User login
Can Lighting Improve Sleep, Mood, and Behavior in Patients With Dementia?
Nonpharmacologic stimulation of the circadian system may benefit people in long-term care facilities.
BALTIMORE—Among patients with Alzheimer’s disease and related dementias, a lighting intervention may improve sleep, mood, and agitation, according to a study presented at the 32nd Annual Meeting of the Associated Professional Sleep Societies.
The intervention “holds considerable promise as a novel, practically applied, nonpharmacologic intervention” for people with dementia who live in long-term care facilities, said Mariana G. Figueiro, PhD, Director of the Lighting Research Center and Professor of Architecture at Rensselaer Polytechnic Institute in Troy, New York.
People with dementia often have problems related to sleep and daytime irritability. A study in office workers found that exposure to light that stimulates the circadian system early in the day is associated with better sleep and improved behavior and mood. To assess whether a lighting intervention that delivers a circadian stimulus may improve sleep and behavior in patients with dementia in long-term care facilities, Dr. Figueiro and colleagues conducted a crossover, repeated-measures, within-subjects study. The study included 43 subjects (31 female) with Alzheimer’s disease or related dementias and Mini-Mental State Examination scores of less than 24.
The intervention consisted of an LED light table and individual room lights that were placed where patients spent most of their waking hours. The lights were turned on when participants woke up and remained on until 6 PM. Participants wore calibrated light meters that monitored their light exposure.
The trial included four weeks with an active circadian stimulus, four weeks with an inactive lighting intervention, and a four-week washout period in between.
In addition, researchers collected subjective measures of sleep disturbances (Pittsburgh Sleep Quality Index [PSQI]), mood (Cornell Scale for Depression in Dementia [CSDD]), and agitation (Cohen-Mansfield Agitation Index [CMAI]) at baseline and during the last week of the active and placebo intervention periods.
The active lighting intervention significantly decreased scores for sleep disturbances, depression, and agitation, compared with placebo. During the active intervention, mean PSQI scores decreased from 10.3 to 6.7, CSDD scores decreased from 10.5 to 7.3, and CMAI scores decreased from 42.9 to 37.4.
A six-month study of the lighting intervention is underway. “A logical next step would be to test the short- and long-term effects of the tailored lighting intervention among those living at home,” Dr. Figueiro and colleagues said.
—Jake Remaly
Suggested Reading
Figueiro MG, Steverson B, Heerwagen J, et al. The impact of daytime light exposures on sleep and mood in office workers. Sleep Health. 2017;3(3):204-215.
Nonpharmacologic stimulation of the circadian system may benefit people in long-term care facilities.
Nonpharmacologic stimulation of the circadian system may benefit people in long-term care facilities.
BALTIMORE—Among patients with Alzheimer’s disease and related dementias, a lighting intervention may improve sleep, mood, and agitation, according to a study presented at the 32nd Annual Meeting of the Associated Professional Sleep Societies.
The intervention “holds considerable promise as a novel, practically applied, nonpharmacologic intervention” for people with dementia who live in long-term care facilities, said Mariana G. Figueiro, PhD, Director of the Lighting Research Center and Professor of Architecture at Rensselaer Polytechnic Institute in Troy, New York.
People with dementia often have problems related to sleep and daytime irritability. A study in office workers found that exposure to light that stimulates the circadian system early in the day is associated with better sleep and improved behavior and mood. To assess whether a lighting intervention that delivers a circadian stimulus may improve sleep and behavior in patients with dementia in long-term care facilities, Dr. Figueiro and colleagues conducted a crossover, repeated-measures, within-subjects study. The study included 43 subjects (31 female) with Alzheimer’s disease or related dementias and Mini-Mental State Examination scores of less than 24.
The intervention consisted of an LED light table and individual room lights that were placed where patients spent most of their waking hours. The lights were turned on when participants woke up and remained on until 6 PM. Participants wore calibrated light meters that monitored their light exposure.
The trial included four weeks with an active circadian stimulus, four weeks with an inactive lighting intervention, and a four-week washout period in between.
In addition, researchers collected subjective measures of sleep disturbances (Pittsburgh Sleep Quality Index [PSQI]), mood (Cornell Scale for Depression in Dementia [CSDD]), and agitation (Cohen-Mansfield Agitation Index [CMAI]) at baseline and during the last week of the active and placebo intervention periods.
The active lighting intervention significantly decreased scores for sleep disturbances, depression, and agitation, compared with placebo. During the active intervention, mean PSQI scores decreased from 10.3 to 6.7, CSDD scores decreased from 10.5 to 7.3, and CMAI scores decreased from 42.9 to 37.4.
A six-month study of the lighting intervention is underway. “A logical next step would be to test the short- and long-term effects of the tailored lighting intervention among those living at home,” Dr. Figueiro and colleagues said.
—Jake Remaly
Suggested Reading
Figueiro MG, Steverson B, Heerwagen J, et al. The impact of daytime light exposures on sleep and mood in office workers. Sleep Health. 2017;3(3):204-215.
BALTIMORE—Among patients with Alzheimer’s disease and related dementias, a lighting intervention may improve sleep, mood, and agitation, according to a study presented at the 32nd Annual Meeting of the Associated Professional Sleep Societies.
The intervention “holds considerable promise as a novel, practically applied, nonpharmacologic intervention” for people with dementia who live in long-term care facilities, said Mariana G. Figueiro, PhD, Director of the Lighting Research Center and Professor of Architecture at Rensselaer Polytechnic Institute in Troy, New York.
People with dementia often have problems related to sleep and daytime irritability. A study in office workers found that exposure to light that stimulates the circadian system early in the day is associated with better sleep and improved behavior and mood. To assess whether a lighting intervention that delivers a circadian stimulus may improve sleep and behavior in patients with dementia in long-term care facilities, Dr. Figueiro and colleagues conducted a crossover, repeated-measures, within-subjects study. The study included 43 subjects (31 female) with Alzheimer’s disease or related dementias and Mini-Mental State Examination scores of less than 24.
The intervention consisted of an LED light table and individual room lights that were placed where patients spent most of their waking hours. The lights were turned on when participants woke up and remained on until 6 PM. Participants wore calibrated light meters that monitored their light exposure.
The trial included four weeks with an active circadian stimulus, four weeks with an inactive lighting intervention, and a four-week washout period in between.
In addition, researchers collected subjective measures of sleep disturbances (Pittsburgh Sleep Quality Index [PSQI]), mood (Cornell Scale for Depression in Dementia [CSDD]), and agitation (Cohen-Mansfield Agitation Index [CMAI]) at baseline and during the last week of the active and placebo intervention periods.
The active lighting intervention significantly decreased scores for sleep disturbances, depression, and agitation, compared with placebo. During the active intervention, mean PSQI scores decreased from 10.3 to 6.7, CSDD scores decreased from 10.5 to 7.3, and CMAI scores decreased from 42.9 to 37.4.
A six-month study of the lighting intervention is underway. “A logical next step would be to test the short- and long-term effects of the tailored lighting intervention among those living at home,” Dr. Figueiro and colleagues said.
—Jake Remaly
Suggested Reading
Figueiro MG, Steverson B, Heerwagen J, et al. The impact of daytime light exposures on sleep and mood in office workers. Sleep Health. 2017;3(3):204-215.
Huntington’s Disease Symptoms Vary by Age of Onset
Earlier age of onset may be associated with higher severity of behavioral symptoms.
MIAMI—The greater the age of Huntington’s disease onset, the lower the likelihood that the patient’s major symptom type at disease presentation will be behavioral or cognitive, according to research presented at the Second Pan American Parkinson’s Disease and Movement Disorders Congress. Increasing age at onset also is associated with a higher likelihood that motor symptoms will be the major symptom type at disease presentation.
Examining Enroll-HD Data
A patient may have subtle changes in movement, thinking, or behavior as early as 20 years before the onset of Huntington’s disease. Allison Daley, a clinical research specialist at Ohio State University in Columbus, and colleagues noted anecdotally that the severity of behavioral symptoms was decreased in older patients with newly diagnosed Huntington’s disease, compared with younger patients. The group set out to investigate the relationship between behavioral symptoms and age at onset of clinical symptoms in Huntington’s disease.
Ms. Daley and colleagues examined data for 8,714 participants registered in the Enroll-HD database as of 2016. They established three categories of patients based on age of onset. Early-onset Huntington’s disease was defined as onset at an age younger than 30. Earlier adult-onset Huntington’s disease was defined as onset between ages 30 and 59. Later adult-onset Huntington’s disease was defined as onset at an age above 59. Ms. Daley’s group examined the frequency and severity of behavioral symptoms at disease presentation in all three groups. They used the Clinical Characteristics form and the Problem Behaviors Assessment form to evaluate symptom presence and severity.
Motor Symptoms More Common in Late-Onset Disease
Of the entire sample, 4,469 participants had manifest Huntington’s disease. Motor symptoms were present in 42% of participants with early-onset Huntington’s disease, 50% of participants with earlier adult-onset Huntington’s disease, and 67% of participants with later adult-onset Huntington’s disease. Cognitive symptoms were recorded in 9% of the early-onset group, 10% of the earlier adult-onset group, and 4% of the later adult-onset group. Behavioral symptoms were observed in 26% of the early-onset group, 19% of the earlier adult-onset group, and 11% of the later adult-onset group.
A one-year increase in age at onset was associated with a 5.5% decrease in the odds of severe behavioral symptom of any type. In addition, a one-year increase in age at onset was associated with a 9.4% decrease in the odds of severe disorientation, an 8.8% decrease in the odds of severe delusions, a 6.8% decrease in the odds of severe obsessive–compulsive behavior, and a 5.8% decrease in the odds of severe apathy.
At baseline, 56% of participants had apathy, 55% had anxiety, 54% had irritability, 51% had depression, 44% had perseverative thinking, and 29% had anger or aggression.
“Specific behavioral symptoms, particularly disorientation, delusions, and obsessive–compulsive behaviors, may tend to manifest more severely in individuals with earlier age at onset. Earlier age at onset may be associated with higher severity of behavioral symptoms overall,” said Ms. Daley. “Further research exploring biologic mechanisms and environmental factors that interact with CAG repeat size to affect symptom presentation in Huntington’s disease at different ages at onset may help identify additional therapeutic strategies and individualized treatment approaches for Huntington’s disease.”
—Erik Greb
Earlier age of onset may be associated with higher severity of behavioral symptoms.
Earlier age of onset may be associated with higher severity of behavioral symptoms.
MIAMI—The greater the age of Huntington’s disease onset, the lower the likelihood that the patient’s major symptom type at disease presentation will be behavioral or cognitive, according to research presented at the Second Pan American Parkinson’s Disease and Movement Disorders Congress. Increasing age at onset also is associated with a higher likelihood that motor symptoms will be the major symptom type at disease presentation.
Examining Enroll-HD Data
A patient may have subtle changes in movement, thinking, or behavior as early as 20 years before the onset of Huntington’s disease. Allison Daley, a clinical research specialist at Ohio State University in Columbus, and colleagues noted anecdotally that the severity of behavioral symptoms was decreased in older patients with newly diagnosed Huntington’s disease, compared with younger patients. The group set out to investigate the relationship between behavioral symptoms and age at onset of clinical symptoms in Huntington’s disease.
Ms. Daley and colleagues examined data for 8,714 participants registered in the Enroll-HD database as of 2016. They established three categories of patients based on age of onset. Early-onset Huntington’s disease was defined as onset at an age younger than 30. Earlier adult-onset Huntington’s disease was defined as onset between ages 30 and 59. Later adult-onset Huntington’s disease was defined as onset at an age above 59. Ms. Daley’s group examined the frequency and severity of behavioral symptoms at disease presentation in all three groups. They used the Clinical Characteristics form and the Problem Behaviors Assessment form to evaluate symptom presence and severity.
Motor Symptoms More Common in Late-Onset Disease
Of the entire sample, 4,469 participants had manifest Huntington’s disease. Motor symptoms were present in 42% of participants with early-onset Huntington’s disease, 50% of participants with earlier adult-onset Huntington’s disease, and 67% of participants with later adult-onset Huntington’s disease. Cognitive symptoms were recorded in 9% of the early-onset group, 10% of the earlier adult-onset group, and 4% of the later adult-onset group. Behavioral symptoms were observed in 26% of the early-onset group, 19% of the earlier adult-onset group, and 11% of the later adult-onset group.
A one-year increase in age at onset was associated with a 5.5% decrease in the odds of severe behavioral symptom of any type. In addition, a one-year increase in age at onset was associated with a 9.4% decrease in the odds of severe disorientation, an 8.8% decrease in the odds of severe delusions, a 6.8% decrease in the odds of severe obsessive–compulsive behavior, and a 5.8% decrease in the odds of severe apathy.
At baseline, 56% of participants had apathy, 55% had anxiety, 54% had irritability, 51% had depression, 44% had perseverative thinking, and 29% had anger or aggression.
“Specific behavioral symptoms, particularly disorientation, delusions, and obsessive–compulsive behaviors, may tend to manifest more severely in individuals with earlier age at onset. Earlier age at onset may be associated with higher severity of behavioral symptoms overall,” said Ms. Daley. “Further research exploring biologic mechanisms and environmental factors that interact with CAG repeat size to affect symptom presentation in Huntington’s disease at different ages at onset may help identify additional therapeutic strategies and individualized treatment approaches for Huntington’s disease.”
—Erik Greb
MIAMI—The greater the age of Huntington’s disease onset, the lower the likelihood that the patient’s major symptom type at disease presentation will be behavioral or cognitive, according to research presented at the Second Pan American Parkinson’s Disease and Movement Disorders Congress. Increasing age at onset also is associated with a higher likelihood that motor symptoms will be the major symptom type at disease presentation.
Examining Enroll-HD Data
A patient may have subtle changes in movement, thinking, or behavior as early as 20 years before the onset of Huntington’s disease. Allison Daley, a clinical research specialist at Ohio State University in Columbus, and colleagues noted anecdotally that the severity of behavioral symptoms was decreased in older patients with newly diagnosed Huntington’s disease, compared with younger patients. The group set out to investigate the relationship between behavioral symptoms and age at onset of clinical symptoms in Huntington’s disease.
Ms. Daley and colleagues examined data for 8,714 participants registered in the Enroll-HD database as of 2016. They established three categories of patients based on age of onset. Early-onset Huntington’s disease was defined as onset at an age younger than 30. Earlier adult-onset Huntington’s disease was defined as onset between ages 30 and 59. Later adult-onset Huntington’s disease was defined as onset at an age above 59. Ms. Daley’s group examined the frequency and severity of behavioral symptoms at disease presentation in all three groups. They used the Clinical Characteristics form and the Problem Behaviors Assessment form to evaluate symptom presence and severity.
Motor Symptoms More Common in Late-Onset Disease
Of the entire sample, 4,469 participants had manifest Huntington’s disease. Motor symptoms were present in 42% of participants with early-onset Huntington’s disease, 50% of participants with earlier adult-onset Huntington’s disease, and 67% of participants with later adult-onset Huntington’s disease. Cognitive symptoms were recorded in 9% of the early-onset group, 10% of the earlier adult-onset group, and 4% of the later adult-onset group. Behavioral symptoms were observed in 26% of the early-onset group, 19% of the earlier adult-onset group, and 11% of the later adult-onset group.
A one-year increase in age at onset was associated with a 5.5% decrease in the odds of severe behavioral symptom of any type. In addition, a one-year increase in age at onset was associated with a 9.4% decrease in the odds of severe disorientation, an 8.8% decrease in the odds of severe delusions, a 6.8% decrease in the odds of severe obsessive–compulsive behavior, and a 5.8% decrease in the odds of severe apathy.
At baseline, 56% of participants had apathy, 55% had anxiety, 54% had irritability, 51% had depression, 44% had perseverative thinking, and 29% had anger or aggression.
“Specific behavioral symptoms, particularly disorientation, delusions, and obsessive–compulsive behaviors, may tend to manifest more severely in individuals with earlier age at onset. Earlier age at onset may be associated with higher severity of behavioral symptoms overall,” said Ms. Daley. “Further research exploring biologic mechanisms and environmental factors that interact with CAG repeat size to affect symptom presentation in Huntington’s disease at different ages at onset may help identify additional therapeutic strategies and individualized treatment approaches for Huntington’s disease.”
—Erik Greb
Tetrad Bodies in Skin
The Diagnosis: Bacterial Infection
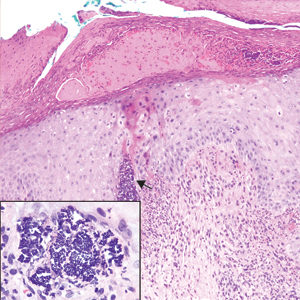
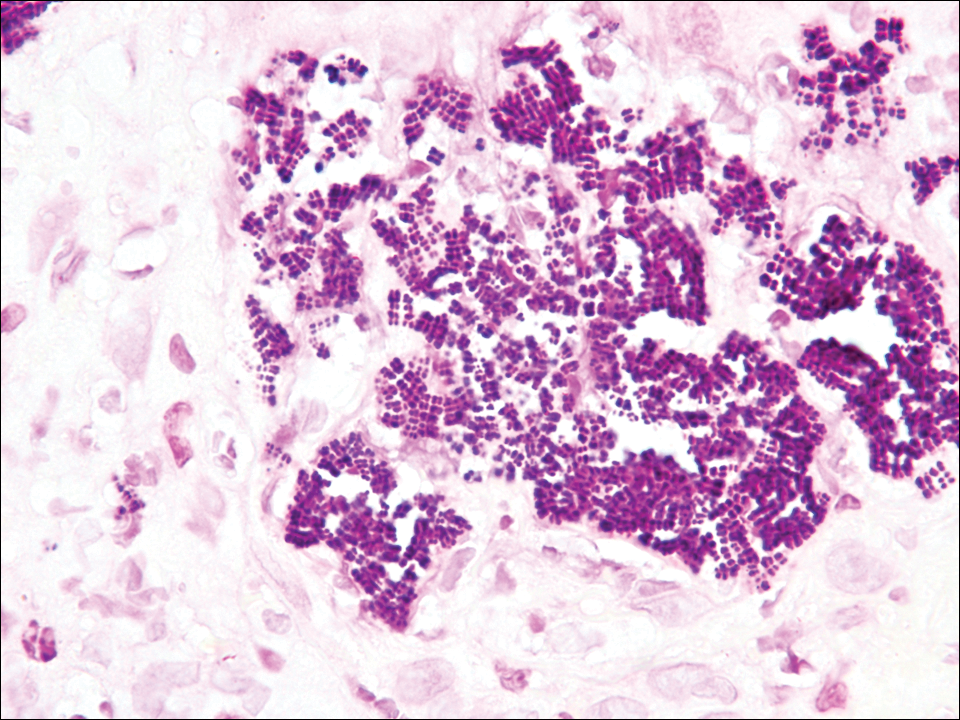
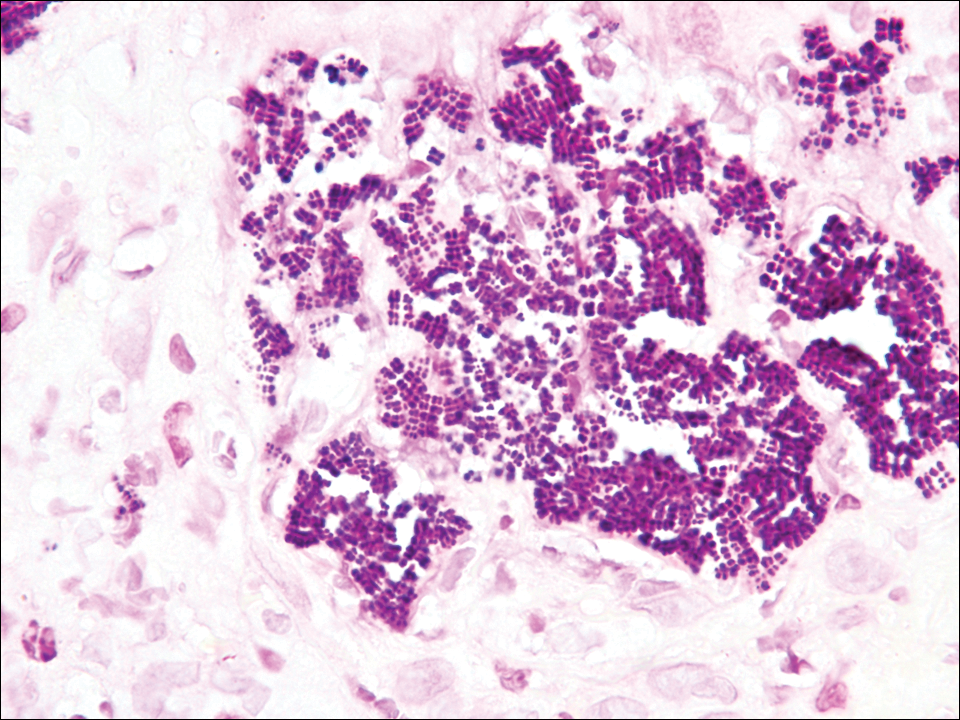
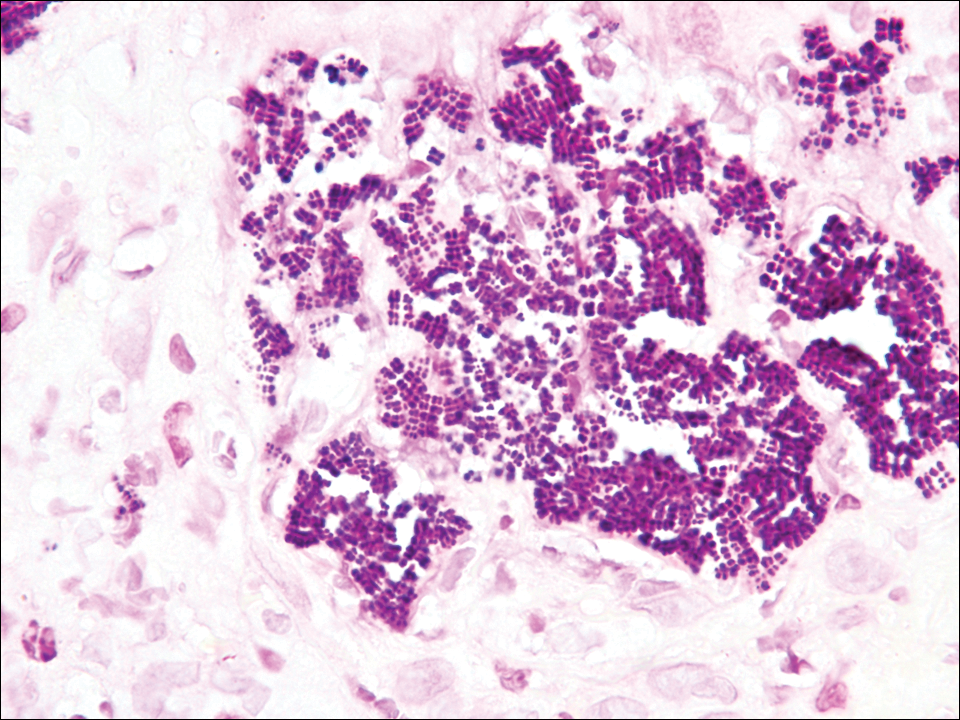
The tetrad arrangement of organisms seen in this case was classic for Micrococcus and Sarcina species. Both are gram-positive cocci that occur in tetrads, but Micrococcus is aerobic and catalase positive, whereas Sarcina species are anaerobic, catalase negative, acidophilic, and form spores in alkaline pH.1 Although difficult to definitively differentiate on light microscopy, micrococci are smaller in size, ranging from 0.5 to 2.0 μm, and occur in tight clusters, as seen in this case (quiz images), in contrast to Sarcina species, which are relatively larger (1.8-3.0 μm).2 Sarcinae typically are found in soil and air, are considered pathogenic, and are associated with gastric symptoms (Sarcina ventriculi).1Sarcina species also are reported to colonize the skin of patients with diabetes mellitus, but no pathogenic activity is known in the skin.3Micrococcus species, with the majority being Micrococcus luteus, are part of the normal flora of the human skin as well as the oral and nasal cavities. Occasional reports of pneumonia, endocarditis, meningitis, arthritis, endophthalmitis, and sepsis have been reported in immunocompromised individuals.4 In the skin, Micrococcus is a commensal organism; however, Micrococcus sedentarius has been associated with pitted keratolysis, and reports of Micrococcus folliculitis in human immunodeficiency virus patients also are described in the literature.5,6 Micrococci are considered opportunistic bacteria and may worsen and prolong a localized cutaneous infection caused by other organisms under favorable conditions.7Micrococcus luteus is one of the most common bacteria cultured from skin and soft tissue infections caused by fungal organisms.8 Depending on the immune status of an individual, use of broad-spectrum antibiotic and/or elimination of favorable milieu (ie, primary pathogen, breaks in skin) usually treats the infection.
