User login
Medtronic to discontinue SmartPill capsule
a spokesperson for its manufacturer, Medtronic, confirmed.
In a June 22 email, company representative Oded Cojocaru stated that the decision followed “several months of ongoing challenges with reliable supply of critical components to our SmartPill motility testing system.”
The SmartPill motility testing system’s maturity “means we cannot source an alternative supplier for the specialized components required to manufacture the SmartPill capsules and recorders. As a result, we have made the difficult decision to discontinue global sales,” Mr. Cojocaru said.
Customers have been notified and all sales of the device will be discontinued across all clinical applications when available inventory is exhausted, which is expected to occur in September. Medtronic has no plans to develop an alternative to the device.
Braden Kuo, MD, of Massachusetts General Hospital, Boston, a motility specialist who took part in the SmartPill’s development and testing at various stages, said that Medtronic’s decision to discontinue the device was already known among his GI colleagues, and was the subject of concern as there is no analogous Food and Drug Administration–approved device on the market.
While the device’s clinical adoption “is not extremely widespread,” Dr. Kuo said, thousands of SmartPills are still used in GI clinics every year, and insurance tends to cover their use, especially in major metropolitan areas.
Originally developed by the SmartPill Corporation of Buffalo, N.Y., the device was first cleared by the FDA in 2006 for the evaluation of colonic transit time in patients with chronic constipation and suspected gastroparesis. Six years later that company was sold to Given Imaging, an Israeli firm making ingestible capsule endoscopy devices with cameras. In 2015, Given Imaging was purchased by Medtronic.
The SmartPill is ingested under clinical supervision, after which a patient can return home and allow the capsule to pass naturally through the body over a period of days. It is used in tandem with proprietary monitoring hardware, software, and a special food product. Known limitations of the device include that it can be difficult for some patients to swallow, and that it can get stuck in the lower digestive tract. Its use is contraindicated in patients with dysphagia, stricture, or bowel obstruction.
“Many motility doctors and some general GI docs find this test helpful,” said Dr. Kuo, who formerly served as a scientific adviser to SmartPill and later ran trials of the technology for Medtronic. It is useful as an alternative to costlier scintigraphy, he said, or to follow up after a negative endoscopy result.
The SmartPill has also been fruitful for GI research, Dr. Kuo added, because the capsule is easy to administer, compared with nonambulatory ways of studying motility, which limited enrollment. “Now we can do studies with several hundred people, because this is much more easily tolerated, and we’ve made a lot of interesting insights about GI physiology and pathophysiology as a result of this technology.”
During its 17 years on the market, Dr. Kuo said, the SmartPill has helped galvanize interest in other capsule applications, including for drug delivery, imaging and sampling.
Jack Semler, PhD, the former chief technology officer of SmartPill and who alongside Dr. Kuo has coauthored some 40 papers on the SmartPill, said he, too, lamented the decision by Medtronic. “The company has only so many resources to devote to upgrading technology and those resources just aren’t available for this particular product,” he speculated. Nonetheless, Dr. Semler said, “I still feel there is a real untapped potential.”
Dr. Kuo and Dr. Semler both disclosed previous paid work for SmartPill and Medtronic. Both are currently consulting for Atmo Biosciences, a company that is developing a different motility capsule technology.
a spokesperson for its manufacturer, Medtronic, confirmed.
In a June 22 email, company representative Oded Cojocaru stated that the decision followed “several months of ongoing challenges with reliable supply of critical components to our SmartPill motility testing system.”
The SmartPill motility testing system’s maturity “means we cannot source an alternative supplier for the specialized components required to manufacture the SmartPill capsules and recorders. As a result, we have made the difficult decision to discontinue global sales,” Mr. Cojocaru said.
Customers have been notified and all sales of the device will be discontinued across all clinical applications when available inventory is exhausted, which is expected to occur in September. Medtronic has no plans to develop an alternative to the device.
Braden Kuo, MD, of Massachusetts General Hospital, Boston, a motility specialist who took part in the SmartPill’s development and testing at various stages, said that Medtronic’s decision to discontinue the device was already known among his GI colleagues, and was the subject of concern as there is no analogous Food and Drug Administration–approved device on the market.
While the device’s clinical adoption “is not extremely widespread,” Dr. Kuo said, thousands of SmartPills are still used in GI clinics every year, and insurance tends to cover their use, especially in major metropolitan areas.
Originally developed by the SmartPill Corporation of Buffalo, N.Y., the device was first cleared by the FDA in 2006 for the evaluation of colonic transit time in patients with chronic constipation and suspected gastroparesis. Six years later that company was sold to Given Imaging, an Israeli firm making ingestible capsule endoscopy devices with cameras. In 2015, Given Imaging was purchased by Medtronic.
The SmartPill is ingested under clinical supervision, after which a patient can return home and allow the capsule to pass naturally through the body over a period of days. It is used in tandem with proprietary monitoring hardware, software, and a special food product. Known limitations of the device include that it can be difficult for some patients to swallow, and that it can get stuck in the lower digestive tract. Its use is contraindicated in patients with dysphagia, stricture, or bowel obstruction.
“Many motility doctors and some general GI docs find this test helpful,” said Dr. Kuo, who formerly served as a scientific adviser to SmartPill and later ran trials of the technology for Medtronic. It is useful as an alternative to costlier scintigraphy, he said, or to follow up after a negative endoscopy result.
The SmartPill has also been fruitful for GI research, Dr. Kuo added, because the capsule is easy to administer, compared with nonambulatory ways of studying motility, which limited enrollment. “Now we can do studies with several hundred people, because this is much more easily tolerated, and we’ve made a lot of interesting insights about GI physiology and pathophysiology as a result of this technology.”
During its 17 years on the market, Dr. Kuo said, the SmartPill has helped galvanize interest in other capsule applications, including for drug delivery, imaging and sampling.
Jack Semler, PhD, the former chief technology officer of SmartPill and who alongside Dr. Kuo has coauthored some 40 papers on the SmartPill, said he, too, lamented the decision by Medtronic. “The company has only so many resources to devote to upgrading technology and those resources just aren’t available for this particular product,” he speculated. Nonetheless, Dr. Semler said, “I still feel there is a real untapped potential.”
Dr. Kuo and Dr. Semler both disclosed previous paid work for SmartPill and Medtronic. Both are currently consulting for Atmo Biosciences, a company that is developing a different motility capsule technology.
a spokesperson for its manufacturer, Medtronic, confirmed.
In a June 22 email, company representative Oded Cojocaru stated that the decision followed “several months of ongoing challenges with reliable supply of critical components to our SmartPill motility testing system.”
The SmartPill motility testing system’s maturity “means we cannot source an alternative supplier for the specialized components required to manufacture the SmartPill capsules and recorders. As a result, we have made the difficult decision to discontinue global sales,” Mr. Cojocaru said.
Customers have been notified and all sales of the device will be discontinued across all clinical applications when available inventory is exhausted, which is expected to occur in September. Medtronic has no plans to develop an alternative to the device.
Braden Kuo, MD, of Massachusetts General Hospital, Boston, a motility specialist who took part in the SmartPill’s development and testing at various stages, said that Medtronic’s decision to discontinue the device was already known among his GI colleagues, and was the subject of concern as there is no analogous Food and Drug Administration–approved device on the market.
While the device’s clinical adoption “is not extremely widespread,” Dr. Kuo said, thousands of SmartPills are still used in GI clinics every year, and insurance tends to cover their use, especially in major metropolitan areas.
Originally developed by the SmartPill Corporation of Buffalo, N.Y., the device was first cleared by the FDA in 2006 for the evaluation of colonic transit time in patients with chronic constipation and suspected gastroparesis. Six years later that company was sold to Given Imaging, an Israeli firm making ingestible capsule endoscopy devices with cameras. In 2015, Given Imaging was purchased by Medtronic.
The SmartPill is ingested under clinical supervision, after which a patient can return home and allow the capsule to pass naturally through the body over a period of days. It is used in tandem with proprietary monitoring hardware, software, and a special food product. Known limitations of the device include that it can be difficult for some patients to swallow, and that it can get stuck in the lower digestive tract. Its use is contraindicated in patients with dysphagia, stricture, or bowel obstruction.
“Many motility doctors and some general GI docs find this test helpful,” said Dr. Kuo, who formerly served as a scientific adviser to SmartPill and later ran trials of the technology for Medtronic. It is useful as an alternative to costlier scintigraphy, he said, or to follow up after a negative endoscopy result.
The SmartPill has also been fruitful for GI research, Dr. Kuo added, because the capsule is easy to administer, compared with nonambulatory ways of studying motility, which limited enrollment. “Now we can do studies with several hundred people, because this is much more easily tolerated, and we’ve made a lot of interesting insights about GI physiology and pathophysiology as a result of this technology.”
During its 17 years on the market, Dr. Kuo said, the SmartPill has helped galvanize interest in other capsule applications, including for drug delivery, imaging and sampling.
Jack Semler, PhD, the former chief technology officer of SmartPill and who alongside Dr. Kuo has coauthored some 40 papers on the SmartPill, said he, too, lamented the decision by Medtronic. “The company has only so many resources to devote to upgrading technology and those resources just aren’t available for this particular product,” he speculated. Nonetheless, Dr. Semler said, “I still feel there is a real untapped potential.”
Dr. Kuo and Dr. Semler both disclosed previous paid work for SmartPill and Medtronic. Both are currently consulting for Atmo Biosciences, a company that is developing a different motility capsule technology.
Low-calorie tastes sweeter with a little salt
Low-calorie tastes sweeter with a little salt
Diet and sugar-free foods and drinks seem like a good idea, but it’s hard to get past that strange aftertaste, right? It’s the calling card for the noncaloric aspartame- and stevia-containing sweeteners that we consume to make us feel like we can have the best of both worlds.
That weird lingering taste can be a total turn-off for some (raises hand), but researchers have found an almost facepalm solution to the not-so-sweet problem, and it’s salt.
Now, the concept of sweet and salty is not a far-fetched partnership when it comes to snack consumption (try M&Ms in your popcorn). The researchers at Almendra, a manufacturer of stevia sweeteners, put that iconic flavor pair to the test by adding mineral salts that have some nutritional value to lessen the effect of a stevia compound, rebaudioside A, found in noncaloric sweeteners.
The researchers added in magnesium chloride, calcium chloride, and potassium chloride separately to lessen rebaudioside A’s intensity, but they needed so much salt that it killed the sweet taste completely. A blend of the three mineral salts, however, reduced the lingering taste by 79% and improved the real sugar-like taste. The researchers tried this blend in reduced-calorie orange juice and a citrus-flavored soft drink, improving the taste in both.
The salty and sweet match comes in for the win once again. This time helping against the fight of obesity instead of making it worse.
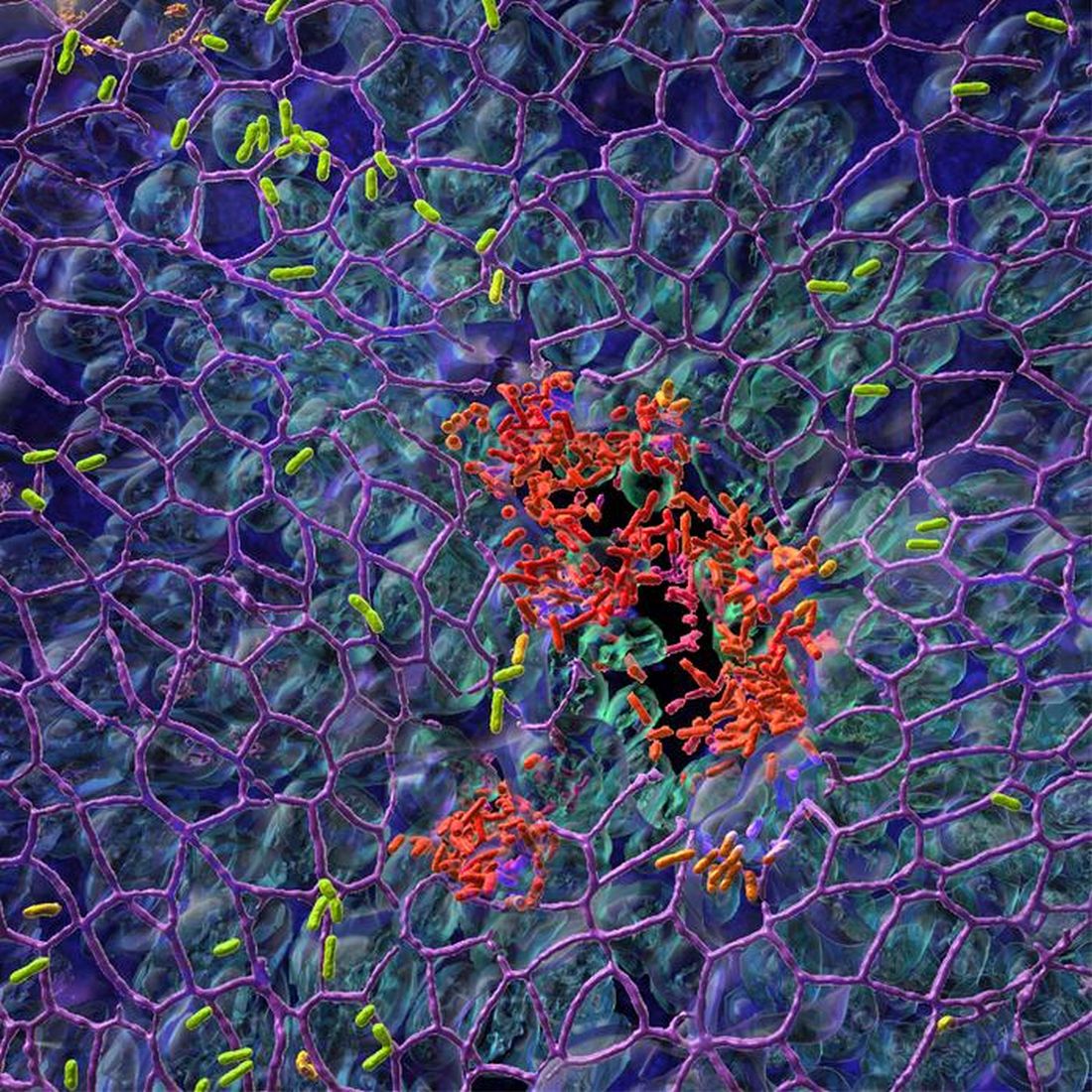
Pseudomonas’ Achilles’ heel is more of an Achilles’ genetic switch
Today, on the long-awaited return of “Bacteria vs. the World,” we meet one of the rock stars of infectious disease.
LOTME: Through the use of imaginary technology, we’re talking to Pseudomonas aeruginosa. Thanks for joining us on such short notice, after Neisseria gonorrhoeae canceled at the last minute.
P. aeruginosa: No problem. I think we can all guess what that little devil is up to.
LOTME: Bacterial resistance to antibiotics is a huge problem for our species. What makes you so hard to fight?
P. aeruginosa: We’ve been trying to keep that a secret, actually, but now that researchers in Switzerland and Denmark seem to have figured it out, I guess it’s okay for me to spill the beans.
LOTME: Beans? What do beans have to do with it?
P. aeruginosa: Nothing, it’s just a colloquial expression that means I’m sharing previously private information.
LOTME: Sure, we knew that. Please, continue your spilling.
P. aeruginosa: The secret is … Well, let’s just say we were a little worried when the Clash released “Should I Stay or Should I Go” back in the 1980s.
LOTME: The Clash? Now we’re really confused.
P. aeruginosa: The answer to their question, “Should I stay or should I go? is yes. Successful invasion of a human is all about division of labor. “While one fraction of the bacterial population adheres to the mucosal surface and forms a biofilm, the other subpopulation spreads to distant tissue sites,” is how the investigators described it. We can increase surface colonization by using a “job-sharing” process, they said, and even resist antibiotics because most of us remain in the protective biofilm.
LOTME: And they say you guys don’t have brains.
P. aeruginosa: But wait, there’s more. We don’t just divide the labor randomly. After the initial colonization we form two functionally distinct subpopulations. One has high levels of the bacterial signaling molecule c-di-GMP and stays put to work on the biofilm. The other group, with low levels of c-di-GMP, heads out to the surrounding tissue to continue the colonization. As project leader Urs Jenal put it, “By identifying the genetic switch, we have tracked down the Achilles heel of the pathogen.”
LOTME: Pretty clever stuff, for humans, anyway.
P. aeruginosa: We agree, but now that you know our secret, we can’t let you share it.
LOTME: Wait! The journal article’s already been published. Your secret is out. You can’t stop that by infecting me.
P. aeruginosa: True enough, but are you familiar with the fable of the scorpion and the frog? It’s our nature.
LOTME: Nooooo! N. gonorrhoeae wouldn’t have done this!
What a pain in the Butt
Businesses rise and businesses fall. We all know that one cursed location, that spot in town where we see businesses move in and close up in a matter of months. At the same time, though, there are also businesses that have been around as long as anyone can remember, pillars of the community.
Corydon, IN., likely has a few such long-lived shops, but it is officially down one 70-year-old family business as of late April, with the unfortunate passing of beloved local pharmacy Butt Drugs. Prescription pick-up in rear.
The business dates back to 1952, when it was founded as William H. Butt Drugs. We’re sure William Butt was never teased about his last name. Nope. No one would ever do that. After he passed the store to his children, it underwent a stint as Butt Rexall Drugs. When the shop was passed down to its third-generation and ultimately final owner, Katie Butt Beckort, she decided to simplify the name. Get right down to the bottom of things, as it were.
Butt Drugs was a popular spot, featuring an old-school soda fountain and themed souvenirs. According to Ms. Butt Beckort, people would come from miles away to buy “I love Butt Drugs” T-shirts, magnets, and so on. Yes, they knew perfectly well what they were sitting on.
So, if was such a hit, why did it close? Butt Drugs may have a hilarious name and merchandise to match, but the pharmacy portion of the pharmacy had been losing money for years. You know, the actual point of the business. As with so many things, we can blame it on the insurance companies. More than half the drugs that passed through Butt Drugs’ doors were sold at a loss, because the insurance companies refused to reimburse the store more than the wholesale price of the drug. Not even a good butt drug could clear up that financial diarrhea.
And so, we’ve lost Butt Drugs forever. Spicy food enthusiasts, coffee drinkers, and all patrons of Taco Bell, take a moment to reflect and mourn on what you’ve lost. No more Butt Drugs to relieve your suffering. A true kick in the butt indeed.
Low-calorie tastes sweeter with a little salt
Diet and sugar-free foods and drinks seem like a good idea, but it’s hard to get past that strange aftertaste, right? It’s the calling card for the noncaloric aspartame- and stevia-containing sweeteners that we consume to make us feel like we can have the best of both worlds.
That weird lingering taste can be a total turn-off for some (raises hand), but researchers have found an almost facepalm solution to the not-so-sweet problem, and it’s salt.
Now, the concept of sweet and salty is not a far-fetched partnership when it comes to snack consumption (try M&Ms in your popcorn). The researchers at Almendra, a manufacturer of stevia sweeteners, put that iconic flavor pair to the test by adding mineral salts that have some nutritional value to lessen the effect of a stevia compound, rebaudioside A, found in noncaloric sweeteners.
The researchers added in magnesium chloride, calcium chloride, and potassium chloride separately to lessen rebaudioside A’s intensity, but they needed so much salt that it killed the sweet taste completely. A blend of the three mineral salts, however, reduced the lingering taste by 79% and improved the real sugar-like taste. The researchers tried this blend in reduced-calorie orange juice and a citrus-flavored soft drink, improving the taste in both.
The salty and sweet match comes in for the win once again. This time helping against the fight of obesity instead of making it worse.
Pseudomonas’ Achilles’ heel is more of an Achilles’ genetic switch
Today, on the long-awaited return of “Bacteria vs. the World,” we meet one of the rock stars of infectious disease.
LOTME: Through the use of imaginary technology, we’re talking to Pseudomonas aeruginosa. Thanks for joining us on such short notice, after Neisseria gonorrhoeae canceled at the last minute.
P. aeruginosa: No problem. I think we can all guess what that little devil is up to.
LOTME: Bacterial resistance to antibiotics is a huge problem for our species. What makes you so hard to fight?
P. aeruginosa: We’ve been trying to keep that a secret, actually, but now that researchers in Switzerland and Denmark seem to have figured it out, I guess it’s okay for me to spill the beans.
LOTME: Beans? What do beans have to do with it?
P. aeruginosa: Nothing, it’s just a colloquial expression that means I’m sharing previously private information.
LOTME: Sure, we knew that. Please, continue your spilling.
P. aeruginosa: The secret is … Well, let’s just say we were a little worried when the Clash released “Should I Stay or Should I Go” back in the 1980s.
LOTME: The Clash? Now we’re really confused.
P. aeruginosa: The answer to their question, “Should I stay or should I go? is yes. Successful invasion of a human is all about division of labor. “While one fraction of the bacterial population adheres to the mucosal surface and forms a biofilm, the other subpopulation spreads to distant tissue sites,” is how the investigators described it. We can increase surface colonization by using a “job-sharing” process, they said, and even resist antibiotics because most of us remain in the protective biofilm.
LOTME: And they say you guys don’t have brains.
P. aeruginosa: But wait, there’s more. We don’t just divide the labor randomly. After the initial colonization we form two functionally distinct subpopulations. One has high levels of the bacterial signaling molecule c-di-GMP and stays put to work on the biofilm. The other group, with low levels of c-di-GMP, heads out to the surrounding tissue to continue the colonization. As project leader Urs Jenal put it, “By identifying the genetic switch, we have tracked down the Achilles heel of the pathogen.”
LOTME: Pretty clever stuff, for humans, anyway.
P. aeruginosa: We agree, but now that you know our secret, we can’t let you share it.
LOTME: Wait! The journal article’s already been published. Your secret is out. You can’t stop that by infecting me.
P. aeruginosa: True enough, but are you familiar with the fable of the scorpion and the frog? It’s our nature.
LOTME: Nooooo! N. gonorrhoeae wouldn’t have done this!
What a pain in the Butt
Businesses rise and businesses fall. We all know that one cursed location, that spot in town where we see businesses move in and close up in a matter of months. At the same time, though, there are also businesses that have been around as long as anyone can remember, pillars of the community.
Corydon, IN., likely has a few such long-lived shops, but it is officially down one 70-year-old family business as of late April, with the unfortunate passing of beloved local pharmacy Butt Drugs. Prescription pick-up in rear.
The business dates back to 1952, when it was founded as William H. Butt Drugs. We’re sure William Butt was never teased about his last name. Nope. No one would ever do that. After he passed the store to his children, it underwent a stint as Butt Rexall Drugs. When the shop was passed down to its third-generation and ultimately final owner, Katie Butt Beckort, she decided to simplify the name. Get right down to the bottom of things, as it were.
Butt Drugs was a popular spot, featuring an old-school soda fountain and themed souvenirs. According to Ms. Butt Beckort, people would come from miles away to buy “I love Butt Drugs” T-shirts, magnets, and so on. Yes, they knew perfectly well what they were sitting on.
So, if was such a hit, why did it close? Butt Drugs may have a hilarious name and merchandise to match, but the pharmacy portion of the pharmacy had been losing money for years. You know, the actual point of the business. As with so many things, we can blame it on the insurance companies. More than half the drugs that passed through Butt Drugs’ doors were sold at a loss, because the insurance companies refused to reimburse the store more than the wholesale price of the drug. Not even a good butt drug could clear up that financial diarrhea.
And so, we’ve lost Butt Drugs forever. Spicy food enthusiasts, coffee drinkers, and all patrons of Taco Bell, take a moment to reflect and mourn on what you’ve lost. No more Butt Drugs to relieve your suffering. A true kick in the butt indeed.
Low-calorie tastes sweeter with a little salt
Diet and sugar-free foods and drinks seem like a good idea, but it’s hard to get past that strange aftertaste, right? It’s the calling card for the noncaloric aspartame- and stevia-containing sweeteners that we consume to make us feel like we can have the best of both worlds.
That weird lingering taste can be a total turn-off for some (raises hand), but researchers have found an almost facepalm solution to the not-so-sweet problem, and it’s salt.
