User login
Chest imaging guidelines released for pediatric COVID-19
Differences are emerging between chest imaging findings in adults and children with COVID-19 pneumonia, according to a new international consensus statement published online April 23 in Radiology: Cardiothoracic Imaging.
“Chest imaging plays an important role in evaluation of pediatric patients with COVID-19, however there is currently little information available describing imaging manifestations of pediatric COVID-19 and even less discussing utilization of imaging studies in pediatric patients,” write Alexandra M. Foust, DO, from the Department of Radiology, Boston Children’s Hospital and Harvard Medical School, Massachusetts, and colleagues.
The authors wrote the consensus statement to help clinicians evaluate children with potential COVID-19, interpret chest imaging findings, and determine the best treatment for these patients.
As a dedicated pediatric radiologist in tertiary care, senior author Edward Y. Lee, MD, MPH, also from Boston Children’s Hospital, said he works with many international pediatric chest radiologists, and the document provides an international perspective. Information on chest imaging for pediatric patients with COVID-19 is scarce, and clinicians are clamoring for information to inform clinical decisions, he said. He noted that the recommendations are practical and easy to use.
The first step in evaluating a child with suspected COVID-19 is to consider the larger clinical picture. “You really have to look at the patient as a person, and when you look at them, [consider] their underlying risk factors – some people we know are prone to have more serious infection from COVID-19 because they have underlying medical problems,” Lee said.
Certain findings on chest x-ray (CXR) are more specific for COVID-19 pneumonia, whereas CT is better for characterizing and confirming and for differentiating one lung infection from another, Lee explained.
Structured reporting
Toward this end, the authors developed tables that provide standardized language to describe imaging findings in patients with suspected COVID-19 pneumonia. Advantages of this type of “structured reporting” include improved understanding and clarity between the radiologist and the ordering provider.
The authors note that structured reporting is likely to be most useful in regions where COVID-19 is highly prevalent. The COVID-19 imaging presentation in children overlaps with some other ailments, including influenza, e-cigarette vaping–associated lung injury, and eosinophilic lung disease. Thus, the use of structured reporting in low-incidence settings could lead to false positive findings.
Commonly seen CXR findings in children with COVID-19 pneumonia include bilaterally distributed peripheral and/or subpleural ground-glass opacities (GGOs) and/or consolidation. Nonspecific findings include “unilateral peripheral or peripheral and central ground-glass opacities and/or consolidation; bilateral peribronchial thickening and/or peribronchial opacities; and multifocal or diffuse GGOs and/or consolidation without specific distribution.”
On CT, commonly seen findings in pediatric COVID-19 pneumonia include “bilateral, peripheral and/or subpleural GGOs and/or consolidation in lower lobe predominant pattern; and ‘halo’ sign early” in the disease course. Indeterminate CT findings include “unilateral peripheral or peripheral and central GGOs and/or consolidation; bilateral peribronchial thickening and/or peribronchial opacities; multivocal or diffuse GGOs and/or consolidation without specific distribution; and ‘crazy paving’ sign.”
Imaging recommendations
Initial chest imaging is not generally recommended for screening of symptomatic or asymptomatic children with suspected COVID-19, nor for children with mild clinical symptoms unless the child is at risk for disease progression or worsens clinically.
An initial CXR may be appropriate for children with moderate to severe clinical symptoms – regardless of whether they have COVID-19 – and the patient may undergo a chest CT if the results could influence clinical management.
A repeat reverse transcription polymerase chain reaction (RT-PCR) test for COVID-19 should be considered for children with moderate to severe symptoms whose initial laboratory result was negative but whose chest imaging findings are consistent with COVID-19.
Chest imaging may be used as a first step in the workup for suspected COVID-19 patients in resource-constrained environments where rapid triage may be needed to spare other resources, such as hospital beds and staffing.
It may be appropriate to conduct sequential CXR examinations for pediatric patients with COVID-19 to assess therapeutic response, evaluate clinical worsening, or determine positioning of life support devices, according to the authors.
Post-recovery follow-up chest imaging is not recommended for asymptomatic pediatric patients after recovery from disease that followed a mild course. Post-recovery imaging may be appropriate for asymptomatic children who initially had moderate to severe illness; the decision should be based on clinical concern that the patient may develop long-term lung injury.
Post-recovery follow-up imaging may be appropriate for children whose symptoms persist or worsen regardless of initial illness severity.
Lee and coauthors have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Differences are emerging between chest imaging findings in adults and children with COVID-19 pneumonia, according to a new international consensus statement published online April 23 in Radiology: Cardiothoracic Imaging.
“Chest imaging plays an important role in evaluation of pediatric patients with COVID-19, however there is currently little information available describing imaging manifestations of pediatric COVID-19 and even less discussing utilization of imaging studies in pediatric patients,” write Alexandra M. Foust, DO, from the Department of Radiology, Boston Children’s Hospital and Harvard Medical School, Massachusetts, and colleagues.
The authors wrote the consensus statement to help clinicians evaluate children with potential COVID-19, interpret chest imaging findings, and determine the best treatment for these patients.
As a dedicated pediatric radiologist in tertiary care, senior author Edward Y. Lee, MD, MPH, also from Boston Children’s Hospital, said he works with many international pediatric chest radiologists, and the document provides an international perspective. Information on chest imaging for pediatric patients with COVID-19 is scarce, and clinicians are clamoring for information to inform clinical decisions, he said. He noted that the recommendations are practical and easy to use.
The first step in evaluating a child with suspected COVID-19 is to consider the larger clinical picture. “You really have to look at the patient as a person, and when you look at them, [consider] their underlying risk factors – some people we know are prone to have more serious infection from COVID-19 because they have underlying medical problems,” Lee said.
Certain findings on chest x-ray (CXR) are more specific for COVID-19 pneumonia, whereas CT is better for characterizing and confirming and for differentiating one lung infection from another, Lee explained.
Structured reporting
Toward this end, the authors developed tables that provide standardized language to describe imaging findings in patients with suspected COVID-19 pneumonia. Advantages of this type of “structured reporting” include improved understanding and clarity between the radiologist and the ordering provider.
The authors note that structured reporting is likely to be most useful in regions where COVID-19 is highly prevalent. The COVID-19 imaging presentation in children overlaps with some other ailments, including influenza, e-cigarette vaping–associated lung injury, and eosinophilic lung disease. Thus, the use of structured reporting in low-incidence settings could lead to false positive findings.
Commonly seen CXR findings in children with COVID-19 pneumonia include bilaterally distributed peripheral and/or subpleural ground-glass opacities (GGOs) and/or consolidation. Nonspecific findings include “unilateral peripheral or peripheral and central ground-glass opacities and/or consolidation; bilateral peribronchial thickening and/or peribronchial opacities; and multifocal or diffuse GGOs and/or consolidation without specific distribution.”
On CT, commonly seen findings in pediatric COVID-19 pneumonia include “bilateral, peripheral and/or subpleural GGOs and/or consolidation in lower lobe predominant pattern; and ‘halo’ sign early” in the disease course. Indeterminate CT findings include “unilateral peripheral or peripheral and central GGOs and/or consolidation; bilateral peribronchial thickening and/or peribronchial opacities; multivocal or diffuse GGOs and/or consolidation without specific distribution; and ‘crazy paving’ sign.”
Imaging recommendations
Initial chest imaging is not generally recommended for screening of symptomatic or asymptomatic children with suspected COVID-19, nor for children with mild clinical symptoms unless the child is at risk for disease progression or worsens clinically.
An initial CXR may be appropriate for children with moderate to severe clinical symptoms – regardless of whether they have COVID-19 – and the patient may undergo a chest CT if the results could influence clinical management.
A repeat reverse transcription polymerase chain reaction (RT-PCR) test for COVID-19 should be considered for children with moderate to severe symptoms whose initial laboratory result was negative but whose chest imaging findings are consistent with COVID-19.
Chest imaging may be used as a first step in the workup for suspected COVID-19 patients in resource-constrained environments where rapid triage may be needed to spare other resources, such as hospital beds and staffing.
It may be appropriate to conduct sequential CXR examinations for pediatric patients with COVID-19 to assess therapeutic response, evaluate clinical worsening, or determine positioning of life support devices, according to the authors.
Post-recovery follow-up chest imaging is not recommended for asymptomatic pediatric patients after recovery from disease that followed a mild course. Post-recovery imaging may be appropriate for asymptomatic children who initially had moderate to severe illness; the decision should be based on clinical concern that the patient may develop long-term lung injury.
Post-recovery follow-up imaging may be appropriate for children whose symptoms persist or worsen regardless of initial illness severity.
Lee and coauthors have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Differences are emerging between chest imaging findings in adults and children with COVID-19 pneumonia, according to a new international consensus statement published online April 23 in Radiology: Cardiothoracic Imaging.
“Chest imaging plays an important role in evaluation of pediatric patients with COVID-19, however there is currently little information available describing imaging manifestations of pediatric COVID-19 and even less discussing utilization of imaging studies in pediatric patients,” write Alexandra M. Foust, DO, from the Department of Radiology, Boston Children’s Hospital and Harvard Medical School, Massachusetts, and colleagues.
The authors wrote the consensus statement to help clinicians evaluate children with potential COVID-19, interpret chest imaging findings, and determine the best treatment for these patients.
As a dedicated pediatric radiologist in tertiary care, senior author Edward Y. Lee, MD, MPH, also from Boston Children’s Hospital, said he works with many international pediatric chest radiologists, and the document provides an international perspective. Information on chest imaging for pediatric patients with COVID-19 is scarce, and clinicians are clamoring for information to inform clinical decisions, he said. He noted that the recommendations are practical and easy to use.
The first step in evaluating a child with suspected COVID-19 is to consider the larger clinical picture. “You really have to look at the patient as a person, and when you look at them, [consider] their underlying risk factors – some people we know are prone to have more serious infection from COVID-19 because they have underlying medical problems,” Lee said.
Certain findings on chest x-ray (CXR) are more specific for COVID-19 pneumonia, whereas CT is better for characterizing and confirming and for differentiating one lung infection from another, Lee explained.
Structured reporting
Toward this end, the authors developed tables that provide standardized language to describe imaging findings in patients with suspected COVID-19 pneumonia. Advantages of this type of “structured reporting” include improved understanding and clarity between the radiologist and the ordering provider.
The authors note that structured reporting is likely to be most useful in regions where COVID-19 is highly prevalent. The COVID-19 imaging presentation in children overlaps with some other ailments, including influenza, e-cigarette vaping–associated lung injury, and eosinophilic lung disease. Thus, the use of structured reporting in low-incidence settings could lead to false positive findings.
Commonly seen CXR findings in children with COVID-19 pneumonia include bilaterally distributed peripheral and/or subpleural ground-glass opacities (GGOs) and/or consolidation. Nonspecific findings include “unilateral peripheral or peripheral and central ground-glass opacities and/or consolidation; bilateral peribronchial thickening and/or peribronchial opacities; and multifocal or diffuse GGOs and/or consolidation without specific distribution.”
On CT, commonly seen findings in pediatric COVID-19 pneumonia include “bilateral, peripheral and/or subpleural GGOs and/or consolidation in lower lobe predominant pattern; and ‘halo’ sign early” in the disease course. Indeterminate CT findings include “unilateral peripheral or peripheral and central GGOs and/or consolidation; bilateral peribronchial thickening and/or peribronchial opacities; multivocal or diffuse GGOs and/or consolidation without specific distribution; and ‘crazy paving’ sign.”
Imaging recommendations
Initial chest imaging is not generally recommended for screening of symptomatic or asymptomatic children with suspected COVID-19, nor for children with mild clinical symptoms unless the child is at risk for disease progression or worsens clinically.
An initial CXR may be appropriate for children with moderate to severe clinical symptoms – regardless of whether they have COVID-19 – and the patient may undergo a chest CT if the results could influence clinical management.
A repeat reverse transcription polymerase chain reaction (RT-PCR) test for COVID-19 should be considered for children with moderate to severe symptoms whose initial laboratory result was negative but whose chest imaging findings are consistent with COVID-19.
Chest imaging may be used as a first step in the workup for suspected COVID-19 patients in resource-constrained environments where rapid triage may be needed to spare other resources, such as hospital beds and staffing.
It may be appropriate to conduct sequential CXR examinations for pediatric patients with COVID-19 to assess therapeutic response, evaluate clinical worsening, or determine positioning of life support devices, according to the authors.
Post-recovery follow-up chest imaging is not recommended for asymptomatic pediatric patients after recovery from disease that followed a mild course. Post-recovery imaging may be appropriate for asymptomatic children who initially had moderate to severe illness; the decision should be based on clinical concern that the patient may develop long-term lung injury.
Post-recovery follow-up imaging may be appropriate for children whose symptoms persist or worsen regardless of initial illness severity.
Lee and coauthors have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Hospitals update hydroxychloroquine protocols after FDA warning
Across the country, hospitals are incorporating Friday’s warning from the US Food and Drug Administration (FDA) about the risks of prescribing hydroxychloroquine and chloroquine for COVID-19 into their treatment protocols.
For some hospitals, the message affirmed the cautious approach they were already taking with hydroxychloroquine. “From a New York state or Northwell perspective, there is no major change,” said Onisis Stefas, PharmD, vice president of pharmacy at Northwell Health in New York. “We were not prescribing it out in the community very early on because of the concerns associated with the heart arrhythmias.”
Brigham and Women’s Hospital in Boston, Massachusetts, is currently in the process of updating its publicly available COVID-19 protocols website “to incorporate the FDA’s updated safety assessment and ongoing clinical trials,” a hospital spokesperson told Medscape Medical News. Prior to the updates, the treatment protocols indicated that hydroxychloroquine should only be considered after weighing the risks and benefits for patients who are not candidates for other clinical trials and meet a specific set of health criteria.
