User login
The child with hypertension: Diagnosis and management
This transcript has been edited for clarity. The transcript and an accompanying video first appeared on Medscape.com.
Justin L. Berk, MD, MPH, MBA: Welcome back to The Cribsiders, our video recap of our pediatric medicine podcast. We interview leading experts in the field to bring clinical pearls and practice-changing knowledge, and answer lingering questions about core topics in pediatric medicine. Chris, what is our topic today?
Christopher J. Chiu, MD: I was really happy to be able to talk about our recent episode with Dr. Carissa Baker-Smith, a pediatric cardiologist and director of the Nemours preventive cardiology program. She helped us review the pediatric screening guidelines for blood pressure, including initial workup and treatment.
Dr. Berk: This was a really great episode that a lot of people found really helpful. What were some of the key takeaway pearls that you think listeners would be interested in?
Dr. Chiu: We talked about when and how we should be checking blood pressures in children. Blood pressure should be checked at every well-child visit starting at age 3. But if they have other risk factors like kidney disease or a condition such as coarctation of the aorta, then blood pressure should be checked at every visit.
Dr. Berk: One thing she spoke about was how blood pressures should be measured. How should we be checking blood pressures in the clinic?
Dr. Chiu: Clinic blood pressures are usually checked with oscillometric devices. They can differ by manufacturer, but basically they find a mean arterial pressure and then each device has a method of calculating systolic and diastolic pressures. Now after that, if the child’s blood pressure is maybe abnormal, you want to double-check a manual blood pressure using Korotkoff sounds to confirm the blood pressure.
She reminded us that blood pressure should be measured with the child sitting with their back supported, feet flat on the floor, and arm at the level of the heart. Make sure you use the right size cuff. The bladder of the cuff should be 40% of the width of the arm, and about 80%-100% of the arm circumference. She recommends sizing up if you have to.
Dr. Berk: Accuracy of blood pressure management was a really important point, especially for diagnosis at this stage. Can you walk us through what we learned about diagnosis of hypertension?
Dr. Chiu: The definitions of hypertension come from the Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents. Up until the age of 13, they define prehypertension as systolic and diastolic blood pressures between the 90th and 95th percentile, or if the blood pressure exceeds 120/80 mm Hg. Hypertension is defined when blood pressure reaches the 95th percentile. Now age 13 is when it gets a little hazy. Many changes in the guidelines happen at age 13, when hypertension starts being defined by adult guidelines. The 2017 adult hypertension guidelines define stage 1 hypertension as 130/89 to 139/89, and stage 2 hypertension as greater than 140/90.
Dr. Berk: How about workup of hypertension? The work of pediatric hypertension is always a little bit complex. What are some of the pearls you took away?
Dr. Chui: She talked about tailoring the workup to the child. So when we’re doing our workup, obviously physical exam should be the first thing we do. You have to assess and compare pulses, which is one of the most important parts of the initial evaluation. Obviously, looking at coarctation of the aorta, but also looking for things like a cushingoid appearance. If the child is less than 6 years of age, she recommends a referral to nephrology for more comprehensive renovascular workup, which probably will include renal ultrasound, urinalysis, metabolic panel, and thyroid studies.
We have to be cognizant of secondary causes of hypertension, such as endocrine tumors, hyperthyroidism, aortic disease, or even medication-induced hypertension. She told us that in the majority of these cases, especially with our obese older children, primary hypertension or essential hypertension is the most likely cause.
Dr. Berk: That was my big takeaway. If they’re really young, they need a big workup, but otherwise it is likely primary hypertension. What did we learn about treatment?
Dr. Chui: Just as we tailor our assessment to the child, we also have to tailor treatment. We know that lifestyle modification is usually the first line of treatment, especially for primary hypertension, and Dr. Baker-Smith tells us that we really need to perform counseling that meets the patient where they are. So if they like dancing to the newest TikTok trends or music videos, maybe we can encourage them to move more that way. Using our motivational interviewing skills is really key here.
If you want to start medication, Dr. Baker-Smith uses things like low-dose ACE inhibitors or calcium channel blockers, but obviously it’ll be tailored to the patient and any underlying conditions.
Dr. Berk: That’s great – a lot of wonderful pearls on the diagnosis and management of pediatric hypertension. Thank you for joining us for another video recap of The Cribsiders pediatric podcast. You can download the full podcast, Off the Cuff: Managing Pediatric Hypertension in Your Primary Care Clinic, on any podcast player, or check out our website at www.theCribsiders.com.
Christopher J. Chiu, MD, is assistant professor, department of internal medicine, division of general internal medicine, Ohio State University, Columbus; lead physician, general internal medicine, OSU Outpatient Care East; department of internal medicine, division of general internal medicine, Ohio State University Wexner Medical Center. Dr. Chiu has disclosed no relevant financial relationships. Justin L. Berk, MD, MPH, MBA, is assistant professor, department of medicine; assistant professor, department of pediatrics, Brown University, Providence, R.I.
This transcript has been edited for clarity. The transcript and an accompanying video first appeared on Medscape.com.
Justin L. Berk, MD, MPH, MBA: Welcome back to The Cribsiders, our video recap of our pediatric medicine podcast. We interview leading experts in the field to bring clinical pearls and practice-changing knowledge, and answer lingering questions about core topics in pediatric medicine. Chris, what is our topic today?
Christopher J. Chiu, MD: I was really happy to be able to talk about our recent episode with Dr. Carissa Baker-Smith, a pediatric cardiologist and director of the Nemours preventive cardiology program. She helped us review the pediatric screening guidelines for blood pressure, including initial workup and treatment.
Dr. Berk: This was a really great episode that a lot of people found really helpful. What were some of the key takeaway pearls that you think listeners would be interested in?
Dr. Chiu: We talked about when and how we should be checking blood pressures in children. Blood pressure should be checked at every well-child visit starting at age 3. But if they have other risk factors like kidney disease or a condition such as coarctation of the aorta, then blood pressure should be checked at every visit.
Dr. Berk: One thing she spoke about was how blood pressures should be measured. How should we be checking blood pressures in the clinic?
Dr. Chiu: Clinic blood pressures are usually checked with oscillometric devices. They can differ by manufacturer, but basically they find a mean arterial pressure and then each device has a method of calculating systolic and diastolic pressures. Now after that, if the child’s blood pressure is maybe abnormal, you want to double-check a manual blood pressure using Korotkoff sounds to confirm the blood pressure.
She reminded us that blood pressure should be measured with the child sitting with their back supported, feet flat on the floor, and arm at the level of the heart. Make sure you use the right size cuff. The bladder of the cuff should be 40% of the width of the arm, and about 80%-100% of the arm circumference. She recommends sizing up if you have to.
Dr. Berk: Accuracy of blood pressure management was a really important point, especially for diagnosis at this stage. Can you walk us through what we learned about diagnosis of hypertension?
Dr. Chiu: The definitions of hypertension come from the Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents. Up until the age of 13, they define prehypertension as systolic and diastolic blood pressures between the 90th and 95th percentile, or if the blood pressure exceeds 120/80 mm Hg. Hypertension is defined when blood pressure reaches the 95th percentile. Now age 13 is when it gets a little hazy. Many changes in the guidelines happen at age 13, when hypertension starts being defined by adult guidelines. The 2017 adult hypertension guidelines define stage 1 hypertension as 130/89 to 139/89, and stage 2 hypertension as greater than 140/90.
Dr. Berk: How about workup of hypertension? The work of pediatric hypertension is always a little bit complex. What are some of the pearls you took away?
Dr. Chui: She talked about tailoring the workup to the child. So when we’re doing our workup, obviously physical exam should be the first thing we do. You have to assess and compare pulses, which is one of the most important parts of the initial evaluation. Obviously, looking at coarctation of the aorta, but also looking for things like a cushingoid appearance. If the child is less than 6 years of age, she recommends a referral to nephrology for more comprehensive renovascular workup, which probably will include renal ultrasound, urinalysis, metabolic panel, and thyroid studies.
We have to be cognizant of secondary causes of hypertension, such as endocrine tumors, hyperthyroidism, aortic disease, or even medication-induced hypertension. She told us that in the majority of these cases, especially with our obese older children, primary hypertension or essential hypertension is the most likely cause.
Dr. Berk: That was my big takeaway. If they’re really young, they need a big workup, but otherwise it is likely primary hypertension. What did we learn about treatment?
Dr. Chui: Just as we tailor our assessment to the child, we also have to tailor treatment. We know that lifestyle modification is usually the first line of treatment, especially for primary hypertension, and Dr. Baker-Smith tells us that we really need to perform counseling that meets the patient where they are. So if they like dancing to the newest TikTok trends or music videos, maybe we can encourage them to move more that way. Using our motivational interviewing skills is really key here.
If you want to start medication, Dr. Baker-Smith uses things like low-dose ACE inhibitors or calcium channel blockers, but obviously it’ll be tailored to the patient and any underlying conditions.
Dr. Berk: That’s great – a lot of wonderful pearls on the diagnosis and management of pediatric hypertension. Thank you for joining us for another video recap of The Cribsiders pediatric podcast. You can download the full podcast, Off the Cuff: Managing Pediatric Hypertension in Your Primary Care Clinic, on any podcast player, or check out our website at www.theCribsiders.com.
Christopher J. Chiu, MD, is assistant professor, department of internal medicine, division of general internal medicine, Ohio State University, Columbus; lead physician, general internal medicine, OSU Outpatient Care East; department of internal medicine, division of general internal medicine, Ohio State University Wexner Medical Center. Dr. Chiu has disclosed no relevant financial relationships. Justin L. Berk, MD, MPH, MBA, is assistant professor, department of medicine; assistant professor, department of pediatrics, Brown University, Providence, R.I.
This transcript has been edited for clarity. The transcript and an accompanying video first appeared on Medscape.com.
Justin L. Berk, MD, MPH, MBA: Welcome back to The Cribsiders, our video recap of our pediatric medicine podcast. We interview leading experts in the field to bring clinical pearls and practice-changing knowledge, and answer lingering questions about core topics in pediatric medicine. Chris, what is our topic today?
Christopher J. Chiu, MD: I was really happy to be able to talk about our recent episode with Dr. Carissa Baker-Smith, a pediatric cardiologist and director of the Nemours preventive cardiology program. She helped us review the pediatric screening guidelines for blood pressure, including initial workup and treatment.
Dr. Berk: This was a really great episode that a lot of people found really helpful. What were some of the key takeaway pearls that you think listeners would be interested in?
Dr. Chiu: We talked about when and how we should be checking blood pressures in children. Blood pressure should be checked at every well-child visit starting at age 3. But if they have other risk factors like kidney disease or a condition such as coarctation of the aorta, then blood pressure should be checked at every visit.
Dr. Berk: One thing she spoke about was how blood pressures should be measured. How should we be checking blood pressures in the clinic?
Dr. Chiu: Clinic blood pressures are usually checked with oscillometric devices. They can differ by manufacturer, but basically they find a mean arterial pressure and then each device has a method of calculating systolic and diastolic pressures. Now after that, if the child’s blood pressure is maybe abnormal, you want to double-check a manual blood pressure using Korotkoff sounds to confirm the blood pressure.
She reminded us that blood pressure should be measured with the child sitting with their back supported, feet flat on the floor, and arm at the level of the heart. Make sure you use the right size cuff. The bladder of the cuff should be 40% of the width of the arm, and about 80%-100% of the arm circumference. She recommends sizing up if you have to.
Dr. Berk: Accuracy of blood pressure management was a really important point, especially for diagnosis at this stage. Can you walk us through what we learned about diagnosis of hypertension?
Dr. Chiu: The definitions of hypertension come from the Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents. Up until the age of 13, they define prehypertension as systolic and diastolic blood pressures between the 90th and 95th percentile, or if the blood pressure exceeds 120/80 mm Hg. Hypertension is defined when blood pressure reaches the 95th percentile. Now age 13 is when it gets a little hazy. Many changes in the guidelines happen at age 13, when hypertension starts being defined by adult guidelines. The 2017 adult hypertension guidelines define stage 1 hypertension as 130/89 to 139/89, and stage 2 hypertension as greater than 140/90.
Dr. Berk: How about workup of hypertension? The work of pediatric hypertension is always a little bit complex. What are some of the pearls you took away?
Dr. Chui: She talked about tailoring the workup to the child. So when we’re doing our workup, obviously physical exam should be the first thing we do. You have to assess and compare pulses, which is one of the most important parts of the initial evaluation. Obviously, looking at coarctation of the aorta, but also looking for things like a cushingoid appearance. If the child is less than 6 years of age, she recommends a referral to nephrology for more comprehensive renovascular workup, which probably will include renal ultrasound, urinalysis, metabolic panel, and thyroid studies.
We have to be cognizant of secondary causes of hypertension, such as endocrine tumors, hyperthyroidism, aortic disease, or even medication-induced hypertension. She told us that in the majority of these cases, especially with our obese older children, primary hypertension or essential hypertension is the most likely cause.
Dr. Berk: That was my big takeaway. If they’re really young, they need a big workup, but otherwise it is likely primary hypertension. What did we learn about treatment?
Dr. Chui: Just as we tailor our assessment to the child, we also have to tailor treatment. We know that lifestyle modification is usually the first line of treatment, especially for primary hypertension, and Dr. Baker-Smith tells us that we really need to perform counseling that meets the patient where they are. So if they like dancing to the newest TikTok trends or music videos, maybe we can encourage them to move more that way. Using our motivational interviewing skills is really key here.
If you want to start medication, Dr. Baker-Smith uses things like low-dose ACE inhibitors or calcium channel blockers, but obviously it’ll be tailored to the patient and any underlying conditions.
Dr. Berk: That’s great – a lot of wonderful pearls on the diagnosis and management of pediatric hypertension. Thank you for joining us for another video recap of The Cribsiders pediatric podcast. You can download the full podcast, Off the Cuff: Managing Pediatric Hypertension in Your Primary Care Clinic, on any podcast player, or check out our website at www.theCribsiders.com.
Christopher J. Chiu, MD, is assistant professor, department of internal medicine, division of general internal medicine, Ohio State University, Columbus; lead physician, general internal medicine, OSU Outpatient Care East; department of internal medicine, division of general internal medicine, Ohio State University Wexner Medical Center. Dr. Chiu has disclosed no relevant financial relationships. Justin L. Berk, MD, MPH, MBA, is assistant professor, department of medicine; assistant professor, department of pediatrics, Brown University, Providence, R.I.
Understanding the Intersection of Homelessness and Justice Involvement: Enhancing Veteran Suicide Prevention Through VA Programming
Despite the success of several US Department of Veterans Affairs (VA) initiatives in facilitating psychosocial functioning, rehabilitation, and re-entry among veterans experiencing homelessness and/or interactions with the criminal justice system (ie, justice-involved veterans), suicide risk among these veterans remains a significant public health concern. Rates of suicide among veterans experiencing homelessness are more than double that of veterans with no history of homelessness.1 Similarly, justice-involved veterans experience myriad mental health concerns, including elevated rates of psychiatric symptoms, suicidal thoughts, and self-directed violence relative to those with no history of criminal justice involvement.2
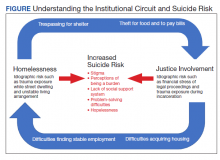
In addition, a bidirectional relationship between criminal justice involvement and homelessness, often called the “institutional circuit,” is well established. Criminal justice involvement can directly result in difficulty finding housing.3 For example, veterans may have their lease agreement denied based solely on their history of criminogenic behavior. Moreover, criminal justice involvement can indirectly impact a veteran’s ability to maintain housing. Indeed, justice-involved veterans can experience difficulty attaining and sustaining employment, which in turn can result in financial difficulties, including inability to afford rental or mortgage payments.
Similarly, those at risk for or experiencing housing instability may resort to criminogenic behavior to survive in the context of limited psychosocial resources.4-6 For instance, a veteran experiencing homelessness may seek refuge from inclement weather in a heated apartment stairwell and subsequently be charged with trespassing. Similarly, these veterans also may resort to theft to eat or pay bills. To this end, homelessness and justice involvement are likely a deleterious cycle that is difficult for the veteran to escape.
Unfortunately, the concurrent impact of housing insecurity and criminal justice involvement often serves to further exacerbate mental health sequelae, including suicide risk (Figure).7 In addition to precipitating frustration and helplessness among veterans who are navigating these stressors, these social determinants of health can engender a perception that the veteran is a burden to those in their support system. For example, these veterans may depend on friends or family to procure housing or transportation assistance for a job, medical appointments, and court hearings.
Furthermore, homelessness and justice involvement can impact veterans’ interpersonal relationships. For instance, veterans with a history of criminal justice involvement may feel stigmatized and ostracized from their social support system. Justice-involved veterans sometimes endorse being labeled an offender, which can result in perceptions that one is poorly perceived by others and generally seen as a bad person.8 In addition, the conditions of a justice-involved veteran’s probation or parole may further exacerbate social relationships. For example, veterans with histories of engaging in intimate partner violence may lose visitation rights with their children, further reinforcing negative views of self and impacting the veterans’ family network.
As such, these homeless and justice-involved veterans may lack a meaningful social support system when navigating psychosocial stressors. Because hopelessness, burdensomeness, and perceptions that one lacks a social support network are potential drivers of suicidal self-directed violence among these populations, facilitating access to and engagement in health (eg, psychotherapy, medication management) and social (eg, case management, transitional housing) services is necessary to enhance veteran suicide prevention efforts.9
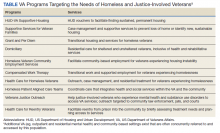
Several VA homeless and justice-related programs have been developed to meet the needs of these veterans (Table). Such programs offer direct access to health and social services capable of addressing mental health symptoms and suicide risk. Moreover, these programs support veterans at various intercepts, or points at which there is an opportunity to identify those at elevated risk and provide access to evidence-based care. For instance, VA homeless programs exist tailored toward those currently, or at risk for, experiencing homelessness. Additionally, VA justice-related programs can target intercepts prior to jail or prison, such as working with crisis intervention teams or diversion courts as well as intercepts following release, such as providing services to facilitate postincarceration reentry. Even VA programs that do not directly administer mental health intervention (eg, Grant and Per Diem, Veterans Justice Outreach) serve as critical points of contact that can connect these veterans to evidence-based suicide prevention treatments (eg, Cognitive Behavioral Therapy for Suicide Prevention; pharmacotherapy) in the VA or the community.
