User login
Study indicates parent-reported penicillin allergy in question
, according to David Vyles, DO, and his associates at the Medical College of Wisconsin, Milwaukee.
Because there is no process to safely and rapidly diagnose true penicillin allergy in a critical care setting, pediatric providers are reluctant to prescribe penicillin to children with a reported allergy. In this study, a three-tier penicillin testing process was used to evaluate the accuracy of a parent-reported penicillin allergy questionnaire in identifying children likely to be at low risk for penicillin allergy in an ED setting.
“Our results in the current study highlight that the high percentage of patients reporting a penicillin allergy to medical providers are likely inconsistent with true allergy,” concluded Dr. Vyles and his associates.
Read more at Pediatrics (2017. doi: 10.1542/peds.2017-0471).
, according to David Vyles, DO, and his associates at the Medical College of Wisconsin, Milwaukee.
Because there is no process to safely and rapidly diagnose true penicillin allergy in a critical care setting, pediatric providers are reluctant to prescribe penicillin to children with a reported allergy. In this study, a three-tier penicillin testing process was used to evaluate the accuracy of a parent-reported penicillin allergy questionnaire in identifying children likely to be at low risk for penicillin allergy in an ED setting.
“Our results in the current study highlight that the high percentage of patients reporting a penicillin allergy to medical providers are likely inconsistent with true allergy,” concluded Dr. Vyles and his associates.
Read more at Pediatrics (2017. doi: 10.1542/peds.2017-0471).
, according to David Vyles, DO, and his associates at the Medical College of Wisconsin, Milwaukee.
Because there is no process to safely and rapidly diagnose true penicillin allergy in a critical care setting, pediatric providers are reluctant to prescribe penicillin to children with a reported allergy. In this study, a three-tier penicillin testing process was used to evaluate the accuracy of a parent-reported penicillin allergy questionnaire in identifying children likely to be at low risk for penicillin allergy in an ED setting.
“Our results in the current study highlight that the high percentage of patients reporting a penicillin allergy to medical providers are likely inconsistent with true allergy,” concluded Dr. Vyles and his associates.
Read more at Pediatrics (2017. doi: 10.1542/peds.2017-0471).
FROM PEDIATRICS
Daily probiotics have no effect on infections causing child care absences
Results of a double-blind, placebo-controlled study do not support use of probiotics to prevent upper respiratory and gastrointestinal infections in children aged 8-14 months at enrollment, as the probiotics did not reduce infection-related child care absences.
In the study of 290 Danish infants randomly allocated to receive a placebo or a combination of Bifidobacterium animalis subsp lactis (BB-12) and Lactobacillus rhamnosus (LGG) in a dose of 109 colony-forming units of each daily for a 6-month intervention period, there were no differences in absences from child care between the two groups (1.14 days; 95% confidence interval, −0.55 to 2.82), reported Rikke Pilmann Laursen, MSc, and her associates at the University of Copenhagen (Pediatrics. 2017. doi: 10.1542/peds.2017-0735).
Infants were a mean 10 months old at baseline, and 47% were still breastfeeding. The mean age at breastfeeding discontinuation was 12 months.
In terms of the number of children with one or more episodes of an upper respiratory tract infection, the LGG and BB-12 vs. placebo odds ratio was 1.22 (95% CI, 0.74-2.00; P = .43). The number of children with one or more episodes of diarrhea in the LGG and BB-12 vs. placebo odds ratio was 1.42 (95% CI, 0.88-2.32; P = .15).
The effect of probiotics in preventing infections in preschool-aged children has been explored in several studies and recent reviews, suggesting an effect specifically on upper respiratory tract and GI infections in small children. This study diverges in that it examined the effect of a combination of probiotics on absences from child care related to those infections in infants aged 8-14 months at the time of enrollment, whereas previous studies focused on children older than 1 year.
This study was funded by Innovation Fund Denmark, the University of Copenhagen, and Chr Hansen A/S. Dr. Kim Fleischer Michaelsen and Dr. Christian Mølgaard received a grant from Chr Hansen for the current study. None of the other investigators had any relevant financial disclosures.
Any intervention that can prevent child care–associated illnesses can have economic and educational implications, as well as public health ones. However, in the Laursen et al. study, almost 47% of the infants enrolled were breastfed, as opposed to previous studies in which the children participating generally were over 1 year old.
Given the positive effects of breastfeeding in preventing infections and the high percentage of infants who were breastfed in this study, it may be harder to distinguish the effects of the probiotic supplement in the Laursen et al. study. Indirectly, this study suggests additional information on the relative value of a probiotic intervention, compared with breastfeeding and diet, is warranted, and perhaps there is another reason to encourage breastfeeding as long as possible.
Michael D. Cabana, MD, MPH, is a professor of pediatrics, epidemiology and biostatistics and a member of the faculty at the Philip R. Lee Institute for Health Policy Studies at the University of California, San Francisco. Daniel J. Merenstein, MD, is an associate professor of family medicine at Georgetown University, Washington. Pharmavite, Bayer, and Sanofi have provided Georgetown University with consulting funding. Both physicians, who commented in an editorial accompanying the article by Laursen et al. (Pediatrics. 2017. doi: 10.1542/peds.2017-1729), disclosed no financial relationships relevant to this article. Dr. Merenstein has been an expert witness for Proctor & Gamble while Dr. Cabana has served as a consultant for BioGaia, Nestle, Mead Johnson, and Wyeth.
Any intervention that can prevent child care–associated illnesses can have economic and educational implications, as well as public health ones. However, in the Laursen et al. study, almost 47% of the infants enrolled were breastfed, as opposed to previous studies in which the children participating generally were over 1 year old.
Given the positive effects of breastfeeding in preventing infections and the high percentage of infants who were breastfed in this study, it may be harder to distinguish the effects of the probiotic supplement in the Laursen et al. study. Indirectly, this study suggests additional information on the relative value of a probiotic intervention, compared with breastfeeding and diet, is warranted, and perhaps there is another reason to encourage breastfeeding as long as possible.
Michael D. Cabana, MD, MPH, is a professor of pediatrics, epidemiology and biostatistics and a member of the faculty at the Philip R. Lee Institute for Health Policy Studies at the University of California, San Francisco. Daniel J. Merenstein, MD, is an associate professor of family medicine at Georgetown University, Washington. Pharmavite, Bayer, and Sanofi have provided Georgetown University with consulting funding. Both physicians, who commented in an editorial accompanying the article by Laursen et al. (Pediatrics. 2017. doi: 10.1542/peds.2017-1729), disclosed no financial relationships relevant to this article. Dr. Merenstein has been an expert witness for Proctor & Gamble while Dr. Cabana has served as a consultant for BioGaia, Nestle, Mead Johnson, and Wyeth.
Any intervention that can prevent child care–associated illnesses can have economic and educational implications, as well as public health ones. However, in the Laursen et al. study, almost 47% of the infants enrolled were breastfed, as opposed to previous studies in which the children participating generally were over 1 year old.
Given the positive effects of breastfeeding in preventing infections and the high percentage of infants who were breastfed in this study, it may be harder to distinguish the effects of the probiotic supplement in the Laursen et al. study. Indirectly, this study suggests additional information on the relative value of a probiotic intervention, compared with breastfeeding and diet, is warranted, and perhaps there is another reason to encourage breastfeeding as long as possible.
Michael D. Cabana, MD, MPH, is a professor of pediatrics, epidemiology and biostatistics and a member of the faculty at the Philip R. Lee Institute for Health Policy Studies at the University of California, San Francisco. Daniel J. Merenstein, MD, is an associate professor of family medicine at Georgetown University, Washington. Pharmavite, Bayer, and Sanofi have provided Georgetown University with consulting funding. Both physicians, who commented in an editorial accompanying the article by Laursen et al. (Pediatrics. 2017. doi: 10.1542/peds.2017-1729), disclosed no financial relationships relevant to this article. Dr. Merenstein has been an expert witness for Proctor & Gamble while Dr. Cabana has served as a consultant for BioGaia, Nestle, Mead Johnson, and Wyeth.
Results of a double-blind, placebo-controlled study do not support use of probiotics to prevent upper respiratory and gastrointestinal infections in children aged 8-14 months at enrollment, as the probiotics did not reduce infection-related child care absences.
In the study of 290 Danish infants randomly allocated to receive a placebo or a combination of Bifidobacterium animalis subsp lactis (BB-12) and Lactobacillus rhamnosus (LGG) in a dose of 109 colony-forming units of each daily for a 6-month intervention period, there were no differences in absences from child care between the two groups (1.14 days; 95% confidence interval, −0.55 to 2.82), reported Rikke Pilmann Laursen, MSc, and her associates at the University of Copenhagen (Pediatrics. 2017. doi: 10.1542/peds.2017-0735).
Infants were a mean 10 months old at baseline, and 47% were still breastfeeding. The mean age at breastfeeding discontinuation was 12 months.
In terms of the number of children with one or more episodes of an upper respiratory tract infection, the LGG and BB-12 vs. placebo odds ratio was 1.22 (95% CI, 0.74-2.00; P = .43). The number of children with one or more episodes of diarrhea in the LGG and BB-12 vs. placebo odds ratio was 1.42 (95% CI, 0.88-2.32; P = .15).
The effect of probiotics in preventing infections in preschool-aged children has been explored in several studies and recent reviews, suggesting an effect specifically on upper respiratory tract and GI infections in small children. This study diverges in that it examined the effect of a combination of probiotics on absences from child care related to those infections in infants aged 8-14 months at the time of enrollment, whereas previous studies focused on children older than 1 year.
This study was funded by Innovation Fund Denmark, the University of Copenhagen, and Chr Hansen A/S. Dr. Kim Fleischer Michaelsen and Dr. Christian Mølgaard received a grant from Chr Hansen for the current study. None of the other investigators had any relevant financial disclosures.
Results of a double-blind, placebo-controlled study do not support use of probiotics to prevent upper respiratory and gastrointestinal infections in children aged 8-14 months at enrollment, as the probiotics did not reduce infection-related child care absences.
In the study of 290 Danish infants randomly allocated to receive a placebo or a combination of Bifidobacterium animalis subsp lactis (BB-12) and Lactobacillus rhamnosus (LGG) in a dose of 109 colony-forming units of each daily for a 6-month intervention period, there were no differences in absences from child care between the two groups (1.14 days; 95% confidence interval, −0.55 to 2.82), reported Rikke Pilmann Laursen, MSc, and her associates at the University of Copenhagen (Pediatrics. 2017. doi: 10.1542/peds.2017-0735).
Infants were a mean 10 months old at baseline, and 47% were still breastfeeding. The mean age at breastfeeding discontinuation was 12 months.
In terms of the number of children with one or more episodes of an upper respiratory tract infection, the LGG and BB-12 vs. placebo odds ratio was 1.22 (95% CI, 0.74-2.00; P = .43). The number of children with one or more episodes of diarrhea in the LGG and BB-12 vs. placebo odds ratio was 1.42 (95% CI, 0.88-2.32; P = .15).
The effect of probiotics in preventing infections in preschool-aged children has been explored in several studies and recent reviews, suggesting an effect specifically on upper respiratory tract and GI infections in small children. This study diverges in that it examined the effect of a combination of probiotics on absences from child care related to those infections in infants aged 8-14 months at the time of enrollment, whereas previous studies focused on children older than 1 year.
This study was funded by Innovation Fund Denmark, the University of Copenhagen, and Chr Hansen A/S. Dr. Kim Fleischer Michaelsen and Dr. Christian Mølgaard received a grant from Chr Hansen for the current study. None of the other investigators had any relevant financial disclosures.
FROM PEDIATRICS
Key clinical point:
Major finding: Intention-to-treat analysis showed no difference between the probiotics and placebo study groups.
Data source: A randomized, double-blind, placebo-controlled study of 290 infants aged 8-14 months at enrollment.
Disclosures: This study was funded by Innovation Fund Denmark, the University of Copenhagen, and Chr Hansen A/S. Dr. Kim Fleischer Michaelsen and Dr. Christian Mølgaard received a grant from Chr Hansen for the current study. None of the other investigators had any relevant financial disclosures.
How Low Should You Go? Optimizing BP in CKD
Q) I hear providers quote different numbers for target blood pressure in kidney patients. Which are correct?
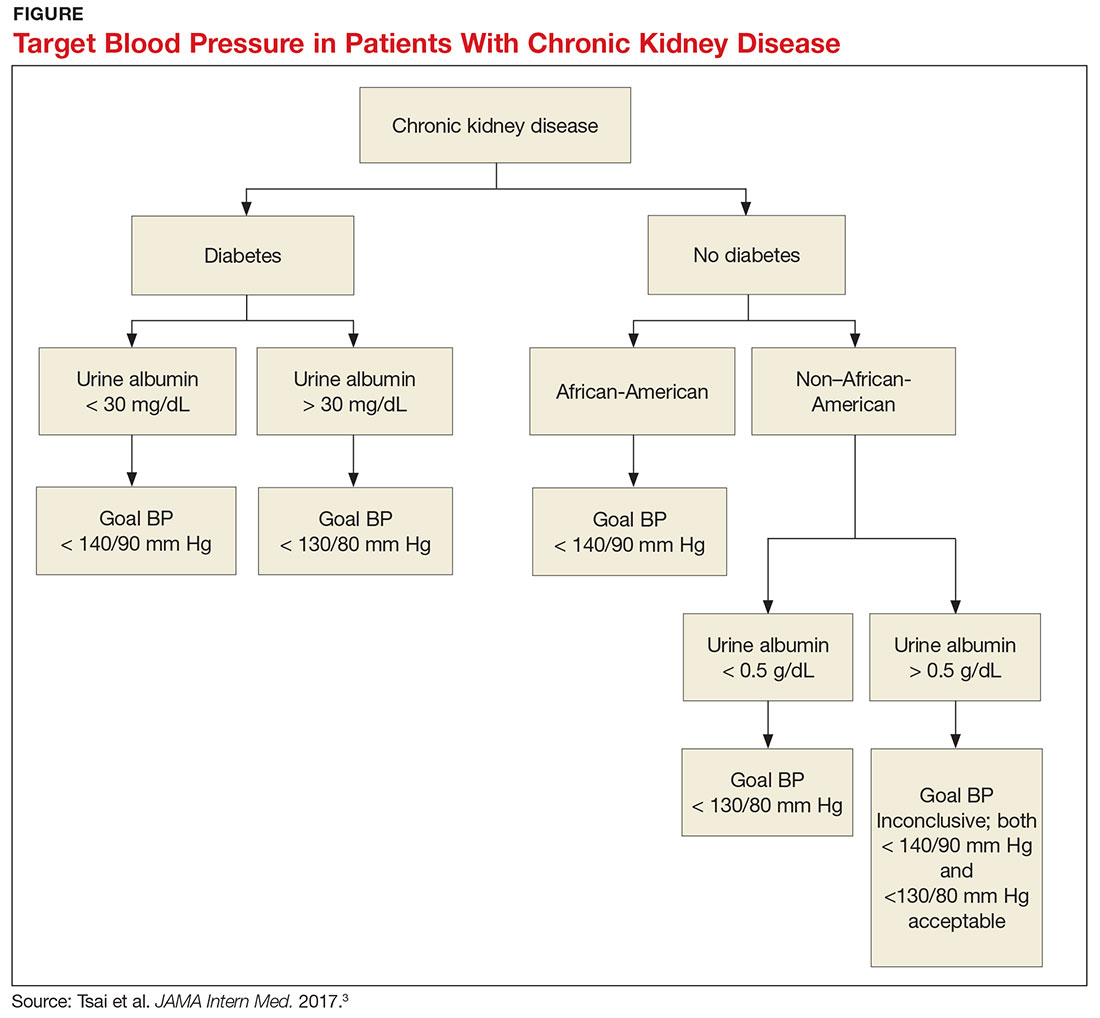
The answer to this question starts with the word “meta-analysis”—but don’t stop reading! We’ll get down to the basics quickly. Determining the goal blood pressure (BP) for patients with chronic kidney disease (CKD) comes down to three questions.
1. Does the patient have diabetes? The National Kidney Foundation states that the goal BP for a patient with type 2 diabetes, CKD, and urine albumin > 30 mg/dL is < 140/90 mm Hg.1 This is in line with the JNC-8 recommendations for patients with hypertension and CKD, which do not take urine albumin level into consideration.2 It is important to recognize that while many patients with CKD do not have diabetes, those who do have a worse prognosis.3
2. Is the patient African-American? A meta-analysis of nine randomized clinical trials found that lowering BP to < 130/80 mm Hg was linked to a slower decline in glomerular filtration rate (GFR) in non-African-American patients.3 But this BP was not beneficial for African-American patients; in fact, it actually caused a faster decline in GFR.3 Therefore, target BP for African-American patients should be < 140/90 mm Hg.
3. Does the patient have significant albuminuria? An additional subgroup analysis for patients with high levels of proteinuria (defined as > 1 g/d) yielded inconclusive results.3 Patients with proteinuria > 1 g/d tended to have a slower decline in GFR with intensive BP control.3 Proteinuria > 0.5 g/d was correlated with a slowed progression to end-stage renal disease with intensive BP control.3 Again, these were trends and not statistically significant. So, for patients with high levels of proteinuria, it will not hurt to achieve a BP < 130/80 mm Hg, but there is no statistically significant difference between BP < 130/80 mm Hg and BP < 140/90 mm Hg.
What, then, are the recommendations for an African-American patient with significant proteinuria? While not addressed directly in the analysis, the study results suggest that the goal should still be < 140/90 mm Hg, since the link between race and changes in GFR is statistically significant and the effects of proteinuria are not. Although the recommendations from this review are many, the main points are summarized in the Figure.—RC
Rebecca Clawson, MAT, PA-C
Instructor, PA Program, LSU Health Shreveport, Louisiana
1. Kidney Disease: Improving Global Outcomes (KDIGO) CKD work group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Inter Suppl. 2013;3(1):1-150.
2. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-520.
3. Tsai WC, Wu HY, Peng YS, et al. Association of intensive blood pressure control and kidney disease progression in nondiabetic patients with chronic kidney disease: a systematic review and meta-analysis. JAMA Intern Med. 2017;177:792-799.
Q) I hear providers quote different numbers for target blood pressure in kidney patients. Which are correct?
The answer to this question starts with the word “meta-analysis”—but don’t stop reading! We’ll get down to the basics quickly. Determining the goal blood pressure (BP) for patients with chronic kidney disease (CKD) comes down to three questions.
1. Does the patient have diabetes? The National Kidney Foundation states that the goal BP for a patient with type 2 diabetes, CKD, and urine albumin > 30 mg/dL is < 140/90 mm Hg.1 This is in line with the JNC-8 recommendations for patients with hypertension and CKD, which do not take urine albumin level into consideration.2 It is important to recognize that while many patients with CKD do not have diabetes, those who do have a worse prognosis.3
2. Is the patient African-American? A meta-analysis of nine randomized clinical trials found that lowering BP to < 130/80 mm Hg was linked to a slower decline in glomerular filtration rate (GFR) in non-African-American patients.3 But this BP was not beneficial for African-American patients; in fact, it actually caused a faster decline in GFR.3 Therefore, target BP for African-American patients should be < 140/90 mm Hg.
3. Does the patient have significant albuminuria? An additional subgroup analysis for patients with high levels of proteinuria (defined as > 1 g/d) yielded inconclusive results.3 Patients with proteinuria > 1 g/d tended to have a slower decline in GFR with intensive BP control.3 Proteinuria > 0.5 g/d was correlated with a slowed progression to end-stage renal disease with intensive BP control.3 Again, these were trends and not statistically significant. So, for patients with high levels of proteinuria, it will not hurt to achieve a BP < 130/80 mm Hg, but there is no statistically significant difference between BP < 130/80 mm Hg and BP < 140/90 mm Hg.
What, then, are the recommendations for an African-American patient with significant proteinuria? While not addressed directly in the analysis, the study results suggest that the goal should still be < 140/90 mm Hg, since the link between race and changes in GFR is statistically significant and the effects of proteinuria are not. Although the recommendations from this review are many, the main points are summarized in the Figure.—RC
Rebecca Clawson, MAT, PA-C
Instructor, PA Program, LSU Health Shreveport, Louisiana
Q) I hear providers quote different numbers for target blood pressure in kidney patients. Which are correct?
The answer to this question starts with the word “meta-analysis”—but don’t stop reading! We’ll get down to the basics quickly. Determining the goal blood pressure (BP) for patients with chronic kidney disease (CKD) comes down to three questions.
1. Does the patient have diabetes? The National Kidney Foundation states that the goal BP for a patient with type 2 diabetes, CKD, and urine albumin > 30 mg/dL is < 140/90 mm Hg.1 This is in line with the JNC-8 recommendations for patients with hypertension and CKD, which do not take urine albumin level into consideration.2 It is important to recognize that while many patients with CKD do not have diabetes, those who do have a worse prognosis.3
2. Is the patient African-American? A meta-analysis of nine randomized clinical trials found that lowering BP to < 130/80 mm Hg was linked to a slower decline in glomerular filtration rate (GFR) in non-African-American patients.3 But this BP was not beneficial for African-American patients; in fact, it actually caused a faster decline in GFR.3 Therefore, target BP for African-American patients should be < 140/90 mm Hg.
3. Does the patient have significant albuminuria? An additional subgroup analysis for patients with high levels of proteinuria (defined as > 1 g/d) yielded inconclusive results.3 Patients with proteinuria > 1 g/d tended to have a slower decline in GFR with intensive BP control.3 Proteinuria > 0.5 g/d was correlated with a slowed progression to end-stage renal disease with intensive BP control.3 Again, these were trends and not statistically significant. So, for patients with high levels of proteinuria, it will not hurt to achieve a BP < 130/80 mm Hg, but there is no statistically significant difference between BP < 130/80 mm Hg and BP < 140/90 mm Hg.
What, then, are the recommendations for an African-American patient with significant proteinuria? While not addressed directly in the analysis, the study results suggest that the goal should still be < 140/90 mm Hg, since the link between race and changes in GFR is statistically significant and the effects of proteinuria are not. Although the recommendations from this review are many, the main points are summarized in the Figure.—RC
Rebecca Clawson, MAT, PA-C
Instructor, PA Program, LSU Health Shreveport, Louisiana
1. Kidney Disease: Improving Global Outcomes (KDIGO) CKD work group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Inter Suppl. 2013;3(1):1-150.
2. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-520.
3. Tsai WC, Wu HY, Peng YS, et al. Association of intensive blood pressure control and kidney disease progression in nondiabetic patients with chronic kidney disease: a systematic review and meta-analysis. JAMA Intern Med. 2017;177:792-799.
1. Kidney Disease: Improving Global Outcomes (KDIGO) CKD work group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Inter Suppl. 2013;3(1):1-150.
2. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-520.
3. Tsai WC, Wu HY, Peng YS, et al. Association of intensive blood pressure control and kidney disease progression in nondiabetic patients with chronic kidney disease: a systematic review and meta-analysis. JAMA Intern Med. 2017;177:792-799.
AHRQ identifies interventions, drugs that best target diabetic neuropathy
Contextual influences of trainee characteristics and daily workload on trainee learning preferences
We previously identified key domains of attending attributes for successful rounds1 and adapted them to represent the trainees’ perspective: Teaching Process (eg, sharing decision-making process, physical exam skills), Learning Environment (eg, being approachable, respectful), Role Modeling (eg, teaching by example, bedside manner), and Team Management (eg, efficiency, providing autonomy). Though all domains are necessary, the relative importance may change in response to external pressures. Inpatient service demands and time constraints fluctuate daily due to patient admissions and discharges, educational conference schedules, and concurrent outpatient clinic responsibilities.2–4 Furthermore, the 2011 Accreditation Council for Graduate Medical Education (ACGME) duty hour rules placed greater time pressure on inpatient ward attending rounds.5 It is plausible that these pressures affect trainees’ needs and priorities during rounds.
Therefore, we sought to refine our understanding of the learners’ needs during ward rounds. Because we were interested in the contextual influences of trainee characteristics and workload on their preferences, we used the principles of ecological momentary assessment (EMA) to design a novel system to assess daily changes in trainee priorities and associated workload.
METHODS
Design, Participants, and Setting
In a prospective observational study, we assessed trainee priorities during inpatient rounds. Participants included third- and fourth-year medical students in the University of Alabama at Birmingham (UAB) School of Medicine (Birmingham campus) and residents in the Tinsley Harrison Internal Medicine Residency Training Program assigned to inpatient general medicine ward services from September 2010 to February 2011 (except from December 20, 2010, to January 3, 2011). Three training sites were included in this study: UAB Hospital (>1000-bed, university-based hospital), Birmingham Veterans Affairs Medical Center (300-bed), and Cooper Green Hospital (40-bed county hospital). Each site housed 4 or 5 general medicine ward teams, composed of 1–3 medical students (third or fourth year), 2 first-year residents, 1 upper level resident (postgraduate year 2–4), and 1 attending physician.
Trainees were recruited to participate via e-mail and verbal announcements during program conferences. Participation was voluntary and responses were confidential. As an incentive, the team submitting the highest number of cards per site each month received 1 free lunch. Institutional review boards of all 3 participating hospitals approved this study.
Assessment
Our original domains of attending rounds were derived from groupings and ratings of specific teaching characteristics by attending physicians, residents, and students.1 However, because our goal was to understand the learners’ perspective of successful ward rounds, we revised these domains by limiting the algorithm to data on groupings and ratings by residents and students only. This process resulted in the domains used in this study (Appendix).
We used EMA principles to create a novel system to assess daily variation in trainees’ prioritization of these domains and workload.6,7 EMA-derived assessment tools collect data frequently (several times per week, up to multiple times per day) to identify time-sensitive fluctuations. We designed a pocket-sized daily assessment card for trainees to complete each day after rounds (Figure 1). Trainees were asked to indicate the most important domain for successful ward rounds to them that day and provide individual characteristics (ie, sex and training level) and data on factors we hypothesized were related to perceived work load (ie, patient census, day of call cycle, and number of team members absent on rounds that day). We anticipated the Expectations domain would not be responsive to daily changes in workload because expectations are usually set once on the first day of the rotation, and thus we did not include this domain in our final assessment tool. Assessment cards and locked receptacles were kept in team workrooms for ease of accessibility; cards were collected twice monthly. All data were anonymous.
Analysis
Our unit of analysis was the EMA card. We examined associations between daily domain priority with respondent demographics and workload information using Pearson’s chi-squared analyses, adjusted for clustering effects by team. α was set at 0.05. All analyses were performed by using Stata 13.0 (Stata Statistical Software: Release 13; College Station, TX).
RESULTS
Sex and training level were associated with prioritization of teaching domains. Male trainees were more likely to choose Team Management (P = 0.01) or Teaching Process (P = 0.04) as their preferred domain. Medical students valued Teaching Process 42% of the time, compared with 23% for interns and 21% for upper level residents (P = 0.005). The opposite trend emerged for Team Management: as training level increased, the importance of Team Management increased (P < 0.001). There were no significant trends by training level for the Role Modeling and Learning Environment domains.
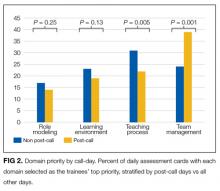
Domain priority was also associated with workload characteristics. On post-call days, Team Management (P < 0.001) was more likely to be selected as the most important domain, but on other days, Teaching Process (P = 0.005) was more often selected (Figure 2). Trainees also selected Team Management as the most important domain with an increasing number of team members absent (P = 0.001), and as the teams’ overall patient census increased (P < 0.001). The Learning Environment and Role Modeling domains’ importance did not vary by call-day or patient census.
DISCUSSION
We used a novel approach to assess contextual factors affecting trainee prioritization of 4 domains that contribute to successful inpatient internal medicine attending rounds. We found training level and workload demands were associated with prioritization of teaching domains. Prioritization of Teaching Process, exemplified by setting aside time to teach, demonstrating physical exam skills, and clear delineation of the attending’s thought process, was inversely associated with training level. On the days with highest workload, Team Management was most likely to be prioritized. Our findings suggest that attending physicians should consider adapting rounding style based on team members’ training levels and workload.
Prior work has described teaching and rounding styles, influences, and priorities in response to workload from the attending physician’s perspective,8–11 and our study extends these reports by providing the complementary perspective of trainees. On days with high workload, trainees prefer the Team Management domain, characterized by organized and efficient rounds, agreement on a clear and consistent plan of care, and being allowed independence and time during rounds to meet other responsibilities.1 These findings support an “empowerment style,” defined by Goldszmidt et al. as using integrated teaching and oversight strategies to support trainees’ progressive independence.9 Though some attending physicians report shifting to a more direct patient care style on days with a high patient census,9 our results suggest that learners instead prefer more independence, being empowered to perform more direct care. While there is an increasing pressure to heighten attending supervision due to concerns about patient safety, restricted work hours, and litigation,12 trainees value being part of the care process and being included as integral members of the care team, which may actually mitigate patient safety risks.8
Our results are consistent with prior studies, reporting that learners at different levels of training have different instructional needs: medical students seek more teaching, and senior residents sought an efficient leader.13,14 Taken together, these studies suggest that attending physicians should tailor rounds to the level of the trainee. For example, it may be beneficial for the attending physician to spend time outside of rounds with students to teach medical knowledge. During rounds, the entire group benefits most from modeling clinical reasoning, discussing new medical evidence, and demonstrating communication skills and leadership.
Our study has limitations. Though our study was performed before the 2011 ACGME duty hour restrictions,5 our results are likely of greater importance and relevance, as our findings ultimately highlight the competing demands of time vs duty. Also, while our study was performed at a single institution, potentially limiting generalizability, we included 3 types of training hospitals, a university, veterans and a county hospital, and found no differences between sites. Additionally, we collected over 1,000 cards over the course of 6 months, assessing rounds of over 50 different attending physicians, suggesting broader applicability. Our overall response rate was low, a typical signal for respondent bias, but because we collected daily assessments, standard interpretation of response rates referring to a one-time survey do not apply.15 We believe we achieved an adequate sample, as the majority of teams participated, the respondent demographics were proportional to the base population eligible to participate, and we received a similar number of cards on all months. Finally, although we were unable to account for clustering effects by individual respondents because response cards were anonymous, we adjusted for clustering effects by team.
Attending physicians may use our findings to adapt teaching techniques to appeal to specific training levels and to external pressures during teaching rounds. Focusing and investing time in teaching medical knowledge and clinical reasoning tailored to each level of learner is paramount on most days. However, days with a high workload may require emphasis on delegating clear, rational treatment plans, when learners are less receptive to traditional didactic methods.
Disclosure
An abstract based on the current analysis was presented at the Society of General Internal Medicine 34th Annual Meeting, April 2011, Phoenix, AZ. Dr. Brita Roy is supported by grant number K12HS023000 from the Agency for Healthcare Research and Quality. The authors have no conflicts to disclose. The opinions expressed in this article are those of the authors alone and do not reflect the views of the Department of Veterans Affairs or the Agency for Healthcare Research and Quality.
1. Roy B, Salanitro AH, Willett L, et al. Using cognitive mapping to identify attributes contributing to successful ward-attending rounds -- a resident and student perspective. J Gen Intern Med. 2010;25(S3):2. PubMed
2. Ben-Menachem T, Estrada C, Young MJ, et al. Balancing service and education: improving internal medicine residencies in the managed care era. Am J Med. 1996;100(2):224–229. PubMed
3. Drolet BC, Bishop KD. Unintended consequences of duty hours regulation. Acad Med. 2012;87(6):680. PubMed
4. Drolet BC, Spalluto LB, Fischer SA. Residents’ perspectives on ACGME regulation of supervision and duty hours--a national survey. N Engl J Med. 2010;363(23):e34. PubMed
5. Nasca TJ, Day SH, Amis ES, Jr. The new recommendations on duty hours from the ACGME Task Force. N Engl J Med. 2010;363(2):e3. PubMed
6. Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32. PubMed
7. Moskowitz DS, Young SN. Ecological momentary assessment: what it is and why it is a method of the future in clinical psychopharmacology. J Psychiatry Neurosci. 2006;31(1):13–20. PubMed
8. Wingo MT, Halvorsen AJ, Beckman TJ, Johnson MG, Reed DA. Associations between attending physician workload, teaching effectiveness, and patient safety. J Hosp Med. 2016;11(3):169–173. PubMed
9. Goldszmidt M, Faden L, Dornan T, van Merriënboer J, Bordage G, Lingard L. Attending physician variability: a model of four supervisory styles. Acad Med. 2015;90(11):1541–1546. PubMed
10. Kennedy TJ, Lingard L, Baker GR, Kitchen L, Regehr G. Clinical oversight: conceptualizing the relationship between supervision and safety. J Gen Intern Med. 2007;22(8):1080–1085. PubMed
11. Irby DM. How attending physicians make instructional decisions when conducting teaching rounds. Acad Med. 1992;67(10):630–638. PubMed
12. Kennedy TJ, Regehr G, Baker GR, Lingard LA. Progressive independence in clinical training: a tradition worth defending? Acad Med. 2005;80(10):S106–S111. PubMed
13. Tariq M, Motiwala A, Ali SU, Riaz M, Awan S, Akhter J. The learners’ perspective on internal medicine ward rounds: a cross-sectional study. BMC Med Educ. 2010;10:53. PubMed
14. Certain LK, Guarino AJ, Greenwald JL. Effective multilevel teaching techniques on attending rounds: a pilot survey and systematic review of the literature. Med Teach. 2011;33(12):e644–e650. PubMed
15. Stone AA, Shiffman S. Capturing momentary, self-report data: A proposal for reporting guidelines. Ann Behav Med. 2002;24(3):236–243. PubMed
We previously identified key domains of attending attributes for successful rounds1 and adapted them to represent the trainees’ perspective: Teaching Process (eg, sharing decision-making process, physical exam skills), Learning Environment (eg, being approachable, respectful), Role Modeling (eg, teaching by example, bedside manner), and Team Management (eg, efficiency, providing autonomy). Though all domains are necessary, the relative importance may change in response to external pressures. Inpatient service demands and time constraints fluctuate daily due to patient admissions and discharges, educational conference schedules, and concurrent outpatient clinic responsibilities.2–4 Furthermore, the 2011 Accreditation Council for Graduate Medical Education (ACGME) duty hour rules placed greater time pressure on inpatient ward attending rounds.5 It is plausible that these pressures affect trainees’ needs and priorities during rounds.
Therefore, we sought to refine our understanding of the learners’ needs during ward rounds. Because we were interested in the contextual influences of trainee characteristics and workload on their preferences, we used the principles of ecological momentary assessment (EMA) to design a novel system to assess daily changes in trainee priorities and associated workload.
METHODS
Design, Participants, and Setting
In a prospective observational study, we assessed trainee priorities during inpatient rounds. Participants included third- and fourth-year medical students in the University of Alabama at Birmingham (UAB) School of Medicine (Birmingham campus) and residents in the Tinsley Harrison Internal Medicine Residency Training Program assigned to inpatient general medicine ward services from September 2010 to February 2011 (except from December 20, 2010, to January 3, 2011). Three training sites were included in this study: UAB Hospital (>1000-bed, university-based hospital), Birmingham Veterans Affairs Medical Center (300-bed), and Cooper Green Hospital (40-bed county hospital). Each site housed 4 or 5 general medicine ward teams, composed of 1–3 medical students (third or fourth year), 2 first-year residents, 1 upper level resident (postgraduate year 2–4), and 1 attending physician.
