User login
Alan F. Schatzberg, MD, on the state of psychiatry
For this Psychiatry Leaders’ Perspectives, Awais Aftab, MD, interviewed Alan F. Schatzberg, MD. Dr. Schatzberg is the Kenneth T. Norris, Jr., Professor of Psychiatry and Behavioral Sciences at Stanford University. He served as the Chair of the Department at Stanford until 2010 and currently directs the Stanford Mood Disorders Center. He was the 136th president of the American Psychiatric Association (APA) (2009-2010). He has been an active investigator in the biology and psychopharmacology of depressive disorders, and has authored more than 700 publications and abstracts, including Schatzberg’s Manual of Clinical Psychopharmacology. Dr. Schatzberg is also the coeditor of the Textbook of Psychopharmacology with Charles B. Nemeroff, MD, PhD. He is a Past President of the American College of Neuropsychopharmacology (ACNP) and the Society of Biological Psychiatry, and was also the Secretary-General of the International Society of Psychoneuroendocrinology (ISPNE). In 2003, he was elected to the Institute of Medicine of the National Academy of Sciences (National Academy of Medicine). He has received numerous prestigious awards, including the 2005 Distinguished Service in Psychiatry Award from the American College of Psychiatrists, the 2005 Falcone Award from the National Alliance for Research in Schizophrenia and Affective Disorders, the 2014 Kraepelin Gold Medal from the Max Planck Institute of Psychiatry, the 2015 Gold Medal from the Society of Biological Psychiatry, the 2015 Lifetime Achievement Award of the ISPNE, the 2017 Julius Axelrod Mentorship Award from the ACNP, the 2018 Donald Klein, MD, Lifetime Achievement Award from the American Society of Clinical Psychopharmacology, and the 2018 Jules Marmor, MD, Award for Biopsychosocial Research from the APA.
Dr. Aftab: You have devoted much of your career to the development of psychopharmacology. What is your perspective on where the field of psychopharmacology stands at present, especially amid the widespread recognition of “treatment resistance” as a pervasive phenomenon and the scarcity of validated neurobiologic etiological models for psychiatric disorders?
Dr. Schatzberg: We have made considerable progress in the development of new classes of agents for major depression, but as we develop new agents, we still see a large percentage of patients who do not seem to demonstrate adequate responses, particularly in major depressive disorder. This has driven us to look for agents that work differently than previous ones. Although we have some new agents with seeming efficacy and newer mechanisms of action, eg, esketamine, these have largely been derived from clinical, often serendipitous, observations of antidepressant effects rather than from prospective development based on a known pharmacological effect or a biological construct of the disorder. Another intriguing and possibly effective anxiolytic and antidepressive agent is psilocybin, whose potential use is largely derived from clinicians who found it helpful in their practices in combination with psychotherapy. These 2 demonstrate how as we branch out into new territory, we find ourselves moving more and more toward drugs of known clinical risk; eg, mind-altering agents or drugs of abuse. These agents may offer risk-benefit ratios that can ultimately prove to be less attractive than what we might have wanted when we ventured on the journey. Unfortunately, there has been little dialogue about the limitations of several of these agents.
In the case of esketamine, the notion has been that the drug is a blocker of the N-methyl-
One approach that has been applied recently is target validation that purports to use functional MRI to assess behavioral and cognitive effects of drugs to allow inferences regarding efficacy in specific disorders. As we have discussed in a recent paper published in the American Journal of Psychiatry,4 this can be quite misleading and may provide both false positive and negative information. From my perspective, these tests do not appear sensitive enough to screen for patients having a disorder, nor for assessing possible drug effects in those patients. Thus, it is unclear if they can provide answers today that we can be confident in.
Continue to: Dr. Aftab...
Dr. Aftab: What do you see as some of the strengths of psychiatry as a profession?
Dr. Schatzberg: Psychiatry as a specialty combines 2 major perspectives—psychological processes and psychobiology—to develop methods for treating patients who suffer from disorders of the mind/brain. It is the most challenging of our specialties because we cannot study the brain directly. We cannot do procedures as we do in cardiology and pulmonology because they may prove dangerously invasive. That hands-off approach limits us, but for the curious it provides an opportunity to begin to unravel the processes that underlie brain functioning. Fortunately, we have therapies—both psychosocial and somatic—that can provide great relief to patients. These can be shown to be effective in sufficient numbers of patients to help many.
Dr. Aftab: Are there ways in which the status quo in psychiatry falls short of the ideal? What are our areas of relative weakness?
Dr. Schatzberg: We need to train our residents in a host of approaches, and not just medications and psychotherapy. They need to understand the basis of brain stimulation approaches (such as repetitive transcranial magnetic stimulation) as well as know how to apply them. We need to train residents more in substance abuse problems and the biology of addiction if they are to better understand the risks of certain new classes of medication. Lastly, we need to train residents in the application of genomics, proteomics, and brain imaging to somatic treatment development.
Dr. Aftab: What is your perception of the threats that psychiatry faces or is likely to face in the future?
Dr. Schatzberg: The biggest threats come from ourselves. We need to do better with our classification approaches, such as the Diagnostic and Statistical Manual of Mental Disorders or the Research Domain Criteria. They need to become more rapidly adaptive to research in the field. We need to be more open to looking at what is a potentially dangerous trend in developing drugs of abuse and mind-altering drugs as therapeutics. We need to be able to demonstrate that telepsychiatry can be as effective as face-to-face treatment and should be reimbursed. Lastly, we need to develop better models for taking care of the psychiatric patient. We have too many patients and not enough psychiatrists.
Dr. Aftab: What do you envision for the future of psychiatry? What sort of opportunities lie ahead for us?
Dr. Schatzberg: I see the future as bright. Over the past 10 years, led by efforts at the APA, some while I was President, reimbursement has increased dramatically. Over the past 10 years, we have done well developing some new drugs and somatic therapies, and these will continue. Less than a decade ago, large pharmaceutical had abandoned psychiatric drug development and investment into biotech start-ups had waned to near zero. However, the last year few years have seen a dramatic surge in investment, and these should yield novel agents and ones that may be combined with innovative biomarkers as companions.
1. Williams NR, Heifets BD, Blasey C, et al. Attenuation of antidepressant effects of ketamine by opioid receptor antagonism. Am J Psychiatry. 2018;175(12):1205-1215. doi:10.1176/appi.ajp.2018.18020138
2. Williams NR, Heifets BD, Bentzley BS, et al. Attenuation of antidepressant and antisuicidal effects of ketamine by opioid receptor antagonism. Mol Psychiatry. 2019;24(12):1779-1786. doi:10.1038/s41380-019-0503-4
3. Bonaventura J, Lam S, Carlton M, et al. Pharmacological and behavioral divergence of ketamine enantiomers: implications for abuse liability. Mol Psychiatry. 2021;10.1038/s41380-021-01093-2. doi:10.1038/s41380-021-01093-2
4. Schatzberg AF. Can target engagement studies miss their targets and mislead drug development? Am J Psychiatry. 2021;178(5):372-374. doi:10.1176/appi.ajp.2020.21030247
For this Psychiatry Leaders’ Perspectives, Awais Aftab, MD, interviewed Alan F. Schatzberg, MD. Dr. Schatzberg is the Kenneth T. Norris, Jr., Professor of Psychiatry and Behavioral Sciences at Stanford University. He served as the Chair of the Department at Stanford until 2010 and currently directs the Stanford Mood Disorders Center. He was the 136th president of the American Psychiatric Association (APA) (2009-2010). He has been an active investigator in the biology and psychopharmacology of depressive disorders, and has authored more than 700 publications and abstracts, including Schatzberg’s Manual of Clinical Psychopharmacology. Dr. Schatzberg is also the coeditor of the Textbook of Psychopharmacology with Charles B. Nemeroff, MD, PhD. He is a Past President of the American College of Neuropsychopharmacology (ACNP) and the Society of Biological Psychiatry, and was also the Secretary-General of the International Society of Psychoneuroendocrinology (ISPNE). In 2003, he was elected to the Institute of Medicine of the National Academy of Sciences (National Academy of Medicine). He has received numerous prestigious awards, including the 2005 Distinguished Service in Psychiatry Award from the American College of Psychiatrists, the 2005 Falcone Award from the National Alliance for Research in Schizophrenia and Affective Disorders, the 2014 Kraepelin Gold Medal from the Max Planck Institute of Psychiatry, the 2015 Gold Medal from the Society of Biological Psychiatry, the 2015 Lifetime Achievement Award of the ISPNE, the 2017 Julius Axelrod Mentorship Award from the ACNP, the 2018 Donald Klein, MD, Lifetime Achievement Award from the American Society of Clinical Psychopharmacology, and the 2018 Jules Marmor, MD, Award for Biopsychosocial Research from the APA.
Dr. Aftab: You have devoted much of your career to the development of psychopharmacology. What is your perspective on where the field of psychopharmacology stands at present, especially amid the widespread recognition of “treatment resistance” as a pervasive phenomenon and the scarcity of validated neurobiologic etiological models for psychiatric disorders?
Dr. Schatzberg: We have made considerable progress in the development of new classes of agents for major depression, but as we develop new agents, we still see a large percentage of patients who do not seem to demonstrate adequate responses, particularly in major depressive disorder. This has driven us to look for agents that work differently than previous ones. Although we have some new agents with seeming efficacy and newer mechanisms of action, eg, esketamine, these have largely been derived from clinical, often serendipitous, observations of antidepressant effects rather than from prospective development based on a known pharmacological effect or a biological construct of the disorder. Another intriguing and possibly effective anxiolytic and antidepressive agent is psilocybin, whose potential use is largely derived from clinicians who found it helpful in their practices in combination with psychotherapy. These 2 demonstrate how as we branch out into new territory, we find ourselves moving more and more toward drugs of known clinical risk; eg, mind-altering agents or drugs of abuse. These agents may offer risk-benefit ratios that can ultimately prove to be less attractive than what we might have wanted when we ventured on the journey. Unfortunately, there has been little dialogue about the limitations of several of these agents.
In the case of esketamine, the notion has been that the drug is a blocker of the N-methyl-
One approach that has been applied recently is target validation that purports to use functional MRI to assess behavioral and cognitive effects of drugs to allow inferences regarding efficacy in specific disorders. As we have discussed in a recent paper published in the American Journal of Psychiatry,4 this can be quite misleading and may provide both false positive and negative information. From my perspective, these tests do not appear sensitive enough to screen for patients having a disorder, nor for assessing possible drug effects in those patients. Thus, it is unclear if they can provide answers today that we can be confident in.
Continue to: Dr. Aftab...
Dr. Aftab: What do you see as some of the strengths of psychiatry as a profession?
Dr. Schatzberg: Psychiatry as a specialty combines 2 major perspectives—psychological processes and psychobiology—to develop methods for treating patients who suffer from disorders of the mind/brain. It is the most challenging of our specialties because we cannot study the brain directly. We cannot do procedures as we do in cardiology and pulmonology because they may prove dangerously invasive. That hands-off approach limits us, but for the curious it provides an opportunity to begin to unravel the processes that underlie brain functioning. Fortunately, we have therapies—both psychosocial and somatic—that can provide great relief to patients. These can be shown to be effective in sufficient numbers of patients to help many.
Dr. Aftab: Are there ways in which the status quo in psychiatry falls short of the ideal? What are our areas of relative weakness?
Dr. Schatzberg: We need to train our residents in a host of approaches, and not just medications and psychotherapy. They need to understand the basis of brain stimulation approaches (such as repetitive transcranial magnetic stimulation) as well as know how to apply them. We need to train residents more in substance abuse problems and the biology of addiction if they are to better understand the risks of certain new classes of medication. Lastly, we need to train residents in the application of genomics, proteomics, and brain imaging to somatic treatment development.
Dr. Aftab: What is your perception of the threats that psychiatry faces or is likely to face in the future?
Dr. Schatzberg: The biggest threats come from ourselves. We need to do better with our classification approaches, such as the Diagnostic and Statistical Manual of Mental Disorders or the Research Domain Criteria. They need to become more rapidly adaptive to research in the field. We need to be more open to looking at what is a potentially dangerous trend in developing drugs of abuse and mind-altering drugs as therapeutics. We need to be able to demonstrate that telepsychiatry can be as effective as face-to-face treatment and should be reimbursed. Lastly, we need to develop better models for taking care of the psychiatric patient. We have too many patients and not enough psychiatrists.
Dr. Aftab: What do you envision for the future of psychiatry? What sort of opportunities lie ahead for us?
Dr. Schatzberg: I see the future as bright. Over the past 10 years, led by efforts at the APA, some while I was President, reimbursement has increased dramatically. Over the past 10 years, we have done well developing some new drugs and somatic therapies, and these will continue. Less than a decade ago, large pharmaceutical had abandoned psychiatric drug development and investment into biotech start-ups had waned to near zero. However, the last year few years have seen a dramatic surge in investment, and these should yield novel agents and ones that may be combined with innovative biomarkers as companions.
For this Psychiatry Leaders’ Perspectives, Awais Aftab, MD, interviewed Alan F. Schatzberg, MD. Dr. Schatzberg is the Kenneth T. Norris, Jr., Professor of Psychiatry and Behavioral Sciences at Stanford University. He served as the Chair of the Department at Stanford until 2010 and currently directs the Stanford Mood Disorders Center. He was the 136th president of the American Psychiatric Association (APA) (2009-2010). He has been an active investigator in the biology and psychopharmacology of depressive disorders, and has authored more than 700 publications and abstracts, including Schatzberg’s Manual of Clinical Psychopharmacology. Dr. Schatzberg is also the coeditor of the Textbook of Psychopharmacology with Charles B. Nemeroff, MD, PhD. He is a Past President of the American College of Neuropsychopharmacology (ACNP) and the Society of Biological Psychiatry, and was also the Secretary-General of the International Society of Psychoneuroendocrinology (ISPNE). In 2003, he was elected to the Institute of Medicine of the National Academy of Sciences (National Academy of Medicine). He has received numerous prestigious awards, including the 2005 Distinguished Service in Psychiatry Award from the American College of Psychiatrists, the 2005 Falcone Award from the National Alliance for Research in Schizophrenia and Affective Disorders, the 2014 Kraepelin Gold Medal from the Max Planck Institute of Psychiatry, the 2015 Gold Medal from the Society of Biological Psychiatry, the 2015 Lifetime Achievement Award of the ISPNE, the 2017 Julius Axelrod Mentorship Award from the ACNP, the 2018 Donald Klein, MD, Lifetime Achievement Award from the American Society of Clinical Psychopharmacology, and the 2018 Jules Marmor, MD, Award for Biopsychosocial Research from the APA.
Dr. Aftab: You have devoted much of your career to the development of psychopharmacology. What is your perspective on where the field of psychopharmacology stands at present, especially amid the widespread recognition of “treatment resistance” as a pervasive phenomenon and the scarcity of validated neurobiologic etiological models for psychiatric disorders?
Dr. Schatzberg: We have made considerable progress in the development of new classes of agents for major depression, but as we develop new agents, we still see a large percentage of patients who do not seem to demonstrate adequate responses, particularly in major depressive disorder. This has driven us to look for agents that work differently than previous ones. Although we have some new agents with seeming efficacy and newer mechanisms of action, eg, esketamine, these have largely been derived from clinical, often serendipitous, observations of antidepressant effects rather than from prospective development based on a known pharmacological effect or a biological construct of the disorder. Another intriguing and possibly effective anxiolytic and antidepressive agent is psilocybin, whose potential use is largely derived from clinicians who found it helpful in their practices in combination with psychotherapy. These 2 demonstrate how as we branch out into new territory, we find ourselves moving more and more toward drugs of known clinical risk; eg, mind-altering agents or drugs of abuse. These agents may offer risk-benefit ratios that can ultimately prove to be less attractive than what we might have wanted when we ventured on the journey. Unfortunately, there has been little dialogue about the limitations of several of these agents.
In the case of esketamine, the notion has been that the drug is a blocker of the N-methyl-
One approach that has been applied recently is target validation that purports to use functional MRI to assess behavioral and cognitive effects of drugs to allow inferences regarding efficacy in specific disorders. As we have discussed in a recent paper published in the American Journal of Psychiatry,4 this can be quite misleading and may provide both false positive and negative information. From my perspective, these tests do not appear sensitive enough to screen for patients having a disorder, nor for assessing possible drug effects in those patients. Thus, it is unclear if they can provide answers today that we can be confident in.
Continue to: Dr. Aftab...
Dr. Aftab: What do you see as some of the strengths of psychiatry as a profession?
Dr. Schatzberg: Psychiatry as a specialty combines 2 major perspectives—psychological processes and psychobiology—to develop methods for treating patients who suffer from disorders of the mind/brain. It is the most challenging of our specialties because we cannot study the brain directly. We cannot do procedures as we do in cardiology and pulmonology because they may prove dangerously invasive. That hands-off approach limits us, but for the curious it provides an opportunity to begin to unravel the processes that underlie brain functioning. Fortunately, we have therapies—both psychosocial and somatic—that can provide great relief to patients. These can be shown to be effective in sufficient numbers of patients to help many.
Dr. Aftab: Are there ways in which the status quo in psychiatry falls short of the ideal? What are our areas of relative weakness?
Dr. Schatzberg: We need to train our residents in a host of approaches, and not just medications and psychotherapy. They need to understand the basis of brain stimulation approaches (such as repetitive transcranial magnetic stimulation) as well as know how to apply them. We need to train residents more in substance abuse problems and the biology of addiction if they are to better understand the risks of certain new classes of medication. Lastly, we need to train residents in the application of genomics, proteomics, and brain imaging to somatic treatment development.
Dr. Aftab: What is your perception of the threats that psychiatry faces or is likely to face in the future?
Dr. Schatzberg: The biggest threats come from ourselves. We need to do better with our classification approaches, such as the Diagnostic and Statistical Manual of Mental Disorders or the Research Domain Criteria. They need to become more rapidly adaptive to research in the field. We need to be more open to looking at what is a potentially dangerous trend in developing drugs of abuse and mind-altering drugs as therapeutics. We need to be able to demonstrate that telepsychiatry can be as effective as face-to-face treatment and should be reimbursed. Lastly, we need to develop better models for taking care of the psychiatric patient. We have too many patients and not enough psychiatrists.
Dr. Aftab: What do you envision for the future of psychiatry? What sort of opportunities lie ahead for us?
Dr. Schatzberg: I see the future as bright. Over the past 10 years, led by efforts at the APA, some while I was President, reimbursement has increased dramatically. Over the past 10 years, we have done well developing some new drugs and somatic therapies, and these will continue. Less than a decade ago, large pharmaceutical had abandoned psychiatric drug development and investment into biotech start-ups had waned to near zero. However, the last year few years have seen a dramatic surge in investment, and these should yield novel agents and ones that may be combined with innovative biomarkers as companions.
1. Williams NR, Heifets BD, Blasey C, et al. Attenuation of antidepressant effects of ketamine by opioid receptor antagonism. Am J Psychiatry. 2018;175(12):1205-1215. doi:10.1176/appi.ajp.2018.18020138
2. Williams NR, Heifets BD, Bentzley BS, et al. Attenuation of antidepressant and antisuicidal effects of ketamine by opioid receptor antagonism. Mol Psychiatry. 2019;24(12):1779-1786. doi:10.1038/s41380-019-0503-4
3. Bonaventura J, Lam S, Carlton M, et al. Pharmacological and behavioral divergence of ketamine enantiomers: implications for abuse liability. Mol Psychiatry. 2021;10.1038/s41380-021-01093-2. doi:10.1038/s41380-021-01093-2
4. Schatzberg AF. Can target engagement studies miss their targets and mislead drug development? Am J Psychiatry. 2021;178(5):372-374. doi:10.1176/appi.ajp.2020.21030247
1. Williams NR, Heifets BD, Blasey C, et al. Attenuation of antidepressant effects of ketamine by opioid receptor antagonism. Am J Psychiatry. 2018;175(12):1205-1215. doi:10.1176/appi.ajp.2018.18020138
2. Williams NR, Heifets BD, Bentzley BS, et al. Attenuation of antidepressant and antisuicidal effects of ketamine by opioid receptor antagonism. Mol Psychiatry. 2019;24(12):1779-1786. doi:10.1038/s41380-019-0503-4
3. Bonaventura J, Lam S, Carlton M, et al. Pharmacological and behavioral divergence of ketamine enantiomers: implications for abuse liability. Mol Psychiatry. 2021;10.1038/s41380-021-01093-2. doi:10.1038/s41380-021-01093-2
4. Schatzberg AF. Can target engagement studies miss their targets and mislead drug development? Am J Psychiatry. 2021;178(5):372-374. doi:10.1176/appi.ajp.2020.21030247
Racial disparities in perinatal mental health care during COVID-19
Perinatal mental health disorders such as perinatal depression are common complications of pregnancy1 and cause significant disability in mothers and children.2 Yet despite facing higher 12-month rates of depression than White women,3 Black and Hispanic women are less likely than White women to be diagnosed with and receive treatment for postpartum depression.4
In addition to leading to >800,000 deaths in the United States alone (as of mid-December 2021),5 COVID-19 has disrupted health care delivery, including perinatal mental health services.6 Emerging data also describe neuropsychiatric effects of COVID-19 on both infected and uninfected individuals.7 Because Black and Hispanic individuals bear a disproportionate burden of COVID-19,8 compared to White women, women of color stand to be more adversely impacted by the direct effects of the disease as well as by related disruptions in perinatal psychiatry services.
Reasons for perinatal health disparities are multifactorial, complex, and interrelated. Disparities, which can be seen as proportionate differences in access by members of minority groups compared with groups in the majority, are related to differences in mental health screening, health care accessibility, and decisions to initiate treatment. In this commentary, we define “women of color” as non-White women, and focus on how traditional barriers to perinatal mental health treatment in women of color are exacerbated in the era of COVID-19. We focus primarily on postpartum depression because it is the peripartum mental health disorder with the highest likelihood of uptake in screening and treatment practices; however, disparities may be present in other mental health disorders during this period.
Gaps in screening and identification
Postpartum depression is a source of mitigatable risk for mother and neonate in the peripartum period, and the topic of screening for its presence arises in educational and best practices materials for primary care, OB-GYN, and pediatric care clinicians. Despite considerable evidence demonstrating better outcomes (for mother and child) with early detection and treatment of perinatal mental health disorders, racial and ethnic disparities persist in the screening process. At baseline, Black, Asian, and American Indian and Alaska Native women are less likely than White women to be screened for depression.9 Research shows that screening practices differ based on type of clinic, with one study noting that patients of family physicians were more likely to be screened for perinatal depression than were patients of OB-GYNs or nursing midwives.9 Even after adjusting for clinic type, racial differences in screening persist, with fewer women of color screened than their White counterparts.9 The literature consistently shows that within the same care settings, physicians deliver less information, less supportive talk, and less evidence-based treatment to Black and Hispanic patients and patients of lower economic status.10-12 Patient-clinician ethnic concordance is shown to positively impact the therapeutic relationship; at present, depressive symptoms are underrecognized in people of color, for whom referral to psychiatric care may be further compounded by inadequate knowledge of psychiatric resources.10-13
Data from Medicaid programs reveal that compared to White women, Black women are less likely to attend postpartum visits, which leads to a downstream effect on the ability to identify Black women with mental health disorders during the postpartum period.14 In addition to experiencing fewer opportunities for detection, women of color are more likely to report somatic symptoms of depression, which may not be detected in routinely employed perinatal depression screening tools.15
Continue to: Disparities in accessibility and treatment...
Disparities in accessibility and treatment
Black women are more likely to present in crisis and, hence, to acute care settings, which is likely related to disparities in screening and early detection.16,17 In a recent study investigating racial and ethnic differences in postpartum depression care, Chan et al16 found that Black women experience higher rates of hospital-based care compared with other racial groups. This study highlights the unavailability or inaccessibility of primary preventive measures to women in racial minority groups, which supports earlier studies that reported a correlation between access to care and severity of illness.16 Women in crisis may experience magnified disparities in access to high-quality care as they encounter institutional racism, potential loss of parental rights, and barriers due to insurance status.17,18 Furthermore, access to care for patients who are members of racial minority groups is limited in settings where culturally competent practices are absent or diminished, or discriminatory procedures are implicitly accepted and prevalent.12,19-22 The adverse impact of language constraints on accessibility of care is also well-documented, with recommendations such as ready access to interpreters to mitigate against miscommunications.23
Black and Hispanic women also experience significant delays between the time of delivery and treatment initiation.4 Studies of postpartum depression detection and treatment in specialty and primary care clinics show that, even when they desire treatment, women of color are less likely than White women to be offered treatment for postpartum depression.24 In terms of treatment options, research suggests women of color prefer psychotherapy over medication management.25,26 However, studies show that White women are more likely to be referred to psychotherapy.27 Research also reveals that Black and Hispanic women who are receptive to psychotropic medications have reduced rates of medication refills,4 which suggests that in these patients, counseling and monitoring adverse effects is suboptimal. In terms of treatment for substance use disorders (SUDs), after adjusting for maternal characteristics, Black and Hispanic women are significantly less likely to receive medication-assisted treatment (MAT) in pregnancy,28 and MAT is significantly less likely to be available in neighborhoods more densely populated by individuals of color.29,30
Several studies have explored possible explanations for discrepancies in treatment, including cultural expectations, differences in socioeconomic class, and racism. The stigma associated with psychiatric illness, misinformation about psychiatric treatments, and financial limitations have a substantial bearing on a patient’s willingness or ability to engage in psychiatric care.25 Regarding SUDs, a fear of legal reprisal is likely to deter women of color from seeking care.31 Such fears are not unfounded; research has demonstrated that interactions with Child Protective Services are increased among women of color compared to White women in similar situations.32
Furthermore, there is evidence that women of color receive less practical support, such as childcare, breastfeeding support, and transportation, during the postpartum period. Despite the preponderance of literature demonstrating the psychological benefits of breastfeeding,33,34 structural and psychosocial barriers appear to disproportionately affect breastfeeding rates in Hispanic, Black, American Indian, and Native women, with Black women experiencing the lowest rates of breastfeeding overall.35 Women in minority groups additionally experience disproportionate uncertainty about employment-based breastfeeding regulations.35,36 Specifically, many low-income jobs are not covered under the Family and Medical Leave Act, and compared to White women, Black women return to work on average 2 weeks earlier to jobs that are less welcoming to breastfeeding.35 In addition, insufficient education and support from health care settings and counselors play significant roles in disincentivizing women in minority groups from engaging in recommended breastfeeding and childcare practices.37,38
Continue to: COVID-19’s influence on these disparities...
