User login
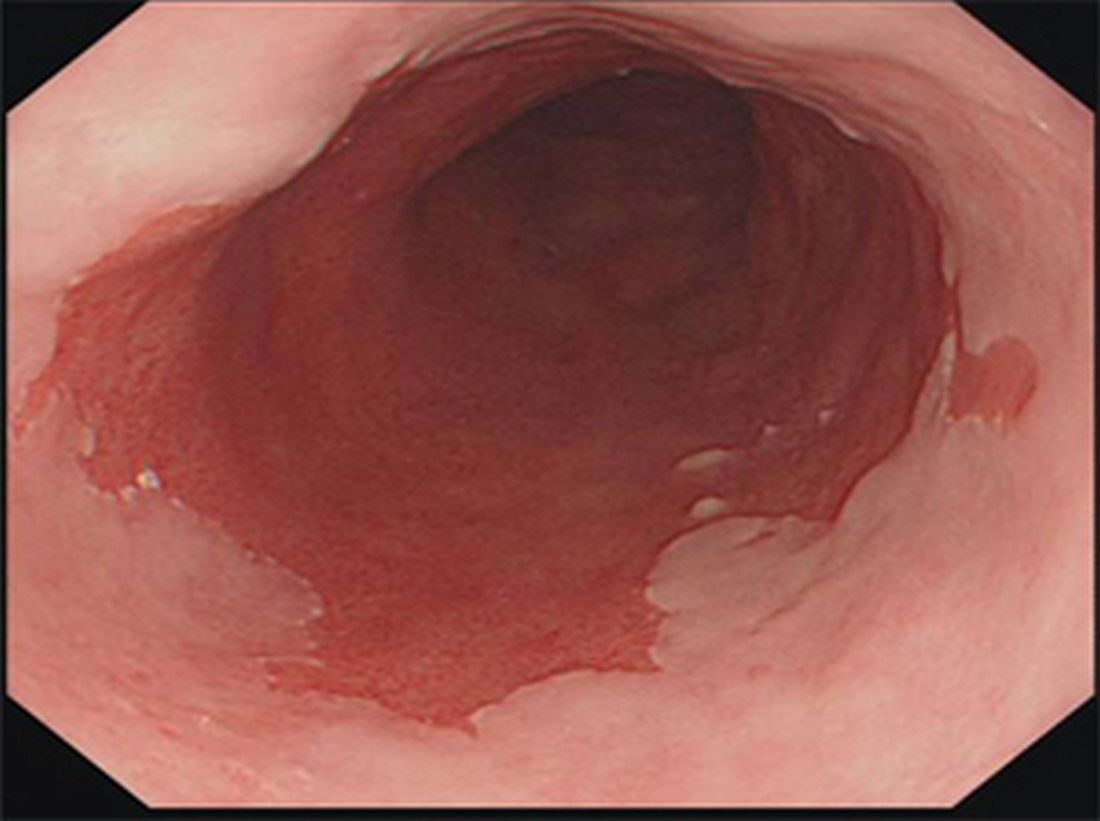
Colorectal tumors: ESD passes long-term test
Endoscopic submucosal dissection (ESD) of superficial colorectal tumors has a favorable long-term outcome, with 94.6% overall survival and 100% disease-specific survival at a median 79 months of follow-up, reported Kenjiro Shigita, MD, of the department of gastroenterology and metabolism, Hiroshima (Japan) University Hospital, and his associates.
The technique is more complicated than endoscopic mucosal resection, but continued advances in the technology and increasingly available training have made it safer than it was, Dr. Shigita and associates wrote (Gastrointest Endosc. 2017. doi: 10.1016/j.gie.2016.07.044).
The study “shows what is possible with an aggressive endoscopic approach,” Dr. Allen added.
Dr. Shigita and associates analyzed data from 222 patients (224 tumors) at their institution for a minimum of 5 years, or until death (median 79 months). Overall survival was 94.6%, and disease-specific survival was 100%.
Patients received follow-up colonoscopy at 1 year if they had a histologic complete resection, defined as horizontal margin negative and vertical margin negative. Those with a histologic positive margin underwent additional colonoscopies at 6 months and 1 year following the ESD procedure.
The en bloc resection rate was 89.7% (201/224), the histologic complete resection rate was 85.7% (192/224), and the R0 resection rate was 83.0% (186/224). R0 was defined as histologic complete resection and no risk of lymph node metastasis as determined by histologic examination.
Delayed bleeding occurred in 6.3% of cases (14/224) and perforation in 5.4% (12/224). All of the adverse events were successfully managed during the procedure.
In 201 tumors, no further surgical resection was performed. In this sample, the local recurrence rate was 1.5%, and none were metastatic. Of these procedures, 179 were en bloc, while 22 were piecemeal. Only one of the en bloc procedures had a recurrence (0.6%), compared with two of the piecemeal procedures (9.1%, P = .038), the authors wrote.
Dr. Allen noted the importance of management and follow-up care of patients. “The authors were careful in deciding which patients needed traditional surgery in addition to endoscopic resection. Also there was careful follow-up with endoscopic surveillance to be sure resection was complete,” he said.
The study is limited by the fact that it is retrospective and was performed at a single center, and the authors stressed the importance of surveillance. “The possibility of local recurrence should be taken into account after piecemeal resection or histologic incomplete resection, and the likelihood of metachronous tumors should be considered,” the authors wrote.
The study is intriguing and warrants further investigation. “This approach should be carefully evaluated with U.S.-based studies and advanced endoscopic training offered,” Dr. Allen said.
Endoscopic submucosal dissection (ESD) of superficial colorectal tumors has a favorable long-term outcome, with 94.6% overall survival and 100% disease-specific survival at a median 79 months of follow-up, reported Kenjiro Shigita, MD, of the department of gastroenterology and metabolism, Hiroshima (Japan) University Hospital, and his associates.
The technique is more complicated than endoscopic mucosal resection, but continued advances in the technology and increasingly available training have made it safer than it was, Dr. Shigita and associates wrote (Gastrointest Endosc. 2017. doi: 10.1016/j.gie.2016.07.044).
The study “shows what is possible with an aggressive endoscopic approach,” Dr. Allen added.
Dr. Shigita and associates analyzed data from 222 patients (224 tumors) at their institution for a minimum of 5 years, or until death (median 79 months). Overall survival was 94.6%, and disease-specific survival was 100%.
Patients received follow-up colonoscopy at 1 year if they had a histologic complete resection, defined as horizontal margin negative and vertical margin negative. Those with a histologic positive margin underwent additional colonoscopies at 6 months and 1 year following the ESD procedure.
The en bloc resection rate was 89.7% (201/224), the histologic complete resection rate was 85.7% (192/224), and the R0 resection rate was 83.0% (186/224). R0 was defined as histologic complete resection and no risk of lymph node metastasis as determined by histologic examination.
Delayed bleeding occurred in 6.3% of cases (14/224) and perforation in 5.4% (12/224). All of the adverse events were successfully managed during the procedure.
In 201 tumors, no further surgical resection was performed. In this sample, the local recurrence rate was 1.5%, and none were metastatic. Of these procedures, 179 were en bloc, while 22 were piecemeal. Only one of the en bloc procedures had a recurrence (0.6%), compared with two of the piecemeal procedures (9.1%, P = .038), the authors wrote.
Dr. Allen noted the importance of management and follow-up care of patients. “The authors were careful in deciding which patients needed traditional surgery in addition to endoscopic resection. Also there was careful follow-up with endoscopic surveillance to be sure resection was complete,” he said.
The study is limited by the fact that it is retrospective and was performed at a single center, and the authors stressed the importance of surveillance. “The possibility of local recurrence should be taken into account after piecemeal resection or histologic incomplete resection, and the likelihood of metachronous tumors should be considered,” the authors wrote.
The study is intriguing and warrants further investigation. “This approach should be carefully evaluated with U.S.-based studies and advanced endoscopic training offered,” Dr. Allen said.
Endoscopic submucosal dissection (ESD) of superficial colorectal tumors has a favorable long-term outcome, with 94.6% overall survival and 100% disease-specific survival at a median 79 months of follow-up, reported Kenjiro Shigita, MD, of the department of gastroenterology and metabolism, Hiroshima (Japan) University Hospital, and his associates.
The technique is more complicated than endoscopic mucosal resection, but continued advances in the technology and increasingly available training have made it safer than it was, Dr. Shigita and associates wrote (Gastrointest Endosc. 2017. doi: 10.1016/j.gie.2016.07.044).
The study “shows what is possible with an aggressive endoscopic approach,” Dr. Allen added.
Dr. Shigita and associates analyzed data from 222 patients (224 tumors) at their institution for a minimum of 5 years, or until death (median 79 months). Overall survival was 94.6%, and disease-specific survival was 100%.
Patients received follow-up colonoscopy at 1 year if they had a histologic complete resection, defined as horizontal margin negative and vertical margin negative. Those with a histologic positive margin underwent additional colonoscopies at 6 months and 1 year following the ESD procedure.
The en bloc resection rate was 89.7% (201/224), the histologic complete resection rate was 85.7% (192/224), and the R0 resection rate was 83.0% (186/224). R0 was defined as histologic complete resection and no risk of lymph node metastasis as determined by histologic examination.
Delayed bleeding occurred in 6.3% of cases (14/224) and perforation in 5.4% (12/224). All of the adverse events were successfully managed during the procedure.
In 201 tumors, no further surgical resection was performed. In this sample, the local recurrence rate was 1.5%, and none were metastatic. Of these procedures, 179 were en bloc, while 22 were piecemeal. Only one of the en bloc procedures had a recurrence (0.6%), compared with two of the piecemeal procedures (9.1%, P = .038), the authors wrote.
Dr. Allen noted the importance of management and follow-up care of patients. “The authors were careful in deciding which patients needed traditional surgery in addition to endoscopic resection. Also there was careful follow-up with endoscopic surveillance to be sure resection was complete,” he said.
The study is limited by the fact that it is retrospective and was performed at a single center, and the authors stressed the importance of surveillance. “The possibility of local recurrence should be taken into account after piecemeal resection or histologic incomplete resection, and the likelihood of metachronous tumors should be considered,” the authors wrote.
The study is intriguing and warrants further investigation. “This approach should be carefully evaluated with U.S.-based studies and advanced endoscopic training offered,” Dr. Allen said.
FROM GASTROINTESTINAL ENDOSCOPY
Key clinical point: Endoscopic submucosal dissection is safe and effective when done by well-trained endoscopists.
Major finding: After 5 or more years, disease-specific survival was 100%.
Data source: Retrospective study of 222 patients at a single center.
Disclosures: The study was funded by the Japan Agency for Medical Research and Development. The authors of the study reported having no financial disclosures. Dr Allen reported having no financial disclosures.
David Hafler, MD
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Barrett’s esophagus: Cancer risk is highest in first year after diagnosis
The highest risk of diagnosis with esophageal adenocarcinoma occurs in the first month after diagnosis with Barrett’s esophagus (BE).
Further, the risk of this type of esophageal cancer is lower than previously believed after that first year, according to a study of 7,932 Swedish residents who were diagnosed with BE from 2006 to 2013.
Esophageal adenocarcinoma (EA) is the most common type of esophageal cancer in the United States, and more than half of patients present with late-stage disease. “The connection between BE and EA is well known, and risk factors for both conditions remain vastly the same, including male sex, age over 50 years, central obesity, and symptomatic GERD [gastroesophageal reflux disease],” Dr. Holmberg said in an interview.
“In order to reduce mortality from esophageal cancer through surveillance and early treatment, we need to improve on BE screening programs,” he said. He also noted that, of all EA cases in Sweden, where screening for BE itself is not recommended in national guidelines, an “astonishing” 97% were diagnosed in patients with previously unknown BE.
Screening programs urge regular endoscopic surveillance in nondysplastic BE patients, but Dr. Holmberg said that their cost-effectiveness is questionable. Complicating matters, there has been conflicting research about the risk of EA that these patients actually face.
As the new study notes, patients with BE were previously thought to face a 30-125 times greater relative risk of EA than the general population did and a mean annual risk of 0.5%. But, recent studies in Europe and the U.S. have suggested that the risk is lower, with an estimated annual risk range of 0.12%-0.18%.
