User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
‘A huge deal’: Millions have long COVID, and more are expected
with symptoms that have lasted 3 months or longer, according to the latest U.S. government survey done in October. More than a quarter say their condition is severe enough to significantly limit their day-to-day activities – yet the problem is only barely starting to get the attention of employers, the health care system, and policymakers.
With no cure or treatment in sight, long COVID is already burdening not only the health care system, but also the economy – and that burden is set to grow. Many experts worry about the possible long-term ripple effects, from increased spending on medical care costs to lost wages due to not being able to work, as well as the policy implications that come with addressing these issues.
“At this point, anyone who’s looking at this seriously would say this is a huge deal,” says senior Brookings Institution fellow Katie Bach, the author of a study that analyzed long COVID’s impact on the labor market.
“We need a real concerted focus on treating these people, which means both research and the clinical side, and figuring out how to build a labor market that is more inclusive of people with disabilities,” she said.
It’s not only that many people are affected. It’s that they are often affected for months and possibly even years.
The U.S. government figures suggest more than 18 million people could have symptoms of long COVID right now. The latest Household Pulse Survey by the Census Bureau and the National Center for Health Statistics takes data from 41,415 people.
A preprint of a study by researchers from City University of New York, posted on medRxiv in September and based on a similar population survey done between June 30 and July 2, drew comparable results. The study has not been peer reviewed.
More than 7% of all those who answered said they had long COVID at the time of the survey, which the researchers said corresponded to approximately 18.5 million U.S. adults. The same study found that a quarter of those, or an estimated 4.7 million adults, said their daily activities were impacted “a lot.”
This can translate into pain not only for the patients, but for governments and employers, too.
In high-income countries around the world, government surveys and other studies are shedding light on the extent to which post-COVID-19 symptoms – commonly known as long COVID – are affecting populations. While results vary, they generally fall within similar ranges.
The World Health Organization estimates that between 10% and 20% of those with COVID-19 go on to have an array of medium- to long-term post-COVID-19 symptoms that range from mild to debilitating. The U.S. Government Accountability Office puts that estimate at 10% to 30%; one of the latest studies published at the end of October in The Journal of the American Medical Association found that 15% of U.S. adults who had tested positive for COVID-19 reported current long COVID symptoms. Elsewhere, a study from the Netherlands published in The Lancet in August found that one in eight COVID-19 cases, or 12.7%, were likely to become long COVID.
“It’s very clear that the condition is devastating people’s lives and livelihoods,” WHO Director-General Tedros Adhanom Ghebreyesus wrote in an article for The Guardian newspaper in October.
“The world has already lost a significant number of the workforce to illness, death, fatigue, unplanned retirement due to an increase in long-term disability, which not only impacts the health system, but is a hit to the overarching economy … the impact of long COVID for all countries is very serious and needs immediate and sustained action equivalent to its scale.”
Global snapshot: Lasting symptoms, impact on activities
Patients describe a spectrum of persistent issues, with extreme fatigue, brain fog or cognitive problems, and shortness of breath among the most common complaints. Many also have manageable symptoms that worsen significantly after even mild physical or mental exertion.
Women appear almost twice as likely as men to get long COVID. Many patients have other medical conditions and disabilities that make them more vulnerable to the condition. Those who face greater obstacles accessing health care due to discrimination or socioeconomic inequity are at higher risk as well.
While many are older, a large number are also in their prime working age. The Census Bureau data show that people ages 40-49 are more likely than any other group to get long COVID, which has broader implications for labor markets and the global economy. Already, experts have estimated that long COVID is likely to cost the U.S. trillions of dollars and affect multiple industries.
“Whether they’re in the financial world, the medical system, lawyers, they’re telling me they’re sitting at the computer screen and they’re unable to process the data,” said Zachary Schwartz, MD, medical director for Vancouver General Hospital’s Post-COVID-19 Recovery Clinic.
“That is what’s most distressing for people, in that they’re not working, they’re not making money, and they don’t know when, or if, they’re going to get better.”
Nearly a third of respondents in the Census Bureau’s Household Pulse Survey who said they have had COVID-19 reported symptoms that lasted 3 months or longer. People between the ages of 30 and 59 were the most affected, with about 32% reporting symptoms. Across the entire adult U.S. population, the survey found that 1 in 7 adults have had long COVID at some point during the pandemic, with about 1 in 18 saying it limited their activity to some degree, and 1 in 50 saying they have faced “a lot” of limits on their activities. Any way these numbers are dissected, long COVID has impacted a large swath of the population.
Yet research into the causes and possible treatments of long COVID is just getting underway.
“The amount of energy and time devoted to it is way, way less than it should, given how many people are likely affected,” said David Cutler, PhD, professor of economics at Harvard University, Cambridge, Mass., who has written about the economic cost of long COVID. “We’re way, way underdoing it here. And I think that’s really a terrible thing.”
Population surveys and studies from around the world show that long COVID lives up to its name, with people reporting serious symptoms for months on end.
In October, Statistics Canada and the Public Health Agency of Canada published early results from a questionnaire done between spring and summer 2022 that found just under 15% of adults who had a confirmed or suspected case of COVID-19 went on to have new or continuing symptoms 3 or more months later. Nearly half, or 47.3%, dealt with symptoms that lasted a year or more. More than one in five said their symptoms “often or always” limited their day-to-day activities, which included routine tasks such as preparing meals, doing errands and chores, and basic functions such as personal care and moving around in their homes.
Nearly three-quarters of workers or students said they missed an average of 20 days of work or school.
“We haven’t yet been able to determine exactly when symptoms resolve,” said Rainu Kaushal, MD, the senior associate dean for clinical research at Weill Cornell Medicine in New York. She is co-leading a national study on long COVID in adults and children, funded by the National Institutes of Health RECOVER Initiative.
“But there does seem to be, for many of the milder symptoms, resolution at about 4-6 weeks. There seems to be a second point of resolution around 6 months for certain symptoms, and then some symptoms do seem to be permanent, and those tend to be patients who have underlying conditions,” she said.
Reducing the risk
Given all the data so far, experts recommend urgent policy changes to help people with long COVID.
“The population needs to be prepared, that understanding long COVID is going to be a very long and difficult process,” said Alexander Charney, MD, PhD, associate professor and the lead principal investigator of the RECOVER adult cohort at Icahn School of Medicine at Mount Sinai in New York. He said the government can do a great deal to help, including setting up a network of connected clinics treating long COVID, standardizing best practices, and sharing information.
“That would go a long way towards making sure that every person feels like they’re not too far away from a clinic where they can get treated for this particular condition,” he said.
But the only known way to prevent long COVID is to prevent COVID-19 infections in the first place, experts say. That means equitable access to tests, therapeutics, and vaccines.
“I will say that avoiding COVID remains the best treatment in the arsenal right now,” said Dr. Kaushal. This means masking, avoiding crowded places with poor ventilation and high exposure risk, and being up to date on vaccinations, she said.
A number of papers – including a large U.K. study published in May 2022, another one from July, and the JAMA study from October – all suggest that vaccinations can help reduce the risk of long COVID.
“I am absolutely of the belief that vaccination has reduced the incidence and overall amount of long COVID … [and is] still by far the best thing the public can do,” said Dr. Schwartz.
A version of this article first appeared on WebMD.com.
with symptoms that have lasted 3 months or longer, according to the latest U.S. government survey done in October. More than a quarter say their condition is severe enough to significantly limit their day-to-day activities – yet the problem is only barely starting to get the attention of employers, the health care system, and policymakers.
With no cure or treatment in sight, long COVID is already burdening not only the health care system, but also the economy – and that burden is set to grow. Many experts worry about the possible long-term ripple effects, from increased spending on medical care costs to lost wages due to not being able to work, as well as the policy implications that come with addressing these issues.
“At this point, anyone who’s looking at this seriously would say this is a huge deal,” says senior Brookings Institution fellow Katie Bach, the author of a study that analyzed long COVID’s impact on the labor market.
“We need a real concerted focus on treating these people, which means both research and the clinical side, and figuring out how to build a labor market that is more inclusive of people with disabilities,” she said.
It’s not only that many people are affected. It’s that they are often affected for months and possibly even years.
The U.S. government figures suggest more than 18 million people could have symptoms of long COVID right now. The latest Household Pulse Survey by the Census Bureau and the National Center for Health Statistics takes data from 41,415 people.
A preprint of a study by researchers from City University of New York, posted on medRxiv in September and based on a similar population survey done between June 30 and July 2, drew comparable results. The study has not been peer reviewed.
More than 7% of all those who answered said they had long COVID at the time of the survey, which the researchers said corresponded to approximately 18.5 million U.S. adults. The same study found that a quarter of those, or an estimated 4.7 million adults, said their daily activities were impacted “a lot.”
This can translate into pain not only for the patients, but for governments and employers, too.
In high-income countries around the world, government surveys and other studies are shedding light on the extent to which post-COVID-19 symptoms – commonly known as long COVID – are affecting populations. While results vary, they generally fall within similar ranges.
The World Health Organization estimates that between 10% and 20% of those with COVID-19 go on to have an array of medium- to long-term post-COVID-19 symptoms that range from mild to debilitating. The U.S. Government Accountability Office puts that estimate at 10% to 30%; one of the latest studies published at the end of October in The Journal of the American Medical Association found that 15% of U.S. adults who had tested positive for COVID-19 reported current long COVID symptoms. Elsewhere, a study from the Netherlands published in The Lancet in August found that one in eight COVID-19 cases, or 12.7%, were likely to become long COVID.
“It’s very clear that the condition is devastating people’s lives and livelihoods,” WHO Director-General Tedros Adhanom Ghebreyesus wrote in an article for The Guardian newspaper in October.
“The world has already lost a significant number of the workforce to illness, death, fatigue, unplanned retirement due to an increase in long-term disability, which not only impacts the health system, but is a hit to the overarching economy … the impact of long COVID for all countries is very serious and needs immediate and sustained action equivalent to its scale.”
Global snapshot: Lasting symptoms, impact on activities
Patients describe a spectrum of persistent issues, with extreme fatigue, brain fog or cognitive problems, and shortness of breath among the most common complaints. Many also have manageable symptoms that worsen significantly after even mild physical or mental exertion.
Women appear almost twice as likely as men to get long COVID. Many patients have other medical conditions and disabilities that make them more vulnerable to the condition. Those who face greater obstacles accessing health care due to discrimination or socioeconomic inequity are at higher risk as well.
While many are older, a large number are also in their prime working age. The Census Bureau data show that people ages 40-49 are more likely than any other group to get long COVID, which has broader implications for labor markets and the global economy. Already, experts have estimated that long COVID is likely to cost the U.S. trillions of dollars and affect multiple industries.
“Whether they’re in the financial world, the medical system, lawyers, they’re telling me they’re sitting at the computer screen and they’re unable to process the data,” said Zachary Schwartz, MD, medical director for Vancouver General Hospital’s Post-COVID-19 Recovery Clinic.
“That is what’s most distressing for people, in that they’re not working, they’re not making money, and they don’t know when, or if, they’re going to get better.”
Nearly a third of respondents in the Census Bureau’s Household Pulse Survey who said they have had COVID-19 reported symptoms that lasted 3 months or longer. People between the ages of 30 and 59 were the most affected, with about 32% reporting symptoms. Across the entire adult U.S. population, the survey found that 1 in 7 adults have had long COVID at some point during the pandemic, with about 1 in 18 saying it limited their activity to some degree, and 1 in 50 saying they have faced “a lot” of limits on their activities. Any way these numbers are dissected, long COVID has impacted a large swath of the population.
Yet research into the causes and possible treatments of long COVID is just getting underway.
“The amount of energy and time devoted to it is way, way less than it should, given how many people are likely affected,” said David Cutler, PhD, professor of economics at Harvard University, Cambridge, Mass., who has written about the economic cost of long COVID. “We’re way, way underdoing it here. And I think that’s really a terrible thing.”
Population surveys and studies from around the world show that long COVID lives up to its name, with people reporting serious symptoms for months on end.
In October, Statistics Canada and the Public Health Agency of Canada published early results from a questionnaire done between spring and summer 2022 that found just under 15% of adults who had a confirmed or suspected case of COVID-19 went on to have new or continuing symptoms 3 or more months later. Nearly half, or 47.3%, dealt with symptoms that lasted a year or more. More than one in five said their symptoms “often or always” limited their day-to-day activities, which included routine tasks such as preparing meals, doing errands and chores, and basic functions such as personal care and moving around in their homes.
Nearly three-quarters of workers or students said they missed an average of 20 days of work or school.
“We haven’t yet been able to determine exactly when symptoms resolve,” said Rainu Kaushal, MD, the senior associate dean for clinical research at Weill Cornell Medicine in New York. She is co-leading a national study on long COVID in adults and children, funded by the National Institutes of Health RECOVER Initiative.
“But there does seem to be, for many of the milder symptoms, resolution at about 4-6 weeks. There seems to be a second point of resolution around 6 months for certain symptoms, and then some symptoms do seem to be permanent, and those tend to be patients who have underlying conditions,” she said.
Reducing the risk
Given all the data so far, experts recommend urgent policy changes to help people with long COVID.
“The population needs to be prepared, that understanding long COVID is going to be a very long and difficult process,” said Alexander Charney, MD, PhD, associate professor and the lead principal investigator of the RECOVER adult cohort at Icahn School of Medicine at Mount Sinai in New York. He said the government can do a great deal to help, including setting up a network of connected clinics treating long COVID, standardizing best practices, and sharing information.
“That would go a long way towards making sure that every person feels like they’re not too far away from a clinic where they can get treated for this particular condition,” he said.
But the only known way to prevent long COVID is to prevent COVID-19 infections in the first place, experts say. That means equitable access to tests, therapeutics, and vaccines.
“I will say that avoiding COVID remains the best treatment in the arsenal right now,” said Dr. Kaushal. This means masking, avoiding crowded places with poor ventilation and high exposure risk, and being up to date on vaccinations, she said.
A number of papers – including a large U.K. study published in May 2022, another one from July, and the JAMA study from October – all suggest that vaccinations can help reduce the risk of long COVID.
“I am absolutely of the belief that vaccination has reduced the incidence and overall amount of long COVID … [and is] still by far the best thing the public can do,” said Dr. Schwartz.
A version of this article first appeared on WebMD.com.
with symptoms that have lasted 3 months or longer, according to the latest U.S. government survey done in October. More than a quarter say their condition is severe enough to significantly limit their day-to-day activities – yet the problem is only barely starting to get the attention of employers, the health care system, and policymakers.
With no cure or treatment in sight, long COVID is already burdening not only the health care system, but also the economy – and that burden is set to grow. Many experts worry about the possible long-term ripple effects, from increased spending on medical care costs to lost wages due to not being able to work, as well as the policy implications that come with addressing these issues.
“At this point, anyone who’s looking at this seriously would say this is a huge deal,” says senior Brookings Institution fellow Katie Bach, the author of a study that analyzed long COVID’s impact on the labor market.
“We need a real concerted focus on treating these people, which means both research and the clinical side, and figuring out how to build a labor market that is more inclusive of people with disabilities,” she said.
It’s not only that many people are affected. It’s that they are often affected for months and possibly even years.
The U.S. government figures suggest more than 18 million people could have symptoms of long COVID right now. The latest Household Pulse Survey by the Census Bureau and the National Center for Health Statistics takes data from 41,415 people.
A preprint of a study by researchers from City University of New York, posted on medRxiv in September and based on a similar population survey done between June 30 and July 2, drew comparable results. The study has not been peer reviewed.
More than 7% of all those who answered said they had long COVID at the time of the survey, which the researchers said corresponded to approximately 18.5 million U.S. adults. The same study found that a quarter of those, or an estimated 4.7 million adults, said their daily activities were impacted “a lot.”
This can translate into pain not only for the patients, but for governments and employers, too.
In high-income countries around the world, government surveys and other studies are shedding light on the extent to which post-COVID-19 symptoms – commonly known as long COVID – are affecting populations. While results vary, they generally fall within similar ranges.
The World Health Organization estimates that between 10% and 20% of those with COVID-19 go on to have an array of medium- to long-term post-COVID-19 symptoms that range from mild to debilitating. The U.S. Government Accountability Office puts that estimate at 10% to 30%; one of the latest studies published at the end of October in The Journal of the American Medical Association found that 15% of U.S. adults who had tested positive for COVID-19 reported current long COVID symptoms. Elsewhere, a study from the Netherlands published in The Lancet in August found that one in eight COVID-19 cases, or 12.7%, were likely to become long COVID.
“It’s very clear that the condition is devastating people’s lives and livelihoods,” WHO Director-General Tedros Adhanom Ghebreyesus wrote in an article for The Guardian newspaper in October.
