User login
Study confirms link between PAP apnea treatment and dementia onset
Obstructive sleep apnea (OSA) treatment with positive airway pressure (PAP) therapy was associated with a lower odds of incident Alzheimer’s disease and other dementia in a large retrospective cohort study of Medicare patients with the sleep disorder.
The study builds on research linking OSA to poor cognitive outcomes and dementia syndromes. With use of a 5% random sample of Medicare beneficiaries (more than 2.7 million) and their claims data, investigators identified approximately 53,000 who had an OSA diagnosis prior to 2011.
Of these Medicare beneficiaries, 78% with OSA were identified as “PAP-treated” based on having at least one durable medical equipment claim for PAP equipment. And of those treated, 74% were identified as “PAP adherent” based on having more than two PAP equipment claims separated by at least a month, said Galit Levi Dunietz, PhD, MPH, at the virtual annual meeting of the Associated Professional Sleep Societies.
Dr. Dunietz and her coinvestigators used logistic regression to examine the associations between PAP treatment and PAP treatment adherence, and incident ICD-9 diagnoses of Alzheimer’s disease (AD), mild cognitive impairment (MCI), and dementia not otherwise specified (DNOS) over the period 2011-2013.
After adjustments for potential confounders (age, sex, race, stroke, hypertension, cardiovascular disease, and depression), OSA treatment was associated with a significantly lower odds of a diagnosis of AD (odds ratio, 0.78; 95% confidence interval 0.69-0.89) or DNOS (OR, 0.69; 95% CI, 0.55-0.85), as well as nonsignificantly lower odds of MCI diagnosis (OR, 0.82; 95% CI, 0.66-1.02).
“People who are treated for OSA have a 22% reduced odds of being diagnosed with AD and a 31% reduced odds of getting DNOS,” said Dr. Dunietz, from the University of Michigan in Ann Arbor, in an interview after the meeting. “The 18% reduced odds of mild cognitive disorder is not really significant because the upper bound is 1.02, but we consider it approaching significance.”
Adherence to treatment was significantly associated with lower odds of AD, but not with significantly lower odds of DNOS or MCI, she said. OSA was confirmed by ICD-9 diagnosis codes plus the presence of relevant polysomnography current procedural terminology code.
All told, the findings “suggest that PAP therapy for OSA may lower short-term risk for dementia in older persons,” Dr. Dunietz and her co-nvestigators said in their poster presentation. “If a causal pathway exists between OSA and dementia, treatment of OSA may offer new opportunities to improve cognitive outcomes in older adults with OSA.”
Andrew W. Varga, MD, of the division of pulmonary, critical care, and sleep medicine at the Icahn School of Medicine at Mount Sinai and the Mount Sinai Integrative Sleep Center, both in New York, said that cognitive impairment is now a recognized clinical consequence of OSA and that OSA treatment could be a target for the prevention of cognitive impairment and Alzheimer’s disease in particular.
“I absolutely bring it up with patients in their 60s and 70s. I’m honest – I say, there seems to be more and more evidence for links between apnea and Alzheimer’s in particular. I tell them we don’t know 100% whether PAP reverses any of this, but it stands to reason that it does,” said Dr. Varga, who was asked to comment on the study and related research.
An analysis published several years ago in Neurology from the Alzheimer’s Disease Neuroimaging Initiative cohort found that patients with self-reported sleep apnea had a younger age of MCI or AD onset (about 10 years) and that patients who used continuous positive airway pressure had a delayed age of onset. “Those who had a subjective diagnosis of sleep apnea and who also reported using CPAP as treatment seemed to go in the opposite direction,” said Dr. Varga, a coauthor of that study. “They had an onset of AD that looked just like people who had no sleep apnea.”
While this study was limited by sleep apnea being self-reported – and by the lack of severity data – the newly reported study may be limited by the use of ICD codes and the fact that OSA is often entered into patient’s chart before diagnosis is confirmed through a sleep study, Dr. Varga said.
“The field is mature enough that we should be thinking of doing honest and rigorous clinical trials for sleep apnea with cognitive outcomes being a main measure of interest,” he said. “The issue we’re struggling with in the field is that such a trial would not be short.”
There are several theories for the link between OSA and cognitive impairment, he said, including disruptions in sleep architecture leading to increased production of amyloid and tau and/or decreased “clearance” of extracellular amyloid, neuronal sensitivity to hypoxia, and cardiovascular comorbidities.
Dr. Dunietz’s study was supported by The American Academy of Sleep Medicine Foundation. She reported having no disclosures. Dr. Varga said he has no relevant disclosures.
Obstructive sleep apnea (OSA) treatment with positive airway pressure (PAP) therapy was associated with a lower odds of incident Alzheimer’s disease and other dementia in a large retrospective cohort study of Medicare patients with the sleep disorder.
The study builds on research linking OSA to poor cognitive outcomes and dementia syndromes. With use of a 5% random sample of Medicare beneficiaries (more than 2.7 million) and their claims data, investigators identified approximately 53,000 who had an OSA diagnosis prior to 2011.
Of these Medicare beneficiaries, 78% with OSA were identified as “PAP-treated” based on having at least one durable medical equipment claim for PAP equipment. And of those treated, 74% were identified as “PAP adherent” based on having more than two PAP equipment claims separated by at least a month, said Galit Levi Dunietz, PhD, MPH, at the virtual annual meeting of the Associated Professional Sleep Societies.
Dr. Dunietz and her coinvestigators used logistic regression to examine the associations between PAP treatment and PAP treatment adherence, and incident ICD-9 diagnoses of Alzheimer’s disease (AD), mild cognitive impairment (MCI), and dementia not otherwise specified (DNOS) over the period 2011-2013.
After adjustments for potential confounders (age, sex, race, stroke, hypertension, cardiovascular disease, and depression), OSA treatment was associated with a significantly lower odds of a diagnosis of AD (odds ratio, 0.78; 95% confidence interval 0.69-0.89) or DNOS (OR, 0.69; 95% CI, 0.55-0.85), as well as nonsignificantly lower odds of MCI diagnosis (OR, 0.82; 95% CI, 0.66-1.02).
“People who are treated for OSA have a 22% reduced odds of being diagnosed with AD and a 31% reduced odds of getting DNOS,” said Dr. Dunietz, from the University of Michigan in Ann Arbor, in an interview after the meeting. “The 18% reduced odds of mild cognitive disorder is not really significant because the upper bound is 1.02, but we consider it approaching significance.”
Adherence to treatment was significantly associated with lower odds of AD, but not with significantly lower odds of DNOS or MCI, she said. OSA was confirmed by ICD-9 diagnosis codes plus the presence of relevant polysomnography current procedural terminology code.
All told, the findings “suggest that PAP therapy for OSA may lower short-term risk for dementia in older persons,” Dr. Dunietz and her co-nvestigators said in their poster presentation. “If a causal pathway exists between OSA and dementia, treatment of OSA may offer new opportunities to improve cognitive outcomes in older adults with OSA.”
Andrew W. Varga, MD, of the division of pulmonary, critical care, and sleep medicine at the Icahn School of Medicine at Mount Sinai and the Mount Sinai Integrative Sleep Center, both in New York, said that cognitive impairment is now a recognized clinical consequence of OSA and that OSA treatment could be a target for the prevention of cognitive impairment and Alzheimer’s disease in particular.
“I absolutely bring it up with patients in their 60s and 70s. I’m honest – I say, there seems to be more and more evidence for links between apnea and Alzheimer’s in particular. I tell them we don’t know 100% whether PAP reverses any of this, but it stands to reason that it does,” said Dr. Varga, who was asked to comment on the study and related research.
An analysis published several years ago in Neurology from the Alzheimer’s Disease Neuroimaging Initiative cohort found that patients with self-reported sleep apnea had a younger age of MCI or AD onset (about 10 years) and that patients who used continuous positive airway pressure had a delayed age of onset. “Those who had a subjective diagnosis of sleep apnea and who also reported using CPAP as treatment seemed to go in the opposite direction,” said Dr. Varga, a coauthor of that study. “They had an onset of AD that looked just like people who had no sleep apnea.”
While this study was limited by sleep apnea being self-reported – and by the lack of severity data – the newly reported study may be limited by the use of ICD codes and the fact that OSA is often entered into patient’s chart before diagnosis is confirmed through a sleep study, Dr. Varga said.
“The field is mature enough that we should be thinking of doing honest and rigorous clinical trials for sleep apnea with cognitive outcomes being a main measure of interest,” he said. “The issue we’re struggling with in the field is that such a trial would not be short.”
There are several theories for the link between OSA and cognitive impairment, he said, including disruptions in sleep architecture leading to increased production of amyloid and tau and/or decreased “clearance” of extracellular amyloid, neuronal sensitivity to hypoxia, and cardiovascular comorbidities.
Dr. Dunietz’s study was supported by The American Academy of Sleep Medicine Foundation. She reported having no disclosures. Dr. Varga said he has no relevant disclosures.
Obstructive sleep apnea (OSA) treatment with positive airway pressure (PAP) therapy was associated with a lower odds of incident Alzheimer’s disease and other dementia in a large retrospective cohort study of Medicare patients with the sleep disorder.
The study builds on research linking OSA to poor cognitive outcomes and dementia syndromes. With use of a 5% random sample of Medicare beneficiaries (more than 2.7 million) and their claims data, investigators identified approximately 53,000 who had an OSA diagnosis prior to 2011.
Of these Medicare beneficiaries, 78% with OSA were identified as “PAP-treated” based on having at least one durable medical equipment claim for PAP equipment. And of those treated, 74% were identified as “PAP adherent” based on having more than two PAP equipment claims separated by at least a month, said Galit Levi Dunietz, PhD, MPH, at the virtual annual meeting of the Associated Professional Sleep Societies.
Dr. Dunietz and her coinvestigators used logistic regression to examine the associations between PAP treatment and PAP treatment adherence, and incident ICD-9 diagnoses of Alzheimer’s disease (AD), mild cognitive impairment (MCI), and dementia not otherwise specified (DNOS) over the period 2011-2013.
After adjustments for potential confounders (age, sex, race, stroke, hypertension, cardiovascular disease, and depression), OSA treatment was associated with a significantly lower odds of a diagnosis of AD (odds ratio, 0.78; 95% confidence interval 0.69-0.89) or DNOS (OR, 0.69; 95% CI, 0.55-0.85), as well as nonsignificantly lower odds of MCI diagnosis (OR, 0.82; 95% CI, 0.66-1.02).
“People who are treated for OSA have a 22% reduced odds of being diagnosed with AD and a 31% reduced odds of getting DNOS,” said Dr. Dunietz, from the University of Michigan in Ann Arbor, in an interview after the meeting. “The 18% reduced odds of mild cognitive disorder is not really significant because the upper bound is 1.02, but we consider it approaching significance.”
Adherence to treatment was significantly associated with lower odds of AD, but not with significantly lower odds of DNOS or MCI, she said. OSA was confirmed by ICD-9 diagnosis codes plus the presence of relevant polysomnography current procedural terminology code.
All told, the findings “suggest that PAP therapy for OSA may lower short-term risk for dementia in older persons,” Dr. Dunietz and her co-nvestigators said in their poster presentation. “If a causal pathway exists between OSA and dementia, treatment of OSA may offer new opportunities to improve cognitive outcomes in older adults with OSA.”
Andrew W. Varga, MD, of the division of pulmonary, critical care, and sleep medicine at the Icahn School of Medicine at Mount Sinai and the Mount Sinai Integrative Sleep Center, both in New York, said that cognitive impairment is now a recognized clinical consequence of OSA and that OSA treatment could be a target for the prevention of cognitive impairment and Alzheimer’s disease in particular.
“I absolutely bring it up with patients in their 60s and 70s. I’m honest – I say, there seems to be more and more evidence for links between apnea and Alzheimer’s in particular. I tell them we don’t know 100% whether PAP reverses any of this, but it stands to reason that it does,” said Dr. Varga, who was asked to comment on the study and related research.
An analysis published several years ago in Neurology from the Alzheimer’s Disease Neuroimaging Initiative cohort found that patients with self-reported sleep apnea had a younger age of MCI or AD onset (about 10 years) and that patients who used continuous positive airway pressure had a delayed age of onset. “Those who had a subjective diagnosis of sleep apnea and who also reported using CPAP as treatment seemed to go in the opposite direction,” said Dr. Varga, a coauthor of that study. “They had an onset of AD that looked just like people who had no sleep apnea.”
While this study was limited by sleep apnea being self-reported – and by the lack of severity data – the newly reported study may be limited by the use of ICD codes and the fact that OSA is often entered into patient’s chart before diagnosis is confirmed through a sleep study, Dr. Varga said.
“The field is mature enough that we should be thinking of doing honest and rigorous clinical trials for sleep apnea with cognitive outcomes being a main measure of interest,” he said. “The issue we’re struggling with in the field is that such a trial would not be short.”
There are several theories for the link between OSA and cognitive impairment, he said, including disruptions in sleep architecture leading to increased production of amyloid and tau and/or decreased “clearance” of extracellular amyloid, neuronal sensitivity to hypoxia, and cardiovascular comorbidities.
Dr. Dunietz’s study was supported by The American Academy of Sleep Medicine Foundation. She reported having no disclosures. Dr. Varga said he has no relevant disclosures.
FROM SLEEP 2020
More dairy lowers risk of falls, fractures in frail elderly
Consuming more milk, cheese, or yogurt might be a simple, low-cost way to boost bone health and prevent some falls and fractures in older people living in long-term care facilities, according to a new randomized study from Australia.
“Supplementation using dairy foods is likely to be an effective, safe, widely available, and low cost means of curtailing the public health burden of fractures,” said Sandra Iuliano, PhD, from the University of Melbourne, who presented the findings during the virtual American Society of Bone and Mineral Research 2020 annual meeting.
The researchers randomized 60 old-age institutions to provide residents with their usual menus or a diet with more milk, cheese, or yogurt for 2 years.
The residents with the altered menus increased their dairy consumption from 2 servings/day to 3.5 servings/day, which was reflected in a greater intake of calcium and protein, along with fewer falls, total fractures, and hip fractures than in the control group.
“This is the first randomized trial to show a benefit of dairy food intake on risk of fractures,” Walter Willett, MD, DrPH, professor of nutrition and epidemiology at the Harvard School of Public Health, Boston, said in an interview.
The results are “not surprising” because supplements of calcium plus vitamin D have reduced the risk of fractures in a similar population of older residents living in special living facilities, said Dr. Willett, coauthor of a recent review article, “Milk and Health,” published in the New England Journal of Medicine.
“It is important for everyone to have adequate intake of calcium and vitamin D,” he said. However, “it isn’t clear whether it is better to ensure this clinically by supplements, overall healthy diet, or extra dairy intake,” he added, noting that consuming the amount of dairy given in this Australian study is not environmentally sustainable.
Clifford Rosen, MD, professor of medicine, Tufts University, Boston, said in an interview that the Australian researchers studied the impact of increased dietary calcium and protein, not the impact of vitamin D via supplements.
“This is progress toward getting interventions to our most needy residents to prevent fractures – probably the most compelling data that we have had in a number of years,” he noted.
The current study shows “it’s not [the] vitamin D,” because the residents had initial low calcium levels but normal vitamin D levels. “For too long we’ve been stuck on the idea that it is [increasing] vitamin D in the elderly that causes a reduction in fractures,” said Dr. Rosen. “The data are not very supportive of it, but people continue to think that’s the most important element.”
On the other hand, the current study raises certain questions. “What we don’t know is, is it the calcium, or is it the protein, or the combination, that had an impact?”
Would upping dairy decrease falls?
Older adults living in institutions have a high risk of falls and fractures, including hip fractures, and “malnutrition is common,” said Dr. Iuliano during her presentation.
Prior studies have reported that such residents have a daily dietary calcium intake of 635 mg (half the recommended 1,300 mg), a protein intake of 0.8 g/kg body weight (less than the recommended 1 g/kg body weight), and a dairy intake of 1.5 servings (about a third of the recommended amount), she said.
The group hypothesized that upping dairy intake of elderly residents living in long-term care institutions would reduce the risk of fractures. They performed a 2-year cluster-randomized trial in 60 facilities in Melbourne and surrounding areas.
Half gave their 3,301 residents menus with a higher dairy content, and the other half gave their 3,894 residents (controls) the usual menus.
The residents in both groups had similar characteristics: they were a mean age of 87 years and 68% were women. A subgroup had blood tests and bone morphology studies at baseline and 1 year.
Researchers verified nutrient intake by analyzing the menus and doing plate waste analysis for a subgroup, and they determined the number of falls and fractures from incident and hospital x-ray reports, respectively.
One-third fewer fractures in the higher-dairy group
At the study start, residents in both groups had similar vitamin D levels (72 nmol/L) and bone morphology. They were consuming two servings of dairy food and drink a day, where a serving was 250 mL of milk (including lactose-free milk) or 200 g of yogurt or 40 g of cheese.
Their initial daily calcium intake was 650 mg, which stayed the same in the control group, but increased to >1100 mg in the intervention group.
Their initial daily protein intake was around 59 g, which remained the same in the control group, but increased to about 72 grams (1.1 g/kg body weight) in the intervention group.
At 2 years, the 1.5 servings/day increase in dairy intake in the control versus intervention group was associated with an 11% reduction in falls (62% vs. 57%), a 33% reduction in fractures (5.2% vs. 3.7%), a 46% reduction in hip fractures (2.4% vs. 1.3%), and no difference in mortality (28% in both groups).
The intervention was also associated with a slowing in bone loss and an increase in insulinlike growth factor–1.
Four dairy servings a day “is high”
Dr. Willett said that “it is reasonable for seniors to take one or two servings of dairy per day, but four servings per day, as in this study, is probably not necessary.”
Moreover, “dairy production has a major impact on greenhouse gas emissions, and even two servings per day would not be environmentally sustainable if everyone were to consume this amount,” he observed.
“Because the world is facing an existential threat from climate change, general advice to consume high amounts of dairy products would be irresponsible as we can get all essential nutrients from other sources,” he added. “That said, modest amounts of dairy foods, such as one to two servings per day could be reasonable. There is some suggestive evidence that dairy in the form of yogurt may have particular benefits.”
The study was funded by Melbourne University and various dietary councils. Dr. Iuliano reported receiving lecture fees from Abbott. Dr. Rosen and Dr. Willett reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Consuming more milk, cheese, or yogurt might be a simple, low-cost way to boost bone health and prevent some falls and fractures in older people living in long-term care facilities, according to a new randomized study from Australia.
“Supplementation using dairy foods is likely to be an effective, safe, widely available, and low cost means of curtailing the public health burden of fractures,” said Sandra Iuliano, PhD, from the University of Melbourne, who presented the findings during the virtual American Society of Bone and Mineral Research 2020 annual meeting.
The researchers randomized 60 old-age institutions to provide residents with their usual menus or a diet with more milk, cheese, or yogurt for 2 years.
The residents with the altered menus increased their dairy consumption from 2 servings/day to 3.5 servings/day, which was reflected in a greater intake of calcium and protein, along with fewer falls, total fractures, and hip fractures than in the control group.
“This is the first randomized trial to show a benefit of dairy food intake on risk of fractures,” Walter Willett, MD, DrPH, professor of nutrition and epidemiology at the Harvard School of Public Health, Boston, said in an interview.
The results are “not surprising” because supplements of calcium plus vitamin D have reduced the risk of fractures in a similar population of older residents living in special living facilities, said Dr. Willett, coauthor of a recent review article, “Milk and Health,” published in the New England Journal of Medicine.
“It is important for everyone to have adequate intake of calcium and vitamin D,” he said. However, “it isn’t clear whether it is better to ensure this clinically by supplements, overall healthy diet, or extra dairy intake,” he added, noting that consuming the amount of dairy given in this Australian study is not environmentally sustainable.
Clifford Rosen, MD, professor of medicine, Tufts University, Boston, said in an interview that the Australian researchers studied the impact of increased dietary calcium and protein, not the impact of vitamin D via supplements.
“This is progress toward getting interventions to our most needy residents to prevent fractures – probably the most compelling data that we have had in a number of years,” he noted.
The current study shows “it’s not [the] vitamin D,” because the residents had initial low calcium levels but normal vitamin D levels. “For too long we’ve been stuck on the idea that it is [increasing] vitamin D in the elderly that causes a reduction in fractures,” said Dr. Rosen. “The data are not very supportive of it, but people continue to think that’s the most important element.”
On the other hand, the current study raises certain questions. “What we don’t know is, is it the calcium, or is it the protein, or the combination, that had an impact?”
Would upping dairy decrease falls?
Older adults living in institutions have a high risk of falls and fractures, including hip fractures, and “malnutrition is common,” said Dr. Iuliano during her presentation.
Prior studies have reported that such residents have a daily dietary calcium intake of 635 mg (half the recommended 1,300 mg), a protein intake of 0.8 g/kg body weight (less than the recommended 1 g/kg body weight), and a dairy intake of 1.5 servings (about a third of the recommended amount), she said.
The group hypothesized that upping dairy intake of elderly residents living in long-term care institutions would reduce the risk of fractures. They performed a 2-year cluster-randomized trial in 60 facilities in Melbourne and surrounding areas.
Half gave their 3,301 residents menus with a higher dairy content, and the other half gave their 3,894 residents (controls) the usual menus.
The residents in both groups had similar characteristics: they were a mean age of 87 years and 68% were women. A subgroup had blood tests and bone morphology studies at baseline and 1 year.
Researchers verified nutrient intake by analyzing the menus and doing plate waste analysis for a subgroup, and they determined the number of falls and fractures from incident and hospital x-ray reports, respectively.
One-third fewer fractures in the higher-dairy group
At the study start, residents in both groups had similar vitamin D levels (72 nmol/L) and bone morphology. They were consuming two servings of dairy food and drink a day, where a serving was 250 mL of milk (including lactose-free milk) or 200 g of yogurt or 40 g of cheese.
Their initial daily calcium intake was 650 mg, which stayed the same in the control group, but increased to >1100 mg in the intervention group.
Their initial daily protein intake was around 59 g, which remained the same in the control group, but increased to about 72 grams (1.1 g/kg body weight) in the intervention group.
At 2 years, the 1.5 servings/day increase in dairy intake in the control versus intervention group was associated with an 11% reduction in falls (62% vs. 57%), a 33% reduction in fractures (5.2% vs. 3.7%), a 46% reduction in hip fractures (2.4% vs. 1.3%), and no difference in mortality (28% in both groups).
The intervention was also associated with a slowing in bone loss and an increase in insulinlike growth factor–1.
Four dairy servings a day “is high”
Dr. Willett said that “it is reasonable for seniors to take one or two servings of dairy per day, but four servings per day, as in this study, is probably not necessary.”
Moreover, “dairy production has a major impact on greenhouse gas emissions, and even two servings per day would not be environmentally sustainable if everyone were to consume this amount,” he observed.
“Because the world is facing an existential threat from climate change, general advice to consume high amounts of dairy products would be irresponsible as we can get all essential nutrients from other sources,” he added. “That said, modest amounts of dairy foods, such as one to two servings per day could be reasonable. There is some suggestive evidence that dairy in the form of yogurt may have particular benefits.”
The study was funded by Melbourne University and various dietary councils. Dr. Iuliano reported receiving lecture fees from Abbott. Dr. Rosen and Dr. Willett reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Consuming more milk, cheese, or yogurt might be a simple, low-cost way to boost bone health and prevent some falls and fractures in older people living in long-term care facilities, according to a new randomized study from Australia.
“Supplementation using dairy foods is likely to be an effective, safe, widely available, and low cost means of curtailing the public health burden of fractures,” said Sandra Iuliano, PhD, from the University of Melbourne, who presented the findings during the virtual American Society of Bone and Mineral Research 2020 annual meeting.
The researchers randomized 60 old-age institutions to provide residents with their usual menus or a diet with more milk, cheese, or yogurt for 2 years.
The residents with the altered menus increased their dairy consumption from 2 servings/day to 3.5 servings/day, which was reflected in a greater intake of calcium and protein, along with fewer falls, total fractures, and hip fractures than in the control group.
“This is the first randomized trial to show a benefit of dairy food intake on risk of fractures,” Walter Willett, MD, DrPH, professor of nutrition and epidemiology at the Harvard School of Public Health, Boston, said in an interview.
The results are “not surprising” because supplements of calcium plus vitamin D have reduced the risk of fractures in a similar population of older residents living in special living facilities, said Dr. Willett, coauthor of a recent review article, “Milk and Health,” published in the New England Journal of Medicine.
“It is important for everyone to have adequate intake of calcium and vitamin D,” he said. However, “it isn’t clear whether it is better to ensure this clinically by supplements, overall healthy diet, or extra dairy intake,” he added, noting that consuming the amount of dairy given in this Australian study is not environmentally sustainable.
Clifford Rosen, MD, professor of medicine, Tufts University, Boston, said in an interview that the Australian researchers studied the impact of increased dietary calcium and protein, not the impact of vitamin D via supplements.
“This is progress toward getting interventions to our most needy residents to prevent fractures – probably the most compelling data that we have had in a number of years,” he noted.
The current study shows “it’s not [the] vitamin D,” because the residents had initial low calcium levels but normal vitamin D levels. “For too long we’ve been stuck on the idea that it is [increasing] vitamin D in the elderly that causes a reduction in fractures,” said Dr. Rosen. “The data are not very supportive of it, but people continue to think that’s the most important element.”
On the other hand, the current study raises certain questions. “What we don’t know is, is it the calcium, or is it the protein, or the combination, that had an impact?”
Would upping dairy decrease falls?
Older adults living in institutions have a high risk of falls and fractures, including hip fractures, and “malnutrition is common,” said Dr. Iuliano during her presentation.
Prior studies have reported that such residents have a daily dietary calcium intake of 635 mg (half the recommended 1,300 mg), a protein intake of 0.8 g/kg body weight (less than the recommended 1 g/kg body weight), and a dairy intake of 1.5 servings (about a third of the recommended amount), she said.
The group hypothesized that upping dairy intake of elderly residents living in long-term care institutions would reduce the risk of fractures. They performed a 2-year cluster-randomized trial in 60 facilities in Melbourne and surrounding areas.
Half gave their 3,301 residents menus with a higher dairy content, and the other half gave their 3,894 residents (controls) the usual menus.
The residents in both groups had similar characteristics: they were a mean age of 87 years and 68% were women. A subgroup had blood tests and bone morphology studies at baseline and 1 year.
Researchers verified nutrient intake by analyzing the menus and doing plate waste analysis for a subgroup, and they determined the number of falls and fractures from incident and hospital x-ray reports, respectively.
One-third fewer fractures in the higher-dairy group
At the study start, residents in both groups had similar vitamin D levels (72 nmol/L) and bone morphology. They were consuming two servings of dairy food and drink a day, where a serving was 250 mL of milk (including lactose-free milk) or 200 g of yogurt or 40 g of cheese.
Their initial daily calcium intake was 650 mg, which stayed the same in the control group, but increased to >1100 mg in the intervention group.
Their initial daily protein intake was around 59 g, which remained the same in the control group, but increased to about 72 grams (1.1 g/kg body weight) in the intervention group.
At 2 years, the 1.5 servings/day increase in dairy intake in the control versus intervention group was associated with an 11% reduction in falls (62% vs. 57%), a 33% reduction in fractures (5.2% vs. 3.7%), a 46% reduction in hip fractures (2.4% vs. 1.3%), and no difference in mortality (28% in both groups).
The intervention was also associated with a slowing in bone loss and an increase in insulinlike growth factor–1.
Four dairy servings a day “is high”
Dr. Willett said that “it is reasonable for seniors to take one or two servings of dairy per day, but four servings per day, as in this study, is probably not necessary.”
Moreover, “dairy production has a major impact on greenhouse gas emissions, and even two servings per day would not be environmentally sustainable if everyone were to consume this amount,” he observed.
“Because the world is facing an existential threat from climate change, general advice to consume high amounts of dairy products would be irresponsible as we can get all essential nutrients from other sources,” he added. “That said, modest amounts of dairy foods, such as one to two servings per day could be reasonable. There is some suggestive evidence that dairy in the form of yogurt may have particular benefits.”
The study was funded by Melbourne University and various dietary councils. Dr. Iuliano reported receiving lecture fees from Abbott. Dr. Rosen and Dr. Willett reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM ASBMR 2020
VA Looks to Increase Real-World Impact of Clinical Research
The US Department of Veterans Affairs (VA) is embracing clinical trials with a focus on oncology, and patients will benefit from new priorities and programs, VA officials reported at the Association of VA Hematology/Oncology (AVAHO) virtual meeting. “The whole model is one that is far more proactive,” said Carolyn Clancy, MD, Under Secretary for Health for Discovery, Education, and Affiliate Networks.
