User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Three stages to COVID-19 brain damage, new review suggests
In stage 1, viral damage is limited to epithelial cells of the nose and mouth, and in stage 2 blood clots that form in the lungs may travel to the brain, leading to stroke. In stage 3, the virus crosses the blood-brain barrier and invades the brain.
“Our major take-home points are that patients with COVID-19 symptoms, such as shortness of breath, headache, or dizziness, may have neurological symptoms that, at the time of hospitalization, might not be noticed or prioritized, or whose neurological symptoms may become apparent only after they leave the hospital,” lead author Majid Fotuhi, MD, PhD, medical director of NeuroGrow Brain Fitness Center in McLean, Va., said.
“Hospitalized patients with COVID-19 should have a neurological evaluation and ideally a brain MRI before leaving the hospital; and, if there are abnormalities, they should follow up with a neurologist in 3-4 months,” said Dr. Fotuhi, who is also affiliate staff at Johns Hopkins Medicine, Baltimore.
The review was published online June 8 in the Journal of Alzheimer’s Disease.
Wreaks CNS havoc
It has become “increasingly evident” that SARS-CoV-2 can cause neurologic manifestations, including anosmia, seizures, stroke, confusion, encephalopathy, and total paralysis, the authors wrote.
They noted that SARS-CoV-2 binds to ACE2, which facilitates the conversion of angiotensin II to angiotensin. After ACE2 has bound to respiratory epithelial cells and then to epithelial cells in blood vessels, SARS-CoV-2 triggers the formation of a “cytokine storm.”
These cytokines, in turn, increase vascular permeability, edema, and widespread inflammation, as well as triggering “hypercoagulation cascades,” which cause small and large blood clots that affect multiple organs.
If SARS-CoV-2 crosses the blood-brain barrier, directly entering the brain, it can contribute to demyelination or neurodegeneration.
“We very thoroughly reviewed the literature published between Jan. 1 and May 1, 2020, about neurological issues [in COVID-19] and what I found interesting is that so many neurological things can happen due to a virus which is so small,” said Dr. Fotuhi.
“This virus’ DNA has such limited information, and yet it can wreak havoc on our nervous system because it kicks off such a potent defense system in our body that damages our nervous system,” he said.
Three-stage classification
- Stage 1: The extent of SARS-CoV-2 binding to the ACE2 receptors is limited to the nasal and gustatory epithelial cells, with the cytokine storm remaining “low and controlled.” During this stage, patients may experience smell or taste impairments, but often recover without any interventions.
- Stage 2: A “robust immune response” is activated by the virus, leading to inflammation in the blood vessels, increased hypercoagulability factors, and the formation of blood clots in cerebral arteries and veins. The patient may therefore experience either large or small strokes. Additional stage 2 symptoms include fatigue, hemiplegia, sensory loss, , tetraplegia, , or ataxia.
- Stage 3: The cytokine storm in the blood vessels is so severe that it causes an “explosive inflammatory response” and penetrates the blood-brain barrier, leading to the entry of cytokines, blood components, and viral particles into the brain parenchyma and causing neuronal cell death and encephalitis. This stage can be characterized by seizures, confusion, , coma, loss of consciousness, or death.
“Patients in stage 3 are more likely to have long-term consequences, because there is evidence that the virus particles have actually penetrated the brain, and we know that SARS-CoV-2 can remain dormant in neurons for many years,” said Dr. Fotuhi.
“Studies of coronaviruses have shown a link between the viruses and the risk of multiple sclerosis or Parkinson’s disease even decades later,” he added.
“Based on several reports in recent months, between 36% to 55% of patients with COVID-19 that are hospitalized have some neurological symptoms, but if you don’t look for them, you won’t see them,” Dr. Fotuhi noted.
As a result, patients should be monitored over time after discharge, as they may develop cognitive dysfunction down the road.
Additionally, “it is imperative for patients [hospitalized with COVID-19] to get a baseline MRI before leaving the hospital so that we have a starting point for future evaluation and treatment,” said Dr. Fotuhi.
“The good news is that neurological manifestations of COVID-19 are treatable,” and “can improve with intensive training,” including lifestyle changes – such as a heart-healthy diet, regular physical activity, stress reduction, improved sleep, biofeedback, and brain rehabilitation, Dr. Fotuhi added.
Routine MRI not necessary
Kenneth Tyler, MD, chair of the department of neurology at the University of Colorado at Denver, Aurora, disagreed that all hospitalized patients with COVID-19 should routinely receive an MRI.
“Whenever you are using a piece of equipment on patients who are COVID-19 infected, you risk introducing the infection to uninfected patients,” he said. Instead, “the indication is in patients who develop unexplained neurological manifestations – altered mental status or focal seizures, for example – because in those cases, you do need to understand whether there are underlying structural abnormalities,” said Dr. Tyler, who was not involved in the review.
Also commenting on the review, Vanja Douglas, MD, associate professor of clinical neurology, University of California, San Francisco, described the review as “thorough” and suggested it may “help us understand how to design observational studies to test whether the associations are due to severe respiratory illness or are specific to SARS-CoV-2 infection.”
Dr. Douglas, who was not involved in the review, added that it is “helpful in giving us a sense of which neurologic syndromes have been observed in COVID-19 patients, and therefore which patients neurologists may want to screen more carefully during the pandemic.”
The study had no specific funding. Dr. Fotuhi disclosed no relevant financial relationships. One coauthor reported receiving consulting fees as a member of the scientific advisory board for Brainreader and reports royalties for expert witness consultation in conjunction with Neurevolution. Dr. Tyler and Dr. Douglas disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
In stage 1, viral damage is limited to epithelial cells of the nose and mouth, and in stage 2 blood clots that form in the lungs may travel to the brain, leading to stroke. In stage 3, the virus crosses the blood-brain barrier and invades the brain.
“Our major take-home points are that patients with COVID-19 symptoms, such as shortness of breath, headache, or dizziness, may have neurological symptoms that, at the time of hospitalization, might not be noticed or prioritized, or whose neurological symptoms may become apparent only after they leave the hospital,” lead author Majid Fotuhi, MD, PhD, medical director of NeuroGrow Brain Fitness Center in McLean, Va., said.
“Hospitalized patients with COVID-19 should have a neurological evaluation and ideally a brain MRI before leaving the hospital; and, if there are abnormalities, they should follow up with a neurologist in 3-4 months,” said Dr. Fotuhi, who is also affiliate staff at Johns Hopkins Medicine, Baltimore.
The review was published online June 8 in the Journal of Alzheimer’s Disease.
Wreaks CNS havoc
It has become “increasingly evident” that SARS-CoV-2 can cause neurologic manifestations, including anosmia, seizures, stroke, confusion, encephalopathy, and total paralysis, the authors wrote.
They noted that SARS-CoV-2 binds to ACE2, which facilitates the conversion of angiotensin II to angiotensin. After ACE2 has bound to respiratory epithelial cells and then to epithelial cells in blood vessels, SARS-CoV-2 triggers the formation of a “cytokine storm.”
These cytokines, in turn, increase vascular permeability, edema, and widespread inflammation, as well as triggering “hypercoagulation cascades,” which cause small and large blood clots that affect multiple organs.
If SARS-CoV-2 crosses the blood-brain barrier, directly entering the brain, it can contribute to demyelination or neurodegeneration.
“We very thoroughly reviewed the literature published between Jan. 1 and May 1, 2020, about neurological issues [in COVID-19] and what I found interesting is that so many neurological things can happen due to a virus which is so small,” said Dr. Fotuhi.
“This virus’ DNA has such limited information, and yet it can wreak havoc on our nervous system because it kicks off such a potent defense system in our body that damages our nervous system,” he said.
Three-stage classification
- Stage 1: The extent of SARS-CoV-2 binding to the ACE2 receptors is limited to the nasal and gustatory epithelial cells, with the cytokine storm remaining “low and controlled.” During this stage, patients may experience smell or taste impairments, but often recover without any interventions.
- Stage 2: A “robust immune response” is activated by the virus, leading to inflammation in the blood vessels, increased hypercoagulability factors, and the formation of blood clots in cerebral arteries and veins. The patient may therefore experience either large or small strokes. Additional stage 2 symptoms include fatigue, hemiplegia, sensory loss, , tetraplegia, , or ataxia.
- Stage 3: The cytokine storm in the blood vessels is so severe that it causes an “explosive inflammatory response” and penetrates the blood-brain barrier, leading to the entry of cytokines, blood components, and viral particles into the brain parenchyma and causing neuronal cell death and encephalitis. This stage can be characterized by seizures, confusion, , coma, loss of consciousness, or death.
“Patients in stage 3 are more likely to have long-term consequences, because there is evidence that the virus particles have actually penetrated the brain, and we know that SARS-CoV-2 can remain dormant in neurons for many years,” said Dr. Fotuhi.
“Studies of coronaviruses have shown a link between the viruses and the risk of multiple sclerosis or Parkinson’s disease even decades later,” he added.
“Based on several reports in recent months, between 36% to 55% of patients with COVID-19 that are hospitalized have some neurological symptoms, but if you don’t look for them, you won’t see them,” Dr. Fotuhi noted.
As a result, patients should be monitored over time after discharge, as they may develop cognitive dysfunction down the road.
Additionally, “it is imperative for patients [hospitalized with COVID-19] to get a baseline MRI before leaving the hospital so that we have a starting point for future evaluation and treatment,” said Dr. Fotuhi.
“The good news is that neurological manifestations of COVID-19 are treatable,” and “can improve with intensive training,” including lifestyle changes – such as a heart-healthy diet, regular physical activity, stress reduction, improved sleep, biofeedback, and brain rehabilitation, Dr. Fotuhi added.
Routine MRI not necessary
Kenneth Tyler, MD, chair of the department of neurology at the University of Colorado at Denver, Aurora, disagreed that all hospitalized patients with COVID-19 should routinely receive an MRI.
“Whenever you are using a piece of equipment on patients who are COVID-19 infected, you risk introducing the infection to uninfected patients,” he said. Instead, “the indication is in patients who develop unexplained neurological manifestations – altered mental status or focal seizures, for example – because in those cases, you do need to understand whether there are underlying structural abnormalities,” said Dr. Tyler, who was not involved in the review.
Also commenting on the review, Vanja Douglas, MD, associate professor of clinical neurology, University of California, San Francisco, described the review as “thorough” and suggested it may “help us understand how to design observational studies to test whether the associations are due to severe respiratory illness or are specific to SARS-CoV-2 infection.”
Dr. Douglas, who was not involved in the review, added that it is “helpful in giving us a sense of which neurologic syndromes have been observed in COVID-19 patients, and therefore which patients neurologists may want to screen more carefully during the pandemic.”
The study had no specific funding. Dr. Fotuhi disclosed no relevant financial relationships. One coauthor reported receiving consulting fees as a member of the scientific advisory board for Brainreader and reports royalties for expert witness consultation in conjunction with Neurevolution. Dr. Tyler and Dr. Douglas disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
In stage 1, viral damage is limited to epithelial cells of the nose and mouth, and in stage 2 blood clots that form in the lungs may travel to the brain, leading to stroke. In stage 3, the virus crosses the blood-brain barrier and invades the brain.
“Our major take-home points are that patients with COVID-19 symptoms, such as shortness of breath, headache, or dizziness, may have neurological symptoms that, at the time of hospitalization, might not be noticed or prioritized, or whose neurological symptoms may become apparent only after they leave the hospital,” lead author Majid Fotuhi, MD, PhD, medical director of NeuroGrow Brain Fitness Center in McLean, Va., said.
“Hospitalized patients with COVID-19 should have a neurological evaluation and ideally a brain MRI before leaving the hospital; and, if there are abnormalities, they should follow up with a neurologist in 3-4 months,” said Dr. Fotuhi, who is also affiliate staff at Johns Hopkins Medicine, Baltimore.
The review was published online June 8 in the Journal of Alzheimer’s Disease.
Wreaks CNS havoc
It has become “increasingly evident” that SARS-CoV-2 can cause neurologic manifestations, including anosmia, seizures, stroke, confusion, encephalopathy, and total paralysis, the authors wrote.
They noted that SARS-CoV-2 binds to ACE2, which facilitates the conversion of angiotensin II to angiotensin. After ACE2 has bound to respiratory epithelial cells and then to epithelial cells in blood vessels, SARS-CoV-2 triggers the formation of a “cytokine storm.”
These cytokines, in turn, increase vascular permeability, edema, and widespread inflammation, as well as triggering “hypercoagulation cascades,” which cause small and large blood clots that affect multiple organs.
If SARS-CoV-2 crosses the blood-brain barrier, directly entering the brain, it can contribute to demyelination or neurodegeneration.
“We very thoroughly reviewed the literature published between Jan. 1 and May 1, 2020, about neurological issues [in COVID-19] and what I found interesting is that so many neurological things can happen due to a virus which is so small,” said Dr. Fotuhi.
“This virus’ DNA has such limited information, and yet it can wreak havoc on our nervous system because it kicks off such a potent defense system in our body that damages our nervous system,” he said.
Three-stage classification
- Stage 1: The extent of SARS-CoV-2 binding to the ACE2 receptors is limited to the nasal and gustatory epithelial cells, with the cytokine storm remaining “low and controlled.” During this stage, patients may experience smell or taste impairments, but often recover without any interventions.
- Stage 2: A “robust immune response” is activated by the virus, leading to inflammation in the blood vessels, increased hypercoagulability factors, and the formation of blood clots in cerebral arteries and veins. The patient may therefore experience either large or small strokes. Additional stage 2 symptoms include fatigue, hemiplegia, sensory loss, , tetraplegia, , or ataxia.
- Stage 3: The cytokine storm in the blood vessels is so severe that it causes an “explosive inflammatory response” and penetrates the blood-brain barrier, leading to the entry of cytokines, blood components, and viral particles into the brain parenchyma and causing neuronal cell death and encephalitis. This stage can be characterized by seizures, confusion, , coma, loss of consciousness, or death.
“Patients in stage 3 are more likely to have long-term consequences, because there is evidence that the virus particles have actually penetrated the brain, and we know that SARS-CoV-2 can remain dormant in neurons for many years,” said Dr. Fotuhi.
“Studies of coronaviruses have shown a link between the viruses and the risk of multiple sclerosis or Parkinson’s disease even decades later,” he added.
“Based on several reports in recent months, between 36% to 55% of patients with COVID-19 that are hospitalized have some neurological symptoms, but if you don’t look for them, you won’t see them,” Dr. Fotuhi noted.
As a result, patients should be monitored over time after discharge, as they may develop cognitive dysfunction down the road.
Additionally, “it is imperative for patients [hospitalized with COVID-19] to get a baseline MRI before leaving the hospital so that we have a starting point for future evaluation and treatment,” said Dr. Fotuhi.
“The good news is that neurological manifestations of COVID-19 are treatable,” and “can improve with intensive training,” including lifestyle changes – such as a heart-healthy diet, regular physical activity, stress reduction, improved sleep, biofeedback, and brain rehabilitation, Dr. Fotuhi added.
Routine MRI not necessary
Kenneth Tyler, MD, chair of the department of neurology at the University of Colorado at Denver, Aurora, disagreed that all hospitalized patients with COVID-19 should routinely receive an MRI.
“Whenever you are using a piece of equipment on patients who are COVID-19 infected, you risk introducing the infection to uninfected patients,” he said. Instead, “the indication is in patients who develop unexplained neurological manifestations – altered mental status or focal seizures, for example – because in those cases, you do need to understand whether there are underlying structural abnormalities,” said Dr. Tyler, who was not involved in the review.
Also commenting on the review, Vanja Douglas, MD, associate professor of clinical neurology, University of California, San Francisco, described the review as “thorough” and suggested it may “help us understand how to design observational studies to test whether the associations are due to severe respiratory illness or are specific to SARS-CoV-2 infection.”
Dr. Douglas, who was not involved in the review, added that it is “helpful in giving us a sense of which neurologic syndromes have been observed in COVID-19 patients, and therefore which patients neurologists may want to screen more carefully during the pandemic.”
The study had no specific funding. Dr. Fotuhi disclosed no relevant financial relationships. One coauthor reported receiving consulting fees as a member of the scientific advisory board for Brainreader and reports royalties for expert witness consultation in conjunction with Neurevolution. Dr. Tyler and Dr. Douglas disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The wave of the future
Longtime CEO bids farewell to SHM
Changing times
After more than 20 years, my leadership role as CEO at the Society of Hospital Medicine (SHM) has ended with the transition to Dr. Eric Howell as the new SHM CEO on July 1, 2020. Looking back, I think we can all be proud of how we have helped to shape the specialty of hospital medicine over these two decades and of how strong SHM has become to support our new specialty.
In 2000, few people knew what a hospitalist was (or more importantly what we could become) and the specialty of hospital medicine had not even been named yet. Today the reputation of SHM is firmly established and the specialty has been defined by a unique curriculum through the Core Competencies in Hospital Medicine for both adult and pediatric patients, and by several textbooks in hospital medicine. There are divisions or departments of hospital medicine at many hospitals and academic medical centers. We even managed to convince the American Board of Internal Medicine, the American Board of Family Medicine, and the American Board of Medical Specialties to create a credential of Focused Practice in Hospital Medicine as the first-ever certification not tied to specific fellowship training.
To recognize the contributions of our members, SHM has established Awards of Excellence and the Fellow and Senior Fellow in Hospital Medicine (FHM and SFHM) designations. We have gone from a small national association in Philadelphia to create 68 active chapters and more than 20 Special Interest Groups. In my time at SHM I have attended more than 75-chapter meetings and met with thousands of hospitalists in 46 states. We now have over 20,000 members at SHM, making us the fastest growing medical specialty ever.