Because of the rarity of infections caused and being part of the normal flora, the clinical implications of subtyping and sensitivity studies via culture or molecular studies may not be important; however, incidental presence of these organisms with unfamiliar morphology may cause confusion for the dermatopathologist. An extremely small size (0.5-2.0 μm) compared to red blood cells (7-8 μm) and white blood cells (10-12 μm) in a tight tetrad arrangement should raise the suspicion for Micrococcus.1 The refractive nature of these organisms from a thick extracellular layer can mimic fungus or plant matter; a negative Grocott-Gomori methenamine-silver stain in this case helped in not only differentiating but also ruling out secondary fungal infection. Finally, a Gram stain with violet staining of these organisms reaffirmed the diagnosis of gram-positive bacterial organisms, most consistent with Micrococcus species (Figure 1). Culture studies were not performed because of contamination of the tissue specimen and resolution of the patient's symptoms.
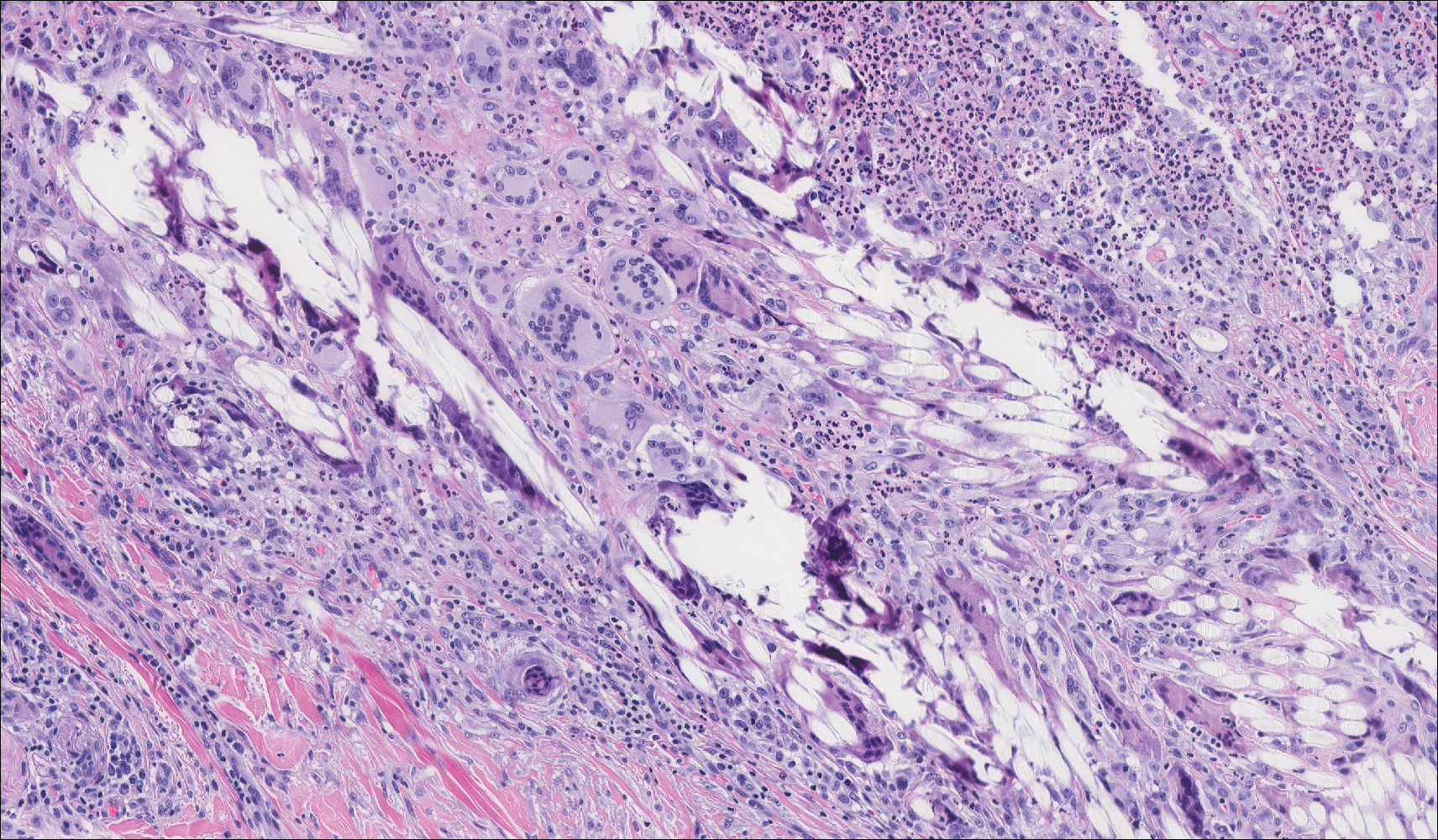
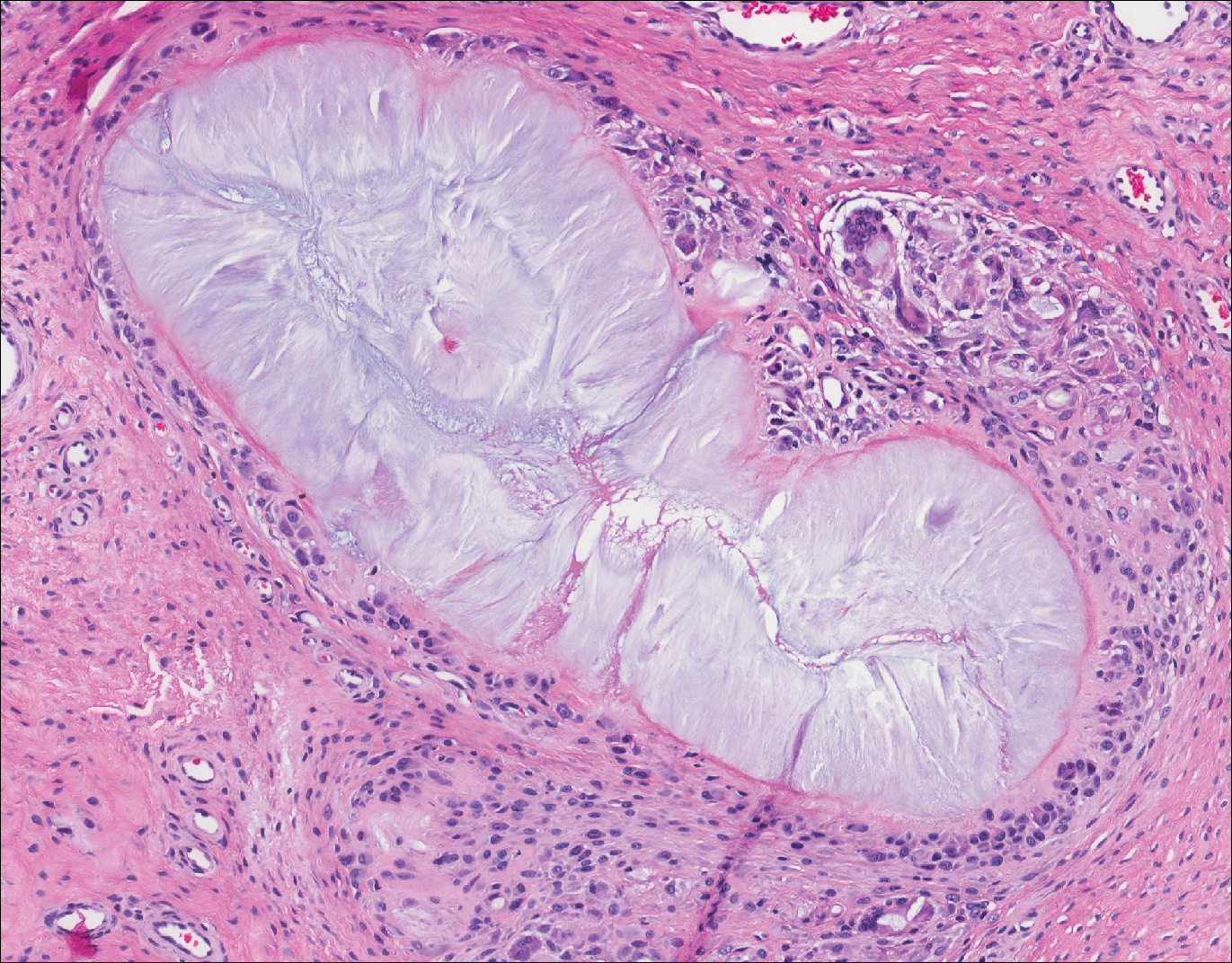
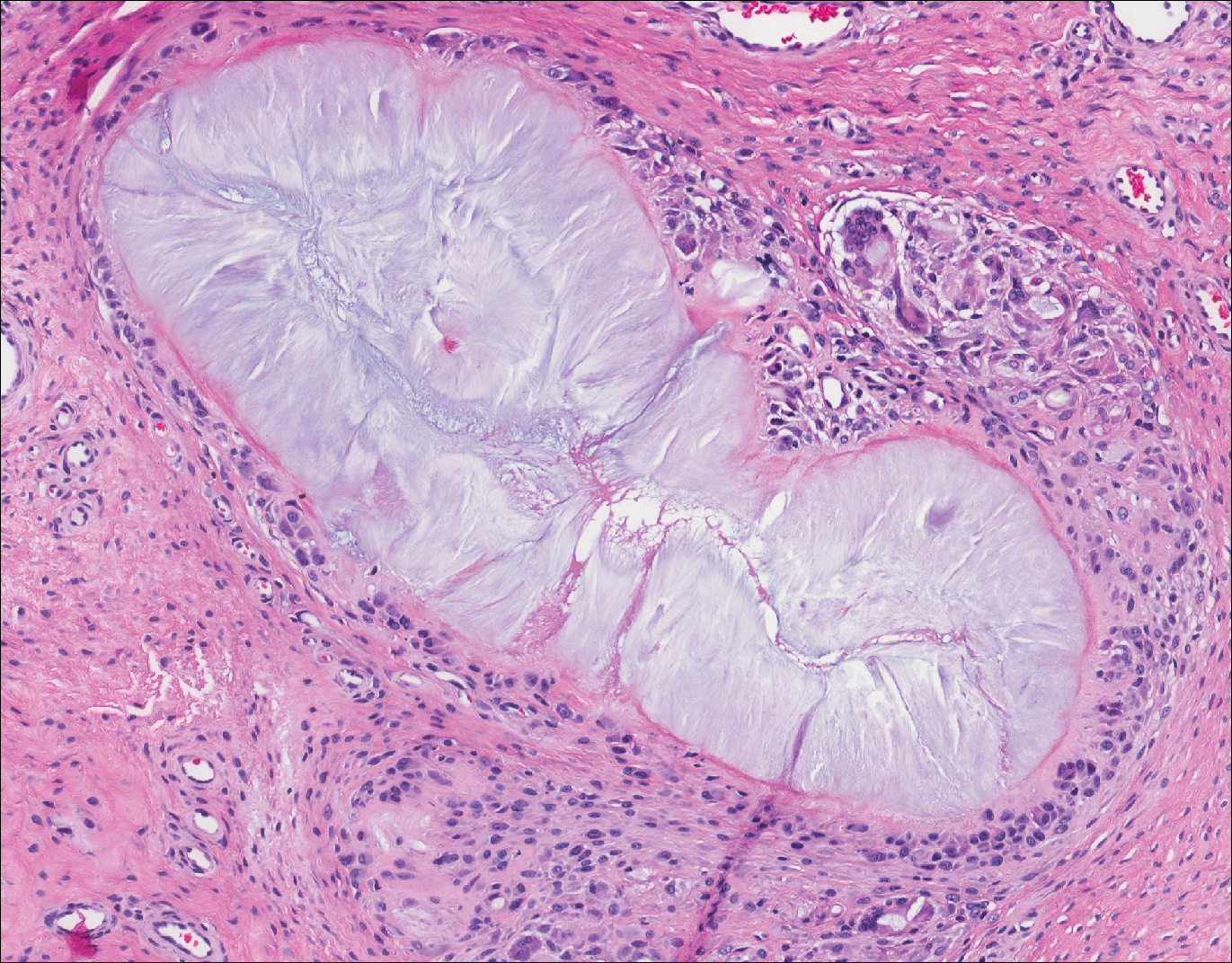
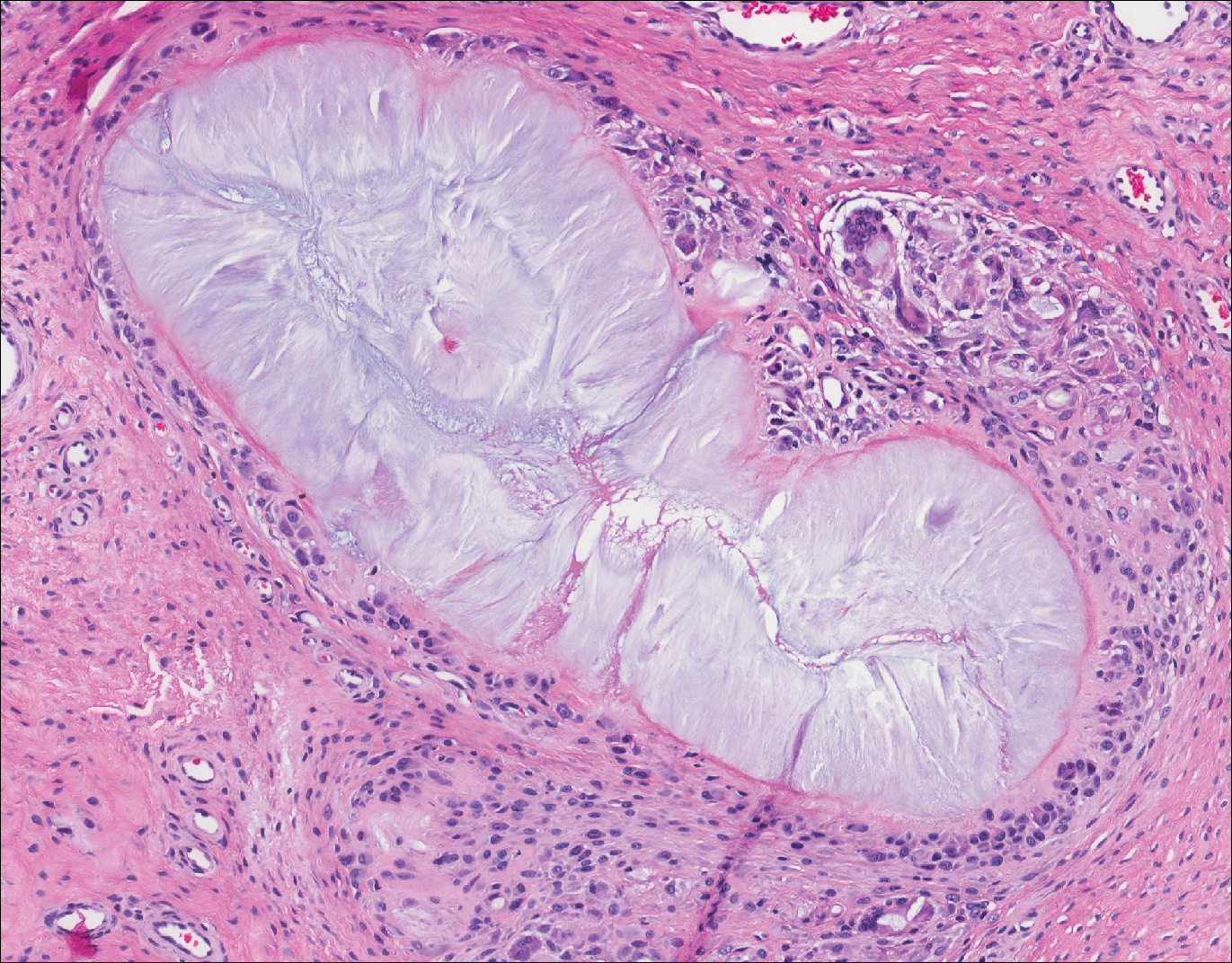
The presence of foreign material in the skin may be traumatic, occupational, cosmetic, iatrogenic, or self-inflicted, including a wide variety of substances that appear in different morphological forms on hematoxylin and eosin (H&E)-stained sections, depending on their structure and physiochemical properties.9 Although not all foreign bodies may polarize, examining the sample under polarized light is considered an important step to narrow down the differential diagnosis. The tissue reaction is primarily dependent on the nature of the substance and duration, consisting of histiocytes, macrophages, plasma cells, lymphocytes, and fibrosis.9 Activated histiocytes, multinucleated giant cells, and granulomas are classic findings that generally are seen surrounding and engulfing the foreign material (Figure 2). In addition to foreign material, substances such as calcium salts, urate crystals, extruded keratin, ruptured cysts, and hair follicles may act as foreign materials and can incite a tissue response.9 Absence of histiocytic response, granuloma formation, and fibrosis in a lesion of 1 month's duration made the tetrad bodies unlikely to be foreign material.
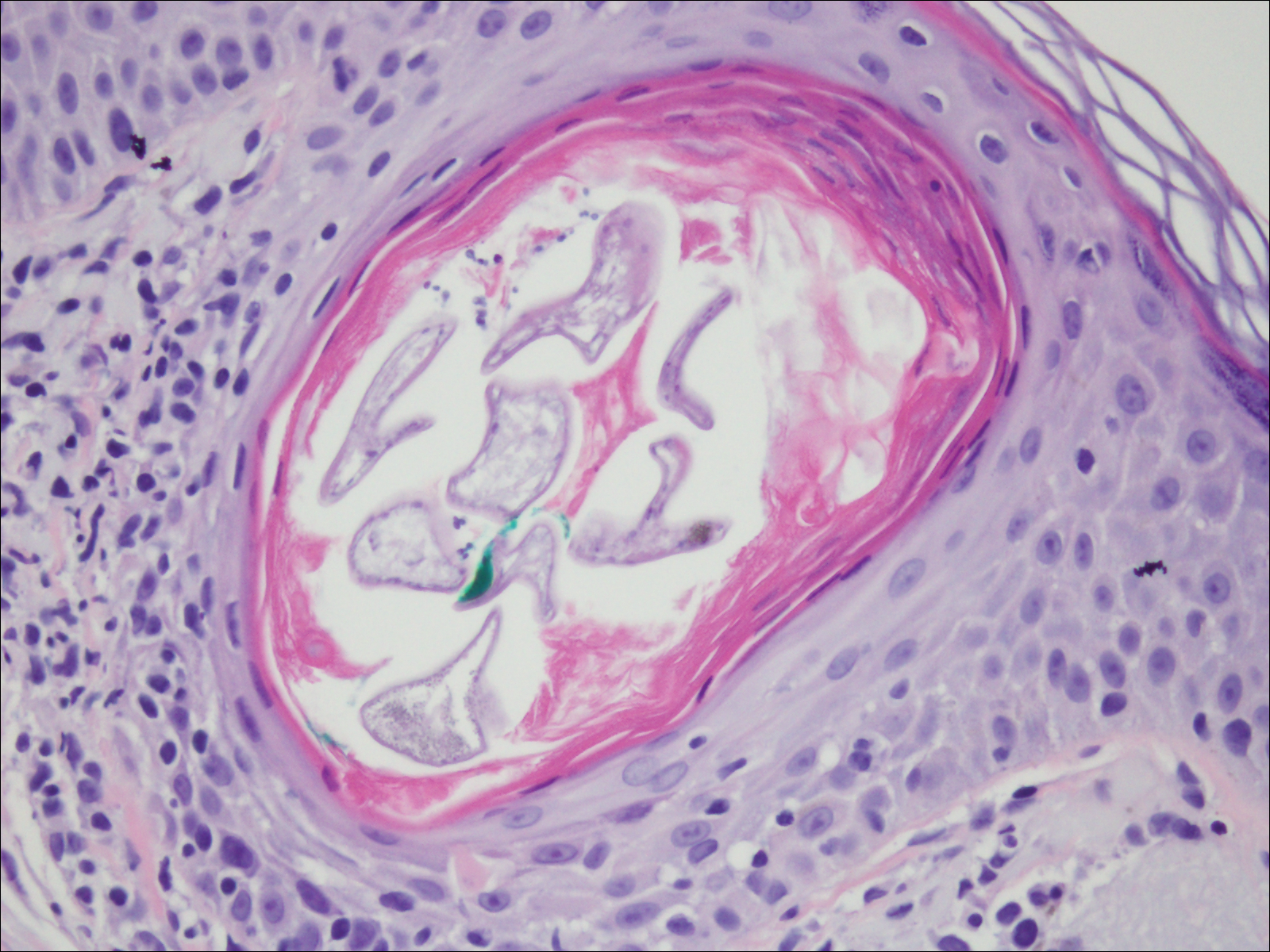
Demodex mites are superficial inhabitants of human skin that are acquired shortly after birth, live in or near pilosebaceous units, and obtain nourishment from skin cells and sebum.10,11 The mites can be recovered on 10% of skin biopsies, most commonly on the face due to high sebum production.10 Adult mites range from 0.1 to 0.4 mm in length and are round to oval in shape. Females lay eggs inside the hair follicle or sebaceous glands.11 They usually are asymptomatic, but their infestation may become pathogenic, especially in immunocompromised individuals.10 The clinical picture may resemble bacterial folliculitis, rosacea, and perioral dermatitis, while histology typically is characterized by spongiosis, lymphohistiocytic inflammation around infested follicles, and mite(s) in follicular infundibula (Figure 3). Sometimes the protrusion of mites and keratin from the follicles is seen as follicular spines on histology and referred to as pityriasis folliculorum.
