User login
FDA: More metformin extended-release tablets recalled
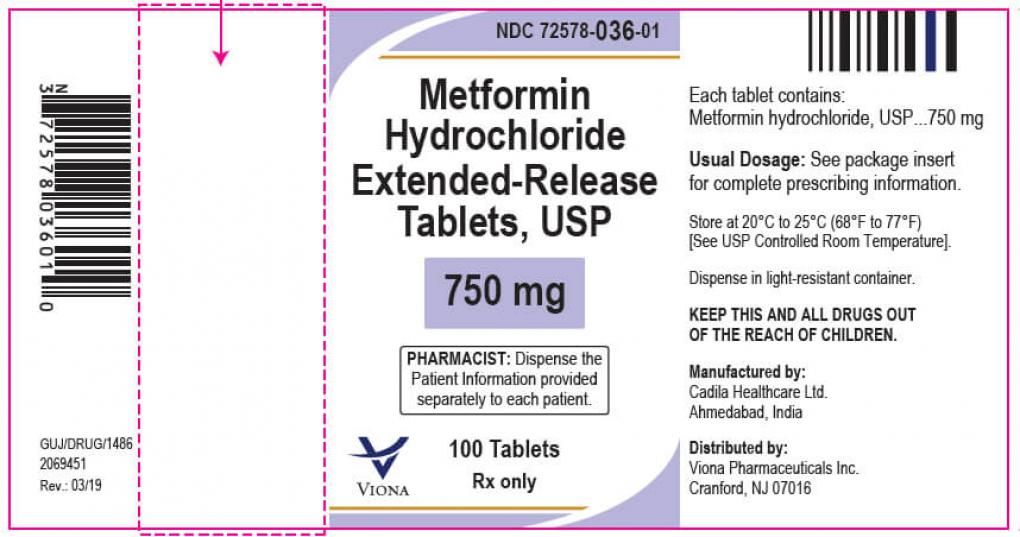
Two lots of metformin HCl extended-release tablets have been recalled by Viona Pharmaceuticals because unacceptable levels of nitrosodimethylamine (NDMA), a likely carcinogen, were found in the 750-mg tablets.
According to a June 11 alert from the Food and Drug Administration, the affected lot numbers are M915601 and M915602.
This generic product was made by Cadila Healthcare, Ahmedabad, India, in November 2019 with an expiration date of October 2021, and distributed throughout the United States. The pill is white to off-white, capsule-shaped, uncoated tablets, debossed with “Z”, “C” on one side and “20” on the other side.
No adverse events related to the lots involved in the recall have been reported, the FDA said. It also recommends that clinicians continue to prescribe metformin when clinically appropriate.
In late 2019, the FDA announced it had become aware of NDMA in some metformin products in other countries. The agency immediately began testing to determine whether the metformin in the U.S. supply was at risk, as part of the ongoing investigation into nitrosamine impurities across medication types, which included recalls of hypertension and heartburn medications within the past 3 years.
In February 2020, the FDA reported that they hadn’t found NDMA levels that exceeded the acceptable daily intake. But starting in May 2020, voluntary recalls by, numerous manufacturers have been announced as levels of the compound exceeded that cutoff.
Two lots of metformin HCl extended-release tablets have been recalled by Viona Pharmaceuticals because unacceptable levels of nitrosodimethylamine (NDMA), a likely carcinogen, were found in the 750-mg tablets.
According to a June 11 alert from the Food and Drug Administration, the affected lot numbers are M915601 and M915602.
This generic product was made by Cadila Healthcare, Ahmedabad, India, in November 2019 with an expiration date of October 2021, and distributed throughout the United States. The pill is white to off-white, capsule-shaped, uncoated tablets, debossed with “Z”, “C” on one side and “20” on the other side.
No adverse events related to the lots involved in the recall have been reported, the FDA said. It also recommends that clinicians continue to prescribe metformin when clinically appropriate.
In late 2019, the FDA announced it had become aware of NDMA in some metformin products in other countries. The agency immediately began testing to determine whether the metformin in the U.S. supply was at risk, as part of the ongoing investigation into nitrosamine impurities across medication types, which included recalls of hypertension and heartburn medications within the past 3 years.
In February 2020, the FDA reported that they hadn’t found NDMA levels that exceeded the acceptable daily intake. But starting in May 2020, voluntary recalls by, numerous manufacturers have been announced as levels of the compound exceeded that cutoff.
Two lots of metformin HCl extended-release tablets have been recalled by Viona Pharmaceuticals because unacceptable levels of nitrosodimethylamine (NDMA), a likely carcinogen, were found in the 750-mg tablets.
According to a June 11 alert from the Food and Drug Administration, the affected lot numbers are M915601 and M915602.
This generic product was made by Cadila Healthcare, Ahmedabad, India, in November 2019 with an expiration date of October 2021, and distributed throughout the United States. The pill is white to off-white, capsule-shaped, uncoated tablets, debossed with “Z”, “C” on one side and “20” on the other side.
No adverse events related to the lots involved in the recall have been reported, the FDA said. It also recommends that clinicians continue to prescribe metformin when clinically appropriate.
In late 2019, the FDA announced it had become aware of NDMA in some metformin products in other countries. The agency immediately began testing to determine whether the metformin in the U.S. supply was at risk, as part of the ongoing investigation into nitrosamine impurities across medication types, which included recalls of hypertension and heartburn medications within the past 3 years.
In February 2020, the FDA reported that they hadn’t found NDMA levels that exceeded the acceptable daily intake. But starting in May 2020, voluntary recalls by, numerous manufacturers have been announced as levels of the compound exceeded that cutoff.
FROM THE FOOD AND DRUG ADMINISTRATION
Surgical outcomes favor addition of nivolumab to neoadjuvant chemo in resectable lung cancers
The addition of nivolumab to neoadjuvant chemotherapy did not impede the feasibility or timing of surgery in patients with resectable lung cancer, according to results from the phase 3 CheckMate 816 trial.
Adding nivolumab to chemotherapy was tolerable and did not increase the rate of surgical complications, investigator Jonathan Spicer, FRCPC, MD, PhD, of McGill University, Montreal, said in his presentation at the annual meeting of the American Society of Clinical Oncology.
His presentation comes about 2 months after the reporting of primary endpoint results of CheckMate 816 (NCT02998528). CheckMate 816 demonstrated that adding nivolumab to neoadjuvant chemotherapy significantly improved pathological complete response (pCR) in patients with resectable non–small cell lung cancer (NSCLC), according to results presented earlier at the American Association for Cancer Research annual meeting.
“The safety and surgical outcome data reported thus far from CheckMate 816, along with significant improvement in pathological complete response, support nivolumab in combination with chemotherapy as an attractive neoadjuvant option for patients with resectable NSCLC,” said Dr. Spicer (Abstract 8503).
Building on previous experience
The CheckMate 816 study builds on extensive experience in advanced NSCLC that has consistently shown better outcomes, including overall survival, with combinations of chemotherapy and immuno-oncology (IO) agents, compared to chemotherapy alone, said discussant Valerie W. Rusch, MD, of Memorial Sloan Kettering Cancer Center in New York.
Dr. Rusch called out “salient and interesting results” regarding surgical management in CheckMate 816, including a lower rate of surgery cancellations and shorter surgical duration in the chemotherapy-plus-IO arm, compared to the chemotherapy-alone arm.
Furthermore, fewer patients required a pneumonectomy and more patients had a complete resection in the chemotherapy-plus-IO arm, compared to chemotherapy alone, she noted.
“These excellent surgical results, along with the data previously presented at AACR regarding the primary endpoint, help to establish a new standard of neoadjuvant care,” Dr. Rusch said in her presentation.
Study details
CheckMate 816 included 358 patients with newly diagnosed, resectable, stage IB-IIIA NSCLC, Eastern Cooperative Oncology Group (ECOG) performance status of 0-1, and no known EGFR mutations or ALK alterations. Patients were randomized to receive nivolumab and platinum-doublet chemotherapy (nivolumab/chemotherapy) or chemotherapy alone every 3 weeks, with surgery to be performed within 6 weeks of the last dose of neoadjuvant treatment.
The median age of patients was 64 years in the nivolumab/chemotherapy arm and 65 years in the chemotherapy-alone arm. About one-third of patients had ECOG performance status of one, and about half had squamous tumor histology, Dr. Spicer said in his report. Almost two-thirds of patients had stage IIIA disease.
In the study results previously presented at the AACR meeting, both pCR and major pathologic response were significantly better following neoadjuvant chemotherapy and IO treatment, compared to chemotherapy alone.
In the intention-to-treat analysis, 24.0% of patients treated with nivolumab/chemotherapy achieved a pCR, compared to 2.2% in the chemotherapy arm, amounting to an approximate 12-fold increase in pCR, Dr. Spicer said. Similarly, the rate of major pathologic response in the intention-to-treat analysis was 36.9% and 8.9% for the nivolumab/chemotherapy and chemotherapy arms, respectively.
Surgical results
In his ASCO presentation, Dr. Spicer reported that definitive surgery was canceled in 16% of patients in the nivolumab/chemotherapy arm, and 21% of the chemotherapy arm. Reasons for surgery cancellation generally included patients declining surgery, unresectable disease, and poor lung function. “Cancellation of surgery due to neoadjuvant therapy toxicity was rare,” Dr. Spicer said in his presentation.
Among patients who did proceed to surgery, the median duration of the procedure was 184 minutes in the nivolumab/chemotherapy arm and 217 minutes in the chemotherapy arm. That half-hour difference in favor of the combination arm suggests that the complexity of surgery was not increased by the addition of nivolumab, Dr. Spicer said.
Median time to surgery was about 5 weeks in both arms, which was “well within accepted standards for a neoadjuvant therapeutic approach,” Dr. Spicer said. Most delays beyond 6 weeks were due to administrative issues, and occurred in similar proportions (21% of the nivolumab/chemotherapy arm and 18% of the chemotherapy arm).
The addition of nivolumab to chemotherapy improved pCR rates regardless of baseline stage of disease, according to Dr. Spicer. Furthermore, the depth of pathological regression in the primary tumor was “dramatically different” across stage groupings, he said. Median residual viable tumor percentage in stage IB/II patients was 28% for nivolumab/chemotherapy and 79% for chemotherapy, and in stage IIIA patients, it was 8% for nivolumab/chemotherapy and 70% for chemotherapy.
Overall, thoracotomy was the most frequent surgical approach in this international phase 3 trial, Dr. Spicer said. However, among patients with stage IIIA disease, minimally invasive approaches were used 30% of the time in the nivolumab/chemotherapy arm and 19% in the chemotherapy arm. Conversely, the rate of conversion from a minimally invasive to open approach in patients with stage IIIA disease was 11% for nivolumab/chemotherapy and 20% for chemotherapy alone.
Lobectomy was more frequent in the nivolumab/chemotherapy arm (77%) compared to the chemotherapy arm (61%), a difference that Dr. Spicer described as clinically important. He said the difference appears to be attributable to a lower rate of pneumonectomy in the nivolumab/chemotherapy arm (17%) than in the chemotherapy arm (25%).
Despite less extensive lung resection being required, the rate of R0 resection was numerically higher in the nivolumab/chemotherapy arm (83%) than in the chemotherapy arm (78%), said Dr. Spicer.
Length of hospital stay was “within expected ranges” from geographic regions represented in the trial, Dr. Spicer said. Median length of stay was 4.0 and 6.0 days, respectively, for nivolumab/chemotherapy and chemotherapy alone in North America, 9.5 and 13.0 days in Europe, and 11.0 and 13.0 days in Asia.
Likewise, 90-day surgical complications were well within expected ranges, according to the investigator, with anemia, pain, and wound complications being the most commonly reported. Rates were generally similar between study arms, other than a twofold higher rate of pain in the chemotherapy arm, possibly due to the lower rate of minimally invasive surgery or higher rate of conversion to an open procedure, compared to the nivolumab/chemotherapy arm, he said.
Awaiting survival
Rates of 30- and 90-day mortality are expected to be evaluated when survival endpoints are available, according to Dr. Spicer. Beyond pCR rate, event-free survival is also a primary endpoint of the study, while overall survival is a secondary endpoint.
The study was supported by Bristol Myers Squibb. Dr. Spicer reported disclosures related to AstraZeneca, Bristol Myers Squibb Foundation, Merck, and Roche. Dr. Rusch reported research funding with Genelux and Genentech, and travel expenses from Intuitive Surgical.
The addition of nivolumab to neoadjuvant chemotherapy did not impede the feasibility or timing of surgery in patients with resectable lung cancer, according to results from the phase 3 CheckMate 816 trial.
Adding nivolumab to chemotherapy was tolerable and did not increase the rate of surgical complications, investigator Jonathan Spicer, FRCPC, MD, PhD, of McGill University, Montreal, said in his presentation at the annual meeting of the American Society of Clinical Oncology.
His presentation comes about 2 months after the reporting of primary endpoint results of CheckMate 816 (NCT02998528). CheckMate 816 demonstrated that adding nivolumab to neoadjuvant chemotherapy significantly improved pathological complete response (pCR) in patients with resectable non–small cell lung cancer (NSCLC), according to results presented earlier at the American Association for Cancer Research annual meeting.
“The safety and surgical outcome data reported thus far from CheckMate 816, along with significant improvement in pathological complete response, support nivolumab in combination with chemotherapy as an attractive neoadjuvant option for patients with resectable NSCLC,” said Dr. Spicer (Abstract 8503).
Building on previous experience
The CheckMate 816 study builds on extensive experience in advanced NSCLC that has consistently shown better outcomes, including overall survival, with combinations of chemotherapy and immuno-oncology (IO) agents, compared to chemotherapy alone, said discussant Valerie W. Rusch, MD, of Memorial Sloan Kettering Cancer Center in New York.
Dr. Rusch called out “salient and interesting results” regarding surgical management in CheckMate 816, including a lower rate of surgery cancellations and shorter surgical duration in the chemotherapy-plus-IO arm, compared to the chemotherapy-alone arm.
Furthermore, fewer patients required a pneumonectomy and more patients had a complete resection in the chemotherapy-plus-IO arm, compared to chemotherapy alone, she noted.
“These excellent surgical results, along with the data previously presented at AACR regarding the primary endpoint, help to establish a new standard of neoadjuvant care,” Dr. Rusch said in her presentation.
Study details
CheckMate 816 included 358 patients with newly diagnosed, resectable, stage IB-IIIA NSCLC, Eastern Cooperative Oncology Group (ECOG) performance status of 0-1, and no known EGFR mutations or ALK alterations. Patients were randomized to receive nivolumab and platinum-doublet chemotherapy (nivolumab/chemotherapy) or chemotherapy alone every 3 weeks, with surgery to be performed within 6 weeks of the last dose of neoadjuvant treatment.
The median age of patients was 64 years in the nivolumab/chemotherapy arm and 65 years in the chemotherapy-alone arm. About one-third of patients had ECOG performance status of one, and about half had squamous tumor histology, Dr. Spicer said in his report. Almost two-thirds of patients had stage IIIA disease.
In the study results previously presented at the AACR meeting, both pCR and major pathologic response were significantly better following neoadjuvant chemotherapy and IO treatment, compared to chemotherapy alone.
