User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Six healthy lifestyle habits linked to slowed memory decline
Investigators found that a healthy diet, cognitive activity, regular physical exercise, not smoking, and abstaining from alcohol were significantly linked to slowed cognitive decline irrespective of APOE4 status.
After adjusting for health and socioeconomic factors, investigators found that each individual healthy behavior was associated with a slower-than-average decline in memory over a decade. A healthy diet emerged as the strongest deterrent, followed by cognitive activity and physical exercise.
“A healthy lifestyle is associated with slower memory decline, even in the presence of the APOE4 allele,” study investigators led by Jianping Jia, MD, PhD, of the Innovation Center for Neurological Disorders and the department of neurology, Xuan Wu Hospital, Capital Medical University, Beijing, write.
“This study might offer important information to protect older adults against memory decline,” they add.
The study was published online in the BMJ.
Preventing memory decline
Memory “continuously declines as people age,” but age-related memory decline is not necessarily a prodrome of dementia and can “merely be senescent forgetfulness,” the investigators note. This can be “reversed or [can] become stable,” instead of progressing to a pathologic state.
Factors affecting memory include aging, APOE4 genotype, chronic diseases, and lifestyle patterns, with lifestyle “receiving increasing attention as a modifiable behavior.”
Nevertheless, few studies have focused on the impact of lifestyle on memory, and those that have are mostly cross-sectional and also “did not consider the interaction between a healthy lifestyle and genetic risk,” the researchers note.
To investigate, the researchers conducted a longitudinal study, known as the China Cognition and Aging Study, that considered genetic risk as well as lifestyle factors.
The study began in 2009 and concluded in 2019. Participants were evaluated and underwent neuropsychological testing in 2012, 2014, 2016, and at the study’s conclusion.
Participants (n = 29,072; mean [SD] age, 72.23 [6.61] years; 48.54% women; 20.43% APOE4 carriers) were required to have normal cognitive function at baseline. Data on those whose condition progressed to mild cognitive impairment (MCI) or dementia during the follow-up period were excluded after their diagnosis.
The Mini–Mental State Examination was used to assess global cognitive function. Memory function was assessed using the World Health Organization/University of California, Los Angeles Auditory Verbal Learning Test.
“Lifestyle” consisted of six modifiable factors: physical exercise (weekly frequency and total time), smoking (current, former, or never-smokers), alcohol consumption (never drank, drank occasionally, low to excess drinking, and heavy drinking), diet (daily intake of 12 food items: fruits, vegetables, fish, meat, dairy products, salt, oil, eggs, cereals, legumes, nuts, tea), cognitive activity (writing, reading, playing cards, mahjong, other games), and social contact (participating in meetings, attending parties, visiting friends/relatives, traveling, chatting online).
Participants’ lifestyles were scored on the basis of the number of healthy factors they engaged in.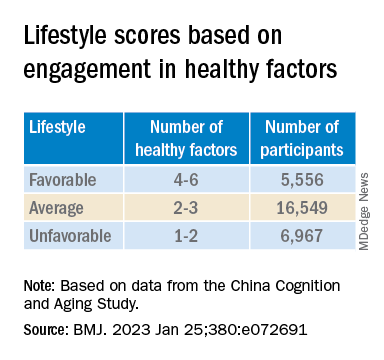
Participants were also stratified by APOE genotype into APOE4 carriers and noncarriers.
Demographic and other items of health information, including the presence of medical illness, were used as covariates. The researchers also included the “learning effect of each participant as a covariate, due to repeated cognitive assessments.”
Important for public health
During the 10-year period, 7,164 participants died, and 3,567 stopped participating.
Participants in the favorable and average groups showed slower memory decline per increased year of age (0.007 [0.005-0.009], P < .001; and 0.002 [0 .000-0.003], P = .033 points higher, respectively), compared with those in the unfavorable group.
Healthy diet had the strongest protective effect on memory.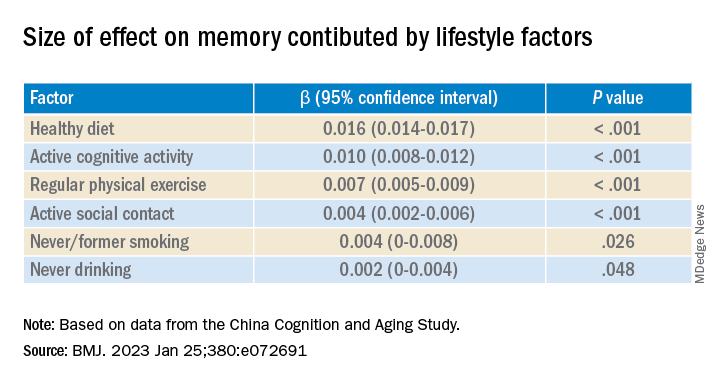
Memory decline occurred faster in APOE4 vesus non-APOE4 carriers (0.002 points/year [95% confidence interval, 0.001-0.003]; P = .007).
But APOE4 carriers with favorable and average lifestyles showed slower memory decline (0.027 [0.023-0.031] and 0.014 [0.010-0.019], respectively), compared with those with unfavorable lifestyles. Similar findings were obtained in non-APOE4 carriers.
Those with favorable or average lifestyle were respectively almost 90% and 30% less likely to develop dementia or MCI, compared with those with an unfavorable lifestyle.
The authors acknowledge the study’s limitations, including its observational design and the potential for measurement errors, owing to self-reporting of lifestyle factors. Additionally, some participants did not return for follow-up evaluations, leading to potential selection bias.
Nevertheless, the findings “might offer important information for public health to protect older [people] against memory decline,” they note – especially since the study “provides evidence that these effects also include individuals with the APOE4 allele.”
‘Important, encouraging’ research
In a comment, Severine Sabia, PhD, a senior researcher at the Université Paris Cité, INSERM Institut National de la Santé et de la Recherche Medicalé, France, called the findings “important and encouraging.”
However, said Dr. Sabia, who was not involved with the study, “there remain important research questions that need to be investigated in order to identify key behaviors: which combination, the cutoff of risk, and when to intervene.”
Future research on prevention “should examine a wider range of possible risk factors” and should also “identify specific exposures associated with the greatest risk, while also considering the risk threshold and age at exposure for each one.”
In an accompanying editorial, Dr. Sabia and co-author Archana Singh-Manoux, PhD, note that the risk of cognitive decline and dementia are probably determined by multiple factors.
They liken it to the “multifactorial risk paradigm introduced by the Framingham study,” which has “led to a substantial reduction in cardiovascular disease.” A similar approach could be used with dementia prevention, they suggest.
The authors received support from the Xuanwu Hospital of Capital Medical University for the submitted work. One of the authors received a grant from the French National Research Agency. The other authors have disclosed no relevant financial relationships. Dr. Sabia received grant funding from the French National Research Agency. Dr. Singh-Manoux received grants from the National Institute on Aging of the National Institutes of Health.
A version of this article first appeared on Medscape.com.
Investigators found that a healthy diet, cognitive activity, regular physical exercise, not smoking, and abstaining from alcohol were significantly linked to slowed cognitive decline irrespective of APOE4 status.
After adjusting for health and socioeconomic factors, investigators found that each individual healthy behavior was associated with a slower-than-average decline in memory over a decade. A healthy diet emerged as the strongest deterrent, followed by cognitive activity and physical exercise.
“A healthy lifestyle is associated with slower memory decline, even in the presence of the APOE4 allele,” study investigators led by Jianping Jia, MD, PhD, of the Innovation Center for Neurological Disorders and the department of neurology, Xuan Wu Hospital, Capital Medical University, Beijing, write.
“This study might offer important information to protect older adults against memory decline,” they add.
The study was published online in the BMJ.
Preventing memory decline
Memory “continuously declines as people age,” but age-related memory decline is not necessarily a prodrome of dementia and can “merely be senescent forgetfulness,” the investigators note. This can be “reversed or [can] become stable,” instead of progressing to a pathologic state.
Factors affecting memory include aging, APOE4 genotype, chronic diseases, and lifestyle patterns, with lifestyle “receiving increasing attention as a modifiable behavior.”
Nevertheless, few studies have focused on the impact of lifestyle on memory, and those that have are mostly cross-sectional and also “did not consider the interaction between a healthy lifestyle and genetic risk,” the researchers note.
To investigate, the researchers conducted a longitudinal study, known as the China Cognition and Aging Study, that considered genetic risk as well as lifestyle factors.
The study began in 2009 and concluded in 2019. Participants were evaluated and underwent neuropsychological testing in 2012, 2014, 2016, and at the study’s conclusion.
Participants (n = 29,072; mean [SD] age, 72.23 [6.61] years; 48.54% women; 20.43% APOE4 carriers) were required to have normal cognitive function at baseline. Data on those whose condition progressed to mild cognitive impairment (MCI) or dementia during the follow-up period were excluded after their diagnosis.
The Mini–Mental State Examination was used to assess global cognitive function. Memory function was assessed using the World Health Organization/University of California, Los Angeles Auditory Verbal Learning Test.
“Lifestyle” consisted of six modifiable factors: physical exercise (weekly frequency and total time), smoking (current, former, or never-smokers), alcohol consumption (never drank, drank occasionally, low to excess drinking, and heavy drinking), diet (daily intake of 12 food items: fruits, vegetables, fish, meat, dairy products, salt, oil, eggs, cereals, legumes, nuts, tea), cognitive activity (writing, reading, playing cards, mahjong, other games), and social contact (participating in meetings, attending parties, visiting friends/relatives, traveling, chatting online).
Participants’ lifestyles were scored on the basis of the number of healthy factors they engaged in.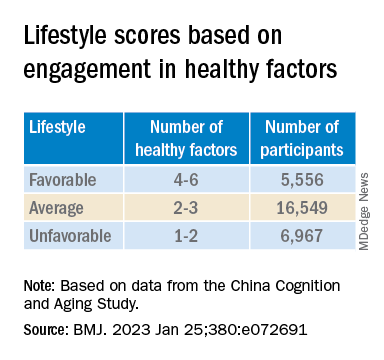
Participants were also stratified by APOE genotype into APOE4 carriers and noncarriers.
Demographic and other items of health information, including the presence of medical illness, were used as covariates. The researchers also included the “learning effect of each participant as a covariate, due to repeated cognitive assessments.”
Important for public health
During the 10-year period, 7,164 participants died, and 3,567 stopped participating.
Participants in the favorable and average groups showed slower memory decline per increased year of age (0.007 [0.005-0.009], P < .001; and 0.002 [0 .000-0.003], P = .033 points higher, respectively), compared with those in the unfavorable group.
Healthy diet had the strongest protective effect on memory.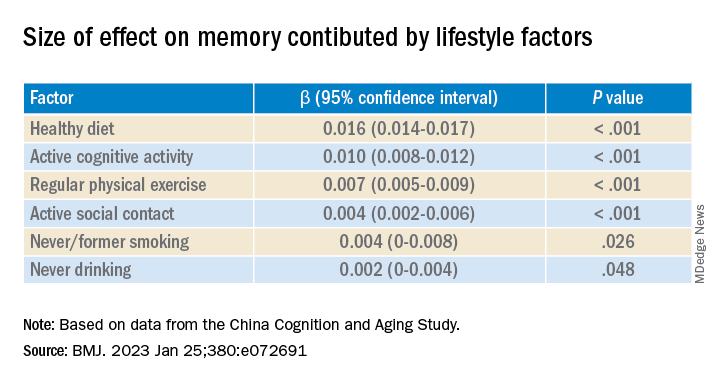
Memory decline occurred faster in APOE4 vesus non-APOE4 carriers (0.002 points/year [95% confidence interval, 0.001-0.003]; P = .007).
But APOE4 carriers with favorable and average lifestyles showed slower memory decline (0.027 [0.023-0.031] and 0.014 [0.010-0.019], respectively), compared with those with unfavorable lifestyles. Similar findings were obtained in non-APOE4 carriers.
Those with favorable or average lifestyle were respectively almost 90% and 30% less likely to develop dementia or MCI, compared with those with an unfavorable lifestyle.
The authors acknowledge the study’s limitations, including its observational design and the potential for measurement errors, owing to self-reporting of lifestyle factors. Additionally, some participants did not return for follow-up evaluations, leading to potential selection bias.
Nevertheless, the findings “might offer important information for public health to protect older [people] against memory decline,” they note – especially since the study “provides evidence that these effects also include individuals with the APOE4 allele.”
‘Important, encouraging’ research
In a comment, Severine Sabia, PhD, a senior researcher at the Université Paris Cité, INSERM Institut National de la Santé et de la Recherche Medicalé, France, called the findings “important and encouraging.”
However, said Dr. Sabia, who was not involved with the study, “there remain important research questions that need to be investigated in order to identify key behaviors: which combination, the cutoff of risk, and when to intervene.”
Future research on prevention “should examine a wider range of possible risk factors” and should also “identify specific exposures associated with the greatest risk, while also considering the risk threshold and age at exposure for each one.”
In an accompanying editorial, Dr. Sabia and co-author Archana Singh-Manoux, PhD, note that the risk of cognitive decline and dementia are probably determined by multiple factors.
They liken it to the “multifactorial risk paradigm introduced by the Framingham study,” which has “led to a substantial reduction in cardiovascular disease.” A similar approach could be used with dementia prevention, they suggest.
The authors received support from the Xuanwu Hospital of Capital Medical University for the submitted work. One of the authors received a grant from the French National Research Agency. The other authors have disclosed no relevant financial relationships. Dr. Sabia received grant funding from the French National Research Agency. Dr. Singh-Manoux received grants from the National Institute on Aging of the National Institutes of Health.
A version of this article first appeared on Medscape.com.
Investigators found that a healthy diet, cognitive activity, regular physical exercise, not smoking, and abstaining from alcohol were significantly linked to slowed cognitive decline irrespective of APOE4 status.
After adjusting for health and socioeconomic factors, investigators found that each individual healthy behavior was associated with a slower-than-average decline in memory over a decade. A healthy diet emerged as the strongest deterrent, followed by cognitive activity and physical exercise.
“A healthy lifestyle is associated with slower memory decline, even in the presence of the APOE4 allele,” study investigators led by Jianping Jia, MD, PhD, of the Innovation Center for Neurological Disorders and the department of neurology, Xuan Wu Hospital, Capital Medical University, Beijing, write.
“This study might offer important information to protect older adults against memory decline,” they add.
The study was published online in the BMJ.
Preventing memory decline
Memory “continuously declines as people age,” but age-related memory decline is not necessarily a prodrome of dementia and can “merely be senescent forgetfulness,” the investigators note. This can be “reversed or [can] become stable,” instead of progressing to a pathologic state.
Factors affecting memory include aging, APOE4 genotype, chronic diseases, and lifestyle patterns, with lifestyle “receiving increasing attention as a modifiable behavior.”
Nevertheless, few studies have focused on the impact of lifestyle on memory, and those that have are mostly cross-sectional and also “did not consider the interaction between a healthy lifestyle and genetic risk,” the researchers note.
To investigate, the researchers conducted a longitudinal study, known as the China Cognition and Aging Study, that considered genetic risk as well as lifestyle factors.
The study began in 2009 and concluded in 2019. Participants were evaluated and underwent neuropsychological testing in 2012, 2014, 2016, and at the study’s conclusion.
Participants (n = 29,072; mean [SD] age, 72.23 [6.61] years; 48.54% women; 20.43% APOE4 carriers) were required to have normal cognitive function at baseline. Data on those whose condition progressed to mild cognitive impairment (MCI) or dementia during the follow-up period were excluded after their diagnosis.
The Mini–Mental State Examination was used to assess global cognitive function. Memory function was assessed using the World Health Organization/University of California, Los Angeles Auditory Verbal Learning Test.
“Lifestyle” consisted of six modifiable factors: physical exercise (weekly frequency and total time), smoking (current, former, or never-smokers), alcohol consumption (never drank, drank occasionally, low to excess drinking, and heavy drinking), diet (daily intake of 12 food items: fruits, vegetables, fish, meat, dairy products, salt, oil, eggs, cereals, legumes, nuts, tea), cognitive activity (writing, reading, playing cards, mahjong, other games), and social contact (participating in meetings, attending parties, visiting friends/relatives, traveling, chatting online).
Participants’ lifestyles were scored on the basis of the number of healthy factors they engaged in.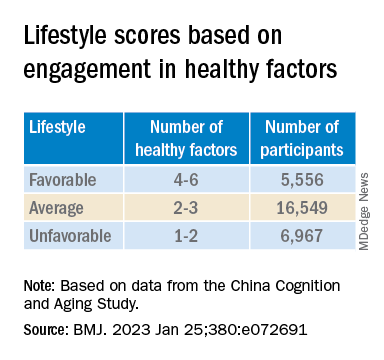
Participants were also stratified by APOE genotype into APOE4 carriers and noncarriers.
Demographic and other items of health information, including the presence of medical illness, were used as covariates. The researchers also included the “learning effect of each participant as a covariate, due to repeated cognitive assessments.”
Important for public health
During the 10-year period, 7,164 participants died, and 3,567 stopped participating.
Participants in the favorable and average groups showed slower memory decline per increased year of age (0.007 [0.005-0.009], P < .001; and 0.002 [0 .000-0.003], P = .033 points higher, respectively), compared with those in the unfavorable group.
Healthy diet had the strongest protective effect on memory.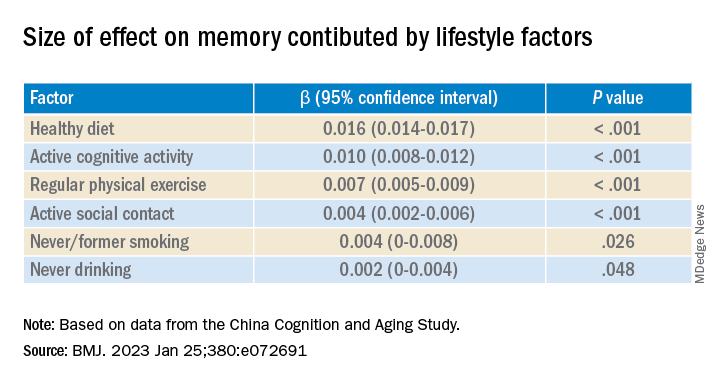
Memory decline occurred faster in APOE4 vesus non-APOE4 carriers (0.002 points/year [95% confidence interval, 0.001-0.003]; P = .007).
But APOE4 carriers with favorable and average lifestyles showed slower memory decline (0.027 [0.023-0.031] and 0.014 [0.010-0.019], respectively), compared with those with unfavorable lifestyles. Similar findings were obtained in non-APOE4 carriers.
Those with favorable or average lifestyle were respectively almost 90% and 30% less likely to develop dementia or MCI, compared with those with an unfavorable lifestyle.
The authors acknowledge the study’s limitations, including its observational design and the potential for measurement errors, owing to self-reporting of lifestyle factors. Additionally, some participants did not return for follow-up evaluations, leading to potential selection bias.
Nevertheless, the findings “might offer important information for public health to protect older [people] against memory decline,” they note – especially since the study “provides evidence that these effects also include individuals with the APOE4 allele.”
‘Important, encouraging’ research
In a comment, Severine Sabia, PhD, a senior researcher at the Université Paris Cité, INSERM Institut National de la Santé et de la Recherche Medicalé, France, called the findings “important and encouraging.”
However, said Dr. Sabia, who was not involved with the study, “there remain important research questions that need to be investigated in order to identify key behaviors: which combination, the cutoff of risk, and when to intervene.”
Future research on prevention “should examine a wider range of possible risk factors” and should also “identify specific exposures associated with the greatest risk, while also considering the risk threshold and age at exposure for each one.”
In an accompanying editorial, Dr. Sabia and co-author Archana Singh-Manoux, PhD, note that the risk of cognitive decline and dementia are probably determined by multiple factors.
They liken it to the “multifactorial risk paradigm introduced by the Framingham study,” which has “led to a substantial reduction in cardiovascular disease.” A similar approach could be used with dementia prevention, they suggest.
The authors received support from the Xuanwu Hospital of Capital Medical University for the submitted work. One of the authors received a grant from the French National Research Agency. The other authors have disclosed no relevant financial relationships. Dr. Sabia received grant funding from the French National Research Agency. Dr. Singh-Manoux received grants from the National Institute on Aging of the National Institutes of Health.
A version of this article first appeared on Medscape.com.
FROM THE BMJ
Even one head injury boosts all-cause mortality risk
An analysis of more than 13,000 adult participants in the Atherosclerosis Risk in Communities (ARIC) study showed a dose-response pattern in which one head injury was linked to a 66% increased risk for all-cause mortality, and two or more head injuries were associated with twice the risk in comparison with no head injuries.
These findings underscore the importance of preventing head injuries and of swift clinical intervention once a head injury occurs, lead author Holly Elser, MD, PhD, department of neurology, Hospital of the University of Pennsylvania, Philadelphia, told this news organization.
“Clinicians should counsel patients who are at risk for falls about head injuries and ensure patients are promptly evaluated in the hospital setting if they do have a fall – especially with loss of consciousness or other symptoms, such as headache or dizziness,” Dr. Elser added.
The findings were published online in JAMA Neurology.
Consistent evidence
There is “pretty consistent evidence” that mortality rates are increased in the short term after head injury, predominantly among hospitalized patients, Dr. Elser noted.
“But there’s less evidence about the long-term mortality implications of head injuries and less evidence from adults living in the community,” she added.
The analysis included 13,037 participants in the ARIC study, an ongoing study involving adults aged 45-65 years who were recruited from four geographically and racially diverse U.S. communities. The mean age at baseline (1987-1989) was 54 years; 57.7% were women; and 27.9% were Black.
Study participants are followed at routine in-person visits and semiannually via telephone.
Data on head injuries came from hospital diagnostic codes and self-reports. These reports included information on the number of injuries and whether the injury required medical care and involved loss of consciousness.
During the 27-year follow-up, 18.4% of the study sample had at least one head injury. Injuries occurred more frequently among women, which may reflect the predominance of women in the study population, said Dr. Elser.
Overall, about 56% of participants died during the study period. The estimated median amount of survival time after head injury was 4.7 years.
The most common causes of death were neoplasm, cardiovascular disease, and neurologic disorders. Regarding specific neurologic causes of death, the researchers found that 62.2% of deaths were due to neurodegenerative disease among individuals with head injury, vs. 51.4% among those without head injury.
This, said Dr. Elser, raises the possibility of reverse causality. “If you have a neurodegenerative disorder like Alzheimer’s disease dementia or Parkinson’s disease that leads to difficulty walking, you may be more likely to fall and have a head injury. The head injury in turn may lead to increased mortality,” she noted.
