User login
Is the keto diet effective for refractory chronic migraine?
Key clinical point: A 3-month ketogenic diet (KD) resulted in a reduction of painful symptoms of drug refractory chronic migraine.
Major finding: KD significantly reduced the number of migraine days/month from a median of 30 days to 7.5 days (P less than .0001), hours of migraine/day from a median of 24 hours to 5.5 hours (P less than .0016), and pain level at maximum value for 83% of participants that improved for 55% of them (P less than .0024). The median number of drugs taken in a month reduced from 30 to 6 doses.
Study details: This open-label, single-arm clinical trial assessed 38 patients with refractory chronic migraine who adopted a KD for 3 months.
Disclosures: No source of funding was declared. The authors declared no conflicts of interest.
Source: Bongiovanni D et al. Neurol Sci. 2021 Feb 1. doi: 10.1007/s10072-021-05078-5.
Key clinical point: A 3-month ketogenic diet (KD) resulted in a reduction of painful symptoms of drug refractory chronic migraine.
Major finding: KD significantly reduced the number of migraine days/month from a median of 30 days to 7.5 days (P less than .0001), hours of migraine/day from a median of 24 hours to 5.5 hours (P less than .0016), and pain level at maximum value for 83% of participants that improved for 55% of them (P less than .0024). The median number of drugs taken in a month reduced from 30 to 6 doses.
Study details: This open-label, single-arm clinical trial assessed 38 patients with refractory chronic migraine who adopted a KD for 3 months.
Disclosures: No source of funding was declared. The authors declared no conflicts of interest.
Source: Bongiovanni D et al. Neurol Sci. 2021 Feb 1. doi: 10.1007/s10072-021-05078-5.
Key clinical point: A 3-month ketogenic diet (KD) resulted in a reduction of painful symptoms of drug refractory chronic migraine.
Major finding: KD significantly reduced the number of migraine days/month from a median of 30 days to 7.5 days (P less than .0001), hours of migraine/day from a median of 24 hours to 5.5 hours (P less than .0016), and pain level at maximum value for 83% of participants that improved for 55% of them (P less than .0024). The median number of drugs taken in a month reduced from 30 to 6 doses.
Study details: This open-label, single-arm clinical trial assessed 38 patients with refractory chronic migraine who adopted a KD for 3 months.
Disclosures: No source of funding was declared. The authors declared no conflicts of interest.
Source: Bongiovanni D et al. Neurol Sci. 2021 Feb 1. doi: 10.1007/s10072-021-05078-5.
Galcanezumab may alleviate severity and symptoms of migraine
Key clinical point: Galcanezumab reduces the frequency of migraine headache days and may also potentially decrease disabling non-pain symptoms on days when migraine is present in patients with episodic and chronic migraine.
Major finding: Galcanezumab doses of 120 and 240 mg were superior to placebo in reducing the number of monthly migraine days with nausea and/or vomiting in both episodic and chronic migraine studies (all P less than .001). Both doses of galcanezumab were associated with a significant reduction in migraine headache days with photophobia and phonophobia vs. placebo in episodic (P less than .001) and chronic (P less than .001 for galcanezumab 120 mg; P =.001 for galcanezumab 240 mg) migraine studies.
Study details: A post hoc analysis of phase 3 randomized clinical trials EVOLVE-1, EVOLVE-2, and REGAIN that included a total of 2,289 patients with episodic or chronic migraine with or without aura.
Disclosures: This study was funded by Eli Lilly and Company, Indianapolis, IN, USA. K Day, VL Stauffer, V Skljarevski, M Rettiganti, E Pearlman, and SK Aurora reported being current/former full-time employees and/or minor stockholders of Eli Lilly and Company. M Ament reported being a consultant and/or on speaker bureaus for Eli Lilly and Company and others.
Source: Ament M et al. J Headache Pain. 2021 Feb 6. doi: 10.1186/s10194-021-01215-9.
Key clinical point: Galcanezumab reduces the frequency of migraine headache days and may also potentially decrease disabling non-pain symptoms on days when migraine is present in patients with episodic and chronic migraine.
Major finding: Galcanezumab doses of 120 and 240 mg were superior to placebo in reducing the number of monthly migraine days with nausea and/or vomiting in both episodic and chronic migraine studies (all P less than .001). Both doses of galcanezumab were associated with a significant reduction in migraine headache days with photophobia and phonophobia vs. placebo in episodic (P less than .001) and chronic (P less than .001 for galcanezumab 120 mg; P =.001 for galcanezumab 240 mg) migraine studies.
Study details: A post hoc analysis of phase 3 randomized clinical trials EVOLVE-1, EVOLVE-2, and REGAIN that included a total of 2,289 patients with episodic or chronic migraine with or without aura.
Disclosures: This study was funded by Eli Lilly and Company, Indianapolis, IN, USA. K Day, VL Stauffer, V Skljarevski, M Rettiganti, E Pearlman, and SK Aurora reported being current/former full-time employees and/or minor stockholders of Eli Lilly and Company. M Ament reported being a consultant and/or on speaker bureaus for Eli Lilly and Company and others.
Source: Ament M et al. J Headache Pain. 2021 Feb 6. doi: 10.1186/s10194-021-01215-9.
Key clinical point: Galcanezumab reduces the frequency of migraine headache days and may also potentially decrease disabling non-pain symptoms on days when migraine is present in patients with episodic and chronic migraine.
Major finding: Galcanezumab doses of 120 and 240 mg were superior to placebo in reducing the number of monthly migraine days with nausea and/or vomiting in both episodic and chronic migraine studies (all P less than .001). Both doses of galcanezumab were associated with a significant reduction in migraine headache days with photophobia and phonophobia vs. placebo in episodic (P less than .001) and chronic (P less than .001 for galcanezumab 120 mg; P =.001 for galcanezumab 240 mg) migraine studies.
Study details: A post hoc analysis of phase 3 randomized clinical trials EVOLVE-1, EVOLVE-2, and REGAIN that included a total of 2,289 patients with episodic or chronic migraine with or without aura.
Disclosures: This study was funded by Eli Lilly and Company, Indianapolis, IN, USA. K Day, VL Stauffer, V Skljarevski, M Rettiganti, E Pearlman, and SK Aurora reported being current/former full-time employees and/or minor stockholders of Eli Lilly and Company. M Ament reported being a consultant and/or on speaker bureaus for Eli Lilly and Company and others.
Source: Ament M et al. J Headache Pain. 2021 Feb 6. doi: 10.1186/s10194-021-01215-9.
Lasmiditan demonstrates superior pain freedom at 2 hours in at least 2 of 3 migraine attacks
Key clinical point: Lasmiditan is effective in the treatment of an acute migraine attack and demonstrates consistency of response across multiple migraine attacks
Major finding: Lasmiditan doses of 100 and 200 mg were superior to placebo for pain freedom at 2 hours during the first attack (odds ratio [OR], 3.8 and 4.6, respectively; P less than .001) and in at least 2 of 3 attacks (OR, 3.8 and 7.2, respectively; P less than .001). The incidence of severe adverse events was similar across treatment groups.
Study details: Findings are from CENTURION, a phase 3 study that randomly assigned patients with migraine with/without aura to either of 3 treatment groups for 4 attacks: lasmiditan 200 mg (n=536), lasmiditan 100 mg (n=539), or control (n=538).
Disclosures: The CENTURION study was sponsored by Eli Lilly and Company. Some authors including the lead author were full-time employees and minor stockholders at Eli Lilly and Company. Some authors reported receiving speaker fees and honorariums from different sources.
Source: Ashina M et al. Cephalalgia. 2021 Feb 4. doi: 10.1177/0333102421989232.
Key clinical point: Lasmiditan is effective in the treatment of an acute migraine attack and demonstrates consistency of response across multiple migraine attacks
Major finding: Lasmiditan doses of 100 and 200 mg were superior to placebo for pain freedom at 2 hours during the first attack (odds ratio [OR], 3.8 and 4.6, respectively; P less than .001) and in at least 2 of 3 attacks (OR, 3.8 and 7.2, respectively; P less than .001). The incidence of severe adverse events was similar across treatment groups.
Study details: Findings are from CENTURION, a phase 3 study that randomly assigned patients with migraine with/without aura to either of 3 treatment groups for 4 attacks: lasmiditan 200 mg (n=536), lasmiditan 100 mg (n=539), or control (n=538).
Disclosures: The CENTURION study was sponsored by Eli Lilly and Company. Some authors including the lead author were full-time employees and minor stockholders at Eli Lilly and Company. Some authors reported receiving speaker fees and honorariums from different sources.
Source: Ashina M et al. Cephalalgia. 2021 Feb 4. doi: 10.1177/0333102421989232.
Key clinical point: Lasmiditan is effective in the treatment of an acute migraine attack and demonstrates consistency of response across multiple migraine attacks
Major finding: Lasmiditan doses of 100 and 200 mg were superior to placebo for pain freedom at 2 hours during the first attack (odds ratio [OR], 3.8 and 4.6, respectively; P less than .001) and in at least 2 of 3 attacks (OR, 3.8 and 7.2, respectively; P less than .001). The incidence of severe adverse events was similar across treatment groups.
Study details: Findings are from CENTURION, a phase 3 study that randomly assigned patients with migraine with/without aura to either of 3 treatment groups for 4 attacks: lasmiditan 200 mg (n=536), lasmiditan 100 mg (n=539), or control (n=538).
Disclosures: The CENTURION study was sponsored by Eli Lilly and Company. Some authors including the lead author were full-time employees and minor stockholders at Eli Lilly and Company. Some authors reported receiving speaker fees and honorariums from different sources.
Source: Ashina M et al. Cephalalgia. 2021 Feb 4. doi: 10.1177/0333102421989232.
Hyperkeratotic Nummular Plaques on the Upper Trunk
The Diagnosis: Extragenital Lichen Sclerosus Et Atrophicus
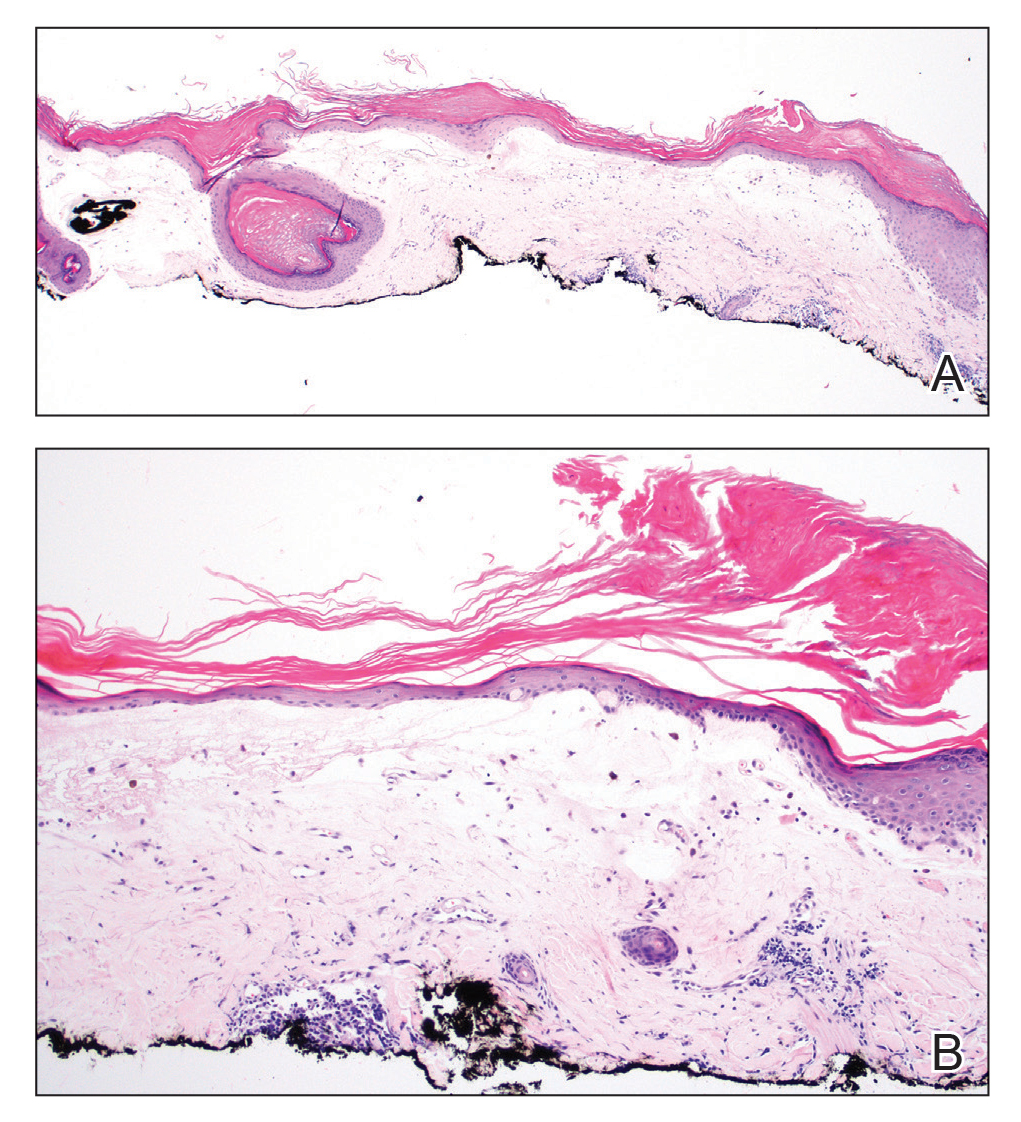
Histopathologic evaluation revealed hyperkeratosis, follicular plugging, epidermal atrophy, and homogenization of papillary dermal collagen with an underlying lymphocytic infiltrate (Figure 1). Direct immunofluorescence of a plaque with a superimposed bulla was negative for deposition of C3, IgG, IgA, IgM, or fibrinogen. Accordingly, clinicopathologic correlation supported a diagnosis of extragenital lichen sclerosus et atrophicus (LSA). Of note, the patient's history of genital irritation was due to genital LSA that preceded the extragenital manifestations.
Lichen sclerosus et atrophicus is an inflammatory dermatosis that typically presents as atrophic white papules of the anogenital area that coalesce into pruritic plaques; the exact etiology remains to be elucidated, yet various circulating autoantibodies have been identified, suggesting a role for autoimmunity.1,2 Lichen sclerosus et atrophicus is more common in women than in men, with a bimodal peak in the age of onset affecting postmenopausal and prepubertal populations.1 In women, affected areas include the labia minora and majora, clitoris, perineum, and perianal skin; LSA spares the mucosal surfaces of the vagina and cervix.2 In men, uncircumscribed genital skin more commonly is affected. Involvement is localized to the foreskin and glans with occasional urethral involvement.2
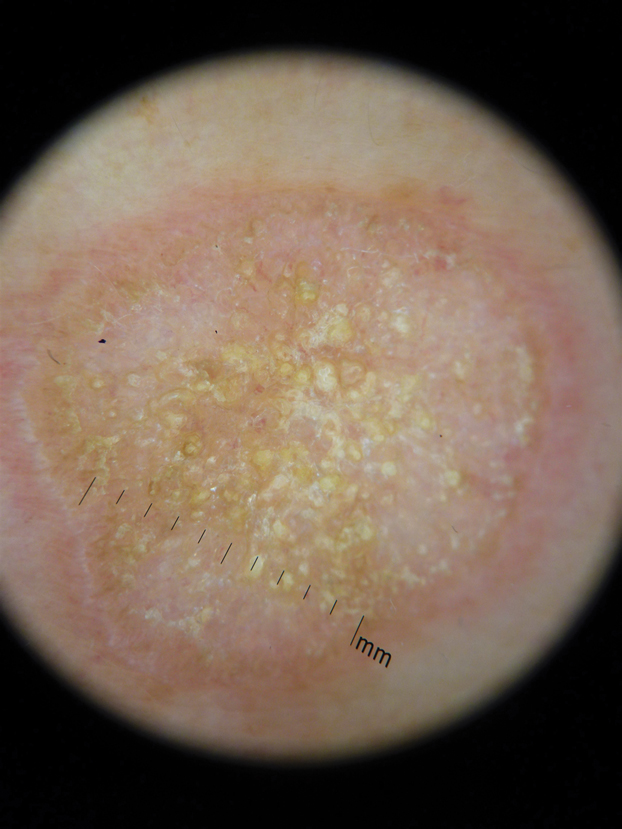
In contrast, extragenital LSA tends to present as asymptomatic papules and plaques that develop atrophy with time, involving the back, shoulders, neck, chest, thighs, axillae, and flexural wrists2,3; an erythematous rim often is present,4 and hyperkeratosis with follicular plugging may be prominent.5 Our patient's case emphasizes the predilection of plaques for the chest and intermammary skin (Figure 2A). Approximately 15% of LSA cases have extragenital involvement, and extragenital-limited disease accounts for roughly 5% of cases.6,7 Unlike genital LSA, extragenital disease has not been associated with an increased risk for squamous cell carcinoma.1 Bullae formation within plaques of genital or extragenital LSA has been reported3,8 and is exemplified in our patient (Figure 2B). Intralesional bullae formation likely is due to a combination of internal and external factors, mainly the inability to withstand shear forces due to an atrophic epidermis with basal vacuolar injury overlying an edematous papillary dermis with altered collagen.8 Dermatoscopic findings may aid in recognizing extragenital LSA9,10; our patient's plaques demonstrated the characteristic findings of comedolike openings, structureless white areas, and pink borders (Figure 3).
The clinical differential diagnosis for well-demarcated, pink, scaly plaques is broad. Nummular eczema usually presents as coin-shaped eczematous plaques on the dorsal aspects of the hands or lower extremities, and histology shows epidermal spongiosis.11 Nummular eczema may be considered due to the striking round morphology of various plaques, yet our patient's presentation was better served by a consideration of several papulosquamous disorders.
