User login
Confronting the NASH epidemic together
. The recommendations from this meeting have been copublished in Gastroenterology along with three other leading journals: Diabetes Care, Metabolism: Clinical and Experimental, and Obesity: The Journal of the Obesity Society.
Key findings from this special report include the following:
- Patients with obesity or type 2 diabetes are at a higher risk of developing NAFLD/NASH with diabetes being a major risk factor for worse disease severity and progression to cirrhosis (permanent damage to the liver).
- Primary care providers are critical to managing this growing epidemic. They should be the first line for screening patients at risk, stratifying patients based on their risk for advanced fibrosis, and providing effective management and referrals.
- The guiding principle for risk stratification is to rule out advanced fibrosis by simple, noninvasive fibrosis scores (such as NAFLD fibrosis score or Fibrosis-4 Index). Patients at intermediate or high risk may require further assessment with a second-line test – evaluation with elastography or by serum marker test with direct measures of fibrogenesis.
- Because NAFLD is not an isolated disease but a component of cardiometabolic abnormalities typically associated with obesity, insulin resistance, and type 2 diabetes, the cornerstone of therapy is lifestyle-based therapies (altered diet – such as reduced-calorie or Mediterranean diets – and regular, moderate physical activity), as well as replacing obesogenic medications, to decrease body weight and improve cardiometabolic health. Patients with diabetes who also have NASH may benefit from certain antidiabetic medications (such as pioglitazone and semaglutide) that treat not only their diabetes but also reverse steatohepatitis and improve cardiometabolic health.
- Optimal care of patients with NAFLD and NASH requires collaboration among primary care providers, endocrinologists, diabetologists, obesity medicine specialists, gastroenterologists, and hepatologists to tackle both the liver manifestations of the disease and the comorbid metabolic syndrome and cardiovascular risk, as well as screening and treating other comorbid conditions (such as obstructive sleep apnea).
. The recommendations from this meeting have been copublished in Gastroenterology along with three other leading journals: Diabetes Care, Metabolism: Clinical and Experimental, and Obesity: The Journal of the Obesity Society.
Key findings from this special report include the following:
- Patients with obesity or type 2 diabetes are at a higher risk of developing NAFLD/NASH with diabetes being a major risk factor for worse disease severity and progression to cirrhosis (permanent damage to the liver).
- Primary care providers are critical to managing this growing epidemic. They should be the first line for screening patients at risk, stratifying patients based on their risk for advanced fibrosis, and providing effective management and referrals.
- The guiding principle for risk stratification is to rule out advanced fibrosis by simple, noninvasive fibrosis scores (such as NAFLD fibrosis score or Fibrosis-4 Index). Patients at intermediate or high risk may require further assessment with a second-line test – evaluation with elastography or by serum marker test with direct measures of fibrogenesis.
- Because NAFLD is not an isolated disease but a component of cardiometabolic abnormalities typically associated with obesity, insulin resistance, and type 2 diabetes, the cornerstone of therapy is lifestyle-based therapies (altered diet – such as reduced-calorie or Mediterranean diets – and regular, moderate physical activity), as well as replacing obesogenic medications, to decrease body weight and improve cardiometabolic health. Patients with diabetes who also have NASH may benefit from certain antidiabetic medications (such as pioglitazone and semaglutide) that treat not only their diabetes but also reverse steatohepatitis and improve cardiometabolic health.
- Optimal care of patients with NAFLD and NASH requires collaboration among primary care providers, endocrinologists, diabetologists, obesity medicine specialists, gastroenterologists, and hepatologists to tackle both the liver manifestations of the disease and the comorbid metabolic syndrome and cardiovascular risk, as well as screening and treating other comorbid conditions (such as obstructive sleep apnea).
. The recommendations from this meeting have been copublished in Gastroenterology along with three other leading journals: Diabetes Care, Metabolism: Clinical and Experimental, and Obesity: The Journal of the Obesity Society.
Key findings from this special report include the following:
- Patients with obesity or type 2 diabetes are at a higher risk of developing NAFLD/NASH with diabetes being a major risk factor for worse disease severity and progression to cirrhosis (permanent damage to the liver).
- Primary care providers are critical to managing this growing epidemic. They should be the first line for screening patients at risk, stratifying patients based on their risk for advanced fibrosis, and providing effective management and referrals.
- The guiding principle for risk stratification is to rule out advanced fibrosis by simple, noninvasive fibrosis scores (such as NAFLD fibrosis score or Fibrosis-4 Index). Patients at intermediate or high risk may require further assessment with a second-line test – evaluation with elastography or by serum marker test with direct measures of fibrogenesis.
- Because NAFLD is not an isolated disease but a component of cardiometabolic abnormalities typically associated with obesity, insulin resistance, and type 2 diabetes, the cornerstone of therapy is lifestyle-based therapies (altered diet – such as reduced-calorie or Mediterranean diets – and regular, moderate physical activity), as well as replacing obesogenic medications, to decrease body weight and improve cardiometabolic health. Patients with diabetes who also have NASH may benefit from certain antidiabetic medications (such as pioglitazone and semaglutide) that treat not only their diabetes but also reverse steatohepatitis and improve cardiometabolic health.
- Optimal care of patients with NAFLD and NASH requires collaboration among primary care providers, endocrinologists, diabetologists, obesity medicine specialists, gastroenterologists, and hepatologists to tackle both the liver manifestations of the disease and the comorbid metabolic syndrome and cardiovascular risk, as well as screening and treating other comorbid conditions (such as obstructive sleep apnea).
Politics or protection? What’s behind the push for boosters?
That plan, which was first announced on Aug. 18, has raised eyebrows because it comes in advance of regulatory reviews by the Food and Drug Administration and recommendations from the Centers for Disease Control and Prevention. Those reviews are needed to determine whether third doses of these vaccines are effective or even safe. The move could have important legal ramifications for doctors and patients, too.
On Aug. 31, two high-level officials in the FDA’s Office of Vaccines Research and Review abruptly resigned amid reports that they were angry that the Biden administration was making decisions that should be left up to that agency.
So far, data show that the vaccines are highly effective at preventing the most severe consequences of COVID-19 – hospitalization and death – even regarding the Delta variant. The World Health Organization has urged wealthy nations such as the United States not to offer boosters so that the limited supply of vaccines can be directed to countries with fewer resources.
White House supports boosters
In a recent press briefing, Jeff Zients, the White House COVID-19 response coordinator, defended the move.
“You know, the booster decision, which you referenced ... was made by and announced by the nation’s leading public health officials, including Dr. Walensky; Dr. Fauci; Surgeon General Vivek Murthy; Dr. Janet Woodcock; the FDA acting commissioner, Dr. Francis Collins; Dr. Kessler; and others,” Mr. Zients said.
“And as our medical experts laid out, having reviewed all of the available data, it is in their clinical judgment that it is time to prepare Americans for a booster shot.”
He said a target date of Sept. 20 was announced so as to give states and practitioners time to prepare. He also said the move to give boosters was meant to help the United States stay ahead of a rapidly changing virus. Mr. Zients added that whether boosters will be administered starting on Sept. 20 depends on the FDA’s and CDC’s giving the go-ahead.
“Booster doses are going to be handled the same way all vaccines are handled,” said Kristen Nordlund, a CDC spokesperson. “Companies will have to provide data to FDA. FDA will have to make a decision and authorize the use of those, and ACIP [the Advisory Committee on Immunization Practices] will have to look at the evidence as well and make recommendations on top of FDA’s regulatory action,” she said.
Ms. Nordlund agreed that the planned Sept. 20 start date for boosters was something to which they aspired and was not necessarily set.
Historically, the FDA has needed at least 4 months to review a change to a vaccine’s approval, even on an accelerated schedule. Reviewers use that time to assess data regarding individual patients in a study, to review raw data, and essentially to check a drug company’s math and conclusions. The Biden administration’s timeline would shorten that review period from months to just a few weeks.
‘FDA in a very difficult position’
After the FDA approves, the ACIP of the CDC must meet to review the evidence and make recommendations on the use of the boosters in the United States.
Pfizer says it completed its submission for a supplemental biologics license application to the FDA on Aug. 27. To meet a Sept. 20 timeline, the entire process would have to be completed within 3 weeks.
“I don’t think that was handled, you know, ideally,” said Peter Lurie, MD, president of the Center for Science in the Public Interest and former associate commissioner of public health strategy and analysis at the FDA.
“It puts FDA in a very difficult position,” Dr. Lurie said. “It’s almost as if the decision has been made and they’re just checking a box, and that is, you know, contrary to the what FDA – at least the internal people at FDA – have been trying to do for ages.”
He said the agency took great pains with the emergency use authorizations and the full approvals of the vaccines to work as rapidly but thoroughly as possible. They did not skip steps.
“I think all of that reflected very well on the agency,” Dr. Lurie said. “And I think it worked out well in terms of trust in the vaccines.”
Although additional doses of vaccine are expected to be safe, little is known about side effects or adverse events after a third dose.
“It’s critical to wait for additional data and regulatory allowance for booster doses,” Sara Oliver, MD, a member of the CDC’s epidemic intelligence service, said in an Aug. 30 presentation to the ACIP, which is charged with making recommendations for use of all vaccines in the United States.
Boosters already being given
But after the White House announced that boosters were on the way, many people are not waiting.
Many health care practitioners and pharmacies have already been giving people third doses of vaccines, even if they are not among the immunocompromised – the group for which the shots are currently approved.
“You can walk into a pharmacy and ask for a third dose. Depending on which pharmacy you go to, you may get it,” said Helen Talbot, MD, associate professor of medicine at Vanderbilt University, Nashville, Tenn., and a member of the ACIP.
She says she has a friend who recently went for a checkup and was offered a third dose. His physician is already giving extra doses to everyone who is older than 65.
Dr. Talbot said that in fairness, pharmacies in the United States are throwing away doses of vaccine because they are expiring before they get used.
“Many of us may or may not be ready to give a third dose but would rather give someone a third dose than throw a vaccine away,” she said.
Consequences of a third shot
But giving or getting a third dose before approval by the FDA may have legal consequences.
In the ACIP meeting on Aug. 30, Demetre Daskalakis, MD, who leads vaccine equity efforts at the CDC, cautioned that physicians who give extra doses of the vaccine before the FDA and CDC have signed off may be in violation of practitioner agreements with the federal government and might not be covered by the federal PREP Act. The PREP Act provides immunity from lawsuits for people who administer COVID-19 vaccines and compensates patients in the event of injury. Patients who get a vaccine and suffer a rare but serious side effect may lose the ability to claim compensation offered by the act.
“Many of us gasped when he said that,” Dr. Talbot said, “because that’s a big deal.”
The ACIP signaled that it is considering recommending boosters for a much narrower slice of the American population than the Biden administration has suggested.
They said that so far, the data point only to the need for boosters for seniors, who are the patients most likely to experience breakthrough infections that require hospitalization, and health care workers, who are needed now more than ever and cannot work if they’re sick.
In a White House news briefing Aug. 31, CDC Director Rochelle Walensky, MD, was asked about the ACIP’s conclusions and whether she believed there were enough data to recommend booster shots for most Americans 8 months after their last dose.
“The ACIP did not review international data that actually has led us to be even more concerned about increased risk of vaccine effectiveness waning against hospitalization, severe disease, and death. They will be reviewing that as well,” she said.
A version of this article first appeared on Medscape.com.
That plan, which was first announced on Aug. 18, has raised eyebrows because it comes in advance of regulatory reviews by the Food and Drug Administration and recommendations from the Centers for Disease Control and Prevention. Those reviews are needed to determine whether third doses of these vaccines are effective or even safe. The move could have important legal ramifications for doctors and patients, too.
On Aug. 31, two high-level officials in the FDA’s Office of Vaccines Research and Review abruptly resigned amid reports that they were angry that the Biden administration was making decisions that should be left up to that agency.
So far, data show that the vaccines are highly effective at preventing the most severe consequences of COVID-19 – hospitalization and death – even regarding the Delta variant. The World Health Organization has urged wealthy nations such as the United States not to offer boosters so that the limited supply of vaccines can be directed to countries with fewer resources.
White House supports boosters
In a recent press briefing, Jeff Zients, the White House COVID-19 response coordinator, defended the move.
“You know, the booster decision, which you referenced ... was made by and announced by the nation’s leading public health officials, including Dr. Walensky; Dr. Fauci; Surgeon General Vivek Murthy; Dr. Janet Woodcock; the FDA acting commissioner, Dr. Francis Collins; Dr. Kessler; and others,” Mr. Zients said.
“And as our medical experts laid out, having reviewed all of the available data, it is in their clinical judgment that it is time to prepare Americans for a booster shot.”
He said a target date of Sept. 20 was announced so as to give states and practitioners time to prepare. He also said the move to give boosters was meant to help the United States stay ahead of a rapidly changing virus. Mr. Zients added that whether boosters will be administered starting on Sept. 20 depends on the FDA’s and CDC’s giving the go-ahead.
“Booster doses are going to be handled the same way all vaccines are handled,” said Kristen Nordlund, a CDC spokesperson. “Companies will have to provide data to FDA. FDA will have to make a decision and authorize the use of those, and ACIP [the Advisory Committee on Immunization Practices] will have to look at the evidence as well and make recommendations on top of FDA’s regulatory action,” she said.
Ms. Nordlund agreed that the planned Sept. 20 start date for boosters was something to which they aspired and was not necessarily set.
Historically, the FDA has needed at least 4 months to review a change to a vaccine’s approval, even on an accelerated schedule. Reviewers use that time to assess data regarding individual patients in a study, to review raw data, and essentially to check a drug company’s math and conclusions. The Biden administration’s timeline would shorten that review period from months to just a few weeks.
‘FDA in a very difficult position’
After the FDA approves, the ACIP of the CDC must meet to review the evidence and make recommendations on the use of the boosters in the United States.
Pfizer says it completed its submission for a supplemental biologics license application to the FDA on Aug. 27. To meet a Sept. 20 timeline, the entire process would have to be completed within 3 weeks.
“I don’t think that was handled, you know, ideally,” said Peter Lurie, MD, president of the Center for Science in the Public Interest and former associate commissioner of public health strategy and analysis at the FDA.
“It puts FDA in a very difficult position,” Dr. Lurie said. “It’s almost as if the decision has been made and they’re just checking a box, and that is, you know, contrary to the what FDA – at least the internal people at FDA – have been trying to do for ages.”
He said the agency took great pains with the emergency use authorizations and the full approvals of the vaccines to work as rapidly but thoroughly as possible. They did not skip steps.
“I think all of that reflected very well on the agency,” Dr. Lurie said. “And I think it worked out well in terms of trust in the vaccines.”
Although additional doses of vaccine are expected to be safe, little is known about side effects or adverse events after a third dose.
“It’s critical to wait for additional data and regulatory allowance for booster doses,” Sara Oliver, MD, a member of the CDC’s epidemic intelligence service, said in an Aug. 30 presentation to the ACIP, which is charged with making recommendations for use of all vaccines in the United States.
Boosters already being given
But after the White House announced that boosters were on the way, many people are not waiting.
Many health care practitioners and pharmacies have already been giving people third doses of vaccines, even if they are not among the immunocompromised – the group for which the shots are currently approved.
“You can walk into a pharmacy and ask for a third dose. Depending on which pharmacy you go to, you may get it,” said Helen Talbot, MD, associate professor of medicine at Vanderbilt University, Nashville, Tenn., and a member of the ACIP.
She says she has a friend who recently went for a checkup and was offered a third dose. His physician is already giving extra doses to everyone who is older than 65.
Dr. Talbot said that in fairness, pharmacies in the United States are throwing away doses of vaccine because they are expiring before they get used.
“Many of us may or may not be ready to give a third dose but would rather give someone a third dose than throw a vaccine away,” she said.
Consequences of a third shot
But giving or getting a third dose before approval by the FDA may have legal consequences.
In the ACIP meeting on Aug. 30, Demetre Daskalakis, MD, who leads vaccine equity efforts at the CDC, cautioned that physicians who give extra doses of the vaccine before the FDA and CDC have signed off may be in violation of practitioner agreements with the federal government and might not be covered by the federal PREP Act. The PREP Act provides immunity from lawsuits for people who administer COVID-19 vaccines and compensates patients in the event of injury. Patients who get a vaccine and suffer a rare but serious side effect may lose the ability to claim compensation offered by the act.
“Many of us gasped when he said that,” Dr. Talbot said, “because that’s a big deal.”
The ACIP signaled that it is considering recommending boosters for a much narrower slice of the American population than the Biden administration has suggested.
They said that so far, the data point only to the need for boosters for seniors, who are the patients most likely to experience breakthrough infections that require hospitalization, and health care workers, who are needed now more than ever and cannot work if they’re sick.
In a White House news briefing Aug. 31, CDC Director Rochelle Walensky, MD, was asked about the ACIP’s conclusions and whether she believed there were enough data to recommend booster shots for most Americans 8 months after their last dose.
“The ACIP did not review international data that actually has led us to be even more concerned about increased risk of vaccine effectiveness waning against hospitalization, severe disease, and death. They will be reviewing that as well,” she said.
A version of this article first appeared on Medscape.com.
That plan, which was first announced on Aug. 18, has raised eyebrows because it comes in advance of regulatory reviews by the Food and Drug Administration and recommendations from the Centers for Disease Control and Prevention. Those reviews are needed to determine whether third doses of these vaccines are effective or even safe. The move could have important legal ramifications for doctors and patients, too.
On Aug. 31, two high-level officials in the FDA’s Office of Vaccines Research and Review abruptly resigned amid reports that they were angry that the Biden administration was making decisions that should be left up to that agency.
So far, data show that the vaccines are highly effective at preventing the most severe consequences of COVID-19 – hospitalization and death – even regarding the Delta variant. The World Health Organization has urged wealthy nations such as the United States not to offer boosters so that the limited supply of vaccines can be directed to countries with fewer resources.
White House supports boosters
In a recent press briefing, Jeff Zients, the White House COVID-19 response coordinator, defended the move.