“The world has already lost a significant number of the workforce to illness, death, fatigue, unplanned retirement due to an increase in long-term disability, which not only impacts the health system, but is a hit to the overarching economy … the impact of long COVID for all countries is very serious and needs immediate and sustained action equivalent to its scale.”
Global snapshot: Lasting symptoms, impact on activities
Patients describe a spectrum of persistent issues, with extreme fatigue, brain fog or cognitive problems, and shortness of breath among the most common complaints. Many also have manageable symptoms that worsen significantly after even mild physical or mental exertion.
Women appear almost twice as likely as men to get long COVID. Many patients have other medical conditions and disabilities that make them more vulnerable to the condition. Those who face greater obstacles accessing health care due to discrimination or socioeconomic inequity are at higher risk as well.
While many are older, a large number are also in their prime working age. The Census Bureau data show that people ages 40-49 are more likely than any other group to get long COVID, which has broader implications for labor markets and the global economy. Already, experts have estimated that long COVID is likely to cost the U.S. trillions of dollars and affect multiple industries.
“Whether they’re in the financial world, the medical system, lawyers, they’re telling me they’re sitting at the computer screen and they’re unable to process the data,” said Zachary Schwartz, MD, medical director for Vancouver General Hospital’s Post-COVID-19 Recovery Clinic.
“That is what’s most distressing for people, in that they’re not working, they’re not making money, and they don’t know when, or if, they’re going to get better.”
Nearly a third of respondents in the Census Bureau’s Household Pulse Survey who said they have had COVID-19 reported symptoms that lasted 3 months or longer. People between the ages of 30 and 59 were the most affected, with about 32% reporting symptoms. Across the entire adult U.S. population, the survey found that 1 in 7 adults have had long COVID at some point during the pandemic, with about 1 in 18 saying it limited their activity to some degree, and 1 in 50 saying they have faced “a lot” of limits on their activities. Any way these numbers are dissected, long COVID has impacted a large swath of the population.
Yet research into the causes and possible treatments of long COVID is just getting underway.
“The amount of energy and time devoted to it is way, way less than it should, given how many people are likely affected,” said David Cutler, PhD, professor of economics at Harvard University, Cambridge, Mass., who has written about the economic cost of long COVID. “We’re way, way underdoing it here. And I think that’s really a terrible thing.”
Population surveys and studies from around the world show that long COVID lives up to its name, with people reporting serious symptoms for months on end.
In October, Statistics Canada and the Public Health Agency of Canada published early results from a questionnaire done between spring and summer 2022 that found just under 15% of adults who had a confirmed or suspected case of COVID-19 went on to have new or continuing symptoms 3 or more months later. Nearly half, or 47.3%, dealt with symptoms that lasted a year or more. More than one in five said their symptoms “often or always” limited their day-to-day activities, which included routine tasks such as preparing meals, doing errands and chores, and basic functions such as personal care and moving around in their homes.
Nearly three-quarters of workers or students said they missed an average of 20 days of work or school.
“We haven’t yet been able to determine exactly when symptoms resolve,” said Rainu Kaushal, MD, the senior associate dean for clinical research at Weill Cornell Medicine in New York. She is co-leading a national study on long COVID in adults and children, funded by the National Institutes of Health RECOVER Initiative.
“But there does seem to be, for many of the milder symptoms, resolution at about 4-6 weeks. There seems to be a second point of resolution around 6 months for certain symptoms, and then some symptoms do seem to be permanent, and those tend to be patients who have underlying conditions,” she said.
Reducing the risk
Given all the data so far, experts recommend urgent policy changes to help people with long COVID.
“The population needs to be prepared, that understanding long COVID is going to be a very long and difficult process,” said Alexander Charney, MD, PhD, associate professor and the lead principal investigator of the RECOVER adult cohort at Icahn School of Medicine at Mount Sinai in New York. He said the government can do a great deal to help, including setting up a network of connected clinics treating long COVID, standardizing best practices, and sharing information.
“That would go a long way towards making sure that every person feels like they’re not too far away from a clinic where they can get treated for this particular condition,” he said.
But the only known way to prevent long COVID is to prevent COVID-19 infections in the first place, experts say. That means equitable access to tests, therapeutics, and vaccines.
“I will say that avoiding COVID remains the best treatment in the arsenal right now,” said Dr. Kaushal. This means masking, avoiding crowded places with poor ventilation and high exposure risk, and being up to date on vaccinations, she said.
A number of papers – including a large U.K. study published in May 2022, another one from July, and the JAMA study from October – all suggest that vaccinations can help reduce the risk of long COVID.
“I am absolutely of the belief that vaccination has reduced the incidence and overall amount of long COVID … [and is] still by far the best thing the public can do,” said Dr. Schwartz.
A version of this article first appeared on WebMD.com.
U.S. dementia rate drops as education, women’s employment rises
new research shows. New data from the Health and Retirement Study, a nationally representative survey, show that the prevalence of dementia among individuals aged 65 and older dropped from 12.2% in 2000 to 8.5% in 2016 – a 30.1% decrease. In men, the prevalence of dementia fell from 10.2% to 7.0%, while for women, it declined from 13.6% to 9.7%, researchers reported. Their finding were published online in PNAS.
The study also revealed that the proportion of college-educated men in the sample increased from 21.5% in 2000 to 33.7% in 2016, while the proportion of college-educated women increased from 12.3% in 2000 to 23% in 2016.
The findings also show a decline in the dementia prevalence in non-Hispanic Black men, which dropped from 17.2% to 9.9%, a decrease of 42.6%. In non-Hispanic White men, dementia declined 9.3% to 6.6%, or 29.0%.
The investigators also found a substantial increase in the level of education between 2000 and 2016. In addition, they found that, among 74- to 84-year-old women in 2000, 29.5% had worked for more than 30 years during their lifetime versus 59.0% in 2016.
The investigators speculated that the decline in dementia prevalence reflects larger socioeconomic changes in the United States as well as prevention strategies to reduce cardiovascular disease.
A person born around 1920, for example, would have had greater exposure to the Great Depression, while someone born in 1936 would have benefited more from the changes in living standards in the years following World War II, they noted.
“There’s a need for more research on the effect of employment on cognitive reserve. It’s plausible that working is good for your mental cognitive abilities,” said study investigator Péter Hudomiet, PhD, from the RAND Corporation, adding that there may also be benefits that extend beyond working years. It’s possible that women’s greater participation in the workforce gives them more chances to establish relationships that in some cases last well into retirement and provide essential social connection. It’s well known that social isolation has a negative impact on cognition.
“It’s plausible that working is good for your mental cognitive abilities,” he added.
The investigators noted that it is beyond the scope of their study to draw definitive conclusions about the causes of the decline, but they observed that positive trends in employment and standard of living make sense. “They would suggest that as schooling levels continue to rise in the U.S. population in younger generations, the prevalence of dementia would continue to decrease.
The investigators report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research shows. New data from the Health and Retirement Study, a nationally representative survey, show that the prevalence of dementia among individuals aged 65 and older dropped from 12.2% in 2000 to 8.5% in 2016 – a 30.1% decrease. In men, the prevalence of dementia fell from 10.2% to 7.0%, while for women, it declined from 13.6% to 9.7%, researchers reported. Their finding were published online in PNAS.
The study also revealed that the proportion of college-educated men in the sample increased from 21.5% in 2000 to 33.7% in 2016, while the proportion of college-educated women increased from 12.3% in 2000 to 23% in 2016.
The findings also show a decline in the dementia prevalence in non-Hispanic Black men, which dropped from 17.2% to 9.9%, a decrease of 42.6%. In non-Hispanic White men, dementia declined 9.3% to 6.6%, or 29.0%.
The investigators also found a substantial increase in the level of education between 2000 and 2016. In addition, they found that, among 74- to 84-year-old women in 2000, 29.5% had worked for more than 30 years during their lifetime versus 59.0% in 2016.
The investigators speculated that the decline in dementia prevalence reflects larger socioeconomic changes in the United States as well as prevention strategies to reduce cardiovascular disease.
A person born around 1920, for example, would have had greater exposure to the Great Depression, while someone born in 1936 would have benefited more from the changes in living standards in the years following World War II, they noted.
“There’s a need for more research on the effect of employment on cognitive reserve. It’s plausible that working is good for your mental cognitive abilities,” said study investigator Péter Hudomiet, PhD, from the RAND Corporation, adding that there may also be benefits that extend beyond working years. It’s possible that women’s greater participation in the workforce gives them more chances to establish relationships that in some cases last well into retirement and provide essential social connection. It’s well known that social isolation has a negative impact on cognition.
“It’s plausible that working is good for your mental cognitive abilities,” he added.
The investigators noted that it is beyond the scope of their study to draw definitive conclusions about the causes of the decline, but they observed that positive trends in employment and standard of living make sense. “They would suggest that as schooling levels continue to rise in the U.S. population in younger generations, the prevalence of dementia would continue to decrease.
The investigators report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research shows. New data from the Health and Retirement Study, a nationally representative survey, show that the prevalence of dementia among individuals aged 65 and older dropped from 12.2% in 2000 to 8.5% in 2016 – a 30.1% decrease. In men, the prevalence of dementia fell from 10.2% to 7.0%, while for women, it declined from 13.6% to 9.7%, researchers reported. Their finding were published online in PNAS.
The study also revealed that the proportion of college-educated men in the sample increased from 21.5% in 2000 to 33.7% in 2016, while the proportion of college-educated women increased from 12.3% in 2000 to 23% in 2016.
The findings also show a decline in the dementia prevalence in non-Hispanic Black men, which dropped from 17.2% to 9.9%, a decrease of 42.6%. In non-Hispanic White men, dementia declined 9.3% to 6.6%, or 29.0%.
The investigators also found a substantial increase in the level of education between 2000 and 2016. In addition, they found that, among 74- to 84-year-old women in 2000, 29.5% had worked for more than 30 years during their lifetime versus 59.0% in 2016.
The investigators speculated that the decline in dementia prevalence reflects larger socioeconomic changes in the United States as well as prevention strategies to reduce cardiovascular disease.
A person born around 1920, for example, would have had greater exposure to the Great Depression, while someone born in 1936 would have benefited more from the changes in living standards in the years following World War II, they noted.
“There’s a need for more research on the effect of employment on cognitive reserve. It’s plausible that working is good for your mental cognitive abilities,” said study investigator Péter Hudomiet, PhD, from the RAND Corporation, adding that there may also be benefits that extend beyond working years. It’s possible that women’s greater participation in the workforce gives them more chances to establish relationships that in some cases last well into retirement and provide essential social connection. It’s well known that social isolation has a negative impact on cognition.
“It’s plausible that working is good for your mental cognitive abilities,” he added.
The investigators noted that it is beyond the scope of their study to draw definitive conclusions about the causes of the decline, but they observed that positive trends in employment and standard of living make sense. “They would suggest that as schooling levels continue to rise in the U.S. population in younger generations, the prevalence of dementia would continue to decrease.
The investigators report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
From PNAS
Is there a doctor on the plane? Tips for providing in-flight assistance
In most cases, passengers on an airline flight are representative of the general population, which means that anyone could have an emergency at any time.
as determined on the basis of in-flight medical emergencies that resulted in calls to a physician-directed medical communications center, said Amy Faith Ho, MD, MPH of Integrative Emergency Services, Dallas–Fort Worth, in a presentation at the annual meeting of the American College of Emergency Physicians.
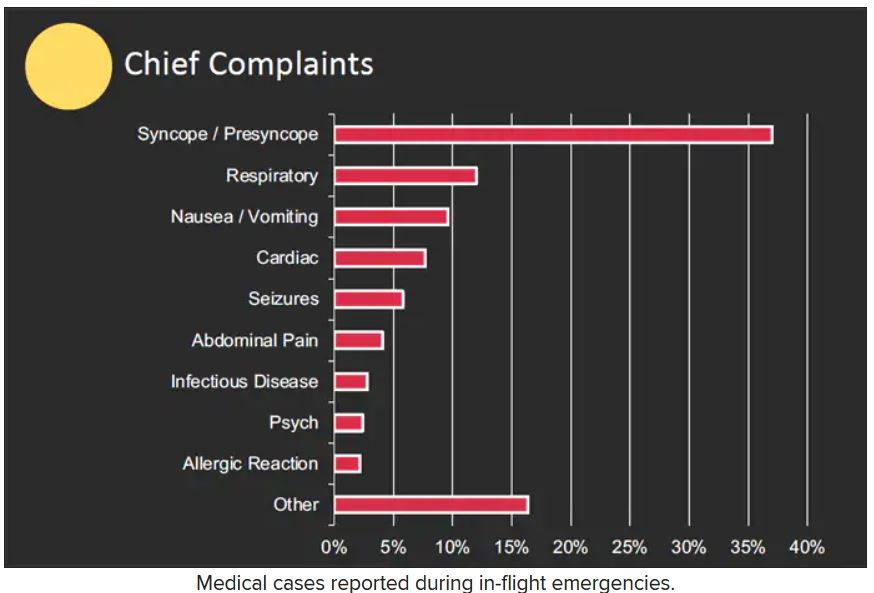
The study authors reviewed records of 11,920 in-flight medical emergencies between Jan. 1, 2008, and Oct. 31, 2010. The data showed that physician passengers provided medical assistance in nearly half of in-flight emergencies (48.1%) and that flights were diverted because of the emergency in 7.3% of cases.
The majority of the in-flight emergencies involved syncope or presyncope (37.4% of cases), followed by respiratory symptoms (12.1%) and nausea or vomiting (9.5%), according to the study.
When a physician is faced with an in-flight emergency, the medical team includes the physician himself, medical ground control, and the flight attendants, said Dr. Ho. Requirements may vary among airlines, but all flight attendants will be trained in cardiopulmonary resuscitation (CPR) or basic life support, as well as use of automated external defibrillators (AEDs).
Physician call centers (medical ground control) can provide additional assistance remotely, she said.
The in-flight medical bag
Tools in a physician’s in-flight toolbox start with the first-aid kit. Airplanes also have an emergency medical kit (EMK), an oxygen tank, and an AED.
The minimum EMK contents are mandated by the Federal Aviation Administration, said Dr. Ho. The standard equipment includes a stethoscope, a sphygmomanometer, and three sizes of oropharyngeal airways. Other items include self-inflating manual resuscitation devices and CPR masks in thee sizes, alcohol sponges, gloves, adhesive tape, scissors, a tourniquet, as well as saline solution, needles, syringes, and an intravenous administration set consisting of tubing and two Y connectors.
An EMK also should contain the following medications: nonnarcotic analgesic tablets, antihistamine tablets, an injectable antihistamine, atropine, aspirin tablets, a bronchodilator, and epinephrine (both 1:1000; 1 injectable cc and 1:10,000; two injectable cc). Nitroglycerin tablets and 5 cc of 20 mg/mL injectable cardiac lidocaine are part of the mandated kit as well, according to Dr. Ho.
Some airlines carry additional supplies on all their flights, said Dr. Ho. Notably, American Airlines and British Airways carry EpiPens for adults and children, as well as opioid reversal medication (naloxone) and glucose for managing low blood sugar. American Airlines and Delta stock antiemetics, and Delta also carries naloxone. British Airways is unique in stocking additional cardiac medications, both oral and injectable.
How to handle an in-flight emergency
Physicians should always carry a copy of their medical license when traveling for documentation by the airline if they assist in a medical emergency during a flight, Dr. Ho emphasized. “Staff” personnel should be used. These include the flight attendants, medical ground control, and other passengers who might have useful skills, such as nursing, the ability to perform CPR, or therapy/counseling to calm a frightened patient. If needed, “crowdsource additional supplies from passengers,” such as a glucometer or pulse oximeter.
Legal lessons
Physicians are not obligated to assist during an in-flight medical emergency, said Dr. Ho. Legal jurisdiction can vary. In the United States, a bystander who assists in an emergency is generally protected by Good Samaritan laws; for international airlines, the laws may vary; those where the airline is based usually apply.
The Aviation Medical Assistance Act, passed in 1998, protects individuals from being sued for negligence while providing medical assistance, “unless the individual, while rendering such assistance, is guilty of gross negligence of willful misconduct,” Dr. Ho noted. The Aviation Medical Assistance Act also protects the airline itself “if the carrier in good faith believes that the passenger is a medically qualified individual.”
Dr. Ho disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In most cases, passengers on an airline flight are representative of the general population, which means that anyone could have an emergency at any time.
as determined on the basis of in-flight medical emergencies that resulted in calls to a physician-directed medical communications center, said Amy Faith Ho, MD, MPH of Integrative Emergency Services, Dallas–Fort Worth, in a presentation at the annual meeting of the American College of Emergency Physicians.
The study authors reviewed records of 11,920 in-flight medical emergencies between Jan. 1, 2008, and Oct. 31, 2010. The data showed that physician passengers provided medical assistance in nearly half of in-flight emergencies (48.1%) and that flights were diverted because of the emergency in 7.3% of cases.