Trainees were recruited to participate via e-mail and verbal announcements during program conferences. Participation was voluntary and responses were confidential. As an incentive, the team submitting the highest number of cards per site each month received 1 free lunch. Institutional review boards of all 3 participating hospitals approved this study.
Assessment
Our original domains of attending rounds were derived from groupings and ratings of specific teaching characteristics by attending physicians, residents, and students.1 However, because our goal was to understand the learners’ perspective of successful ward rounds, we revised these domains by limiting the algorithm to data on groupings and ratings by residents and students only. This process resulted in the domains used in this study (Appendix).
We used EMA principles to create a novel system to assess daily variation in trainees’ prioritization of these domains and workload.6,7 EMA-derived assessment tools collect data frequently (several times per week, up to multiple times per day) to identify time-sensitive fluctuations. We designed a pocket-sized daily assessment card for trainees to complete each day after rounds (Figure 1). Trainees were asked to indicate the most important domain for successful ward rounds to them that day and provide individual characteristics (ie, sex and training level) and data on factors we hypothesized were related to perceived work load (ie, patient census, day of call cycle, and number of team members absent on rounds that day). We anticipated the Expectations domain would not be responsive to daily changes in workload because expectations are usually set once on the first day of the rotation, and thus we did not include this domain in our final assessment tool. Assessment cards and locked receptacles were kept in team workrooms for ease of accessibility; cards were collected twice monthly. All data were anonymous.
Analysis
Our unit of analysis was the EMA card. We examined associations between daily domain priority with respondent demographics and workload information using Pearson’s chi-squared analyses, adjusted for clustering effects by team. α was set at 0.05. All analyses were performed by using Stata 13.0 (Stata Statistical Software: Release 13; College Station, TX).
RESULTS
Sex and training level were associated with prioritization of teaching domains. Male trainees were more likely to choose Team Management (P = 0.01) or Teaching Process (P = 0.04) as their preferred domain. Medical students valued Teaching Process 42% of the time, compared with 23% for interns and 21% for upper level residents (P = 0.005). The opposite trend emerged for Team Management: as training level increased, the importance of Team Management increased (P < 0.001). There were no significant trends by training level for the Role Modeling and Learning Environment domains.
Domain priority was also associated with workload characteristics. On post-call days, Team Management (P < 0.001) was more likely to be selected as the most important domain, but on other days, Teaching Process (P = 0.005) was more often selected (Figure 2). Trainees also selected Team Management as the most important domain with an increasing number of team members absent (P = 0.001), and as the teams’ overall patient census increased (P < 0.001). The Learning Environment and Role Modeling domains’ importance did not vary by call-day or patient census.
DISCUSSION
We used a novel approach to assess contextual factors affecting trainee prioritization of 4 domains that contribute to successful inpatient internal medicine attending rounds. We found training level and workload demands were associated with prioritization of teaching domains. Prioritization of Teaching Process, exemplified by setting aside time to teach, demonstrating physical exam skills, and clear delineation of the attending’s thought process, was inversely associated with training level. On the days with highest workload, Team Management was most likely to be prioritized. Our findings suggest that attending physicians should consider adapting rounding style based on team members’ training levels and workload.
Prior work has described teaching and rounding styles, influences, and priorities in response to workload from the attending physician’s perspective,8–11 and our study extends these reports by providing the complementary perspective of trainees. On days with high workload, trainees prefer the Team Management domain, characterized by organized and efficient rounds, agreement on a clear and consistent plan of care, and being allowed independence and time during rounds to meet other responsibilities.1 These findings support an “empowerment style,” defined by Goldszmidt et al. as using integrated teaching and oversight strategies to support trainees’ progressive independence.9 Though some attending physicians report shifting to a more direct patient care style on days with a high patient census,9 our results suggest that learners instead prefer more independence, being empowered to perform more direct care. While there is an increasing pressure to heighten attending supervision due to concerns about patient safety, restricted work hours, and litigation,12 trainees value being part of the care process and being included as integral members of the care team, which may actually mitigate patient safety risks.8
Our results are consistent with prior studies, reporting that learners at different levels of training have different instructional needs: medical students seek more teaching, and senior residents sought an efficient leader.13,14 Taken together, these studies suggest that attending physicians should tailor rounds to the level of the trainee. For example, it may be beneficial for the attending physician to spend time outside of rounds with students to teach medical knowledge. During rounds, the entire group benefits most from modeling clinical reasoning, discussing new medical evidence, and demonstrating communication skills and leadership.
Our study has limitations. Though our study was performed before the 2011 ACGME duty hour restrictions,5 our results are likely of greater importance and relevance, as our findings ultimately highlight the competing demands of time vs duty. Also, while our study was performed at a single institution, potentially limiting generalizability, we included 3 types of training hospitals, a university, veterans and a county hospital, and found no differences between sites. Additionally, we collected over 1,000 cards over the course of 6 months, assessing rounds of over 50 different attending physicians, suggesting broader applicability. Our overall response rate was low, a typical signal for respondent bias, but because we collected daily assessments, standard interpretation of response rates referring to a one-time survey do not apply.15 We believe we achieved an adequate sample, as the majority of teams participated, the respondent demographics were proportional to the base population eligible to participate, and we received a similar number of cards on all months. Finally, although we were unable to account for clustering effects by individual respondents because response cards were anonymous, we adjusted for clustering effects by team.
Attending physicians may use our findings to adapt teaching techniques to appeal to specific training levels and to external pressures during teaching rounds. Focusing and investing time in teaching medical knowledge and clinical reasoning tailored to each level of learner is paramount on most days. However, days with a high workload may require emphasis on delegating clear, rational treatment plans, when learners are less receptive to traditional didactic methods.
Disclosure
An abstract based on the current analysis was presented at the Society of General Internal Medicine 34th Annual Meeting, April 2011, Phoenix, AZ. Dr. Brita Roy is supported by grant number K12HS023000 from the Agency for Healthcare Research and Quality. The authors have no conflicts to disclose. The opinions expressed in this article are those of the authors alone and do not reflect the views of the Department of Veterans Affairs or the Agency for Healthcare Research and Quality.
We previously identified key domains of attending attributes for successful rounds1 and adapted them to represent the trainees’ perspective: Teaching Process (eg, sharing decision-making process, physical exam skills), Learning Environment (eg, being approachable, respectful), Role Modeling (eg, teaching by example, bedside manner), and Team Management (eg, efficiency, providing autonomy). Though all domains are necessary, the relative importance may change in response to external pressures. Inpatient service demands and time constraints fluctuate daily due to patient admissions and discharges, educational conference schedules, and concurrent outpatient clinic responsibilities.2–4 Furthermore, the 2011 Accreditation Council for Graduate Medical Education (ACGME) duty hour rules placed greater time pressure on inpatient ward attending rounds.5 It is plausible that these pressures affect trainees’ needs and priorities during rounds.
Therefore, we sought to refine our understanding of the learners’ needs during ward rounds. Because we were interested in the contextual influences of trainee characteristics and workload on their preferences, we used the principles of ecological momentary assessment (EMA) to design a novel system to assess daily changes in trainee priorities and associated workload.
METHODS
Design, Participants, and Setting
In a prospective observational study, we assessed trainee priorities during inpatient rounds. Participants included third- and fourth-year medical students in the University of Alabama at Birmingham (UAB) School of Medicine (Birmingham campus) and residents in the Tinsley Harrison Internal Medicine Residency Training Program assigned to inpatient general medicine ward services from September 2010 to February 2011 (except from December 20, 2010, to January 3, 2011). Three training sites were included in this study: UAB Hospital (>1000-bed, university-based hospital), Birmingham Veterans Affairs Medical Center (300-bed), and Cooper Green Hospital (40-bed county hospital). Each site housed 4 or 5 general medicine ward teams, composed of 1–3 medical students (third or fourth year), 2 first-year residents, 1 upper level resident (postgraduate year 2–4), and 1 attending physician.
Trainees were recruited to participate via e-mail and verbal announcements during program conferences. Participation was voluntary and responses were confidential. As an incentive, the team submitting the highest number of cards per site each month received 1 free lunch. Institutional review boards of all 3 participating hospitals approved this study.
Assessment
Our original domains of attending rounds were derived from groupings and ratings of specific teaching characteristics by attending physicians, residents, and students.1 However, because our goal was to understand the learners’ perspective of successful ward rounds, we revised these domains by limiting the algorithm to data on groupings and ratings by residents and students only. This process resulted in the domains used in this study (Appendix).
We used EMA principles to create a novel system to assess daily variation in trainees’ prioritization of these domains and workload.6,7 EMA-derived assessment tools collect data frequently (several times per week, up to multiple times per day) to identify time-sensitive fluctuations. We designed a pocket-sized daily assessment card for trainees to complete each day after rounds (Figure 1). Trainees were asked to indicate the most important domain for successful ward rounds to them that day and provide individual characteristics (ie, sex and training level) and data on factors we hypothesized were related to perceived work load (ie, patient census, day of call cycle, and number of team members absent on rounds that day). We anticipated the Expectations domain would not be responsive to daily changes in workload because expectations are usually set once on the first day of the rotation, and thus we did not include this domain in our final assessment tool. Assessment cards and locked receptacles were kept in team workrooms for ease of accessibility; cards were collected twice monthly. All data were anonymous.
Analysis
Our unit of analysis was the EMA card. We examined associations between daily domain priority with respondent demographics and workload information using Pearson’s chi-squared analyses, adjusted for clustering effects by team. α was set at 0.05. All analyses were performed by using Stata 13.0 (Stata Statistical Software: Release 13; College Station, TX).
RESULTS
Sex and training level were associated with prioritization of teaching domains. Male trainees were more likely to choose Team Management (P = 0.01) or Teaching Process (P = 0.04) as their preferred domain. Medical students valued Teaching Process 42% of the time, compared with 23% for interns and 21% for upper level residents (P = 0.005). The opposite trend emerged for Team Management: as training level increased, the importance of Team Management increased (P < 0.001). There were no significant trends by training level for the Role Modeling and Learning Environment domains.
Domain priority was also associated with workload characteristics. On post-call days, Team Management (P < 0.001) was more likely to be selected as the most important domain, but on other days, Teaching Process (P = 0.005) was more often selected (Figure 2). Trainees also selected Team Management as the most important domain with an increasing number of team members absent (P = 0.001), and as the teams’ overall patient census increased (P < 0.001). The Learning Environment and Role Modeling domains’ importance did not vary by call-day or patient census.
DISCUSSION
We used a novel approach to assess contextual factors affecting trainee prioritization of 4 domains that contribute to successful inpatient internal medicine attending rounds. We found training level and workload demands were associated with prioritization of teaching domains. Prioritization of Teaching Process, exemplified by setting aside time to teach, demonstrating physical exam skills, and clear delineation of the attending’s thought process, was inversely associated with training level. On the days with highest workload, Team Management was most likely to be prioritized. Our findings suggest that attending physicians should consider adapting rounding style based on team members’ training levels and workload.
Prior work has described teaching and rounding styles, influences, and priorities in response to workload from the attending physician’s perspective,8–11 and our study extends these reports by providing the complementary perspective of trainees. On days with high workload, trainees prefer the Team Management domain, characterized by organized and efficient rounds, agreement on a clear and consistent plan of care, and being allowed independence and time during rounds to meet other responsibilities.1 These findings support an “empowerment style,” defined by Goldszmidt et al. as using integrated teaching and oversight strategies to support trainees’ progressive independence.9 Though some attending physicians report shifting to a more direct patient care style on days with a high patient census,9 our results suggest that learners instead prefer more independence, being empowered to perform more direct care. While there is an increasing pressure to heighten attending supervision due to concerns about patient safety, restricted work hours, and litigation,12 trainees value being part of the care process and being included as integral members of the care team, which may actually mitigate patient safety risks.8
Our results are consistent with prior studies, reporting that learners at different levels of training have different instructional needs: medical students seek more teaching, and senior residents sought an efficient leader.13,14 Taken together, these studies suggest that attending physicians should tailor rounds to the level of the trainee. For example, it may be beneficial for the attending physician to spend time outside of rounds with students to teach medical knowledge. During rounds, the entire group benefits most from modeling clinical reasoning, discussing new medical evidence, and demonstrating communication skills and leadership.
Our study has limitations. Though our study was performed before the 2011 ACGME duty hour restrictions,5 our results are likely of greater importance and relevance, as our findings ultimately highlight the competing demands of time vs duty. Also, while our study was performed at a single institution, potentially limiting generalizability, we included 3 types of training hospitals, a university, veterans and a county hospital, and found no differences between sites. Additionally, we collected over 1,000 cards over the course of 6 months, assessing rounds of over 50 different attending physicians, suggesting broader applicability. Our overall response rate was low, a typical signal for respondent bias, but because we collected daily assessments, standard interpretation of response rates referring to a one-time survey do not apply.15 We believe we achieved an adequate sample, as the majority of teams participated, the respondent demographics were proportional to the base population eligible to participate, and we received a similar number of cards on all months. Finally, although we were unable to account for clustering effects by individual respondents because response cards were anonymous, we adjusted for clustering effects by team.
Attending physicians may use our findings to adapt teaching techniques to appeal to specific training levels and to external pressures during teaching rounds. Focusing and investing time in teaching medical knowledge and clinical reasoning tailored to each level of learner is paramount on most days. However, days with a high workload may require emphasis on delegating clear, rational treatment plans, when learners are less receptive to traditional didactic methods.
Disclosure
An abstract based on the current analysis was presented at the Society of General Internal Medicine 34th Annual Meeting, April 2011, Phoenix, AZ. Dr. Brita Roy is supported by grant number K12HS023000 from the Agency for Healthcare Research and Quality. The authors have no conflicts to disclose. The opinions expressed in this article are those of the authors alone and do not reflect the views of the Department of Veterans Affairs or the Agency for Healthcare Research and Quality.
1. Roy B, Salanitro AH, Willett L, et al. Using cognitive mapping to identify attributes contributing to successful ward-attending rounds -- a resident and student perspective. J Gen Intern Med. 2010;25(S3):2. PubMed
2. Ben-Menachem T, Estrada C, Young MJ, et al. Balancing service and education: improving internal medicine residencies in the managed care era. Am J Med. 1996;100(2):224–229. PubMed
3. Drolet BC, Bishop KD. Unintended consequences of duty hours regulation. Acad Med. 2012;87(6):680. PubMed
4. Drolet BC, Spalluto LB, Fischer SA. Residents’ perspectives on ACGME regulation of supervision and duty hours--a national survey. N Engl J Med. 2010;363(23):e34. PubMed
5. Nasca TJ, Day SH, Amis ES, Jr. The new recommendations on duty hours from the ACGME Task Force. N Engl J Med. 2010;363(2):e3. PubMed
6. Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32. PubMed
7. Moskowitz DS, Young SN. Ecological momentary assessment: what it is and why it is a method of the future in clinical psychopharmacology. J Psychiatry Neurosci. 2006;31(1):13–20. PubMed
8. Wingo MT, Halvorsen AJ, Beckman TJ, Johnson MG, Reed DA. Associations between attending physician workload, teaching effectiveness, and patient safety. J Hosp Med. 2016;11(3):169–173. PubMed
9. Goldszmidt M, Faden L, Dornan T, van Merriënboer J, Bordage G, Lingard L. Attending physician variability: a model of four supervisory styles. Acad Med. 2015;90(11):1541–1546. PubMed
10. Kennedy TJ, Lingard L, Baker GR, Kitchen L, Regehr G. Clinical oversight: conceptualizing the relationship between supervision and safety. J Gen Intern Med. 2007;22(8):1080–1085. PubMed
11. Irby DM. How attending physicians make instructional decisions when conducting teaching rounds. Acad Med. 1992;67(10):630–638. PubMed
12. Kennedy TJ, Regehr G, Baker GR, Lingard LA. Progressive independence in clinical training: a tradition worth defending? Acad Med. 2005;80(10):S106–S111. PubMed
13. Tariq M, Motiwala A, Ali SU, Riaz M, Awan S, Akhter J. The learners’ perspective on internal medicine ward rounds: a cross-sectional study. BMC Med Educ. 2010;10:53. PubMed
14. Certain LK, Guarino AJ, Greenwald JL. Effective multilevel teaching techniques on attending rounds: a pilot survey and systematic review of the literature. Med Teach. 2011;33(12):e644–e650. PubMed
15. Stone AA, Shiffman S. Capturing momentary, self-report data: A proposal for reporting guidelines. Ann Behav Med. 2002;24(3):236–243. PubMed
1. Roy B, Salanitro AH, Willett L, et al. Using cognitive mapping to identify attributes contributing to successful ward-attending rounds -- a resident and student perspective. J Gen Intern Med. 2010;25(S3):2. PubMed
2. Ben-Menachem T, Estrada C, Young MJ, et al. Balancing service and education: improving internal medicine residencies in the managed care era. Am J Med. 1996;100(2):224–229. PubMed
3. Drolet BC, Bishop KD. Unintended consequences of duty hours regulation. Acad Med. 2012;87(6):680. PubMed
4. Drolet BC, Spalluto LB, Fischer SA. Residents’ perspectives on ACGME regulation of supervision and duty hours--a national survey. N Engl J Med. 2010;363(23):e34. PubMed
5. Nasca TJ, Day SH, Amis ES, Jr. The new recommendations on duty hours from the ACGME Task Force. N Engl J Med. 2010;363(2):e3. PubMed
6. Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32. PubMed
7. Moskowitz DS, Young SN. Ecological momentary assessment: what it is and why it is a method of the future in clinical psychopharmacology. J Psychiatry Neurosci. 2006;31(1):13–20. PubMed
8. Wingo MT, Halvorsen AJ, Beckman TJ, Johnson MG, Reed DA. Associations between attending physician workload, teaching effectiveness, and patient safety. J Hosp Med. 2016;11(3):169–173. PubMed
9. Goldszmidt M, Faden L, Dornan T, van Merriënboer J, Bordage G, Lingard L. Attending physician variability: a model of four supervisory styles. Acad Med. 2015;90(11):1541–1546. PubMed
10. Kennedy TJ, Lingard L, Baker GR, Kitchen L, Regehr G. Clinical oversight: conceptualizing the relationship between supervision and safety. J Gen Intern Med. 2007;22(8):1080–1085. PubMed
11. Irby DM. How attending physicians make instructional decisions when conducting teaching rounds. Acad Med. 1992;67(10):630–638. PubMed
12. Kennedy TJ, Regehr G, Baker GR, Lingard LA. Progressive independence in clinical training: a tradition worth defending? Acad Med. 2005;80(10):S106–S111. PubMed
13. Tariq M, Motiwala A, Ali SU, Riaz M, Awan S, Akhter J. The learners’ perspective on internal medicine ward rounds: a cross-sectional study. BMC Med Educ. 2010;10:53. PubMed
14. Certain LK, Guarino AJ, Greenwald JL. Effective multilevel teaching techniques on attending rounds: a pilot survey and systematic review of the literature. Med Teach. 2011;33(12):e644–e650. PubMed
15. Stone AA, Shiffman S. Capturing momentary, self-report data: A proposal for reporting guidelines. Ann Behav Med. 2002;24(3):236–243. PubMed
© 2017 Society of Hospital Medicine
Drug granted PRIME access as treatment for DLBCL
The European Medicines Agency (EMA) has granted polatuzumab vedotin access to the agency’s PRIority MEdicines (PRIME) program.
