User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Inpatient sodium imbalances linked to adverse COVID-19 outcomes
Both high and low serum sodium levels are associated with adverse outcomes for hospitalized patients with COVID-19, new research suggests.
In the retrospective study of 488 patients hospitalized with COVID-19 at one of two London hospitals between February and May 2020, hypernatremia (defined as serum sodium level >145 mmol/L) at any time point during hospital stay was associated with a threefold increase in inpatient mortality.
Hyponatremia (serum sodium level <135 mmol/L) was associated with twice the likelihood of requiring advanced ventilatory support. In-hospital mortality was also increased among patients with hypovolemic hyponatremia.
“Serum sodium values could be used in clinical practice to identify patients with COVID-19 at high risk of poor outcomes who would benefit from more intensive monitoring and judicious rehydration,” Ploutarchos Tzoulis, MD, PhD, and colleagues wrote in their article, which was published online on Feb. 24, 2021, in the Journal of Clinical Endocrinology and Metabolism.
The findings will be presented at the upcoming news conference held by the Endocrine Society
Should sodium be included in a risk calculator for COVID-19?
Dr. Tzoulis, professor of endocrinology at the University College London Medical School, said in an interview that “sodium could be incorporated in risk calculators across other routine biomarkers, such as white cell count, lymphocytes, and CRP [C-reactive protein], in order to provide a tool for dynamic risk stratification throughout the clinical course of COVID-19 and assist clinical decision-making.”
Moreover, he said, “we should follow less conservative strategies in the rate and amount of fluid resuscitation in order to prevent hypernatremia, which is induced by negative fluid balance and can often be iatrogenic.”
Asked to comment, Steven Q. Simpson, MD, professor of medicine in the division of pulmonary, critical care, and sleep medicine at the University of Kansas, Kansas City, said that the article is missing key results that would assist in interpreting of the findings.
“Data regarding diuretic use and sparing of fluid administration are not in the paper. ... It is simply not possible to tell whether serum sodium is a ‘predictor’ ... or if it is a side effect of other issues or actions taken by physicians in patients who are progressing poorly.
“To say that sodium needs to be included in a risk calculator is to subtly suggest that there is some causal association with mortality, and that has quite clearly not been established,” stressed Dr. Simpson, who is president of the American College of Chest Physicians but was not speaking for the organization.
He added: “The data are interesting, but not actionable. It is common practice in critical care medicine to adjust water and salt intake to maintain serum sodium within the normal range, so the paper really doesn’t change any behavior.”
Dr. Tzoulis said in an interview that, despite not having electronic medical record data on diuretic use or fluid input and output, “our acute physicians and intensivists at both study sites have been adamant that they’ve not routinely used diuretics in COVID-19 patients. Diuretics have been sparingly used in our cohort, and also the frequency of pulmonary edema was reported as below 5%.”
Regarding volume of fluid intake, Dr. Tzoulis noted, “At our hospital sites, the strategy has been that of cautious fluid resuscitation. In fact, the amount of fluid given has been reported by our physicians and intensivists as ‘on purpose much more conservative than the usual one adopted in patients with community-acquired pneumonia at risk of respiratory failure.’ ”
Hyper- and hyponatremia linked to adverse COVID-19 outcomes
In the study, 5.3% of the 488 patients had hypernatremia at hospital presentation, and 24.6% had hyponatremia. Of note, only 19% of those with hyponatremia underwent laboratory workup to determine the etiology. Of those, three quarters had hypovolemic hyponatremia, determined on the basis of a urinary sodium cutoff of 30 mmol/L.
The total in-hospital mortality rate was 31.1%. There was a strong, although nonsignificant, trend toward higher mortality in association with sodium status at admission. Death rates were 28.4%, 30.8%, and 46.1% for those who were normonatremic, hyponatremic, and hypernatremic, respectively (P = .07). Baseline serum sodium levels didn’t differ between survivors (137 mmol/L) and nonsurvivors (138 mmol/L).
In multivariable analysis, the occurrence of hypernatremia at any point during the first 5 days in the hospital was among three independent risk factors for higher in-hospital mortality (adjusted hazard ratio, 2.74; P = .02). The other risk factors were older age and higher CRP level.
Overall, hyponatremia was not associated with death (P = .41).
During hospitalization, 37.9% of patients remained normonatremic; 36.9% experienced hyponatremia; 10.9% had hypernatremia; and 14.3% had both conditions at some point during their stay.
In-hospital mortality was 21% among those with normonatremia, compared with 56.6% for those with hypernatremia (odds ratio, 3.05; P = .0038) and 45.7% for those with both (OR, 2.25; P < .0001).
The 28.3% mortality rate in the overall group that experienced hyponatremia didn’t differ significantly from the 21.1% in the normonatremic group (OR, 1.34; P = .16). However, the death rate was 40.9% among the subgroup that developed hypovolemic hyponatremia, significantly higher than the normonatremic group (OR, 2.59, P = .0017).
The incidence of hyponatremia decreased from 24.6% at admission to 14.1% 5 days later, whereas the frequency of hypernatremia rose from 5.3% to 13.8%.
Key finding: Link between hospital-acquired hypernatremia and death
“The key novel finding of our study was that hospital-acquired hypernatremia, rather than hypernatremia at admission, was a predictor for in-hospital mortality, with the worst prognosis being reported in patients with the largest increase in serum sodium in the first 5 days of hospitalization,” noted Dr. Tzoulis and colleagues.
Hypernatremia was present in 29.6% of nonsurvivors, compared with 5.2% in survivors.
Among 120 patients with hyponatremia at admission, 31.7% received advanced respiratory support, compared with 17.5% and 7.7% of those with normonatremia or hypernatremia, respectively (OR, 2.18; P = .0011).
In contrast, there was no difference in the proportions needing ventilatory support between those with hypernatremia and those with normonatremia (16.7% vs. 12.4%; OR, 1.44; P = .39).
Acute kidney injury occurred in 181 patients (37.1%). It was not related to serum sodium concentration at any time point.
Dr. Tzoulis and Dr. Simpson disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Both high and low serum sodium levels are associated with adverse outcomes for hospitalized patients with COVID-19, new research suggests.
In the retrospective study of 488 patients hospitalized with COVID-19 at one of two London hospitals between February and May 2020, hypernatremia (defined as serum sodium level >145 mmol/L) at any time point during hospital stay was associated with a threefold increase in inpatient mortality.
Hyponatremia (serum sodium level <135 mmol/L) was associated with twice the likelihood of requiring advanced ventilatory support. In-hospital mortality was also increased among patients with hypovolemic hyponatremia.
“Serum sodium values could be used in clinical practice to identify patients with COVID-19 at high risk of poor outcomes who would benefit from more intensive monitoring and judicious rehydration,” Ploutarchos Tzoulis, MD, PhD, and colleagues wrote in their article, which was published online on Feb. 24, 2021, in the Journal of Clinical Endocrinology and Metabolism.
The findings will be presented at the upcoming news conference held by the Endocrine Society
Should sodium be included in a risk calculator for COVID-19?
Dr. Tzoulis, professor of endocrinology at the University College London Medical School, said in an interview that “sodium could be incorporated in risk calculators across other routine biomarkers, such as white cell count, lymphocytes, and CRP [C-reactive protein], in order to provide a tool for dynamic risk stratification throughout the clinical course of COVID-19 and assist clinical decision-making.”
Moreover, he said, “we should follow less conservative strategies in the rate and amount of fluid resuscitation in order to prevent hypernatremia, which is induced by negative fluid balance and can often be iatrogenic.”
Asked to comment, Steven Q. Simpson, MD, professor of medicine in the division of pulmonary, critical care, and sleep medicine at the University of Kansas, Kansas City, said that the article is missing key results that would assist in interpreting of the findings.
“Data regarding diuretic use and sparing of fluid administration are not in the paper. ... It is simply not possible to tell whether serum sodium is a ‘predictor’ ... or if it is a side effect of other issues or actions taken by physicians in patients who are progressing poorly.
“To say that sodium needs to be included in a risk calculator is to subtly suggest that there is some causal association with mortality, and that has quite clearly not been established,” stressed Dr. Simpson, who is president of the American College of Chest Physicians but was not speaking for the organization.
He added: “The data are interesting, but not actionable. It is common practice in critical care medicine to adjust water and salt intake to maintain serum sodium within the normal range, so the paper really doesn’t change any behavior.”
Dr. Tzoulis said in an interview that, despite not having electronic medical record data on diuretic use or fluid input and output, “our acute physicians and intensivists at both study sites have been adamant that they’ve not routinely used diuretics in COVID-19 patients. Diuretics have been sparingly used in our cohort, and also the frequency of pulmonary edema was reported as below 5%.”
Regarding volume of fluid intake, Dr. Tzoulis noted, “At our hospital sites, the strategy has been that of cautious fluid resuscitation. In fact, the amount of fluid given has been reported by our physicians and intensivists as ‘on purpose much more conservative than the usual one adopted in patients with community-acquired pneumonia at risk of respiratory failure.’ ”
Hyper- and hyponatremia linked to adverse COVID-19 outcomes
In the study, 5.3% of the 488 patients had hypernatremia at hospital presentation, and 24.6% had hyponatremia. Of note, only 19% of those with hyponatremia underwent laboratory workup to determine the etiology. Of those, three quarters had hypovolemic hyponatremia, determined on the basis of a urinary sodium cutoff of 30 mmol/L.
The total in-hospital mortality rate was 31.1%. There was a strong, although nonsignificant, trend toward higher mortality in association with sodium status at admission. Death rates were 28.4%, 30.8%, and 46.1% for those who were normonatremic, hyponatremic, and hypernatremic, respectively (P = .07). Baseline serum sodium levels didn’t differ between survivors (137 mmol/L) and nonsurvivors (138 mmol/L).
In multivariable analysis, the occurrence of hypernatremia at any point during the first 5 days in the hospital was among three independent risk factors for higher in-hospital mortality (adjusted hazard ratio, 2.74; P = .02). The other risk factors were older age and higher CRP level.
Overall, hyponatremia was not associated with death (P = .41).
During hospitalization, 37.9% of patients remained normonatremic; 36.9% experienced hyponatremia; 10.9% had hypernatremia; and 14.3% had both conditions at some point during their stay.
In-hospital mortality was 21% among those with normonatremia, compared with 56.6% for those with hypernatremia (odds ratio, 3.05; P = .0038) and 45.7% for those with both (OR, 2.25; P < .0001).
The 28.3% mortality rate in the overall group that experienced hyponatremia didn’t differ significantly from the 21.1% in the normonatremic group (OR, 1.34; P = .16). However, the death rate was 40.9% among the subgroup that developed hypovolemic hyponatremia, significantly higher than the normonatremic group (OR, 2.59, P = .0017).
The incidence of hyponatremia decreased from 24.6% at admission to 14.1% 5 days later, whereas the frequency of hypernatremia rose from 5.3% to 13.8%.
Key finding: Link between hospital-acquired hypernatremia and death
“The key novel finding of our study was that hospital-acquired hypernatremia, rather than hypernatremia at admission, was a predictor for in-hospital mortality, with the worst prognosis being reported in patients with the largest increase in serum sodium in the first 5 days of hospitalization,” noted Dr. Tzoulis and colleagues.
Hypernatremia was present in 29.6% of nonsurvivors, compared with 5.2% in survivors.
Among 120 patients with hyponatremia at admission, 31.7% received advanced respiratory support, compared with 17.5% and 7.7% of those with normonatremia or hypernatremia, respectively (OR, 2.18; P = .0011).
In contrast, there was no difference in the proportions needing ventilatory support between those with hypernatremia and those with normonatremia (16.7% vs. 12.4%; OR, 1.44; P = .39).
Acute kidney injury occurred in 181 patients (37.1%). It was not related to serum sodium concentration at any time point.
Dr. Tzoulis and Dr. Simpson disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Both high and low serum sodium levels are associated with adverse outcomes for hospitalized patients with COVID-19, new research suggests.
In the retrospective study of 488 patients hospitalized with COVID-19 at one of two London hospitals between February and May 2020, hypernatremia (defined as serum sodium level >145 mmol/L) at any time point during hospital stay was associated with a threefold increase in inpatient mortality.
Hyponatremia (serum sodium level <135 mmol/L) was associated with twice the likelihood of requiring advanced ventilatory support. In-hospital mortality was also increased among patients with hypovolemic hyponatremia.
“Serum sodium values could be used in clinical practice to identify patients with COVID-19 at high risk of poor outcomes who would benefit from more intensive monitoring and judicious rehydration,” Ploutarchos Tzoulis, MD, PhD, and colleagues wrote in their article, which was published online on Feb. 24, 2021, in the Journal of Clinical Endocrinology and Metabolism.
The findings will be presented at the upcoming news conference held by the Endocrine Society
Should sodium be included in a risk calculator for COVID-19?
Dr. Tzoulis, professor of endocrinology at the University College London Medical School, said in an interview that “sodium could be incorporated in risk calculators across other routine biomarkers, such as white cell count, lymphocytes, and CRP [C-reactive protein], in order to provide a tool for dynamic risk stratification throughout the clinical course of COVID-19 and assist clinical decision-making.”
Moreover, he said, “we should follow less conservative strategies in the rate and amount of fluid resuscitation in order to prevent hypernatremia, which is induced by negative fluid balance and can often be iatrogenic.”
Asked to comment, Steven Q. Simpson, MD, professor of medicine in the division of pulmonary, critical care, and sleep medicine at the University of Kansas, Kansas City, said that the article is missing key results that would assist in interpreting of the findings.
“Data regarding diuretic use and sparing of fluid administration are not in the paper. ... It is simply not possible to tell whether serum sodium is a ‘predictor’ ... or if it is a side effect of other issues or actions taken by physicians in patients who are progressing poorly.
“To say that sodium needs to be included in a risk calculator is to subtly suggest that there is some causal association with mortality, and that has quite clearly not been established,” stressed Dr. Simpson, who is president of the American College of Chest Physicians but was not speaking for the organization.
He added: “The data are interesting, but not actionable. It is common practice in critical care medicine to adjust water and salt intake to maintain serum sodium within the normal range, so the paper really doesn’t change any behavior.”
Dr. Tzoulis said in an interview that, despite not having electronic medical record data on diuretic use or fluid input and output, “our acute physicians and intensivists at both study sites have been adamant that they’ve not routinely used diuretics in COVID-19 patients. Diuretics have been sparingly used in our cohort, and also the frequency of pulmonary edema was reported as below 5%.”
Regarding volume of fluid intake, Dr. Tzoulis noted, “At our hospital sites, the strategy has been that of cautious fluid resuscitation. In fact, the amount of fluid given has been reported by our physicians and intensivists as ‘on purpose much more conservative than the usual one adopted in patients with community-acquired pneumonia at risk of respiratory failure.’ ”
Hyper- and hyponatremia linked to adverse COVID-19 outcomes
In the study, 5.3% of the 488 patients had hypernatremia at hospital presentation, and 24.6% had hyponatremia. Of note, only 19% of those with hyponatremia underwent laboratory workup to determine the etiology. Of those, three quarters had hypovolemic hyponatremia, determined on the basis of a urinary sodium cutoff of 30 mmol/L.
The total in-hospital mortality rate was 31.1%. There was a strong, although nonsignificant, trend toward higher mortality in association with sodium status at admission. Death rates were 28.4%, 30.8%, and 46.1% for those who were normonatremic, hyponatremic, and hypernatremic, respectively (P = .07). Baseline serum sodium levels didn’t differ between survivors (137 mmol/L) and nonsurvivors (138 mmol/L).
In multivariable analysis, the occurrence of hypernatremia at any point during the first 5 days in the hospital was among three independent risk factors for higher in-hospital mortality (adjusted hazard ratio, 2.74; P = .02). The other risk factors were older age and higher CRP level.
Overall, hyponatremia was not associated with death (P = .41).
During hospitalization, 37.9% of patients remained normonatremic; 36.9% experienced hyponatremia; 10.9% had hypernatremia; and 14.3% had both conditions at some point during their stay.
In-hospital mortality was 21% among those with normonatremia, compared with 56.6% for those with hypernatremia (odds ratio, 3.05; P = .0038) and 45.7% for those with both (OR, 2.25; P < .0001).
The 28.3% mortality rate in the overall group that experienced hyponatremia didn’t differ significantly from the 21.1% in the normonatremic group (OR, 1.34; P = .16). However, the death rate was 40.9% among the subgroup that developed hypovolemic hyponatremia, significantly higher than the normonatremic group (OR, 2.59, P = .0017).
The incidence of hyponatremia decreased from 24.6% at admission to 14.1% 5 days later, whereas the frequency of hypernatremia rose from 5.3% to 13.8%.
Key finding: Link between hospital-acquired hypernatremia and death
“The key novel finding of our study was that hospital-acquired hypernatremia, rather than hypernatremia at admission, was a predictor for in-hospital mortality, with the worst prognosis being reported in patients with the largest increase in serum sodium in the first 5 days of hospitalization,” noted Dr. Tzoulis and colleagues.
Hypernatremia was present in 29.6% of nonsurvivors, compared with 5.2% in survivors.
Among 120 patients with hyponatremia at admission, 31.7% received advanced respiratory support, compared with 17.5% and 7.7% of those with normonatremia or hypernatremia, respectively (OR, 2.18; P = .0011).
