User login
Failed First Metatarsophalangeal Arthroplasty Salvaged by Hamstring Interposition Arthroplasty: Metallic Debris From Grommets
joint, arthroplasty, implant, metallic debris, grommets, titanium, synovitis, foot
joint, arthroplasty, implant, metallic debris, grommets, titanium, synovitis, foot
joint, arthroplasty, implant, metallic debris, grommets, titanium, synovitis, foot
New and Noteworthy Information—April 2014
Little evidence suggests that most complementary or alternative medicine therapies treat the symptoms of multiple sclerosis (MS), according to an American Academy of Neurology guideline published March 25 in Neurology. Oral cannabis and oral medical marijuana spray, however, may ease patients’ reported symptoms of spasticity, pain related to spasticity, and frequent urination in MS. Not enough evidence is available to show whether smoking marijuana helps treat MS symptoms, according to the guideline. The authors concluded that magnetic therapy is probably effective for fatigue and probably ineffective for depression. Fish oil is probably ineffective for relapses, disability, fatigue, MRI lesions, and quality of life, according to the guideline. In addition, evidence indicates that ginkgo biloba is ineffective for cognition and possibly effective for fatigue, said the authors.
People who develop diabetes and high blood pressure in middle age are more likely to have brain cell loss and problems with memory and thinking skills than people who never have diabetes or high blood pressure or who develop them in old age, according to a study published online ahead of print March 19 in Neurology. Investigators evaluated the thinking and memory skills of 1,437 people (average age, 80), conducted brain scans, and reviewed participants’ medical records to determine whether the latter had been diagnosed with diabetes or high blood pressure in middle age or later. Midlife diabetes was associated with subcortical infarctions, reduced hippocampal volume, reduced whole brain volume, and prevalent mild cognitive impairment. Midlife hypertension was associated with infarctions and white matter hyperintensity volume.
Each 15-minute decrease in treatment delay may provide a patient an average equivalent of one month of additional disability-free life, according to a study published online ahead of print March 13 in Stroke. Researchers examined observational prospective data for 2,258 consecutive stroke patients treated with IV thrombolysis to determine distributions of age, sex, stroke severity, onset-to-treatment times, and three-month modified Rankin Scale score in daily clinical practice. The investigators found that for every one-minute reduction in onset-to-treatment time, patients gained an average 1.8 days of healthy life. Although all patients benefited from faster treatment, younger patients with longer life expectancies gained a little more than older patients. Women gained slightly more than men throughout their longer lifetimes. The awareness of the importance of speed could promote practice change, said the authors.
The FDA has approved extended-release Qudexy XR (topiramate) capsules as initial monotherapy in patients 10 or older with partial-onset seizures or primary generalized tonic-clonic seizures. The drug also received approval as adjunctive therapy in patients age 2 or older with partial-onset seizures, primary generalized tonic-clonic seizures, and seizures associated with Lennox–Gastaut syndrome. In a randomized, double-blind, placebo-controlled study, the drug demonstrated favorable safety and tolerability in patients with refractory partial-onset seizures. The extended-release formulation was associated with a significantly greater median percent reduction from baseline in seizure frequency, compared with placebo (39.5% vs 21.7%) after 11 weeks of treatment. Upsher-Smith Laboratories, headquartered in Maple Grove, Minnesota, manufactures the drug and expects it to be available during the second quarter of 2014.
The FDA has approved the Cefaly medical device as a preventive treatment for migraine headaches. The product is the first transcutaneous electrical nerve stimulation device specifically authorized for use before the onset of pain. The product is a small, portable, battery-powered unit resembling a plastic headband worn across the forehead once per day for 20 minutes. The device applies an electric current to the skin and underlying tissues to stimulate branches of the trigeminal nerve. In a study including 67 participants, patients who used Cefaly had significantly fewer days with migraines per month and used less migraine attack medication, compared with patients who used a placebo device. STX-Med, which is headquartered in Herstal, Liege, Belgium, manufactures the device, which is indicated for patients 18 and older.
Children with autism who are fed infant formula containing soy protein rather than milk protein may have a higher rate of seizures, according to research published March 12 in PLOS One. Researchers analyzed medical record data for 1,949 children with autism, including information on infant formula use, seizure incidence, the specific type of seizure exhibited, and IQ. Soy-based formula was given in 17.5% of the study population. About 13% of the subjects were female. The researchers found a 2.6-fold higher rate of febrile seizures (4.2% vs 1.6%), a 2.1-fold higher rate of epilepsy comorbidity (3.6% vs 1.7%), and a fourfold higher rate of simple partial seizures (1.2% vs 0.3%) in the children with autism who were fed soy-based formula. No statistically significant associations were found with other outcomes.
For patients with Alzheimer’s disease, levels of markers of neuronal injury in the spinal fluid may decrease as symptoms of memory loss and mental decline appear, according to research published March 5 in Science Translational Medicine. Investigators studied data from the Dominantly Inherited Alzheimer’s Network, which includes participants from families with genetic mutations that cause rare inherited forms of Alzheimer’s disease. The group examined levels of tau, p-tau, and visinin-like protein-1 (VILIP-1). Asymptomatic mutation carriers had elevated concentrations of CSF tau, p-tau181, and VILIP-1 10 to 20 years before their estimated age at symptom onset and before cognitive deficits were detected. The concentrations of CSF biomarkers of neuronal injury or death decreased after their estimated age at symptom onset, suggesting a slowing of acute neurodegenerative processes with symptomatic disease progression.
Men with poor cardiovascular fitness or a low IQ at age 18 are more likely to develop dementia before age 60, investigators reported online ahead of print March 6 in Brain. The researchers conducted a population-based cohort study of more than 1.1 million Swedish male conscripts (age 18) who underwent conscription exams between 1968 and 2005. Participants were followed for as long as 42 years. In fully adjusted models, low cardiovascular fitness and cognitive performance at age 18 were associated with increased risk for future early-onset dementia and mild cognitive impairment, compared with high cardiovascular fitness and cognitive performance. Poor performance on cardiovascular fitness and cognitive tests was associated with a greater-than-sevenfold and a greater than eightfold increased risk of early-onset dementia and early-onset mild cognitive impairment, respectively.
A test that detects low levels of prion protein in the blood may accurately screen for infection with the agent responsible for variant Creutzfeldt-Jakob disease (vCJD), according to a study published online ahead of print March 3 in JAMA Neurology. Researchers performed the test on samples from national blood collection and prion disease centers in the US and the UK. The samples were taken from healthy donors, patients with nonprion neurodegenerative disease, patients in whom a prion disease diagnosis was likely, and patients with confirmed vCJD. The assay’s specificity was confirmed as 100% in a healthy UK cohort. No potentially cross-reactive blood samples from patients with nonprion neurodegenerative diseases tested positive. Two patients with sporadic CJD tested positive. The authors’ previous sensitivity estimate was reconfirmed but not refined.
The FDA has approved Neuraceq (florbetaben F18 injection) for PET imaging of the brain to estimate beta-amyloid neuritic plaque density in adults with cognitive impairment who are being evaluated for Alzheimer’s disease and other causes of cognitive decline. The approval is based on safety data from 872 patients who participated in global clinical trials, and on three studies that examined images from adults with a range of cognitive function. Images were analyzed from 82 subjects with postmortem confirmation of the presence or absence of beta-amyloid neuritic plaques. Correlation of the visual PET interpretation with histopathology in these 82 brains demonstrated that Neuraceq (Piramal Imaging; Boston) accurately detects moderate to frequent beta-amyloid neuritic plaques in the brain.
A combination of human umbilical cord blood cells (hUCBs) and granulocyte colony stimulating factor (G-CSF) may provide more benefit for patients with traumatic brain injury (TBI) than either therapy alone, according to research published March 12 in PLOS One. Adult rats underwent moderate TBI and, seven days later, were treated with saline alone, G-CSF and saline, hUCB and saline, or hUCB and G-CSF. The rats treated with saline exhibited widespread neuroinflammation, impaired endogenous neurogenesis, and severe hippocampal cell loss. hUCB monotherapy suppressed neuroinflammation, nearly normalized neurogenesis, and reduced hippocampal cell loss, compared with saline alone. G-CSF monotherapy produced partial and short-lived benefits characterized by low levels of neuroinflammation, modest neurogenesis, and moderate reduction of hippocampal cell loss. Combined therapy robustly dampened neuroinflammation, enhanced endogenous neurogenesis, and reduced hippocampal cell loss.
The ability to learn new information may be significantly poorer among patients with Parkinson’s disease than among healthy individuals, according to research published online ahead of print February 24 in Movement Disorders. Investigators examined 27 patients with Parkinson’s disease without dementia and 27 age-, gender-, and education-matched healthy controls with a neuropsychologic test battery designed to assess new learning and memory. The researchers found a significant difference in the groups’ ability to learn a list of 10 semantically related words. Once the groups were equated on learning abilities, the investigators found no significant difference between patients with Parkinson’s disease and controls in recall or recognition of the newly learned material. The memory deficit in nondemented patients with Parkinson’s disease largely results from a deficit in learning new information, said the authors.
Chronic sleep loss may lead to irreversible physical damage to and loss of brain cells, according to research published March 19 in the Journal of Neuroscience. Investigators examined mice following periods of normal rest, short wakefulness, or extended wakefulness to model shift workers’ typical sleep patterns. In response to short-term sleep loss, locus coeruleus neurons upregulated the sirtuin type 3 (SirT3) protein, which protects neurons from metabolic injury. After several days of shift worker sleep patterns, locus coeruleus neurons in the mice had reduced SirT3 and increased cell death. In addition, oxidative stress and acetylation of mitochondrial proteins increased. The mice lost 25% of their locus coeruleus neurons. “This is the first report that sleep loss can actually result in a loss of neurons,” said the authors.
—Erik Greb
Little evidence suggests that most complementary or alternative medicine therapies treat the symptoms of multiple sclerosis (MS), according to an American Academy of Neurology guideline published March 25 in Neurology. Oral cannabis and oral medical marijuana spray, however, may ease patients’ reported symptoms of spasticity, pain related to spasticity, and frequent urination in MS. Not enough evidence is available to show whether smoking marijuana helps treat MS symptoms, according to the guideline. The authors concluded that magnetic therapy is probably effective for fatigue and probably ineffective for depression. Fish oil is probably ineffective for relapses, disability, fatigue, MRI lesions, and quality of life, according to the guideline. In addition, evidence indicates that ginkgo biloba is ineffective for cognition and possibly effective for fatigue, said the authors.
People who develop diabetes and high blood pressure in middle age are more likely to have brain cell loss and problems with memory and thinking skills than people who never have diabetes or high blood pressure or who develop them in old age, according to a study published online ahead of print March 19 in Neurology. Investigators evaluated the thinking and memory skills of 1,437 people (average age, 80), conducted brain scans, and reviewed participants’ medical records to determine whether the latter had been diagnosed with diabetes or high blood pressure in middle age or later. Midlife diabetes was associated with subcortical infarctions, reduced hippocampal volume, reduced whole brain volume, and prevalent mild cognitive impairment. Midlife hypertension was associated with infarctions and white matter hyperintensity volume.
Each 15-minute decrease in treatment delay may provide a patient an average equivalent of one month of additional disability-free life, according to a study published online ahead of print March 13 in Stroke. Researchers examined observational prospective data for 2,258 consecutive stroke patients treated with IV thrombolysis to determine distributions of age, sex, stroke severity, onset-to-treatment times, and three-month modified Rankin Scale score in daily clinical practice. The investigators found that for every one-minute reduction in onset-to-treatment time, patients gained an average 1.8 days of healthy life. Although all patients benefited from faster treatment, younger patients with longer life expectancies gained a little more than older patients. Women gained slightly more than men throughout their longer lifetimes. The awareness of the importance of speed could promote practice change, said the authors.
The FDA has approved extended-release Qudexy XR (topiramate) capsules as initial monotherapy in patients 10 or older with partial-onset seizures or primary generalized tonic-clonic seizures. The drug also received approval as adjunctive therapy in patients age 2 or older with partial-onset seizures, primary generalized tonic-clonic seizures, and seizures associated with Lennox–Gastaut syndrome. In a randomized, double-blind, placebo-controlled study, the drug demonstrated favorable safety and tolerability in patients with refractory partial-onset seizures. The extended-release formulation was associated with a significantly greater median percent reduction from baseline in seizure frequency, compared with placebo (39.5% vs 21.7%) after 11 weeks of treatment. Upsher-Smith Laboratories, headquartered in Maple Grove, Minnesota, manufactures the drug and expects it to be available during the second quarter of 2014.
The FDA has approved the Cefaly medical device as a preventive treatment for migraine headaches. The product is the first transcutaneous electrical nerve stimulation device specifically authorized for use before the onset of pain. The product is a small, portable, battery-powered unit resembling a plastic headband worn across the forehead once per day for 20 minutes. The device applies an electric current to the skin and underlying tissues to stimulate branches of the trigeminal nerve. In a study including 67 participants, patients who used Cefaly had significantly fewer days with migraines per month and used less migraine attack medication, compared with patients who used a placebo device. STX-Med, which is headquartered in Herstal, Liege, Belgium, manufactures the device, which is indicated for patients 18 and older.
Children with autism who are fed infant formula containing soy protein rather than milk protein may have a higher rate of seizures, according to research published March 12 in PLOS One. Researchers analyzed medical record data for 1,949 children with autism, including information on infant formula use, seizure incidence, the specific type of seizure exhibited, and IQ. Soy-based formula was given in 17.5% of the study population. About 13% of the subjects were female. The researchers found a 2.6-fold higher rate of febrile seizures (4.2% vs 1.6%), a 2.1-fold higher rate of epilepsy comorbidity (3.6% vs 1.7%), and a fourfold higher rate of simple partial seizures (1.2% vs 0.3%) in the children with autism who were fed soy-based formula. No statistically significant associations were found with other outcomes.
For patients with Alzheimer’s disease, levels of markers of neuronal injury in the spinal fluid may decrease as symptoms of memory loss and mental decline appear, according to research published March 5 in Science Translational Medicine. Investigators studied data from the Dominantly Inherited Alzheimer’s Network, which includes participants from families with genetic mutations that cause rare inherited forms of Alzheimer’s disease. The group examined levels of tau, p-tau, and visinin-like protein-1 (VILIP-1). Asymptomatic mutation carriers had elevated concentrations of CSF tau, p-tau181, and VILIP-1 10 to 20 years before their estimated age at symptom onset and before cognitive deficits were detected. The concentrations of CSF biomarkers of neuronal injury or death decreased after their estimated age at symptom onset, suggesting a slowing of acute neurodegenerative processes with symptomatic disease progression.