The access is for polatuzumab vedotin when used in combination with rituximab and bendamustine for the treatment of relapsed or refractory diffuse large B-cell lymphoma (DLBCL).
Polatuzumab vedotin is an anti-CD79b antibody drug conjugate consisting of an anti-CD79b monoclonal antibody that is linked to a microtubule-disrupting agent.
Polatuzumab vedotin is being developed by Roche utilizing Seattle Genetics’ technology.
The goal of the EMA’s PRIME program is to accelerate the development of therapies that may offer a major advantage over existing treatments or benefit patients with no treatment options.
Through PRIME, the EMA offers early and enhanced support to developers in order to optimize development plans and speed regulatory evaluations to potentially bring therapies to patients more quickly.
To be accepted for PRIME, a therapy must demonstrate the potential to benefit patients with unmet medical need through early clinical or nonclinical data.
The acceptance of polatuzumab vedotin in the PRIME program was supported by results from the phase 2 component of the GO29365 study.
Results from this trial were recently presented at the 22nd Congress of the European Hematology Association (EHA) as abstract S468. ![]()
The European Medicines Agency (EMA) has granted polatuzumab vedotin access to the agency’s PRIority MEdicines (PRIME) program.
The access is for polatuzumab vedotin when used in combination with rituximab and bendamustine for the treatment of relapsed or refractory diffuse large B-cell lymphoma (DLBCL).
Polatuzumab vedotin is an anti-CD79b antibody drug conjugate consisting of an anti-CD79b monoclonal antibody that is linked to a microtubule-disrupting agent.
Polatuzumab vedotin is being developed by Roche utilizing Seattle Genetics’ technology.
The goal of the EMA’s PRIME program is to accelerate the development of therapies that may offer a major advantage over existing treatments or benefit patients with no treatment options.
Through PRIME, the EMA offers early and enhanced support to developers in order to optimize development plans and speed regulatory evaluations to potentially bring therapies to patients more quickly.
To be accepted for PRIME, a therapy must demonstrate the potential to benefit patients with unmet medical need through early clinical or nonclinical data.
The acceptance of polatuzumab vedotin in the PRIME program was supported by results from the phase 2 component of the GO29365 study.
Results from this trial were recently presented at the 22nd Congress of the European Hematology Association (EHA) as abstract S468. ![]()
The European Medicines Agency (EMA) has granted polatuzumab vedotin access to the agency’s PRIority MEdicines (PRIME) program.
The access is for polatuzumab vedotin when used in combination with rituximab and bendamustine for the treatment of relapsed or refractory diffuse large B-cell lymphoma (DLBCL).
Polatuzumab vedotin is an anti-CD79b antibody drug conjugate consisting of an anti-CD79b monoclonal antibody that is linked to a microtubule-disrupting agent.
Polatuzumab vedotin is being developed by Roche utilizing Seattle Genetics’ technology.
The goal of the EMA’s PRIME program is to accelerate the development of therapies that may offer a major advantage over existing treatments or benefit patients with no treatment options.
Through PRIME, the EMA offers early and enhanced support to developers in order to optimize development plans and speed regulatory evaluations to potentially bring therapies to patients more quickly.
To be accepted for PRIME, a therapy must demonstrate the potential to benefit patients with unmet medical need through early clinical or nonclinical data.
The acceptance of polatuzumab vedotin in the PRIME program was supported by results from the phase 2 component of the GO29365 study.
Results from this trial were recently presented at the 22nd Congress of the European Hematology Association (EHA) as abstract S468. ![]()
Writing: Do Make a MEAL of It!
Writing for publication fulfills a professional obligation to contribute to the body of knowledge. In the past decade, we’ve seen increases in the number of journals and in the number of NPs and PAs—providing more publishing opportunities and more potential authors. Yet many of my colleagues have little interest in publishing; perhaps they fear the writing process or believe they lack the skills to compose a manuscript.
How, then, do we cajole them into sharing their expertise in written form? Much has been written about why you should write.1,2 What is needed is guidance on the process to help overcome the common barriers to success in publishing. If it’s been a long time since you were in school at all—or at least since you took English Composition 101—allow me to offer a solid starting point for the journey of writing.
A manuscript, in essence, is a collection of paragraphs that follow a traditional flow. But to be sufficiently developed, paragraphs must (1) contain a main idea, (2) be structurally coherent, and (3) maintain a sense of unity around the idea.3 Once authors master the composition of a strong paragraph, the development of the manuscript comes naturally. Here are seven tips—four on content development and three on form—for compiling a manuscript worthy of publication and personal pride.
1. Start strong. Everyone understands the importance of grabbing a reader’s attention right out of the gate, right? A strong topic sentence does more than introduce the subject; it sets the tone for those that follow. A short sentence at the beginning of a paragraph establishes an understanding that a discussion will follow—and offers a preview of what the discussion will entail. But writers need not be limited; a topic sentence can take the form of a question or be placed later in the paragraph. Less experienced authors may prefer to open the paragraph with the topic sentence, however, as this allows for a quick assessment of whether the subsequent sentences follow logically. In other words, start simple—there is room to grow as you gain confidence with writing.
2. Use the MEAL plan. A paragraph should extend from the topic sentence. Collectively, the paragraph’s sentences should follow the steps outlined in the “MEAL plan,” a valuable resource conceptualized by the Duke University Thompson Writing Program.4 The “M” stands for the main topic; “E,” for the evidence that supports or refutes the topic sentence; “A,” for analysis and its importance; and “L,” for the link back to the larger claim (ie, the overall topic of the paper).
Using the MEAL approach is relatively straightforward. Picture yourself as the sender of a message; the reader is your recipient. You need to convey the information to your reader so that he or she understands it.
Limiting the number of words in a sentence and the number of sentences in a paragraph may help. Exceedingly long sentences are cumbersome and threaten to muddle the author’s message. They also pose the risk for improper noun/verb agreement, irregular punctuation, and hindered readability. (But then, what are editors for?)
A paragraph presents a well-formulated argument; one that contains only two sentences is unlikely to support the author’s assertion. Novice writers, however, often go to the other extreme, which dilutes the point. As a rule of thumb, if you can speak the entire paragraph with a single breath, the length is adequate. Reading your work aloud also helps identify hidden hazards.
3. Make connections. The result would be confusing and nonsensical. Similarly, you wouldn’t conclude your paragraph before you’ve started it. Imagine if you tried to clean out a wound after applying a dressing. The key to a good paragraph is cohesion.
If you’re scratching your head at the previous paragraph, you take my next point: All sentences within a paragraph should have a natural flow. In a well-developed paragraph, each sentence directly relates to the one before and the one after; they work together to convey your point. If the topic sentence contains an assertion, the following sentences provide supporting evidence. In medical writing, this evidence comes from citations to published literature.
If you are using the MEAL plan, you have an outline for how to support your topic sentence in a logical manner. You can then link sentences by capitalizing on words or phrases to form bridges that carry the reader through the paragraph.5 These links are created through repetition of key words or through parallel grammatical forms.
4. Pump the brakes. No one likes an abrupt stop. When you’re winding down on a paragraph, you need to signal to the reader that you’re going to shift gears. The last sentence of a paragraph should serve as a natural transition to the next paragraph.6 Equally important is the transition line at the beginning of the next paragraph.
Regardless of where the transition occurs, the goal remains to help the reader follow your logic. A subsequent paragraph can extend or refute the argument that has been presented, or it can introduce an entirely new point. No matter what, you want the reader to be prepared for a change in focus and to stay with you through your transition to a new perspective or subtopic.
On the other hand, if the argument is exhausted—it stops. When your discussion is complete, the transition to the next paragraph is very different (eg, “In summary…”). This is an appropriate time to move to a new paragraph and new section.
Speaking of a new section, let’s switch our focus to form.
5. Take action. There are two types of “voice” in communication: active, in which the subject is taking some form of action (eg, You are reading this article), and passive, in which the action is performed upon the subject (eg, This article is being read by you). Active voice is preferred for several reasons—namely, clarity and space. An active sentence identifies who is doing what. The same conclusion may be reached through a passive sentence, with some effort on the reader’s part—but active sentences tend to be more concise. They also convey a sense of immediacy, hopefully drawing the reader into your article.
6. Punctuate like a pro. Punctuation is important! It provides structure, improving clarity and comprehension. Can you fathom the confusion that would occur if an author misused (or failed to use) appropriate punctuation?
Thankfully, rules regarding punctuation have not changed much over the past century. One notable exception is use of the serial (or “Oxford”) comma, which incites passionate debate among both amateur and professional linguists.7 (For the record, this publication uses the Oxford comma. Just ask the editors: Karen, Ann, and Amy.)
A full review of punctuation is beyond the scope of this article; however, be it known that the most problematic marks—the ones to double-check in your own writing—are the apostrophe (plural or singular possessive use), the semi-colon, the comma (or lack of), and quotation marks.8 To improve your punctuation, obtain a basic grammar handbook or search online.
7. Don’t volley with verbs. Verb tense should remain consistent throughout the paragraph.9 Paragraphs with multiple verb tenses bounce the reader’s mind back and forth. It’s like watching a ping pong match, but less enjoyable.
To check for consistency, print the manuscript and mix the order of the pages. Circle the verbs. Look at the circled words and assess the tense of each. Then, repair the damage.
It is easier to identify these types of problems with a manuscript when you’re reading the pages out of order. Editors will tell you that it is difficult to focus on particulars when you are distracted by the content of the paper. Out-of-order pages are harder to read for “sense,” so you can focus on tense, voice, and punctuation.
In conclusion, I hope I’ve helped you see that writing is a process—some say a craft—but it is one that anyone can tackle with the right mindset and preparation. Most authors have a key message; they may just need help expressing it. Starting with small elements, such as the paragraph, helps the author deliver the message clearly.
1. Danielsen RD. I’d like to write a medical article, but …. Clinician Reviews. 2013;23(12):11-12.
2. Onieal ME. Be the change you wish to see. Clinician Reviews. 2015;25(7):8-9.
3. Monmouth University Tutoring and Writing Services. Paragraphs. www.monmouth.edu/uploadedFiles/Resources_for_Writers/The_Writing_Process/Paragraphs2013.pdf. Accessed June 1, 2017.
4. Duke University Thompson Writing Program. Paragraphing: The MEAL Plan. https://twp.duke.edu/sites/twp.duke.edu/files/file-attachments/meal-plan.original.pdf. Accessed June 1, 2017.
5. Purdue Online Writing Lab. On paragraphs. https://owl.english.purdue.edu/owl/resource/606/01/. Accessed June 1, 2017.
6. The Writing Center at UNC–Chapel Hill. Transitions. http://writingcenter.unc.edu/handouts/transitions/. Accessed June 1, 2017.
7. Edwards A. What is the Oxford comma and why do people care so much about it? www.grammarly.com/blog/what-is-the-oxford-comma-and-why-do-people-care-so-much-about-it/. Accessed June 1, 2017.
8. Endpaper: the Paperblanks blog. Writing Wednesday: 3 most commonly misused punctuation marks. February 1, 2017. http://blog.paperblanks.com/2017/02/writing-wednesday-3-most-commonly-misused-punctuation-marks/. Accessed June 1, 2017.
9. Towson University Online Writing Support. Verb tense consistency. https://webapps.towson.edu/ows/tenseconsistency.htm. Accessed June 1, 2017.
Writing for publication fulfills a professional obligation to contribute to the body of knowledge. In the past decade, we’ve seen increases in the number of journals and in the number of NPs and PAs—providing more publishing opportunities and more potential authors. Yet many of my colleagues have little interest in publishing; perhaps they fear the writing process or believe they lack the skills to compose a manuscript.
How, then, do we cajole them into sharing their expertise in written form? Much has been written about why you should write.1,2 What is needed is guidance on the process to help overcome the common barriers to success in publishing. If it’s been a long time since you were in school at all—or at least since you took English Composition 101—allow me to offer a solid starting point for the journey of writing.
A manuscript, in essence, is a collection of paragraphs that follow a traditional flow. But to be sufficiently developed, paragraphs must (1) contain a main idea, (2) be structurally coherent, and (3) maintain a sense of unity around the idea.3 Once authors master the composition of a strong paragraph, the development of the manuscript comes naturally. Here are seven tips—four on content development and three on form—for compiling a manuscript worthy of publication and personal pride.
1. Start strong. Everyone understands the importance of grabbing a reader’s attention right out of the gate, right? A strong topic sentence does more than introduce the subject; it sets the tone for those that follow. A short sentence at the beginning of a paragraph establishes an understanding that a discussion will follow—and offers a preview of what the discussion will entail. But writers need not be limited; a topic sentence can take the form of a question or be placed later in the paragraph. Less experienced authors may prefer to open the paragraph with the topic sentence, however, as this allows for a quick assessment of whether the subsequent sentences follow logically. In other words, start simple—there is room to grow as you gain confidence with writing.
2. Use the MEAL plan. A paragraph should extend from the topic sentence. Collectively, the paragraph’s sentences should follow the steps outlined in the “MEAL plan,” a valuable resource conceptualized by the Duke University Thompson Writing Program.4 The “M” stands for the main topic; “E,” for the evidence that supports or refutes the topic sentence; “A,” for analysis and its importance; and “L,” for the link back to the larger claim (ie, the overall topic of the paper).
Using the MEAL approach is relatively straightforward. Picture yourself as the sender of a message; the reader is your recipient. You need to convey the information to your reader so that he or she understands it.
Limiting the number of words in a sentence and the number of sentences in a paragraph may help. Exceedingly long sentences are cumbersome and threaten to muddle the author’s message. They also pose the risk for improper noun/verb agreement, irregular punctuation, and hindered readability. (But then, what are editors for?)
A paragraph presents a well-formulated argument; one that contains only two sentences is unlikely to support the author’s assertion. Novice writers, however, often go to the other extreme, which dilutes the point. As a rule of thumb, if you can speak the entire paragraph with a single breath, the length is adequate. Reading your work aloud also helps identify hidden hazards.
3. Make connections. The result would be confusing and nonsensical. Similarly, you wouldn’t conclude your paragraph before you’ve started it. Imagine if you tried to clean out a wound after applying a dressing. The key to a good paragraph is cohesion.
If you’re scratching your head at the previous paragraph, you take my next point: All sentences within a paragraph should have a natural flow. In a well-developed paragraph, each sentence directly relates to the one before and the one after; they work together to convey your point. If the topic sentence contains an assertion, the following sentences provide supporting evidence. In medical writing, this evidence comes from citations to published literature.
If you are using the MEAL plan, you have an outline for how to support your topic sentence in a logical manner. You can then link sentences by capitalizing on words or phrases to form bridges that carry the reader through the paragraph.5 These links are created through repetition of key words or through parallel grammatical forms.
4. Pump the brakes. No one likes an abrupt stop. When you’re winding down on a paragraph, you need to signal to the reader that you’re going to shift gears. The last sentence of a paragraph should serve as a natural transition to the next paragraph.6 Equally important is the transition line at the beginning of the next paragraph.
Regardless of where the transition occurs, the goal remains to help the reader follow your logic. A subsequent paragraph can extend or refute the argument that has been presented, or it can introduce an entirely new point. No matter what, you want the reader to be prepared for a change in focus and to stay with you through your transition to a new perspective or subtopic.
On the other hand, if the argument is exhausted—it stops. When your discussion is complete, the transition to the next paragraph is very different (eg, “In summary…”). This is an appropriate time to move to a new paragraph and new section.
Speaking of a new section, let’s switch our focus to form.
5. Take action. There are two types of “voice” in communication: active, in which the subject is taking some form of action (eg, You are reading this article), and passive, in which the action is performed upon the subject (eg, This article is being read by you). Active voice is preferred for several reasons—namely, clarity and space. An active sentence identifies who is doing what. The same conclusion may be reached through a passive sentence, with some effort on the reader’s part—but active sentences tend to be more concise. They also convey a sense of immediacy, hopefully drawing the reader into your article.
6. Punctuate like a pro. Punctuation is important! It provides structure, improving clarity and comprehension. Can you fathom the confusion that would occur if an author misused (or failed to use) appropriate punctuation?
Thankfully, rules regarding punctuation have not changed much over the past century. One notable exception is use of the serial (or “Oxford”) comma, which incites passionate debate among both amateur and professional linguists.7 (For the record, this publication uses the Oxford comma. Just ask the editors: Karen, Ann, and Amy.)