Deposits of urate crystals in skin occur from the elevated serum uric acid levels in gout. The cutaneous deposits are mainly in the dermis and subcutaneous tissue and are extremely painful.12 Urate crystals get dissolved during formalin fixation and leave needlelike clefts in a homogenous, lightly basophilic material on H&E slide (Figure 4). For the same reason, polarized microscopy also is not helpful despite the birefringent nature of urate crystals.12
Fungal yeast forms appear round to oval under light microscopy, ranging from 2 to 100 μm in size.13 The common superficial forms involving the epidermis or hair follicles similar to the current case of bacterial infection include Malassezia and dermatophyte infections. Malassezia is part of the normal flora of sebum-rich areas of skin and is associated with superficial infections such as folliculitis, atopic dermatitis, psoriasis, seborrheic dermatitis, and dandruff.14Malassezia appear as clusters of yeast cells that are pleomorphic and round to oval in shape, ranging from 2 to 6 μm in size. It forms hyphae in its pathogenic form and gives rise to the classic spaghetti and meatball-like appearance that can be highlighted by periodic acid-Schiff (Figure 5) and Grocott-Gomori methenamine-silver special stains. Dermatophytes include 3 genera--Trichophyton, Microsporum, and Epidermophyton--with at least 40 species that causes skin infections in humans.14 Fungal spores and hyphae forms are restricted to the stratum corneum. The hyphae forms may not be apparent on H&E stain, and periodic acid-Schiff staining is helpful in visualizing the fungal elements. The presence of neutrophils in the corneal layer, basket weave hyperkeratosis, and presence of fungal hyphae within the corneal layer fissures (sandwich sign) are clues to the dermatophyte infection.15 Other smaller fungi such as Histoplasma capsulatum (2-4 μm), Candida (3-5 μm), and Pneumocystis (2-5 μm) species can be found in skin in disseminated infections, usually affecting immunocompromised individuals.13Histoplasma is a basophilic yeast that exhibits narrow-based budding and appears clustered within or outside of macrophages. Candida species generally are dimorphic, and yeasts are found intermingled with filamentous forms. Pneumocystis infection in skin is extremely rare, and the fungi appear as spherical or crescent-shaped bodies in a foamy amorphous material.16

- Al Rasheed MR, Senseng CG. Sarcina ventriculi: review of the literature. Arch Pathol Lab Med. 2016;140:1441-1445.
- Lam-Himlin D, Tsiatis AC, Montgomery E, et al. Sarcina organisms in the gastrointestinal tract: a clinicopathologic and molecular study. Am J Surg Pathol. 2011;35:1700-1705.
- Somerville DA, Lancaster-Smith M. The aerobic cutaneous microflora of diabetic subjects. Br J Dermatol. 1973;89:395-400.
- Hetem DJ, Rooijakkers S, Ekkelenkamp MB. Staphylococci and Micrococci. In: Cohen J, Powderly WG, Opal SM, eds. Infectious Diseases. 4th ed. Vol 2. New York, NY: Elsevier; 2017:1509-1522.
- Nordstrom KM, McGinley KJ, Cappiello L, et al. Pitted keratolysis. the role of Micrococcus sedentarius. Arch Dermatol. 1987;123:1320-1325.
- Smith KJ, Neafie R, Yeager J, et al. Micrococcus folliculitis in HIV-1 disease. Br J Dermatol. 1999;141:558-561.
- van Rensburg JJ, Lin H, Gao X, et al. The human skin microbiome associates with the outcome of and is influenced by bacterial infection. mBio. 2015;6:E01315-15. doi:10.1128/mBio.01315-15.
- Chuku A, Nwankiti OO. Association of bacteria with fungal infection of skin and soft tissue lesions in plateau state, Nigeria. Br Microbiol Res J. 2013;3:470-477.
- Molina-Ruiz AM, Requena L. Foreign body granulomas. Dermatol Clin. 2015;33:497-523.
- Elston CA, Elston DM. Demodex mites. Clin Dermatol. 2014;32:739-743.
- Rather PA, Hassan I. Human Demodex mite: the versatile mite of dermatological importance. Indian J Dermatol. 2014;59:60-66.
- Gaviria JL, Ortega VG, Gaona J, et al. Unusual dermatological manifestations of gout: review of literature and a case report. Plast Reconstr Surg Glob Open. 2015;3:E445.
- Guarner J, Brandt ME. Histopathologic diagnosis of fungal infections in the 21st century. Clin Microbiol Rev. 2011;24:247-280.
- White TC, Findley K, Dawson TL Jr, et al. Fungi on the skin: dermatophytes and Malassezia. Cold Spring Harb Perspect Med. 2014;4. pii:a019802. doi:10.1101/cshperspect.a019802.
- Gottlieb GJ, Ackerman AB. The "sandwich sign" of dermatophytosis. Am J Dermatopathol. 1986;8:347.
- Hennessey NP, Parro EL, Cockerell CJ. Cutaneous Pneumocystis carinii infection in patients with acquired immunodeficiency syndrome. Arch Dermatol. 1991;127:1699-1701.
The Diagnosis: Bacterial Infection
The tetrad arrangement of organisms seen in this case was classic for Micrococcus and Sarcina species. Both are gram-positive cocci that occur in tetrads, but Micrococcus is aerobic and catalase positive, whereas Sarcina species are anaerobic, catalase negative, acidophilic, and form spores in alkaline pH.1 Although difficult to definitively differentiate on light microscopy, micrococci are smaller in size, ranging from 0.5 to 2.0 μm, and occur in tight clusters, as seen in this case (quiz images), in contrast to Sarcina species, which are relatively larger (1.8-3.0 μm).2 Sarcinae typically are found in soil and air, are considered pathogenic, and are associated with gastric symptoms (Sarcina ventriculi).1Sarcina species also are reported to colonize the skin of patients with diabetes mellitus, but no pathogenic activity is known in the skin.3Micrococcus species, with the majority being Micrococcus luteus, are part of the normal flora of the human skin as well as the oral and nasal cavities. Occasional reports of pneumonia, endocarditis, meningitis, arthritis, endophthalmitis, and sepsis have been reported in immunocompromised individuals.4 In the skin, Micrococcus is a commensal organism; however, Micrococcus sedentarius has been associated with pitted keratolysis, and reports of Micrococcus folliculitis in human immunodeficiency virus patients also are described in the literature.5,6 Micrococci are considered opportunistic bacteria and may worsen and prolong a localized cutaneous infection caused by other organisms under favorable conditions.7Micrococcus luteus is one of the most common bacteria cultured from skin and soft tissue infections caused by fungal organisms.8 Depending on the immune status of an individual, use of broad-spectrum antibiotic and/or elimination of favorable milieu (ie, primary pathogen, breaks in skin) usually treats the infection.
Because of the rarity of infections caused and being part of the normal flora, the clinical implications of subtyping and sensitivity studies via culture or molecular studies may not be important; however, incidental presence of these organisms with unfamiliar morphology may cause confusion for the dermatopathologist. An extremely small size (0.5-2.0 μm) compared to red blood cells (7-8 μm) and white blood cells (10-12 μm) in a tight tetrad arrangement should raise the suspicion for Micrococcus.1 The refractive nature of these organisms from a thick extracellular layer can mimic fungus or plant matter; a negative Grocott-Gomori methenamine-silver stain in this case helped in not only differentiating but also ruling out secondary fungal infection. Finally, a Gram stain with violet staining of these organisms reaffirmed the diagnosis of gram-positive bacterial organisms, most consistent with Micrococcus species (Figure 1). Culture studies were not performed because of contamination of the tissue specimen and resolution of the patient's symptoms.
The presence of foreign material in the skin may be traumatic, occupational, cosmetic, iatrogenic, or self-inflicted, including a wide variety of substances that appear in different morphological forms on hematoxylin and eosin (H&E)-stained sections, depending on their structure and physiochemical properties.9 Although not all foreign bodies may polarize, examining the sample under polarized light is considered an important step to narrow down the differential diagnosis. The tissue reaction is primarily dependent on the nature of the substance and duration, consisting of histiocytes, macrophages, plasma cells, lymphocytes, and fibrosis.9 Activated histiocytes, multinucleated giant cells, and granulomas are classic findings that generally are seen surrounding and engulfing the foreign material (Figure 2). In addition to foreign material, substances such as calcium salts, urate crystals, extruded keratin, ruptured cysts, and hair follicles may act as foreign materials and can incite a tissue response.9 Absence of histiocytic response, granuloma formation, and fibrosis in a lesion of 1 month's duration made the tetrad bodies unlikely to be foreign material.
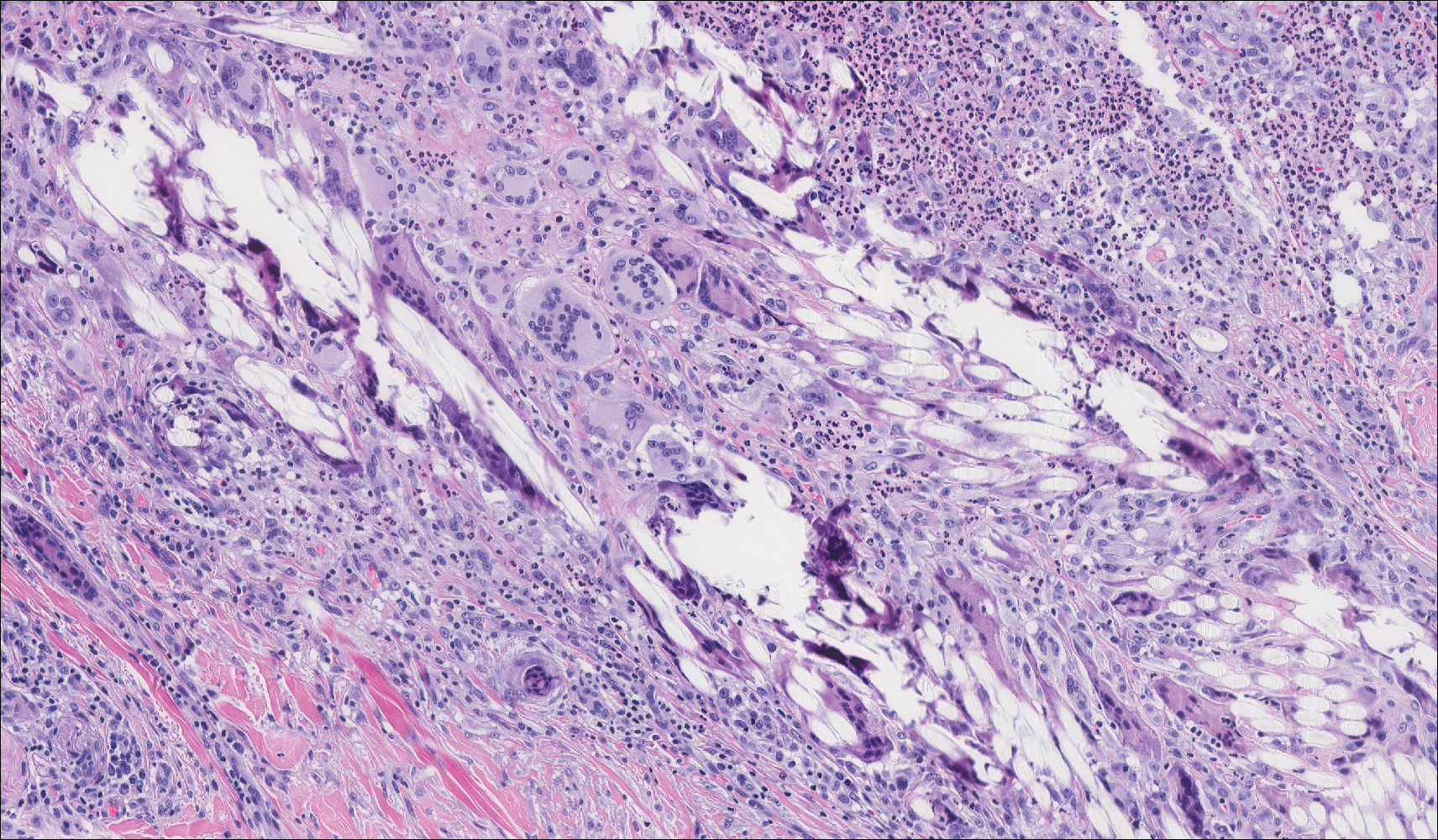
Demodex mites are superficial inhabitants of human skin that are acquired shortly after birth, live in or near pilosebaceous units, and obtain nourishment from skin cells and sebum.10,11 The mites can be recovered on 10% of skin biopsies, most commonly on the face due to high sebum production.10 Adult mites range from 0.1 to 0.4 mm in length and are round to oval in shape. Females lay eggs inside the hair follicle or sebaceous glands.11 They usually are asymptomatic, but their infestation may become pathogenic, especially in immunocompromised individuals.10 The clinical picture may resemble bacterial folliculitis, rosacea, and perioral dermatitis, while histology typically is characterized by spongiosis, lymphohistiocytic inflammation around infested follicles, and mite(s) in follicular infundibula (Figure 3). Sometimes the protrusion of mites and keratin from the follicles is seen as follicular spines on histology and referred to as pityriasis folliculorum.
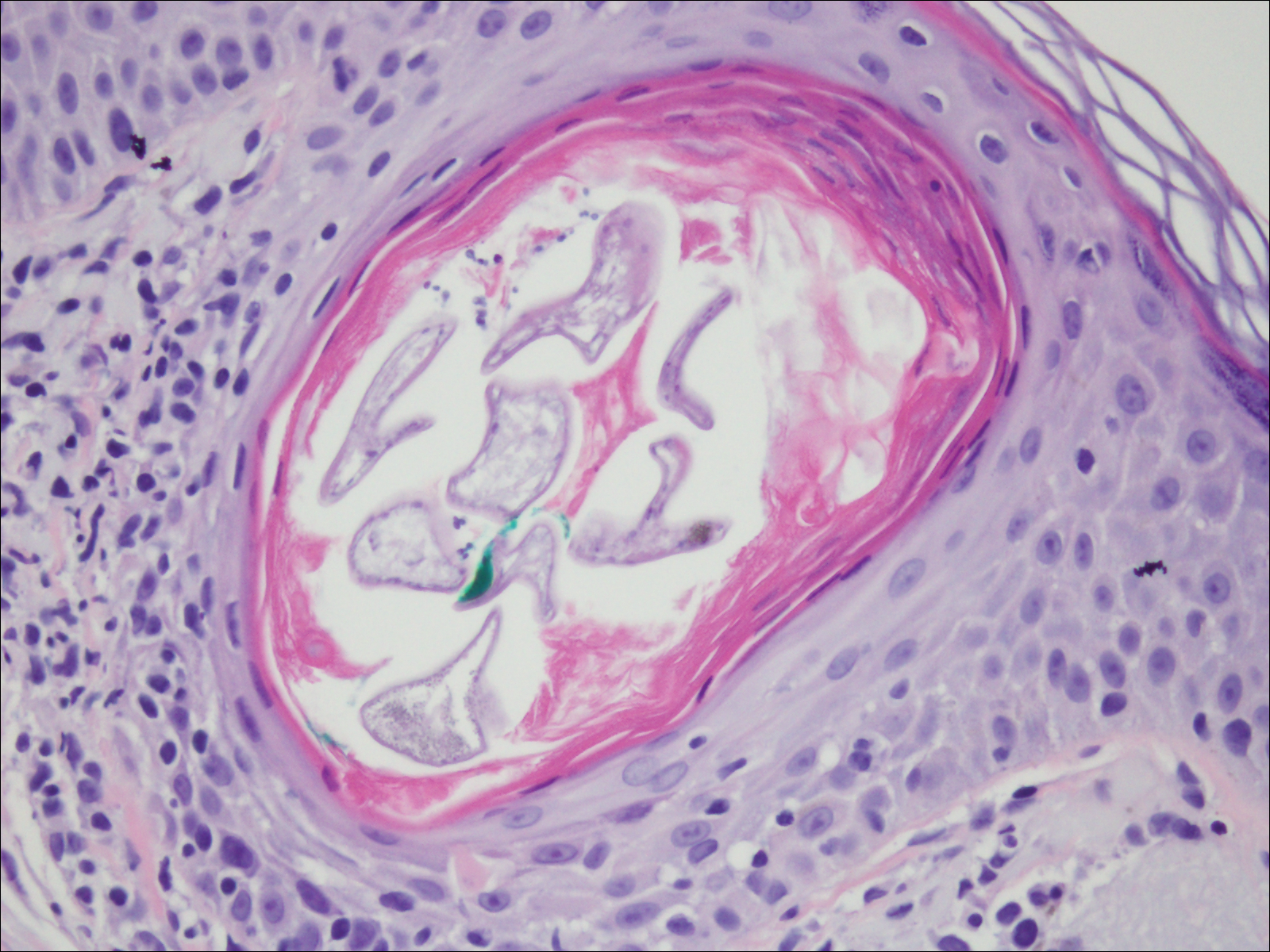
Deposits of urate crystals in skin occur from the elevated serum uric acid levels in gout. The cutaneous deposits are mainly in the dermis and subcutaneous tissue and are extremely painful.12 Urate crystals get dissolved during formalin fixation and leave needlelike clefts in a homogenous, lightly basophilic material on H&E slide (Figure 4). For the same reason, polarized microscopy also is not helpful despite the birefringent nature of urate crystals.12
Fungal yeast forms appear round to oval under light microscopy, ranging from 2 to 100 μm in size.13 The common superficial forms involving the epidermis or hair follicles similar to the current case of bacterial infection include Malassezia and dermatophyte infections. Malassezia is part of the normal flora of sebum-rich areas of skin and is associated with superficial infections such as folliculitis, atopic dermatitis, psoriasis, seborrheic dermatitis, and dandruff.14Malassezia appear as clusters of yeast cells that are pleomorphic and round to oval in shape, ranging from 2 to 6 μm in size. It forms hyphae in its pathogenic form and gives rise to the classic spaghetti and meatball-like appearance that can be highlighted by periodic acid-Schiff (Figure 5) and Grocott-Gomori methenamine-silver special stains. Dermatophytes include 3 genera--Trichophyton, Microsporum, and Epidermophyton--with at least 40 species that causes skin infections in humans.14 Fungal spores and hyphae forms are restricted to the stratum corneum. The hyphae forms may not be apparent on H&E stain, and periodic acid-Schiff staining is helpful in visualizing the fungal elements. The presence of neutrophils in the corneal layer, basket weave hyperkeratosis, and presence of fungal hyphae within the corneal layer fissures (sandwich sign) are clues to the dermatophyte infection.15 Other smaller fungi such as Histoplasma capsulatum (2-4 μm), Candida (3-5 μm), and Pneumocystis (2-5 μm) species can be found in skin in disseminated infections, usually affecting immunocompromised individuals.13Histoplasma is a basophilic yeast that exhibits narrow-based budding and appears clustered within or outside of macrophages. Candida species generally are dimorphic, and yeasts are found intermingled with filamentous forms. Pneumocystis infection in skin is extremely rare, and the fungi appear as spherical or crescent-shaped bodies in a foamy amorphous material.16

The Diagnosis: Bacterial Infection
The tetrad arrangement of organisms seen in this case was classic for Micrococcus and Sarcina species. Both are gram-positive cocci that occur in tetrads, but Micrococcus is aerobic and catalase positive, whereas Sarcina species are anaerobic, catalase negative, acidophilic, and form spores in alkaline pH.1 Although difficult to definitively differentiate on light microscopy, micrococci are smaller in size, ranging from 0.5 to 2.0 μm, and occur in tight clusters, as seen in this case (quiz images), in contrast to Sarcina species, which are relatively larger (1.8-3.0 μm).2 Sarcinae typically are found in soil and air, are considered pathogenic, and are associated with gastric symptoms (Sarcina ventriculi).1Sarcina species also are reported to colonize the skin of patients with diabetes mellitus, but no pathogenic activity is known in the skin.3Micrococcus species, with the majority being Micrococcus luteus, are part of the normal flora of the human skin as well as the oral and nasal cavities. Occasional reports of pneumonia, endocarditis, meningitis, arthritis, endophthalmitis, and sepsis have been reported in immunocompromised individuals.4 In the skin, Micrococcus is a commensal organism; however, Micrococcus sedentarius has been associated with pitted keratolysis, and reports of Micrococcus folliculitis in human immunodeficiency virus patients also are described in the literature.5,6 Micrococci are considered opportunistic bacteria and may worsen and prolong a localized cutaneous infection caused by other organisms under favorable conditions.7Micrococcus luteus is one of the most common bacteria cultured from skin and soft tissue infections caused by fungal organisms.8 Depending on the immune status of an individual, use of broad-spectrum antibiotic and/or elimination of favorable milieu (ie, primary pathogen, breaks in skin) usually treats the infection.
Because of the rarity of infections caused and being part of the normal flora, the clinical implications of subtyping and sensitivity studies via culture or molecular studies may not be important; however, incidental presence of these organisms with unfamiliar morphology may cause confusion for the dermatopathologist. An extremely small size (0.5-2.0 μm) compared to red blood cells (7-8 μm) and white blood cells (10-12 μm) in a tight tetrad arrangement should raise the suspicion for Micrococcus.1 The refractive nature of these organisms from a thick extracellular layer can mimic fungus or plant matter; a negative Grocott-Gomori methenamine-silver stain in this case helped in not only differentiating but also ruling out secondary fungal infection. Finally, a Gram stain with violet staining of these organisms reaffirmed the diagnosis of gram-positive bacterial organisms, most consistent with Micrococcus species (Figure 1). Culture studies were not performed because of contamination of the tissue specimen and resolution of the patient's symptoms.
The presence of foreign material in the skin may be traumatic, occupational, cosmetic, iatrogenic, or self-inflicted, including a wide variety of substances that appear in different morphological forms on hematoxylin and eosin (H&E)-stained sections, depending on their structure and physiochemical properties.9 Although not all foreign bodies may polarize, examining the sample under polarized light is considered an important step to narrow down the differential diagnosis. The tissue reaction is primarily dependent on the nature of the substance and duration, consisting of histiocytes, macrophages, plasma cells, lymphocytes, and fibrosis.9 Activated histiocytes, multinucleated giant cells, and granulomas are classic findings that generally are seen surrounding and engulfing the foreign material (Figure 2). In addition to foreign material, substances such as calcium salts, urate crystals, extruded keratin, ruptured cysts, and hair follicles may act as foreign materials and can incite a tissue response.9 Absence of histiocytic response, granuloma formation, and fibrosis in a lesion of 1 month's duration made the tetrad bodies unlikely to be foreign material.