According to Clancy, the department’s top research priority is to increase veteran access to high-quality clinical trials. “Priority number 2 is increasing the real-world impact of VA research,” she said. “Our commitment to veterans and the taxpayers is to reverse and shorten the [research-to-implementation] timeline. And the third priority is to put VA data to work for veterans, not just through people who work in VA and Veterans Health Administration, but through other researchers who can have access to them.”
To meet these goals, VA is engaging in multiple research programs and collaborations. Rachel B. Ramoni, DMD, ScD, the VA chief research and development officer, highlighted a number of the projects in a separate AVAHO meeting presentation, including:
- The National Cancer Institute and VA Interagency Group to Accelerate Trials Enrollment (NAVIGATE), an interagency collaboration between the VA and the National Cancer Institute (NCI). This program established a network of sites to help enrolled veterans take part in NCI-supported clinical trials. “It really got up and running in 2018, and I’m proud to say that over 250 veterans have been enrolled, and enrollment exceeds that at non-NAVIGATE sites,” Ramoni reported. “Clearly, the additional support that these sites are getting is really helping to achieve the outcome of getting more veterans access to these trials.” However, she said, some areas of the nation aren’t yet covered by the program.
- The Precision Oncology Program for Cancer of the Prostate (POPCaP), established through a partnership with the Prostate Cancer Foundation. The foundation provided a $50 million investment. “This program ensures that veterans, no matter where they are, get best-in-class prostate cancer care,” Ramoni explained. “The initial focus was ensuring that men get sequencing if they have metastatic prostate cancer, and that they get access to clinical trials. The really distinguishing factor about POPCaP is that it has built a vibrant community of clinicians, researchers and program offices. The whole is much greater than the sum of its parts.” More POPCaP hubs are in development, she said.
- PATCH (Prostate Cancer Analysis for Therapy Choice), a program funded by the VA and the Prostate Cancer Foundation. “The whole purpose of PATCH is to create this network of sites to systematically go through different clinical trials that are biomarker-driven,” Ramoni said. “One of the great things about PATCH is that it’s leveraging the genetics databases to help proactively identify men who might qualify for these trials and to find them wherever they might be across the system so they have access to these trials.” She also praised the program’s commitment to collaboration and mentorship. “If you’re new to putting together clinical trials concepts or to submitting merit proposals to VA for funding, PATCH is a great place to get into a community that’s supportive and wants to help you succeed.”
- The VA Phenomics Library. This library, based at the Boston VA Medical Center, focuses on improving the analysis of “messy” electronic health record data, Ramoni noted. “There are automated algorithms that go through and help you clean up that data to make sense of it,” she said. “The problem is that it’s really been an every-person-for-himself-or-herself system. Each researcher who needed these phenotypes was creating his or her own.” The Phenomics Library will promote sharing “so there’s not going to be as much wasted time duplicating effort,” she said. “By the end of fiscal year 2021, we will have over 1,000 curated phenotypes in there. We hope that will be a great resource for the oncology community as well as many other communities.”
- Access to Clinical Trials (ACT) for Veterans. “This program, which began a couple of years ago, has really succeeded,” Ramoni said. “We were focusing on decreasing the time it takes to start up multi-site industry trials. When we got started with ACT, it was taking over 200 days to get started. And now, just a couple years later, we are well under 100 days, which is within industry standards.” Also, she said, the VA established a Partnered Research Program office, “which serves to interact with our industry partners and really guide them through the VA system, which can be complex if you’re approaching it for the first time.”
In a separate presentation, Krissa Caroff, MS, CPC, program manager of the Partnered Research Program, said it had quickened the process of implementing clinical trials by tackling roadblocks such as the need for multiple master agreements to be signed. Central coordination has been key, she said, “and we are working closely to ensure that we when have a multisite trial, all the VA sites are utilizing the same single IRB [institutional review board]. We’ve also identified the critical information that we need to collect from industry in order for us to evaluate a trial.”
What’s next? “We really are going to be focusing on oncology trials,” Ramoni insisted. “This is a high priority for us.” She added: “Please share your feedback and experiences with us. And also please communicate amongst your colleagues within your organization to explain how we’re standardizing things within VA.”
The speakers reported no relevant disclosures.
The US Department of Veterans Affairs (VA) is embracing clinical trials with a focus on oncology, and patients will benefit from new priorities and programs, VA officials reported at the Association of VA Hematology/Oncology (AVAHO) virtual meeting. “The whole model is one that is far more proactive,” said Carolyn Clancy, MD, Under Secretary for Health for Discovery, Education, and Affiliate Networks.
According to Clancy, the department’s top research priority is to increase veteran access to high-quality clinical trials. “Priority number 2 is increasing the real-world impact of VA research,” she said. “Our commitment to veterans and the taxpayers is to reverse and shorten the [research-to-implementation] timeline. And the third priority is to put VA data to work for veterans, not just through people who work in VA and Veterans Health Administration, but through other researchers who can have access to them.”
To meet these goals, VA is engaging in multiple research programs and collaborations. Rachel B. Ramoni, DMD, ScD, the VA chief research and development officer, highlighted a number of the projects in a separate AVAHO meeting presentation, including:
- The National Cancer Institute and VA Interagency Group to Accelerate Trials Enrollment (NAVIGATE), an interagency collaboration between the VA and the National Cancer Institute (NCI). This program established a network of sites to help enrolled veterans take part in NCI-supported clinical trials. “It really got up and running in 2018, and I’m proud to say that over 250 veterans have been enrolled, and enrollment exceeds that at non-NAVIGATE sites,” Ramoni reported. “Clearly, the additional support that these sites are getting is really helping to achieve the outcome of getting more veterans access to these trials.” However, she said, some areas of the nation aren’t yet covered by the program.
- The Precision Oncology Program for Cancer of the Prostate (POPCaP), established through a partnership with the Prostate Cancer Foundation. The foundation provided a $50 million investment. “This program ensures that veterans, no matter where they are, get best-in-class prostate cancer care,” Ramoni explained. “The initial focus was ensuring that men get sequencing if they have metastatic prostate cancer, and that they get access to clinical trials. The really distinguishing factor about POPCaP is that it has built a vibrant community of clinicians, researchers and program offices. The whole is much greater than the sum of its parts.” More POPCaP hubs are in development, she said.
- PATCH (Prostate Cancer Analysis for Therapy Choice), a program funded by the VA and the Prostate Cancer Foundation. “The whole purpose of PATCH is to create this network of sites to systematically go through different clinical trials that are biomarker-driven,” Ramoni said. “One of the great things about PATCH is that it’s leveraging the genetics databases to help proactively identify men who might qualify for these trials and to find them wherever they might be across the system so they have access to these trials.” She also praised the program’s commitment to collaboration and mentorship. “If you’re new to putting together clinical trials concepts or to submitting merit proposals to VA for funding, PATCH is a great place to get into a community that’s supportive and wants to help you succeed.”
- The VA Phenomics Library. This library, based at the Boston VA Medical Center, focuses on improving the analysis of “messy” electronic health record data, Ramoni noted. “There are automated algorithms that go through and help you clean up that data to make sense of it,” she said. “The problem is that it’s really been an every-person-for-himself-or-herself system. Each researcher who needed these phenotypes was creating his or her own.” The Phenomics Library will promote sharing “so there’s not going to be as much wasted time duplicating effort,” she said. “By the end of fiscal year 2021, we will have over 1,000 curated phenotypes in there. We hope that will be a great resource for the oncology community as well as many other communities.”
- Access to Clinical Trials (ACT) for Veterans. “This program, which began a couple of years ago, has really succeeded,” Ramoni said. “We were focusing on decreasing the time it takes to start up multi-site industry trials. When we got started with ACT, it was taking over 200 days to get started. And now, just a couple years later, we are well under 100 days, which is within industry standards.” Also, she said, the VA established a Partnered Research Program office, “which serves to interact with our industry partners and really guide them through the VA system, which can be complex if you’re approaching it for the first time.”
In a separate presentation, Krissa Caroff, MS, CPC, program manager of the Partnered Research Program, said it had quickened the process of implementing clinical trials by tackling roadblocks such as the need for multiple master agreements to be signed. Central coordination has been key, she said, “and we are working closely to ensure that we when have a multisite trial, all the VA sites are utilizing the same single IRB [institutional review board]. We’ve also identified the critical information that we need to collect from industry in order for us to evaluate a trial.”
What’s next? “We really are going to be focusing on oncology trials,” Ramoni insisted. “This is a high priority for us.” She added: “Please share your feedback and experiences with us. And also please communicate amongst your colleagues within your organization to explain how we’re standardizing things within VA.”
The speakers reported no relevant disclosures.
The US Department of Veterans Affairs (VA) is embracing clinical trials with a focus on oncology, and patients will benefit from new priorities and programs, VA officials reported at the Association of VA Hematology/Oncology (AVAHO) virtual meeting. “The whole model is one that is far more proactive,” said Carolyn Clancy, MD, Under Secretary for Health for Discovery, Education, and Affiliate Networks.
According to Clancy, the department’s top research priority is to increase veteran access to high-quality clinical trials. “Priority number 2 is increasing the real-world impact of VA research,” she said. “Our commitment to veterans and the taxpayers is to reverse and shorten the [research-to-implementation] timeline. And the third priority is to put VA data to work for veterans, not just through people who work in VA and Veterans Health Administration, but through other researchers who can have access to them.”
To meet these goals, VA is engaging in multiple research programs and collaborations. Rachel B. Ramoni, DMD, ScD, the VA chief research and development officer, highlighted a number of the projects in a separate AVAHO meeting presentation, including:
- The National Cancer Institute and VA Interagency Group to Accelerate Trials Enrollment (NAVIGATE), an interagency collaboration between the VA and the National Cancer Institute (NCI). This program established a network of sites to help enrolled veterans take part in NCI-supported clinical trials. “It really got up and running in 2018, and I’m proud to say that over 250 veterans have been enrolled, and enrollment exceeds that at non-NAVIGATE sites,” Ramoni reported. “Clearly, the additional support that these sites are getting is really helping to achieve the outcome of getting more veterans access to these trials.” However, she said, some areas of the nation aren’t yet covered by the program.
- The Precision Oncology Program for Cancer of the Prostate (POPCaP), established through a partnership with the Prostate Cancer Foundation. The foundation provided a $50 million investment. “This program ensures that veterans, no matter where they are, get best-in-class prostate cancer care,” Ramoni explained. “The initial focus was ensuring that men get sequencing if they have metastatic prostate cancer, and that they get access to clinical trials. The really distinguishing factor about POPCaP is that it has built a vibrant community of clinicians, researchers and program offices. The whole is much greater than the sum of its parts.” More POPCaP hubs are in development, she said.
- PATCH (Prostate Cancer Analysis for Therapy Choice), a program funded by the VA and the Prostate Cancer Foundation. “The whole purpose of PATCH is to create this network of sites to systematically go through different clinical trials that are biomarker-driven,” Ramoni said. “One of the great things about PATCH is that it’s leveraging the genetics databases to help proactively identify men who might qualify for these trials and to find them wherever they might be across the system so they have access to these trials.” She also praised the program’s commitment to collaboration and mentorship. “If you’re new to putting together clinical trials concepts or to submitting merit proposals to VA for funding, PATCH is a great place to get into a community that’s supportive and wants to help you succeed.”
- The VA Phenomics Library. This library, based at the Boston VA Medical Center, focuses on improving the analysis of “messy” electronic health record data, Ramoni noted. “There are automated algorithms that go through and help you clean up that data to make sense of it,” she said. “The problem is that it’s really been an every-person-for-himself-or-herself system. Each researcher who needed these phenotypes was creating his or her own.” The Phenomics Library will promote sharing “so there’s not going to be as much wasted time duplicating effort,” she said. “By the end of fiscal year 2021, we will have over 1,000 curated phenotypes in there. We hope that will be a great resource for the oncology community as well as many other communities.”
- Access to Clinical Trials (ACT) for Veterans. “This program, which began a couple of years ago, has really succeeded,” Ramoni said. “We were focusing on decreasing the time it takes to start up multi-site industry trials. When we got started with ACT, it was taking over 200 days to get started. And now, just a couple years later, we are well under 100 days, which is within industry standards.” Also, she said, the VA established a Partnered Research Program office, “which serves to interact with our industry partners and really guide them through the VA system, which can be complex if you’re approaching it for the first time.”
In a separate presentation, Krissa Caroff, MS, CPC, program manager of the Partnered Research Program, said it had quickened the process of implementing clinical trials by tackling roadblocks such as the need for multiple master agreements to be signed. Central coordination has been key, she said, “and we are working closely to ensure that we when have a multisite trial, all the VA sites are utilizing the same single IRB [institutional review board]. We’ve also identified the critical information that we need to collect from industry in order for us to evaluate a trial.”
What’s next? “We really are going to be focusing on oncology trials,” Ramoni insisted. “This is a high priority for us.” She added: “Please share your feedback and experiences with us. And also please communicate amongst your colleagues within your organization to explain how we’re standardizing things within VA.”
The speakers reported no relevant disclosures.
Researchers examine learning curve for gender-affirming vaginoplasty
research suggests. For one surgeon, certain adverse events, including the need for revision surgery, were less likely after 50 cases.
“As surgical programs evolve, the important question becomes: At what case threshold are cases performed safely, efficiently, and with favorable outcomes?” said Cecile A. Ferrando, MD, MPH, program director of the female pelvic medicine and reconstructive surgery fellowship at Cleveland Clinic and director of the transgender surgery and medicine program in the Cleveland Clinic’s Center for LGBT Care.
The answer could guide training for future surgeons, Dr. Ferrando said at the virtual annual scientific meeting of the Society of Gynecologic Surgeons. Future studies should include patient-centered outcomes and data from multiple centers, other doctors said.
Transgender women who opt to surgically transition may undergo vaginoplasty. Although many reports describe surgical techniques, “there is a paucity of evidence-based data as well as few reports on outcomes,” Dr. Ferrando noted.
To describe perioperative adverse events related to vaginoplasty performed for gender affirmation and determine a minimum number of cases needed to reduce their likelihood, Dr. Ferrando performed a retrospective study of 76 patients. The patients underwent surgery between December 2015 and March 2019 and had 6-month postoperative outcomes available. Dr. Ferrando performed the procedures.
Dr. Ferrando evaluated outcomes after increments of 10 cases. After 50 cases, the median surgical time decreased to approximately 180 minutes, which an informal survey of surgeons suggested was efficient, and the rates of adverse events were similar to those in other studies. Dr. Ferrando compared outcomes from the first 50 cases with outcomes from the 26 cases that followed.
Overall, the patients had a mean age of 41 years. The first 50 patients were older on average (44 years vs. 35 years). About 83% underwent full-depth vaginoplasty. The incidence of intraoperative and immediate postoperative events was low and did not differ between the two groups. Rates of delayed postoperative events – those occurring 30 or more days after surgery – did significantly differ between the two groups, however.
After 50 cases, there was a lower incidence of urinary stream abnormalities (7.7% vs. 16.3%), introital stenosis (3.9% vs. 12%), and revision surgery (that is, elective, cosmetic, or functional revision within 6 months; 19.2% vs. 44%), compared with the first 50 cases.
The study did not include patient-centered outcomes and the results may have limited generalizability, Dr. Ferrando noted. “The incidence of serious adverse events related to vaginoplasty is low while minor events are common,” she said. “A 50-case minimum may be an adequate case number target for postgraduate trainees learning how to do this surgery.”
“I learned that the incidence of serious complications, like injuries during the surgery, or serious events immediately after surgery was quite low, which was reassuring,” Dr. Ferrando said in a later interview. “The cosmetic result and detail that is involved with the surgery – something that is very important to patients – that skill set takes time and experience to refine.”
Subsequent studies should include patient-centered outcomes, which may help surgeons understand potential “sources of consternation for patients,” such as persistent corporal tissue, poor aesthetics, vaginal stenosis, urinary meatus location, and clitoral hooding, Joseph J. Pariser, MD, commented in an interview. Dr. Pariser, a urologist who specializes in gender care at the University of Minnesota in Minneapolis, in 2019 reviewed safety outcomes from published case series.
“In my own practice, precise placement of the urethra, familiarity with landmarks during canal dissection, and rapidity of working through steps of the surgery have all dramatically improved as our experience at University of Minnesota performing primary vaginoplasty has grown,” Dr. Pariser said.
Optimal case thresholds may vary depending on a surgeon’s background, Rachel M. Whynott, MD, a reproductive endocrinology and infertility fellow at the University of Iowa in Iowa City, said in an interview. At the University of Kansas in Kansas City, a multidisciplinary team that includes a gynecologist, a reconstructive urologist, and a plastic surgeon performs the procedure.
Dr. Whynott and colleagues recently published a retrospective study that evaluated surgical aptitude over time in a male-to-female penoscrotal vaginoplasty program . Their analysis of 43 cases identified a learning curve that was reflected in overall time in the operating room and time to neoclitoral sensation.
Investigators are “trying to add to the growing body of literature about this procedure and how we can best go about improving outcomes for our patients and improving this surgery,” Dr. Whynott said. A study that includes data from multiple centers would be useful, she added.
Dr. Ferrando disclosed authorship royalties from UpToDate. Dr. Pariser and Dr. Whynott had no relevant financial disclosures.
SOURCE: Ferrando C. SGS 2020, Abstract 09.
research suggests. For one surgeon, certain adverse events, including the need for revision surgery, were less likely after 50 cases.
“As surgical programs evolve, the important question becomes: At what case threshold are cases performed safely, efficiently, and with favorable outcomes?” said Cecile A. Ferrando, MD, MPH, program director of the female pelvic medicine and reconstructive surgery fellowship at Cleveland Clinic and director of the transgender surgery and medicine program in the Cleveland Clinic’s Center for LGBT Care.
The answer could guide training for future surgeons, Dr. Ferrando said at the virtual annual scientific meeting of the Society of Gynecologic Surgeons. Future studies should include patient-centered outcomes and data from multiple centers, other doctors said.
Transgender women who opt to surgically transition may undergo vaginoplasty. Although many reports describe surgical techniques, “there is a paucity of evidence-based data as well as few reports on outcomes,” Dr. Ferrando noted.
To describe perioperative adverse events related to vaginoplasty performed for gender affirmation and determine a minimum number of cases needed to reduce their likelihood, Dr. Ferrando performed a retrospective study of 76 patients. The patients underwent surgery between December 2015 and March 2019 and had 6-month postoperative outcomes available. Dr. Ferrando performed the procedures.
Dr. Ferrando evaluated outcomes after increments of 10 cases. After 50 cases, the median surgical time decreased to approximately 180 minutes, which an informal survey of surgeons suggested was efficient, and the rates of adverse events were similar to those in other studies. Dr. Ferrando compared outcomes from the first 50 cases with outcomes from the 26 cases that followed.
Overall, the patients had a mean age of 41 years. The first 50 patients were older on average (44 years vs. 35 years). About 83% underwent full-depth vaginoplasty. The incidence of intraoperative and immediate postoperative events was low and did not differ between the two groups. Rates of delayed postoperative events – those occurring 30 or more days after surgery – did significantly differ between the two groups, however.
After 50 cases, there was a lower incidence of urinary stream abnormalities (7.7% vs. 16.3%), introital stenosis (3.9% vs. 12%), and revision surgery (that is, elective, cosmetic, or functional revision within 6 months; 19.2% vs. 44%), compared with the first 50 cases.
The study did not include patient-centered outcomes and the results may have limited generalizability, Dr. Ferrando noted. “The incidence of serious adverse events related to vaginoplasty is low while minor events are common,” she said. “A 50-case minimum may be an adequate case number target for postgraduate trainees learning how to do this surgery.”
“I learned that the incidence of serious complications, like injuries during the surgery, or serious events immediately after surgery was quite low, which was reassuring,” Dr. Ferrando said in a later interview. “The cosmetic result and detail that is involved with the surgery – something that is very important to patients – that skill set takes time and experience to refine.”
Subsequent studies should include patient-centered outcomes, which may help surgeons understand potential “sources of consternation for patients,” such as persistent corporal tissue, poor aesthetics, vaginal stenosis, urinary meatus location, and clitoral hooding, Joseph J. Pariser, MD, commented in an interview. Dr. Pariser, a urologist who specializes in gender care at the University of Minnesota in Minneapolis, in 2019 reviewed safety outcomes from published case series.
“In my own practice, precise placement of the urethra, familiarity with landmarks during canal dissection, and rapidity of working through steps of the surgery have all dramatically improved as our experience at University of Minnesota performing primary vaginoplasty has grown,” Dr. Pariser said.
Optimal case thresholds may vary depending on a surgeon’s background, Rachel M. Whynott, MD, a reproductive endocrinology and infertility fellow at the University of Iowa in Iowa City, said in an interview. At the University of Kansas in Kansas City, a multidisciplinary team that includes a gynecologist, a reconstructive urologist, and a plastic surgeon performs the procedure.
Dr. Whynott and colleagues recently published a retrospective study that evaluated surgical aptitude over time in a male-to-female penoscrotal vaginoplasty program . Their analysis of 43 cases identified a learning curve that was reflected in overall time in the operating room and time to neoclitoral sensation.
Investigators are “trying to add to the growing body of literature about this procedure and how we can best go about improving outcomes for our patients and improving this surgery,” Dr. Whynott said. A study that includes data from multiple centers would be useful, she added.
Dr. Ferrando disclosed authorship royalties from UpToDate. Dr. Pariser and Dr. Whynott had no relevant financial disclosures.
SOURCE: Ferrando C. SGS 2020, Abstract 09.
research suggests. For one surgeon, certain adverse events, including the need for revision surgery, were less likely after 50 cases.
“As surgical programs evolve, the important question becomes: At what case threshold are cases performed safely, efficiently, and with favorable outcomes?” said Cecile A. Ferrando, MD, MPH, program director of the female pelvic medicine and reconstructive surgery fellowship at Cleveland Clinic and director of the transgender surgery and medicine program in the Cleveland Clinic’s Center for LGBT Care.
The answer could guide training for future surgeons, Dr. Ferrando said at the virtual annual scientific meeting of the Society of Gynecologic Surgeons. Future studies should include patient-centered outcomes and data from multiple centers, other doctors said.
Transgender women who opt to surgically transition may undergo vaginoplasty. Although many reports describe surgical techniques, “there is a paucity of evidence-based data as well as few reports on outcomes,” Dr. Ferrando noted.
To describe perioperative adverse events related to vaginoplasty performed for gender affirmation and determine a minimum number of cases needed to reduce their likelihood, Dr. Ferrando performed a retrospective study of 76 patients. The patients underwent surgery between December 2015 and March 2019 and had 6-month postoperative outcomes available. Dr. Ferrando performed the procedures.
Dr. Ferrando evaluated outcomes after increments of 10 cases. After 50 cases, the median surgical time decreased to approximately 180 minutes, which an informal survey of surgeons suggested was efficient, and the rates of adverse events were similar to those in other studies. Dr. Ferrando compared outcomes from the first 50 cases with outcomes from the 26 cases that followed.
Overall, the patients had a mean age of 41 years. The first 50 patients were older on average (44 years vs. 35 years). About 83% underwent full-depth vaginoplasty. The incidence of intraoperative and immediate postoperative events was low and did not differ between the two groups. Rates of delayed postoperative events – those occurring 30 or more days after surgery – did significantly differ between the two groups, however.
After 50 cases, there was a lower incidence of urinary stream abnormalities (7.7% vs. 16.3%), introital stenosis (3.9% vs. 12%), and revision surgery (that is, elective, cosmetic, or functional revision within 6 months; 19.2% vs. 44%), compared with the first 50 cases.
The study did not include patient-centered outcomes and the results may have limited generalizability, Dr. Ferrando noted. “The incidence of serious adverse events related to vaginoplasty is low while minor events are common,” she said. “A 50-case minimum may be an adequate case number target for postgraduate trainees learning how to do this surgery.”
“I learned that the incidence of serious complications, like injuries during the surgery, or serious events immediately after surgery was quite low, which was reassuring,” Dr. Ferrando said in a later interview. “The cosmetic result and detail that is involved with the surgery – something that is very important to patients – that skill set takes time and experience to refine.”
Subsequent studies should include patient-centered outcomes, which may help surgeons understand potential “sources of consternation for patients,” such as persistent corporal tissue, poor aesthetics, vaginal stenosis, urinary meatus location, and clitoral hooding, Joseph J. Pariser, MD, commented in an interview. Dr. Pariser, a urologist who specializes in gender care at the University of Minnesota in Minneapolis, in 2019 reviewed safety outcomes from published case series.
“In my own practice, precise placement of the urethra, familiarity with landmarks during canal dissection, and rapidity of working through steps of the surgery have all dramatically improved as our experience at University of Minnesota performing primary vaginoplasty has grown,” Dr. Pariser said.
Optimal case thresholds may vary depending on a surgeon’s background, Rachel M. Whynott, MD, a reproductive endocrinology and infertility fellow at the University of Iowa in Iowa City, said in an interview. At the University of Kansas in Kansas City, a multidisciplinary team that includes a gynecologist, a reconstructive urologist, and a plastic surgeon performs the procedure.
Dr. Whynott and colleagues recently published a retrospective study that evaluated surgical aptitude over time in a male-to-female penoscrotal vaginoplasty program . Their analysis of 43 cases identified a learning curve that was reflected in overall time in the operating room and time to neoclitoral sensation.
Investigators are “trying to add to the growing body of literature about this procedure and how we can best go about improving outcomes for our patients and improving this surgery,” Dr. Whynott said. A study that includes data from multiple centers would be useful, she added.
Dr. Ferrando disclosed authorship royalties from UpToDate. Dr. Pariser and Dr. Whynott had no relevant financial disclosures.
SOURCE: Ferrando C. SGS 2020, Abstract 09.
FROM SGS 2020
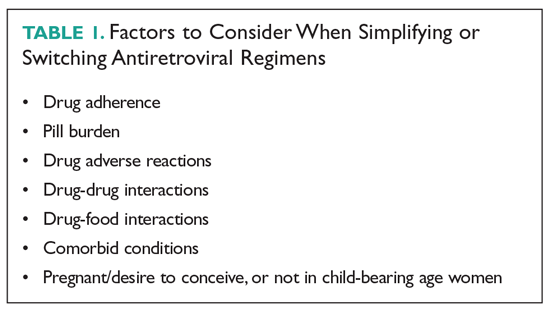
Simplifying or Switching Antiretroviral Therapy in Treatment-Experienced Adults Living With HIV
A 57-year-old man living with HIV has been followed at a local infectious disease clinic for more than 15 years. He acquired HIV disease through heterosexual contact. He lives alone and works at a convenience store; he has not been sexually active for the past 5 years. He smokes 10 cigarettes a day, but does not drink alcohol or use illicit drugs. He had been on coformulated emtricitabine/tenofovir disoproxil fumarate (TDF) and coformulated lopinavir/ritonavir, which he had taken conscientiously, since May 2008, without noticing any adverse reactions from this regimen. His HIV viral load had been undetectable, and his CD4 count had hovered between 600 and 700 cells/µL. Although he was on atorvastatin for dyslipidemia, his fasting lipid profile, performed in 2018, revealed a total cholesterol level of 200 mg/dL;triglyceride, 247 mg/dL; high-density lipoprotein (HDL), 43 mg/dL; and low-density lipoprotein (LDL), 132 mg/dL. In April 2019, his HIV regimen was switched to bictegravir/emtricitabine/tenofovir alafenamide (TAF). Blood tests performed in December 2019 revealed undetectable HIV viral load; an increased CD4 count to 849 cell/µL; total cholesterol, 140 mg/dL; triglyceride, 115 mg/dL; HDL, 60 mg/dL; and LDL, 90 mg/dL.
SIMPLIFYING ART
Virologically Suppressed Patients Without Drug-Resistant Virus
Treatment adherence is of paramount importance to ensure treatment success. Patients with a viral load that is undetectable or nearly undetectable without drug resistance could be taking ART regimens consisting of more than 1 pill and/or that require more than once-daily dosing. Decreasing pill burden or dosing frequency can help to improve adherence to treatment. In addition, older-generation ART agents are usually more toxic and less potent than newer-generation agents, so another important objective of switching older drugs to newer drugs is to decrease adverse reactions and improve virologic suppression. Selection of an ART regimen should be guided by the results of resistance testing (genotyping and phenotyping tests) and previous treatment history. After switching a patient’s ART regimen, plasma HIV viral load and CD4 count should be closely monitored.2 The following 3-drug, single-tablet, once-daily ART regimens can be used in patients who are virologically stable (ordered chronologically by FDA approval dates).