Lichen planus (LP) presents as intensely pruritic, violaceous, polygonal, flat-topped papules with overlying reticular white lines, or Wickham striae, that favor the flexural wrists, lower back, and lower extremities. Lichen planus also may have oral and genital mucosal involvement. Similar to LSA, LP is more common in women and preferentially affects the postmenopausal population.12 Additionally, hypertrophic LP may obscure Wickham striae and mimic extragenital LSA; distinguishing features of hypertrophic LP are intense pruritus and a predilection for the shins. Histology is defined by orthohyperkeratosis, hypergranulosis, sawtooth acanthosis, and vacuolar degeneration of the basal layer with Civatte bodies or dyskeratotic basal keratinocytes overlying a characteristic bandlike infiltrate of lymphocytes.12
Lichen simplex chronicus (LSC) is characterized by intense pruritus and presents as hyperkeratotic plaques with a predilection for accessible regions such as the posterior neck and extremities.13 The striking annular demarcation of this case makes LSC unlikely. Comparable to LSA and LP, LSC also may present with both genital and extragenital findings. Histology of LSC is characterized by irregular acanthosis or thickening of the epidermis with vertical streaking of collagen and vascular bundles of the papillary dermis.13
Subacute cutaneous lupus erythematosus (SCLE) is important to consider for a new papulosquamous eruption with a predilection for the sun-exposed skin of a middle-aged woman. The presence of papules on the volar wrist and history of genital irritation, however, make this entity less likely. Similar to LSA, histologic examination of SCLE reveals epidermal atrophy, basal layer degeneration, and papillary dermal edema with lymphocytic inflammation. However, SCLE lacks the band of inflammation underlying pale homogenized papillary dermal collagen, the most distinguishing feature of LSA; instead, SCLE shows superficial and deep perivascular and periadnexal lymphocytes and mucin in the dermis.14
Lichen sclerosus et atrophicus may be chronic and progressive in nature or cycle through remissions and relapses.2 Treatment is not curative, and management is directed to alleviating symptoms and preventing the progression of disease. First-line management of extragenital LSA is potent topical steroids.1 Adjuvant topical calcineurin inhibitors may be used as steroid-sparing agents.2 Phototherapy is a second-line therapy and even narrowband UVB phototherapy has demonstrated efficacy in managing extragenital LSA.15,16 Our patient was started on mometasone ointment and calcipotriene cream with slight improvement after a 6-month trial. Ongoing management is focused on optimizing application of topical therapies.
- Powell JJ, Wojnarowska F. Lichen sclerosus. Lancet. 1999;353:1777-1783.
- Fistarol SK, Itin PH. Diagnosis and treatment of lichen sclerosus. Am J Clin Dermatol. 2013;14:27-47.
- Meffert JJ, Davis BM, Grimwood RE. Lichen sclerosus. J Am Acad Dermatol. 1995;32:393-416.
- Surkan M, Hull P. A case of lichen sclerosus et atrophicus with distinct erythematous borders. J Cutan Med Surg. 2015;19:600-603.
- Kimura A, Kambe N, Satoh T, et al. Follicular keratosis and bullous formation are typical signs of extragenital lichen sclerosus. J Dermatol. 2011;38:834-836.
- Meyrick Thomas RH, Ridley CM, McGibbon DH, et al. Lichen sclerosus et atrophicus and autoimmunity: a study of 350 women. Br J Dermatol. 1988;118:41-46.
- Wallace HJ. Lichen sclerosus et atrophicus. Trans St Johns Hosp Dermatol Soc. 1971;57:9-30.
- Hallel-Halevy D, Grunwald MH, Yerushalmi J, et al. Bullous lichen sclerosus et atrophicus. J Am Acad Dermatol. 1998;39:500-501.
- Garrido-Ríos AA, Álvarez-Garrido H, Sanz-Muñoz C, et al. Dermoscopy of extragenital lichen sclerosus. Arch Dermatol. 2009;145:1468.
- Larre Borges A, Tiodorovic-Zivkovic D, Lallas A, et al. Clinical, dermoscopic and histopathologic features of genital and extragenital lichen sclerosus. J Eur Acad Dermatol Venereol. 2013;27:1433-1439.
- Rudikoff D. Differential diagnosis of round or discoid lesions. Clin Dermatol. 2011;29:489-497.
- Boyd AS, Neldner KH. Lichen planus. J Am Acad Dermatol. 1991;25:593-619.
- Shaffer B, Beerman H. Lichen simplex chronicus and its variants: a discussion of certain psychodynamic mechanisms and clinical and histopathologic correlations. AMA Arch Derm Syphilol. 1951;64:340-351.
- Walling HW, Sontheimer RD. Cutaneous lupus erythematosus. Am J Clin Dermatol. 2009;10:365-381.
- Sauder MB, Linzon-Smith J, Beecker J. Extragenital bullous lichen sclerosus. J Am Acad Dermatol. 2014;71:981-984.
- Colbert RL, Chiang MP, Carlin CS, et al. Progressive extragenital lichen sclerosus successfully treated with narrowband UV-B phototherapy. Arch Dermatol. 2007;143:19-20.
The Diagnosis: Extragenital Lichen Sclerosus Et Atrophicus
Histopathologic evaluation revealed hyperkeratosis, follicular plugging, epidermal atrophy, and homogenization of papillary dermal collagen with an underlying lymphocytic infiltrate (Figure 1). Direct immunofluorescence of a plaque with a superimposed bulla was negative for deposition of C3, IgG, IgA, IgM, or fibrinogen. Accordingly, clinicopathologic correlation supported a diagnosis of extragenital lichen sclerosus et atrophicus (LSA). Of note, the patient's history of genital irritation was due to genital LSA that preceded the extragenital manifestations.
Lichen sclerosus et atrophicus is an inflammatory dermatosis that typically presents as atrophic white papules of the anogenital area that coalesce into pruritic plaques; the exact etiology remains to be elucidated, yet various circulating autoantibodies have been identified, suggesting a role for autoimmunity.1,2 Lichen sclerosus et atrophicus is more common in women than in men, with a bimodal peak in the age of onset affecting postmenopausal and prepubertal populations.1 In women, affected areas include the labia minora and majora, clitoris, perineum, and perianal skin; LSA spares the mucosal surfaces of the vagina and cervix.2 In men, uncircumscribed genital skin more commonly is affected. Involvement is localized to the foreskin and glans with occasional urethral involvement.2
In contrast, extragenital LSA tends to present as asymptomatic papules and plaques that develop atrophy with time, involving the back, shoulders, neck, chest, thighs, axillae, and flexural wrists2,3; an erythematous rim often is present,4 and hyperkeratosis with follicular plugging may be prominent.5 Our patient's case emphasizes the predilection of plaques for the chest and intermammary skin (Figure 2A). Approximately 15% of LSA cases have extragenital involvement, and extragenital-limited disease accounts for roughly 5% of cases.6,7 Unlike genital LSA, extragenital disease has not been associated with an increased risk for squamous cell carcinoma.1 Bullae formation within plaques of genital or extragenital LSA has been reported3,8 and is exemplified in our patient (Figure 2B). Intralesional bullae formation likely is due to a combination of internal and external factors, mainly the inability to withstand shear forces due to an atrophic epidermis with basal vacuolar injury overlying an edematous papillary dermis with altered collagen.8 Dermatoscopic findings may aid in recognizing extragenital LSA9,10; our patient's plaques demonstrated the characteristic findings of comedolike openings, structureless white areas, and pink borders (Figure 3).
The clinical differential diagnosis for well-demarcated, pink, scaly plaques is broad. Nummular eczema usually presents as coin-shaped eczematous plaques on the dorsal aspects of the hands or lower extremities, and histology shows epidermal spongiosis.11 Nummular eczema may be considered due to the striking round morphology of various plaques, yet our patient's presentation was better served by a consideration of several papulosquamous disorders.
Lichen planus (LP) presents as intensely pruritic, violaceous, polygonal, flat-topped papules with overlying reticular white lines, or Wickham striae, that favor the flexural wrists, lower back, and lower extremities. Lichen planus also may have oral and genital mucosal involvement. Similar to LSA, LP is more common in women and preferentially affects the postmenopausal population.12 Additionally, hypertrophic LP may obscure Wickham striae and mimic extragenital LSA; distinguishing features of hypertrophic LP are intense pruritus and a predilection for the shins. Histology is defined by orthohyperkeratosis, hypergranulosis, sawtooth acanthosis, and vacuolar degeneration of the basal layer with Civatte bodies or dyskeratotic basal keratinocytes overlying a characteristic bandlike infiltrate of lymphocytes.12
Lichen simplex chronicus (LSC) is characterized by intense pruritus and presents as hyperkeratotic plaques with a predilection for accessible regions such as the posterior neck and extremities.13 The striking annular demarcation of this case makes LSC unlikely. Comparable to LSA and LP, LSC also may present with both genital and extragenital findings. Histology of LSC is characterized by irregular acanthosis or thickening of the epidermis with vertical streaking of collagen and vascular bundles of the papillary dermis.13
Subacute cutaneous lupus erythematosus (SCLE) is important to consider for a new papulosquamous eruption with a predilection for the sun-exposed skin of a middle-aged woman. The presence of papules on the volar wrist and history of genital irritation, however, make this entity less likely. Similar to LSA, histologic examination of SCLE reveals epidermal atrophy, basal layer degeneration, and papillary dermal edema with lymphocytic inflammation. However, SCLE lacks the band of inflammation underlying pale homogenized papillary dermal collagen, the most distinguishing feature of LSA; instead, SCLE shows superficial and deep perivascular and periadnexal lymphocytes and mucin in the dermis.14
Lichen sclerosus et atrophicus may be chronic and progressive in nature or cycle through remissions and relapses.2 Treatment is not curative, and management is directed to alleviating symptoms and preventing the progression of disease. First-line management of extragenital LSA is potent topical steroids.1 Adjuvant topical calcineurin inhibitors may be used as steroid-sparing agents.2 Phototherapy is a second-line therapy and even narrowband UVB phototherapy has demonstrated efficacy in managing extragenital LSA.15,16 Our patient was started on mometasone ointment and calcipotriene cream with slight improvement after a 6-month trial. Ongoing management is focused on optimizing application of topical therapies.
The Diagnosis: Extragenital Lichen Sclerosus Et Atrophicus
Histopathologic evaluation revealed hyperkeratosis, follicular plugging, epidermal atrophy, and homogenization of papillary dermal collagen with an underlying lymphocytic infiltrate (Figure 1). Direct immunofluorescence of a plaque with a superimposed bulla was negative for deposition of C3, IgG, IgA, IgM, or fibrinogen. Accordingly, clinicopathologic correlation supported a diagnosis of extragenital lichen sclerosus et atrophicus (LSA). Of note, the patient's history of genital irritation was due to genital LSA that preceded the extragenital manifestations.
Lichen sclerosus et atrophicus is an inflammatory dermatosis that typically presents as atrophic white papules of the anogenital area that coalesce into pruritic plaques; the exact etiology remains to be elucidated, yet various circulating autoantibodies have been identified, suggesting a role for autoimmunity.1,2 Lichen sclerosus et atrophicus is more common in women than in men, with a bimodal peak in the age of onset affecting postmenopausal and prepubertal populations.1 In women, affected areas include the labia minora and majora, clitoris, perineum, and perianal skin; LSA spares the mucosal surfaces of the vagina and cervix.2 In men, uncircumscribed genital skin more commonly is affected. Involvement is localized to the foreskin and glans with occasional urethral involvement.2
In contrast, extragenital LSA tends to present as asymptomatic papules and plaques that develop atrophy with time, involving the back, shoulders, neck, chest, thighs, axillae, and flexural wrists2,3; an erythematous rim often is present,4 and hyperkeratosis with follicular plugging may be prominent.5 Our patient's case emphasizes the predilection of plaques for the chest and intermammary skin (Figure 2A). Approximately 15% of LSA cases have extragenital involvement, and extragenital-limited disease accounts for roughly 5% of cases.6,7 Unlike genital LSA, extragenital disease has not been associated with an increased risk for squamous cell carcinoma.1 Bullae formation within plaques of genital or extragenital LSA has been reported3,8 and is exemplified in our patient (Figure 2B). Intralesional bullae formation likely is due to a combination of internal and external factors, mainly the inability to withstand shear forces due to an atrophic epidermis with basal vacuolar injury overlying an edematous papillary dermis with altered collagen.8 Dermatoscopic findings may aid in recognizing extragenital LSA9,10; our patient's plaques demonstrated the characteristic findings of comedolike openings, structureless white areas, and pink borders (Figure 3).
The clinical differential diagnosis for well-demarcated, pink, scaly plaques is broad. Nummular eczema usually presents as coin-shaped eczematous plaques on the dorsal aspects of the hands or lower extremities, and histology shows epidermal spongiosis.11 Nummular eczema may be considered due to the striking round morphology of various plaques, yet our patient's presentation was better served by a consideration of several papulosquamous disorders.
Lichen planus (LP) presents as intensely pruritic, violaceous, polygonal, flat-topped papules with overlying reticular white lines, or Wickham striae, that favor the flexural wrists, lower back, and lower extremities. Lichen planus also may have oral and genital mucosal involvement. Similar to LSA, LP is more common in women and preferentially affects the postmenopausal population.12 Additionally, hypertrophic LP may obscure Wickham striae and mimic extragenital LSA; distinguishing features of hypertrophic LP are intense pruritus and a predilection for the shins. Histology is defined by orthohyperkeratosis, hypergranulosis, sawtooth acanthosis, and vacuolar degeneration of the basal layer with Civatte bodies or dyskeratotic basal keratinocytes overlying a characteristic bandlike infiltrate of lymphocytes.12
Lichen simplex chronicus (LSC) is characterized by intense pruritus and presents as hyperkeratotic plaques with a predilection for accessible regions such as the posterior neck and extremities.13 The striking annular demarcation of this case makes LSC unlikely. Comparable to LSA and LP, LSC also may present with both genital and extragenital findings. Histology of LSC is characterized by irregular acanthosis or thickening of the epidermis with vertical streaking of collagen and vascular bundles of the papillary dermis.13
Subacute cutaneous lupus erythematosus (SCLE) is important to consider for a new papulosquamous eruption with a predilection for the sun-exposed skin of a middle-aged woman. The presence of papules on the volar wrist and history of genital irritation, however, make this entity less likely. Similar to LSA, histologic examination of SCLE reveals epidermal atrophy, basal layer degeneration, and papillary dermal edema with lymphocytic inflammation. However, SCLE lacks the band of inflammation underlying pale homogenized papillary dermal collagen, the most distinguishing feature of LSA; instead, SCLE shows superficial and deep perivascular and periadnexal lymphocytes and mucin in the dermis.14
Lichen sclerosus et atrophicus may be chronic and progressive in nature or cycle through remissions and relapses.2 Treatment is not curative, and management is directed to alleviating symptoms and preventing the progression of disease. First-line management of extragenital LSA is potent topical steroids.1 Adjuvant topical calcineurin inhibitors may be used as steroid-sparing agents.2 Phototherapy is a second-line therapy and even narrowband UVB phototherapy has demonstrated efficacy in managing extragenital LSA.15,16 Our patient was started on mometasone ointment and calcipotriene cream with slight improvement after a 6-month trial. Ongoing management is focused on optimizing application of topical therapies.
- Powell JJ, Wojnarowska F. Lichen sclerosus. Lancet. 1999;353:1777-1783.
- Fistarol SK, Itin PH. Diagnosis and treatment of lichen sclerosus. Am J Clin Dermatol. 2013;14:27-47.
- Meffert JJ, Davis BM, Grimwood RE. Lichen sclerosus. J Am Acad Dermatol. 1995;32:393-416.
- Surkan M, Hull P. A case of lichen sclerosus et atrophicus with distinct erythematous borders. J Cutan Med Surg. 2015;19:600-603.
- Kimura A, Kambe N, Satoh T, et al. Follicular keratosis and bullous formation are typical signs of extragenital lichen sclerosus. J Dermatol. 2011;38:834-836.
- Meyrick Thomas RH, Ridley CM, McGibbon DH, et al. Lichen sclerosus et atrophicus and autoimmunity: a study of 350 women. Br J Dermatol. 1988;118:41-46.
- Wallace HJ. Lichen sclerosus et atrophicus. Trans St Johns Hosp Dermatol Soc. 1971;57:9-30.
- Hallel-Halevy D, Grunwald MH, Yerushalmi J, et al. Bullous lichen sclerosus et atrophicus. J Am Acad Dermatol. 1998;39:500-501.
- Garrido-Ríos AA, Álvarez-Garrido H, Sanz-Muñoz C, et al. Dermoscopy of extragenital lichen sclerosus. Arch Dermatol. 2009;145:1468.
- Larre Borges A, Tiodorovic-Zivkovic D, Lallas A, et al. Clinical, dermoscopic and histopathologic features of genital and extragenital lichen sclerosus. J Eur Acad Dermatol Venereol. 2013;27:1433-1439.
- Rudikoff D. Differential diagnosis of round or discoid lesions. Clin Dermatol. 2011;29:489-497.
- Boyd AS, Neldner KH. Lichen planus. J Am Acad Dermatol. 1991;25:593-619.
- Shaffer B, Beerman H. Lichen simplex chronicus and its variants: a discussion of certain psychodynamic mechanisms and clinical and histopathologic correlations. AMA Arch Derm Syphilol. 1951;64:340-351.
- Walling HW, Sontheimer RD. Cutaneous lupus erythematosus. Am J Clin Dermatol. 2009;10:365-381.
- Sauder MB, Linzon-Smith J, Beecker J. Extragenital bullous lichen sclerosus. J Am Acad Dermatol. 2014;71:981-984.