COVID-19’s influence on these disparities
The COVID-19 pandemic has disproportionately impacted individuals of color. Black communities have experienced a higher rate of COVID-19 infection and a higher rate of death attributed to COVID-19, even after adjusting for age, poverty, medical comorbidities, and epidemic duration.39 The reasons for the disproportionate effects of the pandemic are complex and deeply ingrained in society.39 Emerging data indicate that COVID-19 might also lead to increased levels of psychological distress, anxiety, and depression in pregnant women33,40,41 and in Black women in particular.42 A survey of 913 pregnant women in Philadelphia conducted in May 2020 found significantly higher rates of anxiety and depression among Black women compared with White women, even after controlling for maternal age, gestational age, socioeconomic status, and marital status.42 A cross-sectional study of 163 women found that during the perinatal period, women of color were more likely than their White counterparts to experience negative changes in their mental health.43 These differences are concerning because pregnant women who experience high levels of stress during the pandemic are at high risk for preterm delivery and perinatal complications.44
Women of color may be disproportionately excluded by models of care that have become commonplace during the pandemic. Remote obstetric care became more common during the COVID-19 pandemic45; however, Black and Hispanic patients have been less likely than White patients to use telehealth services.46 Whether the differences are related to a lower likelihood of having a usual source of care, less access to digital resources, decreased awareness of the availability of telehealth, or less familiarity with digital technology, the common factor in all of the hypothesized reasons is structural racism.46 This is despite the fact that pregnant Black women report higher rates of concern than their White peers regarding the quality of their prenatal care during the pandemic.42 In a small study that surveyed 100 women about their preference for obstetric care, a significantly higher proportion of White women preferred virtual visits, with non-White women preferring in-person visits.47 Reasons cited for preferring virtual visits included convenience, safety with respect to viral transmission, compatibility with working from home, and less time waiting for the clinician; reasons cited for preferring in-person visits included a feeling of missing out on important parts of care, receiving less clinician attention, and having less of a connection with their clinician during virtual visits.47 Women of color have lower rates of perinatal depression screening than their White counterparts,9 and less frequent telehealth visits might lead to a further reduction in the detection and treatment of depression and other mental health conditions in this population.
Along with increasing telehealth services during the pandemic, many hospitals implemented stricter visitation policies for patients, including women giving birth, with the potential for greater detrimental impact on women of color. Before the pandemic, a survey of >2,500 women found that up to 10% of Black women reported experiencing racism during hospitalization for obstetrics-related care.48 These women also reported barriers to open and supportive communication with their clinicians.48 A recent study by Gur et al42 found that pregnant Black women reported more worries about the birthing experience during the pandemic than White women. In a setting with restricted visitors, all women are at risk for having a lonelier birth experience, but women of color who are already concerned about barriers to communication and racist care practices also must contend with their lived experience of systemic inequity, barriers to communication, and concerns about frank racism, without the support and potential advocacy they may usually rely upon to get them through medical experiences. Furthermore, pregnant women with mental illness are at greater risk for pregnancy complications. Together, these data suggest that women in minority groups who are pregnant and have mental illness are particularly vulnerable and are at greater risk without social support and advocacy during hospitalization.
The postpartum period is accompanied by unique concerns in terms of breastfeeding and social support for women of color. Women in minority groups had lower breastfeeding rates before the pandemic. Several studies looked at the impact of COVID-19 and associated restrictions on breastfeeding. In the United Kingdom, women in minority groups were more likely to stop breastfeeding due to the challenges of COVID-19–related restrictions.49 Compared with White women, these women were also more likely to report less practical support for breastfeeding during the pandemic.49 Other factors associated with low breastfeeding rates include lower levels of education and stressful living conditions.49 Though these factors were present before COVID-19, the pandemic has exacerbated these differences. Taken together, the evidence points to a role of long-standing structural and systemic inequity and racism in the health and wellbeing of women in minority groups.
A look towards solutions
Although perinatal mental health racial disparities predate the COVID-19 pandemic, differences in access to screening, identification, and treatment for mental health disorders place pregnant women of color and their children at heightened risk for poor health outcomes compared to their White counterparts during and after the pandemic. Despite the advent and progression of telehealth, existing race-based differences appear to have been maintained or exacerbated. The reasons for disparities are multifactorial and interrelated, and some of the outcomes perpetuate certain drivers of racism, which in turn drive continued inequity. Given the symptoms of depression, it is especially worrisome that clinicians may expect vulnerable women with illness-induced amotivation, anhedonia, and apathy to advocate for their own care.
Overall, the evidence confirms an imperative need—before, during, and after the COVID-19 pandemic—to provide education in mental health and cultural competency to clinicians such as obstetricians and pediatricians, who are more likely to have the first contact with women with perinatal depression. Health systems and government agencies also bear a responsibility to provide avenues for perinatal care clinicians to receive training and to increase access to culturally appropriate treatments through policy and structural changes.
Bottom Line
Racial disparities in perinatal mental health care persist despite widespread incorporation of telehealth into psychiatric services. Until causal factors are appropriately addressed through education, implementation, and structural changes, the benefits that have accompanied expanded psychiatric services via telehealth may only serve to exacerbate these differences.
1. Woody CA, Ferrari AJ, Siskind DJ, et al. A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J Affect Disord. 2017;219:86-92.
2. Slomian J, Honvo G, Emonts P, et al. Consequences of maternal postpartum depression: a systematic review of maternal and infant outcomes. Womens Health (Lond). 2019;15:174550651984404.
3. Kurz B, Hesselbrock M. Ethnic differences in mental health symptomatology and mental health care utilization among WIC mothers. Social Work in Mental Health. 2006;4(3):1-21.
4. Kozhimannil KB, Trinacty CM, Busch AB, et al. Racial and ethnic disparities in postpartum depression care among low-income women. Psychiatr Serv. 2011;62(6):619-625.
5. COVID-19 global cases. Coronavirus Resource Center for Systems Science and Engineering. Johns Hopkins University. Accessed December 10, 2021. https://coronavirus.jhu.edu/map.html
6. Gressier F, Mezzacappa A, Lasica PA, et al. COVID outbreak is changing our practices of perinatal psychiatry. Arch Womens Ment Health. 2020;23(6):791-792.
7. Troyer EA, Kohn JN, Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav Immun. 2020;87:34-39.
8. COVID-19: Data. NYC Health. Accessed February 3, 2021. https://www1.nyc.gov/site/doh/covid/covid-19-data.page
9. Sidebottom A, Vacquier M, LaRusso E, et al. Perinatal depression screening practices in a large health system: identifying current state and assessing opportunities to provide more equitable care. Arch Womens Ment Health. 2021;24(1):133-144.
10. Ma A, Sanchez A, Ma M. The impact of patient-provider race/ethnicity concordance on provider visits: updated evidence from the medical expenditure panel survey. J Racial Ethn Health Disparities. 2019;6(5):1011-1020.
11. Greenwood BN, Hardeman RR, Huang L, et al. Physician-patient racial concordance and disparities in birthing mortality for newborns. Proc Natl Acad Sci USA. 2020;117(35):21194-21200.
12. Chaudron LH, Kitzman HJ, Peifer KL, et al. Self-recognition of and provider response to maternal depressive symptoms in low-income Hispanic women. J Womens Health (Larchmt). 2005;14(4):331-338.
13. Institute of Medicine. Unequal treatment: confronting racial and ethnic disparities in health care. The National Academies Press; 2003. Accessed December 7, 2021. https://www.nap.edu/catalog/12875/unequal-treatment-confronting-racial-and-ethnic-disparities-in-health-care
14. Thiel de Bocanegra H, Braughton M, Bradsberry M, et al. Racial and ethnic disparities in postpartum care and contraception in California’s Medicaid program. Am J Obstet Gynecol. 2017;217(1):47.e1-47.e7.
15. Nadeem E, Lange JM, Miranda J. Perceived need for care among low-income immigrant and U.S.-born Black and Latina women with depression. J Womens Health (Larchmt). 2009;18(3):369-375.
16. Chan AL, Guo N, Popat R, et al. Racial and ethnic disparities in hospital-based care associated with postpartum depression. J Racial Ethn Health Disparities. 2021;8(1):220-229.
17. Kopelman R, Moel J, Mertens C, et al. Barriers to care for antenatal depression. Psychiatr Serv. 2008;59(4):429-432.
18. Kimerling R, Baumrind N. Access to specialty mental health services among women in California. Psychiatr Serv. 2005;56(6):729-734.
19. Ta Park V, Goyal D, Nguyen T, et al. Postpartum traditions, mental health, and help-seeking considerations among Vietnamese American women: a mixed-methods pilot study. J Behav Health Serv Res. 2017;44(3):428-441.
20. Chen F, Fryer GE Jr, Phillips RL Jr, et al. Patients’ beliefs about racism, preferences for physician race, and satisfaction with care. Ann Fam Med. 2005;3(2):138-143.
21. Holopainen D. The experience of seeking help for postnatal depression. Aust J Adv Nurs. 2002;19(3):39-44.
22. Alvidrez J, Azocar F. Distressed women’s clinic patients: preferences for mental health treatments and perceived obstacles. Gen Hosp Psychiatry. 1999;21(5):340-347.
23. Lara-Cinisomo S, Clark CT, Wood J. Increasing diagnosis and treatment of perinatal depression in Latinas and African American women: addressing stigma is not enough. Womens Health Issues. 2018;28(3):201-204.
24. Zittel-Palamara K, Rockmaker JR, Schwabel KM, et al. Desired assistance versus care received for postpartum depression: access to care differences by race. Arch Womens Ment Health. 2008;11(2):81-92.
25. Dennis CL, Chung-Lee L. Postpartum depression help-seeking barriers and maternal treatment preferences: a qualitative systematic review. Birth. 2006;33(4):323-331.
26. Cooper LA, Gonzales JJ, Gallo JJ, et al. The acceptability of treatment for depression among African American, Hispanic, and white primary care patients. Med Care. 2003;41(4):479-489.
27. House TS, Alnajjar E, Mulekar M, et al. Mommy meltdown: understanding racial differences between black and white women in attitudes about postpartum depression and treatment modalities. J Clin Gynecol Obstet. 2020;9(3):37-42.
28. Schiff DM, Nielsen T, Hoeppner BB, et al. Assessment of racial and ethnic disparities in the use of medication to treat opioid use disorder among pregnant women in Massachusetts. JAMA Netw Open. 2020;3(5):e205734.
29. Hansen H, Siegel C, Wanderling J, et al. Buprenorphine and methadone treatment for opioid dependence by income, ethnicity, and race of neighborhoods in New York City. Drug Alcohol Depend. 2016;164:14-21.
30. Goedel WC, Shapiro A, Cerdá M, et al. Association of racial/ethnic segregation with treatment capacity for opioid use disorder in counties in the United States. JAMA Netw Open. 2020;3(4):e203711.
31. Stone R. Pregnant women and substance use: fear, stigma, and barriers to care. Health Justice. 2015;3:2.
32. Roberts SC, Nuru-Jeter A. Universal screening for alcohol and drug use and racial disparities in child protective services reporting. J Behav Health Serv Res. 2012;39(1):3-16.

33. Krol KM, Grossmann T. Psychological effects of breastfeeding on children and mothers. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2018;61(8):977-985.
34. Evans K, Labbok M, Abrahams SW. WIC and breastfeeding support services: does the mix of services offered vary with race and ethnicity? Breastfeed Med. 2011;6(6):401-406.
35. Jones KM, Power ML, Queenan JT, et al. Racial and ethnic disparities in breastfeeding. Breastfeed Med. 2015;10(4):186-196.
36. Hohl S, Thompson B, Escareño M, et al. Cultural norms in conflict: breastfeeding among Hispanic immigrants in rural Washington state. Matern Child Health J. 2016;20(7):1549-1557.
37. McKinney CO, Hahn-Holbrook J, Chase-Lansdale PL, et al. Racial and ethnic differences in breastfeeding. Pediatrics. 2016;138(2):e20152388.
38. Louis-Jacques A, Deubel TF, Taylor M, et al. Racial and ethnic disparities in U.S. breastfeeding and implications for maternal and child health outcomes. Semin Perinatol. 2017;41(5):299-307.
39. Millett GA, Jones AT, Benkeser D, et al. Assessing differential impacts of COVID-19 on black communities. Ann Epidemiol. 2020;47:37-44.
40. Fan S, Guan J, Cao L, et al. Psychological effects caused by COVID-19 pandemic on pregnant women: a systematic review with meta-analysis. Asian J Psychiatr. 2021;56:102533.
41. Robinson GE, Benders-Hadi N, Conteh N, et al. Psychological impact of COVID-19 on pregnancy. J Nerv Ment Dis. 2021;209(6):396-397.
42. Gur RE, White LK, Waller R, et al. The disproportionate burden of the COVID-19 pandemic among pregnant Black women. Psychiatry Res. 2020;293:113475.
43. Masters GA, Asipenko E, Bergman AL, et al. Impact of the COVID-19 pandemic on mental health, access to care, and health disparities in the perinatal period. J Psychiatr Res. 2021;137:126-130.
44. Preis H, Mahaffey B, Pati S, et al. Adverse perinatal outcomes predicted by prenatal maternal stress among U.S. women at the COVID-19 pandemic onset. Ann Behav Med. 2021;55(3):179-191.
45. Fryer K, Delgado A, Foti T, et al. Implementation of obstetric telehealth during COVID-19 and beyond. Matern Child Health J. 2020;24(9):1104-1110.
46. Weber E, Miller SJ, Astha V, et al. Characteristics of telehealth users in NYC for COVID-related care during the coronavirus pandemic. J Am Med Inform Assoc. 2020;27(12):1949-1954.
47. Sullivan MW, Kanbergs AN, Burdette ER, et al. Acceptability of virtual prenatal care: thinking beyond the pandemic. J Matern Fetal Neonatal Med. 2021:1-4.
48. National Partnership for Women & Families. Listening to Black mothers in California. Issue Brief. September 2018. Accessed December 7, 2021. https://www.nationalpartnership.org/our-work/resources/health-care/maternity/listening-to-black-mothers-in-california.pdf
49. Brown A, Shenker N. Experiences of breastfeeding during COVID-19: lessons for future practical and emotional support. Matern Child Nutr. 2021;17(1):e13088.
Perinatal mental health disorders such as perinatal depression are common complications of pregnancy1 and cause significant disability in mothers and children.2 Yet despite facing higher 12-month rates of depression than White women,3 Black and Hispanic women are less likely than White women to be diagnosed with and receive treatment for postpartum depression.4
In addition to leading to >800,000 deaths in the United States alone (as of mid-December 2021),5 COVID-19 has disrupted health care delivery, including perinatal mental health services.6 Emerging data also describe neuropsychiatric effects of COVID-19 on both infected and uninfected individuals.7 Because Black and Hispanic individuals bear a disproportionate burden of COVID-19,8 compared to White women, women of color stand to be more adversely impacted by the direct effects of the disease as well as by related disruptions in perinatal psychiatry services.
Reasons for perinatal health disparities are multifactorial, complex, and interrelated. Disparities, which can be seen as proportionate differences in access by members of minority groups compared with groups in the majority, are related to differences in mental health screening, health care accessibility, and decisions to initiate treatment. In this commentary, we define “women of color” as non-White women, and focus on how traditional barriers to perinatal mental health treatment in women of color are exacerbated in the era of COVID-19. We focus primarily on postpartum depression because it is the peripartum mental health disorder with the highest likelihood of uptake in screening and treatment practices; however, disparities may be present in other mental health disorders during this period.
Gaps in screening and identification
Postpartum depression is a source of mitigatable risk for mother and neonate in the peripartum period, and the topic of screening for its presence arises in educational and best practices materials for primary care, OB-GYN, and pediatric care clinicians. Despite considerable evidence demonstrating better outcomes (for mother and child) with early detection and treatment of perinatal mental health disorders, racial and ethnic disparities persist in the screening process. At baseline, Black, Asian, and American Indian and Alaska Native women are less likely than White women to be screened for depression.9 Research shows that screening practices differ based on type of clinic, with one study noting that patients of family physicians were more likely to be screened for perinatal depression than were patients of OB-GYNs or nursing midwives.9 Even after adjusting for clinic type, racial differences in screening persist, with fewer women of color screened than their White counterparts.9 The literature consistently shows that within the same care settings, physicians deliver less information, less supportive talk, and less evidence-based treatment to Black and Hispanic patients and patients of lower economic status.10-12 Patient-clinician ethnic concordance is shown to positively impact the therapeutic relationship; at present, depressive symptoms are underrecognized in people of color, for whom referral to psychiatric care may be further compounded by inadequate knowledge of psychiatric resources.10-13
Data from Medicaid programs reveal that compared to White women, Black women are less likely to attend postpartum visits, which leads to a downstream effect on the ability to identify Black women with mental health disorders during the postpartum period.14 In addition to experiencing fewer opportunities for detection, women of color are more likely to report somatic symptoms of depression, which may not be detected in routinely employed perinatal depression screening tools.15
Continue to: Disparities in accessibility and treatment...
Disparities in accessibility and treatment
Black women are more likely to present in crisis and, hence, to acute care settings, which is likely related to disparities in screening and early detection.16,17 In a recent study investigating racial and ethnic differences in postpartum depression care, Chan et al16 found that Black women experience higher rates of hospital-based care compared with other racial groups. This study highlights the unavailability or inaccessibility of primary preventive measures to women in racial minority groups, which supports earlier studies that reported a correlation between access to care and severity of illness.16 Women in crisis may experience magnified disparities in access to high-quality care as they encounter institutional racism, potential loss of parental rights, and barriers due to insurance status.17,18 Furthermore, access to care for patients who are members of racial minority groups is limited in settings where culturally competent practices are absent or diminished, or discriminatory procedures are implicitly accepted and prevalent.12,19-22 The adverse impact of language constraints on accessibility of care is also well-documented, with recommendations such as ready access to interpreters to mitigate against miscommunications.23
Black and Hispanic women also experience significant delays between the time of delivery and treatment initiation.4 Studies of postpartum depression detection and treatment in specialty and primary care clinics show that, even when they desire treatment, women of color are less likely than White women to be offered treatment for postpartum depression.24 In terms of treatment options, research suggests women of color prefer psychotherapy over medication management.25,26 However, studies show that White women are more likely to be referred to psychotherapy.27 Research also reveals that Black and Hispanic women who are receptive to psychotropic medications have reduced rates of medication refills,4 which suggests that in these patients, counseling and monitoring adverse effects is suboptimal. In terms of treatment for substance use disorders (SUDs), after adjusting for maternal characteristics, Black and Hispanic women are significantly less likely to receive medication-assisted treatment (MAT) in pregnancy,28 and MAT is significantly less likely to be available in neighborhoods more densely populated by individuals of color.29,30
Several studies have explored possible explanations for discrepancies in treatment, including cultural expectations, differences in socioeconomic class, and racism. The stigma associated with psychiatric illness, misinformation about psychiatric treatments, and financial limitations have a substantial bearing on a patient’s willingness or ability to engage in psychiatric care.25 Regarding SUDs, a fear of legal reprisal is likely to deter women of color from seeking care.31 Such fears are not unfounded; research has demonstrated that interactions with Child Protective Services are increased among women of color compared to White women in similar situations.32
Furthermore, there is evidence that women of color receive less practical support, such as childcare, breastfeeding support, and transportation, during the postpartum period. Despite the preponderance of literature demonstrating the psychological benefits of breastfeeding,33,34 structural and psychosocial barriers appear to disproportionately affect breastfeeding rates in Hispanic, Black, American Indian, and Native women, with Black women experiencing the lowest rates of breastfeeding overall.35 Women in minority groups additionally experience disproportionate uncertainty about employment-based breastfeeding regulations.35,36 Specifically, many low-income jobs are not covered under the Family and Medical Leave Act, and compared to White women, Black women return to work on average 2 weeks earlier to jobs that are less welcoming to breastfeeding.35 In addition, insufficient education and support from health care settings and counselors play significant roles in disincentivizing women in minority groups from engaging in recommended breastfeeding and childcare practices.37,38
Continue to: COVID-19’s influence on these disparities...
COVID-19’s influence on these disparities
The COVID-19 pandemic has disproportionately impacted individuals of color. Black communities have experienced a higher rate of COVID-19 infection and a higher rate of death attributed to COVID-19, even after adjusting for age, poverty, medical comorbidities, and epidemic duration.39 The reasons for the disproportionate effects of the pandemic are complex and deeply ingrained in society.39 Emerging data indicate that COVID-19 might also lead to increased levels of psychological distress, anxiety, and depression in pregnant women33,40,41 and in Black women in particular.42 A survey of 913 pregnant women in Philadelphia conducted in May 2020 found significantly higher rates of anxiety and depression among Black women compared with White women, even after controlling for maternal age, gestational age, socioeconomic status, and marital status.42 A cross-sectional study of 163 women found that during the perinatal period, women of color were more likely than their White counterparts to experience negative changes in their mental health.43 These differences are concerning because pregnant women who experience high levels of stress during the pandemic are at high risk for preterm delivery and perinatal complications.44
Women of color may be disproportionately excluded by models of care that have become commonplace during the pandemic. Remote obstetric care became more common during the COVID-19 pandemic45; however, Black and Hispanic patients have been less likely than White patients to use telehealth services.46 Whether the differences are related to a lower likelihood of having a usual source of care, less access to digital resources, decreased awareness of the availability of telehealth, or less familiarity with digital technology, the common factor in all of the hypothesized reasons is structural racism.46 This is despite the fact that pregnant Black women report higher rates of concern than their White peers regarding the quality of their prenatal care during the pandemic.42 In a small study that surveyed 100 women about their preference for obstetric care, a significantly higher proportion of White women preferred virtual visits, with non-White women preferring in-person visits.47 Reasons cited for preferring virtual visits included convenience, safety with respect to viral transmission, compatibility with working from home, and less time waiting for the clinician; reasons cited for preferring in-person visits included a feeling of missing out on important parts of care, receiving less clinician attention, and having less of a connection with their clinician during virtual visits.47 Women of color have lower rates of perinatal depression screening than their White counterparts,9 and less frequent telehealth visits might lead to a further reduction in the detection and treatment of depression and other mental health conditions in this population.
Along with increasing telehealth services during the pandemic, many hospitals implemented stricter visitation policies for patients, including women giving birth, with the potential for greater detrimental impact on women of color. Before the pandemic, a survey of >2,500 women found that up to 10% of Black women reported experiencing racism during hospitalization for obstetrics-related care.48 These women also reported barriers to open and supportive communication with their clinicians.48 A recent study by Gur et al42 found that pregnant Black women reported more worries about the birthing experience during the pandemic than White women. In a setting with restricted visitors, all women are at risk for having a lonelier birth experience, but women of color who are already concerned about barriers to communication and racist care practices also must contend with their lived experience of systemic inequity, barriers to communication, and concerns about frank racism, without the support and potential advocacy they may usually rely upon to get them through medical experiences. Furthermore, pregnant women with mental illness are at greater risk for pregnancy complications. Together, these data suggest that women in minority groups who are pregnant and have mental illness are particularly vulnerable and are at greater risk without social support and advocacy during hospitalization.
The postpartum period is accompanied by unique concerns in terms of breastfeeding and social support for women of color. Women in minority groups had lower breastfeeding rates before the pandemic. Several studies looked at the impact of COVID-19 and associated restrictions on breastfeeding. In the United Kingdom, women in minority groups were more likely to stop breastfeeding due to the challenges of COVID-19–related restrictions.49 Compared with White women, these women were also more likely to report less practical support for breastfeeding during the pandemic.49 Other factors associated with low breastfeeding rates include lower levels of education and stressful living conditions.49 Though these factors were present before COVID-19, the pandemic has exacerbated these differences. Taken together, the evidence points to a role of long-standing structural and systemic inequity and racism in the health and wellbeing of women in minority groups.
A look towards solutions
Although perinatal mental health racial disparities predate the COVID-19 pandemic, differences in access to screening, identification, and treatment for mental health disorders place pregnant women of color and their children at heightened risk for poor health outcomes compared to their White counterparts during and after the pandemic. Despite the advent and progression of telehealth, existing race-based differences appear to have been maintained or exacerbated. The reasons for disparities are multifactorial and interrelated, and some of the outcomes perpetuate certain drivers of racism, which in turn drive continued inequity. Given the symptoms of depression, it is especially worrisome that clinicians may expect vulnerable women with illness-induced amotivation, anhedonia, and apathy to advocate for their own care.
Overall, the evidence confirms an imperative need—before, during, and after the COVID-19 pandemic—to provide education in mental health and cultural competency to clinicians such as obstetricians and pediatricians, who are more likely to have the first contact with women with perinatal depression. Health systems and government agencies also bear a responsibility to provide avenues for perinatal care clinicians to receive training and to increase access to culturally appropriate treatments through policy and structural changes.
Bottom Line
Racial disparities in perinatal mental health care persist despite widespread incorporation of telehealth into psychiatric services. Until causal factors are appropriately addressed through education, implementation, and structural changes, the benefits that have accompanied expanded psychiatric services via telehealth may only serve to exacerbate these differences.
Perinatal mental health disorders such as perinatal depression are common complications of pregnancy1 and cause significant disability in mothers and children.2 Yet despite facing higher 12-month rates of depression than White women,3 Black and Hispanic women are less likely than White women to be diagnosed with and receive treatment for postpartum depression.4
In addition to leading to >800,000 deaths in the United States alone (as of mid-December 2021),5 COVID-19 has disrupted health care delivery, including perinatal mental health services.6 Emerging data also describe neuropsychiatric effects of COVID-19 on both infected and uninfected individuals.7 Because Black and Hispanic individuals bear a disproportionate burden of COVID-19,8 compared to White women, women of color stand to be more adversely impacted by the direct effects of the disease as well as by related disruptions in perinatal psychiatry services.
Reasons for perinatal health disparities are multifactorial, complex, and interrelated. Disparities, which can be seen as proportionate differences in access by members of minority groups compared with groups in the majority, are related to differences in mental health screening, health care accessibility, and decisions to initiate treatment. In this commentary, we define “women of color” as non-White women, and focus on how traditional barriers to perinatal mental health treatment in women of color are exacerbated in the era of COVID-19. We focus primarily on postpartum depression because it is the peripartum mental health disorder with the highest likelihood of uptake in screening and treatment practices; however, disparities may be present in other mental health disorders during this period.
Gaps in screening and identification
Postpartum depression is a source of mitigatable risk for mother and neonate in the peripartum period, and the topic of screening for its presence arises in educational and best practices materials for primary care, OB-GYN, and pediatric care clinicians. Despite considerable evidence demonstrating better outcomes (for mother and child) with early detection and treatment of perinatal mental health disorders, racial and ethnic disparities persist in the screening process. At baseline, Black, Asian, and American Indian and Alaska Native women are less likely than White women to be screened for depression.9 Research shows that screening practices differ based on type of clinic, with one study noting that patients of family physicians were more likely to be screened for perinatal depression than were patients of OB-GYNs or nursing midwives.9 Even after adjusting for clinic type, racial differences in screening persist, with fewer women of color screened than their White counterparts.9 The literature consistently shows that within the same care settings, physicians deliver less information, less supportive talk, and less evidence-based treatment to Black and Hispanic patients and patients of lower economic status.10-12 Patient-clinician ethnic concordance is shown to positively impact the therapeutic relationship; at present, depressive symptoms are underrecognized in people of color, for whom referral to psychiatric care may be further compounded by inadequate knowledge of psychiatric resources.10-13
Data from Medicaid programs reveal that compared to White women, Black women are less likely to attend postpartum visits, which leads to a downstream effect on the ability to identify Black women with mental health disorders during the postpartum period.14 In addition to experiencing fewer opportunities for detection, women of color are more likely to report somatic symptoms of depression, which may not be detected in routinely employed perinatal depression screening tools.15
Continue to: Disparities in accessibility and treatment...
