User login
Surgeon General scolds docs for failing to help patients quit smoking
The U.S. Surgeon General is calling on all physicians to help patients stop smoking, noting that two-thirds of adult smokers say they want to quit, but only 40% report that their doctor has advised them to stop.
“I’ve got to own this as the nation’s doctor, and our health providers in this room and in this country need to own this stat,” said Surgeon General Jerome Adams, MD, at a press briefing releasing a new report on smoking cessation.
“Smoking is the No. 1 preventable cause of death, disease, and disability in the United States,” he said. “So why are 40% of our health providers out there not advising smokers to quit when they come in?”
In the first U.S. Surgeon General report on smoking cessation in 30 years, the 700-page report suggests smoking cessation-related quality measures that include physician reimbursement would increase treatment.
The evidence also suggests that using electronic health records to prompt clinicians to inquire about smoking would increase cessation treatment.
EHRs could be used to “empower and enable” physicians to advise people to quit, said Dr. Adams. Physicians also need “the education and the confidence to be able to have that conversation, because too many of them look at someone and say: ‘Nope, too hard, too much effort, no, that’s not what they’re here for today,’ ” he said.
However, “simply asking, advising, and referring can be enough to get someone on the pathway to quitting,” Dr. Adams said.
34 million still smoke
The new report is the first on the topic released since 1990, and the 34th on tobacco control since the first one was issued in 1964, said Dr. Adams. Since that first report, adult smoking has declined 70%, but some 34 million Americans (14%) still smoke, he said.
In addition, Dr. Adams said that many subpopulations have been left behind, noting: “Cigarette smoking remains highest among LGBTQ adults, people with disabilities or limitations, American Indians and Alaska Natives, and people with mental health conditions or substance use disorders.”
He also noted that 40% of cigarettes are consumed by those with a mental illness or a substance use disorder.
Quitting is beneficial at any age and can add as much as a decade to life expectancy, the report notes. Quitting also reduces the risk of 12 cancers, cuts the risk of chronic obstructive pulmonary disease, and reduces cardiovascular and stroke morbidity and mortality.
Pregnant women who quit also reduce their own morbidity and mortality risk and that of unborn children and infants, the report says.
“We know more about the science of quitting than ever before. We can, and must, do more to ensure that evidence-based cessation treatments are reaching the people that need them,” said Dr. Adams.
Less than one-third of those who have quit have used Food and Drug Administration–approved cessation medications or behavioral counseling, Dr. Adams said.
Barriers to care
Despite the existence of five nicotine replacement therapies and two nonnicotine oral medications, and more widespread availability of proven counseling methods – including web- or text-based programs – barriers to access remain.
These include a lack of insurance coverage for comprehensive, evidence-based smoking cessation treatment, which, when offered, increases availability and use.
“These are cost-effective interventions,” said Dr. Adams. “It’s penny wise and pound foolish to not give someone access to what we know works,” he said.
Because of the diversity of e-cigarette products and the variety of ways they are used, coupled with little research, it’s not currently possible to determine whether they are, or are not, useful smoking cessation tools, the report notes.
However, experts who compiled the report found some evidence to suggest that e-cigarettes containing nicotine may be “associated with increased smoking cessation compared with the use of e-cigarettes not containing nicotine.”
Asked whether the report’s conclusions might be interpreted as supportive of e-cigarettes, Dr. Adams said the report focused on smoking cessation, not initiation.
“I’m terribly concerned about the clear data that shows youth are initiating tobacco product use with e-cigarettes,” he said.
The Trump administration’s current proposal to partially restrict sales of some flavored e-cigarettes “reflects the science,” and “a balance between a desire to really make sure that people aren’t initiating with these products, but also a desire to again try to maintain a pathway for adults who want to use these products to quit to use them,” Dr. Adams said.
The focus, said Dr. Adams, should not be on e-cigarettes and whether they do, or do not, work.
“People want to quit,” he said. “We know what works. Not enough of them are getting it, and there are terrible disparities in who is and who is not getting access to effective and evidence-based treatment – that’s the story here.”
This article first appeared on Medscape.com.
The U.S. Surgeon General is calling on all physicians to help patients stop smoking, noting that two-thirds of adult smokers say they want to quit, but only 40% report that their doctor has advised them to stop.
“I’ve got to own this as the nation’s doctor, and our health providers in this room and in this country need to own this stat,” said Surgeon General Jerome Adams, MD, at a press briefing releasing a new report on smoking cessation.
“Smoking is the No. 1 preventable cause of death, disease, and disability in the United States,” he said. “So why are 40% of our health providers out there not advising smokers to quit when they come in?”
In the first U.S. Surgeon General report on smoking cessation in 30 years, the 700-page report suggests smoking cessation-related quality measures that include physician reimbursement would increase treatment.
The evidence also suggests that using electronic health records to prompt clinicians to inquire about smoking would increase cessation treatment.
EHRs could be used to “empower and enable” physicians to advise people to quit, said Dr. Adams. Physicians also need “the education and the confidence to be able to have that conversation, because too many of them look at someone and say: ‘Nope, too hard, too much effort, no, that’s not what they’re here for today,’ ” he said.
However, “simply asking, advising, and referring can be enough to get someone on the pathway to quitting,” Dr. Adams said.
34 million still smoke
The new report is the first on the topic released since 1990, and the 34th on tobacco control since the first one was issued in 1964, said Dr. Adams. Since that first report, adult smoking has declined 70%, but some 34 million Americans (14%) still smoke, he said.
In addition, Dr. Adams said that many subpopulations have been left behind, noting: “Cigarette smoking remains highest among LGBTQ adults, people with disabilities or limitations, American Indians and Alaska Natives, and people with mental health conditions or substance use disorders.”
He also noted that 40% of cigarettes are consumed by those with a mental illness or a substance use disorder.
Quitting is beneficial at any age and can add as much as a decade to life expectancy, the report notes. Quitting also reduces the risk of 12 cancers, cuts the risk of chronic obstructive pulmonary disease, and reduces cardiovascular and stroke morbidity and mortality.
Pregnant women who quit also reduce their own morbidity and mortality risk and that of unborn children and infants, the report says.
“We know more about the science of quitting than ever before. We can, and must, do more to ensure that evidence-based cessation treatments are reaching the people that need them,” said Dr. Adams.
Less than one-third of those who have quit have used Food and Drug Administration–approved cessation medications or behavioral counseling, Dr. Adams said.
Barriers to care
Despite the existence of five nicotine replacement therapies and two nonnicotine oral medications, and more widespread availability of proven counseling methods – including web- or text-based programs – barriers to access remain.
These include a lack of insurance coverage for comprehensive, evidence-based smoking cessation treatment, which, when offered, increases availability and use.
“These are cost-effective interventions,” said Dr. Adams. “It’s penny wise and pound foolish to not give someone access to what we know works,” he said.
Because of the diversity of e-cigarette products and the variety of ways they are used, coupled with little research, it’s not currently possible to determine whether they are, or are not, useful smoking cessation tools, the report notes.
However, experts who compiled the report found some evidence to suggest that e-cigarettes containing nicotine may be “associated with increased smoking cessation compared with the use of e-cigarettes not containing nicotine.”
Asked whether the report’s conclusions might be interpreted as supportive of e-cigarettes, Dr. Adams said the report focused on smoking cessation, not initiation.
“I’m terribly concerned about the clear data that shows youth are initiating tobacco product use with e-cigarettes,” he said.
The Trump administration’s current proposal to partially restrict sales of some flavored e-cigarettes “reflects the science,” and “a balance between a desire to really make sure that people aren’t initiating with these products, but also a desire to again try to maintain a pathway for adults who want to use these products to quit to use them,” Dr. Adams said.
The focus, said Dr. Adams, should not be on e-cigarettes and whether they do, or do not, work.
“People want to quit,” he said. “We know what works. Not enough of them are getting it, and there are terrible disparities in who is and who is not getting access to effective and evidence-based treatment – that’s the story here.”
This article first appeared on Medscape.com.
The U.S. Surgeon General is calling on all physicians to help patients stop smoking, noting that two-thirds of adult smokers say they want to quit, but only 40% report that their doctor has advised them to stop.
“I’ve got to own this as the nation’s doctor, and our health providers in this room and in this country need to own this stat,” said Surgeon General Jerome Adams, MD, at a press briefing releasing a new report on smoking cessation.
“Smoking is the No. 1 preventable cause of death, disease, and disability in the United States,” he said. “So why are 40% of our health providers out there not advising smokers to quit when they come in?”
In the first U.S. Surgeon General report on smoking cessation in 30 years, the 700-page report suggests smoking cessation-related quality measures that include physician reimbursement would increase treatment.
The evidence also suggests that using electronic health records to prompt clinicians to inquire about smoking would increase cessation treatment.
EHRs could be used to “empower and enable” physicians to advise people to quit, said Dr. Adams. Physicians also need “the education and the confidence to be able to have that conversation, because too many of them look at someone and say: ‘Nope, too hard, too much effort, no, that’s not what they’re here for today,’ ” he said.
However, “simply asking, advising, and referring can be enough to get someone on the pathway to quitting,” Dr. Adams said.
34 million still smoke
The new report is the first on the topic released since 1990, and the 34th on tobacco control since the first one was issued in 1964, said Dr. Adams. Since that first report, adult smoking has declined 70%, but some 34 million Americans (14%) still smoke, he said.
In addition, Dr. Adams said that many subpopulations have been left behind, noting: “Cigarette smoking remains highest among LGBTQ adults, people with disabilities or limitations, American Indians and Alaska Natives, and people with mental health conditions or substance use disorders.”
He also noted that 40% of cigarettes are consumed by those with a mental illness or a substance use disorder.
Quitting is beneficial at any age and can add as much as a decade to life expectancy, the report notes. Quitting also reduces the risk of 12 cancers, cuts the risk of chronic obstructive pulmonary disease, and reduces cardiovascular and stroke morbidity and mortality.
Pregnant women who quit also reduce their own morbidity and mortality risk and that of unborn children and infants, the report says.
“We know more about the science of quitting than ever before. We can, and must, do more to ensure that evidence-based cessation treatments are reaching the people that need them,” said Dr. Adams.
Less than one-third of those who have quit have used Food and Drug Administration–approved cessation medications or behavioral counseling, Dr. Adams said.
Barriers to care
Despite the existence of five nicotine replacement therapies and two nonnicotine oral medications, and more widespread availability of proven counseling methods – including web- or text-based programs – barriers to access remain.
These include a lack of insurance coverage for comprehensive, evidence-based smoking cessation treatment, which, when offered, increases availability and use.
“These are cost-effective interventions,” said Dr. Adams. “It’s penny wise and pound foolish to not give someone access to what we know works,” he said.
Because of the diversity of e-cigarette products and the variety of ways they are used, coupled with little research, it’s not currently possible to determine whether they are, or are not, useful smoking cessation tools, the report notes.
However, experts who compiled the report found some evidence to suggest that e-cigarettes containing nicotine may be “associated with increased smoking cessation compared with the use of e-cigarettes not containing nicotine.”
Asked whether the report’s conclusions might be interpreted as supportive of e-cigarettes, Dr. Adams said the report focused on smoking cessation, not initiation.
“I’m terribly concerned about the clear data that shows youth are initiating tobacco product use with e-cigarettes,” he said.
The Trump administration’s current proposal to partially restrict sales of some flavored e-cigarettes “reflects the science,” and “a balance between a desire to really make sure that people aren’t initiating with these products, but also a desire to again try to maintain a pathway for adults who want to use these products to quit to use them,” Dr. Adams said.
The focus, said Dr. Adams, should not be on e-cigarettes and whether they do, or do not, work.
“People want to quit,” he said. “We know what works. Not enough of them are getting it, and there are terrible disparities in who is and who is not getting access to effective and evidence-based treatment – that’s the story here.”
This article first appeared on Medscape.com.
What will it take to lower the cost of insulin in the United States?
Mayo Clinic hematologist S. Vincent Rajkumar, MD, argues in a new commentary.
The High Cost of Insulin in the United States: An Urgent Call to Action was published in the January 2020 issue of the Mayo Clinic Proceedings by Dr. Rajkumar, professor of medicine at the Mayo Clinic, Rochester, Minn., who specializes in treating myeloma and, more recently, has become an expert in drug pricing.
He also presented the information in a YouTube video.
As has been widely reported and examined by Congress in the past few years, the cost of insulin in the United States has risen at a far higher rate than inflation. For example, the list price of a single vial of Humalog jumped from $21 in 1999 to $275 in 2019, a far higher price than anywhere else in the world.
Stories of one in four patients having to ration their insulin use because of cost, and of some dying, have fueled protests, leading to legislative efforts and to a few initiatives by some of the manufacturers to address the cost problem.