- Colbert RL, Chiang MP, Carlin CS, et al. Progressive extragenital lichen sclerosus successfully treated with narrowband UV-B phototherapy. Arch Dermatol. 2007;143:19-20.
- Powell JJ, Wojnarowska F. Lichen sclerosus. Lancet. 1999;353:1777-1783.
- Fistarol SK, Itin PH. Diagnosis and treatment of lichen sclerosus. Am J Clin Dermatol. 2013;14:27-47.
- Meffert JJ, Davis BM, Grimwood RE. Lichen sclerosus. J Am Acad Dermatol. 1995;32:393-416.
- Surkan M, Hull P. A case of lichen sclerosus et atrophicus with distinct erythematous borders. J Cutan Med Surg. 2015;19:600-603.
- Kimura A, Kambe N, Satoh T, et al. Follicular keratosis and bullous formation are typical signs of extragenital lichen sclerosus. J Dermatol. 2011;38:834-836.
- Meyrick Thomas RH, Ridley CM, McGibbon DH, et al. Lichen sclerosus et atrophicus and autoimmunity: a study of 350 women. Br J Dermatol. 1988;118:41-46.
- Wallace HJ. Lichen sclerosus et atrophicus. Trans St Johns Hosp Dermatol Soc. 1971;57:9-30.
- Hallel-Halevy D, Grunwald MH, Yerushalmi J, et al. Bullous lichen sclerosus et atrophicus. J Am Acad Dermatol. 1998;39:500-501.
- Garrido-Ríos AA, Álvarez-Garrido H, Sanz-Muñoz C, et al. Dermoscopy of extragenital lichen sclerosus. Arch Dermatol. 2009;145:1468.
- Larre Borges A, Tiodorovic-Zivkovic D, Lallas A, et al. Clinical, dermoscopic and histopathologic features of genital and extragenital lichen sclerosus. J Eur Acad Dermatol Venereol. 2013;27:1433-1439.
- Rudikoff D. Differential diagnosis of round or discoid lesions. Clin Dermatol. 2011;29:489-497.
- Boyd AS, Neldner KH. Lichen planus. J Am Acad Dermatol. 1991;25:593-619.
- Shaffer B, Beerman H. Lichen simplex chronicus and its variants: a discussion of certain psychodynamic mechanisms and clinical and histopathologic correlations. AMA Arch Derm Syphilol. 1951;64:340-351.
- Walling HW, Sontheimer RD. Cutaneous lupus erythematosus. Am J Clin Dermatol. 2009;10:365-381.
- Sauder MB, Linzon-Smith J, Beecker J. Extragenital bullous lichen sclerosus. J Am Acad Dermatol. 2014;71:981-984.
- Colbert RL, Chiang MP, Carlin CS, et al. Progressive extragenital lichen sclerosus successfully treated with narrowband UV-B phototherapy. Arch Dermatol. 2007;143:19-20.
A 48-year-old woman with a history of type 2 diabetes mellitus and nonalcoholic steatohepatitis presented with papules and plaques on the upper trunk, proximal extremities, and volar wrists. Clear fluid–filled bullae occasionally developed within the plaques and subsequently ruptured and healed. Aside from intermittent lesion tenderness and irritation with the formation and rupture of the bullae, the patient’s plaques were asymptomatic, and she specifically denied pruritus. A review of systems revealed a history of genital irritation evaluated by a gynecologist; nystatin–triamcinolone cream 0.1% applied as needed provided relief. The patient denied any recent flares or any new or changing oral mucosa findings or symptoms, preceding medications, or family history of similar lesions. Physical examination revealed well-demarcated, round, pink plaques with keratotic scale scattered across the upper trunk and central chest. The bilateral volar wrists were surfaced by well-circumscribed, thin, pink to violaceous, hyperkeratotic papules.
Genetic testing for breast and ovarian cancer: What has changed and what still needs to change?
Investigators found racial and ethnic disparities in genetic testing as well as “persistent underuse” of testing in patients with ovarian cancer.
The team also discovered that most pathogenic variant (PV) results were in 20 genes associated with breast and/or ovarian cancer, and testing other genes largely revealed variants of uncertain significance (VUS).
Allison W. Kurian, MD, of Stanford (Calif.) University, and colleagues recounted these findings in the Journal of Clinical Oncology.
Because of improvements in sequencing technology, competition among commercial purveyors, and declining cost, genetic testing has been increasingly available to clinicians for patient management and cancer prevention (JAMA. 2015 Sep 8;314[10]:997-8). Although germline testing can guide therapy for several solid tumors, there is little research about how often and how well it is used in practice.
For their study, Dr. Kurian and colleagues used a SEER Genetic Testing Linkage Demonstration Project in a population-based assessment of testing for cancer risk. The investigators analyzed 7-year trends in testing among all women diagnosed with breast or ovarian cancer in Georgia or California from 2013 to 2017, reviewing testing patterns and result interpretation from 2012 to 2019.
Before analyzing the data, the investigators made the following hypotheses:
- Multigene panels (MGP) would entirely replace testing for BRCA1/2 only.
- Testing underutilization in patients with ovarian cancer would improve over time.
- More patients would be tested at lower levels of pretest risk for PVs.
- Sociodemographic differences in testing trends would not be observed.
- Detection of PVs and VUS would increase.
- Racial and ethnic disparities in rates of VUS would diminish.
Study conduct
The investigators examined genetic tests performed from 2012 through the beginning of 2019 at major commercial laboratories and linked that information with data in the SEER registries in Georgia and California on all breast and ovarian cancer patients diagnosed between 2013 and 2017. There were few criteria for exclusion.
Genetic testing results were categorized as identifying a PV or likely PV, VUS, or benign or likely benign mutation by American College of Medical Genetics criteria. When a patient had genetic testing on more than one occasion, the most recent test was used.
If a PV was identified, the types of PVs were grouped according to the level of evidence that supported pathogenicity into the following categories:
- BRCA1 or BRCA2 mutations.
- PVs in other genes designated by the National Comprehensive Cancer Network as associated with breast or ovarian cancer (e.g., ATM, BARD1, BRIP1, CDH1, CHEK2, EPCAM, MLH1, MSH2, MSH6, NBN, NF1, PALB2, MS2, PTEN, RAD51C, RAD51D, STK11, and TP53).
- PVs in other actionable genes (e.g., APC, BMPR1A, MEN1, MUTYH, NF2, RB1, RET, SDHAF2, SDHB, SDHC, SDHD, SMAD4, TSC1, TSC2, and VHL).
- Any other tested genes.
The investigators also tabulated instances in which genetic testing identified a VUS in any gene but no PV. If a VUS was identified originally and was reclassified more recently into the “PV/likely PV” or “benign/likely benign” categories, only the resolved categorization was recorded.
The authors evaluated clinical and sociodemographic correlates of testing trends for breast and ovarian cancer, assessing the relationship between race, age, and geographic site in receipt of any test or type of test.
Among laboratories, the investigators examined trends in the number of genes tested, associations with sociodemographic factors, categories of test results, and whether trends differed by race or ethnicity.
Findings, by hypothesis
Hypothesis #1: MGP will entirely replace testing for BRCA1/2 only.
About 25% of tested patients with breast cancer diagnosed in early 2013 received MGP, compared with more than 80% of those diagnosed in late 2017.
The trend for ovarian cancer was similar. About 40% of patients diagnosed in early 2013 received MGP, compared with more than 90% diagnosed in late 2017. These trends were similar in California and Georgia.
From 2012 to 2019, there was a consistent upward trend in gene number for patients with breast cancer (mean, 19) or ovarian cancer (mean, 21), from approximately 10 genes to 35 genes.
Hypothesis #2: Underutilization of testing in patients with ovarian cancer will improve.
Among the 187,535 patients with breast cancer and the 14,689 patients with ovarian cancer diagnosed in Georgia or California from 2013 through 2017, on average, testing rates increased 2% per year.
In all, 25.2% of breast cancer patients and 34.3% of ovarian cancer patients had genetic testing on one (87.3%) or more (12.7%) occasions.
Prior research suggested that, in 2013 and 2014, 31% of women with ovarian cancer had genetic testing (JAMA Oncol. 2018 Aug 1;4[8]:1066-72/ J Clin Oncol. 2019 May 20;37[15]:1305-15).
The investigators therefore concluded that underutilization of genetic testing in ovarian cancer did not improve substantially during the 7-year interval analyzed.
Hypothesis #3: More patients will be tested at lower levels of pretest risk.
These data were more difficult to abstract from the SEER database, but older patients were more likely to be tested in later years.
In patients older than 60 years of age (who accounted for more than 50% of both cancer cohorts), testing rates increased from 11.1% to 14.9% for breast cancer and 25.3% to 31.4% for ovarian cancer. By contrast, patients younger than 45 years of age were less than 15% of the sample and had lower testing rates over time.
There were no substantial changes in testing rates by other clinical variables. Therefore, in concert with the age-related testing trends, it is likely that women were tested for genetic mutations at increasingly lower levels of pretest risk.
Hypothesis #4: Sociodemographic differences in testing trends will not be observed.
Among patients with breast cancer, approximately 31% of those who had genetic testing were uninsured, 31% had Medicaid, and 26% had private insurance, Medicare, or other insurance.
For patients with ovarian cancer, approximately 28% were uninsured, 27% had Medicaid, and 39% had private insurance, Medicare, or other insurance.
The authors had previously found that less testing was associated with Black race, greater poverty, and less insurance coverage (J Clin Oncol. 2019 May 20;37[15]:1305-15). However, they noted no changes in testing rates by sociodemographic variables over time.
Hypothesis #5: Detection of both PVs and VUS will increase.
The proportion of tested breast cancer patients with PVs in BRCA1/2 decreased from 7.5% to 5.0% (P < .001), whereas PV yield for the two other clinically salient categories (breast or ovarian and other actionable genes) increased.
The proportion of PVs in any breast or ovarian gene increased from 1.3% to 4.6%, and the proportion in any other actionable gene increased from 0.3% to 1.3%.
For breast cancer patients, VUS-only rates increased from 8.5% in early 2013 to 22.4% in late 2017.
For ovarian cancer patients, the yield of PVs in BRCA1/2 decreased from 15.7% to 12.4% (P < .001), whereas the PV yield for breast or ovarian genes increased from 3.9% to 4.3%, and the yield for other actionable genes increased from 0.3% to 2.0%.
In ovarian cancer patients, the PV or VUS-only result rate increased from 30.8% in early 2013 to 43.0% in late 2017, entirely due to the increase in VUS-only rates. VUS were identified in 8.1% of patients diagnosed in early 2013 and increased to 28.3% in patients diagnosed in late 2017.
Hypothesis #6: Racial or ethnic disparities in rates of VUS will diminish.
Among patients with breast cancer, racial or ethnic differences in PV rates were small and did not change over time. For patients with ovarian cancer, PV rates across racial or ethnic groups diminished over time.
However, for both breast and ovarian cancer patients, there were large differences in VUS-only rates by race and ethnicity that persisted during the interval studied.
In 2017, for patients with breast cancer, VUS-only rates were substantially higher in Asian (42.4%), Black (36.6%), and Hispanic (27.7%) patients than in non-Hispanic White patients (24.5%, P < .001).
Similar trends were noted for patients with ovarian cancer. VUS-only rates were substantially higher in Asian (47.8%), Black (46.0%), and Hispanic (36.8%) patients than in non-Hispanic White patients (24.6%, P < .001).
Multivariable logistic regressions were performed separately for tested patients with breast cancer and ovarian cancer, and the results showed no significant interaction between race or ethnicity and date. Therefore, there was no significant change in racial or ethnic differences in VUS-only results across the study period.
Where these findings leave clinicians in 2021
Among the patients studied, there was:
- Marked expansion in the number of genes sequenced.
- A likely modest trend toward testing patients with lower pretest risk of a PV.
- No sociodemographic differences in testing trends.
- A small increase in PV rates and a substantial increase in VUS-only rates.
- Near-complete replacement of selective testing by MGP.
For patients with breast cancer, the proportion of all PVs that were in BRCA1/2 fell substantially. Adoption of MGP testing doubled the probability of detecting a PV in other tested genes. Most of the increase was in genes with an established breast or ovarian cancer association, with fewer PVs found in other actionable genes and very few PVs in other tested genes.
Contrary to their hypothesis, the authors observed a sustained undertesting of patients with ovarian cancer. Only 34.3% performed versus nearly 100% recommended, with little change since 2014.
This finding is surprising – and tremendously disappointing – since the prevalence of BRCA1/2 PVs is higher in ovarian cancer than in other cancers (Gynecol Oncol. 2017 Nov;147[2]:375-380), and germline-targeted therapy with PARP inhibitors has been approved for use since 2014.
Furthermore, insurance carriers provide coverage for genetic testing in most patients with carcinoma of the ovary, fallopian tube, and/or peritoneum.
Action plans: Less could be more
During the period analyzed, the increase in VUS-only results dramatically outpaced the increase in PVs.
Since there is a substantially larger volume of clinical genetic testing in non-Hispanic White patients with breast or ovarian cancer, the spectrum of normal variation is less well-defined in other racial or ethnic groups.
The study showed a widening of the “racial-ethnic VUS gap,” with Black and Asian patients having nearly twofold more VUS, although they were not tested for more genes than non-Hispanic White patients.
This is problematic on several levels. Identification of a VUS is challenging for communicating results to and recommending cascade testing for family members.
There is worrisome information regarding overtreatment or counseling of VUS patients about their results. For example, the PROMPT registry showed that 10%-15% of women with PV/VUS in genes not associated with a high risk of ovarian cancer underwent oophorectomy without a clear indication for the procedure.
Although population-based testing might augment the available data on the spectrum of normal variation in racial and ethnic minorities, it would likely exacerbate the proliferation of VUS over PVs.
It is essential to accelerate ongoing approaches to VUS reclassification.
In addition, the authors suggest that it may be time to reverse the trend in increasing the number of genes tested in MGPs. Their rationale is that, in Georgia and California, most PVs among patients with breast and ovarian cancer were identified in 20 genes (ATM, BARD1, BRCA1, BRCA2, BRIP1, CDH1, CHEK2, EPCAM, MLH1, MSH2, MSH6, NBN, NF1, PMS2, PALB2, PTEN, RAD51C, RAD51D, STK11, and TP53).
If the Georgia and California data are representative of a more generalized pattern, a panel of 20 breast cancer– and/or ovarian cancer–associated genes may be ideal for maximizing the yield of clinically relevant PVs and minimizing VUS results for all patients.
Finally, defining the patient, clinician, and health care system factors that impede widespread genetic testing for ovarian cancer patients must be prioritized. As the authors suggest, quality improvement efforts should focus on getting a lot closer to testing rates of 100% for patients with ovarian cancer and building the database that will help sort VUS in minority patients into their proper context of pathogenicity, rather than adding more genes per test.
This research was supported by the National Cancer Institute, the Centers for Disease Control and Prevention, and the California Department of Public Health. The authors disclosed relationships with Myriad Genetics, Ambry Genetics, Color Genomics, GeneDx/BioReference, InVitae, Genentech, Genomic Health, Roche/Genentech, Oncoquest, Tesaro, and Karyopharm Therapeutics.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
Investigators found racial and ethnic disparities in genetic testing as well as “persistent underuse” of testing in patients with ovarian cancer.
The team also discovered that most pathogenic variant (PV) results were in 20 genes associated with breast and/or ovarian cancer, and testing other genes largely revealed variants of uncertain significance (VUS).
Allison W. Kurian, MD, of Stanford (Calif.) University, and colleagues recounted these findings in the Journal of Clinical Oncology.
Because of improvements in sequencing technology, competition among commercial purveyors, and declining cost, genetic testing has been increasingly available to clinicians for patient management and cancer prevention (JAMA. 2015 Sep 8;314[10]:997-8). Although germline testing can guide therapy for several solid tumors, there is little research about how often and how well it is used in practice.
For their study, Dr. Kurian and colleagues used a SEER Genetic Testing Linkage Demonstration Project in a population-based assessment of testing for cancer risk. The investigators analyzed 7-year trends in testing among all women diagnosed with breast or ovarian cancer in Georgia or California from 2013 to 2017, reviewing testing patterns and result interpretation from 2012 to 2019.
Before analyzing the data, the investigators made the following hypotheses:
- Multigene panels (MGP) would entirely replace testing for BRCA1/2 only.
- Testing underutilization in patients with ovarian cancer would improve over time.
- More patients would be tested at lower levels of pretest risk for PVs.
- Sociodemographic differences in testing trends would not be observed.
- Detection of PVs and VUS would increase.
- Racial and ethnic disparities in rates of VUS would diminish.
Study conduct
The investigators examined genetic tests performed from 2012 through the beginning of 2019 at major commercial laboratories and linked that information with data in the SEER registries in Georgia and California on all breast and ovarian cancer patients diagnosed between 2013 and 2017. There were few criteria for exclusion.
Genetic testing results were categorized as identifying a PV or likely PV, VUS, or benign or likely benign mutation by American College of Medical Genetics criteria. When a patient had genetic testing on more than one occasion, the most recent test was used.
If a PV was identified, the types of PVs were grouped according to the level of evidence that supported pathogenicity into the following categories:
- BRCA1 or BRCA2 mutations.
- PVs in other genes designated by the National Comprehensive Cancer Network as associated with breast or ovarian cancer (e.g., ATM, BARD1, BRIP1, CDH1, CHEK2, EPCAM, MLH1, MSH2, MSH6, NBN, NF1, PALB2, MS2, PTEN, RAD51C, RAD51D, STK11, and TP53).