Dr. Holmberg said he and his colleagues launched the new study to better understand the risk in the first year after BE diagnosis.
The researchers used the Swedish National Patient Register to track 7,932 Swedish residents who were diagnosed with BE from 2006 to 2013. About two-thirds were male, and the median age at BE diagnosis was 66 years.
The findings appear in the European Journal of Cancer (2017;75:41-6). Of the patients with BE, 89 new cases of EA were diagnosed 62% of the time within a year of BE diagnosis.
Over a median follow-up of 2.13 person-years, the overall incidence of EA in the patients with BE was 1.47 (95% CI, 0.91-2.02) per 1,000 person-years. That is the equivalent of an annual risk of 0.15%.
The highest incidence rate by far was in the period of 7 to 30 days after diagnosis at 15.53 (95% CI, 4.77-26.29). The incident rates varied from 1.44 to 4.10 (95% CI, 0.00-7.38) for other periods (31-100 days, 101 days to 6 months, over 6 months to 1 year, over 1 year to 3 years, over 3 years to end of follow-up).
How should physicians interpret the study findings and look forward? “Nondysplastic BE represents almost 80% of all BE,” Dr. Holmberg said, but “nondiscriminatory long-term surveillance in nondysplastic BE is not cost-efficient.”
However, while this is “the group with the least risk of EA development, it still generates a large chunk of all EA cases. It is likely that future management of nondysplastic BE will include more risk factors than just degree of dysplasia.”
He added that “individuals with multiple risk factors, such as Caucasian males, age over 50 years, obesity, symptomatic reflux, and with long-segment nondysplastic BE would likely benefit more from more frequent surveillance or even prophylactic treatment with radio-frequency ablation compared to individuals without those risk factors.”
The study was funded by the Swedish Cancer Society and the Swedish Research Council. The authors report no relevant disclosures.
The highest risk of diagnosis with esophageal adenocarcinoma occurs in the first month after diagnosis with Barrett’s esophagus (BE).
Further, the risk of this type of esophageal cancer is lower than previously believed after that first year, according to a study of 7,932 Swedish residents who were diagnosed with BE from 2006 to 2013.
Esophageal adenocarcinoma (EA) is the most common type of esophageal cancer in the United States, and more than half of patients present with late-stage disease. “The connection between BE and EA is well known, and risk factors for both conditions remain vastly the same, including male sex, age over 50 years, central obesity, and symptomatic GERD [gastroesophageal reflux disease],” Dr. Holmberg said in an interview.
“In order to reduce mortality from esophageal cancer through surveillance and early treatment, we need to improve on BE screening programs,” he said. He also noted that, of all EA cases in Sweden, where screening for BE itself is not recommended in national guidelines, an “astonishing” 97% were diagnosed in patients with previously unknown BE.
Screening programs urge regular endoscopic surveillance in nondysplastic BE patients, but Dr. Holmberg said that their cost-effectiveness is questionable. Complicating matters, there has been conflicting research about the risk of EA that these patients actually face.
As the new study notes, patients with BE were previously thought to face a 30-125 times greater relative risk of EA than the general population did and a mean annual risk of 0.5%. But, recent studies in Europe and the U.S. have suggested that the risk is lower, with an estimated annual risk range of 0.12%-0.18%.
Dr. Holmberg said he and his colleagues launched the new study to better understand the risk in the first year after BE diagnosis.
The researchers used the Swedish National Patient Register to track 7,932 Swedish residents who were diagnosed with BE from 2006 to 2013. About two-thirds were male, and the median age at BE diagnosis was 66 years.
The findings appear in the European Journal of Cancer (2017;75:41-6). Of the patients with BE, 89 new cases of EA were diagnosed 62% of the time within a year of BE diagnosis.
Over a median follow-up of 2.13 person-years, the overall incidence of EA in the patients with BE was 1.47 (95% CI, 0.91-2.02) per 1,000 person-years. That is the equivalent of an annual risk of 0.15%.
The highest incidence rate by far was in the period of 7 to 30 days after diagnosis at 15.53 (95% CI, 4.77-26.29). The incident rates varied from 1.44 to 4.10 (95% CI, 0.00-7.38) for other periods (31-100 days, 101 days to 6 months, over 6 months to 1 year, over 1 year to 3 years, over 3 years to end of follow-up).
How should physicians interpret the study findings and look forward? “Nondysplastic BE represents almost 80% of all BE,” Dr. Holmberg said, but “nondiscriminatory long-term surveillance in nondysplastic BE is not cost-efficient.”
However, while this is “the group with the least risk of EA development, it still generates a large chunk of all EA cases. It is likely that future management of nondysplastic BE will include more risk factors than just degree of dysplasia.”
He added that “individuals with multiple risk factors, such as Caucasian males, age over 50 years, obesity, symptomatic reflux, and with long-segment nondysplastic BE would likely benefit more from more frequent surveillance or even prophylactic treatment with radio-frequency ablation compared to individuals without those risk factors.”
The study was funded by the Swedish Cancer Society and the Swedish Research Council. The authors report no relevant disclosures.
The highest risk of diagnosis with esophageal adenocarcinoma occurs in the first month after diagnosis with Barrett’s esophagus (BE).
Further, the risk of this type of esophageal cancer is lower than previously believed after that first year, according to a study of 7,932 Swedish residents who were diagnosed with BE from 2006 to 2013.
Esophageal adenocarcinoma (EA) is the most common type of esophageal cancer in the United States, and more than half of patients present with late-stage disease. “The connection between BE and EA is well known, and risk factors for both conditions remain vastly the same, including male sex, age over 50 years, central obesity, and symptomatic GERD [gastroesophageal reflux disease],” Dr. Holmberg said in an interview.
“In order to reduce mortality from esophageal cancer through surveillance and early treatment, we need to improve on BE screening programs,” he said. He also noted that, of all EA cases in Sweden, where screening for BE itself is not recommended in national guidelines, an “astonishing” 97% were diagnosed in patients with previously unknown BE.
Screening programs urge regular endoscopic surveillance in nondysplastic BE patients, but Dr. Holmberg said that their cost-effectiveness is questionable. Complicating matters, there has been conflicting research about the risk of EA that these patients actually face.
As the new study notes, patients with BE were previously thought to face a 30-125 times greater relative risk of EA than the general population did and a mean annual risk of 0.5%. But, recent studies in Europe and the U.S. have suggested that the risk is lower, with an estimated annual risk range of 0.12%-0.18%.
Dr. Holmberg said he and his colleagues launched the new study to better understand the risk in the first year after BE diagnosis.
The researchers used the Swedish National Patient Register to track 7,932 Swedish residents who were diagnosed with BE from 2006 to 2013. About two-thirds were male, and the median age at BE diagnosis was 66 years.
The findings appear in the European Journal of Cancer (2017;75:41-6). Of the patients with BE, 89 new cases of EA were diagnosed 62% of the time within a year of BE diagnosis.
Over a median follow-up of 2.13 person-years, the overall incidence of EA in the patients with BE was 1.47 (95% CI, 0.91-2.02) per 1,000 person-years. That is the equivalent of an annual risk of 0.15%.
The highest incidence rate by far was in the period of 7 to 30 days after diagnosis at 15.53 (95% CI, 4.77-26.29). The incident rates varied from 1.44 to 4.10 (95% CI, 0.00-7.38) for other periods (31-100 days, 101 days to 6 months, over 6 months to 1 year, over 1 year to 3 years, over 3 years to end of follow-up).
How should physicians interpret the study findings and look forward? “Nondysplastic BE represents almost 80% of all BE,” Dr. Holmberg said, but “nondiscriminatory long-term surveillance in nondysplastic BE is not cost-efficient.”
However, while this is “the group with the least risk of EA development, it still generates a large chunk of all EA cases. It is likely that future management of nondysplastic BE will include more risk factors than just degree of dysplasia.”
He added that “individuals with multiple risk factors, such as Caucasian males, age over 50 years, obesity, symptomatic reflux, and with long-segment nondysplastic BE would likely benefit more from more frequent surveillance or even prophylactic treatment with radio-frequency ablation compared to individuals without those risk factors.”
The study was funded by the Swedish Cancer Society and the Swedish Research Council. The authors report no relevant disclosures.
FROM THE EUROPEAN JOURNAL OF CANCER
Key clinical point: While their overall risk over the short term is low, patients with Barrett’s esophagus are especially likely to be diagnosed with esophageal adenocarcinoma in the first weeks after Barrett’s diagnosis.
Major finding: Over a median of 2.13 person-years, the annual risk of esophageal adenocarcinoma diagnosis was 0.15% in patients with Barrett’s esophagus, but the incidence rate was especially high (15.53; 95% confidence interval, 4.77-26.29) from 7 to 30 days after Barrett’s diagnosis, compared with rates of 1.44-4.10 (95% CI, 0.00-7.38) for later periods.
Data source: A population-centered analysis of 7,932 Swedish residents diagnosed with Barrett’s esophagus from 2006 to 2013.
Disclosures: The study was funded by the Swedish Cancer Society and the Swedish Research Council. The authors report no relevant disclosures.
Miami Breast Cancer Symposium to explore treatment controversies
FROM MBCC (FRONTLINE MEDICAL NEWS) – Oncology Practice will be on site this coming week at the Miami Breast Cancer Symposium in Miami Beach, reporting on the latest in multidisciplinary management of breast cancer patients. Sessions will highlight updates in systemic therapy, immunology and immunotherapy, and overcoming therapeutic resistance, as well as explore treatment controversies, such as omitting anthracyclines, extended-field radiation therapy, and who should be receiving extended hormonal therapy. The symposium, hosted by Physicians’ Education Resource, begins Thursday, March 9. Our team will provide daily coverage of the following presentations and more:
Overcoming Resistance to HER2 Targeted Therapy
Mark D. Pegram, MD
Overcoming Resistance to Endocrine Ablative Therapy
William J. Gradishar, MD
Medical Crossfire: Is Extended Field Radiation Therapy Ready for Prime Time?
Lawrence J. Solin, MD, & Thomas A. Buchholz, MD
Raising the Therapeutic Index for HER2+ Targeted Therapy: Can We Safely Omit
Anthracyclines?
Sara Hurvitz, MD
Update on Neoadjuvant Treatment Strategies in HER2+ Breast Cancer
Debu Tripathy, MD
Update on PARP Inhibitors in Breast Cancer
Kimberly L. Blackwell, MD
Update on Immunology and Immunotherapy in Breast Cancer
Elizabeth Mittendorf, MD, PhD
Medical Crossfire: Is Extended Hormonal Therapy Required for Everyone?
William J. Gradishar, MD, & Sara Hurvitz, MD
FROM MBCC (FRONTLINE MEDICAL NEWS) – Oncology Practice will be on site this coming week at the Miami Breast Cancer Symposium in Miami Beach, reporting on the latest in multidisciplinary management of breast cancer patients. Sessions will highlight updates in systemic therapy, immunology and immunotherapy, and overcoming therapeutic resistance, as well as explore treatment controversies, such as omitting anthracyclines, extended-field radiation therapy, and who should be receiving extended hormonal therapy. The symposium, hosted by Physicians’ Education Resource, begins Thursday, March 9. Our team will provide daily coverage of the following presentations and more:
Overcoming Resistance to HER2 Targeted Therapy
Mark D. Pegram, MD
Overcoming Resistance to Endocrine Ablative Therapy
William J. Gradishar, MD
Medical Crossfire: Is Extended Field Radiation Therapy Ready for Prime Time?
Lawrence J. Solin, MD, & Thomas A. Buchholz, MD
Raising the Therapeutic Index for HER2+ Targeted Therapy: Can We Safely Omit
Anthracyclines?
Sara Hurvitz, MD
Update on Neoadjuvant Treatment Strategies in HER2+ Breast Cancer
Debu Tripathy, MD
Update on PARP Inhibitors in Breast Cancer
Kimberly L. Blackwell, MD
Update on Immunology and Immunotherapy in Breast Cancer
Elizabeth Mittendorf, MD, PhD
Medical Crossfire: Is Extended Hormonal Therapy Required for Everyone?
