User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
Tyranny by the numbers
“How come you retired?” I asked.
A few years my junior, Marty had taught in public school forever. “It was the MCAS,” he said. That’s the Massachusetts Comprehensive Assessment System, a standardized test meant to gauge student performance and teacher competence.
“They demanded that my students test at a fifth-grade level,” Marty said. “But they were all at a second-grade level.
“Plus, I had been teaching for thirty years, and some kid right out of college was telling me how to do my job. So I left.”
Of course, this tale will sound familiar to physicians. Pay for performance. Bean counters calling the shots. Dismissal of clinical experience as useless and self-serving.
A recent book lays it all out: Jerry Z. Muller’s The Tyranny of Metrics. This book is punchy, witty, and succinct – you can read it in a day. A historian of economics and culture, Muller shows the extent of what I had guessed at from chats with people in different fields. In all of these, if you don’t count it, it doesn’t count.
Metrics, it is assumed, are “hard” and “objective.” They must “replace judgment based on experience with standardized measurement.” Their promise is transparency, efficiency, accountability.
Muller began to study this when he became chair of his academic department. He thought his job was to nurture scholars and help students learn, only to find much of his time taken up with feeding often worthless data to remote administrators. He traces the metrical impulse, at root, to lack of trust. It’s not only doctors whom society doesn’t trust, but experts of all kinds.
Principal agents ... “employed in institutions are not to be trusted … their activity must be monitored and measured ... those measures need to be transparent to those without firsthand knowledge of the institutions ... and ... pecuniary rewards and punishments are the best way to motivate ‘agents.’ ”
What this analysis ignores, argues Muller, is that professionals respond not just to “extrinsic motivation[s]” (money) but to intrinsic ones: commitment to profession and clients, doing the right thing, making people happier and better, being recognized and honored by peers, doing interesting and stimulating work. When society denigrates and dismisses those considerations, professionals become demoralized. They leave, or they learn to game the system.
Muller gives many examples. Punish hospitals for readmissions within 30 days of discharge? Fine – readmit patients under “observation status” and call them outpatients. Dock hospitals for deaths within 30 days of leaving? Keep the respirator on for an extra day, and let the patient die on day 31. Risky case? Don’t operate. “Juking the stats” – arresting many small-fry drug pushers instead of focusing on the kingpins. Does U.S. News and World Report rank a college higher for classes with under 20 students? Schedule seminars with a maximum of 19. (My example, not Muller’s.) Teach to the MCAS (unless, like Marty, you decide that’s hopeless and just quit). Buff the numbers.
You know the drill. And if you need to learn it to succeed – or not be judged a failure – you’ll learn it.
Studies show that “pay for performance” often doesn’t work. Metric advocates ignore these and call for more studies. In Muller’s words, “Metric fixation, which aspires to imitate science, too often resembles faith.”
Muller argues with balance and nuance. He affirms that objective measurement has helped sweep away old dogmas no one had ever tested and culled markedly substandard teachers. But he shows that over the past 30 years just counting what you know how to count, counting things that cannot be counted, and privileging belief over disconfirming evidence has conferred on metrics “elements of a cult,” whose baleful effects doctors and others toiling in their professional vineyards know too well.
Faith in metrics will wane and its cult will pass away, though likely well after we have done so ourselves. At some point, so-called situated knowledge – what people who actually do something know – will again be valued.
In the meantime, please rate this column highly (give it a 6 on a scale of 1-5), and confirm that there are no barriers to your implementing its wisdom, which comes unsullied by any financial conflicts of interest.
And check out Muller’s book. You have nothing to lose but your chains.
Measurement without meaning is tyranny!
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at amazon.com and barnesandnoble.com. Write to him at dermnews@mdedge.com.
“How come you retired?” I asked.
A few years my junior, Marty had taught in public school forever. “It was the MCAS,” he said. That’s the Massachusetts Comprehensive Assessment System, a standardized test meant to gauge student performance and teacher competence.
“They demanded that my students test at a fifth-grade level,” Marty said. “But they were all at a second-grade level.
“Plus, I had been teaching for thirty years, and some kid right out of college was telling me how to do my job. So I left.”
Of course, this tale will sound familiar to physicians. Pay for performance. Bean counters calling the shots. Dismissal of clinical experience as useless and self-serving.
A recent book lays it all out: Jerry Z. Muller’s The Tyranny of Metrics. This book is punchy, witty, and succinct – you can read it in a day. A historian of economics and culture, Muller shows the extent of what I had guessed at from chats with people in different fields. In all of these, if you don’t count it, it doesn’t count.
Metrics, it is assumed, are “hard” and “objective.” They must “replace judgment based on experience with standardized measurement.” Their promise is transparency, efficiency, accountability.
Muller began to study this when he became chair of his academic department. He thought his job was to nurture scholars and help students learn, only to find much of his time taken up with feeding often worthless data to remote administrators. He traces the metrical impulse, at root, to lack of trust. It’s not only doctors whom society doesn’t trust, but experts of all kinds.
Principal agents ... “employed in institutions are not to be trusted … their activity must be monitored and measured ... those measures need to be transparent to those without firsthand knowledge of the institutions ... and ... pecuniary rewards and punishments are the best way to motivate ‘agents.’ ”
What this analysis ignores, argues Muller, is that professionals respond not just to “extrinsic motivation[s]” (money) but to intrinsic ones: commitment to profession and clients, doing the right thing, making people happier and better, being recognized and honored by peers, doing interesting and stimulating work. When society denigrates and dismisses those considerations, professionals become demoralized. They leave, or they learn to game the system.
Muller gives many examples. Punish hospitals for readmissions within 30 days of discharge? Fine – readmit patients under “observation status” and call them outpatients. Dock hospitals for deaths within 30 days of leaving? Keep the respirator on for an extra day, and let the patient die on day 31. Risky case? Don’t operate. “Juking the stats” – arresting many small-fry drug pushers instead of focusing on the kingpins. Does U.S. News and World Report rank a college higher for classes with under 20 students? Schedule seminars with a maximum of 19. (My example, not Muller’s.) Teach to the MCAS (unless, like Marty, you decide that’s hopeless and just quit). Buff the numbers.
You know the drill. And if you need to learn it to succeed – or not be judged a failure – you’ll learn it.
Studies show that “pay for performance” often doesn’t work. Metric advocates ignore these and call for more studies. In Muller’s words, “Metric fixation, which aspires to imitate science, too often resembles faith.”
Muller argues with balance and nuance. He affirms that objective measurement has helped sweep away old dogmas no one had ever tested and culled markedly substandard teachers. But he shows that over the past 30 years just counting what you know how to count, counting things that cannot be counted, and privileging belief over disconfirming evidence has conferred on metrics “elements of a cult,” whose baleful effects doctors and others toiling in their professional vineyards know too well.
Faith in metrics will wane and its cult will pass away, though likely well after we have done so ourselves. At some point, so-called situated knowledge – what people who actually do something know – will again be valued.
In the meantime, please rate this column highly (give it a 6 on a scale of 1-5), and confirm that there are no barriers to your implementing its wisdom, which comes unsullied by any financial conflicts of interest.
And check out Muller’s book. You have nothing to lose but your chains.
Measurement without meaning is tyranny!
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at amazon.com and barnesandnoble.com. Write to him at dermnews@mdedge.com.
“How come you retired?” I asked.
A few years my junior, Marty had taught in public school forever. “It was the MCAS,” he said. That’s the Massachusetts Comprehensive Assessment System, a standardized test meant to gauge student performance and teacher competence.
“They demanded that my students test at a fifth-grade level,” Marty said. “But they were all at a second-grade level.
“Plus, I had been teaching for thirty years, and some kid right out of college was telling me how to do my job. So I left.”
Of course, this tale will sound familiar to physicians. Pay for performance. Bean counters calling the shots. Dismissal of clinical experience as useless and self-serving.
A recent book lays it all out: Jerry Z. Muller’s The Tyranny of Metrics. This book is punchy, witty, and succinct – you can read it in a day. A historian of economics and culture, Muller shows the extent of what I had guessed at from chats with people in different fields. In all of these, if you don’t count it, it doesn’t count.
Metrics, it is assumed, are “hard” and “objective.” They must “replace judgment based on experience with standardized measurement.” Their promise is transparency, efficiency, accountability.
Muller began to study this when he became chair of his academic department. He thought his job was to nurture scholars and help students learn, only to find much of his time taken up with feeding often worthless data to remote administrators. He traces the metrical impulse, at root, to lack of trust. It’s not only doctors whom society doesn’t trust, but experts of all kinds.
Principal agents ... “employed in institutions are not to be trusted … their activity must be monitored and measured ... those measures need to be transparent to those without firsthand knowledge of the institutions ... and ... pecuniary rewards and punishments are the best way to motivate ‘agents.’ ”
What this analysis ignores, argues Muller, is that professionals respond not just to “extrinsic motivation[s]” (money) but to intrinsic ones: commitment to profession and clients, doing the right thing, making people happier and better, being recognized and honored by peers, doing interesting and stimulating work. When society denigrates and dismisses those considerations, professionals become demoralized. They leave, or they learn to game the system.
Muller gives many examples. Punish hospitals for readmissions within 30 days of discharge? Fine – readmit patients under “observation status” and call them outpatients. Dock hospitals for deaths within 30 days of leaving? Keep the respirator on for an extra day, and let the patient die on day 31. Risky case? Don’t operate. “Juking the stats” – arresting many small-fry drug pushers instead of focusing on the kingpins. Does U.S. News and World Report rank a college higher for classes with under 20 students? Schedule seminars with a maximum of 19. (My example, not Muller’s.) Teach to the MCAS (unless, like Marty, you decide that’s hopeless and just quit). Buff the numbers.
You know the drill. And if you need to learn it to succeed – or not be judged a failure – you’ll learn it.
Studies show that “pay for performance” often doesn’t work. Metric advocates ignore these and call for more studies. In Muller’s words, “Metric fixation, which aspires to imitate science, too often resembles faith.”
