User login
Is COVID-19 accelerating progress toward high-value care?
As Rachna Rawal, MD, was donning her personal protective equipment (PPE), a process that has become deeply ingrained into her muscle memory, a nurse approached her to ask, “Hey, for Mr. Smith, any chance we can time these labs to be done together with his medication administration? We’ve been in and out of that room a few times already.”
As someone who embraces high-value care, this simple suggestion surprised her. What an easy strategy to minimize room entry with full PPE, lab testing, and patient interruptions. That same day, someone else asked, “Do we need overnight vitals?”
COVID-19 has forced hospitalists to reconsider almost every aspect of care. It feels like every decision we make including things we do routinely – labs, vital signs, imaging – needs to be reassessed to determine the actual benefit to the patient balanced against concerns about staff safety, dwindling PPE supplies, and medication reserves. We are all faced with frequently answering the question, “How will this intervention help the patient?” This question lies at the heart of delivering high-value care.
High-value care is providing the best care possible through efficient use of resources, achieving optimal results for each patient. While high-value care has become a prominent focus over the past decade, COVID-19’s high transmissibility without a cure – and associated scarcity of health care resources – have sparked additional discussions on the front lines about promoting patient outcomes while avoiding waste. Clinicians may not have realized that these were high-value care conversations.
The United States’ health care quality and cost crises, worsened in the face of the current pandemic, have been glaringly apparent for years. Our country is spending more money on health care than anywhere else in the world without desired improvements in patient outcomes. A 2019 JAMA study found that 25% of all health care spending, an estimated $760 to $935 billion, is considered waste, and a significant proportion of this waste is due to repetitive care, overuse and unnecessary care in the U.S.1
Examples of low-value care tests include ordering daily labs in stable medicine inpatients, routine urine electrolytes in acute kidney injury, and folate testing in anemia. The Choosing Wisely® national campaign, Journal of Hospital Medicine’s “Things We Do For No Reason,” and JAMA Internal Medicine’s “Teachable Moment” series have provided guidance on areas where common testing or interventions may not benefit patient outcomes.
The COVID-19 pandemic has raised questions related to other widely-utilized practices: Can medication times be readjusted to allow only one entry into the room? Will these labs or imaging studies actually change management? Are vital checks every 4 hours needed?
Why did it take the COVID-19 threat to our medical system to force many of us to have these discussions? Despite prior efforts to integrate high-value care into hospital practices, long-standing habits and deep-seeded culture are challenging to overcome. Once clinicians develop practice habits, these behaviors tend to persist throughout their careers.2 In many ways, COVID-19 was like hitting a “reset button” as health care professionals were forced to rapidly confront their deeply-ingrained hospital practices and habits. From new protocols for patient rounding to universal masking and social distancing to ground-breaking strategies like awake proning, the response to COVID-19 has represented an unprecedented rapid shift in practice. Previously, consequences of overuse were too downstream or too abstract for clinicians to see in real-time. However, now the ramifications of these choices hit closer to home with obvious potential consequences – like spreading a terrifying virus.
There are three interventions that hospitalists should consider implementing immediately in the COVID-19 era that accelerate us toward high-value care. Routine lab tests, imaging, and overnight vitals represent opportunities to provide patient-centered care while also remaining cognizant of resource utilization.
One area in hospital medicine that has proven challenging to significantly change practice has been routine daily labs. Patients on a general medical inpatient service who are clinically stable generally do not benefit from routine lab work.3 Avoiding these tests does not increase mortality or length of stay in clinically stable patients.3 However, despite this evidence, many patients with COVID-19 and other conditions experience lab draws that are not timed together and are done each morning out of “routine.” Choosing Wisely® recommendations from the Society of Hospital Medicine encourage clinicians to question routine lab work for COVID-19 patients and to consider batching them, if possible.3,4 In COVID-19 patients, the risks of not batching tests are magnified, both in terms of the patient-centered experience and for clinician safety. In essence, COVID-19 has pushed us to consider the elements of safety, PPE conservation and other factors, rather than making decisions based solely on their own comfort, convenience, or historical practice.
Clinicians are also reconsidering the necessity of imaging during the pandemic. The “Things We Do For No Reason” article on “Choosing Wisely® in the COVID-19 era” highlights this well.4 It is more important now than ever to decide whether the timing and type of imaging will change management for your patient. Questions to ask include: Can a portable x-ray be used to avoid patient travel and will that CT scan help your patient? A posterior-anterior/lateral x-ray can potentially provide more information depending on the clinical scenario. However, we now need to assess if that extra information is going to impact patient management. Downstream consequences of these decisions include not only risks to the patient but also infectious exposures for staff and others during patient travel.
Lastly, overnight vital sign checks are another intervention we should analyze through this high-value care lens. The Journal of Hospital Medicine released a “Things We Do For No Reason” article about minimizing overnight vitals to promote uninterrupted sleep at night.5 Deleterious effects of interrupting the sleep of our patients include delirium and patient dissatisfaction.5 Studies have shown the benefits of this approach, yet the shift away from routine overnight vitals has not yet widely occurred.
COVID-19 has pressed us to save PPE and minimize exposure risk; hence, some centers are coordinating the timing of vitals with medication administration times, when feasible. In the stable patient recovering from COVID-19, overnight vitals may not be necessary, particularly if remote monitoring is available. This accomplishes multiple goals: Providing high quality patient care, reducing resource utilization, and minimizing patient nighttime interruptions – all culminating in high-value care.
Even though the COVID-19 pandemic has brought unforeseen emotional, physical, and financial challenges for the health care system and its workers, there may be a silver lining. The pandemic has sparked high-value care discussions, and the urgency of the crisis may be instilling new practices in our daily work. This virus has indeed left a terrible wake of destruction, but may also be a nudge to permanently change our culture of overuse to help us shape the habits of all trainees during this tumultuous time. This experience will hopefully culminate in a culture in which clinicians routinely ask, “How will this intervention help the patient?”
Dr. Rawal is clinical assistant professor of medicine, University of Pittsburgh. Dr. Linker is assistant professor of medicine, Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York. Dr. Moriates is associate professor of internal medicine, Dell Medical School at the University of Texas at Austin.
References
1. Shrank W et al. Waste in The US healthcare system. JAMA. 2019;322(15):1501-9.
2. Chen C et al. Spending patterns in region of residency training and subsequent expenditures for care provided by practicing physicians for Medicare beneficiaries. JAMA. 2014;312(22):2385-93.
3. Eaton KP et al. Evidence-based guidelines to eliminate repetitive laboratory testing. JAMA Intern Med. 2017;177(12):1833-9.
4. Cho H et al. Choosing Wisely in the COVID-19 Era: Preventing harm to healthcare workers. J Hosp Med. 2020;15(6):360-2.
5. Orlov N and Arora V. Things we do for no reason: Routine overnight vital sign checks. J Hosp Med. 2020;15(5):272-27.
As Rachna Rawal, MD, was donning her personal protective equipment (PPE), a process that has become deeply ingrained into her muscle memory, a nurse approached her to ask, “Hey, for Mr. Smith, any chance we can time these labs to be done together with his medication administration? We’ve been in and out of that room a few times already.”
As someone who embraces high-value care, this simple suggestion surprised her. What an easy strategy to minimize room entry with full PPE, lab testing, and patient interruptions. That same day, someone else asked, “Do we need overnight vitals?”
COVID-19 has forced hospitalists to reconsider almost every aspect of care. It feels like every decision we make including things we do routinely – labs, vital signs, imaging – needs to be reassessed to determine the actual benefit to the patient balanced against concerns about staff safety, dwindling PPE supplies, and medication reserves. We are all faced with frequently answering the question, “How will this intervention help the patient?” This question lies at the heart of delivering high-value care.
High-value care is providing the best care possible through efficient use of resources, achieving optimal results for each patient. While high-value care has become a prominent focus over the past decade, COVID-19’s high transmissibility without a cure – and associated scarcity of health care resources – have sparked additional discussions on the front lines about promoting patient outcomes while avoiding waste. Clinicians may not have realized that these were high-value care conversations.
The United States’ health care quality and cost crises, worsened in the face of the current pandemic, have been glaringly apparent for years. Our country is spending more money on health care than anywhere else in the world without desired improvements in patient outcomes. A 2019 JAMA study found that 25% of all health care spending, an estimated $760 to $935 billion, is considered waste, and a significant proportion of this waste is due to repetitive care, overuse and unnecessary care in the U.S.1
Examples of low-value care tests include ordering daily labs in stable medicine inpatients, routine urine electrolytes in acute kidney injury, and folate testing in anemia. The Choosing Wisely® national campaign, Journal of Hospital Medicine’s “Things We Do For No Reason,” and JAMA Internal Medicine’s “Teachable Moment” series have provided guidance on areas where common testing or interventions may not benefit patient outcomes.
The COVID-19 pandemic has raised questions related to other widely-utilized practices: Can medication times be readjusted to allow only one entry into the room? Will these labs or imaging studies actually change management? Are vital checks every 4 hours needed?
Why did it take the COVID-19 threat to our medical system to force many of us to have these discussions? Despite prior efforts to integrate high-value care into hospital practices, long-standing habits and deep-seeded culture are challenging to overcome. Once clinicians develop practice habits, these behaviors tend to persist throughout their careers.2 In many ways, COVID-19 was like hitting a “reset button” as health care professionals were forced to rapidly confront their deeply-ingrained hospital practices and habits. From new protocols for patient rounding to universal masking and social distancing to ground-breaking strategies like awake proning, the response to COVID-19 has represented an unprecedented rapid shift in practice. Previously, consequences of overuse were too downstream or too abstract for clinicians to see in real-time. However, now the ramifications of these choices hit closer to home with obvious potential consequences – like spreading a terrifying virus.
There are three interventions that hospitalists should consider implementing immediately in the COVID-19 era that accelerate us toward high-value care. Routine lab tests, imaging, and overnight vitals represent opportunities to provide patient-centered care while also remaining cognizant of resource utilization.
One area in hospital medicine that has proven challenging to significantly change practice has been routine daily labs. Patients on a general medical inpatient service who are clinically stable generally do not benefit from routine lab work.3 Avoiding these tests does not increase mortality or length of stay in clinically stable patients.3 However, despite this evidence, many patients with COVID-19 and other conditions experience lab draws that are not timed together and are done each morning out of “routine.” Choosing Wisely® recommendations from the Society of Hospital Medicine encourage clinicians to question routine lab work for COVID-19 patients and to consider batching them, if possible.3,4 In COVID-19 patients, the risks of not batching tests are magnified, both in terms of the patient-centered experience and for clinician safety. In essence, COVID-19 has pushed us to consider the elements of safety, PPE conservation and other factors, rather than making decisions based solely on their own comfort, convenience, or historical practice.
Clinicians are also reconsidering the necessity of imaging during the pandemic. The “Things We Do For No Reason” article on “Choosing Wisely® in the COVID-19 era” highlights this well.4 It is more important now than ever to decide whether the timing and type of imaging will change management for your patient. Questions to ask include: Can a portable x-ray be used to avoid patient travel and will that CT scan help your patient? A posterior-anterior/lateral x-ray can potentially provide more information depending on the clinical scenario. However, we now need to assess if that extra information is going to impact patient management. Downstream consequences of these decisions include not only risks to the patient but also infectious exposures for staff and others during patient travel.
Lastly, overnight vital sign checks are another intervention we should analyze through this high-value care lens. The Journal of Hospital Medicine released a “Things We Do For No Reason” article about minimizing overnight vitals to promote uninterrupted sleep at night.5 Deleterious effects of interrupting the sleep of our patients include delirium and patient dissatisfaction.5 Studies have shown the benefits of this approach, yet the shift away from routine overnight vitals has not yet widely occurred.
COVID-19 has pressed us to save PPE and minimize exposure risk; hence, some centers are coordinating the timing of vitals with medication administration times, when feasible. In the stable patient recovering from COVID-19, overnight vitals may not be necessary, particularly if remote monitoring is available. This accomplishes multiple goals: Providing high quality patient care, reducing resource utilization, and minimizing patient nighttime interruptions – all culminating in high-value care.
Even though the COVID-19 pandemic has brought unforeseen emotional, physical, and financial challenges for the health care system and its workers, there may be a silver lining. The pandemic has sparked high-value care discussions, and the urgency of the crisis may be instilling new practices in our daily work. This virus has indeed left a terrible wake of destruction, but may also be a nudge to permanently change our culture of overuse to help us shape the habits of all trainees during this tumultuous time. This experience will hopefully culminate in a culture in which clinicians routinely ask, “How will this intervention help the patient?”
Dr. Rawal is clinical assistant professor of medicine, University of Pittsburgh. Dr. Linker is assistant professor of medicine, Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York. Dr. Moriates is associate professor of internal medicine, Dell Medical School at the University of Texas at Austin.
References
1. Shrank W et al. Waste in The US healthcare system. JAMA. 2019;322(15):1501-9.
2. Chen C et al. Spending patterns in region of residency training and subsequent expenditures for care provided by practicing physicians for Medicare beneficiaries. JAMA. 2014;312(22):2385-93.
3. Eaton KP et al. Evidence-based guidelines to eliminate repetitive laboratory testing. JAMA Intern Med. 2017;177(12):1833-9.
4. Cho H et al. Choosing Wisely in the COVID-19 Era: Preventing harm to healthcare workers. J Hosp Med. 2020;15(6):360-2.
5. Orlov N and Arora V. Things we do for no reason: Routine overnight vital sign checks. J Hosp Med. 2020;15(5):272-27.
As Rachna Rawal, MD, was donning her personal protective equipment (PPE), a process that has become deeply ingrained into her muscle memory, a nurse approached her to ask, “Hey, for Mr. Smith, any chance we can time these labs to be done together with his medication administration? We’ve been in and out of that room a few times already.”
As someone who embraces high-value care, this simple suggestion surprised her. What an easy strategy to minimize room entry with full PPE, lab testing, and patient interruptions. That same day, someone else asked, “Do we need overnight vitals?”
COVID-19 has forced hospitalists to reconsider almost every aspect of care. It feels like every decision we make including things we do routinely – labs, vital signs, imaging – needs to be reassessed to determine the actual benefit to the patient balanced against concerns about staff safety, dwindling PPE supplies, and medication reserves. We are all faced with frequently answering the question, “How will this intervention help the patient?” This question lies at the heart of delivering high-value care.
High-value care is providing the best care possible through efficient use of resources, achieving optimal results for each patient. While high-value care has become a prominent focus over the past decade, COVID-19’s high transmissibility without a cure – and associated scarcity of health care resources – have sparked additional discussions on the front lines about promoting patient outcomes while avoiding waste. Clinicians may not have realized that these were high-value care conversations.
The United States’ health care quality and cost crises, worsened in the face of the current pandemic, have been glaringly apparent for years. Our country is spending more money on health care than anywhere else in the world without desired improvements in patient outcomes. A 2019 JAMA study found that 25% of all health care spending, an estimated $760 to $935 billion, is considered waste, and a significant proportion of this waste is due to repetitive care, overuse and unnecessary care in the U.S.1
Examples of low-value care tests include ordering daily labs in stable medicine inpatients, routine urine electrolytes in acute kidney injury, and folate testing in anemia. The Choosing Wisely® national campaign, Journal of Hospital Medicine’s “Things We Do For No Reason,” and JAMA Internal Medicine’s “Teachable Moment” series have provided guidance on areas where common testing or interventions may not benefit patient outcomes.
The COVID-19 pandemic has raised questions related to other widely-utilized practices: Can medication times be readjusted to allow only one entry into the room? Will these labs or imaging studies actually change management? Are vital checks every 4 hours needed?
Why did it take the COVID-19 threat to our medical system to force many of us to have these discussions? Despite prior efforts to integrate high-value care into hospital practices, long-standing habits and deep-seeded culture are challenging to overcome. Once clinicians develop practice habits, these behaviors tend to persist throughout their careers.2 In many ways, COVID-19 was like hitting a “reset button” as health care professionals were forced to rapidly confront their deeply-ingrained hospital practices and habits. From new protocols for patient rounding to universal masking and social distancing to ground-breaking strategies like awake proning, the response to COVID-19 has represented an unprecedented rapid shift in practice. Previously, consequences of overuse were too downstream or too abstract for clinicians to see in real-time. However, now the ramifications of these choices hit closer to home with obvious potential consequences – like spreading a terrifying virus.
There are three interventions that hospitalists should consider implementing immediately in the COVID-19 era that accelerate us toward high-value care. Routine lab tests, imaging, and overnight vitals represent opportunities to provide patient-centered care while also remaining cognizant of resource utilization.
One area in hospital medicine that has proven challenging to significantly change practice has been routine daily labs. Patients on a general medical inpatient service who are clinically stable generally do not benefit from routine lab work.3 Avoiding these tests does not increase mortality or length of stay in clinically stable patients.3 However, despite this evidence, many patients with COVID-19 and other conditions experience lab draws that are not timed together and are done each morning out of “routine.” Choosing Wisely® recommendations from the Society of Hospital Medicine encourage clinicians to question routine lab work for COVID-19 patients and to consider batching them, if possible.3,4 In COVID-19 patients, the risks of not batching tests are magnified, both in terms of the patient-centered experience and for clinician safety. In essence, COVID-19 has pushed us to consider the elements of safety, PPE conservation and other factors, rather than making decisions based solely on their own comfort, convenience, or historical practice.