In contrast, there was no difference in the proportions needing ventilatory support between those with hypernatremia and those with normonatremia (16.7% vs. 12.4%; OR, 1.44; P = .39).
Acute kidney injury occurred in 181 patients (37.1%). It was not related to serum sodium concentration at any time point.
Dr. Tzoulis and Dr. Simpson disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Inclusivity needed in PHM fellowships
A year and a half ago, I found myself seated in a crowded hall at the national Pediatric Hospital Medicine (PHM) conference. Throughout the conference, trainees like me were warmly welcomed into small groups and lunch tables. I tried to keep my cool while PHM “celebrities” chatted with me in the elevator. Most sessions were prepared with plenty of chairs, and those that were not encouraged latecomers to grab a spot on the floor or the back wall – the more the merrier.
The intention of this “advice for applicants” meeting was to inspire and guide our next steps toward fellowship, but a discomforting reality loomed over us. It was the first year graduating pediatricians could not choose PHM board certification via the practice pathway – we needed an invitation in the form of a fellowship match.
The “hidden curriculum” was not subtle: People who scored a seat would keep their options open within the field of PHM, and those who did not had a murkier future. This message stood in stark contrast to the PHM inclusivity I had experienced all conference, and planted seeds of doubt: Was I welcome here? Did I “deserve” a seat?
I found the experience as a PHM fellowship applicant to be uncomfortable, and my all-too familiar friend “imposter syndrome” set up camp in my brain and made herself at home. I had no way of knowing how many programs to apply to, how many to interview at, or the chances of my matching at all. Once on the interview trail, I realized I was not alone in my discomfort – most applicants harbored some trepidation, and no one truly knew how the chips would fall on Match Day.
I am thrilled and relieved to have come out the other end in a great position. The team I work with and learn from is phenomenal. I am grateful that ACGME accreditation ensures structures are in place for fellows to be supported in their academic and educational efforts and have full confidence that the skills I gain in fellowship will help me contribute to progression of the field of PHM and improve my performance as a clinician-educator.
Sadly, each year PHM match day celebrations are dampened by the knowledge that a large portion of our colleagues are being left out in the cold with an “unmatched” notification in their inboxes. Approximately 200 graduating pediatricians become pediatric hospitalists each year,1 but only 68 fellowship positions were available in the United States for matriculation in 2020.2 In 2019, PHM fellowship candidates navigated the 6-month application journey with aspirations to further their training in the profession they love. Of the candidates who submitted a rank list committing to 2 or more years in PHM fellowship, 35% were denied.
Unfortunately, despite expansion of PHM fellowship programs and fifteen seats added from last year, we learned this December that there still are not enough positions to welcome qualified applicants with open arms: Thirty-three percent of candidates ranked PHM programs first in the NRMP but did not match – the highest unmatched percentage out of all pediatric subspecialties.3
The NRMP report shared a glimpse of our colleagues who received interview invitations and submitted a rank list, but this is likely an underestimation of pediatric graduates who wanted to obtain PHM board certification and wound up on a different path. Some residents anticipated the stiff competition and delayed their plans to apply for fellowship, while others matched into another subspecialty that was able to accommodate them. Many pediatric graduates joined the workforce directly as pediatric hospitalists knowing the practice pathway to certification is not available to them. Along with other physicians without board certification in PHM, they shoulder concerns of being withheld from professional advancement opportunities.
For the foreseeable future it is clear that pediatric hospitalists without board certification will be a large part of our community, and are crucial to providing high-quality care to hospitalized children nationally. In 2019, a national survey of pediatric hospital medicine groups revealed that 50% of pediatric hospitalist hires came directly out of residency, and only 8% of hires were fellowship trained.4 The same report revealed that 26% of physicians were board-certified.These percentages are likely to change over the next 5 years as the window of practice pathway certification closes and fellowship programs continue to expand. Only time will tell what the national prevalence of board-certified pediatric hospitalists settles out to be.
Historically, PHM fellowship graduates have assumed roles that include teaching and research responsibilities, and ACGME fellowship requirements have ensured that trainees graduate with skills in medical education and scholarship, and need only 4 weeks of training to be done in a community hospital.5 Pediatric hospitalists who do not pursue board certification are seeing the growing pool of PHM fellowship graduates prepared for positions in academic institutions. It is reasonable that they harbor concerns about being siloed toward primarily community hospital roles, and for community hospitalists to feel that this structure undervalues their role within the field of PHM.
At a time when inclusivity and community in medicine are receiving much-needed recognition, the current fellowship application climate has potential to create division within the PHM community. Newly graduating pediatric residents are among the populations disproportionately affected by the practice pathway cutoff. Like other subspecialties with ever-climbing steps up the “ivory tower” of academia and specialization within medicine, the inherent structure of the training pathway makes navigating it more difficult for pediatricians with professional, geographic, and economic diversity or constraints.
Med-Peds–trained colleagues have the added challenge of finding a fellowship position that is willing and able to support their concurrent internal medicine goals. International medical graduates make up about 20% of graduating residents each year, and just 11% of matched PHM fellows.3,6 Similarly, while DO medical graduates make up 20% of pediatric residents in the United States, only 10% of matched PHM fellows were DOs.3,6 New pediatricians with families or financial insecurity may be unable to invest in an expensive application process, move to a new city, and accept less than half of the average starting salary of a pediatric hospitalist for 2-3 years.7
The prevalence of implicit bias in medicine is well documented, and there is growing evidence that it negatively impacts candidate selection in medical education and contributes to minorities being underrepresented in the physician workforce.8 We must recognize the ways that adding a competitive costly hurdle may risk conflict with our mission to encourage diversity of representation within PHM leadership positions.
We have not yet successfully bridged the gap between qualified PHM fellowship candidates and available fellowship positions. I worry that this gap and the lack of transparency surrounding it is resulting in one portion of new pediatricians being welcomed by the subspecialty, and others feeling unsupported and alienated by the larger PHM community as early career physicians.
Right now, the only solution available is expansion of fellowship programs. We see progress with the new addition of fellowship positions every year, but finding funding for each position is often a lengthy endeavor, and the COVID-19 pandemic has tightened the purse strings of many children’s hospitals. It may be many years before the number of available fellowship positions more closely approximates the 200 pediatricians that become hospitalists each year.
The most equitable solution would be offering other avenues to board certification while this gap is being bridged, either by extending the practice pathway option, or making a third pathway that requires less institutional funding per fellow, but still incentivizes institutional investment in fellowship positions and resources (e.g., a pathway requiring some number of years in practice, plus 1 year in fellowship centered around a nonclinical academic curriculum).
In the absence of the solutions above, we collectively hold the responsibility of maintaining inclusivity and support of our PHM colleagues with and without board certification. One important strategy provided by Dr. Gregory Welsh9 is to incorporate community hospital medicine rotations into residency training. Sharing this side of PHM with residents may help some graduates avoid a training pathway they may not want or need. More importantly, it would raise trainee exposure and interest toward a service that is both expansive – approximately 70% of pediatric hospitalists practice in a community hospital – and crucial to children’s health nationally.
Pediatric hospitalists who are not eligible for board certification are vital and valued members of the PHM community, and as such need to maintain representation within PHM leadership. Professional development opportunities need to remain accessible outside of fellowship. The blossoming of virtual conferences and Zoom meet-ups in the face of the COVID-19 pandemic have shown us that with innovation (and a good Internet connection), networking and mentorship can be accomplished across thousands of miles.
While there’s great diversity within PHM, this subspecialty has a history of attracting pediatricians with some common core qualities: Grit, creativity, and the belief that a strong team is far greater than the sum of its parts. I have confidence that if we approach this PHM transition period with transparency about our goals and challenges, this community can emerge from it strong and united.
Dr. Ezzio is a first-year pediatric hospital medicine fellow at Helen DeVos Children’s Hospital in Grand Rapids, Mich. Her interests include medical education and advocacy. Dr. Ezzio would like to thank Dr. Jeri Kessenich and Dr. Rachel “Danielle” Fisher for their assistance in revising the article. To submit to, or for inquiries about, our PHM Fellows Column, please contact our Pediatrics Editor, Dr. Anika Kumar (KumarA4@ccf.org).
References
1. Leyenaar JK and Fritner MP. Graduating pediatric residents entering the hospital medicine workforce, 2006-2015. Acad Pediatr. 2018 Mar;18(2):200-7.
2. National Resident Matching Program. Results and data: Specialties matching service 2020 appointment year. Washington, DC 2020.
3. National Resident Matching Program. Results and data: Specialties matching service 2021 appointment year. Washington, DC 2021.
4. 2020 State of Hospital Medicine report. Society of Hospital Medicine. 2020.
5. Oshimura JM et al. Current roles and perceived needs of pediatric hospital medicine fellowship graduates. Hosp Pediatr. 2016;6(10):633-7.
6. National Resident Matching Program. Results and data: 2020 main residency match. Washington, DC 2020.
7. American Academy of Pediatrics Annual Survey of graduating residents 2003-2020.
8. Quinn Capers IV. How clinicians and educators can mitigate implicit bias in patient care and candidate selection in medical education. American Thoracic Society Scholar. 2020 Jun;1(3):211-17.
9. Welsh G. The importance of community pediatric hospital medicine. The Hospitalist. 2021 Jan;25(1):27.
A year and a half ago, I found myself seated in a crowded hall at the national Pediatric Hospital Medicine (PHM) conference. Throughout the conference, trainees like me were warmly welcomed into small groups and lunch tables. I tried to keep my cool while PHM “celebrities” chatted with me in the elevator. Most sessions were prepared with plenty of chairs, and those that were not encouraged latecomers to grab a spot on the floor or the back wall – the more the merrier.
The intention of this “advice for applicants” meeting was to inspire and guide our next steps toward fellowship, but a discomforting reality loomed over us. It was the first year graduating pediatricians could not choose PHM board certification via the practice pathway – we needed an invitation in the form of a fellowship match.
The “hidden curriculum” was not subtle: People who scored a seat would keep their options open within the field of PHM, and those who did not had a murkier future. This message stood in stark contrast to the PHM inclusivity I had experienced all conference, and planted seeds of doubt: Was I welcome here? Did I “deserve” a seat?
I found the experience as a PHM fellowship applicant to be uncomfortable, and my all-too familiar friend “imposter syndrome” set up camp in my brain and made herself at home. I had no way of knowing how many programs to apply to, how many to interview at, or the chances of my matching at all. Once on the interview trail, I realized I was not alone in my discomfort – most applicants harbored some trepidation, and no one truly knew how the chips would fall on Match Day.
I am thrilled and relieved to have come out the other end in a great position. The team I work with and learn from is phenomenal. I am grateful that ACGME accreditation ensures structures are in place for fellows to be supported in their academic and educational efforts and have full confidence that the skills I gain in fellowship will help me contribute to progression of the field of PHM and improve my performance as a clinician-educator.
Sadly, each year PHM match day celebrations are dampened by the knowledge that a large portion of our colleagues are being left out in the cold with an “unmatched” notification in their inboxes. Approximately 200 graduating pediatricians become pediatric hospitalists each year,1 but only 68 fellowship positions were available in the United States for matriculation in 2020.2 In 2019, PHM fellowship candidates navigated the 6-month application journey with aspirations to further their training in the profession they love. Of the candidates who submitted a rank list committing to 2 or more years in PHM fellowship, 35% were denied.
Unfortunately, despite expansion of PHM fellowship programs and fifteen seats added from last year, we learned this December that there still are not enough positions to welcome qualified applicants with open arms: Thirty-three percent of candidates ranked PHM programs first in the NRMP but did not match – the highest unmatched percentage out of all pediatric subspecialties.3
The NRMP report shared a glimpse of our colleagues who received interview invitations and submitted a rank list, but this is likely an underestimation of pediatric graduates who wanted to obtain PHM board certification and wound up on a different path. Some residents anticipated the stiff competition and delayed their plans to apply for fellowship, while others matched into another subspecialty that was able to accommodate them. Many pediatric graduates joined the workforce directly as pediatric hospitalists knowing the practice pathway to certification is not available to them. Along with other physicians without board certification in PHM, they shoulder concerns of being withheld from professional advancement opportunities.
For the foreseeable future it is clear that pediatric hospitalists without board certification will be a large part of our community, and are crucial to providing high-quality care to hospitalized children nationally. In 2019, a national survey of pediatric hospital medicine groups revealed that 50% of pediatric hospitalist hires came directly out of residency, and only 8% of hires were fellowship trained.4 The same report revealed that 26% of physicians were board-certified.These percentages are likely to change over the next 5 years as the window of practice pathway certification closes and fellowship programs continue to expand. Only time will tell what the national prevalence of board-certified pediatric hospitalists settles out to be.
Historically, PHM fellowship graduates have assumed roles that include teaching and research responsibilities, and ACGME fellowship requirements have ensured that trainees graduate with skills in medical education and scholarship, and need only 4 weeks of training to be done in a community hospital.5 Pediatric hospitalists who do not pursue board certification are seeing the growing pool of PHM fellowship graduates prepared for positions in academic institutions. It is reasonable that they harbor concerns about being siloed toward primarily community hospital roles, and for community hospitalists to feel that this structure undervalues their role within the field of PHM.
At a time when inclusivity and community in medicine are receiving much-needed recognition, the current fellowship application climate has potential to create division within the PHM community. Newly graduating pediatric residents are among the populations disproportionately affected by the practice pathway cutoff. Like other subspecialties with ever-climbing steps up the “ivory tower” of academia and specialization within medicine, the inherent structure of the training pathway makes navigating it more difficult for pediatricians with professional, geographic, and economic diversity or constraints.
Med-Peds–trained colleagues have the added challenge of finding a fellowship position that is willing and able to support their concurrent internal medicine goals. International medical graduates make up about 20% of graduating residents each year, and just 11% of matched PHM fellows.3,6 Similarly, while DO medical graduates make up 20% of pediatric residents in the United States, only 10% of matched PHM fellows were DOs.3,6 New pediatricians with families or financial insecurity may be unable to invest in an expensive application process, move to a new city, and accept less than half of the average starting salary of a pediatric hospitalist for 2-3 years.7
The prevalence of implicit bias in medicine is well documented, and there is growing evidence that it negatively impacts candidate selection in medical education and contributes to minorities being underrepresented in the physician workforce.8 We must recognize the ways that adding a competitive costly hurdle may risk conflict with our mission to encourage diversity of representation within PHM leadership positions.
We have not yet successfully bridged the gap between qualified PHM fellowship candidates and available fellowship positions. I worry that this gap and the lack of transparency surrounding it is resulting in one portion of new pediatricians being welcomed by the subspecialty, and others feeling unsupported and alienated by the larger PHM community as early career physicians.
Right now, the only solution available is expansion of fellowship programs. We see progress with the new addition of fellowship positions every year, but finding funding for each position is often a lengthy endeavor, and the COVID-19 pandemic has tightened the purse strings of many children’s hospitals. It may be many years before the number of available fellowship positions more closely approximates the 200 pediatricians that become hospitalists each year.
The most equitable solution would be offering other avenues to board certification while this gap is being bridged, either by extending the practice pathway option, or making a third pathway that requires less institutional funding per fellow, but still incentivizes institutional investment in fellowship positions and resources (e.g., a pathway requiring some number of years in practice, plus 1 year in fellowship centered around a nonclinical academic curriculum).
In the absence of the solutions above, we collectively hold the responsibility of maintaining inclusivity and support of our PHM colleagues with and without board certification. One important strategy provided by Dr. Gregory Welsh9 is to incorporate community hospital medicine rotations into residency training. Sharing this side of PHM with residents may help some graduates avoid a training pathway they may not want or need. More importantly, it would raise trainee exposure and interest toward a service that is both expansive – approximately 70% of pediatric hospitalists practice in a community hospital – and crucial to children’s health nationally.
Pediatric hospitalists who are not eligible for board certification are vital and valued members of the PHM community, and as such need to maintain representation within PHM leadership. Professional development opportunities need to remain accessible outside of fellowship. The blossoming of virtual conferences and Zoom meet-ups in the face of the COVID-19 pandemic have shown us that with innovation (and a good Internet connection), networking and mentorship can be accomplished across thousands of miles.
While there’s great diversity within PHM, this subspecialty has a history of attracting pediatricians with some common core qualities: Grit, creativity, and the belief that a strong team is far greater than the sum of its parts. I have confidence that if we approach this PHM transition period with transparency about our goals and challenges, this community can emerge from it strong and united.
Dr. Ezzio is a first-year pediatric hospital medicine fellow at Helen DeVos Children’s Hospital in Grand Rapids, Mich. Her interests include medical education and advocacy. Dr. Ezzio would like to thank Dr. Jeri Kessenich and Dr. Rachel “Danielle” Fisher for their assistance in revising the article. To submit to, or for inquiries about, our PHM Fellows Column, please contact our Pediatrics Editor, Dr. Anika Kumar (KumarA4@ccf.org).
References
1. Leyenaar JK and Fritner MP. Graduating pediatric residents entering the hospital medicine workforce, 2006-2015. Acad Pediatr. 2018 Mar;18(2):200-7.
2. National Resident Matching Program. Results and data: Specialties matching service 2020 appointment year. Washington, DC 2020.
3. National Resident Matching Program. Results and data: Specialties matching service 2021 appointment year. Washington, DC 2021.