In the intention-to-treat analysis, 24.0% of patients treated with nivolumab/chemotherapy achieved a pCR, compared to 2.2% in the chemotherapy arm, amounting to an approximate 12-fold increase in pCR, Dr. Spicer said. Similarly, the rate of major pathologic response in the intention-to-treat analysis was 36.9% and 8.9% for the nivolumab/chemotherapy and chemotherapy arms, respectively.
Surgical results
In his ASCO presentation, Dr. Spicer reported that definitive surgery was canceled in 16% of patients in the nivolumab/chemotherapy arm, and 21% of the chemotherapy arm. Reasons for surgery cancellation generally included patients declining surgery, unresectable disease, and poor lung function. “Cancellation of surgery due to neoadjuvant therapy toxicity was rare,” Dr. Spicer said in his presentation.
Among patients who did proceed to surgery, the median duration of the procedure was 184 minutes in the nivolumab/chemotherapy arm and 217 minutes in the chemotherapy arm. That half-hour difference in favor of the combination arm suggests that the complexity of surgery was not increased by the addition of nivolumab, Dr. Spicer said.
Median time to surgery was about 5 weeks in both arms, which was “well within accepted standards for a neoadjuvant therapeutic approach,” Dr. Spicer said. Most delays beyond 6 weeks were due to administrative issues, and occurred in similar proportions (21% of the nivolumab/chemotherapy arm and 18% of the chemotherapy arm).
The addition of nivolumab to chemotherapy improved pCR rates regardless of baseline stage of disease, according to Dr. Spicer. Furthermore, the depth of pathological regression in the primary tumor was “dramatically different” across stage groupings, he said. Median residual viable tumor percentage in stage IB/II patients was 28% for nivolumab/chemotherapy and 79% for chemotherapy, and in stage IIIA patients, it was 8% for nivolumab/chemotherapy and 70% for chemotherapy.
Overall, thoracotomy was the most frequent surgical approach in this international phase 3 trial, Dr. Spicer said. However, among patients with stage IIIA disease, minimally invasive approaches were used 30% of the time in the nivolumab/chemotherapy arm and 19% in the chemotherapy arm. Conversely, the rate of conversion from a minimally invasive to open approach in patients with stage IIIA disease was 11% for nivolumab/chemotherapy and 20% for chemotherapy alone.
Lobectomy was more frequent in the nivolumab/chemotherapy arm (77%) compared to the chemotherapy arm (61%), a difference that Dr. Spicer described as clinically important. He said the difference appears to be attributable to a lower rate of pneumonectomy in the nivolumab/chemotherapy arm (17%) than in the chemotherapy arm (25%).
Despite less extensive lung resection being required, the rate of R0 resection was numerically higher in the nivolumab/chemotherapy arm (83%) than in the chemotherapy arm (78%), said Dr. Spicer.
Length of hospital stay was “within expected ranges” from geographic regions represented in the trial, Dr. Spicer said. Median length of stay was 4.0 and 6.0 days, respectively, for nivolumab/chemotherapy and chemotherapy alone in North America, 9.5 and 13.0 days in Europe, and 11.0 and 13.0 days in Asia.
Likewise, 90-day surgical complications were well within expected ranges, according to the investigator, with anemia, pain, and wound complications being the most commonly reported. Rates were generally similar between study arms, other than a twofold higher rate of pain in the chemotherapy arm, possibly due to the lower rate of minimally invasive surgery or higher rate of conversion to an open procedure, compared to the nivolumab/chemotherapy arm, he said.
Awaiting survival
Rates of 30- and 90-day mortality are expected to be evaluated when survival endpoints are available, according to Dr. Spicer. Beyond pCR rate, event-free survival is also a primary endpoint of the study, while overall survival is a secondary endpoint.
The study was supported by Bristol Myers Squibb. Dr. Spicer reported disclosures related to AstraZeneca, Bristol Myers Squibb Foundation, Merck, and Roche. Dr. Rusch reported research funding with Genelux and Genentech, and travel expenses from Intuitive Surgical.
The addition of nivolumab to neoadjuvant chemotherapy did not impede the feasibility or timing of surgery in patients with resectable lung cancer, according to results from the phase 3 CheckMate 816 trial.
Adding nivolumab to chemotherapy was tolerable and did not increase the rate of surgical complications, investigator Jonathan Spicer, FRCPC, MD, PhD, of McGill University, Montreal, said in his presentation at the annual meeting of the American Society of Clinical Oncology.
His presentation comes about 2 months after the reporting of primary endpoint results of CheckMate 816 (NCT02998528). CheckMate 816 demonstrated that adding nivolumab to neoadjuvant chemotherapy significantly improved pathological complete response (pCR) in patients with resectable non–small cell lung cancer (NSCLC), according to results presented earlier at the American Association for Cancer Research annual meeting.
“The safety and surgical outcome data reported thus far from CheckMate 816, along with significant improvement in pathological complete response, support nivolumab in combination with chemotherapy as an attractive neoadjuvant option for patients with resectable NSCLC,” said Dr. Spicer (Abstract 8503).
Building on previous experience
The CheckMate 816 study builds on extensive experience in advanced NSCLC that has consistently shown better outcomes, including overall survival, with combinations of chemotherapy and immuno-oncology (IO) agents, compared to chemotherapy alone, said discussant Valerie W. Rusch, MD, of Memorial Sloan Kettering Cancer Center in New York.
Dr. Rusch called out “salient and interesting results” regarding surgical management in CheckMate 816, including a lower rate of surgery cancellations and shorter surgical duration in the chemotherapy-plus-IO arm, compared to the chemotherapy-alone arm.
Furthermore, fewer patients required a pneumonectomy and more patients had a complete resection in the chemotherapy-plus-IO arm, compared to chemotherapy alone, she noted.
“These excellent surgical results, along with the data previously presented at AACR regarding the primary endpoint, help to establish a new standard of neoadjuvant care,” Dr. Rusch said in her presentation.
Study details
CheckMate 816 included 358 patients with newly diagnosed, resectable, stage IB-IIIA NSCLC, Eastern Cooperative Oncology Group (ECOG) performance status of 0-1, and no known EGFR mutations or ALK alterations. Patients were randomized to receive nivolumab and platinum-doublet chemotherapy (nivolumab/chemotherapy) or chemotherapy alone every 3 weeks, with surgery to be performed within 6 weeks of the last dose of neoadjuvant treatment.
The median age of patients was 64 years in the nivolumab/chemotherapy arm and 65 years in the chemotherapy-alone arm. About one-third of patients had ECOG performance status of one, and about half had squamous tumor histology, Dr. Spicer said in his report. Almost two-thirds of patients had stage IIIA disease.
In the study results previously presented at the AACR meeting, both pCR and major pathologic response were significantly better following neoadjuvant chemotherapy and IO treatment, compared to chemotherapy alone.
In the intention-to-treat analysis, 24.0% of patients treated with nivolumab/chemotherapy achieved a pCR, compared to 2.2% in the chemotherapy arm, amounting to an approximate 12-fold increase in pCR, Dr. Spicer said. Similarly, the rate of major pathologic response in the intention-to-treat analysis was 36.9% and 8.9% for the nivolumab/chemotherapy and chemotherapy arms, respectively.
Surgical results
In his ASCO presentation, Dr. Spicer reported that definitive surgery was canceled in 16% of patients in the nivolumab/chemotherapy arm, and 21% of the chemotherapy arm. Reasons for surgery cancellation generally included patients declining surgery, unresectable disease, and poor lung function. “Cancellation of surgery due to neoadjuvant therapy toxicity was rare,” Dr. Spicer said in his presentation.
Among patients who did proceed to surgery, the median duration of the procedure was 184 minutes in the nivolumab/chemotherapy arm and 217 minutes in the chemotherapy arm. That half-hour difference in favor of the combination arm suggests that the complexity of surgery was not increased by the addition of nivolumab, Dr. Spicer said.
Median time to surgery was about 5 weeks in both arms, which was “well within accepted standards for a neoadjuvant therapeutic approach,” Dr. Spicer said. Most delays beyond 6 weeks were due to administrative issues, and occurred in similar proportions (21% of the nivolumab/chemotherapy arm and 18% of the chemotherapy arm).
The addition of nivolumab to chemotherapy improved pCR rates regardless of baseline stage of disease, according to Dr. Spicer. Furthermore, the depth of pathological regression in the primary tumor was “dramatically different” across stage groupings, he said. Median residual viable tumor percentage in stage IB/II patients was 28% for nivolumab/chemotherapy and 79% for chemotherapy, and in stage IIIA patients, it was 8% for nivolumab/chemotherapy and 70% for chemotherapy.
Overall, thoracotomy was the most frequent surgical approach in this international phase 3 trial, Dr. Spicer said. However, among patients with stage IIIA disease, minimally invasive approaches were used 30% of the time in the nivolumab/chemotherapy arm and 19% in the chemotherapy arm. Conversely, the rate of conversion from a minimally invasive to open approach in patients with stage IIIA disease was 11% for nivolumab/chemotherapy and 20% for chemotherapy alone.
Lobectomy was more frequent in the nivolumab/chemotherapy arm (77%) compared to the chemotherapy arm (61%), a difference that Dr. Spicer described as clinically important. He said the difference appears to be attributable to a lower rate of pneumonectomy in the nivolumab/chemotherapy arm (17%) than in the chemotherapy arm (25%).
Despite less extensive lung resection being required, the rate of R0 resection was numerically higher in the nivolumab/chemotherapy arm (83%) than in the chemotherapy arm (78%), said Dr. Spicer.
Length of hospital stay was “within expected ranges” from geographic regions represented in the trial, Dr. Spicer said. Median length of stay was 4.0 and 6.0 days, respectively, for nivolumab/chemotherapy and chemotherapy alone in North America, 9.5 and 13.0 days in Europe, and 11.0 and 13.0 days in Asia.
Likewise, 90-day surgical complications were well within expected ranges, according to the investigator, with anemia, pain, and wound complications being the most commonly reported. Rates were generally similar between study arms, other than a twofold higher rate of pain in the chemotherapy arm, possibly due to the lower rate of minimally invasive surgery or higher rate of conversion to an open procedure, compared to the nivolumab/chemotherapy arm, he said.
Awaiting survival
Rates of 30- and 90-day mortality are expected to be evaluated when survival endpoints are available, according to Dr. Spicer. Beyond pCR rate, event-free survival is also a primary endpoint of the study, while overall survival is a secondary endpoint.
The study was supported by Bristol Myers Squibb. Dr. Spicer reported disclosures related to AstraZeneca, Bristol Myers Squibb Foundation, Merck, and Roche. Dr. Rusch reported research funding with Genelux and Genentech, and travel expenses from Intuitive Surgical.
FROM ASCO 2021
Schizophrenia meds a key contributor to cognitive impairment
Anticholinergic medication burden from antipsychotics, antidepressants, and other psychotropics has a cumulative effect of worsening cognitive function in patients with schizophrenia, new research indicates.
“The link between long-term use of anticholinergic medications and cognitive impairment is well-known and growing,” lead researcher Yash Joshi, MD, department of psychiatry, University of California, San Diego, said in an interview.
“While this association is relevant for everyone, it is particularly important for those living with schizophrenia, who often struggle with cognitive difficulties conferred by the illness itself,” said Dr. Joshi.
“Brain health in schizophrenia is a game of inches, and even small negative effects on cognitive functioning through anticholinergic medication burden may have large impacts on patients’ lives,” he added.
The study was published online May 14 in the American Journal of Psychiatry.
‘Striking’ results
Dr. Joshi and colleagues set out to comprehensively characterize how the cumulative anticholinergic burden from different classes of medications affect cognition in patients with schizophrenia.
They assessed medical records, including all prescribed medications, for 1,120 adults with a diagnosis of schizophrenia or schizoaffective disorder.
For each participant, prescribed medications were rated and summed using a modified anticholinergic cognitive burden (ACB) scale. Cognitive functioning was assessed by performance on domains of the Penn Computerized Neurocognitive Battery (PCNB).
The investigators found that 63% of participants had an ACB score of at least 3, which is “striking,” said Dr. Joshi, given that previous studies have shown that an ACB score of 3 in a healthy, older adult is associated with cognitive dysfunction and a 50% increased risk of developing dementia.
About one-quarter of participants had an ACB score of 6 or higher.
Yet, these high ACB scores are not hard to achieve in routine psychiatric care, the researchers note.
For example, a patient taking olanzapine daily to ease symptoms of psychosis would have an ACB score of 3; if hydroxyzine was added for anxiety or insomnia, the patient’s ACB score would rise to 6, they point out.
Lightening the load
Antipsychotics contributed more than half of the anticholinergic burden, while traditional anticholinergics, antidepressants, mood stabilizers, and benzodiazepines accounted for the remainder.
“It is easy even for well-meaning clinicians to inadvertently contribute to anticholinergic medication burden through routine and appropriate care. The unique finding here is that this burden comes from medications we don’t usually think of as typical anticholinergic agents,” senior author Gregory Light, PhD, with University of California, San Diego, said in a news release.
Anticholinergic medication burden was significantly associated with generalized impairments in cognitive functioning across all cognitive domains on the PCNB with comparable magnitude and after controlling for multiple proxies of functioning or disease severity.
Higher anticholinergic medication burden was associated with worse cognitive performance. The PCNB global cognitive averages for none, low, average, high, and very high anticholinergic burdens were, respectively (in z values), -0.51, -0.70, -0.85, -0.96, and -1.15.
The results suggest “total cumulative anticholinergic burden – rather than anticholinergic burden attributable to a specific antipsychotic or psychotropic medication class – is a key contributor to cognitive impairment in schizophrenia,” the researchers write.
“The results imply that if it is clinically safe and practical,” said Dr. Joshi.
“This may be accomplished by reducing overall polypharmacy or transitioning to equivalent medications with lower overall anticholinergic burden. While ‘traditional’ anticholinergic medications should always be scrutinized, all medications should be carefully evaluated to understand whether they contribute to cumulative anticholinergic medication burden,” he added.
Confirmatory findings
Commenting on the study for this news organization, Jessica Gannon, MD, assistant professor of psychiatry, University of Pittsburgh, said the author’s findings “aren’t surprising, but the work that they did was pretty comprehensive [and] further fleshed out some of our concerns about the impact of anticholinergics on cognitive function in patients with schizophrenia.”
“We certainly have to use some of these medications for patients, like antipsychotics that do have some anticholinergic burden associated with them. We don’t really have other options,” Dr. Gannon said.
“But certainly I think this calls us to be better stewards of medication in general. And when we prescribe for comorbid conditions, like depression and anxiety, we should be careful in our prescribing practices, try not to prescribe an anticholinergic medication, and, if they have been prescribed, to deprescribe them,” Dr. Gannon added.
The study was supported by grants from the National Institute of Mental Health; the Sidney R. Baer, Jr. Foundation; the Brain and Behavior Research Foundation; the VISN-22 Mental Illness Research, Education, and Clinical Center; and the Department of Veterans Affairs. Dr. Joshi and Dr. Gannon have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Anticholinergic medication burden from antipsychotics, antidepressants, and other psychotropics has a cumulative effect of worsening cognitive function in patients with schizophrenia, new research indicates.
“The link between long-term use of anticholinergic medications and cognitive impairment is well-known and growing,” lead researcher Yash Joshi, MD, department of psychiatry, University of California, San Diego, said in an interview.