Muller argues with balance and nuance. He affirms that objective measurement has helped sweep away old dogmas no one had ever tested and culled markedly substandard teachers. But he shows that over the past 30 years just counting what you know how to count, counting things that cannot be counted, and privileging belief over disconfirming evidence has conferred on metrics “elements of a cult,” whose baleful effects doctors and others toiling in their professional vineyards know too well.
Faith in metrics will wane and its cult will pass away, though likely well after we have done so ourselves. At some point, so-called situated knowledge – what people who actually do something know – will again be valued.
In the meantime, please rate this column highly (give it a 6 on a scale of 1-5), and confirm that there are no barriers to your implementing its wisdom, which comes unsullied by any financial conflicts of interest.
And check out Muller’s book. You have nothing to lose but your chains.
Measurement without meaning is tyranny!
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at amazon.com and barnesandnoble.com. Write to him at dermnews@mdedge.com.
SPRINT MIND with extension planned
Also today, medical ethics and economics, PTSD after traumatic brain injury may be predicted by race and ethnicity, and aspirin for primary cardiovascular prevention.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, medical ethics and economics, PTSD after traumatic brain injury may be predicted by race and ethnicity, and aspirin for primary cardiovascular prevention.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, medical ethics and economics, PTSD after traumatic brain injury may be predicted by race and ethnicity, and aspirin for primary cardiovascular prevention.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Clinical benefits persist 5 years after thymectomy for myasthenia gravis
Thymectomy may continue to benefit patients with myasthenia gravis 5 years after the procedure, according to an extension study published in Lancet Neurology.
The study evaluated the clinical status, medication requirements, and adverse events of patients with myasthenia gravis who completed a randomized controlled trial of thymectomy plus prednisone versus prednisone alone and agreed to participate in a rater-blinded 2-year extension.
“Thymectomy within the first few years of the disease course in addition to prednisone therapy confers benefits that persist for 5 years ... in patients with generalized nonthymomatous myasthenia gravis,” said lead study author Gil I. Wolfe, MD, chair of the department of neurology at the University at Buffalo in New York, and his research colleagues. “Results from the extension study provide further support for the use of thymectomy in management of myasthenia gravis and should encourage serious consideration of this treatment option in discussions between clinicians and their patients,” they wrote. “Our results should lead to revision of clinical guidelines in favor of thymectomy and could potentially reverse downward trends in the use of thymectomy in overall management of myasthenia gravis.”
The main 3-year results of the Thymectomy Trial in Nonthymomatous Myasthenia Gravis Patients Receiving Prednisone (MGTX) were reported in 2016; the international trial found that thymectomy plus prednisone was superior to prednisone alone at 3 years (N Engl J Med. 2016 Aug 11;375[6]:511-22). The extension study aimed to assess the durability of the treatment response.
MGTX enrolled patients aged 18-65 years who had generalized nonthymomatous myasthenia gravis of less than 5 years’ duration and Myasthenia Gravis Foundation of America Clinical Classification Class II-IV disease. Of 111 patients who completed MGTX, 68 entered the extension study, and 50 completed the 60-month assessment (24 patients in the prednisone alone group and 26 patients in the prednisone plus thymectomy group).
At 5 years, patients in the thymectomy plus prednisone group had significantly lower time-weighted average Quantitative Myasthenia Gravis (QMG) scores (5.47 vs. 9.34) and mean alternate-day prednisone doses (24 mg vs. 48 mg), compared with patients who received prednisone alone. Twelve of 35 patients in the thymectomy group and 14 of 33 patients in the prednisone group had at least one adverse event by month 60. No treatment-related deaths occurred in the extension phase.
At 5 years, significantly more patients who underwent thymectomy had minimal manifestation status (i.e., no functional limitations from the disease other than some muscle weakness) – 88% versus 58%. The corresponding figures at 3 years were 67% and 47%.
In addition, 3-year and 5-year data indicate that the need for hospitalization is reduced after surgery, compared with medical therapy alone, Dr. Wolfe said.
Two patients in each treatment arm had an increase of 2 points or more in the QMG score, indicating clinical worsening.
“Our current findings reinforce the benefit of thymectomy seen in [MGTX], dispelling doubts about the procedure’s benefits and how long those benefits last,” said Dr. Wolfe. “We do hope that the new findings help reverse the apparent reluctance to do thymectomy and that the proportion of patients with myasthenia gravis who undergo thymectomy will increase.”
The authors noted that the small sample size of the extension study may limit its generalizability.
The study received funding from the National Institutes of Health. Dr. Wolfe reported grants from the NIH, the Muscular Dystrophy Association, the Myasthenia Gravis Foundation of America, CSL-Behring, and ArgenX, as well as personal fees from Grifols, Shire, and Alexion Pharmaceuticals. Coauthors reported working with and receiving funds from agencies, foundations, and pharmaceutical companies.
SOURCE: Wolfe GI et al. Lancet Neurol. 2019 Jan 25. doi: 10.1016/S1474-4422(18)30392-2.
Thymectomy may continue to benefit patients with myasthenia gravis 5 years after the procedure, according to an extension study published in Lancet Neurology.
The study evaluated the clinical status, medication requirements, and adverse events of patients with myasthenia gravis who completed a randomized controlled trial of thymectomy plus prednisone versus prednisone alone and agreed to participate in a rater-blinded 2-year extension.
“Thymectomy within the first few years of the disease course in addition to prednisone therapy confers benefits that persist for 5 years ... in patients with generalized nonthymomatous myasthenia gravis,” said lead study author Gil I. Wolfe, MD, chair of the department of neurology at the University at Buffalo in New York, and his research colleagues. “Results from the extension study provide further support for the use of thymectomy in management of myasthenia gravis and should encourage serious consideration of this treatment option in discussions between clinicians and their patients,” they wrote. “Our results should lead to revision of clinical guidelines in favor of thymectomy and could potentially reverse downward trends in the use of thymectomy in overall management of myasthenia gravis.”
The main 3-year results of the Thymectomy Trial in Nonthymomatous Myasthenia Gravis Patients Receiving Prednisone (MGTX) were reported in 2016; the international trial found that thymectomy plus prednisone was superior to prednisone alone at 3 years (N Engl J Med. 2016 Aug 11;375[6]:511-22). The extension study aimed to assess the durability of the treatment response.
MGTX enrolled patients aged 18-65 years who had generalized nonthymomatous myasthenia gravis of less than 5 years’ duration and Myasthenia Gravis Foundation of America Clinical Classification Class II-IV disease. Of 111 patients who completed MGTX, 68 entered the extension study, and 50 completed the 60-month assessment (24 patients in the prednisone alone group and 26 patients in the prednisone plus thymectomy group).
At 5 years, patients in the thymectomy plus prednisone group had significantly lower time-weighted average Quantitative Myasthenia Gravis (QMG) scores (5.47 vs. 9.34) and mean alternate-day prednisone doses (24 mg vs. 48 mg), compared with patients who received prednisone alone. Twelve of 35 patients in the thymectomy group and 14 of 33 patients in the prednisone group had at least one adverse event by month 60. No treatment-related deaths occurred in the extension phase.
At 5 years, significantly more patients who underwent thymectomy had minimal manifestation status (i.e., no functional limitations from the disease other than some muscle weakness) – 88% versus 58%. The corresponding figures at 3 years were 67% and 47%.
In addition, 3-year and 5-year data indicate that the need for hospitalization is reduced after surgery, compared with medical therapy alone, Dr. Wolfe said.
Two patients in each treatment arm had an increase of 2 points or more in the QMG score, indicating clinical worsening.
“Our current findings reinforce the benefit of thymectomy seen in [MGTX], dispelling doubts about the procedure’s benefits and how long those benefits last,” said Dr. Wolfe. “We do hope that the new findings help reverse the apparent reluctance to do thymectomy and that the proportion of patients with myasthenia gravis who undergo thymectomy will increase.”
The authors noted that the small sample size of the extension study may limit its generalizability.
The study received funding from the National Institutes of Health. Dr. Wolfe reported grants from the NIH, the Muscular Dystrophy Association, the Myasthenia Gravis Foundation of America, CSL-Behring, and ArgenX, as well as personal fees from Grifols, Shire, and Alexion Pharmaceuticals. Coauthors reported working with and receiving funds from agencies, foundations, and pharmaceutical companies.
SOURCE: Wolfe GI et al. Lancet Neurol. 2019 Jan 25. doi: 10.1016/S1474-4422(18)30392-2.
Thymectomy may continue to benefit patients with myasthenia gravis 5 years after the procedure, according to an extension study published in Lancet Neurology.
The study evaluated the clinical status, medication requirements, and adverse events of patients with myasthenia gravis who completed a randomized controlled trial of thymectomy plus prednisone versus prednisone alone and agreed to participate in a rater-blinded 2-year extension.
“Thymectomy within the first few years of the disease course in addition to prednisone therapy confers benefits that persist for 5 years ... in patients with generalized nonthymomatous myasthenia gravis,” said lead study author Gil I. Wolfe, MD, chair of the department of neurology at the University at Buffalo in New York, and his research colleagues. “Results from the extension study provide further support for the use of thymectomy in management of myasthenia gravis and should encourage serious consideration of this treatment option in discussions between clinicians and their patients,” they wrote. “Our results should lead to revision of clinical guidelines in favor of thymectomy and could potentially reverse downward trends in the use of thymectomy in overall management of myasthenia gravis.”
The main 3-year results of the Thymectomy Trial in Nonthymomatous Myasthenia Gravis Patients Receiving Prednisone (MGTX) were reported in 2016; the international trial found that thymectomy plus prednisone was superior to prednisone alone at 3 years (N Engl J Med. 2016 Aug 11;375[6]:511-22). The extension study aimed to assess the durability of the treatment response.
MGTX enrolled patients aged 18-65 years who had generalized nonthymomatous myasthenia gravis of less than 5 years’ duration and Myasthenia Gravis Foundation of America Clinical Classification Class II-IV disease. Of 111 patients who completed MGTX, 68 entered the extension study, and 50 completed the 60-month assessment (24 patients in the prednisone alone group and 26 patients in the prednisone plus thymectomy group).