Disparities in accessibility and treatment
Black women are more likely to present in crisis and, hence, to acute care settings, which is likely related to disparities in screening and early detection.16,17 In a recent study investigating racial and ethnic differences in postpartum depression care, Chan et al16 found that Black women experience higher rates of hospital-based care compared with other racial groups. This study highlights the unavailability or inaccessibility of primary preventive measures to women in racial minority groups, which supports earlier studies that reported a correlation between access to care and severity of illness.16 Women in crisis may experience magnified disparities in access to high-quality care as they encounter institutional racism, potential loss of parental rights, and barriers due to insurance status.17,18 Furthermore, access to care for patients who are members of racial minority groups is limited in settings where culturally competent practices are absent or diminished, or discriminatory procedures are implicitly accepted and prevalent.12,19-22 The adverse impact of language constraints on accessibility of care is also well-documented, with recommendations such as ready access to interpreters to mitigate against miscommunications.23
Black and Hispanic women also experience significant delays between the time of delivery and treatment initiation.4 Studies of postpartum depression detection and treatment in specialty and primary care clinics show that, even when they desire treatment, women of color are less likely than White women to be offered treatment for postpartum depression.24 In terms of treatment options, research suggests women of color prefer psychotherapy over medication management.25,26 However, studies show that White women are more likely to be referred to psychotherapy.27 Research also reveals that Black and Hispanic women who are receptive to psychotropic medications have reduced rates of medication refills,4 which suggests that in these patients, counseling and monitoring adverse effects is suboptimal. In terms of treatment for substance use disorders (SUDs), after adjusting for maternal characteristics, Black and Hispanic women are significantly less likely to receive medication-assisted treatment (MAT) in pregnancy,28 and MAT is significantly less likely to be available in neighborhoods more densely populated by individuals of color.29,30
Several studies have explored possible explanations for discrepancies in treatment, including cultural expectations, differences in socioeconomic class, and racism. The stigma associated with psychiatric illness, misinformation about psychiatric treatments, and financial limitations have a substantial bearing on a patient’s willingness or ability to engage in psychiatric care.25 Regarding SUDs, a fear of legal reprisal is likely to deter women of color from seeking care.31 Such fears are not unfounded; research has demonstrated that interactions with Child Protective Services are increased among women of color compared to White women in similar situations.32
Furthermore, there is evidence that women of color receive less practical support, such as childcare, breastfeeding support, and transportation, during the postpartum period. Despite the preponderance of literature demonstrating the psychological benefits of breastfeeding,33,34 structural and psychosocial barriers appear to disproportionately affect breastfeeding rates in Hispanic, Black, American Indian, and Native women, with Black women experiencing the lowest rates of breastfeeding overall.35 Women in minority groups additionally experience disproportionate uncertainty about employment-based breastfeeding regulations.35,36 Specifically, many low-income jobs are not covered under the Family and Medical Leave Act, and compared to White women, Black women return to work on average 2 weeks earlier to jobs that are less welcoming to breastfeeding.35 In addition, insufficient education and support from health care settings and counselors play significant roles in disincentivizing women in minority groups from engaging in recommended breastfeeding and childcare practices.37,38
Continue to: COVID-19’s influence on these disparities...
COVID-19’s influence on these disparities
The COVID-19 pandemic has disproportionately impacted individuals of color. Black communities have experienced a higher rate of COVID-19 infection and a higher rate of death attributed to COVID-19, even after adjusting for age, poverty, medical comorbidities, and epidemic duration.39 The reasons for the disproportionate effects of the pandemic are complex and deeply ingrained in society.39 Emerging data indicate that COVID-19 might also lead to increased levels of psychological distress, anxiety, and depression in pregnant women33,40,41 and in Black women in particular.42 A survey of 913 pregnant women in Philadelphia conducted in May 2020 found significantly higher rates of anxiety and depression among Black women compared with White women, even after controlling for maternal age, gestational age, socioeconomic status, and marital status.42 A cross-sectional study of 163 women found that during the perinatal period, women of color were more likely than their White counterparts to experience negative changes in their mental health.43 These differences are concerning because pregnant women who experience high levels of stress during the pandemic are at high risk for preterm delivery and perinatal complications.44
Women of color may be disproportionately excluded by models of care that have become commonplace during the pandemic. Remote obstetric care became more common during the COVID-19 pandemic45; however, Black and Hispanic patients have been less likely than White patients to use telehealth services.46 Whether the differences are related to a lower likelihood of having a usual source of care, less access to digital resources, decreased awareness of the availability of telehealth, or less familiarity with digital technology, the common factor in all of the hypothesized reasons is structural racism.46 This is despite the fact that pregnant Black women report higher rates of concern than their White peers regarding the quality of their prenatal care during the pandemic.42 In a small study that surveyed 100 women about their preference for obstetric care, a significantly higher proportion of White women preferred virtual visits, with non-White women preferring in-person visits.47 Reasons cited for preferring virtual visits included convenience, safety with respect to viral transmission, compatibility with working from home, and less time waiting for the clinician; reasons cited for preferring in-person visits included a feeling of missing out on important parts of care, receiving less clinician attention, and having less of a connection with their clinician during virtual visits.47 Women of color have lower rates of perinatal depression screening than their White counterparts,9 and less frequent telehealth visits might lead to a further reduction in the detection and treatment of depression and other mental health conditions in this population.
Along with increasing telehealth services during the pandemic, many hospitals implemented stricter visitation policies for patients, including women giving birth, with the potential for greater detrimental impact on women of color. Before the pandemic, a survey of >2,500 women found that up to 10% of Black women reported experiencing racism during hospitalization for obstetrics-related care.48 These women also reported barriers to open and supportive communication with their clinicians.48 A recent study by Gur et al42 found that pregnant Black women reported more worries about the birthing experience during the pandemic than White women. In a setting with restricted visitors, all women are at risk for having a lonelier birth experience, but women of color who are already concerned about barriers to communication and racist care practices also must contend with their lived experience of systemic inequity, barriers to communication, and concerns about frank racism, without the support and potential advocacy they may usually rely upon to get them through medical experiences. Furthermore, pregnant women with mental illness are at greater risk for pregnancy complications. Together, these data suggest that women in minority groups who are pregnant and have mental illness are particularly vulnerable and are at greater risk without social support and advocacy during hospitalization.
The postpartum period is accompanied by unique concerns in terms of breastfeeding and social support for women of color. Women in minority groups had lower breastfeeding rates before the pandemic. Several studies looked at the impact of COVID-19 and associated restrictions on breastfeeding. In the United Kingdom, women in minority groups were more likely to stop breastfeeding due to the challenges of COVID-19–related restrictions.49 Compared with White women, these women were also more likely to report less practical support for breastfeeding during the pandemic.49 Other factors associated with low breastfeeding rates include lower levels of education and stressful living conditions.49 Though these factors were present before COVID-19, the pandemic has exacerbated these differences. Taken together, the evidence points to a role of long-standing structural and systemic inequity and racism in the health and wellbeing of women in minority groups.
A look towards solutions
Although perinatal mental health racial disparities predate the COVID-19 pandemic, differences in access to screening, identification, and treatment for mental health disorders place pregnant women of color and their children at heightened risk for poor health outcomes compared to their White counterparts during and after the pandemic. Despite the advent and progression of telehealth, existing race-based differences appear to have been maintained or exacerbated. The reasons for disparities are multifactorial and interrelated, and some of the outcomes perpetuate certain drivers of racism, which in turn drive continued inequity. Given the symptoms of depression, it is especially worrisome that clinicians may expect vulnerable women with illness-induced amotivation, anhedonia, and apathy to advocate for their own care.
Overall, the evidence confirms an imperative need—before, during, and after the COVID-19 pandemic—to provide education in mental health and cultural competency to clinicians such as obstetricians and pediatricians, who are more likely to have the first contact with women with perinatal depression. Health systems and government agencies also bear a responsibility to provide avenues for perinatal care clinicians to receive training and to increase access to culturally appropriate treatments through policy and structural changes.
Bottom Line
Racial disparities in perinatal mental health care persist despite widespread incorporation of telehealth into psychiatric services. Until causal factors are appropriately addressed through education, implementation, and structural changes, the benefits that have accompanied expanded psychiatric services via telehealth may only serve to exacerbate these differences.
1. Woody CA, Ferrari AJ, Siskind DJ, et al. A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J Affect Disord. 2017;219:86-92.
2. Slomian J, Honvo G, Emonts P, et al. Consequences of maternal postpartum depression: a systematic review of maternal and infant outcomes. Womens Health (Lond). 2019;15:174550651984404.
3. Kurz B, Hesselbrock M. Ethnic differences in mental health symptomatology and mental health care utilization among WIC mothers. Social Work in Mental Health. 2006;4(3):1-21.
4. Kozhimannil KB, Trinacty CM, Busch AB, et al. Racial and ethnic disparities in postpartum depression care among low-income women. Psychiatr Serv. 2011;62(6):619-625.
5. COVID-19 global cases. Coronavirus Resource Center for Systems Science and Engineering. Johns Hopkins University. Accessed December 10, 2021. https://coronavirus.jhu.edu/map.html
6. Gressier F, Mezzacappa A, Lasica PA, et al. COVID outbreak is changing our practices of perinatal psychiatry. Arch Womens Ment Health. 2020;23(6):791-792.
7. Troyer EA, Kohn JN, Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav Immun. 2020;87:34-39.
8. COVID-19: Data. NYC Health. Accessed February 3, 2021. https://www1.nyc.gov/site/doh/covid/covid-19-data.page
9. Sidebottom A, Vacquier M, LaRusso E, et al. Perinatal depression screening practices in a large health system: identifying current state and assessing opportunities to provide more equitable care. Arch Womens Ment Health. 2021;24(1):133-144.
10. Ma A, Sanchez A, Ma M. The impact of patient-provider race/ethnicity concordance on provider visits: updated evidence from the medical expenditure panel survey. J Racial Ethn Health Disparities. 2019;6(5):1011-1020.
11. Greenwood BN, Hardeman RR, Huang L, et al. Physician-patient racial concordance and disparities in birthing mortality for newborns. Proc Natl Acad Sci USA. 2020;117(35):21194-21200.
12. Chaudron LH, Kitzman HJ, Peifer KL, et al. Self-recognition of and provider response to maternal depressive symptoms in low-income Hispanic women. J Womens Health (Larchmt). 2005;14(4):331-338.
13. Institute of Medicine. Unequal treatment: confronting racial and ethnic disparities in health care. The National Academies Press; 2003. Accessed December 7, 2021. https://www.nap.edu/catalog/12875/unequal-treatment-confronting-racial-and-ethnic-disparities-in-health-care
14. Thiel de Bocanegra H, Braughton M, Bradsberry M, et al. Racial and ethnic disparities in postpartum care and contraception in California’s Medicaid program. Am J Obstet Gynecol. 2017;217(1):47.e1-47.e7.
15. Nadeem E, Lange JM, Miranda J. Perceived need for care among low-income immigrant and U.S.-born Black and Latina women with depression. J Womens Health (Larchmt). 2009;18(3):369-375.
16. Chan AL, Guo N, Popat R, et al. Racial and ethnic disparities in hospital-based care associated with postpartum depression. J Racial Ethn Health Disparities. 2021;8(1):220-229.
17. Kopelman R, Moel J, Mertens C, et al. Barriers to care for antenatal depression. Psychiatr Serv. 2008;59(4):429-432.
18. Kimerling R, Baumrind N. Access to specialty mental health services among women in California. Psychiatr Serv. 2005;56(6):729-734.
19. Ta Park V, Goyal D, Nguyen T, et al. Postpartum traditions, mental health, and help-seeking considerations among Vietnamese American women: a mixed-methods pilot study. J Behav Health Serv Res. 2017;44(3):428-441.
20. Chen F, Fryer GE Jr, Phillips RL Jr, et al. Patients’ beliefs about racism, preferences for physician race, and satisfaction with care. Ann Fam Med. 2005;3(2):138-143.
21. Holopainen D. The experience of seeking help for postnatal depression. Aust J Adv Nurs. 2002;19(3):39-44.
22. Alvidrez J, Azocar F. Distressed women’s clinic patients: preferences for mental health treatments and perceived obstacles. Gen Hosp Psychiatry. 1999;21(5):340-347.
23. Lara-Cinisomo S, Clark CT, Wood J. Increasing diagnosis and treatment of perinatal depression in Latinas and African American women: addressing stigma is not enough. Womens Health Issues. 2018;28(3):201-204.
24. Zittel-Palamara K, Rockmaker JR, Schwabel KM, et al. Desired assistance versus care received for postpartum depression: access to care differences by race. Arch Womens Ment Health. 2008;11(2):81-92.
25. Dennis CL, Chung-Lee L. Postpartum depression help-seeking barriers and maternal treatment preferences: a qualitative systematic review. Birth. 2006;33(4):323-331.
26. Cooper LA, Gonzales JJ, Gallo JJ, et al. The acceptability of treatment for depression among African American, Hispanic, and white primary care patients. Med Care. 2003;41(4):479-489.
27. House TS, Alnajjar E, Mulekar M, et al. Mommy meltdown: understanding racial differences between black and white women in attitudes about postpartum depression and treatment modalities. J Clin Gynecol Obstet. 2020;9(3):37-42.
28. Schiff DM, Nielsen T, Hoeppner BB, et al. Assessment of racial and ethnic disparities in the use of medication to treat opioid use disorder among pregnant women in Massachusetts. JAMA Netw Open. 2020;3(5):e205734.
29. Hansen H, Siegel C, Wanderling J, et al. Buprenorphine and methadone treatment for opioid dependence by income, ethnicity, and race of neighborhoods in New York City. Drug Alcohol Depend. 2016;164:14-21.
30. Goedel WC, Shapiro A, Cerdá M, et al. Association of racial/ethnic segregation with treatment capacity for opioid use disorder in counties in the United States. JAMA Netw Open. 2020;3(4):e203711.
31. Stone R. Pregnant women and substance use: fear, stigma, and barriers to care. Health Justice. 2015;3:2.
32. Roberts SC, Nuru-Jeter A. Universal screening for alcohol and drug use and racial disparities in child protective services reporting. J Behav Health Serv Res. 2012;39(1):3-16.

33. Krol KM, Grossmann T. Psychological effects of breastfeeding on children and mothers. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2018;61(8):977-985.
34. Evans K, Labbok M, Abrahams SW. WIC and breastfeeding support services: does the mix of services offered vary with race and ethnicity? Breastfeed Med. 2011;6(6):401-406.
35. Jones KM, Power ML, Queenan JT, et al. Racial and ethnic disparities in breastfeeding. Breastfeed Med. 2015;10(4):186-196.
36. Hohl S, Thompson B, Escareño M, et al. Cultural norms in conflict: breastfeeding among Hispanic immigrants in rural Washington state. Matern Child Health J. 2016;20(7):1549-1557.
37. McKinney CO, Hahn-Holbrook J, Chase-Lansdale PL, et al. Racial and ethnic differences in breastfeeding. Pediatrics. 2016;138(2):e20152388.
38. Louis-Jacques A, Deubel TF, Taylor M, et al. Racial and ethnic disparities in U.S. breastfeeding and implications for maternal and child health outcomes. Semin Perinatol. 2017;41(5):299-307.
39. Millett GA, Jones AT, Benkeser D, et al. Assessing differential impacts of COVID-19 on black communities. Ann Epidemiol. 2020;47:37-44.
40. Fan S, Guan J, Cao L, et al. Psychological effects caused by COVID-19 pandemic on pregnant women: a systematic review with meta-analysis. Asian J Psychiatr. 2021;56:102533.
41. Robinson GE, Benders-Hadi N, Conteh N, et al. Psychological impact of COVID-19 on pregnancy. J Nerv Ment Dis. 2021;209(6):396-397.
42. Gur RE, White LK, Waller R, et al. The disproportionate burden of the COVID-19 pandemic among pregnant Black women. Psychiatry Res. 2020;293:113475.
43. Masters GA, Asipenko E, Bergman AL, et al. Impact of the COVID-19 pandemic on mental health, access to care, and health disparities in the perinatal period. J Psychiatr Res. 2021;137:126-130.
44. Preis H, Mahaffey B, Pati S, et al. Adverse perinatal outcomes predicted by prenatal maternal stress among U.S. women at the COVID-19 pandemic onset. Ann Behav Med. 2021;55(3):179-191.
45. Fryer K, Delgado A, Foti T, et al. Implementation of obstetric telehealth during COVID-19 and beyond. Matern Child Health J. 2020;24(9):1104-1110.
46. Weber E, Miller SJ, Astha V, et al. Characteristics of telehealth users in NYC for COVID-related care during the coronavirus pandemic. J Am Med Inform Assoc. 2020;27(12):1949-1954.
47. Sullivan MW, Kanbergs AN, Burdette ER, et al. Acceptability of virtual prenatal care: thinking beyond the pandemic. J Matern Fetal Neonatal Med. 2021:1-4.
48. National Partnership for Women & Families. Listening to Black mothers in California. Issue Brief. September 2018. Accessed December 7, 2021. https://www.nationalpartnership.org/our-work/resources/health-care/maternity/listening-to-black-mothers-in-california.pdf
49. Brown A, Shenker N. Experiences of breastfeeding during COVID-19: lessons for future practical and emotional support. Matern Child Nutr. 2021;17(1):e13088.
1. Woody CA, Ferrari AJ, Siskind DJ, et al. A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J Affect Disord. 2017;219:86-92.
2. Slomian J, Honvo G, Emonts P, et al. Consequences of maternal postpartum depression: a systematic review of maternal and infant outcomes. Womens Health (Lond). 2019;15:174550651984404.
3. Kurz B, Hesselbrock M. Ethnic differences in mental health symptomatology and mental health care utilization among WIC mothers. Social Work in Mental Health. 2006;4(3):1-21.
4. Kozhimannil KB, Trinacty CM, Busch AB, et al. Racial and ethnic disparities in postpartum depression care among low-income women. Psychiatr Serv. 2011;62(6):619-625.
5. COVID-19 global cases. Coronavirus Resource Center for Systems Science and Engineering. Johns Hopkins University. Accessed December 10, 2021. https://coronavirus.jhu.edu/map.html
6. Gressier F, Mezzacappa A, Lasica PA, et al. COVID outbreak is changing our practices of perinatal psychiatry. Arch Womens Ment Health. 2020;23(6):791-792.
7. Troyer EA, Kohn JN, Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav Immun. 2020;87:34-39.
8. COVID-19: Data. NYC Health. Accessed February 3, 2021. https://www1.nyc.gov/site/doh/covid/covid-19-data.page
9. Sidebottom A, Vacquier M, LaRusso E, et al. Perinatal depression screening practices in a large health system: identifying current state and assessing opportunities to provide more equitable care. Arch Womens Ment Health. 2021;24(1):133-144.
10. Ma A, Sanchez A, Ma M. The impact of patient-provider race/ethnicity concordance on provider visits: updated evidence from the medical expenditure panel survey. J Racial Ethn Health Disparities. 2019;6(5):1011-1020.
11. Greenwood BN, Hardeman RR, Huang L, et al. Physician-patient racial concordance and disparities in birthing mortality for newborns. Proc Natl Acad Sci USA. 2020;117(35):21194-21200.
12. Chaudron LH, Kitzman HJ, Peifer KL, et al. Self-recognition of and provider response to maternal depressive symptoms in low-income Hispanic women. J Womens Health (Larchmt). 2005;14(4):331-338.
13. Institute of Medicine. Unequal treatment: confronting racial and ethnic disparities in health care. The National Academies Press; 2003. Accessed December 7, 2021. https://www.nap.edu/catalog/12875/unequal-treatment-confronting-racial-and-ethnic-disparities-in-health-care
14. Thiel de Bocanegra H, Braughton M, Bradsberry M, et al. Racial and ethnic disparities in postpartum care and contraception in California’s Medicaid program. Am J Obstet Gynecol. 2017;217(1):47.e1-47.e7.
15. Nadeem E, Lange JM, Miranda J. Perceived need for care among low-income immigrant and U.S.-born Black and Latina women with depression. J Womens Health (Larchmt). 2009;18(3):369-375.
16. Chan AL, Guo N, Popat R, et al. Racial and ethnic disparities in hospital-based care associated with postpartum depression. J Racial Ethn Health Disparities. 2021;8(1):220-229.
17. Kopelman R, Moel J, Mertens C, et al. Barriers to care for antenatal depression. Psychiatr Serv. 2008;59(4):429-432.
18. Kimerling R, Baumrind N. Access to specialty mental health services among women in California. Psychiatr Serv. 2005;56(6):729-734.
19. Ta Park V, Goyal D, Nguyen T, et al. Postpartum traditions, mental health, and help-seeking considerations among Vietnamese American women: a mixed-methods pilot study. J Behav Health Serv Res. 2017;44(3):428-441.
20. Chen F, Fryer GE Jr, Phillips RL Jr, et al. Patients’ beliefs about racism, preferences for physician race, and satisfaction with care. Ann Fam Med. 2005;3(2):138-143.
21. Holopainen D. The experience of seeking help for postnatal depression. Aust J Adv Nurs. 2002;19(3):39-44.
22. Alvidrez J, Azocar F. Distressed women’s clinic patients: preferences for mental health treatments and perceived obstacles. Gen Hosp Psychiatry. 1999;21(5):340-347.
23. Lara-Cinisomo S, Clark CT, Wood J. Increasing diagnosis and treatment of perinatal depression in Latinas and African American women: addressing stigma is not enough. Womens Health Issues. 2018;28(3):201-204.
24. Zittel-Palamara K, Rockmaker JR, Schwabel KM, et al. Desired assistance versus care received for postpartum depression: access to care differences by race. Arch Womens Ment Health. 2008;11(2):81-92.
25. Dennis CL, Chung-Lee L. Postpartum depression help-seeking barriers and maternal treatment preferences: a qualitative systematic review. Birth. 2006;33(4):323-331.
26. Cooper LA, Gonzales JJ, Gallo JJ, et al. The acceptability of treatment for depression among African American, Hispanic, and white primary care patients. Med Care. 2003;41(4):479-489.
27. House TS, Alnajjar E, Mulekar M, et al. Mommy meltdown: understanding racial differences between black and white women in attitudes about postpartum depression and treatment modalities. J Clin Gynecol Obstet. 2020;9(3):37-42.
28. Schiff DM, Nielsen T, Hoeppner BB, et al. Assessment of racial and ethnic disparities in the use of medication to treat opioid use disorder among pregnant women in Massachusetts. JAMA Netw Open. 2020;3(5):e205734.
29. Hansen H, Siegel C, Wanderling J, et al. Buprenorphine and methadone treatment for opioid dependence by income, ethnicity, and race of neighborhoods in New York City. Drug Alcohol Depend. 2016;164:14-21.
30. Goedel WC, Shapiro A, Cerdá M, et al. Association of racial/ethnic segregation with treatment capacity for opioid use disorder in counties in the United States. JAMA Netw Open. 2020;3(4):e203711.
31. Stone R. Pregnant women and substance use: fear, stigma, and barriers to care. Health Justice. 2015;3:2.
32. Roberts SC, Nuru-Jeter A. Universal screening for alcohol and drug use and racial disparities in child protective services reporting. J Behav Health Serv Res. 2012;39(1):3-16.

33. Krol KM, Grossmann T. Psychological effects of breastfeeding on children and mothers. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2018;61(8):977-985.
34. Evans K, Labbok M, Abrahams SW. WIC and breastfeeding support services: does the mix of services offered vary with race and ethnicity? Breastfeed Med. 2011;6(6):401-406.
35. Jones KM, Power ML, Queenan JT, et al. Racial and ethnic disparities in breastfeeding. Breastfeed Med. 2015;10(4):186-196.
36. Hohl S, Thompson B, Escareño M, et al. Cultural norms in conflict: breastfeeding among Hispanic immigrants in rural Washington state. Matern Child Health J. 2016;20(7):1549-1557.
37. McKinney CO, Hahn-Holbrook J, Chase-Lansdale PL, et al. Racial and ethnic differences in breastfeeding. Pediatrics. 2016;138(2):e20152388.
38. Louis-Jacques A, Deubel TF, Taylor M, et al. Racial and ethnic disparities in U.S. breastfeeding and implications for maternal and child health outcomes. Semin Perinatol. 2017;41(5):299-307.
39. Millett GA, Jones AT, Benkeser D, et al. Assessing differential impacts of COVID-19 on black communities. Ann Epidemiol. 2020;47:37-44.
40. Fan S, Guan J, Cao L, et al. Psychological effects caused by COVID-19 pandemic on pregnant women: a systematic review with meta-analysis. Asian J Psychiatr. 2021;56:102533.
41. Robinson GE, Benders-Hadi N, Conteh N, et al. Psychological impact of COVID-19 on pregnancy. J Nerv Ment Dis. 2021;209(6):396-397.
42. Gur RE, White LK, Waller R, et al. The disproportionate burden of the COVID-19 pandemic among pregnant Black women. Psychiatry Res. 2020;293:113475.
43. Masters GA, Asipenko E, Bergman AL, et al. Impact of the COVID-19 pandemic on mental health, access to care, and health disparities in the perinatal period. J Psychiatr Res. 2021;137:126-130.
44. Preis H, Mahaffey B, Pati S, et al. Adverse perinatal outcomes predicted by prenatal maternal stress among U.S. women at the COVID-19 pandemic onset. Ann Behav Med. 2021;55(3):179-191.
45. Fryer K, Delgado A, Foti T, et al. Implementation of obstetric telehealth during COVID-19 and beyond. Matern Child Health J. 2020;24(9):1104-1110.
46. Weber E, Miller SJ, Astha V, et al. Characteristics of telehealth users in NYC for COVID-related care during the coronavirus pandemic. J Am Med Inform Assoc. 2020;27(12):1949-1954.
47. Sullivan MW, Kanbergs AN, Burdette ER, et al. Acceptability of virtual prenatal care: thinking beyond the pandemic. J Matern Fetal Neonatal Med. 2021:1-4.
48. National Partnership for Women & Families. Listening to Black mothers in California. Issue Brief. September 2018. Accessed December 7, 2021. https://www.nationalpartnership.org/our-work/resources/health-care/maternity/listening-to-black-mothers-in-california.pdf
49. Brown A, Shenker N. Experiences of breastfeeding during COVID-19: lessons for future practical and emotional support. Matern Child Nutr. 2021;17(1):e13088.
Most Americans approve of the death penalty. Do you?
As a health care provider, I have always been interested in topics that concern incarcerated citizens, whether the discussion is related to the pursuit of aggressive care or jurisprudence in general. Additionally, I have followed the issue of capital punishment for most of my career, wondering if our democracy would continue this form of punishment for violent crimes.
In the early 2000s, public opinion moved away from capital punishment. The days of executing violent criminals such as Ted Bundy (who was killed in the electric chair in 1989) seemed to be in the rearview mirror. The ability of prison systems to obtain drugs for execution had become arduous, and Americans appeared disinterested in continuing with the process. Slowly, states began opting out of executions. Currently, 27 U.S. states offer the death penalty as an option at prosecution.
Botched executions
So far in 2021, 11 prisoners have been put to death by the federal government as well as five states, using either a one-drug or three-drug intravenous protocol. Of those prisoners, one was female.
The length of time from sentencing to date of execution varied from a low of 9 years to a high of 29 years, according to the Death Penalty Information Center. Of the executions performed this year, one was considered “botched.” The victim convulsed and vomited for several minutes before his ultimate demise. In fact, in the history of using the death penalty, from 1890 to 2010, approximately 3% of total executions (276 prisoners) were botched. They involved failed electric shocks, convulsions, labored breathing, and in one particularly horrific incident, a victim who was shot in the hip and abdomen by a firing squad and took several minutes to die.