The warning is a timely and important synthesis of what physicians know about the drugs so far and how cautiously clinicians across the country should be using them, said Rajesh T. Gandhi, MD, infectious diseases physician at Massachusetts General Hospital (MGH), Boston, professor of medicine at Harvard Medical School, member of the Infectious Diseases Society of America (IDSA), and chair-elect of the HIV Medicine Association.
“I think to be honest it’s a really important message to the public and clinicians across the country,” said Gandhi. “Because we all know there is just a ton of discussion around this drug ... and it came out fairly and said what we know right now.”
The two antimalarial drugs have been at the center of much political debate and scientific scrutiny in recent weeks, following President Trump’s endorsement and the FDA’s emergency use authorization for the two medications in March. Hospitals across the country had incorporated hydroxychloroquine and chloroquine into their constantly evolving treatment protocols for patients with COVID-19.
But the evidence that these drugs actually help treat COVID-19 remains scant. Some small studies suggest the therapies help patients with COVID-19, while others conclude the drugs have no effect or even harm patients. In the United States, medical societies including the American Heart Association have also warned about the serious cardiac issues that can accompany these drugs for some patients.
In the new warning, the FDA said it “cautions against use of hydroxychloroquine or chloroquine for COVID-19 patients outside of the hospital setting or a clinical trial” and urged “close supervision” of patients treated with these therapies, citing cardiac side effects.
The FDA also said it is aware that the outpatient prescription of these medications has increased since its March authorization, but the drugs still have not been shown to be safe or effective in treating or preventing COVID-19.
The FDA announcement is consistent with protocols established by the National Institutes of Health and IDSA earlier this month that recommend against using hydroxychloroquine or chloroquine, except when these drugs are administered as part of a clinical trial.
“We agree wholeheartedly with the FDA and have been hoping that the FDA would in fact issue that kind of clarification,” said Samuel Brown, MD, study committee cochair of the ORCHID clinical trial, a multicenter, blinded study investigating the safety and efficacy of hydroxychloroquine. These medications need to be tested in clinical trials that are able to focus closely on safety monitoring, he said. Experts at Vanderbilt University, one of the medical centers participating in the ORCHID clinical trial, decided before Tennessee had any cases of COVID-19 that unproven therapies like hydroxychloroquine would only be available through clinical trials, said Wesley Self, MD, associate professor of emergency medicine at Vanderbilt University, Nashville, Tennessee, and chair of the ORCHID study committee.
Northwell Health, like other hospitals in New York, has been following a March executive order issued by Governor Andrew Cuomo limiting the use of these drugs for COVID-19 outside of clinical trials, said Stefas. At Northwell Health, patients with COVID-19 only receive hydroxychloroquine or chloroquine when treated in hospital, where they can be closely monitored, or as part of a clinical trial. The hospital system’s protocols currently do not recommend pairing hydroxychloroquine with azithromycin, said Stefas. The new FDA announcement is “very similar” to New York’s existing executive order, he said. “Reading through this reinforces a lot of what we originally thought.”
At MGH in Boston, the FDA safety warning is in line with and “solidifies” the hospital’s evolving protocols, said Gandhi. Clinicians at MGH have been steadily moving away from prescribing hydroxychloroquine outside of clinical trials as the efficacy has remained murky, the serious side effects have become more evident, and clinical trials to assess the drug have gotten underway in recent weeks, he said. Given the conflicting evidence, Gandhi feels the use of these drugs needs to be focused in clinical trials, where scientists can truly evaluate how much they help or harm.
“We know fundamentally that’s the way to do this,” Gandhi said. “We also don’t know that it doesn’t work, so it is ethical and incumbent upon us to do a study,” Gandhi said.
Other hospitals are already heeding the FDA’s warning. At UW Medicine in Washington state, for example, hydroxychloroquine was considered a possible treatment for COVID-19 prior to the FDA’s recent announcement. “Based on FDA guidance, hydroxychloroquine is no longer recommended as therapy for COVID-19 unless done through a clinical trial,” said Tim Dellit, MD, chief medical officer for UW Medicine.
Michigan Medicine stopped using hydroxychloroquine and azithromycin (both separately and in combination) about a month ago, said Daniel Kaul, MD, a professor of infectious disease at the University of Michigan. “When we reviewed the data that was available in more detail, we realized that it was essentially uninterpretable,” he said. As of Monday, the only patients receiving this drug at Michigan Medicine are those enrolled in the ORCHID clinical trial.
But that does not seem to be the case everywhere. Most patients transferred to Michigan Medicine from other hospitals have received these drugs, indicating they are still being widely used, said Kaul. “I think this FDA guidance is appropriate and may reduce usage of this drug and make people more aware of the potential side effects both in inpatient and outpatient settings.”
Hopefully, the FDA guidance will help slow the use of these drugs outside the appropriate clinical trial setting, said Kaul. “I think that the kind of politicization of this drug, which is pretty much unprecedented in my experience, created a really harmful environment where calm decision making and assessment of the relative risks and benefits became somewhat impossible,” said Kaul.
This article first appeared on Medscape.com.
Across the country, hospitals are incorporating Friday’s warning from the US Food and Drug Administration (FDA) about the risks of prescribing hydroxychloroquine and chloroquine for COVID-19 into their treatment protocols.
For some hospitals, the message affirmed the cautious approach they were already taking with hydroxychloroquine. “From a New York state or Northwell perspective, there is no major change,” said Onisis Stefas, PharmD, vice president of pharmacy at Northwell Health in New York. “We were not prescribing it out in the community very early on because of the concerns associated with the heart arrhythmias.”
Brigham and Women’s Hospital in Boston, Massachusetts, is currently in the process of updating its publicly available COVID-19 protocols website “to incorporate the FDA’s updated safety assessment and ongoing clinical trials,” a hospital spokesperson told Medscape Medical News. Prior to the updates, the treatment protocols indicated that hydroxychloroquine should only be considered after weighing the risks and benefits for patients who are not candidates for other clinical trials and meet a specific set of health criteria.
The warning is a timely and important synthesis of what physicians know about the drugs so far and how cautiously clinicians across the country should be using them, said Rajesh T. Gandhi, MD, infectious diseases physician at Massachusetts General Hospital (MGH), Boston, professor of medicine at Harvard Medical School, member of the Infectious Diseases Society of America (IDSA), and chair-elect of the HIV Medicine Association.
“I think to be honest it’s a really important message to the public and clinicians across the country,” said Gandhi. “Because we all know there is just a ton of discussion around this drug ... and it came out fairly and said what we know right now.”
The two antimalarial drugs have been at the center of much political debate and scientific scrutiny in recent weeks, following President Trump’s endorsement and the FDA’s emergency use authorization for the two medications in March. Hospitals across the country had incorporated hydroxychloroquine and chloroquine into their constantly evolving treatment protocols for patients with COVID-19.
But the evidence that these drugs actually help treat COVID-19 remains scant. Some small studies suggest the therapies help patients with COVID-19, while others conclude the drugs have no effect or even harm patients. In the United States, medical societies including the American Heart Association have also warned about the serious cardiac issues that can accompany these drugs for some patients.
In the new warning, the FDA said it “cautions against use of hydroxychloroquine or chloroquine for COVID-19 patients outside of the hospital setting or a clinical trial” and urged “close supervision” of patients treated with these therapies, citing cardiac side effects.
The FDA also said it is aware that the outpatient prescription of these medications has increased since its March authorization, but the drugs still have not been shown to be safe or effective in treating or preventing COVID-19.
The FDA announcement is consistent with protocols established by the National Institutes of Health and IDSA earlier this month that recommend against using hydroxychloroquine or chloroquine, except when these drugs are administered as part of a clinical trial.
“We agree wholeheartedly with the FDA and have been hoping that the FDA would in fact issue that kind of clarification,” said Samuel Brown, MD, study committee cochair of the ORCHID clinical trial, a multicenter, blinded study investigating the safety and efficacy of hydroxychloroquine. These medications need to be tested in clinical trials that are able to focus closely on safety monitoring, he said. Experts at Vanderbilt University, one of the medical centers participating in the ORCHID clinical trial, decided before Tennessee had any cases of COVID-19 that unproven therapies like hydroxychloroquine would only be available through clinical trials, said Wesley Self, MD, associate professor of emergency medicine at Vanderbilt University, Nashville, Tennessee, and chair of the ORCHID study committee.
Northwell Health, like other hospitals in New York, has been following a March executive order issued by Governor Andrew Cuomo limiting the use of these drugs for COVID-19 outside of clinical trials, said Stefas. At Northwell Health, patients with COVID-19 only receive hydroxychloroquine or chloroquine when treated in hospital, where they can be closely monitored, or as part of a clinical trial. The hospital system’s protocols currently do not recommend pairing hydroxychloroquine with azithromycin, said Stefas. The new FDA announcement is “very similar” to New York’s existing executive order, he said. “Reading through this reinforces a lot of what we originally thought.”
At MGH in Boston, the FDA safety warning is in line with and “solidifies” the hospital’s evolving protocols, said Gandhi. Clinicians at MGH have been steadily moving away from prescribing hydroxychloroquine outside of clinical trials as the efficacy has remained murky, the serious side effects have become more evident, and clinical trials to assess the drug have gotten underway in recent weeks, he said. Given the conflicting evidence, Gandhi feels the use of these drugs needs to be focused in clinical trials, where scientists can truly evaluate how much they help or harm.
“We know fundamentally that’s the way to do this,” Gandhi said. “We also don’t know that it doesn’t work, so it is ethical and incumbent upon us to do a study,” Gandhi said.
Other hospitals are already heeding the FDA’s warning. At UW Medicine in Washington state, for example, hydroxychloroquine was considered a possible treatment for COVID-19 prior to the FDA’s recent announcement. “Based on FDA guidance, hydroxychloroquine is no longer recommended as therapy for COVID-19 unless done through a clinical trial,” said Tim Dellit, MD, chief medical officer for UW Medicine.
Michigan Medicine stopped using hydroxychloroquine and azithromycin (both separately and in combination) about a month ago, said Daniel Kaul, MD, a professor of infectious disease at the University of Michigan. “When we reviewed the data that was available in more detail, we realized that it was essentially uninterpretable,” he said. As of Monday, the only patients receiving this drug at Michigan Medicine are those enrolled in the ORCHID clinical trial.
But that does not seem to be the case everywhere. Most patients transferred to Michigan Medicine from other hospitals have received these drugs, indicating they are still being widely used, said Kaul. “I think this FDA guidance is appropriate and may reduce usage of this drug and make people more aware of the potential side effects both in inpatient and outpatient settings.”
Hopefully, the FDA guidance will help slow the use of these drugs outside the appropriate clinical trial setting, said Kaul. “I think that the kind of politicization of this drug, which is pretty much unprecedented in my experience, created a really harmful environment where calm decision making and assessment of the relative risks and benefits became somewhat impossible,” said Kaul.
This article first appeared on Medscape.com.
Across the country, hospitals are incorporating Friday’s warning from the US Food and Drug Administration (FDA) about the risks of prescribing hydroxychloroquine and chloroquine for COVID-19 into their treatment protocols.
For some hospitals, the message affirmed the cautious approach they were already taking with hydroxychloroquine. “From a New York state or Northwell perspective, there is no major change,” said Onisis Stefas, PharmD, vice president of pharmacy at Northwell Health in New York. “We were not prescribing it out in the community very early on because of the concerns associated with the heart arrhythmias.”
Brigham and Women’s Hospital in Boston, Massachusetts, is currently in the process of updating its publicly available COVID-19 protocols website “to incorporate the FDA’s updated safety assessment and ongoing clinical trials,” a hospital spokesperson told Medscape Medical News. Prior to the updates, the treatment protocols indicated that hydroxychloroquine should only be considered after weighing the risks and benefits for patients who are not candidates for other clinical trials and meet a specific set of health criteria.
The warning is a timely and important synthesis of what physicians know about the drugs so far and how cautiously clinicians across the country should be using them, said Rajesh T. Gandhi, MD, infectious diseases physician at Massachusetts General Hospital (MGH), Boston, professor of medicine at Harvard Medical School, member of the Infectious Diseases Society of America (IDSA), and chair-elect of the HIV Medicine Association.
“I think to be honest it’s a really important message to the public and clinicians across the country,” said Gandhi. “Because we all know there is just a ton of discussion around this drug ... and it came out fairly and said what we know right now.”
The two antimalarial drugs have been at the center of much political debate and scientific scrutiny in recent weeks, following President Trump’s endorsement and the FDA’s emergency use authorization for the two medications in March. Hospitals across the country had incorporated hydroxychloroquine and chloroquine into their constantly evolving treatment protocols for patients with COVID-19.
But the evidence that these drugs actually help treat COVID-19 remains scant. Some small studies suggest the therapies help patients with COVID-19, while others conclude the drugs have no effect or even harm patients. In the United States, medical societies including the American Heart Association have also warned about the serious cardiac issues that can accompany these drugs for some patients.
In the new warning, the FDA said it “cautions against use of hydroxychloroquine or chloroquine for COVID-19 patients outside of the hospital setting or a clinical trial” and urged “close supervision” of patients treated with these therapies, citing cardiac side effects.
The FDA also said it is aware that the outpatient prescription of these medications has increased since its March authorization, but the drugs still have not been shown to be safe or effective in treating or preventing COVID-19.
The FDA announcement is consistent with protocols established by the National Institutes of Health and IDSA earlier this month that recommend against using hydroxychloroquine or chloroquine, except when these drugs are administered as part of a clinical trial.