When I started at the National Association of Inpatient Physicians (NAIP) our only meeting was an annual CME meeting for about 150-200 people. We now hold a national meeting every year for more than 4,000 attendees that is the “Center of the Universe for Hospital Medicine.” Understanding that we needed to educate the people who will lead change in our health care system, we developed from scratch a set of Leadership Academies that has already educated more than 2,500 hospitalist leaders. To train the educators in quality improvement in medical education we developed our Quality and Safety Educator Academy (QSEA) programs, and to promote career development of academic hospitalists we created our Academic Hospitalist Academy.
SHM is the leader in adult in-practice learning, specifically designed for hospitalists. SHM members have access to a state-of-the-art comprehensive hospitalist-based online education system as well as board review and maintenance of certification (MOC) review tools in our SPARK program, specifically for hospital medicine.
In the area of quality improvement, most medical societies convene a panel of experts, develop guidelines, publish them, and hope that change will occur. SHM has been much more proactive, creating the Center for Quality Improvement that has raised more than $10 million and developed Quality Improvement programs in more than 400 hospitals over the years, winning the prestigious Eisenberg Award along the way.
When I started at NAIP in 2000, our only communication tools were a 4-page newsletter and an email listserv. Along the way we have developed a broadly read newsmagazine (The Hospitalist), a well-recognized peer reviewed journal (Journal of Hospital Medicine), a robust website, and a significant social media presence.
From the very early days we knew that our specialty would not be totally successful by only facing inward. Change was coming to our health care system and hospitalists were going to be right in the middle. Despite our young age and limited resources, we have always hit above our weight class in advocacy. We actively participated in the development of the Affordable Care Act (Obamacare), making suggestions in payment reform, expanding the workforce with visa reform, and expanding the team of clinicians. Along the way SHM members rose to run the Centers for Medicare & Medicaid Services (CMS) and the Food and Drug Administration (FDA), and serve as U.S. Surgeon General.
Today in these troubled times, SHM continues to be a positive voice in promoting the use of PPE, the need for increased COVID-19 testing, and the recognition of our nation’s 60,000 hospitalists as essential frontline workers in the COVID-19 pandemic. With its longstanding role in promoting diversity and overcoming social injustice, SHM has had a positive national voice during the protests over police brutality.
We have proved to be a good partner with many other organizations and consistently were invited to partner in coalitions with the ED physicians (ACEP), the critical care docs (SCCM), the hospitals (AHA), the house of medicine (AMA), other internists (ACP), surgeons (ACS), and pediatricians (AAP), and so many other much more established societies, because we could be an active, flexible, and knowledgeable partner for more than 20 years.
Today, SHM and hospital medicine are clearly recognized as a force in the rapidly evolving health care system. With this comes not only influence but also responsibility, and I am certain the SHM Board, membership, and staff are ready for this challenge. The economic toll of our current pandemic will see colleges and other major companies and institutions go out of business and leave the landscape. SHM has a deep foundation and a well of strength to call on and will survive and thrive into the future.
SHM has been a good fit for me professionally and personally. Many of my skills and strengths have served SHM in our “early” years. I am very proud of what we have been able to accomplish TOGETHER. In the end it is the people I have been fortunate enough to meet and work with throughout these past 20 years that will stay with me, many of whom are lifelong friends. My mother, even today at 93, has always asked me to leave anything I do better off than when I came in the door. As I look back at my time helping to shape and lead SHM, I am sure I have answered my mother’s challenge and more.
I look forward to seeing many of you at a future SHM meeting and reveling in the way that hospitalists will actively play an important role in shaping our health care system in the future.
Dr. Wellikson is retiring as CEO of SHM.
Live long and prosper
Back in 2000, I was extremely fortunate to land my dream job as a hospitalist at Johns Hopkins Bayview in Baltimore. That dream exceeded my wildest aspirations. During my 20-year career as faculty in the Johns Hopkins School of Medicine I grew our tiny, 4 physician hospitalist group at Johns Hopkins Bayview into a multihospital program, complete with more than 150 physicians. That exceedingly rewarding work helped to shape the field of hospital medicine nationally and provided the foundation for my promotion to professor of medicine at Johns Hopkins in 2016.
Most professionals are lucky if they find one inspiring institution; I have found two. SHM has been my professional home since I became a hospitalist in 2000, and in that time I have dedicated as much creative energy to SHM as I have at Johns Hopkins.
Even at this time when the medical profession, and the entire world, has been rocked by the coronavirus, the fundamentals that have made SHM so successful will serve us well through the effects of this pandemic and beyond. It takes a skilled leader to nurture a professional society through the growth from only a few hundred members to thousands upon thousands, and at the same time crafting the profession into one of quality and high impact. These past 22 years Dr. Larry Wellikson, our retiring CEO, has skillfully accomplished just that by building lasting programs and people.
As you might imagine, my approach will work to add onto the legacy that Larry has left us. Yes, we will have to adapt SHM to the realities of the near future: virtual meetings, in-person events (yes, those will return one day) with appropriate social distancing until the coronavirus has faded, modified chapter meetings, and more. Someday the world will find a new normal, and SHM will evolve to meet the needs of our members and the patients we serve.
Through this pandemic and beyond, my vision – in partnership with the Board of Directors – will be to:
- Continue the work to enhance member engagement. We are primarily a membership organization, after all.
- Maintain our profession’s leadership role in the care continuum, particularly acute care.
- Be a deliberate sponsor of diversity and inclusion. I believe social justice is a moral imperative, and good business.
- Invest in teams: Chapters, special interest groups, and committees are key to success.
- Be financially prudent, so that this organization can serve its members through the best of times and those most challenging times.
Back in 2000 I joined my dream society, the Society of Hospital Medicine. That society exceeded my wildest aspirations. During my 20-year membership I started an SHM Chapter, was a leader in the Leadership Academies, joined the Board of Directors, participated in Annual Conferences, and helped lead the SHM Center for Quality Improvement. That exceedingly rewarding partnership helped shape the field of hospital medicine nationally and provided the foundation for my next role at SHM. I am excited and grateful to be the CEO of SHM.
I’ll end with something I use every day – “Eric Howell’s Core Values”:
- Make the world a better place.
- Invest in people.
- Be ethical and transparent.
- Do what you love.
- Try to use Star Trek references whenever possible. (Okay, this last one is not really a core value, but maybe a character trait?) At least the Vulcan greeting is appropriate for our times: Live long and prosper.
Dr. Howell is the new CEO for SHM as of July 1, 2020.
Longtime CEO bids farewell to SHM
Longtime CEO bids farewell to SHM
Changing times
After more than 20 years, my leadership role as CEO at the Society of Hospital Medicine (SHM) has ended with the transition to Dr. Eric Howell as the new SHM CEO on July 1, 2020. Looking back, I think we can all be proud of how we have helped to shape the specialty of hospital medicine over these two decades and of how strong SHM has become to support our new specialty.
In 2000, few people knew what a hospitalist was (or more importantly what we could become) and the specialty of hospital medicine had not even been named yet. Today the reputation of SHM is firmly established and the specialty has been defined by a unique curriculum through the Core Competencies in Hospital Medicine for both adult and pediatric patients, and by several textbooks in hospital medicine. There are divisions or departments of hospital medicine at many hospitals and academic medical centers. We even managed to convince the American Board of Internal Medicine, the American Board of Family Medicine, and the American Board of Medical Specialties to create a credential of Focused Practice in Hospital Medicine as the first-ever certification not tied to specific fellowship training.
To recognize the contributions of our members, SHM has established Awards of Excellence and the Fellow and Senior Fellow in Hospital Medicine (FHM and SFHM) designations. We have gone from a small national association in Philadelphia to create 68 active chapters and more than 20 Special Interest Groups. In my time at SHM I have attended more than 75-chapter meetings and met with thousands of hospitalists in 46 states. We now have over 20,000 members at SHM, making us the fastest growing medical specialty ever.
When I started at the National Association of Inpatient Physicians (NAIP) our only meeting was an annual CME meeting for about 150-200 people. We now hold a national meeting every year for more than 4,000 attendees that is the “Center of the Universe for Hospital Medicine.” Understanding that we needed to educate the people who will lead change in our health care system, we developed from scratch a set of Leadership Academies that has already educated more than 2,500 hospitalist leaders. To train the educators in quality improvement in medical education we developed our Quality and Safety Educator Academy (QSEA) programs, and to promote career development of academic hospitalists we created our Academic Hospitalist Academy.
SHM is the leader in adult in-practice learning, specifically designed for hospitalists. SHM members have access to a state-of-the-art comprehensive hospitalist-based online education system as well as board review and maintenance of certification (MOC) review tools in our SPARK program, specifically for hospital medicine.
In the area of quality improvement, most medical societies convene a panel of experts, develop guidelines, publish them, and hope that change will occur. SHM has been much more proactive, creating the Center for Quality Improvement that has raised more than $10 million and developed Quality Improvement programs in more than 400 hospitals over the years, winning the prestigious Eisenberg Award along the way.
When I started at NAIP in 2000, our only communication tools were a 4-page newsletter and an email listserv. Along the way we have developed a broadly read newsmagazine (The Hospitalist), a well-recognized peer reviewed journal (Journal of Hospital Medicine), a robust website, and a significant social media presence.
From the very early days we knew that our specialty would not be totally successful by only facing inward. Change was coming to our health care system and hospitalists were going to be right in the middle. Despite our young age and limited resources, we have always hit above our weight class in advocacy. We actively participated in the development of the Affordable Care Act (Obamacare), making suggestions in payment reform, expanding the workforce with visa reform, and expanding the team of clinicians. Along the way SHM members rose to run the Centers for Medicare & Medicaid Services (CMS) and the Food and Drug Administration (FDA), and serve as U.S. Surgeon General.
Today in these troubled times, SHM continues to be a positive voice in promoting the use of PPE, the need for increased COVID-19 testing, and the recognition of our nation’s 60,000 hospitalists as essential frontline workers in the COVID-19 pandemic. With its longstanding role in promoting diversity and overcoming social injustice, SHM has had a positive national voice during the protests over police brutality.
We have proved to be a good partner with many other organizations and consistently were invited to partner in coalitions with the ED physicians (ACEP), the critical care docs (SCCM), the hospitals (AHA), the house of medicine (AMA), other internists (ACP), surgeons (ACS), and pediatricians (AAP), and so many other much more established societies, because we could be an active, flexible, and knowledgeable partner for more than 20 years.
Today, SHM and hospital medicine are clearly recognized as a force in the rapidly evolving health care system. With this comes not only influence but also responsibility, and I am certain the SHM Board, membership, and staff are ready for this challenge. The economic toll of our current pandemic will see colleges and other major companies and institutions go out of business and leave the landscape. SHM has a deep foundation and a well of strength to call on and will survive and thrive into the future.
SHM has been a good fit for me professionally and personally. Many of my skills and strengths have served SHM in our “early” years. I am very proud of what we have been able to accomplish TOGETHER. In the end it is the people I have been fortunate enough to meet and work with throughout these past 20 years that will stay with me, many of whom are lifelong friends. My mother, even today at 93, has always asked me to leave anything I do better off than when I came in the door. As I look back at my time helping to shape and lead SHM, I am sure I have answered my mother’s challenge and more.
I look forward to seeing many of you at a future SHM meeting and reveling in the way that hospitalists will actively play an important role in shaping our health care system in the future.
Dr. Wellikson is retiring as CEO of SHM.
Live long and prosper
Back in 2000, I was extremely fortunate to land my dream job as a hospitalist at Johns Hopkins Bayview in Baltimore. That dream exceeded my wildest aspirations. During my 20-year career as faculty in the Johns Hopkins School of Medicine I grew our tiny, 4 physician hospitalist group at Johns Hopkins Bayview into a multihospital program, complete with more than 150 physicians. That exceedingly rewarding work helped to shape the field of hospital medicine nationally and provided the foundation for my promotion to professor of medicine at Johns Hopkins in 2016.
Most professionals are lucky if they find one inspiring institution; I have found two. SHM has been my professional home since I became a hospitalist in 2000, and in that time I have dedicated as much creative energy to SHM as I have at Johns Hopkins.
Even at this time when the medical profession, and the entire world, has been rocked by the coronavirus, the fundamentals that have made SHM so successful will serve us well through the effects of this pandemic and beyond. It takes a skilled leader to nurture a professional society through the growth from only a few hundred members to thousands upon thousands, and at the same time crafting the profession into one of quality and high impact. These past 22 years Dr. Larry Wellikson, our retiring CEO, has skillfully accomplished just that by building lasting programs and people.
As you might imagine, my approach will work to add onto the legacy that Larry has left us. Yes, we will have to adapt SHM to the realities of the near future: virtual meetings, in-person events (yes, those will return one day) with appropriate social distancing until the coronavirus has faded, modified chapter meetings, and more. Someday the world will find a new normal, and SHM will evolve to meet the needs of our members and the patients we serve.
Through this pandemic and beyond, my vision – in partnership with the Board of Directors – will be to:
- Continue the work to enhance member engagement. We are primarily a membership organization, after all.
- Maintain our profession’s leadership role in the care continuum, particularly acute care.
- Be a deliberate sponsor of diversity and inclusion. I believe social justice is a moral imperative, and good business.
- Invest in teams: Chapters, special interest groups, and committees are key to success.
- Be financially prudent, so that this organization can serve its members through the best of times and those most challenging times.
Back in 2000 I joined my dream society, the Society of Hospital Medicine. That society exceeded my wildest aspirations. During my 20-year membership I started an SHM Chapter, was a leader in the Leadership Academies, joined the Board of Directors, participated in Annual Conferences, and helped lead the SHM Center for Quality Improvement. That exceedingly rewarding partnership helped shape the field of hospital medicine nationally and provided the foundation for my next role at SHM. I am excited and grateful to be the CEO of SHM.
I’ll end with something I use every day – “Eric Howell’s Core Values”:
- Make the world a better place.
- Invest in people.
- Be ethical and transparent.
- Do what you love.
- Try to use Star Trek references whenever possible. (Okay, this last one is not really a core value, but maybe a character trait?) At least the Vulcan greeting is appropriate for our times: Live long and prosper.
Dr. Howell is the new CEO for SHM as of July 1, 2020.
Changing times
After more than 20 years, my leadership role as CEO at the Society of Hospital Medicine (SHM) has ended with the transition to Dr. Eric Howell as the new SHM CEO on July 1, 2020. Looking back, I think we can all be proud of how we have helped to shape the specialty of hospital medicine over these two decades and of how strong SHM has become to support our new specialty.
In 2000, few people knew what a hospitalist was (or more importantly what we could become) and the specialty of hospital medicine had not even been named yet. Today the reputation of SHM is firmly established and the specialty has been defined by a unique curriculum through the Core Competencies in Hospital Medicine for both adult and pediatric patients, and by several textbooks in hospital medicine. There are divisions or departments of hospital medicine at many hospitals and academic medical centers. We even managed to convince the American Board of Internal Medicine, the American Board of Family Medicine, and the American Board of Medical Specialties to create a credential of Focused Practice in Hospital Medicine as the first-ever certification not tied to specific fellowship training.
To recognize the contributions of our members, SHM has established Awards of Excellence and the Fellow and Senior Fellow in Hospital Medicine (FHM and SFHM) designations. We have gone from a small national association in Philadelphia to create 68 active chapters and more than 20 Special Interest Groups. In my time at SHM I have attended more than 75-chapter meetings and met with thousands of hospitalists in 46 states. We now have over 20,000 members at SHM, making us the fastest growing medical specialty ever.
When I started at the National Association of Inpatient Physicians (NAIP) our only meeting was an annual CME meeting for about 150-200 people. We now hold a national meeting every year for more than 4,000 attendees that is the “Center of the Universe for Hospital Medicine.” Understanding that we needed to educate the people who will lead change in our health care system, we developed from scratch a set of Leadership Academies that has already educated more than 2,500 hospitalist leaders. To train the educators in quality improvement in medical education we developed our Quality and Safety Educator Academy (QSEA) programs, and to promote career development of academic hospitalists we created our Academic Hospitalist Academy.
SHM is the leader in adult in-practice learning, specifically designed for hospitalists. SHM members have access to a state-of-the-art comprehensive hospitalist-based online education system as well as board review and maintenance of certification (MOC) review tools in our SPARK program, specifically for hospital medicine.
In the area of quality improvement, most medical societies convene a panel of experts, develop guidelines, publish them, and hope that change will occur. SHM has been much more proactive, creating the Center for Quality Improvement that has raised more than $10 million and developed Quality Improvement programs in more than 400 hospitals over the years, winning the prestigious Eisenberg Award along the way.
When I started at NAIP in 2000, our only communication tools were a 4-page newsletter and an email listserv. Along the way we have developed a broadly read newsmagazine (The Hospitalist), a well-recognized peer reviewed journal (Journal of Hospital Medicine), a robust website, and a significant social media presence.
From the very early days we knew that our specialty would not be totally successful by only facing inward. Change was coming to our health care system and hospitalists were going to be right in the middle. Despite our young age and limited resources, we have always hit above our weight class in advocacy. We actively participated in the development of the Affordable Care Act (Obamacare), making suggestions in payment reform, expanding the workforce with visa reform, and expanding the team of clinicians. Along the way SHM members rose to run the Centers for Medicare & Medicaid Services (CMS) and the Food and Drug Administration (FDA), and serve as U.S. Surgeon General.