Now, the concept of sweet and salty is not a far-fetched partnership when it comes to snack consumption (try M&Ms in your popcorn). The researchers at Almendra, a manufacturer of stevia sweeteners, put that iconic flavor pair to the test by adding mineral salts that have some nutritional value to lessen the effect of a stevia compound, rebaudioside A, found in noncaloric sweeteners.
The researchers added in magnesium chloride, calcium chloride, and potassium chloride separately to lessen rebaudioside A’s intensity, but they needed so much salt that it killed the sweet taste completely. A blend of the three mineral salts, however, reduced the lingering taste by 79% and improved the real sugar-like taste. The researchers tried this blend in reduced-calorie orange juice and a citrus-flavored soft drink, improving the taste in both.
The salty and sweet match comes in for the win once again. This time helping against the fight of obesity instead of making it worse.
Pseudomonas’ Achilles’ heel is more of an Achilles’ genetic switch
Today, on the long-awaited return of “Bacteria vs. the World,” we meet one of the rock stars of infectious disease.
LOTME: Through the use of imaginary technology, we’re talking to Pseudomonas aeruginosa. Thanks for joining us on such short notice, after Neisseria gonorrhoeae canceled at the last minute.
P. aeruginosa: No problem. I think we can all guess what that little devil is up to.
LOTME: Bacterial resistance to antibiotics is a huge problem for our species. What makes you so hard to fight?
P. aeruginosa: We’ve been trying to keep that a secret, actually, but now that researchers in Switzerland and Denmark seem to have figured it out, I guess it’s okay for me to spill the beans.
LOTME: Beans? What do beans have to do with it?
P. aeruginosa: Nothing, it’s just a colloquial expression that means I’m sharing previously private information.
LOTME: Sure, we knew that. Please, continue your spilling.
P. aeruginosa: The secret is … Well, let’s just say we were a little worried when the Clash released “Should I Stay or Should I Go” back in the 1980s.
LOTME: The Clash? Now we’re really confused.
P. aeruginosa: The answer to their question, “Should I stay or should I go? is yes. Successful invasion of a human is all about division of labor. “While one fraction of the bacterial population adheres to the mucosal surface and forms a biofilm, the other subpopulation spreads to distant tissue sites,” is how the investigators described it. We can increase surface colonization by using a “job-sharing” process, they said, and even resist antibiotics because most of us remain in the protective biofilm.
LOTME: And they say you guys don’t have brains.
P. aeruginosa: But wait, there’s more. We don’t just divide the labor randomly. After the initial colonization we form two functionally distinct subpopulations. One has high levels of the bacterial signaling molecule c-di-GMP and stays put to work on the biofilm. The other group, with low levels of c-di-GMP, heads out to the surrounding tissue to continue the colonization. As project leader Urs Jenal put it, “By identifying the genetic switch, we have tracked down the Achilles heel of the pathogen.”
LOTME: Pretty clever stuff, for humans, anyway.
P. aeruginosa: We agree, but now that you know our secret, we can’t let you share it.
LOTME: Wait! The journal article’s already been published. Your secret is out. You can’t stop that by infecting me.
P. aeruginosa: True enough, but are you familiar with the fable of the scorpion and the frog? It’s our nature.
LOTME: Nooooo! N. gonorrhoeae wouldn’t have done this!
What a pain in the Butt
Businesses rise and businesses fall. We all know that one cursed location, that spot in town where we see businesses move in and close up in a matter of months. At the same time, though, there are also businesses that have been around as long as anyone can remember, pillars of the community.
Corydon, IN., likely has a few such long-lived shops, but it is officially down one 70-year-old family business as of late April, with the unfortunate passing of beloved local pharmacy Butt Drugs. Prescription pick-up in rear.
The business dates back to 1952, when it was founded as William H. Butt Drugs. We’re sure William Butt was never teased about his last name. Nope. No one would ever do that. After he passed the store to his children, it underwent a stint as Butt Rexall Drugs. When the shop was passed down to its third-generation and ultimately final owner, Katie Butt Beckort, she decided to simplify the name. Get right down to the bottom of things, as it were.
Butt Drugs was a popular spot, featuring an old-school soda fountain and themed souvenirs. According to Ms. Butt Beckort, people would come from miles away to buy “I love Butt Drugs” T-shirts, magnets, and so on. Yes, they knew perfectly well what they were sitting on.
So, if was such a hit, why did it close? Butt Drugs may have a hilarious name and merchandise to match, but the pharmacy portion of the pharmacy had been losing money for years. You know, the actual point of the business. As with so many things, we can blame it on the insurance companies. More than half the drugs that passed through Butt Drugs’ doors were sold at a loss, because the insurance companies refused to reimburse the store more than the wholesale price of the drug. Not even a good butt drug could clear up that financial diarrhea.
And so, we’ve lost Butt Drugs forever. Spicy food enthusiasts, coffee drinkers, and all patrons of Taco Bell, take a moment to reflect and mourn on what you’ve lost. No more Butt Drugs to relieve your suffering. A true kick in the butt indeed.
Proposal to cap Part B pay on some drugs draws opposition
An influential panel proposed capping Medicare Part B pay for some drugs, arguing this would remove financial incentives to use more costly medicines when there are less expensive equivalents.
Medical groups have objected to both this recommendation from the Medicare Payment Advisory Commission (MedPAC) and the panel’s underlying premise. MedPAC said financial as well as clinical factors can come into play in clinicians’ choices of drugs for patients.
In an interview, Christina Downey, MD, chair of the Government Affairs Committee of the American College of Rheumatology, said physicians in her field cannot switch patients’ medicines to try to make a profit.
“Patients only respond to the drugs that they respond to,” Dr. Downey said. “It’s frankly very insulting to say that physicians just force patients to go on medicines that are going to make them a bunch of money.”
In a June report to Congress, MedPAC recommended reducing the add-on payment for many drugs given in hospitals and clinics, which are thus covered by Part B, as part of a package of suggestions for addressing rising costs. Part B drug spending grew about 9% annually between 2009 and 2021, rising from $15.4 billion to $42.9 billion, MedPAC said.
Medicare’s current Part B drug pricing model starts with the reported average sales price (ASP) and then adds about 4.3% or 6%, depending on current budget-sequester law, to the cost of medicines.
MedPAC members voted 17-0 in April in favor of a general recommendation to revise the Part B payment approach. In the June report, MedPAC fleshes out this idea. It mentions a model in which the add-on Part B payment would be the lesser of either 6% of the ASP, 3% plus $24, or $220.
The majority of Part B drug administrations are for very low-priced drugs, MedPAC said. But for some of the more costly ones, annual prices can be more than $400,000 per patient, and future launch prices may be even higher for certain types of products, such as gene therapies, MedPAC said.
“There is no evidence that the costs of a drug’s administration are proportionate to the price of the drug,” MedPAC said.
Concerns about how well Medicare covers the cost of drug administration should be addressed through other pathways, such as the American Medical
Association’s Specialty Society Relative Value Scale Update Committee (RUC), MedPAC said. AMA’s RUC advises the Centers for Medicare & Medicaid Services on the physician fee schedule.
Congress is not obliged to act on or to even consider MedPAC’s work. In general, lawmakers and CMS often pay heed to the panel’s recommendations, sometimes incorporating them into new policy.
But this new MedPAC Part B recommendation has drawn strong opposition, similar to the response to a 2016 CMS plan to cut the Part B add-on payment. That plan, which CMS later abandoned, would have cut the markup on Part B drugs to 2.5% and added a flat fee to cover administration costs.
Why not focus on PBMs instead?
The timing of the MedPAC recommendation is poor, given that CMS already is trying to implement the Inflation Reduction Act and create a new system of direct Medicare drug price negotiations, as ordered by Congress, said Madelaine A. Feldman, MD, a rheumatologist based in New Orleans.
A better approach for lowering drug prices would be to focus more on the operations of pharmacy benefit managers (PBMs), said Dr. Feldman, who also is vice president for advocacy and government affairs for the Coalition of State Rheumatology Organizations. A pending bipartisan Senate bill, for example, would prohibit PBM compensation based on the price of a drug as a condition of entering into a contract with a Medicare Part D plan.
Congress needs to take steps to unlink the profits of PBMs from higher drug prices, Dr. Feldman said.
“Until that happens, we can put all the lipstick we want on this big pig, but it’s not going to really fix the problem,” she said.
Reduced pay for drugs acquired through 340B program?
In an interview about the new MedPAC proposal, Ted Okon, executive director of the Community Oncology Alliance, urged renewed attention to what he sees as unintended consequences of the 340B discount drug program.
Under this program, certain hospitals can acquire drugs at steeply reduced prices, but they are not obliged to share those discounts with patients. Hospitals that participate in the 340B program can gain funds when patients and their insurers, including Medicare, pay more for the medicines hospitals and other organizations acquired with the 340B discount. Hospitals say they use the money from the 340B program to expand resources in their communities.
But rapid growth of the program in recent years has led to questions, especially about the role of contract pharmacies that manage the program. Congress created the 340B program in 1992 as a workaround to then new rules on Medicaid drug coverage.
In 2021, participating hospitals and clinics and organizations purchased about $44 billion worth of medicines through the 340B drug program. This was an increase of 16% from the previous year, according to a report from the nonprofit Commonwealth Fund. The number of sites, including hospitals and pharmacies, enrolled in the 340B program rose from 8,100 in 2000 to 50,000 by 2020, the report said.
MedPAC in 2016 urged CMS to reduce the amount Medicare pays for drugs acquired through the 340B program. CMS did so during the Trump administration, a policy later defended by the Biden administration.
But the U.S. Supreme Court last year said Medicare erred in its approach to making this cut, as earlier reported. Federal law required that the Department of Health and Human Services conduct a survey to support such a step, and HHS did not do this, the court said. CMS thus was ordered to return Medicare to the ASP+6% payment model for drugs purchased through the 340B discount program.
In the June report, though, MedPAC stuck by its 2016 recommendation that Medicare reduce its payments for drugs purchased through the 340B discount program despite this setback.
“We continue to believe that this approach is appropriate, and the specific level of payment reduction could be considered further as newer data become available,” MedPAC said.
Hospital, PhRMA split
Hospitals would certainly contest any renewed bid by CMS to drop Medicare’s pay for drugs purchased through the 340B program. The American Hospital Association objected to the MedPAC proposal regarding the add-on payment in Part B drug pricing.
MedPAC commissioners discussed this idea at a January meeting, prompting a February letter from the AHA to the panel. Like Dr. Feldman, AHA said it would be “premature” to launch into a revision of Part B drug pricing while the impact of the IRA on drug prices was still unclear.
AHA also noted that a reduction in Part B drug reimbursement would “shift the responsibility for the rapid increase in drug prices away from drug manufacturers, and instead places the burden on hospitals and patients.”
But the AHA gave a much warmer reception to another proposal MedPAC considered this year and that it included in its June report, which is a plan to address the high cost of certain drugs of as yet unconfirmed clinical benefit.
In April, the AHA said it supports a move toward a “value-based approach” in certain cases in which first-in-class medicines are sold under U.S. Food and Drug Administration’s accelerated approvals. Medicare could then cap payment for such drugs that have excessively high launch prices and uncertain clinical benefit, AHA said.
In the June report, MedPAC recommended that Medicare be able to place such a limit on Part B payments in certain cases, including ones in which companies do not meet FDA deadlines for postmarketing confirmatory trials.
The Pharmaceutical Research and Manufacturers of America (PhRMA) objected to this proposed change. The trade group for drugmakers said the FDA often revises and extends enrollment milestones for pending confirmatory trials when companies hit snags, such as challenges in enrolling patients, PhRMA said.
Reducing Part B payment for drugs for which confirmatory trials have been delayed would have a “disproportionate impact” on smaller and rural communities, where independent practices struggle to keep their doors open as it is, PhRMA spokeswoman Nicole Longo wrote in a blog post.
“If physicians can’t afford to administer a medicine, then they won’t and that means their patients won’t have access to them either,” Ms. Longo wrote.
A version of this article first appeared on Medscape.com.
An influential panel proposed capping Medicare Part B pay for some drugs, arguing this would remove financial incentives to use more costly medicines when there are less expensive equivalents.
Medical groups have objected to both this recommendation from the Medicare Payment Advisory Commission (MedPAC) and the panel’s underlying premise. MedPAC said financial as well as clinical factors can come into play in clinicians’ choices of drugs for patients.
In an interview, Christina Downey, MD, chair of the Government Affairs Committee of the American College of Rheumatology, said physicians in her field cannot switch patients’ medicines to try to make a profit.
“Patients only respond to the drugs that they respond to,” Dr. Downey said. “It’s frankly very insulting to say that physicians just force patients to go on medicines that are going to make them a bunch of money.”
In a June report to Congress, MedPAC recommended reducing the add-on payment for many drugs given in hospitals and clinics, which are thus covered by Part B, as part of a package of suggestions for addressing rising costs. Part B drug spending grew about 9% annually between 2009 and 2021, rising from $15.4 billion to $42.9 billion, MedPAC said.
Medicare’s current Part B drug pricing model starts with the reported average sales price (ASP) and then adds about 4.3% or 6%, depending on current budget-sequester law, to the cost of medicines.
MedPAC members voted 17-0 in April in favor of a general recommendation to revise the Part B payment approach. In the June report, MedPAC fleshes out this idea. It mentions a model in which the add-on Part B payment would be the lesser of either 6% of the ASP, 3% plus $24, or $220.
The majority of Part B drug administrations are for very low-priced drugs, MedPAC said. But for some of the more costly ones, annual prices can be more than $400,000 per patient, and future launch prices may be even higher for certain types of products, such as gene therapies, MedPAC said.
“There is no evidence that the costs of a drug’s administration are proportionate to the price of the drug,” MedPAC said.
Concerns about how well Medicare covers the cost of drug administration should be addressed through other pathways, such as the American Medical
Association’s Specialty Society Relative Value Scale Update Committee (RUC), MedPAC said. AMA’s RUC advises the Centers for Medicare & Medicaid Services on the physician fee schedule.
Congress is not obliged to act on or to even consider MedPAC’s work. In general, lawmakers and CMS often pay heed to the panel’s recommendations, sometimes incorporating them into new policy.
But this new MedPAC Part B recommendation has drawn strong opposition, similar to the response to a 2016 CMS plan to cut the Part B add-on payment. That plan, which CMS later abandoned, would have cut the markup on Part B drugs to 2.5% and added a flat fee to cover administration costs.
Why not focus on PBMs instead?
The timing of the MedPAC recommendation is poor, given that CMS already is trying to implement the Inflation Reduction Act and create a new system of direct Medicare drug price negotiations, as ordered by Congress, said Madelaine A. Feldman, MD, a rheumatologist based in New Orleans.
A better approach for lowering drug prices would be to focus more on the operations of pharmacy benefit managers (PBMs), said Dr. Feldman, who also is vice president for advocacy and government affairs for the Coalition of State Rheumatology Organizations. A pending bipartisan Senate bill, for example, would prohibit PBM compensation based on the price of a drug as a condition of entering into a contract with a Medicare Part D plan.
Congress needs to take steps to unlink the profits of PBMs from higher drug prices, Dr. Feldman said.
“Until that happens, we can put all the lipstick we want on this big pig, but it’s not going to really fix the problem,” she said.
Reduced pay for drugs acquired through 340B program?
In an interview about the new MedPAC proposal, Ted Okon, executive director of the Community Oncology Alliance, urged renewed attention to what he sees as unintended consequences of the 340B discount drug program.
Under this program, certain hospitals can acquire drugs at steeply reduced prices, but they are not obliged to share those discounts with patients. Hospitals that participate in the 340B program can gain funds when patients and their insurers, including Medicare, pay more for the medicines hospitals and other organizations acquired with the 340B discount. Hospitals say they use the money from the 340B program to expand resources in their communities.
But rapid growth of the program in recent years has led to questions, especially about the role of contract pharmacies that manage the program. Congress created the 340B program in 1992 as a workaround to then new rules on Medicaid drug coverage.
In 2021, participating hospitals and clinics and organizations purchased about $44 billion worth of medicines through the 340B drug program. This was an increase of 16% from the previous year, according to a report from the nonprofit Commonwealth Fund. The number of sites, including hospitals and pharmacies, enrolled in the 340B program rose from 8,100 in 2000 to 50,000 by 2020, the report said.
MedPAC in 2016 urged CMS to reduce the amount Medicare pays for drugs acquired through the 340B program. CMS did so during the Trump administration, a policy later defended by the Biden administration.
But the U.S. Supreme Court last year said Medicare erred in its approach to making this cut, as earlier reported. Federal law required that the Department of Health and Human Services conduct a survey to support such a step, and HHS did not do this, the court said. CMS thus was ordered to return Medicare to the ASP+6% payment model for drugs purchased through the 340B discount program.
In the June report, though, MedPAC stuck by its 2016 recommendation that Medicare reduce its payments for drugs purchased through the 340B discount program despite this setback.
“We continue to believe that this approach is appropriate, and the specific level of payment reduction could be considered further as newer data become available,” MedPAC said.
Hospital, PhRMA split
Hospitals would certainly contest any renewed bid by CMS to drop Medicare’s pay for drugs purchased through the 340B program. The American Hospital Association objected to the MedPAC proposal regarding the add-on payment in Part B drug pricing.
MedPAC commissioners discussed this idea at a January meeting, prompting a February letter from the AHA to the panel. Like Dr. Feldman, AHA said it would be “premature” to launch into a revision of Part B drug pricing while the impact of the IRA on drug prices was still unclear.
AHA also noted that a reduction in Part B drug reimbursement would “shift the responsibility for the rapid increase in drug prices away from drug manufacturers, and instead places the burden on hospitals and patients.”
But the AHA gave a much warmer reception to another proposal MedPAC considered this year and that it included in its June report, which is a plan to address the high cost of certain drugs of as yet unconfirmed clinical benefit.
In April, the AHA said it supports a move toward a “value-based approach” in certain cases in which first-in-class medicines are sold under U.S. Food and Drug Administration’s accelerated approvals. Medicare could then cap payment for such drugs that have excessively high launch prices and uncertain clinical benefit, AHA said.
In the June report, MedPAC recommended that Medicare be able to place such a limit on Part B payments in certain cases, including ones in which companies do not meet FDA deadlines for postmarketing confirmatory trials.
The Pharmaceutical Research and Manufacturers of America (PhRMA) objected to this proposed change. The trade group for drugmakers said the FDA often revises and extends enrollment milestones for pending confirmatory trials when companies hit snags, such as challenges in enrolling patients, PhRMA said.
Reducing Part B payment for drugs for which confirmatory trials have been delayed would have a “disproportionate impact” on smaller and rural communities, where independent practices struggle to keep their doors open as it is, PhRMA spokeswoman Nicole Longo wrote in a blog post.
“If physicians can’t afford to administer a medicine, then they won’t and that means their patients won’t have access to them either,” Ms. Longo wrote.
A version of this article first appeared on Medscape.com.
An influential panel proposed capping Medicare Part B pay for some drugs, arguing this would remove financial incentives to use more costly medicines when there are less expensive equivalents.
Medical groups have objected to both this recommendation from the Medicare Payment Advisory Commission (MedPAC) and the panel’s underlying premise. MedPAC said financial as well as clinical factors can come into play in clinicians’ choices of drugs for patients.
In an interview, Christina Downey, MD, chair of the Government Affairs Committee of the American College of Rheumatology, said physicians in her field cannot switch patients’ medicines to try to make a profit.
“Patients only respond to the drugs that they respond to,” Dr. Downey said. “It’s frankly very insulting to say that physicians just force patients to go on medicines that are going to make them a bunch of money.”
In a June report to Congress, MedPAC recommended reducing the add-on payment for many drugs given in hospitals and clinics, which are thus covered by Part B, as part of a package of suggestions for addressing rising costs. Part B drug spending grew about 9% annually between 2009 and 2021, rising from $15.4 billion to $42.9 billion, MedPAC said.
Medicare’s current Part B drug pricing model starts with the reported average sales price (ASP) and then adds about 4.3% or 6%, depending on current budget-sequester law, to the cost of medicines.
MedPAC members voted 17-0 in April in favor of a general recommendation to revise the Part B payment approach. In the June report, MedPAC fleshes out this idea. It mentions a model in which the add-on Part B payment would be the lesser of either 6% of the ASP, 3% plus $24, or $220.
The majority of Part B drug administrations are for very low-priced drugs, MedPAC said. But for some of the more costly ones, annual prices can be more than $400,000 per patient, and future launch prices may be even higher for certain types of products, such as gene therapies, MedPAC said.
“There is no evidence that the costs of a drug’s administration are proportionate to the price of the drug,” MedPAC said.
Concerns about how well Medicare covers the cost of drug administration should be addressed through other pathways, such as the American Medical
Association’s Specialty Society Relative Value Scale Update Committee (RUC), MedPAC said. AMA’s RUC advises the Centers for Medicare & Medicaid Services on the physician fee schedule.
Congress is not obliged to act on or to even consider MedPAC’s work. In general, lawmakers and CMS often pay heed to the panel’s recommendations, sometimes incorporating them into new policy.
But this new MedPAC Part B recommendation has drawn strong opposition, similar to the response to a 2016 CMS plan to cut the Part B add-on payment. That plan, which CMS later abandoned, would have cut the markup on Part B drugs to 2.5% and added a flat fee to cover administration costs.
Why not focus on PBMs instead?
The timing of the MedPAC recommendation is poor, given that CMS already is trying to implement the Inflation Reduction Act and create a new system of direct Medicare drug price negotiations, as ordered by Congress, said Madelaine A. Feldman, MD, a rheumatologist based in New Orleans.
A better approach for lowering drug prices would be to focus more on the operations of pharmacy benefit managers (PBMs), said Dr. Feldman, who also is vice president for advocacy and government affairs for the Coalition of State Rheumatology Organizations. A pending bipartisan Senate bill, for example, would prohibit PBM compensation based on the price of a drug as a condition of entering into a contract with a Medicare Part D plan.
Congress needs to take steps to unlink the profits of PBMs from higher drug prices, Dr. Feldman said.
“Until that happens, we can put all the lipstick we want on this big pig, but it’s not going to really fix the problem,” she said.
Reduced pay for drugs acquired through 340B program?
In an interview about the new MedPAC proposal, Ted Okon, executive director of the Community Oncology Alliance, urged renewed attention to what he sees as unintended consequences of the 340B discount drug program.
Under this program, certain hospitals can acquire drugs at steeply reduced prices, but they are not obliged to share those discounts with patients. Hospitals that participate in the 340B program can gain funds when patients and their insurers, including Medicare, pay more for the medicines hospitals and other organizations acquired with the 340B discount. Hospitals say they use the money from the 340B program to expand resources in their communities.
But rapid growth of the program in recent years has led to questions, especially about the role of contract pharmacies that manage the program. Congress created the 340B program in 1992 as a workaround to then new rules on Medicaid drug coverage.
In 2021, participating hospitals and clinics and organizations purchased about $44 billion worth of medicines through the 340B drug program. This was an increase of 16% from the previous year, according to a report from the nonprofit Commonwealth Fund. The number of sites, including hospitals and pharmacies, enrolled in the 340B program rose from 8,100 in 2000 to 50,000 by 2020, the report said.
MedPAC in 2016 urged CMS to reduce the amount Medicare pays for drugs acquired through the 340B program. CMS did so during the Trump administration, a policy later defended by the Biden administration.
But the U.S. Supreme Court last year said Medicare erred in its approach to making this cut, as earlier reported. Federal law required that the Department of Health and Human Services conduct a survey to support such a step, and HHS did not do this, the court said. CMS thus was ordered to return Medicare to the ASP+6% payment model for drugs purchased through the 340B discount program.
In the June report, though, MedPAC stuck by its 2016 recommendation that Medicare reduce its payments for drugs purchased through the 340B discount program despite this setback.
“We continue to believe that this approach is appropriate, and the specific level of payment reduction could be considered further as newer data become available,” MedPAC said.
Hospital, PhRMA split
Hospitals would certainly contest any renewed bid by CMS to drop Medicare’s pay for drugs purchased through the 340B program. The American Hospital Association objected to the MedPAC proposal regarding the add-on payment in Part B drug pricing.
MedPAC commissioners discussed this idea at a January meeting, prompting a February letter from the AHA to the panel. Like Dr. Feldman, AHA said it would be “premature” to launch into a revision of Part B drug pricing while the impact of the IRA on drug prices was still unclear.