Collective advocacy
Much of the blame has been placed on the manufacturers for charging such high prices and on the pharmacy benefit managers (PBMs) – also known as “middlemen” – for incentivizing higher-priced products on formularies through rebates. Those are major factors, Dr. Rajkumar argues, but they are not the only ones.
“There is no one reason why this is happening, and no one solution. It’s very complicated. It’s multiple factors all playing together. The only way to tackle it is to really understand it 360,” he said in an interview.
This is true of drug prices overall in the United States, but insulin is a special case. The current analog formulations have not changed in more than 20 years, yet only in the past 5 years have a handful of biosimilar and generic versions started to appear from the same manufacturers as the branded products.
“Insulin is a window into what’s wrong with the pharma industry. ... It’s the best example of how the system is broken,” Dr. Rajkumar stressed.
Physicians can help ease the problem, he said, by becoming educated about drug prices, taking cost into account when prescribing, and routinely discussing prescription drug affordability with patients.
Resources such as www.goodrx.com and www.blinkhealth.com provide information about drug prices and pharmacies that offer drugs at the lowest prices.
“Doctors need to not be suspicious of biosimilars and generics,” he emphasized.
Physicians can also advocate for policies that will lower insulin prices, and their institutions can establish preferences for lower-cost biosimilars in formularies.
“Our individual and collective advocacy gives voice to the needs of our patients,” Dr. Rajkumar emphasized.
‘Everyone in the supply chain benefits’
In his commentary, Dr. Rajkumar lists six major reasons for the high cost of insulin:
1. People with type 1 diabetes are a “vulnerable population” who will die without insulin and are therefore willing to pay a high price to stay alive.
2. Just three manufacturers – Eli Lilly, Novo Nordisk, and Sanofi-Aventis – control nearly the entire insulin market in the United States, with no regulations to cap or control the prices they can charge.
3. The manufacturers continually file new patents for existing insulin products – 70 in the case of Lantus, for example – that provide additional years of monopoly protection from competition.
4. Although the Food and Drug Administration has been receptive to approving insulin biosimilars, it still requires manufacturers to go through a long and cumbersome process to obtain licensure, sometimes taking as long as 10 years.
5.PBMs, paid by insurance companies to negotiate prices with retail pharmacies and pharmaceutical companies (through rebates), stand to benefit from higher, not lower, list prices.
6. Pharmaceutical companies have vast lobbying power.
In regard to the fifth point, about PBMs, Dr. Rajkumar said, “It’s not just the PBMs – it’s the whole supply chain. It’s hard to put a finger on the source of the problem. There’s no transparency in any of the arrangements for you to know why only certain drugs are on a given formulary of an insurance company or PBM. But we do know that, in general, the whole supply chain benefits from the higher list price. Everyone.”
‘Authorized generic’ insulins
That is why Dr. Rajkumar is not convinced that Eli Lilly’s recent launch of half-priced “authorized generic” insulins – first the Lispro injection in March 2019, and then two combination pen products in January 2020 – or Novo Nordisk’s My$99Insulin program and “follow-on” authorized generic versions of Novolog and NovoLog Mix, launched Jan. 2, 2020, will have a huge impact.
“It’s common sense. If Apple made the same iPhone for two different prices, who would pay the full price? It gives you a window into asking what is wrong with the system that allows that? To pay for the higher-priced product, somebody is being paid,” he said.
Indeed, in December 2019, the offices of Sen. Elizabeth Warren (D-MA) and Sen. Richard Blumenthal (D-CT) issued a report from a survey of 400 pharmacies nationwide that found that 83% of the less expensive authorized generic Insulin Lispro was not in stock.
More than two-thirds of pharmacies reported they could not order the product.
“Eli Lilly has failed to take consequential steps – such as simply lowering the list price of Humalog, as it has in foreign markets – to provide lower-cost access to this important diabetes drug,” according to the senators’ report, which concludes by urging Eli Lilly to lower the list price of its insulin and calling for Congress to take steps to enact systemic change to reduce drug prices nationwide.
Asked for comment, Dani Barnhizer, Eli Lilly’s manager of global diabetes communications, said, “Like Senators Warren and Blumenthal, Lilly would like to see even broader use of Insulin Lispro injection because it’s a real solution that can lower copays for people living with diabetes.”
“But the Senators’ paper failed to identify the system challenges that have inhibited access to this lower list price product,” Ms. Barnhizer said. “Payers determine an individual’s premiums and copays, which are subsidized by rebates that pharmaceutical companies pay. And many payers prioritize these rebates to lower premiums instead of offering low copays for chronic medications such as insulin.
“It’s why only one in four people using Medicare Part D, and one in five with commercial plans, have coverage for Insulin Lispro injection. That will not change until payers prioritize providing consistent, affordable insulin copays,” she added.
However, Ms. Barnhizer also noted, “It is not unusual for pharmacies to not stock a medicine. Any pharmacy can place an order for Insulin Lispro injection, with delivery in 1-2 days. All major U.S. wholesalers are now distributing Insulin Lispro injection.”
She also said that people who earn 400% or less of the federal poverty level may be eligible for free insulin, and that Lilly can provide free insulin to anyone in emergency situations. (Novo Nordisk offers that as well.)
Asked why Lilly does not simply lower the price of all their insulins, Ms. Barnhizer responded: “Cutting the list prices would significantly disrupt access to branded insulins, which thousands of insured patients depend on. Launching lower-priced insulin options is a less disruptive approach to help reduce the amount people pay at the pharmacy for people who need the help.”
Government role needed
In addition to the recommendations for physicians and their institutions, Dr. Rajkumar listed several potential policy-level solutions:
1. At the state and federal level, regulations should protect against excessive drug launch prices through the same type of value-based pricing approaches used in other developed countries. “Capping the maximum price increases to the rate of inflation is needed and can happen only through state and/or federal legislation,” he wrote.
Although some may see this as antithetical to “free market” economics, Dr. Rajkumar points out that, in the case of many prescription drugs, including insulin, “we not only have an unregulated monopoly, but it’s a prolonged unregulated monopoly for a lifesaving product, not a luxury item.”
“When you grant monopoly protection and put a barrier on competition, that’s not a free market. People have always had regulations on monopolies. Unregulated monopoly is a recipe for high prices. You have to have some regulation that protects citizens from exploitation.”
And here, he believes, the United States could adopt price negotiations as practiced in Europe and other parts of the world, but which are currently forbidden in the United States.
“Other countries negotiate the price in exchange for monopoly protection. You don’t have to reinvent the wheel,” he said.
2. Reform of the regulatory and legal processes to ease the path for approval of generics and biosimilars to enter the market. This could include reciprocal approval so that biosimilars approved in Canada or the European Union could automatically be granted FDA approval in the United States.
3. Reform of the patent system to prevent overpatenting and patent abuse, by capping patent life to 7-10 years and forbidding use of additional patents as a way of prolonging market exclusivity.
To this point, Barnhizer pointed out that “none of the Lilly insulins are patent protected. Our most commonly used insulin, Humalog U-100, lost patent protection in 2014.”
4. A nongovernmental agency should oversee pricing and make recommendations to Medicare and insurers on the maximum price of new and existing drugs, including insulin. One body poised to do that work is the Institute for Clinical and Economic Review, which receives 77% of its funding from nonprofit foundations. “I have worked with them and they are the best there is,” Dr. Rajkumar said.
5. Any rebates paid by manufacturers to PBMs should be transparent to all stakeholders, including patients.
6. Nonprofit generic manufacturing should be established. The Mayo Clinic has recently partnered with Intermountain Healthcare and several other organizations in creating Civica Rx, a nonprofit generic company.
7. Measures and laws that provide access to insulin in emergency situations are needed, particularly for people with type 1 diabetes.
Recent proposed and enacted legislation has been aimed at some of these goals.
The Insulin Price Reduction Act, introduced in October 2019 and just endorsed by the American Diabetes Association, would reduce insulin costs by providing incentives for manufacturers to revert to the 2006 list price of all insulins.
The Affordable Insulin Approvals Now Act, introduced in July 2019, aims to speed up approvals of generic and biosimilar insulins.
And in May 2019, the state of Colorado passed a bill to cap patient copays for insulin at $100 a month, and similar legislation has been introduced in several other states.
Dr. Rajkumar says that an overall fix will require changes at the federal level.
But, he said, they do not need to happen all at once.
“There are a number of changes that need to happen, but we can do one legislation at a time. ... I’m optimistic that something will happen. This is a national conversation. Both sides of the aisle want to do something about it. People are indeed feeling the pinch, so maybe something will get done,” he said.
Dr. Rajkumar has reported no relevant financial relationships.
This article first appeared on Medscape.com.
Mayo Clinic hematologist S. Vincent Rajkumar, MD, argues in a new commentary.
The High Cost of Insulin in the United States: An Urgent Call to Action was published in the January 2020 issue of the Mayo Clinic Proceedings by Dr. Rajkumar, professor of medicine at the Mayo Clinic, Rochester, Minn., who specializes in treating myeloma and, more recently, has become an expert in drug pricing.
He also presented the information in a YouTube video.
As has been widely reported and examined by Congress in the past few years, the cost of insulin in the United States has risen at a far higher rate than inflation. For example, the list price of a single vial of Humalog jumped from $21 in 1999 to $275 in 2019, a far higher price than anywhere else in the world.
Stories of one in four patients having to ration their insulin use because of cost, and of some dying, have fueled protests, leading to legislative efforts and to a few initiatives by some of the manufacturers to address the cost problem.
Collective advocacy
Much of the blame has been placed on the manufacturers for charging such high prices and on the pharmacy benefit managers (PBMs) – also known as “middlemen” – for incentivizing higher-priced products on formularies through rebates. Those are major factors, Dr. Rajkumar argues, but they are not the only ones.
“There is no one reason why this is happening, and no one solution. It’s very complicated. It’s multiple factors all playing together. The only way to tackle it is to really understand it 360,” he said in an interview.
This is true of drug prices overall in the United States, but insulin is a special case. The current analog formulations have not changed in more than 20 years, yet only in the past 5 years have a handful of biosimilar and generic versions started to appear from the same manufacturers as the branded products.
“Insulin is a window into what’s wrong with the pharma industry. ... It’s the best example of how the system is broken,” Dr. Rajkumar stressed.
Physicians can help ease the problem, he said, by becoming educated about drug prices, taking cost into account when prescribing, and routinely discussing prescription drug affordability with patients.
Resources such as www.goodrx.com and www.blinkhealth.com provide information about drug prices and pharmacies that offer drugs at the lowest prices.
“Doctors need to not be suspicious of biosimilars and generics,” he emphasized.
Physicians can also advocate for policies that will lower insulin prices, and their institutions can establish preferences for lower-cost biosimilars in formularies.
“Our individual and collective advocacy gives voice to the needs of our patients,” Dr. Rajkumar emphasized.
‘Everyone in the supply chain benefits’
In his commentary, Dr. Rajkumar lists six major reasons for the high cost of insulin:
1. People with type 1 diabetes are a “vulnerable population” who will die without insulin and are therefore willing to pay a high price to stay alive.
2. Just three manufacturers – Eli Lilly, Novo Nordisk, and Sanofi-Aventis – control nearly the entire insulin market in the United States, with no regulations to cap or control the prices they can charge.
3. The manufacturers continually file new patents for existing insulin products – 70 in the case of Lantus, for example – that provide additional years of monopoly protection from competition.
4. Although the Food and Drug Administration has been receptive to approving insulin biosimilars, it still requires manufacturers to go through a long and cumbersome process to obtain licensure, sometimes taking as long as 10 years.
5.PBMs, paid by insurance companies to negotiate prices with retail pharmacies and pharmaceutical companies (through rebates), stand to benefit from higher, not lower, list prices.
6. Pharmaceutical companies have vast lobbying power.
In regard to the fifth point, about PBMs, Dr. Rajkumar said, “It’s not just the PBMs – it’s the whole supply chain. It’s hard to put a finger on the source of the problem. There’s no transparency in any of the arrangements for you to know why only certain drugs are on a given formulary of an insurance company or PBM. But we do know that, in general, the whole supply chain benefits from the higher list price. Everyone.”
‘Authorized generic’ insulins
That is why Dr. Rajkumar is not convinced that Eli Lilly’s recent launch of half-priced “authorized generic” insulins – first the Lispro injection in March 2019, and then two combination pen products in January 2020 – or Novo Nordisk’s My$99Insulin program and “follow-on” authorized generic versions of Novolog and NovoLog Mix, launched Jan. 2, 2020, will have a huge impact.
“It’s common sense. If Apple made the same iPhone for two different prices, who would pay the full price? It gives you a window into asking what is wrong with the system that allows that? To pay for the higher-priced product, somebody is being paid,” he said.