A full review of punctuation is beyond the scope of this article; however, be it known that the most problematic marks—the ones to double-check in your own writing—are the apostrophe (plural or singular possessive use), the semi-colon, the comma (or lack of), and quotation marks.8 To improve your punctuation, obtain a basic grammar handbook or search online.
7. Don’t volley with verbs. Verb tense should remain consistent throughout the paragraph.9 Paragraphs with multiple verb tenses bounce the reader’s mind back and forth. It’s like watching a ping pong match, but less enjoyable.
To check for consistency, print the manuscript and mix the order of the pages. Circle the verbs. Look at the circled words and assess the tense of each. Then, repair the damage.
It is easier to identify these types of problems with a manuscript when you’re reading the pages out of order. Editors will tell you that it is difficult to focus on particulars when you are distracted by the content of the paper. Out-of-order pages are harder to read for “sense,” so you can focus on tense, voice, and punctuation.
In conclusion, I hope I’ve helped you see that writing is a process—some say a craft—but it is one that anyone can tackle with the right mindset and preparation. Most authors have a key message; they may just need help expressing it. Starting with small elements, such as the paragraph, helps the author deliver the message clearly.
Writing for publication fulfills a professional obligation to contribute to the body of knowledge. In the past decade, we’ve seen increases in the number of journals and in the number of NPs and PAs—providing more publishing opportunities and more potential authors. Yet many of my colleagues have little interest in publishing; perhaps they fear the writing process or believe they lack the skills to compose a manuscript.
How, then, do we cajole them into sharing their expertise in written form? Much has been written about why you should write.1,2 What is needed is guidance on the process to help overcome the common barriers to success in publishing. If it’s been a long time since you were in school at all—or at least since you took English Composition 101—allow me to offer a solid starting point for the journey of writing.
A manuscript, in essence, is a collection of paragraphs that follow a traditional flow. But to be sufficiently developed, paragraphs must (1) contain a main idea, (2) be structurally coherent, and (3) maintain a sense of unity around the idea.3 Once authors master the composition of a strong paragraph, the development of the manuscript comes naturally. Here are seven tips—four on content development and three on form—for compiling a manuscript worthy of publication and personal pride.
1. Start strong. Everyone understands the importance of grabbing a reader’s attention right out of the gate, right? A strong topic sentence does more than introduce the subject; it sets the tone for those that follow. A short sentence at the beginning of a paragraph establishes an understanding that a discussion will follow—and offers a preview of what the discussion will entail. But writers need not be limited; a topic sentence can take the form of a question or be placed later in the paragraph. Less experienced authors may prefer to open the paragraph with the topic sentence, however, as this allows for a quick assessment of whether the subsequent sentences follow logically. In other words, start simple—there is room to grow as you gain confidence with writing.
2. Use the MEAL plan. A paragraph should extend from the topic sentence. Collectively, the paragraph’s sentences should follow the steps outlined in the “MEAL plan,” a valuable resource conceptualized by the Duke University Thompson Writing Program.4 The “M” stands for the main topic; “E,” for the evidence that supports or refutes the topic sentence; “A,” for analysis and its importance; and “L,” for the link back to the larger claim (ie, the overall topic of the paper).
Using the MEAL approach is relatively straightforward. Picture yourself as the sender of a message; the reader is your recipient. You need to convey the information to your reader so that he or she understands it.
Limiting the number of words in a sentence and the number of sentences in a paragraph may help. Exceedingly long sentences are cumbersome and threaten to muddle the author’s message. They also pose the risk for improper noun/verb agreement, irregular punctuation, and hindered readability. (But then, what are editors for?)
A paragraph presents a well-formulated argument; one that contains only two sentences is unlikely to support the author’s assertion. Novice writers, however, often go to the other extreme, which dilutes the point. As a rule of thumb, if you can speak the entire paragraph with a single breath, the length is adequate. Reading your work aloud also helps identify hidden hazards.
3. Make connections. The result would be confusing and nonsensical. Similarly, you wouldn’t conclude your paragraph before you’ve started it. Imagine if you tried to clean out a wound after applying a dressing. The key to a good paragraph is cohesion.
If you’re scratching your head at the previous paragraph, you take my next point: All sentences within a paragraph should have a natural flow. In a well-developed paragraph, each sentence directly relates to the one before and the one after; they work together to convey your point. If the topic sentence contains an assertion, the following sentences provide supporting evidence. In medical writing, this evidence comes from citations to published literature.
If you are using the MEAL plan, you have an outline for how to support your topic sentence in a logical manner. You can then link sentences by capitalizing on words or phrases to form bridges that carry the reader through the paragraph.5 These links are created through repetition of key words or through parallel grammatical forms.
4. Pump the brakes. No one likes an abrupt stop. When you’re winding down on a paragraph, you need to signal to the reader that you’re going to shift gears. The last sentence of a paragraph should serve as a natural transition to the next paragraph.6 Equally important is the transition line at the beginning of the next paragraph.
Regardless of where the transition occurs, the goal remains to help the reader follow your logic. A subsequent paragraph can extend or refute the argument that has been presented, or it can introduce an entirely new point. No matter what, you want the reader to be prepared for a change in focus and to stay with you through your transition to a new perspective or subtopic.
On the other hand, if the argument is exhausted—it stops. When your discussion is complete, the transition to the next paragraph is very different (eg, “In summary…”). This is an appropriate time to move to a new paragraph and new section.
Speaking of a new section, let’s switch our focus to form.
5. Take action. There are two types of “voice” in communication: active, in which the subject is taking some form of action (eg, You are reading this article), and passive, in which the action is performed upon the subject (eg, This article is being read by you). Active voice is preferred for several reasons—namely, clarity and space. An active sentence identifies who is doing what. The same conclusion may be reached through a passive sentence, with some effort on the reader’s part—but active sentences tend to be more concise. They also convey a sense of immediacy, hopefully drawing the reader into your article.
6. Punctuate like a pro. Punctuation is important! It provides structure, improving clarity and comprehension. Can you fathom the confusion that would occur if an author misused (or failed to use) appropriate punctuation?
Thankfully, rules regarding punctuation have not changed much over the past century. One notable exception is use of the serial (or “Oxford”) comma, which incites passionate debate among both amateur and professional linguists.7 (For the record, this publication uses the Oxford comma. Just ask the editors: Karen, Ann, and Amy.)
A full review of punctuation is beyond the scope of this article; however, be it known that the most problematic marks—the ones to double-check in your own writing—are the apostrophe (plural or singular possessive use), the semi-colon, the comma (or lack of), and quotation marks.8 To improve your punctuation, obtain a basic grammar handbook or search online.
7. Don’t volley with verbs. Verb tense should remain consistent throughout the paragraph.9 Paragraphs with multiple verb tenses bounce the reader’s mind back and forth. It’s like watching a ping pong match, but less enjoyable.
To check for consistency, print the manuscript and mix the order of the pages. Circle the verbs. Look at the circled words and assess the tense of each. Then, repair the damage.
It is easier to identify these types of problems with a manuscript when you’re reading the pages out of order. Editors will tell you that it is difficult to focus on particulars when you are distracted by the content of the paper. Out-of-order pages are harder to read for “sense,” so you can focus on tense, voice, and punctuation.
In conclusion, I hope I’ve helped you see that writing is a process—some say a craft—but it is one that anyone can tackle with the right mindset and preparation. Most authors have a key message; they may just need help expressing it. Starting with small elements, such as the paragraph, helps the author deliver the message clearly.
1. Danielsen RD. I’d like to write a medical article, but …. Clinician Reviews. 2013;23(12):11-12.
2. Onieal ME. Be the change you wish to see. Clinician Reviews. 2015;25(7):8-9.
3. Monmouth University Tutoring and Writing Services. Paragraphs. www.monmouth.edu/uploadedFiles/Resources_for_Writers/The_Writing_Process/Paragraphs2013.pdf. Accessed June 1, 2017.
4. Duke University Thompson Writing Program. Paragraphing: The MEAL Plan. https://twp.duke.edu/sites/twp.duke.edu/files/file-attachments/meal-plan.original.pdf. Accessed June 1, 2017.
5. Purdue Online Writing Lab. On paragraphs. https://owl.english.purdue.edu/owl/resource/606/01/. Accessed June 1, 2017.
6. The Writing Center at UNC–Chapel Hill. Transitions. http://writingcenter.unc.edu/handouts/transitions/. Accessed June 1, 2017.
7. Edwards A. What is the Oxford comma and why do people care so much about it? www.grammarly.com/blog/what-is-the-oxford-comma-and-why-do-people-care-so-much-about-it/. Accessed June 1, 2017.
8. Endpaper: the Paperblanks blog. Writing Wednesday: 3 most commonly misused punctuation marks. February 1, 2017. http://blog.paperblanks.com/2017/02/writing-wednesday-3-most-commonly-misused-punctuation-marks/. Accessed June 1, 2017.
9. Towson University Online Writing Support. Verb tense consistency. https://webapps.towson.edu/ows/tenseconsistency.htm. Accessed June 1, 2017.
1. Danielsen RD. I’d like to write a medical article, but …. Clinician Reviews. 2013;23(12):11-12.
2. Onieal ME. Be the change you wish to see. Clinician Reviews. 2015;25(7):8-9.
3. Monmouth University Tutoring and Writing Services. Paragraphs. www.monmouth.edu/uploadedFiles/Resources_for_Writers/The_Writing_Process/Paragraphs2013.pdf. Accessed June 1, 2017.
4. Duke University Thompson Writing Program. Paragraphing: The MEAL Plan. https://twp.duke.edu/sites/twp.duke.edu/files/file-attachments/meal-plan.original.pdf. Accessed June 1, 2017.
5. Purdue Online Writing Lab. On paragraphs. https://owl.english.purdue.edu/owl/resource/606/01/. Accessed June 1, 2017.
6. The Writing Center at UNC–Chapel Hill. Transitions. http://writingcenter.unc.edu/handouts/transitions/. Accessed June 1, 2017.
7. Edwards A. What is the Oxford comma and why do people care so much about it? www.grammarly.com/blog/what-is-the-oxford-comma-and-why-do-people-care-so-much-about-it/. Accessed June 1, 2017.
8. Endpaper: the Paperblanks blog. Writing Wednesday: 3 most commonly misused punctuation marks. February 1, 2017. http://blog.paperblanks.com/2017/02/writing-wednesday-3-most-commonly-misused-punctuation-marks/. Accessed June 1, 2017.
9. Towson University Online Writing Support. Verb tense consistency. https://webapps.towson.edu/ows/tenseconsistency.htm. Accessed June 1, 2017.
‘Chronic Lyme’: Serious bacterial infections reported with unproven treatments
Unproven treatments for so-called chronic Lyme disease can cause serious, even fatal, complications, according to five case reports published in the Morbidity and Mortality Weekly Report.
“Patients, clinicians, and public health practitioners should be aware that treatments for chronic Lyme disease can carry serious risks,” the authors wrote.
Chronic Lyme disease is a nonspecific diagnosis that has no consistent definition. Some clinicians use this label for patients who have a variety of debilitating conditions such as fatigue, generalized pain, and neurologic symptoms, even in the absence of laboratory evidence of Borrelia burgdorferi infection, objective signs of infection, or a history of tick exposure. People who support this diagnosis mistakenly believe that B. burgdorferi can cause longstanding disabling symptoms even when standard testing for the organism is negative, when the truth is that tests for the organism become more sensitive the longer the infection persists, according to Natalie S. Marzec, MD, a resident in preventive medicine at the University of Colorado, Aurora, and her associates.
Patients who cannot obtain symptom relief with conventional clinicians may consult “practitioners who might identify themselves as Lyme disease specialists (‘Lyme literate’ doctors) or from complementary and alternative medicine clinics,” where they are diagnosed with chronic Lyme disease. Such patients have been offered unproven treatments, including extended courses of intravenous antibiotics, infusions of hydrogen peroxide, immunoglobulin therapy, hyperbaric oxygen treatment, electromagnetic frequency therapy, garlic supplements, colloidal silver, and stem-cell transplantation.
Dr. Marzec and her associates presented case reports of five such patients diagnosed with chronic Lyme disease who sustained serious harm from such treatments (MMWR 2017;66[23]:607-9).
A woman in her late 30s with fatigue and joint pain was given a peripherally inserted central catheter (PICC) for IV delivery of ceftriaxone and cefotaxime. After 3 weeks, she developed fever, rash, hypotension, and tachycardia. In the intensive care unit (ICU), she was given broad-spectrum IV antibiotics and vasopressors, and was mechanically ventilated, but died of septic shock related to catheter-associated bacteremia.
An adolescent was told at an alternative medicine clinic that her years of muscle and joint pain, backaches, headaches, and lethargy were due to chronic Lyme disease. A PICC was placed to deliver IV antibiotics for 5 months. She developed pallor, chills, fever, hypotension, and tachycardia consistent with septic shock. Cultures demonstrated Acinetobacter species in her blood and on the PICC, and she required several weeks of ICU care.
A woman in her late 40s was diagnosed as having chronic Lyme disease based on unvalidated tests and was treated for months with intramuscular penicillin, IV ceftriazone, and IV azithromycin administered through a tunneled IV catheter; as well as doxycycline, and the antiparasitic drug tinidazole. She was hospitalized for back pain, shortness of breath, and malaise, and cultures of the catheter and her blood yielded Pseudomonas aeruginosa. She was found to have osteodiscitis caused by the same organism, with destruction of the 9th and 10th vertebrae, and was treated, and her back pain eventually improved.
A woman in her 50s was diagnosed as having amyotrophic lateral sclerosis, but sought a second opinion and was told that she had chronic Lyme disease (along with babesiosis, and Rocky Mountain spotted fever). She was treated with herbs and homeopathic remedies, followed by intensive antimicrobial and antiviral therapies. She developed intractable Clostridium difficile colitis that lasted for 2 years until she died from complications related to amyotrophic lateral sclerosis.
A woman in her 60s who had autoimmune neutropenia, mixed connective tissue disease, and degenerative arthritis was told her neuropathy was due to chronic Lyme disease. She was treated with immunoglobulin administered through an implanted subcutaneous port. After years of treatments, she was hospitalized for fever and back pain, had blood cultures positive for methicillin-sensitive Staphylococcus aureus, was found to have inflammation of the lumbar facet joints, epidural space, and paraspinal muscles – and eventually required surgical drainage of a paraspinal abscess.
“These cases highlight the severity and scope of adverse effects that can be caused by the use of unproven treatments for chronic Lyme disease,” Dr. Marzec and her associates said.
This work was supported by the CDC. Dr. Marzec and her associates reported having no relevant financial disclosures.
Unproven treatments for so-called chronic Lyme disease can cause serious, even fatal, complications, according to five case reports published in the Morbidity and Mortality Weekly Report.
“Patients, clinicians, and public health practitioners should be aware that treatments for chronic Lyme disease can carry serious risks,” the authors wrote.
Chronic Lyme disease is a nonspecific diagnosis that has no consistent definition. Some clinicians use this label for patients who have a variety of debilitating conditions such as fatigue, generalized pain, and neurologic symptoms, even in the absence of laboratory evidence of Borrelia burgdorferi infection, objective signs of infection, or a history of tick exposure. People who support this diagnosis mistakenly believe that B. burgdorferi can cause longstanding disabling symptoms even when standard testing for the organism is negative, when the truth is that tests for the organism become more sensitive the longer the infection persists, according to Natalie S. Marzec, MD, a resident in preventive medicine at the University of Colorado, Aurora, and her associates.
Patients who cannot obtain symptom relief with conventional clinicians may consult “practitioners who might identify themselves as Lyme disease specialists (‘Lyme literate’ doctors) or from complementary and alternative medicine clinics,” where they are diagnosed with chronic Lyme disease. Such patients have been offered unproven treatments, including extended courses of intravenous antibiotics, infusions of hydrogen peroxide, immunoglobulin therapy, hyperbaric oxygen treatment, electromagnetic frequency therapy, garlic supplements, colloidal silver, and stem-cell transplantation.
Dr. Marzec and her associates presented case reports of five such patients diagnosed with chronic Lyme disease who sustained serious harm from such treatments (MMWR 2017;66[23]:607-9).
A woman in her late 30s with fatigue and joint pain was given a peripherally inserted central catheter (PICC) for IV delivery of ceftriaxone and cefotaxime. After 3 weeks, she developed fever, rash, hypotension, and tachycardia. In the intensive care unit (ICU), she was given broad-spectrum IV antibiotics and vasopressors, and was mechanically ventilated, but died of septic shock related to catheter-associated bacteremia.
An adolescent was told at an alternative medicine clinic that her years of muscle and joint pain, backaches, headaches, and lethargy were due to chronic Lyme disease. A PICC was placed to deliver IV antibiotics for 5 months. She developed pallor, chills, fever, hypotension, and tachycardia consistent with septic shock. Cultures demonstrated Acinetobacter species in her blood and on the PICC, and she required several weeks of ICU care.
A woman in her late 40s was diagnosed as having chronic Lyme disease based on unvalidated tests and was treated for months with intramuscular penicillin, IV ceftriazone, and IV azithromycin administered through a tunneled IV catheter; as well as doxycycline, and the antiparasitic drug tinidazole. She was hospitalized for back pain, shortness of breath, and malaise, and cultures of the catheter and her blood yielded Pseudomonas aeruginosa. She was found to have osteodiscitis caused by the same organism, with destruction of the 9th and 10th vertebrae, and was treated, and her back pain eventually improved.
A woman in her 50s was diagnosed as having amyotrophic lateral sclerosis, but sought a second opinion and was told that she had chronic Lyme disease (along with babesiosis, and Rocky Mountain spotted fever). She was treated with herbs and homeopathic remedies, followed by intensive antimicrobial and antiviral therapies. She developed intractable Clostridium difficile colitis that lasted for 2 years until she died from complications related to amyotrophic lateral sclerosis.