However, she stressed that the data on cause-specific mortality are exploratory. “Our research motivates future studies that really examine this time-dependent relationship between neurodegenerative disease and head injuries,” Dr. Elser said.
Dose-dependent response
In the unadjusted analysis, the hazard ratio of mortality among individuals with head injury was 2.21 (95% confidence interval, 2.09-2.34) compared with those who did not have head injury.
The association remained significant with adjustment for sociodemographic factors (HR, 1.99; 95% CI, 1.88-2.11) and with additional adjustment for vascular risk factors (HR, 1.92; 95% CI, 1.81-2.03).
The findings also showed a dose-response pattern in the association of head injuries with mortality. Compared with participants who did not have head injury, the HR was 1.66 (95% CI, 1.56-1.77) for those with one head injury and 2.11 (95% CI, 1.89-2.37) for those with two or more head injuries.
“It’s not as though once you’ve had one head injury, you’ve accrued all the damage you possibly can. We see pretty clearly here that recurrent head injury further increased the rate of deaths from all causes,” said Dr. Elser.
Injury severity was determined from hospital diagnostic codes using established algorithms. Results showed that mortality rates were increased with even mild head injury.
Interestingly, the association between head injury and all-cause mortality was weaker among those whose injuries were self-reported. One possibility is that these injuries were less severe, Dr. Elser noted.
“If you have head injury that’s mild enough that you don’t need to go to the hospital, it’s probably going to confer less long-term health risks than one that’s severe enough that you needed to be examined in an acute care setting,” she said.
Results were similar by race and for sex. “Even though there were more women with head injuries, the rate of mortality associated with head injury doesn’t differ from the rate among men,” Dr. Elser reported.
However, the association was stronger among those younger than 54 years at baseline (HR, 2.26) compared with older individuals (HR, 2.0) in the model that adjusted for demographics and lifestyle factors.
This may be explained by the reference group (those without a head injury) – the mortality rate was in general higher for the older participants, said Dr. Elser. It could also be that younger adults are more likely to have severe head injuries from, for example, motor vehicle accidents or violence, she added.
These new findings underscore the importance of public health measures, such as seatbelt laws, to reduce head injuries, the investigators note.
They add that clinicians with patients at risk for head injuries may recommend steps to lessen the risk of falls, such as having access to durable medical equipment, and ensuring driver safety.
Shorter life span
Commenting for this news organization, Frank Conidi, MD, director of the Florida Center for Headache and Sports Neurology in Port St. Lucie and past president of the Florida Society of Neurology, said the large number of participants “adds validity” to the finding that individuals with head injury are likely to have a shorter life span than those who do not suffer head trauma – and that this “was not purely by chance or from other causes.”
However, patients may not have accurately reported head injuries, in which case the rate of injury in the self-report subgroup would not reflect the actual incidence, noted Dr. Conidi, who was not involved with the research.
“In my practice, most patients have little knowledge as to the signs and symptoms of concussion and traumatic brain injury. Most think there needs to be some form of loss of consciousness to have a head injury, which is of course not true,” he said.
Dr. Conidi added that the finding of a higher incidence of death from neurodegenerative disorders supports the generally accepted consensus view that about 30% of patients with traumatic brain injury experience progression of symptoms and are at risk for early dementia.
The ARIC study is supported by the National Heart, Lung, and Blood Institute. Dr. Elser and Dr. Conidi have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
An analysis of more than 13,000 adult participants in the Atherosclerosis Risk in Communities (ARIC) study showed a dose-response pattern in which one head injury was linked to a 66% increased risk for all-cause mortality, and two or more head injuries were associated with twice the risk in comparison with no head injuries.
These findings underscore the importance of preventing head injuries and of swift clinical intervention once a head injury occurs, lead author Holly Elser, MD, PhD, department of neurology, Hospital of the University of Pennsylvania, Philadelphia, told this news organization.
“Clinicians should counsel patients who are at risk for falls about head injuries and ensure patients are promptly evaluated in the hospital setting if they do have a fall – especially with loss of consciousness or other symptoms, such as headache or dizziness,” Dr. Elser added.
The findings were published online in JAMA Neurology.
Consistent evidence
There is “pretty consistent evidence” that mortality rates are increased in the short term after head injury, predominantly among hospitalized patients, Dr. Elser noted.
“But there’s less evidence about the long-term mortality implications of head injuries and less evidence from adults living in the community,” she added.
The analysis included 13,037 participants in the ARIC study, an ongoing study involving adults aged 45-65 years who were recruited from four geographically and racially diverse U.S. communities. The mean age at baseline (1987-1989) was 54 years; 57.7% were women; and 27.9% were Black.
Study participants are followed at routine in-person visits and semiannually via telephone.
Data on head injuries came from hospital diagnostic codes and self-reports. These reports included information on the number of injuries and whether the injury required medical care and involved loss of consciousness.
During the 27-year follow-up, 18.4% of the study sample had at least one head injury. Injuries occurred more frequently among women, which may reflect the predominance of women in the study population, said Dr. Elser.
Overall, about 56% of participants died during the study period. The estimated median amount of survival time after head injury was 4.7 years.
The most common causes of death were neoplasm, cardiovascular disease, and neurologic disorders. Regarding specific neurologic causes of death, the researchers found that 62.2% of deaths were due to neurodegenerative disease among individuals with head injury, vs. 51.4% among those without head injury.
This, said Dr. Elser, raises the possibility of reverse causality. “If you have a neurodegenerative disorder like Alzheimer’s disease dementia or Parkinson’s disease that leads to difficulty walking, you may be more likely to fall and have a head injury. The head injury in turn may lead to increased mortality,” she noted.
However, she stressed that the data on cause-specific mortality are exploratory. “Our research motivates future studies that really examine this time-dependent relationship between neurodegenerative disease and head injuries,” Dr. Elser said.
Dose-dependent response
In the unadjusted analysis, the hazard ratio of mortality among individuals with head injury was 2.21 (95% confidence interval, 2.09-2.34) compared with those who did not have head injury.
The association remained significant with adjustment for sociodemographic factors (HR, 1.99; 95% CI, 1.88-2.11) and with additional adjustment for vascular risk factors (HR, 1.92; 95% CI, 1.81-2.03).
The findings also showed a dose-response pattern in the association of head injuries with mortality. Compared with participants who did not have head injury, the HR was 1.66 (95% CI, 1.56-1.77) for those with one head injury and 2.11 (95% CI, 1.89-2.37) for those with two or more head injuries.
“It’s not as though once you’ve had one head injury, you’ve accrued all the damage you possibly can. We see pretty clearly here that recurrent head injury further increased the rate of deaths from all causes,” said Dr. Elser.
Injury severity was determined from hospital diagnostic codes using established algorithms. Results showed that mortality rates were increased with even mild head injury.
Interestingly, the association between head injury and all-cause mortality was weaker among those whose injuries were self-reported. One possibility is that these injuries were less severe, Dr. Elser noted.
“If you have head injury that’s mild enough that you don’t need to go to the hospital, it’s probably going to confer less long-term health risks than one that’s severe enough that you needed to be examined in an acute care setting,” she said.
Results were similar by race and for sex. “Even though there were more women with head injuries, the rate of mortality associated with head injury doesn’t differ from the rate among men,” Dr. Elser reported.
However, the association was stronger among those younger than 54 years at baseline (HR, 2.26) compared with older individuals (HR, 2.0) in the model that adjusted for demographics and lifestyle factors.
This may be explained by the reference group (those without a head injury) – the mortality rate was in general higher for the older participants, said Dr. Elser. It could also be that younger adults are more likely to have severe head injuries from, for example, motor vehicle accidents or violence, she added.
These new findings underscore the importance of public health measures, such as seatbelt laws, to reduce head injuries, the investigators note.
They add that clinicians with patients at risk for head injuries may recommend steps to lessen the risk of falls, such as having access to durable medical equipment, and ensuring driver safety.
Shorter life span
Commenting for this news organization, Frank Conidi, MD, director of the Florida Center for Headache and Sports Neurology in Port St. Lucie and past president of the Florida Society of Neurology, said the large number of participants “adds validity” to the finding that individuals with head injury are likely to have a shorter life span than those who do not suffer head trauma – and that this “was not purely by chance or from other causes.”
However, patients may not have accurately reported head injuries, in which case the rate of injury in the self-report subgroup would not reflect the actual incidence, noted Dr. Conidi, who was not involved with the research.
“In my practice, most patients have little knowledge as to the signs and symptoms of concussion and traumatic brain injury. Most think there needs to be some form of loss of consciousness to have a head injury, which is of course not true,” he said.
Dr. Conidi added that the finding of a higher incidence of death from neurodegenerative disorders supports the generally accepted consensus view that about 30% of patients with traumatic brain injury experience progression of symptoms and are at risk for early dementia.
The ARIC study is supported by the National Heart, Lung, and Blood Institute. Dr. Elser and Dr. Conidi have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
An analysis of more than 13,000 adult participants in the Atherosclerosis Risk in Communities (ARIC) study showed a dose-response pattern in which one head injury was linked to a 66% increased risk for all-cause mortality, and two or more head injuries were associated with twice the risk in comparison with no head injuries.
These findings underscore the importance of preventing head injuries and of swift clinical intervention once a head injury occurs, lead author Holly Elser, MD, PhD, department of neurology, Hospital of the University of Pennsylvania, Philadelphia, told this news organization.
“Clinicians should counsel patients who are at risk for falls about head injuries and ensure patients are promptly evaluated in the hospital setting if they do have a fall – especially with loss of consciousness or other symptoms, such as headache or dizziness,” Dr. Elser added.
The findings were published online in JAMA Neurology.
Consistent evidence
There is “pretty consistent evidence” that mortality rates are increased in the short term after head injury, predominantly among hospitalized patients, Dr. Elser noted.
“But there’s less evidence about the long-term mortality implications of head injuries and less evidence from adults living in the community,” she added.
The analysis included 13,037 participants in the ARIC study, an ongoing study involving adults aged 45-65 years who were recruited from four geographically and racially diverse U.S. communities. The mean age at baseline (1987-1989) was 54 years; 57.7% were women; and 27.9% were Black.
Study participants are followed at routine in-person visits and semiannually via telephone.
Data on head injuries came from hospital diagnostic codes and self-reports. These reports included information on the number of injuries and whether the injury required medical care and involved loss of consciousness.
During the 27-year follow-up, 18.4% of the study sample had at least one head injury. Injuries occurred more frequently among women, which may reflect the predominance of women in the study population, said Dr. Elser.
Overall, about 56% of participants died during the study period. The estimated median amount of survival time after head injury was 4.7 years.
The most common causes of death were neoplasm, cardiovascular disease, and neurologic disorders. Regarding specific neurologic causes of death, the researchers found that 62.2% of deaths were due to neurodegenerative disease among individuals with head injury, vs. 51.4% among those without head injury.
This, said Dr. Elser, raises the possibility of reverse causality. “If you have a neurodegenerative disorder like Alzheimer’s disease dementia or Parkinson’s disease that leads to difficulty walking, you may be more likely to fall and have a head injury. The head injury in turn may lead to increased mortality,” she noted.
However, she stressed that the data on cause-specific mortality are exploratory. “Our research motivates future studies that really examine this time-dependent relationship between neurodegenerative disease and head injuries,” Dr. Elser said.
Dose-dependent response
In the unadjusted analysis, the hazard ratio of mortality among individuals with head injury was 2.21 (95% confidence interval, 2.09-2.34) compared with those who did not have head injury.
The association remained significant with adjustment for sociodemographic factors (HR, 1.99; 95% CI, 1.88-2.11) and with additional adjustment for vascular risk factors (HR, 1.92; 95% CI, 1.81-2.03).
The findings also showed a dose-response pattern in the association of head injuries with mortality. Compared with participants who did not have head injury, the HR was 1.66 (95% CI, 1.56-1.77) for those with one head injury and 2.11 (95% CI, 1.89-2.37) for those with two or more head injuries.
“It’s not as though once you’ve had one head injury, you’ve accrued all the damage you possibly can. We see pretty clearly here that recurrent head injury further increased the rate of deaths from all causes,” said Dr. Elser.
Injury severity was determined from hospital diagnostic codes using established algorithms. Results showed that mortality rates were increased with even mild head injury.
Interestingly, the association between head injury and all-cause mortality was weaker among those whose injuries were self-reported. One possibility is that these injuries were less severe, Dr. Elser noted.
“If you have head injury that’s mild enough that you don’t need to go to the hospital, it’s probably going to confer less long-term health risks than one that’s severe enough that you needed to be examined in an acute care setting,” she said.
Results were similar by race and for sex. “Even though there were more women with head injuries, the rate of mortality associated with head injury doesn’t differ from the rate among men,” Dr. Elser reported.
However, the association was stronger among those younger than 54 years at baseline (HR, 2.26) compared with older individuals (HR, 2.0) in the model that adjusted for demographics and lifestyle factors.
This may be explained by the reference group (those without a head injury) – the mortality rate was in general higher for the older participants, said Dr. Elser. It could also be that younger adults are more likely to have severe head injuries from, for example, motor vehicle accidents or violence, she added.
These new findings underscore the importance of public health measures, such as seatbelt laws, to reduce head injuries, the investigators note.
They add that clinicians with patients at risk for head injuries may recommend steps to lessen the risk of falls, such as having access to durable medical equipment, and ensuring driver safety.
Shorter life span
Commenting for this news organization, Frank Conidi, MD, director of the Florida Center for Headache and Sports Neurology in Port St. Lucie and past president of the Florida Society of Neurology, said the large number of participants “adds validity” to the finding that individuals with head injury are likely to have a shorter life span than those who do not suffer head trauma – and that this “was not purely by chance or from other causes.”
However, patients may not have accurately reported head injuries, in which case the rate of injury in the self-report subgroup would not reflect the actual incidence, noted Dr. Conidi, who was not involved with the research.
“In my practice, most patients have little knowledge as to the signs and symptoms of concussion and traumatic brain injury. Most think there needs to be some form of loss of consciousness to have a head injury, which is of course not true,” he said.
Dr. Conidi added that the finding of a higher incidence of death from neurodegenerative disorders supports the generally accepted consensus view that about 30% of patients with traumatic brain injury experience progression of symptoms and are at risk for early dementia.
The ARIC study is supported by the National Heart, Lung, and Blood Institute. Dr. Elser and Dr. Conidi have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM JAMA NEUROLOGY
Don’t cross the friends line with patients
All that moving can make it hard to maintain friendships. Factor in the challenges from the pandemic, and a physician’s life can be lonely. So, when a patient invites you for coffee or a game of pickleball, do you accept? For almost one-third of the physicians who responded to the Medscape Physician Friendships: The Joys and Challenges 2022, the answer might be yes.
About 29% said they develop friendships with patients. However, a lot depends on the circumstances. As one physician in the report said: “I have been a pediatrician for 35 years, and my patients have grown up and become productive adults in our small, rural, isolated area. You can’t help but know almost everyone.”
As the daughter of a cardiologist, Nishi Mehta, MD, a radiologist and founder of the largest physician-only Facebook group in the country, grew up with that small-town-everyone-knows-the-doctor model.
“When I was a kid, I’d go to the mall, and my friends and I would play a game: How long before a patient [of my dad’s] comes up to me?” she said. At the time, Dr. Mehta was embarrassed, but now she marvels that her dad knew his patients so well that they would recognize his daughter in crowded suburban mall.
In other instances, a physician may develop a friendly relationship after a patient leaves their care. For example, Leo Nissola, MD, now a full-time researcher and immunotherapy scientist in San Francisco, has stayed in touch with some of the patients he treated while at the University of Texas MD Anderson Cancer Center, Houston.
Dr. Nissola said it was important to stay connected with the patients he had meaningful relationships with. “It becomes challenging, though, when a former patient asks for medical advice.” At that moment, “you have to be explicitly clear that the relationship has changed.”
A hard line in the sand
The blurring of lines is one reason many doctors refuse to befriend patients, even after they are no longer treating them. The American College of Physicians Ethics Manual advises against treating anyone with whom you have a close relationship, including family and friends.
“Friendships can get in the way of patients being honest with you, which can interfere with medical care,” Dr. Mehta said. “If a patient has a concern related to something they wouldn’t want you to know as friends, it can get awkward. They may elect not to tell you.”
And on the flip side, friendship can provide a view into your private life that you may not welcome in the exam room.
“Let’s say you go out for drinks [with a patient], and you’re up late, but you have surgery the next day,” said Brandi Ring, MD, an ob.gyn. and the associate medical director at the Center for Children and Women in Houston. Now, one of your patients knows you were out until midnight when you had to be in the OR at 5:00 a.m.
Worse still, your relationship could color your decisions about a patient’s care, even unconsciously. It can be hard to maintain objectivity when you have an emotional investment in someone’s well-being.
“We don’t necessarily treat family and friends to the standards of medical care,” said Dr. Ring. “We go above and beyond. We might order more tests and more scans. We don’t always follow the guidelines, especially in critical illness.”
For all these reasons and more, the ACP advises against treating friends.
Put physician before friend
But adhering to those guidelines can lead physicians to make some painful decisions. Cutting yourself off from the possibility of friendship is never easy, and the Medscape report found that physicians tend to have fewer friends than the average American.
“Especially earlier in my practice, when I was a young parent, and I would see a lot of other young parents in the same stage in life, I’d think, ‘In other circumstances, I would be hanging out at the park with this person,’ “ said Kathleen Rowland, MD, a family medicine physician and vice chair of education in the department of family medicine at Rush University, Chicago. “But the hard part is, the doctor-patient relationship always comes first.”
To a certain extent, one’s specialty may determine the feasibility of becoming friends with a patient. While Dr. Mehta has never done so, as a radiologist, she doesn’t usually see patients repeatedly. Likewise, a young gerontologist may have little in common with his octogenarian patients. And an older pediatrician is not in the same life stage as his patients’ sleep-deprived new parents, possibly making them less attractive friends.
However, practicing family medicine is all about long-term physician-patient relationships. Getting to know patients and their families over many years can lead to a certain intimacy. Dr. Rowland said that, while a wonderful part of being a physician is getting that unique trust whereby patients tell you all sorts of things about their lives, she’s never gone down the friendship path.
“There’s the assumption I’ll take care of someone for a long period of time, and their partner and their kids, maybe another generation or two,” Dr. Rowland said. “People really do rely on that relationship to contribute to their health.”
Worse, nowadays, when people may be starved for connection, many patients want to feel emotionally close and cared for by their doctor, so it’d be easy to cross the line. While patients deserve a compassionate, caring doctor, the physician is left to walk the line between those boundaries. Dr. Rowland said, “It’s up to the clinician to say: ‘My role is as a doctor. You deserve caring friends, but I have to order your mammogram and your blood counts. My role is different.’ ”
Friendly but not friends
It can be tricky to navigate the boundary between a cordial, warm relationship with a patient and that patient inviting you to their daughter’s wedding.
“People may mistake being pleasant and friendly for being friends,” said Larry Blosser, MD, chief medical officer at Central Ohio Primary Care, Westerville. In his position, he sometimes hears from patients who have misunderstood their relationship with a doctor in the practice. When that happens, he advises the physician to consider the persona they’re presenting to the patient. If you’re overly friendly, there’s the potential for confusion, but you can’t be aloof and cold, he said.
Maintaining that awareness helps to prevent a patient’s offhand invitation to catch a movie or go on a hike. And verbalizing it to your patients can make your relationship clear from the get-go.
“I tell patients we’re a team. I’m the captain, and they’re my MVP. When the match is over, whatever the results, we’re done,” said Karenne Fru, MD, PhD, a fertility specialist at Oma Fertility Atlanta. Making deep connections is essential to her practice, so Dr. Fru structures her patient interactions carefully. “Infertility is such an isolating experience. While you’re with us, we care about what’s going on in your life, your pets, and your mom’s chemo. We need mutual trust for you to be compliant with the care.”
However, that approach won’t work when you see patients regularly, as with family practice or specialties that see the same patients repeatedly throughout the year. In those circumstances, the match is never over but one in which the onus is on the physician to establish a friendly yet professional rapport without letting your self-interest, loneliness, or lack of friends interfere.
“It’s been a very difficult couple of years for a lot of us. Depending on what kind of clinical work we do, some of us took care of healthy people that got very sick or passed away,” Dr. Rowland said. “Having the chance to reconnect with people and reestablish some of that closeness, both physical and emotional, is going to be good for us.”
Just continue conveying warm, trusting compassion for your patients without blurring the friend lines.
A version of this article first appeared on Medscape.com.
All that moving can make it hard to maintain friendships. Factor in the challenges from the pandemic, and a physician’s life can be lonely. So, when a patient invites you for coffee or a game of pickleball, do you accept? For almost one-third of the physicians who responded to the Medscape Physician Friendships: The Joys and Challenges 2022, the answer might be yes.
About 29% said they develop friendships with patients. However, a lot depends on the circumstances. As one physician in the report said: “I have been a pediatrician for 35 years, and my patients have grown up and become productive adults in our small, rural, isolated area. You can’t help but know almost everyone.”
As the daughter of a cardiologist, Nishi Mehta, MD, a radiologist and founder of the largest physician-only Facebook group in the country, grew up with that small-town-everyone-knows-the-doctor model.
“When I was a kid, I’d go to the mall, and my friends and I would play a game: How long before a patient [of my dad’s] comes up to me?” she said. At the time, Dr. Mehta was embarrassed, but now she marvels that her dad knew his patients so well that they would recognize his daughter in crowded suburban mall.
In other instances, a physician may develop a friendly relationship after a patient leaves their care. For example, Leo Nissola, MD, now a full-time researcher and immunotherapy scientist in San Francisco, has stayed in touch with some of the patients he treated while at the University of Texas MD Anderson Cancer Center, Houston.
Dr. Nissola said it was important to stay connected with the patients he had meaningful relationships with. “It becomes challenging, though, when a former patient asks for medical advice.” At that moment, “you have to be explicitly clear that the relationship has changed.”
A hard line in the sand
The blurring of lines is one reason many doctors refuse to befriend patients, even after they are no longer treating them. The American College of Physicians Ethics Manual advises against treating anyone with whom you have a close relationship, including family and friends.
“Friendships can get in the way of patients being honest with you, which can interfere with medical care,” Dr. Mehta said. “If a patient has a concern related to something they wouldn’t want you to know as friends, it can get awkward. They may elect not to tell you.”
And on the flip side, friendship can provide a view into your private life that you may not welcome in the exam room.
