User login
ApoB may better predict mortality risk in statin-treated patients
A new study shows apolipoprotein B (apoB) and non-HDL cholesterol – but not LDL cholesterol – are associated with increased risk for all-cause mortality and myocardial infarction in patients taking statins.
Moreover, apoB was a more accurate marker of all-cause mortality risk than non-HDL or LDL cholesterol and was more accurate at identifying MI risk than LDL cholesterol.
“Any patient that comes to a doctor for evaluation, if statin treatment is sufficient, the doctor should look not only at LDL cholesterol but HDL cholesterol and apoB, if its available – that is the take-home message,” senior author Børge Grønne Nordestgaard, MD, DMSC, University of Copenhagen, said in an interview.
The findings are very relevant to clinical practice because international guidelines focus on LDL cholesterol and “many doctors are brainwashed that that is the only thing they should look at, just to keep LDL cholesterol down,” he said. “I’ve worked for years with triglyceride lipoproteins, what I call remnant cholesterol, and I think that the risk is very high also when you have high remnant cholesterol.”
Previous work has shown that apoB and non-HDL cholesterol better reflect atherosclerotic cardiovascular disease risk than LDL cholesterol. This is the first study, however, to show that elevated apoB and non-HDL cholesterol are associated with a higher risk for all-cause death in statin-treated patients with low LDL cholesterol, Dr. Nordestgaard noted.
The investigators compared outcomes among 13,015 statin-treated participants in the Copenhagen General Population Study using median baseline values of 92 mg/dL for apoB, 3.1 mmol/L (120 mg/dL) for non-HDL cholesterol, and 2.3 mmol/L (89 mg/dL) for LDL cholesterol. Over a median follow-up of 8 years, there were 2,499 deaths and 537 MIs.
As reported in the Journal of the American College of Cardiology, discordant apoB above the median with LDL cholesterol below was associated with a 21% increased risk for all-cause mortality (hazard ratio, 1.21; 95% confidence interval, 1.07-1.36) and 49% increased risk for MI (HR, 1.49; 95% CI, 1.15-1.92), compared with concordant apoB and LDL cholesterol below the medians.
Similar results were found for discordant non-HDL cholesterol above the median with low LDL cholesterol for all-cause mortality (HR, 1.18; 95% CI, 1.02-1.36) and MI (1.78; 95% CI, 1.35-2.34).
No such associations with mortality or MI were observed when LDL cholesterol was above the median and apoB or non-HDL below.
Additional analyses showed that high apoB with low non-HDL cholesterol was associated with a higher risk for all-cause mortality (HR, 1.21; 95% CI, 1.03-1.41), whereas high non-HDL cholesterol with low apoB was associated with a lower risk (HR, 0.75; 95% CI, 0.62-0.92).
Current guidelines define apoB greater than 130 mg/dL as a risk modifier in patients not using statins but, the authors wrote, “based on our results, the threshold for apoB as a risk modifier in statin-treated patients should be closer to 92 mg/dL than to 130 mg/dL.”
In an accompanying editorial, Neil J. Stone, MD, and Donald Lloyd-Jones, MD, both from Northwestern University, Chicago, said that American and European guidelines acknowledge the usefulness of apoB and non-HDL cholesterol in their risk algorithms and as possible targets to indicate efficacy, but don’t give a strong recommendation for apoB to assess residual risk.
“This paper suggests that, in the next iteration, we’ve got to give a stronger thought to measuring apoB for residual risk in those with secondary prevention,” Dr. Stone, vice chair of the 2018 American Heart Association/ACC cholesterol guidelines, said in an interview.
“The whole part of the guidelines was not to focus on any one number but to focus on the clinical risk as a whole,” he said. “You can enlarge your understanding of the patient by looking at their non-HDL, which you have anyway, and in certain circumstances, for example, people with metabolic syndrome, diabetes, obesity, or high triglycerides, those people might very well benefit from an apoB to further understand their risk. This paper simply highlights that and, therefore, was very valuable.”
Dr. Stone and Dr. Lloyd-Jones, however, pointed out that statin use was self-reported and information was lacking on adherence, dose intensity, and the amount of LDL cholesterol lowering from baseline. LDL cholesterol levels were also above current recommendations for optimizing risk reduction. “If statin dosing and LDL [cholesterol] were not optimized already, then there may have been ‘room’ for non-HDL [cholesterol] and apoB to add value in understanding residual risk,” they wrote.