4. 2020 State of Hospital Medicine report. Society of Hospital Medicine. 2020.
5. Oshimura JM et al. Current roles and perceived needs of pediatric hospital medicine fellowship graduates. Hosp Pediatr. 2016;6(10):633-7.
6. National Resident Matching Program. Results and data: 2020 main residency match. Washington, DC 2020.
7. American Academy of Pediatrics Annual Survey of graduating residents 2003-2020.
8. Quinn Capers IV. How clinicians and educators can mitigate implicit bias in patient care and candidate selection in medical education. American Thoracic Society Scholar. 2020 Jun;1(3):211-17.
9. Welsh G. The importance of community pediatric hospital medicine. The Hospitalist. 2021 Jan;25(1):27.
A year and a half ago, I found myself seated in a crowded hall at the national Pediatric Hospital Medicine (PHM) conference. Throughout the conference, trainees like me were warmly welcomed into small groups and lunch tables. I tried to keep my cool while PHM “celebrities” chatted with me in the elevator. Most sessions were prepared with plenty of chairs, and those that were not encouraged latecomers to grab a spot on the floor or the back wall – the more the merrier.
The intention of this “advice for applicants” meeting was to inspire and guide our next steps toward fellowship, but a discomforting reality loomed over us. It was the first year graduating pediatricians could not choose PHM board certification via the practice pathway – we needed an invitation in the form of a fellowship match.
The “hidden curriculum” was not subtle: People who scored a seat would keep their options open within the field of PHM, and those who did not had a murkier future. This message stood in stark contrast to the PHM inclusivity I had experienced all conference, and planted seeds of doubt: Was I welcome here? Did I “deserve” a seat?
I found the experience as a PHM fellowship applicant to be uncomfortable, and my all-too familiar friend “imposter syndrome” set up camp in my brain and made herself at home. I had no way of knowing how many programs to apply to, how many to interview at, or the chances of my matching at all. Once on the interview trail, I realized I was not alone in my discomfort – most applicants harbored some trepidation, and no one truly knew how the chips would fall on Match Day.
I am thrilled and relieved to have come out the other end in a great position. The team I work with and learn from is phenomenal. I am grateful that ACGME accreditation ensures structures are in place for fellows to be supported in their academic and educational efforts and have full confidence that the skills I gain in fellowship will help me contribute to progression of the field of PHM and improve my performance as a clinician-educator.
Sadly, each year PHM match day celebrations are dampened by the knowledge that a large portion of our colleagues are being left out in the cold with an “unmatched” notification in their inboxes. Approximately 200 graduating pediatricians become pediatric hospitalists each year,1 but only 68 fellowship positions were available in the United States for matriculation in 2020.2 In 2019, PHM fellowship candidates navigated the 6-month application journey with aspirations to further their training in the profession they love. Of the candidates who submitted a rank list committing to 2 or more years in PHM fellowship, 35% were denied.
Unfortunately, despite expansion of PHM fellowship programs and fifteen seats added from last year, we learned this December that there still are not enough positions to welcome qualified applicants with open arms: Thirty-three percent of candidates ranked PHM programs first in the NRMP but did not match – the highest unmatched percentage out of all pediatric subspecialties.3
The NRMP report shared a glimpse of our colleagues who received interview invitations and submitted a rank list, but this is likely an underestimation of pediatric graduates who wanted to obtain PHM board certification and wound up on a different path. Some residents anticipated the stiff competition and delayed their plans to apply for fellowship, while others matched into another subspecialty that was able to accommodate them. Many pediatric graduates joined the workforce directly as pediatric hospitalists knowing the practice pathway to certification is not available to them. Along with other physicians without board certification in PHM, they shoulder concerns of being withheld from professional advancement opportunities.
For the foreseeable future it is clear that pediatric hospitalists without board certification will be a large part of our community, and are crucial to providing high-quality care to hospitalized children nationally. In 2019, a national survey of pediatric hospital medicine groups revealed that 50% of pediatric hospitalist hires came directly out of residency, and only 8% of hires were fellowship trained.4 The same report revealed that 26% of physicians were board-certified.These percentages are likely to change over the next 5 years as the window of practice pathway certification closes and fellowship programs continue to expand. Only time will tell what the national prevalence of board-certified pediatric hospitalists settles out to be.
Historically, PHM fellowship graduates have assumed roles that include teaching and research responsibilities, and ACGME fellowship requirements have ensured that trainees graduate with skills in medical education and scholarship, and need only 4 weeks of training to be done in a community hospital.5 Pediatric hospitalists who do not pursue board certification are seeing the growing pool of PHM fellowship graduates prepared for positions in academic institutions. It is reasonable that they harbor concerns about being siloed toward primarily community hospital roles, and for community hospitalists to feel that this structure undervalues their role within the field of PHM.
At a time when inclusivity and community in medicine are receiving much-needed recognition, the current fellowship application climate has potential to create division within the PHM community. Newly graduating pediatric residents are among the populations disproportionately affected by the practice pathway cutoff. Like other subspecialties with ever-climbing steps up the “ivory tower” of academia and specialization within medicine, the inherent structure of the training pathway makes navigating it more difficult for pediatricians with professional, geographic, and economic diversity or constraints.
Med-Peds–trained colleagues have the added challenge of finding a fellowship position that is willing and able to support their concurrent internal medicine goals. International medical graduates make up about 20% of graduating residents each year, and just 11% of matched PHM fellows.3,6 Similarly, while DO medical graduates make up 20% of pediatric residents in the United States, only 10% of matched PHM fellows were DOs.3,6 New pediatricians with families or financial insecurity may be unable to invest in an expensive application process, move to a new city, and accept less than half of the average starting salary of a pediatric hospitalist for 2-3 years.7
The prevalence of implicit bias in medicine is well documented, and there is growing evidence that it negatively impacts candidate selection in medical education and contributes to minorities being underrepresented in the physician workforce.8 We must recognize the ways that adding a competitive costly hurdle may risk conflict with our mission to encourage diversity of representation within PHM leadership positions.
We have not yet successfully bridged the gap between qualified PHM fellowship candidates and available fellowship positions. I worry that this gap and the lack of transparency surrounding it is resulting in one portion of new pediatricians being welcomed by the subspecialty, and others feeling unsupported and alienated by the larger PHM community as early career physicians.
Right now, the only solution available is expansion of fellowship programs. We see progress with the new addition of fellowship positions every year, but finding funding for each position is often a lengthy endeavor, and the COVID-19 pandemic has tightened the purse strings of many children’s hospitals. It may be many years before the number of available fellowship positions more closely approximates the 200 pediatricians that become hospitalists each year.
The most equitable solution would be offering other avenues to board certification while this gap is being bridged, either by extending the practice pathway option, or making a third pathway that requires less institutional funding per fellow, but still incentivizes institutional investment in fellowship positions and resources (e.g., a pathway requiring some number of years in practice, plus 1 year in fellowship centered around a nonclinical academic curriculum).
In the absence of the solutions above, we collectively hold the responsibility of maintaining inclusivity and support of our PHM colleagues with and without board certification. One important strategy provided by Dr. Gregory Welsh9 is to incorporate community hospital medicine rotations into residency training. Sharing this side of PHM with residents may help some graduates avoid a training pathway they may not want or need. More importantly, it would raise trainee exposure and interest toward a service that is both expansive – approximately 70% of pediatric hospitalists practice in a community hospital – and crucial to children’s health nationally.
Pediatric hospitalists who are not eligible for board certification are vital and valued members of the PHM community, and as such need to maintain representation within PHM leadership. Professional development opportunities need to remain accessible outside of fellowship. The blossoming of virtual conferences and Zoom meet-ups in the face of the COVID-19 pandemic have shown us that with innovation (and a good Internet connection), networking and mentorship can be accomplished across thousands of miles.
While there’s great diversity within PHM, this subspecialty has a history of attracting pediatricians with some common core qualities: Grit, creativity, and the belief that a strong team is far greater than the sum of its parts. I have confidence that if we approach this PHM transition period with transparency about our goals and challenges, this community can emerge from it strong and united.
Dr. Ezzio is a first-year pediatric hospital medicine fellow at Helen DeVos Children’s Hospital in Grand Rapids, Mich. Her interests include medical education and advocacy. Dr. Ezzio would like to thank Dr. Jeri Kessenich and Dr. Rachel “Danielle” Fisher for their assistance in revising the article. To submit to, or for inquiries about, our PHM Fellows Column, please contact our Pediatrics Editor, Dr. Anika Kumar (KumarA4@ccf.org).
References
1. Leyenaar JK and Fritner MP. Graduating pediatric residents entering the hospital medicine workforce, 2006-2015. Acad Pediatr. 2018 Mar;18(2):200-7.
2. National Resident Matching Program. Results and data: Specialties matching service 2020 appointment year. Washington, DC 2020.
3. National Resident Matching Program. Results and data: Specialties matching service 2021 appointment year. Washington, DC 2021.
4. 2020 State of Hospital Medicine report. Society of Hospital Medicine. 2020.
5. Oshimura JM et al. Current roles and perceived needs of pediatric hospital medicine fellowship graduates. Hosp Pediatr. 2016;6(10):633-7.
6. National Resident Matching Program. Results and data: 2020 main residency match. Washington, DC 2020.
7. American Academy of Pediatrics Annual Survey of graduating residents 2003-2020.
8. Quinn Capers IV. How clinicians and educators can mitigate implicit bias in patient care and candidate selection in medical education. American Thoracic Society Scholar. 2020 Jun;1(3):211-17.
9. Welsh G. The importance of community pediatric hospital medicine. The Hospitalist. 2021 Jan;25(1):27.
Delay surgery by 7 weeks after COVID-19 diagnosis, study shows
Seven weeks appears to be the ideal amount of time to delay surgery, when possible, after someone tests positive for COVID-19, researchers in the United Kingdom report.
Risk for death was about 3.5 to 4 times higher in the first 6 weeks after surgery among more than 3,000 people with a preoperative COVID-19 diagnosis compared with patients without COVID-19. After 7 weeks, the 30-day mortality rate dropped to a baseline level.
The study was published online March 9 in Anaesthesia.
Surgery should be further delayed for people who remain symptomatic at 7 weeks post diagnosis, lead author Dmitri Nepogodiev, MBChB, said in an interview.
“In this group we recommend waiting until COVID-19 symptoms resolve, if possible. However, our study did not capture specific data on long COVID … so we are unable to make specific recommendations for this group,” said Dr. Nepogodiev, research fellow at the NIHR Global Health Research Unit on Global Surgery at the University of Birmingham (England).
“This should be an area for future research,” he added.
The international, multicenter, prospective cohort study is notable for its sheer size – more than 15,000 investigators reported outcomes for 140,231 surgical patients from 1,674 hospitals across 116 countries. In total, 2.2% of these patients tested positive for SARS-CoV-2 prior to surgery.
Surgery of any type performed in October 2020 was assessed. A greater proportion of patients with a preoperative COVID-19 diagnosis had emergency surgery, 44%, compared with 30% of people who never had a COVID-19 diagnosis.
Most patients were asymptomatic at the time of surgery, either because they never experienced COVID-19 symptoms or their symptoms resolved. The 30-day mortality rate was the primary outcome.
Death rates among surgical patients with preoperative COVID-19 diagnosis
Comparing the timing of surgery after COVID-19 diagnosis vs. 30-day mortality yielded the following results:
- 0 to 2 weeks – 9.1% mortality.
- 3 to 4 weeks – 6.9%.
- 5 to 6 weeks – 5.5%.
- 7 weeks or longer – 2.0%..
For comparison, the 30-day mortality rate for surgical patients without a preoperative COVID-19 diagnosis was 1.4%. A COVID-19 diagnosis more than 7 weeks before surgery did not make a significant difference on outcomes.
The ‘why’ remains unknown
The reasons for the association between a COVID-19 diagnosis and higher postoperative death rates remain unknown. However, Dr. Nepogodiev speculated that it could be related to “some degree of lung injury, even if patients are initially asymptomatic.”
Intubation and mechanical ventilation during surgery could exacerbate the existing lung injury, he said, thereby leading to more severe COVID-19.
In fact, Dr. Nepogodiev and colleagues found that postoperative pulmonary complications followed a pattern similar to the findings on death. They reported higher rates of pneumonia, acute respiratory distress syndrome, and unexpected reventilation in the first 6 weeks following a COVID-19 diagnosis. Again, at 7 weeks and beyond, the rates returned to be relatively the same as those for people who never had COVID-19.
“Waiting for 7 or more weeks may allow time for the initial COVID-19 injury to resolve,” Dr. Nepogodiev said.
‘An important study’
“This is an important study of postoperative mortality among patients recovered from COVID-19,” Adrian Diaz, MD, MPH, said in an interview when asked to comment.
The large cohort and numerous practice settings are among the strengths of the research, said Dr. Diaz, of the University of Michigan Institute for Healthcare Policy and Innovation in Ann Arbor. He was lead author of a June 2020 review article on elective surgery in the time of COVID-19, published in The American Journal of Surgery.
“As with nearly all studies of this nature, results must be interpreted on a case-by-case basis for individual patients. However, this study does add important information for patients and providers in helping them have an informed discussion on the timing of surgery,” said Dr. Diaz, a fellow in the Center for Healthcare Outcomes and Policy and a resident in general surgery at the Ohio State University, Columbus.
Dr. Nepogodiev and colleagues included both urgent and elective surgeries in the study. Dr. Diaz said this was a potential limitation because emergency operations “should never be delayed, by definition.” Lack of indications for the surgeries and information on cause of death were additional limitations.
Future research should evaluate any benefit in delaying surgery longer than 7 or more weeks, Dr. Diaz added, perhaps looking specifically at 10, 12, or 14 weeks, or considering outcomes as a continuous variable. This would help health care providers “garner more insight into risk and benefits of delaying surgery beyond 7 weeks.”
Dr. Nepogodiev and Dr. Diaz disclosed no relevant financial relationships. The study had multiple funding sources, including the National Institute for Health Research Global Health Research Unit, the Association of Upper Gastrointestinal Surgeons, the British Association of Surgical Oncology, and Medtronic.
A version of this article first appeared on Medscape.com.
Seven weeks appears to be the ideal amount of time to delay surgery, when possible, after someone tests positive for COVID-19, researchers in the United Kingdom report.
Risk for death was about 3.5 to 4 times higher in the first 6 weeks after surgery among more than 3,000 people with a preoperative COVID-19 diagnosis compared with patients without COVID-19. After 7 weeks, the 30-day mortality rate dropped to a baseline level.
The study was published online March 9 in Anaesthesia.
Surgery should be further delayed for people who remain symptomatic at 7 weeks post diagnosis, lead author Dmitri Nepogodiev, MBChB, said in an interview.
“In this group we recommend waiting until COVID-19 symptoms resolve, if possible. However, our study did not capture specific data on long COVID … so we are unable to make specific recommendations for this group,” said Dr. Nepogodiev, research fellow at the NIHR Global Health Research Unit on Global Surgery at the University of Birmingham (England).
“This should be an area for future research,” he added.
The international, multicenter, prospective cohort study is notable for its sheer size – more than 15,000 investigators reported outcomes for 140,231 surgical patients from 1,674 hospitals across 116 countries. In total, 2.2% of these patients tested positive for SARS-CoV-2 prior to surgery.
Surgery of any type performed in October 2020 was assessed. A greater proportion of patients with a preoperative COVID-19 diagnosis had emergency surgery, 44%, compared with 30% of people who never had a COVID-19 diagnosis.
Most patients were asymptomatic at the time of surgery, either because they never experienced COVID-19 symptoms or their symptoms resolved. The 30-day mortality rate was the primary outcome.
Death rates among surgical patients with preoperative COVID-19 diagnosis
Comparing the timing of surgery after COVID-19 diagnosis vs. 30-day mortality yielded the following results:
- 0 to 2 weeks – 9.1% mortality.
- 3 to 4 weeks – 6.9%.
- 5 to 6 weeks – 5.5%.
- 7 weeks or longer – 2.0%..
For comparison, the 30-day mortality rate for surgical patients without a preoperative COVID-19 diagnosis was 1.4%. A COVID-19 diagnosis more than 7 weeks before surgery did not make a significant difference on outcomes.
The ‘why’ remains unknown
The reasons for the association between a COVID-19 diagnosis and higher postoperative death rates remain unknown. However, Dr. Nepogodiev speculated that it could be related to “some degree of lung injury, even if patients are initially asymptomatic.”
Intubation and mechanical ventilation during surgery could exacerbate the existing lung injury, he said, thereby leading to more severe COVID-19.
In fact, Dr. Nepogodiev and colleagues found that postoperative pulmonary complications followed a pattern similar to the findings on death. They reported higher rates of pneumonia, acute respiratory distress syndrome, and unexpected reventilation in the first 6 weeks following a COVID-19 diagnosis. Again, at 7 weeks and beyond, the rates returned to be relatively the same as those for people who never had COVID-19.
“Waiting for 7 or more weeks may allow time for the initial COVID-19 injury to resolve,” Dr. Nepogodiev said.
‘An important study’
“This is an important study of postoperative mortality among patients recovered from COVID-19,” Adrian Diaz, MD, MPH, said in an interview when asked to comment.
