the number of manageable predisaster stressors and the risk for postdisaster MDD.
The investigators explain that these findings are particularly relevant in light of the COVID-19 pandemic and the current focus on racial and economic inequality in the United States. “The findings highlight the sectors of the population that are at greatest risk,” Dr. Buka said. “And those are the ones who’ve had more challenging and traumatic lives and more hardship.
“So it certainly calls for greater concentration of psychiatric services in traditionally underserved areas, because those are also areas that have greater histories of trauma.”
“Fascinating” research
Commenting on the findings fin an interview, Patricia A. Resick, PhD, who was not involved in the study, said she found the research fascinating.
“The fact that they had preexisting data and then had the wherewithal to go back after the earthquake is quite amazing,” she said.
The findings came as little surprise to Dr. Resick, professor of psychiatry and behavioral sciences at Duke University Medical Center in Durham, N.C.
“I think most people are in agreement that the more stress you have, the more likely you are to get PTSD when you experience a traumatic stressor,” she said.
Treating these individuals remains a challenge, Dr. Resick noted, though knowing their history of stressors and traumas is an important starting point.
“We have to get a good history and figure out where to start treating them, because we always want to start with the event that causes the most PTSD symptoms,” she explained.
She also characterized the issue as being as much a public health concern as one for psychiatrists. “These are people you will want to have surveillance on and encourage them to get help,” Dr. Resick added.
Dr. Fernandez agreed.
“In the face of a disaster,” she said, “there needs to be more attention paid to vulnerable populations, because they likely don’t have the support they need.
“At the clinical level, these findings help the clinician know which patients are more likely to need more intensive services,” Dr. Buka added. “And the more trauma and hardship they’ve experienced, the more attention they need and the less likely they’re going to be able to cope and manage on their own.”
The study was funded by the U.S. National Institute of Mental Health and FONDEF Chile. Dr. Fernandez, Dr. Buka, and Dr. Resick have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The famous quote from the German philosopher Friedrich Nietzsche, “That which does not kill us makes us stronger,” may not be true after all – at least when it comes to mental health.
Results of a new study show that individuals who have a history of a stressful life events are more likely to develop posttraumatic stress disorder (PTSD) and/or major depressive disorder (MDD) following a major natural disaster than their counterparts who do not have such a history.
The investigation of more than a thousand Chilean residents – all of whom experienced one of the most powerful earthquakes in the country’s history – showed that the odds of developing postdisaster PTSD or MDD increased according to the number of predisaster stressors participants had experienced.
“We’ve learned that Nietzsche was wrong in this case and that the people who have had prior stressful and traumatic histories were more likely to develop PTSD and depression than those with fewer, study investigator Stephen L. Buka, PhD, professor of epidemiology at Brown University, Providence, Rhode Island, said in an interview.
The study was published online June 11 in the British Journal of Psychiatry.
Stress inoculation hypothesis
The so-called stress inoculation hypothesis proposes that individuals who experience manageable stressors may be able to better cope with subsequent stressors, inasmuch as such experience affords them opportunities to practice effective coping skills and develop a sense of mastery over stressors.
, particularly with respect to such common mental health disorders as MDD and PTSD. Although less severe day-to-day stressors may be easier to cope with, major trauma can overwhelm an individual’s coping mechanisms.
Findings from previous research have been mixed. Some studiessuggest that prior stressors can increase the risk of developing later psychiatric disorders. On the other hand, previous research has also shown that exposure to prior trauma alone does not predict subsequent PTSD.
Given these contradictions, the investigators wanted to determine whether a history of prior stressors was associated with psychiatric resilience among individuals who had no psychiatric history of MDD or PTSD.
“Only a small minority of people who have experienced a traumatic event go on to develop PTSD or MDD,” said lead author Cristina Fernandez, PhD, a psychiatric epidemiologist at the PAHO/WHO Collaborating Center for Research on Psychiatric Epidemiology and Mental Health, Brown University, Providence, R.I.
“So most people are resilient and move on without developing these disorders. But what is unique about this minority of individuals that makes them more susceptible to developing these disorders?” she continued. “It’s one of the most significant questions in the PTSD literature,” she added.
The analysis included data from 10 sites in the Chilean cities of Concepción and Talcahuano that had participated in the PREDICT investigation, a prospective cohort study that sought to predict mental health outcomes among primary care patients.
While the PREDICT study was being conducted, in February 2010, a major earthquake struck the coast of central Chile, killing more than 500 people and displacing 800,000. Concepción and Talcahuano experienced the most damage from the earthquake and its subsequent effects, including a tsunami that ravaged Talcahuano.
Dose-dependent effect
At baseline and 1 year after the disaster, all participants completed the Composite International Diagnostic Interview, which assesses for the presence of PTSD and/or MDD. Participants also completed the List of Threatening Experiences, a 12-item questionnaire that measures major stressful life events.
Of 3,000 participants who initially agreed to take part in the trial, 1708 completed both the predisaster assessment in 2003 and the postdisaster assessment in 2011, 1 year after the earthquake and tsunami occurred. After excluding for a variety other criteria, 1,160 individuals were included in the final analysis.
“As it turns out, it was a very natural experiment,” said Dr. Buka. “We had a group of people whose past traumatic experiences we knew about, and then they were all subjected to this terrible earthquake, and then we were able to look forward into time and see who did and didn’t develop PTSD and MDD.”
When the study began in 2003, none of the 1,160 participants had a history of PTSD or MDD. After the 2010 earthquake, 9.1% of the survivors (n = 106) were diagnosed with PTSD, and 14.4% were diagnosed with MDD (n = 167).
Further analyses showed that prior disaster exposure was not a significant predictor of postdisaster PTSD. Nevertheless, for every unit increase in prior nondisaster stressors, the odds of developing postdisaster PTSD increased (odds ratio, 1.21; 95% confidence interval, 1.08-1.37; P = .001).
When categorizing predisaster stressors, the investigators found that individuals who had four or more predisaster stressors had a significantly greater chance of developing postdisaster PTSD than those with no predisaster stressors (OR, 2.77; 95% CI, 1.52 – 5.04).
Similar logistic regression analyses were performed for MDD, with comparable results. Although prior disaster exposure was not a significant predictor of postdisaster MDD, each one-unit increase in prior nondisaster stressors increased the odds of developing postdisaster MDD by 16% (OR, 1.16; 95% CI, 1.06-1.27; P = .001).
Categorization of these stressors revealed that experiencing any number of stressors significantly increased the odds of developing postdisaster MDD in a dose-response fashion.
In other words, every predisaster stressor – even a single one – increased an individual’s risk of developing postdisaster MDD, and each additional stressor further increased the risk.
Predisaster stressors
Interestingly, the study also showed that the risk of developing both PTSD and MDD was particularly high among those who had experienced multiple predisaster stressors, such as serious illness or injury, death of a loved one, divorce, unemployment, financial struggles, legal troubles, or the loss of a valuable possession.
These findings, the researchers note, demonstrate that a history of stressors increases what they called “stress sensitization,” which may make individuals more vulnerable to the negative effects of subsequent stressors rather than more resilient.
As such, individuals who have experienced several stressors over the course of a lifetime are at higher risk of developing a psychiatric disorder.
This was the case with PTSD, in which exposure to at least four previous manageable stressors was associated with greater odds of developing postdisaster PTSD. For MDD, on the other hand, there was a distinct dose-response relationship between the number of manageable predisaster stressors and the risk for postdisaster MDD.
The investigators explain that these findings are particularly relevant in light of the COVID-19 pandemic and the current focus on racial and economic inequality in the United States. “The findings highlight the sectors of the population that are at greatest risk,” Dr. Buka said. “And those are the ones who’ve had more challenging and traumatic lives and more hardship.
“So it certainly calls for greater concentration of psychiatric services in traditionally underserved areas, because those are also areas that have greater histories of trauma.”
“Fascinating” research
Commenting on the findings fin an interview, Patricia A. Resick, PhD, who was not involved in the study, said she found the research fascinating.
“The fact that they had preexisting data and then had the wherewithal to go back after the earthquake is quite amazing,” she said.
The findings came as little surprise to Dr. Resick, professor of psychiatry and behavioral sciences at Duke University Medical Center in Durham, N.C.
“I think most people are in agreement that the more stress you have, the more likely you are to get PTSD when you experience a traumatic stressor,” she said.
Treating these individuals remains a challenge, Dr. Resick noted, though knowing their history of stressors and traumas is an important starting point.
“We have to get a good history and figure out where to start treating them, because we always want to start with the event that causes the most PTSD symptoms,” she explained.
She also characterized the issue as being as much a public health concern as one for psychiatrists. “These are people you will want to have surveillance on and encourage them to get help,” Dr. Resick added.
Dr. Fernandez agreed.
“In the face of a disaster,” she said, “there needs to be more attention paid to vulnerable populations, because they likely don’t have the support they need.
“At the clinical level, these findings help the clinician know which patients are more likely to need more intensive services,” Dr. Buka added. “And the more trauma and hardship they’ve experienced, the more attention they need and the less likely they’re going to be able to cope and manage on their own.”
The study was funded by the U.S. National Institute of Mental Health and FONDEF Chile. Dr. Fernandez, Dr. Buka, and Dr. Resick have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The famous quote from the German philosopher Friedrich Nietzsche, “That which does not kill us makes us stronger,” may not be true after all – at least when it comes to mental health.
Results of a new study show that individuals who have a history of a stressful life events are more likely to develop posttraumatic stress disorder (PTSD) and/or major depressive disorder (MDD) following a major natural disaster than their counterparts who do not have such a history.
The investigation of more than a thousand Chilean residents – all of whom experienced one of the most powerful earthquakes in the country’s history – showed that the odds of developing postdisaster PTSD or MDD increased according to the number of predisaster stressors participants had experienced.
“We’ve learned that Nietzsche was wrong in this case and that the people who have had prior stressful and traumatic histories were more likely to develop PTSD and depression than those with fewer, study investigator Stephen L. Buka, PhD, professor of epidemiology at Brown University, Providence, Rhode Island, said in an interview.
The study was published online June 11 in the British Journal of Psychiatry.
Stress inoculation hypothesis
The so-called stress inoculation hypothesis proposes that individuals who experience manageable stressors may be able to better cope with subsequent stressors, inasmuch as such experience affords them opportunities to practice effective coping skills and develop a sense of mastery over stressors.
, particularly with respect to such common mental health disorders as MDD and PTSD. Although less severe day-to-day stressors may be easier to cope with, major trauma can overwhelm an individual’s coping mechanisms.
Findings from previous research have been mixed. Some studiessuggest that prior stressors can increase the risk of developing later psychiatric disorders. On the other hand, previous research has also shown that exposure to prior trauma alone does not predict subsequent PTSD.
Given these contradictions, the investigators wanted to determine whether a history of prior stressors was associated with psychiatric resilience among individuals who had no psychiatric history of MDD or PTSD.
“Only a small minority of people who have experienced a traumatic event go on to develop PTSD or MDD,” said lead author Cristina Fernandez, PhD, a psychiatric epidemiologist at the PAHO/WHO Collaborating Center for Research on Psychiatric Epidemiology and Mental Health, Brown University, Providence, R.I.
“So most people are resilient and move on without developing these disorders. But what is unique about this minority of individuals that makes them more susceptible to developing these disorders?” she continued. “It’s one of the most significant questions in the PTSD literature,” she added.
The analysis included data from 10 sites in the Chilean cities of Concepción and Talcahuano that had participated in the PREDICT investigation, a prospective cohort study that sought to predict mental health outcomes among primary care patients.
While the PREDICT study was being conducted, in February 2010, a major earthquake struck the coast of central Chile, killing more than 500 people and displacing 800,000. Concepción and Talcahuano experienced the most damage from the earthquake and its subsequent effects, including a tsunami that ravaged Talcahuano.
Dose-dependent effect
At baseline and 1 year after the disaster, all participants completed the Composite International Diagnostic Interview, which assesses for the presence of PTSD and/or MDD. Participants also completed the List of Threatening Experiences, a 12-item questionnaire that measures major stressful life events.
Of 3,000 participants who initially agreed to take part in the trial, 1708 completed both the predisaster assessment in 2003 and the postdisaster assessment in 2011, 1 year after the earthquake and tsunami occurred. After excluding for a variety other criteria, 1,160 individuals were included in the final analysis.
“As it turns out, it was a very natural experiment,” said Dr. Buka. “We had a group of people whose past traumatic experiences we knew about, and then they were all subjected to this terrible earthquake, and then we were able to look forward into time and see who did and didn’t develop PTSD and MDD.”
When the study began in 2003, none of the 1,160 participants had a history of PTSD or MDD. After the 2010 earthquake, 9.1% of the survivors (n = 106) were diagnosed with PTSD, and 14.4% were diagnosed with MDD (n = 167).
Further analyses showed that prior disaster exposure was not a significant predictor of postdisaster PTSD. Nevertheless, for every unit increase in prior nondisaster stressors, the odds of developing postdisaster PTSD increased (odds ratio, 1.21; 95% confidence interval, 1.08-1.37; P = .001).
When categorizing predisaster stressors, the investigators found that individuals who had four or more predisaster stressors had a significantly greater chance of developing postdisaster PTSD than those with no predisaster stressors (OR, 2.77; 95% CI, 1.52 – 5.04).
Similar logistic regression analyses were performed for MDD, with comparable results. Although prior disaster exposure was not a significant predictor of postdisaster MDD, each one-unit increase in prior nondisaster stressors increased the odds of developing postdisaster MDD by 16% (OR, 1.16; 95% CI, 1.06-1.27; P = .001).
Categorization of these stressors revealed that experiencing any number of stressors significantly increased the odds of developing postdisaster MDD in a dose-response fashion.
In other words, every predisaster stressor – even a single one – increased an individual’s risk of developing postdisaster MDD, and each additional stressor further increased the risk.
Predisaster stressors
Interestingly, the study also showed that the risk of developing both PTSD and MDD was particularly high among those who had experienced multiple predisaster stressors, such as serious illness or injury, death of a loved one, divorce, unemployment, financial struggles, legal troubles, or the loss of a valuable possession.
These findings, the researchers note, demonstrate that a history of stressors increases what they called “stress sensitization,” which may make individuals more vulnerable to the negative effects of subsequent stressors rather than more resilient.
As such, individuals who have experienced several stressors over the course of a lifetime are at higher risk of developing a psychiatric disorder.
This was the case with PTSD, in which exposure to at least four previous manageable stressors was associated with greater odds of developing postdisaster PTSD. For MDD, on the other hand, there was a distinct dose-response relationship between the number of manageable predisaster stressors and the risk for postdisaster MDD.