AHA also noted that a reduction in Part B drug reimbursement would “shift the responsibility for the rapid increase in drug prices away from drug manufacturers, and instead places the burden on hospitals and patients.”
But the AHA gave a much warmer reception to another proposal MedPAC considered this year and that it included in its June report, which is a plan to address the high cost of certain drugs of as yet unconfirmed clinical benefit.
In April, the AHA said it supports a move toward a “value-based approach” in certain cases in which first-in-class medicines are sold under U.S. Food and Drug Administration’s accelerated approvals. Medicare could then cap payment for such drugs that have excessively high launch prices and uncertain clinical benefit, AHA said.
In the June report, MedPAC recommended that Medicare be able to place such a limit on Part B payments in certain cases, including ones in which companies do not meet FDA deadlines for postmarketing confirmatory trials.
The Pharmaceutical Research and Manufacturers of America (PhRMA) objected to this proposed change. The trade group for drugmakers said the FDA often revises and extends enrollment milestones for pending confirmatory trials when companies hit snags, such as challenges in enrolling patients, PhRMA said.
Reducing Part B payment for drugs for which confirmatory trials have been delayed would have a “disproportionate impact” on smaller and rural communities, where independent practices struggle to keep their doors open as it is, PhRMA spokeswoman Nicole Longo wrote in a blog post.
“If physicians can’t afford to administer a medicine, then they won’t and that means their patients won’t have access to them either,” Ms. Longo wrote.
A version of this article first appeared on Medscape.com.
How physician-inventors create new, life-saving products
WakeMed emergency department physician and medical director, Graham Snyder, MD, has seen his fair share of deaths: an average of one or two per day. That’s part of the job. Some of the deaths were the result of risky behavior, ongoing health problems, and other natural causes.
But what he didn’t find acceptable was losing a 6-year-old girl in a backyard pool drowning at what was meant to be a celebratory birthday party and family reunion.
“There were aunts and uncles and brothers and sisters and cousins, and the pool was packed, and they’re having a great time. One of the parents looked over and saw that she was swimming around underneath but acting weird. A relative pulled her up by the arm, and she was dead,” he said. “What nobody could tell me, and what they’ll live with the rest of their life, is how long was she under water?”
So Dr. Snyder invented a solution. The catch: The goal: Improving systemic and “unsolvable” issues that harm society.
The cool part: Any MD with an idea can get in on the game.
Keeping little heads above water
Drowning is the leading cause of death in young children ages 1-4 years, and the second leading cause for children ages 5-14 years. The issue, Dr. Snyder explained, is not that rescuers couldn’t get to these children in time. “It’s that nobody knew to start looking.”
Dr. Snyder created a collar that alerts those around the swimmer that they are in trouble. The SEAL SwimSafe drowning prevention technology sets off an alarm system if a child is under water for too long. The necklace has been used to protect more than 10,000 children, including at larger swim facilities, such as the YMCA.
When Dr. Snyder first started pursuing his invention, he asked himself two key questions: “Has someone already tried this? And if they did, why did they not succeed?” These questions help counteract the potential arrogance, he says, with imagining that you are the first person to have a certain idea. And using whatever reason others didn’t succeed as your “secret sauce” helps lead to more success. He also had to consider obstacles. People might resist wearing a collar or necklace while swimming or putting one on their child, like the reluctance around wearing bicycle helmets when they gained popularity in the 1980s. He concluded that the collars would work best at larger facilities, where they were mandated.
Another obstacle was false alarms. “It was possible to trigger a false alarm, and that could really scare people,” Dr. Snyder said. He is still considering systems to prevent the collars from being stolen or from “13-year-old boys hiding them in the water drain and making everyone really scared when an alarm is going off.”
The demand is real, however, and is based on alarming data. Safe Kids has reported that 66% of natural water drownings and around half of pool drownings happened with an adult supervising. They added, however, that supervision is often lacking or insufficient, such as a parent not being within arm’s reach of a young kid. As Dr. Snyder told reporters in a 2018 story, even the most well-intentioned parents still “miss something” sometimes, and this technology is for that moment.
“This is a completely solvable problem, but not a flip-a-switch, one and done,” he said, pointing to his product as a part of a more comprehensive approach, such as in Europe, where mandated public school swimming lessons are helping to decrease drowning deaths.
The pandemic slowed progress for the SEAL SwimSafe collar, which is currently waiting on a new funder or investor to take the reins. But the concept is alive and well with competitors pursuing related ideas. Dr. Snyder is holding out hope that entrepreneurs, scientists, public health workers, researchers, and others will be interested in continuing this work.
Eliminating the stigma of incontinence
Ever had an accident before making it to the bathroom? So have two-thirds of adult women, and almost one-third of older men. Incontinence is linked to a wide variety of conditions, from pelvic-floor trauma to neurological issues to diabetes, and others. Urologist Jessica Lubahn, MD, in Portland, Ore., saw one too many patients feeling this type of shame, unaware that the condition was so common. In addition, she personally experienced childbirth-related incontinence, and helped a relative who was having incontinence after prostate cancer surgery.
“He had a great result, but he had confided in me ... it was one of the only times in his life that he’s been truly depressed,” Dr. Lubahn said. “It’s not even the amount of leakage, but the smell, the stigma is so embarrassing, that not only is it an inconvenience, but [it affects] your entire psyche.” She thought there had to be a better solution than the “demeaning” act of wearing adult diapers.
Noting the explosion of the period panty industry in the past decade, Dr. Lubahn wanted to “destigmatize” incontinence in the same way menstruation education and products have been. She created ONDR incontinence underwear, specifically meant for urine, to ease the mental and physical burden on her patients and many others.
Dr. Lubahn said a process happens when you decide to start talking about the product you want to make rather than trying to find answers on your own. “A lot of people are so afraid to talk about their ideas because they’re afraid it’s going to get stolen or scooped, or it might fail,” she said. “I just openly discussed it, kind of like cocktail party conversation – ‘Wouldn’t it be funny if you just pee into your underwear?’ ” She noticed each connection led to finding more people to help her along her journey.
Dr. Lubahn studied the apparel industry, learning that overseas manufacturers were more helpful and cost-effective. She navigated issues such as a special stitch that prevented leakage and other details. She was also intent on using eco-friendly products that offset the environmental impact of pads, liners, and diapers. She said there’s a strong entrepreneurship community that can help other physician-inventors get grants, be part of accelerator programs, and receive support.
Six years after the original idea, Dr. Lubahn’s product was released in 2020. She now sells eight types of underwear for women and men’s boxer briefs. She wears them herself daily.
Deterring carjackers, saving lives
In 2022, carjackings tripled in Chicago and Memphis. The areas have the highest rates in 30 cities that the Council on Criminal Justice analyzed in a report on pandemic crime rates. According to the report, nearly 40% of offenders used a firearm, more than a quarter of victims were injured, and only around half of the vehicles taken were recovered. In addition, vehicles are sometimes used in secondary crimes, such as drive-by shootings. William Yates, MD, former trauma surgeon, now turned hair restoration surgeon in Chicago, saw the evidence of those crimes daily.
“I was perplexed by carjacking because there wasn’t any answer, and it just kept getting worse and worse. A lot of innocent people were being affected,” he said. “I was seeing deaths – needless. If you give them any push back at all, they will shoot you.”
As a deterrent to counter this “easy crime,” he invented the Yates Device, an alarm system designed to prevent or interrupt carjacking. The driver can activate a switch located beneath the foot pedal or an app on the phone to trigger a programmed high-decibel alarm. Critically, it allows the carjacker to drive a safe distance away from the victim before it starts going off.
The alarm “turns your car into a very noisy Christmas tree on a time delay,” Dr. Yates explained. An external siren blares “stolen vehicle” repeatedly. A camera records everything in the car. Lights flash. Only the original driver can turn off the system. Later, once the car is abandoned, the police can help recover the vehicle.
In Dr. Yates’ experience, the invention process takes longer than you think. He worked through earlier iterations with strobe lights, but these could lead to bystanders getting hurt if the carjacker couldn’t see, for example. Developing the final product and applying for patents was a two-part process.
“The first is part is a pending patent phase, which secures your place in line,” he said. “After 1 year, we filed the utility patent as the final documentation that the invention is truly unique. That has been in process for a year now and the attorneys say we should receive approval soon.”
The product has initially been tested in seven cars for about 1 year. Dr. Yates is measuring how the system performs in all types of weather, including Chicago’s below-zero temperatures. The product is not available to the public for purchase yet because Dr. Yates is still seeking funding to have it mass produced, but it is currently being evaluated by Korean automakers for their car manufacturers.
“Everybody was saying ‘Let’s do something about this,’ but I didn’t see anybody doing anything yet,” Dr. Yates recalled. In the surgeon’s lounge, everybody has ideas. “You go around the room, and every doctor would have five ideas that would make them the richest doctor, but nobody takes it beyond that stage – talk. You have to synthesize that into a plan, to take action.”
Dr. Yates said that many doctors have the intellect to invent, but they aren’t in a network like entrepreneurs to bring their ideas to life.
For Dr. Yates, it takes a curious mindset to solve these daunting problems. “I’m always curious, always looking for how to improve something, to get better outcomes you have to be asking questions and just never let it go.”
A version of this article originally appeared on Medscape.com.
WakeMed emergency department physician and medical director, Graham Snyder, MD, has seen his fair share of deaths: an average of one or two per day. That’s part of the job. Some of the deaths were the result of risky behavior, ongoing health problems, and other natural causes.
But what he didn’t find acceptable was losing a 6-year-old girl in a backyard pool drowning at what was meant to be a celebratory birthday party and family reunion.
“There were aunts and uncles and brothers and sisters and cousins, and the pool was packed, and they’re having a great time. One of the parents looked over and saw that she was swimming around underneath but acting weird. A relative pulled her up by the arm, and she was dead,” he said. “What nobody could tell me, and what they’ll live with the rest of their life, is how long was she under water?”
So Dr. Snyder invented a solution. The catch: The goal: Improving systemic and “unsolvable” issues that harm society.
The cool part: Any MD with an idea can get in on the game.
Keeping little heads above water
Drowning is the leading cause of death in young children ages 1-4 years, and the second leading cause for children ages 5-14 years. The issue, Dr. Snyder explained, is not that rescuers couldn’t get to these children in time. “It’s that nobody knew to start looking.”
Dr. Snyder created a collar that alerts those around the swimmer that they are in trouble. The SEAL SwimSafe drowning prevention technology sets off an alarm system if a child is under water for too long. The necklace has been used to protect more than 10,000 children, including at larger swim facilities, such as the YMCA.
When Dr. Snyder first started pursuing his invention, he asked himself two key questions: “Has someone already tried this? And if they did, why did they not succeed?” These questions help counteract the potential arrogance, he says, with imagining that you are the first person to have a certain idea. And using whatever reason others didn’t succeed as your “secret sauce” helps lead to more success. He also had to consider obstacles. People might resist wearing a collar or necklace while swimming or putting one on their child, like the reluctance around wearing bicycle helmets when they gained popularity in the 1980s. He concluded that the collars would work best at larger facilities, where they were mandated.
Another obstacle was false alarms. “It was possible to trigger a false alarm, and that could really scare people,” Dr. Snyder said. He is still considering systems to prevent the collars from being stolen or from “13-year-old boys hiding them in the water drain and making everyone really scared when an alarm is going off.”
The demand is real, however, and is based on alarming data. Safe Kids has reported that 66% of natural water drownings and around half of pool drownings happened with an adult supervising. They added, however, that supervision is often lacking or insufficient, such as a parent not being within arm’s reach of a young kid. As Dr. Snyder told reporters in a 2018 story, even the most well-intentioned parents still “miss something” sometimes, and this technology is for that moment.
“This is a completely solvable problem, but not a flip-a-switch, one and done,” he said, pointing to his product as a part of a more comprehensive approach, such as in Europe, where mandated public school swimming lessons are helping to decrease drowning deaths.
The pandemic slowed progress for the SEAL SwimSafe collar, which is currently waiting on a new funder or investor to take the reins. But the concept is alive and well with competitors pursuing related ideas. Dr. Snyder is holding out hope that entrepreneurs, scientists, public health workers, researchers, and others will be interested in continuing this work.
Eliminating the stigma of incontinence
Ever had an accident before making it to the bathroom? So have two-thirds of adult women, and almost one-third of older men. Incontinence is linked to a wide variety of conditions, from pelvic-floor trauma to neurological issues to diabetes, and others. Urologist Jessica Lubahn, MD, in Portland, Ore., saw one too many patients feeling this type of shame, unaware that the condition was so common. In addition, she personally experienced childbirth-related incontinence, and helped a relative who was having incontinence after prostate cancer surgery.
“He had a great result, but he had confided in me ... it was one of the only times in his life that he’s been truly depressed,” Dr. Lubahn said. “It’s not even the amount of leakage, but the smell, the stigma is so embarrassing, that not only is it an inconvenience, but [it affects] your entire psyche.” She thought there had to be a better solution than the “demeaning” act of wearing adult diapers.
Noting the explosion of the period panty industry in the past decade, Dr. Lubahn wanted to “destigmatize” incontinence in the same way menstruation education and products have been. She created ONDR incontinence underwear, specifically meant for urine, to ease the mental and physical burden on her patients and many others.
Dr. Lubahn said a process happens when you decide to start talking about the product you want to make rather than trying to find answers on your own. “A lot of people are so afraid to talk about their ideas because they’re afraid it’s going to get stolen or scooped, or it might fail,” she said. “I just openly discussed it, kind of like cocktail party conversation – ‘Wouldn’t it be funny if you just pee into your underwear?’ ” She noticed each connection led to finding more people to help her along her journey.
Dr. Lubahn studied the apparel industry, learning that overseas manufacturers were more helpful and cost-effective. She navigated issues such as a special stitch that prevented leakage and other details. She was also intent on using eco-friendly products that offset the environmental impact of pads, liners, and diapers. She said there’s a strong entrepreneurship community that can help other physician-inventors get grants, be part of accelerator programs, and receive support.
Six years after the original idea, Dr. Lubahn’s product was released in 2020. She now sells eight types of underwear for women and men’s boxer briefs. She wears them herself daily.
Deterring carjackers, saving lives
In 2022, carjackings tripled in Chicago and Memphis. The areas have the highest rates in 30 cities that the Council on Criminal Justice analyzed in a report on pandemic crime rates. According to the report, nearly 40% of offenders used a firearm, more than a quarter of victims were injured, and only around half of the vehicles taken were recovered. In addition, vehicles are sometimes used in secondary crimes, such as drive-by shootings. William Yates, MD, former trauma surgeon, now turned hair restoration surgeon in Chicago, saw the evidence of those crimes daily.
“I was perplexed by carjacking because there wasn’t any answer, and it just kept getting worse and worse. A lot of innocent people were being affected,” he said. “I was seeing deaths – needless. If you give them any push back at all, they will shoot you.”
As a deterrent to counter this “easy crime,” he invented the Yates Device, an alarm system designed to prevent or interrupt carjacking. The driver can activate a switch located beneath the foot pedal or an app on the phone to trigger a programmed high-decibel alarm. Critically, it allows the carjacker to drive a safe distance away from the victim before it starts going off.
The alarm “turns your car into a very noisy Christmas tree on a time delay,” Dr. Yates explained. An external siren blares “stolen vehicle” repeatedly. A camera records everything in the car. Lights flash. Only the original driver can turn off the system. Later, once the car is abandoned, the police can help recover the vehicle.
In Dr. Yates’ experience, the invention process takes longer than you think. He worked through earlier iterations with strobe lights, but these could lead to bystanders getting hurt if the carjacker couldn’t see, for example. Developing the final product and applying for patents was a two-part process.
“The first is part is a pending patent phase, which secures your place in line,” he said. “After 1 year, we filed the utility patent as the final documentation that the invention is truly unique. That has been in process for a year now and the attorneys say we should receive approval soon.”
The product has initially been tested in seven cars for about 1 year. Dr. Yates is measuring how the system performs in all types of weather, including Chicago’s below-zero temperatures. The product is not available to the public for purchase yet because Dr. Yates is still seeking funding to have it mass produced, but it is currently being evaluated by Korean automakers for their car manufacturers.
“Everybody was saying ‘Let’s do something about this,’ but I didn’t see anybody doing anything yet,” Dr. Yates recalled. In the surgeon’s lounge, everybody has ideas. “You go around the room, and every doctor would have five ideas that would make them the richest doctor, but nobody takes it beyond that stage – talk. You have to synthesize that into a plan, to take action.”
Dr. Yates said that many doctors have the intellect to invent, but they aren’t in a network like entrepreneurs to bring their ideas to life.
For Dr. Yates, it takes a curious mindset to solve these daunting problems. “I’m always curious, always looking for how to improve something, to get better outcomes you have to be asking questions and just never let it go.”
A version of this article originally appeared on Medscape.com.
WakeMed emergency department physician and medical director, Graham Snyder, MD, has seen his fair share of deaths: an average of one or two per day. That’s part of the job. Some of the deaths were the result of risky behavior, ongoing health problems, and other natural causes.
But what he didn’t find acceptable was losing a 6-year-old girl in a backyard pool drowning at what was meant to be a celebratory birthday party and family reunion.
“There were aunts and uncles and brothers and sisters and cousins, and the pool was packed, and they’re having a great time. One of the parents looked over and saw that she was swimming around underneath but acting weird. A relative pulled her up by the arm, and she was dead,” he said. “What nobody could tell me, and what they’ll live with the rest of their life, is how long was she under water?”
So Dr. Snyder invented a solution. The catch: The goal: Improving systemic and “unsolvable” issues that harm society.
The cool part: Any MD with an idea can get in on the game.
Keeping little heads above water
Drowning is the leading cause of death in young children ages 1-4 years, and the second leading cause for children ages 5-14 years. The issue, Dr. Snyder explained, is not that rescuers couldn’t get to these children in time. “It’s that nobody knew to start looking.”
Dr. Snyder created a collar that alerts those around the swimmer that they are in trouble. The SEAL SwimSafe drowning prevention technology sets off an alarm system if a child is under water for too long. The necklace has been used to protect more than 10,000 children, including at larger swim facilities, such as the YMCA.
When Dr. Snyder first started pursuing his invention, he asked himself two key questions: “Has someone already tried this? And if they did, why did they not succeed?” These questions help counteract the potential arrogance, he says, with imagining that you are the first person to have a certain idea. And using whatever reason others didn’t succeed as your “secret sauce” helps lead to more success. He also had to consider obstacles. People might resist wearing a collar or necklace while swimming or putting one on their child, like the reluctance around wearing bicycle helmets when they gained popularity in the 1980s. He concluded that the collars would work best at larger facilities, where they were mandated.
Another obstacle was false alarms. “It was possible to trigger a false alarm, and that could really scare people,” Dr. Snyder said. He is still considering systems to prevent the collars from being stolen or from “13-year-old boys hiding them in the water drain and making everyone really scared when an alarm is going off.”
The demand is real, however, and is based on alarming data. Safe Kids has reported that 66% of natural water drownings and around half of pool drownings happened with an adult supervising. They added, however, that supervision is often lacking or insufficient, such as a parent not being within arm’s reach of a young kid. As Dr. Snyder told reporters in a 2018 story, even the most well-intentioned parents still “miss something” sometimes, and this technology is for that moment.
“This is a completely solvable problem, but not a flip-a-switch, one and done,” he said, pointing to his product as a part of a more comprehensive approach, such as in Europe, where mandated public school swimming lessons are helping to decrease drowning deaths.
The pandemic slowed progress for the SEAL SwimSafe collar, which is currently waiting on a new funder or investor to take the reins. But the concept is alive and well with competitors pursuing related ideas. Dr. Snyder is holding out hope that entrepreneurs, scientists, public health workers, researchers, and others will be interested in continuing this work.
Eliminating the stigma of incontinence
Ever had an accident before making it to the bathroom? So have two-thirds of adult women, and almost one-third of older men. Incontinence is linked to a wide variety of conditions, from pelvic-floor trauma to neurological issues to diabetes, and others. Urologist Jessica Lubahn, MD, in Portland, Ore., saw one too many patients feeling this type of shame, unaware that the condition was so common. In addition, she personally experienced childbirth-related incontinence, and helped a relative who was having incontinence after prostate cancer surgery.
“He had a great result, but he had confided in me ... it was one of the only times in his life that he’s been truly depressed,” Dr. Lubahn said. “It’s not even the amount of leakage, but the smell, the stigma is so embarrassing, that not only is it an inconvenience, but [it affects] your entire psyche.” She thought there had to be a better solution than the “demeaning” act of wearing adult diapers.
Noting the explosion of the period panty industry in the past decade, Dr. Lubahn wanted to “destigmatize” incontinence in the same way menstruation education and products have been. She created ONDR incontinence underwear, specifically meant for urine, to ease the mental and physical burden on her patients and many others.
Dr. Lubahn said a process happens when you decide to start talking about the product you want to make rather than trying to find answers on your own. “A lot of people are so afraid to talk about their ideas because they’re afraid it’s going to get stolen or scooped, or it might fail,” she said. “I just openly discussed it, kind of like cocktail party conversation – ‘Wouldn’t it be funny if you just pee into your underwear?’ ” She noticed each connection led to finding more people to help her along her journey.
Dr. Lubahn studied the apparel industry, learning that overseas manufacturers were more helpful and cost-effective. She navigated issues such as a special stitch that prevented leakage and other details. She was also intent on using eco-friendly products that offset the environmental impact of pads, liners, and diapers. She said there’s a strong entrepreneurship community that can help other physician-inventors get grants, be part of accelerator programs, and receive support.
Six years after the original idea, Dr. Lubahn’s product was released in 2020. She now sells eight types of underwear for women and men’s boxer briefs. She wears them herself daily.
Deterring carjackers, saving lives
In 2022, carjackings tripled in Chicago and Memphis. The areas have the highest rates in 30 cities that the Council on Criminal Justice analyzed in a report on pandemic crime rates. According to the report, nearly 40% of offenders used a firearm, more than a quarter of victims were injured, and only around half of the vehicles taken were recovered. In addition, vehicles are sometimes used in secondary crimes, such as drive-by shootings. William Yates, MD, former trauma surgeon, now turned hair restoration surgeon in Chicago, saw the evidence of those crimes daily.
“I was perplexed by carjacking because there wasn’t any answer, and it just kept getting worse and worse. A lot of innocent people were being affected,” he said. “I was seeing deaths – needless. If you give them any push back at all, they will shoot you.”
As a deterrent to counter this “easy crime,” he invented the Yates Device, an alarm system designed to prevent or interrupt carjacking. The driver can activate a switch located beneath the foot pedal or an app on the phone to trigger a programmed high-decibel alarm. Critically, it allows the carjacker to drive a safe distance away from the victim before it starts going off.
The alarm “turns your car into a very noisy Christmas tree on a time delay,” Dr. Yates explained. An external siren blares “stolen vehicle” repeatedly. A camera records everything in the car. Lights flash. Only the original driver can turn off the system. Later, once the car is abandoned, the police can help recover the vehicle.
In Dr. Yates’ experience, the invention process takes longer than you think. He worked through earlier iterations with strobe lights, but these could lead to bystanders getting hurt if the carjacker couldn’t see, for example. Developing the final product and applying for patents was a two-part process.
“The first is part is a pending patent phase, which secures your place in line,” he said. “After 1 year, we filed the utility patent as the final documentation that the invention is truly unique. That has been in process for a year now and the attorneys say we should receive approval soon.”
The product has initially been tested in seven cars for about 1 year. Dr. Yates is measuring how the system performs in all types of weather, including Chicago’s below-zero temperatures. The product is not available to the public for purchase yet because Dr. Yates is still seeking funding to have it mass produced, but it is currently being evaluated by Korean automakers for their car manufacturers.
“Everybody was saying ‘Let’s do something about this,’ but I didn’t see anybody doing anything yet,” Dr. Yates recalled. In the surgeon’s lounge, everybody has ideas. “You go around the room, and every doctor would have five ideas that would make them the richest doctor, but nobody takes it beyond that stage – talk. You have to synthesize that into a plan, to take action.”
Dr. Yates said that many doctors have the intellect to invent, but they aren’t in a network like entrepreneurs to bring their ideas to life.