The large cohort and numerous practice settings are among the strengths of the research, said Dr. Diaz, of the University of Michigan Institute for Healthcare Policy and Innovation in Ann Arbor. He was lead author of a June 2020 review article on elective surgery in the time of COVID-19, published in The American Journal of Surgery.
“As with nearly all studies of this nature, results must be interpreted on a case-by-case basis for individual patients. However, this study does add important information for patients and providers in helping them have an informed discussion on the timing of surgery,” said Dr. Diaz, a fellow in the Center for Healthcare Outcomes and Policy and a resident in general surgery at the Ohio State University, Columbus.
Dr. Nepogodiev and colleagues included both urgent and elective surgeries in the study. Dr. Diaz said this was a potential limitation because emergency operations “should never be delayed, by definition.” Lack of indications for the surgeries and information on cause of death were additional limitations.
Future research should evaluate any benefit in delaying surgery longer than 7 or more weeks, Dr. Diaz added, perhaps looking specifically at 10, 12, or 14 weeks, or considering outcomes as a continuous variable. This would help health care providers “garner more insight into risk and benefits of delaying surgery beyond 7 weeks.”
Dr. Nepogodiev and Dr. Diaz disclosed no relevant financial relationships. The study had multiple funding sources, including the National Institute for Health Research Global Health Research Unit, the Association of Upper Gastrointestinal Surgeons, the British Association of Surgical Oncology, and Medtronic.
A version of this article first appeared on Medscape.com.
Seven weeks appears to be the ideal amount of time to delay surgery, when possible, after someone tests positive for COVID-19, researchers in the United Kingdom report.
Risk for death was about 3.5 to 4 times higher in the first 6 weeks after surgery among more than 3,000 people with a preoperative COVID-19 diagnosis compared with patients without COVID-19. After 7 weeks, the 30-day mortality rate dropped to a baseline level.
The study was published online March 9 in Anaesthesia.
Surgery should be further delayed for people who remain symptomatic at 7 weeks post diagnosis, lead author Dmitri Nepogodiev, MBChB, said in an interview.
“In this group we recommend waiting until COVID-19 symptoms resolve, if possible. However, our study did not capture specific data on long COVID … so we are unable to make specific recommendations for this group,” said Dr. Nepogodiev, research fellow at the NIHR Global Health Research Unit on Global Surgery at the University of Birmingham (England).
“This should be an area for future research,” he added.
The international, multicenter, prospective cohort study is notable for its sheer size – more than 15,000 investigators reported outcomes for 140,231 surgical patients from 1,674 hospitals across 116 countries. In total, 2.2% of these patients tested positive for SARS-CoV-2 prior to surgery.
Surgery of any type performed in October 2020 was assessed. A greater proportion of patients with a preoperative COVID-19 diagnosis had emergency surgery, 44%, compared with 30% of people who never had a COVID-19 diagnosis.
Most patients were asymptomatic at the time of surgery, either because they never experienced COVID-19 symptoms or their symptoms resolved. The 30-day mortality rate was the primary outcome.
Death rates among surgical patients with preoperative COVID-19 diagnosis
Comparing the timing of surgery after COVID-19 diagnosis vs. 30-day mortality yielded the following results:
- 0 to 2 weeks – 9.1% mortality.
- 3 to 4 weeks – 6.9%.
- 5 to 6 weeks – 5.5%.
- 7 weeks or longer – 2.0%..
For comparison, the 30-day mortality rate for surgical patients without a preoperative COVID-19 diagnosis was 1.4%. A COVID-19 diagnosis more than 7 weeks before surgery did not make a significant difference on outcomes.
The ‘why’ remains unknown
The reasons for the association between a COVID-19 diagnosis and higher postoperative death rates remain unknown. However, Dr. Nepogodiev speculated that it could be related to “some degree of lung injury, even if patients are initially asymptomatic.”
Intubation and mechanical ventilation during surgery could exacerbate the existing lung injury, he said, thereby leading to more severe COVID-19.
In fact, Dr. Nepogodiev and colleagues found that postoperative pulmonary complications followed a pattern similar to the findings on death. They reported higher rates of pneumonia, acute respiratory distress syndrome, and unexpected reventilation in the first 6 weeks following a COVID-19 diagnosis. Again, at 7 weeks and beyond, the rates returned to be relatively the same as those for people who never had COVID-19.
“Waiting for 7 or more weeks may allow time for the initial COVID-19 injury to resolve,” Dr. Nepogodiev said.
‘An important study’
“This is an important study of postoperative mortality among patients recovered from COVID-19,” Adrian Diaz, MD, MPH, said in an interview when asked to comment.
The large cohort and numerous practice settings are among the strengths of the research, said Dr. Diaz, of the University of Michigan Institute for Healthcare Policy and Innovation in Ann Arbor. He was lead author of a June 2020 review article on elective surgery in the time of COVID-19, published in The American Journal of Surgery.
“As with nearly all studies of this nature, results must be interpreted on a case-by-case basis for individual patients. However, this study does add important information for patients and providers in helping them have an informed discussion on the timing of surgery,” said Dr. Diaz, a fellow in the Center for Healthcare Outcomes and Policy and a resident in general surgery at the Ohio State University, Columbus.
Dr. Nepogodiev and colleagues included both urgent and elective surgeries in the study. Dr. Diaz said this was a potential limitation because emergency operations “should never be delayed, by definition.” Lack of indications for the surgeries and information on cause of death were additional limitations.
Future research should evaluate any benefit in delaying surgery longer than 7 or more weeks, Dr. Diaz added, perhaps looking specifically at 10, 12, or 14 weeks, or considering outcomes as a continuous variable. This would help health care providers “garner more insight into risk and benefits of delaying surgery beyond 7 weeks.”
Dr. Nepogodiev and Dr. Diaz disclosed no relevant financial relationships. The study had multiple funding sources, including the National Institute for Health Research Global Health Research Unit, the Association of Upper Gastrointestinal Surgeons, the British Association of Surgical Oncology, and Medtronic.
A version of this article first appeared on Medscape.com.
Palliative care and hospital medicine partnerships in the pandemic
Patients dying without their loved ones, families forced to remotely decide goals of care without the physical presence or human connection of the care team, overworked staff physically isolated from their critically ill patients, and at-risk community members with uncertain and undocumented goals for care are among the universal challenges confronted by hospitals and hospitalists during this COVID-19 pandemic. Partnerships among hospital medicine (HM) and palliative care (PC) teams at Dell Medical School/Dell Seton Medical Center thrive on mutually shared core values of patient centered care – compassion, empathy, and humanity.
A key PC-HM collaboration was adapting our multidisciplinary huddle to focus on communication effectiveness and efficiency in the medical intensive care unit (MICU). Expanded interprofessional and cross-specialty collaboration promoted streamlined, succinct, and standardized communication with patients’ families while their loved ones were critically ill with COVID-19. The PC team attended daily MICU multidisciplinary huddles, attentive to both the medical and psychosocial updates for each patient. During huddles, residents or HM providers were asked to end their presentation with a clinical status “headline” and solicited feedback from the multidisciplinary team before messaging to the family. The PC team then communicated with families a succinct and cohesive medical update and continuously explored goals of care. This allowed the HM team, often overwhelmed with admissions, co-managing intensive care patients, and facilitating safe discharges, to focus on urgent issues while PC provided continuity and personalized support for patients and families. PC’s ability to synthesize and summarize clinical information from multiple teams and then provide cohesive updates in patient-friendly language modeled important communication skills for learners and simultaneously benefited HM providers.
Our chaplains, too, were central to facilitating timely, proactive conversations and documentation of Medical Power of Attorney (MPOA) for patients with COVID-19 admitted to our hospital. HM prioritized early admission conversations with patients to counsel them on severity of illness, prognosis based on risk factors, to elucidate wishes for intubation or resuscitation, and to capture their desired medical decision maker. HM was notified of all COVID and PUI admissions, allowing us to speak with even critically ill patients in the ER or ICU prior to intubation in order to quickly and accurately capture patients’ wishes for treatment and delegate decision makers. Our chaplains supported and supplemented these efforts by diligently and dutifully soliciting, hearing, and documenting patient MPOA delegates, with over 50% MPOA completion by 24 hours of hospitalization.
Another early PC-HM project, “Meet My Loved One,” was adapted from the University of Alabama at Birmingham Palliative and Comfort Unit. The absence of families visiting the ICU and sharing pictures, stories, anecdotes of our patients left a deeply felt, dehumanizing void in the halls and rooms of our hospital. To fill this space with life and humanity, furloughed medical students on their “transition of care” electives contacted family members of their “continuity” patients focusing primarily on those patients expected to have prolonged ICU or hospital stays and solicited personal, humanizing information about our patients. Questions included: “What is your loved one’s preferred name or nickname?” and “What are three things we should know to take better care of your loved one?” With family permission, we posted this information on the door outside the patient’s room. Nursing staff, in particular, appreciated getting to know their patients more personally and families appreciated the staff’s desire to know their loved one as an individual.
It is also important to acknowledge setbacks. Early efforts to engage technology proved more foe than friend. We continue to struggle with using our iPads for video visits. Most of our families prefer “WhatsApp” for video communication, which is not compatible with operating systems on early versions of the iPad, which were generously and widely donated by local school systems. Desperate to allow families to connect, many providers resorted to using personal devices to facilitate video visits and family meetings. And we discovered that many video visits caused more not less family angst, especially for critically ill patients. Families often required preparation and coaching on what to expect and how to interact with intubated, sedated, proned, and paralyzed loved ones.
Our hospital medicine and palliative care teams have an established strong partnership. The COVID-19 pandemic created novel communication challenges but our shared mission toward patient-centered care allowed us to effectively collaborate to bring the patients goals of care to the forefront aligning patients, families, physicians, nurses, and staff during the COVID-19 surge.
Dr. Johnston is associate professor at Dell Medical School at The University of Texas in Austin. She practices hospital medicine and inpatient palliative care at Dell Seton Medical Center. Dr. Cooremans is a resident physician at Dell Medical School. Dr. Salib is the internal medicine clerkship director and an associate professor at Dell Medical School. Dr. Nieto is an assistant professor and associate chief of the Division of Hospital Medicine at Dell Medical School. Dr. Patel is an assistant professor at Dell Medical School. This article is part of a series written by members of the Division of Hospital Medicine at Dell Medical School, exploring lessons learned from the coronavirus pandemic and outlining an approach for creating COVID-19 Centers of Excellence. The article first appeared in The Hospital Leader, the official blog of SHM.
Patients dying without their loved ones, families forced to remotely decide goals of care without the physical presence or human connection of the care team, overworked staff physically isolated from their critically ill patients, and at-risk community members with uncertain and undocumented goals for care are among the universal challenges confronted by hospitals and hospitalists during this COVID-19 pandemic. Partnerships among hospital medicine (HM) and palliative care (PC) teams at Dell Medical School/Dell Seton Medical Center thrive on mutually shared core values of patient centered care – compassion, empathy, and humanity.
A key PC-HM collaboration was adapting our multidisciplinary huddle to focus on communication effectiveness and efficiency in the medical intensive care unit (MICU). Expanded interprofessional and cross-specialty collaboration promoted streamlined, succinct, and standardized communication with patients’ families while their loved ones were critically ill with COVID-19. The PC team attended daily MICU multidisciplinary huddles, attentive to both the medical and psychosocial updates for each patient. During huddles, residents or HM providers were asked to end their presentation with a clinical status “headline” and solicited feedback from the multidisciplinary team before messaging to the family. The PC team then communicated with families a succinct and cohesive medical update and continuously explored goals of care. This allowed the HM team, often overwhelmed with admissions, co-managing intensive care patients, and facilitating safe discharges, to focus on urgent issues while PC provided continuity and personalized support for patients and families. PC’s ability to synthesize and summarize clinical information from multiple teams and then provide cohesive updates in patient-friendly language modeled important communication skills for learners and simultaneously benefited HM providers.
Our chaplains, too, were central to facilitating timely, proactive conversations and documentation of Medical Power of Attorney (MPOA) for patients with COVID-19 admitted to our hospital. HM prioritized early admission conversations with patients to counsel them on severity of illness, prognosis based on risk factors, to elucidate wishes for intubation or resuscitation, and to capture their desired medical decision maker. HM was notified of all COVID and PUI admissions, allowing us to speak with even critically ill patients in the ER or ICU prior to intubation in order to quickly and accurately capture patients’ wishes for treatment and delegate decision makers. Our chaplains supported and supplemented these efforts by diligently and dutifully soliciting, hearing, and documenting patient MPOA delegates, with over 50% MPOA completion by 24 hours of hospitalization.
Another early PC-HM project, “Meet My Loved One,” was adapted from the University of Alabama at Birmingham Palliative and Comfort Unit. The absence of families visiting the ICU and sharing pictures, stories, anecdotes of our patients left a deeply felt, dehumanizing void in the halls and rooms of our hospital. To fill this space with life and humanity, furloughed medical students on their “transition of care” electives contacted family members of their “continuity” patients focusing primarily on those patients expected to have prolonged ICU or hospital stays and solicited personal, humanizing information about our patients. Questions included: “What is your loved one’s preferred name or nickname?” and “What are three things we should know to take better care of your loved one?” With family permission, we posted this information on the door outside the patient’s room. Nursing staff, in particular, appreciated getting to know their patients more personally and families appreciated the staff’s desire to know their loved one as an individual.
It is also important to acknowledge setbacks. Early efforts to engage technology proved more foe than friend. We continue to struggle with using our iPads for video visits. Most of our families prefer “WhatsApp” for video communication, which is not compatible with operating systems on early versions of the iPad, which were generously and widely donated by local school systems. Desperate to allow families to connect, many providers resorted to using personal devices to facilitate video visits and family meetings. And we discovered that many video visits caused more not less family angst, especially for critically ill patients. Families often required preparation and coaching on what to expect and how to interact with intubated, sedated, proned, and paralyzed loved ones.
Our hospital medicine and palliative care teams have an established strong partnership. The COVID-19 pandemic created novel communication challenges but our shared mission toward patient-centered care allowed us to effectively collaborate to bring the patients goals of care to the forefront aligning patients, families, physicians, nurses, and staff during the COVID-19 surge.
Dr. Johnston is associate professor at Dell Medical School at The University of Texas in Austin. She practices hospital medicine and inpatient palliative care at Dell Seton Medical Center. Dr. Cooremans is a resident physician at Dell Medical School. Dr. Salib is the internal medicine clerkship director and an associate professor at Dell Medical School. Dr. Nieto is an assistant professor and associate chief of the Division of Hospital Medicine at Dell Medical School. Dr. Patel is an assistant professor at Dell Medical School. This article is part of a series written by members of the Division of Hospital Medicine at Dell Medical School, exploring lessons learned from the coronavirus pandemic and outlining an approach for creating COVID-19 Centers of Excellence. The article first appeared in The Hospital Leader, the official blog of SHM.
Patients dying without their loved ones, families forced to remotely decide goals of care without the physical presence or human connection of the care team, overworked staff physically isolated from their critically ill patients, and at-risk community members with uncertain and undocumented goals for care are among the universal challenges confronted by hospitals and hospitalists during this COVID-19 pandemic. Partnerships among hospital medicine (HM) and palliative care (PC) teams at Dell Medical School/Dell Seton Medical Center thrive on mutually shared core values of patient centered care – compassion, empathy, and humanity.
A key PC-HM collaboration was adapting our multidisciplinary huddle to focus on communication effectiveness and efficiency in the medical intensive care unit (MICU). Expanded interprofessional and cross-specialty collaboration promoted streamlined, succinct, and standardized communication with patients’ families while their loved ones were critically ill with COVID-19. The PC team attended daily MICU multidisciplinary huddles, attentive to both the medical and psychosocial updates for each patient. During huddles, residents or HM providers were asked to end their presentation with a clinical status “headline” and solicited feedback from the multidisciplinary team before messaging to the family. The PC team then communicated with families a succinct and cohesive medical update and continuously explored goals of care. This allowed the HM team, often overwhelmed with admissions, co-managing intensive care patients, and facilitating safe discharges, to focus on urgent issues while PC provided continuity and personalized support for patients and families. PC’s ability to synthesize and summarize clinical information from multiple teams and then provide cohesive updates in patient-friendly language modeled important communication skills for learners and simultaneously benefited HM providers.
Our chaplains, too, were central to facilitating timely, proactive conversations and documentation of Medical Power of Attorney (MPOA) for patients with COVID-19 admitted to our hospital. HM prioritized early admission conversations with patients to counsel them on severity of illness, prognosis based on risk factors, to elucidate wishes for intubation or resuscitation, and to capture their desired medical decision maker. HM was notified of all COVID and PUI admissions, allowing us to speak with even critically ill patients in the ER or ICU prior to intubation in order to quickly and accurately capture patients’ wishes for treatment and delegate decision makers. Our chaplains supported and supplemented these efforts by diligently and dutifully soliciting, hearing, and documenting patient MPOA delegates, with over 50% MPOA completion by 24 hours of hospitalization.