“We agree wholeheartedly with the FDA and have been hoping that the FDA would in fact issue that kind of clarification,” said Samuel Brown, MD, study committee cochair of the ORCHID clinical trial, a multicenter, blinded study investigating the safety and efficacy of hydroxychloroquine. These medications need to be tested in clinical trials that are able to focus closely on safety monitoring, he said. Experts at Vanderbilt University, one of the medical centers participating in the ORCHID clinical trial, decided before Tennessee had any cases of COVID-19 that unproven therapies like hydroxychloroquine would only be available through clinical trials, said Wesley Self, MD, associate professor of emergency medicine at Vanderbilt University, Nashville, Tennessee, and chair of the ORCHID study committee.
Northwell Health, like other hospitals in New York, has been following a March executive order issued by Governor Andrew Cuomo limiting the use of these drugs for COVID-19 outside of clinical trials, said Stefas. At Northwell Health, patients with COVID-19 only receive hydroxychloroquine or chloroquine when treated in hospital, where they can be closely monitored, or as part of a clinical trial. The hospital system’s protocols currently do not recommend pairing hydroxychloroquine with azithromycin, said Stefas. The new FDA announcement is “very similar” to New York’s existing executive order, he said. “Reading through this reinforces a lot of what we originally thought.”
At MGH in Boston, the FDA safety warning is in line with and “solidifies” the hospital’s evolving protocols, said Gandhi. Clinicians at MGH have been steadily moving away from prescribing hydroxychloroquine outside of clinical trials as the efficacy has remained murky, the serious side effects have become more evident, and clinical trials to assess the drug have gotten underway in recent weeks, he said. Given the conflicting evidence, Gandhi feels the use of these drugs needs to be focused in clinical trials, where scientists can truly evaluate how much they help or harm.
“We know fundamentally that’s the way to do this,” Gandhi said. “We also don’t know that it doesn’t work, so it is ethical and incumbent upon us to do a study,” Gandhi said.
Other hospitals are already heeding the FDA’s warning. At UW Medicine in Washington state, for example, hydroxychloroquine was considered a possible treatment for COVID-19 prior to the FDA’s recent announcement. “Based on FDA guidance, hydroxychloroquine is no longer recommended as therapy for COVID-19 unless done through a clinical trial,” said Tim Dellit, MD, chief medical officer for UW Medicine.
Michigan Medicine stopped using hydroxychloroquine and azithromycin (both separately and in combination) about a month ago, said Daniel Kaul, MD, a professor of infectious disease at the University of Michigan. “When we reviewed the data that was available in more detail, we realized that it was essentially uninterpretable,” he said. As of Monday, the only patients receiving this drug at Michigan Medicine are those enrolled in the ORCHID clinical trial.
But that does not seem to be the case everywhere. Most patients transferred to Michigan Medicine from other hospitals have received these drugs, indicating they are still being widely used, said Kaul. “I think this FDA guidance is appropriate and may reduce usage of this drug and make people more aware of the potential side effects both in inpatient and outpatient settings.”
Hopefully, the FDA guidance will help slow the use of these drugs outside the appropriate clinical trial setting, said Kaul. “I think that the kind of politicization of this drug, which is pretty much unprecedented in my experience, created a really harmful environment where calm decision making and assessment of the relative risks and benefits became somewhat impossible,” said Kaul.
This article first appeared on Medscape.com.
Contact tracing, isolation have impact, study shows
A far-reaching surveillance initiative was implemented in Shenzhen, China, to isolate and contact trace people suspected of having the COVID-19 coronavirus. This initiative led to faster confirmation of new cases and reduced the window of time during which people were infectious in the community. This potentially reduced the number of new infections that arose from each case, according to a study of patients and contacts over 4 weeks (Lancet Infect Dis. 2020 Apr 27. doi: 10.1016/S1473-3099[20]30287-5).
“The experience of COVID-19 in the city of Shenzhen may demonstrate the huge scale of testing and contact tracing that’s needed to reduce the virus spreading,” said study coauthor Ting Ma, PhD, of Harbin Institute of Technology at Shenzhen.
Dr. Ma acknowledged that some of the measures the program used, such as isolating people outside their homes, may be difficult to impose in other countries, “but we urge governments to consider our findings in the global response to COVID-19.”
The study followed 391 coronavirus cases and 1,286 close contacts identified by the Shenzhen Center for Disease Control and Prevention from Jan. 14 to Feb. 12 this year. The study showed that contact tracing led to confirming new diagnoses within 3.2 days on average vs. 5.5 for symptom-based surveillance, and reduced the time it took to isolate newly infected people by 2 days, from an average of 4.6 to 2.7 days. Eighty-seven people were diagnosed with COVID-19 after they were contact traced and tested. Twenty percent of them had no symptoms, and 29% had no fever. Three deaths occurred in the group during the study period.
The surveillance program was comprehensive and intense. On Jan. 8, the Shenzhen CDC started monitoring travelers from Hubei province, of which Wuhan is the capital, for symptoms of COVID-19. Shenzhen is a city of about 12.5 million people in southeastern China, near Hong Kong, and is about 560 miles south of Wuhan. Over the next 2 weeks, the Shenzhen CDC expanded that surveillance program to all travelers from Hubei regardless of symptoms, along with local hospital patients and people detected by fever screenings at area clinics.
Suspected cases and close contacts underwent nasal-swab testing at 40 different locations in the city. The program identified close contacts through contact tracing, and included anyone who lived in the same dwelling, shared a meal, traveled, or had a social interaction with an index 2 days before symptoms appeared. Casual contacts and some close contacts, such as clinic nurses, who wore masks during the encounters were excluded.
“To achieve similar results, other countries might be able to combine near-universal testing and intensive contact tracing with social distancing and partial lockdowns,” said Dr. Ma. “Although no lockdown measures were introduced in Shenzhen until the end of our study period, Wuhan’s lockdown could have significantly restricted the spread of coronavirus to Shenzhen.”
The researchers noted that children are as susceptible to the virus as are adults, even though their symptoms are not as severe as those of adults. The rate of infection in children 10 and younger was similar to the overall infection rate, 7.4% vs. 6.6%, so the researchers noted that surveillance measures should target them as well.
“This study to me confirms a lot of what we’ve already known,” Aaron E. Glatt, MD, chairman of medicine and an epidemiologist at Mount Sinai South Nassau in Oceanside, N.Y., said in an interview. “It’s an elegant study, but at the same time it sends us a message that we’re at a critical point of time for us to intervene and prevent cases at the very beginning.”
He acknowledged that the Shenzhen effort was intense. “It’s always a resource-intense requirement to do such extensive contact tracing, but that doesn’t mean it shouldn’t be done to the best of your ability to do so,” he said. He was struck by the low relative rate of infection among contacts in the study – around 7%. “There are differences obviously in infection rates in every outbreak,” he said. “Every individual has their own particular infection rate. While we can take ranges and statistical guesses for every individual patient, it could be very high or very low, and that’s most critical to nip it in the bud.”
Lead author Qifang Bi and study coauthors had no financial relationships to disclose.
SOURCE: Bi Q et al. Lancet Infect Dis. 2020 Apr 27. doi: 10.1016/S1473-3099(20)30287-5.
A far-reaching surveillance initiative was implemented in Shenzhen, China, to isolate and contact trace people suspected of having the COVID-19 coronavirus. This initiative led to faster confirmation of new cases and reduced the window of time during which people were infectious in the community. This potentially reduced the number of new infections that arose from each case, according to a study of patients and contacts over 4 weeks (Lancet Infect Dis. 2020 Apr 27. doi: 10.1016/S1473-3099[20]30287-5).
“The experience of COVID-19 in the city of Shenzhen may demonstrate the huge scale of testing and contact tracing that’s needed to reduce the virus spreading,” said study coauthor Ting Ma, PhD, of Harbin Institute of Technology at Shenzhen.
Dr. Ma acknowledged that some of the measures the program used, such as isolating people outside their homes, may be difficult to impose in other countries, “but we urge governments to consider our findings in the global response to COVID-19.”
The study followed 391 coronavirus cases and 1,286 close contacts identified by the Shenzhen Center for Disease Control and Prevention from Jan. 14 to Feb. 12 this year. The study showed that contact tracing led to confirming new diagnoses within 3.2 days on average vs. 5.5 for symptom-based surveillance, and reduced the time it took to isolate newly infected people by 2 days, from an average of 4.6 to 2.7 days. Eighty-seven people were diagnosed with COVID-19 after they were contact traced and tested. Twenty percent of them had no symptoms, and 29% had no fever. Three deaths occurred in the group during the study period.
The surveillance program was comprehensive and intense. On Jan. 8, the Shenzhen CDC started monitoring travelers from Hubei province, of which Wuhan is the capital, for symptoms of COVID-19. Shenzhen is a city of about 12.5 million people in southeastern China, near Hong Kong, and is about 560 miles south of Wuhan. Over the next 2 weeks, the Shenzhen CDC expanded that surveillance program to all travelers from Hubei regardless of symptoms, along with local hospital patients and people detected by fever screenings at area clinics.
Suspected cases and close contacts underwent nasal-swab testing at 40 different locations in the city. The program identified close contacts through contact tracing, and included anyone who lived in the same dwelling, shared a meal, traveled, or had a social interaction with an index 2 days before symptoms appeared. Casual contacts and some close contacts, such as clinic nurses, who wore masks during the encounters were excluded.
“To achieve similar results, other countries might be able to combine near-universal testing and intensive contact tracing with social distancing and partial lockdowns,” said Dr. Ma. “Although no lockdown measures were introduced in Shenzhen until the end of our study period, Wuhan’s lockdown could have significantly restricted the spread of coronavirus to Shenzhen.”
The researchers noted that children are as susceptible to the virus as are adults, even though their symptoms are not as severe as those of adults. The rate of infection in children 10 and younger was similar to the overall infection rate, 7.4% vs. 6.6%, so the researchers noted that surveillance measures should target them as well.
“This study to me confirms a lot of what we’ve already known,” Aaron E. Glatt, MD, chairman of medicine and an epidemiologist at Mount Sinai South Nassau in Oceanside, N.Y., said in an interview. “It’s an elegant study, but at the same time it sends us a message that we’re at a critical point of time for us to intervene and prevent cases at the very beginning.”
He acknowledged that the Shenzhen effort was intense. “It’s always a resource-intense requirement to do such extensive contact tracing, but that doesn’t mean it shouldn’t be done to the best of your ability to do so,” he said. He was struck by the low relative rate of infection among contacts in the study – around 7%. “There are differences obviously in infection rates in every outbreak,” he said. “Every individual has their own particular infection rate. While we can take ranges and statistical guesses for every individual patient, it could be very high or very low, and that’s most critical to nip it in the bud.”
Lead author Qifang Bi and study coauthors had no financial relationships to disclose.
SOURCE: Bi Q et al. Lancet Infect Dis. 2020 Apr 27. doi: 10.1016/S1473-3099(20)30287-5.
A far-reaching surveillance initiative was implemented in Shenzhen, China, to isolate and contact trace people suspected of having the COVID-19 coronavirus. This initiative led to faster confirmation of new cases and reduced the window of time during which people were infectious in the community. This potentially reduced the number of new infections that arose from each case, according to a study of patients and contacts over 4 weeks (Lancet Infect Dis. 2020 Apr 27. doi: 10.1016/S1473-3099[20]30287-5).
“The experience of COVID-19 in the city of Shenzhen may demonstrate the huge scale of testing and contact tracing that’s needed to reduce the virus spreading,” said study coauthor Ting Ma, PhD, of Harbin Institute of Technology at Shenzhen.
Dr. Ma acknowledged that some of the measures the program used, such as isolating people outside their homes, may be difficult to impose in other countries, “but we urge governments to consider our findings in the global response to COVID-19.”
The study followed 391 coronavirus cases and 1,286 close contacts identified by the Shenzhen Center for Disease Control and Prevention from Jan. 14 to Feb. 12 this year. The study showed that contact tracing led to confirming new diagnoses within 3.2 days on average vs. 5.5 for symptom-based surveillance, and reduced the time it took to isolate newly infected people by 2 days, from an average of 4.6 to 2.7 days. Eighty-seven people were diagnosed with COVID-19 after they were contact traced and tested. Twenty percent of them had no symptoms, and 29% had no fever. Three deaths occurred in the group during the study period.
The surveillance program was comprehensive and intense. On Jan. 8, the Shenzhen CDC started monitoring travelers from Hubei province, of which Wuhan is the capital, for symptoms of COVID-19. Shenzhen is a city of about 12.5 million people in southeastern China, near Hong Kong, and is about 560 miles south of Wuhan. Over the next 2 weeks, the Shenzhen CDC expanded that surveillance program to all travelers from Hubei regardless of symptoms, along with local hospital patients and people detected by fever screenings at area clinics.
Suspected cases and close contacts underwent nasal-swab testing at 40 different locations in the city. The program identified close contacts through contact tracing, and included anyone who lived in the same dwelling, shared a meal, traveled, or had a social interaction with an index 2 days before symptoms appeared. Casual contacts and some close contacts, such as clinic nurses, who wore masks during the encounters were excluded.
“To achieve similar results, other countries might be able to combine near-universal testing and intensive contact tracing with social distancing and partial lockdowns,” said Dr. Ma. “Although no lockdown measures were introduced in Shenzhen until the end of our study period, Wuhan’s lockdown could have significantly restricted the spread of coronavirus to Shenzhen.”
The researchers noted that children are as susceptible to the virus as are adults, even though their symptoms are not as severe as those of adults. The rate of infection in children 10 and younger was similar to the overall infection rate, 7.4% vs. 6.6%, so the researchers noted that surveillance measures should target them as well.