“You know, the booster decision, which you referenced ... was made by and announced by the nation’s leading public health officials, including Dr. Walensky; Dr. Fauci; Surgeon General Vivek Murthy; Dr. Janet Woodcock; the FDA acting commissioner, Dr. Francis Collins; Dr. Kessler; and others,” Mr. Zients said.
“And as our medical experts laid out, having reviewed all of the available data, it is in their clinical judgment that it is time to prepare Americans for a booster shot.”
He said a target date of Sept. 20 was announced so as to give states and practitioners time to prepare. He also said the move to give boosters was meant to help the United States stay ahead of a rapidly changing virus. Mr. Zients added that whether boosters will be administered starting on Sept. 20 depends on the FDA’s and CDC’s giving the go-ahead.
“Booster doses are going to be handled the same way all vaccines are handled,” said Kristen Nordlund, a CDC spokesperson. “Companies will have to provide data to FDA. FDA will have to make a decision and authorize the use of those, and ACIP [the Advisory Committee on Immunization Practices] will have to look at the evidence as well and make recommendations on top of FDA’s regulatory action,” she said.
Ms. Nordlund agreed that the planned Sept. 20 start date for boosters was something to which they aspired and was not necessarily set.
Historically, the FDA has needed at least 4 months to review a change to a vaccine’s approval, even on an accelerated schedule. Reviewers use that time to assess data regarding individual patients in a study, to review raw data, and essentially to check a drug company’s math and conclusions. The Biden administration’s timeline would shorten that review period from months to just a few weeks.
‘FDA in a very difficult position’
After the FDA approves, the ACIP of the CDC must meet to review the evidence and make recommendations on the use of the boosters in the United States.
Pfizer says it completed its submission for a supplemental biologics license application to the FDA on Aug. 27. To meet a Sept. 20 timeline, the entire process would have to be completed within 3 weeks.
“I don’t think that was handled, you know, ideally,” said Peter Lurie, MD, president of the Center for Science in the Public Interest and former associate commissioner of public health strategy and analysis at the FDA.
“It puts FDA in a very difficult position,” Dr. Lurie said. “It’s almost as if the decision has been made and they’re just checking a box, and that is, you know, contrary to the what FDA – at least the internal people at FDA – have been trying to do for ages.”
He said the agency took great pains with the emergency use authorizations and the full approvals of the vaccines to work as rapidly but thoroughly as possible. They did not skip steps.
“I think all of that reflected very well on the agency,” Dr. Lurie said. “And I think it worked out well in terms of trust in the vaccines.”
Although additional doses of vaccine are expected to be safe, little is known about side effects or adverse events after a third dose.
“It’s critical to wait for additional data and regulatory allowance for booster doses,” Sara Oliver, MD, a member of the CDC’s epidemic intelligence service, said in an Aug. 30 presentation to the ACIP, which is charged with making recommendations for use of all vaccines in the United States.
Boosters already being given
But after the White House announced that boosters were on the way, many people are not waiting.
Many health care practitioners and pharmacies have already been giving people third doses of vaccines, even if they are not among the immunocompromised – the group for which the shots are currently approved.
“You can walk into a pharmacy and ask for a third dose. Depending on which pharmacy you go to, you may get it,” said Helen Talbot, MD, associate professor of medicine at Vanderbilt University, Nashville, Tenn., and a member of the ACIP.
She says she has a friend who recently went for a checkup and was offered a third dose. His physician is already giving extra doses to everyone who is older than 65.
Dr. Talbot said that in fairness, pharmacies in the United States are throwing away doses of vaccine because they are expiring before they get used.
“Many of us may or may not be ready to give a third dose but would rather give someone a third dose than throw a vaccine away,” she said.
Consequences of a third shot
But giving or getting a third dose before approval by the FDA may have legal consequences.
In the ACIP meeting on Aug. 30, Demetre Daskalakis, MD, who leads vaccine equity efforts at the CDC, cautioned that physicians who give extra doses of the vaccine before the FDA and CDC have signed off may be in violation of practitioner agreements with the federal government and might not be covered by the federal PREP Act. The PREP Act provides immunity from lawsuits for people who administer COVID-19 vaccines and compensates patients in the event of injury. Patients who get a vaccine and suffer a rare but serious side effect may lose the ability to claim compensation offered by the act.
“Many of us gasped when he said that,” Dr. Talbot said, “because that’s a big deal.”
The ACIP signaled that it is considering recommending boosters for a much narrower slice of the American population than the Biden administration has suggested.
They said that so far, the data point only to the need for boosters for seniors, who are the patients most likely to experience breakthrough infections that require hospitalization, and health care workers, who are needed now more than ever and cannot work if they’re sick.
In a White House news briefing Aug. 31, CDC Director Rochelle Walensky, MD, was asked about the ACIP’s conclusions and whether she believed there were enough data to recommend booster shots for most Americans 8 months after their last dose.
“The ACIP did not review international data that actually has led us to be even more concerned about increased risk of vaccine effectiveness waning against hospitalization, severe disease, and death. They will be reviewing that as well,” she said.
A version of this article first appeared on Medscape.com.
WHO tracking new COVID-19 variant called Mu
The variant, also known as B.1.621, was first identified in Colombia in January. It has now been detected in 43 countries and was added to the WHO’s “variant of interest” list Aug. 30.
“The Mu variant has a constellation of mutations that indicate potential properties of immune escape,” the WHO wrote in its weekly COVID-19 update on Aug 31.
Preliminary data suggests that the Mu variant may be able to evade antibodies at levels similar to the Beta variant, the WHO wrote, though more studies are needed. The Beta variant, also known as B.1.351, was first detected in South Africa and has shown some ability to evade vaccines.
As of Aug. 29, the global prevalence of the Mu variant appears to be less than 0.1%. But its prevalence in South America has “consistently increased,” the WHO wrote, now making up 39% of cases in Colombia and 13% of cases in Ecuador.
More than 4,700 cases of the Mu variant have been identified worldwide through genomic sequencing, according to Outbreak.info, an open-source database operated by Scripps Research. The United States has identified 2,011 of these cases, with 348 in California. As of Sept. 2, only one state -- Nebraska -- had not yet reported a Mu case.
“At the moment, it looks like there’s genuine cause for concern in USA, Central America, and South America, but as we saw with Delta, a potent variant can traverse the globe in the blink of an eye,” Danny Altmann, PhD, an immunologist at Imperial College London, told The Telegraph.
The WHO is monitoring nine variants with genetic mutations that could make them more transmissible, lead to more severe disease, and help them evade vaccines. The Delta variant, which is now a dominant form of the virus in the United States and worldwide, has led to a surge in cases and hospitalizations this summer.
In its report, the WHO said it would monitor the Mu variant for changes, “particularly with the co-circulation of the Delta variant.”
“Mu looks potentially good at immune evasion,” Dr. Altmann told The Telegraph. “For my taste, it’s a stark reminder that this isn’t by any means over. On a planet of 4.4 million-plus new infections per week, there are new variants popping up all the time, and little reason to feel complacent.”
A version of this article first appeared on WebMD.com.
The variant, also known as B.1.621, was first identified in Colombia in January. It has now been detected in 43 countries and was added to the WHO’s “variant of interest” list Aug. 30.
“The Mu variant has a constellation of mutations that indicate potential properties of immune escape,” the WHO wrote in its weekly COVID-19 update on Aug 31.
Preliminary data suggests that the Mu variant may be able to evade antibodies at levels similar to the Beta variant, the WHO wrote, though more studies are needed. The Beta variant, also known as B.1.351, was first detected in South Africa and has shown some ability to evade vaccines.
As of Aug. 29, the global prevalence of the Mu variant appears to be less than 0.1%. But its prevalence in South America has “consistently increased,” the WHO wrote, now making up 39% of cases in Colombia and 13% of cases in Ecuador.
More than 4,700 cases of the Mu variant have been identified worldwide through genomic sequencing, according to Outbreak.info, an open-source database operated by Scripps Research. The United States has identified 2,011 of these cases, with 348 in California. As of Sept. 2, only one state -- Nebraska -- had not yet reported a Mu case.
“At the moment, it looks like there’s genuine cause for concern in USA, Central America, and South America, but as we saw with Delta, a potent variant can traverse the globe in the blink of an eye,” Danny Altmann, PhD, an immunologist at Imperial College London, told The Telegraph.
The WHO is monitoring nine variants with genetic mutations that could make them more transmissible, lead to more severe disease, and help them evade vaccines. The Delta variant, which is now a dominant form of the virus in the United States and worldwide, has led to a surge in cases and hospitalizations this summer.
In its report, the WHO said it would monitor the Mu variant for changes, “particularly with the co-circulation of the Delta variant.”
“Mu looks potentially good at immune evasion,” Dr. Altmann told The Telegraph. “For my taste, it’s a stark reminder that this isn’t by any means over. On a planet of 4.4 million-plus new infections per week, there are new variants popping up all the time, and little reason to feel complacent.”
A version of this article first appeared on WebMD.com.
The variant, also known as B.1.621, was first identified in Colombia in January. It has now been detected in 43 countries and was added to the WHO’s “variant of interest” list Aug. 30.
“The Mu variant has a constellation of mutations that indicate potential properties of immune escape,” the WHO wrote in its weekly COVID-19 update on Aug 31.
Preliminary data suggests that the Mu variant may be able to evade antibodies at levels similar to the Beta variant, the WHO wrote, though more studies are needed. The Beta variant, also known as B.1.351, was first detected in South Africa and has shown some ability to evade vaccines.
As of Aug. 29, the global prevalence of the Mu variant appears to be less than 0.1%. But its prevalence in South America has “consistently increased,” the WHO wrote, now making up 39% of cases in Colombia and 13% of cases in Ecuador.
More than 4,700 cases of the Mu variant have been identified worldwide through genomic sequencing, according to Outbreak.info, an open-source database operated by Scripps Research. The United States has identified 2,011 of these cases, with 348 in California. As of Sept. 2, only one state -- Nebraska -- had not yet reported a Mu case.
“At the moment, it looks like there’s genuine cause for concern in USA, Central America, and South America, but as we saw with Delta, a potent variant can traverse the globe in the blink of an eye,” Danny Altmann, PhD, an immunologist at Imperial College London, told The Telegraph.
The WHO is monitoring nine variants with genetic mutations that could make them more transmissible, lead to more severe disease, and help them evade vaccines. The Delta variant, which is now a dominant form of the virus in the United States and worldwide, has led to a surge in cases and hospitalizations this summer.
In its report, the WHO said it would monitor the Mu variant for changes, “particularly with the co-circulation of the Delta variant.”
“Mu looks potentially good at immune evasion,” Dr. Altmann told The Telegraph. “For my taste, it’s a stark reminder that this isn’t by any means over. On a planet of 4.4 million-plus new infections per week, there are new variants popping up all the time, and little reason to feel complacent.”
A version of this article first appeared on WebMD.com.
A long look at long haulers
With the number of pediatric infections with SARS-CoV-2 rising it is not surprising that children with persistent symptoms are beginning to accumulate. Who are these pediatric “long haulers” and do they differ from their adult counterparts? The answer is far from clear because the terms “long COVID” and “long hauler” are not well defined. But, I suspect we will find that they will be similar in most respects.
In a recent Guest Essay in the New York Times, two medical school professors attempt to inject some common sense into the long hauler phenomenon. (“The Truth About Long Covid is Complicated. Better Treatment Isn’t,” Adam Gaffney and Zackary Berger, The New York Times, Aug. 18, 2021).
The authors divide the patients with long COVID into three categories. The first includes those who are complaining of persistent cough and fatigue for up to 3 months, a not unexpected course for patients recovering from a significant respiratory illness like pneumonia.
The second group comprises patients who developed acute respiratory distress syndrome during the course of their SARS-CoV-2 infection. These unfortunate individuals likely incurred lung damage that may have triggered renal damage and delirium and may never regain full function.
The third group of patients reports a wide variety of less specific symptoms including, but not limited to, severe fatigue, brain fog, shortness of breath, gastrointestinal symptoms, chronic pain, and palpitations.
The authors of the essay refer to several studies in which there was little if any correlation between these patients’ complaints and their antibody levels. In fact, one study of adolescents found that in a group with similar symptoms many of the individuals had no serologic evidence of SARS-CoV-2 infection.
Unfortunately, the lay public, the media, and some physicians make no distinction between these three groups and lump them all under the same long COVID umbrella. The resulting confusion seeds unwarranted anxiety among the first and third groups and may prevent some individuals from receiving the appropriate attention they deserve.
I suspect that like me, many of you see some similarities between this third group of long COVID patients and adolescents whose persistent symptoms don’t quite fit with their primary illness. Patients labeled as having post-concussion syndrome or “chronic Lyme disease” come immediately to mind. In both conditions, many of the patients had little if any evidence of severe insult from the initial event but continue to complain about a variety of symptoms including severe fatigue and brain fog.
We have done a very poor job of properly managing these patients. And there are a lot of them. A large part of the problem is labeling. In the old days one might have said these patients were having “psychosomatic” symptoms. But, while it may be an accurate description, like the term “retardation” it has been permanently tarnished. Fortunately, most of us are smart enough to avoid telling these patients that it is all in their heads.
However, convincing an individual that many of his symptoms may be the result of the psychological insult from the original disease compounded by other stresses and lifestyle factors can be a difficult sell. The task is made particularly difficult when there continue to be physicians who will miss or ignore the obvious and embark on therapeutic endeavors that are not only ineffective but can serve as a distraction from the real work of listening to and engaging these patients whose suffering may be just as real as that of those long haulers with structural damage.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
With the number of pediatric infections with SARS-CoV-2 rising it is not surprising that children with persistent symptoms are beginning to accumulate. Who are these pediatric “long haulers” and do they differ from their adult counterparts? The answer is far from clear because the terms “long COVID” and “long hauler” are not well defined. But, I suspect we will find that they will be similar in most respects.
In a recent Guest Essay in the New York Times, two medical school professors attempt to inject some common sense into the long hauler phenomenon. (“The Truth About Long Covid is Complicated. Better Treatment Isn’t,” Adam Gaffney and Zackary Berger, The New York Times, Aug. 18, 2021).
The authors divide the patients with long COVID into three categories. The first includes those who are complaining of persistent cough and fatigue for up to 3 months, a not unexpected course for patients recovering from a significant respiratory illness like pneumonia.
The second group comprises patients who developed acute respiratory distress syndrome during the course of their SARS-CoV-2 infection. These unfortunate individuals likely incurred lung damage that may have triggered renal damage and delirium and may never regain full function.
The third group of patients reports a wide variety of less specific symptoms including, but not limited to, severe fatigue, brain fog, shortness of breath, gastrointestinal symptoms, chronic pain, and palpitations.
The authors of the essay refer to several studies in which there was little if any correlation between these patients’ complaints and their antibody levels. In fact, one study of adolescents found that in a group with similar symptoms many of the individuals had no serologic evidence of SARS-CoV-2 infection.
Unfortunately, the lay public, the media, and some physicians make no distinction between these three groups and lump them all under the same long COVID umbrella. The resulting confusion seeds unwarranted anxiety among the first and third groups and may prevent some individuals from receiving the appropriate attention they deserve.
I suspect that like me, many of you see some similarities between this third group of long COVID patients and adolescents whose persistent symptoms don’t quite fit with their primary illness. Patients labeled as having post-concussion syndrome or “chronic Lyme disease” come immediately to mind. In both conditions, many of the patients had little if any evidence of severe insult from the initial event but continue to complain about a variety of symptoms including severe fatigue and brain fog.
We have done a very poor job of properly managing these patients. And there are a lot of them. A large part of the problem is labeling. In the old days one might have said these patients were having “psychosomatic” symptoms. But, while it may be an accurate description, like the term “retardation” it has been permanently tarnished. Fortunately, most of us are smart enough to avoid telling these patients that it is all in their heads.
However, convincing an individual that many of his symptoms may be the result of the psychological insult from the original disease compounded by other stresses and lifestyle factors can be a difficult sell. The task is made particularly difficult when there continue to be physicians who will miss or ignore the obvious and embark on therapeutic endeavors that are not only ineffective but can serve as a distraction from the real work of listening to and engaging these patients whose suffering may be just as real as that of those long haulers with structural damage.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
With the number of pediatric infections with SARS-CoV-2 rising it is not surprising that children with persistent symptoms are beginning to accumulate. Who are these pediatric “long haulers” and do they differ from their adult counterparts? The answer is far from clear because the terms “long COVID” and “long hauler” are not well defined. But, I suspect we will find that they will be similar in most respects.
In a recent Guest Essay in the New York Times, two medical school professors attempt to inject some common sense into the long hauler phenomenon. (“The Truth About Long Covid is Complicated. Better Treatment Isn’t,” Adam Gaffney and Zackary Berger, The New York Times, Aug. 18, 2021).
The authors divide the patients with long COVID into three categories. The first includes those who are complaining of persistent cough and fatigue for up to 3 months, a not unexpected course for patients recovering from a significant respiratory illness like pneumonia.
The second group comprises patients who developed acute respiratory distress syndrome during the course of their SARS-CoV-2 infection. These unfortunate individuals likely incurred lung damage that may have triggered renal damage and delirium and may never regain full function.
The third group of patients reports a wide variety of less specific symptoms including, but not limited to, severe fatigue, brain fog, shortness of breath, gastrointestinal symptoms, chronic pain, and palpitations.
The authors of the essay refer to several studies in which there was little if any correlation between these patients’ complaints and their antibody levels. In fact, one study of adolescents found that in a group with similar symptoms many of the individuals had no serologic evidence of SARS-CoV-2 infection.
Unfortunately, the lay public, the media, and some physicians make no distinction between these three groups and lump them all under the same long COVID umbrella. The resulting confusion seeds unwarranted anxiety among the first and third groups and may prevent some individuals from receiving the appropriate attention they deserve.
