User login
Adding lymphopenia component ‘improves’ FLIPI
Incorporating lymphopenia into the Follicular Lymphoma International Prognostic Index (FLIPI) can improve prognostication, according to researchers.
The team added lymphopenia as a point in a revised FLIPI scoring system, called FLIPI-L, and found the new system could better predict overall survival (OS), progression-free survival, and histologic transformation in patients with follicular lymphoma.
George Yang, MD, of Moffitt Cancer Center in Tampa, Fla., and his colleagues described results with the FLIPI-L in a letter published in Blood Cancer Journal.
“Prior studies have demonstrated that lymphopenia was associated with worsened OS in [follicular lymphoma],” Dr. Yang and his colleagues wrote. “Therefore, we hypothesized that lymphopenia may be integrated with existing FLIPI to better stratify long-term survival outcomes and predict for transformation.”
The researchers tested this theory in 736 follicular lymphoma patients who were followed for a median of 72 months (range, 2-211 months). The 5-year OS in this cohort was 81.3%, the 10-year OS was 67.3%, and 18% of patients experienced transformation to high-grade lymphoma.
The researchers defined absolute lymphopenia as less than 1.0 × 109 lymphocytes per liter. In multivariate analyses, lymphopenia was an independent predictor of OS (hazard ratio, 1.74; P less than .01) and transformation (odds ratio, 2.1; P less than .01).
To incorporate lymphopenia into the FLIPI, the researchers created a model in which 1 point was given for each of the standard FLIPI components (age, Ann Arbor stage, number of nodal areas, lactate dehydrogenase, and hemoglobin level), and one point was given for the presence of lymphopenia. Patients in the low-risk FLIPI-L category had 0-1 points, those in the intermediate-risk category had 2-3 points, and patients in the high-risk FLIPI-L category had 4-6 points.
Using the original FLIPI, the 5-year OS was 91% in the low-risk group (0-1), 82.7% in the intermediate-risk group (2), and 66% in the high-risk group (3-5). The 10-year OS was 80.4%, 66%, and 45.8%, respectively.
Using the FLIPI-L, the 5-year OS was 94.5% in the low-risk group (0-1), 89% in the intermediate-risk group (2-3), and 61% in the high-risk group (4-6). The 10-year OS was 83.9%, 68.5%, and 34.5%, respectively.
In a univariate Cox regression analysis of OS, each point increase in FLIPI-L score was associated with a significant increase in hazard ratio. For example, the hazard ratio was 3.4 for patients with a FLIPI-L score of 1 and 30.9 for those with a FLIPI-L score of 6 (P less than .02 for all FLIPI-L scores). Conversely, increases in hazard ratio were not significant with the original FLIPI (P greater than .05 for all FLIPI scores).
The FLIPI-L was prognostic for OS in different treatment groups. In patients who received rituximab alone, radiation alone, or rituximab plus chemotherapy, the scoring system differentiated low-, intermediate-, and high-risk groups (P less than .04). In patients under observation, the FLIPI-L distinguished low/intermediate-risk and high-risk groups (P less than .01).
For patients who progressed within 24 months, the FLIPI-L was more predictive of progression-free survival (P = .05) than was the original FLIPI (P = .11).
Increasing FLIPI-L was an independent predictor of transformation, both when assessed as a continuous variable (P less than .01) and stepwise for FLIPI-L 3-5 (P = .004-.01). The original FLIPI, on the other hand, was not an independent predictor of transformation.
“Our analysis of a lymphopenia cutoff as an addition to the original FLIPI is simple yet improves risk stratification to differentiate between prognostic groups and, importantly, to predict transformation,” Dr. Yang and his colleagues wrote.
The authors reported having no conflicts of interest.
SOURCE: Yang G et al. Blood Cancer J. 2020 Jan 2;9(12):104. doi: 10.1038/s41408-019-0269-6.
Incorporating lymphopenia into the Follicular Lymphoma International Prognostic Index (FLIPI) can improve prognostication, according to researchers.
The team added lymphopenia as a point in a revised FLIPI scoring system, called FLIPI-L, and found the new system could better predict overall survival (OS), progression-free survival, and histologic transformation in patients with follicular lymphoma.
George Yang, MD, of Moffitt Cancer Center in Tampa, Fla., and his colleagues described results with the FLIPI-L in a letter published in Blood Cancer Journal.
“Prior studies have demonstrated that lymphopenia was associated with worsened OS in [follicular lymphoma],” Dr. Yang and his colleagues wrote. “Therefore, we hypothesized that lymphopenia may be integrated with existing FLIPI to better stratify long-term survival outcomes and predict for transformation.”
The researchers tested this theory in 736 follicular lymphoma patients who were followed for a median of 72 months (range, 2-211 months). The 5-year OS in this cohort was 81.3%, the 10-year OS was 67.3%, and 18% of patients experienced transformation to high-grade lymphoma.
The researchers defined absolute lymphopenia as less than 1.0 × 109 lymphocytes per liter. In multivariate analyses, lymphopenia was an independent predictor of OS (hazard ratio, 1.74; P less than .01) and transformation (odds ratio, 2.1; P less than .01).
To incorporate lymphopenia into the FLIPI, the researchers created a model in which 1 point was given for each of the standard FLIPI components (age, Ann Arbor stage, number of nodal areas, lactate dehydrogenase, and hemoglobin level), and one point was given for the presence of lymphopenia. Patients in the low-risk FLIPI-L category had 0-1 points, those in the intermediate-risk category had 2-3 points, and patients in the high-risk FLIPI-L category had 4-6 points.
Using the original FLIPI, the 5-year OS was 91% in the low-risk group (0-1), 82.7% in the intermediate-risk group (2), and 66% in the high-risk group (3-5). The 10-year OS was 80.4%, 66%, and 45.8%, respectively.
Using the FLIPI-L, the 5-year OS was 94.5% in the low-risk group (0-1), 89% in the intermediate-risk group (2-3), and 61% in the high-risk group (4-6). The 10-year OS was 83.9%, 68.5%, and 34.5%, respectively.
In a univariate Cox regression analysis of OS, each point increase in FLIPI-L score was associated with a significant increase in hazard ratio. For example, the hazard ratio was 3.4 for patients with a FLIPI-L score of 1 and 30.9 for those with a FLIPI-L score of 6 (P less than .02 for all FLIPI-L scores). Conversely, increases in hazard ratio were not significant with the original FLIPI (P greater than .05 for all FLIPI scores).
The FLIPI-L was prognostic for OS in different treatment groups. In patients who received rituximab alone, radiation alone, or rituximab plus chemotherapy, the scoring system differentiated low-, intermediate-, and high-risk groups (P less than .04). In patients under observation, the FLIPI-L distinguished low/intermediate-risk and high-risk groups (P less than .01).
For patients who progressed within 24 months, the FLIPI-L was more predictive of progression-free survival (P = .05) than was the original FLIPI (P = .11).
Increasing FLIPI-L was an independent predictor of transformation, both when assessed as a continuous variable (P less than .01) and stepwise for FLIPI-L 3-5 (P = .004-.01). The original FLIPI, on the other hand, was not an independent predictor of transformation.
“Our analysis of a lymphopenia cutoff as an addition to the original FLIPI is simple yet improves risk stratification to differentiate between prognostic groups and, importantly, to predict transformation,” Dr. Yang and his colleagues wrote.
The authors reported having no conflicts of interest.
SOURCE: Yang G et al. Blood Cancer J. 2020 Jan 2;9(12):104. doi: 10.1038/s41408-019-0269-6.
Incorporating lymphopenia into the Follicular Lymphoma International Prognostic Index (FLIPI) can improve prognostication, according to researchers.
The team added lymphopenia as a point in a revised FLIPI scoring system, called FLIPI-L, and found the new system could better predict overall survival (OS), progression-free survival, and histologic transformation in patients with follicular lymphoma.
George Yang, MD, of Moffitt Cancer Center in Tampa, Fla., and his colleagues described results with the FLIPI-L in a letter published in Blood Cancer Journal.
“Prior studies have demonstrated that lymphopenia was associated with worsened OS in [follicular lymphoma],” Dr. Yang and his colleagues wrote. “Therefore, we hypothesized that lymphopenia may be integrated with existing FLIPI to better stratify long-term survival outcomes and predict for transformation.”
The researchers tested this theory in 736 follicular lymphoma patients who were followed for a median of 72 months (range, 2-211 months). The 5-year OS in this cohort was 81.3%, the 10-year OS was 67.3%, and 18% of patients experienced transformation to high-grade lymphoma.
The researchers defined absolute lymphopenia as less than 1.0 × 109 lymphocytes per liter. In multivariate analyses, lymphopenia was an independent predictor of OS (hazard ratio, 1.74; P less than .01) and transformation (odds ratio, 2.1; P less than .01).
To incorporate lymphopenia into the FLIPI, the researchers created a model in which 1 point was given for each of the standard FLIPI components (age, Ann Arbor stage, number of nodal areas, lactate dehydrogenase, and hemoglobin level), and one point was given for the presence of lymphopenia. Patients in the low-risk FLIPI-L category had 0-1 points, those in the intermediate-risk category had 2-3 points, and patients in the high-risk FLIPI-L category had 4-6 points.
Using the original FLIPI, the 5-year OS was 91% in the low-risk group (0-1), 82.7% in the intermediate-risk group (2), and 66% in the high-risk group (3-5). The 10-year OS was 80.4%, 66%, and 45.8%, respectively.
Using the FLIPI-L, the 5-year OS was 94.5% in the low-risk group (0-1), 89% in the intermediate-risk group (2-3), and 61% in the high-risk group (4-6). The 10-year OS was 83.9%, 68.5%, and 34.5%, respectively.
In a univariate Cox regression analysis of OS, each point increase in FLIPI-L score was associated with a significant increase in hazard ratio. For example, the hazard ratio was 3.4 for patients with a FLIPI-L score of 1 and 30.9 for those with a FLIPI-L score of 6 (P less than .02 for all FLIPI-L scores). Conversely, increases in hazard ratio were not significant with the original FLIPI (P greater than .05 for all FLIPI scores).
The FLIPI-L was prognostic for OS in different treatment groups. In patients who received rituximab alone, radiation alone, or rituximab plus chemotherapy, the scoring system differentiated low-, intermediate-, and high-risk groups (P less than .04). In patients under observation, the FLIPI-L distinguished low/intermediate-risk and high-risk groups (P less than .01).
For patients who progressed within 24 months, the FLIPI-L was more predictive of progression-free survival (P = .05) than was the original FLIPI (P = .11).
Increasing FLIPI-L was an independent predictor of transformation, both when assessed as a continuous variable (P less than .01) and stepwise for FLIPI-L 3-5 (P = .004-.01). The original FLIPI, on the other hand, was not an independent predictor of transformation.
“Our analysis of a lymphopenia cutoff as an addition to the original FLIPI is simple yet improves risk stratification to differentiate between prognostic groups and, importantly, to predict transformation,” Dr. Yang and his colleagues wrote.
The authors reported having no conflicts of interest.
SOURCE: Yang G et al. Blood Cancer J. 2020 Jan 2;9(12):104. doi: 10.1038/s41408-019-0269-6.
FROM BLOOD CANCER JOURNAL
Infant deaths from birth defects decline, but some disparities widen
according to the Centers for Disease Control and Prevention.
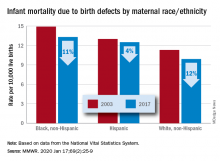
The total rate of IMBD dropped from 12.2 cases per 10,000 live births in 2003 to 11 cases per 10,000 in 2017, with decreases occurring “across the categories of maternal race/ethnicity, infant sex, and infant age at death,” Lynn M. Almli, PhD, of the CDC’s National Center on Birth Defects and Developmental Disabilities and associates wrote in the Morbidity and Mortality Weekly Report.
Rates were down for infants of white non-Hispanic, black non-Hispanic, and Hispanic mothers, but disparities among races/ethnicities persisted or even increased. The IMBD rate for infants born to Hispanic mothers, which was 15% higher than that of infants born to white mothers in 2003, was 26% higher by 2017. The difference between infants born to black mothers and those born to whites rose from 32% in 2003 to 34% in 2017, the investigators reported.
The disparities were even greater among subgroups of infants categorized by gestational age. From 2003 to 2017, IMBD rates dropped by 20% for infants in the youngest group (20-27 weeks), 25% for infants in the oldest group (41-44 weeks), and 29% among those born at 39-40 weeks, they said.
For moderate- and late-preterm infants, however, IMBD rates went up: Infants born at 32-33 weeks and 34-36 weeks each had an increase of 17% over the study period, Dr. Almli and associates noted, based on data from the National Vital Statistics System.
“The observed differences in IMBD rates by race/ethnicity might be influenced by access to and utilization of health care before and during pregnancy, prenatal screening, losses of pregnancies with fetal anomalies, and insurance type,” they wrote, and trends by gestational age “could be influenced by the quantity and quality of care for infants born before 30 weeks’ gestation, compared with that of those born closer to term.”
Birth defects occur in approximately 3% of all births in the United States but accounted for 20% of infant deaths during 2003-2017, the investigators wrote, suggesting that “the results from this analysis can inform future research into areas where efforts to reduce IMBD rates are needed.”
SOURCE: Almli LM et al. MMWR. 2020 Jan 17;69(2):25-9.
according to the Centers for Disease Control and Prevention.
The total rate of IMBD dropped from 12.2 cases per 10,000 live births in 2003 to 11 cases per 10,000 in 2017, with decreases occurring “across the categories of maternal race/ethnicity, infant sex, and infant age at death,” Lynn M. Almli, PhD, of the CDC’s National Center on Birth Defects and Developmental Disabilities and associates wrote in the Morbidity and Mortality Weekly Report.