William J. Gradishar, MD, & Sara Hurvitz, MD
FROM MBCC (FRONTLINE MEDICAL NEWS) – Oncology Practice will be on site this coming week at the Miami Breast Cancer Symposium in Miami Beach, reporting on the latest in multidisciplinary management of breast cancer patients. Sessions will highlight updates in systemic therapy, immunology and immunotherapy, and overcoming therapeutic resistance, as well as explore treatment controversies, such as omitting anthracyclines, extended-field radiation therapy, and who should be receiving extended hormonal therapy. The symposium, hosted by Physicians’ Education Resource, begins Thursday, March 9. Our team will provide daily coverage of the following presentations and more:
Overcoming Resistance to HER2 Targeted Therapy
Mark D. Pegram, MD
Overcoming Resistance to Endocrine Ablative Therapy
William J. Gradishar, MD
Medical Crossfire: Is Extended Field Radiation Therapy Ready for Prime Time?
Lawrence J. Solin, MD, & Thomas A. Buchholz, MD
Raising the Therapeutic Index for HER2+ Targeted Therapy: Can We Safely Omit
Anthracyclines?
Sara Hurvitz, MD
Update on Neoadjuvant Treatment Strategies in HER2+ Breast Cancer
Debu Tripathy, MD
Update on PARP Inhibitors in Breast Cancer
Kimberly L. Blackwell, MD
Update on Immunology and Immunotherapy in Breast Cancer
Elizabeth Mittendorf, MD, PhD
Medical Crossfire: Is Extended Hormonal Therapy Required for Everyone?
William J. Gradishar, MD, & Sara Hurvitz, MD
Voclosporin linked to threefold increase in lupus nephritis remission
Treatment with the investigational calcineurin inhibitor voclosporin is associated with a significant, threefold-higher rate of complete remission for lupus nephritis, compared with the current standard of care, according to 48-week data from the AURA-LV (Aurinia Urinary Protein Reduction Active–Lupus With Voclosporin) study.
In a company release, manufacturer Aurinia Pharmaceuticals presented the results of the international phase IIb controlled trial involving 265 patients with active lupus nephritis from 20 countries, which they say has now met its primary and secondary endpoints.
After 48 weeks, 49% of patients in the low-dose group and 40% in the high-dose group had achieved complete remission, compared with 24% in the control group (P less than .001 for low-dose vs. control; P = .026 for high-dose vs. control). This represented a threefold-higher remission rate for the low-dose group (odds ratio, 3.21) and a twofold-higher rate for the high-dose group (OR, 2.1), compared with controls.
Complete remission was defined as a composite endpoint that included urine protein/creatinine ratio of 0.5 mg/mg or less; normal, stable renal function; presence of sustained, low dose steroids; and no administration of rescue medications.
Partial remission – defined as at least a 50% reduction in urine protein/creatinine ratio with no concomitant use of rescue medication – was seen in 68% of patients in the low-dose voclosporin group, 72% of patients in the high-dose group, and 48% of patients in the control arm (P = .007 for low-dose vs. control; P = .002 for high-dose vs. control).
Investigators said there were no unexpected safety signals from voclosporin, but there were three deaths and one malignancy reported in the control arm after the study treatment period ended.
Brad Rovin, MD, of Ohio State University in Columbus said in the company’s statement that current treatments for this severe complication of systemic lupus erythematosus are toxic, and complete renal response rates are low.
“The AURA trial’s long-term results convincingly demonstrate that the addition of voclosporin to standard of care treatment is superior to standard of care alone,” Dr. Rovin said. “This is an impressive renal response rate, and these results may shift the treatment paradigm of lupus nephritis.”
Aurinia’s chief medical officer, Neil Solomons, MD, said in the release that the results provide the company with confidence that they can now execute a successful phase III program.
The 24-week results of the study – in which all primary and the 24-week secondary endpoints were also met – were released in November 2016.
Treatment with the investigational calcineurin inhibitor voclosporin is associated with a significant, threefold-higher rate of complete remission for lupus nephritis, compared with the current standard of care, according to 48-week data from the AURA-LV (Aurinia Urinary Protein Reduction Active–Lupus With Voclosporin) study.
In a company release, manufacturer Aurinia Pharmaceuticals presented the results of the international phase IIb controlled trial involving 265 patients with active lupus nephritis from 20 countries, which they say has now met its primary and secondary endpoints.
After 48 weeks, 49% of patients in the low-dose group and 40% in the high-dose group had achieved complete remission, compared with 24% in the control group (P less than .001 for low-dose vs. control; P = .026 for high-dose vs. control). This represented a threefold-higher remission rate for the low-dose group (odds ratio, 3.21) and a twofold-higher rate for the high-dose group (OR, 2.1), compared with controls.
Complete remission was defined as a composite endpoint that included urine protein/creatinine ratio of 0.5 mg/mg or less; normal, stable renal function; presence of sustained, low dose steroids; and no administration of rescue medications.
Partial remission – defined as at least a 50% reduction in urine protein/creatinine ratio with no concomitant use of rescue medication – was seen in 68% of patients in the low-dose voclosporin group, 72% of patients in the high-dose group, and 48% of patients in the control arm (P = .007 for low-dose vs. control; P = .002 for high-dose vs. control).
Investigators said there were no unexpected safety signals from voclosporin, but there were three deaths and one malignancy reported in the control arm after the study treatment period ended.
Brad Rovin, MD, of Ohio State University in Columbus said in the company’s statement that current treatments for this severe complication of systemic lupus erythematosus are toxic, and complete renal response rates are low.
“The AURA trial’s long-term results convincingly demonstrate that the addition of voclosporin to standard of care treatment is superior to standard of care alone,” Dr. Rovin said. “This is an impressive renal response rate, and these results may shift the treatment paradigm of lupus nephritis.”
Aurinia’s chief medical officer, Neil Solomons, MD, said in the release that the results provide the company with confidence that they can now execute a successful phase III program.
The 24-week results of the study – in which all primary and the 24-week secondary endpoints were also met – were released in November 2016.
Treatment with the investigational calcineurin inhibitor voclosporin is associated with a significant, threefold-higher rate of complete remission for lupus nephritis, compared with the current standard of care, according to 48-week data from the AURA-LV (Aurinia Urinary Protein Reduction Active–Lupus With Voclosporin) study.
In a company release, manufacturer Aurinia Pharmaceuticals presented the results of the international phase IIb controlled trial involving 265 patients with active lupus nephritis from 20 countries, which they say has now met its primary and secondary endpoints.
After 48 weeks, 49% of patients in the low-dose group and 40% in the high-dose group had achieved complete remission, compared with 24% in the control group (P less than .001 for low-dose vs. control; P = .026 for high-dose vs. control). This represented a threefold-higher remission rate for the low-dose group (odds ratio, 3.21) and a twofold-higher rate for the high-dose group (OR, 2.1), compared with controls.
Complete remission was defined as a composite endpoint that included urine protein/creatinine ratio of 0.5 mg/mg or less; normal, stable renal function; presence of sustained, low dose steroids; and no administration of rescue medications.
Partial remission – defined as at least a 50% reduction in urine protein/creatinine ratio with no concomitant use of rescue medication – was seen in 68% of patients in the low-dose voclosporin group, 72% of patients in the high-dose group, and 48% of patients in the control arm (P = .007 for low-dose vs. control; P = .002 for high-dose vs. control).
Investigators said there were no unexpected safety signals from voclosporin, but there were three deaths and one malignancy reported in the control arm after the study treatment period ended.
Brad Rovin, MD, of Ohio State University in Columbus said in the company’s statement that current treatments for this severe complication of systemic lupus erythematosus are toxic, and complete renal response rates are low.
“The AURA trial’s long-term results convincingly demonstrate that the addition of voclosporin to standard of care treatment is superior to standard of care alone,” Dr. Rovin said. “This is an impressive renal response rate, and these results may shift the treatment paradigm of lupus nephritis.”
Aurinia’s chief medical officer, Neil Solomons, MD, said in the release that the results provide the company with confidence that they can now execute a successful phase III program.
The 24-week results of the study – in which all primary and the 24-week secondary endpoints were also met – were released in November 2016.
Key clinical point:
Major finding: Nearly half of patients treated with the lower dose of investigational calcineurin inhibitor voclosporin achieved complete remission compared to one-quarter of patients in the control group.
Data source: The AURA-LV phase IIb controlled study involving 265 patients with active lupus nephritis.
Disclosures: The results were presented in a company release from manufacturer Aurinia Pharmaceuticals.
Neuropsychiatric Strategies May Benefit Patients With Refractory Epilepsy
HOUSTON—Treating psychiatric symptoms in patients with refractory epilepsy is likely to improve the overall course of the disease, as well as patients’ quality of life, according to an overview provided at the 70th Annual Meeting of the American Epilepsy Society.
Epilepsy “is not necessarily a neurologic disease with psychiatric comorbidity. Maybe there is something in the interface … that is really our target,” he said.
Epilepsy and psychiatry have considerable symptom overlap, Dr. Salpekar noted. For example, someone with a seizure focus in the amygdala might have an aura of anxiety or overwhelming fear that resembles the early stages of a panic attack.
Neurologists should aim to treat seizures and psychiatric symptoms. “Think about psychiatric symptoms as clues that we have not treated the entire disease yet,” Dr. Salpekar said. “We want to use our anticonvulsants to treat the entire disease, and maybe that will lead to improved seizure control.”
A Bidirectional Relationship
Understanding the bidirectional relationship between neuropsychiatric disorders and epilepsy is key to treatment. “Not only are you more likely to be depressed if you have epilepsy, but you are more likely to have epilepsy or develop seizures if you are depressed,” Dr. Salpekar said. This finding represents “a paradigm shift … in how we interpret what this illness could be.”
In addition, ADHD increases the likelihood of seizures, and one study found that 28% of children with ADHD who underwent polysomnography had centrotemporal spikes. Other research suggests that patients with epilepsy may have structural changes and cognitive symptoms prior to their first identified seizures.
Antiepileptic drugs (AEDs) effectively treat psychiatric symptoms, including impulsivity, rage outbursts, and mood lability. “In the psychiatric world, we depend upon these [drugs] all the time,” Dr. Salpekar said. “Maybe there are relationships between seizure control and behavior control that are more clear-cut than we have thought.”
Treatment Options
Dr. Salpekar and colleagues in 2006 conducted a review of patients with epilepsy and comorbid bipolar spectrum disorder. They reviewed cases to see whether treatment with AEDs improved bipolar symptoms, such as mood lability, impulsivity, rage outbursts, and extreme irritability, as well as seizures. They found that carbamazepine, divalproex sodium, lamotrigine, and oxcarbazepine monotherapies were associated with better psychiatric symptom ratings, compared with other monotherapies. In many cases, the drugs appeared to treat epilepsy and mood disorder simultaneously. The findings suggest that AEDs can “bridge the gap between epilepsy or seizure counts and psychiatric symptoms” and that neurologists should “aim for broad-spectrum treatment,” he said.
Psychiatric symptoms sometimes may be related to AEDs. If an AED causes depressive symptoms or irritability, neurologists should try to remove it. In addition, benzodiazepine withdrawal may cause depression, and this effect may occur in certain patients due to their metabolism. “If someone is a fast metabolizer, and they are taking b.i.d. clonazepam, what happens if it wears off?” In those cases, behavior problems may occur late in the afternoon when serum drug concentrations are lowest.
Many GABAergic drugs have been reported to improve anxiety. Gabapentin also has been reported to improve social phobia and chronic pain. Potential negative effects of GABAergic drugs include depression, sedation, mood lability, and hyperactivity.
Among antiglutamatergic drugs, lamotrigine may be the best evidence-based option for improving mood or depression. Lamotrigine, however, may promote mania in patients with a propensity for bipolar spectrum disorder.
Among drugs with other mechanisms of action, carbamazepine is known to be a mood stabilizer, and eslicarbazepine may have the same effect. Levetiracetam may cause irritability, but the drug also may improve mood in some cases. “There are positives and negatives with any of our AEDs,” Dr. Salpekar said.
An Important Question to Ask Patients
Patients with severe refractory epilepsy often have depression, and treating depression may improve their quality of life dramatically. “When all else fails, at the very least, we want to identify if depression is present because we can do something about that most of the time,” Dr. Salpekar said.
Many depression screening tools are available, but the important thing is to broach the subject. “I would encourage all of you to ask one question of your patients. Just say, ‘Are you depressed?’ That might be all you have to do.”