I suspect that like me, many of you see some similarities between this third group of long COVID patients and adolescents whose persistent symptoms don’t quite fit with their primary illness. Patients labeled as having post-concussion syndrome or “chronic Lyme disease” come immediately to mind. In both conditions, many of the patients had little if any evidence of severe insult from the initial event but continue to complain about a variety of symptoms including severe fatigue and brain fog.
We have done a very poor job of properly managing these patients. And there are a lot of them. A large part of the problem is labeling. In the old days one might have said these patients were having “psychosomatic” symptoms. But, while it may be an accurate description, like the term “retardation” it has been permanently tarnished. Fortunately, most of us are smart enough to avoid telling these patients that it is all in their heads.
However, convincing an individual that many of his symptoms may be the result of the psychological insult from the original disease compounded by other stresses and lifestyle factors can be a difficult sell. The task is made particularly difficult when there continue to be physicians who will miss or ignore the obvious and embark on therapeutic endeavors that are not only ineffective but can serve as a distraction from the real work of listening to and engaging these patients whose suffering may be just as real as that of those long haulers with structural damage.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
COVID-19 disease may actually cause preeclampsia, suggests study
New evidence strongly suggests that COVID-19 disease causes an increased risk of preeclampsia and preterm birth in those who have an infection while pregnant, according to a retrospective observational study published in the American Journal of Obstetrics and Gynecology. Though the study was observational, its primary finding was a dose-response relationship between the severity of COVID-19 disease and the likelihood of preeclampsia or preterm birth, fulfilling a key criterion for establishing causality in an association.
“The fact that 43% (13/30) of the cases of preeclampsia diagnosed after SARS-Cov-2 infection were preterm preeclampsia (< 37 weeks) suggests that COVID-19 may be a cause for medically indicated preterm birth that contributes to the excess preterm birth delivery rate previously reported,” wrote Jonathan Lai, MD, of the Fetal Medicine Research Institute of King’s College Hospital, London, and colleagues. The study also found an increased likelihood of COVID-19 disease in those who had preeclampsia before their infection. “Whether preeclampsia can predispose COVID-19 some cases, or that the two conditions may co-occur because they share similar risk factors requires further investigation,” the authors wrote.
It’s also unclear whether the increased risk of pre-eclampsia is contributing to the higher preterm birth risk, according to Linda Eckert, MD, a professor of Ob.Gyn. at The University of Washington who specializes in maternal immunization.
“COVID is linked to preeclampsia in this study, and COVID is linked to preterm birth,” Dr. Eckert said in an interview. “The question of whether preeclampsia leading to preterm birth is also linked to infection is not possible to tease out in this study as all the factors are likely interrelated. There is a relationship between COVID and preterm birth absent preeclampsia.”
The researchers retrospectively examined data from 1,223 pregnant women who tested positive for SARS-CoV-2 between February 2020 and March 2021 at any of 14 National Health Service maternity hospitals in the United Kingdom. The researchers compared the severity of disease among the women with their risk of preeclampsia as a primary outcome, followed by the outcomes of preterm birth and gestational age at delivery.
COVID-19 infections were classified as asymptomatic, mild illness (lacking shortness of breath, dyspnea, or abnormal chest imaging), moderate illness (evidence of lower respiratory disease but an oxygen saturation of at least 94%), and severe illness (requiring “high dependency or intensive care secondary to respiratory impairment/failure or multiorgan dysfunction”).
The researchers adjusted their analysis of preeclampsia to account for prior risk of preeclampsia based on maternal characteristics and medical history. Analysis of preterm birth risk included adjustment for maternal age, weight, height, race, method of conception, chronic hypertension, smoking, and diabetes.
Preeclampsia occurred in 4.2% of the women, and 17.6% of the women had a preterm birth. In addition, 1.3% of the cohort had a miscarriage, and there were 10 (0.81%) fetal deaths. Since 21 cases of preeclampsia occurred before the women tested positive, the researchers removed those cases from the analysis. Among the remaining 30 cases, 13 women had preterm preeclampsia and 17 had term preeclampsia.
When the researchers compared the study population’s risk of preeclampsia with that of a separate population with similar risk factors, they found a dose-response increased risk in those with COVID-19 infections. While 1.9% of asymptomatic patients had preeclampsia, incidence was 2.2% in patients with mild disease, 5.7% in those with moderate disease, and 11.1% in those with severe disease. Women with severe COVID-19 tended to be older and to have a higher body mass index.
After adjustments, women were nearly five times more likely to develop preeclampsia if they had severe COVID-19 compared to women with asymptomatic infection (adjusted relative risk [aRR] = 4.9). Those with moderate or severe disease had triple the risk of preeclampsia compared to those with mild or asymptomatic infection (aRR = 3.3).
To investigate whether having preeclampsia predisposes women to develop COVID-19 disease, the researchers compared the women who had preeclampsia before their infection with women in the study who never developed preeclampsia. Although they found a trend toward higher risk of moderate or severe COVID-19 following preeclampsia, the association was not significant before or after adjustment.
The researchers also found a dose-response relationship in risk of preterm birth. While 11.7% of asymptomatic patients had preterm birth, the incidence was 12.8% in those with mild COVID-19, 29.9% in those with moderate disease, and 69.4% in those with severe disease. Women with severe disease were more than five times more likely to have a preterm birth than were women with an asymptomatic infection (aRR = 5.64), and the risk of preterm birth was 2.5 times greater in women with moderate disease (aRR = 2.47).
“Moreover, there was a dose-response relationship between gestational age at delivery and the severity of SARS-CoV-2 infection,” the authors reported. Mean gestational age at delivery was 38.7 weeks in asymptomatic women compared to 37.5 weeks for those with moderate disease and 33 weeks in those with severe disease (P < .001).
”The more severe the infection with SARS-CoV-2, the greater the risk of preeclampsia and preterm birth,” the authors wrote. “SARS-CoV-2 infection can lead to endothelial dysfunction, intravascular inflammation, proteinuria, activation of thrombin, and hypertension, which are all features of preeclampsia. Therefore, a causal relationship must be considered.”
A dose-response association is only one criterion for causality, however, so it’s still premature to say definitively that a causal relationship exists, Dr. Eckert said.
“More investigation in different populations across different ethnicities is needed before causality can be confidently assured,” she said.
Anthony Sciscione, DO, director of maternal-fetal medicine and the ob.gyn. residency at ChristianaCare in Delaware, agreed that the precise relationship between the two remains unresolved.
”We don’t know what causes preeclampsia,” but “we strongly suspect it has to do with a placental dysfunction, or endothelial dysfunction, and it’s really clear that women who get COVID have a much higher risk of preeclampsia,” Dr. Sciscione said in an interview. It’s possible that no real relationship exists between the two (or that greater surveillance of women with COVID-19 is picking up the relationship) but it’s more likely that one of two other situations is happening, Dr. Sciscione said. Either COVID-19 involves a syndrome that looks like preeclampsia in pregnant women, or the disease “leads to the cascade that causes preeclampsia,” he said.
One clear clinical implication of these findings is that “women who have severe COVID early in pregnancy may need to be watched more closely for signs of developing preeclampsia” and that “women with severe COVID are more likely to have preterm births,” Dr. Eckert said. “This absolutely lends support to the need for pregnant individuals to receive a COVID vaccine.”
Dr. Sciscione said his experience counseling pregnant patients about the vaccine has made it clear that patients generally want to do what’s safest for their babies and may feel uneasiness about the safety of the vaccine. “The truth is, now there’s mounting evidence that there are fetal effects, not just maternal effects” from COVID-19 disease. He added that preterm birth is associated with a variety of long-term adverse outcomes, such as cerebral palsy and learning disabilities.
“At this time it’s critically important that women be offered and get the vaccine because we know that people that are vaccinated don’t get as sick,” Dr. Sciscione said.
The research was funded by the Fetal Medicine Foundation and the National Institutes of Health. The authors and Dr. Eckert have no disclosures. Dr. Sciscione is the associate editor of the American Journal of Obstetrics and Gynecology, where the study appeared.
New evidence strongly suggests that COVID-19 disease causes an increased risk of preeclampsia and preterm birth in those who have an infection while pregnant, according to a retrospective observational study published in the American Journal of Obstetrics and Gynecology. Though the study was observational, its primary finding was a dose-response relationship between the severity of COVID-19 disease and the likelihood of preeclampsia or preterm birth, fulfilling a key criterion for establishing causality in an association.
“The fact that 43% (13/30) of the cases of preeclampsia diagnosed after SARS-Cov-2 infection were preterm preeclampsia (< 37 weeks) suggests that COVID-19 may be a cause for medically indicated preterm birth that contributes to the excess preterm birth delivery rate previously reported,” wrote Jonathan Lai, MD, of the Fetal Medicine Research Institute of King’s College Hospital, London, and colleagues. The study also found an increased likelihood of COVID-19 disease in those who had preeclampsia before their infection. “Whether preeclampsia can predispose COVID-19 some cases, or that the two conditions may co-occur because they share similar risk factors requires further investigation,” the authors wrote.
It’s also unclear whether the increased risk of pre-eclampsia is contributing to the higher preterm birth risk, according to Linda Eckert, MD, a professor of Ob.Gyn. at The University of Washington who specializes in maternal immunization.
“COVID is linked to preeclampsia in this study, and COVID is linked to preterm birth,” Dr. Eckert said in an interview. “The question of whether preeclampsia leading to preterm birth is also linked to infection is not possible to tease out in this study as all the factors are likely interrelated. There is a relationship between COVID and preterm birth absent preeclampsia.”
The researchers retrospectively examined data from 1,223 pregnant women who tested positive for SARS-CoV-2 between February 2020 and March 2021 at any of 14 National Health Service maternity hospitals in the United Kingdom. The researchers compared the severity of disease among the women with their risk of preeclampsia as a primary outcome, followed by the outcomes of preterm birth and gestational age at delivery.
COVID-19 infections were classified as asymptomatic, mild illness (lacking shortness of breath, dyspnea, or abnormal chest imaging), moderate illness (evidence of lower respiratory disease but an oxygen saturation of at least 94%), and severe illness (requiring “high dependency or intensive care secondary to respiratory impairment/failure or multiorgan dysfunction”).
The researchers adjusted their analysis of preeclampsia to account for prior risk of preeclampsia based on maternal characteristics and medical history. Analysis of preterm birth risk included adjustment for maternal age, weight, height, race, method of conception, chronic hypertension, smoking, and diabetes.
Preeclampsia occurred in 4.2% of the women, and 17.6% of the women had a preterm birth. In addition, 1.3% of the cohort had a miscarriage, and there were 10 (0.81%) fetal deaths. Since 21 cases of preeclampsia occurred before the women tested positive, the researchers removed those cases from the analysis. Among the remaining 30 cases, 13 women had preterm preeclampsia and 17 had term preeclampsia.
When the researchers compared the study population’s risk of preeclampsia with that of a separate population with similar risk factors, they found a dose-response increased risk in those with COVID-19 infections. While 1.9% of asymptomatic patients had preeclampsia, incidence was 2.2% in patients with mild disease, 5.7% in those with moderate disease, and 11.1% in those with severe disease. Women with severe COVID-19 tended to be older and to have a higher body mass index.
After adjustments, women were nearly five times more likely to develop preeclampsia if they had severe COVID-19 compared to women with asymptomatic infection (adjusted relative risk [aRR] = 4.9). Those with moderate or severe disease had triple the risk of preeclampsia compared to those with mild or asymptomatic infection (aRR = 3.3).
To investigate whether having preeclampsia predisposes women to develop COVID-19 disease, the researchers compared the women who had preeclampsia before their infection with women in the study who never developed preeclampsia. Although they found a trend toward higher risk of moderate or severe COVID-19 following preeclampsia, the association was not significant before or after adjustment.
The researchers also found a dose-response relationship in risk of preterm birth. While 11.7% of asymptomatic patients had preterm birth, the incidence was 12.8% in those with mild COVID-19, 29.9% in those with moderate disease, and 69.4% in those with severe disease. Women with severe disease were more than five times more likely to have a preterm birth than were women with an asymptomatic infection (aRR = 5.64), and the risk of preterm birth was 2.5 times greater in women with moderate disease (aRR = 2.47).
“Moreover, there was a dose-response relationship between gestational age at delivery and the severity of SARS-CoV-2 infection,” the authors reported. Mean gestational age at delivery was 38.7 weeks in asymptomatic women compared to 37.5 weeks for those with moderate disease and 33 weeks in those with severe disease (P < .001).
”The more severe the infection with SARS-CoV-2, the greater the risk of preeclampsia and preterm birth,” the authors wrote. “SARS-CoV-2 infection can lead to endothelial dysfunction, intravascular inflammation, proteinuria, activation of thrombin, and hypertension, which are all features of preeclampsia. Therefore, a causal relationship must be considered.”
A dose-response association is only one criterion for causality, however, so it’s still premature to say definitively that a causal relationship exists, Dr. Eckert said.
“More investigation in different populations across different ethnicities is needed before causality can be confidently assured,” she said.
Anthony Sciscione, DO, director of maternal-fetal medicine and the ob.gyn. residency at ChristianaCare in Delaware, agreed that the precise relationship between the two remains unresolved.
”We don’t know what causes preeclampsia,” but “we strongly suspect it has to do with a placental dysfunction, or endothelial dysfunction, and it’s really clear that women who get COVID have a much higher risk of preeclampsia,” Dr. Sciscione said in an interview. It’s possible that no real relationship exists between the two (or that greater surveillance of women with COVID-19 is picking up the relationship) but it’s more likely that one of two other situations is happening, Dr. Sciscione said. Either COVID-19 involves a syndrome that looks like preeclampsia in pregnant women, or the disease “leads to the cascade that causes preeclampsia,” he said.
One clear clinical implication of these findings is that “women who have severe COVID early in pregnancy may need to be watched more closely for signs of developing preeclampsia” and that “women with severe COVID are more likely to have preterm births,” Dr. Eckert said. “This absolutely lends support to the need for pregnant individuals to receive a COVID vaccine.”
Dr. Sciscione said his experience counseling pregnant patients about the vaccine has made it clear that patients generally want to do what’s safest for their babies and may feel uneasiness about the safety of the vaccine. “The truth is, now there’s mounting evidence that there are fetal effects, not just maternal effects” from COVID-19 disease. He added that preterm birth is associated with a variety of long-term adverse outcomes, such as cerebral palsy and learning disabilities.
“At this time it’s critically important that women be offered and get the vaccine because we know that people that are vaccinated don’t get as sick,” Dr. Sciscione said.
The research was funded by the Fetal Medicine Foundation and the National Institutes of Health. The authors and Dr. Eckert have no disclosures. Dr. Sciscione is the associate editor of the American Journal of Obstetrics and Gynecology, where the study appeared.
New evidence strongly suggests that COVID-19 disease causes an increased risk of preeclampsia and preterm birth in those who have an infection while pregnant, according to a retrospective observational study published in the American Journal of Obstetrics and Gynecology. Though the study was observational, its primary finding was a dose-response relationship between the severity of COVID-19 disease and the likelihood of preeclampsia or preterm birth, fulfilling a key criterion for establishing causality in an association.
“The fact that 43% (13/30) of the cases of preeclampsia diagnosed after SARS-Cov-2 infection were preterm preeclampsia (< 37 weeks) suggests that COVID-19 may be a cause for medically indicated preterm birth that contributes to the excess preterm birth delivery rate previously reported,” wrote Jonathan Lai, MD, of the Fetal Medicine Research Institute of King’s College Hospital, London, and colleagues. The study also found an increased likelihood of COVID-19 disease in those who had preeclampsia before their infection. “Whether preeclampsia can predispose COVID-19 some cases, or that the two conditions may co-occur because they share similar risk factors requires further investigation,” the authors wrote.
It’s also unclear whether the increased risk of pre-eclampsia is contributing to the higher preterm birth risk, according to Linda Eckert, MD, a professor of Ob.Gyn. at The University of Washington who specializes in maternal immunization.
“COVID is linked to preeclampsia in this study, and COVID is linked to preterm birth,” Dr. Eckert said in an interview. “The question of whether preeclampsia leading to preterm birth is also linked to infection is not possible to tease out in this study as all the factors are likely interrelated. There is a relationship between COVID and preterm birth absent preeclampsia.”
The researchers retrospectively examined data from 1,223 pregnant women who tested positive for SARS-CoV-2 between February 2020 and March 2021 at any of 14 National Health Service maternity hospitals in the United Kingdom. The researchers compared the severity of disease among the women with their risk of preeclampsia as a primary outcome, followed by the outcomes of preterm birth and gestational age at delivery.
COVID-19 infections were classified as asymptomatic, mild illness (lacking shortness of breath, dyspnea, or abnormal chest imaging), moderate illness (evidence of lower respiratory disease but an oxygen saturation of at least 94%), and severe illness (requiring “high dependency or intensive care secondary to respiratory impairment/failure or multiorgan dysfunction”).
The researchers adjusted their analysis of preeclampsia to account for prior risk of preeclampsia based on maternal characteristics and medical history. Analysis of preterm birth risk included adjustment for maternal age, weight, height, race, method of conception, chronic hypertension, smoking, and diabetes.
Preeclampsia occurred in 4.2% of the women, and 17.6% of the women had a preterm birth. In addition, 1.3% of the cohort had a miscarriage, and there were 10 (0.81%) fetal deaths. Since 21 cases of preeclampsia occurred before the women tested positive, the researchers removed those cases from the analysis. Among the remaining 30 cases, 13 women had preterm preeclampsia and 17 had term preeclampsia.
When the researchers compared the study population’s risk of preeclampsia with that of a separate population with similar risk factors, they found a dose-response increased risk in those with COVID-19 infections. While 1.9% of asymptomatic patients had preeclampsia, incidence was 2.2% in patients with mild disease, 5.7% in those with moderate disease, and 11.1% in those with severe disease. Women with severe COVID-19 tended to be older and to have a higher body mass index.
After adjustments, women were nearly five times more likely to develop preeclampsia if they had severe COVID-19 compared to women with asymptomatic infection (adjusted relative risk [aRR] = 4.9). Those with moderate or severe disease had triple the risk of preeclampsia compared to those with mild or asymptomatic infection (aRR = 3.3).