Rates were down for infants of white non-Hispanic, black non-Hispanic, and Hispanic mothers, but disparities among races/ethnicities persisted or even increased. The IMBD rate for infants born to Hispanic mothers, which was 15% higher than that of infants born to white mothers in 2003, was 26% higher by 2017. The difference between infants born to black mothers and those born to whites rose from 32% in 2003 to 34% in 2017, the investigators reported.
The disparities were even greater among subgroups of infants categorized by gestational age. From 2003 to 2017, IMBD rates dropped by 20% for infants in the youngest group (20-27 weeks), 25% for infants in the oldest group (41-44 weeks), and 29% among those born at 39-40 weeks, they said.
For moderate- and late-preterm infants, however, IMBD rates went up: Infants born at 32-33 weeks and 34-36 weeks each had an increase of 17% over the study period, Dr. Almli and associates noted, based on data from the National Vital Statistics System.
“The observed differences in IMBD rates by race/ethnicity might be influenced by access to and utilization of health care before and during pregnancy, prenatal screening, losses of pregnancies with fetal anomalies, and insurance type,” they wrote, and trends by gestational age “could be influenced by the quantity and quality of care for infants born before 30 weeks’ gestation, compared with that of those born closer to term.”
Birth defects occur in approximately 3% of all births in the United States but accounted for 20% of infant deaths during 2003-2017, the investigators wrote, suggesting that “the results from this analysis can inform future research into areas where efforts to reduce IMBD rates are needed.”
SOURCE: Almli LM et al. MMWR. 2020 Jan 17;69(2):25-9.
according to the Centers for Disease Control and Prevention.
The total rate of IMBD dropped from 12.2 cases per 10,000 live births in 2003 to 11 cases per 10,000 in 2017, with decreases occurring “across the categories of maternal race/ethnicity, infant sex, and infant age at death,” Lynn M. Almli, PhD, of the CDC’s National Center on Birth Defects and Developmental Disabilities and associates wrote in the Morbidity and Mortality Weekly Report.
Rates were down for infants of white non-Hispanic, black non-Hispanic, and Hispanic mothers, but disparities among races/ethnicities persisted or even increased. The IMBD rate for infants born to Hispanic mothers, which was 15% higher than that of infants born to white mothers in 2003, was 26% higher by 2017. The difference between infants born to black mothers and those born to whites rose from 32% in 2003 to 34% in 2017, the investigators reported.
The disparities were even greater among subgroups of infants categorized by gestational age. From 2003 to 2017, IMBD rates dropped by 20% for infants in the youngest group (20-27 weeks), 25% for infants in the oldest group (41-44 weeks), and 29% among those born at 39-40 weeks, they said.
For moderate- and late-preterm infants, however, IMBD rates went up: Infants born at 32-33 weeks and 34-36 weeks each had an increase of 17% over the study period, Dr. Almli and associates noted, based on data from the National Vital Statistics System.
“The observed differences in IMBD rates by race/ethnicity might be influenced by access to and utilization of health care before and during pregnancy, prenatal screening, losses of pregnancies with fetal anomalies, and insurance type,” they wrote, and trends by gestational age “could be influenced by the quantity and quality of care for infants born before 30 weeks’ gestation, compared with that of those born closer to term.”
Birth defects occur in approximately 3% of all births in the United States but accounted for 20% of infant deaths during 2003-2017, the investigators wrote, suggesting that “the results from this analysis can inform future research into areas where efforts to reduce IMBD rates are needed.”
SOURCE: Almli LM et al. MMWR. 2020 Jan 17;69(2):25-9.
FROM MMWR
AFib link with titin mutations warrants selected genetic testing
NATIONAL HARBOR, MD. – Testing to identify mutations in the gene that codes for the muscle protein titin is now a reasonable step in routine clinical practice for selected people with either early-onset atrial fibrillation (AFib) or a family history of atrial fibrillation, or other cardiac disorders that have been strongly linked with titin-gene mutations, Patrick T. Ellinor, MD, said at the annual International AF Symposium.
About one out of every 250 people carries a loss of function (LOF) mutation in one of their TTN genes that codes for the titin protein, making these mutations about as common as mutations for familial hypercholesterolemia, noted Dr. Ellinor, professor of medicine at Harvard Medical School in Boston and director of the Cardiovascular Disease Initiative at the Broad Institute in Cambridge, Mass. TTN LOF mutations are “bad and very frequent,” he said in an interview. “This is evolving quickly as we start to appreciate how frequent these mutations are.”
Several commercial genetic testing companies now offer testing of blood specimens for TTN LOF mutations, often as part of an “arrhythmia test” panel, with a turnaround time of about 4 weeks at a cost to the patient of about $100, noted Dr. Ellinor, who said that he has begun to discuss such testing with a small number of patients in his practice. “It’s reasonable for selected people; the jury is still out on which ones,” a subject that guideline writers will soon need to address, he said.
Patients already diagnosed with early-onset atrial fibrillation (AFib) could benefit from knowing if they had a TTN LOF mutation because that diagnosis would warrant a magnetic resonance scan to look for “subtle myopathies” not detectable with echocardiography, Dr. Ellinor explained. Identification of a TTN LOF would also be a reason to then test the patient’s children. “Perhaps we should offer testing to everyone 40 years old or younger with AFib,” Dr. Ellinor suggested. Many of these patients are now getting genetic testing for TTN on their own “whether or not their physician wants it done,” he noted.
The most recent, and perhaps most persuasive evidence for the link between TTN LOF mutations and AFib came from a recent report from Dr. Ellinor and associates that examined genome-wide associations in 1,546 people with AFib and 41,593 controls using information contained in the UK Biobank, which holds complete gene sequencing data for about half a million U.K. residents (Circ Res. 2020 Jan 17;126[2]: 200-9). The results showed that just under 0.5% of the entire population carried a TTN LOF mutation, and among patients with AFib the prevalence of a TTN LOF mutation was about 2%, but among people who carry this type of mutation 14% were diagnosed with AFib. This penetrance of 14% for AFib among people with a TTN LOF mutation makes AFib the most frequent clinical consequence identified so far for people with this type of mutation. Other cardiac disorders linked with TTN LOF mutations include heart failure and nonischemic cardiomyopathy. The Biobank study findings showed a penetrance for heart failure of about 7% among those with a TTN LOF mutation, and a penetrance of these mutations for nonischemic cardiomyopathy of about 3%.
Dr. Ellinor cited three other recently published studies with consistent results documenting a strong link between TTN LOF mutations and AFib: a study he worked on with lead author Seung H. Choi, Ph.D., and associates that ran an analysis on 2,781 AFib patients and 4,959 controls in a U.S. database of people who underwent whole-genome sequencing (JAMA. 2018 Dec 11; 320[22]:2354-64); a study of 24 Danish families with clusters of three or more affected members with AFib as well as 399 Danish residents with lone, early-onset AFib (Nat Commun. 2018 Oct 17;9[1]:4316); and a study of 25 patients with “very early onset” (less than 45 years old) AFib, which identified four of the 25 patients with a TTN LOF mutation (Circ Genom Precis Med. 2019 Nov 12[11]; 526-8).
Titin is the largest protein in humans and is critical for normal myocardial function. Titin acts as a molecular scaffold for sarcomere assembly and signaling, providing passive stiffness to the sarcomere. Mutations in TTN have been associated with tibial muscular dystrophy, hypertrophic cardiomyopathy, and dilated cardiomyopathy. The relationship now established between TTN mutations and AFib, cardiomyopathy, and heart failure may in the future help explain the tight clinical association of AFib and heart failure, Dr. Ellinor noted. The TTN gene is also notable as the largest gene in the human genome.
Dr. Ellinor has received research funding from Bayer, and he has served as an adviser or consultant to Bayer, Quest Diagnostics, and Novartis.
SOURCE: Choi SH et al. Circ Res. 2020 Jan 17;126[2]: 200-9.
NATIONAL HARBOR, MD. – Testing to identify mutations in the gene that codes for the muscle protein titin is now a reasonable step in routine clinical practice for selected people with either early-onset atrial fibrillation (AFib) or a family history of atrial fibrillation, or other cardiac disorders that have been strongly linked with titin-gene mutations, Patrick T. Ellinor, MD, said at the annual International AF Symposium.
About one out of every 250 people carries a loss of function (LOF) mutation in one of their TTN genes that codes for the titin protein, making these mutations about as common as mutations for familial hypercholesterolemia, noted Dr. Ellinor, professor of medicine at Harvard Medical School in Boston and director of the Cardiovascular Disease Initiative at the Broad Institute in Cambridge, Mass. TTN LOF mutations are “bad and very frequent,” he said in an interview. “This is evolving quickly as we start to appreciate how frequent these mutations are.”
Several commercial genetic testing companies now offer testing of blood specimens for TTN LOF mutations, often as part of an “arrhythmia test” panel, with a turnaround time of about 4 weeks at a cost to the patient of about $100, noted Dr. Ellinor, who said that he has begun to discuss such testing with a small number of patients in his practice. “It’s reasonable for selected people; the jury is still out on which ones,” a subject that guideline writers will soon need to address, he said.
Patients already diagnosed with early-onset atrial fibrillation (AFib) could benefit from knowing if they had a TTN LOF mutation because that diagnosis would warrant a magnetic resonance scan to look for “subtle myopathies” not detectable with echocardiography, Dr. Ellinor explained. Identification of a TTN LOF would also be a reason to then test the patient’s children. “Perhaps we should offer testing to everyone 40 years old or younger with AFib,” Dr. Ellinor suggested. Many of these patients are now getting genetic testing for TTN on their own “whether or not their physician wants it done,” he noted.
The most recent, and perhaps most persuasive evidence for the link between TTN LOF mutations and AFib came from a recent report from Dr. Ellinor and associates that examined genome-wide associations in 1,546 people with AFib and 41,593 controls using information contained in the UK Biobank, which holds complete gene sequencing data for about half a million U.K. residents (Circ Res. 2020 Jan 17;126[2]: 200-9). The results showed that just under 0.5% of the entire population carried a TTN LOF mutation, and among patients with AFib the prevalence of a TTN LOF mutation was about 2%, but among people who carry this type of mutation 14% were diagnosed with AFib. This penetrance of 14% for AFib among people with a TTN LOF mutation makes AFib the most frequent clinical consequence identified so far for people with this type of mutation. Other cardiac disorders linked with TTN LOF mutations include heart failure and nonischemic cardiomyopathy. The Biobank study findings showed a penetrance for heart failure of about 7% among those with a TTN LOF mutation, and a penetrance of these mutations for nonischemic cardiomyopathy of about 3%.
Dr. Ellinor cited three other recently published studies with consistent results documenting a strong link between TTN LOF mutations and AFib: a study he worked on with lead author Seung H. Choi, Ph.D., and associates that ran an analysis on 2,781 AFib patients and 4,959 controls in a U.S. database of people who underwent whole-genome sequencing (JAMA. 2018 Dec 11; 320[22]:2354-64); a study of 24 Danish families with clusters of three or more affected members with AFib as well as 399 Danish residents with lone, early-onset AFib (Nat Commun. 2018 Oct 17;9[1]:4316); and a study of 25 patients with “very early onset” (less than 45 years old) AFib, which identified four of the 25 patients with a TTN LOF mutation (Circ Genom Precis Med. 2019 Nov 12[11]; 526-8).
Titin is the largest protein in humans and is critical for normal myocardial function. Titin acts as a molecular scaffold for sarcomere assembly and signaling, providing passive stiffness to the sarcomere. Mutations in TTN have been associated with tibial muscular dystrophy, hypertrophic cardiomyopathy, and dilated cardiomyopathy. The relationship now established between TTN mutations and AFib, cardiomyopathy, and heart failure may in the future help explain the tight clinical association of AFib and heart failure, Dr. Ellinor noted. The TTN gene is also notable as the largest gene in the human genome.
Dr. Ellinor has received research funding from Bayer, and he has served as an adviser or consultant to Bayer, Quest Diagnostics, and Novartis.
SOURCE: Choi SH et al. Circ Res. 2020 Jan 17;126[2]: 200-9.
NATIONAL HARBOR, MD. – Testing to identify mutations in the gene that codes for the muscle protein titin is now a reasonable step in routine clinical practice for selected people with either early-onset atrial fibrillation (AFib) or a family history of atrial fibrillation, or other cardiac disorders that have been strongly linked with titin-gene mutations, Patrick T. Ellinor, MD, said at the annual International AF Symposium.
About one out of every 250 people carries a loss of function (LOF) mutation in one of their TTN genes that codes for the titin protein, making these mutations about as common as mutations for familial hypercholesterolemia, noted Dr. Ellinor, professor of medicine at Harvard Medical School in Boston and director of the Cardiovascular Disease Initiative at the Broad Institute in Cambridge, Mass. TTN LOF mutations are “bad and very frequent,” he said in an interview. “This is evolving quickly as we start to appreciate how frequent these mutations are.”
Several commercial genetic testing companies now offer testing of blood specimens for TTN LOF mutations, often as part of an “arrhythmia test” panel, with a turnaround time of about 4 weeks at a cost to the patient of about $100, noted Dr. Ellinor, who said that he has begun to discuss such testing with a small number of patients in his practice. “It’s reasonable for selected people; the jury is still out on which ones,” a subject that guideline writers will soon need to address, he said.