“Let’s say you go out for drinks [with a patient], and you’re up late, but you have surgery the next day,” said Brandi Ring, MD, an ob.gyn. and the associate medical director at the Center for Children and Women in Houston. Now, one of your patients knows you were out until midnight when you had to be in the OR at 5:00 a.m.
Worse still, your relationship could color your decisions about a patient’s care, even unconsciously. It can be hard to maintain objectivity when you have an emotional investment in someone’s well-being.
“We don’t necessarily treat family and friends to the standards of medical care,” said Dr. Ring. “We go above and beyond. We might order more tests and more scans. We don’t always follow the guidelines, especially in critical illness.”
For all these reasons and more, the ACP advises against treating friends.
Put physician before friend
But adhering to those guidelines can lead physicians to make some painful decisions. Cutting yourself off from the possibility of friendship is never easy, and the Medscape report found that physicians tend to have fewer friends than the average American.
“Especially earlier in my practice, when I was a young parent, and I would see a lot of other young parents in the same stage in life, I’d think, ‘In other circumstances, I would be hanging out at the park with this person,’ “ said Kathleen Rowland, MD, a family medicine physician and vice chair of education in the department of family medicine at Rush University, Chicago. “But the hard part is, the doctor-patient relationship always comes first.”
To a certain extent, one’s specialty may determine the feasibility of becoming friends with a patient. While Dr. Mehta has never done so, as a radiologist, she doesn’t usually see patients repeatedly. Likewise, a young gerontologist may have little in common with his octogenarian patients. And an older pediatrician is not in the same life stage as his patients’ sleep-deprived new parents, possibly making them less attractive friends.
However, practicing family medicine is all about long-term physician-patient relationships. Getting to know patients and their families over many years can lead to a certain intimacy. Dr. Rowland said that, while a wonderful part of being a physician is getting that unique trust whereby patients tell you all sorts of things about their lives, she’s never gone down the friendship path.
“There’s the assumption I’ll take care of someone for a long period of time, and their partner and their kids, maybe another generation or two,” Dr. Rowland said. “People really do rely on that relationship to contribute to their health.”
Worse, nowadays, when people may be starved for connection, many patients want to feel emotionally close and cared for by their doctor, so it’d be easy to cross the line. While patients deserve a compassionate, caring doctor, the physician is left to walk the line between those boundaries. Dr. Rowland said, “It’s up to the clinician to say: ‘My role is as a doctor. You deserve caring friends, but I have to order your mammogram and your blood counts. My role is different.’ ”
Friendly but not friends
It can be tricky to navigate the boundary between a cordial, warm relationship with a patient and that patient inviting you to their daughter’s wedding.
“People may mistake being pleasant and friendly for being friends,” said Larry Blosser, MD, chief medical officer at Central Ohio Primary Care, Westerville. In his position, he sometimes hears from patients who have misunderstood their relationship with a doctor in the practice. When that happens, he advises the physician to consider the persona they’re presenting to the patient. If you’re overly friendly, there’s the potential for confusion, but you can’t be aloof and cold, he said.
Maintaining that awareness helps to prevent a patient’s offhand invitation to catch a movie or go on a hike. And verbalizing it to your patients can make your relationship clear from the get-go.
“I tell patients we’re a team. I’m the captain, and they’re my MVP. When the match is over, whatever the results, we’re done,” said Karenne Fru, MD, PhD, a fertility specialist at Oma Fertility Atlanta. Making deep connections is essential to her practice, so Dr. Fru structures her patient interactions carefully. “Infertility is such an isolating experience. While you’re with us, we care about what’s going on in your life, your pets, and your mom’s chemo. We need mutual trust for you to be compliant with the care.”
However, that approach won’t work when you see patients regularly, as with family practice or specialties that see the same patients repeatedly throughout the year. In those circumstances, the match is never over but one in which the onus is on the physician to establish a friendly yet professional rapport without letting your self-interest, loneliness, or lack of friends interfere.
“It’s been a very difficult couple of years for a lot of us. Depending on what kind of clinical work we do, some of us took care of healthy people that got very sick or passed away,” Dr. Rowland said. “Having the chance to reconnect with people and reestablish some of that closeness, both physical and emotional, is going to be good for us.”
Just continue conveying warm, trusting compassion for your patients without blurring the friend lines.
A version of this article first appeared on Medscape.com.
All that moving can make it hard to maintain friendships. Factor in the challenges from the pandemic, and a physician’s life can be lonely. So, when a patient invites you for coffee or a game of pickleball, do you accept? For almost one-third of the physicians who responded to the Medscape Physician Friendships: The Joys and Challenges 2022, the answer might be yes.
About 29% said they develop friendships with patients. However, a lot depends on the circumstances. As one physician in the report said: “I have been a pediatrician for 35 years, and my patients have grown up and become productive adults in our small, rural, isolated area. You can’t help but know almost everyone.”
As the daughter of a cardiologist, Nishi Mehta, MD, a radiologist and founder of the largest physician-only Facebook group in the country, grew up with that small-town-everyone-knows-the-doctor model.
“When I was a kid, I’d go to the mall, and my friends and I would play a game: How long before a patient [of my dad’s] comes up to me?” she said. At the time, Dr. Mehta was embarrassed, but now she marvels that her dad knew his patients so well that they would recognize his daughter in crowded suburban mall.
In other instances, a physician may develop a friendly relationship after a patient leaves their care. For example, Leo Nissola, MD, now a full-time researcher and immunotherapy scientist in San Francisco, has stayed in touch with some of the patients he treated while at the University of Texas MD Anderson Cancer Center, Houston.
Dr. Nissola said it was important to stay connected with the patients he had meaningful relationships with. “It becomes challenging, though, when a former patient asks for medical advice.” At that moment, “you have to be explicitly clear that the relationship has changed.”
A hard line in the sand
The blurring of lines is one reason many doctors refuse to befriend patients, even after they are no longer treating them. The American College of Physicians Ethics Manual advises against treating anyone with whom you have a close relationship, including family and friends.
“Friendships can get in the way of patients being honest with you, which can interfere with medical care,” Dr. Mehta said. “If a patient has a concern related to something they wouldn’t want you to know as friends, it can get awkward. They may elect not to tell you.”
And on the flip side, friendship can provide a view into your private life that you may not welcome in the exam room.
“Let’s say you go out for drinks [with a patient], and you’re up late, but you have surgery the next day,” said Brandi Ring, MD, an ob.gyn. and the associate medical director at the Center for Children and Women in Houston. Now, one of your patients knows you were out until midnight when you had to be in the OR at 5:00 a.m.
Worse still, your relationship could color your decisions about a patient’s care, even unconsciously. It can be hard to maintain objectivity when you have an emotional investment in someone’s well-being.
“We don’t necessarily treat family and friends to the standards of medical care,” said Dr. Ring. “We go above and beyond. We might order more tests and more scans. We don’t always follow the guidelines, especially in critical illness.”
For all these reasons and more, the ACP advises against treating friends.
Put physician before friend
But adhering to those guidelines can lead physicians to make some painful decisions. Cutting yourself off from the possibility of friendship is never easy, and the Medscape report found that physicians tend to have fewer friends than the average American.
“Especially earlier in my practice, when I was a young parent, and I would see a lot of other young parents in the same stage in life, I’d think, ‘In other circumstances, I would be hanging out at the park with this person,’ “ said Kathleen Rowland, MD, a family medicine physician and vice chair of education in the department of family medicine at Rush University, Chicago. “But the hard part is, the doctor-patient relationship always comes first.”
To a certain extent, one’s specialty may determine the feasibility of becoming friends with a patient. While Dr. Mehta has never done so, as a radiologist, she doesn’t usually see patients repeatedly. Likewise, a young gerontologist may have little in common with his octogenarian patients. And an older pediatrician is not in the same life stage as his patients’ sleep-deprived new parents, possibly making them less attractive friends.
However, practicing family medicine is all about long-term physician-patient relationships. Getting to know patients and their families over many years can lead to a certain intimacy. Dr. Rowland said that, while a wonderful part of being a physician is getting that unique trust whereby patients tell you all sorts of things about their lives, she’s never gone down the friendship path.
“There’s the assumption I’ll take care of someone for a long period of time, and their partner and their kids, maybe another generation or two,” Dr. Rowland said. “People really do rely on that relationship to contribute to their health.”
Worse, nowadays, when people may be starved for connection, many patients want to feel emotionally close and cared for by their doctor, so it’d be easy to cross the line. While patients deserve a compassionate, caring doctor, the physician is left to walk the line between those boundaries. Dr. Rowland said, “It’s up to the clinician to say: ‘My role is as a doctor. You deserve caring friends, but I have to order your mammogram and your blood counts. My role is different.’ ”
Friendly but not friends
It can be tricky to navigate the boundary between a cordial, warm relationship with a patient and that patient inviting you to their daughter’s wedding.
“People may mistake being pleasant and friendly for being friends,” said Larry Blosser, MD, chief medical officer at Central Ohio Primary Care, Westerville. In his position, he sometimes hears from patients who have misunderstood their relationship with a doctor in the practice. When that happens, he advises the physician to consider the persona they’re presenting to the patient. If you’re overly friendly, there’s the potential for confusion, but you can’t be aloof and cold, he said.
Maintaining that awareness helps to prevent a patient’s offhand invitation to catch a movie or go on a hike. And verbalizing it to your patients can make your relationship clear from the get-go.
“I tell patients we’re a team. I’m the captain, and they’re my MVP. When the match is over, whatever the results, we’re done,” said Karenne Fru, MD, PhD, a fertility specialist at Oma Fertility Atlanta. Making deep connections is essential to her practice, so Dr. Fru structures her patient interactions carefully. “Infertility is such an isolating experience. While you’re with us, we care about what’s going on in your life, your pets, and your mom’s chemo. We need mutual trust for you to be compliant with the care.”
However, that approach won’t work when you see patients regularly, as with family practice or specialties that see the same patients repeatedly throughout the year. In those circumstances, the match is never over but one in which the onus is on the physician to establish a friendly yet professional rapport without letting your self-interest, loneliness, or lack of friends interfere.
“It’s been a very difficult couple of years for a lot of us. Depending on what kind of clinical work we do, some of us took care of healthy people that got very sick or passed away,” Dr. Rowland said. “Having the chance to reconnect with people and reestablish some of that closeness, both physical and emotional, is going to be good for us.”
Just continue conveying warm, trusting compassion for your patients without blurring the friend lines.
A version of this article first appeared on Medscape.com.
Pediatricians, specialists largely agree on ASD diagnoses
General pediatricians and a multidisciplinary team of specialists agreed most of the time on which children should be diagnosed with autism spectrum disorder (ASD), data from a new study suggest.
But when it came to ruling out ASD, the agreement rate was much lower.
The study by Melanie Penner, MSc, MD, with the Autism Research Centre at Bloorview Research Institute, Toronto, and colleagues found that 89% of the time when a physician determined a child had ASD, the multidisciplinary team agreed. But when a pediatrician thought a child did not have ASD, the multidisciplinary team agreed only 60% of the time. The study was published in JAMA Network Open.
Multidisciplinary team model can’t keep up with demand
The findings are important as many guidelines recommend multidisciplinary teams (MDTs) for all ASD diagnostic assessment. However, the resources for this model can’t meet the demand of children needing a diagnosis and can lead to long waits for ASD therapies.
In Canada, the researchers note, the average wait time from referral to receipt of ASD diagnosis has been reported as 7 months and “has likely lengthened since the COVID-19 pandemic.”
Jennifer Gerdts, PhD, an attending psychologist at the Seattle Children’s Autism Center, said in an interview that the wait there for diagnosis in children older than 4 is “multiple years,” a length of time that’s common across the United States. Meanwhile, in many states families can’t access services without a diagnosis.
Expanding capacity with diagnoses by general pediatricians may improve access, but the diagnostic accuracy is critical.
Dr. Gerdts, who was not part of the study, said this research is “hugely important in the work that is under way to build community capacity for diagnostic evaluation.”
She said this study shows that not all diagnoses need the resources of a multiple-disciplinary team and that “pediatricians can do it, too, and they can do it pretty accurately.” Dr. Gerdts evaluates children for autism and helps train pediatricians to make diagnoses.
Pediatricians, specialist team completed blinded assessments
The 17 pediatricians in the study and the specialist team independently completed blinded assessment and each recorded a decision on whether the child had ASD. The prospective diagnostic study was conducted in a specialist assessment center in Toronto and in general pediatrician practices in Ontario from June 2016 to March 2020.
Children were younger than 5.5 years, did not have an ASD diagnosis and were referred because there was a development concern. The pediatricians referred 106 children (75% boys; average age, 3.5 years). More than half (57%) of the participating children were from minority racial and ethnic groups.
The children were randomly assigned to two groups: One included children who had their MDT visits before their pediatrician assessment and the other group included those who had their MDT visits after their pediatrician assessment.
The MDT diagnosed more than two-thirds of the children (68%) with ASD.
Sensitivity and specificity of the pediatrician assessments, compared with that of the specialist team, were 0.75 (95% confidence interval, 0.67-0.83) and 0.79 (95% CI, 0.62-0.91), respectively.
A look at pediatricians’ accuracy
Pediatricians reported the decisions they would have made had the child not been in the study.
- In 69% of the true-positive cases, pediatricians would have given an ASD diagnosis.
- In 44% of true-negative cases, they would have told the family the child did not have autism; in 30% of those case, they would give alternative diagnoses (most commonly ADHD and language delay).
- The pediatrician would have diagnosed ASD in only one of the seven false-positive cases and would refer those patients to a subspecialist 71% of the time.
- In false-negative cases, the pediatrician would incorrectly tell the family the child does not have autism 44% of the time.
Regarding the false-negative cases, the authors wrote, “more caution is needed for pediatricians when definitively ruling out ASD, which might result in diagnostic delays.”
Confidence is key
Physician confidence was also correlated with accuracy.
The authors wrote: “Among true-positive cases (MDT and pediatrician agree the child has ASD), the pediatrician was certain or very certain 80% of the time (43 cases) and the MDT was certain or very certain 96% of the time (52 cases). As such, if pediatricians conferred ASD diagnoses when feeling certain or very certain, they would make 46 correct diagnoses and 2 incorrect diagnoses.”
The high accuracy of diagnosis when physicians are confident suggests “listening to that sense of certainty is important,” Dr. Gerdts said. Conversely, these numbers show when a physician is uncertain about diagnosing ASD, they should listen to that instinct, too, and refer.
The results of the study support having general pediatricians diagnose and move forward with their patients when the signs of ASD are more definitive, saving the less-certain cases for the more resource-intensive teams to diagnose. Many states are moving toward that “tiered” system, Dr. Gerdts said.
“For many, and in fact most children, general pediatricians are pretty accurate when making an autism diagnosis,” she said.
“Let’s get [general pediatricians] confident in recognizing when this is outside their skill and ability level,” she said. “If you’re not sure, it is better to refer them on than to misdiagnose them.”
The important missing piece she said is how to support them “so they don’t feel pressure to make that call,” Dr. Gerdts said.
This project was funded by a grant from the Bloorview Research Institute, a grant from the Canadian Institutes of Health Research and a grant from the Canadian Institutes of Health. Three coauthors consult for and receive grants from several pharmaceutical companies and other organizations. Dr. Gerdts declared no relevant financial relationships.
General pediatricians and a multidisciplinary team of specialists agreed most of the time on which children should be diagnosed with autism spectrum disorder (ASD), data from a new study suggest.
But when it came to ruling out ASD, the agreement rate was much lower.
The study by Melanie Penner, MSc, MD, with the Autism Research Centre at Bloorview Research Institute, Toronto, and colleagues found that 89% of the time when a physician determined a child had ASD, the multidisciplinary team agreed. But when a pediatrician thought a child did not have ASD, the multidisciplinary team agreed only 60% of the time. The study was published in JAMA Network Open.
Multidisciplinary team model can’t keep up with demand
The findings are important as many guidelines recommend multidisciplinary teams (MDTs) for all ASD diagnostic assessment. However, the resources for this model can’t meet the demand of children needing a diagnosis and can lead to long waits for ASD therapies.
In Canada, the researchers note, the average wait time from referral to receipt of ASD diagnosis has been reported as 7 months and “has likely lengthened since the COVID-19 pandemic.”
Jennifer Gerdts, PhD, an attending psychologist at the Seattle Children’s Autism Center, said in an interview that the wait there for diagnosis in children older than 4 is “multiple years,” a length of time that’s common across the United States. Meanwhile, in many states families can’t access services without a diagnosis.
Expanding capacity with diagnoses by general pediatricians may improve access, but the diagnostic accuracy is critical.
Dr. Gerdts, who was not part of the study, said this research is “hugely important in the work that is under way to build community capacity for diagnostic evaluation.”
She said this study shows that not all diagnoses need the resources of a multiple-disciplinary team and that “pediatricians can do it, too, and they can do it pretty accurately.” Dr. Gerdts evaluates children for autism and helps train pediatricians to make diagnoses.
Pediatricians, specialist team completed blinded assessments
The 17 pediatricians in the study and the specialist team independently completed blinded assessment and each recorded a decision on whether the child had ASD. The prospective diagnostic study was conducted in a specialist assessment center in Toronto and in general pediatrician practices in Ontario from June 2016 to March 2020.
Children were younger than 5.5 years, did not have an ASD diagnosis and were referred because there was a development concern. The pediatricians referred 106 children (75% boys; average age, 3.5 years). More than half (57%) of the participating children were from minority racial and ethnic groups.
The children were randomly assigned to two groups: One included children who had their MDT visits before their pediatrician assessment and the other group included those who had their MDT visits after their pediatrician assessment.
The MDT diagnosed more than two-thirds of the children (68%) with ASD.
Sensitivity and specificity of the pediatrician assessments, compared with that of the specialist team, were 0.75 (95% confidence interval, 0.67-0.83) and 0.79 (95% CI, 0.62-0.91), respectively.
A look at pediatricians’ accuracy
Pediatricians reported the decisions they would have made had the child not been in the study.
- In 69% of the true-positive cases, pediatricians would have given an ASD diagnosis.
- In 44% of true-negative cases, they would have told the family the child did not have autism; in 30% of those case, they would give alternative diagnoses (most commonly ADHD and language delay).
- The pediatrician would have diagnosed ASD in only one of the seven false-positive cases and would refer those patients to a subspecialist 71% of the time.
- In false-negative cases, the pediatrician would incorrectly tell the family the child does not have autism 44% of the time.
Regarding the false-negative cases, the authors wrote, “more caution is needed for pediatricians when definitively ruling out ASD, which might result in diagnostic delays.”
Confidence is key
Physician confidence was also correlated with accuracy.
The authors wrote: “Among true-positive cases (MDT and pediatrician agree the child has ASD), the pediatrician was certain or very certain 80% of the time (43 cases) and the MDT was certain or very certain 96% of the time (52 cases). As such, if pediatricians conferred ASD diagnoses when feeling certain or very certain, they would make 46 correct diagnoses and 2 incorrect diagnoses.”
The high accuracy of diagnosis when physicians are confident suggests “listening to that sense of certainty is important,” Dr. Gerdts said. Conversely, these numbers show when a physician is uncertain about diagnosing ASD, they should listen to that instinct, too, and refer.
The results of the study support having general pediatricians diagnose and move forward with their patients when the signs of ASD are more definitive, saving the less-certain cases for the more resource-intensive teams to diagnose. Many states are moving toward that “tiered” system, Dr. Gerdts said.
“For many, and in fact most children, general pediatricians are pretty accurate when making an autism diagnosis,” she said.
“Let’s get [general pediatricians] confident in recognizing when this is outside their skill and ability level,” she said. “If you’re not sure, it is better to refer them on than to misdiagnose them.”
The important missing piece she said is how to support them “so they don’t feel pressure to make that call,” Dr. Gerdts said.
This project was funded by a grant from the Bloorview Research Institute, a grant from the Canadian Institutes of Health Research and a grant from the Canadian Institutes of Health. Three coauthors consult for and receive grants from several pharmaceutical companies and other organizations. Dr. Gerdts declared no relevant financial relationships.
General pediatricians and a multidisciplinary team of specialists agreed most of the time on which children should be diagnosed with autism spectrum disorder (ASD), data from a new study suggest.
But when it came to ruling out ASD, the agreement rate was much lower.
The study by Melanie Penner, MSc, MD, with the Autism Research Centre at Bloorview Research Institute, Toronto, and colleagues found that 89% of the time when a physician determined a child had ASD, the multidisciplinary team agreed. But when a pediatrician thought a child did not have ASD, the multidisciplinary team agreed only 60% of the time. The study was published in JAMA Network Open.
Multidisciplinary team model can’t keep up with demand
The findings are important as many guidelines recommend multidisciplinary teams (MDTs) for all ASD diagnostic assessment. However, the resources for this model can’t meet the demand of children needing a diagnosis and can lead to long waits for ASD therapies.
In Canada, the researchers note, the average wait time from referral to receipt of ASD diagnosis has been reported as 7 months and “has likely lengthened since the COVID-19 pandemic.”
Jennifer Gerdts, PhD, an attending psychologist at the Seattle Children’s Autism Center, said in an interview that the wait there for diagnosis in children older than 4 is “multiple years,” a length of time that’s common across the United States. Meanwhile, in many states families can’t access services without a diagnosis.
Expanding capacity with diagnoses by general pediatricians may improve access, but the diagnostic accuracy is critical.
Dr. Gerdts, who was not part of the study, said this research is “hugely important in the work that is under way to build community capacity for diagnostic evaluation.”
She said this study shows that not all diagnoses need the resources of a multiple-disciplinary team and that “pediatricians can do it, too, and they can do it pretty accurately.” Dr. Gerdts evaluates children for autism and helps train pediatricians to make diagnoses.
Pediatricians, specialist team completed blinded assessments
The 17 pediatricians in the study and the specialist team independently completed blinded assessment and each recorded a decision on whether the child had ASD. The prospective diagnostic study was conducted in a specialist assessment center in Toronto and in general pediatrician practices in Ontario from June 2016 to March 2020.
Children were younger than 5.5 years, did not have an ASD diagnosis and were referred because there was a development concern. The pediatricians referred 106 children (75% boys; average age, 3.5 years). More than half (57%) of the participating children were from minority racial and ethnic groups.
The children were randomly assigned to two groups: One included children who had their MDT visits before their pediatrician assessment and the other group included those who had their MDT visits after their pediatrician assessment.
The MDT diagnosed more than two-thirds of the children (68%) with ASD.