Efavirenz/Emtricitabine/TDF (Atripla)
Coformulated efavirenz/emtricitabine/TDF was the first single-tablet, once-daily, fixed-dose combination approved by the FDA (July 2006). Approval was based on a 48- week clinical trial involving 244 adults with HIV infection that showed that 80% of participants achieved a marked reduction in HIV viral load and a significant increase in CD4 cell count.3 Of the 3 components, efavirenz has unique central nervous system (CNS) adverse effects that could reduce adherence. Patients who were started on this fixed-dose combination commonly reported dizziness, headache, nightmare, insomnia, and impaired concentration.4 However, the CNS side effects resolved within the first 4 weeks of therapy, and less than 5% of patients quit taking the drug. Primate studies showed efavirenz is teratogenic, but studies in pregnant women did not find efavirenz to be more teratogenic than other ART agents.5
Emtricitabine/Rilpivirine/TDF (Complera)
Coformulated emtricitabine/rilpivirine/TDF was approved based on data from two 48-week, phase 3, double-blind, randomized controlled trials (ECHO and THRIVE) that evaluated the safety and efficacy of rilpivirine compared to efavirenz among treatment-naive adults with HIV infection.7,8 Rilpivirine is well tolerated and causes fewer CNS symptoms compared to efavirenz. The main caveat for rilpivirine is drug-drug interactions. It should not be coadministered with CYP inducers, such as rifampin, phenytoin, or St. John’s wort, as coadministration can cause subtherapeutic blood levels of rilpivirine. Because increased levels of rilpivirine can prolong QTc on electrocardiogram (ECG), an ECG should be obtained before starting an ART regimen that contains rilpivirine, especially in the presence of CYP 3A4 inhibitors.9
Elvitegravir/Cobicistat/Emtricitabine/TDF (Stribild)
This coformulation was approved based on data from 2 randomized, double-blind, controlled trials, Study 102 and Study 103, in treatment-naive patients with HIV (n = 1408). In Study 102, participants were randomized to receive either elvitegravir/cobicistat/emtricitabine/TDF or efavirenz/emtricitabine/TDF (Atripla).10 In Study 103, participants were randomized to receive either elvitegravir/cobicistat/emtricitabine/TDF or atazanavir + ritonavir + emtricitabine/TDF. In both studies, the primary endpoint was virologic success (HIV-1 RNA < 50 copies/mL) at 48 weeks, and elvitegravir/cobicistat/emtricitabine/TDF was noninferior compared to the other regimens.11
Abacavir/Dolutegravir/Lamivudine (Triumeq)
Approval of abacavir/dolutegravir/lamivudine (Triumeq) in August 2014 was based on SINGLE, a noninferiority trial involving 833 treatment-naive adults that compared dolutegravir and abacavir/lamivudine (the separate components of Triumeq) to efavirenz/emtricitabine/TDF. At 96 weeks, more patients in the dolutegravir and abacavir/lamivudine arm achieved an undetectable HIV viral load (80% versus 72%).13
Elvitegravir/Cobicistat/Emtricitabine/TAF (Genvoya)
Approval of coformulated elvitegravir/cobicistat/emtricitabine/TAF was supported by data from two 48-week phase 3, double-blind studies (Studies 104 and 111) involving 1733 treatment-naive patients that compared the regimen to elvitegravir/cobicistat/emtricitabine/TDF (Stribild). Both studies demonstrated that elvitegravir/cobicistat/emtricitabine/TAF was statistically noninferior, and it was favored in regard to certain renal and bone laboratory parameters.15 Studies comparing TAF and TDF have demonstrated that TAF is less likely to cause loss of bone mineral density and nephrotoxicity compared to TDF.16,17
Emtricitabine/Rilpivirine/TAF (Odefsey)
Coformulated emtricitabine/rilpivirine/TAF was approved based, in part, on positive bioequivalence studies demonstrating that it achieved similar drug levels of emtricitabine and TAF as coformulated elvitegravir/cobicistat/emtricitabine/TAF and similar drug levels of rilpivirine as individually dosed rilpivirine.18 The safety, efficacy, and tolerability of this coformulation is supported by clinical studies of rilpivirine-based therapy and emtricitabine/TAF-based therapy in a range of patients with HIV.18
Bictegravir/Emtricitabine/TAF (Biktarvy)
The coformulation bictegravir/emtricitabine/TAF was approved based on 4 phase 3 studies: Studies 1489 and 1490 in treatment-naive adults, and Studies 1844 and 1878 in virologically suppressed adults. In Study 1489, 629 treatment-naive adults were randomized 1:1 to receive coformulated bictegravir/emtricitabine/TAF or coformulated abacavir/dolutegravir/lamivudine. At week 48, similar percentages of patients in each arm achieved the primary endpoint of HIV-1 RNA < 50 copies/mL. In Study 1490, 645 treatment-naive adults were randomized 1:1 to receive coformulated bictegravir/emtricitabine/TAF or dolutegravir + emtricitabine/TAF. At week 48, similar percentages of patients in each arm achieved the primary endpoint of virologic success (HIV-1 RNA < 50 copies/mL).19,20
Darunavir/Cobicistat/Emtricitabine/TAF (Symtuza)
Approval of coformulated darunavir/cobicistat/emtricitabine/TAF was based on data from two 48-week, noninferiority, phase 3 studies that assessed the safety and efficacy of the coformulation versus a control regimen (darunavir/cobicistat plus emtricitabine/TDF) in adults with no prior ART history (AMBER) and in virologically suppressed adults (EMERALD). In the randomized, double-blind, multicenter controlled AMBER trial, at week 48, 91.4% of patients in the study group and 88.4% in the control group achieved viral suppression (HIV-1 RNA < 50 copies/mL), and virologic failure rates were low in both groups (HIV-1 RNA ≥ 50 copies/mL; 4.4% versus 3.3%, respectively).21
Doravirine/Lamivudine/TDF (Delstrigo)
Coformulated doravirine/lamivudine/TDF was approved based on data from 2 randomized, double-blind, controlled phase 3 trials, DRIVE-AHEAD and DRIVE-FORWARD. The former trial compared coformulated doravirine/lamivudine/TDF with efavirenz/emtricitabine/TDF in 728 treatment-naive patients. At 48 weeks, 84.3% in the doravirine/lamivudine/TDF arm and 80.8% in the efavirenz/emtricitabine/TDF arm met the primary endpoint of HIV-1 RNA < 50 copies/mL. Thus, doravirine/lamivudine/TDF showed sustained viral suppression and noninferiority compared to efavirenz/emtricitabine/TDF.23 The DRIVE-FORWARD trial investigated doravirine compared with ritonavir-boosted darunavir, each in combination with 2 NRTIs (TDF with emtricitabine or abacavir with lamivudine). At week 48, 84% of patients in the doravirine arm and 80% in the ritonavir-boosted darunavir arm achieved the primary endpoint of HIV-1 RNA < 50 copies/mL.24
Two-Drug, Single-Tablet, Once-Daily Regimens
Experts have long recommended that optimal treatment of HIV must consist of 3 active drugs, with trials both in the United States and Europe demonstrating decreased morbidity and mortality with 3-drug therapy.25,26 However, newer, more potent 2-drug therapy is giving more choices to people living with HIV. The single-tablet, 2-drug regimens currently available are dolutegravir/rilpivirine and dolutegravir/lamivudine. There are theoretical benefits of 2-drug therapy, such as minimizing long-term toxicities, avoidance of some drug-drug interactions, and preservation of drugs for future treatment options. At this time, a 2-drug simplification regimen can be a viable option for selected virologically stable populations.
Dolutegravir/Rilpivirine (Juluca)
Dolutegravir/rilpivirine has been shown to be noninferior to standard therapy at 48-weeks, although it is associated with a higher discontinuation rate because of side effects.27 This option can be particularly useful in patients who have contraindications to NRTIs or renal dysfunction, but it has been studied only in patients without resistance who are already virologically suppressed. Ongoing studies are looking at 2-versus 3-drug therapies for HIV treatment-experienced patients. Most of these use PIs as a backbone because of their potency and high barrier to resistance. The advent of second-generation integrase inhibitors offers additional options.
Dolutegravir/Lamivudine (Dovato)
The GEMINI-1 and GEMINI-2 trials demonstrated that dolutegravir/lamivudine was noninferior to dolutegravir/TDF/emtricitabine.28 Based on these 2 studies, new guidelines have added dolutegravir/lamivudine as a recommended first-line therapy. For now, the recommendation is to use dolutegravir/lamivudine in individuals where NRTIs are contraindicated, and it should not be used in patients with chronic hepatitis B. Additionally, 3 studies have demonstrated the safety and efficacy of switching to dolutegravir/lamivudine.29-31 In the TANGO trial, neither virologic failures nor resistant virus were identified at 48 weeks following the switch.32 Although there are benefits of simplification with this regimen, including lower toxicity, lower costs, and saving other NRTIs in case of resistance, there should be no rush to switch patients to a 2-drug regimen. This is a viable strategy in patients without baseline resistance who have preserved T-cells and do not have hepatitis B.
SWITCHING ART AGENTS IN SELECTED CLINICAL SCENARIOS
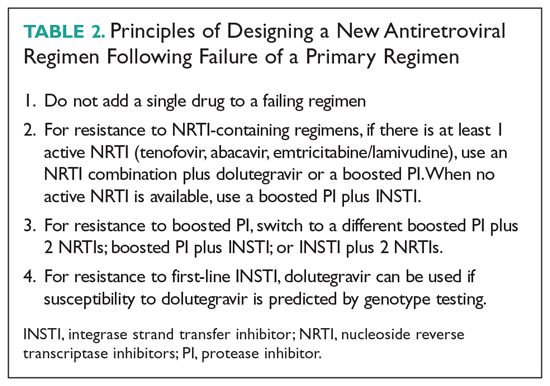
Virologic Failure
One of the main goals of ART is maximal and durable suppression of HIV viral load to prevent the development of drug-resistant mutations.2 When patients are unable to achieve durable virologic suppression or have virologic rebound, the cause of virologic failure needs to be investigated. Virologic failure is defined as the inability to achieve or maintain viral suppression to a level below 200 copies/mL, whereas rebound is defined as an HIV RNA level exceeding 200 copies/mL after virologic suppression.33 A common cause of virologic failure is patient nonadherence, which can be related to a range of factors, including psychosocial issues and affordability of medications. Innate viral resistance can be the result of transmitted drug resistance at the time of infection or be acquired during unsuppressed viral replication secondary to inherent error-prone reverse transcriptase.33 Pharmacokinetic factors that affect blood levels of ART, such as drug-drug interactions, also can be a key factor in HIV drug resistance.
Patients With Limited Treatment Options
Despite advances in ART, some patients exhaust the existing regimens, leading to development of multidrug resistance and limited treatment options. In light of the treatment challenges in this group of patients, the FDA has recently approved 2 antiretroviral agents to target multidrug-resistant HIV: ibalizumab and fostemsavir.
Pregnancy
ART is used during pregnancy to maintain the pregnant woman’s health and to prevent perinatal transmission. Pregnancy can present unique challenges to effective ART, and therapy decisions should be made based on short-term and long-term safety data, pharmacokinetics, and tolerability. With few exceptions, women who are on a stable ART regimen and present for care should continue the same regimen.38 Key exceptions, due to increased toxicity, include didanosine, indinavir, nelfinavir, stavudine, and treatment-dose ritonavir. Cobicistat-based regimens (atazanavir, darunavir, elvitegravir) have altered pharmacokinetics during the second and third trimesters of pregnancy, leading to reduced mean steady-state minimum concentrations.39 Because increasing plasma HIV RNA level is associated with transmission to infants, women continuing cobicistat-based ART treatments should undergo more frequent viral load measurements.40 If viral rebound occurs late in pregnancy, especially shortly before delivery, achieving viral suppression can be more difficult. Therefore, women on a suppressed ART regimen containing cobicistat should consider switching to a different recommended regimen.38
Geriatric Populations
Although HIV is seen predominantly in younger patients, 48% of persons living with HIV are older than 50 years and 8% are 65 years of age or older.46 With effective antiretroviral treatment, we will continue to see an aging population of people living with HIV. There are no specific guidelines regarding the treatment of older adults, but HIV treatment can have its own challenges. Physiologic declines in renal function occur with aging, which can be compounded by an increasing prevalence of diabetes and decreased muscle mass, making estimations of renal function unreliable.47 Physiologic changes with age, such as decline in renal and hepatic function, decreasing metabolism via cytochrome P450, and body composition, influence drug pharmacokinetics and can in turn potentiate drug toxicities.48 Comorbid states and polypharmacy can complicate care. The prevalence of polypharmacy in the elderly is high, 93%, and is increasing.49,50 A study found that in those aged 65 years or older with HIV, 65% had at least 1 potential drug-drug interaction, and 6.6% had a potential severe drug-drug interaction.50 These patients are thus at risk of poor drug adherence, which in HIV therapy can lead to rebound viremia and resistance.
Renal Insufficiency
Several commonly used ART agents have nephrotoxic potential. The most common manifestations of nephrotoxicity are tubular toxicity, crystal nephropathy, and interstitial nephritis. Of these, acute tubular toxicity caused by TDF is the most widely reported. About 2% of those taking TDF developed treatment-limiting renal insufficiency, manifested as Fanconi syndrome.53 Higher plasma levels of TDF are associated with increased nephrotoxicity.55 Guidelines recommend switching from TDF if the estimated glomerular filtration rate (eGFR) declines by > 25% or the eGFr is < 60/mL/min/1.73 m2. Wever et al reports that in TDF-associated nephrotoxicity, only 42% of patients reached their pre-TDF eGFR.54TAF, a prodrug of TDF, is associated with reduced levels of TDF and is hypothesized to have fewer adverse effects.55 A pooled analysis comparing renal adverse effects of TDF and TAF reported no cases of renal dysfunction in the TAF group, supporting its safety; however, acute kidney injury has also been reported with TAF.56,57 Switching from TDF to TAF in patients with renal dysfunction has been shown to lead to improvement in proteinuria, but the impact remains unclear.53
Dyslipidemia and Cardiovascular Risk
Aside from the traditional cardiovascular risks, PIs, TAF, and efavirenz can negatively affect the lipid profile, with changes in LDL and triglycerides appearing as early as 2 weeks after initiating therapy. An observational study from Spain showed that treatment with TAF worsens the lipid profile in comparison to patients treated with TDF for elvitegravir/cobicistat-based therapies; patients on TAF were twice as likely to need lipid-lower drugs in comparison to those in the TDF arm.61 Similarly, patients who changed from a TDF-based regimen to TAF for improved renal and bone safety profiles had significant changes in both total cholesterol and LDL.65Other NRTIs do not negatively affect lipid profile. Although NNRTIs can increase LDL, this is usually offset by an increase in HDL.62 Of the NNRTIs, the incidence of increased LDL is higher with efavirenz, but it also can cause an increase in HDL; in contrast, patients switched from efavirenz to rilpivirine have a better lipid profile.63,64 PIs, especially older ones such as lopinavir/ritonavir, are associated with lipid abnormalities. For patients who develop dyslipidemia as a result of using older PIs, switching to a darunavir or atazanavir regimen or even integrase inhibitors, which are considered lipid neutral, is recommended.63 When making adjustments in ART, care should be taken in prescribing abacavir to individuals with risk factors for coronary artery disease. Although there is no consensus, some randomized controlled trials suggested an association between myocardial infarction and abacavir, whereas others have not.66,67
HIV and Hepatis B Co-infection
In patients with HIV and hepatitis B co-infection, ART regimens should contain 1 drug that is active against hepatitis B (lamivudine, emtricitabine, TDF, or TAF). Clinicians should monitor liver function for hepatitis B reactivation and liver function when a regimen that contains anti-hepatitis B drugs is stopped because discontinuation of these regimens can result in acute, and sometimes fatal, liver damage.2
Financial Considerations
With out-of-pocket expenses and co-pays, some patients may have to switch ART regimens for financial reasons. Additionally, switching to generic versions of ART has been proposed as a means of saving resources for government programs already facing budgetary constraints. A study published in 2013 using generic-based ART versus branded ART showed a potential savings of almost $1 billion per year.68 A key barrier to the use of generic-based ART is patient skepticism regarding the performance of these medications. Branded ART regimens are also co-formulated, creating the perception that taking more pills will lead to noncompliance and therefore place the patient at risk of viral rebound. In a study from France, only 17% of patients were willing to switch to generic medications if doing so increased pill burden.69 In the same study, 75% physicians were generally willing to prescribe generics; however, that number dropped to 26% if the patient’s pill burden would increase.69 Paradoxically, because of the patchwork of insurance, government assistance, Medicaid, and Medicare, changing to generic-based ART may increase patients’ co-pays.
1. Benson CA, Gandhi RT, et al. Antiretroviral drugs for treatment and prevention of HIV infection in adults. 2018 recommendations of the International Antiviral Society-USA Panel. JAMA. 2018; 320:379-396.
2. Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents living with HIV. http://www.aidsinfo.nih.gov/ContentFiles/ AdultandAdolescentGL.pdf. Accessed July 14, 2020.
3. FDA approves the first once-a-day three-drug combination tablet for treatment of HIV-1. https://aidsinfo.nih.gov/news/769/fda-approves-the-first-once-a-day-three-drug-combination-tablet-for-treatment-of-hiv-1. Accessed July 14, 2020.
4. Apostolova N, Funes HA, Blas-Garcia A, et al. Efavirenz and the CNS: what we already know and questions that need to be answered. J Antimicrob Chemother. 2015;70:2693-2708.
5. de Béthune MP. Non-nucleoside reverse transcriptase inhibitors (NNRTIs), their discovery, development, and use in the treatment of HIV-1 infection: a review of the last 20 years (1989-2009). Antiviral Res. 2010;85:75-90.
6. Carey D, Puls R, Amin J, et al. Efficacy and safety of efanvirenz 400mg daily versus 600 mg daily: 96-week data from the randomized, double-blind, placebo-controlled, non-inferiority ENCORE1 study. Lancet Infect Dis. 2015;15:793-802.
7. Molina JM, Cahn P, Grinsztejn B, et al; ECHO study group. Rilpivirine versus efavirenz with tenofovir and emtricitabine in treatment-naive adults infected with HIV-1 (ECHO): a phase 3 randomised double-blind active-controlled trial. Lancet. 2011;378:238-246.
8. Cohen CJ, Andrade-Villanueva J, Clotet B, et al. THRIVE study group Rilpivirine versus efavirenz with two background nucleoside or nucleotide reverse transcriptase inhibitors in treatment-naive adults infected with HIV-1 (THRIVE): a phase 3, randomised, non-inferiority trial. Lancet. 2011;378:229-237.
9. James C, Preninger L, Sweet M. Rilpivirine: A second-generation nonnucleoside reverse transcriptase inhibitor. Am J Health Syst Pharm. 2012;69:857-861.
10. Zolopa A, Sax PE, DeJesus E, et al. GS-US-236-0102 Study Team A randomized double-blind comparison of coformulated elvitegravir/cobicistat/emtricitabine/tenofovir disoproxil fumarate versus efavirenz/emtricitabine/tenofovir disoproxil fumarate for initial treatment of HIV-1 infection: analysis of week 96 results. J Acquir Immune Defic Syndr. 2013;63:96-100.
11. DeJesus E, Rockstroh JK, Henry K, et al. GS-236-0103 Study Team Co-formulated elvitegravir, cobicistat, emtricitabine, and tenofovir disoproxil fumarate versus ritonavir-boosted atazanavir plus co-formulated emtricitabine and tenofovir disoproxil fumarate for initial treatment of HIV-1 infection: a randomised, double-blind, phase 3, non-inferiority trial. Lancet. 2012;379:2429-2438.
12. Sherman EM, et al. Cobicistat: review of a pharmacokinetic enhancer for HIV infection. Clin Ther. 2015;37:1876-1893.
13. Walmsley S, Baumgarten A, Berenguer J, et al. Dolutegravir plus abacavir/lamivudine for the treatment of HIV-1 infection in antiretroviral therapy-naive patients: week 96 and week 144 results from the SINGLE randomized clinical trial. J Acquir Immune Defic Syndr. 2015;70:515-519.
14. Barbarino JM, Kroetz DL, Altman RB, Klein TE. PharmGKB summary: abacavir pathway. Pharmacogenet Genomics. 2014;24:276-282.
15. Sax PE, Wohl DA, Yin MT, et al. Tenofovir alafenamide versus tenofovir disoproxil fumarate, coformulated with elvitegravir, cobicistat, and emtricitabine, for initial treatment of HIV-1 infection: two randomized, double-blind, phase 3, non-inferiority trials. Lancet. 2015;385:2606–2615.
16. DeJesus E, Haas B, Segal-Maurer S, et al. Superior efficacy and improved renal and bone safety after switching from a tenofovir disoproxil fumarate regimen to a tenofovir alafenamide-based regimen through 96 weeks of treatment. AIDS Res Hum Retroviruses. 2016;34:337-342.
17. Maggiolo F, Rizzardini G, Raff F, et al. Bone mineral density in virologically suppressed people aged 60 years or older with HIV-1 switching from a regimen containing tenofovir disoproxil fumarate to an elvitegravir, cobicistat, emtricitabine, and tenofovir alafenamide single-tablet regimen: a multicentre, open-label, phase 3b, randomised trial. Lancet HIV. 2019;6: e655-e666.
18. Ogbuagu O. Rilpivirine, emtricitabine and tenofovir alafenamide: single-tablet combination for the treatment of HIV-1 infection in selected patients. Expert Rev Anti Infect Ther. 2016;;14:1113-1126.
19. Gallant J, Lazzarin A, Mills A, et al. Bictegravir, emtricitabine, and tenofovir alafenamide versus dolutegravir, abacavir, and lamivudine for initial treatment of HIV-1 infection (GS-US-380-1489): a double-blind, multicentre, phase 3, randomised controlled non-inferiority trial. Lancet. 2017;390:2063-2072.
20. Sax PE, Pozniak A, Montes ML, et al. Coformulated bictegravir, emtricitabine, and tenofovir alafenamide versus dolutegravir with emtricitabine and tenofovir alafenamide, for the initial treatment of HIV-1 infection (GS-US-1490): a randomised, double-blind, multicenter, phase 3, non-inferiority trial. Lancet. 2017;390:2073-2082.
21. Eron JJ, Orkin C, Gallant J, et al. A week-48 randomized phase-3 trial of darunavir/cobicistat/emtricitabine/tenofovir alafenamide in treatment-naive HIV-1 patients. AIDS. 2018;32:1431-1442.
22. Orkin C, Molina JM, Negredo E, et al;. EMERALD study group. Efficacy and safety of switching from boosted protease inhibitors plus emtricitabine/tenofovir disoproxil fumarate regimens to the once-daily complete HIV-1 regimen of darunavir/cobicistat/emtricitabine/tenofovir alafenamide (D/C/F/TAF) in virologically suppressed, HIV-1-infected adults through 48 weeks (EMERALD): a phase 3, randomized, non-inferiority trial. Lancet HIV. 2018;5:e23-e34.
23. Orkin C, Squires KE, Molina JM, et al. Doravirine/lamivudine/tenofovir disoproxil fumarate is non-inferior to efavirenz/emtricitabine/tenofovir disoproxil fumarate in treatment-naive adults with human immunodeficiency virus-1 infection: week 48 results of the DRIVE-AHEAD Trial. Clin Infect Dis. 2019;68:535-544.
24. Molina JM, Squires K, Sax PE, et al. Doravirine versus ritonavir-boosted darunavir in antiretroviral-naive adults with HIV-1 (DRIVE-FORWARD): 48-week results of a randomised, double-blind, phase 3, non-inferiority trial. Lancet HIV. 2018;5:e211-e220.
25. Palella FJ, Delaney KM, Moorman ACE, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med. 1998;338:853-860.
26. Mocroft A, Vella S, Benfiedl TL. Changing patterns of mortality across Europe in patients infected with HIV-1. Lancet. 1998;3552:1725-1730.
27. Libre JM, Hugh CC, Castelli F, et al. Efficacy, safety, and tolerability of dolutegravir-rilpivirine for the maintenance of virological suppression in adults with HIV-1: phase 3, randomized, noninferiority SWORD-1 and SWORD-2 studies. Lancet. 2018;391:839-849.
28. Cahn P, Madero JS, Arribas JR, et al. Durable efficacy of dolutegravir plus lamivudine in antiretroviral treatment-naive adults with HIV-1 infection: 96-week results from the GEMINI-1 and GEMINI-2 randomized clinical trials. J Acquir Immune Defic Syndr. 2020;83:310-318.
29. Joly V, Burdet C, Landman R, et al. Dolutegravir and lamivudine maintenance therapy in HIV-1 virologically suppressed patients: results of the ANRS 167 trial (LAMIDOL). J Antimicrob Chemother. 2019;74:739-745.
30. Li JZ, Sax PE, Marconi VC, et al. No significant changes to residual viremia after switch to dolutegravir and lamivudine in a randomized trial. Open Forum Infect Dis. 2019;6:ofz056.
31. Taiwo BO, Marconi VC, Verzins B, et al. Dolutegravir plus lamivudine maintains human immunodeficiency virus-1 suppression through week 48 in a pilot randomized trial. Clin Infect Dis. 2018;66:1794-1979.
32. Van Wyk J, Ajana F, Bisshop F, et al. Efficacy and safety of switching to dolutegravir/lamivudine fixed-dose 2-drug regimen vs continuing a tenofovir alafenamide–based 3- or 4-drug regimen for maintenance of virologic suppression in adults living with human immunodeficiency virus type 1: phase 3, randomized, noninferiority TANGO Study. Clin Infect Dis. Jan 6;ciz1243. doi: 10.1093/cid/ciz1243.
33. Cutrell J, Jodlowski T, Bedimo R. The management of treatment-experienced HIV patients (including virologic failure and switches). Ther Adv Infectious Dis. 2020;7:1-15.
34. Devereux, HL, Youle, M, Johnson, MA, et al. Rapid decline in detectability of HIV-1 drug resistance mutations after stopping therapy. AIDS. 1999;13:F123-F127.
35. Gatanaga H, Tsukada K, Honda H, et al. Detection of HIV type 1 load by the Roche Cobas TaqMan assay in patients with viral loads previously undetectable by the Roche Cobas Amplicor Monitor. Clin Infect Dis. 2009;48:260-262.
36. Emu B, Fessel J, Schrader S, et al. Phase 3 study of ibalizumab for multidrug-resistant HIV-1. N Engl J Med. 2018;379:645-654.
37. Kozal M, Aberg J, Pialoux G, et al. Fostemsavir in adults with multidrug-resistant HIV-1 infection. N Engl J Med. 2020; 382:1232-1243.
38. Department of Health and Human Services (HHS) Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission. recommendations for use of antiretroviral drugs in pregnant HIV-1-infected women for maternal health and interventions to reduce perinatal HIV transmission in the United States. http://aidsinfo.nih.gov/guidelines/html/3/perinatal-guidelines/0/ Accessed on July 13, 2020.
39. Boyd SD, Sampson MR, Viswanathan P, et al. Cobicistat-containing antiretroviral regimens are not recommended during pregnancy: viewpoint. AIDS. 2019;33:1089-1093.
40. Garcia PM, Kalish LA, Pitt J, et al. Maternal levels of plasma human immunodeficiency virus type 1 RNA and the risk of perinatal transmission. N Engl J Med. 1999;341:394-402.
41. Stek A, Best BM, Wang J, et al. Pharmacokinetics of once versus twice daily darunavir In pregnant HIV-infected women. J Acquir Immune Defic Syndr. 2015;70:33-41.
42. Stek A, Best B, Capparelli E, et al. Pharmacokinetics of increased dose darunavir during late pregnancy and postpartum. Presented at: 23rd Conference on Retroviruses and Opportunistic Infections. 2016. Boston, MA.
43. Mirochnick M, Best BM, Stek AM, et al. Atazanavir pharmacokinetics with and without tenofovir during pregnancy. J Acquir Immune Defic Syndr. 2011;56:412-419.
44. Schalkwijk S, Colbers A, Konopnicki D, et al. Lowered rilpivirine exposure during third trimester of pregnancy in HIV-1-positive women. Clin Infect Dis. 2017;65:1335-1341.