Patients already diagnosed with early-onset atrial fibrillation (AFib) could benefit from knowing if they had a TTN LOF mutation because that diagnosis would warrant a magnetic resonance scan to look for “subtle myopathies” not detectable with echocardiography, Dr. Ellinor explained. Identification of a TTN LOF would also be a reason to then test the patient’s children. “Perhaps we should offer testing to everyone 40 years old or younger with AFib,” Dr. Ellinor suggested. Many of these patients are now getting genetic testing for TTN on their own “whether or not their physician wants it done,” he noted.
The most recent, and perhaps most persuasive evidence for the link between TTN LOF mutations and AFib came from a recent report from Dr. Ellinor and associates that examined genome-wide associations in 1,546 people with AFib and 41,593 controls using information contained in the UK Biobank, which holds complete gene sequencing data for about half a million U.K. residents (Circ Res. 2020 Jan 17;126[2]: 200-9). The results showed that just under 0.5% of the entire population carried a TTN LOF mutation, and among patients with AFib the prevalence of a TTN LOF mutation was about 2%, but among people who carry this type of mutation 14% were diagnosed with AFib. This penetrance of 14% for AFib among people with a TTN LOF mutation makes AFib the most frequent clinical consequence identified so far for people with this type of mutation. Other cardiac disorders linked with TTN LOF mutations include heart failure and nonischemic cardiomyopathy. The Biobank study findings showed a penetrance for heart failure of about 7% among those with a TTN LOF mutation, and a penetrance of these mutations for nonischemic cardiomyopathy of about 3%.
Dr. Ellinor cited three other recently published studies with consistent results documenting a strong link between TTN LOF mutations and AFib: a study he worked on with lead author Seung H. Choi, Ph.D., and associates that ran an analysis on 2,781 AFib patients and 4,959 controls in a U.S. database of people who underwent whole-genome sequencing (JAMA. 2018 Dec 11; 320[22]:2354-64); a study of 24 Danish families with clusters of three or more affected members with AFib as well as 399 Danish residents with lone, early-onset AFib (Nat Commun. 2018 Oct 17;9[1]:4316); and a study of 25 patients with “very early onset” (less than 45 years old) AFib, which identified four of the 25 patients with a TTN LOF mutation (Circ Genom Precis Med. 2019 Nov 12[11]; 526-8).
Titin is the largest protein in humans and is critical for normal myocardial function. Titin acts as a molecular scaffold for sarcomere assembly and signaling, providing passive stiffness to the sarcomere. Mutations in TTN have been associated with tibial muscular dystrophy, hypertrophic cardiomyopathy, and dilated cardiomyopathy. The relationship now established between TTN mutations and AFib, cardiomyopathy, and heart failure may in the future help explain the tight clinical association of AFib and heart failure, Dr. Ellinor noted. The TTN gene is also notable as the largest gene in the human genome.
Dr. Ellinor has received research funding from Bayer, and he has served as an adviser or consultant to Bayer, Quest Diagnostics, and Novartis.
SOURCE: Choi SH et al. Circ Res. 2020 Jan 17;126[2]: 200-9.
REPORTING FROM THE AF SYMPOSIUM 2020
Hospitalist movers and shakers – January 2020
Hyung (Harry) Cho, MD, SFHM, and Christopher Moriates, MD, SFHM, have been honored by Modern Healthcare as two of 25 emerging young executives in health care management.
Dr. Cho is chief value officer for NYC Health and Hospitals, where his focus is on eliminating unnecessary testing and treatments within the New York City public health system, which includes 11 hospitals and five post-acute care facilities. Before landing with NYC Health and Hospitals, Dr. Cho was director of quality, safety and value at the Icahn School of Medicine at Mount Sinai, New York.
Dr. Moriates is assistant dean for health care and value at the University of Texas at Austin’s Dell Medical School, where he has created the Discovering Value-Based Health Care online learning platform. In addition, Dr. Moriates has helped design a care model to enhance the treatment of patients who suffer from opioid use disorder. Prior to arriving at Dell, he helped create curriculum to educate students about costs and value at the University of California, San Francisco.
Trina Abla, DO, was appointed chief medical officer at Mercy Catholic Medical Center in Darby, Pa. A practicing hospitalist, Dr. Abla will be in charge of the hospital budget, the recruiting and training of physicians, and maintaining safety standards and quality care at the facility.
Prior to taking the position at Mercy Catholic, Dr. Abla was chief quality officer and associate CMO at Penn State Health St. Joseph in Reading, Pa.
Ghania El Akiki, MD, has been named to the board of advisors at Beth Israel Deaconess Hospital in Needham, Mass. Dr. Akiki is chief of hospitalist services at Beth Israel Deaconess, landing there after a fellowship in geriatrics at Beth Israel Deaconess Medical Center.
Dr. Akiki completed a physician leadership program at BID Medical Center in 2018, and serves as instructor of medicine at Harvard Medical School, Boston.
Michael Schandorf-Lartey, MD, has been named the chief medical officer at Doctors Hospital in Sarasota, Fla. Dr. Schandorf-Lartey has been a hospitalist at Doctors Hospital for the past 12 years.
In his time at Doctors, Dr. Schandorf-Lartey also has been chief of medicine, president-elect, and president of the medical staff. A native of Ghana, he has had experience working in rural and urban hospitals in Africa before coming to the United States.
Michael Roberts, MD, was named chief of staff at East Alabama Medical Center in Opeleika, Ala. He has been part of EAMC since 2008, when he became a hospitalist there through Internal Medicine Associates.
As chief of staff, Dr. Roberts will work with different components of the medical staff and serve as a liaison between the hospital board and its staff; assist in developing policies alongside the chief medical officer; and serve on many of the medical staff’s committees.
Brian Dawson, MD, has been named chief medical officer for Ballad Health, Southwest Region, based in Johnson City, Tenn. Dr. Dawson will lead Ballad Health locations in Washington County, which include Franklin Woods Community Hospital, Johnson City Medical Center, Niswonger Children Hospital, and Woodridge Hospital.
Dr. Dawson comes to Ballad Health after serving as vice president at VEP Healthcare, where he focused on contract management for the emergency medicine and hospitalist firm. Previously, he was chief of staff and Northeast regional director for emergency medicine at Johnston Memorial Hospital, Abington, Va.
Eagle Telemedicine (Atlanta, Ga.) recently agreed to begin a telehospitalist program at Jersey Community Hospital in Jerseyville, Ill. Eagle Telemedicine offers telehospitalist services to more than 150 hospitals nationwide.
A rural facility with fewer than 50 beds, JCH will use Eagle to make up for the lack of a full-time, onsite hospitalist program, taking strain off of physicians handling emergency calls. At JCH, telehospitalists work closely with onsite nurse practitioners to guide patients through their hospital stay.
Hyung (Harry) Cho, MD, SFHM, and Christopher Moriates, MD, SFHM, have been honored by Modern Healthcare as two of 25 emerging young executives in health care management.
Dr. Cho is chief value officer for NYC Health and Hospitals, where his focus is on eliminating unnecessary testing and treatments within the New York City public health system, which includes 11 hospitals and five post-acute care facilities. Before landing with NYC Health and Hospitals, Dr. Cho was director of quality, safety and value at the Icahn School of Medicine at Mount Sinai, New York.
Dr. Moriates is assistant dean for health care and value at the University of Texas at Austin’s Dell Medical School, where he has created the Discovering Value-Based Health Care online learning platform. In addition, Dr. Moriates has helped design a care model to enhance the treatment of patients who suffer from opioid use disorder. Prior to arriving at Dell, he helped create curriculum to educate students about costs and value at the University of California, San Francisco.
Trina Abla, DO, was appointed chief medical officer at Mercy Catholic Medical Center in Darby, Pa. A practicing hospitalist, Dr. Abla will be in charge of the hospital budget, the recruiting and training of physicians, and maintaining safety standards and quality care at the facility.
Prior to taking the position at Mercy Catholic, Dr. Abla was chief quality officer and associate CMO at Penn State Health St. Joseph in Reading, Pa.
Ghania El Akiki, MD, has been named to the board of advisors at Beth Israel Deaconess Hospital in Needham, Mass. Dr. Akiki is chief of hospitalist services at Beth Israel Deaconess, landing there after a fellowship in geriatrics at Beth Israel Deaconess Medical Center.
Dr. Akiki completed a physician leadership program at BID Medical Center in 2018, and serves as instructor of medicine at Harvard Medical School, Boston.
Michael Schandorf-Lartey, MD, has been named the chief medical officer at Doctors Hospital in Sarasota, Fla. Dr. Schandorf-Lartey has been a hospitalist at Doctors Hospital for the past 12 years.
In his time at Doctors, Dr. Schandorf-Lartey also has been chief of medicine, president-elect, and president of the medical staff. A native of Ghana, he has had experience working in rural and urban hospitals in Africa before coming to the United States.
Michael Roberts, MD, was named chief of staff at East Alabama Medical Center in Opeleika, Ala. He has been part of EAMC since 2008, when he became a hospitalist there through Internal Medicine Associates.
As chief of staff, Dr. Roberts will work with different components of the medical staff and serve as a liaison between the hospital board and its staff; assist in developing policies alongside the chief medical officer; and serve on many of the medical staff’s committees.
Brian Dawson, MD, has been named chief medical officer for Ballad Health, Southwest Region, based in Johnson City, Tenn. Dr. Dawson will lead Ballad Health locations in Washington County, which include Franklin Woods Community Hospital, Johnson City Medical Center, Niswonger Children Hospital, and Woodridge Hospital.
Dr. Dawson comes to Ballad Health after serving as vice president at VEP Healthcare, where he focused on contract management for the emergency medicine and hospitalist firm. Previously, he was chief of staff and Northeast regional director for emergency medicine at Johnston Memorial Hospital, Abington, Va.
Eagle Telemedicine (Atlanta, Ga.) recently agreed to begin a telehospitalist program at Jersey Community Hospital in Jerseyville, Ill. Eagle Telemedicine offers telehospitalist services to more than 150 hospitals nationwide.
A rural facility with fewer than 50 beds, JCH will use Eagle to make up for the lack of a full-time, onsite hospitalist program, taking strain off of physicians handling emergency calls. At JCH, telehospitalists work closely with onsite nurse practitioners to guide patients through their hospital stay.
Hyung (Harry) Cho, MD, SFHM, and Christopher Moriates, MD, SFHM, have been honored by Modern Healthcare as two of 25 emerging young executives in health care management.
Dr. Cho is chief value officer for NYC Health and Hospitals, where his focus is on eliminating unnecessary testing and treatments within the New York City public health system, which includes 11 hospitals and five post-acute care facilities. Before landing with NYC Health and Hospitals, Dr. Cho was director of quality, safety and value at the Icahn School of Medicine at Mount Sinai, New York.
Dr. Moriates is assistant dean for health care and value at the University of Texas at Austin’s Dell Medical School, where he has created the Discovering Value-Based Health Care online learning platform. In addition, Dr. Moriates has helped design a care model to enhance the treatment of patients who suffer from opioid use disorder. Prior to arriving at Dell, he helped create curriculum to educate students about costs and value at the University of California, San Francisco.
Trina Abla, DO, was appointed chief medical officer at Mercy Catholic Medical Center in Darby, Pa. A practicing hospitalist, Dr. Abla will be in charge of the hospital budget, the recruiting and training of physicians, and maintaining safety standards and quality care at the facility.
Prior to taking the position at Mercy Catholic, Dr. Abla was chief quality officer and associate CMO at Penn State Health St. Joseph in Reading, Pa.
Ghania El Akiki, MD, has been named to the board of advisors at Beth Israel Deaconess Hospital in Needham, Mass. Dr. Akiki is chief of hospitalist services at Beth Israel Deaconess, landing there after a fellowship in geriatrics at Beth Israel Deaconess Medical Center.
Dr. Akiki completed a physician leadership program at BID Medical Center in 2018, and serves as instructor of medicine at Harvard Medical School, Boston.
Michael Schandorf-Lartey, MD, has been named the chief medical officer at Doctors Hospital in Sarasota, Fla. Dr. Schandorf-Lartey has been a hospitalist at Doctors Hospital for the past 12 years.
In his time at Doctors, Dr. Schandorf-Lartey also has been chief of medicine, president-elect, and president of the medical staff. A native of Ghana, he has had experience working in rural and urban hospitals in Africa before coming to the United States.
Michael Roberts, MD, was named chief of staff at East Alabama Medical Center in Opeleika, Ala. He has been part of EAMC since 2008, when he became a hospitalist there through Internal Medicine Associates.
As chief of staff, Dr. Roberts will work with different components of the medical staff and serve as a liaison between the hospital board and its staff; assist in developing policies alongside the chief medical officer; and serve on many of the medical staff’s committees.
Brian Dawson, MD, has been named chief medical officer for Ballad Health, Southwest Region, based in Johnson City, Tenn. Dr. Dawson will lead Ballad Health locations in Washington County, which include Franklin Woods Community Hospital, Johnson City Medical Center, Niswonger Children Hospital, and Woodridge Hospital.
Dr. Dawson comes to Ballad Health after serving as vice president at VEP Healthcare, where he focused on contract management for the emergency medicine and hospitalist firm. Previously, he was chief of staff and Northeast regional director for emergency medicine at Johnston Memorial Hospital, Abington, Va.
Eagle Telemedicine (Atlanta, Ga.) recently agreed to begin a telehospitalist program at Jersey Community Hospital in Jerseyville, Ill. Eagle Telemedicine offers telehospitalist services to more than 150 hospitals nationwide.
A rural facility with fewer than 50 beds, JCH will use Eagle to make up for the lack of a full-time, onsite hospitalist program, taking strain off of physicians handling emergency calls. At JCH, telehospitalists work closely with onsite nurse practitioners to guide patients through their hospital stay.