For Dr. Yates, it takes a curious mindset to solve these daunting problems. “I’m always curious, always looking for how to improve something, to get better outcomes you have to be asking questions and just never let it go.”
A version of this article originally appeared on Medscape.com.
Cutting-edge nasal tech could usher in a new era of medicine
Noses are like caverns – twisting, turning, no two exactly the same. But if you nose past anyone’s nostrils, you’ll discover a surprisingly sprawling space.
“The size of the nasal cavity is about the same as a large handkerchief,” said Hugh Smyth, PhD, a professor of molecular pharmaceutics and drug delivery at the University of Texas at Austin.
“It’s very accessible tissue, and it has a lot of blood flow,” said Dr. Smyth. “The speed of onset can often be as fast as injections, sometimes even faster.”
It’s nothing new to get medicines via your nose. For decades, we’ve squirted various sprays into our nostrils to treat local maladies like allergies or infections. Even the ancients saw wisdom in the nasal route.
But recently, the nose has gained scientific attention as a gateway to the rest of the body – even the brain, a notoriously difficult target.
The upshot: Someday, inhaling therapies could be as routine as swallowing pills.
The nasal route is quick, needle free, and user friendly, and it often requires a smaller dose than other methods, since the drug doesn’t have to pass through the digestive tract, losing potency during digestion.
But there are challenges.
How hard can it be?
Old-school nasal sprayers, mostly unchanged since the 1800s, aren’t cut out for deep-nose delivery. “The technology is relatively limited because you’ve just got a single spray nozzle,” said Michael Hindle, PhD, a professor of pharmaceutics at Virginia Commonwealth University, Richmond.
These traditional devices (similar to perfume sprayers) don’t consistently push meds past the lower to middle sections inside the nose, called the nasal valve – if they do so at all: In a 2020 Rhinology study (doi: 10.4193/Rhin18.304) conventional nasal sprays only reached this first segment of the nose, a less-than-ideal spot to land.
Inside the nasal valve, the surface is skin-like and doesn’t absorb very well. Its narrow design slows airflow, preventing particles from moving to deeper regions, where tissue is vascular and porous like the lungs. And even if this structural roadblock is surpassed, other hurdles remain.
The nose is designed to keep stuff out. Nose hair, cilia, mucus, sneezing, coughing – all make “distributing drugs evenly across the nasal cavity difficult,” said Dr. Smyth. “The spray gets filtered out before it reaches those deeper zones,” potentially dripping out of the nostrils instead of being absorbed.
Complicating matters is how every person’s nose is different. In a 2018 study, Dr. Smyth and a research team created three dimensional–printed models of people’s nasal cavities. They varied widely. “Nasal cavities are very different in size, length, and internal geometry,” he said. “This makes it challenging to target specific areas.”
Although carefully positioning the spray nozzle can help, even something as minor as sniffing too hard (constricting the nostrils) can keep sprays from reaching the absorptive deeper regions.
Still, the benefits are enough to compel researchers to find a way in.
“This really is a drug delivery challenge we’ve been wrestling with,” said Dr. Hindle. “It’s not new formulations we hear about. It’s new devices and delivery methods trying to target the different nasal regions.”
Delivering the goods
In the late aughts, John Hoekman was a graduate student in the University of Washington’s pharmaceutics program, studying nasal drug delivery. In his experiments, he noticed that drugs distributed differently, depending on the region targeted – aiming for the upper nasal cavity led to a spike in absorption.
The results convinced Mr. Hoekman to stake his future on nasal drug delivery.
In 2008, while still in graduate school, he started his own company, now known as Impel Pharmaceuticals. In 2021, Impel released its first product: Trudhesa, a nasal spray for migraines. Although the drug itself – dihydroergotamine mesylate – was hardly novel, used for migraine relief since 1946 (Headache. 2020 Jan;60[1]:40-57), it was usually delivered through an intravenous line, often in the ED.
But with Mr. Hoekman’s POD device – short for precision olfactory delivery – the drug can be given by the patient, via the nose. This generally means faster, more reliable relief, with fewer side effects. “We were able to lower the dose and improve the overall absorption,” said Mr. Hoekman.
The POD’s nozzle is engineered to spray a soft, narrow plume. It’s gas propelled, so patients don’t have to breathe in any special way to ensure delivery. The drug can zip right through the nasal valve into the upper nasal cavity.
Another company – OptiNose – has a “bidirectional” delivery method that propels drugs, either liquid or dry powder, deep into the nose.
“You insert the nozzle into your nose, and as you blow through the mouthpiece, your soft palate closes,” said Dr. Hindle. With the throat sealed off, “the only place for the drug to go is into one nostril and out the other, coating both sides of the nasal passageways.”
The device is only available for Onzetra Xsail, a powder for migraines. But another application is on its way.
In May, OptiNose announced that the FDA is reviewing Xhance, which uses the system to direct a steroid to the sinuses. In a clinical trial, patients with chronic sinusitis who tried the drug-device combo saw a decline in congestion, facial pain, and inflammation.
Targeting the brain
Both of those migraine drugs – Trudhesa and Onzetra Xsail – are thought to penetrate the upper nasal cavity. That’s where you’ll find the olfactory zone, a sheet of neurons that connects to the olfactory bulb. Located behind the eyes, these two nerve bundles detect odors.
“The olfactory region is almost like a back door to the brain,” said Mr. Hoekman.
By bypassing the blood-brain barrier, it offers a direct pathway – the only direct pathway, actually – between an exposed area of the body and the brain. Meaning it can ferry drugs straight from the nasal cavity to the central nervous system.
Nose-to-brain treatments could be game-changing for central nervous system disorders, such as Parkinson’s disease, Alzheimer’s, or anxiety.
But reaching the olfactory zone is notoriously hard. “The vasculature in your nose is like a big freeway, and the olfactory tract is like a side alley,” explained Mr. Hoekman. “It’s very limiting in what it will allow through.” The region is also small, occupying only 3%-10% of the nasal cavity’s surface area.
Again, POD means “precision olfactory delivery.” But the device isn’t quite as laser focused on the region as its name implies. “We’re not at the stage where we’re able to exclusively deliver to one target site in the nose,” said Dr. Hindle.
While wending its way toward the olfactory zone, some of the drug will be absorbed by other regions, then circulate throughout the body.
“About 59% of the drug that we put into the upper nasal space gets absorbed into the bloodstream,” said Mr. Hoekman.
Janssen Pharmaceuticals’ Spravato – a nasal spray for drug-resistant depression – is thought to work similarly: Some goes straight to the brain via the olfactory nerves, while the rest takes a more roundabout route, passing through the blood vessels to circulate in your system.
A needle-free option
Sometimes, the bloodstream is the main target. Because the nose’s middle and upper stretches are so vascular, drugs can be rapidly absorbed.
This is especially valuable for time-sensitive conditions. “If you give something nasally, you can have peak uptake in 15-30 minutes,” said Mr. Hoekman.
Take Narcan nasal spray, which delivers a burst of naloxone to quickly reverse the effects of opioid an overdose. Or Noctiva nasal spray. Taken just half an hour before bed, it can prevent frequent nighttime urination.
There’s also a group of seizure-stopping sprays, known as “rescue treatments.” One works by temporarily loosening the space between nasal cells, allowing the seizure drug to be quickly absorbed through the vessels.
This systemic access also has potential for drugs that would otherwise have to be injected, such as biologics.
The same goes for vaccines. Mucosal tissue inside the nasal cavity offers direct access to the infection-fighting lymphatic system, making the nose a prime target for inoculation against certain viruses.
Inhaling protection against viruses
Despite the recent surge of interest, nasal vaccines faced a rocky start. After the first nasal flu vaccine hit the market in 2001, it was pulled due to potential toxicity and reports of Bell’s palsy, a type of facial paralysis.
FluMist came in 2003 and has been plagued by problems ever since. Because it contains a weakened live virus, flu-like side effects can occur. And it doesn’t always work. During the 2016-2017 flu season, FluMist protected only 3% of kids, prompting the Centers for Disease Control and Prevention to advise against the nasal route that year.
Why FluMist can be so hit-or-miss is poorly understood. But generally, the nose can pose an effectiveness challenge. “The nose is highly cycling,” said Dr. Hindle. “Anything we deposit usually gets transported out within 15-20 minutes.”
For kids – big fans of not using needles – chronically runny noses can be an issue. “You squirt it in the nose, and it will probably just come back out in their snot,” said Jay Kolls, MD, a professor of medicine and pediatrics at Tulane University, New Orleans, who is developing an intranasal pneumonia vaccine.
Even so, nasal vaccines became a hot topic among researchers after the world was shut down by a virus that invades through the nose.
“We realized that intramuscular vaccines were effective at preventing severe disease, but they weren’t that effective at preventing transmission,” said Michael Diamond, MD, PhD, an immunologist at Washington University in St. Louis.
Nasal vaccines could solve that problem by putting an immune barrier at the point of entry, denying access to the rest of the body. “You squash the infection early enough that it not only prevents disease,” said Dr. Kolls, “but potentially prevents transmission.”
And yes, a nasal COVID vaccine is on the way
In March 2020, Dr. Diamond’s team began exploring a nasal COVID vaccine. Promising results in animals prompted a vaccine development company to license the technology. The resulting nasal vaccine – the first for COVID – has been approved in India, both as a primary vaccine and a booster.
It works by stimulating an influx of IgA, a type of antibody found in the nasal passages, and production of resident memory T cells, immune cells on standby just beneath the surface tissue in the nose.
By contrast, injected vaccines generate mostly IgG antibodies, which struggle to enter the respiratory tract. Only a tiny fraction – an estimated 1% – typically reach the nose.
Nasal vaccines could also be used along with shots. The latter could prime the whole body to fight back, while a nasal spritz could pull that immune protection to the mucosal surfaces.
Nasal technology could yield more effective vaccines for infections like tuberculosis or malaria, or even safeguard against new – sometimes surprising – conditions.
In a 2021 Nature study, an intranasal vaccine derived from fentanyl was better at preventing overdose than an injected vaccine. “Through some clever chemistry, the drug [in the vaccine] isn’t fentanyl anymore,” said study author Elizabeth Norton, PhD, an assistant professor of microbiology and immunology at Tulane University. “But the immune system still has an antibody response to it.”
Novel applications like this represent the future of nasal drug delivery.
“We’re not going to innovate in asthma or COPD. We’re not going to innovate in local delivery to the nose,” said Dr. Hindle. “Innovation will only come if we look to treat new conditions.”
A version of this article originally appeared on WebMD.com.
Noses are like caverns – twisting, turning, no two exactly the same. But if you nose past anyone’s nostrils, you’ll discover a surprisingly sprawling space.
“The size of the nasal cavity is about the same as a large handkerchief,” said Hugh Smyth, PhD, a professor of molecular pharmaceutics and drug delivery at the University of Texas at Austin.
“It’s very accessible tissue, and it has a lot of blood flow,” said Dr. Smyth. “The speed of onset can often be as fast as injections, sometimes even faster.”
It’s nothing new to get medicines via your nose. For decades, we’ve squirted various sprays into our nostrils to treat local maladies like allergies or infections. Even the ancients saw wisdom in the nasal route.
But recently, the nose has gained scientific attention as a gateway to the rest of the body – even the brain, a notoriously difficult target.
The upshot: Someday, inhaling therapies could be as routine as swallowing pills.
The nasal route is quick, needle free, and user friendly, and it often requires a smaller dose than other methods, since the drug doesn’t have to pass through the digestive tract, losing potency during digestion.
But there are challenges.
How hard can it be?
Old-school nasal sprayers, mostly unchanged since the 1800s, aren’t cut out for deep-nose delivery. “The technology is relatively limited because you’ve just got a single spray nozzle,” said Michael Hindle, PhD, a professor of pharmaceutics at Virginia Commonwealth University, Richmond.
These traditional devices (similar to perfume sprayers) don’t consistently push meds past the lower to middle sections inside the nose, called the nasal valve – if they do so at all: In a 2020 Rhinology study (doi: 10.4193/Rhin18.304) conventional nasal sprays only reached this first segment of the nose, a less-than-ideal spot to land.
Inside the nasal valve, the surface is skin-like and doesn’t absorb very well. Its narrow design slows airflow, preventing particles from moving to deeper regions, where tissue is vascular and porous like the lungs. And even if this structural roadblock is surpassed, other hurdles remain.
The nose is designed to keep stuff out. Nose hair, cilia, mucus, sneezing, coughing – all make “distributing drugs evenly across the nasal cavity difficult,” said Dr. Smyth. “The spray gets filtered out before it reaches those deeper zones,” potentially dripping out of the nostrils instead of being absorbed.
Complicating matters is how every person’s nose is different. In a 2018 study, Dr. Smyth and a research team created three dimensional–printed models of people’s nasal cavities. They varied widely. “Nasal cavities are very different in size, length, and internal geometry,” he said. “This makes it challenging to target specific areas.”
Although carefully positioning the spray nozzle can help, even something as minor as sniffing too hard (constricting the nostrils) can keep sprays from reaching the absorptive deeper regions.
Still, the benefits are enough to compel researchers to find a way in.
“This really is a drug delivery challenge we’ve been wrestling with,” said Dr. Hindle. “It’s not new formulations we hear about. It’s new devices and delivery methods trying to target the different nasal regions.”
Delivering the goods
In the late aughts, John Hoekman was a graduate student in the University of Washington’s pharmaceutics program, studying nasal drug delivery. In his experiments, he noticed that drugs distributed differently, depending on the region targeted – aiming for the upper nasal cavity led to a spike in absorption.
The results convinced Mr. Hoekman to stake his future on nasal drug delivery.
In 2008, while still in graduate school, he started his own company, now known as Impel Pharmaceuticals. In 2021, Impel released its first product: Trudhesa, a nasal spray for migraines. Although the drug itself – dihydroergotamine mesylate – was hardly novel, used for migraine relief since 1946 (Headache. 2020 Jan;60[1]:40-57), it was usually delivered through an intravenous line, often in the ED.
But with Mr. Hoekman’s POD device – short for precision olfactory delivery – the drug can be given by the patient, via the nose. This generally means faster, more reliable relief, with fewer side effects. “We were able to lower the dose and improve the overall absorption,” said Mr. Hoekman.
The POD’s nozzle is engineered to spray a soft, narrow plume. It’s gas propelled, so patients don’t have to breathe in any special way to ensure delivery. The drug can zip right through the nasal valve into the upper nasal cavity.
Another company – OptiNose – has a “bidirectional” delivery method that propels drugs, either liquid or dry powder, deep into the nose.
“You insert the nozzle into your nose, and as you blow through the mouthpiece, your soft palate closes,” said Dr. Hindle. With the throat sealed off, “the only place for the drug to go is into one nostril and out the other, coating both sides of the nasal passageways.”
The device is only available for Onzetra Xsail, a powder for migraines. But another application is on its way.
In May, OptiNose announced that the FDA is reviewing Xhance, which uses the system to direct a steroid to the sinuses. In a clinical trial, patients with chronic sinusitis who tried the drug-device combo saw a decline in congestion, facial pain, and inflammation.
Targeting the brain
Both of those migraine drugs – Trudhesa and Onzetra Xsail – are thought to penetrate the upper nasal cavity. That’s where you’ll find the olfactory zone, a sheet of neurons that connects to the olfactory bulb. Located behind the eyes, these two nerve bundles detect odors.
“The olfactory region is almost like a back door to the brain,” said Mr. Hoekman.
By bypassing the blood-brain barrier, it offers a direct pathway – the only direct pathway, actually – between an exposed area of the body and the brain. Meaning it can ferry drugs straight from the nasal cavity to the central nervous system.
Nose-to-brain treatments could be game-changing for central nervous system disorders, such as Parkinson’s disease, Alzheimer’s, or anxiety.
But reaching the olfactory zone is notoriously hard. “The vasculature in your nose is like a big freeway, and the olfactory tract is like a side alley,” explained Mr. Hoekman. “It’s very limiting in what it will allow through.” The region is also small, occupying only 3%-10% of the nasal cavity’s surface area.
Again, POD means “precision olfactory delivery.” But the device isn’t quite as laser focused on the region as its name implies. “We’re not at the stage where we’re able to exclusively deliver to one target site in the nose,” said Dr. Hindle.
While wending its way toward the olfactory zone, some of the drug will be absorbed by other regions, then circulate throughout the body.
“About 59% of the drug that we put into the upper nasal space gets absorbed into the bloodstream,” said Mr. Hoekman.
Janssen Pharmaceuticals’ Spravato – a nasal spray for drug-resistant depression – is thought to work similarly: Some goes straight to the brain via the olfactory nerves, while the rest takes a more roundabout route, passing through the blood vessels to circulate in your system.
A needle-free option
Sometimes, the bloodstream is the main target. Because the nose’s middle and upper stretches are so vascular, drugs can be rapidly absorbed.
This is especially valuable for time-sensitive conditions. “If you give something nasally, you can have peak uptake in 15-30 minutes,” said Mr. Hoekman.
Take Narcan nasal spray, which delivers a burst of naloxone to quickly reverse the effects of opioid an overdose. Or Noctiva nasal spray. Taken just half an hour before bed, it can prevent frequent nighttime urination.
There’s also a group of seizure-stopping sprays, known as “rescue treatments.” One works by temporarily loosening the space between nasal cells, allowing the seizure drug to be quickly absorbed through the vessels.
This systemic access also has potential for drugs that would otherwise have to be injected, such as biologics.
The same goes for vaccines. Mucosal tissue inside the nasal cavity offers direct access to the infection-fighting lymphatic system, making the nose a prime target for inoculation against certain viruses.
Inhaling protection against viruses
Despite the recent surge of interest, nasal vaccines faced a rocky start. After the first nasal flu vaccine hit the market in 2001, it was pulled due to potential toxicity and reports of Bell’s palsy, a type of facial paralysis.
FluMist came in 2003 and has been plagued by problems ever since. Because it contains a weakened live virus, flu-like side effects can occur. And it doesn’t always work. During the 2016-2017 flu season, FluMist protected only 3% of kids, prompting the Centers for Disease Control and Prevention to advise against the nasal route that year.
Why FluMist can be so hit-or-miss is poorly understood. But generally, the nose can pose an effectiveness challenge. “The nose is highly cycling,” said Dr. Hindle. “Anything we deposit usually gets transported out within 15-20 minutes.”
For kids – big fans of not using needles – chronically runny noses can be an issue. “You squirt it in the nose, and it will probably just come back out in their snot,” said Jay Kolls, MD, a professor of medicine and pediatrics at Tulane University, New Orleans, who is developing an intranasal pneumonia vaccine.
Even so, nasal vaccines became a hot topic among researchers after the world was shut down by a virus that invades through the nose.
“We realized that intramuscular vaccines were effective at preventing severe disease, but they weren’t that effective at preventing transmission,” said Michael Diamond, MD, PhD, an immunologist at Washington University in St. Louis.
Nasal vaccines could solve that problem by putting an immune barrier at the point of entry, denying access to the rest of the body. “You squash the infection early enough that it not only prevents disease,” said Dr. Kolls, “but potentially prevents transmission.”
And yes, a nasal COVID vaccine is on the way
In March 2020, Dr. Diamond’s team began exploring a nasal COVID vaccine. Promising results in animals prompted a vaccine development company to license the technology. The resulting nasal vaccine – the first for COVID – has been approved in India, both as a primary vaccine and a booster.
It works by stimulating an influx of IgA, a type of antibody found in the nasal passages, and production of resident memory T cells, immune cells on standby just beneath the surface tissue in the nose.
By contrast, injected vaccines generate mostly IgG antibodies, which struggle to enter the respiratory tract. Only a tiny fraction – an estimated 1% – typically reach the nose.
Nasal vaccines could also be used along with shots. The latter could prime the whole body to fight back, while a nasal spritz could pull that immune protection to the mucosal surfaces.
Nasal technology could yield more effective vaccines for infections like tuberculosis or malaria, or even safeguard against new – sometimes surprising – conditions.
In a 2021 Nature study, an intranasal vaccine derived from fentanyl was better at preventing overdose than an injected vaccine. “Through some clever chemistry, the drug [in the vaccine] isn’t fentanyl anymore,” said study author Elizabeth Norton, PhD, an assistant professor of microbiology and immunology at Tulane University. “But the immune system still has an antibody response to it.”
Novel applications like this represent the future of nasal drug delivery.
“We’re not going to innovate in asthma or COPD. We’re not going to innovate in local delivery to the nose,” said Dr. Hindle. “Innovation will only come if we look to treat new conditions.”
A version of this article originally appeared on WebMD.com.
Noses are like caverns – twisting, turning, no two exactly the same. But if you nose past anyone’s nostrils, you’ll discover a surprisingly sprawling space.
“The size of the nasal cavity is about the same as a large handkerchief,” said Hugh Smyth, PhD, a professor of molecular pharmaceutics and drug delivery at the University of Texas at Austin.
“It’s very accessible tissue, and it has a lot of blood flow,” said Dr. Smyth. “The speed of onset can often be as fast as injections, sometimes even faster.”
It’s nothing new to get medicines via your nose. For decades, we’ve squirted various sprays into our nostrils to treat local maladies like allergies or infections. Even the ancients saw wisdom in the nasal route.
But recently, the nose has gained scientific attention as a gateway to the rest of the body – even the brain, a notoriously difficult target.
The upshot: Someday, inhaling therapies could be as routine as swallowing pills.
The nasal route is quick, needle free, and user friendly, and it often requires a smaller dose than other methods, since the drug doesn’t have to pass through the digestive tract, losing potency during digestion.
But there are challenges.
How hard can it be?
Old-school nasal sprayers, mostly unchanged since the 1800s, aren’t cut out for deep-nose delivery. “The technology is relatively limited because you’ve just got a single spray nozzle,” said Michael Hindle, PhD, a professor of pharmaceutics at Virginia Commonwealth University, Richmond.
These traditional devices (similar to perfume sprayers) don’t consistently push meds past the lower to middle sections inside the nose, called the nasal valve – if they do so at all: In a 2020 Rhinology study (doi: 10.4193/Rhin18.304) conventional nasal sprays only reached this first segment of the nose, a less-than-ideal spot to land.
Inside the nasal valve, the surface is skin-like and doesn’t absorb very well. Its narrow design slows airflow, preventing particles from moving to deeper regions, where tissue is vascular and porous like the lungs. And even if this structural roadblock is surpassed, other hurdles remain.
The nose is designed to keep stuff out. Nose hair, cilia, mucus, sneezing, coughing – all make “distributing drugs evenly across the nasal cavity difficult,” said Dr. Smyth. “The spray gets filtered out before it reaches those deeper zones,” potentially dripping out of the nostrils instead of being absorbed.
Complicating matters is how every person’s nose is different. In a 2018 study, Dr. Smyth and a research team created three dimensional–printed models of people’s nasal cavities. They varied widely. “Nasal cavities are very different in size, length, and internal geometry,” he said. “This makes it challenging to target specific areas.”
Although carefully positioning the spray nozzle can help, even something as minor as sniffing too hard (constricting the nostrils) can keep sprays from reaching the absorptive deeper regions.
Still, the benefits are enough to compel researchers to find a way in.
“This really is a drug delivery challenge we’ve been wrestling with,” said Dr. Hindle. “It’s not new formulations we hear about. It’s new devices and delivery methods trying to target the different nasal regions.”
Delivering the goods
In the late aughts, John Hoekman was a graduate student in the University of Washington’s pharmaceutics program, studying nasal drug delivery. In his experiments, he noticed that drugs distributed differently, depending on the region targeted – aiming for the upper nasal cavity led to a spike in absorption.
The results convinced Mr. Hoekman to stake his future on nasal drug delivery.
In 2008, while still in graduate school, he started his own company, now known as Impel Pharmaceuticals. In 2021, Impel released its first product: Trudhesa, a nasal spray for migraines. Although the drug itself – dihydroergotamine mesylate – was hardly novel, used for migraine relief since 1946 (Headache. 2020 Jan;60[1]:40-57), it was usually delivered through an intravenous line, often in the ED.
But with Mr. Hoekman’s POD device – short for precision olfactory delivery – the drug can be given by the patient, via the nose. This generally means faster, more reliable relief, with fewer side effects. “We were able to lower the dose and improve the overall absorption,” said Mr. Hoekman.
