User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
FDA authorizes intradermal use of Jynneos vaccine for monkeypox
The Food and Drug Administration on Aug. 9 authorized intradermal administration of the Jynneos vaccine for the treatment of monkeypox. The process, approved specifically for high-risk patients, was passed under the administration’s Emergency Use Authorization. It follows the decision on Aug. 4 by the U.S. Department of Health and Human Services to declare monkeypox a public health emergency. Intradermal administration will allow providers to get five doses out of a one-dose vial.
This news organization will update this article as more information becomes available.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration on Aug. 9 authorized intradermal administration of the Jynneos vaccine for the treatment of monkeypox. The process, approved specifically for high-risk patients, was passed under the administration’s Emergency Use Authorization. It follows the decision on Aug. 4 by the U.S. Department of Health and Human Services to declare monkeypox a public health emergency. Intradermal administration will allow providers to get five doses out of a one-dose vial.
This news organization will update this article as more information becomes available.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration on Aug. 9 authorized intradermal administration of the Jynneos vaccine for the treatment of monkeypox. The process, approved specifically for high-risk patients, was passed under the administration’s Emergency Use Authorization. It follows the decision on Aug. 4 by the U.S. Department of Health and Human Services to declare monkeypox a public health emergency. Intradermal administration will allow providers to get five doses out of a one-dose vial.
This news organization will update this article as more information becomes available.
A version of this article first appeared on Medscape.com.
Children and COVID: Severe illness rising as vaccination effort stalls
, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
After new child cases jumped by 22% during the week of July 15-21, the two successive weeks have produced increases of 3.9% (July 22-29) and 1.2% (July 30-Aug. 4). The latest weekly count from all states and territories still reporting was 96,599, the AAP and CHA said in their weekly COVID report, noting that several states have stopped reporting child cases and that others are reporting every other week.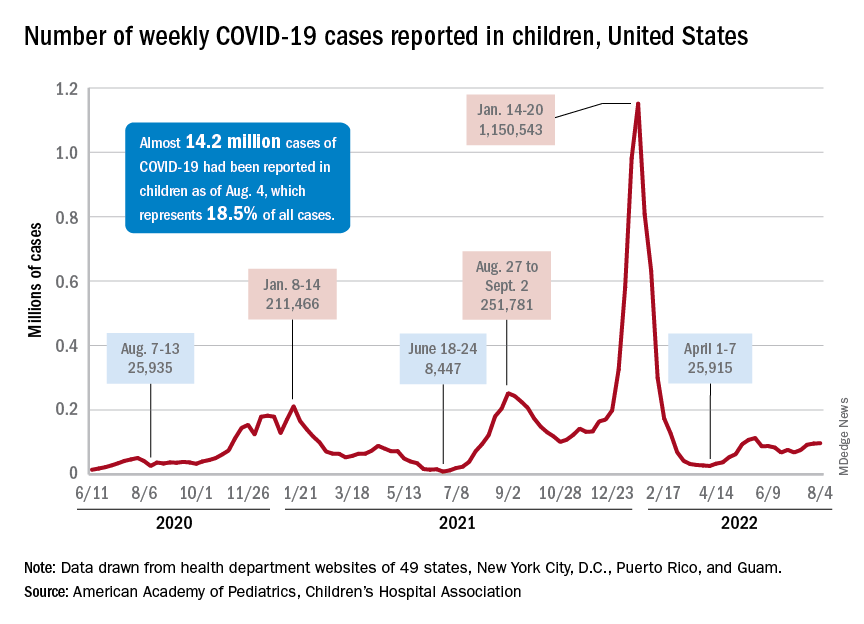
The deceleration in new cases, however, does not apply to emergency department visits and hospital admissions. The proportion of ED visits with diagnosed COVID rose steadily throughout June and July, as 7-day averages went from 2.6% on June 1 to 6.3% on July 31 for children aged 0-11 years, from 2.1% to 3.1% for children aged 12-15, and from 2.4% to 3.5% for 16- to 17-year-olds, according to data from the Centers for Disease Control and Prevention.
The rate of new admissions with confirmed COVID, which reached 0.46 per 100,000 population for children aged 0-17 years on July 30, has more than tripled since early April, when it had fallen to 0.13 per 100,000 in the wake of the Omicron surge, the CDC reported on its COVID Data Tracker.
A smaller but more detailed sample of children from the COVID-19–Associated Hospitalization Network (COVID-NET), which covers nearly 100 counties in 14 states, indicates that the increase in new admissions is occurring almost entirely among children aged 0-4 years, who had a rate of 5.6 per 100,000 for the week of July 17-23, compared with 0.8 per 100,000 for 5- to 11-year-olds and 1.5 per 100,000 for those aged 12-17, the CDC said.
Vaccine’s summer rollout gets lukewarm reception
As a group, children aged 0-4 years have not exactly flocked to the COVID-19 vaccine. As of Aug. 2 – about 6 weeks since the vaccine was authorized for children aged 6 months to 4 years – just 3.8% of those eligible had received at least one dose. Among children aged 5-11 the corresponding number on Aug. 2 was 37.4%, and for those aged 12-17 years it was 70.3%, the CDC data show.
That 3.8% of children aged less than 5 years represents almost 756,000 initial doses. That compares with over 6 million children aged 5-11 years who had received at least one dose through the first 6 weeks of their vaccination experience and over 5 million children aged 12-15, according to the COVID Data Tracker.
, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
After new child cases jumped by 22% during the week of July 15-21, the two successive weeks have produced increases of 3.9% (July 22-29) and 1.2% (July 30-Aug. 4). The latest weekly count from all states and territories still reporting was 96,599, the AAP and CHA said in their weekly COVID report, noting that several states have stopped reporting child cases and that others are reporting every other week.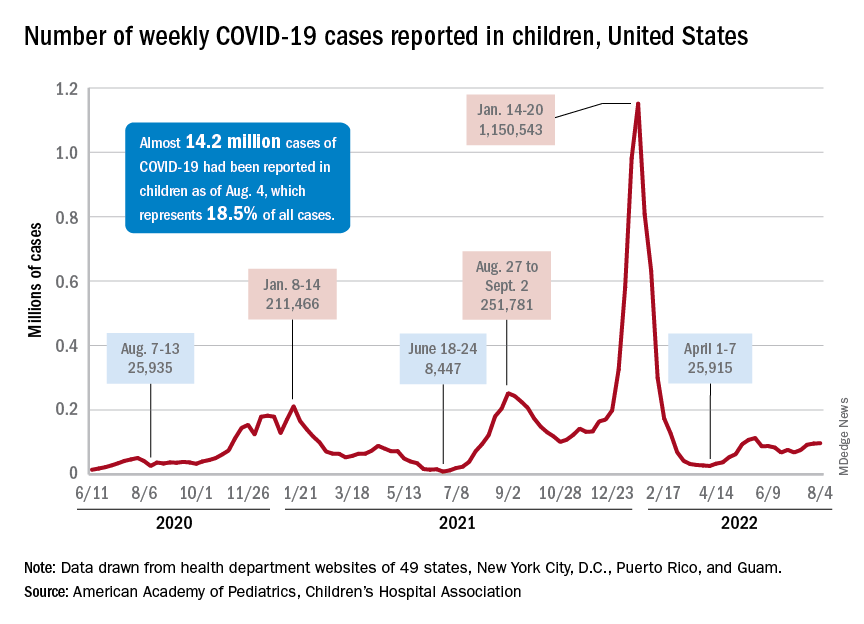
The deceleration in new cases, however, does not apply to emergency department visits and hospital admissions. The proportion of ED visits with diagnosed COVID rose steadily throughout June and July, as 7-day averages went from 2.6% on June 1 to 6.3% on July 31 for children aged 0-11 years, from 2.1% to 3.1% for children aged 12-15, and from 2.4% to 3.5% for 16- to 17-year-olds, according to data from the Centers for Disease Control and Prevention.
The rate of new admissions with confirmed COVID, which reached 0.46 per 100,000 population for children aged 0-17 years on July 30, has more than tripled since early April, when it had fallen to 0.13 per 100,000 in the wake of the Omicron surge, the CDC reported on its COVID Data Tracker.
A smaller but more detailed sample of children from the COVID-19–Associated Hospitalization Network (COVID-NET), which covers nearly 100 counties in 14 states, indicates that the increase in new admissions is occurring almost entirely among children aged 0-4 years, who had a rate of 5.6 per 100,000 for the week of July 17-23, compared with 0.8 per 100,000 for 5- to 11-year-olds and 1.5 per 100,000 for those aged 12-17, the CDC said.
Vaccine’s summer rollout gets lukewarm reception
As a group, children aged 0-4 years have not exactly flocked to the COVID-19 vaccine. As of Aug. 2 – about 6 weeks since the vaccine was authorized for children aged 6 months to 4 years – just 3.8% of those eligible had received at least one dose. Among children aged 5-11 the corresponding number on Aug. 2 was 37.4%, and for those aged 12-17 years it was 70.3%, the CDC data show.
That 3.8% of children aged less than 5 years represents almost 756,000 initial doses. That compares with over 6 million children aged 5-11 years who had received at least one dose through the first 6 weeks of their vaccination experience and over 5 million children aged 12-15, according to the COVID Data Tracker.
, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
After new child cases jumped by 22% during the week of July 15-21, the two successive weeks have produced increases of 3.9% (July 22-29) and 1.2% (July 30-Aug. 4). The latest weekly count from all states and territories still reporting was 96,599, the AAP and CHA said in their weekly COVID report, noting that several states have stopped reporting child cases and that others are reporting every other week.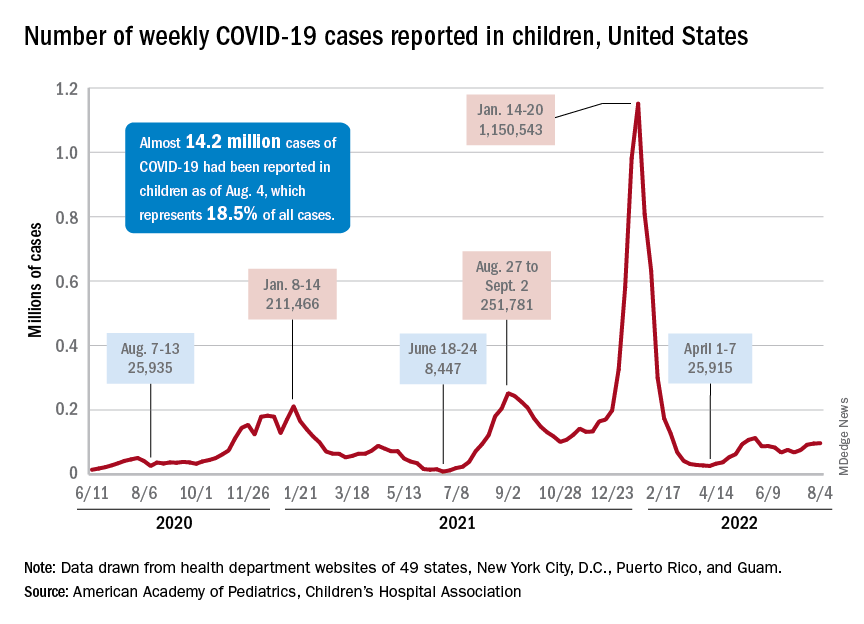
The deceleration in new cases, however, does not apply to emergency department visits and hospital admissions. The proportion of ED visits with diagnosed COVID rose steadily throughout June and July, as 7-day averages went from 2.6% on June 1 to 6.3% on July 31 for children aged 0-11 years, from 2.1% to 3.1% for children aged 12-15, and from 2.4% to 3.5% for 16- to 17-year-olds, according to data from the Centers for Disease Control and Prevention.
The rate of new admissions with confirmed COVID, which reached 0.46 per 100,000 population for children aged 0-17 years on July 30, has more than tripled since early April, when it had fallen to 0.13 per 100,000 in the wake of the Omicron surge, the CDC reported on its COVID Data Tracker.
A smaller but more detailed sample of children from the COVID-19–Associated Hospitalization Network (COVID-NET), which covers nearly 100 counties in 14 states, indicates that the increase in new admissions is occurring almost entirely among children aged 0-4 years, who had a rate of 5.6 per 100,000 for the week of July 17-23, compared with 0.8 per 100,000 for 5- to 11-year-olds and 1.5 per 100,000 for those aged 12-17, the CDC said.
Vaccine’s summer rollout gets lukewarm reception
As a group, children aged 0-4 years have not exactly flocked to the COVID-19 vaccine. As of Aug. 2 – about 6 weeks since the vaccine was authorized for children aged 6 months to 4 years – just 3.8% of those eligible had received at least one dose. Among children aged 5-11 the corresponding number on Aug. 2 was 37.4%, and for those aged 12-17 years it was 70.3%, the CDC data show.
That 3.8% of children aged less than 5 years represents almost 756,000 initial doses. That compares with over 6 million children aged 5-11 years who had received at least one dose through the first 6 weeks of their vaccination experience and over 5 million children aged 12-15, according to the COVID Data Tracker.
Updates on treatment/prevention of VTE in cancer patients
Updated clinical practice guidelines for the treatment and prevention of venous thromboembolism for patients with cancer, including those with cancer and COVID-19, have been released by the International Initiative on Thrombosis and Cancer (ITAC), an academic working group of VTE experts.
“Because patients with cancer have a baseline increased risk of VTE, compared with patients without cancer, the combination of both COVID-19 and cancer – and its effect on VTE risk and treatment – is of concern,” said the authors, led by Dominique Farge, MD, PhD, Nord Universite de Paris.
they added.
The new guidelines were published online in The Lancet Oncology.
“Cancer-associated VTE remains an important clinical problem, associated with increased morbidity and mortality,” Dr. Farge and colleagues observed.
“The ITAC guidelines’ companion free web-based mobile application will assist the practicing clinician with decision making at various levels to provide optimal care of patients with cancer to treat and prevent VTE,” they emphasized. More information is available at itaccme.com.
Cancer patients with COVID
The new section of the guidelines notes that the treatment and prevention of VTE for cancer patients infected with SARS-CoV-2 remain the same as for patients without COVID.
Whether or not cancer patients with COVID-19 are hospitalized, have been discharged, or are ambulatory, they should be assessed for the risk of VTE, as should any other patient. For cancer patients with COVID-19 who are hospitalized, pharmacologic prophylaxis should be given at the same dose and anticoagulant type as for hospitalized cancer patients who do not have COVID-19.
Following discharge, VTE prophylaxis is not advised for cancer patients infected with SARS-CoV-2, and routine primary pharmacologic prophylaxis of VTE for ambulatory patients with COVID-19 is also not recommended, the authors noted.
Initial treatment of established VTE
Initial treatment of established VTE for up to 10 days of anticoagulation should include low-molecular-weight heparin (LMWH) when creatinine clearance is at least 30 mL/min.
“A regimen of LMWH, taken once per day, is recommended unless a twice-per-day regimen is required because of patients’ characteristics,” the authors noted. These characteristics include a high risk of bleeding, moderate renal failure, and the need for technical intervention, including surgery.
If a twice-a-day regimen is required, only enoxaparin at a dose of 1 mg/kg twice daily can be used, the authors cautioned.
For patients with a low risk of gastrointestinal or genitourinary bleeding, rivaroxaban (Xarelto) or apixaban (Eliquis) can be given in the first 10 days, as well as edoxaban (Lixiana). The latter should be started after at least 5 days of parenteral anticoagulation, provided creatinine clearance is at least 30 mL/min.
“Unfractionated heparin as well as fondaparinux (GlaxoSmithKline) can be also used for the initial treatment of established VTE when LMWH or direct oral anticoagulants are contraindicated,” Dr. Farge and colleagues wrote.
Thrombolysis can be considered on a case-by-case basis, although physicians must pay attention to specific contraindications, especially bleeding risk.
“In the initial treatment of VTE, inferior vena cava filters might be considered when anticoagulant treatment is contraindicated or, in the case of pulmonary embolism, when recurrence occurs under optimal anticoagulation,” the authors noted.
Maintenance VTE treatment
For maintenance therapy, which the authors define as early maintenance for up to 6 months and long-term maintenance beyond 6 months, they point out that LMWHs are preferred over vitamin K antagonists for the treatment of VTE when the creatinine clearance is again at least 30 mL/min.
Any of the direct oral anticoagulants (DOAs) – edoxaban, rivaroxaban, or apixaban – is also recommended for the same patients, provided there is no risk of inducing a strong drug-drug interaction or GI absorption is impaired.
However, the DOAs should be used with caution for patients with GI malignancies, especially upper GI cancers, because data show there is an increased risk of GI bleeding with both edoxaban and rivaroxaban.
“LMWH or direct oral anticoagulants should be used for a minimum of 6 months to treat established VTE in patients with cancer,” the authors wrote.
“After 6 months, termination or continuation of anticoagulation (LMWH, direct oral anticoagulants, or vitamin K antagonists) should be based on individual evaluation of the benefit-risk ratio,” they added.
Treatment of VTE recurrence
The guideline authors explain that three options can be considered in the event of VTE recurrence. These include an increase in the LMWH dose by 20%-25%, or a switch to a DOA, or, if patients are taking a DOA, a switch to an LMWH. If the patient is taking a vitamin K antagonist, it can be switched to either an LMWH or a DOA.
For treatment of catheter-related thrombosis, anticoagulant treatment is recommended for a minimum of 3 months and as long as the central venous catheter is in place. In this setting, the LMWHs are recommended.
The central venous catheter can be kept in place if it is functional, well positioned, and is not infected, provided there is good resolution of symptoms under close surveillance while anticoagulants are being administered.
In surgically treated patients, the LMWH, given once a day, to patients with a serum creatinine concentration of at least 30 mL/min can be used to prevent VTE. Alternatively, VTE can be prevented by the use low-dose unfractionated heparin, given three times a day.