45. Zash R, Holmes L, Diseko M, et al. Neural-tube defects and antiretroviral treatment regimens in Botswana. N Engl J Med. 2019;381:827-840.
46. Centers for Disease Control and Prevention. HIV Surveillance Report, 2017; vol. 29. www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published November 2018.
47. Rhee MS, Greenblatt DJ. Pharmacologic consideration for the use of antiretroviral agents in the elderly. J Clin Pharmacol. 2008;481212-1225.
48. Nguyen, N, Holodniy M. HIV infection in the elderly. Clin Interv Aging. 2008;3:453-472.
49. Gleason LJ, Luque AE, Shah K. Polypharmacy in the HIV-infected older adult population. Clin Interv Aging. 2013;8749-763.
50. Bastida C, Grau A, Marquez M, et al. Polypharmacy and potential drug-drug interactions in an HIV-infected elderly population. Farm Hosp. 2017;41:618-624.
51. Brown TT, Hoy J, Borderi M, et al. Recommendations for evaluation and management of bone disease in HIV. Clin Infect Dis. 2015;60:1242-1251.
52. Mocroft A, Lundgren JD, Ross M, et al. Cumulative and current exposure to potentially nephrotoxic antiretrovirals and development of chronic kidney disease in HIV-positive individuals with a normal baseline estimated glomerular filtration rate: a prospective international cohort study. Lancet HIV. 2016;3:e23-32.
53. Ryom L, Mocroft A, Kirk O, et al. D:A:D Study Group. Association between antiretroviral exposure and renal impairment among HIV-positive persons with normal baseline renal function: the D:A:D study. J Infect Dis. 2013;207:1359.
54. Wever K, van Agtmael MA, Carr A. Incomplete reversibility of tenofovir related renal toxicity in HIV-infected men. J Acquir Immune Defic Syndr. 2010;55:78-81.
55. Hall AM, Hendry BM, Nitsch D, Connolly JO. Tenofovir-associated kidney toxicity in HIV-infected patients: a review of the evidence. Am J Kidney Dis. 2011; 57:773-780.
56. Gupta SK, Post FA, Arribas JR, et al. Renal safety of tenofovir alafenamide vs. tenofovir disoproxil fumarate: a pooled analysis of 26 clinical trials. AIDS. 2019;33:1455-1465.
57. Novick TK, Choi MJ, Rosenberg AZ, et al, Tenofovir alafenamide nephrotoxicity in an HIV-positive patient: A case report. Medicine (Baltimore). 2017;96:e8046.
58. Surial B, Ledergerber B, Calmy A, et al. Swiss HIV Cohort Study, changes in renal function after switching from TDF to TAF in HIV-infected individuals: a prospective cohort study. J Infect Dis. jiaa125, https://doi.org/10.1093/infdis/jiaa125.
59. McLaughlin MM, Guerrero AJ, Merker A. Renal effects of non-tenofovir antiretroviral therapy in patients living with HIV. Drugs Context. 2018;7:212519.
60. German P, Liu H, Szwarcberg J, et al. Effect of cobicistat on glomerular filtration rate in subjects with normal and impaired renal function. J Acquir Immune Defic Syndr. 2012;61:32-40.
61. Cid-Silva P, Fernandez-Bargiela N, Margusino-Framinan L, et al. Treatment with tenofovir alafenamide fumarate worsens the lipid profile of HIV-infected patients versus treatment with tenofovir disoproxil fumarate, each coformulated with elvitegravir, cobicistat, and emtricitabine. Basic Clin Pharmacol Toxicol. 2019;124:479-490.
62. Fontas E, van Leth F, Sabin CA, et al. Lipid profiles in HIV-infected patients receiving combination antiretroviral therapy: are different antiretroviral drugs associated with different lipid profiles?. J Infect Dis. 2004;189:1056-1074.
63. Tebas P, Sension M, Arribas J, et al. Lipid levels and changes in body fat distribution in treatment-naive, HIV-1-Infected adults treated with rilpivirine or Efavirenz for 96 weeks in the ECHO and THRIVE trials. Clin Infect Dis. 2014;59:425-434.
64. Taramasso L, Tatarelli P, Ricci E, et al. Improvement of lipid profile after switching from efavirenz or ritonavir-boosted protease inhibitors to rilpivirine or once-daily integrase inhibitors: results from a large observational cohort study (SCOLTA). BMC Infect Dis. 2018;18:357.
65. Lacey A, Savinelli, S, Barco, EA, et al. The UCD ID Cohort Study; Investigating the effect of antiretroviral switch to tenofovir alafenamide on lipid profiles in people living with HIV. AIDS. 2020;341161-1170.
66. Marcus JL, Neugebauer RS, Leyden WA, et al. Use of abacavir and risk of cardiovascular disease among HIV-infected individuals. J Acquir Immune Defic Syndr. 2016;71:413-419.
67. Ribaudo HJ, Benson CA, Zheng Y, et al. No risk of myocardial infarction associated with initial antiretroviral treatment containing abacavir: short and long-term results from ACTG A5001/ALLRT. Clin Infect Dis. 2011;52:929-940.
68. Walensky RP, Sax PE, Nakamura YM, et al. Economic savings versus health losses: the cost-effectiveness of generic antiretroviral therapy in the United States. Ann Intern Med. 2013;158:84-92.
69. Jacomet C, Allavena C, Peyrol F, et al. Perception of antiretroviral generic medicines: one-day survey of HIV-infected patients and their physicians in France. PLoS One. 2015;10:e0117214-e0117214.
A 57-year-old man living with HIV has been followed at a local infectious disease clinic for more than 15 years. He acquired HIV disease through heterosexual contact. He lives alone and works at a convenience store; he has not been sexually active for the past 5 years. He smokes 10 cigarettes a day, but does not drink alcohol or use illicit drugs. He had been on coformulated emtricitabine/tenofovir disoproxil fumarate (TDF) and coformulated lopinavir/ritonavir, which he had taken conscientiously, since May 2008, without noticing any adverse reactions from this regimen. His HIV viral load had been undetectable, and his CD4 count had hovered between 600 and 700 cells/µL. Although he was on atorvastatin for dyslipidemia, his fasting lipid profile, performed in 2018, revealed a total cholesterol level of 200 mg/dL;triglyceride, 247 mg/dL; high-density lipoprotein (HDL), 43 mg/dL; and low-density lipoprotein (LDL), 132 mg/dL. In April 2019, his HIV regimen was switched to bictegravir/emtricitabine/tenofovir alafenamide (TAF). Blood tests performed in December 2019 revealed undetectable HIV viral load; an increased CD4 count to 849 cell/µL; total cholesterol, 140 mg/dL; triglyceride, 115 mg/dL; HDL, 60 mg/dL; and LDL, 90 mg/dL.
SIMPLIFYING ART
Virologically Suppressed Patients Without Drug-Resistant Virus
Treatment adherence is of paramount importance to ensure treatment success. Patients with a viral load that is undetectable or nearly undetectable without drug resistance could be taking ART regimens consisting of more than 1 pill and/or that require more than once-daily dosing. Decreasing pill burden or dosing frequency can help to improve adherence to treatment. In addition, older-generation ART agents are usually more toxic and less potent than newer-generation agents, so another important objective of switching older drugs to newer drugs is to decrease adverse reactions and improve virologic suppression. Selection of an ART regimen should be guided by the results of resistance testing (genotyping and phenotyping tests) and previous treatment history. After switching a patient’s ART regimen, plasma HIV viral load and CD4 count should be closely monitored.2 The following 3-drug, single-tablet, once-daily ART regimens can be used in patients who are virologically stable (ordered chronologically by FDA approval dates).
Efavirenz/Emtricitabine/TDF (Atripla)
Coformulated efavirenz/emtricitabine/TDF was the first single-tablet, once-daily, fixed-dose combination approved by the FDA (July 2006). Approval was based on a 48- week clinical trial involving 244 adults with HIV infection that showed that 80% of participants achieved a marked reduction in HIV viral load and a significant increase in CD4 cell count.3 Of the 3 components, efavirenz has unique central nervous system (CNS) adverse effects that could reduce adherence. Patients who were started on this fixed-dose combination commonly reported dizziness, headache, nightmare, insomnia, and impaired concentration.4 However, the CNS side effects resolved within the first 4 weeks of therapy, and less than 5% of patients quit taking the drug. Primate studies showed efavirenz is teratogenic, but studies in pregnant women did not find efavirenz to be more teratogenic than other ART agents.5
Emtricitabine/Rilpivirine/TDF (Complera)
Coformulated emtricitabine/rilpivirine/TDF was approved based on data from two 48-week, phase 3, double-blind, randomized controlled trials (ECHO and THRIVE) that evaluated the safety and efficacy of rilpivirine compared to efavirenz among treatment-naive adults with HIV infection.7,8 Rilpivirine is well tolerated and causes fewer CNS symptoms compared to efavirenz. The main caveat for rilpivirine is drug-drug interactions. It should not be coadministered with CYP inducers, such as rifampin, phenytoin, or St. John’s wort, as coadministration can cause subtherapeutic blood levels of rilpivirine. Because increased levels of rilpivirine can prolong QTc on electrocardiogram (ECG), an ECG should be obtained before starting an ART regimen that contains rilpivirine, especially in the presence of CYP 3A4 inhibitors.9
Elvitegravir/Cobicistat/Emtricitabine/TDF (Stribild)
This coformulation was approved based on data from 2 randomized, double-blind, controlled trials, Study 102 and Study 103, in treatment-naive patients with HIV (n = 1408). In Study 102, participants were randomized to receive either elvitegravir/cobicistat/emtricitabine/TDF or efavirenz/emtricitabine/TDF (Atripla).10 In Study 103, participants were randomized to receive either elvitegravir/cobicistat/emtricitabine/TDF or atazanavir + ritonavir + emtricitabine/TDF. In both studies, the primary endpoint was virologic success (HIV-1 RNA < 50 copies/mL) at 48 weeks, and elvitegravir/cobicistat/emtricitabine/TDF was noninferior compared to the other regimens.11
Abacavir/Dolutegravir/Lamivudine (Triumeq)
Approval of abacavir/dolutegravir/lamivudine (Triumeq) in August 2014 was based on SINGLE, a noninferiority trial involving 833 treatment-naive adults that compared dolutegravir and abacavir/lamivudine (the separate components of Triumeq) to efavirenz/emtricitabine/TDF. At 96 weeks, more patients in the dolutegravir and abacavir/lamivudine arm achieved an undetectable HIV viral load (80% versus 72%).13
Elvitegravir/Cobicistat/Emtricitabine/TAF (Genvoya)
Approval of coformulated elvitegravir/cobicistat/emtricitabine/TAF was supported by data from two 48-week phase 3, double-blind studies (Studies 104 and 111) involving 1733 treatment-naive patients that compared the regimen to elvitegravir/cobicistat/emtricitabine/TDF (Stribild). Both studies demonstrated that elvitegravir/cobicistat/emtricitabine/TAF was statistically noninferior, and it was favored in regard to certain renal and bone laboratory parameters.15 Studies comparing TAF and TDF have demonstrated that TAF is less likely to cause loss of bone mineral density and nephrotoxicity compared to TDF.16,17
Emtricitabine/Rilpivirine/TAF (Odefsey)
Coformulated emtricitabine/rilpivirine/TAF was approved based, in part, on positive bioequivalence studies demonstrating that it achieved similar drug levels of emtricitabine and TAF as coformulated elvitegravir/cobicistat/emtricitabine/TAF and similar drug levels of rilpivirine as individually dosed rilpivirine.18 The safety, efficacy, and tolerability of this coformulation is supported by clinical studies of rilpivirine-based therapy and emtricitabine/TAF-based therapy in a range of patients with HIV.18
Bictegravir/Emtricitabine/TAF (Biktarvy)
The coformulation bictegravir/emtricitabine/TAF was approved based on 4 phase 3 studies: Studies 1489 and 1490 in treatment-naive adults, and Studies 1844 and 1878 in virologically suppressed adults. In Study 1489, 629 treatment-naive adults were randomized 1:1 to receive coformulated bictegravir/emtricitabine/TAF or coformulated abacavir/dolutegravir/lamivudine. At week 48, similar percentages of patients in each arm achieved the primary endpoint of HIV-1 RNA < 50 copies/mL. In Study 1490, 645 treatment-naive adults were randomized 1:1 to receive coformulated bictegravir/emtricitabine/TAF or dolutegravir + emtricitabine/TAF. At week 48, similar percentages of patients in each arm achieved the primary endpoint of virologic success (HIV-1 RNA < 50 copies/mL).19,20
Darunavir/Cobicistat/Emtricitabine/TAF (Symtuza)
Approval of coformulated darunavir/cobicistat/emtricitabine/TAF was based on data from two 48-week, noninferiority, phase 3 studies that assessed the safety and efficacy of the coformulation versus a control regimen (darunavir/cobicistat plus emtricitabine/TDF) in adults with no prior ART history (AMBER) and in virologically suppressed adults (EMERALD). In the randomized, double-blind, multicenter controlled AMBER trial, at week 48, 91.4% of patients in the study group and 88.4% in the control group achieved viral suppression (HIV-1 RNA < 50 copies/mL), and virologic failure rates were low in both groups (HIV-1 RNA ≥ 50 copies/mL; 4.4% versus 3.3%, respectively).21
Doravirine/Lamivudine/TDF (Delstrigo)
Coformulated doravirine/lamivudine/TDF was approved based on data from 2 randomized, double-blind, controlled phase 3 trials, DRIVE-AHEAD and DRIVE-FORWARD. The former trial compared coformulated doravirine/lamivudine/TDF with efavirenz/emtricitabine/TDF in 728 treatment-naive patients. At 48 weeks, 84.3% in the doravirine/lamivudine/TDF arm and 80.8% in the efavirenz/emtricitabine/TDF arm met the primary endpoint of HIV-1 RNA < 50 copies/mL. Thus, doravirine/lamivudine/TDF showed sustained viral suppression and noninferiority compared to efavirenz/emtricitabine/TDF.23 The DRIVE-FORWARD trial investigated doravirine compared with ritonavir-boosted darunavir, each in combination with 2 NRTIs (TDF with emtricitabine or abacavir with lamivudine). At week 48, 84% of patients in the doravirine arm and 80% in the ritonavir-boosted darunavir arm achieved the primary endpoint of HIV-1 RNA < 50 copies/mL.24
Two-Drug, Single-Tablet, Once-Daily Regimens
Experts have long recommended that optimal treatment of HIV must consist of 3 active drugs, with trials both in the United States and Europe demonstrating decreased morbidity and mortality with 3-drug therapy.25,26 However, newer, more potent 2-drug therapy is giving more choices to people living with HIV. The single-tablet, 2-drug regimens currently available are dolutegravir/rilpivirine and dolutegravir/lamivudine. There are theoretical benefits of 2-drug therapy, such as minimizing long-term toxicities, avoidance of some drug-drug interactions, and preservation of drugs for future treatment options. At this time, a 2-drug simplification regimen can be a viable option for selected virologically stable populations.
Dolutegravir/Rilpivirine (Juluca)
Dolutegravir/rilpivirine has been shown to be noninferior to standard therapy at 48-weeks, although it is associated with a higher discontinuation rate because of side effects.27 This option can be particularly useful in patients who have contraindications to NRTIs or renal dysfunction, but it has been studied only in patients without resistance who are already virologically suppressed. Ongoing studies are looking at 2-versus 3-drug therapies for HIV treatment-experienced patients. Most of these use PIs as a backbone because of their potency and high barrier to resistance. The advent of second-generation integrase inhibitors offers additional options.
Dolutegravir/Lamivudine (Dovato)
The GEMINI-1 and GEMINI-2 trials demonstrated that dolutegravir/lamivudine was noninferior to dolutegravir/TDF/emtricitabine.28 Based on these 2 studies, new guidelines have added dolutegravir/lamivudine as a recommended first-line therapy. For now, the recommendation is to use dolutegravir/lamivudine in individuals where NRTIs are contraindicated, and it should not be used in patients with chronic hepatitis B. Additionally, 3 studies have demonstrated the safety and efficacy of switching to dolutegravir/lamivudine.29-31 In the TANGO trial, neither virologic failures nor resistant virus were identified at 48 weeks following the switch.32 Although there are benefits of simplification with this regimen, including lower toxicity, lower costs, and saving other NRTIs in case of resistance, there should be no rush to switch patients to a 2-drug regimen. This is a viable strategy in patients without baseline resistance who have preserved T-cells and do not have hepatitis B.
SWITCHING ART AGENTS IN SELECTED CLINICAL SCENARIOS
Virologic Failure
One of the main goals of ART is maximal and durable suppression of HIV viral load to prevent the development of drug-resistant mutations.2 When patients are unable to achieve durable virologic suppression or have virologic rebound, the cause of virologic failure needs to be investigated. Virologic failure is defined as the inability to achieve or maintain viral suppression to a level below 200 copies/mL, whereas rebound is defined as an HIV RNA level exceeding 200 copies/mL after virologic suppression.33 A common cause of virologic failure is patient nonadherence, which can be related to a range of factors, including psychosocial issues and affordability of medications. Innate viral resistance can be the result of transmitted drug resistance at the time of infection or be acquired during unsuppressed viral replication secondary to inherent error-prone reverse transcriptase.33 Pharmacokinetic factors that affect blood levels of ART, such as drug-drug interactions, also can be a key factor in HIV drug resistance.
Patients With Limited Treatment Options
Despite advances in ART, some patients exhaust the existing regimens, leading to development of multidrug resistance and limited treatment options. In light of the treatment challenges in this group of patients, the FDA has recently approved 2 antiretroviral agents to target multidrug-resistant HIV: ibalizumab and fostemsavir.
Pregnancy
ART is used during pregnancy to maintain the pregnant woman’s health and to prevent perinatal transmission. Pregnancy can present unique challenges to effective ART, and therapy decisions should be made based on short-term and long-term safety data, pharmacokinetics, and tolerability. With few exceptions, women who are on a stable ART regimen and present for care should continue the same regimen.38 Key exceptions, due to increased toxicity, include didanosine, indinavir, nelfinavir, stavudine, and treatment-dose ritonavir. Cobicistat-based regimens (atazanavir, darunavir, elvitegravir) have altered pharmacokinetics during the second and third trimesters of pregnancy, leading to reduced mean steady-state minimum concentrations.39 Because increasing plasma HIV RNA level is associated with transmission to infants, women continuing cobicistat-based ART treatments should undergo more frequent viral load measurements.40 If viral rebound occurs late in pregnancy, especially shortly before delivery, achieving viral suppression can be more difficult. Therefore, women on a suppressed ART regimen containing cobicistat should consider switching to a different recommended regimen.38
Geriatric Populations
Although HIV is seen predominantly in younger patients, 48% of persons living with HIV are older than 50 years and 8% are 65 years of age or older.46 With effective antiretroviral treatment, we will continue to see an aging population of people living with HIV. There are no specific guidelines regarding the treatment of older adults, but HIV treatment can have its own challenges. Physiologic declines in renal function occur with aging, which can be compounded by an increasing prevalence of diabetes and decreased muscle mass, making estimations of renal function unreliable.47 Physiologic changes with age, such as decline in renal and hepatic function, decreasing metabolism via cytochrome P450, and body composition, influence drug pharmacokinetics and can in turn potentiate drug toxicities.48 Comorbid states and polypharmacy can complicate care. The prevalence of polypharmacy in the elderly is high, 93%, and is increasing.49,50 A study found that in those aged 65 years or older with HIV, 65% had at least 1 potential drug-drug interaction, and 6.6% had a potential severe drug-drug interaction.50 These patients are thus at risk of poor drug adherence, which in HIV therapy can lead to rebound viremia and resistance.
Renal Insufficiency
Several commonly used ART agents have nephrotoxic potential. The most common manifestations of nephrotoxicity are tubular toxicity, crystal nephropathy, and interstitial nephritis. Of these, acute tubular toxicity caused by TDF is the most widely reported. About 2% of those taking TDF developed treatment-limiting renal insufficiency, manifested as Fanconi syndrome.53 Higher plasma levels of TDF are associated with increased nephrotoxicity.55 Guidelines recommend switching from TDF if the estimated glomerular filtration rate (eGFR) declines by > 25% or the eGFr is < 60/mL/min/1.73 m2. Wever et al reports that in TDF-associated nephrotoxicity, only 42% of patients reached their pre-TDF eGFR.54TAF, a prodrug of TDF, is associated with reduced levels of TDF and is hypothesized to have fewer adverse effects.55 A pooled analysis comparing renal adverse effects of TDF and TAF reported no cases of renal dysfunction in the TAF group, supporting its safety; however, acute kidney injury has also been reported with TAF.56,57 Switching from TDF to TAF in patients with renal dysfunction has been shown to lead to improvement in proteinuria, but the impact remains unclear.53
Dyslipidemia and Cardiovascular Risk
Aside from the traditional cardiovascular risks, PIs, TAF, and efavirenz can negatively affect the lipid profile, with changes in LDL and triglycerides appearing as early as 2 weeks after initiating therapy. An observational study from Spain showed that treatment with TAF worsens the lipid profile in comparison to patients treated with TDF for elvitegravir/cobicistat-based therapies; patients on TAF were twice as likely to need lipid-lower drugs in comparison to those in the TDF arm.61 Similarly, patients who changed from a TDF-based regimen to TAF for improved renal and bone safety profiles had significant changes in both total cholesterol and LDL.65Other NRTIs do not negatively affect lipid profile. Although NNRTIs can increase LDL, this is usually offset by an increase in HDL.62 Of the NNRTIs, the incidence of increased LDL is higher with efavirenz, but it also can cause an increase in HDL; in contrast, patients switched from efavirenz to rilpivirine have a better lipid profile.63,64 PIs, especially older ones such as lopinavir/ritonavir, are associated with lipid abnormalities. For patients who develop dyslipidemia as a result of using older PIs, switching to a darunavir or atazanavir regimen or even integrase inhibitors, which are considered lipid neutral, is recommended.63 When making adjustments in ART, care should be taken in prescribing abacavir to individuals with risk factors for coronary artery disease. Although there is no consensus, some randomized controlled trials suggested an association between myocardial infarction and abacavir, whereas others have not.66,67
HIV and Hepatis B Co-infection
In patients with HIV and hepatitis B co-infection, ART regimens should contain 1 drug that is active against hepatitis B (lamivudine, emtricitabine, TDF, or TAF). Clinicians should monitor liver function for hepatitis B reactivation and liver function when a regimen that contains anti-hepatitis B drugs is stopped because discontinuation of these regimens can result in acute, and sometimes fatal, liver damage.2
Financial Considerations
With out-of-pocket expenses and co-pays, some patients may have to switch ART regimens for financial reasons. Additionally, switching to generic versions of ART has been proposed as a means of saving resources for government programs already facing budgetary constraints. A study published in 2013 using generic-based ART versus branded ART showed a potential savings of almost $1 billion per year.68 A key barrier to the use of generic-based ART is patient skepticism regarding the performance of these medications. Branded ART regimens are also co-formulated, creating the perception that taking more pills will lead to noncompliance and therefore place the patient at risk of viral rebound. In a study from France, only 17% of patients were willing to switch to generic medications if doing so increased pill burden.69 In the same study, 75% physicians were generally willing to prescribe generics; however, that number dropped to 26% if the patient’s pill burden would increase.69 Paradoxically, because of the patchwork of insurance, government assistance, Medicaid, and Medicare, changing to generic-based ART may increase patients’ co-pays.
A 57-year-old man living with HIV has been followed at a local infectious disease clinic for more than 15 years. He acquired HIV disease through heterosexual contact. He lives alone and works at a convenience store; he has not been sexually active for the past 5 years. He smokes 10 cigarettes a day, but does not drink alcohol or use illicit drugs. He had been on coformulated emtricitabine/tenofovir disoproxil fumarate (TDF) and coformulated lopinavir/ritonavir, which he had taken conscientiously, since May 2008, without noticing any adverse reactions from this regimen. His HIV viral load had been undetectable, and his CD4 count had hovered between 600 and 700 cells/µL. Although he was on atorvastatin for dyslipidemia, his fasting lipid profile, performed in 2018, revealed a total cholesterol level of 200 mg/dL;triglyceride, 247 mg/dL; high-density lipoprotein (HDL), 43 mg/dL; and low-density lipoprotein (LDL), 132 mg/dL. In April 2019, his HIV regimen was switched to bictegravir/emtricitabine/tenofovir alafenamide (TAF). Blood tests performed in December 2019 revealed undetectable HIV viral load; an increased CD4 count to 849 cell/µL; total cholesterol, 140 mg/dL; triglyceride, 115 mg/dL; HDL, 60 mg/dL; and LDL, 90 mg/dL.
SIMPLIFYING ART
Virologically Suppressed Patients Without Drug-Resistant Virus
Treatment adherence is of paramount importance to ensure treatment success. Patients with a viral load that is undetectable or nearly undetectable without drug resistance could be taking ART regimens consisting of more than 1 pill and/or that require more than once-daily dosing. Decreasing pill burden or dosing frequency can help to improve adherence to treatment. In addition, older-generation ART agents are usually more toxic and less potent than newer-generation agents, so another important objective of switching older drugs to newer drugs is to decrease adverse reactions and improve virologic suppression. Selection of an ART regimen should be guided by the results of resistance testing (genotyping and phenotyping tests) and previous treatment history. After switching a patient’s ART regimen, plasma HIV viral load and CD4 count should be closely monitored.2 The following 3-drug, single-tablet, once-daily ART regimens can be used in patients who are virologically stable (ordered chronologically by FDA approval dates).