Men with poor cardiovascular fitness or a low IQ at age 18 are more likely to develop dementia before age 60, investigators reported online ahead of print March 6 in Brain. The researchers conducted a population-based cohort study of more than 1.1 million Swedish male conscripts (age 18) who underwent conscription exams between 1968 and 2005. Participants were followed for as long as 42 years. In fully adjusted models, low cardiovascular fitness and cognitive performance at age 18 were associated with increased risk for future early-onset dementia and mild cognitive impairment, compared with high cardiovascular fitness and cognitive performance. Poor performance on cardiovascular fitness and cognitive tests was associated with a greater-than-sevenfold and a greater than eightfold increased risk of early-onset dementia and early-onset mild cognitive impairment, respectively.
A test that detects low levels of prion protein in the blood may accurately screen for infection with the agent responsible for variant Creutzfeldt-Jakob disease (vCJD), according to a study published online ahead of print March 3 in JAMA Neurology. Researchers performed the test on samples from national blood collection and prion disease centers in the US and the UK. The samples were taken from healthy donors, patients with nonprion neurodegenerative disease, patients in whom a prion disease diagnosis was likely, and patients with confirmed vCJD. The assay’s specificity was confirmed as 100% in a healthy UK cohort. No potentially cross-reactive blood samples from patients with nonprion neurodegenerative diseases tested positive. Two patients with sporadic CJD tested positive. The authors’ previous sensitivity estimate was reconfirmed but not refined.
The FDA has approved Neuraceq (florbetaben F18 injection) for PET imaging of the brain to estimate beta-amyloid neuritic plaque density in adults with cognitive impairment who are being evaluated for Alzheimer’s disease and other causes of cognitive decline. The approval is based on safety data from 872 patients who participated in global clinical trials, and on three studies that examined images from adults with a range of cognitive function. Images were analyzed from 82 subjects with postmortem confirmation of the presence or absence of beta-amyloid neuritic plaques. Correlation of the visual PET interpretation with histopathology in these 82 brains demonstrated that Neuraceq (Piramal Imaging; Boston) accurately detects moderate to frequent beta-amyloid neuritic plaques in the brain.
A combination of human umbilical cord blood cells (hUCBs) and granulocyte colony stimulating factor (G-CSF) may provide more benefit for patients with traumatic brain injury (TBI) than either therapy alone, according to research published March 12 in PLOS One. Adult rats underwent moderate TBI and, seven days later, were treated with saline alone, G-CSF and saline, hUCB and saline, or hUCB and G-CSF. The rats treated with saline exhibited widespread neuroinflammation, impaired endogenous neurogenesis, and severe hippocampal cell loss. hUCB monotherapy suppressed neuroinflammation, nearly normalized neurogenesis, and reduced hippocampal cell loss, compared with saline alone. G-CSF monotherapy produced partial and short-lived benefits characterized by low levels of neuroinflammation, modest neurogenesis, and moderate reduction of hippocampal cell loss. Combined therapy robustly dampened neuroinflammation, enhanced endogenous neurogenesis, and reduced hippocampal cell loss.
The ability to learn new information may be significantly poorer among patients with Parkinson’s disease than among healthy individuals, according to research published online ahead of print February 24 in Movement Disorders. Investigators examined 27 patients with Parkinson’s disease without dementia and 27 age-, gender-, and education-matched healthy controls with a neuropsychologic test battery designed to assess new learning and memory. The researchers found a significant difference in the groups’ ability to learn a list of 10 semantically related words. Once the groups were equated on learning abilities, the investigators found no significant difference between patients with Parkinson’s disease and controls in recall or recognition of the newly learned material. The memory deficit in nondemented patients with Parkinson’s disease largely results from a deficit in learning new information, said the authors.
Chronic sleep loss may lead to irreversible physical damage to and loss of brain cells, according to research published March 19 in the Journal of Neuroscience. Investigators examined mice following periods of normal rest, short wakefulness, or extended wakefulness to model shift workers’ typical sleep patterns. In response to short-term sleep loss, locus coeruleus neurons upregulated the sirtuin type 3 (SirT3) protein, which protects neurons from metabolic injury. After several days of shift worker sleep patterns, locus coeruleus neurons in the mice had reduced SirT3 and increased cell death. In addition, oxidative stress and acetylation of mitochondrial proteins increased. The mice lost 25% of their locus coeruleus neurons. “This is the first report that sleep loss can actually result in a loss of neurons,” said the authors.
—Erik Greb
Little evidence suggests that most complementary or alternative medicine therapies treat the symptoms of multiple sclerosis (MS), according to an American Academy of Neurology guideline published March 25 in Neurology. Oral cannabis and oral medical marijuana spray, however, may ease patients’ reported symptoms of spasticity, pain related to spasticity, and frequent urination in MS. Not enough evidence is available to show whether smoking marijuana helps treat MS symptoms, according to the guideline. The authors concluded that magnetic therapy is probably effective for fatigue and probably ineffective for depression. Fish oil is probably ineffective for relapses, disability, fatigue, MRI lesions, and quality of life, according to the guideline. In addition, evidence indicates that ginkgo biloba is ineffective for cognition and possibly effective for fatigue, said the authors.
People who develop diabetes and high blood pressure in middle age are more likely to have brain cell loss and problems with memory and thinking skills than people who never have diabetes or high blood pressure or who develop them in old age, according to a study published online ahead of print March 19 in Neurology. Investigators evaluated the thinking and memory skills of 1,437 people (average age, 80), conducted brain scans, and reviewed participants’ medical records to determine whether the latter had been diagnosed with diabetes or high blood pressure in middle age or later. Midlife diabetes was associated with subcortical infarctions, reduced hippocampal volume, reduced whole brain volume, and prevalent mild cognitive impairment. Midlife hypertension was associated with infarctions and white matter hyperintensity volume.
Each 15-minute decrease in treatment delay may provide a patient an average equivalent of one month of additional disability-free life, according to a study published online ahead of print March 13 in Stroke. Researchers examined observational prospective data for 2,258 consecutive stroke patients treated with IV thrombolysis to determine distributions of age, sex, stroke severity, onset-to-treatment times, and three-month modified Rankin Scale score in daily clinical practice. The investigators found that for every one-minute reduction in onset-to-treatment time, patients gained an average 1.8 days of healthy life. Although all patients benefited from faster treatment, younger patients with longer life expectancies gained a little more than older patients. Women gained slightly more than men throughout their longer lifetimes. The awareness of the importance of speed could promote practice change, said the authors.
The FDA has approved extended-release Qudexy XR (topiramate) capsules as initial monotherapy in patients 10 or older with partial-onset seizures or primary generalized tonic-clonic seizures. The drug also received approval as adjunctive therapy in patients age 2 or older with partial-onset seizures, primary generalized tonic-clonic seizures, and seizures associated with Lennox–Gastaut syndrome. In a randomized, double-blind, placebo-controlled study, the drug demonstrated favorable safety and tolerability in patients with refractory partial-onset seizures. The extended-release formulation was associated with a significantly greater median percent reduction from baseline in seizure frequency, compared with placebo (39.5% vs 21.7%) after 11 weeks of treatment. Upsher-Smith Laboratories, headquartered in Maple Grove, Minnesota, manufactures the drug and expects it to be available during the second quarter of 2014.
The FDA has approved the Cefaly medical device as a preventive treatment for migraine headaches. The product is the first transcutaneous electrical nerve stimulation device specifically authorized for use before the onset of pain. The product is a small, portable, battery-powered unit resembling a plastic headband worn across the forehead once per day for 20 minutes. The device applies an electric current to the skin and underlying tissues to stimulate branches of the trigeminal nerve. In a study including 67 participants, patients who used Cefaly had significantly fewer days with migraines per month and used less migraine attack medication, compared with patients who used a placebo device. STX-Med, which is headquartered in Herstal, Liege, Belgium, manufactures the device, which is indicated for patients 18 and older.
Children with autism who are fed infant formula containing soy protein rather than milk protein may have a higher rate of seizures, according to research published March 12 in PLOS One. Researchers analyzed medical record data for 1,949 children with autism, including information on infant formula use, seizure incidence, the specific type of seizure exhibited, and IQ. Soy-based formula was given in 17.5% of the study population. About 13% of the subjects were female. The researchers found a 2.6-fold higher rate of febrile seizures (4.2% vs 1.6%), a 2.1-fold higher rate of epilepsy comorbidity (3.6% vs 1.7%), and a fourfold higher rate of simple partial seizures (1.2% vs 0.3%) in the children with autism who were fed soy-based formula. No statistically significant associations were found with other outcomes.
For patients with Alzheimer’s disease, levels of markers of neuronal injury in the spinal fluid may decrease as symptoms of memory loss and mental decline appear, according to research published March 5 in Science Translational Medicine. Investigators studied data from the Dominantly Inherited Alzheimer’s Network, which includes participants from families with genetic mutations that cause rare inherited forms of Alzheimer’s disease. The group examined levels of tau, p-tau, and visinin-like protein-1 (VILIP-1). Asymptomatic mutation carriers had elevated concentrations of CSF tau, p-tau181, and VILIP-1 10 to 20 years before their estimated age at symptom onset and before cognitive deficits were detected. The concentrations of CSF biomarkers of neuronal injury or death decreased after their estimated age at symptom onset, suggesting a slowing of acute neurodegenerative processes with symptomatic disease progression.
Men with poor cardiovascular fitness or a low IQ at age 18 are more likely to develop dementia before age 60, investigators reported online ahead of print March 6 in Brain. The researchers conducted a population-based cohort study of more than 1.1 million Swedish male conscripts (age 18) who underwent conscription exams between 1968 and 2005. Participants were followed for as long as 42 years. In fully adjusted models, low cardiovascular fitness and cognitive performance at age 18 were associated with increased risk for future early-onset dementia and mild cognitive impairment, compared with high cardiovascular fitness and cognitive performance. Poor performance on cardiovascular fitness and cognitive tests was associated with a greater-than-sevenfold and a greater than eightfold increased risk of early-onset dementia and early-onset mild cognitive impairment, respectively.
A test that detects low levels of prion protein in the blood may accurately screen for infection with the agent responsible for variant Creutzfeldt-Jakob disease (vCJD), according to a study published online ahead of print March 3 in JAMA Neurology. Researchers performed the test on samples from national blood collection and prion disease centers in the US and the UK. The samples were taken from healthy donors, patients with nonprion neurodegenerative disease, patients in whom a prion disease diagnosis was likely, and patients with confirmed vCJD. The assay’s specificity was confirmed as 100% in a healthy UK cohort. No potentially cross-reactive blood samples from patients with nonprion neurodegenerative diseases tested positive. Two patients with sporadic CJD tested positive. The authors’ previous sensitivity estimate was reconfirmed but not refined.
The FDA has approved Neuraceq (florbetaben F18 injection) for PET imaging of the brain to estimate beta-amyloid neuritic plaque density in adults with cognitive impairment who are being evaluated for Alzheimer’s disease and other causes of cognitive decline. The approval is based on safety data from 872 patients who participated in global clinical trials, and on three studies that examined images from adults with a range of cognitive function. Images were analyzed from 82 subjects with postmortem confirmation of the presence or absence of beta-amyloid neuritic plaques. Correlation of the visual PET interpretation with histopathology in these 82 brains demonstrated that Neuraceq (Piramal Imaging; Boston) accurately detects moderate to frequent beta-amyloid neuritic plaques in the brain.
A combination of human umbilical cord blood cells (hUCBs) and granulocyte colony stimulating factor (G-CSF) may provide more benefit for patients with traumatic brain injury (TBI) than either therapy alone, according to research published March 12 in PLOS One. Adult rats underwent moderate TBI and, seven days later, were treated with saline alone, G-CSF and saline, hUCB and saline, or hUCB and G-CSF. The rats treated with saline exhibited widespread neuroinflammation, impaired endogenous neurogenesis, and severe hippocampal cell loss. hUCB monotherapy suppressed neuroinflammation, nearly normalized neurogenesis, and reduced hippocampal cell loss, compared with saline alone. G-CSF monotherapy produced partial and short-lived benefits characterized by low levels of neuroinflammation, modest neurogenesis, and moderate reduction of hippocampal cell loss. Combined therapy robustly dampened neuroinflammation, enhanced endogenous neurogenesis, and reduced hippocampal cell loss.
The ability to learn new information may be significantly poorer among patients with Parkinson’s disease than among healthy individuals, according to research published online ahead of print February 24 in Movement Disorders. Investigators examined 27 patients with Parkinson’s disease without dementia and 27 age-, gender-, and education-matched healthy controls with a neuropsychologic test battery designed to assess new learning and memory. The researchers found a significant difference in the groups’ ability to learn a list of 10 semantically related words. Once the groups were equated on learning abilities, the investigators found no significant difference between patients with Parkinson’s disease and controls in recall or recognition of the newly learned material. The memory deficit in nondemented patients with Parkinson’s disease largely results from a deficit in learning new information, said the authors.
Chronic sleep loss may lead to irreversible physical damage to and loss of brain cells, according to research published March 19 in the Journal of Neuroscience. Investigators examined mice following periods of normal rest, short wakefulness, or extended wakefulness to model shift workers’ typical sleep patterns. In response to short-term sleep loss, locus coeruleus neurons upregulated the sirtuin type 3 (SirT3) protein, which protects neurons from metabolic injury. After several days of shift worker sleep patterns, locus coeruleus neurons in the mice had reduced SirT3 and increased cell death. In addition, oxidative stress and acetylation of mitochondrial proteins increased. The mice lost 25% of their locus coeruleus neurons. “This is the first report that sleep loss can actually result in a loss of neurons,” said the authors.
—Erik Greb
Iatrogenic Transection of the Peroneal and Partial Transection of the Tibial Nerve During Arthroscopic Lateral Meniscal Debridement and Removal of Osteochondral Fragment
Atypical Presentation of Soft-Tissue Mass With Gonococcal Infection in the Hand
Effect of Capsulotomy on Hip Stability—A Consideration During Hip Arthroscopy
Hookahs vs cigarettes: What to tell patients
How to discuss sex with elderly patients
› Keep in mind that elderly patients may want to discuss matters of sexuality but can also be embarrassed, fearful, or reluctant to do so with a younger caregiver. C
› Consider making a patient’s sexual history part of your general health screening, perhaps using the PLISSIT model for facilitating discussion. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Sexuality is a central aspect of being human. It encompasses sex, gender identities and roles, sexual orientation, pleasure, eroticism, and intimacy, and is a major contributor to an individual’s quality of life and sense of wellbeing.1,2 Positive sexual relationships and behaviors are integral to maintaining good health and general well-being later in life, as well.2,3 Cynthia Graber, a reporter with Scientific American, reported that sex is a key reason retirees have a happy life.4
While there is a decline in sexual activity with age, a great number of men and women continue to engage in vaginal or anal intercourse, oral sex, and masturbation into the eighth and ninth decades of life.2,5 In a survey conducted among married men and women, about 90% of respondents between the ages of 60 and 64 and almost 30% of those older than age 80 said they were still sexually active.2 Another study reported that 62% of men and 30% of women 80 to 102 years of age were still sexually active.6 However, sexuality is rarely discussed with the elderly, and most physicians are unsure about how to handle such conversations.7
The baby boomer population is aging in the United States and elsewhere. By 2030, 20% of the US population will be ≥65 years old, and 4% (3 million) will be lesbian, gay, bisexual, transgender, and queer (LGBTQ) elderly adults.3,8 Given the impact of sex on maintaining quality of life, it is important for health care providers to be comfortable discussing sexuality with the elderly.9
Barriers to discussing sexuality
Physician barriers
Primary care physicians typically are the first point of contact for elderly adults experiencing health problems, including sexual dysfunction. According to the American Psychological Association, sex is not discussed enough with the elderly. Most physicians do not address sexual health proactively, and rarely do they include a sexual history as part of general health screening in the elderly.2,10,11 Inadequate training of physicians in sexual health is likely a contributing factor.5 Physicians also often feel discomfort when discussing such matters with patients of the opposite sex.12 (For a suggested approach to these conversations, see “Discussing sexuality with elderly patients: Getting beyond ‘don’t ask, don’t tell,” below.) With the increasing number of LGBTQ elderly adults, physicians should not assume their patients have any particular sexual behavior or orientation. This will help elderly LGBTQ patients feel more comfortable discussing their sexual health needs.8
The PLISSIT model, developed in 1976 by clinical psychologist Dr. Jack Annon, can facilitate a discussion of sexuality with elderly patients.11,13 First, the healthcare provider seeks permission (P) to discuss sexuality with the patient. After permission is given, the provider can share limited information (LI) about sexual issues that affect the older adult. Next, the provider may offer specific suggestions (SS) to improve sexual health or resolve problems. Finally, referral for intensive therapy (IT) may be needed for someone whose sexual dysfunction goes beyond the scope of the health care provider’s expertise. In 2000, open-ended questions were added to the PLISSIT model to more effectively guide an assessment of sexuality in older adults13,14:
• Can you tell me how you express your sexuality?