Within these programs, several suicide prevention efforts also are currently underway. In particular, the VA has mandated routine screening for suicide risk. This includes screening for the presence of elevations in acute risk (eg, suicidal intent, recent suicide attempt) and, within the context of acute risk, conducting a comprehensive risk evaluation that captures veterans’ risk and protective factors as well as access to lethal means. These clinical data are used to determine the veteran’s severity of acute and chronic risk and match them to an appropriate intervention.
Despite these ongoing efforts, several gaps in understanding exist, such as for example, elucidating the potential role of traditional VA homeless and justice-related programming in reducing risk for suicide.10 Additional research specific to suicide prevention programming among these populations also remains important.11 In particular, no examination to date has evaluated national rates of suicide risk assessment within these settings or elucidated if specific subsets of homeless and justice-involved veterans may be less likely to receive suicide risk screening. For instance, understanding whether homeless veterans accessing mental health services are more likely to be screened for suicide risk relative to homeless veterans accessing care in other VA settings (eg, emergency services). Moreover, the effectiveness of existing suicide-focused evidence-based treatments among homeless and justice-involved veterans remains unknown. Such research may reveal a need to adapt existing interventions, such as safety planning, to the idiographic needs of homeless or justice-involved veterans in order to improve effectiveness.10 Finally, social determinants of health, such as race, ethnicity, gender, and rurality may confer additional risk coupled with difficulties accessing and engaging in care within these populations.11 As such, research specific to these veteran populations and their inherent suicide prevention needs may further inform suicide prevention efforts.
Despite these gaps, it is important to acknowledge ongoing research and programmatic efforts focused on enhancing mental health and suicide prevention practices within VA settings. For example, efforts led by Temblique and colleagues acknowledge not only challenges to the execution of suicide prevention efforts in VA homeless programs, but also potential methods of enhancing care, including additional training in suicide risk screening and evaluation due to provider discomfort.12 Such quality improvement projects are paramount in their potential to identify gaps in health service delivery and thus potentially save veteran lives.
The VA currently has several programs focused on enhancing care for homeless and justice-involved veterans, and many incorporate suicide prevention initiatives. Further understanding of factors that may impact health service delivery of suicide risk assessment and intervention among these populations may be beneficial in order to enhance veteran suicide prevention efforts.
1. McCarthy JF, Bossarte RM, Katz IR, et al. Predictive modeling and concentration of the risk of suicide: implications for preventive interventions in the US Department of Veterans Affairs. Am J Public Health. 2015;105(9):1935-1942. doi:10.2105/AJPH.2015.302737
2. Holliday R, Hoffmire CA, Martin WB, Hoff RA, Monteith LL. Associations between justice involvement and PTSD and depressive symptoms, suicidal ideation, and suicide attempt among post-9/11 veterans. Psychol Trauma. 2021;13(7):730-739. doi:10.1037/tra0001038
3. Tsai J, Rosenheck RA. Risk factors for homelessness among US veterans. Epidemiol Rev. 2015;37:177-195. doi:10.1093/epirev/mxu004
4. Fischer PJ. Criminal activity among the homeless: a study of arrests in Baltimore. Hosp Community Psychiatry. 1988;39(1):46-51. doi:10.1176/ps.39.1.46
5. McCarthy B, Hagan J. Homelessness: a criminogenic situation? Br J Criminol. 1991;31(4):393–410.doi:10.1093/oxfordjournals.bjc.a048137
6. Solomon P, Draine J. Issues in serving the forensic client. Soc Work. 1995;40(1):25-33.
7. Holliday R, Forster JE, Desai A, et al. Association of lifetime homelessness and justice involvement with psychiatric symptoms, suicidal ideation, and suicide attempt among post-9/11 veterans. J Psychiatr Res. 2021;144:455-461. doi:10.1016/j.jpsychires.2021.11.007
8. Desai A, Holliday R, Borges LM, et al. Facilitating successful reentry among justice-involved veterans: the role of veteran and offender identity. J Psychiatr Pract. 2021;27(1):52-60. Published 2021 Jan 21. doi:10.1097/PRA.0000000000000520
9. Holliday R, Martin WB, Monteith LL, Clark SC, LePage JP. Suicide among justice-involved veterans: a brief overview of extant research, theoretical conceptualization, and recommendations for future research. J Soc Distress Homeless. 2021;30(1):41-49. doi: 10.1080/10530789.2019.1711306
10. Hoffberg AS, Spitzer E, Mackelprang JL, Farro SA, Brenner LA. Suicidal self-directed violence among homeless US veterans: a systematic review. Suicide Life Threat Behav. 2018;48(4):481-498. doi:10.1111/sltb.12369
11. Holliday R, Liu S, Brenner LA, et al. Preventing suicide among homeless veterans: a consensus statement by the Veterans Affairs Suicide Prevention Among Veterans Experiencing Homelessness Workgroup. Med Care. 2021;59(suppl 2):S103-S105. doi:10.1097/MLR.0000000000001399.
12. Temblique EKR, Foster K, Fujimoto J, Kopelson K, Borthick KM, et al. Addressing the mental health crisis: a one year review of a nationally-led intervention to improve suicide prevention screening at a large homeless veterans clinic. Fed Pract. 2022;39(1):12-18. doi:10.12788/fp.0215
Despite the success of several US Department of Veterans Affairs (VA) initiatives in facilitating psychosocial functioning, rehabilitation, and re-entry among veterans experiencing homelessness and/or interactions with the criminal justice system (ie, justice-involved veterans), suicide risk among these veterans remains a significant public health concern. Rates of suicide among veterans experiencing homelessness are more than double that of veterans with no history of homelessness.1 Similarly, justice-involved veterans experience myriad mental health concerns, including elevated rates of psychiatric symptoms, suicidal thoughts, and self-directed violence relative to those with no history of criminal justice involvement.2
In addition, a bidirectional relationship between criminal justice involvement and homelessness, often called the “institutional circuit,” is well established. Criminal justice involvement can directly result in difficulty finding housing.3 For example, veterans may have their lease agreement denied based solely on their history of criminogenic behavior. Moreover, criminal justice involvement can indirectly impact a veteran’s ability to maintain housing. Indeed, justice-involved veterans can experience difficulty attaining and sustaining employment, which in turn can result in financial difficulties, including inability to afford rental or mortgage payments.
Similarly, those at risk for or experiencing housing instability may resort to criminogenic behavior to survive in the context of limited psychosocial resources.4-6 For instance, a veteran experiencing homelessness may seek refuge from inclement weather in a heated apartment stairwell and subsequently be charged with trespassing. Similarly, these veterans also may resort to theft to eat or pay bills. To this end, homelessness and justice involvement are likely a deleterious cycle that is difficult for the veteran to escape.
Unfortunately, the concurrent impact of housing insecurity and criminal justice involvement often serves to further exacerbate mental health sequelae, including suicide risk (Figure).7 In addition to precipitating frustration and helplessness among veterans who are navigating these stressors, these social determinants of health can engender a perception that the veteran is a burden to those in their support system. For example, these veterans may depend on friends or family to procure housing or transportation assistance for a job, medical appointments, and court hearings.
Furthermore, homelessness and justice involvement can impact veterans’ interpersonal relationships. For instance, veterans with a history of criminal justice involvement may feel stigmatized and ostracized from their social support system. Justice-involved veterans sometimes endorse being labeled an offender, which can result in perceptions that one is poorly perceived by others and generally seen as a bad person.8 In addition, the conditions of a justice-involved veteran’s probation or parole may further exacerbate social relationships. For example, veterans with histories of engaging in intimate partner violence may lose visitation rights with their children, further reinforcing negative views of self and impacting the veterans’ family network.
As such, these homeless and justice-involved veterans may lack a meaningful social support system when navigating psychosocial stressors. Because hopelessness, burdensomeness, and perceptions that one lacks a social support network are potential drivers of suicidal self-directed violence among these populations, facilitating access to and engagement in health (eg, psychotherapy, medication management) and social (eg, case management, transitional housing) services is necessary to enhance veteran suicide prevention efforts.9
Several VA homeless and justice-related programs have been developed to meet the needs of these veterans (Table). Such programs offer direct access to health and social services capable of addressing mental health symptoms and suicide risk. Moreover, these programs support veterans at various intercepts, or points at which there is an opportunity to identify those at elevated risk and provide access to evidence-based care. For instance, VA homeless programs exist tailored toward those currently, or at risk for, experiencing homelessness. Additionally, VA justice-related programs can target intercepts prior to jail or prison, such as working with crisis intervention teams or diversion courts as well as intercepts following release, such as providing services to facilitate postincarceration reentry. Even VA programs that do not directly administer mental health intervention (eg, Grant and Per Diem, Veterans Justice Outreach) serve as critical points of contact that can connect these veterans to evidence-based suicide prevention treatments (eg, Cognitive Behavioral Therapy for Suicide Prevention; pharmacotherapy) in the VA or the community.
Within these programs, several suicide prevention efforts also are currently underway. In particular, the VA has mandated routine screening for suicide risk. This includes screening for the presence of elevations in acute risk (eg, suicidal intent, recent suicide attempt) and, within the context of acute risk, conducting a comprehensive risk evaluation that captures veterans’ risk and protective factors as well as access to lethal means. These clinical data are used to determine the veteran’s severity of acute and chronic risk and match them to an appropriate intervention.
Despite these ongoing efforts, several gaps in understanding exist, such as for example, elucidating the potential role of traditional VA homeless and justice-related programming in reducing risk for suicide.10 Additional research specific to suicide prevention programming among these populations also remains important.11 In particular, no examination to date has evaluated national rates of suicide risk assessment within these settings or elucidated if specific subsets of homeless and justice-involved veterans may be less likely to receive suicide risk screening. For instance, understanding whether homeless veterans accessing mental health services are more likely to be screened for suicide risk relative to homeless veterans accessing care in other VA settings (eg, emergency services). Moreover, the effectiveness of existing suicide-focused evidence-based treatments among homeless and justice-involved veterans remains unknown. Such research may reveal a need to adapt existing interventions, such as safety planning, to the idiographic needs of homeless or justice-involved veterans in order to improve effectiveness.10 Finally, social determinants of health, such as race, ethnicity, gender, and rurality may confer additional risk coupled with difficulties accessing and engaging in care within these populations.11 As such, research specific to these veteran populations and their inherent suicide prevention needs may further inform suicide prevention efforts.
Despite these gaps, it is important to acknowledge ongoing research and programmatic efforts focused on enhancing mental health and suicide prevention practices within VA settings. For example, efforts led by Temblique and colleagues acknowledge not only challenges to the execution of suicide prevention efforts in VA homeless programs, but also potential methods of enhancing care, including additional training in suicide risk screening and evaluation due to provider discomfort.12 Such quality improvement projects are paramount in their potential to identify gaps in health service delivery and thus potentially save veteran lives.
The VA currently has several programs focused on enhancing care for homeless and justice-involved veterans, and many incorporate suicide prevention initiatives. Further understanding of factors that may impact health service delivery of suicide risk assessment and intervention among these populations may be beneficial in order to enhance veteran suicide prevention efforts.
Despite the success of several US Department of Veterans Affairs (VA) initiatives in facilitating psychosocial functioning, rehabilitation, and re-entry among veterans experiencing homelessness and/or interactions with the criminal justice system (ie, justice-involved veterans), suicide risk among these veterans remains a significant public health concern. Rates of suicide among veterans experiencing homelessness are more than double that of veterans with no history of homelessness.1 Similarly, justice-involved veterans experience myriad mental health concerns, including elevated rates of psychiatric symptoms, suicidal thoughts, and self-directed violence relative to those with no history of criminal justice involvement.2
In addition, a bidirectional relationship between criminal justice involvement and homelessness, often called the “institutional circuit,” is well established. Criminal justice involvement can directly result in difficulty finding housing.3 For example, veterans may have their lease agreement denied based solely on their history of criminogenic behavior. Moreover, criminal justice involvement can indirectly impact a veteran’s ability to maintain housing. Indeed, justice-involved veterans can experience difficulty attaining and sustaining employment, which in turn can result in financial difficulties, including inability to afford rental or mortgage payments.
Similarly, those at risk for or experiencing housing instability may resort to criminogenic behavior to survive in the context of limited psychosocial resources.4-6 For instance, a veteran experiencing homelessness may seek refuge from inclement weather in a heated apartment stairwell and subsequently be charged with trespassing. Similarly, these veterans also may resort to theft to eat or pay bills. To this end, homelessness and justice involvement are likely a deleterious cycle that is difficult for the veteran to escape.
Unfortunately, the concurrent impact of housing insecurity and criminal justice involvement often serves to further exacerbate mental health sequelae, including suicide risk (Figure).7 In addition to precipitating frustration and helplessness among veterans who are navigating these stressors, these social determinants of health can engender a perception that the veteran is a burden to those in their support system. For example, these veterans may depend on friends or family to procure housing or transportation assistance for a job, medical appointments, and court hearings.
Furthermore, homelessness and justice involvement can impact veterans’ interpersonal relationships. For instance, veterans with a history of criminal justice involvement may feel stigmatized and ostracized from their social support system. Justice-involved veterans sometimes endorse being labeled an offender, which can result in perceptions that one is poorly perceived by others and generally seen as a bad person.8 In addition, the conditions of a justice-involved veteran’s probation or parole may further exacerbate social relationships. For example, veterans with histories of engaging in intimate partner violence may lose visitation rights with their children, further reinforcing negative views of self and impacting the veterans’ family network.
As such, these homeless and justice-involved veterans may lack a meaningful social support system when navigating psychosocial stressors. Because hopelessness, burdensomeness, and perceptions that one lacks a social support network are potential drivers of suicidal self-directed violence among these populations, facilitating access to and engagement in health (eg, psychotherapy, medication management) and social (eg, case management, transitional housing) services is necessary to enhance veteran suicide prevention efforts.9
Several VA homeless and justice-related programs have been developed to meet the needs of these veterans (Table). Such programs offer direct access to health and social services capable of addressing mental health symptoms and suicide risk. Moreover, these programs support veterans at various intercepts, or points at which there is an opportunity to identify those at elevated risk and provide access to evidence-based care. For instance, VA homeless programs exist tailored toward those currently, or at risk for, experiencing homelessness. Additionally, VA justice-related programs can target intercepts prior to jail or prison, such as working with crisis intervention teams or diversion courts as well as intercepts following release, such as providing services to facilitate postincarceration reentry. Even VA programs that do not directly administer mental health intervention (eg, Grant and Per Diem, Veterans Justice Outreach) serve as critical points of contact that can connect these veterans to evidence-based suicide prevention treatments (eg, Cognitive Behavioral Therapy for Suicide Prevention; pharmacotherapy) in the VA or the community.
Within these programs, several suicide prevention efforts also are currently underway. In particular, the VA has mandated routine screening for suicide risk. This includes screening for the presence of elevations in acute risk (eg, suicidal intent, recent suicide attempt) and, within the context of acute risk, conducting a comprehensive risk evaluation that captures veterans’ risk and protective factors as well as access to lethal means. These clinical data are used to determine the veteran’s severity of acute and chronic risk and match them to an appropriate intervention.
Despite these ongoing efforts, several gaps in understanding exist, such as for example, elucidating the potential role of traditional VA homeless and justice-related programming in reducing risk for suicide.10 Additional research specific to suicide prevention programming among these populations also remains important.11 In particular, no examination to date has evaluated national rates of suicide risk assessment within these settings or elucidated if specific subsets of homeless and justice-involved veterans may be less likely to receive suicide risk screening. For instance, understanding whether homeless veterans accessing mental health services are more likely to be screened for suicide risk relative to homeless veterans accessing care in other VA settings (eg, emergency services). Moreover, the effectiveness of existing suicide-focused evidence-based treatments among homeless and justice-involved veterans remains unknown. Such research may reveal a need to adapt existing interventions, such as safety planning, to the idiographic needs of homeless or justice-involved veterans in order to improve effectiveness.10 Finally, social determinants of health, such as race, ethnicity, gender, and rurality may confer additional risk coupled with difficulties accessing and engaging in care within these populations.11 As such, research specific to these veteran populations and their inherent suicide prevention needs may further inform suicide prevention efforts.
Despite these gaps, it is important to acknowledge ongoing research and programmatic efforts focused on enhancing mental health and suicide prevention practices within VA settings. For example, efforts led by Temblique and colleagues acknowledge not only challenges to the execution of suicide prevention efforts in VA homeless programs, but also potential methods of enhancing care, including additional training in suicide risk screening and evaluation due to provider discomfort.12 Such quality improvement projects are paramount in their potential to identify gaps in health service delivery and thus potentially save veteran lives.
The VA currently has several programs focused on enhancing care for homeless and justice-involved veterans, and many incorporate suicide prevention initiatives. Further understanding of factors that may impact health service delivery of suicide risk assessment and intervention among these populations may be beneficial in order to enhance veteran suicide prevention efforts.