GAO Finds DoD Can Do More to Recruit and Retain Physicians and Dentists
Is the US Department of Defense (DoD) doing enough—or the right things—to attract and keep physicians and dentists? According to a new report by the Government Accountability Office (GAO), although the DoD is hitting the mark in some areas, there’s room for improvement in others.
It’s a crucial question. The GAO reported in 2018 that DoD officials cited “a number of challenges” that made it difficult to attract and retain physicians and dentists, such as national shortages and competition with the private sector. Indeed, military health system physicians and dentists make less than do their counterparts in the private sector, the GAO says. For 21 of 27 specialties studied in the new report, the maximum cash compensation was less than the civilian median within 4 officer pay grades (O-3 to O-6). Moreover, cash compensation even for the most senior military physicians and dentists was less than that of the civilian median at “key retention points,” such as after physicians and dentists fulfill their initial active-duty service.
The DoD provides “substantial” deferred and noncash benefits, the GAO notes, such as retirement pensions and tuition-free education, but adds that the value to service members is “difficult to determine.” The DoD also recruits with a package of incentives, including multi-year retention bonuses.
In general, the GAO found, the DoD applies several “effective human capital management” principles. For instance, it relies on clearly defined criteria on when to use incentives (such as rules-based pay plans). It also identifies and evaluates unique staffing situations. For example, to attract physicians and dentists in “critically short wartime specialties,” it offers a Critical Wartime Skills Accession Bonus.
However, the report says, the DoD does not consistently collect information that could help inform its recruitment/retention decisions. At the time of the study, the DoD had not identified replacement costs for physicians or dentists as it does, for instance, with nuclear propulsion personnel. Nor did it gather current and historical retention information. Specifically, the GAO report says, Navy and Air Force officials said they don’t have readily available information to determine the percentage of those who accepted a retention bonus. Conversely, Army officials don’t have a framework in place that uses retention information to determine the effectiveness of retention bonuses (as do the Navy, Marine Corps, and Air Force).
Extending Service Obligations
The DoD is considering extending service obligations for students receiving DoD-funded assistance for physician or dentist education. Students in the DoD scholarship program have a 2-year minimum service obligation, with 6months of active-duty service obligations for each 6 months of benefits received. Medical students attending the Uniformed Services University of the Health Sciences (USUHS), have a 7-year active-duty service obligation.
The GAO held 8 focus groups with students and found 68% of USUHS students and 46% of scholarship students would be willing to accept 1 more year of obligation (although only 34% and 16%, respectively, would agree to 2). The participants expressed concern that longer service obligations would delay their eligibility for retention bonuses—resulting in a reduction of cash compensation over the course of a career. However, 80% and 63%, respectively, would accept an additional year of service obligation if accompanied by additional cash incentives.
Further, the GAO notes, longer obligations could have “unintended consequences.” For example, students might decide to separate and train in a civilian program after 1 or more tours as general medical officers to complete their active duty service obligation, decline further medical training and specialization via a military fellowship program, or separate from the military sooner than planned.
Potential Reductions in Health Care Force
The DoD, according to the report, also is considering reducing the overall number of active-duty physicians, including “targeted reductions” to certain specialties, raising concerns among participants in all 8 focus groups.
Given that the DoD spends millions of dollars annually to train medical and dental students and that almost half of the special pay budget is dedicated to retaining them once they’re fully trained, consistently collecting information to help inform investment decisions is “critical to ensuring the efficiency of these significant resources,” the GAO says. Collecting such information, the GAO says, and using it, would help inform its decision making. For instance, such information would help officials decide whether it would be more cost effective to focus on retaining medical personnel rather than training new staff.
Retaining “top talent,” the DoD says, is “essential to sustaining mission readiness that is adaptable and responsive.” The GAO report cites a 2012 study that found compensation for military physicians had “a large impact on the decision to remain in the military in the first unobligated year of service and just a small impact on retention in the years afterward.”
DoD officials told the GAO that budget considerations and statutory limitations hinder their ability to change the rate of special and incentive pays. The GAO calls these “valid considerations” but suggests that collecting information on replacement costs, retention, and civilian wages would allow DoD departments to “provide greater stewardship of available funding by ensuring its efficient application.” It may be, the GAO says, that retaining fully trained physicians within the DoD is “highly economical.”. Most important, using such data to inform investment decisions will allow the DoD to “efficiently and effectively meet its mission of providing health care during times of war and peace.”
In response to the GAO findings, DoD officials have a group working on a plan to recruit and retain critical specialties, which will be released by June 2020. They also concurred with other GAO recommendations, saying changes will be made within 2 years.
Is the US Department of Defense (DoD) doing enough—or the right things—to attract and keep physicians and dentists? According to a new report by the Government Accountability Office (GAO), although the DoD is hitting the mark in some areas, there’s room for improvement in others.
It’s a crucial question. The GAO reported in 2018 that DoD officials cited “a number of challenges” that made it difficult to attract and retain physicians and dentists, such as national shortages and competition with the private sector. Indeed, military health system physicians and dentists make less than do their counterparts in the private sector, the GAO says. For 21 of 27 specialties studied in the new report, the maximum cash compensation was less than the civilian median within 4 officer pay grades (O-3 to O-6). Moreover, cash compensation even for the most senior military physicians and dentists was less than that of the civilian median at “key retention points,” such as after physicians and dentists fulfill their initial active-duty service.
The DoD provides “substantial” deferred and noncash benefits, the GAO notes, such as retirement pensions and tuition-free education, but adds that the value to service members is “difficult to determine.” The DoD also recruits with a package of incentives, including multi-year retention bonuses.
In general, the GAO found, the DoD applies several “effective human capital management” principles. For instance, it relies on clearly defined criteria on when to use incentives (such as rules-based pay plans). It also identifies and evaluates unique staffing situations. For example, to attract physicians and dentists in “critically short wartime specialties,” it offers a Critical Wartime Skills Accession Bonus.
However, the report says, the DoD does not consistently collect information that could help inform its recruitment/retention decisions. At the time of the study, the DoD had not identified replacement costs for physicians or dentists as it does, for instance, with nuclear propulsion personnel. Nor did it gather current and historical retention information. Specifically, the GAO report says, Navy and Air Force officials said they don’t have readily available information to determine the percentage of those who accepted a retention bonus. Conversely, Army officials don’t have a framework in place that uses retention information to determine the effectiveness of retention bonuses (as do the Navy, Marine Corps, and Air Force).
Extending Service Obligations
The DoD is considering extending service obligations for students receiving DoD-funded assistance for physician or dentist education. Students in the DoD scholarship program have a 2-year minimum service obligation, with 6months of active-duty service obligations for each 6 months of benefits received. Medical students attending the Uniformed Services University of the Health Sciences (USUHS), have a 7-year active-duty service obligation.
The GAO held 8 focus groups with students and found 68% of USUHS students and 46% of scholarship students would be willing to accept 1 more year of obligation (although only 34% and 16%, respectively, would agree to 2). The participants expressed concern that longer service obligations would delay their eligibility for retention bonuses—resulting in a reduction of cash compensation over the course of a career. However, 80% and 63%, respectively, would accept an additional year of service obligation if accompanied by additional cash incentives.
Further, the GAO notes, longer obligations could have “unintended consequences.” For example, students might decide to separate and train in a civilian program after 1 or more tours as general medical officers to complete their active duty service obligation, decline further medical training and specialization via a military fellowship program, or separate from the military sooner than planned.
Potential Reductions in Health Care Force
The DoD, according to the report, also is considering reducing the overall number of active-duty physicians, including “targeted reductions” to certain specialties, raising concerns among participants in all 8 focus groups.
Given that the DoD spends millions of dollars annually to train medical and dental students and that almost half of the special pay budget is dedicated to retaining them once they’re fully trained, consistently collecting information to help inform investment decisions is “critical to ensuring the efficiency of these significant resources,” the GAO says. Collecting such information, the GAO says, and using it, would help inform its decision making. For instance, such information would help officials decide whether it would be more cost effective to focus on retaining medical personnel rather than training new staff.
Retaining “top talent,” the DoD says, is “essential to sustaining mission readiness that is adaptable and responsive.” The GAO report cites a 2012 study that found compensation for military physicians had “a large impact on the decision to remain in the military in the first unobligated year of service and just a small impact on retention in the years afterward.”
DoD officials told the GAO that budget considerations and statutory limitations hinder their ability to change the rate of special and incentive pays. The GAO calls these “valid considerations” but suggests that collecting information on replacement costs, retention, and civilian wages would allow DoD departments to “provide greater stewardship of available funding by ensuring its efficient application.” It may be, the GAO says, that retaining fully trained physicians within the DoD is “highly economical.”. Most important, using such data to inform investment decisions will allow the DoD to “efficiently and effectively meet its mission of providing health care during times of war and peace.”
In response to the GAO findings, DoD officials have a group working on a plan to recruit and retain critical specialties, which will be released by June 2020. They also concurred with other GAO recommendations, saying changes will be made within 2 years.
Is the US Department of Defense (DoD) doing enough—or the right things—to attract and keep physicians and dentists? According to a new report by the Government Accountability Office (GAO), although the DoD is hitting the mark in some areas, there’s room for improvement in others.
It’s a crucial question. The GAO reported in 2018 that DoD officials cited “a number of challenges” that made it difficult to attract and retain physicians and dentists, such as national shortages and competition with the private sector. Indeed, military health system physicians and dentists make less than do their counterparts in the private sector, the GAO says. For 21 of 27 specialties studied in the new report, the maximum cash compensation was less than the civilian median within 4 officer pay grades (O-3 to O-6). Moreover, cash compensation even for the most senior military physicians and dentists was less than that of the civilian median at “key retention points,” such as after physicians and dentists fulfill their initial active-duty service.
The DoD provides “substantial” deferred and noncash benefits, the GAO notes, such as retirement pensions and tuition-free education, but adds that the value to service members is “difficult to determine.” The DoD also recruits with a package of incentives, including multi-year retention bonuses.
In general, the GAO found, the DoD applies several “effective human capital management” principles. For instance, it relies on clearly defined criteria on when to use incentives (such as rules-based pay plans). It also identifies and evaluates unique staffing situations. For example, to attract physicians and dentists in “critically short wartime specialties,” it offers a Critical Wartime Skills Accession Bonus.
However, the report says, the DoD does not consistently collect information that could help inform its recruitment/retention decisions. At the time of the study, the DoD had not identified replacement costs for physicians or dentists as it does, for instance, with nuclear propulsion personnel. Nor did it gather current and historical retention information. Specifically, the GAO report says, Navy and Air Force officials said they don’t have readily available information to determine the percentage of those who accepted a retention bonus. Conversely, Army officials don’t have a framework in place that uses retention information to determine the effectiveness of retention bonuses (as do the Navy, Marine Corps, and Air Force).
Extending Service Obligations
The DoD is considering extending service obligations for students receiving DoD-funded assistance for physician or dentist education. Students in the DoD scholarship program have a 2-year minimum service obligation, with 6months of active-duty service obligations for each 6 months of benefits received. Medical students attending the Uniformed Services University of the Health Sciences (USUHS), have a 7-year active-duty service obligation.
The GAO held 8 focus groups with students and found 68% of USUHS students and 46% of scholarship students would be willing to accept 1 more year of obligation (although only 34% and 16%, respectively, would agree to 2). The participants expressed concern that longer service obligations would delay their eligibility for retention bonuses—resulting in a reduction of cash compensation over the course of a career. However, 80% and 63%, respectively, would accept an additional year of service obligation if accompanied by additional cash incentives.
Further, the GAO notes, longer obligations could have “unintended consequences.” For example, students might decide to separate and train in a civilian program after 1 or more tours as general medical officers to complete their active duty service obligation, decline further medical training and specialization via a military fellowship program, or separate from the military sooner than planned.
Potential Reductions in Health Care Force
The DoD, according to the report, also is considering reducing the overall number of active-duty physicians, including “targeted reductions” to certain specialties, raising concerns among participants in all 8 focus groups.
Given that the DoD spends millions of dollars annually to train medical and dental students and that almost half of the special pay budget is dedicated to retaining them once they’re fully trained, consistently collecting information to help inform investment decisions is “critical to ensuring the efficiency of these significant resources,” the GAO says. Collecting such information, the GAO says, and using it, would help inform its decision making. For instance, such information would help officials decide whether it would be more cost effective to focus on retaining medical personnel rather than training new staff.
Retaining “top talent,” the DoD says, is “essential to sustaining mission readiness that is adaptable and responsive.” The GAO report cites a 2012 study that found compensation for military physicians had “a large impact on the decision to remain in the military in the first unobligated year of service and just a small impact on retention in the years afterward.”
DoD officials told the GAO that budget considerations and statutory limitations hinder their ability to change the rate of special and incentive pays. The GAO calls these “valid considerations” but suggests that collecting information on replacement costs, retention, and civilian wages would allow DoD departments to “provide greater stewardship of available funding by ensuring its efficient application.” It may be, the GAO says, that retaining fully trained physicians within the DoD is “highly economical.”. Most important, using such data to inform investment decisions will allow the DoD to “efficiently and effectively meet its mission of providing health care during times of war and peace.”
In response to the GAO findings, DoD officials have a group working on a plan to recruit and retain critical specialties, which will be released by June 2020. They also concurred with other GAO recommendations, saying changes will be made within 2 years.
Second U.S. coronavirus patient confirmed
at a Jan. 24, 2020, press briefing.
The first U.S. case, a traveler who entered the United States at Seattle-Tacoma International Airport, was confirmed on Jan. 20.