Efavirenz/Emtricitabine/TDF (Atripla)
Coformulated efavirenz/emtricitabine/TDF was the first single-tablet, once-daily, fixed-dose combination approved by the FDA (July 2006). Approval was based on a 48- week clinical trial involving 244 adults with HIV infection that showed that 80% of participants achieved a marked reduction in HIV viral load and a significant increase in CD4 cell count.3 Of the 3 components, efavirenz has unique central nervous system (CNS) adverse effects that could reduce adherence. Patients who were started on this fixed-dose combination commonly reported dizziness, headache, nightmare, insomnia, and impaired concentration.4 However, the CNS side effects resolved within the first 4 weeks of therapy, and less than 5% of patients quit taking the drug. Primate studies showed efavirenz is teratogenic, but studies in pregnant women did not find efavirenz to be more teratogenic than other ART agents.5
Emtricitabine/Rilpivirine/TDF (Complera)
Coformulated emtricitabine/rilpivirine/TDF was approved based on data from two 48-week, phase 3, double-blind, randomized controlled trials (ECHO and THRIVE) that evaluated the safety and efficacy of rilpivirine compared to efavirenz among treatment-naive adults with HIV infection.7,8 Rilpivirine is well tolerated and causes fewer CNS symptoms compared to efavirenz. The main caveat for rilpivirine is drug-drug interactions. It should not be coadministered with CYP inducers, such as rifampin, phenytoin, or St. John’s wort, as coadministration can cause subtherapeutic blood levels of rilpivirine. Because increased levels of rilpivirine can prolong QTc on electrocardiogram (ECG), an ECG should be obtained before starting an ART regimen that contains rilpivirine, especially in the presence of CYP 3A4 inhibitors.9
Elvitegravir/Cobicistat/Emtricitabine/TDF (Stribild)
This coformulation was approved based on data from 2 randomized, double-blind, controlled trials, Study 102 and Study 103, in treatment-naive patients with HIV (n = 1408). In Study 102, participants were randomized to receive either elvitegravir/cobicistat/emtricitabine/TDF or efavirenz/emtricitabine/TDF (Atripla).10 In Study 103, participants were randomized to receive either elvitegravir/cobicistat/emtricitabine/TDF or atazanavir + ritonavir + emtricitabine/TDF. In both studies, the primary endpoint was virologic success (HIV-1 RNA < 50 copies/mL) at 48 weeks, and elvitegravir/cobicistat/emtricitabine/TDF was noninferior compared to the other regimens.11
Abacavir/Dolutegravir/Lamivudine (Triumeq)
Approval of abacavir/dolutegravir/lamivudine (Triumeq) in August 2014 was based on SINGLE, a noninferiority trial involving 833 treatment-naive adults that compared dolutegravir and abacavir/lamivudine (the separate components of Triumeq) to efavirenz/emtricitabine/TDF. At 96 weeks, more patients in the dolutegravir and abacavir/lamivudine arm achieved an undetectable HIV viral load (80% versus 72%).13
Elvitegravir/Cobicistat/Emtricitabine/TAF (Genvoya)
Approval of coformulated elvitegravir/cobicistat/emtricitabine/TAF was supported by data from two 48-week phase 3, double-blind studies (Studies 104 and 111) involving 1733 treatment-naive patients that compared the regimen to elvitegravir/cobicistat/emtricitabine/TDF (Stribild). Both studies demonstrated that elvitegravir/cobicistat/emtricitabine/TAF was statistically noninferior, and it was favored in regard to certain renal and bone laboratory parameters.15 Studies comparing TAF and TDF have demonstrated that TAF is less likely to cause loss of bone mineral density and nephrotoxicity compared to TDF.16,17
Emtricitabine/Rilpivirine/TAF (Odefsey)
Coformulated emtricitabine/rilpivirine/TAF was approved based, in part, on positive bioequivalence studies demonstrating that it achieved similar drug levels of emtricitabine and TAF as coformulated elvitegravir/cobicistat/emtricitabine/TAF and similar drug levels of rilpivirine as individually dosed rilpivirine.18 The safety, efficacy, and tolerability of this coformulation is supported by clinical studies of rilpivirine-based therapy and emtricitabine/TAF-based therapy in a range of patients with HIV.18
Bictegravir/Emtricitabine/TAF (Biktarvy)
The coformulation bictegravir/emtricitabine/TAF was approved based on 4 phase 3 studies: Studies 1489 and 1490 in treatment-naive adults, and Studies 1844 and 1878 in virologically suppressed adults. In Study 1489, 629 treatment-naive adults were randomized 1:1 to receive coformulated bictegravir/emtricitabine/TAF or coformulated abacavir/dolutegravir/lamivudine. At week 48, similar percentages of patients in each arm achieved the primary endpoint of HIV-1 RNA < 50 copies/mL. In Study 1490, 645 treatment-naive adults were randomized 1:1 to receive coformulated bictegravir/emtricitabine/TAF or dolutegravir + emtricitabine/TAF. At week 48, similar percentages of patients in each arm achieved the primary endpoint of virologic success (HIV-1 RNA < 50 copies/mL).19,20
Darunavir/Cobicistat/Emtricitabine/TAF (Symtuza)
Approval of coformulated darunavir/cobicistat/emtricitabine/TAF was based on data from two 48-week, noninferiority, phase 3 studies that assessed the safety and efficacy of the coformulation versus a control regimen (darunavir/cobicistat plus emtricitabine/TDF) in adults with no prior ART history (AMBER) and in virologically suppressed adults (EMERALD). In the randomized, double-blind, multicenter controlled AMBER trial, at week 48, 91.4% of patients in the study group and 88.4% in the control group achieved viral suppression (HIV-1 RNA < 50 copies/mL), and virologic failure rates were low in both groups (HIV-1 RNA ≥ 50 copies/mL; 4.4% versus 3.3%, respectively).21
Doravirine/Lamivudine/TDF (Delstrigo)
Coformulated doravirine/lamivudine/TDF was approved based on data from 2 randomized, double-blind, controlled phase 3 trials, DRIVE-AHEAD and DRIVE-FORWARD. The former trial compared coformulated doravirine/lamivudine/TDF with efavirenz/emtricitabine/TDF in 728 treatment-naive patients. At 48 weeks, 84.3% in the doravirine/lamivudine/TDF arm and 80.8% in the efavirenz/emtricitabine/TDF arm met the primary endpoint of HIV-1 RNA < 50 copies/mL. Thus, doravirine/lamivudine/TDF showed sustained viral suppression and noninferiority compared to efavirenz/emtricitabine/TDF.23 The DRIVE-FORWARD trial investigated doravirine compared with ritonavir-boosted darunavir, each in combination with 2 NRTIs (TDF with emtricitabine or abacavir with lamivudine). At week 48, 84% of patients in the doravirine arm and 80% in the ritonavir-boosted darunavir arm achieved the primary endpoint of HIV-1 RNA < 50 copies/mL.24
Two-Drug, Single-Tablet, Once-Daily Regimens
Experts have long recommended that optimal treatment of HIV must consist of 3 active drugs, with trials both in the United States and Europe demonstrating decreased morbidity and mortality with 3-drug therapy.25,26 However, newer, more potent 2-drug therapy is giving more choices to people living with HIV. The single-tablet, 2-drug regimens currently available are dolutegravir/rilpivirine and dolutegravir/lamivudine. There are theoretical benefits of 2-drug therapy, such as minimizing long-term toxicities, avoidance of some drug-drug interactions, and preservation of drugs for future treatment options. At this time, a 2-drug simplification regimen can be a viable option for selected virologically stable populations.
Dolutegravir/Rilpivirine (Juluca)
Dolutegravir/rilpivirine has been shown to be noninferior to standard therapy at 48-weeks, although it is associated with a higher discontinuation rate because of side effects.27 This option can be particularly useful in patients who have contraindications to NRTIs or renal dysfunction, but it has been studied only in patients without resistance who are already virologically suppressed. Ongoing studies are looking at 2-versus 3-drug therapies for HIV treatment-experienced patients. Most of these use PIs as a backbone because of their potency and high barrier to resistance. The advent of second-generation integrase inhibitors offers additional options.
Dolutegravir/Lamivudine (Dovato)
The GEMINI-1 and GEMINI-2 trials demonstrated that dolutegravir/lamivudine was noninferior to dolutegravir/TDF/emtricitabine.28 Based on these 2 studies, new guidelines have added dolutegravir/lamivudine as a recommended first-line therapy. For now, the recommendation is to use dolutegravir/lamivudine in individuals where NRTIs are contraindicated, and it should not be used in patients with chronic hepatitis B. Additionally, 3 studies have demonstrated the safety and efficacy of switching to dolutegravir/lamivudine.29-31 In the TANGO trial, neither virologic failures nor resistant virus were identified at 48 weeks following the switch.32 Although there are benefits of simplification with this regimen, including lower toxicity, lower costs, and saving other NRTIs in case of resistance, there should be no rush to switch patients to a 2-drug regimen. This is a viable strategy in patients without baseline resistance who have preserved T-cells and do not have hepatitis B.
SWITCHING ART AGENTS IN SELECTED CLINICAL SCENARIOS
Virologic Failure
One of the main goals of ART is maximal and durable suppression of HIV viral load to prevent the development of drug-resistant mutations.2 When patients are unable to achieve durable virologic suppression or have virologic rebound, the cause of virologic failure needs to be investigated. Virologic failure is defined as the inability to achieve or maintain viral suppression to a level below 200 copies/mL, whereas rebound is defined as an HIV RNA level exceeding 200 copies/mL after virologic suppression.33 A common cause of virologic failure is patient nonadherence, which can be related to a range of factors, including psychosocial issues and affordability of medications. Innate viral resistance can be the result of transmitted drug resistance at the time of infection or be acquired during unsuppressed viral replication secondary to inherent error-prone reverse transcriptase.33 Pharmacokinetic factors that affect blood levels of ART, such as drug-drug interactions, also can be a key factor in HIV drug resistance.
Patients With Limited Treatment Options
Despite advances in ART, some patients exhaust the existing regimens, leading to development of multidrug resistance and limited treatment options. In light of the treatment challenges in this group of patients, the FDA has recently approved 2 antiretroviral agents to target multidrug-resistant HIV: ibalizumab and fostemsavir.
Pregnancy
ART is used during pregnancy to maintain the pregnant woman’s health and to prevent perinatal transmission. Pregnancy can present unique challenges to effective ART, and therapy decisions should be made based on short-term and long-term safety data, pharmacokinetics, and tolerability. With few exceptions, women who are on a stable ART regimen and present for care should continue the same regimen.38 Key exceptions, due to increased toxicity, include didanosine, indinavir, nelfinavir, stavudine, and treatment-dose ritonavir. Cobicistat-based regimens (atazanavir, darunavir, elvitegravir) have altered pharmacokinetics during the second and third trimesters of pregnancy, leading to reduced mean steady-state minimum concentrations.39 Because increasing plasma HIV RNA level is associated with transmission to infants, women continuing cobicistat-based ART treatments should undergo more frequent viral load measurements.40 If viral rebound occurs late in pregnancy, especially shortly before delivery, achieving viral suppression can be more difficult. Therefore, women on a suppressed ART regimen containing cobicistat should consider switching to a different recommended regimen.38
Geriatric Populations
Although HIV is seen predominantly in younger patients, 48% of persons living with HIV are older than 50 years and 8% are 65 years of age or older.46 With effective antiretroviral treatment, we will continue to see an aging population of people living with HIV. There are no specific guidelines regarding the treatment of older adults, but HIV treatment can have its own challenges. Physiologic declines in renal function occur with aging, which can be compounded by an increasing prevalence of diabetes and decreased muscle mass, making estimations of renal function unreliable.47 Physiologic changes with age, such as decline in renal and hepatic function, decreasing metabolism via cytochrome P450, and body composition, influence drug pharmacokinetics and can in turn potentiate drug toxicities.48 Comorbid states and polypharmacy can complicate care. The prevalence of polypharmacy in the elderly is high, 93%, and is increasing.49,50 A study found that in those aged 65 years or older with HIV, 65% had at least 1 potential drug-drug interaction, and 6.6% had a potential severe drug-drug interaction.50 These patients are thus at risk of poor drug adherence, which in HIV therapy can lead to rebound viremia and resistance.
Renal Insufficiency
Several commonly used ART agents have nephrotoxic potential. The most common manifestations of nephrotoxicity are tubular toxicity, crystal nephropathy, and interstitial nephritis. Of these, acute tubular toxicity caused by TDF is the most widely reported. About 2% of those taking TDF developed treatment-limiting renal insufficiency, manifested as Fanconi syndrome.53 Higher plasma levels of TDF are associated with increased nephrotoxicity.55 Guidelines recommend switching from TDF if the estimated glomerular filtration rate (eGFR) declines by > 25% or the eGFr is < 60/mL/min/1.73 m2. Wever et al reports that in TDF-associated nephrotoxicity, only 42% of patients reached their pre-TDF eGFR.54TAF, a prodrug of TDF, is associated with reduced levels of TDF and is hypothesized to have fewer adverse effects.55 A pooled analysis comparing renal adverse effects of TDF and TAF reported no cases of renal dysfunction in the TAF group, supporting its safety; however, acute kidney injury has also been reported with TAF.56,57 Switching from TDF to TAF in patients with renal dysfunction has been shown to lead to improvement in proteinuria, but the impact remains unclear.53
Dyslipidemia and Cardiovascular Risk
Aside from the traditional cardiovascular risks, PIs, TAF, and efavirenz can negatively affect the lipid profile, with changes in LDL and triglycerides appearing as early as 2 weeks after initiating therapy. An observational study from Spain showed that treatment with TAF worsens the lipid profile in comparison to patients treated with TDF for elvitegravir/cobicistat-based therapies; patients on TAF were twice as likely to need lipid-lower drugs in comparison to those in the TDF arm.61 Similarly, patients who changed from a TDF-based regimen to TAF for improved renal and bone safety profiles had significant changes in both total cholesterol and LDL.65Other NRTIs do not negatively affect lipid profile. Although NNRTIs can increase LDL, this is usually offset by an increase in HDL.62 Of the NNRTIs, the incidence of increased LDL is higher with efavirenz, but it also can cause an increase in HDL; in contrast, patients switched from efavirenz to rilpivirine have a better lipid profile.63,64 PIs, especially older ones such as lopinavir/ritonavir, are associated with lipid abnormalities. For patients who develop dyslipidemia as a result of using older PIs, switching to a darunavir or atazanavir regimen or even integrase inhibitors, which are considered lipid neutral, is recommended.63 When making adjustments in ART, care should be taken in prescribing abacavir to individuals with risk factors for coronary artery disease. Although there is no consensus, some randomized controlled trials suggested an association between myocardial infarction and abacavir, whereas others have not.66,67
HIV and Hepatis B Co-infection
In patients with HIV and hepatitis B co-infection, ART regimens should contain 1 drug that is active against hepatitis B (lamivudine, emtricitabine, TDF, or TAF). Clinicians should monitor liver function for hepatitis B reactivation and liver function when a regimen that contains anti-hepatitis B drugs is stopped because discontinuation of these regimens can result in acute, and sometimes fatal, liver damage.2
Financial Considerations
With out-of-pocket expenses and co-pays, some patients may have to switch ART regimens for financial reasons. Additionally, switching to generic versions of ART has been proposed as a means of saving resources for government programs already facing budgetary constraints. A study published in 2013 using generic-based ART versus branded ART showed a potential savings of almost $1 billion per year.68 A key barrier to the use of generic-based ART is patient skepticism regarding the performance of these medications. Branded ART regimens are also co-formulated, creating the perception that taking more pills will lead to noncompliance and therefore place the patient at risk of viral rebound. In a study from France, only 17% of patients were willing to switch to generic medications if doing so increased pill burden.69 In the same study, 75% physicians were generally willing to prescribe generics; however, that number dropped to 26% if the patient’s pill burden would increase.69 Paradoxically, because of the patchwork of insurance, government assistance, Medicaid, and Medicare, changing to generic-based ART may increase patients’ co-pays.
1. Benson CA, Gandhi RT, et al. Antiretroviral drugs for treatment and prevention of HIV infection in adults. 2018 recommendations of the International Antiviral Society-USA Panel. JAMA. 2018; 320:379-396.
2. Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents living with HIV. http://www.aidsinfo.nih.gov/ContentFiles/ AdultandAdolescentGL.pdf. Accessed July 14, 2020.
3. FDA approves the first once-a-day three-drug combination tablet for treatment of HIV-1. https://aidsinfo.nih.gov/news/769/fda-approves-the-first-once-a-day-three-drug-combination-tablet-for-treatment-of-hiv-1. Accessed July 14, 2020.
4. Apostolova N, Funes HA, Blas-Garcia A, et al. Efavirenz and the CNS: what we already know and questions that need to be answered. J Antimicrob Chemother. 2015;70:2693-2708.
5. de Béthune MP. Non-nucleoside reverse transcriptase inhibitors (NNRTIs), their discovery, development, and use in the treatment of HIV-1 infection: a review of the last 20 years (1989-2009). Antiviral Res. 2010;85:75-90.
6. Carey D, Puls R, Amin J, et al. Efficacy and safety of efanvirenz 400mg daily versus 600 mg daily: 96-week data from the randomized, double-blind, placebo-controlled, non-inferiority ENCORE1 study. Lancet Infect Dis. 2015;15:793-802.
7. Molina JM, Cahn P, Grinsztejn B, et al; ECHO study group. Rilpivirine versus efavirenz with tenofovir and emtricitabine in treatment-naive adults infected with HIV-1 (ECHO): a phase 3 randomised double-blind active-controlled trial. Lancet. 2011;378:238-246.
8. Cohen CJ, Andrade-Villanueva J, Clotet B, et al. THRIVE study group Rilpivirine versus efavirenz with two background nucleoside or nucleotide reverse transcriptase inhibitors in treatment-naive adults infected with HIV-1 (THRIVE): a phase 3, randomised, non-inferiority trial. Lancet. 2011;378:229-237.
9. James C, Preninger L, Sweet M. Rilpivirine: A second-generation nonnucleoside reverse transcriptase inhibitor. Am J Health Syst Pharm. 2012;69:857-861.
10. Zolopa A, Sax PE, DeJesus E, et al. GS-US-236-0102 Study Team A randomized double-blind comparison of coformulated elvitegravir/cobicistat/emtricitabine/tenofovir disoproxil fumarate versus efavirenz/emtricitabine/tenofovir disoproxil fumarate for initial treatment of HIV-1 infection: analysis of week 96 results. J Acquir Immune Defic Syndr. 2013;63:96-100.
11. DeJesus E, Rockstroh JK, Henry K, et al. GS-236-0103 Study Team Co-formulated elvitegravir, cobicistat, emtricitabine, and tenofovir disoproxil fumarate versus ritonavir-boosted atazanavir plus co-formulated emtricitabine and tenofovir disoproxil fumarate for initial treatment of HIV-1 infection: a randomised, double-blind, phase 3, non-inferiority trial. Lancet. 2012;379:2429-2438.
12. Sherman EM, et al. Cobicistat: review of a pharmacokinetic enhancer for HIV infection. Clin Ther. 2015;37:1876-1893.
13. Walmsley S, Baumgarten A, Berenguer J, et al. Dolutegravir plus abacavir/lamivudine for the treatment of HIV-1 infection in antiretroviral therapy-naive patients: week 96 and week 144 results from the SINGLE randomized clinical trial. J Acquir Immune Defic Syndr. 2015;70:515-519.
14. Barbarino JM, Kroetz DL, Altman RB, Klein TE. PharmGKB summary: abacavir pathway. Pharmacogenet Genomics. 2014;24:276-282.
15. Sax PE, Wohl DA, Yin MT, et al. Tenofovir alafenamide versus tenofovir disoproxil fumarate, coformulated with elvitegravir, cobicistat, and emtricitabine, for initial treatment of HIV-1 infection: two randomized, double-blind, phase 3, non-inferiority trials. Lancet. 2015;385:2606–2615.
16. DeJesus E, Haas B, Segal-Maurer S, et al. Superior efficacy and improved renal and bone safety after switching from a tenofovir disoproxil fumarate regimen to a tenofovir alafenamide-based regimen through 96 weeks of treatment. AIDS Res Hum Retroviruses. 2016;34:337-342.
17. Maggiolo F, Rizzardini G, Raff F, et al. Bone mineral density in virologically suppressed people aged 60 years or older with HIV-1 switching from a regimen containing tenofovir disoproxil fumarate to an elvitegravir, cobicistat, emtricitabine, and tenofovir alafenamide single-tablet regimen: a multicentre, open-label, phase 3b, randomised trial. Lancet HIV. 2019;6: e655-e666.
18. Ogbuagu O. Rilpivirine, emtricitabine and tenofovir alafenamide: single-tablet combination for the treatment of HIV-1 infection in selected patients. Expert Rev Anti Infect Ther. 2016;;14:1113-1126.
19. Gallant J, Lazzarin A, Mills A, et al. Bictegravir, emtricitabine, and tenofovir alafenamide versus dolutegravir, abacavir, and lamivudine for initial treatment of HIV-1 infection (GS-US-380-1489): a double-blind, multicentre, phase 3, randomised controlled non-inferiority trial. Lancet. 2017;390:2063-2072.
20. Sax PE, Pozniak A, Montes ML, et al. Coformulated bictegravir, emtricitabine, and tenofovir alafenamide versus dolutegravir with emtricitabine and tenofovir alafenamide, for the initial treatment of HIV-1 infection (GS-US-1490): a randomised, double-blind, multicenter, phase 3, non-inferiority trial. Lancet. 2017;390:2073-2082.
21. Eron JJ, Orkin C, Gallant J, et al. A week-48 randomized phase-3 trial of darunavir/cobicistat/emtricitabine/tenofovir alafenamide in treatment-naive HIV-1 patients. AIDS. 2018;32:1431-1442.
22. Orkin C, Molina JM, Negredo E, et al;. EMERALD study group. Efficacy and safety of switching from boosted protease inhibitors plus emtricitabine/tenofovir disoproxil fumarate regimens to the once-daily complete HIV-1 regimen of darunavir/cobicistat/emtricitabine/tenofovir alafenamide (D/C/F/TAF) in virologically suppressed, HIV-1-infected adults through 48 weeks (EMERALD): a phase 3, randomized, non-inferiority trial. Lancet HIV. 2018;5:e23-e34.
23. Orkin C, Squires KE, Molina JM, et al. Doravirine/lamivudine/tenofovir disoproxil fumarate is non-inferior to efavirenz/emtricitabine/tenofovir disoproxil fumarate in treatment-naive adults with human immunodeficiency virus-1 infection: week 48 results of the DRIVE-AHEAD Trial. Clin Infect Dis. 2019;68:535-544.
24. Molina JM, Squires K, Sax PE, et al. Doravirine versus ritonavir-boosted darunavir in antiretroviral-naive adults with HIV-1 (DRIVE-FORWARD): 48-week results of a randomised, double-blind, phase 3, non-inferiority trial. Lancet HIV. 2018;5:e211-e220.
25. Palella FJ, Delaney KM, Moorman ACE, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med. 1998;338:853-860.
26. Mocroft A, Vella S, Benfiedl TL. Changing patterns of mortality across Europe in patients infected with HIV-1. Lancet. 1998;3552:1725-1730.
27. Libre JM, Hugh CC, Castelli F, et al. Efficacy, safety, and tolerability of dolutegravir-rilpivirine for the maintenance of virological suppression in adults with HIV-1: phase 3, randomized, noninferiority SWORD-1 and SWORD-2 studies. Lancet. 2018;391:839-849.
28. Cahn P, Madero JS, Arribas JR, et al. Durable efficacy of dolutegravir plus lamivudine in antiretroviral treatment-naive adults with HIV-1 infection: 96-week results from the GEMINI-1 and GEMINI-2 randomized clinical trials. J Acquir Immune Defic Syndr. 2020;83:310-318.
29. Joly V, Burdet C, Landman R, et al. Dolutegravir and lamivudine maintenance therapy in HIV-1 virologically suppressed patients: results of the ANRS 167 trial (LAMIDOL). J Antimicrob Chemother. 2019;74:739-745.
30. Li JZ, Sax PE, Marconi VC, et al. No significant changes to residual viremia after switch to dolutegravir and lamivudine in a randomized trial. Open Forum Infect Dis. 2019;6:ofz056.
31. Taiwo BO, Marconi VC, Verzins B, et al. Dolutegravir plus lamivudine maintains human immunodeficiency virus-1 suppression through week 48 in a pilot randomized trial. Clin Infect Dis. 2018;66:1794-1979.
32. Van Wyk J, Ajana F, Bisshop F, et al. Efficacy and safety of switching to dolutegravir/lamivudine fixed-dose 2-drug regimen vs continuing a tenofovir alafenamide–based 3- or 4-drug regimen for maintenance of virologic suppression in adults living with human immunodeficiency virus type 1: phase 3, randomized, noninferiority TANGO Study. Clin Infect Dis. Jan 6;ciz1243. doi: 10.1093/cid/ciz1243.
33. Cutrell J, Jodlowski T, Bedimo R. The management of treatment-experienced HIV patients (including virologic failure and switches). Ther Adv Infectious Dis. 2020;7:1-15.
34. Devereux, HL, Youle, M, Johnson, MA, et al. Rapid decline in detectability of HIV-1 drug resistance mutations after stopping therapy. AIDS. 1999;13:F123-F127.
35. Gatanaga H, Tsukada K, Honda H, et al. Detection of HIV type 1 load by the Roche Cobas TaqMan assay in patients with viral loads previously undetectable by the Roche Cobas Amplicor Monitor. Clin Infect Dis. 2009;48:260-262.
36. Emu B, Fessel J, Schrader S, et al. Phase 3 study of ibalizumab for multidrug-resistant HIV-1. N Engl J Med. 2018;379:645-654.
37. Kozal M, Aberg J, Pialoux G, et al. Fostemsavir in adults with multidrug-resistant HIV-1 infection. N Engl J Med. 2020; 382:1232-1243.
38. Department of Health and Human Services (HHS) Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission. recommendations for use of antiretroviral drugs in pregnant HIV-1-infected women for maternal health and interventions to reduce perinatal HIV transmission in the United States. http://aidsinfo.nih.gov/guidelines/html/3/perinatal-guidelines/0/ Accessed on July 13, 2020.
39. Boyd SD, Sampson MR, Viswanathan P, et al. Cobicistat-containing antiretroviral regimens are not recommended during pregnancy: viewpoint. AIDS. 2019;33:1089-1093.
40. Garcia PM, Kalish LA, Pitt J, et al. Maternal levels of plasma human immunodeficiency virus type 1 RNA and the risk of perinatal transmission. N Engl J Med. 1999;341:394-402.
41. Stek A, Best BM, Wang J, et al. Pharmacokinetics of once versus twice daily darunavir In pregnant HIV-infected women. J Acquir Immune Defic Syndr. 2015;70:33-41.
42. Stek A, Best B, Capparelli E, et al. Pharmacokinetics of increased dose darunavir during late pregnancy and postpartum. Presented at: 23rd Conference on Retroviruses and Opportunistic Infections. 2016. Boston, MA.
43. Mirochnick M, Best BM, Stek AM, et al. Atazanavir pharmacokinetics with and without tenofovir during pregnancy. J Acquir Immune Defic Syndr. 2011;56:412-419.
44. Schalkwijk S, Colbers A, Konopnicki D, et al. Lowered rilpivirine exposure during third trimester of pregnancy in HIV-1-positive women. Clin Infect Dis. 2017;65:1335-1341.
45. Zash R, Holmes L, Diseko M, et al. Neural-tube defects and antiretroviral treatment regimens in Botswana. N Engl J Med. 2019;381:827-840.
46. Centers for Disease Control and Prevention. HIV Surveillance Report, 2017; vol. 29. www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published November 2018.
47. Rhee MS, Greenblatt DJ. Pharmacologic consideration for the use of antiretroviral agents in the elderly. J Clin Pharmacol. 2008;481212-1225.
48. Nguyen, N, Holodniy M. HIV infection in the elderly. Clin Interv Aging. 2008;3:453-472.
49. Gleason LJ, Luque AE, Shah K. Polypharmacy in the HIV-infected older adult population. Clin Interv Aging. 2013;8749-763.
50. Bastida C, Grau A, Marquez M, et al. Polypharmacy and potential drug-drug interactions in an HIV-infected elderly population. Farm Hosp. 2017;41:618-624.
51. Brown TT, Hoy J, Borderi M, et al. Recommendations for evaluation and management of bone disease in HIV. Clin Infect Dis. 2015;60:1242-1251.
52. Mocroft A, Lundgren JD, Ross M, et al. Cumulative and current exposure to potentially nephrotoxic antiretrovirals and development of chronic kidney disease in HIV-positive individuals with a normal baseline estimated glomerular filtration rate: a prospective international cohort study. Lancet HIV. 2016;3:e23-32.
53. Ryom L, Mocroft A, Kirk O, et al. D:A:D Study Group. Association between antiretroviral exposure and renal impairment among HIV-positive persons with normal baseline renal function: the D:A:D study. J Infect Dis. 2013;207:1359.
54. Wever K, van Agtmael MA, Carr A. Incomplete reversibility of tenofovir related renal toxicity in HIV-infected men. J Acquir Immune Defic Syndr. 2010;55:78-81.
55. Hall AM, Hendry BM, Nitsch D, Connolly JO. Tenofovir-associated kidney toxicity in HIV-infected patients: a review of the evidence. Am J Kidney Dis. 2011; 57:773-780.
56. Gupta SK, Post FA, Arribas JR, et al. Renal safety of tenofovir alafenamide vs. tenofovir disoproxil fumarate: a pooled analysis of 26 clinical trials. AIDS. 2019;33:1455-1465.
57. Novick TK, Choi MJ, Rosenberg AZ, et al, Tenofovir alafenamide nephrotoxicity in an HIV-positive patient: A case report. Medicine (Baltimore). 2017;96:e8046.
58. Surial B, Ledergerber B, Calmy A, et al. Swiss HIV Cohort Study, changes in renal function after switching from TDF to TAF in HIV-infected individuals: a prospective cohort study. J Infect Dis. jiaa125, https://doi.org/10.1093/infdis/jiaa125.
59. McLaughlin MM, Guerrero AJ, Merker A. Renal effects of non-tenofovir antiretroviral therapy in patients living with HIV. Drugs Context. 2018;7:212519.
60. German P, Liu H, Szwarcberg J, et al. Effect of cobicistat on glomerular filtration rate in subjects with normal and impaired renal function. J Acquir Immune Defic Syndr. 2012;61:32-40.
61. Cid-Silva P, Fernandez-Bargiela N, Margusino-Framinan L, et al. Treatment with tenofovir alafenamide fumarate worsens the lipid profile of HIV-infected patients versus treatment with tenofovir disoproxil fumarate, each coformulated with elvitegravir, cobicistat, and emtricitabine. Basic Clin Pharmacol Toxicol. 2019;124:479-490.
62. Fontas E, van Leth F, Sabin CA, et al. Lipid profiles in HIV-infected patients receiving combination antiretroviral therapy: are different antiretroviral drugs associated with different lipid profiles?. J Infect Dis. 2004;189:1056-1074.
63. Tebas P, Sension M, Arribas J, et al. Lipid levels and changes in body fat distribution in treatment-naive, HIV-1-Infected adults treated with rilpivirine or Efavirenz for 96 weeks in the ECHO and THRIVE trials. Clin Infect Dis. 2014;59:425-434.