One of the more difficult tasks for conducting an execution is intravenous access, with acquisition of an intravenous site proving to be a common issue. Another concern involves intravenous efficacy, or failure of the site to remain patent until death is achieved. That is why a few states that still practice capital punishment have returned to an electric chair option for execution (the method is chosen by the prisoner).
Majority favor capital punishment
But why do most Americans believe we need the death penalty? According to a 2021 poll by the Pew Research Center, 60% of U.S. citizens favor the use of capital punishment for those convicted of murder, including 27% who strongly favor its use. About 4 in 10 oppose the punishment, but only 15% are strongly opposed. The belief of those who favor retaining execution is that use of the death penalty deters violent crime.
Surprisingly, the American South has both the highest murder rate in the country and the highest percentage of executions. This geographic area encompasses 81% of the nation’s executions. A 2012 National Research Council poll determined that studies claiming the death penalty deters violent crime are “fundamentally flawed.” States that have abolished the death penalty do not show an increase in murder rates; in fact, the opposite is true, the organization concluded.
Since 1990, states without death penalty punishment have had consistently lower murder rates than those that retain capital punishment.
Where does that leave us?
Place my attitude in the column labeled “undecided.” I would love to believe capital punishment is a deterrent to violent crime, yet statistics do not prove the hypothesis to be true. We live in one of the more violent times in history, with mass shootings becoming commonplace. Large-scale retail theft has also been on the rise, especially in recent weeks.
The idea of severe punishment for heinous crime appeals to me, yet in 2001 Timothy McVeigh was executed after eating ice cream and gazing at the moon. His treatment before execution and the length of time he served were in opposition to other inmates sentenced to death. This, despite being punished for killing 168 people (including 19 children) in the Oklahoma City bombings.
I know we cannot be complacent. Violent crime needs to be reduced, and Americans need to feel safe. The process for achieving that goal? You tell me.
Nurses in prisons
About 1% of employed nurses (i.e., close to 21,000) in the United States work in prisons. This figure does not include the many LPNs and unlicensed assistive personnel who are also working in the field and may underrepresent actual numbers.
Correctional nurses have their own scope and standards of practice. They demonstrate superb assessment skills and organization.
If you can hire a correctional nurse, or even aspire to be one, do not hesitate. Patients will thank you.
A version of this article first appeared on Medscape.com.
As a health care provider, I have always been interested in topics that concern incarcerated citizens, whether the discussion is related to the pursuit of aggressive care or jurisprudence in general. Additionally, I have followed the issue of capital punishment for most of my career, wondering if our democracy would continue this form of punishment for violent crimes.
In the early 2000s, public opinion moved away from capital punishment. The days of executing violent criminals such as Ted Bundy (who was killed in the electric chair in 1989) seemed to be in the rearview mirror. The ability of prison systems to obtain drugs for execution had become arduous, and Americans appeared disinterested in continuing with the process. Slowly, states began opting out of executions. Currently, 27 U.S. states offer the death penalty as an option at prosecution.
Botched executions
So far in 2021, 11 prisoners have been put to death by the federal government as well as five states, using either a one-drug or three-drug intravenous protocol. Of those prisoners, one was female.
The length of time from sentencing to date of execution varied from a low of 9 years to a high of 29 years, according to the Death Penalty Information Center. Of the executions performed this year, one was considered “botched.” The victim convulsed and vomited for several minutes before his ultimate demise. In fact, in the history of using the death penalty, from 1890 to 2010, approximately 3% of total executions (276 prisoners) were botched. They involved failed electric shocks, convulsions, labored breathing, and in one particularly horrific incident, a victim who was shot in the hip and abdomen by a firing squad and took several minutes to die.
One of the more difficult tasks for conducting an execution is intravenous access, with acquisition of an intravenous site proving to be a common issue. Another concern involves intravenous efficacy, or failure of the site to remain patent until death is achieved. That is why a few states that still practice capital punishment have returned to an electric chair option for execution (the method is chosen by the prisoner).
Majority favor capital punishment
But why do most Americans believe we need the death penalty? According to a 2021 poll by the Pew Research Center, 60% of U.S. citizens favor the use of capital punishment for those convicted of murder, including 27% who strongly favor its use. About 4 in 10 oppose the punishment, but only 15% are strongly opposed. The belief of those who favor retaining execution is that use of the death penalty deters violent crime.
Surprisingly, the American South has both the highest murder rate in the country and the highest percentage of executions. This geographic area encompasses 81% of the nation’s executions. A 2012 National Research Council poll determined that studies claiming the death penalty deters violent crime are “fundamentally flawed.” States that have abolished the death penalty do not show an increase in murder rates; in fact, the opposite is true, the organization concluded.
Since 1990, states without death penalty punishment have had consistently lower murder rates than those that retain capital punishment.
Where does that leave us?
Place my attitude in the column labeled “undecided.” I would love to believe capital punishment is a deterrent to violent crime, yet statistics do not prove the hypothesis to be true. We live in one of the more violent times in history, with mass shootings becoming commonplace. Large-scale retail theft has also been on the rise, especially in recent weeks.
The idea of severe punishment for heinous crime appeals to me, yet in 2001 Timothy McVeigh was executed after eating ice cream and gazing at the moon. His treatment before execution and the length of time he served were in opposition to other inmates sentenced to death. This, despite being punished for killing 168 people (including 19 children) in the Oklahoma City bombings.
I know we cannot be complacent. Violent crime needs to be reduced, and Americans need to feel safe. The process for achieving that goal? You tell me.
Nurses in prisons
About 1% of employed nurses (i.e., close to 21,000) in the United States work in prisons. This figure does not include the many LPNs and unlicensed assistive personnel who are also working in the field and may underrepresent actual numbers.
Correctional nurses have their own scope and standards of practice. They demonstrate superb assessment skills and organization.
If you can hire a correctional nurse, or even aspire to be one, do not hesitate. Patients will thank you.
A version of this article first appeared on Medscape.com.
As a health care provider, I have always been interested in topics that concern incarcerated citizens, whether the discussion is related to the pursuit of aggressive care or jurisprudence in general. Additionally, I have followed the issue of capital punishment for most of my career, wondering if our democracy would continue this form of punishment for violent crimes.
In the early 2000s, public opinion moved away from capital punishment. The days of executing violent criminals such as Ted Bundy (who was killed in the electric chair in 1989) seemed to be in the rearview mirror. The ability of prison systems to obtain drugs for execution had become arduous, and Americans appeared disinterested in continuing with the process. Slowly, states began opting out of executions. Currently, 27 U.S. states offer the death penalty as an option at prosecution.
Botched executions
So far in 2021, 11 prisoners have been put to death by the federal government as well as five states, using either a one-drug or three-drug intravenous protocol. Of those prisoners, one was female.
The length of time from sentencing to date of execution varied from a low of 9 years to a high of 29 years, according to the Death Penalty Information Center. Of the executions performed this year, one was considered “botched.” The victim convulsed and vomited for several minutes before his ultimate demise. In fact, in the history of using the death penalty, from 1890 to 2010, approximately 3% of total executions (276 prisoners) were botched. They involved failed electric shocks, convulsions, labored breathing, and in one particularly horrific incident, a victim who was shot in the hip and abdomen by a firing squad and took several minutes to die.
One of the more difficult tasks for conducting an execution is intravenous access, with acquisition of an intravenous site proving to be a common issue. Another concern involves intravenous efficacy, or failure of the site to remain patent until death is achieved. That is why a few states that still practice capital punishment have returned to an electric chair option for execution (the method is chosen by the prisoner).
Majority favor capital punishment
But why do most Americans believe we need the death penalty? According to a 2021 poll by the Pew Research Center, 60% of U.S. citizens favor the use of capital punishment for those convicted of murder, including 27% who strongly favor its use. About 4 in 10 oppose the punishment, but only 15% are strongly opposed. The belief of those who favor retaining execution is that use of the death penalty deters violent crime.
Surprisingly, the American South has both the highest murder rate in the country and the highest percentage of executions. This geographic area encompasses 81% of the nation’s executions. A 2012 National Research Council poll determined that studies claiming the death penalty deters violent crime are “fundamentally flawed.” States that have abolished the death penalty do not show an increase in murder rates; in fact, the opposite is true, the organization concluded.
Since 1990, states without death penalty punishment have had consistently lower murder rates than those that retain capital punishment.
Where does that leave us?
Place my attitude in the column labeled “undecided.” I would love to believe capital punishment is a deterrent to violent crime, yet statistics do not prove the hypothesis to be true. We live in one of the more violent times in history, with mass shootings becoming commonplace. Large-scale retail theft has also been on the rise, especially in recent weeks.
The idea of severe punishment for heinous crime appeals to me, yet in 2001 Timothy McVeigh was executed after eating ice cream and gazing at the moon. His treatment before execution and the length of time he served were in opposition to other inmates sentenced to death. This, despite being punished for killing 168 people (including 19 children) in the Oklahoma City bombings.
I know we cannot be complacent. Violent crime needs to be reduced, and Americans need to feel safe. The process for achieving that goal? You tell me.
Nurses in prisons
About 1% of employed nurses (i.e., close to 21,000) in the United States work in prisons. This figure does not include the many LPNs and unlicensed assistive personnel who are also working in the field and may underrepresent actual numbers.
Correctional nurses have their own scope and standards of practice. They demonstrate superb assessment skills and organization.
If you can hire a correctional nurse, or even aspire to be one, do not hesitate. Patients will thank you.
A version of this article first appeared on Medscape.com.
Treating homeless patients: Book offers key insights
As a psychiatrist dedicated to working with people who are experiencing homelessness, I was very impressed with the new book edited by Col. (Ret.) Elspeth Cameron Ritchie, MD, MPH, and Maria D. Llorente, MD, about treating and providing services to this vulnerable population.
The book, “Clinical Management of the Homeless Patient: Social, Psychiatric, and Medical Issues” (Cham, Switzerland: Springer Nature Switzerland, 2021), offers an in-depth review and analysis of the biopsychosocial complexities that affect how medical and behavioral health conditions present in those who are unhoused. Notably, the book recommends with great sensitivity best practices to address these conditions with care, understanding, and love.
This text, invaluable in particular for those of us clinicians who work with people experiencing homelessness (PEH), provides a historical context of homelessness in the United States, an evaluation of the current state, and indispensable guidance for medical and behavioral health practitioners, case managers, housing navigators, and policy makers alike. It also serves as an inspiring source for those who are considering work in the public sector while reminding those of us in the field why we continue to do this challenging and rewarding work.
Tips can provide hope to clinicians
The volume is divided into four clear sections that are easy to navigate depending on your area of expertise and interest. Each chapter consolidates an extensive literature review into an intriguing and thought-provoking analysis. Part I, “The Big Picture – Social and Medical Issues,” focuses on conditions that disproportionately affect those who are unhoused. The authors offer a glimpse into the unique challenges of managing routine health conditions. They also detail the practical knowledge that’s needed to best care for our most vulnerable neighbors; for example, promoting a shared decision-making model; simplifying treatment plans; prescribing, when possible, medications that are dosed daily – instead of multiple times per day; allowing for walk-in appointments; and addressing cultural, linguistic, and educational barriers.
Most chapters highlight informative case examples that bring the text to life. It can be heartbreaking to recognize and witness the inhumane conditions in which PEH live, and these practical tips and suggestions for future policies based on best practices can help prevent burnout and provide hope for those who care for this community.
Part II, “Psychiatric Issues and Treatments,” presents a brief yet comprehensive history on homelessness, beginning with the deep shame that PEH experienced in Colonial times as the result of cultural and religious influences. Sadly, that negative judgment continues to this day.
The authors also explain how deinstitutionalization and transinstitutionalization have shaped the current state of homelessness, including why many PEH receive their care in emergency departments while incarcerated. This section highlights the barriers of care that are created not just by the patient, but also by the clinicians and systems of care – and what’s needed practically to overcome those challenges.
I appreciate the chapter on substance use disorders. It reminds us that the most commonly used substance among PEH is tobacco, which has serious health effects and for which we have treatment; nevertheless, . This section also provides examples of the trauma-informed language to use when addressing difficult and sometimes stigmatizing topics, such as survival sex and trauma history.
The evidence-based discussion continues in Part III with a focus on topics that everyone working with PEH should understand, including food insecurity, the criminal justice system, and sex trafficking. Part IV highlights best practices that should be replicated in every community, including Housing First approaches, medical respite care, and multiple Veterans Administration programs.
Throughout the text, major themes reverberate across the chapters, beginning with empathy. All who work with PEH must understand the conditions and challenges PEH face every day that affect their physical and mental health. The authors offer a stark and pointed reminder that being unhoused amounts to a full-time job just to meet basic needs. In addition, the devastating role of trauma and structural racism in creating and promoting the conditions that lead someone to be unhoused cannot be underestimated.
Fortunately, the primary aim of the book is to highlight solutions, and it’s here that the book shines. While some interventions are well-known, such as the importance of working in multidisciplinary teams, building trust and rapport with our patients, and urging clinicians and institutions to examine their own judgments and biases that might interfere with humane treatment, other suggestions will lead some readers into new territory. The authors, for example, maintain that we need more data and evidence-based research that include PEH. They also make a case for more preventive care and enhanced professional education for all health care workers that centers on trauma-informed care, social determinants of health, and the unique needs of especially vulnerable communities, such as the unhoused LBGTQ+ community and policies that promote best practices, such as Housing First. The book is a stirring read. It offers both inspiration and practical guidance for all who are currently working with or interested in caring for people experiencing homelessness.
Dr. Bird is a psychiatrist with Alameda County Health Care for the Homeless and the TRUST Clinic in Oakland, Calif. She also is a cofounder of StreetHealth, a backpack street medicine team that provides psychiatric and substance use disorder treatment to people experiencing homelessness in downtown Oakland.
Dr. Bird has no disclosures.
As a psychiatrist dedicated to working with people who are experiencing homelessness, I was very impressed with the new book edited by Col. (Ret.) Elspeth Cameron Ritchie, MD, MPH, and Maria D. Llorente, MD, about treating and providing services to this vulnerable population.
The book, “Clinical Management of the Homeless Patient: Social, Psychiatric, and Medical Issues” (Cham, Switzerland: Springer Nature Switzerland, 2021), offers an in-depth review and analysis of the biopsychosocial complexities that affect how medical and behavioral health conditions present in those who are unhoused. Notably, the book recommends with great sensitivity best practices to address these conditions with care, understanding, and love.
This text, invaluable in particular for those of us clinicians who work with people experiencing homelessness (PEH), provides a historical context of homelessness in the United States, an evaluation of the current state, and indispensable guidance for medical and behavioral health practitioners, case managers, housing navigators, and policy makers alike. It also serves as an inspiring source for those who are considering work in the public sector while reminding those of us in the field why we continue to do this challenging and rewarding work.
Tips can provide hope to clinicians
The volume is divided into four clear sections that are easy to navigate depending on your area of expertise and interest. Each chapter consolidates an extensive literature review into an intriguing and thought-provoking analysis. Part I, “The Big Picture – Social and Medical Issues,” focuses on conditions that disproportionately affect those who are unhoused. The authors offer a glimpse into the unique challenges of managing routine health conditions. They also detail the practical knowledge that’s needed to best care for our most vulnerable neighbors; for example, promoting a shared decision-making model; simplifying treatment plans; prescribing, when possible, medications that are dosed daily – instead of multiple times per day; allowing for walk-in appointments; and addressing cultural, linguistic, and educational barriers.
Most chapters highlight informative case examples that bring the text to life. It can be heartbreaking to recognize and witness the inhumane conditions in which PEH live, and these practical tips and suggestions for future policies based on best practices can help prevent burnout and provide hope for those who care for this community.
Part II, “Psychiatric Issues and Treatments,” presents a brief yet comprehensive history on homelessness, beginning with the deep shame that PEH experienced in Colonial times as the result of cultural and religious influences. Sadly, that negative judgment continues to this day.
The authors also explain how deinstitutionalization and transinstitutionalization have shaped the current state of homelessness, including why many PEH receive their care in emergency departments while incarcerated. This section highlights the barriers of care that are created not just by the patient, but also by the clinicians and systems of care – and what’s needed practically to overcome those challenges.
I appreciate the chapter on substance use disorders. It reminds us that the most commonly used substance among PEH is tobacco, which has serious health effects and for which we have treatment; nevertheless, . This section also provides examples of the trauma-informed language to use when addressing difficult and sometimes stigmatizing topics, such as survival sex and trauma history.
The evidence-based discussion continues in Part III with a focus on topics that everyone working with PEH should understand, including food insecurity, the criminal justice system, and sex trafficking. Part IV highlights best practices that should be replicated in every community, including Housing First approaches, medical respite care, and multiple Veterans Administration programs.
Throughout the text, major themes reverberate across the chapters, beginning with empathy. All who work with PEH must understand the conditions and challenges PEH face every day that affect their physical and mental health. The authors offer a stark and pointed reminder that being unhoused amounts to a full-time job just to meet basic needs. In addition, the devastating role of trauma and structural racism in creating and promoting the conditions that lead someone to be unhoused cannot be underestimated.
Fortunately, the primary aim of the book is to highlight solutions, and it’s here that the book shines. While some interventions are well-known, such as the importance of working in multidisciplinary teams, building trust and rapport with our patients, and urging clinicians and institutions to examine their own judgments and biases that might interfere with humane treatment, other suggestions will lead some readers into new territory. The authors, for example, maintain that we need more data and evidence-based research that include PEH. They also make a case for more preventive care and enhanced professional education for all health care workers that centers on trauma-informed care, social determinants of health, and the unique needs of especially vulnerable communities, such as the unhoused LBGTQ+ community and policies that promote best practices, such as Housing First. The book is a stirring read. It offers both inspiration and practical guidance for all who are currently working with or interested in caring for people experiencing homelessness.
Dr. Bird is a psychiatrist with Alameda County Health Care for the Homeless and the TRUST Clinic in Oakland, Calif. She also is a cofounder of StreetHealth, a backpack street medicine team that provides psychiatric and substance use disorder treatment to people experiencing homelessness in downtown Oakland.
Dr. Bird has no disclosures.
As a psychiatrist dedicated to working with people who are experiencing homelessness, I was very impressed with the new book edited by Col. (Ret.) Elspeth Cameron Ritchie, MD, MPH, and Maria D. Llorente, MD, about treating and providing services to this vulnerable population.
The book, “Clinical Management of the Homeless Patient: Social, Psychiatric, and Medical Issues” (Cham, Switzerland: Springer Nature Switzerland, 2021), offers an in-depth review and analysis of the biopsychosocial complexities that affect how medical and behavioral health conditions present in those who are unhoused. Notably, the book recommends with great sensitivity best practices to address these conditions with care, understanding, and love.
This text, invaluable in particular for those of us clinicians who work with people experiencing homelessness (PEH), provides a historical context of homelessness in the United States, an evaluation of the current state, and indispensable guidance for medical and behavioral health practitioners, case managers, housing navigators, and policy makers alike. It also serves as an inspiring source for those who are considering work in the public sector while reminding those of us in the field why we continue to do this challenging and rewarding work.
Tips can provide hope to clinicians
The volume is divided into four clear sections that are easy to navigate depending on your area of expertise and interest. Each chapter consolidates an extensive literature review into an intriguing and thought-provoking analysis. Part I, “The Big Picture – Social and Medical Issues,” focuses on conditions that disproportionately affect those who are unhoused. The authors offer a glimpse into the unique challenges of managing routine health conditions. They also detail the practical knowledge that’s needed to best care for our most vulnerable neighbors; for example, promoting a shared decision-making model; simplifying treatment plans; prescribing, when possible, medications that are dosed daily – instead of multiple times per day; allowing for walk-in appointments; and addressing cultural, linguistic, and educational barriers.
Most chapters highlight informative case examples that bring the text to life. It can be heartbreaking to recognize and witness the inhumane conditions in which PEH live, and these practical tips and suggestions for future policies based on best practices can help prevent burnout and provide hope for those who care for this community.
Part II, “Psychiatric Issues and Treatments,” presents a brief yet comprehensive history on homelessness, beginning with the deep shame that PEH experienced in Colonial times as the result of cultural and religious influences. Sadly, that negative judgment continues to this day.
The authors also explain how deinstitutionalization and transinstitutionalization have shaped the current state of homelessness, including why many PEH receive their care in emergency departments while incarcerated. This section highlights the barriers of care that are created not just by the patient, but also by the clinicians and systems of care – and what’s needed practically to overcome those challenges.
I appreciate the chapter on substance use disorders. It reminds us that the most commonly used substance among PEH is tobacco, which has serious health effects and for which we have treatment; nevertheless, . This section also provides examples of the trauma-informed language to use when addressing difficult and sometimes stigmatizing topics, such as survival sex and trauma history.
The evidence-based discussion continues in Part III with a focus on topics that everyone working with PEH should understand, including food insecurity, the criminal justice system, and sex trafficking. Part IV highlights best practices that should be replicated in every community, including Housing First approaches, medical respite care, and multiple Veterans Administration programs.
Throughout the text, major themes reverberate across the chapters, beginning with empathy. All who work with PEH must understand the conditions and challenges PEH face every day that affect their physical and mental health. The authors offer a stark and pointed reminder that being unhoused amounts to a full-time job just to meet basic needs. In addition, the devastating role of trauma and structural racism in creating and promoting the conditions that lead someone to be unhoused cannot be underestimated.
Fortunately, the primary aim of the book is to highlight solutions, and it’s here that the book shines. While some interventions are well-known, such as the importance of working in multidisciplinary teams, building trust and rapport with our patients, and urging clinicians and institutions to examine their own judgments and biases that might interfere with humane treatment, other suggestions will lead some readers into new territory. The authors, for example, maintain that we need more data and evidence-based research that include PEH. They also make a case for more preventive care and enhanced professional education for all health care workers that centers on trauma-informed care, social determinants of health, and the unique needs of especially vulnerable communities, such as the unhoused LBGTQ+ community and policies that promote best practices, such as Housing First. The book is a stirring read. It offers both inspiration and practical guidance for all who are currently working with or interested in caring for people experiencing homelessness.
Dr. Bird is a psychiatrist with Alameda County Health Care for the Homeless and the TRUST Clinic in Oakland, Calif. She also is a cofounder of StreetHealth, a backpack street medicine team that provides psychiatric and substance use disorder treatment to people experiencing homelessness in downtown Oakland.
Dr. Bird has no disclosures.
How do digital technologies affect young people’s mental health?
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
For almost all of us, “screen time”—time spent using a device with a screen such as a smartphone, computer, television, or video game console—has become a large part of our daily lives. This is very much the case for children and adolescents. In the United States, children ages 8 to 12 years spend an average of 4 to 6 hours each day watching or using screens, and teens spend up to 9 hours.1 Because young people are continually adopting newer forms of entertainment and technologies, new digital technologies are an ongoing source of concern for parents and clinicians alike.2 Studies have suggested that excessive screen time is associated with numerous psychiatric symptoms and disorders, including poor sleep, weight gain, anxiety, depression, and attention-deficit/hyperactive disorder.3,4 However, a recent systematic review and meta-analysis found that individuals’ self-reports of media use were rarely an accurate reflection of their actual, logged media use, and that measures of problematic media use had an even weaker association with usage logs.5 Therefore, it is crucial to have an accurate understanding of how children and adolescents are affected by new technologies. In this article, we discuss a recent study that investigated variations in adolescents’ mental health over time, and the association of their mental health and their use of digital technologies.
Results were mixed
Vuorre et al6 conducted a study to examine a possible shift in the associations between adolescents’ technology use and mental health outcomes. To investigate whether technology engagement and mental health outcomes changed over time, these researchers evaluated the impact not only of smartphones and social media, but also of television, which in the mid- to late-20th century elicited comparable levels of academic, public, and policy concern about its potential impact on child development. They analyzed data from 3 large-scale studies of adolescents living in the United States (Monitoring the Future and Youth Risk Behavior Surveillance System) and the United Kingdom (Understanding Society) that included a total of 430,561 participants.
The results were mixed across types of technology and mental health outcomes. Television and social media were found to have a direct correlation with conduct problems and emotional problems. Suicidal ideation and behavior were associated with digital device use; however, no correlation was found between depression and technology use. Regarding social media use, researchers found that its association with conduct problems remained stable, decreased with depression, and increased with emotional problems. The magnitudes of the observed changes over time were small. These researchers concluded there is “little evidence for increases in the associations between adolescents’ technology engagement and mental health [problems]” and “drawing firm conclusions about changes in ... associations with mental health may be premature.”6
Future directions
The study by Vuorre et al6 has opened the door to better analysis of the association between screen use and mental health outcomes. More robust, detailed studies are required to fully understand the varying impact of technologies on the lives of children and adolescents. Collaborative efforts by technology companies and researchers can help to determine the impact of technology on young people’s mental health.
1. American Academy of Child & Adolescent Psychiatry. Screen time and children. Updated February 2020. Accessed October 7, 2021. http://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFF-Guide/Children-And-Watching-TV-054.aspx
2. Orben A. The Sisyphean cycle of technology panics. Perspect Psychol Sci. 2020;15(5):1143-1157.
3. Paulich KN, Ross JM, Lessem JM, et al. Screen time and early adolescent mental health, academic, and social outcomes in 9- and 10-year old children: utilizing the Adolescent Brain Cognitive Development (ABCD) Study. PLoS One. 2021;16(9):e0256591. doi: 10.1371/journal.pone.0256591
4. Twenge JM, Campbell WK. Associations between screen time and lower psychological well-being among children and adolescents: evidence from a population-based study. Prev Med Rep. 2018;12:271-283. doi: 10.1016/j.pmedr.2018.10.003
5. Parry DA, Davidson BI, Sewall CJR, et al. A systematic review and meta-analysis of discrepancies between logged and self-reported digital media use. Nat Hum Behav. 2021;5(11):1535-1547.
6. Vuorre M, Orben A, Przybylski AK. There is no evidence that associations between adolescents’ digital technology engagement and mental health problems have increased. Clin Psychol Sci. 2021;9(5):823-835.
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
For almost all of us, “screen time”—time spent using a device with a screen such as a smartphone, computer, television, or video game console—has become a large part of our daily lives. This is very much the case for children and adolescents. In the United States, children ages 8 to 12 years spend an average of 4 to 6 hours each day watching or using screens, and teens spend up to 9 hours.1 Because young people are continually adopting newer forms of entertainment and technologies, new digital technologies are an ongoing source of concern for parents and clinicians alike.2 Studies have suggested that excessive screen time is associated with numerous psychiatric symptoms and disorders, including poor sleep, weight gain, anxiety, depression, and attention-deficit/hyperactive disorder.3,4 However, a recent systematic review and meta-analysis found that individuals’ self-reports of media use were rarely an accurate reflection of their actual, logged media use, and that measures of problematic media use had an even weaker association with usage logs.5 Therefore, it is crucial to have an accurate understanding of how children and adolescents are affected by new technologies. In this article, we discuss a recent study that investigated variations in adolescents’ mental health over time, and the association of their mental health and their use of digital technologies.
Results were mixed
Vuorre et al6 conducted a study to examine a possible shift in the associations between adolescents’ technology use and mental health outcomes. To investigate whether technology engagement and mental health outcomes changed over time, these researchers evaluated the impact not only of smartphones and social media, but also of television, which in the mid- to late-20th century elicited comparable levels of academic, public, and policy concern about its potential impact on child development. They analyzed data from 3 large-scale studies of adolescents living in the United States (Monitoring the Future and Youth Risk Behavior Surveillance System) and the United Kingdom (Understanding Society) that included a total of 430,561 participants.