Depression may be more common in patients with temporal lobe foci, and evidence suggests that adults with left foci have an increased likelihood of depression. Waxman and Geschwind observed that patients with temporal lobe epilepsy may have an increased preoccupation with philosophical, moral, or religious issues, which also can be characteristic of manic episodes, Dr. Salpekar said.
Dr. Salpekar and colleagues conducted a study of children with medically refractory epilepsy who presented for surgical evaluation to assess whether psychiatric symptoms differed according to seizure focus. Researchers reviewed case records for 40 patients. Patients with suspected temporal lobe foci had more behavioral problems and were more likely to have a diagnosis of depression, compared with children with extratemporal foci. This finding “lends some credence to our idea that temporal lobe foci are worse … in terms of depression,” he said.
Treating Depression
Neurologists can follow practical steps to address depression. First, determine whether symptoms are attributable to drug side effects. Then, address lifestyle factors, including sleep, exercise, and diet, and consider social stressors, such as family members or employers who do not appreciate the patient’s cognitive or physical limitations. Neurologists should identify targets that help measure whether treatment is working and consider whether low doses of adjunctive AEDs may help treat psychiatric symptoms. Finally, neurologists may consider prescribing an antidepressant. “If you are going to use an antidepressant, get comfortable, skilled, and knowledgeable about using one of them,” he said.
Studies have provided data regarding the use of antidepressants in patients with epilepsy. In an observational pediatric study, 36 patients who received fluoxetine or sertraline improved clinically, whereas two patients who received fluoxetine or sertraline had worsened seizures. Studies also have provided evidence for the use of citalopram and sertraline in adults with epilepsy. Other studies regarding the treatment of depression in epilepsy are ongoing.
Selective serotonin reuptake inhibitors (SSRIs) entail a low risk of lowering seizure threshold, as do certain antipsychotics (eg, haloperidol, risperidone, and aripiprazole). Methylphenidate is considered safe and is widely used for children with epilepsy and comorbid ADHD.
Nonmedical treatment also can benefit patients. Social skills groups, overnight camps, and cognitive behavioral therapy may be effective options. Vocational support also is important. “Meaningful activity can … tip the balance into more functionality,” he said. “Think about seizure control and behavior control as partners,” Dr. Salpekar concluded. “Think about treating both of these types of targets as working together to improve the entire illness.”
—Jake Remaly
Suggested Reading
Hermann BP, Dabbs K, Becker T, et al. Brain development in children with new onset epilepsy: a prospective controlled cohort investigation. Epilepsia. 2010;51(10):2038-2046.
Hesdorffer DC, Hauser WA, Olafsson E, et al. Depression and suicide attempt as risk factors for incident unprovoked seizures. Ann Neurol. 2006;59(1):35-41.
Salpekar JA. Mood disorders in epilepsy. Focus. 2016;14(4):465-472.
Salpekar JA, Berl MM, Havens K, et al. Psychiatric symptoms in children prior to epilepsy surgery differ according to suspected seizure focus. Epilepsia. 2013;54(6):1074-1082.
Salpekar JA, Conry JA, Doss W, et al. Clinical experience with anticonvulsant medication in pediatric epilepsy and comorbid bipolar spectrum disorder. Epilepsy Behav. 2006;9(2):327-334.
Silvestri R, Gagliano A, Calarese T, et al. Ictal and interictal EEG abnormalities in ADHD children recorded over night by video-polysomnography. Epilepsy Res. 2007;75(2-3):130-137.
Waxman SG, Geschwind N. The interictal behavior syndrome of temporal lobe epilepsy. Arch Gen Psychiatry. 1975;32(12):1580-1586.
HOUSTON—Treating psychiatric symptoms in patients with refractory epilepsy is likely to improve the overall course of the disease, as well as patients’ quality of life, according to an overview provided at the 70th Annual Meeting of the American Epilepsy Society.
Epilepsy “is not necessarily a neurologic disease with psychiatric comorbidity. Maybe there is something in the interface … that is really our target,” he said.
Epilepsy and psychiatry have considerable symptom overlap, Dr. Salpekar noted. For example, someone with a seizure focus in the amygdala might have an aura of anxiety or overwhelming fear that resembles the early stages of a panic attack.
Neurologists should aim to treat seizures and psychiatric symptoms. “Think about psychiatric symptoms as clues that we have not treated the entire disease yet,” Dr. Salpekar said. “We want to use our anticonvulsants to treat the entire disease, and maybe that will lead to improved seizure control.”
A Bidirectional Relationship
Understanding the bidirectional relationship between neuropsychiatric disorders and epilepsy is key to treatment. “Not only are you more likely to be depressed if you have epilepsy, but you are more likely to have epilepsy or develop seizures if you are depressed,” Dr. Salpekar said. This finding represents “a paradigm shift … in how we interpret what this illness could be.”
In addition, ADHD increases the likelihood of seizures, and one study found that 28% of children with ADHD who underwent polysomnography had centrotemporal spikes. Other research suggests that patients with epilepsy may have structural changes and cognitive symptoms prior to their first identified seizures.
Antiepileptic drugs (AEDs) effectively treat psychiatric symptoms, including impulsivity, rage outbursts, and mood lability. “In the psychiatric world, we depend upon these [drugs] all the time,” Dr. Salpekar said. “Maybe there are relationships between seizure control and behavior control that are more clear-cut than we have thought.”
Treatment Options
Dr. Salpekar and colleagues in 2006 conducted a review of patients with epilepsy and comorbid bipolar spectrum disorder. They reviewed cases to see whether treatment with AEDs improved bipolar symptoms, such as mood lability, impulsivity, rage outbursts, and extreme irritability, as well as seizures. They found that carbamazepine, divalproex sodium, lamotrigine, and oxcarbazepine monotherapies were associated with better psychiatric symptom ratings, compared with other monotherapies. In many cases, the drugs appeared to treat epilepsy and mood disorder simultaneously. The findings suggest that AEDs can “bridge the gap between epilepsy or seizure counts and psychiatric symptoms” and that neurologists should “aim for broad-spectrum treatment,” he said.
Psychiatric symptoms sometimes may be related to AEDs. If an AED causes depressive symptoms or irritability, neurologists should try to remove it. In addition, benzodiazepine withdrawal may cause depression, and this effect may occur in certain patients due to their metabolism. “If someone is a fast metabolizer, and they are taking b.i.d. clonazepam, what happens if it wears off?” In those cases, behavior problems may occur late in the afternoon when serum drug concentrations are lowest.
Many GABAergic drugs have been reported to improve anxiety. Gabapentin also has been reported to improve social phobia and chronic pain. Potential negative effects of GABAergic drugs include depression, sedation, mood lability, and hyperactivity.
Among antiglutamatergic drugs, lamotrigine may be the best evidence-based option for improving mood or depression. Lamotrigine, however, may promote mania in patients with a propensity for bipolar spectrum disorder.
Among drugs with other mechanisms of action, carbamazepine is known to be a mood stabilizer, and eslicarbazepine may have the same effect. Levetiracetam may cause irritability, but the drug also may improve mood in some cases. “There are positives and negatives with any of our AEDs,” Dr. Salpekar said.
An Important Question to Ask Patients
Patients with severe refractory epilepsy often have depression, and treating depression may improve their quality of life dramatically. “When all else fails, at the very least, we want to identify if depression is present because we can do something about that most of the time,” Dr. Salpekar said.
Many depression screening tools are available, but the important thing is to broach the subject. “I would encourage all of you to ask one question of your patients. Just say, ‘Are you depressed?’ That might be all you have to do.”
Depression may be more common in patients with temporal lobe foci, and evidence suggests that adults with left foci have an increased likelihood of depression. Waxman and Geschwind observed that patients with temporal lobe epilepsy may have an increased preoccupation with philosophical, moral, or religious issues, which also can be characteristic of manic episodes, Dr. Salpekar said.
Dr. Salpekar and colleagues conducted a study of children with medically refractory epilepsy who presented for surgical evaluation to assess whether psychiatric symptoms differed according to seizure focus. Researchers reviewed case records for 40 patients. Patients with suspected temporal lobe foci had more behavioral problems and were more likely to have a diagnosis of depression, compared with children with extratemporal foci. This finding “lends some credence to our idea that temporal lobe foci are worse … in terms of depression,” he said.
Treating Depression
Neurologists can follow practical steps to address depression. First, determine whether symptoms are attributable to drug side effects. Then, address lifestyle factors, including sleep, exercise, and diet, and consider social stressors, such as family members or employers who do not appreciate the patient’s cognitive or physical limitations. Neurologists should identify targets that help measure whether treatment is working and consider whether low doses of adjunctive AEDs may help treat psychiatric symptoms. Finally, neurologists may consider prescribing an antidepressant. “If you are going to use an antidepressant, get comfortable, skilled, and knowledgeable about using one of them,” he said.
Studies have provided data regarding the use of antidepressants in patients with epilepsy. In an observational pediatric study, 36 patients who received fluoxetine or sertraline improved clinically, whereas two patients who received fluoxetine or sertraline had worsened seizures. Studies also have provided evidence for the use of citalopram and sertraline in adults with epilepsy. Other studies regarding the treatment of depression in epilepsy are ongoing.
Selective serotonin reuptake inhibitors (SSRIs) entail a low risk of lowering seizure threshold, as do certain antipsychotics (eg, haloperidol, risperidone, and aripiprazole). Methylphenidate is considered safe and is widely used for children with epilepsy and comorbid ADHD.
Nonmedical treatment also can benefit patients. Social skills groups, overnight camps, and cognitive behavioral therapy may be effective options. Vocational support also is important. “Meaningful activity can … tip the balance into more functionality,” he said. “Think about seizure control and behavior control as partners,” Dr. Salpekar concluded. “Think about treating both of these types of targets as working together to improve the entire illness.”
—Jake Remaly
Suggested Reading
Hermann BP, Dabbs K, Becker T, et al. Brain development in children with new onset epilepsy: a prospective controlled cohort investigation. Epilepsia. 2010;51(10):2038-2046.
Hesdorffer DC, Hauser WA, Olafsson E, et al. Depression and suicide attempt as risk factors for incident unprovoked seizures. Ann Neurol. 2006;59(1):35-41.
Salpekar JA. Mood disorders in epilepsy. Focus. 2016;14(4):465-472.
Salpekar JA, Berl MM, Havens K, et al. Psychiatric symptoms in children prior to epilepsy surgery differ according to suspected seizure focus. Epilepsia. 2013;54(6):1074-1082.
Salpekar JA, Conry JA, Doss W, et al. Clinical experience with anticonvulsant medication in pediatric epilepsy and comorbid bipolar spectrum disorder. Epilepsy Behav. 2006;9(2):327-334.
Silvestri R, Gagliano A, Calarese T, et al. Ictal and interictal EEG abnormalities in ADHD children recorded over night by video-polysomnography. Epilepsy Res. 2007;75(2-3):130-137.
Waxman SG, Geschwind N. The interictal behavior syndrome of temporal lobe epilepsy. Arch Gen Psychiatry. 1975;32(12):1580-1586.
HOUSTON—Treating psychiatric symptoms in patients with refractory epilepsy is likely to improve the overall course of the disease, as well as patients’ quality of life, according to an overview provided at the 70th Annual Meeting of the American Epilepsy Society.
Epilepsy “is not necessarily a neurologic disease with psychiatric comorbidity. Maybe there is something in the interface … that is really our target,” he said.
Epilepsy and psychiatry have considerable symptom overlap, Dr. Salpekar noted. For example, someone with a seizure focus in the amygdala might have an aura of anxiety or overwhelming fear that resembles the early stages of a panic attack.
Neurologists should aim to treat seizures and psychiatric symptoms. “Think about psychiatric symptoms as clues that we have not treated the entire disease yet,” Dr. Salpekar said. “We want to use our anticonvulsants to treat the entire disease, and maybe that will lead to improved seizure control.”
A Bidirectional Relationship
Understanding the bidirectional relationship between neuropsychiatric disorders and epilepsy is key to treatment. “Not only are you more likely to be depressed if you have epilepsy, but you are more likely to have epilepsy or develop seizures if you are depressed,” Dr. Salpekar said. This finding represents “a paradigm shift … in how we interpret what this illness could be.”