“This study to me confirms a lot of what we’ve already known,” Aaron E. Glatt, MD, chairman of medicine and an epidemiologist at Mount Sinai South Nassau in Oceanside, N.Y., said in an interview. “It’s an elegant study, but at the same time it sends us a message that we’re at a critical point of time for us to intervene and prevent cases at the very beginning.”
He acknowledged that the Shenzhen effort was intense. “It’s always a resource-intense requirement to do such extensive contact tracing, but that doesn’t mean it shouldn’t be done to the best of your ability to do so,” he said. He was struck by the low relative rate of infection among contacts in the study – around 7%. “There are differences obviously in infection rates in every outbreak,” he said. “Every individual has their own particular infection rate. While we can take ranges and statistical guesses for every individual patient, it could be very high or very low, and that’s most critical to nip it in the bud.”
Lead author Qifang Bi and study coauthors had no financial relationships to disclose.
SOURCE: Bi Q et al. Lancet Infect Dis. 2020 Apr 27. doi: 10.1016/S1473-3099(20)30287-5.
FROM LANCET INFECTIOUS DISEASE
Acute kidney injury in children hospitalized with diarrheal illness in the U.S.
Clinical question: To determine the incidence and consequences of acute kidney injury among children hospitalized with diarrheal illness in the United States.
Background: Diarrheal illness is the fourth leading cause of death for children younger than 5 years and the fifth leading cause of years of life lost globally. In the United States, diarrheal illness remains a leading cause of hospital admission among young children. Complications of severe diarrheal illness include hypovolemic acute kidney injury (AKI). Hospitalized children who develop AKI experience longer hospital stays and higher mortality. Additionally, children who experience AKI are at increased risk for chronic kidney disease (CKD), hypertension, and proteinuria.
Study design: Retrospective cohort study.
Setting: Kids’ Inpatient Database (KID) from 2009 and 2012. The authors used secondary International Classification of Diseases, Ninth Revision (ICD-9) diagnoses of AKI to identify patients.
Synopsis: The authors reviewed all patients with diarrhea and found that the incidence of AKI in children hospitalized was 0.8%. Those with infectious diarrhea had an incidence of 1% and with noninfectious diarrhea had an incidence of 0.6%. There was a higher incidence of dialysis-requiring AKI in patients with infectious diarrhea. The odds of developing AKI increased with older age in both infectious and noninfectious diarrheal illnesses. As compared with noninfectious diarrheal illness, infectious diarrheal illness was associated with higher odds of AKI (odds ratio, 2.1; 95% confidence interval, 1.7-2.7). Irrespective of diarrhea type, hematologic and rheumatologic conditions, solid organ transplant, CKD, and hypertension were associated with higher odds of developing AKI. AKI in infectious diarrheal illness was also associated with other renal or genitourinary abnormalities, whereas AKI in noninfectious diarrheal illness was associated with diabetes, cardiovascular, and neurologic conditions.
Hospitalizations for diarrheal illness complicated by AKI were associated with higher mortality, prolonged LOS, and higher hospital cost with odds of death increased eightfold with AKI, mean hospital stay was prolonged by 3 days, and costs increased by greater than $9,000 per hospital stay. The development of AKI in hospitalized diarrheal illness was associated with an up to 11-fold increase in the odds of in-hospital mortality for infectious (OR, 10.8; 95% CI, 3.4-34.3) and noninfectious diarrheal illness (OR, 7.0; 95% CI, 3.1-15.7).
The strengths of this study include broad representation of hospitals caring for children across the United States. The study was limited by its use of ICD-9 codes which may misidentify AKI. The authors were unable to determine if identifying AKI could improve outcomes for patients with diarrheal illness.
Bottom line: AKI in diarrhea illnesses is relatively rare. Close attention should be given to AKI in patients with certain serious comorbid illnesses.
Article citation: Bradshaw C, Han J, Chertow GM, Long J, Sutherland SM, Anand S. Acute Kidney Injury in Children Hospitalized With Diarrheal Illness in the United States. Hosp Pediatr. 2019 Dec;9(12):933-941.
Dr. Kumar is a pediatric hospitalist at Cleveland Clinic Children’s. She is a clinical assistant professor of pediatrics at Case Western Reserve University, and serves as the pediatrics editor for The Hospitalist.
Clinical question: To determine the incidence and consequences of acute kidney injury among children hospitalized with diarrheal illness in the United States.
Background: Diarrheal illness is the fourth leading cause of death for children younger than 5 years and the fifth leading cause of years of life lost globally. In the United States, diarrheal illness remains a leading cause of hospital admission among young children. Complications of severe diarrheal illness include hypovolemic acute kidney injury (AKI). Hospitalized children who develop AKI experience longer hospital stays and higher mortality. Additionally, children who experience AKI are at increased risk for chronic kidney disease (CKD), hypertension, and proteinuria.
Study design: Retrospective cohort study.
Setting: Kids’ Inpatient Database (KID) from 2009 and 2012. The authors used secondary International Classification of Diseases, Ninth Revision (ICD-9) diagnoses of AKI to identify patients.
Synopsis: The authors reviewed all patients with diarrhea and found that the incidence of AKI in children hospitalized was 0.8%. Those with infectious diarrhea had an incidence of 1% and with noninfectious diarrhea had an incidence of 0.6%. There was a higher incidence of dialysis-requiring AKI in patients with infectious diarrhea. The odds of developing AKI increased with older age in both infectious and noninfectious diarrheal illnesses. As compared with noninfectious diarrheal illness, infectious diarrheal illness was associated with higher odds of AKI (odds ratio, 2.1; 95% confidence interval, 1.7-2.7). Irrespective of diarrhea type, hematologic and rheumatologic conditions, solid organ transplant, CKD, and hypertension were associated with higher odds of developing AKI. AKI in infectious diarrheal illness was also associated with other renal or genitourinary abnormalities, whereas AKI in noninfectious diarrheal illness was associated with diabetes, cardiovascular, and neurologic conditions.
Hospitalizations for diarrheal illness complicated by AKI were associated with higher mortality, prolonged LOS, and higher hospital cost with odds of death increased eightfold with AKI, mean hospital stay was prolonged by 3 days, and costs increased by greater than $9,000 per hospital stay. The development of AKI in hospitalized diarrheal illness was associated with an up to 11-fold increase in the odds of in-hospital mortality for infectious (OR, 10.8; 95% CI, 3.4-34.3) and noninfectious diarrheal illness (OR, 7.0; 95% CI, 3.1-15.7).
The strengths of this study include broad representation of hospitals caring for children across the United States. The study was limited by its use of ICD-9 codes which may misidentify AKI. The authors were unable to determine if identifying AKI could improve outcomes for patients with diarrheal illness.
Bottom line: AKI in diarrhea illnesses is relatively rare. Close attention should be given to AKI in patients with certain serious comorbid illnesses.
Article citation: Bradshaw C, Han J, Chertow GM, Long J, Sutherland SM, Anand S. Acute Kidney Injury in Children Hospitalized With Diarrheal Illness in the United States. Hosp Pediatr. 2019 Dec;9(12):933-941.
Dr. Kumar is a pediatric hospitalist at Cleveland Clinic Children’s. She is a clinical assistant professor of pediatrics at Case Western Reserve University, and serves as the pediatrics editor for The Hospitalist.
Clinical question: To determine the incidence and consequences of acute kidney injury among children hospitalized with diarrheal illness in the United States.
Background: Diarrheal illness is the fourth leading cause of death for children younger than 5 years and the fifth leading cause of years of life lost globally. In the United States, diarrheal illness remains a leading cause of hospital admission among young children. Complications of severe diarrheal illness include hypovolemic acute kidney injury (AKI). Hospitalized children who develop AKI experience longer hospital stays and higher mortality. Additionally, children who experience AKI are at increased risk for chronic kidney disease (CKD), hypertension, and proteinuria.
Study design: Retrospective cohort study.
Setting: Kids’ Inpatient Database (KID) from 2009 and 2012. The authors used secondary International Classification of Diseases, Ninth Revision (ICD-9) diagnoses of AKI to identify patients.
Synopsis: The authors reviewed all patients with diarrhea and found that the incidence of AKI in children hospitalized was 0.8%. Those with infectious diarrhea had an incidence of 1% and with noninfectious diarrhea had an incidence of 0.6%. There was a higher incidence of dialysis-requiring AKI in patients with infectious diarrhea. The odds of developing AKI increased with older age in both infectious and noninfectious diarrheal illnesses. As compared with noninfectious diarrheal illness, infectious diarrheal illness was associated with higher odds of AKI (odds ratio, 2.1; 95% confidence interval, 1.7-2.7). Irrespective of diarrhea type, hematologic and rheumatologic conditions, solid organ transplant, CKD, and hypertension were associated with higher odds of developing AKI. AKI in infectious diarrheal illness was also associated with other renal or genitourinary abnormalities, whereas AKI in noninfectious diarrheal illness was associated with diabetes, cardiovascular, and neurologic conditions.
Hospitalizations for diarrheal illness complicated by AKI were associated with higher mortality, prolonged LOS, and higher hospital cost with odds of death increased eightfold with AKI, mean hospital stay was prolonged by 3 days, and costs increased by greater than $9,000 per hospital stay. The development of AKI in hospitalized diarrheal illness was associated with an up to 11-fold increase in the odds of in-hospital mortality for infectious (OR, 10.8; 95% CI, 3.4-34.3) and noninfectious diarrheal illness (OR, 7.0; 95% CI, 3.1-15.7).
The strengths of this study include broad representation of hospitals caring for children across the United States. The study was limited by its use of ICD-9 codes which may misidentify AKI. The authors were unable to determine if identifying AKI could improve outcomes for patients with diarrheal illness.
Bottom line: AKI in diarrhea illnesses is relatively rare. Close attention should be given to AKI in patients with certain serious comorbid illnesses.
Article citation: Bradshaw C, Han J, Chertow GM, Long J, Sutherland SM, Anand S. Acute Kidney Injury in Children Hospitalized With Diarrheal Illness in the United States. Hosp Pediatr. 2019 Dec;9(12):933-941.
Dr. Kumar is a pediatric hospitalist at Cleveland Clinic Children’s. She is a clinical assistant professor of pediatrics at Case Western Reserve University, and serves as the pediatrics editor for The Hospitalist.
SGLT2 inhibitor ertugliflozin shows no CV death or renal benefit
The sodium-glucose transporter 2 (SGLT-2) inhibitor ertugliflozin broke ranks with the other drugs in its class and failed to produce statistically significant drops in the both the combined incidence of cardiovascular (CV) death or heart failure hospitalization, and the rate of adverse renal outcomes, in the mandated CV outcomes trial run for ertugliflozin with more than 8,200 patients with type 2 diabetes and established CV disease.
Merck, one of the companies that markets the drug, announced the topline results in a quarterly financial report released on April 28, 2020.
According to the report, the results from the ertugliflozin cardiovascular outcomes trial “achieved its primary endpoint of noninferiority for major adverse CV events (MACE), compared to placebo in patients with type 2 diabetes mellitus and established atherosclerotic CV disease,” but “the key secondary endpoints of superiority” of ertugliflozin, compared with placebo, “for time to the composite of CV death or hospitalization for heart failure, CV death alone, and the composite of renal death, dialysis/transplant or doubling of serum creatinine from baseline were not met.”
However, the report added that, “while not a prespecified hypothesis for statistical testing, a reduction in hospitalization for heart failure was observed” with ertugliflozin treatment, and the report further said that the drug’s safety profile in the trial “was consistent with that reported in previous studies.” The statement closed by saying that detailed results from the trial are scheduled to be presented on June 16, 2020, at the virtual American Diabetes Association’s 80th Scientific Sessions.
These results came from the VERTIS CV (Evaluation of Ertugliflozin EffIcacy and Safety Cardiovascular Outcomes) trial, which researchers said in 2018 had administered at least one investigational dose to 8,238 randomized patients at centers in any of 34 countries during two enrollment periods in 2013-2015 and 2016-2017 (Am Heart J. 2018 Dec;206:11-23). The tested agent, ertugliflozin (Steglatro) received Food and Drug Administration marketing approval late in 2017 for the indication of improving glycemic control in patients with type 2 diabetes.
The FDA mandated cardiovascular outcomes trials for new glycemic control drugs in guidance the agency issued in 2008 (the FDA released in March 2020 a draft of updated guidance on this topic).
Other FDA-approved agents from the SGLT2 inhibitor class include canagliflozin (Invokana), dapagliflozin (Farxiga), and empagliflozin (Jardiance), and all three showed evidence for a statistically significant effect on reducing the incidence of CV disease death and heart failure hospitalizations, as well as renal complications (Can J Diabetes. 2020 Feb;44[1]:61-7). The evidence showing that several SGLT2 drugs have important and consistent effects on endpoints like CV death, heart failure hospitalizations, and renal complications has helped propel this class of agents to the forefront of glycemic control treatments. More recently, one agent from this group, dapagliflozin, also significantly cut the rate of heart failure worsening or CV disease death in patients with heart failure with reduced ejection fraction but without diabetes (N Engl J Med. 2019 Nov 21;381[21]:1995-2008). Based on this evidence, the FDA is currently considering adding a new indication for dapagliflozin that would also label it for use in patients with heart failure with reduced ejection fraction but without diabetes.
The sodium-glucose transporter 2 (SGLT-2) inhibitor ertugliflozin broke ranks with the other drugs in its class and failed to produce statistically significant drops in the both the combined incidence of cardiovascular (CV) death or heart failure hospitalization, and the rate of adverse renal outcomes, in the mandated CV outcomes trial run for ertugliflozin with more than 8,200 patients with type 2 diabetes and established CV disease.
Merck, one of the companies that markets the drug, announced the topline results in a quarterly financial report released on April 28, 2020.