Today in these troubled times, SHM continues to be a positive voice in promoting the use of PPE, the need for increased COVID-19 testing, and the recognition of our nation’s 60,000 hospitalists as essential frontline workers in the COVID-19 pandemic. With its longstanding role in promoting diversity and overcoming social injustice, SHM has had a positive national voice during the protests over police brutality.
We have proved to be a good partner with many other organizations and consistently were invited to partner in coalitions with the ED physicians (ACEP), the critical care docs (SCCM), the hospitals (AHA), the house of medicine (AMA), other internists (ACP), surgeons (ACS), and pediatricians (AAP), and so many other much more established societies, because we could be an active, flexible, and knowledgeable partner for more than 20 years.
Today, SHM and hospital medicine are clearly recognized as a force in the rapidly evolving health care system. With this comes not only influence but also responsibility, and I am certain the SHM Board, membership, and staff are ready for this challenge. The economic toll of our current pandemic will see colleges and other major companies and institutions go out of business and leave the landscape. SHM has a deep foundation and a well of strength to call on and will survive and thrive into the future.
SHM has been a good fit for me professionally and personally. Many of my skills and strengths have served SHM in our “early” years. I am very proud of what we have been able to accomplish TOGETHER. In the end it is the people I have been fortunate enough to meet and work with throughout these past 20 years that will stay with me, many of whom are lifelong friends. My mother, even today at 93, has always asked me to leave anything I do better off than when I came in the door. As I look back at my time helping to shape and lead SHM, I am sure I have answered my mother’s challenge and more.
I look forward to seeing many of you at a future SHM meeting and reveling in the way that hospitalists will actively play an important role in shaping our health care system in the future.
Dr. Wellikson is retiring as CEO of SHM.
Live long and prosper
Back in 2000, I was extremely fortunate to land my dream job as a hospitalist at Johns Hopkins Bayview in Baltimore. That dream exceeded my wildest aspirations. During my 20-year career as faculty in the Johns Hopkins School of Medicine I grew our tiny, 4 physician hospitalist group at Johns Hopkins Bayview into a multihospital program, complete with more than 150 physicians. That exceedingly rewarding work helped to shape the field of hospital medicine nationally and provided the foundation for my promotion to professor of medicine at Johns Hopkins in 2016.
Most professionals are lucky if they find one inspiring institution; I have found two. SHM has been my professional home since I became a hospitalist in 2000, and in that time I have dedicated as much creative energy to SHM as I have at Johns Hopkins.
Even at this time when the medical profession, and the entire world, has been rocked by the coronavirus, the fundamentals that have made SHM so successful will serve us well through the effects of this pandemic and beyond. It takes a skilled leader to nurture a professional society through the growth from only a few hundred members to thousands upon thousands, and at the same time crafting the profession into one of quality and high impact. These past 22 years Dr. Larry Wellikson, our retiring CEO, has skillfully accomplished just that by building lasting programs and people.
As you might imagine, my approach will work to add onto the legacy that Larry has left us. Yes, we will have to adapt SHM to the realities of the near future: virtual meetings, in-person events (yes, those will return one day) with appropriate social distancing until the coronavirus has faded, modified chapter meetings, and more. Someday the world will find a new normal, and SHM will evolve to meet the needs of our members and the patients we serve.
Through this pandemic and beyond, my vision – in partnership with the Board of Directors – will be to:
- Continue the work to enhance member engagement. We are primarily a membership organization, after all.
- Maintain our profession’s leadership role in the care continuum, particularly acute care.
- Be a deliberate sponsor of diversity and inclusion. I believe social justice is a moral imperative, and good business.
- Invest in teams: Chapters, special interest groups, and committees are key to success.
- Be financially prudent, so that this organization can serve its members through the best of times and those most challenging times.
Back in 2000 I joined my dream society, the Society of Hospital Medicine. That society exceeded my wildest aspirations. During my 20-year membership I started an SHM Chapter, was a leader in the Leadership Academies, joined the Board of Directors, participated in Annual Conferences, and helped lead the SHM Center for Quality Improvement. That exceedingly rewarding partnership helped shape the field of hospital medicine nationally and provided the foundation for my next role at SHM. I am excited and grateful to be the CEO of SHM.
I’ll end with something I use every day – “Eric Howell’s Core Values”:
- Make the world a better place.
- Invest in people.
- Be ethical and transparent.
- Do what you love.
- Try to use Star Trek references whenever possible. (Okay, this last one is not really a core value, but maybe a character trait?) At least the Vulcan greeting is appropriate for our times: Live long and prosper.
Dr. Howell is the new CEO for SHM as of July 1, 2020.
Pride profile: Keshav Khanijow, MD
Keshav Khanijow, MD, is a hospitalist at Northwestern Memorial Hospital and assistant professor at Northwestern University, Chicago. Originally from the San Francisco Bay area, he studied anthropology as an undergrad at Johns Hopkins University, Baltimore, then went to medical school at the University of California, San Francisco, followed by internal medicine residency and a hospital medicine fellowship at Johns Hopkins Bayview Medical Center. He came out as gay in 2006 as an undergrad. He is a founding member of the Society of Hospital Medicine’s LGBTQ+ Task Force and is involved with SHM’s Diversity and Inclusion Special Interest Group.
What challenges have you faced because of your sexual orientation in the different stages of your career, from training to now as a practicing physician?
In my early training, there weren’t a lot of accessible LGBTQ role models to talk about balancing my personal identities with my professional aspirations. Being a double minority as both South Asian and a gay male, made it that much more difficult. “What is it like to work in health care as a gay cismale? Will being out on my personal statement affect my entry into medical school? Should I list my LGBTQ activism activities or not?” Those were important to me.
And did you make your activism known?
Thankfully, I did. I joke that my application might as well have been printed on rainbow paper, if you will. I decided to be out because I wanted to be part of an environment that would accept me for who I was. But it was a difficult decision.
In medical school at UCSF, it’s San Francisco, so they were a little ahead of the game. They had a lot of social networking opportunities with LGBTQ and ally faculty. Those connections were important in helping me explore different fields, and I even got to write my first publication. That said, networking could sometimes be challenging, especially when it came to residency interviews. While many people would talk about family activities and engagements, I’d only been out to my family for a few years. As such, there would be somewhat of a disconnect. On the flip side, there were LGBTQ celebrations and cultural concepts important to me, but I couldn’t always connect on those fronts either.
When it comes to patients, I do have a bit of a higher-pitched voice, and my mannerisms can be gender nonconforming. While it did make me the target of some cruel middle school humor, I’ve come to be proud of myself, mannerisms and all. That said, I have had patients make remarks to me about being gay, whether it be positive or negative. For LGBTQ patients, they’re like, “this is great, I have a gay doctor. They’ll know a bit more about what I’m talking about or be able to relate to the community pressures I face.”
But sometimes homophobic patients can be a bit more cold. I’ve never had anyone say that they don’t want to have me as their physician, but I definitely have patients who disagree with me and say, essentially, “oh well, you don’t know what you’re talking about because you’re gay.” Of course, there have also been comments based on my ethnicity as well.
What specific progress could you point to that you’ve seen over the course of your training and your career so far with regard to LGBTQ health care workers’ experience and LGBTQ patients?
When I was in college, there was a case in 2007 where a woman wasn’t able to see her partner or children before dying in a Florida hospital. Since then, there’s been great strides with a 2011 executive order extending hospital visitation rights to LGBTQ families. In 2013, there was the legalization of same-sex marriage. More recently, in June 2020, the Supreme Court extended protections against workplace discrimination to LGBTQ employees.
But there are certain things that continue to be problems, such as the recent Final Rule from the Department of Health & Human Services that fails to protect our LGBTQ patients and friends against discrimination in health care.
Can you remember a specific episode with a patient who was in the LGBTQ community that was particularly satisfying or moving?
There are two that I think about. In medical school, I was working in a more conservative area of California, and there was a patient who identified as lesbian. She felt more able to talk about her fears of raising a family in a conservative area. She even said, “I feel you can understand the stuff, I can talk to you a bit more about it freely, which is really nice.” Later on, I was able to see them on another rotation I was on, after she’d had a baby with her partner. I was honored that they considered me a part of their family’s journey.
A couple years ago as an attending hospitalist, I had a gay male patient that came in for hepatitis A treatment. Although we typically think of hepatitis A as a foodborne illness, oral-anal sex (rimming) is also a risk factor. After having an open discussion with him about his sexual practices, I said, “it was probably an STI in your case,” and was able to give him guidelines on how to prevent giving it to anyone else during the recovery period. He was very appreciative, and I was glad to have been there for that patient.
What is SHM’s role in regard to improving the care of LGBTQ patients, improving inclusiveness for LGBTQ health professionals?
Continuing to have educational activities, whether it be lectures at the annual conference or online learning modules, will be critical to care for our LGBTQ patients. With regard to membership, we need to make sure that hospitalists feel included and protected. To this end, our Diversity and Inclusion Special Interest Group was working toward having gender-neutral bathrooms and personal pronoun tags for the in-person 2020 annual conference before it was converted to an online format.
Does it ever get tiring for you to work on “social issues” in addition to strictly medical issues?
I will say I definitely experienced a moment in time during residency where I had to take a step back and recenter myself. Sometimes, realizing how much work needs to get done, coupled with the challenges of one’s personal life, can be daunting. That said, I can only stare at a problem so long before needing to work on creating a solution. At the end of the day I didn’t want to run away from these newfound problems of exclusion – I wanted to be a part of the solution.
In my hospital medicine fellowship, I was lucky to have Flora Kisuule, MD, as a mentor who encouraged me to take my prior work with LGBTQ health and leverage it into hospital medicine projects. As such, I was able to combine a topic I was passionate about with my interests in research and teaching so that they work synergistically. After all, the social issues affect our medical histories, just as our medical issues affect our social being. They go hand in hand.
Keshav Khanijow, MD, is a hospitalist at Northwestern Memorial Hospital and assistant professor at Northwestern University, Chicago. Originally from the San Francisco Bay area, he studied anthropology as an undergrad at Johns Hopkins University, Baltimore, then went to medical school at the University of California, San Francisco, followed by internal medicine residency and a hospital medicine fellowship at Johns Hopkins Bayview Medical Center. He came out as gay in 2006 as an undergrad. He is a founding member of the Society of Hospital Medicine’s LGBTQ+ Task Force and is involved with SHM’s Diversity and Inclusion Special Interest Group.
What challenges have you faced because of your sexual orientation in the different stages of your career, from training to now as a practicing physician?
In my early training, there weren’t a lot of accessible LGBTQ role models to talk about balancing my personal identities with my professional aspirations. Being a double minority as both South Asian and a gay male, made it that much more difficult. “What is it like to work in health care as a gay cismale? Will being out on my personal statement affect my entry into medical school? Should I list my LGBTQ activism activities or not?” Those were important to me.
And did you make your activism known?
Thankfully, I did. I joke that my application might as well have been printed on rainbow paper, if you will. I decided to be out because I wanted to be part of an environment that would accept me for who I was. But it was a difficult decision.
In medical school at UCSF, it’s San Francisco, so they were a little ahead of the game. They had a lot of social networking opportunities with LGBTQ and ally faculty. Those connections were important in helping me explore different fields, and I even got to write my first publication. That said, networking could sometimes be challenging, especially when it came to residency interviews. While many people would talk about family activities and engagements, I’d only been out to my family for a few years. As such, there would be somewhat of a disconnect. On the flip side, there were LGBTQ celebrations and cultural concepts important to me, but I couldn’t always connect on those fronts either.
When it comes to patients, I do have a bit of a higher-pitched voice, and my mannerisms can be gender nonconforming. While it did make me the target of some cruel middle school humor, I’ve come to be proud of myself, mannerisms and all. That said, I have had patients make remarks to me about being gay, whether it be positive or negative. For LGBTQ patients, they’re like, “this is great, I have a gay doctor. They’ll know a bit more about what I’m talking about or be able to relate to the community pressures I face.”
But sometimes homophobic patients can be a bit more cold. I’ve never had anyone say that they don’t want to have me as their physician, but I definitely have patients who disagree with me and say, essentially, “oh well, you don’t know what you’re talking about because you’re gay.” Of course, there have also been comments based on my ethnicity as well.
What specific progress could you point to that you’ve seen over the course of your training and your career so far with regard to LGBTQ health care workers’ experience and LGBTQ patients?
When I was in college, there was a case in 2007 where a woman wasn’t able to see her partner or children before dying in a Florida hospital. Since then, there’s been great strides with a 2011 executive order extending hospital visitation rights to LGBTQ families. In 2013, there was the legalization of same-sex marriage. More recently, in June 2020, the Supreme Court extended protections against workplace discrimination to LGBTQ employees.
But there are certain things that continue to be problems, such as the recent Final Rule from the Department of Health & Human Services that fails to protect our LGBTQ patients and friends against discrimination in health care.
Can you remember a specific episode with a patient who was in the LGBTQ community that was particularly satisfying or moving?
There are two that I think about. In medical school, I was working in a more conservative area of California, and there was a patient who identified as lesbian. She felt more able to talk about her fears of raising a family in a conservative area. She even said, “I feel you can understand the stuff, I can talk to you a bit more about it freely, which is really nice.” Later on, I was able to see them on another rotation I was on, after she’d had a baby with her partner. I was honored that they considered me a part of their family’s journey.
A couple years ago as an attending hospitalist, I had a gay male patient that came in for hepatitis A treatment. Although we typically think of hepatitis A as a foodborne illness, oral-anal sex (rimming) is also a risk factor. After having an open discussion with him about his sexual practices, I said, “it was probably an STI in your case,” and was able to give him guidelines on how to prevent giving it to anyone else during the recovery period. He was very appreciative, and I was glad to have been there for that patient.
What is SHM’s role in regard to improving the care of LGBTQ patients, improving inclusiveness for LGBTQ health professionals?
Continuing to have educational activities, whether it be lectures at the annual conference or online learning modules, will be critical to care for our LGBTQ patients. With regard to membership, we need to make sure that hospitalists feel included and protected. To this end, our Diversity and Inclusion Special Interest Group was working toward having gender-neutral bathrooms and personal pronoun tags for the in-person 2020 annual conference before it was converted to an online format.
Does it ever get tiring for you to work on “social issues” in addition to strictly medical issues?
I will say I definitely experienced a moment in time during residency where I had to take a step back and recenter myself. Sometimes, realizing how much work needs to get done, coupled with the challenges of one’s personal life, can be daunting. That said, I can only stare at a problem so long before needing to work on creating a solution. At the end of the day I didn’t want to run away from these newfound problems of exclusion – I wanted to be a part of the solution.
In my hospital medicine fellowship, I was lucky to have Flora Kisuule, MD, as a mentor who encouraged me to take my prior work with LGBTQ health and leverage it into hospital medicine projects. As such, I was able to combine a topic I was passionate about with my interests in research and teaching so that they work synergistically. After all, the social issues affect our medical histories, just as our medical issues affect our social being. They go hand in hand.
Keshav Khanijow, MD, is a hospitalist at Northwestern Memorial Hospital and assistant professor at Northwestern University, Chicago. Originally from the San Francisco Bay area, he studied anthropology as an undergrad at Johns Hopkins University, Baltimore, then went to medical school at the University of California, San Francisco, followed by internal medicine residency and a hospital medicine fellowship at Johns Hopkins Bayview Medical Center. He came out as gay in 2006 as an undergrad. He is a founding member of the Society of Hospital Medicine’s LGBTQ+ Task Force and is involved with SHM’s Diversity and Inclusion Special Interest Group.
What challenges have you faced because of your sexual orientation in the different stages of your career, from training to now as a practicing physician?
In my early training, there weren’t a lot of accessible LGBTQ role models to talk about balancing my personal identities with my professional aspirations. Being a double minority as both South Asian and a gay male, made it that much more difficult. “What is it like to work in health care as a gay cismale? Will being out on my personal statement affect my entry into medical school? Should I list my LGBTQ activism activities or not?” Those were important to me.
And did you make your activism known?
Thankfully, I did. I joke that my application might as well have been printed on rainbow paper, if you will. I decided to be out because I wanted to be part of an environment that would accept me for who I was. But it was a difficult decision.
In medical school at UCSF, it’s San Francisco, so they were a little ahead of the game. They had a lot of social networking opportunities with LGBTQ and ally faculty. Those connections were important in helping me explore different fields, and I even got to write my first publication. That said, networking could sometimes be challenging, especially when it came to residency interviews. While many people would talk about family activities and engagements, I’d only been out to my family for a few years. As such, there would be somewhat of a disconnect. On the flip side, there were LGBTQ celebrations and cultural concepts important to me, but I couldn’t always connect on those fronts either.
When it comes to patients, I do have a bit of a higher-pitched voice, and my mannerisms can be gender nonconforming. While it did make me the target of some cruel middle school humor, I’ve come to be proud of myself, mannerisms and all. That said, I have had patients make remarks to me about being gay, whether it be positive or negative. For LGBTQ patients, they’re like, “this is great, I have a gay doctor. They’ll know a bit more about what I’m talking about or be able to relate to the community pressures I face.”
But sometimes homophobic patients can be a bit more cold. I’ve never had anyone say that they don’t want to have me as their physician, but I definitely have patients who disagree with me and say, essentially, “oh well, you don’t know what you’re talking about because you’re gay.” Of course, there have also been comments based on my ethnicity as well.
What specific progress could you point to that you’ve seen over the course of your training and your career so far with regard to LGBTQ health care workers’ experience and LGBTQ patients?
When I was in college, there was a case in 2007 where a woman wasn’t able to see her partner or children before dying in a Florida hospital. Since then, there’s been great strides with a 2011 executive order extending hospital visitation rights to LGBTQ families. In 2013, there was the legalization of same-sex marriage. More recently, in June 2020, the Supreme Court extended protections against workplace discrimination to LGBTQ employees.