The investigators explain that these findings are particularly relevant in light of the COVID-19 pandemic and the current focus on racial and economic inequality in the United States. “The findings highlight the sectors of the population that are at greatest risk,” Dr. Buka said. “And those are the ones who’ve had more challenging and traumatic lives and more hardship.
“So it certainly calls for greater concentration of psychiatric services in traditionally underserved areas, because those are also areas that have greater histories of trauma.”
“Fascinating” research
Commenting on the findings fin an interview, Patricia A. Resick, PhD, who was not involved in the study, said she found the research fascinating.
“The fact that they had preexisting data and then had the wherewithal to go back after the earthquake is quite amazing,” she said.
The findings came as little surprise to Dr. Resick, professor of psychiatry and behavioral sciences at Duke University Medical Center in Durham, N.C.
“I think most people are in agreement that the more stress you have, the more likely you are to get PTSD when you experience a traumatic stressor,” she said.
Treating these individuals remains a challenge, Dr. Resick noted, though knowing their history of stressors and traumas is an important starting point.
“We have to get a good history and figure out where to start treating them, because we always want to start with the event that causes the most PTSD symptoms,” she explained.
She also characterized the issue as being as much a public health concern as one for psychiatrists. “These are people you will want to have surveillance on and encourage them to get help,” Dr. Resick added.
Dr. Fernandez agreed.
“In the face of a disaster,” she said, “there needs to be more attention paid to vulnerable populations, because they likely don’t have the support they need.
“At the clinical level, these findings help the clinician know which patients are more likely to need more intensive services,” Dr. Buka added. “And the more trauma and hardship they’ve experienced, the more attention they need and the less likely they’re going to be able to cope and manage on their own.”
The study was funded by the U.S. National Institute of Mental Health and FONDEF Chile. Dr. Fernandez, Dr. Buka, and Dr. Resick have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Will primary care physicians be COVID-19’s next victims?
In a recently published editorial, Tom Frieden, MD, MPH, former head of the Centers for Disease Control and Prevention, argued that primary care is in deep trouble, its long-standing financial problems exacerbated by the fallout from the COVID-19 pandemic. Those arguments resonated with Kenny Lin, MD, MPH, a family physician, professor at Georgetown University School of Medicine, and a regular contributor to Medscape. He spoke with Dr. Frieden about his concerns.
Dr. Lin: Why did you feel that it was important to write this piece focused on primary care?
Dr. Frieden: I’m glad you asked that question. Given all that is going on, one might ask, what is the importance of primary care? We’ve got this epidemic going on that requires public health and hospital systems. Why voice concern about primary care now?
It’s really striking to see that the number of visits has plummeted. Because of our payment structure, that means incomes have plummeted. We’re hearing about doctors’ offices getting boarded up and shuttering. As I write in the piece, it’s one thing for a theater or a restaurant or another important community entity to shut because of economic downturn, and these are real losses, but to lose their only primary care practice or one of the few in an area really is a matter of life and death for many communities.
Dr. Lin: I agree. In my own practice we haven’t had to furlough anyone, but we’ve put people on forced paid time off. We’ve been reallocating physicians to other parts of our health system. It is definitely a concern. A solo practitioner or someone in a rural practice would most likely be even much more heavily hit. You’ve argued that the neglect of our public health system on a national level has led to many preventable deaths from COVID-19. Do you feel that something similar has happened in primary care? How could a stronger, better-funded primary care infrastructure better prepare us for the next pandemic?
Dr. Frieden: All over the world, we see an overemphasis on hospital care and an underemphasis on primary care, outpatient care, family medicine. As a result, we pay more. We have larger risks, and we don’t prevent diseases that we could prevent. It’s fundamentally about the economic incentives of our health care system. Of course, that often reflects the political reality of different profit centers and cost centers of care. That won’t change with tweaking around the edges. It will only change if we change the way we pay for health care. Money talks. We need to start paying at least part of what we pay based on health outcomes.
Many years ago a colleague and I wrote an article, “Health Care as If Health Mattered.” If you step back and look at how we pay for health care, very little, if any, of our payment structure is based on how much health the care system delivers. Part of that can be addressed by going to capitated models, which I think do better. But you have also got to put into those capitated systems some quality and outcome measures that are both valid and not too burdensome to report on. That’s not easy. We could talk a lot about some of the information systems and payment systems, but I think the bottom line is that we need to be able to deal not only with health emergencies, but also with preventive care, care of chronic diseases, and behavioral health care in ways that maximize health.
One of the ways to do that is simple, monthly, capitated payments along with what I call a registry-based outcomes system.
I’m a tuberculosis specialist by training. In tuberculosis there really is a great information system. We track every single patient who has been diagnosed, and we hold every clinician accountable for whether or not they’ve successfully treated that patient. An optimal health care system should do the same with treatment of hypertension, diabetes, seizure disorder, and other common conditions in which treatment makes a really big difference. Preventive care, especially vaccine delivery, is another example.
I understand that physicians will point out that patients may not come in for that care, or they’re hard to deal with, or they refuse recommended treatment. We don’t expect 100%. But we should expect that, if we’re paying for health care, we should get health.
To do that, I think we need much more support for primary care, both in terms of the absolute amount of dollars going in and the administrative support. Some of our systems are so complicated that you can’t manage them without a billing department. How does a one- or two-physician practice deal with systems that will take dozens of hours a week to manage? You have to deal with the administrative complexity, the structure of the incentives, and the structure of care.
I think these are all things that we have to address. But for a minute, let’s helicopter up and look at the big picture. Without additional help from Congress, tens of thousands of primary care physicians could go out of business in the coming weeks. This is a crisis, and this will be very hard to rebuild. We don’t have a strong, resilient primary care infrastructure today, and if we’re not careful it’ll be even weaker as we try to rebuild.
It has been encouraging to see some of the care innovations that have occurred in response to the pandemic. I’m particularly encouraged by the widespread interest in and support for telemedicine. Telemedicine is a very important way of making care safer, more accessible, less expensive, more efficient. There have been a lot of restrictions on it, not just in the United States but globally, for many years. It’s really interesting to see those restrictions rapidly change. I give credit to the Centers for Medicare & Medicaid Services for quick changes in this area.
Now, telemedicine isn’t a cure-all. There are lots of things you can’t do from a distance. It’s a pale reflection of reality, compared with an in-person first visit with a patient. But it’s a whole lot better than nothing. If we look at some of the best health systems in the United States, they’ve gone to as much as 80% of clinical visits done by telemedicine. I don’t think we’re going to go back. Even if COVID is no longer the threat that it is today, if you can do things more quickly, more efficiently, and more conveniently for both patients and doctors, do them. Obviously, it won’t be all visits, but it could be a large proportion of visits and an important part of strengthening our primary care system.
My initiative, Resolve to Save Lives, which is part of the global health organization Vital Strategies, has done work in the area of public health around the world. I am really struck by how weak primary care systems are in so many countries. Strong primary care systems are the exception rather than the rule, but they’re also a best buy in health care. They’re crucially important, and they’re going to work differently in different countries, in different states, in different communities. We need to do a better job of supporting primary care, building primary care, and paying for primary care.
Dr. Lin: You’ve identified two needs. The immediate need is that primary care practices need revenue now to not have to close in the immediate aftermath or the ongoing COVID epidemic, but also there’s the long term, the percentage of health care dollars that are going to primary care in the long term. You pointed out in your article that currently 5% or less of health care spending is in primary care, which is a lot less percentage-wise than in many other countries. I think the question always comes up is that we want to increase that share, but the money has to come from somewhere. Where is that extra money going to come from? Dr. Frieden: I’m not an expert in health care finance, but one thing I’ve learned over the years is that one person’s waste, fraud, and abuse is somebody else’s profit center. It’s not going to be easy. On the one hand, we do need to think about more efficient ways to organize primary care; on the other hand, we have to figure out a way to internalize some of the savings. If you give good primary care and, therefore, someone doesn’t get hospitalized, you can actually lose money in the current system, whereas you’re saving the system a lot of money by preventing that hospitalization.
I think our health system does have significant inefficiencies in terms of the number of tests and interventions that are done that are really not proven to help patients. It has been demonstrated for decades now that the usual economic incentives don’t operate in health care. In health care, supply often generates demand. The number of gallbladder operations is proportional not to population but to the number of gallbladder surgeons. That’s a problem, and it’s a problem that we’re going to have to assess. “Gatekeeper” is an unpleasant word, but if a primary care practitioner could be the advocate for patients so that we’re not pushing for patients to get more care or to get less care but to get the right care, we have the potential to reduce costs while improving quality.
Dr. Lin: You accurately point out that the fee-for-service payment system has been the major culprit in the declining revenues of primary care practices since the start of the pandemic. But for the majority of primary care physicians, including myself, fee-for-service is all that we’ve ever known. Do you think that primary care is ready for such an abrupt financing change, particularly in a very short period of time?Dr. Frieden: You’re certainly accurate in saying that nothing about health care finance is easy. Trying to address these problems at the national or state level has been extremely difficult. I think that the pilot programs in Medicare are very important. Medicaid is a particular challenge because it’s a state-based program and many of the costs are driven by nursing home and long-term care. When you take those costs out, the actual funding per patient or per provider is quite low in most places.
It’s hard enough to reorganize if you’ve got ample resources, but to reorganize when they are insufficient is particularly hard. I would say only that there are no quick and simple answers to this question, but there is a widespread understanding that what we’re doing now doesn’t make sense. We pay top dollar and we get – despite fantastic doctors and fantastic hospitals – lousy outcomes. I’m a public health physician. I’m an internal medicine and infectious disease specialist. Fundamentally, I look at the data. If you think of our health care system as a patient, the patient is not doing well. We’re not functional to the degree we need to be, particularly when you think of what an enormous outlier our per capita expenditures are [compared with other developed countries] – almost twice the average upper-income country and 25% more than any other upper-income country.
Now, anyone who tells you that change is going to be pain-free is not leveling with you. In addition to things like telemedicine, we have to make much more use of team-based care and task sharing. There are lots of things that doctors are doing these days that they really shouldn’t.
Dr. Lin: In your recent op-ed, you noted the pivot to telehealth that primary care practices have made very quickly in response to the pandemic. That certainly was the experience for my practice. But what are some other strategies that you think are important to support the goal of better care delivery in our primary care practices?Dr. Frieden: Another really important innovation is team-based care. There are lots of things that doctors are doing today that nurses, nurse practitioners, physician assistants, and community health workers can do better and for less money. Frankly, I think that should increase the job satisfaction of physicians, to be doing work that is specific to the physician, requiring either more patient interaction or advanced reasoning or experience.
In my own field of tuberculosis control, I learned how to treat tuberculosis because the nurse at the TB clinic kept correcting me because that’s all she did. She did tuberculosis care, so she had seen everything. Even though I’d finished an infectious disease fellowship and internal medicine residency, the public health nurse knew TB a whole lot better than I did.
Similarly, as we work on hypertension control, you can protocolize most of this care and do a much better job. That’s been proven for more than 40 years, and yet we still don’t do it.
One of the big parts of being able to do more with the same or fewer resources is going to be more team-based care. That’s really a task-sharing approach. I think of that as a triple win: You get better care for lower costs with more employment. What’s not to like?
Dr. Lin: I’m hopeful, as you are, that many of these innovations that have been made by necessity will persist beyond the duration of COVID-19. As you said, the health care system has been really difficult to change, and it often takes something like this to galvanize enough consensus that things need to change.
Dr. Frieden: I think the bottom line here is that we should pay our primary health care providers to keep us healthy and ensure that we have a payment system that lets them do that without risking bankruptcy. That’s not too much to ask of our system. It’s important for our health. It’s important for our economy. It’s important for our communities.
Dr. Lin teaches family medicine, preventive medicine, and health policy at Georgetown University School of Medicine. He is deputy editor of the journal American Family Physician. Follow him on Twitter. He has served as a director, officer, partner, employee, adviser, consultant, or trustee for MedStar Georgetown University Hospital and received income in an amount equal to or greater than $250 from UpToDate, Wiley-Blackwell, and American Academy of Family Physicians.
Dr. Frieden is a physician with advanced training in internal medicine, infectious disease, public health, and epidemiology. He has served as director of the Centers for Disease Control and Prevention and as commissioner of the New York City Health Department. Currently he is president and CEO of Resolve to Save Lives. Follow him on Twitter. Thomas R. Frieden, MD, MPH, has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
In a recently published editorial, Tom Frieden, MD, MPH, former head of the Centers for Disease Control and Prevention, argued that primary care is in deep trouble, its long-standing financial problems exacerbated by the fallout from the COVID-19 pandemic. Those arguments resonated with Kenny Lin, MD, MPH, a family physician, professor at Georgetown University School of Medicine, and a regular contributor to Medscape. He spoke with Dr. Frieden about his concerns.
Dr. Lin: Why did you feel that it was important to write this piece focused on primary care?
Dr. Frieden: I’m glad you asked that question. Given all that is going on, one might ask, what is the importance of primary care? We’ve got this epidemic going on that requires public health and hospital systems. Why voice concern about primary care now?
It’s really striking to see that the number of visits has plummeted. Because of our payment structure, that means incomes have plummeted. We’re hearing about doctors’ offices getting boarded up and shuttering. As I write in the piece, it’s one thing for a theater or a restaurant or another important community entity to shut because of economic downturn, and these are real losses, but to lose their only primary care practice or one of the few in an area really is a matter of life and death for many communities.
Dr. Lin: I agree. In my own practice we haven’t had to furlough anyone, but we’ve put people on forced paid time off. We’ve been reallocating physicians to other parts of our health system. It is definitely a concern. A solo practitioner or someone in a rural practice would most likely be even much more heavily hit. You’ve argued that the neglect of our public health system on a national level has led to many preventable deaths from COVID-19. Do you feel that something similar has happened in primary care? How could a stronger, better-funded primary care infrastructure better prepare us for the next pandemic?
Dr. Frieden: All over the world, we see an overemphasis on hospital care and an underemphasis on primary care, outpatient care, family medicine. As a result, we pay more. We have larger risks, and we don’t prevent diseases that we could prevent. It’s fundamentally about the economic incentives of our health care system. Of course, that often reflects the political reality of different profit centers and cost centers of care. That won’t change with tweaking around the edges. It will only change if we change the way we pay for health care. Money talks. We need to start paying at least part of what we pay based on health outcomes.