1. McCarthy JF, Bossarte RM, Katz IR, et al. Predictive modeling and concentration of the risk of suicide: implications for preventive interventions in the US Department of Veterans Affairs. Am J Public Health. 2015;105(9):1935-1942. doi:10.2105/AJPH.2015.302737
2. Holliday R, Hoffmire CA, Martin WB, Hoff RA, Monteith LL. Associations between justice involvement and PTSD and depressive symptoms, suicidal ideation, and suicide attempt among post-9/11 veterans. Psychol Trauma. 2021;13(7):730-739. doi:10.1037/tra0001038
3. Tsai J, Rosenheck RA. Risk factors for homelessness among US veterans. Epidemiol Rev. 2015;37:177-195. doi:10.1093/epirev/mxu004
4. Fischer PJ. Criminal activity among the homeless: a study of arrests in Baltimore. Hosp Community Psychiatry. 1988;39(1):46-51. doi:10.1176/ps.39.1.46
5. McCarthy B, Hagan J. Homelessness: a criminogenic situation? Br J Criminol. 1991;31(4):393–410.doi:10.1093/oxfordjournals.bjc.a048137
6. Solomon P, Draine J. Issues in serving the forensic client. Soc Work. 1995;40(1):25-33.
7. Holliday R, Forster JE, Desai A, et al. Association of lifetime homelessness and justice involvement with psychiatric symptoms, suicidal ideation, and suicide attempt among post-9/11 veterans. J Psychiatr Res. 2021;144:455-461. doi:10.1016/j.jpsychires.2021.11.007
8. Desai A, Holliday R, Borges LM, et al. Facilitating successful reentry among justice-involved veterans: the role of veteran and offender identity. J Psychiatr Pract. 2021;27(1):52-60. Published 2021 Jan 21. doi:10.1097/PRA.0000000000000520
9. Holliday R, Martin WB, Monteith LL, Clark SC, LePage JP. Suicide among justice-involved veterans: a brief overview of extant research, theoretical conceptualization, and recommendations for future research. J Soc Distress Homeless. 2021;30(1):41-49. doi: 10.1080/10530789.2019.1711306
10. Hoffberg AS, Spitzer E, Mackelprang JL, Farro SA, Brenner LA. Suicidal self-directed violence among homeless US veterans: a systematic review. Suicide Life Threat Behav. 2018;48(4):481-498. doi:10.1111/sltb.12369
11. Holliday R, Liu S, Brenner LA, et al. Preventing suicide among homeless veterans: a consensus statement by the Veterans Affairs Suicide Prevention Among Veterans Experiencing Homelessness Workgroup. Med Care. 2021;59(suppl 2):S103-S105. doi:10.1097/MLR.0000000000001399.
12. Temblique EKR, Foster K, Fujimoto J, Kopelson K, Borthick KM, et al. Addressing the mental health crisis: a one year review of a nationally-led intervention to improve suicide prevention screening at a large homeless veterans clinic. Fed Pract. 2022;39(1):12-18. doi:10.12788/fp.0215
1. McCarthy JF, Bossarte RM, Katz IR, et al. Predictive modeling and concentration of the risk of suicide: implications for preventive interventions in the US Department of Veterans Affairs. Am J Public Health. 2015;105(9):1935-1942. doi:10.2105/AJPH.2015.302737
2. Holliday R, Hoffmire CA, Martin WB, Hoff RA, Monteith LL. Associations between justice involvement and PTSD and depressive symptoms, suicidal ideation, and suicide attempt among post-9/11 veterans. Psychol Trauma. 2021;13(7):730-739. doi:10.1037/tra0001038
3. Tsai J, Rosenheck RA. Risk factors for homelessness among US veterans. Epidemiol Rev. 2015;37:177-195. doi:10.1093/epirev/mxu004
4. Fischer PJ. Criminal activity among the homeless: a study of arrests in Baltimore. Hosp Community Psychiatry. 1988;39(1):46-51. doi:10.1176/ps.39.1.46
5. McCarthy B, Hagan J. Homelessness: a criminogenic situation? Br J Criminol. 1991;31(4):393–410.doi:10.1093/oxfordjournals.bjc.a048137
6. Solomon P, Draine J. Issues in serving the forensic client. Soc Work. 1995;40(1):25-33.
7. Holliday R, Forster JE, Desai A, et al. Association of lifetime homelessness and justice involvement with psychiatric symptoms, suicidal ideation, and suicide attempt among post-9/11 veterans. J Psychiatr Res. 2021;144:455-461. doi:10.1016/j.jpsychires.2021.11.007
8. Desai A, Holliday R, Borges LM, et al. Facilitating successful reentry among justice-involved veterans: the role of veteran and offender identity. J Psychiatr Pract. 2021;27(1):52-60. Published 2021 Jan 21. doi:10.1097/PRA.0000000000000520
9. Holliday R, Martin WB, Monteith LL, Clark SC, LePage JP. Suicide among justice-involved veterans: a brief overview of extant research, theoretical conceptualization, and recommendations for future research. J Soc Distress Homeless. 2021;30(1):41-49. doi: 10.1080/10530789.2019.1711306
10. Hoffberg AS, Spitzer E, Mackelprang JL, Farro SA, Brenner LA. Suicidal self-directed violence among homeless US veterans: a systematic review. Suicide Life Threat Behav. 2018;48(4):481-498. doi:10.1111/sltb.12369
11. Holliday R, Liu S, Brenner LA, et al. Preventing suicide among homeless veterans: a consensus statement by the Veterans Affairs Suicide Prevention Among Veterans Experiencing Homelessness Workgroup. Med Care. 2021;59(suppl 2):S103-S105. doi:10.1097/MLR.0000000000001399.
12. Temblique EKR, Foster K, Fujimoto J, Kopelson K, Borthick KM, et al. Addressing the mental health crisis: a one year review of a nationally-led intervention to improve suicide prevention screening at a large homeless veterans clinic. Fed Pract. 2022;39(1):12-18. doi:10.12788/fp.0215
A Simple Message
I do not usually have difficulty writing editorials. However, this month was different. I kept coming up with grand ideas that flopped. First, I thought I would write a column entitled, “For What Should We Hope For?” When I started exploring the concept of hope, I quickly learned that there was extensive literature from multiple disciplines and even several centers and research projects dedicated to studying it.1 It seemed unlikely that I would have anything worthwhile to add to that literature. Then I thought I would discuss new year’s resolutions for federal practitioners. There was not much written about that topic, yet it seemed to be overly self-indulgent and superficial to discuss eating less and exercising more amid a pandemic and a climate change crisis. Finally, I wanted to opine on the futility of telling people to be resilient when we are all exhausted and demoralized, and yet that seemed too ponderous and paradoxical for our beleaguered state. With the third strike, I finally realized I was trying too hard. And perhaps that was exactly what I needed to say, at least to myself, and maybe some readers would benefit from reading that simple message as well.
I was surprised—though I probably should not have been given the explosion of media—to find that Americans were surveyed about what months they hate most. A 2021 poll of more than 15,000 adults found that January was the most disliked month.2 It’s not hard to figure out why. Characterized by a postholiday let down, these months in the middle of winter marked by either too much precipitation or if you live in the West not enough; short days and gray nights that are dark and cold. It is a long time to wait before spring with few holidays to break up the quotidian routine of work and school. January is a hard enough month in a good or even ordinary year. And 2022 is shaping up to be neither. We are entering the third year of a prolonged pandemic. Every time we have hope we are coming to the end of this long ordeal or at least things are moving toward normality, a new variant emerges, and we are back to living in fear and uncertainty.
COVID-19 is only the most relentless and deadly of our current disasters: There are rumors of wars, tornadoes, droughts, floods, shootings in schools and churches, political turmoil, and police violence. American society and the very planet seem to be in a perilous situation more than ever. No wonder then, that in the last month, several people have asked me, “Do you think this is the end of the world?” I suppose they think I am so old that I have become wise. And though I should cite a brilliant philosopher or renowned theologian: I am going to revert to my youth as a rock musician and quote R.E.M.: “It is the end of the world as we know it.” And “most of us do not feel fine!”
The world of 2022 is far more constricted and confined than it was before we heard the word COVID-19. We have less freedom of movement and fewer opportunities for companionship and gathering, for advancement and enjoyment. To thrive, and even to survive, in this cramped existence of limited possibilities, we need different values and attitudes than those that made us happy and successful in the open, hurried world before 2019. No generation since World War II has confronted such shortages of automobiles, paper goods, food, and even medicines as we have.
That is the first of the important simple messages I want to convey. Find something to be grateful for: your loved ones, your companion animals, your friends. Cherish the rainy or sunny day depending on how your climate has changed. Treasure the most basic and enduring pleasures, homemade cookies, favorite music, talking to a good friend even virtually, reading an actual book on a Sunday afternoon. These are things even the pandemic cannot take away from us unless we let our own inability to accept the conditions of our time ruin even what the meager, harsh Master of History has spared us.
The second of these simple messages is even more essential to finding any peace or joy in our current tense and somber existence: to show compassion for others and kindness to yourself. The most consistent report I have heard from people all over the country is that their fellow citizens are angry and selfish. We all understand, and even in some measure empathize with this the frustration and impatience with all the extraordinary pressure of having to function under these challenging conditions. Though we can take it out on the stranger at the grocery store or the family of the patient who has different views of masks and vaccines; it likely will not make the line shorter, the family any less demanding or seemingly unreasonable and probably will waste the little energy we have left to get home with the groceries or take care of the patient.
You never know what burden the person annoying you is carrying; it may perhaps be heavier than yours. And how we react to each other makes the weight of world weariness we all bear either easier or harder to shoulder. It sounds trite and trivial to say, yet tell people you care, and value, and love them. Although no less than Pope Francis in a Christmas present to marriages under strain from the stress of the pandemic that the 3 key words to remember are please, sorry, and thank you.3 I am applying that sage advice liberally to all relationships and interactions in the daily grind of work and home. The cost is little, the reward priceless.
It is good and right to have high hopes. We all need to take care of ourselves, whether we make resolutions to do so or not. Though more than anything else what we need is to be kind to ourselves. It is presumptuous of me to tell you what wellness means for your individual struggle, as it is inhuman of me to deign to tell you to be resilient when many of you face intolerable working conditions.4 As Jackson Browne sang in “Rock Me on the Water”, “Everyone must have some thought that’s going to pull them through somehow. Find your own thought, the reason you keep getting up and going to care for patients who increasingly respond with the rage of denial and resentment. Amid what morally distressed public health professionals have called so many unnecessary deaths,choose what gives you reason to keep serving that other side of this life full of healing.5 And if like so many of my fellow health care professionals, you are so spent and bent, that you feel that you can no longer practice without becoming someone you do not want to be, then let go with grace, get the help you deserve and perhaps one day when rested and mended, find another way to give.6
I rarely self-disclose but I want to end this column with a personal story that exemplifies more than all these words living this simple message. My spouse is a health care practitioner at a Veterans Affairs medical center. Like all of you on the front lines they work far too long hours in difficult conditions, with challenging patients and not enough staff to care for them. My partner had not an hour to get any gifts for me or our furry children. On Christmas Eve, before a long shift, they went to a packed Walgreens to buy our huskies each a toy and me a pair of fuzzy slippers. We sat by the tree and opened the hastily wrapped packages, and nothing could have been more memorable or meaningful. All of us at Federal Practitioner wish you, our readers, find in 2022 many such moments to sustain you.
1. The Center for the Advanced Study and Practice of Hope. T Denny Sanford School of Social and Family Dynamics, Arizona State University. Accessed January 3, 2022. https://thesanfordschool.asu.edu/research/centers-initiatives/hope-center
2. Ballard J. What is America’s favorite (and least favorite) month?” Published March 1, 2021. Accessed January 3, 2022. https://today.yougov.com/topics/lifestyle/articles-reports/2021/03/01/favorite-least-favorite-month-poll
3. Winlfield N. Pope’s 3 key words for a marriage: ‘please, thanks sorry.’ Associated Press. December 26, 2021. Accessed January 3, 2022. https://apnews.com/article/pope-francis-lifestyle-religion-relationships-couples-23c81169982e50c35d1c1fc7bfef8cbc
4. Dineen K. Why resilience isn’t always the answer to coping with challenging times. Published September 29, 2020. Accessed January 3, 2022. https://theconversation.com/why-resilience-isnt-always-the-answer-to-coping-with-challenging-times-145796
5. Caldwell T. ‘Everyone of those deaths is unnecessary,’ expert says of rising COVID-19 U.S. death toll as tens of millions remain unvaccinated. Published October 3, 2021. Accessed December 29, 2021. https://www.cnn.com/2021/10/03/health/us-coronavirus-sunday/index.html 6. Yong E. Why healthcare professionals are quitting in droves. The Atlantic. November 16, 2021. Accessed December 29, 2021. https://www.theatlantic.com/health/archive/2021/11/the-mass-exodus-of-americas-health-care-workers/620713/
I do not usually have difficulty writing editorials. However, this month was different. I kept coming up with grand ideas that flopped. First, I thought I would write a column entitled, “For What Should We Hope For?” When I started exploring the concept of hope, I quickly learned that there was extensive literature from multiple disciplines and even several centers and research projects dedicated to studying it.1 It seemed unlikely that I would have anything worthwhile to add to that literature. Then I thought I would discuss new year’s resolutions for federal practitioners. There was not much written about that topic, yet it seemed to be overly self-indulgent and superficial to discuss eating less and exercising more amid a pandemic and a climate change crisis. Finally, I wanted to opine on the futility of telling people to be resilient when we are all exhausted and demoralized, and yet that seemed too ponderous and paradoxical for our beleaguered state. With the third strike, I finally realized I was trying too hard. And perhaps that was exactly what I needed to say, at least to myself, and maybe some readers would benefit from reading that simple message as well.
I was surprised—though I probably should not have been given the explosion of media—to find that Americans were surveyed about what months they hate most. A 2021 poll of more than 15,000 adults found that January was the most disliked month.2 It’s not hard to figure out why. Characterized by a postholiday let down, these months in the middle of winter marked by either too much precipitation or if you live in the West not enough; short days and gray nights that are dark and cold. It is a long time to wait before spring with few holidays to break up the quotidian routine of work and school. January is a hard enough month in a good or even ordinary year. And 2022 is shaping up to be neither. We are entering the third year of a prolonged pandemic. Every time we have hope we are coming to the end of this long ordeal or at least things are moving toward normality, a new variant emerges, and we are back to living in fear and uncertainty.
COVID-19 is only the most relentless and deadly of our current disasters: There are rumors of wars, tornadoes, droughts, floods, shootings in schools and churches, political turmoil, and police violence. American society and the very planet seem to be in a perilous situation more than ever. No wonder then, that in the last month, several people have asked me, “Do you think this is the end of the world?” I suppose they think I am so old that I have become wise. And though I should cite a brilliant philosopher or renowned theologian: I am going to revert to my youth as a rock musician and quote R.E.M.: “It is the end of the world as we know it.” And “most of us do not feel fine!”
The world of 2022 is far more constricted and confined than it was before we heard the word COVID-19. We have less freedom of movement and fewer opportunities for companionship and gathering, for advancement and enjoyment. To thrive, and even to survive, in this cramped existence of limited possibilities, we need different values and attitudes than those that made us happy and successful in the open, hurried world before 2019. No generation since World War II has confronted such shortages of automobiles, paper goods, food, and even medicines as we have.
That is the first of the important simple messages I want to convey. Find something to be grateful for: your loved ones, your companion animals, your friends. Cherish the rainy or sunny day depending on how your climate has changed. Treasure the most basic and enduring pleasures, homemade cookies, favorite music, talking to a good friend even virtually, reading an actual book on a Sunday afternoon. These are things even the pandemic cannot take away from us unless we let our own inability to accept the conditions of our time ruin even what the meager, harsh Master of History has spared us.
The second of these simple messages is even more essential to finding any peace or joy in our current tense and somber existence: to show compassion for others and kindness to yourself. The most consistent report I have heard from people all over the country is that their fellow citizens are angry and selfish. We all understand, and even in some measure empathize with this the frustration and impatience with all the extraordinary pressure of having to function under these challenging conditions. Though we can take it out on the stranger at the grocery store or the family of the patient who has different views of masks and vaccines; it likely will not make the line shorter, the family any less demanding or seemingly unreasonable and probably will waste the little energy we have left to get home with the groceries or take care of the patient.
You never know what burden the person annoying you is carrying; it may perhaps be heavier than yours. And how we react to each other makes the weight of world weariness we all bear either easier or harder to shoulder. It sounds trite and trivial to say, yet tell people you care, and value, and love them. Although no less than Pope Francis in a Christmas present to marriages under strain from the stress of the pandemic that the 3 key words to remember are please, sorry, and thank you.3 I am applying that sage advice liberally to all relationships and interactions in the daily grind of work and home. The cost is little, the reward priceless.
It is good and right to have high hopes. We all need to take care of ourselves, whether we make resolutions to do so or not. Though more than anything else what we need is to be kind to ourselves. It is presumptuous of me to tell you what wellness means for your individual struggle, as it is inhuman of me to deign to tell you to be resilient when many of you face intolerable working conditions.4 As Jackson Browne sang in “Rock Me on the Water”, “Everyone must have some thought that’s going to pull them through somehow. Find your own thought, the reason you keep getting up and going to care for patients who increasingly respond with the rage of denial and resentment. Amid what morally distressed public health professionals have called so many unnecessary deaths,choose what gives you reason to keep serving that other side of this life full of healing.5 And if like so many of my fellow health care professionals, you are so spent and bent, that you feel that you can no longer practice without becoming someone you do not want to be, then let go with grace, get the help you deserve and perhaps one day when rested and mended, find another way to give.6
I rarely self-disclose but I want to end this column with a personal story that exemplifies more than all these words living this simple message. My spouse is a health care practitioner at a Veterans Affairs medical center. Like all of you on the front lines they work far too long hours in difficult conditions, with challenging patients and not enough staff to care for them. My partner had not an hour to get any gifts for me or our furry children. On Christmas Eve, before a long shift, they went to a packed Walgreens to buy our huskies each a toy and me a pair of fuzzy slippers. We sat by the tree and opened the hastily wrapped packages, and nothing could have been more memorable or meaningful. All of us at Federal Practitioner wish you, our readers, find in 2022 many such moments to sustain you.