• What concerns or questions do you have about fulfilling your continuing sexual needs?
• In what ways has your sexual relationship with your partner changed as you have aged?
Many physicians have only a vague understanding of the sexual needs of the elderly, and some may even consider sexuality among elderly people a taboo.5 The reality is that elderly adults need to be touched, held, and feel loved, and this does not diminish with age.15-17 Unfortunately, many healthcare professionals have a mindset of, “I don’t want to think about my parents having sex, let alone my grandparents.” It is critical that physicians address intimacy needs as part of a medical assessment of the elderly.
Loss of physical and emotional intimacy is profound and often ignored as a source of suffering for the elderly. Most elderly patients want to discuss sexual issues with their physician, according to the Global Study of Sexual Attitudes among men and women ages 40 to 80 years.18 Surprisingly, even geriatricians often fail to take a sexual history of their patients. In one study, only 57% of 120 geriatricians surveyed routinely took a sexual history, even though 97% of them believed that patients with sexual problems should be managed further.1
Patient barriers
Even given a desire to discuss sexual concerns with their health care provider, elderly patients can be reluctant due to embarrassment or a fear of sexuality. Others may hesitate because their caregiver is younger than they or is of the opposite sex.19,20 The attitude of a medical professional has a powerful impact on the sexual attitudes and behaviors of elderly patients, and on their level of comfort in discussing sexual issues.21 Elderly patients do not usually complain to their physicians about sexual dysfunctions; 92% of men and 96% of women who reported at least one sexual problem in a survey had not sought help at all.18
Addressing issues in sexual dysfunction
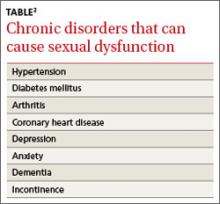
Though sexual desires and needs may not decline with age, sexual function might, for any number of reasons.1,2,7 Many chronic diseases are known to interfere with sexual function (TABLE).2 Polypharmacy can lead to physical challenges, cognitive changes, and impaired sexual arousal, especially in men.3 However, the reason cited most often for absence of sexual activity is lack of a partner or a willing partner.2 Unfortunately as one ages, the chance of finding a partner diminishes. Hence the need to discuss alternative expressions of sexuality that may not require a partner.3 Many elderly individuals enjoy masturbation as a form of sexual expression.
Men and women have different sexual problems, but they are all treatable. For instance, with normal aging, levels of testosterone in men and estrogen in women decrease.5,15 Despite the number of sexual health dysfunctions, only 14% of men and 1% of women use medications to treat them.2,5 With men who have erectile dysfunction, discuss possible testosterone replacement or medication. For women with postmenopausal (atrophic) vaginitis, estrogen therapy or a lubricant (for those with contraindication to estrogen therapy) can improve sexual function. Anorgasmia and low libido are other concerns for postmenopausal women, and may warrant gynecologic referral.
For elderly adults moving into assisted living or a nursing home, the transition can signal the end of a sexual life.16,22 There is limited opportunity for men and women in residential settings to engage in sexual activity, in part due to a lack of privacy.23 The nursing home is still a home, and facility staff should provide opportunities for privacy and intimacy. In a study conducted in a residential setting, more than 25% of those ages 65 to 85 reported an active sex life, while 90% of those surveyed had sexual thoughts and fantasies.22 Of course, many elderly adults enter residential settings without a partner. They should be allowed to engage in sexual activities if they can understand, consent to, and form a relationship. Sexual needs remain even in those with dementia. But cognitive impairment frequently manifests as inappropriate sexual behavior. A study of cognitively impaired older adults revealed that 1.8% had displayed sexually inappropriate verbal or physical behavior.24 In these situations, a behavior medicine specialist can be of great help.
Health risks of sexual activity in the elderly
In 2011, the Centers for Disease Control and Prevention reported that 5% of new human immunodeficiency virus (HIV) cases occurred in those ≥55 years, and almost 2% of new diagnoses were in the those ≥65 years.25 Sexually active elderly individuals are at risk for acquiring HIV, in part because they do not consider themselves to be at risk for sexually transmitted diseases (STDs).26 They also might not have received education about the importance of condom use.11,26 In addition, prescribing erectile dysfunction medications for men and hormone replacement therapy for women might have played a part in increasing STDs among the elderly, particularly Chlamydia and HIV.27 The long-term effects of STDs left untreated can easily be mistaken for other symptoms or diseases of aging, which further underscores the importance of discussing sexuality with elderly patients.
CORRESPONDENCE
Folashade Omole, MD, FAAFP, 1513 East Cleveland Avenue, Building 100, Suite 300-A, East Point, GA 30344; fomole@msm.edu
1. Balami JS. Are geriatricians guilty of failure to take a sexual history? J Clin Gerontol Geriatr. 2011;2:17-20.
2. Lindau ST, Schumm LP, Laumann EO, et al. A study of sexuality and health among older adults in the United States. N Engl J Med. 2007;357:762-774.
3. Bradford A, Meston CM. Senior sexual health: The effects of aging on sexuality. In: VandeCreek L, Petersen FL, Bley JW, eds. Innovations in Clinical Practice: Focus on Sexual Health. Sarasota, FL: Professional Resource Press; 2007:35-45.
4. Graber C. Sex keeps elderly happier in marriage. Scientific American.
Available at: http://www.scientificamerican.com/podcast/episode/sex-keeps-elderly-happier-in-marria-11-11-29. Accessed March 26, 2014.
5. Hinchliff S, Gott M. Seeking medical help for sexual concerns in mid- and later life: a review of the literature. J Sex Res. 2011;48:106-117.
6. Tobin JM, Harindra V. Attendance by older patients at a genitourinary medicine clinic. Sex Transm Infect. 2001;77:289-291.
7. Bauer M, McAuliffe L, Nay R. Sexuality, health care and the older person: an overview of the literature. Int J Older People Nurs. 2007;2:63-68.
8. Wallace SP, Cochran SD, Durazo EM, et al. The health of aging lesbian, gay and bisexual adults in California. Policy Brief UCLA Cent Health Policy Res. 2011;(PB2011-2):1-8.
9. Henry J, McNab W. Forever young: a health promotion focus on sexuality and aging. Gerontol Geriatr Education. 2003;23:57-74.
10. Gott M, Hinchliff S, Galena E. General practitioner attitudes to discussing sexual health issues with older people. Soc Sci Med. 2004;58:2093-2103.
11. Nusbaum MR, Hamilton CD. The proactive sexual health history. Am Fam Physician. 2002;66:1705-1712.
12. Burd ID, Nevadunsky N, Bachmann G. Impact of physician gender on sexual history taking in a multispecialty practice. J Sex Med. 2006;3:194-200.
13. Kazer MW. Sexuality Assessment for Older Adults. Hartford Institute for Geriatric Nursing Web site. Available at: http://consultgerirn.org/uploads/File/trythis/try_this_10.pdf. Updated 2012. Accessed March 14, 2014.
14. Wallace MA. Assessment of sexual health in older adults. Am J Nursing. 2012;108:52-60.
15. Sexuality in later life. National Institute on Aging Web site. Available at: http://www.nia.nih.gov/health/publication/sexualitylater-life. Updated March 11, 2014. Accessed March 21, 2014.
16. Hajjar RR, Kamel HK. Sexuality in the nursing home, part 1: attitudes and barriers to sexual expression. J Am Med Dir Assoc. 2004;5(2 suppl):S42-S47.
17. Bildtgård T. The sexuality of elderly people on film—visual limitations. J Aging Identity. 2000;5:169-183.
18. Moreira ED Jr, Brock G, Glasser DB, et al; GSSAB Investigators’ Group. Help-seeking behaviour for sexual problems: the global study of sexual attitudes and behaviors. Int J Clin Pract. 2005;59:6-16.
19. Gott M, Hinchliff S. Barriers to seeking treatment for sexual problems in primary care: a qualitative study with older people. Fam Pract. 2003;20:690-695.
20. Politi MC, Clark MA, Armstrong G, et al. Patient-provider communication about sexual health among unmarried middle-aged and older women. J Gen Intern Med. 2009;24:511-516.
21. Bouman W, Arcelus J, Benbow S. Nottingham study of sexuality & ageing (NoSSA I). Attitudes regarding sexuality and older people: a review of the literature. Sex Relationship Ther. 2006;21:149-161.
22. Low LPL, Lui MHL, Lee DTF, et al. Promoting awareness of sexuality of older people in residential care. Electronic J Human Sexuality. 2005;8:8-16.
23. Rheaume C, Mitty E. Sexuality and intimacy in older adults. Geriatr Nurs. 2008;29:342-349.
24. Nagaratnam N, Gayagay G Jr. Hypersexuality in nursing care facilities—a descriptive study. Arch Gerontol Geriatr. 2002;35:195-203.
25. HIV among older Americans. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/hiv/risk/age/olderamericans/. Updated December 23, 2013. Accessed February 28, 2014.
26. Nguyen N, Holodniy M. HIV infection in the elderly. Clin Interv Aging. 2008;3:453-472.
27. Jena AB, Goldman DP, Kamdar A, et al. Sexually transmitted diseases among users of erectile dysfunction drugs: analysis of claims data. Ann Intern Med. 2010;153:1-7.
› Keep in mind that elderly patients may want to discuss matters of sexuality but can also be embarrassed, fearful, or reluctant to do so with a younger caregiver. C
› Consider making a patient’s sexual history part of your general health screening, perhaps using the PLISSIT model for facilitating discussion. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Sexuality is a central aspect of being human. It encompasses sex, gender identities and roles, sexual orientation, pleasure, eroticism, and intimacy, and is a major contributor to an individual’s quality of life and sense of wellbeing.1,2 Positive sexual relationships and behaviors are integral to maintaining good health and general well-being later in life, as well.2,3 Cynthia Graber, a reporter with Scientific American, reported that sex is a key reason retirees have a happy life.4
While there is a decline in sexual activity with age, a great number of men and women continue to engage in vaginal or anal intercourse, oral sex, and masturbation into the eighth and ninth decades of life.2,5 In a survey conducted among married men and women, about 90% of respondents between the ages of 60 and 64 and almost 30% of those older than age 80 said they were still sexually active.2 Another study reported that 62% of men and 30% of women 80 to 102 years of age were still sexually active.6 However, sexuality is rarely discussed with the elderly, and most physicians are unsure about how to handle such conversations.7
The baby boomer population is aging in the United States and elsewhere. By 2030, 20% of the US population will be ≥65 years old, and 4% (3 million) will be lesbian, gay, bisexual, transgender, and queer (LGBTQ) elderly adults.3,8 Given the impact of sex on maintaining quality of life, it is important for health care providers to be comfortable discussing sexuality with the elderly.9
Barriers to discussing sexuality
Physician barriers
Primary care physicians typically are the first point of contact for elderly adults experiencing health problems, including sexual dysfunction. According to the American Psychological Association, sex is not discussed enough with the elderly. Most physicians do not address sexual health proactively, and rarely do they include a sexual history as part of general health screening in the elderly.2,10,11 Inadequate training of physicians in sexual health is likely a contributing factor.5 Physicians also often feel discomfort when discussing such matters with patients of the opposite sex.12 (For a suggested approach to these conversations, see “Discussing sexuality with elderly patients: Getting beyond ‘don’t ask, don’t tell,” below.) With the increasing number of LGBTQ elderly adults, physicians should not assume their patients have any particular sexual behavior or orientation. This will help elderly LGBTQ patients feel more comfortable discussing their sexual health needs.8
The PLISSIT model, developed in 1976 by clinical psychologist Dr. Jack Annon, can facilitate a discussion of sexuality with elderly patients.11,13 First, the healthcare provider seeks permission (P) to discuss sexuality with the patient. After permission is given, the provider can share limited information (LI) about sexual issues that affect the older adult. Next, the provider may offer specific suggestions (SS) to improve sexual health or resolve problems. Finally, referral for intensive therapy (IT) may be needed for someone whose sexual dysfunction goes beyond the scope of the health care provider’s expertise. In 2000, open-ended questions were added to the PLISSIT model to more effectively guide an assessment of sexuality in older adults13,14:
• Can you tell me how you express your sexuality?
• What concerns or questions do you have about fulfilling your continuing sexual needs?
• In what ways has your sexual relationship with your partner changed as you have aged?
Many physicians have only a vague understanding of the sexual needs of the elderly, and some may even consider sexuality among elderly people a taboo.5 The reality is that elderly adults need to be touched, held, and feel loved, and this does not diminish with age.15-17 Unfortunately, many healthcare professionals have a mindset of, “I don’t want to think about my parents having sex, let alone my grandparents.” It is critical that physicians address intimacy needs as part of a medical assessment of the elderly.