The POD’s nozzle is engineered to spray a soft, narrow plume. It’s gas propelled, so patients don’t have to breathe in any special way to ensure delivery. The drug can zip right through the nasal valve into the upper nasal cavity.
Another company – OptiNose – has a “bidirectional” delivery method that propels drugs, either liquid or dry powder, deep into the nose.
“You insert the nozzle into your nose, and as you blow through the mouthpiece, your soft palate closes,” said Dr. Hindle. With the throat sealed off, “the only place for the drug to go is into one nostril and out the other, coating both sides of the nasal passageways.”
The device is only available for Onzetra Xsail, a powder for migraines. But another application is on its way.
In May, OptiNose announced that the FDA is reviewing Xhance, which uses the system to direct a steroid to the sinuses. In a clinical trial, patients with chronic sinusitis who tried the drug-device combo saw a decline in congestion, facial pain, and inflammation.
Targeting the brain
Both of those migraine drugs – Trudhesa and Onzetra Xsail – are thought to penetrate the upper nasal cavity. That’s where you’ll find the olfactory zone, a sheet of neurons that connects to the olfactory bulb. Located behind the eyes, these two nerve bundles detect odors.
“The olfactory region is almost like a back door to the brain,” said Mr. Hoekman.
By bypassing the blood-brain barrier, it offers a direct pathway – the only direct pathway, actually – between an exposed area of the body and the brain. Meaning it can ferry drugs straight from the nasal cavity to the central nervous system.
Nose-to-brain treatments could be game-changing for central nervous system disorders, such as Parkinson’s disease, Alzheimer’s, or anxiety.
But reaching the olfactory zone is notoriously hard. “The vasculature in your nose is like a big freeway, and the olfactory tract is like a side alley,” explained Mr. Hoekman. “It’s very limiting in what it will allow through.” The region is also small, occupying only 3%-10% of the nasal cavity’s surface area.
Again, POD means “precision olfactory delivery.” But the device isn’t quite as laser focused on the region as its name implies. “We’re not at the stage where we’re able to exclusively deliver to one target site in the nose,” said Dr. Hindle.
While wending its way toward the olfactory zone, some of the drug will be absorbed by other regions, then circulate throughout the body.
“About 59% of the drug that we put into the upper nasal space gets absorbed into the bloodstream,” said Mr. Hoekman.
Janssen Pharmaceuticals’ Spravato – a nasal spray for drug-resistant depression – is thought to work similarly: Some goes straight to the brain via the olfactory nerves, while the rest takes a more roundabout route, passing through the blood vessels to circulate in your system.
A needle-free option
Sometimes, the bloodstream is the main target. Because the nose’s middle and upper stretches are so vascular, drugs can be rapidly absorbed.
This is especially valuable for time-sensitive conditions. “If you give something nasally, you can have peak uptake in 15-30 minutes,” said Mr. Hoekman.
Take Narcan nasal spray, which delivers a burst of naloxone to quickly reverse the effects of opioid an overdose. Or Noctiva nasal spray. Taken just half an hour before bed, it can prevent frequent nighttime urination.
There’s also a group of seizure-stopping sprays, known as “rescue treatments.” One works by temporarily loosening the space between nasal cells, allowing the seizure drug to be quickly absorbed through the vessels.
This systemic access also has potential for drugs that would otherwise have to be injected, such as biologics.
The same goes for vaccines. Mucosal tissue inside the nasal cavity offers direct access to the infection-fighting lymphatic system, making the nose a prime target for inoculation against certain viruses.
Inhaling protection against viruses
Despite the recent surge of interest, nasal vaccines faced a rocky start. After the first nasal flu vaccine hit the market in 2001, it was pulled due to potential toxicity and reports of Bell’s palsy, a type of facial paralysis.
FluMist came in 2003 and has been plagued by problems ever since. Because it contains a weakened live virus, flu-like side effects can occur. And it doesn’t always work. During the 2016-2017 flu season, FluMist protected only 3% of kids, prompting the Centers for Disease Control and Prevention to advise against the nasal route that year.
Why FluMist can be so hit-or-miss is poorly understood. But generally, the nose can pose an effectiveness challenge. “The nose is highly cycling,” said Dr. Hindle. “Anything we deposit usually gets transported out within 15-20 minutes.”
For kids – big fans of not using needles – chronically runny noses can be an issue. “You squirt it in the nose, and it will probably just come back out in their snot,” said Jay Kolls, MD, a professor of medicine and pediatrics at Tulane University, New Orleans, who is developing an intranasal pneumonia vaccine.
Even so, nasal vaccines became a hot topic among researchers after the world was shut down by a virus that invades through the nose.
“We realized that intramuscular vaccines were effective at preventing severe disease, but they weren’t that effective at preventing transmission,” said Michael Diamond, MD, PhD, an immunologist at Washington University in St. Louis.
Nasal vaccines could solve that problem by putting an immune barrier at the point of entry, denying access to the rest of the body. “You squash the infection early enough that it not only prevents disease,” said Dr. Kolls, “but potentially prevents transmission.”
And yes, a nasal COVID vaccine is on the way
In March 2020, Dr. Diamond’s team began exploring a nasal COVID vaccine. Promising results in animals prompted a vaccine development company to license the technology. The resulting nasal vaccine – the first for COVID – has been approved in India, both as a primary vaccine and a booster.
It works by stimulating an influx of IgA, a type of antibody found in the nasal passages, and production of resident memory T cells, immune cells on standby just beneath the surface tissue in the nose.
By contrast, injected vaccines generate mostly IgG antibodies, which struggle to enter the respiratory tract. Only a tiny fraction – an estimated 1% – typically reach the nose.
Nasal vaccines could also be used along with shots. The latter could prime the whole body to fight back, while a nasal spritz could pull that immune protection to the mucosal surfaces.
Nasal technology could yield more effective vaccines for infections like tuberculosis or malaria, or even safeguard against new – sometimes surprising – conditions.
In a 2021 Nature study, an intranasal vaccine derived from fentanyl was better at preventing overdose than an injected vaccine. “Through some clever chemistry, the drug [in the vaccine] isn’t fentanyl anymore,” said study author Elizabeth Norton, PhD, an assistant professor of microbiology and immunology at Tulane University. “But the immune system still has an antibody response to it.”
Novel applications like this represent the future of nasal drug delivery.
“We’re not going to innovate in asthma or COPD. We’re not going to innovate in local delivery to the nose,” said Dr. Hindle. “Innovation will only come if we look to treat new conditions.”
A version of this article originally appeared on WebMD.com.
Time to prescribe sauna bathing for cardiovascular health?
Is it time to start recommending regular sauna bathing to improve heart health?
While a post-workout sauna can compound the benefits of exercise, the hormetic effects of heat therapy alone can produce significant gains for microvascular and endothelial function, no workout required.
“There’s enough evidence to say that regular sauna use improves cardiovascular health,” Matthew S. Ganio, PhD, a professor of exercise science at the University of Arkansas in Fayetteville, who studies thermoregulatory responses and cardiovascular health, said.
“The more they used it, the greater the reduction in cardiovascular events like heart attack. But you don’t need to be in there more than 20-30 minutes. That’s where it seemed to have the best effect,” Dr. Ganio said, adding that studies have shown a dose-response.
A prospective cohort study published in 2015 in JAMA Internal Medicine included 20 years of data on more than 2,300 Finnish men who regularly sauna bathed. The researchers found that among participants who sat in saunas more frequently, rates of death from heart disease and stroke were lower than among those who did so less often.
Cutaneous vasodilation
The body experiences several physiologic changes when exposed to heat therapy of any kind, including sauna, hot water submerging, shortwave diathermy, and heat wrapping. Many of these changes involve elements of the cardiovascular system, said Earric Lee, PhD, an exercise physiologist and postdoctoral researcher at the University of Jyväskylä in Finland, who has studied the effects of sauna on cardiovascular health.
The mechanisms by which heat therapy improves cardiovascular fitness have not been determined, as few studies of sauna bathing have been conducted to this degree. One driver appears to be cutaneous vasodilation. To cool the body when exposed to extreme external heat, cutaneous vessels dilate and push blood to the skin, which lowers body temperature, increases heart rate, and delivers oxygen to muscles in the limbs in a way similar to aerobic exercise.
Sauna bathing has similar effects on heart rate and cardiac output. Studies have shown it can improve the circulation of blood through the body, as well as vascular endothelial function, which is closely tied to vascular tone.
“Increased cardiac output is one of the physiologic reasons sauna is good for heart health,” Dr. Ganio said.
During a sauna session, cardiac output can increase by as much as 70% in relation to elevated heart rate. And while heart rate and cardiac output rise, stroke volume remains stable. As stroke volume increases, the effort that muscle must exert increases. When heart rate rises, stroke volume often falls, which subjects the heart to less of a workout and reduces the amount of oxygen and blood circulating throughout the body.
Heat therapy also temporarily increases blood pressure, but in a way similar to exercise, which supports better long-term heart health, said Christopher Minson, PhD, the Kenneth M. and Kenda H. Singer Endowed Professor of Human Physiology at the University of Oregon in Eugene.
A small study of 19 healthy adults that was published in Complementary Therapies in Medicine in 2019 found that blood pressure and heart rate rose during a 25-minute sauna session as they might during moderate exercise, equivalent to an exercise load of about 60-100 watts. These parameters then steadily decreased for 30 minutes after the sauna. An earlier study found that in the long term, blood pressure was lower after a sauna than before a sauna.
Upregulated heat shock proteins
Both aerobic exercise and heat stress from sauna bathing increase the activity of heat shock proteins. A 2021 review published in Experimental Gerontology found that heat shock proteins become elevated in cells within 30 minutes of exposure to heat and remain elevated over time – an effect similar to exercise.
“Saunas increase heat shock proteins that break down old, dysfunctional proteins and then protect new proteins from becoming dysfunctional,” Hunter S. Waldman, PhD, an assistant professor of exercise science at the University of North Alabama in Florence, said. This effect is one way sauna bathing may quell systemic inflammation, Dr. Waldman said.
According to a 2018 review published in BioMed Research International, an abundance of heat shock proteins may increase exercise tolerance. The researchers concluded that the positive stress associated with elevated body temperature could help people be physically active for longer periods.
Added stress, especially heat-related strain, is not good for everyone, however. Dr. Waldman cautioned that heat exposure, be it through a sauna, hot tub, or other source, can be harmful for pregnant women and children and can be dangerous for people who have low blood pressure, since blood pressure often drops to rates that are lower than before taking a sauna. It also can impair semen quality for months after exposure, so people who are trying to conceive should avoid sauna bathing.
Anyone who has been diagnosed with a heart condition, including cardiac arrhythmia, coronary artery disease, and congestive heart failure, should always consult their physician prior to using sauna for the first time or before using it habitually, Dr. Lee said.
Effects compounded by exercise
Dr. Minson stressed that any type of heat therapy should be part of a lifestyle that includes mostly healthy habits overall, especially a regular exercise regime when possible.
“You have to have everything else working as well: finding time to relax, not being overly stressed, staying hydrated – all those things are critical with any exercise training and heat therapy program,” he said.
Dr. Lee said it’s easy to overhype the benefits of sauna bathing and agreed the practice should be used in tandem with other therapies, not as a replacement. So far, stacking research has shown it to be an effective extension of aerobic exercise.
A June 2023 review published in Mayo Clinic Proceedings found that while sauna bathing can produce benefits on its own, a post-workout sauna can extend the benefits of exercise. As a result, the researchers concluded, saunas likely provide the most benefit when combined with aerobic and strength training.
While some of the benefits of exercise overlap those associated with sauna bathing, “you’re going to get some benefits with exercise that you’re never going to get with sauna,” Dr. Ganio said.
For instance, strength training or aerobic exercise usually results in muscle contractions, which sauna bathing does not produce.
If a person is impaired in a way that makes exercise difficult, taking a sauna after aerobic activity can extend the cardiovascular benefits of the workout, even if muscle-building does not occur, Dr. Lee said.
“All other things considered, especially with aerobic exercise, it is very comparable, so we can look at adding sauna bathing post exercise as a way to lengthen the aerobic exercise workout,” he said. “It’s not to the same degree, but you can get many of the ranging benefits of exercising simply by going into the sauna.”
The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Is it time to start recommending regular sauna bathing to improve heart health?
While a post-workout sauna can compound the benefits of exercise, the hormetic effects of heat therapy alone can produce significant gains for microvascular and endothelial function, no workout required.
“There’s enough evidence to say that regular sauna use improves cardiovascular health,” Matthew S. Ganio, PhD, a professor of exercise science at the University of Arkansas in Fayetteville, who studies thermoregulatory responses and cardiovascular health, said.
“The more they used it, the greater the reduction in cardiovascular events like heart attack. But you don’t need to be in there more than 20-30 minutes. That’s where it seemed to have the best effect,” Dr. Ganio said, adding that studies have shown a dose-response.
A prospective cohort study published in 2015 in JAMA Internal Medicine included 20 years of data on more than 2,300 Finnish men who regularly sauna bathed. The researchers found that among participants who sat in saunas more frequently, rates of death from heart disease and stroke were lower than among those who did so less often.
Cutaneous vasodilation
The body experiences several physiologic changes when exposed to heat therapy of any kind, including sauna, hot water submerging, shortwave diathermy, and heat wrapping. Many of these changes involve elements of the cardiovascular system, said Earric Lee, PhD, an exercise physiologist and postdoctoral researcher at the University of Jyväskylä in Finland, who has studied the effects of sauna on cardiovascular health.
The mechanisms by which heat therapy improves cardiovascular fitness have not been determined, as few studies of sauna bathing have been conducted to this degree. One driver appears to be cutaneous vasodilation. To cool the body when exposed to extreme external heat, cutaneous vessels dilate and push blood to the skin, which lowers body temperature, increases heart rate, and delivers oxygen to muscles in the limbs in a way similar to aerobic exercise.
Sauna bathing has similar effects on heart rate and cardiac output. Studies have shown it can improve the circulation of blood through the body, as well as vascular endothelial function, which is closely tied to vascular tone.
“Increased cardiac output is one of the physiologic reasons sauna is good for heart health,” Dr. Ganio said.
During a sauna session, cardiac output can increase by as much as 70% in relation to elevated heart rate. And while heart rate and cardiac output rise, stroke volume remains stable. As stroke volume increases, the effort that muscle must exert increases. When heart rate rises, stroke volume often falls, which subjects the heart to less of a workout and reduces the amount of oxygen and blood circulating throughout the body.
Heat therapy also temporarily increases blood pressure, but in a way similar to exercise, which supports better long-term heart health, said Christopher Minson, PhD, the Kenneth M. and Kenda H. Singer Endowed Professor of Human Physiology at the University of Oregon in Eugene.
A small study of 19 healthy adults that was published in Complementary Therapies in Medicine in 2019 found that blood pressure and heart rate rose during a 25-minute sauna session as they might during moderate exercise, equivalent to an exercise load of about 60-100 watts. These parameters then steadily decreased for 30 minutes after the sauna. An earlier study found that in the long term, blood pressure was lower after a sauna than before a sauna.
Upregulated heat shock proteins
Both aerobic exercise and heat stress from sauna bathing increase the activity of heat shock proteins. A 2021 review published in Experimental Gerontology found that heat shock proteins become elevated in cells within 30 minutes of exposure to heat and remain elevated over time – an effect similar to exercise.
“Saunas increase heat shock proteins that break down old, dysfunctional proteins and then protect new proteins from becoming dysfunctional,” Hunter S. Waldman, PhD, an assistant professor of exercise science at the University of North Alabama in Florence, said. This effect is one way sauna bathing may quell systemic inflammation, Dr. Waldman said.
According to a 2018 review published in BioMed Research International, an abundance of heat shock proteins may increase exercise tolerance. The researchers concluded that the positive stress associated with elevated body temperature could help people be physically active for longer periods.
Added stress, especially heat-related strain, is not good for everyone, however. Dr. Waldman cautioned that heat exposure, be it through a sauna, hot tub, or other source, can be harmful for pregnant women and children and can be dangerous for people who have low blood pressure, since blood pressure often drops to rates that are lower than before taking a sauna. It also can impair semen quality for months after exposure, so people who are trying to conceive should avoid sauna bathing.
Anyone who has been diagnosed with a heart condition, including cardiac arrhythmia, coronary artery disease, and congestive heart failure, should always consult their physician prior to using sauna for the first time or before using it habitually, Dr. Lee said.
Effects compounded by exercise
Dr. Minson stressed that any type of heat therapy should be part of a lifestyle that includes mostly healthy habits overall, especially a regular exercise regime when possible.
“You have to have everything else working as well: finding time to relax, not being overly stressed, staying hydrated – all those things are critical with any exercise training and heat therapy program,” he said.
Dr. Lee said it’s easy to overhype the benefits of sauna bathing and agreed the practice should be used in tandem with other therapies, not as a replacement. So far, stacking research has shown it to be an effective extension of aerobic exercise.
A June 2023 review published in Mayo Clinic Proceedings found that while sauna bathing can produce benefits on its own, a post-workout sauna can extend the benefits of exercise. As a result, the researchers concluded, saunas likely provide the most benefit when combined with aerobic and strength training.
While some of the benefits of exercise overlap those associated with sauna bathing, “you’re going to get some benefits with exercise that you’re never going to get with sauna,” Dr. Ganio said.
For instance, strength training or aerobic exercise usually results in muscle contractions, which sauna bathing does not produce.
If a person is impaired in a way that makes exercise difficult, taking a sauna after aerobic activity can extend the cardiovascular benefits of the workout, even if muscle-building does not occur, Dr. Lee said.
“All other things considered, especially with aerobic exercise, it is very comparable, so we can look at adding sauna bathing post exercise as a way to lengthen the aerobic exercise workout,” he said. “It’s not to the same degree, but you can get many of the ranging benefits of exercising simply by going into the sauna.”
The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Is it time to start recommending regular sauna bathing to improve heart health?
While a post-workout sauna can compound the benefits of exercise, the hormetic effects of heat therapy alone can produce significant gains for microvascular and endothelial function, no workout required.
“There’s enough evidence to say that regular sauna use improves cardiovascular health,” Matthew S. Ganio, PhD, a professor of exercise science at the University of Arkansas in Fayetteville, who studies thermoregulatory responses and cardiovascular health, said.
“The more they used it, the greater the reduction in cardiovascular events like heart attack. But you don’t need to be in there more than 20-30 minutes. That’s where it seemed to have the best effect,” Dr. Ganio said, adding that studies have shown a dose-response.
A prospective cohort study published in 2015 in JAMA Internal Medicine included 20 years of data on more than 2,300 Finnish men who regularly sauna bathed. The researchers found that among participants who sat in saunas more frequently, rates of death from heart disease and stroke were lower than among those who did so less often.
Cutaneous vasodilation
The body experiences several physiologic changes when exposed to heat therapy of any kind, including sauna, hot water submerging, shortwave diathermy, and heat wrapping. Many of these changes involve elements of the cardiovascular system, said Earric Lee, PhD, an exercise physiologist and postdoctoral researcher at the University of Jyväskylä in Finland, who has studied the effects of sauna on cardiovascular health.
The mechanisms by which heat therapy improves cardiovascular fitness have not been determined, as few studies of sauna bathing have been conducted to this degree. One driver appears to be cutaneous vasodilation. To cool the body when exposed to extreme external heat, cutaneous vessels dilate and push blood to the skin, which lowers body temperature, increases heart rate, and delivers oxygen to muscles in the limbs in a way similar to aerobic exercise.
Sauna bathing has similar effects on heart rate and cardiac output. Studies have shown it can improve the circulation of blood through the body, as well as vascular endothelial function, which is closely tied to vascular tone.
“Increased cardiac output is one of the physiologic reasons sauna is good for heart health,” Dr. Ganio said.
During a sauna session, cardiac output can increase by as much as 70% in relation to elevated heart rate. And while heart rate and cardiac output rise, stroke volume remains stable. As stroke volume increases, the effort that muscle must exert increases. When heart rate rises, stroke volume often falls, which subjects the heart to less of a workout and reduces the amount of oxygen and blood circulating throughout the body.
Heat therapy also temporarily increases blood pressure, but in a way similar to exercise, which supports better long-term heart health, said Christopher Minson, PhD, the Kenneth M. and Kenda H. Singer Endowed Professor of Human Physiology at the University of Oregon in Eugene.
A small study of 19 healthy adults that was published in Complementary Therapies in Medicine in 2019 found that blood pressure and heart rate rose during a 25-minute sauna session as they might during moderate exercise, equivalent to an exercise load of about 60-100 watts. These parameters then steadily decreased for 30 minutes after the sauna. An earlier study found that in the long term, blood pressure was lower after a sauna than before a sauna.
Upregulated heat shock proteins
Both aerobic exercise and heat stress from sauna bathing increase the activity of heat shock proteins. A 2021 review published in Experimental Gerontology found that heat shock proteins become elevated in cells within 30 minutes of exposure to heat and remain elevated over time – an effect similar to exercise.
“Saunas increase heat shock proteins that break down old, dysfunctional proteins and then protect new proteins from becoming dysfunctional,” Hunter S. Waldman, PhD, an assistant professor of exercise science at the University of North Alabama in Florence, said. This effect is one way sauna bathing may quell systemic inflammation, Dr. Waldman said.
According to a 2018 review published in BioMed Research International, an abundance of heat shock proteins may increase exercise tolerance. The researchers concluded that the positive stress associated with elevated body temperature could help people be physically active for longer periods.
Added stress, especially heat-related strain, is not good for everyone, however. Dr. Waldman cautioned that heat exposure, be it through a sauna, hot tub, or other source, can be harmful for pregnant women and children and can be dangerous for people who have low blood pressure, since blood pressure often drops to rates that are lower than before taking a sauna. It also can impair semen quality for months after exposure, so people who are trying to conceive should avoid sauna bathing.
Anyone who has been diagnosed with a heart condition, including cardiac arrhythmia, coronary artery disease, and congestive heart failure, should always consult their physician prior to using sauna for the first time or before using it habitually, Dr. Lee said.
Effects compounded by exercise
Dr. Minson stressed that any type of heat therapy should be part of a lifestyle that includes mostly healthy habits overall, especially a regular exercise regime when possible.
“You have to have everything else working as well: finding time to relax, not being overly stressed, staying hydrated – all those things are critical with any exercise training and heat therapy program,” he said.
Dr. Lee said it’s easy to overhype the benefits of sauna bathing and agreed the practice should be used in tandem with other therapies, not as a replacement. So far, stacking research has shown it to be an effective extension of aerobic exercise.
A June 2023 review published in Mayo Clinic Proceedings found that while sauna bathing can produce benefits on its own, a post-workout sauna can extend the benefits of exercise. As a result, the researchers concluded, saunas likely provide the most benefit when combined with aerobic and strength training.
While some of the benefits of exercise overlap those associated with sauna bathing, “you’re going to get some benefits with exercise that you’re never going to get with sauna,” Dr. Ganio said.
For instance, strength training or aerobic exercise usually results in muscle contractions, which sauna bathing does not produce.
If a person is impaired in a way that makes exercise difficult, taking a sauna after aerobic activity can extend the cardiovascular benefits of the workout, even if muscle-building does not occur, Dr. Lee said.
“All other things considered, especially with aerobic exercise, it is very comparable, so we can look at adding sauna bathing post exercise as a way to lengthen the aerobic exercise workout,” he said. “It’s not to the same degree, but you can get many of the ranging benefits of exercising simply by going into the sauna.”
The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Tips for addressing uptick in mental health visits: Primary care providers collaborate, innovate
This growth in the number of patients needing behavioral health–related care is likely driven by multiple factors, including a shortage of mental health care providers, an increasing incidence of psychiatric illness, and destigmatization of mental health in general, suggested Swetha P. Iruku, MD, MPH, associate professor of family medicine and community health at the University of Pennsylvania and Penn Medicine family physician in Philadelphia.
The Centers for Disease Control and Prevention noted that “the COVID-19 pandemic has been associated with mental health challenges related to the morbidity and mortality caused by the disease and to mitigation activities, including the impact of physical distancing and stay-at-home orders,” in a Morbidity and Mortality Weekly Report.
From June 24 to 30, 2020, U.S. adults reported considerably elevated adverse mental health conditions associated with COVID-19, and symptoms of anxiety disorder and depressive disorder climbed during the months of April through June of the same year, compared with the same period in 2019, they wrote.