64. Taramasso L, Tatarelli P, Ricci E, et al. Improvement of lipid profile after switching from efavirenz or ritonavir-boosted protease inhibitors to rilpivirine or once-daily integrase inhibitors: results from a large observational cohort study (SCOLTA). BMC Infect Dis. 2018;18:357.
65. Lacey A, Savinelli, S, Barco, EA, et al. The UCD ID Cohort Study; Investigating the effect of antiretroviral switch to tenofovir alafenamide on lipid profiles in people living with HIV. AIDS. 2020;341161-1170.
66. Marcus JL, Neugebauer RS, Leyden WA, et al. Use of abacavir and risk of cardiovascular disease among HIV-infected individuals. J Acquir Immune Defic Syndr. 2016;71:413-419.
67. Ribaudo HJ, Benson CA, Zheng Y, et al. No risk of myocardial infarction associated with initial antiretroviral treatment containing abacavir: short and long-term results from ACTG A5001/ALLRT. Clin Infect Dis. 2011;52:929-940.
68. Walensky RP, Sax PE, Nakamura YM, et al. Economic savings versus health losses: the cost-effectiveness of generic antiretroviral therapy in the United States. Ann Intern Med. 2013;158:84-92.
69. Jacomet C, Allavena C, Peyrol F, et al. Perception of antiretroviral generic medicines: one-day survey of HIV-infected patients and their physicians in France. PLoS One. 2015;10:e0117214-e0117214.
1. Benson CA, Gandhi RT, et al. Antiretroviral drugs for treatment and prevention of HIV infection in adults. 2018 recommendations of the International Antiviral Society-USA Panel. JAMA. 2018; 320:379-396.
2. Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents living with HIV. http://www.aidsinfo.nih.gov/ContentFiles/ AdultandAdolescentGL.pdf. Accessed July 14, 2020.
3. FDA approves the first once-a-day three-drug combination tablet for treatment of HIV-1. https://aidsinfo.nih.gov/news/769/fda-approves-the-first-once-a-day-three-drug-combination-tablet-for-treatment-of-hiv-1. Accessed July 14, 2020.
4. Apostolova N, Funes HA, Blas-Garcia A, et al. Efavirenz and the CNS: what we already know and questions that need to be answered. J Antimicrob Chemother. 2015;70:2693-2708.
5. de Béthune MP. Non-nucleoside reverse transcriptase inhibitors (NNRTIs), their discovery, development, and use in the treatment of HIV-1 infection: a review of the last 20 years (1989-2009). Antiviral Res. 2010;85:75-90.
6. Carey D, Puls R, Amin J, et al. Efficacy and safety of efanvirenz 400mg daily versus 600 mg daily: 96-week data from the randomized, double-blind, placebo-controlled, non-inferiority ENCORE1 study. Lancet Infect Dis. 2015;15:793-802.
7. Molina JM, Cahn P, Grinsztejn B, et al; ECHO study group. Rilpivirine versus efavirenz with tenofovir and emtricitabine in treatment-naive adults infected with HIV-1 (ECHO): a phase 3 randomised double-blind active-controlled trial. Lancet. 2011;378:238-246.
8. Cohen CJ, Andrade-Villanueva J, Clotet B, et al. THRIVE study group Rilpivirine versus efavirenz with two background nucleoside or nucleotide reverse transcriptase inhibitors in treatment-naive adults infected with HIV-1 (THRIVE): a phase 3, randomised, non-inferiority trial. Lancet. 2011;378:229-237.
9. James C, Preninger L, Sweet M. Rilpivirine: A second-generation nonnucleoside reverse transcriptase inhibitor. Am J Health Syst Pharm. 2012;69:857-861.
10. Zolopa A, Sax PE, DeJesus E, et al. GS-US-236-0102 Study Team A randomized double-blind comparison of coformulated elvitegravir/cobicistat/emtricitabine/tenofovir disoproxil fumarate versus efavirenz/emtricitabine/tenofovir disoproxil fumarate for initial treatment of HIV-1 infection: analysis of week 96 results. J Acquir Immune Defic Syndr. 2013;63:96-100.
11. DeJesus E, Rockstroh JK, Henry K, et al. GS-236-0103 Study Team Co-formulated elvitegravir, cobicistat, emtricitabine, and tenofovir disoproxil fumarate versus ritonavir-boosted atazanavir plus co-formulated emtricitabine and tenofovir disoproxil fumarate for initial treatment of HIV-1 infection: a randomised, double-blind, phase 3, non-inferiority trial. Lancet. 2012;379:2429-2438.
12. Sherman EM, et al. Cobicistat: review of a pharmacokinetic enhancer for HIV infection. Clin Ther. 2015;37:1876-1893.
13. Walmsley S, Baumgarten A, Berenguer J, et al. Dolutegravir plus abacavir/lamivudine for the treatment of HIV-1 infection in antiretroviral therapy-naive patients: week 96 and week 144 results from the SINGLE randomized clinical trial. J Acquir Immune Defic Syndr. 2015;70:515-519.
14. Barbarino JM, Kroetz DL, Altman RB, Klein TE. PharmGKB summary: abacavir pathway. Pharmacogenet Genomics. 2014;24:276-282.
15. Sax PE, Wohl DA, Yin MT, et al. Tenofovir alafenamide versus tenofovir disoproxil fumarate, coformulated with elvitegravir, cobicistat, and emtricitabine, for initial treatment of HIV-1 infection: two randomized, double-blind, phase 3, non-inferiority trials. Lancet. 2015;385:2606–2615.
16. DeJesus E, Haas B, Segal-Maurer S, et al. Superior efficacy and improved renal and bone safety after switching from a tenofovir disoproxil fumarate regimen to a tenofovir alafenamide-based regimen through 96 weeks of treatment. AIDS Res Hum Retroviruses. 2016;34:337-342.
17. Maggiolo F, Rizzardini G, Raff F, et al. Bone mineral density in virologically suppressed people aged 60 years or older with HIV-1 switching from a regimen containing tenofovir disoproxil fumarate to an elvitegravir, cobicistat, emtricitabine, and tenofovir alafenamide single-tablet regimen: a multicentre, open-label, phase 3b, randomised trial. Lancet HIV. 2019;6: e655-e666.
18. Ogbuagu O. Rilpivirine, emtricitabine and tenofovir alafenamide: single-tablet combination for the treatment of HIV-1 infection in selected patients. Expert Rev Anti Infect Ther. 2016;;14:1113-1126.
19. Gallant J, Lazzarin A, Mills A, et al. Bictegravir, emtricitabine, and tenofovir alafenamide versus dolutegravir, abacavir, and lamivudine for initial treatment of HIV-1 infection (GS-US-380-1489): a double-blind, multicentre, phase 3, randomised controlled non-inferiority trial. Lancet. 2017;390:2063-2072.
20. Sax PE, Pozniak A, Montes ML, et al. Coformulated bictegravir, emtricitabine, and tenofovir alafenamide versus dolutegravir with emtricitabine and tenofovir alafenamide, for the initial treatment of HIV-1 infection (GS-US-1490): a randomised, double-blind, multicenter, phase 3, non-inferiority trial. Lancet. 2017;390:2073-2082.
21. Eron JJ, Orkin C, Gallant J, et al. A week-48 randomized phase-3 trial of darunavir/cobicistat/emtricitabine/tenofovir alafenamide in treatment-naive HIV-1 patients. AIDS. 2018;32:1431-1442.
22. Orkin C, Molina JM, Negredo E, et al;. EMERALD study group. Efficacy and safety of switching from boosted protease inhibitors plus emtricitabine/tenofovir disoproxil fumarate regimens to the once-daily complete HIV-1 regimen of darunavir/cobicistat/emtricitabine/tenofovir alafenamide (D/C/F/TAF) in virologically suppressed, HIV-1-infected adults through 48 weeks (EMERALD): a phase 3, randomized, non-inferiority trial. Lancet HIV. 2018;5:e23-e34.
23. Orkin C, Squires KE, Molina JM, et al. Doravirine/lamivudine/tenofovir disoproxil fumarate is non-inferior to efavirenz/emtricitabine/tenofovir disoproxil fumarate in treatment-naive adults with human immunodeficiency virus-1 infection: week 48 results of the DRIVE-AHEAD Trial. Clin Infect Dis. 2019;68:535-544.
24. Molina JM, Squires K, Sax PE, et al. Doravirine versus ritonavir-boosted darunavir in antiretroviral-naive adults with HIV-1 (DRIVE-FORWARD): 48-week results of a randomised, double-blind, phase 3, non-inferiority trial. Lancet HIV. 2018;5:e211-e220.
25. Palella FJ, Delaney KM, Moorman ACE, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med. 1998;338:853-860.
26. Mocroft A, Vella S, Benfiedl TL. Changing patterns of mortality across Europe in patients infected with HIV-1. Lancet. 1998;3552:1725-1730.
27. Libre JM, Hugh CC, Castelli F, et al. Efficacy, safety, and tolerability of dolutegravir-rilpivirine for the maintenance of virological suppression in adults with HIV-1: phase 3, randomized, noninferiority SWORD-1 and SWORD-2 studies. Lancet. 2018;391:839-849.
28. Cahn P, Madero JS, Arribas JR, et al. Durable efficacy of dolutegravir plus lamivudine in antiretroviral treatment-naive adults with HIV-1 infection: 96-week results from the GEMINI-1 and GEMINI-2 randomized clinical trials. J Acquir Immune Defic Syndr. 2020;83:310-318.
29. Joly V, Burdet C, Landman R, et al. Dolutegravir and lamivudine maintenance therapy in HIV-1 virologically suppressed patients: results of the ANRS 167 trial (LAMIDOL). J Antimicrob Chemother. 2019;74:739-745.
30. Li JZ, Sax PE, Marconi VC, et al. No significant changes to residual viremia after switch to dolutegravir and lamivudine in a randomized trial. Open Forum Infect Dis. 2019;6:ofz056.
31. Taiwo BO, Marconi VC, Verzins B, et al. Dolutegravir plus lamivudine maintains human immunodeficiency virus-1 suppression through week 48 in a pilot randomized trial. Clin Infect Dis. 2018;66:1794-1979.
32. Van Wyk J, Ajana F, Bisshop F, et al. Efficacy and safety of switching to dolutegravir/lamivudine fixed-dose 2-drug regimen vs continuing a tenofovir alafenamide–based 3- or 4-drug regimen for maintenance of virologic suppression in adults living with human immunodeficiency virus type 1: phase 3, randomized, noninferiority TANGO Study. Clin Infect Dis. Jan 6;ciz1243. doi: 10.1093/cid/ciz1243.
33. Cutrell J, Jodlowski T, Bedimo R. The management of treatment-experienced HIV patients (including virologic failure and switches). Ther Adv Infectious Dis. 2020;7:1-15.
34. Devereux, HL, Youle, M, Johnson, MA, et al. Rapid decline in detectability of HIV-1 drug resistance mutations after stopping therapy. AIDS. 1999;13:F123-F127.
35. Gatanaga H, Tsukada K, Honda H, et al. Detection of HIV type 1 load by the Roche Cobas TaqMan assay in patients with viral loads previously undetectable by the Roche Cobas Amplicor Monitor. Clin Infect Dis. 2009;48:260-262.
36. Emu B, Fessel J, Schrader S, et al. Phase 3 study of ibalizumab for multidrug-resistant HIV-1. N Engl J Med. 2018;379:645-654.
37. Kozal M, Aberg J, Pialoux G, et al. Fostemsavir in adults with multidrug-resistant HIV-1 infection. N Engl J Med. 2020; 382:1232-1243.
38. Department of Health and Human Services (HHS) Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission. recommendations for use of antiretroviral drugs in pregnant HIV-1-infected women for maternal health and interventions to reduce perinatal HIV transmission in the United States. http://aidsinfo.nih.gov/guidelines/html/3/perinatal-guidelines/0/ Accessed on July 13, 2020.
39. Boyd SD, Sampson MR, Viswanathan P, et al. Cobicistat-containing antiretroviral regimens are not recommended during pregnancy: viewpoint. AIDS. 2019;33:1089-1093.
40. Garcia PM, Kalish LA, Pitt J, et al. Maternal levels of plasma human immunodeficiency virus type 1 RNA and the risk of perinatal transmission. N Engl J Med. 1999;341:394-402.
41. Stek A, Best BM, Wang J, et al. Pharmacokinetics of once versus twice daily darunavir In pregnant HIV-infected women. J Acquir Immune Defic Syndr. 2015;70:33-41.
42. Stek A, Best B, Capparelli E, et al. Pharmacokinetics of increased dose darunavir during late pregnancy and postpartum. Presented at: 23rd Conference on Retroviruses and Opportunistic Infections. 2016. Boston, MA.
43. Mirochnick M, Best BM, Stek AM, et al. Atazanavir pharmacokinetics with and without tenofovir during pregnancy. J Acquir Immune Defic Syndr. 2011;56:412-419.
44. Schalkwijk S, Colbers A, Konopnicki D, et al. Lowered rilpivirine exposure during third trimester of pregnancy in HIV-1-positive women. Clin Infect Dis. 2017;65:1335-1341.
45. Zash R, Holmes L, Diseko M, et al. Neural-tube defects and antiretroviral treatment regimens in Botswana. N Engl J Med. 2019;381:827-840.
46. Centers for Disease Control and Prevention. HIV Surveillance Report, 2017; vol. 29. www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published November 2018.
47. Rhee MS, Greenblatt DJ. Pharmacologic consideration for the use of antiretroviral agents in the elderly. J Clin Pharmacol. 2008;481212-1225.
48. Nguyen, N, Holodniy M. HIV infection in the elderly. Clin Interv Aging. 2008;3:453-472.
49. Gleason LJ, Luque AE, Shah K. Polypharmacy in the HIV-infected older adult population. Clin Interv Aging. 2013;8749-763.
50. Bastida C, Grau A, Marquez M, et al. Polypharmacy and potential drug-drug interactions in an HIV-infected elderly population. Farm Hosp. 2017;41:618-624.
51. Brown TT, Hoy J, Borderi M, et al. Recommendations for evaluation and management of bone disease in HIV. Clin Infect Dis. 2015;60:1242-1251.
52. Mocroft A, Lundgren JD, Ross M, et al. Cumulative and current exposure to potentially nephrotoxic antiretrovirals and development of chronic kidney disease in HIV-positive individuals with a normal baseline estimated glomerular filtration rate: a prospective international cohort study. Lancet HIV. 2016;3:e23-32.
53. Ryom L, Mocroft A, Kirk O, et al. D:A:D Study Group. Association between antiretroviral exposure and renal impairment among HIV-positive persons with normal baseline renal function: the D:A:D study. J Infect Dis. 2013;207:1359.
54. Wever K, van Agtmael MA, Carr A. Incomplete reversibility of tenofovir related renal toxicity in HIV-infected men. J Acquir Immune Defic Syndr. 2010;55:78-81.
55. Hall AM, Hendry BM, Nitsch D, Connolly JO. Tenofovir-associated kidney toxicity in HIV-infected patients: a review of the evidence. Am J Kidney Dis. 2011; 57:773-780.
56. Gupta SK, Post FA, Arribas JR, et al. Renal safety of tenofovir alafenamide vs. tenofovir disoproxil fumarate: a pooled analysis of 26 clinical trials. AIDS. 2019;33:1455-1465.
57. Novick TK, Choi MJ, Rosenberg AZ, et al, Tenofovir alafenamide nephrotoxicity in an HIV-positive patient: A case report. Medicine (Baltimore). 2017;96:e8046.
58. Surial B, Ledergerber B, Calmy A, et al. Swiss HIV Cohort Study, changes in renal function after switching from TDF to TAF in HIV-infected individuals: a prospective cohort study. J Infect Dis. jiaa125, https://doi.org/10.1093/infdis/jiaa125.
59. McLaughlin MM, Guerrero AJ, Merker A. Renal effects of non-tenofovir antiretroviral therapy in patients living with HIV. Drugs Context. 2018;7:212519.
60. German P, Liu H, Szwarcberg J, et al. Effect of cobicistat on glomerular filtration rate in subjects with normal and impaired renal function. J Acquir Immune Defic Syndr. 2012;61:32-40.
61. Cid-Silva P, Fernandez-Bargiela N, Margusino-Framinan L, et al. Treatment with tenofovir alafenamide fumarate worsens the lipid profile of HIV-infected patients versus treatment with tenofovir disoproxil fumarate, each coformulated with elvitegravir, cobicistat, and emtricitabine. Basic Clin Pharmacol Toxicol. 2019;124:479-490.
62. Fontas E, van Leth F, Sabin CA, et al. Lipid profiles in HIV-infected patients receiving combination antiretroviral therapy: are different antiretroviral drugs associated with different lipid profiles?. J Infect Dis. 2004;189:1056-1074.
63. Tebas P, Sension M, Arribas J, et al. Lipid levels and changes in body fat distribution in treatment-naive, HIV-1-Infected adults treated with rilpivirine or Efavirenz for 96 weeks in the ECHO and THRIVE trials. Clin Infect Dis. 2014;59:425-434.
64. Taramasso L, Tatarelli P, Ricci E, et al. Improvement of lipid profile after switching from efavirenz or ritonavir-boosted protease inhibitors to rilpivirine or once-daily integrase inhibitors: results from a large observational cohort study (SCOLTA). BMC Infect Dis. 2018;18:357.
65. Lacey A, Savinelli, S, Barco, EA, et al. The UCD ID Cohort Study; Investigating the effect of antiretroviral switch to tenofovir alafenamide on lipid profiles in people living with HIV. AIDS. 2020;341161-1170.
66. Marcus JL, Neugebauer RS, Leyden WA, et al. Use of abacavir and risk of cardiovascular disease among HIV-infected individuals. J Acquir Immune Defic Syndr. 2016;71:413-419.
67. Ribaudo HJ, Benson CA, Zheng Y, et al. No risk of myocardial infarction associated with initial antiretroviral treatment containing abacavir: short and long-term results from ACTG A5001/ALLRT. Clin Infect Dis. 2011;52:929-940.
68. Walensky RP, Sax PE, Nakamura YM, et al. Economic savings versus health losses: the cost-effectiveness of generic antiretroviral therapy in the United States. Ann Intern Med. 2013;158:84-92.
69. Jacomet C, Allavena C, Peyrol F, et al. Perception of antiretroviral generic medicines: one-day survey of HIV-infected patients and their physicians in France. PLoS One. 2015;10:e0117214-e0117214.
Is vertical transmission of SARS-CoV-2 possible? Is that the right question?
Pique-Regi R, Romero R, Tarca AL, et al. Does the human placenta express the canonical cell entry mediators for SARS CoV-2? eLife. 2020;9:e58716.
EXPERT COMMENTARY
Maternal infection with the novel SARS-CoV-2 virus has been associated with severe maternal morbidity and mortality causing adverse pregnancy outcomes, such as preterm birth and, potentially, stillbirth, with vertical transmission of the virus to the fetus possible.1,2
Uniquely, maternal physiology supports both pro- and anti-inflammatory states within pregnancy—a system that not only must protect the mother but also must tolerate a semi-allogenic fetus. Studies demonstrate that the first and third trimesters are pro-inflammatory, while the second trimester is thought to be anti-inflammatory.3 Since the discovery of the SARS-CoV-2 virus, the question surrounding vertical transmission (infectivity from mother to fetus via the placenta) has occupied the imagination of physicians, scientists, and pregnant women. Importantly, the virus is transmitted to human cells via the ACE2 (angiotensin-converting enzyme 2) receptor, which aids in viral cell attachment. ACE2 receptors are expressed in placental stromal cells, perivascular cells of decidua, cytotrophoblast and syncytiotrophoblast,4 as well as blood vessel endothelium and vascular smooth muscle from both primary and secondary villi.
Details of the study
In their recent study, Pique-Regi and colleagues used single-cell RNA sequencing data to investigate whether the receptors responsible for SARS-CoV-2 infection are expressed in the human placenta.5 Their findings suggest that TMPRSS2 is present in insufficient quantity in the placenta to make vertical transmission possible and/or clinically relevant. Thus, despite the presence of ACE2 receptors in placental tissue, without the enzymatic assistance of a helper protein like TMPRSS2 (transmembrane protease, serine 2), vertical transmission is highly unlikely. The researchers found that there was negligible co-transcription for ACE2 and TMPRSS2 in the placenta and that placental tissue lacks the mRNA necessary to produce the enzyme; they concluded that the likelihood of vertical transmission to the fetus was therefore unlikely.
As a caveat to their research, the authors noted that:
- transcription levels do not always correlate with protein expression
- it is possible that a noncanonical cell-entry mediator facilitates entry
- individuals with complications related to the renin-angiotensin-aldosterone system (such as hypertensive disease) may have alterations to the expression of ACE2.
Study strengths and limitations
Methods for this study reveal that the researchers examined 32 placentas, all taken in the third trimester (32.9-39.1 weeks), with a median gestational age of 36.9 weeks. Notably, 81.3% of placentas were from Black women, 6.2% from White women, and 12.5% from Other women. The median maternal age was 25 years, median body mass index was 27.8 kg/m2, and 84.4% of women were multiparous. While this sample was not representative of race, gestational age, or parity, it is difficult to know whether those selection biases would have changed the researchers' findings.
The question regarding vertical transmission is one not answered solely on the basis of RNA sequencing data. Clinically, we know that neonates of mothers infected with SARS-CoV-2 have been born with immunoglobulin M antibodies, indicating antenatal exposure to the virus.6,7 In addition, infants have tested positive immediately after birth for coronavirus disease 2019 (COVID-19) via nasopharyngeal swab and amniotic fluid, and there are ample cases of histologic and polymerase chain reaction evidence of placental infection.8,9 We also know that inflammatory damage to the placenta could possibly break down the placental barrier.10
The destruction that SARS-CoV-2 often leaves in its wake is devastating for the maternal-fetal dyad. The effects of maternal infection on the placenta—where additional research is needed—can be profound, causing profuse endothelial damage, vascular malperfusion, thrombi, and infarcts, all of which can be lethal to some developing fetuses.
While the study by Pique-Regi and colleagues is an important contribution to the literature, it does not satisfactorily answer the question regarding vertical transmission. More research is needed, especially regarding maternal infection in the first and second trimesters, on the effects on placental vasculature (and timing of infection in each trimester), the potential breakdown of the maternal-fetal barrier, and, most important, the clinical courses and outcomes in both mother and infant.
JANE VAN DIS, MD
- Khalil A, Kalafat E, Benlioglu C, et al. SARS-CoV-2 infection in pregnancy: a systematic review and meta-analysis of clinical features and pregnancy outcomes. EClinical Medicine. 2020;25:100446.
- Khalil A, von Dadelszen P, Draycott T, et al. Change in the incidence of stillbirth and preterm delivery during the COVID-19 pandemic. JAMA. 2020;324:705-706.
- Liu H, Wang LL, Zhao SJ, et al. Why are pregnant women susceptible to COVID-19? An immunological viewpoint. J Reprod Immunol. 2020;139;103122.
- Li M, Chen L, Zhang J, et al. The SARS-CoV-2 receptor ACE2 expression of maternal-fetal interface and fetal organs by single-cell transcriptome study. PLoS One. 2020;15:e0230295.
- Pique-Regi R, Romero R, Tarca AL, et al. Does the human placenta express the canonical cell entry mediators for SARS-CoV-2? eLife. 2020;9:e58716.
- Zeng H, Xu C, Fan J, et al. Antibodies in infants born to mothers with COVID-19 pneumonia. JAMA. 2020;323:1848-1849.
- Dong L, Tian J, He S, et al. Possible vertical transmission of SARS-CoV-2 from an infected mother to her newborn. JAMA. 2020;323:1846-1848.
- Kotlyar A, Grechukhina O, Chen A, et al. Vertical transmission of COVID-19: a systematic review and meta-analysis. Am J Obstet Gynecol. 2020;S0002-9378(20)30823-1.
- Richtmann R, Torloni MR, Oyamada Otani AR, et al. Fetal deaths in pregnancies with SARS-CoV-2 infection in Brazil: a case series. Case Rep Womens Health. 2020;e00243.
- Wang C, Zhou YH, Yang HX, et al. Intrauterine vertical transmission of SARS-CoV-2: what we know so far. Ultrasound Obstet Gynecol. 2020;55:724-725.
Pique-Regi R, Romero R, Tarca AL, et al. Does the human placenta express the canonical cell entry mediators for SARS CoV-2? eLife. 2020;9:e58716.
EXPERT COMMENTARY
Maternal infection with the novel SARS-CoV-2 virus has been associated with severe maternal morbidity and mortality causing adverse pregnancy outcomes, such as preterm birth and, potentially, stillbirth, with vertical transmission of the virus to the fetus possible.1,2
Uniquely, maternal physiology supports both pro- and anti-inflammatory states within pregnancy—a system that not only must protect the mother but also must tolerate a semi-allogenic fetus. Studies demonstrate that the first and third trimesters are pro-inflammatory, while the second trimester is thought to be anti-inflammatory.3 Since the discovery of the SARS-CoV-2 virus, the question surrounding vertical transmission (infectivity from mother to fetus via the placenta) has occupied the imagination of physicians, scientists, and pregnant women. Importantly, the virus is transmitted to human cells via the ACE2 (angiotensin-converting enzyme 2) receptor, which aids in viral cell attachment. ACE2 receptors are expressed in placental stromal cells, perivascular cells of decidua, cytotrophoblast and syncytiotrophoblast,4 as well as blood vessel endothelium and vascular smooth muscle from both primary and secondary villi.
Details of the study
In their recent study, Pique-Regi and colleagues used single-cell RNA sequencing data to investigate whether the receptors responsible for SARS-CoV-2 infection are expressed in the human placenta.5 Their findings suggest that TMPRSS2 is present in insufficient quantity in the placenta to make vertical transmission possible and/or clinically relevant. Thus, despite the presence of ACE2 receptors in placental tissue, without the enzymatic assistance of a helper protein like TMPRSS2 (transmembrane protease, serine 2), vertical transmission is highly unlikely. The researchers found that there was negligible co-transcription for ACE2 and TMPRSS2 in the placenta and that placental tissue lacks the mRNA necessary to produce the enzyme; they concluded that the likelihood of vertical transmission to the fetus was therefore unlikely.
As a caveat to their research, the authors noted that:
- transcription levels do not always correlate with protein expression
- it is possible that a noncanonical cell-entry mediator facilitates entry
- individuals with complications related to the renin-angiotensin-aldosterone system (such as hypertensive disease) may have alterations to the expression of ACE2.
Study strengths and limitations
Methods for this study reveal that the researchers examined 32 placentas, all taken in the third trimester (32.9-39.1 weeks), with a median gestational age of 36.9 weeks. Notably, 81.3% of placentas were from Black women, 6.2% from White women, and 12.5% from Other women. The median maternal age was 25 years, median body mass index was 27.8 kg/m2, and 84.4% of women were multiparous. While this sample was not representative of race, gestational age, or parity, it is difficult to know whether those selection biases would have changed the researchers' findings.
The question regarding vertical transmission is one not answered solely on the basis of RNA sequencing data. Clinically, we know that neonates of mothers infected with SARS-CoV-2 have been born with immunoglobulin M antibodies, indicating antenatal exposure to the virus.6,7 In addition, infants have tested positive immediately after birth for coronavirus disease 2019 (COVID-19) via nasopharyngeal swab and amniotic fluid, and there are ample cases of histologic and polymerase chain reaction evidence of placental infection.8,9 We also know that inflammatory damage to the placenta could possibly break down the placental barrier.10
The destruction that SARS-CoV-2 often leaves in its wake is devastating for the maternal-fetal dyad. The effects of maternal infection on the placenta—where additional research is needed—can be profound, causing profuse endothelial damage, vascular malperfusion, thrombi, and infarcts, all of which can be lethal to some developing fetuses.
While the study by Pique-Regi and colleagues is an important contribution to the literature, it does not satisfactorily answer the question regarding vertical transmission. More research is needed, especially regarding maternal infection in the first and second trimesters, on the effects on placental vasculature (and timing of infection in each trimester), the potential breakdown of the maternal-fetal barrier, and, most important, the clinical courses and outcomes in both mother and infant.
JANE VAN DIS, MD
Pique-Regi R, Romero R, Tarca AL, et al. Does the human placenta express the canonical cell entry mediators for SARS CoV-2? eLife. 2020;9:e58716.