The majority of the in-flight emergencies involved syncope or presyncope (37.4% of cases), followed by respiratory symptoms (12.1%) and nausea or vomiting (9.5%), according to the study.
When a physician is faced with an in-flight emergency, the medical team includes the physician himself, medical ground control, and the flight attendants, said Dr. Ho. Requirements may vary among airlines, but all flight attendants will be trained in cardiopulmonary resuscitation (CPR) or basic life support, as well as use of automated external defibrillators (AEDs).
Physician call centers (medical ground control) can provide additional assistance remotely, she said.
The in-flight medical bag
Tools in a physician’s in-flight toolbox start with the first-aid kit. Airplanes also have an emergency medical kit (EMK), an oxygen tank, and an AED.
The minimum EMK contents are mandated by the Federal Aviation Administration, said Dr. Ho. The standard equipment includes a stethoscope, a sphygmomanometer, and three sizes of oropharyngeal airways. Other items include self-inflating manual resuscitation devices and CPR masks in thee sizes, alcohol sponges, gloves, adhesive tape, scissors, a tourniquet, as well as saline solution, needles, syringes, and an intravenous administration set consisting of tubing and two Y connectors.
An EMK also should contain the following medications: nonnarcotic analgesic tablets, antihistamine tablets, an injectable antihistamine, atropine, aspirin tablets, a bronchodilator, and epinephrine (both 1:1000; 1 injectable cc and 1:10,000; two injectable cc). Nitroglycerin tablets and 5 cc of 20 mg/mL injectable cardiac lidocaine are part of the mandated kit as well, according to Dr. Ho.
Some airlines carry additional supplies on all their flights, said Dr. Ho. Notably, American Airlines and British Airways carry EpiPens for adults and children, as well as opioid reversal medication (naloxone) and glucose for managing low blood sugar. American Airlines and Delta stock antiemetics, and Delta also carries naloxone. British Airways is unique in stocking additional cardiac medications, both oral and injectable.
How to handle an in-flight emergency
Physicians should always carry a copy of their medical license when traveling for documentation by the airline if they assist in a medical emergency during a flight, Dr. Ho emphasized. “Staff” personnel should be used. These include the flight attendants, medical ground control, and other passengers who might have useful skills, such as nursing, the ability to perform CPR, or therapy/counseling to calm a frightened patient. If needed, “crowdsource additional supplies from passengers,” such as a glucometer or pulse oximeter.
Legal lessons
Physicians are not obligated to assist during an in-flight medical emergency, said Dr. Ho. Legal jurisdiction can vary. In the United States, a bystander who assists in an emergency is generally protected by Good Samaritan laws; for international airlines, the laws may vary; those where the airline is based usually apply.
The Aviation Medical Assistance Act, passed in 1998, protects individuals from being sued for negligence while providing medical assistance, “unless the individual, while rendering such assistance, is guilty of gross negligence of willful misconduct,” Dr. Ho noted. The Aviation Medical Assistance Act also protects the airline itself “if the carrier in good faith believes that the passenger is a medically qualified individual.”
Dr. Ho disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In most cases, passengers on an airline flight are representative of the general population, which means that anyone could have an emergency at any time.
as determined on the basis of in-flight medical emergencies that resulted in calls to a physician-directed medical communications center, said Amy Faith Ho, MD, MPH of Integrative Emergency Services, Dallas–Fort Worth, in a presentation at the annual meeting of the American College of Emergency Physicians.
The study authors reviewed records of 11,920 in-flight medical emergencies between Jan. 1, 2008, and Oct. 31, 2010. The data showed that physician passengers provided medical assistance in nearly half of in-flight emergencies (48.1%) and that flights were diverted because of the emergency in 7.3% of cases.
The majority of the in-flight emergencies involved syncope or presyncope (37.4% of cases), followed by respiratory symptoms (12.1%) and nausea or vomiting (9.5%), according to the study.
When a physician is faced with an in-flight emergency, the medical team includes the physician himself, medical ground control, and the flight attendants, said Dr. Ho. Requirements may vary among airlines, but all flight attendants will be trained in cardiopulmonary resuscitation (CPR) or basic life support, as well as use of automated external defibrillators (AEDs).
Physician call centers (medical ground control) can provide additional assistance remotely, she said.
The in-flight medical bag
Tools in a physician’s in-flight toolbox start with the first-aid kit. Airplanes also have an emergency medical kit (EMK), an oxygen tank, and an AED.
The minimum EMK contents are mandated by the Federal Aviation Administration, said Dr. Ho. The standard equipment includes a stethoscope, a sphygmomanometer, and three sizes of oropharyngeal airways. Other items include self-inflating manual resuscitation devices and CPR masks in thee sizes, alcohol sponges, gloves, adhesive tape, scissors, a tourniquet, as well as saline solution, needles, syringes, and an intravenous administration set consisting of tubing and two Y connectors.
An EMK also should contain the following medications: nonnarcotic analgesic tablets, antihistamine tablets, an injectable antihistamine, atropine, aspirin tablets, a bronchodilator, and epinephrine (both 1:1000; 1 injectable cc and 1:10,000; two injectable cc). Nitroglycerin tablets and 5 cc of 20 mg/mL injectable cardiac lidocaine are part of the mandated kit as well, according to Dr. Ho.
Some airlines carry additional supplies on all their flights, said Dr. Ho. Notably, American Airlines and British Airways carry EpiPens for adults and children, as well as opioid reversal medication (naloxone) and glucose for managing low blood sugar. American Airlines and Delta stock antiemetics, and Delta also carries naloxone. British Airways is unique in stocking additional cardiac medications, both oral and injectable.
How to handle an in-flight emergency
Physicians should always carry a copy of their medical license when traveling for documentation by the airline if they assist in a medical emergency during a flight, Dr. Ho emphasized. “Staff” personnel should be used. These include the flight attendants, medical ground control, and other passengers who might have useful skills, such as nursing, the ability to perform CPR, or therapy/counseling to calm a frightened patient. If needed, “crowdsource additional supplies from passengers,” such as a glucometer or pulse oximeter.
Legal lessons
Physicians are not obligated to assist during an in-flight medical emergency, said Dr. Ho. Legal jurisdiction can vary. In the United States, a bystander who assists in an emergency is generally protected by Good Samaritan laws; for international airlines, the laws may vary; those where the airline is based usually apply.
The Aviation Medical Assistance Act, passed in 1998, protects individuals from being sued for negligence while providing medical assistance, “unless the individual, while rendering such assistance, is guilty of gross negligence of willful misconduct,” Dr. Ho noted. The Aviation Medical Assistance Act also protects the airline itself “if the carrier in good faith believes that the passenger is a medically qualified individual.”
Dr. Ho disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ACEP 2022
Meditation equal to first-line medication for anxiety
“I would encourage clinicians to list meditation training as one possible treatment option for patients who are diagnosed with anxiety disorders. Doctors should feel comfortable recommending in-person, group-based meditation classes,” study investigator Elizabeth A. Hoge, MD, director, Anxiety Disorders Research Program, Georgetown University Medical Center, Washington, told this news organization.
The findings were published online in JAMA Psychiatry.
Screening recommended
Anxiety disorders, including generalized anxiety, social anxiety, panic disorder, and agoraphobia, are the most common type of mental disorder, affecting an estimated 301 million people worldwide. Owing to their high prevalence, the United States Preventive Services Task Force recommends screening for anxiety disorders.
Effective treatments for anxiety disorders include medications and cognitive-behavioral therapy. However, not all patients have access to these interventions, respond to them, or are comfortable seeking care in a psychiatric setting.
Mindfulness meditation, which has risen in popularity in recent years, may help people experiencing intrusive, anxious thoughts. “By practicing mindfulness meditation, people learn not to be overwhelmed by those thoughts,” said Dr. Hoge.
The study included 276 adult patients with an anxiety disorder, mostly generalized anxiety or social anxiety. The mean age of the study population was 33 years; 75% were women, 59% were White, 15% were Black, and 20% were Asian.
Researchers randomly assigned 136 patients to receive MBSR and 140 to receive the selective serotonin reuptake inhibitor escitalopram, a first-line medication for treating anxiety disorders.
The MBSR intervention included a weekly 2.5-hour class and a day-long weekend class. Participants also completed daily 45-minute guided meditation sessions at home. They learned mindfulness meditation exercises, including breath awareness, body scanning, and mindful movement.
Those in the escitalopram group initially received 10 mg of the oral drug daily. The dose was increased to 20 mg daily at week 2 if well tolerated.
The primary outcome was the score on the Clinical Global Impression of Severity (CGI-S) scale for anxiety, assessed by clinicians blinded to treatment allocation. This instrument measures overall symptom severity on a scale from 1 (not at all ill) to 7 (most extremely ill) and can be used to assess different types of anxiety disorders, said Dr. Hoge.
Among the 208 participants who completed the study, the baseline mean CGI-S score was 4.44 for MBSR and 4.51 for escitalopram. At week 8, on the CGI-S scale, the MBSR group’s score improved by a mean of 1.35 points, and the escitalopram group’s score improved by 1.43 points (difference of –0.07; 95% CI, –0.38 to 0.23; P = .65).
The lower end of the confidence interval (–0.38) was smaller than the prespecified noninferiority margin of –0.495, indicating noninferiority of MBSR, compared with escitalopram.
Remarkable results
“What was remarkable was that the medication worked great, like it always does, but the meditation also worked great; we saw about a 30% drop in symptoms for both groups,” said Dr. Hoge. “That helps us know that meditation, and in particular mindfulness meditation, could be useful as a first-line treatment for patients with anxiety disorders.”
The patient-reported outcome of the Overall Anxiety Severity and Impairment Scale also showed no significant group differences. “It’s important to have the self-reports, because that gives us two ways to look at the information,” said Dr. Hoge.
Anecdotally, participants noted that the meditation helped with their personal relationships and with being “kinder to themselves,” said Dr. Hoge. “In meditation, there’s an implicit teaching to be accepting and nonjudgmental towards your own thoughts, and that teaches people to be more self-compassionate.”
Just over 78% of patients in the escitalopram group had at least one treatment-related adverse event (AE), which included sleep disturbances, nausea, fatigue, and headache, compared with 15.4% in the MBSR group.
The most common AE in the meditation group was anxiety, which is “counterintuitive” but represents “a momentary anxiety,” said Dr. Hoge. “People who are meditating have feelings come up that maybe they didn’t pay attention to before. This gives them an opportunity to process through those emotions.”
Fatigue was the next most common AE for meditators, which “makes sense,” since they’re putting away their phones and not being stimulated, said Dr. Hoge.
MBSR was delivered in person, which limits extrapolation to mindfulness apps or programs delivered over the internet. Dr. Hoge believes apps would likely be less effective because they don’t have the face-to-face component, instructors available for consultation, or fellow participants contributing group support.
But online classes might work if “the exact same class,” including all its components, is moved online, she said.
MBSR is available in all major U.S. cities, doesn’t require finding a therapist, and is available outside a mental health environment – for example, at yoga centers and some places of employment. Anyone can learn MBSR, although it takes time and commitment, said Dr. Hoge.
A time-tested intervention
Commenting on the study, psychiatrist Gregory Scott Brown, MD, affiliate faculty, University of Texas Dell Medical School, and author of “The Self-Healing Mind: An Essential Five-Step Practice for Overcoming Anxiety and Depression and Revitalizing Your Life,” said the results aren’t surprising inasmuch as mindfulness, including spirituality, breath work, and meditation, is a “time-tested and evidence-based” intervention.
“I’m encouraged by the fact studies like this are now being conducted and there’s more evidence that supports these mindfulness-based interventions, so they can start to make their way into standard-of-care treatments.” he said.
He noted that mindfulness can produce “long-term, sustainable improvements” and that the 45-minute daily home exercise included in the study “is not a huge time commitment when you talk about benefits you can potentially glean from incorporating that time.”
Because most study participants were women and “men are anxious too,” Dr. Brown said he would like to see the study replicated “with a more diverse pool of participants.”
The study was supported by the Patient-Centered Outcomes Research Institute. Dr. Hoge and Dr. Brown have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
“I would encourage clinicians to list meditation training as one possible treatment option for patients who are diagnosed with anxiety disorders. Doctors should feel comfortable recommending in-person, group-based meditation classes,” study investigator Elizabeth A. Hoge, MD, director, Anxiety Disorders Research Program, Georgetown University Medical Center, Washington, told this news organization.
The findings were published online in JAMA Psychiatry.
Screening recommended
Anxiety disorders, including generalized anxiety, social anxiety, panic disorder, and agoraphobia, are the most common type of mental disorder, affecting an estimated 301 million people worldwide. Owing to their high prevalence, the United States Preventive Services Task Force recommends screening for anxiety disorders.
Effective treatments for anxiety disorders include medications and cognitive-behavioral therapy. However, not all patients have access to these interventions, respond to them, or are comfortable seeking care in a psychiatric setting.
Mindfulness meditation, which has risen in popularity in recent years, may help people experiencing intrusive, anxious thoughts. “By practicing mindfulness meditation, people learn not to be overwhelmed by those thoughts,” said Dr. Hoge.
The study included 276 adult patients with an anxiety disorder, mostly generalized anxiety or social anxiety. The mean age of the study population was 33 years; 75% were women, 59% were White, 15% were Black, and 20% were Asian.
Researchers randomly assigned 136 patients to receive MBSR and 140 to receive the selective serotonin reuptake inhibitor escitalopram, a first-line medication for treating anxiety disorders.
The MBSR intervention included a weekly 2.5-hour class and a day-long weekend class. Participants also completed daily 45-minute guided meditation sessions at home. They learned mindfulness meditation exercises, including breath awareness, body scanning, and mindful movement.
Those in the escitalopram group initially received 10 mg of the oral drug daily. The dose was increased to 20 mg daily at week 2 if well tolerated.
The primary outcome was the score on the Clinical Global Impression of Severity (CGI-S) scale for anxiety, assessed by clinicians blinded to treatment allocation. This instrument measures overall symptom severity on a scale from 1 (not at all ill) to 7 (most extremely ill) and can be used to assess different types of anxiety disorders, said Dr. Hoge.
Among the 208 participants who completed the study, the baseline mean CGI-S score was 4.44 for MBSR and 4.51 for escitalopram. At week 8, on the CGI-S scale, the MBSR group’s score improved by a mean of 1.35 points, and the escitalopram group’s score improved by 1.43 points (difference of –0.07; 95% CI, –0.38 to 0.23; P = .65).
The lower end of the confidence interval (–0.38) was smaller than the prespecified noninferiority margin of –0.495, indicating noninferiority of MBSR, compared with escitalopram.
Remarkable results
“What was remarkable was that the medication worked great, like it always does, but the meditation also worked great; we saw about a 30% drop in symptoms for both groups,” said Dr. Hoge. “That helps us know that meditation, and in particular mindfulness meditation, could be useful as a first-line treatment for patients with anxiety disorders.”
The patient-reported outcome of the Overall Anxiety Severity and Impairment Scale also showed no significant group differences. “It’s important to have the self-reports, because that gives us two ways to look at the information,” said Dr. Hoge.
Anecdotally, participants noted that the meditation helped with their personal relationships and with being “kinder to themselves,” said Dr. Hoge. “In meditation, there’s an implicit teaching to be accepting and nonjudgmental towards your own thoughts, and that teaches people to be more self-compassionate.”
Just over 78% of patients in the escitalopram group had at least one treatment-related adverse event (AE), which included sleep disturbances, nausea, fatigue, and headache, compared with 15.4% in the MBSR group.
The most common AE in the meditation group was anxiety, which is “counterintuitive” but represents “a momentary anxiety,” said Dr. Hoge. “People who are meditating have feelings come up that maybe they didn’t pay attention to before. This gives them an opportunity to process through those emotions.”
Fatigue was the next most common AE for meditators, which “makes sense,” since they’re putting away their phones and not being stimulated, said Dr. Hoge.
MBSR was delivered in person, which limits extrapolation to mindfulness apps or programs delivered over the internet. Dr. Hoge believes apps would likely be less effective because they don’t have the face-to-face component, instructors available for consultation, or fellow participants contributing group support.
But online classes might work if “the exact same class,” including all its components, is moved online, she said.
MBSR is available in all major U.S. cities, doesn’t require finding a therapist, and is available outside a mental health environment – for example, at yoga centers and some places of employment. Anyone can learn MBSR, although it takes time and commitment, said Dr. Hoge.
A time-tested intervention
Commenting on the study, psychiatrist Gregory Scott Brown, MD, affiliate faculty, University of Texas Dell Medical School, and author of “The Self-Healing Mind: An Essential Five-Step Practice for Overcoming Anxiety and Depression and Revitalizing Your Life,” said the results aren’t surprising inasmuch as mindfulness, including spirituality, breath work, and meditation, is a “time-tested and evidence-based” intervention.