A Chicago resident returning from Wuhan, China, on Jan. 13, 2020, developed symptoms of the disease and contacted her health care clinician and is currently being treated in isolation at an unnamed hospital, according to Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the CDC. The patient, a woman in her 60s, is in stable condition and remains hospitalized. She was not symptomatic on her flight to Chicago but developed symptoms in the following days after her return from Wuhan. She had limited contacts after her return, and all potential contacts are being tracked.
Dr. Messonnier said the CDC expects more cases in the United States but stressed that, although this is a serious public health threat, the risk to the American public is low. She noted that the situation is evolving rapidly and that the CDC is following the developments hour by hour.
Jennifer Layden, MD, PhD, chief medical officer and state epidemiologist with the Illinois Department of Public Health, said public health preparations made it possible to quickly identify and arrange appropriate hospitalization for this patient. Allison Arwady, MD, Chicago Department of Health commissioner, said the Illinois Department of Health partnered with the CDC to test specimens quickly, which led to the diagnosis in this patient.
So far, 63 U.S. patients have been investigated for possible infection with the 2019-nCoV; 11 so far have tested negative and 2 have tested positive. Testing of the remaining potential cases and others is ongoing.
Currently, samples from patients with suspected 2010-nCoV infections are being sent to the CDC for testing, Dr. Messonnier said. The turnaround for testing is currently 4-6 hours. Respiratory samples and some blood samples are being tested by the CDC labs.
The CDC is developing diagnostic kits for public health authorities in the United States for local testing and will work with the World Health Organization to make these kits available to the international community when possible.
Dr. Messonnier said that, at present, the incubation period for this disease appears to be about 14 days, but she suggested that further study will be required to identify the range of time for contagion. She also said it is premature to compare the 2019-nCoV with previous coronavirus outbreaks, such as severe acute respiratory syndrome (SARS) or Middle East respiratory syndrome (MERS), in terms of contagion or fatality rates.
Meanwhile, Andrew D. Mesecar, PhD, the Walther Professor in Cancer Structural Biology and head of the department of biochemistry at Purdue University, West Lafayette, Ind., said on Jan. 24 in a news release that 2019-nCoV is genetically similar to the SARS variant. “MERS virus and the SARS virus are more different genetically,” noted Dr. Mesecar, whose team received the genome of 2019-nCoV on Jan. 17 and analyzed it the next day. “But the Wuhan virus is genetically almost identical to the SARS virus and, therefore, it is expected to look and act nearly the same. In another week or two, we’ll be able to begin to see if the virus is mutating.”
Dr. Messonnier said that nonessential travel to Wuhan is not recommended. In addition, she said, and all other visitors to China need to take appropriate precautions, such as handwashing and avoiding other individuals with respiratory illness.
Screenings at five U.S. airports will continue. So far, approximately 200 flights and 2,000 travelers have been screened as of Jan. 23. No cases were reported, but one traveler has been identified for further for evaluation. Possible contacts with those suspected of infection have been identified and alerted in 22 states.
The CDC will continue to update the public and will post information on the CDC newsroom website.
at a Jan. 24, 2020, press briefing.
The first U.S. case, a traveler who entered the United States at Seattle-Tacoma International Airport, was confirmed on Jan. 20.
A Chicago resident returning from Wuhan, China, on Jan. 13, 2020, developed symptoms of the disease and contacted her health care clinician and is currently being treated in isolation at an unnamed hospital, according to Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the CDC. The patient, a woman in her 60s, is in stable condition and remains hospitalized. She was not symptomatic on her flight to Chicago but developed symptoms in the following days after her return from Wuhan. She had limited contacts after her return, and all potential contacts are being tracked.
Dr. Messonnier said the CDC expects more cases in the United States but stressed that, although this is a serious public health threat, the risk to the American public is low. She noted that the situation is evolving rapidly and that the CDC is following the developments hour by hour.
Jennifer Layden, MD, PhD, chief medical officer and state epidemiologist with the Illinois Department of Public Health, said public health preparations made it possible to quickly identify and arrange appropriate hospitalization for this patient. Allison Arwady, MD, Chicago Department of Health commissioner, said the Illinois Department of Health partnered with the CDC to test specimens quickly, which led to the diagnosis in this patient.
So far, 63 U.S. patients have been investigated for possible infection with the 2019-nCoV; 11 so far have tested negative and 2 have tested positive. Testing of the remaining potential cases and others is ongoing.
Currently, samples from patients with suspected 2010-nCoV infections are being sent to the CDC for testing, Dr. Messonnier said. The turnaround for testing is currently 4-6 hours. Respiratory samples and some blood samples are being tested by the CDC labs.
The CDC is developing diagnostic kits for public health authorities in the United States for local testing and will work with the World Health Organization to make these kits available to the international community when possible.
Dr. Messonnier said that, at present, the incubation period for this disease appears to be about 14 days, but she suggested that further study will be required to identify the range of time for contagion. She also said it is premature to compare the 2019-nCoV with previous coronavirus outbreaks, such as severe acute respiratory syndrome (SARS) or Middle East respiratory syndrome (MERS), in terms of contagion or fatality rates.
Meanwhile, Andrew D. Mesecar, PhD, the Walther Professor in Cancer Structural Biology and head of the department of biochemistry at Purdue University, West Lafayette, Ind., said on Jan. 24 in a news release that 2019-nCoV is genetically similar to the SARS variant. “MERS virus and the SARS virus are more different genetically,” noted Dr. Mesecar, whose team received the genome of 2019-nCoV on Jan. 17 and analyzed it the next day. “But the Wuhan virus is genetically almost identical to the SARS virus and, therefore, it is expected to look and act nearly the same. In another week or two, we’ll be able to begin to see if the virus is mutating.”
Dr. Messonnier said that nonessential travel to Wuhan is not recommended. In addition, she said, and all other visitors to China need to take appropriate precautions, such as handwashing and avoiding other individuals with respiratory illness.
Screenings at five U.S. airports will continue. So far, approximately 200 flights and 2,000 travelers have been screened as of Jan. 23. No cases were reported, but one traveler has been identified for further for evaluation. Possible contacts with those suspected of infection have been identified and alerted in 22 states.
The CDC will continue to update the public and will post information on the CDC newsroom website.
at a Jan. 24, 2020, press briefing.
The first U.S. case, a traveler who entered the United States at Seattle-Tacoma International Airport, was confirmed on Jan. 20.
A Chicago resident returning from Wuhan, China, on Jan. 13, 2020, developed symptoms of the disease and contacted her health care clinician and is currently being treated in isolation at an unnamed hospital, according to Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the CDC. The patient, a woman in her 60s, is in stable condition and remains hospitalized. She was not symptomatic on her flight to Chicago but developed symptoms in the following days after her return from Wuhan. She had limited contacts after her return, and all potential contacts are being tracked.
Dr. Messonnier said the CDC expects more cases in the United States but stressed that, although this is a serious public health threat, the risk to the American public is low. She noted that the situation is evolving rapidly and that the CDC is following the developments hour by hour.
Jennifer Layden, MD, PhD, chief medical officer and state epidemiologist with the Illinois Department of Public Health, said public health preparations made it possible to quickly identify and arrange appropriate hospitalization for this patient. Allison Arwady, MD, Chicago Department of Health commissioner, said the Illinois Department of Health partnered with the CDC to test specimens quickly, which led to the diagnosis in this patient.
So far, 63 U.S. patients have been investigated for possible infection with the 2019-nCoV; 11 so far have tested negative and 2 have tested positive. Testing of the remaining potential cases and others is ongoing.
Currently, samples from patients with suspected 2010-nCoV infections are being sent to the CDC for testing, Dr. Messonnier said. The turnaround for testing is currently 4-6 hours. Respiratory samples and some blood samples are being tested by the CDC labs.
The CDC is developing diagnostic kits for public health authorities in the United States for local testing and will work with the World Health Organization to make these kits available to the international community when possible.
Dr. Messonnier said that, at present, the incubation period for this disease appears to be about 14 days, but she suggested that further study will be required to identify the range of time for contagion. She also said it is premature to compare the 2019-nCoV with previous coronavirus outbreaks, such as severe acute respiratory syndrome (SARS) or Middle East respiratory syndrome (MERS), in terms of contagion or fatality rates.
Meanwhile, Andrew D. Mesecar, PhD, the Walther Professor in Cancer Structural Biology and head of the department of biochemistry at Purdue University, West Lafayette, Ind., said on Jan. 24 in a news release that 2019-nCoV is genetically similar to the SARS variant. “MERS virus and the SARS virus are more different genetically,” noted Dr. Mesecar, whose team received the genome of 2019-nCoV on Jan. 17 and analyzed it the next day. “But the Wuhan virus is genetically almost identical to the SARS virus and, therefore, it is expected to look and act nearly the same. In another week or two, we’ll be able to begin to see if the virus is mutating.”
Dr. Messonnier said that nonessential travel to Wuhan is not recommended. In addition, she said, and all other visitors to China need to take appropriate precautions, such as handwashing and avoiding other individuals with respiratory illness.
Screenings at five U.S. airports will continue. So far, approximately 200 flights and 2,000 travelers have been screened as of Jan. 23. No cases were reported, but one traveler has been identified for further for evaluation. Possible contacts with those suspected of infection have been identified and alerted in 22 states.
The CDC will continue to update the public and will post information on the CDC newsroom website.
FDA: Cybersecurity vulnerabilities identified in GE Healthcare monitoring devices
The Food and Drug Administration has issued a warning that certain GE Healthcare Clinical Information Central Stations and Telemetry Servers have cybersecurity vulnerabilities that may introduce risk to monitored patients.
silence alarms, generate false alarms, and interfere with alarms of patient monitors connected to these devices, according to an “Urgent Medical Device Correction” letter issued by GE Healthcare in November 2019.
The affected devices are the ApexPro Telemetry Server and CARESCAPE Telemetry Server, the CARESCAPE Central Station (CSCS) version 1, and the CIC Pro Clinical Information Center Central Station version 1. These devices are used in health care facilities for displaying information, such as the patient’s physiological parameters, and for monitoring patient status from a central location in a facility.
No adverse events related to the vulnerabilities have been reported to the FDA. Health care facility staff should update their devices when GE Healthcare issues a software patch that addresses the vulnerability, separate the network connecting patient monitors using affected devices from the rest of the hospital, and use firewalls and other means to minimize the risk of remote or local network attacks.
“The FDA takes reports of cybersecurity vulnerabilities in medical devices seriously and will continue to work with GE Healthcare as the firm develops software patches to correct these vulnerabilities as soon as possible. The FDA will continue to assess new information concerning the vulnerabilities and will keep the public informed if significant new information becomes available,” the FDA said in the Safety Communication.
The Food and Drug Administration has issued a warning that certain GE Healthcare Clinical Information Central Stations and Telemetry Servers have cybersecurity vulnerabilities that may introduce risk to monitored patients.
silence alarms, generate false alarms, and interfere with alarms of patient monitors connected to these devices, according to an “Urgent Medical Device Correction” letter issued by GE Healthcare in November 2019.
The affected devices are the ApexPro Telemetry Server and CARESCAPE Telemetry Server, the CARESCAPE Central Station (CSCS) version 1, and the CIC Pro Clinical Information Center Central Station version 1. These devices are used in health care facilities for displaying information, such as the patient’s physiological parameters, and for monitoring patient status from a central location in a facility.
No adverse events related to the vulnerabilities have been reported to the FDA. Health care facility staff should update their devices when GE Healthcare issues a software patch that addresses the vulnerability, separate the network connecting patient monitors using affected devices from the rest of the hospital, and use firewalls and other means to minimize the risk of remote or local network attacks.
“The FDA takes reports of cybersecurity vulnerabilities in medical devices seriously and will continue to work with GE Healthcare as the firm develops software patches to correct these vulnerabilities as soon as possible. The FDA will continue to assess new information concerning the vulnerabilities and will keep the public informed if significant new information becomes available,” the FDA said in the Safety Communication.
The Food and Drug Administration has issued a warning that certain GE Healthcare Clinical Information Central Stations and Telemetry Servers have cybersecurity vulnerabilities that may introduce risk to monitored patients.
silence alarms, generate false alarms, and interfere with alarms of patient monitors connected to these devices, according to an “Urgent Medical Device Correction” letter issued by GE Healthcare in November 2019.
The affected devices are the ApexPro Telemetry Server and CARESCAPE Telemetry Server, the CARESCAPE Central Station (CSCS) version 1, and the CIC Pro Clinical Information Center Central Station version 1. These devices are used in health care facilities for displaying information, such as the patient’s physiological parameters, and for monitoring patient status from a central location in a facility.
No adverse events related to the vulnerabilities have been reported to the FDA. Health care facility staff should update their devices when GE Healthcare issues a software patch that addresses the vulnerability, separate the network connecting patient monitors using affected devices from the rest of the hospital, and use firewalls and other means to minimize the risk of remote or local network attacks.
“The FDA takes reports of cybersecurity vulnerabilities in medical devices seriously and will continue to work with GE Healthcare as the firm develops software patches to correct these vulnerabilities as soon as possible. The FDA will continue to assess new information concerning the vulnerabilities and will keep the public informed if significant new information becomes available,” the FDA said in the Safety Communication.
Neurologic disease doesn’t discriminate against anyone
In 1982, I went to my first concert. It was Rush, on their “Signals” tour, and I loved it. In fact, I went back and saw them again about a year later. I bought a concert T-shirt at the first one. I still have it somewhere, though I am pretty sure it hasn’t fit me in years.
I loved their music before the concert, enjoyed it even more afterwards, and still do. Their albums are all on my computer and phone, and part of the daily soundtrack of my life when working at my desk, driving, and walking (I’m trying to fit back in the shirt).
On Jan. 7, 2020, Neil Peart, the trio’s remarkably gifted drummer, died of a neurologic disease.