“Pharmacological prophylaxis should be started 2-12 h preoperatively and continued for at least 7–10 days,” Dr. Farge and colleagues advised. In this setting, there is insufficient evidence to support the use of fondaparinux or a DOA as an alternative to an LMWH for the prophylaxis of postoperative VTE. “Use of the highest prophylactic dose of LMWH to prevent postoperative VTE in patients with cancer is recommended,” the authors advised.
Furthermore, extended prophylaxis of at least 4 weeks with LMWH is advised to prevent postoperative VTE after major abdominal or pelvic surgery. Mechanical methods are not recommended except when pharmacologic methods are contraindicated. Inferior vena cava filters are also not recommended for routine prophylaxis.
Patients with reduced mobility
For medically treated hospitalized patients with cancer whose mobility is reduced, the authors recommend prophylaxis with either an LMWH or fondaparinux, provided their creatinine clearance is at least 30 mL/min. These patients can also be treated with unfractionated heparin, they add.
In contrast, DOAs are not recommended – at least not routinely – in this setting, the authors cautioned. Primary pharmacologic prophylaxis of VTE with either LMWH or DOAs – either rivaroxaban or apixaban – is indicated in ambulatory patients with locally advanced or metastatic pancreatic cancer who are receiving systemic anticancer therapy, provided they are at low risk of bleeding.
However, primary pharmacologic prophylaxis with LMWH is not recommended outside of a clinical trial for patients with locally advanced or metastatic lung cancer who are undergoing systemic anticancer therapy, even for patients who are at low risk of bleeding.
For ambulatory patients who are receiving systemic anticancer therapy and who are at intermediate risk of VTE, primary prophylaxis with rivaroxaban or apixaban is recommended for those with myeloma who are receiving immunomodulatory therapy plus steroids or other systemic therapies.
In this setting, oral anticoagulants should consist of a vitamin K antagonist, given at low or therapeutic doses, or apixaban, given at prophylactic doses. Alternatively, LMWH, given at prophylactic doses, or low-dose aspirin, given at a dose of 100 mg/day, can be used.
Catheter-related thrombosis
Use of anticoagulation for routine prophylaxis of catheter-related thrombosis is not recommended. Catheters should be inserted on the right side in the jugular vein, and the distal extremity of the central catheter should be located at the junction of the superior vena cava and the right atrium. “In patients requiring central venous catheters, we suggest the use of implanted ports over peripheral inserted central catheter lines,” the authors noted.
The authors described a number of unique situations regarding the treatment of VTE. These situations include patients with a brain tumor, for whom treatment of established VTE should favor either LMWH or a DOA. The authors also recommended the use of LMWH or unfractionated heparin, started postoperatively, for the prevention of VTE for patients undergoing neurosurgery.
In contrast, pharmacologic prophylaxis of VTE in medically treated patients with a brain tumor who are not undergoing neurosurgery is not recommended. “In the presence of severe renal failure...we suggest using unfractionated heparin followed by early vitamin K antagonists (possibly from day 1) or LMWH adjusted to anti-Xa concentration of the treatment of established VTE,” Dr. Farge and colleagues wrote.
Anticoagulant treatment is also recommended for a minimum of 3 months for children with symptomatic catheter-related thrombosis and as long as the central venous catheter is in place. For children with acute lymphoblastic leukemia who are undergoing induction chemotherapy, LMWH is also recommended as thromboprophylaxis.
For children who require a central venous catheter, the authors suggested that physicians use implanted ports over peripherally inserted central lines.
A version of this article first appeared on Medscape.com.
Updated clinical practice guidelines for the treatment and prevention of venous thromboembolism for patients with cancer, including those with cancer and COVID-19, have been released by the International Initiative on Thrombosis and Cancer (ITAC), an academic working group of VTE experts.
“Because patients with cancer have a baseline increased risk of VTE, compared with patients without cancer, the combination of both COVID-19 and cancer – and its effect on VTE risk and treatment – is of concern,” said the authors, led by Dominique Farge, MD, PhD, Nord Universite de Paris.
they added.
The new guidelines were published online in The Lancet Oncology.
“Cancer-associated VTE remains an important clinical problem, associated with increased morbidity and mortality,” Dr. Farge and colleagues observed.
“The ITAC guidelines’ companion free web-based mobile application will assist the practicing clinician with decision making at various levels to provide optimal care of patients with cancer to treat and prevent VTE,” they emphasized. More information is available at itaccme.com.
Cancer patients with COVID
The new section of the guidelines notes that the treatment and prevention of VTE for cancer patients infected with SARS-CoV-2 remain the same as for patients without COVID.
Whether or not cancer patients with COVID-19 are hospitalized, have been discharged, or are ambulatory, they should be assessed for the risk of VTE, as should any other patient. For cancer patients with COVID-19 who are hospitalized, pharmacologic prophylaxis should be given at the same dose and anticoagulant type as for hospitalized cancer patients who do not have COVID-19.
Following discharge, VTE prophylaxis is not advised for cancer patients infected with SARS-CoV-2, and routine primary pharmacologic prophylaxis of VTE for ambulatory patients with COVID-19 is also not recommended, the authors noted.
Initial treatment of established VTE
Initial treatment of established VTE for up to 10 days of anticoagulation should include low-molecular-weight heparin (LMWH) when creatinine clearance is at least 30 mL/min.
“A regimen of LMWH, taken once per day, is recommended unless a twice-per-day regimen is required because of patients’ characteristics,” the authors noted. These characteristics include a high risk of bleeding, moderate renal failure, and the need for technical intervention, including surgery.
If a twice-a-day regimen is required, only enoxaparin at a dose of 1 mg/kg twice daily can be used, the authors cautioned.
For patients with a low risk of gastrointestinal or genitourinary bleeding, rivaroxaban (Xarelto) or apixaban (Eliquis) can be given in the first 10 days, as well as edoxaban (Lixiana). The latter should be started after at least 5 days of parenteral anticoagulation, provided creatinine clearance is at least 30 mL/min.
“Unfractionated heparin as well as fondaparinux (GlaxoSmithKline) can be also used for the initial treatment of established VTE when LMWH or direct oral anticoagulants are contraindicated,” Dr. Farge and colleagues wrote.
Thrombolysis can be considered on a case-by-case basis, although physicians must pay attention to specific contraindications, especially bleeding risk.
“In the initial treatment of VTE, inferior vena cava filters might be considered when anticoagulant treatment is contraindicated or, in the case of pulmonary embolism, when recurrence occurs under optimal anticoagulation,” the authors noted.
Maintenance VTE treatment
For maintenance therapy, which the authors define as early maintenance for up to 6 months and long-term maintenance beyond 6 months, they point out that LMWHs are preferred over vitamin K antagonists for the treatment of VTE when the creatinine clearance is again at least 30 mL/min.
Any of the direct oral anticoagulants (DOAs) – edoxaban, rivaroxaban, or apixaban – is also recommended for the same patients, provided there is no risk of inducing a strong drug-drug interaction or GI absorption is impaired.
However, the DOAs should be used with caution for patients with GI malignancies, especially upper GI cancers, because data show there is an increased risk of GI bleeding with both edoxaban and rivaroxaban.
“LMWH or direct oral anticoagulants should be used for a minimum of 6 months to treat established VTE in patients with cancer,” the authors wrote.
“After 6 months, termination or continuation of anticoagulation (LMWH, direct oral anticoagulants, or vitamin K antagonists) should be based on individual evaluation of the benefit-risk ratio,” they added.
Treatment of VTE recurrence
The guideline authors explain that three options can be considered in the event of VTE recurrence. These include an increase in the LMWH dose by 20%-25%, or a switch to a DOA, or, if patients are taking a DOA, a switch to an LMWH. If the patient is taking a vitamin K antagonist, it can be switched to either an LMWH or a DOA.
For treatment of catheter-related thrombosis, anticoagulant treatment is recommended for a minimum of 3 months and as long as the central venous catheter is in place. In this setting, the LMWHs are recommended.
The central venous catheter can be kept in place if it is functional, well positioned, and is not infected, provided there is good resolution of symptoms under close surveillance while anticoagulants are being administered.
In surgically treated patients, the LMWH, given once a day, to patients with a serum creatinine concentration of at least 30 mL/min can be used to prevent VTE. Alternatively, VTE can be prevented by the use low-dose unfractionated heparin, given three times a day.
“Pharmacological prophylaxis should be started 2-12 h preoperatively and continued for at least 7–10 days,” Dr. Farge and colleagues advised. In this setting, there is insufficient evidence to support the use of fondaparinux or a DOA as an alternative to an LMWH for the prophylaxis of postoperative VTE. “Use of the highest prophylactic dose of LMWH to prevent postoperative VTE in patients with cancer is recommended,” the authors advised.
Furthermore, extended prophylaxis of at least 4 weeks with LMWH is advised to prevent postoperative VTE after major abdominal or pelvic surgery. Mechanical methods are not recommended except when pharmacologic methods are contraindicated. Inferior vena cava filters are also not recommended for routine prophylaxis.
Patients with reduced mobility
For medically treated hospitalized patients with cancer whose mobility is reduced, the authors recommend prophylaxis with either an LMWH or fondaparinux, provided their creatinine clearance is at least 30 mL/min. These patients can also be treated with unfractionated heparin, they add.
In contrast, DOAs are not recommended – at least not routinely – in this setting, the authors cautioned. Primary pharmacologic prophylaxis of VTE with either LMWH or DOAs – either rivaroxaban or apixaban – is indicated in ambulatory patients with locally advanced or metastatic pancreatic cancer who are receiving systemic anticancer therapy, provided they are at low risk of bleeding.
However, primary pharmacologic prophylaxis with LMWH is not recommended outside of a clinical trial for patients with locally advanced or metastatic lung cancer who are undergoing systemic anticancer therapy, even for patients who are at low risk of bleeding.
For ambulatory patients who are receiving systemic anticancer therapy and who are at intermediate risk of VTE, primary prophylaxis with rivaroxaban or apixaban is recommended for those with myeloma who are receiving immunomodulatory therapy plus steroids or other systemic therapies.
In this setting, oral anticoagulants should consist of a vitamin K antagonist, given at low or therapeutic doses, or apixaban, given at prophylactic doses. Alternatively, LMWH, given at prophylactic doses, or low-dose aspirin, given at a dose of 100 mg/day, can be used.
Catheter-related thrombosis
Use of anticoagulation for routine prophylaxis of catheter-related thrombosis is not recommended. Catheters should be inserted on the right side in the jugular vein, and the distal extremity of the central catheter should be located at the junction of the superior vena cava and the right atrium. “In patients requiring central venous catheters, we suggest the use of implanted ports over peripheral inserted central catheter lines,” the authors noted.
The authors described a number of unique situations regarding the treatment of VTE. These situations include patients with a brain tumor, for whom treatment of established VTE should favor either LMWH or a DOA. The authors also recommended the use of LMWH or unfractionated heparin, started postoperatively, for the prevention of VTE for patients undergoing neurosurgery.
In contrast, pharmacologic prophylaxis of VTE in medically treated patients with a brain tumor who are not undergoing neurosurgery is not recommended. “In the presence of severe renal failure...we suggest using unfractionated heparin followed by early vitamin K antagonists (possibly from day 1) or LMWH adjusted to anti-Xa concentration of the treatment of established VTE,” Dr. Farge and colleagues wrote.
Anticoagulant treatment is also recommended for a minimum of 3 months for children with symptomatic catheter-related thrombosis and as long as the central venous catheter is in place. For children with acute lymphoblastic leukemia who are undergoing induction chemotherapy, LMWH is also recommended as thromboprophylaxis.
For children who require a central venous catheter, the authors suggested that physicians use implanted ports over peripherally inserted central lines.
A version of this article first appeared on Medscape.com.
Updated clinical practice guidelines for the treatment and prevention of venous thromboembolism for patients with cancer, including those with cancer and COVID-19, have been released by the International Initiative on Thrombosis and Cancer (ITAC), an academic working group of VTE experts.
“Because patients with cancer have a baseline increased risk of VTE, compared with patients without cancer, the combination of both COVID-19 and cancer – and its effect on VTE risk and treatment – is of concern,” said the authors, led by Dominique Farge, MD, PhD, Nord Universite de Paris.
they added.
The new guidelines were published online in The Lancet Oncology.
“Cancer-associated VTE remains an important clinical problem, associated with increased morbidity and mortality,” Dr. Farge and colleagues observed.
“The ITAC guidelines’ companion free web-based mobile application will assist the practicing clinician with decision making at various levels to provide optimal care of patients with cancer to treat and prevent VTE,” they emphasized. More information is available at itaccme.com.
Cancer patients with COVID
The new section of the guidelines notes that the treatment and prevention of VTE for cancer patients infected with SARS-CoV-2 remain the same as for patients without COVID.
Whether or not cancer patients with COVID-19 are hospitalized, have been discharged, or are ambulatory, they should be assessed for the risk of VTE, as should any other patient. For cancer patients with COVID-19 who are hospitalized, pharmacologic prophylaxis should be given at the same dose and anticoagulant type as for hospitalized cancer patients who do not have COVID-19.
Following discharge, VTE prophylaxis is not advised for cancer patients infected with SARS-CoV-2, and routine primary pharmacologic prophylaxis of VTE for ambulatory patients with COVID-19 is also not recommended, the authors noted.
Initial treatment of established VTE
Initial treatment of established VTE for up to 10 days of anticoagulation should include low-molecular-weight heparin (LMWH) when creatinine clearance is at least 30 mL/min.
“A regimen of LMWH, taken once per day, is recommended unless a twice-per-day regimen is required because of patients’ characteristics,” the authors noted. These characteristics include a high risk of bleeding, moderate renal failure, and the need for technical intervention, including surgery.
If a twice-a-day regimen is required, only enoxaparin at a dose of 1 mg/kg twice daily can be used, the authors cautioned.
For patients with a low risk of gastrointestinal or genitourinary bleeding, rivaroxaban (Xarelto) or apixaban (Eliquis) can be given in the first 10 days, as well as edoxaban (Lixiana). The latter should be started after at least 5 days of parenteral anticoagulation, provided creatinine clearance is at least 30 mL/min.
“Unfractionated heparin as well as fondaparinux (GlaxoSmithKline) can be also used for the initial treatment of established VTE when LMWH or direct oral anticoagulants are contraindicated,” Dr. Farge and colleagues wrote.
Thrombolysis can be considered on a case-by-case basis, although physicians must pay attention to specific contraindications, especially bleeding risk.
“In the initial treatment of VTE, inferior vena cava filters might be considered when anticoagulant treatment is contraindicated or, in the case of pulmonary embolism, when recurrence occurs under optimal anticoagulation,” the authors noted.
Maintenance VTE treatment
For maintenance therapy, which the authors define as early maintenance for up to 6 months and long-term maintenance beyond 6 months, they point out that LMWHs are preferred over vitamin K antagonists for the treatment of VTE when the creatinine clearance is again at least 30 mL/min.
Any of the direct oral anticoagulants (DOAs) – edoxaban, rivaroxaban, or apixaban – is also recommended for the same patients, provided there is no risk of inducing a strong drug-drug interaction or GI absorption is impaired.
However, the DOAs should be used with caution for patients with GI malignancies, especially upper GI cancers, because data show there is an increased risk of GI bleeding with both edoxaban and rivaroxaban.
“LMWH or direct oral anticoagulants should be used for a minimum of 6 months to treat established VTE in patients with cancer,” the authors wrote.
“After 6 months, termination or continuation of anticoagulation (LMWH, direct oral anticoagulants, or vitamin K antagonists) should be based on individual evaluation of the benefit-risk ratio,” they added.
Treatment of VTE recurrence
The guideline authors explain that three options can be considered in the event of VTE recurrence. These include an increase in the LMWH dose by 20%-25%, or a switch to a DOA, or, if patients are taking a DOA, a switch to an LMWH. If the patient is taking a vitamin K antagonist, it can be switched to either an LMWH or a DOA.
For treatment of catheter-related thrombosis, anticoagulant treatment is recommended for a minimum of 3 months and as long as the central venous catheter is in place. In this setting, the LMWHs are recommended.
The central venous catheter can be kept in place if it is functional, well positioned, and is not infected, provided there is good resolution of symptoms under close surveillance while anticoagulants are being administered.
In surgically treated patients, the LMWH, given once a day, to patients with a serum creatinine concentration of at least 30 mL/min can be used to prevent VTE. Alternatively, VTE can be prevented by the use low-dose unfractionated heparin, given three times a day.
“Pharmacological prophylaxis should be started 2-12 h preoperatively and continued for at least 7–10 days,” Dr. Farge and colleagues advised. In this setting, there is insufficient evidence to support the use of fondaparinux or a DOA as an alternative to an LMWH for the prophylaxis of postoperative VTE. “Use of the highest prophylactic dose of LMWH to prevent postoperative VTE in patients with cancer is recommended,” the authors advised.
Furthermore, extended prophylaxis of at least 4 weeks with LMWH is advised to prevent postoperative VTE after major abdominal or pelvic surgery. Mechanical methods are not recommended except when pharmacologic methods are contraindicated. Inferior vena cava filters are also not recommended for routine prophylaxis.
Patients with reduced mobility
For medically treated hospitalized patients with cancer whose mobility is reduced, the authors recommend prophylaxis with either an LMWH or fondaparinux, provided their creatinine clearance is at least 30 mL/min. These patients can also be treated with unfractionated heparin, they add.
In contrast, DOAs are not recommended – at least not routinely – in this setting, the authors cautioned. Primary pharmacologic prophylaxis of VTE with either LMWH or DOAs – either rivaroxaban or apixaban – is indicated in ambulatory patients with locally advanced or metastatic pancreatic cancer who are receiving systemic anticancer therapy, provided they are at low risk of bleeding.
However, primary pharmacologic prophylaxis with LMWH is not recommended outside of a clinical trial for patients with locally advanced or metastatic lung cancer who are undergoing systemic anticancer therapy, even for patients who are at low risk of bleeding.