According to the report, the results from the ertugliflozin cardiovascular outcomes trial “achieved its primary endpoint of noninferiority for major adverse CV events (MACE), compared to placebo in patients with type 2 diabetes mellitus and established atherosclerotic CV disease,” but “the key secondary endpoints of superiority” of ertugliflozin, compared with placebo, “for time to the composite of CV death or hospitalization for heart failure, CV death alone, and the composite of renal death, dialysis/transplant or doubling of serum creatinine from baseline were not met.”
However, the report added that, “while not a prespecified hypothesis for statistical testing, a reduction in hospitalization for heart failure was observed” with ertugliflozin treatment, and the report further said that the drug’s safety profile in the trial “was consistent with that reported in previous studies.” The statement closed by saying that detailed results from the trial are scheduled to be presented on June 16, 2020, at the virtual American Diabetes Association’s 80th Scientific Sessions.
These results came from the VERTIS CV (Evaluation of Ertugliflozin EffIcacy and Safety Cardiovascular Outcomes) trial, which researchers said in 2018 had administered at least one investigational dose to 8,238 randomized patients at centers in any of 34 countries during two enrollment periods in 2013-2015 and 2016-2017 (Am Heart J. 2018 Dec;206:11-23). The tested agent, ertugliflozin (Steglatro) received Food and Drug Administration marketing approval late in 2017 for the indication of improving glycemic control in patients with type 2 diabetes.
The FDA mandated cardiovascular outcomes trials for new glycemic control drugs in guidance the agency issued in 2008 (the FDA released in March 2020 a draft of updated guidance on this topic).
Other FDA-approved agents from the SGLT2 inhibitor class include canagliflozin (Invokana), dapagliflozin (Farxiga), and empagliflozin (Jardiance), and all three showed evidence for a statistically significant effect on reducing the incidence of CV disease death and heart failure hospitalizations, as well as renal complications (Can J Diabetes. 2020 Feb;44[1]:61-7). The evidence showing that several SGLT2 drugs have important and consistent effects on endpoints like CV death, heart failure hospitalizations, and renal complications has helped propel this class of agents to the forefront of glycemic control treatments. More recently, one agent from this group, dapagliflozin, also significantly cut the rate of heart failure worsening or CV disease death in patients with heart failure with reduced ejection fraction but without diabetes (N Engl J Med. 2019 Nov 21;381[21]:1995-2008). Based on this evidence, the FDA is currently considering adding a new indication for dapagliflozin that would also label it for use in patients with heart failure with reduced ejection fraction but without diabetes.
The sodium-glucose transporter 2 (SGLT-2) inhibitor ertugliflozin broke ranks with the other drugs in its class and failed to produce statistically significant drops in the both the combined incidence of cardiovascular (CV) death or heart failure hospitalization, and the rate of adverse renal outcomes, in the mandated CV outcomes trial run for ertugliflozin with more than 8,200 patients with type 2 diabetes and established CV disease.
Merck, one of the companies that markets the drug, announced the topline results in a quarterly financial report released on April 28, 2020.
According to the report, the results from the ertugliflozin cardiovascular outcomes trial “achieved its primary endpoint of noninferiority for major adverse CV events (MACE), compared to placebo in patients with type 2 diabetes mellitus and established atherosclerotic CV disease,” but “the key secondary endpoints of superiority” of ertugliflozin, compared with placebo, “for time to the composite of CV death or hospitalization for heart failure, CV death alone, and the composite of renal death, dialysis/transplant or doubling of serum creatinine from baseline were not met.”
However, the report added that, “while not a prespecified hypothesis for statistical testing, a reduction in hospitalization for heart failure was observed” with ertugliflozin treatment, and the report further said that the drug’s safety profile in the trial “was consistent with that reported in previous studies.” The statement closed by saying that detailed results from the trial are scheduled to be presented on June 16, 2020, at the virtual American Diabetes Association’s 80th Scientific Sessions.
These results came from the VERTIS CV (Evaluation of Ertugliflozin EffIcacy and Safety Cardiovascular Outcomes) trial, which researchers said in 2018 had administered at least one investigational dose to 8,238 randomized patients at centers in any of 34 countries during two enrollment periods in 2013-2015 and 2016-2017 (Am Heart J. 2018 Dec;206:11-23). The tested agent, ertugliflozin (Steglatro) received Food and Drug Administration marketing approval late in 2017 for the indication of improving glycemic control in patients with type 2 diabetes.
The FDA mandated cardiovascular outcomes trials for new glycemic control drugs in guidance the agency issued in 2008 (the FDA released in March 2020 a draft of updated guidance on this topic).
Other FDA-approved agents from the SGLT2 inhibitor class include canagliflozin (Invokana), dapagliflozin (Farxiga), and empagliflozin (Jardiance), and all three showed evidence for a statistically significant effect on reducing the incidence of CV disease death and heart failure hospitalizations, as well as renal complications (Can J Diabetes. 2020 Feb;44[1]:61-7). The evidence showing that several SGLT2 drugs have important and consistent effects on endpoints like CV death, heart failure hospitalizations, and renal complications has helped propel this class of agents to the forefront of glycemic control treatments. More recently, one agent from this group, dapagliflozin, also significantly cut the rate of heart failure worsening or CV disease death in patients with heart failure with reduced ejection fraction but without diabetes (N Engl J Med. 2019 Nov 21;381[21]:1995-2008). Based on this evidence, the FDA is currently considering adding a new indication for dapagliflozin that would also label it for use in patients with heart failure with reduced ejection fraction but without diabetes.
Consensus recommendations on AMI management during COVID-19
A consensus statement from the American College of Cardiology (ACC), the American College of Emergency Physicians (ACEP), and the Society for Cardiovascular Angiography & Interventions (SCAI) outlines recommendations for a systematic approach for the care of patients with an acute myocardial infarction (AMI) during the COVID-19 pandemic.
The statement was published in the Journal of the American College of Cardiology.
During the COVID-19 pandemic, percutaneous coronary intervention (PCI) remains the standard of care for patients with ST-segment elevation MI (STEMI) at PCI-capable hospitals when it can be provided in a timely fashion in a dedicated cardiac catheterization laboratory with an expert care team wearing personal protection equipment (PPE), the writing group advised.
“A fibrinolysis-based strategy may be entertained at non-PCI capable referral hospitals or in specific situations where primary PCI cannot be executed or is not deemed the best option,” they said.
SCAI President Ehtisham Mahmud, MD, of the University of California, San Diego, and the writing group also said that clinicians should recognize that cardiovascular manifestations of COVID-19 are “complex” in patients presenting with AMI, myocarditis simulating a STEMI, stress cardiomyopathy, nonischemic cardiomyopathy, coronary spasm, or nonspecific myocardial injury.
A “broad differential diagnosis for ST elevations (including COVID-associated myocarditis) should be considered in the ED prior to choosing a reperfusion strategy,” they advised.
In the absence of hemodynamic instability or ongoing ischemic symptoms, non-STEMI patients with known or suspected COVID-19 are best managed with an initial medical stabilization strategy, the group said.
They also said it is “imperative that health care workers use appropriate PPE for all invasive procedures during this pandemic” and that new rapid COVID-19 testing be “expeditiously” disseminated to all hospitals that manage patients with AMI.
Major challenges are that the prevalence of the COVID-19 in the United States remains unknown and there is the risk for asymptomatic spread.
The writing group said it’s “critical” to “inform the public that we can minimize exposure to the coronavirus so they can continue to call the Emergency Medical System (EMS) for acute ischemic heart disease symptoms and therefore get the appropriate level of cardiac care that their presentation warrants.”
This research had no commercial funding. Dr. Mahmud reported receiving clinical trial research support from Corindus, Abbott Vascular, and CSI; consulting with Medtronic; and consulting and equity with Abiomed. A complete list of author disclosures is included with the original article.
A version of this article originally appeared on Medscape.com.
A consensus statement from the American College of Cardiology (ACC), the American College of Emergency Physicians (ACEP), and the Society for Cardiovascular Angiography & Interventions (SCAI) outlines recommendations for a systematic approach for the care of patients with an acute myocardial infarction (AMI) during the COVID-19 pandemic.
The statement was published in the Journal of the American College of Cardiology.
During the COVID-19 pandemic, percutaneous coronary intervention (PCI) remains the standard of care for patients with ST-segment elevation MI (STEMI) at PCI-capable hospitals when it can be provided in a timely fashion in a dedicated cardiac catheterization laboratory with an expert care team wearing personal protection equipment (PPE), the writing group advised.
“A fibrinolysis-based strategy may be entertained at non-PCI capable referral hospitals or in specific situations where primary PCI cannot be executed or is not deemed the best option,” they said.
SCAI President Ehtisham Mahmud, MD, of the University of California, San Diego, and the writing group also said that clinicians should recognize that cardiovascular manifestations of COVID-19 are “complex” in patients presenting with AMI, myocarditis simulating a STEMI, stress cardiomyopathy, nonischemic cardiomyopathy, coronary spasm, or nonspecific myocardial injury.
A “broad differential diagnosis for ST elevations (including COVID-associated myocarditis) should be considered in the ED prior to choosing a reperfusion strategy,” they advised.
In the absence of hemodynamic instability or ongoing ischemic symptoms, non-STEMI patients with known or suspected COVID-19 are best managed with an initial medical stabilization strategy, the group said.
They also said it is “imperative that health care workers use appropriate PPE for all invasive procedures during this pandemic” and that new rapid COVID-19 testing be “expeditiously” disseminated to all hospitals that manage patients with AMI.
Major challenges are that the prevalence of the COVID-19 in the United States remains unknown and there is the risk for asymptomatic spread.
The writing group said it’s “critical” to “inform the public that we can minimize exposure to the coronavirus so they can continue to call the Emergency Medical System (EMS) for acute ischemic heart disease symptoms and therefore get the appropriate level of cardiac care that their presentation warrants.”
This research had no commercial funding. Dr. Mahmud reported receiving clinical trial research support from Corindus, Abbott Vascular, and CSI; consulting with Medtronic; and consulting and equity with Abiomed. A complete list of author disclosures is included with the original article.
A version of this article originally appeared on Medscape.com.
A consensus statement from the American College of Cardiology (ACC), the American College of Emergency Physicians (ACEP), and the Society for Cardiovascular Angiography & Interventions (SCAI) outlines recommendations for a systematic approach for the care of patients with an acute myocardial infarction (AMI) during the COVID-19 pandemic.
The statement was published in the Journal of the American College of Cardiology.
During the COVID-19 pandemic, percutaneous coronary intervention (PCI) remains the standard of care for patients with ST-segment elevation MI (STEMI) at PCI-capable hospitals when it can be provided in a timely fashion in a dedicated cardiac catheterization laboratory with an expert care team wearing personal protection equipment (PPE), the writing group advised.
“A fibrinolysis-based strategy may be entertained at non-PCI capable referral hospitals or in specific situations where primary PCI cannot be executed or is not deemed the best option,” they said.
SCAI President Ehtisham Mahmud, MD, of the University of California, San Diego, and the writing group also said that clinicians should recognize that cardiovascular manifestations of COVID-19 are “complex” in patients presenting with AMI, myocarditis simulating a STEMI, stress cardiomyopathy, nonischemic cardiomyopathy, coronary spasm, or nonspecific myocardial injury.
A “broad differential diagnosis for ST elevations (including COVID-associated myocarditis) should be considered in the ED prior to choosing a reperfusion strategy,” they advised.
In the absence of hemodynamic instability or ongoing ischemic symptoms, non-STEMI patients with known or suspected COVID-19 are best managed with an initial medical stabilization strategy, the group said.
They also said it is “imperative that health care workers use appropriate PPE for all invasive procedures during this pandemic” and that new rapid COVID-19 testing be “expeditiously” disseminated to all hospitals that manage patients with AMI.
Major challenges are that the prevalence of the COVID-19 in the United States remains unknown and there is the risk for asymptomatic spread.
The writing group said it’s “critical” to “inform the public that we can minimize exposure to the coronavirus so they can continue to call the Emergency Medical System (EMS) for acute ischemic heart disease symptoms and therefore get the appropriate level of cardiac care that their presentation warrants.”
This research had no commercial funding. Dr. Mahmud reported receiving clinical trial research support from Corindus, Abbott Vascular, and CSI; consulting with Medtronic; and consulting and equity with Abiomed. A complete list of author disclosures is included with the original article.
A version of this article originally appeared on Medscape.com.
Compounded analgesic topical creams offer no benefit in treatment of localized chronic pain
Background: Federal health system programs, including TRICARE for military personnel, spent $259 million in 2013 and $746 million in 2014 for compounded analgesic medications despite a dearth of efficacy data. The purpose of this trial was to evaluate the efficacy and functional impact of this class of medications for chronic localized pain.
Study design: Randomized, double-blind, parallel trial.
Setting: Walter Reed National Military Medical Center.
Synopsis: A total of 339 patients with at least mild, chronic localized pain were allocated to three subgroups of 133 patients based on pain type; neuropathic, nociceptive, or mixed pain. The patients in the neuropathic pain arm received a compounded formulation containing 10% ketamine, 6% gabapentin, 0.2% clonidine, and 2% lidocaine; in the nociceptive pain arm, a formulation containing 10% ketoprofen, 2% baclofen, 2% cyclobenzaprine, and 2% lidocaine; and in the mixed pain arm, a formulation containing 10% ketamine, 6% gabapentin, 3% diclofenac, 2% baclofen, 2% cyclobenzaprine, and 2% lidocaine. Half of the patients in each subgroup received the compounded formulation and the other half received placebo.
The primary outcome was the average pain score at 1 month follow-up, based on self-recorded arithmetic mean pain scores in the preceding week. Secondary outcomes included mean worst pain over the past week, functional improvement (assessed by validated Short-Form 36 Health Survey scores), and satisfaction (measured on a 1 to 5 Likert scale) with the individual treatment regimen.