EXPERT COMMENTARY
Maternal infection with the novel SARS-CoV-2 virus has been associated with severe maternal morbidity and mortality causing adverse pregnancy outcomes, such as preterm birth and, potentially, stillbirth, with vertical transmission of the virus to the fetus possible.1,2
Uniquely, maternal physiology supports both pro- and anti-inflammatory states within pregnancy—a system that not only must protect the mother but also must tolerate a semi-allogenic fetus. Studies demonstrate that the first and third trimesters are pro-inflammatory, while the second trimester is thought to be anti-inflammatory.3 Since the discovery of the SARS-CoV-2 virus, the question surrounding vertical transmission (infectivity from mother to fetus via the placenta) has occupied the imagination of physicians, scientists, and pregnant women. Importantly, the virus is transmitted to human cells via the ACE2 (angiotensin-converting enzyme 2) receptor, which aids in viral cell attachment. ACE2 receptors are expressed in placental stromal cells, perivascular cells of decidua, cytotrophoblast and syncytiotrophoblast,4 as well as blood vessel endothelium and vascular smooth muscle from both primary and secondary villi.
Details of the study
In their recent study, Pique-Regi and colleagues used single-cell RNA sequencing data to investigate whether the receptors responsible for SARS-CoV-2 infection are expressed in the human placenta.5 Their findings suggest that TMPRSS2 is present in insufficient quantity in the placenta to make vertical transmission possible and/or clinically relevant. Thus, despite the presence of ACE2 receptors in placental tissue, without the enzymatic assistance of a helper protein like TMPRSS2 (transmembrane protease, serine 2), vertical transmission is highly unlikely. The researchers found that there was negligible co-transcription for ACE2 and TMPRSS2 in the placenta and that placental tissue lacks the mRNA necessary to produce the enzyme; they concluded that the likelihood of vertical transmission to the fetus was therefore unlikely.
As a caveat to their research, the authors noted that:
- transcription levels do not always correlate with protein expression
- it is possible that a noncanonical cell-entry mediator facilitates entry
- individuals with complications related to the renin-angiotensin-aldosterone system (such as hypertensive disease) may have alterations to the expression of ACE2.
Study strengths and limitations
Methods for this study reveal that the researchers examined 32 placentas, all taken in the third trimester (32.9-39.1 weeks), with a median gestational age of 36.9 weeks. Notably, 81.3% of placentas were from Black women, 6.2% from White women, and 12.5% from Other women. The median maternal age was 25 years, median body mass index was 27.8 kg/m2, and 84.4% of women were multiparous. While this sample was not representative of race, gestational age, or parity, it is difficult to know whether those selection biases would have changed the researchers' findings.
The question regarding vertical transmission is one not answered solely on the basis of RNA sequencing data. Clinically, we know that neonates of mothers infected with SARS-CoV-2 have been born with immunoglobulin M antibodies, indicating antenatal exposure to the virus.6,7 In addition, infants have tested positive immediately after birth for coronavirus disease 2019 (COVID-19) via nasopharyngeal swab and amniotic fluid, and there are ample cases of histologic and polymerase chain reaction evidence of placental infection.8,9 We also know that inflammatory damage to the placenta could possibly break down the placental barrier.10
The destruction that SARS-CoV-2 often leaves in its wake is devastating for the maternal-fetal dyad. The effects of maternal infection on the placenta—where additional research is needed—can be profound, causing profuse endothelial damage, vascular malperfusion, thrombi, and infarcts, all of which can be lethal to some developing fetuses.
While the study by Pique-Regi and colleagues is an important contribution to the literature, it does not satisfactorily answer the question regarding vertical transmission. More research is needed, especially regarding maternal infection in the first and second trimesters, on the effects on placental vasculature (and timing of infection in each trimester), the potential breakdown of the maternal-fetal barrier, and, most important, the clinical courses and outcomes in both mother and infant.
JANE VAN DIS, MD
- Khalil A, Kalafat E, Benlioglu C, et al. SARS-CoV-2 infection in pregnancy: a systematic review and meta-analysis of clinical features and pregnancy outcomes. EClinical Medicine. 2020;25:100446.
- Khalil A, von Dadelszen P, Draycott T, et al. Change in the incidence of stillbirth and preterm delivery during the COVID-19 pandemic. JAMA. 2020;324:705-706.
- Liu H, Wang LL, Zhao SJ, et al. Why are pregnant women susceptible to COVID-19? An immunological viewpoint. J Reprod Immunol. 2020;139;103122.
- Li M, Chen L, Zhang J, et al. The SARS-CoV-2 receptor ACE2 expression of maternal-fetal interface and fetal organs by single-cell transcriptome study. PLoS One. 2020;15:e0230295.
- Pique-Regi R, Romero R, Tarca AL, et al. Does the human placenta express the canonical cell entry mediators for SARS-CoV-2? eLife. 2020;9:e58716.
- Zeng H, Xu C, Fan J, et al. Antibodies in infants born to mothers with COVID-19 pneumonia. JAMA. 2020;323:1848-1849.
- Dong L, Tian J, He S, et al. Possible vertical transmission of SARS-CoV-2 from an infected mother to her newborn. JAMA. 2020;323:1846-1848.
- Kotlyar A, Grechukhina O, Chen A, et al. Vertical transmission of COVID-19: a systematic review and meta-analysis. Am J Obstet Gynecol. 2020;S0002-9378(20)30823-1.
- Richtmann R, Torloni MR, Oyamada Otani AR, et al. Fetal deaths in pregnancies with SARS-CoV-2 infection in Brazil: a case series. Case Rep Womens Health. 2020;e00243.
- Wang C, Zhou YH, Yang HX, et al. Intrauterine vertical transmission of SARS-CoV-2: what we know so far. Ultrasound Obstet Gynecol. 2020;55:724-725.
- Khalil A, Kalafat E, Benlioglu C, et al. SARS-CoV-2 infection in pregnancy: a systematic review and meta-analysis of clinical features and pregnancy outcomes. EClinical Medicine. 2020;25:100446.
- Khalil A, von Dadelszen P, Draycott T, et al. Change in the incidence of stillbirth and preterm delivery during the COVID-19 pandemic. JAMA. 2020;324:705-706.
- Liu H, Wang LL, Zhao SJ, et al. Why are pregnant women susceptible to COVID-19? An immunological viewpoint. J Reprod Immunol. 2020;139;103122.
- Li M, Chen L, Zhang J, et al. The SARS-CoV-2 receptor ACE2 expression of maternal-fetal interface and fetal organs by single-cell transcriptome study. PLoS One. 2020;15:e0230295.
- Pique-Regi R, Romero R, Tarca AL, et al. Does the human placenta express the canonical cell entry mediators for SARS-CoV-2? eLife. 2020;9:e58716.
- Zeng H, Xu C, Fan J, et al. Antibodies in infants born to mothers with COVID-19 pneumonia. JAMA. 2020;323:1848-1849.
- Dong L, Tian J, He S, et al. Possible vertical transmission of SARS-CoV-2 from an infected mother to her newborn. JAMA. 2020;323:1846-1848.
- Kotlyar A, Grechukhina O, Chen A, et al. Vertical transmission of COVID-19: a systematic review and meta-analysis. Am J Obstet Gynecol. 2020;S0002-9378(20)30823-1.
- Richtmann R, Torloni MR, Oyamada Otani AR, et al. Fetal deaths in pregnancies with SARS-CoV-2 infection in Brazil: a case series. Case Rep Womens Health. 2020;e00243.
- Wang C, Zhou YH, Yang HX, et al. Intrauterine vertical transmission of SARS-CoV-2: what we know so far. Ultrasound Obstet Gynecol. 2020;55:724-725.
Watch for nonsuicidal self-injury in girls with ADHD, comorbidities
Recent studies constitute a clarion call for clinicians to routinely screen adolescents with ADHD for nonsuicidal self-injury (NSSI) and its risk factors, Judit Balazs, MD, PhD, said at the virtual congress of the European College of Neuropsychopharmacology.
She was lead author of one of these studies, which drew a remarkable and disturbing conclusion: “We found – and it’s a very alarming result – that more than 70% of those people who had ADHD and [nonsuicidal self-injury] were girls. The girls with ADHD seem to be a high-risk population,” observed Dr. Balazs, professor and chair of the department of developmental psychology at Eotvos Lorand University, Budapest.
NSSI first became a specific diagnosis in the DSM-5. It is defined as deliberate, nonculturally sanctioned, nonsuicidal self-injury on at least five occasions within the past year and carried out with the aim of improving one’s emotional state as a result. The prevalence of NSSI among the general population of adolescents is high, with various investigators reporting rates of 15%-45%. Among adolescents with mental disorders, the reported prevalence climbs to 40%-80%. even though it’s now clear that many cases of pediatric-onset ADHD continue on well into adulthood, albeit often undiagnosed.
Whether NSSI and suicidal behavior are actually the same entity is currently a topic of intense research, according to Dr. Balazs, who is both a child and adolescent psychiatrist, as well as an adult psychiatrist.
She presented highlights of her cross-sectional study of 202 adolescent inpatients, 51% of them female, at the Vadaskert Child and Adolescent Psychiatry Hospital, a tertiary care center in Budapest. Using the structured diagnostic Mini International Neuropsychiatric Interview for Children and Adolescents (MINI Kid) and the self-rated Deliberate Self-Harm Inventory, Dr. Balazs and her coinvestigators determined that 52 of the adolescents, including 23 boys and 29 girls, met full diagnostic criteria for ADHD and another 77 demonstrated more than five subthreshold ADHD symptoms.
Strikingly, 35 of the 52 teens diagnosed with ADHD, or 67%, had current NSSI. Only 10 of these patients were boys. The other 25, or 71% of the total, were girls.
Psychiatric comorbidities proved to be the rule rather than the exception in the adolescent inpatients with ADHD plus NSSI. Among these inpatients, 94% had a history of suicidal behavior. In addition, 66% carried the diagnosis of oppositional defiant disorder, 63% generalized anxiety disorder, 60% had a psychotic disorder, and 51% had experienced a manic episode. Among them, 49% were diagnosed with social anxiety disorder, 46% with obsessive-compulsive disorder, 31% with panic disorder, 23% with conduct disorder, and an equal percentage with agoraphobia. Furthermore, 43% had a major depressive disorder and 34%, dysthymia. Alcohol abuse or dependence was present in 20%, and an equal percentage had psychoactive substance use disorder.
Dr. Balazs said she and her coinvestigators were surprised by the high prevalence of symptoms of comorbid psychotic disorder in conjunction with NSSI and ADHD. One possible explanation, she opined, is that as inpatients the study participants were at the more severe end of the disease spectrum, and some patients may have been admitted not solely because of the severity of their comorbidities. Another possibility is that, in some cases, what was labeled psychotic disorder may actually have been prodromal unipolar depression.
A key finding in Dr. Balazs’s study was that, according to a regression analysis, the relationship between ADHD and NSSI was mediated entirely by the symptoms of the ADHD comorbidities. Specifically, the significant risk factors for NSSI in patients with ADHD were affective disorders, suicidality, and psychotic disorders in both sexes, with the addition of comorbid alcohol abuse or dependence in girls only. There was no evidence of a direct causal relationship between ADHD, per se, and NSSI.
‘Findings warrant further investigation’
The study, which looks at the association between NSSI and adolescents is interesting, yet preliminary, said David Fassler, MD, in an interview.
“The authors conclude that girls with ADHD are at particularly high risk of NSSI,” said Dr. Fassler, clinical professor of psychiatry at the University of Vermont, Burlington. Dr. Fassler was not involved with the study.
“It is limited by sample size, acuity, and the incidence of comorbidities,” said Dr. Fassler, who had no conflicts of interest. “Nonetheless, the findings are intriguing and warrant further investigation with larger samples in diverse clinical settings.”
The study was supported by the Hungarian Scientific Research Fund. In addition, Dr. Balazs received funding from the Hungarian Academy of Sciences. The full details of the study have been published (BMC Psychiatry. 2018 Feb 6;18[1]:34).
SOURCE: Balazs J et al. ECNP 2020, Abstract EDU.02.
Recent studies constitute a clarion call for clinicians to routinely screen adolescents with ADHD for nonsuicidal self-injury (NSSI) and its risk factors, Judit Balazs, MD, PhD, said at the virtual congress of the European College of Neuropsychopharmacology.
She was lead author of one of these studies, which drew a remarkable and disturbing conclusion: “We found – and it’s a very alarming result – that more than 70% of those people who had ADHD and [nonsuicidal self-injury] were girls. The girls with ADHD seem to be a high-risk population,” observed Dr. Balazs, professor and chair of the department of developmental psychology at Eotvos Lorand University, Budapest.
NSSI first became a specific diagnosis in the DSM-5. It is defined as deliberate, nonculturally sanctioned, nonsuicidal self-injury on at least five occasions within the past year and carried out with the aim of improving one’s emotional state as a result. The prevalence of NSSI among the general population of adolescents is high, with various investigators reporting rates of 15%-45%. Among adolescents with mental disorders, the reported prevalence climbs to 40%-80%. even though it’s now clear that many cases of pediatric-onset ADHD continue on well into adulthood, albeit often undiagnosed.
Whether NSSI and suicidal behavior are actually the same entity is currently a topic of intense research, according to Dr. Balazs, who is both a child and adolescent psychiatrist, as well as an adult psychiatrist.
She presented highlights of her cross-sectional study of 202 adolescent inpatients, 51% of them female, at the Vadaskert Child and Adolescent Psychiatry Hospital, a tertiary care center in Budapest. Using the structured diagnostic Mini International Neuropsychiatric Interview for Children and Adolescents (MINI Kid) and the self-rated Deliberate Self-Harm Inventory, Dr. Balazs and her coinvestigators determined that 52 of the adolescents, including 23 boys and 29 girls, met full diagnostic criteria for ADHD and another 77 demonstrated more than five subthreshold ADHD symptoms.
Strikingly, 35 of the 52 teens diagnosed with ADHD, or 67%, had current NSSI. Only 10 of these patients were boys. The other 25, or 71% of the total, were girls.
Psychiatric comorbidities proved to be the rule rather than the exception in the adolescent inpatients with ADHD plus NSSI. Among these inpatients, 94% had a history of suicidal behavior. In addition, 66% carried the diagnosis of oppositional defiant disorder, 63% generalized anxiety disorder, 60% had a psychotic disorder, and 51% had experienced a manic episode. Among them, 49% were diagnosed with social anxiety disorder, 46% with obsessive-compulsive disorder, 31% with panic disorder, 23% with conduct disorder, and an equal percentage with agoraphobia. Furthermore, 43% had a major depressive disorder and 34%, dysthymia. Alcohol abuse or dependence was present in 20%, and an equal percentage had psychoactive substance use disorder.
Dr. Balazs said she and her coinvestigators were surprised by the high prevalence of symptoms of comorbid psychotic disorder in conjunction with NSSI and ADHD. One possible explanation, she opined, is that as inpatients the study participants were at the more severe end of the disease spectrum, and some patients may have been admitted not solely because of the severity of their comorbidities. Another possibility is that, in some cases, what was labeled psychotic disorder may actually have been prodromal unipolar depression.
A key finding in Dr. Balazs’s study was that, according to a regression analysis, the relationship between ADHD and NSSI was mediated entirely by the symptoms of the ADHD comorbidities. Specifically, the significant risk factors for NSSI in patients with ADHD were affective disorders, suicidality, and psychotic disorders in both sexes, with the addition of comorbid alcohol abuse or dependence in girls only. There was no evidence of a direct causal relationship between ADHD, per se, and NSSI.
‘Findings warrant further investigation’
The study, which looks at the association between NSSI and adolescents is interesting, yet preliminary, said David Fassler, MD, in an interview.
“The authors conclude that girls with ADHD are at particularly high risk of NSSI,” said Dr. Fassler, clinical professor of psychiatry at the University of Vermont, Burlington. Dr. Fassler was not involved with the study.
“It is limited by sample size, acuity, and the incidence of comorbidities,” said Dr. Fassler, who had no conflicts of interest. “Nonetheless, the findings are intriguing and warrant further investigation with larger samples in diverse clinical settings.”
The study was supported by the Hungarian Scientific Research Fund. In addition, Dr. Balazs received funding from the Hungarian Academy of Sciences. The full details of the study have been published (BMC Psychiatry. 2018 Feb 6;18[1]:34).
SOURCE: Balazs J et al. ECNP 2020, Abstract EDU.02.
Recent studies constitute a clarion call for clinicians to routinely screen adolescents with ADHD for nonsuicidal self-injury (NSSI) and its risk factors, Judit Balazs, MD, PhD, said at the virtual congress of the European College of Neuropsychopharmacology.
She was lead author of one of these studies, which drew a remarkable and disturbing conclusion: “We found – and it’s a very alarming result – that more than 70% of those people who had ADHD and [nonsuicidal self-injury] were girls. The girls with ADHD seem to be a high-risk population,” observed Dr. Balazs, professor and chair of the department of developmental psychology at Eotvos Lorand University, Budapest.
NSSI first became a specific diagnosis in the DSM-5. It is defined as deliberate, nonculturally sanctioned, nonsuicidal self-injury on at least five occasions within the past year and carried out with the aim of improving one’s emotional state as a result. The prevalence of NSSI among the general population of adolescents is high, with various investigators reporting rates of 15%-45%. Among adolescents with mental disorders, the reported prevalence climbs to 40%-80%. even though it’s now clear that many cases of pediatric-onset ADHD continue on well into adulthood, albeit often undiagnosed.
Whether NSSI and suicidal behavior are actually the same entity is currently a topic of intense research, according to Dr. Balazs, who is both a child and adolescent psychiatrist, as well as an adult psychiatrist.
She presented highlights of her cross-sectional study of 202 adolescent inpatients, 51% of them female, at the Vadaskert Child and Adolescent Psychiatry Hospital, a tertiary care center in Budapest. Using the structured diagnostic Mini International Neuropsychiatric Interview for Children and Adolescents (MINI Kid) and the self-rated Deliberate Self-Harm Inventory, Dr. Balazs and her coinvestigators determined that 52 of the adolescents, including 23 boys and 29 girls, met full diagnostic criteria for ADHD and another 77 demonstrated more than five subthreshold ADHD symptoms.
Strikingly, 35 of the 52 teens diagnosed with ADHD, or 67%, had current NSSI. Only 10 of these patients were boys. The other 25, or 71% of the total, were girls.
Psychiatric comorbidities proved to be the rule rather than the exception in the adolescent inpatients with ADHD plus NSSI. Among these inpatients, 94% had a history of suicidal behavior. In addition, 66% carried the diagnosis of oppositional defiant disorder, 63% generalized anxiety disorder, 60% had a psychotic disorder, and 51% had experienced a manic episode. Among them, 49% were diagnosed with social anxiety disorder, 46% with obsessive-compulsive disorder, 31% with panic disorder, 23% with conduct disorder, and an equal percentage with agoraphobia. Furthermore, 43% had a major depressive disorder and 34%, dysthymia. Alcohol abuse or dependence was present in 20%, and an equal percentage had psychoactive substance use disorder.
Dr. Balazs said she and her coinvestigators were surprised by the high prevalence of symptoms of comorbid psychotic disorder in conjunction with NSSI and ADHD. One possible explanation, she opined, is that as inpatients the study participants were at the more severe end of the disease spectrum, and some patients may have been admitted not solely because of the severity of their comorbidities. Another possibility is that, in some cases, what was labeled psychotic disorder may actually have been prodromal unipolar depression.
A key finding in Dr. Balazs’s study was that, according to a regression analysis, the relationship between ADHD and NSSI was mediated entirely by the symptoms of the ADHD comorbidities. Specifically, the significant risk factors for NSSI in patients with ADHD were affective disorders, suicidality, and psychotic disorders in both sexes, with the addition of comorbid alcohol abuse or dependence in girls only. There was no evidence of a direct causal relationship between ADHD, per se, and NSSI.
‘Findings warrant further investigation’
The study, which looks at the association between NSSI and adolescents is interesting, yet preliminary, said David Fassler, MD, in an interview.
“The authors conclude that girls with ADHD are at particularly high risk of NSSI,” said Dr. Fassler, clinical professor of psychiatry at the University of Vermont, Burlington. Dr. Fassler was not involved with the study.
“It is limited by sample size, acuity, and the incidence of comorbidities,” said Dr. Fassler, who had no conflicts of interest. “Nonetheless, the findings are intriguing and warrant further investigation with larger samples in diverse clinical settings.”
The study was supported by the Hungarian Scientific Research Fund. In addition, Dr. Balazs received funding from the Hungarian Academy of Sciences. The full details of the study have been published (BMC Psychiatry. 2018 Feb 6;18[1]:34).
SOURCE: Balazs J et al. ECNP 2020, Abstract EDU.02.
FROM ECNP 2020
AGA addresses postendoscopy esophageal adenocarcinoma
The American Gastroenterological Association has published a clinical practice update that characterizes postendoscopy esophageal adenocarcinoma (EAC) and offers recommendations to improve endoscopic detection of dysplastic and neoplastic lesions in patients with Barrett’s esophagus.
While emerging technologies may improve detection rates in the future, short-term progress will depend on human expertise, reported lead author Sachin Wani, MD, of the University of Colorado at Denver, Aurora, and colleagues.
Writing in Gastroenterology, Dr. Wani and colleagues noted that EAC incidence has increased sevenfold over the past 4 decades, and 40% of patients with EAC have advanced disease at diagnosis, with a “dismal” 5-year survival rate.
Attempts to catch EAC earlier through Barrett’s esophagus surveillance endoscopy have been generally fallen short, the investigators added. They discussed a variety of obstacles to success, including divergence from recommended screening timelines, nonadherence to the Seattle biopsy protocol, sampling errors, and variability of dysplastic tissue interpretation between pathologists.
“Even in the face of suboptimal impact of current strategies on population-based EAC mortality, medical societies consistently recommend [Barrett’s esophagus] screening and surveillance,” the investigators wrote. “In this context, similar to postcolonoscopy colorectal cancer, the concept of missed EAC is gaining importance in endoscopic Barrett’s esophagus screening and surveillance.”
In the present update, the investigators first aimed to standardize definitions of postendoscopy and interval EAC.
“We propose that postendoscopy EAC be defined as EAC and/or [Barrett’s esophagus]–related high-grade dysplasia identified within a finite time period (typically 1 year) following a nondiagnostic endoscopy,” the investigators wrote. “Interval EAC may be defined as EAC or [Barrett’s esophagus]–related high-grade dysplasia diagnosed after a negative screening or surveillance endoscopy before the date of the next recommended test.”
The latter definition, the investigators noted, was written with acknowledgment of emerging, noninvasive, nonendoscopic screening tools.
Next, Dr. Wani and colleagues dove deeper into the incidence of postendoscopy EAC in the Barrett’s esophagus population. Across multiple cohort studies and meta-analyses, incidence within 1 year of screening endoscopy ranged widely, from 3% to 25%. Data from Barrett’s esophagus patients undergoing endoscopic eradication therapy suggest that incidence of postendoscopy EAC may be greatest within 1-2 years of complete eradication of intestinal metaplasia; one meta-analysis involving 22 studies reported that the risk of EAC was 92% higher within the first year of eradication, compared with subsequent years.
“These data support that high-grade dysplasia/EAC identified within 1 year after complete eradication of intestinal metaplasia likely represents missed and/or incompletely treated prevalent disease rather than recurrent or incident neoplasia,” the investigators wrote.
In support of this conclusion, Dr. Wani and colleagues drew upon data from colorectal cancer screening programs, which suggest that 89% of postcolonoscopy colorectal cancers “may be avoidable, attributable to technical endoscopic factors, compromised decision-making, and administrative factors.”
Regulatory agencies measure quality of colorectal cancer screening programs with adenoma detection rate, which has been shown to correlate inversely with colorectal cancer and mortality; but no analogous measure has been established for Barrett’s esophagus screening. Candidate quality markers include neoplasia detection rate and dysplasia detection rate, though more work is needed to confirm their reliability.
“While easier to measure, compared to postendoscopy EAC rates, neoplasia detection rate remains a surrogate endoscopy quality marker in Barrett’s esophagus surveillance, while postendoscopy EAC rates serve as a true outcome measure that matters clinically,” the investigators wrote.
Dr. Wani and colleagues proposed four clinical strategies that may immediately improve quality of Barrett’s esophagus screening.
- First, they recommended “assiduous identification and photo-documentation of esophageal landmarks” coupled with lesion descriptions that adhere to Prague and Paris classification schemes, along with resection or referral upon identification.
- Second, they called for consistent use of high-definition white-light endoscopy and virtual chromoendoscopy.
- Third, they suggested that endoscopists “spend adequate time for inspection,” with biopsies taken in accordance with the Seattle protocol.
- Fourth, Dr. Wani and colleagues suggested that all practices conducting Barrett’s esophagus screening and surveillance establish continuously active quality control programs.
The investigators concluded the clinical practice update with a discussion of future directions.
“Prospective trials are needed to evaluate the impact of better dissemination of guidelines and quality indicators, improved endoscopic dysplasia detection using interactive web-based educational tools, advanced imaging techniques with artificial intelligence, and improved sampling modalities that reduce sampling errors,” they wrote. “Finally, increased emphasis is needed on improving training in both the cognitive and procedural aspects of [Barrett’s esophagus] endoscopy through structured educational programs among trainees and practicing endoscopists.”
The study was supported by the University of Colorado department of medicine’s Outstanding Early Scholars Program. The investigators disclosed relationships with Medtronic, Boston Scientific, Ironwood, and others.
SOURCE: Wani S et al. Gastroenterology. 2020 Jul 13. doi: 10.1053/j.gastro.2020.06.089.
The American Gastroenterological Association has published a clinical practice update that characterizes postendoscopy esophageal adenocarcinoma (EAC) and offers recommendations to improve endoscopic detection of dysplastic and neoplastic lesions in patients with Barrett’s esophagus.
While emerging technologies may improve detection rates in the future, short-term progress will depend on human expertise, reported lead author Sachin Wani, MD, of the University of Colorado at Denver, Aurora, and colleagues.
Writing in Gastroenterology, Dr. Wani and colleagues noted that EAC incidence has increased sevenfold over the past 4 decades, and 40% of patients with EAC have advanced disease at diagnosis, with a “dismal” 5-year survival rate.
Attempts to catch EAC earlier through Barrett’s esophagus surveillance endoscopy have been generally fallen short, the investigators added. They discussed a variety of obstacles to success, including divergence from recommended screening timelines, nonadherence to the Seattle biopsy protocol, sampling errors, and variability of dysplastic tissue interpretation between pathologists.
“Even in the face of suboptimal impact of current strategies on population-based EAC mortality, medical societies consistently recommend [Barrett’s esophagus] screening and surveillance,” the investigators wrote. “In this context, similar to postcolonoscopy colorectal cancer, the concept of missed EAC is gaining importance in endoscopic Barrett’s esophagus screening and surveillance.”
In the present update, the investigators first aimed to standardize definitions of postendoscopy and interval EAC.
“We propose that postendoscopy EAC be defined as EAC and/or [Barrett’s esophagus]–related high-grade dysplasia identified within a finite time period (typically 1 year) following a nondiagnostic endoscopy,” the investigators wrote. “Interval EAC may be defined as EAC or [Barrett’s esophagus]–related high-grade dysplasia diagnosed after a negative screening or surveillance endoscopy before the date of the next recommended test.”
The latter definition, the investigators noted, was written with acknowledgment of emerging, noninvasive, nonendoscopic screening tools.
Next, Dr. Wani and colleagues dove deeper into the incidence of postendoscopy EAC in the Barrett’s esophagus population. Across multiple cohort studies and meta-analyses, incidence within 1 year of screening endoscopy ranged widely, from 3% to 25%. Data from Barrett’s esophagus patients undergoing endoscopic eradication therapy suggest that incidence of postendoscopy EAC may be greatest within 1-2 years of complete eradication of intestinal metaplasia; one meta-analysis involving 22 studies reported that the risk of EAC was 92% higher within the first year of eradication, compared with subsequent years.
“These data support that high-grade dysplasia/EAC identified within 1 year after complete eradication of intestinal metaplasia likely represents missed and/or incompletely treated prevalent disease rather than recurrent or incident neoplasia,” the investigators wrote.
In support of this conclusion, Dr. Wani and colleagues drew upon data from colorectal cancer screening programs, which suggest that 89% of postcolonoscopy colorectal cancers “may be avoidable, attributable to technical endoscopic factors, compromised decision-making, and administrative factors.”
Regulatory agencies measure quality of colorectal cancer screening programs with adenoma detection rate, which has been shown to correlate inversely with colorectal cancer and mortality; but no analogous measure has been established for Barrett’s esophagus screening. Candidate quality markers include neoplasia detection rate and dysplasia detection rate, though more work is needed to confirm their reliability.