Another early PC-HM project, “Meet My Loved One,” was adapted from the University of Alabama at Birmingham Palliative and Comfort Unit. The absence of families visiting the ICU and sharing pictures, stories, anecdotes of our patients left a deeply felt, dehumanizing void in the halls and rooms of our hospital. To fill this space with life and humanity, furloughed medical students on their “transition of care” electives contacted family members of their “continuity” patients focusing primarily on those patients expected to have prolonged ICU or hospital stays and solicited personal, humanizing information about our patients. Questions included: “What is your loved one’s preferred name or nickname?” and “What are three things we should know to take better care of your loved one?” With family permission, we posted this information on the door outside the patient’s room. Nursing staff, in particular, appreciated getting to know their patients more personally and families appreciated the staff’s desire to know their loved one as an individual.
It is also important to acknowledge setbacks. Early efforts to engage technology proved more foe than friend. We continue to struggle with using our iPads for video visits. Most of our families prefer “WhatsApp” for video communication, which is not compatible with operating systems on early versions of the iPad, which were generously and widely donated by local school systems. Desperate to allow families to connect, many providers resorted to using personal devices to facilitate video visits and family meetings. And we discovered that many video visits caused more not less family angst, especially for critically ill patients. Families often required preparation and coaching on what to expect and how to interact with intubated, sedated, proned, and paralyzed loved ones.
Our hospital medicine and palliative care teams have an established strong partnership. The COVID-19 pandemic created novel communication challenges but our shared mission toward patient-centered care allowed us to effectively collaborate to bring the patients goals of care to the forefront aligning patients, families, physicians, nurses, and staff during the COVID-19 surge.
Dr. Johnston is associate professor at Dell Medical School at The University of Texas in Austin. She practices hospital medicine and inpatient palliative care at Dell Seton Medical Center. Dr. Cooremans is a resident physician at Dell Medical School. Dr. Salib is the internal medicine clerkship director and an associate professor at Dell Medical School. Dr. Nieto is an assistant professor and associate chief of the Division of Hospital Medicine at Dell Medical School. Dr. Patel is an assistant professor at Dell Medical School. This article is part of a series written by members of the Division of Hospital Medicine at Dell Medical School, exploring lessons learned from the coronavirus pandemic and outlining an approach for creating COVID-19 Centers of Excellence. The article first appeared in The Hospital Leader, the official blog of SHM.
CDC data strengthen link between obesity and severe COVID
Officials have previously linked being overweight or obese to a greater risk for more severe COVID-19. A report today from the U.S. Centers for Disease Control and Prevention adds numbers and some nuance to the association.
Data from nearly 150,000 U.S. adults hospitalized with COVID-19 nationwide indicate that risk for more severe disease outcomes increases along with body mass index (BMI). The risk of COVID-19–related hospitalization and death associated with obesity was particularly high among people younger than 65.
“As clinicians develop care plans for COVID-19 patients, they should consider the risk for severe outcomes in patients with higher BMIs, especially for those with severe obesity,” the researchers note. They add that their findings suggest “progressively intensive management of COVID-19 might be needed for patients with more severe obesity.”
People with COVID-19 close to the border between a healthy and overweight BMI – from 23.7 kg/m2 to 25.9 kg/m2 – had the lowest risks for adverse outcomes.
The study was published online today in Morbidity and Mortality Weekly Report.
Greater need for critical care
The risk of ICU admission was particularly associated with severe obesity. For example, those with a BMI in the 40-44.9 kg/m2 category had a 6% increased risk, which jumped to 16% higher among those with a BMI of 45 or greater.
Compared to people with a healthy BMI, the need for invasive mechanical ventilation was 12% more likely among overweight adults with a BMI of 25-29.2. The risked jumped to 108% greater among the most obese people, those with a BMI of 45 or greater, lead CDC researcher Lyudmyla Kompaniyets, PhD, and colleagues reported.
Moreover, the risks for hospitalization and death increased in a dose-response relationship with obesity.
For example, risks of being hospitalized were 7% greater for adults with a BMI between 30 and 34.9 and climbed to 33% greater for those with a BMI of 45. Risks were calculated as adjusted relative risks compared with people with a healthy BMI between 18.5 and 24.9.
Interestingly, being underweight was associated with elevated risk for COVID-19 hospitalization as well. For example, people with a BMI of less than 18.5 had a 20% greater chance of admission vs. people in the healthy BMI range. Unknown underlying medical conditions or issues related to nutrition or immune function could be contributing factors, the researchers note.
Elevated risk of dying
The risk of death in adults with obesity ranged from 8% higher in the 30-34.9 range up to 61% greater for those with a BMI of 45.
Chronic inflammation or impaired lung function from excess weight are possible reasons that higher BMI imparts greater risk, the researchers note.
The CDC researchers evaluated 148,494 adults from 238 hospitals participating in PHD-SR database. Because the study was limited to people hospitalized with COVID-19, the findings may not apply to all adults with COVID-19.
Another potential limitation is that investigators were unable to calculate BMI for all patients in the database because about 28% of participating hospitals did not report height and weight.
The study authors had no relevant financial relationships to disclose.
A version of this article first appeared on Medscape.com.
Officials have previously linked being overweight or obese to a greater risk for more severe COVID-19. A report today from the U.S. Centers for Disease Control and Prevention adds numbers and some nuance to the association.
Data from nearly 150,000 U.S. adults hospitalized with COVID-19 nationwide indicate that risk for more severe disease outcomes increases along with body mass index (BMI). The risk of COVID-19–related hospitalization and death associated with obesity was particularly high among people younger than 65.
“As clinicians develop care plans for COVID-19 patients, they should consider the risk for severe outcomes in patients with higher BMIs, especially for those with severe obesity,” the researchers note. They add that their findings suggest “progressively intensive management of COVID-19 might be needed for patients with more severe obesity.”
People with COVID-19 close to the border between a healthy and overweight BMI – from 23.7 kg/m2 to 25.9 kg/m2 – had the lowest risks for adverse outcomes.
The study was published online today in Morbidity and Mortality Weekly Report.
Greater need for critical care
The risk of ICU admission was particularly associated with severe obesity. For example, those with a BMI in the 40-44.9 kg/m2 category had a 6% increased risk, which jumped to 16% higher among those with a BMI of 45 or greater.
Compared to people with a healthy BMI, the need for invasive mechanical ventilation was 12% more likely among overweight adults with a BMI of 25-29.2. The risked jumped to 108% greater among the most obese people, those with a BMI of 45 or greater, lead CDC researcher Lyudmyla Kompaniyets, PhD, and colleagues reported.
Moreover, the risks for hospitalization and death increased in a dose-response relationship with obesity.
For example, risks of being hospitalized were 7% greater for adults with a BMI between 30 and 34.9 and climbed to 33% greater for those with a BMI of 45. Risks were calculated as adjusted relative risks compared with people with a healthy BMI between 18.5 and 24.9.
Interestingly, being underweight was associated with elevated risk for COVID-19 hospitalization as well. For example, people with a BMI of less than 18.5 had a 20% greater chance of admission vs. people in the healthy BMI range. Unknown underlying medical conditions or issues related to nutrition or immune function could be contributing factors, the researchers note.
Elevated risk of dying
The risk of death in adults with obesity ranged from 8% higher in the 30-34.9 range up to 61% greater for those with a BMI of 45.
Chronic inflammation or impaired lung function from excess weight are possible reasons that higher BMI imparts greater risk, the researchers note.
The CDC researchers evaluated 148,494 adults from 238 hospitals participating in PHD-SR database. Because the study was limited to people hospitalized with COVID-19, the findings may not apply to all adults with COVID-19.
Another potential limitation is that investigators were unable to calculate BMI for all patients in the database because about 28% of participating hospitals did not report height and weight.
The study authors had no relevant financial relationships to disclose.
A version of this article first appeared on Medscape.com.
Officials have previously linked being overweight or obese to a greater risk for more severe COVID-19. A report today from the U.S. Centers for Disease Control and Prevention adds numbers and some nuance to the association.
Data from nearly 150,000 U.S. adults hospitalized with COVID-19 nationwide indicate that risk for more severe disease outcomes increases along with body mass index (BMI). The risk of COVID-19–related hospitalization and death associated with obesity was particularly high among people younger than 65.
“As clinicians develop care plans for COVID-19 patients, they should consider the risk for severe outcomes in patients with higher BMIs, especially for those with severe obesity,” the researchers note. They add that their findings suggest “progressively intensive management of COVID-19 might be needed for patients with more severe obesity.”
People with COVID-19 close to the border between a healthy and overweight BMI – from 23.7 kg/m2 to 25.9 kg/m2 – had the lowest risks for adverse outcomes.
The study was published online today in Morbidity and Mortality Weekly Report.
Greater need for critical care
The risk of ICU admission was particularly associated with severe obesity. For example, those with a BMI in the 40-44.9 kg/m2 category had a 6% increased risk, which jumped to 16% higher among those with a BMI of 45 or greater.
Compared to people with a healthy BMI, the need for invasive mechanical ventilation was 12% more likely among overweight adults with a BMI of 25-29.2. The risked jumped to 108% greater among the most obese people, those with a BMI of 45 or greater, lead CDC researcher Lyudmyla Kompaniyets, PhD, and colleagues reported.
Moreover, the risks for hospitalization and death increased in a dose-response relationship with obesity.
For example, risks of being hospitalized were 7% greater for adults with a BMI between 30 and 34.9 and climbed to 33% greater for those with a BMI of 45. Risks were calculated as adjusted relative risks compared with people with a healthy BMI between 18.5 and 24.9.
Interestingly, being underweight was associated with elevated risk for COVID-19 hospitalization as well. For example, people with a BMI of less than 18.5 had a 20% greater chance of admission vs. people in the healthy BMI range. Unknown underlying medical conditions or issues related to nutrition or immune function could be contributing factors, the researchers note.
Elevated risk of dying
The risk of death in adults with obesity ranged from 8% higher in the 30-34.9 range up to 61% greater for those with a BMI of 45.
Chronic inflammation or impaired lung function from excess weight are possible reasons that higher BMI imparts greater risk, the researchers note.
The CDC researchers evaluated 148,494 adults from 238 hospitals participating in PHD-SR database. Because the study was limited to people hospitalized with COVID-19, the findings may not apply to all adults with COVID-19.
Another potential limitation is that investigators were unable to calculate BMI for all patients in the database because about 28% of participating hospitals did not report height and weight.
The study authors had no relevant financial relationships to disclose.
A version of this article first appeared on Medscape.com.
Decline in weekly child COVID-19 cases has almost stopped
A third COVID-19 vaccine is now in circulation and states are starting to drop mask mandates, but the latest decline in weekly child cases barely registers as a decline, according to new data from the American Academy of Pediatrics and the Children’s Hospital Association.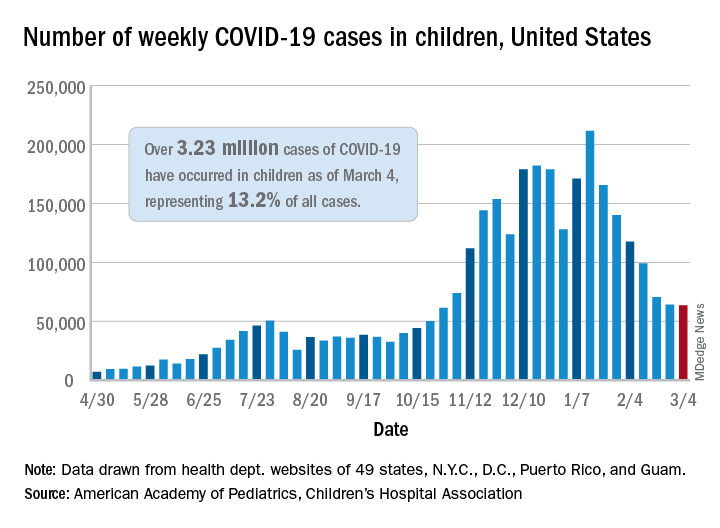
That’s only 702 cases – a drop of just 1.1% – the smallest by far since weekly cases peaked in mid-January, the AAP and CHA said in their weekly COVID-19 report. Since that peak, the last 7 weeks of declines have looked like this: 21.7%, 15.3%, 16.2%, 15.7%, 28.7%, 9.0%, and 1.1%.
Meanwhile, children’s share of the COVID-19 burden increased to its highest point ever: 18.0% of all new cases occurred in children during the week ending March 4, climbing from 15.7% the week before and eclipsing the previous high of 16.9%. Cumulatively, the 3.23 million cases in children represent 13.2% of all COVID-19 cases reported in 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
At the state level, the new leader in cumulative share of cases is Vermont at 19.4%, which just edged past Wyoming’s 19.3% as of the week ending March 4. The other states above 18% are Alaska (19.2%) and South Carolina (18.2%). The lowest rates can be found in Florida (8.1%), New Jersey (10.2%), Iowa (10.4%), and Utah (10.5%), the AAP and CHA said.
The overall rate of COVID-19 cases nationwide was 4,294 cases per 100,000 children as of March 4, up from 4,209 per 100,000 the week before. That measure had doubled between Dec. 3 (1,941 per 100,000) and Feb. 4 (3,899) but has only risen about 10% in the last month, the AAP/CHA data show.
Perhaps the most surprising news of the week involves the number of COVID-19 deaths in children, which went from 256 the previous week to 253 after Ohio made a downward revision of its mortality data. So far, children represent just 0.06% of all coronavirus-related deaths, a figure that has held steady since last summer in the 43 states (along with New York City and Guam) that are reporting mortality data by age, the AAP and CHA said.
A third COVID-19 vaccine is now in circulation and states are starting to drop mask mandates, but the latest decline in weekly child cases barely registers as a decline, according to new data from the American Academy of Pediatrics and the Children’s Hospital Association.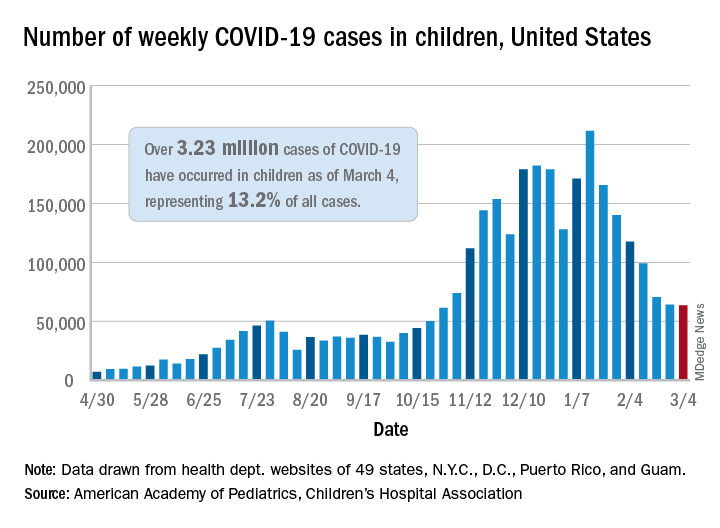
That’s only 702 cases – a drop of just 1.1% – the smallest by far since weekly cases peaked in mid-January, the AAP and CHA said in their weekly COVID-19 report. Since that peak, the last 7 weeks of declines have looked like this: 21.7%, 15.3%, 16.2%, 15.7%, 28.7%, 9.0%, and 1.1%.
Meanwhile, children’s share of the COVID-19 burden increased to its highest point ever: 18.0% of all new cases occurred in children during the week ending March 4, climbing from 15.7% the week before and eclipsing the previous high of 16.9%. Cumulatively, the 3.23 million cases in children represent 13.2% of all COVID-19 cases reported in 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
At the state level, the new leader in cumulative share of cases is Vermont at 19.4%, which just edged past Wyoming’s 19.3% as of the week ending March 4. The other states above 18% are Alaska (19.2%) and South Carolina (18.2%). The lowest rates can be found in Florida (8.1%), New Jersey (10.2%), Iowa (10.4%), and Utah (10.5%), the AAP and CHA said.
The overall rate of COVID-19 cases nationwide was 4,294 cases per 100,000 children as of March 4, up from 4,209 per 100,000 the week before. That measure had doubled between Dec. 3 (1,941 per 100,000) and Feb. 4 (3,899) but has only risen about 10% in the last month, the AAP/CHA data show.
Perhaps the most surprising news of the week involves the number of COVID-19 deaths in children, which went from 256 the previous week to 253 after Ohio made a downward revision of its mortality data. So far, children represent just 0.06% of all coronavirus-related deaths, a figure that has held steady since last summer in the 43 states (along with New York City and Guam) that are reporting mortality data by age, the AAP and CHA said.
A third COVID-19 vaccine is now in circulation and states are starting to drop mask mandates, but the latest decline in weekly child cases barely registers as a decline, according to new data from the American Academy of Pediatrics and the Children’s Hospital Association.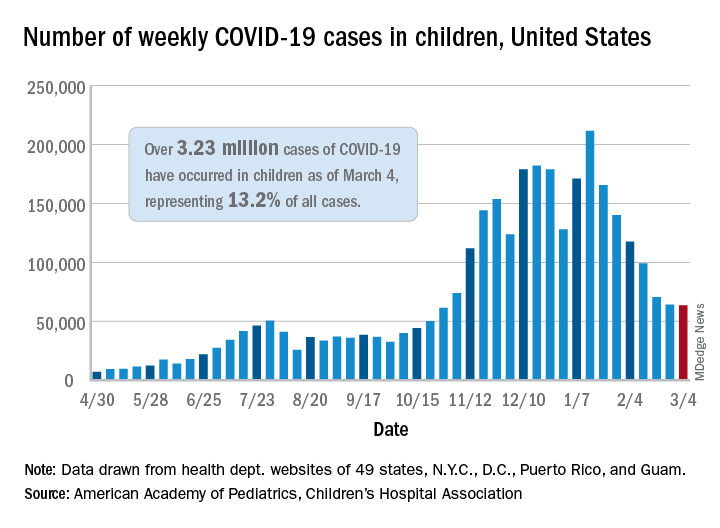
That’s only 702 cases – a drop of just 1.1% – the smallest by far since weekly cases peaked in mid-January, the AAP and CHA said in their weekly COVID-19 report. Since that peak, the last 7 weeks of declines have looked like this: 21.7%, 15.3%, 16.2%, 15.7%, 28.7%, 9.0%, and 1.1%.