Sensitivity and specificity of the pediatrician assessments, compared with that of the specialist team, were 0.75 (95% confidence interval, 0.67-0.83) and 0.79 (95% CI, 0.62-0.91), respectively.
A look at pediatricians’ accuracy
Pediatricians reported the decisions they would have made had the child not been in the study.
- In 69% of the true-positive cases, pediatricians would have given an ASD diagnosis.
- In 44% of true-negative cases, they would have told the family the child did not have autism; in 30% of those case, they would give alternative diagnoses (most commonly ADHD and language delay).
- The pediatrician would have diagnosed ASD in only one of the seven false-positive cases and would refer those patients to a subspecialist 71% of the time.
- In false-negative cases, the pediatrician would incorrectly tell the family the child does not have autism 44% of the time.
Regarding the false-negative cases, the authors wrote, “more caution is needed for pediatricians when definitively ruling out ASD, which might result in diagnostic delays.”
Confidence is key
Physician confidence was also correlated with accuracy.
The authors wrote: “Among true-positive cases (MDT and pediatrician agree the child has ASD), the pediatrician was certain or very certain 80% of the time (43 cases) and the MDT was certain or very certain 96% of the time (52 cases). As such, if pediatricians conferred ASD diagnoses when feeling certain or very certain, they would make 46 correct diagnoses and 2 incorrect diagnoses.”
The high accuracy of diagnosis when physicians are confident suggests “listening to that sense of certainty is important,” Dr. Gerdts said. Conversely, these numbers show when a physician is uncertain about diagnosing ASD, they should listen to that instinct, too, and refer.
The results of the study support having general pediatricians diagnose and move forward with their patients when the signs of ASD are more definitive, saving the less-certain cases for the more resource-intensive teams to diagnose. Many states are moving toward that “tiered” system, Dr. Gerdts said.
“For many, and in fact most children, general pediatricians are pretty accurate when making an autism diagnosis,” she said.
“Let’s get [general pediatricians] confident in recognizing when this is outside their skill and ability level,” she said. “If you’re not sure, it is better to refer them on than to misdiagnose them.”
The important missing piece she said is how to support them “so they don’t feel pressure to make that call,” Dr. Gerdts said.
This project was funded by a grant from the Bloorview Research Institute, a grant from the Canadian Institutes of Health Research and a grant from the Canadian Institutes of Health. Three coauthors consult for and receive grants from several pharmaceutical companies and other organizations. Dr. Gerdts declared no relevant financial relationships.
FROM JAMA NETWORK OPEN
Nine more minutes a day of vigorous exercise tied to better cognition
such as running and cycling, plays in brain health.
“Even minor differences in daily behavior appeared meaningful for cognition in this study,” researcher John J. Mitchell, MSci and PhD candidate, Medical Research Council, London, told this news organization.
The findings were published online in the Journal of Epidemiology and Community Health.
Research gap
Previous research has linked physical activity (PA) with increased cognitive reserve, which delays the onset of cognitive decline in later life. But disentangling the most important components of PA for cognition – such as intensity and volume – has not been well researched.
Previous studies didn’t capture sleep time, which typically takes up the largest component of the day. Sleep is “acutely relevant” when examining cognition, the investigators noted.
In addition, studies in this area often focus on just one or two activity components of the day, which “neglects the growing awareness” that movements “are all tightly interlinked,” said Mr. Mitchell.
The new study included 4,481 participants in the British Cohort Study who were born in 1970 across England, Scotland, and Wales. The participants were followed throughout childhood and adulthood.
The median age of the participants was 47 years, and they were predominantly White, female (52%), married (66%), and well educated. Most were occasional or nonrisky alcohol consumers, and half had never smoked.
The researchers collected biometric measurements and health, demographic, and lifestyle information. Participants wore a thigh-mounted accelerometer at least 7 consecutive hours a day for up to 7 days to track PA, sedentary behavior (SB), and sleep time.
The device used in the study could detect subtle movements as well as speed of accelerations, said Mr. Mitchell. “From this, we can distinguish MVPA from slow walking, standing, and sitting. It’s the current best practice for detecting the more subtle movements we make, such as brisk walking and stair climbing, beyond just ‘exercise,’ “ he added.
Light intensity PA (LIPA) describes movement such as walking and moving around the house or office, while MVPA includes activities such as brisk walking and running that accelerate the heart rate. SB, defined as time spent sitting or lying, is distinguished from standing by the thigh inclination.
On an average day, the cohort spent 51 minutes in MVPA; 5 hours, 42 minutes in LIPA; 9 hours, 16 minutes in SB; and 8 hours, 11 minutes sleeping.
Researchers calculated an overall global score for verbal memory and executive function.
The study used “compositional data analysis,” a statistical method that can examine the associations of cognition and PA in the context of all components of daily movement.
The analysis revealed a positive association between MVPA and cognition relative to all other behaviors, after adjustment for sociodemographic factors that included sex, age, education, and marital status. But the relationship lessened after further adjustment for health status – for example, cardiovascular disease or disability – and lifestyle factors, such as alcohol consumption and smoking status.
SB relative to all other movements remained positively associated with cognition after full adjustment. This, the authors speculated, may reflect engagement in cognitively stimulating activities such as reading.
To better understand the associations, the researchers used a statistical method to reallocate time in the cohort’s average day from one activity component to another.
“We held two of the components static but moved time between the other two and monitored the theoretical ramifications of that change for cognition,” said Mr. Mitchell.
Real cognitive change
There was a 1.31% improvement in cognition ranking compared to the sample average after replacing 9 minutes of sedentary activity with MVPA (1.31; 95% confidence interval [CI], 0.09-2.50). There was a 1.27% improvement after replacing 7 minutes of LIPA with MVPA, and a 1.2% improvement after replacing 7 minutes of sleep with MVPA.
Individuals might move up from about the 50th percentile to the 51st or 52nd percentile after just 9 minutes of more moderate to vigorous movement in place of sitting, said Mr. Mitchell. “This highlights how even very modest differences in people’s daily movement – less than 10 minutes – is linked to quite real changes in our cognitive health.”
The impact of physical activity appeared greatest on working memory and mental processes, such as planning and organization.
On the other hand, cognition declined by 1%-2% after replacing MVPA with 8 minutes of SB, 6 minutes of LIPA, or 7 minutes of sleep.
The activity tracking device couldn’t determine how well participants slept, which is “a clear limitation” of the study, said Mr. Mitchell. “We have to be cautious when trying to interpret our findings surrounding sleep.”
Another limitation is that despite a large sample size, people of color were underrepresented, limiting the generalizability of the findings. As well, other healthy pursuits – for example, reading – might have contributed to improved cognition.
Important findings
In a comment, Jennifer J. Heisz, PhD, associate professor and Canada research chair in brain health and aging, department of kinesiology, McMaster University, Hamilton, Ont., said the findings from the study are important.
“Through the statistical modelling, the authors demonstrate that swapping just 9 minutes of sedentary behavior with moderate to vigorous physical activity, such as a brisk walk or bike ride, was associated with an increase in cognition.”
She added that this seemed to be especially true for people who sit while at work.
The findings “confer with the growing consensus” that some exercise is better than none when it comes to brain health, said Dr. Heisz.
“Clinicians should encourage their patients to add a brisk, 10-minute walk to their daily routine and break up prolonged sitting with short movement breaks.”
She noted the study was cross-sectional, “so it is not possible to infer causation.”
The study received funding from the Medical Research Council and the British Heart Foundation. Mr. Mitchell and Dr. Heisz have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
such as running and cycling, plays in brain health.
“Even minor differences in daily behavior appeared meaningful for cognition in this study,” researcher John J. Mitchell, MSci and PhD candidate, Medical Research Council, London, told this news organization.
The findings were published online in the Journal of Epidemiology and Community Health.
Research gap
Previous research has linked physical activity (PA) with increased cognitive reserve, which delays the onset of cognitive decline in later life. But disentangling the most important components of PA for cognition – such as intensity and volume – has not been well researched.
Previous studies didn’t capture sleep time, which typically takes up the largest component of the day. Sleep is “acutely relevant” when examining cognition, the investigators noted.
In addition, studies in this area often focus on just one or two activity components of the day, which “neglects the growing awareness” that movements “are all tightly interlinked,” said Mr. Mitchell.
The new study included 4,481 participants in the British Cohort Study who were born in 1970 across England, Scotland, and Wales. The participants were followed throughout childhood and adulthood.
The median age of the participants was 47 years, and they were predominantly White, female (52%), married (66%), and well educated. Most were occasional or nonrisky alcohol consumers, and half had never smoked.
The researchers collected biometric measurements and health, demographic, and lifestyle information. Participants wore a thigh-mounted accelerometer at least 7 consecutive hours a day for up to 7 days to track PA, sedentary behavior (SB), and sleep time.
The device used in the study could detect subtle movements as well as speed of accelerations, said Mr. Mitchell. “From this, we can distinguish MVPA from slow walking, standing, and sitting. It’s the current best practice for detecting the more subtle movements we make, such as brisk walking and stair climbing, beyond just ‘exercise,’ “ he added.
Light intensity PA (LIPA) describes movement such as walking and moving around the house or office, while MVPA includes activities such as brisk walking and running that accelerate the heart rate. SB, defined as time spent sitting or lying, is distinguished from standing by the thigh inclination.
On an average day, the cohort spent 51 minutes in MVPA; 5 hours, 42 minutes in LIPA; 9 hours, 16 minutes in SB; and 8 hours, 11 minutes sleeping.
Researchers calculated an overall global score for verbal memory and executive function.
The study used “compositional data analysis,” a statistical method that can examine the associations of cognition and PA in the context of all components of daily movement.
The analysis revealed a positive association between MVPA and cognition relative to all other behaviors, after adjustment for sociodemographic factors that included sex, age, education, and marital status. But the relationship lessened after further adjustment for health status – for example, cardiovascular disease or disability – and lifestyle factors, such as alcohol consumption and smoking status.
SB relative to all other movements remained positively associated with cognition after full adjustment. This, the authors speculated, may reflect engagement in cognitively stimulating activities such as reading.
To better understand the associations, the researchers used a statistical method to reallocate time in the cohort’s average day from one activity component to another.
“We held two of the components static but moved time between the other two and monitored the theoretical ramifications of that change for cognition,” said Mr. Mitchell.
Real cognitive change
There was a 1.31% improvement in cognition ranking compared to the sample average after replacing 9 minutes of sedentary activity with MVPA (1.31; 95% confidence interval [CI], 0.09-2.50). There was a 1.27% improvement after replacing 7 minutes of LIPA with MVPA, and a 1.2% improvement after replacing 7 minutes of sleep with MVPA.
Individuals might move up from about the 50th percentile to the 51st or 52nd percentile after just 9 minutes of more moderate to vigorous movement in place of sitting, said Mr. Mitchell. “This highlights how even very modest differences in people’s daily movement – less than 10 minutes – is linked to quite real changes in our cognitive health.”
The impact of physical activity appeared greatest on working memory and mental processes, such as planning and organization.
On the other hand, cognition declined by 1%-2% after replacing MVPA with 8 minutes of SB, 6 minutes of LIPA, or 7 minutes of sleep.
The activity tracking device couldn’t determine how well participants slept, which is “a clear limitation” of the study, said Mr. Mitchell. “We have to be cautious when trying to interpret our findings surrounding sleep.”
Another limitation is that despite a large sample size, people of color were underrepresented, limiting the generalizability of the findings. As well, other healthy pursuits – for example, reading – might have contributed to improved cognition.
Important findings
In a comment, Jennifer J. Heisz, PhD, associate professor and Canada research chair in brain health and aging, department of kinesiology, McMaster University, Hamilton, Ont., said the findings from the study are important.
“Through the statistical modelling, the authors demonstrate that swapping just 9 minutes of sedentary behavior with moderate to vigorous physical activity, such as a brisk walk or bike ride, was associated with an increase in cognition.”
She added that this seemed to be especially true for people who sit while at work.
The findings “confer with the growing consensus” that some exercise is better than none when it comes to brain health, said Dr. Heisz.
“Clinicians should encourage their patients to add a brisk, 10-minute walk to their daily routine and break up prolonged sitting with short movement breaks.”
She noted the study was cross-sectional, “so it is not possible to infer causation.”
The study received funding from the Medical Research Council and the British Heart Foundation. Mr. Mitchell and Dr. Heisz have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
such as running and cycling, plays in brain health.
“Even minor differences in daily behavior appeared meaningful for cognition in this study,” researcher John J. Mitchell, MSci and PhD candidate, Medical Research Council, London, told this news organization.
The findings were published online in the Journal of Epidemiology and Community Health.
Research gap
Previous research has linked physical activity (PA) with increased cognitive reserve, which delays the onset of cognitive decline in later life. But disentangling the most important components of PA for cognition – such as intensity and volume – has not been well researched.
Previous studies didn’t capture sleep time, which typically takes up the largest component of the day. Sleep is “acutely relevant” when examining cognition, the investigators noted.
In addition, studies in this area often focus on just one or two activity components of the day, which “neglects the growing awareness” that movements “are all tightly interlinked,” said Mr. Mitchell.
The new study included 4,481 participants in the British Cohort Study who were born in 1970 across England, Scotland, and Wales. The participants were followed throughout childhood and adulthood.
The median age of the participants was 47 years, and they were predominantly White, female (52%), married (66%), and well educated. Most were occasional or nonrisky alcohol consumers, and half had never smoked.
The researchers collected biometric measurements and health, demographic, and lifestyle information. Participants wore a thigh-mounted accelerometer at least 7 consecutive hours a day for up to 7 days to track PA, sedentary behavior (SB), and sleep time.
The device used in the study could detect subtle movements as well as speed of accelerations, said Mr. Mitchell. “From this, we can distinguish MVPA from slow walking, standing, and sitting. It’s the current best practice for detecting the more subtle movements we make, such as brisk walking and stair climbing, beyond just ‘exercise,’ “ he added.
Light intensity PA (LIPA) describes movement such as walking and moving around the house or office, while MVPA includes activities such as brisk walking and running that accelerate the heart rate. SB, defined as time spent sitting or lying, is distinguished from standing by the thigh inclination.
On an average day, the cohort spent 51 minutes in MVPA; 5 hours, 42 minutes in LIPA; 9 hours, 16 minutes in SB; and 8 hours, 11 minutes sleeping.
Researchers calculated an overall global score for verbal memory and executive function.
The study used “compositional data analysis,” a statistical method that can examine the associations of cognition and PA in the context of all components of daily movement.
The analysis revealed a positive association between MVPA and cognition relative to all other behaviors, after adjustment for sociodemographic factors that included sex, age, education, and marital status. But the relationship lessened after further adjustment for health status – for example, cardiovascular disease or disability – and lifestyle factors, such as alcohol consumption and smoking status.
SB relative to all other movements remained positively associated with cognition after full adjustment. This, the authors speculated, may reflect engagement in cognitively stimulating activities such as reading.
To better understand the associations, the researchers used a statistical method to reallocate time in the cohort’s average day from one activity component to another.
“We held two of the components static but moved time between the other two and monitored the theoretical ramifications of that change for cognition,” said Mr. Mitchell.
Real cognitive change
There was a 1.31% improvement in cognition ranking compared to the sample average after replacing 9 minutes of sedentary activity with MVPA (1.31; 95% confidence interval [CI], 0.09-2.50). There was a 1.27% improvement after replacing 7 minutes of LIPA with MVPA, and a 1.2% improvement after replacing 7 minutes of sleep with MVPA.
Individuals might move up from about the 50th percentile to the 51st or 52nd percentile after just 9 minutes of more moderate to vigorous movement in place of sitting, said Mr. Mitchell. “This highlights how even very modest differences in people’s daily movement – less than 10 minutes – is linked to quite real changes in our cognitive health.”
The impact of physical activity appeared greatest on working memory and mental processes, such as planning and organization.
On the other hand, cognition declined by 1%-2% after replacing MVPA with 8 minutes of SB, 6 minutes of LIPA, or 7 minutes of sleep.
The activity tracking device couldn’t determine how well participants slept, which is “a clear limitation” of the study, said Mr. Mitchell. “We have to be cautious when trying to interpret our findings surrounding sleep.”
Another limitation is that despite a large sample size, people of color were underrepresented, limiting the generalizability of the findings. As well, other healthy pursuits – for example, reading – might have contributed to improved cognition.
Important findings
In a comment, Jennifer J. Heisz, PhD, associate professor and Canada research chair in brain health and aging, department of kinesiology, McMaster University, Hamilton, Ont., said the findings from the study are important.
“Through the statistical modelling, the authors demonstrate that swapping just 9 minutes of sedentary behavior with moderate to vigorous physical activity, such as a brisk walk or bike ride, was associated with an increase in cognition.”
She added that this seemed to be especially true for people who sit while at work.
The findings “confer with the growing consensus” that some exercise is better than none when it comes to brain health, said Dr. Heisz.
“Clinicians should encourage their patients to add a brisk, 10-minute walk to their daily routine and break up prolonged sitting with short movement breaks.”
She noted the study was cross-sectional, “so it is not possible to infer causation.”
The study received funding from the Medical Research Council and the British Heart Foundation. Mr. Mitchell and Dr. Heisz have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF EPIDEMIOLOGY AND COMMUNITY HEALTH
The longevity gene: Healthy mutant reverses heart aging
Everybody wants a younger heart
As more people live well past 90, scientists have been taking a closer look at how they’ve been doing it. Mostly it boiled down to genetics. You either had it or you didn’t. Well, a recent study suggests that doesn’t have to be true anymore, at least for the heart.
Scientists from the United Kingdom and Italy found an antiaging gene in some centenarians that has shown possible antiaging effects in mice and in human heart cells. A single administration of the mutant antiaging gene, they found, stopped heart function decay in middle-aged mice and even reversed the biological clock by the human equivalent of 10 years in elderly mice.
When the researchers applied the antiaging gene to samples of human heart cells from elderly people with heart problems, the cells “resumed functioning properly, proving to be more efficient in building new blood vessels,” they said in a written statement. It all kind of sounds like something out of Dr. Frankenstein’s lab.
I want to believe … in better sleep
The “X-Files” theme song plays. Mulder and Scully are sitting in a diner, breakfast laid out around them. The diner is quiet, with only a few people inside.
Mulder: I’m telling you, Scully, there’s something spooky going on here.
Scully: You mean other than the fact that this town in Georgia looks suspiciously like Vancouver?
Mulder: Not one person we spoke to yesterday has gotten a full night’s sleep since the UFO sighting last month. I’m telling you, they’re here, they’re experimenting.
Scully: Do you really want me to do this to you again?
Mulder: Do what again?
Scully: There’s nothing going on here that can’t be explained by the current research. Why, in January 2023 a study was published revealing a link between poor sleep and belief in paranormal phenomena like UFOS, demons, or ghosts. Which probably explains why you’re on your third cup of coffee for the morning.
Mulder: Scully, you’ve literally been abducted by aliens. Do we have to play this game every time?
Scully: Look, it’s simple. In a sample of nearly 9,000 people, nearly two-thirds of those who reported experiencing sleep paralysis or exploding head syndrome reported believing in UFOs and aliens walking amongst humanity, despite making up just 3% of the overall sample.
Furthermore, about 60% of those reporting sleep paralysis also reported believing near-death experiences prove the soul lingers on after death, and those with stronger insomnia symptoms were more likely to believe in the devil.
Mulder: Aha!
Scully: Aha what?
Mulder: You’re a devout Christian. You believe in the devil and the soul.
Scully: Yes, but I don’t let it interfere with a good night’s sleep, Mulder. These people saw something strange, convinced themselves it was a UFO, and now they can’t sleep. It’s a vicious cycle. The study authors even said that people experiencing strange nighttime phenomena could interpret this as evidence of aliens or other paranormal beings, thus making them even more susceptible to further sleep disruption and deepening beliefs. Look who I’m talking to.
Mulder: Always with the facts, eh?
Scully: I am a doctor, after all. And if you want more research into how paranormal belief and poor sleep quality are linked, I’d be happy to dig out the literature, because the truth is out there, Mulder.
Mulder: I hate you sometimes.
It’s ChatGPT’s world. We’re just living in it
Have you heard about ChatGPT? The artificial intelligence chatbot was just launched in November and it’s already more important to the Internet than either Vladimir Putin or “Rick and Morty.”
What’s that? You’re wondering why you should care? Well, excuuuuuse us, but we thought you might want to know that ChatGPT is in the process of taking over the world. Let’s take a quick look at what it’s been up to.
“ChatGPT bot passes law school exam”
“ChatGPT passes MBA exam given by a Wharton professor”
“A freelance writer says ChatGPT wrote a $600 article in just 30 seconds”
And here’s one that might be of interest to those of the health care persuasion: “ChatGPT can pass part of the U.S. Medical Licensing Exam.” See? It’s coming for you, too.
The artificial intelligence known as ChatGPT “performed at >50% accuracy across [the three USMLE] examinations, exceeding 60% in most analyses,” a group of researchers wrote on the preprint server medRxiv, noting that 60% is usually the pass threshold for humans taking the exam in any given year.
ChatGPT was not given any special medical training before the exam, but the investigators pointed out that another AI, PubMedGPT, which is trained exclusively on biomedical domain literature, was only 50.8% accurate on the USMLE. Its reliance on “ongoing academic discourse that tends to be inconclusive, contradictory, or highly conservative or noncommittal in its language” was its undoing, the team suggested.
To top it off, ChatGPT is listed as one of the authors at the top of the medRxiv report, with an acknowledgment at the end saying that “ChatGPT contributed to the writing of several sections of this manuscript.”
We’ve said it before, and no doubt we’ll say it again: We’re doomed.
Everybody wants a younger heart
As more people live well past 90, scientists have been taking a closer look at how they’ve been doing it. Mostly it boiled down to genetics. You either had it or you didn’t. Well, a recent study suggests that doesn’t have to be true anymore, at least for the heart.
Scientists from the United Kingdom and Italy found an antiaging gene in some centenarians that has shown possible antiaging effects in mice and in human heart cells. A single administration of the mutant antiaging gene, they found, stopped heart function decay in middle-aged mice and even reversed the biological clock by the human equivalent of 10 years in elderly mice.
When the researchers applied the antiaging gene to samples of human heart cells from elderly people with heart problems, the cells “resumed functioning properly, proving to be more efficient in building new blood vessels,” they said in a written statement. It all kind of sounds like something out of Dr. Frankenstein’s lab.
I want to believe … in better sleep
The “X-Files” theme song plays. Mulder and Scully are sitting in a diner, breakfast laid out around them. The diner is quiet, with only a few people inside.
Mulder: I’m telling you, Scully, there’s something spooky going on here.