The results were mixed across types of technology and mental health outcomes. Television and social media were found to have a direct correlation with conduct problems and emotional problems. Suicidal ideation and behavior were associated with digital device use; however, no correlation was found between depression and technology use. Regarding social media use, researchers found that its association with conduct problems remained stable, decreased with depression, and increased with emotional problems. The magnitudes of the observed changes over time were small. These researchers concluded there is “little evidence for increases in the associations between adolescents’ technology engagement and mental health [problems]” and “drawing firm conclusions about changes in ... associations with mental health may be premature.”6
Future directions
The study by Vuorre et al6 has opened the door to better analysis of the association between screen use and mental health outcomes. More robust, detailed studies are required to fully understand the varying impact of technologies on the lives of children and adolescents. Collaborative efforts by technology companies and researchers can help to determine the impact of technology on young people’s mental health.
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
For almost all of us, “screen time”—time spent using a device with a screen such as a smartphone, computer, television, or video game console—has become a large part of our daily lives. This is very much the case for children and adolescents. In the United States, children ages 8 to 12 years spend an average of 4 to 6 hours each day watching or using screens, and teens spend up to 9 hours.1 Because young people are continually adopting newer forms of entertainment and technologies, new digital technologies are an ongoing source of concern for parents and clinicians alike.2 Studies have suggested that excessive screen time is associated with numerous psychiatric symptoms and disorders, including poor sleep, weight gain, anxiety, depression, and attention-deficit/hyperactive disorder.3,4 However, a recent systematic review and meta-analysis found that individuals’ self-reports of media use were rarely an accurate reflection of their actual, logged media use, and that measures of problematic media use had an even weaker association with usage logs.5 Therefore, it is crucial to have an accurate understanding of how children and adolescents are affected by new technologies. In this article, we discuss a recent study that investigated variations in adolescents’ mental health over time, and the association of their mental health and their use of digital technologies.
Results were mixed
Vuorre et al6 conducted a study to examine a possible shift in the associations between adolescents’ technology use and mental health outcomes. To investigate whether technology engagement and mental health outcomes changed over time, these researchers evaluated the impact not only of smartphones and social media, but also of television, which in the mid- to late-20th century elicited comparable levels of academic, public, and policy concern about its potential impact on child development. They analyzed data from 3 large-scale studies of adolescents living in the United States (Monitoring the Future and Youth Risk Behavior Surveillance System) and the United Kingdom (Understanding Society) that included a total of 430,561 participants.
The results were mixed across types of technology and mental health outcomes. Television and social media were found to have a direct correlation with conduct problems and emotional problems. Suicidal ideation and behavior were associated with digital device use; however, no correlation was found between depression and technology use. Regarding social media use, researchers found that its association with conduct problems remained stable, decreased with depression, and increased with emotional problems. The magnitudes of the observed changes over time were small. These researchers concluded there is “little evidence for increases in the associations between adolescents’ technology engagement and mental health [problems]” and “drawing firm conclusions about changes in ... associations with mental health may be premature.”6
Future directions
The study by Vuorre et al6 has opened the door to better analysis of the association between screen use and mental health outcomes. More robust, detailed studies are required to fully understand the varying impact of technologies on the lives of children and adolescents. Collaborative efforts by technology companies and researchers can help to determine the impact of technology on young people’s mental health.
1. American Academy of Child & Adolescent Psychiatry. Screen time and children. Updated February 2020. Accessed October 7, 2021. http://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFF-Guide/Children-And-Watching-TV-054.aspx
2. Orben A. The Sisyphean cycle of technology panics. Perspect Psychol Sci. 2020;15(5):1143-1157.
3. Paulich KN, Ross JM, Lessem JM, et al. Screen time and early adolescent mental health, academic, and social outcomes in 9- and 10-year old children: utilizing the Adolescent Brain Cognitive Development (ABCD) Study. PLoS One. 2021;16(9):e0256591. doi: 10.1371/journal.pone.0256591
4. Twenge JM, Campbell WK. Associations between screen time and lower psychological well-being among children and adolescents: evidence from a population-based study. Prev Med Rep. 2018;12:271-283. doi: 10.1016/j.pmedr.2018.10.003
5. Parry DA, Davidson BI, Sewall CJR, et al. A systematic review and meta-analysis of discrepancies between logged and self-reported digital media use. Nat Hum Behav. 2021;5(11):1535-1547.
6. Vuorre M, Orben A, Przybylski AK. There is no evidence that associations between adolescents’ digital technology engagement and mental health problems have increased. Clin Psychol Sci. 2021;9(5):823-835.
1. American Academy of Child & Adolescent Psychiatry. Screen time and children. Updated February 2020. Accessed October 7, 2021. http://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFF-Guide/Children-And-Watching-TV-054.aspx
2. Orben A. The Sisyphean cycle of technology panics. Perspect Psychol Sci. 2020;15(5):1143-1157.
3. Paulich KN, Ross JM, Lessem JM, et al. Screen time and early adolescent mental health, academic, and social outcomes in 9- and 10-year old children: utilizing the Adolescent Brain Cognitive Development (ABCD) Study. PLoS One. 2021;16(9):e0256591. doi: 10.1371/journal.pone.0256591
4. Twenge JM, Campbell WK. Associations between screen time and lower psychological well-being among children and adolescents: evidence from a population-based study. Prev Med Rep. 2018;12:271-283. doi: 10.1016/j.pmedr.2018.10.003
5. Parry DA, Davidson BI, Sewall CJR, et al. A systematic review and meta-analysis of discrepancies between logged and self-reported digital media use. Nat Hum Behav. 2021;5(11):1535-1547.
6. Vuorre M, Orben A, Przybylski AK. There is no evidence that associations between adolescents’ digital technology engagement and mental health problems have increased. Clin Psychol Sci. 2021;9(5):823-835.
Is anosognosia a delusion, a negative symptom, or a cognitive deficit?
Anosognosia is the lack of awareness of a disabling physical or mental illness. The term was coined by Joseph Babinski in 1914 following his observations that patients with left-side paralysis due to right hemisphere stroke do not recognize their hemiplegia and strongly deny that there is anything physically wrong with their body, or that they need treatment or rehabilitation.
Psychiatrists have long observed anosognosia in patients with acute psychoses such as schizophrenia or mania who vehemently deny that there is anything wrong with them, despite experiencing hallucinations, delusions, and/or bizarre behavior. They adamantly refuse medical care and often have to be involuntarily hospitalized to receive urgently needed medications they don’t believe they need.
So is anosognosia in schizophrenia a fixed false belief (delusion), a negative symptom, or a cognitive deficit? Arguments can be made for any of those 3 options, but the evidence suggests that anosognosia is a disorder of consciousness, a “meta-cognitive” deficit, or, as I referred to it in a previous publication, the loss of self-proprioception.1
Anosognosia in neurologic brain disorders
Although right hemispheric stroke is the most common disease state associated with anosognosia,2 other neurologic disorders can be associated with anosognosia, including Anton’s syndrome of cortical blindness,3 traumatic brain injury,4 Wernicke’s aphasia,5 mild cognitive impairment,6 and Alzheimer’s disease.7 In addition to anosognosia, those disorders can be accompanied by indifference to the deficit, which is referred to as “anosodiaphoria.”
The neuroanatomy of anosognosia generally implicates right hemisphere deficits, especially the frontal cortex, the right parietal lobe, the temporoparietal cortex, and the thalamus. It can be conceptualized as a disturbance of “body schema” because all motor and sensory functions of the body have a “representation” in brain structure.
Anosognosia in psychiatric brain disorders
Although schizophrenia is most frequently associated with anosognosia, other psychiatric disorders also exhibit this absence of insight. They include delusional disorder,8 bipolar disorder,9 intellectual disability,10 and personality disorders.11 In all those psychiatric disorders, there is a lack of self-reflection (metacognition). At the neuroanatomical level, most studies have focused on schizophrenia, and abnormalities have been described in the frontal and parietal regions. Significant pathology in the inferior parietal lobe has been identified in schizophrenia.12 However, the right insula, which is connected to multiple neural circuits,13 appears to be intimately associated with anosognosia when impaired. The insula also regulates interoception and a “sense of self.”14 The loss of cortical gray matter in schizophrenia is most pronounced in the insula bilaterally. Another neurologic mechanism associated with anosognosia in schizophrenia is the default mode network (DMN). The DMN, which usually is overactive at rest and is deactivated during a focused activity, is involved in both insight and social cognition.15
Measurement of anosognosia
Several rating scales are used to measure the severity of anosognosia and the loss of insight. They include:
- The Insight and Treatment Attitude Questionnaire16
- The Scale to Assess Unawareness of Mental Disorder17
- The Beck Cognitive Insight Scale,18 the only self-administered scale that measures a patient’s ability to evaluate their psychiatric beliefs and possibly modify them
- The Positive and Negative Syndrome Scale,19 which is the gold standard for measuring the overall severity of schizophrenia, has only 1 item related to insight within the 16-item General Subscale (G12: Lack of judgement and insight).
Continue to: Consequences of anosognosia...
Consequences of anosognosia
Patients with anosognosia neglect themselves both mentally and physically and fail to seek or accept medical attention. Thus, schizophrenia is associated with many serious and damaging consequences due to the lack of self-monitoring or appraising their health needs. The Table summarizes the multiple consequences of anosognosia.
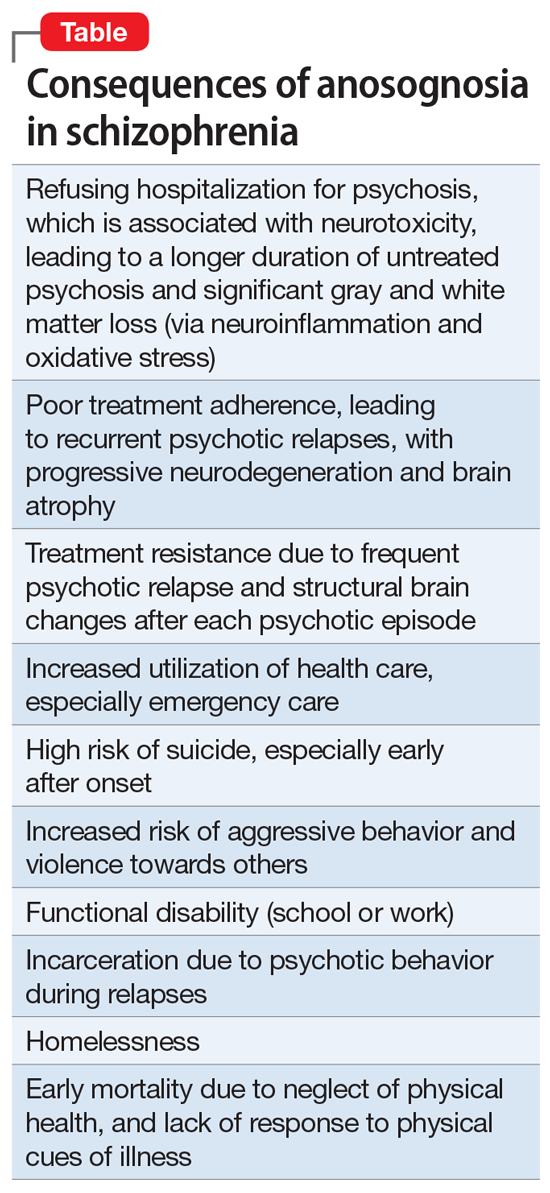
Is anosognosia treatable or irreversible?
Schizophrenia is well established to be a heterogeneous syndrome with hundreds of biotypes that share a similar phenotype of positive, negative, cognitive, mood, and neuromotor symptoms of variable severities.20 This includes anosognosia, which has been reported in 57% to 98% of patients in various studies.21,22
So what happens to anosognosia with antipsychotic therapy? In the first study that used a long-acting injectable (LAI) second-generation antipsychotic (SGA) in first-episode psychosis to ensure full adherence, Emsley et al23 reported a 64% remission rate after 2 years of treatment, and observed that many patients regained their insight after several months of uninterrupted antipsychotic pharmacotherapy. This suggests that avoiding psychotic relapse with uninterrupted antipsychotic therapy with LAIs may help restore insight. I have personally witnessed reversal of anosognosia in patients with first-episode schizophrenia whom I treated with LAI SGAs continuously for several years; these patients not only regained insight into their illness but were able to return to college or to work.
There is also evidence that stroke patients with left-side hemiplegia, or patients with cortical blindness (due to calcarine cortex damage secondary to posterior cerebral artery infarct), who paradoxically deny being blind due to anosognosia, do regain their insight after several months. Cognitive-behavioral therapy (CBT) and adherence therapy, as well as psychoeducation, can help in reversing anosognosia. Bilateral electroconvulsive therapy has been reported to improve insight in schizophrenia. Transcranial magnetic stimulation over the posterior parietal cortex has been reported to restore insight in patients with visuospatial neglect due to a stroke. However, more research targeting anosognosia along with psychotic symptoms is needed. It should be noted that patients with bipolar disorder who have anosognosia during the manic phase of their illness do have insight when they switch to a depressed phase,9 which suggests that anosognosia is reversible in bipolar disorder and is phase-dependent (ie, a state, not a trait, variable).
A symptom of impaired consciousness
A large body of evidence links lesions in the right hemisphere to delusion and to anosognosia.24 Gazzaniga and Miller25 published a book chapter with the provocative title “the left hemisphere does not miss the right hemisphere.” Such right-hemisphere lesions can lead to a disruption of consciousness, leading to anosognosia. Schizophrenia is a pervasive brain syndrome involving multiple brain regions and a wide range of clinical symptoms ranging across psychotic as well as negative and cognitive domains. Anosognosia can be conceptualized as a psychotic symptom (delusion), a negative symptom (self-monitoring deficit), or a cognitive failure. However, anosognosia in schizophrenia can be best understood as a symptom of impaired consciousness and self-pathology,26 where the brain fails to process and recognize one’s mental function, which culminates in faulty reality testing.
Schizophrenia is a neurologic syndrome associated with numerous psychiatric manifestations, and anosognosia is one of its fundamental initial symptoms.
1. Nasrallah HA. Impaired mental proprioception in schizophrenia. Current Psychiatry. 2012;11(8):4-5.
2. Kirsch LP, Mathys C, Papadaki C, et al. Updating beliefs beyond the here-and-now: the counter-factual self in anosognosia for hemiplegia. Brain Commun. 2021;3(2):fcab098. doi: 10.1093/braincomms/fcab098
3. Das JM, Nagvi IA. Anton syndrome. StatPearls Publishing. Updated April 10, 2021. Accessed December 13, 2021. https://www.ncbi.nlm.nih.gov/books/NBK538155/
4. Steward KA, Kretzmer T. Anosognosia in moderate-to-severe traumatic brain injury: a review of prevalence, clinical correlates, and diversity considerations. Clin Neuropsychol. 2021:1-20.
5. Klarendié M, Gorišek VR, Granda G, et al. Auditory agnosia with anosognosia. Cortex. 2021;137:255-270.
6. Bastin C, Giacomelli F, Miévis F, et al. Anosognosia in mild cognitive impairment: lack of awareness of memory difficulties characterizes prodromal Alzheimer’s disease. Front Psychiatry. 202;12:631518.
7. Chen S, Song Y, Xu W, et al; Alzheimer’s Disease Neuroimaging Initiative. Impaired memory awareness and loss integration in self-referential network across the progression of Alzheimer’s disease spectrum. J Alzheimers Dis. 2021;83(1):111-126.
8. Turnbull OH, Fotopoulou A, Solms M. Anosognosia as motivated unawareness: the ‘defence’ hypothesis revisited. Cortex. 2014;61:18-29.
9. Ibrahim SU, Kalyanasundaram VB, Ramanathan SA, et al. Trajectory of insight on various dimensions among bipolar disorder in-patients. Ind Psychiatry J. 2020;29(2):285-292.
10. Levine DN. Unawareness of visual and sensorimotor defects: a hypothesis. Brain Cogn. 1990;13(2):233-281.
11. Pourmohammad P, Imani M, Goodarzi MA, et al. Impaired complex theory of mind and low emotional self-awareness in outpatients with borderline personality disorder compared to healthy controls: a cross-sectional study. J Psychiatr Res. 2021;143:445-450.
12. Torrey EF. Schizophrenia and the inferior parietal lobule. Schizophr Res. 2007;97(1-3):215-225.
13. Dionisio S, Mayoglou L, Cho SM, et al. Connectivity of the human insula: a cortico-cortical evoked potential (CCEP) study. Cortex. 2019;120:419-442.
14. Nord CL, Lawson RP, Dalgleish T. Disrupted dorsal mid-insula activation during interoception across psychiatric disorders. Am J Psychiatry. 2021;178(8):761-770.
15. Glahn DC, Laird AR, Ellison-Wright I, et al. Meta-analysis of gray matter anomalies in schizophrenia: application of anatomic likelihood estimation and network analysis. Biol Psychiatry. 2008;64(9):774-781.
16. McEvoy JP, Freter S, Everett G, et al. Insight and the clinical outcome of schizophrenic patients. J Nerv Ment Dis. 1989;177(1):48-51.
17. Amador XF, Strauss DH, Yale SA, et al. Assessment of insight in psychosis. Am J Psychiatry. 1993;150(6):873-879.
18. Beck AT, Baruch E, Balter JM, et al. A new instrument for measuring insight: the Beck Cognitive Insight Scale. Schizophr Res. 2004;68(2-3):319-329.
19. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261-276.
20. Nasrallah HA. FAST and RAPID: acronyms to prevent brain damage in stroke and psychosis. Current Psychiatry. 2018;17(8):6-8.
21. Buckley PF, Wirshing DA, Bhushan P, et al. Lack of insight in schizophrenia: impact on treatment adherence. CNS Drugs. 2007;21(2):129-141.
22. Lehrer DS, Lorenz J. Anosognosia in schizophrenia: hidden in plain sight. Innov Clin Neurosci. 2014;11(5-6):101-107.
23. Emsley R, Medori R, Koen L, et al. Long-acting injectable risperidone in the treatment of subjects with recent-onset psychosis: a preliminary study. J Clin Psychopharmacol. 2008;28(2):210-213.
24. Gurin L, Blum S. Delusions and the right hemisphere: a review of the case for the right hemisphere as a mediator of reality-based belief. J Neuropsychiatry Clin Neurosci. 2017;29(3):225-235.
25. Gazzaniga MS, Miller M. The left hemisphere does not miss the right hemisphere. In: Laureys S, Tononi G (eds). The Neurology of Consciousness. Cognitive Neuroscience and Neuropathology. Academic Press; 2008:261-270.
26. Cooney JW, Gazzaniga MS. Neurological disorders and the structure of human consciousness. Trends Cogn Sci. 2003;7(4):161-165.
Anosognosia is the lack of awareness of a disabling physical or mental illness. The term was coined by Joseph Babinski in 1914 following his observations that patients with left-side paralysis due to right hemisphere stroke do not recognize their hemiplegia and strongly deny that there is anything physically wrong with their body, or that they need treatment or rehabilitation.
Psychiatrists have long observed anosognosia in patients with acute psychoses such as schizophrenia or mania who vehemently deny that there is anything wrong with them, despite experiencing hallucinations, delusions, and/or bizarre behavior. They adamantly refuse medical care and often have to be involuntarily hospitalized to receive urgently needed medications they don’t believe they need.
So is anosognosia in schizophrenia a fixed false belief (delusion), a negative symptom, or a cognitive deficit? Arguments can be made for any of those 3 options, but the evidence suggests that anosognosia is a disorder of consciousness, a “meta-cognitive” deficit, or, as I referred to it in a previous publication, the loss of self-proprioception.1
Anosognosia in neurologic brain disorders
Although right hemispheric stroke is the most common disease state associated with anosognosia,2 other neurologic disorders can be associated with anosognosia, including Anton’s syndrome of cortical blindness,3 traumatic brain injury,4 Wernicke’s aphasia,5 mild cognitive impairment,6 and Alzheimer’s disease.7 In addition to anosognosia, those disorders can be accompanied by indifference to the deficit, which is referred to as “anosodiaphoria.”
The neuroanatomy of anosognosia generally implicates right hemisphere deficits, especially the frontal cortex, the right parietal lobe, the temporoparietal cortex, and the thalamus. It can be conceptualized as a disturbance of “body schema” because all motor and sensory functions of the body have a “representation” in brain structure.
Anosognosia in psychiatric brain disorders
Although schizophrenia is most frequently associated with anosognosia, other psychiatric disorders also exhibit this absence of insight. They include delusional disorder,8 bipolar disorder,9 intellectual disability,10 and personality disorders.11 In all those psychiatric disorders, there is a lack of self-reflection (metacognition). At the neuroanatomical level, most studies have focused on schizophrenia, and abnormalities have been described in the frontal and parietal regions. Significant pathology in the inferior parietal lobe has been identified in schizophrenia.12 However, the right insula, which is connected to multiple neural circuits,13 appears to be intimately associated with anosognosia when impaired. The insula also regulates interoception and a “sense of self.”14 The loss of cortical gray matter in schizophrenia is most pronounced in the insula bilaterally. Another neurologic mechanism associated with anosognosia in schizophrenia is the default mode network (DMN). The DMN, which usually is overactive at rest and is deactivated during a focused activity, is involved in both insight and social cognition.15
Measurement of anosognosia
Several rating scales are used to measure the severity of anosognosia and the loss of insight. They include:
- The Insight and Treatment Attitude Questionnaire16
- The Scale to Assess Unawareness of Mental Disorder17
- The Beck Cognitive Insight Scale,18 the only self-administered scale that measures a patient’s ability to evaluate their psychiatric beliefs and possibly modify them
- The Positive and Negative Syndrome Scale,19 which is the gold standard for measuring the overall severity of schizophrenia, has only 1 item related to insight within the 16-item General Subscale (G12: Lack of judgement and insight).
Continue to: Consequences of anosognosia...
Consequences of anosognosia
Patients with anosognosia neglect themselves both mentally and physically and fail to seek or accept medical attention. Thus, schizophrenia is associated with many serious and damaging consequences due to the lack of self-monitoring or appraising their health needs. The Table summarizes the multiple consequences of anosognosia.
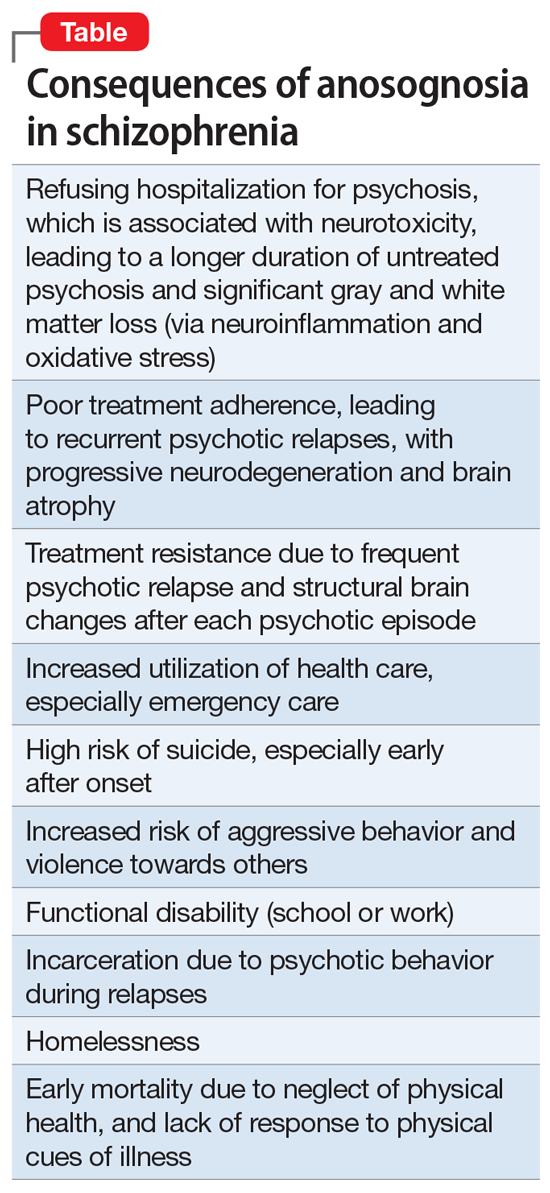
Is anosognosia treatable or irreversible?
Schizophrenia is well established to be a heterogeneous syndrome with hundreds of biotypes that share a similar phenotype of positive, negative, cognitive, mood, and neuromotor symptoms of variable severities.20 This includes anosognosia, which has been reported in 57% to 98% of patients in various studies.21,22
So what happens to anosognosia with antipsychotic therapy? In the first study that used a long-acting injectable (LAI) second-generation antipsychotic (SGA) in first-episode psychosis to ensure full adherence, Emsley et al23 reported a 64% remission rate after 2 years of treatment, and observed that many patients regained their insight after several months of uninterrupted antipsychotic pharmacotherapy. This suggests that avoiding psychotic relapse with uninterrupted antipsychotic therapy with LAIs may help restore insight. I have personally witnessed reversal of anosognosia in patients with first-episode schizophrenia whom I treated with LAI SGAs continuously for several years; these patients not only regained insight into their illness but were able to return to college or to work.
There is also evidence that stroke patients with left-side hemiplegia, or patients with cortical blindness (due to calcarine cortex damage secondary to posterior cerebral artery infarct), who paradoxically deny being blind due to anosognosia, do regain their insight after several months. Cognitive-behavioral therapy (CBT) and adherence therapy, as well as psychoeducation, can help in reversing anosognosia. Bilateral electroconvulsive therapy has been reported to improve insight in schizophrenia. Transcranial magnetic stimulation over the posterior parietal cortex has been reported to restore insight in patients with visuospatial neglect due to a stroke. However, more research targeting anosognosia along with psychotic symptoms is needed. It should be noted that patients with bipolar disorder who have anosognosia during the manic phase of their illness do have insight when they switch to a depressed phase,9 which suggests that anosognosia is reversible in bipolar disorder and is phase-dependent (ie, a state, not a trait, variable).
A symptom of impaired consciousness
A large body of evidence links lesions in the right hemisphere to delusion and to anosognosia.24 Gazzaniga and Miller25 published a book chapter with the provocative title “the left hemisphere does not miss the right hemisphere.” Such right-hemisphere lesions can lead to a disruption of consciousness, leading to anosognosia. Schizophrenia is a pervasive brain syndrome involving multiple brain regions and a wide range of clinical symptoms ranging across psychotic as well as negative and cognitive domains. Anosognosia can be conceptualized as a psychotic symptom (delusion), a negative symptom (self-monitoring deficit), or a cognitive failure. However, anosognosia in schizophrenia can be best understood as a symptom of impaired consciousness and self-pathology,26 where the brain fails to process and recognize one’s mental function, which culminates in faulty reality testing.
Schizophrenia is a neurologic syndrome associated with numerous psychiatric manifestations, and anosognosia is one of its fundamental initial symptoms.
Anosognosia is the lack of awareness of a disabling physical or mental illness. The term was coined by Joseph Babinski in 1914 following his observations that patients with left-side paralysis due to right hemisphere stroke do not recognize their hemiplegia and strongly deny that there is anything physically wrong with their body, or that they need treatment or rehabilitation.