- PVs in other actionable genes (e.g., APC, BMPR1A, MEN1, MUTYH, NF2, RB1, RET, SDHAF2, SDHB, SDHC, SDHD, SMAD4, TSC1, TSC2, and VHL).
- Any other tested genes.
The investigators also tabulated instances in which genetic testing identified a VUS in any gene but no PV. If a VUS was identified originally and was reclassified more recently into the “PV/likely PV” or “benign/likely benign” categories, only the resolved categorization was recorded.
The authors evaluated clinical and sociodemographic correlates of testing trends for breast and ovarian cancer, assessing the relationship between race, age, and geographic site in receipt of any test or type of test.
Among laboratories, the investigators examined trends in the number of genes tested, associations with sociodemographic factors, categories of test results, and whether trends differed by race or ethnicity.
Findings, by hypothesis
Hypothesis #1: MGP will entirely replace testing for BRCA1/2 only.
About 25% of tested patients with breast cancer diagnosed in early 2013 received MGP, compared with more than 80% of those diagnosed in late 2017.
The trend for ovarian cancer was similar. About 40% of patients diagnosed in early 2013 received MGP, compared with more than 90% diagnosed in late 2017. These trends were similar in California and Georgia.
From 2012 to 2019, there was a consistent upward trend in gene number for patients with breast cancer (mean, 19) or ovarian cancer (mean, 21), from approximately 10 genes to 35 genes.
Hypothesis #2: Underutilization of testing in patients with ovarian cancer will improve.
Among the 187,535 patients with breast cancer and the 14,689 patients with ovarian cancer diagnosed in Georgia or California from 2013 through 2017, on average, testing rates increased 2% per year.
In all, 25.2% of breast cancer patients and 34.3% of ovarian cancer patients had genetic testing on one (87.3%) or more (12.7%) occasions.
Prior research suggested that, in 2013 and 2014, 31% of women with ovarian cancer had genetic testing (JAMA Oncol. 2018 Aug 1;4[8]:1066-72/ J Clin Oncol. 2019 May 20;37[15]:1305-15).
The investigators therefore concluded that underutilization of genetic testing in ovarian cancer did not improve substantially during the 7-year interval analyzed.
Hypothesis #3: More patients will be tested at lower levels of pretest risk.
These data were more difficult to abstract from the SEER database, but older patients were more likely to be tested in later years.
In patients older than 60 years of age (who accounted for more than 50% of both cancer cohorts), testing rates increased from 11.1% to 14.9% for breast cancer and 25.3% to 31.4% for ovarian cancer. By contrast, patients younger than 45 years of age were less than 15% of the sample and had lower testing rates over time.
There were no substantial changes in testing rates by other clinical variables. Therefore, in concert with the age-related testing trends, it is likely that women were tested for genetic mutations at increasingly lower levels of pretest risk.
Hypothesis #4: Sociodemographic differences in testing trends will not be observed.
Among patients with breast cancer, approximately 31% of those who had genetic testing were uninsured, 31% had Medicaid, and 26% had private insurance, Medicare, or other insurance.
For patients with ovarian cancer, approximately 28% were uninsured, 27% had Medicaid, and 39% had private insurance, Medicare, or other insurance.
The authors had previously found that less testing was associated with Black race, greater poverty, and less insurance coverage (J Clin Oncol. 2019 May 20;37[15]:1305-15). However, they noted no changes in testing rates by sociodemographic variables over time.
Hypothesis #5: Detection of both PVs and VUS will increase.
The proportion of tested breast cancer patients with PVs in BRCA1/2 decreased from 7.5% to 5.0% (P < .001), whereas PV yield for the two other clinically salient categories (breast or ovarian and other actionable genes) increased.
The proportion of PVs in any breast or ovarian gene increased from 1.3% to 4.6%, and the proportion in any other actionable gene increased from 0.3% to 1.3%.
For breast cancer patients, VUS-only rates increased from 8.5% in early 2013 to 22.4% in late 2017.
For ovarian cancer patients, the yield of PVs in BRCA1/2 decreased from 15.7% to 12.4% (P < .001), whereas the PV yield for breast or ovarian genes increased from 3.9% to 4.3%, and the yield for other actionable genes increased from 0.3% to 2.0%.
In ovarian cancer patients, the PV or VUS-only result rate increased from 30.8% in early 2013 to 43.0% in late 2017, entirely due to the increase in VUS-only rates. VUS were identified in 8.1% of patients diagnosed in early 2013 and increased to 28.3% in patients diagnosed in late 2017.
Hypothesis #6: Racial or ethnic disparities in rates of VUS will diminish.
Among patients with breast cancer, racial or ethnic differences in PV rates were small and did not change over time. For patients with ovarian cancer, PV rates across racial or ethnic groups diminished over time.
However, for both breast and ovarian cancer patients, there were large differences in VUS-only rates by race and ethnicity that persisted during the interval studied.
In 2017, for patients with breast cancer, VUS-only rates were substantially higher in Asian (42.4%), Black (36.6%), and Hispanic (27.7%) patients than in non-Hispanic White patients (24.5%, P < .001).
Similar trends were noted for patients with ovarian cancer. VUS-only rates were substantially higher in Asian (47.8%), Black (46.0%), and Hispanic (36.8%) patients than in non-Hispanic White patients (24.6%, P < .001).
Multivariable logistic regressions were performed separately for tested patients with breast cancer and ovarian cancer, and the results showed no significant interaction between race or ethnicity and date. Therefore, there was no significant change in racial or ethnic differences in VUS-only results across the study period.
Where these findings leave clinicians in 2021
Among the patients studied, there was:
- Marked expansion in the number of genes sequenced.
- A likely modest trend toward testing patients with lower pretest risk of a PV.
- No sociodemographic differences in testing trends.
- A small increase in PV rates and a substantial increase in VUS-only rates.
- Near-complete replacement of selective testing by MGP.
For patients with breast cancer, the proportion of all PVs that were in BRCA1/2 fell substantially. Adoption of MGP testing doubled the probability of detecting a PV in other tested genes. Most of the increase was in genes with an established breast or ovarian cancer association, with fewer PVs found in other actionable genes and very few PVs in other tested genes.
Contrary to their hypothesis, the authors observed a sustained undertesting of patients with ovarian cancer. Only 34.3% performed versus nearly 100% recommended, with little change since 2014.
This finding is surprising – and tremendously disappointing – since the prevalence of BRCA1/2 PVs is higher in ovarian cancer than in other cancers (Gynecol Oncol. 2017 Nov;147[2]:375-380), and germline-targeted therapy with PARP inhibitors has been approved for use since 2014.
Furthermore, insurance carriers provide coverage for genetic testing in most patients with carcinoma of the ovary, fallopian tube, and/or peritoneum.
Action plans: Less could be more
During the period analyzed, the increase in VUS-only results dramatically outpaced the increase in PVs.
Since there is a substantially larger volume of clinical genetic testing in non-Hispanic White patients with breast or ovarian cancer, the spectrum of normal variation is less well-defined in other racial or ethnic groups.
The study showed a widening of the “racial-ethnic VUS gap,” with Black and Asian patients having nearly twofold more VUS, although they were not tested for more genes than non-Hispanic White patients.
This is problematic on several levels. Identification of a VUS is challenging for communicating results to and recommending cascade testing for family members.
There is worrisome information regarding overtreatment or counseling of VUS patients about their results. For example, the PROMPT registry showed that 10%-15% of women with PV/VUS in genes not associated with a high risk of ovarian cancer underwent oophorectomy without a clear indication for the procedure.
Although population-based testing might augment the available data on the spectrum of normal variation in racial and ethnic minorities, it would likely exacerbate the proliferation of VUS over PVs.
It is essential to accelerate ongoing approaches to VUS reclassification.
In addition, the authors suggest that it may be time to reverse the trend in increasing the number of genes tested in MGPs. Their rationale is that, in Georgia and California, most PVs among patients with breast and ovarian cancer were identified in 20 genes (ATM, BARD1, BRCA1, BRCA2, BRIP1, CDH1, CHEK2, EPCAM, MLH1, MSH2, MSH6, NBN, NF1, PMS2, PALB2, PTEN, RAD51C, RAD51D, STK11, and TP53).
If the Georgia and California data are representative of a more generalized pattern, a panel of 20 breast cancer– and/or ovarian cancer–associated genes may be ideal for maximizing the yield of clinically relevant PVs and minimizing VUS results for all patients.
Finally, defining the patient, clinician, and health care system factors that impede widespread genetic testing for ovarian cancer patients must be prioritized. As the authors suggest, quality improvement efforts should focus on getting a lot closer to testing rates of 100% for patients with ovarian cancer and building the database that will help sort VUS in minority patients into their proper context of pathogenicity, rather than adding more genes per test.
This research was supported by the National Cancer Institute, the Centers for Disease Control and Prevention, and the California Department of Public Health. The authors disclosed relationships with Myriad Genetics, Ambry Genetics, Color Genomics, GeneDx/BioReference, InVitae, Genentech, Genomic Health, Roche/Genentech, Oncoquest, Tesaro, and Karyopharm Therapeutics.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
Investigators found racial and ethnic disparities in genetic testing as well as “persistent underuse” of testing in patients with ovarian cancer.
The team also discovered that most pathogenic variant (PV) results were in 20 genes associated with breast and/or ovarian cancer, and testing other genes largely revealed variants of uncertain significance (VUS).
Allison W. Kurian, MD, of Stanford (Calif.) University, and colleagues recounted these findings in the Journal of Clinical Oncology.
Because of improvements in sequencing technology, competition among commercial purveyors, and declining cost, genetic testing has been increasingly available to clinicians for patient management and cancer prevention (JAMA. 2015 Sep 8;314[10]:997-8). Although germline testing can guide therapy for several solid tumors, there is little research about how often and how well it is used in practice.
For their study, Dr. Kurian and colleagues used a SEER Genetic Testing Linkage Demonstration Project in a population-based assessment of testing for cancer risk. The investigators analyzed 7-year trends in testing among all women diagnosed with breast or ovarian cancer in Georgia or California from 2013 to 2017, reviewing testing patterns and result interpretation from 2012 to 2019.
Before analyzing the data, the investigators made the following hypotheses:
- Multigene panels (MGP) would entirely replace testing for BRCA1/2 only.
- Testing underutilization in patients with ovarian cancer would improve over time.
- More patients would be tested at lower levels of pretest risk for PVs.
- Sociodemographic differences in testing trends would not be observed.
- Detection of PVs and VUS would increase.
- Racial and ethnic disparities in rates of VUS would diminish.
Study conduct
The investigators examined genetic tests performed from 2012 through the beginning of 2019 at major commercial laboratories and linked that information with data in the SEER registries in Georgia and California on all breast and ovarian cancer patients diagnosed between 2013 and 2017. There were few criteria for exclusion.
Genetic testing results were categorized as identifying a PV or likely PV, VUS, or benign or likely benign mutation by American College of Medical Genetics criteria. When a patient had genetic testing on more than one occasion, the most recent test was used.
If a PV was identified, the types of PVs were grouped according to the level of evidence that supported pathogenicity into the following categories:
- BRCA1 or BRCA2 mutations.
- PVs in other genes designated by the National Comprehensive Cancer Network as associated with breast or ovarian cancer (e.g., ATM, BARD1, BRIP1, CDH1, CHEK2, EPCAM, MLH1, MSH2, MSH6, NBN, NF1, PALB2, MS2, PTEN, RAD51C, RAD51D, STK11, and TP53).
- PVs in other actionable genes (e.g., APC, BMPR1A, MEN1, MUTYH, NF2, RB1, RET, SDHAF2, SDHB, SDHC, SDHD, SMAD4, TSC1, TSC2, and VHL).
- Any other tested genes.
The investigators also tabulated instances in which genetic testing identified a VUS in any gene but no PV. If a VUS was identified originally and was reclassified more recently into the “PV/likely PV” or “benign/likely benign” categories, only the resolved categorization was recorded.
The authors evaluated clinical and sociodemographic correlates of testing trends for breast and ovarian cancer, assessing the relationship between race, age, and geographic site in receipt of any test or type of test.
Among laboratories, the investigators examined trends in the number of genes tested, associations with sociodemographic factors, categories of test results, and whether trends differed by race or ethnicity.
Findings, by hypothesis
Hypothesis #1: MGP will entirely replace testing for BRCA1/2 only.
About 25% of tested patients with breast cancer diagnosed in early 2013 received MGP, compared with more than 80% of those diagnosed in late 2017.
The trend for ovarian cancer was similar. About 40% of patients diagnosed in early 2013 received MGP, compared with more than 90% diagnosed in late 2017. These trends were similar in California and Georgia.
From 2012 to 2019, there was a consistent upward trend in gene number for patients with breast cancer (mean, 19) or ovarian cancer (mean, 21), from approximately 10 genes to 35 genes.
Hypothesis #2: Underutilization of testing in patients with ovarian cancer will improve.
Among the 187,535 patients with breast cancer and the 14,689 patients with ovarian cancer diagnosed in Georgia or California from 2013 through 2017, on average, testing rates increased 2% per year.
In all, 25.2% of breast cancer patients and 34.3% of ovarian cancer patients had genetic testing on one (87.3%) or more (12.7%) occasions.
Prior research suggested that, in 2013 and 2014, 31% of women with ovarian cancer had genetic testing (JAMA Oncol. 2018 Aug 1;4[8]:1066-72/ J Clin Oncol. 2019 May 20;37[15]:1305-15).
The investigators therefore concluded that underutilization of genetic testing in ovarian cancer did not improve substantially during the 7-year interval analyzed.
Hypothesis #3: More patients will be tested at lower levels of pretest risk.
These data were more difficult to abstract from the SEER database, but older patients were more likely to be tested in later years.
In patients older than 60 years of age (who accounted for more than 50% of both cancer cohorts), testing rates increased from 11.1% to 14.9% for breast cancer and 25.3% to 31.4% for ovarian cancer. By contrast, patients younger than 45 years of age were less than 15% of the sample and had lower testing rates over time.
There were no substantial changes in testing rates by other clinical variables. Therefore, in concert with the age-related testing trends, it is likely that women were tested for genetic mutations at increasingly lower levels of pretest risk.
Hypothesis #4: Sociodemographic differences in testing trends will not be observed.
Among patients with breast cancer, approximately 31% of those who had genetic testing were uninsured, 31% had Medicaid, and 26% had private insurance, Medicare, or other insurance.
For patients with ovarian cancer, approximately 28% were uninsured, 27% had Medicaid, and 39% had private insurance, Medicare, or other insurance.
The authors had previously found that less testing was associated with Black race, greater poverty, and less insurance coverage (J Clin Oncol. 2019 May 20;37[15]:1305-15). However, they noted no changes in testing rates by sociodemographic variables over time.
Hypothesis #5: Detection of both PVs and VUS will increase.
The proportion of tested breast cancer patients with PVs in BRCA1/2 decreased from 7.5% to 5.0% (P < .001), whereas PV yield for the two other clinically salient categories (breast or ovarian and other actionable genes) increased.
The proportion of PVs in any breast or ovarian gene increased from 1.3% to 4.6%, and the proportion in any other actionable gene increased from 0.3% to 1.3%.
For breast cancer patients, VUS-only rates increased from 8.5% in early 2013 to 22.4% in late 2017.
For ovarian cancer patients, the yield of PVs in BRCA1/2 decreased from 15.7% to 12.4% (P < .001), whereas the PV yield for breast or ovarian genes increased from 3.9% to 4.3%, and the yield for other actionable genes increased from 0.3% to 2.0%.
In ovarian cancer patients, the PV or VUS-only result rate increased from 30.8% in early 2013 to 43.0% in late 2017, entirely due to the increase in VUS-only rates. VUS were identified in 8.1% of patients diagnosed in early 2013 and increased to 28.3% in patients diagnosed in late 2017.
Hypothesis #6: Racial or ethnic disparities in rates of VUS will diminish.
Among patients with breast cancer, racial or ethnic differences in PV rates were small and did not change over time. For patients with ovarian cancer, PV rates across racial or ethnic groups diminished over time.
However, for both breast and ovarian cancer patients, there were large differences in VUS-only rates by race and ethnicity that persisted during the interval studied.
In 2017, for patients with breast cancer, VUS-only rates were substantially higher in Asian (42.4%), Black (36.6%), and Hispanic (27.7%) patients than in non-Hispanic White patients (24.5%, P < .001).
Similar trends were noted for patients with ovarian cancer. VUS-only rates were substantially higher in Asian (47.8%), Black (46.0%), and Hispanic (36.8%) patients than in non-Hispanic White patients (24.6%, P < .001).
Multivariable logistic regressions were performed separately for tested patients with breast cancer and ovarian cancer, and the results showed no significant interaction between race or ethnicity and date. Therefore, there was no significant change in racial or ethnic differences in VUS-only results across the study period.
Where these findings leave clinicians in 2021
Among the patients studied, there was:
- Marked expansion in the number of genes sequenced.
- A likely modest trend toward testing patients with lower pretest risk of a PV.
- No sociodemographic differences in testing trends.
- A small increase in PV rates and a substantial increase in VUS-only rates.
- Near-complete replacement of selective testing by MGP.
For patients with breast cancer, the proportion of all PVs that were in BRCA1/2 fell substantially. Adoption of MGP testing doubled the probability of detecting a PV in other tested genes. Most of the increase was in genes with an established breast or ovarian cancer association, with fewer PVs found in other actionable genes and very few PVs in other tested genes.
Contrary to their hypothesis, the authors observed a sustained undertesting of patients with ovarian cancer. Only 34.3% performed versus nearly 100% recommended, with little change since 2014.
This finding is surprising – and tremendously disappointing – since the prevalence of BRCA1/2 PVs is higher in ovarian cancer than in other cancers (Gynecol Oncol. 2017 Nov;147[2]:375-380), and germline-targeted therapy with PARP inhibitors has been approved for use since 2014.
