User login
Acute Hepatitis E Superinfection Reactivates Chronic HBV
Many things can reactivate chronic hepatitis B virus (HBV) infection—withdrawal of antiviral therapy, pregnancy, and chemotherapy, to name a few. So when a patient with stable chronic HBV virus presented with significant hepatitis flare, clinicians from Beth Israel Deaconess Medical Center in Boston, Massachusetts, had a long list to check.
They first ruled out drug-associated hepatotoxicity and screened the patient for common causes of acute hepatitis. Beyond the HBV, the patient did not have other significant medical conditions, had not had close contact with anyone ill, and was not pregnant. Tests were negative for cytomegalovirus, Epstein-Barr syndrome, HIV, hepatitis A, C, and D. The patient tested negative for both antihepatitis E virus (HEV) IgM and IgG in a visit about 9 months before.
However, she reported regularly consuming pork, including a recent barbecue meal. Thus, the clinicians focused on HEV serology, which confirmed that she had an acute HEV infection.
Pigs act as a “natural reservoir” for HEV; contaminated meats and direct contact with animals are the most common causes of HEV human infection in industrialized countries. Recent data reveal the prevalence of HEV antibodies in the US is about 6%, illustrating that it is not as uncommon as it was thought to be. Although there was no direct evidence to confirm the source of her infection, it seemed likely due to the pork consumption.
The patient was started on tenofovir but stopped it 4 months later because she felt well. After a subsequent flare, “repeated counseling” persuaded the patient to start on entecavir, with successful viral suppression.
Hepatitis E superinfection on chronic HBV can contribute to significant morbidity and mortality, the clinicians say, particularly in patients with cirrhosis. Concurrent infection with another viral hepatitis should be considered in both immunodeficient and immunocompetent patients with chronic HBV reactivation.
Source:
Aslam A, Susheela A, Iriana S, Chan SS, Lau D. BMJ Case Rep. 2018;2018. pii: bcr-2017-223616.
doi: 10.1136/bcr-2017-223616.
Many things can reactivate chronic hepatitis B virus (HBV) infection—withdrawal of antiviral therapy, pregnancy, and chemotherapy, to name a few. So when a patient with stable chronic HBV virus presented with significant hepatitis flare, clinicians from Beth Israel Deaconess Medical Center in Boston, Massachusetts, had a long list to check.
They first ruled out drug-associated hepatotoxicity and screened the patient for common causes of acute hepatitis. Beyond the HBV, the patient did not have other significant medical conditions, had not had close contact with anyone ill, and was not pregnant. Tests were negative for cytomegalovirus, Epstein-Barr syndrome, HIV, hepatitis A, C, and D. The patient tested negative for both antihepatitis E virus (HEV) IgM and IgG in a visit about 9 months before.
However, she reported regularly consuming pork, including a recent barbecue meal. Thus, the clinicians focused on HEV serology, which confirmed that she had an acute HEV infection.
Pigs act as a “natural reservoir” for HEV; contaminated meats and direct contact with animals are the most common causes of HEV human infection in industrialized countries. Recent data reveal the prevalence of HEV antibodies in the US is about 6%, illustrating that it is not as uncommon as it was thought to be. Although there was no direct evidence to confirm the source of her infection, it seemed likely due to the pork consumption.
The patient was started on tenofovir but stopped it 4 months later because she felt well. After a subsequent flare, “repeated counseling” persuaded the patient to start on entecavir, with successful viral suppression.
Hepatitis E superinfection on chronic HBV can contribute to significant morbidity and mortality, the clinicians say, particularly in patients with cirrhosis. Concurrent infection with another viral hepatitis should be considered in both immunodeficient and immunocompetent patients with chronic HBV reactivation.
Source:
Aslam A, Susheela A, Iriana S, Chan SS, Lau D. BMJ Case Rep. 2018;2018. pii: bcr-2017-223616.
doi: 10.1136/bcr-2017-223616.
Many things can reactivate chronic hepatitis B virus (HBV) infection—withdrawal of antiviral therapy, pregnancy, and chemotherapy, to name a few. So when a patient with stable chronic HBV virus presented with significant hepatitis flare, clinicians from Beth Israel Deaconess Medical Center in Boston, Massachusetts, had a long list to check.
They first ruled out drug-associated hepatotoxicity and screened the patient for common causes of acute hepatitis. Beyond the HBV, the patient did not have other significant medical conditions, had not had close contact with anyone ill, and was not pregnant. Tests were negative for cytomegalovirus, Epstein-Barr syndrome, HIV, hepatitis A, C, and D. The patient tested negative for both antihepatitis E virus (HEV) IgM and IgG in a visit about 9 months before.
However, she reported regularly consuming pork, including a recent barbecue meal. Thus, the clinicians focused on HEV serology, which confirmed that she had an acute HEV infection.
Pigs act as a “natural reservoir” for HEV; contaminated meats and direct contact with animals are the most common causes of HEV human infection in industrialized countries. Recent data reveal the prevalence of HEV antibodies in the US is about 6%, illustrating that it is not as uncommon as it was thought to be. Although there was no direct evidence to confirm the source of her infection, it seemed likely due to the pork consumption.
The patient was started on tenofovir but stopped it 4 months later because she felt well. After a subsequent flare, “repeated counseling” persuaded the patient to start on entecavir, with successful viral suppression.
Hepatitis E superinfection on chronic HBV can contribute to significant morbidity and mortality, the clinicians say, particularly in patients with cirrhosis. Concurrent infection with another viral hepatitis should be considered in both immunodeficient and immunocompetent patients with chronic HBV reactivation.
Source:
Aslam A, Susheela A, Iriana S, Chan SS, Lau D. BMJ Case Rep. 2018;2018. pii: bcr-2017-223616.
doi: 10.1136/bcr-2017-223616.
Voxelotor benefits adolescents with SCD
STOCKHOLM—An ongoing phase 2 study suggests voxelotor (GBT440) can benefit adolescents with sickle cell disease (SCD).
In the HOPE-KIDS 1 study, voxelotor produced sustained improvements in hemoglobin levels and a reduction in clinical measures of hemolysis in a cohort of adolescents with SCD, most of whom were also receiving hydroxyurea (HU).
The most common adverse events (AEs) related to voxelotor were nausea, vomiting, headache, and rash.
These results were presented in a poster (abstract PF709) at the 23rd Congress of the European Hematology Association (EHA).
HOPE-KIDS 1 is sponsored by Global Blood Therapeutics, Inc.
In this study, researchers are evaluating voxelotor in SCD patients ages 6 to 17. In part A, researchers evaluated a 600 mg daily dose of voxelotor. In part B, they are testing voxelotor at daily doses of 900 mg and 1500 mg in patients ages 12 to 17.
At EHA, the researchers presented data on 25 patients who received voxelotor at 900 mg/day for 24 weeks in part B. Eighty-eight percent of the patients (n=22) were also taking HU.
The patients’ median age was 14 (range, 12-17), and 56% were male. Ninety-six percent (n=24) had the HbSS genotype.
Forty-eight percent of patients had 1 to 4 vaso-occlusive crises (VOCs) in the past year, 8% had more than 4 VOCs, and 44% had 0 VOCs.
At baseline, the median hemoglobin was 8.9 g/dL, the median fetal hemoglobin was 10.8 g/dL, and the median time-averaged mean of maximum velocity was 110 cm/s.
All 25 patients were dosed with voxelotor, and 22 completed 24 weeks of dosing. One patient withdrew consent, 1 was lost to follow-up, and 1 patient discontinued due to noncompliance.
Of the 22 patients who completed 24 weeks of voxelotor treatment, all but 3 were receiving concurrent HU.
Results
Voxelotor-related AEs occurring in at least 2 patients included nausea (12%, n=3), vomiting (8%, n=2), headache (8%, n=2), and rash (8%, n=2).
There was 1 case of grade 3 urticaria, which resolved and did not recur with continued dosing. There were no discontinuations of voxelotor due to AEs.
Patients experienced increased hemoglobin levels and improved clinical measures of hemolysis at 24 weeks, as evaluated by changes from baseline in hemoglobin, percent of reticulocytes, and percent of unconjugated bilirubin.
In all, 43% of patients (9/21) achieved a hemoglobin response (>1 g/dL) at 24 weeks. The median hemoglobin change from baseline was 0.7 g/dL, the median reduction in reticulocytes was 22.9%, and the median reduction in unconjugated bilirubin was 38.6%.
Sixty-two percent of patients (13/21) had a reduction in daily symptoms at 24 weeks, as assessed by total symptom scores (TSS). There was a 39% median reduction in TSS from baseline.
Fifty-five percent of patients (11/20) had a numerical decrease in transcranial doppler (TCD) flow at 24 weeks. Among hemoglobin responders (>1 g/dL), 88% (7/8) had a numerical decrease in TCD at 24 weeks.
“We continue to be encouraged by the results of the ongoing HOPE-KIDS 1 study, which are consistent with inhibition of HbS polymerization by voxelotor and support its ongoing clinical evaluation as a potential disease-modifying therapy for both adults and adolescents with SCD,” said Ted W. Love, MD, president and chief executive officer of Global Blood Therapeutics.
“Results to date support our ongoing development of voxelotor in a broad range of patients, including in our phase 3 HOPE study, which is also evaluating voxelotor at doses of 900 mg and 1500 mg per day in adolescents and adults. We continue to expect to announce top-line clinical data from part A of the HOPE study by the end of this quarter.”
STOCKHOLM—An ongoing phase 2 study suggests voxelotor (GBT440) can benefit adolescents with sickle cell disease (SCD).
In the HOPE-KIDS 1 study, voxelotor produced sustained improvements in hemoglobin levels and a reduction in clinical measures of hemolysis in a cohort of adolescents with SCD, most of whom were also receiving hydroxyurea (HU).
The most common adverse events (AEs) related to voxelotor were nausea, vomiting, headache, and rash.
These results were presented in a poster (abstract PF709) at the 23rd Congress of the European Hematology Association (EHA).
HOPE-KIDS 1 is sponsored by Global Blood Therapeutics, Inc.
In this study, researchers are evaluating voxelotor in SCD patients ages 6 to 17. In part A, researchers evaluated a 600 mg daily dose of voxelotor. In part B, they are testing voxelotor at daily doses of 900 mg and 1500 mg in patients ages 12 to 17.
At EHA, the researchers presented data on 25 patients who received voxelotor at 900 mg/day for 24 weeks in part B. Eighty-eight percent of the patients (n=22) were also taking HU.
The patients’ median age was 14 (range, 12-17), and 56% were male. Ninety-six percent (n=24) had the HbSS genotype.
Forty-eight percent of patients had 1 to 4 vaso-occlusive crises (VOCs) in the past year, 8% had more than 4 VOCs, and 44% had 0 VOCs.
At baseline, the median hemoglobin was 8.9 g/dL, the median fetal hemoglobin was 10.8 g/dL, and the median time-averaged mean of maximum velocity was 110 cm/s.
All 25 patients were dosed with voxelotor, and 22 completed 24 weeks of dosing. One patient withdrew consent, 1 was lost to follow-up, and 1 patient discontinued due to noncompliance.
Of the 22 patients who completed 24 weeks of voxelotor treatment, all but 3 were receiving concurrent HU.
Results
Voxelotor-related AEs occurring in at least 2 patients included nausea (12%, n=3), vomiting (8%, n=2), headache (8%, n=2), and rash (8%, n=2).
There was 1 case of grade 3 urticaria, which resolved and did not recur with continued dosing. There were no discontinuations of voxelotor due to AEs.
Patients experienced increased hemoglobin levels and improved clinical measures of hemolysis at 24 weeks, as evaluated by changes from baseline in hemoglobin, percent of reticulocytes, and percent of unconjugated bilirubin.
In all, 43% of patients (9/21) achieved a hemoglobin response (>1 g/dL) at 24 weeks. The median hemoglobin change from baseline was 0.7 g/dL, the median reduction in reticulocytes was 22.9%, and the median reduction in unconjugated bilirubin was 38.6%.
Sixty-two percent of patients (13/21) had a reduction in daily symptoms at 24 weeks, as assessed by total symptom scores (TSS). There was a 39% median reduction in TSS from baseline.