Clinicians are also reconsidering the necessity of imaging during the pandemic. The “Things We Do For No Reason” article on “Choosing Wisely® in the COVID-19 era” highlights this well.4 It is more important now than ever to decide whether the timing and type of imaging will change management for your patient. Questions to ask include: Can a portable x-ray be used to avoid patient travel and will that CT scan help your patient? A posterior-anterior/lateral x-ray can potentially provide more information depending on the clinical scenario. However, we now need to assess if that extra information is going to impact patient management. Downstream consequences of these decisions include not only risks to the patient but also infectious exposures for staff and others during patient travel.
Lastly, overnight vital sign checks are another intervention we should analyze through this high-value care lens. The Journal of Hospital Medicine released a “Things We Do For No Reason” article about minimizing overnight vitals to promote uninterrupted sleep at night.5 Deleterious effects of interrupting the sleep of our patients include delirium and patient dissatisfaction.5 Studies have shown the benefits of this approach, yet the shift away from routine overnight vitals has not yet widely occurred.
COVID-19 has pressed us to save PPE and minimize exposure risk; hence, some centers are coordinating the timing of vitals with medication administration times, when feasible. In the stable patient recovering from COVID-19, overnight vitals may not be necessary, particularly if remote monitoring is available. This accomplishes multiple goals: Providing high quality patient care, reducing resource utilization, and minimizing patient nighttime interruptions – all culminating in high-value care.
Even though the COVID-19 pandemic has brought unforeseen emotional, physical, and financial challenges for the health care system and its workers, there may be a silver lining. The pandemic has sparked high-value care discussions, and the urgency of the crisis may be instilling new practices in our daily work. This virus has indeed left a terrible wake of destruction, but may also be a nudge to permanently change our culture of overuse to help us shape the habits of all trainees during this tumultuous time. This experience will hopefully culminate in a culture in which clinicians routinely ask, “How will this intervention help the patient?”
Dr. Rawal is clinical assistant professor of medicine, University of Pittsburgh. Dr. Linker is assistant professor of medicine, Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York. Dr. Moriates is associate professor of internal medicine, Dell Medical School at the University of Texas at Austin.
References
1. Shrank W et al. Waste in The US healthcare system. JAMA. 2019;322(15):1501-9.
2. Chen C et al. Spending patterns in region of residency training and subsequent expenditures for care provided by practicing physicians for Medicare beneficiaries. JAMA. 2014;312(22):2385-93.
3. Eaton KP et al. Evidence-based guidelines to eliminate repetitive laboratory testing. JAMA Intern Med. 2017;177(12):1833-9.
4. Cho H et al. Choosing Wisely in the COVID-19 Era: Preventing harm to healthcare workers. J Hosp Med. 2020;15(6):360-2.
5. Orlov N and Arora V. Things we do for no reason: Routine overnight vital sign checks. J Hosp Med. 2020;15(5):272-27.
The journey from burnout to wellbeing
A check-in for you and your peers
COVID-19 did not discriminate when it came to the impact it imposed on our hospitalist community. As the nomenclature moves away from the negative connotations of ‘burnout’ to ‘wellbeing,’ the pandemic has taught us something important about being intentional about our personal health: we must secure our own oxygen masks before helping others.
In February 2020, the Society of Hospital Medicine’s Wellbeing Taskforce efforts quickly changed focus from addressing general wellbeing, to wellbeing during COVID-19. Our Taskforce was commissioned by SHM’s Board with a new charge: Address immediate and ongoing needs of well-being and resiliency support for hospitalists during the COVID-19 pandemic. In this essay, I will discuss how our SHM Wellbeing Taskforce approached the overall topic of wellbeing for hospitalists during the COVID-19 pandemic, including some of our Taskforce group experiences.
The Taskforce started with a framework to aide in cultivating open and authentic conversations within hospital medicine groups. Creating spaces for honest sharing around how providers are doing is a crucial first step to reducing stigma, building mutual support within a group, and elevating issues of wellbeing to the level where structural change can take place. The Taskforce established two objectives for normalizing and mitigating stressors we face as hospitalists during the COVID-19 pandemic:
- Provide a framework for hospitalists to take their own emotional pulse
- Provide an approach to reduce stigma of hospitalists who are suffering from pandemic stress
While a more typical approach to fix stress and burnout is using formal institutional interventions, we used the value and insight provided by SHM’s 7 Drivers of Burnout in Hospital Medicine to help guide the creation of SHM resources in addressing the severe emotional strain being felt across the country by hospitalists. The 7 Drivers support the idea that the social role peers and hospital leaders can make a crucial difference in mitigating stress and burnout. Two examples of social support come to mind from the Wellbeing Taskforce experience:
- Participate in your meetings. One example comes from a member of our group who had underestimated the “healing power” that our group meetings had provided to his psyche. The simple act of participating in our Taskforce meeting and being in the presence of our group had provided such a positive impact that he was better able to face the “death and misery” in his unit with a smile on his face.
- Share what is stressful. The second example of social support comes from an hour of Zoom-based facilitation meetings between the SHM’s Wellbeing Taskforce members and Chapter Leaders in late October. During our Taskforce debrief after the meeting, we came to realize the enormous burden of grief our peers were carrying as one hospitalist had lost a group colleague the previous week due to suicide. Our member who led this meeting was moved – as were we – at how this had impacted his small team, and he was reminded he was not alone.
To form meaningful relationships that foster support, there needs to be a space where people can safely come together at times that initially might feel awkward. After taking steps toward your peers, these conversations can become normalized and contribute to meaningful relationships, providing the opportunity for healthy exchanges on vulnerable topics like emotional and psychological wellbeing. A printable guide for this specific purpose (“HM COVID-19 Check-In Guide for Self and Peers”) was designed to help hospitalists move into safe and supportive conversations with each other. While it is difficult to place a value on the importance these types of conversations have on individual wellbeing, it is known that the quality of a positive work environment where people feel supported can moderate stress, morale, and depression. In other words, hospitalist groups can positively contribute to their social environment during stressful times by sharing meaningful and difficult experiences with one another.
Second, the Taskforce created a social media campaign to provide a public social space for sharing hospitalists’ COVID-19 experiences. We believed that sharing collective experiences with the theme of #YouAreNotAlone and a complementary social media campaign, SHM Cares, on SHM’s social media channels, would further connect the national hospitalist community and provide a different communication pathway to decrease a sense of isolation. This idea came from the second social support idea mentioned earlier to share what is stressful with others in a safe space. We understood that some hospitalists would be more comfortable sharing publicly their comments, photos, and videos in achieving a sense of hospitalist unity.
Using our shared experiences, we identified three pillars for the final structure of the HM COVID-19 Check-In Guide for Self and Peers:
- Pillar 1. Recognize your issues. Recall our oxygen mask metaphor and this is what we mean by recognizing symptoms of new stressors (e.g., sleeplessness, irritability, forgetfulness).
- Pillar 2. Know what to say. A simple open-ended question about how the other person is working through the pandemic is an easy way to start a connection. We learned from a mental health perspective that it is unlikely that you could say anything to make a situation worse by offering a listening ear.
- Pillar 3. Check in with others. Listen to others without trying to fix the person or the situation. When appropriate, offer humorous reflections without diminishing the problem. Be a partner and commit to check in regularly with the other person.
Cultivating human connections outside of your immediate peer group can be valuable and offer additional perspective to stressful situations. For instance, one of my roles as a hospitalist administrator has been offering support by regularly listening as my physicians ‘talk out’ their day confidentially for as long as they needed. Offering open conversation in a safe and confidential way can have a healing effect. As one of my former hospitalists used to say, if issues are not addressed, they will “ooze out somewhere else.”
The HM COVID-19 Check-In Guide for Self and Peers and the SHM Cares social media campaign was the result of the Taskforce’s collective observations to help others normalize the feeling that ‘it’s OK not to be OK.’ Using the pandemic as context, the 7 Drivers of Hospitalist Burnout reminded us that the increased burnout issues we face will require continued attention past the pandemic. The value in cultivating human connections has never been more important. The SHM Wellbeing Taskforce is committed to provide continued resources. Checking in with others and listening to peers are all part of a personal wellbeing and resilience strategy. On behalf of the SHM Wellbeing Taskforce, we hope the information in this article will highlight the importance of continued attention to personal wellbeing during and after the pandemic.
Dr. Robinson received her PhD in organizational learning, performance and change from Colorado State University in 2019. Her dissertation topic was exploring hospitalist burnout, engagement, and social support. She is administrative director of inpatient medicine at St. Mary’s Medical Center in Grand Junction, Colo., a part of SCL Health. She has volunteered in numerous SHM committees, and currently serves on the SHM Wellbeing Taskforce.
A check-in for you and your peers
A check-in for you and your peers
COVID-19 did not discriminate when it came to the impact it imposed on our hospitalist community. As the nomenclature moves away from the negative connotations of ‘burnout’ to ‘wellbeing,’ the pandemic has taught us something important about being intentional about our personal health: we must secure our own oxygen masks before helping others.
In February 2020, the Society of Hospital Medicine’s Wellbeing Taskforce efforts quickly changed focus from addressing general wellbeing, to wellbeing during COVID-19. Our Taskforce was commissioned by SHM’s Board with a new charge: Address immediate and ongoing needs of well-being and resiliency support for hospitalists during the COVID-19 pandemic. In this essay, I will discuss how our SHM Wellbeing Taskforce approached the overall topic of wellbeing for hospitalists during the COVID-19 pandemic, including some of our Taskforce group experiences.
The Taskforce started with a framework to aide in cultivating open and authentic conversations within hospital medicine groups. Creating spaces for honest sharing around how providers are doing is a crucial first step to reducing stigma, building mutual support within a group, and elevating issues of wellbeing to the level where structural change can take place. The Taskforce established two objectives for normalizing and mitigating stressors we face as hospitalists during the COVID-19 pandemic:
- Provide a framework for hospitalists to take their own emotional pulse
- Provide an approach to reduce stigma of hospitalists who are suffering from pandemic stress
While a more typical approach to fix stress and burnout is using formal institutional interventions, we used the value and insight provided by SHM’s 7 Drivers of Burnout in Hospital Medicine to help guide the creation of SHM resources in addressing the severe emotional strain being felt across the country by hospitalists. The 7 Drivers support the idea that the social role peers and hospital leaders can make a crucial difference in mitigating stress and burnout. Two examples of social support come to mind from the Wellbeing Taskforce experience:
- Participate in your meetings. One example comes from a member of our group who had underestimated the “healing power” that our group meetings had provided to his psyche. The simple act of participating in our Taskforce meeting and being in the presence of our group had provided such a positive impact that he was better able to face the “death and misery” in his unit with a smile on his face.
- Share what is stressful. The second example of social support comes from an hour of Zoom-based facilitation meetings between the SHM’s Wellbeing Taskforce members and Chapter Leaders in late October. During our Taskforce debrief after the meeting, we came to realize the enormous burden of grief our peers were carrying as one hospitalist had lost a group colleague the previous week due to suicide. Our member who led this meeting was moved – as were we – at how this had impacted his small team, and he was reminded he was not alone.
To form meaningful relationships that foster support, there needs to be a space where people can safely come together at times that initially might feel awkward. After taking steps toward your peers, these conversations can become normalized and contribute to meaningful relationships, providing the opportunity for healthy exchanges on vulnerable topics like emotional and psychological wellbeing. A printable guide for this specific purpose (“HM COVID-19 Check-In Guide for Self and Peers”) was designed to help hospitalists move into safe and supportive conversations with each other. While it is difficult to place a value on the importance these types of conversations have on individual wellbeing, it is known that the quality of a positive work environment where people feel supported can moderate stress, morale, and depression. In other words, hospitalist groups can positively contribute to their social environment during stressful times by sharing meaningful and difficult experiences with one another.
Second, the Taskforce created a social media campaign to provide a public social space for sharing hospitalists’ COVID-19 experiences. We believed that sharing collective experiences with the theme of #YouAreNotAlone and a complementary social media campaign, SHM Cares, on SHM’s social media channels, would further connect the national hospitalist community and provide a different communication pathway to decrease a sense of isolation. This idea came from the second social support idea mentioned earlier to share what is stressful with others in a safe space. We understood that some hospitalists would be more comfortable sharing publicly their comments, photos, and videos in achieving a sense of hospitalist unity.
Using our shared experiences, we identified three pillars for the final structure of the HM COVID-19 Check-In Guide for Self and Peers:
- Pillar 1. Recognize your issues. Recall our oxygen mask metaphor and this is what we mean by recognizing symptoms of new stressors (e.g., sleeplessness, irritability, forgetfulness).
- Pillar 2. Know what to say. A simple open-ended question about how the other person is working through the pandemic is an easy way to start a connection. We learned from a mental health perspective that it is unlikely that you could say anything to make a situation worse by offering a listening ear.
- Pillar 3. Check in with others. Listen to others without trying to fix the person or the situation. When appropriate, offer humorous reflections without diminishing the problem. Be a partner and commit to check in regularly with the other person.
Cultivating human connections outside of your immediate peer group can be valuable and offer additional perspective to stressful situations. For instance, one of my roles as a hospitalist administrator has been offering support by regularly listening as my physicians ‘talk out’ their day confidentially for as long as they needed. Offering open conversation in a safe and confidential way can have a healing effect. As one of my former hospitalists used to say, if issues are not addressed, they will “ooze out somewhere else.”
The HM COVID-19 Check-In Guide for Self and Peers and the SHM Cares social media campaign was the result of the Taskforce’s collective observations to help others normalize the feeling that ‘it’s OK not to be OK.’ Using the pandemic as context, the 7 Drivers of Hospitalist Burnout reminded us that the increased burnout issues we face will require continued attention past the pandemic. The value in cultivating human connections has never been more important. The SHM Wellbeing Taskforce is committed to provide continued resources. Checking in with others and listening to peers are all part of a personal wellbeing and resilience strategy. On behalf of the SHM Wellbeing Taskforce, we hope the information in this article will highlight the importance of continued attention to personal wellbeing during and after the pandemic.
Dr. Robinson received her PhD in organizational learning, performance and change from Colorado State University in 2019. Her dissertation topic was exploring hospitalist burnout, engagement, and social support. She is administrative director of inpatient medicine at St. Mary’s Medical Center in Grand Junction, Colo., a part of SCL Health. She has volunteered in numerous SHM committees, and currently serves on the SHM Wellbeing Taskforce.
COVID-19 did not discriminate when it came to the impact it imposed on our hospitalist community. As the nomenclature moves away from the negative connotations of ‘burnout’ to ‘wellbeing,’ the pandemic has taught us something important about being intentional about our personal health: we must secure our own oxygen masks before helping others.
In February 2020, the Society of Hospital Medicine’s Wellbeing Taskforce efforts quickly changed focus from addressing general wellbeing, to wellbeing during COVID-19. Our Taskforce was commissioned by SHM’s Board with a new charge: Address immediate and ongoing needs of well-being and resiliency support for hospitalists during the COVID-19 pandemic. In this essay, I will discuss how our SHM Wellbeing Taskforce approached the overall topic of wellbeing for hospitalists during the COVID-19 pandemic, including some of our Taskforce group experiences.
The Taskforce started with a framework to aide in cultivating open and authentic conversations within hospital medicine groups. Creating spaces for honest sharing around how providers are doing is a crucial first step to reducing stigma, building mutual support within a group, and elevating issues of wellbeing to the level where structural change can take place. The Taskforce established two objectives for normalizing and mitigating stressors we face as hospitalists during the COVID-19 pandemic:
- Provide a framework for hospitalists to take their own emotional pulse
- Provide an approach to reduce stigma of hospitalists who are suffering from pandemic stress
While a more typical approach to fix stress and burnout is using formal institutional interventions, we used the value and insight provided by SHM’s 7 Drivers of Burnout in Hospital Medicine to help guide the creation of SHM resources in addressing the severe emotional strain being felt across the country by hospitalists. The 7 Drivers support the idea that the social role peers and hospital leaders can make a crucial difference in mitigating stress and burnout. Two examples of social support come to mind from the Wellbeing Taskforce experience:
- Participate in your meetings. One example comes from a member of our group who had underestimated the “healing power” that our group meetings had provided to his psyche. The simple act of participating in our Taskforce meeting and being in the presence of our group had provided such a positive impact that he was better able to face the “death and misery” in his unit with a smile on his face.
- Share what is stressful. The second example of social support comes from an hour of Zoom-based facilitation meetings between the SHM’s Wellbeing Taskforce members and Chapter Leaders in late October. During our Taskforce debrief after the meeting, we came to realize the enormous burden of grief our peers were carrying as one hospitalist had lost a group colleague the previous week due to suicide. Our member who led this meeting was moved – as were we – at how this had impacted his small team, and he was reminded he was not alone.