For ambulatory patients who are receiving systemic anticancer therapy and who are at intermediate risk of VTE, primary prophylaxis with rivaroxaban or apixaban is recommended for those with myeloma who are receiving immunomodulatory therapy plus steroids or other systemic therapies.
In this setting, oral anticoagulants should consist of a vitamin K antagonist, given at low or therapeutic doses, or apixaban, given at prophylactic doses. Alternatively, LMWH, given at prophylactic doses, or low-dose aspirin, given at a dose of 100 mg/day, can be used.
Catheter-related thrombosis
Use of anticoagulation for routine prophylaxis of catheter-related thrombosis is not recommended. Catheters should be inserted on the right side in the jugular vein, and the distal extremity of the central catheter should be located at the junction of the superior vena cava and the right atrium. “In patients requiring central venous catheters, we suggest the use of implanted ports over peripheral inserted central catheter lines,” the authors noted.
The authors described a number of unique situations regarding the treatment of VTE. These situations include patients with a brain tumor, for whom treatment of established VTE should favor either LMWH or a DOA. The authors also recommended the use of LMWH or unfractionated heparin, started postoperatively, for the prevention of VTE for patients undergoing neurosurgery.
In contrast, pharmacologic prophylaxis of VTE in medically treated patients with a brain tumor who are not undergoing neurosurgery is not recommended. “In the presence of severe renal failure...we suggest using unfractionated heparin followed by early vitamin K antagonists (possibly from day 1) or LMWH adjusted to anti-Xa concentration of the treatment of established VTE,” Dr. Farge and colleagues wrote.
Anticoagulant treatment is also recommended for a minimum of 3 months for children with symptomatic catheter-related thrombosis and as long as the central venous catheter is in place. For children with acute lymphoblastic leukemia who are undergoing induction chemotherapy, LMWH is also recommended as thromboprophylaxis.
For children who require a central venous catheter, the authors suggested that physicians use implanted ports over peripherally inserted central lines.
A version of this article first appeared on Medscape.com.
FROM THE LANCET ONCOLOGY
FDA acts against sales of unapproved mole and skin tag products on Amazon, other sites
according to a press release issued on Aug. 9.
In addition to Amazon.com, the other two companies are Ariella Naturals, and Justified Laboratories.
Currently, no over-the-counter products are FDA-approved for the at-home removal of moles and skin tags, and use of unapproved products could be dangerous to consumers, according to the statement. These products may be sold as ointments, gels, sticks, or liquids, and may contain high concentrations of salicylic acid or other harmful ingredients. Introducing unapproved products in to interstate commerce violates the Federal Food, Drug, and Cosmetic Act.
Two products sold on Amazon are the “Deisana Skin Tag Remover, Mole Remover and Repair Gel Set” and “Skincell Mole Skin Tag Corrector Serum,” according to the letter sent to Amazon.
The warning letters alert the three companies that they have 15 days from receipt to address any violations. However, warning letters are not a final FDA action, according to the statement.
“The agency’s rigorous surveillance works to identify threats to public health and stop these products from reaching our communities,” Donald D. Ashley, JD, director of the Office of Compliance in the FDA’s Center for Drug Evaluation and Research, said in the press release. “This includes where online retailers like Amazon are involved in the interstate sale of unapproved drug products. We will continue to work diligently to ensure that online retailers do not sell products that violate federal law,” he added.
The statement emphasized that moles should be evaluated by a health care professional, as attempts at self-diagnosis and at-home treatment could lead to a delayed cancer diagnosis, and potentially to cancer progression.
Products marketed to consumers for at-home removal of moles, skin tags, and other skin lesions could cause injuries, infections, and scarring, according to a related consumer update first posted by the FDA in June, which was updated after the warning letters were sent out.
Consumers and health care professionals are encouraged to report any adverse events related to mole removal or skin tag removal products to the agency’s MedWatch Adverse Event Reporting program.
The FDA also offers an online guide, BeSafeRx, with advice for consumers about potential risks of using online pharmacies and how to do so safely.
according to a press release issued on Aug. 9.
In addition to Amazon.com, the other two companies are Ariella Naturals, and Justified Laboratories.
Currently, no over-the-counter products are FDA-approved for the at-home removal of moles and skin tags, and use of unapproved products could be dangerous to consumers, according to the statement. These products may be sold as ointments, gels, sticks, or liquids, and may contain high concentrations of salicylic acid or other harmful ingredients. Introducing unapproved products in to interstate commerce violates the Federal Food, Drug, and Cosmetic Act.
Two products sold on Amazon are the “Deisana Skin Tag Remover, Mole Remover and Repair Gel Set” and “Skincell Mole Skin Tag Corrector Serum,” according to the letter sent to Amazon.
The warning letters alert the three companies that they have 15 days from receipt to address any violations. However, warning letters are not a final FDA action, according to the statement.
“The agency’s rigorous surveillance works to identify threats to public health and stop these products from reaching our communities,” Donald D. Ashley, JD, director of the Office of Compliance in the FDA’s Center for Drug Evaluation and Research, said in the press release. “This includes where online retailers like Amazon are involved in the interstate sale of unapproved drug products. We will continue to work diligently to ensure that online retailers do not sell products that violate federal law,” he added.
The statement emphasized that moles should be evaluated by a health care professional, as attempts at self-diagnosis and at-home treatment could lead to a delayed cancer diagnosis, and potentially to cancer progression.
Products marketed to consumers for at-home removal of moles, skin tags, and other skin lesions could cause injuries, infections, and scarring, according to a related consumer update first posted by the FDA in June, which was updated after the warning letters were sent out.
Consumers and health care professionals are encouraged to report any adverse events related to mole removal or skin tag removal products to the agency’s MedWatch Adverse Event Reporting program.
The FDA also offers an online guide, BeSafeRx, with advice for consumers about potential risks of using online pharmacies and how to do so safely.
according to a press release issued on Aug. 9.
In addition to Amazon.com, the other two companies are Ariella Naturals, and Justified Laboratories.
Currently, no over-the-counter products are FDA-approved for the at-home removal of moles and skin tags, and use of unapproved products could be dangerous to consumers, according to the statement. These products may be sold as ointments, gels, sticks, or liquids, and may contain high concentrations of salicylic acid or other harmful ingredients. Introducing unapproved products in to interstate commerce violates the Federal Food, Drug, and Cosmetic Act.
Two products sold on Amazon are the “Deisana Skin Tag Remover, Mole Remover and Repair Gel Set” and “Skincell Mole Skin Tag Corrector Serum,” according to the letter sent to Amazon.
The warning letters alert the three companies that they have 15 days from receipt to address any violations. However, warning letters are not a final FDA action, according to the statement.
“The agency’s rigorous surveillance works to identify threats to public health and stop these products from reaching our communities,” Donald D. Ashley, JD, director of the Office of Compliance in the FDA’s Center for Drug Evaluation and Research, said in the press release. “This includes where online retailers like Amazon are involved in the interstate sale of unapproved drug products. We will continue to work diligently to ensure that online retailers do not sell products that violate federal law,” he added.
The statement emphasized that moles should be evaluated by a health care professional, as attempts at self-diagnosis and at-home treatment could lead to a delayed cancer diagnosis, and potentially to cancer progression.
Products marketed to consumers for at-home removal of moles, skin tags, and other skin lesions could cause injuries, infections, and scarring, according to a related consumer update first posted by the FDA in June, which was updated after the warning letters were sent out.
Consumers and health care professionals are encouraged to report any adverse events related to mole removal or skin tag removal products to the agency’s MedWatch Adverse Event Reporting program.
The FDA also offers an online guide, BeSafeRx, with advice for consumers about potential risks of using online pharmacies and how to do so safely.
Mysterious cases of illness with an unusual cause
So begins the search for evidence.
No relations or common journeys
Between March and July 2021, cases of the bacterial infectious disease sprang up in Georgia, Kansas, Minnesota, and Texas, with the disease being fatal for two of those affected. Usually, cases of melioidosis occur in the United States after traveling to regions where the pathogen is prevalent. However, none of the patients had undertaken any previous international travel.
When the genomes of the bacterial strains (Burkholderia pseudomallei) were sequenced, they showed a high level of concordance, suggesting a common source of infection. The bacterial strain is similar to those that are found in Southeast Asia above all. An imported product from there was taken into consideration as the trigger.
The Centers for Disease Control and Prevention examined blood samples from the patients, as well as samples from the soil, water, food, and household items around their homes.
Aroma spray as a trigger
In October, the cause of the melioidosis was finally identified in the house of the patient from Georgia: an aromatherapy spray. The genetic fingerprint of the bacterial strain matched with that from the other patients. The common trigger was thus discovered.
The contaminated spray, with a lavender-chamomile scent for room fragrancing, was sold between February and October in some branches of Walmart, as well as in their online store. The product was therefore recalled and it was checked whether the ingredients were also being used in other products.
The CDC requested physicians to also take melioidosis into account if they were presented with acute bacterial infections that did not respond to normal antibiotics and to inquire whether the affected room spray had been used.
More information about melioidosis
Melioidosis is an infectious disease affecting humans and animals. The trigger is the bacteria B pseudomallei. The disease appears predominantly in tropical regions, especially in Southeast Asia and northern Australia.
Transmission
The bacteria can be found in contaminated water and soil. It is disseminated between humans and animals through direct contact with the infectious source, such as through inhaling dust particles or water droplets, or through consuming contaminated water or food. Human-to-human transmission is extremely rare. Recently however, tropical saltwater fish were identified as potential carriers.
Symptoms
Melioidosis has a wide range of symptoms, which can lead to its being confused with other diseases such as tuberculosis or other forms of pneumonia. There are different forms of the disease, each with different symptoms.
- Localized infection: localized pain and swelling, fever, ulceration, and abscess.
- Pulmonary infection: cough, chest pain, high fever, headaches, and loss of appetite
- Bacteremia: fever, headaches, breathing problems, stomach discomfort, joint pain, and disorientation.
- Disseminated infection: fever, weight loss, stomach or chest pain, muscle or joint pain, headaches, central nervous system infections, and epileptic seizures.
The incubation time is not clearly defined and can be from 1 day to several years; however, the symptoms mostly emerge 2-4 weeks after exposure. The risk factors include diabetes, high alcohol consumption, chronic pulmonary or kidney disease, and immunodeficiencies.
Diagnosis based on the symptoms is often difficult since the clinical picture is similar to other, more common conditions.
Therapy
If the melioidosis is identified as such, it can be treated with only mildly effective antibiotics, since it has a natural resistance to many commonly used antibiotics. The type of infection and the course of treatment also affects the long-term outcome. Without treatment, 90% of the infections have a fatal outcome. With appropriate treatment, the mortality rate still lies at 40%.
Therapy generally begins with intravenous antibiotic therapy for at least 2-8 weeks (ceftazidime or meropenem). Oral antibiotic therapy then follows for 3-6 months (trimethoprim-sulfamethoxazole or amoxicillin/clavulanic acid). If the patient is allergic to penicillin, alternative antibiotics can be used.
Use as a bioweapon
The CDC classifies B. pseudomallei as a potential pathogen for biological attack (class-B candidate). The agency lists the potential reasons for use as a bioweapon as:
- The pathogen can be found naturally in certain regions.
- The triggered disease can take a serious course and ultimately be fatal without appropriate therapy.
- In the past, the United States has used similar pathogens in wars as bioweapons.
In a potential attack, the pathogen could be spread through air, water, or food, and by doing so, many people would be exposed. Any contact with the bacteria can result in melioidosis. As the bacteria cannot be seen, smelled, or tasted, the biological attack would not be recognized for some time. A certain amount of time can also pass until the pathogen is identified, once fever and respiratory diseases have developed.
In such an emergency, the CDC would collaborate with other federal and local authorities to supply specialized testing laboratories and provide the public with information.
This content was translated from Coliquio. A version appeared on Medscape.com.
So begins the search for evidence.
No relations or common journeys
Between March and July 2021, cases of the bacterial infectious disease sprang up in Georgia, Kansas, Minnesota, and Texas, with the disease being fatal for two of those affected. Usually, cases of melioidosis occur in the United States after traveling to regions where the pathogen is prevalent. However, none of the patients had undertaken any previous international travel.
When the genomes of the bacterial strains (Burkholderia pseudomallei) were sequenced, they showed a high level of concordance, suggesting a common source of infection. The bacterial strain is similar to those that are found in Southeast Asia above all. An imported product from there was taken into consideration as the trigger.
The Centers for Disease Control and Prevention examined blood samples from the patients, as well as samples from the soil, water, food, and household items around their homes.
Aroma spray as a trigger
In October, the cause of the melioidosis was finally identified in the house of the patient from Georgia: an aromatherapy spray. The genetic fingerprint of the bacterial strain matched with that from the other patients. The common trigger was thus discovered.
The contaminated spray, with a lavender-chamomile scent for room fragrancing, was sold between February and October in some branches of Walmart, as well as in their online store. The product was therefore recalled and it was checked whether the ingredients were also being used in other products.
The CDC requested physicians to also take melioidosis into account if they were presented with acute bacterial infections that did not respond to normal antibiotics and to inquire whether the affected room spray had been used.
More information about melioidosis
Melioidosis is an infectious disease affecting humans and animals. The trigger is the bacteria B pseudomallei. The disease appears predominantly in tropical regions, especially in Southeast Asia and northern Australia.
Transmission
The bacteria can be found in contaminated water and soil. It is disseminated between humans and animals through direct contact with the infectious source, such as through inhaling dust particles or water droplets, or through consuming contaminated water or food. Human-to-human transmission is extremely rare. Recently however, tropical saltwater fish were identified as potential carriers.
Symptoms
Melioidosis has a wide range of symptoms, which can lead to its being confused with other diseases such as tuberculosis or other forms of pneumonia. There are different forms of the disease, each with different symptoms.
- Localized infection: localized pain and swelling, fever, ulceration, and abscess.
- Pulmonary infection: cough, chest pain, high fever, headaches, and loss of appetite
- Bacteremia: fever, headaches, breathing problems, stomach discomfort, joint pain, and disorientation.
- Disseminated infection: fever, weight loss, stomach or chest pain, muscle or joint pain, headaches, central nervous system infections, and epileptic seizures.
The incubation time is not clearly defined and can be from 1 day to several years; however, the symptoms mostly emerge 2-4 weeks after exposure. The risk factors include diabetes, high alcohol consumption, chronic pulmonary or kidney disease, and immunodeficiencies.
Diagnosis based on the symptoms is often difficult since the clinical picture is similar to other, more common conditions.
Therapy
If the melioidosis is identified as such, it can be treated with only mildly effective antibiotics, since it has a natural resistance to many commonly used antibiotics. The type of infection and the course of treatment also affects the long-term outcome. Without treatment, 90% of the infections have a fatal outcome. With appropriate treatment, the mortality rate still lies at 40%.
Therapy generally begins with intravenous antibiotic therapy for at least 2-8 weeks (ceftazidime or meropenem). Oral antibiotic therapy then follows for 3-6 months (trimethoprim-sulfamethoxazole or amoxicillin/clavulanic acid). If the patient is allergic to penicillin, alternative antibiotics can be used.
Use as a bioweapon
The CDC classifies B. pseudomallei as a potential pathogen for biological attack (class-B candidate). The agency lists the potential reasons for use as a bioweapon as:
- The pathogen can be found naturally in certain regions.
- The triggered disease can take a serious course and ultimately be fatal without appropriate therapy.
- In the past, the United States has used similar pathogens in wars as bioweapons.
In a potential attack, the pathogen could be spread through air, water, or food, and by doing so, many people would be exposed. Any contact with the bacteria can result in melioidosis. As the bacteria cannot be seen, smelled, or tasted, the biological attack would not be recognized for some time. A certain amount of time can also pass until the pathogen is identified, once fever and respiratory diseases have developed.
In such an emergency, the CDC would collaborate with other federal and local authorities to supply specialized testing laboratories and provide the public with information.
This content was translated from Coliquio. A version appeared on Medscape.com.
So begins the search for evidence.
No relations or common journeys
Between March and July 2021, cases of the bacterial infectious disease sprang up in Georgia, Kansas, Minnesota, and Texas, with the disease being fatal for two of those affected. Usually, cases of melioidosis occur in the United States after traveling to regions where the pathogen is prevalent. However, none of the patients had undertaken any previous international travel.
When the genomes of the bacterial strains (Burkholderia pseudomallei) were sequenced, they showed a high level of concordance, suggesting a common source of infection. The bacterial strain is similar to those that are found in Southeast Asia above all. An imported product from there was taken into consideration as the trigger.
The Centers for Disease Control and Prevention examined blood samples from the patients, as well as samples from the soil, water, food, and household items around their homes.
Aroma spray as a trigger
In October, the cause of the melioidosis was finally identified in the house of the patient from Georgia: an aromatherapy spray. The genetic fingerprint of the bacterial strain matched with that from the other patients. The common trigger was thus discovered.
The contaminated spray, with a lavender-chamomile scent for room fragrancing, was sold between February and October in some branches of Walmart, as well as in their online store. The product was therefore recalled and it was checked whether the ingredients were also being used in other products.
The CDC requested physicians to also take melioidosis into account if they were presented with acute bacterial infections that did not respond to normal antibiotics and to inquire whether the affected room spray had been used.
More information about melioidosis
Melioidosis is an infectious disease affecting humans and animals. The trigger is the bacteria B pseudomallei. The disease appears predominantly in tropical regions, especially in Southeast Asia and northern Australia.
Transmission
The bacteria can be found in contaminated water and soil. It is disseminated between humans and animals through direct contact with the infectious source, such as through inhaling dust particles or water droplets, or through consuming contaminated water or food. Human-to-human transmission is extremely rare. Recently however, tropical saltwater fish were identified as potential carriers.