Loss of physical and emotional intimacy is profound and often ignored as a source of suffering for the elderly. Most elderly patients want to discuss sexual issues with their physician, according to the Global Study of Sexual Attitudes among men and women ages 40 to 80 years.18 Surprisingly, even geriatricians often fail to take a sexual history of their patients. In one study, only 57% of 120 geriatricians surveyed routinely took a sexual history, even though 97% of them believed that patients with sexual problems should be managed further.1
Patient barriers
Even given a desire to discuss sexual concerns with their health care provider, elderly patients can be reluctant due to embarrassment or a fear of sexuality. Others may hesitate because their caregiver is younger than they or is of the opposite sex.19,20 The attitude of a medical professional has a powerful impact on the sexual attitudes and behaviors of elderly patients, and on their level of comfort in discussing sexual issues.21 Elderly patients do not usually complain to their physicians about sexual dysfunctions; 92% of men and 96% of women who reported at least one sexual problem in a survey had not sought help at all.18
Addressing issues in sexual dysfunction
Though sexual desires and needs may not decline with age, sexual function might, for any number of reasons.1,2,7 Many chronic diseases are known to interfere with sexual function (TABLE).2 Polypharmacy can lead to physical challenges, cognitive changes, and impaired sexual arousal, especially in men.3 However, the reason cited most often for absence of sexual activity is lack of a partner or a willing partner.2 Unfortunately as one ages, the chance of finding a partner diminishes. Hence the need to discuss alternative expressions of sexuality that may not require a partner.3 Many elderly individuals enjoy masturbation as a form of sexual expression.
Men and women have different sexual problems, but they are all treatable. For instance, with normal aging, levels of testosterone in men and estrogen in women decrease.5,15 Despite the number of sexual health dysfunctions, only 14% of men and 1% of women use medications to treat them.2,5 With men who have erectile dysfunction, discuss possible testosterone replacement or medication. For women with postmenopausal (atrophic) vaginitis, estrogen therapy or a lubricant (for those with contraindication to estrogen therapy) can improve sexual function. Anorgasmia and low libido are other concerns for postmenopausal women, and may warrant gynecologic referral.
For elderly adults moving into assisted living or a nursing home, the transition can signal the end of a sexual life.16,22 There is limited opportunity for men and women in residential settings to engage in sexual activity, in part due to a lack of privacy.23 The nursing home is still a home, and facility staff should provide opportunities for privacy and intimacy. In a study conducted in a residential setting, more than 25% of those ages 65 to 85 reported an active sex life, while 90% of those surveyed had sexual thoughts and fantasies.22 Of course, many elderly adults enter residential settings without a partner. They should be allowed to engage in sexual activities if they can understand, consent to, and form a relationship. Sexual needs remain even in those with dementia. But cognitive impairment frequently manifests as inappropriate sexual behavior. A study of cognitively impaired older adults revealed that 1.8% had displayed sexually inappropriate verbal or physical behavior.24 In these situations, a behavior medicine specialist can be of great help.
Health risks of sexual activity in the elderly
In 2011, the Centers for Disease Control and Prevention reported that 5% of new human immunodeficiency virus (HIV) cases occurred in those ≥55 years, and almost 2% of new diagnoses were in the those ≥65 years.25 Sexually active elderly individuals are at risk for acquiring HIV, in part because they do not consider themselves to be at risk for sexually transmitted diseases (STDs).26 They also might not have received education about the importance of condom use.11,26 In addition, prescribing erectile dysfunction medications for men and hormone replacement therapy for women might have played a part in increasing STDs among the elderly, particularly Chlamydia and HIV.27 The long-term effects of STDs left untreated can easily be mistaken for other symptoms or diseases of aging, which further underscores the importance of discussing sexuality with elderly patients.
CORRESPONDENCE
Folashade Omole, MD, FAAFP, 1513 East Cleveland Avenue, Building 100, Suite 300-A, East Point, GA 30344; fomole@msm.edu
› Keep in mind that elderly patients may want to discuss matters of sexuality but can also be embarrassed, fearful, or reluctant to do so with a younger caregiver. C
› Consider making a patient’s sexual history part of your general health screening, perhaps using the PLISSIT model for facilitating discussion. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Sexuality is a central aspect of being human. It encompasses sex, gender identities and roles, sexual orientation, pleasure, eroticism, and intimacy, and is a major contributor to an individual’s quality of life and sense of wellbeing.1,2 Positive sexual relationships and behaviors are integral to maintaining good health and general well-being later in life, as well.2,3 Cynthia Graber, a reporter with Scientific American, reported that sex is a key reason retirees have a happy life.4
While there is a decline in sexual activity with age, a great number of men and women continue to engage in vaginal or anal intercourse, oral sex, and masturbation into the eighth and ninth decades of life.2,5 In a survey conducted among married men and women, about 90% of respondents between the ages of 60 and 64 and almost 30% of those older than age 80 said they were still sexually active.2 Another study reported that 62% of men and 30% of women 80 to 102 years of age were still sexually active.6 However, sexuality is rarely discussed with the elderly, and most physicians are unsure about how to handle such conversations.7
The baby boomer population is aging in the United States and elsewhere. By 2030, 20% of the US population will be ≥65 years old, and 4% (3 million) will be lesbian, gay, bisexual, transgender, and queer (LGBTQ) elderly adults.3,8 Given the impact of sex on maintaining quality of life, it is important for health care providers to be comfortable discussing sexuality with the elderly.9
Barriers to discussing sexuality
Physician barriers
Primary care physicians typically are the first point of contact for elderly adults experiencing health problems, including sexual dysfunction. According to the American Psychological Association, sex is not discussed enough with the elderly. Most physicians do not address sexual health proactively, and rarely do they include a sexual history as part of general health screening in the elderly.2,10,11 Inadequate training of physicians in sexual health is likely a contributing factor.5 Physicians also often feel discomfort when discussing such matters with patients of the opposite sex.12 (For a suggested approach to these conversations, see “Discussing sexuality with elderly patients: Getting beyond ‘don’t ask, don’t tell,” below.) With the increasing number of LGBTQ elderly adults, physicians should not assume their patients have any particular sexual behavior or orientation. This will help elderly LGBTQ patients feel more comfortable discussing their sexual health needs.8
The PLISSIT model, developed in 1976 by clinical psychologist Dr. Jack Annon, can facilitate a discussion of sexuality with elderly patients.11,13 First, the healthcare provider seeks permission (P) to discuss sexuality with the patient. After permission is given, the provider can share limited information (LI) about sexual issues that affect the older adult. Next, the provider may offer specific suggestions (SS) to improve sexual health or resolve problems. Finally, referral for intensive therapy (IT) may be needed for someone whose sexual dysfunction goes beyond the scope of the health care provider’s expertise. In 2000, open-ended questions were added to the PLISSIT model to more effectively guide an assessment of sexuality in older adults13,14:
• Can you tell me how you express your sexuality?
• What concerns or questions do you have about fulfilling your continuing sexual needs?
• In what ways has your sexual relationship with your partner changed as you have aged?
Many physicians have only a vague understanding of the sexual needs of the elderly, and some may even consider sexuality among elderly people a taboo.5 The reality is that elderly adults need to be touched, held, and feel loved, and this does not diminish with age.15-17 Unfortunately, many healthcare professionals have a mindset of, “I don’t want to think about my parents having sex, let alone my grandparents.” It is critical that physicians address intimacy needs as part of a medical assessment of the elderly.
Loss of physical and emotional intimacy is profound and often ignored as a source of suffering for the elderly. Most elderly patients want to discuss sexual issues with their physician, according to the Global Study of Sexual Attitudes among men and women ages 40 to 80 years.18 Surprisingly, even geriatricians often fail to take a sexual history of their patients. In one study, only 57% of 120 geriatricians surveyed routinely took a sexual history, even though 97% of them believed that patients with sexual problems should be managed further.1
Patient barriers
Even given a desire to discuss sexual concerns with their health care provider, elderly patients can be reluctant due to embarrassment or a fear of sexuality. Others may hesitate because their caregiver is younger than they or is of the opposite sex.19,20 The attitude of a medical professional has a powerful impact on the sexual attitudes and behaviors of elderly patients, and on their level of comfort in discussing sexual issues.21 Elderly patients do not usually complain to their physicians about sexual dysfunctions; 92% of men and 96% of women who reported at least one sexual problem in a survey had not sought help at all.18
Addressing issues in sexual dysfunction
Though sexual desires and needs may not decline with age, sexual function might, for any number of reasons.1,2,7 Many chronic diseases are known to interfere with sexual function (TABLE).2 Polypharmacy can lead to physical challenges, cognitive changes, and impaired sexual arousal, especially in men.3 However, the reason cited most often for absence of sexual activity is lack of a partner or a willing partner.2 Unfortunately as one ages, the chance of finding a partner diminishes. Hence the need to discuss alternative expressions of sexuality that may not require a partner.3 Many elderly individuals enjoy masturbation as a form of sexual expression.
Men and women have different sexual problems, but they are all treatable. For instance, with normal aging, levels of testosterone in men and estrogen in women decrease.5,15 Despite the number of sexual health dysfunctions, only 14% of men and 1% of women use medications to treat them.2,5 With men who have erectile dysfunction, discuss possible testosterone replacement or medication. For women with postmenopausal (atrophic) vaginitis, estrogen therapy or a lubricant (for those with contraindication to estrogen therapy) can improve sexual function. Anorgasmia and low libido are other concerns for postmenopausal women, and may warrant gynecologic referral.
For elderly adults moving into assisted living or a nursing home, the transition can signal the end of a sexual life.16,22 There is limited opportunity for men and women in residential settings to engage in sexual activity, in part due to a lack of privacy.23 The nursing home is still a home, and facility staff should provide opportunities for privacy and intimacy. In a study conducted in a residential setting, more than 25% of those ages 65 to 85 reported an active sex life, while 90% of those surveyed had sexual thoughts and fantasies.22 Of course, many elderly adults enter residential settings without a partner. They should be allowed to engage in sexual activities if they can understand, consent to, and form a relationship. Sexual needs remain even in those with dementia. But cognitive impairment frequently manifests as inappropriate sexual behavior. A study of cognitively impaired older adults revealed that 1.8% had displayed sexually inappropriate verbal or physical behavior.24 In these situations, a behavior medicine specialist can be of great help.
Health risks of sexual activity in the elderly
In 2011, the Centers for Disease Control and Prevention reported that 5% of new human immunodeficiency virus (HIV) cases occurred in those ≥55 years, and almost 2% of new diagnoses were in the those ≥65 years.25 Sexually active elderly individuals are at risk for acquiring HIV, in part because they do not consider themselves to be at risk for sexually transmitted diseases (STDs).26 They also might not have received education about the importance of condom use.11,26 In addition, prescribing erectile dysfunction medications for men and hormone replacement therapy for women might have played a part in increasing STDs among the elderly, particularly Chlamydia and HIV.27 The long-term effects of STDs left untreated can easily be mistaken for other symptoms or diseases of aging, which further underscores the importance of discussing sexuality with elderly patients.
CORRESPONDENCE
Folashade Omole, MD, FAAFP, 1513 East Cleveland Avenue, Building 100, Suite 300-A, East Point, GA 30344; fomole@msm.edu
1. Balami JS. Are geriatricians guilty of failure to take a sexual history? J Clin Gerontol Geriatr. 2011;2:17-20.
2. Lindau ST, Schumm LP, Laumann EO, et al. A study of sexuality and health among older adults in the United States. N Engl J Med. 2007;357:762-774.
3. Bradford A, Meston CM. Senior sexual health: The effects of aging on sexuality. In: VandeCreek L, Petersen FL, Bley JW, eds. Innovations in Clinical Practice: Focus on Sexual Health. Sarasota, FL: Professional Resource Press; 2007:35-45.
4. Graber C. Sex keeps elderly happier in marriage. Scientific American.
Available at: http://www.scientificamerican.com/podcast/episode/sex-keeps-elderly-happier-in-marria-11-11-29. Accessed March 26, 2014.
5. Hinchliff S, Gott M. Seeking medical help for sexual concerns in mid- and later life: a review of the literature. J Sex Res. 2011;48:106-117.
6. Tobin JM, Harindra V. Attendance by older patients at a genitourinary medicine clinic. Sex Transm Infect. 2001;77:289-291.
7. Bauer M, McAuliffe L, Nay R. Sexuality, health care and the older person: an overview of the literature. Int J Older People Nurs. 2007;2:63-68.
8. Wallace SP, Cochran SD, Durazo EM, et al. The health of aging lesbian, gay and bisexual adults in California. Policy Brief UCLA Cent Health Policy Res. 2011;(PB2011-2):1-8.
9. Henry J, McNab W. Forever young: a health promotion focus on sexuality and aging. Gerontol Geriatr Education. 2003;23:57-74.
10. Gott M, Hinchliff S, Galena E. General practitioner attitudes to discussing sexual health issues with older people. Soc Sci Med. 2004;58:2093-2103.
11. Nusbaum MR, Hamilton CD. The proactive sexual health history. Am Fam Physician. 2002;66:1705-1712.
12. Burd ID, Nevadunsky N, Bachmann G. Impact of physician gender on sexual history taking in a multispecialty practice. J Sex Med. 2006;3:194-200.
13. Kazer MW. Sexuality Assessment for Older Adults. Hartford Institute for Geriatric Nursing Web site. Available at: http://consultgerirn.org/uploads/File/trythis/try_this_10.pdf. Updated 2012. Accessed March 14, 2014.
14. Wallace MA. Assessment of sexual health in older adults. Am J Nursing. 2012;108:52-60.
15. Sexuality in later life. National Institute on Aging Web site. Available at: http://www.nia.nih.gov/health/publication/sexualitylater-life. Updated March 11, 2014. Accessed March 21, 2014.
16. Hajjar RR, Kamel HK. Sexuality in the nursing home, part 1: attitudes and barriers to sexual expression. J Am Med Dir Assoc. 2004;5(2 suppl):S42-S47.
17. Bildtgård T. The sexuality of elderly people on film—visual limitations. J Aging Identity. 2000;5:169-183.
18. Moreira ED Jr, Brock G, Glasser DB, et al; GSSAB Investigators’ Group. Help-seeking behaviour for sexual problems: the global study of sexual attitudes and behaviors. Int J Clin Pract. 2005;59:6-16.
19. Gott M, Hinchliff S. Barriers to seeking treatment for sexual problems in primary care: a qualitative study with older people. Fam Pract. 2003;20:690-695.
20. Politi MC, Clark MA, Armstrong G, et al. Patient-provider communication about sexual health among unmarried middle-aged and older women. J Gen Intern Med. 2009;24:511-516.
21. Bouman W, Arcelus J, Benbow S. Nottingham study of sexuality & ageing (NoSSA I). Attitudes regarding sexuality and older people: a review of the literature. Sex Relationship Ther. 2006;21:149-161.
22. Low LPL, Lui MHL, Lee DTF, et al. Promoting awareness of sexuality of older people in residential care. Electronic J Human Sexuality. 2005;8:8-16.
23. Rheaume C, Mitty E. Sexuality and intimacy in older adults. Geriatr Nurs. 2008;29:342-349.
24. Nagaratnam N, Gayagay G Jr. Hypersexuality in nursing care facilities—a descriptive study. Arch Gerontol Geriatr. 2002;35:195-203.
25. HIV among older Americans. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/hiv/risk/age/olderamericans/. Updated December 23, 2013. Accessed February 28, 2014.
26. Nguyen N, Holodniy M. HIV infection in the elderly. Clin Interv Aging. 2008;3:453-472.
27. Jena AB, Goldman DP, Kamdar A, et al. Sexually transmitted diseases among users of erectile dysfunction drugs: analysis of claims data. Ann Intern Med. 2010;153:1-7.