To form meaningful relationships that foster support, there needs to be a space where people can safely come together at times that initially might feel awkward. After taking steps toward your peers, these conversations can become normalized and contribute to meaningful relationships, providing the opportunity for healthy exchanges on vulnerable topics like emotional and psychological wellbeing. A printable guide for this specific purpose (“HM COVID-19 Check-In Guide for Self and Peers”) was designed to help hospitalists move into safe and supportive conversations with each other. While it is difficult to place a value on the importance these types of conversations have on individual wellbeing, it is known that the quality of a positive work environment where people feel supported can moderate stress, morale, and depression. In other words, hospitalist groups can positively contribute to their social environment during stressful times by sharing meaningful and difficult experiences with one another.
Second, the Taskforce created a social media campaign to provide a public social space for sharing hospitalists’ COVID-19 experiences. We believed that sharing collective experiences with the theme of #YouAreNotAlone and a complementary social media campaign, SHM Cares, on SHM’s social media channels, would further connect the national hospitalist community and provide a different communication pathway to decrease a sense of isolation. This idea came from the second social support idea mentioned earlier to share what is stressful with others in a safe space. We understood that some hospitalists would be more comfortable sharing publicly their comments, photos, and videos in achieving a sense of hospitalist unity.
Using our shared experiences, we identified three pillars for the final structure of the HM COVID-19 Check-In Guide for Self and Peers:
- Pillar 1. Recognize your issues. Recall our oxygen mask metaphor and this is what we mean by recognizing symptoms of new stressors (e.g., sleeplessness, irritability, forgetfulness).
- Pillar 2. Know what to say. A simple open-ended question about how the other person is working through the pandemic is an easy way to start a connection. We learned from a mental health perspective that it is unlikely that you could say anything to make a situation worse by offering a listening ear.
- Pillar 3. Check in with others. Listen to others without trying to fix the person or the situation. When appropriate, offer humorous reflections without diminishing the problem. Be a partner and commit to check in regularly with the other person.
Cultivating human connections outside of your immediate peer group can be valuable and offer additional perspective to stressful situations. For instance, one of my roles as a hospitalist administrator has been offering support by regularly listening as my physicians ‘talk out’ their day confidentially for as long as they needed. Offering open conversation in a safe and confidential way can have a healing effect. As one of my former hospitalists used to say, if issues are not addressed, they will “ooze out somewhere else.”
The HM COVID-19 Check-In Guide for Self and Peers and the SHM Cares social media campaign was the result of the Taskforce’s collective observations to help others normalize the feeling that ‘it’s OK not to be OK.’ Using the pandemic as context, the 7 Drivers of Hospitalist Burnout reminded us that the increased burnout issues we face will require continued attention past the pandemic. The value in cultivating human connections has never been more important. The SHM Wellbeing Taskforce is committed to provide continued resources. Checking in with others and listening to peers are all part of a personal wellbeing and resilience strategy. On behalf of the SHM Wellbeing Taskforce, we hope the information in this article will highlight the importance of continued attention to personal wellbeing during and after the pandemic.
Dr. Robinson received her PhD in organizational learning, performance and change from Colorado State University in 2019. Her dissertation topic was exploring hospitalist burnout, engagement, and social support. She is administrative director of inpatient medicine at St. Mary’s Medical Center in Grand Junction, Colo., a part of SCL Health. She has volunteered in numerous SHM committees, and currently serves on the SHM Wellbeing Taskforce.
Nature or nurture in primary care?
Does the name Bruce Lipton sound familiar to you? Until a few years ago the only bell that it rang with me was that I had a high school classmate named Bruce Lipton. I recall that his father owned the local grocery store and he was one of the most prolific pranksters in a class with a long history of prank playing. If the name dredges up any associations for you it may because you have heard of a PhD biologist who has written and lectured extensively on epigenetics. You may have even read his most widely published book, “The Biology of Belief.” It turns out the Epigenetics Guy and my high school prankster classmate are one and the same.
After decades of separation – he is in California and I’m here in Maine – we have reconnected via Zoom mini reunions that our class has organized to combat the isolation that has descended on us with the pandemic. While I haven’t read his books, I have watched and listened to some of his podcasts and lectures. The devilish twinkle in his eye in the 1950s and 1960s has provided the scaffolding on which he has built a charismatic and persuasive presentation style.
Bruce was no dummy in school but his early career as a cell biologist doing research in stem-cell function was a surprise to all of us. But then high school reunions are often full of surprises and should serve as good reminders of the danger of profiling and pigeon-holing adolescents.
Professor Lipton’s take on epigenetics boils down to the notion that our genome should merely be considered a blueprint and not the final determinant of who we are and what illnesses befall us. His research and observations suggest to him that there are an uncountable number extragenomic factors, including environmental conditions and our belief systems, that can influence how that blueprint is read and the resulting expression of the genes we have inherited.
At face value, Bruce’s basic premise falls very close to some of the conclusions I have toyed with in an attempt to explain what I have observed doing primary care pediatrics. For example, I have trouble blaming the meteoric rise of the ADHD phenomenon on a genetic mutation. I suspect there are likely to be extragenomic forces coming into play, such as sleep deprivation and changing child-rearing practices. In my Oct. 9, 2020, Letters from Maine column I referred to a Swedish twins study that suggested children from a family with a strong history of depression were more likely to develop depression when raised in an adopted family that experienced domestic turmoil. His philosophy also fits with my sense that I have more control over my own health outcomes than many other people.
However, Professor Lipton and I part company (just philosophically that is) when he slips into hyperbole and applies what he terms as the New Biology too broadly. He may be correct that the revolutionary changes which came in the wake of Watson and Crick’s double helix discovery have resulted in a view of pathophysiology that is overly focused on what we are learning about our genome. On the other hand it is refreshing to hear someone with his charismatic and persuasive skills question the status quo.
If you haven’t listened to what he has to say I urge you to browse the Internet and sample some of his talks. I am sure you will find what he has to say stimulating. I doubt you will buy his whole package but I suspect you may find some bits you can agree with.
It still boils down to the old nature versus nurture argument. He’s all in for nurture. I’m still more comfortable straddling the fence.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Does the name Bruce Lipton sound familiar to you? Until a few years ago the only bell that it rang with me was that I had a high school classmate named Bruce Lipton. I recall that his father owned the local grocery store and he was one of the most prolific pranksters in a class with a long history of prank playing. If the name dredges up any associations for you it may because you have heard of a PhD biologist who has written and lectured extensively on epigenetics. You may have even read his most widely published book, “The Biology of Belief.” It turns out the Epigenetics Guy and my high school prankster classmate are one and the same.
After decades of separation – he is in California and I’m here in Maine – we have reconnected via Zoom mini reunions that our class has organized to combat the isolation that has descended on us with the pandemic. While I haven’t read his books, I have watched and listened to some of his podcasts and lectures. The devilish twinkle in his eye in the 1950s and 1960s has provided the scaffolding on which he has built a charismatic and persuasive presentation style.
Bruce was no dummy in school but his early career as a cell biologist doing research in stem-cell function was a surprise to all of us. But then high school reunions are often full of surprises and should serve as good reminders of the danger of profiling and pigeon-holing adolescents.
Professor Lipton’s take on epigenetics boils down to the notion that our genome should merely be considered a blueprint and not the final determinant of who we are and what illnesses befall us. His research and observations suggest to him that there are an uncountable number extragenomic factors, including environmental conditions and our belief systems, that can influence how that blueprint is read and the resulting expression of the genes we have inherited.
At face value, Bruce’s basic premise falls very close to some of the conclusions I have toyed with in an attempt to explain what I have observed doing primary care pediatrics. For example, I have trouble blaming the meteoric rise of the ADHD phenomenon on a genetic mutation. I suspect there are likely to be extragenomic forces coming into play, such as sleep deprivation and changing child-rearing practices. In my Oct. 9, 2020, Letters from Maine column I referred to a Swedish twins study that suggested children from a family with a strong history of depression were more likely to develop depression when raised in an adopted family that experienced domestic turmoil. His philosophy also fits with my sense that I have more control over my own health outcomes than many other people.
However, Professor Lipton and I part company (just philosophically that is) when he slips into hyperbole and applies what he terms as the New Biology too broadly. He may be correct that the revolutionary changes which came in the wake of Watson and Crick’s double helix discovery have resulted in a view of pathophysiology that is overly focused on what we are learning about our genome. On the other hand it is refreshing to hear someone with his charismatic and persuasive skills question the status quo.
If you haven’t listened to what he has to say I urge you to browse the Internet and sample some of his talks. I am sure you will find what he has to say stimulating. I doubt you will buy his whole package but I suspect you may find some bits you can agree with.
It still boils down to the old nature versus nurture argument. He’s all in for nurture. I’m still more comfortable straddling the fence.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Does the name Bruce Lipton sound familiar to you? Until a few years ago the only bell that it rang with me was that I had a high school classmate named Bruce Lipton. I recall that his father owned the local grocery store and he was one of the most prolific pranksters in a class with a long history of prank playing. If the name dredges up any associations for you it may because you have heard of a PhD biologist who has written and lectured extensively on epigenetics. You may have even read his most widely published book, “The Biology of Belief.” It turns out the Epigenetics Guy and my high school prankster classmate are one and the same.
After decades of separation – he is in California and I’m here in Maine – we have reconnected via Zoom mini reunions that our class has organized to combat the isolation that has descended on us with the pandemic. While I haven’t read his books, I have watched and listened to some of his podcasts and lectures. The devilish twinkle in his eye in the 1950s and 1960s has provided the scaffolding on which he has built a charismatic and persuasive presentation style.
Bruce was no dummy in school but his early career as a cell biologist doing research in stem-cell function was a surprise to all of us. But then high school reunions are often full of surprises and should serve as good reminders of the danger of profiling and pigeon-holing adolescents.
Professor Lipton’s take on epigenetics boils down to the notion that our genome should merely be considered a blueprint and not the final determinant of who we are and what illnesses befall us. His research and observations suggest to him that there are an uncountable number extragenomic factors, including environmental conditions and our belief systems, that can influence how that blueprint is read and the resulting expression of the genes we have inherited.
At face value, Bruce’s basic premise falls very close to some of the conclusions I have toyed with in an attempt to explain what I have observed doing primary care pediatrics. For example, I have trouble blaming the meteoric rise of the ADHD phenomenon on a genetic mutation. I suspect there are likely to be extragenomic forces coming into play, such as sleep deprivation and changing child-rearing practices. In my Oct. 9, 2020, Letters from Maine column I referred to a Swedish twins study that suggested children from a family with a strong history of depression were more likely to develop depression when raised in an adopted family that experienced domestic turmoil. His philosophy also fits with my sense that I have more control over my own health outcomes than many other people.
However, Professor Lipton and I part company (just philosophically that is) when he slips into hyperbole and applies what he terms as the New Biology too broadly. He may be correct that the revolutionary changes which came in the wake of Watson and Crick’s double helix discovery have resulted in a view of pathophysiology that is overly focused on what we are learning about our genome. On the other hand it is refreshing to hear someone with his charismatic and persuasive skills question the status quo.
If you haven’t listened to what he has to say I urge you to browse the Internet and sample some of his talks. I am sure you will find what he has to say stimulating. I doubt you will buy his whole package but I suspect you may find some bits you can agree with.
It still boils down to the old nature versus nurture argument. He’s all in for nurture. I’m still more comfortable straddling the fence.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
The Blitz and COVID-19
Lessons from history for hospitalists
The Blitz was a Nazi bombing campaign targeting London. It was designed to break the spirit of the British. Knowing London would be the centerpiece of the campaign, the British rather hastily established several psychiatric hospitals for the expected panic in the streets. However, despite 9 months of bombing, 43,000 civilians killed and 139,000 more wounded, the predicted chaos in the streets did not manifest. Civilians continued to work, industry continued to churn, and eventually, Hitler’s eye turned east toward Russia.
The surprising lack of pandemonium in London inspired Dr. John T. MacCurdy, who chronicled his findings in a book The Structure of Morale, more recently popularized in Malcolm Gladwell’s David and Goliath. A brief summary of Dr. MacCurdy’s theory divides the targeted Londoners into the following categories:
- Direct hit
- Near miss
- Remote miss
The direct hit group was defined as those killed by the bombing. However, As Dr. MacCurdy stated, “The morale of the community depends on the reaction of the survivors…Put this way, the fact is obvious, corpses do not run about spreading panic.”
A near miss were those for whom wounds were inflicted or loved ones were killed. This group felt the real repercussions of the bombing. However, with 139,000 wounded out of a city of 8 million people, they were a small minority.
The majority of Londoners, then, fit into the third group – the remote miss. These people faced a serious fear, but survived, often totally unscathed. The process of facing that fear without having panicked or having been harmed, then, led to “a feeling of excitement with a flavour of invulnerability.”
Therefore, rather than a city of millions running in fear in the streets, requiring military presence to control the chaos, London became a city of people who felt themselves, perhaps, invincible.
A similar threat passed through the world in the first several months of the COVID-19 pandemic. Hospitals were expected to be overrun, and ethics committees convened to discuss allocation of scarce ventilators. However, due, at least in part, to the impressive efforts of the populace of the United States, the majority of civilians did not feel the burden of this frightening disease. Certainly, in a few places, hospitals were overwhelmed, and resources were unavailable due to sheer numbers. These places saw those who suffered direct hits with the highest frequency. However, a disease with an infection fatality ratio recently estimated at 0.5-1%, with a relatively high rate of asymptomatic disease, led to a large majority of people who experienced the first wave of COVID-19 in the United States as a remote miss. COVID-19’s flattened first peak gave much of the population a sense of relief, and, perhaps, a “flavour of invulnerability.”
An anonymous, but concerned, household contact wrote The New York Times and illustrated perfectly the invulnerable feelings of a remote miss:
“I’m doing my best to avoid social contact, along with two other members of my household. We have sufficient supplies for a month. Despite that, one member insists on going out for trivial reasons, such as not liking the kind of apples we have. He’s 92. I’ve tried explaining and cajoling, using graphs and anecdotes to make the danger to all of us seem ‘real.’ It doesn’t take. His risk of death is many times greater than mine, and he’s poking holes in a lifeboat we all have to rely on. What is the correct path?”
American culture expects certainty from science. Therein lies the problem with a new disease no medical provider or researcher had seen prior to November 2019. Action was required in the effort to slow the spread with little to no data as a guide. Therefore, messages that seemed contradictory reached the public. “A mask less than N-95 grade will not protect you,” evolved to, “everyone should wear a homemade cloth mask.” As the pandemic evolved and data was gathered, new recommendations were presented. Unfortunately, such well-meaning and necessary changes led to confusion, mistrust, and conspiracy theories.
Psychologists have weighed in regarding other aspects of our culture that allow for the flourishing of misinformation. A photograph even loosely related to the information presented has been shown to increase the initial sense of trustworthiness. Simple repetition can also make a point seem more trustworthy. As social media pushes the daily deluge of information (with pictures!) to new heights, it is a small wonder misinformation remains in circulation.
Medicine’s response
The science of COVID-19 carries phenomenal uncertainties, but the psychology of those who have suffered direct hits or near misses are the daily bedside challenge of all physicians, but particularly of hospitalists. We live at the front lines of disease – as one colleague put it to me, “we are the watchers on the wall.” Though we do not yet have our hoped-for, evidence-based treatment for this virus, we are familiar with acute illness. We know the rapid change of health to disease, and we know the chronically ill who suffer exacerbations of such illness. Supporting patients and their loved ones through those times is our daily practice.
On the other hand, those who have experienced only remote misses remain vulnerable in this pandemic, despite their feelings of invincibility. Those that feel invincible may be the least interested in our advice. This, too, is no strange position for a physician. We have tools to reach patients who do not reach out to us. Traditional media outlets have been saturated with headlines and talking points about this disease. Physicians who have taken to social media have been met with appreciation in some situations, but ignored, doubted, or shunned in others. In May 2020, NBC News reported an ED doctor’s attempt to dispel some COVID myths on social media. Unfortunately, his remarks were summarily dismissed. Through the frustration, we persevere.
Out of the many responsible authorities who help battle misinformation, the World Health Organization’s mythbusting website (www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters) directly confronts many incorrect circulating ideas. My personal favorite at the time of this writing is: “Being able to hold your breath for 10 seconds or more without coughing or feeling discomfort DOES NOT mean you are free from COVID-19.”
For the policy and communication side of medicine in the midst of this pandemic, I will not claim to have a silver bullet. There are many intelligent, policy-minded people who are working on that very problem. However, as individual practitioners and as individual citizens, I can see two powerful tools that may help us move forward.
1) Confidence and humility: We live in a world of uncertainty, and we struggle against that every day. This pandemic has put our uncertainty clearly on display. However, we may also be confident in providing the best currently known care, even while holding the humility that what we know will likely change. Before COVID-19, we have all seen patients who received multiple different answers from multiple different providers. When I am willing to admit my uncertainty, I have witnessed patients’ skepticism transform into assuming an active role in their care.