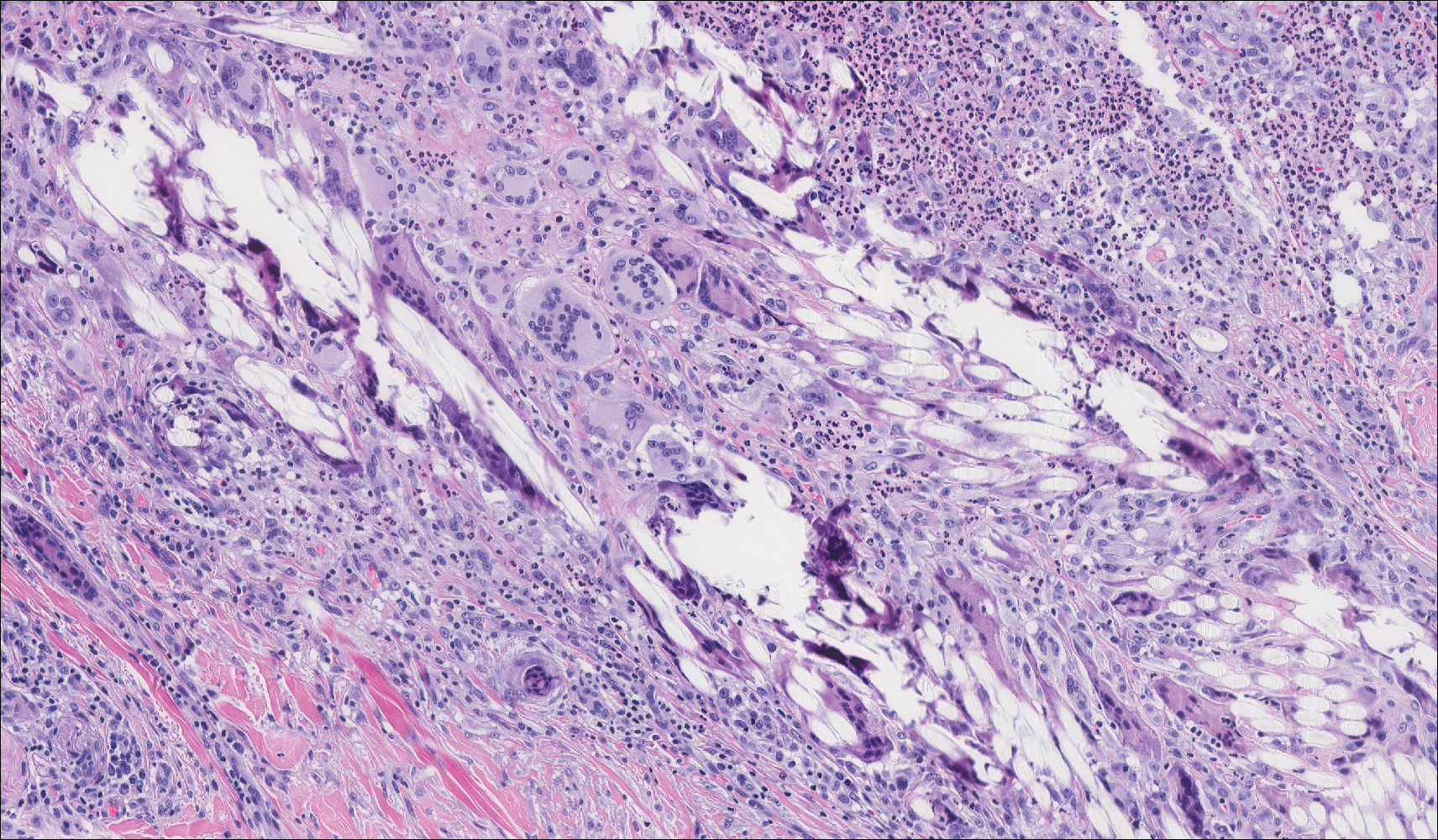
Demodex mites are superficial inhabitants of human skin that are acquired shortly after birth, live in or near pilosebaceous units, and obtain nourishment from skin cells and sebum.10,11 The mites can be recovered on 10% of skin biopsies, most commonly on the face due to high sebum production.10 Adult mites range from 0.1 to 0.4 mm in length and are round to oval in shape. Females lay eggs inside the hair follicle or sebaceous glands.11 They usually are asymptomatic, but their infestation may become pathogenic, especially in immunocompromised individuals.10 The clinical picture may resemble bacterial folliculitis, rosacea, and perioral dermatitis, while histology typically is characterized by spongiosis, lymphohistiocytic inflammation around infested follicles, and mite(s) in follicular infundibula (Figure 3). Sometimes the protrusion of mites and keratin from the follicles is seen as follicular spines on histology and referred to as pityriasis folliculorum.
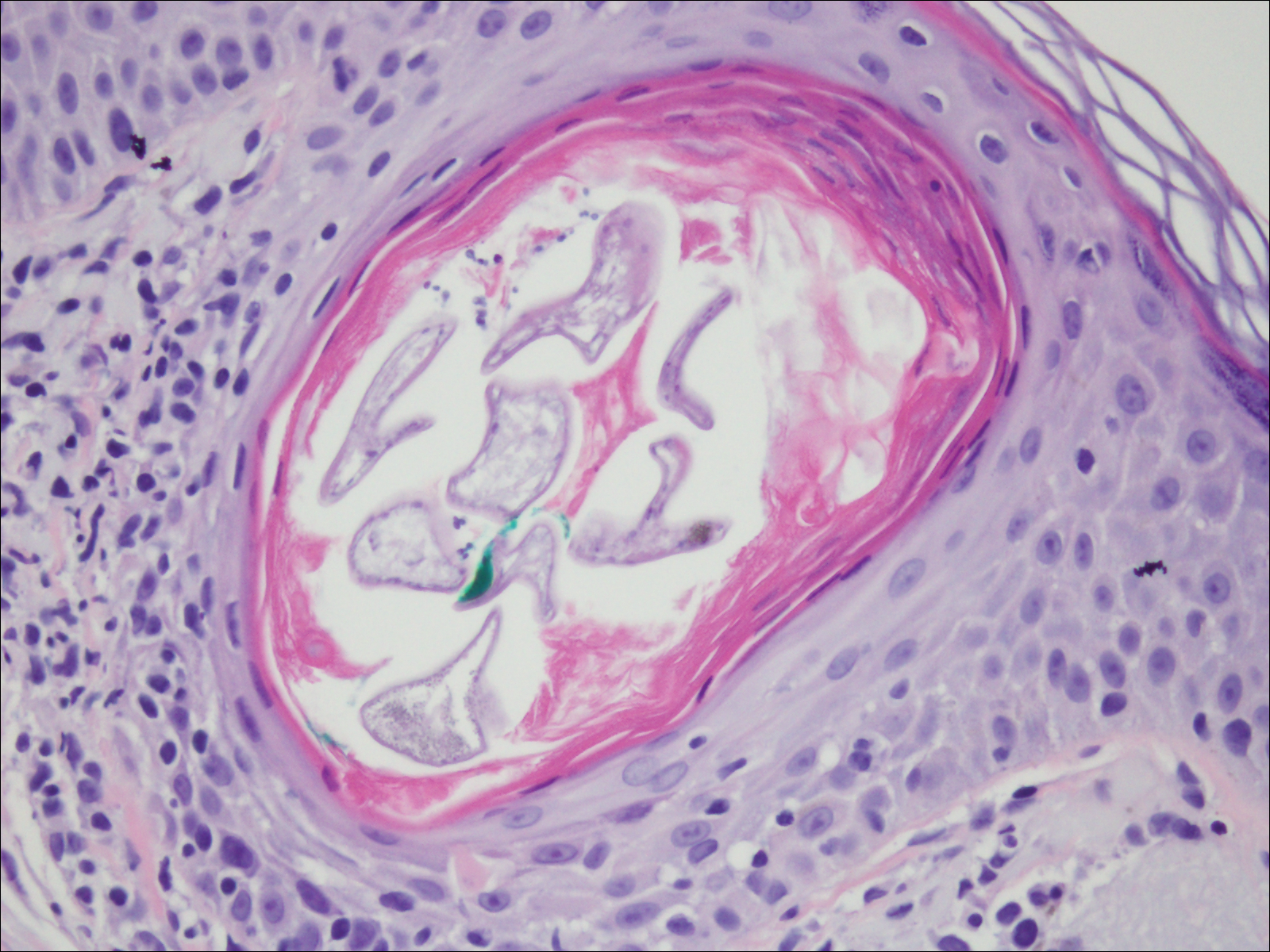
Deposits of urate crystals in skin occur from the elevated serum uric acid levels in gout. The cutaneous deposits are mainly in the dermis and subcutaneous tissue and are extremely painful.12 Urate crystals get dissolved during formalin fixation and leave needlelike clefts in a homogenous, lightly basophilic material on H&E slide (Figure 4). For the same reason, polarized microscopy also is not helpful despite the birefringent nature of urate crystals.12
Fungal yeast forms appear round to oval under light microscopy, ranging from 2 to 100 μm in size.13 The common superficial forms involving the epidermis or hair follicles similar to the current case of bacterial infection include Malassezia and dermatophyte infections. Malassezia is part of the normal flora of sebum-rich areas of skin and is associated with superficial infections such as folliculitis, atopic dermatitis, psoriasis, seborrheic dermatitis, and dandruff.14Malassezia appear as clusters of yeast cells that are pleomorphic and round to oval in shape, ranging from 2 to 6 μm in size. It forms hyphae in its pathogenic form and gives rise to the classic spaghetti and meatball-like appearance that can be highlighted by periodic acid-Schiff (Figure 5) and Grocott-Gomori methenamine-silver special stains. Dermatophytes include 3 genera--Trichophyton, Microsporum, and Epidermophyton--with at least 40 species that causes skin infections in humans.14 Fungal spores and hyphae forms are restricted to the stratum corneum. The hyphae forms may not be apparent on H&E stain, and periodic acid-Schiff staining is helpful in visualizing the fungal elements. The presence of neutrophils in the corneal layer, basket weave hyperkeratosis, and presence of fungal hyphae within the corneal layer fissures (sandwich sign) are clues to the dermatophyte infection.15 Other smaller fungi such as Histoplasma capsulatum (2-4 μm), Candida (3-5 μm), and Pneumocystis (2-5 μm) species can be found in skin in disseminated infections, usually affecting immunocompromised individuals.13Histoplasma is a basophilic yeast that exhibits narrow-based budding and appears clustered within or outside of macrophages. Candida species generally are dimorphic, and yeasts are found intermingled with filamentous forms. Pneumocystis infection in skin is extremely rare, and the fungi appear as spherical or crescent-shaped bodies in a foamy amorphous material.16

- Al Rasheed MR, Senseng CG. Sarcina ventriculi: review of the literature. Arch Pathol Lab Med. 2016;140:1441-1445.
- Lam-Himlin D, Tsiatis AC, Montgomery E, et al. Sarcina organisms in the gastrointestinal tract: a clinicopathologic and molecular study. Am J Surg Pathol. 2011;35:1700-1705.
- Somerville DA, Lancaster-Smith M. The aerobic cutaneous microflora of diabetic subjects. Br J Dermatol. 1973;89:395-400.
- Hetem DJ, Rooijakkers S, Ekkelenkamp MB. Staphylococci and Micrococci. In: Cohen J, Powderly WG, Opal SM, eds. Infectious Diseases. 4th ed. Vol 2. New York, NY: Elsevier; 2017:1509-1522.
- Nordstrom KM, McGinley KJ, Cappiello L, et al. Pitted keratolysis. the role of Micrococcus sedentarius. Arch Dermatol. 1987;123:1320-1325.
- Smith KJ, Neafie R, Yeager J, et al. Micrococcus folliculitis in HIV-1 disease. Br J Dermatol. 1999;141:558-561.
- van Rensburg JJ, Lin H, Gao X, et al. The human skin microbiome associates with the outcome of and is influenced by bacterial infection. mBio. 2015;6:E01315-15. doi:10.1128/mBio.01315-15.
- Chuku A, Nwankiti OO. Association of bacteria with fungal infection of skin and soft tissue lesions in plateau state, Nigeria. Br Microbiol Res J. 2013;3:470-477.
- Molina-Ruiz AM, Requena L. Foreign body granulomas. Dermatol Clin. 2015;33:497-523.
- Elston CA, Elston DM. Demodex mites. Clin Dermatol. 2014;32:739-743.
- Rather PA, Hassan I. Human Demodex mite: the versatile mite of dermatological importance. Indian J Dermatol. 2014;59:60-66.
- Gaviria JL, Ortega VG, Gaona J, et al. Unusual dermatological manifestations of gout: review of literature and a case report. Plast Reconstr Surg Glob Open. 2015;3:E445.
- Guarner J, Brandt ME. Histopathologic diagnosis of fungal infections in the 21st century. Clin Microbiol Rev. 2011;24:247-280.
- White TC, Findley K, Dawson TL Jr, et al. Fungi on the skin: dermatophytes and Malassezia. Cold Spring Harb Perspect Med. 2014;4. pii:a019802. doi:10.1101/cshperspect.a019802.
- Gottlieb GJ, Ackerman AB. The "sandwich sign" of dermatophytosis. Am J Dermatopathol. 1986;8:347.
- Hennessey NP, Parro EL, Cockerell CJ. Cutaneous Pneumocystis carinii infection in patients with acquired immunodeficiency syndrome. Arch Dermatol. 1991;127:1699-1701.
- Al Rasheed MR, Senseng CG. Sarcina ventriculi: review of the literature. Arch Pathol Lab Med. 2016;140:1441-1445.
- Lam-Himlin D, Tsiatis AC, Montgomery E, et al. Sarcina organisms in the gastrointestinal tract: a clinicopathologic and molecular study. Am J Surg Pathol. 2011;35:1700-1705.
- Somerville DA, Lancaster-Smith M. The aerobic cutaneous microflora of diabetic subjects. Br J Dermatol. 1973;89:395-400.
- Hetem DJ, Rooijakkers S, Ekkelenkamp MB. Staphylococci and Micrococci. In: Cohen J, Powderly WG, Opal SM, eds. Infectious Diseases. 4th ed. Vol 2. New York, NY: Elsevier; 2017:1509-1522.
- Nordstrom KM, McGinley KJ, Cappiello L, et al. Pitted keratolysis. the role of Micrococcus sedentarius. Arch Dermatol. 1987;123:1320-1325.
- Smith KJ, Neafie R, Yeager J, et al. Micrococcus folliculitis in HIV-1 disease. Br J Dermatol. 1999;141:558-561.
- van Rensburg JJ, Lin H, Gao X, et al. The human skin microbiome associates with the outcome of and is influenced by bacterial infection. mBio. 2015;6:E01315-15. doi:10.1128/mBio.01315-15.
- Chuku A, Nwankiti OO. Association of bacteria with fungal infection of skin and soft tissue lesions in plateau state, Nigeria. Br Microbiol Res J. 2013;3:470-477.
- Molina-Ruiz AM, Requena L. Foreign body granulomas. Dermatol Clin. 2015;33:497-523.
- Elston CA, Elston DM. Demodex mites. Clin Dermatol. 2014;32:739-743.
- Rather PA, Hassan I. Human Demodex mite: the versatile mite of dermatological importance. Indian J Dermatol. 2014;59:60-66.
- Gaviria JL, Ortega VG, Gaona J, et al. Unusual dermatological manifestations of gout: review of literature and a case report. Plast Reconstr Surg Glob Open. 2015;3:E445.
- Guarner J, Brandt ME. Histopathologic diagnosis of fungal infections in the 21st century. Clin Microbiol Rev. 2011;24:247-280.
- White TC, Findley K, Dawson TL Jr, et al. Fungi on the skin: dermatophytes and Malassezia. Cold Spring Harb Perspect Med. 2014;4. pii:a019802. doi:10.1101/cshperspect.a019802.
- Gottlieb GJ, Ackerman AB. The "sandwich sign" of dermatophytosis. Am J Dermatopathol. 1986;8:347.
- Hennessey NP, Parro EL, Cockerell CJ. Cutaneous Pneumocystis carinii infection in patients with acquired immunodeficiency syndrome. Arch Dermatol. 1991;127:1699-1701.
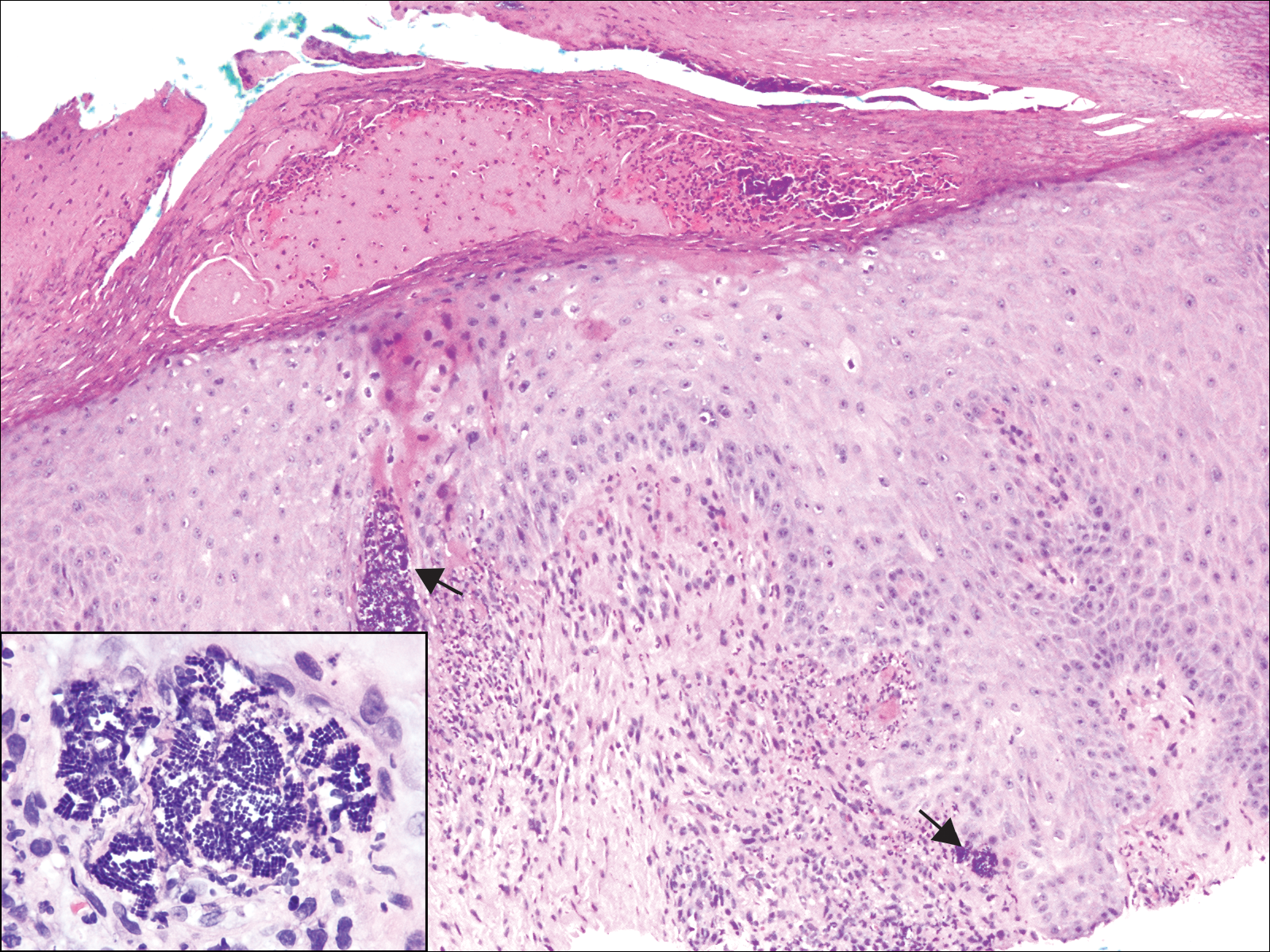
A 72-year-old woman with a medical history notable for multiple sclerosis and intravenous drug abuse presented to the dermatology clinic with a 0.6×0.5-cm, pruritic, wartlike, inflamed, keratotic papule on the palmar aspect of the right finger of more than 1 month's duration. A shave biopsy was performed that showed excoriation with serum crust, parakeratosis, and neutrophilic infiltrate in the papillary dermis. Within the serum crust and at the dermoepidermal junction, clusters of refractive basophilic bodies (arrows) in tetrad arrangement also were noted (inset). The papule resolved after the biopsy without any additional treatment.
Researchers Investigate Nontraditional Methods of Providing CBT-I
Studies compare telehealth with in-person treatment and examine two Internet-based methods of delivering CBT-I.
BALTIMORE—Cognitive behavioral therapy for insomnia (CBT-I) is an effective treatment, but a scarcity of trained clinicians has limited patients’ access to it. Telehealth and Internet-based platforms could broaden access to CBT-I, and investigators presented research on the efficacy of these methods of administration at the 32nd Annual Meeting of the Associated Professional Sleep Societies.
CBT-I by Telehealth Is Noninferior to In-Person CBT-I
Philip Gehrman, PhD, Associate Professor of Psychology at the University of Pennsylvania and the Philadelphia VA Medical Center, and colleagues conducted a cluster-randomized trial to determine whether group CBT-I delivered by telehealth was noninferior to CBT-I delivered in person. Eligible participants were veterans with posttraumatic stress disorder (PTSD) and an Insomnia Severity Index (ISI) score of 15 or higher. The investigators randomized 95 participants in groups of six to eight to group CBT-I in person or by telehealth. The primary outcome was the change in ISI score from baseline to the three-month follow-up. Dr. Gehrman and colleagues defined treatment inferiority as a difference of greater than two points on the ISI score.
Participants’ mean age was 55.6, about 91% of the sample was male, and 42.2% of the sample was African American. The study population generally was overweight and had severe PTSD. Approximately half of the population was receiving one or more psychotropic medication. Forty-six participants were randomized to in-person CBT-I, and 49 were randomized to CBT-I delivered by telehealth.
At three months, the mean change in ISI score was 6.48 for in-person CBT-I and 4.45 for telehealth CBT-I. The difference between groups was outside of the prespecified margin of inferiority, and the researchers concluded that CBT-I delivered by telehealth was noninferior to in-person CBT-I.
The overall effectiveness of both methods of administration was modest, said Dr. Gehrman. The effect size might be greater in a group with fewer comorbidities or in a group that received more treatment sessions, he added. Nevertheless, the results “demonstrate that CBT-I can be effective even in a complex patient population,” he concluded.
SHUTi May Be Inferior to In-Person CBT-I
The online CBT-I intervention Sleep Healthy Using the Internet (SHUTi) has reduced insomnia with effect sizes similar to those of traditional CBT-I. No researchers had compared the two techniques directly, however. Håvard Kallestad, PhD, a clinical psychologist at Saint Olav’s Hospital in Trondheim, Norway, and colleagues examined whether SHUTi was a noninferior treatment for insomnia, compared with in-person CBT-I.
Eligible participants were 18 or older, had a diagnosis of insomnia, had been referred to a sleep clinic, and had access to a computer and adequate computer skills. Participants were randomized to in-person CBT-I or SHUTi. The primary outcome was ISI score, and three therapists assessed participants’ outcomes at baseline, after treatment, and at six months. They defined noninferiority as a difference between treatments of 2 or fewer points on ISI score.
Dr. Kallestad and colleagues randomized 52 participants to in-person CBT-I and 49 to SHUTi. Mean duration of insomnia was about 13 years. Approximately 60% of participants were currently using sleep medication, and about 90% had had previous treatment with sleep medication. After treatment, two patients in the in-person group and five in the SHUTi group were lost to follow-up. At six months, four participants in the in-person group and eight in the SHUTi group were lost to follow-up.
Both study arms had significantly lower ISI scores after treatment and at six months. After treatment, the mean ISI score in the in-person group was 5.1 points lower than in the SHUTi group, indicating that SHUTi was inferior at that time. At six months, mean ISI score was 3.3 points lower in the in-person group than in the SHUTi group. Because part of the confidence interval overlapped with the noninferiority margin, the result was inconclusive.
After treatment, the response rate was 70% in the in-person group and 43% in the SHUTi group. The remission rate was 52% in the in-person group and 18% in the SHUTi group. At six months, the response rate was 65% for the in-person group and 46% for the SHUTi group. The remission rate was 56% in the in-person group and 24% in the SHUTi group.
“SHUTi did not have the same effectiveness in this patient sample, compared with previous studies,” said Dr. Kallestad. One reason could be that previous studies included self-selected participants, rather than patients who had been referred to a sleep clinic. Also, the researchers interviewed all participants at baseline, and SHUTi might have seemed “more limited” in comparison with the interview, Dr. Kallestad concluded.
Digital CBT-I May Prevent Incident Depression
Insomnia is a modifiable risk factor for depression, and research has indicated that CBT-I reduces the severity of depression. Investigators also have shown that digitally delivered CBT-I effectively reduces insomnia and depression. Phillip C. Cheng, PhD, a researcher at the Henry Ford Health System in Detroit, and colleagues sought to determine whether digitally delivered CBT-I could prevent incident depression.
The researchers randomized 658 people with insomnia to Sleepio, an Internet-based CBT-I treatment, or to a control condition of online sleep education. The study’s primary outcome was the Quick Inventory of Depressive Symptomatology (QIDS), and Dr. Cheng’s group defined depression as a score greater than 10 on the QIDS. The researchers also examined participants’ ISI scores and functional outcomes such as work productivity, social functioning, cognitive functioning, and resilience. Assessments were performed at baseline, after treatment, and at one year.
In all, 358 participants were randomized to Sleepio, and 300 were randomized to sleep education. The patient population was predominantly female, was racially diverse, and had a diversity of educational attainment. The demographics of the study arms did not differ significantly.