Scully: You mean other than the fact that this town in Georgia looks suspiciously like Vancouver?
Mulder: Not one person we spoke to yesterday has gotten a full night’s sleep since the UFO sighting last month. I’m telling you, they’re here, they’re experimenting.
Scully: Do you really want me to do this to you again?
Mulder: Do what again?
Scully: There’s nothing going on here that can’t be explained by the current research. Why, in January 2023 a study was published revealing a link between poor sleep and belief in paranormal phenomena like UFOS, demons, or ghosts. Which probably explains why you’re on your third cup of coffee for the morning.
Mulder: Scully, you’ve literally been abducted by aliens. Do we have to play this game every time?
Scully: Look, it’s simple. In a sample of nearly 9,000 people, nearly two-thirds of those who reported experiencing sleep paralysis or exploding head syndrome reported believing in UFOs and aliens walking amongst humanity, despite making up just 3% of the overall sample.
Furthermore, about 60% of those reporting sleep paralysis also reported believing near-death experiences prove the soul lingers on after death, and those with stronger insomnia symptoms were more likely to believe in the devil.
Mulder: Aha!
Scully: Aha what?
Mulder: You’re a devout Christian. You believe in the devil and the soul.
Scully: Yes, but I don’t let it interfere with a good night’s sleep, Mulder. These people saw something strange, convinced themselves it was a UFO, and now they can’t sleep. It’s a vicious cycle. The study authors even said that people experiencing strange nighttime phenomena could interpret this as evidence of aliens or other paranormal beings, thus making them even more susceptible to further sleep disruption and deepening beliefs. Look who I’m talking to.
Mulder: Always with the facts, eh?
Scully: I am a doctor, after all. And if you want more research into how paranormal belief and poor sleep quality are linked, I’d be happy to dig out the literature, because the truth is out there, Mulder.
Mulder: I hate you sometimes.
It’s ChatGPT’s world. We’re just living in it
Have you heard about ChatGPT? The artificial intelligence chatbot was just launched in November and it’s already more important to the Internet than either Vladimir Putin or “Rick and Morty.”
What’s that? You’re wondering why you should care? Well, excuuuuuse us, but we thought you might want to know that ChatGPT is in the process of taking over the world. Let’s take a quick look at what it’s been up to.
“ChatGPT bot passes law school exam”
“ChatGPT passes MBA exam given by a Wharton professor”
“A freelance writer says ChatGPT wrote a $600 article in just 30 seconds”
And here’s one that might be of interest to those of the health care persuasion: “ChatGPT can pass part of the U.S. Medical Licensing Exam.” See? It’s coming for you, too.
The artificial intelligence known as ChatGPT “performed at >50% accuracy across [the three USMLE] examinations, exceeding 60% in most analyses,” a group of researchers wrote on the preprint server medRxiv, noting that 60% is usually the pass threshold for humans taking the exam in any given year.
ChatGPT was not given any special medical training before the exam, but the investigators pointed out that another AI, PubMedGPT, which is trained exclusively on biomedical domain literature, was only 50.8% accurate on the USMLE. Its reliance on “ongoing academic discourse that tends to be inconclusive, contradictory, or highly conservative or noncommittal in its language” was its undoing, the team suggested.
To top it off, ChatGPT is listed as one of the authors at the top of the medRxiv report, with an acknowledgment at the end saying that “ChatGPT contributed to the writing of several sections of this manuscript.”
We’ve said it before, and no doubt we’ll say it again: We’re doomed.
Everybody wants a younger heart
As more people live well past 90, scientists have been taking a closer look at how they’ve been doing it. Mostly it boiled down to genetics. You either had it or you didn’t. Well, a recent study suggests that doesn’t have to be true anymore, at least for the heart.
Scientists from the United Kingdom and Italy found an antiaging gene in some centenarians that has shown possible antiaging effects in mice and in human heart cells. A single administration of the mutant antiaging gene, they found, stopped heart function decay in middle-aged mice and even reversed the biological clock by the human equivalent of 10 years in elderly mice.
When the researchers applied the antiaging gene to samples of human heart cells from elderly people with heart problems, the cells “resumed functioning properly, proving to be more efficient in building new blood vessels,” they said in a written statement. It all kind of sounds like something out of Dr. Frankenstein’s lab.
I want to believe … in better sleep
The “X-Files” theme song plays. Mulder and Scully are sitting in a diner, breakfast laid out around them. The diner is quiet, with only a few people inside.
Mulder: I’m telling you, Scully, there’s something spooky going on here.
Scully: You mean other than the fact that this town in Georgia looks suspiciously like Vancouver?
Mulder: Not one person we spoke to yesterday has gotten a full night’s sleep since the UFO sighting last month. I’m telling you, they’re here, they’re experimenting.
Scully: Do you really want me to do this to you again?
Mulder: Do what again?
Scully: There’s nothing going on here that can’t be explained by the current research. Why, in January 2023 a study was published revealing a link between poor sleep and belief in paranormal phenomena like UFOS, demons, or ghosts. Which probably explains why you’re on your third cup of coffee for the morning.
Mulder: Scully, you’ve literally been abducted by aliens. Do we have to play this game every time?
Scully: Look, it’s simple. In a sample of nearly 9,000 people, nearly two-thirds of those who reported experiencing sleep paralysis or exploding head syndrome reported believing in UFOs and aliens walking amongst humanity, despite making up just 3% of the overall sample.
Furthermore, about 60% of those reporting sleep paralysis also reported believing near-death experiences prove the soul lingers on after death, and those with stronger insomnia symptoms were more likely to believe in the devil.
Mulder: Aha!
Scully: Aha what?
Mulder: You’re a devout Christian. You believe in the devil and the soul.
Scully: Yes, but I don’t let it interfere with a good night’s sleep, Mulder. These people saw something strange, convinced themselves it was a UFO, and now they can’t sleep. It’s a vicious cycle. The study authors even said that people experiencing strange nighttime phenomena could interpret this as evidence of aliens or other paranormal beings, thus making them even more susceptible to further sleep disruption and deepening beliefs. Look who I’m talking to.
Mulder: Always with the facts, eh?
Scully: I am a doctor, after all. And if you want more research into how paranormal belief and poor sleep quality are linked, I’d be happy to dig out the literature, because the truth is out there, Mulder.
Mulder: I hate you sometimes.
It’s ChatGPT’s world. We’re just living in it
Have you heard about ChatGPT? The artificial intelligence chatbot was just launched in November and it’s already more important to the Internet than either Vladimir Putin or “Rick and Morty.”
What’s that? You’re wondering why you should care? Well, excuuuuuse us, but we thought you might want to know that ChatGPT is in the process of taking over the world. Let’s take a quick look at what it’s been up to.
“ChatGPT bot passes law school exam”
“ChatGPT passes MBA exam given by a Wharton professor”
“A freelance writer says ChatGPT wrote a $600 article in just 30 seconds”
And here’s one that might be of interest to those of the health care persuasion: “ChatGPT can pass part of the U.S. Medical Licensing Exam.” See? It’s coming for you, too.
The artificial intelligence known as ChatGPT “performed at >50% accuracy across [the three USMLE] examinations, exceeding 60% in most analyses,” a group of researchers wrote on the preprint server medRxiv, noting that 60% is usually the pass threshold for humans taking the exam in any given year.
ChatGPT was not given any special medical training before the exam, but the investigators pointed out that another AI, PubMedGPT, which is trained exclusively on biomedical domain literature, was only 50.8% accurate on the USMLE. Its reliance on “ongoing academic discourse that tends to be inconclusive, contradictory, or highly conservative or noncommittal in its language” was its undoing, the team suggested.
To top it off, ChatGPT is listed as one of the authors at the top of the medRxiv report, with an acknowledgment at the end saying that “ChatGPT contributed to the writing of several sections of this manuscript.”
We’ve said it before, and no doubt we’ll say it again: We’re doomed.
Canadian guidance recommends reducing alcohol consumption
“Drinking less is better,” says the guidance, which replaces Canada’s 2011 Low-Risk Drinking Guidelines (LRDGs).
Developed in consultation with an executive committee from federal, provincial, and territorial governments; national organizations; three scientific expert panels; and an internal evidence review working group, the guidance presents the following findings:
- Consuming no drinks per week has benefits, such as better health and better sleep, and it’s the only safe option during pregnancy.
- Consuming one or two standard drinks weekly will likely not have alcohol-related consequences.
- Three to six drinks raise the risk of developing breast, colon, and other cancers.
- Seven or more increase the risk of heart disease or stroke.
- Each additional drink “radically increases” the risk of these health consequences.
“Alcohol is more harmful than was previously thought and is a key component of the health of your patients,” Adam Sherk, PhD, a scientist at the Canadian Institute for Substance Use Research at the University of Victoria (B.C.), and a member of the scientific expert panel that contributed to the guidance, said in an interview. “Display and discuss the new guidance with your patients with the main message that drinking less is better.”
Peter Butt, MD, a clinical associate professor at the University of Saskatchewan, Saskatoon, and cochair of the guidance project, said in an interview: “The World Health Organization has identified over 200 ICD-coded conditions associated with alcohol use. This creates many opportunities to inquire into quantity and frequency of alcohol use, relate it to the patient’s health and well-being, and provide advice on reduction.”
“Canada’s Guidance on Alcohol and Health: Final Report” and a related infographic were published online Jan. 17.
Continuum of risk
The impetus for the new guidance came from the fact that “our 2011 LRDGs were no longer current, and there was emerging evidence that people drinking within those levels were coming to harm,” said Dr. Butt.
That evidence indicates that alcohol causes at least seven types of cancer, mostly of the breast or colon; is a risk factor for most types of heart disease; and is a main cause of liver disease. Evidence also indicates that avoiding drinking to the point of intoxication will reduce people’s risk of perpetrating alcohol-related violence.
Responding to the need to accurately quantify the risk, the guidance defines a “standard” drink as 12 oz of beer, cooler, or cider (5% alcohol); 5 oz of wine (12% alcohol); and 1.5 oz of spirits such as whiskey, vodka, or gin (40% alcohol).
Using different mortality risk thresholds, the project’s experts developed the following continuum of risk:
- Low for individuals who consume two standard drinks or fewer per week
- Moderate for those who consume from three to six standard drinks per week
- Increasingly high for those who consume seven standard drinks or more per week
The guidance makes the following observations:
- Consuming more than two standard drinks per drinking occasion is associated with an increased risk of harms to self and others, including injuries and violence.
- When pregnant or trying to get pregnant, no amount of alcohol is safe.
- When breastfeeding, not drinking is safest.
- Above the upper limit of the moderate risk zone, health risks increase more steeply for females than males.
- Far more injuries, violence, and deaths result from men’s alcohol use, especially for per occasion drinking, than from women’s alcohol use.
- Young people should delay alcohol use for as long as possible.
- Individuals should not start to use alcohol or increase their alcohol use for health benefits.
- Any reduction in alcohol use is beneficial.
Other national guidelines
“Countries that haven’t updated their alcohol use guidelines recently should do so, as the evidence regarding alcohol and health has advanced considerably in the past 10 years,” said Dr. Sherk. He acknowledged that “any time health guidance changes substantially, it’s reasonable to expect a period of readjustment.”
“Some will be resistant,” Dr. Butt agreed. “Some professionals will need more education than others on the health effects of alcohol. Some patients will also be more invested in drinking than others. The harm-reduction, risk-zone approach should assist in the process of engaging patients and helping them reduce over time.
“Just as we benefited from the updates done in the United Kingdom, France, and especially Australia, so also researchers elsewhere will critique our work and our approach and make their own decisions on how best to communicate with their public,” Dr. Butt said. He noted that Canada’s contributions regarding the association between alcohol and violence, as well as their sex/gender approach to the evidence, “may influence the next country’s review.”
Commenting on whether the United States should consider changing its guidance, Timothy Brennan, MD, MPH, chief of clinical services for the Addiction Institute of Mount Sinai Health System in New York, said in an interview, “A lot of people will be surprised at the recommended limits on alcohol. Most think that they can have one or two glasses of alcohol per day and not have any increased risk to their health. I think the Canadians deserve credit for putting themselves out there.”
Dr. Brennan said there will “certainly be pushback by the drinking lobby, which is very strong both in the U.S. and in Canada.” In fact, the national trade group Beer Canada was recently quoted as stating that it still supports the 2011 guidelines and that the updating process lacked full transparency and expert technical peer review.
Nevertheless, Dr. Brennan said, “it’s overwhelmingly clear that alcohol affects a ton of different parts of our body, so limiting the amount of alcohol we take in is always going to be a good thing. The Canadian graphic is great because it color-codes the risk. I recommend that clinicians put it up in their offices and begin quantifying the units of alcohol that are going into a patient’s body each day.”
A version of this article originally appeared on Medscape.com.
“Drinking less is better,” says the guidance, which replaces Canada’s 2011 Low-Risk Drinking Guidelines (LRDGs).
Developed in consultation with an executive committee from federal, provincial, and territorial governments; national organizations; three scientific expert panels; and an internal evidence review working group, the guidance presents the following findings:
- Consuming no drinks per week has benefits, such as better health and better sleep, and it’s the only safe option during pregnancy.
- Consuming one or two standard drinks weekly will likely not have alcohol-related consequences.
- Three to six drinks raise the risk of developing breast, colon, and other cancers.
- Seven or more increase the risk of heart disease or stroke.
- Each additional drink “radically increases” the risk of these health consequences.
“Alcohol is more harmful than was previously thought and is a key component of the health of your patients,” Adam Sherk, PhD, a scientist at the Canadian Institute for Substance Use Research at the University of Victoria (B.C.), and a member of the scientific expert panel that contributed to the guidance, said in an interview. “Display and discuss the new guidance with your patients with the main message that drinking less is better.”
Peter Butt, MD, a clinical associate professor at the University of Saskatchewan, Saskatoon, and cochair of the guidance project, said in an interview: “The World Health Organization has identified over 200 ICD-coded conditions associated with alcohol use. This creates many opportunities to inquire into quantity and frequency of alcohol use, relate it to the patient’s health and well-being, and provide advice on reduction.”
“Canada’s Guidance on Alcohol and Health: Final Report” and a related infographic were published online Jan. 17.
Continuum of risk
The impetus for the new guidance came from the fact that “our 2011 LRDGs were no longer current, and there was emerging evidence that people drinking within those levels were coming to harm,” said Dr. Butt.
That evidence indicates that alcohol causes at least seven types of cancer, mostly of the breast or colon; is a risk factor for most types of heart disease; and is a main cause of liver disease. Evidence also indicates that avoiding drinking to the point of intoxication will reduce people’s risk of perpetrating alcohol-related violence.
Responding to the need to accurately quantify the risk, the guidance defines a “standard” drink as 12 oz of beer, cooler, or cider (5% alcohol); 5 oz of wine (12% alcohol); and 1.5 oz of spirits such as whiskey, vodka, or gin (40% alcohol).
Using different mortality risk thresholds, the project’s experts developed the following continuum of risk:
- Low for individuals who consume two standard drinks or fewer per week
- Moderate for those who consume from three to six standard drinks per week
- Increasingly high for those who consume seven standard drinks or more per week
The guidance makes the following observations:
- Consuming more than two standard drinks per drinking occasion is associated with an increased risk of harms to self and others, including injuries and violence.
- When pregnant or trying to get pregnant, no amount of alcohol is safe.
- When breastfeeding, not drinking is safest.
- Above the upper limit of the moderate risk zone, health risks increase more steeply for females than males.
- Far more injuries, violence, and deaths result from men’s alcohol use, especially for per occasion drinking, than from women’s alcohol use.
- Young people should delay alcohol use for as long as possible.
- Individuals should not start to use alcohol or increase their alcohol use for health benefits.
- Any reduction in alcohol use is beneficial.
Other national guidelines
“Countries that haven’t updated their alcohol use guidelines recently should do so, as the evidence regarding alcohol and health has advanced considerably in the past 10 years,” said Dr. Sherk. He acknowledged that “any time health guidance changes substantially, it’s reasonable to expect a period of readjustment.”
“Some will be resistant,” Dr. Butt agreed. “Some professionals will need more education than others on the health effects of alcohol. Some patients will also be more invested in drinking than others. The harm-reduction, risk-zone approach should assist in the process of engaging patients and helping them reduce over time.
“Just as we benefited from the updates done in the United Kingdom, France, and especially Australia, so also researchers elsewhere will critique our work and our approach and make their own decisions on how best to communicate with their public,” Dr. Butt said. He noted that Canada’s contributions regarding the association between alcohol and violence, as well as their sex/gender approach to the evidence, “may influence the next country’s review.”
Commenting on whether the United States should consider changing its guidance, Timothy Brennan, MD, MPH, chief of clinical services for the Addiction Institute of Mount Sinai Health System in New York, said in an interview, “A lot of people will be surprised at the recommended limits on alcohol. Most think that they can have one or two glasses of alcohol per day and not have any increased risk to their health. I think the Canadians deserve credit for putting themselves out there.”
Dr. Brennan said there will “certainly be pushback by the drinking lobby, which is very strong both in the U.S. and in Canada.” In fact, the national trade group Beer Canada was recently quoted as stating that it still supports the 2011 guidelines and that the updating process lacked full transparency and expert technical peer review.
Nevertheless, Dr. Brennan said, “it’s overwhelmingly clear that alcohol affects a ton of different parts of our body, so limiting the amount of alcohol we take in is always going to be a good thing. The Canadian graphic is great because it color-codes the risk. I recommend that clinicians put it up in their offices and begin quantifying the units of alcohol that are going into a patient’s body each day.”
A version of this article originally appeared on Medscape.com.
“Drinking less is better,” says the guidance, which replaces Canada’s 2011 Low-Risk Drinking Guidelines (LRDGs).
Developed in consultation with an executive committee from federal, provincial, and territorial governments; national organizations; three scientific expert panels; and an internal evidence review working group, the guidance presents the following findings:
- Consuming no drinks per week has benefits, such as better health and better sleep, and it’s the only safe option during pregnancy.
- Consuming one or two standard drinks weekly will likely not have alcohol-related consequences.
- Three to six drinks raise the risk of developing breast, colon, and other cancers.
- Seven or more increase the risk of heart disease or stroke.
- Each additional drink “radically increases” the risk of these health consequences.
“Alcohol is more harmful than was previously thought and is a key component of the health of your patients,” Adam Sherk, PhD, a scientist at the Canadian Institute for Substance Use Research at the University of Victoria (B.C.), and a member of the scientific expert panel that contributed to the guidance, said in an interview. “Display and discuss the new guidance with your patients with the main message that drinking less is better.”
Peter Butt, MD, a clinical associate professor at the University of Saskatchewan, Saskatoon, and cochair of the guidance project, said in an interview: “The World Health Organization has identified over 200 ICD-coded conditions associated with alcohol use. This creates many opportunities to inquire into quantity and frequency of alcohol use, relate it to the patient’s health and well-being, and provide advice on reduction.”
“Canada’s Guidance on Alcohol and Health: Final Report” and a related infographic were published online Jan. 17.
Continuum of risk
The impetus for the new guidance came from the fact that “our 2011 LRDGs were no longer current, and there was emerging evidence that people drinking within those levels were coming to harm,” said Dr. Butt.
That evidence indicates that alcohol causes at least seven types of cancer, mostly of the breast or colon; is a risk factor for most types of heart disease; and is a main cause of liver disease. Evidence also indicates that avoiding drinking to the point of intoxication will reduce people’s risk of perpetrating alcohol-related violence.
Responding to the need to accurately quantify the risk, the guidance defines a “standard” drink as 12 oz of beer, cooler, or cider (5% alcohol); 5 oz of wine (12% alcohol); and 1.5 oz of spirits such as whiskey, vodka, or gin (40% alcohol).
Using different mortality risk thresholds, the project’s experts developed the following continuum of risk:
- Low for individuals who consume two standard drinks or fewer per week
- Moderate for those who consume from three to six standard drinks per week
- Increasingly high for those who consume seven standard drinks or more per week
The guidance makes the following observations:
- Consuming more than two standard drinks per drinking occasion is associated with an increased risk of harms to self and others, including injuries and violence.
- When pregnant or trying to get pregnant, no amount of alcohol is safe.
- When breastfeeding, not drinking is safest.
- Above the upper limit of the moderate risk zone, health risks increase more steeply for females than males.
- Far more injuries, violence, and deaths result from men’s alcohol use, especially for per occasion drinking, than from women’s alcohol use.
- Young people should delay alcohol use for as long as possible.
- Individuals should not start to use alcohol or increase their alcohol use for health benefits.
- Any reduction in alcohol use is beneficial.
Other national guidelines
“Countries that haven’t updated their alcohol use guidelines recently should do so, as the evidence regarding alcohol and health has advanced considerably in the past 10 years,” said Dr. Sherk. He acknowledged that “any time health guidance changes substantially, it’s reasonable to expect a period of readjustment.”
“Some will be resistant,” Dr. Butt agreed. “Some professionals will need more education than others on the health effects of alcohol. Some patients will also be more invested in drinking than others. The harm-reduction, risk-zone approach should assist in the process of engaging patients and helping them reduce over time.
“Just as we benefited from the updates done in the United Kingdom, France, and especially Australia, so also researchers elsewhere will critique our work and our approach and make their own decisions on how best to communicate with their public,” Dr. Butt said. He noted that Canada’s contributions regarding the association between alcohol and violence, as well as their sex/gender approach to the evidence, “may influence the next country’s review.”
Commenting on whether the United States should consider changing its guidance, Timothy Brennan, MD, MPH, chief of clinical services for the Addiction Institute of Mount Sinai Health System in New York, said in an interview, “A lot of people will be surprised at the recommended limits on alcohol. Most think that they can have one or two glasses of alcohol per day and not have any increased risk to their health. I think the Canadians deserve credit for putting themselves out there.”
Dr. Brennan said there will “certainly be pushback by the drinking lobby, which is very strong both in the U.S. and in Canada.” In fact, the national trade group Beer Canada was recently quoted as stating that it still supports the 2011 guidelines and that the updating process lacked full transparency and expert technical peer review.
Nevertheless, Dr. Brennan said, “it’s overwhelmingly clear that alcohol affects a ton of different parts of our body, so limiting the amount of alcohol we take in is always going to be a good thing. The Canadian graphic is great because it color-codes the risk. I recommend that clinicians put it up in their offices and begin quantifying the units of alcohol that are going into a patient’s body each day.”
A version of this article originally appeared on Medscape.com.