To investigate whether having preeclampsia predisposes women to develop COVID-19 disease, the researchers compared the women who had preeclampsia before their infection with women in the study who never developed preeclampsia. Although they found a trend toward higher risk of moderate or severe COVID-19 following preeclampsia, the association was not significant before or after adjustment.
The researchers also found a dose-response relationship in risk of preterm birth. While 11.7% of asymptomatic patients had preterm birth, the incidence was 12.8% in those with mild COVID-19, 29.9% in those with moderate disease, and 69.4% in those with severe disease. Women with severe disease were more than five times more likely to have a preterm birth than were women with an asymptomatic infection (aRR = 5.64), and the risk of preterm birth was 2.5 times greater in women with moderate disease (aRR = 2.47).
“Moreover, there was a dose-response relationship between gestational age at delivery and the severity of SARS-CoV-2 infection,” the authors reported. Mean gestational age at delivery was 38.7 weeks in asymptomatic women compared to 37.5 weeks for those with moderate disease and 33 weeks in those with severe disease (P < .001).
”The more severe the infection with SARS-CoV-2, the greater the risk of preeclampsia and preterm birth,” the authors wrote. “SARS-CoV-2 infection can lead to endothelial dysfunction, intravascular inflammation, proteinuria, activation of thrombin, and hypertension, which are all features of preeclampsia. Therefore, a causal relationship must be considered.”
A dose-response association is only one criterion for causality, however, so it’s still premature to say definitively that a causal relationship exists, Dr. Eckert said.
“More investigation in different populations across different ethnicities is needed before causality can be confidently assured,” she said.
Anthony Sciscione, DO, director of maternal-fetal medicine and the ob.gyn. residency at ChristianaCare in Delaware, agreed that the precise relationship between the two remains unresolved.
”We don’t know what causes preeclampsia,” but “we strongly suspect it has to do with a placental dysfunction, or endothelial dysfunction, and it’s really clear that women who get COVID have a much higher risk of preeclampsia,” Dr. Sciscione said in an interview. It’s possible that no real relationship exists between the two (or that greater surveillance of women with COVID-19 is picking up the relationship) but it’s more likely that one of two other situations is happening, Dr. Sciscione said. Either COVID-19 involves a syndrome that looks like preeclampsia in pregnant women, or the disease “leads to the cascade that causes preeclampsia,” he said.
One clear clinical implication of these findings is that “women who have severe COVID early in pregnancy may need to be watched more closely for signs of developing preeclampsia” and that “women with severe COVID are more likely to have preterm births,” Dr. Eckert said. “This absolutely lends support to the need for pregnant individuals to receive a COVID vaccine.”
Dr. Sciscione said his experience counseling pregnant patients about the vaccine has made it clear that patients generally want to do what’s safest for their babies and may feel uneasiness about the safety of the vaccine. “The truth is, now there’s mounting evidence that there are fetal effects, not just maternal effects” from COVID-19 disease. He added that preterm birth is associated with a variety of long-term adverse outcomes, such as cerebral palsy and learning disabilities.
“At this time it’s critically important that women be offered and get the vaccine because we know that people that are vaccinated don’t get as sick,” Dr. Sciscione said.
The research was funded by the Fetal Medicine Foundation and the National Institutes of Health. The authors and Dr. Eckert have no disclosures. Dr. Sciscione is the associate editor of the American Journal of Obstetrics and Gynecology, where the study appeared.
FROM THE JOURNAL OF OBSTETRICS AND GYNECOLOGY
Expert shares vulvovaginal candidiasis treatment pearls
that was approved in June 2021, Aruna Venkatesan, MD, recommends.
“Ibrexafungerp, an inhibitor of beta (1-3)–glucan synthase, is important for many reasons,” Dr. Venkatesan, chief of dermatology and director of the genital dermatology clinic at Santa Clara Valley Medical Center, San Jose, Calif., said during the annual meeting of the Pacific Dermatologic Association. “It’s one of the few drugs that can be used to treat Candida glabrata when C. glabrata is resistant to azoles and echinocandins. As the second-most common Candida species after C. albicans, C. glabrata is more common in immunosuppressed patients and it can cause mucosal and invasive disease, so ibrexafungerp is a welcome addition to our treatment armamentarium,” said Dr. Venkatesan, clinical professor of dermatology (affiliated) at Stanford (Calif.) Hospital and Clinics, adding that that vulvovaginal candidiasis can be tricky to diagnose. “In medical school, we learned that yeast infection in a woman presents as white, curd-like discharge, but that’s actually a minority of patients.”
For a patient who is being treated with topical steroids or estrogen for a genital condition, but is experiencing worsening itch, redness, or thick white discharge, she recommends performing a KOH exam.
“Instead of using a 15-blade scalpel, as we are used to performing on the skin for tinea, take a sterile [cotton swab], and swab the affected area. You can then apply it to a slide and perform a KOH exam as you normally would. Then look for yeast elements under the microscope. I also find it helpful to send for fungal culture to get speciation, especially in someone who’s not responding to therapy. This is because non-albicans yeast can be more resistant to azoles and require a different treatment plan.”
Often, patients with vulvovaginal candidiasis who present to her clinic are referred from an ob.gyn. and other general practitioners because they have failed a topical or oral azole. “I tend to avoid the topicals,” said Dr. Venkatesan, who is also president-elect of the North American chapter of the International Society for the Study of Vulvovaginal Disease. “If the culture shows C. albicans, I usually treat with oral fluconazole, 150 mg or 200 mg once, and consider repeat weekly dosing. Many patients come to me because they have recurrent refractory disease, so giving it once weekly for 6-8 weeks while they work on their potential risk factors such as diabetic blood sugar control is sensible.”
Non-albicans yeast can be resistant to azoles. If the fungal culture shows C. glabrata in such patients, “consider a course of intravaginal boric acid suppositories,” she advised. “These used to be difficult to give patients, because you would either have to send the prescription to a compounding pharmacy, or have the patients buy the capsules and boric acid crystals separately and make them themselves. That always made me nervous because of the chance of errors. The safety and the concern of taking it by mouth is an issue.” But now, intravaginal boric acid suppositories are available on Amazon and other web sites, and are relatively affordable, she said, adding, “just make sure the patient doesn’t take it by mouth as this is very toxic.”
Dr. Venkatesan reported having no financial disclosures.
that was approved in June 2021, Aruna Venkatesan, MD, recommends.
“Ibrexafungerp, an inhibitor of beta (1-3)–glucan synthase, is important for many reasons,” Dr. Venkatesan, chief of dermatology and director of the genital dermatology clinic at Santa Clara Valley Medical Center, San Jose, Calif., said during the annual meeting of the Pacific Dermatologic Association. “It’s one of the few drugs that can be used to treat Candida glabrata when C. glabrata is resistant to azoles and echinocandins. As the second-most common Candida species after C. albicans, C. glabrata is more common in immunosuppressed patients and it can cause mucosal and invasive disease, so ibrexafungerp is a welcome addition to our treatment armamentarium,” said Dr. Venkatesan, clinical professor of dermatology (affiliated) at Stanford (Calif.) Hospital and Clinics, adding that that vulvovaginal candidiasis can be tricky to diagnose. “In medical school, we learned that yeast infection in a woman presents as white, curd-like discharge, but that’s actually a minority of patients.”
For a patient who is being treated with topical steroids or estrogen for a genital condition, but is experiencing worsening itch, redness, or thick white discharge, she recommends performing a KOH exam.
“Instead of using a 15-blade scalpel, as we are used to performing on the skin for tinea, take a sterile [cotton swab], and swab the affected area. You can then apply it to a slide and perform a KOH exam as you normally would. Then look for yeast elements under the microscope. I also find it helpful to send for fungal culture to get speciation, especially in someone who’s not responding to therapy. This is because non-albicans yeast can be more resistant to azoles and require a different treatment plan.”
Often, patients with vulvovaginal candidiasis who present to her clinic are referred from an ob.gyn. and other general practitioners because they have failed a topical or oral azole. “I tend to avoid the topicals,” said Dr. Venkatesan, who is also president-elect of the North American chapter of the International Society for the Study of Vulvovaginal Disease. “If the culture shows C. albicans, I usually treat with oral fluconazole, 150 mg or 200 mg once, and consider repeat weekly dosing. Many patients come to me because they have recurrent refractory disease, so giving it once weekly for 6-8 weeks while they work on their potential risk factors such as diabetic blood sugar control is sensible.”
Non-albicans yeast can be resistant to azoles. If the fungal culture shows C. glabrata in such patients, “consider a course of intravaginal boric acid suppositories,” she advised. “These used to be difficult to give patients, because you would either have to send the prescription to a compounding pharmacy, or have the patients buy the capsules and boric acid crystals separately and make them themselves. That always made me nervous because of the chance of errors. The safety and the concern of taking it by mouth is an issue.” But now, intravaginal boric acid suppositories are available on Amazon and other web sites, and are relatively affordable, she said, adding, “just make sure the patient doesn’t take it by mouth as this is very toxic.”
Dr. Venkatesan reported having no financial disclosures.
that was approved in June 2021, Aruna Venkatesan, MD, recommends.
“Ibrexafungerp, an inhibitor of beta (1-3)–glucan synthase, is important for many reasons,” Dr. Venkatesan, chief of dermatology and director of the genital dermatology clinic at Santa Clara Valley Medical Center, San Jose, Calif., said during the annual meeting of the Pacific Dermatologic Association. “It’s one of the few drugs that can be used to treat Candida glabrata when C. glabrata is resistant to azoles and echinocandins. As the second-most common Candida species after C. albicans, C. glabrata is more common in immunosuppressed patients and it can cause mucosal and invasive disease, so ibrexafungerp is a welcome addition to our treatment armamentarium,” said Dr. Venkatesan, clinical professor of dermatology (affiliated) at Stanford (Calif.) Hospital and Clinics, adding that that vulvovaginal candidiasis can be tricky to diagnose. “In medical school, we learned that yeast infection in a woman presents as white, curd-like discharge, but that’s actually a minority of patients.”
For a patient who is being treated with topical steroids or estrogen for a genital condition, but is experiencing worsening itch, redness, or thick white discharge, she recommends performing a KOH exam.
“Instead of using a 15-blade scalpel, as we are used to performing on the skin for tinea, take a sterile [cotton swab], and swab the affected area. You can then apply it to a slide and perform a KOH exam as you normally would. Then look for yeast elements under the microscope. I also find it helpful to send for fungal culture to get speciation, especially in someone who’s not responding to therapy. This is because non-albicans yeast can be more resistant to azoles and require a different treatment plan.”
Often, patients with vulvovaginal candidiasis who present to her clinic are referred from an ob.gyn. and other general practitioners because they have failed a topical or oral azole. “I tend to avoid the topicals,” said Dr. Venkatesan, who is also president-elect of the North American chapter of the International Society for the Study of Vulvovaginal Disease. “If the culture shows C. albicans, I usually treat with oral fluconazole, 150 mg or 200 mg once, and consider repeat weekly dosing. Many patients come to me because they have recurrent refractory disease, so giving it once weekly for 6-8 weeks while they work on their potential risk factors such as diabetic blood sugar control is sensible.”
Non-albicans yeast can be resistant to azoles. If the fungal culture shows C. glabrata in such patients, “consider a course of intravaginal boric acid suppositories,” she advised. “These used to be difficult to give patients, because you would either have to send the prescription to a compounding pharmacy, or have the patients buy the capsules and boric acid crystals separately and make them themselves. That always made me nervous because of the chance of errors. The safety and the concern of taking it by mouth is an issue.” But now, intravaginal boric acid suppositories are available on Amazon and other web sites, and are relatively affordable, she said, adding, “just make sure the patient doesn’t take it by mouth as this is very toxic.”
Dr. Venkatesan reported having no financial disclosures.
FROM PDA 2021
Ask about itch and joint pain in pediatric psoriasis patients, expert advises
During the annual meeting of the Society for Pediatric Dermatology, Amy S. Paller, MD, MS, marveled on the remarkable advances in the treatment of inflammatory skin disorders during the past 2 decades.
“We’ve come a long way, from disease features being red, thick, and scaly and being treated with nonspecific therapy like topical steroids, keratolytics, and tar, to understanding disease pathogenesis and finding new targeted therapies for inflammatory skin disorders in children,” said Dr. Paller, professor and chair of the department of dermatology at Northwestern University, Chicago. “There are now studies moving forward with gene correction, gene replacement, the gene product replaced, or pathway inhibition to prevent the effects of genetic change.”
Technology is leading the way in generating new therapeutic advances, she continued, beyond traditional “omics” to lipidomics, metabolomics, glycomics, and kinomics. “This has enabled us to find new genetic disorders and their causes, to look at changes in gene expression patterns, and to look at changes in protein expression patterns that give us clues as to how to move forward with better therapy,” she said. “When we’re talking about new insights into pathogenesis-based therapy, we’re talking largely about understanding the pathways that lead to either inflammation or promoting cell proliferation and abnormal differentiation.”
Treating pediatric psoriasis
. “First of all, ask about itch and pain with these patients,” she advised. “Interviews have shown that 61% of children experience some itch, 39% have pain or stinging, and in the ixekizumab trials, 72% had what’s considered meaningful itch, with at least 4 out of 10 (mean intensity 5.3) on the itch numeric rating scale. Little is known about the itch associated with psoriasis and its underlying cause – unrelated to the IL-4/IL-13 pathway activation of atopic dermatitis – but it’s worth asking about. I find that itch of the scalp is especially a problem in psoriasis.”
Physicians should also ask pediatric psoriasis patients about joint pain, because about 1% of them have psoriatic arthritis, which is much less common than in adults, “but important to find and manage,” she added. Dr. Paller recommends the new R-JET rapid joint exam technique, which is accompanied by a three-question survey and body diagram that facilitates identification of true arthritis, “so you can know how quickly to refer”.
Several studies have described an increased risk of metabolic syndrome in adolescents with pediatric psoriasis and now in prepubertal children with the disease. In a recent study of 60 consecutive prepubertal children with psoriasis, 70% of whom had mild disease, 40% were overweight or obese, 53% had central obesity, 27% had high levels of the HOMA-IR (homeostasis model assessment of insulin resistance) despite generally normal levels of fasting glucose, and 30% met criteria for metabolic syndrome.
“This really struck me because our AAD [American Academy of Dermatology] guidelines did not recommend screening for type 2 diabetes in prepubertal children, even if overweight, because the risk is so small,” Dr. Paller said. “This report suggests that we may need to reconsider this recommendation in prepubertal children with psoriasis.”
Meanwhile, the number of medications approved by the Food and Drug Administration and the European Medicines Agency for children with psoriasis who are 6 years of age and above continues to expand, including tumor necrosis factor (TNF) inhibitors, interleukin (IL)-23 inhibitors, and IL-17 inhibitors. Most children can now achieve a PASI 90 within 12 weeks with the IL-23 inhibitor ustekinumab and the IL-17 inhibitors ixekizumab and secukinumab, Dr. Paller said.
In the ixekizumab trial, there are head-to-head comparison data in a European arm that involved the use of etanercept, she said. “What’s most noticeable is the significant difference in those who were able to achieve PASI 90 or above with this IL-17 inhibitor, versus etanercept,” which she added, raises the question of whether aiming for a PASI 75 is adequate, "or should we strive for PASI 90?” A pediatric psoriasis study published in 2020 found that the greatest improvement in quality of life was associated with a PASI 90 and use of systemic treatments.
Looking forward, phase 3 clinical trials are underway in pediatric patients with moderate to severe psoriasis for guselkumab, tildrakizumab, risankizumab, certolizumab, bimekizumab, and brodalumab. “The cost of all of these biologics is high, however. I remind everyone that we still have methotrexate,” she said. “The risk of side effects with our low-dose methotrexate treatment for psoriasis remains low, but methotrexate doesn’t hit these [high] PASI numbers and it’s much slower in its onset than biologics.”
Dr. Paller disclosed that she is a consultant to and/or an investigator for AbbVie, Arena, Bausch, Bristol Myers Squibb, Dermavant, Eli Lilly, Incyte, Forte, LEO Pharma, LifeMax, Pfizer, RAPT Therapeutics, Regeneron, and Sanofi.
Commentary by Robert Sidbury, MD, MPH
Dr. Paller reminds us of some essential features of pediatric psoriasis:
• It can hurt. Ask your patients if it does.
• It can itch. Look for excoriations, especially in the scalp.
• It is often associated with metabolic syndrome, so check relevant biometrics and labs, and consider coincident insulin resistance.
• Our traditional clinical trial target of PASI75, or a 75% reduction in body surface area involvement, is just not good enough. Studies have shown that the most meaningful quality-of-life gains come at PASI90 or above.
• With our newer biologics, such as IL-12/23 blockers (for instance, ustekinumab) and IL-17 blockers (for example, ixekizumab and secukinumab), PASI90 and better is a reasonable expectation, not a pipe dream.
Dr. Sidbury is chief of dermatology at Seattle Children's Hospital and professor, department of pediatrics, University of Washington, Seattle. He is a site principal investigator for dupilumab trials, for which the hospital has a contract with Regeneron.
This article was updated 6/16/22.
During the annual meeting of the Society for Pediatric Dermatology, Amy S. Paller, MD, MS, marveled on the remarkable advances in the treatment of inflammatory skin disorders during the past 2 decades.
“We’ve come a long way, from disease features being red, thick, and scaly and being treated with nonspecific therapy like topical steroids, keratolytics, and tar, to understanding disease pathogenesis and finding new targeted therapies for inflammatory skin disorders in children,” said Dr. Paller, professor and chair of the department of dermatology at Northwestern University, Chicago. “There are now studies moving forward with gene correction, gene replacement, the gene product replaced, or pathway inhibition to prevent the effects of genetic change.”