Indeed, in December 2019, the offices of Sen. Elizabeth Warren (D-MA) and Sen. Richard Blumenthal (D-CT) issued a report from a survey of 400 pharmacies nationwide that found that 83% of the less expensive authorized generic Insulin Lispro was not in stock.
More than two-thirds of pharmacies reported they could not order the product.
“Eli Lilly has failed to take consequential steps – such as simply lowering the list price of Humalog, as it has in foreign markets – to provide lower-cost access to this important diabetes drug,” according to the senators’ report, which concludes by urging Eli Lilly to lower the list price of its insulin and calling for Congress to take steps to enact systemic change to reduce drug prices nationwide.
Asked for comment, Dani Barnhizer, Eli Lilly’s manager of global diabetes communications, said, “Like Senators Warren and Blumenthal, Lilly would like to see even broader use of Insulin Lispro injection because it’s a real solution that can lower copays for people living with diabetes.”
“But the Senators’ paper failed to identify the system challenges that have inhibited access to this lower list price product,” Ms. Barnhizer said. “Payers determine an individual’s premiums and copays, which are subsidized by rebates that pharmaceutical companies pay. And many payers prioritize these rebates to lower premiums instead of offering low copays for chronic medications such as insulin.
“It’s why only one in four people using Medicare Part D, and one in five with commercial plans, have coverage for Insulin Lispro injection. That will not change until payers prioritize providing consistent, affordable insulin copays,” she added.
However, Ms. Barnhizer also noted, “It is not unusual for pharmacies to not stock a medicine. Any pharmacy can place an order for Insulin Lispro injection, with delivery in 1-2 days. All major U.S. wholesalers are now distributing Insulin Lispro injection.”
She also said that people who earn 400% or less of the federal poverty level may be eligible for free insulin, and that Lilly can provide free insulin to anyone in emergency situations. (Novo Nordisk offers that as well.)
Asked why Lilly does not simply lower the price of all their insulins, Ms. Barnhizer responded: “Cutting the list prices would significantly disrupt access to branded insulins, which thousands of insured patients depend on. Launching lower-priced insulin options is a less disruptive approach to help reduce the amount people pay at the pharmacy for people who need the help.”
Government role needed
In addition to the recommendations for physicians and their institutions, Dr. Rajkumar listed several potential policy-level solutions:
1. At the state and federal level, regulations should protect against excessive drug launch prices through the same type of value-based pricing approaches used in other developed countries. “Capping the maximum price increases to the rate of inflation is needed and can happen only through state and/or federal legislation,” he wrote.
Although some may see this as antithetical to “free market” economics, Dr. Rajkumar points out that, in the case of many prescription drugs, including insulin, “we not only have an unregulated monopoly, but it’s a prolonged unregulated monopoly for a lifesaving product, not a luxury item.”
“When you grant monopoly protection and put a barrier on competition, that’s not a free market. People have always had regulations on monopolies. Unregulated monopoly is a recipe for high prices. You have to have some regulation that protects citizens from exploitation.”
And here, he believes, the United States could adopt price negotiations as practiced in Europe and other parts of the world, but which are currently forbidden in the United States.
“Other countries negotiate the price in exchange for monopoly protection. You don’t have to reinvent the wheel,” he said.
2. Reform of the regulatory and legal processes to ease the path for approval of generics and biosimilars to enter the market. This could include reciprocal approval so that biosimilars approved in Canada or the European Union could automatically be granted FDA approval in the United States.
3. Reform of the patent system to prevent overpatenting and patent abuse, by capping patent life to 7-10 years and forbidding use of additional patents as a way of prolonging market exclusivity.
To this point, Barnhizer pointed out that “none of the Lilly insulins are patent protected. Our most commonly used insulin, Humalog U-100, lost patent protection in 2014.”
4. A nongovernmental agency should oversee pricing and make recommendations to Medicare and insurers on the maximum price of new and existing drugs, including insulin. One body poised to do that work is the Institute for Clinical and Economic Review, which receives 77% of its funding from nonprofit foundations. “I have worked with them and they are the best there is,” Dr. Rajkumar said.
5. Any rebates paid by manufacturers to PBMs should be transparent to all stakeholders, including patients.
6. Nonprofit generic manufacturing should be established. The Mayo Clinic has recently partnered with Intermountain Healthcare and several other organizations in creating Civica Rx, a nonprofit generic company.
7. Measures and laws that provide access to insulin in emergency situations are needed, particularly for people with type 1 diabetes.
Recent proposed and enacted legislation has been aimed at some of these goals.
The Insulin Price Reduction Act, introduced in October 2019 and just endorsed by the American Diabetes Association, would reduce insulin costs by providing incentives for manufacturers to revert to the 2006 list price of all insulins.
The Affordable Insulin Approvals Now Act, introduced in July 2019, aims to speed up approvals of generic and biosimilar insulins.
And in May 2019, the state of Colorado passed a bill to cap patient copays for insulin at $100 a month, and similar legislation has been introduced in several other states.
Dr. Rajkumar says that an overall fix will require changes at the federal level.
But, he said, they do not need to happen all at once.
“There are a number of changes that need to happen, but we can do one legislation at a time. ... I’m optimistic that something will happen. This is a national conversation. Both sides of the aisle want to do something about it. People are indeed feeling the pinch, so maybe something will get done,” he said.
Dr. Rajkumar has reported no relevant financial relationships.
This article first appeared on Medscape.com.
Mayo Clinic hematologist S. Vincent Rajkumar, MD, argues in a new commentary.
The High Cost of Insulin in the United States: An Urgent Call to Action was published in the January 2020 issue of the Mayo Clinic Proceedings by Dr. Rajkumar, professor of medicine at the Mayo Clinic, Rochester, Minn., who specializes in treating myeloma and, more recently, has become an expert in drug pricing.
He also presented the information in a YouTube video.
As has been widely reported and examined by Congress in the past few years, the cost of insulin in the United States has risen at a far higher rate than inflation. For example, the list price of a single vial of Humalog jumped from $21 in 1999 to $275 in 2019, a far higher price than anywhere else in the world.
Stories of one in four patients having to ration their insulin use because of cost, and of some dying, have fueled protests, leading to legislative efforts and to a few initiatives by some of the manufacturers to address the cost problem.
Collective advocacy
Much of the blame has been placed on the manufacturers for charging such high prices and on the pharmacy benefit managers (PBMs) – also known as “middlemen” – for incentivizing higher-priced products on formularies through rebates. Those are major factors, Dr. Rajkumar argues, but they are not the only ones.
“There is no one reason why this is happening, and no one solution. It’s very complicated. It’s multiple factors all playing together. The only way to tackle it is to really understand it 360,” he said in an interview.
This is true of drug prices overall in the United States, but insulin is a special case. The current analog formulations have not changed in more than 20 years, yet only in the past 5 years have a handful of biosimilar and generic versions started to appear from the same manufacturers as the branded products.
“Insulin is a window into what’s wrong with the pharma industry. ... It’s the best example of how the system is broken,” Dr. Rajkumar stressed.
Physicians can help ease the problem, he said, by becoming educated about drug prices, taking cost into account when prescribing, and routinely discussing prescription drug affordability with patients.
Resources such as www.goodrx.com and www.blinkhealth.com provide information about drug prices and pharmacies that offer drugs at the lowest prices.
“Doctors need to not be suspicious of biosimilars and generics,” he emphasized.
Physicians can also advocate for policies that will lower insulin prices, and their institutions can establish preferences for lower-cost biosimilars in formularies.
“Our individual and collective advocacy gives voice to the needs of our patients,” Dr. Rajkumar emphasized.
‘Everyone in the supply chain benefits’
In his commentary, Dr. Rajkumar lists six major reasons for the high cost of insulin:
1. People with type 1 diabetes are a “vulnerable population” who will die without insulin and are therefore willing to pay a high price to stay alive.
2. Just three manufacturers – Eli Lilly, Novo Nordisk, and Sanofi-Aventis – control nearly the entire insulin market in the United States, with no regulations to cap or control the prices they can charge.
3. The manufacturers continually file new patents for existing insulin products – 70 in the case of Lantus, for example – that provide additional years of monopoly protection from competition.
4. Although the Food and Drug Administration has been receptive to approving insulin biosimilars, it still requires manufacturers to go through a long and cumbersome process to obtain licensure, sometimes taking as long as 10 years.
5.PBMs, paid by insurance companies to negotiate prices with retail pharmacies and pharmaceutical companies (through rebates), stand to benefit from higher, not lower, list prices.
6. Pharmaceutical companies have vast lobbying power.
In regard to the fifth point, about PBMs, Dr. Rajkumar said, “It’s not just the PBMs – it’s the whole supply chain. It’s hard to put a finger on the source of the problem. There’s no transparency in any of the arrangements for you to know why only certain drugs are on a given formulary of an insurance company or PBM. But we do know that, in general, the whole supply chain benefits from the higher list price. Everyone.”
‘Authorized generic’ insulins
That is why Dr. Rajkumar is not convinced that Eli Lilly’s recent launch of half-priced “authorized generic” insulins – first the Lispro injection in March 2019, and then two combination pen products in January 2020 – or Novo Nordisk’s My$99Insulin program and “follow-on” authorized generic versions of Novolog and NovoLog Mix, launched Jan. 2, 2020, will have a huge impact.
“It’s common sense. If Apple made the same iPhone for two different prices, who would pay the full price? It gives you a window into asking what is wrong with the system that allows that? To pay for the higher-priced product, somebody is being paid,” he said.
Indeed, in December 2019, the offices of Sen. Elizabeth Warren (D-MA) and Sen. Richard Blumenthal (D-CT) issued a report from a survey of 400 pharmacies nationwide that found that 83% of the less expensive authorized generic Insulin Lispro was not in stock.
More than two-thirds of pharmacies reported they could not order the product.
“Eli Lilly has failed to take consequential steps – such as simply lowering the list price of Humalog, as it has in foreign markets – to provide lower-cost access to this important diabetes drug,” according to the senators’ report, which concludes by urging Eli Lilly to lower the list price of its insulin and calling for Congress to take steps to enact systemic change to reduce drug prices nationwide.
Asked for comment, Dani Barnhizer, Eli Lilly’s manager of global diabetes communications, said, “Like Senators Warren and Blumenthal, Lilly would like to see even broader use of Insulin Lispro injection because it’s a real solution that can lower copays for people living with diabetes.”
“But the Senators’ paper failed to identify the system challenges that have inhibited access to this lower list price product,” Ms. Barnhizer said. “Payers determine an individual’s premiums and copays, which are subsidized by rebates that pharmaceutical companies pay. And many payers prioritize these rebates to lower premiums instead of offering low copays for chronic medications such as insulin.
“It’s why only one in four people using Medicare Part D, and one in five with commercial plans, have coverage for Insulin Lispro injection. That will not change until payers prioritize providing consistent, affordable insulin copays,” she added.
However, Ms. Barnhizer also noted, “It is not unusual for pharmacies to not stock a medicine. Any pharmacy can place an order for Insulin Lispro injection, with delivery in 1-2 days. All major U.S. wholesalers are now distributing Insulin Lispro injection.”
She also said that people who earn 400% or less of the federal poverty level may be eligible for free insulin, and that Lilly can provide free insulin to anyone in emergency situations. (Novo Nordisk offers that as well.)
Asked why Lilly does not simply lower the price of all their insulins, Ms. Barnhizer responded: “Cutting the list prices would significantly disrupt access to branded insulins, which thousands of insured patients depend on. Launching lower-priced insulin options is a less disruptive approach to help reduce the amount people pay at the pharmacy for people who need the help.”
Government role needed
In addition to the recommendations for physicians and their institutions, Dr. Rajkumar listed several potential policy-level solutions:
1. At the state and federal level, regulations should protect against excessive drug launch prices through the same type of value-based pricing approaches used in other developed countries. “Capping the maximum price increases to the rate of inflation is needed and can happen only through state and/or federal legislation,” he wrote.
Although some may see this as antithetical to “free market” economics, Dr. Rajkumar points out that, in the case of many prescription drugs, including insulin, “we not only have an unregulated monopoly, but it’s a prolonged unregulated monopoly for a lifesaving product, not a luxury item.”
“When you grant monopoly protection and put a barrier on competition, that’s not a free market. People have always had regulations on monopolies. Unregulated monopoly is a recipe for high prices. You have to have some regulation that protects citizens from exploitation.”
And here, he believes, the United States could adopt price negotiations as practiced in Europe and other parts of the world, but which are currently forbidden in the United States.
“Other countries negotiate the price in exchange for monopoly protection. You don’t have to reinvent the wheel,” he said.
2. Reform of the regulatory and legal processes to ease the path for approval of generics and biosimilars to enter the market. This could include reciprocal approval so that biosimilars approved in Canada or the European Union could automatically be granted FDA approval in the United States.