According to the news, he had a glioblastoma multiforme, a tumor terrifying for its aggressiveness, difficulty of treatment, and lack of preventable risk factors.
The cost of neurologic disease is terrible. Glioblastoma multiforme, unfortunately, is far from rare, nor is it the only one. In recent times, entertainers afflicted with neurologic disease have included Neil Diamond, Linda Ronstadt, Peter Falk, Glen Campbell, Charlton Heston, Gene Siskel, Michael J. Fox, Stephen Hillenburg, Teri Garr, Annette Funicello, Robin Williams, Dudley Moore, and most recently Ozzy Osbourne.
That’s a pretty short list, too, far from all-encompassing. The majority of people with these disorders won’t be in the news. Their everyday struggles, stories, and losses are known only to family, friends, and the medical team doing its best to help.
Medical technology advances every year. In the 22 years since I began practicing, we’ve made remarkable strides in some areas – multiple sclerosis, for example. But our work in so many other areas is nowhere close. The increasing knowledge as to the mechanisms and causes of Alzheimer’s disease have, to date, failed to translate into treatment success.
That’s not to say we should give up. Far from it. Our species has gotten where we are by always wanting to get over the next hill. Initial failures will always outnumber successes. But when you’re a doctor dealing with the very real human cost of neurologic disease, that’s not much consolation. And it’s far less so for the patients and families affected who come to us for help.
We use terms like “burden” or “cost” to discuss the financial aspects of illness, but they often don’t seem adequate to describe the real effects. The emotional damages. The gifted musicians and loved family members lost. Family members struggling with the difficult role of being care givers.
Neurologic disease doesn’t discriminate against anyone, regardless of age, fame, or talent. I’ll stay here and do my best for all of them who come to me. I’m certainly not on the front line of research. That’s incredibly important, but I’ll leave it to others. My work is where the patients are every day.
Thank you for the music, Neil.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
In 1982, I went to my first concert. It was Rush, on their “Signals” tour, and I loved it. In fact, I went back and saw them again about a year later. I bought a concert T-shirt at the first one. I still have it somewhere, though I am pretty sure it hasn’t fit me in years.
I loved their music before the concert, enjoyed it even more afterwards, and still do. Their albums are all on my computer and phone, and part of the daily soundtrack of my life when working at my desk, driving, and walking (I’m trying to fit back in the shirt).
On Jan. 7, 2020, Neil Peart, the trio’s remarkably gifted drummer, died of a neurologic disease.
According to the news, he had a glioblastoma multiforme, a tumor terrifying for its aggressiveness, difficulty of treatment, and lack of preventable risk factors.
The cost of neurologic disease is terrible. Glioblastoma multiforme, unfortunately, is far from rare, nor is it the only one. In recent times, entertainers afflicted with neurologic disease have included Neil Diamond, Linda Ronstadt, Peter Falk, Glen Campbell, Charlton Heston, Gene Siskel, Michael J. Fox, Stephen Hillenburg, Teri Garr, Annette Funicello, Robin Williams, Dudley Moore, and most recently Ozzy Osbourne.
That’s a pretty short list, too, far from all-encompassing. The majority of people with these disorders won’t be in the news. Their everyday struggles, stories, and losses are known only to family, friends, and the medical team doing its best to help.
Medical technology advances every year. In the 22 years since I began practicing, we’ve made remarkable strides in some areas – multiple sclerosis, for example. But our work in so many other areas is nowhere close. The increasing knowledge as to the mechanisms and causes of Alzheimer’s disease have, to date, failed to translate into treatment success.
That’s not to say we should give up. Far from it. Our species has gotten where we are by always wanting to get over the next hill. Initial failures will always outnumber successes. But when you’re a doctor dealing with the very real human cost of neurologic disease, that’s not much consolation. And it’s far less so for the patients and families affected who come to us for help.
We use terms like “burden” or “cost” to discuss the financial aspects of illness, but they often don’t seem adequate to describe the real effects. The emotional damages. The gifted musicians and loved family members lost. Family members struggling with the difficult role of being care givers.
Neurologic disease doesn’t discriminate against anyone, regardless of age, fame, or talent. I’ll stay here and do my best for all of them who come to me. I’m certainly not on the front line of research. That’s incredibly important, but I’ll leave it to others. My work is where the patients are every day.
Thank you for the music, Neil.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
In 1982, I went to my first concert. It was Rush, on their “Signals” tour, and I loved it. In fact, I went back and saw them again about a year later. I bought a concert T-shirt at the first one. I still have it somewhere, though I am pretty sure it hasn’t fit me in years.
I loved their music before the concert, enjoyed it even more afterwards, and still do. Their albums are all on my computer and phone, and part of the daily soundtrack of my life when working at my desk, driving, and walking (I’m trying to fit back in the shirt).
On Jan. 7, 2020, Neil Peart, the trio’s remarkably gifted drummer, died of a neurologic disease.
According to the news, he had a glioblastoma multiforme, a tumor terrifying for its aggressiveness, difficulty of treatment, and lack of preventable risk factors.
The cost of neurologic disease is terrible. Glioblastoma multiforme, unfortunately, is far from rare, nor is it the only one. In recent times, entertainers afflicted with neurologic disease have included Neil Diamond, Linda Ronstadt, Peter Falk, Glen Campbell, Charlton Heston, Gene Siskel, Michael J. Fox, Stephen Hillenburg, Teri Garr, Annette Funicello, Robin Williams, Dudley Moore, and most recently Ozzy Osbourne.
That’s a pretty short list, too, far from all-encompassing. The majority of people with these disorders won’t be in the news. Their everyday struggles, stories, and losses are known only to family, friends, and the medical team doing its best to help.
Medical technology advances every year. In the 22 years since I began practicing, we’ve made remarkable strides in some areas – multiple sclerosis, for example. But our work in so many other areas is nowhere close. The increasing knowledge as to the mechanisms and causes of Alzheimer’s disease have, to date, failed to translate into treatment success.
That’s not to say we should give up. Far from it. Our species has gotten where we are by always wanting to get over the next hill. Initial failures will always outnumber successes. But when you’re a doctor dealing with the very real human cost of neurologic disease, that’s not much consolation. And it’s far less so for the patients and families affected who come to us for help.
We use terms like “burden” or “cost” to discuss the financial aspects of illness, but they often don’t seem adequate to describe the real effects. The emotional damages. The gifted musicians and loved family members lost. Family members struggling with the difficult role of being care givers.
Neurologic disease doesn’t discriminate against anyone, regardless of age, fame, or talent. I’ll stay here and do my best for all of them who come to me. I’m certainly not on the front line of research. That’s incredibly important, but I’ll leave it to others. My work is where the patients are every day.
Thank you for the music, Neil.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
New Vascepa indication opens up treatment to millions; “Most significant event since statins”
The newly approved U.S. indication for icosapent ethyl (Vascepa; Amarin) is broadly in line with the entry criteria for the REDUCE-IT trial and includes a large high-risk primary-prevention population, as well as those with established cardiovascular disease (CVD). The drug, thus, could well be used by millions of patients in the United States alone.
The high-dose, purified eicosapentaenoic acid product was approved last week by the Food and Drug Administration for cardiovascular risk reduction among adults already taking maximally tolerated statins with triglyceride levels of 150 mg/dL or higher who have either established CVD or diabetes and two or more additional risk factors for CVD.
The approval is based largely on the REDUCE-IT trial’s finding of a 25% reduction in risk for major adverse cardiovascular events versus placebo. The FDA stated that the approval is the first for an agent with this specific indication.
Noting that it recognizes the need for additional medical treatments for CVD, the FDA says the new approval “will give patients with elevated triglycerides and other important risk factors, including heart disease, stroke, and diabetes, an adjunctive treatment option that can help decrease their risk of cardiovascular events.”
The drug was unanimously recommended for approval by the FDA’s Endocrinologic and Metabolic Drugs Advisory Committee last month. But while the committee all agreed on its use in patients with established CVD, which made up 70% of the REDUCE-IT population, they were divided on whether the indication should be extended to the high-risk primary-prevention population, who made up just 30% of patients in the study.
Nonetheless, the FDA has gone for a broad indication based on the whole REDUCE-IT population.
In a conference call following the approval, Steven Ketchum, PhD, chief scientific officer at Amarin, pointed out that the primary-prevention population stipulated in the new approval differed very slightly from the REDUCE-IT enrollment criteria.
The trial specified that patients with diabetes should be older than 50 with one other cardiovascular risk factor, whereas the approved population is for diabetes and two cardiovascular risk factors. But as these two risk factors are not specified, they could include age, cigarette smoking, hypertension or use of an antihypertensive agent, low HDL cholesterol, high C-reactive protein, body mass index above 25 kg/m2, renal dysfunction, retinopathy, albuminuria, or an ankle branchial index below 0.9, Dr. Ketchum said.
“So while the label asks for two other risk factors, one of these could be age; so we believe the label is actually slightly broader than the REDUCE-IT inclusion criteria, and doctors have been left with significant leeway to decide which risk factors to consider on top of diabetes.”
Deepak Bhatt, MD, the lead investigator of REDUCE-IT, described the Vascepa approval as “the most significant event in the field of cardiovascular prevention since the introduction of statins nearly 3 decades ago.”
He commended the FDA on “a very evidence-based, prescriber-friendly, and most importantly, patient-friendly label,” which he said was in line with guidelines from multiple professional societies that have already incorporated the REDUCE-IT findings for secondary prevention and diabetic primary prevention.
Dr. Bhatt, who is a professor of medicine at Brigham and Women’s Hospital and Harvard Medical School, Boston, said the label essentially matches the REDUCE-IT population.
“The entry criteria for REDUCE-IT was fasting triglycerides greater than or equal to 150 mg/dL, with a 10% variance allowed (giving a minimum triglyceride value of 135 mg/dL). In actuality, we ended up with about 10% of the population with triglycerides between 100 and 150 mg/dL, and they had a similar degree of benefit as those with higher levels,” he reported.
“In the label, the 150 mg/dL does not specify fasting, and in fact many practices have moved away from fasting lipid measurements for the sake of patient comfort,” Dr. Bhatt added. “On average, nonfasting levels are about 50 mg/dL higher, so the label essentially mirrors those we studied, with the FDA applying good common sense and not being overly dogmatic about the exact wording of the trial inclusion criteria.”
No price change foreseen
Vascepa is already on the market for patients with very high triglyceride levels, and the company says it is not increasing the current price of about $300 a month, which is “relatively low, compared to other new breakthrough drugs.” However, it says it expects sales to grow from vastly increased volume based on the new indication.
Dr. Bhatt noted that REDUCE-IT cost-effectiveness data presented at the recent American Heart Association scientific sessions found the drug to be cost saving in the majority of cases. “That is something that is quite rare in cost-effectiveness research,” he said.
“Now, the key challenge is to identify and treat appropriate patients,” Dr. Bhatt noted. He says this task will largely fall on cardiologists, endocrinologists, and primary care physicians, though stroke neurologists, nephrologists, and vascular medicine specialists will also have patients for whom the data are relevant.
“I believe the drug will ultimately be widely prescribed, initially by subspecialists, but by primary care physicians also. It is overall very well tolerated, safe, and easy to use,” he said. “Much like statin prescription started in subspecialty practices but then became quite common in primary care, I envision the same happening with icosapent ethyl.”
Lipid expert Roger Blumenthal, MD, who was not involved in the REDUCE-IT trial, also welcomed the new approval for Vascepa.
“The indication is very appropriate; it is great to have another disease-modifying medication in our prevention toolkit,” Dr. Blumenthal, who is director of the Johns Hopkins Ciccarone Center for the Prevention of Cardiovascular Disease in Baltimore, said in an interview.
Some still unsure
But not everyone is in full agreement with the broad indication granted.
One expert who has reservations is James de Lemos, MD, professor of medicine at the University of Texas, Dallas, who sat on the FDA advisory committee that assessed the drug last month.
“I would have preferred a narrower label for now, limited to the secondary prevention indication, because I felt that REDUCE-IT did not include sufficient numbers of patients to justify the high-risk primary-prevention indication. We need an adequately powered, randomized, controlled trial to establish the risk/benefit and cost/benefit in primary prevention, and with this broad label, I worry there will be little incentive for the company to pursue this,” Dr. de Lemos commented in an interview.
“This is a slippery slope, and we should not allow broad indications that extend to primary prevention for drugs that were studied in mixed secondary- and primary-prevention patients, with the results driven by the secondary-prevention subset. These two subgroups are fundamentally different populations in whom the pathophysiology and the background treatments are very different,” he added.
However, Dr. de Lemos acknowledged that he would use Vascepa for some high-risk primary-prevention patients in his practice – those with diabetes, high triglycerides, and multiple risk factors. “I just wish we had more data coming so that I could be more certain of the benefit in this group,” he said.
Dr. Bhatt disclosed sitting on advisory boards for Cardax, Cereno Scientific, Medscape Cardiology, PhaseBio, and Regado Biosciences; conducting unfunded research in association with FlowCo, Fractyl, Merck, Novo Nordisk, PLx Pharma, and Takeda; and receiving research funding from Abbott, Afimmune, Amarin, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Chiesi, CSL Behring, Eisai, Ethicon, Ferring Pharmaceuticals, and Forest Laboratories. Dr. De Lemos reported receiving grant and consulting income from Roche Diagnostics and Abbott Diagnostics; and consulting for Ortho Clinical Diagnostics. Dr. Blumenthal has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The newly approved U.S. indication for icosapent ethyl (Vascepa; Amarin) is broadly in line with the entry criteria for the REDUCE-IT trial and includes a large high-risk primary-prevention population, as well as those with established cardiovascular disease (CVD). The drug, thus, could well be used by millions of patients in the United States alone.