Technology is leading the way in generating new therapeutic advances, she continued, beyond traditional “omics” to lipidomics, metabolomics, glycomics, and kinomics. “This has enabled us to find new genetic disorders and their causes, to look at changes in gene expression patterns, and to look at changes in protein expression patterns that give us clues as to how to move forward with better therapy,” she said. “When we’re talking about new insights into pathogenesis-based therapy, we’re talking largely about understanding the pathways that lead to either inflammation or promoting cell proliferation and abnormal differentiation.”
Treating pediatric psoriasis
. “First of all, ask about itch and pain with these patients,” she advised. “Interviews have shown that 61% of children experience some itch, 39% have pain or stinging, and in the ixekizumab trials, 72% had what’s considered meaningful itch, with at least 4 out of 10 (mean intensity 5.3) on the itch numeric rating scale. Little is known about the itch associated with psoriasis and its underlying cause – unrelated to the IL-4/IL-13 pathway activation of atopic dermatitis – but it’s worth asking about. I find that itch of the scalp is especially a problem in psoriasis.”
Physicians should also ask pediatric psoriasis patients about joint pain, because about 1% of them have psoriatic arthritis, which is much less common than in adults, “but important to find and manage,” she added. Dr. Paller recommends the new R-JET rapid joint exam technique, which is accompanied by a three-question survey and body diagram that facilitates identification of true arthritis, “so you can know how quickly to refer”.
Several studies have described an increased risk of metabolic syndrome in adolescents with pediatric psoriasis and now in prepubertal children with the disease. In a recent study of 60 consecutive prepubertal children with psoriasis, 70% of whom had mild disease, 40% were overweight or obese, 53% had central obesity, 27% had high levels of the HOMA-IR (homeostasis model assessment of insulin resistance) despite generally normal levels of fasting glucose, and 30% met criteria for metabolic syndrome.
“This really struck me because our AAD [American Academy of Dermatology] guidelines did not recommend screening for type 2 diabetes in prepubertal children, even if overweight, because the risk is so small,” Dr. Paller said. “This report suggests that we may need to reconsider this recommendation in prepubertal children with psoriasis.”
Meanwhile, the number of medications approved by the Food and Drug Administration and the European Medicines Agency for children with psoriasis who are 6 years of age and above continues to expand, including tumor necrosis factor (TNF) inhibitors, interleukin (IL)-23 inhibitors, and IL-17 inhibitors. Most children can now achieve a PASI 90 within 12 weeks with the IL-23 inhibitor ustekinumab and the IL-17 inhibitors ixekizumab and secukinumab, Dr. Paller said.
In the ixekizumab trial, there are head-to-head comparison data in a European arm that involved the use of etanercept, she said. “What’s most noticeable is the significant difference in those who were able to achieve PASI 90 or above with this IL-17 inhibitor, versus etanercept,” which she added, raises the question of whether aiming for a PASI 75 is adequate, "or should we strive for PASI 90?” A pediatric psoriasis study published in 2020 found that the greatest improvement in quality of life was associated with a PASI 90 and use of systemic treatments.
Looking forward, phase 3 clinical trials are underway in pediatric patients with moderate to severe psoriasis for guselkumab, tildrakizumab, risankizumab, certolizumab, bimekizumab, and brodalumab. “The cost of all of these biologics is high, however. I remind everyone that we still have methotrexate,” she said. “The risk of side effects with our low-dose methotrexate treatment for psoriasis remains low, but methotrexate doesn’t hit these [high] PASI numbers and it’s much slower in its onset than biologics.”
Dr. Paller disclosed that she is a consultant to and/or an investigator for AbbVie, Arena, Bausch, Bristol Myers Squibb, Dermavant, Eli Lilly, Incyte, Forte, LEO Pharma, LifeMax, Pfizer, RAPT Therapeutics, Regeneron, and Sanofi.
Commentary by Robert Sidbury, MD, MPH
Dr. Paller reminds us of some essential features of pediatric psoriasis:
• It can hurt. Ask your patients if it does.
• It can itch. Look for excoriations, especially in the scalp.
• It is often associated with metabolic syndrome, so check relevant biometrics and labs, and consider coincident insulin resistance.
• Our traditional clinical trial target of PASI75, or a 75% reduction in body surface area involvement, is just not good enough. Studies have shown that the most meaningful quality-of-life gains come at PASI90 or above.
• With our newer biologics, such as IL-12/23 blockers (for instance, ustekinumab) and IL-17 blockers (for example, ixekizumab and secukinumab), PASI90 and better is a reasonable expectation, not a pipe dream.
Dr. Sidbury is chief of dermatology at Seattle Children's Hospital and professor, department of pediatrics, University of Washington, Seattle. He is a site principal investigator for dupilumab trials, for which the hospital has a contract with Regeneron.
This article was updated 6/16/22.
During the annual meeting of the Society for Pediatric Dermatology, Amy S. Paller, MD, MS, marveled on the remarkable advances in the treatment of inflammatory skin disorders during the past 2 decades.
“We’ve come a long way, from disease features being red, thick, and scaly and being treated with nonspecific therapy like topical steroids, keratolytics, and tar, to understanding disease pathogenesis and finding new targeted therapies for inflammatory skin disorders in children,” said Dr. Paller, professor and chair of the department of dermatology at Northwestern University, Chicago. “There are now studies moving forward with gene correction, gene replacement, the gene product replaced, or pathway inhibition to prevent the effects of genetic change.”
Technology is leading the way in generating new therapeutic advances, she continued, beyond traditional “omics” to lipidomics, metabolomics, glycomics, and kinomics. “This has enabled us to find new genetic disorders and their causes, to look at changes in gene expression patterns, and to look at changes in protein expression patterns that give us clues as to how to move forward with better therapy,” she said. “When we’re talking about new insights into pathogenesis-based therapy, we’re talking largely about understanding the pathways that lead to either inflammation or promoting cell proliferation and abnormal differentiation.”
Treating pediatric psoriasis
. “First of all, ask about itch and pain with these patients,” she advised. “Interviews have shown that 61% of children experience some itch, 39% have pain or stinging, and in the ixekizumab trials, 72% had what’s considered meaningful itch, with at least 4 out of 10 (mean intensity 5.3) on the itch numeric rating scale. Little is known about the itch associated with psoriasis and its underlying cause – unrelated to the IL-4/IL-13 pathway activation of atopic dermatitis – but it’s worth asking about. I find that itch of the scalp is especially a problem in psoriasis.”
Physicians should also ask pediatric psoriasis patients about joint pain, because about 1% of them have psoriatic arthritis, which is much less common than in adults, “but important to find and manage,” she added. Dr. Paller recommends the new R-JET rapid joint exam technique, which is accompanied by a three-question survey and body diagram that facilitates identification of true arthritis, “so you can know how quickly to refer”.
Several studies have described an increased risk of metabolic syndrome in adolescents with pediatric psoriasis and now in prepubertal children with the disease. In a recent study of 60 consecutive prepubertal children with psoriasis, 70% of whom had mild disease, 40% were overweight or obese, 53% had central obesity, 27% had high levels of the HOMA-IR (homeostasis model assessment of insulin resistance) despite generally normal levels of fasting glucose, and 30% met criteria for metabolic syndrome.
“This really struck me because our AAD [American Academy of Dermatology] guidelines did not recommend screening for type 2 diabetes in prepubertal children, even if overweight, because the risk is so small,” Dr. Paller said. “This report suggests that we may need to reconsider this recommendation in prepubertal children with psoriasis.”
Meanwhile, the number of medications approved by the Food and Drug Administration and the European Medicines Agency for children with psoriasis who are 6 years of age and above continues to expand, including tumor necrosis factor (TNF) inhibitors, interleukin (IL)-23 inhibitors, and IL-17 inhibitors. Most children can now achieve a PASI 90 within 12 weeks with the IL-23 inhibitor ustekinumab and the IL-17 inhibitors ixekizumab and secukinumab, Dr. Paller said.
In the ixekizumab trial, there are head-to-head comparison data in a European arm that involved the use of etanercept, she said. “What’s most noticeable is the significant difference in those who were able to achieve PASI 90 or above with this IL-17 inhibitor, versus etanercept,” which she added, raises the question of whether aiming for a PASI 75 is adequate, "or should we strive for PASI 90?” A pediatric psoriasis study published in 2020 found that the greatest improvement in quality of life was associated with a PASI 90 and use of systemic treatments.
Looking forward, phase 3 clinical trials are underway in pediatric patients with moderate to severe psoriasis for guselkumab, tildrakizumab, risankizumab, certolizumab, bimekizumab, and brodalumab. “The cost of all of these biologics is high, however. I remind everyone that we still have methotrexate,” she said. “The risk of side effects with our low-dose methotrexate treatment for psoriasis remains low, but methotrexate doesn’t hit these [high] PASI numbers and it’s much slower in its onset than biologics.”
Dr. Paller disclosed that she is a consultant to and/or an investigator for AbbVie, Arena, Bausch, Bristol Myers Squibb, Dermavant, Eli Lilly, Incyte, Forte, LEO Pharma, LifeMax, Pfizer, RAPT Therapeutics, Regeneron, and Sanofi.
Commentary by Robert Sidbury, MD, MPH
Dr. Paller reminds us of some essential features of pediatric psoriasis:
• It can hurt. Ask your patients if it does.
• It can itch. Look for excoriations, especially in the scalp.
• It is often associated with metabolic syndrome, so check relevant biometrics and labs, and consider coincident insulin resistance.
• Our traditional clinical trial target of PASI75, or a 75% reduction in body surface area involvement, is just not good enough. Studies have shown that the most meaningful quality-of-life gains come at PASI90 or above.
• With our newer biologics, such as IL-12/23 blockers (for instance, ustekinumab) and IL-17 blockers (for example, ixekizumab and secukinumab), PASI90 and better is a reasonable expectation, not a pipe dream.
Dr. Sidbury is chief of dermatology at Seattle Children's Hospital and professor, department of pediatrics, University of Washington, Seattle. He is a site principal investigator for dupilumab trials, for which the hospital has a contract with Regeneron.
This article was updated 6/16/22.
FROM SPD 2021
High prevalence of Fall Risk–Increasing Drugs in older adults after falls
Background: Falls are the leading cause of unintentional injuries and injury-related deaths among adults aged 65 years and older. FRIDs (such as antidepressants, sedatives-hypnotics, and opioids) continue to be a major contributor for risk of falls. At the same time, little is known about prevalence of use or interventions directed toward reduction of use in older adults presenting with fall.
Study design: Systematic review.
Setting: PubMed and Embase databases were used to search for studies published in English on or before June 30, 2019. Search terms included older adults, falls, medication classes, and hospitalizations among other related terms.
Synopsis: The review included a total of 14 articles (10 observational studies and 4 prospective intervention studies). High prevalence of FRID use (65%-93%) was seen in older adults with fall-related injury. Use of FRIDs continued to remain high at 1 month and 6 months follow-up after a fall. Antidepressants, sedative-hypnotics, opioids, and antipsychotics were the most commonly used FRIDs. Three randomized controlled trials showed no effect of reducing FRID use on reduction in falls. An outpatient clinic pre-post assessment study based on intervention by geriatrician and communication with prescribing physicians led to reduction in FRID use and falls.
Limitations of this review included high risk of bias in observational studies and unclear timeline definitions of interventions or outcome measurements in the intervention studies. In conclusion, there is a significant need for well-designed interventions targeted at reducing FRID use in conjunction with other risk factors to decrease the incidence of falls comprehensively. An aggressive approach directed toward patient education along with primary care communication may be the key to reducing FRID use in this population.
Bottom line: With limited evidence, there is a high prevalence of FRID use in older adults presenting with falls and no reduction in FRID use following the encounter.
Citation: Hart LA et al. Use of fall risk-increasing drugs around a fall-related injury in older adults: A systematic review. J Am Geriatr Soc. 2020 Feb 17. doi: 10.1111/jgs.16369.
Dr. Yarra is a hospitalist and assistant professor of medicine at UK HealthCare, Lexington, Ky.
Background: Falls are the leading cause of unintentional injuries and injury-related deaths among adults aged 65 years and older. FRIDs (such as antidepressants, sedatives-hypnotics, and opioids) continue to be a major contributor for risk of falls. At the same time, little is known about prevalence of use or interventions directed toward reduction of use in older adults presenting with fall.
Study design: Systematic review.
Setting: PubMed and Embase databases were used to search for studies published in English on or before June 30, 2019. Search terms included older adults, falls, medication classes, and hospitalizations among other related terms.
Synopsis: The review included a total of 14 articles (10 observational studies and 4 prospective intervention studies). High prevalence of FRID use (65%-93%) was seen in older adults with fall-related injury. Use of FRIDs continued to remain high at 1 month and 6 months follow-up after a fall. Antidepressants, sedative-hypnotics, opioids, and antipsychotics were the most commonly used FRIDs. Three randomized controlled trials showed no effect of reducing FRID use on reduction in falls. An outpatient clinic pre-post assessment study based on intervention by geriatrician and communication with prescribing physicians led to reduction in FRID use and falls.
Limitations of this review included high risk of bias in observational studies and unclear timeline definitions of interventions or outcome measurements in the intervention studies. In conclusion, there is a significant need for well-designed interventions targeted at reducing FRID use in conjunction with other risk factors to decrease the incidence of falls comprehensively. An aggressive approach directed toward patient education along with primary care communication may be the key to reducing FRID use in this population.
Bottom line: With limited evidence, there is a high prevalence of FRID use in older adults presenting with falls and no reduction in FRID use following the encounter.
Citation: Hart LA et al. Use of fall risk-increasing drugs around a fall-related injury in older adults: A systematic review. J Am Geriatr Soc. 2020 Feb 17. doi: 10.1111/jgs.16369.
Dr. Yarra is a hospitalist and assistant professor of medicine at UK HealthCare, Lexington, Ky.
Background: Falls are the leading cause of unintentional injuries and injury-related deaths among adults aged 65 years and older. FRIDs (such as antidepressants, sedatives-hypnotics, and opioids) continue to be a major contributor for risk of falls. At the same time, little is known about prevalence of use or interventions directed toward reduction of use in older adults presenting with fall.
Study design: Systematic review.
Setting: PubMed and Embase databases were used to search for studies published in English on or before June 30, 2019. Search terms included older adults, falls, medication classes, and hospitalizations among other related terms.
Synopsis: The review included a total of 14 articles (10 observational studies and 4 prospective intervention studies). High prevalence of FRID use (65%-93%) was seen in older adults with fall-related injury. Use of FRIDs continued to remain high at 1 month and 6 months follow-up after a fall. Antidepressants, sedative-hypnotics, opioids, and antipsychotics were the most commonly used FRIDs. Three randomized controlled trials showed no effect of reducing FRID use on reduction in falls. An outpatient clinic pre-post assessment study based on intervention by geriatrician and communication with prescribing physicians led to reduction in FRID use and falls.
Limitations of this review included high risk of bias in observational studies and unclear timeline definitions of interventions or outcome measurements in the intervention studies. In conclusion, there is a significant need for well-designed interventions targeted at reducing FRID use in conjunction with other risk factors to decrease the incidence of falls comprehensively. An aggressive approach directed toward patient education along with primary care communication may be the key to reducing FRID use in this population.
Bottom line: With limited evidence, there is a high prevalence of FRID use in older adults presenting with falls and no reduction in FRID use following the encounter.
Citation: Hart LA et al. Use of fall risk-increasing drugs around a fall-related injury in older adults: A systematic review. J Am Geriatr Soc. 2020 Feb 17. doi: 10.1111/jgs.16369.
Dr. Yarra is a hospitalist and assistant professor of medicine at UK HealthCare, Lexington, Ky.
Pregnancy and parental leave during gastroenterology fellowship training: A program perspective
Due to broad social changes and efforts from leaders in GI, there is renewed interest in family planning and parental leave policies for GI trainees. The American Board of Medical Specialties now permits trainees a minimum of 6 weeks away during training, without automatically requiring an extension of training time or completely depleting vacation time, for boards eligibility.1,2 However, national and institutional guidance for family planning and pregnancy during GI fellowship is lacking. How can gastroenterology fellowship programs support fellows taking parental leave and enact fair policies? We review the scope of the problem, describe our experience in developing resources within our GI fellowship program, and highlight areas that require further development.
The scope of the issue
There is no national data yet on the number of GI fellows that are parents prior to starting fellowship or who become parents during fellowship. We estimate that approximately 25% of fellows enter training as parents or become parents during fellowship, although 40%-50% may have an intention to have children.3,4 Fellows may be worried that they will “fall behind” or be perceived as less committed if they devote time to childrearing or take parental leave.5-7 Indeed, worries about discrimination based on pregnancy and parental leave are borne out by the experiences of older physicians (in particular, female physicians).8,9
State- and institution-specific benefits vary from program to program. Nationally, the Family and Medical Leave Act provides only unpaid leave and applies only to trainees who have been employed for greater than 12 months.10 Benefits may not always be well advertised, and even when they are, trainees (and attendings) may feel uncomfortable taking full advantage. One survey of GIs revealed that, although two-thirds believed that 6-8 weeks of maternity leave was inadequate, half took less than that amount due to fears about financial and professional consequences.8
Pregnancy during GI fellowship is a special concern. GI fellowship consists of long work hours, includes night call, and can be physically demanding. All three of these factors have been associated with preterm delivery, infertility, and miscarriage.11,12 In addition, there are no guidelines for ergonomic adjustments or infection precautions for pregnant endoscopists. We have compiled information about infection prevention guidance in pregnancy (available from the authors on request) derived from guidance from the National Institute for Occupational Safety and Health, which recommends the same precautions for pregnant health care workers as for nonpregnant health care workers.13 In regards to SARS-CoV-2, we believe that the decision to perform procedures on patients with COVID-19 infection should be individualized, although vaccinated endoscopists should be reassured by the exceedingly low rates of infection after vaccination and with appropriate personal protective equipment. Radiation is yet another concern. There are limited data on radiation dosages incurred by workers in the endoscopy suite and no pregnancy-specific data, which may lead trainees to avoid fluoroscopic procedures and unnecessarily double up on lead gowns.8,11,14-17
Breastfeeding accommodations, and access to lactation rooms for trainees, are required by federal law for a minimum of 12 months.18 Should a trainee choose to breastfeed, education of staff and attendings is critical because many may be unaware of the specific needs pertaining to lactation. Staff should be aware that 30-45 minutes are needed to prepare, pump, and store milk. Trainees should not be solely responsible for educating their attendings and staff.