3. Reform of the patent system to prevent overpatenting and patent abuse, by capping patent life to 7-10 years and forbidding use of additional patents as a way of prolonging market exclusivity.
To this point, Barnhizer pointed out that “none of the Lilly insulins are patent protected. Our most commonly used insulin, Humalog U-100, lost patent protection in 2014.”
4. A nongovernmental agency should oversee pricing and make recommendations to Medicare and insurers on the maximum price of new and existing drugs, including insulin. One body poised to do that work is the Institute for Clinical and Economic Review, which receives 77% of its funding from nonprofit foundations. “I have worked with them and they are the best there is,” Dr. Rajkumar said.
5. Any rebates paid by manufacturers to PBMs should be transparent to all stakeholders, including patients.
6. Nonprofit generic manufacturing should be established. The Mayo Clinic has recently partnered with Intermountain Healthcare and several other organizations in creating Civica Rx, a nonprofit generic company.
7. Measures and laws that provide access to insulin in emergency situations are needed, particularly for people with type 1 diabetes.
Recent proposed and enacted legislation has been aimed at some of these goals.
The Insulin Price Reduction Act, introduced in October 2019 and just endorsed by the American Diabetes Association, would reduce insulin costs by providing incentives for manufacturers to revert to the 2006 list price of all insulins.
The Affordable Insulin Approvals Now Act, introduced in July 2019, aims to speed up approvals of generic and biosimilar insulins.
And in May 2019, the state of Colorado passed a bill to cap patient copays for insulin at $100 a month, and similar legislation has been introduced in several other states.
Dr. Rajkumar says that an overall fix will require changes at the federal level.
But, he said, they do not need to happen all at once.
“There are a number of changes that need to happen, but we can do one legislation at a time. ... I’m optimistic that something will happen. This is a national conversation. Both sides of the aisle want to do something about it. People are indeed feeling the pinch, so maybe something will get done,” he said.
Dr. Rajkumar has reported no relevant financial relationships.
This article first appeared on Medscape.com.
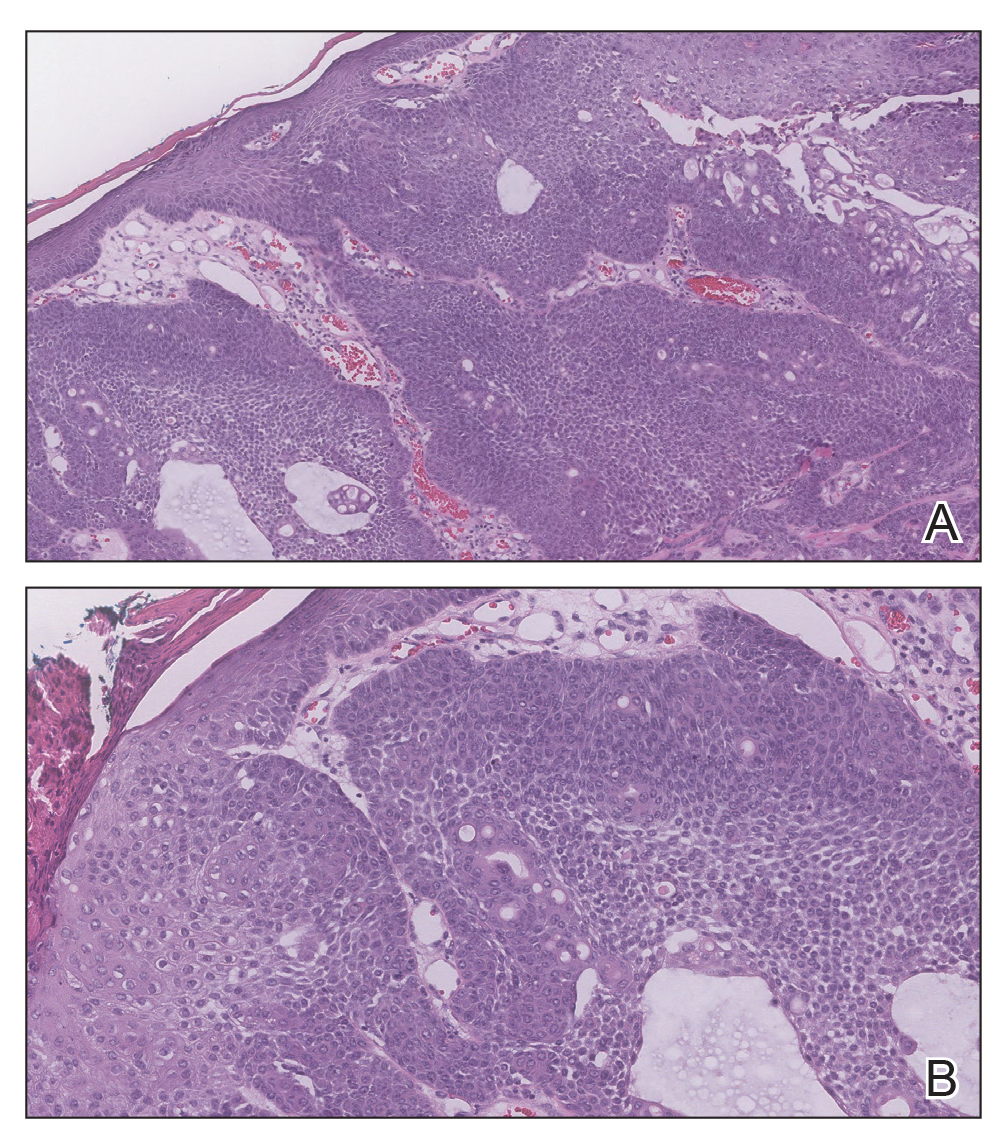
FDA approves first treatment for advanced epithelioid sarcoma
The Food and Drug Administration has granted accelerated approval to tazemetostat (Tazverik) for the treatment of adults and pediatric patients aged 16 years and older with metastatic or locally advanced epithelioid sarcoma not eligible for complete resection.
Approval was based on overall response rate in a trial enrolling 62 patients with metastatic or locally advanced epithelioid sarcoma. The overall response rate was 15%, with 1.6% of patients having a complete response and 13% having a partial response. Of the nine patients that had a response, six (67%) had a response lasting 6 months or longer, the FDA said in a press statement.
The most common side effects for patients taking tazemetostat were pain, fatigue, nausea, decreased appetite, vomiting, and constipation. Patients treated with tazemetostat are at increased risk of developing secondary malignancies, including T-cell lymphoblastic lymphoma, myelodysplastic syndrome, and acute myeloid leukemia.
“Epithelioid sarcoma accounts for less than 1% of all soft-tissue sarcomas,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Oncologic Diseases in the Center for Drug Evaluation and Research. “Until today, there were no treatment options specifically for patients with epithelioid sarcoma. The approval of Tazverik provides a treatment option that specifically targets this disease.”
Tazemetostat must be dispensed with a patient medication guide that describes important information about the drug’s uses and risks, the FDA said.
The Food and Drug Administration has granted accelerated approval to tazemetostat (Tazverik) for the treatment of adults and pediatric patients aged 16 years and older with metastatic or locally advanced epithelioid sarcoma not eligible for complete resection.
Approval was based on overall response rate in a trial enrolling 62 patients with metastatic or locally advanced epithelioid sarcoma. The overall response rate was 15%, with 1.6% of patients having a complete response and 13% having a partial response. Of the nine patients that had a response, six (67%) had a response lasting 6 months or longer, the FDA said in a press statement.
The most common side effects for patients taking tazemetostat were pain, fatigue, nausea, decreased appetite, vomiting, and constipation. Patients treated with tazemetostat are at increased risk of developing secondary malignancies, including T-cell lymphoblastic lymphoma, myelodysplastic syndrome, and acute myeloid leukemia.
“Epithelioid sarcoma accounts for less than 1% of all soft-tissue sarcomas,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Oncologic Diseases in the Center for Drug Evaluation and Research. “Until today, there were no treatment options specifically for patients with epithelioid sarcoma. The approval of Tazverik provides a treatment option that specifically targets this disease.”
Tazemetostat must be dispensed with a patient medication guide that describes important information about the drug’s uses and risks, the FDA said.
The Food and Drug Administration has granted accelerated approval to tazemetostat (Tazverik) for the treatment of adults and pediatric patients aged 16 years and older with metastatic or locally advanced epithelioid sarcoma not eligible for complete resection.
Approval was based on overall response rate in a trial enrolling 62 patients with metastatic or locally advanced epithelioid sarcoma. The overall response rate was 15%, with 1.6% of patients having a complete response and 13% having a partial response. Of the nine patients that had a response, six (67%) had a response lasting 6 months or longer, the FDA said in a press statement.
The most common side effects for patients taking tazemetostat were pain, fatigue, nausea, decreased appetite, vomiting, and constipation. Patients treated with tazemetostat are at increased risk of developing secondary malignancies, including T-cell lymphoblastic lymphoma, myelodysplastic syndrome, and acute myeloid leukemia.
“Epithelioid sarcoma accounts for less than 1% of all soft-tissue sarcomas,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Oncologic Diseases in the Center for Drug Evaluation and Research. “Until today, there were no treatment options specifically for patients with epithelioid sarcoma. The approval of Tazverik provides a treatment option that specifically targets this disease.”
Tazemetostat must be dispensed with a patient medication guide that describes important information about the drug’s uses and risks, the FDA said.
Family-focused therapy linked to longer remissions in youth at risk for bipolar disorder
A 4-month intensive program of family-focused therapy worked better than a less-intensive program in delaying new mood episodes among young people at risk of developing bipolar disorder, new research shows.
“This study extends the results of other randomized clinical trials indicating effects of family psychoeducation and skill training on the long-term trajectory of depressive symptoms in pediatric mood disorders,” wrote David J. Miklowitz, PhD, of the department of psychiatry and biobehavioral sciences at the University of California, Los Angeles, and colleagues. The study was published in JAMA Psychiatry.
For their research, the investigators recruited 127 subjects aged 9-17 years (mean age, 13 years) deemed at high risk for later bipolar I or II disorder for having depression or subthreshold mania along with active mood symptoms and a family history of bipolar disorder. Some 85% of subjects had depression symptoms at enrollment.
Subjects were randomized to 12 sessions over 4 months of family-focused therapy – a psychoeducation, communication, and problem-solving training program incorporating caretakers and also siblings if possible (n = 61) – or to 3 sessions of family-focused therapy and an additional 3 of individual therapy in the same 4-month time frame (n = 66). Medication was allowed for all subjects, and patients were followed for a median 2 years after the intervention. Baseline characteristics, medication use, and dropout rates were similar between the groups.
Both groups saw similarly high rates of new episodes of major depression, mania, or hypomania during follow-up; however, those in the intensive family-focused therapy group saw longer intervals of wellness, with a median 81 weeks (95% confidence interval, 56-123 weeks) from randomization until the first observed mood episode, compared with 63 weeks (95% CI, 44-78 weeks) to an episode for the less-intensive group (P = .03). Dr. Miklowitz and colleagues did not find differences in the severity of mood episodes following either treatment mode or in later conversion to bipolar I or II.
The researchers described as limitations of their study its inability to measure the “temporal relationship between changes in family communication and symptom changes in patients,” which would help answer whether improvements in communication patterns aid symptom regulation, or whether more stable patients are better able to manage difficult family interactions.
Family-focused therapy “may have uniquely enduring effects that extend into the maintenance phase of treatment,” Dr. Miklowitz and colleagues wrote.
The study was funded by the National Institute of Mental Health. Several coauthors, including the lead author, reported receiving research grants from NIMH and other foundations. Two additional coauthors reported receiving pharmaceutical industry funding, including advisory board and consulting fees.
SOURCE: Miklowitz DJ et al. JAMA Psychiatry. 2020 Jan 15. doi: 10.1001/jamapsychiatry.2019.4520.
A 4-month intensive program of family-focused therapy worked better than a less-intensive program in delaying new mood episodes among young people at risk of developing bipolar disorder, new research shows.
“This study extends the results of other randomized clinical trials indicating effects of family psychoeducation and skill training on the long-term trajectory of depressive symptoms in pediatric mood disorders,” wrote David J. Miklowitz, PhD, of the department of psychiatry and biobehavioral sciences at the University of California, Los Angeles, and colleagues. The study was published in JAMA Psychiatry.
For their research, the investigators recruited 127 subjects aged 9-17 years (mean age, 13 years) deemed at high risk for later bipolar I or II disorder for having depression or subthreshold mania along with active mood symptoms and a family history of bipolar disorder. Some 85% of subjects had depression symptoms at enrollment.