Many years ago a colleague and I wrote an article, “Health Care as If Health Mattered.” If you step back and look at how we pay for health care, very little, if any, of our payment structure is based on how much health the care system delivers. Part of that can be addressed by going to capitated models, which I think do better. But you have also got to put into those capitated systems some quality and outcome measures that are both valid and not too burdensome to report on. That’s not easy. We could talk a lot about some of the information systems and payment systems, but I think the bottom line is that we need to be able to deal not only with health emergencies, but also with preventive care, care of chronic diseases, and behavioral health care in ways that maximize health.
One of the ways to do that is simple, monthly, capitated payments along with what I call a registry-based outcomes system.
I’m a tuberculosis specialist by training. In tuberculosis there really is a great information system. We track every single patient who has been diagnosed, and we hold every clinician accountable for whether or not they’ve successfully treated that patient. An optimal health care system should do the same with treatment of hypertension, diabetes, seizure disorder, and other common conditions in which treatment makes a really big difference. Preventive care, especially vaccine delivery, is another example.
I understand that physicians will point out that patients may not come in for that care, or they’re hard to deal with, or they refuse recommended treatment. We don’t expect 100%. But we should expect that, if we’re paying for health care, we should get health.
To do that, I think we need much more support for primary care, both in terms of the absolute amount of dollars going in and the administrative support. Some of our systems are so complicated that you can’t manage them without a billing department. How does a one- or two-physician practice deal with systems that will take dozens of hours a week to manage? You have to deal with the administrative complexity, the structure of the incentives, and the structure of care.
I think these are all things that we have to address. But for a minute, let’s helicopter up and look at the big picture. Without additional help from Congress, tens of thousands of primary care physicians could go out of business in the coming weeks. This is a crisis, and this will be very hard to rebuild. We don’t have a strong, resilient primary care infrastructure today, and if we’re not careful it’ll be even weaker as we try to rebuild.
It has been encouraging to see some of the care innovations that have occurred in response to the pandemic. I’m particularly encouraged by the widespread interest in and support for telemedicine. Telemedicine is a very important way of making care safer, more accessible, less expensive, more efficient. There have been a lot of restrictions on it, not just in the United States but globally, for many years. It’s really interesting to see those restrictions rapidly change. I give credit to the Centers for Medicare & Medicaid Services for quick changes in this area.
Now, telemedicine isn’t a cure-all. There are lots of things you can’t do from a distance. It’s a pale reflection of reality, compared with an in-person first visit with a patient. But it’s a whole lot better than nothing. If we look at some of the best health systems in the United States, they’ve gone to as much as 80% of clinical visits done by telemedicine. I don’t think we’re going to go back. Even if COVID is no longer the threat that it is today, if you can do things more quickly, more efficiently, and more conveniently for both patients and doctors, do them. Obviously, it won’t be all visits, but it could be a large proportion of visits and an important part of strengthening our primary care system.
My initiative, Resolve to Save Lives, which is part of the global health organization Vital Strategies, has done work in the area of public health around the world. I am really struck by how weak primary care systems are in so many countries. Strong primary care systems are the exception rather than the rule, but they’re also a best buy in health care. They’re crucially important, and they’re going to work differently in different countries, in different states, in different communities. We need to do a better job of supporting primary care, building primary care, and paying for primary care.
Dr. Lin: You’ve identified two needs. The immediate need is that primary care practices need revenue now to not have to close in the immediate aftermath or the ongoing COVID epidemic, but also there’s the long term, the percentage of health care dollars that are going to primary care in the long term. You pointed out in your article that currently 5% or less of health care spending is in primary care, which is a lot less percentage-wise than in many other countries. I think the question always comes up is that we want to increase that share, but the money has to come from somewhere. Where is that extra money going to come from? Dr. Frieden: I’m not an expert in health care finance, but one thing I’ve learned over the years is that one person’s waste, fraud, and abuse is somebody else’s profit center. It’s not going to be easy. On the one hand, we do need to think about more efficient ways to organize primary care; on the other hand, we have to figure out a way to internalize some of the savings. If you give good primary care and, therefore, someone doesn’t get hospitalized, you can actually lose money in the current system, whereas you’re saving the system a lot of money by preventing that hospitalization.
I think our health system does have significant inefficiencies in terms of the number of tests and interventions that are done that are really not proven to help patients. It has been demonstrated for decades now that the usual economic incentives don’t operate in health care. In health care, supply often generates demand. The number of gallbladder operations is proportional not to population but to the number of gallbladder surgeons. That’s a problem, and it’s a problem that we’re going to have to assess. “Gatekeeper” is an unpleasant word, but if a primary care practitioner could be the advocate for patients so that we’re not pushing for patients to get more care or to get less care but to get the right care, we have the potential to reduce costs while improving quality.
Dr. Lin: You accurately point out that the fee-for-service payment system has been the major culprit in the declining revenues of primary care practices since the start of the pandemic. But for the majority of primary care physicians, including myself, fee-for-service is all that we’ve ever known. Do you think that primary care is ready for such an abrupt financing change, particularly in a very short period of time?Dr. Frieden: You’re certainly accurate in saying that nothing about health care finance is easy. Trying to address these problems at the national or state level has been extremely difficult. I think that the pilot programs in Medicare are very important. Medicaid is a particular challenge because it’s a state-based program and many of the costs are driven by nursing home and long-term care. When you take those costs out, the actual funding per patient or per provider is quite low in most places.
It’s hard enough to reorganize if you’ve got ample resources, but to reorganize when they are insufficient is particularly hard. I would say only that there are no quick and simple answers to this question, but there is a widespread understanding that what we’re doing now doesn’t make sense. We pay top dollar and we get – despite fantastic doctors and fantastic hospitals – lousy outcomes. I’m a public health physician. I’m an internal medicine and infectious disease specialist. Fundamentally, I look at the data. If you think of our health care system as a patient, the patient is not doing well. We’re not functional to the degree we need to be, particularly when you think of what an enormous outlier our per capita expenditures are [compared with other developed countries] – almost twice the average upper-income country and 25% more than any other upper-income country.
Now, anyone who tells you that change is going to be pain-free is not leveling with you. In addition to things like telemedicine, we have to make much more use of team-based care and task sharing. There are lots of things that doctors are doing these days that they really shouldn’t.
Dr. Lin: In your recent op-ed, you noted the pivot to telehealth that primary care practices have made very quickly in response to the pandemic. That certainly was the experience for my practice. But what are some other strategies that you think are important to support the goal of better care delivery in our primary care practices?Dr. Frieden: Another really important innovation is team-based care. There are lots of things that doctors are doing today that nurses, nurse practitioners, physician assistants, and community health workers can do better and for less money. Frankly, I think that should increase the job satisfaction of physicians, to be doing work that is specific to the physician, requiring either more patient interaction or advanced reasoning or experience.
In my own field of tuberculosis control, I learned how to treat tuberculosis because the nurse at the TB clinic kept correcting me because that’s all she did. She did tuberculosis care, so she had seen everything. Even though I’d finished an infectious disease fellowship and internal medicine residency, the public health nurse knew TB a whole lot better than I did.
Similarly, as we work on hypertension control, you can protocolize most of this care and do a much better job. That’s been proven for more than 40 years, and yet we still don’t do it.
One of the big parts of being able to do more with the same or fewer resources is going to be more team-based care. That’s really a task-sharing approach. I think of that as a triple win: You get better care for lower costs with more employment. What’s not to like?
Dr. Lin: I’m hopeful, as you are, that many of these innovations that have been made by necessity will persist beyond the duration of COVID-19. As you said, the health care system has been really difficult to change, and it often takes something like this to galvanize enough consensus that things need to change.
Dr. Frieden: I think the bottom line here is that we should pay our primary health care providers to keep us healthy and ensure that we have a payment system that lets them do that without risking bankruptcy. That’s not too much to ask of our system. It’s important for our health. It’s important for our economy. It’s important for our communities.
Dr. Lin teaches family medicine, preventive medicine, and health policy at Georgetown University School of Medicine. He is deputy editor of the journal American Family Physician. Follow him on Twitter. He has served as a director, officer, partner, employee, adviser, consultant, or trustee for MedStar Georgetown University Hospital and received income in an amount equal to or greater than $250 from UpToDate, Wiley-Blackwell, and American Academy of Family Physicians.
Dr. Frieden is a physician with advanced training in internal medicine, infectious disease, public health, and epidemiology. He has served as director of the Centers for Disease Control and Prevention and as commissioner of the New York City Health Department. Currently he is president and CEO of Resolve to Save Lives. Follow him on Twitter. Thomas R. Frieden, MD, MPH, has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
In a recently published editorial, Tom Frieden, MD, MPH, former head of the Centers for Disease Control and Prevention, argued that primary care is in deep trouble, its long-standing financial problems exacerbated by the fallout from the COVID-19 pandemic. Those arguments resonated with Kenny Lin, MD, MPH, a family physician, professor at Georgetown University School of Medicine, and a regular contributor to Medscape. He spoke with Dr. Frieden about his concerns.
Dr. Lin: Why did you feel that it was important to write this piece focused on primary care?
Dr. Frieden: I’m glad you asked that question. Given all that is going on, one might ask, what is the importance of primary care? We’ve got this epidemic going on that requires public health and hospital systems. Why voice concern about primary care now?
It’s really striking to see that the number of visits has plummeted. Because of our payment structure, that means incomes have plummeted. We’re hearing about doctors’ offices getting boarded up and shuttering. As I write in the piece, it’s one thing for a theater or a restaurant or another important community entity to shut because of economic downturn, and these are real losses, but to lose their only primary care practice or one of the few in an area really is a matter of life and death for many communities.
Dr. Lin: I agree. In my own practice we haven’t had to furlough anyone, but we’ve put people on forced paid time off. We’ve been reallocating physicians to other parts of our health system. It is definitely a concern. A solo practitioner or someone in a rural practice would most likely be even much more heavily hit. You’ve argued that the neglect of our public health system on a national level has led to many preventable deaths from COVID-19. Do you feel that something similar has happened in primary care? How could a stronger, better-funded primary care infrastructure better prepare us for the next pandemic?
Dr. Frieden: All over the world, we see an overemphasis on hospital care and an underemphasis on primary care, outpatient care, family medicine. As a result, we pay more. We have larger risks, and we don’t prevent diseases that we could prevent. It’s fundamentally about the economic incentives of our health care system. Of course, that often reflects the political reality of different profit centers and cost centers of care. That won’t change with tweaking around the edges. It will only change if we change the way we pay for health care. Money talks. We need to start paying at least part of what we pay based on health outcomes.
Many years ago a colleague and I wrote an article, “Health Care as If Health Mattered.” If you step back and look at how we pay for health care, very little, if any, of our payment structure is based on how much health the care system delivers. Part of that can be addressed by going to capitated models, which I think do better. But you have also got to put into those capitated systems some quality and outcome measures that are both valid and not too burdensome to report on. That’s not easy. We could talk a lot about some of the information systems and payment systems, but I think the bottom line is that we need to be able to deal not only with health emergencies, but also with preventive care, care of chronic diseases, and behavioral health care in ways that maximize health.
One of the ways to do that is simple, monthly, capitated payments along with what I call a registry-based outcomes system.
I’m a tuberculosis specialist by training. In tuberculosis there really is a great information system. We track every single patient who has been diagnosed, and we hold every clinician accountable for whether or not they’ve successfully treated that patient. An optimal health care system should do the same with treatment of hypertension, diabetes, seizure disorder, and other common conditions in which treatment makes a really big difference. Preventive care, especially vaccine delivery, is another example.
I understand that physicians will point out that patients may not come in for that care, or they’re hard to deal with, or they refuse recommended treatment. We don’t expect 100%. But we should expect that, if we’re paying for health care, we should get health.
To do that, I think we need much more support for primary care, both in terms of the absolute amount of dollars going in and the administrative support. Some of our systems are so complicated that you can’t manage them without a billing department. How does a one- or two-physician practice deal with systems that will take dozens of hours a week to manage? You have to deal with the administrative complexity, the structure of the incentives, and the structure of care.
I think these are all things that we have to address. But for a minute, let’s helicopter up and look at the big picture. Without additional help from Congress, tens of thousands of primary care physicians could go out of business in the coming weeks. This is a crisis, and this will be very hard to rebuild. We don’t have a strong, resilient primary care infrastructure today, and if we’re not careful it’ll be even weaker as we try to rebuild.
It has been encouraging to see some of the care innovations that have occurred in response to the pandemic. I’m particularly encouraged by the widespread interest in and support for telemedicine. Telemedicine is a very important way of making care safer, more accessible, less expensive, more efficient. There have been a lot of restrictions on it, not just in the United States but globally, for many years. It’s really interesting to see those restrictions rapidly change. I give credit to the Centers for Medicare & Medicaid Services for quick changes in this area.
Now, telemedicine isn’t a cure-all. There are lots of things you can’t do from a distance. It’s a pale reflection of reality, compared with an in-person first visit with a patient. But it’s a whole lot better than nothing. If we look at some of the best health systems in the United States, they’ve gone to as much as 80% of clinical visits done by telemedicine. I don’t think we’re going to go back. Even if COVID is no longer the threat that it is today, if you can do things more quickly, more efficiently, and more conveniently for both patients and doctors, do them. Obviously, it won’t be all visits, but it could be a large proportion of visits and an important part of strengthening our primary care system.
My initiative, Resolve to Save Lives, which is part of the global health organization Vital Strategies, has done work in the area of public health around the world. I am really struck by how weak primary care systems are in so many countries. Strong primary care systems are the exception rather than the rule, but they’re also a best buy in health care. They’re crucially important, and they’re going to work differently in different countries, in different states, in different communities. We need to do a better job of supporting primary care, building primary care, and paying for primary care.
Dr. Lin: You’ve identified two needs. The immediate need is that primary care practices need revenue now to not have to close in the immediate aftermath or the ongoing COVID epidemic, but also there’s the long term, the percentage of health care dollars that are going to primary care in the long term. You pointed out in your article that currently 5% or less of health care spending is in primary care, which is a lot less percentage-wise than in many other countries. I think the question always comes up is that we want to increase that share, but the money has to come from somewhere. Where is that extra money going to come from? Dr. Frieden: I’m not an expert in health care finance, but one thing I’ve learned over the years is that one person’s waste, fraud, and abuse is somebody else’s profit center. It’s not going to be easy. On the one hand, we do need to think about more efficient ways to organize primary care; on the other hand, we have to figure out a way to internalize some of the savings. If you give good primary care and, therefore, someone doesn’t get hospitalized, you can actually lose money in the current system, whereas you’re saving the system a lot of money by preventing that hospitalization.