Psychiatrists have long observed anosognosia in patients with acute psychoses such as schizophrenia or mania who vehemently deny that there is anything wrong with them, despite experiencing hallucinations, delusions, and/or bizarre behavior. They adamantly refuse medical care and often have to be involuntarily hospitalized to receive urgently needed medications they don’t believe they need.
So is anosognosia in schizophrenia a fixed false belief (delusion), a negative symptom, or a cognitive deficit? Arguments can be made for any of those 3 options, but the evidence suggests that anosognosia is a disorder of consciousness, a “meta-cognitive” deficit, or, as I referred to it in a previous publication, the loss of self-proprioception.1
Anosognosia in neurologic brain disorders
Although right hemispheric stroke is the most common disease state associated with anosognosia,2 other neurologic disorders can be associated with anosognosia, including Anton’s syndrome of cortical blindness,3 traumatic brain injury,4 Wernicke’s aphasia,5 mild cognitive impairment,6 and Alzheimer’s disease.7 In addition to anosognosia, those disorders can be accompanied by indifference to the deficit, which is referred to as “anosodiaphoria.”
The neuroanatomy of anosognosia generally implicates right hemisphere deficits, especially the frontal cortex, the right parietal lobe, the temporoparietal cortex, and the thalamus. It can be conceptualized as a disturbance of “body schema” because all motor and sensory functions of the body have a “representation” in brain structure.
Anosognosia in psychiatric brain disorders
Although schizophrenia is most frequently associated with anosognosia, other psychiatric disorders also exhibit this absence of insight. They include delusional disorder,8 bipolar disorder,9 intellectual disability,10 and personality disorders.11 In all those psychiatric disorders, there is a lack of self-reflection (metacognition). At the neuroanatomical level, most studies have focused on schizophrenia, and abnormalities have been described in the frontal and parietal regions. Significant pathology in the inferior parietal lobe has been identified in schizophrenia.12 However, the right insula, which is connected to multiple neural circuits,13 appears to be intimately associated with anosognosia when impaired. The insula also regulates interoception and a “sense of self.”14 The loss of cortical gray matter in schizophrenia is most pronounced in the insula bilaterally. Another neurologic mechanism associated with anosognosia in schizophrenia is the default mode network (DMN). The DMN, which usually is overactive at rest and is deactivated during a focused activity, is involved in both insight and social cognition.15
Measurement of anosognosia
Several rating scales are used to measure the severity of anosognosia and the loss of insight. They include:
- The Insight and Treatment Attitude Questionnaire16
- The Scale to Assess Unawareness of Mental Disorder17
- The Beck Cognitive Insight Scale,18 the only self-administered scale that measures a patient’s ability to evaluate their psychiatric beliefs and possibly modify them
- The Positive and Negative Syndrome Scale,19 which is the gold standard for measuring the overall severity of schizophrenia, has only 1 item related to insight within the 16-item General Subscale (G12: Lack of judgement and insight).
Continue to: Consequences of anosognosia...
Consequences of anosognosia
Patients with anosognosia neglect themselves both mentally and physically and fail to seek or accept medical attention. Thus, schizophrenia is associated with many serious and damaging consequences due to the lack of self-monitoring or appraising their health needs. The Table summarizes the multiple consequences of anosognosia.
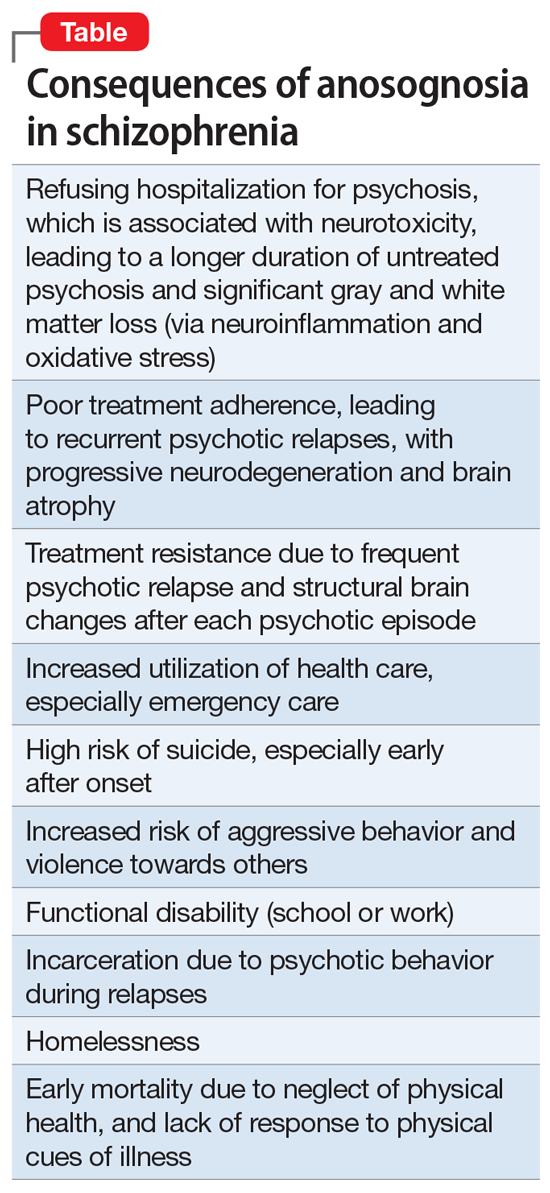
Is anosognosia treatable or irreversible?
Schizophrenia is well established to be a heterogeneous syndrome with hundreds of biotypes that share a similar phenotype of positive, negative, cognitive, mood, and neuromotor symptoms of variable severities.20 This includes anosognosia, which has been reported in 57% to 98% of patients in various studies.21,22
So what happens to anosognosia with antipsychotic therapy? In the first study that used a long-acting injectable (LAI) second-generation antipsychotic (SGA) in first-episode psychosis to ensure full adherence, Emsley et al23 reported a 64% remission rate after 2 years of treatment, and observed that many patients regained their insight after several months of uninterrupted antipsychotic pharmacotherapy. This suggests that avoiding psychotic relapse with uninterrupted antipsychotic therapy with LAIs may help restore insight. I have personally witnessed reversal of anosognosia in patients with first-episode schizophrenia whom I treated with LAI SGAs continuously for several years; these patients not only regained insight into their illness but were able to return to college or to work.
There is also evidence that stroke patients with left-side hemiplegia, or patients with cortical blindness (due to calcarine cortex damage secondary to posterior cerebral artery infarct), who paradoxically deny being blind due to anosognosia, do regain their insight after several months. Cognitive-behavioral therapy (CBT) and adherence therapy, as well as psychoeducation, can help in reversing anosognosia. Bilateral electroconvulsive therapy has been reported to improve insight in schizophrenia. Transcranial magnetic stimulation over the posterior parietal cortex has been reported to restore insight in patients with visuospatial neglect due to a stroke. However, more research targeting anosognosia along with psychotic symptoms is needed. It should be noted that patients with bipolar disorder who have anosognosia during the manic phase of their illness do have insight when they switch to a depressed phase,9 which suggests that anosognosia is reversible in bipolar disorder and is phase-dependent (ie, a state, not a trait, variable).
A symptom of impaired consciousness
A large body of evidence links lesions in the right hemisphere to delusion and to anosognosia.24 Gazzaniga and Miller25 published a book chapter with the provocative title “the left hemisphere does not miss the right hemisphere.” Such right-hemisphere lesions can lead to a disruption of consciousness, leading to anosognosia. Schizophrenia is a pervasive brain syndrome involving multiple brain regions and a wide range of clinical symptoms ranging across psychotic as well as negative and cognitive domains. Anosognosia can be conceptualized as a psychotic symptom (delusion), a negative symptom (self-monitoring deficit), or a cognitive failure. However, anosognosia in schizophrenia can be best understood as a symptom of impaired consciousness and self-pathology,26 where the brain fails to process and recognize one’s mental function, which culminates in faulty reality testing.
Schizophrenia is a neurologic syndrome associated with numerous psychiatric manifestations, and anosognosia is one of its fundamental initial symptoms.
1. Nasrallah HA. Impaired mental proprioception in schizophrenia. Current Psychiatry. 2012;11(8):4-5.
2. Kirsch LP, Mathys C, Papadaki C, et al. Updating beliefs beyond the here-and-now: the counter-factual self in anosognosia for hemiplegia. Brain Commun. 2021;3(2):fcab098. doi: 10.1093/braincomms/fcab098
3. Das JM, Nagvi IA. Anton syndrome. StatPearls Publishing. Updated April 10, 2021. Accessed December 13, 2021. https://www.ncbi.nlm.nih.gov/books/NBK538155/
4. Steward KA, Kretzmer T. Anosognosia in moderate-to-severe traumatic brain injury: a review of prevalence, clinical correlates, and diversity considerations. Clin Neuropsychol. 2021:1-20.
5. Klarendié M, Gorišek VR, Granda G, et al. Auditory agnosia with anosognosia. Cortex. 2021;137:255-270.
6. Bastin C, Giacomelli F, Miévis F, et al. Anosognosia in mild cognitive impairment: lack of awareness of memory difficulties characterizes prodromal Alzheimer’s disease. Front Psychiatry. 202;12:631518.
7. Chen S, Song Y, Xu W, et al; Alzheimer’s Disease Neuroimaging Initiative. Impaired memory awareness and loss integration in self-referential network across the progression of Alzheimer’s disease spectrum. J Alzheimers Dis. 2021;83(1):111-126.
8. Turnbull OH, Fotopoulou A, Solms M. Anosognosia as motivated unawareness: the ‘defence’ hypothesis revisited. Cortex. 2014;61:18-29.
9. Ibrahim SU, Kalyanasundaram VB, Ramanathan SA, et al. Trajectory of insight on various dimensions among bipolar disorder in-patients. Ind Psychiatry J. 2020;29(2):285-292.
10. Levine DN. Unawareness of visual and sensorimotor defects: a hypothesis. Brain Cogn. 1990;13(2):233-281.
11. Pourmohammad P, Imani M, Goodarzi MA, et al. Impaired complex theory of mind and low emotional self-awareness in outpatients with borderline personality disorder compared to healthy controls: a cross-sectional study. J Psychiatr Res. 2021;143:445-450.
12. Torrey EF. Schizophrenia and the inferior parietal lobule. Schizophr Res. 2007;97(1-3):215-225.
13. Dionisio S, Mayoglou L, Cho SM, et al. Connectivity of the human insula: a cortico-cortical evoked potential (CCEP) study. Cortex. 2019;120:419-442.
14. Nord CL, Lawson RP, Dalgleish T. Disrupted dorsal mid-insula activation during interoception across psychiatric disorders. Am J Psychiatry. 2021;178(8):761-770.
15. Glahn DC, Laird AR, Ellison-Wright I, et al. Meta-analysis of gray matter anomalies in schizophrenia: application of anatomic likelihood estimation and network analysis. Biol Psychiatry. 2008;64(9):774-781.
16. McEvoy JP, Freter S, Everett G, et al. Insight and the clinical outcome of schizophrenic patients. J Nerv Ment Dis. 1989;177(1):48-51.
17. Amador XF, Strauss DH, Yale SA, et al. Assessment of insight in psychosis. Am J Psychiatry. 1993;150(6):873-879.
18. Beck AT, Baruch E, Balter JM, et al. A new instrument for measuring insight: the Beck Cognitive Insight Scale. Schizophr Res. 2004;68(2-3):319-329.
19. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261-276.
20. Nasrallah HA. FAST and RAPID: acronyms to prevent brain damage in stroke and psychosis. Current Psychiatry. 2018;17(8):6-8.
21. Buckley PF, Wirshing DA, Bhushan P, et al. Lack of insight in schizophrenia: impact on treatment adherence. CNS Drugs. 2007;21(2):129-141.
22. Lehrer DS, Lorenz J. Anosognosia in schizophrenia: hidden in plain sight. Innov Clin Neurosci. 2014;11(5-6):101-107.
23. Emsley R, Medori R, Koen L, et al. Long-acting injectable risperidone in the treatment of subjects with recent-onset psychosis: a preliminary study. J Clin Psychopharmacol. 2008;28(2):210-213.
24. Gurin L, Blum S. Delusions and the right hemisphere: a review of the case for the right hemisphere as a mediator of reality-based belief. J Neuropsychiatry Clin Neurosci. 2017;29(3):225-235.
25. Gazzaniga MS, Miller M. The left hemisphere does not miss the right hemisphere. In: Laureys S, Tononi G (eds). The Neurology of Consciousness. Cognitive Neuroscience and Neuropathology. Academic Press; 2008:261-270.
26. Cooney JW, Gazzaniga MS. Neurological disorders and the structure of human consciousness. Trends Cogn Sci. 2003;7(4):161-165.
1. Nasrallah HA. Impaired mental proprioception in schizophrenia. Current Psychiatry. 2012;11(8):4-5.
2. Kirsch LP, Mathys C, Papadaki C, et al. Updating beliefs beyond the here-and-now: the counter-factual self in anosognosia for hemiplegia. Brain Commun. 2021;3(2):fcab098. doi: 10.1093/braincomms/fcab098
3. Das JM, Nagvi IA. Anton syndrome. StatPearls Publishing. Updated April 10, 2021. Accessed December 13, 2021. https://www.ncbi.nlm.nih.gov/books/NBK538155/
4. Steward KA, Kretzmer T. Anosognosia in moderate-to-severe traumatic brain injury: a review of prevalence, clinical correlates, and diversity considerations. Clin Neuropsychol. 2021:1-20.
5. Klarendié M, Gorišek VR, Granda G, et al. Auditory agnosia with anosognosia. Cortex. 2021;137:255-270.
6. Bastin C, Giacomelli F, Miévis F, et al. Anosognosia in mild cognitive impairment: lack of awareness of memory difficulties characterizes prodromal Alzheimer’s disease. Front Psychiatry. 202;12:631518.
7. Chen S, Song Y, Xu W, et al; Alzheimer’s Disease Neuroimaging Initiative. Impaired memory awareness and loss integration in self-referential network across the progression of Alzheimer’s disease spectrum. J Alzheimers Dis. 2021;83(1):111-126.
8. Turnbull OH, Fotopoulou A, Solms M. Anosognosia as motivated unawareness: the ‘defence’ hypothesis revisited. Cortex. 2014;61:18-29.
9. Ibrahim SU, Kalyanasundaram VB, Ramanathan SA, et al. Trajectory of insight on various dimensions among bipolar disorder in-patients. Ind Psychiatry J. 2020;29(2):285-292.
10. Levine DN. Unawareness of visual and sensorimotor defects: a hypothesis. Brain Cogn. 1990;13(2):233-281.
11. Pourmohammad P, Imani M, Goodarzi MA, et al. Impaired complex theory of mind and low emotional self-awareness in outpatients with borderline personality disorder compared to healthy controls: a cross-sectional study. J Psychiatr Res. 2021;143:445-450.
12. Torrey EF. Schizophrenia and the inferior parietal lobule. Schizophr Res. 2007;97(1-3):215-225.
13. Dionisio S, Mayoglou L, Cho SM, et al. Connectivity of the human insula: a cortico-cortical evoked potential (CCEP) study. Cortex. 2019;120:419-442.
14. Nord CL, Lawson RP, Dalgleish T. Disrupted dorsal mid-insula activation during interoception across psychiatric disorders. Am J Psychiatry. 2021;178(8):761-770.
15. Glahn DC, Laird AR, Ellison-Wright I, et al. Meta-analysis of gray matter anomalies in schizophrenia: application of anatomic likelihood estimation and network analysis. Biol Psychiatry. 2008;64(9):774-781.
16. McEvoy JP, Freter S, Everett G, et al. Insight and the clinical outcome of schizophrenic patients. J Nerv Ment Dis. 1989;177(1):48-51.
17. Amador XF, Strauss DH, Yale SA, et al. Assessment of insight in psychosis. Am J Psychiatry. 1993;150(6):873-879.
18. Beck AT, Baruch E, Balter JM, et al. A new instrument for measuring insight: the Beck Cognitive Insight Scale. Schizophr Res. 2004;68(2-3):319-329.
19. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261-276.
20. Nasrallah HA. FAST and RAPID: acronyms to prevent brain damage in stroke and psychosis. Current Psychiatry. 2018;17(8):6-8.
21. Buckley PF, Wirshing DA, Bhushan P, et al. Lack of insight in schizophrenia: impact on treatment adherence. CNS Drugs. 2007;21(2):129-141.
22. Lehrer DS, Lorenz J. Anosognosia in schizophrenia: hidden in plain sight. Innov Clin Neurosci. 2014;11(5-6):101-107.
23. Emsley R, Medori R, Koen L, et al. Long-acting injectable risperidone in the treatment of subjects with recent-onset psychosis: a preliminary study. J Clin Psychopharmacol. 2008;28(2):210-213.
24. Gurin L, Blum S. Delusions and the right hemisphere: a review of the case for the right hemisphere as a mediator of reality-based belief. J Neuropsychiatry Clin Neurosci. 2017;29(3):225-235.
25. Gazzaniga MS, Miller M. The left hemisphere does not miss the right hemisphere. In: Laureys S, Tononi G (eds). The Neurology of Consciousness. Cognitive Neuroscience and Neuropathology. Academic Press; 2008:261-270.
26. Cooney JW, Gazzaniga MS. Neurological disorders and the structure of human consciousness. Trends Cogn Sci. 2003;7(4):161-165.
Tap of the brakes on gender-affirming care
In the November 2021 issue of Pediatric News are two stories that on the surface present viewpoints that couldn’t be more divergent. On page 1 under the headline “Gender dysphoria” you will read about a position statement by the Royal Australian and New Zealand College of Psychiatrists (RANZCP) in which they strongly recommend a mental health evaluation for any child or adolescent with gender dysphoria “before any firm decisions are made on whether to prescribe hormonal treatments to transition, or perform surgeries.”
On page 6 is another story titled “Gender-affirming care ‘can save lives’ new research shows” that reports on a research study in which transgender and binary young people who received a year of gender-affirming care experienced less depression and fewer suicidal thoughts. Dr. David J. Inwards-Breland, chief of adolescent and young adult medicine at Rady Children’s Hospital in San Diego and one of the authors of the study is quoted as saying “The younger we can provide gender-affirming care, the less likely [our patients are] to have depression and then negative outcomes.” One can’t avoid the impression that he is in favor of moving ahead without delay in prescribing gender-affirming care.
Where does the new recommendation by the RANZCP fit in with this sense of urgency? Does requiring a mental health evaluation constitute a delay in the institution of gender-affirming care that could increase the risk of negative mental health outcomes for gender dysphoric patients?
In one of the final paragraphs in the Pediatric News article one learns that Dr. Inwards-Breland would agree with the folks of RANZCP. He acknowledges that his study relied on screening and not diagnostic testing and says that “future studies should look at a mental health evaluation and diagnosis by a mental health provider.”
When we drill into the details there are two issues that demand clarification. First, what kind of time course are we talking about for a mental health evaluation? Are we talking weeks, or months, hopefully not years? This of course depends on the availability of mental health services for the specific patient and the depth of the evaluation required. How long a delay is acceptable?
Second, will the evaluation be performed by a provider free of bias? Can it be performed without creating the impression that the patient needs to see a mental health provider because there is something wrong with being trans and we can fix it? One would hope these evaluations would be performed in the spirit of wanting to learn more about the patient with the goal of making the process go more smoothly.
Listening to neighborhood discussions around the fire pit I find that the RANZCP plea for a broader and deeper look at each gender-dysphoric child strikes a chord with the general population. More and more people are realizing that gender-dysphoria happens and that for too long it was closeted with unfortunate consequences. However, there is a feeling, in fact one in which I share, that the rapid rise in its prevalence contains an element of social contagion. And, some irreversible decisions are being made without sufficient consideration. This may or not be a valid concern but it seems to me a thorough and sensitively done mental health evaluation might minimize the collateral damage from some gender-affirming care and at least help those patients for whom it is prescribed transition more smoothly.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
In the November 2021 issue of Pediatric News are two stories that on the surface present viewpoints that couldn’t be more divergent. On page 1 under the headline “Gender dysphoria” you will read about a position statement by the Royal Australian and New Zealand College of Psychiatrists (RANZCP) in which they strongly recommend a mental health evaluation for any child or adolescent with gender dysphoria “before any firm decisions are made on whether to prescribe hormonal treatments to transition, or perform surgeries.”
On page 6 is another story titled “Gender-affirming care ‘can save lives’ new research shows” that reports on a research study in which transgender and binary young people who received a year of gender-affirming care experienced less depression and fewer suicidal thoughts. Dr. David J. Inwards-Breland, chief of adolescent and young adult medicine at Rady Children’s Hospital in San Diego and one of the authors of the study is quoted as saying “The younger we can provide gender-affirming care, the less likely [our patients are] to have depression and then negative outcomes.” One can’t avoid the impression that he is in favor of moving ahead without delay in prescribing gender-affirming care.
Where does the new recommendation by the RANZCP fit in with this sense of urgency? Does requiring a mental health evaluation constitute a delay in the institution of gender-affirming care that could increase the risk of negative mental health outcomes for gender dysphoric patients?
In one of the final paragraphs in the Pediatric News article one learns that Dr. Inwards-Breland would agree with the folks of RANZCP. He acknowledges that his study relied on screening and not diagnostic testing and says that “future studies should look at a mental health evaluation and diagnosis by a mental health provider.”
When we drill into the details there are two issues that demand clarification. First, what kind of time course are we talking about for a mental health evaluation? Are we talking weeks, or months, hopefully not years? This of course depends on the availability of mental health services for the specific patient and the depth of the evaluation required. How long a delay is acceptable?
Second, will the evaluation be performed by a provider free of bias? Can it be performed without creating the impression that the patient needs to see a mental health provider because there is something wrong with being trans and we can fix it? One would hope these evaluations would be performed in the spirit of wanting to learn more about the patient with the goal of making the process go more smoothly.
Listening to neighborhood discussions around the fire pit I find that the RANZCP plea for a broader and deeper look at each gender-dysphoric child strikes a chord with the general population. More and more people are realizing that gender-dysphoria happens and that for too long it was closeted with unfortunate consequences. However, there is a feeling, in fact one in which I share, that the rapid rise in its prevalence contains an element of social contagion. And, some irreversible decisions are being made without sufficient consideration. This may or not be a valid concern but it seems to me a thorough and sensitively done mental health evaluation might minimize the collateral damage from some gender-affirming care and at least help those patients for whom it is prescribed transition more smoothly.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
In the November 2021 issue of Pediatric News are two stories that on the surface present viewpoints that couldn’t be more divergent. On page 1 under the headline “Gender dysphoria” you will read about a position statement by the Royal Australian and New Zealand College of Psychiatrists (RANZCP) in which they strongly recommend a mental health evaluation for any child or adolescent with gender dysphoria “before any firm decisions are made on whether to prescribe hormonal treatments to transition, or perform surgeries.”
On page 6 is another story titled “Gender-affirming care ‘can save lives’ new research shows” that reports on a research study in which transgender and binary young people who received a year of gender-affirming care experienced less depression and fewer suicidal thoughts. Dr. David J. Inwards-Breland, chief of adolescent and young adult medicine at Rady Children’s Hospital in San Diego and one of the authors of the study is quoted as saying “The younger we can provide gender-affirming care, the less likely [our patients are] to have depression and then negative outcomes.” One can’t avoid the impression that he is in favor of moving ahead without delay in prescribing gender-affirming care.
Where does the new recommendation by the RANZCP fit in with this sense of urgency? Does requiring a mental health evaluation constitute a delay in the institution of gender-affirming care that could increase the risk of negative mental health outcomes for gender dysphoric patients?
In one of the final paragraphs in the Pediatric News article one learns that Dr. Inwards-Breland would agree with the folks of RANZCP. He acknowledges that his study relied on screening and not diagnostic testing and says that “future studies should look at a mental health evaluation and diagnosis by a mental health provider.”
When we drill into the details there are two issues that demand clarification. First, what kind of time course are we talking about for a mental health evaluation? Are we talking weeks, or months, hopefully not years? This of course depends on the availability of mental health services for the specific patient and the depth of the evaluation required. How long a delay is acceptable?
Second, will the evaluation be performed by a provider free of bias? Can it be performed without creating the impression that the patient needs to see a mental health provider because there is something wrong with being trans and we can fix it? One would hope these evaluations would be performed in the spirit of wanting to learn more about the patient with the goal of making the process go more smoothly.
Listening to neighborhood discussions around the fire pit I find that the RANZCP plea for a broader and deeper look at each gender-dysphoric child strikes a chord with the general population. More and more people are realizing that gender-dysphoria happens and that for too long it was closeted with unfortunate consequences. However, there is a feeling, in fact one in which I share, that the rapid rise in its prevalence contains an element of social contagion. And, some irreversible decisions are being made without sufficient consideration. This may or not be a valid concern but it seems to me a thorough and sensitively done mental health evaluation might minimize the collateral damage from some gender-affirming care and at least help those patients for whom it is prescribed transition more smoothly.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Benefits of low-dose CT scanning for lung cancer screening explained
According to the Centers for Disease Control and Prevention, lung cancer is the third-most common cancer in the United States and the leading cause of cancer deaths in both men and women. Approximately, 150,000 Americans die every year from this disease.
In fact, it has been shown that low-dose CT scan screening can reduce lung cancer deaths by 20%-30% in high-risk populations.
In the United States, low-dose CT scan screening for lung cancer has largely become the norm. In July 2021, CHEST released new clinical guidelines. These guidelines cover 18 evidence-based recommendations as well as inclusion of further evidence regarding the benefits, risks, and use of CT screening.
In doing the risk assessment of low-dose CT scan as a method of lung cancer screening, meta-analyses were performed on evidence obtained through a literature search using PubMed, Embase, and the Cochrane Library. It was concluded that the benefits outweigh the risks as a method of lung cancer screening and can be utilized in reducing lung cancer deaths.
Low-dose CT scan screening was recommended for the following patients:
- Asymptomatic individuals aged 55-77 years with a history of smoking 30 or more pack-years. (This includes those who continue to smoke or who have quit in the previous 15 years. Annual screening is advised.)
- Asymptomatic individuals aged 55-80 years with a history of smoking 20-30 pack-years who either continue to smoke or have quit in the previous 15 years.
- For asymptomatic individuals who do not meet the above criteria but are predicted to benefit based on life-year gained calculations.
Don’t screen these patients
CT scan screening should not be performed on any person who does not meet any of the above three criteria.
Additionally, if a person has significant comorbidities that would limit their life expectancy, it is recommended not to do CT scan screening. Symptomatic patients should have appropriate diagnostic testing rather than screening.
Additional recommendations from the updated guidelines include developing appropriate counseling strategies as well as deciding what constitutes a positive test.
A positive test should be anything that warrants further evaluation rather than a return to annual screening. It was also advised that overtreatment strategies should be implemented. Additionally, smoking cessation treatment should be provided.
CHEST suggested undertaking a comprehensive approach involving multiple specialists including pulmonologists, radiologists, oncologists, etc. Strategies to ensure compliance with annual screening should also be devised, the guidelines say.
USPSTF’s updated guidelines
It should be noted that the U.S. Preventative Task Force released their own set of updated guidelines in March 2021. In these guidelines, the age at which lung cancer screening should be started was lowered from 55 years to 50 years.
Also, the USPSTF lowered the minimum required smoking history in order to be screened from 30 to 20 pack-years. Their purpose for doing this was to include more high-risk women as well as minorities.