Subjects were randomized to 12 sessions over 4 months of family-focused therapy – a psychoeducation, communication, and problem-solving training program incorporating caretakers and also siblings if possible (n = 61) – or to 3 sessions of family-focused therapy and an additional 3 of individual therapy in the same 4-month time frame (n = 66). Medication was allowed for all subjects, and patients were followed for a median 2 years after the intervention. Baseline characteristics, medication use, and dropout rates were similar between the groups.
Both groups saw similarly high rates of new episodes of major depression, mania, or hypomania during follow-up; however, those in the intensive family-focused therapy group saw longer intervals of wellness, with a median 81 weeks (95% confidence interval, 56-123 weeks) from randomization until the first observed mood episode, compared with 63 weeks (95% CI, 44-78 weeks) to an episode for the less-intensive group (P = .03). Dr. Miklowitz and colleagues did not find differences in the severity of mood episodes following either treatment mode or in later conversion to bipolar I or II.
The researchers described as limitations of their study its inability to measure the “temporal relationship between changes in family communication and symptom changes in patients,” which would help answer whether improvements in communication patterns aid symptom regulation, or whether more stable patients are better able to manage difficult family interactions.
Family-focused therapy “may have uniquely enduring effects that extend into the maintenance phase of treatment,” Dr. Miklowitz and colleagues wrote.
The study was funded by the National Institute of Mental Health. Several coauthors, including the lead author, reported receiving research grants from NIMH and other foundations. Two additional coauthors reported receiving pharmaceutical industry funding, including advisory board and consulting fees.
SOURCE: Miklowitz DJ et al. JAMA Psychiatry. 2020 Jan 15. doi: 10.1001/jamapsychiatry.2019.4520.
A 4-month intensive program of family-focused therapy worked better than a less-intensive program in delaying new mood episodes among young people at risk of developing bipolar disorder, new research shows.
“This study extends the results of other randomized clinical trials indicating effects of family psychoeducation and skill training on the long-term trajectory of depressive symptoms in pediatric mood disorders,” wrote David J. Miklowitz, PhD, of the department of psychiatry and biobehavioral sciences at the University of California, Los Angeles, and colleagues. The study was published in JAMA Psychiatry.
For their research, the investigators recruited 127 subjects aged 9-17 years (mean age, 13 years) deemed at high risk for later bipolar I or II disorder for having depression or subthreshold mania along with active mood symptoms and a family history of bipolar disorder. Some 85% of subjects had depression symptoms at enrollment.
Subjects were randomized to 12 sessions over 4 months of family-focused therapy – a psychoeducation, communication, and problem-solving training program incorporating caretakers and also siblings if possible (n = 61) – or to 3 sessions of family-focused therapy and an additional 3 of individual therapy in the same 4-month time frame (n = 66). Medication was allowed for all subjects, and patients were followed for a median 2 years after the intervention. Baseline characteristics, medication use, and dropout rates were similar between the groups.
Both groups saw similarly high rates of new episodes of major depression, mania, or hypomania during follow-up; however, those in the intensive family-focused therapy group saw longer intervals of wellness, with a median 81 weeks (95% confidence interval, 56-123 weeks) from randomization until the first observed mood episode, compared with 63 weeks (95% CI, 44-78 weeks) to an episode for the less-intensive group (P = .03). Dr. Miklowitz and colleagues did not find differences in the severity of mood episodes following either treatment mode or in later conversion to bipolar I or II.
The researchers described as limitations of their study its inability to measure the “temporal relationship between changes in family communication and symptom changes in patients,” which would help answer whether improvements in communication patterns aid symptom regulation, or whether more stable patients are better able to manage difficult family interactions.
Family-focused therapy “may have uniquely enduring effects that extend into the maintenance phase of treatment,” Dr. Miklowitz and colleagues wrote.
The study was funded by the National Institute of Mental Health. Several coauthors, including the lead author, reported receiving research grants from NIMH and other foundations. Two additional coauthors reported receiving pharmaceutical industry funding, including advisory board and consulting fees.
SOURCE: Miklowitz DJ et al. JAMA Psychiatry. 2020 Jan 15. doi: 10.1001/jamapsychiatry.2019.4520.
FROM JAMA PSYCHIATRY
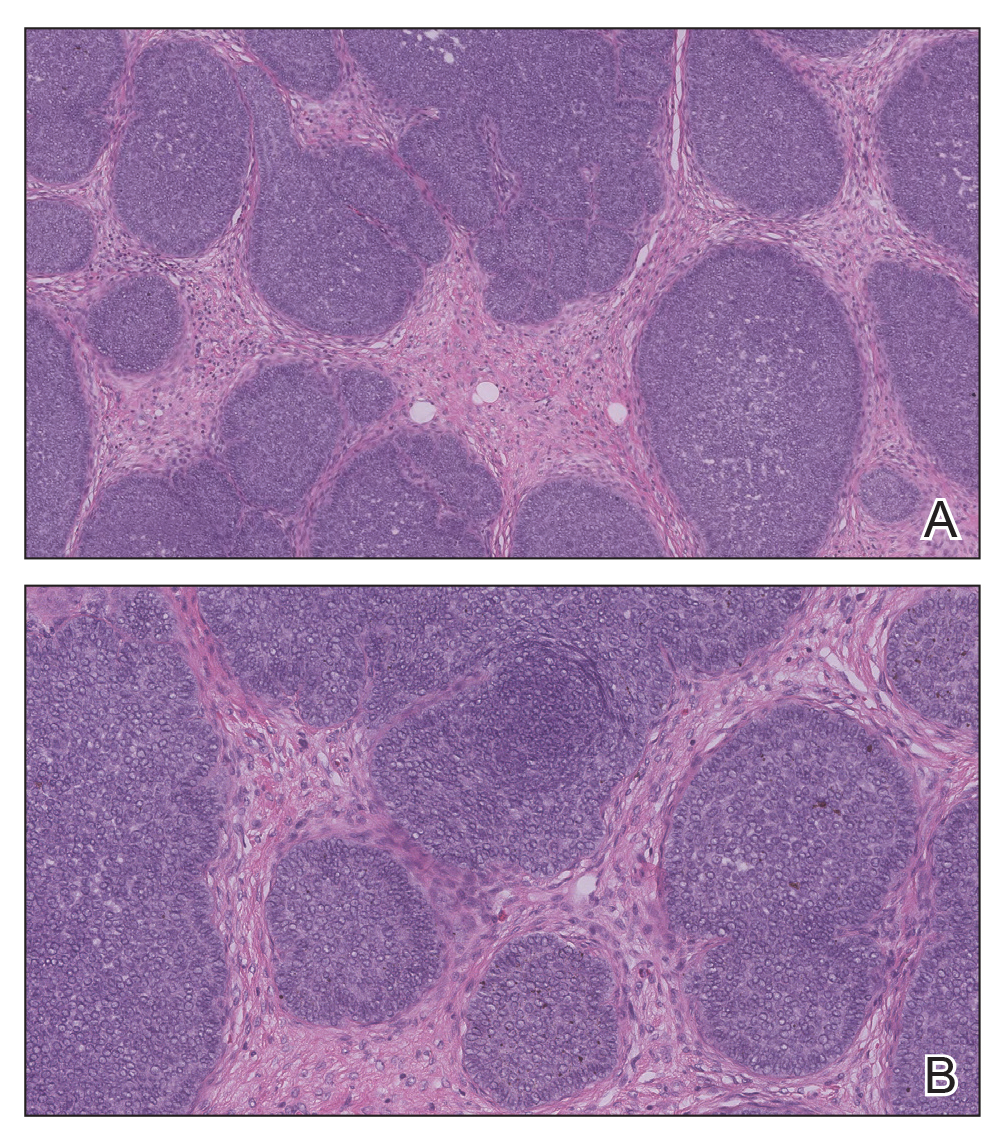
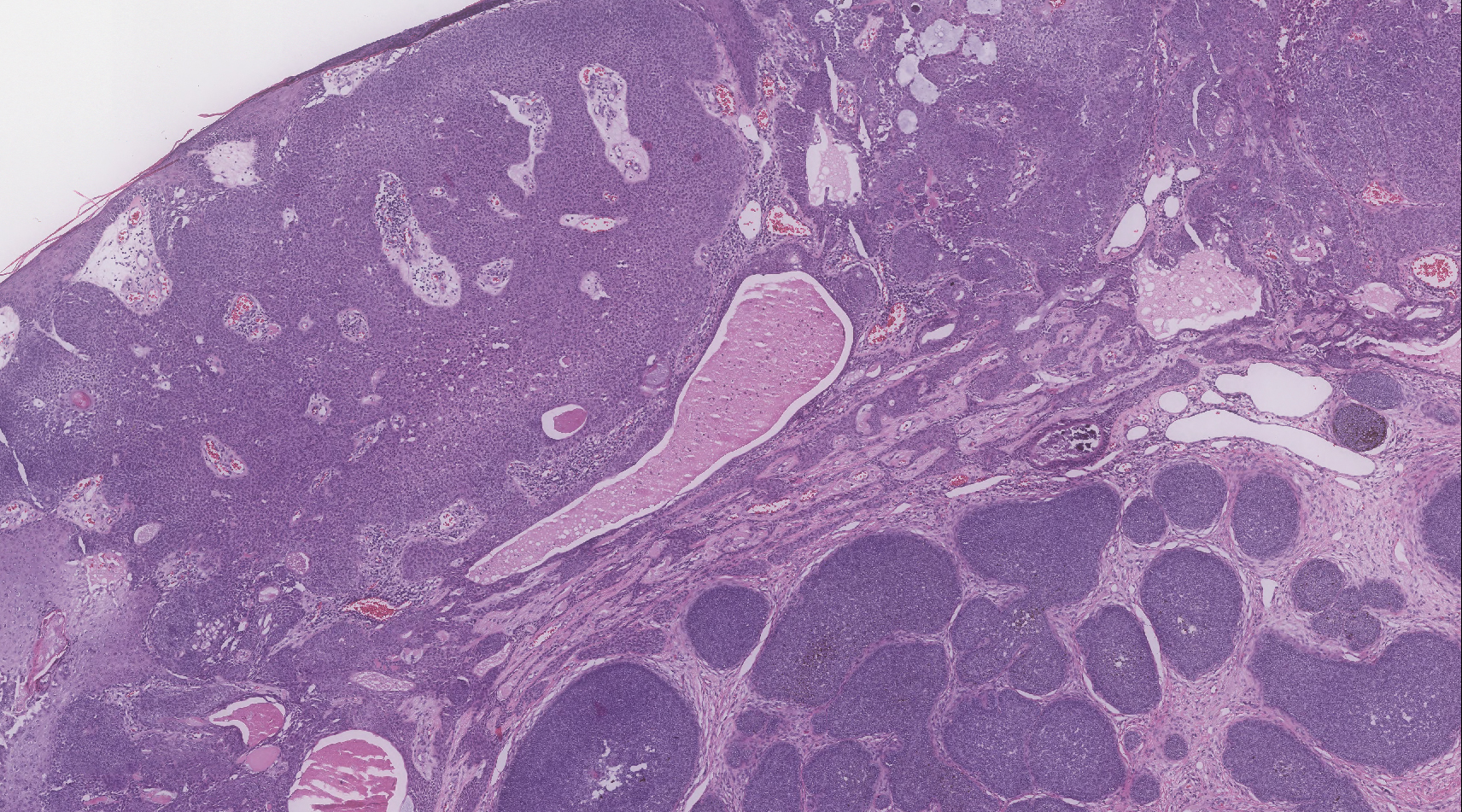
T-VEC plus pembrolizumab yields promising response rate in phase 2 sarcoma study
The combination of oncolytic immunotherapy and an immune checkpoint inhibitor had promising activity in a phase 2 study including patients with previously treated advanced sarcoma, investigators report.
Responses were seen in about one-third of the patients (30%) at 24 weeks after starting treatment with talimogene laherparepvec (T-VEC) and pembrolizumab, according to the investigators, led by Ciara M. Kelly, MBBChBAO, MD, of the department of sarcoma oncology at Memorial Sloan Kettering Cancer Center, New York.
“To our knowledge, this is one of the highest ORRs [objective response rates] reported in an unselected sarcoma-specific study population evaluating the efficacy of combination immunotherapy,” Dr. Kelly and coauthors wrote in JAMA Oncology.
Two of the patients who responded to the combination had previously failed regimens that included an immune checkpoint inhibitor, suggesting T-VEC might be augmenting the efficacy of pembrolizumab, according to the authors.
Among responders, the mean number of prior treatments was one, while by contrast, most of the study cohort (60%) had three or more prior treatments. “This finding supports the rationale to enroll patients with sarcoma in immunotherapy trials earlier in their treatment course,” Dr. Kelly and colleagues wrote.
In studies of immunotherapy in Merkel cell carcinoma and other cancer types, higher response rates have been seen in patients who were naive to chemotherapy, as opposed to those who were refractory to it.