I think our health system does have significant inefficiencies in terms of the number of tests and interventions that are done that are really not proven to help patients. It has been demonstrated for decades now that the usual economic incentives don’t operate in health care. In health care, supply often generates demand. The number of gallbladder operations is proportional not to population but to the number of gallbladder surgeons. That’s a problem, and it’s a problem that we’re going to have to assess. “Gatekeeper” is an unpleasant word, but if a primary care practitioner could be the advocate for patients so that we’re not pushing for patients to get more care or to get less care but to get the right care, we have the potential to reduce costs while improving quality.
Dr. Lin: You accurately point out that the fee-for-service payment system has been the major culprit in the declining revenues of primary care practices since the start of the pandemic. But for the majority of primary care physicians, including myself, fee-for-service is all that we’ve ever known. Do you think that primary care is ready for such an abrupt financing change, particularly in a very short period of time?Dr. Frieden: You’re certainly accurate in saying that nothing about health care finance is easy. Trying to address these problems at the national or state level has been extremely difficult. I think that the pilot programs in Medicare are very important. Medicaid is a particular challenge because it’s a state-based program and many of the costs are driven by nursing home and long-term care. When you take those costs out, the actual funding per patient or per provider is quite low in most places.
It’s hard enough to reorganize if you’ve got ample resources, but to reorganize when they are insufficient is particularly hard. I would say only that there are no quick and simple answers to this question, but there is a widespread understanding that what we’re doing now doesn’t make sense. We pay top dollar and we get – despite fantastic doctors and fantastic hospitals – lousy outcomes. I’m a public health physician. I’m an internal medicine and infectious disease specialist. Fundamentally, I look at the data. If you think of our health care system as a patient, the patient is not doing well. We’re not functional to the degree we need to be, particularly when you think of what an enormous outlier our per capita expenditures are [compared with other developed countries] – almost twice the average upper-income country and 25% more than any other upper-income country.
Now, anyone who tells you that change is going to be pain-free is not leveling with you. In addition to things like telemedicine, we have to make much more use of team-based care and task sharing. There are lots of things that doctors are doing these days that they really shouldn’t.
Dr. Lin: In your recent op-ed, you noted the pivot to telehealth that primary care practices have made very quickly in response to the pandemic. That certainly was the experience for my practice. But what are some other strategies that you think are important to support the goal of better care delivery in our primary care practices?Dr. Frieden: Another really important innovation is team-based care. There are lots of things that doctors are doing today that nurses, nurse practitioners, physician assistants, and community health workers can do better and for less money. Frankly, I think that should increase the job satisfaction of physicians, to be doing work that is specific to the physician, requiring either more patient interaction or advanced reasoning or experience.
In my own field of tuberculosis control, I learned how to treat tuberculosis because the nurse at the TB clinic kept correcting me because that’s all she did. She did tuberculosis care, so she had seen everything. Even though I’d finished an infectious disease fellowship and internal medicine residency, the public health nurse knew TB a whole lot better than I did.
Similarly, as we work on hypertension control, you can protocolize most of this care and do a much better job. That’s been proven for more than 40 years, and yet we still don’t do it.
One of the big parts of being able to do more with the same or fewer resources is going to be more team-based care. That’s really a task-sharing approach. I think of that as a triple win: You get better care for lower costs with more employment. What’s not to like?
Dr. Lin: I’m hopeful, as you are, that many of these innovations that have been made by necessity will persist beyond the duration of COVID-19. As you said, the health care system has been really difficult to change, and it often takes something like this to galvanize enough consensus that things need to change.
Dr. Frieden: I think the bottom line here is that we should pay our primary health care providers to keep us healthy and ensure that we have a payment system that lets them do that without risking bankruptcy. That’s not too much to ask of our system. It’s important for our health. It’s important for our economy. It’s important for our communities.
Dr. Lin teaches family medicine, preventive medicine, and health policy at Georgetown University School of Medicine. He is deputy editor of the journal American Family Physician. Follow him on Twitter. He has served as a director, officer, partner, employee, adviser, consultant, or trustee for MedStar Georgetown University Hospital and received income in an amount equal to or greater than $250 from UpToDate, Wiley-Blackwell, and American Academy of Family Physicians.
Dr. Frieden is a physician with advanced training in internal medicine, infectious disease, public health, and epidemiology. He has served as director of the Centers for Disease Control and Prevention and as commissioner of the New York City Health Department. Currently he is president and CEO of Resolve to Save Lives. Follow him on Twitter. Thomas R. Frieden, MD, MPH, has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
How can we better engage black men as patients?
I’m a black man, husband, father, son, brother, and a board-certified psychiatrist, child and adolescent psychiatry fellow, and addiction medicine fellow. I write this article as the latter, a colleague, from the former’s perspective, which you would not need to verify via Google, social media, or a badge upon meeting me.
July is Minority Mental Health Awareness Month, established to bring awareness to the unique struggles that marginalized groups face concerning mental illness in the United States.
Given the events of the last few months, including a global pandemic and videotaped killings of Ahmaud Arbery and George Floyd, two unarmed black men, America’s structural racism and inequality are being challenged in historic ways. Black people are suffering. In fact, I was not surprised to learn1 that some black families with sons have expanded the “talk” – which traditionally has focused on dealing with police officers – to include vigilantes.
Because of my extensive work with and treatment of men of color, I would like to answer a key question: “How do psychiatrists and other mental health clinicians better engage men of color? Before the “how,” let’s review the state of black men’s mental health.
According to Healthy People 2020, mental disorders are the leading cause of disability in the United States.2 Among those with diagnosable mental disorders, black people are more likely than are their white counterparts to experience severe symptoms and protracted diseases. Roughly 7% of black men meet the criteria for a lifetime prevalence of major depressive disorder.3 Applying that figure to recent national population estimates means that there are 1.4 million black men currently suffering from major depression. Suicide has been on a continued uptrend among black male youth for more than 2 decades. Moreover, given the high rates of stigma and unmet need in this population, it is likely that these figures are even more dire.
Compared with other groups, black men in the United States face a disproportionate burden of preventable morbidity and mortality rates. Of all the health concerns faced by black men, mental health challenges may be among the most stigmatized.4 Evidence suggests that black men have more adverse life experiences than do men of other racial/ethnic groups, and consequently, experience poorer mental health.5 Black men experience high rates of poverty, unemployment, and underemployment, and are incarcerated at much higher rates than those of men of other racial/ethnic groups.6 It is notable that black male youth are often perceived as older by law enforcement, beginning as early as 10 years old, often resulting in negative interactions.7
Despite those challenges, black men are often expected to project strength, they are expected to minimize displays of emotion when off the field or court (i.e., “Just shut up and dribble”), and they are expected to be true versions of folk hero John Henry. This caricature of black males is used at times to validate shootings of unarmed black males (adults and youth).
Black men’s mental health should be a priority for those in the mental health field. This is particularly the case light of our field’s historical involvement in and promotion of stereotyped clinical descriptions of black men and contributing to health disparities that persist. Black men are nearly six times as likely to be diagnosed with schizophrenia as are white men. To read about holdovers from the days of targeted advertising against black protesters of the 1960s and 1970s, check out “The Protest Psychosis” (Beacon Press, 2010) by psychiatrist and anthropologist Jonathan Metzl, MD, PhD. If you go further back in psychiatric history, the late 1800s, you can learn about the devious diagnosis of drapetomania attributed to enslaved people who were seeking freedom.
Those on the front lines providing mental health services should understand black men’s mental health from an ecological perspective. Beyond the emotional burden that mental illness imposes on the individual, there are more considerable interpersonal and societal implications for the state of black men’s mental health. As such, in our full capacity like other men, black men play an essential role within families, churches, neighborhoods, and organizations.
Given our brief review, we can reconsider our question, “How do psychiatrists and mental health clinicians better engage men of color?”
I will suggest a few fundamental principles that honestly can be applied to any patient but should be strongly considered with your black male patients – given they are likely not accustomed to engaging with the health care system, let alone with a mental health clinician:
1. Create a comfortable environment. Because of stigma, persistent myths, and lack of normalcy with talking to a mental health professional, many patients, including black men, do not have a framework for a psychiatric/psychological evaluation or treatment. It would be essential to set the frame of your encounter. Evidence suggests this can improve engagement and follow-up care among black men.8 In addition, keep in mind that “fictive kin”9 tend to play a major role in the transmission of culture, health promotion, and decision-making in the black community. This helps explain why barbershop initiatives10 are effective. If clinicians are able to allow black male patients to feel comfortable, the clinician, too, might become part of that fictive community and enhance the patient-provider relationship.
2. Allow for storytelling. In the age of the checklist, it can be relatively easy to lose sight that our patients, including black men, have their own narratives. Evidence suggests that physicians interrupt patients early and often. Challenge yourself to allow the patient to tell his story. In consideration of an initial evaluation, it may help to begin by first gathering sociodemographic information (i.e. housing, education, employment, family, etc.); doing so will allow the patient time to get comfortable before you assess possible psychiatric symptoms.
3. Confidentiality assurance. Many black men have a distrust for the health care profession; as such, it is vital that clinicians emphasize that their patients’ information and history will be used only to help the patient. It will be important to inform black male patients of their rights, because often in the greater society, their rights seem to be negated.
4. Be aware of nonverbal language. Given black men’s stereotyped roles in society and recognition that they are regularly perceived as threats, many black men have become adept at reading nonverbal cues (i.e., purse clutched, side comment, etc.). In doing so, clinicians must be attuned to their own nonverbal language. For example, a glance at one’s watch might be interpreted as you’re not listening. It would be better to be upfront and candid by saying something like, “I need to check the time,” rather than attempting to be stealth. Being transparent in that way will let the patient know that you will be upfront with him.
5. Be respectful. During an encounter, and in particular when discussing treatment plans, clinicians must allow the patient space to process and be involved in his care. Allowing the patient time to think through how he would want to proceed provides him a sense of personal agency and lets him know that he is capable of improving his mental wellness.
Black male patients need to feel comfortable, safe, able to trust the clinician. They must feel listened to, understood, and respected. This information might help some clinicians better understand what needs to happen between a black male patient and a nonblack clinician so the patient can feel good about his mental health engagement. To some, these recommendations might seem obvious or too simple, yet if we consider the countless reports of poor patient treatment engagement, adherence, and retention, we cannot deny the need for change. Having black male patients disclose important information during encounters could prevent poor clinical interactions that leave them feeling uncomfortable, uncertain, skeptical, disrespected, and further cynical about mental health care.
Dr. Simon practices at Boston Children’s Hospital. He has no disclosures.
References
1. Bunn C. After Arbery shooting, black parents are rethinking “the talk” to explain white vigilantes. NBC News. 2020 May 19.
2. U.S. Department of Health and Human Services. Office of Disease Prevention and Promotion. Healthy People 2020.
3. Ward E and Mangesha M. Am J Orthopsychiatry. 2013 Apr-Jul;83(2 0 3):386-97.
4. Holden KB et al. J Mens health. 2012 Jun 1;9(2):63-9.
5. Brown TH et al. Fam Community Health. 2015 Oct-Dec;38(4):307-18.
6. Jäggi et al. Soc Ment Health. 2016 Nov;6(3):187-296.
7. Goff PA et al. J Pers Soc Psychol. 2014;106(4):526-45.
8. Alsan M et al. National Bureau of Economic Research. NBER Working Paper No. 24787. 2018 Jun. Revised 2019 Aug.
9. Spruill IJ. J Nat Black Nurses Assoc. 2014 Dec;25(2):23-30.
10. Graham LF et al. Am J Mens Health. 2018 Sep;12(5):1307-16.
I’m a black man, husband, father, son, brother, and a board-certified psychiatrist, child and adolescent psychiatry fellow, and addiction medicine fellow. I write this article as the latter, a colleague, from the former’s perspective, which you would not need to verify via Google, social media, or a badge upon meeting me.
July is Minority Mental Health Awareness Month, established to bring awareness to the unique struggles that marginalized groups face concerning mental illness in the United States.
Given the events of the last few months, including a global pandemic and videotaped killings of Ahmaud Arbery and George Floyd, two unarmed black men, America’s structural racism and inequality are being challenged in historic ways. Black people are suffering. In fact, I was not surprised to learn1 that some black families with sons have expanded the “talk” – which traditionally has focused on dealing with police officers – to include vigilantes.
Because of my extensive work with and treatment of men of color, I would like to answer a key question: “How do psychiatrists and other mental health clinicians better engage men of color? Before the “how,” let’s review the state of black men’s mental health.
According to Healthy People 2020, mental disorders are the leading cause of disability in the United States.2 Among those with diagnosable mental disorders, black people are more likely than are their white counterparts to experience severe symptoms and protracted diseases. Roughly 7% of black men meet the criteria for a lifetime prevalence of major depressive disorder.3 Applying that figure to recent national population estimates means that there are 1.4 million black men currently suffering from major depression. Suicide has been on a continued uptrend among black male youth for more than 2 decades. Moreover, given the high rates of stigma and unmet need in this population, it is likely that these figures are even more dire.
Compared with other groups, black men in the United States face a disproportionate burden of preventable morbidity and mortality rates. Of all the health concerns faced by black men, mental health challenges may be among the most stigmatized.4 Evidence suggests that black men have more adverse life experiences than do men of other racial/ethnic groups, and consequently, experience poorer mental health.5 Black men experience high rates of poverty, unemployment, and underemployment, and are incarcerated at much higher rates than those of men of other racial/ethnic groups.6 It is notable that black male youth are often perceived as older by law enforcement, beginning as early as 10 years old, often resulting in negative interactions.7
Despite those challenges, black men are often expected to project strength, they are expected to minimize displays of emotion when off the field or court (i.e., “Just shut up and dribble”), and they are expected to be true versions of folk hero John Henry. This caricature of black males is used at times to validate shootings of unarmed black males (adults and youth).
Black men’s mental health should be a priority for those in the mental health field. This is particularly the case light of our field’s historical involvement in and promotion of stereotyped clinical descriptions of black men and contributing to health disparities that persist. Black men are nearly six times as likely to be diagnosed with schizophrenia as are white men. To read about holdovers from the days of targeted advertising against black protesters of the 1960s and 1970s, check out “The Protest Psychosis” (Beacon Press, 2010) by psychiatrist and anthropologist Jonathan Metzl, MD, PhD. If you go further back in psychiatric history, the late 1800s, you can learn about the devious diagnosis of drapetomania attributed to enslaved people who were seeking freedom.