With the changes, 14.5 million individuals living in the United States would be eligible for lung cancer screening by low-dose CT scan, an increase of 6.5 million people, compared with the previous guidelines.
While only small differences exist between the set of guidelines issued by CHEST and the ones issues by the USPSTF, lung cancer screening is still largely underutilized.
One of the barriers to screening may be patients’ lacking insurance coverage for it. As physicians, we need to advocate for these screening tools to be covered.
Other barriers include lack of patient knowledge regarding low-dose CT scans as a screening tool, patient time, and patient visits with their doctors being too short.
Key message
Part of the duties of physicians is to give our patients the best information. We can reduce lung cancer mortality in high risk patients by performing annual low-dose CT scans.
Whichever set of guidelines we chose to follow, we fail our patients if we don’t follow either set of them. The evidence is clear that a low-dose CT scan is a valuable screening tool to add to our practice of medicine.
Dr. Girgis practices family medicine in South River, N.J., and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, N.J. You can contact her at fpnews@mdedge.com.
According to the Centers for Disease Control and Prevention, lung cancer is the third-most common cancer in the United States and the leading cause of cancer deaths in both men and women. Approximately, 150,000 Americans die every year from this disease.
In fact, it has been shown that low-dose CT scan screening can reduce lung cancer deaths by 20%-30% in high-risk populations.
In the United States, low-dose CT scan screening for lung cancer has largely become the norm. In July 2021, CHEST released new clinical guidelines. These guidelines cover 18 evidence-based recommendations as well as inclusion of further evidence regarding the benefits, risks, and use of CT screening.
In doing the risk assessment of low-dose CT scan as a method of lung cancer screening, meta-analyses were performed on evidence obtained through a literature search using PubMed, Embase, and the Cochrane Library. It was concluded that the benefits outweigh the risks as a method of lung cancer screening and can be utilized in reducing lung cancer deaths.
Low-dose CT scan screening was recommended for the following patients:
- Asymptomatic individuals aged 55-77 years with a history of smoking 30 or more pack-years. (This includes those who continue to smoke or who have quit in the previous 15 years. Annual screening is advised.)
- Asymptomatic individuals aged 55-80 years with a history of smoking 20-30 pack-years who either continue to smoke or have quit in the previous 15 years.
- For asymptomatic individuals who do not meet the above criteria but are predicted to benefit based on life-year gained calculations.
Don’t screen these patients
CT scan screening should not be performed on any person who does not meet any of the above three criteria.
Additionally, if a person has significant comorbidities that would limit their life expectancy, it is recommended not to do CT scan screening. Symptomatic patients should have appropriate diagnostic testing rather than screening.
Additional recommendations from the updated guidelines include developing appropriate counseling strategies as well as deciding what constitutes a positive test.
A positive test should be anything that warrants further evaluation rather than a return to annual screening. It was also advised that overtreatment strategies should be implemented. Additionally, smoking cessation treatment should be provided.
CHEST suggested undertaking a comprehensive approach involving multiple specialists including pulmonologists, radiologists, oncologists, etc. Strategies to ensure compliance with annual screening should also be devised, the guidelines say.
USPSTF’s updated guidelines
It should be noted that the U.S. Preventative Task Force released their own set of updated guidelines in March 2021. In these guidelines, the age at which lung cancer screening should be started was lowered from 55 years to 50 years.
Also, the USPSTF lowered the minimum required smoking history in order to be screened from 30 to 20 pack-years. Their purpose for doing this was to include more high-risk women as well as minorities.
With the changes, 14.5 million individuals living in the United States would be eligible for lung cancer screening by low-dose CT scan, an increase of 6.5 million people, compared with the previous guidelines.
While only small differences exist between the set of guidelines issued by CHEST and the ones issues by the USPSTF, lung cancer screening is still largely underutilized.
One of the barriers to screening may be patients’ lacking insurance coverage for it. As physicians, we need to advocate for these screening tools to be covered.
Other barriers include lack of patient knowledge regarding low-dose CT scans as a screening tool, patient time, and patient visits with their doctors being too short.
Key message
Part of the duties of physicians is to give our patients the best information. We can reduce lung cancer mortality in high risk patients by performing annual low-dose CT scans.
Whichever set of guidelines we chose to follow, we fail our patients if we don’t follow either set of them. The evidence is clear that a low-dose CT scan is a valuable screening tool to add to our practice of medicine.
Dr. Girgis practices family medicine in South River, N.J., and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, N.J. You can contact her at fpnews@mdedge.com.
According to the Centers for Disease Control and Prevention, lung cancer is the third-most common cancer in the United States and the leading cause of cancer deaths in both men and women. Approximately, 150,000 Americans die every year from this disease.
In fact, it has been shown that low-dose CT scan screening can reduce lung cancer deaths by 20%-30% in high-risk populations.
In the United States, low-dose CT scan screening for lung cancer has largely become the norm. In July 2021, CHEST released new clinical guidelines. These guidelines cover 18 evidence-based recommendations as well as inclusion of further evidence regarding the benefits, risks, and use of CT screening.
In doing the risk assessment of low-dose CT scan as a method of lung cancer screening, meta-analyses were performed on evidence obtained through a literature search using PubMed, Embase, and the Cochrane Library. It was concluded that the benefits outweigh the risks as a method of lung cancer screening and can be utilized in reducing lung cancer deaths.
Low-dose CT scan screening was recommended for the following patients:
- Asymptomatic individuals aged 55-77 years with a history of smoking 30 or more pack-years. (This includes those who continue to smoke or who have quit in the previous 15 years. Annual screening is advised.)
- Asymptomatic individuals aged 55-80 years with a history of smoking 20-30 pack-years who either continue to smoke or have quit in the previous 15 years.
- For asymptomatic individuals who do not meet the above criteria but are predicted to benefit based on life-year gained calculations.
Don’t screen these patients
CT scan screening should not be performed on any person who does not meet any of the above three criteria.
Additionally, if a person has significant comorbidities that would limit their life expectancy, it is recommended not to do CT scan screening. Symptomatic patients should have appropriate diagnostic testing rather than screening.
Additional recommendations from the updated guidelines include developing appropriate counseling strategies as well as deciding what constitutes a positive test.
A positive test should be anything that warrants further evaluation rather than a return to annual screening. It was also advised that overtreatment strategies should be implemented. Additionally, smoking cessation treatment should be provided.
CHEST suggested undertaking a comprehensive approach involving multiple specialists including pulmonologists, radiologists, oncologists, etc. Strategies to ensure compliance with annual screening should also be devised, the guidelines say.
USPSTF’s updated guidelines
It should be noted that the U.S. Preventative Task Force released their own set of updated guidelines in March 2021. In these guidelines, the age at which lung cancer screening should be started was lowered from 55 years to 50 years.
Also, the USPSTF lowered the minimum required smoking history in order to be screened from 30 to 20 pack-years. Their purpose for doing this was to include more high-risk women as well as minorities.
With the changes, 14.5 million individuals living in the United States would be eligible for lung cancer screening by low-dose CT scan, an increase of 6.5 million people, compared with the previous guidelines.
While only small differences exist between the set of guidelines issued by CHEST and the ones issues by the USPSTF, lung cancer screening is still largely underutilized.
One of the barriers to screening may be patients’ lacking insurance coverage for it. As physicians, we need to advocate for these screening tools to be covered.
Other barriers include lack of patient knowledge regarding low-dose CT scans as a screening tool, patient time, and patient visits with their doctors being too short.
Key message
Part of the duties of physicians is to give our patients the best information. We can reduce lung cancer mortality in high risk patients by performing annual low-dose CT scans.
Whichever set of guidelines we chose to follow, we fail our patients if we don’t follow either set of them. The evidence is clear that a low-dose CT scan is a valuable screening tool to add to our practice of medicine.
Dr. Girgis practices family medicine in South River, N.J., and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, N.J. You can contact her at fpnews@mdedge.com.
The mess that is matching in psychiatry
The day I interviewed at Johns Hopkins in Baltimore, like every other day of residency interviews, was a very long and draining day.
I started by meeting alone with Philip Slavney, MD, the residency director, who spoke with me about the program and gave me a schedule to follow. I was to meet with residents and psychiatrists, some of whom had graduated from my medical school, and was sent to the Bayview campus a few miles away to have lunch and attend a few meetings. By the time I boarded an Amtrak train at Baltimore Penn Station, I was tired but I liked what I had seen. By the end of the interview season, I had crossed four programs off my list and had decided to rank only three.
In 1987, there were 987 residency positions in psychiatry in the United States, and 83.6% of those positions filled with a combination of U.S. and international medical graduates. Still, this was a risky move; the programs that I decided to rank would fill, but I was matching separately for an internship year in internal medicine in New York and decided that I would rather reapply in a year than risk matching at a program I didn’t want to go to.
I wasn’t quite sure where I wanted to rank Hopkins on my list, so I called Dr. Slavney and said I wanted to come back and meet more members of the department. He did not hide his surprise and was quick to tell me that no one had ever requested a second set of interviews. I mentioned specific people I wanted to meet with, and he was kind enough to accommodate my request and set up a second day of interviews for me.
Needless to say, the residency match felt very personal – at least to me – and although I felt vulnerable, I also felt empowered. Because of the low pay, patients with stigmatized illnesses, and the rampant belief that psychiatry was not “real” medicine and the patients never got better, psychiatry was not a desired specialty.
The residency application process in psychiatry (and every other specialty) has become a much different process. In 2006, the Association of American Medical Colleges called on medical schools to increase their enrollments to address the national shortage of physicians. Soon, there were more medical schools, bigger classes, and more doctors being minted, but the Balanced Budget Act of 1997 prevented a proportional increase in residency positions.
Len Marquez, senior director of government relations at the AAMC noted: “The Resident Physician Shortage Reduction Act of 2021 (S. 834), sponsored by Sen. Robert Menendez (D-N.J.), Sen. John Boozman (R-Ark.), and Majority Leader Sen. Charles Schumer (D-N.Y.), would support 2,000 additional Medicare-supported residency positions each year for 7 years, but Congress has not yet acted on the legislation. We were very pleased that last year, Congress passed the first increase in Medicare-supported graduate medical education in 25 years by including 1,000 new slots as part of the Consolidated Appropriations Act, 2021.”
In addition, the Build Back Better Act, which is currently being debated in Congress, would provide 4,000 more graduate medical education slots, including a specific requirement that 15% of them go to “psychiatry-related residencies,” he added.
Over 90% of graduates from U.S. medical schools currently match into a residency position. That statistic for international medical graduates is notably lower, with perhaps as few as 50% of all applicants matching.
Since 2014, the number of applicants to psychiatry residencies has nearly doubled. For the 2021 match, there were 2,486 applicants applying for 1,858 positions in psychiatry – so 1.34 applicants for each slot. Of the 1,117 senior medical students at U.S. schools who applied to psychiatry residencies, 129 did not match. Overall, 99.8% of residency positions in psychiatry filled.
“It used to be less competitive,” said Kaz J. Nelson, MD, the vice chair for education at the University of Minnesota’s department of psychiatry and behavioral sciences in Minneapolis, adding that interest in psychiatry has increased over the years.
“Interest has skyrocketed as the word has gotten out about how great a field it is. It helps that reimbursements are better, that there is less bias and discrimination against patients with psychiatric issues, and that psychiatric care is seen as a legitimate part of medicine. It has been exciting to watch!” Dr. Nelson said.
The numbers are only one part of the story, however.
Application submission now involves a centralized, electronic process, and it has become easier for applicants to apply to a lot of programs indiscriminately. It’s not unusual for applicants to apply to 70 or more programs. The factors that have limited applications include the cost: Electronic Residency Application Services (ERAS) charges for each application package they send to a program, and applicants traditionally pay to travel to the programs where they interview. This all changed with the 2021 cycle when in-person interviews were halted for the pandemic and interviews became virtual. While I recall applying to 7 residency programs, this year the average number of applications was 54.7 per applicant.
“It used to be that the cap on interviewing was financial,” Dr. Nelson said. “It was discriminatory and favored those who had more money to travel to interviews. There are still the ERAS fees, but COVID has been an equalizer and we are getting more applicants, and interviewing more who are not from Minnesota or the Midwest. We have been working to make our program attractive in terms of diversity, equity, inclusion, and justice. Our hospital is located a mile from where George Floyd was murdered, and it’s our responsibility to lead the effort to ensure the psychiatry workforce is diverse, and inclusive, as possible.”
Daniel E. Gih, MD, is the program director for a new psychiatry residency at the University of Nebraska, Omaha. When the program started in 2019, there were spots for four residents and the program had 588 applications. In 2020, the program grew to five positions and this year there were 553 applicants. Dr. Gih attributed the high number of applications to his program’s strong social media presence.
“Going through the applications and meeting the students are some of the most enjoyable parts of my work,” Dr. Gih said. “I feel guilty though, that I’m likely going to miss a great applicant. Each application averages 35 pages and it’s inevitable that programs have to take shortcuts. Applicants worry that they’ll be ranked by board scores. While we certainly don’t do that here, students might feel ruled out of a program if their numbers aren’t high enough. Furthermore, wealthy students can apply to more programs. The pandemic has really highlighted the inequity issues.”
Dr. Gih noted that the Zoom interview process has not been disappointing: “Two of the people we matched had never been to Omaha, and many expressed concerns about what it is like here. Of course, on Zoom you don’t catch subtle interpersonal issues, but we have been pleasantly surprised that the people we matched were consistent with what we expected. It is exciting to meet the people who will eventually replace us as psychiatrists, they will be here to deal with future challenges!” His enthusiasm was tangible.
While the program directors remain optimistic, the system is not without its stresses, as many programs receive over 1,000 applications.
“This is difficult,” Dr. Nelson said.” It’s wonderful for the programs, but for the medical students, not matching is experienced by them as being catastrophic, so they apply to a lot of programs. Getting this many applications is a challenge, yet I don’t want to interview someone if they are going to rank our program No. 80 on their list!”
Residencies have dealt with the deluge of applicants in a number of ways. Some specialties started a “signal” protocol wherein candidates and programs receive a certain number of tokens to indicate that each would rank the other highly, but psychiatry has not done this. Early on in the Zoom process, multiple applicants would be offered interviews simultaneously, and the interview would be given to the candidate who responded first. Students vented their frustrations on Twitter when they lost interview spots at their coveted programs because they hadn’t checked their email in time or had gone to take a shower.
“The American Association of Directors of Psychiatry Residency Training Programs issued guidelines saying that it is unacceptable to offer interview spots without allowing a reasonable time for the applicant to respond, and that it is not appropriate to offer multiple candidates one spot on a first-come, first-serve basis,” Dr. Nelson explained.
Her program has managed some of the application chaos by using a software program called Scutmonkey, codeveloped by David Ross, MD, PhD, the associate program director of the Yale Adult Psychiatry Residency Program.
“It lets us screen applications for candidates who specifically are interested in being here, and for those who qualify as part of the mission we are trying to fulfill.”
One fourth-year student at a mid-Atlantic medical school who is applying in psychiatry – who I’ll call Sacha to protect his anonymity – applied to 73 psychiatry programs and to date, has interviewed at 6. He describes a stressful, roller coaster experience:
“I got those six interviews right away and that was an amazing start, but then I didn’t get any more. The interviews I had went well, but it has been disappointing not to have more. Some were all-day interviews, while other programs had me meet with residents and attendings for 20 minutes each and it was all done after 2 hours.”
He has mixed opinions about not seeing the schools in person. “There are very heavy pros and cons. I’ve saved thousands of dollars in travel expenses that would have limited my applications, so logistically it’s a dream. On the other hand, I’ve interviewed in cities I have never been to, it’s hard to get a sense of the intangibles of a program, and the shorter interviews feel very impersonal.”
Sacha expressed anxieties about the process. “With so many applicants, it’s difficult for someone with a nontraditional story to get a spot and it’s easier for the programs to toss applications. it’s common enough and everyone has seen someone who has gone through this. At times, we feel powerless; we have no real agency or control. We send stuff out and then we sit in the prayer position and wait.”
I think back on my own application process with a sense of gratitude. I certainly didn’t feel powerless, and in today’s world, postinterview communications with program directors are regulated for both parties. Dr. Slavney was kind enough to humor my request, but I don’t believe this would be feasible in the current environment.
Even though it is wonderful that more doctors have figured out that careers in psychiatry are rewarding, the current situation is overwhelming for both the applicants and the programs. With over 100 applicants for every position – many of whom will have no interest in going to some of the programs they apply to – qualified candidates who go unmatched, and a roulette wheel which requires heavily indebted students to pay to apply, this is simply not sustainable in a country with a shortage of physicians – psychiatrists in particular.
We hear that mid-level practitioners are the answer to our shortages, but perhaps we need to create a system with enough residency positions to accommodate highly trained and qualified physicians in a more inviting and targeted way.
Dinah Miller, MD, is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore. A version of this article first appeared on Medscape.com.
The day I interviewed at Johns Hopkins in Baltimore, like every other day of residency interviews, was a very long and draining day.
I started by meeting alone with Philip Slavney, MD, the residency director, who spoke with me about the program and gave me a schedule to follow. I was to meet with residents and psychiatrists, some of whom had graduated from my medical school, and was sent to the Bayview campus a few miles away to have lunch and attend a few meetings. By the time I boarded an Amtrak train at Baltimore Penn Station, I was tired but I liked what I had seen. By the end of the interview season, I had crossed four programs off my list and had decided to rank only three.
In 1987, there were 987 residency positions in psychiatry in the United States, and 83.6% of those positions filled with a combination of U.S. and international medical graduates. Still, this was a risky move; the programs that I decided to rank would fill, but I was matching separately for an internship year in internal medicine in New York and decided that I would rather reapply in a year than risk matching at a program I didn’t want to go to.
I wasn’t quite sure where I wanted to rank Hopkins on my list, so I called Dr. Slavney and said I wanted to come back and meet more members of the department. He did not hide his surprise and was quick to tell me that no one had ever requested a second set of interviews. I mentioned specific people I wanted to meet with, and he was kind enough to accommodate my request and set up a second day of interviews for me.
Needless to say, the residency match felt very personal – at least to me – and although I felt vulnerable, I also felt empowered. Because of the low pay, patients with stigmatized illnesses, and the rampant belief that psychiatry was not “real” medicine and the patients never got better, psychiatry was not a desired specialty.
The residency application process in psychiatry (and every other specialty) has become a much different process. In 2006, the Association of American Medical Colleges called on medical schools to increase their enrollments to address the national shortage of physicians. Soon, there were more medical schools, bigger classes, and more doctors being minted, but the Balanced Budget Act of 1997 prevented a proportional increase in residency positions.
Len Marquez, senior director of government relations at the AAMC noted: “The Resident Physician Shortage Reduction Act of 2021 (S. 834), sponsored by Sen. Robert Menendez (D-N.J.), Sen. John Boozman (R-Ark.), and Majority Leader Sen. Charles Schumer (D-N.Y.), would support 2,000 additional Medicare-supported residency positions each year for 7 years, but Congress has not yet acted on the legislation. We were very pleased that last year, Congress passed the first increase in Medicare-supported graduate medical education in 25 years by including 1,000 new slots as part of the Consolidated Appropriations Act, 2021.”
In addition, the Build Back Better Act, which is currently being debated in Congress, would provide 4,000 more graduate medical education slots, including a specific requirement that 15% of them go to “psychiatry-related residencies,” he added.
Over 90% of graduates from U.S. medical schools currently match into a residency position. That statistic for international medical graduates is notably lower, with perhaps as few as 50% of all applicants matching.
Since 2014, the number of applicants to psychiatry residencies has nearly doubled. For the 2021 match, there were 2,486 applicants applying for 1,858 positions in psychiatry – so 1.34 applicants for each slot. Of the 1,117 senior medical students at U.S. schools who applied to psychiatry residencies, 129 did not match. Overall, 99.8% of residency positions in psychiatry filled.
“It used to be less competitive,” said Kaz J. Nelson, MD, the vice chair for education at the University of Minnesota’s department of psychiatry and behavioral sciences in Minneapolis, adding that interest in psychiatry has increased over the years.
“Interest has skyrocketed as the word has gotten out about how great a field it is. It helps that reimbursements are better, that there is less bias and discrimination against patients with psychiatric issues, and that psychiatric care is seen as a legitimate part of medicine. It has been exciting to watch!” Dr. Nelson said.
The numbers are only one part of the story, however.
Application submission now involves a centralized, electronic process, and it has become easier for applicants to apply to a lot of programs indiscriminately. It’s not unusual for applicants to apply to 70 or more programs. The factors that have limited applications include the cost: Electronic Residency Application Services (ERAS) charges for each application package they send to a program, and applicants traditionally pay to travel to the programs where they interview. This all changed with the 2021 cycle when in-person interviews were halted for the pandemic and interviews became virtual. While I recall applying to 7 residency programs, this year the average number of applications was 54.7 per applicant.
“It used to be that the cap on interviewing was financial,” Dr. Nelson said. “It was discriminatory and favored those who had more money to travel to interviews. There are still the ERAS fees, but COVID has been an equalizer and we are getting more applicants, and interviewing more who are not from Minnesota or the Midwest. We have been working to make our program attractive in terms of diversity, equity, inclusion, and justice. Our hospital is located a mile from where George Floyd was murdered, and it’s our responsibility to lead the effort to ensure the psychiatry workforce is diverse, and inclusive, as possible.”
Daniel E. Gih, MD, is the program director for a new psychiatry residency at the University of Nebraska, Omaha. When the program started in 2019, there were spots for four residents and the program had 588 applications. In 2020, the program grew to five positions and this year there were 553 applicants. Dr. Gih attributed the high number of applications to his program’s strong social media presence.
“Going through the applications and meeting the students are some of the most enjoyable parts of my work,” Dr. Gih said. “I feel guilty though, that I’m likely going to miss a great applicant. Each application averages 35 pages and it’s inevitable that programs have to take shortcuts. Applicants worry that they’ll be ranked by board scores. While we certainly don’t do that here, students might feel ruled out of a program if their numbers aren’t high enough. Furthermore, wealthy students can apply to more programs. The pandemic has really highlighted the inequity issues.”
Dr. Gih noted that the Zoom interview process has not been disappointing: “Two of the people we matched had never been to Omaha, and many expressed concerns about what it is like here. Of course, on Zoom you don’t catch subtle interpersonal issues, but we have been pleasantly surprised that the people we matched were consistent with what we expected. It is exciting to meet the people who will eventually replace us as psychiatrists, they will be here to deal with future challenges!” His enthusiasm was tangible.
While the program directors remain optimistic, the system is not without its stresses, as many programs receive over 1,000 applications.
“This is difficult,” Dr. Nelson said.” It’s wonderful for the programs, but for the medical students, not matching is experienced by them as being catastrophic, so they apply to a lot of programs. Getting this many applications is a challenge, yet I don’t want to interview someone if they are going to rank our program No. 80 on their list!”
Residencies have dealt with the deluge of applicants in a number of ways. Some specialties started a “signal” protocol wherein candidates and programs receive a certain number of tokens to indicate that each would rank the other highly, but psychiatry has not done this. Early on in the Zoom process, multiple applicants would be offered interviews simultaneously, and the interview would be given to the candidate who responded first. Students vented their frustrations on Twitter when they lost interview spots at their coveted programs because they hadn’t checked their email in time or had gone to take a shower.
“The American Association of Directors of Psychiatry Residency Training Programs issued guidelines saying that it is unacceptable to offer interview spots without allowing a reasonable time for the applicant to respond, and that it is not appropriate to offer multiple candidates one spot on a first-come, first-serve basis,” Dr. Nelson explained.
Her program has managed some of the application chaos by using a software program called Scutmonkey, codeveloped by David Ross, MD, PhD, the associate program director of the Yale Adult Psychiatry Residency Program.
“It lets us screen applications for candidates who specifically are interested in being here, and for those who qualify as part of the mission we are trying to fulfill.”
One fourth-year student at a mid-Atlantic medical school who is applying in psychiatry – who I’ll call Sacha to protect his anonymity – applied to 73 psychiatry programs and to date, has interviewed at 6. He describes a stressful, roller coaster experience:
“I got those six interviews right away and that was an amazing start, but then I didn’t get any more. The interviews I had went well, but it has been disappointing not to have more. Some were all-day interviews, while other programs had me meet with residents and attendings for 20 minutes each and it was all done after 2 hours.”
He has mixed opinions about not seeing the schools in person. “There are very heavy pros and cons. I’ve saved thousands of dollars in travel expenses that would have limited my applications, so logistically it’s a dream. On the other hand, I’ve interviewed in cities I have never been to, it’s hard to get a sense of the intangibles of a program, and the shorter interviews feel very impersonal.”
Sacha expressed anxieties about the process. “With so many applicants, it’s difficult for someone with a nontraditional story to get a spot and it’s easier for the programs to toss applications. it’s common enough and everyone has seen someone who has gone through this. At times, we feel powerless; we have no real agency or control. We send stuff out and then we sit in the prayer position and wait.”
I think back on my own application process with a sense of gratitude. I certainly didn’t feel powerless, and in today’s world, postinterview communications with program directors are regulated for both parties. Dr. Slavney was kind enough to humor my request, but I don’t believe this would be feasible in the current environment.
Even though it is wonderful that more doctors have figured out that careers in psychiatry are rewarding, the current situation is overwhelming for both the applicants and the programs. With over 100 applicants for every position – many of whom will have no interest in going to some of the programs they apply to – qualified candidates who go unmatched, and a roulette wheel which requires heavily indebted students to pay to apply, this is simply not sustainable in a country with a shortage of physicians – psychiatrists in particular.
We hear that mid-level practitioners are the answer to our shortages, but perhaps we need to create a system with enough residency positions to accommodate highly trained and qualified physicians in a more inviting and targeted way.
Dinah Miller, MD, is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore. A version of this article first appeared on Medscape.com.
The day I interviewed at Johns Hopkins in Baltimore, like every other day of residency interviews, was a very long and draining day.
I started by meeting alone with Philip Slavney, MD, the residency director, who spoke with me about the program and gave me a schedule to follow. I was to meet with residents and psychiatrists, some of whom had graduated from my medical school, and was sent to the Bayview campus a few miles away to have lunch and attend a few meetings. By the time I boarded an Amtrak train at Baltimore Penn Station, I was tired but I liked what I had seen. By the end of the interview season, I had crossed four programs off my list and had decided to rank only three.
In 1987, there were 987 residency positions in psychiatry in the United States, and 83.6% of those positions filled with a combination of U.S. and international medical graduates. Still, this was a risky move; the programs that I decided to rank would fill, but I was matching separately for an internship year in internal medicine in New York and decided that I would rather reapply in a year than risk matching at a program I didn’t want to go to.
I wasn’t quite sure where I wanted to rank Hopkins on my list, so I called Dr. Slavney and said I wanted to come back and meet more members of the department. He did not hide his surprise and was quick to tell me that no one had ever requested a second set of interviews. I mentioned specific people I wanted to meet with, and he was kind enough to accommodate my request and set up a second day of interviews for me.
Needless to say, the residency match felt very personal – at least to me – and although I felt vulnerable, I also felt empowered. Because of the low pay, patients with stigmatized illnesses, and the rampant belief that psychiatry was not “real” medicine and the patients never got better, psychiatry was not a desired specialty.
The residency application process in psychiatry (and every other specialty) has become a much different process. In 2006, the Association of American Medical Colleges called on medical schools to increase their enrollments to address the national shortage of physicians. Soon, there were more medical schools, bigger classes, and more doctors being minted, but the Balanced Budget Act of 1997 prevented a proportional increase in residency positions.