Furthermore, insurance carriers provide coverage for genetic testing in most patients with carcinoma of the ovary, fallopian tube, and/or peritoneum.
Action plans: Less could be more
During the period analyzed, the increase in VUS-only results dramatically outpaced the increase in PVs.
Since there is a substantially larger volume of clinical genetic testing in non-Hispanic White patients with breast or ovarian cancer, the spectrum of normal variation is less well-defined in other racial or ethnic groups.
The study showed a widening of the “racial-ethnic VUS gap,” with Black and Asian patients having nearly twofold more VUS, although they were not tested for more genes than non-Hispanic White patients.
This is problematic on several levels. Identification of a VUS is challenging for communicating results to and recommending cascade testing for family members.
There is worrisome information regarding overtreatment or counseling of VUS patients about their results. For example, the PROMPT registry showed that 10%-15% of women with PV/VUS in genes not associated with a high risk of ovarian cancer underwent oophorectomy without a clear indication for the procedure.
Although population-based testing might augment the available data on the spectrum of normal variation in racial and ethnic minorities, it would likely exacerbate the proliferation of VUS over PVs.
It is essential to accelerate ongoing approaches to VUS reclassification.
In addition, the authors suggest that it may be time to reverse the trend in increasing the number of genes tested in MGPs. Their rationale is that, in Georgia and California, most PVs among patients with breast and ovarian cancer were identified in 20 genes (ATM, BARD1, BRCA1, BRCA2, BRIP1, CDH1, CHEK2, EPCAM, MLH1, MSH2, MSH6, NBN, NF1, PMS2, PALB2, PTEN, RAD51C, RAD51D, STK11, and TP53).
If the Georgia and California data are representative of a more generalized pattern, a panel of 20 breast cancer– and/or ovarian cancer–associated genes may be ideal for maximizing the yield of clinically relevant PVs and minimizing VUS results for all patients.
Finally, defining the patient, clinician, and health care system factors that impede widespread genetic testing for ovarian cancer patients must be prioritized. As the authors suggest, quality improvement efforts should focus on getting a lot closer to testing rates of 100% for patients with ovarian cancer and building the database that will help sort VUS in minority patients into their proper context of pathogenicity, rather than adding more genes per test.
This research was supported by the National Cancer Institute, the Centers for Disease Control and Prevention, and the California Department of Public Health. The authors disclosed relationships with Myriad Genetics, Ambry Genetics, Color Genomics, GeneDx/BioReference, InVitae, Genentech, Genomic Health, Roche/Genentech, Oncoquest, Tesaro, and Karyopharm Therapeutics.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Anti-CD20s linked to higher COVID-19 severity in MS
Like other people, a biostatistician told neurologists. With the exception of anti-CD20s, registries also suggest that disease-modifying therapies (DMTs) don’t cause higher degrees of severity.
“It’s good news since it’s important for patients to stay on these treatments,” said Amber Salter, PhD, MPH, an assistant professor at Washington University, St. Louis, in a follow-up interview following her presentation at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Dr. Salter reported on the findings of several MS/COVID-19 registries from around the world, including the COViMS Registry, which is supported by the Consortium of MS Centers, the MS Society of Canada, and the National MS Society. It tracks patients who developed COVID-19 while also having MS, neuromyelitis optica, or MOG antibody disease.
The registry began collecting data in April 2020 and is ongoing. As of Jan. 29, 2021, 2,059 patients had been tracked; 85% of cases were confirmed by laboratory tests. Nearly all patients (97%) were from the United States, with about 21% from New York state. Nearly 76% were female, the average age was 48. About 70% were non-Hispanic White, 18% were African American; 83% had relapsing remitting MS, and 17% had progressive MS.
“We found that 11.5% of MS patients were reported being hospitalized, while 4.2% were admitted to the ICU or ventilated and 3% had died,” Dr. Salter said. Not surprisingly, the death rate was highest (21%) in patients aged 75 years or older, compared with 11% of those aged 65-74 years. Those with more severe cases – those who were nonambulatory – had a death rate of 18%, compared with 0.6% of those who were fully ambulatory and 4% of those who walked with assistance.
“A lot of the risks [for COVID-19 severity] we see in the general population are risks in the MS population,” Dr. Salter said.
Dr. Salter also summarized the results of other international registries. After adjustment, a registry in Italy linked the anti-CD20 drugs ocrelizumab or rituximab (odds ratio, 2.37, P = .015) and recent use of methylprednisolone (OR, 5.2; P = .001) to more severe courses of COVID-19, compared with other DMTs. And a global data-sharing project linked anti-CD20s to more severe outcomes, compared with other DMTs (hospitalization, adjusted prevalence ratio, 1.49; ICU admission, aPR, 2.55; and ventilation, aPR, 3.05).
In an interview, neurologist Lauren Gluck, MD, of Albert Einstein College of Medicine and Montefiore Medical Center, both in New York, cautioned that prescribing anti-CD20s now “requires a more complex informed consent process with patients and outlining of risk as well as strategies to minimize contracting the infection.”
Moving forward, she advised colleagues to “keep treating MS with DMTs. Preventing MS attacks will help keep patients out of the hospital and limit need for high-dose steroids.” And she cautioned that “avoiding action due to inaccurate fear of DMTs and COVID-19 may put your patients at unnecessary risk of relapses and accumulated disability. Educate your patients on the reality of the COVID19 pandemic, their personal risk of exposure, and strategies to minimize their risk.”
Fortunately, vaccinations offer protection against COVID-19 in patients with MS, although patients are clearly concerned about potential risks. “A frequent concern is whether the vaccines are safe for MS patients in general and if they could incite MS relapses,” neurologist Hesham Abboud, MD, PhD, of University Hospitals of Cleveland and Case Western Reserve University, said in an interview. “The American Academy of Neurology guidelines have not found a connection between vaccination and MS relapses. Having COVID-19 infection can trigger MS relapses, so clearly the benefit from the vaccine outweighs any potential risks. Obviously, it is not advisable to take any vaccine during an active relapse, but vaccines are safe otherwise when given during remission.”
Dr. Salter and Dr. Gluck reported no relevant disclosures. Dr. Abboud reports consulting fees from Biogen, Genentech, Bristol-Myers Squibb, Alexion, and Viela Bio. He receives research support from Novartis, Bristol-Myers Squibb, Genentech, and Sanofi-Genzyme.
Like other people, a biostatistician told neurologists. With the exception of anti-CD20s, registries also suggest that disease-modifying therapies (DMTs) don’t cause higher degrees of severity.
“It’s good news since it’s important for patients to stay on these treatments,” said Amber Salter, PhD, MPH, an assistant professor at Washington University, St. Louis, in a follow-up interview following her presentation at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Dr. Salter reported on the findings of several MS/COVID-19 registries from around the world, including the COViMS Registry, which is supported by the Consortium of MS Centers, the MS Society of Canada, and the National MS Society. It tracks patients who developed COVID-19 while also having MS, neuromyelitis optica, or MOG antibody disease.
The registry began collecting data in April 2020 and is ongoing. As of Jan. 29, 2021, 2,059 patients had been tracked; 85% of cases were confirmed by laboratory tests. Nearly all patients (97%) were from the United States, with about 21% from New York state. Nearly 76% were female, the average age was 48. About 70% were non-Hispanic White, 18% were African American; 83% had relapsing remitting MS, and 17% had progressive MS.
“We found that 11.5% of MS patients were reported being hospitalized, while 4.2% were admitted to the ICU or ventilated and 3% had died,” Dr. Salter said. Not surprisingly, the death rate was highest (21%) in patients aged 75 years or older, compared with 11% of those aged 65-74 years. Those with more severe cases – those who were nonambulatory – had a death rate of 18%, compared with 0.6% of those who were fully ambulatory and 4% of those who walked with assistance.
“A lot of the risks [for COVID-19 severity] we see in the general population are risks in the MS population,” Dr. Salter said.
Dr. Salter also summarized the results of other international registries. After adjustment, a registry in Italy linked the anti-CD20 drugs ocrelizumab or rituximab (odds ratio, 2.37, P = .015) and recent use of methylprednisolone (OR, 5.2; P = .001) to more severe courses of COVID-19, compared with other DMTs. And a global data-sharing project linked anti-CD20s to more severe outcomes, compared with other DMTs (hospitalization, adjusted prevalence ratio, 1.49; ICU admission, aPR, 2.55; and ventilation, aPR, 3.05).
In an interview, neurologist Lauren Gluck, MD, of Albert Einstein College of Medicine and Montefiore Medical Center, both in New York, cautioned that prescribing anti-CD20s now “requires a more complex informed consent process with patients and outlining of risk as well as strategies to minimize contracting the infection.”
Moving forward, she advised colleagues to “keep treating MS with DMTs. Preventing MS attacks will help keep patients out of the hospital and limit need for high-dose steroids.” And she cautioned that “avoiding action due to inaccurate fear of DMTs and COVID-19 may put your patients at unnecessary risk of relapses and accumulated disability. Educate your patients on the reality of the COVID19 pandemic, their personal risk of exposure, and strategies to minimize their risk.”
Fortunately, vaccinations offer protection against COVID-19 in patients with MS, although patients are clearly concerned about potential risks. “A frequent concern is whether the vaccines are safe for MS patients in general and if they could incite MS relapses,” neurologist Hesham Abboud, MD, PhD, of University Hospitals of Cleveland and Case Western Reserve University, said in an interview. “The American Academy of Neurology guidelines have not found a connection between vaccination and MS relapses. Having COVID-19 infection can trigger MS relapses, so clearly the benefit from the vaccine outweighs any potential risks. Obviously, it is not advisable to take any vaccine during an active relapse, but vaccines are safe otherwise when given during remission.”
Dr. Salter and Dr. Gluck reported no relevant disclosures. Dr. Abboud reports consulting fees from Biogen, Genentech, Bristol-Myers Squibb, Alexion, and Viela Bio. He receives research support from Novartis, Bristol-Myers Squibb, Genentech, and Sanofi-Genzyme.
Like other people, a biostatistician told neurologists. With the exception of anti-CD20s, registries also suggest that disease-modifying therapies (DMTs) don’t cause higher degrees of severity.
“It’s good news since it’s important for patients to stay on these treatments,” said Amber Salter, PhD, MPH, an assistant professor at Washington University, St. Louis, in a follow-up interview following her presentation at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Dr. Salter reported on the findings of several MS/COVID-19 registries from around the world, including the COViMS Registry, which is supported by the Consortium of MS Centers, the MS Society of Canada, and the National MS Society. It tracks patients who developed COVID-19 while also having MS, neuromyelitis optica, or MOG antibody disease.
The registry began collecting data in April 2020 and is ongoing. As of Jan. 29, 2021, 2,059 patients had been tracked; 85% of cases were confirmed by laboratory tests. Nearly all patients (97%) were from the United States, with about 21% from New York state. Nearly 76% were female, the average age was 48. About 70% were non-Hispanic White, 18% were African American; 83% had relapsing remitting MS, and 17% had progressive MS.
“We found that 11.5% of MS patients were reported being hospitalized, while 4.2% were admitted to the ICU or ventilated and 3% had died,” Dr. Salter said. Not surprisingly, the death rate was highest (21%) in patients aged 75 years or older, compared with 11% of those aged 65-74 years. Those with more severe cases – those who were nonambulatory – had a death rate of 18%, compared with 0.6% of those who were fully ambulatory and 4% of those who walked with assistance.
“A lot of the risks [for COVID-19 severity] we see in the general population are risks in the MS population,” Dr. Salter said.
Dr. Salter also summarized the results of other international registries. After adjustment, a registry in Italy linked the anti-CD20 drugs ocrelizumab or rituximab (odds ratio, 2.37, P = .015) and recent use of methylprednisolone (OR, 5.2; P = .001) to more severe courses of COVID-19, compared with other DMTs. And a global data-sharing project linked anti-CD20s to more severe outcomes, compared with other DMTs (hospitalization, adjusted prevalence ratio, 1.49; ICU admission, aPR, 2.55; and ventilation, aPR, 3.05).
In an interview, neurologist Lauren Gluck, MD, of Albert Einstein College of Medicine and Montefiore Medical Center, both in New York, cautioned that prescribing anti-CD20s now “requires a more complex informed consent process with patients and outlining of risk as well as strategies to minimize contracting the infection.”
Moving forward, she advised colleagues to “keep treating MS with DMTs. Preventing MS attacks will help keep patients out of the hospital and limit need for high-dose steroids.” And she cautioned that “avoiding action due to inaccurate fear of DMTs and COVID-19 may put your patients at unnecessary risk of relapses and accumulated disability. Educate your patients on the reality of the COVID19 pandemic, their personal risk of exposure, and strategies to minimize their risk.”
Fortunately, vaccinations offer protection against COVID-19 in patients with MS, although patients are clearly concerned about potential risks. “A frequent concern is whether the vaccines are safe for MS patients in general and if they could incite MS relapses,” neurologist Hesham Abboud, MD, PhD, of University Hospitals of Cleveland and Case Western Reserve University, said in an interview. “The American Academy of Neurology guidelines have not found a connection between vaccination and MS relapses. Having COVID-19 infection can trigger MS relapses, so clearly the benefit from the vaccine outweighs any potential risks. Obviously, it is not advisable to take any vaccine during an active relapse, but vaccines are safe otherwise when given during remission.”
Dr. Salter and Dr. Gluck reported no relevant disclosures. Dr. Abboud reports consulting fees from Biogen, Genentech, Bristol-Myers Squibb, Alexion, and Viela Bio. He receives research support from Novartis, Bristol-Myers Squibb, Genentech, and Sanofi-Genzyme.
FROM ACTRIMS FORUM 2021
Tocilizumab (Actemra) scores FDA approval for systemic sclerosis–associated interstitial lung disease
The Food and Drug Administration has approved subcutaneously-injected tocilizumab (Actemra) to reduce the rate of pulmonary function decline in systemic sclerosis–associated interstitial lung disease (SSc-ILD) patients, according to a press release from manufacturer Genentech.
Tocilizumab is the first biologic to be approved by the agency for adults with SSc-ILD, a rare and potentially life-threatening condition that may affect up to 80% of SSc patients and lead to lung inflammation and scarring.
The approval was based primarily on data from a phase 3 randomized, double-blind, placebo-controlled clinical trial (the focuSSced trial) that included 212 adults with SSc. Although that study failed to meet its primary endpoint of change from baseline to 48 weeks in the modified Rodnan Skin Score, the researchers observed a significantly reduced lung function decline as measured by forced vital capacity (FVC) and percent predicted forced vital capacity (ppFVC) among tocilizumab-treated patients, compared with those who received placebo. A total of 68 patients (65%) in the tocilizumab group and 68 patients (64%) in the placebo group had SSc-ILD at baseline.
In a subgroup analysis, patients taking tocilizumab had a smaller decline in mean ppFVC, compared with placebo patients (0.07% vs. –6.4%; mean difference, 6.47%), and a smaller decline in FVC (mean change –14 mL vs. –255 mL with placebo; mean difference, 241 mL).
The mean change from baseline to week 48 in modified Rodnan Skin Score was –5.88 for patients on tocilizumab and –3.77 with placebo.
Safety data were similar between tocilizumab and placebo groups through 48 weeks, and similar for patients with and without SSc-ILD. In general, tocilizumab side effects include increased susceptibility to infections, and serious side effects may include stomach tears, hepatotoxicity, and increased risk of cancer and hepatitis B, according to the prescribing information. However, the most common side effects are upper respiratory tract infections, headache, hypertension, and injection-site reactions.
Tocilizumab, an interleukin-6 receptor antagonist, is already approved for the treatment of adult patients with moderately to severely active rheumatoid arthritis, as well as for adult patients with giant cell arteritis; patients aged 2 years and older with active polyarticular juvenile idiopathic arthritis or active systemic juvenile idiopathic arthritis; and adults and pediatric patients 2 years of age and older with chimeric antigen receptor T-cell–induced severe or life-threatening cytokine release syndrome.
Prescribing information is available here.
The Food and Drug Administration has approved subcutaneously-injected tocilizumab (Actemra) to reduce the rate of pulmonary function decline in systemic sclerosis–associated interstitial lung disease (SSc-ILD) patients, according to a press release from manufacturer Genentech.
Tocilizumab is the first biologic to be approved by the agency for adults with SSc-ILD, a rare and potentially life-threatening condition that may affect up to 80% of SSc patients and lead to lung inflammation and scarring.
The approval was based primarily on data from a phase 3 randomized, double-blind, placebo-controlled clinical trial (the focuSSced trial) that included 212 adults with SSc. Although that study failed to meet its primary endpoint of change from baseline to 48 weeks in the modified Rodnan Skin Score, the researchers observed a significantly reduced lung function decline as measured by forced vital capacity (FVC) and percent predicted forced vital capacity (ppFVC) among tocilizumab-treated patients, compared with those who received placebo. A total of 68 patients (65%) in the tocilizumab group and 68 patients (64%) in the placebo group had SSc-ILD at baseline.
In a subgroup analysis, patients taking tocilizumab had a smaller decline in mean ppFVC, compared with placebo patients (0.07% vs. –6.4%; mean difference, 6.47%), and a smaller decline in FVC (mean change –14 mL vs. –255 mL with placebo; mean difference, 241 mL).
The mean change from baseline to week 48 in modified Rodnan Skin Score was –5.88 for patients on tocilizumab and –3.77 with placebo.
Safety data were similar between tocilizumab and placebo groups through 48 weeks, and similar for patients with and without SSc-ILD. In general, tocilizumab side effects include increased susceptibility to infections, and serious side effects may include stomach tears, hepatotoxicity, and increased risk of cancer and hepatitis B, according to the prescribing information. However, the most common side effects are upper respiratory tract infections, headache, hypertension, and injection-site reactions.