Even before the pandemic got underway, multiple studies of national data published this year suggested mental issues were on the rise in the United States. For example, the proportion of adult patient visits to primary care providers that addressed mental health concerns rose from 10.7% to 15.9% from 2006 to 2018, according to research published in Health Affairs. Plus, the number and proportion of pediatric acute care hospitalizations because of mental health diagnoses increased significantly between 2009 and 2019, according to a paper published in JAMA.
“I truly believe that we can’t, as primary care physicians, take care of someone’s physical health without also taking care of their mental health,” Dr. Iruku said in an interview. “It’s all intertwined.”
To rise to this challenge, PCPs first need a collaborative mindset, she suggested, as well as familiarity with available resources, both locally and virtually.
This article examines strategies for managing mental illness in primary care, outlines clinical resources, and reviews related educational opportunities.
In addition, clinical pearls are shared by Dr. Iruku and five other clinicians who provide or have provided mental health care to primary care patients or work in close collaboration with a primary care practice, including a clinical psychologist, a nurse practitioner licensed in psychiatric health, a pediatrician, and a licensed clinical social worker.
Build a network
Most of the providers interviewed cited the importance of collaboration in mental health care, particularly for complex cases.
“I would recommend [that primary care providers get] to know the psychiatric providers [in their area],” said Jessica Viton, DNP, FNP, PMHNP, who delivers mental health care through a community-based primary care practice in Colorado which she requested remain anonymous.
Dr. Iruku suggested making an in-person connection first, if possible.
“So much of what we do is ‘see one, do one, teach one,’ so learn a little bit, then go off and trial,” she said. “[It can be valuable] having someone in your back pocket that you can contact in the case of an emergency, or in a situation where you just don’t know how to tackle it.”
Screen for depression and anxiety
William J. Sieber, PhD, a clinical psychologist, director of integrated behavioral health, and professor in the department of family medicine and public health and the department of psychiatry at the University of California, San Diego, said primary care providers should screen all adult patients for depression and anxiety with the Patient Health Questionnaire (PHQ-9) and General Anxiety Disorder Assessment (GAD-7), respectively.
To save time, he suggested a cascading approach.
“In primary care, everybody’s in a hurry,” Dr. Sieber said. “[With the cascading approach,] the first two items [from each questionnaire] are given, and if a person endorses either of those items … then they are asked to complete the other items.”
Jennifer Mullally, MD, a pediatrician at Sanford Health in Fargo, N.D., uses this cascading approach to depression and anxiety screening with all her patients aged 13-18. For younger kids, she screens only those who present with signs or symptoms of mental health issues, or if the parent shares a concern.
This approach differs slightly from U.S. Preventive Services Task Force recommendations, which suggest screening for anxiety in patients aged 8-18 years and depression in patients aged 12-18 years.
Use other screening tools only as needed
Dr. Sieber, the research director for the division of family medicine at UC San Diego, collaborates regularly with primary care providers via hallway consultations, by sharing cases, and through providing oversight of psychiatric care at 13 primary care practices within the UC San Diego network. He recommended against routine screening beyond depression and anxiety in the primary care setting.
“There are a lot of screening tools,” Dr. Sieber said. “It depends on what you’re presented with. The challenge in primary care is you’re going to see all kinds of things. It’s not like running a depression clinic.”
Other than the PHQ-9 and GAD-7, he suggested primary care providers establish familiarity with screening tools for posttraumatic stress disorder and attention-deficit/hyperactivity disorder, noting again that these should be used only when one of the conditions is already suspected.
Dr. Mullally follows a similar approach with her pediatric population. In addition to the GAD-7, she investigates whether a patient has anxiety with the Screen for Child Anxiety Related Disorders (SCARED). For depression, she couples the PHQ-9 with the Columbia Suicide Severity Rating Scale.
While additional screening tools like these are readily available online, Dr. Viton suggested that they should be employed only if the provider is trained to interpret and respond to those findings, and only if they know which tool to use, and when.
For example, she has recently observed PCPs diagnosing adults with ADHD using a three-question test, when in fact a full-length, standardized instrument should be administered by a provider with necessary training.
She also pointed out that bipolar disorder continues to be underdiagnosed, possibly because of providers detecting depression using a questionnaire like the PHQ-9, while failing to inquire about manic episodes.
Leverage online resources
If depression is confirmed, Dr. Iruku often directs the patient to the Mayo Clinic Depression Medication Choice Decision Aid. This website steers patients through medication options based on their answers to a questionnaire. Choices are listed alongside possible adverse effects.
For clinician use, Dr. Iruku recommended The Waco Guide to Psychopharmacology in Primary Care, which aids clinical decision-making for mental illness and substance abuse. The app processes case details to suggest first-, second-, and third-line pharmacotherapies, as well as modifications based on patient needs.
Even with tools like these, however, a referral may be needed.
“[Primary care providers] may not be the best fit for what the patient is looking for, from a mental health or behavioral standpoint,” Dr. Sieber said.
In this case, he encourages patients to visit Psychology Today, a “quite popular portal” that helps patients locate a suitable provider based on location, insurance, driving radius, and mental health concern. This usually generates 10-20 options, Dr. Sieber said, although results can vary.
“It may be discouraging, because maybe only three [providers] pop up based on your criteria, and the closest one is miles away,” he said.
Consider virtual support
If no local psychiatric help is available, Dr. Sieber suggested virtual support, highlighting that “it’s much easier now than it was 3 or 4 years ago” to connect patients with external mental health care.
But this strategy should be reserved for cases of actual need instead of pure convenience, cautioned Dr. Viton, who noted that virtual visits may fail to capture the nuance of an in-person meeting, as body language, mode of dress, and other clues can provide insights into mental health status.
“Occasionally, I think you do have to have an in-person visit, especially when you’re developing a rapport with someone,” Dr. Viton said.
Claire McArdle, a licensed clinical social worker in Fort Collins, Colo., noted that virtual care from an outside provider may also impede the collaboration needed to effectively address mental illness.
In her 11 years in primary care at Associates in Family Medicine, Ms. McArdle had countless interactions with colleagues seeking support when managing a complex case. “I’m coaching providers, front desk staff, and nursing staff on how to interact with patients [with] behavioral health needs,” she said, citing the multitude of nonmedical factors that need to be considered, such as family relationships and patient preferences.
These unscheduled conversations with colleagues throughout the day are impossible to have when sharing a case with an unknown, remote peer.
Ms. McArdle speaks from experience. She recently resigned from Associates in Family Medicine to start her own private therapy practice after her former employer was acquired by VillageMD, a national provider that terminated employment of most other social workers in the practice and began outsourcing mental health care to Mindoula Health, a virtual provider.
Dr. Sieber offered a similar perspective on in-person collaboration as the psychiatric specialist at his center. He routinely offers on-site support for both providers and patients, serving as “another set of eyes and ears” when there is a concern about patient safety or directly managing care when a patient is hospitalized for mental illness.
While virtual solutions may fall short of in-person management, they can offer care at a scale and cost impossible through traditional practice.
This could even be free. Zero-cost, automated software now allows individuals who are uninsured or unable to afford care at least one avenue to manage their mental health concerns.
For example, Bliss is a free, 8-session, interactive online therapy program for depression that was created by the Centre for Interactive Mental Health Solutions. The program offers a tool for monitoring mood and quizzes to test understanding of personal mental health management, among other features.
More advanced programs are emerging as artificial intelligence (AI) enables dialogues between humans and machines. This is the case with Woebot, an app that asks the user about their mood throughout the day, and responds with evidence-based strategies for managing concerns, all for free at press time.
Keep learning
A range of educational options and professional resources are available for primary care providers who would like to improve their knowledge of mental health care. These include formal fellowships in primary care psychiatry/behavioral health integration, free mental health webinars, and various other opportunities.
Eric Eschweiler, DNP, APRN, FNP-C, PHN, completed the University of California, Irvine, Train New Trainers (TNT) Primary Care Psychiatry (PCP) Fellowship in 2016, when he was working as a solo nurse practitioner.
“I was drowning in practice,” said Dr. Eschweiler, director of nursing and public health outreach services at Riverside-San Bernardino County Indian Health, Grand Terrace, Calif., in an interview. “I was a solo NP. There was no physician on site. We were seeing a lot of [individuals with] schizoaffective [disorder] in downtown San Bernardino, the homeless, unhoused – a lot of substance use. I felt I needed to have the skills to be able to treat them effectively. That’s what the fellowship did.”
The skills Dr. Eschweiler learned from participating in his fellowship allowed him to manage more cases of mental illness without need for referral. When a referral was needed for a complex or severe case, he had the confidence to bridge care and collaborate more effectively with psychiatric specialists.
“It was awesome, because we were able to communicate using the same language,” Dr. Eschweiler said of these collaborations. “It’s [about] talking that same language, starting those initial treatments, and then moving forward with specialty care, and vice versa. [Psychiatric specialists] would send me patients that needed medical care because of the types of medications they were taking. And I was then very well aware of those side effects and other issues that might come up from those treatments. So it’s a two-way street.”
Dr. Eschweiler was so impressed by his fellowship that he has since ushered multiple providers through the program since transitioning to an administrative role as director of nursing.
In Fargo, where psychiatric care is sparse and wait times for referral can be months long, Dr. Mullally, like Dr. Eschweiler, knew that she needed more training in mental health.
“I don’t feel like we get enough training in residency,” Dr. Mullally said. “So you do need to look at your options for further CME.”
Out of several CME courses she has taken to further her understanding of pediatric psychiatry, Dr. Mullally recommended The Reach Institute above all others, as their courses involve in-depth discussions and valuable handouts, particularly for medication selection.
“I think that a lot of the other CMEs tend to involve a lot more PowerPoint presentations,” Dr. Mullally said. “And you don’t necessarily leave with a lot of good documents. I still use my Reach handouts. I have them sitting right next to me. I use them every single day.”
Providers interested in The Reach Institute, however, should be prepared to invest both time and money, she added, citing a 2-3 day commitment, and calling it “not cheap.” To overcome these barriers, she suggested that providers get their institution to support their attendance.
For a lighter commitment, Dr. Iruku recommended the American Academy of Family Physicians CME portal, as this offers 13 online, accredited courses covering a range of topics, from adolescent health to substance abuse disorders.
Dr. Sieber suggested that primary care providers join the Collaborative Family Healthcare Association, which aims to integrate physical and behavioral health in routine practice. CFHA, of which he is a member, offers a “bevy of different resources” for interested providers, including a conference in Phoenix this October.
The interviewees disclosed no conflicts of interest.
This growth in the number of patients needing behavioral health–related care is likely driven by multiple factors, including a shortage of mental health care providers, an increasing incidence of psychiatric illness, and destigmatization of mental health in general, suggested Swetha P. Iruku, MD, MPH, associate professor of family medicine and community health at the University of Pennsylvania and Penn Medicine family physician in Philadelphia.
The Centers for Disease Control and Prevention noted that “the COVID-19 pandemic has been associated with mental health challenges related to the morbidity and mortality caused by the disease and to mitigation activities, including the impact of physical distancing and stay-at-home orders,” in a Morbidity and Mortality Weekly Report.
From June 24 to 30, 2020, U.S. adults reported considerably elevated adverse mental health conditions associated with COVID-19, and symptoms of anxiety disorder and depressive disorder climbed during the months of April through June of the same year, compared with the same period in 2019, they wrote.
Even before the pandemic got underway, multiple studies of national data published this year suggested mental issues were on the rise in the United States. For example, the proportion of adult patient visits to primary care providers that addressed mental health concerns rose from 10.7% to 15.9% from 2006 to 2018, according to research published in Health Affairs. Plus, the number and proportion of pediatric acute care hospitalizations because of mental health diagnoses increased significantly between 2009 and 2019, according to a paper published in JAMA.
“I truly believe that we can’t, as primary care physicians, take care of someone’s physical health without also taking care of their mental health,” Dr. Iruku said in an interview. “It’s all intertwined.”
To rise to this challenge, PCPs first need a collaborative mindset, she suggested, as well as familiarity with available resources, both locally and virtually.
This article examines strategies for managing mental illness in primary care, outlines clinical resources, and reviews related educational opportunities.
In addition, clinical pearls are shared by Dr. Iruku and five other clinicians who provide or have provided mental health care to primary care patients or work in close collaboration with a primary care practice, including a clinical psychologist, a nurse practitioner licensed in psychiatric health, a pediatrician, and a licensed clinical social worker.
Build a network
Most of the providers interviewed cited the importance of collaboration in mental health care, particularly for complex cases.
“I would recommend [that primary care providers get] to know the psychiatric providers [in their area],” said Jessica Viton, DNP, FNP, PMHNP, who delivers mental health care through a community-based primary care practice in Colorado which she requested remain anonymous.
Dr. Iruku suggested making an in-person connection first, if possible.
“So much of what we do is ‘see one, do one, teach one,’ so learn a little bit, then go off and trial,” she said. “[It can be valuable] having someone in your back pocket that you can contact in the case of an emergency, or in a situation where you just don’t know how to tackle it.”
Screen for depression and anxiety
William J. Sieber, PhD, a clinical psychologist, director of integrated behavioral health, and professor in the department of family medicine and public health and the department of psychiatry at the University of California, San Diego, said primary care providers should screen all adult patients for depression and anxiety with the Patient Health Questionnaire (PHQ-9) and General Anxiety Disorder Assessment (GAD-7), respectively.
To save time, he suggested a cascading approach.
“In primary care, everybody’s in a hurry,” Dr. Sieber said. “[With the cascading approach,] the first two items [from each questionnaire] are given, and if a person endorses either of those items … then they are asked to complete the other items.”
Jennifer Mullally, MD, a pediatrician at Sanford Health in Fargo, N.D., uses this cascading approach to depression and anxiety screening with all her patients aged 13-18. For younger kids, she screens only those who present with signs or symptoms of mental health issues, or if the parent shares a concern.
This approach differs slightly from U.S. Preventive Services Task Force recommendations, which suggest screening for anxiety in patients aged 8-18 years and depression in patients aged 12-18 years.
Use other screening tools only as needed
Dr. Sieber, the research director for the division of family medicine at UC San Diego, collaborates regularly with primary care providers via hallway consultations, by sharing cases, and through providing oversight of psychiatric care at 13 primary care practices within the UC San Diego network. He recommended against routine screening beyond depression and anxiety in the primary care setting.
“There are a lot of screening tools,” Dr. Sieber said. “It depends on what you’re presented with. The challenge in primary care is you’re going to see all kinds of things. It’s not like running a depression clinic.”
Other than the PHQ-9 and GAD-7, he suggested primary care providers establish familiarity with screening tools for posttraumatic stress disorder and attention-deficit/hyperactivity disorder, noting again that these should be used only when one of the conditions is already suspected.
Dr. Mullally follows a similar approach with her pediatric population. In addition to the GAD-7, she investigates whether a patient has anxiety with the Screen for Child Anxiety Related Disorders (SCARED). For depression, she couples the PHQ-9 with the Columbia Suicide Severity Rating Scale.
While additional screening tools like these are readily available online, Dr. Viton suggested that they should be employed only if the provider is trained to interpret and respond to those findings, and only if they know which tool to use, and when.
For example, she has recently observed PCPs diagnosing adults with ADHD using a three-question test, when in fact a full-length, standardized instrument should be administered by a provider with necessary training.
She also pointed out that bipolar disorder continues to be underdiagnosed, possibly because of providers detecting depression using a questionnaire like the PHQ-9, while failing to inquire about manic episodes.
Leverage online resources
If depression is confirmed, Dr. Iruku often directs the patient to the Mayo Clinic Depression Medication Choice Decision Aid. This website steers patients through medication options based on their answers to a questionnaire. Choices are listed alongside possible adverse effects.
For clinician use, Dr. Iruku recommended The Waco Guide to Psychopharmacology in Primary Care, which aids clinical decision-making for mental illness and substance abuse. The app processes case details to suggest first-, second-, and third-line pharmacotherapies, as well as modifications based on patient needs.
Even with tools like these, however, a referral may be needed.
“[Primary care providers] may not be the best fit for what the patient is looking for, from a mental health or behavioral standpoint,” Dr. Sieber said.
In this case, he encourages patients to visit Psychology Today, a “quite popular portal” that helps patients locate a suitable provider based on location, insurance, driving radius, and mental health concern. This usually generates 10-20 options, Dr. Sieber said, although results can vary.
“It may be discouraging, because maybe only three [providers] pop up based on your criteria, and the closest one is miles away,” he said.
Consider virtual support
If no local psychiatric help is available, Dr. Sieber suggested virtual support, highlighting that “it’s much easier now than it was 3 or 4 years ago” to connect patients with external mental health care.
But this strategy should be reserved for cases of actual need instead of pure convenience, cautioned Dr. Viton, who noted that virtual visits may fail to capture the nuance of an in-person meeting, as body language, mode of dress, and other clues can provide insights into mental health status.
“Occasionally, I think you do have to have an in-person visit, especially when you’re developing a rapport with someone,” Dr. Viton said.
Claire McArdle, a licensed clinical social worker in Fort Collins, Colo., noted that virtual care from an outside provider may also impede the collaboration needed to effectively address mental illness.
In her 11 years in primary care at Associates in Family Medicine, Ms. McArdle had countless interactions with colleagues seeking support when managing a complex case. “I’m coaching providers, front desk staff, and nursing staff on how to interact with patients [with] behavioral health needs,” she said, citing the multitude of nonmedical factors that need to be considered, such as family relationships and patient preferences.
These unscheduled conversations with colleagues throughout the day are impossible to have when sharing a case with an unknown, remote peer.
Ms. McArdle speaks from experience. She recently resigned from Associates in Family Medicine to start her own private therapy practice after her former employer was acquired by VillageMD, a national provider that terminated employment of most other social workers in the practice and began outsourcing mental health care to Mindoula Health, a virtual provider.
Dr. Sieber offered a similar perspective on in-person collaboration as the psychiatric specialist at his center. He routinely offers on-site support for both providers and patients, serving as “another set of eyes and ears” when there is a concern about patient safety or directly managing care when a patient is hospitalized for mental illness.
While virtual solutions may fall short of in-person management, they can offer care at a scale and cost impossible through traditional practice.
This could even be free. Zero-cost, automated software now allows individuals who are uninsured or unable to afford care at least one avenue to manage their mental health concerns.
For example, Bliss is a free, 8-session, interactive online therapy program for depression that was created by the Centre for Interactive Mental Health Solutions. The program offers a tool for monitoring mood and quizzes to test understanding of personal mental health management, among other features.
More advanced programs are emerging as artificial intelligence (AI) enables dialogues between humans and machines. This is the case with Woebot, an app that asks the user about their mood throughout the day, and responds with evidence-based strategies for managing concerns, all for free at press time.
Keep learning
A range of educational options and professional resources are available for primary care providers who would like to improve their knowledge of mental health care. These include formal fellowships in primary care psychiatry/behavioral health integration, free mental health webinars, and various other opportunities.
Eric Eschweiler, DNP, APRN, FNP-C, PHN, completed the University of California, Irvine, Train New Trainers (TNT) Primary Care Psychiatry (PCP) Fellowship in 2016, when he was working as a solo nurse practitioner.
“I was drowning in practice,” said Dr. Eschweiler, director of nursing and public health outreach services at Riverside-San Bernardino County Indian Health, Grand Terrace, Calif., in an interview. “I was a solo NP. There was no physician on site. We were seeing a lot of [individuals with] schizoaffective [disorder] in downtown San Bernardino, the homeless, unhoused – a lot of substance use. I felt I needed to have the skills to be able to treat them effectively. That’s what the fellowship did.”
The skills Dr. Eschweiler learned from participating in his fellowship allowed him to manage more cases of mental illness without need for referral. When a referral was needed for a complex or severe case, he had the confidence to bridge care and collaborate more effectively with psychiatric specialists.
“It was awesome, because we were able to communicate using the same language,” Dr. Eschweiler said of these collaborations. “It’s [about] talking that same language, starting those initial treatments, and then moving forward with specialty care, and vice versa. [Psychiatric specialists] would send me patients that needed medical care because of the types of medications they were taking. And I was then very well aware of those side effects and other issues that might come up from those treatments. So it’s a two-way street.”
Dr. Eschweiler was so impressed by his fellowship that he has since ushered multiple providers through the program since transitioning to an administrative role as director of nursing.
In Fargo, where psychiatric care is sparse and wait times for referral can be months long, Dr. Mullally, like Dr. Eschweiler, knew that she needed more training in mental health.
“I don’t feel like we get enough training in residency,” Dr. Mullally said. “So you do need to look at your options for further CME.”
Out of several CME courses she has taken to further her understanding of pediatric psychiatry, Dr. Mullally recommended The Reach Institute above all others, as their courses involve in-depth discussions and valuable handouts, particularly for medication selection.
“I think that a lot of the other CMEs tend to involve a lot more PowerPoint presentations,” Dr. Mullally said. “And you don’t necessarily leave with a lot of good documents. I still use my Reach handouts. I have them sitting right next to me. I use them every single day.”
Providers interested in The Reach Institute, however, should be prepared to invest both time and money, she added, citing a 2-3 day commitment, and calling it “not cheap.” To overcome these barriers, she suggested that providers get their institution to support their attendance.
For a lighter commitment, Dr. Iruku recommended the American Academy of Family Physicians CME portal, as this offers 13 online, accredited courses covering a range of topics, from adolescent health to substance abuse disorders.
Dr. Sieber suggested that primary care providers join the Collaborative Family Healthcare Association, which aims to integrate physical and behavioral health in routine practice. CFHA, of which he is a member, offers a “bevy of different resources” for interested providers, including a conference in Phoenix this October.
The interviewees disclosed no conflicts of interest.
This growth in the number of patients needing behavioral health–related care is likely driven by multiple factors, including a shortage of mental health care providers, an increasing incidence of psychiatric illness, and destigmatization of mental health in general, suggested Swetha P. Iruku, MD, MPH, associate professor of family medicine and community health at the University of Pennsylvania and Penn Medicine family physician in Philadelphia.
The Centers for Disease Control and Prevention noted that “the COVID-19 pandemic has been associated with mental health challenges related to the morbidity and mortality caused by the disease and to mitigation activities, including the impact of physical distancing and stay-at-home orders,” in a Morbidity and Mortality Weekly Report.
From June 24 to 30, 2020, U.S. adults reported considerably elevated adverse mental health conditions associated with COVID-19, and symptoms of anxiety disorder and depressive disorder climbed during the months of April through June of the same year, compared with the same period in 2019, they wrote.
Even before the pandemic got underway, multiple studies of national data published this year suggested mental issues were on the rise in the United States. For example, the proportion of adult patient visits to primary care providers that addressed mental health concerns rose from 10.7% to 15.9% from 2006 to 2018, according to research published in Health Affairs. Plus, the number and proportion of pediatric acute care hospitalizations because of mental health diagnoses increased significantly between 2009 and 2019, according to a paper published in JAMA.
“I truly believe that we can’t, as primary care physicians, take care of someone’s physical health without also taking care of their mental health,” Dr. Iruku said in an interview. “It’s all intertwined.”
To rise to this challenge, PCPs first need a collaborative mindset, she suggested, as well as familiarity with available resources, both locally and virtually.
This article examines strategies for managing mental illness in primary care, outlines clinical resources, and reviews related educational opportunities.
In addition, clinical pearls are shared by Dr. Iruku and five other clinicians who provide or have provided mental health care to primary care patients or work in close collaboration with a primary care practice, including a clinical psychologist, a nurse practitioner licensed in psychiatric health, a pediatrician, and a licensed clinical social worker.
Build a network
Most of the providers interviewed cited the importance of collaboration in mental health care, particularly for complex cases.
“I would recommend [that primary care providers get] to know the psychiatric providers [in their area],” said Jessica Viton, DNP, FNP, PMHNP, who delivers mental health care through a community-based primary care practice in Colorado which she requested remain anonymous.
Dr. Iruku suggested making an in-person connection first, if possible.
“So much of what we do is ‘see one, do one, teach one,’ so learn a little bit, then go off and trial,” she said. “[It can be valuable] having someone in your back pocket that you can contact in the case of an emergency, or in a situation where you just don’t know how to tackle it.”