Symptoms
Melioidosis has a wide range of symptoms, which can lead to its being confused with other diseases such as tuberculosis or other forms of pneumonia. There are different forms of the disease, each with different symptoms.
- Localized infection: localized pain and swelling, fever, ulceration, and abscess.
- Pulmonary infection: cough, chest pain, high fever, headaches, and loss of appetite
- Bacteremia: fever, headaches, breathing problems, stomach discomfort, joint pain, and disorientation.
- Disseminated infection: fever, weight loss, stomach or chest pain, muscle or joint pain, headaches, central nervous system infections, and epileptic seizures.
The incubation time is not clearly defined and can be from 1 day to several years; however, the symptoms mostly emerge 2-4 weeks after exposure. The risk factors include diabetes, high alcohol consumption, chronic pulmonary or kidney disease, and immunodeficiencies.
Diagnosis based on the symptoms is often difficult since the clinical picture is similar to other, more common conditions.
Therapy
If the melioidosis is identified as such, it can be treated with only mildly effective antibiotics, since it has a natural resistance to many commonly used antibiotics. The type of infection and the course of treatment also affects the long-term outcome. Without treatment, 90% of the infections have a fatal outcome. With appropriate treatment, the mortality rate still lies at 40%.
Therapy generally begins with intravenous antibiotic therapy for at least 2-8 weeks (ceftazidime or meropenem). Oral antibiotic therapy then follows for 3-6 months (trimethoprim-sulfamethoxazole or amoxicillin/clavulanic acid). If the patient is allergic to penicillin, alternative antibiotics can be used.
Use as a bioweapon
The CDC classifies B. pseudomallei as a potential pathogen for biological attack (class-B candidate). The agency lists the potential reasons for use as a bioweapon as:
- The pathogen can be found naturally in certain regions.
- The triggered disease can take a serious course and ultimately be fatal without appropriate therapy.
- In the past, the United States has used similar pathogens in wars as bioweapons.
In a potential attack, the pathogen could be spread through air, water, or food, and by doing so, many people would be exposed. Any contact with the bacteria can result in melioidosis. As the bacteria cannot be seen, smelled, or tasted, the biological attack would not be recognized for some time. A certain amount of time can also pass until the pathogen is identified, once fever and respiratory diseases have developed.
In such an emergency, the CDC would collaborate with other federal and local authorities to supply specialized testing laboratories and provide the public with information.
This content was translated from Coliquio. A version appeared on Medscape.com.
CV admissions on the rise in Americans with cancer
Although cardiovascular disease (CVD) is known to often strike the mortal blow in patients with cancer, a national analysis puts in stark relief the burden of CV-related hospitalizations in this vulnerable population.
, whereas admissions fell 10.9% among those without cancer.
Admissions increased steadily across all cancer types, except prostate cancer, with heart failure being the most common reason for admission.
“Hospital admissions is really important because we know that the size of this group is increasing, given that they live longer and many of the treatments that we offer cause cardiovascular disease or increase the risk of having cardiovascular events. So, from a health care planning perspective, I think it’s really important to see what the burden is likely to be in the next few years,” senior author Mamas Mamas, MD, Keele University, England, told this news organization.
For physicians and the wider population, he said, the findings underscore the need to shift the conversation from saying that patients with cancer are at increased CVD risk to asking how to mitigate this risk. “Because I would say that this increase in cardiovascular admissions, that’s a failure from a preventative perspective.”
The study was published in the European Heart Journal: Quality of Care & Clinical Outcomes.
Individual cancer types
The researchers, led by Ofer Kobo, MD, also with Keele University, used the National Inpatient Sample to identify 42.5 million weighted cases of CV admissions for acute myocardial infarction (AMI), pulmonary embolism, ischemic stroke, heart failure, atrial fibrillation (AFib) or atrial flutter, and intracranial hemorrhage from January 2004 to December 2017. Of these, 1.9 million had a record of cancer.
Patients with cancer were older; had a higher prevalence of valvular disease, anemia, and coagulopathy; and had a lower prevalence of hypertension, diabetes mellitus, and obesity than did patients without cancer.
The most common cancer type was hematologic cancers (26.1%), followed by lung (18.7%), gastrointestinal (12.4%), prostate (11.6%), breast (6.7%), and other in 24.4%.
The admission rate increased across all six admission causes – between 7% for AMI and ischemic stroke and 46% for AFib.
Heart failure was the chief reason for admission among all patients. Annual rates per 100,000 U.S. population increased in patients with cancer (from 13.6 to 16.6; P for trend = .02) and declined in those without (from 352.2 to 349.8; P for trend < .001).
“In the past, patients would be started on medications, and perhaps the importance of monitoring [left ventricular] LV function wasn’t as widely known, whereas now we’re much more aggressive in looking at it and much more aggressive at trying to prevent it,” Dr. Mamas said. “But even with this greater identification and attempting to modify regimens, we’re still getting quite substantial increases in heart failure admissions in this population. And what really surprised me is that it wasn’t just in the breast cancer population, but it was nearly across the board.”
He noted that patients are at highest risk from CV events within the first 2 years of cancer diagnosis. “So that’s really the time where you’ve got to be really aggressive in looking and working up their cardiovascular profile.”
Patients with hematologic cancers (9.7-13.5), lung (7.4-8.9), and gastrointestinal cancer (4.6-6.3) had the highest crude admission rates of CV hospitalizations per 100,000 U.S. population.
The CV admission rate went up from 2.5 to 3.7 per 100,000 U.S. population for breast cancer, and in prostate cancer, the rate dropped from 5.8 to 4.8 per 100,000 U.S. population.
Of note, patients with hematologic cancers also had the highest rate of heart failure hospitalization across all cancer types, which, coupled with their increasing admission rates, likely reflects their exposure to a “constellation of cardiotoxic therapies” as well as pathologic processes related to the cancers themselves, the authors suggest.
In-hospital mortality rates were higher among patients with cancer than those without, ranging from 5% for patients with breast cancer to 9.6% for patients with lung cancer versus 4.2% for those without cancer.
Among patients with cancer, the odds ratio for mortality was highest in those admitted with AFib (4.43), followed by pulmonary embolism (2.36), AMI (2.31), ischemic stroke (2.29), and heart failure (2.24).
In line with prior work and general population trends, in-hospital deaths in primary CV admissions trended lower among patients with cancer over the study period.
Mitigating risk
Commenting on the study, Joerg Herrmann, MD, director of the cardio-oncology clinic at Mayo Clinic, Rochester, Minn., said that the data are “extremely important” because they reflect admissions during a new era of cancer therapy. “Targeted therapies all came out about the turn of the millennium, so we’re not really looking at cancer patients treated with only old and ancient strategies.”
This may be one reason for the increased admissions, but because the study lacked information on specific cancer treatments and the date of cancer diagnosis, it’s not possible to tease out whether the uptick is related to cardiotoxicity or because the oncology outcomes have improved so much that this is a growing population, he said.
One clear implication, however, is that whoever is working on the hospital service will see more patients with a cancer diagnosis, Dr. Herrmann observed.
“Though some may have tried to maybe not get involved with this topic as much, it really calls for some broader scope to get familiar with this very entity,” he said. “And that plays out, in particular, in those patients with a diagnosis of active cancer.”
Dr. Herrmann and colleagues previously reported that patients with active leukemia or lymphoma who were hospitalized with acute coronary syndrome were less likely to receive guideline-directed therapies, even at the Mayo Clinic.
Similarly, a 2020 report by Dr. Mamas and colleagues found that patients with a variety of active cancers derived similar benefit from primary percutaneous coronary intervention for ST-segment–elevation MI as those without cancer but received the treatment less commonly.
Although there’s a greater appreciation that patients with cancer benefit equally from aggressive treatment, much more can be done to mitigate CV risk, Dr. Mamas noted. Valuable coronary information captured by MRI and CT done as part of the cancer investigation is often overlooked. For example, “we know that breast calcification and vascular calcification in the breast are very strong predictors of cardiovascular outcomes and yet people aren’t using this information.”
There are numerous shared risk factors in the development of cancer and coronary artery disease, and patients with cancer often have much worse CV risk profiles but aren’t routinely risk stratified from a CV perspective, he said.
Dr. Mamas said that his team is also studying whether CVD risk prediction tools like the Framingham Risk Score, which were derived from noncancer populations, work as well in patients with cancer. “Often, when you look at the performance of these tools in populations that weren’t covered, they’re much worse.”
“A lot of cancer survivors worry about the recurrence of their cancer and will religiously go and have repeated scans, religiously check themselves, and have all these investigations but don’t think about the actual risk that is greater for them, which is cardiovascular risk,” he said.
The authors report no study funding or relevant financial relationships.
A version of this article first appeared on Medscape.com.
Although cardiovascular disease (CVD) is known to often strike the mortal blow in patients with cancer, a national analysis puts in stark relief the burden of CV-related hospitalizations in this vulnerable population.
, whereas admissions fell 10.9% among those without cancer.
Admissions increased steadily across all cancer types, except prostate cancer, with heart failure being the most common reason for admission.
“Hospital admissions is really important because we know that the size of this group is increasing, given that they live longer and many of the treatments that we offer cause cardiovascular disease or increase the risk of having cardiovascular events. So, from a health care planning perspective, I think it’s really important to see what the burden is likely to be in the next few years,” senior author Mamas Mamas, MD, Keele University, England, told this news organization.
For physicians and the wider population, he said, the findings underscore the need to shift the conversation from saying that patients with cancer are at increased CVD risk to asking how to mitigate this risk. “Because I would say that this increase in cardiovascular admissions, that’s a failure from a preventative perspective.”
The study was published in the European Heart Journal: Quality of Care & Clinical Outcomes.
Individual cancer types
The researchers, led by Ofer Kobo, MD, also with Keele University, used the National Inpatient Sample to identify 42.5 million weighted cases of CV admissions for acute myocardial infarction (AMI), pulmonary embolism, ischemic stroke, heart failure, atrial fibrillation (AFib) or atrial flutter, and intracranial hemorrhage from January 2004 to December 2017. Of these, 1.9 million had a record of cancer.
Patients with cancer were older; had a higher prevalence of valvular disease, anemia, and coagulopathy; and had a lower prevalence of hypertension, diabetes mellitus, and obesity than did patients without cancer.
The most common cancer type was hematologic cancers (26.1%), followed by lung (18.7%), gastrointestinal (12.4%), prostate (11.6%), breast (6.7%), and other in 24.4%.
The admission rate increased across all six admission causes – between 7% for AMI and ischemic stroke and 46% for AFib.
Heart failure was the chief reason for admission among all patients. Annual rates per 100,000 U.S. population increased in patients with cancer (from 13.6 to 16.6; P for trend = .02) and declined in those without (from 352.2 to 349.8; P for trend < .001).
“In the past, patients would be started on medications, and perhaps the importance of monitoring [left ventricular] LV function wasn’t as widely known, whereas now we’re much more aggressive in looking at it and much more aggressive at trying to prevent it,” Dr. Mamas said. “But even with this greater identification and attempting to modify regimens, we’re still getting quite substantial increases in heart failure admissions in this population. And what really surprised me is that it wasn’t just in the breast cancer population, but it was nearly across the board.”
He noted that patients are at highest risk from CV events within the first 2 years of cancer diagnosis. “So that’s really the time where you’ve got to be really aggressive in looking and working up their cardiovascular profile.”
Patients with hematologic cancers (9.7-13.5), lung (7.4-8.9), and gastrointestinal cancer (4.6-6.3) had the highest crude admission rates of CV hospitalizations per 100,000 U.S. population.
The CV admission rate went up from 2.5 to 3.7 per 100,000 U.S. population for breast cancer, and in prostate cancer, the rate dropped from 5.8 to 4.8 per 100,000 U.S. population.
Of note, patients with hematologic cancers also had the highest rate of heart failure hospitalization across all cancer types, which, coupled with their increasing admission rates, likely reflects their exposure to a “constellation of cardiotoxic therapies” as well as pathologic processes related to the cancers themselves, the authors suggest.
In-hospital mortality rates were higher among patients with cancer than those without, ranging from 5% for patients with breast cancer to 9.6% for patients with lung cancer versus 4.2% for those without cancer.
Among patients with cancer, the odds ratio for mortality was highest in those admitted with AFib (4.43), followed by pulmonary embolism (2.36), AMI (2.31), ischemic stroke (2.29), and heart failure (2.24).
In line with prior work and general population trends, in-hospital deaths in primary CV admissions trended lower among patients with cancer over the study period.
Mitigating risk
Commenting on the study, Joerg Herrmann, MD, director of the cardio-oncology clinic at Mayo Clinic, Rochester, Minn., said that the data are “extremely important” because they reflect admissions during a new era of cancer therapy. “Targeted therapies all came out about the turn of the millennium, so we’re not really looking at cancer patients treated with only old and ancient strategies.”
This may be one reason for the increased admissions, but because the study lacked information on specific cancer treatments and the date of cancer diagnosis, it’s not possible to tease out whether the uptick is related to cardiotoxicity or because the oncology outcomes have improved so much that this is a growing population, he said.
One clear implication, however, is that whoever is working on the hospital service will see more patients with a cancer diagnosis, Dr. Herrmann observed.
“Though some may have tried to maybe not get involved with this topic as much, it really calls for some broader scope to get familiar with this very entity,” he said. “And that plays out, in particular, in those patients with a diagnosis of active cancer.”
Dr. Herrmann and colleagues previously reported that patients with active leukemia or lymphoma who were hospitalized with acute coronary syndrome were less likely to receive guideline-directed therapies, even at the Mayo Clinic.
Similarly, a 2020 report by Dr. Mamas and colleagues found that patients with a variety of active cancers derived similar benefit from primary percutaneous coronary intervention for ST-segment–elevation MI as those without cancer but received the treatment less commonly.
Although there’s a greater appreciation that patients with cancer benefit equally from aggressive treatment, much more can be done to mitigate CV risk, Dr. Mamas noted. Valuable coronary information captured by MRI and CT done as part of the cancer investigation is often overlooked. For example, “we know that breast calcification and vascular calcification in the breast are very strong predictors of cardiovascular outcomes and yet people aren’t using this information.”
There are numerous shared risk factors in the development of cancer and coronary artery disease, and patients with cancer often have much worse CV risk profiles but aren’t routinely risk stratified from a CV perspective, he said.
Dr. Mamas said that his team is also studying whether CVD risk prediction tools like the Framingham Risk Score, which were derived from noncancer populations, work as well in patients with cancer. “Often, when you look at the performance of these tools in populations that weren’t covered, they’re much worse.”
“A lot of cancer survivors worry about the recurrence of their cancer and will religiously go and have repeated scans, religiously check themselves, and have all these investigations but don’t think about the actual risk that is greater for them, which is cardiovascular risk,” he said.
The authors report no study funding or relevant financial relationships.
A version of this article first appeared on Medscape.com.
Although cardiovascular disease (CVD) is known to often strike the mortal blow in patients with cancer, a national analysis puts in stark relief the burden of CV-related hospitalizations in this vulnerable population.
, whereas admissions fell 10.9% among those without cancer.
Admissions increased steadily across all cancer types, except prostate cancer, with heart failure being the most common reason for admission.
“Hospital admissions is really important because we know that the size of this group is increasing, given that they live longer and many of the treatments that we offer cause cardiovascular disease or increase the risk of having cardiovascular events. So, from a health care planning perspective, I think it’s really important to see what the burden is likely to be in the next few years,” senior author Mamas Mamas, MD, Keele University, England, told this news organization.
For physicians and the wider population, he said, the findings underscore the need to shift the conversation from saying that patients with cancer are at increased CVD risk to asking how to mitigate this risk. “Because I would say that this increase in cardiovascular admissions, that’s a failure from a preventative perspective.”
The study was published in the European Heart Journal: Quality of Care & Clinical Outcomes.
Individual cancer types
The researchers, led by Ofer Kobo, MD, also with Keele University, used the National Inpatient Sample to identify 42.5 million weighted cases of CV admissions for acute myocardial infarction (AMI), pulmonary embolism, ischemic stroke, heart failure, atrial fibrillation (AFib) or atrial flutter, and intracranial hemorrhage from January 2004 to December 2017. Of these, 1.9 million had a record of cancer.
Patients with cancer were older; had a higher prevalence of valvular disease, anemia, and coagulopathy; and had a lower prevalence of hypertension, diabetes mellitus, and obesity than did patients without cancer.
The most common cancer type was hematologic cancers (26.1%), followed by lung (18.7%), gastrointestinal (12.4%), prostate (11.6%), breast (6.7%), and other in 24.4%.
The admission rate increased across all six admission causes – between 7% for AMI and ischemic stroke and 46% for AFib.
Heart failure was the chief reason for admission among all patients. Annual rates per 100,000 U.S. population increased in patients with cancer (from 13.6 to 16.6; P for trend = .02) and declined in those without (from 352.2 to 349.8; P for trend < .001).
“In the past, patients would be started on medications, and perhaps the importance of monitoring [left ventricular] LV function wasn’t as widely known, whereas now we’re much more aggressive in looking at it and much more aggressive at trying to prevent it,” Dr. Mamas said. “But even with this greater identification and attempting to modify regimens, we’re still getting quite substantial increases in heart failure admissions in this population. And what really surprised me is that it wasn’t just in the breast cancer population, but it was nearly across the board.”
He noted that patients are at highest risk from CV events within the first 2 years of cancer diagnosis. “So that’s really the time where you’ve got to be really aggressive in looking and working up their cardiovascular profile.”
Patients with hematologic cancers (9.7-13.5), lung (7.4-8.9), and gastrointestinal cancer (4.6-6.3) had the highest crude admission rates of CV hospitalizations per 100,000 U.S. population.
The CV admission rate went up from 2.5 to 3.7 per 100,000 U.S. population for breast cancer, and in prostate cancer, the rate dropped from 5.8 to 4.8 per 100,000 U.S. population.