Patients had small improvements in average pain scores at 1 month in the compounded formulation and placebo subgroups in all pain type categories. No significant differences were noted in the average pain scores compared to baseline, functional improvement or satisfaction in the compounded formulation and placebo groups of the total cohort or in any of the subgroups.
Bottom line: Compounded topical analgesics are costly and ineffective in the treatment of all types of chronic localized pain.
Citation: Brutcher RE et al. Compounded topical pain creams to treat localized chronic pain. Ann Intern Med. 2019;170(5):309-18.
Dr. Lambert is a hospital medicine clinician and addiction medicine specialist in the division of hospital medicine at Massachusetts General Hospital.
Background: Federal health system programs, including TRICARE for military personnel, spent $259 million in 2013 and $746 million in 2014 for compounded analgesic medications despite a dearth of efficacy data. The purpose of this trial was to evaluate the efficacy and functional impact of this class of medications for chronic localized pain.
Study design: Randomized, double-blind, parallel trial.
Setting: Walter Reed National Military Medical Center.
Synopsis: A total of 339 patients with at least mild, chronic localized pain were allocated to three subgroups of 133 patients based on pain type; neuropathic, nociceptive, or mixed pain. The patients in the neuropathic pain arm received a compounded formulation containing 10% ketamine, 6% gabapentin, 0.2% clonidine, and 2% lidocaine; in the nociceptive pain arm, a formulation containing 10% ketoprofen, 2% baclofen, 2% cyclobenzaprine, and 2% lidocaine; and in the mixed pain arm, a formulation containing 10% ketamine, 6% gabapentin, 3% diclofenac, 2% baclofen, 2% cyclobenzaprine, and 2% lidocaine. Half of the patients in each subgroup received the compounded formulation and the other half received placebo.
The primary outcome was the average pain score at 1 month follow-up, based on self-recorded arithmetic mean pain scores in the preceding week. Secondary outcomes included mean worst pain over the past week, functional improvement (assessed by validated Short-Form 36 Health Survey scores), and satisfaction (measured on a 1 to 5 Likert scale) with the individual treatment regimen.
Patients had small improvements in average pain scores at 1 month in the compounded formulation and placebo subgroups in all pain type categories. No significant differences were noted in the average pain scores compared to baseline, functional improvement or satisfaction in the compounded formulation and placebo groups of the total cohort or in any of the subgroups.
Bottom line: Compounded topical analgesics are costly and ineffective in the treatment of all types of chronic localized pain.
Citation: Brutcher RE et al. Compounded topical pain creams to treat localized chronic pain. Ann Intern Med. 2019;170(5):309-18.
Dr. Lambert is a hospital medicine clinician and addiction medicine specialist in the division of hospital medicine at Massachusetts General Hospital.
Background: Federal health system programs, including TRICARE for military personnel, spent $259 million in 2013 and $746 million in 2014 for compounded analgesic medications despite a dearth of efficacy data. The purpose of this trial was to evaluate the efficacy and functional impact of this class of medications for chronic localized pain.
Study design: Randomized, double-blind, parallel trial.
Setting: Walter Reed National Military Medical Center.
Synopsis: A total of 339 patients with at least mild, chronic localized pain were allocated to three subgroups of 133 patients based on pain type; neuropathic, nociceptive, or mixed pain. The patients in the neuropathic pain arm received a compounded formulation containing 10% ketamine, 6% gabapentin, 0.2% clonidine, and 2% lidocaine; in the nociceptive pain arm, a formulation containing 10% ketoprofen, 2% baclofen, 2% cyclobenzaprine, and 2% lidocaine; and in the mixed pain arm, a formulation containing 10% ketamine, 6% gabapentin, 3% diclofenac, 2% baclofen, 2% cyclobenzaprine, and 2% lidocaine. Half of the patients in each subgroup received the compounded formulation and the other half received placebo.
The primary outcome was the average pain score at 1 month follow-up, based on self-recorded arithmetic mean pain scores in the preceding week. Secondary outcomes included mean worst pain over the past week, functional improvement (assessed by validated Short-Form 36 Health Survey scores), and satisfaction (measured on a 1 to 5 Likert scale) with the individual treatment regimen.
Patients had small improvements in average pain scores at 1 month in the compounded formulation and placebo subgroups in all pain type categories. No significant differences were noted in the average pain scores compared to baseline, functional improvement or satisfaction in the compounded formulation and placebo groups of the total cohort or in any of the subgroups.
Bottom line: Compounded topical analgesics are costly and ineffective in the treatment of all types of chronic localized pain.
Citation: Brutcher RE et al. Compounded topical pain creams to treat localized chronic pain. Ann Intern Med. 2019;170(5):309-18.
Dr. Lambert is a hospital medicine clinician and addiction medicine specialist in the division of hospital medicine at Massachusetts General Hospital.
Observation pathway safely reduces acute pancreatitis hospitalization rate
For patients diagnosed with mild acute pancreatitis (AP) in the ED, an observation pathway may significantly reduce hospitalization rate and associated costs without compromising patient safety or quality of care, according to investigators.
Over a 2-year period, the observation pathway at Beth Israel Deaconess Medical Center, Boston, reduced hospitalizations by 31.2%, reported lead author Awais Ahmed, MD, of Harvard Medical School, Boston, and colleagues.
“AP carries a significant burden on the health care system, accounting for the third most common reason for gastrointestinal-related admissions in the United States,” the investigators wrote in the Journal of Clinical Gastroenterology. “As such, streamlining care for AP patients to reduce admissions can reduce the associated financial burden.”
The investigators’ efforts to reduce admissions for patients with AP began in 2016, when they first implemented an observation pathway at Beth Israel. This 6-month pilot study demonstrated proof of concept because it reduced admissions by 22.2% and shortened average length of stay without negatively affecting rates of mortality or readmission.
Based on these encouraging results, the hospital implemented the observation pathway as a standard of care. The present study analyzed 2 years of data from patients diagnosed with AP following the end of the pilot study. The primary outcome was hospitalization rate. Secondary outcomes included health care utilization, 30-day mortality rate, 30-day readmission rate, and median length of stay.
Patients with mild AP entered the observation pathway at the discretion of the supervising clinician, as well as based on absence of exclusion criteria, such as end organ damage, chronic pancreatitis, cholangitis, and other considerations.
Over 2 years, 165 patients were diagnosed with AP in the ED, of whom 118 (71.5%) had mild AP. From this latter group, 54 (45.8%) entered the observation pathway, while 64 (54.2%) were admitted as inpatients, primarily (n = 58) because of exclusion criteria. Within the observation group, 45 out of 54 patients (83.3%) successfully completed the pathway and were discharged. Six of these patients were readmitted within 30 days. Among the 9 patients who did not complete the pathway, 6 failed to meet discharge criteria, resulting in admission, whereas 3 patients left the hospital against medical advice.
Combining data from this 2-year period and the pilot study, the hospitalization rate for mild AP was reduced by 31.2%. In the present study, hospitalization was reduced by 27% for patients with AP of any severity. This figure was steady over a 3-year period, at 25.8%.
Median length of stay for patients with mild AP was significantly shorter in the present study’s observation pathway than in a historical cohort (19.9 vs. 72.0 hours); this remained significant when also including patients from the pilot study (21.2 vs. 72.0 hours). Compared with the historic cohort, patients in the observation had significantly fewer radiographic studies, and more patients were discharged in less than 24 hours. Meanwhile, 30-day readmission and mortality rates remained unchanged.
“In summary, our long-term data of a single center emergency department–based observation management pathway for mild AP demonstrates durability over more than 2 years in maintaining its objective of reducing hospitalization,” the investigators concluded. “This is associated with a [shorter] length of stay, and reduced health care resource utilization, suggesting a possible decrease in financial cost of managing mild AP, without affecting readmission rates or mortality.”
These findings encourage further research, the investigators suggested, while noting that the observation pathway may not be appropriate for all treatment centers.
“The generalizability of the pathway is limited, given its single center location, and tertiary environment,” the investigators wrote. “Smaller hospitals, lacking multidisciplinary support for complications of AP, may find it challenging to implement such a pathway, and thus triage these patients for inpatient admission at their facility or to nearby tertiary centers.”The investigators reported no conflicts of interest.
SOURCE: Ahmed A et al. J Clin Gastroenterol. 2020 Apr 14. doi: 10.1097/MCG.0000000000001354.
For patients diagnosed with mild acute pancreatitis (AP) in the ED, an observation pathway may significantly reduce hospitalization rate and associated costs without compromising patient safety or quality of care, according to investigators.
Over a 2-year period, the observation pathway at Beth Israel Deaconess Medical Center, Boston, reduced hospitalizations by 31.2%, reported lead author Awais Ahmed, MD, of Harvard Medical School, Boston, and colleagues.
“AP carries a significant burden on the health care system, accounting for the third most common reason for gastrointestinal-related admissions in the United States,” the investigators wrote in the Journal of Clinical Gastroenterology. “As such, streamlining care for AP patients to reduce admissions can reduce the associated financial burden.”
The investigators’ efforts to reduce admissions for patients with AP began in 2016, when they first implemented an observation pathway at Beth Israel. This 6-month pilot study demonstrated proof of concept because it reduced admissions by 22.2% and shortened average length of stay without negatively affecting rates of mortality or readmission.
Based on these encouraging results, the hospital implemented the observation pathway as a standard of care. The present study analyzed 2 years of data from patients diagnosed with AP following the end of the pilot study. The primary outcome was hospitalization rate. Secondary outcomes included health care utilization, 30-day mortality rate, 30-day readmission rate, and median length of stay.
Patients with mild AP entered the observation pathway at the discretion of the supervising clinician, as well as based on absence of exclusion criteria, such as end organ damage, chronic pancreatitis, cholangitis, and other considerations.
Over 2 years, 165 patients were diagnosed with AP in the ED, of whom 118 (71.5%) had mild AP. From this latter group, 54 (45.8%) entered the observation pathway, while 64 (54.2%) were admitted as inpatients, primarily (n = 58) because of exclusion criteria. Within the observation group, 45 out of 54 patients (83.3%) successfully completed the pathway and were discharged. Six of these patients were readmitted within 30 days. Among the 9 patients who did not complete the pathway, 6 failed to meet discharge criteria, resulting in admission, whereas 3 patients left the hospital against medical advice.
Combining data from this 2-year period and the pilot study, the hospitalization rate for mild AP was reduced by 31.2%. In the present study, hospitalization was reduced by 27% for patients with AP of any severity. This figure was steady over a 3-year period, at 25.8%.
Median length of stay for patients with mild AP was significantly shorter in the present study’s observation pathway than in a historical cohort (19.9 vs. 72.0 hours); this remained significant when also including patients from the pilot study (21.2 vs. 72.0 hours). Compared with the historic cohort, patients in the observation had significantly fewer radiographic studies, and more patients were discharged in less than 24 hours. Meanwhile, 30-day readmission and mortality rates remained unchanged.
“In summary, our long-term data of a single center emergency department–based observation management pathway for mild AP demonstrates durability over more than 2 years in maintaining its objective of reducing hospitalization,” the investigators concluded. “This is associated with a [shorter] length of stay, and reduced health care resource utilization, suggesting a possible decrease in financial cost of managing mild AP, without affecting readmission rates or mortality.”
These findings encourage further research, the investigators suggested, while noting that the observation pathway may not be appropriate for all treatment centers.
“The generalizability of the pathway is limited, given its single center location, and tertiary environment,” the investigators wrote. “Smaller hospitals, lacking multidisciplinary support for complications of AP, may find it challenging to implement such a pathway, and thus triage these patients for inpatient admission at their facility or to nearby tertiary centers.”The investigators reported no conflicts of interest.
SOURCE: Ahmed A et al. J Clin Gastroenterol. 2020 Apr 14. doi: 10.1097/MCG.0000000000001354.
For patients diagnosed with mild acute pancreatitis (AP) in the ED, an observation pathway may significantly reduce hospitalization rate and associated costs without compromising patient safety or quality of care, according to investigators.
Over a 2-year period, the observation pathway at Beth Israel Deaconess Medical Center, Boston, reduced hospitalizations by 31.2%, reported lead author Awais Ahmed, MD, of Harvard Medical School, Boston, and colleagues.
“AP carries a significant burden on the health care system, accounting for the third most common reason for gastrointestinal-related admissions in the United States,” the investigators wrote in the Journal of Clinical Gastroenterology. “As such, streamlining care for AP patients to reduce admissions can reduce the associated financial burden.”
The investigators’ efforts to reduce admissions for patients with AP began in 2016, when they first implemented an observation pathway at Beth Israel. This 6-month pilot study demonstrated proof of concept because it reduced admissions by 22.2% and shortened average length of stay without negatively affecting rates of mortality or readmission.
Based on these encouraging results, the hospital implemented the observation pathway as a standard of care. The present study analyzed 2 years of data from patients diagnosed with AP following the end of the pilot study. The primary outcome was hospitalization rate. Secondary outcomes included health care utilization, 30-day mortality rate, 30-day readmission rate, and median length of stay.
Patients with mild AP entered the observation pathway at the discretion of the supervising clinician, as well as based on absence of exclusion criteria, such as end organ damage, chronic pancreatitis, cholangitis, and other considerations.
Over 2 years, 165 patients were diagnosed with AP in the ED, of whom 118 (71.5%) had mild AP. From this latter group, 54 (45.8%) entered the observation pathway, while 64 (54.2%) were admitted as inpatients, primarily (n = 58) because of exclusion criteria. Within the observation group, 45 out of 54 patients (83.3%) successfully completed the pathway and were discharged. Six of these patients were readmitted within 30 days. Among the 9 patients who did not complete the pathway, 6 failed to meet discharge criteria, resulting in admission, whereas 3 patients left the hospital against medical advice.