The editorialists suggested that sequential use, rather than regular use, of apoB and non-HDL cholesterol may be best and that incorporating this information may be particularly beneficial for patients with metabolic disorders and elevated triglycerides after statin therapy.
“Maybe this paper is a wake-up call that there are other markers out there that can tell you that you still have higher risk and need to tighten up lifestyle and maybe be more adherent,” Dr. Stone said. “I think this is a wonderful chance to say that preventive cardiology isn’t just ‘set it and forget it’.”
C. Noel Bairey Merz, MD, who coauthored the 2018 cholesterol guidelines, agreed there’s “an overexuberant focus on LDL [cholesterol] for residual risk” and highlighted a recent systematic review of statins, ezetimibe, and PCSK9 cardiovascular outcomes trials that showed very little gain from aggressively driving down LDL below 100 mg/dL, unless the patient is at extremely high risk.
“If I, as a treating cardiologist who spends a lot of time on lipids, had a patient on a high-intensity statin and they didn’t drop [their LDL cholesterol] 50% and I already had them going to cardiac rehab and they were already losing weight, would I measure apoB? Yeah, I might, to motivate them to do more or to take Vascepa,” she said.
“This study is a useful addition to a relatively important problem, which is residual risk, and really supports personalized or precision medicine,” added Bairey Merz, MD, Cedars-Sinai Medical Center, Los Angeles. “But now we have to do the work and do an intervention trial in these people and see whether these markers make a difference.”
The study was supported by Herlev and Gentofte Hospital’s Research Fund and the department of clinical biochemistry, Herlev and Gentofte Hospital, Copenhagen University Hospital. Dr. Nordestgaard has had consultancies or talks sponsored by AstraZeneca, Sanofi, Regeneron, Akcea, Amarin, Amgen, Esperion, Kowa, Novartis, Novo Nordisk, and Silence Therapeutics. All other authors, Dr. Stone, and Dr. Lloyd-Jones reported no conflicts. Dr. Merz reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
A new study shows apolipoprotein B (apoB) and non-HDL cholesterol – but not LDL cholesterol – are associated with increased risk for all-cause mortality and myocardial infarction in patients taking statins.
Moreover, apoB was a more accurate marker of all-cause mortality risk than non-HDL or LDL cholesterol and was more accurate at identifying MI risk than LDL cholesterol.
“Any patient that comes to a doctor for evaluation, if statin treatment is sufficient, the doctor should look not only at LDL cholesterol but HDL cholesterol and apoB, if its available – that is the take-home message,” senior author Børge Grønne Nordestgaard, MD, DMSC, University of Copenhagen, said in an interview.
The findings are very relevant to clinical practice because international guidelines focus on LDL cholesterol and “many doctors are brainwashed that that is the only thing they should look at, just to keep LDL cholesterol down,” he said. “I’ve worked for years with triglyceride lipoproteins, what I call remnant cholesterol, and I think that the risk is very high also when you have high remnant cholesterol.”
Previous work has shown that apoB and non-HDL cholesterol better reflect atherosclerotic cardiovascular disease risk than LDL cholesterol. This is the first study, however, to show that elevated apoB and non-HDL cholesterol are associated with a higher risk for all-cause death in statin-treated patients with low LDL cholesterol, Dr. Nordestgaard noted.
The investigators compared outcomes among 13,015 statin-treated participants in the Copenhagen General Population Study using median baseline values of 92 mg/dL for apoB, 3.1 mmol/L (120 mg/dL) for non-HDL cholesterol, and 2.3 mmol/L (89 mg/dL) for LDL cholesterol. Over a median follow-up of 8 years, there were 2,499 deaths and 537 MIs.
As reported in the Journal of the American College of Cardiology, discordant apoB above the median with LDL cholesterol below was associated with a 21% increased risk for all-cause mortality (hazard ratio, 1.21; 95% confidence interval, 1.07-1.36) and 49% increased risk for MI (HR, 1.49; 95% CI, 1.15-1.92), compared with concordant apoB and LDL cholesterol below the medians.
Similar results were found for discordant non-HDL cholesterol above the median with low LDL cholesterol for all-cause mortality (HR, 1.18; 95% CI, 1.02-1.36) and MI (1.78; 95% CI, 1.35-2.34).