“While this association is relevant for everyone, it is particularly important for those living with schizophrenia, who often struggle with cognitive difficulties conferred by the illness itself,” said Dr. Joshi.
“Brain health in schizophrenia is a game of inches, and even small negative effects on cognitive functioning through anticholinergic medication burden may have large impacts on patients’ lives,” he added.
The study was published online May 14 in the American Journal of Psychiatry.
‘Striking’ results
Dr. Joshi and colleagues set out to comprehensively characterize how the cumulative anticholinergic burden from different classes of medications affect cognition in patients with schizophrenia.
They assessed medical records, including all prescribed medications, for 1,120 adults with a diagnosis of schizophrenia or schizoaffective disorder.
For each participant, prescribed medications were rated and summed using a modified anticholinergic cognitive burden (ACB) scale. Cognitive functioning was assessed by performance on domains of the Penn Computerized Neurocognitive Battery (PCNB).
The investigators found that 63% of participants had an ACB score of at least 3, which is “striking,” said Dr. Joshi, given that previous studies have shown that an ACB score of 3 in a healthy, older adult is associated with cognitive dysfunction and a 50% increased risk of developing dementia.
About one-quarter of participants had an ACB score of 6 or higher.
Yet, these high ACB scores are not hard to achieve in routine psychiatric care, the researchers note.
For example, a patient taking olanzapine daily to ease symptoms of psychosis would have an ACB score of 3; if hydroxyzine was added for anxiety or insomnia, the patient’s ACB score would rise to 6, they point out.
Lightening the load
Antipsychotics contributed more than half of the anticholinergic burden, while traditional anticholinergics, antidepressants, mood stabilizers, and benzodiazepines accounted for the remainder.
“It is easy even for well-meaning clinicians to inadvertently contribute to anticholinergic medication burden through routine and appropriate care. The unique finding here is that this burden comes from medications we don’t usually think of as typical anticholinergic agents,” senior author Gregory Light, PhD, with University of California, San Diego, said in a news release.
Anticholinergic medication burden was significantly associated with generalized impairments in cognitive functioning across all cognitive domains on the PCNB with comparable magnitude and after controlling for multiple proxies of functioning or disease severity.
Higher anticholinergic medication burden was associated with worse cognitive performance. The PCNB global cognitive averages for none, low, average, high, and very high anticholinergic burdens were, respectively (in z values), -0.51, -0.70, -0.85, -0.96, and -1.15.
The results suggest “total cumulative anticholinergic burden – rather than anticholinergic burden attributable to a specific antipsychotic or psychotropic medication class – is a key contributor to cognitive impairment in schizophrenia,” the researchers write.
“The results imply that if it is clinically safe and practical,” said Dr. Joshi.
“This may be accomplished by reducing overall polypharmacy or transitioning to equivalent medications with lower overall anticholinergic burden. While ‘traditional’ anticholinergic medications should always be scrutinized, all medications should be carefully evaluated to understand whether they contribute to cumulative anticholinergic medication burden,” he added.
Confirmatory findings
Commenting on the study for this news organization, Jessica Gannon, MD, assistant professor of psychiatry, University of Pittsburgh, said the author’s findings “aren’t surprising, but the work that they did was pretty comprehensive [and] further fleshed out some of our concerns about the impact of anticholinergics on cognitive function in patients with schizophrenia.”
“We certainly have to use some of these medications for patients, like antipsychotics that do have some anticholinergic burden associated with them. We don’t really have other options,” Dr. Gannon said.
“But certainly I think this calls us to be better stewards of medication in general. And when we prescribe for comorbid conditions, like depression and anxiety, we should be careful in our prescribing practices, try not to prescribe an anticholinergic medication, and, if they have been prescribed, to deprescribe them,” Dr. Gannon added.
The study was supported by grants from the National Institute of Mental Health; the Sidney R. Baer, Jr. Foundation; the Brain and Behavior Research Foundation; the VISN-22 Mental Illness Research, Education, and Clinical Center; and the Department of Veterans Affairs. Dr. Joshi and Dr. Gannon have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Anticholinergic medication burden from antipsychotics, antidepressants, and other psychotropics has a cumulative effect of worsening cognitive function in patients with schizophrenia, new research indicates.
“The link between long-term use of anticholinergic medications and cognitive impairment is well-known and growing,” lead researcher Yash Joshi, MD, department of psychiatry, University of California, San Diego, said in an interview.
“While this association is relevant for everyone, it is particularly important for those living with schizophrenia, who often struggle with cognitive difficulties conferred by the illness itself,” said Dr. Joshi.
“Brain health in schizophrenia is a game of inches, and even small negative effects on cognitive functioning through anticholinergic medication burden may have large impacts on patients’ lives,” he added.
The study was published online May 14 in the American Journal of Psychiatry.
‘Striking’ results
Dr. Joshi and colleagues set out to comprehensively characterize how the cumulative anticholinergic burden from different classes of medications affect cognition in patients with schizophrenia.
They assessed medical records, including all prescribed medications, for 1,120 adults with a diagnosis of schizophrenia or schizoaffective disorder.
For each participant, prescribed medications were rated and summed using a modified anticholinergic cognitive burden (ACB) scale. Cognitive functioning was assessed by performance on domains of the Penn Computerized Neurocognitive Battery (PCNB).
The investigators found that 63% of participants had an ACB score of at least 3, which is “striking,” said Dr. Joshi, given that previous studies have shown that an ACB score of 3 in a healthy, older adult is associated with cognitive dysfunction and a 50% increased risk of developing dementia.
About one-quarter of participants had an ACB score of 6 or higher.
Yet, these high ACB scores are not hard to achieve in routine psychiatric care, the researchers note.
For example, a patient taking olanzapine daily to ease symptoms of psychosis would have an ACB score of 3; if hydroxyzine was added for anxiety or insomnia, the patient’s ACB score would rise to 6, they point out.
Lightening the load
Antipsychotics contributed more than half of the anticholinergic burden, while traditional anticholinergics, antidepressants, mood stabilizers, and benzodiazepines accounted for the remainder.
“It is easy even for well-meaning clinicians to inadvertently contribute to anticholinergic medication burden through routine and appropriate care. The unique finding here is that this burden comes from medications we don’t usually think of as typical anticholinergic agents,” senior author Gregory Light, PhD, with University of California, San Diego, said in a news release.
Anticholinergic medication burden was significantly associated with generalized impairments in cognitive functioning across all cognitive domains on the PCNB with comparable magnitude and after controlling for multiple proxies of functioning or disease severity.
Higher anticholinergic medication burden was associated with worse cognitive performance. The PCNB global cognitive averages for none, low, average, high, and very high anticholinergic burdens were, respectively (in z values), -0.51, -0.70, -0.85, -0.96, and -1.15.
The results suggest “total cumulative anticholinergic burden – rather than anticholinergic burden attributable to a specific antipsychotic or psychotropic medication class – is a key contributor to cognitive impairment in schizophrenia,” the researchers write.
“The results imply that if it is clinically safe and practical,” said Dr. Joshi.
“This may be accomplished by reducing overall polypharmacy or transitioning to equivalent medications with lower overall anticholinergic burden. While ‘traditional’ anticholinergic medications should always be scrutinized, all medications should be carefully evaluated to understand whether they contribute to cumulative anticholinergic medication burden,” he added.
Confirmatory findings
Commenting on the study for this news organization, Jessica Gannon, MD, assistant professor of psychiatry, University of Pittsburgh, said the author’s findings “aren’t surprising, but the work that they did was pretty comprehensive [and] further fleshed out some of our concerns about the impact of anticholinergics on cognitive function in patients with schizophrenia.”
“We certainly have to use some of these medications for patients, like antipsychotics that do have some anticholinergic burden associated with them. We don’t really have other options,” Dr. Gannon said.
“But certainly I think this calls us to be better stewards of medication in general. And when we prescribe for comorbid conditions, like depression and anxiety, we should be careful in our prescribing practices, try not to prescribe an anticholinergic medication, and, if they have been prescribed, to deprescribe them,” Dr. Gannon added.
The study was supported by grants from the National Institute of Mental Health; the Sidney R. Baer, Jr. Foundation; the Brain and Behavior Research Foundation; the VISN-22 Mental Illness Research, Education, and Clinical Center; and the Department of Veterans Affairs. Dr. Joshi and Dr. Gannon have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Choosing the right R-CHOP dosage for elderly patients with DLBCL
Physicians often face the choice of whether to treat elderly patients with diffuse large B-cell lymphoma (DLBCL) with a full or reduced dose intensity (DI) of R-CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone + rituximab), according to Edward J. Bataillard of the Imperial College Healthcare National Health Service Trust, London, and colleagues.
To address this issue, the researchers conducted a systematic review assessing the impact of R-CHOP DI on DLBCL survival outcomes, according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses for Protocols (PRISMA-P) guidelines. They found that greater than 80 years of age is an important cutoff for treating patients with a reduced R-CHOP dosage, according to their results, published in Blood Advances (2021;5[9]:2426-37).
Cutoff at 80 years of age
Their final review comprised 13 studies including 5,188 patients. Overall, the lower DI (intended or relative) was associated with inferior survival in seven of nine studies reporting crude survival analyses. In addition, most studies and those larger studies of higher quality showed poorer outcomes associated with reduced R-CHOP DI.
However, in subgroups of patients aged 80 years or more, survival was not consistently affected by the use of lower dosage R-CHOP, according to the researchers.
“We found evidence of improved survival with higher RDIs (up to R-CHOP-21) in those aged < 80 years, but the literature to date does not support full-dose intensity in those 80 years [or older],” they stated.
However, the researchers concluded that: “In the absence of improved options beyond R-CHOP in DLBCL over the past 20 years, prospective studies of DI are warranted, despite the recognized challenges involved.”
Two of the authors reported being previously employed by Roche. A third served as a consultant and adviser and received honoraria from Roche and other pharmaceutical companies. Several authors reported disclosures related to multiple other pharmaceutical companies.
Physicians often face the choice of whether to treat elderly patients with diffuse large B-cell lymphoma (DLBCL) with a full or reduced dose intensity (DI) of R-CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone + rituximab), according to Edward J. Bataillard of the Imperial College Healthcare National Health Service Trust, London, and colleagues.
To address this issue, the researchers conducted a systematic review assessing the impact of R-CHOP DI on DLBCL survival outcomes, according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses for Protocols (PRISMA-P) guidelines. They found that greater than 80 years of age is an important cutoff for treating patients with a reduced R-CHOP dosage, according to their results, published in Blood Advances (2021;5[9]:2426-37).
Cutoff at 80 years of age
Their final review comprised 13 studies including 5,188 patients. Overall, the lower DI (intended or relative) was associated with inferior survival in seven of nine studies reporting crude survival analyses. In addition, most studies and those larger studies of higher quality showed poorer outcomes associated with reduced R-CHOP DI.
However, in subgroups of patients aged 80 years or more, survival was not consistently affected by the use of lower dosage R-CHOP, according to the researchers.
“We found evidence of improved survival with higher RDIs (up to R-CHOP-21) in those aged < 80 years, but the literature to date does not support full-dose intensity in those 80 years [or older],” they stated.
However, the researchers concluded that: “In the absence of improved options beyond R-CHOP in DLBCL over the past 20 years, prospective studies of DI are warranted, despite the recognized challenges involved.”
Two of the authors reported being previously employed by Roche. A third served as a consultant and adviser and received honoraria from Roche and other pharmaceutical companies. Several authors reported disclosures related to multiple other pharmaceutical companies.
Physicians often face the choice of whether to treat elderly patients with diffuse large B-cell lymphoma (DLBCL) with a full or reduced dose intensity (DI) of R-CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone + rituximab), according to Edward J. Bataillard of the Imperial College Healthcare National Health Service Trust, London, and colleagues.
To address this issue, the researchers conducted a systematic review assessing the impact of R-CHOP DI on DLBCL survival outcomes, according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses for Protocols (PRISMA-P) guidelines. They found that greater than 80 years of age is an important cutoff for treating patients with a reduced R-CHOP dosage, according to their results, published in Blood Advances (2021;5[9]:2426-37).
Cutoff at 80 years of age
Their final review comprised 13 studies including 5,188 patients. Overall, the lower DI (intended or relative) was associated with inferior survival in seven of nine studies reporting crude survival analyses. In addition, most studies and those larger studies of higher quality showed poorer outcomes associated with reduced R-CHOP DI.
However, in subgroups of patients aged 80 years or more, survival was not consistently affected by the use of lower dosage R-CHOP, according to the researchers.
“We found evidence of improved survival with higher RDIs (up to R-CHOP-21) in those aged < 80 years, but the literature to date does not support full-dose intensity in those 80 years [or older],” they stated.
However, the researchers concluded that: “In the absence of improved options beyond R-CHOP in DLBCL over the past 20 years, prospective studies of DI are warranted, despite the recognized challenges involved.”
Two of the authors reported being previously employed by Roche. A third served as a consultant and adviser and received honoraria from Roche and other pharmaceutical companies. Several authors reported disclosures related to multiple other pharmaceutical companies.
FROM BLOOD ADVANCES
‘Remarkable’ response to diabetes drug in resistant bipolar depression
Treating insulin resistance may improve treatment-resistant bipolar depression, early research suggests.
In a randomized, placebo-controlled trial, treatment with the diabetes drug metformin reversed insulin resistance in 50% of patients, and this reversal was associated with significant improvement of depressive symptoms. One patient randomly assigned to placebo also achieved a reversal of insulin resistance and improved depressive symptoms.
“The study needs replication, but this early clinical trial suggests that the mitigation of insulin resistance by metformin significantly improves depressive symptoms in a significant percentage of treatment resistant bipolar patients,” presenting author Jessica M. Gannon, MD, University of Pittsburgh Medical Center (UPMC), said in an interview.
“It looks like in treatment-resistant bipolar depression, treating insulin resistance is a way to get people well again, to get out of their depression,” principal investigator Cynthia Calkin, MD, Dalhousie University, Halifax, N.S., added.
The findings were presented at the virtual American Society of Clinical Psychopharmacology 2021 Annual Meeting.
Chronic inflammation
The study was a joint effort by UPMC and Dalhousie University and was sponsored by the Stanley Medical Research Institute.
Patients with bipolar disorder (BD) who are obese tend to have more serious illness, with a more chronic course, more rapid cycling, and more morbidity. These patients also fail to respond to lithium, Dr. Calkin said.
“Untreated hyperinsulinemia could be contributing to a state of chronic inflammation and be involved in disease progression. So the question for me was, if we treat this insulin resistance, would patients get better?” she said.
Dr. Calkin said investigators used metformin because it is already used by psychiatrists for weight management in patients on antipsychotics.
“I wanted to test the drug that would work to reverse insulin resistance and that psychiatrists would be comfortable prescribing,” she said.
The 26-week study randomly assigned 20 patients to receive metformin and 25 patients to placebo.
All participants were 18 years and older, had a diagnosis of BD I or II, and had nonremitting BD defined by moderate depressive symptoms as measured on the Montgomery-Asberg Depression Rating Scale (MADRS) score of 15 or greater, despite being on optimal, guideline-compatible treatment.
All patients were stable, were on optimal doses of mood-stabilizing medications for at least 4 weeks prior to study entry, and had insulin resistance as defined by a Homeostatic Model Assessment for Insulin Resistance (HOMA-IR) ≥1.8.