But there are certain things that continue to be problems, such as the recent Final Rule from the Department of Health & Human Services that fails to protect our LGBTQ patients and friends against discrimination in health care.
Can you remember a specific episode with a patient who was in the LGBTQ community that was particularly satisfying or moving?
There are two that I think about. In medical school, I was working in a more conservative area of California, and there was a patient who identified as lesbian. She felt more able to talk about her fears of raising a family in a conservative area. She even said, “I feel you can understand the stuff, I can talk to you a bit more about it freely, which is really nice.” Later on, I was able to see them on another rotation I was on, after she’d had a baby with her partner. I was honored that they considered me a part of their family’s journey.
A couple years ago as an attending hospitalist, I had a gay male patient that came in for hepatitis A treatment. Although we typically think of hepatitis A as a foodborne illness, oral-anal sex (rimming) is also a risk factor. After having an open discussion with him about his sexual practices, I said, “it was probably an STI in your case,” and was able to give him guidelines on how to prevent giving it to anyone else during the recovery period. He was very appreciative, and I was glad to have been there for that patient.
What is SHM’s role in regard to improving the care of LGBTQ patients, improving inclusiveness for LGBTQ health professionals?
Continuing to have educational activities, whether it be lectures at the annual conference or online learning modules, will be critical to care for our LGBTQ patients. With regard to membership, we need to make sure that hospitalists feel included and protected. To this end, our Diversity and Inclusion Special Interest Group was working toward having gender-neutral bathrooms and personal pronoun tags for the in-person 2020 annual conference before it was converted to an online format.
Does it ever get tiring for you to work on “social issues” in addition to strictly medical issues?
I will say I definitely experienced a moment in time during residency where I had to take a step back and recenter myself. Sometimes, realizing how much work needs to get done, coupled with the challenges of one’s personal life, can be daunting. That said, I can only stare at a problem so long before needing to work on creating a solution. At the end of the day I didn’t want to run away from these newfound problems of exclusion – I wanted to be a part of the solution.
In my hospital medicine fellowship, I was lucky to have Flora Kisuule, MD, as a mentor who encouraged me to take my prior work with LGBTQ health and leverage it into hospital medicine projects. As such, I was able to combine a topic I was passionate about with my interests in research and teaching so that they work synergistically. After all, the social issues affect our medical histories, just as our medical issues affect our social being. They go hand in hand.
Managing pain expectations is key to enhanced recovery
Planning for reduced use of opioids in pain management involves identifying appropriate patients and managing their expectations, according to according to Timothy E. Miller, MB, ChB, FRCA, of Duke University, Durham, N.C., who is president of the American Society for Enhanced Recovery.
, he said in a presentation at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education.
Dr. Miller shared a treatment algorithm for achieving optimal analgesia in patients after colorectal surgery that combines intravenous or oral analgesia with local anesthetics and additional nonopioid options. The algorithm involves choosing NSAIDs, acetaminophen, or gabapentin for IV/oral use. In addition, options for local anesthetic include with a choice of single-shot transversus abdominis plane (TAP) block.
Careful patient selection is key to an opioid-free or opioid reduced anesthetic strategy, Dr. Miller said. The appropriate patients have “no chronic opioids, no anxiety, and the desire to avoid opioid side effects,” he said.
Opioid-free or opioid-reduced strategies include realigning patient expectations to prepare for pain at a level of 2-4 on a scale of 10 as “expected and reasonable,” he said. Patients given no opioids or reduced opioids may report cramping after laparoscopic surgery, as well as shoulder pain that is referred from the CO2 bubble under the diaphragm, he said. However, opioids don’t treat the shoulder pain well, and “walking or changing position usually relieves this pain,” and it usually resolves within 24 hours, Dr. Miller noted. “Just letting the patient know what is expected in terms of pain relief in their recovery is hugely important,” he said.
The optimal analgesia after surgery is a plan that combines optimized patient comfort with the fastest functional recovery and the fewest side effects, he emphasized.
Optimized patient comfort includes optimal pain ratings at rest and with movement, a decreasing impact of pain on emotion, function, and sleep disruption, and an improvement in the patient experience, he said. The fastest functional recovery is defined as a return to drinking liquids, eating solid foods, performing activities of daily living, and maintaining normal bladder, bowel, and cognitive function. Side effects to be considered in analgesia included nausea, vomiting, sedation, ileus, itching, dizziness, and delirium, he said.
In an unpublished study, Dr. Miller and colleagues eliminated opioids intraoperatively in a series of 56 cases of laparoscopic cholecystectomy and found significantly less opioids needed in the postanesthesia care unit (PACU). In addition, opioid-free patients had significantly shorter length of stay in the PACU, he said. “We are writing this up for publication and looking into doing larger studies,” Dr. Miller said.
Questions include whether the opioid-free technique translates more broadly, he said.
In addition, it is important to continue to collect data and study methods to treat pain and reduce opioid use perioperatively, Dr. Miller said. Some ongoing concerns include data surrounding the use of gabapentin and possible association with respiratory depression, he noted. Several meta-analyses have suggested that “gabapentinoids (gabapentin, pregabalin) when given as a single dose preoperatively are associated with a decrease in postoperative pain and opioid consumption at 24 hours,” said Dr. Miller. “When gabapentinoids are included in multimodal analgesic regimens, intraoperative opioids must be reduced, and increased vigilance for respiratory depression may be warranted, especially in elderly patients,” he said.
Overall, opioid-free anesthesia is both feasible and appropriate in certain patient populations, Dr. Miller concluded. “Implement your pathway and measure your outcomes with timely feedback so you can revise your protocol based on data,” he emphasized.
Global Academy for Medical Education and this news organization are owned by the same parent company.
Dr. Miller disclosed relationships with Edwards Lifesciences, and serving as a board member for the Perioperative Quality Initiative and as a founding member of the Morpheus Consortium.
Planning for reduced use of opioids in pain management involves identifying appropriate patients and managing their expectations, according to according to Timothy E. Miller, MB, ChB, FRCA, of Duke University, Durham, N.C., who is president of the American Society for Enhanced Recovery.
, he said in a presentation at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education.
Dr. Miller shared a treatment algorithm for achieving optimal analgesia in patients after colorectal surgery that combines intravenous or oral analgesia with local anesthetics and additional nonopioid options. The algorithm involves choosing NSAIDs, acetaminophen, or gabapentin for IV/oral use. In addition, options for local anesthetic include with a choice of single-shot transversus abdominis plane (TAP) block.
Careful patient selection is key to an opioid-free or opioid reduced anesthetic strategy, Dr. Miller said. The appropriate patients have “no chronic opioids, no anxiety, and the desire to avoid opioid side effects,” he said.
Opioid-free or opioid-reduced strategies include realigning patient expectations to prepare for pain at a level of 2-4 on a scale of 10 as “expected and reasonable,” he said. Patients given no opioids or reduced opioids may report cramping after laparoscopic surgery, as well as shoulder pain that is referred from the CO2 bubble under the diaphragm, he said. However, opioids don’t treat the shoulder pain well, and “walking or changing position usually relieves this pain,” and it usually resolves within 24 hours, Dr. Miller noted. “Just letting the patient know what is expected in terms of pain relief in their recovery is hugely important,” he said.
The optimal analgesia after surgery is a plan that combines optimized patient comfort with the fastest functional recovery and the fewest side effects, he emphasized.
Optimized patient comfort includes optimal pain ratings at rest and with movement, a decreasing impact of pain on emotion, function, and sleep disruption, and an improvement in the patient experience, he said. The fastest functional recovery is defined as a return to drinking liquids, eating solid foods, performing activities of daily living, and maintaining normal bladder, bowel, and cognitive function. Side effects to be considered in analgesia included nausea, vomiting, sedation, ileus, itching, dizziness, and delirium, he said.
In an unpublished study, Dr. Miller and colleagues eliminated opioids intraoperatively in a series of 56 cases of laparoscopic cholecystectomy and found significantly less opioids needed in the postanesthesia care unit (PACU). In addition, opioid-free patients had significantly shorter length of stay in the PACU, he said. “We are writing this up for publication and looking into doing larger studies,” Dr. Miller said.
Questions include whether the opioid-free technique translates more broadly, he said.
In addition, it is important to continue to collect data and study methods to treat pain and reduce opioid use perioperatively, Dr. Miller said. Some ongoing concerns include data surrounding the use of gabapentin and possible association with respiratory depression, he noted. Several meta-analyses have suggested that “gabapentinoids (gabapentin, pregabalin) when given as a single dose preoperatively are associated with a decrease in postoperative pain and opioid consumption at 24 hours,” said Dr. Miller. “When gabapentinoids are included in multimodal analgesic regimens, intraoperative opioids must be reduced, and increased vigilance for respiratory depression may be warranted, especially in elderly patients,” he said.
Overall, opioid-free anesthesia is both feasible and appropriate in certain patient populations, Dr. Miller concluded. “Implement your pathway and measure your outcomes with timely feedback so you can revise your protocol based on data,” he emphasized.
Global Academy for Medical Education and this news organization are owned by the same parent company.
Dr. Miller disclosed relationships with Edwards Lifesciences, and serving as a board member for the Perioperative Quality Initiative and as a founding member of the Morpheus Consortium.
Planning for reduced use of opioids in pain management involves identifying appropriate patients and managing their expectations, according to according to Timothy E. Miller, MB, ChB, FRCA, of Duke University, Durham, N.C., who is president of the American Society for Enhanced Recovery.
, he said in a presentation at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education.
Dr. Miller shared a treatment algorithm for achieving optimal analgesia in patients after colorectal surgery that combines intravenous or oral analgesia with local anesthetics and additional nonopioid options. The algorithm involves choosing NSAIDs, acetaminophen, or gabapentin for IV/oral use. In addition, options for local anesthetic include with a choice of single-shot transversus abdominis plane (TAP) block.
Careful patient selection is key to an opioid-free or opioid reduced anesthetic strategy, Dr. Miller said. The appropriate patients have “no chronic opioids, no anxiety, and the desire to avoid opioid side effects,” he said.
Opioid-free or opioid-reduced strategies include realigning patient expectations to prepare for pain at a level of 2-4 on a scale of 10 as “expected and reasonable,” he said. Patients given no opioids or reduced opioids may report cramping after laparoscopic surgery, as well as shoulder pain that is referred from the CO2 bubble under the diaphragm, he said. However, opioids don’t treat the shoulder pain well, and “walking or changing position usually relieves this pain,” and it usually resolves within 24 hours, Dr. Miller noted. “Just letting the patient know what is expected in terms of pain relief in their recovery is hugely important,” he said.
The optimal analgesia after surgery is a plan that combines optimized patient comfort with the fastest functional recovery and the fewest side effects, he emphasized.
Optimized patient comfort includes optimal pain ratings at rest and with movement, a decreasing impact of pain on emotion, function, and sleep disruption, and an improvement in the patient experience, he said. The fastest functional recovery is defined as a return to drinking liquids, eating solid foods, performing activities of daily living, and maintaining normal bladder, bowel, and cognitive function. Side effects to be considered in analgesia included nausea, vomiting, sedation, ileus, itching, dizziness, and delirium, he said.
In an unpublished study, Dr. Miller and colleagues eliminated opioids intraoperatively in a series of 56 cases of laparoscopic cholecystectomy and found significantly less opioids needed in the postanesthesia care unit (PACU). In addition, opioid-free patients had significantly shorter length of stay in the PACU, he said. “We are writing this up for publication and looking into doing larger studies,” Dr. Miller said.
Questions include whether the opioid-free technique translates more broadly, he said.
In addition, it is important to continue to collect data and study methods to treat pain and reduce opioid use perioperatively, Dr. Miller said. Some ongoing concerns include data surrounding the use of gabapentin and possible association with respiratory depression, he noted. Several meta-analyses have suggested that “gabapentinoids (gabapentin, pregabalin) when given as a single dose preoperatively are associated with a decrease in postoperative pain and opioid consumption at 24 hours,” said Dr. Miller. “When gabapentinoids are included in multimodal analgesic regimens, intraoperative opioids must be reduced, and increased vigilance for respiratory depression may be warranted, especially in elderly patients,” he said.
Overall, opioid-free anesthesia is both feasible and appropriate in certain patient populations, Dr. Miller concluded. “Implement your pathway and measure your outcomes with timely feedback so you can revise your protocol based on data,” he emphasized.
Global Academy for Medical Education and this news organization are owned by the same parent company.
Dr. Miller disclosed relationships with Edwards Lifesciences, and serving as a board member for the Perioperative Quality Initiative and as a founding member of the Morpheus Consortium.
FROM MISS
Phase 3 COVID-19 vaccine trials launching in July, expert says
The race to develop a SARS-CoV-2 vaccine is unlike any other global research and development effort in modern medicine.
According to Paul A. Offit, MD, there are now 120 Investigational New Drug applications to the Food and Drug Administration for these vaccines, and researchers at more than 70 companies across the globe are interested in making a vaccine. The Biomedical Advanced Research and Development Authority (BARDA) has awarded $2.5 billion to five different pharmaceutical companies to make a vaccine.
“The good news is that the new coronavirus is relatively stable,” Dr. Offit, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia, said during the virtual Pediatric Dermatology 2020: Best Practices and Innovations Conference. “Although it is a single-stranded RNA virus, it does mutate to some extent, but it doesn’t look like it’s going to mutate away from the vaccine. So, this is not going to be like influenza virus, where you must give a vaccine every year. I think we can make a vaccine that will last for several years. And we know the protein we’re interested in. We’re interested in antibodies directed against the spike glycoprotein, which is abundantly present on the surface of the virus. We know that if we make an antibody response to that protein, we can therefore prevent infection.”
Some research groups are interested in developing a whole, killed virus like those used in the inactivated polio vaccine, and vaccines for hepatitis A virus and rabies, said Dr. Offit, who is a member of Accelerating COVID-19 Technical Innovations And Vaccines, a public-private partnership formed by the National Institutes of Health. Other groups are interested in making a live-attenuated vaccine like those for measles, mumps, and rubella. “Some are interested in using a vectored vaccine, where you take a virus that is relatively weak and doesn’t cause disease in people, like vesicular stomatitis virus, and then clone into that the gene that codes for this coronavirus spike protein, which is the way that we made the Ebola virus vaccine,” Dr. Offit said. “Those approaches have all been used before, with success.”
Novel approaches are also being employed to make this vaccine, including using a replication-defective adenovirus. “That means that the virus can’t reproduce itself, but it can make proteins,” he explained. “There are some proteins that are made, but most aren’t. Therefore, the virus can’t reproduce itself. We’ll see whether or not that [approach] works, but it’s never been used before.”
Another approach is to inject messenger RNA that codes for the coronavirus spike protein, where that genetic material is translated into the spike protein. The other platform being evaluated is a DNA vaccine, in which “you give DNA which is coded for that spike protein, which is transcribed to messenger RNA and then is translated to other proteins.”
Typical vaccine development involves animal models to prove the concept, dose-ranging studies in humans, and progressively larger safety and immunogenicity studies in hundreds of thousands of people. Next come phase 3 studies, “where the proof is in the pudding,” he said. “These are large, prospective placebo-controlled trials to prove that the vaccine is safe. This is the only way whether you can prove or not a vaccine is effective.”
“Some companies may branch out on their own and do smaller studies than that,” he said. “We’ll see how this plays out. Keep your eyes open for that, because you really want to make sure you have a fairly large phase 3 trial. That’s the best way to show whether something works and whether it’s safe.”
The tried and true vaccines that emerge from the effort will not be FDA-licensed products. Rather, they will be approved products under the Emergency Use Authorization program. “Ever since the 1950s, every vaccine that has been used in the U.S. has been under the auspices of FDA licensure,” said Dr. Offit, who is also professor of pediatrics and the Maurice R. Hilleman professor of vaccinology at the University of Pennsylvania, Philadelphia. “That’s not going to be true here. The FDA is involved every step of the way but here they have a somewhat lighter touch.”
A few candidate vaccines are being mass-produced at risk, “meaning they’re being produced not knowing whether these vaccines are safe and effective yet or not,” he said. “But when they’re shown in a phase 3 trial to be safe and effective, you will have already produced it, and then it’s much easier to roll it out to the general public the minute you’ve shown that it works. This is what we did for the polio vaccine back in the 1950s. We mass-produced that vaccine at risk.”
Dr. Offit emphasized the importance of managing expectations once a COVID-19 vaccine gets approved for use. “Regarding safety, these vaccines will be tested in tens of thousands of people, not tens of millions of people, so although you can disprove a relatively uncommon side effect preapproval, you’re not going to disprove a rare side effect preapproval. You’re only going to know that post approval. I think we need to make people aware of that and to let them know that through groups like the Vaccine Safety Datalink, we’re going to be monitoring these vaccines once they’re approved.”
Regarding efficacy, he continued, “we’re not going know about the rates of immunity initially; we’re only going to know about that after the vaccine [has been administered]. My guess is the protection is going to be short lived and incomplete. By short lived, I mean that protection would last for years but not decades. By incomplete, I mean that protection will be against moderate to severe disease, which is fine. You don’t need protection against all of the disease; it’s hard to do that with respiratory viruses. That means you can keep people out of the hospital, and you can keep them from dying. That’s the main goal.”
Dr. Offit closed his remarks by noting that much is at stake in this effort to develop a vaccine so quickly and that it “could go one of two ways. We could find that the vaccine is a lifesaver, and [that] we can finally end this awful pandemic. Or, if we cut corners and don’t prove that the vaccines are safe and effective as we should before they’re released, we could shake what is a fragile vaccine confidence in this country. Hopefully, it doesn’t play out that way.”