1. Balami JS. Are geriatricians guilty of failure to take a sexual history? J Clin Gerontol Geriatr. 2011;2:17-20.
2. Lindau ST, Schumm LP, Laumann EO, et al. A study of sexuality and health among older adults in the United States. N Engl J Med. 2007;357:762-774.
3. Bradford A, Meston CM. Senior sexual health: The effects of aging on sexuality. In: VandeCreek L, Petersen FL, Bley JW, eds. Innovations in Clinical Practice: Focus on Sexual Health. Sarasota, FL: Professional Resource Press; 2007:35-45.
4. Graber C. Sex keeps elderly happier in marriage. Scientific American.
Available at: http://www.scientificamerican.com/podcast/episode/sex-keeps-elderly-happier-in-marria-11-11-29. Accessed March 26, 2014.
5. Hinchliff S, Gott M. Seeking medical help for sexual concerns in mid- and later life: a review of the literature. J Sex Res. 2011;48:106-117.
6. Tobin JM, Harindra V. Attendance by older patients at a genitourinary medicine clinic. Sex Transm Infect. 2001;77:289-291.
7. Bauer M, McAuliffe L, Nay R. Sexuality, health care and the older person: an overview of the literature. Int J Older People Nurs. 2007;2:63-68.
8. Wallace SP, Cochran SD, Durazo EM, et al. The health of aging lesbian, gay and bisexual adults in California. Policy Brief UCLA Cent Health Policy Res. 2011;(PB2011-2):1-8.
9. Henry J, McNab W. Forever young: a health promotion focus on sexuality and aging. Gerontol Geriatr Education. 2003;23:57-74.
10. Gott M, Hinchliff S, Galena E. General practitioner attitudes to discussing sexual health issues with older people. Soc Sci Med. 2004;58:2093-2103.
11. Nusbaum MR, Hamilton CD. The proactive sexual health history. Am Fam Physician. 2002;66:1705-1712.
12. Burd ID, Nevadunsky N, Bachmann G. Impact of physician gender on sexual history taking in a multispecialty practice. J Sex Med. 2006;3:194-200.
13. Kazer MW. Sexuality Assessment for Older Adults. Hartford Institute for Geriatric Nursing Web site. Available at: http://consultgerirn.org/uploads/File/trythis/try_this_10.pdf. Updated 2012. Accessed March 14, 2014.
14. Wallace MA. Assessment of sexual health in older adults. Am J Nursing. 2012;108:52-60.
15. Sexuality in later life. National Institute on Aging Web site. Available at: http://www.nia.nih.gov/health/publication/sexualitylater-life. Updated March 11, 2014. Accessed March 21, 2014.
16. Hajjar RR, Kamel HK. Sexuality in the nursing home, part 1: attitudes and barriers to sexual expression. J Am Med Dir Assoc. 2004;5(2 suppl):S42-S47.
17. Bildtgård T. The sexuality of elderly people on film—visual limitations. J Aging Identity. 2000;5:169-183.
18. Moreira ED Jr, Brock G, Glasser DB, et al; GSSAB Investigators’ Group. Help-seeking behaviour for sexual problems: the global study of sexual attitudes and behaviors. Int J Clin Pract. 2005;59:6-16.
19. Gott M, Hinchliff S. Barriers to seeking treatment for sexual problems in primary care: a qualitative study with older people. Fam Pract. 2003;20:690-695.
20. Politi MC, Clark MA, Armstrong G, et al. Patient-provider communication about sexual health among unmarried middle-aged and older women. J Gen Intern Med. 2009;24:511-516.
21. Bouman W, Arcelus J, Benbow S. Nottingham study of sexuality & ageing (NoSSA I). Attitudes regarding sexuality and older people: a review of the literature. Sex Relationship Ther. 2006;21:149-161.
22. Low LPL, Lui MHL, Lee DTF, et al. Promoting awareness of sexuality of older people in residential care. Electronic J Human Sexuality. 2005;8:8-16.
23. Rheaume C, Mitty E. Sexuality and intimacy in older adults. Geriatr Nurs. 2008;29:342-349.
24. Nagaratnam N, Gayagay G Jr. Hypersexuality in nursing care facilities—a descriptive study. Arch Gerontol Geriatr. 2002;35:195-203.
25. HIV among older Americans. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/hiv/risk/age/olderamericans/. Updated December 23, 2013. Accessed February 28, 2014.
26. Nguyen N, Holodniy M. HIV infection in the elderly. Clin Interv Aging. 2008;3:453-472.
27. Jena AB, Goldman DP, Kamdar A, et al. Sexually transmitted diseases among users of erectile dysfunction drugs: analysis of claims data. Ann Intern Med. 2010;153:1-7.
How do hydrochlorothiazide and chlorthalidone compare for treating hypertension?
Both medications reduce theincidence of cardiovascular events in patients with hypertension, but chlorthalidone may confer additional cardiovascular risk reduction (strength of recommendation [SOR]: B, conflicting network meta-analysis and cohort studies). (No head-to-head studies of hydrochlorothiazide [HCTZ] and chlorthalidone have been done.)
Serious hypokalemia and hyponatremia can occur with either medication; it is unclear if the rates of these adverse effects are the same at equivalent doses. Patients taking chlorthalidone are less likely to need a second antihypertensive medication but more likely to be nonadherent than patients taking HCTZ (SOR: B, cohort studies).
EVIDENCE SUMMARY
A network meta-analysis—designed to compare 2 interventions that haven’t been studied head-to-head—examined 9 trials that evaluated cardiovascular outcomes in 18,000 patients taking HCTZ and 60,000 patients taking chlorthalidone against outcomes for placebo or other antihypertensive agents.1 Daily doses ranged from 12.5 to 25 mg for HCTZ and 12.5 to 100 mg for chlorthalidone (although most patients taking chlorthalidone were on 12.5-25 mg).
In a drug-adjusted analysis using shared comparator medications, chlorthalidone proved superior to HCTZ in reducing the risk of both heart failure (relative risk [RR]=0.77; 95% confidence interval [CI], 0.61-0.98) and combined cardiovascular events—myocardial infarction (MI), stroke, a new diagnosis of coronary artery disease, and new-onset congestive heart failure (RR=0.79; 95% CI, 0.72-0.88).
After adjusting for achieved blood pressure, chlorthalidone was still associated with lower rates of cardiovascular events than HCTZ (RR=0.82; 95% CI, 0.70-0.97). Relative to HCTZ, the number needed to treat with chlorthalidone to prevent 1 additional cardiovascular event over 5 years was 27. Because network meta-analyses draw from a wider body of research than standard meta-analyses, they may be weakened by increased variability in study design and patient demographics.
But another study shows no significant difference in cardiovascular outcomes
A subsequent retrospective cohort study didn’t find a significant difference in cardiovascular outcomes between HCTZ and chlorthalidone. The study compared pooled cardiovascular outcomes (MI, heart failure, and stroke) in 10,400 patients recently started on chlorthalidone and 19,500 started on HCTZ.2 Initial doses were typically either 25 mg chlorthalidone (70% of patients on chlorthalidone) or 12.5 mg HCTZ (67% of patients on HCTZ). The median follow-up was about a year, but lasted as long as 5 years in some cases.
The 2 groups showed no significant difference in cardiovascular events (3.2 events per 100 person-years for chlorthalidone compared with 3.4 for HCTZ; adjusted hazard ratio [aHR]=0.93; 95% CI, 0.81-1.06).
Serious hypokalemia and hyponatremia are risks
Patients taking chlorthalidone were more likely to be hospitalized for hypokalemia (0.69 per 100 person-years vs 0.27 for HCTZ; aHR=3.1; 95% CI, 2.0-4.6; number needed to harm [NNH]=238 in 1 year) or hyponatremia (0.69 per 100 person-years vs 0.49 for HCTZ; aHR=1.7; 95% CI, 1.2-2.3; NNH=434 in 1 year).2 However, the all-cause hospitalization rates for the 2 drugs were the same (aHR=1.0; 95% CI, 0.93-1.07).
Lower systolic BP and serum potassium found with chlorthalidone
A smaller retrospective cohort analysis (6441 participants who received either chlorthalidone or HCTZ starting at 50 mg and stepped once to 100 mg) also assessed the difference in cardiovascular events between patients taking the 2 drugs.3 (Cardiovascular events were defined as pooled MIs, onset of angina or peripheral artery occlusive disease, or need for coronary artery bypass.) Although significant reductions in pooled events occurred in both groups over the 7-year study, these reductions were significantly lower in the chlorthalidone group than in the HCTZ group (aHR=0.79; 95% CI, 0.68-0.92).
Systolic blood pressures were statistically lower in the chlorthalidone group during Years 1 through 5 but not in Years 6 and 7 (difference 2-4 mm Hg). Serum potassium was also lower in patients taking chlorthalidone (3.8 mEq/L on chlorthalidone vs 4.0 mEq/L on HCTZ after 7 years; P<.05).
Chlorthalidone users more responsive, but less adherent than HCTZ users
A retrospective cohort study investigated medication tolerance in veterans who had recently started either HCTZ (120,000 patients) or chlorthalidone (2200 patients) and were followed for a year.4 Most received doses between 12.5 and 25 mg of active drug.
One primary outcome was “nonpersistence,” defined as failure to refill the medication after double the number of days as the initial prescription. The other was “insufficient response,” defined as the need to start another antihypertensive medication. Chlorthalidone users were less likely than HCTZ users to have an insufficient response (odds ratio [OR]=0.71; 95% CI, 0.63-0.80) but more likely to exhibit nonpersistence (OR=1.6; 95% CI, 1.5-1.8).
RECOMMENDATIONS
For primary hypertension, the United Kingdom’s National Institute for Health and Care Excellence (NICE) recommends diuretic monotherapy in patients older than 55 years who are poor candidates for calcium channel blockers.5 If a diuretic is to be initiated or changed, NICE recommends chlorthalidone (12.5-25 mg daily) or indapamide (1.5-2.5 mg daily) in preference to HCTZ. The guideline set forth in the eighth annual report of the United States Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure makes no distinction between chlorthalidone and HCTZ; it refers only to “thiazidetype diuretics.” Thiazide-type diuretics are listed as one option (along with angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and calcium channel blockers) for initial monotherapy in nonblack patients.6
1. Roush GC, Holford TR, Guddati AK. Chlorthalidone compared with hydrochlorothiazide in reducing cardiovascular events: systematic review and network meta-analyses. Hypertension. 2012;59:1110–1117.
2. Dhalla IA, Gomes T, Yao Z, et al. Chlorthalidone versus hydrochlorothiazide for the treatment of hypertension in older adults: a population-based cohort study. Ann Intern Med. 2013;158:447–455.
3. Dorsh MP, Gillespie BW, Erickson SR, et al. Chlorthalidone reduces cardiovascular events compared with hydrochlorothiazide: a retrospective cohort analysis. Hypertension. 2011;57:689–694.
4. Lund BC, Ernst ME. The comparative effectiveness of hydrochlorothiazide and chlorthalidone in an observational cohort of veterans. J Clin Hypertension. 2012;14:623–629.
5. Hypertension: clinical management of primary hypertension in adults. (NICE Clinical Guideline 127). National Institute for Health and Care Excellence Web site. London, UK: National Institute for Health and Care Excellence; 2011. Available at: www.nice.org.UK/guidance/CG127. Accessed December 16, 2013.
6. James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC8). JAMA. 2014;311:507-520.
Both medications reduce theincidence of cardiovascular events in patients with hypertension, but chlorthalidone may confer additional cardiovascular risk reduction (strength of recommendation [SOR]: B, conflicting network meta-analysis and cohort studies). (No head-to-head studies of hydrochlorothiazide [HCTZ] and chlorthalidone have been done.)
Serious hypokalemia and hyponatremia can occur with either medication; it is unclear if the rates of these adverse effects are the same at equivalent doses. Patients taking chlorthalidone are less likely to need a second antihypertensive medication but more likely to be nonadherent than patients taking HCTZ (SOR: B, cohort studies).
EVIDENCE SUMMARY
A network meta-analysis—designed to compare 2 interventions that haven’t been studied head-to-head—examined 9 trials that evaluated cardiovascular outcomes in 18,000 patients taking HCTZ and 60,000 patients taking chlorthalidone against outcomes for placebo or other antihypertensive agents.1 Daily doses ranged from 12.5 to 25 mg for HCTZ and 12.5 to 100 mg for chlorthalidone (although most patients taking chlorthalidone were on 12.5-25 mg).
In a drug-adjusted analysis using shared comparator medications, chlorthalidone proved superior to HCTZ in reducing the risk of both heart failure (relative risk [RR]=0.77; 95% confidence interval [CI], 0.61-0.98) and combined cardiovascular events—myocardial infarction (MI), stroke, a new diagnosis of coronary artery disease, and new-onset congestive heart failure (RR=0.79; 95% CI, 0.72-0.88).
After adjusting for achieved blood pressure, chlorthalidone was still associated with lower rates of cardiovascular events than HCTZ (RR=0.82; 95% CI, 0.70-0.97). Relative to HCTZ, the number needed to treat with chlorthalidone to prevent 1 additional cardiovascular event over 5 years was 27. Because network meta-analyses draw from a wider body of research than standard meta-analyses, they may be weakened by increased variability in study design and patient demographics.
But another study shows no significant difference in cardiovascular outcomes
A subsequent retrospective cohort study didn’t find a significant difference in cardiovascular outcomes between HCTZ and chlorthalidone. The study compared pooled cardiovascular outcomes (MI, heart failure, and stroke) in 10,400 patients recently started on chlorthalidone and 19,500 started on HCTZ.2 Initial doses were typically either 25 mg chlorthalidone (70% of patients on chlorthalidone) or 12.5 mg HCTZ (67% of patients on HCTZ). The median follow-up was about a year, but lasted as long as 5 years in some cases.
The 2 groups showed no significant difference in cardiovascular events (3.2 events per 100 person-years for chlorthalidone compared with 3.4 for HCTZ; adjusted hazard ratio [aHR]=0.93; 95% CI, 0.81-1.06).
Serious hypokalemia and hyponatremia are risks
Patients taking chlorthalidone were more likely to be hospitalized for hypokalemia (0.69 per 100 person-years vs 0.27 for HCTZ; aHR=3.1; 95% CI, 2.0-4.6; number needed to harm [NNH]=238 in 1 year) or hyponatremia (0.69 per 100 person-years vs 0.49 for HCTZ; aHR=1.7; 95% CI, 1.2-2.3; NNH=434 in 1 year).2 However, the all-cause hospitalization rates for the 2 drugs were the same (aHR=1.0; 95% CI, 0.93-1.07).