For those who have suffered a direct hit or a near miss, honest conversations are vital to build a trusting physician-patient relationship. For the remote miss group, speaking candidly about our uncertainty displays our authenticity and helps combat conspiracy-type theories of ulterior motives. This becomes all the more crucial when new technologies are being deployed – for instance, a September 2020 CBS News survey showed only 21% of Americans planned to get a COVID-19 vaccine “as soon as possible.”
2) Insight into our driving emotions: While the near miss patients are likely ready to continue prevention measures, the remote miss group is often more difficult. When we do have the opportunity to discuss actions to impede the virus’ spread with the remote miss group, understanding their potentially unrecognized motivations helps with that conversation. I have shared the story of the London Blitz and the remote miss and seen people connect the dots with their own emotions. Effective counseling – expecting the feelings of invulnerability amongst the remote miss group – can support endurance with prevention measures amongst that group and help flatten the curve.
Communicating our strengths, transparently discussing our weaknesses, and better understanding underlying emotions for ourselves and our patients may help save lives. As physicians, that is our daily practice, unchanged even as medicine takes center stage in our national conversation.
Dr. Walthall completed his internal medicine residency at the Medical University of South Carolina in Charleston, SC. After residency, he joined the faculty at MUSC in the Division of Hospital Medicine. He is also interested in systems-based care and has taken on the role of physician advisor. This essay appeared first on The Hospital Leader, the official blog of SHM.
Lessons from history for hospitalists
Lessons from history for hospitalists
The Blitz was a Nazi bombing campaign targeting London. It was designed to break the spirit of the British. Knowing London would be the centerpiece of the campaign, the British rather hastily established several psychiatric hospitals for the expected panic in the streets. However, despite 9 months of bombing, 43,000 civilians killed and 139,000 more wounded, the predicted chaos in the streets did not manifest. Civilians continued to work, industry continued to churn, and eventually, Hitler’s eye turned east toward Russia.
The surprising lack of pandemonium in London inspired Dr. John T. MacCurdy, who chronicled his findings in a book The Structure of Morale, more recently popularized in Malcolm Gladwell’s David and Goliath. A brief summary of Dr. MacCurdy’s theory divides the targeted Londoners into the following categories:
- Direct hit
- Near miss
- Remote miss
The direct hit group was defined as those killed by the bombing. However, As Dr. MacCurdy stated, “The morale of the community depends on the reaction of the survivors…Put this way, the fact is obvious, corpses do not run about spreading panic.”
A near miss were those for whom wounds were inflicted or loved ones were killed. This group felt the real repercussions of the bombing. However, with 139,000 wounded out of a city of 8 million people, they were a small minority.
The majority of Londoners, then, fit into the third group – the remote miss. These people faced a serious fear, but survived, often totally unscathed. The process of facing that fear without having panicked or having been harmed, then, led to “a feeling of excitement with a flavour of invulnerability.”
Therefore, rather than a city of millions running in fear in the streets, requiring military presence to control the chaos, London became a city of people who felt themselves, perhaps, invincible.
A similar threat passed through the world in the first several months of the COVID-19 pandemic. Hospitals were expected to be overrun, and ethics committees convened to discuss allocation of scarce ventilators. However, due, at least in part, to the impressive efforts of the populace of the United States, the majority of civilians did not feel the burden of this frightening disease. Certainly, in a few places, hospitals were overwhelmed, and resources were unavailable due to sheer numbers. These places saw those who suffered direct hits with the highest frequency. However, a disease with an infection fatality ratio recently estimated at 0.5-1%, with a relatively high rate of asymptomatic disease, led to a large majority of people who experienced the first wave of COVID-19 in the United States as a remote miss. COVID-19’s flattened first peak gave much of the population a sense of relief, and, perhaps, a “flavour of invulnerability.”
An anonymous, but concerned, household contact wrote The New York Times and illustrated perfectly the invulnerable feelings of a remote miss:
“I’m doing my best to avoid social contact, along with two other members of my household. We have sufficient supplies for a month. Despite that, one member insists on going out for trivial reasons, such as not liking the kind of apples we have. He’s 92. I’ve tried explaining and cajoling, using graphs and anecdotes to make the danger to all of us seem ‘real.’ It doesn’t take. His risk of death is many times greater than mine, and he’s poking holes in a lifeboat we all have to rely on. What is the correct path?”
American culture expects certainty from science. Therein lies the problem with a new disease no medical provider or researcher had seen prior to November 2019. Action was required in the effort to slow the spread with little to no data as a guide. Therefore, messages that seemed contradictory reached the public. “A mask less than N-95 grade will not protect you,” evolved to, “everyone should wear a homemade cloth mask.” As the pandemic evolved and data was gathered, new recommendations were presented. Unfortunately, such well-meaning and necessary changes led to confusion, mistrust, and conspiracy theories.
Psychologists have weighed in regarding other aspects of our culture that allow for the flourishing of misinformation. A photograph even loosely related to the information presented has been shown to increase the initial sense of trustworthiness. Simple repetition can also make a point seem more trustworthy. As social media pushes the daily deluge of information (with pictures!) to new heights, it is a small wonder misinformation remains in circulation.
Medicine’s response
The science of COVID-19 carries phenomenal uncertainties, but the psychology of those who have suffered direct hits or near misses are the daily bedside challenge of all physicians, but particularly of hospitalists. We live at the front lines of disease – as one colleague put it to me, “we are the watchers on the wall.” Though we do not yet have our hoped-for, evidence-based treatment for this virus, we are familiar with acute illness. We know the rapid change of health to disease, and we know the chronically ill who suffer exacerbations of such illness. Supporting patients and their loved ones through those times is our daily practice.
On the other hand, those who have experienced only remote misses remain vulnerable in this pandemic, despite their feelings of invincibility. Those that feel invincible may be the least interested in our advice. This, too, is no strange position for a physician. We have tools to reach patients who do not reach out to us. Traditional media outlets have been saturated with headlines and talking points about this disease. Physicians who have taken to social media have been met with appreciation in some situations, but ignored, doubted, or shunned in others. In May 2020, NBC News reported an ED doctor’s attempt to dispel some COVID myths on social media. Unfortunately, his remarks were summarily dismissed. Through the frustration, we persevere.
Out of the many responsible authorities who help battle misinformation, the World Health Organization’s mythbusting website (www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters) directly confronts many incorrect circulating ideas. My personal favorite at the time of this writing is: “Being able to hold your breath for 10 seconds or more without coughing or feeling discomfort DOES NOT mean you are free from COVID-19.”
For the policy and communication side of medicine in the midst of this pandemic, I will not claim to have a silver bullet. There are many intelligent, policy-minded people who are working on that very problem. However, as individual practitioners and as individual citizens, I can see two powerful tools that may help us move forward.
1) Confidence and humility: We live in a world of uncertainty, and we struggle against that every day. This pandemic has put our uncertainty clearly on display. However, we may also be confident in providing the best currently known care, even while holding the humility that what we know will likely change. Before COVID-19, we have all seen patients who received multiple different answers from multiple different providers. When I am willing to admit my uncertainty, I have witnessed patients’ skepticism transform into assuming an active role in their care.
For those who have suffered a direct hit or a near miss, honest conversations are vital to build a trusting physician-patient relationship. For the remote miss group, speaking candidly about our uncertainty displays our authenticity and helps combat conspiracy-type theories of ulterior motives. This becomes all the more crucial when new technologies are being deployed – for instance, a September 2020 CBS News survey showed only 21% of Americans planned to get a COVID-19 vaccine “as soon as possible.”
2) Insight into our driving emotions: While the near miss patients are likely ready to continue prevention measures, the remote miss group is often more difficult. When we do have the opportunity to discuss actions to impede the virus’ spread with the remote miss group, understanding their potentially unrecognized motivations helps with that conversation. I have shared the story of the London Blitz and the remote miss and seen people connect the dots with their own emotions. Effective counseling – expecting the feelings of invulnerability amongst the remote miss group – can support endurance with prevention measures amongst that group and help flatten the curve.
Communicating our strengths, transparently discussing our weaknesses, and better understanding underlying emotions for ourselves and our patients may help save lives. As physicians, that is our daily practice, unchanged even as medicine takes center stage in our national conversation.
Dr. Walthall completed his internal medicine residency at the Medical University of South Carolina in Charleston, SC. After residency, he joined the faculty at MUSC in the Division of Hospital Medicine. He is also interested in systems-based care and has taken on the role of physician advisor. This essay appeared first on The Hospital Leader, the official blog of SHM.
The Blitz was a Nazi bombing campaign targeting London. It was designed to break the spirit of the British. Knowing London would be the centerpiece of the campaign, the British rather hastily established several psychiatric hospitals for the expected panic in the streets. However, despite 9 months of bombing, 43,000 civilians killed and 139,000 more wounded, the predicted chaos in the streets did not manifest. Civilians continued to work, industry continued to churn, and eventually, Hitler’s eye turned east toward Russia.
The surprising lack of pandemonium in London inspired Dr. John T. MacCurdy, who chronicled his findings in a book The Structure of Morale, more recently popularized in Malcolm Gladwell’s David and Goliath. A brief summary of Dr. MacCurdy’s theory divides the targeted Londoners into the following categories:
- Direct hit
- Near miss
- Remote miss
The direct hit group was defined as those killed by the bombing. However, As Dr. MacCurdy stated, “The morale of the community depends on the reaction of the survivors…Put this way, the fact is obvious, corpses do not run about spreading panic.”
A near miss were those for whom wounds were inflicted or loved ones were killed. This group felt the real repercussions of the bombing. However, with 139,000 wounded out of a city of 8 million people, they were a small minority.
The majority of Londoners, then, fit into the third group – the remote miss. These people faced a serious fear, but survived, often totally unscathed. The process of facing that fear without having panicked or having been harmed, then, led to “a feeling of excitement with a flavour of invulnerability.”
Therefore, rather than a city of millions running in fear in the streets, requiring military presence to control the chaos, London became a city of people who felt themselves, perhaps, invincible.
A similar threat passed through the world in the first several months of the COVID-19 pandemic. Hospitals were expected to be overrun, and ethics committees convened to discuss allocation of scarce ventilators. However, due, at least in part, to the impressive efforts of the populace of the United States, the majority of civilians did not feel the burden of this frightening disease. Certainly, in a few places, hospitals were overwhelmed, and resources were unavailable due to sheer numbers. These places saw those who suffered direct hits with the highest frequency. However, a disease with an infection fatality ratio recently estimated at 0.5-1%, with a relatively high rate of asymptomatic disease, led to a large majority of people who experienced the first wave of COVID-19 in the United States as a remote miss. COVID-19’s flattened first peak gave much of the population a sense of relief, and, perhaps, a “flavour of invulnerability.”
An anonymous, but concerned, household contact wrote The New York Times and illustrated perfectly the invulnerable feelings of a remote miss:
“I’m doing my best to avoid social contact, along with two other members of my household. We have sufficient supplies for a month. Despite that, one member insists on going out for trivial reasons, such as not liking the kind of apples we have. He’s 92. I’ve tried explaining and cajoling, using graphs and anecdotes to make the danger to all of us seem ‘real.’ It doesn’t take. His risk of death is many times greater than mine, and he’s poking holes in a lifeboat we all have to rely on. What is the correct path?”
American culture expects certainty from science. Therein lies the problem with a new disease no medical provider or researcher had seen prior to November 2019. Action was required in the effort to slow the spread with little to no data as a guide. Therefore, messages that seemed contradictory reached the public. “A mask less than N-95 grade will not protect you,” evolved to, “everyone should wear a homemade cloth mask.” As the pandemic evolved and data was gathered, new recommendations were presented. Unfortunately, such well-meaning and necessary changes led to confusion, mistrust, and conspiracy theories.
Psychologists have weighed in regarding other aspects of our culture that allow for the flourishing of misinformation. A photograph even loosely related to the information presented has been shown to increase the initial sense of trustworthiness. Simple repetition can also make a point seem more trustworthy. As social media pushes the daily deluge of information (with pictures!) to new heights, it is a small wonder misinformation remains in circulation.
Medicine’s response
The science of COVID-19 carries phenomenal uncertainties, but the psychology of those who have suffered direct hits or near misses are the daily bedside challenge of all physicians, but particularly of hospitalists. We live at the front lines of disease – as one colleague put it to me, “we are the watchers on the wall.” Though we do not yet have our hoped-for, evidence-based treatment for this virus, we are familiar with acute illness. We know the rapid change of health to disease, and we know the chronically ill who suffer exacerbations of such illness. Supporting patients and their loved ones through those times is our daily practice.
On the other hand, those who have experienced only remote misses remain vulnerable in this pandemic, despite their feelings of invincibility. Those that feel invincible may be the least interested in our advice. This, too, is no strange position for a physician. We have tools to reach patients who do not reach out to us. Traditional media outlets have been saturated with headlines and talking points about this disease. Physicians who have taken to social media have been met with appreciation in some situations, but ignored, doubted, or shunned in others. In May 2020, NBC News reported an ED doctor’s attempt to dispel some COVID myths on social media. Unfortunately, his remarks were summarily dismissed. Through the frustration, we persevere.
Out of the many responsible authorities who help battle misinformation, the World Health Organization’s mythbusting website (www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters) directly confronts many incorrect circulating ideas. My personal favorite at the time of this writing is: “Being able to hold your breath for 10 seconds or more without coughing or feeling discomfort DOES NOT mean you are free from COVID-19.”
For the policy and communication side of medicine in the midst of this pandemic, I will not claim to have a silver bullet. There are many intelligent, policy-minded people who are working on that very problem. However, as individual practitioners and as individual citizens, I can see two powerful tools that may help us move forward.
1) Confidence and humility: We live in a world of uncertainty, and we struggle against that every day. This pandemic has put our uncertainty clearly on display. However, we may also be confident in providing the best currently known care, even while holding the humility that what we know will likely change. Before COVID-19, we have all seen patients who received multiple different answers from multiple different providers. When I am willing to admit my uncertainty, I have witnessed patients’ skepticism transform into assuming an active role in their care.
For those who have suffered a direct hit or a near miss, honest conversations are vital to build a trusting physician-patient relationship. For the remote miss group, speaking candidly about our uncertainty displays our authenticity and helps combat conspiracy-type theories of ulterior motives. This becomes all the more crucial when new technologies are being deployed – for instance, a September 2020 CBS News survey showed only 21% of Americans planned to get a COVID-19 vaccine “as soon as possible.”
2) Insight into our driving emotions: While the near miss patients are likely ready to continue prevention measures, the remote miss group is often more difficult. When we do have the opportunity to discuss actions to impede the virus’ spread with the remote miss group, understanding their potentially unrecognized motivations helps with that conversation. I have shared the story of the London Blitz and the remote miss and seen people connect the dots with their own emotions. Effective counseling – expecting the feelings of invulnerability amongst the remote miss group – can support endurance with prevention measures amongst that group and help flatten the curve.
Communicating our strengths, transparently discussing our weaknesses, and better understanding underlying emotions for ourselves and our patients may help save lives. As physicians, that is our daily practice, unchanged even as medicine takes center stage in our national conversation.
Dr. Walthall completed his internal medicine residency at the Medical University of South Carolina in Charleston, SC. After residency, he joined the faculty at MUSC in the Division of Hospital Medicine. He is also interested in systems-based care and has taken on the role of physician advisor. This essay appeared first on The Hospital Leader, the official blog of SHM.
Psychiatric consequences of nitrous oxide abuse
We would like to describe the case of a patient we treated who developed neuropsychiatric symptoms secondary to recreational use of nitrous oxide (N2O).
Mr. N, a 24-year-old military veteran, presented to the emergency department (ED) with symptoms of numbness, tingling of his entire body, and difficulty walking for the past 3 days. His family recently became concerned when they noted changes in his personality and behavior, including increased irritability, verbal aggression, and paranoia. The family reported that before the recent changes, Mr. N had typically been calm and had a pleasant temperament. When Mr. N’s symptoms progressed to difficulty ambulating, his family brought him to the ED for evaluation.
During his interview, Mr. N reported that he started using N2O 2 years ago for recreational purposes because he learned it is legal to purchase and undetectable on a urine drug screen. He said he had been using >100 N2O canisters per day and had spent approximately $15,000 over the past few months. His use had increasingly escalated up to 3 days before his visit to the ED, which was the last day he used N2O.
Mr. N was admitted to the inpatient medical service. Laboratory testing revealed a low-normal vitamin B12 level of 254 pg/mL (normal range: 200 to 900 pg/mL), an elevated methylmalonic acid blood level of 2,491 nmol/L (normal range: 73 to 376 nmol/L), and an elevated homocysteine blood level of 22.4 μmol/L (normal range: 0 to 15 μmol/L). Magnetic resonance imaging studies showed hyperintensity regions on his cervical spine from the C1 to C6 levels. These changes suggested demyelination due to vitamin B12 deficiency from N2O abuse.
Mr. N was started on vitamin B12 injections and physical therapy, which led to the resolution of his concerning neurologic symptoms. A few weeks after admission, he was discharged with outpatient follow-up services. Unfortunately, he was lost to follow-up.