At 5 years, patients in the thymectomy plus prednisone group had significantly lower time-weighted average Quantitative Myasthenia Gravis (QMG) scores (5.47 vs. 9.34) and mean alternate-day prednisone doses (24 mg vs. 48 mg), compared with patients who received prednisone alone. Twelve of 35 patients in the thymectomy group and 14 of 33 patients in the prednisone group had at least one adverse event by month 60. No treatment-related deaths occurred in the extension phase.
At 5 years, significantly more patients who underwent thymectomy had minimal manifestation status (i.e., no functional limitations from the disease other than some muscle weakness) – 88% versus 58%. The corresponding figures at 3 years were 67% and 47%.
In addition, 3-year and 5-year data indicate that the need for hospitalization is reduced after surgery, compared with medical therapy alone, Dr. Wolfe said.
Two patients in each treatment arm had an increase of 2 points or more in the QMG score, indicating clinical worsening.
“Our current findings reinforce the benefit of thymectomy seen in [MGTX], dispelling doubts about the procedure’s benefits and how long those benefits last,” said Dr. Wolfe. “We do hope that the new findings help reverse the apparent reluctance to do thymectomy and that the proportion of patients with myasthenia gravis who undergo thymectomy will increase.”
The authors noted that the small sample size of the extension study may limit its generalizability.
The study received funding from the National Institutes of Health. Dr. Wolfe reported grants from the NIH, the Muscular Dystrophy Association, the Myasthenia Gravis Foundation of America, CSL-Behring, and ArgenX, as well as personal fees from Grifols, Shire, and Alexion Pharmaceuticals. Coauthors reported working with and receiving funds from agencies, foundations, and pharmaceutical companies.
SOURCE: Wolfe GI et al. Lancet Neurol. 2019 Jan 25. doi: 10.1016/S1474-4422(18)30392-2.
FROM LANCET NEUROLOGY
Key clinical point: The benefits of thymectomy for myasthenia gravis persist 5 years after the procedure.
Major finding: Patients who undergo thymectomy and receive prednisone have lower time-weighted average Quantitative Myasthenia Gravis scores (5.47 vs. 9.34) and mean alternate-day prednisone doses (24 mg vs. 48 mg), compared with patients who receive prednisone alone.
Study details: A rater-blinded 2-year extension study that enrolled 68 patients who had completed a 3-year randomized controlled trial.
Disclosures: The study received funding from the National Institutes of Health. Dr. Wolfe reported grants from the NIH, the Muscular Dystrophy Association, the Myasthenia Gravis Foundation of America, CSL-Behring, and ArgenX, as well as personal fees from Grifols, Shire, and Alexion Pharmaceuticals. Other authors reported working with and receiving funds from various agencies, foundations, and pharmaceutical companies.
Source: Wolfe GI et al. Lancet Neurol. 2019 Jan 25. doi: 10.1016/S1474-4422(18)30392-2.
Mild OSA spontaneously resolves in about one-third of young children
CORONADO, CALIF. – results from a single-center study showed.
“OSA affects up to 6% of the pediatric population, and diagnosis of young children can be particularly challenging due to the heterogeneity of presenting symptoms,” Douglas C. von Allmen, MD, said at the Triological Society’s Combined Sections Meeting. “While school-age children may present with snoring, that’s less common in the younger population. Up to one-quarter of infants may have noisy breathing, which may mimic obstructive events throughout the first 3 years of life. Additionally, long-term clinical implications of mild sleep apnea in very young children is unclear.”
According to Dr. von Allmen, a fifth-year otolaryngology resident at the University of Cincinnati, management strategies of children with OSA can include a period of observation, particularly when there’s an absence of concerning findings on polysomnography (PSG), such as hypoventilation or significant hypoxia, or when the primary etiology of the OSA is unknown. “Additionally, few studies at this point have attempted to characterize the natural history of mild OSA in pediatric patients under 3 years of age,” he said.
In an effort to assess the effects of observation on the PSG outcomes of children under 3 years with mild OSA, Dr. Von Allmen and his colleagues performed a retrospective review of 26 children who had an overnight PSG with a follow-up PSG performed 3-12 months later. They excluded patients with neuromuscular disease, tracheostomy, or interstitial lung disease. All PSGs were performed at the Cincinnati Children’s Hospital Medical Center between 2012 and 2017 and were scored by a board-certified sleep physician. The researchers defined mild OSA as at least one, but fewer than five, events per hour. The mean age of the 26 patients was 7 months, 65% were male, 92% were white, and their median body mass index was in the 39th percentile. Comorbidities include laryngomalacia (40%), cardiac disease (40%), allergies (34%), asthma (23%), and Down syndrome (11%).
Between baseline and follow-up, the apnea-hypoapnea index (AHI) trended downward from 4.3 to 3.4 events per hour (P = .19), the obstructive AHI decreased significantly from 2.7 to 1.3 events per hour (P = .013), while the central apnea index also trended downward from 1.4 to 1.2 events per hour (P = .60). The oxyhemoglobin nadir and sleep efficiency did not change significantly, but there was a decrease in the arousal index (from 14.7 to 13 events per hour; P = .027) and in the percentage of REM sleep (from 33% to 30%; P = .008).
As for postobservation OSA severity outcomes, eight patients (31%) resolved spontaneously, one patient progressed from mild to moderate OSA, and the rest remained in their mild OSA state. Subanalysis revealed that OSA resolution rate was 36% in patients with laryngomalacia, compared with 27% in those with no laryngomalacia, a difference that did not reach statistical significance (P = .98).
Dr. von Allmen pointed out that the study cohort had comorbidities which may have contributed to the persistence of OSA. He also acknowledged certain limitations of the study, including its retrospective nature, the potential for selection bias, the small sample size, and the fact that it did not include a control sample of normal children. “The presence of laryngomalacia did not affect the resolution rate in our cohort, but we’ll need larger studies to better elucidate the factors that do affect persistent disease and to identify the optimal timing of intervention in children with mild OSA,” he said.
Dr. von Allmen reported having no financial disclosures. The study received a resident research award at the meeting, which was jointly sponsored by the Triological Society and the American College of Surgeons.
SOURCE: von Allmen DC et al. Triological CSM, Abstracts.
CORONADO, CALIF. – results from a single-center study showed.
“OSA affects up to 6% of the pediatric population, and diagnosis of young children can be particularly challenging due to the heterogeneity of presenting symptoms,” Douglas C. von Allmen, MD, said at the Triological Society’s Combined Sections Meeting. “While school-age children may present with snoring, that’s less common in the younger population. Up to one-quarter of infants may have noisy breathing, which may mimic obstructive events throughout the first 3 years of life. Additionally, long-term clinical implications of mild sleep apnea in very young children is unclear.”
According to Dr. von Allmen, a fifth-year otolaryngology resident at the University of Cincinnati, management strategies of children with OSA can include a period of observation, particularly when there’s an absence of concerning findings on polysomnography (PSG), such as hypoventilation or significant hypoxia, or when the primary etiology of the OSA is unknown. “Additionally, few studies at this point have attempted to characterize the natural history of mild OSA in pediatric patients under 3 years of age,” he said.
In an effort to assess the effects of observation on the PSG outcomes of children under 3 years with mild OSA, Dr. Von Allmen and his colleagues performed a retrospective review of 26 children who had an overnight PSG with a follow-up PSG performed 3-12 months later. They excluded patients with neuromuscular disease, tracheostomy, or interstitial lung disease. All PSGs were performed at the Cincinnati Children’s Hospital Medical Center between 2012 and 2017 and were scored by a board-certified sleep physician. The researchers defined mild OSA as at least one, but fewer than five, events per hour. The mean age of the 26 patients was 7 months, 65% were male, 92% were white, and their median body mass index was in the 39th percentile. Comorbidities include laryngomalacia (40%), cardiac disease (40%), allergies (34%), asthma (23%), and Down syndrome (11%).
Between baseline and follow-up, the apnea-hypoapnea index (AHI) trended downward from 4.3 to 3.4 events per hour (P = .19), the obstructive AHI decreased significantly from 2.7 to 1.3 events per hour (P = .013), while the central apnea index also trended downward from 1.4 to 1.2 events per hour (P = .60). The oxyhemoglobin nadir and sleep efficiency did not change significantly, but there was a decrease in the arousal index (from 14.7 to 13 events per hour; P = .027) and in the percentage of REM sleep (from 33% to 30%; P = .008).
As for postobservation OSA severity outcomes, eight patients (31%) resolved spontaneously, one patient progressed from mild to moderate OSA, and the rest remained in their mild OSA state. Subanalysis revealed that OSA resolution rate was 36% in patients with laryngomalacia, compared with 27% in those with no laryngomalacia, a difference that did not reach statistical significance (P = .98).
Dr. von Allmen pointed out that the study cohort had comorbidities which may have contributed to the persistence of OSA. He also acknowledged certain limitations of the study, including its retrospective nature, the potential for selection bias, the small sample size, and the fact that it did not include a control sample of normal children. “The presence of laryngomalacia did not affect the resolution rate in our cohort, but we’ll need larger studies to better elucidate the factors that do affect persistent disease and to identify the optimal timing of intervention in children with mild OSA,” he said.
Dr. von Allmen reported having no financial disclosures. The study received a resident research award at the meeting, which was jointly sponsored by the Triological Society and the American College of Surgeons.
SOURCE: von Allmen DC et al. Triological CSM, Abstracts.
CORONADO, CALIF. – results from a single-center study showed.
“OSA affects up to 6% of the pediatric population, and diagnosis of young children can be particularly challenging due to the heterogeneity of presenting symptoms,” Douglas C. von Allmen, MD, said at the Triological Society’s Combined Sections Meeting. “While school-age children may present with snoring, that’s less common in the younger population. Up to one-quarter of infants may have noisy breathing, which may mimic obstructive events throughout the first 3 years of life. Additionally, long-term clinical implications of mild sleep apnea in very young children is unclear.”