Meanwhile, children’s share of the COVID-19 burden increased to its highest point ever: 18.0% of all new cases occurred in children during the week ending March 4, climbing from 15.7% the week before and eclipsing the previous high of 16.9%. Cumulatively, the 3.23 million cases in children represent 13.2% of all COVID-19 cases reported in 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
At the state level, the new leader in cumulative share of cases is Vermont at 19.4%, which just edged past Wyoming’s 19.3% as of the week ending March 4. The other states above 18% are Alaska (19.2%) and South Carolina (18.2%). The lowest rates can be found in Florida (8.1%), New Jersey (10.2%), Iowa (10.4%), and Utah (10.5%), the AAP and CHA said.
The overall rate of COVID-19 cases nationwide was 4,294 cases per 100,000 children as of March 4, up from 4,209 per 100,000 the week before. That measure had doubled between Dec. 3 (1,941 per 100,000) and Feb. 4 (3,899) but has only risen about 10% in the last month, the AAP/CHA data show.
Perhaps the most surprising news of the week involves the number of COVID-19 deaths in children, which went from 256 the previous week to 253 after Ohio made a downward revision of its mortality data. So far, children represent just 0.06% of all coronavirus-related deaths, a figure that has held steady since last summer in the 43 states (along with New York City and Guam) that are reporting mortality data by age, the AAP and CHA said.
Call to action on obesity amid COVID-19 pandemic
Hundreds of thousands of deaths worldwide from COVID-19 could have been avoided if obesity rates were lower, a new report says.
An analysis by the World Obesity Federation found that of the 2.5 million COVID-19 deaths reported by the end of February 2021, almost 90% (2.2 million) were in countries where more than half the population is classified as overweight.
The report, released to coincide with World Obesity Day, calls for obesity to be recognized as a disease in its own right around the world, and for people with obesity to be included in priority lists for COVID-19 testing and vaccination.
“Overweight is a highly significant predictor of developing complications from COVID-19, including the need for hospitalization, for intensive care and for mechanical ventilation,” the WOF notes in the report.
It adds that in countries where less than half the adult population is classified as overweight (body mass index > 25 mg/kg2), for example, Vietnam, the likelihood of death from COVID-19 is a small fraction – around one-tenth – of the level seen in countries where more than half the population is classified as overweight.
And while it acknowledges that figures for COVID-19 deaths are affected by the age structure of national populations and a country’s relative wealth and reporting capacity, “our findings appear to be independent of these contributory factors. Furthermore, other studies have found that overweight remains a highly significant predictor of the need for COVID-19 health care after accounting for these other influences.”
As an example, based on the U.K. experience, where an estimated 36% of COVID-19 hospitalizations have been attributed to lack of physical activity and excess body weight, it can be suggested that up to a third of the costs – between $6 trillion and $7 trillion over the longer period – might be attributable to these predisposing risks.
The report said the prevalence of obesity in the United Kingdom is expected to rise from 27.8% in 2016 to more than 35% by 2025.
Rachel Batterham, lead adviser on obesity at the Royal College of Physicians, commented: “The link between high levels of obesity and deaths from COVID-19 in the U.K. is indisputable, as is the urgent need to address the factors that lead so many people to be living with obesity.
“With 30% of COVID-19 hospitalizations in the U.K. directly attributed to overweight and obesity, and three-quarters of all critically ill patients having overweight or obesity, the human and financial costs are high.”
Window of opportunity to prioritize obesity as a disease
WOF says that evolving evidence on the close association between COVID-19 and underlying obesity “provides a new urgency … for political and collective action.”
“Obesity is a disease that does not receive prioritization commensurate with its prevalence and impact, which is rising fastest in emerging economies. It is a gateway to many other noncommunicable diseases and mental-health illness and is now a major factor in COVID-19 complications and mortality.”
The WOF also shows that COVID-19 is not a special case, noting that several other respiratory viruses lead to more severe consequences in people living with excess bodyweight, giving good reasons to expect the next pandemic to have similar effects. “For these reasons we need to recognize overweight as a major risk factor for infectious diseases including respiratory viruses.”
“To prevent pandemic health crises in future requires action now: we call on all readers to support the World Obesity Federation’s call for stronger, more resilient economies that prioritize investment in people’s health.”
There is, it stresses, “a window of opportunity to advocate for, fund and implement these actions in all countries to ensure better, more resilient and sustainable health for all, “now and in our postCOVID-19 future.”
It proposes a ROOTS approach:
- Recognize that obesity is a disease in its own right.
- Obesity monitoring and surveillance must be enhanced.
- Obesity prevention strategies must be developed.
- Treatment of obesity.
- Systems-based approaches should be applied.
A version of this article first appeared on Medscape.com.
Hundreds of thousands of deaths worldwide from COVID-19 could have been avoided if obesity rates were lower, a new report says.
An analysis by the World Obesity Federation found that of the 2.5 million COVID-19 deaths reported by the end of February 2021, almost 90% (2.2 million) were in countries where more than half the population is classified as overweight.
The report, released to coincide with World Obesity Day, calls for obesity to be recognized as a disease in its own right around the world, and for people with obesity to be included in priority lists for COVID-19 testing and vaccination.
“Overweight is a highly significant predictor of developing complications from COVID-19, including the need for hospitalization, for intensive care and for mechanical ventilation,” the WOF notes in the report.
It adds that in countries where less than half the adult population is classified as overweight (body mass index > 25 mg/kg2), for example, Vietnam, the likelihood of death from COVID-19 is a small fraction – around one-tenth – of the level seen in countries where more than half the population is classified as overweight.
And while it acknowledges that figures for COVID-19 deaths are affected by the age structure of national populations and a country’s relative wealth and reporting capacity, “our findings appear to be independent of these contributory factors. Furthermore, other studies have found that overweight remains a highly significant predictor of the need for COVID-19 health care after accounting for these other influences.”
As an example, based on the U.K. experience, where an estimated 36% of COVID-19 hospitalizations have been attributed to lack of physical activity and excess body weight, it can be suggested that up to a third of the costs – between $6 trillion and $7 trillion over the longer period – might be attributable to these predisposing risks.
The report said the prevalence of obesity in the United Kingdom is expected to rise from 27.8% in 2016 to more than 35% by 2025.
Rachel Batterham, lead adviser on obesity at the Royal College of Physicians, commented: “The link between high levels of obesity and deaths from COVID-19 in the U.K. is indisputable, as is the urgent need to address the factors that lead so many people to be living with obesity.
“With 30% of COVID-19 hospitalizations in the U.K. directly attributed to overweight and obesity, and three-quarters of all critically ill patients having overweight or obesity, the human and financial costs are high.”
Window of opportunity to prioritize obesity as a disease
WOF says that evolving evidence on the close association between COVID-19 and underlying obesity “provides a new urgency … for political and collective action.”
“Obesity is a disease that does not receive prioritization commensurate with its prevalence and impact, which is rising fastest in emerging economies. It is a gateway to many other noncommunicable diseases and mental-health illness and is now a major factor in COVID-19 complications and mortality.”
The WOF also shows that COVID-19 is not a special case, noting that several other respiratory viruses lead to more severe consequences in people living with excess bodyweight, giving good reasons to expect the next pandemic to have similar effects. “For these reasons we need to recognize overweight as a major risk factor for infectious diseases including respiratory viruses.”
“To prevent pandemic health crises in future requires action now: we call on all readers to support the World Obesity Federation’s call for stronger, more resilient economies that prioritize investment in people’s health.”
There is, it stresses, “a window of opportunity to advocate for, fund and implement these actions in all countries to ensure better, more resilient and sustainable health for all, “now and in our postCOVID-19 future.”
It proposes a ROOTS approach:
- Recognize that obesity is a disease in its own right.
- Obesity monitoring and surveillance must be enhanced.
- Obesity prevention strategies must be developed.
- Treatment of obesity.
- Systems-based approaches should be applied.
A version of this article first appeared on Medscape.com.
Hundreds of thousands of deaths worldwide from COVID-19 could have been avoided if obesity rates were lower, a new report says.
An analysis by the World Obesity Federation found that of the 2.5 million COVID-19 deaths reported by the end of February 2021, almost 90% (2.2 million) were in countries where more than half the population is classified as overweight.
The report, released to coincide with World Obesity Day, calls for obesity to be recognized as a disease in its own right around the world, and for people with obesity to be included in priority lists for COVID-19 testing and vaccination.
“Overweight is a highly significant predictor of developing complications from COVID-19, including the need for hospitalization, for intensive care and for mechanical ventilation,” the WOF notes in the report.
It adds that in countries where less than half the adult population is classified as overweight (body mass index > 25 mg/kg2), for example, Vietnam, the likelihood of death from COVID-19 is a small fraction – around one-tenth – of the level seen in countries where more than half the population is classified as overweight.
And while it acknowledges that figures for COVID-19 deaths are affected by the age structure of national populations and a country’s relative wealth and reporting capacity, “our findings appear to be independent of these contributory factors. Furthermore, other studies have found that overweight remains a highly significant predictor of the need for COVID-19 health care after accounting for these other influences.”
As an example, based on the U.K. experience, where an estimated 36% of COVID-19 hospitalizations have been attributed to lack of physical activity and excess body weight, it can be suggested that up to a third of the costs – between $6 trillion and $7 trillion over the longer period – might be attributable to these predisposing risks.
The report said the prevalence of obesity in the United Kingdom is expected to rise from 27.8% in 2016 to more than 35% by 2025.
Rachel Batterham, lead adviser on obesity at the Royal College of Physicians, commented: “The link between high levels of obesity and deaths from COVID-19 in the U.K. is indisputable, as is the urgent need to address the factors that lead so many people to be living with obesity.
“With 30% of COVID-19 hospitalizations in the U.K. directly attributed to overweight and obesity, and three-quarters of all critically ill patients having overweight or obesity, the human and financial costs are high.”
Window of opportunity to prioritize obesity as a disease
WOF says that evolving evidence on the close association between COVID-19 and underlying obesity “provides a new urgency … for political and collective action.”
“Obesity is a disease that does not receive prioritization commensurate with its prevalence and impact, which is rising fastest in emerging economies. It is a gateway to many other noncommunicable diseases and mental-health illness and is now a major factor in COVID-19 complications and mortality.”
The WOF also shows that COVID-19 is not a special case, noting that several other respiratory viruses lead to more severe consequences in people living with excess bodyweight, giving good reasons to expect the next pandemic to have similar effects. “For these reasons we need to recognize overweight as a major risk factor for infectious diseases including respiratory viruses.”
“To prevent pandemic health crises in future requires action now: we call on all readers to support the World Obesity Federation’s call for stronger, more resilient economies that prioritize investment in people’s health.”
There is, it stresses, “a window of opportunity to advocate for, fund and implement these actions in all countries to ensure better, more resilient and sustainable health for all, “now and in our postCOVID-19 future.”
It proposes a ROOTS approach:
- Recognize that obesity is a disease in its own right.
- Obesity monitoring and surveillance must be enhanced.
- Obesity prevention strategies must be developed.
- Treatment of obesity.
- Systems-based approaches should be applied.
A version of this article first appeared on Medscape.com.
Who do you call in those late, quiet hours, when all seems lost?
I swear by Apollo Physician and Asclepius and Hygeia and Panacea and all the gods and goddesses, making them my witnesses, that I will fulfill according to my ability and judgment this oath and this covenant.
On my desk sits a bust of Hygeia, a mask from Venice, next to a small sculpture and a figurine of the plague doctor. Nearby, there is a Klimt closeup of Hygeia, a postcard portraying Asclepius, St. Sebastian paintings, and quotes from Maimonides. They whisper secrets and nod to the challenges of the past. These medical specters, ancient voices of the past, keep me grounded. They speak, listen, and elevate me, too. They bring life into my otherwise quiet room.
We all began our careers swearing to Apollo, Asclepius, Hygeia, and Panacea when we recited the Hippocratic Oath. I call upon them, and other gods and totems, and saints and ancient healers, now more than ever. As an atheist, I don’t appeal to them as prayers, but as Hippocrates intended. I look to their supernatural healing powers as a source of strength and as revealers of the natural and observable phenomena.
Apollo was one of the Twelve Olympians, a God of medicine, father of Asclepius. He was a healer, though his arrows also bore the plagues of the Gods.
For centuries, Apollo was found floating above the marble dissection table in the Bologna anatomical theater, guiding students who dove into the secrets of the human body.
Asclepius, son of Apollo, was hailed as a god of medicine. He healed many from plagues at his temples throughout the Ancient Greek and Roman empires. He was mentored in the healing arts by the centaur, Chiron. His many daughters and sons represent various aspects of medicine including cures, healing, recovery, sanitation, and beauty. To Asclepius, temples were places of healing, an ancient ancestor to modern hospitals.
Two of his daughters, Panacea and Hygeia, gave us the healing words of panacea and hygiene. Today, these acts of hygiene, handwashing, mask-wearing, and sanitation are discussed across the world louder than ever. While we’re all wishing for a panacea, we know it will take all the attributes of medicine to get us through this pandemic.
Hospitalists are part of the frontline teams facing this pandemic head-on. Gowning up for MRSA isolation seems quaint nowadays.
My attendings spoke of their fears, up against the unknown while on service in the 1980s, when HIV appeared. 2014 brought the Ebola biocontainment units. Now, this generation works daily against a modern plague, where every day is a risk of exposure. When every patient is in isolation, the garb begins to reflect the PPE that emerged during a 17th-century plague epidemics, the plague doctor outfit.
Godfather II fans recall the famous portrayal of the August 16th festival to San Rocco play out in the streets of New York. For those stricken with COVID-19 and recovered, you emulate San Rocco, in your continued return to service.
The Scuola Grande di San Rocco, in Venice, is the epitome of healing and greatness in one building. Tintoretto, the great Venetian painter, assembled the story of healing through art and portraits of San Rocco. The scuola, a confraternity, was a community of healers, gathered in one place to look after the less fortunate.
Hospitalists march into the hospital risking their lives. We always wear PPE for MRSA, ESBL, or C. diff. And enter reverse isolation rooms wearing N95s for possible TB cases. But those don’t elevate to the volume, to the same fear, as gowning up for COVID-19.
Hospitalists, frontline health care workers, embody the story of San Sebastian, another plague saint who absorbed the arrows, the symbolic plagues, onto his own shoulders so no one else had to bear them. San Sebastian was a Christian persecuted by a Roman emperor once his beliefs were discovered. He is often laden with arrows in spots where buboes would have appeared: the armpits and the groin. His sacrifice for others’ recovery became a symbol of absorbing the plague, the wounds, and the impact of the arrows.
This sacrifice epitomizes the daily work the frontline nurses, ER docs, intensivists, hospitalists, and the entire hospital staff perform daily, bearing the slung arrows of coronavirus.
One of the images I think of frequently during this time lies atop Castel San Angelo in Rome. Built in 161 AD, it has served as a mausoleum, prison, papal residence, and is currently a museum. Atop San’Angelo stands St. Michael, the destroyer of the dragon. He is sheathing his sword in representation of the end of the plague in 590.
The arrows flow, yet the sword will be sheathed. Evil will be halted. The stories of these ancient totems and strength can give us strength as they remind us of the work that was done for centuries: pestilence, famine, war. The great killers never go away completely.
Fast forward to today
These medical specters serve as reminders of what makes the field of medicine so inspiring: the selfless acts, the fortitude of spirit, the healers, the long history, and the shoulders of giants we stand upon. From these stories, we spring the healing waters we bathe in to give us the courage to wake up and care for our patients each day. These specters encourage us to defeat any and all of the scourges that come our way.
I hear and read stories about the frontline heroes, the vaccine makers, the PPE creators, the health care workers, grocery store clerks, and teachers. I’m honored to hear of these stories and your sacrifices. I’m inspired to continue upholding your essence, your fight, and your stories. In keeping with ancient empire metaphors, you are taking the slings of the diseased arrows flying to our brethren as you try to keep yourself and others safe.
The sheathing of this sword will come. These arrows will be silenced. But until then, I lean on these pictures, these stories, and these saints, to give us all the strength to wake up each morning and continue healing.
They serve as reminders of what makes the field of medicine so great: the selfless acts, the fortitude of spirit, the healers, the long history, and the shoulders of giants we stand upon. From these stories spring the healing waters we bathe in to give us the courage to wake up and care for our patients each day and defeat any and all scourges that come our way.
So, who do you call in those late, quiet hours, when all seems lost?
Dr. Messler is the executive director, quality initiatives at Glytec and works as a hospitalist at Morton Plant Hospitalist group in Clearwater, Fla. This essay appeared initially on The Hospital Leader, the official blog of SHM.