Our Experience in Creating a Policy
We developed a formal fellowship program policy on parental leave and pregnancy in the setting of a broader discussion about fellow workload and wellness. We agreed that trainees should be allowed to make changes to their schedule with co-fellows as needed for medical appointments or procedures and that our backup policy should be flexible enough to provide spot coverage for unexpected complications and family emergencies. We also incorporated a GI psychologist to provide wellness resources and suggestions for reducing burnout for our fellows.
We strove to follow certain principles in creating this policy. Trainees who are parents should have a comparable clinical experience to their nonparenting colleagues and should take the lead in rearranging their own schedule. Nonbirthing parents, adopting parents, and parents using surrogacy should be included in any parental leave policy. Fellowship leaders have an important responsibility in helping fellows proactively plan to meet requirements for graduation and maximize learning and exposure (Figure). We also recognized the importance of equitable coverage. For example, there is sometimes a perception that fellows with children “burden” fellows who are not parents.3,19 On the other hand, fellows without children may feel that they are called on more than their colleagues with children to cover those with childcare issues. In addition, as a recent study of general surgery residency program directors indicates, there are complex interpersonal issues that play into a colleague’s willingness to provide coverage.20 It behooves program leadership to be cognizant of group dynamics that might cause conflict over what should be a straightforward coverage situation.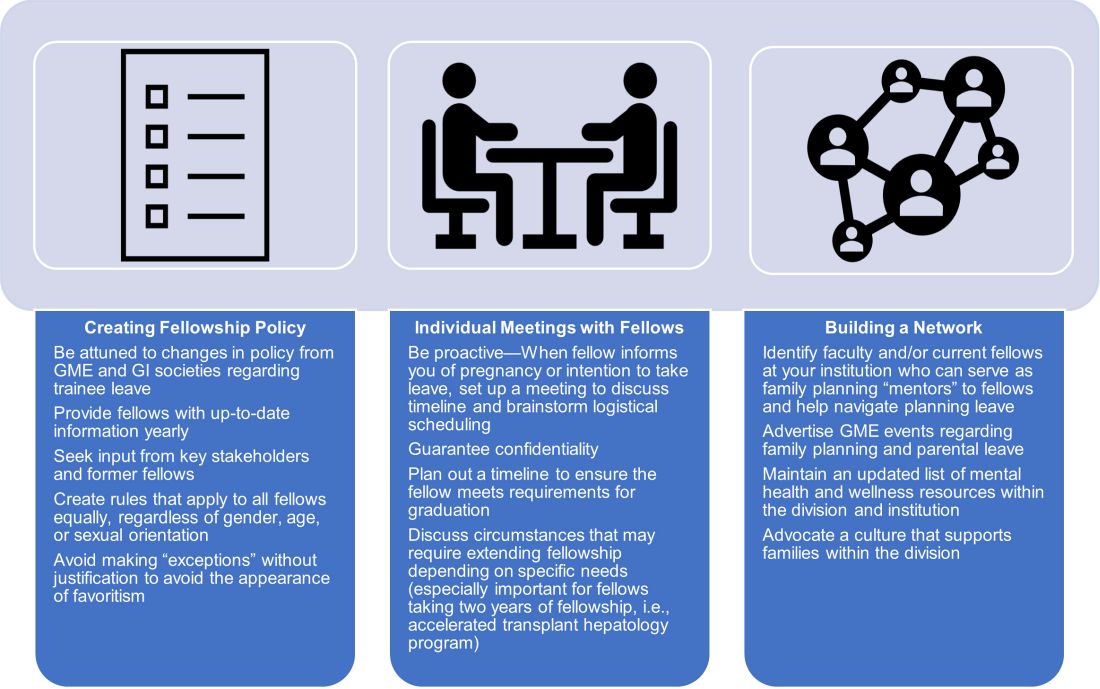
We first researched national and societal guidelines if available, as well as our institution’s graduate medical education (GME) website. We categorized benefits by whether they were federal, state-mandated, or institutional. It is important to note that any concerns about trainee salaries should be discussed with one’s GME office to ensure the leave policy is in accordance with federal funding policies.21 We solicited experiences and advice from former and current fellows who had gone through, or were planning, pregnancy and parental leave. A few faculty members volunteered to serve as a resource for fellows; these “ambassadors” discussed their experiences during a lunchtime panel, as well as offered to provide one-on-one advice and participate in future panels. We also reached out to our infection control experts to review the literature and federal policies on infections of special consideration during pregnancy and endoscopy. As for radiation safety, given the importance of education and active monitoring, we offer the option of reaching out to our radiation safety officer for individualized counseling.22
Based on these efforts, we drafted a written policy designed for pregnant fellows and fellows planning parental leave on expectations for the program and fellows, benefits, and advice, including childcare options, lactation room locations, and financial planning tips. We shared this document with fellows and incorporated feedback. As a “living document” it is subject to change and will be updated as needed (at least annually).
Additional planning considerations for fellows
Research childcare options (ideally 6 months or more before leave).
- Start to explore your institution’s resources for leave and childcare options (daycare waitlists may be greater than 1 year in some cities).
Inform your program director (4-5 months before leave).
- Consider informing your program director about pregnancy at the beginning of the second trimester.
- Discuss Accreditation Council for Graduate Medical Education requirements and scheduling responsibilities.
- Explicitly discuss whether you plan to graduate on time or extend fellowship.
Inform your colleagues and patients (at least 3-4 months before leave).
- If comfortable, consider getting advice from a co-fellow and/or faculty mentor parent to facilitate transition to parenthood.
- When you feel ready, begin trading rotations and calls with co-fellows. If you have a results inbox or pager, discuss who can help cover those during your leave.
- Inform research collaborators about your leave and make preparations to keep projects progressing during your leave.
- If you have “active” clinic patients, when appropriate, begin to inform them that you will be away and provide reassurance that a colleague will be covering you. Leave clear plans with contingencies for these patients in your last progress notes.
Complete institutional paperwork and map out facilities (at least 2-3 months before leave).
- Review your options for using time toward leave, including vacation, research, or Family and Medical Leave Act–provided leave (unpaid), and what paperwork you need to fill out.
- Contact your payroll and/or human resources office to inform them of birth/adoption.
- Research potential program parental benefits, such as dependent daycare and/or health care flexible spending accounts.
- If choosing to breastfeed, explore the lactation rooms that are closest to your workroom and endoscopy suite and determine how much time you will need to set aside for pumping.
Be prepared to make adjustments as needed.
- Endoscopy-heavy rotations may be more difficult in the third trimester of pregnancy.
- Make contingency plans for early or late delivery dates, as well as if you undergo a cesarean that requires additional recovery time.
- Consider scheduling elective rotations (research, clinic) toward the end of leave and for the first month of “return to work.”
- If you plan to join limited clinic or outpatient endoscopy blocks later in your leave, make early arrangements to work regularly with these attendings.
Conclusion
Trainee needs assessments in gastroenterology fellowship similar to those in other specialties should be performed, and are in fact underway.19,23,24 There is a lack of data regarding the availability of fellowship program guidance and, specifically, adherence to required policies, and more data from program directors at a national level need to be collected.20 We recommend that programs engage in identifying specific needs at their institutions with the goal of eventually sharing this knowledge with other programs. Gastroenterology society recommendations for performing endoscopy while pregnant, with regard to ergonomics, infection control, and radiation exposure, would be instrumental. GI fellowships should consolidate institutional knowledge and engage key stakeholders – including trainees, prior trainees, occupational safety experts, radiation safety offices, wellness experts, and GME – to create program-specific policies that are flexible but rigorous and generous but equitable.
Dr. Liu and Dr. Summa are gastroenterology fellows at Northwestern University, Chicago. Dr. Patel is an assistant professor of medicine and a gastroenterology fellowship assistant program director at Northwestern University, Chicago. Dr. Donnan and Dr. Guentner are assistant professors of medicine at Northwestern University. Dr. Kia is an assistant professor of medicine and the gastroenterology fellowship program director at Northwestern University. They have no conflicts of interest to disclose. The authors would like to thank Michelle Clermont, MD, and Maureen K. Bolon, MD, for their discussion and assistance during the drafting of this article.
References
1. Section on Medical Students, Residents, and Fellowship Trainees; Committee on Early Childhood. Pediatrics. 2013;131(2):387-90.
2. American Board of Medical Specialties. ABMS Announces Progressive Leave Policy for Residents and Fellows. July 13, 2020. Accessed May 1, 2021. https://www.abms.org/news-events/abms-announces-progressive-leave-policy-for-residents-and-fellows/.
3. Magudia K et al. J Grad Med Educ. 2020;12(2):162-7.
4. Blair JE et al. Acad Med. 2016;91(7):972-8.
5. Feld LD. Am J Gastroenterol. 2021;116(3):505-8.
6. Roubaud MS. Plast Reconstr Surg Glob Open. 2019. doi: 10.1097/GOX.0000000000002104.
7. Price J, Dunbar K. Gastrointest Endosc. 2009;69(1):121-3.
8. David YN et al. Gastrointest Endosc. 2020;91(6):AB75-AB76.
9. Webb AMB et al. Acad Med J Assoc Am Med Coll. 2019;94(11):1631-4.
10. Weinstein DF et al. N Engl J Med. 2019 Sep 12;381(11):995-7.
11. Anderson M, Goldman RH. JAMA Surg. 2020;155(3):243-9.
12. Palmer KT et al. Occup Environ Med. 2013;70(4):213-22.
13. Siegel JD et al; Healthcare Infection, Control Practices Advisory Committee. Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings (2007). 2007. Last reviewed July 22, 2019. Accessed April 28, 2021. https://www.cdc.gov/infectioncontrol/guidelines/isolation/index.html
14. David YN et al. Am J Gastroenterol. 2021;116(3):539-50.
15. Sethi S et al. Dig Dis Sci. 2019;64(9):2455-66.
16. Alzimami K et al. Gastroenterol Res Pract. 2013;2013:587574.
17. Hayashi S et al. World J Clin Cases. 2018;6(16):1087-93.
18. U.S. Department of Labor, Wage and Hour Division. “Frequently Asked Questions – Break Time for Nursing Mothers.” Accessed May 1, 2021. https://www.dol.gov/agencies/whd/nursing-mothers/faq.
19. Mwakyanjala EJ et al. J Am Heart Assoc. 2019. doi: 10.1161/JAHA.119.012137.
20. Castillo-Angeles M et al. JAMA Surg. 2021 Jul 1;156(7):647-53.
21. Prasad S et al. J Grad Med Educ. 2021 Jun;13(3):349-54.
22. Ho IKH et al. Am J Gastroenterol. 2014;109(8):1180-94.
23. Sherbaf FG et al. AJNR Am J Neuroradiol. 2020;41(8):1348-54.
24. Altieri MS et al. JAMA Surg. 2019;154(10):952-58.
Due to broad social changes and efforts from leaders in GI, there is renewed interest in family planning and parental leave policies for GI trainees. The American Board of Medical Specialties now permits trainees a minimum of 6 weeks away during training, without automatically requiring an extension of training time or completely depleting vacation time, for boards eligibility.1,2 However, national and institutional guidance for family planning and pregnancy during GI fellowship is lacking. How can gastroenterology fellowship programs support fellows taking parental leave and enact fair policies? We review the scope of the problem, describe our experience in developing resources within our GI fellowship program, and highlight areas that require further development.
The scope of the issue
There is no national data yet on the number of GI fellows that are parents prior to starting fellowship or who become parents during fellowship. We estimate that approximately 25% of fellows enter training as parents or become parents during fellowship, although 40%-50% may have an intention to have children.3,4 Fellows may be worried that they will “fall behind” or be perceived as less committed if they devote time to childrearing or take parental leave.5-7 Indeed, worries about discrimination based on pregnancy and parental leave are borne out by the experiences of older physicians (in particular, female physicians).8,9
State- and institution-specific benefits vary from program to program. Nationally, the Family and Medical Leave Act provides only unpaid leave and applies only to trainees who have been employed for greater than 12 months.10 Benefits may not always be well advertised, and even when they are, trainees (and attendings) may feel uncomfortable taking full advantage. One survey of GIs revealed that, although two-thirds believed that 6-8 weeks of maternity leave was inadequate, half took less than that amount due to fears about financial and professional consequences.8
Pregnancy during GI fellowship is a special concern. GI fellowship consists of long work hours, includes night call, and can be physically demanding. All three of these factors have been associated with preterm delivery, infertility, and miscarriage.11,12 In addition, there are no guidelines for ergonomic adjustments or infection precautions for pregnant endoscopists. We have compiled information about infection prevention guidance in pregnancy (available from the authors on request) derived from guidance from the National Institute for Occupational Safety and Health, which recommends the same precautions for pregnant health care workers as for nonpregnant health care workers.13 In regards to SARS-CoV-2, we believe that the decision to perform procedures on patients with COVID-19 infection should be individualized, although vaccinated endoscopists should be reassured by the exceedingly low rates of infection after vaccination and with appropriate personal protective equipment. Radiation is yet another concern. There are limited data on radiation dosages incurred by workers in the endoscopy suite and no pregnancy-specific data, which may lead trainees to avoid fluoroscopic procedures and unnecessarily double up on lead gowns.8,11,14-17
Breastfeeding accommodations, and access to lactation rooms for trainees, are required by federal law for a minimum of 12 months.18 Should a trainee choose to breastfeed, education of staff and attendings is critical because many may be unaware of the specific needs pertaining to lactation. Staff should be aware that 30-45 minutes are needed to prepare, pump, and store milk. Trainees should not be solely responsible for educating their attendings and staff.
Our Experience in Creating a Policy
We developed a formal fellowship program policy on parental leave and pregnancy in the setting of a broader discussion about fellow workload and wellness. We agreed that trainees should be allowed to make changes to their schedule with co-fellows as needed for medical appointments or procedures and that our backup policy should be flexible enough to provide spot coverage for unexpected complications and family emergencies. We also incorporated a GI psychologist to provide wellness resources and suggestions for reducing burnout for our fellows.
We strove to follow certain principles in creating this policy. Trainees who are parents should have a comparable clinical experience to their nonparenting colleagues and should take the lead in rearranging their own schedule. Nonbirthing parents, adopting parents, and parents using surrogacy should be included in any parental leave policy. Fellowship leaders have an important responsibility in helping fellows proactively plan to meet requirements for graduation and maximize learning and exposure (Figure). We also recognized the importance of equitable coverage. For example, there is sometimes a perception that fellows with children “burden” fellows who are not parents.3,19 On the other hand, fellows without children may feel that they are called on more than their colleagues with children to cover those with childcare issues. In addition, as a recent study of general surgery residency program directors indicates, there are complex interpersonal issues that play into a colleague’s willingness to provide coverage.20 It behooves program leadership to be cognizant of group dynamics that might cause conflict over what should be a straightforward coverage situation.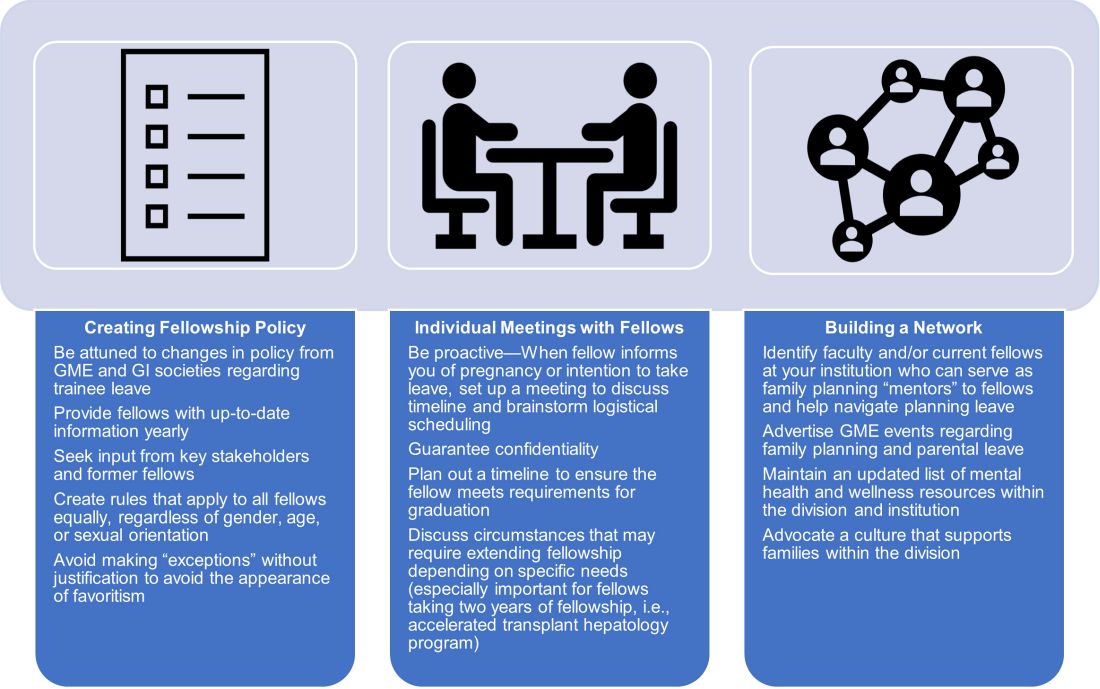
We first researched national and societal guidelines if available, as well as our institution’s graduate medical education (GME) website. We categorized benefits by whether they were federal, state-mandated, or institutional. It is important to note that any concerns about trainee salaries should be discussed with one’s GME office to ensure the leave policy is in accordance with federal funding policies.21 We solicited experiences and advice from former and current fellows who had gone through, or were planning, pregnancy and parental leave. A few faculty members volunteered to serve as a resource for fellows; these “ambassadors” discussed their experiences during a lunchtime panel, as well as offered to provide one-on-one advice and participate in future panels. We also reached out to our infection control experts to review the literature and federal policies on infections of special consideration during pregnancy and endoscopy. As for radiation safety, given the importance of education and active monitoring, we offer the option of reaching out to our radiation safety officer for individualized counseling.22
Based on these efforts, we drafted a written policy designed for pregnant fellows and fellows planning parental leave on expectations for the program and fellows, benefits, and advice, including childcare options, lactation room locations, and financial planning tips. We shared this document with fellows and incorporated feedback. As a “living document” it is subject to change and will be updated as needed (at least annually).