Fifty-five percent of patients (11/20) had a numerical decrease in transcranial doppler (TCD) flow at 24 weeks. Among hemoglobin responders (>1 g/dL), 88% (7/8) had a numerical decrease in TCD at 24 weeks.
“We continue to be encouraged by the results of the ongoing HOPE-KIDS 1 study, which are consistent with inhibition of HbS polymerization by voxelotor and support its ongoing clinical evaluation as a potential disease-modifying therapy for both adults and adolescents with SCD,” said Ted W. Love, MD, president and chief executive officer of Global Blood Therapeutics.
“Results to date support our ongoing development of voxelotor in a broad range of patients, including in our phase 3 HOPE study, which is also evaluating voxelotor at doses of 900 mg and 1500 mg per day in adolescents and adults. We continue to expect to announce top-line clinical data from part A of the HOPE study by the end of this quarter.”
STOCKHOLM—An ongoing phase 2 study suggests voxelotor (GBT440) can benefit adolescents with sickle cell disease (SCD).
In the HOPE-KIDS 1 study, voxelotor produced sustained improvements in hemoglobin levels and a reduction in clinical measures of hemolysis in a cohort of adolescents with SCD, most of whom were also receiving hydroxyurea (HU).
The most common adverse events (AEs) related to voxelotor were nausea, vomiting, headache, and rash.
These results were presented in a poster (abstract PF709) at the 23rd Congress of the European Hematology Association (EHA).
HOPE-KIDS 1 is sponsored by Global Blood Therapeutics, Inc.
In this study, researchers are evaluating voxelotor in SCD patients ages 6 to 17. In part A, researchers evaluated a 600 mg daily dose of voxelotor. In part B, they are testing voxelotor at daily doses of 900 mg and 1500 mg in patients ages 12 to 17.
At EHA, the researchers presented data on 25 patients who received voxelotor at 900 mg/day for 24 weeks in part B. Eighty-eight percent of the patients (n=22) were also taking HU.
The patients’ median age was 14 (range, 12-17), and 56% were male. Ninety-six percent (n=24) had the HbSS genotype.
Forty-eight percent of patients had 1 to 4 vaso-occlusive crises (VOCs) in the past year, 8% had more than 4 VOCs, and 44% had 0 VOCs.
At baseline, the median hemoglobin was 8.9 g/dL, the median fetal hemoglobin was 10.8 g/dL, and the median time-averaged mean of maximum velocity was 110 cm/s.
All 25 patients were dosed with voxelotor, and 22 completed 24 weeks of dosing. One patient withdrew consent, 1 was lost to follow-up, and 1 patient discontinued due to noncompliance.
Of the 22 patients who completed 24 weeks of voxelotor treatment, all but 3 were receiving concurrent HU.
Results
Voxelotor-related AEs occurring in at least 2 patients included nausea (12%, n=3), vomiting (8%, n=2), headache (8%, n=2), and rash (8%, n=2).
There was 1 case of grade 3 urticaria, which resolved and did not recur with continued dosing. There were no discontinuations of voxelotor due to AEs.
Patients experienced increased hemoglobin levels and improved clinical measures of hemolysis at 24 weeks, as evaluated by changes from baseline in hemoglobin, percent of reticulocytes, and percent of unconjugated bilirubin.
In all, 43% of patients (9/21) achieved a hemoglobin response (>1 g/dL) at 24 weeks. The median hemoglobin change from baseline was 0.7 g/dL, the median reduction in reticulocytes was 22.9%, and the median reduction in unconjugated bilirubin was 38.6%.
Sixty-two percent of patients (13/21) had a reduction in daily symptoms at 24 weeks, as assessed by total symptom scores (TSS). There was a 39% median reduction in TSS from baseline.
Fifty-five percent of patients (11/20) had a numerical decrease in transcranial doppler (TCD) flow at 24 weeks. Among hemoglobin responders (>1 g/dL), 88% (7/8) had a numerical decrease in TCD at 24 weeks.
“We continue to be encouraged by the results of the ongoing HOPE-KIDS 1 study, which are consistent with inhibition of HbS polymerization by voxelotor and support its ongoing clinical evaluation as a potential disease-modifying therapy for both adults and adolescents with SCD,” said Ted W. Love, MD, president and chief executive officer of Global Blood Therapeutics.
“Results to date support our ongoing development of voxelotor in a broad range of patients, including in our phase 3 HOPE study, which is also evaluating voxelotor at doses of 900 mg and 1500 mg per day in adolescents and adults. We continue to expect to announce top-line clinical data from part A of the HOPE study by the end of this quarter.”
Ibrutinib sNDA receives priority review
The US Food and Drug Administration (FDA) has accepted for priority review a supplemental new drug application (sNDA) for ibrutinib (Imbruvica®) to be used in combination with rituximab in patients with Waldenström’s macroglobulinemia (WM).
The FDA intends to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
Ibrutinib is a first-in-class Bruton’s tyrosine kinase inhibitor jointly developed and commercialized by Pharmacyclics LLC, an AbbVie company, and Janssen Biotech, Inc.
Ibrutinib is already FDA-approved to treat chronic lymphocytic leukemia/small lymphocytic lymphoma, previously treated mantle cell lymphoma, previously treated marginal zone lymphoma, previously treated chronic graft-versus-host disease, and WM.
If the new sNDA is approved, the use of ibrutinib in WM will extend beyond its current approved use as a single agent.
Phase 3 trial
The sNDA for ibrutinib and rituximab in WM is supported by data from the phase 3 iNNOVATE study. Results from this trial were presented at the 2018 ASCO Annual Meeting (abstract 8003) and were simultaneously published in NEJM.
iNNOVATE is a placebo-controlled, double-blind, phase 3 study that enrolled 150 patients with relapsed/refractory and treatment-naïve WM.
All patients received rituximab at 375 mg/m2 with weekly infusions at weeks 1 to 4 and 17 to 20. They also received either ibrutinib (420 mg) or placebo once daily continuously until criteria for permanent discontinuation were met.
Overall response rates were significantly higher in the ibrutinib arm than the placebo arm—92% and 47%, respectively (P<0.0001). Complete response rates were 3% and 1%, respectively.
The median time to next treatment was not reached for the ibrutinib arm and was 18 months for the placebo arm (hazard ratio=0.096; P<0.0001). Of the patients randomized to ibrutinib plus rituximab, 75% continued on treatment at last follow-up.
The 30-month progression-free survival rates were 82% in the ibrutinib arm and 28% in the placebo arm. The median progression-free survival was not reached in the ibrutinib arm and was 20.3 months in the placebo arm (hazard ratio=0.20; P<0.0001).
The 30-month overall survival rates were 94% in the ibrutinib arm and 92% in the placebo arm.
Grade 3 or higher treatment-emergent adverse events (AEs) occurred in 60% of patients in the ibrutinib arm and 61% in the placebo arm.
Serious AEs occurred in 43% and 33% of patients, respectively. There were no fatal AEs in the ibrutinib arm and 3 in the rituximab arm.
Grade 3 or higher AEs that occurred more frequently in the ibrutinib arm than the placebo arm included atrial fibrillation (12% vs 1%) and hypertension (13% vs 4%).
AEs that occurred less frequently in the ibrutinib arm than the placebo arm included grade 3 or higher infusion reactions (1% vs 16%) and any-grade IgM flare (8% vs 47%).
The US Food and Drug Administration (FDA) has accepted for priority review a supplemental new drug application (sNDA) for ibrutinib (Imbruvica®) to be used in combination with rituximab in patients with Waldenström’s macroglobulinemia (WM).
The FDA intends to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
Ibrutinib is a first-in-class Bruton’s tyrosine kinase inhibitor jointly developed and commercialized by Pharmacyclics LLC, an AbbVie company, and Janssen Biotech, Inc.
Ibrutinib is already FDA-approved to treat chronic lymphocytic leukemia/small lymphocytic lymphoma, previously treated mantle cell lymphoma, previously treated marginal zone lymphoma, previously treated chronic graft-versus-host disease, and WM.
If the new sNDA is approved, the use of ibrutinib in WM will extend beyond its current approved use as a single agent.
Phase 3 trial
The sNDA for ibrutinib and rituximab in WM is supported by data from the phase 3 iNNOVATE study. Results from this trial were presented at the 2018 ASCO Annual Meeting (abstract 8003) and were simultaneously published in NEJM.
iNNOVATE is a placebo-controlled, double-blind, phase 3 study that enrolled 150 patients with relapsed/refractory and treatment-naïve WM.
All patients received rituximab at 375 mg/m2 with weekly infusions at weeks 1 to 4 and 17 to 20. They also received either ibrutinib (420 mg) or placebo once daily continuously until criteria for permanent discontinuation were met.
Overall response rates were significantly higher in the ibrutinib arm than the placebo arm—92% and 47%, respectively (P<0.0001). Complete response rates were 3% and 1%, respectively.
The median time to next treatment was not reached for the ibrutinib arm and was 18 months for the placebo arm (hazard ratio=0.096; P<0.0001). Of the patients randomized to ibrutinib plus rituximab, 75% continued on treatment at last follow-up.
The 30-month progression-free survival rates were 82% in the ibrutinib arm and 28% in the placebo arm. The median progression-free survival was not reached in the ibrutinib arm and was 20.3 months in the placebo arm (hazard ratio=0.20; P<0.0001).
The 30-month overall survival rates were 94% in the ibrutinib arm and 92% in the placebo arm.
Grade 3 or higher treatment-emergent adverse events (AEs) occurred in 60% of patients in the ibrutinib arm and 61% in the placebo arm.
Serious AEs occurred in 43% and 33% of patients, respectively. There were no fatal AEs in the ibrutinib arm and 3 in the rituximab arm.
Grade 3 or higher AEs that occurred more frequently in the ibrutinib arm than the placebo arm included atrial fibrillation (12% vs 1%) and hypertension (13% vs 4%).
AEs that occurred less frequently in the ibrutinib arm than the placebo arm included grade 3 or higher infusion reactions (1% vs 16%) and any-grade IgM flare (8% vs 47%).
The US Food and Drug Administration (FDA) has accepted for priority review a supplemental new drug application (sNDA) for ibrutinib (Imbruvica®) to be used in combination with rituximab in patients with Waldenström’s macroglobulinemia (WM).
The FDA intends to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
Ibrutinib is a first-in-class Bruton’s tyrosine kinase inhibitor jointly developed and commercialized by Pharmacyclics LLC, an AbbVie company, and Janssen Biotech, Inc.
Ibrutinib is already FDA-approved to treat chronic lymphocytic leukemia/small lymphocytic lymphoma, previously treated mantle cell lymphoma, previously treated marginal zone lymphoma, previously treated chronic graft-versus-host disease, and WM.
If the new sNDA is approved, the use of ibrutinib in WM will extend beyond its current approved use as a single agent.
Phase 3 trial
The sNDA for ibrutinib and rituximab in WM is supported by data from the phase 3 iNNOVATE study. Results from this trial were presented at the 2018 ASCO Annual Meeting (abstract 8003) and were simultaneously published in NEJM.
iNNOVATE is a placebo-controlled, double-blind, phase 3 study that enrolled 150 patients with relapsed/refractory and treatment-naïve WM.
All patients received rituximab at 375 mg/m2 with weekly infusions at weeks 1 to 4 and 17 to 20. They also received either ibrutinib (420 mg) or placebo once daily continuously until criteria for permanent discontinuation were met.
Overall response rates were significantly higher in the ibrutinib arm than the placebo arm—92% and 47%, respectively (P<0.0001). Complete response rates were 3% and 1%, respectively.
The median time to next treatment was not reached for the ibrutinib arm and was 18 months for the placebo arm (hazard ratio=0.096; P<0.0001). Of the patients randomized to ibrutinib plus rituximab, 75% continued on treatment at last follow-up.
The 30-month progression-free survival rates were 82% in the ibrutinib arm and 28% in the placebo arm. The median progression-free survival was not reached in the ibrutinib arm and was 20.3 months in the placebo arm (hazard ratio=0.20; P<0.0001).