Lower systolic BP and serum potassium found with chlorthalidone
A smaller retrospective cohort analysis (6441 participants who received either chlorthalidone or HCTZ starting at 50 mg and stepped once to 100 mg) also assessed the difference in cardiovascular events between patients taking the 2 drugs.3 (Cardiovascular events were defined as pooled MIs, onset of angina or peripheral artery occlusive disease, or need for coronary artery bypass.) Although significant reductions in pooled events occurred in both groups over the 7-year study, these reductions were significantly lower in the chlorthalidone group than in the HCTZ group (aHR=0.79; 95% CI, 0.68-0.92).
Systolic blood pressures were statistically lower in the chlorthalidone group during Years 1 through 5 but not in Years 6 and 7 (difference 2-4 mm Hg). Serum potassium was also lower in patients taking chlorthalidone (3.8 mEq/L on chlorthalidone vs 4.0 mEq/L on HCTZ after 7 years; P<.05).
Chlorthalidone users more responsive, but less adherent than HCTZ users
A retrospective cohort study investigated medication tolerance in veterans who had recently started either HCTZ (120,000 patients) or chlorthalidone (2200 patients) and were followed for a year.4 Most received doses between 12.5 and 25 mg of active drug.
One primary outcome was “nonpersistence,” defined as failure to refill the medication after double the number of days as the initial prescription. The other was “insufficient response,” defined as the need to start another antihypertensive medication. Chlorthalidone users were less likely than HCTZ users to have an insufficient response (odds ratio [OR]=0.71; 95% CI, 0.63-0.80) but more likely to exhibit nonpersistence (OR=1.6; 95% CI, 1.5-1.8).
RECOMMENDATIONS
For primary hypertension, the United Kingdom’s National Institute for Health and Care Excellence (NICE) recommends diuretic monotherapy in patients older than 55 years who are poor candidates for calcium channel blockers.5 If a diuretic is to be initiated or changed, NICE recommends chlorthalidone (12.5-25 mg daily) or indapamide (1.5-2.5 mg daily) in preference to HCTZ. The guideline set forth in the eighth annual report of the United States Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure makes no distinction between chlorthalidone and HCTZ; it refers only to “thiazidetype diuretics.” Thiazide-type diuretics are listed as one option (along with angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and calcium channel blockers) for initial monotherapy in nonblack patients.6
Both medications reduce theincidence of cardiovascular events in patients with hypertension, but chlorthalidone may confer additional cardiovascular risk reduction (strength of recommendation [SOR]: B, conflicting network meta-analysis and cohort studies). (No head-to-head studies of hydrochlorothiazide [HCTZ] and chlorthalidone have been done.)
Serious hypokalemia and hyponatremia can occur with either medication; it is unclear if the rates of these adverse effects are the same at equivalent doses. Patients taking chlorthalidone are less likely to need a second antihypertensive medication but more likely to be nonadherent than patients taking HCTZ (SOR: B, cohort studies).
EVIDENCE SUMMARY
A network meta-analysis—designed to compare 2 interventions that haven’t been studied head-to-head—examined 9 trials that evaluated cardiovascular outcomes in 18,000 patients taking HCTZ and 60,000 patients taking chlorthalidone against outcomes for placebo or other antihypertensive agents.1 Daily doses ranged from 12.5 to 25 mg for HCTZ and 12.5 to 100 mg for chlorthalidone (although most patients taking chlorthalidone were on 12.5-25 mg).
In a drug-adjusted analysis using shared comparator medications, chlorthalidone proved superior to HCTZ in reducing the risk of both heart failure (relative risk [RR]=0.77; 95% confidence interval [CI], 0.61-0.98) and combined cardiovascular events—myocardial infarction (MI), stroke, a new diagnosis of coronary artery disease, and new-onset congestive heart failure (RR=0.79; 95% CI, 0.72-0.88).
After adjusting for achieved blood pressure, chlorthalidone was still associated with lower rates of cardiovascular events than HCTZ (RR=0.82; 95% CI, 0.70-0.97). Relative to HCTZ, the number needed to treat with chlorthalidone to prevent 1 additional cardiovascular event over 5 years was 27. Because network meta-analyses draw from a wider body of research than standard meta-analyses, they may be weakened by increased variability in study design and patient demographics.
But another study shows no significant difference in cardiovascular outcomes
A subsequent retrospective cohort study didn’t find a significant difference in cardiovascular outcomes between HCTZ and chlorthalidone. The study compared pooled cardiovascular outcomes (MI, heart failure, and stroke) in 10,400 patients recently started on chlorthalidone and 19,500 started on HCTZ.2 Initial doses were typically either 25 mg chlorthalidone (70% of patients on chlorthalidone) or 12.5 mg HCTZ (67% of patients on HCTZ). The median follow-up was about a year, but lasted as long as 5 years in some cases.
The 2 groups showed no significant difference in cardiovascular events (3.2 events per 100 person-years for chlorthalidone compared with 3.4 for HCTZ; adjusted hazard ratio [aHR]=0.93; 95% CI, 0.81-1.06).
Serious hypokalemia and hyponatremia are risks
Patients taking chlorthalidone were more likely to be hospitalized for hypokalemia (0.69 per 100 person-years vs 0.27 for HCTZ; aHR=3.1; 95% CI, 2.0-4.6; number needed to harm [NNH]=238 in 1 year) or hyponatremia (0.69 per 100 person-years vs 0.49 for HCTZ; aHR=1.7; 95% CI, 1.2-2.3; NNH=434 in 1 year).2 However, the all-cause hospitalization rates for the 2 drugs were the same (aHR=1.0; 95% CI, 0.93-1.07).
Lower systolic BP and serum potassium found with chlorthalidone
A smaller retrospective cohort analysis (6441 participants who received either chlorthalidone or HCTZ starting at 50 mg and stepped once to 100 mg) also assessed the difference in cardiovascular events between patients taking the 2 drugs.3 (Cardiovascular events were defined as pooled MIs, onset of angina or peripheral artery occlusive disease, or need for coronary artery bypass.) Although significant reductions in pooled events occurred in both groups over the 7-year study, these reductions were significantly lower in the chlorthalidone group than in the HCTZ group (aHR=0.79; 95% CI, 0.68-0.92).
Systolic blood pressures were statistically lower in the chlorthalidone group during Years 1 through 5 but not in Years 6 and 7 (difference 2-4 mm Hg). Serum potassium was also lower in patients taking chlorthalidone (3.8 mEq/L on chlorthalidone vs 4.0 mEq/L on HCTZ after 7 years; P<.05).
Chlorthalidone users more responsive, but less adherent than HCTZ users
A retrospective cohort study investigated medication tolerance in veterans who had recently started either HCTZ (120,000 patients) or chlorthalidone (2200 patients) and were followed for a year.4 Most received doses between 12.5 and 25 mg of active drug.
One primary outcome was “nonpersistence,” defined as failure to refill the medication after double the number of days as the initial prescription. The other was “insufficient response,” defined as the need to start another antihypertensive medication. Chlorthalidone users were less likely than HCTZ users to have an insufficient response (odds ratio [OR]=0.71; 95% CI, 0.63-0.80) but more likely to exhibit nonpersistence (OR=1.6; 95% CI, 1.5-1.8).
RECOMMENDATIONS
For primary hypertension, the United Kingdom’s National Institute for Health and Care Excellence (NICE) recommends diuretic monotherapy in patients older than 55 years who are poor candidates for calcium channel blockers.5 If a diuretic is to be initiated or changed, NICE recommends chlorthalidone (12.5-25 mg daily) or indapamide (1.5-2.5 mg daily) in preference to HCTZ. The guideline set forth in the eighth annual report of the United States Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure makes no distinction between chlorthalidone and HCTZ; it refers only to “thiazidetype diuretics.” Thiazide-type diuretics are listed as one option (along with angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and calcium channel blockers) for initial monotherapy in nonblack patients.6
1. Roush GC, Holford TR, Guddati AK. Chlorthalidone compared with hydrochlorothiazide in reducing cardiovascular events: systematic review and network meta-analyses. Hypertension. 2012;59:1110–1117.
2. Dhalla IA, Gomes T, Yao Z, et al. Chlorthalidone versus hydrochlorothiazide for the treatment of hypertension in older adults: a population-based cohort study. Ann Intern Med. 2013;158:447–455.
3. Dorsh MP, Gillespie BW, Erickson SR, et al. Chlorthalidone reduces cardiovascular events compared with hydrochlorothiazide: a retrospective cohort analysis. Hypertension. 2011;57:689–694.
4. Lund BC, Ernst ME. The comparative effectiveness of hydrochlorothiazide and chlorthalidone in an observational cohort of veterans. J Clin Hypertension. 2012;14:623–629.
5. Hypertension: clinical management of primary hypertension in adults. (NICE Clinical Guideline 127). National Institute for Health and Care Excellence Web site. London, UK: National Institute for Health and Care Excellence; 2011. Available at: www.nice.org.UK/guidance/CG127. Accessed December 16, 2013.
6. James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC8). JAMA. 2014;311:507-520.
1. Roush GC, Holford TR, Guddati AK. Chlorthalidone compared with hydrochlorothiazide in reducing cardiovascular events: systematic review and network meta-analyses. Hypertension. 2012;59:1110–1117.
2. Dhalla IA, Gomes T, Yao Z, et al. Chlorthalidone versus hydrochlorothiazide for the treatment of hypertension in older adults: a population-based cohort study. Ann Intern Med. 2013;158:447–455.
3. Dorsh MP, Gillespie BW, Erickson SR, et al. Chlorthalidone reduces cardiovascular events compared with hydrochlorothiazide: a retrospective cohort analysis. Hypertension. 2011;57:689–694.
4. Lund BC, Ernst ME. The comparative effectiveness of hydrochlorothiazide and chlorthalidone in an observational cohort of veterans. J Clin Hypertension. 2012;14:623–629.
5. Hypertension: clinical management of primary hypertension in adults. (NICE Clinical Guideline 127). National Institute for Health and Care Excellence Web site. London, UK: National Institute for Health and Care Excellence; 2011. Available at: www.nice.org.UK/guidance/CG127. Accessed December 16, 2013.
6. James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC8). JAMA. 2014;311:507-520.
Evidence-based answers from the Family Physicians Inquiries Network
Which prophylactic therapies best prevent gout attacks?
Allopurinol and febuxostat reduce the frequency of gout attacks equally after 8 weeks of treatment (strength of recommendation [SOR]: B, multiple randomized control trials [RCTs] with limitations).
Intravenous pegloticase decreases serum uric acid and gout attacks and improves quality of life (QOL) (SOR: A, 2 RCTs).
Colchicine reduces gout attacks when combined with probenecid or allopurinol at the start of urate-lowering therapy (SOR: B, 1 high-quality and 1 low-quality RCT).
EVIDENCE SUMMARY
A 28-week RCT compared the effects of placebo, allopurinol (300 mg/d), and febuxostat (80 mg, 120 mg, and 240 mg) on serum uric acid levels (sUA) and gout attacks in 1067 patients with gout and hyperuricemia (94% male, 78% white, 18 to 85 years of age with mean age ranging from 51 to 54 years ± 12 years in each group).1 Patients also received prophylaxis with either colchicine or naproxen during the first 8 weeks of the study.
During Weeks 1 through 8, investigators found no statistically significant differences in the percentage of patients requiring treatment for gout attacks between the febuxostat 80 mg, allopurinol, and placebo groups (28%, 23%, and 20%, respectively). During Weeks 8 through 28, no statistically significant differences in gout attack rates occurred between the allopurinol and febuxostat groups, although the study didn’t report specific attack rates for this period.
Both allopurinol and all doses of febuxostat reduced sUA to <6 mg/dL more effectively than placebo; more patients treated with febuxostat than allopurinol achieved a uric acid level of less than <6 mg/dL.
Another RCT of 762 mostly white, male patients (mean age 52 years) with gout and sUA >8 mg/dL—35% of whom had renal impairment, defined as creatinine clearance <80 mL/min/1.73m2—also concluded that febuxostat and allopurinol are equally effective in reducing gout attacks (incidence of gout flares during Weeks 9 to 52 was 64% with both febuxostat 80 mg and allopurinol 300 mg).2 The percentage of patients with sUA <6 mg/dL at the last 3 monthly visits was 53% in the febuxostat 80 mg group compared with 21% in the allopurinol 300 mg group (P<.001; number needed to treat [NNT]=4]).
One significant limitation of both RCTs was the fixed dose of allopurinol (300 mg/d). US Food and Drug Administration-approved dosing for allopurinol allows for titration to a maximum of 800 mg/d to achieve serum uric acid <6 mg/dL.
IV pegloticase decreases gout attacks after 3 months, improves quality of life
Pegloticase is an intravenously administered, recombinant form of uricase, the natural enzyme that converts uric acid to more soluble allantoin. Two RCTs compared pegloticase with placebo in a total of 212 patients with gout (mean age 54 to 59 years; 70% to 90% male) intolerant or refractory to allopurinol (defined as baseline sUA of ≥8 mg/dL and at least one of the following: ≥3 self-reported gout flares during the previous 18 months, ≥1 tophi, or gouty arthropathy.
These trials found that treatment with 8 mg of pegloticase every 2 weeks for 6 months initially increased gout flares during Months 1 to 3 (75% with pegloticase, 53% with placebo; P=.02; number needed to harm [NNH]=5) but then decreased the incidence of acute gout attacks during Months 4 to 6 (41% with pegloticase, 67% with placebo; P=.007; NNT=4).3 In addition, pegloticase resulted in statistically significant improvements in QOL measured at the final visit using the Health Assessment Questionnaire (HAQ) pain scale, the HAQ-Disability Index, and the 36-item Short Form Health Survey.
Colchicine plus probenecid or allopurinol reduces gout attacks
One small, low-quality RCT (N=38) found that colchicine 0.5 mg administered 3 times daily effectively prevented gout attacks when administered concomitantly with probenecid initiated to lower urate (gout attacks per month in colchicine and placebo-treated patients, respectively, were 0.19±0.05 and 0.48±0.12; P<.05).4
Another RCT that compared allopurinol with and without colchicine showed that coadministration of colchicine 0.6 mg twice daily reduced gout attacks: 33% of patients treated with colchicine experienced a gout flare compared with 77% of placebo-treated patients (P=.008; NNT=3 over 6 months).5
We identified no RCTs that evaluated the uricosuric agent probenecid and no studies that assessed the use of nonsteroidal anti-inflammatory drugs (NSAIDs) to prevent recurrent gout attacks.
RECOMMENDATIONS
The American College of Rheumatology (ACR) guidelines on managing gout recommend allopurinol or febuxostat as first-line pharmacologic urate-lowering therapy, with a goal of reducing sUA to <6 mg/dL. They recommend probenecid as an alternative if contraindications exist or the patient is intolerant to allopurinol and febuxostat.6 The guidelines note that allopurinol doses may exceed 300 mg/d, even in patients with chronic kidney disease.
The ACR recommends anti-inflammatory prophylaxis with colchicine or NSAIDs upon initiation of urate-lowering therapy. Anti-inflammatory prophylaxis should be continued as long as clinical evidence of continuing gout disease exists and until the sUA target has been acheived.7
1. Schumacher HR Jr, Becker MA, Wortmann RL, et al. Effects of febuxostat versus allopurinol and placebo in reducing serum urate in subjects with hyperuricemia and gout: a 28-week, phase III, randomized, double-blind, parallel-group trial. Arthritis Rheum. 2008;59:1540-1548.