I do not usually have difficulty writing editorials. However, this month was different. I kept coming up with grand ideas that flopped. First, I thought I would write a column entitled, “For What Should We Hope For?” When I started exploring the concept of hope, I quickly learned that there was extensive literature from multiple disciplines and even several centers and research projects dedicated to studying it.1 It seemed unlikely that I would have anything worthwhile to add to that literature. Then I thought I would discuss new year’s resolutions for federal practitioners. There was not much written about that topic, yet it seemed to be overly self-indulgent and superficial to discuss eating less and exercising more amid a pandemic and a climate change crisis. Finally, I wanted to opine on the futility of telling people to be resilient when we are all exhausted and demoralized, and yet that seemed too ponderous and paradoxical for our beleaguered state. With the third strike, I finally realized I was trying too hard. And perhaps that was exactly what I needed to say, at least to myself, and maybe some readers would benefit from reading that simple message as well.
I was surprised—though I probably should not have been given the explosion of media—to find that Americans were surveyed about what months they hate most. A 2021 poll of more than 15,000 adults found that January was the most disliked month.2 It’s not hard to figure out why. Characterized by a postholiday let down, these months in the middle of winter marked by either too much precipitation or if you live in the West not enough; short days and gray nights that are dark and cold. It is a long time to wait before spring with few holidays to break up the quotidian routine of work and school. January is a hard enough month in a good or even ordinary year. And 2022 is shaping up to be neither. We are entering the third year of a prolonged pandemic. Every time we have hope we are coming to the end of this long ordeal or at least things are moving toward normality, a new variant emerges, and we are back to living in fear and uncertainty.
COVID-19 is only the most relentless and deadly of our current disasters: There are rumors of wars, tornadoes, droughts, floods, shootings in schools and churches, political turmoil, and police violence. American society and the very planet seem to be in a perilous situation more than ever. No wonder then, that in the last month, several people have asked me, “Do you think this is the end of the world?” I suppose they think I am so old that I have become wise. And though I should cite a brilliant philosopher or renowned theologian: I am going to revert to my youth as a rock musician and quote R.E.M.: “It is the end of the world as we know it.” And “most of us do not feel fine!”
The world of 2022 is far more constricted and confined than it was before we heard the word COVID-19. We have less freedom of movement and fewer opportunities for companionship and gathering, for advancement and enjoyment. To thrive, and even to survive, in this cramped existence of limited possibilities, we need different values and attitudes than those that made us happy and successful in the open, hurried world before 2019. No generation since World War II has confronted such shortages of automobiles, paper goods, food, and even medicines as we have.
That is the first of the important simple messages I want to convey. Find something to be grateful for: your loved ones, your companion animals, your friends. Cherish the rainy or sunny day depending on how your climate has changed. Treasure the most basic and enduring pleasures, homemade cookies, favorite music, talking to a good friend even virtually, reading an actual book on a Sunday afternoon. These are things even the pandemic cannot take away from us unless we let our own inability to accept the conditions of our time ruin even what the meager, harsh Master of History has spared us.
The second of these simple messages is even more essential to finding any peace or joy in our current tense and somber existence: to show compassion for others and kindness to yourself. The most consistent report I have heard from people all over the country is that their fellow citizens are angry and selfish. We all understand, and even in some measure empathize with this the frustration and impatience with all the extraordinary pressure of having to function under these challenging conditions. Though we can take it out on the stranger at the grocery store or the family of the patient who has different views of masks and vaccines; it likely will not make the line shorter, the family any less demanding or seemingly unreasonable and probably will waste the little energy we have left to get home with the groceries or take care of the patient.
You never know what burden the person annoying you is carrying; it may perhaps be heavier than yours. And how we react to each other makes the weight of world weariness we all bear either easier or harder to shoulder. It sounds trite and trivial to say, yet tell people you care, and value, and love them. Although no less than Pope Francis in a Christmas present to marriages under strain from the stress of the pandemic that the 3 key words to remember are please, sorry, and thank you.3 I am applying that sage advice liberally to all relationships and interactions in the daily grind of work and home. The cost is little, the reward priceless.
It is good and right to have high hopes. We all need to take care of ourselves, whether we make resolutions to do so or not. Though more than anything else what we need is to be kind to ourselves. It is presumptuous of me to tell you what wellness means for your individual struggle, as it is inhuman of me to deign to tell you to be resilient when many of you face intolerable working conditions.4 As Jackson Browne sang in “Rock Me on the Water”, “Everyone must have some thought that’s going to pull them through somehow. Find your own thought, the reason you keep getting up and going to care for patients who increasingly respond with the rage of denial and resentment. Amid what morally distressed public health professionals have called so many unnecessary deaths,choose what gives you reason to keep serving that other side of this life full of healing.5 And if like so many of my fellow health care professionals, you are so spent and bent, that you feel that you can no longer practice without becoming someone you do not want to be, then let go with grace, get the help you deserve and perhaps one day when rested and mended, find another way to give.6
I rarely self-disclose but I want to end this column with a personal story that exemplifies more than all these words living this simple message. My spouse is a health care practitioner at a Veterans Affairs medical center. Like all of you on the front lines they work far too long hours in difficult conditions, with challenging patients and not enough staff to care for them. My partner had not an hour to get any gifts for me or our furry children. On Christmas Eve, before a long shift, they went to a packed Walgreens to buy our huskies each a toy and me a pair of fuzzy slippers. We sat by the tree and opened the hastily wrapped packages, and nothing could have been more memorable or meaningful. All of us at Federal Practitioner wish you, our readers, find in 2022 many such moments to sustain you.
1. The Center for the Advanced Study and Practice of Hope. T Denny Sanford School of Social and Family Dynamics, Arizona State University. Accessed January 3, 2022. https://thesanfordschool.asu.edu/research/centers-initiatives/hope-center
2. Ballard J. What is America’s favorite (and least favorite) month?” Published March 1, 2021. Accessed January 3, 2022. https://today.yougov.com/topics/lifestyle/articles-reports/2021/03/01/favorite-least-favorite-month-poll
3. Winlfield N. Pope’s 3 key words for a marriage: ‘please, thanks sorry.’ Associated Press. December 26, 2021. Accessed January 3, 2022. https://apnews.com/article/pope-francis-lifestyle-religion-relationships-couples-23c81169982e50c35d1c1fc7bfef8cbc
4. Dineen K. Why resilience isn’t always the answer to coping with challenging times. Published September 29, 2020. Accessed January 3, 2022. https://theconversation.com/why-resilience-isnt-always-the-answer-to-coping-with-challenging-times-145796
5. Caldwell T. ‘Everyone of those deaths is unnecessary,’ expert says of rising COVID-19 U.S. death toll as tens of millions remain unvaccinated. Published October 3, 2021. Accessed December 29, 2021. https://www.cnn.com/2021/10/03/health/us-coronavirus-sunday/index.html 6. Yong E. Why healthcare professionals are quitting in droves. The Atlantic. November 16, 2021. Accessed December 29, 2021. https://www.theatlantic.com/health/archive/2021/11/the-mass-exodus-of-americas-health-care-workers/620713/
1. The Center for the Advanced Study and Practice of Hope. T Denny Sanford School of Social and Family Dynamics, Arizona State University. Accessed January 3, 2022. https://thesanfordschool.asu.edu/research/centers-initiatives/hope-center
2. Ballard J. What is America’s favorite (and least favorite) month?” Published March 1, 2021. Accessed January 3, 2022. https://today.yougov.com/topics/lifestyle/articles-reports/2021/03/01/favorite-least-favorite-month-poll
3. Winlfield N. Pope’s 3 key words for a marriage: ‘please, thanks sorry.’ Associated Press. December 26, 2021. Accessed January 3, 2022. https://apnews.com/article/pope-francis-lifestyle-religion-relationships-couples-23c81169982e50c35d1c1fc7bfef8cbc
4. Dineen K. Why resilience isn’t always the answer to coping with challenging times. Published September 29, 2020. Accessed January 3, 2022. https://theconversation.com/why-resilience-isnt-always-the-answer-to-coping-with-challenging-times-145796
5. Caldwell T. ‘Everyone of those deaths is unnecessary,’ expert says of rising COVID-19 U.S. death toll as tens of millions remain unvaccinated. Published October 3, 2021. Accessed December 29, 2021. https://www.cnn.com/2021/10/03/health/us-coronavirus-sunday/index.html 6. Yong E. Why healthcare professionals are quitting in droves. The Atlantic. November 16, 2021. Accessed December 29, 2021. https://www.theatlantic.com/health/archive/2021/11/the-mass-exodus-of-americas-health-care-workers/620713/
Teledermatology During the COVID-19 Pandemic: Lessons Learned and Future Directions
Although teledermatology utilization in the United States traditionally has lagged behind other countries,1,2 the COVID-19 pandemic upended this trend by creating the need for a massive teledermatology experiment. Recently reported survey results from a large representative sample of US dermatologists (5000 participants) on perceptions of teledermatology during COVID-19 indicated that only 14.1% of participants used teledermatology prior to the COVID-19 pandemic vs 54.1% of dermatologists in Europe.2,3 Since the pandemic started, 97% of US dermatologists reported teledermatology use,3 demonstrating a huge shift in utilization. This trend is notable, as teledermatology has been shown to increase access to dermatology in underserved areas, reduce patient travel times, improve patient triage, and even reduce carbon footprints.1,4 Thus, to sustain the momentum, insights from the recent teledermatology experience during the pandemic should inform future development.
Notably, the COVID-19 pandemic led to a rapid shift in focus from store-and-forward teledermatology to live video–based models.1,2 Logistically, live video visits are challenging, require more time and resources, and often are diagnostically limited, with concerns regarding technology, connectivity, reimbursement, and appropriate use.3 Prior to COVID-19, formal Health Insurance Portability and Accountability Act–compliant teledermatology platforms often were costly to establish and maintain, largely relegating use to academic centers and Veterans Affairs hospitals. Thus, many fewer private practice dermatologists had used teledermatology compared to academic dermatologists in the United States (11.4% vs 27.6%).3 Government regulations—a key barrier to the adoption of teledermatology in private practice before COVID-19—were greatly relaxed during the pandemic. The Centers for Medicare and Medicaid Services removed restrictions on where patients could be seen, improved reimbursement for video visits, and allowed the use of platforms that are not Health Insurance Portability and Accountability Act compliant. Many states also relaxed medical licensing rules.
Overall, the general outlook on telehealth seems positive. Reimbursement has been found to be a primary factor in dermatologists’ willingness to use teledermatology.3 Thus, sustainable use of teledermatology likely will depend on continued reimbursement parity for live video as well as store-and-forward consultations, which have several advantages but currently are de-incentivized by low reimbursement. The survey also found that 70% of respondents felt that teledermatology use will continue after COVID-19, while 58% intended to continue use—nearly 5-fold more than before the pandemic.3 We suspect the discrepancy between participants’ predictions regarding future use of teledermatology and their personal intent to use it highlights perceived barriers and limitations of the long-term success of teledermatology. Aside from reimbursement, connectivity and functionality were common concerns, emphasizing the need for innovative technological solutions.3 Moving forward, we anticipate that dermatologists will need to establish consistent workflows to establish consistent triage for the most appropriate visit—in-person visits vs teledermatology, which may include augmented, intelligence-enhanced solutions. Similar to prior clinician perspectives about which types of visits are conducive to teledermatology,2 most survey participants believed virtual visits were effective for acne, routine follow-ups, medication monitoring, and some inflammatory conditions.3
Importantly, we must be mindful of patients who may be left behind by the digital divide, such as those with lack of access to a smartphone or the internet, language barriers, or limited telehealth experience.5 Systems should be designed to provide these patients with technologic and health literacy aid or alternate modalities to access care. For example, structured methods could be introduced to provide training and instructions on how to access phone applications, computer-based programs, and more. Likewise, for those with hearing or vision deficits, it will be important to improve sound amplification and accessibility for headphones or hearing aid connectivity, as well as appropriate font size, button size, and application navigation. In remote areas, existing clinics may be used to help field specialty consultation teleconferences. Certainly, applications and platforms devised for teledermatology must be designed to serve diverse patient groups, with special consideration for the elderly, those who speak languages other than English, and those with disabilities that may make telehealth use more challenging.
Large-scale regulatory changes and reimbursement parity can have a substantial impact on future teledermatology use. Advocacy efforts continue to push for fair valuation of telemedicine, coverage of store-and-forward teledermatology codes, and coverage for all models of care. It is imperative for the dermatology community to continue discussions on implementation and methodology to best leverage this technology for the most patient benefit.
- Tensen E, van der Heijden JP, Jaspers MWM, et al. Two decades of teledermatology: current status and integration in national healthcare systems. Curr Dermatol Rep. 2016;5:96-104.
- Moscarella E, Pasquali P, Cinotti E, et al. A survey on teledermatology use and doctors’ perception in times of COVID-19 [published online August 17, 2020]. J Eur Acad Dermatol Venereol. 2020;34:E772-E773.
- Kennedy J, Arey S, Hopkins Z, et al. Dermatologist perceptions of teledermatology implementation and future use after COVID-19: demographics, barriers, and insights. JAMA Dermatol. 2021;157:595-597.
- Bonsall A. Unleashing carbon emissions savings with regular teledermatology clinics. Clin Exp Dermatol. 2021;46:574-575.
- Bakhtiar M, Elbuluk N, Lipoff JB. The digital divide: how COVID-19’s telemedicine expansion could exacerbate disparities. J Am Acad Dermatol. 2020;83:E345-E346.
Although teledermatology utilization in the United States traditionally has lagged behind other countries,1,2 the COVID-19 pandemic upended this trend by creating the need for a massive teledermatology experiment. Recently reported survey results from a large representative sample of US dermatologists (5000 participants) on perceptions of teledermatology during COVID-19 indicated that only 14.1% of participants used teledermatology prior to the COVID-19 pandemic vs 54.1% of dermatologists in Europe.2,3 Since the pandemic started, 97% of US dermatologists reported teledermatology use,3 demonstrating a huge shift in utilization. This trend is notable, as teledermatology has been shown to increase access to dermatology in underserved areas, reduce patient travel times, improve patient triage, and even reduce carbon footprints.1,4 Thus, to sustain the momentum, insights from the recent teledermatology experience during the pandemic should inform future development.
Notably, the COVID-19 pandemic led to a rapid shift in focus from store-and-forward teledermatology to live video–based models.1,2 Logistically, live video visits are challenging, require more time and resources, and often are diagnostically limited, with concerns regarding technology, connectivity, reimbursement, and appropriate use.3 Prior to COVID-19, formal Health Insurance Portability and Accountability Act–compliant teledermatology platforms often were costly to establish and maintain, largely relegating use to academic centers and Veterans Affairs hospitals. Thus, many fewer private practice dermatologists had used teledermatology compared to academic dermatologists in the United States (11.4% vs 27.6%).3 Government regulations—a key barrier to the adoption of teledermatology in private practice before COVID-19—were greatly relaxed during the pandemic. The Centers for Medicare and Medicaid Services removed restrictions on where patients could be seen, improved reimbursement for video visits, and allowed the use of platforms that are not Health Insurance Portability and Accountability Act compliant. Many states also relaxed medical licensing rules.
Overall, the general outlook on telehealth seems positive. Reimbursement has been found to be a primary factor in dermatologists’ willingness to use teledermatology.3 Thus, sustainable use of teledermatology likely will depend on continued reimbursement parity for live video as well as store-and-forward consultations, which have several advantages but currently are de-incentivized by low reimbursement. The survey also found that 70% of respondents felt that teledermatology use will continue after COVID-19, while 58% intended to continue use—nearly 5-fold more than before the pandemic.3 We suspect the discrepancy between participants’ predictions regarding future use of teledermatology and their personal intent to use it highlights perceived barriers and limitations of the long-term success of teledermatology. Aside from reimbursement, connectivity and functionality were common concerns, emphasizing the need for innovative technological solutions.3 Moving forward, we anticipate that dermatologists will need to establish consistent workflows to establish consistent triage for the most appropriate visit—in-person visits vs teledermatology, which may include augmented, intelligence-enhanced solutions. Similar to prior clinician perspectives about which types of visits are conducive to teledermatology,2 most survey participants believed virtual visits were effective for acne, routine follow-ups, medication monitoring, and some inflammatory conditions.3
Importantly, we must be mindful of patients who may be left behind by the digital divide, such as those with lack of access to a smartphone or the internet, language barriers, or limited telehealth experience.5 Systems should be designed to provide these patients with technologic and health literacy aid or alternate modalities to access care. For example, structured methods could be introduced to provide training and instructions on how to access phone applications, computer-based programs, and more. Likewise, for those with hearing or vision deficits, it will be important to improve sound amplification and accessibility for headphones or hearing aid connectivity, as well as appropriate font size, button size, and application navigation. In remote areas, existing clinics may be used to help field specialty consultation teleconferences. Certainly, applications and platforms devised for teledermatology must be designed to serve diverse patient groups, with special consideration for the elderly, those who speak languages other than English, and those with disabilities that may make telehealth use more challenging.
Large-scale regulatory changes and reimbursement parity can have a substantial impact on future teledermatology use. Advocacy efforts continue to push for fair valuation of telemedicine, coverage of store-and-forward teledermatology codes, and coverage for all models of care. It is imperative for the dermatology community to continue discussions on implementation and methodology to best leverage this technology for the most patient benefit.
Although teledermatology utilization in the United States traditionally has lagged behind other countries,1,2 the COVID-19 pandemic upended this trend by creating the need for a massive teledermatology experiment. Recently reported survey results from a large representative sample of US dermatologists (5000 participants) on perceptions of teledermatology during COVID-19 indicated that only 14.1% of participants used teledermatology prior to the COVID-19 pandemic vs 54.1% of dermatologists in Europe.2,3 Since the pandemic started, 97% of US dermatologists reported teledermatology use,3 demonstrating a huge shift in utilization. This trend is notable, as teledermatology has been shown to increase access to dermatology in underserved areas, reduce patient travel times, improve patient triage, and even reduce carbon footprints.1,4 Thus, to sustain the momentum, insights from the recent teledermatology experience during the pandemic should inform future development.