The 30-month overall survival rates were 94% in the ibrutinib arm and 92% in the placebo arm.
Grade 3 or higher treatment-emergent adverse events (AEs) occurred in 60% of patients in the ibrutinib arm and 61% in the placebo arm.
Serious AEs occurred in 43% and 33% of patients, respectively. There were no fatal AEs in the ibrutinib arm and 3 in the rituximab arm.
Grade 3 or higher AEs that occurred more frequently in the ibrutinib arm than the placebo arm included atrial fibrillation (12% vs 1%) and hypertension (13% vs 4%).
AEs that occurred less frequently in the ibrutinib arm than the placebo arm included grade 3 or higher infusion reactions (1% vs 16%) and any-grade IgM flare (8% vs 47%).
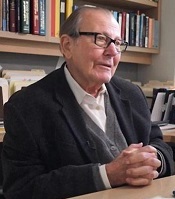
Leading researcher in genetics, hematology dies at 84
George Stamatoyannopoulos, MD, who conducted important research into hemoglobinopathies, passed away this month at the age of 84.
Dr Stamatoyannopoulos’s research encompassed human genetics and hematology, including the structure and function of hemoglobinopathies, the genetics of thalassemia, and the molecular and cellular control of globin gene switching.
For much of his career, Dr Stamatoyannopoulos focused on the development of gene therapy for hemoglobinopathies and other disorders.
Dr Stamatoyannopoulos was born in Athens, Greece, on March 11, 1934. He entered medical school in Athens at age 17 and graduated at the top of his class 7 years later.
After his medical training, Dr Stamatoyannopoulos pursued thesis research on inherited blood disorders, particularly anemias.
Dr Stamatoyannopoulos performed the first large-scale molecular geographical survey of a genetic trait, which revealed the relationship between malaria and both thalassemia and sickle cell traits.
Dr Stamatoyannopoulos also discovered that fetal hemoglobin could ameliorate the effects of thalassemia. His theory that thalassemia and sickle cell anemia could be treated by re-activating fetal hemoglobin has underpinned decades of efforts to cure these disorders.
As a young investigator, Dr Stamatoyannopoulos expanded genetic studies of blood diseases in Greece, where his work drew the attention of medical genetics pioneer Arno Motulsky, MD.
Dr Motulsky recruited Dr Stamatoyannopoulos to the University of Washington (Seattle) in 1964. Dr Stamatoyannopoulos became a full professor there in 1973, founded the Markey Molecular Medicine Center, and was chief of medical genetics from 1989 to 2005.
Dr Stamatoyannopoulos organized the founding of the American Society of Gene and Cell Therapy. His contributions were recognized by establishment of the Stamatoyannopoulos lecture, the society’s highest award.
Dr Stamatoyannopoulos also served as president of the American Society of Hematology (1992) and president of the American Society of Gene and Cell Therapy (1996). He held leadership positions in other medical and scientific societies as well.
Dr Stamatoyannopoulos authored more than 420 scientific papers and 14 books, including The Molecular Basis of Blood Diseases.
Dr Stamatoyannopoulos died June 16, 2018. He is survived by his wife and collaborator Thalia Papayannopoulou, MD, (a professor of medicine and internationally recognized hematologist), 2 sons, and 3 grandchildren.
George Stamatoyannopoulos, MD, who conducted important research into hemoglobinopathies, passed away this month at the age of 84.
Dr Stamatoyannopoulos’s research encompassed human genetics and hematology, including the structure and function of hemoglobinopathies, the genetics of thalassemia, and the molecular and cellular control of globin gene switching.
For much of his career, Dr Stamatoyannopoulos focused on the development of gene therapy for hemoglobinopathies and other disorders.
Dr Stamatoyannopoulos was born in Athens, Greece, on March 11, 1934. He entered medical school in Athens at age 17 and graduated at the top of his class 7 years later.
After his medical training, Dr Stamatoyannopoulos pursued thesis research on inherited blood disorders, particularly anemias.
Dr Stamatoyannopoulos performed the first large-scale molecular geographical survey of a genetic trait, which revealed the relationship between malaria and both thalassemia and sickle cell traits.
Dr Stamatoyannopoulos also discovered that fetal hemoglobin could ameliorate the effects of thalassemia. His theory that thalassemia and sickle cell anemia could be treated by re-activating fetal hemoglobin has underpinned decades of efforts to cure these disorders.
As a young investigator, Dr Stamatoyannopoulos expanded genetic studies of blood diseases in Greece, where his work drew the attention of medical genetics pioneer Arno Motulsky, MD.
Dr Motulsky recruited Dr Stamatoyannopoulos to the University of Washington (Seattle) in 1964. Dr Stamatoyannopoulos became a full professor there in 1973, founded the Markey Molecular Medicine Center, and was chief of medical genetics from 1989 to 2005.
Dr Stamatoyannopoulos organized the founding of the American Society of Gene and Cell Therapy. His contributions were recognized by establishment of the Stamatoyannopoulos lecture, the society’s highest award.
Dr Stamatoyannopoulos also served as president of the American Society of Hematology (1992) and president of the American Society of Gene and Cell Therapy (1996). He held leadership positions in other medical and scientific societies as well.
Dr Stamatoyannopoulos authored more than 420 scientific papers and 14 books, including The Molecular Basis of Blood Diseases.
Dr Stamatoyannopoulos died June 16, 2018. He is survived by his wife and collaborator Thalia Papayannopoulou, MD, (a professor of medicine and internationally recognized hematologist), 2 sons, and 3 grandchildren.
George Stamatoyannopoulos, MD, who conducted important research into hemoglobinopathies, passed away this month at the age of 84.
Dr Stamatoyannopoulos’s research encompassed human genetics and hematology, including the structure and function of hemoglobinopathies, the genetics of thalassemia, and the molecular and cellular control of globin gene switching.
For much of his career, Dr Stamatoyannopoulos focused on the development of gene therapy for hemoglobinopathies and other disorders.
Dr Stamatoyannopoulos was born in Athens, Greece, on March 11, 1934. He entered medical school in Athens at age 17 and graduated at the top of his class 7 years later.
After his medical training, Dr Stamatoyannopoulos pursued thesis research on inherited blood disorders, particularly anemias.
Dr Stamatoyannopoulos performed the first large-scale molecular geographical survey of a genetic trait, which revealed the relationship between malaria and both thalassemia and sickle cell traits.
Dr Stamatoyannopoulos also discovered that fetal hemoglobin could ameliorate the effects of thalassemia. His theory that thalassemia and sickle cell anemia could be treated by re-activating fetal hemoglobin has underpinned decades of efforts to cure these disorders.
As a young investigator, Dr Stamatoyannopoulos expanded genetic studies of blood diseases in Greece, where his work drew the attention of medical genetics pioneer Arno Motulsky, MD.
Dr Motulsky recruited Dr Stamatoyannopoulos to the University of Washington (Seattle) in 1964. Dr Stamatoyannopoulos became a full professor there in 1973, founded the Markey Molecular Medicine Center, and was chief of medical genetics from 1989 to 2005.
Dr Stamatoyannopoulos organized the founding of the American Society of Gene and Cell Therapy. His contributions were recognized by establishment of the Stamatoyannopoulos lecture, the society’s highest award.
Dr Stamatoyannopoulos also served as president of the American Society of Hematology (1992) and president of the American Society of Gene and Cell Therapy (1996). He held leadership positions in other medical and scientific societies as well.
Dr Stamatoyannopoulos authored more than 420 scientific papers and 14 books, including The Molecular Basis of Blood Diseases.
Dr Stamatoyannopoulos died June 16, 2018. He is survived by his wife and collaborator Thalia Papayannopoulou, MD, (a professor of medicine and internationally recognized hematologist), 2 sons, and 3 grandchildren.
Checkpoint inhibitors in autoimmune disease: More flares, better cancer outcomes
AMSTERDAM – In patients with autoimmune diseases, cancer treatment with checkpoint inhibitor immunotherapy increases the risk of flares, but these flares are associated with improved cancer outcomes, according to a multicenter, retrospective study presented at the European Congress of Rheumatology.
“Survival was longer in patients who experienced a flare of their preexisting autoimmune disease or any other immune-related adverse event, but this gain was lost if an immunosuppressive therapy was used,” reported Alice Tison, a resident in rheumatology at the Centre Hospitalier Universitaire, Brest, France.
These were some of the mixed messages from this evaluation, which involved 112 patients with preexisting autoimmune disease (PAD) whose data were collected from 11 tertiary care centers in France. Of the cases of PAD represented, the majority involved joint diseases, including psoriatic arthritis (28%), rheumatoid arthritis (18%), and spondyloarthritis (4.5%). However, other types of PAD, including inflammatory bowel disease (13%), were included in the series.
Only 33% of the patients had active disease at the time that checkpoint inhibitor therapy was initiated, and only 21% were taking an immunosuppressive therapy for their disease. Of those on therapy, the majority were taking steroids, but about a third of those on therapy were taking a disease-modifying antirheumatic drug, such as methotrexate.
With the initiation of checkpoint inhibitors, which were offered primarily for the treatment of melanoma (59%) and non–small cell lung cancer (36%), 42% of patients with PAD developed a disease flare. Of these, 30% were considered severe. Other immune-related events not considered related to the underlying disease, such as colitis, were also observed but at rates not clearly different than those observed in patients without PAD.
The activity of checkpoint inhibitors did not appear to be different than that observed in non-PAD patients. For example, the overall response rate was 48% in those with melanoma and 54% in those with non–small cell lung cancer. After a median of 8 months of follow-up, the median progression-free survival was 12.4 months and 9.7 months for the two diseases, respectively. Median overall survival had not been reached in either disease.
However, those with a flare or another immune-related adverse event had significantly better progression-free survival (P = .016) and overall survival (P = .004) when compared with those who did not flare or have an immune-related adverse event. According to Ms. Tison, this has been reported before, but a more surprising finding was that the gain in progression-free survival and overall survival was lost in those treated with an immunosuppressive drug.
Even though non-PAD patients commonly receive steroids for immune-related adverse events such as colitis, the loss of benefit in PAD patients who received immunosuppressive therapies may be caused by, at least in part, cross-reactivity between tumor antigens and autoantigens, Ms. Tison speculated.
Ms. Tison was cautious in drawing conclusions about specific strategies to optimize benefits from checkpoint inhibitors in PAD based on this limited series of patients. However, she did suggest that discontinuation of immunosuppressive therapies prior to initiating checkpoint inhibitors may be prudent in PAD patients, particularly those with inactive disease.
Overall, she emphasized that checkpoint inhibitors “have revolutionized the management of several cancers” and should not be denied to PAD patients who are otherwise appropriate candidates. Although flares are common, more than half of PAD patients in this series did not flare and flares were mild to moderate in most of those who did.
“The response to checkpoint inhibitors in PAD patients is good,” Ms. Tison advised. For those who do flare, “we need prospective studies to understand which strategies provide a good balance of benefit to risk” for cancer immunotherapy and for the options to manage immune-related adverse events.
The study was not industry funded. Ms. Tison reported no potential conflicts of interest.
SOURCE: Tison A et al. Ann Rheum Dis. 2018;77(Suppl 2):147. EULAR Congress 2018, Abstract OP0196.
AMSTERDAM – In patients with autoimmune diseases, cancer treatment with checkpoint inhibitor immunotherapy increases the risk of flares, but these flares are associated with improved cancer outcomes, according to a multicenter, retrospective study presented at the European Congress of Rheumatology.
“Survival was longer in patients who experienced a flare of their preexisting autoimmune disease or any other immune-related adverse event, but this gain was lost if an immunosuppressive therapy was used,” reported Alice Tison, a resident in rheumatology at the Centre Hospitalier Universitaire, Brest, France.
These were some of the mixed messages from this evaluation, which involved 112 patients with preexisting autoimmune disease (PAD) whose data were collected from 11 tertiary care centers in France. Of the cases of PAD represented, the majority involved joint diseases, including psoriatic arthritis (28%), rheumatoid arthritis (18%), and spondyloarthritis (4.5%). However, other types of PAD, including inflammatory bowel disease (13%), were included in the series.