According to Dr. von Allmen, a fifth-year otolaryngology resident at the University of Cincinnati, management strategies of children with OSA can include a period of observation, particularly when there’s an absence of concerning findings on polysomnography (PSG), such as hypoventilation or significant hypoxia, or when the primary etiology of the OSA is unknown. “Additionally, few studies at this point have attempted to characterize the natural history of mild OSA in pediatric patients under 3 years of age,” he said.
In an effort to assess the effects of observation on the PSG outcomes of children under 3 years with mild OSA, Dr. Von Allmen and his colleagues performed a retrospective review of 26 children who had an overnight PSG with a follow-up PSG performed 3-12 months later. They excluded patients with neuromuscular disease, tracheostomy, or interstitial lung disease. All PSGs were performed at the Cincinnati Children’s Hospital Medical Center between 2012 and 2017 and were scored by a board-certified sleep physician. The researchers defined mild OSA as at least one, but fewer than five, events per hour. The mean age of the 26 patients was 7 months, 65% were male, 92% were white, and their median body mass index was in the 39th percentile. Comorbidities include laryngomalacia (40%), cardiac disease (40%), allergies (34%), asthma (23%), and Down syndrome (11%).
Between baseline and follow-up, the apnea-hypoapnea index (AHI) trended downward from 4.3 to 3.4 events per hour (P = .19), the obstructive AHI decreased significantly from 2.7 to 1.3 events per hour (P = .013), while the central apnea index also trended downward from 1.4 to 1.2 events per hour (P = .60). The oxyhemoglobin nadir and sleep efficiency did not change significantly, but there was a decrease in the arousal index (from 14.7 to 13 events per hour; P = .027) and in the percentage of REM sleep (from 33% to 30%; P = .008).
As for postobservation OSA severity outcomes, eight patients (31%) resolved spontaneously, one patient progressed from mild to moderate OSA, and the rest remained in their mild OSA state. Subanalysis revealed that OSA resolution rate was 36% in patients with laryngomalacia, compared with 27% in those with no laryngomalacia, a difference that did not reach statistical significance (P = .98).
Dr. von Allmen pointed out that the study cohort had comorbidities which may have contributed to the persistence of OSA. He also acknowledged certain limitations of the study, including its retrospective nature, the potential for selection bias, the small sample size, and the fact that it did not include a control sample of normal children. “The presence of laryngomalacia did not affect the resolution rate in our cohort, but we’ll need larger studies to better elucidate the factors that do affect persistent disease and to identify the optimal timing of intervention in children with mild OSA,” he said.
Dr. von Allmen reported having no financial disclosures. The study received a resident research award at the meeting, which was jointly sponsored by the Triological Society and the American College of Surgeons.
SOURCE: von Allmen DC et al. Triological CSM, Abstracts.
REPORTING FROM THE TRIOLOGICAL CSM
Key clinical point: Comorbidities may contribute to the persistence of OSA in young children.
Major finding: OSA spontaneously resolved in 31% of patients.
Study details: A retrospective analysis of 26 children under age 3 years.
Disclosures: The researchers reported having no financial disclosures.
Source: Von Allmen et al. Triological CSM, Abstracts.
Phase 3 studies of antiamyloid Alzheimer’s drug crenezumab stopped
After a disappointing interim analysis, Roche and its collaborator AC Immune are halting two phase 3 trials of the antiamyloid antibody crenezumab.
CREAD 1 and CREAD 2 enrolled patients with prodromal-to-mild sporadic Alzheimer’s disease. The preplanned interim safety and efficacy analysis determined that neither study was likely to meet the primary endpoint of change from baseline on the Clinical Dementia Rating-sum of boxes score.
There were no unexpected safety signals associated with the drug, despite a quadrupling of the phase 3 dose from that used in phase 2. The company in its press release said that it will continue to conduct the Autosomal Dominant Alzheimer’s Disease (ADAD) trial as part of the Alzheimer’s Prevention Initiative (API). ADAD is a large South American trial of crenezumab in Colombian families with familial Alzheimer’s caused by mutations in the presenilin-1 gene (PSEN1).
Roche did not release any data but said the trial results will be discussed at an upcoming scientific meeting.
“While the results with crenezumab are disappointing, they meaningfully contribute to our understanding of Alzheimer’s disease,” Sandra Horning, MD, Roche’s chief medical officer and executive vice president for global development, said in an interview. “We gratefully acknowledge the participants in the CREAD trials and the efforts of everyone involved in this important program.”
The decision was not a surprise to researchers who have followed the antibody’s development. It advanced into phase 3 with lackluster phase 2 cognitive, imaging, and biomarker data. Its selection as the therapeutic agent for the ADAD trial was a key driver in its continued development, securing Roche $100 million in federal funds to help launch ADAD, the first-ever Alzheimer’s primary prevention study.
Despite its failure in sporadic Alzheimer’s, there is still some hope that crenezumab might benefit people with the PSEN1 mutation, said Richard Caselli, MD, professor of neurology at the Mayo Clinic Arizona in Scottsdale and associate director and clinical core director of the Arizona Alzheimer’s Disease Center.
“The Colombian trial is aimed at dominantly-inherited AD due to a PSEN1 mutation, so it is different enough to imagine it still might make a difference in patients in whom amyloid metabolism is actually defective due to functionally altered amyloid precursor protein or gamma secretase,” he said in an interview. “Possibly some might argue that many of the patients in the crenezumab trial likely had additional pathologies so that even if the AD component responded, the overall clinical picture might not reflect it due to the other components. That would be interesting if proven and could even argue against equating young-onset with late-onset AD, at least for clinical purposes, as is currently envisioned.”
Michael Wolfe, PhD, had a different take on the matter.
“Although amyloid-beta [Abeta] production is not necessarily altered in sporadic AD, there is essentially the same pathology, presentation, and progression with familial and sporadic AD, suggesting a common molecular mechanism,” said Dr. Wolfe, who is the Mathias P. Mertes Professor of Medicinal Chemistry at the University of Kansas, Lawrence. “It’s hard to say Abeta is the pathogenic species in familial but not sporadic AD.
“To me, the failures of the antiamyloid approaches are because the drugs are given too late, are targeting the wrong form of Abeta, or are targeting an enzyme [for example, beta secretase1] that has other important functions. Most likely it’s a combination of these reasons. One could argue that even if some form of Abeta is the pathogenic entity, it is not a practical target because intervention may need to be initiated many years before the onset of symptoms.”
Despite the long string of failed antiamyloid antibodies, it’s not yet time to give up on the approach, said James Kupiec, MD, chief medical officer at ProMIS Neurosciences of Toronto.
“I understand where the pessimism [around antiamyloid antibodies] is coming from, and I also understand the enthusiasm from these companies to pursue them,” said Dr. Kupiec, who formerly headed Pfizer’s neuroscience research unit. “Targeting plaque is clearly not going to do the job. But in my opinion, the deeper pathophysiologic questions have not been adequately addressed. I’m not willing to throw in the towel. The correct molecular species [of amyloid] has not been appropriately or adequately tested in studies with monoclonal antibodies.”
The antibodies that have been failing for 5 years now were designed in the early 2000s, Dr. Kupiec pointed out, when knowledge of the various amyloid species was still immature. Newer candidates can target specific conformations of the protein – monomers and oligomers – before they aggregate into insoluble sheets. “Solanezumab was the first of these, paving the way for this new generation of antibodies,” Dr. Kupiec said.
Because they target soluble Abeta, not amyloid plaques, these domain-specific antibodies are less likely to elicit ARIA (amyloid-related imaging abnormalities), the inflammatory reaction that’s been associated with plaque dissolution in other antibody trials. ARIA has been a dose-limiting step for antiamyloid antibodies – one that conformationally targeted antibodies could avoid, Dr. Kupiec said.
“There may be some limited success with the these, and there may be enough of a treatment effect to secure approval,” he said. “The question is: Can we generate a higher effect size with an antibody that is more selective to the toxic forms of Abeta?”
PMN310 is ProMIS’ attempt to thread this needle. In preclinical studies, the antibody did not bind to amyloid monomers, plaques, or vascular Abeta aggregates. The company expects to take this antibody into phase 1 trials later this year.
“If we have a molecule that doesn’t bind to monomers or to plaques, but only to the toxic oligomer, then that is an something well worth testing in the clinic,” he said.
Dr. Caselli and Dr. Wolfe have no financial disclosures.
On behalf of the millions of people living with Alzheimer’s disease and their families that we serve and represent, the Alzheimer’s Association is disappointed to learn that these trials have been stopped.
We learn something from every Alzheimer’s clinical trial. The Alzheimer’s Association looks forward to hearing details of these studies at an upcoming scientific meeting.
More important, we must redouble our efforts to better understand the causes of the disease, and to discover additional therapeutic targets. No stone can be left unturned in the pursuit of better treatments and effective preventions.
The Alzheimer’s Association is investing in research looking at a variety of novel targets for treatment and prevention, including brain inflammation, the life and death cycle of brain cells, how brain cells use different energy sources, and the impact of lifestyle.
• Lifestyle interventions include leading the U.S. POINTER Study.
• To further the study of blood pressure control on reducing risk of mild cognitive impairment and dementia, the Alzheimer’s Association recently announced seed funding of SPRINT MIND 2.0.
• Part The Cloud Translational Research program fills a gap in Alzheimer’s drug development by supporting more than 30 early phase clinical studies.
• The Association is also funding research into the causes of the disease.
The emotional and financial cost of Alzheimer’s is enormous. At the Alzheimer’s Association, we will not stop. We will not slow down in our fight against this terrible disease.
Maria Carrillo, PhD , is the Alzheimer’s Association’s chief science officer.
On behalf of the millions of people living with Alzheimer’s disease and their families that we serve and represent, the Alzheimer’s Association is disappointed to learn that these trials have been stopped.
We learn something from every Alzheimer’s clinical trial. The Alzheimer’s Association looks forward to hearing details of these studies at an upcoming scientific meeting.
More important, we must redouble our efforts to better understand the causes of the disease, and to discover additional therapeutic targets. No stone can be left unturned in the pursuit of better treatments and effective preventions.
The Alzheimer’s Association is investing in research looking at a variety of novel targets for treatment and prevention, including brain inflammation, the life and death cycle of brain cells, how brain cells use different energy sources, and the impact of lifestyle.