Of note, patients with hematologic cancers also had the highest rate of heart failure hospitalization across all cancer types, which, coupled with their increasing admission rates, likely reflects their exposure to a “constellation of cardiotoxic therapies” as well as pathologic processes related to the cancers themselves, the authors suggest.
In-hospital mortality rates were higher among patients with cancer than those without, ranging from 5% for patients with breast cancer to 9.6% for patients with lung cancer versus 4.2% for those without cancer.
Among patients with cancer, the odds ratio for mortality was highest in those admitted with AFib (4.43), followed by pulmonary embolism (2.36), AMI (2.31), ischemic stroke (2.29), and heart failure (2.24).
In line with prior work and general population trends, in-hospital deaths in primary CV admissions trended lower among patients with cancer over the study period.
Mitigating risk
Commenting on the study, Joerg Herrmann, MD, director of the cardio-oncology clinic at Mayo Clinic, Rochester, Minn., said that the data are “extremely important” because they reflect admissions during a new era of cancer therapy. “Targeted therapies all came out about the turn of the millennium, so we’re not really looking at cancer patients treated with only old and ancient strategies.”
This may be one reason for the increased admissions, but because the study lacked information on specific cancer treatments and the date of cancer diagnosis, it’s not possible to tease out whether the uptick is related to cardiotoxicity or because the oncology outcomes have improved so much that this is a growing population, he said.
One clear implication, however, is that whoever is working on the hospital service will see more patients with a cancer diagnosis, Dr. Herrmann observed.
“Though some may have tried to maybe not get involved with this topic as much, it really calls for some broader scope to get familiar with this very entity,” he said. “And that plays out, in particular, in those patients with a diagnosis of active cancer.”
Dr. Herrmann and colleagues previously reported that patients with active leukemia or lymphoma who were hospitalized with acute coronary syndrome were less likely to receive guideline-directed therapies, even at the Mayo Clinic.
Similarly, a 2020 report by Dr. Mamas and colleagues found that patients with a variety of active cancers derived similar benefit from primary percutaneous coronary intervention for ST-segment–elevation MI as those without cancer but received the treatment less commonly.
Although there’s a greater appreciation that patients with cancer benefit equally from aggressive treatment, much more can be done to mitigate CV risk, Dr. Mamas noted. Valuable coronary information captured by MRI and CT done as part of the cancer investigation is often overlooked. For example, “we know that breast calcification and vascular calcification in the breast are very strong predictors of cardiovascular outcomes and yet people aren’t using this information.”
There are numerous shared risk factors in the development of cancer and coronary artery disease, and patients with cancer often have much worse CV risk profiles but aren’t routinely risk stratified from a CV perspective, he said.
Dr. Mamas said that his team is also studying whether CVD risk prediction tools like the Framingham Risk Score, which were derived from noncancer populations, work as well in patients with cancer. “Often, when you look at the performance of these tools in populations that weren’t covered, they’re much worse.”
“A lot of cancer survivors worry about the recurrence of their cancer and will religiously go and have repeated scans, religiously check themselves, and have all these investigations but don’t think about the actual risk that is greater for them, which is cardiovascular risk,” he said.
The authors report no study funding or relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM European Heart Journal: Quality of Care & Clinical Outcomes
How well do vaccines protect against long COVID?
New York City veterinarian Erin Kulick used to be a weekend warrior. Only 2½ years ago, the 38-year-old new mother played ultimate Frisbee and flag football with friends. She went for regular 30-minute runs to burn off stress.
Now, Dr. Kulick is usually so exhausted, she can’t walk nonstop for 15 minutes. She recently tried to take her 4-year-old son, Cooper, to the American Museum of Natural History for his first visit, but ended up on a bench outside the museum, sobbing in the rain, because she couldn’t even get through the first hurdle of standing in line. “I just wanted to be there with my kid,” she said.
Dr. Kulick got sick with COVID-19 at the start of the pandemic in March 2020, 9 months before the first vaccine would be approved. Now she is among the estimated one in five infected Americans, or 19%, whose symptoms developed into long COVID.
Dr. Kulick also is now vaccinated and boosted. Had a vaccine been available sooner, could it have protected her from long COVID?
Evidence is starting to show it’s likely.
“The best way not to have long COVID is not to have COVID at all,” said Leora Horwitz, MD, a professor of population health and medicine at New York University. “To the extent that vaccination can prevent you from getting COVID at all, then it helps to reduce long COVID.”
And People with more serious initial illness appear more likely to have prolonged symptoms, but those with milder disease can certainly get it, too.
“You’re more likely to have long COVID with more severe disease, and we have ample evidence that vaccination reduces the severity of disease,” Dr. Horwitz said. “We also now have quite a lot of evidence that vaccination does reduce your risk of long COVID – probably because it reduces your risk of severe disease.”
There is little consensus about how much vaccines can lower the risk of long-term COVID symptoms, but several studies suggest that number lies anywhere from 15% to more than 80%.
That might seem like a big variation, but infectious disease experts argue that trying to interpret the gap isn’t as important as noticing what’s consistent across all these studies: “Vaccines do offer some protection, but it’s incomplete,” said Ziyad Al-Aly, MD, chief of research and development at the Veterans Affairs St. Louis Health Care System. Dr. Al-Aly, who has led several large studies on long COVID, said focusing on the fact that vaccines do offer some protection is a much better public health message than looking at the different levels of risk.
“Vaccines do a miraculous job for what they were designed to do,” said Dr. Al-Aly. “Vaccines were designed to reduce the risk of hospitalization ... and for that, vaccines are still holding up, even with all the changes in the virus.”
Still, Elena Azzolini, MD, PhD, head of the Humanitas Research Hospital’s vaccination center in Milan, thinks some studies may have underestimated the level of long COVID protection from vaccines because of limits in the study methods, such as not including enough women, who are more affected by long COVID. Her recent study, which looked at 2,560 health care professionals working in nine Italian centers from March 2020 to April 2022, focused on the risk for healthy women and men in their 20s to their 70s.
In the paper, Dr. Azzolini and associates reported that two or three doses of vaccine reduced the risk of hospitalization from COVID-19 from 42% among those who are unvaccinated to 16%-17%. In other words, they found unvaccinated people in the study were nearly three times as likely to have serious symptoms for longer than 4 weeks.
But Dr. Azzolini and Dr. Al-Aly still say that, even for the vaccinated, as long as COVID is around, masks are necessary. That’s because current vaccines don’t do enough to reduce transmission, said Dr. Al-Aly. “The only way that can really help [stop] transmission is covering our nose and mouth with a mask.”
How vaccinations affect people who already have long COVID
Some long COVID patients have said they got better after they get boosted, while some say they’re getting worse, said Dr. Horwitz, who is also a lead investigator at the National Institutes of Health’s flagship RECOVER program, a 4-year research project to study long COVID across the United States. (The NIH is still recruiting volunteers for these studies, which are also open to people who have never had COVID.)
One study published in the British Medical Journal analyzed survey data of more than 28,000 people infected with COVID in the United Kingdom and found a 13% reduction in long-term symptoms after a first dose of the vaccine, although it was unclear from the data if the improvement was sustained.
A second dose was associated with another 8% improvement over a 2-month period. “It’s reassuring that we see an average modest improvement in symptoms, not an average worsening in symptoms,” said Daniel Ayoubkhani, principal statistician at the U.K. Office for National Statistics and lead author of the study. Of course, the experience will differ among different people.
“It doesn’t appear that vaccination is the silver bullet that’s going to eradicate long COVID,” he said, but evidence from multiple studies suggests vaccines may help people with long-term symptoms.
Akiko Iwasaki, PhD, an immunobiologist at Yale University, New Haven, Conn., told a White House summit in July that one of the best ways to prevent long COVID is to develop the next generation of vaccines that also prevent milder cases by blocking transmission in the first place.
Back in New York, Dr. Kulick is now triple vaccinated. She’s due for a fourth dose soon but admits she’s “terrified every time” that she’s going to get sicker.
In her Facebook support group for long COVID, she reads that most people with prolonged symptoms handle it well. She has also noticed some of her symptoms eased after her first two doses of vaccine.
Since being diagnosed, Dr. Kulick learned she has a genetic condition, Ehlers-Danlos syndrome, which affects connective tissues that support skin, joints, organs, and blood vessels, and which her doctors say may have made her more prone to long COVID. She’s also being screened for autoimmune diseases, but for now, the only relief she has found has come from long COVID physical therapy, changes to her diet, and integrative medicine.
Dr. Kulick is still trying to figure out how she can get better while keeping her long hours at her veterinary job – and her health benefits. She is thankful her husband is a devoted caregiver to their son and a professional jazz musician with a schedule that allows for some flexibility.
“But it’s really hard when every week feels like I’ve run a marathon,” she said. “I can barely make it through.”
A version of this article first appeared on WebMD.com.
New York City veterinarian Erin Kulick used to be a weekend warrior. Only 2½ years ago, the 38-year-old new mother played ultimate Frisbee and flag football with friends. She went for regular 30-minute runs to burn off stress.
Now, Dr. Kulick is usually so exhausted, she can’t walk nonstop for 15 minutes. She recently tried to take her 4-year-old son, Cooper, to the American Museum of Natural History for his first visit, but ended up on a bench outside the museum, sobbing in the rain, because she couldn’t even get through the first hurdle of standing in line. “I just wanted to be there with my kid,” she said.
Dr. Kulick got sick with COVID-19 at the start of the pandemic in March 2020, 9 months before the first vaccine would be approved. Now she is among the estimated one in five infected Americans, or 19%, whose symptoms developed into long COVID.
Dr. Kulick also is now vaccinated and boosted. Had a vaccine been available sooner, could it have protected her from long COVID?
Evidence is starting to show it’s likely.
“The best way not to have long COVID is not to have COVID at all,” said Leora Horwitz, MD, a professor of population health and medicine at New York University. “To the extent that vaccination can prevent you from getting COVID at all, then it helps to reduce long COVID.”
And People with more serious initial illness appear more likely to have prolonged symptoms, but those with milder disease can certainly get it, too.
“You’re more likely to have long COVID with more severe disease, and we have ample evidence that vaccination reduces the severity of disease,” Dr. Horwitz said. “We also now have quite a lot of evidence that vaccination does reduce your risk of long COVID – probably because it reduces your risk of severe disease.”
There is little consensus about how much vaccines can lower the risk of long-term COVID symptoms, but several studies suggest that number lies anywhere from 15% to more than 80%.
That might seem like a big variation, but infectious disease experts argue that trying to interpret the gap isn’t as important as noticing what’s consistent across all these studies: “Vaccines do offer some protection, but it’s incomplete,” said Ziyad Al-Aly, MD, chief of research and development at the Veterans Affairs St. Louis Health Care System. Dr. Al-Aly, who has led several large studies on long COVID, said focusing on the fact that vaccines do offer some protection is a much better public health message than looking at the different levels of risk.
“Vaccines do a miraculous job for what they were designed to do,” said Dr. Al-Aly. “Vaccines were designed to reduce the risk of hospitalization ... and for that, vaccines are still holding up, even with all the changes in the virus.”
Still, Elena Azzolini, MD, PhD, head of the Humanitas Research Hospital’s vaccination center in Milan, thinks some studies may have underestimated the level of long COVID protection from vaccines because of limits in the study methods, such as not including enough women, who are more affected by long COVID. Her recent study, which looked at 2,560 health care professionals working in nine Italian centers from March 2020 to April 2022, focused on the risk for healthy women and men in their 20s to their 70s.
In the paper, Dr. Azzolini and associates reported that two or three doses of vaccine reduced the risk of hospitalization from COVID-19 from 42% among those who are unvaccinated to 16%-17%. In other words, they found unvaccinated people in the study were nearly three times as likely to have serious symptoms for longer than 4 weeks.
But Dr. Azzolini and Dr. Al-Aly still say that, even for the vaccinated, as long as COVID is around, masks are necessary. That’s because current vaccines don’t do enough to reduce transmission, said Dr. Al-Aly. “The only way that can really help [stop] transmission is covering our nose and mouth with a mask.”
How vaccinations affect people who already have long COVID
Some long COVID patients have said they got better after they get boosted, while some say they’re getting worse, said Dr. Horwitz, who is also a lead investigator at the National Institutes of Health’s flagship RECOVER program, a 4-year research project to study long COVID across the United States. (The NIH is still recruiting volunteers for these studies, which are also open to people who have never had COVID.)
One study published in the British Medical Journal analyzed survey data of more than 28,000 people infected with COVID in the United Kingdom and found a 13% reduction in long-term symptoms after a first dose of the vaccine, although it was unclear from the data if the improvement was sustained.
A second dose was associated with another 8% improvement over a 2-month period. “It’s reassuring that we see an average modest improvement in symptoms, not an average worsening in symptoms,” said Daniel Ayoubkhani, principal statistician at the U.K. Office for National Statistics and lead author of the study. Of course, the experience will differ among different people.
“It doesn’t appear that vaccination is the silver bullet that’s going to eradicate long COVID,” he said, but evidence from multiple studies suggests vaccines may help people with long-term symptoms.
Akiko Iwasaki, PhD, an immunobiologist at Yale University, New Haven, Conn., told a White House summit in July that one of the best ways to prevent long COVID is to develop the next generation of vaccines that also prevent milder cases by blocking transmission in the first place.
Back in New York, Dr. Kulick is now triple vaccinated. She’s due for a fourth dose soon but admits she’s “terrified every time” that she’s going to get sicker.
In her Facebook support group for long COVID, she reads that most people with prolonged symptoms handle it well. She has also noticed some of her symptoms eased after her first two doses of vaccine.
Since being diagnosed, Dr. Kulick learned she has a genetic condition, Ehlers-Danlos syndrome, which affects connective tissues that support skin, joints, organs, and blood vessels, and which her doctors say may have made her more prone to long COVID. She’s also being screened for autoimmune diseases, but for now, the only relief she has found has come from long COVID physical therapy, changes to her diet, and integrative medicine.
Dr. Kulick is still trying to figure out how she can get better while keeping her long hours at her veterinary job – and her health benefits. She is thankful her husband is a devoted caregiver to their son and a professional jazz musician with a schedule that allows for some flexibility.
“But it’s really hard when every week feels like I’ve run a marathon,” she said. “I can barely make it through.”
A version of this article first appeared on WebMD.com.
New York City veterinarian Erin Kulick used to be a weekend warrior. Only 2½ years ago, the 38-year-old new mother played ultimate Frisbee and flag football with friends. She went for regular 30-minute runs to burn off stress.
Now, Dr. Kulick is usually so exhausted, she can’t walk nonstop for 15 minutes. She recently tried to take her 4-year-old son, Cooper, to the American Museum of Natural History for his first visit, but ended up on a bench outside the museum, sobbing in the rain, because she couldn’t even get through the first hurdle of standing in line. “I just wanted to be there with my kid,” she said.
Dr. Kulick got sick with COVID-19 at the start of the pandemic in March 2020, 9 months before the first vaccine would be approved. Now she is among the estimated one in five infected Americans, or 19%, whose symptoms developed into long COVID.
Dr. Kulick also is now vaccinated and boosted. Had a vaccine been available sooner, could it have protected her from long COVID?
Evidence is starting to show it’s likely.
“The best way not to have long COVID is not to have COVID at all,” said Leora Horwitz, MD, a professor of population health and medicine at New York University. “To the extent that vaccination can prevent you from getting COVID at all, then it helps to reduce long COVID.”
And People with more serious initial illness appear more likely to have prolonged symptoms, but those with milder disease can certainly get it, too.
“You’re more likely to have long COVID with more severe disease, and we have ample evidence that vaccination reduces the severity of disease,” Dr. Horwitz said. “We also now have quite a lot of evidence that vaccination does reduce your risk of long COVID – probably because it reduces your risk of severe disease.”
There is little consensus about how much vaccines can lower the risk of long-term COVID symptoms, but several studies suggest that number lies anywhere from 15% to more than 80%.
That might seem like a big variation, but infectious disease experts argue that trying to interpret the gap isn’t as important as noticing what’s consistent across all these studies: “Vaccines do offer some protection, but it’s incomplete,” said Ziyad Al-Aly, MD, chief of research and development at the Veterans Affairs St. Louis Health Care System. Dr. Al-Aly, who has led several large studies on long COVID, said focusing on the fact that vaccines do offer some protection is a much better public health message than looking at the different levels of risk.
“Vaccines do a miraculous job for what they were designed to do,” said Dr. Al-Aly. “Vaccines were designed to reduce the risk of hospitalization ... and for that, vaccines are still holding up, even with all the changes in the virus.”
Still, Elena Azzolini, MD, PhD, head of the Humanitas Research Hospital’s vaccination center in Milan, thinks some studies may have underestimated the level of long COVID protection from vaccines because of limits in the study methods, such as not including enough women, who are more affected by long COVID. Her recent study, which looked at 2,560 health care professionals working in nine Italian centers from March 2020 to April 2022, focused on the risk for healthy women and men in their 20s to their 70s.
In the paper, Dr. Azzolini and associates reported that two or three doses of vaccine reduced the risk of hospitalization from COVID-19 from 42% among those who are unvaccinated to 16%-17%. In other words, they found unvaccinated people in the study were nearly three times as likely to have serious symptoms for longer than 4 weeks.
But Dr. Azzolini and Dr. Al-Aly still say that, even for the vaccinated, as long as COVID is around, masks are necessary. That’s because current vaccines don’t do enough to reduce transmission, said Dr. Al-Aly. “The only way that can really help [stop] transmission is covering our nose and mouth with a mask.”
How vaccinations affect people who already have long COVID
Some long COVID patients have said they got better after they get boosted, while some say they’re getting worse, said Dr. Horwitz, who is also a lead investigator at the National Institutes of Health’s flagship RECOVER program, a 4-year research project to study long COVID across the United States. (The NIH is still recruiting volunteers for these studies, which are also open to people who have never had COVID.)