“I’m encouraged by the fact studies like this are now being conducted and there’s more evidence that supports these mindfulness-based interventions, so they can start to make their way into standard-of-care treatments.” he said.
He noted that mindfulness can produce “long-term, sustainable improvements” and that the 45-minute daily home exercise included in the study “is not a huge time commitment when you talk about benefits you can potentially glean from incorporating that time.”
Because most study participants were women and “men are anxious too,” Dr. Brown said he would like to see the study replicated “with a more diverse pool of participants.”
The study was supported by the Patient-Centered Outcomes Research Institute. Dr. Hoge and Dr. Brown have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
“I would encourage clinicians to list meditation training as one possible treatment option for patients who are diagnosed with anxiety disorders. Doctors should feel comfortable recommending in-person, group-based meditation classes,” study investigator Elizabeth A. Hoge, MD, director, Anxiety Disorders Research Program, Georgetown University Medical Center, Washington, told this news organization.
The findings were published online in JAMA Psychiatry.
Screening recommended
Anxiety disorders, including generalized anxiety, social anxiety, panic disorder, and agoraphobia, are the most common type of mental disorder, affecting an estimated 301 million people worldwide. Owing to their high prevalence, the United States Preventive Services Task Force recommends screening for anxiety disorders.
Effective treatments for anxiety disorders include medications and cognitive-behavioral therapy. However, not all patients have access to these interventions, respond to them, or are comfortable seeking care in a psychiatric setting.
Mindfulness meditation, which has risen in popularity in recent years, may help people experiencing intrusive, anxious thoughts. “By practicing mindfulness meditation, people learn not to be overwhelmed by those thoughts,” said Dr. Hoge.
The study included 276 adult patients with an anxiety disorder, mostly generalized anxiety or social anxiety. The mean age of the study population was 33 years; 75% were women, 59% were White, 15% were Black, and 20% were Asian.
Researchers randomly assigned 136 patients to receive MBSR and 140 to receive the selective serotonin reuptake inhibitor escitalopram, a first-line medication for treating anxiety disorders.
The MBSR intervention included a weekly 2.5-hour class and a day-long weekend class. Participants also completed daily 45-minute guided meditation sessions at home. They learned mindfulness meditation exercises, including breath awareness, body scanning, and mindful movement.
Those in the escitalopram group initially received 10 mg of the oral drug daily. The dose was increased to 20 mg daily at week 2 if well tolerated.
The primary outcome was the score on the Clinical Global Impression of Severity (CGI-S) scale for anxiety, assessed by clinicians blinded to treatment allocation. This instrument measures overall symptom severity on a scale from 1 (not at all ill) to 7 (most extremely ill) and can be used to assess different types of anxiety disorders, said Dr. Hoge.
Among the 208 participants who completed the study, the baseline mean CGI-S score was 4.44 for MBSR and 4.51 for escitalopram. At week 8, on the CGI-S scale, the MBSR group’s score improved by a mean of 1.35 points, and the escitalopram group’s score improved by 1.43 points (difference of –0.07; 95% CI, –0.38 to 0.23; P = .65).
The lower end of the confidence interval (–0.38) was smaller than the prespecified noninferiority margin of –0.495, indicating noninferiority of MBSR, compared with escitalopram.
Remarkable results
“What was remarkable was that the medication worked great, like it always does, but the meditation also worked great; we saw about a 30% drop in symptoms for both groups,” said Dr. Hoge. “That helps us know that meditation, and in particular mindfulness meditation, could be useful as a first-line treatment for patients with anxiety disorders.”
The patient-reported outcome of the Overall Anxiety Severity and Impairment Scale also showed no significant group differences. “It’s important to have the self-reports, because that gives us two ways to look at the information,” said Dr. Hoge.
Anecdotally, participants noted that the meditation helped with their personal relationships and with being “kinder to themselves,” said Dr. Hoge. “In meditation, there’s an implicit teaching to be accepting and nonjudgmental towards your own thoughts, and that teaches people to be more self-compassionate.”
Just over 78% of patients in the escitalopram group had at least one treatment-related adverse event (AE), which included sleep disturbances, nausea, fatigue, and headache, compared with 15.4% in the MBSR group.
The most common AE in the meditation group was anxiety, which is “counterintuitive” but represents “a momentary anxiety,” said Dr. Hoge. “People who are meditating have feelings come up that maybe they didn’t pay attention to before. This gives them an opportunity to process through those emotions.”
Fatigue was the next most common AE for meditators, which “makes sense,” since they’re putting away their phones and not being stimulated, said Dr. Hoge.
MBSR was delivered in person, which limits extrapolation to mindfulness apps or programs delivered over the internet. Dr. Hoge believes apps would likely be less effective because they don’t have the face-to-face component, instructors available for consultation, or fellow participants contributing group support.
But online classes might work if “the exact same class,” including all its components, is moved online, she said.
MBSR is available in all major U.S. cities, doesn’t require finding a therapist, and is available outside a mental health environment – for example, at yoga centers and some places of employment. Anyone can learn MBSR, although it takes time and commitment, said Dr. Hoge.
A time-tested intervention
Commenting on the study, psychiatrist Gregory Scott Brown, MD, affiliate faculty, University of Texas Dell Medical School, and author of “The Self-Healing Mind: An Essential Five-Step Practice for Overcoming Anxiety and Depression and Revitalizing Your Life,” said the results aren’t surprising inasmuch as mindfulness, including spirituality, breath work, and meditation, is a “time-tested and evidence-based” intervention.
“I’m encouraged by the fact studies like this are now being conducted and there’s more evidence that supports these mindfulness-based interventions, so they can start to make their way into standard-of-care treatments.” he said.
He noted that mindfulness can produce “long-term, sustainable improvements” and that the 45-minute daily home exercise included in the study “is not a huge time commitment when you talk about benefits you can potentially glean from incorporating that time.”
Because most study participants were women and “men are anxious too,” Dr. Brown said he would like to see the study replicated “with a more diverse pool of participants.”
The study was supported by the Patient-Centered Outcomes Research Institute. Dr. Hoge and Dr. Brown have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY
Imaging IDs brain activity related to dissociative symptoms
Results from a neuroimaging study showed that different dissociative symptoms were linked to hyperconnectivity within several key regions of the brain, including the central executive, default, and salience networks as well as decreased connectivity of the central executive and salience networks with other brain areas.
Depersonalization/derealization showed a different brain signature than partially dissociated intrusions, and participants with posttraumatic stress disorder showed a different brain signature, compared with those who had dissociative identity disorder (DID).
“Dissociation is a complex, subjective set of symptoms that are largely experienced internally and, contrary to media portrayal, are not usually overtly observable,” lead author Lauren Lebois, PhD, director of the Dissociative Disorders and Trauma Research Program, McLean Hospital, Belmont, Mass., and assistant professor of psychiatry at Harvard Medical School, Boston, told this news organization.
“However, we have shown that you can objectively measure dissociation and link it to robust brain signatures. We hope these results will encourage clinicians to screen for dissociation and approach reports of these experiences seriously, empathetically, and with awareness that they can be treated effectively,” Dr. Lebois said.
The findings were published online in Neuropsychopharmacology.
Detachment, discontinuity
Pathological dissociation is “the experience of detachment from or discontinuity in one’s internal experience, sense of self, or surroundings” and is common in the aftermath of trauma, the investigators write.
Previous research into trauma-related pathological dissociation suggests it encompasses a range of experiences or “subtypes,” some of which frequently occur in PTSD and DID.
“Depersonalization and derealization involve feelings of detachment or disconnection from one’s sense of self, body, and environment,” the current researchers write. “Individuals report feeling like their body or surroundings are unreal or like they are in a movie.”
Dissociation also includes “experiences of self-alteration common in DID, in which people lose a sense of agency and ownership over their thoughts, emotions, actions, and body [and] experience some thoughts, emotions, etc. as partially dissociated intrusions,” Dr. Lebois said.
She added that dissociative symptoms are “common and disabling.” And dissociation and severe dissociative disorders such as DID “remain at best underappreciated and, at worst, frequently go undiagnosed or misdiagnosed,” with a high cost of stigmatization and misunderstanding preventing individuals from accessing effective treatment.
In addition, “given that DID disproportionately affects women, gender disparity is an important issue in this context,” Dr. Lebois noted.
Her team was motivated to conduct the study “to learn more about how different types of dissociation manifest in brain activity and to help combat the stigma around dissociation and DID.”
Filling the gap
The investigators drew on the “Triple Network” model of psychopathology, which “offers an integrative framework based in systems neuroscience for understanding cognitive and affective dysfunction across psychiatric conditions,” they write.
This model “implicates altered intrinsic organization and interactions between three large-scale brain networks across disorders,” they add.
The brain networks included in the study were the right-lateralized central executive network (rCEN), with the lateral frontoparietal brain region; the medial temporal subnetwork of the default network (tDN), with the medial frontoparietal brain region; and the cingulo-opercular subnetwork (cSN), with the midcingulo-insular brain region.
Previous neuroimaging research into dissociative disorders has implicated altered connectivity in these regions. However, although previous studies covered dissociation subtypes, they did not directly compare these subtypes. This study was designed to fill that gap, the investigators note.
They assessed 91 women with and without a history of childhood trauma, current PTSD, and with varying degrees of dissociation.
This included 19 with conventional PTSD (mean age, 33.4 years), 18 with PTSD dissociative subtype (mean age, 29.5 years), 26 with DID (mean age, 37.4 years), and 28 who acted as the healthy control group (mean age, 32 years).
Participants completed several scales regarding symptoms of PTSD, dissociation, and childhood trauma. They also underwent functional magnetic resonance imaging. Covariates included age, childhood maltreatment, and PTSD severity.
Connectivity alterations
Results showed the rCEN was “most impacted” by pathological dissociation, with 39 clusters linked to connectivity alterations.
Ten clusters within tDN exhibited within-network hyperconnectivity related to dissociation but only of the depersonalization/derealization subtype.
Eight clusters within cSN were linked to dissociation – specifically, within-network hyperconnectivity and decreased connectivity between regions in rCEN with cSN, with “no significant unique contributions of dissociation subtypes,” the researchers report.
“Depersonalization and derealization symptoms were associated with increased communication between a brain network involved in reasoning, attention, inhibition, and working memory and a brain region implicated in out-of-body experiences. This may, in part, contribute to depersonalization/derealization feelings of detachment, strangeness or unreality experienced with your body and surroundings,” Dr. Lebois said.
“In contrast, partially dissociated intrusion symptoms central to DID were linked to increased communication between a brain network involved in autobiographical memory and your sense of self and a brain network involved in reasoning, attention, inhibition, and working memory,” she added.
She noted that this matches how patients with DID describe their mental experiences: as sometimes feeling as if they lost a sense of ownership over their own thoughts and feelings, which can “intrude into their mental landscape.”
In the future, Dr. Lebois hopes that “we may be able to monitor dissociative brain signatures during psychotherapy to help assess recovery or relapse, or we could target brain activity directly with neurofeedback or neuromodulatory techniques as a dissociation treatment in and of itself.”
A first step?
Commenting on the study, Richard Loewenstein, MD, adjunct professor, department of psychiatry, University of Maryland School of Medicine, Baltimore, called the paper a “first step in more sophisticated studies of pathological dissociation using cutting-edge concepts of brain connectivity, methodology based on naturalistic, dimensional symptoms categories, and innovative statistical methods.”
Dr. Loewenstein, who was not involved with the current study, added that there is an “oversimplified conflation of hallucinations and other symptoms of dissociation with psychosis.” So studies may “incorrectly relate phenomena such as racism-based trauma to psychosis, rather than pathological dissociation and racism-based PTSD,” he said.
He noted that the implications are “profound, as pathological dissociation is not treatable with antipsychotic medications and requires treatment with psychotherapy specifically targeting symptoms of pathological dissociation.”
The study was funded by the Julia Kasparian Fund for Neuroscience Research and the National Institute of Mental Health. Dr. Lebois reported unpaid membership on the Scientific Committee for the International Society for the Study of Trauma and Dissociation, grant support from the NIMH and the Julia Kasparian Fund for Neuroscience Research, and spousal IP payments from Vanderbilt University for technology licensed to Acadia Pharmaceuticals unrelated to the present work. The other investigators’ disclosures are listed in the original paper. Dr. Loewenstein has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results from a neuroimaging study showed that different dissociative symptoms were linked to hyperconnectivity within several key regions of the brain, including the central executive, default, and salience networks as well as decreased connectivity of the central executive and salience networks with other brain areas.
Depersonalization/derealization showed a different brain signature than partially dissociated intrusions, and participants with posttraumatic stress disorder showed a different brain signature, compared with those who had dissociative identity disorder (DID).
“Dissociation is a complex, subjective set of symptoms that are largely experienced internally and, contrary to media portrayal, are not usually overtly observable,” lead author Lauren Lebois, PhD, director of the Dissociative Disorders and Trauma Research Program, McLean Hospital, Belmont, Mass., and assistant professor of psychiatry at Harvard Medical School, Boston, told this news organization.
“However, we have shown that you can objectively measure dissociation and link it to robust brain signatures. We hope these results will encourage clinicians to screen for dissociation and approach reports of these experiences seriously, empathetically, and with awareness that they can be treated effectively,” Dr. Lebois said.
The findings were published online in Neuropsychopharmacology.
Detachment, discontinuity
Pathological dissociation is “the experience of detachment from or discontinuity in one’s internal experience, sense of self, or surroundings” and is common in the aftermath of trauma, the investigators write.
Previous research into trauma-related pathological dissociation suggests it encompasses a range of experiences or “subtypes,” some of which frequently occur in PTSD and DID.
“Depersonalization and derealization involve feelings of detachment or disconnection from one’s sense of self, body, and environment,” the current researchers write. “Individuals report feeling like their body or surroundings are unreal or like they are in a movie.”
Dissociation also includes “experiences of self-alteration common in DID, in which people lose a sense of agency and ownership over their thoughts, emotions, actions, and body [and] experience some thoughts, emotions, etc. as partially dissociated intrusions,” Dr. Lebois said.
She added that dissociative symptoms are “common and disabling.” And dissociation and severe dissociative disorders such as DID “remain at best underappreciated and, at worst, frequently go undiagnosed or misdiagnosed,” with a high cost of stigmatization and misunderstanding preventing individuals from accessing effective treatment.
In addition, “given that DID disproportionately affects women, gender disparity is an important issue in this context,” Dr. Lebois noted.
Her team was motivated to conduct the study “to learn more about how different types of dissociation manifest in brain activity and to help combat the stigma around dissociation and DID.”
Filling the gap
The investigators drew on the “Triple Network” model of psychopathology, which “offers an integrative framework based in systems neuroscience for understanding cognitive and affective dysfunction across psychiatric conditions,” they write.
This model “implicates altered intrinsic organization and interactions between three large-scale brain networks across disorders,” they add.
The brain networks included in the study were the right-lateralized central executive network (rCEN), with the lateral frontoparietal brain region; the medial temporal subnetwork of the default network (tDN), with the medial frontoparietal brain region; and the cingulo-opercular subnetwork (cSN), with the midcingulo-insular brain region.
Previous neuroimaging research into dissociative disorders has implicated altered connectivity in these regions. However, although previous studies covered dissociation subtypes, they did not directly compare these subtypes. This study was designed to fill that gap, the investigators note.
They assessed 91 women with and without a history of childhood trauma, current PTSD, and with varying degrees of dissociation.
This included 19 with conventional PTSD (mean age, 33.4 years), 18 with PTSD dissociative subtype (mean age, 29.5 years), 26 with DID (mean age, 37.4 years), and 28 who acted as the healthy control group (mean age, 32 years).
Participants completed several scales regarding symptoms of PTSD, dissociation, and childhood trauma. They also underwent functional magnetic resonance imaging. Covariates included age, childhood maltreatment, and PTSD severity.
Connectivity alterations
Results showed the rCEN was “most impacted” by pathological dissociation, with 39 clusters linked to connectivity alterations.
Ten clusters within tDN exhibited within-network hyperconnectivity related to dissociation but only of the depersonalization/derealization subtype.
Eight clusters within cSN were linked to dissociation – specifically, within-network hyperconnectivity and decreased connectivity between regions in rCEN with cSN, with “no significant unique contributions of dissociation subtypes,” the researchers report.
“Depersonalization and derealization symptoms were associated with increased communication between a brain network involved in reasoning, attention, inhibition, and working memory and a brain region implicated in out-of-body experiences. This may, in part, contribute to depersonalization/derealization feelings of detachment, strangeness or unreality experienced with your body and surroundings,” Dr. Lebois said.