• Lifestyle interventions include leading the U.S. POINTER Study.
• To further the study of blood pressure control on reducing risk of mild cognitive impairment and dementia, the Alzheimer’s Association recently announced seed funding of SPRINT MIND 2.0.
• Part The Cloud Translational Research program fills a gap in Alzheimer’s drug development by supporting more than 30 early phase clinical studies.
• The Association is also funding research into the causes of the disease.
The emotional and financial cost of Alzheimer’s is enormous. At the Alzheimer’s Association, we will not stop. We will not slow down in our fight against this terrible disease.
Maria Carrillo, PhD , is the Alzheimer’s Association’s chief science officer.
On behalf of the millions of people living with Alzheimer’s disease and their families that we serve and represent, the Alzheimer’s Association is disappointed to learn that these trials have been stopped.
We learn something from every Alzheimer’s clinical trial. The Alzheimer’s Association looks forward to hearing details of these studies at an upcoming scientific meeting.
More important, we must redouble our efforts to better understand the causes of the disease, and to discover additional therapeutic targets. No stone can be left unturned in the pursuit of better treatments and effective preventions.
The Alzheimer’s Association is investing in research looking at a variety of novel targets for treatment and prevention, including brain inflammation, the life and death cycle of brain cells, how brain cells use different energy sources, and the impact of lifestyle.
• Lifestyle interventions include leading the U.S. POINTER Study.
• To further the study of blood pressure control on reducing risk of mild cognitive impairment and dementia, the Alzheimer’s Association recently announced seed funding of SPRINT MIND 2.0.
• Part The Cloud Translational Research program fills a gap in Alzheimer’s drug development by supporting more than 30 early phase clinical studies.
• The Association is also funding research into the causes of the disease.
The emotional and financial cost of Alzheimer’s is enormous. At the Alzheimer’s Association, we will not stop. We will not slow down in our fight against this terrible disease.
Maria Carrillo, PhD , is the Alzheimer’s Association’s chief science officer.
After a disappointing interim analysis, Roche and its collaborator AC Immune are halting two phase 3 trials of the antiamyloid antibody crenezumab.
CREAD 1 and CREAD 2 enrolled patients with prodromal-to-mild sporadic Alzheimer’s disease. The preplanned interim safety and efficacy analysis determined that neither study was likely to meet the primary endpoint of change from baseline on the Clinical Dementia Rating-sum of boxes score.
There were no unexpected safety signals associated with the drug, despite a quadrupling of the phase 3 dose from that used in phase 2. The company in its press release said that it will continue to conduct the Autosomal Dominant Alzheimer’s Disease (ADAD) trial as part of the Alzheimer’s Prevention Initiative (API). ADAD is a large South American trial of crenezumab in Colombian families with familial Alzheimer’s caused by mutations in the presenilin-1 gene (PSEN1).
Roche did not release any data but said the trial results will be discussed at an upcoming scientific meeting.
“While the results with crenezumab are disappointing, they meaningfully contribute to our understanding of Alzheimer’s disease,” Sandra Horning, MD, Roche’s chief medical officer and executive vice president for global development, said in an interview. “We gratefully acknowledge the participants in the CREAD trials and the efforts of everyone involved in this important program.”
The decision was not a surprise to researchers who have followed the antibody’s development. It advanced into phase 3 with lackluster phase 2 cognitive, imaging, and biomarker data. Its selection as the therapeutic agent for the ADAD trial was a key driver in its continued development, securing Roche $100 million in federal funds to help launch ADAD, the first-ever Alzheimer’s primary prevention study.
Despite its failure in sporadic Alzheimer’s, there is still some hope that crenezumab might benefit people with the PSEN1 mutation, said Richard Caselli, MD, professor of neurology at the Mayo Clinic Arizona in Scottsdale and associate director and clinical core director of the Arizona Alzheimer’s Disease Center.
“The Colombian trial is aimed at dominantly-inherited AD due to a PSEN1 mutation, so it is different enough to imagine it still might make a difference in patients in whom amyloid metabolism is actually defective due to functionally altered amyloid precursor protein or gamma secretase,” he said in an interview. “Possibly some might argue that many of the patients in the crenezumab trial likely had additional pathologies so that even if the AD component responded, the overall clinical picture might not reflect it due to the other components. That would be interesting if proven and could even argue against equating young-onset with late-onset AD, at least for clinical purposes, as is currently envisioned.”
Michael Wolfe, PhD, had a different take on the matter.
“Although amyloid-beta [Abeta] production is not necessarily altered in sporadic AD, there is essentially the same pathology, presentation, and progression with familial and sporadic AD, suggesting a common molecular mechanism,” said Dr. Wolfe, who is the Mathias P. Mertes Professor of Medicinal Chemistry at the University of Kansas, Lawrence. “It’s hard to say Abeta is the pathogenic species in familial but not sporadic AD.
“To me, the failures of the antiamyloid approaches are because the drugs are given too late, are targeting the wrong form of Abeta, or are targeting an enzyme [for example, beta secretase1] that has other important functions. Most likely it’s a combination of these reasons. One could argue that even if some form of Abeta is the pathogenic entity, it is not a practical target because intervention may need to be initiated many years before the onset of symptoms.”
Despite the long string of failed antiamyloid antibodies, it’s not yet time to give up on the approach, said James Kupiec, MD, chief medical officer at ProMIS Neurosciences of Toronto.
“I understand where the pessimism [around antiamyloid antibodies] is coming from, and I also understand the enthusiasm from these companies to pursue them,” said Dr. Kupiec, who formerly headed Pfizer’s neuroscience research unit. “Targeting plaque is clearly not going to do the job. But in my opinion, the deeper pathophysiologic questions have not been adequately addressed. I’m not willing to throw in the towel. The correct molecular species [of amyloid] has not been appropriately or adequately tested in studies with monoclonal antibodies.”
The antibodies that have been failing for 5 years now were designed in the early 2000s, Dr. Kupiec pointed out, when knowledge of the various amyloid species was still immature. Newer candidates can target specific conformations of the protein – monomers and oligomers – before they aggregate into insoluble sheets. “Solanezumab was the first of these, paving the way for this new generation of antibodies,” Dr. Kupiec said.
Because they target soluble Abeta, not amyloid plaques, these domain-specific antibodies are less likely to elicit ARIA (amyloid-related imaging abnormalities), the inflammatory reaction that’s been associated with plaque dissolution in other antibody trials. ARIA has been a dose-limiting step for antiamyloid antibodies – one that conformationally targeted antibodies could avoid, Dr. Kupiec said.
“There may be some limited success with the these, and there may be enough of a treatment effect to secure approval,” he said. “The question is: Can we generate a higher effect size with an antibody that is more selective to the toxic forms of Abeta?”
PMN310 is ProMIS’ attempt to thread this needle. In preclinical studies, the antibody did not bind to amyloid monomers, plaques, or vascular Abeta aggregates. The company expects to take this antibody into phase 1 trials later this year.
“If we have a molecule that doesn’t bind to monomers or to plaques, but only to the toxic oligomer, then that is an something well worth testing in the clinic,” he said.
Dr. Caselli and Dr. Wolfe have no financial disclosures.
After a disappointing interim analysis, Roche and its collaborator AC Immune are halting two phase 3 trials of the antiamyloid antibody crenezumab.
CREAD 1 and CREAD 2 enrolled patients with prodromal-to-mild sporadic Alzheimer’s disease. The preplanned interim safety and efficacy analysis determined that neither study was likely to meet the primary endpoint of change from baseline on the Clinical Dementia Rating-sum of boxes score.
There were no unexpected safety signals associated with the drug, despite a quadrupling of the phase 3 dose from that used in phase 2. The company in its press release said that it will continue to conduct the Autosomal Dominant Alzheimer’s Disease (ADAD) trial as part of the Alzheimer’s Prevention Initiative (API). ADAD is a large South American trial of crenezumab in Colombian families with familial Alzheimer’s caused by mutations in the presenilin-1 gene (PSEN1).
Roche did not release any data but said the trial results will be discussed at an upcoming scientific meeting.
“While the results with crenezumab are disappointing, they meaningfully contribute to our understanding of Alzheimer’s disease,” Sandra Horning, MD, Roche’s chief medical officer and executive vice president for global development, said in an interview. “We gratefully acknowledge the participants in the CREAD trials and the efforts of everyone involved in this important program.”
The decision was not a surprise to researchers who have followed the antibody’s development. It advanced into phase 3 with lackluster phase 2 cognitive, imaging, and biomarker data. Its selection as the therapeutic agent for the ADAD trial was a key driver in its continued development, securing Roche $100 million in federal funds to help launch ADAD, the first-ever Alzheimer’s primary prevention study.
Despite its failure in sporadic Alzheimer’s, there is still some hope that crenezumab might benefit people with the PSEN1 mutation, said Richard Caselli, MD, professor of neurology at the Mayo Clinic Arizona in Scottsdale and associate director and clinical core director of the Arizona Alzheimer’s Disease Center.
“The Colombian trial is aimed at dominantly-inherited AD due to a PSEN1 mutation, so it is different enough to imagine it still might make a difference in patients in whom amyloid metabolism is actually defective due to functionally altered amyloid precursor protein or gamma secretase,” he said in an interview. “Possibly some might argue that many of the patients in the crenezumab trial likely had additional pathologies so that even if the AD component responded, the overall clinical picture might not reflect it due to the other components. That would be interesting if proven and could even argue against equating young-onset with late-onset AD, at least for clinical purposes, as is currently envisioned.”
Michael Wolfe, PhD, had a different take on the matter.
“Although amyloid-beta [Abeta] production is not necessarily altered in sporadic AD, there is essentially the same pathology, presentation, and progression with familial and sporadic AD, suggesting a common molecular mechanism,” said Dr. Wolfe, who is the Mathias P. Mertes Professor of Medicinal Chemistry at the University of Kansas, Lawrence. “It’s hard to say Abeta is the pathogenic species in familial but not sporadic AD.