No such associations with mortality or MI were observed when LDL cholesterol was above the median and apoB or non-HDL below.
Additional analyses showed that high apoB with low non-HDL cholesterol was associated with a higher risk for all-cause mortality (HR, 1.21; 95% CI, 1.03-1.41), whereas high non-HDL cholesterol with low apoB was associated with a lower risk (HR, 0.75; 95% CI, 0.62-0.92).
Current guidelines define apoB greater than 130 mg/dL as a risk modifier in patients not using statins but, the authors wrote, “based on our results, the threshold for apoB as a risk modifier in statin-treated patients should be closer to 92 mg/dL than to 130 mg/dL.”
In an accompanying editorial, Neil J. Stone, MD, and Donald Lloyd-Jones, MD, both from Northwestern University, Chicago, said that American and European guidelines acknowledge the usefulness of apoB and non-HDL cholesterol in their risk algorithms and as possible targets to indicate efficacy, but don’t give a strong recommendation for apoB to assess residual risk.
“This paper suggests that, in the next iteration, we’ve got to give a stronger thought to measuring apoB for residual risk in those with secondary prevention,” Dr. Stone, vice chair of the 2018 American Heart Association/ACC cholesterol guidelines, said in an interview.
“The whole part of the guidelines was not to focus on any one number but to focus on the clinical risk as a whole,” he said. “You can enlarge your understanding of the patient by looking at their non-HDL, which you have anyway, and in certain circumstances, for example, people with metabolic syndrome, diabetes, obesity, or high triglycerides, those people might very well benefit from an apoB to further understand their risk. This paper simply highlights that and, therefore, was very valuable.”
Dr. Stone and Dr. Lloyd-Jones, however, pointed out that statin use was self-reported and information was lacking on adherence, dose intensity, and the amount of LDL cholesterol lowering from baseline. LDL cholesterol levels were also above current recommendations for optimizing risk reduction. “If statin dosing and LDL [cholesterol] were not optimized already, then there may have been ‘room’ for non-HDL [cholesterol] and apoB to add value in understanding residual risk,” they wrote.
The editorialists suggested that sequential use, rather than regular use, of apoB and non-HDL cholesterol may be best and that incorporating this information may be particularly beneficial for patients with metabolic disorders and elevated triglycerides after statin therapy.
“Maybe this paper is a wake-up call that there are other markers out there that can tell you that you still have higher risk and need to tighten up lifestyle and maybe be more adherent,” Dr. Stone said. “I think this is a wonderful chance to say that preventive cardiology isn’t just ‘set it and forget it’.”
C. Noel Bairey Merz, MD, who coauthored the 2018 cholesterol guidelines, agreed there’s “an overexuberant focus on LDL [cholesterol] for residual risk” and highlighted a recent systematic review of statins, ezetimibe, and PCSK9 cardiovascular outcomes trials that showed very little gain from aggressively driving down LDL below 100 mg/dL, unless the patient is at extremely high risk.
“If I, as a treating cardiologist who spends a lot of time on lipids, had a patient on a high-intensity statin and they didn’t drop [their LDL cholesterol] 50% and I already had them going to cardiac rehab and they were already losing weight, would I measure apoB? Yeah, I might, to motivate them to do more or to take Vascepa,” she said.
“This study is a useful addition to a relatively important problem, which is residual risk, and really supports personalized or precision medicine,” added Bairey Merz, MD, Cedars-Sinai Medical Center, Los Angeles. “But now we have to do the work and do an intervention trial in these people and see whether these markers make a difference.”
The study was supported by Herlev and Gentofte Hospital’s Research Fund and the department of clinical biochemistry, Herlev and Gentofte Hospital, Copenhagen University Hospital. Dr. Nordestgaard has had consultancies or talks sponsored by AstraZeneca, Sanofi, Regeneron, Akcea, Amarin, Amgen, Esperion, Kowa, Novartis, Novo Nordisk, and Silence Therapeutics. All other authors, Dr. Stone, and Dr. Lloyd-Jones reported no conflicts. Dr. Merz reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
A new study shows apolipoprotein B (apoB) and non-HDL cholesterol – but not LDL cholesterol – are associated with increased risk for all-cause mortality and myocardial infarction in patients taking statins.