Those on the front lines providing mental health services should understand black men’s mental health from an ecological perspective. Beyond the emotional burden that mental illness imposes on the individual, there are more considerable interpersonal and societal implications for the state of black men’s mental health. As such, in our full capacity like other men, black men play an essential role within families, churches, neighborhoods, and organizations.
Given our brief review, we can reconsider our question, “How do psychiatrists and mental health clinicians better engage men of color?”
I will suggest a few fundamental principles that honestly can be applied to any patient but should be strongly considered with your black male patients – given they are likely not accustomed to engaging with the health care system, let alone with a mental health clinician:
1. Create a comfortable environment. Because of stigma, persistent myths, and lack of normalcy with talking to a mental health professional, many patients, including black men, do not have a framework for a psychiatric/psychological evaluation or treatment. It would be essential to set the frame of your encounter. Evidence suggests this can improve engagement and follow-up care among black men.8 In addition, keep in mind that “fictive kin”9 tend to play a major role in the transmission of culture, health promotion, and decision-making in the black community. This helps explain why barbershop initiatives10 are effective. If clinicians are able to allow black male patients to feel comfortable, the clinician, too, might become part of that fictive community and enhance the patient-provider relationship.
2. Allow for storytelling. In the age of the checklist, it can be relatively easy to lose sight that our patients, including black men, have their own narratives. Evidence suggests that physicians interrupt patients early and often. Challenge yourself to allow the patient to tell his story. In consideration of an initial evaluation, it may help to begin by first gathering sociodemographic information (i.e. housing, education, employment, family, etc.); doing so will allow the patient time to get comfortable before you assess possible psychiatric symptoms.
3. Confidentiality assurance. Many black men have a distrust for the health care profession; as such, it is vital that clinicians emphasize that their patients’ information and history will be used only to help the patient. It will be important to inform black male patients of their rights, because often in the greater society, their rights seem to be negated.
4. Be aware of nonverbal language. Given black men’s stereotyped roles in society and recognition that they are regularly perceived as threats, many black men have become adept at reading nonverbal cues (i.e., purse clutched, side comment, etc.). In doing so, clinicians must be attuned to their own nonverbal language. For example, a glance at one’s watch might be interpreted as you’re not listening. It would be better to be upfront and candid by saying something like, “I need to check the time,” rather than attempting to be stealth. Being transparent in that way will let the patient know that you will be upfront with him.
5. Be respectful. During an encounter, and in particular when discussing treatment plans, clinicians must allow the patient space to process and be involved in his care. Allowing the patient time to think through how he would want to proceed provides him a sense of personal agency and lets him know that he is capable of improving his mental wellness.
Black male patients need to feel comfortable, safe, able to trust the clinician. They must feel listened to, understood, and respected. This information might help some clinicians better understand what needs to happen between a black male patient and a nonblack clinician so the patient can feel good about his mental health engagement. To some, these recommendations might seem obvious or too simple, yet if we consider the countless reports of poor patient treatment engagement, adherence, and retention, we cannot deny the need for change. Having black male patients disclose important information during encounters could prevent poor clinical interactions that leave them feeling uncomfortable, uncertain, skeptical, disrespected, and further cynical about mental health care.
Dr. Simon practices at Boston Children’s Hospital. He has no disclosures.
References
1. Bunn C. After Arbery shooting, black parents are rethinking “the talk” to explain white vigilantes. NBC News. 2020 May 19.
2. U.S. Department of Health and Human Services. Office of Disease Prevention and Promotion. Healthy People 2020.
3. Ward E and Mangesha M. Am J Orthopsychiatry. 2013 Apr-Jul;83(2 0 3):386-97.
4. Holden KB et al. J Mens health. 2012 Jun 1;9(2):63-9.
5. Brown TH et al. Fam Community Health. 2015 Oct-Dec;38(4):307-18.
6. Jäggi et al. Soc Ment Health. 2016 Nov;6(3):187-296.
7. Goff PA et al. J Pers Soc Psychol. 2014;106(4):526-45.
8. Alsan M et al. National Bureau of Economic Research. NBER Working Paper No. 24787. 2018 Jun. Revised 2019 Aug.
9. Spruill IJ. J Nat Black Nurses Assoc. 2014 Dec;25(2):23-30.
10. Graham LF et al. Am J Mens Health. 2018 Sep;12(5):1307-16.
I’m a black man, husband, father, son, brother, and a board-certified psychiatrist, child and adolescent psychiatry fellow, and addiction medicine fellow. I write this article as the latter, a colleague, from the former’s perspective, which you would not need to verify via Google, social media, or a badge upon meeting me.
July is Minority Mental Health Awareness Month, established to bring awareness to the unique struggles that marginalized groups face concerning mental illness in the United States.
Given the events of the last few months, including a global pandemic and videotaped killings of Ahmaud Arbery and George Floyd, two unarmed black men, America’s structural racism and inequality are being challenged in historic ways. Black people are suffering. In fact, I was not surprised to learn1 that some black families with sons have expanded the “talk” – which traditionally has focused on dealing with police officers – to include vigilantes.
Because of my extensive work with and treatment of men of color, I would like to answer a key question: “How do psychiatrists and other mental health clinicians better engage men of color? Before the “how,” let’s review the state of black men’s mental health.
According to Healthy People 2020, mental disorders are the leading cause of disability in the United States.2 Among those with diagnosable mental disorders, black people are more likely than are their white counterparts to experience severe symptoms and protracted diseases. Roughly 7% of black men meet the criteria for a lifetime prevalence of major depressive disorder.3 Applying that figure to recent national population estimates means that there are 1.4 million black men currently suffering from major depression. Suicide has been on a continued uptrend among black male youth for more than 2 decades. Moreover, given the high rates of stigma and unmet need in this population, it is likely that these figures are even more dire.
Compared with other groups, black men in the United States face a disproportionate burden of preventable morbidity and mortality rates. Of all the health concerns faced by black men, mental health challenges may be among the most stigmatized.4 Evidence suggests that black men have more adverse life experiences than do men of other racial/ethnic groups, and consequently, experience poorer mental health.5 Black men experience high rates of poverty, unemployment, and underemployment, and are incarcerated at much higher rates than those of men of other racial/ethnic groups.6 It is notable that black male youth are often perceived as older by law enforcement, beginning as early as 10 years old, often resulting in negative interactions.7
Despite those challenges, black men are often expected to project strength, they are expected to minimize displays of emotion when off the field or court (i.e., “Just shut up and dribble”), and they are expected to be true versions of folk hero John Henry. This caricature of black males is used at times to validate shootings of unarmed black males (adults and youth).
Black men’s mental health should be a priority for those in the mental health field. This is particularly the case light of our field’s historical involvement in and promotion of stereotyped clinical descriptions of black men and contributing to health disparities that persist. Black men are nearly six times as likely to be diagnosed with schizophrenia as are white men. To read about holdovers from the days of targeted advertising against black protesters of the 1960s and 1970s, check out “The Protest Psychosis” (Beacon Press, 2010) by psychiatrist and anthropologist Jonathan Metzl, MD, PhD. If you go further back in psychiatric history, the late 1800s, you can learn about the devious diagnosis of drapetomania attributed to enslaved people who were seeking freedom.
Those on the front lines providing mental health services should understand black men’s mental health from an ecological perspective. Beyond the emotional burden that mental illness imposes on the individual, there are more considerable interpersonal and societal implications for the state of black men’s mental health. As such, in our full capacity like other men, black men play an essential role within families, churches, neighborhoods, and organizations.
Given our brief review, we can reconsider our question, “How do psychiatrists and mental health clinicians better engage men of color?”
I will suggest a few fundamental principles that honestly can be applied to any patient but should be strongly considered with your black male patients – given they are likely not accustomed to engaging with the health care system, let alone with a mental health clinician:
1. Create a comfortable environment. Because of stigma, persistent myths, and lack of normalcy with talking to a mental health professional, many patients, including black men, do not have a framework for a psychiatric/psychological evaluation or treatment. It would be essential to set the frame of your encounter. Evidence suggests this can improve engagement and follow-up care among black men.8 In addition, keep in mind that “fictive kin”9 tend to play a major role in the transmission of culture, health promotion, and decision-making in the black community. This helps explain why barbershop initiatives10 are effective. If clinicians are able to allow black male patients to feel comfortable, the clinician, too, might become part of that fictive community and enhance the patient-provider relationship.
2. Allow for storytelling. In the age of the checklist, it can be relatively easy to lose sight that our patients, including black men, have their own narratives. Evidence suggests that physicians interrupt patients early and often. Challenge yourself to allow the patient to tell his story. In consideration of an initial evaluation, it may help to begin by first gathering sociodemographic information (i.e. housing, education, employment, family, etc.); doing so will allow the patient time to get comfortable before you assess possible psychiatric symptoms.
3. Confidentiality assurance. Many black men have a distrust for the health care profession; as such, it is vital that clinicians emphasize that their patients’ information and history will be used only to help the patient. It will be important to inform black male patients of their rights, because often in the greater society, their rights seem to be negated.
4. Be aware of nonverbal language. Given black men’s stereotyped roles in society and recognition that they are regularly perceived as threats, many black men have become adept at reading nonverbal cues (i.e., purse clutched, side comment, etc.). In doing so, clinicians must be attuned to their own nonverbal language. For example, a glance at one’s watch might be interpreted as you’re not listening. It would be better to be upfront and candid by saying something like, “I need to check the time,” rather than attempting to be stealth. Being transparent in that way will let the patient know that you will be upfront with him.
5. Be respectful. During an encounter, and in particular when discussing treatment plans, clinicians must allow the patient space to process and be involved in his care. Allowing the patient time to think through how he would want to proceed provides him a sense of personal agency and lets him know that he is capable of improving his mental wellness.
Black male patients need to feel comfortable, safe, able to trust the clinician. They must feel listened to, understood, and respected. This information might help some clinicians better understand what needs to happen between a black male patient and a nonblack clinician so the patient can feel good about his mental health engagement. To some, these recommendations might seem obvious or too simple, yet if we consider the countless reports of poor patient treatment engagement, adherence, and retention, we cannot deny the need for change. Having black male patients disclose important information during encounters could prevent poor clinical interactions that leave them feeling uncomfortable, uncertain, skeptical, disrespected, and further cynical about mental health care.
Dr. Simon practices at Boston Children’s Hospital. He has no disclosures.
References
1. Bunn C. After Arbery shooting, black parents are rethinking “the talk” to explain white vigilantes. NBC News. 2020 May 19.
2. U.S. Department of Health and Human Services. Office of Disease Prevention and Promotion. Healthy People 2020.
3. Ward E and Mangesha M. Am J Orthopsychiatry. 2013 Apr-Jul;83(2 0 3):386-97.
4. Holden KB et al. J Mens health. 2012 Jun 1;9(2):63-9.
5. Brown TH et al. Fam Community Health. 2015 Oct-Dec;38(4):307-18.
6. Jäggi et al. Soc Ment Health. 2016 Nov;6(3):187-296.
7. Goff PA et al. J Pers Soc Psychol. 2014;106(4):526-45.
8. Alsan M et al. National Bureau of Economic Research. NBER Working Paper No. 24787. 2018 Jun. Revised 2019 Aug.
9. Spruill IJ. J Nat Black Nurses Assoc. 2014 Dec;25(2):23-30.
10. Graham LF et al. Am J Mens Health. 2018 Sep;12(5):1307-16.
The merger of personal and professional: A psychologist’s experience with the effects of COVID-19
The concepts of days, weeks, and months have all but lost their meaning during the times of coronavirus. This became all too clear when I found myself weeks into June before realizing that we were in the second half of 2020. The world has been in the grips of COVID-19 (the disease caused by SARS-CoV-2) for over half a year, and the end is still not in sight. Even more chilling is the fact that the virus’s effects will continue to be felt by humanity for years to come.
By now, most of us have been affected by COVID-19, whether directly or indirectly. Consequently, we’ve seen that the psychological toll the pandemic takes is as wide ranging as the disease caused by the novel coronavirus itself. Confusion, denial, fear, anxiety, depression/sadness, and emotional dysregulation have become all too common an experience. Many mental health experts have even likened our psychological response to COVID-19 to that of trauma survivors.
In early 2020, triggered by two separate but related threats. In addition to concerns regarding COVID-19, we also began to experience fear for our physical safety as anti-Chinese sentiment began to rise across the country and the world. Discrimination and acts of violence toward Chinese people worldwide began to spread almost as rapidly as the virus itself. Anxiety and fear became a common daily experience of countless people, myself included.
In late March, amid coping with existing stressors, my situation became significantly worse when my brother, a New York City firefighter, contracted COVID-19 while working on the front lines. Shortly thereafter, my parents, both aged 60 years and older, with whom my brother shares a home, contracted the virus as well. My anxiety triggers related to the spread of the virus and xenophobia suddenly became a distant memory. I now found myself grappling with the much greater fear of losing my entire family.
At the time, the availability of testing was very limited, even for those working on the front lines. Although not without a short delay, my brother was able to access testing through Fire Department of New York connections. After about 3 weeks in self-isolation at home and with the use of over the counter pain relievers, he made a full recovery and returned to work. My parents, on the other hand, were placed at the end of a weeks-long line for testing, during which time their conditions deteriorated. Nine days following the onset of my mother’s symptoms, her condition had gotten so bad, she required hospitalization. Six days later, my father followed suit.
Being in the epicenter of the COVID-19 outbreak, New York hospitals were severely overwhelmed. Upon admission, my mother was held in the ED and other temporary open spaces in the hospital for nearly 24 hours because there was a lack of available patient rooms. During this time, she was packed into small spaces with dozens of other patients afflicted with the same disease. Four days later, she was transferred to a different hospital 10 miles away to make room for new patients. Decisions needed to be made rapidly and often with limited communication, which made for a roller coaster of emotions that would not relent.
Confusion. One of the few things we know with certainty about coronavirus is how much we don’t know. The Centers for Disease Control and Prevention data indicate that older adults with underlying health conditions have worse outcomes. Yet my mother, who is younger and in better physical health than my father, became much sicker in a drastically shorter period of time. Furthermore, my parents’ symptoms were completely inconsistent with one another’s. Based on their symptoms alone, it appeared as though they were suffering with different conditions entirely. My mother experienced body aches and gastrointestinal symptoms, whereas my father developed the typical cough and fever associated with COVID-19. In addition to confusion regarding their symptoms and, therefore, in determining the best at-home supportive care prior to their hospitalizations, the lack of available testing made the very question of whether they even had COVID-19 an uncertainty.