Approximately 1 year later, Mr. N returned to the ED with anxiety and paranoid ideation. Medical workup at the time was normal (including vitamin B12 and methylmalonic acid blood levels). He denied any recent substance use and was admitted voluntarily to the psychiatric unit. He declined the recommended treatment of risperidone. Because he showed no signs or symptoms that warranted involuntary retention, he was discharged. Over the next few months, he had 4 visits to the ED with similar concerns and poor adherence to outpatient treatment.
On Mr. N’s fourth admission, he agreed to a course of long-acting injectable paliperidone and escitalopram to target his psychotic and anxious symptoms. These treatments stabilized him, and he was discharged. Neuropsychological testing later showed impairment across several cognitive domains, including memory, processing speed, attention, and executive functioning.
Continue to: Identifying N2O use
Identifying N2O use. N2O is not detected on routine drug screen panels. Obtaining a careful psychiatric and substance use history, as well as conducting a neurologic assessment, are helpful to identify N2O use. Both acute and chronic inhalation of N2O can result in vitamin B12 deficiency with hematologic (megaloblastic anemia), neurologic (subacute combined degeneration of spinal cord, motor-sensory polyneuropathy), and psychiatric sequelae (memory loss, depression, hypomania, transient psychosis).1 Patients who exhibit these changes warrant workup for vitamin B12 deficiency, which includes testing for B12, homocysteine, and methylmalonic acid blood levels. Magnetic resonance imaging should be considered for patients who exhibit neurologic symptoms.
The means by which N2O causes neuropsychiatric changes have been explored in the literature. There is general consensus that part of N2O’s deleterious effects is due to the inactivation of vitamin B12 by the irreversible oxidation of Cob(I)alamin to Cob(III)alamin.1
Treatment. The recommended treatment is high-dose oral or parenteral vitamin B12.1 Repletion of vitamin B12 is believed to reverse the course of illness. However, our patient’s symptoms of paranoia and delusions persisted despite resolution of his neurologic symptoms after the underlying vitamin B12 deficiency was corrected.
Due to N2O’s wide availability and growing recreational use, it is important for clinicians to ask their patients about their use of this substance. The abuse of N2O remains an important topic that requires further research, particularly in adolescents, who are still undergoing significant brain development.2,3
Daniel Roberts, MD, MSW
PGY-3 Psychiatric Resident
Department of Psychiatry
New York University Grossman School of Medicine
New York, New York
Pantea Farahmand, MA, MD
Assistant Professor
Department of Psychiatry
New York University Grossman School of Medicine
Inpatient Psychiatrist
Veterans Administration New York Harbor Healthcare System
New York, New York
Adam Wolkin, MD
Associate Professor and Vice Chair
New York University Grossman School of Medicine
Associate Chief of Staff for Mental Health
Veterans Administration New York Harbor Healthcare System
New York, New York
Disclosures: The authors report no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
1. Thompson AG, Leite MI, Lunn MP, et al. Whippits, nitrous oxide and the dangers of legal highs. Pract Neurol. 2015;15(3):207-209.
2. Global Drug Survey 2017. Global Drug Survey. Published May 24, 2017. Accessed January 12, 2021. https://www.globaldrugsurvey.com/past-findings/gds2017-launch/results-released/
3. Kaar SJ, Ferris J, Waldron J, et al. Up: the rise of nitrous oxide abuse. An international survey of contemporary nitrous oxide use. J Psychopharmacol. 2016;30(4):395-401.
We would like to describe the case of a patient we treated who developed neuropsychiatric symptoms secondary to recreational use of nitrous oxide (N2O).
Mr. N, a 24-year-old military veteran, presented to the emergency department (ED) with symptoms of numbness, tingling of his entire body, and difficulty walking for the past 3 days. His family recently became concerned when they noted changes in his personality and behavior, including increased irritability, verbal aggression, and paranoia. The family reported that before the recent changes, Mr. N had typically been calm and had a pleasant temperament. When Mr. N’s symptoms progressed to difficulty ambulating, his family brought him to the ED for evaluation.
During his interview, Mr. N reported that he started using N2O 2 years ago for recreational purposes because he learned it is legal to purchase and undetectable on a urine drug screen. He said he had been using >100 N2O canisters per day and had spent approximately $15,000 over the past few months. His use had increasingly escalated up to 3 days before his visit to the ED, which was the last day he used N2O.
Mr. N was admitted to the inpatient medical service. Laboratory testing revealed a low-normal vitamin B12 level of 254 pg/mL (normal range: 200 to 900 pg/mL), an elevated methylmalonic acid blood level of 2,491 nmol/L (normal range: 73 to 376 nmol/L), and an elevated homocysteine blood level of 22.4 μmol/L (normal range: 0 to 15 μmol/L). Magnetic resonance imaging studies showed hyperintensity regions on his cervical spine from the C1 to C6 levels. These changes suggested demyelination due to vitamin B12 deficiency from N2O abuse.
Mr. N was started on vitamin B12 injections and physical therapy, which led to the resolution of his concerning neurologic symptoms. A few weeks after admission, he was discharged with outpatient follow-up services. Unfortunately, he was lost to follow-up.
Approximately 1 year later, Mr. N returned to the ED with anxiety and paranoid ideation. Medical workup at the time was normal (including vitamin B12 and methylmalonic acid blood levels). He denied any recent substance use and was admitted voluntarily to the psychiatric unit. He declined the recommended treatment of risperidone. Because he showed no signs or symptoms that warranted involuntary retention, he was discharged. Over the next few months, he had 4 visits to the ED with similar concerns and poor adherence to outpatient treatment.
On Mr. N’s fourth admission, he agreed to a course of long-acting injectable paliperidone and escitalopram to target his psychotic and anxious symptoms. These treatments stabilized him, and he was discharged. Neuropsychological testing later showed impairment across several cognitive domains, including memory, processing speed, attention, and executive functioning.
Continue to: Identifying N2O use
Identifying N2O use. N2O is not detected on routine drug screen panels. Obtaining a careful psychiatric and substance use history, as well as conducting a neurologic assessment, are helpful to identify N2O use. Both acute and chronic inhalation of N2O can result in vitamin B12 deficiency with hematologic (megaloblastic anemia), neurologic (subacute combined degeneration of spinal cord, motor-sensory polyneuropathy), and psychiatric sequelae (memory loss, depression, hypomania, transient psychosis).1 Patients who exhibit these changes warrant workup for vitamin B12 deficiency, which includes testing for B12, homocysteine, and methylmalonic acid blood levels. Magnetic resonance imaging should be considered for patients who exhibit neurologic symptoms.
The means by which N2O causes neuropsychiatric changes have been explored in the literature. There is general consensus that part of N2O’s deleterious effects is due to the inactivation of vitamin B12 by the irreversible oxidation of Cob(I)alamin to Cob(III)alamin.1
Treatment. The recommended treatment is high-dose oral or parenteral vitamin B12.1 Repletion of vitamin B12 is believed to reverse the course of illness. However, our patient’s symptoms of paranoia and delusions persisted despite resolution of his neurologic symptoms after the underlying vitamin B12 deficiency was corrected.
Due to N2O’s wide availability and growing recreational use, it is important for clinicians to ask their patients about their use of this substance. The abuse of N2O remains an important topic that requires further research, particularly in adolescents, who are still undergoing significant brain development.2,3
Daniel Roberts, MD, MSW
PGY-3 Psychiatric Resident
Department of Psychiatry
New York University Grossman School of Medicine
New York, New York
Pantea Farahmand, MA, MD
Assistant Professor
Department of Psychiatry
New York University Grossman School of Medicine
Inpatient Psychiatrist
Veterans Administration New York Harbor Healthcare System
New York, New York
Adam Wolkin, MD
Associate Professor and Vice Chair
New York University Grossman School of Medicine
Associate Chief of Staff for Mental Health
Veterans Administration New York Harbor Healthcare System
New York, New York
Disclosures: The authors report no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
We would like to describe the case of a patient we treated who developed neuropsychiatric symptoms secondary to recreational use of nitrous oxide (N2O).
Mr. N, a 24-year-old military veteran, presented to the emergency department (ED) with symptoms of numbness, tingling of his entire body, and difficulty walking for the past 3 days. His family recently became concerned when they noted changes in his personality and behavior, including increased irritability, verbal aggression, and paranoia. The family reported that before the recent changes, Mr. N had typically been calm and had a pleasant temperament. When Mr. N’s symptoms progressed to difficulty ambulating, his family brought him to the ED for evaluation.
During his interview, Mr. N reported that he started using N2O 2 years ago for recreational purposes because he learned it is legal to purchase and undetectable on a urine drug screen. He said he had been using >100 N2O canisters per day and had spent approximately $15,000 over the past few months. His use had increasingly escalated up to 3 days before his visit to the ED, which was the last day he used N2O.
Mr. N was admitted to the inpatient medical service. Laboratory testing revealed a low-normal vitamin B12 level of 254 pg/mL (normal range: 200 to 900 pg/mL), an elevated methylmalonic acid blood level of 2,491 nmol/L (normal range: 73 to 376 nmol/L), and an elevated homocysteine blood level of 22.4 μmol/L (normal range: 0 to 15 μmol/L). Magnetic resonance imaging studies showed hyperintensity regions on his cervical spine from the C1 to C6 levels. These changes suggested demyelination due to vitamin B12 deficiency from N2O abuse.
Mr. N was started on vitamin B12 injections and physical therapy, which led to the resolution of his concerning neurologic symptoms. A few weeks after admission, he was discharged with outpatient follow-up services. Unfortunately, he was lost to follow-up.
Approximately 1 year later, Mr. N returned to the ED with anxiety and paranoid ideation. Medical workup at the time was normal (including vitamin B12 and methylmalonic acid blood levels). He denied any recent substance use and was admitted voluntarily to the psychiatric unit. He declined the recommended treatment of risperidone. Because he showed no signs or symptoms that warranted involuntary retention, he was discharged. Over the next few months, he had 4 visits to the ED with similar concerns and poor adherence to outpatient treatment.
On Mr. N’s fourth admission, he agreed to a course of long-acting injectable paliperidone and escitalopram to target his psychotic and anxious symptoms. These treatments stabilized him, and he was discharged. Neuropsychological testing later showed impairment across several cognitive domains, including memory, processing speed, attention, and executive functioning.
Continue to: Identifying N2O use
Identifying N2O use. N2O is not detected on routine drug screen panels. Obtaining a careful psychiatric and substance use history, as well as conducting a neurologic assessment, are helpful to identify N2O use. Both acute and chronic inhalation of N2O can result in vitamin B12 deficiency with hematologic (megaloblastic anemia), neurologic (subacute combined degeneration of spinal cord, motor-sensory polyneuropathy), and psychiatric sequelae (memory loss, depression, hypomania, transient psychosis).1 Patients who exhibit these changes warrant workup for vitamin B12 deficiency, which includes testing for B12, homocysteine, and methylmalonic acid blood levels. Magnetic resonance imaging should be considered for patients who exhibit neurologic symptoms.
The means by which N2O causes neuropsychiatric changes have been explored in the literature. There is general consensus that part of N2O’s deleterious effects is due to the inactivation of vitamin B12 by the irreversible oxidation of Cob(I)alamin to Cob(III)alamin.1
Treatment. The recommended treatment is high-dose oral or parenteral vitamin B12.1 Repletion of vitamin B12 is believed to reverse the course of illness. However, our patient’s symptoms of paranoia and delusions persisted despite resolution of his neurologic symptoms after the underlying vitamin B12 deficiency was corrected.
Due to N2O’s wide availability and growing recreational use, it is important for clinicians to ask their patients about their use of this substance. The abuse of N2O remains an important topic that requires further research, particularly in adolescents, who are still undergoing significant brain development.2,3
Daniel Roberts, MD, MSW
PGY-3 Psychiatric Resident
Department of Psychiatry
New York University Grossman School of Medicine
New York, New York
Pantea Farahmand, MA, MD
Assistant Professor
Department of Psychiatry
New York University Grossman School of Medicine
Inpatient Psychiatrist
Veterans Administration New York Harbor Healthcare System
New York, New York
Adam Wolkin, MD
Associate Professor and Vice Chair
New York University Grossman School of Medicine
Associate Chief of Staff for Mental Health
Veterans Administration New York Harbor Healthcare System
New York, New York
Disclosures: The authors report no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
1. Thompson AG, Leite MI, Lunn MP, et al. Whippits, nitrous oxide and the dangers of legal highs. Pract Neurol. 2015;15(3):207-209.
2. Global Drug Survey 2017. Global Drug Survey. Published May 24, 2017. Accessed January 12, 2021. https://www.globaldrugsurvey.com/past-findings/gds2017-launch/results-released/
3. Kaar SJ, Ferris J, Waldron J, et al. Up: the rise of nitrous oxide abuse. An international survey of contemporary nitrous oxide use. J Psychopharmacol. 2016;30(4):395-401.
1. Thompson AG, Leite MI, Lunn MP, et al. Whippits, nitrous oxide and the dangers of legal highs. Pract Neurol. 2015;15(3):207-209.
2. Global Drug Survey 2017. Global Drug Survey. Published May 24, 2017. Accessed January 12, 2021. https://www.globaldrugsurvey.com/past-findings/gds2017-launch/results-released/
3. Kaar SJ, Ferris J, Waldron J, et al. Up: the rise of nitrous oxide abuse. An international survey of contemporary nitrous oxide use. J Psychopharmacol. 2016;30(4):395-401.
Plagues that will haunt us long after the COVID-19 pandemic is gone
As we struggle to gradually emerge from the horrid coronavirus disease 2019 (COVID-19) pandemic that has disrupted our lives and killed hundreds of thousands of people in the United States, we harbor the hope that life will return to “normal.” But while it will certainly be a great relief to put this deadly virus behind us, many other epidemics will continue to plague our society and taint our culture.
Scientific ingenuity has led to the development of several vaccines in record time (aka “warp speed”) that will help defeat the deadly scourge of COVID-19. The pandemic is likely to peter out 2 years after its onset. We will all be grateful for such a rapid resolution of the worst health crisis the world has faced in a century, which will enable medical, economic, and social recovery. But as we eventually resume our lives and rejoice in resuming the pursuit of happiness, we will quickly realize that all is not well in our society just because the viral pandemic is gone.
Perhaps the ordeal of the COVID-19 pandemic, and the agony that was universally shared, will open our collective eyes to a jarring reality: many other epidemics will continue to permeate society and cause endless grief and suffering to many of our fellow humans. And thanks to our training as psychiatric physicians, we have developed extra “receptors” to the darker side of the human condition. As we help many of our psychiatric patients rendered sicker under the unbearable stress of the pandemic, we must not overlook the plight of so many others who do not show up in our clinics for health care, yet suffer enormously but imperceptibly. And no vaccine can come to the rescue of those who continue to live in quiet desperation.
Long-standing epidemics
It is truly unfortunate that many of the epidemics I am referring to have persisted for so long that they have become “fixtures” of contemporary societies. They have become “endemic epidemics” with no urgency to squelch them, as with the COVID-19 pandemic. The benign neglect that perpetuates these serious epidemics has had a malignant effect of “grudging resignation” that nothing can be done to reverse them. Unlike the viral epidemic that engulfed everyone around the world and triggered a massive and unified push to defeat the virus, these long-standing epidemics continue to afflict subgroups who are left to fend for themselves. These individuals deserve our empathy and warrant our determination to lift them from their miserable existence.
Consider some of the widespread epidemics that preceded the pandemic and will, in all likelihood, persist after the pandemic’s burden is lifted:
- millions of people living in poverty and hunger
- widespread racism
- smoldering social injustice
- appalling human trafficking, especially targeting children and women
- child abuse and neglect that leads to psychosis, depression, and suicide in adulthood
- gun violence, which kills many innocent people
- domestic violence that inflicts both physical and mental harm on families
- suicide, both attempts and completions, which continues to increase annually
- the festering stigma of mental illness that adds insult to injury for psychiatric patients
- alcohol and drug addictions, which destroy lives and corrode the fabric of society
- lack of access to mental health care for millions of people who need it
- lack of parity for psychiatric disorders, which is so unjust for our patients
- venomous political hatred and hyperpartisanship, which permeates our culture and can lead to violence, as we recently witnessed
- physician burnout, due to many causes, even before the stresses of COVID-19
- the ongoing agony of wars and terrorism, including dangerous cyberattacks
- the deleterious effect of social media on everyone, especially children.
Most of these epidemics claim thousands of lives each year, and yet no concerted public health effort is being mounted to counteract them, as we are seeing with the COVID-19 pandemic. Much is being written about each of them, but there has been little tangible action, so they persist. They have become a perpetual underbelly of our society that is essentially ignored or simply given the usual lip service.
It will take a herculean effort by policymakers, the judicial system, the medical establishment, and faith organizations to put an end to these life-threatening epidemics. It may appear too daunting to mount a war on so many fronts, but that should not deter us all from launching a strategic plan to create meaningful tactics and solutions. And just as was done with the COVID-19 pandemic, both mitigation measures as well as effective interventions must be employed in this campaign against the epidemic “hydra.”
Continue to: It is tragic...