“To me, the failures of the antiamyloid approaches are because the drugs are given too late, are targeting the wrong form of Abeta, or are targeting an enzyme [for example, beta secretase1] that has other important functions. Most likely it’s a combination of these reasons. One could argue that even if some form of Abeta is the pathogenic entity, it is not a practical target because intervention may need to be initiated many years before the onset of symptoms.”
Despite the long string of failed antiamyloid antibodies, it’s not yet time to give up on the approach, said James Kupiec, MD, chief medical officer at ProMIS Neurosciences of Toronto.
“I understand where the pessimism [around antiamyloid antibodies] is coming from, and I also understand the enthusiasm from these companies to pursue them,” said Dr. Kupiec, who formerly headed Pfizer’s neuroscience research unit. “Targeting plaque is clearly not going to do the job. But in my opinion, the deeper pathophysiologic questions have not been adequately addressed. I’m not willing to throw in the towel. The correct molecular species [of amyloid] has not been appropriately or adequately tested in studies with monoclonal antibodies.”
The antibodies that have been failing for 5 years now were designed in the early 2000s, Dr. Kupiec pointed out, when knowledge of the various amyloid species was still immature. Newer candidates can target specific conformations of the protein – monomers and oligomers – before they aggregate into insoluble sheets. “Solanezumab was the first of these, paving the way for this new generation of antibodies,” Dr. Kupiec said.
Because they target soluble Abeta, not amyloid plaques, these domain-specific antibodies are less likely to elicit ARIA (amyloid-related imaging abnormalities), the inflammatory reaction that’s been associated with plaque dissolution in other antibody trials. ARIA has been a dose-limiting step for antiamyloid antibodies – one that conformationally targeted antibodies could avoid, Dr. Kupiec said.
“There may be some limited success with the these, and there may be enough of a treatment effect to secure approval,” he said. “The question is: Can we generate a higher effect size with an antibody that is more selective to the toxic forms of Abeta?”
PMN310 is ProMIS’ attempt to thread this needle. In preclinical studies, the antibody did not bind to amyloid monomers, plaques, or vascular Abeta aggregates. The company expects to take this antibody into phase 1 trials later this year.
“If we have a molecule that doesn’t bind to monomers or to plaques, but only to the toxic oligomer, then that is an something well worth testing in the clinic,” he said.
Dr. Caselli and Dr. Wolfe have no financial disclosures.
Revamped A fib guidelines
Also today, family gun ownership is linked to gun deaths among young children, insulin may be toxic to the placenta in early pregnancy, and ticks are the arthropod ride of choice for pathogens.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, family gun ownership is linked to gun deaths among young children, insulin may be toxic to the placenta in early pregnancy, and ticks are the arthropod ride of choice for pathogens.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, family gun ownership is linked to gun deaths among young children, insulin may be toxic to the placenta in early pregnancy, and ticks are the arthropod ride of choice for pathogens.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Tantrum-taming edibles, support gators, and chemo eggs
Chill out, kid
What do you do when your child has constant tantrums? A simple edible could do the trick, according to a Hollywood physician.
The natural medicine physician is in hot (bong) water after recommending marijuana cookies as treatment for a 4-year-old child’s ADHD and bipolar disorder. The icing on the cake (or cookie) is that both diagnoses weren’t even accurate. Perhaps the doctor was sampling his own treatments before the office visit?
The progressive physician has had his license revoked for the “grossly negligent” diagnosis, which he made in 30 minutes without consulting the child’s teachers, his father, or a psychiatrist. Probably not the best way to handle it, said the state medical board. Perhaps he should have suggested some CBD-infused Coke, instead?
Gator saver
Dogs, cats, peacocks – these are the animals that many people with anxiety, depression, and other mental health issues use for emotional support. But now, enter Wally, the emotional support alligator.
Spanning 5 feet long and sporting way too many teeth, Wally is the constant companion of a 65-year-old Pennsylvania man with depression. Wally’s owner decided to forgo pharmacologic treatment for something decidedly more reptilian.
Wally, who was rescued from Florida, loves chicken wings, hugs, and his adopted gator brother, Scrappy. He also has the potential to reach 16 feet long, which is … concerning. Something tells me you can’t take Wally on a plane as a service gator.
But don’t worry, Wally has been approved by a doctor. Rumors that Wally had the doctor’s arm in his jaws before approval are unsubstantiated.
Synergy is not always a good thing
Since it is generally agreed that two heads are better than one, three heads must be even better than two, right? But what if we’re not talking about heads? Suppose, instead, that the subject is global pandemics. Would it be better if three of the greatest threats to humanity’s existence on the planet decided to join forces?
The Lancet Global Syndemic Commission, a group of more than 40 international experts, said that obesity, undernutrition, and climate change “constitute a syndemic, or synergy of epidemics, because they co-occur in time and place, interact with each other to produce complex sequelae, and share common underlying societal drivers” (Lancet. 2019 Jan. 27. doi: 10.1016/S0140-6736[18]32822-8).
It gets better: The commission suggested that the “three interconnected health pandemics [have been] effectively orchestrated by the shadowy manipulations and influence of vested commercial interests – an entity collectively defined as ‘Big Food,’ ” according to Science Alert.
This all seems like a lot to overcome, but we here at LOTME have faith in science, and in the scientists who are working to solve these problems. After all, it’s not like anyone’s out there disregarding the science and saying that this stuff isn’t really happening. … Wait, what? … Climate change deniers? … Really? … The president tweeted what? … We’re doomed.
I prefer my medication sunny side up
Here’s a hypothetical question for you: If you were to have cancer, how would you prefer to be treated? Would you rather go through the rigors of chemotherapy? Or would you rather eat an omelet?
Okay, it probably wouldn’t work quite like that, but a group of physicians from the University of Edinburgh have successfully modified chickens to lay eggs containing a pair of human proteins within the egg white.
One of these proteins has antiviral and anticancer effects, and the other can help damaged tissue repair itself. The researchers added that the protein in the egg white could be modified to make the key ingredients for other protein-based drugs such as Avastin and Herceptin, which are used for treating cancer.
We know what you’re thinking: It’ll probably take a thousand eggs to make one dose – but no, it only takes three. Over the course of a year, one chicken could produce a hundred doses, and do it for far cheaper than is currently possible. We hate jumping on the social media bandwagon here, but frankly, this is an egg worth giving millions of Instagram likes.
Chill out, kid
What do you do when your child has constant tantrums? A simple edible could do the trick, according to a Hollywood physician.
The natural medicine physician is in hot (bong) water after recommending marijuana cookies as treatment for a 4-year-old child’s ADHD and bipolar disorder. The icing on the cake (or cookie) is that both diagnoses weren’t even accurate. Perhaps the doctor was sampling his own treatments before the office visit?
The progressive physician has had his license revoked for the “grossly negligent” diagnosis, which he made in 30 minutes without consulting the child’s teachers, his father, or a psychiatrist. Probably not the best way to handle it, said the state medical board. Perhaps he should have suggested some CBD-infused Coke, instead?
Gator saver
Dogs, cats, peacocks – these are the animals that many people with anxiety, depression, and other mental health issues use for emotional support. But now, enter Wally, the emotional support alligator.
Spanning 5 feet long and sporting way too many teeth, Wally is the constant companion of a 65-year-old Pennsylvania man with depression. Wally’s owner decided to forgo pharmacologic treatment for something decidedly more reptilian.
Wally, who was rescued from Florida, loves chicken wings, hugs, and his adopted gator brother, Scrappy. He also has the potential to reach 16 feet long, which is … concerning. Something tells me you can’t take Wally on a plane as a service gator.
But don’t worry, Wally has been approved by a doctor. Rumors that Wally had the doctor’s arm in his jaws before approval are unsubstantiated.
Synergy is not always a good thing
Since it is generally agreed that two heads are better than one, three heads must be even better than two, right? But what if we’re not talking about heads? Suppose, instead, that the subject is global pandemics. Would it be better if three of the greatest threats to humanity’s existence on the planet decided to join forces?
The Lancet Global Syndemic Commission, a group of more than 40 international experts, said that obesity, undernutrition, and climate change “constitute a syndemic, or synergy of epidemics, because they co-occur in time and place, interact with each other to produce complex sequelae, and share common underlying societal drivers” (Lancet. 2019 Jan. 27. doi: 10.1016/S0140-6736[18]32822-8).
It gets better: The commission suggested that the “three interconnected health pandemics [have been] effectively orchestrated by the shadowy manipulations and influence of vested commercial interests – an entity collectively defined as ‘Big Food,’ ” according to Science Alert.
This all seems like a lot to overcome, but we here at LOTME have faith in science, and in the scientists who are working to solve these problems. After all, it’s not like anyone’s out there disregarding the science and saying that this stuff isn’t really happening. … Wait, what? … Climate change deniers? … Really? … The president tweeted what? … We’re doomed.
I prefer my medication sunny side up
Here’s a hypothetical question for you: If you were to have cancer, how would you prefer to be treated? Would you rather go through the rigors of chemotherapy? Or would you rather eat an omelet?
Okay, it probably wouldn’t work quite like that, but a group of physicians from the University of Edinburgh have successfully modified chickens to lay eggs containing a pair of human proteins within the egg white.
One of these proteins has antiviral and anticancer effects, and the other can help damaged tissue repair itself. The researchers added that the protein in the egg white could be modified to make the key ingredients for other protein-based drugs such as Avastin and Herceptin, which are used for treating cancer.
We know what you’re thinking: It’ll probably take a thousand eggs to make one dose – but no, it only takes three. Over the course of a year, one chicken could produce a hundred doses, and do it for far cheaper than is currently possible. We hate jumping on the social media bandwagon here, but frankly, this is an egg worth giving millions of Instagram likes.
Chill out, kid
What do you do when your child has constant tantrums? A simple edible could do the trick, according to a Hollywood physician.
The natural medicine physician is in hot (bong) water after recommending marijuana cookies as treatment for a 4-year-old child’s ADHD and bipolar disorder. The icing on the cake (or cookie) is that both diagnoses weren’t even accurate. Perhaps the doctor was sampling his own treatments before the office visit?