Moreover, apoB was a more accurate marker of all-cause mortality risk than non-HDL or LDL cholesterol and was more accurate at identifying MI risk than LDL cholesterol.
“Any patient that comes to a doctor for evaluation, if statin treatment is sufficient, the doctor should look not only at LDL cholesterol but HDL cholesterol and apoB, if its available – that is the take-home message,” senior author Børge Grønne Nordestgaard, MD, DMSC, University of Copenhagen, said in an interview.
The findings are very relevant to clinical practice because international guidelines focus on LDL cholesterol and “many doctors are brainwashed that that is the only thing they should look at, just to keep LDL cholesterol down,” he said. “I’ve worked for years with triglyceride lipoproteins, what I call remnant cholesterol, and I think that the risk is very high also when you have high remnant cholesterol.”
Previous work has shown that apoB and non-HDL cholesterol better reflect atherosclerotic cardiovascular disease risk than LDL cholesterol. This is the first study, however, to show that elevated apoB and non-HDL cholesterol are associated with a higher risk for all-cause death in statin-treated patients with low LDL cholesterol, Dr. Nordestgaard noted.
The investigators compared outcomes among 13,015 statin-treated participants in the Copenhagen General Population Study using median baseline values of 92 mg/dL for apoB, 3.1 mmol/L (120 mg/dL) for non-HDL cholesterol, and 2.3 mmol/L (89 mg/dL) for LDL cholesterol. Over a median follow-up of 8 years, there were 2,499 deaths and 537 MIs.
As reported in the Journal of the American College of Cardiology, discordant apoB above the median with LDL cholesterol below was associated with a 21% increased risk for all-cause mortality (hazard ratio, 1.21; 95% confidence interval, 1.07-1.36) and 49% increased risk for MI (HR, 1.49; 95% CI, 1.15-1.92), compared with concordant apoB and LDL cholesterol below the medians.
Similar results were found for discordant non-HDL cholesterol above the median with low LDL cholesterol for all-cause mortality (HR, 1.18; 95% CI, 1.02-1.36) and MI (1.78; 95% CI, 1.35-2.34).
No such associations with mortality or MI were observed when LDL cholesterol was above the median and apoB or non-HDL below.
Additional analyses showed that high apoB with low non-HDL cholesterol was associated with a higher risk for all-cause mortality (HR, 1.21; 95% CI, 1.03-1.41), whereas high non-HDL cholesterol with low apoB was associated with a lower risk (HR, 0.75; 95% CI, 0.62-0.92).
Current guidelines define apoB greater than 130 mg/dL as a risk modifier in patients not using statins but, the authors wrote, “based on our results, the threshold for apoB as a risk modifier in statin-treated patients should be closer to 92 mg/dL than to 130 mg/dL.”
In an accompanying editorial, Neil J. Stone, MD, and Donald Lloyd-Jones, MD, both from Northwestern University, Chicago, said that American and European guidelines acknowledge the usefulness of apoB and non-HDL cholesterol in their risk algorithms and as possible targets to indicate efficacy, but don’t give a strong recommendation for apoB to assess residual risk.
“This paper suggests that, in the next iteration, we’ve got to give a stronger thought to measuring apoB for residual risk in those with secondary prevention,” Dr. Stone, vice chair of the 2018 American Heart Association/ACC cholesterol guidelines, said in an interview.
“The whole part of the guidelines was not to focus on any one number but to focus on the clinical risk as a whole,” he said. “You can enlarge your understanding of the patient by looking at their non-HDL, which you have anyway, and in certain circumstances, for example, people with metabolic syndrome, diabetes, obesity, or high triglycerides, those people might very well benefit from an apoB to further understand their risk. This paper simply highlights that and, therefore, was very valuable.”
Dr. Stone and Dr. Lloyd-Jones, however, pointed out that statin use was self-reported and information was lacking on adherence, dose intensity, and the amount of LDL cholesterol lowering from baseline. LDL cholesterol levels were also above current recommendations for optimizing risk reduction. “If statin dosing and LDL [cholesterol] were not optimized already, then there may have been ‘room’ for non-HDL [cholesterol] and apoB to add value in understanding residual risk,” they wrote.
The editorialists suggested that sequential use, rather than regular use, of apoB and non-HDL cholesterol may be best and that incorporating this information may be particularly beneficial for patients with metabolic disorders and elevated triglycerides after statin therapy.