Characteristics were similar between the two groups, including baseline MADRS scores, body mass index, fasting glucose and insulin serum levels.
Patients were titrated up to 2,000 mg of metformin, which was the full dose, over 2 weeks and then maintained on treatment for a further 24 weeks.
Highly resistant population
The study’s primary outcome measure was change in MADRS score, with a response defined as a 30% reduction in MADRS from baseline.
By week 14, 10 metformin-treated patients (50%) and one patient in the placebo group (4%) no longer met insulin resistance criteria.
“It was a bit of a surprise to me that 50% of patients converted to being insulin sensitive again. When you use metformin to treat diabetes, people respond to it at more than a 50% rate, so I was expecting more people to respond,” Dr. Calkin said.
Nevertheless, the 11 patients who did respond and reversed insulin resistance achieved greater reduction in MADRS scores compared with nonconverters.
“Those who reversed their insulin resistance showed a remarkable resolution in their depressive symptoms. The reduction in MADRS scores began at week six, and were maintained through to the end of the study, and the Cohen’s d effect size for MADRS depression scores for converters was 0.52 at week 14 and 0.55 at week 26,” Dr. Calkin said.
“They were moderately to severely depressed going in, and at the end of the study, they had mild residual depressive symptoms, or they were completely well. These were very treatment-resistant patients.”
“All had failed, on average, eight or nine trials in their lifetime. When they came to us, nothing else would work. That’s one of the remarkable things about our results, just how well they responded when they had not responded to any other psychotropic medications. This approach may be very helpful for some patients,” Dr. Calkin said.
A holistic approach
Commenting on the study, Michael E. Thase, MD, professor of psychiatry, University of Pennsylvania, Philadelphia, said the findings need to be replicated but provide further support for the broader strategy of taking a holistic approach to the care of patients with difficult-to-treat mood disorders.
“Approximately one-half of people with treatment-resistant bipolar depression showed evidence of glucose resistance, and that adjunctive treatment with metformin, a medication that enhances insulin sensitivity, was moderately effective in normalizing glucose metabolism, with about a 50% response rate. Among those who experienced improved glucose regulation, there was a significant reduction in depressive symptoms,” he noted.
The study was funded by the Stanley Medical Research Institute (SMRI). Dr. Calkin and Dr. Thase have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Treating insulin resistance may improve treatment-resistant bipolar depression, early research suggests.
In a randomized, placebo-controlled trial, treatment with the diabetes drug metformin reversed insulin resistance in 50% of patients, and this reversal was associated with significant improvement of depressive symptoms. One patient randomly assigned to placebo also achieved a reversal of insulin resistance and improved depressive symptoms.
“The study needs replication, but this early clinical trial suggests that the mitigation of insulin resistance by metformin significantly improves depressive symptoms in a significant percentage of treatment resistant bipolar patients,” presenting author Jessica M. Gannon, MD, University of Pittsburgh Medical Center (UPMC), said in an interview.
“It looks like in treatment-resistant bipolar depression, treating insulin resistance is a way to get people well again, to get out of their depression,” principal investigator Cynthia Calkin, MD, Dalhousie University, Halifax, N.S., added.
The findings were presented at the virtual American Society of Clinical Psychopharmacology 2021 Annual Meeting.
Chronic inflammation
The study was a joint effort by UPMC and Dalhousie University and was sponsored by the Stanley Medical Research Institute.
Patients with bipolar disorder (BD) who are obese tend to have more serious illness, with a more chronic course, more rapid cycling, and more morbidity. These patients also fail to respond to lithium, Dr. Calkin said.
“Untreated hyperinsulinemia could be contributing to a state of chronic inflammation and be involved in disease progression. So the question for me was, if we treat this insulin resistance, would patients get better?” she said.
Dr. Calkin said investigators used metformin because it is already used by psychiatrists for weight management in patients on antipsychotics.
“I wanted to test the drug that would work to reverse insulin resistance and that psychiatrists would be comfortable prescribing,” she said.
The 26-week study randomly assigned 20 patients to receive metformin and 25 patients to placebo.
All participants were 18 years and older, had a diagnosis of BD I or II, and had nonremitting BD defined by moderate depressive symptoms as measured on the Montgomery-Asberg Depression Rating Scale (MADRS) score of 15 or greater, despite being on optimal, guideline-compatible treatment.
All patients were stable, were on optimal doses of mood-stabilizing medications for at least 4 weeks prior to study entry, and had insulin resistance as defined by a Homeostatic Model Assessment for Insulin Resistance (HOMA-IR) ≥1.8.
Characteristics were similar between the two groups, including baseline MADRS scores, body mass index, fasting glucose and insulin serum levels.
Patients were titrated up to 2,000 mg of metformin, which was the full dose, over 2 weeks and then maintained on treatment for a further 24 weeks.
Highly resistant population
The study’s primary outcome measure was change in MADRS score, with a response defined as a 30% reduction in MADRS from baseline.
By week 14, 10 metformin-treated patients (50%) and one patient in the placebo group (4%) no longer met insulin resistance criteria.
“It was a bit of a surprise to me that 50% of patients converted to being insulin sensitive again. When you use metformin to treat diabetes, people respond to it at more than a 50% rate, so I was expecting more people to respond,” Dr. Calkin said.
Nevertheless, the 11 patients who did respond and reversed insulin resistance achieved greater reduction in MADRS scores compared with nonconverters.
“Those who reversed their insulin resistance showed a remarkable resolution in their depressive symptoms. The reduction in MADRS scores began at week six, and were maintained through to the end of the study, and the Cohen’s d effect size for MADRS depression scores for converters was 0.52 at week 14 and 0.55 at week 26,” Dr. Calkin said.
“They were moderately to severely depressed going in, and at the end of the study, they had mild residual depressive symptoms, or they were completely well. These were very treatment-resistant patients.”
“All had failed, on average, eight or nine trials in their lifetime. When they came to us, nothing else would work. That’s one of the remarkable things about our results, just how well they responded when they had not responded to any other psychotropic medications. This approach may be very helpful for some patients,” Dr. Calkin said.
A holistic approach
Commenting on the study, Michael E. Thase, MD, professor of psychiatry, University of Pennsylvania, Philadelphia, said the findings need to be replicated but provide further support for the broader strategy of taking a holistic approach to the care of patients with difficult-to-treat mood disorders.
“Approximately one-half of people with treatment-resistant bipolar depression showed evidence of glucose resistance, and that adjunctive treatment with metformin, a medication that enhances insulin sensitivity, was moderately effective in normalizing glucose metabolism, with about a 50% response rate. Among those who experienced improved glucose regulation, there was a significant reduction in depressive symptoms,” he noted.
The study was funded by the Stanley Medical Research Institute (SMRI). Dr. Calkin and Dr. Thase have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Treating insulin resistance may improve treatment-resistant bipolar depression, early research suggests.
In a randomized, placebo-controlled trial, treatment with the diabetes drug metformin reversed insulin resistance in 50% of patients, and this reversal was associated with significant improvement of depressive symptoms. One patient randomly assigned to placebo also achieved a reversal of insulin resistance and improved depressive symptoms.
“The study needs replication, but this early clinical trial suggests that the mitigation of insulin resistance by metformin significantly improves depressive symptoms in a significant percentage of treatment resistant bipolar patients,” presenting author Jessica M. Gannon, MD, University of Pittsburgh Medical Center (UPMC), said in an interview.
“It looks like in treatment-resistant bipolar depression, treating insulin resistance is a way to get people well again, to get out of their depression,” principal investigator Cynthia Calkin, MD, Dalhousie University, Halifax, N.S., added.
The findings were presented at the virtual American Society of Clinical Psychopharmacology 2021 Annual Meeting.
Chronic inflammation
The study was a joint effort by UPMC and Dalhousie University and was sponsored by the Stanley Medical Research Institute.
Patients with bipolar disorder (BD) who are obese tend to have more serious illness, with a more chronic course, more rapid cycling, and more morbidity. These patients also fail to respond to lithium, Dr. Calkin said.
“Untreated hyperinsulinemia could be contributing to a state of chronic inflammation and be involved in disease progression. So the question for me was, if we treat this insulin resistance, would patients get better?” she said.
Dr. Calkin said investigators used metformin because it is already used by psychiatrists for weight management in patients on antipsychotics.
“I wanted to test the drug that would work to reverse insulin resistance and that psychiatrists would be comfortable prescribing,” she said.
The 26-week study randomly assigned 20 patients to receive metformin and 25 patients to placebo.
All participants were 18 years and older, had a diagnosis of BD I or II, and had nonremitting BD defined by moderate depressive symptoms as measured on the Montgomery-Asberg Depression Rating Scale (MADRS) score of 15 or greater, despite being on optimal, guideline-compatible treatment.
All patients were stable, were on optimal doses of mood-stabilizing medications for at least 4 weeks prior to study entry, and had insulin resistance as defined by a Homeostatic Model Assessment for Insulin Resistance (HOMA-IR) ≥1.8.
Characteristics were similar between the two groups, including baseline MADRS scores, body mass index, fasting glucose and insulin serum levels.
Patients were titrated up to 2,000 mg of metformin, which was the full dose, over 2 weeks and then maintained on treatment for a further 24 weeks.
Highly resistant population
The study’s primary outcome measure was change in MADRS score, with a response defined as a 30% reduction in MADRS from baseline.
By week 14, 10 metformin-treated patients (50%) and one patient in the placebo group (4%) no longer met insulin resistance criteria.
“It was a bit of a surprise to me that 50% of patients converted to being insulin sensitive again. When you use metformin to treat diabetes, people respond to it at more than a 50% rate, so I was expecting more people to respond,” Dr. Calkin said.
Nevertheless, the 11 patients who did respond and reversed insulin resistance achieved greater reduction in MADRS scores compared with nonconverters.
“Those who reversed their insulin resistance showed a remarkable resolution in their depressive symptoms. The reduction in MADRS scores began at week six, and were maintained through to the end of the study, and the Cohen’s d effect size for MADRS depression scores for converters was 0.52 at week 14 and 0.55 at week 26,” Dr. Calkin said.
“They were moderately to severely depressed going in, and at the end of the study, they had mild residual depressive symptoms, or they were completely well. These were very treatment-resistant patients.”
“All had failed, on average, eight or nine trials in their lifetime. When they came to us, nothing else would work. That’s one of the remarkable things about our results, just how well they responded when they had not responded to any other psychotropic medications. This approach may be very helpful for some patients,” Dr. Calkin said.
A holistic approach
Commenting on the study, Michael E. Thase, MD, professor of psychiatry, University of Pennsylvania, Philadelphia, said the findings need to be replicated but provide further support for the broader strategy of taking a holistic approach to the care of patients with difficult-to-treat mood disorders.
“Approximately one-half of people with treatment-resistant bipolar depression showed evidence of glucose resistance, and that adjunctive treatment with metformin, a medication that enhances insulin sensitivity, was moderately effective in normalizing glucose metabolism, with about a 50% response rate. Among those who experienced improved glucose regulation, there was a significant reduction in depressive symptoms,” he noted.
The study was funded by the Stanley Medical Research Institute (SMRI). Dr. Calkin and Dr. Thase have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FDA approves controversial Alzheimer’s drug aducanumab (Aduhelm)
In November, the Peripheral and Central Nervous System Drugs Advisory Committee voted eight to one against approving the drug because, based on clinical trial results, evidence of efficacy was not strong enough. Two other members said they were uncertain on the issue of efficacy.
In a company release Michel Vounatsos, Biogen’s Chief Executive Officer, said, “this historic moment is the culmination of more than a decade of groundbreaking research in the complex field of Alzheimer’s disease. We believe this first-in-class medicine will transform the treatment of people living with Alzheimer’s disease and spark continuous innovation in the years to come.
Rocky road
The road to approval has been extremely rocky for aducanumab, an anti-amyloid-beta human monoclonal antibody, previously known as BIIB037.
As reported by this news organization, two phase 3 trials evaluating the drug were initially scrapped in March 2019 because of interim futility analysis. At the time, Biogen released a statement saying that aducanumab was unlikely to meet primary endpoints in the ENGAGE and EMERGE randomized controlled trials.
However, in an about-face 7 months later, Biogen and Eisai announced that a new analysis showed the drug met its primary endpoint of reduction in clinical decline, including cognition and function, in the EMERGE trial.
Although ENGAGE still didn’t meet its primary endpoint, data from its new analysis “supported” the EMERGE findings, the drug companies said at the time.
However, 1 year later, a majority of the members of the FDA’s advisory panel were against the drug’s approval. Details of that decision were published online March 30 in the Journal of the American Medical Association.
As reported by this news organization, a Viewpoint written by three of the committee members notes that results from the drug’s only large positive clinical trial fell short.
“There is no persuasive evidence to support approval of aducanumab at this time,” they write.
Groups such as Public Citizen’s Health Research Group not only agree with the Viewpoint’s authors, they also criticized the FDA for its collaboration with the drug’s manufacturers on briefing documents and more.
On April 1, Health Research Group members sent a letter to the U.S. Secretary of Health and Human Services requesting the temporary suspension of the FDA’s neuroscience chief, Bill Dunn, MD, because of his role in supervising the collaboration.
Alzheimer association weighs in
The Alzheimer’s Association has been a proponent of the drug throughout its development.
Ahead of today’s news, the organization noted in a statement that a decision to approve “would be historic” because it would make aducanumab “the first drug to slow Alzheimer’s disease” and would mark the beginning of a new future for AD treatments.
“The Alzheimer’s Association urgently supports FDA approval of the treatment based on clinical trial results that showed a 22% reduction in cognitive and function decline — something that could make a meaningful difference” for patients with AD, it said.
Kristen Clifford, chief program officer for the Alzheimer’s Association, said in an interview at the time that approval would be considered a “victory” for patients with AD and for the field overall.
“For individuals who would potentially be eligible for the treatment, this drug could mean more quality time. Slowing decline, particularly in early diagnosis, could add weeks or months or maybe even years of active life,” Clifford said.
“If approved, this would really be a landmark moment. And it could provide hope for those living with Alzheimer’s and their families,” she added.
Clifford noted that approval of this type of drug would also underscore the importance of early detection for AD. “This treatment would encourage earlier diagnosis of the disease,” she said.
In a new statement released just after approval for aducanumab was announced, the organization said that today’s news is a win-win for all patients with AD and their families.
A version of this article first appeared on Medscape.com.
In November, the Peripheral and Central Nervous System Drugs Advisory Committee voted eight to one against approving the drug because, based on clinical trial results, evidence of efficacy was not strong enough. Two other members said they were uncertain on the issue of efficacy.
In a company release Michel Vounatsos, Biogen’s Chief Executive Officer, said, “this historic moment is the culmination of more than a decade of groundbreaking research in the complex field of Alzheimer’s disease. We believe this first-in-class medicine will transform the treatment of people living with Alzheimer’s disease and spark continuous innovation in the years to come.
Rocky road
The road to approval has been extremely rocky for aducanumab, an anti-amyloid-beta human monoclonal antibody, previously known as BIIB037.
As reported by this news organization, two phase 3 trials evaluating the drug were initially scrapped in March 2019 because of interim futility analysis. At the time, Biogen released a statement saying that aducanumab was unlikely to meet primary endpoints in the ENGAGE and EMERGE randomized controlled trials.