Denial. When my family members first became symptomatic, I found myself in a state of denial not unlike that of individuals experiencing grief. I frequently engaged in both internal and external dialogues in which I would attempt to convince myself of the reasons why my family did not have COVID-19.
“My brother wears PPE while at work.”
“My father’s cough was mild.”
“My mother does not have a cough or a fever.”
Despite knowing better, I was initially unable to accept that everyone in my family had contracted a disease that had already claimed the lives of tens of thousands globally.
Fear. In order to prevent the spread of infection, many hospitals made changes to their visitor policies, placing greater restrictions on who can come and go. This has meant hospital patients who have died from COVID-19 complications have done so separated from their loved ones. After transporting my mother to the hospital ED, I was politely but firmly asked to leave per the new visitor policy. I felt as though there were cinder blocks attached to my feet as I reluctantly walked away, not knowing if it would be the last time I would see her. I experienced a fear and sadness so intense, it continues to elicit an emotional response today as I think back on that moment.
Anxiety. The difference between fear and anxiety is fear is an emotional response to a known threat or danger, and anxiety is a response to an unknown threat or danger. The days that followed my parents’ hospitalizations were riddled with anxiety that would come in waves. How were they doing? Could they breathe? Do the overwhelmed hospital staff have time to take care of them? What can I do to help? Is there anything I can do to help? The worrisome thoughts and unanswerable questions were incessant and seemed unresponsive to my efforts to quell them.
Sadness. To feel sadness is to be human. In my work as a psychologist, I emphasize the value in experiencing this emotion when therapeutically beneficial. This technique is used as part of acceptance and commitment therapy (ACT), which emphasizes the value of being present or in touch with one’s thoughts and emotions, instead of working to eliminate them. During these scary times, I leaned into this notion more than ever. I gave myself permission to not feel okay, to cry more than I had in a long time, and to be unapologetically sad. I flip-flopped between states of near-despair and hopeful, with the switch usually following a call from a member of the hospital care team with updates on my parents’ conditions.
My parents’ road to recovery extended far beyond their discharge from the hospital and was not without incident, but with support and appropriate follow-up care, they have since made full recoveries from COVID-19. Although the relief and happiness this brings me is immeasurable, the experience has left a lasting impression on me as both a person and a psychologist. Speaking as a person, I cannot overstate the value of relying on one’s social support network while coping with stressors related to COVID-19. Whether you are directly or indirectly affected by the disease, the emotional effects can feel equally intense. As in times of happiness and celebration, times of sadness can and should be shared by those who are equipped to provide support. This can be tricky in an era during which isolation is prescribed for our safety, but we have more options today for connecting virtually with others than ever before, including video conferencing, email, and that old friend, the telephone. Furthermore, identify and assert your boundaries. Sometimes, saying no to others is the best way to say yes to yourself. Certain work, chores, and social obligations that can wait, should wait.
As a psychologist, my experience has given me a renewed appreciation for the power of the therapeutic use of self in psychotherapy. The factor with the greatest effects on psychotherapy outcomes is the quality of the therapeutic alliance, a concept introduced by Sigmund Freud in 1912. I believe a therapist’s willingness to show that we, too, experience life’s ups and downs strengthens our ability to demonstrate empathy and further promote a sense of alliance. Therapists are not immune to the effects of COVID-19, and to acknowledge this fact allows us to relate to our patients on a basic human level, which is more important now than ever.
Dr. Tseng, a licensed clinical psychologist, is in private practice in New York. She disclosed no relevant financial relationships.
The concepts of days, weeks, and months have all but lost their meaning during the times of coronavirus. This became all too clear when I found myself weeks into June before realizing that we were in the second half of 2020. The world has been in the grips of COVID-19 (the disease caused by SARS-CoV-2) for over half a year, and the end is still not in sight. Even more chilling is the fact that the virus’s effects will continue to be felt by humanity for years to come.
By now, most of us have been affected by COVID-19, whether directly or indirectly. Consequently, we’ve seen that the psychological toll the pandemic takes is as wide ranging as the disease caused by the novel coronavirus itself. Confusion, denial, fear, anxiety, depression/sadness, and emotional dysregulation have become all too common an experience. Many mental health experts have even likened our psychological response to COVID-19 to that of trauma survivors.
In early 2020, triggered by two separate but related threats. In addition to concerns regarding COVID-19, we also began to experience fear for our physical safety as anti-Chinese sentiment began to rise across the country and the world. Discrimination and acts of violence toward Chinese people worldwide began to spread almost as rapidly as the virus itself. Anxiety and fear became a common daily experience of countless people, myself included.
In late March, amid coping with existing stressors, my situation became significantly worse when my brother, a New York City firefighter, contracted COVID-19 while working on the front lines. Shortly thereafter, my parents, both aged 60 years and older, with whom my brother shares a home, contracted the virus as well. My anxiety triggers related to the spread of the virus and xenophobia suddenly became a distant memory. I now found myself grappling with the much greater fear of losing my entire family.
At the time, the availability of testing was very limited, even for those working on the front lines. Although not without a short delay, my brother was able to access testing through Fire Department of New York connections. After about 3 weeks in self-isolation at home and with the use of over the counter pain relievers, he made a full recovery and returned to work. My parents, on the other hand, were placed at the end of a weeks-long line for testing, during which time their conditions deteriorated. Nine days following the onset of my mother’s symptoms, her condition had gotten so bad, she required hospitalization. Six days later, my father followed suit.
Being in the epicenter of the COVID-19 outbreak, New York hospitals were severely overwhelmed. Upon admission, my mother was held in the ED and other temporary open spaces in the hospital for nearly 24 hours because there was a lack of available patient rooms. During this time, she was packed into small spaces with dozens of other patients afflicted with the same disease. Four days later, she was transferred to a different hospital 10 miles away to make room for new patients. Decisions needed to be made rapidly and often with limited communication, which made for a roller coaster of emotions that would not relent.
Confusion. One of the few things we know with certainty about coronavirus is how much we don’t know. The Centers for Disease Control and Prevention data indicate that older adults with underlying health conditions have worse outcomes. Yet my mother, who is younger and in better physical health than my father, became much sicker in a drastically shorter period of time. Furthermore, my parents’ symptoms were completely inconsistent with one another’s. Based on their symptoms alone, it appeared as though they were suffering with different conditions entirely. My mother experienced body aches and gastrointestinal symptoms, whereas my father developed the typical cough and fever associated with COVID-19. In addition to confusion regarding their symptoms and, therefore, in determining the best at-home supportive care prior to their hospitalizations, the lack of available testing made the very question of whether they even had COVID-19 an uncertainty.
Denial. When my family members first became symptomatic, I found myself in a state of denial not unlike that of individuals experiencing grief. I frequently engaged in both internal and external dialogues in which I would attempt to convince myself of the reasons why my family did not have COVID-19.
“My brother wears PPE while at work.”
“My father’s cough was mild.”
“My mother does not have a cough or a fever.”
Despite knowing better, I was initially unable to accept that everyone in my family had contracted a disease that had already claimed the lives of tens of thousands globally.
Fear. In order to prevent the spread of infection, many hospitals made changes to their visitor policies, placing greater restrictions on who can come and go. This has meant hospital patients who have died from COVID-19 complications have done so separated from their loved ones. After transporting my mother to the hospital ED, I was politely but firmly asked to leave per the new visitor policy. I felt as though there were cinder blocks attached to my feet as I reluctantly walked away, not knowing if it would be the last time I would see her. I experienced a fear and sadness so intense, it continues to elicit an emotional response today as I think back on that moment.
Anxiety. The difference between fear and anxiety is fear is an emotional response to a known threat or danger, and anxiety is a response to an unknown threat or danger. The days that followed my parents’ hospitalizations were riddled with anxiety that would come in waves. How were they doing? Could they breathe? Do the overwhelmed hospital staff have time to take care of them? What can I do to help? Is there anything I can do to help? The worrisome thoughts and unanswerable questions were incessant and seemed unresponsive to my efforts to quell them.
Sadness. To feel sadness is to be human. In my work as a psychologist, I emphasize the value in experiencing this emotion when therapeutically beneficial. This technique is used as part of acceptance and commitment therapy (ACT), which emphasizes the value of being present or in touch with one’s thoughts and emotions, instead of working to eliminate them. During these scary times, I leaned into this notion more than ever. I gave myself permission to not feel okay, to cry more than I had in a long time, and to be unapologetically sad. I flip-flopped between states of near-despair and hopeful, with the switch usually following a call from a member of the hospital care team with updates on my parents’ conditions.
My parents’ road to recovery extended far beyond their discharge from the hospital and was not without incident, but with support and appropriate follow-up care, they have since made full recoveries from COVID-19. Although the relief and happiness this brings me is immeasurable, the experience has left a lasting impression on me as both a person and a psychologist. Speaking as a person, I cannot overstate the value of relying on one’s social support network while coping with stressors related to COVID-19. Whether you are directly or indirectly affected by the disease, the emotional effects can feel equally intense. As in times of happiness and celebration, times of sadness can and should be shared by those who are equipped to provide support. This can be tricky in an era during which isolation is prescribed for our safety, but we have more options today for connecting virtually with others than ever before, including video conferencing, email, and that old friend, the telephone. Furthermore, identify and assert your boundaries. Sometimes, saying no to others is the best way to say yes to yourself. Certain work, chores, and social obligations that can wait, should wait.
As a psychologist, my experience has given me a renewed appreciation for the power of the therapeutic use of self in psychotherapy. The factor with the greatest effects on psychotherapy outcomes is the quality of the therapeutic alliance, a concept introduced by Sigmund Freud in 1912. I believe a therapist’s willingness to show that we, too, experience life’s ups and downs strengthens our ability to demonstrate empathy and further promote a sense of alliance. Therapists are not immune to the effects of COVID-19, and to acknowledge this fact allows us to relate to our patients on a basic human level, which is more important now than ever.
Dr. Tseng, a licensed clinical psychologist, is in private practice in New York. She disclosed no relevant financial relationships.
The concepts of days, weeks, and months have all but lost their meaning during the times of coronavirus. This became all too clear when I found myself weeks into June before realizing that we were in the second half of 2020. The world has been in the grips of COVID-19 (the disease caused by SARS-CoV-2) for over half a year, and the end is still not in sight. Even more chilling is the fact that the virus’s effects will continue to be felt by humanity for years to come.
By now, most of us have been affected by COVID-19, whether directly or indirectly. Consequently, we’ve seen that the psychological toll the pandemic takes is as wide ranging as the disease caused by the novel coronavirus itself. Confusion, denial, fear, anxiety, depression/sadness, and emotional dysregulation have become all too common an experience. Many mental health experts have even likened our psychological response to COVID-19 to that of trauma survivors.
In early 2020, triggered by two separate but related threats. In addition to concerns regarding COVID-19, we also began to experience fear for our physical safety as anti-Chinese sentiment began to rise across the country and the world. Discrimination and acts of violence toward Chinese people worldwide began to spread almost as rapidly as the virus itself. Anxiety and fear became a common daily experience of countless people, myself included.
In late March, amid coping with existing stressors, my situation became significantly worse when my brother, a New York City firefighter, contracted COVID-19 while working on the front lines. Shortly thereafter, my parents, both aged 60 years and older, with whom my brother shares a home, contracted the virus as well. My anxiety triggers related to the spread of the virus and xenophobia suddenly became a distant memory. I now found myself grappling with the much greater fear of losing my entire family.
At the time, the availability of testing was very limited, even for those working on the front lines. Although not without a short delay, my brother was able to access testing through Fire Department of New York connections. After about 3 weeks in self-isolation at home and with the use of over the counter pain relievers, he made a full recovery and returned to work. My parents, on the other hand, were placed at the end of a weeks-long line for testing, during which time their conditions deteriorated. Nine days following the onset of my mother’s symptoms, her condition had gotten so bad, she required hospitalization. Six days later, my father followed suit.
Being in the epicenter of the COVID-19 outbreak, New York hospitals were severely overwhelmed. Upon admission, my mother was held in the ED and other temporary open spaces in the hospital for nearly 24 hours because there was a lack of available patient rooms. During this time, she was packed into small spaces with dozens of other patients afflicted with the same disease. Four days later, she was transferred to a different hospital 10 miles away to make room for new patients. Decisions needed to be made rapidly and often with limited communication, which made for a roller coaster of emotions that would not relent.
Confusion. One of the few things we know with certainty about coronavirus is how much we don’t know. The Centers for Disease Control and Prevention data indicate that older adults with underlying health conditions have worse outcomes. Yet my mother, who is younger and in better physical health than my father, became much sicker in a drastically shorter period of time. Furthermore, my parents’ symptoms were completely inconsistent with one another’s. Based on their symptoms alone, it appeared as though they were suffering with different conditions entirely. My mother experienced body aches and gastrointestinal symptoms, whereas my father developed the typical cough and fever associated with COVID-19. In addition to confusion regarding their symptoms and, therefore, in determining the best at-home supportive care prior to their hospitalizations, the lack of available testing made the very question of whether they even had COVID-19 an uncertainty.
Denial. When my family members first became symptomatic, I found myself in a state of denial not unlike that of individuals experiencing grief. I frequently engaged in both internal and external dialogues in which I would attempt to convince myself of the reasons why my family did not have COVID-19.
“My brother wears PPE while at work.”
“My father’s cough was mild.”
“My mother does not have a cough or a fever.”
Despite knowing better, I was initially unable to accept that everyone in my family had contracted a disease that had already claimed the lives of tens of thousands globally.
Fear. In order to prevent the spread of infection, many hospitals made changes to their visitor policies, placing greater restrictions on who can come and go. This has meant hospital patients who have died from COVID-19 complications have done so separated from their loved ones. After transporting my mother to the hospital ED, I was politely but firmly asked to leave per the new visitor policy. I felt as though there were cinder blocks attached to my feet as I reluctantly walked away, not knowing if it would be the last time I would see her. I experienced a fear and sadness so intense, it continues to elicit an emotional response today as I think back on that moment.
Anxiety. The difference between fear and anxiety is fear is an emotional response to a known threat or danger, and anxiety is a response to an unknown threat or danger. The days that followed my parents’ hospitalizations were riddled with anxiety that would come in waves. How were they doing? Could they breathe? Do the overwhelmed hospital staff have time to take care of them? What can I do to help? Is there anything I can do to help? The worrisome thoughts and unanswerable questions were incessant and seemed unresponsive to my efforts to quell them.