Tocilizumab, an interleukin-6 receptor antagonist, is already approved for the treatment of adult patients with moderately to severely active rheumatoid arthritis, as well as for adult patients with giant cell arteritis; patients aged 2 years and older with active polyarticular juvenile idiopathic arthritis or active systemic juvenile idiopathic arthritis; and adults and pediatric patients 2 years of age and older with chimeric antigen receptor T-cell–induced severe or life-threatening cytokine release syndrome.
Prescribing information is available here.
The Food and Drug Administration has approved subcutaneously-injected tocilizumab (Actemra) to reduce the rate of pulmonary function decline in systemic sclerosis–associated interstitial lung disease (SSc-ILD) patients, according to a press release from manufacturer Genentech.
Tocilizumab is the first biologic to be approved by the agency for adults with SSc-ILD, a rare and potentially life-threatening condition that may affect up to 80% of SSc patients and lead to lung inflammation and scarring.
The approval was based primarily on data from a phase 3 randomized, double-blind, placebo-controlled clinical trial (the focuSSced trial) that included 212 adults with SSc. Although that study failed to meet its primary endpoint of change from baseline to 48 weeks in the modified Rodnan Skin Score, the researchers observed a significantly reduced lung function decline as measured by forced vital capacity (FVC) and percent predicted forced vital capacity (ppFVC) among tocilizumab-treated patients, compared with those who received placebo. A total of 68 patients (65%) in the tocilizumab group and 68 patients (64%) in the placebo group had SSc-ILD at baseline.
In a subgroup analysis, patients taking tocilizumab had a smaller decline in mean ppFVC, compared with placebo patients (0.07% vs. –6.4%; mean difference, 6.47%), and a smaller decline in FVC (mean change –14 mL vs. –255 mL with placebo; mean difference, 241 mL).
The mean change from baseline to week 48 in modified Rodnan Skin Score was –5.88 for patients on tocilizumab and –3.77 with placebo.
Safety data were similar between tocilizumab and placebo groups through 48 weeks, and similar for patients with and without SSc-ILD. In general, tocilizumab side effects include increased susceptibility to infections, and serious side effects may include stomach tears, hepatotoxicity, and increased risk of cancer and hepatitis B, according to the prescribing information. However, the most common side effects are upper respiratory tract infections, headache, hypertension, and injection-site reactions.
Tocilizumab, an interleukin-6 receptor antagonist, is already approved for the treatment of adult patients with moderately to severely active rheumatoid arthritis, as well as for adult patients with giant cell arteritis; patients aged 2 years and older with active polyarticular juvenile idiopathic arthritis or active systemic juvenile idiopathic arthritis; and adults and pediatric patients 2 years of age and older with chimeric antigen receptor T-cell–induced severe or life-threatening cytokine release syndrome.
Prescribing information is available here.
Confirmed: Diet influences colorectal cancer risk
It’s now confirmed: What you eat does affect your risk of developing colorectal cancer (CRC).
An umbrella review of studies and meta-analyses found “convincing evidence of an association between a lower CRC risk and higher intakes of dietary fiber, dietary calcium, and yogurt and lower intakes of alcohol and red meat.”
However, more research is needed to address the link between CRC and other foods, including dairy products, whole grains, processed meat, and specific dietary patterns, the authors conclude.
“We can say that the existing recommendations for diet in the primary prevention of colorectal cancer is confirmed,” said lead author Nathorn Chaiyakunapruk, PharmD, PhD, professor of pharmacology at the University of Utah, Salt Lake City.
“It makes sense to encourage healthy diet, including those rich in fruits, vegetables, grains, and low-fat dairy, and reducing red meat and alcohol intake,” he said in an interview. “However, some of them may not yet have convincing evidence to fully support the claim.”
Other lifestyle factors, including excess weight and physical inactivity, also play a role in cancer risk. Dr. Chaiyakunapruk pointed out that their review was focused only on diet and that they had set out to confirm factors for which there was strong and convincing evidence.
The review was published online in JAMA Network Open.
The umbrella review of 45 meta-analyses found 109 associations. Overall, 35 of these 109 associations (32.1%) were nominally statistically significant, as determined on the basis of random-effects meta-analysis models, the researchers explained.
Convincing evidence was found for an increase in the risk for CRC with higher versus lower red meat consumption and with heavy alcohol intake (defined as more than four drinks per day, compared with no drinks per day or occasional drinks).
In addition, convincing evidence was found for three inverse associations: a decrease in the risk for CRC was associated with higher versus lower intake of total dietary fiber, calcium, and yogurt.
The researchers noted that, although not completely convincing, there was highly suggestive evidence for another association: a link between diet and CRC incidence. A higher intake of total dairy products (e.g., milk, cheese, and yogurt) was associated with significant risk reduction, in comparison with lower intake. A moderate intake of alcohol (from one to three drinks but not more than four per day) was associated with an increase in incidence in comparison with no drinks or an occasional drink.
Evidence suggested a reduced risk in association with several lifestyle behaviors, including adherence to a Mediterranean diet, a healthy diet, a pesco-vegetarian or semivegetarian diet, and the intake of whole grains, nonfermented milk, and supplemental calcium.
The evidence suggested that adherence to a Western diet and intake of processed meat were associated with an increased risk for CRC.
There was weak or no evidence for the remaining associations.
Existing cancer prevention guidelines
The findings support the existing cancer prevention dietary guidance and recommendations from the American Institute for Cancer Research, commented the institute’s director of nutrition programs, Sheena Swanner Patel, MS, RDN. The study confirms that dietary factors play a strong role in lowering CRC risk.
“AICR’s report found strong evidence for whole grains, foods containing dietary fiber, dairy products, and calcium supplements decreasing risk for colorectal cancer,” she said. “Specifically, eating 90 g or three servings of whole grains per day is associated with a 17% decrease in colorectal cancer risk.”
Ms. Patel added that the AICR’s report also suggested there was strong evidence that eating large amounts of red and processed meat, drinking alcohol excessively, and carrying extra body weight increased the risk for CRC.
Many previous studies have suggested a link between diet and CRC risk. One recent study suggested that, among all cancers, CRC has the highest proportion of diet-related cases (38.3%). The next highest were cancers of the mouth, pharynx, and larynx, for which almost 26% of cases were linked to diet, followed by endometrial cancer, postmenopausal breast cancer, and cancers of the kidney, stomach, liver, pancreas, and esophagus.
Neither Dr. Chaiyakunapruk and coauthors nor Ms. Patel disclosed any relevant financial relationships.
A version of this article first appeared on Medscape.com.
It’s now confirmed: What you eat does affect your risk of developing colorectal cancer (CRC).
An umbrella review of studies and meta-analyses found “convincing evidence of an association between a lower CRC risk and higher intakes of dietary fiber, dietary calcium, and yogurt and lower intakes of alcohol and red meat.”
However, more research is needed to address the link between CRC and other foods, including dairy products, whole grains, processed meat, and specific dietary patterns, the authors conclude.
“We can say that the existing recommendations for diet in the primary prevention of colorectal cancer is confirmed,” said lead author Nathorn Chaiyakunapruk, PharmD, PhD, professor of pharmacology at the University of Utah, Salt Lake City.
“It makes sense to encourage healthy diet, including those rich in fruits, vegetables, grains, and low-fat dairy, and reducing red meat and alcohol intake,” he said in an interview. “However, some of them may not yet have convincing evidence to fully support the claim.”
Other lifestyle factors, including excess weight and physical inactivity, also play a role in cancer risk. Dr. Chaiyakunapruk pointed out that their review was focused only on diet and that they had set out to confirm factors for which there was strong and convincing evidence.
The review was published online in JAMA Network Open.
The umbrella review of 45 meta-analyses found 109 associations. Overall, 35 of these 109 associations (32.1%) were nominally statistically significant, as determined on the basis of random-effects meta-analysis models, the researchers explained.
Convincing evidence was found for an increase in the risk for CRC with higher versus lower red meat consumption and with heavy alcohol intake (defined as more than four drinks per day, compared with no drinks per day or occasional drinks).
In addition, convincing evidence was found for three inverse associations: a decrease in the risk for CRC was associated with higher versus lower intake of total dietary fiber, calcium, and yogurt.
The researchers noted that, although not completely convincing, there was highly suggestive evidence for another association: a link between diet and CRC incidence. A higher intake of total dairy products (e.g., milk, cheese, and yogurt) was associated with significant risk reduction, in comparison with lower intake. A moderate intake of alcohol (from one to three drinks but not more than four per day) was associated with an increase in incidence in comparison with no drinks or an occasional drink.
Evidence suggested a reduced risk in association with several lifestyle behaviors, including adherence to a Mediterranean diet, a healthy diet, a pesco-vegetarian or semivegetarian diet, and the intake of whole grains, nonfermented milk, and supplemental calcium.
The evidence suggested that adherence to a Western diet and intake of processed meat were associated with an increased risk for CRC.
There was weak or no evidence for the remaining associations.
Existing cancer prevention guidelines
The findings support the existing cancer prevention dietary guidance and recommendations from the American Institute for Cancer Research, commented the institute’s director of nutrition programs, Sheena Swanner Patel, MS, RDN. The study confirms that dietary factors play a strong role in lowering CRC risk.
“AICR’s report found strong evidence for whole grains, foods containing dietary fiber, dairy products, and calcium supplements decreasing risk for colorectal cancer,” she said. “Specifically, eating 90 g or three servings of whole grains per day is associated with a 17% decrease in colorectal cancer risk.”
Ms. Patel added that the AICR’s report also suggested there was strong evidence that eating large amounts of red and processed meat, drinking alcohol excessively, and carrying extra body weight increased the risk for CRC.
Many previous studies have suggested a link between diet and CRC risk. One recent study suggested that, among all cancers, CRC has the highest proportion of diet-related cases (38.3%). The next highest were cancers of the mouth, pharynx, and larynx, for which almost 26% of cases were linked to diet, followed by endometrial cancer, postmenopausal breast cancer, and cancers of the kidney, stomach, liver, pancreas, and esophagus.
Neither Dr. Chaiyakunapruk and coauthors nor Ms. Patel disclosed any relevant financial relationships.
A version of this article first appeared on Medscape.com.
It’s now confirmed: What you eat does affect your risk of developing colorectal cancer (CRC).
An umbrella review of studies and meta-analyses found “convincing evidence of an association between a lower CRC risk and higher intakes of dietary fiber, dietary calcium, and yogurt and lower intakes of alcohol and red meat.”
However, more research is needed to address the link between CRC and other foods, including dairy products, whole grains, processed meat, and specific dietary patterns, the authors conclude.
“We can say that the existing recommendations for diet in the primary prevention of colorectal cancer is confirmed,” said lead author Nathorn Chaiyakunapruk, PharmD, PhD, professor of pharmacology at the University of Utah, Salt Lake City.
“It makes sense to encourage healthy diet, including those rich in fruits, vegetables, grains, and low-fat dairy, and reducing red meat and alcohol intake,” he said in an interview. “However, some of them may not yet have convincing evidence to fully support the claim.”
Other lifestyle factors, including excess weight and physical inactivity, also play a role in cancer risk. Dr. Chaiyakunapruk pointed out that their review was focused only on diet and that they had set out to confirm factors for which there was strong and convincing evidence.
The review was published online in JAMA Network Open.
The umbrella review of 45 meta-analyses found 109 associations. Overall, 35 of these 109 associations (32.1%) were nominally statistically significant, as determined on the basis of random-effects meta-analysis models, the researchers explained.
Convincing evidence was found for an increase in the risk for CRC with higher versus lower red meat consumption and with heavy alcohol intake (defined as more than four drinks per day, compared with no drinks per day or occasional drinks).
In addition, convincing evidence was found for three inverse associations: a decrease in the risk for CRC was associated with higher versus lower intake of total dietary fiber, calcium, and yogurt.
The researchers noted that, although not completely convincing, there was highly suggestive evidence for another association: a link between diet and CRC incidence. A higher intake of total dairy products (e.g., milk, cheese, and yogurt) was associated with significant risk reduction, in comparison with lower intake. A moderate intake of alcohol (from one to three drinks but not more than four per day) was associated with an increase in incidence in comparison with no drinks or an occasional drink.
Evidence suggested a reduced risk in association with several lifestyle behaviors, including adherence to a Mediterranean diet, a healthy diet, a pesco-vegetarian or semivegetarian diet, and the intake of whole grains, nonfermented milk, and supplemental calcium.
The evidence suggested that adherence to a Western diet and intake of processed meat were associated with an increased risk for CRC.
There was weak or no evidence for the remaining associations.
Existing cancer prevention guidelines
The findings support the existing cancer prevention dietary guidance and recommendations from the American Institute for Cancer Research, commented the institute’s director of nutrition programs, Sheena Swanner Patel, MS, RDN. The study confirms that dietary factors play a strong role in lowering CRC risk.
“AICR’s report found strong evidence for whole grains, foods containing dietary fiber, dairy products, and calcium supplements decreasing risk for colorectal cancer,” she said. “Specifically, eating 90 g or three servings of whole grains per day is associated with a 17% decrease in colorectal cancer risk.”
Ms. Patel added that the AICR’s report also suggested there was strong evidence that eating large amounts of red and processed meat, drinking alcohol excessively, and carrying extra body weight increased the risk for CRC.
Many previous studies have suggested a link between diet and CRC risk. One recent study suggested that, among all cancers, CRC has the highest proportion of diet-related cases (38.3%). The next highest were cancers of the mouth, pharynx, and larynx, for which almost 26% of cases were linked to diet, followed by endometrial cancer, postmenopausal breast cancer, and cancers of the kidney, stomach, liver, pancreas, and esophagus.
Neither Dr. Chaiyakunapruk and coauthors nor Ms. Patel disclosed any relevant financial relationships.
A version of this article first appeared on Medscape.com.
What drives treatment satisfaction among adults with atopic dermatitis?
.
Satisfaction scores were higher when specialists prescribed systemic therapy, but were lower when nonspecialists prescribed systemic therapy and when specialists prescribed only topical therapy.
Those are among key findings from an analysis of the Medical Expenditure Panel Surveys reported by Brian T. Cheng during a late-breaking research session at the Revolutionizing Atopic Dermatitis virtual symposium.
“AD management is complex,” said Mr. Cheng, a medical student at Northwestern University, Chicago. “It includes patient education about trigger avoidance, over-the-counter and prescription topical therapies, as well as systemic therapies. Previous studies have shown major decrements to quality of life as well as atopic and non-atopic comorbidities in these patients. The burden of AD and their comorbidities, as well as their management, may impact patient satisfaction.”
Prior studies have demonstrated that patient satisfaction is associated with improvements in clinical outcomes, increased patient retention, and reduced malpractice claims (Br J Dermatol. 2001 Oct;145[4]:617-23, Arch Dermatol 2008 Feb;144[2]:263-5). However, since data on patient satisfaction in AD are limited, Mr. Cheng and the study’s senior author, Jonathan I. Silverberg, MD, PhD, MPH, set out to examine overall patient satisfaction among adults with AD, to determine associations of patient satisfaction with patterns of health care utilization, and to identify predictors of higher satisfaction among these adults.
The researchers conducted a cross-sectional retrospective analysis of 3,810 patients from the 2000-2015 Medical Expenditure Panel Surveys, representative surveys of the U.S. noninstitutionalized population conducted annually by the Agency for Healthcare Research and Quality. They used ICD-9 codes 691 and 692 to determine AD diagnosis and five Consumer Assessment of Health Plans Survey (CAHPS) questions to assess patients’ satisfaction with their clinicians. “These questions have been extensively validated to correlate with global satisfaction,” Mr. Cheng said. “These are not disease-specific and allow for comparison across multiple diseases.”
Next, the researchers created a composite satisfaction score based on the methods of Anthony Jerant, MD, of the University of California, Davis, and colleagues. They adjusted each question in the CAHPS survey to have an equal weight and then summed these into a composite satisfaction score. “We examined patient satisfaction comparing across diseases, and based on the guidelines from the AHRQ to isolate that impact of patient-physician interaction, we adjusted for sociodemographics, mental and physical health status, self-reported health rating, as well as multimorbidity and comorbid diseases.”
Compared with adults who are healthy, adults with AD had lower patient satisfaction overall. “Moreover, people with AD had lower satisfaction compared to those with psoriasis, which may reflect more substantial itch burden as well as the greater comorbid disease challenges in management,” Mr. Cheng said. “It may also reflect the renaissance in psoriasis treatment over the last 10-20 years, giving a wider spectrum of treatment and thus a higher patient satisfaction.”
Among adults with AD, lower satisfaction was consistent across all domains of CAHPS. For the question of “How often health providers listen carefully to you” the adjusted OR (aOR) was 0.87 (P = .008). For the question of “How often health providers explain things in a way that was easy to understand” the aOR was 0.89 (P = .003). For the question of “How often health providers spent enough time with you” the aOR was 0.86 (P = .0001). For “How often providers showed respect for what you had to say” the aOR was 0.91 (P = .02).
Recognizing that treatment regimens are complex and used differently by provider type, the researchers examined interactions between specialists (dermatologists and allergists) and treatment type. “Previous studies found dermatologists treat more severe, chronic AD,” Mr. Cheng said. “We found here that there was lower satisfaction among those treated with topical therapy and by specialists, which may reflect inadequate disease control. We also found lower satisfaction among those treated with systemic therapy by primary care physicians. This may reflect that these patients are not achieving optimal therapy. We found that satisfaction was highest among those treated with systemic therapy and by dermatologists and allergists.”