The race to develop a SARS-CoV-2 vaccine is unlike any other global research and development effort in modern medicine.
According to Paul A. Offit, MD, there are now 120 Investigational New Drug applications to the Food and Drug Administration for these vaccines, and researchers at more than 70 companies across the globe are interested in making a vaccine. The Biomedical Advanced Research and Development Authority (BARDA) has awarded $2.5 billion to five different pharmaceutical companies to make a vaccine.
“The good news is that the new coronavirus is relatively stable,” Dr. Offit, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia, said during the virtual Pediatric Dermatology 2020: Best Practices and Innovations Conference. “Although it is a single-stranded RNA virus, it does mutate to some extent, but it doesn’t look like it’s going to mutate away from the vaccine. So, this is not going to be like influenza virus, where you must give a vaccine every year. I think we can make a vaccine that will last for several years. And we know the protein we’re interested in. We’re interested in antibodies directed against the spike glycoprotein, which is abundantly present on the surface of the virus. We know that if we make an antibody response to that protein, we can therefore prevent infection.”
Some research groups are interested in developing a whole, killed virus like those used in the inactivated polio vaccine, and vaccines for hepatitis A virus and rabies, said Dr. Offit, who is a member of Accelerating COVID-19 Technical Innovations And Vaccines, a public-private partnership formed by the National Institutes of Health. Other groups are interested in making a live-attenuated vaccine like those for measles, mumps, and rubella. “Some are interested in using a vectored vaccine, where you take a virus that is relatively weak and doesn’t cause disease in people, like vesicular stomatitis virus, and then clone into that the gene that codes for this coronavirus spike protein, which is the way that we made the Ebola virus vaccine,” Dr. Offit said. “Those approaches have all been used before, with success.”
Novel approaches are also being employed to make this vaccine, including using a replication-defective adenovirus. “That means that the virus can’t reproduce itself, but it can make proteins,” he explained. “There are some proteins that are made, but most aren’t. Therefore, the virus can’t reproduce itself. We’ll see whether or not that [approach] works, but it’s never been used before.”
Another approach is to inject messenger RNA that codes for the coronavirus spike protein, where that genetic material is translated into the spike protein. The other platform being evaluated is a DNA vaccine, in which “you give DNA which is coded for that spike protein, which is transcribed to messenger RNA and then is translated to other proteins.”
Typical vaccine development involves animal models to prove the concept, dose-ranging studies in humans, and progressively larger safety and immunogenicity studies in hundreds of thousands of people. Next come phase 3 studies, “where the proof is in the pudding,” he said. “These are large, prospective placebo-controlled trials to prove that the vaccine is safe. This is the only way whether you can prove or not a vaccine is effective.”
“Some companies may branch out on their own and do smaller studies than that,” he said. “We’ll see how this plays out. Keep your eyes open for that, because you really want to make sure you have a fairly large phase 3 trial. That’s the best way to show whether something works and whether it’s safe.”
The tried and true vaccines that emerge from the effort will not be FDA-licensed products. Rather, they will be approved products under the Emergency Use Authorization program. “Ever since the 1950s, every vaccine that has been used in the U.S. has been under the auspices of FDA licensure,” said Dr. Offit, who is also professor of pediatrics and the Maurice R. Hilleman professor of vaccinology at the University of Pennsylvania, Philadelphia. “That’s not going to be true here. The FDA is involved every step of the way but here they have a somewhat lighter touch.”
A few candidate vaccines are being mass-produced at risk, “meaning they’re being produced not knowing whether these vaccines are safe and effective yet or not,” he said. “But when they’re shown in a phase 3 trial to be safe and effective, you will have already produced it, and then it’s much easier to roll it out to the general public the minute you’ve shown that it works. This is what we did for the polio vaccine back in the 1950s. We mass-produced that vaccine at risk.”
Dr. Offit emphasized the importance of managing expectations once a COVID-19 vaccine gets approved for use. “Regarding safety, these vaccines will be tested in tens of thousands of people, not tens of millions of people, so although you can disprove a relatively uncommon side effect preapproval, you’re not going to disprove a rare side effect preapproval. You’re only going to know that post approval. I think we need to make people aware of that and to let them know that through groups like the Vaccine Safety Datalink, we’re going to be monitoring these vaccines once they’re approved.”
Regarding efficacy, he continued, “we’re not going know about the rates of immunity initially; we’re only going to know about that after the vaccine [has been administered]. My guess is the protection is going to be short lived and incomplete. By short lived, I mean that protection would last for years but not decades. By incomplete, I mean that protection will be against moderate to severe disease, which is fine. You don’t need protection against all of the disease; it’s hard to do that with respiratory viruses. That means you can keep people out of the hospital, and you can keep them from dying. That’s the main goal.”
Dr. Offit closed his remarks by noting that much is at stake in this effort to develop a vaccine so quickly and that it “could go one of two ways. We could find that the vaccine is a lifesaver, and [that] we can finally end this awful pandemic. Or, if we cut corners and don’t prove that the vaccines are safe and effective as we should before they’re released, we could shake what is a fragile vaccine confidence in this country. Hopefully, it doesn’t play out that way.”
The race to develop a SARS-CoV-2 vaccine is unlike any other global research and development effort in modern medicine.
According to Paul A. Offit, MD, there are now 120 Investigational New Drug applications to the Food and Drug Administration for these vaccines, and researchers at more than 70 companies across the globe are interested in making a vaccine. The Biomedical Advanced Research and Development Authority (BARDA) has awarded $2.5 billion to five different pharmaceutical companies to make a vaccine.
“The good news is that the new coronavirus is relatively stable,” Dr. Offit, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia, said during the virtual Pediatric Dermatology 2020: Best Practices and Innovations Conference. “Although it is a single-stranded RNA virus, it does mutate to some extent, but it doesn’t look like it’s going to mutate away from the vaccine. So, this is not going to be like influenza virus, where you must give a vaccine every year. I think we can make a vaccine that will last for several years. And we know the protein we’re interested in. We’re interested in antibodies directed against the spike glycoprotein, which is abundantly present on the surface of the virus. We know that if we make an antibody response to that protein, we can therefore prevent infection.”
Some research groups are interested in developing a whole, killed virus like those used in the inactivated polio vaccine, and vaccines for hepatitis A virus and rabies, said Dr. Offit, who is a member of Accelerating COVID-19 Technical Innovations And Vaccines, a public-private partnership formed by the National Institutes of Health. Other groups are interested in making a live-attenuated vaccine like those for measles, mumps, and rubella. “Some are interested in using a vectored vaccine, where you take a virus that is relatively weak and doesn’t cause disease in people, like vesicular stomatitis virus, and then clone into that the gene that codes for this coronavirus spike protein, which is the way that we made the Ebola virus vaccine,” Dr. Offit said. “Those approaches have all been used before, with success.”
Novel approaches are also being employed to make this vaccine, including using a replication-defective adenovirus. “That means that the virus can’t reproduce itself, but it can make proteins,” he explained. “There are some proteins that are made, but most aren’t. Therefore, the virus can’t reproduce itself. We’ll see whether or not that [approach] works, but it’s never been used before.”
Another approach is to inject messenger RNA that codes for the coronavirus spike protein, where that genetic material is translated into the spike protein. The other platform being evaluated is a DNA vaccine, in which “you give DNA which is coded for that spike protein, which is transcribed to messenger RNA and then is translated to other proteins.”
Typical vaccine development involves animal models to prove the concept, dose-ranging studies in humans, and progressively larger safety and immunogenicity studies in hundreds of thousands of people. Next come phase 3 studies, “where the proof is in the pudding,” he said. “These are large, prospective placebo-controlled trials to prove that the vaccine is safe. This is the only way whether you can prove or not a vaccine is effective.”
“Some companies may branch out on their own and do smaller studies than that,” he said. “We’ll see how this plays out. Keep your eyes open for that, because you really want to make sure you have a fairly large phase 3 trial. That’s the best way to show whether something works and whether it’s safe.”
The tried and true vaccines that emerge from the effort will not be FDA-licensed products. Rather, they will be approved products under the Emergency Use Authorization program. “Ever since the 1950s, every vaccine that has been used in the U.S. has been under the auspices of FDA licensure,” said Dr. Offit, who is also professor of pediatrics and the Maurice R. Hilleman professor of vaccinology at the University of Pennsylvania, Philadelphia. “That’s not going to be true here. The FDA is involved every step of the way but here they have a somewhat lighter touch.”
A few candidate vaccines are being mass-produced at risk, “meaning they’re being produced not knowing whether these vaccines are safe and effective yet or not,” he said. “But when they’re shown in a phase 3 trial to be safe and effective, you will have already produced it, and then it’s much easier to roll it out to the general public the minute you’ve shown that it works. This is what we did for the polio vaccine back in the 1950s. We mass-produced that vaccine at risk.”
Dr. Offit emphasized the importance of managing expectations once a COVID-19 vaccine gets approved for use. “Regarding safety, these vaccines will be tested in tens of thousands of people, not tens of millions of people, so although you can disprove a relatively uncommon side effect preapproval, you’re not going to disprove a rare side effect preapproval. You’re only going to know that post approval. I think we need to make people aware of that and to let them know that through groups like the Vaccine Safety Datalink, we’re going to be monitoring these vaccines once they’re approved.”
Regarding efficacy, he continued, “we’re not going know about the rates of immunity initially; we’re only going to know about that after the vaccine [has been administered]. My guess is the protection is going to be short lived and incomplete. By short lived, I mean that protection would last for years but not decades. By incomplete, I mean that protection will be against moderate to severe disease, which is fine. You don’t need protection against all of the disease; it’s hard to do that with respiratory viruses. That means you can keep people out of the hospital, and you can keep them from dying. That’s the main goal.”
Dr. Offit closed his remarks by noting that much is at stake in this effort to develop a vaccine so quickly and that it “could go one of two ways. We could find that the vaccine is a lifesaver, and [that] we can finally end this awful pandemic. Or, if we cut corners and don’t prove that the vaccines are safe and effective as we should before they’re released, we could shake what is a fragile vaccine confidence in this country. Hopefully, it doesn’t play out that way.”
FROM PEDIATRIC DERMATOLOGY 2020
Many physicians live within their means and save, survey shows
Although about two of five physicians report a net worth of between $1 million and $5 million, half are under the million dollars and about half believe in living at or below their means, according to the latest Medscape Physician Debt and Net Worth Report 2020.

Along with that somewhat prudent lifestyle comes savings, with
Those habits may help some navigate the financial upheaval in medicine brought about by COVID-19.
The survey responses on salary, debt, and net worth from more than 17,000 physicians spanning 30 specialties were collected prior to Feb. 11, before COVID-19 was declared a pandemic.
The authors of the report note that by some estimates, primary care offices have seen a 55% drop in revenue because of the pandemic, and specialists have been hard hit with the suspension of most elective procedures.
Primary care offices are seeing fewer patients and are limiting hours, and some offices have been forced to close. Others have stemmed the losses by introducing telemedicine options.
Before COVID-19, average incomes had continued to rise – this year to $243,000 (a 2.5% boost from last year’s $237,000) for primary care physicians and $346,000 for specialists (a 1.5% rise from last year’s $341,000).
About half of physicians (42%) reported a net worth of $1 million to $5 million, and 8% reported a net worth of more than $5 million. Fifty percent of physicians had a net worth of less than $1 million.
Those figures varied greatly by specialty. Among specialists, orthopedists were most likely (at 19%) to top the $5 million level, followed by plastic surgeons and gastroenterologists (both at 16%).
Conversely, 46% of family physicians and 44% of pediatricians reported that their net worth was under $500,000.
Gender gaps were also apparent in the data, especially at the highest levels. Twice as many male physicians (10%) as their female counterparts (5%) had a net worth of more than $5 million.
43% live below their means
Asked about habits regarding saving, 43% of physicians reported they live below their means. Half said they live at their means, and 7% said they live above their means.
Joel Greenwald, MD, CEO of Greenwald Wealth Management in St. Louis Park, Minn., recommends in the report trying to save 20% of annual gross salary.
More than a third of physicians who responded (39%) said they put more than $2,000/month into tax-deferred retirement or college savings, but Dr. Greenwald acknowledged that this may become more challenging.
“Many have seen the employer match in their retirement plans reduced or eliminated through the end of 2020, with what comes in 2021 as yet undefined,” he said.
A smaller percentage (26%) answered that they put more than $2,000 a month into a taxable retirement or college savings account each month.
Home size by specialty
Mortgages on a primary residence were the top reasons for debt (63%), followed by car loans (37%), personal education loans (26%), and credit card balances (25%).
Half of specialists and 61% of primary care physicians live in homes with up to 3,000 square feet. Only 7% of PCPs and 12% of specialists live in homes with 5000 square feet or more.
At 22%, plastic surgeons and orthopedists were the most likely groups to have houses with the largest square footage, according to the survey.
About one in four physicians in five specialties (urology, cardiology, plastic surgery, otolaryngology, and critical care) reported that they had mortgages of more than $500,000.
Standard financial advice, the report authors note, is that a mortgage should take up no more than 28% of monthly gross income.
Another large source of debt came from student loans. Close to 80% of graduating medical students have educational debt. The average balance for graduating students in 2018 was $196,520, the report authors state.
Those in physical medicine/rehabilitation and family medicine were most likely to still be paying off student debt (34% said they were). Conversely, half as many nephrologists and rheumatologists (15%) and gastroenterologists (14%) reported that they were paying off educational debt.
Only 11% of physicians said they were currently free of any debt.
Most physicians in the survey (72%) reported that they had not experienced a significant financial loss in the past year.
For those who did experience such a loss, the top reason given was related to a bad investment or the stock market (9%).
Cost-cutting strategies
Revenue reduction will likely lead to spending less this year as the pandemic challenges continue.
Survey respondents offered their most effective cost-cutting strategies.
A hospitalist said, “Half of every bonus goes into the investment account, no matter how much.”
“We add an extra amount to the principal of our monthly mortgage payment,” an internist said.
A pediatrician offered, “I bring my lunch to work every day and don’t eat in restaurants often.”
This article first appeared on Medscape.com.
Although about two of five physicians report a net worth of between $1 million and $5 million, half are under the million dollars and about half believe in living at or below their means, according to the latest Medscape Physician Debt and Net Worth Report 2020.

Along with that somewhat prudent lifestyle comes savings, with
Those habits may help some navigate the financial upheaval in medicine brought about by COVID-19.
The survey responses on salary, debt, and net worth from more than 17,000 physicians spanning 30 specialties were collected prior to Feb. 11, before COVID-19 was declared a pandemic.
The authors of the report note that by some estimates, primary care offices have seen a 55% drop in revenue because of the pandemic, and specialists have been hard hit with the suspension of most elective procedures.
Primary care offices are seeing fewer patients and are limiting hours, and some offices have been forced to close. Others have stemmed the losses by introducing telemedicine options.
Before COVID-19, average incomes had continued to rise – this year to $243,000 (a 2.5% boost from last year’s $237,000) for primary care physicians and $346,000 for specialists (a 1.5% rise from last year’s $341,000).
About half of physicians (42%) reported a net worth of $1 million to $5 million, and 8% reported a net worth of more than $5 million. Fifty percent of physicians had a net worth of less than $1 million.
Those figures varied greatly by specialty. Among specialists, orthopedists were most likely (at 19%) to top the $5 million level, followed by plastic surgeons and gastroenterologists (both at 16%).
Conversely, 46% of family physicians and 44% of pediatricians reported that their net worth was under $500,000.
Gender gaps were also apparent in the data, especially at the highest levels. Twice as many male physicians (10%) as their female counterparts (5%) had a net worth of more than $5 million.
43% live below their means
Asked about habits regarding saving, 43% of physicians reported they live below their means. Half said they live at their means, and 7% said they live above their means.
Joel Greenwald, MD, CEO of Greenwald Wealth Management in St. Louis Park, Minn., recommends in the report trying to save 20% of annual gross salary.
More than a third of physicians who responded (39%) said they put more than $2,000/month into tax-deferred retirement or college savings, but Dr. Greenwald acknowledged that this may become more challenging.
“Many have seen the employer match in their retirement plans reduced or eliminated through the end of 2020, with what comes in 2021 as yet undefined,” he said.
A smaller percentage (26%) answered that they put more than $2,000 a month into a taxable retirement or college savings account each month.
Home size by specialty
Mortgages on a primary residence were the top reasons for debt (63%), followed by car loans (37%), personal education loans (26%), and credit card balances (25%).
Half of specialists and 61% of primary care physicians live in homes with up to 3,000 square feet. Only 7% of PCPs and 12% of specialists live in homes with 5000 square feet or more.
At 22%, plastic surgeons and orthopedists were the most likely groups to have houses with the largest square footage, according to the survey.
About one in four physicians in five specialties (urology, cardiology, plastic surgery, otolaryngology, and critical care) reported that they had mortgages of more than $500,000.
Standard financial advice, the report authors note, is that a mortgage should take up no more than 28% of monthly gross income.
Another large source of debt came from student loans. Close to 80% of graduating medical students have educational debt. The average balance for graduating students in 2018 was $196,520, the report authors state.
Those in physical medicine/rehabilitation and family medicine were most likely to still be paying off student debt (34% said they were). Conversely, half as many nephrologists and rheumatologists (15%) and gastroenterologists (14%) reported that they were paying off educational debt.
Only 11% of physicians said they were currently free of any debt.
Most physicians in the survey (72%) reported that they had not experienced a significant financial loss in the past year.