“While easier to measure, compared to postendoscopy EAC rates, neoplasia detection rate remains a surrogate endoscopy quality marker in Barrett’s esophagus surveillance, while postendoscopy EAC rates serve as a true outcome measure that matters clinically,” the investigators wrote.
Dr. Wani and colleagues proposed four clinical strategies that may immediately improve quality of Barrett’s esophagus screening.
- First, they recommended “assiduous identification and photo-documentation of esophageal landmarks” coupled with lesion descriptions that adhere to Prague and Paris classification schemes, along with resection or referral upon identification.
- Second, they called for consistent use of high-definition white-light endoscopy and virtual chromoendoscopy.
- Third, they suggested that endoscopists “spend adequate time for inspection,” with biopsies taken in accordance with the Seattle protocol.
- Fourth, Dr. Wani and colleagues suggested that all practices conducting Barrett’s esophagus screening and surveillance establish continuously active quality control programs.
The investigators concluded the clinical practice update with a discussion of future directions.
“Prospective trials are needed to evaluate the impact of better dissemination of guidelines and quality indicators, improved endoscopic dysplasia detection using interactive web-based educational tools, advanced imaging techniques with artificial intelligence, and improved sampling modalities that reduce sampling errors,” they wrote. “Finally, increased emphasis is needed on improving training in both the cognitive and procedural aspects of [Barrett’s esophagus] endoscopy through structured educational programs among trainees and practicing endoscopists.”
The study was supported by the University of Colorado department of medicine’s Outstanding Early Scholars Program. The investigators disclosed relationships with Medtronic, Boston Scientific, Ironwood, and others.
SOURCE: Wani S et al. Gastroenterology. 2020 Jul 13. doi: 10.1053/j.gastro.2020.06.089.
The American Gastroenterological Association has published a clinical practice update that characterizes postendoscopy esophageal adenocarcinoma (EAC) and offers recommendations to improve endoscopic detection of dysplastic and neoplastic lesions in patients with Barrett’s esophagus.
While emerging technologies may improve detection rates in the future, short-term progress will depend on human expertise, reported lead author Sachin Wani, MD, of the University of Colorado at Denver, Aurora, and colleagues.
Writing in Gastroenterology, Dr. Wani and colleagues noted that EAC incidence has increased sevenfold over the past 4 decades, and 40% of patients with EAC have advanced disease at diagnosis, with a “dismal” 5-year survival rate.
Attempts to catch EAC earlier through Barrett’s esophagus surveillance endoscopy have been generally fallen short, the investigators added. They discussed a variety of obstacles to success, including divergence from recommended screening timelines, nonadherence to the Seattle biopsy protocol, sampling errors, and variability of dysplastic tissue interpretation between pathologists.
“Even in the face of suboptimal impact of current strategies on population-based EAC mortality, medical societies consistently recommend [Barrett’s esophagus] screening and surveillance,” the investigators wrote. “In this context, similar to postcolonoscopy colorectal cancer, the concept of missed EAC is gaining importance in endoscopic Barrett’s esophagus screening and surveillance.”
In the present update, the investigators first aimed to standardize definitions of postendoscopy and interval EAC.
“We propose that postendoscopy EAC be defined as EAC and/or [Barrett’s esophagus]–related high-grade dysplasia identified within a finite time period (typically 1 year) following a nondiagnostic endoscopy,” the investigators wrote. “Interval EAC may be defined as EAC or [Barrett’s esophagus]–related high-grade dysplasia diagnosed after a negative screening or surveillance endoscopy before the date of the next recommended test.”
The latter definition, the investigators noted, was written with acknowledgment of emerging, noninvasive, nonendoscopic screening tools.
Next, Dr. Wani and colleagues dove deeper into the incidence of postendoscopy EAC in the Barrett’s esophagus population. Across multiple cohort studies and meta-analyses, incidence within 1 year of screening endoscopy ranged widely, from 3% to 25%. Data from Barrett’s esophagus patients undergoing endoscopic eradication therapy suggest that incidence of postendoscopy EAC may be greatest within 1-2 years of complete eradication of intestinal metaplasia; one meta-analysis involving 22 studies reported that the risk of EAC was 92% higher within the first year of eradication, compared with subsequent years.
“These data support that high-grade dysplasia/EAC identified within 1 year after complete eradication of intestinal metaplasia likely represents missed and/or incompletely treated prevalent disease rather than recurrent or incident neoplasia,” the investigators wrote.
In support of this conclusion, Dr. Wani and colleagues drew upon data from colorectal cancer screening programs, which suggest that 89% of postcolonoscopy colorectal cancers “may be avoidable, attributable to technical endoscopic factors, compromised decision-making, and administrative factors.”
Regulatory agencies measure quality of colorectal cancer screening programs with adenoma detection rate, which has been shown to correlate inversely with colorectal cancer and mortality; but no analogous measure has been established for Barrett’s esophagus screening. Candidate quality markers include neoplasia detection rate and dysplasia detection rate, though more work is needed to confirm their reliability.
“While easier to measure, compared to postendoscopy EAC rates, neoplasia detection rate remains a surrogate endoscopy quality marker in Barrett’s esophagus surveillance, while postendoscopy EAC rates serve as a true outcome measure that matters clinically,” the investigators wrote.
Dr. Wani and colleagues proposed four clinical strategies that may immediately improve quality of Barrett’s esophagus screening.
- First, they recommended “assiduous identification and photo-documentation of esophageal landmarks” coupled with lesion descriptions that adhere to Prague and Paris classification schemes, along with resection or referral upon identification.
- Second, they called for consistent use of high-definition white-light endoscopy and virtual chromoendoscopy.
- Third, they suggested that endoscopists “spend adequate time for inspection,” with biopsies taken in accordance with the Seattle protocol.
- Fourth, Dr. Wani and colleagues suggested that all practices conducting Barrett’s esophagus screening and surveillance establish continuously active quality control programs.
The investigators concluded the clinical practice update with a discussion of future directions.
“Prospective trials are needed to evaluate the impact of better dissemination of guidelines and quality indicators, improved endoscopic dysplasia detection using interactive web-based educational tools, advanced imaging techniques with artificial intelligence, and improved sampling modalities that reduce sampling errors,” they wrote. “Finally, increased emphasis is needed on improving training in both the cognitive and procedural aspects of [Barrett’s esophagus] endoscopy through structured educational programs among trainees and practicing endoscopists.”
The study was supported by the University of Colorado department of medicine’s Outstanding Early Scholars Program. The investigators disclosed relationships with Medtronic, Boston Scientific, Ironwood, and others.
SOURCE: Wani S et al. Gastroenterology. 2020 Jul 13. doi: 10.1053/j.gastro.2020.06.089.
FROM GASTROENTEROLOGY
FOLFOXIRI tops doublets as bevacizumab backbone for mCRC
investigators reported in the Journal of Clinical Oncology.
In analyzing data from five clinical trials, the investigators found a 4.4-month increase in median overall survival and an 11.6% increase in estimated 5-year overall survival with FOLFOXIRI versus doublets. The trade-off was a higher incidence of grade 3-4 adverse events with FOLFOXIRI.
FOLFOXIRI plus bevacizumab is already included among first-line options in most clinical guidelines and recommendations, but there was no “proper estimation of the magnitude of the overall survival benefit” because trials had other primary endpoints, according to study author Chiara Cremolini, MD, PhD, of University of Pisa (Italy), and colleagues.
“To fully appreciate the cost/benefit balance of this option,” the investigators wanted to see how the numbers played out when overall survival was the primary endpoint, so they pooled individual patient data from the CHARTA, OLIVIA, STEAM, TRIBE, and TRIBE2 trials.
Patient characteristics and treatment
The analysis included 1,697 patients. The median age was 61 years (range, 53-67 years).
About 99% of patients had an Eastern Cooperative Oncology Group performance score of 0 or 1. About 20% had left-sided RAS and BRAF wild-type tumors because of the increased use of anti–epidermal growth factor receptor antibodies as first-line therapy for that indication in recent years.
In all, 846 patients were randomized to FOLFOXIRI plus bevacizumab and 851 to bevacizumab with doublets: 69.9% to FOLFOX (leucovorin, fluorouracil, and oxaliplatin) and 30.1% to FOLFIRI (fluorouracil, leucovorin, and irinotecan).
The duration of induction in all five trials ranged from 4 to 6 months. It was followed by maintenance with a fluoropyrimidine (fluorouracil and leucovorin or capecitabine) plus bevacizumab.
Efficacy and safety
At a median follow-up of 39.9 months, the median overall survival was 28.9 months in the FOLFOXIRI group and 24.5 months in the doublet group (P < .001). The estimated 5-year overall survival rate was 22.3% and 10.7%, respectively.
The median progression-free survival was 12.2 months in the FOLFOXIRI group and 9.9 months in the doublet group (P < .001).
The objective response rate was higher with FOLFOXIRI (64.5% vs. 53.6%, P < .001), as was R0 resection rate (16.4% vs. 11.8%, P = .007).
The FOLFOXIRI group also had a higher incidence of grade 3-4 adverse events, including neutropenia (45.8% vs. 21.5%; P < .001), febrile neutropenia (6.3% vs. 3.7%; P = .019), nausea (5.5% vs. 3.0%; P = .016), mucositis (5.1% vs. 2.9%; P = .024), and diarrhea (17.8% vs. 8.4%; P < .001).
Even so, FOLFOXIRI plus bevacizumab was not associated with a significant increase in toxic deaths (2.3% vs. 1.4%; P = .277).
Patient selection is ‘critical’
Based on their findings, the investigators said the best candidates for first-line FOLFOXIRI plus bevacizumab may be younger patients with an ECOG performance status of 0 or 1 and right-sided and/or RAS-mutated tumors not exposed to a previous oxaliplatin-based adjuvant regimen.
FOLFOXIRI plus bevacizumab did not provide any additional benefit in patients with BRAF-mutant tumors, so the combination shouldn’t be the first choice in this group, the investigators wrote. “FOLFOX plus bevacizumab seems the preferable upfront option.”
For left-sided RAS and BRAF wild-type tumors, a chemotherapy doublet with an anti–epidermal growth factor receptor remains the preferred option, according to the investigators.
“The study does support the use of FOLFOXIRI and bevacizumab as a valuable first-line option, but patient selection is critical because there is a toxicity cost; this efficacy versus toxicity will constantly be a seesaw for us,” commented Aparna Parikh, MD, of Massachusetts General Hospital in Boston, when the study was presented at the American Society of Clinical Oncology annual meeting earlier this year.
There was no external funding for this analysis. Three of the original five trials were sponsored by Roche. The study authors had numerous industry ties. Among others, Dr. Cremolini is a consultant for and reported honoraria and travel expenses from Roche. One author was a Genentech employee. Dr. Parikh disclosed relationships with Lilly, Genentech, and other companies.
SOURCE: Cremolini C et al. J Clin Oncol. 2020 Aug 20. doi: 10.1200/JCO.20.01225.
investigators reported in the Journal of Clinical Oncology.
In analyzing data from five clinical trials, the investigators found a 4.4-month increase in median overall survival and an 11.6% increase in estimated 5-year overall survival with FOLFOXIRI versus doublets. The trade-off was a higher incidence of grade 3-4 adverse events with FOLFOXIRI.
FOLFOXIRI plus bevacizumab is already included among first-line options in most clinical guidelines and recommendations, but there was no “proper estimation of the magnitude of the overall survival benefit” because trials had other primary endpoints, according to study author Chiara Cremolini, MD, PhD, of University of Pisa (Italy), and colleagues.
“To fully appreciate the cost/benefit balance of this option,” the investigators wanted to see how the numbers played out when overall survival was the primary endpoint, so they pooled individual patient data from the CHARTA, OLIVIA, STEAM, TRIBE, and TRIBE2 trials.
Patient characteristics and treatment
The analysis included 1,697 patients. The median age was 61 years (range, 53-67 years).
About 99% of patients had an Eastern Cooperative Oncology Group performance score of 0 or 1. About 20% had left-sided RAS and BRAF wild-type tumors because of the increased use of anti–epidermal growth factor receptor antibodies as first-line therapy for that indication in recent years.
In all, 846 patients were randomized to FOLFOXIRI plus bevacizumab and 851 to bevacizumab with doublets: 69.9% to FOLFOX (leucovorin, fluorouracil, and oxaliplatin) and 30.1% to FOLFIRI (fluorouracil, leucovorin, and irinotecan).
The duration of induction in all five trials ranged from 4 to 6 months. It was followed by maintenance with a fluoropyrimidine (fluorouracil and leucovorin or capecitabine) plus bevacizumab.
Efficacy and safety
At a median follow-up of 39.9 months, the median overall survival was 28.9 months in the FOLFOXIRI group and 24.5 months in the doublet group (P < .001). The estimated 5-year overall survival rate was 22.3% and 10.7%, respectively.
The median progression-free survival was 12.2 months in the FOLFOXIRI group and 9.9 months in the doublet group (P < .001).
The objective response rate was higher with FOLFOXIRI (64.5% vs. 53.6%, P < .001), as was R0 resection rate (16.4% vs. 11.8%, P = .007).
The FOLFOXIRI group also had a higher incidence of grade 3-4 adverse events, including neutropenia (45.8% vs. 21.5%; P < .001), febrile neutropenia (6.3% vs. 3.7%; P = .019), nausea (5.5% vs. 3.0%; P = .016), mucositis (5.1% vs. 2.9%; P = .024), and diarrhea (17.8% vs. 8.4%; P < .001).
Even so, FOLFOXIRI plus bevacizumab was not associated with a significant increase in toxic deaths (2.3% vs. 1.4%; P = .277).
Patient selection is ‘critical’
Based on their findings, the investigators said the best candidates for first-line FOLFOXIRI plus bevacizumab may be younger patients with an ECOG performance status of 0 or 1 and right-sided and/or RAS-mutated tumors not exposed to a previous oxaliplatin-based adjuvant regimen.
FOLFOXIRI plus bevacizumab did not provide any additional benefit in patients with BRAF-mutant tumors, so the combination shouldn’t be the first choice in this group, the investigators wrote. “FOLFOX plus bevacizumab seems the preferable upfront option.”
For left-sided RAS and BRAF wild-type tumors, a chemotherapy doublet with an anti–epidermal growth factor receptor remains the preferred option, according to the investigators.
“The study does support the use of FOLFOXIRI and bevacizumab as a valuable first-line option, but patient selection is critical because there is a toxicity cost; this efficacy versus toxicity will constantly be a seesaw for us,” commented Aparna Parikh, MD, of Massachusetts General Hospital in Boston, when the study was presented at the American Society of Clinical Oncology annual meeting earlier this year.
There was no external funding for this analysis. Three of the original five trials were sponsored by Roche. The study authors had numerous industry ties. Among others, Dr. Cremolini is a consultant for and reported honoraria and travel expenses from Roche. One author was a Genentech employee. Dr. Parikh disclosed relationships with Lilly, Genentech, and other companies.
SOURCE: Cremolini C et al. J Clin Oncol. 2020 Aug 20. doi: 10.1200/JCO.20.01225.
investigators reported in the Journal of Clinical Oncology.
In analyzing data from five clinical trials, the investigators found a 4.4-month increase in median overall survival and an 11.6% increase in estimated 5-year overall survival with FOLFOXIRI versus doublets. The trade-off was a higher incidence of grade 3-4 adverse events with FOLFOXIRI.
FOLFOXIRI plus bevacizumab is already included among first-line options in most clinical guidelines and recommendations, but there was no “proper estimation of the magnitude of the overall survival benefit” because trials had other primary endpoints, according to study author Chiara Cremolini, MD, PhD, of University of Pisa (Italy), and colleagues.
“To fully appreciate the cost/benefit balance of this option,” the investigators wanted to see how the numbers played out when overall survival was the primary endpoint, so they pooled individual patient data from the CHARTA, OLIVIA, STEAM, TRIBE, and TRIBE2 trials.
Patient characteristics and treatment
The analysis included 1,697 patients. The median age was 61 years (range, 53-67 years).
About 99% of patients had an Eastern Cooperative Oncology Group performance score of 0 or 1. About 20% had left-sided RAS and BRAF wild-type tumors because of the increased use of anti–epidermal growth factor receptor antibodies as first-line therapy for that indication in recent years.
In all, 846 patients were randomized to FOLFOXIRI plus bevacizumab and 851 to bevacizumab with doublets: 69.9% to FOLFOX (leucovorin, fluorouracil, and oxaliplatin) and 30.1% to FOLFIRI (fluorouracil, leucovorin, and irinotecan).
The duration of induction in all five trials ranged from 4 to 6 months. It was followed by maintenance with a fluoropyrimidine (fluorouracil and leucovorin or capecitabine) plus bevacizumab.
Efficacy and safety
At a median follow-up of 39.9 months, the median overall survival was 28.9 months in the FOLFOXIRI group and 24.5 months in the doublet group (P < .001). The estimated 5-year overall survival rate was 22.3% and 10.7%, respectively.
The median progression-free survival was 12.2 months in the FOLFOXIRI group and 9.9 months in the doublet group (P < .001).
The objective response rate was higher with FOLFOXIRI (64.5% vs. 53.6%, P < .001), as was R0 resection rate (16.4% vs. 11.8%, P = .007).
The FOLFOXIRI group also had a higher incidence of grade 3-4 adverse events, including neutropenia (45.8% vs. 21.5%; P < .001), febrile neutropenia (6.3% vs. 3.7%; P = .019), nausea (5.5% vs. 3.0%; P = .016), mucositis (5.1% vs. 2.9%; P = .024), and diarrhea (17.8% vs. 8.4%; P < .001).
Even so, FOLFOXIRI plus bevacizumab was not associated with a significant increase in toxic deaths (2.3% vs. 1.4%; P = .277).
Patient selection is ‘critical’
Based on their findings, the investigators said the best candidates for first-line FOLFOXIRI plus bevacizumab may be younger patients with an ECOG performance status of 0 or 1 and right-sided and/or RAS-mutated tumors not exposed to a previous oxaliplatin-based adjuvant regimen.
FOLFOXIRI plus bevacizumab did not provide any additional benefit in patients with BRAF-mutant tumors, so the combination shouldn’t be the first choice in this group, the investigators wrote. “FOLFOX plus bevacizumab seems the preferable upfront option.”
For left-sided RAS and BRAF wild-type tumors, a chemotherapy doublet with an anti–epidermal growth factor receptor remains the preferred option, according to the investigators.
“The study does support the use of FOLFOXIRI and bevacizumab as a valuable first-line option, but patient selection is critical because there is a toxicity cost; this efficacy versus toxicity will constantly be a seesaw for us,” commented Aparna Parikh, MD, of Massachusetts General Hospital in Boston, when the study was presented at the American Society of Clinical Oncology annual meeting earlier this year.
There was no external funding for this analysis. Three of the original five trials were sponsored by Roche. The study authors had numerous industry ties. Among others, Dr. Cremolini is a consultant for and reported honoraria and travel expenses from Roche. One author was a Genentech employee. Dr. Parikh disclosed relationships with Lilly, Genentech, and other companies.
SOURCE: Cremolini C et al. J Clin Oncol. 2020 Aug 20. doi: 10.1200/JCO.20.01225.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Exorcising your ghosts
The COVID-19 pandemic has affected private medical practices on so many levels, not least of which is the loss of employees to illness, fear of illness, early retirement, and other reasons.
If you’re not hip to the slang, “ghosting” is the situation in which an employee disappears without any warning, notice, or explanation. It usually occurs after a candidate accepts a job offer, and you schedule their first day of work. That day dawns, but the new hire never arrives. Less commonly, an employee who has been with you for some time simply stops showing up and cannot be contacted.
Many employers think of ghosting as a relatively new phenomenon, and blame it on the irresponsibility of younger age groups – millennials, in particular. In fact, it has been an issue for many years across all age groups, and employers often share more of the responsibility than they think.
While total prevention is impossible, there are steps you can take as an employer to minimize ghosting in your practice.
- Your hiring process needs to be efficient. If you wait too long to schedule an interview with a promising candidate or to offer them the job, another job offer could lure them away. At the very least, a lengthy process or a lack of transparency may make the applicant apprehensive about accepting a job with you, particularly if other employers are pursuing them.
- Keep applicants in the loop. Follow up with every candidate; let them know where they are in your hiring process. Applicants who have no clue whether they have a shot at the job are going to start looking elsewhere. And make sure they know the job description and starting salary from the outset.
- Talk to new hires before their first day. Contact them personally to see if they have any questions or concerns, and let them know that you’re looking forward to their arrival.
- Once they start, make them feel welcome. An employee’s first few days on the job set the tone for the rest of the employment relationship. During this time, clearly communicate what the employee can expect from you and what you expect from them. Take time to discuss key issues, such as work schedules, timekeeping practices, how performance is measured, and dress codes. Introduce them to coworkers, and get them started shadowing more experienced staff members.
- Take a hard look at your supervision and your supervisors. Business people like to say that employees don’t quit their job, they quit their boss. If an employee quits – with or without notice – it may very well be because of a poor working relationship with you or the supervisor. To be effective, you and your supervisors need to be diligent in setting goals, managing performance, and applying workplace rules and policies. Numerous third-party companies provide training and guidance in these areas when needed.
- Recognize and reward. As I’ve written many times, positive feedback is a simple, low-cost way to improve employee retention. It demonstrates that you value an employee’s contributions and sets an excellent example for other employees. Effective recognition can come from anyone – including patients – and should be given openly. (Another old adage: “Praise publicly, criticize privately.”) It never hurts to catch an employee doing something right and acknowledge it.
- Don’t jump to conclusions. If a new hire or employee is absent without notice, don’t just assume you’ve been ghosted. There may be extenuating circumstances, such as an emergency or illness. In some states, an employee’s absence is protected under a law where the employee may not be required to provide advance notice, and taking adverse action could violate these laws. Establish procedures for attempting to contact absent employees, and make sure you’re complying with all applicable leave laws before taking any action.
If an employee does abandon their job, think before you act. Comply with all applicable laws. Act consistently with how you’ve handled similar situations in the past. Your attorney should be involved, especially if the decision involves termination. Notify the employee in writing. As with all employment decisions, keep adequate documentation in case the decision is ever challenged, or you need it to support future disciplinary decisions.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. He has no disclosures related to this column. Write to him at dermnews@mdedge.com.
The COVID-19 pandemic has affected private medical practices on so many levels, not least of which is the loss of employees to illness, fear of illness, early retirement, and other reasons.
If you’re not hip to the slang, “ghosting” is the situation in which an employee disappears without any warning, notice, or explanation. It usually occurs after a candidate accepts a job offer, and you schedule their first day of work. That day dawns, but the new hire never arrives. Less commonly, an employee who has been with you for some time simply stops showing up and cannot be contacted.
Many employers think of ghosting as a relatively new phenomenon, and blame it on the irresponsibility of younger age groups – millennials, in particular. In fact, it has been an issue for many years across all age groups, and employers often share more of the responsibility than they think.
While total prevention is impossible, there are steps you can take as an employer to minimize ghosting in your practice.
- Your hiring process needs to be efficient. If you wait too long to schedule an interview with a promising candidate or to offer them the job, another job offer could lure them away. At the very least, a lengthy process or a lack of transparency may make the applicant apprehensive about accepting a job with you, particularly if other employers are pursuing them.
- Keep applicants in the loop. Follow up with every candidate; let them know where they are in your hiring process. Applicants who have no clue whether they have a shot at the job are going to start looking elsewhere. And make sure they know the job description and starting salary from the outset.
- Talk to new hires before their first day. Contact them personally to see if they have any questions or concerns, and let them know that you’re looking forward to their arrival.
- Once they start, make them feel welcome. An employee’s first few days on the job set the tone for the rest of the employment relationship. During this time, clearly communicate what the employee can expect from you and what you expect from them. Take time to discuss key issues, such as work schedules, timekeeping practices, how performance is measured, and dress codes. Introduce them to coworkers, and get them started shadowing more experienced staff members.
- Take a hard look at your supervision and your supervisors. Business people like to say that employees don’t quit their job, they quit their boss. If an employee quits – with or without notice – it may very well be because of a poor working relationship with you or the supervisor. To be effective, you and your supervisors need to be diligent in setting goals, managing performance, and applying workplace rules and policies. Numerous third-party companies provide training and guidance in these areas when needed.
- Recognize and reward. As I’ve written many times, positive feedback is a simple, low-cost way to improve employee retention. It demonstrates that you value an employee’s contributions and sets an excellent example for other employees. Effective recognition can come from anyone – including patients – and should be given openly. (Another old adage: “Praise publicly, criticize privately.”) It never hurts to catch an employee doing something right and acknowledge it.
- Don’t jump to conclusions. If a new hire or employee is absent without notice, don’t just assume you’ve been ghosted. There may be extenuating circumstances, such as an emergency or illness. In some states, an employee’s absence is protected under a law where the employee may not be required to provide advance notice, and taking adverse action could violate these laws. Establish procedures for attempting to contact absent employees, and make sure you’re complying with all applicable leave laws before taking any action.
If an employee does abandon their job, think before you act. Comply with all applicable laws. Act consistently with how you’ve handled similar situations in the past. Your attorney should be involved, especially if the decision involves termination. Notify the employee in writing. As with all employment decisions, keep adequate documentation in case the decision is ever challenged, or you need it to support future disciplinary decisions.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. He has no disclosures related to this column. Write to him at dermnews@mdedge.com.
The COVID-19 pandemic has affected private medical practices on so many levels, not least of which is the loss of employees to illness, fear of illness, early retirement, and other reasons.
If you’re not hip to the slang, “ghosting” is the situation in which an employee disappears without any warning, notice, or explanation. It usually occurs after a candidate accepts a job offer, and you schedule their first day of work. That day dawns, but the new hire never arrives. Less commonly, an employee who has been with you for some time simply stops showing up and cannot be contacted.
Many employers think of ghosting as a relatively new phenomenon, and blame it on the irresponsibility of younger age groups – millennials, in particular. In fact, it has been an issue for many years across all age groups, and employers often share more of the responsibility than they think.
While total prevention is impossible, there are steps you can take as an employer to minimize ghosting in your practice.
- Your hiring process needs to be efficient. If you wait too long to schedule an interview with a promising candidate or to offer them the job, another job offer could lure them away. At the very least, a lengthy process or a lack of transparency may make the applicant apprehensive about accepting a job with you, particularly if other employers are pursuing them.
- Keep applicants in the loop. Follow up with every candidate; let them know where they are in your hiring process. Applicants who have no clue whether they have a shot at the job are going to start looking elsewhere. And make sure they know the job description and starting salary from the outset.
- Talk to new hires before their first day. Contact them personally to see if they have any questions or concerns, and let them know that you’re looking forward to their arrival.
- Once they start, make them feel welcome. An employee’s first few days on the job set the tone for the rest of the employment relationship. During this time, clearly communicate what the employee can expect from you and what you expect from them. Take time to discuss key issues, such as work schedules, timekeeping practices, how performance is measured, and dress codes. Introduce them to coworkers, and get them started shadowing more experienced staff members.
- Take a hard look at your supervision and your supervisors. Business people like to say that employees don’t quit their job, they quit their boss. If an employee quits – with or without notice – it may very well be because of a poor working relationship with you or the supervisor. To be effective, you and your supervisors need to be diligent in setting goals, managing performance, and applying workplace rules and policies. Numerous third-party companies provide training and guidance in these areas when needed.
- Recognize and reward. As I’ve written many times, positive feedback is a simple, low-cost way to improve employee retention. It demonstrates that you value an employee’s contributions and sets an excellent example for other employees. Effective recognition can come from anyone – including patients – and should be given openly. (Another old adage: “Praise publicly, criticize privately.”) It never hurts to catch an employee doing something right and acknowledge it.
- Don’t jump to conclusions. If a new hire or employee is absent without notice, don’t just assume you’ve been ghosted. There may be extenuating circumstances, such as an emergency or illness. In some states, an employee’s absence is protected under a law where the employee may not be required to provide advance notice, and taking adverse action could violate these laws. Establish procedures for attempting to contact absent employees, and make sure you’re complying with all applicable leave laws before taking any action.
If an employee does abandon their job, think before you act. Comply with all applicable laws. Act consistently with how you’ve handled similar situations in the past. Your attorney should be involved, especially if the decision involves termination. Notify the employee in writing. As with all employment decisions, keep adequate documentation in case the decision is ever challenged, or you need it to support future disciplinary decisions.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. He has no disclosures related to this column. Write to him at dermnews@mdedge.com.