Screen for depression and anxiety
William J. Sieber, PhD, a clinical psychologist, director of integrated behavioral health, and professor in the department of family medicine and public health and the department of psychiatry at the University of California, San Diego, said primary care providers should screen all adult patients for depression and anxiety with the Patient Health Questionnaire (PHQ-9) and General Anxiety Disorder Assessment (GAD-7), respectively.
To save time, he suggested a cascading approach.
“In primary care, everybody’s in a hurry,” Dr. Sieber said. “[With the cascading approach,] the first two items [from each questionnaire] are given, and if a person endorses either of those items … then they are asked to complete the other items.”
Jennifer Mullally, MD, a pediatrician at Sanford Health in Fargo, N.D., uses this cascading approach to depression and anxiety screening with all her patients aged 13-18. For younger kids, she screens only those who present with signs or symptoms of mental health issues, or if the parent shares a concern.
This approach differs slightly from U.S. Preventive Services Task Force recommendations, which suggest screening for anxiety in patients aged 8-18 years and depression in patients aged 12-18 years.
Use other screening tools only as needed
Dr. Sieber, the research director for the division of family medicine at UC San Diego, collaborates regularly with primary care providers via hallway consultations, by sharing cases, and through providing oversight of psychiatric care at 13 primary care practices within the UC San Diego network. He recommended against routine screening beyond depression and anxiety in the primary care setting.
“There are a lot of screening tools,” Dr. Sieber said. “It depends on what you’re presented with. The challenge in primary care is you’re going to see all kinds of things. It’s not like running a depression clinic.”
Other than the PHQ-9 and GAD-7, he suggested primary care providers establish familiarity with screening tools for posttraumatic stress disorder and attention-deficit/hyperactivity disorder, noting again that these should be used only when one of the conditions is already suspected.
Dr. Mullally follows a similar approach with her pediatric population. In addition to the GAD-7, she investigates whether a patient has anxiety with the Screen for Child Anxiety Related Disorders (SCARED). For depression, she couples the PHQ-9 with the Columbia Suicide Severity Rating Scale.
While additional screening tools like these are readily available online, Dr. Viton suggested that they should be employed only if the provider is trained to interpret and respond to those findings, and only if they know which tool to use, and when.
For example, she has recently observed PCPs diagnosing adults with ADHD using a three-question test, when in fact a full-length, standardized instrument should be administered by a provider with necessary training.
She also pointed out that bipolar disorder continues to be underdiagnosed, possibly because of providers detecting depression using a questionnaire like the PHQ-9, while failing to inquire about manic episodes.
Leverage online resources
If depression is confirmed, Dr. Iruku often directs the patient to the Mayo Clinic Depression Medication Choice Decision Aid. This website steers patients through medication options based on their answers to a questionnaire. Choices are listed alongside possible adverse effects.
For clinician use, Dr. Iruku recommended The Waco Guide to Psychopharmacology in Primary Care, which aids clinical decision-making for mental illness and substance abuse. The app processes case details to suggest first-, second-, and third-line pharmacotherapies, as well as modifications based on patient needs.
Even with tools like these, however, a referral may be needed.
“[Primary care providers] may not be the best fit for what the patient is looking for, from a mental health or behavioral standpoint,” Dr. Sieber said.
In this case, he encourages patients to visit Psychology Today, a “quite popular portal” that helps patients locate a suitable provider based on location, insurance, driving radius, and mental health concern. This usually generates 10-20 options, Dr. Sieber said, although results can vary.
“It may be discouraging, because maybe only three [providers] pop up based on your criteria, and the closest one is miles away,” he said.
Consider virtual support
If no local psychiatric help is available, Dr. Sieber suggested virtual support, highlighting that “it’s much easier now than it was 3 or 4 years ago” to connect patients with external mental health care.
But this strategy should be reserved for cases of actual need instead of pure convenience, cautioned Dr. Viton, who noted that virtual visits may fail to capture the nuance of an in-person meeting, as body language, mode of dress, and other clues can provide insights into mental health status.
“Occasionally, I think you do have to have an in-person visit, especially when you’re developing a rapport with someone,” Dr. Viton said.
Claire McArdle, a licensed clinical social worker in Fort Collins, Colo., noted that virtual care from an outside provider may also impede the collaboration needed to effectively address mental illness.
In her 11 years in primary care at Associates in Family Medicine, Ms. McArdle had countless interactions with colleagues seeking support when managing a complex case. “I’m coaching providers, front desk staff, and nursing staff on how to interact with patients [with] behavioral health needs,” she said, citing the multitude of nonmedical factors that need to be considered, such as family relationships and patient preferences.
These unscheduled conversations with colleagues throughout the day are impossible to have when sharing a case with an unknown, remote peer.
Ms. McArdle speaks from experience. She recently resigned from Associates in Family Medicine to start her own private therapy practice after her former employer was acquired by VillageMD, a national provider that terminated employment of most other social workers in the practice and began outsourcing mental health care to Mindoula Health, a virtual provider.
Dr. Sieber offered a similar perspective on in-person collaboration as the psychiatric specialist at his center. He routinely offers on-site support for both providers and patients, serving as “another set of eyes and ears” when there is a concern about patient safety or directly managing care when a patient is hospitalized for mental illness.
While virtual solutions may fall short of in-person management, they can offer care at a scale and cost impossible through traditional practice.
This could even be free. Zero-cost, automated software now allows individuals who are uninsured or unable to afford care at least one avenue to manage their mental health concerns.
For example, Bliss is a free, 8-session, interactive online therapy program for depression that was created by the Centre for Interactive Mental Health Solutions. The program offers a tool for monitoring mood and quizzes to test understanding of personal mental health management, among other features.
More advanced programs are emerging as artificial intelligence (AI) enables dialogues between humans and machines. This is the case with Woebot, an app that asks the user about their mood throughout the day, and responds with evidence-based strategies for managing concerns, all for free at press time.
Keep learning
A range of educational options and professional resources are available for primary care providers who would like to improve their knowledge of mental health care. These include formal fellowships in primary care psychiatry/behavioral health integration, free mental health webinars, and various other opportunities.
Eric Eschweiler, DNP, APRN, FNP-C, PHN, completed the University of California, Irvine, Train New Trainers (TNT) Primary Care Psychiatry (PCP) Fellowship in 2016, when he was working as a solo nurse practitioner.
“I was drowning in practice,” said Dr. Eschweiler, director of nursing and public health outreach services at Riverside-San Bernardino County Indian Health, Grand Terrace, Calif., in an interview. “I was a solo NP. There was no physician on site. We were seeing a lot of [individuals with] schizoaffective [disorder] in downtown San Bernardino, the homeless, unhoused – a lot of substance use. I felt I needed to have the skills to be able to treat them effectively. That’s what the fellowship did.”
The skills Dr. Eschweiler learned from participating in his fellowship allowed him to manage more cases of mental illness without need for referral. When a referral was needed for a complex or severe case, he had the confidence to bridge care and collaborate more effectively with psychiatric specialists.
“It was awesome, because we were able to communicate using the same language,” Dr. Eschweiler said of these collaborations. “It’s [about] talking that same language, starting those initial treatments, and then moving forward with specialty care, and vice versa. [Psychiatric specialists] would send me patients that needed medical care because of the types of medications they were taking. And I was then very well aware of those side effects and other issues that might come up from those treatments. So it’s a two-way street.”
Dr. Eschweiler was so impressed by his fellowship that he has since ushered multiple providers through the program since transitioning to an administrative role as director of nursing.
In Fargo, where psychiatric care is sparse and wait times for referral can be months long, Dr. Mullally, like Dr. Eschweiler, knew that she needed more training in mental health.
“I don’t feel like we get enough training in residency,” Dr. Mullally said. “So you do need to look at your options for further CME.”
Out of several CME courses she has taken to further her understanding of pediatric psychiatry, Dr. Mullally recommended The Reach Institute above all others, as their courses involve in-depth discussions and valuable handouts, particularly for medication selection.
“I think that a lot of the other CMEs tend to involve a lot more PowerPoint presentations,” Dr. Mullally said. “And you don’t necessarily leave with a lot of good documents. I still use my Reach handouts. I have them sitting right next to me. I use them every single day.”
Providers interested in The Reach Institute, however, should be prepared to invest both time and money, she added, citing a 2-3 day commitment, and calling it “not cheap.” To overcome these barriers, she suggested that providers get their institution to support their attendance.
For a lighter commitment, Dr. Iruku recommended the American Academy of Family Physicians CME portal, as this offers 13 online, accredited courses covering a range of topics, from adolescent health to substance abuse disorders.
Dr. Sieber suggested that primary care providers join the Collaborative Family Healthcare Association, which aims to integrate physical and behavioral health in routine practice. CFHA, of which he is a member, offers a “bevy of different resources” for interested providers, including a conference in Phoenix this October.
The interviewees disclosed no conflicts of interest.
‘Deprescribing’: Should some older adults shed their meds?
Joanne Lynn, MD, has lost track of the number of times in her 40 years as a geriatrician she’s seen a new patient come to her office carrying a bucket full of prescription medications – many of which they don’t need.
Dr. Lynn, who is on the faculty of George Washington University,Washington, recalled one woman who unwittingly was taking two blood pressure medications with different names.
“The risks included all the side effects overdosing carries,” Dr. Lynn said, ranging from blurred vision and crankiness to organ failure and even death.
For doctors with patients who don’t know they’re taking too much of a medication, “you wonder whether the drug is causing the health problems, and it’s a symptom of the wrong medication,” rather than a symptom of an undiagnosed illness, she said.
Patients often assume their health providers check for drug interactions or assess if a medication is no longer needed, and will catch extra prescriptions. That could be a risky assumption. Some doctors may prescribe yet another prescription to manage the side effects of an unnecessary drug, instead of doing a medication review and potentially “deprescribing” or discontinuing, a treatment that’s no longer needed.
About 57% of people age 65 years or older take five or more medications regularly – a concept known as polypharmacy, a study published in 2020 in the Journal of the American Geriatrics Society shows. While doctors prescribe drugs to help patients manage various ailments, as a list of medications grows, so do potential complications.
An older adult might forget to tell their doctor what they’re taking, or maybe they don’t even know what they’re taking or why, Dr. Lynn said.
“In some cases, a doctor just added a drug to treat something, not realizing they were already taking something else for it,” she said. “Of course, the situation of whether these patients can even afford all these drugs matters a lot, too.”
Some older adults may pick and choose which medications to take based on cost, not knowing which prescriptions are necessary, Dr. Lynn said.
Finding the ‘right balance’
Indeed, if given the option, up to 80% of older adults ages 50-80 would be open to stopping one or more of their prescribed medications, according to a 2023 poll by researchers at the University of Michigan, Ann Arbor.
“A lot of drugs that people take might have been appropriate at one point, but might have outlived their usefulness for that individual,” said Michael Steinman, MD, a professor of medicine and a geriatrician at the University of California, San Francisco, and coprincipal investigator of the U.S. Deprescribing Research Network, a doctor group focused on improving medication use for older adults.
“Having fewer medications can actually be beneficial,” he said. “You can take too many medications; you can take too few. The optimal thing is finding what is the right balance for you.”
Defining how many medications is too many depends on each person, which is why caregivers and older adults can ask their doctor for a review of medications that have multiplied over time.
By reevaluating their medications, older adults can actually lower their chances of potentially harmful side effects, and avoid the spiral of being prescribed even more medications, said Sarah Vordenberg, PharmD, MPH, a clinical associate professor at the University of Michigan’s College of Pharmacy, Ann Arbor.
“It’s not really the number of medications, it’s [about] are they inappropriate or unnecessary medications for a patient,” she said.
Patients and caregivers can ask for an honest conversation with their doctor. The University of Michigan poll found that more than 90% of older adults who took prescription medications expected their health care provider to review their medicines during a regular visit.
But doctors often need prompting from patients to start a review.
“The clinical inertia, or maintaining the status quo, unfortunately is a lot of times easier than having time-intensive conversations,” Dr. Vordenberg said.
Ask questions
Sara Merwin spent many years helping manage her parents’ medical appointments and health as they transitioned from living independently in Colorado to a retirement community and finally a nursing home. Ms. Merwin, coauthor of “The Informed Patient,” said her father was taking a long list of medications, and she often asked his primary care doctor for a medication review.
“I felt that my father at his age and his frailty didn’t need as many meds as he was on,” said Ms. Merwin, who lives in Long Island, N.Y. “So we went over his meds, and I asked, ‘Does he really need to be on this?’ ‘Does he really need to be on that?’ ”
She questioned one medication in particular, a statin to lower his cholesterol and risk of a heart attack.
“I thought possibly the statin was causing some myalgia, some muscle aches in his legs, which is why I advocated for coming off it,” she said.
The primary care doctor discontinued the anticholesterol drug.
Local pharmacies can also serve as a starting point for older adults and caregivers, where a pharmacist can give them more information on whether a particular combination of the medications taken may be harmful. In states that allow for pharmacists to prescribe some medications, pharmacists may be able to consolidate some of the medications or advise that a patient stop taking one or more, Dr. Vordenberg said.
“All pharmacists have the training to do a comprehensive medication review,” she said. “All pharmacists have the ability to follow up with the patient to find out how the deprescribing is going.”
Ms. Merwin’s parents received their prescriptions from a “small mom-and-pop pharmacy, where they were on a first-name basis with the pharmacist who really looked out for them. So they had that expertise available to them,” she said.
With information in hand on potentially unnecessary medications, the work of shedding medications should be done along with health care providers, some of whom prescribed the medications in the first place.
Many older adults live in geographically isolated areas without pharmacies, or receive prescriptions from mail-order pharmacies. In this case, Medicare plans offer free medication reviews with a doctor or pharmacist – known as a medication therapy management program – and provide recommendations for taking each drug.
Ms. Merwin’s father died in early 2020. She sometimes questions whether he should have stayed on the statin for longer, or if the doctor agreed too quickly without doing more research. But overall, she doesn’t regret raising the question with his health care providers, and she advises other caregivers and older adults to pay attention to medication lists.
“It’s dangerous to be passive when it comes to one’s health care now,” Ms. Merwin said. “That’s a difficult message for older adults to hear because they have grown up with the primacy of the doctor and the authority of the doctor, as opposed to it being a collaborative relationship.”
A version of this article first appeared on WebMD.com.
Joanne Lynn, MD, has lost track of the number of times in her 40 years as a geriatrician she’s seen a new patient come to her office carrying a bucket full of prescription medications – many of which they don’t need.
Dr. Lynn, who is on the faculty of George Washington University,Washington, recalled one woman who unwittingly was taking two blood pressure medications with different names.
“The risks included all the side effects overdosing carries,” Dr. Lynn said, ranging from blurred vision and crankiness to organ failure and even death.
For doctors with patients who don’t know they’re taking too much of a medication, “you wonder whether the drug is causing the health problems, and it’s a symptom of the wrong medication,” rather than a symptom of an undiagnosed illness, she said.
Patients often assume their health providers check for drug interactions or assess if a medication is no longer needed, and will catch extra prescriptions. That could be a risky assumption. Some doctors may prescribe yet another prescription to manage the side effects of an unnecessary drug, instead of doing a medication review and potentially “deprescribing” or discontinuing, a treatment that’s no longer needed.
About 57% of people age 65 years or older take five or more medications regularly – a concept known as polypharmacy, a study published in 2020 in the Journal of the American Geriatrics Society shows. While doctors prescribe drugs to help patients manage various ailments, as a list of medications grows, so do potential complications.
An older adult might forget to tell their doctor what they’re taking, or maybe they don’t even know what they’re taking or why, Dr. Lynn said.
“In some cases, a doctor just added a drug to treat something, not realizing they were already taking something else for it,” she said. “Of course, the situation of whether these patients can even afford all these drugs matters a lot, too.”
Some older adults may pick and choose which medications to take based on cost, not knowing which prescriptions are necessary, Dr. Lynn said.
Finding the ‘right balance’
Indeed, if given the option, up to 80% of older adults ages 50-80 would be open to stopping one or more of their prescribed medications, according to a 2023 poll by researchers at the University of Michigan, Ann Arbor.
“A lot of drugs that people take might have been appropriate at one point, but might have outlived their usefulness for that individual,” said Michael Steinman, MD, a professor of medicine and a geriatrician at the University of California, San Francisco, and coprincipal investigator of the U.S. Deprescribing Research Network, a doctor group focused on improving medication use for older adults.
“Having fewer medications can actually be beneficial,” he said. “You can take too many medications; you can take too few. The optimal thing is finding what is the right balance for you.”
Defining how many medications is too many depends on each person, which is why caregivers and older adults can ask their doctor for a review of medications that have multiplied over time.
By reevaluating their medications, older adults can actually lower their chances of potentially harmful side effects, and avoid the spiral of being prescribed even more medications, said Sarah Vordenberg, PharmD, MPH, a clinical associate professor at the University of Michigan’s College of Pharmacy, Ann Arbor.
“It’s not really the number of medications, it’s [about] are they inappropriate or unnecessary medications for a patient,” she said.
Patients and caregivers can ask for an honest conversation with their doctor. The University of Michigan poll found that more than 90% of older adults who took prescription medications expected their health care provider to review their medicines during a regular visit.
But doctors often need prompting from patients to start a review.
“The clinical inertia, or maintaining the status quo, unfortunately is a lot of times easier than having time-intensive conversations,” Dr. Vordenberg said.
Ask questions
Sara Merwin spent many years helping manage her parents’ medical appointments and health as they transitioned from living independently in Colorado to a retirement community and finally a nursing home. Ms. Merwin, coauthor of “The Informed Patient,” said her father was taking a long list of medications, and she often asked his primary care doctor for a medication review.
“I felt that my father at his age and his frailty didn’t need as many meds as he was on,” said Ms. Merwin, who lives in Long Island, N.Y. “So we went over his meds, and I asked, ‘Does he really need to be on this?’ ‘Does he really need to be on that?’ ”
She questioned one medication in particular, a statin to lower his cholesterol and risk of a heart attack.
“I thought possibly the statin was causing some myalgia, some muscle aches in his legs, which is why I advocated for coming off it,” she said.
The primary care doctor discontinued the anticholesterol drug.
Local pharmacies can also serve as a starting point for older adults and caregivers, where a pharmacist can give them more information on whether a particular combination of the medications taken may be harmful. In states that allow for pharmacists to prescribe some medications, pharmacists may be able to consolidate some of the medications or advise that a patient stop taking one or more, Dr. Vordenberg said.
“All pharmacists have the training to do a comprehensive medication review,” she said. “All pharmacists have the ability to follow up with the patient to find out how the deprescribing is going.”
Ms. Merwin’s parents received their prescriptions from a “small mom-and-pop pharmacy, where they were on a first-name basis with the pharmacist who really looked out for them. So they had that expertise available to them,” she said.
With information in hand on potentially unnecessary medications, the work of shedding medications should be done along with health care providers, some of whom prescribed the medications in the first place.
Many older adults live in geographically isolated areas without pharmacies, or receive prescriptions from mail-order pharmacies. In this case, Medicare plans offer free medication reviews with a doctor or pharmacist – known as a medication therapy management program – and provide recommendations for taking each drug.
Ms. Merwin’s father died in early 2020. She sometimes questions whether he should have stayed on the statin for longer, or if the doctor agreed too quickly without doing more research. But overall, she doesn’t regret raising the question with his health care providers, and she advises other caregivers and older adults to pay attention to medication lists.
“It’s dangerous to be passive when it comes to one’s health care now,” Ms. Merwin said. “That’s a difficult message for older adults to hear because they have grown up with the primacy of the doctor and the authority of the doctor, as opposed to it being a collaborative relationship.”
A version of this article first appeared on WebMD.com.
Joanne Lynn, MD, has lost track of the number of times in her 40 years as a geriatrician she’s seen a new patient come to her office carrying a bucket full of prescription medications – many of which they don’t need.
Dr. Lynn, who is on the faculty of George Washington University,Washington, recalled one woman who unwittingly was taking two blood pressure medications with different names.
“The risks included all the side effects overdosing carries,” Dr. Lynn said, ranging from blurred vision and crankiness to organ failure and even death.
For doctors with patients who don’t know they’re taking too much of a medication, “you wonder whether the drug is causing the health problems, and it’s a symptom of the wrong medication,” rather than a symptom of an undiagnosed illness, she said.
Patients often assume their health providers check for drug interactions or assess if a medication is no longer needed, and will catch extra prescriptions. That could be a risky assumption. Some doctors may prescribe yet another prescription to manage the side effects of an unnecessary drug, instead of doing a medication review and potentially “deprescribing” or discontinuing, a treatment that’s no longer needed.
About 57% of people age 65 years or older take five or more medications regularly – a concept known as polypharmacy, a study published in 2020 in the Journal of the American Geriatrics Society shows. While doctors prescribe drugs to help patients manage various ailments, as a list of medications grows, so do potential complications.
An older adult might forget to tell their doctor what they’re taking, or maybe they don’t even know what they’re taking or why, Dr. Lynn said.
“In some cases, a doctor just added a drug to treat something, not realizing they were already taking something else for it,” she said. “Of course, the situation of whether these patients can even afford all these drugs matters a lot, too.”
Some older adults may pick and choose which medications to take based on cost, not knowing which prescriptions are necessary, Dr. Lynn said.
Finding the ‘right balance’
Indeed, if given the option, up to 80% of older adults ages 50-80 would be open to stopping one or more of their prescribed medications, according to a 2023 poll by researchers at the University of Michigan, Ann Arbor.
“A lot of drugs that people take might have been appropriate at one point, but might have outlived their usefulness for that individual,” said Michael Steinman, MD, a professor of medicine and a geriatrician at the University of California, San Francisco, and coprincipal investigator of the U.S. Deprescribing Research Network, a doctor group focused on improving medication use for older adults.
“Having fewer medications can actually be beneficial,” he said. “You can take too many medications; you can take too few. The optimal thing is finding what is the right balance for you.”
Defining how many medications is too many depends on each person, which is why caregivers and older adults can ask their doctor for a review of medications that have multiplied over time.
By reevaluating their medications, older adults can actually lower their chances of potentially harmful side effects, and avoid the spiral of being prescribed even more medications, said Sarah Vordenberg, PharmD, MPH, a clinical associate professor at the University of Michigan’s College of Pharmacy, Ann Arbor.
“It’s not really the number of medications, it’s [about] are they inappropriate or unnecessary medications for a patient,” she said.
Patients and caregivers can ask for an honest conversation with their doctor. The University of Michigan poll found that more than 90% of older adults who took prescription medications expected their health care provider to review their medicines during a regular visit.
But doctors often need prompting from patients to start a review.
“The clinical inertia, or maintaining the status quo, unfortunately is a lot of times easier than having time-intensive conversations,” Dr. Vordenberg said.
Ask questions
Sara Merwin spent many years helping manage her parents’ medical appointments and health as they transitioned from living independently in Colorado to a retirement community and finally a nursing home. Ms. Merwin, coauthor of “The Informed Patient,” said her father was taking a long list of medications, and she often asked his primary care doctor for a medication review.
“I felt that my father at his age and his frailty didn’t need as many meds as he was on,” said Ms. Merwin, who lives in Long Island, N.Y. “So we went over his meds, and I asked, ‘Does he really need to be on this?’ ‘Does he really need to be on that?’ ”
She questioned one medication in particular, a statin to lower his cholesterol and risk of a heart attack.
“I thought possibly the statin was causing some myalgia, some muscle aches in his legs, which is why I advocated for coming off it,” she said.
The primary care doctor discontinued the anticholesterol drug.
Local pharmacies can also serve as a starting point for older adults and caregivers, where a pharmacist can give them more information on whether a particular combination of the medications taken may be harmful. In states that allow for pharmacists to prescribe some medications, pharmacists may be able to consolidate some of the medications or advise that a patient stop taking one or more, Dr. Vordenberg said.
“All pharmacists have the training to do a comprehensive medication review,” she said. “All pharmacists have the ability to follow up with the patient to find out how the deprescribing is going.”
Ms. Merwin’s parents received their prescriptions from a “small mom-and-pop pharmacy, where they were on a first-name basis with the pharmacist who really looked out for them. So they had that expertise available to them,” she said.
With information in hand on potentially unnecessary medications, the work of shedding medications should be done along with health care providers, some of whom prescribed the medications in the first place.