Concern grows over ‘medical assistance in dying for mental illness’ law
Canada already has the largest number of deaths by MAID of any nation, with 10,064 in 2021, a 32% increase from 2020. With the addition of serious mental illness (SMI) as an eligible category, the country is on track to have the most liberal assisted-death policy in the world.
Concerns about the additional number of patients who could become eligible for MAID, and a lack of evidence-backed standards from disability rights groups, mental health advocates, First Nations leaders, psychiatrists, and other mental health providers, seems to have led the Canadian government to give the proposed law some sober second thought.
“Listening to experts and Canadians, we believe this date needs to be temporarily delayed,” said David Lametti, Canada’s minister of Justice and attorney general of Canada; Jean-Yves Duclos, minister of Health; and Carolyn Bennett, minister of Mental Health and Addictions, in a Dec. 15, 2022, joint statement.
Canada’s Parliament – which approved the expansion – will now have to vote on whether to okay a pause on the legislation.
However, the Canadian Psychiatric Association has not been calling for a delay in the proposed legislation. In a November 2021 statement, the CPA said it “does not take a position on the legality or morality of MAID,” but added that to deny MAID to people with mental illness was discriminatory, and that, as it was the law, it must be followed.
“CPA has not taken a position about MAID,” the association’s president Gary Chaimowitz, MBChB, told this news organization. “We know this is coming and our organization is trying to get its members ready for what will be most likely the ability of people with mental conditions to be able to request MAID,” said Dr. Chaimowitz, who is also head of forensic psychiatry at St. Joseph’s Healthcare and a professor of psychiatry at McMaster University, both in Hamilton, Ont.
Dr. Chaimowitz acknowledges that “a majority of psychiatrists do not want to be involved in anything to do with MAID.”
“The idea, certainly in psychiatry, is to get people well and we’ve been taught that people dying from a major mental disorder is something that we’re trained to prevent,” he added.
A ‘clinical option’
Assisted medical death is especially fraught in psychiatry, said Rebecca Brendel, MD, president of the American Psychiatric Association. She noted a 25-year life expectancy gap between people with SMI and those who do not have such conditions.
“As a profession we have very serious obligations to advance treatment so that a person with serious mental illness can live [a] full, productive, and healthy [life],” Dr. Brendel, associate director of the Center for Bioethics at Harvard Medical School in Boston, said in an interview.
Under the Canadian proposal, psychiatrists would be allowed to suggest MAID as a “clinical option.”
Harold Braswell, PhD, a fellow with The Hastings Center, a bioethics research institute, calls that problematic.
“It’s not neutral to suggest to someone that it would be theoretically reasonable to end their lives,” Dr. Braswell, associate professor at the Albert Gnaegi Center for Health Care Ethics at Saint Louis University, told this news organization.
It also creates a double standard in the treatment of suicidal ideation, in which suicide prevention is absolute for some, but encouraging it as a possibility for others, he added.
“To have that come from an authority figure is something that’s very harsh and, in my opinion, very potentially destructive,” especially for vulnerable groups, like First Nations people, who already have elevated rates of suicide, said Dr. Braswell.
Fierce debate
Since 2016, Canada has allowed MAID for medical conditions and diseases that will not improve and in cases where the evidence shows that medical providers can accurately predict the condition will not improve.
However, in 2019, a Quebec court ruled that the law unconstitutionally barred euthanasia in people who were not terminally ill. In March 2021, Canada’s criminal code was amended to allow MAID for people whose natural death was not “reasonably foreseeable,” but it excluded SMI for a period of 2 years, ending in March 2023.
The 2-year stay was intended to allow for study and to give mental health providers and MAID assessors time to develop standards.
The federal government charged a 12-member expert panel with determining how to safely allow MAID for SMI. In its final report released in May 2022 it recommended that standards be developed.
The panel acknowledged that for many conditions it may be impossible to make predictions about whether an individual might improve. However, it did not mention SMI.
In those cases, when MAID is requested, “establishing incurability and irreversibility on the basis of the evolution and response to past interventions is necessary,” the panel noted, adding that these are the criteria used by psychiatrists assessing euthanasia requests in the Netherlands and Belgium.
But the notion that mental illness can be irremediable has been fiercely debated.
Soon after the expert report was released, the Center for Addiction and Mental Health in Toronto noted on its website that there are currently “no agreed upon standards for psychiatrists or other health care practitioners to use to determine if a person’s mental illness is ‘grievous and irremediable’ for the purposes of MAID.”
Dr. Chaimowitz acknowledged that “there’s no agreed-upon definition of incurability” in mental illness. Some psychiatrists “will argue that there’s always another treatment that can be attempted,” he said, adding that there has been a lack of consensus on irremediability among CPA members.
Protecting vulnerable populations
Matt Wynia, MD, MPH, FACP, director of the Center for Bioethics and Humanities at the University of Colorado at Denver, Aurora, said the question of irremediability is crucial. “Most people with mental illness do get better, especially if they’re in treatment,” Dr. Wynia said.
For MAID assessors it may be difficult to know when someone has tried all possible treatments, especially given the wide array of options, including psychedelics, said Dr. Wynia.
Dr. Braswell said there is not enough evidence that mental illness is incurable. With SMI, “there’s a lot more potential for the causes of the individual’s suffering to be ameliorated. By offering MAID, you’re going to kill people who might have been able to get out of this through other nonlethal means.”
Currently, MAID is provided for an irremediable medical condition, “in other words, a condition that will not improve and that we can predict will not improve,” said Karandeep S. Gaind, MD, chief of psychiatry at Toronto’s Humber River Hospital and physician chair of the hospital’s MAID team.
“If that’s the premise, then I think we cannot provide MAID for sole mental illness,” Dr. Gaind said. “Because we can’t honestly make those predictions” with mental illness, he added.
Dr. Gaind does not support MAID for mental illness and believes that it will put the vulnerable – including those living in poverty – at particular risk.
With the proposed expansion, MAID is “now becoming something which is being sought as a way to escape a painful life rather than to avoid a painful death,” said Dr. Gaind, who is also a past president of the CPA.
One member of the federal government’s expert panel – Ellen Cohen, who had a psychiatric condition – wrote in The Globe and Mail that she quit early on when it became apparent that the panel was not seriously considering her own experiences or the possibility that poverty and lack of access to care or social supports could strongly influence a request for MAID.
Social determinants of suffering
People with mental illness often are without homes, have substance use disorders, have been stigmatized and discriminated against, and have poor social supports, said Dr. Wynia. “You worry that it’s all of those things that are making them want to end their lives,” he said.
The Daily Mail ran a story in December 2022 about a 65-year-old Canadian who said he’d applied for MAID solely because of fears that his disability benefits for various chronic health conditions were being cut off and that he didn’t want to live in poverty.
A 51-year-old Ontario woman with multiple chemical sensitivities was granted MAID after she said she could not find housing that could keep her safe, according to an August report by CTV News.
Tarek Rajji, MD, chief of the Adult Neurodevelopment and Geriatric Psychiatry Division at CAMH, said social determinants of health need to be considered in standards created to guide MAID for mental illness.
“We’re very mindful of the fact that the suffering, that is, the grievousness that the person is living with, in the context of mental illness, many times is due to the social determinants of their illness and the social determinants of their suffering,” Dr. Rajji said.
Many are also concerned that it will be difficult to separate out suicidality from sheer hopelessness.
The CPA has advised a group that’s working on developing guidelines for MAID in SMI and is also developing a curriculum for mental health providers, Dr. Chaimowitz said. As part of that, there will be a process to ensure that someone who is actively suicidal is not granted MAID.
“I do not believe that it’s contemplated that MAID is going to accelerate or facilitate suicidal ideation,” he said. Someone who is suicidal will be referred to treatment, said Dr. Chaimowitz.
“People with depression often feel hopeless,” and may refuse treatments that have worked in the past, countered Dr. Gaind. Some of his patients “are absolutely convinced that nothing will help,” he said.
Troublesome cases
The expert panel said in its final report that “it is not possible to provide fixed rules for how many attempts at interventions, how many types of interventions, and over how much time,” are necessary to establish “irreversibility” of mental illness.
Dr. Chaimowitz said MAID will not be offered to anyone “refusing treatment for their condition without any good reason.” They will be “unlikely to meet criteria for incurable,” as they will have needed to avail themselves of the array of treatments available, he said.
That would be similar to rules in Belgium and the Netherlands, which allow euthanasia for psychiatric conditions.
An estimated 100-300 psychiatric patients receive euthanasia each year in those countries, according to a 2021 commentary in Psychiatric Times (Jun 7;38[6]) by Mark S. Komrad, MD, a Towson, Maryland-based psychiatrist.
There are still troublesome cases.
As previously reported by this news organization, many in Belgium were distressed recently at the news that a 23-year-old woman who had survived a terrorist attack, Shanti De Corte, requested and was granted euthanasia.
As the deadline for implementation of MAID grew closer, calls for delay grew louder, especially given the lack of concrete standards for providers.
During the waning months of 2022, Dr. Gaind – who said he was suspended from CPA for “unprofessional interactions” and allegedly misrepresenting CPA’s processes and governance matters – announced the launch of a new organization, the Society of Canadian Psychiatry, in November calling for a delay in MAID of at least 1 year so that evidence-based safeguards could be implemented. The petition has been signed by more than 200 psychiatrists, along with several dozen physicians, MAID assessors, and individuals with mental illness and family members.
The Association of Chairs of Psychiatry in Canada, the Canadian Association for Suicide Prevention, the Council of Canadians with Disabilities, a group of indigenous leaders, and the Ontario Association for ACT and FACT, psychiatrists who provide care to individuals with severe mental illness, among other groups, joined the call for a delay.
In its December announcement, the Canadian federal ministers said a factor in seeking a delay was that standards guiding clinicians would not be delivered until at least February – too close to when applications would be opened.
Upon hearing about the federal government’s intentions, the chair of the expert panel, Mona Gupta, MD, told The Canadian Press that she did not think it was necessary to put off implementation because necessary safeguards were already in place.
Dr. Chaimowitz awaits the standards but is optimistic that for mental illness, “the process will be tightly controlled, closely monitored, and open to scrutiny,” he said.
Dr. Braswell is not convinced. The concern is that adding people with mental illness is “going to overload the capacity of the government to monitor this practice,” he said.
Is the United States next?
Although Canada and the United States share a border, it’s unlikely that U.S. states will allow aid in dying for nonterminal illness, much less for psychiatric conditions any time soon, said Dr. Braswell and others.
Ten states – California, Colorado, Hawaii, Maine, Montana, New Jersey, New Mexico, Oregon, Vermont, and Washington – have laws allowing assistance in dying, but for terminal illness only.
In 2016, the APA adopted the American Medical Association policy on medical euthanasia, stating, “that a psychiatrist should not prescribe or administer any intervention to a nonterminally ill person for the purpose of causing death.”
Dr. Brendel said the field is acutely aware that people with mental illness do suffer, but that more work needs to be done – and is being done – on “distinguishing wishes to hasten death or end one’s life from these historical or traditional notions that any premature death is a suicide.”
There is also increasing discussion within the medical community, not just psychiatry, about a physician’s duty to relieve suffering, said Dr. Wynia. “There’s debate basically about whether we stand for preserving life essentially at all costs and never being involved in the taking of life, or whether we stand for reduction of suffering and being the advocate for the patients that we serve,” he said.
“Those are both legitimate,” said Dr. Wynia, adding, “there are good reasons to want both of those to be true.”
“I suspect that 20 years from now we will still be having conversations about how physicians, how psychiatrists ought to participate in preserving life and in shepherding death,” said Dr. Brendel.
But to Dr. Gaind, the debate is not just esoteric, it’s a soon-to-be reality in Canada. “When we’re providing death to people who aren’t dying, to me that’s like providing what amounts to a wrongful death,” he said.
A version of this article originally appeared on Medscape.com.
Canada already has the largest number of deaths by MAID of any nation, with 10,064 in 2021, a 32% increase from 2020. With the addition of serious mental illness (SMI) as an eligible category, the country is on track to have the most liberal assisted-death policy in the world.
Concerns about the additional number of patients who could become eligible for MAID, and a lack of evidence-backed standards from disability rights groups, mental health advocates, First Nations leaders, psychiatrists, and other mental health providers, seems to have led the Canadian government to give the proposed law some sober second thought.
“Listening to experts and Canadians, we believe this date needs to be temporarily delayed,” said David Lametti, Canada’s minister of Justice and attorney general of Canada; Jean-Yves Duclos, minister of Health; and Carolyn Bennett, minister of Mental Health and Addictions, in a Dec. 15, 2022, joint statement.
Canada’s Parliament – which approved the expansion – will now have to vote on whether to okay a pause on the legislation.
However, the Canadian Psychiatric Association has not been calling for a delay in the proposed legislation. In a November 2021 statement, the CPA said it “does not take a position on the legality or morality of MAID,” but added that to deny MAID to people with mental illness was discriminatory, and that, as it was the law, it must be followed.
“CPA has not taken a position about MAID,” the association’s president Gary Chaimowitz, MBChB, told this news organization. “We know this is coming and our organization is trying to get its members ready for what will be most likely the ability of people with mental conditions to be able to request MAID,” said Dr. Chaimowitz, who is also head of forensic psychiatry at St. Joseph’s Healthcare and a professor of psychiatry at McMaster University, both in Hamilton, Ont.
Dr. Chaimowitz acknowledges that “a majority of psychiatrists do not want to be involved in anything to do with MAID.”
“The idea, certainly in psychiatry, is to get people well and we’ve been taught that people dying from a major mental disorder is something that we’re trained to prevent,” he added.
A ‘clinical option’
Assisted medical death is especially fraught in psychiatry, said Rebecca Brendel, MD, president of the American Psychiatric Association. She noted a 25-year life expectancy gap between people with SMI and those who do not have such conditions.
“As a profession we have very serious obligations to advance treatment so that a person with serious mental illness can live [a] full, productive, and healthy [life],” Dr. Brendel, associate director of the Center for Bioethics at Harvard Medical School in Boston, said in an interview.
Under the Canadian proposal, psychiatrists would be allowed to suggest MAID as a “clinical option.”
Harold Braswell, PhD, a fellow with The Hastings Center, a bioethics research institute, calls that problematic.
“It’s not neutral to suggest to someone that it would be theoretically reasonable to end their lives,” Dr. Braswell, associate professor at the Albert Gnaegi Center for Health Care Ethics at Saint Louis University, told this news organization.
It also creates a double standard in the treatment of suicidal ideation, in which suicide prevention is absolute for some, but encouraging it as a possibility for others, he added.
“To have that come from an authority figure is something that’s very harsh and, in my opinion, very potentially destructive,” especially for vulnerable groups, like First Nations people, who already have elevated rates of suicide, said Dr. Braswell.
Fierce debate
Since 2016, Canada has allowed MAID for medical conditions and diseases that will not improve and in cases where the evidence shows that medical providers can accurately predict the condition will not improve.
However, in 2019, a Quebec court ruled that the law unconstitutionally barred euthanasia in people who were not terminally ill. In March 2021, Canada’s criminal code was amended to allow MAID for people whose natural death was not “reasonably foreseeable,” but it excluded SMI for a period of 2 years, ending in March 2023.
The 2-year stay was intended to allow for study and to give mental health providers and MAID assessors time to develop standards.
The federal government charged a 12-member expert panel with determining how to safely allow MAID for SMI. In its final report released in May 2022 it recommended that standards be developed.
The panel acknowledged that for many conditions it may be impossible to make predictions about whether an individual might improve. However, it did not mention SMI.
In those cases, when MAID is requested, “establishing incurability and irreversibility on the basis of the evolution and response to past interventions is necessary,” the panel noted, adding that these are the criteria used by psychiatrists assessing euthanasia requests in the Netherlands and Belgium.
But the notion that mental illness can be irremediable has been fiercely debated.
Soon after the expert report was released, the Center for Addiction and Mental Health in Toronto noted on its website that there are currently “no agreed upon standards for psychiatrists or other health care practitioners to use to determine if a person’s mental illness is ‘grievous and irremediable’ for the purposes of MAID.”
Dr. Chaimowitz acknowledged that “there’s no agreed-upon definition of incurability” in mental illness. Some psychiatrists “will argue that there’s always another treatment that can be attempted,” he said, adding that there has been a lack of consensus on irremediability among CPA members.
Protecting vulnerable populations
Matt Wynia, MD, MPH, FACP, director of the Center for Bioethics and Humanities at the University of Colorado at Denver, Aurora, said the question of irremediability is crucial. “Most people with mental illness do get better, especially if they’re in treatment,” Dr. Wynia said.
For MAID assessors it may be difficult to know when someone has tried all possible treatments, especially given the wide array of options, including psychedelics, said Dr. Wynia.
Dr. Braswell said there is not enough evidence that mental illness is incurable. With SMI, “there’s a lot more potential for the causes of the individual’s suffering to be ameliorated. By offering MAID, you’re going to kill people who might have been able to get out of this through other nonlethal means.”
Currently, MAID is provided for an irremediable medical condition, “in other words, a condition that will not improve and that we can predict will not improve,” said Karandeep S. Gaind, MD, chief of psychiatry at Toronto’s Humber River Hospital and physician chair of the hospital’s MAID team.
“If that’s the premise, then I think we cannot provide MAID for sole mental illness,” Dr. Gaind said. “Because we can’t honestly make those predictions” with mental illness, he added.
Dr. Gaind does not support MAID for mental illness and believes that it will put the vulnerable – including those living in poverty – at particular risk.
With the proposed expansion, MAID is “now becoming something which is being sought as a way to escape a painful life rather than to avoid a painful death,” said Dr. Gaind, who is also a past president of the CPA.
One member of the federal government’s expert panel – Ellen Cohen, who had a psychiatric condition – wrote in The Globe and Mail that she quit early on when it became apparent that the panel was not seriously considering her own experiences or the possibility that poverty and lack of access to care or social supports could strongly influence a request for MAID.
Social determinants of suffering
People with mental illness often are without homes, have substance use disorders, have been stigmatized and discriminated against, and have poor social supports, said Dr. Wynia. “You worry that it’s all of those things that are making them want to end their lives,” he said.
The Daily Mail ran a story in December 2022 about a 65-year-old Canadian who said he’d applied for MAID solely because of fears that his disability benefits for various chronic health conditions were being cut off and that he didn’t want to live in poverty.
A 51-year-old Ontario woman with multiple chemical sensitivities was granted MAID after she said she could not find housing that could keep her safe, according to an August report by CTV News.
Tarek Rajji, MD, chief of the Adult Neurodevelopment and Geriatric Psychiatry Division at CAMH, said social determinants of health need to be considered in standards created to guide MAID for mental illness.
“We’re very mindful of the fact that the suffering, that is, the grievousness that the person is living with, in the context of mental illness, many times is due to the social determinants of their illness and the social determinants of their suffering,” Dr. Rajji said.
Many are also concerned that it will be difficult to separate out suicidality from sheer hopelessness.
The CPA has advised a group that’s working on developing guidelines for MAID in SMI and is also developing a curriculum for mental health providers, Dr. Chaimowitz said. As part of that, there will be a process to ensure that someone who is actively suicidal is not granted MAID.
“I do not believe that it’s contemplated that MAID is going to accelerate or facilitate suicidal ideation,” he said. Someone who is suicidal will be referred to treatment, said Dr. Chaimowitz.
“People with depression often feel hopeless,” and may refuse treatments that have worked in the past, countered Dr. Gaind. Some of his patients “are absolutely convinced that nothing will help,” he said.
Troublesome cases
The expert panel said in its final report that “it is not possible to provide fixed rules for how many attempts at interventions, how many types of interventions, and over how much time,” are necessary to establish “irreversibility” of mental illness.
Dr. Chaimowitz said MAID will not be offered to anyone “refusing treatment for their condition without any good reason.” They will be “unlikely to meet criteria for incurable,” as they will have needed to avail themselves of the array of treatments available, he said.
That would be similar to rules in Belgium and the Netherlands, which allow euthanasia for psychiatric conditions.
An estimated 100-300 psychiatric patients receive euthanasia each year in those countries, according to a 2021 commentary in Psychiatric Times (Jun 7;38[6]) by Mark S. Komrad, MD, a Towson, Maryland-based psychiatrist.
There are still troublesome cases.
As previously reported by this news organization, many in Belgium were distressed recently at the news that a 23-year-old woman who had survived a terrorist attack, Shanti De Corte, requested and was granted euthanasia.
As the deadline for implementation of MAID grew closer, calls for delay grew louder, especially given the lack of concrete standards for providers.
During the waning months of 2022, Dr. Gaind – who said he was suspended from CPA for “unprofessional interactions” and allegedly misrepresenting CPA’s processes and governance matters – announced the launch of a new organization, the Society of Canadian Psychiatry, in November calling for a delay in MAID of at least 1 year so that evidence-based safeguards could be implemented. The petition has been signed by more than 200 psychiatrists, along with several dozen physicians, MAID assessors, and individuals with mental illness and family members.
The Association of Chairs of Psychiatry in Canada, the Canadian Association for Suicide Prevention, the Council of Canadians with Disabilities, a group of indigenous leaders, and the Ontario Association for ACT and FACT, psychiatrists who provide care to individuals with severe mental illness, among other groups, joined the call for a delay.
In its December announcement, the Canadian federal ministers said a factor in seeking a delay was that standards guiding clinicians would not be delivered until at least February – too close to when applications would be opened.
Upon hearing about the federal government’s intentions, the chair of the expert panel, Mona Gupta, MD, told The Canadian Press that she did not think it was necessary to put off implementation because necessary safeguards were already in place.
Dr. Chaimowitz awaits the standards but is optimistic that for mental illness, “the process will be tightly controlled, closely monitored, and open to scrutiny,” he said.
Dr. Braswell is not convinced. The concern is that adding people with mental illness is “going to overload the capacity of the government to monitor this practice,” he said.
Is the United States next?
Although Canada and the United States share a border, it’s unlikely that U.S. states will allow aid in dying for nonterminal illness, much less for psychiatric conditions any time soon, said Dr. Braswell and others.
Ten states – California, Colorado, Hawaii, Maine, Montana, New Jersey, New Mexico, Oregon, Vermont, and Washington – have laws allowing assistance in dying, but for terminal illness only.
In 2016, the APA adopted the American Medical Association policy on medical euthanasia, stating, “that a psychiatrist should not prescribe or administer any intervention to a nonterminally ill person for the purpose of causing death.”
Dr. Brendel said the field is acutely aware that people with mental illness do suffer, but that more work needs to be done – and is being done – on “distinguishing wishes to hasten death or end one’s life from these historical or traditional notions that any premature death is a suicide.”