In addition, ADHD increases the likelihood of seizures, and one study found that 28% of children with ADHD who underwent polysomnography had centrotemporal spikes. Other research suggests that patients with epilepsy may have structural changes and cognitive symptoms prior to their first identified seizures.
Antiepileptic drugs (AEDs) effectively treat psychiatric symptoms, including impulsivity, rage outbursts, and mood lability. “In the psychiatric world, we depend upon these [drugs] all the time,” Dr. Salpekar said. “Maybe there are relationships between seizure control and behavior control that are more clear-cut than we have thought.”
Treatment Options
Dr. Salpekar and colleagues in 2006 conducted a review of patients with epilepsy and comorbid bipolar spectrum disorder. They reviewed cases to see whether treatment with AEDs improved bipolar symptoms, such as mood lability, impulsivity, rage outbursts, and extreme irritability, as well as seizures. They found that carbamazepine, divalproex sodium, lamotrigine, and oxcarbazepine monotherapies were associated with better psychiatric symptom ratings, compared with other monotherapies. In many cases, the drugs appeared to treat epilepsy and mood disorder simultaneously. The findings suggest that AEDs can “bridge the gap between epilepsy or seizure counts and psychiatric symptoms” and that neurologists should “aim for broad-spectrum treatment,” he said.
Psychiatric symptoms sometimes may be related to AEDs. If an AED causes depressive symptoms or irritability, neurologists should try to remove it. In addition, benzodiazepine withdrawal may cause depression, and this effect may occur in certain patients due to their metabolism. “If someone is a fast metabolizer, and they are taking b.i.d. clonazepam, what happens if it wears off?” In those cases, behavior problems may occur late in the afternoon when serum drug concentrations are lowest.
Many GABAergic drugs have been reported to improve anxiety. Gabapentin also has been reported to improve social phobia and chronic pain. Potential negative effects of GABAergic drugs include depression, sedation, mood lability, and hyperactivity.
Among antiglutamatergic drugs, lamotrigine may be the best evidence-based option for improving mood or depression. Lamotrigine, however, may promote mania in patients with a propensity for bipolar spectrum disorder.
Among drugs with other mechanisms of action, carbamazepine is known to be a mood stabilizer, and eslicarbazepine may have the same effect. Levetiracetam may cause irritability, but the drug also may improve mood in some cases. “There are positives and negatives with any of our AEDs,” Dr. Salpekar said.
An Important Question to Ask Patients
Patients with severe refractory epilepsy often have depression, and treating depression may improve their quality of life dramatically. “When all else fails, at the very least, we want to identify if depression is present because we can do something about that most of the time,” Dr. Salpekar said.
Many depression screening tools are available, but the important thing is to broach the subject. “I would encourage all of you to ask one question of your patients. Just say, ‘Are you depressed?’ That might be all you have to do.”
Depression may be more common in patients with temporal lobe foci, and evidence suggests that adults with left foci have an increased likelihood of depression. Waxman and Geschwind observed that patients with temporal lobe epilepsy may have an increased preoccupation with philosophical, moral, or religious issues, which also can be characteristic of manic episodes, Dr. Salpekar said.
Dr. Salpekar and colleagues conducted a study of children with medically refractory epilepsy who presented for surgical evaluation to assess whether psychiatric symptoms differed according to seizure focus. Researchers reviewed case records for 40 patients. Patients with suspected temporal lobe foci had more behavioral problems and were more likely to have a diagnosis of depression, compared with children with extratemporal foci. This finding “lends some credence to our idea that temporal lobe foci are worse … in terms of depression,” he said.
Treating Depression
Neurologists can follow practical steps to address depression. First, determine whether symptoms are attributable to drug side effects. Then, address lifestyle factors, including sleep, exercise, and diet, and consider social stressors, such as family members or employers who do not appreciate the patient’s cognitive or physical limitations. Neurologists should identify targets that help measure whether treatment is working and consider whether low doses of adjunctive AEDs may help treat psychiatric symptoms. Finally, neurologists may consider prescribing an antidepressant. “If you are going to use an antidepressant, get comfortable, skilled, and knowledgeable about using one of them,” he said.
Studies have provided data regarding the use of antidepressants in patients with epilepsy. In an observational pediatric study, 36 patients who received fluoxetine or sertraline improved clinically, whereas two patients who received fluoxetine or sertraline had worsened seizures. Studies also have provided evidence for the use of citalopram and sertraline in adults with epilepsy. Other studies regarding the treatment of depression in epilepsy are ongoing.
Selective serotonin reuptake inhibitors (SSRIs) entail a low risk of lowering seizure threshold, as do certain antipsychotics (eg, haloperidol, risperidone, and aripiprazole). Methylphenidate is considered safe and is widely used for children with epilepsy and comorbid ADHD.
Nonmedical treatment also can benefit patients. Social skills groups, overnight camps, and cognitive behavioral therapy may be effective options. Vocational support also is important. “Meaningful activity can … tip the balance into more functionality,” he said. “Think about seizure control and behavior control as partners,” Dr. Salpekar concluded. “Think about treating both of these types of targets as working together to improve the entire illness.”
—Jake Remaly
Suggested Reading
Hermann BP, Dabbs K, Becker T, et al. Brain development in children with new onset epilepsy: a prospective controlled cohort investigation. Epilepsia. 2010;51(10):2038-2046.
Hesdorffer DC, Hauser WA, Olafsson E, et al. Depression and suicide attempt as risk factors for incident unprovoked seizures. Ann Neurol. 2006;59(1):35-41.
Salpekar JA. Mood disorders in epilepsy. Focus. 2016;14(4):465-472.
Salpekar JA, Berl MM, Havens K, et al. Psychiatric symptoms in children prior to epilepsy surgery differ according to suspected seizure focus. Epilepsia. 2013;54(6):1074-1082.
Salpekar JA, Conry JA, Doss W, et al. Clinical experience with anticonvulsant medication in pediatric epilepsy and comorbid bipolar spectrum disorder. Epilepsy Behav. 2006;9(2):327-334.
Silvestri R, Gagliano A, Calarese T, et al. Ictal and interictal EEG abnormalities in ADHD children recorded over night by video-polysomnography. Epilepsy Res. 2007;75(2-3):130-137.
Waxman SG, Geschwind N. The interictal behavior syndrome of temporal lobe epilepsy. Arch Gen Psychiatry. 1975;32(12):1580-1586.
Outcomes of neoadjuvant therapy vary by subtype in bladder cancer
Clinical outcomes for neoadjuvant chemotherapy (NAC) vary by molecular subtype in muscle-invasive bladder cancer, investigators report.
Researchers classified the subtypes in 223 patients with muscle-invasive bladder cancer (luminal, basal, claudin-low, and luminal-infiltrated) and found response to neoadjuvant cisplatin-based chemotherapy varied by subtype (P = .0001).
“Neoadjuvant chemotherapy improves outcomes in muscle-invasive bladder cancer, but only at 5%-7% for overall survival at 5 years,” study author Roland Seiler, MD, of the University of British Columbia, Vancouver, said in a press briefing held at the 2017 genitourinary cancers symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology. “About 60% of patients still have invasive disease at cystectomy so they are therefore nonresponders, but they still suffer from unnecessary side effects.”
Dr. Seiler explained that molecular subtypes of muscle-invasive bladder cancers had been identified that were based on gene expression. They decided to investigate the impact of different subtyping methods on patient response to NAC with the goal of developing a single sample model for subtyping.
A transcriptome-wide microarray analysis was conducted, using bladder tumor transurethral resection specimens that were obtained from 223 patients prior to receipt of NAC and cystectomy. The specimens were then classified according to four published methods for molecular subtype: University of North Carolina (UNC) dataset, MD Anderson (MDA) dataset, The Cancer Genome Atlas (TCGA) dataset, and the Lund dataset.
A validation set of 82 pre-NAC specimens also was done, with the results compared to non-NAC cohorts in the public domain including 179 cases from TCGA dataset, 107 from the MDA dataset, and 190 from the Lund dataset.
Finally, a genomic classifier was trained to predict the different subtypes in a single sample model and was then validated in both independent NAC and non-NAC datasets.
Investigators found that patients with luminal tumors had the best overall survival and it was independent of NAC. Patients with tumors classified as UNC basal, MDA basal, and TCGA cluster III achieved the greatest improvement in overall survival following NAC as compared with cystectomy alone.
Patients with tumors that were classified as UNC basal, MDA basal and TCGA cluster III achieved the greatest survival benefit following NAC, compared to surgery alone. Tumors that were assigned as UNC claudin-low had the worst overall survival regardless of the type of treatment regimen (P = .005).
“Basal tumors showed the most improvement with neoadjuvant therapy and should be prioritized with this treatment,” said Dr. Seiler. “Whereas for other subtypes we may need novel therapies.”
As discussant for the presentation, Jonathan Rosenberg, MD, of Memorial Sloan Kettering Cancer Center in New York, said that cisplatin “is a toxic therapy and we would love to have a great biomarker to select the right group of patients. Currently using present data, anywhere from 10 to 20 patients need to be treated to save one life.”
He reiterated that these findings confirm that basal tumors appear to benefit significantly from platinum-based chemotherapy and this benefit appears to exist regardless of downstaging.
“However it does not automatically follow that other subtypes do not benefit, and we are not ready to change clinical practice just yet,” Dr. Rosenberg said. “We need to prospectively validate these findings before we implement them into clinical practice.”
Clinical outcomes for neoadjuvant chemotherapy (NAC) vary by molecular subtype in muscle-invasive bladder cancer, investigators report.
Researchers classified the subtypes in 223 patients with muscle-invasive bladder cancer (luminal, basal, claudin-low, and luminal-infiltrated) and found response to neoadjuvant cisplatin-based chemotherapy varied by subtype (P = .0001).
“Neoadjuvant chemotherapy improves outcomes in muscle-invasive bladder cancer, but only at 5%-7% for overall survival at 5 years,” study author Roland Seiler, MD, of the University of British Columbia, Vancouver, said in a press briefing held at the 2017 genitourinary cancers symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology. “About 60% of patients still have invasive disease at cystectomy so they are therefore nonresponders, but they still suffer from unnecessary side effects.”
Dr. Seiler explained that molecular subtypes of muscle-invasive bladder cancers had been identified that were based on gene expression. They decided to investigate the impact of different subtyping methods on patient response to NAC with the goal of developing a single sample model for subtyping.
A transcriptome-wide microarray analysis was conducted, using bladder tumor transurethral resection specimens that were obtained from 223 patients prior to receipt of NAC and cystectomy. The specimens were then classified according to four published methods for molecular subtype: University of North Carolina (UNC) dataset, MD Anderson (MDA) dataset, The Cancer Genome Atlas (TCGA) dataset, and the Lund dataset.
A validation set of 82 pre-NAC specimens also was done, with the results compared to non-NAC cohorts in the public domain including 179 cases from TCGA dataset, 107 from the MDA dataset, and 190 from the Lund dataset.
Finally, a genomic classifier was trained to predict the different subtypes in a single sample model and was then validated in both independent NAC and non-NAC datasets.
Investigators found that patients with luminal tumors had the best overall survival and it was independent of NAC. Patients with tumors classified as UNC basal, MDA basal, and TCGA cluster III achieved the greatest improvement in overall survival following NAC as compared with cystectomy alone.
Patients with tumors that were classified as UNC basal, MDA basal and TCGA cluster III achieved the greatest survival benefit following NAC, compared to surgery alone. Tumors that were assigned as UNC claudin-low had the worst overall survival regardless of the type of treatment regimen (P = .005).
“Basal tumors showed the most improvement with neoadjuvant therapy and should be prioritized with this treatment,” said Dr. Seiler. “Whereas for other subtypes we may need novel therapies.”
As discussant for the presentation, Jonathan Rosenberg, MD, of Memorial Sloan Kettering Cancer Center in New York, said that cisplatin “is a toxic therapy and we would love to have a great biomarker to select the right group of patients. Currently using present data, anywhere from 10 to 20 patients need to be treated to save one life.”
He reiterated that these findings confirm that basal tumors appear to benefit significantly from platinum-based chemotherapy and this benefit appears to exist regardless of downstaging.
“However it does not automatically follow that other subtypes do not benefit, and we are not ready to change clinical practice just yet,” Dr. Rosenberg said. “We need to prospectively validate these findings before we implement them into clinical practice.”