“In contrast, partially dissociated intrusion symptoms central to DID were linked to increased communication between a brain network involved in autobiographical memory and your sense of self and a brain network involved in reasoning, attention, inhibition, and working memory,” she added.
She noted that this matches how patients with DID describe their mental experiences: as sometimes feeling as if they lost a sense of ownership over their own thoughts and feelings, which can “intrude into their mental landscape.”
In the future, Dr. Lebois hopes that “we may be able to monitor dissociative brain signatures during psychotherapy to help assess recovery or relapse, or we could target brain activity directly with neurofeedback or neuromodulatory techniques as a dissociation treatment in and of itself.”
A first step?
Commenting on the study, Richard Loewenstein, MD, adjunct professor, department of psychiatry, University of Maryland School of Medicine, Baltimore, called the paper a “first step in more sophisticated studies of pathological dissociation using cutting-edge concepts of brain connectivity, methodology based on naturalistic, dimensional symptoms categories, and innovative statistical methods.”
Dr. Loewenstein, who was not involved with the current study, added that there is an “oversimplified conflation of hallucinations and other symptoms of dissociation with psychosis.” So studies may “incorrectly relate phenomena such as racism-based trauma to psychosis, rather than pathological dissociation and racism-based PTSD,” he said.
He noted that the implications are “profound, as pathological dissociation is not treatable with antipsychotic medications and requires treatment with psychotherapy specifically targeting symptoms of pathological dissociation.”
The study was funded by the Julia Kasparian Fund for Neuroscience Research and the National Institute of Mental Health. Dr. Lebois reported unpaid membership on the Scientific Committee for the International Society for the Study of Trauma and Dissociation, grant support from the NIMH and the Julia Kasparian Fund for Neuroscience Research, and spousal IP payments from Vanderbilt University for technology licensed to Acadia Pharmaceuticals unrelated to the present work. The other investigators’ disclosures are listed in the original paper. Dr. Loewenstein has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results from a neuroimaging study showed that different dissociative symptoms were linked to hyperconnectivity within several key regions of the brain, including the central executive, default, and salience networks as well as decreased connectivity of the central executive and salience networks with other brain areas.
Depersonalization/derealization showed a different brain signature than partially dissociated intrusions, and participants with posttraumatic stress disorder showed a different brain signature, compared with those who had dissociative identity disorder (DID).
“Dissociation is a complex, subjective set of symptoms that are largely experienced internally and, contrary to media portrayal, are not usually overtly observable,” lead author Lauren Lebois, PhD, director of the Dissociative Disorders and Trauma Research Program, McLean Hospital, Belmont, Mass., and assistant professor of psychiatry at Harvard Medical School, Boston, told this news organization.
“However, we have shown that you can objectively measure dissociation and link it to robust brain signatures. We hope these results will encourage clinicians to screen for dissociation and approach reports of these experiences seriously, empathetically, and with awareness that they can be treated effectively,” Dr. Lebois said.
The findings were published online in Neuropsychopharmacology.
Detachment, discontinuity
Pathological dissociation is “the experience of detachment from or discontinuity in one’s internal experience, sense of self, or surroundings” and is common in the aftermath of trauma, the investigators write.
Previous research into trauma-related pathological dissociation suggests it encompasses a range of experiences or “subtypes,” some of which frequently occur in PTSD and DID.
“Depersonalization and derealization involve feelings of detachment or disconnection from one’s sense of self, body, and environment,” the current researchers write. “Individuals report feeling like their body or surroundings are unreal or like they are in a movie.”
Dissociation also includes “experiences of self-alteration common in DID, in which people lose a sense of agency and ownership over their thoughts, emotions, actions, and body [and] experience some thoughts, emotions, etc. as partially dissociated intrusions,” Dr. Lebois said.
She added that dissociative symptoms are “common and disabling.” And dissociation and severe dissociative disorders such as DID “remain at best underappreciated and, at worst, frequently go undiagnosed or misdiagnosed,” with a high cost of stigmatization and misunderstanding preventing individuals from accessing effective treatment.
In addition, “given that DID disproportionately affects women, gender disparity is an important issue in this context,” Dr. Lebois noted.
Her team was motivated to conduct the study “to learn more about how different types of dissociation manifest in brain activity and to help combat the stigma around dissociation and DID.”
Filling the gap
The investigators drew on the “Triple Network” model of psychopathology, which “offers an integrative framework based in systems neuroscience for understanding cognitive and affective dysfunction across psychiatric conditions,” they write.
This model “implicates altered intrinsic organization and interactions between three large-scale brain networks across disorders,” they add.
The brain networks included in the study were the right-lateralized central executive network (rCEN), with the lateral frontoparietal brain region; the medial temporal subnetwork of the default network (tDN), with the medial frontoparietal brain region; and the cingulo-opercular subnetwork (cSN), with the midcingulo-insular brain region.
Previous neuroimaging research into dissociative disorders has implicated altered connectivity in these regions. However, although previous studies covered dissociation subtypes, they did not directly compare these subtypes. This study was designed to fill that gap, the investigators note.
They assessed 91 women with and without a history of childhood trauma, current PTSD, and with varying degrees of dissociation.
This included 19 with conventional PTSD (mean age, 33.4 years), 18 with PTSD dissociative subtype (mean age, 29.5 years), 26 with DID (mean age, 37.4 years), and 28 who acted as the healthy control group (mean age, 32 years).
Participants completed several scales regarding symptoms of PTSD, dissociation, and childhood trauma. They also underwent functional magnetic resonance imaging. Covariates included age, childhood maltreatment, and PTSD severity.
Connectivity alterations
Results showed the rCEN was “most impacted” by pathological dissociation, with 39 clusters linked to connectivity alterations.
Ten clusters within tDN exhibited within-network hyperconnectivity related to dissociation but only of the depersonalization/derealization subtype.
Eight clusters within cSN were linked to dissociation – specifically, within-network hyperconnectivity and decreased connectivity between regions in rCEN with cSN, with “no significant unique contributions of dissociation subtypes,” the researchers report.
“Depersonalization and derealization symptoms were associated with increased communication between a brain network involved in reasoning, attention, inhibition, and working memory and a brain region implicated in out-of-body experiences. This may, in part, contribute to depersonalization/derealization feelings of detachment, strangeness or unreality experienced with your body and surroundings,” Dr. Lebois said.
“In contrast, partially dissociated intrusion symptoms central to DID were linked to increased communication between a brain network involved in autobiographical memory and your sense of self and a brain network involved in reasoning, attention, inhibition, and working memory,” she added.
She noted that this matches how patients with DID describe their mental experiences: as sometimes feeling as if they lost a sense of ownership over their own thoughts and feelings, which can “intrude into their mental landscape.”
In the future, Dr. Lebois hopes that “we may be able to monitor dissociative brain signatures during psychotherapy to help assess recovery or relapse, or we could target brain activity directly with neurofeedback or neuromodulatory techniques as a dissociation treatment in and of itself.”
A first step?
Commenting on the study, Richard Loewenstein, MD, adjunct professor, department of psychiatry, University of Maryland School of Medicine, Baltimore, called the paper a “first step in more sophisticated studies of pathological dissociation using cutting-edge concepts of brain connectivity, methodology based on naturalistic, dimensional symptoms categories, and innovative statistical methods.”
Dr. Loewenstein, who was not involved with the current study, added that there is an “oversimplified conflation of hallucinations and other symptoms of dissociation with psychosis.” So studies may “incorrectly relate phenomena such as racism-based trauma to psychosis, rather than pathological dissociation and racism-based PTSD,” he said.
He noted that the implications are “profound, as pathological dissociation is not treatable with antipsychotic medications and requires treatment with psychotherapy specifically targeting symptoms of pathological dissociation.”
The study was funded by the Julia Kasparian Fund for Neuroscience Research and the National Institute of Mental Health. Dr. Lebois reported unpaid membership on the Scientific Committee for the International Society for the Study of Trauma and Dissociation, grant support from the NIMH and the Julia Kasparian Fund for Neuroscience Research, and spousal IP payments from Vanderbilt University for technology licensed to Acadia Pharmaceuticals unrelated to the present work. The other investigators’ disclosures are listed in the original paper. Dr. Loewenstein has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NEUROPSYCHOPHARMACOLOGY
ED visits for kids with suicidal thoughts increasing: Study
A new study sheds light on the escalating youth suicide crisis, revealing that emergency room visits for suicidal thoughts among kids and teens steeply increased even before the start of the COVID-19 pandemic.
Emergency room visits for “suicidal ideation” (or suicidal thoughts) among 5- to 19-year-olds increased 59% from 2016 to 2021, and hospitalizations rose 57% from fall 2019 to the fall of 2020, according to the study published in Pediatrics.
“A lot of people have talked about mental health problems in youth during the pandemic, but it was happening before the pandemic,” said author Audrey Brewer, MD, MPH, in a news release from the Ann and Robert H. Lurie Children’s Hospital of Chicago. “This has been an issue for so long, and it’s getting worse.”
Researchers looked at data for 81,105 emergency room visits across 205 Illinois hospitals from 2016 to 2021 for kids between the ages of 5 and 19.
The researchers found “there was a very sharp spike in fall 2019, followed by a similar spike during the pandemic fall of 2020, with the highest number of monthly visits during October 2020,” the authors said. “Youth aged 14-17 years had the highest frequency of [suicidal ideation emergency room] monthly visits, with visits in this group greater than the other age groups combined.”
Last year, the Centers for Disease Control and Prevention announced that suicide is the second leading cause of death among 10- to 19-year-olds.
The new research is being called a benchmark because it evaluates emergency room data for suicidal thoughts – a critical point of care for serving youths’ mental health needs. The data showed that providers were increasingly likely to list suicidal thoughts as the main diagnosis.
“Suicidal ideation can be thought about as two types: actively thinking about suicide or having thoughts, but not having a plan,” Dr. Brewer said in the news release. “That could be the difference in why someone might get admitted to the hospital.”
The researchers hypothesize that care in 2019 (when the initial spike occurred) was delayed in the early days of the pandemic, and that delay possibly contributed to the increase in providers identifying suicidal ideation as the main diagnosis.
“The early pandemic period coincided with constrained access to pediatric mental health services through schools, pediatric primary care homes, and mental health clinics for many children and their families,” the authors wrote. “The proportion of child mental health visits increased relative to other types as patients avoided ED visits during the early wave of the COVID-19 pandemic. Thus, the increase in hospitalizations during fall 2020 may reflect patients’ deferring care until symptoms became even more severe.”
Other health care scholars agreed the study spurred questions about whether the pandemic was truly the source of the crisis.
“Was it the pandemic that exacerbated the increase or is this a growing trend?” wrote Lisa M. Horowitz, PhD, MPH, and Jeffrey A. Bridge, PhD, in a commentary published along with the study. “These rising rates underscore the worsening mental health crisis for youth, as noted by the 2022 Surgeon General report and several youth mental health organizations.”
A version of this article first appeared on WebMD.com.
A new study sheds light on the escalating youth suicide crisis, revealing that emergency room visits for suicidal thoughts among kids and teens steeply increased even before the start of the COVID-19 pandemic.
Emergency room visits for “suicidal ideation” (or suicidal thoughts) among 5- to 19-year-olds increased 59% from 2016 to 2021, and hospitalizations rose 57% from fall 2019 to the fall of 2020, according to the study published in Pediatrics.
“A lot of people have talked about mental health problems in youth during the pandemic, but it was happening before the pandemic,” said author Audrey Brewer, MD, MPH, in a news release from the Ann and Robert H. Lurie Children’s Hospital of Chicago. “This has been an issue for so long, and it’s getting worse.”
Researchers looked at data for 81,105 emergency room visits across 205 Illinois hospitals from 2016 to 2021 for kids between the ages of 5 and 19.
The researchers found “there was a very sharp spike in fall 2019, followed by a similar spike during the pandemic fall of 2020, with the highest number of monthly visits during October 2020,” the authors said. “Youth aged 14-17 years had the highest frequency of [suicidal ideation emergency room] monthly visits, with visits in this group greater than the other age groups combined.”
Last year, the Centers for Disease Control and Prevention announced that suicide is the second leading cause of death among 10- to 19-year-olds.
The new research is being called a benchmark because it evaluates emergency room data for suicidal thoughts – a critical point of care for serving youths’ mental health needs. The data showed that providers were increasingly likely to list suicidal thoughts as the main diagnosis.
“Suicidal ideation can be thought about as two types: actively thinking about suicide or having thoughts, but not having a plan,” Dr. Brewer said in the news release. “That could be the difference in why someone might get admitted to the hospital.”
The researchers hypothesize that care in 2019 (when the initial spike occurred) was delayed in the early days of the pandemic, and that delay possibly contributed to the increase in providers identifying suicidal ideation as the main diagnosis.
“The early pandemic period coincided with constrained access to pediatric mental health services through schools, pediatric primary care homes, and mental health clinics for many children and their families,” the authors wrote. “The proportion of child mental health visits increased relative to other types as patients avoided ED visits during the early wave of the COVID-19 pandemic. Thus, the increase in hospitalizations during fall 2020 may reflect patients’ deferring care until symptoms became even more severe.”
Other health care scholars agreed the study spurred questions about whether the pandemic was truly the source of the crisis.
“Was it the pandemic that exacerbated the increase or is this a growing trend?” wrote Lisa M. Horowitz, PhD, MPH, and Jeffrey A. Bridge, PhD, in a commentary published along with the study. “These rising rates underscore the worsening mental health crisis for youth, as noted by the 2022 Surgeon General report and several youth mental health organizations.”
A version of this article first appeared on WebMD.com.
A new study sheds light on the escalating youth suicide crisis, revealing that emergency room visits for suicidal thoughts among kids and teens steeply increased even before the start of the COVID-19 pandemic.
Emergency room visits for “suicidal ideation” (or suicidal thoughts) among 5- to 19-year-olds increased 59% from 2016 to 2021, and hospitalizations rose 57% from fall 2019 to the fall of 2020, according to the study published in Pediatrics.
“A lot of people have talked about mental health problems in youth during the pandemic, but it was happening before the pandemic,” said author Audrey Brewer, MD, MPH, in a news release from the Ann and Robert H. Lurie Children’s Hospital of Chicago. “This has been an issue for so long, and it’s getting worse.”
Researchers looked at data for 81,105 emergency room visits across 205 Illinois hospitals from 2016 to 2021 for kids between the ages of 5 and 19.
The researchers found “there was a very sharp spike in fall 2019, followed by a similar spike during the pandemic fall of 2020, with the highest number of monthly visits during October 2020,” the authors said. “Youth aged 14-17 years had the highest frequency of [suicidal ideation emergency room] monthly visits, with visits in this group greater than the other age groups combined.”
Last year, the Centers for Disease Control and Prevention announced that suicide is the second leading cause of death among 10- to 19-year-olds.
The new research is being called a benchmark because it evaluates emergency room data for suicidal thoughts – a critical point of care for serving youths’ mental health needs. The data showed that providers were increasingly likely to list suicidal thoughts as the main diagnosis.
“Suicidal ideation can be thought about as two types: actively thinking about suicide or having thoughts, but not having a plan,” Dr. Brewer said in the news release. “That could be the difference in why someone might get admitted to the hospital.”
The researchers hypothesize that care in 2019 (when the initial spike occurred) was delayed in the early days of the pandemic, and that delay possibly contributed to the increase in providers identifying suicidal ideation as the main diagnosis.
“The early pandemic period coincided with constrained access to pediatric mental health services through schools, pediatric primary care homes, and mental health clinics for many children and their families,” the authors wrote. “The proportion of child mental health visits increased relative to other types as patients avoided ED visits during the early wave of the COVID-19 pandemic. Thus, the increase in hospitalizations during fall 2020 may reflect patients’ deferring care until symptoms became even more severe.”
Other health care scholars agreed the study spurred questions about whether the pandemic was truly the source of the crisis.
“Was it the pandemic that exacerbated the increase or is this a growing trend?” wrote Lisa M. Horowitz, PhD, MPH, and Jeffrey A. Bridge, PhD, in a commentary published along with the study. “These rising rates underscore the worsening mental health crisis for youth, as noted by the 2022 Surgeon General report and several youth mental health organizations.”
A version of this article first appeared on WebMD.com.
FROM PEDIATRICS
Nutrition for cognition: A missed opportunity in U.S. seniors?
, new research shows. Researchers assessed the memory function of more than 3,500 persons who used SNAP or did not use SNAP over a period of 20 years. They found that those who didn’t use the food benefits program experienced 2 more years of cognitive aging compared with program users.
Of the 3,555 individuals included in the study, all were eligible to use the benefits, but only 559 did, leaving 2,996 participants who did not take advantage of the program.