There is also increasing discussion within the medical community, not just psychiatry, about a physician’s duty to relieve suffering, said Dr. Wynia. “There’s debate basically about whether we stand for preserving life essentially at all costs and never being involved in the taking of life, or whether we stand for reduction of suffering and being the advocate for the patients that we serve,” he said.
“Those are both legitimate,” said Dr. Wynia, adding, “there are good reasons to want both of those to be true.”
“I suspect that 20 years from now we will still be having conversations about how physicians, how psychiatrists ought to participate in preserving life and in shepherding death,” said Dr. Brendel.
But to Dr. Gaind, the debate is not just esoteric, it’s a soon-to-be reality in Canada. “When we’re providing death to people who aren’t dying, to me that’s like providing what amounts to a wrongful death,” he said.
A version of this article originally appeared on Medscape.com.
Canada already has the largest number of deaths by MAID of any nation, with 10,064 in 2021, a 32% increase from 2020. With the addition of serious mental illness (SMI) as an eligible category, the country is on track to have the most liberal assisted-death policy in the world.
Concerns about the additional number of patients who could become eligible for MAID, and a lack of evidence-backed standards from disability rights groups, mental health advocates, First Nations leaders, psychiatrists, and other mental health providers, seems to have led the Canadian government to give the proposed law some sober second thought.
“Listening to experts and Canadians, we believe this date needs to be temporarily delayed,” said David Lametti, Canada’s minister of Justice and attorney general of Canada; Jean-Yves Duclos, minister of Health; and Carolyn Bennett, minister of Mental Health and Addictions, in a Dec. 15, 2022, joint statement.
Canada’s Parliament – which approved the expansion – will now have to vote on whether to okay a pause on the legislation.
However, the Canadian Psychiatric Association has not been calling for a delay in the proposed legislation. In a November 2021 statement, the CPA said it “does not take a position on the legality or morality of MAID,” but added that to deny MAID to people with mental illness was discriminatory, and that, as it was the law, it must be followed.
“CPA has not taken a position about MAID,” the association’s president Gary Chaimowitz, MBChB, told this news organization. “We know this is coming and our organization is trying to get its members ready for what will be most likely the ability of people with mental conditions to be able to request MAID,” said Dr. Chaimowitz, who is also head of forensic psychiatry at St. Joseph’s Healthcare and a professor of psychiatry at McMaster University, both in Hamilton, Ont.
Dr. Chaimowitz acknowledges that “a majority of psychiatrists do not want to be involved in anything to do with MAID.”
“The idea, certainly in psychiatry, is to get people well and we’ve been taught that people dying from a major mental disorder is something that we’re trained to prevent,” he added.
A ‘clinical option’
Assisted medical death is especially fraught in psychiatry, said Rebecca Brendel, MD, president of the American Psychiatric Association. She noted a 25-year life expectancy gap between people with SMI and those who do not have such conditions.
“As a profession we have very serious obligations to advance treatment so that a person with serious mental illness can live [a] full, productive, and healthy [life],” Dr. Brendel, associate director of the Center for Bioethics at Harvard Medical School in Boston, said in an interview.
Under the Canadian proposal, psychiatrists would be allowed to suggest MAID as a “clinical option.”
Harold Braswell, PhD, a fellow with The Hastings Center, a bioethics research institute, calls that problematic.
“It’s not neutral to suggest to someone that it would be theoretically reasonable to end their lives,” Dr. Braswell, associate professor at the Albert Gnaegi Center for Health Care Ethics at Saint Louis University, told this news organization.
It also creates a double standard in the treatment of suicidal ideation, in which suicide prevention is absolute for some, but encouraging it as a possibility for others, he added.
“To have that come from an authority figure is something that’s very harsh and, in my opinion, very potentially destructive,” especially for vulnerable groups, like First Nations people, who already have elevated rates of suicide, said Dr. Braswell.
Fierce debate
Since 2016, Canada has allowed MAID for medical conditions and diseases that will not improve and in cases where the evidence shows that medical providers can accurately predict the condition will not improve.
However, in 2019, a Quebec court ruled that the law unconstitutionally barred euthanasia in people who were not terminally ill. In March 2021, Canada’s criminal code was amended to allow MAID for people whose natural death was not “reasonably foreseeable,” but it excluded SMI for a period of 2 years, ending in March 2023.
The 2-year stay was intended to allow for study and to give mental health providers and MAID assessors time to develop standards.
The federal government charged a 12-member expert panel with determining how to safely allow MAID for SMI. In its final report released in May 2022 it recommended that standards be developed.
The panel acknowledged that for many conditions it may be impossible to make predictions about whether an individual might improve. However, it did not mention SMI.
In those cases, when MAID is requested, “establishing incurability and irreversibility on the basis of the evolution and response to past interventions is necessary,” the panel noted, adding that these are the criteria used by psychiatrists assessing euthanasia requests in the Netherlands and Belgium.
But the notion that mental illness can be irremediable has been fiercely debated.
Soon after the expert report was released, the Center for Addiction and Mental Health in Toronto noted on its website that there are currently “no agreed upon standards for psychiatrists or other health care practitioners to use to determine if a person’s mental illness is ‘grievous and irremediable’ for the purposes of MAID.”
Dr. Chaimowitz acknowledged that “there’s no agreed-upon definition of incurability” in mental illness. Some psychiatrists “will argue that there’s always another treatment that can be attempted,” he said, adding that there has been a lack of consensus on irremediability among CPA members.
Protecting vulnerable populations
Matt Wynia, MD, MPH, FACP, director of the Center for Bioethics and Humanities at the University of Colorado at Denver, Aurora, said the question of irremediability is crucial. “Most people with mental illness do get better, especially if they’re in treatment,” Dr. Wynia said.
For MAID assessors it may be difficult to know when someone has tried all possible treatments, especially given the wide array of options, including psychedelics, said Dr. Wynia.
Dr. Braswell said there is not enough evidence that mental illness is incurable. With SMI, “there’s a lot more potential for the causes of the individual’s suffering to be ameliorated. By offering MAID, you’re going to kill people who might have been able to get out of this through other nonlethal means.”
Currently, MAID is provided for an irremediable medical condition, “in other words, a condition that will not improve and that we can predict will not improve,” said Karandeep S. Gaind, MD, chief of psychiatry at Toronto’s Humber River Hospital and physician chair of the hospital’s MAID team.
“If that’s the premise, then I think we cannot provide MAID for sole mental illness,” Dr. Gaind said. “Because we can’t honestly make those predictions” with mental illness, he added.
Dr. Gaind does not support MAID for mental illness and believes that it will put the vulnerable – including those living in poverty – at particular risk.
With the proposed expansion, MAID is “now becoming something which is being sought as a way to escape a painful life rather than to avoid a painful death,” said Dr. Gaind, who is also a past president of the CPA.
One member of the federal government’s expert panel – Ellen Cohen, who had a psychiatric condition – wrote in The Globe and Mail that she quit early on when it became apparent that the panel was not seriously considering her own experiences or the possibility that poverty and lack of access to care or social supports could strongly influence a request for MAID.
Social determinants of suffering
People with mental illness often are without homes, have substance use disorders, have been stigmatized and discriminated against, and have poor social supports, said Dr. Wynia. “You worry that it’s all of those things that are making them want to end their lives,” he said.
The Daily Mail ran a story in December 2022 about a 65-year-old Canadian who said he’d applied for MAID solely because of fears that his disability benefits for various chronic health conditions were being cut off and that he didn’t want to live in poverty.
A 51-year-old Ontario woman with multiple chemical sensitivities was granted MAID after she said she could not find housing that could keep her safe, according to an August report by CTV News.
Tarek Rajji, MD, chief of the Adult Neurodevelopment and Geriatric Psychiatry Division at CAMH, said social determinants of health need to be considered in standards created to guide MAID for mental illness.
“We’re very mindful of the fact that the suffering, that is, the grievousness that the person is living with, in the context of mental illness, many times is due to the social determinants of their illness and the social determinants of their suffering,” Dr. Rajji said.
Many are also concerned that it will be difficult to separate out suicidality from sheer hopelessness.
The CPA has advised a group that’s working on developing guidelines for MAID in SMI and is also developing a curriculum for mental health providers, Dr. Chaimowitz said. As part of that, there will be a process to ensure that someone who is actively suicidal is not granted MAID.
“I do not believe that it’s contemplated that MAID is going to accelerate or facilitate suicidal ideation,” he said. Someone who is suicidal will be referred to treatment, said Dr. Chaimowitz.
“People with depression often feel hopeless,” and may refuse treatments that have worked in the past, countered Dr. Gaind. Some of his patients “are absolutely convinced that nothing will help,” he said.
Troublesome cases
The expert panel said in its final report that “it is not possible to provide fixed rules for how many attempts at interventions, how many types of interventions, and over how much time,” are necessary to establish “irreversibility” of mental illness.
Dr. Chaimowitz said MAID will not be offered to anyone “refusing treatment for their condition without any good reason.” They will be “unlikely to meet criteria for incurable,” as they will have needed to avail themselves of the array of treatments available, he said.
That would be similar to rules in Belgium and the Netherlands, which allow euthanasia for psychiatric conditions.
An estimated 100-300 psychiatric patients receive euthanasia each year in those countries, according to a 2021 commentary in Psychiatric Times (Jun 7;38[6]) by Mark S. Komrad, MD, a Towson, Maryland-based psychiatrist.
There are still troublesome cases.
As previously reported by this news organization, many in Belgium were distressed recently at the news that a 23-year-old woman who had survived a terrorist attack, Shanti De Corte, requested and was granted euthanasia.
As the deadline for implementation of MAID grew closer, calls for delay grew louder, especially given the lack of concrete standards for providers.
During the waning months of 2022, Dr. Gaind – who said he was suspended from CPA for “unprofessional interactions” and allegedly misrepresenting CPA’s processes and governance matters – announced the launch of a new organization, the Society of Canadian Psychiatry, in November calling for a delay in MAID of at least 1 year so that evidence-based safeguards could be implemented. The petition has been signed by more than 200 psychiatrists, along with several dozen physicians, MAID assessors, and individuals with mental illness and family members.
The Association of Chairs of Psychiatry in Canada, the Canadian Association for Suicide Prevention, the Council of Canadians with Disabilities, a group of indigenous leaders, and the Ontario Association for ACT and FACT, psychiatrists who provide care to individuals with severe mental illness, among other groups, joined the call for a delay.
In its December announcement, the Canadian federal ministers said a factor in seeking a delay was that standards guiding clinicians would not be delivered until at least February – too close to when applications would be opened.
Upon hearing about the federal government’s intentions, the chair of the expert panel, Mona Gupta, MD, told The Canadian Press that she did not think it was necessary to put off implementation because necessary safeguards were already in place.
Dr. Chaimowitz awaits the standards but is optimistic that for mental illness, “the process will be tightly controlled, closely monitored, and open to scrutiny,” he said.
Dr. Braswell is not convinced. The concern is that adding people with mental illness is “going to overload the capacity of the government to monitor this practice,” he said.
Is the United States next?
Although Canada and the United States share a border, it’s unlikely that U.S. states will allow aid in dying for nonterminal illness, much less for psychiatric conditions any time soon, said Dr. Braswell and others.
Ten states – California, Colorado, Hawaii, Maine, Montana, New Jersey, New Mexico, Oregon, Vermont, and Washington – have laws allowing assistance in dying, but for terminal illness only.
In 2016, the APA adopted the American Medical Association policy on medical euthanasia, stating, “that a psychiatrist should not prescribe or administer any intervention to a nonterminally ill person for the purpose of causing death.”
Dr. Brendel said the field is acutely aware that people with mental illness do suffer, but that more work needs to be done – and is being done – on “distinguishing wishes to hasten death or end one’s life from these historical or traditional notions that any premature death is a suicide.”
There is also increasing discussion within the medical community, not just psychiatry, about a physician’s duty to relieve suffering, said Dr. Wynia. “There’s debate basically about whether we stand for preserving life essentially at all costs and never being involved in the taking of life, or whether we stand for reduction of suffering and being the advocate for the patients that we serve,” he said.
“Those are both legitimate,” said Dr. Wynia, adding, “there are good reasons to want both of those to be true.”
“I suspect that 20 years from now we will still be having conversations about how physicians, how psychiatrists ought to participate in preserving life and in shepherding death,” said Dr. Brendel.
But to Dr. Gaind, the debate is not just esoteric, it’s a soon-to-be reality in Canada. “When we’re providing death to people who aren’t dying, to me that’s like providing what amounts to a wrongful death,” he said.
A version of this article originally appeared on Medscape.com.
Depression guidelines fall short in characterizing withdrawal
Previous research suggests that approximately half of patients who discontinue or decrease dosage of antidepressants experience withdrawal symptoms, wrote Anders Sørensen, MD, of Copenhagen University Hospital, and colleagues. These symptoms are diverse and may include flulike symptoms, fatigue, anxiety, and sensations of electric shock, they noted. Most withdrawal effects last for a few weeks, but some persist for months or years, sometimes described as persistent postwithdrawal disorder, they added.
“Symptoms of withdrawal and depression overlap considerably but constitute two fundamentally different clinical conditions, which makes it important to distinguish between the two,” the researchers emphasized.
In a study published in the Journal of Affective Disorders, the researchers identified 21 clinical practice guidelines (CPGs) for depression published between 1998 and 2022. The guidelines were published in the United Kingdom, the United States, Canada, Australia, Singapore, Ireland, and New Zealand. They compared descriptions of withdrawal from antidepressants and calculated the proportion of CPGs with different information.
Overall, 15 of the 21 studies in the review (71%) noted that antidepressants are associated with withdrawal symptoms, but less than half (43%) used the term “withdrawal symptoms,” or similar. Of the nine guidelines that mentioned withdrawal symptoms, five used the term interchangeably with “discontinuation symptoms” and six used the term “discontinuation symptoms” only when discussing antidepressant withdrawal. In addition, six CPGs specifically stated that patients who stop antidepressants can experience withdrawal symptoms, and five stated that these symptoms also can occur in patients who are reducing or tapering their doses.
The type of withdrawal symptoms was mentioned in 10 CPGs, and the other 11 had no information on potential withdrawal symptoms, the researchers noted. Of the CPGs that mentioned symptoms specifically associated with withdrawal, the number of potential symptoms ranged from 4 to 39.
“None of the CPGs provided an exhaustive list of the potential withdrawal symptoms identified in the research literature,” the researchers wrote in their discussion.
Only four of the guidelines (19%) mentioned the overlap in symptoms between withdrawal from antidepressants and depression relapse, and only one provided guidance on distinguishing between the two conditions. Most of the symptoms of withdrawal, when described, were characterized as mild, brief, or self-limiting, the researchers noted.
“Being in withdrawal is a fundamentally different clinical situation than experiencing relapse, requiring two distinctly different treatment approaches,” the researchers emphasized. “Withdrawal reactions that are more severe and longer lasting than currently defined in the CPGs could risk getting misinterpreted as relapse, potentially leading to resumed unnecessary long-term antidepressant treatment in some patients,” they added.
The findings were limited by several factors including the inclusion only of guidelines from English-speaking countries, which may limit generalizability, the researchers noted. Other potential limitations include the subjective judgments involved in creating different guidelines, they said.
However, the results support the need for improved CPGs that help clinicians distinguish potential withdrawal reactions from depression relapse, and the need for more research on optimal dose reduction strategies for antidepressants, they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
Previous research suggests that approximately half of patients who discontinue or decrease dosage of antidepressants experience withdrawal symptoms, wrote Anders Sørensen, MD, of Copenhagen University Hospital, and colleagues. These symptoms are diverse and may include flulike symptoms, fatigue, anxiety, and sensations of electric shock, they noted. Most withdrawal effects last for a few weeks, but some persist for months or years, sometimes described as persistent postwithdrawal disorder, they added.
“Symptoms of withdrawal and depression overlap considerably but constitute two fundamentally different clinical conditions, which makes it important to distinguish between the two,” the researchers emphasized.
In a study published in the Journal of Affective Disorders, the researchers identified 21 clinical practice guidelines (CPGs) for depression published between 1998 and 2022. The guidelines were published in the United Kingdom, the United States, Canada, Australia, Singapore, Ireland, and New Zealand. They compared descriptions of withdrawal from antidepressants and calculated the proportion of CPGs with different information.
Overall, 15 of the 21 studies in the review (71%) noted that antidepressants are associated with withdrawal symptoms, but less than half (43%) used the term “withdrawal symptoms,” or similar. Of the nine guidelines that mentioned withdrawal symptoms, five used the term interchangeably with “discontinuation symptoms” and six used the term “discontinuation symptoms” only when discussing antidepressant withdrawal. In addition, six CPGs specifically stated that patients who stop antidepressants can experience withdrawal symptoms, and five stated that these symptoms also can occur in patients who are reducing or tapering their doses.
The type of withdrawal symptoms was mentioned in 10 CPGs, and the other 11 had no information on potential withdrawal symptoms, the researchers noted. Of the CPGs that mentioned symptoms specifically associated with withdrawal, the number of potential symptoms ranged from 4 to 39.
“None of the CPGs provided an exhaustive list of the potential withdrawal symptoms identified in the research literature,” the researchers wrote in their discussion.
Only four of the guidelines (19%) mentioned the overlap in symptoms between withdrawal from antidepressants and depression relapse, and only one provided guidance on distinguishing between the two conditions. Most of the symptoms of withdrawal, when described, were characterized as mild, brief, or self-limiting, the researchers noted.
“Being in withdrawal is a fundamentally different clinical situation than experiencing relapse, requiring two distinctly different treatment approaches,” the researchers emphasized. “Withdrawal reactions that are more severe and longer lasting than currently defined in the CPGs could risk getting misinterpreted as relapse, potentially leading to resumed unnecessary long-term antidepressant treatment in some patients,” they added.
The findings were limited by several factors including the inclusion only of guidelines from English-speaking countries, which may limit generalizability, the researchers noted. Other potential limitations include the subjective judgments involved in creating different guidelines, they said.
However, the results support the need for improved CPGs that help clinicians distinguish potential withdrawal reactions from depression relapse, and the need for more research on optimal dose reduction strategies for antidepressants, they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
Previous research suggests that approximately half of patients who discontinue or decrease dosage of antidepressants experience withdrawal symptoms, wrote Anders Sørensen, MD, of Copenhagen University Hospital, and colleagues. These symptoms are diverse and may include flulike symptoms, fatigue, anxiety, and sensations of electric shock, they noted. Most withdrawal effects last for a few weeks, but some persist for months or years, sometimes described as persistent postwithdrawal disorder, they added.
“Symptoms of withdrawal and depression overlap considerably but constitute two fundamentally different clinical conditions, which makes it important to distinguish between the two,” the researchers emphasized.
In a study published in the Journal of Affective Disorders, the researchers identified 21 clinical practice guidelines (CPGs) for depression published between 1998 and 2022. The guidelines were published in the United Kingdom, the United States, Canada, Australia, Singapore, Ireland, and New Zealand. They compared descriptions of withdrawal from antidepressants and calculated the proportion of CPGs with different information.
Overall, 15 of the 21 studies in the review (71%) noted that antidepressants are associated with withdrawal symptoms, but less than half (43%) used the term “withdrawal symptoms,” or similar. Of the nine guidelines that mentioned withdrawal symptoms, five used the term interchangeably with “discontinuation symptoms” and six used the term “discontinuation symptoms” only when discussing antidepressant withdrawal. In addition, six CPGs specifically stated that patients who stop antidepressants can experience withdrawal symptoms, and five stated that these symptoms also can occur in patients who are reducing or tapering their doses.
The type of withdrawal symptoms was mentioned in 10 CPGs, and the other 11 had no information on potential withdrawal symptoms, the researchers noted. Of the CPGs that mentioned symptoms specifically associated with withdrawal, the number of potential symptoms ranged from 4 to 39.
“None of the CPGs provided an exhaustive list of the potential withdrawal symptoms identified in the research literature,” the researchers wrote in their discussion.
Only four of the guidelines (19%) mentioned the overlap in symptoms between withdrawal from antidepressants and depression relapse, and only one provided guidance on distinguishing between the two conditions. Most of the symptoms of withdrawal, when described, were characterized as mild, brief, or self-limiting, the researchers noted.
“Being in withdrawal is a fundamentally different clinical situation than experiencing relapse, requiring two distinctly different treatment approaches,” the researchers emphasized. “Withdrawal reactions that are more severe and longer lasting than currently defined in the CPGs could risk getting misinterpreted as relapse, potentially leading to resumed unnecessary long-term antidepressant treatment in some patients,” they added.
The findings were limited by several factors including the inclusion only of guidelines from English-speaking countries, which may limit generalizability, the researchers noted. Other potential limitations include the subjective judgments involved in creating different guidelines, they said.
However, the results support the need for improved CPGs that help clinicians distinguish potential withdrawal reactions from depression relapse, and the need for more research on optimal dose reduction strategies for antidepressants, they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
FROM THE JOURNAL OF AFFECTIVE DISORDERS
Guidelines recommend CBT alone for mild acute depression, more options for more severe cases
The guidelines also state that patients with mild depression should start with CBT alone, and if a patient with moderate to severe depression prefers, they can use a combination of both CBT and an SGA.
These nuanced recommendations contrast sharply with the 2016 ACP guidelines for depression, which lumped all stages and severity levels together, and came with just one recommendation: Clinicians should choose between CBT and an SGA.
More data have come to light over the years, requiring the present update, reported lead author Amir Qaseem, MD, PhD, vice president of Clinical Policy and the Center for Evidence Reviews at the ACP, and adjunct faculty at Thomas Jefferson University, Philadelphia, and colleagues.
In addition to the focus on acute depression, Dr. Qaseem and colleagues highlighted the new guidelines' “consideration of patient values and preferences, and costs,” as well as responses to therapy.
Recommendations were derived from a network meta-analysis that included studies evaluating nonpharmacologic and pharmacologic therapies, the authors wrote in Annals of Internal Medicine. They compared effectiveness across a range of SGAs, “including selective serotonin reuptake inhibitors; serotonin-norepinephrine reuptake inhibitors; and others such as bupropion, mirtazapine, nefazodone, trazodone, vilazodone, and vortioxetine.”
This analysis yielded three pieces of clinical advice.
First, patients in the acute phase of mild depression should receive CBT alone as their initial treatment.
Dr. Qaseem and colleagues noted that many depression studies for pharmacologic therapies excluded these patients in favor of those with moderate to severe depression, leaving an evidence gap.