Only 33% of the patients had active disease at the time that checkpoint inhibitor therapy was initiated, and only 21% were taking an immunosuppressive therapy for their disease. Of those on therapy, the majority were taking steroids, but about a third of those on therapy were taking a disease-modifying antirheumatic drug, such as methotrexate.
With the initiation of checkpoint inhibitors, which were offered primarily for the treatment of melanoma (59%) and non–small cell lung cancer (36%), 42% of patients with PAD developed a disease flare. Of these, 30% were considered severe. Other immune-related events not considered related to the underlying disease, such as colitis, were also observed but at rates not clearly different than those observed in patients without PAD.
The activity of checkpoint inhibitors did not appear to be different than that observed in non-PAD patients. For example, the overall response rate was 48% in those with melanoma and 54% in those with non–small cell lung cancer. After a median of 8 months of follow-up, the median progression-free survival was 12.4 months and 9.7 months for the two diseases, respectively. Median overall survival had not been reached in either disease.
However, those with a flare or another immune-related adverse event had significantly better progression-free survival (P = .016) and overall survival (P = .004) when compared with those who did not flare or have an immune-related adverse event. According to Ms. Tison, this has been reported before, but a more surprising finding was that the gain in progression-free survival and overall survival was lost in those treated with an immunosuppressive drug.
Even though non-PAD patients commonly receive steroids for immune-related adverse events such as colitis, the loss of benefit in PAD patients who received immunosuppressive therapies may be caused by, at least in part, cross-reactivity between tumor antigens and autoantigens, Ms. Tison speculated.
Ms. Tison was cautious in drawing conclusions about specific strategies to optimize benefits from checkpoint inhibitors in PAD based on this limited series of patients. However, she did suggest that discontinuation of immunosuppressive therapies prior to initiating checkpoint inhibitors may be prudent in PAD patients, particularly those with inactive disease.
Overall, she emphasized that checkpoint inhibitors “have revolutionized the management of several cancers” and should not be denied to PAD patients who are otherwise appropriate candidates. Although flares are common, more than half of PAD patients in this series did not flare and flares were mild to moderate in most of those who did.
“The response to checkpoint inhibitors in PAD patients is good,” Ms. Tison advised. For those who do flare, “we need prospective studies to understand which strategies provide a good balance of benefit to risk” for cancer immunotherapy and for the options to manage immune-related adverse events.
The study was not industry funded. Ms. Tison reported no potential conflicts of interest.
SOURCE: Tison A et al. Ann Rheum Dis. 2018;77(Suppl 2):147. EULAR Congress 2018, Abstract OP0196.
AMSTERDAM – In patients with autoimmune diseases, cancer treatment with checkpoint inhibitor immunotherapy increases the risk of flares, but these flares are associated with improved cancer outcomes, according to a multicenter, retrospective study presented at the European Congress of Rheumatology.
“Survival was longer in patients who experienced a flare of their preexisting autoimmune disease or any other immune-related adverse event, but this gain was lost if an immunosuppressive therapy was used,” reported Alice Tison, a resident in rheumatology at the Centre Hospitalier Universitaire, Brest, France.
These were some of the mixed messages from this evaluation, which involved 112 patients with preexisting autoimmune disease (PAD) whose data were collected from 11 tertiary care centers in France. Of the cases of PAD represented, the majority involved joint diseases, including psoriatic arthritis (28%), rheumatoid arthritis (18%), and spondyloarthritis (4.5%). However, other types of PAD, including inflammatory bowel disease (13%), were included in the series.
Only 33% of the patients had active disease at the time that checkpoint inhibitor therapy was initiated, and only 21% were taking an immunosuppressive therapy for their disease. Of those on therapy, the majority were taking steroids, but about a third of those on therapy were taking a disease-modifying antirheumatic drug, such as methotrexate.
With the initiation of checkpoint inhibitors, which were offered primarily for the treatment of melanoma (59%) and non–small cell lung cancer (36%), 42% of patients with PAD developed a disease flare. Of these, 30% were considered severe. Other immune-related events not considered related to the underlying disease, such as colitis, were also observed but at rates not clearly different than those observed in patients without PAD.
The activity of checkpoint inhibitors did not appear to be different than that observed in non-PAD patients. For example, the overall response rate was 48% in those with melanoma and 54% in those with non–small cell lung cancer. After a median of 8 months of follow-up, the median progression-free survival was 12.4 months and 9.7 months for the two diseases, respectively. Median overall survival had not been reached in either disease.
However, those with a flare or another immune-related adverse event had significantly better progression-free survival (P = .016) and overall survival (P = .004) when compared with those who did not flare or have an immune-related adverse event. According to Ms. Tison, this has been reported before, but a more surprising finding was that the gain in progression-free survival and overall survival was lost in those treated with an immunosuppressive drug.
Even though non-PAD patients commonly receive steroids for immune-related adverse events such as colitis, the loss of benefit in PAD patients who received immunosuppressive therapies may be caused by, at least in part, cross-reactivity between tumor antigens and autoantigens, Ms. Tison speculated.
Ms. Tison was cautious in drawing conclusions about specific strategies to optimize benefits from checkpoint inhibitors in PAD based on this limited series of patients. However, she did suggest that discontinuation of immunosuppressive therapies prior to initiating checkpoint inhibitors may be prudent in PAD patients, particularly those with inactive disease.
Overall, she emphasized that checkpoint inhibitors “have revolutionized the management of several cancers” and should not be denied to PAD patients who are otherwise appropriate candidates. Although flares are common, more than half of PAD patients in this series did not flare and flares were mild to moderate in most of those who did.
“The response to checkpoint inhibitors in PAD patients is good,” Ms. Tison advised. For those who do flare, “we need prospective studies to understand which strategies provide a good balance of benefit to risk” for cancer immunotherapy and for the options to manage immune-related adverse events.
The study was not industry funded. Ms. Tison reported no potential conflicts of interest.
SOURCE: Tison A et al. Ann Rheum Dis. 2018;77(Suppl 2):147. EULAR Congress 2018, Abstract OP0196.
REPORTING FROM THE EULAR 2018 CONGRESS
Key clinical point: Cancer patients who take a checkpoint inhibitor and have a preexisting autoimmune disease were significantly more likely to have a disease flare but also a better cancer outcome than were those without preexisting disease.
Major finding: In those with a disease flare, progression-free and overall survival were significantly improved (P = .016 and P = .004, respectively).
Study details: Retrospective multicenter study.
Disclosures: The study was not industry funded. Ms. Tison reported no potential conflicts of interest.
Source: Tison A et al. Ann Rheum Dis. 2018;77(Suppl 2):147. EULAR Congress 2018, Abstract OP0196.
Data suggest harm outweighs benefit of opioids for musculoskeletal pain
AMSTERDAM – Opioids cannot be justified for the routine treatment for musculoskeletal pain because risks outweigh benefits, according to a detailed review of published studies presented at the European Congress of Rheumatology.
“There is very little evidence of benefit for the long-term management of nonmalignant pain, but very good evidence for harm,” reported Blair Smith, MD, head of the population health sciences division, University of Dundee (Scotland).
In the treatment of musculoskeletal pain, the goals are increased function and quality of life, rather than complete relief of pain, according to Dr. Smith. On this basis, opioids are not an appropriate routine therapy. He reported that pain relief is not well documented, while side effects such as sedation, dizziness, and constipation, are likely to be counterproductive to improved outcomes.
There is no absolute contraindication for opioids in the control of chronic musculoskeletal pain, but Dr. Smith’s summary of the data led him to conclude that they should be used judiciously and “only for carefully selected patients.”
Of the many studies he reviewed to draw this conclusion, one of the most recent was identified as the most persuasive. Published earlier this year, the SPACE study is “the first good-quality study of long-term opioid use” in patients with musculoskeletal complaints. It was negative.
“The pain intensity at the end of 12 months of treatment was slightly but significantly worse among those randomized to opioids,” reported Dr. Smith. “There was no difference in patient function, but there was an increased risk of adverse events.”
In the SPACE study, 240 patients with moderate to severe chronic back pain or hip or knee osteoarthritis were randomized to opioid or nonopioid pain management. In the nonopioid group, the first therapeutic step was acetaminophen, but medications could be changed, added, or adjusted within both groups to improve patient response.
At the end of 12 months, a lack of benefit on both pain control and functional improvement from opioids relative to nonopioid treatment was accompanied by a higher rate of adverse effects. This led the authors to conclude that opioids are not supported for musculoskeletal pain.
Not all the evidence argues against opioids for noncancer pain management, according to Dr. Smith, but he emphasized that those who support use of opioids do so for pain control only. They do not confirm an advantage for function and quality of life, which he suggested are the key endpoints. For example, a 2010 Cochrane review concluded from a systematic literature review that there is “weak evidence” for pain relief but inconclusive evidence of an improvement in functioning and quality of life.
Other investigators have drawn the same conclusion, according to Dr. Smith. He cited a statement from the International Association for Study of Pain that advises, “Caution should be used for prescribing opioids for chronic pain.” Although this statement was not specific to musculoskeletal pain, the IASP does specify that pain medications should be employed “to promote increased function and improved quality of life rather than complete relief of pain,” according to Dr. Smith.
Opioid prescriptions for chronic pain have been increasing in Europe as they have in the United States, but Dr. Smith indicated that opioids, if used at all, should be prescribed for very short periods and for very specific goals, particularly improvement in function.
“Probably most important for my [primary care] colleagues, patients prescribed opioids should be evaluated early and frequently to gauge benefit,” Dr. Smith said. Although he believes pain control is an important and worthwhile goal, it must be approached within the context of improved well-being rather than as an isolated endpoint.
SOURCE: Smith B et al. EULAR 2018, Abstract No. SP0073.
AMSTERDAM – Opioids cannot be justified for the routine treatment for musculoskeletal pain because risks outweigh benefits, according to a detailed review of published studies presented at the European Congress of Rheumatology.
“There is very little evidence of benefit for the long-term management of nonmalignant pain, but very good evidence for harm,” reported Blair Smith, MD, head of the population health sciences division, University of Dundee (Scotland).
In the treatment of musculoskeletal pain, the goals are increased function and quality of life, rather than complete relief of pain, according to Dr. Smith. On this basis, opioids are not an appropriate routine therapy. He reported that pain relief is not well documented, while side effects such as sedation, dizziness, and constipation, are likely to be counterproductive to improved outcomes.
There is no absolute contraindication for opioids in the control of chronic musculoskeletal pain, but Dr. Smith’s summary of the data led him to conclude that they should be used judiciously and “only for carefully selected patients.”
Of the many studies he reviewed to draw this conclusion, one of the most recent was identified as the most persuasive. Published earlier this year, the SPACE study is “the first good-quality study of long-term opioid use” in patients with musculoskeletal complaints. It was negative.
“The pain intensity at the end of 12 months of treatment was slightly but significantly worse among those randomized to opioids,” reported Dr. Smith. “There was no difference in patient function, but there was an increased risk of adverse events.”
In the SPACE study, 240 patients with moderate to severe chronic back pain or hip or knee osteoarthritis were randomized to opioid or nonopioid pain management. In the nonopioid group, the first therapeutic step was acetaminophen, but medications could be changed, added, or adjusted within both groups to improve patient response.
At the end of 12 months, a lack of benefit on both pain control and functional improvement from opioids relative to nonopioid treatment was accompanied by a higher rate of adverse effects. This led the authors to conclude that opioids are not supported for musculoskeletal pain.
Not all the evidence argues against opioids for noncancer pain management, according to Dr. Smith, but he emphasized that those who support use of opioids do so for pain control only. They do not confirm an advantage for function and quality of life, which he suggested are the key endpoints. For example, a 2010 Cochrane review concluded from a systematic literature review that there is “weak evidence” for pain relief but inconclusive evidence of an improvement in functioning and quality of life.
Other investigators have drawn the same conclusion, according to Dr. Smith. He cited a statement from the International Association for Study of Pain that advises, “Caution should be used for prescribing opioids for chronic pain.” Although this statement was not specific to musculoskeletal pain, the IASP does specify that pain medications should be employed “to promote increased function and improved quality of life rather than complete relief of pain,” according to Dr. Smith.