Clinical outcomes for neoadjuvant chemotherapy (NAC) vary by molecular subtype in muscle-invasive bladder cancer, investigators report.
Researchers classified the subtypes in 223 patients with muscle-invasive bladder cancer (luminal, basal, claudin-low, and luminal-infiltrated) and found response to neoadjuvant cisplatin-based chemotherapy varied by subtype (P = .0001).
“Neoadjuvant chemotherapy improves outcomes in muscle-invasive bladder cancer, but only at 5%-7% for overall survival at 5 years,” study author Roland Seiler, MD, of the University of British Columbia, Vancouver, said in a press briefing held at the 2017 genitourinary cancers symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology. “About 60% of patients still have invasive disease at cystectomy so they are therefore nonresponders, but they still suffer from unnecessary side effects.”
Dr. Seiler explained that molecular subtypes of muscle-invasive bladder cancers had been identified that were based on gene expression. They decided to investigate the impact of different subtyping methods on patient response to NAC with the goal of developing a single sample model for subtyping.
A transcriptome-wide microarray analysis was conducted, using bladder tumor transurethral resection specimens that were obtained from 223 patients prior to receipt of NAC and cystectomy. The specimens were then classified according to four published methods for molecular subtype: University of North Carolina (UNC) dataset, MD Anderson (MDA) dataset, The Cancer Genome Atlas (TCGA) dataset, and the Lund dataset.
A validation set of 82 pre-NAC specimens also was done, with the results compared to non-NAC cohorts in the public domain including 179 cases from TCGA dataset, 107 from the MDA dataset, and 190 from the Lund dataset.
Finally, a genomic classifier was trained to predict the different subtypes in a single sample model and was then validated in both independent NAC and non-NAC datasets.
Investigators found that patients with luminal tumors had the best overall survival and it was independent of NAC. Patients with tumors classified as UNC basal, MDA basal, and TCGA cluster III achieved the greatest improvement in overall survival following NAC as compared with cystectomy alone.
Patients with tumors that were classified as UNC basal, MDA basal and TCGA cluster III achieved the greatest survival benefit following NAC, compared to surgery alone. Tumors that were assigned as UNC claudin-low had the worst overall survival regardless of the type of treatment regimen (P = .005).
“Basal tumors showed the most improvement with neoadjuvant therapy and should be prioritized with this treatment,” said Dr. Seiler. “Whereas for other subtypes we may need novel therapies.”
As discussant for the presentation, Jonathan Rosenberg, MD, of Memorial Sloan Kettering Cancer Center in New York, said that cisplatin “is a toxic therapy and we would love to have a great biomarker to select the right group of patients. Currently using present data, anywhere from 10 to 20 patients need to be treated to save one life.”
He reiterated that these findings confirm that basal tumors appear to benefit significantly from platinum-based chemotherapy and this benefit appears to exist regardless of downstaging.
“However it does not automatically follow that other subtypes do not benefit, and we are not ready to change clinical practice just yet,” Dr. Rosenberg said. “We need to prospectively validate these findings before we implement them into clinical practice.”
FROM THE GENITOURINARY CANCERS SYMPOSIUM
Key clinical point: Clinical outcomes for neoadjuvant chemotherapy (NAC) vary by molecular subtype in muscle-invasive bladder cancer.
Major finding: Luminal tumors had the best overall survival independent of NAC and basal tumors the best response to NAC.
Data source: Experimental study that evaluated the efficacy of NAC in the molecular subtypes of muscle invasive bladder cancer.
Disclosures: The funding source is not disclosed. Dr Seiler has no disclosures. Several of his coauthors report relationships with multiple pharmaceutical companies. Dr Rosenberg reports financial ties to multiple pharmaceutical companies.
Does Patient History Affect the Treatment of Pediatric Refractory Status Epilepticus?
Children with refractory status epilepticus do not receive more timely treatment if they have a prior diagnosis of epilepsy, according to an investigation published January 24 in Neurology. A history of status epilepticus, however, is associated with more timely administration of abortive medication.
Most episodes of pediatric status epilepticus occur in children with no history of seizures. Investigators had not examined whether having a history of seizures or status epilepticus leads to more timely treatment, including escalation of therapy when indicated, and better outcomes.
Iván Sánchez Fernández, MD, Clinical Fellow in Neurology at Boston Children’s Hospital, and colleagues conducted a prospective observational study to compare the management and outcomes of refractory status epilepticus in children with and without a prior diagnosis of epilepsy and with and without a history of status epilepticus. Eligible patients were between ages one month and 21 years and had convulsive seizures at onset that continued after administration of at least two antiepileptic drugs (AEDs).
The investigators enrolled 189 participants (53% male) with a median age of 4.2 years. Eighty-nine (47%) patients had a prior diagnosis of epilepsy. Thirty-four (18%) patients had a history of status epilepticus.
The time to first benzodiazepine was similar in participants with and without a diagnosis of epilepsy (15 minutes vs 16.5 minutes). Patients with a diagnosis of epilepsy received their first nonbenzodiazepine AED later (93 minutes vs 50.5 minutes) and were less likely to receive at least one continuous infusion (39.3% vs 57%). The time to the first continuous infusion, however, was similar in patients with and without a diagnosis of epilepsy (258.5 vs 149 minutes)
Patients with a diagnosis of epilepsy were less likely to be intubated (66.3% vs 83%), had a longer duration of status epilepticus (174 minutes vs 120 minutes), and had a shorter ICU stay (3.9 days vs 5 days). At hospital discharge, patients with a diagnosis of epilepsy were more likely to return to baseline (75% vs 65%) and had lower mortality (0% vs 7%).
Time to the first benzodiazepine was shorter for patients with a history of status epilepticus, compared with patients without (8 minutes vs 20 minutes). The time to first nonbenzodiazepine AED was similar in patients with and without a history of status epilepticus (76.5 minutes vs 65 minutes). Patients with and without a history of status epilepticus were as likely to receive continuous infusions (52.9% vs 47.7%), had a similar time to the first continuous infusion (182 vs 180 minutes), and were as likely to be intubated (82.4% vs 73.5%). Patients with a history of status epilepticus had a longer duration of status epilepticus (150 minutes vs 124.5 minutes) and a shorter ICU stay (5 vs 4.3 days).
At hospital discharge, return to baseline function was similar between patients with and without a history of status epilepticus (76.5% vs 68.4%). The difference between groups in mortality rate was not statistically significant (0% vs 4.5%). The more timely administration of the first benzodiazepine in patients with a history of status epilepticus mainly resulted from cases with onset outside a hospital, while management of status epilepticus with in-hospital onset was similar in patients with and without a history of status epilepticus.
—Erik Greb
Suggested Reading
Sánchez Fernández I, Jackson MC, Abend NS, et al. Refractory status epilepticus in children with and without prior epilepsy or status epilepticus. Neurology. 2017;88(4):386-394.
Children with refractory status epilepticus do not receive more timely treatment if they have a prior diagnosis of epilepsy, according to an investigation published January 24 in Neurology. A history of status epilepticus, however, is associated with more timely administration of abortive medication.
Most episodes of pediatric status epilepticus occur in children with no history of seizures. Investigators had not examined whether having a history of seizures or status epilepticus leads to more timely treatment, including escalation of therapy when indicated, and better outcomes.
Iván Sánchez Fernández, MD, Clinical Fellow in Neurology at Boston Children’s Hospital, and colleagues conducted a prospective observational study to compare the management and outcomes of refractory status epilepticus in children with and without a prior diagnosis of epilepsy and with and without a history of status epilepticus. Eligible patients were between ages one month and 21 years and had convulsive seizures at onset that continued after administration of at least two antiepileptic drugs (AEDs).
The investigators enrolled 189 participants (53% male) with a median age of 4.2 years. Eighty-nine (47%) patients had a prior diagnosis of epilepsy. Thirty-four (18%) patients had a history of status epilepticus.
The time to first benzodiazepine was similar in participants with and without a diagnosis of epilepsy (15 minutes vs 16.5 minutes). Patients with a diagnosis of epilepsy received their first nonbenzodiazepine AED later (93 minutes vs 50.5 minutes) and were less likely to receive at least one continuous infusion (39.3% vs 57%). The time to the first continuous infusion, however, was similar in patients with and without a diagnosis of epilepsy (258.5 vs 149 minutes)
Patients with a diagnosis of epilepsy were less likely to be intubated (66.3% vs 83%), had a longer duration of status epilepticus (174 minutes vs 120 minutes), and had a shorter ICU stay (3.9 days vs 5 days). At hospital discharge, patients with a diagnosis of epilepsy were more likely to return to baseline (75% vs 65%) and had lower mortality (0% vs 7%).
Time to the first benzodiazepine was shorter for patients with a history of status epilepticus, compared with patients without (8 minutes vs 20 minutes). The time to first nonbenzodiazepine AED was similar in patients with and without a history of status epilepticus (76.5 minutes vs 65 minutes). Patients with and without a history of status epilepticus were as likely to receive continuous infusions (52.9% vs 47.7%), had a similar time to the first continuous infusion (182 vs 180 minutes), and were as likely to be intubated (82.4% vs 73.5%). Patients with a history of status epilepticus had a longer duration of status epilepticus (150 minutes vs 124.5 minutes) and a shorter ICU stay (5 vs 4.3 days).
At hospital discharge, return to baseline function was similar between patients with and without a history of status epilepticus (76.5% vs 68.4%). The difference between groups in mortality rate was not statistically significant (0% vs 4.5%). The more timely administration of the first benzodiazepine in patients with a history of status epilepticus mainly resulted from cases with onset outside a hospital, while management of status epilepticus with in-hospital onset was similar in patients with and without a history of status epilepticus.
—Erik Greb
Suggested Reading
Sánchez Fernández I, Jackson MC, Abend NS, et al. Refractory status epilepticus in children with and without prior epilepsy or status epilepticus. Neurology. 2017;88(4):386-394.
Children with refractory status epilepticus do not receive more timely treatment if they have a prior diagnosis of epilepsy, according to an investigation published January 24 in Neurology. A history of status epilepticus, however, is associated with more timely administration of abortive medication.
Most episodes of pediatric status epilepticus occur in children with no history of seizures. Investigators had not examined whether having a history of seizures or status epilepticus leads to more timely treatment, including escalation of therapy when indicated, and better outcomes.
Iván Sánchez Fernández, MD, Clinical Fellow in Neurology at Boston Children’s Hospital, and colleagues conducted a prospective observational study to compare the management and outcomes of refractory status epilepticus in children with and without a prior diagnosis of epilepsy and with and without a history of status epilepticus. Eligible patients were between ages one month and 21 years and had convulsive seizures at onset that continued after administration of at least two antiepileptic drugs (AEDs).
The investigators enrolled 189 participants (53% male) with a median age of 4.2 years. Eighty-nine (47%) patients had a prior diagnosis of epilepsy. Thirty-four (18%) patients had a history of status epilepticus.
The time to first benzodiazepine was similar in participants with and without a diagnosis of epilepsy (15 minutes vs 16.5 minutes). Patients with a diagnosis of epilepsy received their first nonbenzodiazepine AED later (93 minutes vs 50.5 minutes) and were less likely to receive at least one continuous infusion (39.3% vs 57%). The time to the first continuous infusion, however, was similar in patients with and without a diagnosis of epilepsy (258.5 vs 149 minutes)
Patients with a diagnosis of epilepsy were less likely to be intubated (66.3% vs 83%), had a longer duration of status epilepticus (174 minutes vs 120 minutes), and had a shorter ICU stay (3.9 days vs 5 days). At hospital discharge, patients with a diagnosis of epilepsy were more likely to return to baseline (75% vs 65%) and had lower mortality (0% vs 7%).
Time to the first benzodiazepine was shorter for patients with a history of status epilepticus, compared with patients without (8 minutes vs 20 minutes). The time to first nonbenzodiazepine AED was similar in patients with and without a history of status epilepticus (76.5 minutes vs 65 minutes). Patients with and without a history of status epilepticus were as likely to receive continuous infusions (52.9% vs 47.7%), had a similar time to the first continuous infusion (182 vs 180 minutes), and were as likely to be intubated (82.4% vs 73.5%). Patients with a history of status epilepticus had a longer duration of status epilepticus (150 minutes vs 124.5 minutes) and a shorter ICU stay (5 vs 4.3 days).