The present single-institution, phase 2 study by Dr. Kelly and colleagues included 20 adult patients with histologically confirmed locally advanced or metastatic sarcoma. The patients received a fixed dose of pembrolizumab administered intravenously, and had T-VEC injected into palpable lesions, on day 1 of 21-day cycles.
While the ORR was 30% at 24 weeks (7 of 35 patients), an additional patient had a response at 32 weeks, bringing the ORR to 35%, according to the report.
“Maximal response to therapy may take a prolonged period to achieve,” the investigators wrote, noting that the median time to response was 14.4 weeks.
Median duration of response was 56.1 weeks, suggesting the combination provided durable disease control, they added.
Safety was consistent with what was seen in a previous study of T-VEC and pembrolizumab in melanoma. In this sarcoma study, the incidence of grade 3 treatment-related adverse events was 20%, while in studies of conventional chemotherapy in this setting, the rate of those events has been “comparable but generally higher,” the investigators wrote.
Dr. Kelly and colleagues wrote that a randomized clinical trial is the “ideal next step” in the development of the regimen, adding that an expansion of the present phase 2 study is in progress.
The study was funded by Amgen and Merck, with additional grant support from Cycle for Survival and the National Institutes of Health/National Cancer Institute. Dr. Kelly reported disclosures related to Merck, Amgen, Agios Pharmaceuticals, and Exicure. Her coauthors reported disclosures with Regeneron, Novartis, Takeda, and Nektar, among others.
SOURCE: Kelly CM et al. JAMA Oncol. 2020 Jan 23. doi: 10.1001/jamaoncol.2019.6152.
The combination of oncolytic immunotherapy and an immune checkpoint inhibitor had promising activity in a phase 2 study including patients with previously treated advanced sarcoma, investigators report.
Responses were seen in about one-third of the patients (30%) at 24 weeks after starting treatment with talimogene laherparepvec (T-VEC) and pembrolizumab, according to the investigators, led by Ciara M. Kelly, MBBChBAO, MD, of the department of sarcoma oncology at Memorial Sloan Kettering Cancer Center, New York.
“To our knowledge, this is one of the highest ORRs [objective response rates] reported in an unselected sarcoma-specific study population evaluating the efficacy of combination immunotherapy,” Dr. Kelly and coauthors wrote in JAMA Oncology.
Two of the patients who responded to the combination had previously failed regimens that included an immune checkpoint inhibitor, suggesting T-VEC might be augmenting the efficacy of pembrolizumab, according to the authors.
Among responders, the mean number of prior treatments was one, while by contrast, most of the study cohort (60%) had three or more prior treatments. “This finding supports the rationale to enroll patients with sarcoma in immunotherapy trials earlier in their treatment course,” Dr. Kelly and colleagues wrote.
In studies of immunotherapy in Merkel cell carcinoma and other cancer types, higher response rates have been seen in patients who were naive to chemotherapy, as opposed to those who were refractory to it.
The present single-institution, phase 2 study by Dr. Kelly and colleagues included 20 adult patients with histologically confirmed locally advanced or metastatic sarcoma. The patients received a fixed dose of pembrolizumab administered intravenously, and had T-VEC injected into palpable lesions, on day 1 of 21-day cycles.
While the ORR was 30% at 24 weeks (7 of 35 patients), an additional patient had a response at 32 weeks, bringing the ORR to 35%, according to the report.
“Maximal response to therapy may take a prolonged period to achieve,” the investigators wrote, noting that the median time to response was 14.4 weeks.
Median duration of response was 56.1 weeks, suggesting the combination provided durable disease control, they added.
Safety was consistent with what was seen in a previous study of T-VEC and pembrolizumab in melanoma. In this sarcoma study, the incidence of grade 3 treatment-related adverse events was 20%, while in studies of conventional chemotherapy in this setting, the rate of those events has been “comparable but generally higher,” the investigators wrote.
Dr. Kelly and colleagues wrote that a randomized clinical trial is the “ideal next step” in the development of the regimen, adding that an expansion of the present phase 2 study is in progress.
The study was funded by Amgen and Merck, with additional grant support from Cycle for Survival and the National Institutes of Health/National Cancer Institute. Dr. Kelly reported disclosures related to Merck, Amgen, Agios Pharmaceuticals, and Exicure. Her coauthors reported disclosures with Regeneron, Novartis, Takeda, and Nektar, among others.
SOURCE: Kelly CM et al. JAMA Oncol. 2020 Jan 23. doi: 10.1001/jamaoncol.2019.6152.
The combination of oncolytic immunotherapy and an immune checkpoint inhibitor had promising activity in a phase 2 study including patients with previously treated advanced sarcoma, investigators report.
Responses were seen in about one-third of the patients (30%) at 24 weeks after starting treatment with talimogene laherparepvec (T-VEC) and pembrolizumab, according to the investigators, led by Ciara M. Kelly, MBBChBAO, MD, of the department of sarcoma oncology at Memorial Sloan Kettering Cancer Center, New York.
“To our knowledge, this is one of the highest ORRs [objective response rates] reported in an unselected sarcoma-specific study population evaluating the efficacy of combination immunotherapy,” Dr. Kelly and coauthors wrote in JAMA Oncology.
Two of the patients who responded to the combination had previously failed regimens that included an immune checkpoint inhibitor, suggesting T-VEC might be augmenting the efficacy of pembrolizumab, according to the authors.
Among responders, the mean number of prior treatments was one, while by contrast, most of the study cohort (60%) had three or more prior treatments. “This finding supports the rationale to enroll patients with sarcoma in immunotherapy trials earlier in their treatment course,” Dr. Kelly and colleagues wrote.
In studies of immunotherapy in Merkel cell carcinoma and other cancer types, higher response rates have been seen in patients who were naive to chemotherapy, as opposed to those who were refractory to it.
The present single-institution, phase 2 study by Dr. Kelly and colleagues included 20 adult patients with histologically confirmed locally advanced or metastatic sarcoma. The patients received a fixed dose of pembrolizumab administered intravenously, and had T-VEC injected into palpable lesions, on day 1 of 21-day cycles.
While the ORR was 30% at 24 weeks (7 of 35 patients), an additional patient had a response at 32 weeks, bringing the ORR to 35%, according to the report.
“Maximal response to therapy may take a prolonged period to achieve,” the investigators wrote, noting that the median time to response was 14.4 weeks.
Median duration of response was 56.1 weeks, suggesting the combination provided durable disease control, they added.
Safety was consistent with what was seen in a previous study of T-VEC and pembrolizumab in melanoma. In this sarcoma study, the incidence of grade 3 treatment-related adverse events was 20%, while in studies of conventional chemotherapy in this setting, the rate of those events has been “comparable but generally higher,” the investigators wrote.
Dr. Kelly and colleagues wrote that a randomized clinical trial is the “ideal next step” in the development of the regimen, adding that an expansion of the present phase 2 study is in progress.
The study was funded by Amgen and Merck, with additional grant support from Cycle for Survival and the National Institutes of Health/National Cancer Institute. Dr. Kelly reported disclosures related to Merck, Amgen, Agios Pharmaceuticals, and Exicure. Her coauthors reported disclosures with Regeneron, Novartis, Takeda, and Nektar, among others.
SOURCE: Kelly CM et al. JAMA Oncol. 2020 Jan 23. doi: 10.1001/jamaoncol.2019.6152.
FROM JAMA ONCOLOGY
GI societies meet with ABIM
Recently, the leadership of AGA, AASLD, ACG, and ASGE met with Richard Battaglia, MD, the chief medical officer of ABIM, about the status of ABIM’s efforts to move toward a longitudinal testing model, which ABIM describes as “a self-paced pathway for physicians to acquire and demonstrate ongoing knowledge.”
ABIM anticipates that the new option will be available beginning in 2022, in as many specialties as possible. In the meantime, all current MOC program policies remain in effect and ABIM directs diplomates to use the current options to maintain certification.
While we would like to see ABIM waive testing requirements while it works with GI to create a new longitudinal model, ABIM has declined to do so. Notwithstanding this fact, the GI societies are committed to advocating for the needs of gastroenterology while working with ABIM to ensure the new model is relevant to gastroenterology and hepatology.
Recently, the leadership of AGA, AASLD, ACG, and ASGE met with Richard Battaglia, MD, the chief medical officer of ABIM, about the status of ABIM’s efforts to move toward a longitudinal testing model, which ABIM describes as “a self-paced pathway for physicians to acquire and demonstrate ongoing knowledge.”
ABIM anticipates that the new option will be available beginning in 2022, in as many specialties as possible. In the meantime, all current MOC program policies remain in effect and ABIM directs diplomates to use the current options to maintain certification.
While we would like to see ABIM waive testing requirements while it works with GI to create a new longitudinal model, ABIM has declined to do so. Notwithstanding this fact, the GI societies are committed to advocating for the needs of gastroenterology while working with ABIM to ensure the new model is relevant to gastroenterology and hepatology.
Recently, the leadership of AGA, AASLD, ACG, and ASGE met with Richard Battaglia, MD, the chief medical officer of ABIM, about the status of ABIM’s efforts to move toward a longitudinal testing model, which ABIM describes as “a self-paced pathway for physicians to acquire and demonstrate ongoing knowledge.”
ABIM anticipates that the new option will be available beginning in 2022, in as many specialties as possible. In the meantime, all current MOC program policies remain in effect and ABIM directs diplomates to use the current options to maintain certification.
While we would like to see ABIM waive testing requirements while it works with GI to create a new longitudinal model, ABIM has declined to do so. Notwithstanding this fact, the GI societies are committed to advocating for the needs of gastroenterology while working with ABIM to ensure the new model is relevant to gastroenterology and hepatology.
Watch your step (therapy) — understanding ‘fail first’
Sometimes known as “fail first,” step therapy is a tool used by insurance companies that requires patients to fail medications before agreeing to cover a health care provider’s initial treatment recommendation.
Largely affecting patients with inflammatory bowel disease (IBD), step therapy focuses on the use of insurer-preferred treatments rather than effective, patient-centric therapies. In addition to causing many patient hardships and health problems, this protocol allows insurance companies to come between the provider-patient relationship and dictate a patient’s course of treatment.
To help clinicians navigate this challenging landscape, AGA is pleased to offer a new step therapy webpage, gastro.org/step-therapy, that details the step therapy protocol and opportunities to advocate for patient protections.
Additional education modules — including videos, podcasts and other resources — are also available for several states that have implemented safe step therapy laws, including Illinois, New York, and Texas.
Visit the Navigating State Step Therapy Laws program page to learn more:
- What is the step therapy protocol?
- How does step therapy impact a health care provider’s ability to provide patient care?
- Which states have implemented step therapy laws?
- How do state step therapy laws provide physician rights and patient protection?
- Tips to share with your patients.
- What are AGA’s advocacy efforts — and how can I help?
Education modules for additional states will be available in early 2020.
AGA’s Navigating State Step Therapy Laws program is funded by an unrestricted educational grant from Takeda and Pfizer.
ginews@gastro.org
Sometimes known as “fail first,” step therapy is a tool used by insurance companies that requires patients to fail medications before agreeing to cover a health care provider’s initial treatment recommendation.
Largely affecting patients with inflammatory bowel disease (IBD), step therapy focuses on the use of insurer-preferred treatments rather than effective, patient-centric therapies. In addition to causing many patient hardships and health problems, this protocol allows insurance companies to come between the provider-patient relationship and dictate a patient’s course of treatment.
To help clinicians navigate this challenging landscape, AGA is pleased to offer a new step therapy webpage, gastro.org/step-therapy, that details the step therapy protocol and opportunities to advocate for patient protections.
Additional education modules — including videos, podcasts and other resources — are also available for several states that have implemented safe step therapy laws, including Illinois, New York, and Texas.
Visit the Navigating State Step Therapy Laws program page to learn more:
- What is the step therapy protocol?
- How does step therapy impact a health care provider’s ability to provide patient care?
- Which states have implemented step therapy laws?
- How do state step therapy laws provide physician rights and patient protection?
- Tips to share with your patients.
- What are AGA’s advocacy efforts — and how can I help?
Education modules for additional states will be available in early 2020.
AGA’s Navigating State Step Therapy Laws program is funded by an unrestricted educational grant from Takeda and Pfizer.
ginews@gastro.org
Sometimes known as “fail first,” step therapy is a tool used by insurance companies that requires patients to fail medications before agreeing to cover a health care provider’s initial treatment recommendation.
Largely affecting patients with inflammatory bowel disease (IBD), step therapy focuses on the use of insurer-preferred treatments rather than effective, patient-centric therapies. In addition to causing many patient hardships and health problems, this protocol allows insurance companies to come between the provider-patient relationship and dictate a patient’s course of treatment.