A woman in her 60s who had autoimmune neutropenia, mixed connective tissue disease, and degenerative arthritis was told her neuropathy was due to chronic Lyme disease. She was treated with immunoglobulin administered through an implanted subcutaneous port. After years of treatments, she was hospitalized for fever and back pain, had blood cultures positive for methicillin-sensitive Staphylococcus aureus, was found to have inflammation of the lumbar facet joints, epidural space, and paraspinal muscles – and eventually required surgical drainage of a paraspinal abscess.
“These cases highlight the severity and scope of adverse effects that can be caused by the use of unproven treatments for chronic Lyme disease,” Dr. Marzec and her associates said.
This work was supported by the CDC. Dr. Marzec and her associates reported having no relevant financial disclosures.
Unproven treatments for so-called chronic Lyme disease can cause serious, even fatal, complications, according to five case reports published in the Morbidity and Mortality Weekly Report.
“Patients, clinicians, and public health practitioners should be aware that treatments for chronic Lyme disease can carry serious risks,” the authors wrote.
Chronic Lyme disease is a nonspecific diagnosis that has no consistent definition. Some clinicians use this label for patients who have a variety of debilitating conditions such as fatigue, generalized pain, and neurologic symptoms, even in the absence of laboratory evidence of Borrelia burgdorferi infection, objective signs of infection, or a history of tick exposure. People who support this diagnosis mistakenly believe that B. burgdorferi can cause longstanding disabling symptoms even when standard testing for the organism is negative, when the truth is that tests for the organism become more sensitive the longer the infection persists, according to Natalie S. Marzec, MD, a resident in preventive medicine at the University of Colorado, Aurora, and her associates.
Patients who cannot obtain symptom relief with conventional clinicians may consult “practitioners who might identify themselves as Lyme disease specialists (‘Lyme literate’ doctors) or from complementary and alternative medicine clinics,” where they are diagnosed with chronic Lyme disease. Such patients have been offered unproven treatments, including extended courses of intravenous antibiotics, infusions of hydrogen peroxide, immunoglobulin therapy, hyperbaric oxygen treatment, electromagnetic frequency therapy, garlic supplements, colloidal silver, and stem-cell transplantation.
Dr. Marzec and her associates presented case reports of five such patients diagnosed with chronic Lyme disease who sustained serious harm from such treatments (MMWR 2017;66[23]:607-9).
A woman in her late 30s with fatigue and joint pain was given a peripherally inserted central catheter (PICC) for IV delivery of ceftriaxone and cefotaxime. After 3 weeks, she developed fever, rash, hypotension, and tachycardia. In the intensive care unit (ICU), she was given broad-spectrum IV antibiotics and vasopressors, and was mechanically ventilated, but died of septic shock related to catheter-associated bacteremia.
An adolescent was told at an alternative medicine clinic that her years of muscle and joint pain, backaches, headaches, and lethargy were due to chronic Lyme disease. A PICC was placed to deliver IV antibiotics for 5 months. She developed pallor, chills, fever, hypotension, and tachycardia consistent with septic shock. Cultures demonstrated Acinetobacter species in her blood and on the PICC, and she required several weeks of ICU care.
A woman in her late 40s was diagnosed as having chronic Lyme disease based on unvalidated tests and was treated for months with intramuscular penicillin, IV ceftriazone, and IV azithromycin administered through a tunneled IV catheter; as well as doxycycline, and the antiparasitic drug tinidazole. She was hospitalized for back pain, shortness of breath, and malaise, and cultures of the catheter and her blood yielded Pseudomonas aeruginosa. She was found to have osteodiscitis caused by the same organism, with destruction of the 9th and 10th vertebrae, and was treated, and her back pain eventually improved.
A woman in her 50s was diagnosed as having amyotrophic lateral sclerosis, but sought a second opinion and was told that she had chronic Lyme disease (along with babesiosis, and Rocky Mountain spotted fever). She was treated with herbs and homeopathic remedies, followed by intensive antimicrobial and antiviral therapies. She developed intractable Clostridium difficile colitis that lasted for 2 years until she died from complications related to amyotrophic lateral sclerosis.
A woman in her 60s who had autoimmune neutropenia, mixed connective tissue disease, and degenerative arthritis was told her neuropathy was due to chronic Lyme disease. She was treated with immunoglobulin administered through an implanted subcutaneous port. After years of treatments, she was hospitalized for fever and back pain, had blood cultures positive for methicillin-sensitive Staphylococcus aureus, was found to have inflammation of the lumbar facet joints, epidural space, and paraspinal muscles – and eventually required surgical drainage of a paraspinal abscess.
“These cases highlight the severity and scope of adverse effects that can be caused by the use of unproven treatments for chronic Lyme disease,” Dr. Marzec and her associates said.
This work was supported by the CDC. Dr. Marzec and her associates reported having no relevant financial disclosures.
FROM MMWR
Key clinical point: Unproven treatments for so-called chronic Lyme disease cause serious, even fatal, complications.
Major finding:
Data source: Five case reports submitted to the CDC by clinicians, health departments, and individual patients.
Disclosures: This work was supported by the CDC. Dr. Marzec and her associates reported having no relevant financial disclosures.
Early phase III data positive for adalimumab biosimilar, for both psoriasis and PsA
MADRID – To date, an adalimumab biosimilar has proven itself in a large, phase III trial of patients with psoriasis, including a subset with mild to moderate psoriatic arthritis (PsA).
The biosimilar, known as CHS-1420, cleared psoriatic plaques and improved health-related quality of life just as well as adalimumab after 12 weeks of treatment, Barbara Finck, MD, said at the European Congress of Rheumatology. It also suppressed high-sensitivity C-reactive protein (CRP) as well as the originator molecule, she said.
Dr. Finck, the chief medical officer of Coherus Biosciences, the developer of CHS-1420, reported results from the first 16-week phase of the 48-week study. Data are still to come on a 6-week period during which half those taking adalimumab switched to CHS-1420 in a blinded fashion, and 26 weeks of open-label CHS-1420 for all patients.
The study’s primary endpoint was a 75% reduction in the Psoriasis Area and Severity Index (PASI) score (PASI 75) Two additional endpoints were evaluated in patients with PsA: change in the Health Assessment Questionnaire-Disability Index (HAQ-DI) and changes in CRP.
Dr. Finck bemoaned the lack of the clinical rheumatologic endpoint, tender and swollen joint count. “I advocated for this but was unable to convince our dermatology colleagues” to conduct this exam, she said. “I think we have a ways to go to educate our colleagues in this regard.”
The study comprised 545 patients with mild to moderate psoriasis; of these, 127 had PsA. They received subcutaneous injections of either CHS-1420 or adalimumab at identical doses (80 mg at week 1, followed by 40 mg every other week). They were a mean of 44 years o
In the entire study population, treatment with CHS-1420 and adalimumab followed almost identical response curves. By week 4, 22% of the CHS-1420 group and 20% of the adalimumab group had reached a PASI75 response. By week 8, those numbers were 57% and 61%, respectively, and by week 12, they were 69% and 72% – not significantly different.
Response was similar in the subgroup of PsA patients: By week 12, 82% of the CHS-1420 group and 77% of the adalimumab group had reached a PASI 75. PsA patients also responded equally well to both medications on the HAQ-DI by week 12. At baseline, the mean HAQ-DI was about 1 in each group. At 12 weeks, it was reduced by about half a point in both groups. High-sensitivity CRP decreased similarly in the CHS-1420 and adalimumab groups as well (reductions of 8.9 mg/L and 6.3 mg/L, respectively).
Adalimumab, a tumor necrosis factor blocker, is a highly immunogenic molecule, and as such, many patients developed antibodies to both it and to CHS-1420. By week 12, 84% of both treatment groups had developed anti-drug antibodies and 32%, neutralizing antibodies. Among those with PsA, 82% taking CHS-1420 and 88% of those taking adalimumab developed antidrug antibodies. Neutralizing antibodies developed in 33% and 30%, respectively. Neither of these differences was statistically significant.
Other adverse events were similar, Dr. Finck noted. These included nasopharyngitis (9% of both groups), upper respiratory tract infection (6%), injection site reaction (4%), headache (3%), and worsening of psoriasis (1% for CHS-1420, and 3% for adalimumab).
If the switching study data are similarly positive, Coherus expects to file a Biologics License Application with the Food and Drug Administration in early 2018, Dr. Finck said.
msullivan@frontlinemedcom.com
On Twitter @Alz_gal
MADRID – To date, an adalimumab biosimilar has proven itself in a large, phase III trial of patients with psoriasis, including a subset with mild to moderate psoriatic arthritis (PsA).
The biosimilar, known as CHS-1420, cleared psoriatic plaques and improved health-related quality of life just as well as adalimumab after 12 weeks of treatment, Barbara Finck, MD, said at the European Congress of Rheumatology. It also suppressed high-sensitivity C-reactive protein (CRP) as well as the originator molecule, she said.
Dr. Finck, the chief medical officer of Coherus Biosciences, the developer of CHS-1420, reported results from the first 16-week phase of the 48-week study. Data are still to come on a 6-week period during which half those taking adalimumab switched to CHS-1420 in a blinded fashion, and 26 weeks of open-label CHS-1420 for all patients.
The study’s primary endpoint was a 75% reduction in the Psoriasis Area and Severity Index (PASI) score (PASI 75) Two additional endpoints were evaluated in patients with PsA: change in the Health Assessment Questionnaire-Disability Index (HAQ-DI) and changes in CRP.
Dr. Finck bemoaned the lack of the clinical rheumatologic endpoint, tender and swollen joint count. “I advocated for this but was unable to convince our dermatology colleagues” to conduct this exam, she said. “I think we have a ways to go to educate our colleagues in this regard.”
The study comprised 545 patients with mild to moderate psoriasis; of these, 127 had PsA. They received subcutaneous injections of either CHS-1420 or adalimumab at identical doses (80 mg at week 1, followed by 40 mg every other week). They were a mean of 44 years o
In the entire study population, treatment with CHS-1420 and adalimumab followed almost identical response curves. By week 4, 22% of the CHS-1420 group and 20% of the adalimumab group had reached a PASI75 response. By week 8, those numbers were 57% and 61%, respectively, and by week 12, they were 69% and 72% – not significantly different.
Response was similar in the subgroup of PsA patients: By week 12, 82% of the CHS-1420 group and 77% of the adalimumab group had reached a PASI 75. PsA patients also responded equally well to both medications on the HAQ-DI by week 12. At baseline, the mean HAQ-DI was about 1 in each group. At 12 weeks, it was reduced by about half a point in both groups. High-sensitivity CRP decreased similarly in the CHS-1420 and adalimumab groups as well (reductions of 8.9 mg/L and 6.3 mg/L, respectively).
Adalimumab, a tumor necrosis factor blocker, is a highly immunogenic molecule, and as such, many patients developed antibodies to both it and to CHS-1420. By week 12, 84% of both treatment groups had developed anti-drug antibodies and 32%, neutralizing antibodies. Among those with PsA, 82% taking CHS-1420 and 88% of those taking adalimumab developed antidrug antibodies. Neutralizing antibodies developed in 33% and 30%, respectively. Neither of these differences was statistically significant.
Other adverse events were similar, Dr. Finck noted. These included nasopharyngitis (9% of both groups), upper respiratory tract infection (6%), injection site reaction (4%), headache (3%), and worsening of psoriasis (1% for CHS-1420, and 3% for adalimumab).
If the switching study data are similarly positive, Coherus expects to file a Biologics License Application with the Food and Drug Administration in early 2018, Dr. Finck said.
msullivan@frontlinemedcom.com
On Twitter @Alz_gal
MADRID – To date, an adalimumab biosimilar has proven itself in a large, phase III trial of patients with psoriasis, including a subset with mild to moderate psoriatic arthritis (PsA).
The biosimilar, known as CHS-1420, cleared psoriatic plaques and improved health-related quality of life just as well as adalimumab after 12 weeks of treatment, Barbara Finck, MD, said at the European Congress of Rheumatology. It also suppressed high-sensitivity C-reactive protein (CRP) as well as the originator molecule, she said.
Dr. Finck, the chief medical officer of Coherus Biosciences, the developer of CHS-1420, reported results from the first 16-week phase of the 48-week study. Data are still to come on a 6-week period during which half those taking adalimumab switched to CHS-1420 in a blinded fashion, and 26 weeks of open-label CHS-1420 for all patients.
The study’s primary endpoint was a 75% reduction in the Psoriasis Area and Severity Index (PASI) score (PASI 75) Two additional endpoints were evaluated in patients with PsA: change in the Health Assessment Questionnaire-Disability Index (HAQ-DI) and changes in CRP.
Dr. Finck bemoaned the lack of the clinical rheumatologic endpoint, tender and swollen joint count. “I advocated for this but was unable to convince our dermatology colleagues” to conduct this exam, she said. “I think we have a ways to go to educate our colleagues in this regard.”
The study comprised 545 patients with mild to moderate psoriasis; of these, 127 had PsA. They received subcutaneous injections of either CHS-1420 or adalimumab at identical doses (80 mg at week 1, followed by 40 mg every other week). They were a mean of 44 years o
In the entire study population, treatment with CHS-1420 and adalimumab followed almost identical response curves. By week 4, 22% of the CHS-1420 group and 20% of the adalimumab group had reached a PASI75 response. By week 8, those numbers were 57% and 61%, respectively, and by week 12, they were 69% and 72% – not significantly different.
Response was similar in the subgroup of PsA patients: By week 12, 82% of the CHS-1420 group and 77% of the adalimumab group had reached a PASI 75. PsA patients also responded equally well to both medications on the HAQ-DI by week 12. At baseline, the mean HAQ-DI was about 1 in each group. At 12 weeks, it was reduced by about half a point in both groups. High-sensitivity CRP decreased similarly in the CHS-1420 and adalimumab groups as well (reductions of 8.9 mg/L and 6.3 mg/L, respectively).
Adalimumab, a tumor necrosis factor blocker, is a highly immunogenic molecule, and as such, many patients developed antibodies to both it and to CHS-1420. By week 12, 84% of both treatment groups had developed anti-drug antibodies and 32%, neutralizing antibodies. Among those with PsA, 82% taking CHS-1420 and 88% of those taking adalimumab developed antidrug antibodies. Neutralizing antibodies developed in 33% and 30%, respectively. Neither of these differences was statistically significant.
Other adverse events were similar, Dr. Finck noted. These included nasopharyngitis (9% of both groups), upper respiratory tract infection (6%), injection site reaction (4%), headache (3%), and worsening of psoriasis (1% for CHS-1420, and 3% for adalimumab).
If the switching study data are similarly positive, Coherus expects to file a Biologics License Application with the Food and Drug Administration in early 2018, Dr. Finck said.
msullivan@frontlinemedcom.com
On Twitter @Alz_gal
AT THE EULAR 2017 CONGRESS
Key clinical point:
Major finding: By week 12, 69% of those who received CHS-1420 and 72% of those who received adalimumab had reached a PASI75, response rates that were not significantly different.
Data source: The phase III trial randomized 545 patients with psoriasis, including 127 with PsA, to treatment with adalimumab or the biosimilar.
Disclosures: Dr. Finck is chief medical officer of Coherus Biosciences, which is developing CHS-1420.
Endometriomas: Classification and surgical management
Related article:
Endometriosis: Expert answers to 7 crucial questions on diagnosis
Etiology
Endometriomas are extensively described in the literature, and their origin is the subject of several theories. In 1921, Sampson noted luteal membrane and ovarian epithelial tissues within endometriomas and was the first to indicate that endometriomas may result from the invasion of functional cysts by endometrial tissue.2,4,5 In 1979, Czernobilsky and Morris6 found endometrial and oviduct-like epithelium in ovarian endometriosis and concluded that ovarian tissue may be a common histologic precursor. Several other authors subsequently have reported finding different types of tissue within ovarian endometriomas, and not all of these chocolate cysts showed histologic evidence of endometriosis.4,7,8
Read about the classification of endometriomas
Disease classification
Our classification system identifies 2 types of endometriomas on the basis of their etiologies and characteristics. Type I, which arise from endometrial tissue implanted on the ovarian surface, are also called true endometriomas. Invagination of cortex and subsequent hemorrhage from endometrial tissue result in cyst formation. Endometrial tissue (endometrial stroma and glands) is histologically present in all type I endometriomas.1,4,9 These endometriomas usually are small (<5 cm in diameter) and have a densely adherent fibrous capsule.4 Often, there is no clear plane between cyst wall and ovarian stroma.3
Type II endometriomas arise from functional cysts involved in or invaded by cortical or pelvic side-wall endometrial implants or by type I endometriomas. Type II endometriomas are subclassified by the extent of endometrial implant involvement in the cyst wall. Type IIA endometriomas are hemorrhagic cysts with less than 10% of endometrial tissue within the cyst wall. Similar to the functional cysts from which they originate, type IIA endometriomas have a cyst wall that is separated easily from ovarian tissue during surgery.4,7,9 Although type II endometriomas tend to be larger than their type I counterparts, in some cases they are identified at an early stage of 2 to 5 cm. Endometriomas larger than 5 cm are almost always type II.4
Type IIB and IIC endometriomas have endometrial implants and fibrosis within their cyst walls, with progressively more endometrial invasion in type IIC endometriomas (>50%) than in type IIB (10% to 50%). Consequently, type IIB cysts are relatively easy to dissect from ovarian tissue, except adjacent to an endometriotic area where the cyst densely adheres to the ovarian stroma. In type IIC, endometrial tissue more extensively penetrates the capsule, making dissection of diseased tissue from the ovarian stroma more difficult; in fact, separating type IIC cyst wall from ovarian stroma can be as challenging as excising a type I endometrioma.7 In most cases, a type IIC cyst is attached by adhesions and fibrosis to the pelvic side wall or uterus and ruptures during mobilization (TABLE).
