User login
Metformin use may curb BCC risk
in Iceland.
“In addition to general anticarcinogenic effects, metformin has also been shown to directly inhibit the sonic hedgehog pathway, a key pathway in basal cell carcinoma (BCC) pathogenesis,” Jonas A. Adalsteinsson, MD, of the University of Iceland, Reykjavik, and colleagues wrote. “The relationship between metformin and keratinocyte carcinoma has not been well-characterized but is of importance considering that metformin is a commonly prescribed medication.”
They added that the hedgehog pathway inhibitors vismodegib (Erivedge) and sonidegib (Odomzo), approved for treating BCC, “are highly effective for BCC prevention, but their broad use for BCC prophylaxis is limited due to numerous side effects.”
In the study, published in the Journal of the American Academy of Dermatology, the researchers identified 6,880 first-time cancer patients with BCC, squamous cell carcinoma in situ (SCCis), or invasive SCC, and 69,620 population controls using data from the Icelandic Cancer Registry and the Icelandic Prescription Medicine Register between 2003 and 2017. Metformin exposure was defined as having filled at least one prescription of metformin more than 2 years prior to cancer diagnosis. They used grams and daily dose units of metformin in their analysis; one DDU of metformin, “or its average daily maintenance dose when used for its primary indication, is 2 grams,” they noted.
Overall, metformin use was associated with a significantly lower risk of developing BCC, compared with nonuse (adjusted odds ratio, 0.71; 95% confidence interval, 0.61-0.83).
The reduced risk occurred similarly across age and gender subgroups, with the exception of individuals younger than 60 years, the researchers said. “This might signify that metformin has less of a protective effect in younger individuals, but we might also have lacked power in this category.” The association with reduced BCC risk remained significant at all three cumulative dose levels measured: 1-500 DDUs, 501-1,500 DDUs, and more than 1,500 DDUs.
Metformin use was not significantly associated with reduced risk of invasive SCC (aOR, 1.01) and in most cases of SCCis. However, the 501-1,500 DDU dose category was associated with a slight increase in risk of SCCis (aOR, 1.40; 95% CI, 1.00-1.96), “showing a possible increased risk of SCCis,” the authors wrote.
The decrease in BCC risk was seen across all metformin dosing levels, but the reason for this remains unclear, and might be related to a confounding factor that was not considered in this study, the researchers said. “It could also be that metformin’s BCC risk-lowering effect is immediate, with only a low dose being needed to see a clinical benefit.”
The study findings were limited by several factors, including the retrospective design and the inability to adjust for factors including ultraviolet exposure, Fitzpatrick skin type, and comorbidities. The frequent use of metformin by people with type 2 diabetes suggests diabetes itself or other diabetes medications could be possible confounding factors, the researchers wrote.
However, the results were strengthened by the large study population, and the data suggest an association between reduced risk of first-time BCC and metformin use, they added.
“Randomized, prospective trials are required to fully understand the effect metformin has on BCC and SCC risk,” the researchers concluded.
“There is a dire need to reduce incidence of skin cancers in general, and consequently a need for new non-surgical treatment options for keratinocytic nonmelanoma skin cancers,” Amor Khachemoune, MD, a dermatologist at the State University of New York, Brooklyn, and the department of dermatology of the Veteran Affairs NY Harbor Healthcare System, also in Brooklyn, said in an interview.
Dr. Khachemoune, who was not involved with the study, said that he was not surprised by the findings. “Like other well-studied sonic hedgehog inhibitors, vismodegib and sonidegib, metformin has a demonstrated effect on this pathway. The medical community outside of dermatology has extensive experience with the use of metformin for a host of other indications, including its role as anticarcinogenic, so it seemed natural that one would consider widening its use to quell the ever-expanding cases of basal cell carcinomas.”
However, complications from long-term use, though likely rare, could be a limitation in using metformin as a chemoprotective agent, Dr. Khachemoune said. Metformin-associated lactic acidosis is one example of a rare, but potentially life-threatening adverse event.
“Finding the right dosage and having an algorithm for follow up monitoring of side effects would certainly need to be put in place in a standardized way,” he emphasized. “As stated by the authors of this study, more inclusive research involving other groups with nonkeratinocytic malignancies in larger cohorts is needed.”
The study received no outside funding. The researchers and Dr. Khachemoune had no financial conflicts to disclose.
in Iceland.
“In addition to general anticarcinogenic effects, metformin has also been shown to directly inhibit the sonic hedgehog pathway, a key pathway in basal cell carcinoma (BCC) pathogenesis,” Jonas A. Adalsteinsson, MD, of the University of Iceland, Reykjavik, and colleagues wrote. “The relationship between metformin and keratinocyte carcinoma has not been well-characterized but is of importance considering that metformin is a commonly prescribed medication.”
They added that the hedgehog pathway inhibitors vismodegib (Erivedge) and sonidegib (Odomzo), approved for treating BCC, “are highly effective for BCC prevention, but their broad use for BCC prophylaxis is limited due to numerous side effects.”
In the study, published in the Journal of the American Academy of Dermatology, the researchers identified 6,880 first-time cancer patients with BCC, squamous cell carcinoma in situ (SCCis), or invasive SCC, and 69,620 population controls using data from the Icelandic Cancer Registry and the Icelandic Prescription Medicine Register between 2003 and 2017. Metformin exposure was defined as having filled at least one prescription of metformin more than 2 years prior to cancer diagnosis. They used grams and daily dose units of metformin in their analysis; one DDU of metformin, “or its average daily maintenance dose when used for its primary indication, is 2 grams,” they noted.
Overall, metformin use was associated with a significantly lower risk of developing BCC, compared with nonuse (adjusted odds ratio, 0.71; 95% confidence interval, 0.61-0.83).
The reduced risk occurred similarly across age and gender subgroups, with the exception of individuals younger than 60 years, the researchers said. “This might signify that metformin has less of a protective effect in younger individuals, but we might also have lacked power in this category.” The association with reduced BCC risk remained significant at all three cumulative dose levels measured: 1-500 DDUs, 501-1,500 DDUs, and more than 1,500 DDUs.
Metformin use was not significantly associated with reduced risk of invasive SCC (aOR, 1.01) and in most cases of SCCis. However, the 501-1,500 DDU dose category was associated with a slight increase in risk of SCCis (aOR, 1.40; 95% CI, 1.00-1.96), “showing a possible increased risk of SCCis,” the authors wrote.
The decrease in BCC risk was seen across all metformin dosing levels, but the reason for this remains unclear, and might be related to a confounding factor that was not considered in this study, the researchers said. “It could also be that metformin’s BCC risk-lowering effect is immediate, with only a low dose being needed to see a clinical benefit.”
The study findings were limited by several factors, including the retrospective design and the inability to adjust for factors including ultraviolet exposure, Fitzpatrick skin type, and comorbidities. The frequent use of metformin by people with type 2 diabetes suggests diabetes itself or other diabetes medications could be possible confounding factors, the researchers wrote.
However, the results were strengthened by the large study population, and the data suggest an association between reduced risk of first-time BCC and metformin use, they added.
“Randomized, prospective trials are required to fully understand the effect metformin has on BCC and SCC risk,” the researchers concluded.
“There is a dire need to reduce incidence of skin cancers in general, and consequently a need for new non-surgical treatment options for keratinocytic nonmelanoma skin cancers,” Amor Khachemoune, MD, a dermatologist at the State University of New York, Brooklyn, and the department of dermatology of the Veteran Affairs NY Harbor Healthcare System, also in Brooklyn, said in an interview.
Dr. Khachemoune, who was not involved with the study, said that he was not surprised by the findings. “Like other well-studied sonic hedgehog inhibitors, vismodegib and sonidegib, metformin has a demonstrated effect on this pathway. The medical community outside of dermatology has extensive experience with the use of metformin for a host of other indications, including its role as anticarcinogenic, so it seemed natural that one would consider widening its use to quell the ever-expanding cases of basal cell carcinomas.”
However, complications from long-term use, though likely rare, could be a limitation in using metformin as a chemoprotective agent, Dr. Khachemoune said. Metformin-associated lactic acidosis is one example of a rare, but potentially life-threatening adverse event.
“Finding the right dosage and having an algorithm for follow up monitoring of side effects would certainly need to be put in place in a standardized way,” he emphasized. “As stated by the authors of this study, more inclusive research involving other groups with nonkeratinocytic malignancies in larger cohorts is needed.”
The study received no outside funding. The researchers and Dr. Khachemoune had no financial conflicts to disclose.
in Iceland.
“In addition to general anticarcinogenic effects, metformin has also been shown to directly inhibit the sonic hedgehog pathway, a key pathway in basal cell carcinoma (BCC) pathogenesis,” Jonas A. Adalsteinsson, MD, of the University of Iceland, Reykjavik, and colleagues wrote. “The relationship between metformin and keratinocyte carcinoma has not been well-characterized but is of importance considering that metformin is a commonly prescribed medication.”
They added that the hedgehog pathway inhibitors vismodegib (Erivedge) and sonidegib (Odomzo), approved for treating BCC, “are highly effective for BCC prevention, but their broad use for BCC prophylaxis is limited due to numerous side effects.”
In the study, published in the Journal of the American Academy of Dermatology, the researchers identified 6,880 first-time cancer patients with BCC, squamous cell carcinoma in situ (SCCis), or invasive SCC, and 69,620 population controls using data from the Icelandic Cancer Registry and the Icelandic Prescription Medicine Register between 2003 and 2017. Metformin exposure was defined as having filled at least one prescription of metformin more than 2 years prior to cancer diagnosis. They used grams and daily dose units of metformin in their analysis; one DDU of metformin, “or its average daily maintenance dose when used for its primary indication, is 2 grams,” they noted.
Overall, metformin use was associated with a significantly lower risk of developing BCC, compared with nonuse (adjusted odds ratio, 0.71; 95% confidence interval, 0.61-0.83).
The reduced risk occurred similarly across age and gender subgroups, with the exception of individuals younger than 60 years, the researchers said. “This might signify that metformin has less of a protective effect in younger individuals, but we might also have lacked power in this category.” The association with reduced BCC risk remained significant at all three cumulative dose levels measured: 1-500 DDUs, 501-1,500 DDUs, and more than 1,500 DDUs.
Metformin use was not significantly associated with reduced risk of invasive SCC (aOR, 1.01) and in most cases of SCCis. However, the 501-1,500 DDU dose category was associated with a slight increase in risk of SCCis (aOR, 1.40; 95% CI, 1.00-1.96), “showing a possible increased risk of SCCis,” the authors wrote.
The decrease in BCC risk was seen across all metformin dosing levels, but the reason for this remains unclear, and might be related to a confounding factor that was not considered in this study, the researchers said. “It could also be that metformin’s BCC risk-lowering effect is immediate, with only a low dose being needed to see a clinical benefit.”
The study findings were limited by several factors, including the retrospective design and the inability to adjust for factors including ultraviolet exposure, Fitzpatrick skin type, and comorbidities. The frequent use of metformin by people with type 2 diabetes suggests diabetes itself or other diabetes medications could be possible confounding factors, the researchers wrote.
However, the results were strengthened by the large study population, and the data suggest an association between reduced risk of first-time BCC and metformin use, they added.
“Randomized, prospective trials are required to fully understand the effect metformin has on BCC and SCC risk,” the researchers concluded.
“There is a dire need to reduce incidence of skin cancers in general, and consequently a need for new non-surgical treatment options for keratinocytic nonmelanoma skin cancers,” Amor Khachemoune, MD, a dermatologist at the State University of New York, Brooklyn, and the department of dermatology of the Veteran Affairs NY Harbor Healthcare System, also in Brooklyn, said in an interview.
Dr. Khachemoune, who was not involved with the study, said that he was not surprised by the findings. “Like other well-studied sonic hedgehog inhibitors, vismodegib and sonidegib, metformin has a demonstrated effect on this pathway. The medical community outside of dermatology has extensive experience with the use of metformin for a host of other indications, including its role as anticarcinogenic, so it seemed natural that one would consider widening its use to quell the ever-expanding cases of basal cell carcinomas.”
However, complications from long-term use, though likely rare, could be a limitation in using metformin as a chemoprotective agent, Dr. Khachemoune said. Metformin-associated lactic acidosis is one example of a rare, but potentially life-threatening adverse event.
“Finding the right dosage and having an algorithm for follow up monitoring of side effects would certainly need to be put in place in a standardized way,” he emphasized. “As stated by the authors of this study, more inclusive research involving other groups with nonkeratinocytic malignancies in larger cohorts is needed.”
The study received no outside funding. The researchers and Dr. Khachemoune had no financial conflicts to disclose.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
State-of-the-art psych unit designed with recovery in mind
Calming wall colors, nature-themed murals, and soft nighttime lighting are all part of a unique new state-of-the-art inpatient psychiatric unit that focuses especially on children and adolescents who have experienced significant trauma.
The 16-bed unit, which has been in the works for 3½ years and opened June 30 at the University of Maryland Medical Center (UMMC), in Baltimore, Maryland, treats youth aged 5 to 17 years. It has separate wings for younger children and for adolescents.
“We offer a really warm and welcoming environment that we think is going to promote health and healing,” the unit’s head, Sarah Edwards, DO, director of child and adolescent psychiatry at UMMC and assistant professor of psychiatry, University of Maryland School of Medicine (UMSOM), Baltimore, said in an interview.
Previous research shows that 1 in 4 children experience some kind of maltreatment, whether physical, sexual, or emotional, and that 1 in 5 develop a diagnosable mental health disorder.
, Dr. Edwards noted. Recent data show that the rate of suicidal ideation among youth has increased significantly during the COVID-19 crisis.
“Urban children have unfortunately suffered a lot of what we call traumatic stress, so they might be victims of physical or sexual abuse but also face layers of stressful situations – for example, living in unsafe neighborhoods and attending schools that might not be so welcoming and safe,” said Dr. Edwards.
Safety first
Typical conditions treated at the new unit will include depression, anxiety, attention-deficit/hyperactivity disorder, psychotic spectrum, as well as trauma disorders.
Some of these young patients have been through the foster care system and show signs of trauma and poor attachment, Dr. Edwards noted. As a result, they may have difficulty regulating their thoughts and emotions and at times exhibit dangerous behavior.
The new unit is designed both architecturally and clinically to deliver “trauma-informed” care. This type of approach “recognizes the pervasive nature of trauma” and promotes settings that facilitate recovery, Dr. Edwards added.
The idea is to treat individuals “in a way that doesn’t re-traumatize them or make their condition worse,” she added.
Safety is of the utmost importance in the unit, Jill RachBeisel, MD, chief of psychiatry at UMMC and professor and chair in the department of psychiatry at UMSOM, said in an interview.
“Health care workers must recognize and respond to the effects of trauma – and one very important way is to provide care in settings that emphasize physical and emotional safety, which helps instill a sense of control and empowerment,” Dr. RachBeisel said.
Providing youth with options is an important way to provide that sense of control, Dr. Edwards added. For example, residents can choose their own music in their bedroom, such as sounds of nature, running water, or birds chirping. They can also draw or write personal notes on a large whiteboard in their unit.
Circadian-rhythm lighting
Other unique elements of the new unit include walls painted soothing shades and murals of natural scenery, created by a local artist.
These murals perfectly capture “the kind of overall spirit of what we were trying to induce,” said Dr. Edwards.
A part of the unit dubbed the “front porch” has a large mural depicting “a landscape of beautiful trees and water and animals,” she noted. Kids can gather here to relax or just hang out.
The lighting at the unit mirrors circadian rhythms. It’s brighter during the day to promote wakefulness and participation in activities and gradually dims toward the evening hours to help induce restful nighttime sleep.
Safe and empowering and adopt productive behaviors and coping skills, Dr. Edwards noted.
The staff for the interprofessional unit includes psychiatrists, psychologists, psychiatric nurses, occupational therapists, and others trained in pediatric care.
Advice for other centers
“Our new unit is designed to provide the highest standard in mental health care and incorporates a high-tech approach to create a calming, soothing, and engaging setting,” said Dr. RachBeisel.
School-transition specialists help connect discharged patients and their families to vital services and peer support. These services represent “an essential component of the continuum of care” for youth experiencing mental distress, she added.
Other organizations considering establishing a similar type of psychiatric unit should consult all stakeholders.
“We had staff, no matter what their role, be part of every step of this process, including helping with the design, picking out furniture they thought would make the most sense, and helping choose the artwork,” she said.
It is also important to incorporate feedback from youth themselves, Dr. Edwards added.
A version of this article first appeared on Medscape.com.
Calming wall colors, nature-themed murals, and soft nighttime lighting are all part of a unique new state-of-the-art inpatient psychiatric unit that focuses especially on children and adolescents who have experienced significant trauma.
The 16-bed unit, which has been in the works for 3½ years and opened June 30 at the University of Maryland Medical Center (UMMC), in Baltimore, Maryland, treats youth aged 5 to 17 years. It has separate wings for younger children and for adolescents.
“We offer a really warm and welcoming environment that we think is going to promote health and healing,” the unit’s head, Sarah Edwards, DO, director of child and adolescent psychiatry at UMMC and assistant professor of psychiatry, University of Maryland School of Medicine (UMSOM), Baltimore, said in an interview.
Previous research shows that 1 in 4 children experience some kind of maltreatment, whether physical, sexual, or emotional, and that 1 in 5 develop a diagnosable mental health disorder.
, Dr. Edwards noted. Recent data show that the rate of suicidal ideation among youth has increased significantly during the COVID-19 crisis.
“Urban children have unfortunately suffered a lot of what we call traumatic stress, so they might be victims of physical or sexual abuse but also face layers of stressful situations – for example, living in unsafe neighborhoods and attending schools that might not be so welcoming and safe,” said Dr. Edwards.
Safety first
Typical conditions treated at the new unit will include depression, anxiety, attention-deficit/hyperactivity disorder, psychotic spectrum, as well as trauma disorders.
Some of these young patients have been through the foster care system and show signs of trauma and poor attachment, Dr. Edwards noted. As a result, they may have difficulty regulating their thoughts and emotions and at times exhibit dangerous behavior.
The new unit is designed both architecturally and clinically to deliver “trauma-informed” care. This type of approach “recognizes the pervasive nature of trauma” and promotes settings that facilitate recovery, Dr. Edwards added.
The idea is to treat individuals “in a way that doesn’t re-traumatize them or make their condition worse,” she added.
Safety is of the utmost importance in the unit, Jill RachBeisel, MD, chief of psychiatry at UMMC and professor and chair in the department of psychiatry at UMSOM, said in an interview.
“Health care workers must recognize and respond to the effects of trauma – and one very important way is to provide care in settings that emphasize physical and emotional safety, which helps instill a sense of control and empowerment,” Dr. RachBeisel said.
Providing youth with options is an important way to provide that sense of control, Dr. Edwards added. For example, residents can choose their own music in their bedroom, such as sounds of nature, running water, or birds chirping. They can also draw or write personal notes on a large whiteboard in their unit.
Circadian-rhythm lighting
Other unique elements of the new unit include walls painted soothing shades and murals of natural scenery, created by a local artist.
These murals perfectly capture “the kind of overall spirit of what we were trying to induce,” said Dr. Edwards.
A part of the unit dubbed the “front porch” has a large mural depicting “a landscape of beautiful trees and water and animals,” she noted. Kids can gather here to relax or just hang out.
The lighting at the unit mirrors circadian rhythms. It’s brighter during the day to promote wakefulness and participation in activities and gradually dims toward the evening hours to help induce restful nighttime sleep.