Socioeconomic, racial/ethnic, and health care disparities were observed in terms of satisfaction among this cohort. The following characteristics were significantly associated with lower patient satisfaction, compared with the general cohort of adults with AD: poor to low income (aOR, –1.82; P less than .0001), multiracial/other race (aOR, –2.34; P = .0001), Hispanic ethnicity (aOR, –1.40; P = .007), and having no insurance coverage (aOR, –4.53; P less than .0001).
“Moreover, those with multimorbidity had even lower satisfaction,” Mr. Cheng said. “In previous studies, AD has been linked with many other comorbidities. This may reflect that these patients are not being adequately managed overall. So, there’s a need here for multidisciplinary care to ensure that all of these comorbidities and the full spectrum of symptoms are being managed adequately.”
He concluded that future research is needed to determine strategies to optimize patient satisfaction in adults with AD.
“I’m not sure how much more provocative you can get in terms of data,” added Dr. Silverberg, director of clinical research and contact dermatitis at George Washington University, Washington. “It’s really eye-opening. I think many clinicians may feel like they’re doing a perfect job in managing this disease. These data suggest that at least at the national level that may not be the case.”
Mr. Cheng reported having no financial disclosures. Dr. Silverberg reported that he is a consultant to and/or an advisory board member for several pharmaceutical companies. He is also a speaker for Regeneron and Sanofi and has received a grant from Galderma.
.
Satisfaction scores were higher when specialists prescribed systemic therapy, but were lower when nonspecialists prescribed systemic therapy and when specialists prescribed only topical therapy.
Those are among key findings from an analysis of the Medical Expenditure Panel Surveys reported by Brian T. Cheng during a late-breaking research session at the Revolutionizing Atopic Dermatitis virtual symposium.
“AD management is complex,” said Mr. Cheng, a medical student at Northwestern University, Chicago. “It includes patient education about trigger avoidance, over-the-counter and prescription topical therapies, as well as systemic therapies. Previous studies have shown major decrements to quality of life as well as atopic and non-atopic comorbidities in these patients. The burden of AD and their comorbidities, as well as their management, may impact patient satisfaction.”
Prior studies have demonstrated that patient satisfaction is associated with improvements in clinical outcomes, increased patient retention, and reduced malpractice claims (Br J Dermatol. 2001 Oct;145[4]:617-23, Arch Dermatol 2008 Feb;144[2]:263-5). However, since data on patient satisfaction in AD are limited, Mr. Cheng and the study’s senior author, Jonathan I. Silverberg, MD, PhD, MPH, set out to examine overall patient satisfaction among adults with AD, to determine associations of patient satisfaction with patterns of health care utilization, and to identify predictors of higher satisfaction among these adults.
The researchers conducted a cross-sectional retrospective analysis of 3,810 patients from the 2000-2015 Medical Expenditure Panel Surveys, representative surveys of the U.S. noninstitutionalized population conducted annually by the Agency for Healthcare Research and Quality. They used ICD-9 codes 691 and 692 to determine AD diagnosis and five Consumer Assessment of Health Plans Survey (CAHPS) questions to assess patients’ satisfaction with their clinicians. “These questions have been extensively validated to correlate with global satisfaction,” Mr. Cheng said. “These are not disease-specific and allow for comparison across multiple diseases.”
Next, the researchers created a composite satisfaction score based on the methods of Anthony Jerant, MD, of the University of California, Davis, and colleagues. They adjusted each question in the CAHPS survey to have an equal weight and then summed these into a composite satisfaction score. “We examined patient satisfaction comparing across diseases, and based on the guidelines from the AHRQ to isolate that impact of patient-physician interaction, we adjusted for sociodemographics, mental and physical health status, self-reported health rating, as well as multimorbidity and comorbid diseases.”
Compared with adults who are healthy, adults with AD had lower patient satisfaction overall. “Moreover, people with AD had lower satisfaction compared to those with psoriasis, which may reflect more substantial itch burden as well as the greater comorbid disease challenges in management,” Mr. Cheng said. “It may also reflect the renaissance in psoriasis treatment over the last 10-20 years, giving a wider spectrum of treatment and thus a higher patient satisfaction.”
Among adults with AD, lower satisfaction was consistent across all domains of CAHPS. For the question of “How often health providers listen carefully to you” the adjusted OR (aOR) was 0.87 (P = .008). For the question of “How often health providers explain things in a way that was easy to understand” the aOR was 0.89 (P = .003). For the question of “How often health providers spent enough time with you” the aOR was 0.86 (P = .0001). For “How often providers showed respect for what you had to say” the aOR was 0.91 (P = .02).
Recognizing that treatment regimens are complex and used differently by provider type, the researchers examined interactions between specialists (dermatologists and allergists) and treatment type. “Previous studies found dermatologists treat more severe, chronic AD,” Mr. Cheng said. “We found here that there was lower satisfaction among those treated with topical therapy and by specialists, which may reflect inadequate disease control. We also found lower satisfaction among those treated with systemic therapy by primary care physicians. This may reflect that these patients are not achieving optimal therapy. We found that satisfaction was highest among those treated with systemic therapy and by dermatologists and allergists.”
Socioeconomic, racial/ethnic, and health care disparities were observed in terms of satisfaction among this cohort. The following characteristics were significantly associated with lower patient satisfaction, compared with the general cohort of adults with AD: poor to low income (aOR, –1.82; P less than .0001), multiracial/other race (aOR, –2.34; P = .0001), Hispanic ethnicity (aOR, –1.40; P = .007), and having no insurance coverage (aOR, –4.53; P less than .0001).
“Moreover, those with multimorbidity had even lower satisfaction,” Mr. Cheng said. “In previous studies, AD has been linked with many other comorbidities. This may reflect that these patients are not being adequately managed overall. So, there’s a need here for multidisciplinary care to ensure that all of these comorbidities and the full spectrum of symptoms are being managed adequately.”
He concluded that future research is needed to determine strategies to optimize patient satisfaction in adults with AD.
“I’m not sure how much more provocative you can get in terms of data,” added Dr. Silverberg, director of clinical research and contact dermatitis at George Washington University, Washington. “It’s really eye-opening. I think many clinicians may feel like they’re doing a perfect job in managing this disease. These data suggest that at least at the national level that may not be the case.”
Mr. Cheng reported having no financial disclosures. Dr. Silverberg reported that he is a consultant to and/or an advisory board member for several pharmaceutical companies. He is also a speaker for Regeneron and Sanofi and has received a grant from Galderma.
.
Satisfaction scores were higher when specialists prescribed systemic therapy, but were lower when nonspecialists prescribed systemic therapy and when specialists prescribed only topical therapy.
Those are among key findings from an analysis of the Medical Expenditure Panel Surveys reported by Brian T. Cheng during a late-breaking research session at the Revolutionizing Atopic Dermatitis virtual symposium.
“AD management is complex,” said Mr. Cheng, a medical student at Northwestern University, Chicago. “It includes patient education about trigger avoidance, over-the-counter and prescription topical therapies, as well as systemic therapies. Previous studies have shown major decrements to quality of life as well as atopic and non-atopic comorbidities in these patients. The burden of AD and their comorbidities, as well as their management, may impact patient satisfaction.”
Prior studies have demonstrated that patient satisfaction is associated with improvements in clinical outcomes, increased patient retention, and reduced malpractice claims (Br J Dermatol. 2001 Oct;145[4]:617-23, Arch Dermatol 2008 Feb;144[2]:263-5). However, since data on patient satisfaction in AD are limited, Mr. Cheng and the study’s senior author, Jonathan I. Silverberg, MD, PhD, MPH, set out to examine overall patient satisfaction among adults with AD, to determine associations of patient satisfaction with patterns of health care utilization, and to identify predictors of higher satisfaction among these adults.
The researchers conducted a cross-sectional retrospective analysis of 3,810 patients from the 2000-2015 Medical Expenditure Panel Surveys, representative surveys of the U.S. noninstitutionalized population conducted annually by the Agency for Healthcare Research and Quality. They used ICD-9 codes 691 and 692 to determine AD diagnosis and five Consumer Assessment of Health Plans Survey (CAHPS) questions to assess patients’ satisfaction with their clinicians. “These questions have been extensively validated to correlate with global satisfaction,” Mr. Cheng said. “These are not disease-specific and allow for comparison across multiple diseases.”
Next, the researchers created a composite satisfaction score based on the methods of Anthony Jerant, MD, of the University of California, Davis, and colleagues. They adjusted each question in the CAHPS survey to have an equal weight and then summed these into a composite satisfaction score. “We examined patient satisfaction comparing across diseases, and based on the guidelines from the AHRQ to isolate that impact of patient-physician interaction, we adjusted for sociodemographics, mental and physical health status, self-reported health rating, as well as multimorbidity and comorbid diseases.”
Compared with adults who are healthy, adults with AD had lower patient satisfaction overall. “Moreover, people with AD had lower satisfaction compared to those with psoriasis, which may reflect more substantial itch burden as well as the greater comorbid disease challenges in management,” Mr. Cheng said. “It may also reflect the renaissance in psoriasis treatment over the last 10-20 years, giving a wider spectrum of treatment and thus a higher patient satisfaction.”
Among adults with AD, lower satisfaction was consistent across all domains of CAHPS. For the question of “How often health providers listen carefully to you” the adjusted OR (aOR) was 0.87 (P = .008). For the question of “How often health providers explain things in a way that was easy to understand” the aOR was 0.89 (P = .003). For the question of “How often health providers spent enough time with you” the aOR was 0.86 (P = .0001). For “How often providers showed respect for what you had to say” the aOR was 0.91 (P = .02).
Recognizing that treatment regimens are complex and used differently by provider type, the researchers examined interactions between specialists (dermatologists and allergists) and treatment type. “Previous studies found dermatologists treat more severe, chronic AD,” Mr. Cheng said. “We found here that there was lower satisfaction among those treated with topical therapy and by specialists, which may reflect inadequate disease control. We also found lower satisfaction among those treated with systemic therapy by primary care physicians. This may reflect that these patients are not achieving optimal therapy. We found that satisfaction was highest among those treated with systemic therapy and by dermatologists and allergists.”
Socioeconomic, racial/ethnic, and health care disparities were observed in terms of satisfaction among this cohort. The following characteristics were significantly associated with lower patient satisfaction, compared with the general cohort of adults with AD: poor to low income (aOR, –1.82; P less than .0001), multiracial/other race (aOR, –2.34; P = .0001), Hispanic ethnicity (aOR, –1.40; P = .007), and having no insurance coverage (aOR, –4.53; P less than .0001).
“Moreover, those with multimorbidity had even lower satisfaction,” Mr. Cheng said. “In previous studies, AD has been linked with many other comorbidities. This may reflect that these patients are not being adequately managed overall. So, there’s a need here for multidisciplinary care to ensure that all of these comorbidities and the full spectrum of symptoms are being managed adequately.”
He concluded that future research is needed to determine strategies to optimize patient satisfaction in adults with AD.
“I’m not sure how much more provocative you can get in terms of data,” added Dr. Silverberg, director of clinical research and contact dermatitis at George Washington University, Washington. “It’s really eye-opening. I think many clinicians may feel like they’re doing a perfect job in managing this disease. These data suggest that at least at the national level that may not be the case.”
Mr. Cheng reported having no financial disclosures. Dr. Silverberg reported that he is a consultant to and/or an advisory board member for several pharmaceutical companies. He is also a speaker for Regeneron and Sanofi and has received a grant from Galderma.
FROM REVOLUTIONIZING AD 2020
Rather Than Bash the VA, Let’s Learn From Its Successes
A new report by the Veterans Healthcare Policy Institute (VHPI) documents how elements included in many bills passed on Capitol Hill have failed to improve the efficacy of mental health services for our nation’s former service members.1 The authors argue that while these efforts may be well intended, they often compound problems by squandering precious financial resources and stretching an already overtaxed workforce. Clearly, there are shortcomings in the US Department of Veterans Affairs (VA), our nation’s largest integrated health care system, but rather than bash the VA, as the media and Congress tend to favor, let’s learn from its successes as we improve its services.
To do this we must avoid several policy pitfalls. Consider, for example, the VA MISSION Act (38 USC § 1703), which aimed to increase veteran access to quality health care outside the VA system. Studies confirmed that private sector mental health providers are not ready to deliver veteran-specific mental health care.2,3 Indeed, a RAND report found that psychotherapists in the private sector were unlikely to have the requisite skills necessary to deliver high-quality mental health care to service members or veterans.4
The MISSION Act meant to fix this clinical deficit by directing that competency standards be set for non-VA mental health providers who treat veterans for posttraumatic stress disorder (PTSD), traumatic brain injury, and military sexual trauma. But to date, no minimum competency standards have been set for non-VA mental health providers who treat veterans’ common psychological conditions. A license is all they need.
Legislation like the MISSION Act and the newly passed Commander John Scott Hannon Act (38 USC § 101) also assume that veterans who are suicidal or have mental health problems and don’t go to the VA will seek care from private sector providers. Nothing is further from the truth. Many veterans are deeply resistant to seeking mental health care no matter where that care is delivered.4,5 Sometimes veterans believe that mental health problems are a sign of weakness and are loathe to seek help.
To address this issue, the VA pioneered models of integrated mental health and primary care services.6 This means that if a veteran goes to an outpatient primary care clinic at a VA medical facility or community-based outpatient clinic and discusses a mental health or substance abuse problem, the veteran can get immediate care with a mental health provider without making a separate mental health appointment. In addition, the VA already provides routine, annual screening for PTSD and sexual assault as well as depression and substance abuse at all its primary care clinics nationwide. Thanks to comprehensive screening (at a level unknown in most other health care systems) even if a veteran doesn’t spontaneously report a trauma history or mental health distress, VA is able to identify the problem and offer help right in the primary care clinic. This one-stop shopping reduces the shame and stigma of having to make an appointment with a mental health provider, allows treatment to begin immediately, and reduces no shows at follow-up appointments.
Other health care systems are trying to copy the VA model of integrated primary and mental health care, but given our fragmented insurance system, it’s not easy to replicate.7 According to Suzanne Gordon coauthor of the VHPI study, “This VA innovation encourages veterans, socialized by the military to conceal serious mental health problems, to get immediate help. So do many other VA programs, like peer support groups and networks. Legislation needs to strengthen, not weaken, such programs that are almost impossible to reproduce in the private sector.” Outside of VA, mental health challenges faced by veterans likely go undetected, and many veterans will not receive the care that might change, or even save, their lives.
VA best practices include an unprecedented national training initiative on 16 evidence-based psychotherapies that has been in operation for more than a decade.8 These high-quality treatments target debilitating conditions such as depression, PTSD, substance use disorders, insomnia, and chronic pain.9-13 More than 12,700 VA mental health providers have received training in these evidence-based psychotherapies.
“There is no way that non-VA health care systems can ever duplicate the quality of training and supervision that has now been provided, nationally, to VA mental health professionals,” Josef Ruzek, PhD, former Director of the VA National Center for PTSD Dissemination and Training Division told me in a phone conversation (January 14, 2021). “Their program of training and implementation in the very best treatments for veteran mental health conditions stands as an international model of a complex, well-executed, large-scale program to improve mental health service delivery and improve the outcomes of treatment.”
The VA not only paid for the training of these mental health providers, but also contributed substantial efforts to assist in the implementation and sustainability of such practices. These include policy changes mandating their availability at all VA facilities, designation of local evidence-based coordinators at each medical center, and even a nationwide PTSD mentoring program to help PTSD clinic managers make organizational changes and to guide the efforts of any VA clinician seeking advice on how to engage and work with a veteran living with PTSD.14 All these incredible dissemination and implementation endeavors have resulted in a substantial overall decrease in mental health symptoms and substance misuse behaviors and increase in functional outcomes, like improvement in relationship functioning and increase in quality of life for many veterans.
As a trauma psychologist and former VA employee, I urge lawmakers to assure that veterans are not sent to private sector providers who don’t understand their unique needs and aren’t trained to serve them well, and to similarly assure that systems of care are carefully designed to meet the specific needs of veterans.
1. Gordon S, Lemle RB, Ruzek JI, Kudler H. Creating effective solutions, programs, and policies to improve veterans’ mental health care. Published January 2021. Accessed February 22, 2021. https://static1.squarespace.com/static/5b19e25e89c1722037f0fdab/t/6018731daf20e7024b5d6aa8/1612215071469/VHPI_MHReport.pdf
2. Tanielian T, Farris C, Batka C, et al. Ready to serve: community-based provider capacity to deliver culturally competent, quality mental health care to veterans and their families. Published 2014. Accessed February 22, 2021. https://www.rand.org/pubs/research_reports/RR806.html
3. Tanielian T, Farmer CM, Burns RM, et al, Ready or not? Assessing the capacity of New York State health care providers to meet the needs of veterans. Published 2018. Accessed February 22, 2021. https://www.rand.org/pubs/research_reports/RR2298.html.
4. Crawford EF, Elbogen EB, Wagner HR, Kudler H, Calhoun PS, Brancu M, Straits-Troster KA. Surveying treatment preferences in U.S. Iraq-Afghanistan Veterans with PTSD symptoms: a step toward veteran-centered care. J Trauma Stress. 2015 Apr;28(2):118-26. doi: 10.1002/jts.21993.
5. Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine 351:13–22, 2004
6. Zeiss AM, Karlin BE. Integrating mental health and primary care services in the Department of Veterans Affairs Health Care System. J Clin Psychol Med Settings. 2008;15(1):73-78. doi:10.1007/s10880-008-9100-4
7. Gordon S. Wounds of War: How the VA Delivers Health, Healing and Hope to the Nation’s Veterans. Cornell University Press; 2018.