Opioid prescriptions for chronic pain have been increasing in Europe as they have in the United States, but Dr. Smith indicated that opioids, if used at all, should be prescribed for very short periods and for very specific goals, particularly improvement in function.
“Probably most important for my [primary care] colleagues, patients prescribed opioids should be evaluated early and frequently to gauge benefit,” Dr. Smith said. Although he believes pain control is an important and worthwhile goal, it must be approached within the context of improved well-being rather than as an isolated endpoint.
SOURCE: Smith B et al. EULAR 2018, Abstract No. SP0073.
AMSTERDAM – Opioids cannot be justified for the routine treatment for musculoskeletal pain because risks outweigh benefits, according to a detailed review of published studies presented at the European Congress of Rheumatology.
“There is very little evidence of benefit for the long-term management of nonmalignant pain, but very good evidence for harm,” reported Blair Smith, MD, head of the population health sciences division, University of Dundee (Scotland).
In the treatment of musculoskeletal pain, the goals are increased function and quality of life, rather than complete relief of pain, according to Dr. Smith. On this basis, opioids are not an appropriate routine therapy. He reported that pain relief is not well documented, while side effects such as sedation, dizziness, and constipation, are likely to be counterproductive to improved outcomes.
There is no absolute contraindication for opioids in the control of chronic musculoskeletal pain, but Dr. Smith’s summary of the data led him to conclude that they should be used judiciously and “only for carefully selected patients.”
Of the many studies he reviewed to draw this conclusion, one of the most recent was identified as the most persuasive. Published earlier this year, the SPACE study is “the first good-quality study of long-term opioid use” in patients with musculoskeletal complaints. It was negative.
“The pain intensity at the end of 12 months of treatment was slightly but significantly worse among those randomized to opioids,” reported Dr. Smith. “There was no difference in patient function, but there was an increased risk of adverse events.”
In the SPACE study, 240 patients with moderate to severe chronic back pain or hip or knee osteoarthritis were randomized to opioid or nonopioid pain management. In the nonopioid group, the first therapeutic step was acetaminophen, but medications could be changed, added, or adjusted within both groups to improve patient response.
At the end of 12 months, a lack of benefit on both pain control and functional improvement from opioids relative to nonopioid treatment was accompanied by a higher rate of adverse effects. This led the authors to conclude that opioids are not supported for musculoskeletal pain.
Not all the evidence argues against opioids for noncancer pain management, according to Dr. Smith, but he emphasized that those who support use of opioids do so for pain control only. They do not confirm an advantage for function and quality of life, which he suggested are the key endpoints. For example, a 2010 Cochrane review concluded from a systematic literature review that there is “weak evidence” for pain relief but inconclusive evidence of an improvement in functioning and quality of life.
Other investigators have drawn the same conclusion, according to Dr. Smith. He cited a statement from the International Association for Study of Pain that advises, “Caution should be used for prescribing opioids for chronic pain.” Although this statement was not specific to musculoskeletal pain, the IASP does specify that pain medications should be employed “to promote increased function and improved quality of life rather than complete relief of pain,” according to Dr. Smith.
Opioid prescriptions for chronic pain have been increasing in Europe as they have in the United States, but Dr. Smith indicated that opioids, if used at all, should be prescribed for very short periods and for very specific goals, particularly improvement in function.
“Probably most important for my [primary care] colleagues, patients prescribed opioids should be evaluated early and frequently to gauge benefit,” Dr. Smith said. Although he believes pain control is an important and worthwhile goal, it must be approached within the context of improved well-being rather than as an isolated endpoint.
SOURCE: Smith B et al. EULAR 2018, Abstract No. SP0073.
REPORTING FROM THE EULAR 2018 CONGRESS
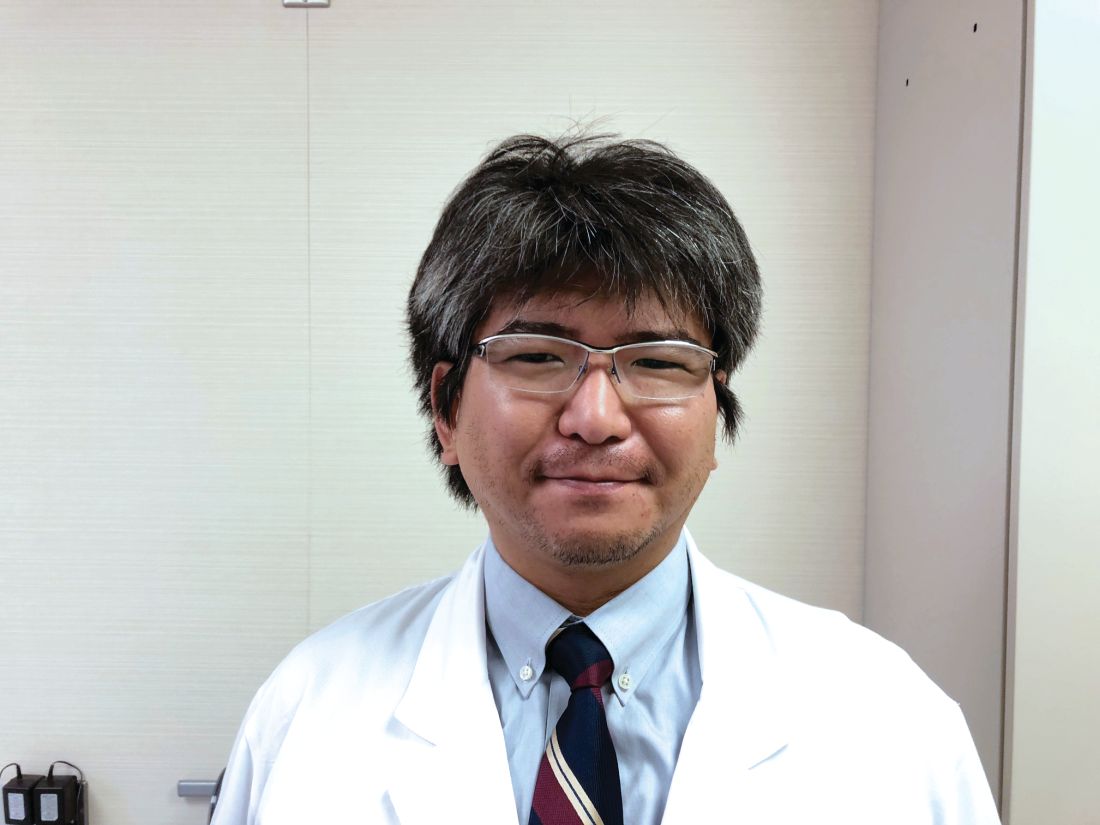
Biologic efficacy differs in psoriatic arthritis by lymphocyte phenotype
AMSTERDAM – In patients with psoriatic arthritis (PsA), new evidence suggests selection of biologic disease-modifying antirheumatic drugs (bDMARDs) might be individualized by T-helper cell phenotype to improve disease control, according to the results of a study presented at the European Congress of Rheumatology.
“Our findings suggest a potential for precision medicine in patients with psoriatic arthritis,” reported Ippei Miyagawa, MD, of the University of Occupational and Environmental Health in Kitakyushu, Japan.
These phenotypes were employed to individualize therapy with the currently available targeted bDMARDs. Patients with a Th1-predominant phenotype received ustekinumab (Stelara), which blocks the p40 subunit of interleukin (IL)-12 and IL-23. Patients with a Th17-predominant phenotype received secukinumab (Cosentyx), which targets IL-17. Patients with the Th1/Th17-high phenotype received either secukinumab or a tumor necrosis factor inhibitor. Patients with the Th1/Th17-low phenotype received a TNF inhibitor.
The 26 patients whose bDMARD therapy was individualized were compared with 38 PsA patients who received bDMARDs selected according to EULAR recommendations. The groups were similar for baseline characteristics.
In both groups, there were significant decreases from baseline in essentially all clinical measures, including the Simplified Disease Activity Index, the Psoriasis Area and Severity Index, and the Patient Global Health Assessment. However, several disease markers suggested greater disease control in those receiving individualized therapy. For example, the Disease Activity Score in 28 joints using erythrocyte sedimentation rate (DAS28-ESR) at 6 months was 0.76 in the Th17-predominant group versus 1.32 in those on an unselected bDMARD therapy (P = .008).
As a proportion of lymphocytes, Th1-predominant cells greater than 1.2% and Th17-predominant cells greater than 1.5% appeared to be sensitive cutoffs for predicting response to ustekinumab and secukinumab, respectively, according to data presented by Dr. Miyagawa. Although the results in this small series of patients are considered preliminary, Dr. Miyagawa said, “We think that this research is the first step toward the future use of precision medicine in PsA.”
Larger studies are needed to verify that lymphocyte phenotyping is an effective and reproducible strategy for individualizing selection of bDMARDs, but Dr. Miyagawa acknowledged other practical barriers to routine clinical application of this strategy. In particular, he called flow cytometry, which was employed in this study to phenotype lymphocyte expression, “complicated” for routine clinical use. However, this study strongly suggests that lymphocyte expression is a predictor of response to the different bDMARDs now available for treatment of PsA.
“The bDMARDs effective in PsA have different targets and may not offer the same degree of efficacy in all patients. Our study suggests an approach to optimal drug selection,” he said.
The study was not industry funded. Dr. Miyagawa reported no relevant financial disclosures.
SOURCE: Miyagawa I et al. Ann Rheum Dis. 2018;77(Suppl 2):206-7. EULAR Congress 2018, Abstract OP0321.
AMSTERDAM – In patients with psoriatic arthritis (PsA), new evidence suggests selection of biologic disease-modifying antirheumatic drugs (bDMARDs) might be individualized by T-helper cell phenotype to improve disease control, according to the results of a study presented at the European Congress of Rheumatology.
“Our findings suggest a potential for precision medicine in patients with psoriatic arthritis,” reported Ippei Miyagawa, MD, of the University of Occupational and Environmental Health in Kitakyushu, Japan.
These phenotypes were employed to individualize therapy with the currently available targeted bDMARDs. Patients with a Th1-predominant phenotype received ustekinumab (Stelara), which blocks the p40 subunit of interleukin (IL)-12 and IL-23. Patients with a Th17-predominant phenotype received secukinumab (Cosentyx), which targets IL-17. Patients with the Th1/Th17-high phenotype received either secukinumab or a tumor necrosis factor inhibitor. Patients with the Th1/Th17-low phenotype received a TNF inhibitor.
The 26 patients whose bDMARD therapy was individualized were compared with 38 PsA patients who received bDMARDs selected according to EULAR recommendations. The groups were similar for baseline characteristics.
In both groups, there were significant decreases from baseline in essentially all clinical measures, including the Simplified Disease Activity Index, the Psoriasis Area and Severity Index, and the Patient Global Health Assessment. However, several disease markers suggested greater disease control in those receiving individualized therapy. For example, the Disease Activity Score in 28 joints using erythrocyte sedimentation rate (DAS28-ESR) at 6 months was 0.76 in the Th17-predominant group versus 1.32 in those on an unselected bDMARD therapy (P = .008).
As a proportion of lymphocytes, Th1-predominant cells greater than 1.2% and Th17-predominant cells greater than 1.5% appeared to be sensitive cutoffs for predicting response to ustekinumab and secukinumab, respectively, according to data presented by Dr. Miyagawa. Although the results in this small series of patients are considered preliminary, Dr. Miyagawa said, “We think that this research is the first step toward the future use of precision medicine in PsA.”
Larger studies are needed to verify that lymphocyte phenotyping is an effective and reproducible strategy for individualizing selection of bDMARDs, but Dr. Miyagawa acknowledged other practical barriers to routine clinical application of this strategy. In particular, he called flow cytometry, which was employed in this study to phenotype lymphocyte expression, “complicated” for routine clinical use. However, this study strongly suggests that lymphocyte expression is a predictor of response to the different bDMARDs now available for treatment of PsA.
“The bDMARDs effective in PsA have different targets and may not offer the same degree of efficacy in all patients. Our study suggests an approach to optimal drug selection,” he said.
The study was not industry funded. Dr. Miyagawa reported no relevant financial disclosures.
SOURCE: Miyagawa I et al. Ann Rheum Dis. 2018;77(Suppl 2):206-7. EULAR Congress 2018, Abstract OP0321.
AMSTERDAM – In patients with psoriatic arthritis (PsA), new evidence suggests selection of biologic disease-modifying antirheumatic drugs (bDMARDs) might be individualized by T-helper cell phenotype to improve disease control, according to the results of a study presented at the European Congress of Rheumatology.
“Our findings suggest a potential for precision medicine in patients with psoriatic arthritis,” reported Ippei Miyagawa, MD, of the University of Occupational and Environmental Health in Kitakyushu, Japan.
These phenotypes were employed to individualize therapy with the currently available targeted bDMARDs. Patients with a Th1-predominant phenotype received ustekinumab (Stelara), which blocks the p40 subunit of interleukin (IL)-12 and IL-23. Patients with a Th17-predominant phenotype received secukinumab (Cosentyx), which targets IL-17. Patients with the Th1/Th17-high phenotype received either secukinumab or a tumor necrosis factor inhibitor. Patients with the Th1/Th17-low phenotype received a TNF inhibitor.
The 26 patients whose bDMARD therapy was individualized were compared with 38 PsA patients who received bDMARDs selected according to EULAR recommendations. The groups were similar for baseline characteristics.
In both groups, there were significant decreases from baseline in essentially all clinical measures, including the Simplified Disease Activity Index, the Psoriasis Area and Severity Index, and the Patient Global Health Assessment. However, several disease markers suggested greater disease control in those receiving individualized therapy. For example, the Disease Activity Score in 28 joints using erythrocyte sedimentation rate (DAS28-ESR) at 6 months was 0.76 in the Th17-predominant group versus 1.32 in those on an unselected bDMARD therapy (P = .008).
As a proportion of lymphocytes, Th1-predominant cells greater than 1.2% and Th17-predominant cells greater than 1.5% appeared to be sensitive cutoffs for predicting response to ustekinumab and secukinumab, respectively, according to data presented by Dr. Miyagawa. Although the results in this small series of patients are considered preliminary, Dr. Miyagawa said, “We think that this research is the first step toward the future use of precision medicine in PsA.”
Larger studies are needed to verify that lymphocyte phenotyping is an effective and reproducible strategy for individualizing selection of bDMARDs, but Dr. Miyagawa acknowledged other practical barriers to routine clinical application of this strategy. In particular, he called flow cytometry, which was employed in this study to phenotype lymphocyte expression, “complicated” for routine clinical use. However, this study strongly suggests that lymphocyte expression is a predictor of response to the different bDMARDs now available for treatment of PsA.
“The bDMARDs effective in PsA have different targets and may not offer the same degree of efficacy in all patients. Our study suggests an approach to optimal drug selection,” he said.
The study was not industry funded. Dr. Miyagawa reported no relevant financial disclosures.
SOURCE: Miyagawa I et al. Ann Rheum Dis. 2018;77(Suppl 2):206-7. EULAR Congress 2018, Abstract OP0321.
REPORTING FROM THE EULAR 2018 CONGRESS
Key clinical point: Lymphocyte profile phenotypes appear to permit individualized biologic therapy in patients with PsA.
Major finding: Therapy individualized for Th17-predominant PsA produced a DAS28 score 0.56 points lower than did nonselected therapy (P = .008).
Study details: A prospective, nonrandomized study of 64 PsA patients with either individualized bDMARD therapy or bDMARDs selected according to EULAR recommendations.
Disclosures: The study was not industry funded. Dr. Miyagawa reported no relevant financial disclosures.
Source: Miyagawa I et al. Ann Rheum Dis. 2018;77(Suppl 2):206-7. EULAR Congress 2018, Abstract OP0321.
Advocate for your LGBTQ patients
June 28, 1969, is the day that many consider to be the origin of the modern LGBTQ (Lesbian, Gay, Bisexual, Transgender, Queer/Questioning) movement.1 At that time, it was not uncommon for police officers to conduct raids on bars frequented by LGBTQ patrons, but this night was different. This night the patrons of the Stonewall Inn fought back. The subsequent violent clashes fueled the national organization of groups concentrated on the goal of advocating for LGBTQ rights. On June 28th, 1970, protests to commemorate the events at Stonewall occurred; many refer to these as the first Pride events. Since then the month of June has been seen as the unofficial Pride month for the LGBTQ community. These events began as demonstrations for equal rights and protections for LGBTQ individuals, but over time, events have grown also to become a celebration of queer lives and sexuality.2
I attended my first Pride event over 10 years ago in support of a friend who had recently come out. He told me that the event was a place where he could proudly be his full self, something that he felt was not safe to do at school or work. When I participated at that event years ago, I began to understand my straight, cisgender privilege: I could walk down the street holding hands with my partner, discuss the details of a first date with colleagues at work, and wear the clothes that aligned with my gender identity without fear of being harassed or attacked. This, I realized, was not the case for everyone. Since attending that Pride event, I have had the opportunity to attend and volunteer at many local Pride events. Some have been in pouring rain, some have been in scorching heat, but all have been rejuvenating, inspiring, and fun! They have been opportunities for me to visibly show support for the local LGBTQ community and meet with other LGBTQ-serving organizations and allies.
Ways to get involved
Find out about local Pride events in your community and consider attending or volunteering. One of the contributing factors to LGBTQ health disparities is limited access to competent care. Many LGBTQ youth and adults have reported experiences of discrimination in the health care setting.3,4 When we, as health care providers, are visible at Pride events, we can have important effects on our local communities by showing them that we recognize and affirm LGBTQ identities.
Consider asking your organization or institution to provide support at local Pride events, post messages of support during Pride month, or host educational sessions about the care of LGBTQ youth.
Dr. Chelvakumar is an attending physician in the division of adolescent medicine at Nationwide Children’s Hospital and an assistant professor of clinical pediatrics at Ohio State University, both in Columbus. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
Resources
Human Rights Campaign/Pride: You can learn more about the history of Pride and events in your state and community at www.hrc.org/pride.
How to contact your elected officials: You can find contact information for your local, state, and federal government representatives at www.usa.gov/elected-officials.
National LGBT Health Education Center: You can find educational resources to help optimize care of LGBT patients at www.lgbthealtheducation.org/.
U.S. Transgender Survey: You can read the report from a survey of almost 28,000 transgender respondents in the U.S. Specific information is available about experiences with health care; state level reports also available at www.ustranssurvey.org/reports/.
References
1. GLAAD Pride Month Resource Kit for Jounalists: www.glaad.org/publications/pridekit
2. Human Rights Campaign: History of LGBT Pride. www.hrc.org/blog/the-history-of-lgbt-pride-from-1970-to-now
3. The Report of the 2015 U.S. Transgender Survey (Washington, DC: National Center for Transgender Equality, 2016).
4. Healthy People 2020: Lesbian, Gay, Bisexual and Transgender Health.
June 28, 1969, is the day that many consider to be the origin of the modern LGBTQ (Lesbian, Gay, Bisexual, Transgender, Queer/Questioning) movement.1 At that time, it was not uncommon for police officers to conduct raids on bars frequented by LGBTQ patrons, but this night was different. This night the patrons of the Stonewall Inn fought back. The subsequent violent clashes fueled the national organization of groups concentrated on the goal of advocating for LGBTQ rights. On June 28th, 1970, protests to commemorate the events at Stonewall occurred; many refer to these as the first Pride events. Since then the month of June has been seen as the unofficial Pride month for the LGBTQ community. These events began as demonstrations for equal rights and protections for LGBTQ individuals, but over time, events have grown also to become a celebration of queer lives and sexuality.2
I attended my first Pride event over 10 years ago in support of a friend who had recently come out. He told me that the event was a place where he could proudly be his full self, something that he felt was not safe to do at school or work. When I participated at that event years ago, I began to understand my straight, cisgender privilege: I could walk down the street holding hands with my partner, discuss the details of a first date with colleagues at work, and wear the clothes that aligned with my gender identity without fear of being harassed or attacked. This, I realized, was not the case for everyone. Since attending that Pride event, I have had the opportunity to attend and volunteer at many local Pride events. Some have been in pouring rain, some have been in scorching heat, but all have been rejuvenating, inspiring, and fun! They have been opportunities for me to visibly show support for the local LGBTQ community and meet with other LGBTQ-serving organizations and allies.
Ways to get involved
Find out about local Pride events in your community and consider attending or volunteering. One of the contributing factors to LGBTQ health disparities is limited access to competent care. Many LGBTQ youth and adults have reported experiences of discrimination in the health care setting.3,4 When we, as health care providers, are visible at Pride events, we can have important effects on our local communities by showing them that we recognize and affirm LGBTQ identities.
Consider asking your organization or institution to provide support at local Pride events, post messages of support during Pride month, or host educational sessions about the care of LGBTQ youth.
Dr. Chelvakumar is an attending physician in the division of adolescent medicine at Nationwide Children’s Hospital and an assistant professor of clinical pediatrics at Ohio State University, both in Columbus. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
Resources
Human Rights Campaign/Pride: You can learn more about the history of Pride and events in your state and community at www.hrc.org/pride.
How to contact your elected officials: You can find contact information for your local, state, and federal government representatives at www.usa.gov/elected-officials.
National LGBT Health Education Center: You can find educational resources to help optimize care of LGBT patients at www.lgbthealtheducation.org/.
U.S. Transgender Survey: You can read the report from a survey of almost 28,000 transgender respondents in the U.S. Specific information is available about experiences with health care; state level reports also available at www.ustranssurvey.org/reports/.
References
1. GLAAD Pride Month Resource Kit for Jounalists: www.glaad.org/publications/pridekit
2. Human Rights Campaign: History of LGBT Pride. www.hrc.org/blog/the-history-of-lgbt-pride-from-1970-to-now
3. The Report of the 2015 U.S. Transgender Survey (Washington, DC: National Center for Transgender Equality, 2016).
4. Healthy People 2020: Lesbian, Gay, Bisexual and Transgender Health.
June 28, 1969, is the day that many consider to be the origin of the modern LGBTQ (Lesbian, Gay, Bisexual, Transgender, Queer/Questioning) movement.1 At that time, it was not uncommon for police officers to conduct raids on bars frequented by LGBTQ patrons, but this night was different. This night the patrons of the Stonewall Inn fought back. The subsequent violent clashes fueled the national organization of groups concentrated on the goal of advocating for LGBTQ rights. On June 28th, 1970, protests to commemorate the events at Stonewall occurred; many refer to these as the first Pride events. Since then the month of June has been seen as the unofficial Pride month for the LGBTQ community. These events began as demonstrations for equal rights and protections for LGBTQ individuals, but over time, events have grown also to become a celebration of queer lives and sexuality.2
I attended my first Pride event over 10 years ago in support of a friend who had recently come out. He told me that the event was a place where he could proudly be his full self, something that he felt was not safe to do at school or work. When I participated at that event years ago, I began to understand my straight, cisgender privilege: I could walk down the street holding hands with my partner, discuss the details of a first date with colleagues at work, and wear the clothes that aligned with my gender identity without fear of being harassed or attacked. This, I realized, was not the case for everyone. Since attending that Pride event, I have had the opportunity to attend and volunteer at many local Pride events. Some have been in pouring rain, some have been in scorching heat, but all have been rejuvenating, inspiring, and fun! They have been opportunities for me to visibly show support for the local LGBTQ community and meet with other LGBTQ-serving organizations and allies.
Ways to get involved
Find out about local Pride events in your community and consider attending or volunteering. One of the contributing factors to LGBTQ health disparities is limited access to competent care. Many LGBTQ youth and adults have reported experiences of discrimination in the health care setting.3,4 When we, as health care providers, are visible at Pride events, we can have important effects on our local communities by showing them that we recognize and affirm LGBTQ identities.
Consider asking your organization or institution to provide support at local Pride events, post messages of support during Pride month, or host educational sessions about the care of LGBTQ youth.
Dr. Chelvakumar is an attending physician in the division of adolescent medicine at Nationwide Children’s Hospital and an assistant professor of clinical pediatrics at Ohio State University, both in Columbus. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
Resources
Human Rights Campaign/Pride: You can learn more about the history of Pride and events in your state and community at www.hrc.org/pride.
How to contact your elected officials: You can find contact information for your local, state, and federal government representatives at www.usa.gov/elected-officials.
National LGBT Health Education Center: You can find educational resources to help optimize care of LGBT patients at www.lgbthealtheducation.org/.
U.S. Transgender Survey: You can read the report from a survey of almost 28,000 transgender respondents in the U.S. Specific information is available about experiences with health care; state level reports also available at www.ustranssurvey.org/reports/.
References
1. GLAAD Pride Month Resource Kit for Jounalists: www.glaad.org/publications/pridekit
2. Human Rights Campaign: History of LGBT Pride. www.hrc.org/blog/the-history-of-lgbt-pride-from-1970-to-now
3. The Report of the 2015 U.S. Transgender Survey (Washington, DC: National Center for Transgender Equality, 2016).
4. Healthy People 2020: Lesbian, Gay, Bisexual and Transgender Health.
PFS does not capture the benefit of PD-1 inhibitors
Median progression-free survival (PFS) based on traditional RECIST criteria did not correlate with overall survival (OS) in a meta-analysis of 12 randomized controlled trials of nivolumab or pembrolizumab monotherapy.
There was no correlation in terms of medians or gains in medians, although hazard ratios for OS and PFS did correlate significantly, said Bishal Gyawali, MD, PhD, of Nagoya (Japan) University Hospital with his associates. “The protective effects of treatment were greater for OS than for PFS,” they concluded in JAMA Network Open. “Progression-free survival cannot adequately capture the benefit of PD-1 inhibitors; thus, OS should remain the gold standard end point for trials of PD-1 inhibitors.”
Progression-free survival often has been used as a surrogate for OS because the latter takes time to ascertain and can be contaminated by crossover or postprogression treatment. However, it can be problematic to assume that the two outcomes correlate. Progression “is defined as an increase in tumor size beyond an arbitrary cutoff and is prone to bias, particularly when the investigators are not blinded,” the researchers noted. Furthermore, PD-1 inhibitors show an “atypical response pattern,” including long durations of response, responses after initial progression (known as pseudoprogression), and even response after treatment cessation.
The analysis, the first to formally compare PFS and OS across PD-1 inhibitors, included 10 randomized, controlled trials comparing nivolumab or pembrolizumab with nonimmunotherapy in adults with solid tumors. Two additional trials evaluated pembrolizumab or nivolumab following treatment with ipilimumab. In all, the studies included 5,417 patients. There was no significant heterogeneity among studies, the researchers said.
Median PFS and median OS correlated poorly, with an R2 value of 0.46 (P = .09). Change in PFS also did not correlate with change in OS (R2 = 0.23; P = .28). In contrast, hazard ratios for PFS and OS correlated significantly (R2 = 0.41; P = .048). The protective effects of treatment were higher for OS than for PFS (pooled HR, 1.2; 95% confidence interval, 1.1-1.3; P = .002).
This might be because traditional RECIST (response evaluation criteria in solid tumors) criteria predate the era of immunotherapy and do not accurately capture disease progression when patients are on immuno-oncologics. For example, pseudoprogression (in which T-cell infiltrates cause the tumor to grow before it shrinks) could be misconstrued as progression. Also, PD-1 inhibitors can continue working even after treatment cessation, which could affect OS more than PFS, the researchers noted.
Regardless, “PD-1 inhibitors may have larger effects on OS than on PFS, which would be unprecedented in oncology therapeutics,” they concluded. “These results support the rationale of using OS as the primary end point of future phase 3 trials of PD-1 inhibitors and discourage the use of PFS as a sole primary end point as the latter may provide misleading information about the efficacy of these drugs.”
Funders included the Laura and John Arnold Foundation, the Harvard Program in Therapeutic Science, and the Engelberg Foundation. The investigators reported having no relevant conflicts of interest. One coinvestigator reported research support from the Laura and John Arnold Foundation. The other investigators had no conflicts.
SOURCE: Gyawali B et al. JAMA Network Open. 2018 June 22. doi: 10.1001/jamanetworkopen.2018.0416.
Median progression-free survival (PFS) based on traditional RECIST criteria did not correlate with overall survival (OS) in a meta-analysis of 12 randomized controlled trials of nivolumab or pembrolizumab monotherapy.
There was no correlation in terms of medians or gains in medians, although hazard ratios for OS and PFS did correlate significantly, said Bishal Gyawali, MD, PhD, of Nagoya (Japan) University Hospital with his associates. “The protective effects of treatment were greater for OS than for PFS,” they concluded in JAMA Network Open. “Progression-free survival cannot adequately capture the benefit of PD-1 inhibitors; thus, OS should remain the gold standard end point for trials of PD-1 inhibitors.”
Progression-free survival often has been used as a surrogate for OS because the latter takes time to ascertain and can be contaminated by crossover or postprogression treatment. However, it can be problematic to assume that the two outcomes correlate. Progression “is defined as an increase in tumor size beyond an arbitrary cutoff and is prone to bias, particularly when the investigators are not blinded,” the researchers noted. Furthermore, PD-1 inhibitors show an “atypical response pattern,” including long durations of response, responses after initial progression (known as pseudoprogression), and even response after treatment cessation.
The analysis, the first to formally compare PFS and OS across PD-1 inhibitors, included 10 randomized, controlled trials comparing nivolumab or pembrolizumab with nonimmunotherapy in adults with solid tumors. Two additional trials evaluated pembrolizumab or nivolumab following treatment with ipilimumab. In all, the studies included 5,417 patients. There was no significant heterogeneity among studies, the researchers said.
Median PFS and median OS correlated poorly, with an R2 value of 0.46 (P = .09). Change in PFS also did not correlate with change in OS (R2 = 0.23; P = .28). In contrast, hazard ratios for PFS and OS correlated significantly (R2 = 0.41; P = .048). The protective effects of treatment were higher for OS than for PFS (pooled HR, 1.2; 95% confidence interval, 1.1-1.3; P = .002).
This might be because traditional RECIST (response evaluation criteria in solid tumors) criteria predate the era of immunotherapy and do not accurately capture disease progression when patients are on immuno-oncologics. For example, pseudoprogression (in which T-cell infiltrates cause the tumor to grow before it shrinks) could be misconstrued as progression. Also, PD-1 inhibitors can continue working even after treatment cessation, which could affect OS more than PFS, the researchers noted.
Regardless, “PD-1 inhibitors may have larger effects on OS than on PFS, which would be unprecedented in oncology therapeutics,” they concluded. “These results support the rationale of using OS as the primary end point of future phase 3 trials of PD-1 inhibitors and discourage the use of PFS as a sole primary end point as the latter may provide misleading information about the efficacy of these drugs.”
Funders included the Laura and John Arnold Foundation, the Harvard Program in Therapeutic Science, and the Engelberg Foundation. The investigators reported having no relevant conflicts of interest. One coinvestigator reported research support from the Laura and John Arnold Foundation. The other investigators had no conflicts.
SOURCE: Gyawali B et al. JAMA Network Open. 2018 June 22. doi: 10.1001/jamanetworkopen.2018.0416.
Median progression-free survival (PFS) based on traditional RECIST criteria did not correlate with overall survival (OS) in a meta-analysis of 12 randomized controlled trials of nivolumab or pembrolizumab monotherapy.
There was no correlation in terms of medians or gains in medians, although hazard ratios for OS and PFS did correlate significantly, said Bishal Gyawali, MD, PhD, of Nagoya (Japan) University Hospital with his associates. “The protective effects of treatment were greater for OS than for PFS,” they concluded in JAMA Network Open. “Progression-free survival cannot adequately capture the benefit of PD-1 inhibitors; thus, OS should remain the gold standard end point for trials of PD-1 inhibitors.”
Progression-free survival often has been used as a surrogate for OS because the latter takes time to ascertain and can be contaminated by crossover or postprogression treatment. However, it can be problematic to assume that the two outcomes correlate. Progression “is defined as an increase in tumor size beyond an arbitrary cutoff and is prone to bias, particularly when the investigators are not blinded,” the researchers noted. Furthermore, PD-1 inhibitors show an “atypical response pattern,” including long durations of response, responses after initial progression (known as pseudoprogression), and even response after treatment cessation.
The analysis, the first to formally compare PFS and OS across PD-1 inhibitors, included 10 randomized, controlled trials comparing nivolumab or pembrolizumab with nonimmunotherapy in adults with solid tumors. Two additional trials evaluated pembrolizumab or nivolumab following treatment with ipilimumab. In all, the studies included 5,417 patients. There was no significant heterogeneity among studies, the researchers said.
Median PFS and median OS correlated poorly, with an R2 value of 0.46 (P = .09). Change in PFS also did not correlate with change in OS (R2 = 0.23; P = .28). In contrast, hazard ratios for PFS and OS correlated significantly (R2 = 0.41; P = .048). The protective effects of treatment were higher for OS than for PFS (pooled HR, 1.2; 95% confidence interval, 1.1-1.3; P = .002).
This might be because traditional RECIST (response evaluation criteria in solid tumors) criteria predate the era of immunotherapy and do not accurately capture disease progression when patients are on immuno-oncologics. For example, pseudoprogression (in which T-cell infiltrates cause the tumor to grow before it shrinks) could be misconstrued as progression. Also, PD-1 inhibitors can continue working even after treatment cessation, which could affect OS more than PFS, the researchers noted.
Regardless, “PD-1 inhibitors may have larger effects on OS than on PFS, which would be unprecedented in oncology therapeutics,” they concluded. “These results support the rationale of using OS as the primary end point of future phase 3 trials of PD-1 inhibitors and discourage the use of PFS as a sole primary end point as the latter may provide misleading information about the efficacy of these drugs.”
Funders included the Laura and John Arnold Foundation, the Harvard Program in Therapeutic Science, and the Engelberg Foundation. The investigators reported having no relevant conflicts of interest. One coinvestigator reported research support from the Laura and John Arnold Foundation. The other investigators had no conflicts.
SOURCE: Gyawali B et al. JAMA Network Open. 2018 June 22. doi: 10.1001/jamanetworkopen.2018.0416.
FROM JAMA NETWORK OPEN
Key clinical point: Overall survival should remain the standard endpoint for trials of PD-1 inhibitors.
Major finding: The protective effects of treatment were higher for OS than for PFS (pooled HR, 1.2; 95% confidence interval, 1.1-1.3; P = .002).
Study details: Systematic review and meta-analysis of 12 randomized, controlled trials.
Disclosures: Funders included the Laura and John Arnold Foundation, the Harvard Program in Therapeutic Science, and the Engelberg Foundation. The investigators reported having no relevant conflicts of interest. One coinvestigator reported research support from the Laura and John Arnold Foundation. The other investigators had no conflicts.
Source: Gyawali B et al. JAMA Network Open. 2018 June 22. doi: 10.1001/jamanetworkopen.2018.0416
Alirocumab’s benefit greater in diabetes patients: ODYSSEY Outcomes
ORLANDO – Higher risk translates to higher benefits. That’s the message of a new analysis of the ODYSSEY Outcomes trial in the PCSK9-inhibitor alirocumab that finds people with diabetes gained about twice the reduction in risk of major adverse cardiac events as their non-diabetic counterparts.
“Patients with diabetes and a recent heart attack are at double the risk of a cardiovascular event in the next 3 years as are nondiabetics, despite guideline-based care,” said study presenting author Kausik Ray, MD, ChB, of the School of Public Health of Imperial College London, in an interview. “These patients in our study had LDL of around 89 mg/dL despite high-intensity statins. Current guidelines recommend a goal of LDL of 55 mg/dL in this group. We brought LDL down to around 38 mg/ dL, and showed that by doing this, diabetics derived a greater reduction in the risk of major cardiovascular events. A greater absolute benefit was observed, and a smaller number needed to treat.”