I swear by Apollo Physician and Asclepius and Hygeia and Panacea and all the gods and goddesses, making them my witnesses, that I will fulfill according to my ability and judgment this oath and this covenant.
On my desk sits a bust of Hygeia, a mask from Venice, next to a small sculpture and a figurine of the plague doctor. Nearby, there is a Klimt closeup of Hygeia, a postcard portraying Asclepius, St. Sebastian paintings, and quotes from Maimonides. They whisper secrets and nod to the challenges of the past. These medical specters, ancient voices of the past, keep me grounded. They speak, listen, and elevate me, too. They bring life into my otherwise quiet room.
We all began our careers swearing to Apollo, Asclepius, Hygeia, and Panacea when we recited the Hippocratic Oath. I call upon them, and other gods and totems, and saints and ancient healers, now more than ever. As an atheist, I don’t appeal to them as prayers, but as Hippocrates intended. I look to their supernatural healing powers as a source of strength and as revealers of the natural and observable phenomena.
Apollo was one of the Twelve Olympians, a God of medicine, father of Asclepius. He was a healer, though his arrows also bore the plagues of the Gods.
For centuries, Apollo was found floating above the marble dissection table in the Bologna anatomical theater, guiding students who dove into the secrets of the human body.
Asclepius, son of Apollo, was hailed as a god of medicine. He healed many from plagues at his temples throughout the Ancient Greek and Roman empires. He was mentored in the healing arts by the centaur, Chiron. His many daughters and sons represent various aspects of medicine including cures, healing, recovery, sanitation, and beauty. To Asclepius, temples were places of healing, an ancient ancestor to modern hospitals.
Two of his daughters, Panacea and Hygeia, gave us the healing words of panacea and hygiene. Today, these acts of hygiene, handwashing, mask-wearing, and sanitation are discussed across the world louder than ever. While we’re all wishing for a panacea, we know it will take all the attributes of medicine to get us through this pandemic.
Hospitalists are part of the frontline teams facing this pandemic head-on. Gowning up for MRSA isolation seems quaint nowadays.
My attendings spoke of their fears, up against the unknown while on service in the 1980s, when HIV appeared. 2014 brought the Ebola biocontainment units. Now, this generation works daily against a modern plague, where every day is a risk of exposure. When every patient is in isolation, the garb begins to reflect the PPE that emerged during a 17th-century plague epidemics, the plague doctor outfit.
Godfather II fans recall the famous portrayal of the August 16th festival to San Rocco play out in the streets of New York. For those stricken with COVID-19 and recovered, you emulate San Rocco, in your continued return to service.
The Scuola Grande di San Rocco, in Venice, is the epitome of healing and greatness in one building. Tintoretto, the great Venetian painter, assembled the story of healing through art and portraits of San Rocco. The scuola, a confraternity, was a community of healers, gathered in one place to look after the less fortunate.
Hospitalists march into the hospital risking their lives. We always wear PPE for MRSA, ESBL, or C. diff. And enter reverse isolation rooms wearing N95s for possible TB cases. But those don’t elevate to the volume, to the same fear, as gowning up for COVID-19.
Hospitalists, frontline health care workers, embody the story of San Sebastian, another plague saint who absorbed the arrows, the symbolic plagues, onto his own shoulders so no one else had to bear them. San Sebastian was a Christian persecuted by a Roman emperor once his beliefs were discovered. He is often laden with arrows in spots where buboes would have appeared: the armpits and the groin. His sacrifice for others’ recovery became a symbol of absorbing the plague, the wounds, and the impact of the arrows.
This sacrifice epitomizes the daily work the frontline nurses, ER docs, intensivists, hospitalists, and the entire hospital staff perform daily, bearing the slung arrows of coronavirus.
One of the images I think of frequently during this time lies atop Castel San Angelo in Rome. Built in 161 AD, it has served as a mausoleum, prison, papal residence, and is currently a museum. Atop San’Angelo stands St. Michael, the destroyer of the dragon. He is sheathing his sword in representation of the end of the plague in 590.
The arrows flow, yet the sword will be sheathed. Evil will be halted. The stories of these ancient totems and strength can give us strength as they remind us of the work that was done for centuries: pestilence, famine, war. The great killers never go away completely.
Fast forward to today
These medical specters serve as reminders of what makes the field of medicine so inspiring: the selfless acts, the fortitude of spirit, the healers, the long history, and the shoulders of giants we stand upon. From these stories, we spring the healing waters we bathe in to give us the courage to wake up and care for our patients each day. These specters encourage us to defeat any and all of the scourges that come our way.
I hear and read stories about the frontline heroes, the vaccine makers, the PPE creators, the health care workers, grocery store clerks, and teachers. I’m honored to hear of these stories and your sacrifices. I’m inspired to continue upholding your essence, your fight, and your stories. In keeping with ancient empire metaphors, you are taking the slings of the diseased arrows flying to our brethren as you try to keep yourself and others safe.
The sheathing of this sword will come. These arrows will be silenced. But until then, I lean on these pictures, these stories, and these saints, to give us all the strength to wake up each morning and continue healing.
They serve as reminders of what makes the field of medicine so great: the selfless acts, the fortitude of spirit, the healers, the long history, and the shoulders of giants we stand upon. From these stories spring the healing waters we bathe in to give us the courage to wake up and care for our patients each day and defeat any and all scourges that come our way.
So, who do you call in those late, quiet hours, when all seems lost?
Dr. Messler is the executive director, quality initiatives at Glytec and works as a hospitalist at Morton Plant Hospitalist group in Clearwater, Fla. This essay appeared initially on The Hospital Leader, the official blog of SHM.
I swear by Apollo Physician and Asclepius and Hygeia and Panacea and all the gods and goddesses, making them my witnesses, that I will fulfill according to my ability and judgment this oath and this covenant.
On my desk sits a bust of Hygeia, a mask from Venice, next to a small sculpture and a figurine of the plague doctor. Nearby, there is a Klimt closeup of Hygeia, a postcard portraying Asclepius, St. Sebastian paintings, and quotes from Maimonides. They whisper secrets and nod to the challenges of the past. These medical specters, ancient voices of the past, keep me grounded. They speak, listen, and elevate me, too. They bring life into my otherwise quiet room.
We all began our careers swearing to Apollo, Asclepius, Hygeia, and Panacea when we recited the Hippocratic Oath. I call upon them, and other gods and totems, and saints and ancient healers, now more than ever. As an atheist, I don’t appeal to them as prayers, but as Hippocrates intended. I look to their supernatural healing powers as a source of strength and as revealers of the natural and observable phenomena.
Apollo was one of the Twelve Olympians, a God of medicine, father of Asclepius. He was a healer, though his arrows also bore the plagues of the Gods.
For centuries, Apollo was found floating above the marble dissection table in the Bologna anatomical theater, guiding students who dove into the secrets of the human body.
Asclepius, son of Apollo, was hailed as a god of medicine. He healed many from plagues at his temples throughout the Ancient Greek and Roman empires. He was mentored in the healing arts by the centaur, Chiron. His many daughters and sons represent various aspects of medicine including cures, healing, recovery, sanitation, and beauty. To Asclepius, temples were places of healing, an ancient ancestor to modern hospitals.
Two of his daughters, Panacea and Hygeia, gave us the healing words of panacea and hygiene. Today, these acts of hygiene, handwashing, mask-wearing, and sanitation are discussed across the world louder than ever. While we’re all wishing for a panacea, we know it will take all the attributes of medicine to get us through this pandemic.
Hospitalists are part of the frontline teams facing this pandemic head-on. Gowning up for MRSA isolation seems quaint nowadays.
My attendings spoke of their fears, up against the unknown while on service in the 1980s, when HIV appeared. 2014 brought the Ebola biocontainment units. Now, this generation works daily against a modern plague, where every day is a risk of exposure. When every patient is in isolation, the garb begins to reflect the PPE that emerged during a 17th-century plague epidemics, the plague doctor outfit.
Godfather II fans recall the famous portrayal of the August 16th festival to San Rocco play out in the streets of New York. For those stricken with COVID-19 and recovered, you emulate San Rocco, in your continued return to service.
The Scuola Grande di San Rocco, in Venice, is the epitome of healing and greatness in one building. Tintoretto, the great Venetian painter, assembled the story of healing through art and portraits of San Rocco. The scuola, a confraternity, was a community of healers, gathered in one place to look after the less fortunate.
Hospitalists march into the hospital risking their lives. We always wear PPE for MRSA, ESBL, or C. diff. And enter reverse isolation rooms wearing N95s for possible TB cases. But those don’t elevate to the volume, to the same fear, as gowning up for COVID-19.
Hospitalists, frontline health care workers, embody the story of San Sebastian, another plague saint who absorbed the arrows, the symbolic plagues, onto his own shoulders so no one else had to bear them. San Sebastian was a Christian persecuted by a Roman emperor once his beliefs were discovered. He is often laden with arrows in spots where buboes would have appeared: the armpits and the groin. His sacrifice for others’ recovery became a symbol of absorbing the plague, the wounds, and the impact of the arrows.
This sacrifice epitomizes the daily work the frontline nurses, ER docs, intensivists, hospitalists, and the entire hospital staff perform daily, bearing the slung arrows of coronavirus.
One of the images I think of frequently during this time lies atop Castel San Angelo in Rome. Built in 161 AD, it has served as a mausoleum, prison, papal residence, and is currently a museum. Atop San’Angelo stands St. Michael, the destroyer of the dragon. He is sheathing his sword in representation of the end of the plague in 590.
The arrows flow, yet the sword will be sheathed. Evil will be halted. The stories of these ancient totems and strength can give us strength as they remind us of the work that was done for centuries: pestilence, famine, war. The great killers never go away completely.
Fast forward to today
These medical specters serve as reminders of what makes the field of medicine so inspiring: the selfless acts, the fortitude of spirit, the healers, the long history, and the shoulders of giants we stand upon. From these stories, we spring the healing waters we bathe in to give us the courage to wake up and care for our patients each day. These specters encourage us to defeat any and all of the scourges that come our way.
I hear and read stories about the frontline heroes, the vaccine makers, the PPE creators, the health care workers, grocery store clerks, and teachers. I’m honored to hear of these stories and your sacrifices. I’m inspired to continue upholding your essence, your fight, and your stories. In keeping with ancient empire metaphors, you are taking the slings of the diseased arrows flying to our brethren as you try to keep yourself and others safe.
The sheathing of this sword will come. These arrows will be silenced. But until then, I lean on these pictures, these stories, and these saints, to give us all the strength to wake up each morning and continue healing.
They serve as reminders of what makes the field of medicine so great: the selfless acts, the fortitude of spirit, the healers, the long history, and the shoulders of giants we stand upon. From these stories spring the healing waters we bathe in to give us the courage to wake up and care for our patients each day and defeat any and all scourges that come our way.
So, who do you call in those late, quiet hours, when all seems lost?
Dr. Messler is the executive director, quality initiatives at Glytec and works as a hospitalist at Morton Plant Hospitalist group in Clearwater, Fla. This essay appeared initially on The Hospital Leader, the official blog of SHM.
Potential COVID-19 variant surge looms over U.S.
Another coronavirus surge may be on the way in the United States as daily COVID-19 cases continue to plateau around 60,000, states begin to lift restrictions, and people embark on spring break trips this week, according to CNN.
Outbreaks will likely stem from the B.1.1.7 variant, which was first identified in the United Kingdom, and gain momentum during the next 6-14 weeks.
“Four weeks ago, the B.1.1.7 variant made up about 1%-4% of the virus that we were seeing in communities across the country. Today it’s up to 30%-40%,” Michael Osterholm, PhD, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, Minneapolis, told NBC’s Meet the Press on March 7.
Dr. Osterholm compared the current situation with the “eye of the hurricane,” where the skies appear clear but more storms are on the way. Across Europe, 27 countries are seeing significant B.1.1.7 case increases, and 10 are getting hit hard, he said.
“What we’ve seen in Europe, when we hit that 50% mark, you see cases surge,” he said. “So right now, we do have to keep America as safe as we can from this virus by not letting up on any of the public health measures we’ve taken.”
In January, the CDC warned that B.1.1.7 variant cases would increase in 2021 and become the dominant variant in the country by this month. The United States has now reported more than 3,000 cases across 46 states, according to the latest CDC tally updated on March 7. More than 600 cases have been found in Florida, followed by more than 400 in Michigan.
The CDC has said the tally doesn’t represent the total number of B.1.1.7 cases in the United States, only the ones that have been identified by analyzing samples through genomic sequencing.
“Where it has hit in the U.K. and now elsewhere in Europe, it has been catastrophic,” Celine Gounder, MD, an infectious disease specialist with New York University Langone Health, told CNN on March 7.
The variant is more transmissible than the original novel coronavirus, and the cases in the United States are “increasing exponentially,” she said.
“It has driven up rates of hospitalizations and deaths and it’s very difficult to control,” Dr. Gounder said.
Vaccination numbers aren’t yet high enough to stop the predicted surge, she added. The United States has shipped more than 116 million vaccine doses, according to the latest CDC update on March 7. Nearly 59 million people have received at least one dose, and 30.6 million people have received two vaccine doses. About 9% of the U.S. population has been fully vaccinated.
States shouldn’t ease restrictions until the vaccination numbers are much higher and daily COVID-19 cases fall below 10,000 – and maybe “considerably less than that,” Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, told CNN on March 4.
Several states have already begun to lift COVID-19 safety protocols, with Texas and Mississippi removing mask mandates last week. Businesses in Texas will be able to reopen at full capacity on March 10. For now, public health officials are urging Americans to continue to wear masks, avoid crowds, and follow social distancing guidelines as vaccines roll out across the country.
“This is sort of like we’ve been running this really long marathon, and we’re 100 yards from the finish line and we sit down and we give up,” Dr. Gounder told CNN on Sunday. ‘We’re almost there, we just need to give ourselves a bit more time to get a larger proportion of the population covered with vaccines.”
A version of this article first appeared on WebMD.com.
Another coronavirus surge may be on the way in the United States as daily COVID-19 cases continue to plateau around 60,000, states begin to lift restrictions, and people embark on spring break trips this week, according to CNN.
Outbreaks will likely stem from the B.1.1.7 variant, which was first identified in the United Kingdom, and gain momentum during the next 6-14 weeks.
“Four weeks ago, the B.1.1.7 variant made up about 1%-4% of the virus that we were seeing in communities across the country. Today it’s up to 30%-40%,” Michael Osterholm, PhD, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, Minneapolis, told NBC’s Meet the Press on March 7.
Dr. Osterholm compared the current situation with the “eye of the hurricane,” where the skies appear clear but more storms are on the way. Across Europe, 27 countries are seeing significant B.1.1.7 case increases, and 10 are getting hit hard, he said.
“What we’ve seen in Europe, when we hit that 50% mark, you see cases surge,” he said. “So right now, we do have to keep America as safe as we can from this virus by not letting up on any of the public health measures we’ve taken.”
In January, the CDC warned that B.1.1.7 variant cases would increase in 2021 and become the dominant variant in the country by this month. The United States has now reported more than 3,000 cases across 46 states, according to the latest CDC tally updated on March 7. More than 600 cases have been found in Florida, followed by more than 400 in Michigan.
The CDC has said the tally doesn’t represent the total number of B.1.1.7 cases in the United States, only the ones that have been identified by analyzing samples through genomic sequencing.
“Where it has hit in the U.K. and now elsewhere in Europe, it has been catastrophic,” Celine Gounder, MD, an infectious disease specialist with New York University Langone Health, told CNN on March 7.
The variant is more transmissible than the original novel coronavirus, and the cases in the United States are “increasing exponentially,” she said.
“It has driven up rates of hospitalizations and deaths and it’s very difficult to control,” Dr. Gounder said.
Vaccination numbers aren’t yet high enough to stop the predicted surge, she added. The United States has shipped more than 116 million vaccine doses, according to the latest CDC update on March 7. Nearly 59 million people have received at least one dose, and 30.6 million people have received two vaccine doses. About 9% of the U.S. population has been fully vaccinated.
States shouldn’t ease restrictions until the vaccination numbers are much higher and daily COVID-19 cases fall below 10,000 – and maybe “considerably less than that,” Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, told CNN on March 4.
Several states have already begun to lift COVID-19 safety protocols, with Texas and Mississippi removing mask mandates last week. Businesses in Texas will be able to reopen at full capacity on March 10. For now, public health officials are urging Americans to continue to wear masks, avoid crowds, and follow social distancing guidelines as vaccines roll out across the country.
“This is sort of like we’ve been running this really long marathon, and we’re 100 yards from the finish line and we sit down and we give up,” Dr. Gounder told CNN on Sunday. ‘We’re almost there, we just need to give ourselves a bit more time to get a larger proportion of the population covered with vaccines.”
A version of this article first appeared on WebMD.com.
Another coronavirus surge may be on the way in the United States as daily COVID-19 cases continue to plateau around 60,000, states begin to lift restrictions, and people embark on spring break trips this week, according to CNN.
Outbreaks will likely stem from the B.1.1.7 variant, which was first identified in the United Kingdom, and gain momentum during the next 6-14 weeks.