One study published in the British Medical Journal analyzed survey data of more than 28,000 people infected with COVID in the United Kingdom and found a 13% reduction in long-term symptoms after a first dose of the vaccine, although it was unclear from the data if the improvement was sustained.
A second dose was associated with another 8% improvement over a 2-month period. “It’s reassuring that we see an average modest improvement in symptoms, not an average worsening in symptoms,” said Daniel Ayoubkhani, principal statistician at the U.K. Office for National Statistics and lead author of the study. Of course, the experience will differ among different people.
“It doesn’t appear that vaccination is the silver bullet that’s going to eradicate long COVID,” he said, but evidence from multiple studies suggests vaccines may help people with long-term symptoms.
Akiko Iwasaki, PhD, an immunobiologist at Yale University, New Haven, Conn., told a White House summit in July that one of the best ways to prevent long COVID is to develop the next generation of vaccines that also prevent milder cases by blocking transmission in the first place.
Back in New York, Dr. Kulick is now triple vaccinated. She’s due for a fourth dose soon but admits she’s “terrified every time” that she’s going to get sicker.
In her Facebook support group for long COVID, she reads that most people with prolonged symptoms handle it well. She has also noticed some of her symptoms eased after her first two doses of vaccine.
Since being diagnosed, Dr. Kulick learned she has a genetic condition, Ehlers-Danlos syndrome, which affects connective tissues that support skin, joints, organs, and blood vessels, and which her doctors say may have made her more prone to long COVID. She’s also being screened for autoimmune diseases, but for now, the only relief she has found has come from long COVID physical therapy, changes to her diet, and integrative medicine.
Dr. Kulick is still trying to figure out how she can get better while keeping her long hours at her veterinary job – and her health benefits. She is thankful her husband is a devoted caregiver to their son and a professional jazz musician with a schedule that allows for some flexibility.
“But it’s really hard when every week feels like I’ve run a marathon,” she said. “I can barely make it through.”
A version of this article first appeared on WebMD.com.
James Roberts, MD, trailblazer in EM, dies at age 76
at the age of 76 years. Dr. Roberts was coauthor of the foundational EM text, Clinical Procedures in Emergency Medicine and Acute Care , and was among the first physicians in the world to be board certified in EM. He was a prominent member of the American College of Emergency Physicians, a long-time contributor and editorial board chair for Emergency Medicine News, and a founding member of the American College of Medical Toxicology. He previously served as chairman of the Mercy Catholic Medical Center emergency department in Philadelphia, and vice chairman of the department of emergency medicine at Drexel University, Philadelphia.
“Dr. Roberts was a prominent EM physician and a pioneer in emergency medicine,” said Robert Glatter, MD, assistant professor of emergency medicine at Hofstra University, Hempstead, N.Y.. “He is a revered and respected figure in emergency medicine.” This sentiment was echoed by his colleagues and former students across the EM world.
“How does one describe a unicorn?” Leslie Dye, MD, past president of the ACMT wrote in a tribute to Dr. Roberts on the ACMT website. “There are existing words, but he should have words that belong solely to him. Compassionate, irreverent, brilliant, funny, sarcastic, HUMBLE, modest, kind, inquisitive, and one of the best doctors I have ever met.”
By all accounts, Dr. Roberts lived his life according to words he wrote in a 2018 column for Emergency Medicine News, “How to Be a Good EP.” “Emergency medicine is not just a job, it’s a lifestyle, but there is more to life than medicine. You can never make up a missed championship soccer game, anniversary, birthday, or chance to take your son or daughter fishing. In a heartbeat your children will be on their own and will likely have trouble finding time for you. Remember that you might need a shift off someday, so be ready to help a colleague with a similar request.”
He is survived by a large extended family, including his daughter Martha, son Matthew, and spouse of more than 40 years, Lydia Forte Roberts.
A version of this article first appeared on Medscape.com.
at the age of 76 years. Dr. Roberts was coauthor of the foundational EM text, Clinical Procedures in Emergency Medicine and Acute Care , and was among the first physicians in the world to be board certified in EM. He was a prominent member of the American College of Emergency Physicians, a long-time contributor and editorial board chair for Emergency Medicine News, and a founding member of the American College of Medical Toxicology. He previously served as chairman of the Mercy Catholic Medical Center emergency department in Philadelphia, and vice chairman of the department of emergency medicine at Drexel University, Philadelphia.
“Dr. Roberts was a prominent EM physician and a pioneer in emergency medicine,” said Robert Glatter, MD, assistant professor of emergency medicine at Hofstra University, Hempstead, N.Y.. “He is a revered and respected figure in emergency medicine.” This sentiment was echoed by his colleagues and former students across the EM world.
“How does one describe a unicorn?” Leslie Dye, MD, past president of the ACMT wrote in a tribute to Dr. Roberts on the ACMT website. “There are existing words, but he should have words that belong solely to him. Compassionate, irreverent, brilliant, funny, sarcastic, HUMBLE, modest, kind, inquisitive, and one of the best doctors I have ever met.”
By all accounts, Dr. Roberts lived his life according to words he wrote in a 2018 column for Emergency Medicine News, “How to Be a Good EP.” “Emergency medicine is not just a job, it’s a lifestyle, but there is more to life than medicine. You can never make up a missed championship soccer game, anniversary, birthday, or chance to take your son or daughter fishing. In a heartbeat your children will be on their own and will likely have trouble finding time for you. Remember that you might need a shift off someday, so be ready to help a colleague with a similar request.”
He is survived by a large extended family, including his daughter Martha, son Matthew, and spouse of more than 40 years, Lydia Forte Roberts.
A version of this article first appeared on Medscape.com.
at the age of 76 years. Dr. Roberts was coauthor of the foundational EM text, Clinical Procedures in Emergency Medicine and Acute Care , and was among the first physicians in the world to be board certified in EM. He was a prominent member of the American College of Emergency Physicians, a long-time contributor and editorial board chair for Emergency Medicine News, and a founding member of the American College of Medical Toxicology. He previously served as chairman of the Mercy Catholic Medical Center emergency department in Philadelphia, and vice chairman of the department of emergency medicine at Drexel University, Philadelphia.
“Dr. Roberts was a prominent EM physician and a pioneer in emergency medicine,” said Robert Glatter, MD, assistant professor of emergency medicine at Hofstra University, Hempstead, N.Y.. “He is a revered and respected figure in emergency medicine.” This sentiment was echoed by his colleagues and former students across the EM world.
“How does one describe a unicorn?” Leslie Dye, MD, past president of the ACMT wrote in a tribute to Dr. Roberts on the ACMT website. “There are existing words, but he should have words that belong solely to him. Compassionate, irreverent, brilliant, funny, sarcastic, HUMBLE, modest, kind, inquisitive, and one of the best doctors I have ever met.”
By all accounts, Dr. Roberts lived his life according to words he wrote in a 2018 column for Emergency Medicine News, “How to Be a Good EP.” “Emergency medicine is not just a job, it’s a lifestyle, but there is more to life than medicine. You can never make up a missed championship soccer game, anniversary, birthday, or chance to take your son or daughter fishing. In a heartbeat your children will be on their own and will likely have trouble finding time for you. Remember that you might need a shift off someday, so be ready to help a colleague with a similar request.”
He is survived by a large extended family, including his daughter Martha, son Matthew, and spouse of more than 40 years, Lydia Forte Roberts.
A version of this article first appeared on Medscape.com.
Patients and doctors trapped in a gray zone when abortion laws and emergency care mandate conflict
Each week, Kim Puterbaugh, MD, sees several pregnant patients at a Cleveland hospital who are experiencing complications involving bleeding or infection. The ob.gyn. has to make quick decisions about how to treat them, including whether to remove the dead or dying fetus to protect the health and life of the mother. Leaving in place a fetus that has no chance of survival dramatically increases the chance of maternal infection and permanent injury.
But now her medical decisions are complicated by Ohio’s new abortion law, which generally prohibits abortions after 6 weeks of pregnancy if cardiac activity is detected in the embryo or fetus – which can persist for hours or days even if a pregnancy has no chance of progressing. Given the new law, University Hospitals Cleveland Medical Center has streamlined its system of having an administrator and legal team on call for Dr. Puterbaugh and other physicians if anyone questions whether the planned treatment is allowed under the law.
Since the Supreme Court erased the constitutional right to abortion in June, Dr. Puterbaugh said these cases put her and doctors like her in an impossible position – squeezing doctors between antiabortion laws in Ohio and other states and the federal Emergency Medical Treatment & Labor Act. That 1986 law requires hospitals and physicians to provide screening and stabilizing treatment – including abortion, if necessary – in emergency situations.
“It’s a challenge to balance both those two things,” said Dr. Puterbaugh, president of the Society of OB/GYN Hospitalists. “But it’s not really a challenge to me because, in my mind, the life and health of the mother always comes first.”
The Biden administration argues that EMTALA trumps state abortion bans in emergency situations. On Aug. 2, the Department of Justice filed a federal lawsuit challenging an Idaho law that bans abortion in nearly all circumstances. The suit claims the law would make it a criminal offense for medical providers to comply with EMTALA’s requirement to provide abortion, if needed, for women experiencing emergency pregnancy complications.
In a July policy guidance and letter, the Department of Health & Human Services reaffirmed that EMTALA requires hospitals and physicians to offer life- or health-saving medical services, including abortion, in emergency situations. The letter refers to situations such as ectopic pregnancies, severe blood pressure spikes known as preeclampsia, and premature ruptures of the membrane causing a woman’s water to break before her pregnancy is viable.
The guidance stressed that this federal requirement supersedes any state laws that bar abortion, and that hospitals and physicians who don’t comply with the federal mandate could face civil fines and termination from the Medicare and Medicaid programs.
There are no known reports so far of EMTALA investigations arising from denial of emergency care in pregnancy situations.
But elected officials in states that have sharply restricted abortion disagree with the federal judgment. Texas Attorney General Ken Paxton sued the Biden administration in July to prevent the federal government from using the EMTALA law to require abortions in emergency cases. The suit claims that EMTALA doesn’t specifically mandate particular medical procedures such as abortion.
Abortion foes argue that state antiabortion laws already include adequate exceptions when a pregnant woman’s life or health is in danger. John Seago, president of Texas Right to Life, said one of Texas’ laws specifies that treatment for ectopic pregnancies or miscarriages is not prohibited. In addition, the law defines a medical emergency allowing abortion as a condition in which a woman is at serious risk of a “substantial impairment of a major bodily function.”
Mr. Seago blamed the news media and medical associations for deliberately sowing confusion about the laws. “The law is very clear,” he said.
Legal wrangling aside, in practice, physicians and hospital lawyers say much depends on the interpretation of vaguely worded exceptions in state abortion bans, and that’s further complicated by the existence of contradictory laws, such as those banning abortion based on cardiac activity. And medical providers don’t want to risk criminal prosecution, fines, and loss of licensure if someone accuses them of violating these confusing laws.
Louise Joy, an attorney in Austin, Tex., who represents hospitals and other health care providers, said her clients perhaps are being overly cautious, but that’s not surprising. “I try to encourage them to do the right thing, but I can’t assure them they’ll be risk free.”
A lot hinges on when a pregnancy-ending complication is deemed an emergency, a moment that is hard to define. Some Missouri women have come to the hospital ED with mild cramping and bleeding and were found to have an ectopic pregnancy that hadn’t ruptured yet, colleagues have told Alison Haddock, MD, a Houston emergency physician who chairs the board of the American College of Emergency Physicians. The standard treatment is to provide the drug methotrexate, which can terminate a pregnancy.
“You’re stable until it ruptures, then it becomes unstable,” she said. “But how unstable do you need to be? The woman’s life is not clearly at risk yet. It’s not clear if EMTALA applies. There will be a lot of gray areas that make it really tough for emergency physicians who want to do what’s right for patients without violating any laws.”
Physicians and hospital attorneys are hoping for clearer federal guidance and guarantees of protection from state prosecutors who might oppose their medical judgment on political grounds.
“This is when we need the federal government to step up and say: ‘Doctors, you must provide the standard of care, and we will prevent the prosecution of anyone who is following appropriate medical practices and doing the right thing for patients,” Ms. Joy said.
They are also hoping that the federal government will proactively investigate without waiting for complaints from individuals whenever appropriate emergency medical care might have been withheld because of the new laws. The New York Times reported in July that a 35-year-old woman in the Dallas–Fort Worth area was denied a dilation and evacuation procedure for her first-trimester miscarriage, despite severe pain and bleeding. The hospital reportedly sent her home with advice to return if she was bleeding heavily. The hospital did not respond to a request for comment for this article.
“If a hospital has a policy saying that when the correct medical procedure for a woman in the emergency department is abortion but physicians can’t do that, that’s a violation of EMTALA that CMS should find actionable,” said Thomas Barker, a former general counsel for the Centers for Medicare & Medicaid Services who advises hospitals on EMTALA compliance issues.
In another potential EMTALA case, Valerie Williams, MD, reported that, after Louisiana implemented its near-total ban on abortion with criminal penalties, her hospital in the New Orleans area blocked her from performing a dilation and evacuation procedure on a pregnant patient whose water broke at 16 weeks. The patient was forced to go through a painful, hours-long labor to deliver a nonviable fetus, with heavy loss of blood.
“This was the first time in my 15-year career that I could not give a patient the care they needed,” Dr. Williams wrote in a court affidavit as part of a case seeking to block the state’s abortion law. “This is a travesty.”
But CMS often relies on state agencies to investigate alleged EMTALA violations. That raises questions about how seriously those investigations will be conducted in states where officials have embraced strict limits on any medical services they deem abortion related.
In July, the Texas Medical Association warned that hospitals are pressing doctors to send pregnant patients with complications home, to wait until they expel the fetus – known as expectant management – rather than treating them at the hospital to remove the fetal remains, according to The Dallas Morning News. In a letter to the Texas Medical Board, the medical association said delayed or denied care risks patients’ future reproductive ability and poses a serious risk to their immediate health.
A study published in the American Journal of Obstetrics and Gynecology found that, after Texas implemented its tight abortion restrictions in September, patients with pregnancy complications experienced much worse outcomes than similar patients in states without abortion bans. Of those treated with expectant management at two major Dallas hospitals, 57% suffered serious complications such as bleeding and infection, compared with 33% who chose immediate pregnancy termination in other states.
Ob.gyns. and emergency physicians say they expect to be on the phone frequently with lawyers to get advice on complying with state antiabortion laws while they are seeing pregnant patients with emergency and near-emergency complications.
“This will endanger women’s lives, no question about it,” Dr. Puterbaugh said.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Each week, Kim Puterbaugh, MD, sees several pregnant patients at a Cleveland hospital who are experiencing complications involving bleeding or infection. The ob.gyn. has to make quick decisions about how to treat them, including whether to remove the dead or dying fetus to protect the health and life of the mother. Leaving in place a fetus that has no chance of survival dramatically increases the chance of maternal infection and permanent injury.
But now her medical decisions are complicated by Ohio’s new abortion law, which generally prohibits abortions after 6 weeks of pregnancy if cardiac activity is detected in the embryo or fetus – which can persist for hours or days even if a pregnancy has no chance of progressing. Given the new law, University Hospitals Cleveland Medical Center has streamlined its system of having an administrator and legal team on call for Dr. Puterbaugh and other physicians if anyone questions whether the planned treatment is allowed under the law.
Since the Supreme Court erased the constitutional right to abortion in June, Dr. Puterbaugh said these cases put her and doctors like her in an impossible position – squeezing doctors between antiabortion laws in Ohio and other states and the federal Emergency Medical Treatment & Labor Act. That 1986 law requires hospitals and physicians to provide screening and stabilizing treatment – including abortion, if necessary – in emergency situations.
“It’s a challenge to balance both those two things,” said Dr. Puterbaugh, president of the Society of OB/GYN Hospitalists. “But it’s not really a challenge to me because, in my mind, the life and health of the mother always comes first.”
The Biden administration argues that EMTALA trumps state abortion bans in emergency situations. On Aug. 2, the Department of Justice filed a federal lawsuit challenging an Idaho law that bans abortion in nearly all circumstances. The suit claims the law would make it a criminal offense for medical providers to comply with EMTALA’s requirement to provide abortion, if needed, for women experiencing emergency pregnancy complications.
In a July policy guidance and letter, the Department of Health & Human Services reaffirmed that EMTALA requires hospitals and physicians to offer life- or health-saving medical services, including abortion, in emergency situations. The letter refers to situations such as ectopic pregnancies, severe blood pressure spikes known as preeclampsia, and premature ruptures of the membrane causing a woman’s water to break before her pregnancy is viable.
The guidance stressed that this federal requirement supersedes any state laws that bar abortion, and that hospitals and physicians who don’t comply with the federal mandate could face civil fines and termination from the Medicare and Medicaid programs.
There are no known reports so far of EMTALA investigations arising from denial of emergency care in pregnancy situations.
But elected officials in states that have sharply restricted abortion disagree with the federal judgment. Texas Attorney General Ken Paxton sued the Biden administration in July to prevent the federal government from using the EMTALA law to require abortions in emergency cases. The suit claims that EMTALA doesn’t specifically mandate particular medical procedures such as abortion.
Abortion foes argue that state antiabortion laws already include adequate exceptions when a pregnant woman’s life or health is in danger. John Seago, president of Texas Right to Life, said one of Texas’ laws specifies that treatment for ectopic pregnancies or miscarriages is not prohibited. In addition, the law defines a medical emergency allowing abortion as a condition in which a woman is at serious risk of a “substantial impairment of a major bodily function.”
Mr. Seago blamed the news media and medical associations for deliberately sowing confusion about the laws. “The law is very clear,” he said.
Legal wrangling aside, in practice, physicians and hospital lawyers say much depends on the interpretation of vaguely worded exceptions in state abortion bans, and that’s further complicated by the existence of contradictory laws, such as those banning abortion based on cardiac activity. And medical providers don’t want to risk criminal prosecution, fines, and loss of licensure if someone accuses them of violating these confusing laws.