Low program participation levels translate into a missed opportunity to prevent dementia, said study investigator Adina Zeki Al Hazzouri, PhD, assistant professor of epidemiology at the Columbia Aging Center at Columbia University Mailman School of Public Health in New York.
She said that prior research has shown that stigma may prevent older Americans from using SNAP. “Educational programs are needed to reduce the stigma that the public holds towards SNAP use,” she said.
Policy change could increase usage among older individuals, Dr. Zeki Al Hazzouri noted. Such changes could include simplifying enrollment and reporting procedures, shortening recertification periods, and increasing benefit levels.
The study was published online in Neurology.
Memory preservation
Dr. Zeki Al Hazzouri and her team assessed respondents from the Health and Retirement Study (HRS), a representative sample of Americans aged 50 and older. All respondents who were eligible to participate in SNAP in 1996 were followed every 2 years until 2016.
At each assessment, HRS respondents completed memory tests, including immediate and delayed word recall. For those who were too impaired to complete the interview, proxy informants – typically, their spouses or family members – assessed the memory and cognition of their family members using validated instruments, such as the 16-item Informant Questionnaire for Cognitive Decline.
Investigators used a validated memory function composite score, which is benchmarked against the memory assessments and evaluations of the Aging, Demographics, and Memory Study (ADAMS) cohort.
The team found that compared with nonusers, SNAP users were more likely to be women, Black, and born in the southern United States. They were less likely to be married and had more chronic conditions, such as high blood pressure, diabetes, cancer, heart problems, psychiatric problems, and arthritis.
One important study limitation was that SNAP use was measured only once during the study, the investigators noted. Ideally, Dr. Zeki Al Hazzouri said, future research would examine cumulative SNAP use history and explore the pathways that might account for the association between SNAP use and memory decline.
While findings suggest that there were no significant differences in baseline memory function between SNAP users and nonusers, users experienced approximately 2 fewer years of cognitive aging over a 10-year period than those who didn’t use the program.
Dr. Zeki Al Hazzouri speculated that SNAP benefits may slow cognitive aging by contributing to overall brain health and that, in comparison with nonusers, SNAP users absorb more nutrients, which promote neuronal integrity.
The investigators theorized that SNAP benefits may reduce stress from financial hardship, which has been linked to premature cognitive aging in other research.
“SNAP may also increase the purchasing power and investment in other health preserving behaviors, but also resulting in better access to care, which may in turn result in better disease management and management of risk factors for cognitive function,” the investigators wrote.
An underutilized program
In an accompanying editorial, Steven Albert, PhD, Philip B. Hallen Endowed Chair in Community Health and Social Justice at the University of Pittsburgh, noted that in 2020, among households with people aged 50 and older in the United States, more than 9 million Americans experienced food insecurity.
Furthermore, he pointed out, research from 2018 showed that 71% of people aged 60 and older who met income eligibility for SNAP did not participate in the program. “SNAP is an underutilized food security program involving substantial income supplements for older people with low incomes.
“Against the backdrop of so many failures of pharmacotherapy for dementia and the so far inexorable increase in the prevalence of dementia due to population aging, are we missing an opportunity to support cognitive health by failing to enroll the 14 million Americans who are over age 60 and eligible for SNAP but who do not participate?” Dr. Albert asked. He suggested that it would be helpful to determine this through a randomized promotion trial.
The study was funded by the National Institute on Aging. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research shows. Researchers assessed the memory function of more than 3,500 persons who used SNAP or did not use SNAP over a period of 20 years. They found that those who didn’t use the food benefits program experienced 2 more years of cognitive aging compared with program users.
Of the 3,555 individuals included in the study, all were eligible to use the benefits, but only 559 did, leaving 2,996 participants who did not take advantage of the program.
Low program participation levels translate into a missed opportunity to prevent dementia, said study investigator Adina Zeki Al Hazzouri, PhD, assistant professor of epidemiology at the Columbia Aging Center at Columbia University Mailman School of Public Health in New York.
She said that prior research has shown that stigma may prevent older Americans from using SNAP. “Educational programs are needed to reduce the stigma that the public holds towards SNAP use,” she said.
Policy change could increase usage among older individuals, Dr. Zeki Al Hazzouri noted. Such changes could include simplifying enrollment and reporting procedures, shortening recertification periods, and increasing benefit levels.
The study was published online in Neurology.
Memory preservation
Dr. Zeki Al Hazzouri and her team assessed respondents from the Health and Retirement Study (HRS), a representative sample of Americans aged 50 and older. All respondents who were eligible to participate in SNAP in 1996 were followed every 2 years until 2016.
At each assessment, HRS respondents completed memory tests, including immediate and delayed word recall. For those who were too impaired to complete the interview, proxy informants – typically, their spouses or family members – assessed the memory and cognition of their family members using validated instruments, such as the 16-item Informant Questionnaire for Cognitive Decline.
Investigators used a validated memory function composite score, which is benchmarked against the memory assessments and evaluations of the Aging, Demographics, and Memory Study (ADAMS) cohort.
The team found that compared with nonusers, SNAP users were more likely to be women, Black, and born in the southern United States. They were less likely to be married and had more chronic conditions, such as high blood pressure, diabetes, cancer, heart problems, psychiatric problems, and arthritis.
One important study limitation was that SNAP use was measured only once during the study, the investigators noted. Ideally, Dr. Zeki Al Hazzouri said, future research would examine cumulative SNAP use history and explore the pathways that might account for the association between SNAP use and memory decline.
While findings suggest that there were no significant differences in baseline memory function between SNAP users and nonusers, users experienced approximately 2 fewer years of cognitive aging over a 10-year period than those who didn’t use the program.
Dr. Zeki Al Hazzouri speculated that SNAP benefits may slow cognitive aging by contributing to overall brain health and that, in comparison with nonusers, SNAP users absorb more nutrients, which promote neuronal integrity.
The investigators theorized that SNAP benefits may reduce stress from financial hardship, which has been linked to premature cognitive aging in other research.
“SNAP may also increase the purchasing power and investment in other health preserving behaviors, but also resulting in better access to care, which may in turn result in better disease management and management of risk factors for cognitive function,” the investigators wrote.
An underutilized program
In an accompanying editorial, Steven Albert, PhD, Philip B. Hallen Endowed Chair in Community Health and Social Justice at the University of Pittsburgh, noted that in 2020, among households with people aged 50 and older in the United States, more than 9 million Americans experienced food insecurity.
Furthermore, he pointed out, research from 2018 showed that 71% of people aged 60 and older who met income eligibility for SNAP did not participate in the program. “SNAP is an underutilized food security program involving substantial income supplements for older people with low incomes.
“Against the backdrop of so many failures of pharmacotherapy for dementia and the so far inexorable increase in the prevalence of dementia due to population aging, are we missing an opportunity to support cognitive health by failing to enroll the 14 million Americans who are over age 60 and eligible for SNAP but who do not participate?” Dr. Albert asked. He suggested that it would be helpful to determine this through a randomized promotion trial.
The study was funded by the National Institute on Aging. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research shows. Researchers assessed the memory function of more than 3,500 persons who used SNAP or did not use SNAP over a period of 20 years. They found that those who didn’t use the food benefits program experienced 2 more years of cognitive aging compared with program users.
Of the 3,555 individuals included in the study, all were eligible to use the benefits, but only 559 did, leaving 2,996 participants who did not take advantage of the program.
Low program participation levels translate into a missed opportunity to prevent dementia, said study investigator Adina Zeki Al Hazzouri, PhD, assistant professor of epidemiology at the Columbia Aging Center at Columbia University Mailman School of Public Health in New York.
She said that prior research has shown that stigma may prevent older Americans from using SNAP. “Educational programs are needed to reduce the stigma that the public holds towards SNAP use,” she said.
Policy change could increase usage among older individuals, Dr. Zeki Al Hazzouri noted. Such changes could include simplifying enrollment and reporting procedures, shortening recertification periods, and increasing benefit levels.
The study was published online in Neurology.
Memory preservation
Dr. Zeki Al Hazzouri and her team assessed respondents from the Health and Retirement Study (HRS), a representative sample of Americans aged 50 and older. All respondents who were eligible to participate in SNAP in 1996 were followed every 2 years until 2016.
At each assessment, HRS respondents completed memory tests, including immediate and delayed word recall. For those who were too impaired to complete the interview, proxy informants – typically, their spouses or family members – assessed the memory and cognition of their family members using validated instruments, such as the 16-item Informant Questionnaire for Cognitive Decline.
Investigators used a validated memory function composite score, which is benchmarked against the memory assessments and evaluations of the Aging, Demographics, and Memory Study (ADAMS) cohort.
The team found that compared with nonusers, SNAP users were more likely to be women, Black, and born in the southern United States. They were less likely to be married and had more chronic conditions, such as high blood pressure, diabetes, cancer, heart problems, psychiatric problems, and arthritis.
One important study limitation was that SNAP use was measured only once during the study, the investigators noted. Ideally, Dr. Zeki Al Hazzouri said, future research would examine cumulative SNAP use history and explore the pathways that might account for the association between SNAP use and memory decline.
While findings suggest that there were no significant differences in baseline memory function between SNAP users and nonusers, users experienced approximately 2 fewer years of cognitive aging over a 10-year period than those who didn’t use the program.
Dr. Zeki Al Hazzouri speculated that SNAP benefits may slow cognitive aging by contributing to overall brain health and that, in comparison with nonusers, SNAP users absorb more nutrients, which promote neuronal integrity.
The investigators theorized that SNAP benefits may reduce stress from financial hardship, which has been linked to premature cognitive aging in other research.
“SNAP may also increase the purchasing power and investment in other health preserving behaviors, but also resulting in better access to care, which may in turn result in better disease management and management of risk factors for cognitive function,” the investigators wrote.
An underutilized program
In an accompanying editorial, Steven Albert, PhD, Philip B. Hallen Endowed Chair in Community Health and Social Justice at the University of Pittsburgh, noted that in 2020, among households with people aged 50 and older in the United States, more than 9 million Americans experienced food insecurity.
Furthermore, he pointed out, research from 2018 showed that 71% of people aged 60 and older who met income eligibility for SNAP did not participate in the program. “SNAP is an underutilized food security program involving substantial income supplements for older people with low incomes.
“Against the backdrop of so many failures of pharmacotherapy for dementia and the so far inexorable increase in the prevalence of dementia due to population aging, are we missing an opportunity to support cognitive health by failing to enroll the 14 million Americans who are over age 60 and eligible for SNAP but who do not participate?” Dr. Albert asked. He suggested that it would be helpful to determine this through a randomized promotion trial.
The study was funded by the National Institute on Aging. The authors reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
From Neurology
Watching violent TV in preschool linked with emotional, behavioral issues at age 12
Preschoolers who watch violent television are more likely to have emotional and behavioral issues at the age of 12, according to investigators.
These findings align with previous studies that have shown the negative effects of watching violent content, reinforcing the importance of restricting childhood screen time, lead author Linda S. Pagani, PhD, of Université de Montréal and colleagues reported.
Past research measured the immediate or short-term effects of seeing violent media. This study examined how TV violence could be leading to issues almost a decade later, the investigators wrote in the Journal of Developmental & Behavioral Pediatrics.
Their study looked at 1,976 children from the Quebec Longitudinal Study of Child Development, a random representative cohort of boys and girls followed since their births in 1997 and 1998.
At the cohort study follow-ups at ages 3.5 and 4.5 years, the parents of these children reported if their kids watched violent TV, showing that about half of them were exposed. At age 12, the same children were scored by their teachers on a range of psychosocial outcomes, including emotional distress, inattentive behavior, disorderly behavior, social withdrawal, classroom engagement, and overall academic achievement. At this second time point, the children also scored themselves on their own academic motivation and confidence in writing.
To adjust for other factors that could be playing a role, the investigators accounted for participant characteristics at various ages between 5 months and 12 years, as well as differences in parenting styles, home environment, and socioeconomic status.
Dr. Pagani noted that these were not “garden-variety” statistical techniques.
“We did them in such a way that we set ourselves up for not finding results,” Dr. Pagani said in an interview. “That’s why this is really interesting.”
She and her colleagues found that watching TV violence during preschool was significantly associated with multiple negative outcomes at age 12.
For girls, negative outcomes included greater emotional distress, less classroom engagement, lower academic achievement, and less academic motivation. Boys showed greater emotional distress, decreased attention, disorderly behavior, social withdrawal, less classroom engagement, lower academic achievement, and less academic motivation.
“As expected, early screen violence exposure seems to come at a cost,” the investigators wrote.
Seeing TV through a child’s eyes
According to Dr. Pagani, many parents think that TV shows watched by preschoolers – like cartoons – are harmless, but these parents need to understand that the brains of children are not yet fully developed.
“The kid has an interpretation that’s very concrete,” Dr. Pagani said. “They don’t have abstract thinking.”
Because of this, kids who see “good guys” beating up “bad guys” don’t understand that the violence is comical and justified; they just see violence being used to address social disagreement, Dr. Pagani said. This leads children to believe that violence is an acceptable way to solve problems in daily life. Children are also more likely to see hostility in others when it isn’t present, leading to conflict.
Although the natural response to these findings is to restrict childhood exposure to violent content, this may be easier said than done, the investigators noted, particularly because TV is no longer the only screen in the home, as it was when this study began. Nowadays, parents need to monitor multiple devices, including smartphones, tablets, and computers, all of which may negatively impact normal brain development.
“People think this technology is innocuous,” Dr. Pagani said. “We are asleep at the wheel.”
She advised parents to wake up and follow the World Health Organization guidelines for sedentary screen time. The guidelines call for no screen time at all until a child is at least 2 years old, and then less than 1 hour per day until age 5.
“It’s the parents who should be in charge,” she said. “They’re the ones who have the cognitive ability to make decisions for their children.”
Choosing quality time over screen time
Loredana Marchica, PhD, of Montreal Children’s Hospital and McGill University, also in Montreal, expressed confidence in the study findings, because the results line up with past research, and because the investigators accounted for other explanations.
There is a “very strong probability” that watching violent TV in preschool leads to psychological issues down the line, Dr. Marchica said.
If a child is exposed to violent content, then parents should help children understand the difference between what happens in TV shows and real life, she added, as this can reduce negative effects on behavior.
“Parents need to explain that it’s a TV show,” Dr. Marchica said. “It’s not real, and if [that violent act] happened in real life, it would actually hurt a person.”
In addition to limiting screen time and explaining any violent content, she encouraged parents to spend quality time with their children, especially during the preschool years.
“Those are the years to fortify the attachment you have with that child,” Dr. Marchica said. “Even 15 minutes a day of quality, interactive play time can make such a difference in their development, their imagination, and their social engagement and abilities.”
Parents should also try to have conversations with their young children, she said, noting that it’s okay to share personal feelings, as this teaches kids how to manage their own emotions.
“Not everything is wonderful in life, and we’re allowed to talk about that,” Dr. Marchica said. “[Parents can say,] ‘Mommy had a bad day today. This bad thing happened. But here’s what I did to make myself feel better.’ ”
Dr. Pagani and coauthors termed their findings “robust,” but also cautioned that, in their correlational study, TV violence cannot be interpreted as causal. In other limitations, they noted that the study relies on a single parent-reported item that yielded a low rate of reported exposure. Or the findings could result from other things, such as family chaos or parenting style or something else.
The longitudinal study was supported by Fondation Lucie et André Chagnon, the Institut de la Statistique du Québec, the Ministère de l’Éducation et de l’Enseignement supérieur, and others. The investigators and Dr. Marchica reported no relevant conflicts of interest.
Preschoolers who watch violent television are more likely to have emotional and behavioral issues at the age of 12, according to investigators.
These findings align with previous studies that have shown the negative effects of watching violent content, reinforcing the importance of restricting childhood screen time, lead author Linda S. Pagani, PhD, of Université de Montréal and colleagues reported.
Past research measured the immediate or short-term effects of seeing violent media. This study examined how TV violence could be leading to issues almost a decade later, the investigators wrote in the Journal of Developmental & Behavioral Pediatrics.
Their study looked at 1,976 children from the Quebec Longitudinal Study of Child Development, a random representative cohort of boys and girls followed since their births in 1997 and 1998.
At the cohort study follow-ups at ages 3.5 and 4.5 years, the parents of these children reported if their kids watched violent TV, showing that about half of them were exposed. At age 12, the same children were scored by their teachers on a range of psychosocial outcomes, including emotional distress, inattentive behavior, disorderly behavior, social withdrawal, classroom engagement, and overall academic achievement. At this second time point, the children also scored themselves on their own academic motivation and confidence in writing.
To adjust for other factors that could be playing a role, the investigators accounted for participant characteristics at various ages between 5 months and 12 years, as well as differences in parenting styles, home environment, and socioeconomic status.