After treatment, the rate of incident depression was 11% in the sleep education group and 6.5% in the Sleepio group. The difference between arms was not statistically significant. At one year, the rate of incident depression was 22% in the sleep education group and 5.1% in the Sleepio group. The difference between arms at one year was statistically significant, as was the change in depression incidence over time in the sleep education group.
Among patients who did not develop depression, ISI score decreased to a value below the cutoff for insomnia, regardless of study arm. ISI score did not change significantly among participants who developed depression, however. Work productivity, social functioning, cognitive functioning, and resilience improved more in the Sleepio group than in the sleep education group.
The results indicate that “digitally delivered CBT-I may prevent incident depression in adults with insomnia,” said Dr. Cheng. Each episode of depression increases the risk of relapse of depression, which underscores the significance of preventing incident depression, he added. Digital CBT-I also appears to reduce the economic burden associated with depression, and further studies could clarify whether it improves resilience, Dr. Cheng concluded.
—Erik Greb
Suggested Reading
Espie CA, Kyle SD, Williams C, et al. A randomized, placebo-controlled trial of online cognitive behavioral therapy for chronic insomnia disorder delivered via an automated media-rich web application. Sleep. 2012;35(6):769-781.
Gehrman P, Shah MT, Miles A, et al. Feasibility of group cognitive-behavioral treatment of insomnia delivered by clinical video telehealth. Telemed J E Health. 2016;22(12):1041-1046.
Hagatun S, Vedaa Ø, Nordgreen T, et al. The short-term efficacy of an unguided internet-based cognitive-behavioral therapy for insomnia: a randomized controlled trial with a six-month nonrandomized follow-up. Behav Sleep Med. 2017 Mar 27 [Epub ahead of print].
Ye YY, Chen NK, Chen J, et al. Internet-based cognitive-behavioural therapy for insomnia (ICBT-i): a meta-analysis of randomised controlled trials. BMJ Open. 2016;6(11):e010707.
Studies compare telehealth with in-person treatment and examine two Internet-based methods of delivering CBT-I.
Studies compare telehealth with in-person treatment and examine two Internet-based methods of delivering CBT-I.
BALTIMORE—Cognitive behavioral therapy for insomnia (CBT-I) is an effective treatment, but a scarcity of trained clinicians has limited patients’ access to it. Telehealth and Internet-based platforms could broaden access to CBT-I, and investigators presented research on the efficacy of these methods of administration at the 32nd Annual Meeting of the Associated Professional Sleep Societies.
CBT-I by Telehealth Is Noninferior to In-Person CBT-I
Philip Gehrman, PhD, Associate Professor of Psychology at the University of Pennsylvania and the Philadelphia VA Medical Center, and colleagues conducted a cluster-randomized trial to determine whether group CBT-I delivered by telehealth was noninferior to CBT-I delivered in person. Eligible participants were veterans with posttraumatic stress disorder (PTSD) and an Insomnia Severity Index (ISI) score of 15 or higher. The investigators randomized 95 participants in groups of six to eight to group CBT-I in person or by telehealth. The primary outcome was the change in ISI score from baseline to the three-month follow-up. Dr. Gehrman and colleagues defined treatment inferiority as a difference of greater than two points on the ISI score.
Participants’ mean age was 55.6, about 91% of the sample was male, and 42.2% of the sample was African American. The study population generally was overweight and had severe PTSD. Approximately half of the population was receiving one or more psychotropic medication. Forty-six participants were randomized to in-person CBT-I, and 49 were randomized to CBT-I delivered by telehealth.
At three months, the mean change in ISI score was 6.48 for in-person CBT-I and 4.45 for telehealth CBT-I. The difference between groups was outside of the prespecified margin of inferiority, and the researchers concluded that CBT-I delivered by telehealth was noninferior to in-person CBT-I.
The overall effectiveness of both methods of administration was modest, said Dr. Gehrman. The effect size might be greater in a group with fewer comorbidities or in a group that received more treatment sessions, he added. Nevertheless, the results “demonstrate that CBT-I can be effective even in a complex patient population,” he concluded.
SHUTi May Be Inferior to In-Person CBT-I
The online CBT-I intervention Sleep Healthy Using the Internet (SHUTi) has reduced insomnia with effect sizes similar to those of traditional CBT-I. No researchers had compared the two techniques directly, however. Håvard Kallestad, PhD, a clinical psychologist at Saint Olav’s Hospital in Trondheim, Norway, and colleagues examined whether SHUTi was a noninferior treatment for insomnia, compared with in-person CBT-I.
Eligible participants were 18 or older, had a diagnosis of insomnia, had been referred to a sleep clinic, and had access to a computer and adequate computer skills. Participants were randomized to in-person CBT-I or SHUTi. The primary outcome was ISI score, and three therapists assessed participants’ outcomes at baseline, after treatment, and at six months. They defined noninferiority as a difference between treatments of 2 or fewer points on ISI score.
Dr. Kallestad and colleagues randomized 52 participants to in-person CBT-I and 49 to SHUTi. Mean duration of insomnia was about 13 years. Approximately 60% of participants were currently using sleep medication, and about 90% had had previous treatment with sleep medication. After treatment, two patients in the in-person group and five in the SHUTi group were lost to follow-up. At six months, four participants in the in-person group and eight in the SHUTi group were lost to follow-up.
Both study arms had significantly lower ISI scores after treatment and at six months. After treatment, the mean ISI score in the in-person group was 5.1 points lower than in the SHUTi group, indicating that SHUTi was inferior at that time. At six months, mean ISI score was 3.3 points lower in the in-person group than in the SHUTi group. Because part of the confidence interval overlapped with the noninferiority margin, the result was inconclusive.
After treatment, the response rate was 70% in the in-person group and 43% in the SHUTi group. The remission rate was 52% in the in-person group and 18% in the SHUTi group. At six months, the response rate was 65% for the in-person group and 46% for the SHUTi group. The remission rate was 56% in the in-person group and 24% in the SHUTi group.
“SHUTi did not have the same effectiveness in this patient sample, compared with previous studies,” said Dr. Kallestad. One reason could be that previous studies included self-selected participants, rather than patients who had been referred to a sleep clinic. Also, the researchers interviewed all participants at baseline, and SHUTi might have seemed “more limited” in comparison with the interview, Dr. Kallestad concluded.
Digital CBT-I May Prevent Incident Depression
Insomnia is a modifiable risk factor for depression, and research has indicated that CBT-I reduces the severity of depression. Investigators also have shown that digitally delivered CBT-I effectively reduces insomnia and depression. Phillip C. Cheng, PhD, a researcher at the Henry Ford Health System in Detroit, and colleagues sought to determine whether digitally delivered CBT-I could prevent incident depression.
The researchers randomized 658 people with insomnia to Sleepio, an Internet-based CBT-I treatment, or to a control condition of online sleep education. The study’s primary outcome was the Quick Inventory of Depressive Symptomatology (QIDS), and Dr. Cheng’s group defined depression as a score greater than 10 on the QIDS. The researchers also examined participants’ ISI scores and functional outcomes such as work productivity, social functioning, cognitive functioning, and resilience. Assessments were performed at baseline, after treatment, and at one year.
In all, 358 participants were randomized to Sleepio, and 300 were randomized to sleep education. The patient population was predominantly female, was racially diverse, and had a diversity of educational attainment. The demographics of the study arms did not differ significantly.
After treatment, the rate of incident depression was 11% in the sleep education group and 6.5% in the Sleepio group. The difference between arms was not statistically significant. At one year, the rate of incident depression was 22% in the sleep education group and 5.1% in the Sleepio group. The difference between arms at one year was statistically significant, as was the change in depression incidence over time in the sleep education group.
Among patients who did not develop depression, ISI score decreased to a value below the cutoff for insomnia, regardless of study arm. ISI score did not change significantly among participants who developed depression, however. Work productivity, social functioning, cognitive functioning, and resilience improved more in the Sleepio group than in the sleep education group.
The results indicate that “digitally delivered CBT-I may prevent incident depression in adults with insomnia,” said Dr. Cheng. Each episode of depression increases the risk of relapse of depression, which underscores the significance of preventing incident depression, he added. Digital CBT-I also appears to reduce the economic burden associated with depression, and further studies could clarify whether it improves resilience, Dr. Cheng concluded.
—Erik Greb
Suggested Reading
Espie CA, Kyle SD, Williams C, et al. A randomized, placebo-controlled trial of online cognitive behavioral therapy for chronic insomnia disorder delivered via an automated media-rich web application. Sleep. 2012;35(6):769-781.
Gehrman P, Shah MT, Miles A, et al. Feasibility of group cognitive-behavioral treatment of insomnia delivered by clinical video telehealth. Telemed J E Health. 2016;22(12):1041-1046.
Hagatun S, Vedaa Ø, Nordgreen T, et al. The short-term efficacy of an unguided internet-based cognitive-behavioral therapy for insomnia: a randomized controlled trial with a six-month nonrandomized follow-up. Behav Sleep Med. 2017 Mar 27 [Epub ahead of print].
Ye YY, Chen NK, Chen J, et al. Internet-based cognitive-behavioural therapy for insomnia (ICBT-i): a meta-analysis of randomised controlled trials. BMJ Open. 2016;6(11):e010707.
BALTIMORE—Cognitive behavioral therapy for insomnia (CBT-I) is an effective treatment, but a scarcity of trained clinicians has limited patients’ access to it. Telehealth and Internet-based platforms could broaden access to CBT-I, and investigators presented research on the efficacy of these methods of administration at the 32nd Annual Meeting of the Associated Professional Sleep Societies.
CBT-I by Telehealth Is Noninferior to In-Person CBT-I
Philip Gehrman, PhD, Associate Professor of Psychology at the University of Pennsylvania and the Philadelphia VA Medical Center, and colleagues conducted a cluster-randomized trial to determine whether group CBT-I delivered by telehealth was noninferior to CBT-I delivered in person. Eligible participants were veterans with posttraumatic stress disorder (PTSD) and an Insomnia Severity Index (ISI) score of 15 or higher. The investigators randomized 95 participants in groups of six to eight to group CBT-I in person or by telehealth. The primary outcome was the change in ISI score from baseline to the three-month follow-up. Dr. Gehrman and colleagues defined treatment inferiority as a difference of greater than two points on the ISI score.
Participants’ mean age was 55.6, about 91% of the sample was male, and 42.2% of the sample was African American. The study population generally was overweight and had severe PTSD. Approximately half of the population was receiving one or more psychotropic medication. Forty-six participants were randomized to in-person CBT-I, and 49 were randomized to CBT-I delivered by telehealth.
At three months, the mean change in ISI score was 6.48 for in-person CBT-I and 4.45 for telehealth CBT-I. The difference between groups was outside of the prespecified margin of inferiority, and the researchers concluded that CBT-I delivered by telehealth was noninferior to in-person CBT-I.
The overall effectiveness of both methods of administration was modest, said Dr. Gehrman. The effect size might be greater in a group with fewer comorbidities or in a group that received more treatment sessions, he added. Nevertheless, the results “demonstrate that CBT-I can be effective even in a complex patient population,” he concluded.
SHUTi May Be Inferior to In-Person CBT-I
The online CBT-I intervention Sleep Healthy Using the Internet (SHUTi) has reduced insomnia with effect sizes similar to those of traditional CBT-I. No researchers had compared the two techniques directly, however. Håvard Kallestad, PhD, a clinical psychologist at Saint Olav’s Hospital in Trondheim, Norway, and colleagues examined whether SHUTi was a noninferior treatment for insomnia, compared with in-person CBT-I.
Eligible participants were 18 or older, had a diagnosis of insomnia, had been referred to a sleep clinic, and had access to a computer and adequate computer skills. Participants were randomized to in-person CBT-I or SHUTi. The primary outcome was ISI score, and three therapists assessed participants’ outcomes at baseline, after treatment, and at six months. They defined noninferiority as a difference between treatments of 2 or fewer points on ISI score.
Dr. Kallestad and colleagues randomized 52 participants to in-person CBT-I and 49 to SHUTi. Mean duration of insomnia was about 13 years. Approximately 60% of participants were currently using sleep medication, and about 90% had had previous treatment with sleep medication. After treatment, two patients in the in-person group and five in the SHUTi group were lost to follow-up. At six months, four participants in the in-person group and eight in the SHUTi group were lost to follow-up.
Both study arms had significantly lower ISI scores after treatment and at six months. After treatment, the mean ISI score in the in-person group was 5.1 points lower than in the SHUTi group, indicating that SHUTi was inferior at that time. At six months, mean ISI score was 3.3 points lower in the in-person group than in the SHUTi group. Because part of the confidence interval overlapped with the noninferiority margin, the result was inconclusive.
After treatment, the response rate was 70% in the in-person group and 43% in the SHUTi group. The remission rate was 52% in the in-person group and 18% in the SHUTi group. At six months, the response rate was 65% for the in-person group and 46% for the SHUTi group. The remission rate was 56% in the in-person group and 24% in the SHUTi group.
“SHUTi did not have the same effectiveness in this patient sample, compared with previous studies,” said Dr. Kallestad. One reason could be that previous studies included self-selected participants, rather than patients who had been referred to a sleep clinic. Also, the researchers interviewed all participants at baseline, and SHUTi might have seemed “more limited” in comparison with the interview, Dr. Kallestad concluded.
Digital CBT-I May Prevent Incident Depression
Insomnia is a modifiable risk factor for depression, and research has indicated that CBT-I reduces the severity of depression. Investigators also have shown that digitally delivered CBT-I effectively reduces insomnia and depression. Phillip C. Cheng, PhD, a researcher at the Henry Ford Health System in Detroit, and colleagues sought to determine whether digitally delivered CBT-I could prevent incident depression.
The researchers randomized 658 people with insomnia to Sleepio, an Internet-based CBT-I treatment, or to a control condition of online sleep education. The study’s primary outcome was the Quick Inventory of Depressive Symptomatology (QIDS), and Dr. Cheng’s group defined depression as a score greater than 10 on the QIDS. The researchers also examined participants’ ISI scores and functional outcomes such as work productivity, social functioning, cognitive functioning, and resilience. Assessments were performed at baseline, after treatment, and at one year.
In all, 358 participants were randomized to Sleepio, and 300 were randomized to sleep education. The patient population was predominantly female, was racially diverse, and had a diversity of educational attainment. The demographics of the study arms did not differ significantly.
After treatment, the rate of incident depression was 11% in the sleep education group and 6.5% in the Sleepio group. The difference between arms was not statistically significant. At one year, the rate of incident depression was 22% in the sleep education group and 5.1% in the Sleepio group. The difference between arms at one year was statistically significant, as was the change in depression incidence over time in the sleep education group.
Among patients who did not develop depression, ISI score decreased to a value below the cutoff for insomnia, regardless of study arm. ISI score did not change significantly among participants who developed depression, however. Work productivity, social functioning, cognitive functioning, and resilience improved more in the Sleepio group than in the sleep education group.
The results indicate that “digitally delivered CBT-I may prevent incident depression in adults with insomnia,” said Dr. Cheng. Each episode of depression increases the risk of relapse of depression, which underscores the significance of preventing incident depression, he added. Digital CBT-I also appears to reduce the economic burden associated with depression, and further studies could clarify whether it improves resilience, Dr. Cheng concluded.
—Erik Greb
Suggested Reading
Espie CA, Kyle SD, Williams C, et al. A randomized, placebo-controlled trial of online cognitive behavioral therapy for chronic insomnia disorder delivered via an automated media-rich web application. Sleep. 2012;35(6):769-781.
Gehrman P, Shah MT, Miles A, et al. Feasibility of group cognitive-behavioral treatment of insomnia delivered by clinical video telehealth. Telemed J E Health. 2016;22(12):1041-1046.
Hagatun S, Vedaa Ø, Nordgreen T, et al. The short-term efficacy of an unguided internet-based cognitive-behavioral therapy for insomnia: a randomized controlled trial with a six-month nonrandomized follow-up. Behav Sleep Med. 2017 Mar 27 [Epub ahead of print].
Ye YY, Chen NK, Chen J, et al. Internet-based cognitive-behavioural therapy for insomnia (ICBT-i): a meta-analysis of randomised controlled trials. BMJ Open. 2016;6(11):e010707.
Outcomes Associated With Shorter Wait Times at a County Hospital Outpatient Dermatology Clinic
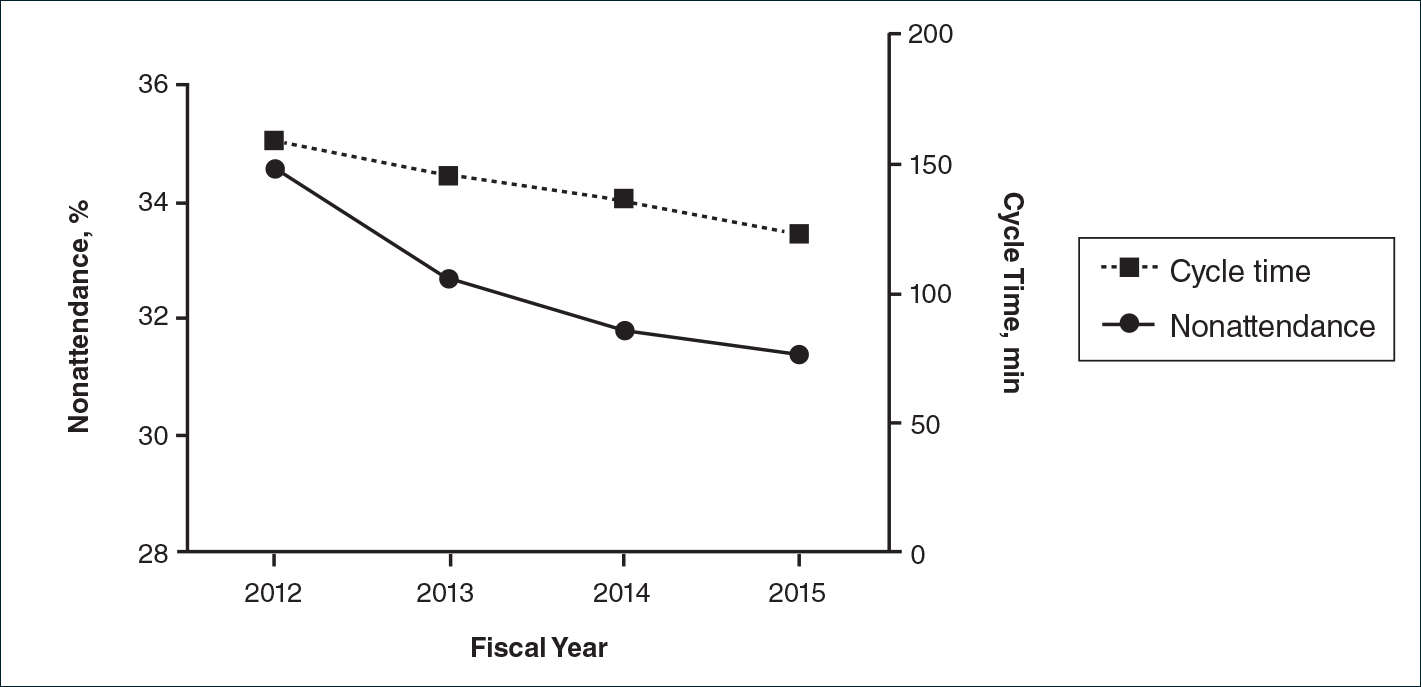
Maximizing productivity is prudent for outpatient subspecialty clinics to improve access to care. The outpatient dermatology clinic at Parkland Health and Hospital System in Dallas, Texas, which is a safety-net hospital in Dallas County, decreased wait times for new patients (from 377 to 48 days) and follow-up patients (from 95 to 34 days) from May 2012 to September 2015.1 Changes in clinic productivity measures that occur with decreased wait times are not well characterized; therefore, we sought to address this knowledge gap. We propose that decreased wait times are associated with improvement in additional clinic productivity measures, specifically decreases in nonattendance and cycle times (defined as time between patient check-in and discharge) as well as increases in referrals.
In our retrospective cohort study of patients seen in the Parkland outpatient dermatology clinic between fiscal year (FY) 2012 and FY 2015 (between October 2011 and September 2015), we collected data on patient nonattendance rates, cycle times, and referral volumes. Categorical variables were compared using χ2 tests, and changes in cycle times were analyzed using 2-way analysis of variance. P<.05 was considered statistically significant.
There were 52,775 scheduled clinic visits from FY 2012 to FY 2015. The overall proportion of patient nonattendance rates decreased from 34.6% (4202/12,141) to 31.4% (4429/14,119)(P<.001)(Figure), despite an increase in completed patient visits during the study period (7939 vs 9690). New patient nonattendance rates decreased from 42.9% (1831/4269) to 30.2% (1474/4874)(P<.001). The number of completed visits for new patients increased from 2438 in FY 2012 to 3400 in FY 2015. Follow-up nonattendance rates increased from 30.1% (2371/7872) to 32.0% (2955/9245)(P<.001). Follow-up completed visits increased from 5501 in FY 2012 to 6290 in FY 2015. Overall, average cycle time showed a trend to decrease from 159 to 123 minutes (22.6%)(Figure). Average cycle times were reduced from 159 to 128 minutes (19.5%) for new patients and from 161 to 115 minutes (28.6%) for follow-up patients (P=.02). Overall, referrals increased by 14.1% (816/5799)(P<.001), which was largely due to the increase in volume of referrals observed between FY 2014 (n=5770) and FY 2015 (n=6615).
We have demonstrated that decreased wait times can be associated with improvements in clinic productivity measures, namely decreased nonattendance rates and cycle times and increased referrals. Patient nonattendance is a burden on clinic resources and has been described in the dermatology clinic setting.2-6 Increased likelihood of nonattendance has been associated with prolonged wait times.3,7 We propose that decreased wait times can lead to diminished nonattendance rates, as patients are more likely to keep their appointments rather than seek other providers for dermatologic care. The difference in trends between new patient and follow-up nonattendance rates may be attributed to the larger relative increase in completed new patient visits compared to follow-ups during the study period.
Furthermore, the decrease in average cycle time reflected our clinic’s ability to see a larger number of patients per clinic, with subsequently shorter wait times. The greater reduction in cycle times for follow-up patients may be attributed to the increased continuity of providers who had previously seen these patients. Although the cycle times may seem high in our clinic compared to other practice settings, we believe that this marker of productivity is widely applicable to various clinic settings, including private practices and other outpatient specialty clinics. Increased clinic referrals can be a downstream effect of decreased wait times due to improvements in access to care, as shown in other specialty clinics.8 Effects of confounding variables on referral volumes, including nationwide health insurance changes during our study period, could not be ruled out.
Limitations of this study include unavailable data on patient and provider satisfaction and changes in patients’ health insurance. This study provides evidence of changes in clinical productivity measures associated with decreased wait times that can demonstrate widespread benefits to the health system.
Acknowledgments
The authors would like to thank Michael Estabrooks, RN, and Trung Vu for providing aggregate data, as well as Linda Hynan, PhD, for statistical advice (all Dallas, Texas).
- O’Brien JC, Chong BF. Reducing outpatient dermatology clinic wait times in a safety net health system in Dallas, Texas. J Am Acad Dermatol. 2016;75:631-632.
- Canizares MJ, Penneys NS. The incidence of nonattendance at an urgent care dermatology clinic. J Am Acad Dermatol. 2002;46:457-459.
- Cohen AD, Dreiher J, Vardy DA, et al. Nonattendance in a dermatology clinic—a large sample analysis. J Eur Acad Dermatol Venereol. 2008;22:1178-1183.
- Resneck JS Jr, Lipton S, Pletcher MJ. Short wait times for patients seeking cosmetic botulinum toxin appointments with dermatologists. J Am Acad Dermatol. 2007;57:985-989.