For those who did experience such a loss, the top reason given was related to a bad investment or the stock market (9%).
Cost-cutting strategies
Revenue reduction will likely lead to spending less this year as the pandemic challenges continue.
Survey respondents offered their most effective cost-cutting strategies.
A hospitalist said, “Half of every bonus goes into the investment account, no matter how much.”
“We add an extra amount to the principal of our monthly mortgage payment,” an internist said.
A pediatrician offered, “I bring my lunch to work every day and don’t eat in restaurants often.”
This article first appeared on Medscape.com.
Although about two of five physicians report a net worth of between $1 million and $5 million, half are under the million dollars and about half believe in living at or below their means, according to the latest Medscape Physician Debt and Net Worth Report 2020.

Along with that somewhat prudent lifestyle comes savings, with
Those habits may help some navigate the financial upheaval in medicine brought about by COVID-19.
The survey responses on salary, debt, and net worth from more than 17,000 physicians spanning 30 specialties were collected prior to Feb. 11, before COVID-19 was declared a pandemic.
The authors of the report note that by some estimates, primary care offices have seen a 55% drop in revenue because of the pandemic, and specialists have been hard hit with the suspension of most elective procedures.
Primary care offices are seeing fewer patients and are limiting hours, and some offices have been forced to close. Others have stemmed the losses by introducing telemedicine options.
Before COVID-19, average incomes had continued to rise – this year to $243,000 (a 2.5% boost from last year’s $237,000) for primary care physicians and $346,000 for specialists (a 1.5% rise from last year’s $341,000).
About half of physicians (42%) reported a net worth of $1 million to $5 million, and 8% reported a net worth of more than $5 million. Fifty percent of physicians had a net worth of less than $1 million.
Those figures varied greatly by specialty. Among specialists, orthopedists were most likely (at 19%) to top the $5 million level, followed by plastic surgeons and gastroenterologists (both at 16%).
Conversely, 46% of family physicians and 44% of pediatricians reported that their net worth was under $500,000.
Gender gaps were also apparent in the data, especially at the highest levels. Twice as many male physicians (10%) as their female counterparts (5%) had a net worth of more than $5 million.
43% live below their means
Asked about habits regarding saving, 43% of physicians reported they live below their means. Half said they live at their means, and 7% said they live above their means.
Joel Greenwald, MD, CEO of Greenwald Wealth Management in St. Louis Park, Minn., recommends in the report trying to save 20% of annual gross salary.
More than a third of physicians who responded (39%) said they put more than $2,000/month into tax-deferred retirement or college savings, but Dr. Greenwald acknowledged that this may become more challenging.
“Many have seen the employer match in their retirement plans reduced or eliminated through the end of 2020, with what comes in 2021 as yet undefined,” he said.
A smaller percentage (26%) answered that they put more than $2,000 a month into a taxable retirement or college savings account each month.
Home size by specialty
Mortgages on a primary residence were the top reasons for debt (63%), followed by car loans (37%), personal education loans (26%), and credit card balances (25%).
Half of specialists and 61% of primary care physicians live in homes with up to 3,000 square feet. Only 7% of PCPs and 12% of specialists live in homes with 5000 square feet or more.
At 22%, plastic surgeons and orthopedists were the most likely groups to have houses with the largest square footage, according to the survey.
About one in four physicians in five specialties (urology, cardiology, plastic surgery, otolaryngology, and critical care) reported that they had mortgages of more than $500,000.
Standard financial advice, the report authors note, is that a mortgage should take up no more than 28% of monthly gross income.
Another large source of debt came from student loans. Close to 80% of graduating medical students have educational debt. The average balance for graduating students in 2018 was $196,520, the report authors state.
Those in physical medicine/rehabilitation and family medicine were most likely to still be paying off student debt (34% said they were). Conversely, half as many nephrologists and rheumatologists (15%) and gastroenterologists (14%) reported that they were paying off educational debt.
Only 11% of physicians said they were currently free of any debt.
Most physicians in the survey (72%) reported that they had not experienced a significant financial loss in the past year.
For those who did experience such a loss, the top reason given was related to a bad investment or the stock market (9%).
Cost-cutting strategies
Revenue reduction will likely lead to spending less this year as the pandemic challenges continue.
Survey respondents offered their most effective cost-cutting strategies.
A hospitalist said, “Half of every bonus goes into the investment account, no matter how much.”
“We add an extra amount to the principal of our monthly mortgage payment,” an internist said.
A pediatrician offered, “I bring my lunch to work every day and don’t eat in restaurants often.”
This article first appeared on Medscape.com.
Pursue multimodal pain management in patients taking opioids
For surgical patients on chronic opioid therapy, , according to Stephanie B. Jones, MD, professor and chair of anesthesiology at Albany Medical College, New York.
“[With] any patient coming in for any sort of surgery, you should be considering multimodal pain management. That applies to the opioid use disorder patient as well,” Dr. Jones said in a presentation at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education.
“The challenge of opioid-tolerant patients or opioid abuse patients is twofold – tolerance and hyperalgesia,” Dr. Jones said. Patient tolerance changes how patients perceive pain and respond to medication. Clinicians need to consider the “opioid debt,” defined as the daily amount of opioid medication required by opioid-dependent patients to maintain their usual prehospitalization opioid levels, she explained. Also consider hyperalgesia, a change in pain perception “resulting in an increase in pain sensitivity to painful stimuli, thereby decreasing the analgesic effects of opioids,” Dr. Jones added.
A multimodal approach to pain management in patients on chronic opioids can include some opioids as appropriate, Dr. Jones said. Modulation of pain may draw on epidurals and nerve blocks, as well as managing CNS perception of pain through opioids or acetaminophen, and also using systemic options such as alpha-2 agonists and tramadol, she said.
Studies have shown that opioid abuse or dependence were associated with increased readmission rates, length of stay, and health care costs in surgery patients, said Dr. Jones. However, switching opioids and managing equivalents is complex, and “equianalgesic conversions serve only as a general guide to estimate opioid dose equivalents,” according to UpToDate’s, “Management of acute pain in the patient chronically using opioids,” she said.
Dr. Jones also addressed the issue of using hospitalization as an opportunity to help patients with untreated opioid use disorder. Medication-assisted options include methadone, buprenorphine, and naltrexone.
“One problem with methadone is that there are a lot of medications interactions,” she said. Buprenorphine has the advantage of being long-lasting, and is formulated with naloxone which deters injection. “Because it is a partial agonist, there is a lower risk of overdose and sedation,” and it has fewer medication interactions. However, some doctors are reluctant to prescribe it and there is some risk of medication diversion, she said.
Naltrexone is newer to the role of treating opioid use disorder, Dr. Jones said. “It can cause acute withdrawal because it is a full opioid antagonist,” she noted. However, naltrexone itself causes no withdrawal if stopped, and no respiratory depression or sedation, said Dr. Jones.
“Utilize addiction services in your hospital if you suspect a patient may be at risk for opioid use disorder,” and engage these services early, she emphasized.
Global Academy for Medical Education and this news organization are owned by the same parent company.
Dr. Jones had no financial conflicts to disclose.
For surgical patients on chronic opioid therapy, , according to Stephanie B. Jones, MD, professor and chair of anesthesiology at Albany Medical College, New York.
“[With] any patient coming in for any sort of surgery, you should be considering multimodal pain management. That applies to the opioid use disorder patient as well,” Dr. Jones said in a presentation at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education.
“The challenge of opioid-tolerant patients or opioid abuse patients is twofold – tolerance and hyperalgesia,” Dr. Jones said. Patient tolerance changes how patients perceive pain and respond to medication. Clinicians need to consider the “opioid debt,” defined as the daily amount of opioid medication required by opioid-dependent patients to maintain their usual prehospitalization opioid levels, she explained. Also consider hyperalgesia, a change in pain perception “resulting in an increase in pain sensitivity to painful stimuli, thereby decreasing the analgesic effects of opioids,” Dr. Jones added.
A multimodal approach to pain management in patients on chronic opioids can include some opioids as appropriate, Dr. Jones said. Modulation of pain may draw on epidurals and nerve blocks, as well as managing CNS perception of pain through opioids or acetaminophen, and also using systemic options such as alpha-2 agonists and tramadol, she said.
Studies have shown that opioid abuse or dependence were associated with increased readmission rates, length of stay, and health care costs in surgery patients, said Dr. Jones. However, switching opioids and managing equivalents is complex, and “equianalgesic conversions serve only as a general guide to estimate opioid dose equivalents,” according to UpToDate’s, “Management of acute pain in the patient chronically using opioids,” she said.
Dr. Jones also addressed the issue of using hospitalization as an opportunity to help patients with untreated opioid use disorder. Medication-assisted options include methadone, buprenorphine, and naltrexone.
“One problem with methadone is that there are a lot of medications interactions,” she said. Buprenorphine has the advantage of being long-lasting, and is formulated with naloxone which deters injection. “Because it is a partial agonist, there is a lower risk of overdose and sedation,” and it has fewer medication interactions. However, some doctors are reluctant to prescribe it and there is some risk of medication diversion, she said.
Naltrexone is newer to the role of treating opioid use disorder, Dr. Jones said. “It can cause acute withdrawal because it is a full opioid antagonist,” she noted. However, naltrexone itself causes no withdrawal if stopped, and no respiratory depression or sedation, said Dr. Jones.
“Utilize addiction services in your hospital if you suspect a patient may be at risk for opioid use disorder,” and engage these services early, she emphasized.
Global Academy for Medical Education and this news organization are owned by the same parent company.
Dr. Jones had no financial conflicts to disclose.
For surgical patients on chronic opioid therapy, , according to Stephanie B. Jones, MD, professor and chair of anesthesiology at Albany Medical College, New York.
“[With] any patient coming in for any sort of surgery, you should be considering multimodal pain management. That applies to the opioid use disorder patient as well,” Dr. Jones said in a presentation at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education.
“The challenge of opioid-tolerant patients or opioid abuse patients is twofold – tolerance and hyperalgesia,” Dr. Jones said. Patient tolerance changes how patients perceive pain and respond to medication. Clinicians need to consider the “opioid debt,” defined as the daily amount of opioid medication required by opioid-dependent patients to maintain their usual prehospitalization opioid levels, she explained. Also consider hyperalgesia, a change in pain perception “resulting in an increase in pain sensitivity to painful stimuli, thereby decreasing the analgesic effects of opioids,” Dr. Jones added.
A multimodal approach to pain management in patients on chronic opioids can include some opioids as appropriate, Dr. Jones said. Modulation of pain may draw on epidurals and nerve blocks, as well as managing CNS perception of pain through opioids or acetaminophen, and also using systemic options such as alpha-2 agonists and tramadol, she said.
Studies have shown that opioid abuse or dependence were associated with increased readmission rates, length of stay, and health care costs in surgery patients, said Dr. Jones. However, switching opioids and managing equivalents is complex, and “equianalgesic conversions serve only as a general guide to estimate opioid dose equivalents,” according to UpToDate’s, “Management of acute pain in the patient chronically using opioids,” she said.
Dr. Jones also addressed the issue of using hospitalization as an opportunity to help patients with untreated opioid use disorder. Medication-assisted options include methadone, buprenorphine, and naltrexone.
“One problem with methadone is that there are a lot of medications interactions,” she said. Buprenorphine has the advantage of being long-lasting, and is formulated with naloxone which deters injection. “Because it is a partial agonist, there is a lower risk of overdose and sedation,” and it has fewer medication interactions. However, some doctors are reluctant to prescribe it and there is some risk of medication diversion, she said.
Naltrexone is newer to the role of treating opioid use disorder, Dr. Jones said. “It can cause acute withdrawal because it is a full opioid antagonist,” she noted. However, naltrexone itself causes no withdrawal if stopped, and no respiratory depression or sedation, said Dr. Jones.
“Utilize addiction services in your hospital if you suspect a patient may be at risk for opioid use disorder,” and engage these services early, she emphasized.
Global Academy for Medical Education and this news organization are owned by the same parent company.
Dr. Jones had no financial conflicts to disclose.
FROM MISS
Treatment developments in obstructive hypertrophic cardiomyopathy (oHCM)
Background: oHCM is characterized by mutations in sarcomeric proteins. Mavacamten is a small-molecule modulator of cardiac myosin, commonly affected in oHCM.
Study design: Open-label, nonrandomized phase 2 trial.
Setting: Five academic medical centers.
Synopsis: A total of 21 patients with oHCM were randomized to cohort A, high-dose mavacamten without additional therapy (beta-blockers, CCBs), or cohort B, low-dose mavacamten plus additional medical therapy. The LVOT gradient at 12 weeks improved in both cohorts: Cohort A had a mean change of –89.5 mm Hg (95% confidence interval, –138.3 to –40.7; P = .008) and cohort B –25.0 mm Hg (95% CI, –47.1 to –3.0, P = .020).
Bottom line: This phase 2 trial provides proof of concept and identified a plasma concentration of mavacamten needed to decrease the LVOT significantly. Phase 3 trials hold significant promise.
Citation: Heitner SB et al. Mavacamten treatment for obstructive hypertrophic cardiomyopathy: A clinical trial. Ann Intern Med. 2019 Apr 30. doi: 10.7326/M18-3016.
Dr. Blount is a hospitalist at the University of Colorado at Denver, Aurora.
Background: oHCM is characterized by mutations in sarcomeric proteins. Mavacamten is a small-molecule modulator of cardiac myosin, commonly affected in oHCM.
Study design: Open-label, nonrandomized phase 2 trial.
Setting: Five academic medical centers.
Synopsis: A total of 21 patients with oHCM were randomized to cohort A, high-dose mavacamten without additional therapy (beta-blockers, CCBs), or cohort B, low-dose mavacamten plus additional medical therapy. The LVOT gradient at 12 weeks improved in both cohorts: Cohort A had a mean change of –89.5 mm Hg (95% confidence interval, –138.3 to –40.7; P = .008) and cohort B –25.0 mm Hg (95% CI, –47.1 to –3.0, P = .020).
Bottom line: This phase 2 trial provides proof of concept and identified a plasma concentration of mavacamten needed to decrease the LVOT significantly. Phase 3 trials hold significant promise.
Citation: Heitner SB et al. Mavacamten treatment for obstructive hypertrophic cardiomyopathy: A clinical trial. Ann Intern Med. 2019 Apr 30. doi: 10.7326/M18-3016.
Dr. Blount is a hospitalist at the University of Colorado at Denver, Aurora.
Background: oHCM is characterized by mutations in sarcomeric proteins. Mavacamten is a small-molecule modulator of cardiac myosin, commonly affected in oHCM.
Study design: Open-label, nonrandomized phase 2 trial.
Setting: Five academic medical centers.
Synopsis: A total of 21 patients with oHCM were randomized to cohort A, high-dose mavacamten without additional therapy (beta-blockers, CCBs), or cohort B, low-dose mavacamten plus additional medical therapy. The LVOT gradient at 12 weeks improved in both cohorts: Cohort A had a mean change of –89.5 mm Hg (95% confidence interval, –138.3 to –40.7; P = .008) and cohort B –25.0 mm Hg (95% CI, –47.1 to –3.0, P = .020).
Bottom line: This phase 2 trial provides proof of concept and identified a plasma concentration of mavacamten needed to decrease the LVOT significantly. Phase 3 trials hold significant promise.
Citation: Heitner SB et al. Mavacamten treatment for obstructive hypertrophic cardiomyopathy: A clinical trial. Ann Intern Med. 2019 Apr 30. doi: 10.7326/M18-3016.
Dr. Blount is a hospitalist at the University of Colorado at Denver, Aurora.
Manage the pandemic with a multidisciplinary coalition
Implement a 6-P framework
The ongoing COVID-19 pandemic, arguably the biggest public health and economic catastrophe of modern times, elevated multiple deficiencies in public health infrastructures across the world, such as a slow or delayed response to suppress and mitigate the virus, an inadequately prepared and protected health care and public health workforce, and decentralized, siloed efforts.1 COVID-19 further highlighted the vulnerabilities of the health care, public health, and economic sectors.2,3 Irrespective of how robust health care systems may have been initially, rapidly spreading and deadly infectious diseases like COVID-19 can quickly derail the system, bringing the workforce and the patients they serve to a breaking point.
Hospital systems in the United States are not only at the crux of the current pandemic but are also well positioned to lead the response to the pandemic. Hospital administrators oversee nearly 33% of national health expenditure that amounts to the hospital-based care in the United States. Additionally, they may have an impact on nearly 30% of the expenditure that is related to physicians, prescriptions, and other facilities.4
The two primary goals underlying our proposed framework to target COVID-19 are based on the World Health Organization recommendations and lessons learned from countries such as South Korea that have successfully implemented these recommendations.5
1. Flatten the curve. According to the WHO and the Centers for Disease Control and Prevention, flattening the curve means that we must do everything that will help us to slow down the rate of infection, so the number of cases do not exceed the capacity of health systems.
2. Establish a standardized, interdisciplinary approach to flattening the curve. Pandemics can have major adverse consequences beyond health outcomes (e.g., economy) that can impact adherence to advisories and introduce multiple unintended consequences (e.g., deferred chronic care, unemployment). Managing the current pandemic and thoughtful consideration of and action regarding its ripple effects is heavily dependent on a standardized, interdisciplinary approach that is monitored, implemented, and evaluated well.
To achieve these two goals, we recommend establishing an interdisciplinary coalition representing multiple sectors. Our 6-P framework described below is intended to guide hospital administrators, to build the coalition, and to achieve these goals.