“Four weeks ago, the B.1.1.7 variant made up about 1%-4% of the virus that we were seeing in communities across the country. Today it’s up to 30%-40%,” Michael Osterholm, PhD, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, Minneapolis, told NBC’s Meet the Press on March 7.
Dr. Osterholm compared the current situation with the “eye of the hurricane,” where the skies appear clear but more storms are on the way. Across Europe, 27 countries are seeing significant B.1.1.7 case increases, and 10 are getting hit hard, he said.
“What we’ve seen in Europe, when we hit that 50% mark, you see cases surge,” he said. “So right now, we do have to keep America as safe as we can from this virus by not letting up on any of the public health measures we’ve taken.”
In January, the CDC warned that B.1.1.7 variant cases would increase in 2021 and become the dominant variant in the country by this month. The United States has now reported more than 3,000 cases across 46 states, according to the latest CDC tally updated on March 7. More than 600 cases have been found in Florida, followed by more than 400 in Michigan.
The CDC has said the tally doesn’t represent the total number of B.1.1.7 cases in the United States, only the ones that have been identified by analyzing samples through genomic sequencing.
“Where it has hit in the U.K. and now elsewhere in Europe, it has been catastrophic,” Celine Gounder, MD, an infectious disease specialist with New York University Langone Health, told CNN on March 7.
The variant is more transmissible than the original novel coronavirus, and the cases in the United States are “increasing exponentially,” she said.
“It has driven up rates of hospitalizations and deaths and it’s very difficult to control,” Dr. Gounder said.
Vaccination numbers aren’t yet high enough to stop the predicted surge, she added. The United States has shipped more than 116 million vaccine doses, according to the latest CDC update on March 7. Nearly 59 million people have received at least one dose, and 30.6 million people have received two vaccine doses. About 9% of the U.S. population has been fully vaccinated.
States shouldn’t ease restrictions until the vaccination numbers are much higher and daily COVID-19 cases fall below 10,000 – and maybe “considerably less than that,” Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, told CNN on March 4.
Several states have already begun to lift COVID-19 safety protocols, with Texas and Mississippi removing mask mandates last week. Businesses in Texas will be able to reopen at full capacity on March 10. For now, public health officials are urging Americans to continue to wear masks, avoid crowds, and follow social distancing guidelines as vaccines roll out across the country.
“This is sort of like we’ve been running this really long marathon, and we’re 100 yards from the finish line and we sit down and we give up,” Dr. Gounder told CNN on Sunday. ‘We’re almost there, we just need to give ourselves a bit more time to get a larger proportion of the population covered with vaccines.”
A version of this article first appeared on WebMD.com.
DOACs offered after heart valve surgery despite absence of data
Direct oral anticoagulants (DOACs) are used in about 1% of patients undergoing surgical mechanical aortic and mitral valve replacement, but in up to 6% of surgical bioprosthetic valve replacements, according to registry data presented at CRT 2021.
In an analysis of the Society of Thoracic Surgery (STS) registry during 2014-2017, DOAC use increased steadily among those undergoing surgical bioprosthetic valve replacement, reaching a number that is potentially clinically significant, according to Ankur Kalra, MD, an interventional cardiologist at Akron General Hospital who has an academic appointment at the Cleveland Clinic.
There was no increase in the use of DOACs observed among patients undergoing mechanical valve replacement, “but even if the number is 1%, they should probably not be used at all until we accrue more data,” Dr. Kalra said.
DOACs discouraged in patients with mechanical or bioprosthetic valves
In Food and Drug Administration labeling, DOACs are contraindicated or not recommended. This can be traced to the randomized RE-ALIGN trial, which was stopped prematurely due to evidence of harm from a DOAC, according to Dr. Kalra.
In RE-ALIGN, which enrolled patients undergoing mechanical aortic or mitral valve replacement, dabigatran was associated not only with more bleeding events than warfarin, but also more thromboembolic events.
There are no randomized data comparing the factor Xa inhibitors rivaroxaban or apixaban to warfarin in heart valve surgery, but Dr. Kalra noted cautionary language is found in the labeling of both, “perhaps due to the RE-ALIGN data.”
Registry shows trends in prescribing
In the STS registry data, 193 (1.1%) of the 18,142 patients undergoing mechanical aortic valve surgery, 139 (1.0%) of the 13,942 patients undergoing mechanical mitral valve surgery, 5,625 (4.7%) of the 116,203 patients undergoing aortic bioprosthetic aortic valve surgery, and 2,180 (5.9%) of the 39,243 patients undergoing bioprosthetic mitral valve surgery were on a DOAC at discharge.
Among those receiving a mechanical value and placed on a DOAC, about two-thirds were on a factor Xa inhibitor rather than dabigatran. For those receiving a bioprosthetic value, the proportion was greater than 80%. Dr. Kalra speculated that the RE-ALIGN trial might be the reason factor Xa inhibitors were favored.
In both types of valves, whether mechanical or bioprosthetic, more comorbidities predicted a greater likelihood of receiving a DOAC rather than warfarin. For those receiving mechanical values, the comorbidities with a significant association with greater DOAC use included hypertension (P = .003), dyslipidemia (P = .02), arrhythmia (P < .001), and peripheral arterial disease (P < 0.001).
The same factors were significant for predicting increased likelihood of a DOAC following bioprosthetic valve replacement, but there were additional factors, including atrial fibrillation independent of other types of arrhythmias (P < .001), a factor not significant for mechanical valves, as well as diabetes (P < .001), cerebrovascular disease (P < .001), dialysis (P < .001), and endocarditis (P < .001).
“This is probably intuitive, but patients who were on a factor Xa inhibitor before their valve replacement were also more likely to be discharged on a factor Xa inhibitor,” Dr. Kalra said at the virtual meeting, sponsored by MedStar Heart & Vascular Institute.
The year-to-year increase in DOAC use among those undergoing bioprosthetic valve replacement over the study period, which was a significant trend, was not observed among those undergoing mechanical valve replacement. Rather, the 1% proportion remained stable over the study period.
“We wanted to look at outcomes, but we found that the STS database, which only includes data out to 30 days, is not structured for this type of analysis,” Dr. Kalra said. He was also concerned about the limitations of a comparison in which 1% of the sample was being compared to 99%.
Expert: One percent is ‘very small number’
David J. Cohen, MD, commented on the 1% figure, which was so low that a moderator questioned whether it could be due mostly to coding errors.
“This is a very, very small number so at some level it is reassuring that it is so low in the mechanical valves,” Dr. Cohen said. However, he was more circumspect about the larger number in bioprosthetic valves.
“I have always thought it was a bit strange there was a warning against using them in bioprosthetic valves, especially in the aortic position,” he said.
“The trials that established the benefits of DOACs were all in nonvalvular atrial fibrillation, but this did not mean non–aortic stenosis; it meant non–mitral valvular. There have been articles written about how that has been misinterpreted,” said Dr. Cohen, director of clinical and outcomes research at the Cardiovascular Research Foundation and director of academic affairs at St. Francis Hospital, Roslyn, N.Y.
For his part, Dr. Kalra reported that he does not consider DOACs in patients who have undergone a surgical mechanical valve replacement. For bioprosthetic valves, he “prefers” warfarin over DOACs.
Overall, the evidence from the registry led Dr. Kalra to suggest that physicians should continue to “exercise caution” in using DOACs instead of warfarin after any surgical valve replacement “until randomized clinical trials provide sufficient evidence” to make a judgment about relative efficacy and safety.
Results of the study were published online as a research letter in Jama Network Open after Dr. Kalra’s presentation. Dr. Kalra and Dr. Cohen report no potential conflicts of interest.
Direct oral anticoagulants (DOACs) are used in about 1% of patients undergoing surgical mechanical aortic and mitral valve replacement, but in up to 6% of surgical bioprosthetic valve replacements, according to registry data presented at CRT 2021.
In an analysis of the Society of Thoracic Surgery (STS) registry during 2014-2017, DOAC use increased steadily among those undergoing surgical bioprosthetic valve replacement, reaching a number that is potentially clinically significant, according to Ankur Kalra, MD, an interventional cardiologist at Akron General Hospital who has an academic appointment at the Cleveland Clinic.
There was no increase in the use of DOACs observed among patients undergoing mechanical valve replacement, “but even if the number is 1%, they should probably not be used at all until we accrue more data,” Dr. Kalra said.
DOACs discouraged in patients with mechanical or bioprosthetic valves
In Food and Drug Administration labeling, DOACs are contraindicated or not recommended. This can be traced to the randomized RE-ALIGN trial, which was stopped prematurely due to evidence of harm from a DOAC, according to Dr. Kalra.
In RE-ALIGN, which enrolled patients undergoing mechanical aortic or mitral valve replacement, dabigatran was associated not only with more bleeding events than warfarin, but also more thromboembolic events.
There are no randomized data comparing the factor Xa inhibitors rivaroxaban or apixaban to warfarin in heart valve surgery, but Dr. Kalra noted cautionary language is found in the labeling of both, “perhaps due to the RE-ALIGN data.”
Registry shows trends in prescribing
In the STS registry data, 193 (1.1%) of the 18,142 patients undergoing mechanical aortic valve surgery, 139 (1.0%) of the 13,942 patients undergoing mechanical mitral valve surgery, 5,625 (4.7%) of the 116,203 patients undergoing aortic bioprosthetic aortic valve surgery, and 2,180 (5.9%) of the 39,243 patients undergoing bioprosthetic mitral valve surgery were on a DOAC at discharge.
Among those receiving a mechanical value and placed on a DOAC, about two-thirds were on a factor Xa inhibitor rather than dabigatran. For those receiving a bioprosthetic value, the proportion was greater than 80%. Dr. Kalra speculated that the RE-ALIGN trial might be the reason factor Xa inhibitors were favored.
In both types of valves, whether mechanical or bioprosthetic, more comorbidities predicted a greater likelihood of receiving a DOAC rather than warfarin. For those receiving mechanical values, the comorbidities with a significant association with greater DOAC use included hypertension (P = .003), dyslipidemia (P = .02), arrhythmia (P < .001), and peripheral arterial disease (P < 0.001).
The same factors were significant for predicting increased likelihood of a DOAC following bioprosthetic valve replacement, but there were additional factors, including atrial fibrillation independent of other types of arrhythmias (P < .001), a factor not significant for mechanical valves, as well as diabetes (P < .001), cerebrovascular disease (P < .001), dialysis (P < .001), and endocarditis (P < .001).
“This is probably intuitive, but patients who were on a factor Xa inhibitor before their valve replacement were also more likely to be discharged on a factor Xa inhibitor,” Dr. Kalra said at the virtual meeting, sponsored by MedStar Heart & Vascular Institute.
The year-to-year increase in DOAC use among those undergoing bioprosthetic valve replacement over the study period, which was a significant trend, was not observed among those undergoing mechanical valve replacement. Rather, the 1% proportion remained stable over the study period.
“We wanted to look at outcomes, but we found that the STS database, which only includes data out to 30 days, is not structured for this type of analysis,” Dr. Kalra said. He was also concerned about the limitations of a comparison in which 1% of the sample was being compared to 99%.
Expert: One percent is ‘very small number’
David J. Cohen, MD, commented on the 1% figure, which was so low that a moderator questioned whether it could be due mostly to coding errors.
“This is a very, very small number so at some level it is reassuring that it is so low in the mechanical valves,” Dr. Cohen said. However, he was more circumspect about the larger number in bioprosthetic valves.
“I have always thought it was a bit strange there was a warning against using them in bioprosthetic valves, especially in the aortic position,” he said.
“The trials that established the benefits of DOACs were all in nonvalvular atrial fibrillation, but this did not mean non–aortic stenosis; it meant non–mitral valvular. There have been articles written about how that has been misinterpreted,” said Dr. Cohen, director of clinical and outcomes research at the Cardiovascular Research Foundation and director of academic affairs at St. Francis Hospital, Roslyn, N.Y.
For his part, Dr. Kalra reported that he does not consider DOACs in patients who have undergone a surgical mechanical valve replacement. For bioprosthetic valves, he “prefers” warfarin over DOACs.
Overall, the evidence from the registry led Dr. Kalra to suggest that physicians should continue to “exercise caution” in using DOACs instead of warfarin after any surgical valve replacement “until randomized clinical trials provide sufficient evidence” to make a judgment about relative efficacy and safety.
Results of the study were published online as a research letter in Jama Network Open after Dr. Kalra’s presentation. Dr. Kalra and Dr. Cohen report no potential conflicts of interest.
Direct oral anticoagulants (DOACs) are used in about 1% of patients undergoing surgical mechanical aortic and mitral valve replacement, but in up to 6% of surgical bioprosthetic valve replacements, according to registry data presented at CRT 2021.
In an analysis of the Society of Thoracic Surgery (STS) registry during 2014-2017, DOAC use increased steadily among those undergoing surgical bioprosthetic valve replacement, reaching a number that is potentially clinically significant, according to Ankur Kalra, MD, an interventional cardiologist at Akron General Hospital who has an academic appointment at the Cleveland Clinic.
There was no increase in the use of DOACs observed among patients undergoing mechanical valve replacement, “but even if the number is 1%, they should probably not be used at all until we accrue more data,” Dr. Kalra said.
DOACs discouraged in patients with mechanical or bioprosthetic valves
In Food and Drug Administration labeling, DOACs are contraindicated or not recommended. This can be traced to the randomized RE-ALIGN trial, which was stopped prematurely due to evidence of harm from a DOAC, according to Dr. Kalra.
In RE-ALIGN, which enrolled patients undergoing mechanical aortic or mitral valve replacement, dabigatran was associated not only with more bleeding events than warfarin, but also more thromboembolic events.
There are no randomized data comparing the factor Xa inhibitors rivaroxaban or apixaban to warfarin in heart valve surgery, but Dr. Kalra noted cautionary language is found in the labeling of both, “perhaps due to the RE-ALIGN data.”
Registry shows trends in prescribing
In the STS registry data, 193 (1.1%) of the 18,142 patients undergoing mechanical aortic valve surgery, 139 (1.0%) of the 13,942 patients undergoing mechanical mitral valve surgery, 5,625 (4.7%) of the 116,203 patients undergoing aortic bioprosthetic aortic valve surgery, and 2,180 (5.9%) of the 39,243 patients undergoing bioprosthetic mitral valve surgery were on a DOAC at discharge.
Among those receiving a mechanical value and placed on a DOAC, about two-thirds were on a factor Xa inhibitor rather than dabigatran. For those receiving a bioprosthetic value, the proportion was greater than 80%. Dr. Kalra speculated that the RE-ALIGN trial might be the reason factor Xa inhibitors were favored.
In both types of valves, whether mechanical or bioprosthetic, more comorbidities predicted a greater likelihood of receiving a DOAC rather than warfarin. For those receiving mechanical values, the comorbidities with a significant association with greater DOAC use included hypertension (P = .003), dyslipidemia (P = .02), arrhythmia (P < .001), and peripheral arterial disease (P < 0.001).
The same factors were significant for predicting increased likelihood of a DOAC following bioprosthetic valve replacement, but there were additional factors, including atrial fibrillation independent of other types of arrhythmias (P < .001), a factor not significant for mechanical valves, as well as diabetes (P < .001), cerebrovascular disease (P < .001), dialysis (P < .001), and endocarditis (P < .001).
“This is probably intuitive, but patients who were on a factor Xa inhibitor before their valve replacement were also more likely to be discharged on a factor Xa inhibitor,” Dr. Kalra said at the virtual meeting, sponsored by MedStar Heart & Vascular Institute.
The year-to-year increase in DOAC use among those undergoing bioprosthetic valve replacement over the study period, which was a significant trend, was not observed among those undergoing mechanical valve replacement. Rather, the 1% proportion remained stable over the study period.
“We wanted to look at outcomes, but we found that the STS database, which only includes data out to 30 days, is not structured for this type of analysis,” Dr. Kalra said. He was also concerned about the limitations of a comparison in which 1% of the sample was being compared to 99%.
Expert: One percent is ‘very small number’
David J. Cohen, MD, commented on the 1% figure, which was so low that a moderator questioned whether it could be due mostly to coding errors.
“This is a very, very small number so at some level it is reassuring that it is so low in the mechanical valves,” Dr. Cohen said. However, he was more circumspect about the larger number in bioprosthetic valves.
“I have always thought it was a bit strange there was a warning against using them in bioprosthetic valves, especially in the aortic position,” he said.
“The trials that established the benefits of DOACs were all in nonvalvular atrial fibrillation, but this did not mean non–aortic stenosis; it meant non–mitral valvular. There have been articles written about how that has been misinterpreted,” said Dr. Cohen, director of clinical and outcomes research at the Cardiovascular Research Foundation and director of academic affairs at St. Francis Hospital, Roslyn, N.Y.
For his part, Dr. Kalra reported that he does not consider DOACs in patients who have undergone a surgical mechanical valve replacement. For bioprosthetic valves, he “prefers” warfarin over DOACs.
Overall, the evidence from the registry led Dr. Kalra to suggest that physicians should continue to “exercise caution” in using DOACs instead of warfarin after any surgical valve replacement “until randomized clinical trials provide sufficient evidence” to make a judgment about relative efficacy and safety.
Results of the study were published online as a research letter in Jama Network Open after Dr. Kalra’s presentation. Dr. Kalra and Dr. Cohen report no potential conflicts of interest.
FROM CRT 2021