Louise Joy, an attorney in Austin, Tex., who represents hospitals and other health care providers, said her clients perhaps are being overly cautious, but that’s not surprising. “I try to encourage them to do the right thing, but I can’t assure them they’ll be risk free.”
A lot hinges on when a pregnancy-ending complication is deemed an emergency, a moment that is hard to define. Some Missouri women have come to the hospital ED with mild cramping and bleeding and were found to have an ectopic pregnancy that hadn’t ruptured yet, colleagues have told Alison Haddock, MD, a Houston emergency physician who chairs the board of the American College of Emergency Physicians. The standard treatment is to provide the drug methotrexate, which can terminate a pregnancy.
“You’re stable until it ruptures, then it becomes unstable,” she said. “But how unstable do you need to be? The woman’s life is not clearly at risk yet. It’s not clear if EMTALA applies. There will be a lot of gray areas that make it really tough for emergency physicians who want to do what’s right for patients without violating any laws.”
Physicians and hospital attorneys are hoping for clearer federal guidance and guarantees of protection from state prosecutors who might oppose their medical judgment on political grounds.
“This is when we need the federal government to step up and say: ‘Doctors, you must provide the standard of care, and we will prevent the prosecution of anyone who is following appropriate medical practices and doing the right thing for patients,” Ms. Joy said.
They are also hoping that the federal government will proactively investigate without waiting for complaints from individuals whenever appropriate emergency medical care might have been withheld because of the new laws. The New York Times reported in July that a 35-year-old woman in the Dallas–Fort Worth area was denied a dilation and evacuation procedure for her first-trimester miscarriage, despite severe pain and bleeding. The hospital reportedly sent her home with advice to return if she was bleeding heavily. The hospital did not respond to a request for comment for this article.
“If a hospital has a policy saying that when the correct medical procedure for a woman in the emergency department is abortion but physicians can’t do that, that’s a violation of EMTALA that CMS should find actionable,” said Thomas Barker, a former general counsel for the Centers for Medicare & Medicaid Services who advises hospitals on EMTALA compliance issues.
In another potential EMTALA case, Valerie Williams, MD, reported that, after Louisiana implemented its near-total ban on abortion with criminal penalties, her hospital in the New Orleans area blocked her from performing a dilation and evacuation procedure on a pregnant patient whose water broke at 16 weeks. The patient was forced to go through a painful, hours-long labor to deliver a nonviable fetus, with heavy loss of blood.
“This was the first time in my 15-year career that I could not give a patient the care they needed,” Dr. Williams wrote in a court affidavit as part of a case seeking to block the state’s abortion law. “This is a travesty.”
But CMS often relies on state agencies to investigate alleged EMTALA violations. That raises questions about how seriously those investigations will be conducted in states where officials have embraced strict limits on any medical services they deem abortion related.
In July, the Texas Medical Association warned that hospitals are pressing doctors to send pregnant patients with complications home, to wait until they expel the fetus – known as expectant management – rather than treating them at the hospital to remove the fetal remains, according to The Dallas Morning News. In a letter to the Texas Medical Board, the medical association said delayed or denied care risks patients’ future reproductive ability and poses a serious risk to their immediate health.
A study published in the American Journal of Obstetrics and Gynecology found that, after Texas implemented its tight abortion restrictions in September, patients with pregnancy complications experienced much worse outcomes than similar patients in states without abortion bans. Of those treated with expectant management at two major Dallas hospitals, 57% suffered serious complications such as bleeding and infection, compared with 33% who chose immediate pregnancy termination in other states.
Ob.gyns. and emergency physicians say they expect to be on the phone frequently with lawyers to get advice on complying with state antiabortion laws while they are seeing pregnant patients with emergency and near-emergency complications.
“This will endanger women’s lives, no question about it,” Dr. Puterbaugh said.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Each week, Kim Puterbaugh, MD, sees several pregnant patients at a Cleveland hospital who are experiencing complications involving bleeding or infection. The ob.gyn. has to make quick decisions about how to treat them, including whether to remove the dead or dying fetus to protect the health and life of the mother. Leaving in place a fetus that has no chance of survival dramatically increases the chance of maternal infection and permanent injury.
But now her medical decisions are complicated by Ohio’s new abortion law, which generally prohibits abortions after 6 weeks of pregnancy if cardiac activity is detected in the embryo or fetus – which can persist for hours or days even if a pregnancy has no chance of progressing. Given the new law, University Hospitals Cleveland Medical Center has streamlined its system of having an administrator and legal team on call for Dr. Puterbaugh and other physicians if anyone questions whether the planned treatment is allowed under the law.
Since the Supreme Court erased the constitutional right to abortion in June, Dr. Puterbaugh said these cases put her and doctors like her in an impossible position – squeezing doctors between antiabortion laws in Ohio and other states and the federal Emergency Medical Treatment & Labor Act. That 1986 law requires hospitals and physicians to provide screening and stabilizing treatment – including abortion, if necessary – in emergency situations.
“It’s a challenge to balance both those two things,” said Dr. Puterbaugh, president of the Society of OB/GYN Hospitalists. “But it’s not really a challenge to me because, in my mind, the life and health of the mother always comes first.”
The Biden administration argues that EMTALA trumps state abortion bans in emergency situations. On Aug. 2, the Department of Justice filed a federal lawsuit challenging an Idaho law that bans abortion in nearly all circumstances. The suit claims the law would make it a criminal offense for medical providers to comply with EMTALA’s requirement to provide abortion, if needed, for women experiencing emergency pregnancy complications.
In a July policy guidance and letter, the Department of Health & Human Services reaffirmed that EMTALA requires hospitals and physicians to offer life- or health-saving medical services, including abortion, in emergency situations. The letter refers to situations such as ectopic pregnancies, severe blood pressure spikes known as preeclampsia, and premature ruptures of the membrane causing a woman’s water to break before her pregnancy is viable.
The guidance stressed that this federal requirement supersedes any state laws that bar abortion, and that hospitals and physicians who don’t comply with the federal mandate could face civil fines and termination from the Medicare and Medicaid programs.
There are no known reports so far of EMTALA investigations arising from denial of emergency care in pregnancy situations.
But elected officials in states that have sharply restricted abortion disagree with the federal judgment. Texas Attorney General Ken Paxton sued the Biden administration in July to prevent the federal government from using the EMTALA law to require abortions in emergency cases. The suit claims that EMTALA doesn’t specifically mandate particular medical procedures such as abortion.
Abortion foes argue that state antiabortion laws already include adequate exceptions when a pregnant woman’s life or health is in danger. John Seago, president of Texas Right to Life, said one of Texas’ laws specifies that treatment for ectopic pregnancies or miscarriages is not prohibited. In addition, the law defines a medical emergency allowing abortion as a condition in which a woman is at serious risk of a “substantial impairment of a major bodily function.”
Mr. Seago blamed the news media and medical associations for deliberately sowing confusion about the laws. “The law is very clear,” he said.
Legal wrangling aside, in practice, physicians and hospital lawyers say much depends on the interpretation of vaguely worded exceptions in state abortion bans, and that’s further complicated by the existence of contradictory laws, such as those banning abortion based on cardiac activity. And medical providers don’t want to risk criminal prosecution, fines, and loss of licensure if someone accuses them of violating these confusing laws.
Louise Joy, an attorney in Austin, Tex., who represents hospitals and other health care providers, said her clients perhaps are being overly cautious, but that’s not surprising. “I try to encourage them to do the right thing, but I can’t assure them they’ll be risk free.”
A lot hinges on when a pregnancy-ending complication is deemed an emergency, a moment that is hard to define. Some Missouri women have come to the hospital ED with mild cramping and bleeding and were found to have an ectopic pregnancy that hadn’t ruptured yet, colleagues have told Alison Haddock, MD, a Houston emergency physician who chairs the board of the American College of Emergency Physicians. The standard treatment is to provide the drug methotrexate, which can terminate a pregnancy.
“You’re stable until it ruptures, then it becomes unstable,” she said. “But how unstable do you need to be? The woman’s life is not clearly at risk yet. It’s not clear if EMTALA applies. There will be a lot of gray areas that make it really tough for emergency physicians who want to do what’s right for patients without violating any laws.”
Physicians and hospital attorneys are hoping for clearer federal guidance and guarantees of protection from state prosecutors who might oppose their medical judgment on political grounds.
“This is when we need the federal government to step up and say: ‘Doctors, you must provide the standard of care, and we will prevent the prosecution of anyone who is following appropriate medical practices and doing the right thing for patients,” Ms. Joy said.
They are also hoping that the federal government will proactively investigate without waiting for complaints from individuals whenever appropriate emergency medical care might have been withheld because of the new laws. The New York Times reported in July that a 35-year-old woman in the Dallas–Fort Worth area was denied a dilation and evacuation procedure for her first-trimester miscarriage, despite severe pain and bleeding. The hospital reportedly sent her home with advice to return if she was bleeding heavily. The hospital did not respond to a request for comment for this article.
“If a hospital has a policy saying that when the correct medical procedure for a woman in the emergency department is abortion but physicians can’t do that, that’s a violation of EMTALA that CMS should find actionable,” said Thomas Barker, a former general counsel for the Centers for Medicare & Medicaid Services who advises hospitals on EMTALA compliance issues.
In another potential EMTALA case, Valerie Williams, MD, reported that, after Louisiana implemented its near-total ban on abortion with criminal penalties, her hospital in the New Orleans area blocked her from performing a dilation and evacuation procedure on a pregnant patient whose water broke at 16 weeks. The patient was forced to go through a painful, hours-long labor to deliver a nonviable fetus, with heavy loss of blood.
“This was the first time in my 15-year career that I could not give a patient the care they needed,” Dr. Williams wrote in a court affidavit as part of a case seeking to block the state’s abortion law. “This is a travesty.”
But CMS often relies on state agencies to investigate alleged EMTALA violations. That raises questions about how seriously those investigations will be conducted in states where officials have embraced strict limits on any medical services they deem abortion related.
In July, the Texas Medical Association warned that hospitals are pressing doctors to send pregnant patients with complications home, to wait until they expel the fetus – known as expectant management – rather than treating them at the hospital to remove the fetal remains, according to The Dallas Morning News. In a letter to the Texas Medical Board, the medical association said delayed or denied care risks patients’ future reproductive ability and poses a serious risk to their immediate health.
A study published in the American Journal of Obstetrics and Gynecology found that, after Texas implemented its tight abortion restrictions in September, patients with pregnancy complications experienced much worse outcomes than similar patients in states without abortion bans. Of those treated with expectant management at two major Dallas hospitals, 57% suffered serious complications such as bleeding and infection, compared with 33% who chose immediate pregnancy termination in other states.
Ob.gyns. and emergency physicians say they expect to be on the phone frequently with lawyers to get advice on complying with state antiabortion laws while they are seeing pregnant patients with emergency and near-emergency complications.
“This will endanger women’s lives, no question about it,” Dr. Puterbaugh said.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
My patient planned to murder me
San Diego internist David B. Bittleman, MD, was finishing an appointment with a patient when the man’s caregiver slipped Dr. Bittleman a note as the patient walked out of the room.
“Call me tomorrow,” the mysterious message read.
Dr. Bittleman phoned the caregiver, who was the patient’s ex-wife, the next day. He assumed she wanted to discuss a routine issue, such as the patient’s treatment. But the reason she wanted to talk privately was far more ominous.
“He wants to kill you,” she said.
Dr. Bittleman was shocked. The caregiver told Dr. Bittleman she believed her ex-husband was serious.
“The ex-wife and two adult sons were very alarmed by his erratic behavior,” Dr. Bittleman recalled. “She made it very clear that he said he planned to kill me. I feared for my life because I took his threat at face value.”
Patient sends alarming message, makes threats
When he went into medicine, Dr. Bittleman never imagined that he’d have to worry about being attacked or killed by a patient.
After spending 20 years in private practice, Dr. Bittleman was excited to accept a position at the Veterans Affairs San Diego health system. His extended family lived in the area, and he looked forward to helping veterans and to working with students, he said.
Dr. Bittleman had practiced primary care at the VA for about 5 years when he encountered the threatening patient, a veteran in his 60’s. The man was suffering from musculoskeletal pain and mental illness.
The patient had taken opioids on and off for many years. Dr. Bittleman felt that to continue the medication would not be safe, considering the man’s lifestyle.
“He had been maintained on oxycodone for chronic pain by previous providers, but I thought that was dangerous, given that he was mixing it with alcohol and marijuana,” he said. “I met with him and a substance use disorder physician for a conference call, and we explained we would need to taper the medication and eventually stop the opioids.”
Dr. Bittleman pleaded with the patient to enter drug rehab, and he offered him inpatient care for treatment of withdrawal. The man refused.
A few weeks later, Dr. Bittleman was checking the health center’s electronic messaging system. He found a disturbing message from the patient.
“You better learn jiu jitsu and hand-to-hand combat if you ever take my opioids away,” the message read. “You better learn how to defend yourself!”
Dr. Bittleman contacted the VA police and reported the message. The patient was interviewed by mental health professionals, but they did not believe he was dangerous, according to Dr. Bittleman.
“They are pretty limited to what they can do,” he said. “At a private practice, the patient might be fired or no longer allowed to come into the building, but the VA is a safety net institution. I’m not sure if he was even reprimanded.”
Two months later, the patient’s ex-wife shared the alarming news that the patient wanted to kill the doctor.
Dr. Bittleman went back to the police. They suggested he file a restraining order, which he sought that afternoon. By the end of the day, the judge had issued the restraining order, according to Dr. Bittleman and court records. The patient could not come within 100 yards of the physician, his clinic, car, or home.
But there was one frightening caveat. The order was temporary. It would last for only 2 weeks. To make the order permanent, Dr. Bittleman would have to go before the judge and argue why it was needed.
He wouldn’t be alone at the hearing. Someone else would be just paces away – the patient who wanted to murder him.
Doctor and patient face off before judge
As the hearing neared, Dr. Bittleman felt anxious, outraged, and fearful. He wondered whether the patient might make good on his threat.
Some colleagues suggested that Bittleman buy a gun, while others recommended he carry pepper spray. Dr. Bittleman had no interest in learning how to use a gun, he said. He took comfort in the fact that there were armed guards and metal detectors in his building, and there was a panic button under his desk.
“I was not sure I wanted to take care of patients anymore, especially chronic pain patients,” he said. “However, I went for some counseling with the Employee Assistance Program, and the therapist was helpful in normalizing my anxiety and acknowledging my fear.”
On the day of the hearing, Dr. Bittleman sat in the back of the courtroom. The patient, who sat near the front, glanced at Dr. Bittleman with a slight smile.
When his case was called, the judge explained that as the plaintiff, the burden was on Dr. Bittleman to prove the patient was a threat to his safety. He provided the judge a copy of the threatening message and a copy of the ex-wife’s note.
After reading the documents, the judge asked the patient to explain his side. The patient complained that the VA had denied him certain benefits and that he was forced to receive mental health treatment rehab that he “didn’t need.” The judge eventually interrupted the man to ask if he had threatened to kill Dr. Bittleman.
“Oh yes, your honor, I did say that, but I was only joking,” he told the judge.
The admission was enough. The judge issued a restraining order against the patient that would last 1 year. He could not have firearms, and if he violated the order, he would be arrested.
The terrifying saga was finally over.
“I never heard from the patient again,” Dr. Bittleman said. “His [care] location was changed, and police were required to come to all his visits with his new provider. I was relieved that if he ever came near me, he was going to jail.”
To raise awareness about such ordeals and the hassles that can follow, Dr. Bittleman wrote an article about his experience, which was published in the Annals of Family Medicine. He continues to treat patients at the VA, including those with chronic pain, but the memory of the menacing patient resurfaces from time to time.
“I do still think about it,” he said. “I know how to use my panic button, and I test it every 90 days. If there is a patient who concerns me, I will have the VA police wait nearby. I am very aware and upset by violence. When I hear about a doctor getting killed, I feel a clutch in my chest. How could I not relate? Here is a doctor who worked hard, who dedicated their life to help patients, and it comes to this? It’s so revolting. It makes me sick.”
Can you identify a violent patient?
Concern over threatening patients has grown across the country after recent violent attacks against physicians in Oklahoma and California. Two physicians were shot to death in June 2022 when a patient opened fire inside a Tulsa medical building. The primary target of the shooting was a surgeon who had performed surgery on the patient. Also in June, two nurses and an emergency physician were stabbed by a patient inside the Encino Hospital Medical Center. They survived.
The attacks raise questions about how to identify potentially violent patients and how to mitigate possible violence.
Threats and violence against health care professionals are nothing new, but they’re finally getting the attention they deserve, says Derek Schaller, MD, an emergency physician and assistant professor of emergency medicine at Central Michigan University in Mount Pleasant.
“Violence against personnel in medicine has been an issue for a long time; it’s just finally making headlines,” he said. “Way back when, it almost seemed like it was part of the job, part of the gig. But it shouldn’t be part of the gig. It’s not something we should be dealing with.”
It’s common for health care professionals and health centers to take a reactive approach to violent patients, but Dr. Schaller encourages a more proactive strategy. Central Michigan University Health, for example, recently studied its past violent encounters and analyzed the characteristics of violent patients. The analysis came after an increase in violent patient episodes at the health center in the past year, Dr. Schaller said.
The study yielded some interesting results, including that a large percentage of patients who became violent in the emergency department did so within the first hour they were in the hospital, he said.
“You would have thought it’s the patients who have been there and have been stuck in the emergency department for a while and who became disgruntled, but that was not the case,” Dr. Schaller said.
He recommends that physicians, medical practices, and hospitals carry out similar assessments of their patient populations and of past violent encounters to determine trends. His institution will be implementing a screening tool in triage to identify patients more likely to become violent so that health care professionals can intervene earlier, he said.