Structure of the pandemic coalition
A successful coalition invites a collaborative partnership involving senior members of respective disciplines, who would provide valuable, complementary perspectives in the coalition. We recommend hospital administrators take a lead in the formation of such a coalition. While we present the stakeholders and their roles below based on their intended influence and impact on the overall outcome of COVID-19, the basic guiding principles behind our 6-P framework remain true for any large-scale population health intervention.
Although several models for staging the transmission of COVID-19 are available, we adopted a four-stage model followed by the Indian Council for Medical Research.6 Irrespective of the origin of the infection, we believe that the four-stage model can cultivate situational awareness that can help guide the strategic design and systematic implementation of interventions.
Our 6-P framework integrates the four-stage model of COVID-19 transmission to identify action items for each stakeholder group and appropriate strategies selected based on the stages targeted.

1. Policy makers: Policy makers at all levels are critical in establishing policies, orders, and advisories, as well as dedicating resources and infrastructure, to enhance adherence to recommendations and guidelines at the community and population levels.7 They can assist hospitals in workforce expansion across county/state/discipline lines (e.g., accelerate the licensing and credentialing process, authorize graduate medical trainees, nurse practitioners, and other allied health professionals). Policy revisions for data sharing, privacy, communication, liability, and telehealth expansion.82. Providers: The health of the health care workforce itself is at risk because of their frontline services. Their buy-in will be crucial in both the formulation and implementation of evidence- and practice-based guidelines.9 Rapid adoption of telehealth for care continuum, policy revisions for elective procedures, visitor restriction, surge, resurge planning, capacity expansion, effective population health management, and working with employee unions, professional staff organizations are few, but very important action items that need to be implemented.
3. Public health authorities: Representation of public health authorities will be crucial in standardizing data collection, management, and reporting; providing up-to-date guidelines and advisories; developing, implementing, and evaluating short- and long-term public health interventions; and preparing and helping communities throughout the course of the pandemic. They also play a key role in identifying and reducing barriers related to the expansion of testing and contact tracing efforts.
4. Payers: In the United States, the Centers for Medicare & Medicaid Services oversees primary federally funded programs and serves as a point of reference for the American health care system. Having representation from all payer sources is crucial for achieving uniformity and standardization of the care process during the pandemic, with particular priority given to individuals and families who may have recently lost their health insurance because of job loss from COVID-19–related business furloughs, layoffs, and closures. Customer outreach initiatives, revision of patients’ out of pocket responsibilities, rapid claim settlement and denial management services, expansion of telehealth, elimination of prior authorization barriers, rapid credentialing of providers, data sharing, and assisting hospital systems in chronic disease management are examples of time-sensitive initiatives that are vital for population health management.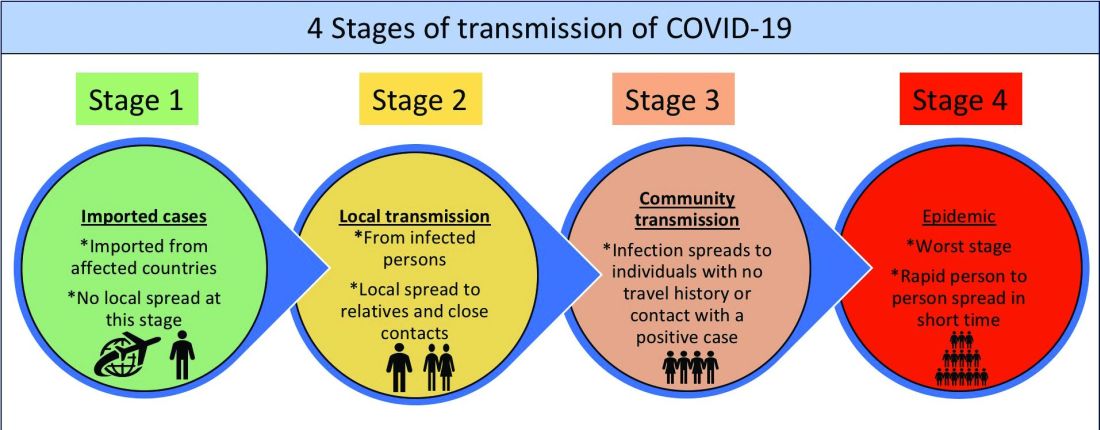
5. Partners: Establishing partnerships with pharma, health IT, labs, device industries, and other ancillary services is important to facilitate rapid innovation, production, and supply of essential medical devices and resources. These partners directly influence the outcomes of the pandemic and long-term health of the society through expansion of testing capability, contact tracing, leveraging technology for expanding access to COVID-19 and non–COVID-19 care, home monitoring of cases, innovation of treatment and prevention, and data sharing. Partners should consider options such as flexible medication delivery, electronic prescription services, and use of drones in supply chain to deliver test kits, test samples, medication, and blood products.
6. People/patients: Lastly and perhaps most critically, the trust, buy-in, and needs of the overall population are needed to enhance adherence to guidelines and recommendations. Many millions more than those who test positive for COVID-19 have and will continue to experience the crippling adverse economic, social, physical, and mental health effects of stay-at-home advisories, business and school closures, and physical distancing orders. Members of each community need to be heard in voicing their concerns and priorities and providing input on public health interventions to enhance acceptance and adherence (e.g., wear mask/face coverings in public, engage in physical distancing, etc.). Special attention should be given to managing chronic or existing medical problems and seek care when needed (e.g., avoid delaying of medical care).
An interdisciplinary and multipronged approach is necessary to address a complex, widespread, disruptive, and deadly pandemic such as COVID-19. The suggested activities put forth in our table are by no means exhaustive, nor do we expect all coalitions to be able to carry them all out. Our intention is that the 6-P framework encourages cross-sector collaboration to facilitate the design, implementation, evaluation, and scalability of preventive and intervention efforts based on the menu of items we have provided. Each coalition may determine which strategies they are able to prioritize and when within the context of specific national, regional, and local advisories, resulting in a tailored approach for each community or region that is thus better positioned for success.
Dr. Lingisetty is a hospitalist and physician executive at Baptist Health System, Little Rock, Ark. He is cofounder/president of SHM’s Arkansas chapter. Dr. Wang is assistant professor in the department of community health sciences at Boston University and adjunct assistant professor of health policy and management at the Harvard School of Public Health. Dr. Palabindala is the medical director, utilization management and physician advisory services, at the University of Mississippi Medical Center, Jackson. He is an associate professor of medicine and academic hospitalist at the University of Mississippi.
References
1. Powles J, Comim F. Public health infrastructure and knowledge, in Smith R et al. “Global Public Goods for Health.” Oxford: Oxford University Press, 2003.
2. Lombardi P, Petroni G. Virus outbreak pushes Italy’s health care system to the brink. Wall Street Journal. 2020 Mar 12. https://www.wsj.com/articles/virus-outbreak-pushes-italys-healthcare-system-to-the-brink-11583968769
3. Davies, R. How coronavirus is affecting the global economy. The Guardian. 2020 Feb 5. https://www.theguardian.com/world/2020/feb/05/coronavirus-global-economy
4. National Center for Health Statistics. FastStats. 2017. https://www.cdc.gov/nchs/fastats/health-expenditures.htm.
5. World Health Organization. Country & Technical Guidance–Coronavirus disease (COVID-19). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance
6. Indian Council of Medical Research. Stages of transmission of COVID-19. https://main.icmr.nic.in/content/covid-19
7. Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19) – Prevention & treatment. 2020 Apr 24. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html
8. Ostriker R. Cutbacks for some doctors and nurses as they battle on the front line. Boston Globe. 2020 Mar 27. https://www.bostonglobe.com/2020/03/27/metro/coronavirus-rages-doctors-hit-with-cuts-compensation/
9. Centers for Medicare & Medicaid Services. News alert. 2020 Mar 26. https://www.cms.gov/newsroom/press-releases/cms-news-alert-march-26-2020
Implement a 6-P framework
Implement a 6-P framework
The ongoing COVID-19 pandemic, arguably the biggest public health and economic catastrophe of modern times, elevated multiple deficiencies in public health infrastructures across the world, such as a slow or delayed response to suppress and mitigate the virus, an inadequately prepared and protected health care and public health workforce, and decentralized, siloed efforts.1 COVID-19 further highlighted the vulnerabilities of the health care, public health, and economic sectors.2,3 Irrespective of how robust health care systems may have been initially, rapidly spreading and deadly infectious diseases like COVID-19 can quickly derail the system, bringing the workforce and the patients they serve to a breaking point.
Hospital systems in the United States are not only at the crux of the current pandemic but are also well positioned to lead the response to the pandemic. Hospital administrators oversee nearly 33% of national health expenditure that amounts to the hospital-based care in the United States. Additionally, they may have an impact on nearly 30% of the expenditure that is related to physicians, prescriptions, and other facilities.4
The two primary goals underlying our proposed framework to target COVID-19 are based on the World Health Organization recommendations and lessons learned from countries such as South Korea that have successfully implemented these recommendations.5
1. Flatten the curve. According to the WHO and the Centers for Disease Control and Prevention, flattening the curve means that we must do everything that will help us to slow down the rate of infection, so the number of cases do not exceed the capacity of health systems.
2. Establish a standardized, interdisciplinary approach to flattening the curve. Pandemics can have major adverse consequences beyond health outcomes (e.g., economy) that can impact adherence to advisories and introduce multiple unintended consequences (e.g., deferred chronic care, unemployment). Managing the current pandemic and thoughtful consideration of and action regarding its ripple effects is heavily dependent on a standardized, interdisciplinary approach that is monitored, implemented, and evaluated well.
To achieve these two goals, we recommend establishing an interdisciplinary coalition representing multiple sectors. Our 6-P framework described below is intended to guide hospital administrators, to build the coalition, and to achieve these goals.
Structure of the pandemic coalition
A successful coalition invites a collaborative partnership involving senior members of respective disciplines, who would provide valuable, complementary perspectives in the coalition. We recommend hospital administrators take a lead in the formation of such a coalition. While we present the stakeholders and their roles below based on their intended influence and impact on the overall outcome of COVID-19, the basic guiding principles behind our 6-P framework remain true for any large-scale population health intervention.
Although several models for staging the transmission of COVID-19 are available, we adopted a four-stage model followed by the Indian Council for Medical Research.6 Irrespective of the origin of the infection, we believe that the four-stage model can cultivate situational awareness that can help guide the strategic design and systematic implementation of interventions.
Our 6-P framework integrates the four-stage model of COVID-19 transmission to identify action items for each stakeholder group and appropriate strategies selected based on the stages targeted.

1. Policy makers: Policy makers at all levels are critical in establishing policies, orders, and advisories, as well as dedicating resources and infrastructure, to enhance adherence to recommendations and guidelines at the community and population levels.7 They can assist hospitals in workforce expansion across county/state/discipline lines (e.g., accelerate the licensing and credentialing process, authorize graduate medical trainees, nurse practitioners, and other allied health professionals). Policy revisions for data sharing, privacy, communication, liability, and telehealth expansion.82. Providers: The health of the health care workforce itself is at risk because of their frontline services. Their buy-in will be crucial in both the formulation and implementation of evidence- and practice-based guidelines.9 Rapid adoption of telehealth for care continuum, policy revisions for elective procedures, visitor restriction, surge, resurge planning, capacity expansion, effective population health management, and working with employee unions, professional staff organizations are few, but very important action items that need to be implemented.
3. Public health authorities: Representation of public health authorities will be crucial in standardizing data collection, management, and reporting; providing up-to-date guidelines and advisories; developing, implementing, and evaluating short- and long-term public health interventions; and preparing and helping communities throughout the course of the pandemic. They also play a key role in identifying and reducing barriers related to the expansion of testing and contact tracing efforts.
4. Payers: In the United States, the Centers for Medicare & Medicaid Services oversees primary federally funded programs and serves as a point of reference for the American health care system. Having representation from all payer sources is crucial for achieving uniformity and standardization of the care process during the pandemic, with particular priority given to individuals and families who may have recently lost their health insurance because of job loss from COVID-19–related business furloughs, layoffs, and closures. Customer outreach initiatives, revision of patients’ out of pocket responsibilities, rapid claim settlement and denial management services, expansion of telehealth, elimination of prior authorization barriers, rapid credentialing of providers, data sharing, and assisting hospital systems in chronic disease management are examples of time-sensitive initiatives that are vital for population health management.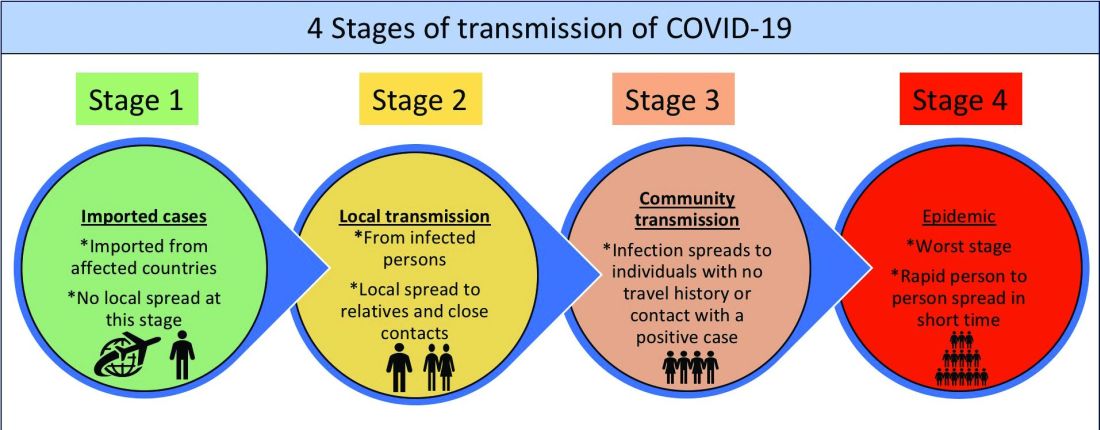
5. Partners: Establishing partnerships with pharma, health IT, labs, device industries, and other ancillary services is important to facilitate rapid innovation, production, and supply of essential medical devices and resources. These partners directly influence the outcomes of the pandemic and long-term health of the society through expansion of testing capability, contact tracing, leveraging technology for expanding access to COVID-19 and non–COVID-19 care, home monitoring of cases, innovation of treatment and prevention, and data sharing. Partners should consider options such as flexible medication delivery, electronic prescription services, and use of drones in supply chain to deliver test kits, test samples, medication, and blood products.
6. People/patients: Lastly and perhaps most critically, the trust, buy-in, and needs of the overall population are needed to enhance adherence to guidelines and recommendations. Many millions more than those who test positive for COVID-19 have and will continue to experience the crippling adverse economic, social, physical, and mental health effects of stay-at-home advisories, business and school closures, and physical distancing orders. Members of each community need to be heard in voicing their concerns and priorities and providing input on public health interventions to enhance acceptance and adherence (e.g., wear mask/face coverings in public, engage in physical distancing, etc.). Special attention should be given to managing chronic or existing medical problems and seek care when needed (e.g., avoid delaying of medical care).
An interdisciplinary and multipronged approach is necessary to address a complex, widespread, disruptive, and deadly pandemic such as COVID-19. The suggested activities put forth in our table are by no means exhaustive, nor do we expect all coalitions to be able to carry them all out. Our intention is that the 6-P framework encourages cross-sector collaboration to facilitate the design, implementation, evaluation, and scalability of preventive and intervention efforts based on the menu of items we have provided. Each coalition may determine which strategies they are able to prioritize and when within the context of specific national, regional, and local advisories, resulting in a tailored approach for each community or region that is thus better positioned for success.
Dr. Lingisetty is a hospitalist and physician executive at Baptist Health System, Little Rock, Ark. He is cofounder/president of SHM’s Arkansas chapter. Dr. Wang is assistant professor in the department of community health sciences at Boston University and adjunct assistant professor of health policy and management at the Harvard School of Public Health. Dr. Palabindala is the medical director, utilization management and physician advisory services, at the University of Mississippi Medical Center, Jackson. He is an associate professor of medicine and academic hospitalist at the University of Mississippi.
References
1. Powles J, Comim F. Public health infrastructure and knowledge, in Smith R et al. “Global Public Goods for Health.” Oxford: Oxford University Press, 2003.
2. Lombardi P, Petroni G. Virus outbreak pushes Italy’s health care system to the brink. Wall Street Journal. 2020 Mar 12. https://www.wsj.com/articles/virus-outbreak-pushes-italys-healthcare-system-to-the-brink-11583968769
3. Davies, R. How coronavirus is affecting the global economy. The Guardian. 2020 Feb 5. https://www.theguardian.com/world/2020/feb/05/coronavirus-global-economy
4. National Center for Health Statistics. FastStats. 2017. https://www.cdc.gov/nchs/fastats/health-expenditures.htm.
5. World Health Organization. Country & Technical Guidance–Coronavirus disease (COVID-19). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance
6. Indian Council of Medical Research. Stages of transmission of COVID-19. https://main.icmr.nic.in/content/covid-19
7. Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19) – Prevention & treatment. 2020 Apr 24. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html
8. Ostriker R. Cutbacks for some doctors and nurses as they battle on the front line. Boston Globe. 2020 Mar 27. https://www.bostonglobe.com/2020/03/27/metro/coronavirus-rages-doctors-hit-with-cuts-compensation/
9. Centers for Medicare & Medicaid Services. News alert. 2020 Mar 26. https://www.cms.gov/newsroom/press-releases/cms-news-alert-march-26-2020
The ongoing COVID-19 pandemic, arguably the biggest public health and economic catastrophe of modern times, elevated multiple deficiencies in public health infrastructures across the world, such as a slow or delayed response to suppress and mitigate the virus, an inadequately prepared and protected health care and public health workforce, and decentralized, siloed efforts.1 COVID-19 further highlighted the vulnerabilities of the health care, public health, and economic sectors.2,3 Irrespective of how robust health care systems may have been initially, rapidly spreading and deadly infectious diseases like COVID-19 can quickly derail the system, bringing the workforce and the patients they serve to a breaking point.