At hospital discharge, return to baseline function was similar between patients with and without a history of status epilepticus (76.5% vs 68.4%). The difference between groups in mortality rate was not statistically significant (0% vs 4.5%). The more timely administration of the first benzodiazepine in patients with a history of status epilepticus mainly resulted from cases with onset outside a hospital, while management of status epilepticus with in-hospital onset was similar in patients with and without a history of status epilepticus.
—Erik Greb
Suggested Reading
Sánchez Fernández I, Jackson MC, Abend NS, et al. Refractory status epilepticus in children with and without prior epilepsy or status epilepticus. Neurology. 2017;88(4):386-394.
When atopic dermatitis is really contact dermatitis
ATLANTA – When patients present with atopic dermatitis that worsens, changes distribution, fails to improve, or immediately rebounds, think contact dermatitis, Luz Fonacier, MD, advised at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
Clinical signs of contact dermatitis include lesions with an atypical distribution/pattern, such as head, eyelid, or cheilitis/perioral predominance, or lesions on the hand or foot. Also elevate your suspicion in patients with therapy-resistant hand eczema, adult- or childhood-onset atopic dermatitis without childhood eczema, as well as in cases of severe or widespread dermatitis prior to initiating a systemic immunosuppressant. The list of potential allergens to consider includes metal (especially nickel, cobalt, and potassium dichromate), fragrances such as formaldehyde and balsam of Peru, preservatives, as well as topical emollients, corticosteroids, antibiotics, and antiseptics.
Dr. Fonacier, professor of medicine at the State University of New York at Stony Brook and section head of allergy at Winthrop University Hospital, Mineola, N.Y., recommends loading acrylates, fragrances, and allergens in an aqueous vehicle immediately before application. She noted that delayed patch test readings are common to metals, topical antibiotics, and topical corticosteroids, and that positive reactions to gold are often not clinically relevant. “The patch test positivity of gold can be as high as 30% in adults and a little bit less in children, but results from two large studies show clinical relevance in only 10%-15% of cases,” she said. A trial of gold avoidance may be warranted in patients with suspected jewelry allergy, facial or eyelid dermatitis, or exposure through gold dental restorations.
She went on to share tips for reading skin patch tests. The first reading should be done after 48 hours, while the second should be done 3, 4, or 7 days after application. “The second reading helps distinguish irritant from allergic responses,” she said. “Thirty percent of negative tests at 48 hours may be positive on delayed readings.” Most true allergic reactions occur between 72 and 96 hours. Allergens that may peak early include thiuram mix, carba mix, and balsam of Peru. Those that disappear after 5 days include balsam of Peru, benzoic acid, disperse blue #124, fragrance mix, mercury, methyldibromo glutaronitrile, phenoxyethanol, and octyl gallate. Delayed patch test reactions after five days include metals (gold potassium dichromate, nickel, and cobalt), topical antibiotics (neomycin and bacitracin) as well as topic corticosteroids.
Resources she recommended to attendees include the American Contact Dermatitis Society and the Contact Dermatitis Institute. Health and safety information about household products can be found here.
Dr. Fonacier disclosed that she has received research and educational grants from Baxter and Genentech. She is also a consultant to Church and Dwight and Regeneron.
ATLANTA – When patients present with atopic dermatitis that worsens, changes distribution, fails to improve, or immediately rebounds, think contact dermatitis, Luz Fonacier, MD, advised at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
Clinical signs of contact dermatitis include lesions with an atypical distribution/pattern, such as head, eyelid, or cheilitis/perioral predominance, or lesions on the hand or foot. Also elevate your suspicion in patients with therapy-resistant hand eczema, adult- or childhood-onset atopic dermatitis without childhood eczema, as well as in cases of severe or widespread dermatitis prior to initiating a systemic immunosuppressant. The list of potential allergens to consider includes metal (especially nickel, cobalt, and potassium dichromate), fragrances such as formaldehyde and balsam of Peru, preservatives, as well as topical emollients, corticosteroids, antibiotics, and antiseptics.
Dr. Fonacier, professor of medicine at the State University of New York at Stony Brook and section head of allergy at Winthrop University Hospital, Mineola, N.Y., recommends loading acrylates, fragrances, and allergens in an aqueous vehicle immediately before application. She noted that delayed patch test readings are common to metals, topical antibiotics, and topical corticosteroids, and that positive reactions to gold are often not clinically relevant. “The patch test positivity of gold can be as high as 30% in adults and a little bit less in children, but results from two large studies show clinical relevance in only 10%-15% of cases,” she said. A trial of gold avoidance may be warranted in patients with suspected jewelry allergy, facial or eyelid dermatitis, or exposure through gold dental restorations.
She went on to share tips for reading skin patch tests. The first reading should be done after 48 hours, while the second should be done 3, 4, or 7 days after application. “The second reading helps distinguish irritant from allergic responses,” she said. “Thirty percent of negative tests at 48 hours may be positive on delayed readings.” Most true allergic reactions occur between 72 and 96 hours. Allergens that may peak early include thiuram mix, carba mix, and balsam of Peru. Those that disappear after 5 days include balsam of Peru, benzoic acid, disperse blue #124, fragrance mix, mercury, methyldibromo glutaronitrile, phenoxyethanol, and octyl gallate. Delayed patch test reactions after five days include metals (gold potassium dichromate, nickel, and cobalt), topical antibiotics (neomycin and bacitracin) as well as topic corticosteroids.
Resources she recommended to attendees include the American Contact Dermatitis Society and the Contact Dermatitis Institute. Health and safety information about household products can be found here.
Dr. Fonacier disclosed that she has received research and educational grants from Baxter and Genentech. She is also a consultant to Church and Dwight and Regeneron.
ATLANTA – When patients present with atopic dermatitis that worsens, changes distribution, fails to improve, or immediately rebounds, think contact dermatitis, Luz Fonacier, MD, advised at the annual meeting of the American Academy of Allergy, Asthma, and Immunology.
Clinical signs of contact dermatitis include lesions with an atypical distribution/pattern, such as head, eyelid, or cheilitis/perioral predominance, or lesions on the hand or foot. Also elevate your suspicion in patients with therapy-resistant hand eczema, adult- or childhood-onset atopic dermatitis without childhood eczema, as well as in cases of severe or widespread dermatitis prior to initiating a systemic immunosuppressant. The list of potential allergens to consider includes metal (especially nickel, cobalt, and potassium dichromate), fragrances such as formaldehyde and balsam of Peru, preservatives, as well as topical emollients, corticosteroids, antibiotics, and antiseptics.
Dr. Fonacier, professor of medicine at the State University of New York at Stony Brook and section head of allergy at Winthrop University Hospital, Mineola, N.Y., recommends loading acrylates, fragrances, and allergens in an aqueous vehicle immediately before application. She noted that delayed patch test readings are common to metals, topical antibiotics, and topical corticosteroids, and that positive reactions to gold are often not clinically relevant. “The patch test positivity of gold can be as high as 30% in adults and a little bit less in children, but results from two large studies show clinical relevance in only 10%-15% of cases,” she said. A trial of gold avoidance may be warranted in patients with suspected jewelry allergy, facial or eyelid dermatitis, or exposure through gold dental restorations.
She went on to share tips for reading skin patch tests. The first reading should be done after 48 hours, while the second should be done 3, 4, or 7 days after application. “The second reading helps distinguish irritant from allergic responses,” she said. “Thirty percent of negative tests at 48 hours may be positive on delayed readings.” Most true allergic reactions occur between 72 and 96 hours. Allergens that may peak early include thiuram mix, carba mix, and balsam of Peru. Those that disappear after 5 days include balsam of Peru, benzoic acid, disperse blue #124, fragrance mix, mercury, methyldibromo glutaronitrile, phenoxyethanol, and octyl gallate. Delayed patch test reactions after five days include metals (gold potassium dichromate, nickel, and cobalt), topical antibiotics (neomycin and bacitracin) as well as topic corticosteroids.
Resources she recommended to attendees include the American Contact Dermatitis Society and the Contact Dermatitis Institute. Health and safety information about household products can be found here.
Dr. Fonacier disclosed that she has received research and educational grants from Baxter and Genentech. She is also a consultant to Church and Dwight and Regeneron.
EXPERT ANALYSIS AT THE 2017 AAAAI ANNUAL MEETING
Online Algorithm Identifies People at Risk of Parkinson’s Disease
The online PREDICT-PD algorithm effectively identifies people at increased risk of Parkinson’s disease, according to research published online ahead of print January 16 in Movement Disorders. The risk scores that the algorithm assigns are significantly associated with intermediate markers of Parkinson’s disease. Higher PREDICT-PD risk score at baseline also is associated with an increased rate of incident Parkinson’s disease.
Previous research with the goal of identifying patients at risk of Parkinson’s disease mainly has focused on people with a family history of the disease, asymptomatic carriers of genes associated with the disease, or people with imaging abnormalities associated with the disease (eg, hyperechogenicity on transcranial sonography). The rarity, the representativeness, and the feasibility of identifying these factors have limited these studies, however.
Internet-Based Testing
To overcome these limitations, Anette-Eleonore Schrag, PhD, Professor of Clinical Neurosciences at University College London, and colleagues developed an online, evidence-based algorithm to identify risk indicators of Parkinson’s disease in the UK population. The investigators used a study website to recruit participants between ages 60 and 80 who did not have Parkinson’s disease, any other movement disorder, or stroke. Participants were prompted to return to the website yearly and complete tests.
Among the tests was a survey that included demographic questions and validated questionnaires about early nonmotor features of and risk factors for Parkinson’s disease (eg, the Hospital Anxiety Depression Scale and the REM sleep behavior disorder Screening Questionnaire [RBDSQ]). Participants also took the Bradykinesia Akinesia Incoordination (BRAIN) test, an online keyboard-tapping task. At baseline and at year three, participants took the University of Pennsylvania Smell Identification Test (UPSIT). The annual survey included a question about whether the participants had received any new diagnoses, including Parkinson’s disease or movement disorder. At year three, participants also gave saliva samples that were genotyped for mutations in exons 8 to 11 of glucocerebrosidase (GBA) and exon 41 in the LRRK2 gene.
The investigators used participants’ early features and risk factors to calculate their risk scores and rank participants according to their risk. Dr. Schrag and colleagues also tested support for enrichment of the population at risk of Parkinson’s disease by examining associations between risk scores and the following intermediate markers of Parkinson’s disease: reduced sense of smell, presence of subjective RBD, and slowing of finger tapping speed.
Risk Scores Were Associated With Incident Disease
The researchers recruited 1,323 eligible volunteers. At baseline, their mean age was 66, and approximately 61% of the population was female. In all, 1,040 of the participants completed follow-up testing at year 1, 939 completed year 2 follow-up, and 846 completed year 3 follow-up. A total of 223 participants completed the baseline assessment only.
Baseline risk scores were associated with significantly higher rates of all intermediate markers of Parkinson’s disease during each year of follow-up. The group of patients at higher risk (ie, those above the 15th percentile) had significantly worse UPSIT score, RBDSQ score, and finger tapping in all years, compared with patients at lower risk (ie, those below the 85th percentile).
Risk scores in the entire sample were strongly associated with intermediate markers of Parkinson’s disease each year. Higher- and lower-risk groups differed significantly in median UPSIT score, RBDSQ score, and mean finger tapping speed in all years of follow-up.
At year 1, three patients had been newly diagnosed with Parkinson’s disease. An additional participant received the diagnosis in year 2, and three other participants received the diagnosis in year 3. All of the participants with newly diagnosed Parkinson’s disease at year 1 were in the higher risk group, and two had also been in the higher risk group at baseline. The participant diagnosed at year 2 was in the higher risk group at baseline, year 1, and year 2. All of the three participants diagnosed by year 3 were in the middle risk group at baseline. “There was substantial heterogeneity in the occurrence of intermediate markers in these individuals,” said the researchers.