Related article:
Imaging the endometrioma and mature cystic teratoma
Presentation and diagnosis
Almost all patients with an endometrioma concurrently have peritoneal endometriosis, which is characterized by dysmenorrhea, dyspareunia, chronic pelvic pain, infertility, and, in some cases, gastrointestinal or genitourinary dysfunction.1 Pelvic examination may reveal an adnexal mass that is an endometrioma, or an endometrioma may appear on imaging obtained in a pelvic pain or infertility work-up. Given its 73% sensitivity, 94% specificity, safety, and low cost, transvaginal ultrasonography is the preferred imaging modality for endometrioma.3 The characteristic ultrasonographic appearance is that of a round, homogeneous, fluid-filled mass with low-level echoes.1 Magnetic resonance imaging is appropriate when a more sensitive imaging modality is indicated, as for a patient with risk factors for malignancy.3,10–12
Read about the surgical management of endometriomas
Surgical management
Indications for surgical excision of endometriomas include pelvic pain, infertility, and prevention and diagnosis of malignancy. Endometriomas may be excised prior to use of assisted reproductive technology.13–15 Medical therapy, such as oral contraceptives, can be used to reduce the size of endometriomas but does not improve fertility.3 Certain ovarian cancers are more common in women with endometriosis, and ovarian tumors are thought to develop in about 1% of ovarian endometriosis cases.1,12 Therefore, endometrioma excision may reduce the risk of malignancy. As with other ovarian cysts, large endometriomas may be excised to reduce the risks of rupture and torsion.
Approach
Laparoscopy is the preferred approach for endometrioma excision. Controversy exists regarding the ideal procedure: complete excision (with stripping of the cyst capsule) or drainage and ablation of the cyst wall. Compared with drainage and ablation, excision reduces recurrence of endometriomas; relieves dysmenorrhea, dyspareunia, pelvic pain, and other symptoms; and improves fertility.13,16 The recurrence rate may be as low as 5.8% with complete excision but is 90% with simple transvaginal aspiration.17,18 If not performed properly, however, cyst capsule stripping may damage nearby ovarian stroma and decrease the ovarian reserve.14 Some authors have advocated combining excision and ablation—performing cystectomy until there is no longer a clear plane between capsule and ovarian stroma and then ablating any remaining endometrial tissue.8
With type I and IIC endometriomas, we have seen the endometrial cyst wall infiltrating the ovarian stroma so deeply there is not always a definable plane. By contrast, type IIA and IIB endometriomas typically have a plane between the cyst wall and the ovarian cortex. In type II endometriomas, endometrial implants on the ovarian cortex infiltrate the plane of the cyst wall such that the juxtaposing lipomatous follicular cyst detaches with minimal intraoperative traction. Portions of type II endometriomas containing fibrosis and adhesions may become more difficult to peel off the cyst wall. For most endometriomas, at least 1 spot is difficult to peel off the ovary, and extra care must be taken at the hilum of ovary to avoid excising healthy ovarian cortex.4,5,7,8
Our surgical approach accounts for the described variations in type I and II endometriomas. Endometrial contents often spill as the endometrioma is dissected off neighboring structures. When possible, endometriomas should be aspirated and irrigated prior to cystectomy to avoid seeding the pelvis and abdomen with spilled endometriotic contents. We use hydrodissection, the injection of dilute vasopressin with a laparoscopic needle, to create a plane between cyst wall and ovarian stroma and strip the cyst capsule with laparoscopic graspers. Type I endometriomas adhere densely to the ovary. Given the presence of fibrosis and adhesions, the cyst is excised in a piecemeal fashion. Care is taken to remove any endometrial implants from the ovary while preserving as much of the ovarian tissue as possible.1
Type II endometriomas are larger cysts originating from the invasion of endometrial implants or type I endometrioma into functional cysts. The difficulty of capsule excision varies according to the extent of endometrial invasion. Type IIA endometriomas contain less than 10% endometrial tissue within the cyst capsule. Thus, the standard ovarian cystectomy stripping technique is successful in removing more than 90% of the cyst capsule. Special care is taken in stripping the residual small portion that involves the endometrial glands and stroma and adheres densely to the ovary.
The larger proportion of endometrial tissue present in type IIB and IIC endometriomas degrades the plane between the cyst capsule and the ovarian stroma, making excision more difficult. Similar to the type I excision, a piecemeal approach is often necessary. If complete stripping of the cyst capsule would result in extensive loss of healthy ovarian tissue, then electrocautery, plasma energy, or laser ablation can be selectively used to destroy focal areas of endometrial invasion. Complete ablation may be difficult, as the endometrioma wall can be up to 5 mm thick.19 For these thick-walled endometriomas, we recommend excision (vs ablation), which lowers the risk of endometrioma recurrence.
Related article:
Endometriosis and pain: Expert answers to 6 questions targeting your management options
- Endometriomas are common adnexal masses in women affected by endometriosis and may exacerbate pelvic pain and impair fertility. Classification of endometriomas into type I and type II,depending on their etiology and characteristics, can guide minimally invasive surgical management.
- Type I endometriomas arise from invagination of endometrial implants on the ovarian cortex, resulting in dense fibrosis and adhesions. These lesions typically require piecemeal excision in order to completely remove the cyst capsule.
- Type II endometriomas result from invasion of endometrial tissue into preexisting functional cysts and are further subclassified by the proportion of cyst capsule containing endometrial tissue (IIA <10%, IIB 10% to 50%, IIC >50%).
- The difficulty of excising type II endometriomas correlates with the degree of endometrial invasion, with type IIA being relatively straightforward and type IIC being as challenging and piecemeal as type I.
- We generally favor complete excision rather than ablation of the cyst capsule, except for when excision would result in an unacceptable loss of healthy ovarian tissue.
Conclusion
Endometriomas, common adnexal masses in women affected by endometriosis, may exacerbate pelvic pain and impair fertility. Gynecologists should be prepared to excise endometriomas completely and exercise care in preserving as much of the ovarian stroma as possible. We classify endometriomas into 2 types: type I, which develop from invagination of endometrial implants in the ovarian cortex, and type II, which stem from invasion of functional cysts by endometrial implants or type I endometrioma. This distinction guides surgical management. We hope this article and its accompanying video will be helpful in guiding laparoscopic excision of type I and II endometriomas.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Nezhat C, Buescher E, Paka C, et al. Video-assisted laparoscopic treatment of endometriosis. In: Nezhat C, Nezhat F, Nezhat C, eds. Nezhat’s Video-Assisted and Robotic-Assisted Laparoscopy and Hysteroscopy. 4th ed. New York, NY: Cambridge University Press; 2013:265–302.
- Burney RO, Giudice LC. Pathogenesis and pathophysiology of endometriosis. Fertil Steril. 2012;98(3):511–519.
- Keyhan S, Hughes C, Price T, Muasher S. An update on surgical versus expectant management of ovarian endometriomas in infertile women. Biomed Res Int. 2015;2015:204792.
- Nezhat F, Nezhat C, Allan CJ, Metzger DA, Sears DL. Clinical and histologic classification of endometriomas. Implications for a mechanism of pathogenesis. J Reprod Med. 1992;37(9):771–776.
- Burney RO, Giudice LC. The pathogenesis of endometriosis. In: Nezhat C, Nezhat F, Nezhat C, eds. Nezhat’s Video-Assisted and Robotic-Assisted Laparoscopy and Hysteroscopy. 4th ed. New York, NY: Cambridge University Press; 2013:252–258.
- Czernobilsky B, Morris WJ. A histologic study of ovarian endometriosis with emphasis on hyperplastic and atypical changes. Obstet Gynecol. 1979;53(3):318–323.
- Nezhat F, Nezhat C, Nezhat C, Admon D. A fresh look at ovarian endometriomas. Contemp Ob Gyn. 1994;39(11):81–94.
- Donnez J, Lousse JC, Jadoul P, Donnez O, Squifflet J. Laparoscopic management of endometriomas using a combined technique of excisional (cystectomy) and ablative surgery. Fertil Steril. 2010;94(1):28–32.
- Nezhat C, Nezhat F, Nezhat C, Seidman DS. Classification of endometriosis. Improving the classification of endometriotic ovarian cysts. Hum Reprod. 1994;9(12):2212–2213.
- Nezhat FR, Pejovic T, Reis FM, Guo SW. The link between endometriosis and ovarian cancer: clinical implications. Int J Gynecol Cancer. 2014;24(4):623–628.
- Nezhat F, Apostol R, Mahmoud M, el Daouk M. Malignant transformation of endometriosis and its clinical significance. Fertil Steril. 2014;102(2):342–344.
- Nezhat FR, Apostal R, Nezhat C, Pejovic T. New insights in the pathophysiology of ovarian cancer and implications for screening and prevention. Am J Obstet Gynecol. 2015;213(3):262–267.
- Hart RJ, Hickey M, Maouris P, Buckett W. Excisional surgery versus ablative surgery for ovarian endometriomata. Cochrane Database Syst Rev. 2008;(2):CD004992.
- Yates J. Endometriosis and infertility: expert answers to 6 questions to help pinpoint the best route to pregnancy. OBG Manag. 2015;27(6):30–35.
- Littman E, Giudice L, Lathi R, Berker B, Milki A, Nezhat C. Role of laparoscopic treatment of endometriosis in patients with failed in vitro fertilization cycles. Fertil Steril. 2005;84(6):1574–1578.
- Exacoustos C, Zupi E, Amadio A, et al. Laparoscopic removal of endometriomas: sonographic evaluation of residual functioning ovarian tissue. Am J Obstet Gynecol. 2004;191(1):68–72.
- Gonçalves FC, Andres MP, Passman LJ, Gonçalves MO, Podgaec S. A systematic review of ultrasonography-guided transvaginal aspiration of recurrent ovarian endometrioma. Int J Gynaecol Obstet. 2016;134(1):3–7.
- Alborzi S, Momtahan M, Parsanezhad ME, Dehbashi S, Zolghadri J, Alborzi S. A prospective, randomized study comparing laparoscopic ovarian cystectomy versus fenestration and coagulation in patients with endometriomas. Fertil Steril. 2004;82(6):1633–1637.
- Nezhat C, Crowgey SR, Garrison CP. Surgical treatment of endometriosis via laser laparoscopy. Fertil Steril. 1986;45(6):778–783.
Related article:
Endometriosis: Expert answers to 7 crucial questions on diagnosis
Etiology
Endometriomas are extensively described in the literature, and their origin is the subject of several theories. In 1921, Sampson noted luteal membrane and ovarian epithelial tissues within endometriomas and was the first to indicate that endometriomas may result from the invasion of functional cysts by endometrial tissue.2,4,5 In 1979, Czernobilsky and Morris6 found endometrial and oviduct-like epithelium in ovarian endometriosis and concluded that ovarian tissue may be a common histologic precursor. Several other authors subsequently have reported finding different types of tissue within ovarian endometriomas, and not all of these chocolate cysts showed histologic evidence of endometriosis.4,7,8
Read about the classification of endometriomas
Disease classification
Our classification system identifies 2 types of endometriomas on the basis of their etiologies and characteristics. Type I, which arise from endometrial tissue implanted on the ovarian surface, are also called true endometriomas. Invagination of cortex and subsequent hemorrhage from endometrial tissue result in cyst formation. Endometrial tissue (endometrial stroma and glands) is histologically present in all type I endometriomas.1,4,9 These endometriomas usually are small (<5 cm in diameter) and have a densely adherent fibrous capsule.4 Often, there is no clear plane between cyst wall and ovarian stroma.3
Type II endometriomas arise from functional cysts involved in or invaded by cortical or pelvic side-wall endometrial implants or by type I endometriomas. Type II endometriomas are subclassified by the extent of endometrial implant involvement in the cyst wall. Type IIA endometriomas are hemorrhagic cysts with less than 10% of endometrial tissue within the cyst wall. Similar to the functional cysts from which they originate, type IIA endometriomas have a cyst wall that is separated easily from ovarian tissue during surgery.4,7,9 Although type II endometriomas tend to be larger than their type I counterparts, in some cases they are identified at an early stage of 2 to 5 cm. Endometriomas larger than 5 cm are almost always type II.4
Type IIB and IIC endometriomas have endometrial implants and fibrosis within their cyst walls, with progressively more endometrial invasion in type IIC endometriomas (>50%) than in type IIB (10% to 50%). Consequently, type IIB cysts are relatively easy to dissect from ovarian tissue, except adjacent to an endometriotic area where the cyst densely adheres to the ovarian stroma. In type IIC, endometrial tissue more extensively penetrates the capsule, making dissection of diseased tissue from the ovarian stroma more difficult; in fact, separating type IIC cyst wall from ovarian stroma can be as challenging as excising a type I endometrioma.7 In most cases, a type IIC cyst is attached by adhesions and fibrosis to the pelvic side wall or uterus and ruptures during mobilization (TABLE).
Related article:
Imaging the endometrioma and mature cystic teratoma
Presentation and diagnosis
Almost all patients with an endometrioma concurrently have peritoneal endometriosis, which is characterized by dysmenorrhea, dyspareunia, chronic pelvic pain, infertility, and, in some cases, gastrointestinal or genitourinary dysfunction.1 Pelvic examination may reveal an adnexal mass that is an endometrioma, or an endometrioma may appear on imaging obtained in a pelvic pain or infertility work-up. Given its 73% sensitivity, 94% specificity, safety, and low cost, transvaginal ultrasonography is the preferred imaging modality for endometrioma.3 The characteristic ultrasonographic appearance is that of a round, homogeneous, fluid-filled mass with low-level echoes.1 Magnetic resonance imaging is appropriate when a more sensitive imaging modality is indicated, as for a patient with risk factors for malignancy.3,10–12
Read about the surgical management of endometriomas
Surgical management
Indications for surgical excision of endometriomas include pelvic pain, infertility, and prevention and diagnosis of malignancy. Endometriomas may be excised prior to use of assisted reproductive technology.13–15 Medical therapy, such as oral contraceptives, can be used to reduce the size of endometriomas but does not improve fertility.3 Certain ovarian cancers are more common in women with endometriosis, and ovarian tumors are thought to develop in about 1% of ovarian endometriosis cases.1,12 Therefore, endometrioma excision may reduce the risk of malignancy. As with other ovarian cysts, large endometriomas may be excised to reduce the risks of rupture and torsion.
Approach
Laparoscopy is the preferred approach for endometrioma excision. Controversy exists regarding the ideal procedure: complete excision (with stripping of the cyst capsule) or drainage and ablation of the cyst wall. Compared with drainage and ablation, excision reduces recurrence of endometriomas; relieves dysmenorrhea, dyspareunia, pelvic pain, and other symptoms; and improves fertility.13,16 The recurrence rate may be as low as 5.8% with complete excision but is 90% with simple transvaginal aspiration.17,18 If not performed properly, however, cyst capsule stripping may damage nearby ovarian stroma and decrease the ovarian reserve.14 Some authors have advocated combining excision and ablation—performing cystectomy until there is no longer a clear plane between capsule and ovarian stroma and then ablating any remaining endometrial tissue.8
With type I and IIC endometriomas, we have seen the endometrial cyst wall infiltrating the ovarian stroma so deeply there is not always a definable plane. By contrast, type IIA and IIB endometriomas typically have a plane between the cyst wall and the ovarian cortex. In type II endometriomas, endometrial implants on the ovarian cortex infiltrate the plane of the cyst wall such that the juxtaposing lipomatous follicular cyst detaches with minimal intraoperative traction. Portions of type II endometriomas containing fibrosis and adhesions may become more difficult to peel off the cyst wall. For most endometriomas, at least 1 spot is difficult to peel off the ovary, and extra care must be taken at the hilum of ovary to avoid excising healthy ovarian cortex.4,5,7,8
Our surgical approach accounts for the described variations in type I and II endometriomas. Endometrial contents often spill as the endometrioma is dissected off neighboring structures. When possible, endometriomas should be aspirated and irrigated prior to cystectomy to avoid seeding the pelvis and abdomen with spilled endometriotic contents. We use hydrodissection, the injection of dilute vasopressin with a laparoscopic needle, to create a plane between cyst wall and ovarian stroma and strip the cyst capsule with laparoscopic graspers. Type I endometriomas adhere densely to the ovary. Given the presence of fibrosis and adhesions, the cyst is excised in a piecemeal fashion. Care is taken to remove any endometrial implants from the ovary while preserving as much of the ovarian tissue as possible.1
Type II endometriomas are larger cysts originating from the invasion of endometrial implants or type I endometrioma into functional cysts. The difficulty of capsule excision varies according to the extent of endometrial invasion. Type IIA endometriomas contain less than 10% endometrial tissue within the cyst capsule. Thus, the standard ovarian cystectomy stripping technique is successful in removing more than 90% of the cyst capsule. Special care is taken in stripping the residual small portion that involves the endometrial glands and stroma and adheres densely to the ovary.
The larger proportion of endometrial tissue present in type IIB and IIC endometriomas degrades the plane between the cyst capsule and the ovarian stroma, making excision more difficult. Similar to the type I excision, a piecemeal approach is often necessary. If complete stripping of the cyst capsule would result in extensive loss of healthy ovarian tissue, then electrocautery, plasma energy, or laser ablation can be selectively used to destroy focal areas of endometrial invasion. Complete ablation may be difficult, as the endometrioma wall can be up to 5 mm thick.19 For these thick-walled endometriomas, we recommend excision (vs ablation), which lowers the risk of endometrioma recurrence.
Related article:
Endometriosis and pain: Expert answers to 6 questions targeting your management options
- Endometriomas are common adnexal masses in women affected by endometriosis and may exacerbate pelvic pain and impair fertility. Classification of endometriomas into type I and type II,depending on their etiology and characteristics, can guide minimally invasive surgical management.
- Type I endometriomas arise from invagination of endometrial implants on the ovarian cortex, resulting in dense fibrosis and adhesions. These lesions typically require piecemeal excision in order to completely remove the cyst capsule.