Hospital systems in the United States are not only at the crux of the current pandemic but are also well positioned to lead the response to the pandemic. Hospital administrators oversee nearly 33% of national health expenditure that amounts to the hospital-based care in the United States. Additionally, they may have an impact on nearly 30% of the expenditure that is related to physicians, prescriptions, and other facilities.4
The two primary goals underlying our proposed framework to target COVID-19 are based on the World Health Organization recommendations and lessons learned from countries such as South Korea that have successfully implemented these recommendations.5
1. Flatten the curve. According to the WHO and the Centers for Disease Control and Prevention, flattening the curve means that we must do everything that will help us to slow down the rate of infection, so the number of cases do not exceed the capacity of health systems.
2. Establish a standardized, interdisciplinary approach to flattening the curve. Pandemics can have major adverse consequences beyond health outcomes (e.g., economy) that can impact adherence to advisories and introduce multiple unintended consequences (e.g., deferred chronic care, unemployment). Managing the current pandemic and thoughtful consideration of and action regarding its ripple effects is heavily dependent on a standardized, interdisciplinary approach that is monitored, implemented, and evaluated well.
To achieve these two goals, we recommend establishing an interdisciplinary coalition representing multiple sectors. Our 6-P framework described below is intended to guide hospital administrators, to build the coalition, and to achieve these goals.
Structure of the pandemic coalition
A successful coalition invites a collaborative partnership involving senior members of respective disciplines, who would provide valuable, complementary perspectives in the coalition. We recommend hospital administrators take a lead in the formation of such a coalition. While we present the stakeholders and their roles below based on their intended influence and impact on the overall outcome of COVID-19, the basic guiding principles behind our 6-P framework remain true for any large-scale population health intervention.
Although several models for staging the transmission of COVID-19 are available, we adopted a four-stage model followed by the Indian Council for Medical Research.6 Irrespective of the origin of the infection, we believe that the four-stage model can cultivate situational awareness that can help guide the strategic design and systematic implementation of interventions.
Our 6-P framework integrates the four-stage model of COVID-19 transmission to identify action items for each stakeholder group and appropriate strategies selected based on the stages targeted.

1. Policy makers: Policy makers at all levels are critical in establishing policies, orders, and advisories, as well as dedicating resources and infrastructure, to enhance adherence to recommendations and guidelines at the community and population levels.7 They can assist hospitals in workforce expansion across county/state/discipline lines (e.g., accelerate the licensing and credentialing process, authorize graduate medical trainees, nurse practitioners, and other allied health professionals). Policy revisions for data sharing, privacy, communication, liability, and telehealth expansion.82. Providers: The health of the health care workforce itself is at risk because of their frontline services. Their buy-in will be crucial in both the formulation and implementation of evidence- and practice-based guidelines.9 Rapid adoption of telehealth for care continuum, policy revisions for elective procedures, visitor restriction, surge, resurge planning, capacity expansion, effective population health management, and working with employee unions, professional staff organizations are few, but very important action items that need to be implemented.
3. Public health authorities: Representation of public health authorities will be crucial in standardizing data collection, management, and reporting; providing up-to-date guidelines and advisories; developing, implementing, and evaluating short- and long-term public health interventions; and preparing and helping communities throughout the course of the pandemic. They also play a key role in identifying and reducing barriers related to the expansion of testing and contact tracing efforts.
4. Payers: In the United States, the Centers for Medicare & Medicaid Services oversees primary federally funded programs and serves as a point of reference for the American health care system. Having representation from all payer sources is crucial for achieving uniformity and standardization of the care process during the pandemic, with particular priority given to individuals and families who may have recently lost their health insurance because of job loss from COVID-19–related business furloughs, layoffs, and closures. Customer outreach initiatives, revision of patients’ out of pocket responsibilities, rapid claim settlement and denial management services, expansion of telehealth, elimination of prior authorization barriers, rapid credentialing of providers, data sharing, and assisting hospital systems in chronic disease management are examples of time-sensitive initiatives that are vital for population health management.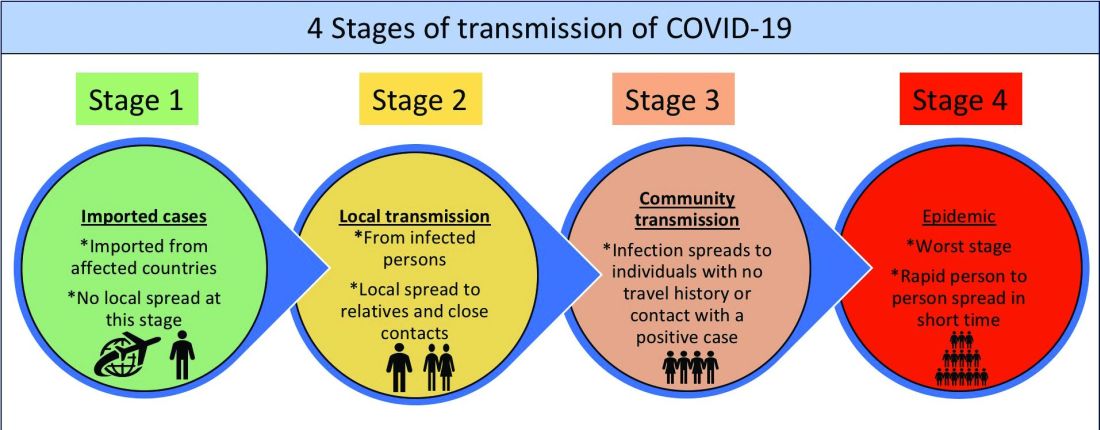
5. Partners: Establishing partnerships with pharma, health IT, labs, device industries, and other ancillary services is important to facilitate rapid innovation, production, and supply of essential medical devices and resources. These partners directly influence the outcomes of the pandemic and long-term health of the society through expansion of testing capability, contact tracing, leveraging technology for expanding access to COVID-19 and non–COVID-19 care, home monitoring of cases, innovation of treatment and prevention, and data sharing. Partners should consider options such as flexible medication delivery, electronic prescription services, and use of drones in supply chain to deliver test kits, test samples, medication, and blood products.
6. People/patients: Lastly and perhaps most critically, the trust, buy-in, and needs of the overall population are needed to enhance adherence to guidelines and recommendations. Many millions more than those who test positive for COVID-19 have and will continue to experience the crippling adverse economic, social, physical, and mental health effects of stay-at-home advisories, business and school closures, and physical distancing orders. Members of each community need to be heard in voicing their concerns and priorities and providing input on public health interventions to enhance acceptance and adherence (e.g., wear mask/face coverings in public, engage in physical distancing, etc.). Special attention should be given to managing chronic or existing medical problems and seek care when needed (e.g., avoid delaying of medical care).
An interdisciplinary and multipronged approach is necessary to address a complex, widespread, disruptive, and deadly pandemic such as COVID-19. The suggested activities put forth in our table are by no means exhaustive, nor do we expect all coalitions to be able to carry them all out. Our intention is that the 6-P framework encourages cross-sector collaboration to facilitate the design, implementation, evaluation, and scalability of preventive and intervention efforts based on the menu of items we have provided. Each coalition may determine which strategies they are able to prioritize and when within the context of specific national, regional, and local advisories, resulting in a tailored approach for each community or region that is thus better positioned for success.
Dr. Lingisetty is a hospitalist and physician executive at Baptist Health System, Little Rock, Ark. He is cofounder/president of SHM’s Arkansas chapter. Dr. Wang is assistant professor in the department of community health sciences at Boston University and adjunct assistant professor of health policy and management at the Harvard School of Public Health. Dr. Palabindala is the medical director, utilization management and physician advisory services, at the University of Mississippi Medical Center, Jackson. He is an associate professor of medicine and academic hospitalist at the University of Mississippi.
References
1. Powles J, Comim F. Public health infrastructure and knowledge, in Smith R et al. “Global Public Goods for Health.” Oxford: Oxford University Press, 2003.
2. Lombardi P, Petroni G. Virus outbreak pushes Italy’s health care system to the brink. Wall Street Journal. 2020 Mar 12. https://www.wsj.com/articles/virus-outbreak-pushes-italys-healthcare-system-to-the-brink-11583968769
3. Davies, R. How coronavirus is affecting the global economy. The Guardian. 2020 Feb 5. https://www.theguardian.com/world/2020/feb/05/coronavirus-global-economy
4. National Center for Health Statistics. FastStats. 2017. https://www.cdc.gov/nchs/fastats/health-expenditures.htm.
5. World Health Organization. Country & Technical Guidance–Coronavirus disease (COVID-19). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance
6. Indian Council of Medical Research. Stages of transmission of COVID-19. https://main.icmr.nic.in/content/covid-19
7. Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19) – Prevention & treatment. 2020 Apr 24. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html
8. Ostriker R. Cutbacks for some doctors and nurses as they battle on the front line. Boston Globe. 2020 Mar 27. https://www.bostonglobe.com/2020/03/27/metro/coronavirus-rages-doctors-hit-with-cuts-compensation/
9. Centers for Medicare & Medicaid Services. News alert. 2020 Mar 26. https://www.cms.gov/newsroom/press-releases/cms-news-alert-march-26-2020
Skin patterns of COVID-19 vary widely
according to Christine Ko, MD.
“Things are very fluid,” Dr. Ko, professor of dermatology and pathology at Yale University, New Haven, Conn., said during the virtual annual meeting of the American Academy of Dermatology. “New studies are coming out daily. Due to the need for rapid dissemination, a lot of the studies are case reports, but there are some nice case series. Another caveat for the literature is that a lot of these cases were not necessarily confirmed with testing for SARS-CoV-2, but some were.”
Dr. Ko framed her remarks largely on a case collection survey of images and clinical data from 375 patients in Spain with suspected or confirmed COVID-19 that was published online April 29, 2020, in the British Journal of Dermatology (doi: 10.1111/bjd.19163). Cutaneous manifestations included early vesicular eruptions mainly on the trunk or limbs (9%), maculopapular (47%) to urticarial lesions (19%) mainly on the trunk, and acral areas of erythema sometimes with vesicles or erosion (perniosis-like) (19%) that seemed to be a later manifestation of COVID-19. Retiform purpura or necrosis (6%) was most concerning in terms of skin disease, with an associated with a mortality of 10%.
On histology, the early vesicular eruptions are typically marked by dyskeratotic keratinocytes, Dr. Ko said, while urticarial lesions are characterized by a mixed dermal infiltrate; maculopapular lesions were a broad category. “There are some case reports that show spongiotic dermatitis or parakeratosis with a lymphocytic infiltrate,” she said. “A caveat to keep in mind is that, although these patients may definitely have COVID-19 and be confirmed to have it by testing, hypersensitivity reactions may be due to the multiple medications they’re on.”
Patients can develop a spectrum of lesions that are suggestive of vascular damage or occlusion, Dr. Ko continued. Livedoid lesions may remain static and not eventuate into necrosis or purpura but will self-resolve. Purpuric lesions and acral gangrene have been described, and these lesions correspond to vascular occlusion on biopsy.
A later manifestation are the so-called “COVID toes” with a superficial and deep lymphocytic infiltrate, as published June 1, 2020, in JAAD Case Reports: (doi: 10.1016/j.jdcr.2020.04.011).
“There are patients in the literature that have slightly different pathology, with lymphocytic inflammation as well as occlusion of vessels,” Dr. Ko said. A paper published June 20, 2020, in the British Journal of Dermatology used immunohistochemical staining against the SARS-CoV-2 spike protein, and biopsies of “COVID toes” had positive staining of endothelial cells, supporting the notion that “COVID toes” are a direct manifestation of viral infection (doi: 10.1111/bjd.19327).
“There’s a lot that we still don’t know, and some patterns are going to be outliers,” Dr. Ko concluded. “[As for] determining which skin manifestations are directly from coronavirus infection within the skin, more study is needed and likely time will tell.” She reported having no financial disclosures relevant to her talk.
according to Christine Ko, MD.
“Things are very fluid,” Dr. Ko, professor of dermatology and pathology at Yale University, New Haven, Conn., said during the virtual annual meeting of the American Academy of Dermatology. “New studies are coming out daily. Due to the need for rapid dissemination, a lot of the studies are case reports, but there are some nice case series. Another caveat for the literature is that a lot of these cases were not necessarily confirmed with testing for SARS-CoV-2, but some were.”
Dr. Ko framed her remarks largely on a case collection survey of images and clinical data from 375 patients in Spain with suspected or confirmed COVID-19 that was published online April 29, 2020, in the British Journal of Dermatology (doi: 10.1111/bjd.19163). Cutaneous manifestations included early vesicular eruptions mainly on the trunk or limbs (9%), maculopapular (47%) to urticarial lesions (19%) mainly on the trunk, and acral areas of erythema sometimes with vesicles or erosion (perniosis-like) (19%) that seemed to be a later manifestation of COVID-19. Retiform purpura or necrosis (6%) was most concerning in terms of skin disease, with an associated with a mortality of 10%.
On histology, the early vesicular eruptions are typically marked by dyskeratotic keratinocytes, Dr. Ko said, while urticarial lesions are characterized by a mixed dermal infiltrate; maculopapular lesions were a broad category. “There are some case reports that show spongiotic dermatitis or parakeratosis with a lymphocytic infiltrate,” she said. “A caveat to keep in mind is that, although these patients may definitely have COVID-19 and be confirmed to have it by testing, hypersensitivity reactions may be due to the multiple medications they’re on.”
Patients can develop a spectrum of lesions that are suggestive of vascular damage or occlusion, Dr. Ko continued. Livedoid lesions may remain static and not eventuate into necrosis or purpura but will self-resolve. Purpuric lesions and acral gangrene have been described, and these lesions correspond to vascular occlusion on biopsy.
A later manifestation are the so-called “COVID toes” with a superficial and deep lymphocytic infiltrate, as published June 1, 2020, in JAAD Case Reports: (doi: 10.1016/j.jdcr.2020.04.011).
“There are patients in the literature that have slightly different pathology, with lymphocytic inflammation as well as occlusion of vessels,” Dr. Ko said. A paper published June 20, 2020, in the British Journal of Dermatology used immunohistochemical staining against the SARS-CoV-2 spike protein, and biopsies of “COVID toes” had positive staining of endothelial cells, supporting the notion that “COVID toes” are a direct manifestation of viral infection (doi: 10.1111/bjd.19327).
“There’s a lot that we still don’t know, and some patterns are going to be outliers,” Dr. Ko concluded. “[As for] determining which skin manifestations are directly from coronavirus infection within the skin, more study is needed and likely time will tell.” She reported having no financial disclosures relevant to her talk.
according to Christine Ko, MD.
“Things are very fluid,” Dr. Ko, professor of dermatology and pathology at Yale University, New Haven, Conn., said during the virtual annual meeting of the American Academy of Dermatology. “New studies are coming out daily. Due to the need for rapid dissemination, a lot of the studies are case reports, but there are some nice case series. Another caveat for the literature is that a lot of these cases were not necessarily confirmed with testing for SARS-CoV-2, but some were.”
Dr. Ko framed her remarks largely on a case collection survey of images and clinical data from 375 patients in Spain with suspected or confirmed COVID-19 that was published online April 29, 2020, in the British Journal of Dermatology (doi: 10.1111/bjd.19163). Cutaneous manifestations included early vesicular eruptions mainly on the trunk or limbs (9%), maculopapular (47%) to urticarial lesions (19%) mainly on the trunk, and acral areas of erythema sometimes with vesicles or erosion (perniosis-like) (19%) that seemed to be a later manifestation of COVID-19. Retiform purpura or necrosis (6%) was most concerning in terms of skin disease, with an associated with a mortality of 10%.
On histology, the early vesicular eruptions are typically marked by dyskeratotic keratinocytes, Dr. Ko said, while urticarial lesions are characterized by a mixed dermal infiltrate; maculopapular lesions were a broad category. “There are some case reports that show spongiotic dermatitis or parakeratosis with a lymphocytic infiltrate,” she said. “A caveat to keep in mind is that, although these patients may definitely have COVID-19 and be confirmed to have it by testing, hypersensitivity reactions may be due to the multiple medications they’re on.”
Patients can develop a spectrum of lesions that are suggestive of vascular damage or occlusion, Dr. Ko continued. Livedoid lesions may remain static and not eventuate into necrosis or purpura but will self-resolve. Purpuric lesions and acral gangrene have been described, and these lesions correspond to vascular occlusion on biopsy.
A later manifestation are the so-called “COVID toes” with a superficial and deep lymphocytic infiltrate, as published June 1, 2020, in JAAD Case Reports: (doi: 10.1016/j.jdcr.2020.04.011).
“There are patients in the literature that have slightly different pathology, with lymphocytic inflammation as well as occlusion of vessels,” Dr. Ko said. A paper published June 20, 2020, in the British Journal of Dermatology used immunohistochemical staining against the SARS-CoV-2 spike protein, and biopsies of “COVID toes” had positive staining of endothelial cells, supporting the notion that “COVID toes” are a direct manifestation of viral infection (doi: 10.1111/bjd.19327).
“There’s a lot that we still don’t know, and some patterns are going to be outliers,” Dr. Ko concluded. “[As for] determining which skin manifestations are directly from coronavirus infection within the skin, more study is needed and likely time will tell.” She reported having no financial disclosures relevant to her talk.
FROM AAD 20