Combining data from this 2-year period and the pilot study, the hospitalization rate for mild AP was reduced by 31.2%. In the present study, hospitalization was reduced by 27% for patients with AP of any severity. This figure was steady over a 3-year period, at 25.8%.
Median length of stay for patients with mild AP was significantly shorter in the present study’s observation pathway than in a historical cohort (19.9 vs. 72.0 hours); this remained significant when also including patients from the pilot study (21.2 vs. 72.0 hours). Compared with the historic cohort, patients in the observation had significantly fewer radiographic studies, and more patients were discharged in less than 24 hours. Meanwhile, 30-day readmission and mortality rates remained unchanged.
“In summary, our long-term data of a single center emergency department–based observation management pathway for mild AP demonstrates durability over more than 2 years in maintaining its objective of reducing hospitalization,” the investigators concluded. “This is associated with a [shorter] length of stay, and reduced health care resource utilization, suggesting a possible decrease in financial cost of managing mild AP, without affecting readmission rates or mortality.”
These findings encourage further research, the investigators suggested, while noting that the observation pathway may not be appropriate for all treatment centers.
“The generalizability of the pathway is limited, given its single center location, and tertiary environment,” the investigators wrote. “Smaller hospitals, lacking multidisciplinary support for complications of AP, may find it challenging to implement such a pathway, and thus triage these patients for inpatient admission at their facility or to nearby tertiary centers.”The investigators reported no conflicts of interest.
SOURCE: Ahmed A et al. J Clin Gastroenterol. 2020 Apr 14. doi: 10.1097/MCG.0000000000001354.
FROM JOURNAL OF CLINICAL GASTROENTEROLOGY
Rural ICU capacity could be strained by COVID-19
The nonmetropolitan, largely rural, areas of the United States have fewer ICU beds than do urban areas, but their populations may be at higher risk for COVID-19 complications, according to the Kaiser Family Foundation.
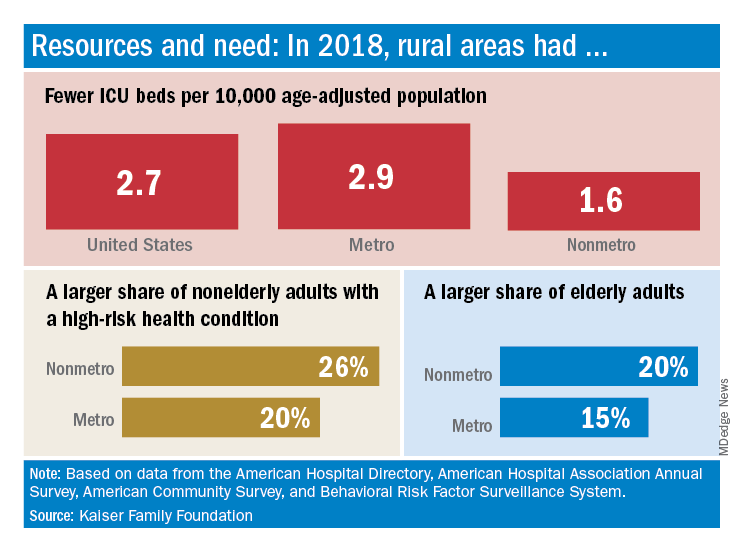
In 2018, the United States had 2.7 ICU beds per 10,000 age-adjusted population, but that number drops to 1.6 beds per 10,000 in nonmetro America and rises to 2.9 per 10,000 in metro areas. Counts for all hospital beds were much closer: 21.6 per 10,000 (rural) and 23.9 per 10,000 (urban), Kaiser investigators reported.
“The novel coronavirus was slower to spread to rural areas in the U.S., but that appears to be changing, with new outbreaks becoming evident in less densely populated parts of the country,” Kendal Orgera and associates said in a recent analysis.
Those rural areas have COVID-19 issues beyond ICU bed counts. Populations in nonmetro areas are less healthy – 26% of adults under age 65 years had a preexisting medical condition in 2018, compared with 20% in metro areas – and older – 20% of people are 65 and older, versus 15% in metro areas, they said.
“If coronavirus continues to spread in rural communities across the U.S., it is possible many [nonmetro] areas will face shortages of ICU beds with limited options to adapt. Patients in rural areas experiencing more severe illnesses may be transferred to hospitals with greater capacity, but if nearby urban areas are also overwhelmed, transfer may not be an option,” Ms. Orgera and associates wrote.
They defined nonmetro counties as those with rural towns of fewer than 2,500 people and/or “urban areas with populations ranging from 2,500 to 49,999 that are not part of larger labor market areas.” The Kaiser analysis involved 2018 data from the American Hospital Association, American Hospital Directory, American Community Survey, and the Behavioral Risk Factor Surveillance System.
The nonmetropolitan, largely rural, areas of the United States have fewer ICU beds than do urban areas, but their populations may be at higher risk for COVID-19 complications, according to the Kaiser Family Foundation.
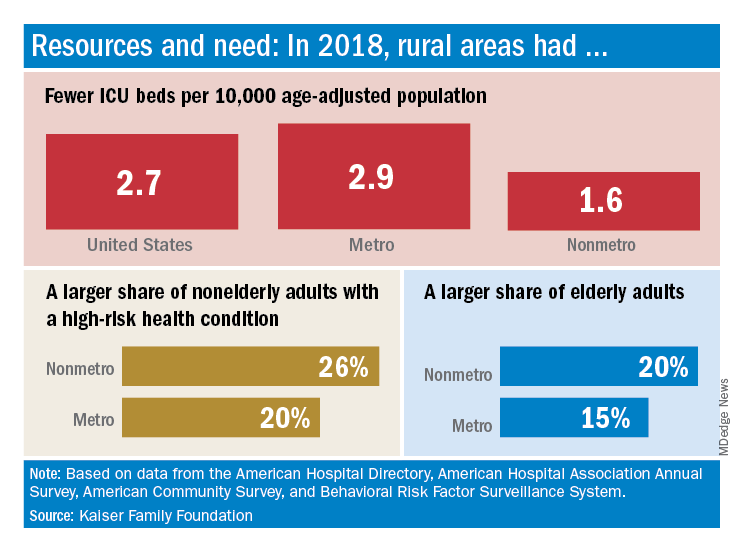
In 2018, the United States had 2.7 ICU beds per 10,000 age-adjusted population, but that number drops to 1.6 beds per 10,000 in nonmetro America and rises to 2.9 per 10,000 in metro areas. Counts for all hospital beds were much closer: 21.6 per 10,000 (rural) and 23.9 per 10,000 (urban), Kaiser investigators reported.
“The novel coronavirus was slower to spread to rural areas in the U.S., but that appears to be changing, with new outbreaks becoming evident in less densely populated parts of the country,” Kendal Orgera and associates said in a recent analysis.
Those rural areas have COVID-19 issues beyond ICU bed counts. Populations in nonmetro areas are less healthy – 26% of adults under age 65 years had a preexisting medical condition in 2018, compared with 20% in metro areas – and older – 20% of people are 65 and older, versus 15% in metro areas, they said.
“If coronavirus continues to spread in rural communities across the U.S., it is possible many [nonmetro] areas will face shortages of ICU beds with limited options to adapt. Patients in rural areas experiencing more severe illnesses may be transferred to hospitals with greater capacity, but if nearby urban areas are also overwhelmed, transfer may not be an option,” Ms. Orgera and associates wrote.
They defined nonmetro counties as those with rural towns of fewer than 2,500 people and/or “urban areas with populations ranging from 2,500 to 49,999 that are not part of larger labor market areas.” The Kaiser analysis involved 2018 data from the American Hospital Association, American Hospital Directory, American Community Survey, and the Behavioral Risk Factor Surveillance System.
The nonmetropolitan, largely rural, areas of the United States have fewer ICU beds than do urban areas, but their populations may be at higher risk for COVID-19 complications, according to the Kaiser Family Foundation.
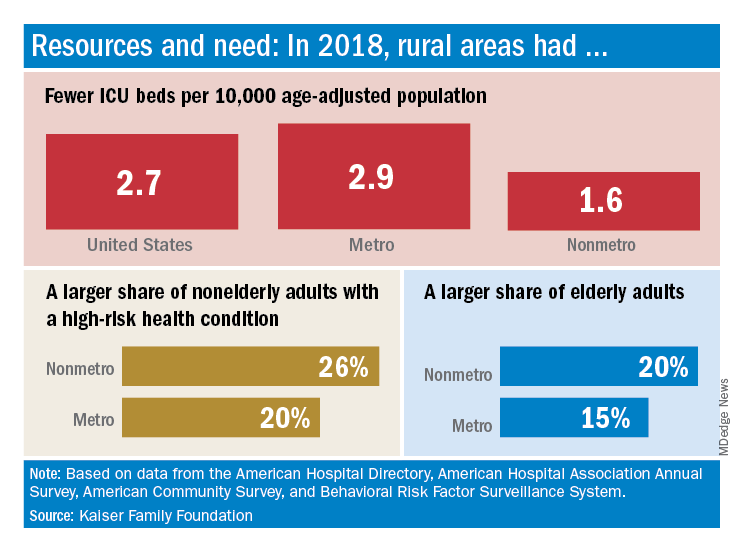
In 2018, the United States had 2.7 ICU beds per 10,000 age-adjusted population, but that number drops to 1.6 beds per 10,000 in nonmetro America and rises to 2.9 per 10,000 in metro areas. Counts for all hospital beds were much closer: 21.6 per 10,000 (rural) and 23.9 per 10,000 (urban), Kaiser investigators reported.
“The novel coronavirus was slower to spread to rural areas in the U.S., but that appears to be changing, with new outbreaks becoming evident in less densely populated parts of the country,” Kendal Orgera and associates said in a recent analysis.
Those rural areas have COVID-19 issues beyond ICU bed counts. Populations in nonmetro areas are less healthy – 26% of adults under age 65 years had a preexisting medical condition in 2018, compared with 20% in metro areas – and older – 20% of people are 65 and older, versus 15% in metro areas, they said.
“If coronavirus continues to spread in rural communities across the U.S., it is possible many [nonmetro] areas will face shortages of ICU beds with limited options to adapt. Patients in rural areas experiencing more severe illnesses may be transferred to hospitals with greater capacity, but if nearby urban areas are also overwhelmed, transfer may not be an option,” Ms. Orgera and associates wrote.
They defined nonmetro counties as those with rural towns of fewer than 2,500 people and/or “urban areas with populations ranging from 2,500 to 49,999 that are not part of larger labor market areas.” The Kaiser analysis involved 2018 data from the American Hospital Association, American Hospital Directory, American Community Survey, and the Behavioral Risk Factor Surveillance System.
Seniors with COVID-19 show unusual symptoms, doctors say
complicating efforts to ensure they get timely and appropriate treatment, according to physicians.
COVID-19 is typically signaled by three symptoms: a fever, an insistent cough, and shortness of breath. But older adults – the age group most at risk of severe complications or death from this condition – may have none of these characteristics.
Instead, seniors may seem “off” – not acting like themselves – early on after being infected by the coronavirus. They may sleep more than usual or stop eating. They may seem unusually apathetic or confused, losing orientation to their surroundings. They may become dizzy and fall. Sometimes, seniors stop speaking or simply collapse.
“With a lot of conditions, older adults don’t present in a typical way, and we’re seeing that with COVID-19 as well,” said Camille Vaughan, MD, section chief of geriatrics and gerontology at Emory University, Atlanta.
The reason has to do with how older bodies respond to illness and infection.
At advanced ages, “someone’s immune response may be blunted and their ability to regulate temperature may be altered,” said Dr. Joseph Ouslander, a professor of geriatric medicine at Florida Atlantic University in Boca Raton.
“Underlying chronic illnesses can mask or interfere with signs of infection,” he said. “Some older people, whether from age-related changes or previous neurologic issues such as a stroke, may have altered cough reflexes. Others with cognitive impairment may not be able to communicate their symptoms.”
Recognizing danger signs is important: If early signs of COVID-19 are missed, seniors may deteriorate before getting needed care. And people may go in and out of their homes without adequate protective measures, risking the spread of infection.
Quratulain Syed, MD, an Atlanta geriatrician, describes a man in his 80s whom she treated in mid-March. Over a period of days, this patient, who had heart disease, diabetes and moderate cognitive impairment, stopped walking and became incontinent and profoundly lethargic. But he didn’t have a fever or a cough. His only respiratory symptom: sneezing off and on.
The man’s elderly spouse called 911 twice. Both times, paramedics checked his vital signs and declared he was OK. After another worried call from the overwhelmed spouse, Dr. Syed insisted the patient be taken to the hospital, where he tested positive for COVID-19.
“I was quite concerned about the paramedics and health aides who’d been in the house and who hadn’t used PPE [personal protective equipment],” Dr. Syed said.
Dr. Sam Torbati, medical director of the emergency department at Cedars-Sinai Medical Center, Los Angeles, describes treating seniors who initially appear to be trauma patients but are found to have COVID-19.
“They get weak and dehydrated,” he said, “and when they stand to walk, they collapse and injure themselves badly.”
Dr. Torbati has seen older adults who are profoundly disoriented and unable to speak and who appear at first to have suffered strokes.
“When we test them, we discover that what’s producing these changes is a central nervous system effect of coronavirus,” he said.
Laura Perry, MD, of the University of California, San Francisco, saw a patient like this several weeks ago. The woman, in her 80s, had what seemed to be a cold before becoming very confused. In the hospital, she couldn’t identify where she was or stay awake during an examination. Dr. Perry diagnosed hypoactive delirium, an altered mental state in which people become inactive and drowsy. The patient tested positive for coronavirus and is still in the ICU.