The high-dose, purified eicosapentaenoic acid product was approved last week by the Food and Drug Administration for cardiovascular risk reduction among adults already taking maximally tolerated statins with triglyceride levels of 150 mg/dL or higher who have either established CVD or diabetes and two or more additional risk factors for CVD.
The approval is based largely on the REDUCE-IT trial’s finding of a 25% reduction in risk for major adverse cardiovascular events versus placebo. The FDA stated that the approval is the first for an agent with this specific indication.
Noting that it recognizes the need for additional medical treatments for CVD, the FDA says the new approval “will give patients with elevated triglycerides and other important risk factors, including heart disease, stroke, and diabetes, an adjunctive treatment option that can help decrease their risk of cardiovascular events.”
The drug was unanimously recommended for approval by the FDA’s Endocrinologic and Metabolic Drugs Advisory Committee last month. But while the committee all agreed on its use in patients with established CVD, which made up 70% of the REDUCE-IT population, they were divided on whether the indication should be extended to the high-risk primary-prevention population, who made up just 30% of patients in the study.
Nonetheless, the FDA has gone for a broad indication based on the whole REDUCE-IT population.
In a conference call following the approval, Steven Ketchum, PhD, chief scientific officer at Amarin, pointed out that the primary-prevention population stipulated in the new approval differed very slightly from the REDUCE-IT enrollment criteria.
The trial specified that patients with diabetes should be older than 50 with one other cardiovascular risk factor, whereas the approved population is for diabetes and two cardiovascular risk factors. But as these two risk factors are not specified, they could include age, cigarette smoking, hypertension or use of an antihypertensive agent, low HDL cholesterol, high C-reactive protein, body mass index above 25 kg/m2, renal dysfunction, retinopathy, albuminuria, or an ankle branchial index below 0.9, Dr. Ketchum said.
“So while the label asks for two other risk factors, one of these could be age; so we believe the label is actually slightly broader than the REDUCE-IT inclusion criteria, and doctors have been left with significant leeway to decide which risk factors to consider on top of diabetes.”
Deepak Bhatt, MD, the lead investigator of REDUCE-IT, described the Vascepa approval as “the most significant event in the field of cardiovascular prevention since the introduction of statins nearly 3 decades ago.”
He commended the FDA on “a very evidence-based, prescriber-friendly, and most importantly, patient-friendly label,” which he said was in line with guidelines from multiple professional societies that have already incorporated the REDUCE-IT findings for secondary prevention and diabetic primary prevention.
Dr. Bhatt, who is a professor of medicine at Brigham and Women’s Hospital and Harvard Medical School, Boston, said the label essentially matches the REDUCE-IT population.
“The entry criteria for REDUCE-IT was fasting triglycerides greater than or equal to 150 mg/dL, with a 10% variance allowed (giving a minimum triglyceride value of 135 mg/dL). In actuality, we ended up with about 10% of the population with triglycerides between 100 and 150 mg/dL, and they had a similar degree of benefit as those with higher levels,” he reported.
“In the label, the 150 mg/dL does not specify fasting, and in fact many practices have moved away from fasting lipid measurements for the sake of patient comfort,” Dr. Bhatt added. “On average, nonfasting levels are about 50 mg/dL higher, so the label essentially mirrors those we studied, with the FDA applying good common sense and not being overly dogmatic about the exact wording of the trial inclusion criteria.”
No price change foreseen
Vascepa is already on the market for patients with very high triglyceride levels, and the company says it is not increasing the current price of about $300 a month, which is “relatively low, compared to other new breakthrough drugs.” However, it says it expects sales to grow from vastly increased volume based on the new indication.
Dr. Bhatt noted that REDUCE-IT cost-effectiveness data presented at the recent American Heart Association scientific sessions found the drug to be cost saving in the majority of cases. “That is something that is quite rare in cost-effectiveness research,” he said.
“Now, the key challenge is to identify and treat appropriate patients,” Dr. Bhatt noted. He says this task will largely fall on cardiologists, endocrinologists, and primary care physicians, though stroke neurologists, nephrologists, and vascular medicine specialists will also have patients for whom the data are relevant.
“I believe the drug will ultimately be widely prescribed, initially by subspecialists, but by primary care physicians also. It is overall very well tolerated, safe, and easy to use,” he said. “Much like statin prescription started in subspecialty practices but then became quite common in primary care, I envision the same happening with icosapent ethyl.”
Lipid expert Roger Blumenthal, MD, who was not involved in the REDUCE-IT trial, also welcomed the new approval for Vascepa.
“The indication is very appropriate; it is great to have another disease-modifying medication in our prevention toolkit,” Dr. Blumenthal, who is director of the Johns Hopkins Ciccarone Center for the Prevention of Cardiovascular Disease in Baltimore, said in an interview.
Some still unsure
But not everyone is in full agreement with the broad indication granted.
One expert who has reservations is James de Lemos, MD, professor of medicine at the University of Texas, Dallas, who sat on the FDA advisory committee that assessed the drug last month.
“I would have preferred a narrower label for now, limited to the secondary prevention indication, because I felt that REDUCE-IT did not include sufficient numbers of patients to justify the high-risk primary-prevention indication. We need an adequately powered, randomized, controlled trial to establish the risk/benefit and cost/benefit in primary prevention, and with this broad label, I worry there will be little incentive for the company to pursue this,” Dr. de Lemos commented in an interview.
“This is a slippery slope, and we should not allow broad indications that extend to primary prevention for drugs that were studied in mixed secondary- and primary-prevention patients, with the results driven by the secondary-prevention subset. These two subgroups are fundamentally different populations in whom the pathophysiology and the background treatments are very different,” he added.
However, Dr. de Lemos acknowledged that he would use Vascepa for some high-risk primary-prevention patients in his practice – those with diabetes, high triglycerides, and multiple risk factors. “I just wish we had more data coming so that I could be more certain of the benefit in this group,” he said.
Dr. Bhatt disclosed sitting on advisory boards for Cardax, Cereno Scientific, Medscape Cardiology, PhaseBio, and Regado Biosciences; conducting unfunded research in association with FlowCo, Fractyl, Merck, Novo Nordisk, PLx Pharma, and Takeda; and receiving research funding from Abbott, Afimmune, Amarin, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Chiesi, CSL Behring, Eisai, Ethicon, Ferring Pharmaceuticals, and Forest Laboratories. Dr. De Lemos reported receiving grant and consulting income from Roche Diagnostics and Abbott Diagnostics; and consulting for Ortho Clinical Diagnostics. Dr. Blumenthal has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The newly approved U.S. indication for icosapent ethyl (Vascepa; Amarin) is broadly in line with the entry criteria for the REDUCE-IT trial and includes a large high-risk primary-prevention population, as well as those with established cardiovascular disease (CVD). The drug, thus, could well be used by millions of patients in the United States alone.
The high-dose, purified eicosapentaenoic acid product was approved last week by the Food and Drug Administration for cardiovascular risk reduction among adults already taking maximally tolerated statins with triglyceride levels of 150 mg/dL or higher who have either established CVD or diabetes and two or more additional risk factors for CVD.
The approval is based largely on the REDUCE-IT trial’s finding of a 25% reduction in risk for major adverse cardiovascular events versus placebo. The FDA stated that the approval is the first for an agent with this specific indication.
Noting that it recognizes the need for additional medical treatments for CVD, the FDA says the new approval “will give patients with elevated triglycerides and other important risk factors, including heart disease, stroke, and diabetes, an adjunctive treatment option that can help decrease their risk of cardiovascular events.”
The drug was unanimously recommended for approval by the FDA’s Endocrinologic and Metabolic Drugs Advisory Committee last month. But while the committee all agreed on its use in patients with established CVD, which made up 70% of the REDUCE-IT population, they were divided on whether the indication should be extended to the high-risk primary-prevention population, who made up just 30% of patients in the study.
Nonetheless, the FDA has gone for a broad indication based on the whole REDUCE-IT population.
In a conference call following the approval, Steven Ketchum, PhD, chief scientific officer at Amarin, pointed out that the primary-prevention population stipulated in the new approval differed very slightly from the REDUCE-IT enrollment criteria.
The trial specified that patients with diabetes should be older than 50 with one other cardiovascular risk factor, whereas the approved population is for diabetes and two cardiovascular risk factors. But as these two risk factors are not specified, they could include age, cigarette smoking, hypertension or use of an antihypertensive agent, low HDL cholesterol, high C-reactive protein, body mass index above 25 kg/m2, renal dysfunction, retinopathy, albuminuria, or an ankle branchial index below 0.9, Dr. Ketchum said.
“So while the label asks for two other risk factors, one of these could be age; so we believe the label is actually slightly broader than the REDUCE-IT inclusion criteria, and doctors have been left with significant leeway to decide which risk factors to consider on top of diabetes.”
Deepak Bhatt, MD, the lead investigator of REDUCE-IT, described the Vascepa approval as “the most significant event in the field of cardiovascular prevention since the introduction of statins nearly 3 decades ago.”
He commended the FDA on “a very evidence-based, prescriber-friendly, and most importantly, patient-friendly label,” which he said was in line with guidelines from multiple professional societies that have already incorporated the REDUCE-IT findings for secondary prevention and diabetic primary prevention.
Dr. Bhatt, who is a professor of medicine at Brigham and Women’s Hospital and Harvard Medical School, Boston, said the label essentially matches the REDUCE-IT population.
“The entry criteria for REDUCE-IT was fasting triglycerides greater than or equal to 150 mg/dL, with a 10% variance allowed (giving a minimum triglyceride value of 135 mg/dL). In actuality, we ended up with about 10% of the population with triglycerides between 100 and 150 mg/dL, and they had a similar degree of benefit as those with higher levels,” he reported.
“In the label, the 150 mg/dL does not specify fasting, and in fact many practices have moved away from fasting lipid measurements for the sake of patient comfort,” Dr. Bhatt added. “On average, nonfasting levels are about 50 mg/dL higher, so the label essentially mirrors those we studied, with the FDA applying good common sense and not being overly dogmatic about the exact wording of the trial inclusion criteria.”
No price change foreseen
Vascepa is already on the market for patients with very high triglyceride levels, and the company says it is not increasing the current price of about $300 a month, which is “relatively low, compared to other new breakthrough drugs.” However, it says it expects sales to grow from vastly increased volume based on the new indication.
Dr. Bhatt noted that REDUCE-IT cost-effectiveness data presented at the recent American Heart Association scientific sessions found the drug to be cost saving in the majority of cases. “That is something that is quite rare in cost-effectiveness research,” he said.
“Now, the key challenge is to identify and treat appropriate patients,” Dr. Bhatt noted. He says this task will largely fall on cardiologists, endocrinologists, and primary care physicians, though stroke neurologists, nephrologists, and vascular medicine specialists will also have patients for whom the data are relevant.
“I believe the drug will ultimately be widely prescribed, initially by subspecialists, but by primary care physicians also. It is overall very well tolerated, safe, and easy to use,” he said. “Much like statin prescription started in subspecialty practices but then became quite common in primary care, I envision the same happening with icosapent ethyl.”
Lipid expert Roger Blumenthal, MD, who was not involved in the REDUCE-IT trial, also welcomed the new approval for Vascepa.
“The indication is very appropriate; it is great to have another disease-modifying medication in our prevention toolkit,” Dr. Blumenthal, who is director of the Johns Hopkins Ciccarone Center for the Prevention of Cardiovascular Disease in Baltimore, said in an interview.
Some still unsure
But not everyone is in full agreement with the broad indication granted.
One expert who has reservations is James de Lemos, MD, professor of medicine at the University of Texas, Dallas, who sat on the FDA advisory committee that assessed the drug last month.
“I would have preferred a narrower label for now, limited to the secondary prevention indication, because I felt that REDUCE-IT did not include sufficient numbers of patients to justify the high-risk primary-prevention indication. We need an adequately powered, randomized, controlled trial to establish the risk/benefit and cost/benefit in primary prevention, and with this broad label, I worry there will be little incentive for the company to pursue this,” Dr. de Lemos commented in an interview.
“This is a slippery slope, and we should not allow broad indications that extend to primary prevention for drugs that were studied in mixed secondary- and primary-prevention patients, with the results driven by the secondary-prevention subset. These two subgroups are fundamentally different populations in whom the pathophysiology and the background treatments are very different,” he added.
However, Dr. de Lemos acknowledged that he would use Vascepa for some high-risk primary-prevention patients in his practice – those with diabetes, high triglycerides, and multiple risk factors. “I just wish we had more data coming so that I could be more certain of the benefit in this group,” he said.
Dr. Bhatt disclosed sitting on advisory boards for Cardax, Cereno Scientific, Medscape Cardiology, PhaseBio, and Regado Biosciences; conducting unfunded research in association with FlowCo, Fractyl, Merck, Novo Nordisk, PLx Pharma, and Takeda; and receiving research funding from Abbott, Afimmune, Amarin, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Chiesi, CSL Behring, Eisai, Ethicon, Ferring Pharmaceuticals, and Forest Laboratories. Dr. De Lemos reported receiving grant and consulting income from Roche Diagnostics and Abbott Diagnostics; and consulting for Ortho Clinical Diagnostics. Dr. Blumenthal has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Blood test may advance diagnosis of GI cancers
SAN FRANCISCO – A new assay based on methylation patterns in plasma cell-free DNA holds promise for improving detection of diverse gastrointestinal (GI) cancers when they are still curable, findings of the Circulating Cell-free Genome Atlas (CCGA) study suggest.