2. Becker MA, Schumacher HR Jr, Wortmann RL, et al. Febuxostat compared with allopurinol in patients with hyperuricemia and gout. N Engl J Med. 2005;353:2450-2461.
3. Sundy JS, Baraf HSB, Yood RA, et al. Efficacy and tolerability of pegloticase for the treatment of chronic gout in patients refractory to conventional treatment: two randomized controlled trials. JAMA. 2011;306:711-720.
4. Paulus HE, Schlosstein LH, Godfrey RG, et al. Prophylactic colchicine therapy of intercritical gout: a placebo-controlled study of probenecid-treated patients. Arthritis Rheum. 1974;17:609-614.
5. Borstad GC, Bryant LR, Abel MP, et al. Colchicine for prophylaxis of acute flares when initiating allopurinol for chronic gouty arthritis. J Rheumatol. 2004;31:2429-2432.
6. Khanna D, Fitzgerald JD, Khanna PP, et al; American College of Rheumatology. 2012 American College of Rheumatology guidelines for management of gout. Part 1: systematic nonpharmacologic and pharmacologic therapeutic approaches to hyperuricemia. Arthritis Care Res (Hoboken). 2012;64:1431-1446.
7. Khanna D, Khanna PP, Fitzgerald JD, et al; American College of Rheumatology. 2012 American College of Rheumatology guidelines for management of gout. Part 2: therapy and anti-inflammatory prophylaxis of acute gouty arthritis. Arthritis Care Res (Hoboken). 2012;64:1447-1461.
Allopurinol and febuxostat reduce the frequency of gout attacks equally after 8 weeks of treatment (strength of recommendation [SOR]: B, multiple randomized control trials [RCTs] with limitations).
Intravenous pegloticase decreases serum uric acid and gout attacks and improves quality of life (QOL) (SOR: A, 2 RCTs).
Colchicine reduces gout attacks when combined with probenecid or allopurinol at the start of urate-lowering therapy (SOR: B, 1 high-quality and 1 low-quality RCT).
EVIDENCE SUMMARY
A 28-week RCT compared the effects of placebo, allopurinol (300 mg/d), and febuxostat (80 mg, 120 mg, and 240 mg) on serum uric acid levels (sUA) and gout attacks in 1067 patients with gout and hyperuricemia (94% male, 78% white, 18 to 85 years of age with mean age ranging from 51 to 54 years ± 12 years in each group).1 Patients also received prophylaxis with either colchicine or naproxen during the first 8 weeks of the study.
During Weeks 1 through 8, investigators found no statistically significant differences in the percentage of patients requiring treatment for gout attacks between the febuxostat 80 mg, allopurinol, and placebo groups (28%, 23%, and 20%, respectively). During Weeks 8 through 28, no statistically significant differences in gout attack rates occurred between the allopurinol and febuxostat groups, although the study didn’t report specific attack rates for this period.
Both allopurinol and all doses of febuxostat reduced sUA to <6 mg/dL more effectively than placebo; more patients treated with febuxostat than allopurinol achieved a uric acid level of less than <6 mg/dL.
Another RCT of 762 mostly white, male patients (mean age 52 years) with gout and sUA >8 mg/dL—35% of whom had renal impairment, defined as creatinine clearance <80 mL/min/1.73m2—also concluded that febuxostat and allopurinol are equally effective in reducing gout attacks (incidence of gout flares during Weeks 9 to 52 was 64% with both febuxostat 80 mg and allopurinol 300 mg).2 The percentage of patients with sUA <6 mg/dL at the last 3 monthly visits was 53% in the febuxostat 80 mg group compared with 21% in the allopurinol 300 mg group (P<.001; number needed to treat [NNT]=4]).
One significant limitation of both RCTs was the fixed dose of allopurinol (300 mg/d). US Food and Drug Administration-approved dosing for allopurinol allows for titration to a maximum of 800 mg/d to achieve serum uric acid <6 mg/dL.
IV pegloticase decreases gout attacks after 3 months, improves quality of life
Pegloticase is an intravenously administered, recombinant form of uricase, the natural enzyme that converts uric acid to more soluble allantoin. Two RCTs compared pegloticase with placebo in a total of 212 patients with gout (mean age 54 to 59 years; 70% to 90% male) intolerant or refractory to allopurinol (defined as baseline sUA of ≥8 mg/dL and at least one of the following: ≥3 self-reported gout flares during the previous 18 months, ≥1 tophi, or gouty arthropathy.
These trials found that treatment with 8 mg of pegloticase every 2 weeks for 6 months initially increased gout flares during Months 1 to 3 (75% with pegloticase, 53% with placebo; P=.02; number needed to harm [NNH]=5) but then decreased the incidence of acute gout attacks during Months 4 to 6 (41% with pegloticase, 67% with placebo; P=.007; NNT=4).3 In addition, pegloticase resulted in statistically significant improvements in QOL measured at the final visit using the Health Assessment Questionnaire (HAQ) pain scale, the HAQ-Disability Index, and the 36-item Short Form Health Survey.
Colchicine plus probenecid or allopurinol reduces gout attacks
One small, low-quality RCT (N=38) found that colchicine 0.5 mg administered 3 times daily effectively prevented gout attacks when administered concomitantly with probenecid initiated to lower urate (gout attacks per month in colchicine and placebo-treated patients, respectively, were 0.19±0.05 and 0.48±0.12; P<.05).4
Another RCT that compared allopurinol with and without colchicine showed that coadministration of colchicine 0.6 mg twice daily reduced gout attacks: 33% of patients treated with colchicine experienced a gout flare compared with 77% of placebo-treated patients (P=.008; NNT=3 over 6 months).5
We identified no RCTs that evaluated the uricosuric agent probenecid and no studies that assessed the use of nonsteroidal anti-inflammatory drugs (NSAIDs) to prevent recurrent gout attacks.
RECOMMENDATIONS
The American College of Rheumatology (ACR) guidelines on managing gout recommend allopurinol or febuxostat as first-line pharmacologic urate-lowering therapy, with a goal of reducing sUA to <6 mg/dL. They recommend probenecid as an alternative if contraindications exist or the patient is intolerant to allopurinol and febuxostat.6 The guidelines note that allopurinol doses may exceed 300 mg/d, even in patients with chronic kidney disease.
The ACR recommends anti-inflammatory prophylaxis with colchicine or NSAIDs upon initiation of urate-lowering therapy. Anti-inflammatory prophylaxis should be continued as long as clinical evidence of continuing gout disease exists and until the sUA target has been acheived.7
Allopurinol and febuxostat reduce the frequency of gout attacks equally after 8 weeks of treatment (strength of recommendation [SOR]: B, multiple randomized control trials [RCTs] with limitations).
Intravenous pegloticase decreases serum uric acid and gout attacks and improves quality of life (QOL) (SOR: A, 2 RCTs).
Colchicine reduces gout attacks when combined with probenecid or allopurinol at the start of urate-lowering therapy (SOR: B, 1 high-quality and 1 low-quality RCT).
EVIDENCE SUMMARY
A 28-week RCT compared the effects of placebo, allopurinol (300 mg/d), and febuxostat (80 mg, 120 mg, and 240 mg) on serum uric acid levels (sUA) and gout attacks in 1067 patients with gout and hyperuricemia (94% male, 78% white, 18 to 85 years of age with mean age ranging from 51 to 54 years ± 12 years in each group).1 Patients also received prophylaxis with either colchicine or naproxen during the first 8 weeks of the study.
During Weeks 1 through 8, investigators found no statistically significant differences in the percentage of patients requiring treatment for gout attacks between the febuxostat 80 mg, allopurinol, and placebo groups (28%, 23%, and 20%, respectively). During Weeks 8 through 28, no statistically significant differences in gout attack rates occurred between the allopurinol and febuxostat groups, although the study didn’t report specific attack rates for this period.
Both allopurinol and all doses of febuxostat reduced sUA to <6 mg/dL more effectively than placebo; more patients treated with febuxostat than allopurinol achieved a uric acid level of less than <6 mg/dL.
Another RCT of 762 mostly white, male patients (mean age 52 years) with gout and sUA >8 mg/dL—35% of whom had renal impairment, defined as creatinine clearance <80 mL/min/1.73m2—also concluded that febuxostat and allopurinol are equally effective in reducing gout attacks (incidence of gout flares during Weeks 9 to 52 was 64% with both febuxostat 80 mg and allopurinol 300 mg).2 The percentage of patients with sUA <6 mg/dL at the last 3 monthly visits was 53% in the febuxostat 80 mg group compared with 21% in the allopurinol 300 mg group (P<.001; number needed to treat [NNT]=4]).
One significant limitation of both RCTs was the fixed dose of allopurinol (300 mg/d). US Food and Drug Administration-approved dosing for allopurinol allows for titration to a maximum of 800 mg/d to achieve serum uric acid <6 mg/dL.
IV pegloticase decreases gout attacks after 3 months, improves quality of life
Pegloticase is an intravenously administered, recombinant form of uricase, the natural enzyme that converts uric acid to more soluble allantoin. Two RCTs compared pegloticase with placebo in a total of 212 patients with gout (mean age 54 to 59 years; 70% to 90% male) intolerant or refractory to allopurinol (defined as baseline sUA of ≥8 mg/dL and at least one of the following: ≥3 self-reported gout flares during the previous 18 months, ≥1 tophi, or gouty arthropathy.
These trials found that treatment with 8 mg of pegloticase every 2 weeks for 6 months initially increased gout flares during Months 1 to 3 (75% with pegloticase, 53% with placebo; P=.02; number needed to harm [NNH]=5) but then decreased the incidence of acute gout attacks during Months 4 to 6 (41% with pegloticase, 67% with placebo; P=.007; NNT=4).3 In addition, pegloticase resulted in statistically significant improvements in QOL measured at the final visit using the Health Assessment Questionnaire (HAQ) pain scale, the HAQ-Disability Index, and the 36-item Short Form Health Survey.
Colchicine plus probenecid or allopurinol reduces gout attacks
One small, low-quality RCT (N=38) found that colchicine 0.5 mg administered 3 times daily effectively prevented gout attacks when administered concomitantly with probenecid initiated to lower urate (gout attacks per month in colchicine and placebo-treated patients, respectively, were 0.19±0.05 and 0.48±0.12; P<.05).4
Another RCT that compared allopurinol with and without colchicine showed that coadministration of colchicine 0.6 mg twice daily reduced gout attacks: 33% of patients treated with colchicine experienced a gout flare compared with 77% of placebo-treated patients (P=.008; NNT=3 over 6 months).5
We identified no RCTs that evaluated the uricosuric agent probenecid and no studies that assessed the use of nonsteroidal anti-inflammatory drugs (NSAIDs) to prevent recurrent gout attacks.
RECOMMENDATIONS
The American College of Rheumatology (ACR) guidelines on managing gout recommend allopurinol or febuxostat as first-line pharmacologic urate-lowering therapy, with a goal of reducing sUA to <6 mg/dL. They recommend probenecid as an alternative if contraindications exist or the patient is intolerant to allopurinol and febuxostat.6 The guidelines note that allopurinol doses may exceed 300 mg/d, even in patients with chronic kidney disease.
The ACR recommends anti-inflammatory prophylaxis with colchicine or NSAIDs upon initiation of urate-lowering therapy. Anti-inflammatory prophylaxis should be continued as long as clinical evidence of continuing gout disease exists and until the sUA target has been acheived.7
1. Schumacher HR Jr, Becker MA, Wortmann RL, et al. Effects of febuxostat versus allopurinol and placebo in reducing serum urate in subjects with hyperuricemia and gout: a 28-week, phase III, randomized, double-blind, parallel-group trial. Arthritis Rheum. 2008;59:1540-1548.
2. Becker MA, Schumacher HR Jr, Wortmann RL, et al. Febuxostat compared with allopurinol in patients with hyperuricemia and gout. N Engl J Med. 2005;353:2450-2461.
3. Sundy JS, Baraf HSB, Yood RA, et al. Efficacy and tolerability of pegloticase for the treatment of chronic gout in patients refractory to conventional treatment: two randomized controlled trials. JAMA. 2011;306:711-720.
4. Paulus HE, Schlosstein LH, Godfrey RG, et al. Prophylactic colchicine therapy of intercritical gout: a placebo-controlled study of probenecid-treated patients. Arthritis Rheum. 1974;17:609-614.
5. Borstad GC, Bryant LR, Abel MP, et al. Colchicine for prophylaxis of acute flares when initiating allopurinol for chronic gouty arthritis. J Rheumatol. 2004;31:2429-2432.
6. Khanna D, Fitzgerald JD, Khanna PP, et al; American College of Rheumatology. 2012 American College of Rheumatology guidelines for management of gout. Part 1: systematic nonpharmacologic and pharmacologic therapeutic approaches to hyperuricemia. Arthritis Care Res (Hoboken). 2012;64:1431-1446.
7. Khanna D, Khanna PP, Fitzgerald JD, et al; American College of Rheumatology. 2012 American College of Rheumatology guidelines for management of gout. Part 2: therapy and anti-inflammatory prophylaxis of acute gouty arthritis. Arthritis Care Res (Hoboken). 2012;64:1447-1461.
1. Schumacher HR Jr, Becker MA, Wortmann RL, et al. Effects of febuxostat versus allopurinol and placebo in reducing serum urate in subjects with hyperuricemia and gout: a 28-week, phase III, randomized, double-blind, parallel-group trial. Arthritis Rheum. 2008;59:1540-1548.
2. Becker MA, Schumacher HR Jr, Wortmann RL, et al. Febuxostat compared with allopurinol in patients with hyperuricemia and gout. N Engl J Med. 2005;353:2450-2461.
3. Sundy JS, Baraf HSB, Yood RA, et al. Efficacy and tolerability of pegloticase for the treatment of chronic gout in patients refractory to conventional treatment: two randomized controlled trials. JAMA. 2011;306:711-720.
4. Paulus HE, Schlosstein LH, Godfrey RG, et al. Prophylactic colchicine therapy of intercritical gout: a placebo-controlled study of probenecid-treated patients. Arthritis Rheum. 1974;17:609-614.
5. Borstad GC, Bryant LR, Abel MP, et al. Colchicine for prophylaxis of acute flares when initiating allopurinol for chronic gouty arthritis. J Rheumatol. 2004;31:2429-2432.
6. Khanna D, Fitzgerald JD, Khanna PP, et al; American College of Rheumatology. 2012 American College of Rheumatology guidelines for management of gout. Part 1: systematic nonpharmacologic and pharmacologic therapeutic approaches to hyperuricemia. Arthritis Care Res (Hoboken). 2012;64:1431-1446.
7. Khanna D, Khanna PP, Fitzgerald JD, et al; American College of Rheumatology. 2012 American College of Rheumatology guidelines for management of gout. Part 2: therapy and anti-inflammatory prophylaxis of acute gouty arthritis. Arthritis Care Res (Hoboken). 2012;64:1447-1461.