“Furthermore, the Clinical Guidelines Committee had concerns about adverse effects of SGAs in these patients and suggests that the use of SGAs as initial treatment of these patients should be based on additional considerations, such as limited access to or cost of CBT, history of moderate or severe major depressive disorder, or patient preferences,” they added.
The committee’s next recommendation, based on moderate-certainty evidence, suggested that CBT alone or an SGA alone should be considered for patients in the acute phase of moderate to severe depression. This call for monotherapy is balanced by a conditional recommendation based on low-certainty evidence that the same group may benefit from initial combination therapy with both CBT and an SGA.
“The informed decision on the options of monotherapy with CBT versus SGAs, or combination therapy, should be personalized and based on discussion of potential treatment benefits, harms, adverse effect profiles, cost, feasibility, patients’ specific symptoms (such as insomnia, hypersomnia, or fluctuation in appetite), comorbidities, concomitant medication use, and patient preferences,” the guidelines state.
The third and final recommendation offers an algorithm for patients who do not respond to initial therapy with an SGA. Multiple pathways are provided: Switch to CBT or augment with CBT; or switch to a different SGA or augment with a second pharmacologic therapy, such as mirtazapine, bupropion, or buspirone.
“These second-line treatment strategies show similar efficacy when compared with each other,” the guidelines committee noted.
Again, the guidelines suggest that second-line choices should be personalized based on the various factors previously discussed.
A timely update
“The new guideline is very different from the last guideline,” said Ryan Mire, MD, president of the ACP and practicing internal medicine physician in Nashville, Tenn. in a written comment. “ACP decided to update the depression guidelines with a focus on acute depression because approximately 70% of patients with major depressive disorder do not achieve remission and remain in the acute phase after the initial pharmacologic treatment attempt. In addition, there is new evidence on second-line treatments since the 2016 ACP guideline was published.”
Neil S. Skolnik, MD, of Thomas Jefferson University, Philadelphia, agreed that the guidelines offer a necessary and fresh perspective on caring for patients with depression.
“These guidelines are a helpful update, assuring us that we are using the latest, evidence-based therapies, and [they] are written in a practical, easy-to-implement manner,” Dr. Skolnik said in a written comment.
“First, the guidelines reaffirm that CBT is an effective first-line option, with or without the concurrent use of an SGA,” Dr. Skolnik said, noting that CBT alone may reduce likelihood of recurrence, compared with an SGA alone. “Many patients do not like the idea of medication, or the potential side effects of medications, and CBT is an evidenced-based approach that can be very helpful for patients.”
Dr. Skolnik also applauded the guidelines authors for offering a clear path forward for patients who do not have full remission after treatment – a common clinical scenario.
He went on to offer some more detailed steps forward.
“If someone chooses to be treated with an SGA alone and has not had much response at all to an initial SGA, usually a selective serotonin reuptake inhibitor, I’ll usually switch to a different SSRI or serotonin and norepinephrine reuptake inhibitor (SNRI) and/or add CBT,” Dr. Skolnik said. “If they have had a partial response, I’ll often encourage CBT and consider the addition of augmentation with an additional medication as discussed in the guidelines.”
Valuable despite the gaps
Other experts expressed mixed impressions of the update, noting both highs and lows.
“Although [this guideline] has some gaps, it is more valuable in several ways than other widely consulted practice guidelines for depression,” wrote Miriam Shuchman, MD and Elia Abi-Jaoude, MSc, MD, PhD, of the University of Toronto, in an accompanying editorial.
Specifically, they praised the publication’s focus on shared decision-making in the treatment planning process.
“This effort to respond to patient preferences is crucial and may even increase the chance that patients will improve with treatment,” they wrote.
They also applauded the ACP’s efforts to recuse any committee members who may have had conflicts of interest “that could affect their judgment about treatments for depression.”
After highlighting these attributes, Dr. Shuchman and Dr. Abi-Jaoude noted that the guidelines still contain “significant gaps.”
Foremost, they pointed out the guidelines' emphasis on CBT to the exclusion of other nonpharmacologic options.
“The guideline does patients a disservice by leaving out several nonmedication treatment options that clinicians can offer as first- or second-line therapies,” they wrote.
This oversight may increase risk that patients simply hop from one SGA to another, which is a common, and often ineffective, strategy, according to Dr. Shuchman and Dr. Abi-Jaoude.
“Patients often go from one drug to the next in the hopes of landing on one that ‘works,’ ” the editorialists wrote. “This narrow clinical approach of pursuing medication-based treatments ignores the ways difficulties in a person’s work or relationships may contribute to their struggles with depression. At a time when the COVID-19 pandemic has underscored the importance of the social context of mental health, clinicians may need to consider other forms of support and tailor prescribing to what is most relevant and accessible for a particular patient.”
Dr. Shuchman and Dr. Abi-Jaoude went on to suggest several nonpharmacologic options beyond CBT, including interpersonal therapy, psychodynamic therapy, problem solving, behavioral activation, and guided self-help.
The other key gap they pointed out relates to withdrawal.
Although the guideline does advise physicians to taper antidepressants to reduce risk of withdrawal, the editorialists suggested that this recommendation lacked sufficient emphasis, as it can be a particularly difficult period in the treatment process.
“Tapering of an antidepressant may need to be done over months or years, not weeks, and a patient may need to visit a compounding pharmacy to obtain doses of a second-generation antidepressant not marketed by drug manufacturers so that prescriptions can be tapered even more slowly,” they suggested.
Financial costs remain unclear
Beyond the above medical considerations, one other piece of the depression puzzle remains unsolved: cost.
In a simultaneously published rapid review, Andreea Dobrescu, MD, PhD, of Cochrane Austria, and colleagues evaluated the relative cost-effectiveness of first- and second-step treatment strategies.
For most comparisons, evidence was insufficient to reach a conclusion, although they suggested that CBT may be more cost effective at the 5-year mark.
“For most pharmacologic and nonpharmacologic interventions for major depressive disorder, evidence was missing or was insufficient to draw conclusions about the cost-effectiveness of first- or second-step treatments for MDD,” Dr. Dobrescu and colleagues wrote. “The strongest evidence (albeit still low certainty of evidence) was for the cost-effectiveness of CBT compared with SGA as a first-step treatment over a 5-year time horizon from the societal and health care sector perspectives. However, this evidence should also be interpreted cautiously considering it is based on a single study.”
When asked about the financial findings, Dr. Mire agreed that more data are needed, especially because CBT and SGA costs range widely. He suggested that cost, for each patient, should be considered in the personalized approach now highlighted by the new guidelines.
The guidelines and the Cochrane cost-effectiveness study were supported by the ACP. The guidelines' authors and other individuals quoted in this article reported no conflicts of interest.
The guidelines also state that patients with mild depression should start with CBT alone, and if a patient with moderate to severe depression prefers, they can use a combination of both CBT and an SGA.
These nuanced recommendations contrast sharply with the 2016 ACP guidelines for depression, which lumped all stages and severity levels together, and came with just one recommendation: Clinicians should choose between CBT and an SGA.
More data have come to light over the years, requiring the present update, reported lead author Amir Qaseem, MD, PhD, vice president of Clinical Policy and the Center for Evidence Reviews at the ACP, and adjunct faculty at Thomas Jefferson University, Philadelphia, and colleagues.
In addition to the focus on acute depression, Dr. Qaseem and colleagues highlighted the new guidelines' “consideration of patient values and preferences, and costs,” as well as responses to therapy.
Recommendations were derived from a network meta-analysis that included studies evaluating nonpharmacologic and pharmacologic therapies, the authors wrote in Annals of Internal Medicine. They compared effectiveness across a range of SGAs, “including selective serotonin reuptake inhibitors; serotonin-norepinephrine reuptake inhibitors; and others such as bupropion, mirtazapine, nefazodone, trazodone, vilazodone, and vortioxetine.”
This analysis yielded three pieces of clinical advice.
First, patients in the acute phase of mild depression should receive CBT alone as their initial treatment.
Dr. Qaseem and colleagues noted that many depression studies for pharmacologic therapies excluded these patients in favor of those with moderate to severe depression, leaving an evidence gap.
“Furthermore, the Clinical Guidelines Committee had concerns about adverse effects of SGAs in these patients and suggests that the use of SGAs as initial treatment of these patients should be based on additional considerations, such as limited access to or cost of CBT, history of moderate or severe major depressive disorder, or patient preferences,” they added.
The committee’s next recommendation, based on moderate-certainty evidence, suggested that CBT alone or an SGA alone should be considered for patients in the acute phase of moderate to severe depression. This call for monotherapy is balanced by a conditional recommendation based on low-certainty evidence that the same group may benefit from initial combination therapy with both CBT and an SGA.
“The informed decision on the options of monotherapy with CBT versus SGAs, or combination therapy, should be personalized and based on discussion of potential treatment benefits, harms, adverse effect profiles, cost, feasibility, patients’ specific symptoms (such as insomnia, hypersomnia, or fluctuation in appetite), comorbidities, concomitant medication use, and patient preferences,” the guidelines state.
The third and final recommendation offers an algorithm for patients who do not respond to initial therapy with an SGA. Multiple pathways are provided: Switch to CBT or augment with CBT; or switch to a different SGA or augment with a second pharmacologic therapy, such as mirtazapine, bupropion, or buspirone.
“These second-line treatment strategies show similar efficacy when compared with each other,” the guidelines committee noted.
Again, the guidelines suggest that second-line choices should be personalized based on the various factors previously discussed.
A timely update
“The new guideline is very different from the last guideline,” said Ryan Mire, MD, president of the ACP and practicing internal medicine physician in Nashville, Tenn. in a written comment. “ACP decided to update the depression guidelines with a focus on acute depression because approximately 70% of patients with major depressive disorder do not achieve remission and remain in the acute phase after the initial pharmacologic treatment attempt. In addition, there is new evidence on second-line treatments since the 2016 ACP guideline was published.”
Neil S. Skolnik, MD, of Thomas Jefferson University, Philadelphia, agreed that the guidelines offer a necessary and fresh perspective on caring for patients with depression.
“These guidelines are a helpful update, assuring us that we are using the latest, evidence-based therapies, and [they] are written in a practical, easy-to-implement manner,” Dr. Skolnik said in a written comment.
“First, the guidelines reaffirm that CBT is an effective first-line option, with or without the concurrent use of an SGA,” Dr. Skolnik said, noting that CBT alone may reduce likelihood of recurrence, compared with an SGA alone. “Many patients do not like the idea of medication, or the potential side effects of medications, and CBT is an evidenced-based approach that can be very helpful for patients.”
Dr. Skolnik also applauded the guidelines authors for offering a clear path forward for patients who do not have full remission after treatment – a common clinical scenario.
He went on to offer some more detailed steps forward.
“If someone chooses to be treated with an SGA alone and has not had much response at all to an initial SGA, usually a selective serotonin reuptake inhibitor, I’ll usually switch to a different SSRI or serotonin and norepinephrine reuptake inhibitor (SNRI) and/or add CBT,” Dr. Skolnik said. “If they have had a partial response, I’ll often encourage CBT and consider the addition of augmentation with an additional medication as discussed in the guidelines.”
Valuable despite the gaps
Other experts expressed mixed impressions of the update, noting both highs and lows.
“Although [this guideline] has some gaps, it is more valuable in several ways than other widely consulted practice guidelines for depression,” wrote Miriam Shuchman, MD and Elia Abi-Jaoude, MSc, MD, PhD, of the University of Toronto, in an accompanying editorial.
Specifically, they praised the publication’s focus on shared decision-making in the treatment planning process.
“This effort to respond to patient preferences is crucial and may even increase the chance that patients will improve with treatment,” they wrote.
They also applauded the ACP’s efforts to recuse any committee members who may have had conflicts of interest “that could affect their judgment about treatments for depression.”
After highlighting these attributes, Dr. Shuchman and Dr. Abi-Jaoude noted that the guidelines still contain “significant gaps.”
Foremost, they pointed out the guidelines' emphasis on CBT to the exclusion of other nonpharmacologic options.
“The guideline does patients a disservice by leaving out several nonmedication treatment options that clinicians can offer as first- or second-line therapies,” they wrote.
This oversight may increase risk that patients simply hop from one SGA to another, which is a common, and often ineffective, strategy, according to Dr. Shuchman and Dr. Abi-Jaoude.
“Patients often go from one drug to the next in the hopes of landing on one that ‘works,’ ” the editorialists wrote. “This narrow clinical approach of pursuing medication-based treatments ignores the ways difficulties in a person’s work or relationships may contribute to their struggles with depression. At a time when the COVID-19 pandemic has underscored the importance of the social context of mental health, clinicians may need to consider other forms of support and tailor prescribing to what is most relevant and accessible for a particular patient.”
Dr. Shuchman and Dr. Abi-Jaoude went on to suggest several nonpharmacologic options beyond CBT, including interpersonal therapy, psychodynamic therapy, problem solving, behavioral activation, and guided self-help.
The other key gap they pointed out relates to withdrawal.
Although the guideline does advise physicians to taper antidepressants to reduce risk of withdrawal, the editorialists suggested that this recommendation lacked sufficient emphasis, as it can be a particularly difficult period in the treatment process.
“Tapering of an antidepressant may need to be done over months or years, not weeks, and a patient may need to visit a compounding pharmacy to obtain doses of a second-generation antidepressant not marketed by drug manufacturers so that prescriptions can be tapered even more slowly,” they suggested.
Financial costs remain unclear
Beyond the above medical considerations, one other piece of the depression puzzle remains unsolved: cost.
In a simultaneously published rapid review, Andreea Dobrescu, MD, PhD, of Cochrane Austria, and colleagues evaluated the relative cost-effectiveness of first- and second-step treatment strategies.
For most comparisons, evidence was insufficient to reach a conclusion, although they suggested that CBT may be more cost effective at the 5-year mark.
“For most pharmacologic and nonpharmacologic interventions for major depressive disorder, evidence was missing or was insufficient to draw conclusions about the cost-effectiveness of first- or second-step treatments for MDD,” Dr. Dobrescu and colleagues wrote. “The strongest evidence (albeit still low certainty of evidence) was for the cost-effectiveness of CBT compared with SGA as a first-step treatment over a 5-year time horizon from the societal and health care sector perspectives. However, this evidence should also be interpreted cautiously considering it is based on a single study.”
When asked about the financial findings, Dr. Mire agreed that more data are needed, especially because CBT and SGA costs range widely. He suggested that cost, for each patient, should be considered in the personalized approach now highlighted by the new guidelines.
The guidelines and the Cochrane cost-effectiveness study were supported by the ACP. The guidelines' authors and other individuals quoted in this article reported no conflicts of interest.
The guidelines also state that patients with mild depression should start with CBT alone, and if a patient with moderate to severe depression prefers, they can use a combination of both CBT and an SGA.
These nuanced recommendations contrast sharply with the 2016 ACP guidelines for depression, which lumped all stages and severity levels together, and came with just one recommendation: Clinicians should choose between CBT and an SGA.
More data have come to light over the years, requiring the present update, reported lead author Amir Qaseem, MD, PhD, vice president of Clinical Policy and the Center for Evidence Reviews at the ACP, and adjunct faculty at Thomas Jefferson University, Philadelphia, and colleagues.
In addition to the focus on acute depression, Dr. Qaseem and colleagues highlighted the new guidelines' “consideration of patient values and preferences, and costs,” as well as responses to therapy.
Recommendations were derived from a network meta-analysis that included studies evaluating nonpharmacologic and pharmacologic therapies, the authors wrote in Annals of Internal Medicine. They compared effectiveness across a range of SGAs, “including selective serotonin reuptake inhibitors; serotonin-norepinephrine reuptake inhibitors; and others such as bupropion, mirtazapine, nefazodone, trazodone, vilazodone, and vortioxetine.”
This analysis yielded three pieces of clinical advice.
First, patients in the acute phase of mild depression should receive CBT alone as their initial treatment.
Dr. Qaseem and colleagues noted that many depression studies for pharmacologic therapies excluded these patients in favor of those with moderate to severe depression, leaving an evidence gap.
“Furthermore, the Clinical Guidelines Committee had concerns about adverse effects of SGAs in these patients and suggests that the use of SGAs as initial treatment of these patients should be based on additional considerations, such as limited access to or cost of CBT, history of moderate or severe major depressive disorder, or patient preferences,” they added.
The committee’s next recommendation, based on moderate-certainty evidence, suggested that CBT alone or an SGA alone should be considered for patients in the acute phase of moderate to severe depression. This call for monotherapy is balanced by a conditional recommendation based on low-certainty evidence that the same group may benefit from initial combination therapy with both CBT and an SGA.
“The informed decision on the options of monotherapy with CBT versus SGAs, or combination therapy, should be personalized and based on discussion of potential treatment benefits, harms, adverse effect profiles, cost, feasibility, patients’ specific symptoms (such as insomnia, hypersomnia, or fluctuation in appetite), comorbidities, concomitant medication use, and patient preferences,” the guidelines state.
The third and final recommendation offers an algorithm for patients who do not respond to initial therapy with an SGA. Multiple pathways are provided: Switch to CBT or augment with CBT; or switch to a different SGA or augment with a second pharmacologic therapy, such as mirtazapine, bupropion, or buspirone.
“These second-line treatment strategies show similar efficacy when compared with each other,” the guidelines committee noted.
Again, the guidelines suggest that second-line choices should be personalized based on the various factors previously discussed.
A timely update
“The new guideline is very different from the last guideline,” said Ryan Mire, MD, president of the ACP and practicing internal medicine physician in Nashville, Tenn. in a written comment. “ACP decided to update the depression guidelines with a focus on acute depression because approximately 70% of patients with major depressive disorder do not achieve remission and remain in the acute phase after the initial pharmacologic treatment attempt. In addition, there is new evidence on second-line treatments since the 2016 ACP guideline was published.”
Neil S. Skolnik, MD, of Thomas Jefferson University, Philadelphia, agreed that the guidelines offer a necessary and fresh perspective on caring for patients with depression.
“These guidelines are a helpful update, assuring us that we are using the latest, evidence-based therapies, and [they] are written in a practical, easy-to-implement manner,” Dr. Skolnik said in a written comment.
“First, the guidelines reaffirm that CBT is an effective first-line option, with or without the concurrent use of an SGA,” Dr. Skolnik said, noting that CBT alone may reduce likelihood of recurrence, compared with an SGA alone. “Many patients do not like the idea of medication, or the potential side effects of medications, and CBT is an evidenced-based approach that can be very helpful for patients.”
Dr. Skolnik also applauded the guidelines authors for offering a clear path forward for patients who do not have full remission after treatment – a common clinical scenario.
He went on to offer some more detailed steps forward.
“If someone chooses to be treated with an SGA alone and has not had much response at all to an initial SGA, usually a selective serotonin reuptake inhibitor, I’ll usually switch to a different SSRI or serotonin and norepinephrine reuptake inhibitor (SNRI) and/or add CBT,” Dr. Skolnik said. “If they have had a partial response, I’ll often encourage CBT and consider the addition of augmentation with an additional medication as discussed in the guidelines.”
Valuable despite the gaps
Other experts expressed mixed impressions of the update, noting both highs and lows.
“Although [this guideline] has some gaps, it is more valuable in several ways than other widely consulted practice guidelines for depression,” wrote Miriam Shuchman, MD and Elia Abi-Jaoude, MSc, MD, PhD, of the University of Toronto, in an accompanying editorial.
Specifically, they praised the publication’s focus on shared decision-making in the treatment planning process.
“This effort to respond to patient preferences is crucial and may even increase the chance that patients will improve with treatment,” they wrote.
They also applauded the ACP’s efforts to recuse any committee members who may have had conflicts of interest “that could affect their judgment about treatments for depression.”
After highlighting these attributes, Dr. Shuchman and Dr. Abi-Jaoude noted that the guidelines still contain “significant gaps.”
Foremost, they pointed out the guidelines' emphasis on CBT to the exclusion of other nonpharmacologic options.
“The guideline does patients a disservice by leaving out several nonmedication treatment options that clinicians can offer as first- or second-line therapies,” they wrote.
This oversight may increase risk that patients simply hop from one SGA to another, which is a common, and often ineffective, strategy, according to Dr. Shuchman and Dr. Abi-Jaoude.
“Patients often go from one drug to the next in the hopes of landing on one that ‘works,’ ” the editorialists wrote. “This narrow clinical approach of pursuing medication-based treatments ignores the ways difficulties in a person’s work or relationships may contribute to their struggles with depression. At a time when the COVID-19 pandemic has underscored the importance of the social context of mental health, clinicians may need to consider other forms of support and tailor prescribing to what is most relevant and accessible for a particular patient.”
Dr. Shuchman and Dr. Abi-Jaoude went on to suggest several nonpharmacologic options beyond CBT, including interpersonal therapy, psychodynamic therapy, problem solving, behavioral activation, and guided self-help.
The other key gap they pointed out relates to withdrawal.
Although the guideline does advise physicians to taper antidepressants to reduce risk of withdrawal, the editorialists suggested that this recommendation lacked sufficient emphasis, as it can be a particularly difficult period in the treatment process.
“Tapering of an antidepressant may need to be done over months or years, not weeks, and a patient may need to visit a compounding pharmacy to obtain doses of a second-generation antidepressant not marketed by drug manufacturers so that prescriptions can be tapered even more slowly,” they suggested.
Financial costs remain unclear
Beyond the above medical considerations, one other piece of the depression puzzle remains unsolved: cost.
In a simultaneously published rapid review, Andreea Dobrescu, MD, PhD, of Cochrane Austria, and colleagues evaluated the relative cost-effectiveness of first- and second-step treatment strategies.
For most comparisons, evidence was insufficient to reach a conclusion, although they suggested that CBT may be more cost effective at the 5-year mark.
“For most pharmacologic and nonpharmacologic interventions for major depressive disorder, evidence was missing or was insufficient to draw conclusions about the cost-effectiveness of first- or second-step treatments for MDD,” Dr. Dobrescu and colleagues wrote. “The strongest evidence (albeit still low certainty of evidence) was for the cost-effectiveness of CBT compared with SGA as a first-step treatment over a 5-year time horizon from the societal and health care sector perspectives. However, this evidence should also be interpreted cautiously considering it is based on a single study.”
When asked about the financial findings, Dr. Mire agreed that more data are needed, especially because CBT and SGA costs range widely. He suggested that cost, for each patient, should be considered in the personalized approach now highlighted by the new guidelines.
The guidelines and the Cochrane cost-effectiveness study were supported by the ACP. The guidelines' authors and other individuals quoted in this article reported no conflicts of interest.
FROM ANNALS OF INTERNAL MEDICINE