It is tragic that so many fellow humans are allowed to suffer or die while the rest of us watch, or worse, turn a blind eye and never get involved. A civilized society must never neglect so many of its suffering citizens. As psychiatrists, we are aware of those human travesties around us, but we are often so overwhelmed with our work and personal responsibilities that few of us are passionately advocating or setting aside some time for those victimized by one or more of these endemic pandemics. And unless we all decide to be actively, meaningfully involved, many lives will continue to be lost every day, but without the daily “casualty count” displayed on television screens, as is the case with COVID-19 causalities.
Regrettably, maybe that old saw is true: out of sight, out of mind.
As we struggle to gradually emerge from the horrid coronavirus disease 2019 (COVID-19) pandemic that has disrupted our lives and killed hundreds of thousands of people in the United States, we harbor the hope that life will return to “normal.” But while it will certainly be a great relief to put this deadly virus behind us, many other epidemics will continue to plague our society and taint our culture.
Scientific ingenuity has led to the development of several vaccines in record time (aka “warp speed”) that will help defeat the deadly scourge of COVID-19. The pandemic is likely to peter out 2 years after its onset. We will all be grateful for such a rapid resolution of the worst health crisis the world has faced in a century, which will enable medical, economic, and social recovery. But as we eventually resume our lives and rejoice in resuming the pursuit of happiness, we will quickly realize that all is not well in our society just because the viral pandemic is gone.
Perhaps the ordeal of the COVID-19 pandemic, and the agony that was universally shared, will open our collective eyes to a jarring reality: many other epidemics will continue to permeate society and cause endless grief and suffering to many of our fellow humans. And thanks to our training as psychiatric physicians, we have developed extra “receptors” to the darker side of the human condition. As we help many of our psychiatric patients rendered sicker under the unbearable stress of the pandemic, we must not overlook the plight of so many others who do not show up in our clinics for health care, yet suffer enormously but imperceptibly. And no vaccine can come to the rescue of those who continue to live in quiet desperation.
Long-standing epidemics
It is truly unfortunate that many of the epidemics I am referring to have persisted for so long that they have become “fixtures” of contemporary societies. They have become “endemic epidemics” with no urgency to squelch them, as with the COVID-19 pandemic. The benign neglect that perpetuates these serious epidemics has had a malignant effect of “grudging resignation” that nothing can be done to reverse them. Unlike the viral epidemic that engulfed everyone around the world and triggered a massive and unified push to defeat the virus, these long-standing epidemics continue to afflict subgroups who are left to fend for themselves. These individuals deserve our empathy and warrant our determination to lift them from their miserable existence.
Consider some of the widespread epidemics that preceded the pandemic and will, in all likelihood, persist after the pandemic’s burden is lifted:
- millions of people living in poverty and hunger
- widespread racism
- smoldering social injustice
- appalling human trafficking, especially targeting children and women
- child abuse and neglect that leads to psychosis, depression, and suicide in adulthood
- gun violence, which kills many innocent people
- domestic violence that inflicts both physical and mental harm on families
- suicide, both attempts and completions, which continues to increase annually
- the festering stigma of mental illness that adds insult to injury for psychiatric patients
- alcohol and drug addictions, which destroy lives and corrode the fabric of society
- lack of access to mental health care for millions of people who need it
- lack of parity for psychiatric disorders, which is so unjust for our patients
- venomous political hatred and hyperpartisanship, which permeates our culture and can lead to violence, as we recently witnessed
- physician burnout, due to many causes, even before the stresses of COVID-19
- the ongoing agony of wars and terrorism, including dangerous cyberattacks
- the deleterious effect of social media on everyone, especially children.
Most of these epidemics claim thousands of lives each year, and yet no concerted public health effort is being mounted to counteract them, as we are seeing with the COVID-19 pandemic. Much is being written about each of them, but there has been little tangible action, so they persist. They have become a perpetual underbelly of our society that is essentially ignored or simply given the usual lip service.
It will take a herculean effort by policymakers, the judicial system, the medical establishment, and faith organizations to put an end to these life-threatening epidemics. It may appear too daunting to mount a war on so many fronts, but that should not deter us all from launching a strategic plan to create meaningful tactics and solutions. And just as was done with the COVID-19 pandemic, both mitigation measures as well as effective interventions must be employed in this campaign against the epidemic “hydra.”
Continue to: It is tragic...
It is tragic that so many fellow humans are allowed to suffer or die while the rest of us watch, or worse, turn a blind eye and never get involved. A civilized society must never neglect so many of its suffering citizens. As psychiatrists, we are aware of those human travesties around us, but we are often so overwhelmed with our work and personal responsibilities that few of us are passionately advocating or setting aside some time for those victimized by one or more of these endemic pandemics. And unless we all decide to be actively, meaningfully involved, many lives will continue to be lost every day, but without the daily “casualty count” displayed on television screens, as is the case with COVID-19 causalities.
Regrettably, maybe that old saw is true: out of sight, out of mind.
As we struggle to gradually emerge from the horrid coronavirus disease 2019 (COVID-19) pandemic that has disrupted our lives and killed hundreds of thousands of people in the United States, we harbor the hope that life will return to “normal.” But while it will certainly be a great relief to put this deadly virus behind us, many other epidemics will continue to plague our society and taint our culture.
Scientific ingenuity has led to the development of several vaccines in record time (aka “warp speed”) that will help defeat the deadly scourge of COVID-19. The pandemic is likely to peter out 2 years after its onset. We will all be grateful for such a rapid resolution of the worst health crisis the world has faced in a century, which will enable medical, economic, and social recovery. But as we eventually resume our lives and rejoice in resuming the pursuit of happiness, we will quickly realize that all is not well in our society just because the viral pandemic is gone.
Perhaps the ordeal of the COVID-19 pandemic, and the agony that was universally shared, will open our collective eyes to a jarring reality: many other epidemics will continue to permeate society and cause endless grief and suffering to many of our fellow humans. And thanks to our training as psychiatric physicians, we have developed extra “receptors” to the darker side of the human condition. As we help many of our psychiatric patients rendered sicker under the unbearable stress of the pandemic, we must not overlook the plight of so many others who do not show up in our clinics for health care, yet suffer enormously but imperceptibly. And no vaccine can come to the rescue of those who continue to live in quiet desperation.
Long-standing epidemics
It is truly unfortunate that many of the epidemics I am referring to have persisted for so long that they have become “fixtures” of contemporary societies. They have become “endemic epidemics” with no urgency to squelch them, as with the COVID-19 pandemic. The benign neglect that perpetuates these serious epidemics has had a malignant effect of “grudging resignation” that nothing can be done to reverse them. Unlike the viral epidemic that engulfed everyone around the world and triggered a massive and unified push to defeat the virus, these long-standing epidemics continue to afflict subgroups who are left to fend for themselves. These individuals deserve our empathy and warrant our determination to lift them from their miserable existence.
Consider some of the widespread epidemics that preceded the pandemic and will, in all likelihood, persist after the pandemic’s burden is lifted:
- millions of people living in poverty and hunger
- widespread racism
- smoldering social injustice
- appalling human trafficking, especially targeting children and women
- child abuse and neglect that leads to psychosis, depression, and suicide in adulthood
- gun violence, which kills many innocent people
- domestic violence that inflicts both physical and mental harm on families
- suicide, both attempts and completions, which continues to increase annually
- the festering stigma of mental illness that adds insult to injury for psychiatric patients
- alcohol and drug addictions, which destroy lives and corrode the fabric of society
- lack of access to mental health care for millions of people who need it
- lack of parity for psychiatric disorders, which is so unjust for our patients
- venomous political hatred and hyperpartisanship, which permeates our culture and can lead to violence, as we recently witnessed
- physician burnout, due to many causes, even before the stresses of COVID-19
- the ongoing agony of wars and terrorism, including dangerous cyberattacks
- the deleterious effect of social media on everyone, especially children.
Most of these epidemics claim thousands of lives each year, and yet no concerted public health effort is being mounted to counteract them, as we are seeing with the COVID-19 pandemic. Much is being written about each of them, but there has been little tangible action, so they persist. They have become a perpetual underbelly of our society that is essentially ignored or simply given the usual lip service.
It will take a herculean effort by policymakers, the judicial system, the medical establishment, and faith organizations to put an end to these life-threatening epidemics. It may appear too daunting to mount a war on so many fronts, but that should not deter us all from launching a strategic plan to create meaningful tactics and solutions. And just as was done with the COVID-19 pandemic, both mitigation measures as well as effective interventions must be employed in this campaign against the epidemic “hydra.”
Continue to: It is tragic...
It is tragic that so many fellow humans are allowed to suffer or die while the rest of us watch, or worse, turn a blind eye and never get involved. A civilized society must never neglect so many of its suffering citizens. As psychiatrists, we are aware of those human travesties around us, but we are often so overwhelmed with our work and personal responsibilities that few of us are passionately advocating or setting aside some time for those victimized by one or more of these endemic pandemics. And unless we all decide to be actively, meaningfully involved, many lives will continue to be lost every day, but without the daily “casualty count” displayed on television screens, as is the case with COVID-19 causalities.
Regrettably, maybe that old saw is true: out of sight, out of mind.
Virtual supervision during the COVID-19 pandemic
The coronavirus disease 2019 (COVID-19) pandemic has fundamentally changed our way of life. It has affected everything from how we go to the grocery store, attend school, worship, and spend time with our loved ones. As vaccinations are becoming available, there’s hope for a time when we can all enjoy a mask-free life again. Despite this, many of us are beginning to sense that the precautions and technology employed in response to COVID-19, and some of the lessons learned as a result, are likely to stay in place long after the virus has been controlled.
Working remotely through audio and visual synchronous communication is now becoming the norm throughout the American workplace and educational system. Hospitals and graduate medical education programs are not exempt from this trend. For at least the foreseeable future, gone are the days of “unsocially distanced” bedside rounds in which 5 to 10 residents and medical students gather around with their attending as a case is presented in front of an agreeable patient.
My experience with ‘virtual’ supervision
Telemedicine has played a key role in the practice of health care during this pandemic, but little has been written about “telesupervision” of residents in the hospital setting. An unprecedented virtual approach to supervising emergency medicine residents was trialed at the University of Alabama a few months prior to my experience with it. This was found to be quite effective and well-received by all involved parties.1
I am a PGY-2 psychiatry resident at ChristianaCare, a large multisite hospital system with more than 1,200 beds that serves the health care needs of Delaware and the surrounding areas. I recently had a novel educational experience working on a busy addiction medicine consult service. On the first day of this rotation, I met with my attending, Dr. Terry Horton, to discuss how the month would proceed. Together we developed a strategy for him to supervise me virtually.
Our arrangement was efficient and simple: I began each day by donning my surgical mask and protective eyewear and reviewing patients that had been placed on the consult list. Dr. Horton and I would have a conversation via telephone early in the morning to discuss the tasks that needed to be completed for the day. I would see and evaluate patients in the standard face-to-face way. After developing a treatment strategy, I contacted Dr. Horton on the phone, presented the patient, shared my plan, and gained information from his experienced perspective.
Then we saw the patient “together.” We used an iPad and Microsoft Teams video conferencing software. The information shared was protected using Microsoft Teams accounts, which were secured with profiles created by our institutional accounts. The iPad was placed on a rolling tripod, and the patient was able to converse with Dr. Horton as though he was physically in the room. I was there to facilitate the call, address any technical issues, and conduct any aspects of a physical exam that could only be done in person. After discussing any other changes to the treatment plan, I placed all medication orders, shared relevant details with nursing staff and other clinicians, wrote my progress note, and rolled my “attending on a stick” over to the next patient. Meanwhile, Dr. Horton was free to respond to pages or any other issues while I worked.
This description of my workflow is not very different from life before the virus. Based on informal feedback gathered from patients, the experience was overall positive. A physician is present; patients feel well cared for, and they look forward to visits and a virtual presence. This virtual approach not only spared unnecessary physical contact, reducing the risk of COVID-19 exposure, it also promoted efficiency.
Continue to: Fortunately, our hospital...
Fortunately, our hospital is surrounded by a solid telecommunications infrastructure. This experience would be limited in more remote areas of the country. At times, sound quality was an issue, which can be especially problematic for certain patients.
Certain psychosocial implications of the pandemic, including (but not limited to)social isolation and financial hardship, are often associated with increased substance use, and early data support the hypothesis that substance use has increased during this period.2 Delaware seems to be included in the national trend. As such, our already-busy service is being stretched even further. Dr. Horton receives calls and is providing critical recommendations continuously throughout the day for multiple hospitals as well as for his outpatient practice. He used to spend a great deal of time traveling between different sites. With increasing need for his expertise, this model became increasingly difficult to practice. Our new model of attending supervision is welcomed in some settings because the attending can virtually be in multiple places at the same time.
For me, this experience has been positive. For a physician in training, virtual rounding can provide a critical balance of autonomy and support. I felt free on the rotation to make my own decisions, but I also did not feel like I was left to care for complicated cases on my own. Furthermore, my education did not suffer. In actuality, the experience enabled me to excel in my training. An attending physician was there for the important steps of plan formulation, but solo problem-solving opportunities were more readily available without his physical presence.
Aside from the medical lessons learned, I believe the participation has given me a glimpse of the future of medical training, health care delivery, and life in the increasingly digital post−COVID-19 world.
Hopefully, my experience will be helpful for other hospital systems as they continue to provide high-quality care to patients and education/training to their resident physicians in the face of the pandemic and the changing landscape of health care.
Acknowledgment
The author thanks Mustafa Mufti, MD, ChristianaCare Psychiatry Residency Program Director; Rachel Bronsther, MD, ChristianaCare Psychiatry Residency Associate Program Director; and Terry Horton, MD, ChristianaCare Addiction Medicine, for their assistance with this article.
1. Schrading WA, Pigott D, Thompson L. Virtual remote attending supervision in an academic emergency department during the COVID-19 pandemic. AEM Educ Train. 2020;4(3):266-269.
2. Czeisler MÉ, Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic - United States, June 24-30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(32):1049-1057.
The coronavirus disease 2019 (COVID-19) pandemic has fundamentally changed our way of life. It has affected everything from how we go to the grocery store, attend school, worship, and spend time with our loved ones. As vaccinations are becoming available, there’s hope for a time when we can all enjoy a mask-free life again. Despite this, many of us are beginning to sense that the precautions and technology employed in response to COVID-19, and some of the lessons learned as a result, are likely to stay in place long after the virus has been controlled.
Working remotely through audio and visual synchronous communication is now becoming the norm throughout the American workplace and educational system. Hospitals and graduate medical education programs are not exempt from this trend. For at least the foreseeable future, gone are the days of “unsocially distanced” bedside rounds in which 5 to 10 residents and medical students gather around with their attending as a case is presented in front of an agreeable patient.
My experience with ‘virtual’ supervision
Telemedicine has played a key role in the practice of health care during this pandemic, but little has been written about “telesupervision” of residents in the hospital setting. An unprecedented virtual approach to supervising emergency medicine residents was trialed at the University of Alabama a few months prior to my experience with it. This was found to be quite effective and well-received by all involved parties.1
I am a PGY-2 psychiatry resident at ChristianaCare, a large multisite hospital system with more than 1,200 beds that serves the health care needs of Delaware and the surrounding areas. I recently had a novel educational experience working on a busy addiction medicine consult service. On the first day of this rotation, I met with my attending, Dr. Terry Horton, to discuss how the month would proceed. Together we developed a strategy for him to supervise me virtually.
Our arrangement was efficient and simple: I began each day by donning my surgical mask and protective eyewear and reviewing patients that had been placed on the consult list. Dr. Horton and I would have a conversation via telephone early in the morning to discuss the tasks that needed to be completed for the day. I would see and evaluate patients in the standard face-to-face way. After developing a treatment strategy, I contacted Dr. Horton on the phone, presented the patient, shared my plan, and gained information from his experienced perspective.
Then we saw the patient “together.” We used an iPad and Microsoft Teams video conferencing software. The information shared was protected using Microsoft Teams accounts, which were secured with profiles created by our institutional accounts. The iPad was placed on a rolling tripod, and the patient was able to converse with Dr. Horton as though he was physically in the room. I was there to facilitate the call, address any technical issues, and conduct any aspects of a physical exam that could only be done in person. After discussing any other changes to the treatment plan, I placed all medication orders, shared relevant details with nursing staff and other clinicians, wrote my progress note, and rolled my “attending on a stick” over to the next patient. Meanwhile, Dr. Horton was free to respond to pages or any other issues while I worked.
This description of my workflow is not very different from life before the virus. Based on informal feedback gathered from patients, the experience was overall positive. A physician is present; patients feel well cared for, and they look forward to visits and a virtual presence. This virtual approach not only spared unnecessary physical contact, reducing the risk of COVID-19 exposure, it also promoted efficiency.
Continue to: Fortunately, our hospital...
Fortunately, our hospital is surrounded by a solid telecommunications infrastructure. This experience would be limited in more remote areas of the country. At times, sound quality was an issue, which can be especially problematic for certain patients.