8. Karlin BE, Cross G. From the laboratory to the therapy room: national dissemination and implementation of evidence-based psychotherapies in the U.S. Department of Veterans Affairs Health Care System. Am Psychol. 2014;69(1):19-33. doi:10.1037/a0033888
9. Stewart MO, Raffa SD, Steele JL, et al. National dissemination of interpersonal psychotherapy for depression in veterans: therapist and patient-level outcomes. J Consult Clin Psychol. 2014;82(6):1201-1206. doi:10.1037/a0037410
10. Karlin BE, Ruzek JI, Chard KM, et al. Dissemination of evidence-based psychological treatments for posttraumatic stress disorder in the Veterans Health Administration. J Trauma Stress. 2010;23(6):663-673. doi:10.1002/jts.20588
11. DeMarce JM, Gnys M, Raffa SD, Kumpula M, Karlin BE. Dissemination of cognitive behavioral therapy for substance use disorders in the Department of Veterans Affairs Health Care System: description and evaluation of veteran outcomes [published online ahead of print, 2019 Oct 23]. Subst Abus. 2019;1-7. doi:10.1080/08897077.2019.1674238
12. Karlin BE, Trockel M, Spira AP, Taylor CB, Manber R. National evaluation of the effectiveness of cognitive behavioral therapy for insomnia among older versus younger veterans. Int J Geriatr Psychiatry. 2015;30(3):308-315. doi:10.1002/gps.4143
13. Stewart MO, Karlin BE, Murphy JL, et al. National dissemination of cognitive-behavioral therapy for chronic pain in veterans: therapist and patient-level outcomes. Clin J Pain. 2015;31(8):722-729. doi:10.1097/AJP.0000000000000151
14. Bernardy NC, Hamblen JL, Friedman MJ, Ruzek JI, McFall ME. Implementation of a posttraumatic stress disorder mentoring program to improve treatment services. Psycholog Trauma. 2011;3(3):292-299. doi:10.1037/a0024847
A new report by the Veterans Healthcare Policy Institute (VHPI) documents how elements included in many bills passed on Capitol Hill have failed to improve the efficacy of mental health services for our nation’s former service members.1 The authors argue that while these efforts may be well intended, they often compound problems by squandering precious financial resources and stretching an already overtaxed workforce. Clearly, there are shortcomings in the US Department of Veterans Affairs (VA), our nation’s largest integrated health care system, but rather than bash the VA, as the media and Congress tend to favor, let’s learn from its successes as we improve its services.
To do this we must avoid several policy pitfalls. Consider, for example, the VA MISSION Act (38 USC § 1703), which aimed to increase veteran access to quality health care outside the VA system. Studies confirmed that private sector mental health providers are not ready to deliver veteran-specific mental health care.2,3 Indeed, a RAND report found that psychotherapists in the private sector were unlikely to have the requisite skills necessary to deliver high-quality mental health care to service members or veterans.4
The MISSION Act meant to fix this clinical deficit by directing that competency standards be set for non-VA mental health providers who treat veterans for posttraumatic stress disorder (PTSD), traumatic brain injury, and military sexual trauma. But to date, no minimum competency standards have been set for non-VA mental health providers who treat veterans’ common psychological conditions. A license is all they need.
Legislation like the MISSION Act and the newly passed Commander John Scott Hannon Act (38 USC § 101) also assume that veterans who are suicidal or have mental health problems and don’t go to the VA will seek care from private sector providers. Nothing is further from the truth. Many veterans are deeply resistant to seeking mental health care no matter where that care is delivered.4,5 Sometimes veterans believe that mental health problems are a sign of weakness and are loathe to seek help.
To address this issue, the VA pioneered models of integrated mental health and primary care services.6 This means that if a veteran goes to an outpatient primary care clinic at a VA medical facility or community-based outpatient clinic and discusses a mental health or substance abuse problem, the veteran can get immediate care with a mental health provider without making a separate mental health appointment. In addition, the VA already provides routine, annual screening for PTSD and sexual assault as well as depression and substance abuse at all its primary care clinics nationwide. Thanks to comprehensive screening (at a level unknown in most other health care systems) even if a veteran doesn’t spontaneously report a trauma history or mental health distress, VA is able to identify the problem and offer help right in the primary care clinic. This one-stop shopping reduces the shame and stigma of having to make an appointment with a mental health provider, allows treatment to begin immediately, and reduces no shows at follow-up appointments.
Other health care systems are trying to copy the VA model of integrated primary and mental health care, but given our fragmented insurance system, it’s not easy to replicate.7 According to Suzanne Gordon coauthor of the VHPI study, “This VA innovation encourages veterans, socialized by the military to conceal serious mental health problems, to get immediate help. So do many other VA programs, like peer support groups and networks. Legislation needs to strengthen, not weaken, such programs that are almost impossible to reproduce in the private sector.” Outside of VA, mental health challenges faced by veterans likely go undetected, and many veterans will not receive the care that might change, or even save, their lives.
VA best practices include an unprecedented national training initiative on 16 evidence-based psychotherapies that has been in operation for more than a decade.8 These high-quality treatments target debilitating conditions such as depression, PTSD, substance use disorders, insomnia, and chronic pain.9-13 More than 12,700 VA mental health providers have received training in these evidence-based psychotherapies.
“There is no way that non-VA health care systems can ever duplicate the quality of training and supervision that has now been provided, nationally, to VA mental health professionals,” Josef Ruzek, PhD, former Director of the VA National Center for PTSD Dissemination and Training Division told me in a phone conversation (January 14, 2021). “Their program of training and implementation in the very best treatments for veteran mental health conditions stands as an international model of a complex, well-executed, large-scale program to improve mental health service delivery and improve the outcomes of treatment.”
The VA not only paid for the training of these mental health providers, but also contributed substantial efforts to assist in the implementation and sustainability of such practices. These include policy changes mandating their availability at all VA facilities, designation of local evidence-based coordinators at each medical center, and even a nationwide PTSD mentoring program to help PTSD clinic managers make organizational changes and to guide the efforts of any VA clinician seeking advice on how to engage and work with a veteran living with PTSD.14 All these incredible dissemination and implementation endeavors have resulted in a substantial overall decrease in mental health symptoms and substance misuse behaviors and increase in functional outcomes, like improvement in relationship functioning and increase in quality of life for many veterans.
As a trauma psychologist and former VA employee, I urge lawmakers to assure that veterans are not sent to private sector providers who don’t understand their unique needs and aren’t trained to serve them well, and to similarly assure that systems of care are carefully designed to meet the specific needs of veterans.
A new report by the Veterans Healthcare Policy Institute (VHPI) documents how elements included in many bills passed on Capitol Hill have failed to improve the efficacy of mental health services for our nation’s former service members.1 The authors argue that while these efforts may be well intended, they often compound problems by squandering precious financial resources and stretching an already overtaxed workforce. Clearly, there are shortcomings in the US Department of Veterans Affairs (VA), our nation’s largest integrated health care system, but rather than bash the VA, as the media and Congress tend to favor, let’s learn from its successes as we improve its services.
To do this we must avoid several policy pitfalls. Consider, for example, the VA MISSION Act (38 USC § 1703), which aimed to increase veteran access to quality health care outside the VA system. Studies confirmed that private sector mental health providers are not ready to deliver veteran-specific mental health care.2,3 Indeed, a RAND report found that psychotherapists in the private sector were unlikely to have the requisite skills necessary to deliver high-quality mental health care to service members or veterans.4
The MISSION Act meant to fix this clinical deficit by directing that competency standards be set for non-VA mental health providers who treat veterans for posttraumatic stress disorder (PTSD), traumatic brain injury, and military sexual trauma. But to date, no minimum competency standards have been set for non-VA mental health providers who treat veterans’ common psychological conditions. A license is all they need.
Legislation like the MISSION Act and the newly passed Commander John Scott Hannon Act (38 USC § 101) also assume that veterans who are suicidal or have mental health problems and don’t go to the VA will seek care from private sector providers. Nothing is further from the truth. Many veterans are deeply resistant to seeking mental health care no matter where that care is delivered.4,5 Sometimes veterans believe that mental health problems are a sign of weakness and are loathe to seek help.
To address this issue, the VA pioneered models of integrated mental health and primary care services.6 This means that if a veteran goes to an outpatient primary care clinic at a VA medical facility or community-based outpatient clinic and discusses a mental health or substance abuse problem, the veteran can get immediate care with a mental health provider without making a separate mental health appointment. In addition, the VA already provides routine, annual screening for PTSD and sexual assault as well as depression and substance abuse at all its primary care clinics nationwide. Thanks to comprehensive screening (at a level unknown in most other health care systems) even if a veteran doesn’t spontaneously report a trauma history or mental health distress, VA is able to identify the problem and offer help right in the primary care clinic. This one-stop shopping reduces the shame and stigma of having to make an appointment with a mental health provider, allows treatment to begin immediately, and reduces no shows at follow-up appointments.
Other health care systems are trying to copy the VA model of integrated primary and mental health care, but given our fragmented insurance system, it’s not easy to replicate.7 According to Suzanne Gordon coauthor of the VHPI study, “This VA innovation encourages veterans, socialized by the military to conceal serious mental health problems, to get immediate help. So do many other VA programs, like peer support groups and networks. Legislation needs to strengthen, not weaken, such programs that are almost impossible to reproduce in the private sector.” Outside of VA, mental health challenges faced by veterans likely go undetected, and many veterans will not receive the care that might change, or even save, their lives.
VA best practices include an unprecedented national training initiative on 16 evidence-based psychotherapies that has been in operation for more than a decade.8 These high-quality treatments target debilitating conditions such as depression, PTSD, substance use disorders, insomnia, and chronic pain.9-13 More than 12,700 VA mental health providers have received training in these evidence-based psychotherapies.
“There is no way that non-VA health care systems can ever duplicate the quality of training and supervision that has now been provided, nationally, to VA mental health professionals,” Josef Ruzek, PhD, former Director of the VA National Center for PTSD Dissemination and Training Division told me in a phone conversation (January 14, 2021). “Their program of training and implementation in the very best treatments for veteran mental health conditions stands as an international model of a complex, well-executed, large-scale program to improve mental health service delivery and improve the outcomes of treatment.”
The VA not only paid for the training of these mental health providers, but also contributed substantial efforts to assist in the implementation and sustainability of such practices. These include policy changes mandating their availability at all VA facilities, designation of local evidence-based coordinators at each medical center, and even a nationwide PTSD mentoring program to help PTSD clinic managers make organizational changes and to guide the efforts of any VA clinician seeking advice on how to engage and work with a veteran living with PTSD.14 All these incredible dissemination and implementation endeavors have resulted in a substantial overall decrease in mental health symptoms and substance misuse behaviors and increase in functional outcomes, like improvement in relationship functioning and increase in quality of life for many veterans.
As a trauma psychologist and former VA employee, I urge lawmakers to assure that veterans are not sent to private sector providers who don’t understand their unique needs and aren’t trained to serve them well, and to similarly assure that systems of care are carefully designed to meet the specific needs of veterans.
1. Gordon S, Lemle RB, Ruzek JI, Kudler H. Creating effective solutions, programs, and policies to improve veterans’ mental health care. Published January 2021. Accessed February 22, 2021. https://static1.squarespace.com/static/5b19e25e89c1722037f0fdab/t/6018731daf20e7024b5d6aa8/1612215071469/VHPI_MHReport.pdf
2. Tanielian T, Farris C, Batka C, et al. Ready to serve: community-based provider capacity to deliver culturally competent, quality mental health care to veterans and their families. Published 2014. Accessed February 22, 2021. https://www.rand.org/pubs/research_reports/RR806.html
3. Tanielian T, Farmer CM, Burns RM, et al, Ready or not? Assessing the capacity of New York State health care providers to meet the needs of veterans. Published 2018. Accessed February 22, 2021. https://www.rand.org/pubs/research_reports/RR2298.html.
4. Crawford EF, Elbogen EB, Wagner HR, Kudler H, Calhoun PS, Brancu M, Straits-Troster KA. Surveying treatment preferences in U.S. Iraq-Afghanistan Veterans with PTSD symptoms: a step toward veteran-centered care. J Trauma Stress. 2015 Apr;28(2):118-26. doi: 10.1002/jts.21993.
5. Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine 351:13–22, 2004
6. Zeiss AM, Karlin BE. Integrating mental health and primary care services in the Department of Veterans Affairs Health Care System. J Clin Psychol Med Settings. 2008;15(1):73-78. doi:10.1007/s10880-008-9100-4
7. Gordon S. Wounds of War: How the VA Delivers Health, Healing and Hope to the Nation’s Veterans. Cornell University Press; 2018.
8. Karlin BE, Cross G. From the laboratory to the therapy room: national dissemination and implementation of evidence-based psychotherapies in the U.S. Department of Veterans Affairs Health Care System. Am Psychol. 2014;69(1):19-33. doi:10.1037/a0033888
9. Stewart MO, Raffa SD, Steele JL, et al. National dissemination of interpersonal psychotherapy for depression in veterans: therapist and patient-level outcomes. J Consult Clin Psychol. 2014;82(6):1201-1206. doi:10.1037/a0037410
10. Karlin BE, Ruzek JI, Chard KM, et al. Dissemination of evidence-based psychological treatments for posttraumatic stress disorder in the Veterans Health Administration. J Trauma Stress. 2010;23(6):663-673. doi:10.1002/jts.20588
11. DeMarce JM, Gnys M, Raffa SD, Kumpula M, Karlin BE. Dissemination of cognitive behavioral therapy for substance use disorders in the Department of Veterans Affairs Health Care System: description and evaluation of veteran outcomes [published online ahead of print, 2019 Oct 23]. Subst Abus. 2019;1-7. doi:10.1080/08897077.2019.1674238
12. Karlin BE, Trockel M, Spira AP, Taylor CB, Manber R. National evaluation of the effectiveness of cognitive behavioral therapy for insomnia among older versus younger veterans. Int J Geriatr Psychiatry. 2015;30(3):308-315. doi:10.1002/gps.4143
13. Stewart MO, Karlin BE, Murphy JL, et al. National dissemination of cognitive-behavioral therapy for chronic pain in veterans: therapist and patient-level outcomes. Clin J Pain. 2015;31(8):722-729. doi:10.1097/AJP.0000000000000151
14. Bernardy NC, Hamblen JL, Friedman MJ, Ruzek JI, McFall ME. Implementation of a posttraumatic stress disorder mentoring program to improve treatment services. Psycholog Trauma. 2011;3(3):292-299. doi:10.1037/a0024847
1. Gordon S, Lemle RB, Ruzek JI, Kudler H. Creating effective solutions, programs, and policies to improve veterans’ mental health care. Published January 2021. Accessed February 22, 2021. https://static1.squarespace.com/static/5b19e25e89c1722037f0fdab/t/6018731daf20e7024b5d6aa8/1612215071469/VHPI_MHReport.pdf
2. Tanielian T, Farris C, Batka C, et al. Ready to serve: community-based provider capacity to deliver culturally competent, quality mental health care to veterans and their families. Published 2014. Accessed February 22, 2021. https://www.rand.org/pubs/research_reports/RR806.html
3. Tanielian T, Farmer CM, Burns RM, et al, Ready or not? Assessing the capacity of New York State health care providers to meet the needs of veterans. Published 2018. Accessed February 22, 2021. https://www.rand.org/pubs/research_reports/RR2298.html.
4. Crawford EF, Elbogen EB, Wagner HR, Kudler H, Calhoun PS, Brancu M, Straits-Troster KA. Surveying treatment preferences in U.S. Iraq-Afghanistan Veterans with PTSD symptoms: a step toward veteran-centered care. J Trauma Stress. 2015 Apr;28(2):118-26. doi: 10.1002/jts.21993.
5. Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine 351:13–22, 2004
6. Zeiss AM, Karlin BE. Integrating mental health and primary care services in the Department of Veterans Affairs Health Care System. J Clin Psychol Med Settings. 2008;15(1):73-78. doi:10.1007/s10880-008-9100-4
7. Gordon S. Wounds of War: How the VA Delivers Health, Healing and Hope to the Nation’s Veterans. Cornell University Press; 2018.
8. Karlin BE, Cross G. From the laboratory to the therapy room: national dissemination and implementation of evidence-based psychotherapies in the U.S. Department of Veterans Affairs Health Care System. Am Psychol. 2014;69(1):19-33. doi:10.1037/a0033888
9. Stewart MO, Raffa SD, Steele JL, et al. National dissemination of interpersonal psychotherapy for depression in veterans: therapist and patient-level outcomes. J Consult Clin Psychol. 2014;82(6):1201-1206. doi:10.1037/a0037410
10. Karlin BE, Ruzek JI, Chard KM, et al. Dissemination of evidence-based psychological treatments for posttraumatic stress disorder in the Veterans Health Administration. J Trauma Stress. 2010;23(6):663-673. doi:10.1002/jts.20588
11. DeMarce JM, Gnys M, Raffa SD, Kumpula M, Karlin BE. Dissemination of cognitive behavioral therapy for substance use disorders in the Department of Veterans Affairs Health Care System: description and evaluation of veteran outcomes [published online ahead of print, 2019 Oct 23]. Subst Abus. 2019;1-7. doi:10.1080/08897077.2019.1674238
12. Karlin BE, Trockel M, Spira AP, Taylor CB, Manber R. National evaluation of the effectiveness of cognitive behavioral therapy for insomnia among older versus younger veterans. Int J Geriatr Psychiatry. 2015;30(3):308-315. doi:10.1002/gps.4143
13. Stewart MO, Karlin BE, Murphy JL, et al. National dissemination of cognitive-behavioral therapy for chronic pain in veterans: therapist and patient-level outcomes. Clin J Pain. 2015;31(8):722-729. doi:10.1097/AJP.0000000000000151
14. Bernardy NC, Hamblen JL, Friedman MJ, Ruzek JI, McFall ME. Implementation of a posttraumatic stress disorder mentoring program to improve treatment services. Psycholog Trauma. 2011;3(3):292-299. doi:10.1037/a0024847