Sadness. To feel sadness is to be human. In my work as a psychologist, I emphasize the value in experiencing this emotion when therapeutically beneficial. This technique is used as part of acceptance and commitment therapy (ACT), which emphasizes the value of being present or in touch with one’s thoughts and emotions, instead of working to eliminate them. During these scary times, I leaned into this notion more than ever. I gave myself permission to not feel okay, to cry more than I had in a long time, and to be unapologetically sad. I flip-flopped between states of near-despair and hopeful, with the switch usually following a call from a member of the hospital care team with updates on my parents’ conditions.
My parents’ road to recovery extended far beyond their discharge from the hospital and was not without incident, but with support and appropriate follow-up care, they have since made full recoveries from COVID-19. Although the relief and happiness this brings me is immeasurable, the experience has left a lasting impression on me as both a person and a psychologist. Speaking as a person, I cannot overstate the value of relying on one’s social support network while coping with stressors related to COVID-19. Whether you are directly or indirectly affected by the disease, the emotional effects can feel equally intense. As in times of happiness and celebration, times of sadness can and should be shared by those who are equipped to provide support. This can be tricky in an era during which isolation is prescribed for our safety, but we have more options today for connecting virtually with others than ever before, including video conferencing, email, and that old friend, the telephone. Furthermore, identify and assert your boundaries. Sometimes, saying no to others is the best way to say yes to yourself. Certain work, chores, and social obligations that can wait, should wait.
As a psychologist, my experience has given me a renewed appreciation for the power of the therapeutic use of self in psychotherapy. The factor with the greatest effects on psychotherapy outcomes is the quality of the therapeutic alliance, a concept introduced by Sigmund Freud in 1912. I believe a therapist’s willingness to show that we, too, experience life’s ups and downs strengthens our ability to demonstrate empathy and further promote a sense of alliance. Therapists are not immune to the effects of COVID-19, and to acknowledge this fact allows us to relate to our patients on a basic human level, which is more important now than ever.
Dr. Tseng, a licensed clinical psychologist, is in private practice in New York. She disclosed no relevant financial relationships.
What COVID-19 has taught us about senior care
Across the globe, there are marked differences in how countries responded to the COVID-19 outbreak, with varying degrees of success in limiting the spread of the virus. Some countries learned important lessons from previous outbreaks, including SARS and MERS, and put policies in place that contributed to lower infection and death rates from COVID-19 in these countries. Others struggled to respond appropriately to the outbreak.
The United States and most of the world was not affected significantly by SARS and MERS. Hence there is a need for different perspectives and observations on lessons that can be learned from this outbreak to help develop effective strategies and policies for the future. It also makes sense to focus intently on the demographic most affected by COVID-19 – the elderly.
Medical care, for the most part, is governed by protocols that clearly detail processes to be followed for the prevention and treatment of disease. Caring for older patients requires going above and beyond the protocols. That is one of the lessons learned from the COVID-19 pandemic – a wake-up call for a more proactive approach for at-risk patients, in this case everyone over the age of 60 years.
In this context, it is important for medical outreach to continue with the senior population long after the pandemic has run its course. Many seniors, particularly those susceptible to other illnesses or exhibiting ongoing issues, would benefit from a consistent and preplanned pattern of contacts by medical professionals and agencies that work with the aging population. These proactive follow-ups can facilitate prevention and treatment and, at the same time, reduce costs that would otherwise increase when health care is reactive.
Lessons in infectious disease containment
As COVID-19 spread globally, there were contrasting responses from individual countries in their efforts to contain the disease. Unfortunately, Italy suffered from its decision to lock down only specific regions of the country initially. The leadership in Italy may have ignored the advice of medical experts and been caught off guard by the intensity of the spread of COVID-19. In fact, they might not have taken strict actions right away because they did not want their responses to be viewed as an overreaction to the disease.
The government decided to shut down areas where the infection rates were high (“red zones”) rather than implement restrictions nationally. This may have inadvertently increased the spread as Italians vacated those “red zones” for other areas of the country not yet affected by COVID-19. Italy’s decentralized health care system also played a part in the effects of the disease, with some regions demonstrating more success in slowing the reach of the disease. According to an article in the Harvard Business Review, the neighboring regions of Lombardy and Veneto applied similar approaches to social distancing and retail closures. Veneto was more proactive, and its response to the outbreak was multipronged, including putting a “strong emphasis on home diagnosis and care” and “specific efforts to monitor and protect health care and other essential workers.” These measures most likely contributed to a slowdown of the spread of the disease in Veneto’s health care facilities, which lessened the load on medical providers.1
Conversely, Taiwan implemented proactive measures swiftly after learning about COVID-19. Taiwan was impacted adversely by the SARS outbreak in 2003 and, afterward, revised their medical policies and procedures to respond quickly to future infectious disease crises. In the beginning, little was known about COVID-19 or how it spread. However, Taiwan’s swift public health response to COVID-19 included early travel restrictions, patient screening, and quarantining of symptomatic patients. The government emphasized education and created real-time digital updates and alerts sent to their citizens, as well as partnering with media to broadcast crucial proactive health information and quickly disproving false information related to COVID-19. They coordinated with organizations throughout the country to increase supplies of personal protective equipment (PPE).2
Although countries and even cities within a country differ in terms of population demographics, health resources, government policies, and cultural practices, initial success stories have some similarities, including the following:
- Early travel restrictions from countries with positive cases, with some circumstances requiring compulsory quarantine periods and testing before entry.
- Extensive testing and proactive tracing of symptomatic cases early. Contacts of people testing positive were also tested, irrespective of being symptomatic or asymptomatic. If testing kits were unavailable, the contacts were self-quarantined.
- Emphasis on avoiding overburdening hospitals by having the public health infrastructure to divert people exhibiting symptoms, including using public health hotlines to send patients to dedicated testing sites and drive-through testing, rather than have patients presenting to emergency rooms and hospitals. This approach protected medical staff from exposure and allowed the focus to remain on treating severe symptomatic patients.
The vastly different response to the COVID-19 outbreak in these two countries illuminates the need for better preparation in the United States. At the onset of this outbreak, emergency room medical professionals, hospitalists, and outpatient primary care providers did not know how to screen for or treat this virus. Additionally, there was limited information on the most effective contact protocols for medical professionals, patients, and visitors. Finally, the lack of PPE and COVID-19 test kits hindered the U.S. response. Once the country is on the road to recovery from COVID-19, it is imperative to set the groundwork to prepare for future outbreaks and create mechanisms to quickly identify vulnerable populations when outbreaks occur.
Senior care in future infectious disease outbreaks
How can medical providers translate lessons learned from this outbreak into improving the quality of care for seniors? The National Institute on Aging (NIA) maintains a website with information about healthy aging. Seniors and their caregivers can use this website to learn more about chronic diseases, lifestyle modifications, disease prevention, and mental health.
In times of a pandemic, this website provides consistent and accurate information and education. One recommendation for reaching the elderly population during future outbreaks is for NIA to develop and implement strategies to increase the use of the website, including adding more audio and visual interfaces and developing a mobile app. Other recommendations for improving the quality of care for seniors include the following:
1. Identify which populations may be most affected when future outbreaks occur.
2. Consider nontraditional platforms, including social media, for communicating with the general population and for medical providers worldwide to learn from each other about new diseases, including the signs, symptoms, and treatment plans. Some medical professionals created specific WhatsApp groups to communicate, and the World Health Organization sent updated information about COVID-19 to anyone who texted them via WhatsApp.3
3. Create a checklist of signs and symptoms related to current infectious diseases and assess every vulnerable patient.
4. Share these guidelines with medical facilities that treat these populations, such as senior care, assisted living and rehabilitation facilities, hospitals, and outpatient treatment centers. Teach the staff at these medical facilities how to screen patients for signs and symptoms of the disease.
5. Implement social isolation strategies, travel and visitor restrictions, and testing and screening as soon as possible at these medical facilities.
6. Recognize that these strategies may affect the psychological and emotional well-being of seniors, increasing their risk for depression and anxiety and negatively affecting their immunity and mental health. Additionally, the use of PPE, either by the medical providers or the patient, may cause anxiety in seniors and those with mild cognitive impairment.
7. Encourage these medical facilities to improve coping strategies with older patients, such as incorporating communication technology that helps seniors stay connected with their families, and participating in physical and mental exercise, as well as religious activities.
8. Ask these medical facilities to create isolation or quarantine rooms for infected seniors.
9. Work with family members to proactively report to medical professionals any symptoms noticed in their senior relatives. Educate seniors to report symptoms earlier.
10. Offer incentives for medical professionals to conduct on-site testing in primary care offices or senior care facilities instead of sending patients to hospital emergency rooms for evaluation. This will only be effective if there are enough test kits available.
11. Urge insurance companies and Medicare to allow additional medical visits for screening vulnerable populations. Encourage the use of telemedicine in place of in-office visits (preferably billed at the same rate as an in-office visit) where appropriate, especially with nonambulatory patients or those with transportation issues. Many insurance companies, including Medicare, approved COVID-19–related coverage of telemedicine in place of office visits to limit the spread of the disease.
12. Provide community health care and integration and better coordination of local, state, and national health care.
13. Hold regular epidemic and pandemic preparedness exercises in every hospital, nursing home, and assisted living facility.
Proactive health care outreach
It is easier to identify the signs and symptoms of already identified infectious diseases as opposed to a novel one like COVID-19. The United States faced a steep learning curve with COVID-19. Hospitalists and other medical professionals were not able to learn about COVID-19 in a journal. At first, they did not know how to screen patients coming into the ER, how to protect staff, or what the treatment plan was for this new disease. As a result, the medical system experienced disorder and confusion. Investing in community health care and better coordination of local, state, and national health care resources is a priority.
The senior citizen population appears to be most vulnerable to this virus and may be just as vulnerable in future outbreaks. Yet the insights gained from this pandemic can lead to a more comprehensive outreach to senior patients and increased screenings for comorbidities and future contagious diseases. An emphasis on proactive health care and outreach for seniors, with a focus on identifying and treating comorbid conditions, improves the medical care system overall and may prevent or slow future community outbreaks.
Dr. Kasarla is a hospitalist with APOGEE Physicians at Wise Surgical at Parkway in Fort Worth, Tex. He did his internal medicine residency at Mercy Hospital & Medical Center, Chicago. Readers can contact him at madhukarreddy.kasarla@apogeephysicians.com. Dr. Devireddy is a family physician at Positive Health Medical Center, Kingston, Jamaica. Contact him at drjaisheel@gmail.com.
References
1. Pisano GP et al. Lessons from Italy’s response to coronavirus. Harvard Business Review. 2020 Mar 27. https://hbr.org/2020/03/lessons-from-italys-response-to-coronavirus.
2. Tu C. Lessons from Taiwan’s experience with COVID-19. New Atlanticist. 2020 Apr 7. https://atlanticcouncil.org/blogs/new-atlanticist/lessons-from-taiwans-experience-with-covid-19/.
3. Newman LH. WhatsApp is at the center of coronavirus response. WIRED. 2020 Mar 20. https://www.wired.com/story/whatsapp-coronavirus-who-information-app/.
Across the globe, there are marked differences in how countries responded to the COVID-19 outbreak, with varying degrees of success in limiting the spread of the virus. Some countries learned important lessons from previous outbreaks, including SARS and MERS, and put policies in place that contributed to lower infection and death rates from COVID-19 in these countries. Others struggled to respond appropriately to the outbreak.
The United States and most of the world was not affected significantly by SARS and MERS. Hence there is a need for different perspectives and observations on lessons that can be learned from this outbreak to help develop effective strategies and policies for the future. It also makes sense to focus intently on the demographic most affected by COVID-19 – the elderly.
Medical care, for the most part, is governed by protocols that clearly detail processes to be followed for the prevention and treatment of disease. Caring for older patients requires going above and beyond the protocols. That is one of the lessons learned from the COVID-19 pandemic – a wake-up call for a more proactive approach for at-risk patients, in this case everyone over the age of 60 years.
In this context, it is important for medical outreach to continue with the senior population long after the pandemic has run its course. Many seniors, particularly those susceptible to other illnesses or exhibiting ongoing issues, would benefit from a consistent and preplanned pattern of contacts by medical professionals and agencies that work with the aging population. These proactive follow-ups can facilitate prevention and treatment and, at the same time, reduce costs that would otherwise increase when health care is reactive.
Lessons in infectious disease containment
As COVID-19 spread globally, there were contrasting responses from individual countries in their efforts to contain the disease. Unfortunately, Italy suffered from its decision to lock down only specific regions of the country initially. The leadership in Italy may have ignored the advice of medical experts and been caught off guard by the intensity of the spread of COVID-19. In fact, they might not have taken strict actions right away because they did not want their responses to be viewed as an overreaction to the disease.
The government decided to shut down areas where the infection rates were high (“red zones”) rather than implement restrictions nationally. This may have inadvertently increased the spread as Italians vacated those “red zones” for other areas of the country not yet affected by COVID-19. Italy’s decentralized health care system also played a part in the effects of the disease, with some regions demonstrating more success in slowing the reach of the disease. According to an article in the Harvard Business Review, the neighboring regions of Lombardy and Veneto applied similar approaches to social distancing and retail closures. Veneto was more proactive, and its response to the outbreak was multipronged, including putting a “strong emphasis on home diagnosis and care” and “specific efforts to monitor and protect health care and other essential workers.” These measures most likely contributed to a slowdown of the spread of the disease in Veneto’s health care facilities, which lessened the load on medical providers.1
Conversely, Taiwan implemented proactive measures swiftly after learning about COVID-19. Taiwan was impacted adversely by the SARS outbreak in 2003 and, afterward, revised their medical policies and procedures to respond quickly to future infectious disease crises. In the beginning, little was known about COVID-19 or how it spread. However, Taiwan’s swift public health response to COVID-19 included early travel restrictions, patient screening, and quarantining of symptomatic patients. The government emphasized education and created real-time digital updates and alerts sent to their citizens, as well as partnering with media to broadcast crucial proactive health information and quickly disproving false information related to COVID-19. They coordinated with organizations throughout the country to increase supplies of personal protective equipment (PPE).2
Although countries and even cities within a country differ in terms of population demographics, health resources, government policies, and cultural practices, initial success stories have some similarities, including the following:
- Early travel restrictions from countries with positive cases, with some circumstances requiring compulsory quarantine periods and testing before entry.
- Extensive testing and proactive tracing of symptomatic cases early. Contacts of people testing positive were also tested, irrespective of being symptomatic or asymptomatic. If testing kits were unavailable, the contacts were self-quarantined.