- Type II endometriomas result from invasion of endometrial tissue into preexisting functional cysts and are further subclassified by the proportion of cyst capsule containing endometrial tissue (IIA <10%, IIB 10% to 50%, IIC >50%).
- The difficulty of excising type II endometriomas correlates with the degree of endometrial invasion, with type IIA being relatively straightforward and type IIC being as challenging and piecemeal as type I.
- We generally favor complete excision rather than ablation of the cyst capsule, except for when excision would result in an unacceptable loss of healthy ovarian tissue.
Conclusion
Endometriomas, common adnexal masses in women affected by endometriosis, may exacerbate pelvic pain and impair fertility. Gynecologists should be prepared to excise endometriomas completely and exercise care in preserving as much of the ovarian stroma as possible. We classify endometriomas into 2 types: type I, which develop from invagination of endometrial implants in the ovarian cortex, and type II, which stem from invasion of functional cysts by endometrial implants or type I endometrioma. This distinction guides surgical management. We hope this article and its accompanying video will be helpful in guiding laparoscopic excision of type I and II endometriomas.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Related article:
Endometriosis: Expert answers to 7 crucial questions on diagnosis
Etiology
Endometriomas are extensively described in the literature, and their origin is the subject of several theories. In 1921, Sampson noted luteal membrane and ovarian epithelial tissues within endometriomas and was the first to indicate that endometriomas may result from the invasion of functional cysts by endometrial tissue.2,4,5 In 1979, Czernobilsky and Morris6 found endometrial and oviduct-like epithelium in ovarian endometriosis and concluded that ovarian tissue may be a common histologic precursor. Several other authors subsequently have reported finding different types of tissue within ovarian endometriomas, and not all of these chocolate cysts showed histologic evidence of endometriosis.4,7,8
Read about the classification of endometriomas
Disease classification
Our classification system identifies 2 types of endometriomas on the basis of their etiologies and characteristics. Type I, which arise from endometrial tissue implanted on the ovarian surface, are also called true endometriomas. Invagination of cortex and subsequent hemorrhage from endometrial tissue result in cyst formation. Endometrial tissue (endometrial stroma and glands) is histologically present in all type I endometriomas.1,4,9 These endometriomas usually are small (<5 cm in diameter) and have a densely adherent fibrous capsule.4 Often, there is no clear plane between cyst wall and ovarian stroma.3
Type II endometriomas arise from functional cysts involved in or invaded by cortical or pelvic side-wall endometrial implants or by type I endometriomas. Type II endometriomas are subclassified by the extent of endometrial implant involvement in the cyst wall. Type IIA endometriomas are hemorrhagic cysts with less than 10% of endometrial tissue within the cyst wall. Similar to the functional cysts from which they originate, type IIA endometriomas have a cyst wall that is separated easily from ovarian tissue during surgery.4,7,9 Although type II endometriomas tend to be larger than their type I counterparts, in some cases they are identified at an early stage of 2 to 5 cm. Endometriomas larger than 5 cm are almost always type II.4
Type IIB and IIC endometriomas have endometrial implants and fibrosis within their cyst walls, with progressively more endometrial invasion in type IIC endometriomas (>50%) than in type IIB (10% to 50%). Consequently, type IIB cysts are relatively easy to dissect from ovarian tissue, except adjacent to an endometriotic area where the cyst densely adheres to the ovarian stroma. In type IIC, endometrial tissue more extensively penetrates the capsule, making dissection of diseased tissue from the ovarian stroma more difficult; in fact, separating type IIC cyst wall from ovarian stroma can be as challenging as excising a type I endometrioma.7 In most cases, a type IIC cyst is attached by adhesions and fibrosis to the pelvic side wall or uterus and ruptures during mobilization (TABLE).
Related article:
Imaging the endometrioma and mature cystic teratoma
Presentation and diagnosis
Almost all patients with an endometrioma concurrently have peritoneal endometriosis, which is characterized by dysmenorrhea, dyspareunia, chronic pelvic pain, infertility, and, in some cases, gastrointestinal or genitourinary dysfunction.1 Pelvic examination may reveal an adnexal mass that is an endometrioma, or an endometrioma may appear on imaging obtained in a pelvic pain or infertility work-up. Given its 73% sensitivity, 94% specificity, safety, and low cost, transvaginal ultrasonography is the preferred imaging modality for endometrioma.3 The characteristic ultrasonographic appearance is that of a round, homogeneous, fluid-filled mass with low-level echoes.1 Magnetic resonance imaging is appropriate when a more sensitive imaging modality is indicated, as for a patient with risk factors for malignancy.3,10–12
Read about the surgical management of endometriomas
Surgical management
Indications for surgical excision of endometriomas include pelvic pain, infertility, and prevention and diagnosis of malignancy. Endometriomas may be excised prior to use of assisted reproductive technology.13–15 Medical therapy, such as oral contraceptives, can be used to reduce the size of endometriomas but does not improve fertility.3 Certain ovarian cancers are more common in women with endometriosis, and ovarian tumors are thought to develop in about 1% of ovarian endometriosis cases.1,12 Therefore, endometrioma excision may reduce the risk of malignancy. As with other ovarian cysts, large endometriomas may be excised to reduce the risks of rupture and torsion.
Approach
Laparoscopy is the preferred approach for endometrioma excision. Controversy exists regarding the ideal procedure: complete excision (with stripping of the cyst capsule) or drainage and ablation of the cyst wall. Compared with drainage and ablation, excision reduces recurrence of endometriomas; relieves dysmenorrhea, dyspareunia, pelvic pain, and other symptoms; and improves fertility.13,16 The recurrence rate may be as low as 5.8% with complete excision but is 90% with simple transvaginal aspiration.17,18 If not performed properly, however, cyst capsule stripping may damage nearby ovarian stroma and decrease the ovarian reserve.14 Some authors have advocated combining excision and ablation—performing cystectomy until there is no longer a clear plane between capsule and ovarian stroma and then ablating any remaining endometrial tissue.8
With type I and IIC endometriomas, we have seen the endometrial cyst wall infiltrating the ovarian stroma so deeply there is not always a definable plane. By contrast, type IIA and IIB endometriomas typically have a plane between the cyst wall and the ovarian cortex. In type II endometriomas, endometrial implants on the ovarian cortex infiltrate the plane of the cyst wall such that the juxtaposing lipomatous follicular cyst detaches with minimal intraoperative traction. Portions of type II endometriomas containing fibrosis and adhesions may become more difficult to peel off the cyst wall. For most endometriomas, at least 1 spot is difficult to peel off the ovary, and extra care must be taken at the hilum of ovary to avoid excising healthy ovarian cortex.4,5,7,8
Our surgical approach accounts for the described variations in type I and II endometriomas. Endometrial contents often spill as the endometrioma is dissected off neighboring structures. When possible, endometriomas should be aspirated and irrigated prior to cystectomy to avoid seeding the pelvis and abdomen with spilled endometriotic contents. We use hydrodissection, the injection of dilute vasopressin with a laparoscopic needle, to create a plane between cyst wall and ovarian stroma and strip the cyst capsule with laparoscopic graspers. Type I endometriomas adhere densely to the ovary. Given the presence of fibrosis and adhesions, the cyst is excised in a piecemeal fashion. Care is taken to remove any endometrial implants from the ovary while preserving as much of the ovarian tissue as possible.1
Type II endometriomas are larger cysts originating from the invasion of endometrial implants or type I endometrioma into functional cysts. The difficulty of capsule excision varies according to the extent of endometrial invasion. Type IIA endometriomas contain less than 10% endometrial tissue within the cyst capsule. Thus, the standard ovarian cystectomy stripping technique is successful in removing more than 90% of the cyst capsule. Special care is taken in stripping the residual small portion that involves the endometrial glands and stroma and adheres densely to the ovary.
The larger proportion of endometrial tissue present in type IIB and IIC endometriomas degrades the plane between the cyst capsule and the ovarian stroma, making excision more difficult. Similar to the type I excision, a piecemeal approach is often necessary. If complete stripping of the cyst capsule would result in extensive loss of healthy ovarian tissue, then electrocautery, plasma energy, or laser ablation can be selectively used to destroy focal areas of endometrial invasion. Complete ablation may be difficult, as the endometrioma wall can be up to 5 mm thick.19 For these thick-walled endometriomas, we recommend excision (vs ablation), which lowers the risk of endometrioma recurrence.
Related article:
Endometriosis and pain: Expert answers to 6 questions targeting your management options
- Endometriomas are common adnexal masses in women affected by endometriosis and may exacerbate pelvic pain and impair fertility. Classification of endometriomas into type I and type II,depending on their etiology and characteristics, can guide minimally invasive surgical management.
- Type I endometriomas arise from invagination of endometrial implants on the ovarian cortex, resulting in dense fibrosis and adhesions. These lesions typically require piecemeal excision in order to completely remove the cyst capsule.
- Type II endometriomas result from invasion of endometrial tissue into preexisting functional cysts and are further subclassified by the proportion of cyst capsule containing endometrial tissue (IIA <10%, IIB 10% to 50%, IIC >50%).
- The difficulty of excising type II endometriomas correlates with the degree of endometrial invasion, with type IIA being relatively straightforward and type IIC being as challenging and piecemeal as type I.
- We generally favor complete excision rather than ablation of the cyst capsule, except for when excision would result in an unacceptable loss of healthy ovarian tissue.
Conclusion
Endometriomas, common adnexal masses in women affected by endometriosis, may exacerbate pelvic pain and impair fertility. Gynecologists should be prepared to excise endometriomas completely and exercise care in preserving as much of the ovarian stroma as possible. We classify endometriomas into 2 types: type I, which develop from invagination of endometrial implants in the ovarian cortex, and type II, which stem from invasion of functional cysts by endometrial implants or type I endometrioma. This distinction guides surgical management. We hope this article and its accompanying video will be helpful in guiding laparoscopic excision of type I and II endometriomas.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Nezhat C, Buescher E, Paka C, et al. Video-assisted laparoscopic treatment of endometriosis. In: Nezhat C, Nezhat F, Nezhat C, eds. Nezhat’s Video-Assisted and Robotic-Assisted Laparoscopy and Hysteroscopy. 4th ed. New York, NY: Cambridge University Press; 2013:265–302.
- Burney RO, Giudice LC. Pathogenesis and pathophysiology of endometriosis. Fertil Steril. 2012;98(3):511–519.
- Keyhan S, Hughes C, Price T, Muasher S. An update on surgical versus expectant management of ovarian endometriomas in infertile women. Biomed Res Int. 2015;2015:204792.
- Nezhat F, Nezhat C, Allan CJ, Metzger DA, Sears DL. Clinical and histologic classification of endometriomas. Implications for a mechanism of pathogenesis. J Reprod Med. 1992;37(9):771–776.
- Burney RO, Giudice LC. The pathogenesis of endometriosis. In: Nezhat C, Nezhat F, Nezhat C, eds. Nezhat’s Video-Assisted and Robotic-Assisted Laparoscopy and Hysteroscopy. 4th ed. New York, NY: Cambridge University Press; 2013:252–258.
- Czernobilsky B, Morris WJ. A histologic study of ovarian endometriosis with emphasis on hyperplastic and atypical changes. Obstet Gynecol. 1979;53(3):318–323.
- Nezhat F, Nezhat C, Nezhat C, Admon D. A fresh look at ovarian endometriomas. Contemp Ob Gyn. 1994;39(11):81–94.
- Donnez J, Lousse JC, Jadoul P, Donnez O, Squifflet J. Laparoscopic management of endometriomas using a combined technique of excisional (cystectomy) and ablative surgery. Fertil Steril. 2010;94(1):28–32.
- Nezhat C, Nezhat F, Nezhat C, Seidman DS. Classification of endometriosis. Improving the classification of endometriotic ovarian cysts. Hum Reprod. 1994;9(12):2212–2213.
- Nezhat FR, Pejovic T, Reis FM, Guo SW. The link between endometriosis and ovarian cancer: clinical implications. Int J Gynecol Cancer. 2014;24(4):623–628.
- Nezhat F, Apostol R, Mahmoud M, el Daouk M. Malignant transformation of endometriosis and its clinical significance. Fertil Steril. 2014;102(2):342–344.
- Nezhat FR, Apostal R, Nezhat C, Pejovic T. New insights in the pathophysiology of ovarian cancer and implications for screening and prevention. Am J Obstet Gynecol. 2015;213(3):262–267.
- Hart RJ, Hickey M, Maouris P, Buckett W. Excisional surgery versus ablative surgery for ovarian endometriomata. Cochrane Database Syst Rev. 2008;(2):CD004992.
- Yates J. Endometriosis and infertility: expert answers to 6 questions to help pinpoint the best route to pregnancy. OBG Manag. 2015;27(6):30–35.
- Littman E, Giudice L, Lathi R, Berker B, Milki A, Nezhat C. Role of laparoscopic treatment of endometriosis in patients with failed in vitro fertilization cycles. Fertil Steril. 2005;84(6):1574–1578.
- Exacoustos C, Zupi E, Amadio A, et al. Laparoscopic removal of endometriomas: sonographic evaluation of residual functioning ovarian tissue. Am J Obstet Gynecol. 2004;191(1):68–72.
- Gonçalves FC, Andres MP, Passman LJ, Gonçalves MO, Podgaec S. A systematic review of ultrasonography-guided transvaginal aspiration of recurrent ovarian endometrioma. Int J Gynaecol Obstet. 2016;134(1):3–7.
- Alborzi S, Momtahan M, Parsanezhad ME, Dehbashi S, Zolghadri J, Alborzi S. A prospective, randomized study comparing laparoscopic ovarian cystectomy versus fenestration and coagulation in patients with endometriomas. Fertil Steril. 2004;82(6):1633–1637.
- Nezhat C, Crowgey SR, Garrison CP. Surgical treatment of endometriosis via laser laparoscopy. Fertil Steril. 1986;45(6):778–783.
- Nezhat C, Buescher E, Paka C, et al. Video-assisted laparoscopic treatment of endometriosis. In: Nezhat C, Nezhat F, Nezhat C, eds. Nezhat’s Video-Assisted and Robotic-Assisted Laparoscopy and Hysteroscopy. 4th ed. New York, NY: Cambridge University Press; 2013:265–302.
- Burney RO, Giudice LC. Pathogenesis and pathophysiology of endometriosis. Fertil Steril. 2012;98(3):511–519.
- Keyhan S, Hughes C, Price T, Muasher S. An update on surgical versus expectant management of ovarian endometriomas in infertile women. Biomed Res Int. 2015;2015:204792.
- Nezhat F, Nezhat C, Allan CJ, Metzger DA, Sears DL. Clinical and histologic classification of endometriomas. Implications for a mechanism of pathogenesis. J Reprod Med. 1992;37(9):771–776.
- Burney RO, Giudice LC. The pathogenesis of endometriosis. In: Nezhat C, Nezhat F, Nezhat C, eds. Nezhat’s Video-Assisted and Robotic-Assisted Laparoscopy and Hysteroscopy. 4th ed. New York, NY: Cambridge University Press; 2013:252–258.
- Czernobilsky B, Morris WJ. A histologic study of ovarian endometriosis with emphasis on hyperplastic and atypical changes. Obstet Gynecol. 1979;53(3):318–323.
- Nezhat F, Nezhat C, Nezhat C, Admon D. A fresh look at ovarian endometriomas. Contemp Ob Gyn. 1994;39(11):81–94.
- Donnez J, Lousse JC, Jadoul P, Donnez O, Squifflet J. Laparoscopic management of endometriomas using a combined technique of excisional (cystectomy) and ablative surgery. Fertil Steril. 2010;94(1):28–32.
- Nezhat C, Nezhat F, Nezhat C, Seidman DS. Classification of endometriosis. Improving the classification of endometriotic ovarian cysts. Hum Reprod. 1994;9(12):2212–2213.
- Nezhat FR, Pejovic T, Reis FM, Guo SW. The link between endometriosis and ovarian cancer: clinical implications. Int J Gynecol Cancer. 2014;24(4):623–628.
- Nezhat F, Apostol R, Mahmoud M, el Daouk M. Malignant transformation of endometriosis and its clinical significance. Fertil Steril. 2014;102(2):342–344.
- Nezhat FR, Apostal R, Nezhat C, Pejovic T. New insights in the pathophysiology of ovarian cancer and implications for screening and prevention. Am J Obstet Gynecol. 2015;213(3):262–267.
- Hart RJ, Hickey M, Maouris P, Buckett W. Excisional surgery versus ablative surgery for ovarian endometriomata. Cochrane Database Syst Rev. 2008;(2):CD004992.
- Yates J. Endometriosis and infertility: expert answers to 6 questions to help pinpoint the best route to pregnancy. OBG Manag. 2015;27(6):30–35.
- Littman E, Giudice L, Lathi R, Berker B, Milki A, Nezhat C. Role of laparoscopic treatment of endometriosis in patients with failed in vitro fertilization cycles. Fertil Steril. 2005;84(6):1574–1578.
- Exacoustos C, Zupi E, Amadio A, et al. Laparoscopic removal of endometriomas: sonographic evaluation of residual functioning ovarian tissue. Am J Obstet Gynecol. 2004;191(1):68–72.
- Gonçalves FC, Andres MP, Passman LJ, Gonçalves MO, Podgaec S. A systematic review of ultrasonography-guided transvaginal aspiration of recurrent ovarian endometrioma. Int J Gynaecol Obstet. 2016;134(1):3–7.
- Alborzi S, Momtahan M, Parsanezhad ME, Dehbashi S, Zolghadri J, Alborzi S. A prospective, randomized study comparing laparoscopic ovarian cystectomy versus fenestration and coagulation in patients with endometriomas. Fertil Steril. 2004;82(6):1633–1637.
- Nezhat C, Crowgey SR, Garrison CP. Surgical treatment of endometriosis via laser laparoscopy. Fertil Steril. 1986;45(6):778–783.
IN THIS ARTICLE