Among 447 patients with GI cancers of varied types and stages, the multicancer assay had sensitivity exceeding 80% for all stages (exceeding 70% for stages I to III) and specificity exceeding 99%, investigators reported at the 2020 GI Cancers Symposium. In addition, the assay correctly determined the tissue of origin about 90% of the time.
“To pursue early detection at a population scale while minimizing harm and cost, several features are important, including a low false-positive rate, a high detection rate, the ability to localize the site of origin of the malignancy, and limiting overdiagnosis,” noted lead investigator Brian M. Wolpin, MD, MPH, director of the Gastrointestinal Cancer Center and director of the Hale Family Center for Pancreatic Cancer Research at Dana-Farber Cancer Institute in Boston. “This multicancer early detection test evaluating cell-free DNA methylation may be a useful test to detect GI cancers and may guide further evaluation and workup.”
About three-quarters of all cancer patients in the study had symptoms that ultimately led to their diagnosis, Dr. Wolpin acknowledged. But the investigators are conducting two large additional studies among asymptomatic populations to better assess the assay’s screening potential: the STRIVE study, which has enrolled nearly 100,000 women undergoing screening mammography, and the SUMMIT study, which is enrolling 50,000 men and women without a known cancer diagnosis, with enrichment of the sample for smokers.
Clinical potential
“The holy grail, of course, is to try to find any test – a blood test, a urine test, a breath test, a stool test – that will allow us to detect cancer at an earlier and more curable stage, and we have hints now that we are headed in the right direction,” session cochair George A. Fisher Jr., MD, PhD, said in an interview. “I don’t know that this is the technology that will do it, but I think it’s superior to the technology just looking at DNA mutations.”
It is a further merit that the assay also has good accuracy in ascertaining the cancer’s tissue of origin, as that should help streamline the diagnostic workup, he agreed.
The assay is already attractive for patients with suspicious lesions or symptoms, but further research will be needed to assess its performance in detecting asymptomatic cancer, and logistic issues would have to be addressed, according to Dr. Fisher of Stanford (Calif.) University.
“As an outright screening test, I don’t think we are there yet. We would have to identify the populations in whom to use the test and come up with some frequency of how often we use it,” he said. Consideration would need to be given to informed consent, especially as some patients may have a positive assay result but a cancer that can’t be found, generating psychological distress.
And cost will come into play. “The problem is, for most stage I cancers you can screen for, they are still very low in likelihood, so you have to screen a lot of people, which means a lot of expense,” he elaborated.
“It will be interesting in the research world to decide when such a test would become a reasonable standard of care, and how regulators will view that and how insurers will view that in terms of cost-efficacy analysis,” Dr. Fisher concluded.
Study details
The CCGA study has enrolled 15,254 participants with and without cancer at 142 U.S and Canadian sites. Participants provide blood samples (at diagnosis for those with cancer) and are followed up for 5 years.
To develop the assay, the investigators performed targeted methylation sequencing of cell-free DNA from plasma and trained an algorithm to use the methylation patterns to detect more than 20 cancer types and classify them based on the organ of origin.
Dr. Wolpin reported results for a CCGA substudy conducted among 2,185 patients with cancer and 2,131 individuals without cancer. About a fifth of the former group had cancers of the GI tract (colon or rectum in 174 patients, pancreas in 123, esophagus in 71, liver or bile duct in 40, stomach in 25, gallbladder in 14). The population was split into training and validation sets.
The assay had a specificity of 99.8% in the entire training set and 99.3% in the entire validation set, corresponding to false-positives in just 0.2% and 0.7% of the individuals without cancer, according to data reported at the symposium, which is sponsored by the American Gastroenterological Association, American Society of Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
For GI cancers, assay sensitivity for stage I-IV disease was 82% in the training set and 81% in the validation set, and sensitivity for stage I-III disease was 73% and 71%, respectively. By specific nonmetastatic stage, sensitivity was about 50% for stage I disease, 75% for stage II disease, and 85% for stage III disease.
Fully 97% of the GI cancers having detectable cell-free DNA were assigned a tissue of origin by the assay. The predicted tissue of origin had an accuracy of 91% in the training set and 89% in the validation set, with similar values across GI cancer types.
Dr. Wolpin disclosed having a relationship with various pharmaceutical companies, including GRAIL, which funded the study. Dr. Fisher disclosed relationships with numerous pharmaceutical companies and that an immediate family member has stock in Seattle Genetics
SOURCE: Wolpin BM et al. 2020 GI Symposium, Abstract 283.
SAN FRANCISCO – A new assay based on methylation patterns in plasma cell-free DNA holds promise for improving detection of diverse gastrointestinal (GI) cancers when they are still curable, findings of the Circulating Cell-free Genome Atlas (CCGA) study suggest.
Among 447 patients with GI cancers of varied types and stages, the multicancer assay had sensitivity exceeding 80% for all stages (exceeding 70% for stages I to III) and specificity exceeding 99%, investigators reported at the 2020 GI Cancers Symposium. In addition, the assay correctly determined the tissue of origin about 90% of the time.
“To pursue early detection at a population scale while minimizing harm and cost, several features are important, including a low false-positive rate, a high detection rate, the ability to localize the site of origin of the malignancy, and limiting overdiagnosis,” noted lead investigator Brian M. Wolpin, MD, MPH, director of the Gastrointestinal Cancer Center and director of the Hale Family Center for Pancreatic Cancer Research at Dana-Farber Cancer Institute in Boston. “This multicancer early detection test evaluating cell-free DNA methylation may be a useful test to detect GI cancers and may guide further evaluation and workup.”
About three-quarters of all cancer patients in the study had symptoms that ultimately led to their diagnosis, Dr. Wolpin acknowledged. But the investigators are conducting two large additional studies among asymptomatic populations to better assess the assay’s screening potential: the STRIVE study, which has enrolled nearly 100,000 women undergoing screening mammography, and the SUMMIT study, which is enrolling 50,000 men and women without a known cancer diagnosis, with enrichment of the sample for smokers.
Clinical potential
“The holy grail, of course, is to try to find any test – a blood test, a urine test, a breath test, a stool test – that will allow us to detect cancer at an earlier and more curable stage, and we have hints now that we are headed in the right direction,” session cochair George A. Fisher Jr., MD, PhD, said in an interview. “I don’t know that this is the technology that will do it, but I think it’s superior to the technology just looking at DNA mutations.”
It is a further merit that the assay also has good accuracy in ascertaining the cancer’s tissue of origin, as that should help streamline the diagnostic workup, he agreed.
The assay is already attractive for patients with suspicious lesions or symptoms, but further research will be needed to assess its performance in detecting asymptomatic cancer, and logistic issues would have to be addressed, according to Dr. Fisher of Stanford (Calif.) University.
“As an outright screening test, I don’t think we are there yet. We would have to identify the populations in whom to use the test and come up with some frequency of how often we use it,” he said. Consideration would need to be given to informed consent, especially as some patients may have a positive assay result but a cancer that can’t be found, generating psychological distress.
And cost will come into play. “The problem is, for most stage I cancers you can screen for, they are still very low in likelihood, so you have to screen a lot of people, which means a lot of expense,” he elaborated.
“It will be interesting in the research world to decide when such a test would become a reasonable standard of care, and how regulators will view that and how insurers will view that in terms of cost-efficacy analysis,” Dr. Fisher concluded.
Study details
The CCGA study has enrolled 15,254 participants with and without cancer at 142 U.S and Canadian sites. Participants provide blood samples (at diagnosis for those with cancer) and are followed up for 5 years.
To develop the assay, the investigators performed targeted methylation sequencing of cell-free DNA from plasma and trained an algorithm to use the methylation patterns to detect more than 20 cancer types and classify them based on the organ of origin.
Dr. Wolpin reported results for a CCGA substudy conducted among 2,185 patients with cancer and 2,131 individuals without cancer. About a fifth of the former group had cancers of the GI tract (colon or rectum in 174 patients, pancreas in 123, esophagus in 71, liver or bile duct in 40, stomach in 25, gallbladder in 14). The population was split into training and validation sets.
The assay had a specificity of 99.8% in the entire training set and 99.3% in the entire validation set, corresponding to false-positives in just 0.2% and 0.7% of the individuals without cancer, according to data reported at the symposium, which is sponsored by the American Gastroenterological Association, American Society of Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
For GI cancers, assay sensitivity for stage I-IV disease was 82% in the training set and 81% in the validation set, and sensitivity for stage I-III disease was 73% and 71%, respectively. By specific nonmetastatic stage, sensitivity was about 50% for stage I disease, 75% for stage II disease, and 85% for stage III disease.
Fully 97% of the GI cancers having detectable cell-free DNA were assigned a tissue of origin by the assay. The predicted tissue of origin had an accuracy of 91% in the training set and 89% in the validation set, with similar values across GI cancer types.
Dr. Wolpin disclosed having a relationship with various pharmaceutical companies, including GRAIL, which funded the study. Dr. Fisher disclosed relationships with numerous pharmaceutical companies and that an immediate family member has stock in Seattle Genetics
SOURCE: Wolpin BM et al. 2020 GI Symposium, Abstract 283.
SAN FRANCISCO – A new assay based on methylation patterns in plasma cell-free DNA holds promise for improving detection of diverse gastrointestinal (GI) cancers when they are still curable, findings of the Circulating Cell-free Genome Atlas (CCGA) study suggest.
Among 447 patients with GI cancers of varied types and stages, the multicancer assay had sensitivity exceeding 80% for all stages (exceeding 70% for stages I to III) and specificity exceeding 99%, investigators reported at the 2020 GI Cancers Symposium. In addition, the assay correctly determined the tissue of origin about 90% of the time.
“To pursue early detection at a population scale while minimizing harm and cost, several features are important, including a low false-positive rate, a high detection rate, the ability to localize the site of origin of the malignancy, and limiting overdiagnosis,” noted lead investigator Brian M. Wolpin, MD, MPH, director of the Gastrointestinal Cancer Center and director of the Hale Family Center for Pancreatic Cancer Research at Dana-Farber Cancer Institute in Boston. “This multicancer early detection test evaluating cell-free DNA methylation may be a useful test to detect GI cancers and may guide further evaluation and workup.”
About three-quarters of all cancer patients in the study had symptoms that ultimately led to their diagnosis, Dr. Wolpin acknowledged. But the investigators are conducting two large additional studies among asymptomatic populations to better assess the assay’s screening potential: the STRIVE study, which has enrolled nearly 100,000 women undergoing screening mammography, and the SUMMIT study, which is enrolling 50,000 men and women without a known cancer diagnosis, with enrichment of the sample for smokers.
Clinical potential
“The holy grail, of course, is to try to find any test – a blood test, a urine test, a breath test, a stool test – that will allow us to detect cancer at an earlier and more curable stage, and we have hints now that we are headed in the right direction,” session cochair George A. Fisher Jr., MD, PhD, said in an interview. “I don’t know that this is the technology that will do it, but I think it’s superior to the technology just looking at DNA mutations.”
It is a further merit that the assay also has good accuracy in ascertaining the cancer’s tissue of origin, as that should help streamline the diagnostic workup, he agreed.
The assay is already attractive for patients with suspicious lesions or symptoms, but further research will be needed to assess its performance in detecting asymptomatic cancer, and logistic issues would have to be addressed, according to Dr. Fisher of Stanford (Calif.) University.
“As an outright screening test, I don’t think we are there yet. We would have to identify the populations in whom to use the test and come up with some frequency of how often we use it,” he said. Consideration would need to be given to informed consent, especially as some patients may have a positive assay result but a cancer that can’t be found, generating psychological distress.
And cost will come into play. “The problem is, for most stage I cancers you can screen for, they are still very low in likelihood, so you have to screen a lot of people, which means a lot of expense,” he elaborated.
“It will be interesting in the research world to decide when such a test would become a reasonable standard of care, and how regulators will view that and how insurers will view that in terms of cost-efficacy analysis,” Dr. Fisher concluded.
Study details
The CCGA study has enrolled 15,254 participants with and without cancer at 142 U.S and Canadian sites. Participants provide blood samples (at diagnosis for those with cancer) and are followed up for 5 years.
To develop the assay, the investigators performed targeted methylation sequencing of cell-free DNA from plasma and trained an algorithm to use the methylation patterns to detect more than 20 cancer types and classify them based on the organ of origin.
Dr. Wolpin reported results for a CCGA substudy conducted among 2,185 patients with cancer and 2,131 individuals without cancer. About a fifth of the former group had cancers of the GI tract (colon or rectum in 174 patients, pancreas in 123, esophagus in 71, liver or bile duct in 40, stomach in 25, gallbladder in 14). The population was split into training and validation sets.
The assay had a specificity of 99.8% in the entire training set and 99.3% in the entire validation set, corresponding to false-positives in just 0.2% and 0.7% of the individuals without cancer, according to data reported at the symposium, which is sponsored by the American Gastroenterological Association, American Society of Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
For GI cancers, assay sensitivity for stage I-IV disease was 82% in the training set and 81% in the validation set, and sensitivity for stage I-III disease was 73% and 71%, respectively. By specific nonmetastatic stage, sensitivity was about 50% for stage I disease, 75% for stage II disease, and 85% for stage III disease.
Fully 97% of the GI cancers having detectable cell-free DNA were assigned a tissue of origin by the assay. The predicted tissue of origin had an accuracy of 91% in the training set and 89% in the validation set, with similar values across GI cancer types.
Dr. Wolpin disclosed having a relationship with various pharmaceutical companies, including GRAIL, which funded the study. Dr. Fisher disclosed relationships with numerous pharmaceutical companies and that an immediate family member has stock in Seattle Genetics
SOURCE: Wolpin BM et al. 2020 GI Symposium, Abstract 283.
REPORTING FROM THE 2020 GI CANCERS SYMPOSIUM