Evidence-based answers from the Family Physicians Inquiries Network
ADHD medication is not working
Welcome to a new column designed to provide practical advice regarding issues related to child mental health. It will be a joint effort, featuring contributions from several child psychiatrists working at the University of Vermont and the Vermont Center for Children, Youth, and Families. While psychopharmacology will certainly be a part of many of the columns, all of us here feel strongly that medications should be only one part of a comprehensive family-oriented plan. We encourage you to submit questions that you would like us address in future issues to obnews@frontlinemedcom.com.
Case summary
A 10-year-old boy presents for a follow-up appointment. He was diagnosed by another pediatrician in the practice 2 months ago with attention-deficit/hyperactivity disorder (ADHD) and now returns to the office with continued symptoms and a complaint from the mother that medication "isn’t working." The boy was started on an extended-release preparation of methylphenidate at 18 mg to take each morning. The child is in the fifth grade and weighs 80 lb (36 kg). He lives with his mother and 8-year-old brother. The father is no longer involved in the patient’s life, which puts added stress on the mother. The diagnosis of ADHD was made by the pediatrician based upon the history, the child’s hyperactive and intrusive behavior in the office, and the results of a standardized rating scale that was completed by the mother, who now requests that the pediatrician "try something different."
Discussion
Many children and adolescents respond extremely well to ADHD medications. Some, however, do not, and the parental complaint that the "medication isn’t working" is a frequent expression heard in pediatrician offices across the country. It is also one of the primary reasons a family is referred to a child psychiatrist. In the course of performing hundreds of these consultations, I have found that there are several possibilities to consider before assuming the medication simply isn’t effective.
We will start with simpler problems and work our way toward more challenging reasons.
• The dose is too low. Methylphenidate often needs to be dosed over 1 mg/kg/day to be effective. If the patient reports minimal response to the medication while experiencing no side effects, an increase may certainly be reasonable.
• The medication is working but wearing off. Despite the advertisements of long-acting stimulants continuing their therapeutic effect for 10-12 hours, many children seem to lose the benefit of the medication much faster. Gathering some data from the school or asking the mother about weekend mornings compared with evenings can be useful. If indeed such a wear-off is found, adding a dose of an immediate-release stimulant in the early afternoon may help.
• Symptoms are being caused by something other than ADHD. Hyperactivity due to exposures such as lead may not change your management of the symptoms, but certainly could necessitate other types of intervention. Chronic sleep problems and inadequate nutrition, especially when it comes to breakfast, also should be queried and can lead to problems with concentration.
• There is psychiatric comorbidity. Unlike many differentials in other specialties, psychiatric differential diagnosis is often a matter of "and" rather than "or." Anxiety disorders, for example, can frequently masquerade as ADHD or be present in addition to ADHD. Oppositional behavior is also very commonly present with ADHD and suggests additional types of treatment.
• There is noncompliance. This problem can surface frequently in two ways. Older children may be responsible at home for taking their medications and forget or refuse to do so. I often ask, "Are you taking the medication every single day?" Diversion is also a potential problem from the parents or for an adolescent. Checking if the refills are occurring on time can provide a clue here, and some states have systems to check for duplicate prescriptions from multiple clinicians.
• Side effects are appearing as untreated ADHD. Sometimes medications are the problem, not the solution, and a failure to recognize this phenomenon can lead to unnecessary and sometimes harmful polypharmacy. Stimulants in some children can lead to increased agitation, anger outbursts, and impulsivity. Trying a medication holiday for several days can sometimes reveal the need to back off rather than add medications.
• Family is expecting improvement for non-ADHD symptoms. Asking what particular behaviors the family is hoping to improve can sometimes expose a situation in which parents expect change in non-ADHD domains. Unfortunately, there is no pill to make kids respect their parents more or want to do their homework. Being clear from the outset about what behaviors are and are not medication responsive can sometimes prevent this problem.
• There is substance abuse. In addition to the potential problem of abuse of the stimulants described previously, other substances such as cannabis can sabotage the benefits of medications.
• There is over-reliance on medications as the sole modality of treatment. ADHD is best treated using a wide range of strategies. Nonpharmacological interventions such as exercise, good nutrition and sleep, parent behavioral training, organizational help, regular reading, screen time reduction, and school supports are critical components of a comprehensive treatment approach.
• There is parental psychopathology. In our opinion, this area is one of the most frequently neglected aspects of child mental health treatment and can have huge implications. ADHD in particular is known to have very high heritability (similar to height). If a mother or father shares the condition, their struggles can frequently contribute to an environment that can exacerbate the child’s symptoms. A pattern in which the ADHD symptoms are more prominent at home compared with school is one clue to look in this direction. When addressing parental psychopathology, it can be important not to come off as blaming the parents for their child’s problems, but rather to convey how challenging dealing with ADHD can be as a parent and how they need to be functioning at their highest mental level as well.
Of course, sometimes the medication truly is not working, and it is time to try something else.
Dr. David C. Rettew is associate professor of psychiatry and pediatrics, director of the child and adolescent psychiatry fellowship, and director of the pediatric psychiatry clinic at the University of Vermont, Burlington.
Welcome to a new column designed to provide practical advice regarding issues related to child mental health. It will be a joint effort, featuring contributions from several child psychiatrists working at the University of Vermont and the Vermont Center for Children, Youth, and Families. While psychopharmacology will certainly be a part of many of the columns, all of us here feel strongly that medications should be only one part of a comprehensive family-oriented plan. We encourage you to submit questions that you would like us address in future issues to obnews@frontlinemedcom.com.
Case summary
A 10-year-old boy presents for a follow-up appointment. He was diagnosed by another pediatrician in the practice 2 months ago with attention-deficit/hyperactivity disorder (ADHD) and now returns to the office with continued symptoms and a complaint from the mother that medication "isn’t working." The boy was started on an extended-release preparation of methylphenidate at 18 mg to take each morning. The child is in the fifth grade and weighs 80 lb (36 kg). He lives with his mother and 8-year-old brother. The father is no longer involved in the patient’s life, which puts added stress on the mother. The diagnosis of ADHD was made by the pediatrician based upon the history, the child’s hyperactive and intrusive behavior in the office, and the results of a standardized rating scale that was completed by the mother, who now requests that the pediatrician "try something different."
Discussion
Many children and adolescents respond extremely well to ADHD medications. Some, however, do not, and the parental complaint that the "medication isn’t working" is a frequent expression heard in pediatrician offices across the country. It is also one of the primary reasons a family is referred to a child psychiatrist. In the course of performing hundreds of these consultations, I have found that there are several possibilities to consider before assuming the medication simply isn’t effective.
We will start with simpler problems and work our way toward more challenging reasons.
• The dose is too low. Methylphenidate often needs to be dosed over 1 mg/kg/day to be effective. If the patient reports minimal response to the medication while experiencing no side effects, an increase may certainly be reasonable.
• The medication is working but wearing off. Despite the advertisements of long-acting stimulants continuing their therapeutic effect for 10-12 hours, many children seem to lose the benefit of the medication much faster. Gathering some data from the school or asking the mother about weekend mornings compared with evenings can be useful. If indeed such a wear-off is found, adding a dose of an immediate-release stimulant in the early afternoon may help.
• Symptoms are being caused by something other than ADHD. Hyperactivity due to exposures such as lead may not change your management of the symptoms, but certainly could necessitate other types of intervention. Chronic sleep problems and inadequate nutrition, especially when it comes to breakfast, also should be queried and can lead to problems with concentration.
• There is psychiatric comorbidity. Unlike many differentials in other specialties, psychiatric differential diagnosis is often a matter of "and" rather than "or." Anxiety disorders, for example, can frequently masquerade as ADHD or be present in addition to ADHD. Oppositional behavior is also very commonly present with ADHD and suggests additional types of treatment.
• There is noncompliance. This problem can surface frequently in two ways. Older children may be responsible at home for taking their medications and forget or refuse to do so. I often ask, "Are you taking the medication every single day?" Diversion is also a potential problem from the parents or for an adolescent. Checking if the refills are occurring on time can provide a clue here, and some states have systems to check for duplicate prescriptions from multiple clinicians.
• Side effects are appearing as untreated ADHD. Sometimes medications are the problem, not the solution, and a failure to recognize this phenomenon can lead to unnecessary and sometimes harmful polypharmacy. Stimulants in some children can lead to increased agitation, anger outbursts, and impulsivity. Trying a medication holiday for several days can sometimes reveal the need to back off rather than add medications.
• Family is expecting improvement for non-ADHD symptoms. Asking what particular behaviors the family is hoping to improve can sometimes expose a situation in which parents expect change in non-ADHD domains. Unfortunately, there is no pill to make kids respect their parents more or want to do their homework. Being clear from the outset about what behaviors are and are not medication responsive can sometimes prevent this problem.
• There is substance abuse. In addition to the potential problem of abuse of the stimulants described previously, other substances such as cannabis can sabotage the benefits of medications.
• There is over-reliance on medications as the sole modality of treatment. ADHD is best treated using a wide range of strategies. Nonpharmacological interventions such as exercise, good nutrition and sleep, parent behavioral training, organizational help, regular reading, screen time reduction, and school supports are critical components of a comprehensive treatment approach.
• There is parental psychopathology. In our opinion, this area is one of the most frequently neglected aspects of child mental health treatment and can have huge implications. ADHD in particular is known to have very high heritability (similar to height). If a mother or father shares the condition, their struggles can frequently contribute to an environment that can exacerbate the child’s symptoms. A pattern in which the ADHD symptoms are more prominent at home compared with school is one clue to look in this direction. When addressing parental psychopathology, it can be important not to come off as blaming the parents for their child’s problems, but rather to convey how challenging dealing with ADHD can be as a parent and how they need to be functioning at their highest mental level as well.
Of course, sometimes the medication truly is not working, and it is time to try something else.
Dr. David C. Rettew is associate professor of psychiatry and pediatrics, director of the child and adolescent psychiatry fellowship, and director of the pediatric psychiatry clinic at the University of Vermont, Burlington.
Welcome to a new column designed to provide practical advice regarding issues related to child mental health. It will be a joint effort, featuring contributions from several child psychiatrists working at the University of Vermont and the Vermont Center for Children, Youth, and Families. While psychopharmacology will certainly be a part of many of the columns, all of us here feel strongly that medications should be only one part of a comprehensive family-oriented plan. We encourage you to submit questions that you would like us address in future issues to obnews@frontlinemedcom.com.
Case summary
A 10-year-old boy presents for a follow-up appointment. He was diagnosed by another pediatrician in the practice 2 months ago with attention-deficit/hyperactivity disorder (ADHD) and now returns to the office with continued symptoms and a complaint from the mother that medication "isn’t working." The boy was started on an extended-release preparation of methylphenidate at 18 mg to take each morning. The child is in the fifth grade and weighs 80 lb (36 kg). He lives with his mother and 8-year-old brother. The father is no longer involved in the patient’s life, which puts added stress on the mother. The diagnosis of ADHD was made by the pediatrician based upon the history, the child’s hyperactive and intrusive behavior in the office, and the results of a standardized rating scale that was completed by the mother, who now requests that the pediatrician "try something different."
Discussion
Many children and adolescents respond extremely well to ADHD medications. Some, however, do not, and the parental complaint that the "medication isn’t working" is a frequent expression heard in pediatrician offices across the country. It is also one of the primary reasons a family is referred to a child psychiatrist. In the course of performing hundreds of these consultations, I have found that there are several possibilities to consider before assuming the medication simply isn’t effective.
We will start with simpler problems and work our way toward more challenging reasons.
• The dose is too low. Methylphenidate often needs to be dosed over 1 mg/kg/day to be effective. If the patient reports minimal response to the medication while experiencing no side effects, an increase may certainly be reasonable.
• The medication is working but wearing off. Despite the advertisements of long-acting stimulants continuing their therapeutic effect for 10-12 hours, many children seem to lose the benefit of the medication much faster. Gathering some data from the school or asking the mother about weekend mornings compared with evenings can be useful. If indeed such a wear-off is found, adding a dose of an immediate-release stimulant in the early afternoon may help.
• Symptoms are being caused by something other than ADHD. Hyperactivity due to exposures such as lead may not change your management of the symptoms, but certainly could necessitate other types of intervention. Chronic sleep problems and inadequate nutrition, especially when it comes to breakfast, also should be queried and can lead to problems with concentration.
• There is psychiatric comorbidity. Unlike many differentials in other specialties, psychiatric differential diagnosis is often a matter of "and" rather than "or." Anxiety disorders, for example, can frequently masquerade as ADHD or be present in addition to ADHD. Oppositional behavior is also very commonly present with ADHD and suggests additional types of treatment.
• There is noncompliance. This problem can surface frequently in two ways. Older children may be responsible at home for taking their medications and forget or refuse to do so. I often ask, "Are you taking the medication every single day?" Diversion is also a potential problem from the parents or for an adolescent. Checking if the refills are occurring on time can provide a clue here, and some states have systems to check for duplicate prescriptions from multiple clinicians.
• Side effects are appearing as untreated ADHD. Sometimes medications are the problem, not the solution, and a failure to recognize this phenomenon can lead to unnecessary and sometimes harmful polypharmacy. Stimulants in some children can lead to increased agitation, anger outbursts, and impulsivity. Trying a medication holiday for several days can sometimes reveal the need to back off rather than add medications.
• Family is expecting improvement for non-ADHD symptoms. Asking what particular behaviors the family is hoping to improve can sometimes expose a situation in which parents expect change in non-ADHD domains. Unfortunately, there is no pill to make kids respect their parents more or want to do their homework. Being clear from the outset about what behaviors are and are not medication responsive can sometimes prevent this problem.
• There is substance abuse. In addition to the potential problem of abuse of the stimulants described previously, other substances such as cannabis can sabotage the benefits of medications.
• There is over-reliance on medications as the sole modality of treatment. ADHD is best treated using a wide range of strategies. Nonpharmacological interventions such as exercise, good nutrition and sleep, parent behavioral training, organizational help, regular reading, screen time reduction, and school supports are critical components of a comprehensive treatment approach.
• There is parental psychopathology. In our opinion, this area is one of the most frequently neglected aspects of child mental health treatment and can have huge implications. ADHD in particular is known to have very high heritability (similar to height). If a mother or father shares the condition, their struggles can frequently contribute to an environment that can exacerbate the child’s symptoms. A pattern in which the ADHD symptoms are more prominent at home compared with school is one clue to look in this direction. When addressing parental psychopathology, it can be important not to come off as blaming the parents for their child’s problems, but rather to convey how challenging dealing with ADHD can be as a parent and how they need to be functioning at their highest mental level as well.
Of course, sometimes the medication truly is not working, and it is time to try something else.
Dr. David C. Rettew is associate professor of psychiatry and pediatrics, director of the child and adolescent psychiatry fellowship, and director of the pediatric psychiatry clinic at the University of Vermont, Burlington.