Notably, the COVID-19 pandemic led to a rapid shift in focus from store-and-forward teledermatology to live video–based models.1,2 Logistically, live video visits are challenging, require more time and resources, and often are diagnostically limited, with concerns regarding technology, connectivity, reimbursement, and appropriate use.3 Prior to COVID-19, formal Health Insurance Portability and Accountability Act–compliant teledermatology platforms often were costly to establish and maintain, largely relegating use to academic centers and Veterans Affairs hospitals. Thus, many fewer private practice dermatologists had used teledermatology compared to academic dermatologists in the United States (11.4% vs 27.6%).3 Government regulations—a key barrier to the adoption of teledermatology in private practice before COVID-19—were greatly relaxed during the pandemic. The Centers for Medicare and Medicaid Services removed restrictions on where patients could be seen, improved reimbursement for video visits, and allowed the use of platforms that are not Health Insurance Portability and Accountability Act compliant. Many states also relaxed medical licensing rules.
Overall, the general outlook on telehealth seems positive. Reimbursement has been found to be a primary factor in dermatologists’ willingness to use teledermatology.3 Thus, sustainable use of teledermatology likely will depend on continued reimbursement parity for live video as well as store-and-forward consultations, which have several advantages but currently are de-incentivized by low reimbursement. The survey also found that 70% of respondents felt that teledermatology use will continue after COVID-19, while 58% intended to continue use—nearly 5-fold more than before the pandemic.3 We suspect the discrepancy between participants’ predictions regarding future use of teledermatology and their personal intent to use it highlights perceived barriers and limitations of the long-term success of teledermatology. Aside from reimbursement, connectivity and functionality were common concerns, emphasizing the need for innovative technological solutions.3 Moving forward, we anticipate that dermatologists will need to establish consistent workflows to establish consistent triage for the most appropriate visit—in-person visits vs teledermatology, which may include augmented, intelligence-enhanced solutions. Similar to prior clinician perspectives about which types of visits are conducive to teledermatology,2 most survey participants believed virtual visits were effective for acne, routine follow-ups, medication monitoring, and some inflammatory conditions.3
Importantly, we must be mindful of patients who may be left behind by the digital divide, such as those with lack of access to a smartphone or the internet, language barriers, or limited telehealth experience.5 Systems should be designed to provide these patients with technologic and health literacy aid or alternate modalities to access care. For example, structured methods could be introduced to provide training and instructions on how to access phone applications, computer-based programs, and more. Likewise, for those with hearing or vision deficits, it will be important to improve sound amplification and accessibility for headphones or hearing aid connectivity, as well as appropriate font size, button size, and application navigation. In remote areas, existing clinics may be used to help field specialty consultation teleconferences. Certainly, applications and platforms devised for teledermatology must be designed to serve diverse patient groups, with special consideration for the elderly, those who speak languages other than English, and those with disabilities that may make telehealth use more challenging.
Large-scale regulatory changes and reimbursement parity can have a substantial impact on future teledermatology use. Advocacy efforts continue to push for fair valuation of telemedicine, coverage of store-and-forward teledermatology codes, and coverage for all models of care. It is imperative for the dermatology community to continue discussions on implementation and methodology to best leverage this technology for the most patient benefit.
- Tensen E, van der Heijden JP, Jaspers MWM, et al. Two decades of teledermatology: current status and integration in national healthcare systems. Curr Dermatol Rep. 2016;5:96-104.
- Moscarella E, Pasquali P, Cinotti E, et al. A survey on teledermatology use and doctors’ perception in times of COVID-19 [published online August 17, 2020]. J Eur Acad Dermatol Venereol. 2020;34:E772-E773.
- Kennedy J, Arey S, Hopkins Z, et al. Dermatologist perceptions of teledermatology implementation and future use after COVID-19: demographics, barriers, and insights. JAMA Dermatol. 2021;157:595-597.
- Bonsall A. Unleashing carbon emissions savings with regular teledermatology clinics. Clin Exp Dermatol. 2021;46:574-575.
- Bakhtiar M, Elbuluk N, Lipoff JB. The digital divide: how COVID-19’s telemedicine expansion could exacerbate disparities. J Am Acad Dermatol. 2020;83:E345-E346.
- Tensen E, van der Heijden JP, Jaspers MWM, et al. Two decades of teledermatology: current status and integration in national healthcare systems. Curr Dermatol Rep. 2016;5:96-104.
- Moscarella E, Pasquali P, Cinotti E, et al. A survey on teledermatology use and doctors’ perception in times of COVID-19 [published online August 17, 2020]. J Eur Acad Dermatol Venereol. 2020;34:E772-E773.
- Kennedy J, Arey S, Hopkins Z, et al. Dermatologist perceptions of teledermatology implementation and future use after COVID-19: demographics, barriers, and insights. JAMA Dermatol. 2021;157:595-597.
- Bonsall A. Unleashing carbon emissions savings with regular teledermatology clinics. Clin Exp Dermatol. 2021;46:574-575.
- Bakhtiar M, Elbuluk N, Lipoff JB. The digital divide: how COVID-19’s telemedicine expansion could exacerbate disparities. J Am Acad Dermatol. 2020;83:E345-E346.
My favorite physical exam pearls
I would like to start the new year off by returning to the past – when the physical exam was emphasized and utilized in decision making. I think a big reason that its use has diminished in recent years is due to the physical exam not having been emphasized in training.
For those seeking to increase their comfort with conducting the physical exam, below are several methods I have found helpful to use in practice.
Examining the pharynx
We were usually taught to ask the patient to say ahhh, with or without a nasty tongue depressor.
When I was on my pediatrics rotation, I was taught to ask the patients to roar like a lion, which always gave a nice look at their posterior pharynx. The kids also really liked doing this, but it might seem a little strange to ask adults to do this.
A technique I have found that works well with adults is to ask them to yawn. I have found that this get me a great look at the pharynx for about half of my patients.
Auscultatory percussion for pleural effusions
Guarino and colleagues described a technique that is easily mastered and very effective for determining the presence of pleural effusions.1 It involves placing the stethoscope 3 cm below the last rib in the mid clavicular line and tapping from the apex down to the last rib.
For patients without effusion, a sharp change to a loud percussion note will occur at the last rib.
If the patient has an effusion, the loud percussion note will start at the top of the effusion.
This method was remarkably successful at finding pleural effusions. In the study, Dr. Guarino found a sensitivity of 96% and a specificity of 100%.
Physical exam for anemia
Look at the nails and see if they look pale. How can we do this?
The first step is to know what your own hematocrit is. You can then compare the color of your nail to that of the patient.
If you have a normal hematocrit and the patient’s nail bed color is lighter than yours, the patient likely has anemia. If you do this frequently, you will get good at estimating hematocrit. This is especially important if you do not have labs readily available.
Another way to assess for anemia is to look at the color tint of the lower conjunctiva. The best way to look for this is to look at whether there is a generous amount of visible capillaries in the lower conjunctiva. Patients without anemia have a darker red color because of these vessels, whereas patients with anemia are a lighter pink.
Strobach and colleagues2 looked at both nail bed rubor and color tint of the lower conjunctiva and found that both reliably predicted presence and degree of anemia.
Determining if clubbing is present
Most physicians are aware of Shamroth sign, and use it to evaluate for clubbing. Shamroth sign is the loss of the diamond that is created by placing the back surfaces of opposite terminal phalanges together.
I have found that it’s easier to diagnose mild clubbing by looking at the finger in profile. If the ratio of the distal phalangeal depth compared to the depth across the distal interphalangeal joint is greater than 1:1, then clubbing is present.3
Pearls
1. Have the patient try yawning to better see the pharynx without using a tongue blade.
2. Try the technique of auscultatory percussion to be more accurate at picking up pleural effusions.
3. Know your hematocrit, so you can better use color shade to assess for anemia.
4. Try looking at fingers in profile to pick up clubbing.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as 3rd-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at imnews@mdedge.com.
References
1. Guarino JR and Guarino JC. Auscultatory percussion: A simple method to detect pleural effusion. J Gen Intern Med. 1994 Feb;9(2):71-4.
2. Strobach RS et al. The value of the physical examination in the diagnosis of anemia. Correlation of the physical findings and the hemoglobin concentration. Arch Intern Med. 1988 Apr;148(4):831-2.
3. Spicknall KE et al. Clubbing: an update on diagnosis, differential diagnosis, pathophysiology, and clinical relevance. J Am Acad Dermatol. 2005 Jun;52(6):1020-8.
I would like to start the new year off by returning to the past – when the physical exam was emphasized and utilized in decision making. I think a big reason that its use has diminished in recent years is due to the physical exam not having been emphasized in training.
For those seeking to increase their comfort with conducting the physical exam, below are several methods I have found helpful to use in practice.
Examining the pharynx
We were usually taught to ask the patient to say ahhh, with or without a nasty tongue depressor.
When I was on my pediatrics rotation, I was taught to ask the patients to roar like a lion, which always gave a nice look at their posterior pharynx. The kids also really liked doing this, but it might seem a little strange to ask adults to do this.
A technique I have found that works well with adults is to ask them to yawn. I have found that this get me a great look at the pharynx for about half of my patients.
Auscultatory percussion for pleural effusions
Guarino and colleagues described a technique that is easily mastered and very effective for determining the presence of pleural effusions.1 It involves placing the stethoscope 3 cm below the last rib in the mid clavicular line and tapping from the apex down to the last rib.
For patients without effusion, a sharp change to a loud percussion note will occur at the last rib.
If the patient has an effusion, the loud percussion note will start at the top of the effusion.
This method was remarkably successful at finding pleural effusions. In the study, Dr. Guarino found a sensitivity of 96% and a specificity of 100%.
Physical exam for anemia
Look at the nails and see if they look pale. How can we do this?
The first step is to know what your own hematocrit is. You can then compare the color of your nail to that of the patient.
If you have a normal hematocrit and the patient’s nail bed color is lighter than yours, the patient likely has anemia. If you do this frequently, you will get good at estimating hematocrit. This is especially important if you do not have labs readily available.
Another way to assess for anemia is to look at the color tint of the lower conjunctiva. The best way to look for this is to look at whether there is a generous amount of visible capillaries in the lower conjunctiva. Patients without anemia have a darker red color because of these vessels, whereas patients with anemia are a lighter pink.
Strobach and colleagues2 looked at both nail bed rubor and color tint of the lower conjunctiva and found that both reliably predicted presence and degree of anemia.
Determining if clubbing is present
Most physicians are aware of Shamroth sign, and use it to evaluate for clubbing. Shamroth sign is the loss of the diamond that is created by placing the back surfaces of opposite terminal phalanges together.
I have found that it’s easier to diagnose mild clubbing by looking at the finger in profile. If the ratio of the distal phalangeal depth compared to the depth across the distal interphalangeal joint is greater than 1:1, then clubbing is present.3
Pearls
1. Have the patient try yawning to better see the pharynx without using a tongue blade.
2. Try the technique of auscultatory percussion to be more accurate at picking up pleural effusions.
3. Know your hematocrit, so you can better use color shade to assess for anemia.
4. Try looking at fingers in profile to pick up clubbing.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as 3rd-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at imnews@mdedge.com.
References
1. Guarino JR and Guarino JC. Auscultatory percussion: A simple method to detect pleural effusion. J Gen Intern Med. 1994 Feb;9(2):71-4.
2. Strobach RS et al. The value of the physical examination in the diagnosis of anemia. Correlation of the physical findings and the hemoglobin concentration. Arch Intern Med. 1988 Apr;148(4):831-2.
3. Spicknall KE et al. Clubbing: an update on diagnosis, differential diagnosis, pathophysiology, and clinical relevance. J Am Acad Dermatol. 2005 Jun;52(6):1020-8.
I would like to start the new year off by returning to the past – when the physical exam was emphasized and utilized in decision making. I think a big reason that its use has diminished in recent years is due to the physical exam not having been emphasized in training.
For those seeking to increase their comfort with conducting the physical exam, below are several methods I have found helpful to use in practice.
Examining the pharynx
We were usually taught to ask the patient to say ahhh, with or without a nasty tongue depressor.
When I was on my pediatrics rotation, I was taught to ask the patients to roar like a lion, which always gave a nice look at their posterior pharynx. The kids also really liked doing this, but it might seem a little strange to ask adults to do this.
A technique I have found that works well with adults is to ask them to yawn. I have found that this get me a great look at the pharynx for about half of my patients.
Auscultatory percussion for pleural effusions
Guarino and colleagues described a technique that is easily mastered and very effective for determining the presence of pleural effusions.1 It involves placing the stethoscope 3 cm below the last rib in the mid clavicular line and tapping from the apex down to the last rib.
For patients without effusion, a sharp change to a loud percussion note will occur at the last rib.
If the patient has an effusion, the loud percussion note will start at the top of the effusion.
This method was remarkably successful at finding pleural effusions. In the study, Dr. Guarino found a sensitivity of 96% and a specificity of 100%.
Physical exam for anemia
Look at the nails and see if they look pale. How can we do this?
The first step is to know what your own hematocrit is. You can then compare the color of your nail to that of the patient.
If you have a normal hematocrit and the patient’s nail bed color is lighter than yours, the patient likely has anemia. If you do this frequently, you will get good at estimating hematocrit. This is especially important if you do not have labs readily available.
Another way to assess for anemia is to look at the color tint of the lower conjunctiva. The best way to look for this is to look at whether there is a generous amount of visible capillaries in the lower conjunctiva. Patients without anemia have a darker red color because of these vessels, whereas patients with anemia are a lighter pink.
Strobach and colleagues2 looked at both nail bed rubor and color tint of the lower conjunctiva and found that both reliably predicted presence and degree of anemia.
Determining if clubbing is present
Most physicians are aware of Shamroth sign, and use it to evaluate for clubbing. Shamroth sign is the loss of the diamond that is created by placing the back surfaces of opposite terminal phalanges together.
I have found that it’s easier to diagnose mild clubbing by looking at the finger in profile. If the ratio of the distal phalangeal depth compared to the depth across the distal interphalangeal joint is greater than 1:1, then clubbing is present.3
Pearls
1. Have the patient try yawning to better see the pharynx without using a tongue blade.
2. Try the technique of auscultatory percussion to be more accurate at picking up pleural effusions.
3. Know your hematocrit, so you can better use color shade to assess for anemia.
4. Try looking at fingers in profile to pick up clubbing.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as 3rd-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at imnews@mdedge.com.
References
1. Guarino JR and Guarino JC. Auscultatory percussion: A simple method to detect pleural effusion. J Gen Intern Med. 1994 Feb;9(2):71-4.
2. Strobach RS et al. The value of the physical examination in the diagnosis of anemia. Correlation of the physical findings and the hemoglobin concentration. Arch Intern Med. 1988 Apr;148(4):831-2.
3. Spicknall KE et al. Clubbing: an update on diagnosis, differential diagnosis, pathophysiology, and clinical relevance. J Am Acad Dermatol. 2005 Jun;52(6):1020-8.
Psychiatry and semantics
I am a psychiatrist, which means I am a mental health professional, which means I work with people with mental illness. Sometimes people with mental health conditions who suffer from mental illness need to take a day off work – also called a mental health day – because they are too symptomatic to work, and sometimes people who don’t have a mental illness need to take a day off work, also called a mental health day, because they are feeling stressed.
Sometimes professional athletes don’t do things they agreed to do in their contracts because they realize that doing these things is very upsetting and will be detrimental to their mental health, or maybe they have a mental illness and doing these things will worsen their mental health condition, which is, in fact, a mental illness. Other times people with mental health conditions need to have pets travel with them because this mitigates the symptoms of their mental illness or perhaps it’s just good for their mental health. And finally, some people suffer from mental illnesses, or sometimes from learning problems, which are severe enough that a person with these conditions has a disability and needs special accommodations to function optimally in educational or occupational settings, or needs public financial support because their difficulties disable them to the point that they can’t work at all.
Is your head spinning yet? who we serve, and differentiating the fact that what someone with a psychiatric disorder needs to do to function or to alleviate emotional suffering may be entirely different from the things that everyone needs to do, regardless of whether they have a psychiatric disorder, to feel their emotional best.
The National Alliance on Mental Illness tells us that one in five Americans are suffering from a mental illness, while the Epidemiologic Catchment Area Program revealed that half of people will meet criteria for a mental illness at some point in their lives. We hear about “the mentally ill” constantly in the news – often in relation to mass shooters or homelessness – yet even psychiatrists might be pressed to define who exactly the “mentally ill” are. And how many of us could not somehow, at some time, find ourselves in 1 of the 157 disorders that DSM-5 lists – down from 365 disorders in the DSM-IV-TR?
Differentiating mental health from mental illness is just the beginning of our semantic confusion. As psychiatrists we treat major depression, and yet the illness “depression,” a syndromic constellation of symptoms, includes the key symptom of sadness. People often say they are “depressed” when they mean they are sad or demoralized, and yet, if their sadness persists in the absence of other symptoms, they may well want, or feel they “should” have medications, even in the absence of a disorder. And maybe those medications help them feel better, so that the presence or absence of a verified illness doesn’t really matter. But if the medications cause adverse reactions, then psychiatry might have done a better job by that person’s sadness. Melancholia, or perhaps any designation than “depression,” with its multiple meanings, might better serve our patients and our profession. This is only one example, as the number of people who tell me they have obsessive-compulsive disorder – or more often announce, “I’m OCD!” because they are well organized in a productive way is remarkable. And while I have treated only a few people who meet the criteria for narcissistic personality disorder, from general conversation it would seem that they are at every dinner table and by every water cooler.
Does it matter? A diagnostic lexicon can be so helpful when it guides treatment, provides a heterogeneous group of patients for research studies, and allows for an understanding of the etiology, course, and prognosis of a given condition. When someone is so depressed that they can’t get out of bed, or is so disorganized that they can’t perform their job and might cause a disturbance in their workplace, it is good to instruct them to take time off work and send them back well with a doctor’s note. But this is different from the person who doesn’t want to face a difficult situation, who simply doesn’t like their job or their boss, or who wants their pet declared an emotional support animal to avoid the fee the airlines charge to bring an animal on board if one does not have a psychiatric diagnosis. Sometimes these lines are blurry – if someone does not want to do something because it makes them anxious, does it matter how deep the pit in their stomach is, or if they are having full-blown panic attacks? When do we agree that their distress is reason to allow them to avoid responsibilities without repercussions versus a violation of their obligations and an infringement on others?