The incidence of independently diagnosed Parkinson’s disease in participants who had been in the higher risk group during three years of follow-up was 1.6% per year and 0.2% across the whole population. Exploratory Cox regression analysis using incident Parkinson’s disease over three years as the outcome indicated an association with baseline risk estimate. In participants for whom GBA and LRRK2 status was known, the association between baseline risk and incident Parkinson’s disease was weaker. But the addition of GBA and LRRK2 variants in the algorithm improved the strength of association between baseline risk and incident Parkinson’s disease. Among the intermediate markers of disease, baseline finger tapping was associated with incident Parkinson’s disease at three years.
Results Could Reflect Selection Bias
“Although only a small number of individuals have been independently diagnosed with Parkinson’s disease during follow-up so far, the overall incidence of 0.2% is consistent with the expected incidence rate in the age group of 60 to 80 from the general population (one to three per 1,000 per year) and supports the representativeness of our sample,” said Dr. Schrag.
The recruitment of participants may have introduced selection bias into the study, she acknowledged. “However, we did not use family history as an entry criterion, and the proportion with a positive family history was lower than in other landmark studies.” The fact that 17% of participants only completed the baseline assessment also may have introduced selection bias, “although there were no differences between those with or without follow-up, meaning that bias as a result of loss to follow-up was less likely.
“This Internet-based approach may be useful for population screening because it can easily be scaled upward,” added Dr. Schrag. “It will allow larger numbers of Parkinson’s disease cases that represent the spectrum of the disease to be identified, rather than what would be possible from cohorts of carriers of specific risk factors.”
—Erik Greb
Suggested Readings
Noyce AJ, R’Bibo L, Peress L, et al. PREDICT-PD: An online approach to prospectively identify risk indicators of Parkinson’s disease. Mov Disord. 2017 Jan 16 [Epub ahead of print].
The online PREDICT-PD algorithm effectively identifies people at increased risk of Parkinson’s disease, according to research published online ahead of print January 16 in Movement Disorders. The risk scores that the algorithm assigns are significantly associated with intermediate markers of Parkinson’s disease. Higher PREDICT-PD risk score at baseline also is associated with an increased rate of incident Parkinson’s disease.
Previous research with the goal of identifying patients at risk of Parkinson’s disease mainly has focused on people with a family history of the disease, asymptomatic carriers of genes associated with the disease, or people with imaging abnormalities associated with the disease (eg, hyperechogenicity on transcranial sonography). The rarity, the representativeness, and the feasibility of identifying these factors have limited these studies, however.
Internet-Based Testing
To overcome these limitations, Anette-Eleonore Schrag, PhD, Professor of Clinical Neurosciences at University College London, and colleagues developed an online, evidence-based algorithm to identify risk indicators of Parkinson’s disease in the UK population. The investigators used a study website to recruit participants between ages 60 and 80 who did not have Parkinson’s disease, any other movement disorder, or stroke. Participants were prompted to return to the website yearly and complete tests.
Among the tests was a survey that included demographic questions and validated questionnaires about early nonmotor features of and risk factors for Parkinson’s disease (eg, the Hospital Anxiety Depression Scale and the REM sleep behavior disorder Screening Questionnaire [RBDSQ]). Participants also took the Bradykinesia Akinesia Incoordination (BRAIN) test, an online keyboard-tapping task. At baseline and at year three, participants took the University of Pennsylvania Smell Identification Test (UPSIT). The annual survey included a question about whether the participants had received any new diagnoses, including Parkinson’s disease or movement disorder. At year three, participants also gave saliva samples that were genotyped for mutations in exons 8 to 11 of glucocerebrosidase (GBA) and exon 41 in the LRRK2 gene.
The investigators used participants’ early features and risk factors to calculate their risk scores and rank participants according to their risk. Dr. Schrag and colleagues also tested support for enrichment of the population at risk of Parkinson’s disease by examining associations between risk scores and the following intermediate markers of Parkinson’s disease: reduced sense of smell, presence of subjective RBD, and slowing of finger tapping speed.
Risk Scores Were Associated With Incident Disease
The researchers recruited 1,323 eligible volunteers. At baseline, their mean age was 66, and approximately 61% of the population was female. In all, 1,040 of the participants completed follow-up testing at year 1, 939 completed year 2 follow-up, and 846 completed year 3 follow-up. A total of 223 participants completed the baseline assessment only.
Baseline risk scores were associated with significantly higher rates of all intermediate markers of Parkinson’s disease during each year of follow-up. The group of patients at higher risk (ie, those above the 15th percentile) had significantly worse UPSIT score, RBDSQ score, and finger tapping in all years, compared with patients at lower risk (ie, those below the 85th percentile).
Risk scores in the entire sample were strongly associated with intermediate markers of Parkinson’s disease each year. Higher- and lower-risk groups differed significantly in median UPSIT score, RBDSQ score, and mean finger tapping speed in all years of follow-up.
At year 1, three patients had been newly diagnosed with Parkinson’s disease. An additional participant received the diagnosis in year 2, and three other participants received the diagnosis in year 3. All of the participants with newly diagnosed Parkinson’s disease at year 1 were in the higher risk group, and two had also been in the higher risk group at baseline. The participant diagnosed at year 2 was in the higher risk group at baseline, year 1, and year 2. All of the three participants diagnosed by year 3 were in the middle risk group at baseline. “There was substantial heterogeneity in the occurrence of intermediate markers in these individuals,” said the researchers.
The incidence of independently diagnosed Parkinson’s disease in participants who had been in the higher risk group during three years of follow-up was 1.6% per year and 0.2% across the whole population. Exploratory Cox regression analysis using incident Parkinson’s disease over three years as the outcome indicated an association with baseline risk estimate. In participants for whom GBA and LRRK2 status was known, the association between baseline risk and incident Parkinson’s disease was weaker. But the addition of GBA and LRRK2 variants in the algorithm improved the strength of association between baseline risk and incident Parkinson’s disease. Among the intermediate markers of disease, baseline finger tapping was associated with incident Parkinson’s disease at three years.
Results Could Reflect Selection Bias
“Although only a small number of individuals have been independently diagnosed with Parkinson’s disease during follow-up so far, the overall incidence of 0.2% is consistent with the expected incidence rate in the age group of 60 to 80 from the general population (one to three per 1,000 per year) and supports the representativeness of our sample,” said Dr. Schrag.
The recruitment of participants may have introduced selection bias into the study, she acknowledged. “However, we did not use family history as an entry criterion, and the proportion with a positive family history was lower than in other landmark studies.” The fact that 17% of participants only completed the baseline assessment also may have introduced selection bias, “although there were no differences between those with or without follow-up, meaning that bias as a result of loss to follow-up was less likely.
“This Internet-based approach may be useful for population screening because it can easily be scaled upward,” added Dr. Schrag. “It will allow larger numbers of Parkinson’s disease cases that represent the spectrum of the disease to be identified, rather than what would be possible from cohorts of carriers of specific risk factors.”
—Erik Greb
Suggested Readings
Noyce AJ, R’Bibo L, Peress L, et al. PREDICT-PD: An online approach to prospectively identify risk indicators of Parkinson’s disease. Mov Disord. 2017 Jan 16 [Epub ahead of print].
The online PREDICT-PD algorithm effectively identifies people at increased risk of Parkinson’s disease, according to research published online ahead of print January 16 in Movement Disorders. The risk scores that the algorithm assigns are significantly associated with intermediate markers of Parkinson’s disease. Higher PREDICT-PD risk score at baseline also is associated with an increased rate of incident Parkinson’s disease.
Previous research with the goal of identifying patients at risk of Parkinson’s disease mainly has focused on people with a family history of the disease, asymptomatic carriers of genes associated with the disease, or people with imaging abnormalities associated with the disease (eg, hyperechogenicity on transcranial sonography). The rarity, the representativeness, and the feasibility of identifying these factors have limited these studies, however.
Internet-Based Testing
To overcome these limitations, Anette-Eleonore Schrag, PhD, Professor of Clinical Neurosciences at University College London, and colleagues developed an online, evidence-based algorithm to identify risk indicators of Parkinson’s disease in the UK population. The investigators used a study website to recruit participants between ages 60 and 80 who did not have Parkinson’s disease, any other movement disorder, or stroke. Participants were prompted to return to the website yearly and complete tests.
Among the tests was a survey that included demographic questions and validated questionnaires about early nonmotor features of and risk factors for Parkinson’s disease (eg, the Hospital Anxiety Depression Scale and the REM sleep behavior disorder Screening Questionnaire [RBDSQ]). Participants also took the Bradykinesia Akinesia Incoordination (BRAIN) test, an online keyboard-tapping task. At baseline and at year three, participants took the University of Pennsylvania Smell Identification Test (UPSIT). The annual survey included a question about whether the participants had received any new diagnoses, including Parkinson’s disease or movement disorder. At year three, participants also gave saliva samples that were genotyped for mutations in exons 8 to 11 of glucocerebrosidase (GBA) and exon 41 in the LRRK2 gene.
The investigators used participants’ early features and risk factors to calculate their risk scores and rank participants according to their risk. Dr. Schrag and colleagues also tested support for enrichment of the population at risk of Parkinson’s disease by examining associations between risk scores and the following intermediate markers of Parkinson’s disease: reduced sense of smell, presence of subjective RBD, and slowing of finger tapping speed.
Risk Scores Were Associated With Incident Disease
The researchers recruited 1,323 eligible volunteers. At baseline, their mean age was 66, and approximately 61% of the population was female. In all, 1,040 of the participants completed follow-up testing at year 1, 939 completed year 2 follow-up, and 846 completed year 3 follow-up. A total of 223 participants completed the baseline assessment only.
Baseline risk scores were associated with significantly higher rates of all intermediate markers of Parkinson’s disease during each year of follow-up. The group of patients at higher risk (ie, those above the 15th percentile) had significantly worse UPSIT score, RBDSQ score, and finger tapping in all years, compared with patients at lower risk (ie, those below the 85th percentile).
Risk scores in the entire sample were strongly associated with intermediate markers of Parkinson’s disease each year. Higher- and lower-risk groups differed significantly in median UPSIT score, RBDSQ score, and mean finger tapping speed in all years of follow-up.
At year 1, three patients had been newly diagnosed with Parkinson’s disease. An additional participant received the diagnosis in year 2, and three other participants received the diagnosis in year 3. All of the participants with newly diagnosed Parkinson’s disease at year 1 were in the higher risk group, and two had also been in the higher risk group at baseline. The participant diagnosed at year 2 was in the higher risk group at baseline, year 1, and year 2. All of the three participants diagnosed by year 3 were in the middle risk group at baseline. “There was substantial heterogeneity in the occurrence of intermediate markers in these individuals,” said the researchers.
The incidence of independently diagnosed Parkinson’s disease in participants who had been in the higher risk group during three years of follow-up was 1.6% per year and 0.2% across the whole population. Exploratory Cox regression analysis using incident Parkinson’s disease over three years as the outcome indicated an association with baseline risk estimate. In participants for whom GBA and LRRK2 status was known, the association between baseline risk and incident Parkinson’s disease was weaker. But the addition of GBA and LRRK2 variants in the algorithm improved the strength of association between baseline risk and incident Parkinson’s disease. Among the intermediate markers of disease, baseline finger tapping was associated with incident Parkinson’s disease at three years.
Results Could Reflect Selection Bias
“Although only a small number of individuals have been independently diagnosed with Parkinson’s disease during follow-up so far, the overall incidence of 0.2% is consistent with the expected incidence rate in the age group of 60 to 80 from the general population (one to three per 1,000 per year) and supports the representativeness of our sample,” said Dr. Schrag.
The recruitment of participants may have introduced selection bias into the study, she acknowledged. “However, we did not use family history as an entry criterion, and the proportion with a positive family history was lower than in other landmark studies.” The fact that 17% of participants only completed the baseline assessment also may have introduced selection bias, “although there were no differences between those with or without follow-up, meaning that bias as a result of loss to follow-up was less likely.
“This Internet-based approach may be useful for population screening because it can easily be scaled upward,” added Dr. Schrag. “It will allow larger numbers of Parkinson’s disease cases that represent the spectrum of the disease to be identified, rather than what would be possible from cohorts of carriers of specific risk factors.”
—Erik Greb
Suggested Readings
Noyce AJ, R’Bibo L, Peress L, et al. PREDICT-PD: An online approach to prospectively identify risk indicators of Parkinson’s disease. Mov Disord. 2017 Jan 16 [Epub ahead of print].