- Tsang MW, Resneck JS Jr. Even patients with changing moles face long dermatology appointment wait-times: a study of simulated patient calls to dermatologists. J Am Acad Dermatol. 2006;55:54-58.
- Rosenbach M, Kagan S, Leventhal S. Dermatology urgent care clinic: a survey of referring physician satisfaction. J Am Acad Dermatol. 2013;69:1067-1069.e1.
- Dickey W, Morrow JI. Can outpatient non-attendance be predicted from the referral letter? an audit of default at neurology clinics. J R Soc Med. 1991;8:662-663.
- Bungard TJ, Smigorowsky MJ, Lalonde LD, et al. Cardiac EASE (Ensuring Access and Speedy Evaluation)—the impact of a single-point-of-entry multidisciplinary outpatient cardiology consultation program on wait times in Canada. Can J Cardiol. 2009;25:697-702.
Maximizing productivity is prudent for outpatient subspecialty clinics to improve access to care. The outpatient dermatology clinic at Parkland Health and Hospital System in Dallas, Texas, which is a safety-net hospital in Dallas County, decreased wait times for new patients (from 377 to 48 days) and follow-up patients (from 95 to 34 days) from May 2012 to September 2015.1 Changes in clinic productivity measures that occur with decreased wait times are not well characterized; therefore, we sought to address this knowledge gap. We propose that decreased wait times are associated with improvement in additional clinic productivity measures, specifically decreases in nonattendance and cycle times (defined as time between patient check-in and discharge) as well as increases in referrals.
In our retrospective cohort study of patients seen in the Parkland outpatient dermatology clinic between fiscal year (FY) 2012 and FY 2015 (between October 2011 and September 2015), we collected data on patient nonattendance rates, cycle times, and referral volumes. Categorical variables were compared using χ2 tests, and changes in cycle times were analyzed using 2-way analysis of variance. P<.05 was considered statistically significant.
There were 52,775 scheduled clinic visits from FY 2012 to FY 2015. The overall proportion of patient nonattendance rates decreased from 34.6% (4202/12,141) to 31.4% (4429/14,119)(P<.001)(Figure), despite an increase in completed patient visits during the study period (7939 vs 9690). New patient nonattendance rates decreased from 42.9% (1831/4269) to 30.2% (1474/4874)(P<.001). The number of completed visits for new patients increased from 2438 in FY 2012 to 3400 in FY 2015. Follow-up nonattendance rates increased from 30.1% (2371/7872) to 32.0% (2955/9245)(P<.001). Follow-up completed visits increased from 5501 in FY 2012 to 6290 in FY 2015. Overall, average cycle time showed a trend to decrease from 159 to 123 minutes (22.6%)(Figure). Average cycle times were reduced from 159 to 128 minutes (19.5%) for new patients and from 161 to 115 minutes (28.6%) for follow-up patients (P=.02). Overall, referrals increased by 14.1% (816/5799)(P<.001), which was largely due to the increase in volume of referrals observed between FY 2014 (n=5770) and FY 2015 (n=6615).
We have demonstrated that decreased wait times can be associated with improvements in clinic productivity measures, namely decreased nonattendance rates and cycle times and increased referrals. Patient nonattendance is a burden on clinic resources and has been described in the dermatology clinic setting.2-6 Increased likelihood of nonattendance has been associated with prolonged wait times.3,7 We propose that decreased wait times can lead to diminished nonattendance rates, as patients are more likely to keep their appointments rather than seek other providers for dermatologic care. The difference in trends between new patient and follow-up nonattendance rates may be attributed to the larger relative increase in completed new patient visits compared to follow-ups during the study period.
Furthermore, the decrease in average cycle time reflected our clinic’s ability to see a larger number of patients per clinic, with subsequently shorter wait times. The greater reduction in cycle times for follow-up patients may be attributed to the increased continuity of providers who had previously seen these patients. Although the cycle times may seem high in our clinic compared to other practice settings, we believe that this marker of productivity is widely applicable to various clinic settings, including private practices and other outpatient specialty clinics. Increased clinic referrals can be a downstream effect of decreased wait times due to improvements in access to care, as shown in other specialty clinics.8 Effects of confounding variables on referral volumes, including nationwide health insurance changes during our study period, could not be ruled out.
Limitations of this study include unavailable data on patient and provider satisfaction and changes in patients’ health insurance. This study provides evidence of changes in clinical productivity measures associated with decreased wait times that can demonstrate widespread benefits to the health system.
Acknowledgments
The authors would like to thank Michael Estabrooks, RN, and Trung Vu for providing aggregate data, as well as Linda Hynan, PhD, for statistical advice (all Dallas, Texas).
Maximizing productivity is prudent for outpatient subspecialty clinics to improve access to care. The outpatient dermatology clinic at Parkland Health and Hospital System in Dallas, Texas, which is a safety-net hospital in Dallas County, decreased wait times for new patients (from 377 to 48 days) and follow-up patients (from 95 to 34 days) from May 2012 to September 2015.1 Changes in clinic productivity measures that occur with decreased wait times are not well characterized; therefore, we sought to address this knowledge gap. We propose that decreased wait times are associated with improvement in additional clinic productivity measures, specifically decreases in nonattendance and cycle times (defined as time between patient check-in and discharge) as well as increases in referrals.
In our retrospective cohort study of patients seen in the Parkland outpatient dermatology clinic between fiscal year (FY) 2012 and FY 2015 (between October 2011 and September 2015), we collected data on patient nonattendance rates, cycle times, and referral volumes. Categorical variables were compared using χ2 tests, and changes in cycle times were analyzed using 2-way analysis of variance. P<.05 was considered statistically significant.
There were 52,775 scheduled clinic visits from FY 2012 to FY 2015. The overall proportion of patient nonattendance rates decreased from 34.6% (4202/12,141) to 31.4% (4429/14,119)(P<.001)(Figure), despite an increase in completed patient visits during the study period (7939 vs 9690). New patient nonattendance rates decreased from 42.9% (1831/4269) to 30.2% (1474/4874)(P<.001). The number of completed visits for new patients increased from 2438 in FY 2012 to 3400 in FY 2015. Follow-up nonattendance rates increased from 30.1% (2371/7872) to 32.0% (2955/9245)(P<.001). Follow-up completed visits increased from 5501 in FY 2012 to 6290 in FY 2015. Overall, average cycle time showed a trend to decrease from 159 to 123 minutes (22.6%)(Figure). Average cycle times were reduced from 159 to 128 minutes (19.5%) for new patients and from 161 to 115 minutes (28.6%) for follow-up patients (P=.02). Overall, referrals increased by 14.1% (816/5799)(P<.001), which was largely due to the increase in volume of referrals observed between FY 2014 (n=5770) and FY 2015 (n=6615).
We have demonstrated that decreased wait times can be associated with improvements in clinic productivity measures, namely decreased nonattendance rates and cycle times and increased referrals. Patient nonattendance is a burden on clinic resources and has been described in the dermatology clinic setting.2-6 Increased likelihood of nonattendance has been associated with prolonged wait times.3,7 We propose that decreased wait times can lead to diminished nonattendance rates, as patients are more likely to keep their appointments rather than seek other providers for dermatologic care. The difference in trends between new patient and follow-up nonattendance rates may be attributed to the larger relative increase in completed new patient visits compared to follow-ups during the study period.
Furthermore, the decrease in average cycle time reflected our clinic’s ability to see a larger number of patients per clinic, with subsequently shorter wait times. The greater reduction in cycle times for follow-up patients may be attributed to the increased continuity of providers who had previously seen these patients. Although the cycle times may seem high in our clinic compared to other practice settings, we believe that this marker of productivity is widely applicable to various clinic settings, including private practices and other outpatient specialty clinics. Increased clinic referrals can be a downstream effect of decreased wait times due to improvements in access to care, as shown in other specialty clinics.8 Effects of confounding variables on referral volumes, including nationwide health insurance changes during our study period, could not be ruled out.
Limitations of this study include unavailable data on patient and provider satisfaction and changes in patients’ health insurance. This study provides evidence of changes in clinical productivity measures associated with decreased wait times that can demonstrate widespread benefits to the health system.
Acknowledgments
The authors would like to thank Michael Estabrooks, RN, and Trung Vu for providing aggregate data, as well as Linda Hynan, PhD, for statistical advice (all Dallas, Texas).
- O’Brien JC, Chong BF. Reducing outpatient dermatology clinic wait times in a safety net health system in Dallas, Texas. J Am Acad Dermatol. 2016;75:631-632.
- Canizares MJ, Penneys NS. The incidence of nonattendance at an urgent care dermatology clinic. J Am Acad Dermatol. 2002;46:457-459.
- Cohen AD, Dreiher J, Vardy DA, et al. Nonattendance in a dermatology clinic—a large sample analysis. J Eur Acad Dermatol Venereol. 2008;22:1178-1183.
- Resneck JS Jr, Lipton S, Pletcher MJ. Short wait times for patients seeking cosmetic botulinum toxin appointments with dermatologists. J Am Acad Dermatol. 2007;57:985-989.
- Tsang MW, Resneck JS Jr. Even patients with changing moles face long dermatology appointment wait-times: a study of simulated patient calls to dermatologists. J Am Acad Dermatol. 2006;55:54-58.
- Rosenbach M, Kagan S, Leventhal S. Dermatology urgent care clinic: a survey of referring physician satisfaction. J Am Acad Dermatol. 2013;69:1067-1069.e1.
- Dickey W, Morrow JI. Can outpatient non-attendance be predicted from the referral letter? an audit of default at neurology clinics. J R Soc Med. 1991;8:662-663.
- Bungard TJ, Smigorowsky MJ, Lalonde LD, et al. Cardiac EASE (Ensuring Access and Speedy Evaluation)—the impact of a single-point-of-entry multidisciplinary outpatient cardiology consultation program on wait times in Canada. Can J Cardiol. 2009;25:697-702.
- O’Brien JC, Chong BF. Reducing outpatient dermatology clinic wait times in a safety net health system in Dallas, Texas. J Am Acad Dermatol. 2016;75:631-632.
- Canizares MJ, Penneys NS. The incidence of nonattendance at an urgent care dermatology clinic. J Am Acad Dermatol. 2002;46:457-459.
- Cohen AD, Dreiher J, Vardy DA, et al. Nonattendance in a dermatology clinic—a large sample analysis. J Eur Acad Dermatol Venereol. 2008;22:1178-1183.
- Resneck JS Jr, Lipton S, Pletcher MJ. Short wait times for patients seeking cosmetic botulinum toxin appointments with dermatologists. J Am Acad Dermatol. 2007;57:985-989.
- Tsang MW, Resneck JS Jr. Even patients with changing moles face long dermatology appointment wait-times: a study of simulated patient calls to dermatologists. J Am Acad Dermatol. 2006;55:54-58.
- Rosenbach M, Kagan S, Leventhal S. Dermatology urgent care clinic: a survey of referring physician satisfaction. J Am Acad Dermatol. 2013;69:1067-1069.e1.
- Dickey W, Morrow JI. Can outpatient non-attendance be predicted from the referral letter? an audit of default at neurology clinics. J R Soc Med. 1991;8:662-663.
- Bungard TJ, Smigorowsky MJ, Lalonde LD, et al. Cardiac EASE (Ensuring Access and Speedy Evaluation)—the impact of a single-point-of-entry multidisciplinary outpatient cardiology consultation program on wait times in Canada. Can J Cardiol. 2009;25:697-702.
Medication app boosts psoriasis patients’ short-term adherence
compared with those who did not use the app.
Treatment adherence remains a challenge in psoriasis, and although the field of electronic health interventions is growing, data on the effectiveness of such interventions are limited, wrote Mathias T. Svendsen, MD, of Odense University Hospital in Denmark, and his colleagues.
In a study published in the British Journal of Dermatology, 134 adults with psoriasis were randomized to use a smartphone app (68) or not (66) that provided daily medication reminders and daily information about the amount of treatment and number of product applications.
The primary outcome measure of treatment adherence was defined as once-daily application of topical medication – calcipotriol/betamethasone dipropionate cutaneous foam – for at least 80% of the days during the treatment period. A computer chip on the medication dispenser tracked patient use of the product and sent usage information to the patient’s smartphone via Bluetooth.
At 4 weeks, 65% of patients who used the app were adherent to treatment, versus 38% of those who didn’t use the app (P = .004).
In addition, patients who used the app showed significant improvement in disease severity, based on the secondary outcome measure of the Lattice System Physician’s Global Assessment (LS-PGA) at 4 weeks, with a mean change in score from baseline of 1.86 in the app group and 1.46 in the non-app group (P = .047). The LS-PGA and the Dermatology Life Quality Index (DLQI) were measured at all visits. No significant differences on the DLQI appeared between the groups.
During a 22-week follow-up completed by 122 patients, the effects were similar, but the differences were not statistically significant at weeks 8 and 26.
The study findings were limited by several factors, including the lack of knowledge of the correct amount of medication needed for the full benefit of the topical treatment and a lack of data on patient satisfaction with the app, the researchers noted. However, the results suggest that a medication reminder app improved disease severity as well as patient adherence rates in the short term, and that “there is potential for implementing patient-supporting apps in the dermatology clinic.”
The study was supported by LEO Pharma and by the Kirsten and Volmer Rask Nielsen’s Foundation; part of Dr. Svendsen’s salary during the study was paid by LEO Pharma, and several coauthors reported relationships with LEO Pharma.
SOURCE: Svendsen MT et al. Br J Dermatol. 2018 Apr 14. doi: 10.1111/bjd.16667.
compared with those who did not use the app.
Treatment adherence remains a challenge in psoriasis, and although the field of electronic health interventions is growing, data on the effectiveness of such interventions are limited, wrote Mathias T. Svendsen, MD, of Odense University Hospital in Denmark, and his colleagues.
In a study published in the British Journal of Dermatology, 134 adults with psoriasis were randomized to use a smartphone app (68) or not (66) that provided daily medication reminders and daily information about the amount of treatment and number of product applications.
The primary outcome measure of treatment adherence was defined as once-daily application of topical medication – calcipotriol/betamethasone dipropionate cutaneous foam – for at least 80% of the days during the treatment period. A computer chip on the medication dispenser tracked patient use of the product and sent usage information to the patient’s smartphone via Bluetooth.
At 4 weeks, 65% of patients who used the app were adherent to treatment, versus 38% of those who didn’t use the app (P = .004).
In addition, patients who used the app showed significant improvement in disease severity, based on the secondary outcome measure of the Lattice System Physician’s Global Assessment (LS-PGA) at 4 weeks, with a mean change in score from baseline of 1.86 in the app group and 1.46 in the non-app group (P = .047). The LS-PGA and the Dermatology Life Quality Index (DLQI) were measured at all visits. No significant differences on the DLQI appeared between the groups.
During a 22-week follow-up completed by 122 patients, the effects were similar, but the differences were not statistically significant at weeks 8 and 26.
The study findings were limited by several factors, including the lack of knowledge of the correct amount of medication needed for the full benefit of the topical treatment and a lack of data on patient satisfaction with the app, the researchers noted. However, the results suggest that a medication reminder app improved disease severity as well as patient adherence rates in the short term, and that “there is potential for implementing patient-supporting apps in the dermatology clinic.”
The study was supported by LEO Pharma and by the Kirsten and Volmer Rask Nielsen’s Foundation; part of Dr. Svendsen’s salary during the study was paid by LEO Pharma, and several coauthors reported relationships with LEO Pharma.
SOURCE: Svendsen MT et al. Br J Dermatol. 2018 Apr 14. doi: 10.1111/bjd.16667.
compared with those who did not use the app.
Treatment adherence remains a challenge in psoriasis, and although the field of electronic health interventions is growing, data on the effectiveness of such interventions are limited, wrote Mathias T. Svendsen, MD, of Odense University Hospital in Denmark, and his colleagues.
In a study published in the British Journal of Dermatology, 134 adults with psoriasis were randomized to use a smartphone app (68) or not (66) that provided daily medication reminders and daily information about the amount of treatment and number of product applications.
The primary outcome measure of treatment adherence was defined as once-daily application of topical medication – calcipotriol/betamethasone dipropionate cutaneous foam – for at least 80% of the days during the treatment period. A computer chip on the medication dispenser tracked patient use of the product and sent usage information to the patient’s smartphone via Bluetooth.
At 4 weeks, 65% of patients who used the app were adherent to treatment, versus 38% of those who didn’t use the app (P = .004).
In addition, patients who used the app showed significant improvement in disease severity, based on the secondary outcome measure of the Lattice System Physician’s Global Assessment (LS-PGA) at 4 weeks, with a mean change in score from baseline of 1.86 in the app group and 1.46 in the non-app group (P = .047). The LS-PGA and the Dermatology Life Quality Index (DLQI) were measured at all visits. No significant differences on the DLQI appeared between the groups.
During a 22-week follow-up completed by 122 patients, the effects were similar, but the differences were not statistically significant at weeks 8 and 26.
The study findings were limited by several factors, including the lack of knowledge of the correct amount of medication needed for the full benefit of the topical treatment and a lack of data on patient satisfaction with the app, the researchers noted. However, the results suggest that a medication reminder app improved disease severity as well as patient adherence rates in the short term, and that “there is potential for implementing patient-supporting apps in the dermatology clinic.”
The study was supported by LEO Pharma and by the Kirsten and Volmer Rask Nielsen’s Foundation; part of Dr. Svendsen’s salary during the study was paid by LEO Pharma, and several coauthors reported relationships with LEO Pharma.
SOURCE: Svendsen MT et al. Br J Dermatol. 2018 Apr 14. doi: 10.1111/bjd.16667.
FROM THE BRITISH JOURNAL OF DERMATOLOGY
Key clinical point: Using a smartphone app helped patients with psoriasis significantly improve their treatment adherence.
Major finding: Significantly more patients who used the app followed their topical treatment plan, compared with the no-app controls (65% vs. 38%).
Study details: The data come from 134 adults with psoriasis who were randomized to use an app or no app for 28 days.
Disclosures: The study was supported by LEO Pharma and by the Kirsten and Volmer Rask Nielsen’s Foundation; part of Dr. Svendsen’s salary during the study was paid by LEO Pharma, and several coauthors reported relationships with LEO Pharma.
Source: Svendsen MT et al. Br J Dermatol. 2018 Apr 14. doi: 10.1111/bjd.16667.
ED visits up for acute pancreatitis linked to younger age, alcohol, chronic disease
, an analysis of a nationally representative database has suggested.
Meanwhile, hospital admissions and length of stay dropped, but ED and inpatient charges increased, according to the analysis by Sushil K. Garg, MD, of the division of gastroenterology and hepatology at the Mayo Clinic, Rochester, Minn., and his coauthors.
“This study identifies important patient populations, specifically young patients with alcohol abuse, to target in order to develop programs to assist in reduction of ED utilization for acute pancreatitis,” Dr. Garg and his colleagues reported in the Journal of Clinical Gastroenterology.
The retrospective analysis was focused on nearly 2.2 million ED visits during 2006-2012 in the National Emergency Department Sample (NEDS) database. The cohort was limited to adults at least 18 years of age with a primary diagnosis of acute pancreatitis.
Overall, there was a nonsignificant 5.5% increase in visits per 10,000 U.S. population during 2006-2012, the researchers found. However, the total number of ED visits in this sample increased significantly – from 292,902 in 2006 to a peak of 326,376, an average rate of increase of 7,213 visits per year (P = .0086), according to the report.
Younger patients had a significant increase in the number of pancreatitis-related ED visits over the study period, while older patients had a significant decrease, according to investigators. Visits were up 9.2% for patients aged 18-44 years and 8.6% for those aged 45-64 but down 13.4% for patients aged 65-84 years and 20.1% for those aged 85 years or older.
The incidence of visits secondary to biliary disease was virtually flat over time, Dr. Garg and his coinvestigators found when looking at visits grouped by the most common presenting etiologies. By contrast, there were significant increases in visits for acute pancreatitis associated with alcohol abuse or chronic pancreatitis.
Specifically, acute pancreatitis associated with biliary disease averaged 20.7% of yearly pancreatitis-related ED visits and did not significantly change over time, the researchers reported.
By contrast, acute pancreatitis associated with alcohol abuse, which accounted for 24.1% of visits on average, increased by 15.9% over the study period, an increase driven by an increase among age groups younger than 65 years.
Acute pancreatitis associated with chronic pancreatitis, which made up 11.5% of visits on average, increased “substantially” in all age groups, according to study authors, with the largest increase in the group aged 45-64 years. Overall, the percentage increase over 7 years was 59.5%.
Rates of hospitalization decreased significantly over time, from 76.2% in 2006 to 72.7% in 2012 (P = .0026), and likewise, the length of stay dropped from 5.36 to 4.64 days (P = .0001), according to the analysis.
Inpatient charges, adjusted for inflation and expressed in 2012 dollars, increased from $32,130.63 to $34,652.00 (P = .0011), an average rate of increase of $489/year.
Predictors of hospitalization included age older than 84 years, alcohol use, smoking, and a Charlson comorbidity score of 1 or greater, according to the results of a multivariate regression analysis.
“Factors which may place patients at higher risk for severe or complicated acute pancreatitis requiring admission, such as obesity, alcohol use, and increasing age, are identified and should be explored in further studies and potentially targeted to improve ED and inpatient care,” Dr. Garg and his coauthors said.
Dr. Garg and his coauthors had no disclosures related to the study.
Help your patients better understand pancreatitis and available tests and treatments by using AGA patient education materials, https://www.gastro.org/practice-guidance/gi-patient-center/topic/pancreatitis.
SOURCE: Garg SK et al. J Clin Gastroenterol. 2018 Apr 6. doi: 10.1097/MCG.0000000000001030.
, an analysis of a nationally representative database has suggested.
Meanwhile, hospital admissions and length of stay dropped, but ED and inpatient charges increased, according to the analysis by Sushil K. Garg, MD, of the division of gastroenterology and hepatology at the Mayo Clinic, Rochester, Minn., and his coauthors.
“This study identifies important patient populations, specifically young patients with alcohol abuse, to target in order to develop programs to assist in reduction of ED utilization for acute pancreatitis,” Dr. Garg and his colleagues reported in the Journal of Clinical Gastroenterology.
The retrospective analysis was focused on nearly 2.2 million ED visits during 2006-2012 in the National Emergency Department Sample (NEDS) database. The cohort was limited to adults at least 18 years of age with a primary diagnosis of acute pancreatitis.
Overall, there was a nonsignificant 5.5% increase in visits per 10,000 U.S. population during 2006-2012, the researchers found. However, the total number of ED visits in this sample increased significantly – from 292,902 in 2006 to a peak of 326,376, an average rate of increase of 7,213 visits per year (P = .0086), according to the report.
Younger patients had a significant increase in the number of pancreatitis-related ED visits over the study period, while older patients had a significant decrease, according to investigators. Visits were up 9.2% for patients aged 18-44 years and 8.6% for those aged 45-64 but down 13.4% for patients aged 65-84 years and 20.1% for those aged 85 years or older.
The incidence of visits secondary to biliary disease was virtually flat over time, Dr. Garg and his coinvestigators found when looking at visits grouped by the most common presenting etiologies. By contrast, there were significant increases in visits for acute pancreatitis associated with alcohol abuse or chronic pancreatitis.
Specifically, acute pancreatitis associated with biliary disease averaged 20.7% of yearly pancreatitis-related ED visits and did not significantly change over time, the researchers reported.
By contrast, acute pancreatitis associated with alcohol abuse, which accounted for 24.1% of visits on average, increased by 15.9% over the study period, an increase driven by an increase among age groups younger than 65 years.
Acute pancreatitis associated with chronic pancreatitis, which made up 11.5% of visits on average, increased “substantially” in all age groups, according to study authors, with the largest increase in the group aged 45-64 years. Overall, the percentage increase over 7 years was 59.5%.