Dr. Pagani noted that these were not “garden-variety” statistical techniques.
“We did them in such a way that we set ourselves up for not finding results,” Dr. Pagani said in an interview. “That’s why this is really interesting.”
She and her colleagues found that watching TV violence during preschool was significantly associated with multiple negative outcomes at age 12.
For girls, negative outcomes included greater emotional distress, less classroom engagement, lower academic achievement, and less academic motivation. Boys showed greater emotional distress, decreased attention, disorderly behavior, social withdrawal, less classroom engagement, lower academic achievement, and less academic motivation.
“As expected, early screen violence exposure seems to come at a cost,” the investigators wrote.
Seeing TV through a child’s eyes
According to Dr. Pagani, many parents think that TV shows watched by preschoolers – like cartoons – are harmless, but these parents need to understand that the brains of children are not yet fully developed.
“The kid has an interpretation that’s very concrete,” Dr. Pagani said. “They don’t have abstract thinking.”
Because of this, kids who see “good guys” beating up “bad guys” don’t understand that the violence is comical and justified; they just see violence being used to address social disagreement, Dr. Pagani said. This leads children to believe that violence is an acceptable way to solve problems in daily life. Children are also more likely to see hostility in others when it isn’t present, leading to conflict.
Although the natural response to these findings is to restrict childhood exposure to violent content, this may be easier said than done, the investigators noted, particularly because TV is no longer the only screen in the home, as it was when this study began. Nowadays, parents need to monitor multiple devices, including smartphones, tablets, and computers, all of which may negatively impact normal brain development.
“People think this technology is innocuous,” Dr. Pagani said. “We are asleep at the wheel.”
She advised parents to wake up and follow the World Health Organization guidelines for sedentary screen time. The guidelines call for no screen time at all until a child is at least 2 years old, and then less than 1 hour per day until age 5.
“It’s the parents who should be in charge,” she said. “They’re the ones who have the cognitive ability to make decisions for their children.”
Choosing quality time over screen time
Loredana Marchica, PhD, of Montreal Children’s Hospital and McGill University, also in Montreal, expressed confidence in the study findings, because the results line up with past research, and because the investigators accounted for other explanations.
There is a “very strong probability” that watching violent TV in preschool leads to psychological issues down the line, Dr. Marchica said.
If a child is exposed to violent content, then parents should help children understand the difference between what happens in TV shows and real life, she added, as this can reduce negative effects on behavior.
“Parents need to explain that it’s a TV show,” Dr. Marchica said. “It’s not real, and if [that violent act] happened in real life, it would actually hurt a person.”
In addition to limiting screen time and explaining any violent content, she encouraged parents to spend quality time with their children, especially during the preschool years.
“Those are the years to fortify the attachment you have with that child,” Dr. Marchica said. “Even 15 minutes a day of quality, interactive play time can make such a difference in their development, their imagination, and their social engagement and abilities.”
Parents should also try to have conversations with their young children, she said, noting that it’s okay to share personal feelings, as this teaches kids how to manage their own emotions.
“Not everything is wonderful in life, and we’re allowed to talk about that,” Dr. Marchica said. “[Parents can say,] ‘Mommy had a bad day today. This bad thing happened. But here’s what I did to make myself feel better.’ ”
Dr. Pagani and coauthors termed their findings “robust,” but also cautioned that, in their correlational study, TV violence cannot be interpreted as causal. In other limitations, they noted that the study relies on a single parent-reported item that yielded a low rate of reported exposure. Or the findings could result from other things, such as family chaos or parenting style or something else.
The longitudinal study was supported by Fondation Lucie et André Chagnon, the Institut de la Statistique du Québec, the Ministère de l’Éducation et de l’Enseignement supérieur, and others. The investigators and Dr. Marchica reported no relevant conflicts of interest.
Preschoolers who watch violent television are more likely to have emotional and behavioral issues at the age of 12, according to investigators.
These findings align with previous studies that have shown the negative effects of watching violent content, reinforcing the importance of restricting childhood screen time, lead author Linda S. Pagani, PhD, of Université de Montréal and colleagues reported.
Past research measured the immediate or short-term effects of seeing violent media. This study examined how TV violence could be leading to issues almost a decade later, the investigators wrote in the Journal of Developmental & Behavioral Pediatrics.
Their study looked at 1,976 children from the Quebec Longitudinal Study of Child Development, a random representative cohort of boys and girls followed since their births in 1997 and 1998.
At the cohort study follow-ups at ages 3.5 and 4.5 years, the parents of these children reported if their kids watched violent TV, showing that about half of them were exposed. At age 12, the same children were scored by their teachers on a range of psychosocial outcomes, including emotional distress, inattentive behavior, disorderly behavior, social withdrawal, classroom engagement, and overall academic achievement. At this second time point, the children also scored themselves on their own academic motivation and confidence in writing.
To adjust for other factors that could be playing a role, the investigators accounted for participant characteristics at various ages between 5 months and 12 years, as well as differences in parenting styles, home environment, and socioeconomic status.
Dr. Pagani noted that these were not “garden-variety” statistical techniques.
“We did them in such a way that we set ourselves up for not finding results,” Dr. Pagani said in an interview. “That’s why this is really interesting.”
She and her colleagues found that watching TV violence during preschool was significantly associated with multiple negative outcomes at age 12.
For girls, negative outcomes included greater emotional distress, less classroom engagement, lower academic achievement, and less academic motivation. Boys showed greater emotional distress, decreased attention, disorderly behavior, social withdrawal, less classroom engagement, lower academic achievement, and less academic motivation.
“As expected, early screen violence exposure seems to come at a cost,” the investigators wrote.
Seeing TV through a child’s eyes
According to Dr. Pagani, many parents think that TV shows watched by preschoolers – like cartoons – are harmless, but these parents need to understand that the brains of children are not yet fully developed.
“The kid has an interpretation that’s very concrete,” Dr. Pagani said. “They don’t have abstract thinking.”
Because of this, kids who see “good guys” beating up “bad guys” don’t understand that the violence is comical and justified; they just see violence being used to address social disagreement, Dr. Pagani said. This leads children to believe that violence is an acceptable way to solve problems in daily life. Children are also more likely to see hostility in others when it isn’t present, leading to conflict.
Although the natural response to these findings is to restrict childhood exposure to violent content, this may be easier said than done, the investigators noted, particularly because TV is no longer the only screen in the home, as it was when this study began. Nowadays, parents need to monitor multiple devices, including smartphones, tablets, and computers, all of which may negatively impact normal brain development.
“People think this technology is innocuous,” Dr. Pagani said. “We are asleep at the wheel.”
She advised parents to wake up and follow the World Health Organization guidelines for sedentary screen time. The guidelines call for no screen time at all until a child is at least 2 years old, and then less than 1 hour per day until age 5.
“It’s the parents who should be in charge,” she said. “They’re the ones who have the cognitive ability to make decisions for their children.”
Choosing quality time over screen time
Loredana Marchica, PhD, of Montreal Children’s Hospital and McGill University, also in Montreal, expressed confidence in the study findings, because the results line up with past research, and because the investigators accounted for other explanations.
There is a “very strong probability” that watching violent TV in preschool leads to psychological issues down the line, Dr. Marchica said.
If a child is exposed to violent content, then parents should help children understand the difference between what happens in TV shows and real life, she added, as this can reduce negative effects on behavior.
“Parents need to explain that it’s a TV show,” Dr. Marchica said. “It’s not real, and if [that violent act] happened in real life, it would actually hurt a person.”
In addition to limiting screen time and explaining any violent content, she encouraged parents to spend quality time with their children, especially during the preschool years.
“Those are the years to fortify the attachment you have with that child,” Dr. Marchica said. “Even 15 minutes a day of quality, interactive play time can make such a difference in their development, their imagination, and their social engagement and abilities.”
Parents should also try to have conversations with their young children, she said, noting that it’s okay to share personal feelings, as this teaches kids how to manage their own emotions.
“Not everything is wonderful in life, and we’re allowed to talk about that,” Dr. Marchica said. “[Parents can say,] ‘Mommy had a bad day today. This bad thing happened. But here’s what I did to make myself feel better.’ ”
Dr. Pagani and coauthors termed their findings “robust,” but also cautioned that, in their correlational study, TV violence cannot be interpreted as causal. In other limitations, they noted that the study relies on a single parent-reported item that yielded a low rate of reported exposure. Or the findings could result from other things, such as family chaos or parenting style or something else.
The longitudinal study was supported by Fondation Lucie et André Chagnon, the Institut de la Statistique du Québec, the Ministère de l’Éducation et de l’Enseignement supérieur, and others. The investigators and Dr. Marchica reported no relevant conflicts of interest.
FROM THE JOURNAL OF DEVELOPMENTAL & BEHAVIORAL PEDIATRICS
Telepsychiatry tips: Etiquette and ethics
From providing virtual therapy sessions to patients in the front seats of their cars, to sessions with patients who turn out to be in another state,
But key practice tips are emerging for the optimization of virtual sessions, said Sanjay Gupta, MD, chief medical officer of the BryLin Behavioral Health System in Buffalo, N.Y., during a presentation on the subject at the 21st Annual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists in Cincinnati, Ohio.
Dr. Gupta noted that while “many pitfalls [may] occur,” an overriding rule that should be emphasized with telepsychiatry is that “[virtual visits] are held to the same standard of care as an in-person visit.” This “rule” needs to be followed diligently, he said, as the key difference in virtual visits is a reduced sense of the formality of a psychotherapy session.
With virtual sessions, the therapeutic experience “can feel kind of trivialized,” said Dr. Gupta, who is also a clinical professor in the department of psychiatry, State University of New York at Buffalo. He noted that it is crucial that “the sacredness of a private setting should not be diluted.”
Challenges in finding that privacy for some, however, lead to the issue of the “patients in cars” scenario, Dr. Gupta said. Still, he added, while psychiatric sessions should never be conducted when a patient is driving, the front seat of a parked car may, for some, be the most private setting available.
“For many patients, their car may be the only private place from which they can take a video call,” Dr. Gupta noted. “Perhaps they are at work and the only way they could fit in the appointment is by going out to their car on their break. Or patients may even be at home, but they’re not alone and need to go out to their car for privacy.”
If the car isn’t being driven, sitting inside it should be fine for virtual therapy, but even there, clinicians should retain a focus on the consistency of care regardless of the setting.
Meanwhile, psychiatrists can take key measures to keep things professional, at least on their end of the session.
Before starting, for instance, keep in mind the patient’s viewing experience, Dr. Gupta suggested. Tips he offered include:
- Keep the background of your video image subtle, with no distractions, such as windows looking out to an ocean or other distracting background elements.
- The camera should be above eye level to suggest a face-to-face conversation more effectively.
- Try not to have other browser windows open and look directly into the camera lens so that the patient knows they have your full attention.
- Try not to take notes or document in the electronic health record during the session, which also can give the impression of being distracted and not listening to the patient.
Psychiatrists should remember that older patients – who may be uncomfortable with email, much less video conferencing – may still struggle with video-calling technology. In such cases, consider:
- Sending the patient instructions in advance of the appointment.
- Have your office hold a “tech check” prior to the appointment to ensure the patient is ready.
- Be prepared to provide troubleshooting.
Whether the patient is tech savvy or not, make sure communication is clear:
- Speak in short sentences on teleconferencing sessions.
- Speak slowly and use a lower frequency.
- Recognize that non-native English speakers may struggle with comprehension, and explore interpreter options.
Dr. Gupta noted that the first minute of the virtual therapy session is crucial in setting the tone.
“The patient wants to hear a professional, confident tone on the other end at the beginning of the session,” he said. “Be warm and respectful throughout the visit, and make sure to explain to the patient how the session will be reconnected if the call is interrupted.”
Clinicians should also make sure to identify the patient’s physical location during the session in case of an emergency, such as the patient becoming suicidal.
Impending ‘telehealth cliff’
Many laws and licensing requirements for telehealth are still relatively loose, falling under the COVID-19 public health emergency (PHE) policies. These policies allow practitioners who are eligible to bill Medicare for telehealth services regardless of where the patient or provider is located, and providers can also deliver telehealth services across state lines, depending on state and federal rules.
However, Dr. Gupta warns that practitioners should be prepared for the potential “telehealth cliff” that is anticipated when those PHE policies are lifted, as barriers in licensing, billing, and other factors, such as HIPAA, are reinstated.
“HIPAA is [flexible] now as long as the public emergency policies exist,” Dr. Gupta said. “However, in noncrisis times, technology will be required to be HIPAA compliant. If you are a solo provider, for instance, you really need to choose a telepsychiatry platform that is HIPAA compliant before that happens.”
While the timing of the “telehealth cliff” is still uncertain, providers have been promised a 60-day advance notice of the PHE end, and at that time, there will be an additional 151-day grace period before the waivers lift.
A key federal measure that could protect more favorable telemedicine policies across state lines, the Temporary Reciprocity to Ensure Access to Treatment Act, currently remains stalled in Congress.
Regardless of those developments, Dr. Gupta underscored that “telepsychiatry is here to stay because the patients and their families like it, and they will be the driving factors.”
He noted that “the future is likely going to be a hybrid model of in-person and virtual visits,” to accommodate the various scenarios in which in-person visits may be preferred or necessary, but many will still likely choose the convenience and greater flexibility of virtual sessions.
Dr. Gupta serves or has served as a speaker or member of a speaker’s bureau for AbbVie, Acadia, Alkermes, Intra-Cellular Therapies, Janssen, Neurocrine, and Otsuka, and serves as a consultant/on an advisory board for Intra-Cellular Therapies.
The Psychopharmacology Update was sponsored by Medscape Live. Medscape Live and this news organization are owned by the same parent company.
From providing virtual therapy sessions to patients in the front seats of their cars, to sessions with patients who turn out to be in another state,
But key practice tips are emerging for the optimization of virtual sessions, said Sanjay Gupta, MD, chief medical officer of the BryLin Behavioral Health System in Buffalo, N.Y., during a presentation on the subject at the 21st Annual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists in Cincinnati, Ohio.
Dr. Gupta noted that while “many pitfalls [may] occur,” an overriding rule that should be emphasized with telepsychiatry is that “[virtual visits] are held to the same standard of care as an in-person visit.” This “rule” needs to be followed diligently, he said, as the key difference in virtual visits is a reduced sense of the formality of a psychotherapy session.
With virtual sessions, the therapeutic experience “can feel kind of trivialized,” said Dr. Gupta, who is also a clinical professor in the department of psychiatry, State University of New York at Buffalo. He noted that it is crucial that “the sacredness of a private setting should not be diluted.”
Challenges in finding that privacy for some, however, lead to the issue of the “patients in cars” scenario, Dr. Gupta said. Still, he added, while psychiatric sessions should never be conducted when a patient is driving, the front seat of a parked car may, for some, be the most private setting available.
“For many patients, their car may be the only private place from which they can take a video call,” Dr. Gupta noted. “Perhaps they are at work and the only way they could fit in the appointment is by going out to their car on their break. Or patients may even be at home, but they’re not alone and need to go out to their car for privacy.”
If the car isn’t being driven, sitting inside it should be fine for virtual therapy, but even there, clinicians should retain a focus on the consistency of care regardless of the setting.
Meanwhile, psychiatrists can take key measures to keep things professional, at least on their end of the session.
Before starting, for instance, keep in mind the patient’s viewing experience, Dr. Gupta suggested. Tips he offered include:
- Keep the background of your video image subtle, with no distractions, such as windows looking out to an ocean or other distracting background elements.
- The camera should be above eye level to suggest a face-to-face conversation more effectively.
- Try not to have other browser windows open and look directly into the camera lens so that the patient knows they have your full attention.
- Try not to take notes or document in the electronic health record during the session, which also can give the impression of being distracted and not listening to the patient.
Psychiatrists should remember that older patients – who may be uncomfortable with email, much less video conferencing – may still struggle with video-calling technology. In such cases, consider:
- Sending the patient instructions in advance of the appointment.
- Have your office hold a “tech check” prior to the appointment to ensure the patient is ready.
- Be prepared to provide troubleshooting.
Whether the patient is tech savvy or not, make sure communication is clear:
- Speak in short sentences on teleconferencing sessions.
- Speak slowly and use a lower frequency.
- Recognize that non-native English speakers may struggle with comprehension, and explore interpreter options.
Dr. Gupta noted that the first minute of the virtual therapy session is crucial in setting the tone.
“The patient wants to hear a professional, confident tone on the other end at the beginning of the session,” he said. “Be warm and respectful throughout the visit, and make sure to explain to the patient how the session will be reconnected if the call is interrupted.”
Clinicians should also make sure to identify the patient’s physical location during the session in case of an emergency, such as the patient becoming suicidal.