Safe and empowering and adopt productive behaviors and coping skills, Dr. Edwards noted.
The staff for the interprofessional unit includes psychiatrists, psychologists, psychiatric nurses, occupational therapists, and others trained in pediatric care.
Advice for other centers
“Our new unit is designed to provide the highest standard in mental health care and incorporates a high-tech approach to create a calming, soothing, and engaging setting,” said Dr. RachBeisel.
School-transition specialists help connect discharged patients and their families to vital services and peer support. These services represent “an essential component of the continuum of care” for youth experiencing mental distress, she added.
Other organizations considering establishing a similar type of psychiatric unit should consult all stakeholders.
“We had staff, no matter what their role, be part of every step of this process, including helping with the design, picking out furniture they thought would make the most sense, and helping choose the artwork,” she said.
It is also important to incorporate feedback from youth themselves, Dr. Edwards added.
A version of this article first appeared on Medscape.com.
Calming wall colors, nature-themed murals, and soft nighttime lighting are all part of a unique new state-of-the-art inpatient psychiatric unit that focuses especially on children and adolescents who have experienced significant trauma.
The 16-bed unit, which has been in the works for 3½ years and opened June 30 at the University of Maryland Medical Center (UMMC), in Baltimore, Maryland, treats youth aged 5 to 17 years. It has separate wings for younger children and for adolescents.
“We offer a really warm and welcoming environment that we think is going to promote health and healing,” the unit’s head, Sarah Edwards, DO, director of child and adolescent psychiatry at UMMC and assistant professor of psychiatry, University of Maryland School of Medicine (UMSOM), Baltimore, said in an interview.
Previous research shows that 1 in 4 children experience some kind of maltreatment, whether physical, sexual, or emotional, and that 1 in 5 develop a diagnosable mental health disorder.
, Dr. Edwards noted. Recent data show that the rate of suicidal ideation among youth has increased significantly during the COVID-19 crisis.
“Urban children have unfortunately suffered a lot of what we call traumatic stress, so they might be victims of physical or sexual abuse but also face layers of stressful situations – for example, living in unsafe neighborhoods and attending schools that might not be so welcoming and safe,” said Dr. Edwards.
Safety first
Typical conditions treated at the new unit will include depression, anxiety, attention-deficit/hyperactivity disorder, psychotic spectrum, as well as trauma disorders.
Some of these young patients have been through the foster care system and show signs of trauma and poor attachment, Dr. Edwards noted. As a result, they may have difficulty regulating their thoughts and emotions and at times exhibit dangerous behavior.
The new unit is designed both architecturally and clinically to deliver “trauma-informed” care. This type of approach “recognizes the pervasive nature of trauma” and promotes settings that facilitate recovery, Dr. Edwards added.
The idea is to treat individuals “in a way that doesn’t re-traumatize them or make their condition worse,” she added.
Safety is of the utmost importance in the unit, Jill RachBeisel, MD, chief of psychiatry at UMMC and professor and chair in the department of psychiatry at UMSOM, said in an interview.
“Health care workers must recognize and respond to the effects of trauma – and one very important way is to provide care in settings that emphasize physical and emotional safety, which helps instill a sense of control and empowerment,” Dr. RachBeisel said.
Providing youth with options is an important way to provide that sense of control, Dr. Edwards added. For example, residents can choose their own music in their bedroom, such as sounds of nature, running water, or birds chirping. They can also draw or write personal notes on a large whiteboard in their unit.
Circadian-rhythm lighting
Other unique elements of the new unit include walls painted soothing shades and murals of natural scenery, created by a local artist.
These murals perfectly capture “the kind of overall spirit of what we were trying to induce,” said Dr. Edwards.
A part of the unit dubbed the “front porch” has a large mural depicting “a landscape of beautiful trees and water and animals,” she noted. Kids can gather here to relax or just hang out.
The lighting at the unit mirrors circadian rhythms. It’s brighter during the day to promote wakefulness and participation in activities and gradually dims toward the evening hours to help induce restful nighttime sleep.
Safe and empowering and adopt productive behaviors and coping skills, Dr. Edwards noted.
The staff for the interprofessional unit includes psychiatrists, psychologists, psychiatric nurses, occupational therapists, and others trained in pediatric care.
Advice for other centers
“Our new unit is designed to provide the highest standard in mental health care and incorporates a high-tech approach to create a calming, soothing, and engaging setting,” said Dr. RachBeisel.
School-transition specialists help connect discharged patients and their families to vital services and peer support. These services represent “an essential component of the continuum of care” for youth experiencing mental distress, she added.
Other organizations considering establishing a similar type of psychiatric unit should consult all stakeholders.
“We had staff, no matter what their role, be part of every step of this process, including helping with the design, picking out furniture they thought would make the most sense, and helping choose the artwork,” she said.
It is also important to incorporate feedback from youth themselves, Dr. Edwards added.
A version of this article first appeared on Medscape.com.
“Enough English” to be at risk
A hectic Friday morning at the hospital seemed less stressful amid morning greetings and humor from colleagues. In a team room full of hospitalists, life and death are often discussed in detail, ranging from medical discussions to joys and frustrations of the day to philosophy, politics, and more. It is almost impossible to miss something interesting.
People breaking into their native languages over the phone call from home always make me smile. The mention of a “complicated Indian patient unable to use interpreter” caught my attention.
My friend and colleague asked if I would be willing to take over the patient since I could speak Hindi. I was doubtful if I would add anything to make a meaningful difference, given the patient wasn’t even participating in a conversation. However, my colleague’s concern for the patient and faith in me was enough to say, “Sure, let me add her to my list.”
At the bedside, it felt like a classic “acute on chronic” hot mess situation. The patient presented with a generalized rash, anasarca, renal failure, multifocal pneumonia, and delirium. All I could gather from the patient were some incomprehensible words that sounded like Hindi. I called the family to obtain some history and to provide updates. Her son was excited to hear from me, and it didn’t take him long to guess that I was from India. But that could still mean that I might speak any of the twenty-two or more Indian languages.
Answering my questions one by one in perfectly understandable English, he was short and sweet. Suspicious of missing out on details, I offered hesitantly, “You could speak in Hindi with me.” Then came a flood of information with the details, concerns, questions, and what was lost in the translation.
We all attend to patients and families with limited English proficiency (LEP), immigrants, and nonimmigrants. LEP is a term used to describe individuals who do not speak English as their primary language and have a limited ability to read, speak, write, or understand English.1 Recent data from the American Community Survey (2005-2009) reports that 8.6% of the population (24 million Americans) have LEP.2 It’s a large and growing population that needs help overcoming language barriers and the appropriate use of professional medical interpreter services – a backbone to safe, quality, and cost-effective patient care.
The following day at bedside rounds, the nurse reported that the patient was looking and responding better. She could cooperate with interpreter services and could speak “some English.” Over the years, one thing that sounds more alarming than “no English” is “some English” or “enough English.” Around noon I received a page that the patient was refusing intravenous Lasix. At the bedside, however, the patient seemed unaware of the perceived refusal. Further discussions with the nurse lead to a familiar culprit, a relatively common gesture in South Asian cultures, a head bobble or shake.
The nurse reported that the patient shook her head side to side, seemed upset, and said “NO” when trying to administer the medication. On the other hand, the patient reported that she was upset to be at the hospital but had “NO” problem with the medicine.
My patient’s “some English” was indeed “enough English” to put her at risk due to medical error, which is highly likely when patients or providers can speak or understand a language to “get by” or to “make do.” Like my patient, the LEP patient population is more likely to experience medical errors, longer hospital stays, hospital-acquired complications, surgical delays, and readmissions. They are also less likely to receive preventive care, have access to regular care, or be satisfied with their care. They are much more likely to have adverse effects from drug complications, poor understanding of diagnoses, a greater risk of being misunderstood by their physicians or ancillary staff, and less likely to follow physician instructions.3-5 One study analyzed over 1,000 adverse-incident reports from six Joint Commission-accredited hospitals for LEP and English-speaking patients and found that 49% of LEP patients experienced physical harm versus 29.5% of English-speaking patients.6
I updated the patient’s LEP status that was missing in the chart, likely due to altered mental status at the time of admission. Reliable language and English proficiency data are usually entered at the patient’s point of entry with documentation of the language services required during the patient-provider encounter. The U.S. Census Bureau’s operational definition for LEP is a patient’s self-assessed ability to speak English less than “very well,” but how well it correlates with a patient’s actual English ability needs more study. Also, one’s self-assessed perception of ability might vary day to day, and language ability, by itself, is not static; it can differ from moment to moment and situation to situation. It may be easier to understand words in English when the situation is simple and less stressful than when things are complicated and stressful.
With a definition of LEP rather vague and the term somewhat derogatory, its meaning is open to interpretation. One study found that though speaking English less than “very well” was the most sensitive measure for identifying all of the patients who reported that they were unable to communicate effectively with their physicians, it was also the least specific.7 This lower specificity could lead to misclassification of some patients as LEP who are, in fact, able to effectively communicate in English with their physicians. This type of misclassification might lead to costly language assistance and carry the potential to cause conflicts between patient and provider. Telling a patient or family that they may have a “limited English proficiency” when they have believed otherwise and feel confident about their skills may come as a challenge. Some patients may also pretend to understand English to avoid being embarrassed about their linguistic abilities or perceive that they might be judged on their abilities in general.
Exiting the room, I gently reminded the RN to use the interpreter services. “Who has never been guilty of using an ad hoc interpreter or rushing through a long interpreter phone call due to time constraints?” I thought. A study from 2011 found that 43% of hospitalized patients with LEP had communicated without an interpreter present during admission, and 40% had communicated without an interpreter present after admission.8 In other words, a system in place does not mean service in use. But, the use of a trained interpreter is not only an obligation for care providers but a right for patients as per legal requirements of Title VI of the Civil Rights Act and the Standards for Culturally and Linguistically Appropriate Services (CLAS) by the Department of Health and Human Services’ (HSS) Office of Minority Health.9 In January 2010, The Joint Commission released a set of new and revised standards for patient-centered communication as part of an initiative to advance effective communication, cultural competence, and patient- and family-centered care.
Despite the requirements and availability of qualified medical interpreter services, there are multiple perceived and experienced barriers to the use of interpreter services. The most common one is that what comes as a free service for patients is a time commitment for providers. A long list of patients, acuity of the situation, and ease of use/availability of translation aids can change the calculus. One may be able to bill a prolonged service code (99354-99357) in addition to the appropriate E/M code, although a patient cannot be billed for the actual service provided by the interpreter. Longstanding CMS policy also permits reimbursement for translation/interpretation activities, so long as they are not included and paid for as part of the rate for direct service.10
The patient, however, insisted that she would rather have her son as the interpreter on the 3-way over the phone (OPI) conference call for interpretation. “He speaks good English and knows my medical history well,” she said. I counseled the patient on the benefits of using interpreter services and explained how to use the call button light and the visual aids.
Placing emphasis on educating patients about the benefits of using, and risks of not using, interpreter services is as essential as emphasizing that care providers use the services. Some patients may voluntarily choose to provide their own interpreter. Use of family members, friends, or unqualified staff as interpreters is one of the most commonly reported causes of errors by frontline staff. Using in-language collateral may help these patients understand how medical interpretation may create a better patient experience and outcome. A short factsheet, in different languages, on qualified interpreters’ expected benefits: meaning-for-meaning communication, impartiality, medical privacy, and improved patient safety and satisfaction, can also come in handy.
However, if the patient still refuses, providers should document the refusal of the offer of free language services, the name of the interpreter designated by the patient, the interpreter’s relationship to the LEP person, and the time or portions of the patient encounter that the interpreter’s services were used. Yet, language interpretation alone can be inadequate without document translation. According to one study, despite the availability of on-site professional interpreter services, hospitalized patients who do not speak English are less likely to have signed consent forms in their medical records.11 Health care professionals, therefore, need well-translated documents to treat LEP patients. Translated documents of consent forms for medical procedures, post-discharge instructions, prescription and medical device labels, and drug usage information may enhance informed decision making, safety and reduce stress and medical errors.
An unpopular and underused service needs it all: availability, convenience, monitoring, reporting, and team effort. Due to the sheer unpopularity and underuse of interpreter services, institutions should enhance ease of availability, monitor the use and quality of interpreter services, and optimize reporting of language-related errors. Ease of availability goes hand in hand with tapping local resources. Over the years, and even more so during the pandemic, in-person interpretation has transitioned to telephonic or video interpretation due to availability, safety, and cost issues. There are challenges in translating a language, and the absence of a visual channel adds another layer of complexity.
The current body of evidence does not indicate a superior interpreting method. Still, in one study providers and interpreters exposed to all three methods were more critical of remote methods and preferred videoconferencing to the telephone as a remote method. The significantly shorter phone interviews raised questions about the prospects of miscommunication in telephonic interpretation, given the absence of a visual channel.12
One way to bypass language barriers is to recognize the value added by hiring and training bilingual health care providers and fostering cultural competence. International medical graduates in many parts of the country aid in closing language barriers. Language-concordant care enhances trust between patients and physicians, optimizes health outcomes, and advances health equity for diverse populations.13-15 The presence of bilingual providers means more effective and timelier communication and improved patient satisfaction. But, according to a Doximity study, there is a significant “language gap” between those languages spoken by physicians and their patients.16 Hospitals, therefore, should assess, qualify, and incentivize staff who can serve as on-site medical interpreters for patients as a means to facilitate language concordant care for LEP patients.
The Agency of Healthcare Research and Quality (AHRQ) also has a guide on how hospitals can better identify, report, monitor, and prevent medical errors in patients with LEP. Included is the TeamSTEPPS LEP module to help develop and deploy a customized plan to train staff in teamwork skills and lead a medical teamwork improvement initiative.17
“Without my family, I was scared that nobody would understand me”
Back to the case. My patient was recovering well, and I was tying up loose ends on the switch day for the hospitalist teams.
“You will likely be discharged in a couple of days,” I said. She and the family were grateful and satisfied with the care. She had used the interpreter services and also received ethnocultural and language concordant and culturally competent care. Reducing language barriers is one of the crucial ways to reduce racial and ethnic disparities in quality of care and health outcomes, and it starts – in many cases – with identifying LEP patients. Proper use and monitoring of interpreter services, reporting language-related errors, hiring and testing bilingual staff’s language proficiency, and educating staff on cultural awareness are essential strategies for caring for LEP patients.
At my weeks’ end, in my handoff note to the incoming providers, I highlighted: “Patient will benefit from a Hindi speaking provider, Limited English Proficiency.”
Dr. Saigal is a hospitalist and clinical assistant professor of medicine in the division of hospital medicine at the Ohio State University Wexner Medical Center, Columbus.
References
1. Questions and Answers. Limited English Proficiency: A federal interagency website. www.lep.gov/commonly-asked-questions.
2. United States Census Bureau. Percent of people 5 years and over who speak English less than ‘very well’. www.census.gov/library/visualizations/interactive/people-that-speak-english-less-than-very-well.html.
3. Jacobs EA, et al. Overcoming language barriers in health care: Costs and benefits of interpreter services. Am J Public Health. 2004;94(5):866–869. doi: 10.2105/ajph.94.5.866.
4. Gandhi TK, et al. Drug complications in outpatients. J Gen Intern Med. 2000;15(3):149–154. doi: 10.1046/j.1525-1497.2000.04199.x.
5. Karliner LS, et al. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42(2):727–754. doi: 10.1111/j.1475-6773.2006.00629.x.
6. Divi C, et al. Language proficiency and adverse events in US hospitals: a pilot study. Int J Qual Health Care. 2007 Apr;19(2):60-7. doi: 10.1093/intqhc/mzl069.
7. Karliner LS, et al. Identification of limited English proficient patients in clinical care. J Gen Intern Med. 2008;23(10):1555-1560. doi:10.1007/s11606-008-0693-y.
8. Schenker Y, et al. Patterns of interpreter use for hospitalized patients with limited English proficiency. J Gen Intern Med. 2011 Jul;26(7):712-7. doi: 10.1007/s11606-010-1619-z.
9. Office of Minority Health, US Department of Health and Human Services. National Standards for Culturally and Linguistically Appropriate Services in Health Care: Final Report. Washington, DC: US Department of Health and Human Services; 2001. https://minorityhealth.hhs.gov/assets/pdf/checked/finalreport.pdf.
10. www.medicaid.gov/medicaid/financial-management/medicaid-administrative-claiming/translation-and-interpretation-services/index.html
11. Schenker Y, et al. The Impact of Language Barriers on Documentation of Informed Consent at a Hospital with On-Site Interpreter Services. J Gen Intern Med. 2007 Nov;22 Suppl 2(Suppl 2):294-9. doi: 10.1007/s11606-007-0359-1.
12. Locatis C, et al. Comparing in-person, video, and telephonic medical interpretation. J Gen Intern Med. 2010;25(4):345-350. doi:10.1007/s11606-009-1236-x.
13. Dunlap JL, et al. The effects of language concordant care on patient satisfaction and clinical understanding for Hispanic pediatric surgery patients. J Pediatr Surg. 2015 Sep;50(9):1586-9. doi: 10.1016/j.jpedsurg.2014.12.020.
14. Diamond L, et al. A Systematic Review of the Impact of Patient–Physician Non-English Language Concordance on Quality of Care and Outcomes. J Gen Intern Med. 2019 Aug;34(8):1591-1606. doi: 10.1007/s11606-019-04847-5.
15. Ngo-Metzger Q, et al. Providing high-quality care for limited English proficient patients: the importance of language concordance and interpreter use. J Gen Intern Med. 2007 Nov;22 Suppl 2(Suppl 2):324-30. doi: 10.1007/s11606-007-0340-z.
16. https://press.doximity.com/articles/first-ever-national-study-to-examine-different-languages-spoken-by-us-doctors.
17. Agency for Healthcare Research and Quality. Patients with Limited English Proficiency. www.ahrq.gov/teamstepps/lep/index.html.
A hectic Friday morning at the hospital seemed less stressful amid morning greetings and humor from colleagues. In a team room full of hospitalists, life and death are often discussed in detail, ranging from medical discussions to joys and frustrations of the day to philosophy, politics, and more. It is almost impossible to miss something interesting.
People breaking into their native languages over the phone call from home always make me smile. The mention of a “complicated Indian patient unable to use interpreter” caught my attention.
My friend and colleague asked if I would be willing to take over the patient since I could speak Hindi. I was doubtful if I would add anything to make a meaningful difference, given the patient wasn’t even participating in a conversation. However, my colleague’s concern for the patient and faith in me was enough to say, “Sure, let me add her to my list.”
At the bedside, it felt like a classic “acute on chronic” hot mess situation. The patient presented with a generalized rash, anasarca, renal failure, multifocal pneumonia, and delirium. All I could gather from the patient were some incomprehensible words that sounded like Hindi. I called the family to obtain some history and to provide updates. Her son was excited to hear from me, and it didn’t take him long to guess that I was from India. But that could still mean that I might speak any of the twenty-two or more Indian languages.
Answering my questions one by one in perfectly understandable English, he was short and sweet. Suspicious of missing out on details, I offered hesitantly, “You could speak in Hindi with me.” Then came a flood of information with the details, concerns, questions, and what was lost in the translation.