The progressive physician has had his license revoked for the “grossly negligent” diagnosis, which he made in 30 minutes without consulting the child’s teachers, his father, or a psychiatrist. Probably not the best way to handle it, said the state medical board. Perhaps he should have suggested some CBD-infused Coke, instead?
Gator saver
Dogs, cats, peacocks – these are the animals that many people with anxiety, depression, and other mental health issues use for emotional support. But now, enter Wally, the emotional support alligator.
Spanning 5 feet long and sporting way too many teeth, Wally is the constant companion of a 65-year-old Pennsylvania man with depression. Wally’s owner decided to forgo pharmacologic treatment for something decidedly more reptilian.
Wally, who was rescued from Florida, loves chicken wings, hugs, and his adopted gator brother, Scrappy. He also has the potential to reach 16 feet long, which is … concerning. Something tells me you can’t take Wally on a plane as a service gator.
But don’t worry, Wally has been approved by a doctor. Rumors that Wally had the doctor’s arm in his jaws before approval are unsubstantiated.
Synergy is not always a good thing
Since it is generally agreed that two heads are better than one, three heads must be even better than two, right? But what if we’re not talking about heads? Suppose, instead, that the subject is global pandemics. Would it be better if three of the greatest threats to humanity’s existence on the planet decided to join forces?
The Lancet Global Syndemic Commission, a group of more than 40 international experts, said that obesity, undernutrition, and climate change “constitute a syndemic, or synergy of epidemics, because they co-occur in time and place, interact with each other to produce complex sequelae, and share common underlying societal drivers” (Lancet. 2019 Jan. 27. doi: 10.1016/S0140-6736[18]32822-8).
It gets better: The commission suggested that the “three interconnected health pandemics [have been] effectively orchestrated by the shadowy manipulations and influence of vested commercial interests – an entity collectively defined as ‘Big Food,’ ” according to Science Alert.
This all seems like a lot to overcome, but we here at LOTME have faith in science, and in the scientists who are working to solve these problems. After all, it’s not like anyone’s out there disregarding the science and saying that this stuff isn’t really happening. … Wait, what? … Climate change deniers? … Really? … The president tweeted what? … We’re doomed.
I prefer my medication sunny side up
Here’s a hypothetical question for you: If you were to have cancer, how would you prefer to be treated? Would you rather go through the rigors of chemotherapy? Or would you rather eat an omelet?
Okay, it probably wouldn’t work quite like that, but a group of physicians from the University of Edinburgh have successfully modified chickens to lay eggs containing a pair of human proteins within the egg white.
One of these proteins has antiviral and anticancer effects, and the other can help damaged tissue repair itself. The researchers added that the protein in the egg white could be modified to make the key ingredients for other protein-based drugs such as Avastin and Herceptin, which are used for treating cancer.
We know what you’re thinking: It’ll probably take a thousand eggs to make one dose – but no, it only takes three. Over the course of a year, one chicken could produce a hundred doses, and do it for far cheaper than is currently possible. We hate jumping on the social media bandwagon here, but frankly, this is an egg worth giving millions of Instagram likes.
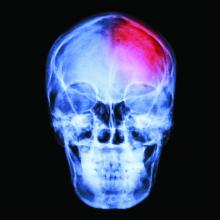
Race/ethnicity, other factors predict PTSD and depression after mild TBI
Civilian patients with mild traumatic brain injury (TBI) who are black, have psychiatric history or lower education, or whose injury was caused by assault might be at greater risk of developing posttraumatic stress disorder or major depression, a longitudinal study suggests.
“Our findings may have implications for surveillance and treatment of mental disorders after TBI,” wrote Murray B. Stein, MD, MPH, and his associates. The study was published Jan. 30 in JAMA Psychiatry.
The researchers looked at the risk factors for and prevalence of posttraumatic stress disorder (PTSD) and major depressive disorder among 1,155 patients. The patients were enrolled at 11 level 1 trauma centers across the United States after they were evaluated for mild TBI in emergency departments as part of a prospective study called Transforming Research and Clinical Knowledge in Traumatic Brain Injury, or TRACK-TBI. The comparison group was 230 patients with nonhead orthopedic trauma injuries, wrote Dr. Stein, distinguished professor of psychiatry and family medicine and public health at the University of California, San Diego, and his associates.
They found that each additional year of education was associated with a significant 11% reduction in the risk of developing PTSD after mild TBI (P = .005). Also, black patients had a greater than fivefold higher risk of PTSD (P less than.001) than that of individuals who were not black.
Among patients with a history of mental illness and those who had experienced their injury as a result of assault or violence – as opposed to a motor vehicle accident or fall, for example – both had a greater than threefold higher risk of developing PTSD (odds ratio, 3.57 and 3.43 respectively). A prior TBI was nonsignificantly associated with an increased risk of developing PTSD.
Lower education duration, being black, or a history of mental illness also were all significantly associated with an increased risk of developing major depressive disorder after mild TBI.
However, duration of lost consciousness or posttraumatic amnesia, evidence of brain injury on CT, or hospitalization did not predict an increased risk of PTSD or major depression.
“Although MDD and PTSD are prevalent after TBI, little is known about which patients are at risk for developing them,” Dr. Stein and his associates wrote.
Noting that having a prior mental health problem was an “exceptionally strong” risk factor for PTSD and MDD after TBI, the authors said this could represent continuation or exacerbation of the prior mental health issue, or the triggering of a new episode in a person with a past history who had recovered.
“However, in either case this finding underscores the importance of clinicians being aware of the mental health history of their patients with [mild TBI], as this information is central to expectations regarding both short-term and long-term outcome,” they wrote.
Dr. Stein and his associates cited as a limitation their reliance on patient or family report. In addition, they said, the elevated risk for mental disorders among black individuals after mild TBI, which was independent of socioeconomic status or cause of injury, was not understood. “Unmeasured covariates may be part of the explanation; this is a topic needing further study,” they wrote.
The study was supported by the National Institutes of Health, the U.S. Department of Defense, Abbott Laboratories, and One Mind. Four authors declared consultancies, advisory board positions, speaking fees, and shares or stock options with the pharmaceutical and private industry. Two authors declared grants from the study sponsors.
SOURCE: Stein MB et al. JAMA Psychiatry. 2019. Jan 30. doi: 10.1001/jamapsychiatry.2018.4288.
Civilian patients with mild traumatic brain injury (TBI) who are black, have psychiatric history or lower education, or whose injury was caused by assault might be at greater risk of developing posttraumatic stress disorder or major depression, a longitudinal study suggests.
“Our findings may have implications for surveillance and treatment of mental disorders after TBI,” wrote Murray B. Stein, MD, MPH, and his associates. The study was published Jan. 30 in JAMA Psychiatry.
The researchers looked at the risk factors for and prevalence of posttraumatic stress disorder (PTSD) and major depressive disorder among 1,155 patients. The patients were enrolled at 11 level 1 trauma centers across the United States after they were evaluated for mild TBI in emergency departments as part of a prospective study called Transforming Research and Clinical Knowledge in Traumatic Brain Injury, or TRACK-TBI. The comparison group was 230 patients with nonhead orthopedic trauma injuries, wrote Dr. Stein, distinguished professor of psychiatry and family medicine and public health at the University of California, San Diego, and his associates.
They found that each additional year of education was associated with a significant 11% reduction in the risk of developing PTSD after mild TBI (P = .005). Also, black patients had a greater than fivefold higher risk of PTSD (P less than.001) than that of individuals who were not black.
Among patients with a history of mental illness and those who had experienced their injury as a result of assault or violence – as opposed to a motor vehicle accident or fall, for example – both had a greater than threefold higher risk of developing PTSD (odds ratio, 3.57 and 3.43 respectively). A prior TBI was nonsignificantly associated with an increased risk of developing PTSD.
Lower education duration, being black, or a history of mental illness also were all significantly associated with an increased risk of developing major depressive disorder after mild TBI.
However, duration of lost consciousness or posttraumatic amnesia, evidence of brain injury on CT, or hospitalization did not predict an increased risk of PTSD or major depression.
“Although MDD and PTSD are prevalent after TBI, little is known about which patients are at risk for developing them,” Dr. Stein and his associates wrote.
Noting that having a prior mental health problem was an “exceptionally strong” risk factor for PTSD and MDD after TBI, the authors said this could represent continuation or exacerbation of the prior mental health issue, or the triggering of a new episode in a person with a past history who had recovered.
“However, in either case this finding underscores the importance of clinicians being aware of the mental health history of their patients with [mild TBI], as this information is central to expectations regarding both short-term and long-term outcome,” they wrote.
Dr. Stein and his associates cited as a limitation their reliance on patient or family report. In addition, they said, the elevated risk for mental disorders among black individuals after mild TBI, which was independent of socioeconomic status or cause of injury, was not understood. “Unmeasured covariates may be part of the explanation; this is a topic needing further study,” they wrote.
The study was supported by the National Institutes of Health, the U.S. Department of Defense, Abbott Laboratories, and One Mind. Four authors declared consultancies, advisory board positions, speaking fees, and shares or stock options with the pharmaceutical and private industry. Two authors declared grants from the study sponsors.
SOURCE: Stein MB et al. JAMA Psychiatry. 2019. Jan 30. doi: 10.1001/jamapsychiatry.2018.4288.
Civilian patients with mild traumatic brain injury (TBI) who are black, have psychiatric history or lower education, or whose injury was caused by assault might be at greater risk of developing posttraumatic stress disorder or major depression, a longitudinal study suggests.
“Our findings may have implications for surveillance and treatment of mental disorders after TBI,” wrote Murray B. Stein, MD, MPH, and his associates. The study was published Jan. 30 in JAMA Psychiatry.
The researchers looked at the risk factors for and prevalence of posttraumatic stress disorder (PTSD) and major depressive disorder among 1,155 patients. The patients were enrolled at 11 level 1 trauma centers across the United States after they were evaluated for mild TBI in emergency departments as part of a prospective study called Transforming Research and Clinical Knowledge in Traumatic Brain Injury, or TRACK-TBI. The comparison group was 230 patients with nonhead orthopedic trauma injuries, wrote Dr. Stein, distinguished professor of psychiatry and family medicine and public health at the University of California, San Diego, and his associates.