Len Marquez, senior director of government relations at the AAMC noted: “The Resident Physician Shortage Reduction Act of 2021 (S. 834), sponsored by Sen. Robert Menendez (D-N.J.), Sen. John Boozman (R-Ark.), and Majority Leader Sen. Charles Schumer (D-N.Y.), would support 2,000 additional Medicare-supported residency positions each year for 7 years, but Congress has not yet acted on the legislation. We were very pleased that last year, Congress passed the first increase in Medicare-supported graduate medical education in 25 years by including 1,000 new slots as part of the Consolidated Appropriations Act, 2021.”
In addition, the Build Back Better Act, which is currently being debated in Congress, would provide 4,000 more graduate medical education slots, including a specific requirement that 15% of them go to “psychiatry-related residencies,” he added.
Over 90% of graduates from U.S. medical schools currently match into a residency position. That statistic for international medical graduates is notably lower, with perhaps as few as 50% of all applicants matching.
Since 2014, the number of applicants to psychiatry residencies has nearly doubled. For the 2021 match, there were 2,486 applicants applying for 1,858 positions in psychiatry – so 1.34 applicants for each slot. Of the 1,117 senior medical students at U.S. schools who applied to psychiatry residencies, 129 did not match. Overall, 99.8% of residency positions in psychiatry filled.
“It used to be less competitive,” said Kaz J. Nelson, MD, the vice chair for education at the University of Minnesota’s department of psychiatry and behavioral sciences in Minneapolis, adding that interest in psychiatry has increased over the years.
“Interest has skyrocketed as the word has gotten out about how great a field it is. It helps that reimbursements are better, that there is less bias and discrimination against patients with psychiatric issues, and that psychiatric care is seen as a legitimate part of medicine. It has been exciting to watch!” Dr. Nelson said.
The numbers are only one part of the story, however.
Application submission now involves a centralized, electronic process, and it has become easier for applicants to apply to a lot of programs indiscriminately. It’s not unusual for applicants to apply to 70 or more programs. The factors that have limited applications include the cost: Electronic Residency Application Services (ERAS) charges for each application package they send to a program, and applicants traditionally pay to travel to the programs where they interview. This all changed with the 2021 cycle when in-person interviews were halted for the pandemic and interviews became virtual. While I recall applying to 7 residency programs, this year the average number of applications was 54.7 per applicant.
“It used to be that the cap on interviewing was financial,” Dr. Nelson said. “It was discriminatory and favored those who had more money to travel to interviews. There are still the ERAS fees, but COVID has been an equalizer and we are getting more applicants, and interviewing more who are not from Minnesota or the Midwest. We have been working to make our program attractive in terms of diversity, equity, inclusion, and justice. Our hospital is located a mile from where George Floyd was murdered, and it’s our responsibility to lead the effort to ensure the psychiatry workforce is diverse, and inclusive, as possible.”
Daniel E. Gih, MD, is the program director for a new psychiatry residency at the University of Nebraska, Omaha. When the program started in 2019, there were spots for four residents and the program had 588 applications. In 2020, the program grew to five positions and this year there were 553 applicants. Dr. Gih attributed the high number of applications to his program’s strong social media presence.
“Going through the applications and meeting the students are some of the most enjoyable parts of my work,” Dr. Gih said. “I feel guilty though, that I’m likely going to miss a great applicant. Each application averages 35 pages and it’s inevitable that programs have to take shortcuts. Applicants worry that they’ll be ranked by board scores. While we certainly don’t do that here, students might feel ruled out of a program if their numbers aren’t high enough. Furthermore, wealthy students can apply to more programs. The pandemic has really highlighted the inequity issues.”
Dr. Gih noted that the Zoom interview process has not been disappointing: “Two of the people we matched had never been to Omaha, and many expressed concerns about what it is like here. Of course, on Zoom you don’t catch subtle interpersonal issues, but we have been pleasantly surprised that the people we matched were consistent with what we expected. It is exciting to meet the people who will eventually replace us as psychiatrists, they will be here to deal with future challenges!” His enthusiasm was tangible.
While the program directors remain optimistic, the system is not without its stresses, as many programs receive over 1,000 applications.
“This is difficult,” Dr. Nelson said.” It’s wonderful for the programs, but for the medical students, not matching is experienced by them as being catastrophic, so they apply to a lot of programs. Getting this many applications is a challenge, yet I don’t want to interview someone if they are going to rank our program No. 80 on their list!”
Residencies have dealt with the deluge of applicants in a number of ways. Some specialties started a “signal” protocol wherein candidates and programs receive a certain number of tokens to indicate that each would rank the other highly, but psychiatry has not done this. Early on in the Zoom process, multiple applicants would be offered interviews simultaneously, and the interview would be given to the candidate who responded first. Students vented their frustrations on Twitter when they lost interview spots at their coveted programs because they hadn’t checked their email in time or had gone to take a shower.
“The American Association of Directors of Psychiatry Residency Training Programs issued guidelines saying that it is unacceptable to offer interview spots without allowing a reasonable time for the applicant to respond, and that it is not appropriate to offer multiple candidates one spot on a first-come, first-serve basis,” Dr. Nelson explained.
Her program has managed some of the application chaos by using a software program called Scutmonkey, codeveloped by David Ross, MD, PhD, the associate program director of the Yale Adult Psychiatry Residency Program.
“It lets us screen applications for candidates who specifically are interested in being here, and for those who qualify as part of the mission we are trying to fulfill.”
One fourth-year student at a mid-Atlantic medical school who is applying in psychiatry – who I’ll call Sacha to protect his anonymity – applied to 73 psychiatry programs and to date, has interviewed at 6. He describes a stressful, roller coaster experience:
“I got those six interviews right away and that was an amazing start, but then I didn’t get any more. The interviews I had went well, but it has been disappointing not to have more. Some were all-day interviews, while other programs had me meet with residents and attendings for 20 minutes each and it was all done after 2 hours.”
He has mixed opinions about not seeing the schools in person. “There are very heavy pros and cons. I’ve saved thousands of dollars in travel expenses that would have limited my applications, so logistically it’s a dream. On the other hand, I’ve interviewed in cities I have never been to, it’s hard to get a sense of the intangibles of a program, and the shorter interviews feel very impersonal.”
Sacha expressed anxieties about the process. “With so many applicants, it’s difficult for someone with a nontraditional story to get a spot and it’s easier for the programs to toss applications. it’s common enough and everyone has seen someone who has gone through this. At times, we feel powerless; we have no real agency or control. We send stuff out and then we sit in the prayer position and wait.”
I think back on my own application process with a sense of gratitude. I certainly didn’t feel powerless, and in today’s world, postinterview communications with program directors are regulated for both parties. Dr. Slavney was kind enough to humor my request, but I don’t believe this would be feasible in the current environment.
Even though it is wonderful that more doctors have figured out that careers in psychiatry are rewarding, the current situation is overwhelming for both the applicants and the programs. With over 100 applicants for every position – many of whom will have no interest in going to some of the programs they apply to – qualified candidates who go unmatched, and a roulette wheel which requires heavily indebted students to pay to apply, this is simply not sustainable in a country with a shortage of physicians – psychiatrists in particular.
We hear that mid-level practitioners are the answer to our shortages, but perhaps we need to create a system with enough residency positions to accommodate highly trained and qualified physicians in a more inviting and targeted way.
Dinah Miller, MD, is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore. A version of this article first appeared on Medscape.com.
COVID-19 and coping with superimposed traumas
While 2022 is lurking around the corner, many of us still have 2020 on our minds. Social media posts are already emerging: “No new years resolutions. It is the circumstances turn to improve [sic],” one post declares. Others proclaim that it is difficult coming to terms with the idea that 2022 is actually pronounced “2020 too.” A critical difference exists between then and now – we have experienced months of living in limbo and rolling with the punches of pandemic life.
In some ways, it has become easy to think of the early pandemic days as a distant memory, yet respect that the impact of 2020 has been indelible for virtually all of us and feels palpable as if it were yesterday.
The year 2020 was marked by the beginning of the COVID-19 pandemic, which was accompanied by extreme uncertainty, loss of all kinds, and emotional turmoil. The early pandemic had a profound economic and social impact, with added stress tethered to political and race-related division in America that created divides among families and friends, and yielded ceaseless discourse related to divergent perspectives. This only exacerbated the stress that came with the pandemic, given that providing support and leaning on one another was more important than ever. All of this was compounded by natural disasters that have plagued the country.
So much was unprecedented. There was a collective sense of feeling “worn down,” and the burnout that was felt was quite profound. Enormous amounts of mental and physical effort were allocated to simply surviving, getting basic needs met, having enough food and supplies, and completing basic tasks. Ordinary relating felt taxing. At this stage of the pandemic, the COVID-19 experience can be conceived of as a traumatic stressor capable of eliciting a traumatic response and exacerbating other mental health symptoms. Our capacity to cope has been diminished. Anxiety rates have soared, as have rates of clinical depression. Those most affected have had lower household incomes, are unmarried, and have experienced pandemic-related stressors. The links between the impact of the pandemic on mental health have been clear.
The pandemic has forced the landscape of social support to dramatically change. Initially, we felt pulled to connect and we leaned into the use of virtual platforms to connect for all matters (simple social gatherings, big birthday events, family reunions, celebration of holidays, work duties, and academic work). However, “Zoom fatigue” began to set in, and our screen time was maxed out. There has been the added dynamic of frontline workers who did not have the option to work virtually or from home. This group largely has felt disconnected from others who didn’t understand the depth of their anxiety and loneliness of their experience. Health care workers have had to make challenging, life-and-death, patient-related decisions that called into question personal morals and ethics all while their own lives were at risk.
Fast-forward to the present, and support systems have either strengthened or worn down – which has yielded a unique dichotomy. Maintaining friendships has either felt of utmost importance given the impact of the disconnect and physical distance or has felt challenging given the mental energy expended from working and connecting virtually. Empathy burnout is also a real and important facet in the equation. We begin to ask the question: Are we checking in with others in the spirit of authentic relating, to cultivate real connection, or to check a box?
Impact of layered traumas
It is interesting to think about the pandemic’s traumatic impact being “superimposed” on top of the “ordinary traumas” experienced outside of the pandemic. We are essentially at the 2-year mark, in some ways have cultivated a sense of resilience and found ways to adapt, and in other ways at times feel right back where we were in early 2020. There were moments that felt hopeful, glimmers of normalcy, and setbacks that all ebbed and flowed – but even so, there have not been many “mental breaks,” only temporary and transient reprieves. Some got sick and died; some recovered; and others are still experiencing long-hauler syndrome and have lingering sequelae. Despite adaptation and resilience, one can’t help but wonder the impact of superimposed traumas on top of this collective trauma. Many of us have not even rebounded from the pandemic, and then are faced with loss, grief, challenges, illness, hard and big life decisions. We are challenged to answer the question: How do we endure in the face of this trauma inception?
It has been a challenging time for all, including those who are ordinarily happy-go-lucky, resilient, and see the glass half-full and are struggling with the idea of struggling. I am no “resilience expert” but gleaned much wisdom from responding to the Surfside, Fla., building collapse. This was a collective trauma that took place in the summer of 2021, and the wisdom of this event highlighted the value of collective healing and unification even in spite of the times. What happened in Surfside was a shock, and the loss was felt by those directly affected, the surrounding community, and those who were part of the disaster response efforts. All of those parties had been processing losses prior to this – loss of normalcy because of the pandemic, loss of people we loved as a result, other personal losses – and this community tragedy was yet another loss to disentangle on top of a period in U.S. history demarcated by a great lack of unity, divisiveness, anger, and hatred. The collapse highlighted the small size yet interconnectedness of the community and the power of connection and authentic relating. It was overwhelming in the moment but extremely heartening and beautiful to see the amount of willingness to drop everything and help. Despite feeling worn down from the pandemic, people drew upon their internal resources, natural goodness, and kindness “reserves” to provide support.
Responding to the collapse highlighted that resilience in the context of collective trauma requires flexibility, embracing uncertainty, cultivating unity, and paying attention to meeting basic needs/self-care. The role of kindness cannot be overemphasized. In the realm of reflecting on the notion of kindness, it is worth noting how much power there is to bearing witness to someone’s experience, especially when they are in pain. People often diminish the role or at the very least do not recognize the power of showing up for someone and just listening. Pandemic resilience, and coping with coalescing traumas, is likely composed of these same facets that were essential in the context of coping with the collapse.
It is not only the immediate impact of a trauma as much as the aftermath that needs to processed and worked through. In one sense, people feel that they should be adjusted to and accustomed to this new reality, and at the same time, one has to remember and reflect on how unnatural this experience has been. There is an impact of a cumulative onslaught of negative events, and it is hard to imagine not being phased, remaining unchanged, or not feeling affected. We may feel hardened and that there are limits to the compassion we have to offer others. We may be feel empathic. There can be desensitization and an apathy to others’ suffering when our patience is worn down and we have limited bandwidth. There are data to support the idea that a level of habituation occurs to individuals who experience multiple traumas, which yields a level of “sensitization” to the negative impact of subsequent events. It becomes easy to make comparisons of suffering. The challenge will be to rise above these and make a conscious effort to connect with who and how we were before we were worn down.
I am still in awe about how much I learned from the victims’ families, survivors, and my colleagues at Surfside – about pain, suffering, loss, resilience, coping, fortitude, and meaning making. We were all forced to think beyond ourselves, show up for others, and unify in a way that remedied this period of fragmentation. With respect to the pandemic and “where we are at now,” some elements of our lives are stabilizing; other aspects feel volatile from the fatigue of what we have been experiencing. This pandemic has not fully abated, but we can find some clarity in the value of setting boundaries and knowing our limits – but not overlooking the power of unity and kindness and the value of the reciprocating those qualities.
Dr. Feldman is a licensed clinical psychologist in private practice in Miami. She is an adjunct professor in the college of psychology at Nova Southeastern University, Fort Lauderdale, Fla., where she teaches clinical psychology doctoral students. She also serves on the board of directors of the Southeast Florida Association for Psychoanalytic Psychology. Dr. Feldman has no disclosures.
While 2022 is lurking around the corner, many of us still have 2020 on our minds. Social media posts are already emerging: “No new years resolutions. It is the circumstances turn to improve [sic],” one post declares. Others proclaim that it is difficult coming to terms with the idea that 2022 is actually pronounced “2020 too.” A critical difference exists between then and now – we have experienced months of living in limbo and rolling with the punches of pandemic life.
In some ways, it has become easy to think of the early pandemic days as a distant memory, yet respect that the impact of 2020 has been indelible for virtually all of us and feels palpable as if it were yesterday.
The year 2020 was marked by the beginning of the COVID-19 pandemic, which was accompanied by extreme uncertainty, loss of all kinds, and emotional turmoil. The early pandemic had a profound economic and social impact, with added stress tethered to political and race-related division in America that created divides among families and friends, and yielded ceaseless discourse related to divergent perspectives. This only exacerbated the stress that came with the pandemic, given that providing support and leaning on one another was more important than ever. All of this was compounded by natural disasters that have plagued the country.
So much was unprecedented. There was a collective sense of feeling “worn down,” and the burnout that was felt was quite profound. Enormous amounts of mental and physical effort were allocated to simply surviving, getting basic needs met, having enough food and supplies, and completing basic tasks. Ordinary relating felt taxing. At this stage of the pandemic, the COVID-19 experience can be conceived of as a traumatic stressor capable of eliciting a traumatic response and exacerbating other mental health symptoms. Our capacity to cope has been diminished. Anxiety rates have soared, as have rates of clinical depression. Those most affected have had lower household incomes, are unmarried, and have experienced pandemic-related stressors. The links between the impact of the pandemic on mental health have been clear.
The pandemic has forced the landscape of social support to dramatically change. Initially, we felt pulled to connect and we leaned into the use of virtual platforms to connect for all matters (simple social gatherings, big birthday events, family reunions, celebration of holidays, work duties, and academic work). However, “Zoom fatigue” began to set in, and our screen time was maxed out. There has been the added dynamic of frontline workers who did not have the option to work virtually or from home. This group largely has felt disconnected from others who didn’t understand the depth of their anxiety and loneliness of their experience. Health care workers have had to make challenging, life-and-death, patient-related decisions that called into question personal morals and ethics all while their own lives were at risk.
Fast-forward to the present, and support systems have either strengthened or worn down – which has yielded a unique dichotomy. Maintaining friendships has either felt of utmost importance given the impact of the disconnect and physical distance or has felt challenging given the mental energy expended from working and connecting virtually. Empathy burnout is also a real and important facet in the equation. We begin to ask the question: Are we checking in with others in the spirit of authentic relating, to cultivate real connection, or to check a box?
Impact of layered traumas
It is interesting to think about the pandemic’s traumatic impact being “superimposed” on top of the “ordinary traumas” experienced outside of the pandemic. We are essentially at the 2-year mark, in some ways have cultivated a sense of resilience and found ways to adapt, and in other ways at times feel right back where we were in early 2020. There were moments that felt hopeful, glimmers of normalcy, and setbacks that all ebbed and flowed – but even so, there have not been many “mental breaks,” only temporary and transient reprieves. Some got sick and died; some recovered; and others are still experiencing long-hauler syndrome and have lingering sequelae. Despite adaptation and resilience, one can’t help but wonder the impact of superimposed traumas on top of this collective trauma. Many of us have not even rebounded from the pandemic, and then are faced with loss, grief, challenges, illness, hard and big life decisions. We are challenged to answer the question: How do we endure in the face of this trauma inception?
It has been a challenging time for all, including those who are ordinarily happy-go-lucky, resilient, and see the glass half-full and are struggling with the idea of struggling. I am no “resilience expert” but gleaned much wisdom from responding to the Surfside, Fla., building collapse. This was a collective trauma that took place in the summer of 2021, and the wisdom of this event highlighted the value of collective healing and unification even in spite of the times. What happened in Surfside was a shock, and the loss was felt by those directly affected, the surrounding community, and those who were part of the disaster response efforts. All of those parties had been processing losses prior to this – loss of normalcy because of the pandemic, loss of people we loved as a result, other personal losses – and this community tragedy was yet another loss to disentangle on top of a period in U.S. history demarcated by a great lack of unity, divisiveness, anger, and hatred. The collapse highlighted the small size yet interconnectedness of the community and the power of connection and authentic relating. It was overwhelming in the moment but extremely heartening and beautiful to see the amount of willingness to drop everything and help. Despite feeling worn down from the pandemic, people drew upon their internal resources, natural goodness, and kindness “reserves” to provide support.
Responding to the collapse highlighted that resilience in the context of collective trauma requires flexibility, embracing uncertainty, cultivating unity, and paying attention to meeting basic needs/self-care. The role of kindness cannot be overemphasized. In the realm of reflecting on the notion of kindness, it is worth noting how much power there is to bearing witness to someone’s experience, especially when they are in pain. People often diminish the role or at the very least do not recognize the power of showing up for someone and just listening. Pandemic resilience, and coping with coalescing traumas, is likely composed of these same facets that were essential in the context of coping with the collapse.
It is not only the immediate impact of a trauma as much as the aftermath that needs to processed and worked through. In one sense, people feel that they should be adjusted to and accustomed to this new reality, and at the same time, one has to remember and reflect on how unnatural this experience has been. There is an impact of a cumulative onslaught of negative events, and it is hard to imagine not being phased, remaining unchanged, or not feeling affected. We may feel hardened and that there are limits to the compassion we have to offer others. We may be feel empathic. There can be desensitization and an apathy to others’ suffering when our patience is worn down and we have limited bandwidth. There are data to support the idea that a level of habituation occurs to individuals who experience multiple traumas, which yields a level of “sensitization” to the negative impact of subsequent events. It becomes easy to make comparisons of suffering. The challenge will be to rise above these and make a conscious effort to connect with who and how we were before we were worn down.
I am still in awe about how much I learned from the victims’ families, survivors, and my colleagues at Surfside – about pain, suffering, loss, resilience, coping, fortitude, and meaning making. We were all forced to think beyond ourselves, show up for others, and unify in a way that remedied this period of fragmentation. With respect to the pandemic and “where we are at now,” some elements of our lives are stabilizing; other aspects feel volatile from the fatigue of what we have been experiencing. This pandemic has not fully abated, but we can find some clarity in the value of setting boundaries and knowing our limits – but not overlooking the power of unity and kindness and the value of the reciprocating those qualities.
Dr. Feldman is a licensed clinical psychologist in private practice in Miami. She is an adjunct professor in the college of psychology at Nova Southeastern University, Fort Lauderdale, Fla., where she teaches clinical psychology doctoral students. She also serves on the board of directors of the Southeast Florida Association for Psychoanalytic Psychology. Dr. Feldman has no disclosures.
While 2022 is lurking around the corner, many of us still have 2020 on our minds. Social media posts are already emerging: “No new years resolutions. It is the circumstances turn to improve [sic],” one post declares. Others proclaim that it is difficult coming to terms with the idea that 2022 is actually pronounced “2020 too.” A critical difference exists between then and now – we have experienced months of living in limbo and rolling with the punches of pandemic life.
In some ways, it has become easy to think of the early pandemic days as a distant memory, yet respect that the impact of 2020 has been indelible for virtually all of us and feels palpable as if it were yesterday.
The year 2020 was marked by the beginning of the COVID-19 pandemic, which was accompanied by extreme uncertainty, loss of all kinds, and emotional turmoil. The early pandemic had a profound economic and social impact, with added stress tethered to political and race-related division in America that created divides among families and friends, and yielded ceaseless discourse related to divergent perspectives. This only exacerbated the stress that came with the pandemic, given that providing support and leaning on one another was more important than ever. All of this was compounded by natural disasters that have plagued the country.
So much was unprecedented. There was a collective sense of feeling “worn down,” and the burnout that was felt was quite profound. Enormous amounts of mental and physical effort were allocated to simply surviving, getting basic needs met, having enough food and supplies, and completing basic tasks. Ordinary relating felt taxing. At this stage of the pandemic, the COVID-19 experience can be conceived of as a traumatic stressor capable of eliciting a traumatic response and exacerbating other mental health symptoms. Our capacity to cope has been diminished. Anxiety rates have soared, as have rates of clinical depression. Those most affected have had lower household incomes, are unmarried, and have experienced pandemic-related stressors. The links between the impact of the pandemic on mental health have been clear.
The pandemic has forced the landscape of social support to dramatically change. Initially, we felt pulled to connect and we leaned into the use of virtual platforms to connect for all matters (simple social gatherings, big birthday events, family reunions, celebration of holidays, work duties, and academic work). However, “Zoom fatigue” began to set in, and our screen time was maxed out. There has been the added dynamic of frontline workers who did not have the option to work virtually or from home. This group largely has felt disconnected from others who didn’t understand the depth of their anxiety and loneliness of their experience. Health care workers have had to make challenging, life-and-death, patient-related decisions that called into question personal morals and ethics all while their own lives were at risk.
Fast-forward to the present, and support systems have either strengthened or worn down – which has yielded a unique dichotomy. Maintaining friendships has either felt of utmost importance given the impact of the disconnect and physical distance or has felt challenging given the mental energy expended from working and connecting virtually. Empathy burnout is also a real and important facet in the equation. We begin to ask the question: Are we checking in with others in the spirit of authentic relating, to cultivate real connection, or to check a box?
Impact of layered traumas
It is interesting to think about the pandemic’s traumatic impact being “superimposed” on top of the “ordinary traumas” experienced outside of the pandemic. We are essentially at the 2-year mark, in some ways have cultivated a sense of resilience and found ways to adapt, and in other ways at times feel right back where we were in early 2020. There were moments that felt hopeful, glimmers of normalcy, and setbacks that all ebbed and flowed – but even so, there have not been many “mental breaks,” only temporary and transient reprieves. Some got sick and died; some recovered; and others are still experiencing long-hauler syndrome and have lingering sequelae. Despite adaptation and resilience, one can’t help but wonder the impact of superimposed traumas on top of this collective trauma. Many of us have not even rebounded from the pandemic, and then are faced with loss, grief, challenges, illness, hard and big life decisions. We are challenged to answer the question: How do we endure in the face of this trauma inception?
It has been a challenging time for all, including those who are ordinarily happy-go-lucky, resilient, and see the glass half-full and are struggling with the idea of struggling. I am no “resilience expert” but gleaned much wisdom from responding to the Surfside, Fla., building collapse. This was a collective trauma that took place in the summer of 2021, and the wisdom of this event highlighted the value of collective healing and unification even in spite of the times. What happened in Surfside was a shock, and the loss was felt by those directly affected, the surrounding community, and those who were part of the disaster response efforts. All of those parties had been processing losses prior to this – loss of normalcy because of the pandemic, loss of people we loved as a result, other personal losses – and this community tragedy was yet another loss to disentangle on top of a period in U.S. history demarcated by a great lack of unity, divisiveness, anger, and hatred. The collapse highlighted the small size yet interconnectedness of the community and the power of connection and authentic relating. It was overwhelming in the moment but extremely heartening and beautiful to see the amount of willingness to drop everything and help. Despite feeling worn down from the pandemic, people drew upon their internal resources, natural goodness, and kindness “reserves” to provide support.
Responding to the collapse highlighted that resilience in the context of collective trauma requires flexibility, embracing uncertainty, cultivating unity, and paying attention to meeting basic needs/self-care. The role of kindness cannot be overemphasized. In the realm of reflecting on the notion of kindness, it is worth noting how much power there is to bearing witness to someone’s experience, especially when they are in pain. People often diminish the role or at the very least do not recognize the power of showing up for someone and just listening. Pandemic resilience, and coping with coalescing traumas, is likely composed of these same facets that were essential in the context of coping with the collapse.
It is not only the immediate impact of a trauma as much as the aftermath that needs to processed and worked through. In one sense, people feel that they should be adjusted to and accustomed to this new reality, and at the same time, one has to remember and reflect on how unnatural this experience has been. There is an impact of a cumulative onslaught of negative events, and it is hard to imagine not being phased, remaining unchanged, or not feeling affected. We may feel hardened and that there are limits to the compassion we have to offer others. We may be feel empathic. There can be desensitization and an apathy to others’ suffering when our patience is worn down and we have limited bandwidth. There are data to support the idea that a level of habituation occurs to individuals who experience multiple traumas, which yields a level of “sensitization” to the negative impact of subsequent events. It becomes easy to make comparisons of suffering. The challenge will be to rise above these and make a conscious effort to connect with who and how we were before we were worn down.
I am still in awe about how much I learned from the victims’ families, survivors, and my colleagues at Surfside – about pain, suffering, loss, resilience, coping, fortitude, and meaning making. We were all forced to think beyond ourselves, show up for others, and unify in a way that remedied this period of fragmentation. With respect to the pandemic and “where we are at now,” some elements of our lives are stabilizing; other aspects feel volatile from the fatigue of what we have been experiencing. This pandemic has not fully abated, but we can find some clarity in the value of setting boundaries and knowing our limits – but not overlooking the power of unity and kindness and the value of the reciprocating those qualities.
Dr. Feldman is a licensed clinical psychologist in private practice in Miami. She is an adjunct professor in the college of psychology at Nova Southeastern University, Fort Lauderdale, Fla., where she teaches clinical psychology doctoral students. She also serves on the board of directors of the Southeast Florida Association for Psychoanalytic Psychology. Dr. Feldman has no disclosures.