We all attend to patients and families with limited English proficiency (LEP), immigrants, and nonimmigrants. LEP is a term used to describe individuals who do not speak English as their primary language and have a limited ability to read, speak, write, or understand English.1 Recent data from the American Community Survey (2005-2009) reports that 8.6% of the population (24 million Americans) have LEP.2 It’s a large and growing population that needs help overcoming language barriers and the appropriate use of professional medical interpreter services – a backbone to safe, quality, and cost-effective patient care.
The following day at bedside rounds, the nurse reported that the patient was looking and responding better. She could cooperate with interpreter services and could speak “some English.” Over the years, one thing that sounds more alarming than “no English” is “some English” or “enough English.” Around noon I received a page that the patient was refusing intravenous Lasix. At the bedside, however, the patient seemed unaware of the perceived refusal. Further discussions with the nurse lead to a familiar culprit, a relatively common gesture in South Asian cultures, a head bobble or shake.
The nurse reported that the patient shook her head side to side, seemed upset, and said “NO” when trying to administer the medication. On the other hand, the patient reported that she was upset to be at the hospital but had “NO” problem with the medicine.
My patient’s “some English” was indeed “enough English” to put her at risk due to medical error, which is highly likely when patients or providers can speak or understand a language to “get by” or to “make do.” Like my patient, the LEP patient population is more likely to experience medical errors, longer hospital stays, hospital-acquired complications, surgical delays, and readmissions. They are also less likely to receive preventive care, have access to regular care, or be satisfied with their care. They are much more likely to have adverse effects from drug complications, poor understanding of diagnoses, a greater risk of being misunderstood by their physicians or ancillary staff, and less likely to follow physician instructions.3-5 One study analyzed over 1,000 adverse-incident reports from six Joint Commission-accredited hospitals for LEP and English-speaking patients and found that 49% of LEP patients experienced physical harm versus 29.5% of English-speaking patients.6
I updated the patient’s LEP status that was missing in the chart, likely due to altered mental status at the time of admission. Reliable language and English proficiency data are usually entered at the patient’s point of entry with documentation of the language services required during the patient-provider encounter. The U.S. Census Bureau’s operational definition for LEP is a patient’s self-assessed ability to speak English less than “very well,” but how well it correlates with a patient’s actual English ability needs more study. Also, one’s self-assessed perception of ability might vary day to day, and language ability, by itself, is not static; it can differ from moment to moment and situation to situation. It may be easier to understand words in English when the situation is simple and less stressful than when things are complicated and stressful.
With a definition of LEP rather vague and the term somewhat derogatory, its meaning is open to interpretation. One study found that though speaking English less than “very well” was the most sensitive measure for identifying all of the patients who reported that they were unable to communicate effectively with their physicians, it was also the least specific.7 This lower specificity could lead to misclassification of some patients as LEP who are, in fact, able to effectively communicate in English with their physicians. This type of misclassification might lead to costly language assistance and carry the potential to cause conflicts between patient and provider. Telling a patient or family that they may have a “limited English proficiency” when they have believed otherwise and feel confident about their skills may come as a challenge. Some patients may also pretend to understand English to avoid being embarrassed about their linguistic abilities or perceive that they might be judged on their abilities in general.
Exiting the room, I gently reminded the RN to use the interpreter services. “Who has never been guilty of using an ad hoc interpreter or rushing through a long interpreter phone call due to time constraints?” I thought. A study from 2011 found that 43% of hospitalized patients with LEP had communicated without an interpreter present during admission, and 40% had communicated without an interpreter present after admission.8 In other words, a system in place does not mean service in use. But, the use of a trained interpreter is not only an obligation for care providers but a right for patients as per legal requirements of Title VI of the Civil Rights Act and the Standards for Culturally and Linguistically Appropriate Services (CLAS) by the Department of Health and Human Services’ (HSS) Office of Minority Health.9 In January 2010, The Joint Commission released a set of new and revised standards for patient-centered communication as part of an initiative to advance effective communication, cultural competence, and patient- and family-centered care.
Despite the requirements and availability of qualified medical interpreter services, there are multiple perceived and experienced barriers to the use of interpreter services. The most common one is that what comes as a free service for patients is a time commitment for providers. A long list of patients, acuity of the situation, and ease of use/availability of translation aids can change the calculus. One may be able to bill a prolonged service code (99354-99357) in addition to the appropriate E/M code, although a patient cannot be billed for the actual service provided by the interpreter. Longstanding CMS policy also permits reimbursement for translation/interpretation activities, so long as they are not included and paid for as part of the rate for direct service.10
The patient, however, insisted that she would rather have her son as the interpreter on the 3-way over the phone (OPI) conference call for interpretation. “He speaks good English and knows my medical history well,” she said. I counseled the patient on the benefits of using interpreter services and explained how to use the call button light and the visual aids.
Placing emphasis on educating patients about the benefits of using, and risks of not using, interpreter services is as essential as emphasizing that care providers use the services. Some patients may voluntarily choose to provide their own interpreter. Use of family members, friends, or unqualified staff as interpreters is one of the most commonly reported causes of errors by frontline staff. Using in-language collateral may help these patients understand how medical interpretation may create a better patient experience and outcome. A short factsheet, in different languages, on qualified interpreters’ expected benefits: meaning-for-meaning communication, impartiality, medical privacy, and improved patient safety and satisfaction, can also come in handy.
However, if the patient still refuses, providers should document the refusal of the offer of free language services, the name of the interpreter designated by the patient, the interpreter’s relationship to the LEP person, and the time or portions of the patient encounter that the interpreter’s services were used. Yet, language interpretation alone can be inadequate without document translation. According to one study, despite the availability of on-site professional interpreter services, hospitalized patients who do not speak English are less likely to have signed consent forms in their medical records.11 Health care professionals, therefore, need well-translated documents to treat LEP patients. Translated documents of consent forms for medical procedures, post-discharge instructions, prescription and medical device labels, and drug usage information may enhance informed decision making, safety and reduce stress and medical errors.
An unpopular and underused service needs it all: availability, convenience, monitoring, reporting, and team effort. Due to the sheer unpopularity and underuse of interpreter services, institutions should enhance ease of availability, monitor the use and quality of interpreter services, and optimize reporting of language-related errors. Ease of availability goes hand in hand with tapping local resources. Over the years, and even more so during the pandemic, in-person interpretation has transitioned to telephonic or video interpretation due to availability, safety, and cost issues. There are challenges in translating a language, and the absence of a visual channel adds another layer of complexity.
The current body of evidence does not indicate a superior interpreting method. Still, in one study providers and interpreters exposed to all three methods were more critical of remote methods and preferred videoconferencing to the telephone as a remote method. The significantly shorter phone interviews raised questions about the prospects of miscommunication in telephonic interpretation, given the absence of a visual channel.12
One way to bypass language barriers is to recognize the value added by hiring and training bilingual health care providers and fostering cultural competence. International medical graduates in many parts of the country aid in closing language barriers. Language-concordant care enhances trust between patients and physicians, optimizes health outcomes, and advances health equity for diverse populations.13-15 The presence of bilingual providers means more effective and timelier communication and improved patient satisfaction. But, according to a Doximity study, there is a significant “language gap” between those languages spoken by physicians and their patients.16 Hospitals, therefore, should assess, qualify, and incentivize staff who can serve as on-site medical interpreters for patients as a means to facilitate language concordant care for LEP patients.
The Agency of Healthcare Research and Quality (AHRQ) also has a guide on how hospitals can better identify, report, monitor, and prevent medical errors in patients with LEP. Included is the TeamSTEPPS LEP module to help develop and deploy a customized plan to train staff in teamwork skills and lead a medical teamwork improvement initiative.17
“Without my family, I was scared that nobody would understand me”
Back to the case. My patient was recovering well, and I was tying up loose ends on the switch day for the hospitalist teams.
“You will likely be discharged in a couple of days,” I said. She and the family were grateful and satisfied with the care. She had used the interpreter services and also received ethnocultural and language concordant and culturally competent care. Reducing language barriers is one of the crucial ways to reduce racial and ethnic disparities in quality of care and health outcomes, and it starts – in many cases – with identifying LEP patients. Proper use and monitoring of interpreter services, reporting language-related errors, hiring and testing bilingual staff’s language proficiency, and educating staff on cultural awareness are essential strategies for caring for LEP patients.
At my weeks’ end, in my handoff note to the incoming providers, I highlighted: “Patient will benefit from a Hindi speaking provider, Limited English Proficiency.”
Dr. Saigal is a hospitalist and clinical assistant professor of medicine in the division of hospital medicine at the Ohio State University Wexner Medical Center, Columbus.
References
1. Questions and Answers. Limited English Proficiency: A federal interagency website. www.lep.gov/commonly-asked-questions.
2. United States Census Bureau. Percent of people 5 years and over who speak English less than ‘very well’. www.census.gov/library/visualizations/interactive/people-that-speak-english-less-than-very-well.html.
3. Jacobs EA, et al. Overcoming language barriers in health care: Costs and benefits of interpreter services. Am J Public Health. 2004;94(5):866–869. doi: 10.2105/ajph.94.5.866.
4. Gandhi TK, et al. Drug complications in outpatients. J Gen Intern Med. 2000;15(3):149–154. doi: 10.1046/j.1525-1497.2000.04199.x.
5. Karliner LS, et al. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42(2):727–754. doi: 10.1111/j.1475-6773.2006.00629.x.
6. Divi C, et al. Language proficiency and adverse events in US hospitals: a pilot study. Int J Qual Health Care. 2007 Apr;19(2):60-7. doi: 10.1093/intqhc/mzl069.
7. Karliner LS, et al. Identification of limited English proficient patients in clinical care. J Gen Intern Med. 2008;23(10):1555-1560. doi:10.1007/s11606-008-0693-y.
8. Schenker Y, et al. Patterns of interpreter use for hospitalized patients with limited English proficiency. J Gen Intern Med. 2011 Jul;26(7):712-7. doi: 10.1007/s11606-010-1619-z.
9. Office of Minority Health, US Department of Health and Human Services. National Standards for Culturally and Linguistically Appropriate Services in Health Care: Final Report. Washington, DC: US Department of Health and Human Services; 2001. https://minorityhealth.hhs.gov/assets/pdf/checked/finalreport.pdf.
10. www.medicaid.gov/medicaid/financial-management/medicaid-administrative-claiming/translation-and-interpretation-services/index.html
11. Schenker Y, et al. The Impact of Language Barriers on Documentation of Informed Consent at a Hospital with On-Site Interpreter Services. J Gen Intern Med. 2007 Nov;22 Suppl 2(Suppl 2):294-9. doi: 10.1007/s11606-007-0359-1.
12. Locatis C, et al. Comparing in-person, video, and telephonic medical interpretation. J Gen Intern Med. 2010;25(4):345-350. doi:10.1007/s11606-009-1236-x.
13. Dunlap JL, et al. The effects of language concordant care on patient satisfaction and clinical understanding for Hispanic pediatric surgery patients. J Pediatr Surg. 2015 Sep;50(9):1586-9. doi: 10.1016/j.jpedsurg.2014.12.020.
14. Diamond L, et al. A Systematic Review of the Impact of Patient–Physician Non-English Language Concordance on Quality of Care and Outcomes. J Gen Intern Med. 2019 Aug;34(8):1591-1606. doi: 10.1007/s11606-019-04847-5.
15. Ngo-Metzger Q, et al. Providing high-quality care for limited English proficient patients: the importance of language concordance and interpreter use. J Gen Intern Med. 2007 Nov;22 Suppl 2(Suppl 2):324-30. doi: 10.1007/s11606-007-0340-z.
16. https://press.doximity.com/articles/first-ever-national-study-to-examine-different-languages-spoken-by-us-doctors.
17. Agency for Healthcare Research and Quality. Patients with Limited English Proficiency. www.ahrq.gov/teamstepps/lep/index.html.
A hectic Friday morning at the hospital seemed less stressful amid morning greetings and humor from colleagues. In a team room full of hospitalists, life and death are often discussed in detail, ranging from medical discussions to joys and frustrations of the day to philosophy, politics, and more. It is almost impossible to miss something interesting.
People breaking into their native languages over the phone call from home always make me smile. The mention of a “complicated Indian patient unable to use interpreter” caught my attention.
My friend and colleague asked if I would be willing to take over the patient since I could speak Hindi. I was doubtful if I would add anything to make a meaningful difference, given the patient wasn’t even participating in a conversation. However, my colleague’s concern for the patient and faith in me was enough to say, “Sure, let me add her to my list.”
At the bedside, it felt like a classic “acute on chronic” hot mess situation. The patient presented with a generalized rash, anasarca, renal failure, multifocal pneumonia, and delirium. All I could gather from the patient were some incomprehensible words that sounded like Hindi. I called the family to obtain some history and to provide updates. Her son was excited to hear from me, and it didn’t take him long to guess that I was from India. But that could still mean that I might speak any of the twenty-two or more Indian languages.
Answering my questions one by one in perfectly understandable English, he was short and sweet. Suspicious of missing out on details, I offered hesitantly, “You could speak in Hindi with me.” Then came a flood of information with the details, concerns, questions, and what was lost in the translation.
We all attend to patients and families with limited English proficiency (LEP), immigrants, and nonimmigrants. LEP is a term used to describe individuals who do not speak English as their primary language and have a limited ability to read, speak, write, or understand English.1 Recent data from the American Community Survey (2005-2009) reports that 8.6% of the population (24 million Americans) have LEP.2 It’s a large and growing population that needs help overcoming language barriers and the appropriate use of professional medical interpreter services – a backbone to safe, quality, and cost-effective patient care.
The following day at bedside rounds, the nurse reported that the patient was looking and responding better. She could cooperate with interpreter services and could speak “some English.” Over the years, one thing that sounds more alarming than “no English” is “some English” or “enough English.” Around noon I received a page that the patient was refusing intravenous Lasix. At the bedside, however, the patient seemed unaware of the perceived refusal. Further discussions with the nurse lead to a familiar culprit, a relatively common gesture in South Asian cultures, a head bobble or shake.
The nurse reported that the patient shook her head side to side, seemed upset, and said “NO” when trying to administer the medication. On the other hand, the patient reported that she was upset to be at the hospital but had “NO” problem with the medicine.
My patient’s “some English” was indeed “enough English” to put her at risk due to medical error, which is highly likely when patients or providers can speak or understand a language to “get by” or to “make do.” Like my patient, the LEP patient population is more likely to experience medical errors, longer hospital stays, hospital-acquired complications, surgical delays, and readmissions. They are also less likely to receive preventive care, have access to regular care, or be satisfied with their care. They are much more likely to have adverse effects from drug complications, poor understanding of diagnoses, a greater risk of being misunderstood by their physicians or ancillary staff, and less likely to follow physician instructions.3-5 One study analyzed over 1,000 adverse-incident reports from six Joint Commission-accredited hospitals for LEP and English-speaking patients and found that 49% of LEP patients experienced physical harm versus 29.5% of English-speaking patients.6
I updated the patient’s LEP status that was missing in the chart, likely due to altered mental status at the time of admission. Reliable language and English proficiency data are usually entered at the patient’s point of entry with documentation of the language services required during the patient-provider encounter. The U.S. Census Bureau’s operational definition for LEP is a patient’s self-assessed ability to speak English less than “very well,” but how well it correlates with a patient’s actual English ability needs more study. Also, one’s self-assessed perception of ability might vary day to day, and language ability, by itself, is not static; it can differ from moment to moment and situation to situation. It may be easier to understand words in English when the situation is simple and less stressful than when things are complicated and stressful.
With a definition of LEP rather vague and the term somewhat derogatory, its meaning is open to interpretation. One study found that though speaking English less than “very well” was the most sensitive measure for identifying all of the patients who reported that they were unable to communicate effectively with their physicians, it was also the least specific.7 This lower specificity could lead to misclassification of some patients as LEP who are, in fact, able to effectively communicate in English with their physicians. This type of misclassification might lead to costly language assistance and carry the potential to cause conflicts between patient and provider. Telling a patient or family that they may have a “limited English proficiency” when they have believed otherwise and feel confident about their skills may come as a challenge. Some patients may also pretend to understand English to avoid being embarrassed about their linguistic abilities or perceive that they might be judged on their abilities in general.
Exiting the room, I gently reminded the RN to use the interpreter services. “Who has never been guilty of using an ad hoc interpreter or rushing through a long interpreter phone call due to time constraints?” I thought. A study from 2011 found that 43% of hospitalized patients with LEP had communicated without an interpreter present during admission, and 40% had communicated without an interpreter present after admission.8 In other words, a system in place does not mean service in use. But, the use of a trained interpreter is not only an obligation for care providers but a right for patients as per legal requirements of Title VI of the Civil Rights Act and the Standards for Culturally and Linguistically Appropriate Services (CLAS) by the Department of Health and Human Services’ (HSS) Office of Minority Health.9 In January 2010, The Joint Commission released a set of new and revised standards for patient-centered communication as part of an initiative to advance effective communication, cultural competence, and patient- and family-centered care.
Despite the requirements and availability of qualified medical interpreter services, there are multiple perceived and experienced barriers to the use of interpreter services. The most common one is that what comes as a free service for patients is a time commitment for providers. A long list of patients, acuity of the situation, and ease of use/availability of translation aids can change the calculus. One may be able to bill a prolonged service code (99354-99357) in addition to the appropriate E/M code, although a patient cannot be billed for the actual service provided by the interpreter. Longstanding CMS policy also permits reimbursement for translation/interpretation activities, so long as they are not included and paid for as part of the rate for direct service.10
The patient, however, insisted that she would rather have her son as the interpreter on the 3-way over the phone (OPI) conference call for interpretation. “He speaks good English and knows my medical history well,” she said. I counseled the patient on the benefits of using interpreter services and explained how to use the call button light and the visual aids.
Placing emphasis on educating patients about the benefits of using, and risks of not using, interpreter services is as essential as emphasizing that care providers use the services. Some patients may voluntarily choose to provide their own interpreter. Use of family members, friends, or unqualified staff as interpreters is one of the most commonly reported causes of errors by frontline staff. Using in-language collateral may help these patients understand how medical interpretation may create a better patient experience and outcome. A short factsheet, in different languages, on qualified interpreters’ expected benefits: meaning-for-meaning communication, impartiality, medical privacy, and improved patient safety and satisfaction, can also come in handy.
However, if the patient still refuses, providers should document the refusal of the offer of free language services, the name of the interpreter designated by the patient, the interpreter’s relationship to the LEP person, and the time or portions of the patient encounter that the interpreter’s services were used. Yet, language interpretation alone can be inadequate without document translation. According to one study, despite the availability of on-site professional interpreter services, hospitalized patients who do not speak English are less likely to have signed consent forms in their medical records.11 Health care professionals, therefore, need well-translated documents to treat LEP patients. Translated documents of consent forms for medical procedures, post-discharge instructions, prescription and medical device labels, and drug usage information may enhance informed decision making, safety and reduce stress and medical errors.
An unpopular and underused service needs it all: availability, convenience, monitoring, reporting, and team effort. Due to the sheer unpopularity and underuse of interpreter services, institutions should enhance ease of availability, monitor the use and quality of interpreter services, and optimize reporting of language-related errors. Ease of availability goes hand in hand with tapping local resources. Over the years, and even more so during the pandemic, in-person interpretation has transitioned to telephonic or video interpretation due to availability, safety, and cost issues. There are challenges in translating a language, and the absence of a visual channel adds another layer of complexity.