They found that each additional year of education was associated with a significant 11% reduction in the risk of developing PTSD after mild TBI (P = .005). Also, black patients had a greater than fivefold higher risk of PTSD (P less than.001) than that of individuals who were not black.
Among patients with a history of mental illness and those who had experienced their injury as a result of assault or violence – as opposed to a motor vehicle accident or fall, for example – both had a greater than threefold higher risk of developing PTSD (odds ratio, 3.57 and 3.43 respectively). A prior TBI was nonsignificantly associated with an increased risk of developing PTSD.
Lower education duration, being black, or a history of mental illness also were all significantly associated with an increased risk of developing major depressive disorder after mild TBI.
However, duration of lost consciousness or posttraumatic amnesia, evidence of brain injury on CT, or hospitalization did not predict an increased risk of PTSD or major depression.
“Although MDD and PTSD are prevalent after TBI, little is known about which patients are at risk for developing them,” Dr. Stein and his associates wrote.
Noting that having a prior mental health problem was an “exceptionally strong” risk factor for PTSD and MDD after TBI, the authors said this could represent continuation or exacerbation of the prior mental health issue, or the triggering of a new episode in a person with a past history who had recovered.
“However, in either case this finding underscores the importance of clinicians being aware of the mental health history of their patients with [mild TBI], as this information is central to expectations regarding both short-term and long-term outcome,” they wrote.
Dr. Stein and his associates cited as a limitation their reliance on patient or family report. In addition, they said, the elevated risk for mental disorders among black individuals after mild TBI, which was independent of socioeconomic status or cause of injury, was not understood. “Unmeasured covariates may be part of the explanation; this is a topic needing further study,” they wrote.
The study was supported by the National Institutes of Health, the U.S. Department of Defense, Abbott Laboratories, and One Mind. Four authors declared consultancies, advisory board positions, speaking fees, and shares or stock options with the pharmaceutical and private industry. Two authors declared grants from the study sponsors.
SOURCE: Stein MB et al. JAMA Psychiatry. 2019. Jan 30. doi: 10.1001/jamapsychiatry.2018.4288.
FROM JAMA PSYCHIATRY
Key clinical point: The findings underscore “the importance of clinicians being aware of the mental health history of their patients with [mild TBI], as this information is central to expectations regarding both short-term and long-term outcome.”
Major finding: Black patients have fivefold higher risk of PTSD after brain injury.
Study details: Longitudinal cohort study of 1,155 patients with mild traumatic brain injury.
Disclosures: The study was supported by the National Institutes of Health, the U.S. Department of Defense, Abbott Laboratories, and One Mind. Four authors declared consultancies, advisory board positions, and speaking fees, shares, or stock options with the pharmaceutical and private industry. Two authors declared grants from the study sponsors.
Source: Stein MB et al. JAMA Psychiatry 2019. Jan 30. doi: 10.1001/jamapsychiatry.2018.4288.
Medical ethics and economics
The balance between medical research and the pharmaceutical world has always been unsettling. The recent spate of articles in the press reporting the large payments by industry to a number of highly paid medical staff of the Memorial Sloan Kettering Cancer Institute in New York has raised again the continuing issue around that relationship.
When large sums of money are paid to medical leaders for serving on advisory boards, it is reasonable to question whom are they representing: industry or medical science. These relationships are not limited to cancer hospitals and can be presumed to pertain to cardiology and other specialties. One need only look at the disclosure statements of contemporary published articles to become aware of the entanglement of science and industry.
There is little question that both industry and science need to interact to focus direct resources to appropriate targets. No one is better able to do that than well informed scientists working in their disease fields. Industry needs scientific input and scientists need the financial resources of industry. I have been able to see that relationship play out to achieve major impacts on heart disease. But corporate decisions also can be driven by market forces and not altruism. Drug and device research has been redirected or stopped as a result of decisions made by sales forces. At other times, drugs that have great potential in the laboratory have been shelved because of a lack of scientific leadership.
So where is the moral and ethical balance? Published disclosures by authors is not much more than a catharsis in the process where action is required. Medical advisory boards are critical for successful drug and device development. That exchange is crucial to move medical science forward, but the large sums of money raise appropriate questions of what is driving the discussion.
At a more grass roots level, the financial role of investigators and hospitals in clinical trials has raised some concern. Traditionally, the institution and investigators have been reimbursed for their time and expense for recruiting and following patients. Patients, of course, are not reimbursed in clinical trials but are placed at considerable risk of an uncertain result. The reimbursements for marginal expenses seem to be appropriate. More recently, payments to physicians and hospitals have been made at current fee schedules for the implantation of a variety of new devices such as pacemakers and valves. In addition, both physicians and hospitals have invested in the financial success of these clinical trials clouding over their altruistic goals. It has been an incentive for recruiting patients for trials and has been a source of considerable revenue both for the physicians and the institution, without informing the patients of their financial relationship to industry. .
There is a lot of money sloshing around in the health care world that has the potential to lead to ethical uncertainty. It is the physician’s responsibility to build up ethical barriers to prevent us from slipping into that morass.
Dr. Goldstein is professor of medicine at Wayne State University and the division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit.
The balance between medical research and the pharmaceutical world has always been unsettling. The recent spate of articles in the press reporting the large payments by industry to a number of highly paid medical staff of the Memorial Sloan Kettering Cancer Institute in New York has raised again the continuing issue around that relationship.
When large sums of money are paid to medical leaders for serving on advisory boards, it is reasonable to question whom are they representing: industry or medical science. These relationships are not limited to cancer hospitals and can be presumed to pertain to cardiology and other specialties. One need only look at the disclosure statements of contemporary published articles to become aware of the entanglement of science and industry.
There is little question that both industry and science need to interact to focus direct resources to appropriate targets. No one is better able to do that than well informed scientists working in their disease fields. Industry needs scientific input and scientists need the financial resources of industry. I have been able to see that relationship play out to achieve major impacts on heart disease. But corporate decisions also can be driven by market forces and not altruism. Drug and device research has been redirected or stopped as a result of decisions made by sales forces. At other times, drugs that have great potential in the laboratory have been shelved because of a lack of scientific leadership.
So where is the moral and ethical balance? Published disclosures by authors is not much more than a catharsis in the process where action is required. Medical advisory boards are critical for successful drug and device development. That exchange is crucial to move medical science forward, but the large sums of money raise appropriate questions of what is driving the discussion.
At a more grass roots level, the financial role of investigators and hospitals in clinical trials has raised some concern. Traditionally, the institution and investigators have been reimbursed for their time and expense for recruiting and following patients. Patients, of course, are not reimbursed in clinical trials but are placed at considerable risk of an uncertain result. The reimbursements for marginal expenses seem to be appropriate. More recently, payments to physicians and hospitals have been made at current fee schedules for the implantation of a variety of new devices such as pacemakers and valves. In addition, both physicians and hospitals have invested in the financial success of these clinical trials clouding over their altruistic goals. It has been an incentive for recruiting patients for trials and has been a source of considerable revenue both for the physicians and the institution, without informing the patients of their financial relationship to industry. .
There is a lot of money sloshing around in the health care world that has the potential to lead to ethical uncertainty. It is the physician’s responsibility to build up ethical barriers to prevent us from slipping into that morass.
Dr. Goldstein is professor of medicine at Wayne State University and the division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit.
The balance between medical research and the pharmaceutical world has always been unsettling. The recent spate of articles in the press reporting the large payments by industry to a number of highly paid medical staff of the Memorial Sloan Kettering Cancer Institute in New York has raised again the continuing issue around that relationship.
When large sums of money are paid to medical leaders for serving on advisory boards, it is reasonable to question whom are they representing: industry or medical science. These relationships are not limited to cancer hospitals and can be presumed to pertain to cardiology and other specialties. One need only look at the disclosure statements of contemporary published articles to become aware of the entanglement of science and industry.
There is little question that both industry and science need to interact to focus direct resources to appropriate targets. No one is better able to do that than well informed scientists working in their disease fields. Industry needs scientific input and scientists need the financial resources of industry. I have been able to see that relationship play out to achieve major impacts on heart disease. But corporate decisions also can be driven by market forces and not altruism. Drug and device research has been redirected or stopped as a result of decisions made by sales forces. At other times, drugs that have great potential in the laboratory have been shelved because of a lack of scientific leadership.
So where is the moral and ethical balance? Published disclosures by authors is not much more than a catharsis in the process where action is required. Medical advisory boards are critical for successful drug and device development. That exchange is crucial to move medical science forward, but the large sums of money raise appropriate questions of what is driving the discussion.
At a more grass roots level, the financial role of investigators and hospitals in clinical trials has raised some concern. Traditionally, the institution and investigators have been reimbursed for their time and expense for recruiting and following patients. Patients, of course, are not reimbursed in clinical trials but are placed at considerable risk of an uncertain result. The reimbursements for marginal expenses seem to be appropriate. More recently, payments to physicians and hospitals have been made at current fee schedules for the implantation of a variety of new devices such as pacemakers and valves. In addition, both physicians and hospitals have invested in the financial success of these clinical trials clouding over their altruistic goals. It has been an incentive for recruiting patients for trials and has been a source of considerable revenue both for the physicians and the institution, without informing the patients of their financial relationship to industry. .
There is a lot of money sloshing around in the health care world that has the potential to lead to ethical uncertainty. It is the physician’s responsibility to build up ethical barriers to prevent us from slipping into that morass.
Dr. Goldstein is professor of medicine at Wayne State University and the division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit.
Physician mothers caring for others at home
Also today, what one neurologist refuses to accept in his office, flu activity increases after 2 weeks of declines, and when sweaty palms are really primary hyperhidrosis.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, what one neurologist refuses to accept in his office, flu activity increases after 2 weeks of declines, and when sweaty palms are really primary hyperhidrosis.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, what one neurologist refuses to accept in his office, flu activity increases after 2 weeks of declines, and when sweaty palms are really primary hyperhidrosis.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify