User login
Tune in to cardiovascular risk in psoriasis
Stay attentive to cardiovascular disease risk in patients with psoriasis because effective treatment of psoriasis could improve their vascular risk as well, said Jeffrey M. Sobell, MD, of Tufts University in Boston.
he said at the Caribbean Dermatology Symposium.
The metabolic syndrome and its associated cardiovascular risk of myocardial infarction and stroke is significantly more prevalent in psoriasis patients, compared with controls, Dr. Sobell said at the meeting, provided by Global Academy for Medical Education.
A possible reason for this link may be that the chronic inflammation associated with psoriasis leads to atherosclerosis, Dr. Sobell noted. The inflammation is evident on PET imaging with a radiolabeled glucose known as fluorodeoxyglucose positron emission tomography–computed tomography (FDG-PET/CT) The technology, first used in cancer and neuroimaging, can detect early subclinical inflammation and allows for exact measurements of inflammatory activity, and measuring inflammation of the aorta can serve as a surrogate marker for treatment, he said.
Treating skin disease appears to impact vascular disease, Dr. Sobell said. In a study published in JAMA Cardiology, researchers followed 115 patients for 1 year using FDG-PET/CT (JAMA Cardiol. 2017. doi: 10.1001/jamacardio.2017.1213)
Overall, when psoriasis improved, so did signs of vascular inflammation. “When the skin is more severe and treated more aggressively with anti-TNF therapy, the reduction in vascular disease is stronger,” Dr. Sobell said.
Data from another large study presented as a late-breaker at the American Academy of Dermatology in 2017 showed that treatment of psoriasis with tumor necrosis factor–alpha inhibitor therapy significantly reduced all-cause mortality in patients with psoriasis or psoriatic arthritis, he noted.
Psoriasis patients often are underscreened for cardiac risk factors, but identifying them can help guide treatment, Dr. Sobell said.
“Dermatologists should at minimum direct patients to primary care physicians for appropriate screening and assessment,” he emphasized.
Dr. Sobell disclosed relationships with Amgen, AbbVie, Celgene, Eli Lilly, Janssen, Merck, Novartis, Regeneron, and Sun Pharma.
Global Academy and this news organization are owned by the same parent company.
Stay attentive to cardiovascular disease risk in patients with psoriasis because effective treatment of psoriasis could improve their vascular risk as well, said Jeffrey M. Sobell, MD, of Tufts University in Boston.
he said at the Caribbean Dermatology Symposium.
The metabolic syndrome and its associated cardiovascular risk of myocardial infarction and stroke is significantly more prevalent in psoriasis patients, compared with controls, Dr. Sobell said at the meeting, provided by Global Academy for Medical Education.
A possible reason for this link may be that the chronic inflammation associated with psoriasis leads to atherosclerosis, Dr. Sobell noted. The inflammation is evident on PET imaging with a radiolabeled glucose known as fluorodeoxyglucose positron emission tomography–computed tomography (FDG-PET/CT) The technology, first used in cancer and neuroimaging, can detect early subclinical inflammation and allows for exact measurements of inflammatory activity, and measuring inflammation of the aorta can serve as a surrogate marker for treatment, he said.
Treating skin disease appears to impact vascular disease, Dr. Sobell said. In a study published in JAMA Cardiology, researchers followed 115 patients for 1 year using FDG-PET/CT (JAMA Cardiol. 2017. doi: 10.1001/jamacardio.2017.1213)
Overall, when psoriasis improved, so did signs of vascular inflammation. “When the skin is more severe and treated more aggressively with anti-TNF therapy, the reduction in vascular disease is stronger,” Dr. Sobell said.
Data from another large study presented as a late-breaker at the American Academy of Dermatology in 2017 showed that treatment of psoriasis with tumor necrosis factor–alpha inhibitor therapy significantly reduced all-cause mortality in patients with psoriasis or psoriatic arthritis, he noted.
Psoriasis patients often are underscreened for cardiac risk factors, but identifying them can help guide treatment, Dr. Sobell said.
“Dermatologists should at minimum direct patients to primary care physicians for appropriate screening and assessment,” he emphasized.
Dr. Sobell disclosed relationships with Amgen, AbbVie, Celgene, Eli Lilly, Janssen, Merck, Novartis, Regeneron, and Sun Pharma.
Global Academy and this news organization are owned by the same parent company.
Stay attentive to cardiovascular disease risk in patients with psoriasis because effective treatment of psoriasis could improve their vascular risk as well, said Jeffrey M. Sobell, MD, of Tufts University in Boston.
he said at the Caribbean Dermatology Symposium.
The metabolic syndrome and its associated cardiovascular risk of myocardial infarction and stroke is significantly more prevalent in psoriasis patients, compared with controls, Dr. Sobell said at the meeting, provided by Global Academy for Medical Education.
A possible reason for this link may be that the chronic inflammation associated with psoriasis leads to atherosclerosis, Dr. Sobell noted. The inflammation is evident on PET imaging with a radiolabeled glucose known as fluorodeoxyglucose positron emission tomography–computed tomography (FDG-PET/CT) The technology, first used in cancer and neuroimaging, can detect early subclinical inflammation and allows for exact measurements of inflammatory activity, and measuring inflammation of the aorta can serve as a surrogate marker for treatment, he said.
Treating skin disease appears to impact vascular disease, Dr. Sobell said. In a study published in JAMA Cardiology, researchers followed 115 patients for 1 year using FDG-PET/CT (JAMA Cardiol. 2017. doi: 10.1001/jamacardio.2017.1213)
Overall, when psoriasis improved, so did signs of vascular inflammation. “When the skin is more severe and treated more aggressively with anti-TNF therapy, the reduction in vascular disease is stronger,” Dr. Sobell said.
Data from another large study presented as a late-breaker at the American Academy of Dermatology in 2017 showed that treatment of psoriasis with tumor necrosis factor–alpha inhibitor therapy significantly reduced all-cause mortality in patients with psoriasis or psoriatic arthritis, he noted.
Psoriasis patients often are underscreened for cardiac risk factors, but identifying them can help guide treatment, Dr. Sobell said.
“Dermatologists should at minimum direct patients to primary care physicians for appropriate screening and assessment,” he emphasized.
Dr. Sobell disclosed relationships with Amgen, AbbVie, Celgene, Eli Lilly, Janssen, Merck, Novartis, Regeneron, and Sun Pharma.
Global Academy and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM THE CARIBBEAN DERMATOLOGY SYMPOSIUM
PAM50-based score identifies low-risk subset with node-positive early-stage breast cancer
The PAM50-based risk of recurrence (ROR) score enabled selection of a subset of patients with estrogen receptor (ER)–positive early-stage breast cancer with node-positive or node-negative disease with an estimated 10-year distant recurrence (DR) absolute risk of less than 5%, investigators reported.
This subset of patients with one to three positive lymph nodes presented a sufficiently low risk of disease recurrence and could safely avoid chemotherapy, reported Anne-Vibeke Laenkholm, MD, and her associates. The report was published in the Journal of Clinical Oncology.
The PAM50-based ROR score (Prosigna Score; Nanostring Technologies, Seattle) is a comparative gene expression profile of the tumor, relative to each of the four PAM50 molecular profiles (luminal A, luminal B, basal, and HER2 enriched) to determine the degree of similarity. The Prosigna assay currently has Food and Drug Administration clearance for prognostic use.
Postmenopausal women diagnosed with ER-positive/HER2-negative early-stage breast cancer in Denmark between 2000 and 2003, and who received adjuvant treatment with tamoxifen or an aromatase inhibitor without chemotherapy were eligible for this cohort study.
The primary endpoint was time to DR, defined as the interval from breast cancer surgery until DR or death as a result of breast cancer. Secondary endpoints included overall survival and time to any recurrence. “The median age of patients was 63 years (range, 50-89 years); 45.5% were node negative, and 54.5% had one to three positive nodes. Tumor characteristics including nodal status, tumor size, malignancy grade, and lymphovascular invasion were all associated with DR, whereas treatment adherence was not,” wrote Dr. Laenkholm of the department of surgical pathology, Zealand University Hospital, Denmark, and her colleagues.
“With a median follow-up of approximately 9 years, 26% of the patients with node-positive disease were categorized as having a low ROR score corresponding to a DR of 3.5% at 10 years compared with those with an intermediate ROR score with a DR of 11.5% and those with a high ROR score corresponding to a DR risk of 22%. In the node-negative group, those with a low ROR score had a 10-year DR risk of 5% and those with an intermediate ROR score had a 7.3% 10-year DR risk, compared with a DR of 17.8% in those with a high ROR score,” Dr. Laenkholm and her associates reported.
The data are entirely prognostic and do not address whether chemotherapy might offer some benefit in a node-positive population (i.e., one to three nodes), or whether adjuvant chemotherapy–associated adverse effects may offset the added benefit, if any, the investigators said.
Nonetheless, genomic assay–based scoring tools are an important aid in clinical decision making readily available to the physician at the patient’s bedside, they said.
Nanostring Technologies funded the study. Laboratory work flow was executed at the department of surgical pathology, Zealand University Hospital. Several authors reported ties with Roche and other pharmaceutical companies.
SOURCE: Laenkholm et al. J Clin Oncol. 2018 Jan 25. doi: 10.1200/JCO.2017.74.6586.
The study by Laenkholm et al. provides encouraging data for the clinical utility of molecular assays to aid decision making for node-positive disease.
The investigators were able to select a subset of patients with node-positive disease with an estimated 10-year distant recurrence risk of less than or equal to 5%, based on the PAM50 risk of recurrence score. It could be argued that the data do not address the issue of whether chemotherapy would offer some benefit (predictive) in a node-positive population; however, a counterargument is that whatever small added benefit may be derived from adjuvant chemotherapy would be offset by adverse effects, resulting in a net gain of zero. The collective data from evaluation of other assays in this population suggest that patients with ER-positive disease, one to three positive nodes, and a low recurrence score can safely avoid adjuvant chemotherapy and receive endocrine therapy alone. This supports the current NCCN guidelines, which indicate the recurrence score assay can be considered in patients with one to three positive nodes. The more definitive answer on whether adjuvant chemotherapy adds benefit to endocrine therapy will be determined from the RxPONDER study, in which patients with ER+ disease, one to three positive nodes, and a recurrence score less than or equal to 25 will be randomly assigned to chemotherapy or not.
Ricardo L. B. Costa, MD, MS, is with the H. Lee Moffitt Cancer Center, Tampa. William J. Gradishar, MD, is with Northwestern University, Chicago. Dr. Costa disclosed ties with Bristol-Myers Squibb. Dr. Gradishar reported having no relevant financial disclosures. Their comments were adapted from an editorial (J Clin Oncol. 2018 Jan 25. doi: 10.1200/JCO.2017.76.9802).
The study by Laenkholm et al. provides encouraging data for the clinical utility of molecular assays to aid decision making for node-positive disease.
The investigators were able to select a subset of patients with node-positive disease with an estimated 10-year distant recurrence risk of less than or equal to 5%, based on the PAM50 risk of recurrence score. It could be argued that the data do not address the issue of whether chemotherapy would offer some benefit (predictive) in a node-positive population; however, a counterargument is that whatever small added benefit may be derived from adjuvant chemotherapy would be offset by adverse effects, resulting in a net gain of zero. The collective data from evaluation of other assays in this population suggest that patients with ER-positive disease, one to three positive nodes, and a low recurrence score can safely avoid adjuvant chemotherapy and receive endocrine therapy alone. This supports the current NCCN guidelines, which indicate the recurrence score assay can be considered in patients with one to three positive nodes. The more definitive answer on whether adjuvant chemotherapy adds benefit to endocrine therapy will be determined from the RxPONDER study, in which patients with ER+ disease, one to three positive nodes, and a recurrence score less than or equal to 25 will be randomly assigned to chemotherapy or not.
Ricardo L. B. Costa, MD, MS, is with the H. Lee Moffitt Cancer Center, Tampa. William J. Gradishar, MD, is with Northwestern University, Chicago. Dr. Costa disclosed ties with Bristol-Myers Squibb. Dr. Gradishar reported having no relevant financial disclosures. Their comments were adapted from an editorial (J Clin Oncol. 2018 Jan 25. doi: 10.1200/JCO.2017.76.9802).
The study by Laenkholm et al. provides encouraging data for the clinical utility of molecular assays to aid decision making for node-positive disease.
The investigators were able to select a subset of patients with node-positive disease with an estimated 10-year distant recurrence risk of less than or equal to 5%, based on the PAM50 risk of recurrence score. It could be argued that the data do not address the issue of whether chemotherapy would offer some benefit (predictive) in a node-positive population; however, a counterargument is that whatever small added benefit may be derived from adjuvant chemotherapy would be offset by adverse effects, resulting in a net gain of zero. The collective data from evaluation of other assays in this population suggest that patients with ER-positive disease, one to three positive nodes, and a low recurrence score can safely avoid adjuvant chemotherapy and receive endocrine therapy alone. This supports the current NCCN guidelines, which indicate the recurrence score assay can be considered in patients with one to three positive nodes. The more definitive answer on whether adjuvant chemotherapy adds benefit to endocrine therapy will be determined from the RxPONDER study, in which patients with ER+ disease, one to three positive nodes, and a recurrence score less than or equal to 25 will be randomly assigned to chemotherapy or not.
Ricardo L. B. Costa, MD, MS, is with the H. Lee Moffitt Cancer Center, Tampa. William J. Gradishar, MD, is with Northwestern University, Chicago. Dr. Costa disclosed ties with Bristol-Myers Squibb. Dr. Gradishar reported having no relevant financial disclosures. Their comments were adapted from an editorial (J Clin Oncol. 2018 Jan 25. doi: 10.1200/JCO.2017.76.9802).
The PAM50-based risk of recurrence (ROR) score enabled selection of a subset of patients with estrogen receptor (ER)–positive early-stage breast cancer with node-positive or node-negative disease with an estimated 10-year distant recurrence (DR) absolute risk of less than 5%, investigators reported.
This subset of patients with one to three positive lymph nodes presented a sufficiently low risk of disease recurrence and could safely avoid chemotherapy, reported Anne-Vibeke Laenkholm, MD, and her associates. The report was published in the Journal of Clinical Oncology.
The PAM50-based ROR score (Prosigna Score; Nanostring Technologies, Seattle) is a comparative gene expression profile of the tumor, relative to each of the four PAM50 molecular profiles (luminal A, luminal B, basal, and HER2 enriched) to determine the degree of similarity. The Prosigna assay currently has Food and Drug Administration clearance for prognostic use.
Postmenopausal women diagnosed with ER-positive/HER2-negative early-stage breast cancer in Denmark between 2000 and 2003, and who received adjuvant treatment with tamoxifen or an aromatase inhibitor without chemotherapy were eligible for this cohort study.
The primary endpoint was time to DR, defined as the interval from breast cancer surgery until DR or death as a result of breast cancer. Secondary endpoints included overall survival and time to any recurrence. “The median age of patients was 63 years (range, 50-89 years); 45.5% were node negative, and 54.5% had one to three positive nodes. Tumor characteristics including nodal status, tumor size, malignancy grade, and lymphovascular invasion were all associated with DR, whereas treatment adherence was not,” wrote Dr. Laenkholm of the department of surgical pathology, Zealand University Hospital, Denmark, and her colleagues.
“With a median follow-up of approximately 9 years, 26% of the patients with node-positive disease were categorized as having a low ROR score corresponding to a DR of 3.5% at 10 years compared with those with an intermediate ROR score with a DR of 11.5% and those with a high ROR score corresponding to a DR risk of 22%. In the node-negative group, those with a low ROR score had a 10-year DR risk of 5% and those with an intermediate ROR score had a 7.3% 10-year DR risk, compared with a DR of 17.8% in those with a high ROR score,” Dr. Laenkholm and her associates reported.
The data are entirely prognostic and do not address whether chemotherapy might offer some benefit in a node-positive population (i.e., one to three nodes), or whether adjuvant chemotherapy–associated adverse effects may offset the added benefit, if any, the investigators said.
Nonetheless, genomic assay–based scoring tools are an important aid in clinical decision making readily available to the physician at the patient’s bedside, they said.
Nanostring Technologies funded the study. Laboratory work flow was executed at the department of surgical pathology, Zealand University Hospital. Several authors reported ties with Roche and other pharmaceutical companies.
SOURCE: Laenkholm et al. J Clin Oncol. 2018 Jan 25. doi: 10.1200/JCO.2017.74.6586.
The PAM50-based risk of recurrence (ROR) score enabled selection of a subset of patients with estrogen receptor (ER)–positive early-stage breast cancer with node-positive or node-negative disease with an estimated 10-year distant recurrence (DR) absolute risk of less than 5%, investigators reported.
This subset of patients with one to three positive lymph nodes presented a sufficiently low risk of disease recurrence and could safely avoid chemotherapy, reported Anne-Vibeke Laenkholm, MD, and her associates. The report was published in the Journal of Clinical Oncology.
The PAM50-based ROR score (Prosigna Score; Nanostring Technologies, Seattle) is a comparative gene expression profile of the tumor, relative to each of the four PAM50 molecular profiles (luminal A, luminal B, basal, and HER2 enriched) to determine the degree of similarity. The Prosigna assay currently has Food and Drug Administration clearance for prognostic use.
Postmenopausal women diagnosed with ER-positive/HER2-negative early-stage breast cancer in Denmark between 2000 and 2003, and who received adjuvant treatment with tamoxifen or an aromatase inhibitor without chemotherapy were eligible for this cohort study.
The primary endpoint was time to DR, defined as the interval from breast cancer surgery until DR or death as a result of breast cancer. Secondary endpoints included overall survival and time to any recurrence. “The median age of patients was 63 years (range, 50-89 years); 45.5% were node negative, and 54.5% had one to three positive nodes. Tumor characteristics including nodal status, tumor size, malignancy grade, and lymphovascular invasion were all associated with DR, whereas treatment adherence was not,” wrote Dr. Laenkholm of the department of surgical pathology, Zealand University Hospital, Denmark, and her colleagues.
“With a median follow-up of approximately 9 years, 26% of the patients with node-positive disease were categorized as having a low ROR score corresponding to a DR of 3.5% at 10 years compared with those with an intermediate ROR score with a DR of 11.5% and those with a high ROR score corresponding to a DR risk of 22%. In the node-negative group, those with a low ROR score had a 10-year DR risk of 5% and those with an intermediate ROR score had a 7.3% 10-year DR risk, compared with a DR of 17.8% in those with a high ROR score,” Dr. Laenkholm and her associates reported.
The data are entirely prognostic and do not address whether chemotherapy might offer some benefit in a node-positive population (i.e., one to three nodes), or whether adjuvant chemotherapy–associated adverse effects may offset the added benefit, if any, the investigators said.
Nonetheless, genomic assay–based scoring tools are an important aid in clinical decision making readily available to the physician at the patient’s bedside, they said.
Nanostring Technologies funded the study. Laboratory work flow was executed at the department of surgical pathology, Zealand University Hospital. Several authors reported ties with Roche and other pharmaceutical companies.
SOURCE: Laenkholm et al. J Clin Oncol. 2018 Jan 25. doi: 10.1200/JCO.2017.74.6586.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: The score enabled selection of a subset of patients with node-positive or node-negative disease with an estimated 10-year DR absolute risk of less than 5%.
Major finding: About 37% of patients with a single positive lymph node and 15% of patients with two positive nodes were identified as low risk by Prosigna, with very favorable outcomes when treated with adjuvant endocrine therapy alone.
Study details: Danish Breast Cancer Cooperative Group database including postmenopausal patients in Denmark diagnosed with ER-positive invasive breast cancer from 2000 through 2003 and treated with endocrine therapy for 5 years.
Disclosures: Nanostring Technologies funded the study. Laboratory work flow was executed at the department of surgical pathology, Zealand University Hospital. Several authors reported ties with Roche and other pharmaceutical companies.
Source: Laenkholm et al. J Clin Oncol. 2018 Jan 25. doi: 10.1200/JCO.2017.74.6586.
Get ready for certolizumab for psoriasis
KAUAI, HAWAII – When certolizumab pegol receives marketing approval for moderate to severe psoriasis – which experts say is a virtual lock – it will offer a singular advantage over current anti–tumor necrosis factor (anti-TNF) biologics: strong evidence of safety in pregnancy.
“ ” Kenneth B. Gordon, MD, observed at the Hawaii Dermatology Seminar provided by the Global Academy for Medical Education/Skin Disease Education Foundation.
Lots of women and their families are understandably deeply concerned about using powerful, transformative medications during pregnancy, even though they know from experience how debilitating inadequately treated psoriasis can be.
“Many women of childbearing potential would find [certolizumab] to be a preferential agent if they’re planning to become pregnant,” said Dr. Gordon, professor and chair of the department of dermatology at the Medical College of Wisconsin, Milwaukee.
He cited the CRIB (A Multicenter, Postmarketing Study Evaluating the Transfer of Cimzia From the Mother to the Infant via the Placenta) study results presented by Alexa B. Kimball, MD, at the 2017 annual meeting of the European Academy of Dermatology and Venereology in Geneva as a major step forward in establishing the safety of certolizumab during pregnancy.
CRIB was a prospective postmarketing pharmacokinetic study that evaluated placental transfer of certolizumab from 16 pregnant women on the biologic to their infants. All of the mothers received their last dose of certolizumab for rheumatoid arthritis or other approved indications within 35 days of delivery. Blood samples were collected from mothers, newborns, and umbilical cords within 1 hour of delivery, and again from the infants at weeks 4 and 8 after delivery.
Only one infant had a detectable plasma level of certolizumab at birth, and it was barely measurable at 0.042 mcg/mL, as compared with 49.4 mcg/mL in the mother’s plasma. This is consistent with the fact that certolizumab’s pegylated arm allows only minimal or no placental transfer from mother to infant, so there is essentially no third trimester in utero fetal exposure. In contrast, as Dr. Kimball noted, other anti-TNF biologics lack a pegylated arm and thus preferentially cross the placenta, creating a theoretical increased risk of maternal pregnancy complications and/or congenital malformations.
Dr. Kimball, professor of dermatology at Harvard Medical School and chief executive officer of Harvard Medical Faculty Physicians at Beth Israel Deaconess Medical Center, both in Boston, also has been deeply involved in an ongoing registry (sponsored by certolizumab manufacturer UCB) of several hundred women on certolizumab in pregnancy. The data have reassuringly shown no increased risk of maternal pregnancy complications such as preeclampsia, gestational diabetes, or preterm birth, nor any increase in or pattern of congenital malformations, compared with background rates in the general population.
Dr. Gordon said that while he understands the concerns, he personally doesn’t think the class-wide safety of TNF inhibitors in pregnancy and lactation is a big issue.
“My argument is that anti-TNF agents have been used very frequently in women of childbearing age, and also in women who are pregnant or lactating. And there have not been any side effect signals from that,” he explained.
The prospects of gaining an expanded indication for certolizumab in psoriasis hinge in part on the impressive results of the pivotal phase 3, randomized, double-blind, placebo-controlled CIMPASI-1 and CIMPASI-2 trials. In CIMPASI-1, the week-48 Psoriasis Area and Severity Index (PASI) 75 and PASI 90 response rates were 87.1% and 60.2%, respectively, in patients on the biologic at 400 mg every 2 weeks; among those on certolizumab at 200 mg every 2 weeks, the rates were 67.2% and 42.8%. In CIMPASI-2, the PASI 75 and PASI 90 rates were 81.3% and 62.0% at 400 mg and 78.7% and 59.6% with 200 mg every 2 weeks.
There were no cases of tuberculosis or any other significant safety concerns through 48 weeks, Dr. Gordon said.
“Certolizumab is coming soon for psoriasis,” predicted Craig L. Leonardi, MD, a psoriasis researcher at Saint Louis University. “The data are very impressive. It’s a high-performance drug. There’s no reason why this drug shouldn’t be approved.”
Since Dr. Kimball’s presentation of the CRIB data at the 2017 annual meeting of the European Academy of Dermatology and Venereology, the study has been published (Ann Rheum Dis. 2018 Feb;77[2]:228-33).
Dr. Gordon reported receiving research support from and serving as a paid consultant to numerous pharmaceutical companies developing new psoriasis therapies.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
KAUAI, HAWAII – When certolizumab pegol receives marketing approval for moderate to severe psoriasis – which experts say is a virtual lock – it will offer a singular advantage over current anti–tumor necrosis factor (anti-TNF) biologics: strong evidence of safety in pregnancy.
“ ” Kenneth B. Gordon, MD, observed at the Hawaii Dermatology Seminar provided by the Global Academy for Medical Education/Skin Disease Education Foundation.
Lots of women and their families are understandably deeply concerned about using powerful, transformative medications during pregnancy, even though they know from experience how debilitating inadequately treated psoriasis can be.
“Many women of childbearing potential would find [certolizumab] to be a preferential agent if they’re planning to become pregnant,” said Dr. Gordon, professor and chair of the department of dermatology at the Medical College of Wisconsin, Milwaukee.
He cited the CRIB (A Multicenter, Postmarketing Study Evaluating the Transfer of Cimzia From the Mother to the Infant via the Placenta) study results presented by Alexa B. Kimball, MD, at the 2017 annual meeting of the European Academy of Dermatology and Venereology in Geneva as a major step forward in establishing the safety of certolizumab during pregnancy.
CRIB was a prospective postmarketing pharmacokinetic study that evaluated placental transfer of certolizumab from 16 pregnant women on the biologic to their infants. All of the mothers received their last dose of certolizumab for rheumatoid arthritis or other approved indications within 35 days of delivery. Blood samples were collected from mothers, newborns, and umbilical cords within 1 hour of delivery, and again from the infants at weeks 4 and 8 after delivery.
Only one infant had a detectable plasma level of certolizumab at birth, and it was barely measurable at 0.042 mcg/mL, as compared with 49.4 mcg/mL in the mother’s plasma. This is consistent with the fact that certolizumab’s pegylated arm allows only minimal or no placental transfer from mother to infant, so there is essentially no third trimester in utero fetal exposure. In contrast, as Dr. Kimball noted, other anti-TNF biologics lack a pegylated arm and thus preferentially cross the placenta, creating a theoretical increased risk of maternal pregnancy complications and/or congenital malformations.
Dr. Kimball, professor of dermatology at Harvard Medical School and chief executive officer of Harvard Medical Faculty Physicians at Beth Israel Deaconess Medical Center, both in Boston, also has been deeply involved in an ongoing registry (sponsored by certolizumab manufacturer UCB) of several hundred women on certolizumab in pregnancy. The data have reassuringly shown no increased risk of maternal pregnancy complications such as preeclampsia, gestational diabetes, or preterm birth, nor any increase in or pattern of congenital malformations, compared with background rates in the general population.
Dr. Gordon said that while he understands the concerns, he personally doesn’t think the class-wide safety of TNF inhibitors in pregnancy and lactation is a big issue.
“My argument is that anti-TNF agents have been used very frequently in women of childbearing age, and also in women who are pregnant or lactating. And there have not been any side effect signals from that,” he explained.
The prospects of gaining an expanded indication for certolizumab in psoriasis hinge in part on the impressive results of the pivotal phase 3, randomized, double-blind, placebo-controlled CIMPASI-1 and CIMPASI-2 trials. In CIMPASI-1, the week-48 Psoriasis Area and Severity Index (PASI) 75 and PASI 90 response rates were 87.1% and 60.2%, respectively, in patients on the biologic at 400 mg every 2 weeks; among those on certolizumab at 200 mg every 2 weeks, the rates were 67.2% and 42.8%. In CIMPASI-2, the PASI 75 and PASI 90 rates were 81.3% and 62.0% at 400 mg and 78.7% and 59.6% with 200 mg every 2 weeks.
There were no cases of tuberculosis or any other significant safety concerns through 48 weeks, Dr. Gordon said.
“Certolizumab is coming soon for psoriasis,” predicted Craig L. Leonardi, MD, a psoriasis researcher at Saint Louis University. “The data are very impressive. It’s a high-performance drug. There’s no reason why this drug shouldn’t be approved.”
Since Dr. Kimball’s presentation of the CRIB data at the 2017 annual meeting of the European Academy of Dermatology and Venereology, the study has been published (Ann Rheum Dis. 2018 Feb;77[2]:228-33).
Dr. Gordon reported receiving research support from and serving as a paid consultant to numerous pharmaceutical companies developing new psoriasis therapies.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
KAUAI, HAWAII – When certolizumab pegol receives marketing approval for moderate to severe psoriasis – which experts say is a virtual lock – it will offer a singular advantage over current anti–tumor necrosis factor (anti-TNF) biologics: strong evidence of safety in pregnancy.
“ ” Kenneth B. Gordon, MD, observed at the Hawaii Dermatology Seminar provided by the Global Academy for Medical Education/Skin Disease Education Foundation.
Lots of women and their families are understandably deeply concerned about using powerful, transformative medications during pregnancy, even though they know from experience how debilitating inadequately treated psoriasis can be.
“Many women of childbearing potential would find [certolizumab] to be a preferential agent if they’re planning to become pregnant,” said Dr. Gordon, professor and chair of the department of dermatology at the Medical College of Wisconsin, Milwaukee.
He cited the CRIB (A Multicenter, Postmarketing Study Evaluating the Transfer of Cimzia From the Mother to the Infant via the Placenta) study results presented by Alexa B. Kimball, MD, at the 2017 annual meeting of the European Academy of Dermatology and Venereology in Geneva as a major step forward in establishing the safety of certolizumab during pregnancy.
CRIB was a prospective postmarketing pharmacokinetic study that evaluated placental transfer of certolizumab from 16 pregnant women on the biologic to their infants. All of the mothers received their last dose of certolizumab for rheumatoid arthritis or other approved indications within 35 days of delivery. Blood samples were collected from mothers, newborns, and umbilical cords within 1 hour of delivery, and again from the infants at weeks 4 and 8 after delivery.
Only one infant had a detectable plasma level of certolizumab at birth, and it was barely measurable at 0.042 mcg/mL, as compared with 49.4 mcg/mL in the mother’s plasma. This is consistent with the fact that certolizumab’s pegylated arm allows only minimal or no placental transfer from mother to infant, so there is essentially no third trimester in utero fetal exposure. In contrast, as Dr. Kimball noted, other anti-TNF biologics lack a pegylated arm and thus preferentially cross the placenta, creating a theoretical increased risk of maternal pregnancy complications and/or congenital malformations.
Dr. Kimball, professor of dermatology at Harvard Medical School and chief executive officer of Harvard Medical Faculty Physicians at Beth Israel Deaconess Medical Center, both in Boston, also has been deeply involved in an ongoing registry (sponsored by certolizumab manufacturer UCB) of several hundred women on certolizumab in pregnancy. The data have reassuringly shown no increased risk of maternal pregnancy complications such as preeclampsia, gestational diabetes, or preterm birth, nor any increase in or pattern of congenital malformations, compared with background rates in the general population.
Dr. Gordon said that while he understands the concerns, he personally doesn’t think the class-wide safety of TNF inhibitors in pregnancy and lactation is a big issue.
“My argument is that anti-TNF agents have been used very frequently in women of childbearing age, and also in women who are pregnant or lactating. And there have not been any side effect signals from that,” he explained.
The prospects of gaining an expanded indication for certolizumab in psoriasis hinge in part on the impressive results of the pivotal phase 3, randomized, double-blind, placebo-controlled CIMPASI-1 and CIMPASI-2 trials. In CIMPASI-1, the week-48 Psoriasis Area and Severity Index (PASI) 75 and PASI 90 response rates were 87.1% and 60.2%, respectively, in patients on the biologic at 400 mg every 2 weeks; among those on certolizumab at 200 mg every 2 weeks, the rates were 67.2% and 42.8%. In CIMPASI-2, the PASI 75 and PASI 90 rates were 81.3% and 62.0% at 400 mg and 78.7% and 59.6% with 200 mg every 2 weeks.
There were no cases of tuberculosis or any other significant safety concerns through 48 weeks, Dr. Gordon said.
“Certolizumab is coming soon for psoriasis,” predicted Craig L. Leonardi, MD, a psoriasis researcher at Saint Louis University. “The data are very impressive. It’s a high-performance drug. There’s no reason why this drug shouldn’t be approved.”
Since Dr. Kimball’s presentation of the CRIB data at the 2017 annual meeting of the European Academy of Dermatology and Venereology, the study has been published (Ann Rheum Dis. 2018 Feb;77[2]:228-33).
Dr. Gordon reported receiving research support from and serving as a paid consultant to numerous pharmaceutical companies developing new psoriasis therapies.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM SDEF HAWAII DERMATOLOGY SEMINAR
Reported penicillin allergies hike inpatient costs
Total inpatient costs for patients who report being allergic to penicillin are much higher than for those who don’t report an allergy, according to a recent systematic review and meta-analysis.
The review, which eventually included 30 articles, found that total inpatient costs ranged from an average $1,145-$4,254 higher per patient with a reported penicillin allergy compared to nonallergic patients, said T. Joseph Mattingly, PharmD, and his associates. Outpatient prescription costs were also estimated to be steeper, running $14-$93 higher per patient who reported a penicillin allergy.
Although 10%-20% of patients report a penicillin allergy, “[a] majority of patients who report PCN [penicillin] allergy are not truly allergic upon confirmatory testing,” Dr. Mattingly and his colleagues wrote.
This overreporting of penicillin allergies is a problem for the patient and the health care system because “reported antibiotic allergies have been associated with suboptimal antibiotic therapy, increased antimicrobial resistance, increased length of stay, increased antibiotic-related adverse events, increased rates of C. difficile infection, intensive care unit (ICU) admission, death, as well as increased treatment cost,” said Dr. Mattingly and his coauthors.
Health care providers often “tend to take reported allergies at face value,” said coauthor Anne Fulton, suggesting that primary care practices can help by considering skin testing for those patients who carry a label of penicillin allergy, but don’t have a documented confirmatory test. The cost for a commonly used skin test for penicillin allergy runs about $200, said Ms. Fulton, a doctoral candidate at the University of Maryland, Baltimore, in an interview.
When conducting the meta-analysis, Dr. Mattingly and his coauthors converted all figures to 2017 U.S. dollars, using Consumer Price Index figures to adjust for inflation. This yields conservative estimates for cost, as drug and health care prices have far outstripped the general rate of inflation during the period in which the studies occurred, Ms. Fulton acknowledged.
The investigators highlighted the need for ongoing study in this area. “To our knowledge, there are no evaluations of long-term outpatient outcomes related to the effects of PCN allergy and the potential impact of delabeling patients who do not have a true allergy,” they wrote.
Ms. Fulton agreed, noting that the studies covered in the meta-analysis were primarily focused on short-term outcomes, though there are many potential long-term benefits to delabeling patients who are not truly penicillin allergic.
For the patient, this includes the opportunity to receive optimal antimicrobial therapy, as well as potential savings in copays and other out-of-pocket expenses for outpatient medications, she said.
As antimicrobial resistance becomes an ever more pressing problem, there are more opportunities for targeted therapy if inappropriate allergy labeling is addressed, Ms. Fulton added.
Further study should use “cost-effectiveness analysis methods that include societal and health sector perspectives capturing immediate and future outcomes and costs to evaluate the use of skin-testing procedures in either inpatient or outpatient settings,” the investigators wrote.
The study was supported by ALK, the manufacturer of Pre-Pen, a commercially available penicillin allergy skin test.
SOURCE: Mattingly TJ et al. J Allergy Clin Immunol Pract. 2018 Jan 31. doi: 10.1016/j.jaip.2017.12.033.
Total inpatient costs for patients who report being allergic to penicillin are much higher than for those who don’t report an allergy, according to a recent systematic review and meta-analysis.
The review, which eventually included 30 articles, found that total inpatient costs ranged from an average $1,145-$4,254 higher per patient with a reported penicillin allergy compared to nonallergic patients, said T. Joseph Mattingly, PharmD, and his associates. Outpatient prescription costs were also estimated to be steeper, running $14-$93 higher per patient who reported a penicillin allergy.
Although 10%-20% of patients report a penicillin allergy, “[a] majority of patients who report PCN [penicillin] allergy are not truly allergic upon confirmatory testing,” Dr. Mattingly and his colleagues wrote.
This overreporting of penicillin allergies is a problem for the patient and the health care system because “reported antibiotic allergies have been associated with suboptimal antibiotic therapy, increased antimicrobial resistance, increased length of stay, increased antibiotic-related adverse events, increased rates of C. difficile infection, intensive care unit (ICU) admission, death, as well as increased treatment cost,” said Dr. Mattingly and his coauthors.
Health care providers often “tend to take reported allergies at face value,” said coauthor Anne Fulton, suggesting that primary care practices can help by considering skin testing for those patients who carry a label of penicillin allergy, but don’t have a documented confirmatory test. The cost for a commonly used skin test for penicillin allergy runs about $200, said Ms. Fulton, a doctoral candidate at the University of Maryland, Baltimore, in an interview.
When conducting the meta-analysis, Dr. Mattingly and his coauthors converted all figures to 2017 U.S. dollars, using Consumer Price Index figures to adjust for inflation. This yields conservative estimates for cost, as drug and health care prices have far outstripped the general rate of inflation during the period in which the studies occurred, Ms. Fulton acknowledged.
The investigators highlighted the need for ongoing study in this area. “To our knowledge, there are no evaluations of long-term outpatient outcomes related to the effects of PCN allergy and the potential impact of delabeling patients who do not have a true allergy,” they wrote.
Ms. Fulton agreed, noting that the studies covered in the meta-analysis were primarily focused on short-term outcomes, though there are many potential long-term benefits to delabeling patients who are not truly penicillin allergic.
For the patient, this includes the opportunity to receive optimal antimicrobial therapy, as well as potential savings in copays and other out-of-pocket expenses for outpatient medications, she said.
As antimicrobial resistance becomes an ever more pressing problem, there are more opportunities for targeted therapy if inappropriate allergy labeling is addressed, Ms. Fulton added.
Further study should use “cost-effectiveness analysis methods that include societal and health sector perspectives capturing immediate and future outcomes and costs to evaluate the use of skin-testing procedures in either inpatient or outpatient settings,” the investigators wrote.
The study was supported by ALK, the manufacturer of Pre-Pen, a commercially available penicillin allergy skin test.
SOURCE: Mattingly TJ et al. J Allergy Clin Immunol Pract. 2018 Jan 31. doi: 10.1016/j.jaip.2017.12.033.
Total inpatient costs for patients who report being allergic to penicillin are much higher than for those who don’t report an allergy, according to a recent systematic review and meta-analysis.
The review, which eventually included 30 articles, found that total inpatient costs ranged from an average $1,145-$4,254 higher per patient with a reported penicillin allergy compared to nonallergic patients, said T. Joseph Mattingly, PharmD, and his associates. Outpatient prescription costs were also estimated to be steeper, running $14-$93 higher per patient who reported a penicillin allergy.
Although 10%-20% of patients report a penicillin allergy, “[a] majority of patients who report PCN [penicillin] allergy are not truly allergic upon confirmatory testing,” Dr. Mattingly and his colleagues wrote.
This overreporting of penicillin allergies is a problem for the patient and the health care system because “reported antibiotic allergies have been associated with suboptimal antibiotic therapy, increased antimicrobial resistance, increased length of stay, increased antibiotic-related adverse events, increased rates of C. difficile infection, intensive care unit (ICU) admission, death, as well as increased treatment cost,” said Dr. Mattingly and his coauthors.
Health care providers often “tend to take reported allergies at face value,” said coauthor Anne Fulton, suggesting that primary care practices can help by considering skin testing for those patients who carry a label of penicillin allergy, but don’t have a documented confirmatory test. The cost for a commonly used skin test for penicillin allergy runs about $200, said Ms. Fulton, a doctoral candidate at the University of Maryland, Baltimore, in an interview.
When conducting the meta-analysis, Dr. Mattingly and his coauthors converted all figures to 2017 U.S. dollars, using Consumer Price Index figures to adjust for inflation. This yields conservative estimates for cost, as drug and health care prices have far outstripped the general rate of inflation during the period in which the studies occurred, Ms. Fulton acknowledged.
The investigators highlighted the need for ongoing study in this area. “To our knowledge, there are no evaluations of long-term outpatient outcomes related to the effects of PCN allergy and the potential impact of delabeling patients who do not have a true allergy,” they wrote.
Ms. Fulton agreed, noting that the studies covered in the meta-analysis were primarily focused on short-term outcomes, though there are many potential long-term benefits to delabeling patients who are not truly penicillin allergic.
For the patient, this includes the opportunity to receive optimal antimicrobial therapy, as well as potential savings in copays and other out-of-pocket expenses for outpatient medications, she said.
As antimicrobial resistance becomes an ever more pressing problem, there are more opportunities for targeted therapy if inappropriate allergy labeling is addressed, Ms. Fulton added.
Further study should use “cost-effectiveness analysis methods that include societal and health sector perspectives capturing immediate and future outcomes and costs to evaluate the use of skin-testing procedures in either inpatient or outpatient settings,” the investigators wrote.
The study was supported by ALK, the manufacturer of Pre-Pen, a commercially available penicillin allergy skin test.
SOURCE: Mattingly TJ et al. J Allergy Clin Immunol Pract. 2018 Jan 31. doi: 10.1016/j.jaip.2017.12.033.
FROM JOURNAL OF ALLERGY AND CLINICAL IMMUNOLOGY: IN PRACTICE
Key clinical point: Inpatient costs were $1,145 – $4,254 higher for those reporting penicillin allergy.
Major finding: Though most studies addressed inpatient admissions, outpatient costs were also significantly higher.
Study details: Systematic review and meta-analysis of 30 articles addressing reported penicillin allergy.
Disclosures: The study was sponsored by ALK.
Source: Mattingly TJ et al. J Allergy Clin Immunol Pract. 2018 Jan 31. doi: 10.1016/j.jaip.2017.12.033.
FDA approves new combination drug for HIV patients
The Food and Drug Administration has approved a combination drug intended to treat HIV-1 infections – bictegravir, emtricitabine, tenofovir alafenamide – in virologically suppressed (HIV-1 RNA less than 50 copies/mL) adults who have no history of antiretroviral treatment or as a replacement for their current antiretroviral regimen.
The approval of the new combination drug (Biktarvy) was based on four active, randomized, controlled trials comprising three double-blind studies and one open label study. After 48 weeks of treatment in all trials, CD4+ cell count was evaluated to determine the efficacy of bictegravir, emtricitabine, tenofovir alafenamide, compared with other antiretroviral therapies.
In trial 1489, patients were randomized 1:1 to receive Biktarvy (n = 314) or ABC/DTG/3TC (abacavir 600 mg/dolutegravir 50 mg/lamivudine 300 mg) (n = 315). Trial 1490 was similar to trial 1489, with patients randomized 1:1 to receive either Biktarvy (n = 320) or DTG + FTC/TAF (dolutegravir + 50 mg, emtricitabine 200 mg/tenofovir alafenamide fumarate 25 mg) (n = 325). In trial 1489, the mean increase in CD4+ count after 48 weeks was 233 cells per mm3 and 229/mm3 in the Biktarvy and ABC/DTG/3TC groups, respectively. Similarly, counts in trial 1490 CD4+ after 48 weeks were 180/mm3 and 201/mm3 in the Biktarvy and DTG + FTC/TAF groups, respectively.
Trial 1844, another randomized trial, was composed of patients who switched to Biktarvy from their older treatment. Patients were randomized 1:1 to the new treatment (n = 282) or their previous antiretroviral regimen (n = 281).
Over 48 weeks, the mean change in CD4+ cell count was –31 cells per mm3 in subjects who switched to Biktarvy and 4/mm3 in subjects who stayed on ABC/DTG/3TC.
The open-label portion of the study, trial 1878, evaluated the safety and efficacy of switching from other retroviral treatments (n = 287) to Biktarvy (n = 290). The average change in CD4+ count after 48 weeks was 25 cells per mm3 who switched to Biktarvy and 0/mm3 who stayed on their previous regimens.
The new combination has received a boxed warning regarding the risk of severe acute exacerbations of hepatitis B that have been reported in patients coinfected with HIV-1 and HBV and have discontinued products containing emtricitabine (FTC) and/or tenofovir disoproxil fumarate (TDF) and may occur with discontinuation of Biktarvy. Such patients should be closely monitored for hepatic function with both clinical and laboratory follow-up for at least several months in patients if they discontinue Biktarvy. If appropriate, antihepatitis B therapy may be warranted.
The approved recommended dosage for bictegravir, emtricitabine, tenofovir alafenamide combination drug is one tablet daily with or without food. More information is available on the FDA website.
The Food and Drug Administration has approved a combination drug intended to treat HIV-1 infections – bictegravir, emtricitabine, tenofovir alafenamide – in virologically suppressed (HIV-1 RNA less than 50 copies/mL) adults who have no history of antiretroviral treatment or as a replacement for their current antiretroviral regimen.
The approval of the new combination drug (Biktarvy) was based on four active, randomized, controlled trials comprising three double-blind studies and one open label study. After 48 weeks of treatment in all trials, CD4+ cell count was evaluated to determine the efficacy of bictegravir, emtricitabine, tenofovir alafenamide, compared with other antiretroviral therapies.
In trial 1489, patients were randomized 1:1 to receive Biktarvy (n = 314) or ABC/DTG/3TC (abacavir 600 mg/dolutegravir 50 mg/lamivudine 300 mg) (n = 315). Trial 1490 was similar to trial 1489, with patients randomized 1:1 to receive either Biktarvy (n = 320) or DTG + FTC/TAF (dolutegravir + 50 mg, emtricitabine 200 mg/tenofovir alafenamide fumarate 25 mg) (n = 325). In trial 1489, the mean increase in CD4+ count after 48 weeks was 233 cells per mm3 and 229/mm3 in the Biktarvy and ABC/DTG/3TC groups, respectively. Similarly, counts in trial 1490 CD4+ after 48 weeks were 180/mm3 and 201/mm3 in the Biktarvy and DTG + FTC/TAF groups, respectively.
Trial 1844, another randomized trial, was composed of patients who switched to Biktarvy from their older treatment. Patients were randomized 1:1 to the new treatment (n = 282) or their previous antiretroviral regimen (n = 281).
Over 48 weeks, the mean change in CD4+ cell count was –31 cells per mm3 in subjects who switched to Biktarvy and 4/mm3 in subjects who stayed on ABC/DTG/3TC.
The open-label portion of the study, trial 1878, evaluated the safety and efficacy of switching from other retroviral treatments (n = 287) to Biktarvy (n = 290). The average change in CD4+ count after 48 weeks was 25 cells per mm3 who switched to Biktarvy and 0/mm3 who stayed on their previous regimens.
The new combination has received a boxed warning regarding the risk of severe acute exacerbations of hepatitis B that have been reported in patients coinfected with HIV-1 and HBV and have discontinued products containing emtricitabine (FTC) and/or tenofovir disoproxil fumarate (TDF) and may occur with discontinuation of Biktarvy. Such patients should be closely monitored for hepatic function with both clinical and laboratory follow-up for at least several months in patients if they discontinue Biktarvy. If appropriate, antihepatitis B therapy may be warranted.
The approved recommended dosage for bictegravir, emtricitabine, tenofovir alafenamide combination drug is one tablet daily with or without food. More information is available on the FDA website.
The Food and Drug Administration has approved a combination drug intended to treat HIV-1 infections – bictegravir, emtricitabine, tenofovir alafenamide – in virologically suppressed (HIV-1 RNA less than 50 copies/mL) adults who have no history of antiretroviral treatment or as a replacement for their current antiretroviral regimen.
The approval of the new combination drug (Biktarvy) was based on four active, randomized, controlled trials comprising three double-blind studies and one open label study. After 48 weeks of treatment in all trials, CD4+ cell count was evaluated to determine the efficacy of bictegravir, emtricitabine, tenofovir alafenamide, compared with other antiretroviral therapies.
In trial 1489, patients were randomized 1:1 to receive Biktarvy (n = 314) or ABC/DTG/3TC (abacavir 600 mg/dolutegravir 50 mg/lamivudine 300 mg) (n = 315). Trial 1490 was similar to trial 1489, with patients randomized 1:1 to receive either Biktarvy (n = 320) or DTG + FTC/TAF (dolutegravir + 50 mg, emtricitabine 200 mg/tenofovir alafenamide fumarate 25 mg) (n = 325). In trial 1489, the mean increase in CD4+ count after 48 weeks was 233 cells per mm3 and 229/mm3 in the Biktarvy and ABC/DTG/3TC groups, respectively. Similarly, counts in trial 1490 CD4+ after 48 weeks were 180/mm3 and 201/mm3 in the Biktarvy and DTG + FTC/TAF groups, respectively.
Trial 1844, another randomized trial, was composed of patients who switched to Biktarvy from their older treatment. Patients were randomized 1:1 to the new treatment (n = 282) or their previous antiretroviral regimen (n = 281).
Over 48 weeks, the mean change in CD4+ cell count was –31 cells per mm3 in subjects who switched to Biktarvy and 4/mm3 in subjects who stayed on ABC/DTG/3TC.
The open-label portion of the study, trial 1878, evaluated the safety and efficacy of switching from other retroviral treatments (n = 287) to Biktarvy (n = 290). The average change in CD4+ count after 48 weeks was 25 cells per mm3 who switched to Biktarvy and 0/mm3 who stayed on their previous regimens.
The new combination has received a boxed warning regarding the risk of severe acute exacerbations of hepatitis B that have been reported in patients coinfected with HIV-1 and HBV and have discontinued products containing emtricitabine (FTC) and/or tenofovir disoproxil fumarate (TDF) and may occur with discontinuation of Biktarvy. Such patients should be closely monitored for hepatic function with both clinical and laboratory follow-up for at least several months in patients if they discontinue Biktarvy. If appropriate, antihepatitis B therapy may be warranted.
The approved recommended dosage for bictegravir, emtricitabine, tenofovir alafenamide combination drug is one tablet daily with or without food. More information is available on the FDA website.
Many prescriptions for older epilepsy patients have potential to interact
A substantial portion of older adults with epilepsy who are on Medicare receive prescriptions for antiepileptic drugs (AEDs) and nonepilepsy drugs (NEDs) that can interact to alter their effectiveness or induce toxicity, according to a retrospective analysis of a claims database.
Up to a quarter of all patients had potential interactions between AED and non-AED prescriptions, and these were more likely to occur for patients with comorbid conditions or those who were eligible for Part D Low Income Subsidy, reported Raymond Edward Faught Jr., MD, a professor in the department of neurology at Emory University, Atlanta, and his colleagues. The study was published in Epilepsia.
Dr. Faught and his coauthors analyzed a 5% random sample of beneficiaries from 2008-2010 Medicare claims who were 67 years or older in 2009 and identified 36,912 prevalent and 3,706 incident epilepsy cases from 2009, both of which were demographically similar. Prevalent cases were defined by the prevalence of epilepsy and seizures with medication, and incident cases had no history of epilepsy or seizure. The research team also compiled a list of interaction risk of AEDs and NED efficacy and rated high risk as potentially life threatening, medium risk as significant, and probable but unspecified risk.
For incident cases, the percentage with concern for drug interaction included 6.9% at high risk, 10.3% at medium risk, and 18.5% with probable but unspecified risk. As a whole, 75.5% had no interaction risk and 24.5% had some risk for interaction. In 18% of incident cases, drug interactions increased the effect of AEDs, while 2.4% decreased AED effect. There were several, specific NEDs that had a documented or probable interaction risk with AEDs. For those on simvastatin, 30.9% were concomitantly prescribed phenytoin, corresponding to 7.6% of all incident cases having a probable but unspecified risk with this combination. Warfarin users also received phenytoin one-third of the time, meaning that 3.6% of all incident cases had a high risk of an interaction with the combination.
A more pronounced effect occurred with drug combinations in prevalent cases. A total of 39% took a drug combination that altered the efficacy of NEDs, whereas 26.2% took combinations that increase the effect of AEDs and 3% had interactions that could decrease AED efficacy.
An increasing number of comorbidities raised the likelihood of having any risk for interaction (odds ratio of 2.14 for one to three comorbidities and 2.73 for four or more), compared with no comorbidities. Eligibility for Part D Low Income Subsidy increased the odds for a high-risk interaction (OR, 2.05) or high-medium risk interaction (OR, 1.44).
The authors cautioned that the list of drug interactions and the associated qualitative rankings reflect their judgment and that they evaluated only concomitant use of the 50 most commonly prescribed NEDs in the patient population. Considering that there are thousands of potential drugs that could interact with AEDs, this represents a limited sample.
The National Institute of Neurological Disorders and Stroke funded the study. Several authors reported financial relationships with pharmaceutical companies that market AEDs.
SOURCE: Faught E et al. Epilepsia. 2008 Feb 7. doi: 10.1111/epi.14010.
A substantial portion of older adults with epilepsy who are on Medicare receive prescriptions for antiepileptic drugs (AEDs) and nonepilepsy drugs (NEDs) that can interact to alter their effectiveness or induce toxicity, according to a retrospective analysis of a claims database.
Up to a quarter of all patients had potential interactions between AED and non-AED prescriptions, and these were more likely to occur for patients with comorbid conditions or those who were eligible for Part D Low Income Subsidy, reported Raymond Edward Faught Jr., MD, a professor in the department of neurology at Emory University, Atlanta, and his colleagues. The study was published in Epilepsia.
Dr. Faught and his coauthors analyzed a 5% random sample of beneficiaries from 2008-2010 Medicare claims who were 67 years or older in 2009 and identified 36,912 prevalent and 3,706 incident epilepsy cases from 2009, both of which were demographically similar. Prevalent cases were defined by the prevalence of epilepsy and seizures with medication, and incident cases had no history of epilepsy or seizure. The research team also compiled a list of interaction risk of AEDs and NED efficacy and rated high risk as potentially life threatening, medium risk as significant, and probable but unspecified risk.
For incident cases, the percentage with concern for drug interaction included 6.9% at high risk, 10.3% at medium risk, and 18.5% with probable but unspecified risk. As a whole, 75.5% had no interaction risk and 24.5% had some risk for interaction. In 18% of incident cases, drug interactions increased the effect of AEDs, while 2.4% decreased AED effect. There were several, specific NEDs that had a documented or probable interaction risk with AEDs. For those on simvastatin, 30.9% were concomitantly prescribed phenytoin, corresponding to 7.6% of all incident cases having a probable but unspecified risk with this combination. Warfarin users also received phenytoin one-third of the time, meaning that 3.6% of all incident cases had a high risk of an interaction with the combination.
A more pronounced effect occurred with drug combinations in prevalent cases. A total of 39% took a drug combination that altered the efficacy of NEDs, whereas 26.2% took combinations that increase the effect of AEDs and 3% had interactions that could decrease AED efficacy.
An increasing number of comorbidities raised the likelihood of having any risk for interaction (odds ratio of 2.14 for one to three comorbidities and 2.73 for four or more), compared with no comorbidities. Eligibility for Part D Low Income Subsidy increased the odds for a high-risk interaction (OR, 2.05) or high-medium risk interaction (OR, 1.44).
The authors cautioned that the list of drug interactions and the associated qualitative rankings reflect their judgment and that they evaluated only concomitant use of the 50 most commonly prescribed NEDs in the patient population. Considering that there are thousands of potential drugs that could interact with AEDs, this represents a limited sample.
The National Institute of Neurological Disorders and Stroke funded the study. Several authors reported financial relationships with pharmaceutical companies that market AEDs.
SOURCE: Faught E et al. Epilepsia. 2008 Feb 7. doi: 10.1111/epi.14010.
A substantial portion of older adults with epilepsy who are on Medicare receive prescriptions for antiepileptic drugs (AEDs) and nonepilepsy drugs (NEDs) that can interact to alter their effectiveness or induce toxicity, according to a retrospective analysis of a claims database.
Up to a quarter of all patients had potential interactions between AED and non-AED prescriptions, and these were more likely to occur for patients with comorbid conditions or those who were eligible for Part D Low Income Subsidy, reported Raymond Edward Faught Jr., MD, a professor in the department of neurology at Emory University, Atlanta, and his colleagues. The study was published in Epilepsia.
Dr. Faught and his coauthors analyzed a 5% random sample of beneficiaries from 2008-2010 Medicare claims who were 67 years or older in 2009 and identified 36,912 prevalent and 3,706 incident epilepsy cases from 2009, both of which were demographically similar. Prevalent cases were defined by the prevalence of epilepsy and seizures with medication, and incident cases had no history of epilepsy or seizure. The research team also compiled a list of interaction risk of AEDs and NED efficacy and rated high risk as potentially life threatening, medium risk as significant, and probable but unspecified risk.
For incident cases, the percentage with concern for drug interaction included 6.9% at high risk, 10.3% at medium risk, and 18.5% with probable but unspecified risk. As a whole, 75.5% had no interaction risk and 24.5% had some risk for interaction. In 18% of incident cases, drug interactions increased the effect of AEDs, while 2.4% decreased AED effect. There were several, specific NEDs that had a documented or probable interaction risk with AEDs. For those on simvastatin, 30.9% were concomitantly prescribed phenytoin, corresponding to 7.6% of all incident cases having a probable but unspecified risk with this combination. Warfarin users also received phenytoin one-third of the time, meaning that 3.6% of all incident cases had a high risk of an interaction with the combination.
A more pronounced effect occurred with drug combinations in prevalent cases. A total of 39% took a drug combination that altered the efficacy of NEDs, whereas 26.2% took combinations that increase the effect of AEDs and 3% had interactions that could decrease AED efficacy.
An increasing number of comorbidities raised the likelihood of having any risk for interaction (odds ratio of 2.14 for one to three comorbidities and 2.73 for four or more), compared with no comorbidities. Eligibility for Part D Low Income Subsidy increased the odds for a high-risk interaction (OR, 2.05) or high-medium risk interaction (OR, 1.44).
The authors cautioned that the list of drug interactions and the associated qualitative rankings reflect their judgment and that they evaluated only concomitant use of the 50 most commonly prescribed NEDs in the patient population. Considering that there are thousands of potential drugs that could interact with AEDs, this represents a limited sample.
The National Institute of Neurological Disorders and Stroke funded the study. Several authors reported financial relationships with pharmaceutical companies that market AEDs.
SOURCE: Faught E et al. Epilepsia. 2008 Feb 7. doi: 10.1111/epi.14010.
FROM EPILEPSIA
Key clinical point:
Major finding: In 18% of incident cases, drug interactions increased the effect of AEDs, while 2.4% decreased AED effect.
Study details: Retrospective analyses of 2008-2010 Medicare claims with a 5% random sample of beneficiaries who were 67 years or older in 2009.
Disclosures: The National Institute of Neurological Disorders and Stroke funded the study. Several authors reported financial relationships with pharmaceutical companies that market AEDs.
Source: Faught E et al. Epilepsia. 2008 Feb 7. doi: 10.1111/epi.14010.
Patient-Specific Implants in Severe Glenoid Bone Loss
ABSTRACT
Complex glenoid bone deformities present the treating surgeon with a complex reconstructive challenge. Although glenoid bone loss can be encountered in the primary setting (degenerative, congenital, post-traumatic), severe glenoid bone loss is encountered in most revision total shoulder arthroplasties. Severe glenoid bone loss is treated with various techniques including hemiarthroplasty, eccentric reaming, and glenoid reconstruction with bone autografts and allografts. Despite encouraging short- to mid-term results reported with these reconstruction techniques, the clinical and radiographic outcomes remain inconsistent and the high number of complications is a concern. To overcome this problem, more recently augmented components and patient specific implants were introduced. Using the computer-aided design and computer-aided manufacturing technology patient-specific implants have been created to reconstruct the glenoid vault in cases of severe glenoid bone loss.
In this article we describe a patient specific glenoid implant, its indication, technical aspects and surgical technique, based on the author's experience as well as a review of the current literature on custom glenoid implants.
Continue to: Total shoulder arthroplasty...
Total shoulder arthroplasty (TSA) is an effective operation for providing pain relief and improving function in patients with end-stage degenerative shoulder disease that is nonresponsive to nonoperative treatments.1-4 With the increasing number of arthroplasties performed, and the expanding indication for shoulder arthroplasty, the number of revision shoulder arthroplasties is also increasing.5-14 Complex glenoid bone deformities present the treating surgeon with a complex reconstructive challenge. Although glenoid bone loss can be seen in the primary setting (degenerative, congenital, and post-traumatic), severe glenoid bone loss is encountered mostly in revision TSAs.
Historically, patients with severe glenoid bone loss were treated with a hemiarthroplasty.15-17 However, due to inferior outcomes associated with the use of shoulder hemiarthroplasties compared with TSA in these cases,18-20 various techniques were developed with the aim of realigning the glenoid axis and securing the implants into the deficient glenoid vault.21-25 Options have included eccentric reaming, glenoid reconstruction with bone autografts and allografts, and more recently augmented components and patient-specific implants. Studies with eccentric reaming and reconstruction with bone graft during complex shoulder arthroplasty have reported encouraging short- to mid-term results, but the clinical and radiographic outcomes remain inconsistent, and the high number of complications is a concern.25-28
Complications with these techniques include component loosening, graft resorption, nonunion, failure of graft incorporation, infection, and instability.25-28
Computer-aided design and computer-aided manufacturing (CAD/CAM) of patient-specific implants have been used successfully by hip arthroplasty surgeons to deal with complex acetabular reconstructions in the setting of severe bone loss. More recently, the same technology has been used to reconstruct the glenoid vault in cases of severe glenoid bone loss.
In this article, we describe a patient-specific glenoid implant, its indication, and both technical aspects and the surgical technique, based on the authors’ experience as well as a review of the current literature on custom glenoid implants.
Continue to: PATIENT-SPECIFIC GLENOID COMPONENT
PATIENT-SPECIFIC GLENOID COMPONENT
The Vault Reconstruction System ([VRS], Zimmer Biomet) is a patient-specific glenoid vault reconstruction system developed with the use of CAD/CAM to address severe glenoid bone loss encountered during shoulder arthroplasty. For several years, the VRS was available only as a custom implant according to the US Food and Drug Administration rules, and therefore its use was limited to a few cases per year. Recently, a 510(k) envelope clearance was granted to use the VRS in reverse TSA to address significant glenoid bone defects.
The VRS is made of porous plasma spray titanium to provide high strength and flexibility, and allows for biologic fixation. This system can accommodate a restricted bone loss envelope of about 50 mm × 50 mm × 35 mm according to the previous experience of the manufacturer in the custom scenario, covering 96% of defects previously addressed. One 6.5-mm nonlocking central screw and a minimum of four 4.75-mm nonlocking or locking peripheral screws are required for optimal fixation of the implant in the native scapula. A custom boss can be added in to enhance fixation in the native scapula when the bone is sufficient. To facilitate the surgical procedure, a trial implant, a bone model of the scapula, and a custom boss reaming guide are 3-dimensional (3-D) and printed in sterilizable material. These are all provided as single-use disposable instruments and can be available for surgeons during both the initial plan review and surgery.
PREOPERATIVE PLANNING
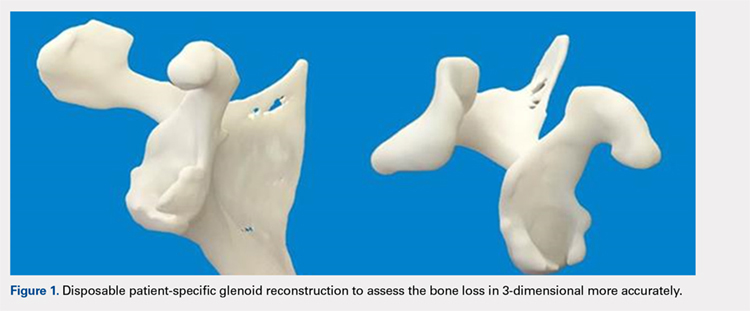
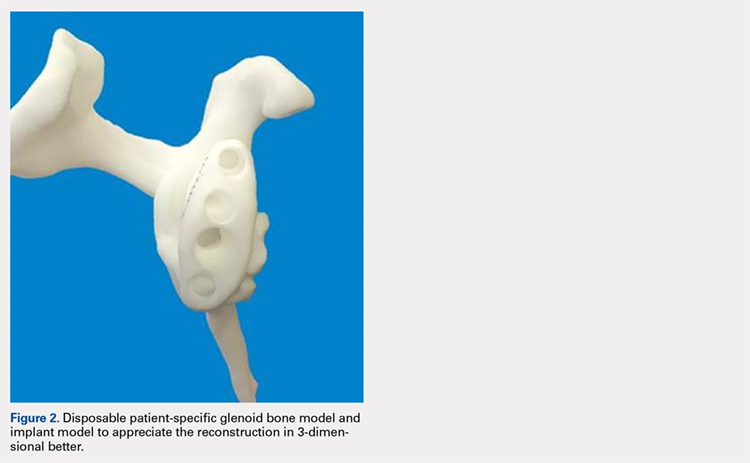
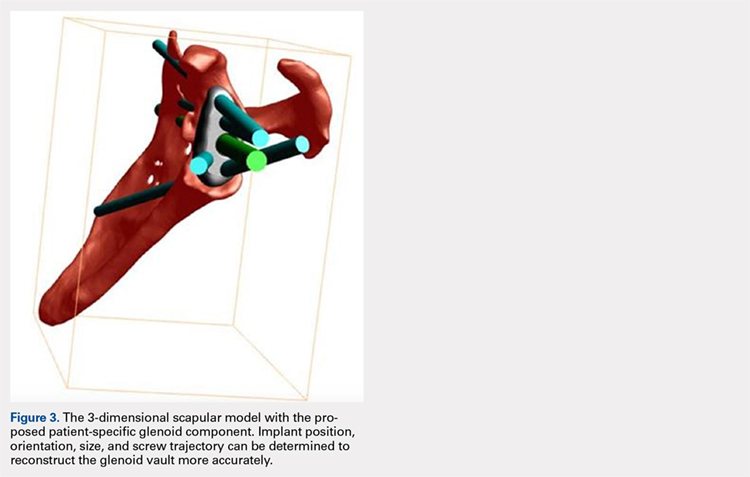
Patients undergo a preoperative fine-cut 2-dimensional computed tomography scan of the scapula and adjacent humerus following a predefined protocol with a slice thickness of 2 mm to 3 mm. An accurate 3-D bone model of the scapula is obtained using a 3-D image processing software system (Figure 1). The 3-D scapular model is used to create a patient-specific glenoid implant proposal that is approved by the surgeon (Figure 2). Implant position, orientation, size, screw trajectory, and recommended bone removal, if necessary, are determined to create a more normal glenohumeral center of rotation and to secure a glenoid implant in severely deficient glenoid bone (Figure 3). Once the implant design is approved by the surgeon, the final patient-specific implant is manufactured.
SURGICAL TECHNIQUE
The exposure of the glenoid is a critical step for the successful implantation of the patient-specific glenoid implant. Soft tissue and scar tissue around the glenoid must be removed to allow for optimal fit of the custom-made reaming guide. Also, removal of the entire capsulolabral complex on the anteroinferior rim of the glenoid is essential to both enhance glenoid exposure and to allow a perfect fit of the guide to the pathologic bone stock. Attention should be paid during débridement and/or implant removal in case of revision, to make sure that no excessive bone is removed because the patient-specific guide is referenced to this anatomy. Excessive bone removal can change the orientation of the patient-specific guide and ultimately the fixation of the implant. Once the custom-made patient-specific guide is positioned, a 3.2-mm Steinmann pin is placed through the inserter for temporary fixation. The pin should engage or perforate the medial cortical wall to ensure that the subsequent reamer has a stable cannula over which to ream. After the glenoid is reamed, the final implant can be placed in the ideal position according to the preoperative planning. A central 6.5-mm nonlocking central screw and 4.75-mm nonlocking or locking peripheral screws are required to complete the fixation of the implant in the native scapula. Once the patient-specific glenoid component is positioned and strongly fixed to the bone, the glenosphere can be positioned according to the preoperative planning, and the reverse shoulder arthroplasty can be completed in the usual fashion.
CASE EXAMPLES
A 68-year-old woman underwent a TSA for end-stage osteoarthritis in 2000. The implant failed due to a cuff failure. The patient underwent several surgeries, including an open cuff repair, with no success. She had no active elevation preoperatively. Because of the significant glenoid bone loss, a patient-specific glenoid reconstruction was planned. Within 24 months after this surgery, the patient was able to get her hand to her head and elevate to 90º (Figures 4A-4F).

Continue to: In October 2013...
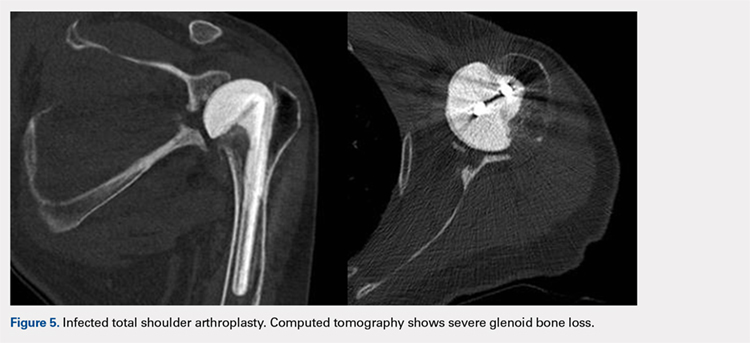
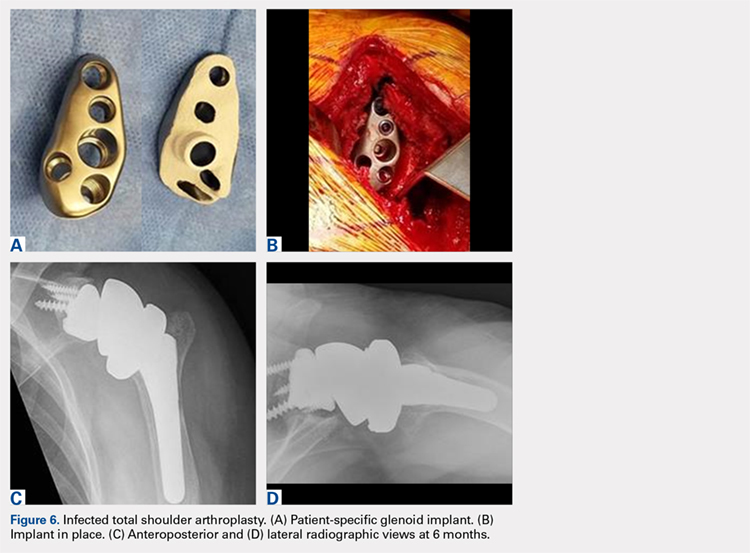
In October 2013, a 68-year-old man underwent a TSA for end-stage osteoarthritis. After 18 months, the implant failed due to active Propionibacterium acnes infection, which required excisional arthroplasty with insertion of an antibiotic spacer. Significant glenoid bone loss (Figure 5) and global soft-tissue deficiency caused substantial disability and led to an indication for a reverse TSA with a patient-specific glenoid vault reconstruction (Figures 6A-6D) after infection eradication. Within 20 months after this surgery, the patient had resumed a satisfactory range of motion (130º forward elevation, 20º external rotation) and outcome.
DISCUSSION
Although glenoid bone loss is often seen in the primary setting (degenerative, congenital, and post-traumatic), severe glenoid bone loss is encountered in most revision TSAs. The best treatment method for massive glenoid bone defects during complex shoulder arthroplasty remains uncertain. Options have included eccentric reaming, glenoid reconstruction with bone allograft and autograft, and more recently augmented components and patient-specific implants.21-25 The advent and availability of CAD/CAM technology have enabled shoulder surgeons to create patient-specific metal solutions to these challenging cases. Currently, only a few reports exist in the literature on patient-specific glenoid components in the setting of severe bone loss.29-32
Chammaa and colleagues29 reported the outcomes of 37 patients with a hip-inspired glenoid component (Total Shoulder Replacement, Stanmore Implants Worldwide). The 5-year results with this implant were promising, with a 16% revision rate and only 1 case of glenoid loosening.
Stoffelen and colleagues30 recently described the successful use of a patient-specific anatomic metal-backed glenoid component for the management of severe glenoid bone loss with excellent results at 2.5 years of follow-up. A different approach was pursued by Gunther and Lynch,31 who reported on 7 patients with a custom inset glenoid implant for deficient glenoid vaults. These circular anatomic, custom-made glenoid components were created with the intention of placing the implants partially inside the glenoid vault and relying partially on sclerotic cortical bone. Despite excellent results at 3 years of follow-up, their use is limited to specific defect geometries and cannot be used in cases of extreme bone loss.
CONCLUSION
We have described the use of a patient-specific glenoid component in 2 patients with severe glenoid bone loss. Despite the satisfactory clinical and short-term radiographic results, we acknowledge that longer-term follow-up is needed to confirm the efficacy of this type of reconstruction. We believe that patient-specific glenoid components represent a valuable addition to the armamentarium of shoulder surgeons who address complex glenoid bone deformities.
1. Chalmers PN, Gupta AK, Rahman Z, Bruce B, Romeo AA, Nicholson GP. Predictors of early complications of total shoulder arthroplasty. J Arthroplasty. 2014;29(4):856-860. doi:10.1016/j.arth.2013.07.002.
2. Deshmukh AV, Koris M, Zurakowski D, Thornhill TS. Total shoulder arthroplasty: long-term survivorship, functional outcome, and quality of life. J Shoulder Elbow Surg. 2005;14(5):471-479. doi:10.1016/j.jse.2005.02.009.
3. Montoya F, Magosch P, Scheiderer B, Lichtenberg S, Melean P, Habermeyer P. Midterm results of a total shoulder prosthesis fixed with a cementless glenoid component. J Shoulder Elbow Surg. 2013;22(5):628-635. doi:10.1016/j.jse.2012.07.005.
4. Torchia ME, Cofield RH, Settergren CR. Total shoulder arthroplasty with the Neer prosthesis: long-term results. J Shoulder Elbow Surg. 1997;6(6):495-505.
5. Antuna SA, Sperling JW, Cofield RH, Rowland CM. Glenoid revision surgery after total shoulder arthroplasty. J Shoulder Elbow Surg. 2001;10(3):217-224. doi:10.1067/mse.2001.113961.
6. Chalmers PN, Rahman Z, Romeo AA, Nicholson GP. Early dislocation after reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23(5):737-744. doi:10.1016/j.jse.2013.08.015.
7. Farng E, Zingmond D, Krenek L, Soohoo NF. Factors predicting complication rates after primary shoulder arthroplasty. J Shoulder Elbow Surg. 2011;20(4):557-563. doi:10.1016/j.jse.2010.11.005.
8. Farshad M, Grogli M, Catanzaro S, Gerber C. Revision of reversed total shoulder arthroplasty. Indications and outcome. BMC Musculoskelet Disord. 2012;13(1):160. doi:10.1186/1471-2474-13-160.
9. Fevang BT, Lie SA, Havelin LI, Skredderstuen A, Furnes O. Risk factors for revision after shoulder arthroplasty: 1,825 shoulder arthroplasties from the Norwegian Arthroplasty Register. Acta Orthop. 2009;80(1):83-91.
10. Fox TJ, Cil A, Sperling JW, Sanchez-Sotelo J, Schleck CD, Cofield RH. Survival of the glenoid component in shoulder arthroplasty. J Shoulder Elbow Surg. 2009;18(6):859-863. doi:10.1016/j.jse.2008.11.020.
11. Rasmussen JV. Outcome and risk of revision following shoulder replacement in patients with glenohumeral osteoarthritis. Acta Orthop Suppl. 2014;85(355 suppl):1-23. doi:10.3109/17453674.2014.922007.
12. Rasmussen JV, Polk A, Brorson S, Sorensen AK, Olsen BS. Patient-reported outcome and risk of revision after shoulder replacement for osteoarthritis. 1,209 cases from the Danish Shoulder Arthroplasty Registry, 2006-2010. Acta Orthop. 2014;85(2):117-122. doi:10.3109/17453674.2014.893497.
13. Sajadi KR, Kwon YW, Zuckerman JD. Revision shoulder arthroplasty: an analysis of indications and outcomes. J Shoulder Elbow Surg. 2010;19(2):308-313. doi:10.1016/j.jse.2009.05.016.
14. Singh JA, Sperling JW, Cofield RH. Revision surgery following total shoulder arthroplasty: analysis of 2588 shoulders over three decades (1976 to 2008). J Bone Joint Surg Br. 2011;93(11):1513-1517. doi:10.1302/0301-620X.93B11.26938.
15. Levine WN, Djurasovic M, Glasson JM, Pollock RG, Flatow EL, Bigliani LU. Hemiarthroplasty for glenohumeral osteoarthritis: results correlated to degree of glenoid wear. J Shoulder Elbow Surg. 1997;6(5):449-454.
16. Levine WN, Fischer CR, Nguyen D, Flatow EL, Ahmad CS, Bigliani LU. Long-term follow-up of shoulder hemiarthroplasty for glenohumeral osteoarthritis. J Bone Joint Surg Am. 2012;94(22):e164. doi:10.2106/JBJS.K.00603.
17. Lynch JR, Franta AK, Montgomery WH, Lenters TR, Mounce D, Matsen FA. Self-assessed outcome at two to four years after shoulder hemiarthroplasty with concentric glenoid reaming. J Bone Joint Surg Am. 2007;89(6):1284-1292. doi:10.2106/JBJS.E.00942.
18. Iannotti JP, Norris TR. Influence of preoperative factors on outcome of shoulder arthroplasty for glenohumeral osteoarthritis. J Bone Joint Surg Am. 2003;85-A(2):251-258.
19. Sperling JW, Cofield RH, Rowland CM. Neer hemiarthroplasty and Neer total shoulder arthroplasty in patients fifty years old or less. Long-term results. J Bone Joint Surg Am. 1998;80(4):464-473.
20. Strauss EJ, Roche C, Flurin PH, Wright T, Zuckerman JD. The glenoid in shoulder arthroplasty. J Shoulder Elbow Surg. 2009;18(5):819-833. doi:10.1016/j.jse.2009.05.008.
21. Cil A, Sperling JW, Cofield RH. Nonstandard glenoid components for bone deficiencies in shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23(7):e149-e157. doi:10.1016/j.jse.2013.09.023.
22. Denard PJ, Walch G. Current concepts in the surgical management of primary glenohumeral arthritis with a biconcave glenoid. J Shoulder Elbow Surg. 2013;22(11):1589-1598. doi:10.1016/j.jse.2013.06.017.
23. Gunther SB, Lynch TL. Total shoulder replacement surgery with custom glenoid implants for severe bone deficiency. J Shoulder Elbow Surg. 2012;21(5):675-684. doi:10.1016/j.jse.2011.03.023.
24. Neer CS, Morrison DS. Glenoid bone-grafting in total shoulder arthroplasty. J Bone Joint Surg Am. 1988;70(8):1154-1162.
25. Steinmann SP, Cofield RH. Bone grafting for glenoid deficiency in total shoulder replacement. J Shoulder Elbow Surg. 2000;9(5):361-367. doi:10.1067/mse.2000.106921.
26. Iannotti JP, Frangiamore SJ. Fate of large structural allograft for treatment of severe uncontained glenoid bone deficiency. J Shoulder Elbow Surg. 2012:21(6):765-771. doi:10.1016/j.jse.2011.08.069.
27. Hill JM, Norris TR. Long-term results of total shoulder arthroplasty following bone-grafting of the glenoid. J Bone Joint Surg Am. 2001;83-A(6):877-883.
28. Hsu JE, Ricchetti ET, Huffman GR, Iannotti JP, Glaser DL. Addressing glenoid bone deficiency and asymptomatic posterior erosion in shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22(9):1298-1308.
29. Chammaa R, Uri O, Lambert S. Primary shoulder arthroplasty using a custom-made hip-inspired implant for the treatment of advanced glenohumeral arthritis in the presence of severe glenoid bone loss. J Shoulder Elbow Surg. 2017;26(1):101-107. doi:10.1016/j.jse.2016.05.027.
30. Stoffelen DV, Eraly K, Debeer P. The use of 3D printing technology in reconstruction of a severe glenoid defect: a case report with 2.5 years of follow-up. J Shoulder Elbow Surg. 2015;24(8):e218-e222. doi:10.1016/j.jse.2015.04.006.
31. Gunther SB, Lynch TL. Total shoulder replacement surgery with custom glenoid implants for severe bone deficiency. J Shoulder Elbow Surg. 2012;21(5):675-684. doi:10.1016/j.jse.2011.03.023.
32. Dines DM, Gulotta L, Craig EV, Dines JS. Novel solution for massive glenoid defects in shoulder arthroplasty: a patient-specific glenoid vault reconstruction system. Am J Orthop. 2017;46(2):104-108.
ABSTRACT
Complex glenoid bone deformities present the treating surgeon with a complex reconstructive challenge. Although glenoid bone loss can be encountered in the primary setting (degenerative, congenital, post-traumatic), severe glenoid bone loss is encountered in most revision total shoulder arthroplasties. Severe glenoid bone loss is treated with various techniques including hemiarthroplasty, eccentric reaming, and glenoid reconstruction with bone autografts and allografts. Despite encouraging short- to mid-term results reported with these reconstruction techniques, the clinical and radiographic outcomes remain inconsistent and the high number of complications is a concern. To overcome this problem, more recently augmented components and patient specific implants were introduced. Using the computer-aided design and computer-aided manufacturing technology patient-specific implants have been created to reconstruct the glenoid vault in cases of severe glenoid bone loss.
In this article we describe a patient specific glenoid implant, its indication, technical aspects and surgical technique, based on the author's experience as well as a review of the current literature on custom glenoid implants.
Continue to: Total shoulder arthroplasty...
Total shoulder arthroplasty (TSA) is an effective operation for providing pain relief and improving function in patients with end-stage degenerative shoulder disease that is nonresponsive to nonoperative treatments.1-4 With the increasing number of arthroplasties performed, and the expanding indication for shoulder arthroplasty, the number of revision shoulder arthroplasties is also increasing.5-14 Complex glenoid bone deformities present the treating surgeon with a complex reconstructive challenge. Although glenoid bone loss can be seen in the primary setting (degenerative, congenital, and post-traumatic), severe glenoid bone loss is encountered mostly in revision TSAs.
Historically, patients with severe glenoid bone loss were treated with a hemiarthroplasty.15-17 However, due to inferior outcomes associated with the use of shoulder hemiarthroplasties compared with TSA in these cases,18-20 various techniques were developed with the aim of realigning the glenoid axis and securing the implants into the deficient glenoid vault.21-25 Options have included eccentric reaming, glenoid reconstruction with bone autografts and allografts, and more recently augmented components and patient-specific implants. Studies with eccentric reaming and reconstruction with bone graft during complex shoulder arthroplasty have reported encouraging short- to mid-term results, but the clinical and radiographic outcomes remain inconsistent, and the high number of complications is a concern.25-28
Complications with these techniques include component loosening, graft resorption, nonunion, failure of graft incorporation, infection, and instability.25-28
Computer-aided design and computer-aided manufacturing (CAD/CAM) of patient-specific implants have been used successfully by hip arthroplasty surgeons to deal with complex acetabular reconstructions in the setting of severe bone loss. More recently, the same technology has been used to reconstruct the glenoid vault in cases of severe glenoid bone loss.
In this article, we describe a patient-specific glenoid implant, its indication, and both technical aspects and the surgical technique, based on the authors’ experience as well as a review of the current literature on custom glenoid implants.
Continue to: PATIENT-SPECIFIC GLENOID COMPONENT
PATIENT-SPECIFIC GLENOID COMPONENT
The Vault Reconstruction System ([VRS], Zimmer Biomet) is a patient-specific glenoid vault reconstruction system developed with the use of CAD/CAM to address severe glenoid bone loss encountered during shoulder arthroplasty. For several years, the VRS was available only as a custom implant according to the US Food and Drug Administration rules, and therefore its use was limited to a few cases per year. Recently, a 510(k) envelope clearance was granted to use the VRS in reverse TSA to address significant glenoid bone defects.
The VRS is made of porous plasma spray titanium to provide high strength and flexibility, and allows for biologic fixation. This system can accommodate a restricted bone loss envelope of about 50 mm × 50 mm × 35 mm according to the previous experience of the manufacturer in the custom scenario, covering 96% of defects previously addressed. One 6.5-mm nonlocking central screw and a minimum of four 4.75-mm nonlocking or locking peripheral screws are required for optimal fixation of the implant in the native scapula. A custom boss can be added in to enhance fixation in the native scapula when the bone is sufficient. To facilitate the surgical procedure, a trial implant, a bone model of the scapula, and a custom boss reaming guide are 3-dimensional (3-D) and printed in sterilizable material. These are all provided as single-use disposable instruments and can be available for surgeons during both the initial plan review and surgery.
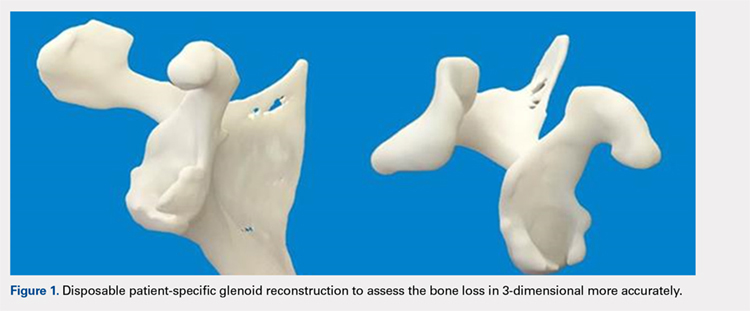
PREOPERATIVE PLANNING
Patients undergo a preoperative fine-cut 2-dimensional computed tomography scan of the scapula and adjacent humerus following a predefined protocol with a slice thickness of 2 mm to 3 mm. An accurate 3-D bone model of the scapula is obtained using a 3-D image processing software system (Figure 1). The 3-D scapular model is used to create a patient-specific glenoid implant proposal that is approved by the surgeon (Figure 2). Implant position, orientation, size, screw trajectory, and recommended bone removal, if necessary, are determined to create a more normal glenohumeral center of rotation and to secure a glenoid implant in severely deficient glenoid bone (Figure 3). Once the implant design is approved by the surgeon, the final patient-specific implant is manufactured.
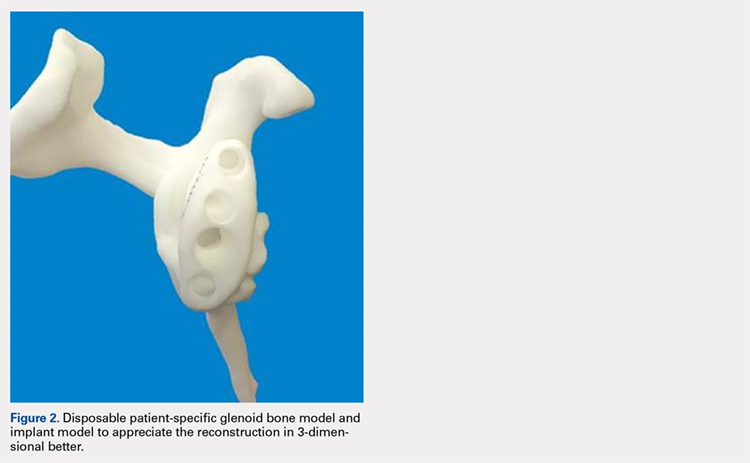
SURGICAL TECHNIQUE
The exposure of the glenoid is a critical step for the successful implantation of the patient-specific glenoid implant. Soft tissue and scar tissue around the glenoid must be removed to allow for optimal fit of the custom-made reaming guide. Also, removal of the entire capsulolabral complex on the anteroinferior rim of the glenoid is essential to both enhance glenoid exposure and to allow a perfect fit of the guide to the pathologic bone stock. Attention should be paid during débridement and/or implant removal in case of revision, to make sure that no excessive bone is removed because the patient-specific guide is referenced to this anatomy. Excessive bone removal can change the orientation of the patient-specific guide and ultimately the fixation of the implant. Once the custom-made patient-specific guide is positioned, a 3.2-mm Steinmann pin is placed through the inserter for temporary fixation. The pin should engage or perforate the medial cortical wall to ensure that the subsequent reamer has a stable cannula over which to ream. After the glenoid is reamed, the final implant can be placed in the ideal position according to the preoperative planning. A central 6.5-mm nonlocking central screw and 4.75-mm nonlocking or locking peripheral screws are required to complete the fixation of the implant in the native scapula. Once the patient-specific glenoid component is positioned and strongly fixed to the bone, the glenosphere can be positioned according to the preoperative planning, and the reverse shoulder arthroplasty can be completed in the usual fashion.
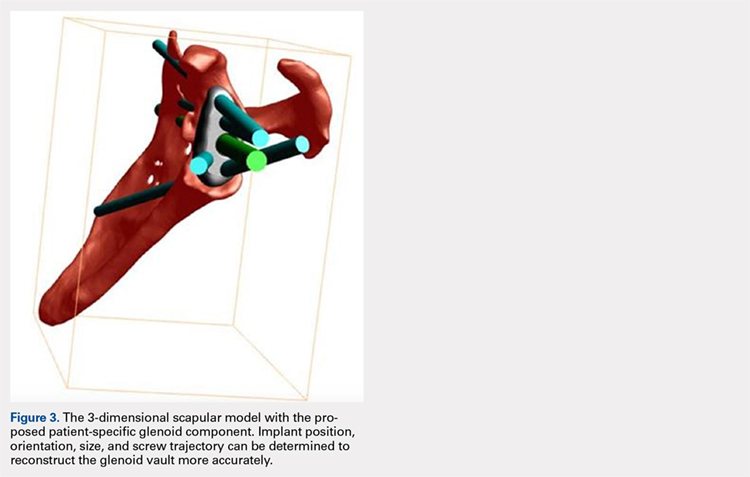
CASE EXAMPLES
A 68-year-old woman underwent a TSA for end-stage osteoarthritis in 2000. The implant failed due to a cuff failure. The patient underwent several surgeries, including an open cuff repair, with no success. She had no active elevation preoperatively. Because of the significant glenoid bone loss, a patient-specific glenoid reconstruction was planned. Within 24 months after this surgery, the patient was able to get her hand to her head and elevate to 90º (Figures 4A-4F).

Continue to: In October 2013...
In October 2013, a 68-year-old man underwent a TSA for end-stage osteoarthritis. After 18 months, the implant failed due to active Propionibacterium acnes infection, which required excisional arthroplasty with insertion of an antibiotic spacer. Significant glenoid bone loss (Figure 5) and global soft-tissue deficiency caused substantial disability and led to an indication for a reverse TSA with a patient-specific glenoid vault reconstruction (Figures 6A-6D) after infection eradication. Within 20 months after this surgery, the patient had resumed a satisfactory range of motion (130º forward elevation, 20º external rotation) and outcome.
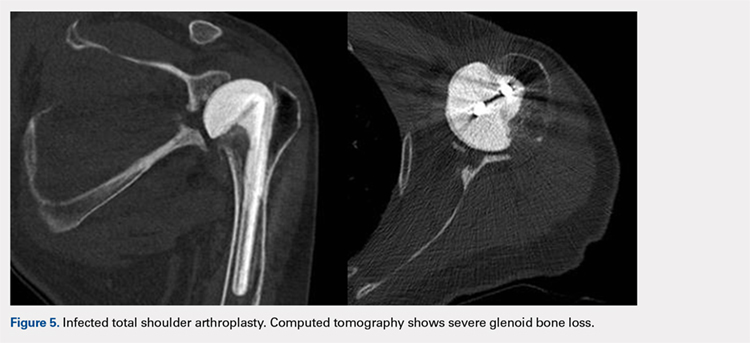
DISCUSSION
Although glenoid bone loss is often seen in the primary setting (degenerative, congenital, and post-traumatic), severe glenoid bone loss is encountered in most revision TSAs. The best treatment method for massive glenoid bone defects during complex shoulder arthroplasty remains uncertain. Options have included eccentric reaming, glenoid reconstruction with bone allograft and autograft, and more recently augmented components and patient-specific implants.21-25 The advent and availability of CAD/CAM technology have enabled shoulder surgeons to create patient-specific metal solutions to these challenging cases. Currently, only a few reports exist in the literature on patient-specific glenoid components in the setting of severe bone loss.29-32
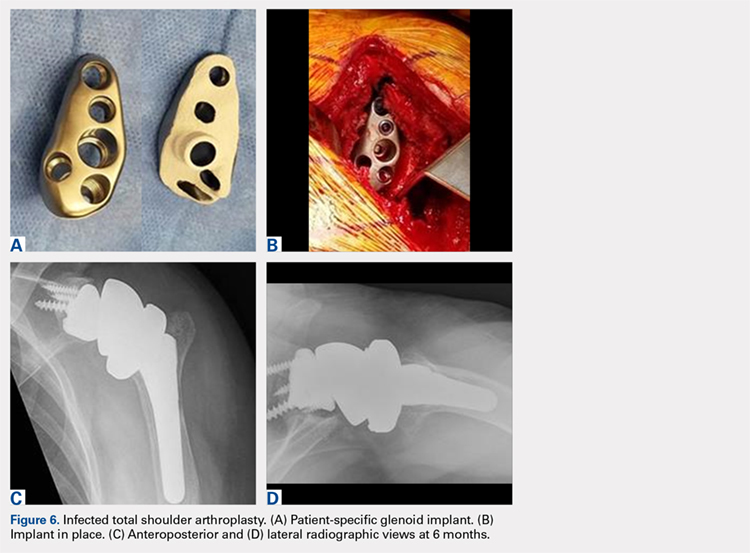
Chammaa and colleagues29 reported the outcomes of 37 patients with a hip-inspired glenoid component (Total Shoulder Replacement, Stanmore Implants Worldwide). The 5-year results with this implant were promising, with a 16% revision rate and only 1 case of glenoid loosening.
Stoffelen and colleagues30 recently described the successful use of a patient-specific anatomic metal-backed glenoid component for the management of severe glenoid bone loss with excellent results at 2.5 years of follow-up. A different approach was pursued by Gunther and Lynch,31 who reported on 7 patients with a custom inset glenoid implant for deficient glenoid vaults. These circular anatomic, custom-made glenoid components were created with the intention of placing the implants partially inside the glenoid vault and relying partially on sclerotic cortical bone. Despite excellent results at 3 years of follow-up, their use is limited to specific defect geometries and cannot be used in cases of extreme bone loss.
CONCLUSION
We have described the use of a patient-specific glenoid component in 2 patients with severe glenoid bone loss. Despite the satisfactory clinical and short-term radiographic results, we acknowledge that longer-term follow-up is needed to confirm the efficacy of this type of reconstruction. We believe that patient-specific glenoid components represent a valuable addition to the armamentarium of shoulder surgeons who address complex glenoid bone deformities.
ABSTRACT
Complex glenoid bone deformities present the treating surgeon with a complex reconstructive challenge. Although glenoid bone loss can be encountered in the primary setting (degenerative, congenital, post-traumatic), severe glenoid bone loss is encountered in most revision total shoulder arthroplasties. Severe glenoid bone loss is treated with various techniques including hemiarthroplasty, eccentric reaming, and glenoid reconstruction with bone autografts and allografts. Despite encouraging short- to mid-term results reported with these reconstruction techniques, the clinical and radiographic outcomes remain inconsistent and the high number of complications is a concern. To overcome this problem, more recently augmented components and patient specific implants were introduced. Using the computer-aided design and computer-aided manufacturing technology patient-specific implants have been created to reconstruct the glenoid vault in cases of severe glenoid bone loss.
In this article we describe a patient specific glenoid implant, its indication, technical aspects and surgical technique, based on the author's experience as well as a review of the current literature on custom glenoid implants.
Continue to: Total shoulder arthroplasty...
Total shoulder arthroplasty (TSA) is an effective operation for providing pain relief and improving function in patients with end-stage degenerative shoulder disease that is nonresponsive to nonoperative treatments.1-4 With the increasing number of arthroplasties performed, and the expanding indication for shoulder arthroplasty, the number of revision shoulder arthroplasties is also increasing.5-14 Complex glenoid bone deformities present the treating surgeon with a complex reconstructive challenge. Although glenoid bone loss can be seen in the primary setting (degenerative, congenital, and post-traumatic), severe glenoid bone loss is encountered mostly in revision TSAs.
Historically, patients with severe glenoid bone loss were treated with a hemiarthroplasty.15-17 However, due to inferior outcomes associated with the use of shoulder hemiarthroplasties compared with TSA in these cases,18-20 various techniques were developed with the aim of realigning the glenoid axis and securing the implants into the deficient glenoid vault.21-25 Options have included eccentric reaming, glenoid reconstruction with bone autografts and allografts, and more recently augmented components and patient-specific implants. Studies with eccentric reaming and reconstruction with bone graft during complex shoulder arthroplasty have reported encouraging short- to mid-term results, but the clinical and radiographic outcomes remain inconsistent, and the high number of complications is a concern.25-28
Complications with these techniques include component loosening, graft resorption, nonunion, failure of graft incorporation, infection, and instability.25-28
Computer-aided design and computer-aided manufacturing (CAD/CAM) of patient-specific implants have been used successfully by hip arthroplasty surgeons to deal with complex acetabular reconstructions in the setting of severe bone loss. More recently, the same technology has been used to reconstruct the glenoid vault in cases of severe glenoid bone loss.
In this article, we describe a patient-specific glenoid implant, its indication, and both technical aspects and the surgical technique, based on the authors’ experience as well as a review of the current literature on custom glenoid implants.
Continue to: PATIENT-SPECIFIC GLENOID COMPONENT
PATIENT-SPECIFIC GLENOID COMPONENT
The Vault Reconstruction System ([VRS], Zimmer Biomet) is a patient-specific glenoid vault reconstruction system developed with the use of CAD/CAM to address severe glenoid bone loss encountered during shoulder arthroplasty. For several years, the VRS was available only as a custom implant according to the US Food and Drug Administration rules, and therefore its use was limited to a few cases per year. Recently, a 510(k) envelope clearance was granted to use the VRS in reverse TSA to address significant glenoid bone defects.
The VRS is made of porous plasma spray titanium to provide high strength and flexibility, and allows for biologic fixation. This system can accommodate a restricted bone loss envelope of about 50 mm × 50 mm × 35 mm according to the previous experience of the manufacturer in the custom scenario, covering 96% of defects previously addressed. One 6.5-mm nonlocking central screw and a minimum of four 4.75-mm nonlocking or locking peripheral screws are required for optimal fixation of the implant in the native scapula. A custom boss can be added in to enhance fixation in the native scapula when the bone is sufficient. To facilitate the surgical procedure, a trial implant, a bone model of the scapula, and a custom boss reaming guide are 3-dimensional (3-D) and printed in sterilizable material. These are all provided as single-use disposable instruments and can be available for surgeons during both the initial plan review and surgery.
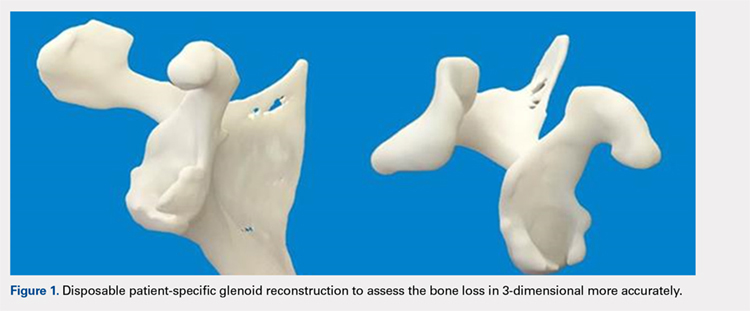
PREOPERATIVE PLANNING
Patients undergo a preoperative fine-cut 2-dimensional computed tomography scan of the scapula and adjacent humerus following a predefined protocol with a slice thickness of 2 mm to 3 mm. An accurate 3-D bone model of the scapula is obtained using a 3-D image processing software system (Figure 1). The 3-D scapular model is used to create a patient-specific glenoid implant proposal that is approved by the surgeon (Figure 2). Implant position, orientation, size, screw trajectory, and recommended bone removal, if necessary, are determined to create a more normal glenohumeral center of rotation and to secure a glenoid implant in severely deficient glenoid bone (Figure 3). Once the implant design is approved by the surgeon, the final patient-specific implant is manufactured.
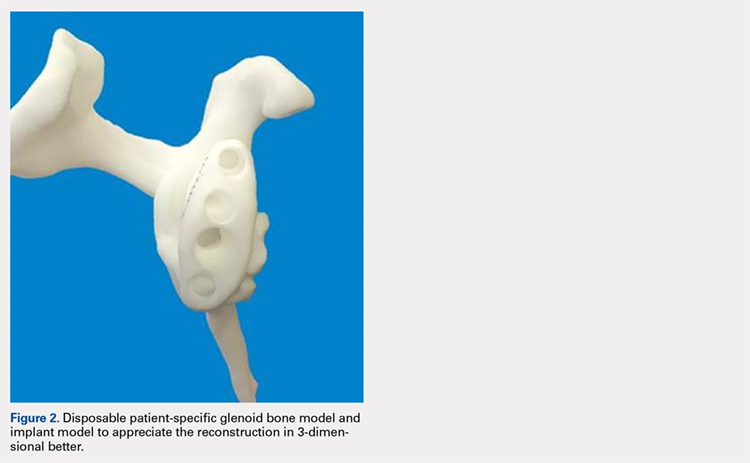
SURGICAL TECHNIQUE
The exposure of the glenoid is a critical step for the successful implantation of the patient-specific glenoid implant. Soft tissue and scar tissue around the glenoid must be removed to allow for optimal fit of the custom-made reaming guide. Also, removal of the entire capsulolabral complex on the anteroinferior rim of the glenoid is essential to both enhance glenoid exposure and to allow a perfect fit of the guide to the pathologic bone stock. Attention should be paid during débridement and/or implant removal in case of revision, to make sure that no excessive bone is removed because the patient-specific guide is referenced to this anatomy. Excessive bone removal can change the orientation of the patient-specific guide and ultimately the fixation of the implant. Once the custom-made patient-specific guide is positioned, a 3.2-mm Steinmann pin is placed through the inserter for temporary fixation. The pin should engage or perforate the medial cortical wall to ensure that the subsequent reamer has a stable cannula over which to ream. After the glenoid is reamed, the final implant can be placed in the ideal position according to the preoperative planning. A central 6.5-mm nonlocking central screw and 4.75-mm nonlocking or locking peripheral screws are required to complete the fixation of the implant in the native scapula. Once the patient-specific glenoid component is positioned and strongly fixed to the bone, the glenosphere can be positioned according to the preoperative planning, and the reverse shoulder arthroplasty can be completed in the usual fashion.
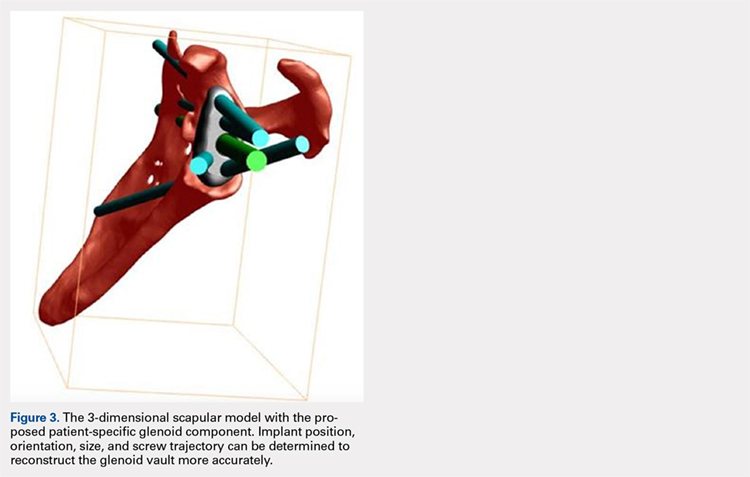
CASE EXAMPLES
A 68-year-old woman underwent a TSA for end-stage osteoarthritis in 2000. The implant failed due to a cuff failure. The patient underwent several surgeries, including an open cuff repair, with no success. She had no active elevation preoperatively. Because of the significant glenoid bone loss, a patient-specific glenoid reconstruction was planned. Within 24 months after this surgery, the patient was able to get her hand to her head and elevate to 90º (Figures 4A-4F).

Continue to: In October 2013...
In October 2013, a 68-year-old man underwent a TSA for end-stage osteoarthritis. After 18 months, the implant failed due to active Propionibacterium acnes infection, which required excisional arthroplasty with insertion of an antibiotic spacer. Significant glenoid bone loss (Figure 5) and global soft-tissue deficiency caused substantial disability and led to an indication for a reverse TSA with a patient-specific glenoid vault reconstruction (Figures 6A-6D) after infection eradication. Within 20 months after this surgery, the patient had resumed a satisfactory range of motion (130º forward elevation, 20º external rotation) and outcome.
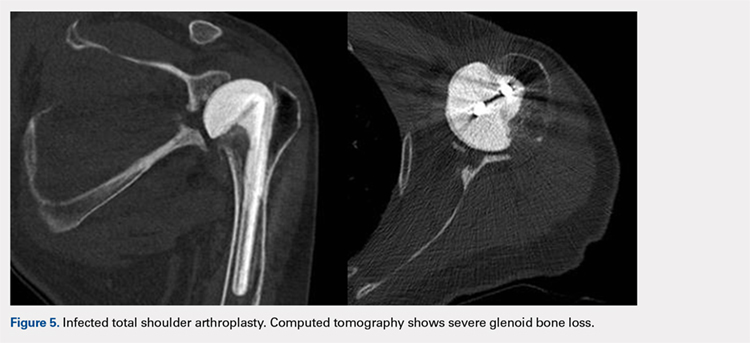
DISCUSSION
Although glenoid bone loss is often seen in the primary setting (degenerative, congenital, and post-traumatic), severe glenoid bone loss is encountered in most revision TSAs. The best treatment method for massive glenoid bone defects during complex shoulder arthroplasty remains uncertain. Options have included eccentric reaming, glenoid reconstruction with bone allograft and autograft, and more recently augmented components and patient-specific implants.21-25 The advent and availability of CAD/CAM technology have enabled shoulder surgeons to create patient-specific metal solutions to these challenging cases. Currently, only a few reports exist in the literature on patient-specific glenoid components in the setting of severe bone loss.29-32
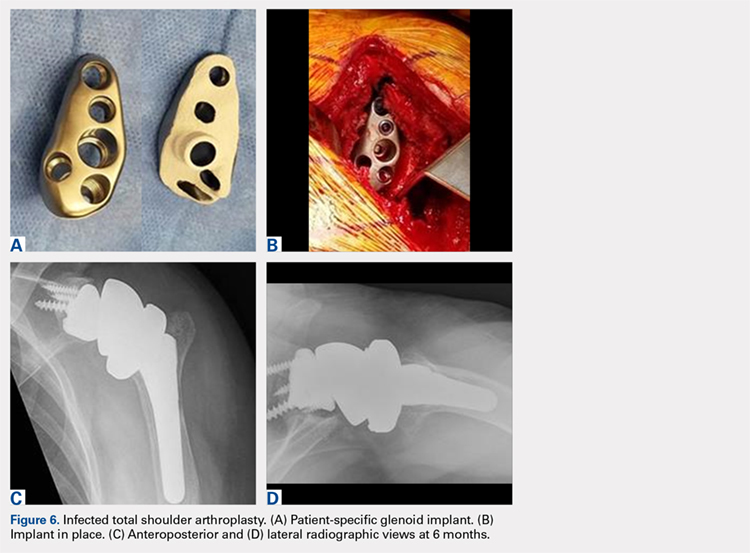
Chammaa and colleagues29 reported the outcomes of 37 patients with a hip-inspired glenoid component (Total Shoulder Replacement, Stanmore Implants Worldwide). The 5-year results with this implant were promising, with a 16% revision rate and only 1 case of glenoid loosening.
Stoffelen and colleagues30 recently described the successful use of a patient-specific anatomic metal-backed glenoid component for the management of severe glenoid bone loss with excellent results at 2.5 years of follow-up. A different approach was pursued by Gunther and Lynch,31 who reported on 7 patients with a custom inset glenoid implant for deficient glenoid vaults. These circular anatomic, custom-made glenoid components were created with the intention of placing the implants partially inside the glenoid vault and relying partially on sclerotic cortical bone. Despite excellent results at 3 years of follow-up, their use is limited to specific defect geometries and cannot be used in cases of extreme bone loss.
CONCLUSION
We have described the use of a patient-specific glenoid component in 2 patients with severe glenoid bone loss. Despite the satisfactory clinical and short-term radiographic results, we acknowledge that longer-term follow-up is needed to confirm the efficacy of this type of reconstruction. We believe that patient-specific glenoid components represent a valuable addition to the armamentarium of shoulder surgeons who address complex glenoid bone deformities.
1. Chalmers PN, Gupta AK, Rahman Z, Bruce B, Romeo AA, Nicholson GP. Predictors of early complications of total shoulder arthroplasty. J Arthroplasty. 2014;29(4):856-860. doi:10.1016/j.arth.2013.07.002.
2. Deshmukh AV, Koris M, Zurakowski D, Thornhill TS. Total shoulder arthroplasty: long-term survivorship, functional outcome, and quality of life. J Shoulder Elbow Surg. 2005;14(5):471-479. doi:10.1016/j.jse.2005.02.009.
3. Montoya F, Magosch P, Scheiderer B, Lichtenberg S, Melean P, Habermeyer P. Midterm results of a total shoulder prosthesis fixed with a cementless glenoid component. J Shoulder Elbow Surg. 2013;22(5):628-635. doi:10.1016/j.jse.2012.07.005.
4. Torchia ME, Cofield RH, Settergren CR. Total shoulder arthroplasty with the Neer prosthesis: long-term results. J Shoulder Elbow Surg. 1997;6(6):495-505.
5. Antuna SA, Sperling JW, Cofield RH, Rowland CM. Glenoid revision surgery after total shoulder arthroplasty. J Shoulder Elbow Surg. 2001;10(3):217-224. doi:10.1067/mse.2001.113961.
6. Chalmers PN, Rahman Z, Romeo AA, Nicholson GP. Early dislocation after reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23(5):737-744. doi:10.1016/j.jse.2013.08.015.
7. Farng E, Zingmond D, Krenek L, Soohoo NF. Factors predicting complication rates after primary shoulder arthroplasty. J Shoulder Elbow Surg. 2011;20(4):557-563. doi:10.1016/j.jse.2010.11.005.
8. Farshad M, Grogli M, Catanzaro S, Gerber C. Revision of reversed total shoulder arthroplasty. Indications and outcome. BMC Musculoskelet Disord. 2012;13(1):160. doi:10.1186/1471-2474-13-160.
9. Fevang BT, Lie SA, Havelin LI, Skredderstuen A, Furnes O. Risk factors for revision after shoulder arthroplasty: 1,825 shoulder arthroplasties from the Norwegian Arthroplasty Register. Acta Orthop. 2009;80(1):83-91.
10. Fox TJ, Cil A, Sperling JW, Sanchez-Sotelo J, Schleck CD, Cofield RH. Survival of the glenoid component in shoulder arthroplasty. J Shoulder Elbow Surg. 2009;18(6):859-863. doi:10.1016/j.jse.2008.11.020.
11. Rasmussen JV. Outcome and risk of revision following shoulder replacement in patients with glenohumeral osteoarthritis. Acta Orthop Suppl. 2014;85(355 suppl):1-23. doi:10.3109/17453674.2014.922007.
12. Rasmussen JV, Polk A, Brorson S, Sorensen AK, Olsen BS. Patient-reported outcome and risk of revision after shoulder replacement for osteoarthritis. 1,209 cases from the Danish Shoulder Arthroplasty Registry, 2006-2010. Acta Orthop. 2014;85(2):117-122. doi:10.3109/17453674.2014.893497.
13. Sajadi KR, Kwon YW, Zuckerman JD. Revision shoulder arthroplasty: an analysis of indications and outcomes. J Shoulder Elbow Surg. 2010;19(2):308-313. doi:10.1016/j.jse.2009.05.016.
14. Singh JA, Sperling JW, Cofield RH. Revision surgery following total shoulder arthroplasty: analysis of 2588 shoulders over three decades (1976 to 2008). J Bone Joint Surg Br. 2011;93(11):1513-1517. doi:10.1302/0301-620X.93B11.26938.
15. Levine WN, Djurasovic M, Glasson JM, Pollock RG, Flatow EL, Bigliani LU. Hemiarthroplasty for glenohumeral osteoarthritis: results correlated to degree of glenoid wear. J Shoulder Elbow Surg. 1997;6(5):449-454.
16. Levine WN, Fischer CR, Nguyen D, Flatow EL, Ahmad CS, Bigliani LU. Long-term follow-up of shoulder hemiarthroplasty for glenohumeral osteoarthritis. J Bone Joint Surg Am. 2012;94(22):e164. doi:10.2106/JBJS.K.00603.
17. Lynch JR, Franta AK, Montgomery WH, Lenters TR, Mounce D, Matsen FA. Self-assessed outcome at two to four years after shoulder hemiarthroplasty with concentric glenoid reaming. J Bone Joint Surg Am. 2007;89(6):1284-1292. doi:10.2106/JBJS.E.00942.
18. Iannotti JP, Norris TR. Influence of preoperative factors on outcome of shoulder arthroplasty for glenohumeral osteoarthritis. J Bone Joint Surg Am. 2003;85-A(2):251-258.
19. Sperling JW, Cofield RH, Rowland CM. Neer hemiarthroplasty and Neer total shoulder arthroplasty in patients fifty years old or less. Long-term results. J Bone Joint Surg Am. 1998;80(4):464-473.
20. Strauss EJ, Roche C, Flurin PH, Wright T, Zuckerman JD. The glenoid in shoulder arthroplasty. J Shoulder Elbow Surg. 2009;18(5):819-833. doi:10.1016/j.jse.2009.05.008.
21. Cil A, Sperling JW, Cofield RH. Nonstandard glenoid components for bone deficiencies in shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23(7):e149-e157. doi:10.1016/j.jse.2013.09.023.
22. Denard PJ, Walch G. Current concepts in the surgical management of primary glenohumeral arthritis with a biconcave glenoid. J Shoulder Elbow Surg. 2013;22(11):1589-1598. doi:10.1016/j.jse.2013.06.017.
23. Gunther SB, Lynch TL. Total shoulder replacement surgery with custom glenoid implants for severe bone deficiency. J Shoulder Elbow Surg. 2012;21(5):675-684. doi:10.1016/j.jse.2011.03.023.
24. Neer CS, Morrison DS. Glenoid bone-grafting in total shoulder arthroplasty. J Bone Joint Surg Am. 1988;70(8):1154-1162.
25. Steinmann SP, Cofield RH. Bone grafting for glenoid deficiency in total shoulder replacement. J Shoulder Elbow Surg. 2000;9(5):361-367. doi:10.1067/mse.2000.106921.
26. Iannotti JP, Frangiamore SJ. Fate of large structural allograft for treatment of severe uncontained glenoid bone deficiency. J Shoulder Elbow Surg. 2012:21(6):765-771. doi:10.1016/j.jse.2011.08.069.
27. Hill JM, Norris TR. Long-term results of total shoulder arthroplasty following bone-grafting of the glenoid. J Bone Joint Surg Am. 2001;83-A(6):877-883.
28. Hsu JE, Ricchetti ET, Huffman GR, Iannotti JP, Glaser DL. Addressing glenoid bone deficiency and asymptomatic posterior erosion in shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22(9):1298-1308.
29. Chammaa R, Uri O, Lambert S. Primary shoulder arthroplasty using a custom-made hip-inspired implant for the treatment of advanced glenohumeral arthritis in the presence of severe glenoid bone loss. J Shoulder Elbow Surg. 2017;26(1):101-107. doi:10.1016/j.jse.2016.05.027.
30. Stoffelen DV, Eraly K, Debeer P. The use of 3D printing technology in reconstruction of a severe glenoid defect: a case report with 2.5 years of follow-up. J Shoulder Elbow Surg. 2015;24(8):e218-e222. doi:10.1016/j.jse.2015.04.006.
31. Gunther SB, Lynch TL. Total shoulder replacement surgery with custom glenoid implants for severe bone deficiency. J Shoulder Elbow Surg. 2012;21(5):675-684. doi:10.1016/j.jse.2011.03.023.
32. Dines DM, Gulotta L, Craig EV, Dines JS. Novel solution for massive glenoid defects in shoulder arthroplasty: a patient-specific glenoid vault reconstruction system. Am J Orthop. 2017;46(2):104-108.
1. Chalmers PN, Gupta AK, Rahman Z, Bruce B, Romeo AA, Nicholson GP. Predictors of early complications of total shoulder arthroplasty. J Arthroplasty. 2014;29(4):856-860. doi:10.1016/j.arth.2013.07.002.
2. Deshmukh AV, Koris M, Zurakowski D, Thornhill TS. Total shoulder arthroplasty: long-term survivorship, functional outcome, and quality of life. J Shoulder Elbow Surg. 2005;14(5):471-479. doi:10.1016/j.jse.2005.02.009.
3. Montoya F, Magosch P, Scheiderer B, Lichtenberg S, Melean P, Habermeyer P. Midterm results of a total shoulder prosthesis fixed with a cementless glenoid component. J Shoulder Elbow Surg. 2013;22(5):628-635. doi:10.1016/j.jse.2012.07.005.
4. Torchia ME, Cofield RH, Settergren CR. Total shoulder arthroplasty with the Neer prosthesis: long-term results. J Shoulder Elbow Surg. 1997;6(6):495-505.
5. Antuna SA, Sperling JW, Cofield RH, Rowland CM. Glenoid revision surgery after total shoulder arthroplasty. J Shoulder Elbow Surg. 2001;10(3):217-224. doi:10.1067/mse.2001.113961.
6. Chalmers PN, Rahman Z, Romeo AA, Nicholson GP. Early dislocation after reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23(5):737-744. doi:10.1016/j.jse.2013.08.015.
7. Farng E, Zingmond D, Krenek L, Soohoo NF. Factors predicting complication rates after primary shoulder arthroplasty. J Shoulder Elbow Surg. 2011;20(4):557-563. doi:10.1016/j.jse.2010.11.005.
8. Farshad M, Grogli M, Catanzaro S, Gerber C. Revision of reversed total shoulder arthroplasty. Indications and outcome. BMC Musculoskelet Disord. 2012;13(1):160. doi:10.1186/1471-2474-13-160.
9. Fevang BT, Lie SA, Havelin LI, Skredderstuen A, Furnes O. Risk factors for revision after shoulder arthroplasty: 1,825 shoulder arthroplasties from the Norwegian Arthroplasty Register. Acta Orthop. 2009;80(1):83-91.
10. Fox TJ, Cil A, Sperling JW, Sanchez-Sotelo J, Schleck CD, Cofield RH. Survival of the glenoid component in shoulder arthroplasty. J Shoulder Elbow Surg. 2009;18(6):859-863. doi:10.1016/j.jse.2008.11.020.
11. Rasmussen JV. Outcome and risk of revision following shoulder replacement in patients with glenohumeral osteoarthritis. Acta Orthop Suppl. 2014;85(355 suppl):1-23. doi:10.3109/17453674.2014.922007.
12. Rasmussen JV, Polk A, Brorson S, Sorensen AK, Olsen BS. Patient-reported outcome and risk of revision after shoulder replacement for osteoarthritis. 1,209 cases from the Danish Shoulder Arthroplasty Registry, 2006-2010. Acta Orthop. 2014;85(2):117-122. doi:10.3109/17453674.2014.893497.
13. Sajadi KR, Kwon YW, Zuckerman JD. Revision shoulder arthroplasty: an analysis of indications and outcomes. J Shoulder Elbow Surg. 2010;19(2):308-313. doi:10.1016/j.jse.2009.05.016.
14. Singh JA, Sperling JW, Cofield RH. Revision surgery following total shoulder arthroplasty: analysis of 2588 shoulders over three decades (1976 to 2008). J Bone Joint Surg Br. 2011;93(11):1513-1517. doi:10.1302/0301-620X.93B11.26938.
15. Levine WN, Djurasovic M, Glasson JM, Pollock RG, Flatow EL, Bigliani LU. Hemiarthroplasty for glenohumeral osteoarthritis: results correlated to degree of glenoid wear. J Shoulder Elbow Surg. 1997;6(5):449-454.
16. Levine WN, Fischer CR, Nguyen D, Flatow EL, Ahmad CS, Bigliani LU. Long-term follow-up of shoulder hemiarthroplasty for glenohumeral osteoarthritis. J Bone Joint Surg Am. 2012;94(22):e164. doi:10.2106/JBJS.K.00603.
17. Lynch JR, Franta AK, Montgomery WH, Lenters TR, Mounce D, Matsen FA. Self-assessed outcome at two to four years after shoulder hemiarthroplasty with concentric glenoid reaming. J Bone Joint Surg Am. 2007;89(6):1284-1292. doi:10.2106/JBJS.E.00942.
18. Iannotti JP, Norris TR. Influence of preoperative factors on outcome of shoulder arthroplasty for glenohumeral osteoarthritis. J Bone Joint Surg Am. 2003;85-A(2):251-258.
19. Sperling JW, Cofield RH, Rowland CM. Neer hemiarthroplasty and Neer total shoulder arthroplasty in patients fifty years old or less. Long-term results. J Bone Joint Surg Am. 1998;80(4):464-473.
20. Strauss EJ, Roche C, Flurin PH, Wright T, Zuckerman JD. The glenoid in shoulder arthroplasty. J Shoulder Elbow Surg. 2009;18(5):819-833. doi:10.1016/j.jse.2009.05.008.
21. Cil A, Sperling JW, Cofield RH. Nonstandard glenoid components for bone deficiencies in shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23(7):e149-e157. doi:10.1016/j.jse.2013.09.023.
22. Denard PJ, Walch G. Current concepts in the surgical management of primary glenohumeral arthritis with a biconcave glenoid. J Shoulder Elbow Surg. 2013;22(11):1589-1598. doi:10.1016/j.jse.2013.06.017.
23. Gunther SB, Lynch TL. Total shoulder replacement surgery with custom glenoid implants for severe bone deficiency. J Shoulder Elbow Surg. 2012;21(5):675-684. doi:10.1016/j.jse.2011.03.023.
24. Neer CS, Morrison DS. Glenoid bone-grafting in total shoulder arthroplasty. J Bone Joint Surg Am. 1988;70(8):1154-1162.
25. Steinmann SP, Cofield RH. Bone grafting for glenoid deficiency in total shoulder replacement. J Shoulder Elbow Surg. 2000;9(5):361-367. doi:10.1067/mse.2000.106921.
26. Iannotti JP, Frangiamore SJ. Fate of large structural allograft for treatment of severe uncontained glenoid bone deficiency. J Shoulder Elbow Surg. 2012:21(6):765-771. doi:10.1016/j.jse.2011.08.069.
27. Hill JM, Norris TR. Long-term results of total shoulder arthroplasty following bone-grafting of the glenoid. J Bone Joint Surg Am. 2001;83-A(6):877-883.
28. Hsu JE, Ricchetti ET, Huffman GR, Iannotti JP, Glaser DL. Addressing glenoid bone deficiency and asymptomatic posterior erosion in shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22(9):1298-1308.
29. Chammaa R, Uri O, Lambert S. Primary shoulder arthroplasty using a custom-made hip-inspired implant for the treatment of advanced glenohumeral arthritis in the presence of severe glenoid bone loss. J Shoulder Elbow Surg. 2017;26(1):101-107. doi:10.1016/j.jse.2016.05.027.
30. Stoffelen DV, Eraly K, Debeer P. The use of 3D printing technology in reconstruction of a severe glenoid defect: a case report with 2.5 years of follow-up. J Shoulder Elbow Surg. 2015;24(8):e218-e222. doi:10.1016/j.jse.2015.04.006.
31. Gunther SB, Lynch TL. Total shoulder replacement surgery with custom glenoid implants for severe bone deficiency. J Shoulder Elbow Surg. 2012;21(5):675-684. doi:10.1016/j.jse.2011.03.023.
32. Dines DM, Gulotta L, Craig EV, Dines JS. Novel solution for massive glenoid defects in shoulder arthroplasty: a patient-specific glenoid vault reconstruction system. Am J Orthop. 2017;46(2):104-108.
TAKE-HOME POINTS
- With the increasing number of arthroplasties performed, and the expanding indication for shoulder arthroplasty, the number of revision shoulder arthroplasties is also increasing.
- Complex glenoid bone defects are sometimes encountered in revision shoulder arthroplasties.
- Glenoid reconstructions with bone graft have reported encouraging short- to mid-term results, but the high number of complications is a concern.
- Using the CAD/CAM technology patient-specific glenoid components have been created to reconstruct the glenoid vault in cases of severe glenoid bone loss.
- Short-term clinical and radiographic results of patient-specific glenoid components are encouraging, however longer-term follow-up are needed to confirm the efficacy of this type of reconstruction.
Bipartisan Senate budget deal boosts health programs
In a rare show of bipartisanship for the mostly polarized 115th Congress, Republican and Democratic Senate leaders announced a 2-year budget deal that would increase federal spending for defense as well as key domestic priorities, including many health programs.
Not in the deal, for which the path to the president’s desk remains unclear, is any bipartisan legislation aimed at shoring up the Affordable Care Act’s individual health insurance marketplaces. Senate Majority Leader Mitch McConnell (R-Ky.) promised Sen. Susan Collins (R-Maine) a vote on health legislation in exchange for her vote for the GOP tax bill in December. So far, that vote has not materialized.
The deal does appear to include almost every other health priority Democrats have been pushing the past several months, including 2 years of renewed funding for community health centers and a series of other health programs Congress failed to provide for before they technically expired last year.
“I believe we have reached a budget deal that neither side loves but both sides can be proud of,” Senate Minority Leader Chuck Schumer (D-N.Y.) said on the Senate floor. “That’s compromise. That’s governing.”
Said McConnell, “This bill represents a significant bipartisan step forward.”
Senate leaders are still negotiating last details of the accord, including the size of a cut to the ACA’s Prevention and Public Health Fund, which would help offset the costs of this legislation.
According to documents circulating on Capitol Hill, the deal includes $6 billion in funding for treatment of mental health issues and opioid addiction, $2 billion in extra funding for the National Institutes of Health, and an additional 4-year extension of the Children’s Health Insurance Program (CHIP), which builds on the 6 years approved by Congress in January.
In the Medicare program, the deal would accelerate the closing of the “doughnut hole” in Medicare drug coverage that requires seniors to pay thousands of dollars out-of-pocket before catastrophic coverage kicks in. It would also repeal the controversial Medicare Independent Payment Advisory Board (IPAB), which is charged with holding down Medicare spending for the federal government if it exceeds a certain level. Members have never been appointed to the board, however, and its use has not so far been triggered by Medicare spending. Both the closure of the doughnut hole and creation of the IPAB were part of the ACA.
The agreement would also fund a host of more limited health programs – some of which are known as “extenders” because they often ride along with other, larger health or spending bills.
Those programs include more than $7 billion in funding for the nation’s federally funded community health centers. The clinics serve 27 million low-income people and saw their funding lapse last fall – a delay advocates said had already complicated budgeting and staffing decisions for many clinics.
And in a victory for the physical therapy industry and patient advocates, the accord would permanently repeal a limit on Medicare’s coverage of physical therapy, speech-language pathology and outpatient treatment. Previously, the program capped coverage after $2,010 worth of occupational therapy and another $2,010 for speech-language therapy and physical therapy combined. But Congress had long taken action to delay those caps or provide exemptions – meaning they had never actually taken effect.
According to an analysis by the nonpartisan Congressional Budget Office, permanently repealing the caps would cost about $6.47 billion over the next decade.
Lawmakers would also forestall cuts mandated by the ACA to reduce the payments made to so-called Disproportionate Share Hospitals, which serve high rates of low-income patients. Those cuts have been delayed continuously since the law’s 2010 passage.
Limited programs are also affected. The deal would fund for 5 years the Maternal, Infant and Early Childhood Home Visiting Program, a program that helps guide low-income, at-risk mothers in parenting. It served about 160,000 families in fiscal year 2016.
“We are relieved that there is a deal for a 5-year reauthorization of MIECHV,” Lori Freeman, CEO of the Association of Maternal & Child Health Programs – an advocacy group – said in an emailed statement. “States, home visitors, and families have been in limbo for the past several months, and this news will bring the stability they need to continue this successful program.”
And the budget deal funds programs that encourage doctors to practice in medically underserved areas, providing just under $500 million over the next 2 years for the National Health Service Corps and another $363 million over 2 years to the Teaching Health Center Graduate Medical Education program, which places medical residents in Community Health Centers.
Kaiser Health News correspondent Emmarie Huetteman contributed to this article. KHN’s coverage of these topics is supported by Heising-Simons Foundation and The David and Lucile Packard Foundation. Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
In a rare show of bipartisanship for the mostly polarized 115th Congress, Republican and Democratic Senate leaders announced a 2-year budget deal that would increase federal spending for defense as well as key domestic priorities, including many health programs.
Not in the deal, for which the path to the president’s desk remains unclear, is any bipartisan legislation aimed at shoring up the Affordable Care Act’s individual health insurance marketplaces. Senate Majority Leader Mitch McConnell (R-Ky.) promised Sen. Susan Collins (R-Maine) a vote on health legislation in exchange for her vote for the GOP tax bill in December. So far, that vote has not materialized.
The deal does appear to include almost every other health priority Democrats have been pushing the past several months, including 2 years of renewed funding for community health centers and a series of other health programs Congress failed to provide for before they technically expired last year.
“I believe we have reached a budget deal that neither side loves but both sides can be proud of,” Senate Minority Leader Chuck Schumer (D-N.Y.) said on the Senate floor. “That’s compromise. That’s governing.”
Said McConnell, “This bill represents a significant bipartisan step forward.”
Senate leaders are still negotiating last details of the accord, including the size of a cut to the ACA’s Prevention and Public Health Fund, which would help offset the costs of this legislation.
According to documents circulating on Capitol Hill, the deal includes $6 billion in funding for treatment of mental health issues and opioid addiction, $2 billion in extra funding for the National Institutes of Health, and an additional 4-year extension of the Children’s Health Insurance Program (CHIP), which builds on the 6 years approved by Congress in January.
In the Medicare program, the deal would accelerate the closing of the “doughnut hole” in Medicare drug coverage that requires seniors to pay thousands of dollars out-of-pocket before catastrophic coverage kicks in. It would also repeal the controversial Medicare Independent Payment Advisory Board (IPAB), which is charged with holding down Medicare spending for the federal government if it exceeds a certain level. Members have never been appointed to the board, however, and its use has not so far been triggered by Medicare spending. Both the closure of the doughnut hole and creation of the IPAB were part of the ACA.
The agreement would also fund a host of more limited health programs – some of which are known as “extenders” because they often ride along with other, larger health or spending bills.
Those programs include more than $7 billion in funding for the nation’s federally funded community health centers. The clinics serve 27 million low-income people and saw their funding lapse last fall – a delay advocates said had already complicated budgeting and staffing decisions for many clinics.
And in a victory for the physical therapy industry and patient advocates, the accord would permanently repeal a limit on Medicare’s coverage of physical therapy, speech-language pathology and outpatient treatment. Previously, the program capped coverage after $2,010 worth of occupational therapy and another $2,010 for speech-language therapy and physical therapy combined. But Congress had long taken action to delay those caps or provide exemptions – meaning they had never actually taken effect.
According to an analysis by the nonpartisan Congressional Budget Office, permanently repealing the caps would cost about $6.47 billion over the next decade.
Lawmakers would also forestall cuts mandated by the ACA to reduce the payments made to so-called Disproportionate Share Hospitals, which serve high rates of low-income patients. Those cuts have been delayed continuously since the law’s 2010 passage.
Limited programs are also affected. The deal would fund for 5 years the Maternal, Infant and Early Childhood Home Visiting Program, a program that helps guide low-income, at-risk mothers in parenting. It served about 160,000 families in fiscal year 2016.
“We are relieved that there is a deal for a 5-year reauthorization of MIECHV,” Lori Freeman, CEO of the Association of Maternal & Child Health Programs – an advocacy group – said in an emailed statement. “States, home visitors, and families have been in limbo for the past several months, and this news will bring the stability they need to continue this successful program.”
And the budget deal funds programs that encourage doctors to practice in medically underserved areas, providing just under $500 million over the next 2 years for the National Health Service Corps and another $363 million over 2 years to the Teaching Health Center Graduate Medical Education program, which places medical residents in Community Health Centers.
Kaiser Health News correspondent Emmarie Huetteman contributed to this article. KHN’s coverage of these topics is supported by Heising-Simons Foundation and The David and Lucile Packard Foundation. Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
In a rare show of bipartisanship for the mostly polarized 115th Congress, Republican and Democratic Senate leaders announced a 2-year budget deal that would increase federal spending for defense as well as key domestic priorities, including many health programs.
Not in the deal, for which the path to the president’s desk remains unclear, is any bipartisan legislation aimed at shoring up the Affordable Care Act’s individual health insurance marketplaces. Senate Majority Leader Mitch McConnell (R-Ky.) promised Sen. Susan Collins (R-Maine) a vote on health legislation in exchange for her vote for the GOP tax bill in December. So far, that vote has not materialized.
The deal does appear to include almost every other health priority Democrats have been pushing the past several months, including 2 years of renewed funding for community health centers and a series of other health programs Congress failed to provide for before they technically expired last year.
“I believe we have reached a budget deal that neither side loves but both sides can be proud of,” Senate Minority Leader Chuck Schumer (D-N.Y.) said on the Senate floor. “That’s compromise. That’s governing.”
Said McConnell, “This bill represents a significant bipartisan step forward.”
Senate leaders are still negotiating last details of the accord, including the size of a cut to the ACA’s Prevention and Public Health Fund, which would help offset the costs of this legislation.
According to documents circulating on Capitol Hill, the deal includes $6 billion in funding for treatment of mental health issues and opioid addiction, $2 billion in extra funding for the National Institutes of Health, and an additional 4-year extension of the Children’s Health Insurance Program (CHIP), which builds on the 6 years approved by Congress in January.
In the Medicare program, the deal would accelerate the closing of the “doughnut hole” in Medicare drug coverage that requires seniors to pay thousands of dollars out-of-pocket before catastrophic coverage kicks in. It would also repeal the controversial Medicare Independent Payment Advisory Board (IPAB), which is charged with holding down Medicare spending for the federal government if it exceeds a certain level. Members have never been appointed to the board, however, and its use has not so far been triggered by Medicare spending. Both the closure of the doughnut hole and creation of the IPAB were part of the ACA.
The agreement would also fund a host of more limited health programs – some of which are known as “extenders” because they often ride along with other, larger health or spending bills.
Those programs include more than $7 billion in funding for the nation’s federally funded community health centers. The clinics serve 27 million low-income people and saw their funding lapse last fall – a delay advocates said had already complicated budgeting and staffing decisions for many clinics.
And in a victory for the physical therapy industry and patient advocates, the accord would permanently repeal a limit on Medicare’s coverage of physical therapy, speech-language pathology and outpatient treatment. Previously, the program capped coverage after $2,010 worth of occupational therapy and another $2,010 for speech-language therapy and physical therapy combined. But Congress had long taken action to delay those caps or provide exemptions – meaning they had never actually taken effect.
According to an analysis by the nonpartisan Congressional Budget Office, permanently repealing the caps would cost about $6.47 billion over the next decade.
Lawmakers would also forestall cuts mandated by the ACA to reduce the payments made to so-called Disproportionate Share Hospitals, which serve high rates of low-income patients. Those cuts have been delayed continuously since the law’s 2010 passage.
Limited programs are also affected. The deal would fund for 5 years the Maternal, Infant and Early Childhood Home Visiting Program, a program that helps guide low-income, at-risk mothers in parenting. It served about 160,000 families in fiscal year 2016.
“We are relieved that there is a deal for a 5-year reauthorization of MIECHV,” Lori Freeman, CEO of the Association of Maternal & Child Health Programs – an advocacy group – said in an emailed statement. “States, home visitors, and families have been in limbo for the past several months, and this news will bring the stability they need to continue this successful program.”
And the budget deal funds programs that encourage doctors to practice in medically underserved areas, providing just under $500 million over the next 2 years for the National Health Service Corps and another $363 million over 2 years to the Teaching Health Center Graduate Medical Education program, which places medical residents in Community Health Centers.
Kaiser Health News correspondent Emmarie Huetteman contributed to this article. KHN’s coverage of these topics is supported by Heising-Simons Foundation and The David and Lucile Packard Foundation. Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Convertible Glenoid Components Facilitate Revisions to Reverse Shoulder Arthroplasty Easier: Retrospective Review of 13 Cases
ABSTRACT
Removal of a cemented glenoid component often leads to massive glenoid bone loss, which makes it difficult to implant a new glenoid baseplate. The purpose of this study was to demonstrate the feasibility of revisions with a completely convertible system and to report clinical and radiographic results of a retrospective review of 13 cases.
Between 2003 and 2011, 104 primary total shoulder arthroplasties (TSAs) were performed with an uncemented glenoid component in our group. Of these patients, 13 (average age, 64 years) were revised to reverse shoulder arthroplasty (RSA) using a modular convertible platform system and were included in this study. Average follow-up after revision was 22 months. Outcome measures included pain, range of motion, Constant-Murley scores, Simple Shoulder Tests, and subjective shoulder values. Active flexion increased significantly from a mean of 93° (range, 30°-120°) to 138° (range, 95°-170°) (P = 0.021), and active external rotation increased significantly from 8° (range, −20°-15°) to 25° (range, −10°-60°). Mean pain scores significantly improved from 4.2 to 13.3 points. The mean Constant Scores improved from 21 (range, 18-32) to 63 (range, 43-90). Subjectively, 12 patients rated their shoulder as better or much better than preoperatively. This retrospective study shows that a complete convertible system facilitates conversion of TSAs to RSAs with excellent pain relief and a significant improvement in shoulder function.
Continue to: Polyethylene glenoid components...
Polyethylene glenoid components are the gold standard in anatomic total shoulder arthroplasty (TSA). However, even though TSA survivorship exceeds 95% at 10-year follow-up,1 glenoid component loosening remains the main complication and the weak link in these implants. This complication accounts for 25% of all complications related to TSA in the literature.2 In most cases, glenoid component loosening is not isolated but combined with a rotator cuff tear, glenohumeral instability, or component malposition.
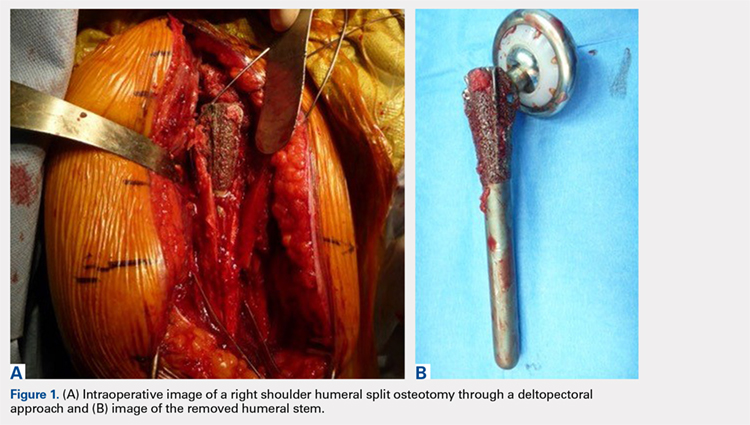
We hypothesized that a completely convertible platform system on both the humeral and the glenoid side could facilitate the revision of a failed TSA to a RSA. This would enable the surgeon to leave the humeral stem and the glenoid baseplate in place, avoiding the difficulty of stem removal and the reimplantation of a glenoid component, especially in osteoporotic glenoid bone and elderly patients. The revision procedure would then only consist of replacing the humeral head by a metallic tray and polyethylene bearing on the humeral side and by impacting a glenosphere on the glenoid baseplate (Figures 2A, 2B).
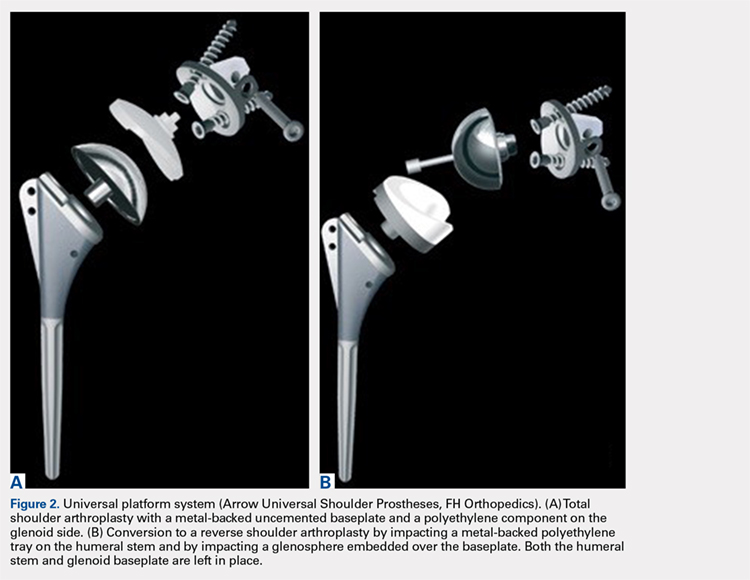
The purpose of this study was to demonstrate the feasibility of revisions with this completely convertible system and to report clinical and radiographic results of a retrospective review of 13 cases.
MATERIALS AND METHODS
PATIENT SELECTION
Between 2003 and 2011, 104 primary TSAs were performed with an uncemented glenoid component in our group. Of these patients, 18 underwent revision (17.3%). Among these 18 patients, 13 were revised to RSA using a modular convertible platform system and were included in this study, while 5 patients were revised to another TSA (2 dissociations of the polyethylene glenoid implant, 2 excessively low implantations of the glenoid baseplate, and 1 glenoid loosening). The mean age of the 13 patients (9 women, 4 men) included in this retrospective study at the time of revision was 64 years (range, 50-75 years). The reasons for revision surgery were rotator cuff tear (5, among which 2 were posterosuperior tears, and 3 were tears of the subscapularis), dislocations (5 posterior and 1 anterior, among which 4 had a B2 or C glenoid), suprascapular nerve paralysis (1), and dissociation of the polyethylene (1). The initial TSA was indicated for primary osteoarthritis with a normal cuff (9), primary osteoarthritis with a reparable cuff tear (2), posttraumatic osteoarthritis (1), and chronic dislocation (1). The right dominant shoulder was involved in 10 cases. The mean time interval between the primary TSA and the revision was 15 months (range, 1-61 months).
OPERATIVE TECHNIQUE
PREOPERATIVE PLANNING
Revision of a failed TSA is always a difficult challenge, and evaluation of bone loss on both the humeral and the glenoid sides, as well as the status of the cuff, is mandatory, even with a completely convertible arthroplasty system. The surgeon must be prepared to remove the humeral stem in case reduction of the joint is impossible. We systematically performed standard radiographs (anteroposterior, axillary, and outlet views) and computed tomography (CT) scans in order to assess both the version and positioning, as well as potential signs of loosening of the implants and the status of the cuff (continuity, degree of muscle trophicity, and fatty infiltration). A preoperative leucocyte count, sedimentation rate, and C-reactive protein rates were requested in every revision case, even if a mechanical etiology was strongly suspected.
Continue to: REVISION PROCEDURE
REVISION PROCEDURE
All the implants that had been used in the primary TSAs were Arrow Universal Shoulder Prostheses (FH Orthopedics). All revisions were performed through the previous deltopectoral approach in the beach chair position under general anesthesia with an interscalene block. Adhesions of the deep part of the deltoid were carefully released. The conjoint tendon was released, and the location of the musculocutaneous and axillary nerves was identified before any retractor was placed. In the 10 cases where the subscapularis was intact, it was peeled off the medial border of the bicipital groove to obtain sufficient length for a tension-free reinsertion.
The anatomical head of the humeral implant was disconnected from the stem and removed. All stems were found to be well fixed; there were no cases of loosening or evidence of infection. A circumferential capsular release was systematically carried out. The polyethylene glenoid onlay was then unlocked from the baseplate.
The quality of the fixation of the glenoid baseplate was systematically evaluated; no screw was found to be loose, and the fixation of all baseplates was stable. Therefore, there was no need to revise the glenoid baseplate, even when its position was considered excessively retroverted (Glenoid B2) or high. A glenosphere was impacted on the baseplate, and a polyethylene humeral bearing was then implanted on the humeral stem. The thinnest polyethylene bearing available (number 0) was chosen in all cases, and a size 36 glenosphere was chosen in 12 out of 13 cases. Intraoperative stability of the implant was satisfactory, and no impingement was found posteriorly, anteriorly, or inferiorly.
In one case, the humeral stem was a first-generation humeral implant which was not compatible with the new-generation humeral bearing, and the humeral stem had to be replaced.
In 2 cases, reduction of the RSA was either impossible or felt to be too tight, even after extensive soft-tissue release and resection of the remaining supraspinatus. The main reason for this was an excessively proud humeral stem because of an onlay polyethylene humeral bearing instead of an inlay design. However, removal of the uncemented humeral stem was always possible with no osteotomy or cortical window of the humeral shaft as the humeral stem has been designed with a bone ingrowth surface only on the metaphyseal part with a smooth surface on diaphyseal part. After removal of the stem, a small amount of humeral metaphysis was cut, and a new humeral stem was press-fit in a lower position. This allowed restoration of an appropriate tension of the soft tissue and, therefore, an easier reduction. The subscapularis was medialized and reinserted transosseously when possible with a double-row repair. In 3 cases, the subscapularis was torn and retracted at the level of the glenoid, or impossible to identify to allow its reinsertion.
Continue to: According to our infectious disease department...
According to our infectious disease department, we made a minimum of 5 cultures for each revision case looking for a possible low-grade infection. All cultures in our group are held for 14 days to assess for Propionibacterium acnes.
POSTOPERATIVE MANAGEMENT
A shoulder splint in neutral rotation was used for the first 4 weeks. Passive range of motion (ROM) was started immediately with pendulum exercises and passive anterior elevation. Active assisted and active ROM were allowed after 4 weeks, and physiotherapy was continued for 6 months. Elderly patients were referred to a center of rehabilitation. We found only 1 or 2 positive cultures (Propionibacterium acnes) for 4 patients, and we decided to consider them as a contamination. None of the patients were treated with antibiotics.
CLINICAL AND RADIOLOGICAL ASSESSMENT
Clinical evaluation included pre- and postoperative pain scores (visual analog scale [VAS]), ROM, the Constant-Murley13 score, the Simple Shoulder Test (SST),14 and the subjective shoulder value.15 Subjective satisfaction was assessed by asking the patients at follow-up how they felt compared with before surgery and was graded using a 4-point scale: 1, much better; 2, better; 3, the same; and 4, worse. Radiographic evaluation was performed on pre- and postoperative standard anteroposterior, outlet, and axillary views. Radiographs were reviewed to determine the presence of glenohumeral subluxation, periprosthetic lucency, component shift in position, and scapular notching.
STATISTICAL ANALYSIS
Descriptive statistics are reported as mean (range) for continuous measures and number (percentage) for discrete variables. The Wilcoxon signed-rank test was used for preoperative vs postoperative changes. The alpha level for all tests was set at 0.05 for statistical significance.
RESULTS
CLINICAL OUTCOME
At a mean of 22 months (range, 7-38 months) follow-up after revision, active ROM was significantly improved. Active flexion increased significantly from a mean of 93° (range, 30°-120°) to 138° (range, 95°-170°) (P = 0.021). Active external rotation with the elbow on the side increased significantly from 8° (range, −20°-15°) to 25° (range, −10°-60°) (P = 0.034), and increased with the arm held at 90° abduction from 13° (range, 0°-20°) to 49° (range, 0°-80°) (P = 0.025). Mean pain scores improved from 4.2 to 13.3 points (P < 0.001). VAS improved significantly from 9 to 1 (P < 0.0001). The mean Constant Scores improved from 21 (range, 18-32) to 63 (range, 43-90) (P = 0.006). The final SST was 7 per 12. Subjectively, 4 patients rated their shoulder as much better, 8 as better, and 1 as the same as preoperatively. No intra- or postoperative complications, including infections, were observed. The mean duration of the procedure was 60 minutes (range, 30-75 minutes).
Continue to: RADIOLOGICAL OUTCOME
RADIOLOGICAL OUTCOME
No periprosthetic lucency or shift in component was observed at the last follow-up. There was no scapular notching. No resorption of the tuberosities, and no fractures of the acromion or the scapular spine were observed.
DISCUSSION
In this retrospective study, failure of TSA with a metal-backed glenoid implant was successfully revised to RSA. In 10 patients, the use of a universal platform system allowed an easier conversion without removal of the humeral stem or the glenoid component (Figures 3A-3D). Twelve of the 13 patients were satisfied or very satisfied at the last follow-up. None of the patients were in pain, and the mean Constant score was 63. In all the cases, the glenoid baseplate was not changed. In 3 cases the humeral stem was changed without any fracture of the tuberosities of need for an osteotomy. This greatly simplified the revision procedure, as glenoid revisions can be very challenging. Indeed, it is often difficult to assess precisely preoperatively the remaining glenoid bone stock after removal of the glenoid component and the cement. Many therapeutic options to deal with glenoid loosening have been reported in the literature: glenoid bone reconstruction after glenoid component removal and revision to a hemiarthroplasty (HA),10,16-18 glenoid bone reconstruction after glenoid component removal and revision to a new TSA with a cemented glenoid implant,16,17,19,20 and glenoid reconstruction after glenoid component removal and revision to a RSA.12,21 These authors reported that glenoid reconstruction frequently necessitates an iliac bone graft associated with a special design of the baseplate with a long post fixed into the native glenoid bone. However, sometimes implantation of an uncemented glenoid component can be unstable with a high risk of early mobilization of the implant, and 2 steps may be necessary. Conversion to a HA,10,16-18 or a TSA16,17,19,20 with a new cemented implant have both been associated with poor clinical outcome, with a high rate of recurrent glenoid loosening for the TSAs.
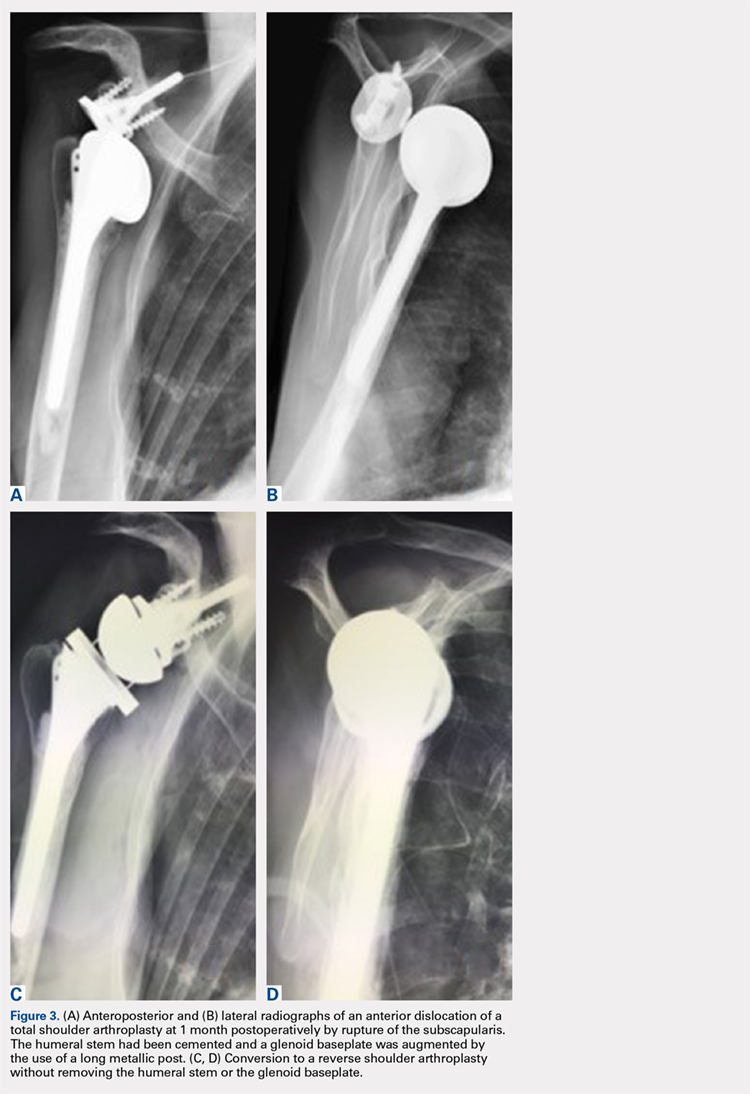
In our retrospective study, we reported no intra- or postoperative complications. Flury and colleagues22 reported a complication rate of 38% in 21 patients after conversion from a TSA to a RSA with a mean follow-up of 46 months. They removed all the components of the prosthesis with a crack or fracture of the humerus and/or the glenoid. Ortmaier and colleagues23 reported a rate of complication of 22.7% during the conversion of TSA to RSA. They did an osteotomy of the humeral diaphysis to extract the stem in 40% of cases and had to remove the glenoid cement in 86% of cases with severe damage of the glenoid bone in 10% of cases. Fewer complications were found in our study, as we did not need any procedure such as humeral osteotomy, cerclage, bone grafting, and/or reconstruction of the glenoid. The short operative time and the absence of extensive soft-tissue dissection, thanks to a standard deltopectoral approach, could explain the absence of infection in our series.
Other authors shared our strategy of a universal convertible system and reported their results in the literature. Castagna and colleagues24 in 2013 reported the clinical and radiological results of conversions of HA or TSA to RSA using a modular, convertible system (SMR Shoulder System, Lima Corporate). In their series, only 8 cases of TSAs were converted to RSA. They preserved, in each case, the humeral stem and the glenoid baseplate. There were no intra- or postoperative complications. The mean VAS score decreased from 8 to 2. Weber-Spickschen and colleague25 reported recently in 2015 the same experience with the same system (SMR Shoulder System). They reviewed 15 conversions of TSAs to RSAs without any removal of the implants at a mean 43-month follow-up. They reported excellent pain relief (VAS decreased from 8 to 1) and improvement in shoulder function with a low rate of complications.
Kany and colleagues26 in 2015 had already reported the advantages of a shoulder platform system for revisions. In their series, the authors included cases of failure of HAs and TSAs with loose cemented glenoids and metal-backed glenoids. The clinical and radiological results were similar, with a final Constant score of 60 (range, 42-85) and a similar rate of humeral stems which had to be changed (24%). These stems were replaced either because they were too proud or because there was not enough space to add an onlay polyethylene socket.
Continue to: Despite the encouraging results...
Despite the encouraging results reported in this study, there are some limitations. Firstly, no control group was used. Attempting to address this issue, we compared our results with the literature. Secondly, the number of patients in our study was small. Finally, the follow-up duration (mean 22 months) did not provide long-term outcomes.
CONCLUSION
This retrospective study shows that a complete convertible system facilitates conversion of TSAs to RSAs with excellent pain relief and a significant improvement in shoulder function. A platform system on both the humeral and the glenoid side reduces the operative time of the conversion with a low risk of complications.
1. Brenner BC, Ferlic DC, Clayton ML, Dennis DA. Survivorship of unconstrained total shoulder arthroplasty. J Bone Joint Surg Am. 1989;71(9):1289-1296.
2. Budge MD, Nolan EM, Heisey MH, Baker K, Wiater JM. Results of total shoulder arthroplasty with a monoblock porous tantalum glenoid component: a prospective minimum 2-year follow-up study. J Shoulder Elbow Surg. 2013;22(4):535-541. doi:10.1016/j.jse.2012.06.001.
3. Chin PY, Sperling JW, Cofield RH, Schleck C. Complications of total shoulder arthroplasty: are they fewer or different? J Shoulder Elbow Surg. 2006;15(1):19-22. doi:10.1016/j.jse.2005.05.005.
4. Torchia ME, Cofield RH, Settergren CR. Total shoulder arthroplasty with the Neer prosthesis: long-term results. J Shoulder Elbow Surg. 1997;6(6):495-505.
5. Wirth MA, Rockwood CA Jr. Complications of total shoulder-replacement surgery. J Bone Joint Surg Am. 1996;78(4):603-616.
6. Gohlke F, Rolf O. Revision of failed fracture hemiarthroplasties to reverse total shoulder prosthesis through the transhumeral approach: method incorporating a pectoralis-major-pedicled bone window. Oper Orthop Traumatol. 2007;19(2):185-208. doi:10.1007/s00064-007-1202-x.
7. Goldberg SH, Cohen MS, Young M, Bradnock B. Thermal tissue damage caused by ultrasonic cement removal from the humerus. J Bone Joint Surg Am. 2005;87(3):583-591. doi:10.2106/JBJS.D.01966.
8. Sperling JW, Cofield RH. Humeral windows in revision shoulder arthroplasty. J Shoulder Elbow Surg. 2005;14(3):258-263. doi:10.1016/j.jse.2004.09.004.
9. Chacon A, Virani N, Shannon R, Levy JC, Pupello D, Frankle M. Revision arthroplasty with use of a reverse shoulder prosthesis-allograft composite. J Bone Joint Surg Am. 2009;91(1):119-127. doi:10.2106/JBJS.H.00094.
10. Iannotti JP, Frangiamore SJ. Fate of large structural allograft for treatment of severe uncontained glenoid bone deficiency. J Shoulder Elbow Surg. 2012;21(6):765-771. doi:10.1016/j.jse.2011.08.069.
11. Kelly JD 2nd, Zhao JX, Hobgood ER, Norris TR. Clinical results of revision shoulder arthroplasty using the reverse prosthesis. J Shoulder Elbow Surg. 2012;21(11):1516-1525. doi:10.1016/j.jse.2011.11.021.
12. Melis B, Bonnevialle N, Neyton L, et al. Glenoid loosening and failure in anatomical total shoulder arthroplasty: is revision with a reverse shoulder arthroplasty a reliable option? J Shoulder Elbow Surg. 2012;21(3):342-349. doi:10.1016/j.jse.2011.05.021.
13. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;(214):160-164.
14. Matsen FA 3rd, Ziegler DW, DeBartolo SE. Patient self-assessment of health status and function in glenohumeral degenerative joint disease. J Shoulder Elbow Surg. 1995;4(5):345-351.
15. Gilbart MK, Gerber C. Comparison of the subjective shoulder value and the Constant score. J Shoulder Elbow Surg. 2007;16(6):717-721. doi:10.1016/j.jse.2007.02.123.
16. Antuna SA, Sperling JW, Cofield RH, Rowland CM. Glenoid revision surgery after total shoulder arthroplasty. J Shoulder Elbow Surg. 2001;10(3):217-224. doi:10.1067/mse.2001.113961.
17. Cofield RH, Edgerton BC. Total shoulder arthroplasty: complications and revision surgery. Instr Course Lect. 1990;39:449-462.
18. Neyton L, Walch G, Nove-Josserand L, Edwards TB. Glenoid corticocancellous bone grafting after glenoid component removal in the treatment of glenoid loosening. J Shoulder Elbow Surg. 2006;15(2):173-179. doi:10.1016/j.jse.2005.07.010.
19. Bonnevialle N, Melis B, Neyton L, et al. Aseptic glenoid loosening or failure in total shoulder arthroplasty: revision with glenoid reimplantation. J Shoulder Elbow Surg. 2013;22(6):745-751. doi:10.1016/j.jse.2012.08.009.
20. Rodosky MW, Bigliani LU. Indications for glenoid resurfacing in shoulder arthroplasty. J Shoulder Elbow Surg. 1996;5(3):231-248.
21. Bateman E, Donald SM. Reconstruction of massive uncontained glenoid defects using a combined autograft-allograft construct with reverse shoulder arthroplasty: preliminary results. J Shoulder Elbow Surg. 2012;21(7):925-934. doi:10.1016/j.jse.2011.07.009.
22. Flury MP, Frey P, Goldhahn J, Schwyzer HK, Simmen BR. Reverse shoulder arthroplasty as a salvage procedure for failed conventional shoulder replacement due to cuff failure--midterm results. Int Orthop. 2011;35(1):53-60. doi:10.1007/s00264-010-0990-z.
23. Ortmaier R, Resch H, Hitzl W, et al. Reverse shoulder arthroplasty combined with latissimus dorsi transfer using the bone-chip technique. Int Orthop. 2013;38(3):1-7. doi:10.1007/s00264-013-2139-3.
24. Castagna A, Delcogliano M, de Caro F, et al. Conversion of shoulder arthroplasty to reverse implants: clinical and radiological results using a modular system. Int Orthop. 2013;37(7):1297-1305. doi:10.1007/s00264-013-1907-4.
25. Weber-Spickschen TS, Alfke D, Agneskirchner JD. The use of a modular system to convert an anatomical total shoulder arthroplasty to a reverse shoulder arthroplasty: Clinical and radiological results. Bone Joint J. 2015;97-B(12):1662-1667. doi:10.1302/0301-620X.97B12.35176.
26. Kany J, Amouyel T, Flamand O, Katz D, Valenti P. A convertible shoulder system: is it useful in total shoulder arthroplasty revisions? Int Orthop. 2015;39(2):299-304. doi:10.1007/s00264-014-2563-z.
ABSTRACT
Removal of a cemented glenoid component often leads to massive glenoid bone loss, which makes it difficult to implant a new glenoid baseplate. The purpose of this study was to demonstrate the feasibility of revisions with a completely convertible system and to report clinical and radiographic results of a retrospective review of 13 cases.
Between 2003 and 2011, 104 primary total shoulder arthroplasties (TSAs) were performed with an uncemented glenoid component in our group. Of these patients, 13 (average age, 64 years) were revised to reverse shoulder arthroplasty (RSA) using a modular convertible platform system and were included in this study. Average follow-up after revision was 22 months. Outcome measures included pain, range of motion, Constant-Murley scores, Simple Shoulder Tests, and subjective shoulder values. Active flexion increased significantly from a mean of 93° (range, 30°-120°) to 138° (range, 95°-170°) (P = 0.021), and active external rotation increased significantly from 8° (range, −20°-15°) to 25° (range, −10°-60°). Mean pain scores significantly improved from 4.2 to 13.3 points. The mean Constant Scores improved from 21 (range, 18-32) to 63 (range, 43-90). Subjectively, 12 patients rated their shoulder as better or much better than preoperatively. This retrospective study shows that a complete convertible system facilitates conversion of TSAs to RSAs with excellent pain relief and a significant improvement in shoulder function.
Continue to: Polyethylene glenoid components...
Polyethylene glenoid components are the gold standard in anatomic total shoulder arthroplasty (TSA). However, even though TSA survivorship exceeds 95% at 10-year follow-up,1 glenoid component loosening remains the main complication and the weak link in these implants. This complication accounts for 25% of all complications related to TSA in the literature.2 In most cases, glenoid component loosening is not isolated but combined with a rotator cuff tear, glenohumeral instability, or component malposition.
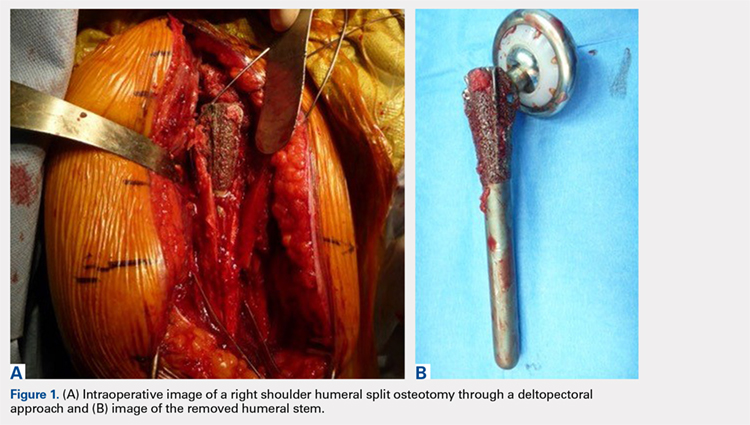
We hypothesized that a completely convertible platform system on both the humeral and the glenoid side could facilitate the revision of a failed TSA to a RSA. This would enable the surgeon to leave the humeral stem and the glenoid baseplate in place, avoiding the difficulty of stem removal and the reimplantation of a glenoid component, especially in osteoporotic glenoid bone and elderly patients. The revision procedure would then only consist of replacing the humeral head by a metallic tray and polyethylene bearing on the humeral side and by impacting a glenosphere on the glenoid baseplate (Figures 2A, 2B).
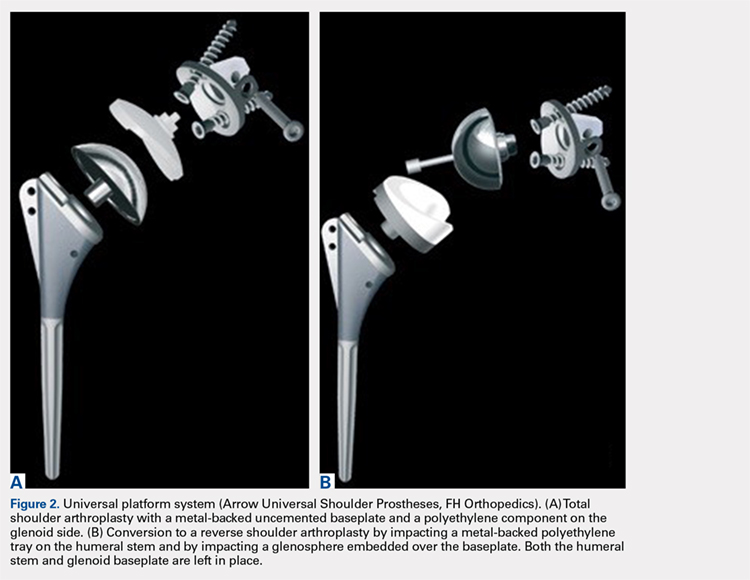
The purpose of this study was to demonstrate the feasibility of revisions with this completely convertible system and to report clinical and radiographic results of a retrospective review of 13 cases.
MATERIALS AND METHODS
PATIENT SELECTION
Between 2003 and 2011, 104 primary TSAs were performed with an uncemented glenoid component in our group. Of these patients, 18 underwent revision (17.3%). Among these 18 patients, 13 were revised to RSA using a modular convertible platform system and were included in this study, while 5 patients were revised to another TSA (2 dissociations of the polyethylene glenoid implant, 2 excessively low implantations of the glenoid baseplate, and 1 glenoid loosening). The mean age of the 13 patients (9 women, 4 men) included in this retrospective study at the time of revision was 64 years (range, 50-75 years). The reasons for revision surgery were rotator cuff tear (5, among which 2 were posterosuperior tears, and 3 were tears of the subscapularis), dislocations (5 posterior and 1 anterior, among which 4 had a B2 or C glenoid), suprascapular nerve paralysis (1), and dissociation of the polyethylene (1). The initial TSA was indicated for primary osteoarthritis with a normal cuff (9), primary osteoarthritis with a reparable cuff tear (2), posttraumatic osteoarthritis (1), and chronic dislocation (1). The right dominant shoulder was involved in 10 cases. The mean time interval between the primary TSA and the revision was 15 months (range, 1-61 months).
OPERATIVE TECHNIQUE
PREOPERATIVE PLANNING
Revision of a failed TSA is always a difficult challenge, and evaluation of bone loss on both the humeral and the glenoid sides, as well as the status of the cuff, is mandatory, even with a completely convertible arthroplasty system. The surgeon must be prepared to remove the humeral stem in case reduction of the joint is impossible. We systematically performed standard radiographs (anteroposterior, axillary, and outlet views) and computed tomography (CT) scans in order to assess both the version and positioning, as well as potential signs of loosening of the implants and the status of the cuff (continuity, degree of muscle trophicity, and fatty infiltration). A preoperative leucocyte count, sedimentation rate, and C-reactive protein rates were requested in every revision case, even if a mechanical etiology was strongly suspected.
Continue to: REVISION PROCEDURE
REVISION PROCEDURE
All the implants that had been used in the primary TSAs were Arrow Universal Shoulder Prostheses (FH Orthopedics). All revisions were performed through the previous deltopectoral approach in the beach chair position under general anesthesia with an interscalene block. Adhesions of the deep part of the deltoid were carefully released. The conjoint tendon was released, and the location of the musculocutaneous and axillary nerves was identified before any retractor was placed. In the 10 cases where the subscapularis was intact, it was peeled off the medial border of the bicipital groove to obtain sufficient length for a tension-free reinsertion.
The anatomical head of the humeral implant was disconnected from the stem and removed. All stems were found to be well fixed; there were no cases of loosening or evidence of infection. A circumferential capsular release was systematically carried out. The polyethylene glenoid onlay was then unlocked from the baseplate.
The quality of the fixation of the glenoid baseplate was systematically evaluated; no screw was found to be loose, and the fixation of all baseplates was stable. Therefore, there was no need to revise the glenoid baseplate, even when its position was considered excessively retroverted (Glenoid B2) or high. A glenosphere was impacted on the baseplate, and a polyethylene humeral bearing was then implanted on the humeral stem. The thinnest polyethylene bearing available (number 0) was chosen in all cases, and a size 36 glenosphere was chosen in 12 out of 13 cases. Intraoperative stability of the implant was satisfactory, and no impingement was found posteriorly, anteriorly, or inferiorly.
In one case, the humeral stem was a first-generation humeral implant which was not compatible with the new-generation humeral bearing, and the humeral stem had to be replaced.
In 2 cases, reduction of the RSA was either impossible or felt to be too tight, even after extensive soft-tissue release and resection of the remaining supraspinatus. The main reason for this was an excessively proud humeral stem because of an onlay polyethylene humeral bearing instead of an inlay design. However, removal of the uncemented humeral stem was always possible with no osteotomy or cortical window of the humeral shaft as the humeral stem has been designed with a bone ingrowth surface only on the metaphyseal part with a smooth surface on diaphyseal part. After removal of the stem, a small amount of humeral metaphysis was cut, and a new humeral stem was press-fit in a lower position. This allowed restoration of an appropriate tension of the soft tissue and, therefore, an easier reduction. The subscapularis was medialized and reinserted transosseously when possible with a double-row repair. In 3 cases, the subscapularis was torn and retracted at the level of the glenoid, or impossible to identify to allow its reinsertion.
Continue to: According to our infectious disease department...
According to our infectious disease department, we made a minimum of 5 cultures for each revision case looking for a possible low-grade infection. All cultures in our group are held for 14 days to assess for Propionibacterium acnes.
POSTOPERATIVE MANAGEMENT
A shoulder splint in neutral rotation was used for the first 4 weeks. Passive range of motion (ROM) was started immediately with pendulum exercises and passive anterior elevation. Active assisted and active ROM were allowed after 4 weeks, and physiotherapy was continued for 6 months. Elderly patients were referred to a center of rehabilitation. We found only 1 or 2 positive cultures (Propionibacterium acnes) for 4 patients, and we decided to consider them as a contamination. None of the patients were treated with antibiotics.
CLINICAL AND RADIOLOGICAL ASSESSMENT
Clinical evaluation included pre- and postoperative pain scores (visual analog scale [VAS]), ROM, the Constant-Murley13 score, the Simple Shoulder Test (SST),14 and the subjective shoulder value.15 Subjective satisfaction was assessed by asking the patients at follow-up how they felt compared with before surgery and was graded using a 4-point scale: 1, much better; 2, better; 3, the same; and 4, worse. Radiographic evaluation was performed on pre- and postoperative standard anteroposterior, outlet, and axillary views. Radiographs were reviewed to determine the presence of glenohumeral subluxation, periprosthetic lucency, component shift in position, and scapular notching.
STATISTICAL ANALYSIS
Descriptive statistics are reported as mean (range) for continuous measures and number (percentage) for discrete variables. The Wilcoxon signed-rank test was used for preoperative vs postoperative changes. The alpha level for all tests was set at 0.05 for statistical significance.
RESULTS
CLINICAL OUTCOME
At a mean of 22 months (range, 7-38 months) follow-up after revision, active ROM was significantly improved. Active flexion increased significantly from a mean of 93° (range, 30°-120°) to 138° (range, 95°-170°) (P = 0.021). Active external rotation with the elbow on the side increased significantly from 8° (range, −20°-15°) to 25° (range, −10°-60°) (P = 0.034), and increased with the arm held at 90° abduction from 13° (range, 0°-20°) to 49° (range, 0°-80°) (P = 0.025). Mean pain scores improved from 4.2 to 13.3 points (P < 0.001). VAS improved significantly from 9 to 1 (P < 0.0001). The mean Constant Scores improved from 21 (range, 18-32) to 63 (range, 43-90) (P = 0.006). The final SST was 7 per 12. Subjectively, 4 patients rated their shoulder as much better, 8 as better, and 1 as the same as preoperatively. No intra- or postoperative complications, including infections, were observed. The mean duration of the procedure was 60 minutes (range, 30-75 minutes).
Continue to: RADIOLOGICAL OUTCOME
RADIOLOGICAL OUTCOME
No periprosthetic lucency or shift in component was observed at the last follow-up. There was no scapular notching. No resorption of the tuberosities, and no fractures of the acromion or the scapular spine were observed.
DISCUSSION
In this retrospective study, failure of TSA with a metal-backed glenoid implant was successfully revised to RSA. In 10 patients, the use of a universal platform system allowed an easier conversion without removal of the humeral stem or the glenoid component (Figures 3A-3D). Twelve of the 13 patients were satisfied or very satisfied at the last follow-up. None of the patients were in pain, and the mean Constant score was 63. In all the cases, the glenoid baseplate was not changed. In 3 cases the humeral stem was changed without any fracture of the tuberosities of need for an osteotomy. This greatly simplified the revision procedure, as glenoid revisions can be very challenging. Indeed, it is often difficult to assess precisely preoperatively the remaining glenoid bone stock after removal of the glenoid component and the cement. Many therapeutic options to deal with glenoid loosening have been reported in the literature: glenoid bone reconstruction after glenoid component removal and revision to a hemiarthroplasty (HA),10,16-18 glenoid bone reconstruction after glenoid component removal and revision to a new TSA with a cemented glenoid implant,16,17,19,20 and glenoid reconstruction after glenoid component removal and revision to a RSA.12,21 These authors reported that glenoid reconstruction frequently necessitates an iliac bone graft associated with a special design of the baseplate with a long post fixed into the native glenoid bone. However, sometimes implantation of an uncemented glenoid component can be unstable with a high risk of early mobilization of the implant, and 2 steps may be necessary. Conversion to a HA,10,16-18 or a TSA16,17,19,20 with a new cemented implant have both been associated with poor clinical outcome, with a high rate of recurrent glenoid loosening for the TSAs.
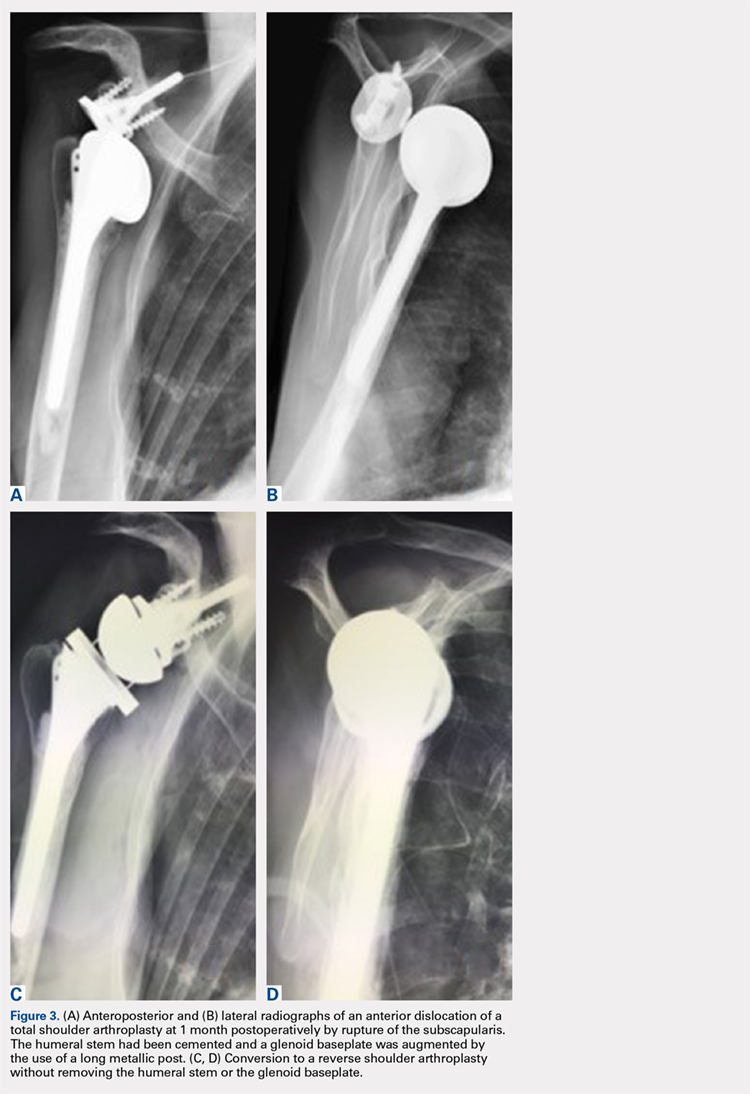
In our retrospective study, we reported no intra- or postoperative complications. Flury and colleagues22 reported a complication rate of 38% in 21 patients after conversion from a TSA to a RSA with a mean follow-up of 46 months. They removed all the components of the prosthesis with a crack or fracture of the humerus and/or the glenoid. Ortmaier and colleagues23 reported a rate of complication of 22.7% during the conversion of TSA to RSA. They did an osteotomy of the humeral diaphysis to extract the stem in 40% of cases and had to remove the glenoid cement in 86% of cases with severe damage of the glenoid bone in 10% of cases. Fewer complications were found in our study, as we did not need any procedure such as humeral osteotomy, cerclage, bone grafting, and/or reconstruction of the glenoid. The short operative time and the absence of extensive soft-tissue dissection, thanks to a standard deltopectoral approach, could explain the absence of infection in our series.
Other authors shared our strategy of a universal convertible system and reported their results in the literature. Castagna and colleagues24 in 2013 reported the clinical and radiological results of conversions of HA or TSA to RSA using a modular, convertible system (SMR Shoulder System, Lima Corporate). In their series, only 8 cases of TSAs were converted to RSA. They preserved, in each case, the humeral stem and the glenoid baseplate. There were no intra- or postoperative complications. The mean VAS score decreased from 8 to 2. Weber-Spickschen and colleague25 reported recently in 2015 the same experience with the same system (SMR Shoulder System). They reviewed 15 conversions of TSAs to RSAs without any removal of the implants at a mean 43-month follow-up. They reported excellent pain relief (VAS decreased from 8 to 1) and improvement in shoulder function with a low rate of complications.
Kany and colleagues26 in 2015 had already reported the advantages of a shoulder platform system for revisions. In their series, the authors included cases of failure of HAs and TSAs with loose cemented glenoids and metal-backed glenoids. The clinical and radiological results were similar, with a final Constant score of 60 (range, 42-85) and a similar rate of humeral stems which had to be changed (24%). These stems were replaced either because they were too proud or because there was not enough space to add an onlay polyethylene socket.
Continue to: Despite the encouraging results...
Despite the encouraging results reported in this study, there are some limitations. Firstly, no control group was used. Attempting to address this issue, we compared our results with the literature. Secondly, the number of patients in our study was small. Finally, the follow-up duration (mean 22 months) did not provide long-term outcomes.
CONCLUSION
This retrospective study shows that a complete convertible system facilitates conversion of TSAs to RSAs with excellent pain relief and a significant improvement in shoulder function. A platform system on both the humeral and the glenoid side reduces the operative time of the conversion with a low risk of complications.
ABSTRACT
Removal of a cemented glenoid component often leads to massive glenoid bone loss, which makes it difficult to implant a new glenoid baseplate. The purpose of this study was to demonstrate the feasibility of revisions with a completely convertible system and to report clinical and radiographic results of a retrospective review of 13 cases.
Between 2003 and 2011, 104 primary total shoulder arthroplasties (TSAs) were performed with an uncemented glenoid component in our group. Of these patients, 13 (average age, 64 years) were revised to reverse shoulder arthroplasty (RSA) using a modular convertible platform system and were included in this study. Average follow-up after revision was 22 months. Outcome measures included pain, range of motion, Constant-Murley scores, Simple Shoulder Tests, and subjective shoulder values. Active flexion increased significantly from a mean of 93° (range, 30°-120°) to 138° (range, 95°-170°) (P = 0.021), and active external rotation increased significantly from 8° (range, −20°-15°) to 25° (range, −10°-60°). Mean pain scores significantly improved from 4.2 to 13.3 points. The mean Constant Scores improved from 21 (range, 18-32) to 63 (range, 43-90). Subjectively, 12 patients rated their shoulder as better or much better than preoperatively. This retrospective study shows that a complete convertible system facilitates conversion of TSAs to RSAs with excellent pain relief and a significant improvement in shoulder function.
Continue to: Polyethylene glenoid components...
Polyethylene glenoid components are the gold standard in anatomic total shoulder arthroplasty (TSA). However, even though TSA survivorship exceeds 95% at 10-year follow-up,1 glenoid component loosening remains the main complication and the weak link in these implants. This complication accounts for 25% of all complications related to TSA in the literature.2 In most cases, glenoid component loosening is not isolated but combined with a rotator cuff tear, glenohumeral instability, or component malposition.
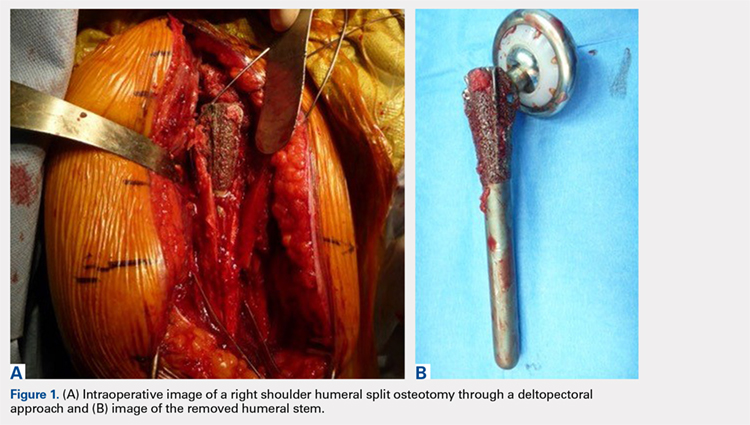
We hypothesized that a completely convertible platform system on both the humeral and the glenoid side could facilitate the revision of a failed TSA to a RSA. This would enable the surgeon to leave the humeral stem and the glenoid baseplate in place, avoiding the difficulty of stem removal and the reimplantation of a glenoid component, especially in osteoporotic glenoid bone and elderly patients. The revision procedure would then only consist of replacing the humeral head by a metallic tray and polyethylene bearing on the humeral side and by impacting a glenosphere on the glenoid baseplate (Figures 2A, 2B).
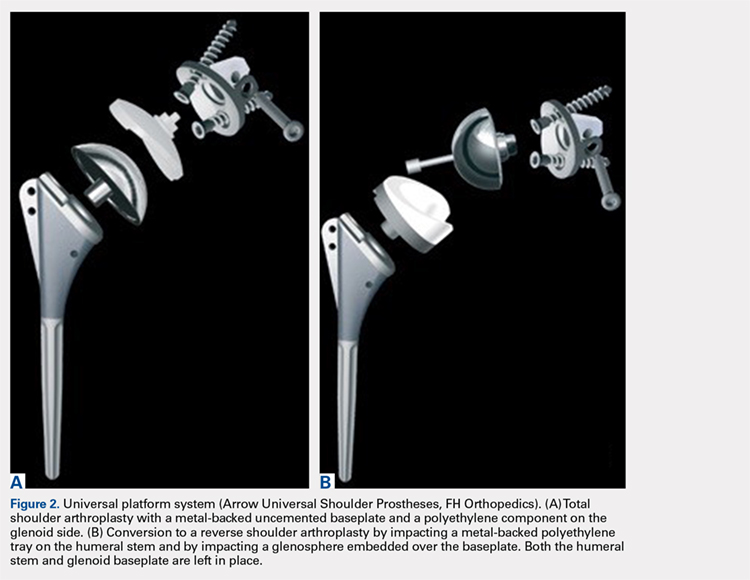
The purpose of this study was to demonstrate the feasibility of revisions with this completely convertible system and to report clinical and radiographic results of a retrospective review of 13 cases.
MATERIALS AND METHODS
PATIENT SELECTION
Between 2003 and 2011, 104 primary TSAs were performed with an uncemented glenoid component in our group. Of these patients, 18 underwent revision (17.3%). Among these 18 patients, 13 were revised to RSA using a modular convertible platform system and were included in this study, while 5 patients were revised to another TSA (2 dissociations of the polyethylene glenoid implant, 2 excessively low implantations of the glenoid baseplate, and 1 glenoid loosening). The mean age of the 13 patients (9 women, 4 men) included in this retrospective study at the time of revision was 64 years (range, 50-75 years). The reasons for revision surgery were rotator cuff tear (5, among which 2 were posterosuperior tears, and 3 were tears of the subscapularis), dislocations (5 posterior and 1 anterior, among which 4 had a B2 or C glenoid), suprascapular nerve paralysis (1), and dissociation of the polyethylene (1). The initial TSA was indicated for primary osteoarthritis with a normal cuff (9), primary osteoarthritis with a reparable cuff tear (2), posttraumatic osteoarthritis (1), and chronic dislocation (1). The right dominant shoulder was involved in 10 cases. The mean time interval between the primary TSA and the revision was 15 months (range, 1-61 months).
OPERATIVE TECHNIQUE
PREOPERATIVE PLANNING
Revision of a failed TSA is always a difficult challenge, and evaluation of bone loss on both the humeral and the glenoid sides, as well as the status of the cuff, is mandatory, even with a completely convertible arthroplasty system. The surgeon must be prepared to remove the humeral stem in case reduction of the joint is impossible. We systematically performed standard radiographs (anteroposterior, axillary, and outlet views) and computed tomography (CT) scans in order to assess both the version and positioning, as well as potential signs of loosening of the implants and the status of the cuff (continuity, degree of muscle trophicity, and fatty infiltration). A preoperative leucocyte count, sedimentation rate, and C-reactive protein rates were requested in every revision case, even if a mechanical etiology was strongly suspected.
Continue to: REVISION PROCEDURE
REVISION PROCEDURE
All the implants that had been used in the primary TSAs were Arrow Universal Shoulder Prostheses (FH Orthopedics). All revisions were performed through the previous deltopectoral approach in the beach chair position under general anesthesia with an interscalene block. Adhesions of the deep part of the deltoid were carefully released. The conjoint tendon was released, and the location of the musculocutaneous and axillary nerves was identified before any retractor was placed. In the 10 cases where the subscapularis was intact, it was peeled off the medial border of the bicipital groove to obtain sufficient length for a tension-free reinsertion.
The anatomical head of the humeral implant was disconnected from the stem and removed. All stems were found to be well fixed; there were no cases of loosening or evidence of infection. A circumferential capsular release was systematically carried out. The polyethylene glenoid onlay was then unlocked from the baseplate.
The quality of the fixation of the glenoid baseplate was systematically evaluated; no screw was found to be loose, and the fixation of all baseplates was stable. Therefore, there was no need to revise the glenoid baseplate, even when its position was considered excessively retroverted (Glenoid B2) or high. A glenosphere was impacted on the baseplate, and a polyethylene humeral bearing was then implanted on the humeral stem. The thinnest polyethylene bearing available (number 0) was chosen in all cases, and a size 36 glenosphere was chosen in 12 out of 13 cases. Intraoperative stability of the implant was satisfactory, and no impingement was found posteriorly, anteriorly, or inferiorly.
In one case, the humeral stem was a first-generation humeral implant which was not compatible with the new-generation humeral bearing, and the humeral stem had to be replaced.
In 2 cases, reduction of the RSA was either impossible or felt to be too tight, even after extensive soft-tissue release and resection of the remaining supraspinatus. The main reason for this was an excessively proud humeral stem because of an onlay polyethylene humeral bearing instead of an inlay design. However, removal of the uncemented humeral stem was always possible with no osteotomy or cortical window of the humeral shaft as the humeral stem has been designed with a bone ingrowth surface only on the metaphyseal part with a smooth surface on diaphyseal part. After removal of the stem, a small amount of humeral metaphysis was cut, and a new humeral stem was press-fit in a lower position. This allowed restoration of an appropriate tension of the soft tissue and, therefore, an easier reduction. The subscapularis was medialized and reinserted transosseously when possible with a double-row repair. In 3 cases, the subscapularis was torn and retracted at the level of the glenoid, or impossible to identify to allow its reinsertion.
Continue to: According to our infectious disease department...
According to our infectious disease department, we made a minimum of 5 cultures for each revision case looking for a possible low-grade infection. All cultures in our group are held for 14 days to assess for Propionibacterium acnes.
POSTOPERATIVE MANAGEMENT
A shoulder splint in neutral rotation was used for the first 4 weeks. Passive range of motion (ROM) was started immediately with pendulum exercises and passive anterior elevation. Active assisted and active ROM were allowed after 4 weeks, and physiotherapy was continued for 6 months. Elderly patients were referred to a center of rehabilitation. We found only 1 or 2 positive cultures (Propionibacterium acnes) for 4 patients, and we decided to consider them as a contamination. None of the patients were treated with antibiotics.
CLINICAL AND RADIOLOGICAL ASSESSMENT
Clinical evaluation included pre- and postoperative pain scores (visual analog scale [VAS]), ROM, the Constant-Murley13 score, the Simple Shoulder Test (SST),14 and the subjective shoulder value.15 Subjective satisfaction was assessed by asking the patients at follow-up how they felt compared with before surgery and was graded using a 4-point scale: 1, much better; 2, better; 3, the same; and 4, worse. Radiographic evaluation was performed on pre- and postoperative standard anteroposterior, outlet, and axillary views. Radiographs were reviewed to determine the presence of glenohumeral subluxation, periprosthetic lucency, component shift in position, and scapular notching.
STATISTICAL ANALYSIS
Descriptive statistics are reported as mean (range) for continuous measures and number (percentage) for discrete variables. The Wilcoxon signed-rank test was used for preoperative vs postoperative changes. The alpha level for all tests was set at 0.05 for statistical significance.
RESULTS
CLINICAL OUTCOME
At a mean of 22 months (range, 7-38 months) follow-up after revision, active ROM was significantly improved. Active flexion increased significantly from a mean of 93° (range, 30°-120°) to 138° (range, 95°-170°) (P = 0.021). Active external rotation with the elbow on the side increased significantly from 8° (range, −20°-15°) to 25° (range, −10°-60°) (P = 0.034), and increased with the arm held at 90° abduction from 13° (range, 0°-20°) to 49° (range, 0°-80°) (P = 0.025). Mean pain scores improved from 4.2 to 13.3 points (P < 0.001). VAS improved significantly from 9 to 1 (P < 0.0001). The mean Constant Scores improved from 21 (range, 18-32) to 63 (range, 43-90) (P = 0.006). The final SST was 7 per 12. Subjectively, 4 patients rated their shoulder as much better, 8 as better, and 1 as the same as preoperatively. No intra- or postoperative complications, including infections, were observed. The mean duration of the procedure was 60 minutes (range, 30-75 minutes).
Continue to: RADIOLOGICAL OUTCOME
RADIOLOGICAL OUTCOME
No periprosthetic lucency or shift in component was observed at the last follow-up. There was no scapular notching. No resorption of the tuberosities, and no fractures of the acromion or the scapular spine were observed.
DISCUSSION
In this retrospective study, failure of TSA with a metal-backed glenoid implant was successfully revised to RSA. In 10 patients, the use of a universal platform system allowed an easier conversion without removal of the humeral stem or the glenoid component (Figures 3A-3D). Twelve of the 13 patients were satisfied or very satisfied at the last follow-up. None of the patients were in pain, and the mean Constant score was 63. In all the cases, the glenoid baseplate was not changed. In 3 cases the humeral stem was changed without any fracture of the tuberosities of need for an osteotomy. This greatly simplified the revision procedure, as glenoid revisions can be very challenging. Indeed, it is often difficult to assess precisely preoperatively the remaining glenoid bone stock after removal of the glenoid component and the cement. Many therapeutic options to deal with glenoid loosening have been reported in the literature: glenoid bone reconstruction after glenoid component removal and revision to a hemiarthroplasty (HA),10,16-18 glenoid bone reconstruction after glenoid component removal and revision to a new TSA with a cemented glenoid implant,16,17,19,20 and glenoid reconstruction after glenoid component removal and revision to a RSA.12,21 These authors reported that glenoid reconstruction frequently necessitates an iliac bone graft associated with a special design of the baseplate with a long post fixed into the native glenoid bone. However, sometimes implantation of an uncemented glenoid component can be unstable with a high risk of early mobilization of the implant, and 2 steps may be necessary. Conversion to a HA,10,16-18 or a TSA16,17,19,20 with a new cemented implant have both been associated with poor clinical outcome, with a high rate of recurrent glenoid loosening for the TSAs.
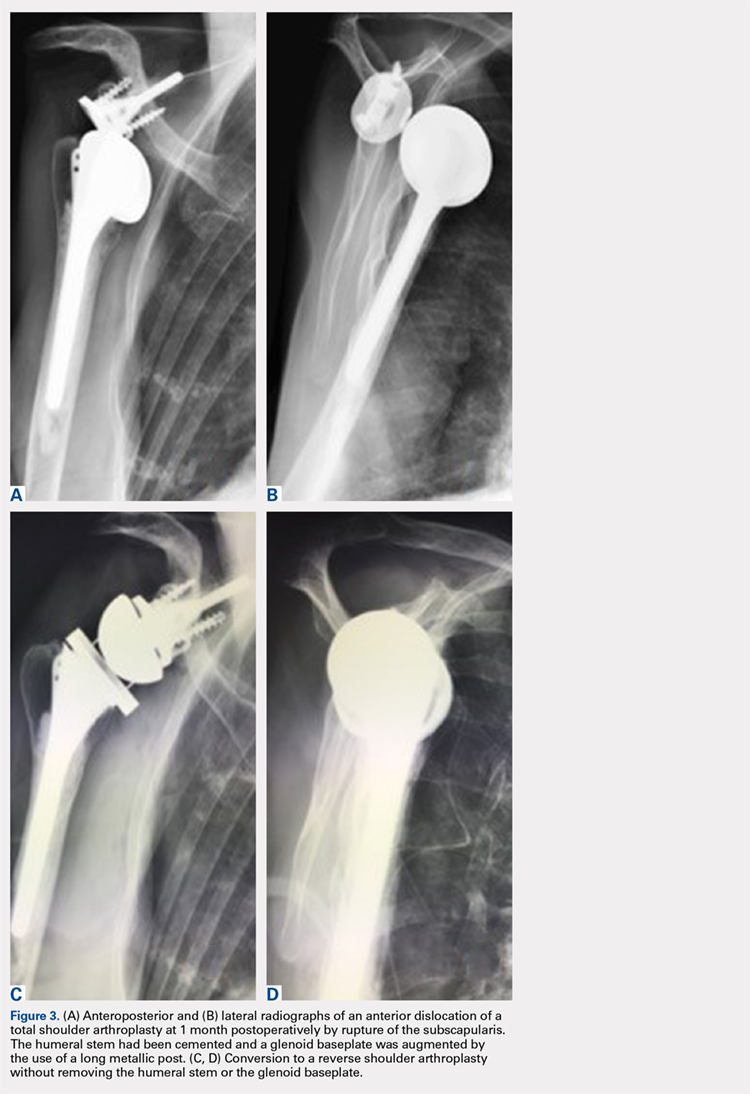
In our retrospective study, we reported no intra- or postoperative complications. Flury and colleagues22 reported a complication rate of 38% in 21 patients after conversion from a TSA to a RSA with a mean follow-up of 46 months. They removed all the components of the prosthesis with a crack or fracture of the humerus and/or the glenoid. Ortmaier and colleagues23 reported a rate of complication of 22.7% during the conversion of TSA to RSA. They did an osteotomy of the humeral diaphysis to extract the stem in 40% of cases and had to remove the glenoid cement in 86% of cases with severe damage of the glenoid bone in 10% of cases. Fewer complications were found in our study, as we did not need any procedure such as humeral osteotomy, cerclage, bone grafting, and/or reconstruction of the glenoid. The short operative time and the absence of extensive soft-tissue dissection, thanks to a standard deltopectoral approach, could explain the absence of infection in our series.
Other authors shared our strategy of a universal convertible system and reported their results in the literature. Castagna and colleagues24 in 2013 reported the clinical and radiological results of conversions of HA or TSA to RSA using a modular, convertible system (SMR Shoulder System, Lima Corporate). In their series, only 8 cases of TSAs were converted to RSA. They preserved, in each case, the humeral stem and the glenoid baseplate. There were no intra- or postoperative complications. The mean VAS score decreased from 8 to 2. Weber-Spickschen and colleague25 reported recently in 2015 the same experience with the same system (SMR Shoulder System). They reviewed 15 conversions of TSAs to RSAs without any removal of the implants at a mean 43-month follow-up. They reported excellent pain relief (VAS decreased from 8 to 1) and improvement in shoulder function with a low rate of complications.
Kany and colleagues26 in 2015 had already reported the advantages of a shoulder platform system for revisions. In their series, the authors included cases of failure of HAs and TSAs with loose cemented glenoids and metal-backed glenoids. The clinical and radiological results were similar, with a final Constant score of 60 (range, 42-85) and a similar rate of humeral stems which had to be changed (24%). These stems were replaced either because they were too proud or because there was not enough space to add an onlay polyethylene socket.
Continue to: Despite the encouraging results...
Despite the encouraging results reported in this study, there are some limitations. Firstly, no control group was used. Attempting to address this issue, we compared our results with the literature. Secondly, the number of patients in our study was small. Finally, the follow-up duration (mean 22 months) did not provide long-term outcomes.
CONCLUSION
This retrospective study shows that a complete convertible system facilitates conversion of TSAs to RSAs with excellent pain relief and a significant improvement in shoulder function. A platform system on both the humeral and the glenoid side reduces the operative time of the conversion with a low risk of complications.
1. Brenner BC, Ferlic DC, Clayton ML, Dennis DA. Survivorship of unconstrained total shoulder arthroplasty. J Bone Joint Surg Am. 1989;71(9):1289-1296.
2. Budge MD, Nolan EM, Heisey MH, Baker K, Wiater JM. Results of total shoulder arthroplasty with a monoblock porous tantalum glenoid component: a prospective minimum 2-year follow-up study. J Shoulder Elbow Surg. 2013;22(4):535-541. doi:10.1016/j.jse.2012.06.001.
3. Chin PY, Sperling JW, Cofield RH, Schleck C. Complications of total shoulder arthroplasty: are they fewer or different? J Shoulder Elbow Surg. 2006;15(1):19-22. doi:10.1016/j.jse.2005.05.005.
4. Torchia ME, Cofield RH, Settergren CR. Total shoulder arthroplasty with the Neer prosthesis: long-term results. J Shoulder Elbow Surg. 1997;6(6):495-505.
5. Wirth MA, Rockwood CA Jr. Complications of total shoulder-replacement surgery. J Bone Joint Surg Am. 1996;78(4):603-616.
6. Gohlke F, Rolf O. Revision of failed fracture hemiarthroplasties to reverse total shoulder prosthesis through the transhumeral approach: method incorporating a pectoralis-major-pedicled bone window. Oper Orthop Traumatol. 2007;19(2):185-208. doi:10.1007/s00064-007-1202-x.
7. Goldberg SH, Cohen MS, Young M, Bradnock B. Thermal tissue damage caused by ultrasonic cement removal from the humerus. J Bone Joint Surg Am. 2005;87(3):583-591. doi:10.2106/JBJS.D.01966.
8. Sperling JW, Cofield RH. Humeral windows in revision shoulder arthroplasty. J Shoulder Elbow Surg. 2005;14(3):258-263. doi:10.1016/j.jse.2004.09.004.
9. Chacon A, Virani N, Shannon R, Levy JC, Pupello D, Frankle M. Revision arthroplasty with use of a reverse shoulder prosthesis-allograft composite. J Bone Joint Surg Am. 2009;91(1):119-127. doi:10.2106/JBJS.H.00094.
10. Iannotti JP, Frangiamore SJ. Fate of large structural allograft for treatment of severe uncontained glenoid bone deficiency. J Shoulder Elbow Surg. 2012;21(6):765-771. doi:10.1016/j.jse.2011.08.069.
11. Kelly JD 2nd, Zhao JX, Hobgood ER, Norris TR. Clinical results of revision shoulder arthroplasty using the reverse prosthesis. J Shoulder Elbow Surg. 2012;21(11):1516-1525. doi:10.1016/j.jse.2011.11.021.
12. Melis B, Bonnevialle N, Neyton L, et al. Glenoid loosening and failure in anatomical total shoulder arthroplasty: is revision with a reverse shoulder arthroplasty a reliable option? J Shoulder Elbow Surg. 2012;21(3):342-349. doi:10.1016/j.jse.2011.05.021.
13. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;(214):160-164.
14. Matsen FA 3rd, Ziegler DW, DeBartolo SE. Patient self-assessment of health status and function in glenohumeral degenerative joint disease. J Shoulder Elbow Surg. 1995;4(5):345-351.
15. Gilbart MK, Gerber C. Comparison of the subjective shoulder value and the Constant score. J Shoulder Elbow Surg. 2007;16(6):717-721. doi:10.1016/j.jse.2007.02.123.
16. Antuna SA, Sperling JW, Cofield RH, Rowland CM. Glenoid revision surgery after total shoulder arthroplasty. J Shoulder Elbow Surg. 2001;10(3):217-224. doi:10.1067/mse.2001.113961.
17. Cofield RH, Edgerton BC. Total shoulder arthroplasty: complications and revision surgery. Instr Course Lect. 1990;39:449-462.
18. Neyton L, Walch G, Nove-Josserand L, Edwards TB. Glenoid corticocancellous bone grafting after glenoid component removal in the treatment of glenoid loosening. J Shoulder Elbow Surg. 2006;15(2):173-179. doi:10.1016/j.jse.2005.07.010.
19. Bonnevialle N, Melis B, Neyton L, et al. Aseptic glenoid loosening or failure in total shoulder arthroplasty: revision with glenoid reimplantation. J Shoulder Elbow Surg. 2013;22(6):745-751. doi:10.1016/j.jse.2012.08.009.
20. Rodosky MW, Bigliani LU. Indications for glenoid resurfacing in shoulder arthroplasty. J Shoulder Elbow Surg. 1996;5(3):231-248.
21. Bateman E, Donald SM. Reconstruction of massive uncontained glenoid defects using a combined autograft-allograft construct with reverse shoulder arthroplasty: preliminary results. J Shoulder Elbow Surg. 2012;21(7):925-934. doi:10.1016/j.jse.2011.07.009.
22. Flury MP, Frey P, Goldhahn J, Schwyzer HK, Simmen BR. Reverse shoulder arthroplasty as a salvage procedure for failed conventional shoulder replacement due to cuff failure--midterm results. Int Orthop. 2011;35(1):53-60. doi:10.1007/s00264-010-0990-z.
23. Ortmaier R, Resch H, Hitzl W, et al. Reverse shoulder arthroplasty combined with latissimus dorsi transfer using the bone-chip technique. Int Orthop. 2013;38(3):1-7. doi:10.1007/s00264-013-2139-3.
24. Castagna A, Delcogliano M, de Caro F, et al. Conversion of shoulder arthroplasty to reverse implants: clinical and radiological results using a modular system. Int Orthop. 2013;37(7):1297-1305. doi:10.1007/s00264-013-1907-4.
25. Weber-Spickschen TS, Alfke D, Agneskirchner JD. The use of a modular system to convert an anatomical total shoulder arthroplasty to a reverse shoulder arthroplasty: Clinical and radiological results. Bone Joint J. 2015;97-B(12):1662-1667. doi:10.1302/0301-620X.97B12.35176.
26. Kany J, Amouyel T, Flamand O, Katz D, Valenti P. A convertible shoulder system: is it useful in total shoulder arthroplasty revisions? Int Orthop. 2015;39(2):299-304. doi:10.1007/s00264-014-2563-z.
1. Brenner BC, Ferlic DC, Clayton ML, Dennis DA. Survivorship of unconstrained total shoulder arthroplasty. J Bone Joint Surg Am. 1989;71(9):1289-1296.
2. Budge MD, Nolan EM, Heisey MH, Baker K, Wiater JM. Results of total shoulder arthroplasty with a monoblock porous tantalum glenoid component: a prospective minimum 2-year follow-up study. J Shoulder Elbow Surg. 2013;22(4):535-541. doi:10.1016/j.jse.2012.06.001.
3. Chin PY, Sperling JW, Cofield RH, Schleck C. Complications of total shoulder arthroplasty: are they fewer or different? J Shoulder Elbow Surg. 2006;15(1):19-22. doi:10.1016/j.jse.2005.05.005.
4. Torchia ME, Cofield RH, Settergren CR. Total shoulder arthroplasty with the Neer prosthesis: long-term results. J Shoulder Elbow Surg. 1997;6(6):495-505.
5. Wirth MA, Rockwood CA Jr. Complications of total shoulder-replacement surgery. J Bone Joint Surg Am. 1996;78(4):603-616.
6. Gohlke F, Rolf O. Revision of failed fracture hemiarthroplasties to reverse total shoulder prosthesis through the transhumeral approach: method incorporating a pectoralis-major-pedicled bone window. Oper Orthop Traumatol. 2007;19(2):185-208. doi:10.1007/s00064-007-1202-x.
7. Goldberg SH, Cohen MS, Young M, Bradnock B. Thermal tissue damage caused by ultrasonic cement removal from the humerus. J Bone Joint Surg Am. 2005;87(3):583-591. doi:10.2106/JBJS.D.01966.
8. Sperling JW, Cofield RH. Humeral windows in revision shoulder arthroplasty. J Shoulder Elbow Surg. 2005;14(3):258-263. doi:10.1016/j.jse.2004.09.004.
9. Chacon A, Virani N, Shannon R, Levy JC, Pupello D, Frankle M. Revision arthroplasty with use of a reverse shoulder prosthesis-allograft composite. J Bone Joint Surg Am. 2009;91(1):119-127. doi:10.2106/JBJS.H.00094.
10. Iannotti JP, Frangiamore SJ. Fate of large structural allograft for treatment of severe uncontained glenoid bone deficiency. J Shoulder Elbow Surg. 2012;21(6):765-771. doi:10.1016/j.jse.2011.08.069.
11. Kelly JD 2nd, Zhao JX, Hobgood ER, Norris TR. Clinical results of revision shoulder arthroplasty using the reverse prosthesis. J Shoulder Elbow Surg. 2012;21(11):1516-1525. doi:10.1016/j.jse.2011.11.021.
12. Melis B, Bonnevialle N, Neyton L, et al. Glenoid loosening and failure in anatomical total shoulder arthroplasty: is revision with a reverse shoulder arthroplasty a reliable option? J Shoulder Elbow Surg. 2012;21(3):342-349. doi:10.1016/j.jse.2011.05.021.
13. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;(214):160-164.
14. Matsen FA 3rd, Ziegler DW, DeBartolo SE. Patient self-assessment of health status and function in glenohumeral degenerative joint disease. J Shoulder Elbow Surg. 1995;4(5):345-351.
15. Gilbart MK, Gerber C. Comparison of the subjective shoulder value and the Constant score. J Shoulder Elbow Surg. 2007;16(6):717-721. doi:10.1016/j.jse.2007.02.123.
16. Antuna SA, Sperling JW, Cofield RH, Rowland CM. Glenoid revision surgery after total shoulder arthroplasty. J Shoulder Elbow Surg. 2001;10(3):217-224. doi:10.1067/mse.2001.113961.
17. Cofield RH, Edgerton BC. Total shoulder arthroplasty: complications and revision surgery. Instr Course Lect. 1990;39:449-462.
18. Neyton L, Walch G, Nove-Josserand L, Edwards TB. Glenoid corticocancellous bone grafting after glenoid component removal in the treatment of glenoid loosening. J Shoulder Elbow Surg. 2006;15(2):173-179. doi:10.1016/j.jse.2005.07.010.
19. Bonnevialle N, Melis B, Neyton L, et al. Aseptic glenoid loosening or failure in total shoulder arthroplasty: revision with glenoid reimplantation. J Shoulder Elbow Surg. 2013;22(6):745-751. doi:10.1016/j.jse.2012.08.009.
20. Rodosky MW, Bigliani LU. Indications for glenoid resurfacing in shoulder arthroplasty. J Shoulder Elbow Surg. 1996;5(3):231-248.
21. Bateman E, Donald SM. Reconstruction of massive uncontained glenoid defects using a combined autograft-allograft construct with reverse shoulder arthroplasty: preliminary results. J Shoulder Elbow Surg. 2012;21(7):925-934. doi:10.1016/j.jse.2011.07.009.
22. Flury MP, Frey P, Goldhahn J, Schwyzer HK, Simmen BR. Reverse shoulder arthroplasty as a salvage procedure for failed conventional shoulder replacement due to cuff failure--midterm results. Int Orthop. 2011;35(1):53-60. doi:10.1007/s00264-010-0990-z.
23. Ortmaier R, Resch H, Hitzl W, et al. Reverse shoulder arthroplasty combined with latissimus dorsi transfer using the bone-chip technique. Int Orthop. 2013;38(3):1-7. doi:10.1007/s00264-013-2139-3.
24. Castagna A, Delcogliano M, de Caro F, et al. Conversion of shoulder arthroplasty to reverse implants: clinical and radiological results using a modular system. Int Orthop. 2013;37(7):1297-1305. doi:10.1007/s00264-013-1907-4.
25. Weber-Spickschen TS, Alfke D, Agneskirchner JD. The use of a modular system to convert an anatomical total shoulder arthroplasty to a reverse shoulder arthroplasty: Clinical and radiological results. Bone Joint J. 2015;97-B(12):1662-1667. doi:10.1302/0301-620X.97B12.35176.
26. Kany J, Amouyel T, Flamand O, Katz D, Valenti P. A convertible shoulder system: is it useful in total shoulder arthroplasty revisions? Int Orthop. 2015;39(2):299-304. doi:10.1007/s00264-014-2563-z.
TAKE-HOME POINTS
- Full polyethylene is the gold standard, but the revision of glenoid loosening leads a difficult reconstruction of a glenoid bone.
- A complete convertible system facilitates the revision and decreases the rate of complications.
- The functional and subjective results of the revision are good.
- During the revision, the metalback was well fixed without any sign of loosening.
- In 3 cases the humeral stem was changed; in 2 cases there was no space to reduce (onlay system) and in 1 case it was an older design, nonadapted.
MedPAC: Medicare hospital readmissions program is working
WASHINGTON – The Medicare Hospital Readmissions Reduction Program is working, according to an original analysis of Medicare claims data presented at a meeting of the Medicare Payment Advisory Commission.
“First, readmissions declined,” MedPAC staff member Jeff Stensland, PhD, said during a congressionally mandated staff report to the commissioners. “Second, while observation stays increased, they did not fully offset the decrease in readmissions. Third, while [emergency department] visits also increased, those increases appear to largely be due to factors other than the readmission program. And fourth, in addition, all the evidence we examined suggests that the readmissions program did not result in increased mortality.”
including a reduction in readmissions and patients spending less time in the hospital with “at least equal outcomes,” Dr. Stensland said at the meeting.
Taxpayers benefited from a $2 billion reduction in spending on readmissions, which will “help extend the viability of the Medicare Trust Fund.” He noted that improvements to the program will be discussed at future MedPAC meetings.
Not all MedPAC commissioners agreed with the staff analysis.
David Nerenz, PhD, of the Henry Ford Health System, Detroit, also was not convinced the program was having an impact, noting that hospital readmissions began to decline even before the program started.
In looking at a graph presented that showed this trend, “I was impressed by the fact that the trend line started coming down all the way to the left side of the graph, and what my eye was impressed with was more just the continuation rather than a change, so I guess I feel cautious saying the program had certain effects because they certainly don’t jump off the graph visually,” Dr. Nerenz said. “I’m not disputing the numbers, but to say just as a clear unqualified conclusion the program reduced readmissions, I’m not so sure.”
It is likely premature to make any firm conclusions about how effectively this program decreases unnecessary utilization of hospitals. However, it is heartening to know that it did not increase mortality. The one variable that would best control readmissions is patient education. What constitutes an emergency requiring hospital evaluation and potential admission is often not explained to the patient by you and me.
It is likely premature to make any firm conclusions about how effectively this program decreases unnecessary utilization of hospitals. However, it is heartening to know that it did not increase mortality. The one variable that would best control readmissions is patient education. What constitutes an emergency requiring hospital evaluation and potential admission is often not explained to the patient by you and me.
It is likely premature to make any firm conclusions about how effectively this program decreases unnecessary utilization of hospitals. However, it is heartening to know that it did not increase mortality. The one variable that would best control readmissions is patient education. What constitutes an emergency requiring hospital evaluation and potential admission is often not explained to the patient by you and me.
WASHINGTON – The Medicare Hospital Readmissions Reduction Program is working, according to an original analysis of Medicare claims data presented at a meeting of the Medicare Payment Advisory Commission.
“First, readmissions declined,” MedPAC staff member Jeff Stensland, PhD, said during a congressionally mandated staff report to the commissioners. “Second, while observation stays increased, they did not fully offset the decrease in readmissions. Third, while [emergency department] visits also increased, those increases appear to largely be due to factors other than the readmission program. And fourth, in addition, all the evidence we examined suggests that the readmissions program did not result in increased mortality.”
including a reduction in readmissions and patients spending less time in the hospital with “at least equal outcomes,” Dr. Stensland said at the meeting.
Taxpayers benefited from a $2 billion reduction in spending on readmissions, which will “help extend the viability of the Medicare Trust Fund.” He noted that improvements to the program will be discussed at future MedPAC meetings.
Not all MedPAC commissioners agreed with the staff analysis.
David Nerenz, PhD, of the Henry Ford Health System, Detroit, also was not convinced the program was having an impact, noting that hospital readmissions began to decline even before the program started.
In looking at a graph presented that showed this trend, “I was impressed by the fact that the trend line started coming down all the way to the left side of the graph, and what my eye was impressed with was more just the continuation rather than a change, so I guess I feel cautious saying the program had certain effects because they certainly don’t jump off the graph visually,” Dr. Nerenz said. “I’m not disputing the numbers, but to say just as a clear unqualified conclusion the program reduced readmissions, I’m not so sure.”
WASHINGTON – The Medicare Hospital Readmissions Reduction Program is working, according to an original analysis of Medicare claims data presented at a meeting of the Medicare Payment Advisory Commission.
“First, readmissions declined,” MedPAC staff member Jeff Stensland, PhD, said during a congressionally mandated staff report to the commissioners. “Second, while observation stays increased, they did not fully offset the decrease in readmissions. Third, while [emergency department] visits also increased, those increases appear to largely be due to factors other than the readmission program. And fourth, in addition, all the evidence we examined suggests that the readmissions program did not result in increased mortality.”
including a reduction in readmissions and patients spending less time in the hospital with “at least equal outcomes,” Dr. Stensland said at the meeting.
Taxpayers benefited from a $2 billion reduction in spending on readmissions, which will “help extend the viability of the Medicare Trust Fund.” He noted that improvements to the program will be discussed at future MedPAC meetings.
Not all MedPAC commissioners agreed with the staff analysis.
David Nerenz, PhD, of the Henry Ford Health System, Detroit, also was not convinced the program was having an impact, noting that hospital readmissions began to decline even before the program started.
In looking at a graph presented that showed this trend, “I was impressed by the fact that the trend line started coming down all the way to the left side of the graph, and what my eye was impressed with was more just the continuation rather than a change, so I guess I feel cautious saying the program had certain effects because they certainly don’t jump off the graph visually,” Dr. Nerenz said. “I’m not disputing the numbers, but to say just as a clear unqualified conclusion the program reduced readmissions, I’m not so sure.”
REPORTING FROM MEDPAC