The current body of evidence does not indicate a superior interpreting method. Still, in one study providers and interpreters exposed to all three methods were more critical of remote methods and preferred videoconferencing to the telephone as a remote method. The significantly shorter phone interviews raised questions about the prospects of miscommunication in telephonic interpretation, given the absence of a visual channel.12
One way to bypass language barriers is to recognize the value added by hiring and training bilingual health care providers and fostering cultural competence. International medical graduates in many parts of the country aid in closing language barriers. Language-concordant care enhances trust between patients and physicians, optimizes health outcomes, and advances health equity for diverse populations.13-15 The presence of bilingual providers means more effective and timelier communication and improved patient satisfaction. But, according to a Doximity study, there is a significant “language gap” between those languages spoken by physicians and their patients.16 Hospitals, therefore, should assess, qualify, and incentivize staff who can serve as on-site medical interpreters for patients as a means to facilitate language concordant care for LEP patients.
The Agency of Healthcare Research and Quality (AHRQ) also has a guide on how hospitals can better identify, report, monitor, and prevent medical errors in patients with LEP. Included is the TeamSTEPPS LEP module to help develop and deploy a customized plan to train staff in teamwork skills and lead a medical teamwork improvement initiative.17
“Without my family, I was scared that nobody would understand me”
Back to the case. My patient was recovering well, and I was tying up loose ends on the switch day for the hospitalist teams.
“You will likely be discharged in a couple of days,” I said. She and the family were grateful and satisfied with the care. She had used the interpreter services and also received ethnocultural and language concordant and culturally competent care. Reducing language barriers is one of the crucial ways to reduce racial and ethnic disparities in quality of care and health outcomes, and it starts – in many cases – with identifying LEP patients. Proper use and monitoring of interpreter services, reporting language-related errors, hiring and testing bilingual staff’s language proficiency, and educating staff on cultural awareness are essential strategies for caring for LEP patients.
At my weeks’ end, in my handoff note to the incoming providers, I highlighted: “Patient will benefit from a Hindi speaking provider, Limited English Proficiency.”
Dr. Saigal is a hospitalist and clinical assistant professor of medicine in the division of hospital medicine at the Ohio State University Wexner Medical Center, Columbus.
References
1. Questions and Answers. Limited English Proficiency: A federal interagency website. www.lep.gov/commonly-asked-questions.
2. United States Census Bureau. Percent of people 5 years and over who speak English less than ‘very well’. www.census.gov/library/visualizations/interactive/people-that-speak-english-less-than-very-well.html.
3. Jacobs EA, et al. Overcoming language barriers in health care: Costs and benefits of interpreter services. Am J Public Health. 2004;94(5):866–869. doi: 10.2105/ajph.94.5.866.
4. Gandhi TK, et al. Drug complications in outpatients. J Gen Intern Med. 2000;15(3):149–154. doi: 10.1046/j.1525-1497.2000.04199.x.
5. Karliner LS, et al. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42(2):727–754. doi: 10.1111/j.1475-6773.2006.00629.x.
6. Divi C, et al. Language proficiency and adverse events in US hospitals: a pilot study. Int J Qual Health Care. 2007 Apr;19(2):60-7. doi: 10.1093/intqhc/mzl069.
7. Karliner LS, et al. Identification of limited English proficient patients in clinical care. J Gen Intern Med. 2008;23(10):1555-1560. doi:10.1007/s11606-008-0693-y.
8. Schenker Y, et al. Patterns of interpreter use for hospitalized patients with limited English proficiency. J Gen Intern Med. 2011 Jul;26(7):712-7. doi: 10.1007/s11606-010-1619-z.
9. Office of Minority Health, US Department of Health and Human Services. National Standards for Culturally and Linguistically Appropriate Services in Health Care: Final Report. Washington, DC: US Department of Health and Human Services; 2001. https://minorityhealth.hhs.gov/assets/pdf/checked/finalreport.pdf.
10. www.medicaid.gov/medicaid/financial-management/medicaid-administrative-claiming/translation-and-interpretation-services/index.html
11. Schenker Y, et al. The Impact of Language Barriers on Documentation of Informed Consent at a Hospital with On-Site Interpreter Services. J Gen Intern Med. 2007 Nov;22 Suppl 2(Suppl 2):294-9. doi: 10.1007/s11606-007-0359-1.
12. Locatis C, et al. Comparing in-person, video, and telephonic medical interpretation. J Gen Intern Med. 2010;25(4):345-350. doi:10.1007/s11606-009-1236-x.
13. Dunlap JL, et al. The effects of language concordant care on patient satisfaction and clinical understanding for Hispanic pediatric surgery patients. J Pediatr Surg. 2015 Sep;50(9):1586-9. doi: 10.1016/j.jpedsurg.2014.12.020.
14. Diamond L, et al. A Systematic Review of the Impact of Patient–Physician Non-English Language Concordance on Quality of Care and Outcomes. J Gen Intern Med. 2019 Aug;34(8):1591-1606. doi: 10.1007/s11606-019-04847-5.
15. Ngo-Metzger Q, et al. Providing high-quality care for limited English proficient patients: the importance of language concordance and interpreter use. J Gen Intern Med. 2007 Nov;22 Suppl 2(Suppl 2):324-30. doi: 10.1007/s11606-007-0340-z.
16. https://press.doximity.com/articles/first-ever-national-study-to-examine-different-languages-spoken-by-us-doctors.
17. Agency for Healthcare Research and Quality. Patients with Limited English Proficiency. www.ahrq.gov/teamstepps/lep/index.html.
Do patients with cancer need a third shot of COVID vaccine?
Patients with cancer have shown varying responses to COVID-19 vaccination, with good responses in patients with solid tumors (even while on systemic therapy) and poor responses in patients with blood cancers, particularly those on immunosuppressive therapies.
The data are evolving to show factors associated with a poor response but are not strong enough yet to recommend booster shots, say researchers.
The work is defining who will likely need a COVID vaccine booster when they become available. “It’s definitely not all cancer patients,” said Dimpy Shah, MD, PhD, a cancer epidemiologist at the Mays Cancer Center, University of Texas, San Antonio.
Public anxiously awaiting boosters
Boosters aren’t recommended in the United States at the moment, in large part because the Emergency Use Authorization under which the vaccines are being administered allows for only two shots of the Pfizer and Moderna vaccines and one shot of the Johnson & Johnson vaccine.
Even so, regulators and policymakers are “keenly aware that physicians and patients alike are anxious to get going and start doing boosters,” Dr. Shah said. There’s concern that antibody response might wane over time, perhaps even more quickly in patients with cancer.
Pfizer is already in talks with the U.S. Food and Drug Administration to authorize a third dose of its vaccine in the United States. Guidelines could very well change in coming months, said Ghady Haidar, MD, a specialist in infectious diseases and cancer at the University of Pittsburgh.
However, it’s still early in the game, and it’s not clear yet if boosters are necessary in cancer, Dr. Haidar said in an interview.
For one thing, it’s unknown if poor antibody response really means that patients aren’t protected, he explained. The vaccines elicit T-cell responses that could protect patients regardless of antibody levels. It’s also unclear if antibody titer levels are clinically relevant, and there hasn’t been much indication yet that less-than-robust vaccine responses translate to worse COVID outcomes in patients with cancer.
Those and other questions are areas of active investigation by Dr. Shah, Dr. Haidar, and others. Dozens of clinical trials are investigating vaccine response in patients with cancer, including the use of boosters.
Meanwhile, some cancer patients aren’t waiting around for more study results. “I get many, many emails a day” about booster shots, Dr. Haidar said. “We recommend against” them for now but some people bend the rules and get an extra shot anyway. “I get it. People are apprehensive.”
Three COVID deaths despite full vaccination
The vaccine clinical trials had fewer patients with cancer, so researchers are moving fast to backfill the data. Although there is some variation in what’s being reported, an overall picture is slowly emerging.
Dr. Shah and her team reported on responses to the mRNA COVID vaccines from Pfizer and Moderna and found a 94% seroconversion rate in 131 patients with cancer 3-4 weeks after their second dose of vaccine. They also found good responses among patients on cytotoxic chemotherapy within 6 months of their first vaccine dose, although their antibody titer levels were significantly lower than seen in other patients with cancer.
Investigators from Montefiore Medical Center in New York City also recently reported a 94% seroconversion rate among 200 patients with cancer, including 98% seroconversion in patients with solid tumors. Rates were lower in patients with blood cancers but were still 85% overall, with 70% conversion among patients on anti-CD20 therapies and 73% among stem cell transplant patients.
Dr. Haidar’s group reported a seroconversion rate of 82.4% among patients with solid tumors but only 54.7% among those with blood cancer. Risk factors for poor response included treatment with antimetabolites and anti-CD20 therapies, and, in the solid tumor group, radiation therapy, likely because of its overall toxicity and impact on lymphocyte function.
Israeli investigators reported in May a 90% seroconversion rate after two doses of the Pfizer vaccine among 102 patients with solid tumors on active treatment, which compared favorably to the 100% conversion rate in healthy controls, but they noted that antibody titers were considerably lower in patients with cancer.
The only variable associated with lower titer levels was combined use of chemotherapy and immunotherapy, they noted. There were also three women on dose-dense chemotherapy for breast cancer who did not produce any antibodies.
In a study limited to patients with blood cancers, a Lithuanian team recently reported that among 885 patients, those on Bruton tyrosine kinase inhibitors, ruxolitinib (Jakafi), venetoclax (Venclexta), or anti-CD20 therapies mounted almost no antibody response to the Pfizer vaccine.
The Lithuanian group also reported nine breakthrough COVID infections among their fully vaccinated blood cancer patients, including three deaths.
A team from the Icahn School of Medicine at Mount Sinai, New York reported that more than 15% of 260 patients with multiple myeloma also had no response to the Pfizer or Moderna vaccine; they were on BCMA-targeted therapy or anti-CD38 monoclonal antibody therapy at the time of vaccination, but a few had undergone CAR-T cell therapy more than 3 months beforehand.
Heated debate about antibody testing
Despite these reports of some patients with cancer having poorer responses, there’s some uncertainty over the benefit of giving a third (booster) shot.
There’s the question about the clinical relevance of antibody titer levels, and very little work has been done to date on cellular T-cell immunity from the vaccines.
“Right now, we are using titer levels like they actually mean something when they might not,” said Ravi Parikh, MD, a genitourinary and thoracic oncologist at the University of Pennsylvania, Philadelphia, who co-wrote an editorial that accompanies the Israeli report.
That’s one of the reasons why the FDA and others do not currently recommend antibody tests for COVID vaccine decisions outside of a clinical trial, but not everyone agrees with that position.
There’s been “a lot of heated debate in the medical community” over the issue, Dr. Haidar said.
The Icahn team, for instance, said that their results “underscore the need for routine serological monitoring of [multiple myeloma] patients following COVID-19 vaccination” to see if they might still need to mask-up and socially distance.
There is precedence, too, for vaccine boosters in cancer. As Dr. Parikh noted in his editorial, guidelines recommend revaccination after stem cell transplant for meningococcus, tetanus, and varicella, and other infections.
In France, COVID booster shots are already standard care for patients on dialysis and those on anti-CD20 agents, as well as for solid organ transplant recipients, for whom the literature supporting the benefit of COVID boosters is much more evolved than in cancer.
Israel has also authorized vaccine boosters for immunocompromised patients, including those with cancer, according to news reports.
It is also almost certain that the FDA will grant a formal approval for the COVID vaccines, at which point doctors will be free to administer boosters as they see fit.
“People are going to have to think really hard about what to do with them” if guidance hasn’t changed by then, Dr. Haidar said.
As the story unfolds, Dr. Haidar and others said in an interview that the take-home message for oncologists remains largely what it has been – namely to get patients vaccinated but also to consider masks and social distancing afterward for those at risk of a poor response.
Dr. Shah, Dr. Haidar, and Dr. Parikh have disclosed no relevant financial relationships. Dr. Parikh is a regular contributor to Medscape Oncology.
A version of this article first appeared on Medscape.com.
Patients with cancer have shown varying responses to COVID-19 vaccination, with good responses in patients with solid tumors (even while on systemic therapy) and poor responses in patients with blood cancers, particularly those on immunosuppressive therapies.
The data are evolving to show factors associated with a poor response but are not strong enough yet to recommend booster shots, say researchers.
The work is defining who will likely need a COVID vaccine booster when they become available. “It’s definitely not all cancer patients,” said Dimpy Shah, MD, PhD, a cancer epidemiologist at the Mays Cancer Center, University of Texas, San Antonio.
Public anxiously awaiting boosters
Boosters aren’t recommended in the United States at the moment, in large part because the Emergency Use Authorization under which the vaccines are being administered allows for only two shots of the Pfizer and Moderna vaccines and one shot of the Johnson & Johnson vaccine.
Even so, regulators and policymakers are “keenly aware that physicians and patients alike are anxious to get going and start doing boosters,” Dr. Shah said. There’s concern that antibody response might wane over time, perhaps even more quickly in patients with cancer.
Pfizer is already in talks with the U.S. Food and Drug Administration to authorize a third dose of its vaccine in the United States. Guidelines could very well change in coming months, said Ghady Haidar, MD, a specialist in infectious diseases and cancer at the University of Pittsburgh.
However, it’s still early in the game, and it’s not clear yet if boosters are necessary in cancer, Dr. Haidar said in an interview.
For one thing, it’s unknown if poor antibody response really means that patients aren’t protected, he explained. The vaccines elicit T-cell responses that could protect patients regardless of antibody levels. It’s also unclear if antibody titer levels are clinically relevant, and there hasn’t been much indication yet that less-than-robust vaccine responses translate to worse COVID outcomes in patients with cancer.
Those and other questions are areas of active investigation by Dr. Shah, Dr. Haidar, and others. Dozens of clinical trials are investigating vaccine response in patients with cancer, including the use of boosters.
Meanwhile, some cancer patients aren’t waiting around for more study results. “I get many, many emails a day” about booster shots, Dr. Haidar said. “We recommend against” them for now but some people bend the rules and get an extra shot anyway. “I get it. People are apprehensive.”
Three COVID deaths despite full vaccination
The vaccine clinical trials had fewer patients with cancer, so researchers are moving fast to backfill the data. Although there is some variation in what’s being reported, an overall picture is slowly emerging.
Dr. Shah and her team reported on responses to the mRNA COVID vaccines from Pfizer and Moderna and found a 94% seroconversion rate in 131 patients with cancer 3-4 weeks after their second dose of vaccine. They also found good responses among patients on cytotoxic chemotherapy within 6 months of their first vaccine dose, although their antibody titer levels were significantly lower than seen in other patients with cancer.
Investigators from Montefiore Medical Center in New York City also recently reported a 94% seroconversion rate among 200 patients with cancer, including 98% seroconversion in patients with solid tumors. Rates were lower in patients with blood cancers but were still 85% overall, with 70% conversion among patients on anti-CD20 therapies and 73% among stem cell transplant patients.
Dr. Haidar’s group reported a seroconversion rate of 82.4% among patients with solid tumors but only 54.7% among those with blood cancer. Risk factors for poor response included treatment with antimetabolites and anti-CD20 therapies, and, in the solid tumor group, radiation therapy, likely because of its overall toxicity and impact on lymphocyte function.
Israeli investigators reported in May a 90% seroconversion rate after two doses of the Pfizer vaccine among 102 patients with solid tumors on active treatment, which compared favorably to the 100% conversion rate in healthy controls, but they noted that antibody titers were considerably lower in patients with cancer.
The only variable associated with lower titer levels was combined use of chemotherapy and immunotherapy, they noted. There were also three women on dose-dense chemotherapy for breast cancer who did not produce any antibodies.
In a study limited to patients with blood cancers, a Lithuanian team recently reported that among 885 patients, those on Bruton tyrosine kinase inhibitors, ruxolitinib (Jakafi), venetoclax (Venclexta), or anti-CD20 therapies mounted almost no antibody response to the Pfizer vaccine.
The Lithuanian group also reported nine breakthrough COVID infections among their fully vaccinated blood cancer patients, including three deaths.
A team from the Icahn School of Medicine at Mount Sinai, New York reported that more than 15% of 260 patients with multiple myeloma also had no response to the Pfizer or Moderna vaccine; they were on BCMA-targeted therapy or anti-CD38 monoclonal antibody therapy at the time of vaccination, but a few had undergone CAR-T cell therapy more than 3 months beforehand.
Heated debate about antibody testing
Despite these reports of some patients with cancer having poorer responses, there’s some uncertainty over the benefit of giving a third (booster) shot.
There’s the question about the clinical relevance of antibody titer levels, and very little work has been done to date on cellular T-cell immunity from the vaccines.
“Right now, we are using titer levels like they actually mean something when they might not,” said Ravi Parikh, MD, a genitourinary and thoracic oncologist at the University of Pennsylvania, Philadelphia, who co-wrote an editorial that accompanies the Israeli report.
That’s one of the reasons why the FDA and others do not currently recommend antibody tests for COVID vaccine decisions outside of a clinical trial, but not everyone agrees with that position.
There’s been “a lot of heated debate in the medical community” over the issue, Dr. Haidar said.
The Icahn team, for instance, said that their results “underscore the need for routine serological monitoring of [multiple myeloma] patients following COVID-19 vaccination” to see if they might still need to mask-up and socially distance.
There is precedence, too, for vaccine boosters in cancer. As Dr. Parikh noted in his editorial, guidelines recommend revaccination after stem cell transplant for meningococcus, tetanus, and varicella, and other infections.
In France, COVID booster shots are already standard care for patients on dialysis and those on anti-CD20 agents, as well as for solid organ transplant recipients, for whom the literature supporting the benefit of COVID boosters is much more evolved than in cancer.
Israel has also authorized vaccine boosters for immunocompromised patients, including those with cancer, according to news reports.
It is also almost certain that the FDA will grant a formal approval for the COVID vaccines, at which point doctors will be free to administer boosters as they see fit.
“People are going to have to think really hard about what to do with them” if guidance hasn’t changed by then, Dr. Haidar said.
As the story unfolds, Dr. Haidar and others said in an interview that the take-home message for oncologists remains largely what it has been – namely to get patients vaccinated but also to consider masks and social distancing afterward for those at risk of a poor response.
Dr. Shah, Dr. Haidar, and Dr. Parikh have disclosed no relevant financial relationships. Dr. Parikh is a regular contributor to Medscape Oncology.
A version of this article first appeared on Medscape.com.
Patients with cancer have shown varying responses to COVID-19 vaccination, with good responses in patients with solid tumors (even while on systemic therapy) and poor responses in patients with blood cancers, particularly those on immunosuppressive therapies.
The data are evolving to show factors associated with a poor response but are not strong enough yet to recommend booster shots, say researchers.
The work is defining who will likely need a COVID vaccine booster when they become available. “It’s definitely not all cancer patients,” said Dimpy Shah, MD, PhD, a cancer epidemiologist at the Mays Cancer Center, University of Texas, San Antonio.
Public anxiously awaiting boosters
Boosters aren’t recommended in the United States at the moment, in large part because the Emergency Use Authorization under which the vaccines are being administered allows for only two shots of the Pfizer and Moderna vaccines and one shot of the Johnson & Johnson vaccine.
Even so, regulators and policymakers are “keenly aware that physicians and patients alike are anxious to get going and start doing boosters,” Dr. Shah said. There’s concern that antibody response might wane over time, perhaps even more quickly in patients with cancer.
Pfizer is already in talks with the U.S. Food and Drug Administration to authorize a third dose of its vaccine in the United States. Guidelines could very well change in coming months, said Ghady Haidar, MD, a specialist in infectious diseases and cancer at the University of Pittsburgh.
However, it’s still early in the game, and it’s not clear yet if boosters are necessary in cancer, Dr. Haidar said in an interview.
For one thing, it’s unknown if poor antibody response really means that patients aren’t protected, he explained. The vaccines elicit T-cell responses that could protect patients regardless of antibody levels. It’s also unclear if antibody titer levels are clinically relevant, and there hasn’t been much indication yet that less-than-robust vaccine responses translate to worse COVID outcomes in patients with cancer.
Those and other questions are areas of active investigation by Dr. Shah, Dr. Haidar, and others. Dozens of clinical trials are investigating vaccine response in patients with cancer, including the use of boosters.
Meanwhile, some cancer patients aren’t waiting around for more study results. “I get many, many emails a day” about booster shots, Dr. Haidar said. “We recommend against” them for now but some people bend the rules and get an extra shot anyway. “I get it. People are apprehensive.”
Three COVID deaths despite full vaccination
The vaccine clinical trials had fewer patients with cancer, so researchers are moving fast to backfill the data. Although there is some variation in what’s being reported, an overall picture is slowly emerging.
Dr. Shah and her team reported on responses to the mRNA COVID vaccines from Pfizer and Moderna and found a 94% seroconversion rate in 131 patients with cancer 3-4 weeks after their second dose of vaccine. They also found good responses among patients on cytotoxic chemotherapy within 6 months of their first vaccine dose, although their antibody titer levels were significantly lower than seen in other patients with cancer.
Investigators from Montefiore Medical Center in New York City also recently reported a 94% seroconversion rate among 200 patients with cancer, including 98% seroconversion in patients with solid tumors. Rates were lower in patients with blood cancers but were still 85% overall, with 70% conversion among patients on anti-CD20 therapies and 73% among stem cell transplant patients.
Dr. Haidar’s group reported a seroconversion rate of 82.4% among patients with solid tumors but only 54.7% among those with blood cancer. Risk factors for poor response included treatment with antimetabolites and anti-CD20 therapies, and, in the solid tumor group, radiation therapy, likely because of its overall toxicity and impact on lymphocyte function.
Israeli investigators reported in May a 90% seroconversion rate after two doses of the Pfizer vaccine among 102 patients with solid tumors on active treatment, which compared favorably to the 100% conversion rate in healthy controls, but they noted that antibody titers were considerably lower in patients with cancer.
The only variable associated with lower titer levels was combined use of chemotherapy and immunotherapy, they noted. There were also three women on dose-dense chemotherapy for breast cancer who did not produce any antibodies.
In a study limited to patients with blood cancers, a Lithuanian team recently reported that among 885 patients, those on Bruton tyrosine kinase inhibitors, ruxolitinib (Jakafi), venetoclax (Venclexta), or anti-CD20 therapies mounted almost no antibody response to the Pfizer vaccine.
The Lithuanian group also reported nine breakthrough COVID infections among their fully vaccinated blood cancer patients, including three deaths.
A team from the Icahn School of Medicine at Mount Sinai, New York reported that more than 15% of 260 patients with multiple myeloma also had no response to the Pfizer or Moderna vaccine; they were on BCMA-targeted therapy or anti-CD38 monoclonal antibody therapy at the time of vaccination, but a few had undergone CAR-T cell therapy more than 3 months beforehand.
Heated debate about antibody testing
Despite these reports of some patients with cancer having poorer responses, there’s some uncertainty over the benefit of giving a third (booster) shot.
There’s the question about the clinical relevance of antibody titer levels, and very little work has been done to date on cellular T-cell immunity from the vaccines.
“Right now, we are using titer levels like they actually mean something when they might not,” said Ravi Parikh, MD, a genitourinary and thoracic oncologist at the University of Pennsylvania, Philadelphia, who co-wrote an editorial that accompanies the Israeli report.
That’s one of the reasons why the FDA and others do not currently recommend antibody tests for COVID vaccine decisions outside of a clinical trial, but not everyone agrees with that position.
There’s been “a lot of heated debate in the medical community” over the issue, Dr. Haidar said.
The Icahn team, for instance, said that their results “underscore the need for routine serological monitoring of [multiple myeloma] patients following COVID-19 vaccination” to see if they might still need to mask-up and socially distance.
There is precedence, too, for vaccine boosters in cancer. As Dr. Parikh noted in his editorial, guidelines recommend revaccination after stem cell transplant for meningococcus, tetanus, and varicella, and other infections.
In France, COVID booster shots are already standard care for patients on dialysis and those on anti-CD20 agents, as well as for solid organ transplant recipients, for whom the literature supporting the benefit of COVID boosters is much more evolved than in cancer.
Israel has also authorized vaccine boosters for immunocompromised patients, including those with cancer, according to news reports.
It is also almost certain that the FDA will grant a formal approval for the COVID vaccines, at which point doctors will be free to administer boosters as they see fit.
“People are going to have to think really hard about what to do with them” if guidance hasn’t changed by then, Dr. Haidar said.
As the story unfolds, Dr. Haidar and others said in an interview that the take-home message for oncologists remains largely what it has been – namely to get patients vaccinated but also to consider masks and social distancing afterward for those at risk of a poor response.
Dr. Shah, Dr. Haidar, and Dr. Parikh have disclosed no relevant financial relationships. Dr. Parikh is a regular contributor to Medscape Oncology.
A version of this article first appeared on Medscape.com.
Long COVID symptoms reported by 6% of pediatric patients
The prevalence of long COVID in children has been unclear, and is complicated by the lack of a consistent definition, said Anna Funk, PhD, an epidemiologist at the University of Calgary (Alba.), during her online presentation of the findings at the 31st European Congress of Clinical Microbiology & Infectious Diseases.
In the several small studies conducted to date, rates range from 0% to 67% 2-4 months after infection, Dr. Funk reported.
To examine prevalence, she and her colleagues, as part of the Pediatric Emergency Research Network (PERN) global research consortium, assessed more than 10,500 children who were screened for SARS-CoV-2 when they presented to the ED at 1 of 41 study sites in 10 countries – Australia, Canada, Indonesia, the United States, plus three countries in Latin America and three in Western Europe – from March 2020 to June 15, 2021.
PERN researchers are following up with the more than 3,100 children who tested positive 14, 30, and 90 days after testing, tracking respiratory, neurologic, and psychobehavioral sequelae.
Dr. Funk presented data on the 1,884 children who tested positive for SARS-CoV-2 before Jan. 20, 2021, and who had completed 90-day follow-up; 447 of those children were hospitalized and 1,437 were not.
Symptoms were reported more often by children admitted to the hospital than not admitted (9.8% vs. 4.6%). Common persistent symptoms were respiratory in 2% of cases, systemic (such as fatigue and fever) in 2%, neurologic (such as headache, seizures, and continued loss of taste or smell) in 1%, and psychological (such as new-onset depression and anxiety) in 1%.
“This study provides the first good epidemiological data on persistent symptoms among SARS-CoV-2–infected children, regardless of severity,” said Kevin Messacar, MD, a pediatric infectious disease clinician and researcher at Children’s Hospital Colorado in Aurora, who was not involved in the study.
And the findings show that, although severe COVID and chronic symptoms are less common in children than in adults, they are “not nonexistent and need to be taken seriously,” he said in an interview.
After adjustment for country of enrollment, children aged 10-17 years were more likely to experience persistent symptoms than children younger than 1 year (odds ratio, 2.4; P = .002).
Hospitalized children were more than twice as likely to experience persistent symptoms as nonhospitalized children (OR, 2.5; P < .001). And children who presented to the ED with at least seven symptoms were four times more likely to have long-term symptoms than those who presented with fewer symptoms (OR, 4.02; P = .01).
‘Some reassurance’
“Given that COVID is new and is known to have acute cardiac and neurologic effects, particularly in children with [multisystem inflammatory syndrome], there were initially concerns about persistent cardiovascular and neurologic effects in any infected child,” Dr. Messacar explained. “These data provide some reassurance that this is uncommon among children with mild or moderate infections who are not hospitalized.”
But “the risk is not zero,” he added. “Getting children vaccinated when it is available to them and taking precautions to prevent unvaccinated children getting COVID is the best way to reduce the risk of severe disease or persistent symptoms.”
The study was limited by its lack of data on variants, reliance on self-reported symptoms, and a population drawn solely from EDs, Dr. Funk acknowledged.
No external funding source was noted. Dr. Messacar and Dr. Funk disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The prevalence of long COVID in children has been unclear, and is complicated by the lack of a consistent definition, said Anna Funk, PhD, an epidemiologist at the University of Calgary (Alba.), during her online presentation of the findings at the 31st European Congress of Clinical Microbiology & Infectious Diseases.
In the several small studies conducted to date, rates range from 0% to 67% 2-4 months after infection, Dr. Funk reported.
To examine prevalence, she and her colleagues, as part of the Pediatric Emergency Research Network (PERN) global research consortium, assessed more than 10,500 children who were screened for SARS-CoV-2 when they presented to the ED at 1 of 41 study sites in 10 countries – Australia, Canada, Indonesia, the United States, plus three countries in Latin America and three in Western Europe – from March 2020 to June 15, 2021.
PERN researchers are following up with the more than 3,100 children who tested positive 14, 30, and 90 days after testing, tracking respiratory, neurologic, and psychobehavioral sequelae.
Dr. Funk presented data on the 1,884 children who tested positive for SARS-CoV-2 before Jan. 20, 2021, and who had completed 90-day follow-up; 447 of those children were hospitalized and 1,437 were not.
Symptoms were reported more often by children admitted to the hospital than not admitted (9.8% vs. 4.6%). Common persistent symptoms were respiratory in 2% of cases, systemic (such as fatigue and fever) in 2%, neurologic (such as headache, seizures, and continued loss of taste or smell) in 1%, and psychological (such as new-onset depression and anxiety) in 1%.
“This study provides the first good epidemiological data on persistent symptoms among SARS-CoV-2–infected children, regardless of severity,” said Kevin Messacar, MD, a pediatric infectious disease clinician and researcher at Children’s Hospital Colorado in Aurora, who was not involved in the study.
And the findings show that, although severe COVID and chronic symptoms are less common in children than in adults, they are “not nonexistent and need to be taken seriously,” he said in an interview.
After adjustment for country of enrollment, children aged 10-17 years were more likely to experience persistent symptoms than children younger than 1 year (odds ratio, 2.4; P = .002).
Hospitalized children were more than twice as likely to experience persistent symptoms as nonhospitalized children (OR, 2.5; P < .001). And children who presented to the ED with at least seven symptoms were four times more likely to have long-term symptoms than those who presented with fewer symptoms (OR, 4.02; P = .01).
‘Some reassurance’
“Given that COVID is new and is known to have acute cardiac and neurologic effects, particularly in children with [multisystem inflammatory syndrome], there were initially concerns about persistent cardiovascular and neurologic effects in any infected child,” Dr. Messacar explained. “These data provide some reassurance that this is uncommon among children with mild or moderate infections who are not hospitalized.”
But “the risk is not zero,” he added. “Getting children vaccinated when it is available to them and taking precautions to prevent unvaccinated children getting COVID is the best way to reduce the risk of severe disease or persistent symptoms.”
The study was limited by its lack of data on variants, reliance on self-reported symptoms, and a population drawn solely from EDs, Dr. Funk acknowledged.
No external funding source was noted. Dr. Messacar and Dr. Funk disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The prevalence of long COVID in children has been unclear, and is complicated by the lack of a consistent definition, said Anna Funk, PhD, an epidemiologist at the University of Calgary (Alba.), during her online presentation of the findings at the 31st European Congress of Clinical Microbiology & Infectious Diseases.
In the several small studies conducted to date, rates range from 0% to 67% 2-4 months after infection, Dr. Funk reported.
To examine prevalence, she and her colleagues, as part of the Pediatric Emergency Research Network (PERN) global research consortium, assessed more than 10,500 children who were screened for SARS-CoV-2 when they presented to the ED at 1 of 41 study sites in 10 countries – Australia, Canada, Indonesia, the United States, plus three countries in Latin America and three in Western Europe – from March 2020 to June 15, 2021.
PERN researchers are following up with the more than 3,100 children who tested positive 14, 30, and 90 days after testing, tracking respiratory, neurologic, and psychobehavioral sequelae.
Dr. Funk presented data on the 1,884 children who tested positive for SARS-CoV-2 before Jan. 20, 2021, and who had completed 90-day follow-up; 447 of those children were hospitalized and 1,437 were not.
Symptoms were reported more often by children admitted to the hospital than not admitted (9.8% vs. 4.6%). Common persistent symptoms were respiratory in 2% of cases, systemic (such as fatigue and fever) in 2%, neurologic (such as headache, seizures, and continued loss of taste or smell) in 1%, and psychological (such as new-onset depression and anxiety) in 1%.
“This study provides the first good epidemiological data on persistent symptoms among SARS-CoV-2–infected children, regardless of severity,” said Kevin Messacar, MD, a pediatric infectious disease clinician and researcher at Children’s Hospital Colorado in Aurora, who was not involved in the study.
And the findings show that, although severe COVID and chronic symptoms are less common in children than in adults, they are “not nonexistent and need to be taken seriously,” he said in an interview.
After adjustment for country of enrollment, children aged 10-17 years were more likely to experience persistent symptoms than children younger than 1 year (odds ratio, 2.4; P = .002).
Hospitalized children were more than twice as likely to experience persistent symptoms as nonhospitalized children (OR, 2.5; P < .001). And children who presented to the ED with at least seven symptoms were four times more likely to have long-term symptoms than those who presented with fewer symptoms (OR, 4.02; P = .01).
‘Some reassurance’
“Given that COVID is new and is known to have acute cardiac and neurologic effects, particularly in children with [multisystem inflammatory syndrome], there were initially concerns about persistent cardiovascular and neurologic effects in any infected child,” Dr. Messacar explained. “These data provide some reassurance that this is uncommon among children with mild or moderate infections who are not hospitalized.”
But “the risk is not zero,” he added. “Getting children vaccinated when it is available to them and taking precautions to prevent unvaccinated children getting COVID is the best way to reduce the risk of severe disease or persistent symptoms.”
The study was limited by its lack of data on variants, reliance on self-reported symptoms, and a population drawn solely from EDs, Dr. Funk acknowledged.
No external funding source was noted. Dr. Messacar and Dr. Funk disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New agents for youth-onset type 2 diabetes ‘finally in sight’
There are limited treatment options for children and youth with type 2 diabetes, but a few novel therapies beyond metformin are on the horizon, experts said at the annual scientific sessions of the American Diabetes Association.
“Type 2 diabetes in youth only emerged as a well-recognized pediatric medical problem in the 1990s and the first decade of the 21st century,” session chair Kenneth C. Copeland, MD, said in an interview.
“Fortunately, a number of clinical trials of antidiabetic pharmacologic agents in diabetic youth have now been completed, demonstrating both safety and efficacy, and at long last, a ... variety of agents are finally in sight,” he noted.
Type 2 diabetes in youth is profoundly different from type 2 diabetes in adults, added Dr. Copeland, pediatrics professor emeritus, University of Oklahoma, Oklahoma City. In youth, its course is typically aggressive and refractive to treatment.
Concerted efforts at lifestyle intervention are important but insufficient, and a response to metformin, even when initiated at diagnosis, is often short lived, he added.
Because of the rapid glycemic deterioration that is typical of type 2 diabetes in youth and leads to the full array of diabetic complications, early aggressive pharmacologic treatment is indicated.
“We all look forward to this next decade ushering in new treatment options, spanning the spectrum from obesity prevention to complex pharmacologic intervention,” Dr. Copeland summarized.
Increasing prevalence of T2D in youth, limited therapies
Rates of type 2 diabetes in youth continue to increase, especially among non-White groups, and most of these individuals have less than optimal diabetes control, Elvira Isganaitis, MD, MPH, a pediatric endocrinologist at the Joslin Diabetes Center and assistant professor of pediatrics at Harvard Medical School, both in Boston, told the meeting.
Although the Food and Drug Administration has approved more than 25 drugs to treat type 2 diabetes in adults, “unfortunately,” metformin is the only oral medication approved to treat the disease in a pediatric population, “and a majority of youth either do not respond to it or do not tolerate it,” she said in an interview.
Dr. Copeland observed that “the TODAY study demonstrated conclusively that, despite an often dramatic initial improvement in glycemic control upon initiation of pharmacologic and lifestyle intervention, this initial response was followed by a rapid deterioration of beta-cell function and glycemic failure, indicating that additional pharmacologic agents were sorely needed for this population.”
The RISE study also showed that, compared with adults, youth had more rapid beta-cell deterioration despite treatment.
Until the June 2019 FDA approval of the injectable glucagonlike peptide–1 receptor agonist liraglutide (Victoza, Novo Nordisk) for children 10 years or older, “except for insulin, metformin was the only antidiabetic medication available for use in youth, severely limiting treatment options,” he added.
Liraglutide ‘a huge breakthrough,’ other options on the horizon
The FDA approval of liraglutide was “a huge breakthrough” as the first noninsulin drug for pediatric type 2 diabetes since metformin was approved for pediatric use in 2000, Dr. Isganaitis said.
The ELLIPSE study, on which the approval was based, showed liraglutide was effective at lowering hemoglobin A1c and was generally well tolerated, although it was associated with a higher incidence of gastrointestinal symptoms.
In December 2020, the FDA also approved liraglutide (Saxenda) for the treatment of obesity in youth age 12 and older (at a dose of 3 mg as opposed to the 1.8-mg dose of liraglutide [Victoza]), “which is wonderful news considering that the majority of pediatric patients with type 2 diabetes also have obesity,” Dr. Isganaitis added.
“The results of studies of liraglutide on glycemia in diabetic youth are impressive, with both an additional benefit of weight loss and without unacceptable identified risks or side effects,” Dr. Copeland concurred.
Waiting in the wings
Dr. Isganaitis reported that a few phase 3 clinical trials of other therapies for pediatric patients with type 2 diabetes are in the wings.
The 24-week phase 3 T2GO clinical trial of the sodium-glucose cotransporter 2 inhibitor dapagliflozin (AstraZeneca) versus placebo in 72 patients with type 2 diabetes aged 10-24 years was completed in April 2020, and the data are being analyzed.
An AstraZeneca-sponsored phase 3 trial of the safety and efficacy of a weekly injection of the GLP-1 receptor agonist exenatide in 10- to 17-year-olds with type 2 diabetes (n = 82) has also been completed and data are being analyzed.
A Takeda-sponsored phase 3 pediatric study of the dipeptidyl peptidase–4 inhibitor alogliptin in 10- to 17-year-olds with type 2 diabetes (n = 150) is estimated to be completed by February 2022.
And the phase 3 DINAMO trial, sponsored by Boehringer Ingelheim, which is evaluating the efficacy and safety of the SGLT2 inhibitor empagliflozin (10 mg/25 mg) versus the DPP-4 inhibitor linagliptin (5 mg) versus placebo over 26 weeks in 10- to 17-year-olds with type 2 diabetes (estimated 186 participants), is expected to be completed in May 2023.
“I hope that these medications will demonstrate efficacy and allow pediatric patients with type 2 diabetes to have more treatment options,” Dr. Isganaitis concluded.
Type 2 diabetes more aggressive than type 1 diabetes in kids
According to Dr. Isganaitis, “there is a widely held misconception among the general public and even among some physicians that type 2 diabetes is somehow less worrisome or ‘milder’ than a diagnosis of type 1 diabetes.”
However, the risk of complications and severe morbidity is higher with a diagnosis of type 2 diabetes versus type 1 diabetes in a child, so “this condition needs to be managed intensively with a multidisciplinary team including pediatric endocrinology, nutrition [support], diabetes educators, and mental health support,” she emphasized.
Many people also believe that “type 2 diabetes in kids is a ‘lifestyle disease,’ ” she continued, “but in fact, there is a strong role for genetics.”
The ADA Presidents’ Select Abstract “paints a picture of youth-onset type 2 diabetes as a disease intermediate in extremity between monogenic diabetes [caused by mutations in a single gene] and type 2 diabetes [caused by multiple genes and lifestyle factors such as obesity], in which genetic variants in both insulin secretion and insulin response pathways are implicated.”
Along the same lines, Dr. Isganaitis presented an oral abstract at the meeting that showed that, among youth with newly diagnosed type 2 diabetes, those whose mothers had diabetes had faster disease progression and earlier onset of diabetes complications.
Dr. Isganaitis has reported no relevant financial relationships. Dr. Copeland has reported serving on data monitoring committees for Boehringer Ingelheim and Novo Nordisk, and on an advisory committee for a research study for Daiichi Sankyo.
A version of this article first appeared on Medscape.com.
There are limited treatment options for children and youth with type 2 diabetes, but a few novel therapies beyond metformin are on the horizon, experts said at the annual scientific sessions of the American Diabetes Association.
“Type 2 diabetes in youth only emerged as a well-recognized pediatric medical problem in the 1990s and the first decade of the 21st century,” session chair Kenneth C. Copeland, MD, said in an interview.
“Fortunately, a number of clinical trials of antidiabetic pharmacologic agents in diabetic youth have now been completed, demonstrating both safety and efficacy, and at long last, a ... variety of agents are finally in sight,” he noted.
Type 2 diabetes in youth is profoundly different from type 2 diabetes in adults, added Dr. Copeland, pediatrics professor emeritus, University of Oklahoma, Oklahoma City. In youth, its course is typically aggressive and refractive to treatment.
Concerted efforts at lifestyle intervention are important but insufficient, and a response to metformin, even when initiated at diagnosis, is often short lived, he added.
Because of the rapid glycemic deterioration that is typical of type 2 diabetes in youth and leads to the full array of diabetic complications, early aggressive pharmacologic treatment is indicated.
“We all look forward to this next decade ushering in new treatment options, spanning the spectrum from obesity prevention to complex pharmacologic intervention,” Dr. Copeland summarized.
Increasing prevalence of T2D in youth, limited therapies
Rates of type 2 diabetes in youth continue to increase, especially among non-White groups, and most of these individuals have less than optimal diabetes control, Elvira Isganaitis, MD, MPH, a pediatric endocrinologist at the Joslin Diabetes Center and assistant professor of pediatrics at Harvard Medical School, both in Boston, told the meeting.
Although the Food and Drug Administration has approved more than 25 drugs to treat type 2 diabetes in adults, “unfortunately,” metformin is the only oral medication approved to treat the disease in a pediatric population, “and a majority of youth either do not respond to it or do not tolerate it,” she said in an interview.
Dr. Copeland observed that “the TODAY study demonstrated conclusively that, despite an often dramatic initial improvement in glycemic control upon initiation of pharmacologic and lifestyle intervention, this initial response was followed by a rapid deterioration of beta-cell function and glycemic failure, indicating that additional pharmacologic agents were sorely needed for this population.”
The RISE study also showed that, compared with adults, youth had more rapid beta-cell deterioration despite treatment.
Until the June 2019 FDA approval of the injectable glucagonlike peptide–1 receptor agonist liraglutide (Victoza, Novo Nordisk) for children 10 years or older, “except for insulin, metformin was the only antidiabetic medication available for use in youth, severely limiting treatment options,” he added.
Liraglutide ‘a huge breakthrough,’ other options on the horizon
The FDA approval of liraglutide was “a huge breakthrough” as the first noninsulin drug for pediatric type 2 diabetes since metformin was approved for pediatric use in 2000, Dr. Isganaitis said.
The ELLIPSE study, on which the approval was based, showed liraglutide was effective at lowering hemoglobin A1c and was generally well tolerated, although it was associated with a higher incidence of gastrointestinal symptoms.
In December 2020, the FDA also approved liraglutide (Saxenda) for the treatment of obesity in youth age 12 and older (at a dose of 3 mg as opposed to the 1.8-mg dose of liraglutide [Victoza]), “which is wonderful news considering that the majority of pediatric patients with type 2 diabetes also have obesity,” Dr. Isganaitis added.
“The results of studies of liraglutide on glycemia in diabetic youth are impressive, with both an additional benefit of weight loss and without unacceptable identified risks or side effects,” Dr. Copeland concurred.
Waiting in the wings
Dr. Isganaitis reported that a few phase 3 clinical trials of other therapies for pediatric patients with type 2 diabetes are in the wings.
The 24-week phase 3 T2GO clinical trial of the sodium-glucose cotransporter 2 inhibitor dapagliflozin (AstraZeneca) versus placebo in 72 patients with type 2 diabetes aged 10-24 years was completed in April 2020, and the data are being analyzed.
An AstraZeneca-sponsored phase 3 trial of the safety and efficacy of a weekly injection of the GLP-1 receptor agonist exenatide in 10- to 17-year-olds with type 2 diabetes (n = 82) has also been completed and data are being analyzed.
A Takeda-sponsored phase 3 pediatric study of the dipeptidyl peptidase–4 inhibitor alogliptin in 10- to 17-year-olds with type 2 diabetes (n = 150) is estimated to be completed by February 2022.
And the phase 3 DINAMO trial, sponsored by Boehringer Ingelheim, which is evaluating the efficacy and safety of the SGLT2 inhibitor empagliflozin (10 mg/25 mg) versus the DPP-4 inhibitor linagliptin (5 mg) versus placebo over 26 weeks in 10- to 17-year-olds with type 2 diabetes (estimated 186 participants), is expected to be completed in May 2023.
“I hope that these medications will demonstrate efficacy and allow pediatric patients with type 2 diabetes to have more treatment options,” Dr. Isganaitis concluded.
Type 2 diabetes more aggressive than type 1 diabetes in kids
According to Dr. Isganaitis, “there is a widely held misconception among the general public and even among some physicians that type 2 diabetes is somehow less worrisome or ‘milder’ than a diagnosis of type 1 diabetes.”
However, the risk of complications and severe morbidity is higher with a diagnosis of type 2 diabetes versus type 1 diabetes in a child, so “this condition needs to be managed intensively with a multidisciplinary team including pediatric endocrinology, nutrition [support], diabetes educators, and mental health support,” she emphasized.
Many people also believe that “type 2 diabetes in kids is a ‘lifestyle disease,’ ” she continued, “but in fact, there is a strong role for genetics.”
The ADA Presidents’ Select Abstract “paints a picture of youth-onset type 2 diabetes as a disease intermediate in extremity between monogenic diabetes [caused by mutations in a single gene] and type 2 diabetes [caused by multiple genes and lifestyle factors such as obesity], in which genetic variants in both insulin secretion and insulin response pathways are implicated.”
Along the same lines, Dr. Isganaitis presented an oral abstract at the meeting that showed that, among youth with newly diagnosed type 2 diabetes, those whose mothers had diabetes had faster disease progression and earlier onset of diabetes complications.
Dr. Isganaitis has reported no relevant financial relationships. Dr. Copeland has reported serving on data monitoring committees for Boehringer Ingelheim and Novo Nordisk, and on an advisory committee for a research study for Daiichi Sankyo.
A version of this article first appeared on Medscape.com.
There are limited treatment options for children and youth with type 2 diabetes, but a few novel therapies beyond metformin are on the horizon, experts said at the annual scientific sessions of the American Diabetes Association.
“Type 2 diabetes in youth only emerged as a well-recognized pediatric medical problem in the 1990s and the first decade of the 21st century,” session chair Kenneth C. Copeland, MD, said in an interview.
“Fortunately, a number of clinical trials of antidiabetic pharmacologic agents in diabetic youth have now been completed, demonstrating both safety and efficacy, and at long last, a ... variety of agents are finally in sight,” he noted.
Type 2 diabetes in youth is profoundly different from type 2 diabetes in adults, added Dr. Copeland, pediatrics professor emeritus, University of Oklahoma, Oklahoma City. In youth, its course is typically aggressive and refractive to treatment.
Concerted efforts at lifestyle intervention are important but insufficient, and a response to metformin, even when initiated at diagnosis, is often short lived, he added.
Because of the rapid glycemic deterioration that is typical of type 2 diabetes in youth and leads to the full array of diabetic complications, early aggressive pharmacologic treatment is indicated.
“We all look forward to this next decade ushering in new treatment options, spanning the spectrum from obesity prevention to complex pharmacologic intervention,” Dr. Copeland summarized.
Increasing prevalence of T2D in youth, limited therapies
Rates of type 2 diabetes in youth continue to increase, especially among non-White groups, and most of these individuals have less than optimal diabetes control, Elvira Isganaitis, MD, MPH, a pediatric endocrinologist at the Joslin Diabetes Center and assistant professor of pediatrics at Harvard Medical School, both in Boston, told the meeting.
Although the Food and Drug Administration has approved more than 25 drugs to treat type 2 diabetes in adults, “unfortunately,” metformin is the only oral medication approved to treat the disease in a pediatric population, “and a majority of youth either do not respond to it or do not tolerate it,” she said in an interview.
Dr. Copeland observed that “the TODAY study demonstrated conclusively that, despite an often dramatic initial improvement in glycemic control upon initiation of pharmacologic and lifestyle intervention, this initial response was followed by a rapid deterioration of beta-cell function and glycemic failure, indicating that additional pharmacologic agents were sorely needed for this population.”
The RISE study also showed that, compared with adults, youth had more rapid beta-cell deterioration despite treatment.
Until the June 2019 FDA approval of the injectable glucagonlike peptide–1 receptor agonist liraglutide (Victoza, Novo Nordisk) for children 10 years or older, “except for insulin, metformin was the only antidiabetic medication available for use in youth, severely limiting treatment options,” he added.
Liraglutide ‘a huge breakthrough,’ other options on the horizon
The FDA approval of liraglutide was “a huge breakthrough” as the first noninsulin drug for pediatric type 2 diabetes since metformin was approved for pediatric use in 2000, Dr. Isganaitis said.
The ELLIPSE study, on which the approval was based, showed liraglutide was effective at lowering hemoglobin A1c and was generally well tolerated, although it was associated with a higher incidence of gastrointestinal symptoms.
In December 2020, the FDA also approved liraglutide (Saxenda) for the treatment of obesity in youth age 12 and older (at a dose of 3 mg as opposed to the 1.8-mg dose of liraglutide [Victoza]), “which is wonderful news considering that the majority of pediatric patients with type 2 diabetes also have obesity,” Dr. Isganaitis added.
“The results of studies of liraglutide on glycemia in diabetic youth are impressive, with both an additional benefit of weight loss and without unacceptable identified risks or side effects,” Dr. Copeland concurred.
Waiting in the wings
Dr. Isganaitis reported that a few phase 3 clinical trials of other therapies for pediatric patients with type 2 diabetes are in the wings.
The 24-week phase 3 T2GO clinical trial of the sodium-glucose cotransporter 2 inhibitor dapagliflozin (AstraZeneca) versus placebo in 72 patients with type 2 diabetes aged 10-24 years was completed in April 2020, and the data are being analyzed.
An AstraZeneca-sponsored phase 3 trial of the safety and efficacy of a weekly injection of the GLP-1 receptor agonist exenatide in 10- to 17-year-olds with type 2 diabetes (n = 82) has also been completed and data are being analyzed.
A Takeda-sponsored phase 3 pediatric study of the dipeptidyl peptidase–4 inhibitor alogliptin in 10- to 17-year-olds with type 2 diabetes (n = 150) is estimated to be completed by February 2022.
And the phase 3 DINAMO trial, sponsored by Boehringer Ingelheim, which is evaluating the efficacy and safety of the SGLT2 inhibitor empagliflozin (10 mg/25 mg) versus the DPP-4 inhibitor linagliptin (5 mg) versus placebo over 26 weeks in 10- to 17-year-olds with type 2 diabetes (estimated 186 participants), is expected to be completed in May 2023.
“I hope that these medications will demonstrate efficacy and allow pediatric patients with type 2 diabetes to have more treatment options,” Dr. Isganaitis concluded.
Type 2 diabetes more aggressive than type 1 diabetes in kids
According to Dr. Isganaitis, “there is a widely held misconception among the general public and even among some physicians that type 2 diabetes is somehow less worrisome or ‘milder’ than a diagnosis of type 1 diabetes.”
However, the risk of complications and severe morbidity is higher with a diagnosis of type 2 diabetes versus type 1 diabetes in a child, so “this condition needs to be managed intensively with a multidisciplinary team including pediatric endocrinology, nutrition [support], diabetes educators, and mental health support,” she emphasized.
Many people also believe that “type 2 diabetes in kids is a ‘lifestyle disease,’ ” she continued, “but in fact, there is a strong role for genetics.”
The ADA Presidents’ Select Abstract “paints a picture of youth-onset type 2 diabetes as a disease intermediate in extremity between monogenic diabetes [caused by mutations in a single gene] and type 2 diabetes [caused by multiple genes and lifestyle factors such as obesity], in which genetic variants in both insulin secretion and insulin response pathways are implicated.”
Along the same lines, Dr. Isganaitis presented an oral abstract at the meeting that showed that, among youth with newly diagnosed type 2 diabetes, those whose mothers had diabetes had faster disease progression and earlier onset of diabetes complications.
Dr. Isganaitis has reported no relevant financial relationships. Dr. Copeland has reported serving on data monitoring committees for Boehringer Ingelheim and Novo Nordisk, and on an advisory committee for a research study for Daiichi Sankyo.
A version of this article first appeared on Medscape.com.
Contraceptive counseling for transmasculine patients
One of the most common reasons patients seek care from an ob.gyn. is for contraceptive counseling and family planning. While prescribing contraceptives for cisgender patients is often part of the daily routine for ob.gyns., many are unfamiliar with counseling and options for patients who identify as transgender. In a survey of practicing ob.gyns. in nine academic centers, 80% did not receive training on caring for transgender patients.1 Other studies have found that 5.5%-9% of transgender men have reported that a clinician informed them that testosterone was a contraceptive.2,3
Testosterone is not a reliable form of contraception and, in fact, testosterone is considered category X, as it can induce labial fusion, produce abnormal vaginal development, cause a persistent urogenital sinus, and cause clitoromegaly in the developing fetus. Given the teratogenic effects of testosterone, it is imperative that patients who do not desire pregnancy receive appropriate contraceptive options. Counseling of patients should be individualized and start by taking a comprehensive sexual history. Such strategies include using gender-inclusive language, avoiding assumptions about sexual orientation, and obtaining an anatomic inventory of both the patient and their partner(s).4 While a majority of patients achieve amenorrhea while taking testosterone, it is important to discuss the need for contraception if patients are engaging in penile-vaginal intercourse. According to a study of 41 transmasculine patients who achieved pregnancy, one-third of pregnancies were unplanned. Another study reported that 20% of transmasculine patients were taking testosterone and amenorrheic at the time of conception.2
Contraindications to certain types of contraception, such as a history of a thromboembolic event precluding a patient from using combined oral contraceptives, still apply. Transmasculine patients have additional concerns that providers should be aware of and sensitive to when prescribing contraceptives. Gender dysphoria may be exacerbated by contraceptive options that require a pelvic exam or procedure, such as an intrauterine device. For patients that desire an IUD but experience heightened distress in anticipation of the procedure, premedication with anxiolytics or topical anesthetics are reasonable options.4 Using an adequate amount of lubricant and a small speculum may also make the exam more comfortable for patients, especially if patients do not engage in receptive frontal intercourse. Of note, certain types of IUDs, such as the Paragard, may cause pelvic cramping or abnormal bleeding, which could be a trigger for dysphoria. Patients may also experience worsening dysphoria by repeatedly taking a medication that is often associated with cisgender women, such as combined oral contraceptives (COCs). Furthermore, patients may want to avoid COCs secondary to concerns about potential feminizing effects of these hormones and their counteraction of masculinizing effects of testosterone. While COCs act to lower androgen levels by increasing sex hormone–binding globulin, which subsequently binds to testosterone, the amount of estrogen in the pill does not contribute significantly to inhibiting masculinization, and patients should be counseled accordingly.4,5 Side effects such as breast tenderness, which is common among COCs and other estrogen-containing contraceptives, can increase dysphoria and make chest binding more painful. In patients who undergo gender-affirming mastectomies, these effects are less pronounced, however, there may be residual breast tissue left behind which can still produce tenderness and pain.
Sterilization is also a reasonable option in transmasculine patients desiring permanent contraception. Similar to sterilization counseling in cisgender women, a discussion about the irreversibility of the procedure and rates of regret should occur. Transmasculine patients may seek hysterectomy for contraception and to avoid further pelvic exams, cervical cancer screening, pelvic cramping, and/or uterine bleeding. Providers should be knowledgeable about the World Professional Association for Transgender Health standards of care for gender-affirming hysterectomies and counsel patients appropriately.
In summary, transmasculine and all gender-diverse patients deserve the same comprehensive care that their cisgender counterparts receive. Even if the ob.gyn. is not the prescribing physician for testosterone, we all must have a basic understanding of the effects of testosterone and provide appropriate contraceptive services and family planning options to patients when indicated.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa.
References
1. Unger CA. J Women’s Health. 2015;24(2):114-8.
2. Abern L and Maguire K. Obstet Gynecol. 2018;131:65S.
3. Light A et al. Contraception. 2018;98:266-9.
4. Krempasky C et al. Am J Obstet Gynecol. 2020;222(2):134-43.
5. Goodman NF et al. Endocrin Pract. 2015:21(11):1291-300.
One of the most common reasons patients seek care from an ob.gyn. is for contraceptive counseling and family planning. While prescribing contraceptives for cisgender patients is often part of the daily routine for ob.gyns., many are unfamiliar with counseling and options for patients who identify as transgender. In a survey of practicing ob.gyns. in nine academic centers, 80% did not receive training on caring for transgender patients.1 Other studies have found that 5.5%-9% of transgender men have reported that a clinician informed them that testosterone was a contraceptive.2,3
Testosterone is not a reliable form of contraception and, in fact, testosterone is considered category X, as it can induce labial fusion, produce abnormal vaginal development, cause a persistent urogenital sinus, and cause clitoromegaly in the developing fetus. Given the teratogenic effects of testosterone, it is imperative that patients who do not desire pregnancy receive appropriate contraceptive options. Counseling of patients should be individualized and start by taking a comprehensive sexual history. Such strategies include using gender-inclusive language, avoiding assumptions about sexual orientation, and obtaining an anatomic inventory of both the patient and their partner(s).4 While a majority of patients achieve amenorrhea while taking testosterone, it is important to discuss the need for contraception if patients are engaging in penile-vaginal intercourse. According to a study of 41 transmasculine patients who achieved pregnancy, one-third of pregnancies were unplanned. Another study reported that 20% of transmasculine patients were taking testosterone and amenorrheic at the time of conception.2
Contraindications to certain types of contraception, such as a history of a thromboembolic event precluding a patient from using combined oral contraceptives, still apply. Transmasculine patients have additional concerns that providers should be aware of and sensitive to when prescribing contraceptives. Gender dysphoria may be exacerbated by contraceptive options that require a pelvic exam or procedure, such as an intrauterine device. For patients that desire an IUD but experience heightened distress in anticipation of the procedure, premedication with anxiolytics or topical anesthetics are reasonable options.4 Using an adequate amount of lubricant and a small speculum may also make the exam more comfortable for patients, especially if patients do not engage in receptive frontal intercourse. Of note, certain types of IUDs, such as the Paragard, may cause pelvic cramping or abnormal bleeding, which could be a trigger for dysphoria. Patients may also experience worsening dysphoria by repeatedly taking a medication that is often associated with cisgender women, such as combined oral contraceptives (COCs). Furthermore, patients may want to avoid COCs secondary to concerns about potential feminizing effects of these hormones and their counteraction of masculinizing effects of testosterone. While COCs act to lower androgen levels by increasing sex hormone–binding globulin, which subsequently binds to testosterone, the amount of estrogen in the pill does not contribute significantly to inhibiting masculinization, and patients should be counseled accordingly.4,5 Side effects such as breast tenderness, which is common among COCs and other estrogen-containing contraceptives, can increase dysphoria and make chest binding more painful. In patients who undergo gender-affirming mastectomies, these effects are less pronounced, however, there may be residual breast tissue left behind which can still produce tenderness and pain.
Sterilization is also a reasonable option in transmasculine patients desiring permanent contraception. Similar to sterilization counseling in cisgender women, a discussion about the irreversibility of the procedure and rates of regret should occur. Transmasculine patients may seek hysterectomy for contraception and to avoid further pelvic exams, cervical cancer screening, pelvic cramping, and/or uterine bleeding. Providers should be knowledgeable about the World Professional Association for Transgender Health standards of care for gender-affirming hysterectomies and counsel patients appropriately.
In summary, transmasculine and all gender-diverse patients deserve the same comprehensive care that their cisgender counterparts receive. Even if the ob.gyn. is not the prescribing physician for testosterone, we all must have a basic understanding of the effects of testosterone and provide appropriate contraceptive services and family planning options to patients when indicated.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa.
References
1. Unger CA. J Women’s Health. 2015;24(2):114-8.
2. Abern L and Maguire K. Obstet Gynecol. 2018;131:65S.
3. Light A et al. Contraception. 2018;98:266-9.
4. Krempasky C et al. Am J Obstet Gynecol. 2020;222(2):134-43.
5. Goodman NF et al. Endocrin Pract. 2015:21(11):1291-300.
One of the most common reasons patients seek care from an ob.gyn. is for contraceptive counseling and family planning. While prescribing contraceptives for cisgender patients is often part of the daily routine for ob.gyns., many are unfamiliar with counseling and options for patients who identify as transgender. In a survey of practicing ob.gyns. in nine academic centers, 80% did not receive training on caring for transgender patients.1 Other studies have found that 5.5%-9% of transgender men have reported that a clinician informed them that testosterone was a contraceptive.2,3
Testosterone is not a reliable form of contraception and, in fact, testosterone is considered category X, as it can induce labial fusion, produce abnormal vaginal development, cause a persistent urogenital sinus, and cause clitoromegaly in the developing fetus. Given the teratogenic effects of testosterone, it is imperative that patients who do not desire pregnancy receive appropriate contraceptive options. Counseling of patients should be individualized and start by taking a comprehensive sexual history. Such strategies include using gender-inclusive language, avoiding assumptions about sexual orientation, and obtaining an anatomic inventory of both the patient and their partner(s).4 While a majority of patients achieve amenorrhea while taking testosterone, it is important to discuss the need for contraception if patients are engaging in penile-vaginal intercourse. According to a study of 41 transmasculine patients who achieved pregnancy, one-third of pregnancies were unplanned. Another study reported that 20% of transmasculine patients were taking testosterone and amenorrheic at the time of conception.2
Contraindications to certain types of contraception, such as a history of a thromboembolic event precluding a patient from using combined oral contraceptives, still apply. Transmasculine patients have additional concerns that providers should be aware of and sensitive to when prescribing contraceptives. Gender dysphoria may be exacerbated by contraceptive options that require a pelvic exam or procedure, such as an intrauterine device. For patients that desire an IUD but experience heightened distress in anticipation of the procedure, premedication with anxiolytics or topical anesthetics are reasonable options.4 Using an adequate amount of lubricant and a small speculum may also make the exam more comfortable for patients, especially if patients do not engage in receptive frontal intercourse. Of note, certain types of IUDs, such as the Paragard, may cause pelvic cramping or abnormal bleeding, which could be a trigger for dysphoria. Patients may also experience worsening dysphoria by repeatedly taking a medication that is often associated with cisgender women, such as combined oral contraceptives (COCs). Furthermore, patients may want to avoid COCs secondary to concerns about potential feminizing effects of these hormones and their counteraction of masculinizing effects of testosterone. While COCs act to lower androgen levels by increasing sex hormone–binding globulin, which subsequently binds to testosterone, the amount of estrogen in the pill does not contribute significantly to inhibiting masculinization, and patients should be counseled accordingly.4,5 Side effects such as breast tenderness, which is common among COCs and other estrogen-containing contraceptives, can increase dysphoria and make chest binding more painful. In patients who undergo gender-affirming mastectomies, these effects are less pronounced, however, there may be residual breast tissue left behind which can still produce tenderness and pain.
Sterilization is also a reasonable option in transmasculine patients desiring permanent contraception. Similar to sterilization counseling in cisgender women, a discussion about the irreversibility of the procedure and rates of regret should occur. Transmasculine patients may seek hysterectomy for contraception and to avoid further pelvic exams, cervical cancer screening, pelvic cramping, and/or uterine bleeding. Providers should be knowledgeable about the World Professional Association for Transgender Health standards of care for gender-affirming hysterectomies and counsel patients appropriately.
In summary, transmasculine and all gender-diverse patients deserve the same comprehensive care that their cisgender counterparts receive. Even if the ob.gyn. is not the prescribing physician for testosterone, we all must have a basic understanding of the effects of testosterone and provide appropriate contraceptive services and family planning options to patients when indicated.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa.
References
1. Unger CA. J Women’s Health. 2015;24(2):114-8.
2. Abern L and Maguire K. Obstet Gynecol. 2018;131:65S.
3. Light A et al. Contraception. 2018;98:266-9.
4. Krempasky C et al. Am J Obstet Gynecol. 2020;222(2):134-43.
5. Goodman NF et al. Endocrin Pract. 2015:21(11):1291-300.
Cancer mortality continues to drop in females as breast cancer reversal looms
Overall cancer mortality in females continues to decrease in the United States, but “previous declining trends in death rates slowed” for breast cancer in recent years, according to an annual report by several national organizations.
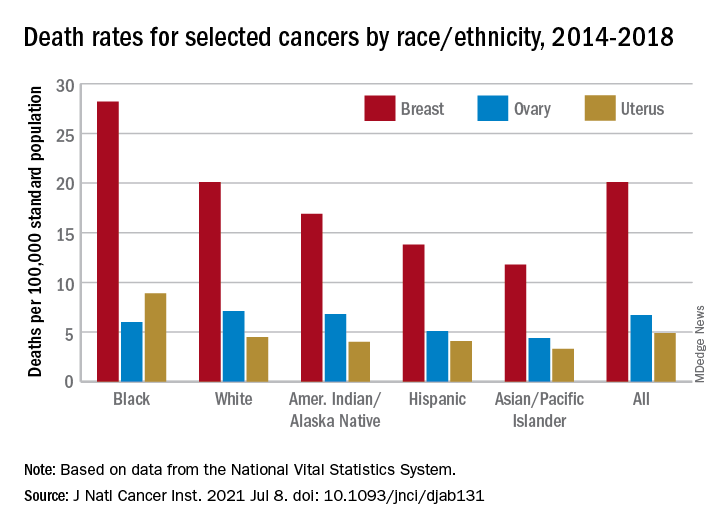
The analysis of long-term trends in cancer death rates shows that a decline of 1.4% per year from 2001 to 2016 accelerated to 2.1% per year in 2016-2018, the American Cancer Society, Centers for Disease Control and Prevention, National Cancer Institute, and the North American Association of Central Cancer Registries said.
Decreases in overall cancer mortality were seen in females of all races and ethnic groups over the most recent 5-year period included in the report, 2014-2018, varying from –1.6% per year in both non-Hispanic Blacks and Whites to –0.9% for non-Hispanic American Indians/Alaska Natives (AI/ANs), Farhad Islami, MD, PhD, of the American Cancer Society, Atlanta, and associates said in the Journal of the National Cancer Institute.
Over those 5 years, death rates fell for 14 of the 20 most common cancers in females; increased for liver, uterus, brain, pancreas, and soft tissue including heart; and remained stable for cancers of the oral cavity/pharynx, they reported.
Breast cancer was among those that declined, but the rate of that decline has been slowing. Mortality declined by an average of 2.3% per year in 2003-2007, by 1.6% a year in 2007-2014, and by just 1.0% annually during 2014-2018, based on data from the National Center for Health Statistics’ National Vital Statistics System.
Mortality from all cancers in 2014-2018 was 133.5 deaths per 100,000 standard population, with the racial/ethnic gap ranging from 85.4 per 100,000 (non-Hispanic Asian/Pacific Islander) to 154.9 (non-Hispanic Black), Dr. Islami and associates said.
Melanoma had the largest decline in mortality over that period among the 20 most common cancers in females, falling by an average of 4.4% per year, with lung cancer next at 4.3%. Among those with increased death rates, uterine cancer saw the largest rise at 2.0% a year, the research team said.
The deaths caused by cancer of the uterus were most common in non-Hispanic Black females, 8.9 per 100,000 population, followed by non-Hispanic White (4.5), Hispanic (4.1), non-Hispanic AI/AN (4.0), and non-Hispanic Asian/Pacific Islander (3.3), they reported.
“Long-term increasing trends in uterine cancer death rates parallel trends in incidence, although death rates are increasing at a somewhat faster rate. Increasing uterine cancer incidence has been attributed to increasing obesity prevalence and decreased use of combined hormone replacement therapy,” Dr. Islami and associates pointed out.
Breast cancer deaths also were most common among Blacks in 2014-2018, occurring at a rate of 28.2 per 100,000, as were deaths from cancer of the cervix (3.4 per 100,000), while ovarian cancers deaths were highest in White females (7.1 per 100,000), the researchers noted.
The continuing racial and ethnic disparity “largely reflects a combination of multiple intertwined factors” of tumor biology, diagnosis, treatment, and systemic discrimination, they wrote, adding that Black persons “are more likely to have a higher exposure to some cancer risk factors and limited access to healthy food, safe places for physical activity, and evidence-based cancer preventive services.”
The report was funded by the four participating groups. Six of the 12 investigators are employees of the American Cancer Society whose salaries are solely paid by the society; the other authors had no conflicts of interest to disclose.
Overall cancer mortality in females continues to decrease in the United States, but “previous declining trends in death rates slowed” for breast cancer in recent years, according to an annual report by several national organizations.
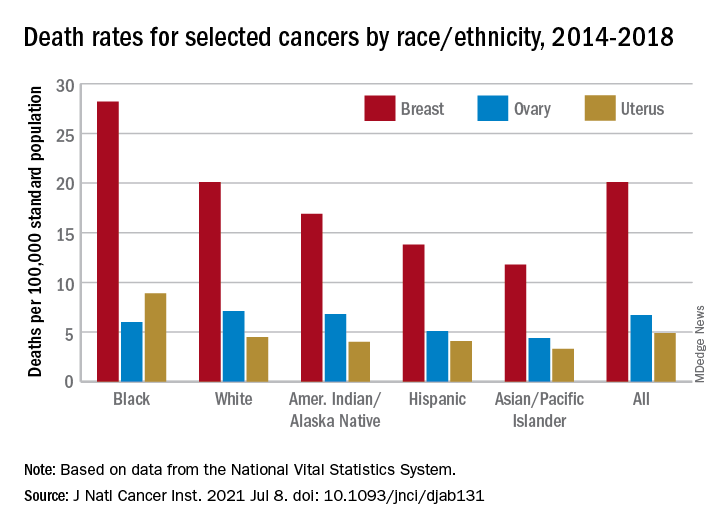
The analysis of long-term trends in cancer death rates shows that a decline of 1.4% per year from 2001 to 2016 accelerated to 2.1% per year in 2016-2018, the American Cancer Society, Centers for Disease Control and Prevention, National Cancer Institute, and the North American Association of Central Cancer Registries said.
Decreases in overall cancer mortality were seen in females of all races and ethnic groups over the most recent 5-year period included in the report, 2014-2018, varying from –1.6% per year in both non-Hispanic Blacks and Whites to –0.9% for non-Hispanic American Indians/Alaska Natives (AI/ANs), Farhad Islami, MD, PhD, of the American Cancer Society, Atlanta, and associates said in the Journal of the National Cancer Institute.
Over those 5 years, death rates fell for 14 of the 20 most common cancers in females; increased for liver, uterus, brain, pancreas, and soft tissue including heart; and remained stable for cancers of the oral cavity/pharynx, they reported.
Breast cancer was among those that declined, but the rate of that decline has been slowing. Mortality declined by an average of 2.3% per year in 2003-2007, by 1.6% a year in 2007-2014, and by just 1.0% annually during 2014-2018, based on data from the National Center for Health Statistics’ National Vital Statistics System.
Mortality from all cancers in 2014-2018 was 133.5 deaths per 100,000 standard population, with the racial/ethnic gap ranging from 85.4 per 100,000 (non-Hispanic Asian/Pacific Islander) to 154.9 (non-Hispanic Black), Dr. Islami and associates said.
Melanoma had the largest decline in mortality over that period among the 20 most common cancers in females, falling by an average of 4.4% per year, with lung cancer next at 4.3%. Among those with increased death rates, uterine cancer saw the largest rise at 2.0% a year, the research team said.
The deaths caused by cancer of the uterus were most common in non-Hispanic Black females, 8.9 per 100,000 population, followed by non-Hispanic White (4.5), Hispanic (4.1), non-Hispanic AI/AN (4.0), and non-Hispanic Asian/Pacific Islander (3.3), they reported.
“Long-term increasing trends in uterine cancer death rates parallel trends in incidence, although death rates are increasing at a somewhat faster rate. Increasing uterine cancer incidence has been attributed to increasing obesity prevalence and decreased use of combined hormone replacement therapy,” Dr. Islami and associates pointed out.
Breast cancer deaths also were most common among Blacks in 2014-2018, occurring at a rate of 28.2 per 100,000, as were deaths from cancer of the cervix (3.4 per 100,000), while ovarian cancers deaths were highest in White females (7.1 per 100,000), the researchers noted.
The continuing racial and ethnic disparity “largely reflects a combination of multiple intertwined factors” of tumor biology, diagnosis, treatment, and systemic discrimination, they wrote, adding that Black persons “are more likely to have a higher exposure to some cancer risk factors and limited access to healthy food, safe places for physical activity, and evidence-based cancer preventive services.”
The report was funded by the four participating groups. Six of the 12 investigators are employees of the American Cancer Society whose salaries are solely paid by the society; the other authors had no conflicts of interest to disclose.
Overall cancer mortality in females continues to decrease in the United States, but “previous declining trends in death rates slowed” for breast cancer in recent years, according to an annual report by several national organizations.
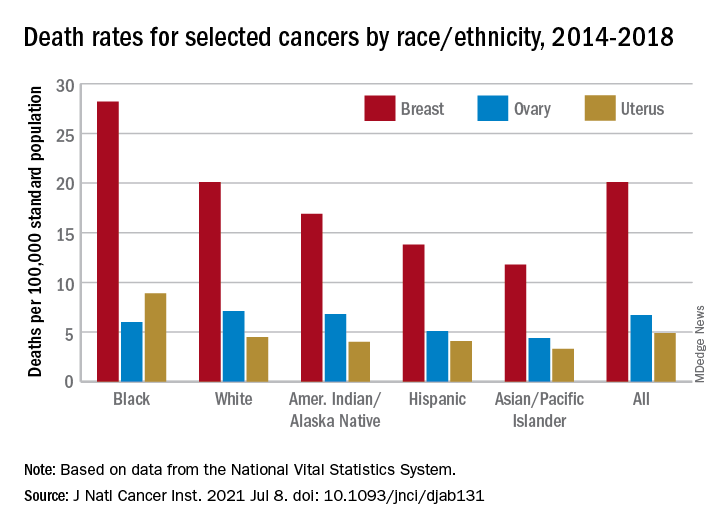
The analysis of long-term trends in cancer death rates shows that a decline of 1.4% per year from 2001 to 2016 accelerated to 2.1% per year in 2016-2018, the American Cancer Society, Centers for Disease Control and Prevention, National Cancer Institute, and the North American Association of Central Cancer Registries said.
Decreases in overall cancer mortality were seen in females of all races and ethnic groups over the most recent 5-year period included in the report, 2014-2018, varying from –1.6% per year in both non-Hispanic Blacks and Whites to –0.9% for non-Hispanic American Indians/Alaska Natives (AI/ANs), Farhad Islami, MD, PhD, of the American Cancer Society, Atlanta, and associates said in the Journal of the National Cancer Institute.
Over those 5 years, death rates fell for 14 of the 20 most common cancers in females; increased for liver, uterus, brain, pancreas, and soft tissue including heart; and remained stable for cancers of the oral cavity/pharynx, they reported.
Breast cancer was among those that declined, but the rate of that decline has been slowing. Mortality declined by an average of 2.3% per year in 2003-2007, by 1.6% a year in 2007-2014, and by just 1.0% annually during 2014-2018, based on data from the National Center for Health Statistics’ National Vital Statistics System.
Mortality from all cancers in 2014-2018 was 133.5 deaths per 100,000 standard population, with the racial/ethnic gap ranging from 85.4 per 100,000 (non-Hispanic Asian/Pacific Islander) to 154.9 (non-Hispanic Black), Dr. Islami and associates said.
Melanoma had the largest decline in mortality over that period among the 20 most common cancers in females, falling by an average of 4.4% per year, with lung cancer next at 4.3%. Among those with increased death rates, uterine cancer saw the largest rise at 2.0% a year, the research team said.
The deaths caused by cancer of the uterus were most common in non-Hispanic Black females, 8.9 per 100,000 population, followed by non-Hispanic White (4.5), Hispanic (4.1), non-Hispanic AI/AN (4.0), and non-Hispanic Asian/Pacific Islander (3.3), they reported.
“Long-term increasing trends in uterine cancer death rates parallel trends in incidence, although death rates are increasing at a somewhat faster rate. Increasing uterine cancer incidence has been attributed to increasing obesity prevalence and decreased use of combined hormone replacement therapy,” Dr. Islami and associates pointed out.
Breast cancer deaths also were most common among Blacks in 2014-2018, occurring at a rate of 28.2 per 100,000, as were deaths from cancer of the cervix (3.4 per 100,000), while ovarian cancers deaths were highest in White females (7.1 per 100,000), the researchers noted.
The continuing racial and ethnic disparity “largely reflects a combination of multiple intertwined factors” of tumor biology, diagnosis, treatment, and systemic discrimination, they wrote, adding that Black persons “are more likely to have a higher exposure to some cancer risk factors and limited access to healthy food, safe places for physical activity, and evidence-based cancer preventive services.”
The report was funded by the four participating groups. Six of the 12 investigators are employees of the American Cancer Society whose salaries are solely paid by the society; the other authors had no conflicts of interest to disclose.
FROM THE JOURNAL OF THE NATIONAL CANCER INSTITUTE
Rising rates of T1D in children: Is COVID to blame?
In early 2020, the COVID-19 pandemic changed everything about life as we know it, with widespread shutdowns across the globe. The U.S. health care system quickly adapted, pivoting to telehealth visits when able and proactively managing outpatient conditions to prevent overwhelming hospital resources and utilization. Meanwhile, at my practice, the typical rate of about one new-onset pediatric type 1 diabetes (T1D) case per week increased to about two per week.
However, the new diabetes cases continued to accumulate, and I saw more patients being diagnosed who did not have a known family history of autoimmunity. I began to ask friends at other centers whether they were noticing the same trend.
One colleague documented a 36% increase in her large center compared with the previous year. Another noted a 40% rise at his children’s hospital. We observed that there was often a respiratory illness reported several weeks before presenting with T1D. Sometimes the child was known to be COVID-positive. Sometimes the child had not been tested. Sometimes we suspected that COVID had been a preceding illness and then found negative SARS-CoV-2 antibodies – but we were not certain whether the result was meaningful given the time lapsed since infection.
Soon, reports emerged of large increases in severe diabetic ketoacidosis (DKA) and hyperglycemic hyperosmolar state at initial presentation, a trend reported in other countries.
Is COVID-19 a trigger for T1D?
There is known precedent for increased risk for T1D after viral infections in patients who are already genetically susceptible. Mechanisms of immune-mediated islet cell failure would make sense following SARS-CoV-2 infection; direct islet toxicity was noted with SARS-CoV-1 and has been suspected with SARS-CoV-2 but not proven. Some have suggested that hypercoagulability with COVID-19 may lead to ischemic damage to the pancreas.
With multiple potential pathways for islet damage, increases in insulin-dependent diabetes would logically follow. Still, whether this is the case remains unclear. There is not yet definitive evidence that there is uptake of SARS-CoV-2 via receptors in the pancreatic beta cells.
Our current understanding of T1D pathogenesis is that susceptible individuals develop autoimmunity in response to an environmental trigger, with beta-cell failure developing over months to years. Perhaps vulnerable patients with genetic risk for pancreatic autoimmunity were stressed by SARS-CoV-2 infection and were diagnosed earlier than they might have been, showing some lead-time bias. Adult patients with COVID-19 demonstrated hyperglycemia that has been reversible in some cases, like the stress hyperglycemia seen with other infections and surgery in response to proinflammatory states.
The true question seems to be whether there is a unique type of diabetes related to direct viral toxicity. Do newly diagnosed patients have measurable traditional antibodies, like anti-glutamic acid decarboxylase or anti-islet cell antibodies? Is there proof of preceding SARS-CoV-2 infection? In the new cases that I thought were unusual at first glance, I found typical pancreatic autoimmunity and negative SARS-CoV-2 antibodies. The small cohorts reported thus far have had similar findings.
A stronger case can be made for the risk of developing diabetes (types 1 and 2) with rapid weight gain. Another marked pattern that pediatric endocrinologists have observed has been increased weight gain in children with closed schools, decreased activity, and more social isolation. I have seen weight change as great as 100 lb in a teen over the past year; 30- to 50-lb weight increases over the course of the pandemic have been common. Considering the “accelerator hypothesis” of faster onset of type 2 diabetes with rapid weight gain, implications for hastening of T1D with weight gain have also been considered. The full impact of these dramatic weight changes will take time to understand.
The true story may not emerge for years
Anecdotes and theoretical concerns may give us pause, but they are far from scientific truth. Efforts are underway to explore this perceived trend with international registries, including the CoviDIAB Registry as well as T1D Exchange. The true story may not emerge until years have passed to see the cumulative fallout of COVID-19. Regardless, these troubling observations should be considered as pandemic safeguards continue to loosen.
While pediatric mortality from COVID-19 has been relatively low (though sadly not zero), some have placed too little focus on possible morbidity. Long-term effects like long COVID and neuropsychiatric sequelae are becoming evident in all populations, including children. If a lifelong illness like diabetes can be directly linked to COVID-19, protecting children from infection with measures like masks becomes all the more crucial until vaccines are more readily available. Despite our rapid progress with understanding COVID-19 disease, there is still much left to learn.
A version of this article first appeared on Medscape.com.
In early 2020, the COVID-19 pandemic changed everything about life as we know it, with widespread shutdowns across the globe. The U.S. health care system quickly adapted, pivoting to telehealth visits when able and proactively managing outpatient conditions to prevent overwhelming hospital resources and utilization. Meanwhile, at my practice, the typical rate of about one new-onset pediatric type 1 diabetes (T1D) case per week increased to about two per week.
However, the new diabetes cases continued to accumulate, and I saw more patients being diagnosed who did not have a known family history of autoimmunity. I began to ask friends at other centers whether they were noticing the same trend.
One colleague documented a 36% increase in her large center compared with the previous year. Another noted a 40% rise at his children’s hospital. We observed that there was often a respiratory illness reported several weeks before presenting with T1D. Sometimes the child was known to be COVID-positive. Sometimes the child had not been tested. Sometimes we suspected that COVID had been a preceding illness and then found negative SARS-CoV-2 antibodies – but we were not certain whether the result was meaningful given the time lapsed since infection.
Soon, reports emerged of large increases in severe diabetic ketoacidosis (DKA) and hyperglycemic hyperosmolar state at initial presentation, a trend reported in other countries.
Is COVID-19 a trigger for T1D?
There is known precedent for increased risk for T1D after viral infections in patients who are already genetically susceptible. Mechanisms of immune-mediated islet cell failure would make sense following SARS-CoV-2 infection; direct islet toxicity was noted with SARS-CoV-1 and has been suspected with SARS-CoV-2 but not proven. Some have suggested that hypercoagulability with COVID-19 may lead to ischemic damage to the pancreas.
With multiple potential pathways for islet damage, increases in insulin-dependent diabetes would logically follow. Still, whether this is the case remains unclear. There is not yet definitive evidence that there is uptake of SARS-CoV-2 via receptors in the pancreatic beta cells.
Our current understanding of T1D pathogenesis is that susceptible individuals develop autoimmunity in response to an environmental trigger, with beta-cell failure developing over months to years. Perhaps vulnerable patients with genetic risk for pancreatic autoimmunity were stressed by SARS-CoV-2 infection and were diagnosed earlier than they might have been, showing some lead-time bias. Adult patients with COVID-19 demonstrated hyperglycemia that has been reversible in some cases, like the stress hyperglycemia seen with other infections and surgery in response to proinflammatory states.
The true question seems to be whether there is a unique type of diabetes related to direct viral toxicity. Do newly diagnosed patients have measurable traditional antibodies, like anti-glutamic acid decarboxylase or anti-islet cell antibodies? Is there proof of preceding SARS-CoV-2 infection? In the new cases that I thought were unusual at first glance, I found typical pancreatic autoimmunity and negative SARS-CoV-2 antibodies. The small cohorts reported thus far have had similar findings.
A stronger case can be made for the risk of developing diabetes (types 1 and 2) with rapid weight gain. Another marked pattern that pediatric endocrinologists have observed has been increased weight gain in children with closed schools, decreased activity, and more social isolation. I have seen weight change as great as 100 lb in a teen over the past year; 30- to 50-lb weight increases over the course of the pandemic have been common. Considering the “accelerator hypothesis” of faster onset of type 2 diabetes with rapid weight gain, implications for hastening of T1D with weight gain have also been considered. The full impact of these dramatic weight changes will take time to understand.
The true story may not emerge for years
Anecdotes and theoretical concerns may give us pause, but they are far from scientific truth. Efforts are underway to explore this perceived trend with international registries, including the CoviDIAB Registry as well as T1D Exchange. The true story may not emerge until years have passed to see the cumulative fallout of COVID-19. Regardless, these troubling observations should be considered as pandemic safeguards continue to loosen.
While pediatric mortality from COVID-19 has been relatively low (though sadly not zero), some have placed too little focus on possible morbidity. Long-term effects like long COVID and neuropsychiatric sequelae are becoming evident in all populations, including children. If a lifelong illness like diabetes can be directly linked to COVID-19, protecting children from infection with measures like masks becomes all the more crucial until vaccines are more readily available. Despite our rapid progress with understanding COVID-19 disease, there is still much left to learn.
A version of this article first appeared on Medscape.com.
In early 2020, the COVID-19 pandemic changed everything about life as we know it, with widespread shutdowns across the globe. The U.S. health care system quickly adapted, pivoting to telehealth visits when able and proactively managing outpatient conditions to prevent overwhelming hospital resources and utilization. Meanwhile, at my practice, the typical rate of about one new-onset pediatric type 1 diabetes (T1D) case per week increased to about two per week.
However, the new diabetes cases continued to accumulate, and I saw more patients being diagnosed who did not have a known family history of autoimmunity. I began to ask friends at other centers whether they were noticing the same trend.
One colleague documented a 36% increase in her large center compared with the previous year. Another noted a 40% rise at his children’s hospital. We observed that there was often a respiratory illness reported several weeks before presenting with T1D. Sometimes the child was known to be COVID-positive. Sometimes the child had not been tested. Sometimes we suspected that COVID had been a preceding illness and then found negative SARS-CoV-2 antibodies – but we were not certain whether the result was meaningful given the time lapsed since infection.
Soon, reports emerged of large increases in severe diabetic ketoacidosis (DKA) and hyperglycemic hyperosmolar state at initial presentation, a trend reported in other countries.
Is COVID-19 a trigger for T1D?
There is known precedent for increased risk for T1D after viral infections in patients who are already genetically susceptible. Mechanisms of immune-mediated islet cell failure would make sense following SARS-CoV-2 infection; direct islet toxicity was noted with SARS-CoV-1 and has been suspected with SARS-CoV-2 but not proven. Some have suggested that hypercoagulability with COVID-19 may lead to ischemic damage to the pancreas.
With multiple potential pathways for islet damage, increases in insulin-dependent diabetes would logically follow. Still, whether this is the case remains unclear. There is not yet definitive evidence that there is uptake of SARS-CoV-2 via receptors in the pancreatic beta cells.
Our current understanding of T1D pathogenesis is that susceptible individuals develop autoimmunity in response to an environmental trigger, with beta-cell failure developing over months to years. Perhaps vulnerable patients with genetic risk for pancreatic autoimmunity were stressed by SARS-CoV-2 infection and were diagnosed earlier than they might have been, showing some lead-time bias. Adult patients with COVID-19 demonstrated hyperglycemia that has been reversible in some cases, like the stress hyperglycemia seen with other infections and surgery in response to proinflammatory states.
The true question seems to be whether there is a unique type of diabetes related to direct viral toxicity. Do newly diagnosed patients have measurable traditional antibodies, like anti-glutamic acid decarboxylase or anti-islet cell antibodies? Is there proof of preceding SARS-CoV-2 infection? In the new cases that I thought were unusual at first glance, I found typical pancreatic autoimmunity and negative SARS-CoV-2 antibodies. The small cohorts reported thus far have had similar findings.
A stronger case can be made for the risk of developing diabetes (types 1 and 2) with rapid weight gain. Another marked pattern that pediatric endocrinologists have observed has been increased weight gain in children with closed schools, decreased activity, and more social isolation. I have seen weight change as great as 100 lb in a teen over the past year; 30- to 50-lb weight increases over the course of the pandemic have been common. Considering the “accelerator hypothesis” of faster onset of type 2 diabetes with rapid weight gain, implications for hastening of T1D with weight gain have also been considered. The full impact of these dramatic weight changes will take time to understand.
The true story may not emerge for years
Anecdotes and theoretical concerns may give us pause, but they are far from scientific truth. Efforts are underway to explore this perceived trend with international registries, including the CoviDIAB Registry as well as T1D Exchange. The true story may not emerge until years have passed to see the cumulative fallout of COVID-19. Regardless, these troubling observations should be considered as pandemic safeguards continue to loosen.
While pediatric mortality from COVID-19 has been relatively low (though sadly not zero), some have placed too little focus on possible morbidity. Long-term effects like long COVID and neuropsychiatric sequelae are becoming evident in all populations, including children. If a lifelong illness like diabetes can be directly linked to COVID-19, protecting children from infection with measures like masks becomes all the more crucial until vaccines are more readily available. Despite our rapid progress with understanding COVID-19 disease, there is still much left to learn.
A version of this article first appeared on Medscape.com.
Latest FDA pembrolizumab approval expands label to cutaneous SCCs
The
The July 6 approval for the programmed death–1 inhibitor follows a June FDA approval for pembrolizumab monotherapy in patients with recurrent or metastatic cSCC disease not curable by surgery or radiation. Both approvals, pembrolizumab’s first for cSCC, are based on findings from the second interim analysis of the phase 2, multicenter, open-label KEYNOTE-629 trial.
The objective response rate in the cohort of 54 patients with locally advanced disease was 50%, including a complete response rate of 17% and a partial response rate of 33%. Duration of response was 6 months or longer in 81% of the 27 responders, and 12 months or longer in 37% of responders. After a median follow-up of 13.4 months, median duration of response had not yet been reached.
Pembrolizumab has previously received FDA approvals, either as monotherapy or in combination with other agents, for the treatment of numerous cancer types, including certain melanomas, non–small cell lung cancers, head and neck SCCs, classical Hodgkin lymphomas, primary mediastinal large B-cell lymphomas, urothelial carcinomas, microsatellite instability–high or mismatch repair–deficient cancers, and gastric, esophageal, cervical, hepatocellular, Merkel cell, renal cell, tumor mutational burden–high, and triple-negative breast cancers.
Patients in the KEYNOTE-629 trial received pembrolizumab at a dose of 200 mg IV every 3 weeks for 24 months or until documented disease progression or unacceptable toxicity.
Adverse reactions occurring in patients with recurrent or metastatic cSCC or locally advanced cSCC in KEYNOTE-629 were similar to those observed in patients with melanoma or non–small cell lung cancer who were treated with pembrolizumab monotherapy in previous trials.
The checkpoint inhibitor can cause immune-mediated adverse reactions, which may be severe or fatal, according to Merck, the drug’s manufacturer. The reactions can occur in any organ system or tissue and can affect more than one body system simultaneously.
“Immune-mediated adverse reactions can occur at any time during or after treatment with Keytruda, including pneumonitis, colitis, hepatitis, endocrinopathies, nephritis, dermatologic reactions, solid organ transplant rejection, and complications of allogeneic hematopoietic stem cell transplantation,” Merck explained in a press release, noting that “early identification and management of immune-mediated adverse reactions are essential to ensure safe use of Keytruda.”
Depending on the severity of any reaction, treatment should be withheld or permanently discontinued, and corticosteroids administered if appropriate, Merck stated.
The
The July 6 approval for the programmed death–1 inhibitor follows a June FDA approval for pembrolizumab monotherapy in patients with recurrent or metastatic cSCC disease not curable by surgery or radiation. Both approvals, pembrolizumab’s first for cSCC, are based on findings from the second interim analysis of the phase 2, multicenter, open-label KEYNOTE-629 trial.
The objective response rate in the cohort of 54 patients with locally advanced disease was 50%, including a complete response rate of 17% and a partial response rate of 33%. Duration of response was 6 months or longer in 81% of the 27 responders, and 12 months or longer in 37% of responders. After a median follow-up of 13.4 months, median duration of response had not yet been reached.
Pembrolizumab has previously received FDA approvals, either as monotherapy or in combination with other agents, for the treatment of numerous cancer types, including certain melanomas, non–small cell lung cancers, head and neck SCCs, classical Hodgkin lymphomas, primary mediastinal large B-cell lymphomas, urothelial carcinomas, microsatellite instability–high or mismatch repair–deficient cancers, and gastric, esophageal, cervical, hepatocellular, Merkel cell, renal cell, tumor mutational burden–high, and triple-negative breast cancers.
Patients in the KEYNOTE-629 trial received pembrolizumab at a dose of 200 mg IV every 3 weeks for 24 months or until documented disease progression or unacceptable toxicity.
Adverse reactions occurring in patients with recurrent or metastatic cSCC or locally advanced cSCC in KEYNOTE-629 were similar to those observed in patients with melanoma or non–small cell lung cancer who were treated with pembrolizumab monotherapy in previous trials.
The checkpoint inhibitor can cause immune-mediated adverse reactions, which may be severe or fatal, according to Merck, the drug’s manufacturer. The reactions can occur in any organ system or tissue and can affect more than one body system simultaneously.
“Immune-mediated adverse reactions can occur at any time during or after treatment with Keytruda, including pneumonitis, colitis, hepatitis, endocrinopathies, nephritis, dermatologic reactions, solid organ transplant rejection, and complications of allogeneic hematopoietic stem cell transplantation,” Merck explained in a press release, noting that “early identification and management of immune-mediated adverse reactions are essential to ensure safe use of Keytruda.”
Depending on the severity of any reaction, treatment should be withheld or permanently discontinued, and corticosteroids administered if appropriate, Merck stated.
The
The July 6 approval for the programmed death–1 inhibitor follows a June FDA approval for pembrolizumab monotherapy in patients with recurrent or metastatic cSCC disease not curable by surgery or radiation. Both approvals, pembrolizumab’s first for cSCC, are based on findings from the second interim analysis of the phase 2, multicenter, open-label KEYNOTE-629 trial.
The objective response rate in the cohort of 54 patients with locally advanced disease was 50%, including a complete response rate of 17% and a partial response rate of 33%. Duration of response was 6 months or longer in 81% of the 27 responders, and 12 months or longer in 37% of responders. After a median follow-up of 13.4 months, median duration of response had not yet been reached.
Pembrolizumab has previously received FDA approvals, either as monotherapy or in combination with other agents, for the treatment of numerous cancer types, including certain melanomas, non–small cell lung cancers, head and neck SCCs, classical Hodgkin lymphomas, primary mediastinal large B-cell lymphomas, urothelial carcinomas, microsatellite instability–high or mismatch repair–deficient cancers, and gastric, esophageal, cervical, hepatocellular, Merkel cell, renal cell, tumor mutational burden–high, and triple-negative breast cancers.
Patients in the KEYNOTE-629 trial received pembrolizumab at a dose of 200 mg IV every 3 weeks for 24 months or until documented disease progression or unacceptable toxicity.
Adverse reactions occurring in patients with recurrent or metastatic cSCC or locally advanced cSCC in KEYNOTE-629 were similar to those observed in patients with melanoma or non–small cell lung cancer who were treated with pembrolizumab monotherapy in previous trials.
The checkpoint inhibitor can cause immune-mediated adverse reactions, which may be severe or fatal, according to Merck, the drug’s manufacturer. The reactions can occur in any organ system or tissue and can affect more than one body system simultaneously.
“Immune-mediated adverse reactions can occur at any time during or after treatment with Keytruda, including pneumonitis, colitis, hepatitis, endocrinopathies, nephritis, dermatologic reactions, solid organ transplant rejection, and complications of allogeneic hematopoietic stem cell transplantation,” Merck explained in a press release, noting that “early identification and management of immune-mediated adverse reactions are essential to ensure safe use of Keytruda.”
Depending on the severity of any reaction, treatment should be withheld or permanently discontinued, and corticosteroids administered if appropriate, Merck stated.