Impending ‘telehealth cliff’
Many laws and licensing requirements for telehealth are still relatively loose, falling under the COVID-19 public health emergency (PHE) policies. These policies allow practitioners who are eligible to bill Medicare for telehealth services regardless of where the patient or provider is located, and providers can also deliver telehealth services across state lines, depending on state and federal rules.
However, Dr. Gupta warns that practitioners should be prepared for the potential “telehealth cliff” that is anticipated when those PHE policies are lifted, as barriers in licensing, billing, and other factors, such as HIPAA, are reinstated.
“HIPAA is [flexible] now as long as the public emergency policies exist,” Dr. Gupta said. “However, in noncrisis times, technology will be required to be HIPAA compliant. If you are a solo provider, for instance, you really need to choose a telepsychiatry platform that is HIPAA compliant before that happens.”
While the timing of the “telehealth cliff” is still uncertain, providers have been promised a 60-day advance notice of the PHE end, and at that time, there will be an additional 151-day grace period before the waivers lift.
A key federal measure that could protect more favorable telemedicine policies across state lines, the Temporary Reciprocity to Ensure Access to Treatment Act, currently remains stalled in Congress.
Regardless of those developments, Dr. Gupta underscored that “telepsychiatry is here to stay because the patients and their families like it, and they will be the driving factors.”
He noted that “the future is likely going to be a hybrid model of in-person and virtual visits,” to accommodate the various scenarios in which in-person visits may be preferred or necessary, but many will still likely choose the convenience and greater flexibility of virtual sessions.
Dr. Gupta serves or has served as a speaker or member of a speaker’s bureau for AbbVie, Acadia, Alkermes, Intra-Cellular Therapies, Janssen, Neurocrine, and Otsuka, and serves as a consultant/on an advisory board for Intra-Cellular Therapies.
The Psychopharmacology Update was sponsored by Medscape Live. Medscape Live and this news organization are owned by the same parent company.
From providing virtual therapy sessions to patients in the front seats of their cars, to sessions with patients who turn out to be in another state,
But key practice tips are emerging for the optimization of virtual sessions, said Sanjay Gupta, MD, chief medical officer of the BryLin Behavioral Health System in Buffalo, N.Y., during a presentation on the subject at the 21st Annual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists in Cincinnati, Ohio.
Dr. Gupta noted that while “many pitfalls [may] occur,” an overriding rule that should be emphasized with telepsychiatry is that “[virtual visits] are held to the same standard of care as an in-person visit.” This “rule” needs to be followed diligently, he said, as the key difference in virtual visits is a reduced sense of the formality of a psychotherapy session.
With virtual sessions, the therapeutic experience “can feel kind of trivialized,” said Dr. Gupta, who is also a clinical professor in the department of psychiatry, State University of New York at Buffalo. He noted that it is crucial that “the sacredness of a private setting should not be diluted.”
Challenges in finding that privacy for some, however, lead to the issue of the “patients in cars” scenario, Dr. Gupta said. Still, he added, while psychiatric sessions should never be conducted when a patient is driving, the front seat of a parked car may, for some, be the most private setting available.
“For many patients, their car may be the only private place from which they can take a video call,” Dr. Gupta noted. “Perhaps they are at work and the only way they could fit in the appointment is by going out to their car on their break. Or patients may even be at home, but they’re not alone and need to go out to their car for privacy.”
If the car isn’t being driven, sitting inside it should be fine for virtual therapy, but even there, clinicians should retain a focus on the consistency of care regardless of the setting.
Meanwhile, psychiatrists can take key measures to keep things professional, at least on their end of the session.
Before starting, for instance, keep in mind the patient’s viewing experience, Dr. Gupta suggested. Tips he offered include:
- Keep the background of your video image subtle, with no distractions, such as windows looking out to an ocean or other distracting background elements.
- The camera should be above eye level to suggest a face-to-face conversation more effectively.
- Try not to have other browser windows open and look directly into the camera lens so that the patient knows they have your full attention.
- Try not to take notes or document in the electronic health record during the session, which also can give the impression of being distracted and not listening to the patient.
Psychiatrists should remember that older patients – who may be uncomfortable with email, much less video conferencing – may still struggle with video-calling technology. In such cases, consider:
- Sending the patient instructions in advance of the appointment.
- Have your office hold a “tech check” prior to the appointment to ensure the patient is ready.
- Be prepared to provide troubleshooting.
Whether the patient is tech savvy or not, make sure communication is clear:
- Speak in short sentences on teleconferencing sessions.
- Speak slowly and use a lower frequency.
- Recognize that non-native English speakers may struggle with comprehension, and explore interpreter options.
Dr. Gupta noted that the first minute of the virtual therapy session is crucial in setting the tone.
“The patient wants to hear a professional, confident tone on the other end at the beginning of the session,” he said. “Be warm and respectful throughout the visit, and make sure to explain to the patient how the session will be reconnected if the call is interrupted.”
Clinicians should also make sure to identify the patient’s physical location during the session in case of an emergency, such as the patient becoming suicidal.
Impending ‘telehealth cliff’
Many laws and licensing requirements for telehealth are still relatively loose, falling under the COVID-19 public health emergency (PHE) policies. These policies allow practitioners who are eligible to bill Medicare for telehealth services regardless of where the patient or provider is located, and providers can also deliver telehealth services across state lines, depending on state and federal rules.
However, Dr. Gupta warns that practitioners should be prepared for the potential “telehealth cliff” that is anticipated when those PHE policies are lifted, as barriers in licensing, billing, and other factors, such as HIPAA, are reinstated.
“HIPAA is [flexible] now as long as the public emergency policies exist,” Dr. Gupta said. “However, in noncrisis times, technology will be required to be HIPAA compliant. If you are a solo provider, for instance, you really need to choose a telepsychiatry platform that is HIPAA compliant before that happens.”
While the timing of the “telehealth cliff” is still uncertain, providers have been promised a 60-day advance notice of the PHE end, and at that time, there will be an additional 151-day grace period before the waivers lift.
A key federal measure that could protect more favorable telemedicine policies across state lines, the Temporary Reciprocity to Ensure Access to Treatment Act, currently remains stalled in Congress.
Regardless of those developments, Dr. Gupta underscored that “telepsychiatry is here to stay because the patients and their families like it, and they will be the driving factors.”
He noted that “the future is likely going to be a hybrid model of in-person and virtual visits,” to accommodate the various scenarios in which in-person visits may be preferred or necessary, but many will still likely choose the convenience and greater flexibility of virtual sessions.
Dr. Gupta serves or has served as a speaker or member of a speaker’s bureau for AbbVie, Acadia, Alkermes, Intra-Cellular Therapies, Janssen, Neurocrine, and Otsuka, and serves as a consultant/on an advisory board for Intra-Cellular Therapies.
The Psychopharmacology Update was sponsored by Medscape Live. Medscape Live and this news organization are owned by the same parent company.
FROM PSYCHOPHARMACOLOGY UPDATE
A new ultrabrief screening scale for pediatric OCD
Obsessive-compulsive disorder (OCD) affects 1-2% of the population. The disorder is characterized by recurrent intrusive unwanted thoughts (obsessions) that cause significant distress and anxiety, and behavioral or mental rituals (compulsions) that are performed to reduce distress stemming from obsessions. OCD may onset at any time in life, but most commonly begins in childhood or in early adulthood.
Cognitive behavioral therapy (CBT) with exposure and response prevention is an empirically based and highly effective treatment for OCD. However, most youth with OCD do not receive any treatment, which is related to a shortage of mental health care providers with expertise in assessment and treatment of the disorder, and misdiagnosis of the disorder is all too prevalent.
Aside from the subjective emotional toll associated with OCD, individuals living with this disorder frequently experience interpersonal, academic, and vocational impairments. Nevertheless, OCD is often overlooked or misdiagnosed. This may be more pronounced in youth with OCD, particularly in primary health care settings and large nonspecialized medical institutions. In fact, research indicates that pediatric OCD is often underrecognized even among mental health professionals. This situation is not new, and in fact the National Institute for Health and Care Excellence (NICE) in the United Kingdom stated that there is an urgent need to develop brief reliable screeners for OCD nearly 20 years ago.
Although there were several attempts to develop brief screening scales for adults and youth with OCD, none of them were found to be suitable for use as rapid screening tools in nonspecialized settings. One of the primary reasons is that OCD is associated with different “themes” or dimensions. For example, a child with OCD may engage in cleaning rituals because the context (or dimension) of their obsessions is contamination concerns. Another child with OCD, who may suffer from similar overall symptom severity, may primarily engage in checking rituals which are related with obsessions associated with fear of being responsible for harm. Therefore, one child with OCD may score very high on items assessing one dimension (e.g., contamination concerns), but very low on another dimension (e.g., harm obsessions).
This results in a known challenge in the assessment and psychometrics of self-report (as opposed to clinician administered) measures of OCD. Secondly, development of such measures requires very large carefully screened samples of individuals with OCD, with other disorders, and those without a known psychological disorder – which may be more challenging than requiring adult participants.
To accomplish this, we harmonized data from several sites that included three samples of carefully screened youths with OCD, with other disorders, and without known disorders who completed multiple self-report questionnaires, including the 21-item Obsessive-Compulsive Inventory – Child Version (OCI-CV).
Utilizing psychometric analyses including factor analyses, invariance analyses, and item response theory methodologies, we were able to develop an ultrabrief measure extracted from the OCI-CV: the 5-item Obsessive-Compulsive Inventory – Child Version (OCI-CV-5). This very brief self-report measure was found to have very good psychometric properties including a sensitive and specific clinical cutoff score. Youth who score at or above the cutoff score are nearly 21 times more likely to meet criteria for OCD.
This measure corresponds to a need to rapidly screen for OCD in children in nonspecialized settings, including community mental health clinics, primary care settings, and pediatric treatment facilities. However, it is important to note it is not a diagnostic measure. The measure is intended to identify youth who should be referred to a mental health care professional to conduct a diagnostic interview.
Dr. Abramovitch is a clinical psychologist and neuropsychologist based in Austin, Tex., and an associate professor at Texas State University. Dr. Abramowitz is professor and director of clinical training in the Anxiety and Stress Lab at University of North Carolina at Chapel Hill. Dr. McKay is professor of psychology at Fordham University, Bronx, N.Y.
Obsessive-compulsive disorder (OCD) affects 1-2% of the population. The disorder is characterized by recurrent intrusive unwanted thoughts (obsessions) that cause significant distress and anxiety, and behavioral or mental rituals (compulsions) that are performed to reduce distress stemming from obsessions. OCD may onset at any time in life, but most commonly begins in childhood or in early adulthood.
Cognitive behavioral therapy (CBT) with exposure and response prevention is an empirically based and highly effective treatment for OCD. However, most youth with OCD do not receive any treatment, which is related to a shortage of mental health care providers with expertise in assessment and treatment of the disorder, and misdiagnosis of the disorder is all too prevalent.
Aside from the subjective emotional toll associated with OCD, individuals living with this disorder frequently experience interpersonal, academic, and vocational impairments. Nevertheless, OCD is often overlooked or misdiagnosed. This may be more pronounced in youth with OCD, particularly in primary health care settings and large nonspecialized medical institutions. In fact, research indicates that pediatric OCD is often underrecognized even among mental health professionals. This situation is not new, and in fact the National Institute for Health and Care Excellence (NICE) in the United Kingdom stated that there is an urgent need to develop brief reliable screeners for OCD nearly 20 years ago.
Although there were several attempts to develop brief screening scales for adults and youth with OCD, none of them were found to be suitable for use as rapid screening tools in nonspecialized settings. One of the primary reasons is that OCD is associated with different “themes” or dimensions. For example, a child with OCD may engage in cleaning rituals because the context (or dimension) of their obsessions is contamination concerns. Another child with OCD, who may suffer from similar overall symptom severity, may primarily engage in checking rituals which are related with obsessions associated with fear of being responsible for harm. Therefore, one child with OCD may score very high on items assessing one dimension (e.g., contamination concerns), but very low on another dimension (e.g., harm obsessions).
This results in a known challenge in the assessment and psychometrics of self-report (as opposed to clinician administered) measures of OCD. Secondly, development of such measures requires very large carefully screened samples of individuals with OCD, with other disorders, and those without a known psychological disorder – which may be more challenging than requiring adult participants.
To accomplish this, we harmonized data from several sites that included three samples of carefully screened youths with OCD, with other disorders, and without known disorders who completed multiple self-report questionnaires, including the 21-item Obsessive-Compulsive Inventory – Child Version (OCI-CV).
Utilizing psychometric analyses including factor analyses, invariance analyses, and item response theory methodologies, we were able to develop an ultrabrief measure extracted from the OCI-CV: the 5-item Obsessive-Compulsive Inventory – Child Version (OCI-CV-5). This very brief self-report measure was found to have very good psychometric properties including a sensitive and specific clinical cutoff score. Youth who score at or above the cutoff score are nearly 21 times more likely to meet criteria for OCD.
This measure corresponds to a need to rapidly screen for OCD in children in nonspecialized settings, including community mental health clinics, primary care settings, and pediatric treatment facilities. However, it is important to note it is not a diagnostic measure. The measure is intended to identify youth who should be referred to a mental health care professional to conduct a diagnostic interview.
Dr. Abramovitch is a clinical psychologist and neuropsychologist based in Austin, Tex., and an associate professor at Texas State University. Dr. Abramowitz is professor and director of clinical training in the Anxiety and Stress Lab at University of North Carolina at Chapel Hill. Dr. McKay is professor of psychology at Fordham University, Bronx, N.Y.
Obsessive-compulsive disorder (OCD) affects 1-2% of the population. The disorder is characterized by recurrent intrusive unwanted thoughts (obsessions) that cause significant distress and anxiety, and behavioral or mental rituals (compulsions) that are performed to reduce distress stemming from obsessions. OCD may onset at any time in life, but most commonly begins in childhood or in early adulthood.
Cognitive behavioral therapy (CBT) with exposure and response prevention is an empirically based and highly effective treatment for OCD. However, most youth with OCD do not receive any treatment, which is related to a shortage of mental health care providers with expertise in assessment and treatment of the disorder, and misdiagnosis of the disorder is all too prevalent.
Aside from the subjective emotional toll associated with OCD, individuals living with this disorder frequently experience interpersonal, academic, and vocational impairments. Nevertheless, OCD is often overlooked or misdiagnosed. This may be more pronounced in youth with OCD, particularly in primary health care settings and large nonspecialized medical institutions. In fact, research indicates that pediatric OCD is often underrecognized even among mental health professionals. This situation is not new, and in fact the National Institute for Health and Care Excellence (NICE) in the United Kingdom stated that there is an urgent need to develop brief reliable screeners for OCD nearly 20 years ago.
Although there were several attempts to develop brief screening scales for adults and youth with OCD, none of them were found to be suitable for use as rapid screening tools in nonspecialized settings. One of the primary reasons is that OCD is associated with different “themes” or dimensions. For example, a child with OCD may engage in cleaning rituals because the context (or dimension) of their obsessions is contamination concerns. Another child with OCD, who may suffer from similar overall symptom severity, may primarily engage in checking rituals which are related with obsessions associated with fear of being responsible for harm. Therefore, one child with OCD may score very high on items assessing one dimension (e.g., contamination concerns), but very low on another dimension (e.g., harm obsessions).
This results in a known challenge in the assessment and psychometrics of self-report (as opposed to clinician administered) measures of OCD. Secondly, development of such measures requires very large carefully screened samples of individuals with OCD, with other disorders, and those without a known psychological disorder – which may be more challenging than requiring adult participants.
To accomplish this, we harmonized data from several sites that included three samples of carefully screened youths with OCD, with other disorders, and without known disorders who completed multiple self-report questionnaires, including the 21-item Obsessive-Compulsive Inventory – Child Version (OCI-CV).
Utilizing psychometric analyses including factor analyses, invariance analyses, and item response theory methodologies, we were able to develop an ultrabrief measure extracted from the OCI-CV: the 5-item Obsessive-Compulsive Inventory – Child Version (OCI-CV-5). This very brief self-report measure was found to have very good psychometric properties including a sensitive and specific clinical cutoff score. Youth who score at or above the cutoff score are nearly 21 times more likely to meet criteria for OCD.
This measure corresponds to a need to rapidly screen for OCD in children in nonspecialized settings, including community mental health clinics, primary care settings, and pediatric treatment facilities. However, it is important to note it is not a diagnostic measure. The measure is intended to identify youth who should be referred to a mental health care professional to conduct a diagnostic interview.
Dr. Abramovitch is a clinical psychologist and neuropsychologist based in Austin, Tex., and an associate professor at Texas State University. Dr. Abramowitz is professor and director of clinical training in the Anxiety and Stress Lab at University of North Carolina at Chapel Hill. Dr. McKay is professor of psychology at Fordham University, Bronx, N.Y.