Certain psychosocial implications of the pandemic, including (but not limited to)social isolation and financial hardship, are often associated with increased substance use, and early data support the hypothesis that substance use has increased during this period.2 Delaware seems to be included in the national trend. As such, our already-busy service is being stretched even further. Dr. Horton receives calls and is providing critical recommendations continuously throughout the day for multiple hospitals as well as for his outpatient practice. He used to spend a great deal of time traveling between different sites. With increasing need for his expertise, this model became increasingly difficult to practice. Our new model of attending supervision is welcomed in some settings because the attending can virtually be in multiple places at the same time.
For me, this experience has been positive. For a physician in training, virtual rounding can provide a critical balance of autonomy and support. I felt free on the rotation to make my own decisions, but I also did not feel like I was left to care for complicated cases on my own. Furthermore, my education did not suffer. In actuality, the experience enabled me to excel in my training. An attending physician was there for the important steps of plan formulation, but solo problem-solving opportunities were more readily available without his physical presence.
Aside from the medical lessons learned, I believe the participation has given me a glimpse of the future of medical training, health care delivery, and life in the increasingly digital post−COVID-19 world.
Hopefully, my experience will be helpful for other hospital systems as they continue to provide high-quality care to patients and education/training to their resident physicians in the face of the pandemic and the changing landscape of health care.
Acknowledgment
The author thanks Mustafa Mufti, MD, ChristianaCare Psychiatry Residency Program Director; Rachel Bronsther, MD, ChristianaCare Psychiatry Residency Associate Program Director; and Terry Horton, MD, ChristianaCare Addiction Medicine, for their assistance with this article.
The coronavirus disease 2019 (COVID-19) pandemic has fundamentally changed our way of life. It has affected everything from how we go to the grocery store, attend school, worship, and spend time with our loved ones. As vaccinations are becoming available, there’s hope for a time when we can all enjoy a mask-free life again. Despite this, many of us are beginning to sense that the precautions and technology employed in response to COVID-19, and some of the lessons learned as a result, are likely to stay in place long after the virus has been controlled.
Working remotely through audio and visual synchronous communication is now becoming the norm throughout the American workplace and educational system. Hospitals and graduate medical education programs are not exempt from this trend. For at least the foreseeable future, gone are the days of “unsocially distanced” bedside rounds in which 5 to 10 residents and medical students gather around with their attending as a case is presented in front of an agreeable patient.
My experience with ‘virtual’ supervision
Telemedicine has played a key role in the practice of health care during this pandemic, but little has been written about “telesupervision” of residents in the hospital setting. An unprecedented virtual approach to supervising emergency medicine residents was trialed at the University of Alabama a few months prior to my experience with it. This was found to be quite effective and well-received by all involved parties.1
I am a PGY-2 psychiatry resident at ChristianaCare, a large multisite hospital system with more than 1,200 beds that serves the health care needs of Delaware and the surrounding areas. I recently had a novel educational experience working on a busy addiction medicine consult service. On the first day of this rotation, I met with my attending, Dr. Terry Horton, to discuss how the month would proceed. Together we developed a strategy for him to supervise me virtually.
Our arrangement was efficient and simple: I began each day by donning my surgical mask and protective eyewear and reviewing patients that had been placed on the consult list. Dr. Horton and I would have a conversation via telephone early in the morning to discuss the tasks that needed to be completed for the day. I would see and evaluate patients in the standard face-to-face way. After developing a treatment strategy, I contacted Dr. Horton on the phone, presented the patient, shared my plan, and gained information from his experienced perspective.
Then we saw the patient “together.” We used an iPad and Microsoft Teams video conferencing software. The information shared was protected using Microsoft Teams accounts, which were secured with profiles created by our institutional accounts. The iPad was placed on a rolling tripod, and the patient was able to converse with Dr. Horton as though he was physically in the room. I was there to facilitate the call, address any technical issues, and conduct any aspects of a physical exam that could only be done in person. After discussing any other changes to the treatment plan, I placed all medication orders, shared relevant details with nursing staff and other clinicians, wrote my progress note, and rolled my “attending on a stick” over to the next patient. Meanwhile, Dr. Horton was free to respond to pages or any other issues while I worked.
This description of my workflow is not very different from life before the virus. Based on informal feedback gathered from patients, the experience was overall positive. A physician is present; patients feel well cared for, and they look forward to visits and a virtual presence. This virtual approach not only spared unnecessary physical contact, reducing the risk of COVID-19 exposure, it also promoted efficiency.
Continue to: Fortunately, our hospital...
Fortunately, our hospital is surrounded by a solid telecommunications infrastructure. This experience would be limited in more remote areas of the country. At times, sound quality was an issue, which can be especially problematic for certain patients.
Certain psychosocial implications of the pandemic, including (but not limited to)social isolation and financial hardship, are often associated with increased substance use, and early data support the hypothesis that substance use has increased during this period.2 Delaware seems to be included in the national trend. As such, our already-busy service is being stretched even further. Dr. Horton receives calls and is providing critical recommendations continuously throughout the day for multiple hospitals as well as for his outpatient practice. He used to spend a great deal of time traveling between different sites. With increasing need for his expertise, this model became increasingly difficult to practice. Our new model of attending supervision is welcomed in some settings because the attending can virtually be in multiple places at the same time.
For me, this experience has been positive. For a physician in training, virtual rounding can provide a critical balance of autonomy and support. I felt free on the rotation to make my own decisions, but I also did not feel like I was left to care for complicated cases on my own. Furthermore, my education did not suffer. In actuality, the experience enabled me to excel in my training. An attending physician was there for the important steps of plan formulation, but solo problem-solving opportunities were more readily available without his physical presence.
Aside from the medical lessons learned, I believe the participation has given me a glimpse of the future of medical training, health care delivery, and life in the increasingly digital post−COVID-19 world.
Hopefully, my experience will be helpful for other hospital systems as they continue to provide high-quality care to patients and education/training to their resident physicians in the face of the pandemic and the changing landscape of health care.
Acknowledgment
The author thanks Mustafa Mufti, MD, ChristianaCare Psychiatry Residency Program Director; Rachel Bronsther, MD, ChristianaCare Psychiatry Residency Associate Program Director; and Terry Horton, MD, ChristianaCare Addiction Medicine, for their assistance with this article.
1. Schrading WA, Pigott D, Thompson L. Virtual remote attending supervision in an academic emergency department during the COVID-19 pandemic. AEM Educ Train. 2020;4(3):266-269.
2. Czeisler MÉ, Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic - United States, June 24-30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(32):1049-1057.
1. Schrading WA, Pigott D, Thompson L. Virtual remote attending supervision in an academic emergency department during the COVID-19 pandemic. AEM Educ Train. 2020;4(3):266-269.
2. Czeisler MÉ, Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic - United States, June 24-30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(32):1049-1057.
Finding fulfillment in a psychiatry clinical teaching role
On my third day as a PGY-4 junior attending on the inpatient psychiatric ward, 2 new PGY-1 residents, 2 medical students, and I stood in the wee hours of the morning, preparing to meet with our attending to begin rounds. I took the opportunity to discuss potential antipsychotic selection for one of our patients. I questioned the students to gauge their level of knowledge on antipsychotics in general, and did some “thinking out loud” about what our possible options could be. We discussed which antipsychotics are considered “weight-neutral” and which ones require caloric intake for adequate absorption. We discussed what other laboratory tests we should consider upon initiating the hypothetical medication. While discussing these things, I was suddenly taken aback to see that every member of my team was diligently taking notes and hanging on my every word!
Lessons from my teaching experiences
Taking on the role of junior attending has made me reflect on a few things about the transition that I will undergo at the end of this year, from resident to attending. First, teaching makes me keen to really sharpen my own knowledge, so that I can provide accurate information with confidence and ease. Making valid clinical decisions is a basic attending skill, but eloquently explaining clinical decisions to trainees with varying levels of background knowledge is a unique teaching attending necessity.
Second, I had this amazing feeling of helping patients beyond those currently in my care, since disseminating useful clinical information will allow trainees to better prepare to treat their own patients later. Random hypothetical situations presented by my attendings through the years may have seemed tangentially related to rounds at the time, but were meant to prepare me for actual future decisions (for example, “What would you change if this patient’s renal impairment were more severe?”). These teaching moments strengthen problem-solving skills and help us get as much benefit as possible from each case. The service to future patients extends to students who aren’t pursuing careers in psychiatry, because the skills they learn during a psychiatry rotation will help them connect with patients in any setting.
Third, I realized that teaching has the power to actively shape the future of medicine. What my attendings have taught me through the years is echoed and amplified in my teaching, and supplemented with my own readings and practice patterns.
Fourth, I noted what a privilege it is to be in a field with such attentive and eager trainees; as teachers in medicine, we truly get to work with the cream of the crop, which is a joy and a great responsibility. Working with such highly motivated and attentive students can be intimidating, but as I realized later in the morning, when asked about the complete indications for gabapentin, I realized I’m comfortable saying, “I don’t know, let’s look it up together!”
My fifth and final realization from this exciting teaching experience was that as an attending, I will need to help manage the wellness and growth of my trainees. Attendings must strike a balance between pushing learners to gain mastery while protecting them from excessive stress. I am so grateful for the perceptiveness of my attendings and their ability to adapt to the demands of a clinical environment while maintaining a strong focus on teaching. I have often told PGY-1 residents, when they face feelings of inadequacy for early mistakes, “You have 4 whole years to learn how to do this job!”
These are the moments that make me appreciate the fulfillment that can come from teaching residents and medical students, and really put into perspective how far I’ve come as a trainee. Not long ago, I was one of those medical students scribbling notes while my attending effortlessly spouted medical knowledge, and I was worried I’d never learn the difference between clonidine and clozapine.
On my third day as a PGY-4 junior attending on the inpatient psychiatric ward, 2 new PGY-1 residents, 2 medical students, and I stood in the wee hours of the morning, preparing to meet with our attending to begin rounds. I took the opportunity to discuss potential antipsychotic selection for one of our patients. I questioned the students to gauge their level of knowledge on antipsychotics in general, and did some “thinking out loud” about what our possible options could be. We discussed which antipsychotics are considered “weight-neutral” and which ones require caloric intake for adequate absorption. We discussed what other laboratory tests we should consider upon initiating the hypothetical medication. While discussing these things, I was suddenly taken aback to see that every member of my team was diligently taking notes and hanging on my every word!
Lessons from my teaching experiences
Taking on the role of junior attending has made me reflect on a few things about the transition that I will undergo at the end of this year, from resident to attending. First, teaching makes me keen to really sharpen my own knowledge, so that I can provide accurate information with confidence and ease. Making valid clinical decisions is a basic attending skill, but eloquently explaining clinical decisions to trainees with varying levels of background knowledge is a unique teaching attending necessity.
Second, I had this amazing feeling of helping patients beyond those currently in my care, since disseminating useful clinical information will allow trainees to better prepare to treat their own patients later. Random hypothetical situations presented by my attendings through the years may have seemed tangentially related to rounds at the time, but were meant to prepare me for actual future decisions (for example, “What would you change if this patient’s renal impairment were more severe?”). These teaching moments strengthen problem-solving skills and help us get as much benefit as possible from each case. The service to future patients extends to students who aren’t pursuing careers in psychiatry, because the skills they learn during a psychiatry rotation will help them connect with patients in any setting.
Third, I realized that teaching has the power to actively shape the future of medicine. What my attendings have taught me through the years is echoed and amplified in my teaching, and supplemented with my own readings and practice patterns.
Fourth, I noted what a privilege it is to be in a field with such attentive and eager trainees; as teachers in medicine, we truly get to work with the cream of the crop, which is a joy and a great responsibility. Working with such highly motivated and attentive students can be intimidating, but as I realized later in the morning, when asked about the complete indications for gabapentin, I realized I’m comfortable saying, “I don’t know, let’s look it up together!”
My fifth and final realization from this exciting teaching experience was that as an attending, I will need to help manage the wellness and growth of my trainees. Attendings must strike a balance between pushing learners to gain mastery while protecting them from excessive stress. I am so grateful for the perceptiveness of my attendings and their ability to adapt to the demands of a clinical environment while maintaining a strong focus on teaching. I have often told PGY-1 residents, when they face feelings of inadequacy for early mistakes, “You have 4 whole years to learn how to do this job!”
These are the moments that make me appreciate the fulfillment that can come from teaching residents and medical students, and really put into perspective how far I’ve come as a trainee. Not long ago, I was one of those medical students scribbling notes while my attending effortlessly spouted medical knowledge, and I was worried I’d never learn the difference between clonidine and clozapine.
On my third day as a PGY-4 junior attending on the inpatient psychiatric ward, 2 new PGY-1 residents, 2 medical students, and I stood in the wee hours of the morning, preparing to meet with our attending to begin rounds. I took the opportunity to discuss potential antipsychotic selection for one of our patients. I questioned the students to gauge their level of knowledge on antipsychotics in general, and did some “thinking out loud” about what our possible options could be. We discussed which antipsychotics are considered “weight-neutral” and which ones require caloric intake for adequate absorption. We discussed what other laboratory tests we should consider upon initiating the hypothetical medication. While discussing these things, I was suddenly taken aback to see that every member of my team was diligently taking notes and hanging on my every word!
Lessons from my teaching experiences
Taking on the role of junior attending has made me reflect on a few things about the transition that I will undergo at the end of this year, from resident to attending. First, teaching makes me keen to really sharpen my own knowledge, so that I can provide accurate information with confidence and ease. Making valid clinical decisions is a basic attending skill, but eloquently explaining clinical decisions to trainees with varying levels of background knowledge is a unique teaching attending necessity.
Second, I had this amazing feeling of helping patients beyond those currently in my care, since disseminating useful clinical information will allow trainees to better prepare to treat their own patients later. Random hypothetical situations presented by my attendings through the years may have seemed tangentially related to rounds at the time, but were meant to prepare me for actual future decisions (for example, “What would you change if this patient’s renal impairment were more severe?”). These teaching moments strengthen problem-solving skills and help us get as much benefit as possible from each case. The service to future patients extends to students who aren’t pursuing careers in psychiatry, because the skills they learn during a psychiatry rotation will help them connect with patients in any setting.
Third, I realized that teaching has the power to actively shape the future of medicine. What my attendings have taught me through the years is echoed and amplified in my teaching, and supplemented with my own readings and practice patterns.
Fourth, I noted what a privilege it is to be in a field with such attentive and eager trainees; as teachers in medicine, we truly get to work with the cream of the crop, which is a joy and a great responsibility. Working with such highly motivated and attentive students can be intimidating, but as I realized later in the morning, when asked about the complete indications for gabapentin, I realized I’m comfortable saying, “I don’t know, let’s look it up together!”
My fifth and final realization from this exciting teaching experience was that as an attending, I will need to help manage the wellness and growth of my trainees. Attendings must strike a balance between pushing learners to gain mastery while protecting them from excessive stress. I am so grateful for the perceptiveness of my attendings and their ability to adapt to the demands of a clinical environment while maintaining a strong focus on teaching. I have often told PGY-1 residents, when they face feelings of inadequacy for early mistakes, “You have 4 whole years to learn how to do this job!”
These are the moments that make me appreciate the fulfillment that can come from teaching residents and medical students, and really put into perspective how far I’ve come as a trainee. Not long ago, I was one of those medical students scribbling notes while my attending effortlessly spouted medical knowledge, and I was worried I’d never learn the difference between clonidine and clozapine.
Dermatology history: University Hospital ‘Saint Louis,’ Paris
The Hospital “Saint Louis” was founded in 1607 by King Henry IV of France to relieve overcrowding of Parisian hospitals during the plague epidemic of 1605-1606. He named it Saint-Louis in memory of his grandfather, King Louis IX.
Today, the Hospital Saint-Louis, a registered historic monument, is used for administrative activities.

Since 1980, a modern building has hosted all the activities of the University Hospital Center, which belongs to the University of Paris 7.

In addition to dermatology, the main departments include hematology and bone marrow transplantation, hemato-oncology, general surgery, endocrinology, gastroenterology, clinical immunology, internal medicine, and nephrology. Saint-Louis Hospital employs 2,500 people, including a medical staff of 1,000. It houses the Institute Inserm U976 – a public research unit that is part of the National Health and Medical Research Institute, which focuses on human immunology, physiopathology and immunotherapy – as well as the René-Touraine Foundation, a private non-profit organization that brings together dermatologists, scientists, pharmaceutical companies, and health authorities to support therapeutic progress in dermatology.
Saint-Louis Hospital is known for its long tradition in hematology; it is the site of the first successful allogeneic bone marrow transplant in 1958, performed by Georges Mathé, MD, Professor Jean Bernard, and one of the recipients of the 1980 Nobel Prize in Medicine, Professor Jean Dausset. The hospital is known for not only its activity in dermatology care and research (such as oncodermatology and inflammatory diseases) but also its long tradition of teaching in dermatology and venereology.