Diagnoses offer solace to some patients: There is a name for their suffering, available treatment, and often others with the same condition to look to for guidance and community. For others, a psychiatric diagnosis is a source of shame, a label they see as damaging to their character and sometimes to their careers – including in medicine – where we have been particularly unsympathetic to those who announce a psychiatric history.
In some cultures, the label itself decreases someone’s attractiveness as a potential marriage partner. We would all like to see the stigma of mental illness vanish, but we have a long way to go.
Psychiatric diagnoses move over time and with our politics and culture. This is good; we don’t hold on to what we learn to be untrue. But they may well add to issues of inequity. Those who can afford to pay for expensive educational assessments can request educational accommodations, including untimed standardized tests. This advantage may not be available to those without the resources to pay for these evaluations, and one might wonder why all comers can’t take untimed tests so as not to favor the privileged. Psychiatry has long been accused of diagnosing people of color with poor prognosis illnesses and women with conditions that imply emotional weakness.
While our diagnoses have clinical utility, it is unfortunate that they have come to be about reimbursement. A diagnosis needs to be assigned for insurers to pay for care, and so we create diagnostic categories to allow for treatment. Is this reasonable? Do we need to say that someone who is suffering after the death of a loved one has a mental illness in order to allow them to seek relief from their suffering? It leads us to believe that all suffering is about pathology, that we should expect pain-free emotional lives. Perhaps we need a diagnostic category of psychic pain, not otherwise specified, to allow for treatment for those who simply ache.
Mental illness is about interventions to alleviate the suffering of those with disorders. Mental health is about interventions that may benefit everyone, whether they suffer from a mental illness or not. Sleep, nutrition, exercise, sunlight, nature, entertainment and escape, yoga, meditation, vacations in beautiful places with loving people – these are things that potentially help us all whether we do or do not have an illness. With so much confusion about what it is we do, and about who “should” get help, who can get help, who might want help, and where they should go to seek help, perhaps it would be better if our lingo were more precise.
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). The has a private practice and is assistant professor of psychiatry ad behavioral sciences at Johns Hopkins University, both in Baltimore. She has no disclosures.
I am a psychiatrist, which means I am a mental health professional, which means I work with people with mental illness. Sometimes people with mental health conditions who suffer from mental illness need to take a day off work – also called a mental health day – because they are too symptomatic to work, and sometimes people who don’t have a mental illness need to take a day off work, also called a mental health day, because they are feeling stressed.
Sometimes professional athletes don’t do things they agreed to do in their contracts because they realize that doing these things is very upsetting and will be detrimental to their mental health, or maybe they have a mental illness and doing these things will worsen their mental health condition, which is, in fact, a mental illness. Other times people with mental health conditions need to have pets travel with them because this mitigates the symptoms of their mental illness or perhaps it’s just good for their mental health. And finally, some people suffer from mental illnesses, or sometimes from learning problems, which are severe enough that a person with these conditions has a disability and needs special accommodations to function optimally in educational or occupational settings, or needs public financial support because their difficulties disable them to the point that they can’t work at all.
Is your head spinning yet? who we serve, and differentiating the fact that what someone with a psychiatric disorder needs to do to function or to alleviate emotional suffering may be entirely different from the things that everyone needs to do, regardless of whether they have a psychiatric disorder, to feel their emotional best.
The National Alliance on Mental Illness tells us that one in five Americans are suffering from a mental illness, while the Epidemiologic Catchment Area Program revealed that half of people will meet criteria for a mental illness at some point in their lives. We hear about “the mentally ill” constantly in the news – often in relation to mass shooters or homelessness – yet even psychiatrists might be pressed to define who exactly the “mentally ill” are. And how many of us could not somehow, at some time, find ourselves in 1 of the 157 disorders that DSM-5 lists – down from 365 disorders in the DSM-IV-TR?
Differentiating mental health from mental illness is just the beginning of our semantic confusion. As psychiatrists we treat major depression, and yet the illness “depression,” a syndromic constellation of symptoms, includes the key symptom of sadness. People often say they are “depressed” when they mean they are sad or demoralized, and yet, if their sadness persists in the absence of other symptoms, they may well want, or feel they “should” have medications, even in the absence of a disorder. And maybe those medications help them feel better, so that the presence or absence of a verified illness doesn’t really matter. But if the medications cause adverse reactions, then psychiatry might have done a better job by that person’s sadness. Melancholia, or perhaps any designation than “depression,” with its multiple meanings, might better serve our patients and our profession. This is only one example, as the number of people who tell me they have obsessive-compulsive disorder – or more often announce, “I’m OCD!” because they are well organized in a productive way is remarkable. And while I have treated only a few people who meet the criteria for narcissistic personality disorder, from general conversation it would seem that they are at every dinner table and by every water cooler.
Does it matter? A diagnostic lexicon can be so helpful when it guides treatment, provides a heterogeneous group of patients for research studies, and allows for an understanding of the etiology, course, and prognosis of a given condition. When someone is so depressed that they can’t get out of bed, or is so disorganized that they can’t perform their job and might cause a disturbance in their workplace, it is good to instruct them to take time off work and send them back well with a doctor’s note. But this is different from the person who doesn’t want to face a difficult situation, who simply doesn’t like their job or their boss, or who wants their pet declared an emotional support animal to avoid the fee the airlines charge to bring an animal on board if one does not have a psychiatric diagnosis. Sometimes these lines are blurry – if someone does not want to do something because it makes them anxious, does it matter how deep the pit in their stomach is, or if they are having full-blown panic attacks? When do we agree that their distress is reason to allow them to avoid responsibilities without repercussions versus a violation of their obligations and an infringement on others?
Diagnoses offer solace to some patients: There is a name for their suffering, available treatment, and often others with the same condition to look to for guidance and community. For others, a psychiatric diagnosis is a source of shame, a label they see as damaging to their character and sometimes to their careers – including in medicine – where we have been particularly unsympathetic to those who announce a psychiatric history.
In some cultures, the label itself decreases someone’s attractiveness as a potential marriage partner. We would all like to see the stigma of mental illness vanish, but we have a long way to go.
Psychiatric diagnoses move over time and with our politics and culture. This is good; we don’t hold on to what we learn to be untrue. But they may well add to issues of inequity. Those who can afford to pay for expensive educational assessments can request educational accommodations, including untimed standardized tests. This advantage may not be available to those without the resources to pay for these evaluations, and one might wonder why all comers can’t take untimed tests so as not to favor the privileged. Psychiatry has long been accused of diagnosing people of color with poor prognosis illnesses and women with conditions that imply emotional weakness.
While our diagnoses have clinical utility, it is unfortunate that they have come to be about reimbursement. A diagnosis needs to be assigned for insurers to pay for care, and so we create diagnostic categories to allow for treatment. Is this reasonable? Do we need to say that someone who is suffering after the death of a loved one has a mental illness in order to allow them to seek relief from their suffering? It leads us to believe that all suffering is about pathology, that we should expect pain-free emotional lives. Perhaps we need a diagnostic category of psychic pain, not otherwise specified, to allow for treatment for those who simply ache.
Mental illness is about interventions to alleviate the suffering of those with disorders. Mental health is about interventions that may benefit everyone, whether they suffer from a mental illness or not. Sleep, nutrition, exercise, sunlight, nature, entertainment and escape, yoga, meditation, vacations in beautiful places with loving people – these are things that potentially help us all whether we do or do not have an illness. With so much confusion about what it is we do, and about who “should” get help, who can get help, who might want help, and where they should go to seek help, perhaps it would be better if our lingo were more precise.
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). The has a private practice and is assistant professor of psychiatry ad behavioral sciences at Johns Hopkins University, both in Baltimore. She has no disclosures.
I am a psychiatrist, which means I am a mental health professional, which means I work with people with mental illness. Sometimes people with mental health conditions who suffer from mental illness need to take a day off work – also called a mental health day – because they are too symptomatic to work, and sometimes people who don’t have a mental illness need to take a day off work, also called a mental health day, because they are feeling stressed.
Sometimes professional athletes don’t do things they agreed to do in their contracts because they realize that doing these things is very upsetting and will be detrimental to their mental health, or maybe they have a mental illness and doing these things will worsen their mental health condition, which is, in fact, a mental illness. Other times people with mental health conditions need to have pets travel with them because this mitigates the symptoms of their mental illness or perhaps it’s just good for their mental health. And finally, some people suffer from mental illnesses, or sometimes from learning problems, which are severe enough that a person with these conditions has a disability and needs special accommodations to function optimally in educational or occupational settings, or needs public financial support because their difficulties disable them to the point that they can’t work at all.
Is your head spinning yet? who we serve, and differentiating the fact that what someone with a psychiatric disorder needs to do to function or to alleviate emotional suffering may be entirely different from the things that everyone needs to do, regardless of whether they have a psychiatric disorder, to feel their emotional best.
The National Alliance on Mental Illness tells us that one in five Americans are suffering from a mental illness, while the Epidemiologic Catchment Area Program revealed that half of people will meet criteria for a mental illness at some point in their lives. We hear about “the mentally ill” constantly in the news – often in relation to mass shooters or homelessness – yet even psychiatrists might be pressed to define who exactly the “mentally ill” are. And how many of us could not somehow, at some time, find ourselves in 1 of the 157 disorders that DSM-5 lists – down from 365 disorders in the DSM-IV-TR?
Differentiating mental health from mental illness is just the beginning of our semantic confusion. As psychiatrists we treat major depression, and yet the illness “depression,” a syndromic constellation of symptoms, includes the key symptom of sadness. People often say they are “depressed” when they mean they are sad or demoralized, and yet, if their sadness persists in the absence of other symptoms, they may well want, or feel they “should” have medications, even in the absence of a disorder. And maybe those medications help them feel better, so that the presence or absence of a verified illness doesn’t really matter. But if the medications cause adverse reactions, then psychiatry might have done a better job by that person’s sadness. Melancholia, or perhaps any designation than “depression,” with its multiple meanings, might better serve our patients and our profession. This is only one example, as the number of people who tell me they have obsessive-compulsive disorder – or more often announce, “I’m OCD!” because they are well organized in a productive way is remarkable. And while I have treated only a few people who meet the criteria for narcissistic personality disorder, from general conversation it would seem that they are at every dinner table and by every water cooler.
Does it matter? A diagnostic lexicon can be so helpful when it guides treatment, provides a heterogeneous group of patients for research studies, and allows for an understanding of the etiology, course, and prognosis of a given condition. When someone is so depressed that they can’t get out of bed, or is so disorganized that they can’t perform their job and might cause a disturbance in their workplace, it is good to instruct them to take time off work and send them back well with a doctor’s note. But this is different from the person who doesn’t want to face a difficult situation, who simply doesn’t like their job or their boss, or who wants their pet declared an emotional support animal to avoid the fee the airlines charge to bring an animal on board if one does not have a psychiatric diagnosis. Sometimes these lines are blurry – if someone does not want to do something because it makes them anxious, does it matter how deep the pit in their stomach is, or if they are having full-blown panic attacks? When do we agree that their distress is reason to allow them to avoid responsibilities without repercussions versus a violation of their obligations and an infringement on others?
Diagnoses offer solace to some patients: There is a name for their suffering, available treatment, and often others with the same condition to look to for guidance and community. For others, a psychiatric diagnosis is a source of shame, a label they see as damaging to their character and sometimes to their careers – including in medicine – where we have been particularly unsympathetic to those who announce a psychiatric history.
In some cultures, the label itself decreases someone’s attractiveness as a potential marriage partner. We would all like to see the stigma of mental illness vanish, but we have a long way to go.
Psychiatric diagnoses move over time and with our politics and culture. This is good; we don’t hold on to what we learn to be untrue. But they may well add to issues of inequity. Those who can afford to pay for expensive educational assessments can request educational accommodations, including untimed standardized tests. This advantage may not be available to those without the resources to pay for these evaluations, and one might wonder why all comers can’t take untimed tests so as not to favor the privileged. Psychiatry has long been accused of diagnosing people of color with poor prognosis illnesses and women with conditions that imply emotional weakness.
While our diagnoses have clinical utility, it is unfortunate that they have come to be about reimbursement. A diagnosis needs to be assigned for insurers to pay for care, and so we create diagnostic categories to allow for treatment. Is this reasonable? Do we need to say that someone who is suffering after the death of a loved one has a mental illness in order to allow them to seek relief from their suffering? It leads us to believe that all suffering is about pathology, that we should expect pain-free emotional lives. Perhaps we need a diagnostic category of psychic pain, not otherwise specified, to allow for treatment for those who simply ache.
Mental illness is about interventions to alleviate the suffering of those with disorders. Mental health is about interventions that may benefit everyone, whether they suffer from a mental illness or not. Sleep, nutrition, exercise, sunlight, nature, entertainment and escape, yoga, meditation, vacations in beautiful places with loving people – these are things that potentially help us all whether we do or do not have an illness. With so much confusion about what it is we do, and about who “should” get help, who can get help, who might want help, and where they should go to seek help, perhaps it would be better if our lingo were more precise.
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). The has a private practice and is assistant professor of psychiatry ad behavioral sciences at Johns Hopkins University, both in Baltimore. She has no disclosures.
10 reasons why Omicron could cause big destruction
As a physician first and a mental health clinician second, I hope to provide factual medical information on the Omicron variant to my patients, family members, and friends. I also try to remain curious instead of angry about why some choose not to vaccinate.
The most effective way to encourage people to obtain a vaccination is to use communication free of judgment and criticism, which allows a safe space for the unvaccinated to express their motivations and fears behind their current choice of not vaccinating and explore possible barriers to an alternative option that could lead to vaccination.
As an adult psychiatrist, ADHD specialist, and amateur COVID-19 expert, I’d like to offer 10 reasons why Omicron – which ironically means “small” in Latin, can still cause big destruction. Please share these 10 reasons with your patients.
- If you are not vaccinated, this virus will find you within the next few weeks and likely lead to severe symptoms.
- Long-haul symptoms from COVID-19 infection are still possible even for people who contract a milder case of the Omicron variant.
- The monoclonal antibody and antiviral treatments recently approved by the Food and Drug Administration for pre-exposure prevention of COVID-19 are limited. For many reasons, now is not the best time to play Russian roulette and intentionally get infected with a “mild” variant.
- There are not enough testing sites or over-the-counter rapid COVID tests available to keep up with the demand, and the latter are cost prohibitive for many people.
- Emergency care during the next few weeks for unforeseen non–COVID-related illnesses, such as a sudden heart attack or stroke, may be affected by the shortage of medical providers because of illness, quarantine, and burnout.
- There will be fewer first responders, including EMTs, police officers, and firefighters, because of COVID quarantines from illness and exposure.
- Although most Americans oppose temporary shutdowns, de facto shutdowns might be necessary because of the absence of healthy, COVID-negative individuals to maintain a functional society.
- Omicron math is deceiving, since the risk of hospitalization with Omicron appears to be far lower than with the Delta variant. However, the higher volume of infections with Omicron will offset the lower severity leading to comparable numbers of hospitalizations.
- Omicron has made it difficult for some schools to reopen after the holiday break, and reopening might become even more difficult as the surge progresses. Many schools already were in desperate need of substitute teachers, bus drivers, and additional staff necessary for COVID safety precautions before the emergence of the Omicron variant.
- And, for a less altruistic reason, as if the nine reasons above weren’t enough – if infections continue, especially among the unvaccinated – where the virus mutates the most – this can lead to a trifecta variant that not only evades the immune system and is highly infectious but causes severe disease in both the unvaccinated as well as the vaccinated.
Because of its extremely high transmissibility, the Omicron variant – layered atop Delta – presents great risk to us as a society. We must do all we can as clinicians to educate our patients so that they can protect themselves and their families.
Dr. Abraham is a psychiatrist in private practice in Philadelphia. She has no disclosures.
As a physician first and a mental health clinician second, I hope to provide factual medical information on the Omicron variant to my patients, family members, and friends. I also try to remain curious instead of angry about why some choose not to vaccinate.
The most effective way to encourage people to obtain a vaccination is to use communication free of judgment and criticism, which allows a safe space for the unvaccinated to express their motivations and fears behind their current choice of not vaccinating and explore possible barriers to an alternative option that could lead to vaccination.
As an adult psychiatrist, ADHD specialist, and amateur COVID-19 expert, I’d like to offer 10 reasons why Omicron – which ironically means “small” in Latin, can still cause big destruction. Please share these 10 reasons with your patients.
- If you are not vaccinated, this virus will find you within the next few weeks and likely lead to severe symptoms.
- Long-haul symptoms from COVID-19 infection are still possible even for people who contract a milder case of the Omicron variant.
- The monoclonal antibody and antiviral treatments recently approved by the Food and Drug Administration for pre-exposure prevention of COVID-19 are limited. For many reasons, now is not the best time to play Russian roulette and intentionally get infected with a “mild” variant.
- There are not enough testing sites or over-the-counter rapid COVID tests available to keep up with the demand, and the latter are cost prohibitive for many people.
- Emergency care during the next few weeks for unforeseen non–COVID-related illnesses, such as a sudden heart attack or stroke, may be affected by the shortage of medical providers because of illness, quarantine, and burnout.
- There will be fewer first responders, including EMTs, police officers, and firefighters, because of COVID quarantines from illness and exposure.
- Although most Americans oppose temporary shutdowns, de facto shutdowns might be necessary because of the absence of healthy, COVID-negative individuals to maintain a functional society.
- Omicron math is deceiving, since the risk of hospitalization with Omicron appears to be far lower than with the Delta variant. However, the higher volume of infections with Omicron will offset the lower severity leading to comparable numbers of hospitalizations.
- Omicron has made it difficult for some schools to reopen after the holiday break, and reopening might become even more difficult as the surge progresses. Many schools already were in desperate need of substitute teachers, bus drivers, and additional staff necessary for COVID safety precautions before the emergence of the Omicron variant.