- Emphasis on avoiding overburdening hospitals by having the public health infrastructure to divert people exhibiting symptoms, including using public health hotlines to send patients to dedicated testing sites and drive-through testing, rather than have patients presenting to emergency rooms and hospitals. This approach protected medical staff from exposure and allowed the focus to remain on treating severe symptomatic patients.
The vastly different response to the COVID-19 outbreak in these two countries illuminates the need for better preparation in the United States. At the onset of this outbreak, emergency room medical professionals, hospitalists, and outpatient primary care providers did not know how to screen for or treat this virus. Additionally, there was limited information on the most effective contact protocols for medical professionals, patients, and visitors. Finally, the lack of PPE and COVID-19 test kits hindered the U.S. response. Once the country is on the road to recovery from COVID-19, it is imperative to set the groundwork to prepare for future outbreaks and create mechanisms to quickly identify vulnerable populations when outbreaks occur.
Senior care in future infectious disease outbreaks
How can medical providers translate lessons learned from this outbreak into improving the quality of care for seniors? The National Institute on Aging (NIA) maintains a website with information about healthy aging. Seniors and their caregivers can use this website to learn more about chronic diseases, lifestyle modifications, disease prevention, and mental health.
In times of a pandemic, this website provides consistent and accurate information and education. One recommendation for reaching the elderly population during future outbreaks is for NIA to develop and implement strategies to increase the use of the website, including adding more audio and visual interfaces and developing a mobile app. Other recommendations for improving the quality of care for seniors include the following:
1. Identify which populations may be most affected when future outbreaks occur.
2. Consider nontraditional platforms, including social media, for communicating with the general population and for medical providers worldwide to learn from each other about new diseases, including the signs, symptoms, and treatment plans. Some medical professionals created specific WhatsApp groups to communicate, and the World Health Organization sent updated information about COVID-19 to anyone who texted them via WhatsApp.3
3. Create a checklist of signs and symptoms related to current infectious diseases and assess every vulnerable patient.
4. Share these guidelines with medical facilities that treat these populations, such as senior care, assisted living and rehabilitation facilities, hospitals, and outpatient treatment centers. Teach the staff at these medical facilities how to screen patients for signs and symptoms of the disease.
5. Implement social isolation strategies, travel and visitor restrictions, and testing and screening as soon as possible at these medical facilities.
6. Recognize that these strategies may affect the psychological and emotional well-being of seniors, increasing their risk for depression and anxiety and negatively affecting their immunity and mental health. Additionally, the use of PPE, either by the medical providers or the patient, may cause anxiety in seniors and those with mild cognitive impairment.
7. Encourage these medical facilities to improve coping strategies with older patients, such as incorporating communication technology that helps seniors stay connected with their families, and participating in physical and mental exercise, as well as religious activities.
8. Ask these medical facilities to create isolation or quarantine rooms for infected seniors.
9. Work with family members to proactively report to medical professionals any symptoms noticed in their senior relatives. Educate seniors to report symptoms earlier.
10. Offer incentives for medical professionals to conduct on-site testing in primary care offices or senior care facilities instead of sending patients to hospital emergency rooms for evaluation. This will only be effective if there are enough test kits available.
11. Urge insurance companies and Medicare to allow additional medical visits for screening vulnerable populations. Encourage the use of telemedicine in place of in-office visits (preferably billed at the same rate as an in-office visit) where appropriate, especially with nonambulatory patients or those with transportation issues. Many insurance companies, including Medicare, approved COVID-19–related coverage of telemedicine in place of office visits to limit the spread of the disease.
12. Provide community health care and integration and better coordination of local, state, and national health care.
13. Hold regular epidemic and pandemic preparedness exercises in every hospital, nursing home, and assisted living facility.
Proactive health care outreach
It is easier to identify the signs and symptoms of already identified infectious diseases as opposed to a novel one like COVID-19. The United States faced a steep learning curve with COVID-19. Hospitalists and other medical professionals were not able to learn about COVID-19 in a journal. At first, they did not know how to screen patients coming into the ER, how to protect staff, or what the treatment plan was for this new disease. As a result, the medical system experienced disorder and confusion. Investing in community health care and better coordination of local, state, and national health care resources is a priority.
The senior citizen population appears to be most vulnerable to this virus and may be just as vulnerable in future outbreaks. Yet the insights gained from this pandemic can lead to a more comprehensive outreach to senior patients and increased screenings for comorbidities and future contagious diseases. An emphasis on proactive health care and outreach for seniors, with a focus on identifying and treating comorbid conditions, improves the medical care system overall and may prevent or slow future community outbreaks.
Dr. Kasarla is a hospitalist with APOGEE Physicians at Wise Surgical at Parkway in Fort Worth, Tex. He did his internal medicine residency at Mercy Hospital & Medical Center, Chicago. Readers can contact him at madhukarreddy.kasarla@apogeephysicians.com. Dr. Devireddy is a family physician at Positive Health Medical Center, Kingston, Jamaica. Contact him at drjaisheel@gmail.com.
References
1. Pisano GP et al. Lessons from Italy’s response to coronavirus. Harvard Business Review. 2020 Mar 27. https://hbr.org/2020/03/lessons-from-italys-response-to-coronavirus.
2. Tu C. Lessons from Taiwan’s experience with COVID-19. New Atlanticist. 2020 Apr 7. https://atlanticcouncil.org/blogs/new-atlanticist/lessons-from-taiwans-experience-with-covid-19/.
3. Newman LH. WhatsApp is at the center of coronavirus response. WIRED. 2020 Mar 20. https://www.wired.com/story/whatsapp-coronavirus-who-information-app/.
Across the globe, there are marked differences in how countries responded to the COVID-19 outbreak, with varying degrees of success in limiting the spread of the virus. Some countries learned important lessons from previous outbreaks, including SARS and MERS, and put policies in place that contributed to lower infection and death rates from COVID-19 in these countries. Others struggled to respond appropriately to the outbreak.
The United States and most of the world was not affected significantly by SARS and MERS. Hence there is a need for different perspectives and observations on lessons that can be learned from this outbreak to help develop effective strategies and policies for the future. It also makes sense to focus intently on the demographic most affected by COVID-19 – the elderly.
Medical care, for the most part, is governed by protocols that clearly detail processes to be followed for the prevention and treatment of disease. Caring for older patients requires going above and beyond the protocols. That is one of the lessons learned from the COVID-19 pandemic – a wake-up call for a more proactive approach for at-risk patients, in this case everyone over the age of 60 years.
In this context, it is important for medical outreach to continue with the senior population long after the pandemic has run its course. Many seniors, particularly those susceptible to other illnesses or exhibiting ongoing issues, would benefit from a consistent and preplanned pattern of contacts by medical professionals and agencies that work with the aging population. These proactive follow-ups can facilitate prevention and treatment and, at the same time, reduce costs that would otherwise increase when health care is reactive.
Lessons in infectious disease containment
As COVID-19 spread globally, there were contrasting responses from individual countries in their efforts to contain the disease. Unfortunately, Italy suffered from its decision to lock down only specific regions of the country initially. The leadership in Italy may have ignored the advice of medical experts and been caught off guard by the intensity of the spread of COVID-19. In fact, they might not have taken strict actions right away because they did not want their responses to be viewed as an overreaction to the disease.
The government decided to shut down areas where the infection rates were high (“red zones”) rather than implement restrictions nationally. This may have inadvertently increased the spread as Italians vacated those “red zones” for other areas of the country not yet affected by COVID-19. Italy’s decentralized health care system also played a part in the effects of the disease, with some regions demonstrating more success in slowing the reach of the disease. According to an article in the Harvard Business Review, the neighboring regions of Lombardy and Veneto applied similar approaches to social distancing and retail closures. Veneto was more proactive, and its response to the outbreak was multipronged, including putting a “strong emphasis on home diagnosis and care” and “specific efforts to monitor and protect health care and other essential workers.” These measures most likely contributed to a slowdown of the spread of the disease in Veneto’s health care facilities, which lessened the load on medical providers.1
Conversely, Taiwan implemented proactive measures swiftly after learning about COVID-19. Taiwan was impacted adversely by the SARS outbreak in 2003 and, afterward, revised their medical policies and procedures to respond quickly to future infectious disease crises. In the beginning, little was known about COVID-19 or how it spread. However, Taiwan’s swift public health response to COVID-19 included early travel restrictions, patient screening, and quarantining of symptomatic patients. The government emphasized education and created real-time digital updates and alerts sent to their citizens, as well as partnering with media to broadcast crucial proactive health information and quickly disproving false information related to COVID-19. They coordinated with organizations throughout the country to increase supplies of personal protective equipment (PPE).2
Although countries and even cities within a country differ in terms of population demographics, health resources, government policies, and cultural practices, initial success stories have some similarities, including the following:
- Early travel restrictions from countries with positive cases, with some circumstances requiring compulsory quarantine periods and testing before entry.
- Extensive testing and proactive tracing of symptomatic cases early. Contacts of people testing positive were also tested, irrespective of being symptomatic or asymptomatic. If testing kits were unavailable, the contacts were self-quarantined.
- Emphasis on avoiding overburdening hospitals by having the public health infrastructure to divert people exhibiting symptoms, including using public health hotlines to send patients to dedicated testing sites and drive-through testing, rather than have patients presenting to emergency rooms and hospitals. This approach protected medical staff from exposure and allowed the focus to remain on treating severe symptomatic patients.
The vastly different response to the COVID-19 outbreak in these two countries illuminates the need for better preparation in the United States. At the onset of this outbreak, emergency room medical professionals, hospitalists, and outpatient primary care providers did not know how to screen for or treat this virus. Additionally, there was limited information on the most effective contact protocols for medical professionals, patients, and visitors. Finally, the lack of PPE and COVID-19 test kits hindered the U.S. response. Once the country is on the road to recovery from COVID-19, it is imperative to set the groundwork to prepare for future outbreaks and create mechanisms to quickly identify vulnerable populations when outbreaks occur.
Senior care in future infectious disease outbreaks
How can medical providers translate lessons learned from this outbreak into improving the quality of care for seniors? The National Institute on Aging (NIA) maintains a website with information about healthy aging. Seniors and their caregivers can use this website to learn more about chronic diseases, lifestyle modifications, disease prevention, and mental health.
In times of a pandemic, this website provides consistent and accurate information and education. One recommendation for reaching the elderly population during future outbreaks is for NIA to develop and implement strategies to increase the use of the website, including adding more audio and visual interfaces and developing a mobile app. Other recommendations for improving the quality of care for seniors include the following:
1. Identify which populations may be most affected when future outbreaks occur.
2. Consider nontraditional platforms, including social media, for communicating with the general population and for medical providers worldwide to learn from each other about new diseases, including the signs, symptoms, and treatment plans. Some medical professionals created specific WhatsApp groups to communicate, and the World Health Organization sent updated information about COVID-19 to anyone who texted them via WhatsApp.3
3. Create a checklist of signs and symptoms related to current infectious diseases and assess every vulnerable patient.
4. Share these guidelines with medical facilities that treat these populations, such as senior care, assisted living and rehabilitation facilities, hospitals, and outpatient treatment centers. Teach the staff at these medical facilities how to screen patients for signs and symptoms of the disease.
5. Implement social isolation strategies, travel and visitor restrictions, and testing and screening as soon as possible at these medical facilities.
6. Recognize that these strategies may affect the psychological and emotional well-being of seniors, increasing their risk for depression and anxiety and negatively affecting their immunity and mental health. Additionally, the use of PPE, either by the medical providers or the patient, may cause anxiety in seniors and those with mild cognitive impairment.
7. Encourage these medical facilities to improve coping strategies with older patients, such as incorporating communication technology that helps seniors stay connected with their families, and participating in physical and mental exercise, as well as religious activities.
8. Ask these medical facilities to create isolation or quarantine rooms for infected seniors.
9. Work with family members to proactively report to medical professionals any symptoms noticed in their senior relatives. Educate seniors to report symptoms earlier.
10. Offer incentives for medical professionals to conduct on-site testing in primary care offices or senior care facilities instead of sending patients to hospital emergency rooms for evaluation. This will only be effective if there are enough test kits available.
11. Urge insurance companies and Medicare to allow additional medical visits for screening vulnerable populations. Encourage the use of telemedicine in place of in-office visits (preferably billed at the same rate as an in-office visit) where appropriate, especially with nonambulatory patients or those with transportation issues. Many insurance companies, including Medicare, approved COVID-19–related coverage of telemedicine in place of office visits to limit the spread of the disease.
12. Provide community health care and integration and better coordination of local, state, and national health care.
13. Hold regular epidemic and pandemic preparedness exercises in every hospital, nursing home, and assisted living facility.
Proactive health care outreach
It is easier to identify the signs and symptoms of already identified infectious diseases as opposed to a novel one like COVID-19. The United States faced a steep learning curve with COVID-19. Hospitalists and other medical professionals were not able to learn about COVID-19 in a journal. At first, they did not know how to screen patients coming into the ER, how to protect staff, or what the treatment plan was for this new disease. As a result, the medical system experienced disorder and confusion. Investing in community health care and better coordination of local, state, and national health care resources is a priority.
The senior citizen population appears to be most vulnerable to this virus and may be just as vulnerable in future outbreaks. Yet the insights gained from this pandemic can lead to a more comprehensive outreach to senior patients and increased screenings for comorbidities and future contagious diseases. An emphasis on proactive health care and outreach for seniors, with a focus on identifying and treating comorbid conditions, improves the medical care system overall and may prevent or slow future community outbreaks.
Dr. Kasarla is a hospitalist with APOGEE Physicians at Wise Surgical at Parkway in Fort Worth, Tex. He did his internal medicine residency at Mercy Hospital & Medical Center, Chicago. Readers can contact him at madhukarreddy.kasarla@apogeephysicians.com. Dr. Devireddy is a family physician at Positive Health Medical Center, Kingston, Jamaica. Contact him at drjaisheel@gmail.com.
References
1. Pisano GP et al. Lessons from Italy’s response to coronavirus. Harvard Business Review. 2020 Mar 27. https://hbr.org/2020/03/lessons-from-italys-response-to-coronavirus.
2. Tu C. Lessons from Taiwan’s experience with COVID-19. New Atlanticist. 2020 Apr 7. https://atlanticcouncil.org/blogs/new-atlanticist/lessons-from-taiwans-experience-with-covid-19/.
3. Newman LH. WhatsApp is at the center of coronavirus response. WIRED. 2020 Mar 20. https://www.wired.com/story/whatsapp-coronavirus-who-information-app/.