To help clinicians navigate this challenging landscape, AGA is pleased to offer a new step therapy webpage, gastro.org/step-therapy, that details the step therapy protocol and opportunities to advocate for patient protections.
Additional education modules — including videos, podcasts and other resources — are also available for several states that have implemented safe step therapy laws, including Illinois, New York, and Texas.
Visit the Navigating State Step Therapy Laws program page to learn more:
- What is the step therapy protocol?
- How does step therapy impact a health care provider’s ability to provide patient care?
- Which states have implemented step therapy laws?
- How do state step therapy laws provide physician rights and patient protection?
- Tips to share with your patients.
- What are AGA’s advocacy efforts — and how can I help?
Education modules for additional states will be available in early 2020.
AGA’s Navigating State Step Therapy Laws program is funded by an unrestricted educational grant from Takeda and Pfizer.
ginews@gastro.org
Friable Scalp Nodule
The Diagnosis: Adnexal Neoplasm Arising in a Nevus Sebaceus
Biopsy of the lesion showed a proliferation of basaloid-appearing cells with focal ductal differentiation and ulceration consistent with poroma (Figure 1). Due to the superficial nature of the biopsy, the pathologist recommended excision to ensure complete removal and to rule out a well-differentiated porocarcinoma. Excision of the lesion showed large basaloid aggregates with a hypercellular stroma and a surrounding papillomatous epidermis with well-developed sebaceous lobules consistent with a trichoblastoma and a nevus sebaceus, respectively (Figure 2). There also was evidence of poroma; however, there were no findings concerning for porocarcinoma, which could lead to metastasis (Figure 3).
Nevus sebaceus is a benign, hamartomatous, congenital growth that occurs in approximately 1% of patients presenting to dermatology offices. It usually presents as a single asymptomatic plaque on the scalp (62.5%) or face (24.5%) that changes in morphology over its lifetime.1,2 In children, a nevus manifests as a yellowish, smooth, waxy skin lesion. As the sebaceous glands become more developed during adolescence, the lesion takes on more of a verrucous appearance and also can darken.
Although nevus sebaceus is benign, it may give rise to both benign and malignant neoplasms. In a 2014 study of 707 cases of nevus sebaceus, 21.4% developed secondary neoplasms, 88% of which were benign.2 The origins of these neoplasms can be epithelial, sebaceous, apocrine, and/or follicular. The 3 most common secondary neoplasms found in nevus sebaceus are trichoblastoma (34.7%), syringocystadenoma papilliferum (24.7%), and apocrine/eccrine adenoma (10%), all of which are benign.2 Trichoblastomas represent a type of hair follicle tumor. Malignant lesions manifest in approximately 2.5% of cases, with basal cell carcinoma (BCC) being the most common (5.3% of all neoplasms), followed by squamous cell carcinoma (2.7% of all neoplasms).2 Differentiating BCC from trichoblastoma can be difficult, but histologically BCCs usually have tumor stromal clefting while trichoblastomas do not.3 The incidence of secondary tumors in nevus sebaceus displays a strong correlation with age; thus, the highest proportion of neoplasms occur in adults.
Treatment of nevus sebaceus depends on the patient's age. In children, because of the low probability of secondary neoplasms, observation in lieu of surgical excision is a common approach. In adults, the approach typically is surgical excision or close follow-up, as there is a concern for secondary neoplasm and the potential for malignant degeneration.
A nevus sebaceus leading to 2 or more tumors within the same lesion is rare (seen in only 4.2% of lesions). The most common combination is trichoblastoma with syringocystadenoma papilliferum (0.6% of all cases).2 Poromas represent sweat gland tumors that usually appear on the soles (65%) or palms (10%).4 It is uncommon for these neoplasms to manifest on the scalp or within a nevus sebaceus. Three independent studies (N=596; N=707; N=450) did not report any occurrences of eccrine poroma.1,2,5 Eccrine poroma in conjunction with nodular trichoblastoma arising in a nevus sebaceus is unusual, and definitive excision should be strongly considered because of the possibility to develop a porocarcinoma.6
Atypical fibroxanthoma presents on sun-exposed areas as an exophytic nodule or plaque that frequently ulcerates. Pathology of this tumor shows a spindled cell proliferation that can stain positively for CD10 and procollagen 1. Basal cell carcinoma presents as a pearly papule or nodule displaying basaloid-appearing aggregates with tumor stromal clefting and can stain with Ber-EP4. Cylindromas typically present on the scalp as large rubbery-appearing plaques and nodules. Cylindromas usually present as a solitary tumor, but in the familial form there can be clusters of multiple nodules. Metastatic renal cell carcinoma frequently appears as a bleeding nodule on the scalp in patients with known renal cell cancer or as the initial presentation.
- Cribier B, Scrivener Y, Grosshans E. Tumors arising in nevus sebaceus: a study of 596 cases. J Am Acad Dermatol. 2000;42(pt 1):263-268.
- Idriss MH, Elston DM. Secondary neoplasms associated with nevus sebaceus of Jadassohn: a study of 707 cases. J Am Acad Dermatol. 2014;70:332-337.
- Wang E, Lee JS, Kazakov DV. A rare combination of sebaceoma with carcinomatous change (sebaceous carcinoma), trichoblastoma, and poroma arising from a nevus sebaceus. J Cutan Pathol. 2013;40:676-682.
- Bae MI, Cho TH, Shin MK, et al. An unusual clinical presentation of eccrine poroma occurring on the auricle. Indian J Dermatol. 2015;60:523.
- Hsu MC, Liau JY, Hong JL, et al. Secondary neoplasms arising from nevus sebaceus: a retrospective study of 450 cases in Taiwan. J Dermatol. 2016;43:175-180.
- Takhan II, Domingo J. Metastasizing eccrine porocarcinoma developing in a sebaceous nevus of Jadassohn. report of a case. Arch Dermatol. 1985;121:413-415.
The Diagnosis: Adnexal Neoplasm Arising in a Nevus Sebaceus
Biopsy of the lesion showed a proliferation of basaloid-appearing cells with focal ductal differentiation and ulceration consistent with poroma (Figure 1). Due to the superficial nature of the biopsy, the pathologist recommended excision to ensure complete removal and to rule out a well-differentiated porocarcinoma. Excision of the lesion showed large basaloid aggregates with a hypercellular stroma and a surrounding papillomatous epidermis with well-developed sebaceous lobules consistent with a trichoblastoma and a nevus sebaceus, respectively (Figure 2). There also was evidence of poroma; however, there were no findings concerning for porocarcinoma, which could lead to metastasis (Figure 3).
Nevus sebaceus is a benign, hamartomatous, congenital growth that occurs in approximately 1% of patients presenting to dermatology offices. It usually presents as a single asymptomatic plaque on the scalp (62.5%) or face (24.5%) that changes in morphology over its lifetime.1,2 In children, a nevus manifests as a yellowish, smooth, waxy skin lesion. As the sebaceous glands become more developed during adolescence, the lesion takes on more of a verrucous appearance and also can darken.
Although nevus sebaceus is benign, it may give rise to both benign and malignant neoplasms. In a 2014 study of 707 cases of nevus sebaceus, 21.4% developed secondary neoplasms, 88% of which were benign.2 The origins of these neoplasms can be epithelial, sebaceous, apocrine, and/or follicular. The 3 most common secondary neoplasms found in nevus sebaceus are trichoblastoma (34.7%), syringocystadenoma papilliferum (24.7%), and apocrine/eccrine adenoma (10%), all of which are benign.2 Trichoblastomas represent a type of hair follicle tumor. Malignant lesions manifest in approximately 2.5% of cases, with basal cell carcinoma (BCC) being the most common (5.3% of all neoplasms), followed by squamous cell carcinoma (2.7% of all neoplasms).2 Differentiating BCC from trichoblastoma can be difficult, but histologically BCCs usually have tumor stromal clefting while trichoblastomas do not.3 The incidence of secondary tumors in nevus sebaceus displays a strong correlation with age; thus, the highest proportion of neoplasms occur in adults.
Treatment of nevus sebaceus depends on the patient's age. In children, because of the low probability of secondary neoplasms, observation in lieu of surgical excision is a common approach. In adults, the approach typically is surgical excision or close follow-up, as there is a concern for secondary neoplasm and the potential for malignant degeneration.
A nevus sebaceus leading to 2 or more tumors within the same lesion is rare (seen in only 4.2% of lesions). The most common combination is trichoblastoma with syringocystadenoma papilliferum (0.6% of all cases).2 Poromas represent sweat gland tumors that usually appear on the soles (65%) or palms (10%).4 It is uncommon for these neoplasms to manifest on the scalp or within a nevus sebaceus. Three independent studies (N=596; N=707; N=450) did not report any occurrences of eccrine poroma.1,2,5 Eccrine poroma in conjunction with nodular trichoblastoma arising in a nevus sebaceus is unusual, and definitive excision should be strongly considered because of the possibility to develop a porocarcinoma.6
Atypical fibroxanthoma presents on sun-exposed areas as an exophytic nodule or plaque that frequently ulcerates. Pathology of this tumor shows a spindled cell proliferation that can stain positively for CD10 and procollagen 1. Basal cell carcinoma presents as a pearly papule or nodule displaying basaloid-appearing aggregates with tumor stromal clefting and can stain with Ber-EP4. Cylindromas typically present on the scalp as large rubbery-appearing plaques and nodules. Cylindromas usually present as a solitary tumor, but in the familial form there can be clusters of multiple nodules. Metastatic renal cell carcinoma frequently appears as a bleeding nodule on the scalp in patients with known renal cell cancer or as the initial presentation.
The Diagnosis: Adnexal Neoplasm Arising in a Nevus Sebaceus
Biopsy of the lesion showed a proliferation of basaloid-appearing cells with focal ductal differentiation and ulceration consistent with poroma (Figure 1). Due to the superficial nature of the biopsy, the pathologist recommended excision to ensure complete removal and to rule out a well-differentiated porocarcinoma. Excision of the lesion showed large basaloid aggregates with a hypercellular stroma and a surrounding papillomatous epidermis with well-developed sebaceous lobules consistent with a trichoblastoma and a nevus sebaceus, respectively (Figure 2). There also was evidence of poroma; however, there were no findings concerning for porocarcinoma, which could lead to metastasis (Figure 3).
Nevus sebaceus is a benign, hamartomatous, congenital growth that occurs in approximately 1% of patients presenting to dermatology offices. It usually presents as a single asymptomatic plaque on the scalp (62.5%) or face (24.5%) that changes in morphology over its lifetime.1,2 In children, a nevus manifests as a yellowish, smooth, waxy skin lesion. As the sebaceous glands become more developed during adolescence, the lesion takes on more of a verrucous appearance and also can darken.
Although nevus sebaceus is benign, it may give rise to both benign and malignant neoplasms. In a 2014 study of 707 cases of nevus sebaceus, 21.4% developed secondary neoplasms, 88% of which were benign.2 The origins of these neoplasms can be epithelial, sebaceous, apocrine, and/or follicular. The 3 most common secondary neoplasms found in nevus sebaceus are trichoblastoma (34.7%), syringocystadenoma papilliferum (24.7%), and apocrine/eccrine adenoma (10%), all of which are benign.2 Trichoblastomas represent a type of hair follicle tumor. Malignant lesions manifest in approximately 2.5% of cases, with basal cell carcinoma (BCC) being the most common (5.3% of all neoplasms), followed by squamous cell carcinoma (2.7% of all neoplasms).2 Differentiating BCC from trichoblastoma can be difficult, but histologically BCCs usually have tumor stromal clefting while trichoblastomas do not.3 The incidence of secondary tumors in nevus sebaceus displays a strong correlation with age; thus, the highest proportion of neoplasms occur in adults.
Treatment of nevus sebaceus depends on the patient's age. In children, because of the low probability of secondary neoplasms, observation in lieu of surgical excision is a common approach. In adults, the approach typically is surgical excision or close follow-up, as there is a concern for secondary neoplasm and the potential for malignant degeneration.
A nevus sebaceus leading to 2 or more tumors within the same lesion is rare (seen in only 4.2% of lesions). The most common combination is trichoblastoma with syringocystadenoma papilliferum (0.6% of all cases).2 Poromas represent sweat gland tumors that usually appear on the soles (65%) or palms (10%).4 It is uncommon for these neoplasms to manifest on the scalp or within a nevus sebaceus. Three independent studies (N=596; N=707; N=450) did not report any occurrences of eccrine poroma.1,2,5 Eccrine poroma in conjunction with nodular trichoblastoma arising in a nevus sebaceus is unusual, and definitive excision should be strongly considered because of the possibility to develop a porocarcinoma.6
Atypical fibroxanthoma presents on sun-exposed areas as an exophytic nodule or plaque that frequently ulcerates. Pathology of this tumor shows a spindled cell proliferation that can stain positively for CD10 and procollagen 1. Basal cell carcinoma presents as a pearly papule or nodule displaying basaloid-appearing aggregates with tumor stromal clefting and can stain with Ber-EP4. Cylindromas typically present on the scalp as large rubbery-appearing plaques and nodules. Cylindromas usually present as a solitary tumor, but in the familial form there can be clusters of multiple nodules. Metastatic renal cell carcinoma frequently appears as a bleeding nodule on the scalp in patients with known renal cell cancer or as the initial presentation.