Rates of hospitalization decreased significantly over time, from 76.2% in 2006 to 72.7% in 2012 (P = .0026), and likewise, the length of stay dropped from 5.36 to 4.64 days (P = .0001), according to the analysis.
Inpatient charges, adjusted for inflation and expressed in 2012 dollars, increased from $32,130.63 to $34,652.00 (P = .0011), an average rate of increase of $489/year.
Predictors of hospitalization included age older than 84 years, alcohol use, smoking, and a Charlson comorbidity score of 1 or greater, according to the results of a multivariate regression analysis.
“Factors which may place patients at higher risk for severe or complicated acute pancreatitis requiring admission, such as obesity, alcohol use, and increasing age, are identified and should be explored in further studies and potentially targeted to improve ED and inpatient care,” Dr. Garg and his coauthors said.
Dr. Garg and his coauthors had no disclosures related to the study.
Help your patients better understand pancreatitis and available tests and treatments by using AGA patient education materials, https://www.gastro.org/practice-guidance/gi-patient-center/topic/pancreatitis.
SOURCE: Garg SK et al. J Clin Gastroenterol. 2018 Apr 6. doi: 10.1097/MCG.0000000000001030.
, an analysis of a nationally representative database has suggested.
Meanwhile, hospital admissions and length of stay dropped, but ED and inpatient charges increased, according to the analysis by Sushil K. Garg, MD, of the division of gastroenterology and hepatology at the Mayo Clinic, Rochester, Minn., and his coauthors.
“This study identifies important patient populations, specifically young patients with alcohol abuse, to target in order to develop programs to assist in reduction of ED utilization for acute pancreatitis,” Dr. Garg and his colleagues reported in the Journal of Clinical Gastroenterology.
The retrospective analysis was focused on nearly 2.2 million ED visits during 2006-2012 in the National Emergency Department Sample (NEDS) database. The cohort was limited to adults at least 18 years of age with a primary diagnosis of acute pancreatitis.
Overall, there was a nonsignificant 5.5% increase in visits per 10,000 U.S. population during 2006-2012, the researchers found. However, the total number of ED visits in this sample increased significantly – from 292,902 in 2006 to a peak of 326,376, an average rate of increase of 7,213 visits per year (P = .0086), according to the report.
Younger patients had a significant increase in the number of pancreatitis-related ED visits over the study period, while older patients had a significant decrease, according to investigators. Visits were up 9.2% for patients aged 18-44 years and 8.6% for those aged 45-64 but down 13.4% for patients aged 65-84 years and 20.1% for those aged 85 years or older.
The incidence of visits secondary to biliary disease was virtually flat over time, Dr. Garg and his coinvestigators found when looking at visits grouped by the most common presenting etiologies. By contrast, there were significant increases in visits for acute pancreatitis associated with alcohol abuse or chronic pancreatitis.
Specifically, acute pancreatitis associated with biliary disease averaged 20.7% of yearly pancreatitis-related ED visits and did not significantly change over time, the researchers reported.
By contrast, acute pancreatitis associated with alcohol abuse, which accounted for 24.1% of visits on average, increased by 15.9% over the study period, an increase driven by an increase among age groups younger than 65 years.
Acute pancreatitis associated with chronic pancreatitis, which made up 11.5% of visits on average, increased “substantially” in all age groups, according to study authors, with the largest increase in the group aged 45-64 years. Overall, the percentage increase over 7 years was 59.5%.
Rates of hospitalization decreased significantly over time, from 76.2% in 2006 to 72.7% in 2012 (P = .0026), and likewise, the length of stay dropped from 5.36 to 4.64 days (P = .0001), according to the analysis.
Inpatient charges, adjusted for inflation and expressed in 2012 dollars, increased from $32,130.63 to $34,652.00 (P = .0011), an average rate of increase of $489/year.
Predictors of hospitalization included age older than 84 years, alcohol use, smoking, and a Charlson comorbidity score of 1 or greater, according to the results of a multivariate regression analysis.
“Factors which may place patients at higher risk for severe or complicated acute pancreatitis requiring admission, such as obesity, alcohol use, and increasing age, are identified and should be explored in further studies and potentially targeted to improve ED and inpatient care,” Dr. Garg and his coauthors said.
Dr. Garg and his coauthors had no disclosures related to the study.
Help your patients better understand pancreatitis and available tests and treatments by using AGA patient education materials, https://www.gastro.org/practice-guidance/gi-patient-center/topic/pancreatitis.
SOURCE: Garg SK et al. J Clin Gastroenterol. 2018 Apr 6. doi: 10.1097/MCG.0000000000001030.
Acne and Rosacea - July 2018 Supplement
Acne & Rosacea is a supplement addressing quality of life, pathogenesis, and treatment of acne and rosacea, with an introduction from Julie C. Harper, M.D. "I am pleased to have so many thought-provoking articles to review on the subjects of acne and rosacea. Our understanding of hese common but life-changing conditions is improving, but there is still a long way to go."
Highlights include:
- New standard classification, pathophysiology of rosacea announced
- Clinicians persist in prescribing antibiotics for acne
- Rosacea tied to physical and psychological comorbidities
Click here to download this supplement.
Acne & Rosacea is a supplement addressing quality of life, pathogenesis, and treatment of acne and rosacea, with an introduction from Julie C. Harper, M.D. "I am pleased to have so many thought-provoking articles to review on the subjects of acne and rosacea. Our understanding of hese common but life-changing conditions is improving, but there is still a long way to go."
Highlights include:
- New standard classification, pathophysiology of rosacea announced
- Clinicians persist in prescribing antibiotics for acne
- Rosacea tied to physical and psychological comorbidities
Click here to download this supplement.
Acne & Rosacea is a supplement addressing quality of life, pathogenesis, and treatment of acne and rosacea, with an introduction from Julie C. Harper, M.D. "I am pleased to have so many thought-provoking articles to review on the subjects of acne and rosacea. Our understanding of hese common but life-changing conditions is improving, but there is still a long way to go."
Highlights include:
- New standard classification, pathophysiology of rosacea announced
- Clinicians persist in prescribing antibiotics for acne
- Rosacea tied to physical and psychological comorbidities
Click here to download this supplement.
Atopic Dermatitis Pipeline
Just when you might have thought dermatologic therapies were peaking, along came another banner year in atopic dermatitis (AD). Last year we saw the landmark launch of dupilumab, the first US Food and Drug Administration (FDA)–approved biologic therapy for AD. Dupilumab addresses a novel mechanism of AD in adults by blocking IL-4 and IL-13, which both play a central role in the type 2 helper T cell (TH2) axis on the dual development of barrier-impaired skin and aberrant immune response including IgE to cutaneous aggravating agents with resultant inflammation. Additional information has shown direct effects to reduce itch in AD.1 A 12-week study of dupilumab monotherapy showed that 85% (47/55) of treated patients had at least a 50% reduction in Eczema Area and Severity Index (EASI) score and 40% (22/55) were clear or almost clear on the investigator global assessment. With concomitant corticosteroid therapy, 100% of patients achieved EASI-50.2 Also notable, 2017 ushered in the appearance of a novel iteration of the 30-year-old concept of phosphodiesterase inhibition with the approval of the topical agent crisaborole for AD treatment in patients 2 years and older, which has been shown to be effective in both children and adults.3,4 However, despite these leaps of advancement in the care of AD, by no means has the condition been cured.
Atopic dermatitis has remained an incurable disease due to many factors: (1) variable immunologic and environmental triggers and patient disease course; (2) intolerance to therapeutic agents, including an enhanced sense of stinging and/or reactivity; (3) poor access to novel therapies among underserved patient populations; (4) lack of available data and information on variable treatment response by ethnicity and race; and (5) the absence of biologic treatments for severe childhood AD to modify long-term recurrence and progression of atopy, which is probably the most important issue, as the majority of AD cases start in children 5 years and younger.
Instituting a treatment today to provide children with disease-free skin for a lifetime truly is the Holy Grail in pediatric dermatology. To aid in the progress toward this goal, a deeper understanding of the manifestation of pediatric versus adult AD is now being investigated. It is clear that with adult chronicity, type 1 helper T cell (TH1) axis activity and prolonged defects are triggered in barrier maturation; however, recent data have started to demonstrate that the youngest patients have different issues in lipid maturation and lack TH1 activation. In particular, fatty acyl-CoA reductase 2 and fatty acid 2-hydroxylase is preferentially downregulated in children.5 It appears that the young immune system may be ripe for immune modification, which previously has been demonstrated with wild-type viral infections of varicella in children.6 However, future research will focus on what kind of tweaks to the immune system are required.
To encapsulate the AD pipeline, we will review drug trials that are in active recruitment as well as recently published data, which constitute an exciting group full of modifications of current therapies and agents with novel mechanisms of action.
Therapies targeting new mechanisms of action include Janus kinase (JAK) inhibitors, which have shown promising results for alopecia areata and vitiligo vulgaris. These agents may create selective modification of the immune system and are being tested topically and orally (Clinicaltrials.gov identifier NCT03011892).
Another mechanism that currently is being studied includes a topical IL-4 and IL-13 inhibitor, which would hopefully mimic the efficacy of dupilumab, antioxidant therapies, and antimicrobials (NCT03351777, NCT03381625, NCT02910011).
Data on the outcome of a phase 3 trial of dupilumab in adolescents has been released but not yet published by the manufacturer and shows promising results in children aged 12 to 17 years, both in reduction of EASI score and in achieving clear or almost clear skin.11 Interestingly, limited data available from a press release reported similar results with dupilumab injection every 2 weeks versus every 4 weeks, which may give alternative dosing regimens in this age group once approved11; however, publication has yet to occur for the latter data.
Other mechanistic agents include blockade of cytokines and interleukins, particularly those involved in type 2 helper T cell (TH2) activity, such as thymic stromal lymphopoietin (a cytokine), as well as targeted single inhibition of IL-4, IL-5, IL-13, and IL-31 and/or their receptors. Nemolizumab, an anti–IL-31 receptor A antibody, is showing promise in the control of AD-associated itch and reduction in EASI
The future of AD therapy is anyone’s guess. Having entered the biologic era with dupilumab, we have a high bar set for efficacy and safety of AD therapies, yet there remains a core group of AD patients who have not yet achieved clearance or refuse injectables; therefore, adjunctive or alternative therapeutics are still needed. Furthermore, we still have not identified who will best benefit long-term from systemic intervention and how to best effect long-term disease control with biologics or novel agents, and choosing the therapy based on patient disease characteristics or serotyping has not yet come of age. It is exciting to think about what next year will bring!
- Xu X, Zheng Y, Zhang X, et al. Efficacy and safety of dupilumab for the treatment of moderate-to-severe atopic dermatitis in adults. Oncotarget. 2017;8:108480-108491.
- Beck LA, Thaçi D, Hamilton JD, et al. Dupilumab treatment in adults with moderate-to-severe atopic dermatitis. N Engl J Med. 2014;371:130-139.
- Murrell D, Gebauer K, Spelman L, et al. Crisaborole topical ointment, 2% in adults with atopic dermatitis: a phase 2a, vehicle-controlled, proof-of-concept study. J Drugs Dermatol. 2015;14:1108-1112.
- Paller AS, Tom WL, Lebwohl MG, et al. Efficacy and safety of crisaborole ointment, a novel, nonsteroidal phosphodiesterase 4 (PDE4) inhibitor for the topical treatment of atopic dermatitis (AD) in children and adults. J Am Acad Dermatol. 2016;75:494-503.e6.
- Brunner PM, Israel A, Zhang N, et al. Early-onset pediatric atopic dermatitis is characterized by TH2/TH17/TH22-centered inflammation and lipid alterations. J Allergy Clin Immunol. 2018;141:2094-2106.
- Silverberg JI, Kleiman E, Silverberg NB, et al. Chickenpox in childhood is associated with decreased atopic disorders, IgE, allergic sensitization, and leukocyte subsets. Pediatr Allergy Immunol. 2012;23:50-58.
- Paller AS, Kabashima K, Bieber T. Therapeutic pipeline for atopic dermatitis: end of the drought? Allergy Clin Immunol. 2017;140:633-643.
- Renert-Yuval Y, Guttman-Yassky E. Systemic therapies in atopic dermatitis: the pipeline. Clin Dermatol. 2017;35:387-397.
- Bissonnette R, Papp KA, Poulin Y, et al. Topical tofacitinib for atopic dermatitis: a phase IIa randomized trial. Br J Dermatol. 2016;175:902-911.
- Guttman-Yassky E, Silverberg JI, Nemoto O, et al. Baricitinib in adult patients with moderate-to-severe atopic dermatitis: a phase 2 parallel, double-blinded, randomized placebo-controlled multiple-dose study [published online February 1, 2018]. J Am Acad Dermatol. doi: 10.1016/j.jaad.2018.01.018.
- Dupixent (dupilumab) showed positive phase 3 results in adolescents with inadequately controlled moderate-to-severe atopic dermatitis [press release]. Tarrytown, NY: Sanofi; May 16, 2018. https://www.prnewswire.com/news-releases/dupixent-dupilumab-showed-positive-phase-3-results-in-adolescents-with-inadequately-controlled-moderate-to-severe-atopic-dermatitis-300649146.html. Accessed July 11, 2018.
- Ruzicka T, Hanifin JM, Furue M, et al. Anti–interleukin-31 receptor A antibody for atopic dermatitis. N Engl J Med. 2017;376:826-835.
Just when you might have thought dermatologic therapies were peaking, along came another banner year in atopic dermatitis (AD). Last year we saw the landmark launch of dupilumab, the first US Food and Drug Administration (FDA)–approved biologic therapy for AD. Dupilumab addresses a novel mechanism of AD in adults by blocking IL-4 and IL-13, which both play a central role in the type 2 helper T cell (TH2) axis on the dual development of barrier-impaired skin and aberrant immune response including IgE to cutaneous aggravating agents with resultant inflammation. Additional information has shown direct effects to reduce itch in AD.1 A 12-week study of dupilumab monotherapy showed that 85% (47/55) of treated patients had at least a 50% reduction in Eczema Area and Severity Index (EASI) score and 40% (22/55) were clear or almost clear on the investigator global assessment. With concomitant corticosteroid therapy, 100% of patients achieved EASI-50.2 Also notable, 2017 ushered in the appearance of a novel iteration of the 30-year-old concept of phosphodiesterase inhibition with the approval of the topical agent crisaborole for AD treatment in patients 2 years and older, which has been shown to be effective in both children and adults.3,4 However, despite these leaps of advancement in the care of AD, by no means has the condition been cured.
Atopic dermatitis has remained an incurable disease due to many factors: (1) variable immunologic and environmental triggers and patient disease course; (2) intolerance to therapeutic agents, including an enhanced sense of stinging and/or reactivity; (3) poor access to novel therapies among underserved patient populations; (4) lack of available data and information on variable treatment response by ethnicity and race; and (5) the absence of biologic treatments for severe childhood AD to modify long-term recurrence and progression of atopy, which is probably the most important issue, as the majority of AD cases start in children 5 years and younger.
Instituting a treatment today to provide children with disease-free skin for a lifetime truly is the Holy Grail in pediatric dermatology. To aid in the progress toward this goal, a deeper understanding of the manifestation of pediatric versus adult AD is now being investigated. It is clear that with adult chronicity, type 1 helper T cell (TH1) axis activity and prolonged defects are triggered in barrier maturation; however, recent data have started to demonstrate that the youngest patients have different issues in lipid maturation and lack TH1 activation. In particular, fatty acyl-CoA reductase 2 and fatty acid 2-hydroxylase is preferentially downregulated in children.5 It appears that the young immune system may be ripe for immune modification, which previously has been demonstrated with wild-type viral infections of varicella in children.6 However, future research will focus on what kind of tweaks to the immune system are required.
To encapsulate the AD pipeline, we will review drug trials that are in active recruitment as well as recently published data, which constitute an exciting group full of modifications of current therapies and agents with novel mechanisms of action.
Therapies targeting new mechanisms of action include Janus kinase (JAK) inhibitors, which have shown promising results for alopecia areata and vitiligo vulgaris. These agents may create selective modification of the immune system and are being tested topically and orally (Clinicaltrials.gov identifier NCT03011892).
Another mechanism that currently is being studied includes a topical IL-4 and IL-13 inhibitor, which would hopefully mimic the efficacy of dupilumab, antioxidant therapies, and antimicrobials (NCT03351777, NCT03381625, NCT02910011).
Data on the outcome of a phase 3 trial of dupilumab in adolescents has been released but not yet published by the manufacturer and shows promising results in children aged 12 to 17 years, both in reduction of EASI score and in achieving clear or almost clear skin.11 Interestingly, limited data available from a press release reported similar results with dupilumab injection every 2 weeks versus every 4 weeks, which may give alternative dosing regimens in this age group once approved11; however, publication has yet to occur for the latter data.
Other mechanistic agents include blockade of cytokines and interleukins, particularly those involved in type 2 helper T cell (TH2) activity, such as thymic stromal lymphopoietin (a cytokine), as well as targeted single inhibition of IL-4, IL-5, IL-13, and IL-31 and/or their receptors. Nemolizumab, an anti–IL-31 receptor A antibody, is showing promise in the control of AD-associated itch and reduction in EASI
The future of AD therapy is anyone’s guess. Having entered the biologic era with dupilumab, we have a high bar set for efficacy and safety of AD therapies, yet there remains a core group of AD patients who have not yet achieved clearance or refuse injectables; therefore, adjunctive or alternative therapeutics are still needed. Furthermore, we still have not identified who will best benefit long-term from systemic intervention and how to best effect long-term disease control with biologics or novel agents, and choosing the therapy based on patient disease characteristics or serotyping has not yet come of age. It is exciting to think about what next year will bring!
Just when you might have thought dermatologic therapies were peaking, along came another banner year in atopic dermatitis (AD). Last year we saw the landmark launch of dupilumab, the first US Food and Drug Administration (FDA)–approved biologic therapy for AD. Dupilumab addresses a novel mechanism of AD in adults by blocking IL-4 and IL-13, which both play a central role in the type 2 helper T cell (TH2) axis on the dual development of barrier-impaired skin and aberrant immune response including IgE to cutaneous aggravating agents with resultant inflammation. Additional information has shown direct effects to reduce itch in AD.1 A 12-week study of dupilumab monotherapy showed that 85% (47/55) of treated patients had at least a 50% reduction in Eczema Area and Severity Index (EASI) score and 40% (22/55) were clear or almost clear on the investigator global assessment. With concomitant corticosteroid therapy, 100% of patients achieved EASI-50.2 Also notable, 2017 ushered in the appearance of a novel iteration of the 30-year-old concept of phosphodiesterase inhibition with the approval of the topical agent crisaborole for AD treatment in patients 2 years and older, which has been shown to be effective in both children and adults.3,4 However, despite these leaps of advancement in the care of AD, by no means has the condition been cured.
Atopic dermatitis has remained an incurable disease due to many factors: (1) variable immunologic and environmental triggers and patient disease course; (2) intolerance to therapeutic agents, including an enhanced sense of stinging and/or reactivity; (3) poor access to novel therapies among underserved patient populations; (4) lack of available data and information on variable treatment response by ethnicity and race; and (5) the absence of biologic treatments for severe childhood AD to modify long-term recurrence and progression of atopy, which is probably the most important issue, as the majority of AD cases start in children 5 years and younger.
Instituting a treatment today to provide children with disease-free skin for a lifetime truly is the Holy Grail in pediatric dermatology. To aid in the progress toward this goal, a deeper understanding of the manifestation of pediatric versus adult AD is now being investigated. It is clear that with adult chronicity, type 1 helper T cell (TH1) axis activity and prolonged defects are triggered in barrier maturation; however, recent data have started to demonstrate that the youngest patients have different issues in lipid maturation and lack TH1 activation. In particular, fatty acyl-CoA reductase 2 and fatty acid 2-hydroxylase is preferentially downregulated in children.5 It appears that the young immune system may be ripe for immune modification, which previously has been demonstrated with wild-type viral infections of varicella in children.6 However, future research will focus on what kind of tweaks to the immune system are required.
To encapsulate the AD pipeline, we will review drug trials that are in active recruitment as well as recently published data, which constitute an exciting group full of modifications of current therapies and agents with novel mechanisms of action.
Therapies targeting new mechanisms of action include Janus kinase (JAK) inhibitors, which have shown promising results for alopecia areata and vitiligo vulgaris. These agents may create selective modification of the immune system and are being tested topically and orally (Clinicaltrials.gov identifier NCT03011892).
Another mechanism that currently is being studied includes a topical IL-4 and IL-13 inhibitor, which would hopefully mimic the efficacy of dupilumab, antioxidant therapies, and antimicrobials (NCT03351777, NCT03381625, NCT02910011).
Data on the outcome of a phase 3 trial of dupilumab in adolescents has been released but not yet published by the manufacturer and shows promising results in children aged 12 to 17 years, both in reduction of EASI score and in achieving clear or almost clear skin.11 Interestingly, limited data available from a press release reported similar results with dupilumab injection every 2 weeks versus every 4 weeks, which may give alternative dosing regimens in this age group once approved11; however, publication has yet to occur for the latter data.
Other mechanistic agents include blockade of cytokines and interleukins, particularly those involved in type 2 helper T cell (TH2) activity, such as thymic stromal lymphopoietin (a cytokine), as well as targeted single inhibition of IL-4, IL-5, IL-13, and IL-31 and/or their receptors. Nemolizumab, an anti–IL-31 receptor A antibody, is showing promise in the control of AD-associated itch and reduction in EASI
The future of AD therapy is anyone’s guess. Having entered the biologic era with dupilumab, we have a high bar set for efficacy and safety of AD therapies, yet there remains a core group of AD patients who have not yet achieved clearance or refuse injectables; therefore, adjunctive or alternative therapeutics are still needed. Furthermore, we still have not identified who will best benefit long-term from systemic intervention and how to best effect long-term disease control with biologics or novel agents, and choosing the therapy based on patient disease characteristics or serotyping has not yet come of age. It is exciting to think about what next year will bring!
- Xu X, Zheng Y, Zhang X, et al. Efficacy and safety of dupilumab for the treatment of moderate-to-severe atopic dermatitis in adults. Oncotarget. 2017;8:108480-108491.
- Beck LA, Thaçi D, Hamilton JD, et al. Dupilumab treatment in adults with moderate-to-severe atopic dermatitis. N Engl J Med. 2014;371:130-139.
- Murrell D, Gebauer K, Spelman L, et al. Crisaborole topical ointment, 2% in adults with atopic dermatitis: a phase 2a, vehicle-controlled, proof-of-concept study. J Drugs Dermatol. 2015;14:1108-1112.
- Paller AS, Tom WL, Lebwohl MG, et al. Efficacy and safety of crisaborole ointment, a novel, nonsteroidal phosphodiesterase 4 (PDE4) inhibitor for the topical treatment of atopic dermatitis (AD) in children and adults. J Am Acad Dermatol. 2016;75:494-503.e6.
- Brunner PM, Israel A, Zhang N, et al. Early-onset pediatric atopic dermatitis is characterized by TH2/TH17/TH22-centered inflammation and lipid alterations. J Allergy Clin Immunol. 2018;141:2094-2106.
- Silverberg JI, Kleiman E, Silverberg NB, et al. Chickenpox in childhood is associated with decreased atopic disorders, IgE, allergic sensitization, and leukocyte subsets. Pediatr Allergy Immunol. 2012;23:50-58.
- Paller AS, Kabashima K, Bieber T. Therapeutic pipeline for atopic dermatitis: end of the drought? Allergy Clin Immunol. 2017;140:633-643.