Over the last four centuries, great physicians have practiced their art here and many professors, and clinicians at Saint-Louis Hospital have authored publications and developed manuals of dermatology that have been translated across five continents. Many diseases and semiology signs in dermatology were first described by physicians from this hospital, their names familiar to dermatologists worldwide: Jean-Louis-Marc Alibert, MD; Jean Guillaume Auguste Lugol, MD; Laurent-Théodore Biett, MD; Pierre-Antoine-Ernest Bazin, MD; Pierre Louis Alphée Cazenave, MD; François Henri Hallopeau, MD; Léon Lortat-Jacob, MD; Henri-Alexandre Danlos, MD; Ernest Besnier, MD; Jean Baptiste Emile Vidal, MD; Ferdinand-Jean Darier, MD; Louis Brocq, MD; Bernard Felix Duperrat, MD; Gaston Auguste Milian, MD; Albert Sézary, MD; Achille Civatte, MD; Raymond Sabouraud, MD; Henri Gougerot, MD; Albert Touraine, MD; Arnault Tzanck, MD; and Robert Degos, MD, among others.
The Henri-Feulard library – known as the “Dermatology Wax Museum” – is a fascinating place that houses the world’s largest collection of 4,807 wax casts dedicated to teaching skin diseases and venereal diseases.
The library next to the museum contains numerous outstanding ancient works on dermatology and sexually transmitted diseases, including first issues of dermatology journals from the 19th century and rare dermatology textbooks published in the last 2 centuries.
The recently renovated museum hosts national and international dermatological meetings and is also where the hospital’s dermatology staff meets weekly.
In the dermatology department at Saint-Louis Hospital, patient care is provided in two hospital areas with 18 beds each and a day hospital with 8 beds for patients with inflammatory and dysimmune dermatoses, including a special room with a bathtub for the management of patients with severe genodermatoses. The department is a referral center for genodermatoses and a dedicated center for autoimmune bullous diseases.
Patients with all types of skin tumors, particularly melanomas, carcinomas, sarcomas, and cutaneous lymphomas, are treated at the oncodermatology center, which has a 10-bed day hospital and a very active consultation service. The Saint-Louis Hospital dermatology department is also a National Reference Center for cutaneous lymphomas, providing four Multidisciplinary Consultation Meetings, a national MCM for cutaneous lymphomas, and a multidisciplinary MCM for the diagnosis and treatment of side effects of new targeted therapies and immunotherapies for cancers.
The dermatology polyclinic, an outpatient clinic, provides 54,000 consultations per year. It includes a very active general consultation service, including a wide variety of specialized consultations for atopic dermatitis, psoriasis, hand dermatitis, hidradenitis suppurativa, internal medicine/dermatology, bullous diseases, keloids, angiomas, leprosy, genodermatoses, and medical mycology.
Anonymous, free screening services are available at the Sexually Transmitted Diseases Center through “CeGIDD,” a free center for HIV/AIDS screening and specialized consultations in venereology and mucosal pathologies.
The surgical activity of the department is provided in the Center of Dermo-Surgery. Dedicated medical and paramedical consultations ensure the management of ulcers and therapeutic baths for patients and families with refractory scabies.
The technical platform includes an allergology consultation, a phototherapy center, a Fotofinder diagnosis, a photodynamic therapy unit, and a confocal microscopy unit. The department, completed in September 2019 with a laser center with four devices, also works in close collaboration with the Sabouraud Center, created by Dr. Sabouraud and dedicated to the investigation and treatment of scalp diseases.
We are absolutely aware that working in a hospital so rich in past personalities and discoveries and part of the history of dermatology is not only a huge honor requiring a special commitment to continue the tradition of research and excellence in dermatology initiated hundreds of years ago, but also an important responsibility to focus all our efforts on teaching dermatology to next generations in France and around the world. It is also our responsibility to pursue this historic tradition of excellence by developing dynamic translational research activities that lead to innovations in the field of dermatology.
Professor Bagot is head of the dermatology department of University Hospital Saint-Louis, Paris. Dr. Ionescu is a specialist in dermatology and venereology in the department of dermatology at University Hospital Saint-Louis in Paris and is a member of the Dermatology News editorial board. Write to them at dermnews@mdedge.com.
The Hospital “Saint Louis” was founded in 1607 by King Henry IV of France to relieve overcrowding of Parisian hospitals during the plague epidemic of 1605-1606. He named it Saint-Louis in memory of his grandfather, King Louis IX.
Today, the Hospital Saint-Louis, a registered historic monument, is used for administrative activities.

Since 1980, a modern building has hosted all the activities of the University Hospital Center, which belongs to the University of Paris 7.

In addition to dermatology, the main departments include hematology and bone marrow transplantation, hemato-oncology, general surgery, endocrinology, gastroenterology, clinical immunology, internal medicine, and nephrology. Saint-Louis Hospital employs 2,500 people, including a medical staff of 1,000. It houses the Institute Inserm U976 – a public research unit that is part of the National Health and Medical Research Institute, which focuses on human immunology, physiopathology and immunotherapy – as well as the René-Touraine Foundation, a private non-profit organization that brings together dermatologists, scientists, pharmaceutical companies, and health authorities to support therapeutic progress in dermatology.
Saint-Louis Hospital is known for its long tradition in hematology; it is the site of the first successful allogeneic bone marrow transplant in 1958, performed by Georges Mathé, MD, Professor Jean Bernard, and one of the recipients of the 1980 Nobel Prize in Medicine, Professor Jean Dausset. The hospital is known for not only its activity in dermatology care and research (such as oncodermatology and inflammatory diseases) but also its long tradition of teaching in dermatology and venereology.
Over the last four centuries, great physicians have practiced their art here and many professors, and clinicians at Saint-Louis Hospital have authored publications and developed manuals of dermatology that have been translated across five continents. Many diseases and semiology signs in dermatology were first described by physicians from this hospital, their names familiar to dermatologists worldwide: Jean-Louis-Marc Alibert, MD; Jean Guillaume Auguste Lugol, MD; Laurent-Théodore Biett, MD; Pierre-Antoine-Ernest Bazin, MD; Pierre Louis Alphée Cazenave, MD; François Henri Hallopeau, MD; Léon Lortat-Jacob, MD; Henri-Alexandre Danlos, MD; Ernest Besnier, MD; Jean Baptiste Emile Vidal, MD; Ferdinand-Jean Darier, MD; Louis Brocq, MD; Bernard Felix Duperrat, MD; Gaston Auguste Milian, MD; Albert Sézary, MD; Achille Civatte, MD; Raymond Sabouraud, MD; Henri Gougerot, MD; Albert Touraine, MD; Arnault Tzanck, MD; and Robert Degos, MD, among others.
The Henri-Feulard library – known as the “Dermatology Wax Museum” – is a fascinating place that houses the world’s largest collection of 4,807 wax casts dedicated to teaching skin diseases and venereal diseases.
The library next to the museum contains numerous outstanding ancient works on dermatology and sexually transmitted diseases, including first issues of dermatology journals from the 19th century and rare dermatology textbooks published in the last 2 centuries.
The recently renovated museum hosts national and international dermatological meetings and is also where the hospital’s dermatology staff meets weekly.
In the dermatology department at Saint-Louis Hospital, patient care is provided in two hospital areas with 18 beds each and a day hospital with 8 beds for patients with inflammatory and dysimmune dermatoses, including a special room with a bathtub for the management of patients with severe genodermatoses. The department is a referral center for genodermatoses and a dedicated center for autoimmune bullous diseases.
Patients with all types of skin tumors, particularly melanomas, carcinomas, sarcomas, and cutaneous lymphomas, are treated at the oncodermatology center, which has a 10-bed day hospital and a very active consultation service. The Saint-Louis Hospital dermatology department is also a National Reference Center for cutaneous lymphomas, providing four Multidisciplinary Consultation Meetings, a national MCM for cutaneous lymphomas, and a multidisciplinary MCM for the diagnosis and treatment of side effects of new targeted therapies and immunotherapies for cancers.
The dermatology polyclinic, an outpatient clinic, provides 54,000 consultations per year. It includes a very active general consultation service, including a wide variety of specialized consultations for atopic dermatitis, psoriasis, hand dermatitis, hidradenitis suppurativa, internal medicine/dermatology, bullous diseases, keloids, angiomas, leprosy, genodermatoses, and medical mycology.
Anonymous, free screening services are available at the Sexually Transmitted Diseases Center through “CeGIDD,” a free center for HIV/AIDS screening and specialized consultations in venereology and mucosal pathologies.
The surgical activity of the department is provided in the Center of Dermo-Surgery. Dedicated medical and paramedical consultations ensure the management of ulcers and therapeutic baths for patients and families with refractory scabies.
The technical platform includes an allergology consultation, a phototherapy center, a Fotofinder diagnosis, a photodynamic therapy unit, and a confocal microscopy unit. The department, completed in September 2019 with a laser center with four devices, also works in close collaboration with the Sabouraud Center, created by Dr. Sabouraud and dedicated to the investigation and treatment of scalp diseases.
We are absolutely aware that working in a hospital so rich in past personalities and discoveries and part of the history of dermatology is not only a huge honor requiring a special commitment to continue the tradition of research and excellence in dermatology initiated hundreds of years ago, but also an important responsibility to focus all our efforts on teaching dermatology to next generations in France and around the world. It is also our responsibility to pursue this historic tradition of excellence by developing dynamic translational research activities that lead to innovations in the field of dermatology.
Professor Bagot is head of the dermatology department of University Hospital Saint-Louis, Paris. Dr. Ionescu is a specialist in dermatology and venereology in the department of dermatology at University Hospital Saint-Louis in Paris and is a member of the Dermatology News editorial board. Write to them at dermnews@mdedge.com.
The Hospital “Saint Louis” was founded in 1607 by King Henry IV of France to relieve overcrowding of Parisian hospitals during the plague epidemic of 1605-1606. He named it Saint-Louis in memory of his grandfather, King Louis IX.
Today, the Hospital Saint-Louis, a registered historic monument, is used for administrative activities.

Since 1980, a modern building has hosted all the activities of the University Hospital Center, which belongs to the University of Paris 7.

In addition to dermatology, the main departments include hematology and bone marrow transplantation, hemato-oncology, general surgery, endocrinology, gastroenterology, clinical immunology, internal medicine, and nephrology. Saint-Louis Hospital employs 2,500 people, including a medical staff of 1,000. It houses the Institute Inserm U976 – a public research unit that is part of the National Health and Medical Research Institute, which focuses on human immunology, physiopathology and immunotherapy – as well as the René-Touraine Foundation, a private non-profit organization that brings together dermatologists, scientists, pharmaceutical companies, and health authorities to support therapeutic progress in dermatology.
Saint-Louis Hospital is known for its long tradition in hematology; it is the site of the first successful allogeneic bone marrow transplant in 1958, performed by Georges Mathé, MD, Professor Jean Bernard, and one of the recipients of the 1980 Nobel Prize in Medicine, Professor Jean Dausset. The hospital is known for not only its activity in dermatology care and research (such as oncodermatology and inflammatory diseases) but also its long tradition of teaching in dermatology and venereology.
Over the last four centuries, great physicians have practiced their art here and many professors, and clinicians at Saint-Louis Hospital have authored publications and developed manuals of dermatology that have been translated across five continents. Many diseases and semiology signs in dermatology were first described by physicians from this hospital, their names familiar to dermatologists worldwide: Jean-Louis-Marc Alibert, MD; Jean Guillaume Auguste Lugol, MD; Laurent-Théodore Biett, MD; Pierre-Antoine-Ernest Bazin, MD; Pierre Louis Alphée Cazenave, MD; François Henri Hallopeau, MD; Léon Lortat-Jacob, MD; Henri-Alexandre Danlos, MD; Ernest Besnier, MD; Jean Baptiste Emile Vidal, MD; Ferdinand-Jean Darier, MD; Louis Brocq, MD; Bernard Felix Duperrat, MD; Gaston Auguste Milian, MD; Albert Sézary, MD; Achille Civatte, MD; Raymond Sabouraud, MD; Henri Gougerot, MD; Albert Touraine, MD; Arnault Tzanck, MD; and Robert Degos, MD, among others.
The Henri-Feulard library – known as the “Dermatology Wax Museum” – is a fascinating place that houses the world’s largest collection of 4,807 wax casts dedicated to teaching skin diseases and venereal diseases.
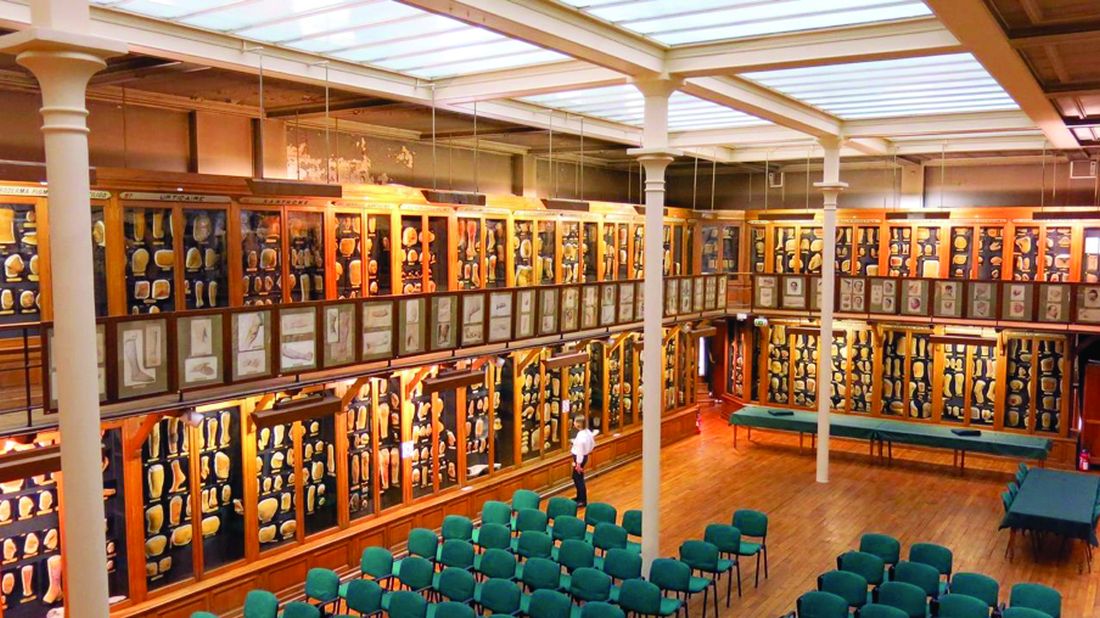
The library next to the museum contains numerous outstanding ancient works on dermatology and sexually transmitted diseases, including first issues of dermatology journals from the 19th century and rare dermatology textbooks published in the last 2 centuries.
The recently renovated museum hosts national and international dermatological meetings and is also where the hospital’s dermatology staff meets weekly.
In the dermatology department at Saint-Louis Hospital, patient care is provided in two hospital areas with 18 beds each and a day hospital with 8 beds for patients with inflammatory and dysimmune dermatoses, including a special room with a bathtub for the management of patients with severe genodermatoses. The department is a referral center for genodermatoses and a dedicated center for autoimmune bullous diseases.
Patients with all types of skin tumors, particularly melanomas, carcinomas, sarcomas, and cutaneous lymphomas, are treated at the oncodermatology center, which has a 10-bed day hospital and a very active consultation service. The Saint-Louis Hospital dermatology department is also a National Reference Center for cutaneous lymphomas, providing four Multidisciplinary Consultation Meetings, a national MCM for cutaneous lymphomas, and a multidisciplinary MCM for the diagnosis and treatment of side effects of new targeted therapies and immunotherapies for cancers.
The dermatology polyclinic, an outpatient clinic, provides 54,000 consultations per year. It includes a very active general consultation service, including a wide variety of specialized consultations for atopic dermatitis, psoriasis, hand dermatitis, hidradenitis suppurativa, internal medicine/dermatology, bullous diseases, keloids, angiomas, leprosy, genodermatoses, and medical mycology.
Anonymous, free screening services are available at the Sexually Transmitted Diseases Center through “CeGIDD,” a free center for HIV/AIDS screening and specialized consultations in venereology and mucosal pathologies.
The surgical activity of the department is provided in the Center of Dermo-Surgery. Dedicated medical and paramedical consultations ensure the management of ulcers and therapeutic baths for patients and families with refractory scabies.
The technical platform includes an allergology consultation, a phototherapy center, a Fotofinder diagnosis, a photodynamic therapy unit, and a confocal microscopy unit. The department, completed in September 2019 with a laser center with four devices, also works in close collaboration with the Sabouraud Center, created by Dr. Sabouraud and dedicated to the investigation and treatment of scalp diseases.
We are absolutely aware that working in a hospital so rich in past personalities and discoveries and part of the history of dermatology is not only a huge honor requiring a special commitment to continue the tradition of research and excellence in dermatology initiated hundreds of years ago, but also an important responsibility to focus all our efforts on teaching dermatology to next generations in France and around the world. It is also our responsibility to pursue this historic tradition of excellence by developing dynamic translational research activities that lead to innovations in the field of dermatology.
Professor Bagot is head of the dermatology department of University Hospital Saint-Louis, Paris. Dr. Ionescu is a specialist in dermatology and venereology in the department of dermatology at University Hospital Saint-Louis in Paris and is a member of the Dermatology News editorial board. Write to them at dermnews@mdedge.com.