However, in an about-face 7 months later, Biogen and Eisai announced that a new analysis showed the drug met its primary endpoint of reduction in clinical decline, including cognition and function, in the EMERGE trial.
Although ENGAGE still didn’t meet its primary endpoint, data from its new analysis “supported” the EMERGE findings, the drug companies said at the time.
However, 1 year later, a majority of the members of the FDA’s advisory panel were against the drug’s approval. Details of that decision were published online March 30 in the Journal of the American Medical Association.
As reported by this news organization, a Viewpoint written by three of the committee members notes that results from the drug’s only large positive clinical trial fell short.
“There is no persuasive evidence to support approval of aducanumab at this time,” they write.
Groups such as Public Citizen’s Health Research Group not only agree with the Viewpoint’s authors, they also criticized the FDA for its collaboration with the drug’s manufacturers on briefing documents and more.
On April 1, Health Research Group members sent a letter to the U.S. Secretary of Health and Human Services requesting the temporary suspension of the FDA’s neuroscience chief, Bill Dunn, MD, because of his role in supervising the collaboration.
Alzheimer association weighs in
The Alzheimer’s Association has been a proponent of the drug throughout its development.
Ahead of today’s news, the organization noted in a statement that a decision to approve “would be historic” because it would make aducanumab “the first drug to slow Alzheimer’s disease” and would mark the beginning of a new future for AD treatments.
“The Alzheimer’s Association urgently supports FDA approval of the treatment based on clinical trial results that showed a 22% reduction in cognitive and function decline — something that could make a meaningful difference” for patients with AD, it said.
Kristen Clifford, chief program officer for the Alzheimer’s Association, said in an interview at the time that approval would be considered a “victory” for patients with AD and for the field overall.
“For individuals who would potentially be eligible for the treatment, this drug could mean more quality time. Slowing decline, particularly in early diagnosis, could add weeks or months or maybe even years of active life,” Clifford said.
“If approved, this would really be a landmark moment. And it could provide hope for those living with Alzheimer’s and their families,” she added.
Clifford noted that approval of this type of drug would also underscore the importance of early detection for AD. “This treatment would encourage earlier diagnosis of the disease,” she said.
In a new statement released just after approval for aducanumab was announced, the organization said that today’s news is a win-win for all patients with AD and their families.
A version of this article first appeared on Medscape.com.
In November, the Peripheral and Central Nervous System Drugs Advisory Committee voted eight to one against approving the drug because, based on clinical trial results, evidence of efficacy was not strong enough. Two other members said they were uncertain on the issue of efficacy.
In a company release Michel Vounatsos, Biogen’s Chief Executive Officer, said, “this historic moment is the culmination of more than a decade of groundbreaking research in the complex field of Alzheimer’s disease. We believe this first-in-class medicine will transform the treatment of people living with Alzheimer’s disease and spark continuous innovation in the years to come.
Rocky road
The road to approval has been extremely rocky for aducanumab, an anti-amyloid-beta human monoclonal antibody, previously known as BIIB037.
As reported by this news organization, two phase 3 trials evaluating the drug were initially scrapped in March 2019 because of interim futility analysis. At the time, Biogen released a statement saying that aducanumab was unlikely to meet primary endpoints in the ENGAGE and EMERGE randomized controlled trials.
However, in an about-face 7 months later, Biogen and Eisai announced that a new analysis showed the drug met its primary endpoint of reduction in clinical decline, including cognition and function, in the EMERGE trial.
Although ENGAGE still didn’t meet its primary endpoint, data from its new analysis “supported” the EMERGE findings, the drug companies said at the time.
However, 1 year later, a majority of the members of the FDA’s advisory panel were against the drug’s approval. Details of that decision were published online March 30 in the Journal of the American Medical Association.
As reported by this news organization, a Viewpoint written by three of the committee members notes that results from the drug’s only large positive clinical trial fell short.
“There is no persuasive evidence to support approval of aducanumab at this time,” they write.
Groups such as Public Citizen’s Health Research Group not only agree with the Viewpoint’s authors, they also criticized the FDA for its collaboration with the drug’s manufacturers on briefing documents and more.
On April 1, Health Research Group members sent a letter to the U.S. Secretary of Health and Human Services requesting the temporary suspension of the FDA’s neuroscience chief, Bill Dunn, MD, because of his role in supervising the collaboration.
Alzheimer association weighs in
The Alzheimer’s Association has been a proponent of the drug throughout its development.
Ahead of today’s news, the organization noted in a statement that a decision to approve “would be historic” because it would make aducanumab “the first drug to slow Alzheimer’s disease” and would mark the beginning of a new future for AD treatments.
“The Alzheimer’s Association urgently supports FDA approval of the treatment based on clinical trial results that showed a 22% reduction in cognitive and function decline — something that could make a meaningful difference” for patients with AD, it said.
Kristen Clifford, chief program officer for the Alzheimer’s Association, said in an interview at the time that approval would be considered a “victory” for patients with AD and for the field overall.
“For individuals who would potentially be eligible for the treatment, this drug could mean more quality time. Slowing decline, particularly in early diagnosis, could add weeks or months or maybe even years of active life,” Clifford said.
“If approved, this would really be a landmark moment. And it could provide hope for those living with Alzheimer’s and their families,” she added.
Clifford noted that approval of this type of drug would also underscore the importance of early detection for AD. “This treatment would encourage earlier diagnosis of the disease,” she said.
In a new statement released just after approval for aducanumab was announced, the organization said that today’s news is a win-win for all patients with AD and their families.
A version of this article first appeared on Medscape.com.
Pregnancy effect on chemotherapy does not affect maternal breast cancer outcomes
Reassuring news for women who receive a diagnosis of breast cancer during pregnancy: Pregnancy-induced alterations in the pharmacokinetics of chemotherapy do not appear to compromise outcomes for the mother.
That’s according to investigators who reviewed registry data on 662 pregnant women and 2,081 nonpregnant women with a diagnosis of breast cancer. After a median follow-up of 66 months, there were no significant differences in either disease-free survival (DFS) or overall survival (OS), and women who received more than 60% of their chemotherapy doses during pregnancy had survival comparable to that of nonpregnant women, reported Frédéric Amant, MD, PhD, of University Hospitals Leuven (Belgium).
“These results support initiation of chemotherapy for breast cancer during pregnancy where indicated for oncological reasons,” they reported in a poster discussion session at the American Society of Clinical Oncology annual meeting. (Abstract 515).
Although in general a diagnosis of breast cancer during pregnancy does not appear to affect the mother’s prognosis when standard therapy is used, “caution is warranted as gestational changes in pharmacokinetics with respect to the distribution, metabolism, and excretion of drugs may lead to reduced chemotherapy concentration in pregnant patients,” the authors wrote.
To get a better picture of the prognosis for women diagnosed with breast cancer during pregnancy, the investigators created a cohort of patients from two multicenter registries: the International Network of Cancer, Infertility, and Pregnancy and the German Breast Group. Both registries collect data retrospectively and prospectively,
They used propensity scoring to smooth out differences in the baseline characteristics of pregnant women and nonpregnant controls.
The median age at diagnosis was 34 year for pregnant women, and 38 years for controls. Pregnant women were more likely than were controls to have stage II disease (60.1% vs. 56, 1%, P = .035), grade 3 tumors (74% vs. 62.2%, P < .001), hormone receptor–negative breast tumors (48.4% vs. 30%), and triple-negative breast cancer (38.9% vs. 26.9%, P < .001).
In Cox proportional hazard regression analysis controlling for age, stage, grade, hormone receptor status, HER2 status and histology, there were no significant differences between pregnant women and controls in either DFS (hazard ratio [HR] 1.02, P = .83) or OS (HR 1.08, P = .57).
As noted before, a subgroup analysis of 339 women who received more than 60% of their assigned chemotherapy doses during pregnancy also showed that survival was not significantly different from that of nonpregnant women (HR for DFS 0,71, P = .13; HR for OS 0.85, P = .39).
Termination does not benefit the mother
“Thanks to the important work of Dr. Amant in the INCIP [International Network on Cancer, Infertility, and Pregnancy] network and others around the world, we now have sufficient data to know that it’s safe to treat breast cancer during pregnancy, and that the prognosis of breast cancer during pregnancy is comparable to nonpregnant controls if we adjust for certain characteristics such as age and others,” said Fatima Cardoso, MD, of Champalimaud Clinical Center in Lisbon, Portugal, the invited discussant.
“With this and other studies, we can come to the conclusion that pregnancy-induced alterations in the chemotherapy concentration due to altered pharmacokinetics does not seem to affect maternal prognosis, and therefore we should initiate treatment of breast cancer during wherever it’s indicated for oncological reasons, knowing that you can only use chemotherapy during the second or third trimester,” she said.
Dr. Cardoso emphasized that breast cancer during pregnancy is a rare situation requiring that treatment be given in a specialized center by an experienced multidisciplinary team, and that interrupting the pregnancy does not improve the mother’s prognosis.
“We have to spread the word to all health professionals who come across these women to stop advising them to immediately terminate pregnancy. For the children, the most important take-home message is avoid prematurely delivery,” she said.
Treatment for women with a diagnosis of breast cancer during pregnancy should be similar to that for nonpregnant women, with the exception of endocrine therapy and anti-HER2 agents, which should be withheld until after delivery, she added.
The study was supported by the European Research Council, Research Foundation Flanders, and Kom op tegen kanker (Stand Up to Cancer). Dr. Amant disclosed a consulting or advisory role for AstraZeneca and Clovis Oncology. Dr. Cardoso disclosed consulting or advisory roles and travel support from multiple companies.
Reassuring news for women who receive a diagnosis of breast cancer during pregnancy: Pregnancy-induced alterations in the pharmacokinetics of chemotherapy do not appear to compromise outcomes for the mother.
That’s according to investigators who reviewed registry data on 662 pregnant women and 2,081 nonpregnant women with a diagnosis of breast cancer. After a median follow-up of 66 months, there were no significant differences in either disease-free survival (DFS) or overall survival (OS), and women who received more than 60% of their chemotherapy doses during pregnancy had survival comparable to that of nonpregnant women, reported Frédéric Amant, MD, PhD, of University Hospitals Leuven (Belgium).
“These results support initiation of chemotherapy for breast cancer during pregnancy where indicated for oncological reasons,” they reported in a poster discussion session at the American Society of Clinical Oncology annual meeting. (Abstract 515).
Although in general a diagnosis of breast cancer during pregnancy does not appear to affect the mother’s prognosis when standard therapy is used, “caution is warranted as gestational changes in pharmacokinetics with respect to the distribution, metabolism, and excretion of drugs may lead to reduced chemotherapy concentration in pregnant patients,” the authors wrote.
To get a better picture of the prognosis for women diagnosed with breast cancer during pregnancy, the investigators created a cohort of patients from two multicenter registries: the International Network of Cancer, Infertility, and Pregnancy and the German Breast Group. Both registries collect data retrospectively and prospectively,
They used propensity scoring to smooth out differences in the baseline characteristics of pregnant women and nonpregnant controls.
The median age at diagnosis was 34 year for pregnant women, and 38 years for controls. Pregnant women were more likely than were controls to have stage II disease (60.1% vs. 56, 1%, P = .035), grade 3 tumors (74% vs. 62.2%, P < .001), hormone receptor–negative breast tumors (48.4% vs. 30%), and triple-negative breast cancer (38.9% vs. 26.9%, P < .001).
In Cox proportional hazard regression analysis controlling for age, stage, grade, hormone receptor status, HER2 status and histology, there were no significant differences between pregnant women and controls in either DFS (hazard ratio [HR] 1.02, P = .83) or OS (HR 1.08, P = .57).
As noted before, a subgroup analysis of 339 women who received more than 60% of their assigned chemotherapy doses during pregnancy also showed that survival was not significantly different from that of nonpregnant women (HR for DFS 0,71, P = .13; HR for OS 0.85, P = .39).
Termination does not benefit the mother
“Thanks to the important work of Dr. Amant in the INCIP [International Network on Cancer, Infertility, and Pregnancy] network and others around the world, we now have sufficient data to know that it’s safe to treat breast cancer during pregnancy, and that the prognosis of breast cancer during pregnancy is comparable to nonpregnant controls if we adjust for certain characteristics such as age and others,” said Fatima Cardoso, MD, of Champalimaud Clinical Center in Lisbon, Portugal, the invited discussant.
“With this and other studies, we can come to the conclusion that pregnancy-induced alterations in the chemotherapy concentration due to altered pharmacokinetics does not seem to affect maternal prognosis, and therefore we should initiate treatment of breast cancer during wherever it’s indicated for oncological reasons, knowing that you can only use chemotherapy during the second or third trimester,” she said.
Dr. Cardoso emphasized that breast cancer during pregnancy is a rare situation requiring that treatment be given in a specialized center by an experienced multidisciplinary team, and that interrupting the pregnancy does not improve the mother’s prognosis.
“We have to spread the word to all health professionals who come across these women to stop advising them to immediately terminate pregnancy. For the children, the most important take-home message is avoid prematurely delivery,” she said.
Treatment for women with a diagnosis of breast cancer during pregnancy should be similar to that for nonpregnant women, with the exception of endocrine therapy and anti-HER2 agents, which should be withheld until after delivery, she added.
The study was supported by the European Research Council, Research Foundation Flanders, and Kom op tegen kanker (Stand Up to Cancer). Dr. Amant disclosed a consulting or advisory role for AstraZeneca and Clovis Oncology. Dr. Cardoso disclosed consulting or advisory roles and travel support from multiple companies.
Reassuring news for women who receive a diagnosis of breast cancer during pregnancy: Pregnancy-induced alterations in the pharmacokinetics of chemotherapy do not appear to compromise outcomes for the mother.
That’s according to investigators who reviewed registry data on 662 pregnant women and 2,081 nonpregnant women with a diagnosis of breast cancer. After a median follow-up of 66 months, there were no significant differences in either disease-free survival (DFS) or overall survival (OS), and women who received more than 60% of their chemotherapy doses during pregnancy had survival comparable to that of nonpregnant women, reported Frédéric Amant, MD, PhD, of University Hospitals Leuven (Belgium).
“These results support initiation of chemotherapy for breast cancer during pregnancy where indicated for oncological reasons,” they reported in a poster discussion session at the American Society of Clinical Oncology annual meeting. (Abstract 515).
Although in general a diagnosis of breast cancer during pregnancy does not appear to affect the mother’s prognosis when standard therapy is used, “caution is warranted as gestational changes in pharmacokinetics with respect to the distribution, metabolism, and excretion of drugs may lead to reduced chemotherapy concentration in pregnant patients,” the authors wrote.
To get a better picture of the prognosis for women diagnosed with breast cancer during pregnancy, the investigators created a cohort of patients from two multicenter registries: the International Network of Cancer, Infertility, and Pregnancy and the German Breast Group. Both registries collect data retrospectively and prospectively,
They used propensity scoring to smooth out differences in the baseline characteristics of pregnant women and nonpregnant controls.
The median age at diagnosis was 34 year for pregnant women, and 38 years for controls. Pregnant women were more likely than were controls to have stage II disease (60.1% vs. 56, 1%, P = .035), grade 3 tumors (74% vs. 62.2%, P < .001), hormone receptor–negative breast tumors (48.4% vs. 30%), and triple-negative breast cancer (38.9% vs. 26.9%, P < .001).