- Cribier B, Scrivener Y, Grosshans E. Tumors arising in nevus sebaceus: a study of 596 cases. J Am Acad Dermatol. 2000;42(pt 1):263-268.
- Idriss MH, Elston DM. Secondary neoplasms associated with nevus sebaceus of Jadassohn: a study of 707 cases. J Am Acad Dermatol. 2014;70:332-337.
- Wang E, Lee JS, Kazakov DV. A rare combination of sebaceoma with carcinomatous change (sebaceous carcinoma), trichoblastoma, and poroma arising from a nevus sebaceus. J Cutan Pathol. 2013;40:676-682.
- Bae MI, Cho TH, Shin MK, et al. An unusual clinical presentation of eccrine poroma occurring on the auricle. Indian J Dermatol. 2015;60:523.
- Hsu MC, Liau JY, Hong JL, et al. Secondary neoplasms arising from nevus sebaceus: a retrospective study of 450 cases in Taiwan. J Dermatol. 2016;43:175-180.
- Takhan II, Domingo J. Metastasizing eccrine porocarcinoma developing in a sebaceous nevus of Jadassohn. report of a case. Arch Dermatol. 1985;121:413-415.
- Cribier B, Scrivener Y, Grosshans E. Tumors arising in nevus sebaceus: a study of 596 cases. J Am Acad Dermatol. 2000;42(pt 1):263-268.
- Idriss MH, Elston DM. Secondary neoplasms associated with nevus sebaceus of Jadassohn: a study of 707 cases. J Am Acad Dermatol. 2014;70:332-337.
- Wang E, Lee JS, Kazakov DV. A rare combination of sebaceoma with carcinomatous change (sebaceous carcinoma), trichoblastoma, and poroma arising from a nevus sebaceus. J Cutan Pathol. 2013;40:676-682.
- Bae MI, Cho TH, Shin MK, et al. An unusual clinical presentation of eccrine poroma occurring on the auricle. Indian J Dermatol. 2015;60:523.
- Hsu MC, Liau JY, Hong JL, et al. Secondary neoplasms arising from nevus sebaceus: a retrospective study of 450 cases in Taiwan. J Dermatol. 2016;43:175-180.
- Takhan II, Domingo J. Metastasizing eccrine porocarcinoma developing in a sebaceous nevus of Jadassohn. report of a case. Arch Dermatol. 1985;121:413-415.
A 75-year-old woman presented with an enlarging plaque on the scalp of 5 years' duration. Physical examination revealed a 5.6.2 ×2.9-cm, tan-colored, verrucous plaque with an overlying pink friable nodule on the left occipital scalp. The lesion was not painful or pruritic, and the patient did not have any constitutional symptoms such as fever, night sweats, or weight loss. The patient denied prior tanning bed use and reported intermittent sun exposure over her lifetime. She denied any prior surgical intervention. There was no family history of similar lesions.
Highlights from AGA’s FDA engagement
AGA members and staff worked closely with representatives across the FDA on a number of key issues impacting gastroenterologists including duodenoscope reprocessing, fecal microbiota transplantation and new drug approvals for GI indications.
Center for Devices and Radiological Health (CDRH). The issue of duodenoscope reprocessing regained national attention when a safety communication issued by CDRH was covered by the New York Times.
The safety communication had noted that about one in 20 samples collected from reprocessed duodenoscopes tested positive for high-concern organisms such as E. coli and Pseudomonas aeruginosa.
AGA partnered with ACG, ASGE and SGNA to develop a letter to the editor and provided insights to AGA members in subsequent communications. CDRH issued another safety communication in August recommending a transition to disposable-component duodenoscopes and convened a public advisory committee meeting in November where AGA gave public testimony including several overarching principles for the evolution of clinical practice focusing on patient safety and outcomes. AGA has been at the forefront of this issue since risk of infection transmission during ERCP first came to light in 2015, and we will continue to work closely with FDA and industry to ensure solutions, like the recently approved disposable scopes and parts, meet the needs of our members.
Center for Biologics Evaluation and Research (CBER). Though it is not an approved therapy for Clostridioides difficile infection (CDI), FDA permits the use of fecal microbiota transplantation (FMT) for CDI unresponsive to standard antibiotic therapies under a temporary “enforcement policy” that has been in place since 2013. In response to concerns from the physician community that patient access to FMT may be discontinued once manufactured microbiota-based products come to market, AGA reengaged CBER in dialogue about the future of FMT through a meeting with CBER Director Peter Marks and eight senior CBER officials. In response to a June safety alert reporting a patient death from FMT using donor stool that was not screened for extended-spectrum beta-lactamase (ESBL)-producing E. coli, AGA requested clarification from CBER on new donor screening requirements announced for those who hold investigational new drug permits for FMT. Most recently, AGA was the only professional society to give public testimony at a November public hearing on the use of FMT to treat CDI. AGA will continue to engage CBER as the agency works to finalize its policy on FMT.
Center for Drug Evaluation and Research (CDER). AGA organized two joint scientific sessions at Digestive Disease Week® 2019 with representatives from CDER’s Division of Gastrointestinal and Inborn Errors Products: the inaugural FDA Town Hall and a session on controversies around measuring drug toxicity. The FDA Town Hall, which will continue at DDW 2020, featured four FDA speakers providing the data and rationale behind recent GI drug approvals. The session titled, “Controversies Around Measuring Drug Toxicity” gave FDA and gastroenterologists’ perspectives on 5-HT3 antagonists (e.g., alosetron) and 5-HT4 agonists (e.g., prucalopride), as well as proton pump inhibitors. These sessions aimed to promote an interchange of ideas among regulators, clinicians and pharmaceutical manufacturers to advance the development and use of new therapies for GI disorders.
AGA members and staff worked closely with representatives across the FDA on a number of key issues impacting gastroenterologists including duodenoscope reprocessing, fecal microbiota transplantation and new drug approvals for GI indications.
Center for Devices and Radiological Health (CDRH). The issue of duodenoscope reprocessing regained national attention when a safety communication issued by CDRH was covered by the New York Times.
The safety communication had noted that about one in 20 samples collected from reprocessed duodenoscopes tested positive for high-concern organisms such as E. coli and Pseudomonas aeruginosa.
AGA partnered with ACG, ASGE and SGNA to develop a letter to the editor and provided insights to AGA members in subsequent communications. CDRH issued another safety communication in August recommending a transition to disposable-component duodenoscopes and convened a public advisory committee meeting in November where AGA gave public testimony including several overarching principles for the evolution of clinical practice focusing on patient safety and outcomes. AGA has been at the forefront of this issue since risk of infection transmission during ERCP first came to light in 2015, and we will continue to work closely with FDA and industry to ensure solutions, like the recently approved disposable scopes and parts, meet the needs of our members.
Center for Biologics Evaluation and Research (CBER). Though it is not an approved therapy for Clostridioides difficile infection (CDI), FDA permits the use of fecal microbiota transplantation (FMT) for CDI unresponsive to standard antibiotic therapies under a temporary “enforcement policy” that has been in place since 2013. In response to concerns from the physician community that patient access to FMT may be discontinued once manufactured microbiota-based products come to market, AGA reengaged CBER in dialogue about the future of FMT through a meeting with CBER Director Peter Marks and eight senior CBER officials. In response to a June safety alert reporting a patient death from FMT using donor stool that was not screened for extended-spectrum beta-lactamase (ESBL)-producing E. coli, AGA requested clarification from CBER on new donor screening requirements announced for those who hold investigational new drug permits for FMT. Most recently, AGA was the only professional society to give public testimony at a November public hearing on the use of FMT to treat CDI. AGA will continue to engage CBER as the agency works to finalize its policy on FMT.
Center for Drug Evaluation and Research (CDER). AGA organized two joint scientific sessions at Digestive Disease Week® 2019 with representatives from CDER’s Division of Gastrointestinal and Inborn Errors Products: the inaugural FDA Town Hall and a session on controversies around measuring drug toxicity. The FDA Town Hall, which will continue at DDW 2020, featured four FDA speakers providing the data and rationale behind recent GI drug approvals. The session titled, “Controversies Around Measuring Drug Toxicity” gave FDA and gastroenterologists’ perspectives on 5-HT3 antagonists (e.g., alosetron) and 5-HT4 agonists (e.g., prucalopride), as well as proton pump inhibitors. These sessions aimed to promote an interchange of ideas among regulators, clinicians and pharmaceutical manufacturers to advance the development and use of new therapies for GI disorders.
AGA members and staff worked closely with representatives across the FDA on a number of key issues impacting gastroenterologists including duodenoscope reprocessing, fecal microbiota transplantation and new drug approvals for GI indications.
Center for Devices and Radiological Health (CDRH). The issue of duodenoscope reprocessing regained national attention when a safety communication issued by CDRH was covered by the New York Times.
The safety communication had noted that about one in 20 samples collected from reprocessed duodenoscopes tested positive for high-concern organisms such as E. coli and Pseudomonas aeruginosa.
AGA partnered with ACG, ASGE and SGNA to develop a letter to the editor and provided insights to AGA members in subsequent communications. CDRH issued another safety communication in August recommending a transition to disposable-component duodenoscopes and convened a public advisory committee meeting in November where AGA gave public testimony including several overarching principles for the evolution of clinical practice focusing on patient safety and outcomes. AGA has been at the forefront of this issue since risk of infection transmission during ERCP first came to light in 2015, and we will continue to work closely with FDA and industry to ensure solutions, like the recently approved disposable scopes and parts, meet the needs of our members.
Center for Biologics Evaluation and Research (CBER). Though it is not an approved therapy for Clostridioides difficile infection (CDI), FDA permits the use of fecal microbiota transplantation (FMT) for CDI unresponsive to standard antibiotic therapies under a temporary “enforcement policy” that has been in place since 2013. In response to concerns from the physician community that patient access to FMT may be discontinued once manufactured microbiota-based products come to market, AGA reengaged CBER in dialogue about the future of FMT through a meeting with CBER Director Peter Marks and eight senior CBER officials. In response to a June safety alert reporting a patient death from FMT using donor stool that was not screened for extended-spectrum beta-lactamase (ESBL)-producing E. coli, AGA requested clarification from CBER on new donor screening requirements announced for those who hold investigational new drug permits for FMT. Most recently, AGA was the only professional society to give public testimony at a November public hearing on the use of FMT to treat CDI. AGA will continue to engage CBER as the agency works to finalize its policy on FMT.
Center for Drug Evaluation and Research (CDER). AGA organized two joint scientific sessions at Digestive Disease Week® 2019 with representatives from CDER’s Division of Gastrointestinal and Inborn Errors Products: the inaugural FDA Town Hall and a session on controversies around measuring drug toxicity. The FDA Town Hall, which will continue at DDW 2020, featured four FDA speakers providing the data and rationale behind recent GI drug approvals. The session titled, “Controversies Around Measuring Drug Toxicity” gave FDA and gastroenterologists’ perspectives on 5-HT3 antagonists (e.g., alosetron) and 5-HT4 agonists (e.g., prucalopride), as well as proton pump inhibitors. These sessions aimed to promote an interchange of ideas among regulators, clinicians and pharmaceutical manufacturers to advance the development and use of new therapies for GI disorders.
Many children who present to headache clinics have joint hypermobility
Key clinical point: About one-quarter of pediatric patients with headache have joint hypermobility.
Major finding: Among children with headache and joint hypermobility, 80% had severe headache disability.
Study details: A prospective, single-center study of 76 children with headache.
Disclosures: The study was not supported by funding, and the investigators had no disclosures.
Citation: Sahjwani D et al. CNS 2019, Abstract 101.
Key clinical point: About one-quarter of pediatric patients with headache have joint hypermobility.
Major finding: Among children with headache and joint hypermobility, 80% had severe headache disability.
Study details: A prospective, single-center study of 76 children with headache.
Disclosures: The study was not supported by funding, and the investigators had no disclosures.
Citation: Sahjwani D et al. CNS 2019, Abstract 101.
Key clinical point: About one-quarter of pediatric patients with headache have joint hypermobility.
Major finding: Among children with headache and joint hypermobility, 80% had severe headache disability.
Study details: A prospective, single-center study of 76 children with headache.
Disclosures: The study was not supported by funding, and the investigators had no disclosures.
Citation: Sahjwani D et al. CNS 2019, Abstract 101.