Dr. Ray presented the study findings, a prespecified analysis of results of ODYSSEY Outcomes, at the annual scientific sessions of the American Diabetes Association.
The trial randomly assigned 18,924 patients with recent acute coronary syndrome and LDL cholesterol of at least 70 mg/dL, despite maximum statin therapy, to 75 mg of alirocumab every 2 weeks or placebo. Doses of alirocumab were increased blindly, to 150 mg, to reach LDL cholesterol levels of 25-50 mg/dL.
During a median 2.8 years of follow-up, the overall cumulative rate of major cardiac adverse events (coronary heart disease death, nonfatal MI, ischemic stroke, or hospitalization for unstable angina) occurred in 9.5% of the overall population randomized to alirocumab and 11.1% of those on placebo, for an absolute risk reduction of 1.6% and a statistically significant and clinically meaningful 15% reduction in relative risk. The results were presented at the annual scientific sessions of the American College of Cardiology in March.
In the current analysis, in patients with diabetes, the cumulative rate of incidents was 14.1% (380 of 2,693) with alirocumab and 16.4% (452 of 2,751) with placebo, for an ARR of 2.3%.
The ARRs for the prediabetes and normoglycemia groups were both 1.2%.
Dr. Ray noted that there’s no sign that the drug works differently in patients with diabetes. “The drug works in the same way and as effectively in everyone: LDL came down by 64% at 16 weeks in everyone. But absolute risk depends upon absolute risk to start with. So, in higher-risk patients, the absolute benefit is greater.”
According to Dr. Ray, the number needed to treat is 43 over 30 months for people with diabetes and 73 over 30 months for people without diabetes.
Prediman K. Shah, MD, director of the Oppenheimer Atherosclerosis Research Center at Cedars-Sinai Medical Center and professor of medicine at the University of California, Los Angeles, questioned the cost effectiveness of the medication in an interview.
“Even among the diabetics, the absolute risk reduction is about 2%, which is underwhelming considering the high cost,” he said. “If the cost were to drop to levels closer to cost of statins, such a small risk reduction may be worth the expense.”
Insurers have been skeptical of covering alirocumab because of its $14,000/year cost. However, Sanofi and Regeneron, which jointly market alirocumab, announced in March 2018 that they “will offer U.S. payers that agree to reduce burdensome access barriers for high-risk patients a further reduced net price for Praluent Injection (alirocumab) in alignment with a new value assessment for high-risk patients from the [United States].”
In response, Dr. Ray said “the benefits quoted are time-to-first-event, and these are modest. But if you look at recurrent events, which represent the natural course of disease, then the benefits and absolute benefits are greater. These are add-on therapies and will never be used in every single patient at current cost.”
Glen J. Pearson, PharmD, of the University of Alberta, Edmonton, said in an interview that, “while these absolute numbers do seem relatively small, it must be remembered that these patients are already receiving very effective therapies to reduce their risk of future cardiovascular outcomes.”
ODYSSEY Outcomes was funded by Sanofi and Regeneron. The presenter reports various disclosures including consulting and research support relationships with Sanofi and Regeneron. The other study authors report various disclosures. Dr. Pearson reports no relevant disclosures. Dr. Shah reports receiving grant support from Sanofi Regeneron.
SOURCE: Ray K et al. ADA 2018, Abstract 6-LB.
ORLANDO – Higher risk translates to higher benefits. That’s the message of a new analysis of the ODYSSEY Outcomes trial in the PCSK9-inhibitor alirocumab that finds people with diabetes gained about twice the reduction in risk of major adverse cardiac events as their non-diabetic counterparts.
“Patients with diabetes and a recent heart attack are at double the risk of a cardiovascular event in the next 3 years as are nondiabetics, despite guideline-based care,” said study presenting author Kausik Ray, MD, ChB, of the School of Public Health of Imperial College London, in an interview. “These patients in our study had LDL of around 89 mg/dL despite high-intensity statins. Current guidelines recommend a goal of LDL of 55 mg/dL in this group. We brought LDL down to around 38 mg/ dL, and showed that by doing this, diabetics derived a greater reduction in the risk of major cardiovascular events. A greater absolute benefit was observed, and a smaller number needed to treat.”
Dr. Ray presented the study findings, a prespecified analysis of results of ODYSSEY Outcomes, at the annual scientific sessions of the American Diabetes Association.
The trial randomly assigned 18,924 patients with recent acute coronary syndrome and LDL cholesterol of at least 70 mg/dL, despite maximum statin therapy, to 75 mg of alirocumab every 2 weeks or placebo. Doses of alirocumab were increased blindly, to 150 mg, to reach LDL cholesterol levels of 25-50 mg/dL.
During a median 2.8 years of follow-up, the overall cumulative rate of major cardiac adverse events (coronary heart disease death, nonfatal MI, ischemic stroke, or hospitalization for unstable angina) occurred in 9.5% of the overall population randomized to alirocumab and 11.1% of those on placebo, for an absolute risk reduction of 1.6% and a statistically significant and clinically meaningful 15% reduction in relative risk. The results were presented at the annual scientific sessions of the American College of Cardiology in March.
In the current analysis, in patients with diabetes, the cumulative rate of incidents was 14.1% (380 of 2,693) with alirocumab and 16.4% (452 of 2,751) with placebo, for an ARR of 2.3%.
The ARRs for the prediabetes and normoglycemia groups were both 1.2%.
Dr. Ray noted that there’s no sign that the drug works differently in patients with diabetes. “The drug works in the same way and as effectively in everyone: LDL came down by 64% at 16 weeks in everyone. But absolute risk depends upon absolute risk to start with. So, in higher-risk patients, the absolute benefit is greater.”
According to Dr. Ray, the number needed to treat is 43 over 30 months for people with diabetes and 73 over 30 months for people without diabetes.
Prediman K. Shah, MD, director of the Oppenheimer Atherosclerosis Research Center at Cedars-Sinai Medical Center and professor of medicine at the University of California, Los Angeles, questioned the cost effectiveness of the medication in an interview.
“Even among the diabetics, the absolute risk reduction is about 2%, which is underwhelming considering the high cost,” he said. “If the cost were to drop to levels closer to cost of statins, such a small risk reduction may be worth the expense.”
Insurers have been skeptical of covering alirocumab because of its $14,000/year cost. However, Sanofi and Regeneron, which jointly market alirocumab, announced in March 2018 that they “will offer U.S. payers that agree to reduce burdensome access barriers for high-risk patients a further reduced net price for Praluent Injection (alirocumab) in alignment with a new value assessment for high-risk patients from the [United States].”
In response, Dr. Ray said “the benefits quoted are time-to-first-event, and these are modest. But if you look at recurrent events, which represent the natural course of disease, then the benefits and absolute benefits are greater. These are add-on therapies and will never be used in every single patient at current cost.”
Glen J. Pearson, PharmD, of the University of Alberta, Edmonton, said in an interview that, “while these absolute numbers do seem relatively small, it must be remembered that these patients are already receiving very effective therapies to reduce their risk of future cardiovascular outcomes.”
ODYSSEY Outcomes was funded by Sanofi and Regeneron. The presenter reports various disclosures including consulting and research support relationships with Sanofi and Regeneron. The other study authors report various disclosures. Dr. Pearson reports no relevant disclosures. Dr. Shah reports receiving grant support from Sanofi Regeneron.
SOURCE: Ray K et al. ADA 2018, Abstract 6-LB.
ORLANDO – Higher risk translates to higher benefits. That’s the message of a new analysis of the ODYSSEY Outcomes trial in the PCSK9-inhibitor alirocumab that finds people with diabetes gained about twice the reduction in risk of major adverse cardiac events as their non-diabetic counterparts.
“Patients with diabetes and a recent heart attack are at double the risk of a cardiovascular event in the next 3 years as are nondiabetics, despite guideline-based care,” said study presenting author Kausik Ray, MD, ChB, of the School of Public Health of Imperial College London, in an interview. “These patients in our study had LDL of around 89 mg/dL despite high-intensity statins. Current guidelines recommend a goal of LDL of 55 mg/dL in this group. We brought LDL down to around 38 mg/ dL, and showed that by doing this, diabetics derived a greater reduction in the risk of major cardiovascular events. A greater absolute benefit was observed, and a smaller number needed to treat.”
Dr. Ray presented the study findings, a prespecified analysis of results of ODYSSEY Outcomes, at the annual scientific sessions of the American Diabetes Association.
The trial randomly assigned 18,924 patients with recent acute coronary syndrome and LDL cholesterol of at least 70 mg/dL, despite maximum statin therapy, to 75 mg of alirocumab every 2 weeks or placebo. Doses of alirocumab were increased blindly, to 150 mg, to reach LDL cholesterol levels of 25-50 mg/dL.
During a median 2.8 years of follow-up, the overall cumulative rate of major cardiac adverse events (coronary heart disease death, nonfatal MI, ischemic stroke, or hospitalization for unstable angina) occurred in 9.5% of the overall population randomized to alirocumab and 11.1% of those on placebo, for an absolute risk reduction of 1.6% and a statistically significant and clinically meaningful 15% reduction in relative risk. The results were presented at the annual scientific sessions of the American College of Cardiology in March.
In the current analysis, in patients with diabetes, the cumulative rate of incidents was 14.1% (380 of 2,693) with alirocumab and 16.4% (452 of 2,751) with placebo, for an ARR of 2.3%.
The ARRs for the prediabetes and normoglycemia groups were both 1.2%.
Dr. Ray noted that there’s no sign that the drug works differently in patients with diabetes. “The drug works in the same way and as effectively in everyone: LDL came down by 64% at 16 weeks in everyone. But absolute risk depends upon absolute risk to start with. So, in higher-risk patients, the absolute benefit is greater.”
According to Dr. Ray, the number needed to treat is 43 over 30 months for people with diabetes and 73 over 30 months for people without diabetes.
Prediman K. Shah, MD, director of the Oppenheimer Atherosclerosis Research Center at Cedars-Sinai Medical Center and professor of medicine at the University of California, Los Angeles, questioned the cost effectiveness of the medication in an interview.
“Even among the diabetics, the absolute risk reduction is about 2%, which is underwhelming considering the high cost,” he said. “If the cost were to drop to levels closer to cost of statins, such a small risk reduction may be worth the expense.”
Insurers have been skeptical of covering alirocumab because of its $14,000/year cost. However, Sanofi and Regeneron, which jointly market alirocumab, announced in March 2018 that they “will offer U.S. payers that agree to reduce burdensome access barriers for high-risk patients a further reduced net price for Praluent Injection (alirocumab) in alignment with a new value assessment for high-risk patients from the [United States].”
In response, Dr. Ray said “the benefits quoted are time-to-first-event, and these are modest. But if you look at recurrent events, which represent the natural course of disease, then the benefits and absolute benefits are greater. These are add-on therapies and will never be used in every single patient at current cost.”
Glen J. Pearson, PharmD, of the University of Alberta, Edmonton, said in an interview that, “while these absolute numbers do seem relatively small, it must be remembered that these patients are already receiving very effective therapies to reduce their risk of future cardiovascular outcomes.”
ODYSSEY Outcomes was funded by Sanofi and Regeneron. The presenter reports various disclosures including consulting and research support relationships with Sanofi and Regeneron. The other study authors report various disclosures. Dr. Pearson reports no relevant disclosures. Dr. Shah reports receiving grant support from Sanofi Regeneron.
SOURCE: Ray K et al. ADA 2018, Abstract 6-LB.
REPORTING FROM ADA 2018
Key clinical point:
Major finding: Over a median 34-month period, patients with diabetes who took alirocumab had a 2.3% absolute risk reduction in major cardiac adverse events incidents. Counterparts without diabetes had an ARR of 1.2%.
Study details: ODYSSEY Outcomes, a double-blind, randomized trial of nearly 19,000 patients with a recent acute coronary syndrome and an LDL cholesterol level of 70 mg/dL or more despite intensive statin therapy.
Disclosures: The study was funded by Sanofi and Regeneron Pharmaceuticals, and many study authors disclose financial relationships with the companies.
Source: Ray K et al. ADA 2018, Abstract 6-LB.