In Cox proportional hazard regression analysis controlling for age, stage, grade, hormone receptor status, HER2 status and histology, there were no significant differences between pregnant women and controls in either DFS (hazard ratio [HR] 1.02, P = .83) or OS (HR 1.08, P = .57).
As noted before, a subgroup analysis of 339 women who received more than 60% of their assigned chemotherapy doses during pregnancy also showed that survival was not significantly different from that of nonpregnant women (HR for DFS 0,71, P = .13; HR for OS 0.85, P = .39).
Termination does not benefit the mother
“Thanks to the important work of Dr. Amant in the INCIP [International Network on Cancer, Infertility, and Pregnancy] network and others around the world, we now have sufficient data to know that it’s safe to treat breast cancer during pregnancy, and that the prognosis of breast cancer during pregnancy is comparable to nonpregnant controls if we adjust for certain characteristics such as age and others,” said Fatima Cardoso, MD, of Champalimaud Clinical Center in Lisbon, Portugal, the invited discussant.
“With this and other studies, we can come to the conclusion that pregnancy-induced alterations in the chemotherapy concentration due to altered pharmacokinetics does not seem to affect maternal prognosis, and therefore we should initiate treatment of breast cancer during wherever it’s indicated for oncological reasons, knowing that you can only use chemotherapy during the second or third trimester,” she said.
Dr. Cardoso emphasized that breast cancer during pregnancy is a rare situation requiring that treatment be given in a specialized center by an experienced multidisciplinary team, and that interrupting the pregnancy does not improve the mother’s prognosis.
“We have to spread the word to all health professionals who come across these women to stop advising them to immediately terminate pregnancy. For the children, the most important take-home message is avoid prematurely delivery,” she said.
Treatment for women with a diagnosis of breast cancer during pregnancy should be similar to that for nonpregnant women, with the exception of endocrine therapy and anti-HER2 agents, which should be withheld until after delivery, she added.
The study was supported by the European Research Council, Research Foundation Flanders, and Kom op tegen kanker (Stand Up to Cancer). Dr. Amant disclosed a consulting or advisory role for AstraZeneca and Clovis Oncology. Dr. Cardoso disclosed consulting or advisory roles and travel support from multiple companies.
FROM ASCO 2021
KRAS inhibitor improved survival in phase 2 lung cancer trial
The first KRAS inhibitor approved for the treatment of lung cancer provided a clinically meaningful overall survival benefit in an updated analysis of a phase 2 study.
Treatment with sotorasib yielded a median overall survival (OS) of 12.5 months in patients with previously treated KRAS p.G12C-mutated non-small cell lung cancer (NSCLC), according to an analysis of the phase 2 CodeBreaK 100 trial data presented at the American Society of Clinical Oncology Annual Meeting.
Median progression-free survival (PFS) was 6.8 months in this update, which included a median follow-up of more than 15 months, according to investigator Ferdinandos Skoulidis, MD, PhD, assistant professor of thoracic/head and neck medical oncology at the University of Texas MD Anderson Cancer Center in Houston.
Efficacy responses
The confirmed objective response rate was 37.1%, including a 3.2% complete response rate and a median duration of response of 11.1 months, according to the report by Dr. Skoulidis.
In exploratory analyses, the benefit of sotorasib was consistent across patient subgroups, Dr. Skoulidis said in his presentation (Abstract 9003).
In particular, efficacy was observed in subgroups with co-occurring mutations in TP53, STK11, and KEAP1, which are molecular indicators of suboptimal outcomes on standard systemic treatments, according to Dr. Skoulidis.
This update on the registrational phase 2 CodeBreaK100 trial, published concurrently in the New England Journal of Medicine , came just one week after the U.S. Food and Drug Administration (FDA) granted accelerated approval to sotorasib.
Sotorasib was approved for the treatment of patients with previously treated KRAS G12C‑mutated locally advanced or metastatic NSCLC on the basis of previously reported results from CodeBreaK100.
This sotorasib indication represents a “historic milestone,” Dr. Skoulidis said in an interview.
No previously studied selective KRAS inhibitor has been approved despite scientific research efforts that stretch back nearly four decades, he explained.
“In a way, one can say that we have dealt KRAS-mutant lung cancer a knockdown blow, however, I should point out that the fight is not over,” he added.
“These clinical results will no doubt spearhead and galvanize further efforts to develop even more effective therapeutic combinations in the future, as well as identify and either forestall or overcome the eventual development of acquired resistance,” he said.
Only 1 out of 8 patients
The KRAS p.G12C mutation is present in about 13% of lung adenocarcinomas, or about one in every eight patients with nonsquamous NSCLC, Dr. Skoulidis said in the interview.
“We are estimating that this is in the region of 13,000 patients newly diagnosed every year in the U.S., and approximately 13,000 patients or so that are currently being treated in the second- or third-line setting,” he said.
The CodeBreaK100 trial included 126 patients with locally advanced or metastatic NSCLC and KRAS p.G12C mutation who had progressed on prior systemic therapies. About 43% had one prior line of treatment, while 35% had two lines, and 22% had three lines. A total of 81% had previously received both platinum-based chemotherapy and PD-1/PD-L1 axis inhibitors.
Most treatment-related adverse events in the study were grade 1-2 and generally manageable, according to Dr. Skoulidis. About 20% of patients experienced grade 3 treatment-related adverse events, which were mostly diarrhea or increases in aspartate aminotransferase and alanine aminotransferase levels. A grade 4 treatment-related adverse event, pneumonitis and dyspnea, was reported in one patient or approximately 1%.
Confirmatory trial
Although CodeBreak100 is not a randomized trial, the median OS of 12.5 months compares favorably to median OS times in the range of 7.9-10.3 months reported in randomized phase 3 clinical trials and subgroup analysis of randomized phase 3 trials of docetaxel for patients with KRAS-mutant lung adenocarcinoma, Dr. Skoulidis said in a question-and-answer session.
A confirmatory phase 3 CodeBreaK200 trial of sotorasib versus docetaxel in patients with previously treated KRAS p.G12C-mutated NSCLC is underway. That trial is evaluating PFS as a primary endpoint and OS as a secondary endpoint.
“If the same magnitude of benefit, 12.5 months median overall survival, is confirmed in the larger phase 3 clinical trial, as a clinician I would consider that beneficial for patients, compared to the standard of care,” Dr. Skoulidis said during the session.
Mature data
The updated analysis of the phase 2 CodeBreaK100 study is notable for its mature OS data, updated safety and the first molecular subgroup analyses, according to discussant Christine Marie Lovly, MD, PhD, of the division of hematology-oncology at Vanderbilt University Medical Center in Nashville.
“The objective response rate was 37.1%,” she added. “This is a little bit lower than we’re used to for targeted therapies, but remember, this is a different mutation and a very different class of drugs.”
The KRAS G12C inhibitors, several of which are under clinical development, are not tyrosine kinase inhibitors (TKIs), but rather allele-specific inhibitors that target mutant KRAS, trapping it in an inactive conformation, she explained.
Dr. Lovly referenced the exploratory analyses demonstrating efficacy in molecularly defined subgroups, calling it “interesting” that there was no difference in objective response rate between TP53 wild type and mutant tumors.
“We do have data that mutant TP53 seems to confer inferior outcomes for EGFR TKI-directed therapy in patients with EGFR-mutant lung cancer,” she said.
CodeBreaK100 was supported by Amgen, Inc. and partly by a National Institutes of Health Cancer Center Support Grant at Memorial Sloan Kettering Cancer Center.
Dr. Skoulidis reported honoraria from Bristol-Myers Squibb; research funding from AIMM Therapeutics and Amgen; and travel, accommodations, or expenses from Tango Therapeutics. Dr. Lovly reported disclosures related to Amgen, AstraZeneca, Genentech, Novartis, and Pfizer, among others.
The first KRAS inhibitor approved for the treatment of lung cancer provided a clinically meaningful overall survival benefit in an updated analysis of a phase 2 study.
Treatment with sotorasib yielded a median overall survival (OS) of 12.5 months in patients with previously treated KRAS p.G12C-mutated non-small cell lung cancer (NSCLC), according to an analysis of the phase 2 CodeBreaK 100 trial data presented at the American Society of Clinical Oncology Annual Meeting.
Median progression-free survival (PFS) was 6.8 months in this update, which included a median follow-up of more than 15 months, according to investigator Ferdinandos Skoulidis, MD, PhD, assistant professor of thoracic/head and neck medical oncology at the University of Texas MD Anderson Cancer Center in Houston.
Efficacy responses
The confirmed objective response rate was 37.1%, including a 3.2% complete response rate and a median duration of response of 11.1 months, according to the report by Dr. Skoulidis.
In exploratory analyses, the benefit of sotorasib was consistent across patient subgroups, Dr. Skoulidis said in his presentation (Abstract 9003).
In particular, efficacy was observed in subgroups with co-occurring mutations in TP53, STK11, and KEAP1, which are molecular indicators of suboptimal outcomes on standard systemic treatments, according to Dr. Skoulidis.
This update on the registrational phase 2 CodeBreaK100 trial, published concurrently in the New England Journal of Medicine , came just one week after the U.S. Food and Drug Administration (FDA) granted accelerated approval to sotorasib.
Sotorasib was approved for the treatment of patients with previously treated KRAS G12C‑mutated locally advanced or metastatic NSCLC on the basis of previously reported results from CodeBreaK100.
This sotorasib indication represents a “historic milestone,” Dr. Skoulidis said in an interview.
No previously studied selective KRAS inhibitor has been approved despite scientific research efforts that stretch back nearly four decades, he explained.
“In a way, one can say that we have dealt KRAS-mutant lung cancer a knockdown blow, however, I should point out that the fight is not over,” he added.
“These clinical results will no doubt spearhead and galvanize further efforts to develop even more effective therapeutic combinations in the future, as well as identify and either forestall or overcome the eventual development of acquired resistance,” he said.
Only 1 out of 8 patients
The KRAS p.G12C mutation is present in about 13% of lung adenocarcinomas, or about one in every eight patients with nonsquamous NSCLC, Dr. Skoulidis said in the interview.
“We are estimating that this is in the region of 13,000 patients newly diagnosed every year in the U.S., and approximately 13,000 patients or so that are currently being treated in the second- or third-line setting,” he said.
The CodeBreaK100 trial included 126 patients with locally advanced or metastatic NSCLC and KRAS p.G12C mutation who had progressed on prior systemic therapies. About 43% had one prior line of treatment, while 35% had two lines, and 22% had three lines. A total of 81% had previously received both platinum-based chemotherapy and PD-1/PD-L1 axis inhibitors.
Most treatment-related adverse events in the study were grade 1-2 and generally manageable, according to Dr. Skoulidis. About 20% of patients experienced grade 3 treatment-related adverse events, which were mostly diarrhea or increases in aspartate aminotransferase and alanine aminotransferase levels. A grade 4 treatment-related adverse event, pneumonitis and dyspnea, was reported in one patient or approximately 1%.
Confirmatory trial
Although CodeBreak100 is not a randomized trial, the median OS of 12.5 months compares favorably to median OS times in the range of 7.9-10.3 months reported in randomized phase 3 clinical trials and subgroup analysis of randomized phase 3 trials of docetaxel for patients with KRAS-mutant lung adenocarcinoma, Dr. Skoulidis said in a question-and-answer session.
A confirmatory phase 3 CodeBreaK200 trial of sotorasib versus docetaxel in patients with previously treated KRAS p.G12C-mutated NSCLC is underway. That trial is evaluating PFS as a primary endpoint and OS as a secondary endpoint.
“If the same magnitude of benefit, 12.5 months median overall survival, is confirmed in the larger phase 3 clinical trial, as a clinician I would consider that beneficial for patients, compared to the standard of care,” Dr. Skoulidis said during the session.
Mature data
The updated analysis of the phase 2 CodeBreaK100 study is notable for its mature OS data, updated safety and the first molecular subgroup analyses, according to discussant Christine Marie Lovly, MD, PhD, of the division of hematology-oncology at Vanderbilt University Medical Center in Nashville.
“The objective response rate was 37.1%,” she added. “This is a little bit lower than we’re used to for targeted therapies, but remember, this is a different mutation and a very different class of drugs.”
The KRAS G12C inhibitors, several of which are under clinical development, are not tyrosine kinase inhibitors (TKIs), but rather allele-specific inhibitors that target mutant KRAS, trapping it in an inactive conformation, she explained.
Dr. Lovly referenced the exploratory analyses demonstrating efficacy in molecularly defined subgroups, calling it “interesting” that there was no difference in objective response rate between TP53 wild type and mutant tumors.
“We do have data that mutant TP53 seems to confer inferior outcomes for EGFR TKI-directed therapy in patients with EGFR-mutant lung cancer,” she said.
CodeBreaK100 was supported by Amgen, Inc. and partly by a National Institutes of Health Cancer Center Support Grant at Memorial Sloan Kettering Cancer Center.
Dr. Skoulidis reported honoraria from Bristol-Myers Squibb; research funding from AIMM Therapeutics and Amgen; and travel, accommodations, or expenses from Tango Therapeutics. Dr. Lovly reported disclosures related to Amgen, AstraZeneca, Genentech, Novartis, and Pfizer, among others.
The first KRAS inhibitor approved for the treatment of lung cancer provided a clinically meaningful overall survival benefit in an updated analysis of a phase 2 study.
Treatment with sotorasib yielded a median overall survival (OS) of 12.5 months in patients with previously treated KRAS p.G12C-mutated non-small cell lung cancer (NSCLC), according to an analysis of the phase 2 CodeBreaK 100 trial data presented at the American Society of Clinical Oncology Annual Meeting.
Median progression-free survival (PFS) was 6.8 months in this update, which included a median follow-up of more than 15 months, according to investigator Ferdinandos Skoulidis, MD, PhD, assistant professor of thoracic/head and neck medical oncology at the University of Texas MD Anderson Cancer Center in Houston.
Efficacy responses
The confirmed objective response rate was 37.1%, including a 3.2% complete response rate and a median duration of response of 11.1 months, according to the report by Dr. Skoulidis.
In exploratory analyses, the benefit of sotorasib was consistent across patient subgroups, Dr. Skoulidis said in his presentation (Abstract 9003).
In particular, efficacy was observed in subgroups with co-occurring mutations in TP53, STK11, and KEAP1, which are molecular indicators of suboptimal outcomes on standard systemic treatments, according to Dr. Skoulidis.
This update on the registrational phase 2 CodeBreaK100 trial, published concurrently in the New England Journal of Medicine , came just one week after the U.S. Food and Drug Administration (FDA) granted accelerated approval to sotorasib.
Sotorasib was approved for the treatment of patients with previously treated KRAS G12C‑mutated locally advanced or metastatic NSCLC on the basis of previously reported results from CodeBreaK100.
This sotorasib indication represents a “historic milestone,” Dr. Skoulidis said in an interview.
No previously studied selective KRAS inhibitor has been approved despite scientific research efforts that stretch back nearly four decades, he explained.
“In a way, one can say that we have dealt KRAS-mutant lung cancer a knockdown blow, however, I should point out that the fight is not over,” he added.