Such a screening tool is already demonstrating success in a variety of medical settings.
About 10 years ago, a research team led by Son Chae Kim, PhD, RN, found that the 10-item Aggressive Behavior Risk Assessment Tool (ABRAT) was able to identify potentially violent patients with reasonable sensitivity and specificity in hospital medical-surgical units.
Subsequently, the tool was modified for long-term care facilities, and again, researchers found that ABRAT was able to identify potentially violent residents with reasonable sensitivity and specificity, said Dr. Kim, ABRAT developer and a professor at Point Loma Nazarene University, San Diego.
In 2021, researchers embedded the checklist into an electronic health record (EHR) system and tested ABRAT in emergency departments.
“Currently, we are working with computer programmers to build an app that would make the ABRAT very easy to use in conjunction with EHR,” Dr. Kim said. “Instead of a nurse searching the EHR to find out if the patient has history of mental illness or aggressive behavior in the past, the app would automatically search the EHR and combine the nurse’s quick observation whether the patient is confused, agitated, staring, or threatening, to automatically calculate the violence risk.”
Dr. Kim and her team also developed a tool called VEST (Violent Event Severity Tool), a standardized objective workplace violence severity assessment. They are working with programmers to incorporate VEST into the app as well.
Dr. Kim’s hope is that the ABRAT tool can be modified for use in a range of health care settings.
A version of this article first appeared on Medscape.com.
San Diego internist David B. Bittleman, MD, was finishing an appointment with a patient when the man’s caregiver slipped Dr. Bittleman a note as the patient walked out of the room.
“Call me tomorrow,” the mysterious message read.
Dr. Bittleman phoned the caregiver, who was the patient’s ex-wife, the next day. He assumed she wanted to discuss a routine issue, such as the patient’s treatment. But the reason she wanted to talk privately was far more ominous.
“He wants to kill you,” she said.
Dr. Bittleman was shocked. The caregiver told Dr. Bittleman she believed her ex-husband was serious.
“The ex-wife and two adult sons were very alarmed by his erratic behavior,” Dr. Bittleman recalled. “She made it very clear that he said he planned to kill me. I feared for my life because I took his threat at face value.”
Patient sends alarming message, makes threats
When he went into medicine, Dr. Bittleman never imagined that he’d have to worry about being attacked or killed by a patient.
After spending 20 years in private practice, Dr. Bittleman was excited to accept a position at the Veterans Affairs San Diego health system. His extended family lived in the area, and he looked forward to helping veterans and to working with students, he said.
Dr. Bittleman had practiced primary care at the VA for about 5 years when he encountered the threatening patient, a veteran in his 60’s. The man was suffering from musculoskeletal pain and mental illness.
The patient had taken opioids on and off for many years. Dr. Bittleman felt that to continue the medication would not be safe, considering the man’s lifestyle.
“He had been maintained on oxycodone for chronic pain by previous providers, but I thought that was dangerous, given that he was mixing it with alcohol and marijuana,” he said. “I met with him and a substance use disorder physician for a conference call, and we explained we would need to taper the medication and eventually stop the opioids.”
Dr. Bittleman pleaded with the patient to enter drug rehab, and he offered him inpatient care for treatment of withdrawal. The man refused.
A few weeks later, Dr. Bittleman was checking the health center’s electronic messaging system. He found a disturbing message from the patient.
“You better learn jiu jitsu and hand-to-hand combat if you ever take my opioids away,” the message read. “You better learn how to defend yourself!”
Dr. Bittleman contacted the VA police and reported the message. The patient was interviewed by mental health professionals, but they did not believe he was dangerous, according to Dr. Bittleman.
“They are pretty limited to what they can do,” he said. “At a private practice, the patient might be fired or no longer allowed to come into the building, but the VA is a safety net institution. I’m not sure if he was even reprimanded.”
Two months later, the patient’s ex-wife shared the alarming news that the patient wanted to kill the doctor.
Dr. Bittleman went back to the police. They suggested he file a restraining order, which he sought that afternoon. By the end of the day, the judge had issued the restraining order, according to Dr. Bittleman and court records. The patient could not come within 100 yards of the physician, his clinic, car, or home.
But there was one frightening caveat. The order was temporary. It would last for only 2 weeks. To make the order permanent, Dr. Bittleman would have to go before the judge and argue why it was needed.
He wouldn’t be alone at the hearing. Someone else would be just paces away – the patient who wanted to murder him.
Doctor and patient face off before judge
As the hearing neared, Dr. Bittleman felt anxious, outraged, and fearful. He wondered whether the patient might make good on his threat.
Some colleagues suggested that Bittleman buy a gun, while others recommended he carry pepper spray. Dr. Bittleman had no interest in learning how to use a gun, he said. He took comfort in the fact that there were armed guards and metal detectors in his building, and there was a panic button under his desk.
“I was not sure I wanted to take care of patients anymore, especially chronic pain patients,” he said. “However, I went for some counseling with the Employee Assistance Program, and the therapist was helpful in normalizing my anxiety and acknowledging my fear.”
On the day of the hearing, Dr. Bittleman sat in the back of the courtroom. The patient, who sat near the front, glanced at Dr. Bittleman with a slight smile.
When his case was called, the judge explained that as the plaintiff, the burden was on Dr. Bittleman to prove the patient was a threat to his safety. He provided the judge a copy of the threatening message and a copy of the ex-wife’s note.
After reading the documents, the judge asked the patient to explain his side. The patient complained that the VA had denied him certain benefits and that he was forced to receive mental health treatment rehab that he “didn’t need.” The judge eventually interrupted the man to ask if he had threatened to kill Dr. Bittleman.
“Oh yes, your honor, I did say that, but I was only joking,” he told the judge.
The admission was enough. The judge issued a restraining order against the patient that would last 1 year. He could not have firearms, and if he violated the order, he would be arrested.
The terrifying saga was finally over.
“I never heard from the patient again,” Dr. Bittleman said. “His [care] location was changed, and police were required to come to all his visits with his new provider. I was relieved that if he ever came near me, he was going to jail.”
To raise awareness about such ordeals and the hassles that can follow, Dr. Bittleman wrote an article about his experience, which was published in the Annals of Family Medicine. He continues to treat patients at the VA, including those with chronic pain, but the memory of the menacing patient resurfaces from time to time.
“I do still think about it,” he said. “I know how to use my panic button, and I test it every 90 days. If there is a patient who concerns me, I will have the VA police wait nearby. I am very aware and upset by violence. When I hear about a doctor getting killed, I feel a clutch in my chest. How could I not relate? Here is a doctor who worked hard, who dedicated their life to help patients, and it comes to this? It’s so revolting. It makes me sick.”
Can you identify a violent patient?
Concern over threatening patients has grown across the country after recent violent attacks against physicians in Oklahoma and California. Two physicians were shot to death in June 2022 when a patient opened fire inside a Tulsa medical building. The primary target of the shooting was a surgeon who had performed surgery on the patient. Also in June, two nurses and an emergency physician were stabbed by a patient inside the Encino Hospital Medical Center. They survived.
The attacks raise questions about how to identify potentially violent patients and how to mitigate possible violence.
Threats and violence against health care professionals are nothing new, but they’re finally getting the attention they deserve, says Derek Schaller, MD, an emergency physician and assistant professor of emergency medicine at Central Michigan University in Mount Pleasant.
“Violence against personnel in medicine has been an issue for a long time; it’s just finally making headlines,” he said. “Way back when, it almost seemed like it was part of the job, part of the gig. But it shouldn’t be part of the gig. It’s not something we should be dealing with.”
It’s common for health care professionals and health centers to take a reactive approach to violent patients, but Dr. Schaller encourages a more proactive strategy. Central Michigan University Health, for example, recently studied its past violent encounters and analyzed the characteristics of violent patients. The analysis came after an increase in violent patient episodes at the health center in the past year, Dr. Schaller said.
The study yielded some interesting results, including that a large percentage of patients who became violent in the emergency department did so within the first hour they were in the hospital, he said.
“You would have thought it’s the patients who have been there and have been stuck in the emergency department for a while and who became disgruntled, but that was not the case,” Dr. Schaller said.
He recommends that physicians, medical practices, and hospitals carry out similar assessments of their patient populations and of past violent encounters to determine trends. His institution will be implementing a screening tool in triage to identify patients more likely to become violent so that health care professionals can intervene earlier, he said.
Such a screening tool is already demonstrating success in a variety of medical settings.
About 10 years ago, a research team led by Son Chae Kim, PhD, RN, found that the 10-item Aggressive Behavior Risk Assessment Tool (ABRAT) was able to identify potentially violent patients with reasonable sensitivity and specificity in hospital medical-surgical units.
Subsequently, the tool was modified for long-term care facilities, and again, researchers found that ABRAT was able to identify potentially violent residents with reasonable sensitivity and specificity, said Dr. Kim, ABRAT developer and a professor at Point Loma Nazarene University, San Diego.
In 2021, researchers embedded the checklist into an electronic health record (EHR) system and tested ABRAT in emergency departments.
“Currently, we are working with computer programmers to build an app that would make the ABRAT very easy to use in conjunction with EHR,” Dr. Kim said. “Instead of a nurse searching the EHR to find out if the patient has history of mental illness or aggressive behavior in the past, the app would automatically search the EHR and combine the nurse’s quick observation whether the patient is confused, agitated, staring, or threatening, to automatically calculate the violence risk.”
Dr. Kim and her team also developed a tool called VEST (Violent Event Severity Tool), a standardized objective workplace violence severity assessment. They are working with programmers to incorporate VEST into the app as well.
Dr. Kim’s hope is that the ABRAT tool can be modified for use in a range of health care settings.
A version of this article first appeared on Medscape.com.
San Diego internist David B. Bittleman, MD, was finishing an appointment with a patient when the man’s caregiver slipped Dr. Bittleman a note as the patient walked out of the room.
“Call me tomorrow,” the mysterious message read.
Dr. Bittleman phoned the caregiver, who was the patient’s ex-wife, the next day. He assumed she wanted to discuss a routine issue, such as the patient’s treatment. But the reason she wanted to talk privately was far more ominous.
“He wants to kill you,” she said.
Dr. Bittleman was shocked. The caregiver told Dr. Bittleman she believed her ex-husband was serious.
“The ex-wife and two adult sons were very alarmed by his erratic behavior,” Dr. Bittleman recalled. “She made it very clear that he said he planned to kill me. I feared for my life because I took his threat at face value.”
Patient sends alarming message, makes threats
When he went into medicine, Dr. Bittleman never imagined that he’d have to worry about being attacked or killed by a patient.
After spending 20 years in private practice, Dr. Bittleman was excited to accept a position at the Veterans Affairs San Diego health system. His extended family lived in the area, and he looked forward to helping veterans and to working with students, he said.
Dr. Bittleman had practiced primary care at the VA for about 5 years when he encountered the threatening patient, a veteran in his 60’s. The man was suffering from musculoskeletal pain and mental illness.
The patient had taken opioids on and off for many years. Dr. Bittleman felt that to continue the medication would not be safe, considering the man’s lifestyle.
“He had been maintained on oxycodone for chronic pain by previous providers, but I thought that was dangerous, given that he was mixing it with alcohol and marijuana,” he said. “I met with him and a substance use disorder physician for a conference call, and we explained we would need to taper the medication and eventually stop the opioids.”
Dr. Bittleman pleaded with the patient to enter drug rehab, and he offered him inpatient care for treatment of withdrawal. The man refused.
A few weeks later, Dr. Bittleman was checking the health center’s electronic messaging system. He found a disturbing message from the patient.
“You better learn jiu jitsu and hand-to-hand combat if you ever take my opioids away,” the message read. “You better learn how to defend yourself!”
Dr. Bittleman contacted the VA police and reported the message. The patient was interviewed by mental health professionals, but they did not believe he was dangerous, according to Dr. Bittleman.
“They are pretty limited to what they can do,” he said. “At a private practice, the patient might be fired or no longer allowed to come into the building, but the VA is a safety net institution. I’m not sure if he was even reprimanded.”
Two months later, the patient’s ex-wife shared the alarming news that the patient wanted to kill the doctor.
Dr. Bittleman went back to the police. They suggested he file a restraining order, which he sought that afternoon. By the end of the day, the judge had issued the restraining order, according to Dr. Bittleman and court records. The patient could not come within 100 yards of the physician, his clinic, car, or home.
But there was one frightening caveat. The order was temporary. It would last for only 2 weeks. To make the order permanent, Dr. Bittleman would have to go before the judge and argue why it was needed.
He wouldn’t be alone at the hearing. Someone else would be just paces away – the patient who wanted to murder him.
Doctor and patient face off before judge
As the hearing neared, Dr. Bittleman felt anxious, outraged, and fearful. He wondered whether the patient might make good on his threat.
Some colleagues suggested that Bittleman buy a gun, while others recommended he carry pepper spray. Dr. Bittleman had no interest in learning how to use a gun, he said. He took comfort in the fact that there were armed guards and metal detectors in his building, and there was a panic button under his desk.
“I was not sure I wanted to take care of patients anymore, especially chronic pain patients,” he said. “However, I went for some counseling with the Employee Assistance Program, and the therapist was helpful in normalizing my anxiety and acknowledging my fear.”
On the day of the hearing, Dr. Bittleman sat in the back of the courtroom. The patient, who sat near the front, glanced at Dr. Bittleman with a slight smile.
When his case was called, the judge explained that as the plaintiff, the burden was on Dr. Bittleman to prove the patient was a threat to his safety. He provided the judge a copy of the threatening message and a copy of the ex-wife’s note.
After reading the documents, the judge asked the patient to explain his side. The patient complained that the VA had denied him certain benefits and that he was forced to receive mental health treatment rehab that he “didn’t need.” The judge eventually interrupted the man to ask if he had threatened to kill Dr. Bittleman.
“Oh yes, your honor, I did say that, but I was only joking,” he told the judge.
The admission was enough. The judge issued a restraining order against the patient that would last 1 year. He could not have firearms, and if he violated the order, he would be arrested.
The terrifying saga was finally over.
“I never heard from the patient again,” Dr. Bittleman said. “His [care] location was changed, and police were required to come to all his visits with his new provider. I was relieved that if he ever came near me, he was going to jail.”
To raise awareness about such ordeals and the hassles that can follow, Dr. Bittleman wrote an article about his experience, which was published in the Annals of Family Medicine. He continues to treat patients at the VA, including those with chronic pain, but the memory of the menacing patient resurfaces from time to time.
“I do still think about it,” he said. “I know how to use my panic button, and I test it every 90 days. If there is a patient who concerns me, I will have the VA police wait nearby. I am very aware and upset by violence. When I hear about a doctor getting killed, I feel a clutch in my chest. How could I not relate? Here is a doctor who worked hard, who dedicated their life to help patients, and it comes to this? It’s so revolting. It makes me sick.”
Can you identify a violent patient?
Concern over threatening patients has grown across the country after recent violent attacks against physicians in Oklahoma and California. Two physicians were shot to death in June 2022 when a patient opened fire inside a Tulsa medical building. The primary target of the shooting was a surgeon who had performed surgery on the patient. Also in June, two nurses and an emergency physician were stabbed by a patient inside the Encino Hospital Medical Center. They survived.
The attacks raise questions about how to identify potentially violent patients and how to mitigate possible violence.
Threats and violence against health care professionals are nothing new, but they’re finally getting the attention they deserve, says Derek Schaller, MD, an emergency physician and assistant professor of emergency medicine at Central Michigan University in Mount Pleasant.
“Violence against personnel in medicine has been an issue for a long time; it’s just finally making headlines,” he said. “Way back when, it almost seemed like it was part of the job, part of the gig. But it shouldn’t be part of the gig. It’s not something we should be dealing with.”
It’s common for health care professionals and health centers to take a reactive approach to violent patients, but Dr. Schaller encourages a more proactive strategy. Central Michigan University Health, for example, recently studied its past violent encounters and analyzed the characteristics of violent patients. The analysis came after an increase in violent patient episodes at the health center in the past year, Dr. Schaller said.
The study yielded some interesting results, including that a large percentage of patients who became violent in the emergency department did so within the first hour they were in the hospital, he said.
“You would have thought it’s the patients who have been there and have been stuck in the emergency department for a while and who became disgruntled, but that was not the case,” Dr. Schaller said.
He recommends that physicians, medical practices, and hospitals carry out similar assessments of their patient populations and of past violent encounters to determine trends. His institution will be implementing a screening tool in triage to identify patients more likely to become violent so that health care professionals can intervene earlier, he said.
Such a screening tool is already demonstrating success in a variety of medical settings.
About 10 years ago, a research team led by Son Chae Kim, PhD, RN, found that the 10-item Aggressive Behavior Risk Assessment Tool (ABRAT) was able to identify potentially violent patients with reasonable sensitivity and specificity in hospital medical-surgical units.
Subsequently, the tool was modified for long-term care facilities, and again, researchers found that ABRAT was able to identify potentially violent residents with reasonable sensitivity and specificity, said Dr. Kim, ABRAT developer and a professor at Point Loma Nazarene University, San Diego.
In 2021, researchers embedded the checklist into an electronic health record (EHR) system and tested ABRAT in emergency departments.
“Currently, we are working with computer programmers to build an app that would make the ABRAT very easy to use in conjunction with EHR,” Dr. Kim said. “Instead of a nurse searching the EHR to find out if the patient has history of mental illness or aggressive behavior in the past, the app would automatically search the EHR and combine the nurse’s quick observation whether the patient is confused, agitated, staring, or threatening, to automatically calculate the violence risk.”
Dr. Kim and her team also developed a tool called VEST (Violent Event Severity Tool), a standardized objective workplace violence severity assessment. They are working with programmers to incorporate VEST into the app as well.
Dr. Kim’s hope is that the ABRAT tool can be modified for use in a range of health care settings.
A version of this article first appeared on Medscape.com.