Many older adults live in geographically isolated areas without pharmacies, or receive prescriptions from mail-order pharmacies. In this case, Medicare plans offer free medication reviews with a doctor or pharmacist – known as a medication therapy management program – and provide recommendations for taking each drug.
Ms. Merwin’s father died in early 2020. She sometimes questions whether he should have stayed on the statin for longer, or if the doctor agreed too quickly without doing more research. But overall, she doesn’t regret raising the question with his health care providers, and she advises other caregivers and older adults to pay attention to medication lists.
“It’s dangerous to be passive when it comes to one’s health care now,” Ms. Merwin said. “That’s a difficult message for older adults to hear because they have grown up with the primacy of the doctor and the authority of the doctor, as opposed to it being a collaborative relationship.”
A version of this article first appeared on WebMD.com.
FDA warns of tattoo ink tied to dangerous infections
The Food and Drug Administration draft guidance released recently on possible contamination of tattoo ink was not concerning Whitney Donohue, 34, owner of Forget Me Not Tattoo in Billings, Mont.
“I get our ink directly through the manufacturer – not at a store or through Amazon or eBay,” she said. “You never know if it’s going to be repackaged.”
Tattoo artists themselves, she said, regulate the quality of ink they use.
Still, the threat is real, said Bruce Brod, MD, a clinical professor of dermatology at the University of Pennsylvania Health System. “I’ve seen several different infections from tattooing, and they are from organisms that tend to contaminate things in damp, liquid-type environments.”
, dermatologists said.
“Tattooing involves puncturing the epidermis about 100 times per second with needles and depositing ink 1.5 to 2 millimeters below the surface of the skin, deep into the dermis,” the guidance states. “Contaminated tattoo ink can cause infections and serious injuries. Because these inks are injected, pathogens or other harmful substances in these inks can travel from the injection site through the blood and lymphatic systems to other parts of the body.”
The guidance comes as body art continues to get more popular. According to a 2019 poll, 30% of Americans had at least one tattoo – up from 21% in 2012. Forty percent of people 18-34 and 36% of those ages 35-54 had at least one tattoo. And though they are commonplace, tattoos come with medical risks that should be known beforehand, doctors said.
Commonly reported symptoms of tattoo ink–associated infections include rashes, blisters, painful nodules, and severe abscesses. One of the most common bacteria found in contaminated tattoo ink is nontuberculous mycobacteria, which is related to the bacteria that causes tuberculosis and can be found in soil and water.
The guidance lists several unsanitary manufacturing conditions that may lead to ink contamination, including:
- Preparing or packing of tattoo inks in facilities that are hard to sanitize, such as carpeted areas
- Ink or ink components left uncovered, especially near open air ducts
- Unsanitary mixing of tattoo inks, including with unclean utensils or containers
- Lack of appropriate attire by staff, failure to use hairnets, lab coats, aprons, gowns, masks, or gloves
“Infections will often spread along the drainage channels in the skin and create squiggly, uneven lines of big red, lumpy nodules,” Dr. Brod said.
Between 2003 and 2023, there were 18 recalls of tattoo inks that were contaminated with various microorganisms, according to the FDA. In May 2019, the FDA issued a safety alert advising consumers, tattoo artists, and retailers to avoid using or selling certain tattoo inks contaminated with microorganisms.
Reputable ink manufacturers use a process called gamma radiation, which refers to electromagnetic radiation of high frequencies to kill microorganisms in the ink and its packaging.
Most of the trustworthy, high-quality ink manufacturers are well-known among tattoo artists, Ms. Donohue said.
While she has seen customers with sensitive skin have allergic reactions, she has not seen someone come back with an infection in her 9 years working in the tattoo industry.
Because tattoo ink is considered a cosmetic product, there is not much regulatory oversight involved, which means the sterility and quality of ingredients vary, said Teo Soleymani, MD, an assistant clinical professor of dermatology and dermatological surgery at the UCLA David Geffen School of Medicine.
“Cosmeceuticals aren’t regulated by the FDA like prescription medication,” he said. “What we’ve seen many times is inadvertent contamination during the application process or contamination while the inks are being made.”
In years past, unclean needles spreading hepatitis and HIV were more of a concern, but those rates have dropped significantly, Dr. Soleymani said.
The infections that have increased are from rare bacteria that exist in stagnant water. And they are injected into a part of the body that allows them to evade the immune system, he said: shallow enough that there aren’t many associated blood vessels, but not still below the layer of skin that gets sloughed off every 28 days.
Sometimes, antibiotics alone won’t cut it, and the tattoo will require surgical removal.
“The aesthetic you were going for has to be not only removed, but you’re left with a surgical scar,” Dr. Soleymani said. “Tattoos can be beautiful, but they can come with unwanted visitors that can cause months of misery.”
A version of this article first appeared on WebMD.com.
The Food and Drug Administration draft guidance released recently on possible contamination of tattoo ink was not concerning Whitney Donohue, 34, owner of Forget Me Not Tattoo in Billings, Mont.
“I get our ink directly through the manufacturer – not at a store or through Amazon or eBay,” she said. “You never know if it’s going to be repackaged.”
Tattoo artists themselves, she said, regulate the quality of ink they use.
Still, the threat is real, said Bruce Brod, MD, a clinical professor of dermatology at the University of Pennsylvania Health System. “I’ve seen several different infections from tattooing, and they are from organisms that tend to contaminate things in damp, liquid-type environments.”
, dermatologists said.
“Tattooing involves puncturing the epidermis about 100 times per second with needles and depositing ink 1.5 to 2 millimeters below the surface of the skin, deep into the dermis,” the guidance states. “Contaminated tattoo ink can cause infections and serious injuries. Because these inks are injected, pathogens or other harmful substances in these inks can travel from the injection site through the blood and lymphatic systems to other parts of the body.”
The guidance comes as body art continues to get more popular. According to a 2019 poll, 30% of Americans had at least one tattoo – up from 21% in 2012. Forty percent of people 18-34 and 36% of those ages 35-54 had at least one tattoo. And though they are commonplace, tattoos come with medical risks that should be known beforehand, doctors said.
Commonly reported symptoms of tattoo ink–associated infections include rashes, blisters, painful nodules, and severe abscesses. One of the most common bacteria found in contaminated tattoo ink is nontuberculous mycobacteria, which is related to the bacteria that causes tuberculosis and can be found in soil and water.
The guidance lists several unsanitary manufacturing conditions that may lead to ink contamination, including:
- Preparing or packing of tattoo inks in facilities that are hard to sanitize, such as carpeted areas
- Ink or ink components left uncovered, especially near open air ducts
- Unsanitary mixing of tattoo inks, including with unclean utensils or containers
- Lack of appropriate attire by staff, failure to use hairnets, lab coats, aprons, gowns, masks, or gloves
“Infections will often spread along the drainage channels in the skin and create squiggly, uneven lines of big red, lumpy nodules,” Dr. Brod said.
Between 2003 and 2023, there were 18 recalls of tattoo inks that were contaminated with various microorganisms, according to the FDA. In May 2019, the FDA issued a safety alert advising consumers, tattoo artists, and retailers to avoid using or selling certain tattoo inks contaminated with microorganisms.
Reputable ink manufacturers use a process called gamma radiation, which refers to electromagnetic radiation of high frequencies to kill microorganisms in the ink and its packaging.
Most of the trustworthy, high-quality ink manufacturers are well-known among tattoo artists, Ms. Donohue said.
While she has seen customers with sensitive skin have allergic reactions, she has not seen someone come back with an infection in her 9 years working in the tattoo industry.
Because tattoo ink is considered a cosmetic product, there is not much regulatory oversight involved, which means the sterility and quality of ingredients vary, said Teo Soleymani, MD, an assistant clinical professor of dermatology and dermatological surgery at the UCLA David Geffen School of Medicine.
“Cosmeceuticals aren’t regulated by the FDA like prescription medication,” he said. “What we’ve seen many times is inadvertent contamination during the application process or contamination while the inks are being made.”
In years past, unclean needles spreading hepatitis and HIV were more of a concern, but those rates have dropped significantly, Dr. Soleymani said.
The infections that have increased are from rare bacteria that exist in stagnant water. And they are injected into a part of the body that allows them to evade the immune system, he said: shallow enough that there aren’t many associated blood vessels, but not still below the layer of skin that gets sloughed off every 28 days.
Sometimes, antibiotics alone won’t cut it, and the tattoo will require surgical removal.
“The aesthetic you were going for has to be not only removed, but you’re left with a surgical scar,” Dr. Soleymani said. “Tattoos can be beautiful, but they can come with unwanted visitors that can cause months of misery.”
A version of this article first appeared on WebMD.com.
The Food and Drug Administration draft guidance released recently on possible contamination of tattoo ink was not concerning Whitney Donohue, 34, owner of Forget Me Not Tattoo in Billings, Mont.
“I get our ink directly through the manufacturer – not at a store or through Amazon or eBay,” she said. “You never know if it’s going to be repackaged.”
Tattoo artists themselves, she said, regulate the quality of ink they use.
Still, the threat is real, said Bruce Brod, MD, a clinical professor of dermatology at the University of Pennsylvania Health System. “I’ve seen several different infections from tattooing, and they are from organisms that tend to contaminate things in damp, liquid-type environments.”
, dermatologists said.
“Tattooing involves puncturing the epidermis about 100 times per second with needles and depositing ink 1.5 to 2 millimeters below the surface of the skin, deep into the dermis,” the guidance states. “Contaminated tattoo ink can cause infections and serious injuries. Because these inks are injected, pathogens or other harmful substances in these inks can travel from the injection site through the blood and lymphatic systems to other parts of the body.”
The guidance comes as body art continues to get more popular. According to a 2019 poll, 30% of Americans had at least one tattoo – up from 21% in 2012. Forty percent of people 18-34 and 36% of those ages 35-54 had at least one tattoo. And though they are commonplace, tattoos come with medical risks that should be known beforehand, doctors said.
Commonly reported symptoms of tattoo ink–associated infections include rashes, blisters, painful nodules, and severe abscesses. One of the most common bacteria found in contaminated tattoo ink is nontuberculous mycobacteria, which is related to the bacteria that causes tuberculosis and can be found in soil and water.
The guidance lists several unsanitary manufacturing conditions that may lead to ink contamination, including:
- Preparing or packing of tattoo inks in facilities that are hard to sanitize, such as carpeted areas
- Ink or ink components left uncovered, especially near open air ducts
- Unsanitary mixing of tattoo inks, including with unclean utensils or containers
- Lack of appropriate attire by staff, failure to use hairnets, lab coats, aprons, gowns, masks, or gloves
“Infections will often spread along the drainage channels in the skin and create squiggly, uneven lines of big red, lumpy nodules,” Dr. Brod said.
Between 2003 and 2023, there were 18 recalls of tattoo inks that were contaminated with various microorganisms, according to the FDA. In May 2019, the FDA issued a safety alert advising consumers, tattoo artists, and retailers to avoid using or selling certain tattoo inks contaminated with microorganisms.
Reputable ink manufacturers use a process called gamma radiation, which refers to electromagnetic radiation of high frequencies to kill microorganisms in the ink and its packaging.
Most of the trustworthy, high-quality ink manufacturers are well-known among tattoo artists, Ms. Donohue said.
While she has seen customers with sensitive skin have allergic reactions, she has not seen someone come back with an infection in her 9 years working in the tattoo industry.
Because tattoo ink is considered a cosmetic product, there is not much regulatory oversight involved, which means the sterility and quality of ingredients vary, said Teo Soleymani, MD, an assistant clinical professor of dermatology and dermatological surgery at the UCLA David Geffen School of Medicine.
“Cosmeceuticals aren’t regulated by the FDA like prescription medication,” he said. “What we’ve seen many times is inadvertent contamination during the application process or contamination while the inks are being made.”
In years past, unclean needles spreading hepatitis and HIV were more of a concern, but those rates have dropped significantly, Dr. Soleymani said.
The infections that have increased are from rare bacteria that exist in stagnant water. And they are injected into a part of the body that allows them to evade the immune system, he said: shallow enough that there aren’t many associated blood vessels, but not still below the layer of skin that gets sloughed off every 28 days.
Sometimes, antibiotics alone won’t cut it, and the tattoo will require surgical removal.
“The aesthetic you were going for has to be not only removed, but you’re left with a surgical scar,” Dr. Soleymani said. “Tattoos can be beautiful, but they can come with unwanted visitors that can cause months of misery.”
A version of this article first appeared on WebMD.com.
International rights group calls out United States for allowing hospitals to push millions into debt
Human Rights Watch, the nonprofit that for decades has called attention to the victims of war, famine, and political repression around the world, is taking aim at U.S. hospitals for pushing millions of American patients into debt.
In a new report, the group calls for stronger government action to protect Americans from aggressive billing and debt collection by nonprofit hospitals, which Human Rights Watch said are systematically undermining patients’ human rights.
“Given the high prevalence of hospital-related medical debt in the U.S., this system is clearly not working,” concludes the report, which draws extensively on an ongoing investigation of medical debt by KFF Health News and NPR.
The report continues: “The U.S. model of subsidizing privately operated hospitals with tax exemptions in the hope that they will increase the accessibility of hospital care for un- and underinsured patients allows for abusive medical billing and debt collection practices and undermines human rights, including the right to health.”
Nationwide, about 100 million people – or 41% of adults – have some form of health care debt, a KFF survey conducted for the KFF Health News–NPR project found. And while patient debt is being driven by a range of medical and dental bills, polls and studies suggest hospitals are a major contributor.
About a third of U.S. adults with health care debt owed money for hospitalization, KFF’s polling found. Close to half of those owed at least $5,000. About a quarter owed $10,000 or more.
The scale of this crisis – which is unparalleled among wealthy nations – compelled Human Rights Watch to release the new report, said researcher Matt McConnell, its author. “Historically, Human Rights Watch has been an organization that has focused on international human rights issues,” he said. “But on medical debt, the U.S. is a real outlier. What you see is a system that privileges a few but creates large barriers to people accessing basic health rights.”
Hospital industry officials defend their work, citing hospitals’ broader work to help the communities they serve. “As a field, hospitals provide more benefit to their communities than any other sector in health care,” Melinda Hatton, general counsel at the American Hospital Association, wrote in a response to the Human Right Watch report.
Federal law requires private, tax-exempt hospitals – which make up more than half the nation’s medical centers – to provide care at no cost or at a discount to low-income patients. But reporting by KFF Health News and others has found that many hospitals make this aid difficult for patients to get.
At the same time, thousands of medical centers – including many tax-exempt ones – engage in aggressive debt collection tactics to pursue patients, including garnishing patients’ wages, placing liens on their homes, or selling their debt to third-party debt collectors.
Overall, KFF Health News found that most of the nation’s approximately 5,100 hospitals serving the general public have policies to use legal action or other aggressive tactics against patients. And one in five will deny nonemergency care to people with outstanding debt.
“Medical debt is drowning many low-income and working families while hospitals continue to benefit from nonprofit tax status as they pursue families for medical debt,” said Marceline White, executive director of Economic Action Maryland. The advocacy group has helped enact tighter rules to ensure Maryland hospitals make financial assistance more easily accessible and to restrict hospitals from some aggressive debt collection tactics, such as placing liens on patients’ homes.
Similar efforts are underway in other states, including Colorado, New Mexico, New York, Oregon, and Washington. But many patient and consumer advocates say stronger federal action is needed to expand patient protections.
The Human Rights Watch report – titled “In Sheep’s Clothing: United States’ Poorly Regulated Nonprofit Hospitals Undermine Health Care Access” – lists more than a dozen recommendations. These include:
- Congress should pass legislation to ensure that hospitals provide at least the same amount of charity care as they receive in public subsidies.
- The IRS should set uniform national standards on patients’ eligibility for financial assistance at nonprofit hospitals. Currently, hospitals are free to set their own standards, resulting in widespread variation, which can confuse patients.
- The Consumer Financial Protection Bureau, a federal watchdog agency, should crack down on debt collectors that do not ensure that patients have been screened for financial assistance before being pursued.
- The federal Centers for Medicare & Medicaid Services, which administers the two mammoth public insurance programs, should penalize hospitals that do not provide adequate financial assistance to patients.
“Nonprofit hospitals are contributing to medical debt and engaging in abusive billing and debt collection practices,” Mr. McConnell said. “The reason this keeps happening is the absence of clear guidelines and the federal government’s inadequate enforcement of existing regulations.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF – the independent source for health policy research, polling, and journalism.
Human Rights Watch, the nonprofit that for decades has called attention to the victims of war, famine, and political repression around the world, is taking aim at U.S. hospitals for pushing millions of American patients into debt.
In a new report, the group calls for stronger government action to protect Americans from aggressive billing and debt collection by nonprofit hospitals, which Human Rights Watch said are systematically undermining patients’ human rights.
“Given the high prevalence of hospital-related medical debt in the U.S., this system is clearly not working,” concludes the report, which draws extensively on an ongoing investigation of medical debt by KFF Health News and NPR.
The report continues: “The U.S. model of subsidizing privately operated hospitals with tax exemptions in the hope that they will increase the accessibility of hospital care for un- and underinsured patients allows for abusive medical billing and debt collection practices and undermines human rights, including the right to health.”
Nationwide, about 100 million people – or 41% of adults – have some form of health care debt, a KFF survey conducted for the KFF Health News–NPR project found. And while patient debt is being driven by a range of medical and dental bills, polls and studies suggest hospitals are a major contributor.
About a third of U.S. adults with health care debt owed money for hospitalization, KFF’s polling found. Close to half of those owed at least $5,000. About a quarter owed $10,000 or more.
The scale of this crisis – which is unparalleled among wealthy nations – compelled Human Rights Watch to release the new report, said researcher Matt McConnell, its author. “Historically, Human Rights Watch has been an organization that has focused on international human rights issues,” he said. “But on medical debt, the U.S. is a real outlier. What you see is a system that privileges a few but creates large barriers to people accessing basic health rights.”
Hospital industry officials defend their work, citing hospitals’ broader work to help the communities they serve. “As a field, hospitals provide more benefit to their communities than any other sector in health care,” Melinda Hatton, general counsel at the American Hospital Association, wrote in a response to the Human Right Watch report.
Federal law requires private, tax-exempt hospitals – which make up more than half the nation’s medical centers – to provide care at no cost or at a discount to low-income patients. But reporting by KFF Health News and others has found that many hospitals make this aid difficult for patients to get.
At the same time, thousands of medical centers – including many tax-exempt ones – engage in aggressive debt collection tactics to pursue patients, including garnishing patients’ wages, placing liens on their homes, or selling their debt to third-party debt collectors.
Overall, KFF Health News found that most of the nation’s approximately 5,100 hospitals serving the general public have policies to use legal action or other aggressive tactics against patients. And one in five will deny nonemergency care to people with outstanding debt.
“Medical debt is drowning many low-income and working families while hospitals continue to benefit from nonprofit tax status as they pursue families for medical debt,” said Marceline White, executive director of Economic Action Maryland. The advocacy group has helped enact tighter rules to ensure Maryland hospitals make financial assistance more easily accessible and to restrict hospitals from some aggressive debt collection tactics, such as placing liens on patients’ homes.
Similar efforts are underway in other states, including Colorado, New Mexico, New York, Oregon, and Washington. But many patient and consumer advocates say stronger federal action is needed to expand patient protections.
The Human Rights Watch report – titled “In Sheep’s Clothing: United States’ Poorly Regulated Nonprofit Hospitals Undermine Health Care Access” – lists more than a dozen recommendations. These include:
- Congress should pass legislation to ensure that hospitals provide at least the same amount of charity care as they receive in public subsidies.
- The IRS should set uniform national standards on patients’ eligibility for financial assistance at nonprofit hospitals. Currently, hospitals are free to set their own standards, resulting in widespread variation, which can confuse patients.
- The Consumer Financial Protection Bureau, a federal watchdog agency, should crack down on debt collectors that do not ensure that patients have been screened for financial assistance before being pursued.
- The federal Centers for Medicare & Medicaid Services, which administers the two mammoth public insurance programs, should penalize hospitals that do not provide adequate financial assistance to patients.
“Nonprofit hospitals are contributing to medical debt and engaging in abusive billing and debt collection practices,” Mr. McConnell said. “The reason this keeps happening is the absence of clear guidelines and the federal government’s inadequate enforcement of existing regulations.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF – the independent source for health policy research, polling, and journalism.
Human Rights Watch, the nonprofit that for decades has called attention to the victims of war, famine, and political repression around the world, is taking aim at U.S. hospitals for pushing millions of American patients into debt.
In a new report, the group calls for stronger government action to protect Americans from aggressive billing and debt collection by nonprofit hospitals, which Human Rights Watch said are systematically undermining patients’ human rights.
“Given the high prevalence of hospital-related medical debt in the U.S., this system is clearly not working,” concludes the report, which draws extensively on an ongoing investigation of medical debt by KFF Health News and NPR.
The report continues: “The U.S. model of subsidizing privately operated hospitals with tax exemptions in the hope that they will increase the accessibility of hospital care for un- and underinsured patients allows for abusive medical billing and debt collection practices and undermines human rights, including the right to health.”
Nationwide, about 100 million people – or 41% of adults – have some form of health care debt, a KFF survey conducted for the KFF Health News–NPR project found. And while patient debt is being driven by a range of medical and dental bills, polls and studies suggest hospitals are a major contributor.
About a third of U.S. adults with health care debt owed money for hospitalization, KFF’s polling found. Close to half of those owed at least $5,000. About a quarter owed $10,000 or more.
The scale of this crisis – which is unparalleled among wealthy nations – compelled Human Rights Watch to release the new report, said researcher Matt McConnell, its author. “Historically, Human Rights Watch has been an organization that has focused on international human rights issues,” he said. “But on medical debt, the U.S. is a real outlier. What you see is a system that privileges a few but creates large barriers to people accessing basic health rights.”
Hospital industry officials defend their work, citing hospitals’ broader work to help the communities they serve. “As a field, hospitals provide more benefit to their communities than any other sector in health care,” Melinda Hatton, general counsel at the American Hospital Association, wrote in a response to the Human Right Watch report.
Federal law requires private, tax-exempt hospitals – which make up more than half the nation’s medical centers – to provide care at no cost or at a discount to low-income patients. But reporting by KFF Health News and others has found that many hospitals make this aid difficult for patients to get.
At the same time, thousands of medical centers – including many tax-exempt ones – engage in aggressive debt collection tactics to pursue patients, including garnishing patients’ wages, placing liens on their homes, or selling their debt to third-party debt collectors.
Overall, KFF Health News found that most of the nation’s approximately 5,100 hospitals serving the general public have policies to use legal action or other aggressive tactics against patients. And one in five will deny nonemergency care to people with outstanding debt.
“Medical debt is drowning many low-income and working families while hospitals continue to benefit from nonprofit tax status as they pursue families for medical debt,” said Marceline White, executive director of Economic Action Maryland. The advocacy group has helped enact tighter rules to ensure Maryland hospitals make financial assistance more easily accessible and to restrict hospitals from some aggressive debt collection tactics, such as placing liens on patients’ homes.
Similar efforts are underway in other states, including Colorado, New Mexico, New York, Oregon, and Washington. But many patient and consumer advocates say stronger federal action is needed to expand patient protections.
The Human Rights Watch report – titled “In Sheep’s Clothing: United States’ Poorly Regulated Nonprofit Hospitals Undermine Health Care Access” – lists more than a dozen recommendations. These include:
- Congress should pass legislation to ensure that hospitals provide at least the same amount of charity care as they receive in public subsidies.
- The IRS should set uniform national standards on patients’ eligibility for financial assistance at nonprofit hospitals. Currently, hospitals are free to set their own standards, resulting in widespread variation, which can confuse patients.
- The Consumer Financial Protection Bureau, a federal watchdog agency, should crack down on debt collectors that do not ensure that patients have been screened for financial assistance before being pursued.
- The federal Centers for Medicare & Medicaid Services, which administers the two mammoth public insurance programs, should penalize hospitals that do not provide adequate financial assistance to patients.
“Nonprofit hospitals are contributing to medical debt and engaging in abusive billing and debt collection practices,” Mr. McConnell said. “The reason this keeps happening is the absence of clear guidelines and the federal government’s inadequate enforcement of existing regulations.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF – the independent source for health policy research, polling, and journalism.