“These clinical results will no doubt spearhead and galvanize further efforts to develop even more effective therapeutic combinations in the future, as well as identify and either forestall or overcome the eventual development of acquired resistance,” he said.
Only 1 out of 8 patients
The KRAS p.G12C mutation is present in about 13% of lung adenocarcinomas, or about one in every eight patients with nonsquamous NSCLC, Dr. Skoulidis said in the interview.
“We are estimating that this is in the region of 13,000 patients newly diagnosed every year in the U.S., and approximately 13,000 patients or so that are currently being treated in the second- or third-line setting,” he said.
The CodeBreaK100 trial included 126 patients with locally advanced or metastatic NSCLC and KRAS p.G12C mutation who had progressed on prior systemic therapies. About 43% had one prior line of treatment, while 35% had two lines, and 22% had three lines. A total of 81% had previously received both platinum-based chemotherapy and PD-1/PD-L1 axis inhibitors.
Most treatment-related adverse events in the study were grade 1-2 and generally manageable, according to Dr. Skoulidis. About 20% of patients experienced grade 3 treatment-related adverse events, which were mostly diarrhea or increases in aspartate aminotransferase and alanine aminotransferase levels. A grade 4 treatment-related adverse event, pneumonitis and dyspnea, was reported in one patient or approximately 1%.
Confirmatory trial
Although CodeBreak100 is not a randomized trial, the median OS of 12.5 months compares favorably to median OS times in the range of 7.9-10.3 months reported in randomized phase 3 clinical trials and subgroup analysis of randomized phase 3 trials of docetaxel for patients with KRAS-mutant lung adenocarcinoma, Dr. Skoulidis said in a question-and-answer session.
A confirmatory phase 3 CodeBreaK200 trial of sotorasib versus docetaxel in patients with previously treated KRAS p.G12C-mutated NSCLC is underway. That trial is evaluating PFS as a primary endpoint and OS as a secondary endpoint.
“If the same magnitude of benefit, 12.5 months median overall survival, is confirmed in the larger phase 3 clinical trial, as a clinician I would consider that beneficial for patients, compared to the standard of care,” Dr. Skoulidis said during the session.
Mature data
The updated analysis of the phase 2 CodeBreaK100 study is notable for its mature OS data, updated safety and the first molecular subgroup analyses, according to discussant Christine Marie Lovly, MD, PhD, of the division of hematology-oncology at Vanderbilt University Medical Center in Nashville.
“The objective response rate was 37.1%,” she added. “This is a little bit lower than we’re used to for targeted therapies, but remember, this is a different mutation and a very different class of drugs.”
The KRAS G12C inhibitors, several of which are under clinical development, are not tyrosine kinase inhibitors (TKIs), but rather allele-specific inhibitors that target mutant KRAS, trapping it in an inactive conformation, she explained.
Dr. Lovly referenced the exploratory analyses demonstrating efficacy in molecularly defined subgroups, calling it “interesting” that there was no difference in objective response rate between TP53 wild type and mutant tumors.
“We do have data that mutant TP53 seems to confer inferior outcomes for EGFR TKI-directed therapy in patients with EGFR-mutant lung cancer,” she said.
CodeBreaK100 was supported by Amgen, Inc. and partly by a National Institutes of Health Cancer Center Support Grant at Memorial Sloan Kettering Cancer Center.
Dr. Skoulidis reported honoraria from Bristol-Myers Squibb; research funding from AIMM Therapeutics and Amgen; and travel, accommodations, or expenses from Tango Therapeutics. Dr. Lovly reported disclosures related to Amgen, AstraZeneca, Genentech, Novartis, and Pfizer, among others.
FROM ASCO 2021
NSCLC: Immune-related AEs during checkpoint inhibitor therapy may predict outcomes
Experiencing an immune-related adverse event during checkpoint inhibitor treatment may predict outcomes in patients with non-small cell lung cancer, exploratory analyses of phase 3 trials suggest.
Immune-related adverse events (irAEs) were tied to longer overall survival (OS) in exploratory pooled analyses of three phase 3 clinical trials evaluating atezolizumab-based regimens, according to investigator Mark A. Socinski, MD, of AdventHealth Cancer Institute, Orlando, Fla.
Median OS approached 26 months for patients who received first-line atezolizumab and experienced an irAE, compared with just 13 months for those who did not experience an irAE, according to results reported at the American Society of Clinical Oncology Annual Meeting (Abstract 9002).
Atezolizumab-treated patients with grade 3 or greater irAEs had the shortest OS, shorter than those atezolizumab-treated patients who experienced grade 1-2 irAEs or no irAEs at all. That short OS may be due to treatment interruptions or discontinuations, said Dr. Socinski.
“Data from these analyses suggest an association between irAEs and efficacy in patients with [non-small cell cancer] NSCLC,” he stated in his presentation of the results.
A lot more to learn about irAEs
Similar linkages between irAEs and outcomes were observed in pooled analyses of patients enrolled in the control arms of the phase 3 trials, with a median OS of about 20 months for control patients experiencing an irAE, versus about 13 months for those who did not.
That linkage in the control arm prompted a question from an ASCO attendee about why an effect of irAEs, commonly associated with immune checkpoint inhibitor therapy, would be evident in analyses of patients who did not receive those agents.
In his response, Dr. Socinski characterized the finding as “a surprise” and said the finding may either reflect how adverse events are characterized or how chemotherapy impacts the immune system.
“I don’t know that our definition of irAEs is perfect,” he said, “and maybe we don’t understand what impact chemotherapy may have on the immune system, and may actually engender what historically we’ve always seen as an adverse event, but didn’t necessarily classify as an immune-related adverse event.”
More work is needed to better understand the connection between irAES and outcomes, and whether anything can be done as a result of that improved understanding, said discussant Mary Weber Redman, PhD.
“The question is, ‘what is actionable?’” added Dr. Redman, a biostatistician at the Fred Hutchinson Cancer Research Center, Seattle.
A firmer understanding of the relationship between irAEs and outcomes could change how clinicians monitor patients for irAEs, lead to better prediction of which patients may experience higher grade irAEs, and ultimately impact treatment selection potentially to avoid those higher grade events, Dr. Redman said in her remarks.
“Doing these types of analyses are quite important, because we have to look at the breadth of information that we have to be able to interpret that and think about what are future questions,” she said in the question-and-answer session accompanying Dr. Socinski’s presentation.
“I think the key is that we shouldn’t use these analyses to be definitive, but we should use them as to be hypothesis generating,” she added.
More evidence to link irAEs and outcomes
Immune-related AEs caused by off-target immune and inflammatory activity have been reported in up to 80% of patients receiving immune checkpoint inhibitors as monotherapy and up to 95% in combination regimens, Dr. Socinski said in his presentation.
“Increasing evidence suggests that the occurrence of immune-related adverse events with PD-L1 or PD-1 inhibitor therapy may be predictive of improved outcomes in cancers such as NSCLC, “ he added.
In their exploratory pooled analyses, Dr. Socinski and co-investigators looked at data from the phase 3 IMpower130 and IMpower132 trials, which evaluated first-line atezolizumab and chemotherapy for NSCLC, and the phase 3 IMpower150 trial, which evaluated atezolizumab plus chemotherapy with or without bevacizumab.
In all, they analyzed data for 1,557 atezolizumab-treated patients, and 900 patients who had been in the control arms of the studies.
Forty-eight percent of atezolizumab-treated patients experienced irAEs of any grade, while 11% experienced irAEs of grade 3-5, according to the presented data. In the control arm, 32% experienced irAEs of any grade and 5% experienced grade 3-5 irAEs.
The most common irAEs of any grade were rash, hepatitis, and hypothyroidism, occurring in 28%, 15%, and 12% of atezolizumab-treated patients, respectively.
Median OS in the atezolizumab arm was 25.7 months for patients with irAEs and 13.0 for patients with no irAEs, with a hazard ratio (HR) of 0.69 using a time-dependent Cox model.
Median OS in the control arm was 20.2 months for patients with irAEs and 12.8 months for patients with no irAEs, with an HR of 0.82.
The overall response rate (ORR) in the atezolizumab arm was 61.1% for patients with irAEs and 37.2% for those without irAEs; in the control arm, ORR was 42.2% for patients with irAEs and 34.0% for those with no irAEs.
Atezolizumab-treated patients who experienced grade 3-5 irAEs had the shortest OS, according to Dr. Socinski. The HRs for OS at 1, 3, 6, and 12 months in atezolizumab-treated patients with grade 3-5 irAEs (compared with those without irAEs) ranged from 1.25 to 0.87. By contrast, HRs at those time points for patients with grade 1-2 irAEs ranged from 0.78 to 0.72, Dr. Socinski said.
Dr. Socinski reported disclosures related to AstraZeneca/MedImmune, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Celgene, Genentech, Guardant Health, Janssen, Lilly, Merck, Novartis, Roche/Genentech, and Spectrum Pharmaceuticals. Dr. Redman reported a consulting or advisory role with AstraZeneca.
Experiencing an immune-related adverse event during checkpoint inhibitor treatment may predict outcomes in patients with non-small cell lung cancer, exploratory analyses of phase 3 trials suggest.
Immune-related adverse events (irAEs) were tied to longer overall survival (OS) in exploratory pooled analyses of three phase 3 clinical trials evaluating atezolizumab-based regimens, according to investigator Mark A. Socinski, MD, of AdventHealth Cancer Institute, Orlando, Fla.
Median OS approached 26 months for patients who received first-line atezolizumab and experienced an irAE, compared with just 13 months for those who did not experience an irAE, according to results reported at the American Society of Clinical Oncology Annual Meeting (Abstract 9002).
Atezolizumab-treated patients with grade 3 or greater irAEs had the shortest OS, shorter than those atezolizumab-treated patients who experienced grade 1-2 irAEs or no irAEs at all. That short OS may be due to treatment interruptions or discontinuations, said Dr. Socinski.
“Data from these analyses suggest an association between irAEs and efficacy in patients with [non-small cell cancer] NSCLC,” he stated in his presentation of the results.
A lot more to learn about irAEs
Similar linkages between irAEs and outcomes were observed in pooled analyses of patients enrolled in the control arms of the phase 3 trials, with a median OS of about 20 months for control patients experiencing an irAE, versus about 13 months for those who did not.
That linkage in the control arm prompted a question from an ASCO attendee about why an effect of irAEs, commonly associated with immune checkpoint inhibitor therapy, would be evident in analyses of patients who did not receive those agents.
In his response, Dr. Socinski characterized the finding as “a surprise” and said the finding may either reflect how adverse events are characterized or how chemotherapy impacts the immune system.
“I don’t know that our definition of irAEs is perfect,” he said, “and maybe we don’t understand what impact chemotherapy may have on the immune system, and may actually engender what historically we’ve always seen as an adverse event, but didn’t necessarily classify as an immune-related adverse event.”
More work is needed to better understand the connection between irAES and outcomes, and whether anything can be done as a result of that improved understanding, said discussant Mary Weber Redman, PhD.
“The question is, ‘what is actionable?’” added Dr. Redman, a biostatistician at the Fred Hutchinson Cancer Research Center, Seattle.
A firmer understanding of the relationship between irAEs and outcomes could change how clinicians monitor patients for irAEs, lead to better prediction of which patients may experience higher grade irAEs, and ultimately impact treatment selection potentially to avoid those higher grade events, Dr. Redman said in her remarks.
“Doing these types of analyses are quite important, because we have to look at the breadth of information that we have to be able to interpret that and think about what are future questions,” she said in the question-and-answer session accompanying Dr. Socinski’s presentation.
“I think the key is that we shouldn’t use these analyses to be definitive, but we should use them as to be hypothesis generating,” she added.
More evidence to link irAEs and outcomes
Immune-related AEs caused by off-target immune and inflammatory activity have been reported in up to 80% of patients receiving immune checkpoint inhibitors as monotherapy and up to 95% in combination regimens, Dr. Socinski said in his presentation.
“Increasing evidence suggests that the occurrence of immune-related adverse events with PD-L1 or PD-1 inhibitor therapy may be predictive of improved outcomes in cancers such as NSCLC, “ he added.
In their exploratory pooled analyses, Dr. Socinski and co-investigators looked at data from the phase 3 IMpower130 and IMpower132 trials, which evaluated first-line atezolizumab and chemotherapy for NSCLC, and the phase 3 IMpower150 trial, which evaluated atezolizumab plus chemotherapy with or without bevacizumab.
In all, they analyzed data for 1,557 atezolizumab-treated patients, and 900 patients who had been in the control arms of the studies.
Forty-eight percent of atezolizumab-treated patients experienced irAEs of any grade, while 11% experienced irAEs of grade 3-5, according to the presented data. In the control arm, 32% experienced irAEs of any grade and 5% experienced grade 3-5 irAEs.
The most common irAEs of any grade were rash, hepatitis, and hypothyroidism, occurring in 28%, 15%, and 12% of atezolizumab-treated patients, respectively.
Median OS in the atezolizumab arm was 25.7 months for patients with irAEs and 13.0 for patients with no irAEs, with a hazard ratio (HR) of 0.69 using a time-dependent Cox model.
Median OS in the control arm was 20.2 months for patients with irAEs and 12.8 months for patients with no irAEs, with an HR of 0.82.
The overall response rate (ORR) in the atezolizumab arm was 61.1% for patients with irAEs and 37.2% for those without irAEs; in the control arm, ORR was 42.2% for patients with irAEs and 34.0% for those with no irAEs.
Atezolizumab-treated patients who experienced grade 3-5 irAEs had the shortest OS, according to Dr. Socinski. The HRs for OS at 1, 3, 6, and 12 months in atezolizumab-treated patients with grade 3-5 irAEs (compared with those without irAEs) ranged from 1.25 to 0.87. By contrast, HRs at those time points for patients with grade 1-2 irAEs ranged from 0.78 to 0.72, Dr. Socinski said.
Dr. Socinski reported disclosures related to AstraZeneca/MedImmune, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Celgene, Genentech, Guardant Health, Janssen, Lilly, Merck, Novartis, Roche/Genentech, and Spectrum Pharmaceuticals. Dr. Redman reported a consulting or advisory role with AstraZeneca.
Experiencing an immune-related adverse event during checkpoint inhibitor treatment may predict outcomes in patients with non-small cell lung cancer, exploratory analyses of phase 3 trials suggest.
Immune-related adverse events (irAEs) were tied to longer overall survival (OS) in exploratory pooled analyses of three phase 3 clinical trials evaluating atezolizumab-based regimens, according to investigator Mark A. Socinski, MD, of AdventHealth Cancer Institute, Orlando, Fla.
Median OS approached 26 months for patients who received first-line atezolizumab and experienced an irAE, compared with just 13 months for those who did not experience an irAE, according to results reported at the American Society of Clinical Oncology Annual Meeting (Abstract 9002).
Atezolizumab-treated patients with grade 3 or greater irAEs had the shortest OS, shorter than those atezolizumab-treated patients who experienced grade 1-2 irAEs or no irAEs at all. That short OS may be due to treatment interruptions or discontinuations, said Dr. Socinski.
“Data from these analyses suggest an association between irAEs and efficacy in patients with [non-small cell cancer] NSCLC,” he stated in his presentation of the results.
A lot more to learn about irAEs
Similar linkages between irAEs and outcomes were observed in pooled analyses of patients enrolled in the control arms of the phase 3 trials, with a median OS of about 20 months for control patients experiencing an irAE, versus about 13 months for those who did not.