Anthony Perry, MD, of the department of geriatric medicine at Rush University Medical Center in Chicago, tells of an 81-year-old woman with nausea, vomiting, and diarrhea who tested positive for COVID-19 in the emergency room. After receiving intravenous fluids, oxygen, and medication for her intestinal upset, she returned home after 2 days and is doing well.
Another 80-year-old Rush patient with similar symptoms – nausea and vomiting, but no cough, fever, or shortness of breath – is in intensive care after getting a positive COVID-19 test and due to be put on a ventilator. The difference? This patient is frail with “a lot of cardiovascular disease,” Dr. Perry said. Other than that, it’s not yet clear why some older patients do well while others do not.
So far, reports of cases like these have been anecdotal. But a few physicians are trying to gather more systematic information.
In Switzerland, Sylvain Nguyen, MD, a geriatrician at the University of Lausanne Hospital Center, put together a list of typical and atypical symptoms in older COVID-19 patients for a paper to be published in the Revue Médicale Suisse. Included on the atypical list are changes in a patient’s usual status, delirium, falls, fatigue, lethargy, low blood pressure, painful swallowing, fainting, diarrhea, nausea, vomiting, abdominal pain, and the loss of smell and taste.
Data come from hospitals and nursing homes in Switzerland, Italy, and France, Dr. Nguyen said in an email.
On the front lines, physicians need to make sure they carefully assess an older patient’s symptoms.
“While we have to have a high suspicion of COVID-19 because it’s so dangerous in the older population, there are many other things to consider,” said Kathleen Unroe, MD, a geriatrician at Indiana University, Indianapolis.
Seniors may also do poorly because their routines have changed. In nursing homes and most assisted living centers, activities have stopped and “residents are going to get weaker and more deconditioned because they’re not walking to and from the dining hall,” she said.
At home, isolated seniors may not be getting as much help with medication management or other essential needs from family members who are keeping their distance, other experts suggested. Or they may have become apathetic or depressed.
“I’d want to know ‘What’s the potential this person has had an exposure [to the coronavirus], especially in the last 2 weeks?’ ” said Dr. Vaughan of Emory. “Do they have home health personnel coming in? Have they gotten together with other family members? Are chronic conditions being controlled? Is there another diagnosis that seems more likely?”
“Someone may be just having a bad day. But if they’re not themselves for a couple of days, absolutely reach out to a primary care doctor or a local health system hotline to see if they meet the threshold for [coronavirus] testing,” Dr. Vaughan advised. “Be persistent. If you get a ‘no’ the first time and things aren’t improving, call back and ask again.”
Kaiser Health News (khn.org) is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
complicating efforts to ensure they get timely and appropriate treatment, according to physicians.
COVID-19 is typically signaled by three symptoms: a fever, an insistent cough, and shortness of breath. But older adults – the age group most at risk of severe complications or death from this condition – may have none of these characteristics.
Instead, seniors may seem “off” – not acting like themselves – early on after being infected by the coronavirus. They may sleep more than usual or stop eating. They may seem unusually apathetic or confused, losing orientation to their surroundings. They may become dizzy and fall. Sometimes, seniors stop speaking or simply collapse.
“With a lot of conditions, older adults don’t present in a typical way, and we’re seeing that with COVID-19 as well,” said Camille Vaughan, MD, section chief of geriatrics and gerontology at Emory University, Atlanta.
The reason has to do with how older bodies respond to illness and infection.
At advanced ages, “someone’s immune response may be blunted and their ability to regulate temperature may be altered,” said Dr. Joseph Ouslander, a professor of geriatric medicine at Florida Atlantic University in Boca Raton.
“Underlying chronic illnesses can mask or interfere with signs of infection,” he said. “Some older people, whether from age-related changes or previous neurologic issues such as a stroke, may have altered cough reflexes. Others with cognitive impairment may not be able to communicate their symptoms.”
Recognizing danger signs is important: If early signs of COVID-19 are missed, seniors may deteriorate before getting needed care. And people may go in and out of their homes without adequate protective measures, risking the spread of infection.
Quratulain Syed, MD, an Atlanta geriatrician, describes a man in his 80s whom she treated in mid-March. Over a period of days, this patient, who had heart disease, diabetes and moderate cognitive impairment, stopped walking and became incontinent and profoundly lethargic. But he didn’t have a fever or a cough. His only respiratory symptom: sneezing off and on.
The man’s elderly spouse called 911 twice. Both times, paramedics checked his vital signs and declared he was OK. After another worried call from the overwhelmed spouse, Dr. Syed insisted the patient be taken to the hospital, where he tested positive for COVID-19.
“I was quite concerned about the paramedics and health aides who’d been in the house and who hadn’t used PPE [personal protective equipment],” Dr. Syed said.
Dr. Sam Torbati, medical director of the emergency department at Cedars-Sinai Medical Center, Los Angeles, describes treating seniors who initially appear to be trauma patients but are found to have COVID-19.
“They get weak and dehydrated,” he said, “and when they stand to walk, they collapse and injure themselves badly.”
Dr. Torbati has seen older adults who are profoundly disoriented and unable to speak and who appear at first to have suffered strokes.
“When we test them, we discover that what’s producing these changes is a central nervous system effect of coronavirus,” he said.
Laura Perry, MD, of the University of California, San Francisco, saw a patient like this several weeks ago. The woman, in her 80s, had what seemed to be a cold before becoming very confused. In the hospital, she couldn’t identify where she was or stay awake during an examination. Dr. Perry diagnosed hypoactive delirium, an altered mental state in which people become inactive and drowsy. The patient tested positive for coronavirus and is still in the ICU.
Anthony Perry, MD, of the department of geriatric medicine at Rush University Medical Center in Chicago, tells of an 81-year-old woman with nausea, vomiting, and diarrhea who tested positive for COVID-19 in the emergency room. After receiving intravenous fluids, oxygen, and medication for her intestinal upset, she returned home after 2 days and is doing well.
Another 80-year-old Rush patient with similar symptoms – nausea and vomiting, but no cough, fever, or shortness of breath – is in intensive care after getting a positive COVID-19 test and due to be put on a ventilator. The difference? This patient is frail with “a lot of cardiovascular disease,” Dr. Perry said. Other than that, it’s not yet clear why some older patients do well while others do not.
So far, reports of cases like these have been anecdotal. But a few physicians are trying to gather more systematic information.
In Switzerland, Sylvain Nguyen, MD, a geriatrician at the University of Lausanne Hospital Center, put together a list of typical and atypical symptoms in older COVID-19 patients for a paper to be published in the Revue Médicale Suisse. Included on the atypical list are changes in a patient’s usual status, delirium, falls, fatigue, lethargy, low blood pressure, painful swallowing, fainting, diarrhea, nausea, vomiting, abdominal pain, and the loss of smell and taste.
Data come from hospitals and nursing homes in Switzerland, Italy, and France, Dr. Nguyen said in an email.
On the front lines, physicians need to make sure they carefully assess an older patient’s symptoms.
“While we have to have a high suspicion of COVID-19 because it’s so dangerous in the older population, there are many other things to consider,” said Kathleen Unroe, MD, a geriatrician at Indiana University, Indianapolis.
Seniors may also do poorly because their routines have changed. In nursing homes and most assisted living centers, activities have stopped and “residents are going to get weaker and more deconditioned because they’re not walking to and from the dining hall,” she said.
At home, isolated seniors may not be getting as much help with medication management or other essential needs from family members who are keeping their distance, other experts suggested. Or they may have become apathetic or depressed.
“I’d want to know ‘What’s the potential this person has had an exposure [to the coronavirus], especially in the last 2 weeks?’ ” said Dr. Vaughan of Emory. “Do they have home health personnel coming in? Have they gotten together with other family members? Are chronic conditions being controlled? Is there another diagnosis that seems more likely?”
“Someone may be just having a bad day. But if they’re not themselves for a couple of days, absolutely reach out to a primary care doctor or a local health system hotline to see if they meet the threshold for [coronavirus] testing,” Dr. Vaughan advised. “Be persistent. If you get a ‘no’ the first time and things aren’t improving, call back and ask again.”
Kaiser Health News (khn.org) is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
complicating efforts to ensure they get timely and appropriate treatment, according to physicians.
COVID-19 is typically signaled by three symptoms: a fever, an insistent cough, and shortness of breath. But older adults – the age group most at risk of severe complications or death from this condition – may have none of these characteristics.
Instead, seniors may seem “off” – not acting like themselves – early on after being infected by the coronavirus. They may sleep more than usual or stop eating. They may seem unusually apathetic or confused, losing orientation to their surroundings. They may become dizzy and fall. Sometimes, seniors stop speaking or simply collapse.
“With a lot of conditions, older adults don’t present in a typical way, and we’re seeing that with COVID-19 as well,” said Camille Vaughan, MD, section chief of geriatrics and gerontology at Emory University, Atlanta.
The reason has to do with how older bodies respond to illness and infection.
At advanced ages, “someone’s immune response may be blunted and their ability to regulate temperature may be altered,” said Dr. Joseph Ouslander, a professor of geriatric medicine at Florida Atlantic University in Boca Raton.
“Underlying chronic illnesses can mask or interfere with signs of infection,” he said. “Some older people, whether from age-related changes or previous neurologic issues such as a stroke, may have altered cough reflexes. Others with cognitive impairment may not be able to communicate their symptoms.”
Recognizing danger signs is important: If early signs of COVID-19 are missed, seniors may deteriorate before getting needed care. And people may go in and out of their homes without adequate protective measures, risking the spread of infection.
Quratulain Syed, MD, an Atlanta geriatrician, describes a man in his 80s whom she treated in mid-March. Over a period of days, this patient, who had heart disease, diabetes and moderate cognitive impairment, stopped walking and became incontinent and profoundly lethargic. But he didn’t have a fever or a cough. His only respiratory symptom: sneezing off and on.
The man’s elderly spouse called 911 twice. Both times, paramedics checked his vital signs and declared he was OK. After another worried call from the overwhelmed spouse, Dr. Syed insisted the patient be taken to the hospital, where he tested positive for COVID-19.
“I was quite concerned about the paramedics and health aides who’d been in the house and who hadn’t used PPE [personal protective equipment],” Dr. Syed said.
Dr. Sam Torbati, medical director of the emergency department at Cedars-Sinai Medical Center, Los Angeles, describes treating seniors who initially appear to be trauma patients but are found to have COVID-19.
“They get weak and dehydrated,” he said, “and when they stand to walk, they collapse and injure themselves badly.”
Dr. Torbati has seen older adults who are profoundly disoriented and unable to speak and who appear at first to have suffered strokes.
“When we test them, we discover that what’s producing these changes is a central nervous system effect of coronavirus,” he said.
Laura Perry, MD, of the University of California, San Francisco, saw a patient like this several weeks ago. The woman, in her 80s, had what seemed to be a cold before becoming very confused. In the hospital, she couldn’t identify where she was or stay awake during an examination. Dr. Perry diagnosed hypoactive delirium, an altered mental state in which people become inactive and drowsy. The patient tested positive for coronavirus and is still in the ICU.
Anthony Perry, MD, of the department of geriatric medicine at Rush University Medical Center in Chicago, tells of an 81-year-old woman with nausea, vomiting, and diarrhea who tested positive for COVID-19 in the emergency room. After receiving intravenous fluids, oxygen, and medication for her intestinal upset, she returned home after 2 days and is doing well.
Another 80-year-old Rush patient with similar symptoms – nausea and vomiting, but no cough, fever, or shortness of breath – is in intensive care after getting a positive COVID-19 test and due to be put on a ventilator. The difference? This patient is frail with “a lot of cardiovascular disease,” Dr. Perry said. Other than that, it’s not yet clear why some older patients do well while others do not.
So far, reports of cases like these have been anecdotal. But a few physicians are trying to gather more systematic information.
In Switzerland, Sylvain Nguyen, MD, a geriatrician at the University of Lausanne Hospital Center, put together a list of typical and atypical symptoms in older COVID-19 patients for a paper to be published in the Revue Médicale Suisse. Included on the atypical list are changes in a patient’s usual status, delirium, falls, fatigue, lethargy, low blood pressure, painful swallowing, fainting, diarrhea, nausea, vomiting, abdominal pain, and the loss of smell and taste.
Data come from hospitals and nursing homes in Switzerland, Italy, and France, Dr. Nguyen said in an email.
On the front lines, physicians need to make sure they carefully assess an older patient’s symptoms.
“While we have to have a high suspicion of COVID-19 because it’s so dangerous in the older population, there are many other things to consider,” said Kathleen Unroe, MD, a geriatrician at Indiana University, Indianapolis.
Seniors may also do poorly because their routines have changed. In nursing homes and most assisted living centers, activities have stopped and “residents are going to get weaker and more deconditioned because they’re not walking to and from the dining hall,” she said.
At home, isolated seniors may not be getting as much help with medication management or other essential needs from family members who are keeping their distance, other experts suggested. Or they may have become apathetic or depressed.
“I’d want to know ‘What’s the potential this person has had an exposure [to the coronavirus], especially in the last 2 weeks?’ ” said Dr. Vaughan of Emory. “Do they have home health personnel coming in? Have they gotten together with other family members? Are chronic conditions being controlled? Is there another diagnosis that seems more likely?”
“Someone may be just having a bad day. But if they’re not themselves for a couple of days, absolutely reach out to a primary care doctor or a local health system hotline to see if they meet the threshold for [coronavirus] testing,” Dr. Vaughan advised. “Be persistent. If you get a ‘no’ the first time and things aren’t improving, call back and ask again.”
Kaiser Health News (khn.org) is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.