Additional planning considerations for fellows
Research childcare options (ideally 6 months or more before leave).
- Start to explore your institution’s resources for leave and childcare options (daycare waitlists may be greater than 1 year in some cities).
Inform your program director (4-5 months before leave).
- Consider informing your program director about pregnancy at the beginning of the second trimester.
- Discuss Accreditation Council for Graduate Medical Education requirements and scheduling responsibilities.
- Explicitly discuss whether you plan to graduate on time or extend fellowship.
Inform your colleagues and patients (at least 3-4 months before leave).
- If comfortable, consider getting advice from a co-fellow and/or faculty mentor parent to facilitate transition to parenthood.
- When you feel ready, begin trading rotations and calls with co-fellows. If you have a results inbox or pager, discuss who can help cover those during your leave.
- Inform research collaborators about your leave and make preparations to keep projects progressing during your leave.
- If you have “active” clinic patients, when appropriate, begin to inform them that you will be away and provide reassurance that a colleague will be covering you. Leave clear plans with contingencies for these patients in your last progress notes.
Complete institutional paperwork and map out facilities (at least 2-3 months before leave).
- Review your options for using time toward leave, including vacation, research, or Family and Medical Leave Act–provided leave (unpaid), and what paperwork you need to fill out.
- Contact your payroll and/or human resources office to inform them of birth/adoption.
- Research potential program parental benefits, such as dependent daycare and/or health care flexible spending accounts.
- If choosing to breastfeed, explore the lactation rooms that are closest to your workroom and endoscopy suite and determine how much time you will need to set aside for pumping.
Be prepared to make adjustments as needed.
- Endoscopy-heavy rotations may be more difficult in the third trimester of pregnancy.
- Make contingency plans for early or late delivery dates, as well as if you undergo a cesarean that requires additional recovery time.
- Consider scheduling elective rotations (research, clinic) toward the end of leave and for the first month of “return to work.”
- If you plan to join limited clinic or outpatient endoscopy blocks later in your leave, make early arrangements to work regularly with these attendings.
Conclusion
Trainee needs assessments in gastroenterology fellowship similar to those in other specialties should be performed, and are in fact underway.19,23,24 There is a lack of data regarding the availability of fellowship program guidance and, specifically, adherence to required policies, and more data from program directors at a national level need to be collected.20 We recommend that programs engage in identifying specific needs at their institutions with the goal of eventually sharing this knowledge with other programs. Gastroenterology society recommendations for performing endoscopy while pregnant, with regard to ergonomics, infection control, and radiation exposure, would be instrumental. GI fellowships should consolidate institutional knowledge and engage key stakeholders – including trainees, prior trainees, occupational safety experts, radiation safety offices, wellness experts, and GME – to create program-specific policies that are flexible but rigorous and generous but equitable.
Dr. Liu and Dr. Summa are gastroenterology fellows at Northwestern University, Chicago. Dr. Patel is an assistant professor of medicine and a gastroenterology fellowship assistant program director at Northwestern University, Chicago. Dr. Donnan and Dr. Guentner are assistant professors of medicine at Northwestern University. Dr. Kia is an assistant professor of medicine and the gastroenterology fellowship program director at Northwestern University. They have no conflicts of interest to disclose. The authors would like to thank Michelle Clermont, MD, and Maureen K. Bolon, MD, for their discussion and assistance during the drafting of this article.
References
1. Section on Medical Students, Residents, and Fellowship Trainees; Committee on Early Childhood. Pediatrics. 2013;131(2):387-90.
2. American Board of Medical Specialties. ABMS Announces Progressive Leave Policy for Residents and Fellows. July 13, 2020. Accessed May 1, 2021. https://www.abms.org/news-events/abms-announces-progressive-leave-policy-for-residents-and-fellows/.
3. Magudia K et al. J Grad Med Educ. 2020;12(2):162-7.
4. Blair JE et al. Acad Med. 2016;91(7):972-8.
5. Feld LD. Am J Gastroenterol. 2021;116(3):505-8.
6. Roubaud MS. Plast Reconstr Surg Glob Open. 2019. doi: 10.1097/GOX.0000000000002104.
7. Price J, Dunbar K. Gastrointest Endosc. 2009;69(1):121-3.
8. David YN et al. Gastrointest Endosc. 2020;91(6):AB75-AB76.
9. Webb AMB et al. Acad Med J Assoc Am Med Coll. 2019;94(11):1631-4.
10. Weinstein DF et al. N Engl J Med. 2019 Sep 12;381(11):995-7.
11. Anderson M, Goldman RH. JAMA Surg. 2020;155(3):243-9.
12. Palmer KT et al. Occup Environ Med. 2013;70(4):213-22.
13. Siegel JD et al; Healthcare Infection, Control Practices Advisory Committee. Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings (2007). 2007. Last reviewed July 22, 2019. Accessed April 28, 2021. https://www.cdc.gov/infectioncontrol/guidelines/isolation/index.html
14. David YN et al. Am J Gastroenterol. 2021;116(3):539-50.
15. Sethi S et al. Dig Dis Sci. 2019;64(9):2455-66.
16. Alzimami K et al. Gastroenterol Res Pract. 2013;2013:587574.
17. Hayashi S et al. World J Clin Cases. 2018;6(16):1087-93.
18. U.S. Department of Labor, Wage and Hour Division. “Frequently Asked Questions – Break Time for Nursing Mothers.” Accessed May 1, 2021. https://www.dol.gov/agencies/whd/nursing-mothers/faq.
19. Mwakyanjala EJ et al. J Am Heart Assoc. 2019. doi: 10.1161/JAHA.119.012137.
20. Castillo-Angeles M et al. JAMA Surg. 2021 Jul 1;156(7):647-53.
21. Prasad S et al. J Grad Med Educ. 2021 Jun;13(3):349-54.
22. Ho IKH et al. Am J Gastroenterol. 2014;109(8):1180-94.
23. Sherbaf FG et al. AJNR Am J Neuroradiol. 2020;41(8):1348-54.
24. Altieri MS et al. JAMA Surg. 2019;154(10):952-58.
Due to broad social changes and efforts from leaders in GI, there is renewed interest in family planning and parental leave policies for GI trainees. The American Board of Medical Specialties now permits trainees a minimum of 6 weeks away during training, without automatically requiring an extension of training time or completely depleting vacation time, for boards eligibility.1,2 However, national and institutional guidance for family planning and pregnancy during GI fellowship is lacking. How can gastroenterology fellowship programs support fellows taking parental leave and enact fair policies? We review the scope of the problem, describe our experience in developing resources within our GI fellowship program, and highlight areas that require further development.
The scope of the issue
There is no national data yet on the number of GI fellows that are parents prior to starting fellowship or who become parents during fellowship. We estimate that approximately 25% of fellows enter training as parents or become parents during fellowship, although 40%-50% may have an intention to have children.3,4 Fellows may be worried that they will “fall behind” or be perceived as less committed if they devote time to childrearing or take parental leave.5-7 Indeed, worries about discrimination based on pregnancy and parental leave are borne out by the experiences of older physicians (in particular, female physicians).8,9
State- and institution-specific benefits vary from program to program. Nationally, the Family and Medical Leave Act provides only unpaid leave and applies only to trainees who have been employed for greater than 12 months.10 Benefits may not always be well advertised, and even when they are, trainees (and attendings) may feel uncomfortable taking full advantage. One survey of GIs revealed that, although two-thirds believed that 6-8 weeks of maternity leave was inadequate, half took less than that amount due to fears about financial and professional consequences.8
Pregnancy during GI fellowship is a special concern. GI fellowship consists of long work hours, includes night call, and can be physically demanding. All three of these factors have been associated with preterm delivery, infertility, and miscarriage.11,12 In addition, there are no guidelines for ergonomic adjustments or infection precautions for pregnant endoscopists. We have compiled information about infection prevention guidance in pregnancy (available from the authors on request) derived from guidance from the National Institute for Occupational Safety and Health, which recommends the same precautions for pregnant health care workers as for nonpregnant health care workers.13 In regards to SARS-CoV-2, we believe that the decision to perform procedures on patients with COVID-19 infection should be individualized, although vaccinated endoscopists should be reassured by the exceedingly low rates of infection after vaccination and with appropriate personal protective equipment. Radiation is yet another concern. There are limited data on radiation dosages incurred by workers in the endoscopy suite and no pregnancy-specific data, which may lead trainees to avoid fluoroscopic procedures and unnecessarily double up on lead gowns.8,11,14-17
Breastfeeding accommodations, and access to lactation rooms for trainees, are required by federal law for a minimum of 12 months.18 Should a trainee choose to breastfeed, education of staff and attendings is critical because many may be unaware of the specific needs pertaining to lactation. Staff should be aware that 30-45 minutes are needed to prepare, pump, and store milk. Trainees should not be solely responsible for educating their attendings and staff.
Our Experience in Creating a Policy
We developed a formal fellowship program policy on parental leave and pregnancy in the setting of a broader discussion about fellow workload and wellness. We agreed that trainees should be allowed to make changes to their schedule with co-fellows as needed for medical appointments or procedures and that our backup policy should be flexible enough to provide spot coverage for unexpected complications and family emergencies. We also incorporated a GI psychologist to provide wellness resources and suggestions for reducing burnout for our fellows.
We strove to follow certain principles in creating this policy. Trainees who are parents should have a comparable clinical experience to their nonparenting colleagues and should take the lead in rearranging their own schedule. Nonbirthing parents, adopting parents, and parents using surrogacy should be included in any parental leave policy. Fellowship leaders have an important responsibility in helping fellows proactively plan to meet requirements for graduation and maximize learning and exposure (Figure). We also recognized the importance of equitable coverage. For example, there is sometimes a perception that fellows with children “burden” fellows who are not parents.3,19 On the other hand, fellows without children may feel that they are called on more than their colleagues with children to cover those with childcare issues. In addition, as a recent study of general surgery residency program directors indicates, there are complex interpersonal issues that play into a colleague’s willingness to provide coverage.20 It behooves program leadership to be cognizant of group dynamics that might cause conflict over what should be a straightforward coverage situation.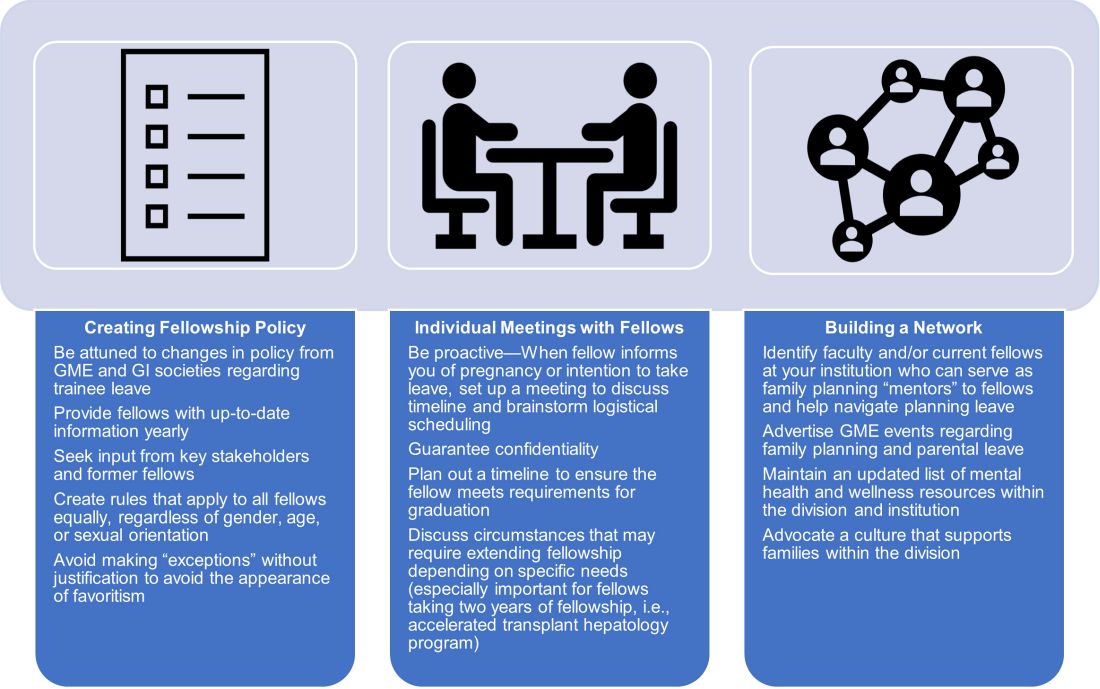
We first researched national and societal guidelines if available, as well as our institution’s graduate medical education (GME) website. We categorized benefits by whether they were federal, state-mandated, or institutional. It is important to note that any concerns about trainee salaries should be discussed with one’s GME office to ensure the leave policy is in accordance with federal funding policies.21 We solicited experiences and advice from former and current fellows who had gone through, or were planning, pregnancy and parental leave. A few faculty members volunteered to serve as a resource for fellows; these “ambassadors” discussed their experiences during a lunchtime panel, as well as offered to provide one-on-one advice and participate in future panels. We also reached out to our infection control experts to review the literature and federal policies on infections of special consideration during pregnancy and endoscopy. As for radiation safety, given the importance of education and active monitoring, we offer the option of reaching out to our radiation safety officer for individualized counseling.22
Based on these efforts, we drafted a written policy designed for pregnant fellows and fellows planning parental leave on expectations for the program and fellows, benefits, and advice, including childcare options, lactation room locations, and financial planning tips. We shared this document with fellows and incorporated feedback. As a “living document” it is subject to change and will be updated as needed (at least annually).
Additional planning considerations for fellows
Research childcare options (ideally 6 months or more before leave).
- Start to explore your institution’s resources for leave and childcare options (daycare waitlists may be greater than 1 year in some cities).
Inform your program director (4-5 months before leave).
- Consider informing your program director about pregnancy at the beginning of the second trimester.
- Discuss Accreditation Council for Graduate Medical Education requirements and scheduling responsibilities.
- Explicitly discuss whether you plan to graduate on time or extend fellowship.
Inform your colleagues and patients (at least 3-4 months before leave).
- If comfortable, consider getting advice from a co-fellow and/or faculty mentor parent to facilitate transition to parenthood.
- When you feel ready, begin trading rotations and calls with co-fellows. If you have a results inbox or pager, discuss who can help cover those during your leave.
- Inform research collaborators about your leave and make preparations to keep projects progressing during your leave.
- If you have “active” clinic patients, when appropriate, begin to inform them that you will be away and provide reassurance that a colleague will be covering you. Leave clear plans with contingencies for these patients in your last progress notes.
Complete institutional paperwork and map out facilities (at least 2-3 months before leave).
- Review your options for using time toward leave, including vacation, research, or Family and Medical Leave Act–provided leave (unpaid), and what paperwork you need to fill out.
- Contact your payroll and/or human resources office to inform them of birth/adoption.
- Research potential program parental benefits, such as dependent daycare and/or health care flexible spending accounts.
- If choosing to breastfeed, explore the lactation rooms that are closest to your workroom and endoscopy suite and determine how much time you will need to set aside for pumping.
Be prepared to make adjustments as needed.
- Endoscopy-heavy rotations may be more difficult in the third trimester of pregnancy.
- Make contingency plans for early or late delivery dates, as well as if you undergo a cesarean that requires additional recovery time.
- Consider scheduling elective rotations (research, clinic) toward the end of leave and for the first month of “return to work.”
- If you plan to join limited clinic or outpatient endoscopy blocks later in your leave, make early arrangements to work regularly with these attendings.
Conclusion
Trainee needs assessments in gastroenterology fellowship similar to those in other specialties should be performed, and are in fact underway.19,23,24 There is a lack of data regarding the availability of fellowship program guidance and, specifically, adherence to required policies, and more data from program directors at a national level need to be collected.20 We recommend that programs engage in identifying specific needs at their institutions with the goal of eventually sharing this knowledge with other programs. Gastroenterology society recommendations for performing endoscopy while pregnant, with regard to ergonomics, infection control, and radiation exposure, would be instrumental. GI fellowships should consolidate institutional knowledge and engage key stakeholders – including trainees, prior trainees, occupational safety experts, radiation safety offices, wellness experts, and GME – to create program-specific policies that are flexible but rigorous and generous but equitable.
Dr. Liu and Dr. Summa are gastroenterology fellows at Northwestern University, Chicago. Dr. Patel is an assistant professor of medicine and a gastroenterology fellowship assistant program director at Northwestern University, Chicago. Dr. Donnan and Dr. Guentner are assistant professors of medicine at Northwestern University. Dr. Kia is an assistant professor of medicine and the gastroenterology fellowship program director at Northwestern University. They have no conflicts of interest to disclose. The authors would like to thank Michelle Clermont, MD, and Maureen K. Bolon, MD, for their discussion and assistance during the drafting of this article.
References
1. Section on Medical Students, Residents, and Fellowship Trainees; Committee on Early Childhood. Pediatrics. 2013;131(2):387-90.
2. American Board of Medical Specialties. ABMS Announces Progressive Leave Policy for Residents and Fellows. July 13, 2020. Accessed May 1, 2021. https://www.abms.org/news-events/abms-announces-progressive-leave-policy-for-residents-and-fellows/.