- Renert-Yuval Y, Guttman-Yassky E. Systemic therapies in atopic dermatitis: the pipeline. Clin Dermatol. 2017;35:387-397.
- Bissonnette R, Papp KA, Poulin Y, et al. Topical tofacitinib for atopic dermatitis: a phase IIa randomized trial. Br J Dermatol. 2016;175:902-911.
- Guttman-Yassky E, Silverberg JI, Nemoto O, et al. Baricitinib in adult patients with moderate-to-severe atopic dermatitis: a phase 2 parallel, double-blinded, randomized placebo-controlled multiple-dose study [published online February 1, 2018]. J Am Acad Dermatol. doi: 10.1016/j.jaad.2018.01.018.
- Dupixent (dupilumab) showed positive phase 3 results in adolescents with inadequately controlled moderate-to-severe atopic dermatitis [press release]. Tarrytown, NY: Sanofi; May 16, 2018. https://www.prnewswire.com/news-releases/dupixent-dupilumab-showed-positive-phase-3-results-in-adolescents-with-inadequately-controlled-moderate-to-severe-atopic-dermatitis-300649146.html. Accessed July 11, 2018.
- Ruzicka T, Hanifin JM, Furue M, et al. Anti–interleukin-31 receptor A antibody for atopic dermatitis. N Engl J Med. 2017;376:826-835.
- Xu X, Zheng Y, Zhang X, et al. Efficacy and safety of dupilumab for the treatment of moderate-to-severe atopic dermatitis in adults. Oncotarget. 2017;8:108480-108491.
- Beck LA, Thaçi D, Hamilton JD, et al. Dupilumab treatment in adults with moderate-to-severe atopic dermatitis. N Engl J Med. 2014;371:130-139.
- Murrell D, Gebauer K, Spelman L, et al. Crisaborole topical ointment, 2% in adults with atopic dermatitis: a phase 2a, vehicle-controlled, proof-of-concept study. J Drugs Dermatol. 2015;14:1108-1112.
- Paller AS, Tom WL, Lebwohl MG, et al. Efficacy and safety of crisaborole ointment, a novel, nonsteroidal phosphodiesterase 4 (PDE4) inhibitor for the topical treatment of atopic dermatitis (AD) in children and adults. J Am Acad Dermatol. 2016;75:494-503.e6.
- Brunner PM, Israel A, Zhang N, et al. Early-onset pediatric atopic dermatitis is characterized by TH2/TH17/TH22-centered inflammation and lipid alterations. J Allergy Clin Immunol. 2018;141:2094-2106.
- Silverberg JI, Kleiman E, Silverberg NB, et al. Chickenpox in childhood is associated with decreased atopic disorders, IgE, allergic sensitization, and leukocyte subsets. Pediatr Allergy Immunol. 2012;23:50-58.
- Paller AS, Kabashima K, Bieber T. Therapeutic pipeline for atopic dermatitis: end of the drought? Allergy Clin Immunol. 2017;140:633-643.
- Renert-Yuval Y, Guttman-Yassky E. Systemic therapies in atopic dermatitis: the pipeline. Clin Dermatol. 2017;35:387-397.
- Bissonnette R, Papp KA, Poulin Y, et al. Topical tofacitinib for atopic dermatitis: a phase IIa randomized trial. Br J Dermatol. 2016;175:902-911.
- Guttman-Yassky E, Silverberg JI, Nemoto O, et al. Baricitinib in adult patients with moderate-to-severe atopic dermatitis: a phase 2 parallel, double-blinded, randomized placebo-controlled multiple-dose study [published online February 1, 2018]. J Am Acad Dermatol. doi: 10.1016/j.jaad.2018.01.018.
- Dupixent (dupilumab) showed positive phase 3 results in adolescents with inadequately controlled moderate-to-severe atopic dermatitis [press release]. Tarrytown, NY: Sanofi; May 16, 2018. https://www.prnewswire.com/news-releases/dupixent-dupilumab-showed-positive-phase-3-results-in-adolescents-with-inadequately-controlled-moderate-to-severe-atopic-dermatitis-300649146.html. Accessed July 11, 2018.
- Ruzicka T, Hanifin JM, Furue M, et al. Anti–interleukin-31 receptor A antibody for atopic dermatitis. N Engl J Med. 2017;376:826-835.
Louis Johnson: First Cold War SecDef
The VA Medical Center in Clarksburg, West Virginia, is named in honor of Louis Arthur Johnson, the Secretary of Defense under President Truman. Johnson cultivated a diversity of viewpoints and experiences before becoming Secretary of Defense. He was born in Roanoke, Virginia, in 1891, and he earned a law degree from the University of Virginia. Two years later, he began his foray into politics with election to the West Virginia House of Delegates, where he acted as Majority Floor Leader and Chair of the Judiciary Committee.1
Johnson served as an Infantry Captain in France during World War I, fighting in the Meuse-Argonne Offensive and earning the Legion of Honor of France. During his service, he gained insight into the military logistics by presenting a lengthy report on Army management and materiel requisition to the War Department—a foreshadowing of his eventual commitment to military budget restructuring as Secretary of Defense. After returning from the war, he practiced law and focused his efforts on aiding veterans, eventually securing the role of National Commander of the American Legion.1
Johnson was Assistant Secretary of War from 1937 to 1940 under President Franklin D. Roosevelt. Johnson frequently disagreed with the policies of Harry Hines Woodring, the acting Secretary of War who was a committed isolationist. While Johnson was adamant about providing military assistance to Great Britain during World War II, Woodring’s isolationism prevailed. However, in 1940, the fall of France forced the US to re-examine its defenses. Woodring resigned, and an eager Johnson was ready to take his place to re-instill confidence in the nation’s defenses against foreign threats.2
His enthusiasm was short-lived. President Roosevelt instead chose to appoint Henry Stimson as Secretary of Defense. Johnson felt betrayed.2 Johnson served as the personal representative of President Roosevelt in India, where he forged a lasting friendship with Jawaharlal Nehru, the first Prime Minister of India.
The 1948 presidential campaign was Johnson’s turn of fate. He aggressively raised funds for President Truman’s campaign and explicitly communicated his interest in serving as Secretary of Defense to the President, emphasizing that his goals for the nation’s defense were in line with those of Truman. Both favored aggressive elimination of unnecessary spending as well as unification of the military to minimize redundancies. In 1949, President Truman asked Johnson to replace James V. Forrestal, the acting Secretary of Defense.1
Johnson’s legacy as Defense Secretary was controversial from the beginning. His overarching goal was to cut any military spending that he deemed superfluous, proclaiming that taxpayers would receive “a dollar’s worth of defense for every dollar spent.”1 He and President Truman were confident that the atomic bomb would curtail most foreign aggression.
He faced enormous push back from military leaders in charge of ambitious expansion projects. The animosity amplified abruptly when Johnson canceled construction of the aircraft carrier USS United States, a multiyear construction effort by the US Navy already in progress. Johnson had not consulted with Congress or the Department of the Navy before announcing this cancellation. John L. Sullivan, the Secretary of the Navy, resigned in exasperation amidst the confusion and voiced his concerns about the future of the nation’s defense.1
Other branches of the military also experienced reductions, fueling an atmosphere of competition for limited funds. The “Revolt of the Admirals” that followed the scrapping of the United States was a salient example of this struggle, as leaders of the Navy and Air Force bitterly quarreled to earn Johnson’s approval for their respective expenses. Tensions rose to a peak in June 1949, when the House Committee on Armed Services commissioned a formal investigation of malfeasance against Secretary Johnson and the Air Force Secretary, likely at the behest of the Navy. These hearings challenged the entirety of Johnson’s platform, criticizing him for the United States cancellation, the feasibility of deterring foreign aggression with nuclear deterrence, and his overarching plan for military unification. After a lengthy series of charges, Johnson survived as the Committee found no convincing evidence of malfeasance. They also chose to support his plans for military unification, albeit with an admonition against aggressive, hasty overunification. Although Johnson had originally intended to eliminate waste and promote cohesiveness by establishing a more unified defense, his budget cuts had the unfortunate effect of creating deep rifts between the branches of the military.1
Johnson supported the establishment of the North Atlantic Treaty Organization (NATO) and the unified efforts of Soviet containment. However, in August 1949 the Soviets shocked the world with a successful atomic bomb test, and the Communists emerged victorious in the Chinese Civil War. In response, President Truman—with Johnson’s support—definitively called for development of the hydrogen bomb. In collaboration with the State Department, Johnson coauthored NSC 68, a top-secret report detailing nuclear expansion, Soviet containment, and aid to allies that laid the groundwork for militarization from the Cold War to the collapse of the Soviet Union in the 1990s.1
Despite the mounting threats, Johnson remained steadfast in his commitment to defense budgeting. The consequences of his economizing were felt at the beginning of the Korean War, as US and South Korean forces lacked adequate supplies to hold back the advance from the North Koreans. The rearguard operations that ensued proved to be extremely costly, and Johnson was forced to acknowledge that, “we have reached the point where the military considerations clearly outweigh the fiscal considerations.”4,5 In response to widespread public outcry over the progress in Korea, Truman asked Johnson to resign as Secretary of Defense, paving the way for George Marshall, General of the Army.
With his resignation, Johnson saw the end of his career in politics. He died in 1966 of a stroke but not before the Louis A. Johnson VA Medical Center, was dedicated in his honor on December 7, 1950.6
Despite the controversies surrounding his tenure, Johnson prioritized the well-being of the US more than anything else. At the end of his term, he solemnly paraphrased Macbeth, “When the hurly burly’s done and the battle is won, I trust the historian will find my record of performance creditable, my services honest and faithful commensurate with the trust that was placed in me and in the best interests of peace and our national defense.”
About this column
This column provides biographical sketches of the namesakes of military and VA health care facilities. To learn more about the individual your facility was named for or to offer a topic suggestion, contact us at fedprac@frontlinemedcom.com or on Facebook.
1. US Department of Defense, Office of the Secretary of Defense, Historical Office. Louis A. Johnson – Harry S. Truman Administration. http://history.defense.gov/Multimedia/Biographies/Article-View/Article/571265/. Accessed June 20, 2018.
2. Master of the Pentagon, Time. 1949;53(23).
3. LaFeber W. America, Russia, and the Cold War, 1945-1992. 7th edition New York: McGraw-Hill; 1993.
4. Zabecki DT. Stand or die—1950 defense of Korea’s Pusan perimeter. http://www.historynet.com/magazines/military_history. Published May 1, 2009. Accessed June 20, 2018.
5. McFarland KD, Roll DL. Louis Johnson and the Arming of America: The Roosevelt And Truman Years. Bloomington, IN: Indiana University Press; 2005.
6. US Department of Veterans Affairs. Louis A. Johnson Medical Center. https://www.clarksburg.va.gov/about/history.asp. Updated June 9, 2015. Accessed June 20, 2018.
The VA Medical Center in Clarksburg, West Virginia, is named in honor of Louis Arthur Johnson, the Secretary of Defense under President Truman. Johnson cultivated a diversity of viewpoints and experiences before becoming Secretary of Defense. He was born in Roanoke, Virginia, in 1891, and he earned a law degree from the University of Virginia. Two years later, he began his foray into politics with election to the West Virginia House of Delegates, where he acted as Majority Floor Leader and Chair of the Judiciary Committee.1
Johnson served as an Infantry Captain in France during World War I, fighting in the Meuse-Argonne Offensive and earning the Legion of Honor of France. During his service, he gained insight into the military logistics by presenting a lengthy report on Army management and materiel requisition to the War Department—a foreshadowing of his eventual commitment to military budget restructuring as Secretary of Defense. After returning from the war, he practiced law and focused his efforts on aiding veterans, eventually securing the role of National Commander of the American Legion.1
Johnson was Assistant Secretary of War from 1937 to 1940 under President Franklin D. Roosevelt. Johnson frequently disagreed with the policies of Harry Hines Woodring, the acting Secretary of War who was a committed isolationist. While Johnson was adamant about providing military assistance to Great Britain during World War II, Woodring’s isolationism prevailed. However, in 1940, the fall of France forced the US to re-examine its defenses. Woodring resigned, and an eager Johnson was ready to take his place to re-instill confidence in the nation’s defenses against foreign threats.2
His enthusiasm was short-lived. President Roosevelt instead chose to appoint Henry Stimson as Secretary of Defense. Johnson felt betrayed.2 Johnson served as the personal representative of President Roosevelt in India, where he forged a lasting friendship with Jawaharlal Nehru, the first Prime Minister of India.
The 1948 presidential campaign was Johnson’s turn of fate. He aggressively raised funds for President Truman’s campaign and explicitly communicated his interest in serving as Secretary of Defense to the President, emphasizing that his goals for the nation’s defense were in line with those of Truman. Both favored aggressive elimination of unnecessary spending as well as unification of the military to minimize redundancies. In 1949, President Truman asked Johnson to replace James V. Forrestal, the acting Secretary of Defense.1
Johnson’s legacy as Defense Secretary was controversial from the beginning. His overarching goal was to cut any military spending that he deemed superfluous, proclaiming that taxpayers would receive “a dollar’s worth of defense for every dollar spent.”1 He and President Truman were confident that the atomic bomb would curtail most foreign aggression.
He faced enormous push back from military leaders in charge of ambitious expansion projects. The animosity amplified abruptly when Johnson canceled construction of the aircraft carrier USS United States, a multiyear construction effort by the US Navy already in progress. Johnson had not consulted with Congress or the Department of the Navy before announcing this cancellation. John L. Sullivan, the Secretary of the Navy, resigned in exasperation amidst the confusion and voiced his concerns about the future of the nation’s defense.1
Other branches of the military also experienced reductions, fueling an atmosphere of competition for limited funds. The “Revolt of the Admirals” that followed the scrapping of the United States was a salient example of this struggle, as leaders of the Navy and Air Force bitterly quarreled to earn Johnson’s approval for their respective expenses. Tensions rose to a peak in June 1949, when the House Committee on Armed Services commissioned a formal investigation of malfeasance against Secretary Johnson and the Air Force Secretary, likely at the behest of the Navy. These hearings challenged the entirety of Johnson’s platform, criticizing him for the United States cancellation, the feasibility of deterring foreign aggression with nuclear deterrence, and his overarching plan for military unification. After a lengthy series of charges, Johnson survived as the Committee found no convincing evidence of malfeasance. They also chose to support his plans for military unification, albeit with an admonition against aggressive, hasty overunification. Although Johnson had originally intended to eliminate waste and promote cohesiveness by establishing a more unified defense, his budget cuts had the unfortunate effect of creating deep rifts between the branches of the military.1
Johnson supported the establishment of the North Atlantic Treaty Organization (NATO) and the unified efforts of Soviet containment. However, in August 1949 the Soviets shocked the world with a successful atomic bomb test, and the Communists emerged victorious in the Chinese Civil War. In response, President Truman—with Johnson’s support—definitively called for development of the hydrogen bomb. In collaboration with the State Department, Johnson coauthored NSC 68, a top-secret report detailing nuclear expansion, Soviet containment, and aid to allies that laid the groundwork for militarization from the Cold War to the collapse of the Soviet Union in the 1990s.1
Despite the mounting threats, Johnson remained steadfast in his commitment to defense budgeting. The consequences of his economizing were felt at the beginning of the Korean War, as US and South Korean forces lacked adequate supplies to hold back the advance from the North Koreans. The rearguard operations that ensued proved to be extremely costly, and Johnson was forced to acknowledge that, “we have reached the point where the military considerations clearly outweigh the fiscal considerations.”4,5 In response to widespread public outcry over the progress in Korea, Truman asked Johnson to resign as Secretary of Defense, paving the way for George Marshall, General of the Army.
With his resignation, Johnson saw the end of his career in politics. He died in 1966 of a stroke but not before the Louis A. Johnson VA Medical Center, was dedicated in his honor on December 7, 1950.6
Despite the controversies surrounding his tenure, Johnson prioritized the well-being of the US more than anything else. At the end of his term, he solemnly paraphrased Macbeth, “When the hurly burly’s done and the battle is won, I trust the historian will find my record of performance creditable, my services honest and faithful commensurate with the trust that was placed in me and in the best interests of peace and our national defense.”
About this column
This column provides biographical sketches of the namesakes of military and VA health care facilities. To learn more about the individual your facility was named for or to offer a topic suggestion, contact us at fedprac@frontlinemedcom.com or on Facebook.
The VA Medical Center in Clarksburg, West Virginia, is named in honor of Louis Arthur Johnson, the Secretary of Defense under President Truman. Johnson cultivated a diversity of viewpoints and experiences before becoming Secretary of Defense. He was born in Roanoke, Virginia, in 1891, and he earned a law degree from the University of Virginia. Two years later, he began his foray into politics with election to the West Virginia House of Delegates, where he acted as Majority Floor Leader and Chair of the Judiciary Committee.1
Johnson served as an Infantry Captain in France during World War I, fighting in the Meuse-Argonne Offensive and earning the Legion of Honor of France. During his service, he gained insight into the military logistics by presenting a lengthy report on Army management and materiel requisition to the War Department—a foreshadowing of his eventual commitment to military budget restructuring as Secretary of Defense. After returning from the war, he practiced law and focused his efforts on aiding veterans, eventually securing the role of National Commander of the American Legion.1
Johnson was Assistant Secretary of War from 1937 to 1940 under President Franklin D. Roosevelt. Johnson frequently disagreed with the policies of Harry Hines Woodring, the acting Secretary of War who was a committed isolationist. While Johnson was adamant about providing military assistance to Great Britain during World War II, Woodring’s isolationism prevailed. However, in 1940, the fall of France forced the US to re-examine its defenses. Woodring resigned, and an eager Johnson was ready to take his place to re-instill confidence in the nation’s defenses against foreign threats.2
His enthusiasm was short-lived. President Roosevelt instead chose to appoint Henry Stimson as Secretary of Defense. Johnson felt betrayed.2 Johnson served as the personal representative of President Roosevelt in India, where he forged a lasting friendship with Jawaharlal Nehru, the first Prime Minister of India.
The 1948 presidential campaign was Johnson’s turn of fate. He aggressively raised funds for President Truman’s campaign and explicitly communicated his interest in serving as Secretary of Defense to the President, emphasizing that his goals for the nation’s defense were in line with those of Truman. Both favored aggressive elimination of unnecessary spending as well as unification of the military to minimize redundancies. In 1949, President Truman asked Johnson to replace James V. Forrestal, the acting Secretary of Defense.1
Johnson’s legacy as Defense Secretary was controversial from the beginning. His overarching goal was to cut any military spending that he deemed superfluous, proclaiming that taxpayers would receive “a dollar’s worth of defense for every dollar spent.”1 He and President Truman were confident that the atomic bomb would curtail most foreign aggression.
He faced enormous push back from military leaders in charge of ambitious expansion projects. The animosity amplified abruptly when Johnson canceled construction of the aircraft carrier USS United States, a multiyear construction effort by the US Navy already in progress. Johnson had not consulted with Congress or the Department of the Navy before announcing this cancellation. John L. Sullivan, the Secretary of the Navy, resigned in exasperation amidst the confusion and voiced his concerns about the future of the nation’s defense.1
Other branches of the military also experienced reductions, fueling an atmosphere of competition for limited funds. The “Revolt of the Admirals” that followed the scrapping of the United States was a salient example of this struggle, as leaders of the Navy and Air Force bitterly quarreled to earn Johnson’s approval for their respective expenses. Tensions rose to a peak in June 1949, when the House Committee on Armed Services commissioned a formal investigation of malfeasance against Secretary Johnson and the Air Force Secretary, likely at the behest of the Navy. These hearings challenged the entirety of Johnson’s platform, criticizing him for the United States cancellation, the feasibility of deterring foreign aggression with nuclear deterrence, and his overarching plan for military unification. After a lengthy series of charges, Johnson survived as the Committee found no convincing evidence of malfeasance. They also chose to support his plans for military unification, albeit with an admonition against aggressive, hasty overunification. Although Johnson had originally intended to eliminate waste and promote cohesiveness by establishing a more unified defense, his budget cuts had the unfortunate effect of creating deep rifts between the branches of the military.1
Johnson supported the establishment of the North Atlantic Treaty Organization (NATO) and the unified efforts of Soviet containment. However, in August 1949 the Soviets shocked the world with a successful atomic bomb test, and the Communists emerged victorious in the Chinese Civil War. In response, President Truman—with Johnson’s support—definitively called for development of the hydrogen bomb. In collaboration with the State Department, Johnson coauthored NSC 68, a top-secret report detailing nuclear expansion, Soviet containment, and aid to allies that laid the groundwork for militarization from the Cold War to the collapse of the Soviet Union in the 1990s.1
Despite the mounting threats, Johnson remained steadfast in his commitment to defense budgeting. The consequences of his economizing were felt at the beginning of the Korean War, as US and South Korean forces lacked adequate supplies to hold back the advance from the North Koreans. The rearguard operations that ensued proved to be extremely costly, and Johnson was forced to acknowledge that, “we have reached the point where the military considerations clearly outweigh the fiscal considerations.”4,5 In response to widespread public outcry over the progress in Korea, Truman asked Johnson to resign as Secretary of Defense, paving the way for George Marshall, General of the Army.
With his resignation, Johnson saw the end of his career in politics. He died in 1966 of a stroke but not before the Louis A. Johnson VA Medical Center, was dedicated in his honor on December 7, 1950.6
Despite the controversies surrounding his tenure, Johnson prioritized the well-being of the US more than anything else. At the end of his term, he solemnly paraphrased Macbeth, “When the hurly burly’s done and the battle is won, I trust the historian will find my record of performance creditable, my services honest and faithful commensurate with the trust that was placed in me and in the best interests of peace and our national defense.”
About this column
This column provides biographical sketches of the namesakes of military and VA health care facilities. To learn more about the individual your facility was named for or to offer a topic suggestion, contact us at fedprac@frontlinemedcom.com or on Facebook.
1. US Department of Defense, Office of the Secretary of Defense, Historical Office. Louis A. Johnson – Harry S. Truman Administration. http://history.defense.gov/Multimedia/Biographies/Article-View/Article/571265/. Accessed June 20, 2018.
2. Master of the Pentagon, Time. 1949;53(23).
3. LaFeber W. America, Russia, and the Cold War, 1945-1992. 7th edition New York: McGraw-Hill; 1993.
4. Zabecki DT. Stand or die—1950 defense of Korea’s Pusan perimeter. http://www.historynet.com/magazines/military_history. Published May 1, 2009. Accessed June 20, 2018.
5. McFarland KD, Roll DL. Louis Johnson and the Arming of America: The Roosevelt And Truman Years. Bloomington, IN: Indiana University Press; 2005.
6. US Department of Veterans Affairs. Louis A. Johnson Medical Center. https://www.clarksburg.va.gov/about/history.asp. Updated June 9, 2015. Accessed June 20, 2018.
1. US Department of Defense, Office of the Secretary of Defense, Historical Office. Louis A. Johnson – Harry S. Truman Administration. http://history.defense.gov/Multimedia/Biographies/Article-View/Article/571265/. Accessed June 20, 2018.
2. Master of the Pentagon, Time. 1949;53(23).
3. LaFeber W. America, Russia, and the Cold War, 1945-1992. 7th edition New York: McGraw-Hill; 1993.
4. Zabecki DT. Stand or die—1950 defense of Korea’s Pusan perimeter. http://www.historynet.com/magazines/military_history. Published May 1, 2009. Accessed June 20, 2018.
5. McFarland KD, Roll DL. Louis Johnson and the Arming of America: The Roosevelt And Truman Years. Bloomington, IN: Indiana University Press; 2005.
6. US Department of Veterans Affairs. Louis A. Johnson Medical Center. https://www.clarksburg.va.gov/about/history.asp. Updated June 9, 2015. Accessed June 20, 2018.