That linkage in the control arm prompted a question from an ASCO attendee about why an effect of irAEs, commonly associated with immune checkpoint inhibitor therapy, would be evident in analyses of patients who did not receive those agents.
In his response, Dr. Socinski characterized the finding as “a surprise” and said the finding may either reflect how adverse events are characterized or how chemotherapy impacts the immune system.
“I don’t know that our definition of irAEs is perfect,” he said, “and maybe we don’t understand what impact chemotherapy may have on the immune system, and may actually engender what historically we’ve always seen as an adverse event, but didn’t necessarily classify as an immune-related adverse event.”
More work is needed to better understand the connection between irAES and outcomes, and whether anything can be done as a result of that improved understanding, said discussant Mary Weber Redman, PhD.
“The question is, ‘what is actionable?’” added Dr. Redman, a biostatistician at the Fred Hutchinson Cancer Research Center, Seattle.
A firmer understanding of the relationship between irAEs and outcomes could change how clinicians monitor patients for irAEs, lead to better prediction of which patients may experience higher grade irAEs, and ultimately impact treatment selection potentially to avoid those higher grade events, Dr. Redman said in her remarks.
“Doing these types of analyses are quite important, because we have to look at the breadth of information that we have to be able to interpret that and think about what are future questions,” she said in the question-and-answer session accompanying Dr. Socinski’s presentation.
“I think the key is that we shouldn’t use these analyses to be definitive, but we should use them as to be hypothesis generating,” she added.
More evidence to link irAEs and outcomes
Immune-related AEs caused by off-target immune and inflammatory activity have been reported in up to 80% of patients receiving immune checkpoint inhibitors as monotherapy and up to 95% in combination regimens, Dr. Socinski said in his presentation.
“Increasing evidence suggests that the occurrence of immune-related adverse events with PD-L1 or PD-1 inhibitor therapy may be predictive of improved outcomes in cancers such as NSCLC, “ he added.
In their exploratory pooled analyses, Dr. Socinski and co-investigators looked at data from the phase 3 IMpower130 and IMpower132 trials, which evaluated first-line atezolizumab and chemotherapy for NSCLC, and the phase 3 IMpower150 trial, which evaluated atezolizumab plus chemotherapy with or without bevacizumab.
In all, they analyzed data for 1,557 atezolizumab-treated patients, and 900 patients who had been in the control arms of the studies.
Forty-eight percent of atezolizumab-treated patients experienced irAEs of any grade, while 11% experienced irAEs of grade 3-5, according to the presented data. In the control arm, 32% experienced irAEs of any grade and 5% experienced grade 3-5 irAEs.
The most common irAEs of any grade were rash, hepatitis, and hypothyroidism, occurring in 28%, 15%, and 12% of atezolizumab-treated patients, respectively.
Median OS in the atezolizumab arm was 25.7 months for patients with irAEs and 13.0 for patients with no irAEs, with a hazard ratio (HR) of 0.69 using a time-dependent Cox model.
Median OS in the control arm was 20.2 months for patients with irAEs and 12.8 months for patients with no irAEs, with an HR of 0.82.
The overall response rate (ORR) in the atezolizumab arm was 61.1% for patients with irAEs and 37.2% for those without irAEs; in the control arm, ORR was 42.2% for patients with irAEs and 34.0% for those with no irAEs.
Atezolizumab-treated patients who experienced grade 3-5 irAEs had the shortest OS, according to Dr. Socinski. The HRs for OS at 1, 3, 6, and 12 months in atezolizumab-treated patients with grade 3-5 irAEs (compared with those without irAEs) ranged from 1.25 to 0.87. By contrast, HRs at those time points for patients with grade 1-2 irAEs ranged from 0.78 to 0.72, Dr. Socinski said.
Dr. Socinski reported disclosures related to AstraZeneca/MedImmune, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Celgene, Genentech, Guardant Health, Janssen, Lilly, Merck, Novartis, Roche/Genentech, and Spectrum Pharmaceuticals. Dr. Redman reported a consulting or advisory role with AstraZeneca.
REPORTING FROM ASCO 2021
Drug conjugate extends life in HER2+ end-stage metastatic colorectal cancer
, according to a phase 2 report.
Among the 53 patients with the highest expression in the study – defined as 3+ expression on immune histochemical staining or 2+ with positive in situ hybridization – median progression median progression-free survival (mPFS) was 6.9 months after failure of a median of four prior regimens.
With standard drugs, mPFS would be expected to be about 2 months or less, said investigator Kanwal Pratap Singh Raghav, MD, an associate professor of GI medical oncology at MD Anderson Cancer Center, Houston.
Many of the 86 study participants were enrolled at MD Anderson, and “they all derived some benefit from the conjugate. “It’s fairly well tolerated,” and “our experience has been pretty good; I think it’s actually a pretty good drug,” Dr. Raghav said shortly before presenting the findings at the American Society of Clinical Oncology Annual Meeting.
HER2 is over-expressed in about 5% of colorectal cancer patients. The conjugate is a kind of “smart bomb” for them that combines the anti-HER2 antibody trastuzumab (Herceptin) with a potent topoisomerase I inhibitor. The trastuzumab portion of the combination zeros in on cancer cells expressing HER2, delivering the cytotoxic agent directly to them.
“The amount of [cytotoxic] drug delivered by the antibody inside the cell is far in excess” to the standard approach of delivering chemotherapy agents individually, Dr. Raghav said.
“Single-agent treatments targeting HER2 only have modest activity. Seeing a response rate of [almost] 50% in colorectal cancer tumors that have high expression of HER2 is very exciting,” Muhammad Beg, MD, a GI oncologist and associate professor at UT Southwestern Medical Center, Dallas, said when asked for comment.
Trastuzumab deruxtecan already is approved for metastatic HER2-positive breast cancer after at least two anti-HER2-based regimens and locally advanced or metastatic HER2-positive gastric or gastroesophageal junction adenocarcinoma after a prior trastuzumab-based regime.
The phase 2 study, dubbed DESTINY-CRC01, divided patients by HER2 expression. In addition to the 53 “high-expressors,” there were 15 medium-expressors – defined as 2+ on immunohistochemical staining and no in situ hybridization – and 18 low-expressors with 1+ HER2 expression.
The patients had run out of other options, having experienced progression on 2 to 11 previous regimens. All participants had been on the topoisomerase I inhibitor irinotecan before, and almost a third of the high-expressors had been on anti-HER2 regimen.
They were treated with 6.4 mg/kg trastuzumab deruxtecan every 3 weeks for a median of 3 months. There was no control group.
The overall response rate was 45.3% among high-expressors. In addition to the mPFS of 6.9 months, median overall survival was 15.5 months. Among those on prior anti-HER2 therapy, the overall response rate was 43.8%.
Benefit was minimal in the lower-expression groups, with a mPFS of 2.1 months and overall survival of 7.3 months in medium-expressors and a mPFS of 1.4 months and overall survival of 7.7 months in low-expressors.
Sixty-five percent of patients (56) had treatment-emergent grade 3 or worse adverse events, most commonly hematologic and gastrointestinal; 13 subjects (15.1%) discontinued due to adverse events.
Eight patients (9.3%) developed interstitial lung disease, a particular concern with trastuzumab deruxtecan; it was fatal for three. “We need to study the lung toxicity. It will become a bigger factor as we think about using this drug for earlier lines of treatment,” Dr. Beg noted.
The median age in the study was 58.5 years, just over half the subjects were men, and more than 90% had left-sided colon or rectum cancer.
The next step in development is a randomized trial in unresectable/metastatic HER2-positive colorectal cancer dubbed DESTINY-CRC02, comparing the 6.4 mg dose with 5.4 mg. It’s already started recruiting.
The work was funded by trastuzumab deruxtecan maker Daiichi Sankyo. Dr. Raghav is an advisor and researcher for the company; Dr. Beg had no relationships with it.
, according to a phase 2 report.
Among the 53 patients with the highest expression in the study – defined as 3+ expression on immune histochemical staining or 2+ with positive in situ hybridization – median progression median progression-free survival (mPFS) was 6.9 months after failure of a median of four prior regimens.
With standard drugs, mPFS would be expected to be about 2 months or less, said investigator Kanwal Pratap Singh Raghav, MD, an associate professor of GI medical oncology at MD Anderson Cancer Center, Houston.
Many of the 86 study participants were enrolled at MD Anderson, and “they all derived some benefit from the conjugate. “It’s fairly well tolerated,” and “our experience has been pretty good; I think it’s actually a pretty good drug,” Dr. Raghav said shortly before presenting the findings at the American Society of Clinical Oncology Annual Meeting.
HER2 is over-expressed in about 5% of colorectal cancer patients. The conjugate is a kind of “smart bomb” for them that combines the anti-HER2 antibody trastuzumab (Herceptin) with a potent topoisomerase I inhibitor. The trastuzumab portion of the combination zeros in on cancer cells expressing HER2, delivering the cytotoxic agent directly to them.
“The amount of [cytotoxic] drug delivered by the antibody inside the cell is far in excess” to the standard approach of delivering chemotherapy agents individually, Dr. Raghav said.
“Single-agent treatments targeting HER2 only have modest activity. Seeing a response rate of [almost] 50% in colorectal cancer tumors that have high expression of HER2 is very exciting,” Muhammad Beg, MD, a GI oncologist and associate professor at UT Southwestern Medical Center, Dallas, said when asked for comment.
Trastuzumab deruxtecan already is approved for metastatic HER2-positive breast cancer after at least two anti-HER2-based regimens and locally advanced or metastatic HER2-positive gastric or gastroesophageal junction adenocarcinoma after a prior trastuzumab-based regime.
The phase 2 study, dubbed DESTINY-CRC01, divided patients by HER2 expression. In addition to the 53 “high-expressors,” there were 15 medium-expressors – defined as 2+ on immunohistochemical staining and no in situ hybridization – and 18 low-expressors with 1+ HER2 expression.
The patients had run out of other options, having experienced progression on 2 to 11 previous regimens. All participants had been on the topoisomerase I inhibitor irinotecan before, and almost a third of the high-expressors had been on anti-HER2 regimen.
They were treated with 6.4 mg/kg trastuzumab deruxtecan every 3 weeks for a median of 3 months. There was no control group.
The overall response rate was 45.3% among high-expressors. In addition to the mPFS of 6.9 months, median overall survival was 15.5 months. Among those on prior anti-HER2 therapy, the overall response rate was 43.8%.
Benefit was minimal in the lower-expression groups, with a mPFS of 2.1 months and overall survival of 7.3 months in medium-expressors and a mPFS of 1.4 months and overall survival of 7.7 months in low-expressors.
Sixty-five percent of patients (56) had treatment-emergent grade 3 or worse adverse events, most commonly hematologic and gastrointestinal; 13 subjects (15.1%) discontinued due to adverse events.
Eight patients (9.3%) developed interstitial lung disease, a particular concern with trastuzumab deruxtecan; it was fatal for three. “We need to study the lung toxicity. It will become a bigger factor as we think about using this drug for earlier lines of treatment,” Dr. Beg noted.
The median age in the study was 58.5 years, just over half the subjects were men, and more than 90% had left-sided colon or rectum cancer.
The next step in development is a randomized trial in unresectable/metastatic HER2-positive colorectal cancer dubbed DESTINY-CRC02, comparing the 6.4 mg dose with 5.4 mg. It’s already started recruiting.
The work was funded by trastuzumab deruxtecan maker Daiichi Sankyo. Dr. Raghav is an advisor and researcher for the company; Dr. Beg had no relationships with it.
, according to a phase 2 report.
Among the 53 patients with the highest expression in the study – defined as 3+ expression on immune histochemical staining or 2+ with positive in situ hybridization – median progression median progression-free survival (mPFS) was 6.9 months after failure of a median of four prior regimens.
With standard drugs, mPFS would be expected to be about 2 months or less, said investigator Kanwal Pratap Singh Raghav, MD, an associate professor of GI medical oncology at MD Anderson Cancer Center, Houston.
Many of the 86 study participants were enrolled at MD Anderson, and “they all derived some benefit from the conjugate. “It’s fairly well tolerated,” and “our experience has been pretty good; I think it’s actually a pretty good drug,” Dr. Raghav said shortly before presenting the findings at the American Society of Clinical Oncology Annual Meeting.
HER2 is over-expressed in about 5% of colorectal cancer patients. The conjugate is a kind of “smart bomb” for them that combines the anti-HER2 antibody trastuzumab (Herceptin) with a potent topoisomerase I inhibitor. The trastuzumab portion of the combination zeros in on cancer cells expressing HER2, delivering the cytotoxic agent directly to them.
“The amount of [cytotoxic] drug delivered by the antibody inside the cell is far in excess” to the standard approach of delivering chemotherapy agents individually, Dr. Raghav said.
“Single-agent treatments targeting HER2 only have modest activity. Seeing a response rate of [almost] 50% in colorectal cancer tumors that have high expression of HER2 is very exciting,” Muhammad Beg, MD, a GI oncologist and associate professor at UT Southwestern Medical Center, Dallas, said when asked for comment.
Trastuzumab deruxtecan already is approved for metastatic HER2-positive breast cancer after at least two anti-HER2-based regimens and locally advanced or metastatic HER2-positive gastric or gastroesophageal junction adenocarcinoma after a prior trastuzumab-based regime.
The phase 2 study, dubbed DESTINY-CRC01, divided patients by HER2 expression. In addition to the 53 “high-expressors,” there were 15 medium-expressors – defined as 2+ on immunohistochemical staining and no in situ hybridization – and 18 low-expressors with 1+ HER2 expression.
The patients had run out of other options, having experienced progression on 2 to 11 previous regimens. All participants had been on the topoisomerase I inhibitor irinotecan before, and almost a third of the high-expressors had been on anti-HER2 regimen.
They were treated with 6.4 mg/kg trastuzumab deruxtecan every 3 weeks for a median of 3 months. There was no control group.
The overall response rate was 45.3% among high-expressors. In addition to the mPFS of 6.9 months, median overall survival was 15.5 months. Among those on prior anti-HER2 therapy, the overall response rate was 43.8%.
Benefit was minimal in the lower-expression groups, with a mPFS of 2.1 months and overall survival of 7.3 months in medium-expressors and a mPFS of 1.4 months and overall survival of 7.7 months in low-expressors.
Sixty-five percent of patients (56) had treatment-emergent grade 3 or worse adverse events, most commonly hematologic and gastrointestinal; 13 subjects (15.1%) discontinued due to adverse events.
Eight patients (9.3%) developed interstitial lung disease, a particular concern with trastuzumab deruxtecan; it was fatal for three. “We need to study the lung toxicity. It will become a bigger factor as we think about using this drug for earlier lines of treatment,” Dr. Beg noted.
The median age in the study was 58.5 years, just over half the subjects were men, and more than 90% had left-sided colon or rectum cancer.
The next step in development is a randomized trial in unresectable/metastatic HER2-positive colorectal cancer dubbed DESTINY-CRC02, comparing the 6.4 mg dose with 5.4 mg. It’s already started recruiting.
The work was funded by trastuzumab deruxtecan maker Daiichi Sankyo. Dr. Raghav is an advisor and researcher for the company; Dr. Beg had no relationships with it.
FROM ASCO 2021