- And, for a less altruistic reason, as if the nine reasons above weren’t enough – if infections continue, especially among the unvaccinated – where the virus mutates the most – this can lead to a trifecta variant that not only evades the immune system and is highly infectious but causes severe disease in both the unvaccinated as well as the vaccinated.
Because of its extremely high transmissibility, the Omicron variant – layered atop Delta – presents great risk to us as a society. We must do all we can as clinicians to educate our patients so that they can protect themselves and their families.
Dr. Abraham is a psychiatrist in private practice in Philadelphia. She has no disclosures.
As a physician first and a mental health clinician second, I hope to provide factual medical information on the Omicron variant to my patients, family members, and friends. I also try to remain curious instead of angry about why some choose not to vaccinate.
The most effective way to encourage people to obtain a vaccination is to use communication free of judgment and criticism, which allows a safe space for the unvaccinated to express their motivations and fears behind their current choice of not vaccinating and explore possible barriers to an alternative option that could lead to vaccination.
As an adult psychiatrist, ADHD specialist, and amateur COVID-19 expert, I’d like to offer 10 reasons why Omicron – which ironically means “small” in Latin, can still cause big destruction. Please share these 10 reasons with your patients.
- If you are not vaccinated, this virus will find you within the next few weeks and likely lead to severe symptoms.
- Long-haul symptoms from COVID-19 infection are still possible even for people who contract a milder case of the Omicron variant.
- The monoclonal antibody and antiviral treatments recently approved by the Food and Drug Administration for pre-exposure prevention of COVID-19 are limited. For many reasons, now is not the best time to play Russian roulette and intentionally get infected with a “mild” variant.
- There are not enough testing sites or over-the-counter rapid COVID tests available to keep up with the demand, and the latter are cost prohibitive for many people.
- Emergency care during the next few weeks for unforeseen non–COVID-related illnesses, such as a sudden heart attack or stroke, may be affected by the shortage of medical providers because of illness, quarantine, and burnout.
- There will be fewer first responders, including EMTs, police officers, and firefighters, because of COVID quarantines from illness and exposure.
- Although most Americans oppose temporary shutdowns, de facto shutdowns might be necessary because of the absence of healthy, COVID-negative individuals to maintain a functional society.
- Omicron math is deceiving, since the risk of hospitalization with Omicron appears to be far lower than with the Delta variant. However, the higher volume of infections with Omicron will offset the lower severity leading to comparable numbers of hospitalizations.
- Omicron has made it difficult for some schools to reopen after the holiday break, and reopening might become even more difficult as the surge progresses. Many schools already were in desperate need of substitute teachers, bus drivers, and additional staff necessary for COVID safety precautions before the emergence of the Omicron variant.
- And, for a less altruistic reason, as if the nine reasons above weren’t enough – if infections continue, especially among the unvaccinated – where the virus mutates the most – this can lead to a trifecta variant that not only evades the immune system and is highly infectious but causes severe disease in both the unvaccinated as well as the vaccinated.
Because of its extremely high transmissibility, the Omicron variant – layered atop Delta – presents great risk to us as a society. We must do all we can as clinicians to educate our patients so that they can protect themselves and their families.
Dr. Abraham is a psychiatrist in private practice in Philadelphia. She has no disclosures.
Surgeon General releases child mental health call to action
The nation’s Surgeon General, Vice Admiral Vivek H. Murthy, MD, MBA, recently released an advisory report on the current state of youth mental health and recommendations to improve well-being. This action follows a number of emergency declarations that have been made by professional organizations such as the American Academy of Child and Adolescent Psychiatry (AACAP), the American Academy of Pediatrics (AAP), and other health care groups to raise awareness about the alarming increase of depression, suicide, anxiety, and other mental health problems in youth.
These reports can be helpful in focusing attention and resources for important public health problems. Many still reference the 1999 report from former Surgeon General David Satcher, MD, PhD, which offered a number of eye-opening statistics regarding the prevalence of mental health conditions and the amount of disability associated with them.
Sadly, the present report indicates that many of these indices have grown worse in the past 20 years. For example, the advisory notes that, even before COVID-19, fully half of female high school students reported persistent feelings of sadness or hopelessness (up 40% from 2009). The report then goes on to cite a number of studies documenting even further rises in youth mental health problems associated with the pandemic.
Most of the advisory, however, is devoted to actions that can be taken by different groups, including young people themselves, parents, educators, the government, and even social media and video game companies, to support mental health and well-being. Multiple online resources are provided at the end of each of these sections.
One of the segments is aimed at health care organizations and professionals. While first making a fairly sweeping statement that “our health care system today is not set up optimally to support the mental health and well-being of children and youth,” this part then outlines five broad recommendations that might help improve the fit. These include the following.
- Increase prevention efforts, such as coordination to enrichment programs and referrals for economic and legal supports for families in need.
- Screen routinely for mental health conditions and link those who screen in with appropriate care.
- Identify mental health needs in parents and caregivers such as depression and substance use that can have negative effects on children.
- Increase partnerships between health care groups and community organizations.
- Build multidisciplinary teams that are culturally appropriate and maximally engage children and caretakers in the decision-making process.
The current report is downloadable for free (see reference below) and it is certainly worthwhile for pediatricians to take a look. Dr. Murthy writes, regarding the current state of mental health, that “it would be a tragedy if we beat back one public health crisis only to allow another to grow in its place.”
The report also outlines specific areas where additional research is needed, such as data on racial and sexual minorities and research on innovative and scalable therapies. In addition to the online resources that are provided, the report is backed by over 250 references.
Since its release, the report has generally been well received, and, indeed, there is much to support. The well-known Child Mind Institute in New York tweeted that “this document is a wake-up call for the country and a long-overdue statement of leadership from the federal government.”
Many of the recommendations are admittedly somewhat commons sense, but there are some that are much less so. For example, one recommendation to youth themselves is to serve others – something that may first come across as counterintuitive but can indeed help children and adolescents develop a sense of purpose and self-worth. The call for pediatric health care professionals to screen parents in addition to the patients themselves will likely result in some debate as well. The recommendation to reduce access to lethal means, including the specific naming of firearms, is also a welcome addition. This report also rightly puts a spotlight on the role of societal factors such as racism and poverty in the development of mental health problems and in getting access to quality treatment.
Also worth noting is how much of the advisory examined the role of media in both the problem and the solution. While recognizing that technology, smartphones, and social media are here to stay, a number of suggestions were given to parents, media organizations, journalists, and entertainment companies to reduce the negative impacts these mediums can have. Explicitly recognized in the report is that “there can be tension between what’s best for the technology company and what’s best for the individual user or society.” Also acknowledged was that the link between media of various types and mental health is complex and inconsistent with there being a strong need for additional work in this area when it comes to academic research as well as product development within these companies themselves.
Yet while there is much to like about the advisory, there remain some areas that seem lacking. For example, the text about what causes mental health conditions gets a little dualistic in mentioning biological and environmental factors without much appreciation that these are hardly independent domains. Perhaps more substantially, there was surprisingly little airtime devoted to an enormous issue that underlies so many other challenges related to mental health care – namely an inadequate workforce that gets smaller by the minute. The topic was treated much too superficially with lots of vague calls to “expand” the workforce that lacked substance or detail.
Overall, however, the new Surgeon General’s Advisory is a welcome document that offers updated knowledge of our current challenges and provides practical responses that truly could make a difference. Now all we have to do is put these recommendations into action.
Dr. Rettew is a child and adolescent psychiatrist and medical director of Lane County Behavioral Health in Eugene, Ore. His latest book is “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood.” You can follow him on Twitter and Facebook @PediPsych.
Reference
“Protecting Youth Mental Health – The U.S. Surgeon General’s Advisory,” U.S. Department of Health & Human Services (2021).
The nation’s Surgeon General, Vice Admiral Vivek H. Murthy, MD, MBA, recently released an advisory report on the current state of youth mental health and recommendations to improve well-being. This action follows a number of emergency declarations that have been made by professional organizations such as the American Academy of Child and Adolescent Psychiatry (AACAP), the American Academy of Pediatrics (AAP), and other health care groups to raise awareness about the alarming increase of depression, suicide, anxiety, and other mental health problems in youth.
These reports can be helpful in focusing attention and resources for important public health problems. Many still reference the 1999 report from former Surgeon General David Satcher, MD, PhD, which offered a number of eye-opening statistics regarding the prevalence of mental health conditions and the amount of disability associated with them.
Sadly, the present report indicates that many of these indices have grown worse in the past 20 years. For example, the advisory notes that, even before COVID-19, fully half of female high school students reported persistent feelings of sadness or hopelessness (up 40% from 2009). The report then goes on to cite a number of studies documenting even further rises in youth mental health problems associated with the pandemic.
Most of the advisory, however, is devoted to actions that can be taken by different groups, including young people themselves, parents, educators, the government, and even social media and video game companies, to support mental health and well-being. Multiple online resources are provided at the end of each of these sections.
One of the segments is aimed at health care organizations and professionals. While first making a fairly sweeping statement that “our health care system today is not set up optimally to support the mental health and well-being of children and youth,” this part then outlines five broad recommendations that might help improve the fit. These include the following.
- Increase prevention efforts, such as coordination to enrichment programs and referrals for economic and legal supports for families in need.
- Screen routinely for mental health conditions and link those who screen in with appropriate care.
- Identify mental health needs in parents and caregivers such as depression and substance use that can have negative effects on children.
- Increase partnerships between health care groups and community organizations.
- Build multidisciplinary teams that are culturally appropriate and maximally engage children and caretakers in the decision-making process.
The current report is downloadable for free (see reference below) and it is certainly worthwhile for pediatricians to take a look. Dr. Murthy writes, regarding the current state of mental health, that “it would be a tragedy if we beat back one public health crisis only to allow another to grow in its place.”
The report also outlines specific areas where additional research is needed, such as data on racial and sexual minorities and research on innovative and scalable therapies. In addition to the online resources that are provided, the report is backed by over 250 references.
Since its release, the report has generally been well received, and, indeed, there is much to support. The well-known Child Mind Institute in New York tweeted that “this document is a wake-up call for the country and a long-overdue statement of leadership from the federal government.”
Many of the recommendations are admittedly somewhat commons sense, but there are some that are much less so. For example, one recommendation to youth themselves is to serve others – something that may first come across as counterintuitive but can indeed help children and adolescents develop a sense of purpose and self-worth. The call for pediatric health care professionals to screen parents in addition to the patients themselves will likely result in some debate as well. The recommendation to reduce access to lethal means, including the specific naming of firearms, is also a welcome addition. This report also rightly puts a spotlight on the role of societal factors such as racism and poverty in the development of mental health problems and in getting access to quality treatment.
Also worth noting is how much of the advisory examined the role of media in both the problem and the solution. While recognizing that technology, smartphones, and social media are here to stay, a number of suggestions were given to parents, media organizations, journalists, and entertainment companies to reduce the negative impacts these mediums can have. Explicitly recognized in the report is that “there can be tension between what’s best for the technology company and what’s best for the individual user or society.” Also acknowledged was that the link between media of various types and mental health is complex and inconsistent with there being a strong need for additional work in this area when it comes to academic research as well as product development within these companies themselves.
Yet while there is much to like about the advisory, there remain some areas that seem lacking. For example, the text about what causes mental health conditions gets a little dualistic in mentioning biological and environmental factors without much appreciation that these are hardly independent domains. Perhaps more substantially, there was surprisingly little airtime devoted to an enormous issue that underlies so many other challenges related to mental health care – namely an inadequate workforce that gets smaller by the minute. The topic was treated much too superficially with lots of vague calls to “expand” the workforce that lacked substance or detail.
Overall, however, the new Surgeon General’s Advisory is a welcome document that offers updated knowledge of our current challenges and provides practical responses that truly could make a difference. Now all we have to do is put these recommendations into action.
Dr. Rettew is a child and adolescent psychiatrist and medical director of Lane County Behavioral Health in Eugene, Ore. His latest book is “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood.” You can follow him on Twitter and Facebook @PediPsych.
Reference
“Protecting Youth Mental Health – The U.S. Surgeon General’s Advisory,” U.S. Department of Health & Human Services (2021).
The nation’s Surgeon General, Vice Admiral Vivek H. Murthy, MD, MBA, recently released an advisory report on the current state of youth mental health and recommendations to improve well-being. This action follows a number of emergency declarations that have been made by professional organizations such as the American Academy of Child and Adolescent Psychiatry (AACAP), the American Academy of Pediatrics (AAP), and other health care groups to raise awareness about the alarming increase of depression, suicide, anxiety, and other mental health problems in youth.
These reports can be helpful in focusing attention and resources for important public health problems. Many still reference the 1999 report from former Surgeon General David Satcher, MD, PhD, which offered a number of eye-opening statistics regarding the prevalence of mental health conditions and the amount of disability associated with them.
Sadly, the present report indicates that many of these indices have grown worse in the past 20 years. For example, the advisory notes that, even before COVID-19, fully half of female high school students reported persistent feelings of sadness or hopelessness (up 40% from 2009). The report then goes on to cite a number of studies documenting even further rises in youth mental health problems associated with the pandemic.
Most of the advisory, however, is devoted to actions that can be taken by different groups, including young people themselves, parents, educators, the government, and even social media and video game companies, to support mental health and well-being. Multiple online resources are provided at the end of each of these sections.
One of the segments is aimed at health care organizations and professionals. While first making a fairly sweeping statement that “our health care system today is not set up optimally to support the mental health and well-being of children and youth,” this part then outlines five broad recommendations that might help improve the fit. These include the following.
- Increase prevention efforts, such as coordination to enrichment programs and referrals for economic and legal supports for families in need.
- Screen routinely for mental health conditions and link those who screen in with appropriate care.
- Identify mental health needs in parents and caregivers such as depression and substance use that can have negative effects on children.
- Increase partnerships between health care groups and community organizations.
- Build multidisciplinary teams that are culturally appropriate and maximally engage children and caretakers in the decision-making process.
The current report is downloadable for free (see reference below) and it is certainly worthwhile for pediatricians to take a look. Dr. Murthy writes, regarding the current state of mental health, that “it would be a tragedy if we beat back one public health crisis only to allow another to grow in its place.”
The report also outlines specific areas where additional research is needed, such as data on racial and sexual minorities and research on innovative and scalable therapies. In addition to the online resources that are provided, the report is backed by over 250 references.
Since its release, the report has generally been well received, and, indeed, there is much to support. The well-known Child Mind Institute in New York tweeted that “this document is a wake-up call for the country and a long-overdue statement of leadership from the federal government.”
Many of the recommendations are admittedly somewhat commons sense, but there are some that are much less so. For example, one recommendation to youth themselves is to serve others – something that may first come across as counterintuitive but can indeed help children and adolescents develop a sense of purpose and self-worth. The call for pediatric health care professionals to screen parents in addition to the patients themselves will likely result in some debate as well. The recommendation to reduce access to lethal means, including the specific naming of firearms, is also a welcome addition. This report also rightly puts a spotlight on the role of societal factors such as racism and poverty in the development of mental health problems and in getting access to quality treatment.
Also worth noting is how much of the advisory examined the role of media in both the problem and the solution. While recognizing that technology, smartphones, and social media are here to stay, a number of suggestions were given to parents, media organizations, journalists, and entertainment companies to reduce the negative impacts these mediums can have. Explicitly recognized in the report is that “there can be tension between what’s best for the technology company and what’s best for the individual user or society.” Also acknowledged was that the link between media of various types and mental health is complex and inconsistent with there being a strong need for additional work in this area when it comes to academic research as well as product development within these companies themselves.
Yet while there is much to like about the advisory, there remain some areas that seem lacking. For example, the text about what causes mental health conditions gets a little dualistic in mentioning biological and environmental factors without much appreciation that these are hardly independent domains. Perhaps more substantially, there was surprisingly little airtime devoted to an enormous issue that underlies so many other challenges related to mental health care – namely an inadequate workforce that gets smaller by the minute. The topic was treated much too superficially with lots of vague calls to “expand” the workforce that lacked substance or detail.
Overall, however, the new Surgeon General’s Advisory is a welcome document that offers updated knowledge of our current challenges and provides practical responses that truly could make a difference. Now all we have to do is put these recommendations into action.
Dr. Rettew is a child and adolescent psychiatrist and medical director of Lane County Behavioral Health in Eugene, Ore. His latest book is “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood.” You can follow him on Twitter and Facebook @PediPsych.
Reference
“Protecting Youth Mental Health – The U.S. Surgeon General’s Advisory,” U.S. Department of Health & Human Services (2021).
Confusing messages on COVID taking a psychological toll
The Centers for Disease Control and Prevention’s decision to shorten the length of isolation time for asymptomatic Americans with COVID-19, regardless of their vaccination status, to 5 days from 10 days is confusing. I hope the agency reconsiders this decision.
After all, one of the CDC’s key messages during this pandemic has been that even people with asymptomatic COVID who have been vaccinated and boosted can transmit the disease. So it seems to me that the Dec. 27, 2021, recommendation about shortening the isolation time for COVID-19–positive people, like the agency’s earlier guidance encouraging people who are vaccinated to stop wearing masks while in indoor settings, runs contrary to good public health principles.
As an expert in human behavior, I am worried about the impact of these confusing messages on the psyche of people in general, as well as on our patients.
Mental health impact
Soon after the United States went on lockdown in March 2020, I wrote about the likelihood of a pandemic of PTSD, anxiety, and depression that would occur in the wake of rising COVID-19 rates. Well, it happened.
Many people have felt a sense of existential despair, depression, and anxiety. As we head into year No. 3 of disruption of our daily lives – and face the loss of more than 825,000 Americans to COVID – we continue to navigate this uncertainty. And now we must deal with Omicron, a variant that is so highly transmissible that it is apparently able to, in some cases, evade two-dose regimens of mRNA vaccines, boosters, and immunity from past infections, according to a report from Imperial College London. Yet, we are being told by some that Omicron might be less severe, compared with other variants. I worry that this assessment is misleading. In that same report, the Imperial College said it “found no evidence” that Omicron is less virulent than Delta, based on the risk of hospitalization and symptom status.