3. Magudia K et al. J Grad Med Educ. 2020;12(2):162-7.
4. Blair JE et al. Acad Med. 2016;91(7):972-8.
5. Feld LD. Am J Gastroenterol. 2021;116(3):505-8.
6. Roubaud MS. Plast Reconstr Surg Glob Open. 2019. doi: 10.1097/GOX.0000000000002104.
7. Price J, Dunbar K. Gastrointest Endosc. 2009;69(1):121-3.
8. David YN et al. Gastrointest Endosc. 2020;91(6):AB75-AB76.
9. Webb AMB et al. Acad Med J Assoc Am Med Coll. 2019;94(11):1631-4.
10. Weinstein DF et al. N Engl J Med. 2019 Sep 12;381(11):995-7.
11. Anderson M, Goldman RH. JAMA Surg. 2020;155(3):243-9.
12. Palmer KT et al. Occup Environ Med. 2013;70(4):213-22.
13. Siegel JD et al; Healthcare Infection, Control Practices Advisory Committee. Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings (2007). 2007. Last reviewed July 22, 2019. Accessed April 28, 2021. https://www.cdc.gov/infectioncontrol/guidelines/isolation/index.html
14. David YN et al. Am J Gastroenterol. 2021;116(3):539-50.
15. Sethi S et al. Dig Dis Sci. 2019;64(9):2455-66.
16. Alzimami K et al. Gastroenterol Res Pract. 2013;2013:587574.
17. Hayashi S et al. World J Clin Cases. 2018;6(16):1087-93.
18. U.S. Department of Labor, Wage and Hour Division. “Frequently Asked Questions – Break Time for Nursing Mothers.” Accessed May 1, 2021. https://www.dol.gov/agencies/whd/nursing-mothers/faq.
19. Mwakyanjala EJ et al. J Am Heart Assoc. 2019. doi: 10.1161/JAHA.119.012137.
20. Castillo-Angeles M et al. JAMA Surg. 2021 Jul 1;156(7):647-53.
21. Prasad S et al. J Grad Med Educ. 2021 Jun;13(3):349-54.
22. Ho IKH et al. Am J Gastroenterol. 2014;109(8):1180-94.
23. Sherbaf FG et al. AJNR Am J Neuroradiol. 2020;41(8):1348-54.
24. Altieri MS et al. JAMA Surg. 2019;154(10):952-58.
COVID-19 linked to baby bust in high-income countries
In an assessment of the pandemic’s early effects, Arnstein Aassve, PhD, and colleagues found a significant COVID-19–related decline in crude birth rates (CBRs) in 7 of 22 high-income countries, particularly in Southwestern Europe.
Dr. Aassve, an economist at the Carlo F. Dondena Center for Research on Social Dynamics and Public Policy at the Università Commerciale Luigi Bocconi, Milan, and colleagues report the results in an article published online August 30 in the Proceedings of the National Academy of Sciences.
Defining the start of the COVID-19 pandemic as February 2020, the study identifies strong declines in Italy (-9.1%), Hungary (-8.5%), Spain (-8.4%), and Portugal (-6.6%) beyond those predicted by past trends. In the United States, CBRs fell by 7.1% relative to 2019 for births occurring in Nov. and Dec. 2020 following conceptions in February and March of that year.
Significant declines in CBR also occurred in Belgium, Austria, and Singapore.
A year-to-year comparison of the mean for monthly CBRs per 1,000 population before and during the pandemic suggests a negative difference for all countries studied except for Denmark, Finland, Germany, and the Netherlands, Dr. Aassve and colleagues write. These findings may have policy implications for childcare, housing, and the labor market.
The Milan researchers compared monthly vital statistics data on live births from the international Human Fertility Database for the period of Jan. 2016 to March 2021. These figures reflect conceptions carried to term between April 2015 and June 2020. The 22 countries in the analysis represent 37% of the total reported COVID-19 cases and 34% of deaths worldwide.
The study findings align with surveys on “fertility intentions” collected early in the first COVID-19 wave in Germany, France, Spain, and the United Kingdom. These surveys indicated that 73% of people who were planning pregnancies in 2020 either decided to delay the pregnancy or they abandoned their plans.
“The popular media speculated that the lockdown would lead to a baby boom, as couples spent more time together,” Dr. Aassve told this news organization. “There’s very little evidence of this when you look to previous disasters and shocks, and the first data suggest more of an immediate collapse than a boom. But as you also see from the paper, the collapse is not seen everywhere.” Other current studies suggest the fertility drop is immediate but temporary, says Dr. Aassve, who is also a professor of demography.
Interestingly, Dr. Aassve and colleagues found that CBRs were relatively stable in Northern Europe. The authors point to supportive social and family policies in that region that might have reduced the effect of the pandemic on births. “These factors are likely to affect CBRs in the subsequent pandemic waves,” they write. They call for future studies to assess the full population implications of the pandemic, the moderating impact of policy interventions, and the nexus between short- and long-run effects in relation to the various waves of the COVID-19 pandemic.
Rebounds
Some regions have already reported a rebound from the COVID-19 fertility trough. Molly J. Stout, MD, director of maternal fetal medicine at the University of Michigan, Ann Arbor, and colleagues used electronic medical records to predict a surge in births after the initial decline.
“The surge we’ve seen at the end of this summer is exceeding the usual annual birth rate, as predicted,” she said in an interview. “But I think there’ll be a return to normal after this transient escalation. I don’t think birth rates will stay elevated above the normal because the birth surge is a temporary response to an event, although there will likely be regional differences.”
Looking ahead, Dr. Stout, who was not involved in Dr. Aassve’s analysis, is not certain how a fourth pandemic wave might ultimately modify a couple’s overall family size. But the toll the health crisis has taken on working women who have been forced to withdraw from the economy because of a lack of childcare points to a societal need that should be addressed.
According to Philip N. Cohen, PhD, a professor of sociology at the University of Maryland, College Park, who’s been tracking fertility trends since the onset of the COVID-19 emergency, the pandemic has combined a health crisis with an economic crisis, along with “the additional factor of social distancing and isolation, which all contributed to the decline in birth rates. Some people changed their plans to hold off on having children, while others didn’t get pregnant because they weren’t socializing and meeting people as much.”
Dr. Cohen, who was not involved in the study by Dr. Aassve and associates, said his provisional data show that although in many places, birth rates have rebounded more or less to prepandemic levels after a nadir around Jan. 2021, some areas of the United States still show substantially lower rates, including California, Hawaii, and Oregon.
As to the duration of the pandemic effect, Dr. Aassve cautions that his group’s estimates refer to the first wave only. “We then have the second, third, and currently the fourth wave. We can’t be sure about the impact of these waves on fertility since the data are not there yet, but I’d be surprised if they didn’t continue to have an impact on fertility rates,” he said.
Dr. Cohen agreed: “Some people who delayed childbearing will make up the delay. However, whenever there’s a delay, there’s inevitably some portion of the decline that’s not recouped.”
As for the wider effect across the world, Dr. Aassve said his team’s figures derive from high-income countries where data are readily available. For middle- and low-income countries, fewer data exist, and the quality of those data is not as good.
The lessons from this and other upheavals teach us that unforeseen shocks almost always have a negative impact on fertility, says Dr. Aassve. “[B]ut these effects may be separate from existing declining trends. The issue here is that those overall declining trends may be driven by other factors. In contrast, the shock of the pandemic is short-lived, and we may return to normal rather quickly. But if the pandemic also impacts other societal structures, such as the occupational and industrial sectors, then the pandemic might exacerbate the negative trend.”
The study was supported by funding from the European Research Council for funding under the European Union’s Horizon 2020 Research and Innovation Programme. The study authors, Dr. Stout, and Dr. Cohen have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In an assessment of the pandemic’s early effects, Arnstein Aassve, PhD, and colleagues found a significant COVID-19–related decline in crude birth rates (CBRs) in 7 of 22 high-income countries, particularly in Southwestern Europe.
Dr. Aassve, an economist at the Carlo F. Dondena Center for Research on Social Dynamics and Public Policy at the Università Commerciale Luigi Bocconi, Milan, and colleagues report the results in an article published online August 30 in the Proceedings of the National Academy of Sciences.
Defining the start of the COVID-19 pandemic as February 2020, the study identifies strong declines in Italy (-9.1%), Hungary (-8.5%), Spain (-8.4%), and Portugal (-6.6%) beyond those predicted by past trends. In the United States, CBRs fell by 7.1% relative to 2019 for births occurring in Nov. and Dec. 2020 following conceptions in February and March of that year.
Significant declines in CBR also occurred in Belgium, Austria, and Singapore.
A year-to-year comparison of the mean for monthly CBRs per 1,000 population before and during the pandemic suggests a negative difference for all countries studied except for Denmark, Finland, Germany, and the Netherlands, Dr. Aassve and colleagues write. These findings may have policy implications for childcare, housing, and the labor market.
The Milan researchers compared monthly vital statistics data on live births from the international Human Fertility Database for the period of Jan. 2016 to March 2021. These figures reflect conceptions carried to term between April 2015 and June 2020. The 22 countries in the analysis represent 37% of the total reported COVID-19 cases and 34% of deaths worldwide.
The study findings align with surveys on “fertility intentions” collected early in the first COVID-19 wave in Germany, France, Spain, and the United Kingdom. These surveys indicated that 73% of people who were planning pregnancies in 2020 either decided to delay the pregnancy or they abandoned their plans.
“The popular media speculated that the lockdown would lead to a baby boom, as couples spent more time together,” Dr. Aassve told this news organization. “There’s very little evidence of this when you look to previous disasters and shocks, and the first data suggest more of an immediate collapse than a boom. But as you also see from the paper, the collapse is not seen everywhere.” Other current studies suggest the fertility drop is immediate but temporary, says Dr. Aassve, who is also a professor of demography.
Interestingly, Dr. Aassve and colleagues found that CBRs were relatively stable in Northern Europe. The authors point to supportive social and family policies in that region that might have reduced the effect of the pandemic on births. “These factors are likely to affect CBRs in the subsequent pandemic waves,” they write. They call for future studies to assess the full population implications of the pandemic, the moderating impact of policy interventions, and the nexus between short- and long-run effects in relation to the various waves of the COVID-19 pandemic.
Rebounds
Some regions have already reported a rebound from the COVID-19 fertility trough. Molly J. Stout, MD, director of maternal fetal medicine at the University of Michigan, Ann Arbor, and colleagues used electronic medical records to predict a surge in births after the initial decline.
“The surge we’ve seen at the end of this summer is exceeding the usual annual birth rate, as predicted,” she said in an interview. “But I think there’ll be a return to normal after this transient escalation. I don’t think birth rates will stay elevated above the normal because the birth surge is a temporary response to an event, although there will likely be regional differences.”
Looking ahead, Dr. Stout, who was not involved in Dr. Aassve’s analysis, is not certain how a fourth pandemic wave might ultimately modify a couple’s overall family size. But the toll the health crisis has taken on working women who have been forced to withdraw from the economy because of a lack of childcare points to a societal need that should be addressed.
According to Philip N. Cohen, PhD, a professor of sociology at the University of Maryland, College Park, who’s been tracking fertility trends since the onset of the COVID-19 emergency, the pandemic has combined a health crisis with an economic crisis, along with “the additional factor of social distancing and isolation, which all contributed to the decline in birth rates. Some people changed their plans to hold off on having children, while others didn’t get pregnant because they weren’t socializing and meeting people as much.”
Dr. Cohen, who was not involved in the study by Dr. Aassve and associates, said his provisional data show that although in many places, birth rates have rebounded more or less to prepandemic levels after a nadir around Jan. 2021, some areas of the United States still show substantially lower rates, including California, Hawaii, and Oregon.
As to the duration of the pandemic effect, Dr. Aassve cautions that his group’s estimates refer to the first wave only. “We then have the second, third, and currently the fourth wave. We can’t be sure about the impact of these waves on fertility since the data are not there yet, but I’d be surprised if they didn’t continue to have an impact on fertility rates,” he said.
Dr. Cohen agreed: “Some people who delayed childbearing will make up the delay. However, whenever there’s a delay, there’s inevitably some portion of the decline that’s not recouped.”
As for the wider effect across the world, Dr. Aassve said his team’s figures derive from high-income countries where data are readily available. For middle- and low-income countries, fewer data exist, and the quality of those data is not as good.
The lessons from this and other upheavals teach us that unforeseen shocks almost always have a negative impact on fertility, says Dr. Aassve. “[B]ut these effects may be separate from existing declining trends. The issue here is that those overall declining trends may be driven by other factors. In contrast, the shock of the pandemic is short-lived, and we may return to normal rather quickly. But if the pandemic also impacts other societal structures, such as the occupational and industrial sectors, then the pandemic might exacerbate the negative trend.”
The study was supported by funding from the European Research Council for funding under the European Union’s Horizon 2020 Research and Innovation Programme. The study authors, Dr. Stout, and Dr. Cohen have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In an assessment of the pandemic’s early effects, Arnstein Aassve, PhD, and colleagues found a significant COVID-19–related decline in crude birth rates (CBRs) in 7 of 22 high-income countries, particularly in Southwestern Europe.
Dr. Aassve, an economist at the Carlo F. Dondena Center for Research on Social Dynamics and Public Policy at the Università Commerciale Luigi Bocconi, Milan, and colleagues report the results in an article published online August 30 in the Proceedings of the National Academy of Sciences.
Defining the start of the COVID-19 pandemic as February 2020, the study identifies strong declines in Italy (-9.1%), Hungary (-8.5%), Spain (-8.4%), and Portugal (-6.6%) beyond those predicted by past trends. In the United States, CBRs fell by 7.1% relative to 2019 for births occurring in Nov. and Dec. 2020 following conceptions in February and March of that year.
Significant declines in CBR also occurred in Belgium, Austria, and Singapore.
A year-to-year comparison of the mean for monthly CBRs per 1,000 population before and during the pandemic suggests a negative difference for all countries studied except for Denmark, Finland, Germany, and the Netherlands, Dr. Aassve and colleagues write. These findings may have policy implications for childcare, housing, and the labor market.
The Milan researchers compared monthly vital statistics data on live births from the international Human Fertility Database for the period of Jan. 2016 to March 2021. These figures reflect conceptions carried to term between April 2015 and June 2020. The 22 countries in the analysis represent 37% of the total reported COVID-19 cases and 34% of deaths worldwide.
The study findings align with surveys on “fertility intentions” collected early in the first COVID-19 wave in Germany, France, Spain, and the United Kingdom. These surveys indicated that 73% of people who were planning pregnancies in 2020 either decided to delay the pregnancy or they abandoned their plans.
“The popular media speculated that the lockdown would lead to a baby boom, as couples spent more time together,” Dr. Aassve told this news organization. “There’s very little evidence of this when you look to previous disasters and shocks, and the first data suggest more of an immediate collapse than a boom. But as you also see from the paper, the collapse is not seen everywhere.” Other current studies suggest the fertility drop is immediate but temporary, says Dr. Aassve, who is also a professor of demography.
Interestingly, Dr. Aassve and colleagues found that CBRs were relatively stable in Northern Europe. The authors point to supportive social and family policies in that region that might have reduced the effect of the pandemic on births. “These factors are likely to affect CBRs in the subsequent pandemic waves,” they write. They call for future studies to assess the full population implications of the pandemic, the moderating impact of policy interventions, and the nexus between short- and long-run effects in relation to the various waves of the COVID-19 pandemic.
Rebounds
Some regions have already reported a rebound from the COVID-19 fertility trough. Molly J. Stout, MD, director of maternal fetal medicine at the University of Michigan, Ann Arbor, and colleagues used electronic medical records to predict a surge in births after the initial decline.
“The surge we’ve seen at the end of this summer is exceeding the usual annual birth rate, as predicted,” she said in an interview. “But I think there’ll be a return to normal after this transient escalation. I don’t think birth rates will stay elevated above the normal because the birth surge is a temporary response to an event, although there will likely be regional differences.”
Looking ahead, Dr. Stout, who was not involved in Dr. Aassve’s analysis, is not certain how a fourth pandemic wave might ultimately modify a couple’s overall family size. But the toll the health crisis has taken on working women who have been forced to withdraw from the economy because of a lack of childcare points to a societal need that should be addressed.
According to Philip N. Cohen, PhD, a professor of sociology at the University of Maryland, College Park, who’s been tracking fertility trends since the onset of the COVID-19 emergency, the pandemic has combined a health crisis with an economic crisis, along with “the additional factor of social distancing and isolation, which all contributed to the decline in birth rates. Some people changed their plans to hold off on having children, while others didn’t get pregnant because they weren’t socializing and meeting people as much.”
Dr. Cohen, who was not involved in the study by Dr. Aassve and associates, said his provisional data show that although in many places, birth rates have rebounded more or less to prepandemic levels after a nadir around Jan. 2021, some areas of the United States still show substantially lower rates, including California, Hawaii, and Oregon.
As to the duration of the pandemic effect, Dr. Aassve cautions that his group’s estimates refer to the first wave only. “We then have the second, third, and currently the fourth wave. We can’t be sure about the impact of these waves on fertility since the data are not there yet, but I’d be surprised if they didn’t continue to have an impact on fertility rates,” he said.
Dr. Cohen agreed: “Some people who delayed childbearing will make up the delay. However, whenever there’s a delay, there’s inevitably some portion of the decline that’s not recouped.”
As for the wider effect across the world, Dr. Aassve said his team’s figures derive from high-income countries where data are readily available. For middle- and low-income countries, fewer data exist, and the quality of those data is not as good.
The lessons from this and other upheavals teach us that unforeseen shocks almost always have a negative impact on fertility, says Dr. Aassve. “[B]ut these effects may be separate from existing declining trends. The issue here is that those overall declining trends may be driven by other factors. In contrast, the shock of the pandemic is short-lived, and we may return to normal rather quickly. But if the pandemic also impacts other societal structures, such as the occupational and industrial sectors, then the pandemic might exacerbate the negative trend.”
The study was supported by funding from the European Research Council for funding under the European Union’s Horizon 2020 Research and Innovation Programme. The study authors, Dr. Stout, and Dr. Cohen have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.