Meanwhile, animal studies suggest that the Omicron variant might lead to less lung damage than previous variants. A preprint article that is being considered for publication by a Nature Portfolio journal suggests that hamsters and mice infected with the Omicron variant do not have as much lung damage as those infected with other variants. More data need to come in for us to get a true understanding of Omicron’s virulence and transmissibility. We should keep an eye on Israel, which is launching a clinical trial of a second booster, or fourth mRNA shot.
As clinicians, we should give our patients and other people with whom we come in contact a sense of hope. In addition to urging people to get boosters, let’s tell them to err on the side of safety when it comes to this pandemic. That means encouraging them to remain isolated for longer than 5 days – until they test negative for COVID. It also means encouraging patients to wear high-quality face masks while inside public spaces – even in the absence of mandates. I have found it heartbreaking to watch televised broadcasts of sporting events held at some stadiums across the country where masks are not being worn. This absence of face coverings is counterintuitive at a time when some Broadway shows are closing. Even the great Radio City Rockettes shut down their holiday shows early in December 2021 because of COVID.
And, as I’ve argued before, we must not give up on unvaccinated people. I have had success in changing the minds of a few patients and some acquaintances with gentle, respectful prodding and vaccine education.
I would also like to see public health principles implemented in our schools and colleges. To protect the health of our children and young adults, we must continue to be nimble – which means school districts should implement layered prevention strategies, as the CDC recommends. This includes not only encouraging eligible staff members and students to get vaccinated, but requiring face masks inside school facilities, maintaining a physical distance of at least 3 feet, “screening testing, ventilation, handwashing, and staying home when sick.”
Furthermore, in deciding whether schools should remain open or be closed after positive COVID cases are discovered, officials should look at the vaccine demographics of that particular school. For example, if 15% of students are vaccinated in one school and 70% are vaccinated in another, the judgment would be different. Of course, it’s clearly best for schools to remain open, but perhaps closing them temporarily – perhaps for a week or 10 days – should be on the table if infection rates reach a certain level.
Now that we know more and have the benefit of getting more than 200 million Americans fully vaccinated, we can be far more selective about closings and openings. An important part of our strategy must be to communicate honestly with the public about which measures are best for safety. As a key tenet of cognitive-behavioral therapy tells us, “all-or-nothing” thinking is not productive. That should also be the case with our approach to managing COVID-19.
We don’t know the future of the pandemic. Yes, it will end, and possibly COVID will become endemic – like the flu. However, in the meantime, in addition to promoting vaccinations and boosters, we must rigorously encourage our patients to follow public health standards of masking, social distancing, and closing down businesses – and schools – temporarily.
This pandemic has taken a horrendous mental health toll on all of us – especially our patients and frontline health care workers. I’ve spoken with numerous people who were anxious, depressed, and showed signs of PTSD in early 2020; after they got vaccinated, COVID spread diminished, and as public health protocols began to lift, so did their spirits. Clearly for some, the benefit of psychiatric/psychological care centering on the pandemic has proven invaluable. In some ways, the pandemic has brought to the surface the importance of mental health care and removed some of the stigma from mental illness. And that’s a good thing.
Dr. London is a practicing psychiatrist who has been a newspaper columnist for 35 years, specializing in writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
The Centers for Disease Control and Prevention’s decision to shorten the length of isolation time for asymptomatic Americans with COVID-19, regardless of their vaccination status, to 5 days from 10 days is confusing. I hope the agency reconsiders this decision.
After all, one of the CDC’s key messages during this pandemic has been that even people with asymptomatic COVID who have been vaccinated and boosted can transmit the disease. So it seems to me that the Dec. 27, 2021, recommendation about shortening the isolation time for COVID-19–positive people, like the agency’s earlier guidance encouraging people who are vaccinated to stop wearing masks while in indoor settings, runs contrary to good public health principles.
As an expert in human behavior, I am worried about the impact of these confusing messages on the psyche of people in general, as well as on our patients.
Mental health impact
Soon after the United States went on lockdown in March 2020, I wrote about the likelihood of a pandemic of PTSD, anxiety, and depression that would occur in the wake of rising COVID-19 rates. Well, it happened.
Many people have felt a sense of existential despair, depression, and anxiety. As we head into year No. 3 of disruption of our daily lives – and face the loss of more than 825,000 Americans to COVID – we continue to navigate this uncertainty. And now we must deal with Omicron, a variant that is so highly transmissible that it is apparently able to, in some cases, evade two-dose regimens of mRNA vaccines, boosters, and immunity from past infections, according to a report from Imperial College London. Yet, we are being told by some that Omicron might be less severe, compared with other variants. I worry that this assessment is misleading. In that same report, the Imperial College said it “found no evidence” that Omicron is less virulent than Delta, based on the risk of hospitalization and symptom status.
Meanwhile, animal studies suggest that the Omicron variant might lead to less lung damage than previous variants. A preprint article that is being considered for publication by a Nature Portfolio journal suggests that hamsters and mice infected with the Omicron variant do not have as much lung damage as those infected with other variants. More data need to come in for us to get a true understanding of Omicron’s virulence and transmissibility. We should keep an eye on Israel, which is launching a clinical trial of a second booster, or fourth mRNA shot.
As clinicians, we should give our patients and other people with whom we come in contact a sense of hope. In addition to urging people to get boosters, let’s tell them to err on the side of safety when it comes to this pandemic. That means encouraging them to remain isolated for longer than 5 days – until they test negative for COVID. It also means encouraging patients to wear high-quality face masks while inside public spaces – even in the absence of mandates. I have found it heartbreaking to watch televised broadcasts of sporting events held at some stadiums across the country where masks are not being worn. This absence of face coverings is counterintuitive at a time when some Broadway shows are closing. Even the great Radio City Rockettes shut down their holiday shows early in December 2021 because of COVID.
And, as I’ve argued before, we must not give up on unvaccinated people. I have had success in changing the minds of a few patients and some acquaintances with gentle, respectful prodding and vaccine education.
I would also like to see public health principles implemented in our schools and colleges. To protect the health of our children and young adults, we must continue to be nimble – which means school districts should implement layered prevention strategies, as the CDC recommends. This includes not only encouraging eligible staff members and students to get vaccinated, but requiring face masks inside school facilities, maintaining a physical distance of at least 3 feet, “screening testing, ventilation, handwashing, and staying home when sick.”
Furthermore, in deciding whether schools should remain open or be closed after positive COVID cases are discovered, officials should look at the vaccine demographics of that particular school. For example, if 15% of students are vaccinated in one school and 70% are vaccinated in another, the judgment would be different. Of course, it’s clearly best for schools to remain open, but perhaps closing them temporarily – perhaps for a week or 10 days – should be on the table if infection rates reach a certain level.
Now that we know more and have the benefit of getting more than 200 million Americans fully vaccinated, we can be far more selective about closings and openings. An important part of our strategy must be to communicate honestly with the public about which measures are best for safety. As a key tenet of cognitive-behavioral therapy tells us, “all-or-nothing” thinking is not productive. That should also be the case with our approach to managing COVID-19.
We don’t know the future of the pandemic. Yes, it will end, and possibly COVID will become endemic – like the flu. However, in the meantime, in addition to promoting vaccinations and boosters, we must rigorously encourage our patients to follow public health standards of masking, social distancing, and closing down businesses – and schools – temporarily.
This pandemic has taken a horrendous mental health toll on all of us – especially our patients and frontline health care workers. I’ve spoken with numerous people who were anxious, depressed, and showed signs of PTSD in early 2020; after they got vaccinated, COVID spread diminished, and as public health protocols began to lift, so did their spirits. Clearly for some, the benefit of psychiatric/psychological care centering on the pandemic has proven invaluable. In some ways, the pandemic has brought to the surface the importance of mental health care and removed some of the stigma from mental illness. And that’s a good thing.
Dr. London is a practicing psychiatrist who has been a newspaper columnist for 35 years, specializing in writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
The Centers for Disease Control and Prevention’s decision to shorten the length of isolation time for asymptomatic Americans with COVID-19, regardless of their vaccination status, to 5 days from 10 days is confusing. I hope the agency reconsiders this decision.
After all, one of the CDC’s key messages during this pandemic has been that even people with asymptomatic COVID who have been vaccinated and boosted can transmit the disease. So it seems to me that the Dec. 27, 2021, recommendation about shortening the isolation time for COVID-19–positive people, like the agency’s earlier guidance encouraging people who are vaccinated to stop wearing masks while in indoor settings, runs contrary to good public health principles.
As an expert in human behavior, I am worried about the impact of these confusing messages on the psyche of people in general, as well as on our patients.
Mental health impact
Soon after the United States went on lockdown in March 2020, I wrote about the likelihood of a pandemic of PTSD, anxiety, and depression that would occur in the wake of rising COVID-19 rates. Well, it happened.
Many people have felt a sense of existential despair, depression, and anxiety. As we head into year No. 3 of disruption of our daily lives – and face the loss of more than 825,000 Americans to COVID – we continue to navigate this uncertainty. And now we must deal with Omicron, a variant that is so highly transmissible that it is apparently able to, in some cases, evade two-dose regimens of mRNA vaccines, boosters, and immunity from past infections, according to a report from Imperial College London. Yet, we are being told by some that Omicron might be less severe, compared with other variants. I worry that this assessment is misleading. In that same report, the Imperial College said it “found no evidence” that Omicron is less virulent than Delta, based on the risk of hospitalization and symptom status.
Meanwhile, animal studies suggest that the Omicron variant might lead to less lung damage than previous variants. A preprint article that is being considered for publication by a Nature Portfolio journal suggests that hamsters and mice infected with the Omicron variant do not have as much lung damage as those infected with other variants. More data need to come in for us to get a true understanding of Omicron’s virulence and transmissibility. We should keep an eye on Israel, which is launching a clinical trial of a second booster, or fourth mRNA shot.
As clinicians, we should give our patients and other people with whom we come in contact a sense of hope. In addition to urging people to get boosters, let’s tell them to err on the side of safety when it comes to this pandemic. That means encouraging them to remain isolated for longer than 5 days – until they test negative for COVID. It also means encouraging patients to wear high-quality face masks while inside public spaces – even in the absence of mandates. I have found it heartbreaking to watch televised broadcasts of sporting events held at some stadiums across the country where masks are not being worn. This absence of face coverings is counterintuitive at a time when some Broadway shows are closing. Even the great Radio City Rockettes shut down their holiday shows early in December 2021 because of COVID.
And, as I’ve argued before, we must not give up on unvaccinated people. I have had success in changing the minds of a few patients and some acquaintances with gentle, respectful prodding and vaccine education.
I would also like to see public health principles implemented in our schools and colleges. To protect the health of our children and young adults, we must continue to be nimble – which means school districts should implement layered prevention strategies, as the CDC recommends. This includes not only encouraging eligible staff members and students to get vaccinated, but requiring face masks inside school facilities, maintaining a physical distance of at least 3 feet, “screening testing, ventilation, handwashing, and staying home when sick.”
Furthermore, in deciding whether schools should remain open or be closed after positive COVID cases are discovered, officials should look at the vaccine demographics of that particular school. For example, if 15% of students are vaccinated in one school and 70% are vaccinated in another, the judgment would be different. Of course, it’s clearly best for schools to remain open, but perhaps closing them temporarily – perhaps for a week or 10 days – should be on the table if infection rates reach a certain level.
Now that we know more and have the benefit of getting more than 200 million Americans fully vaccinated, we can be far more selective about closings and openings. An important part of our strategy must be to communicate honestly with the public about which measures are best for safety. As a key tenet of cognitive-behavioral therapy tells us, “all-or-nothing” thinking is not productive. That should also be the case with our approach to managing COVID-19.
We don’t know the future of the pandemic. Yes, it will end, and possibly COVID will become endemic – like the flu. However, in the meantime, in addition to promoting vaccinations and boosters, we must rigorously encourage our patients to follow public health standards of masking, social distancing, and closing down businesses – and schools – temporarily.
This pandemic has taken a horrendous mental health toll on all of us – especially our patients and frontline health care workers. I’ve spoken with numerous people who were anxious, depressed, and showed signs of PTSD in early 2020; after they got vaccinated, COVID spread diminished, and as public health protocols began to lift, so did their spirits. Clearly for some, the benefit of psychiatric/psychological care centering on the pandemic has proven invaluable. In some ways, the pandemic has brought to the surface the importance of mental health care and removed some of the stigma from mental illness. And that’s a good thing.
Dr. London is a practicing psychiatrist who has been a newspaper columnist for 35 years, specializing in writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
The present and future of virtual care in GI
The rapid and unprecedented expansion of virtual care in response to COVID-19 is likely to leave a permanent mark on how health care is delivered. While this expansion has been critical in the near term in caring for our patients while minimizing risk of exposure during the pandemic, it is vital to be forward thinking in considering the ongoing value of virtual care in optimizing routine patient care and in reaching our high-need patients in rural and other underserved areas. We are likely to hear more in the coming months regarding the short- and long-term impacts of virtual care expansion as we transition away from COVID and begin to consider how to maximize use of virtual care in our routine practice. Many questions remain, including defining the optimal balance between virtual and in-person care, assessing whether virtual care is a substitute for in-person care or simply additive, and understanding the impacts of virtual care on outcomes. On the latter questions, a recent study from Kaiser Permanente Northern California found that primary care visits conducted virtually resulted in modestly higher rates of follow-up outpatient office visits than initial in-person visits, but no significant difference in 7-day ED visits or hospitalizations. Whether these results are generalizable to GI patient populations is unclear.
Highlights from this month’s issue of GIHN include a study evaluating the impact of a “virtual” liver transplant center on access to liver transplant listing among patients in rural areas, another suggesting lower serologic response to COVID-19 vaccines among patients with IBD, a new AGA Clinical Practice Update: Commentary offering tips regarding surveillance after endoscopic submucosal dissection for dysplasia and early-stage GI cancer, and results from a phase 3 clinical trial demonstrating the efficacy of upadacitinib for treatment of moderate to severe ulcerative colitis.
And while the winter weather here in Michigan may suggest otherwise, DDW 2022 is just around the corner – registration opens on Jan. 19, and we look forward to the GI community coming together, whether in person in sunny San Diego or virtually at home or office, for this hybrid conference.
Megan A. Adams, MD, JD, MSc
Editor in Chief
The rapid and unprecedented expansion of virtual care in response to COVID-19 is likely to leave a permanent mark on how health care is delivered. While this expansion has been critical in the near term in caring for our patients while minimizing risk of exposure during the pandemic, it is vital to be forward thinking in considering the ongoing value of virtual care in optimizing routine patient care and in reaching our high-need patients in rural and other underserved areas. We are likely to hear more in the coming months regarding the short- and long-term impacts of virtual care expansion as we transition away from COVID and begin to consider how to maximize use of virtual care in our routine practice. Many questions remain, including defining the optimal balance between virtual and in-person care, assessing whether virtual care is a substitute for in-person care or simply additive, and understanding the impacts of virtual care on outcomes. On the latter questions, a recent study from Kaiser Permanente Northern California found that primary care visits conducted virtually resulted in modestly higher rates of follow-up outpatient office visits than initial in-person visits, but no significant difference in 7-day ED visits or hospitalizations. Whether these results are generalizable to GI patient populations is unclear.
Highlights from this month’s issue of GIHN include a study evaluating the impact of a “virtual” liver transplant center on access to liver transplant listing among patients in rural areas, another suggesting lower serologic response to COVID-19 vaccines among patients with IBD, a new AGA Clinical Practice Update: Commentary offering tips regarding surveillance after endoscopic submucosal dissection for dysplasia and early-stage GI cancer, and results from a phase 3 clinical trial demonstrating the efficacy of upadacitinib for treatment of moderate to severe ulcerative colitis.
And while the winter weather here in Michigan may suggest otherwise, DDW 2022 is just around the corner – registration opens on Jan. 19, and we look forward to the GI community coming together, whether in person in sunny San Diego or virtually at home or office, for this hybrid conference.
Megan A. Adams, MD, JD, MSc
Editor in Chief
The rapid and unprecedented expansion of virtual care in response to COVID-19 is likely to leave a permanent mark on how health care is delivered. While this expansion has been critical in the near term in caring for our patients while minimizing risk of exposure during the pandemic, it is vital to be forward thinking in considering the ongoing value of virtual care in optimizing routine patient care and in reaching our high-need patients in rural and other underserved areas. We are likely to hear more in the coming months regarding the short- and long-term impacts of virtual care expansion as we transition away from COVID and begin to consider how to maximize use of virtual care in our routine practice. Many questions remain, including defining the optimal balance between virtual and in-person care, assessing whether virtual care is a substitute for in-person care or simply additive, and understanding the impacts of virtual care on outcomes. On the latter questions, a recent study from Kaiser Permanente Northern California found that primary care visits conducted virtually resulted in modestly higher rates of follow-up outpatient office visits than initial in-person visits, but no significant difference in 7-day ED visits or hospitalizations. Whether these results are generalizable to GI patient populations is unclear.
Highlights from this month’s issue of GIHN include a study evaluating the impact of a “virtual” liver transplant center on access to liver transplant listing among patients in rural areas, another suggesting lower serologic response to COVID-19 vaccines among patients with IBD, a new AGA Clinical Practice Update: Commentary offering tips regarding surveillance after endoscopic submucosal dissection for dysplasia and early-stage GI cancer, and results from a phase 3 clinical trial demonstrating the efficacy of upadacitinib for treatment of moderate to severe ulcerative colitis.
And while the winter weather here in Michigan may suggest otherwise, DDW 2022 is just around the corner – registration opens on Jan. 19, and we look forward to the GI community coming together, whether in person in sunny San Diego or virtually at home or office, for this hybrid conference.
Megan A. Adams, MD, JD, MSc
Editor in Chief