“Maybe this paper is a wake-up call that there are other markers out there that can tell you that you still have higher risk and need to tighten up lifestyle and maybe be more adherent,” Dr. Stone said. “I think this is a wonderful chance to say that preventive cardiology isn’t just ‘set it and forget it’.”
C. Noel Bairey Merz, MD, who coauthored the 2018 cholesterol guidelines, agreed there’s “an overexuberant focus on LDL [cholesterol] for residual risk” and highlighted a recent systematic review of statins, ezetimibe, and PCSK9 cardiovascular outcomes trials that showed very little gain from aggressively driving down LDL below 100 mg/dL, unless the patient is at extremely high risk.
“If I, as a treating cardiologist who spends a lot of time on lipids, had a patient on a high-intensity statin and they didn’t drop [their LDL cholesterol] 50% and I already had them going to cardiac rehab and they were already losing weight, would I measure apoB? Yeah, I might, to motivate them to do more or to take Vascepa,” she said.
“This study is a useful addition to a relatively important problem, which is residual risk, and really supports personalized or precision medicine,” added Bairey Merz, MD, Cedars-Sinai Medical Center, Los Angeles. “But now we have to do the work and do an intervention trial in these people and see whether these markers make a difference.”
The study was supported by Herlev and Gentofte Hospital’s Research Fund and the department of clinical biochemistry, Herlev and Gentofte Hospital, Copenhagen University Hospital. Dr. Nordestgaard has had consultancies or talks sponsored by AstraZeneca, Sanofi, Regeneron, Akcea, Amarin, Amgen, Esperion, Kowa, Novartis, Novo Nordisk, and Silence Therapeutics. All other authors, Dr. Stone, and Dr. Lloyd-Jones reported no conflicts. Dr. Merz reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
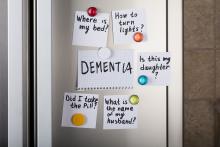
Cannabinoids promising for improving appetite, behavior in dementia
For patients with dementia, cannabinoids may be a promising intervention for treating neuropsychiatric symptoms (NPS) and the refusing of food, new research suggests.
Results of a systematic literature review, presented at the 2021 meeting of the American Association for Geriatric Psychiatry, showed that cannabinoids were associated with reduced agitation, longer sleep, and lower NPS. They were also linked to increased meal consumption and weight gain.
Refusing food is a common problem for patients with dementia, often resulting in worsening sleep, agitation, and mood, study investigator Niraj Asthana, MD, a second-year resident in the department of psychiatry, University of California, San Diego, said in an interview. Dr. Asthana noted that certain cannabinoid analogues are now used to stimulate appetite for patients undergoing chemotherapy.
Filling a treatment gap
After years of legal and other problems affecting cannabinoid research, there is renewed interest in investigating its use for patients with dementia. Early evidence suggests that cannabinoids may also be beneficial for pain, sleep, and aggression.
The researchers noted that cannabinoids may be especially valuable in areas where there are currently limited therapies, including food refusal and NPS.
“Unfortunately, there are limited treatments available for food refusal, so we’re left with appetite stimulants and electroconvulsive therapy, and although atypical antipsychotics are commonly used to treat NPS, they’re associated with an increased risk of serious adverse events and mortality in older patients,” said Dr. Asthana.
Dr. Asthana and colleague Dan Sewell, MD, carried out a systematic literature review of relevant studies of the use of cannabinoids for dementia patients.
“We found there are lot of studies, but they’re small scale; I’d say the largest was probably about 50 patients, with most studies having 10-50 patients,” said Dr. Asthana. In part, this may be because, until very recently, research on cannabinoids was controversial.
To review the current literature on the potential applications of cannabinoids in the treatment of food refusal and NPS in dementia patients, the researchers conducted a literature review.
They identified 23 relevant studies of the use of synthetic cannabinoids, including dronabinol and nabilone, for dementia patients. These products contain tetrahydrocannabinol (THC), the main psychoactive compound in cannabis.
More research coming
Several studies showed that cannabinoid use was associated with reduced nighttime motor activity, improved sleep duration, reduced agitation, and lower Neuropsychiatric Inventory scores.
One crossover placebo-controlled trial showed an overall increase in body weight among dementia patients who took dronabinol.
This suggests there might be something to the “colloquial cultural association between cannabinoids and the munchies,” said Dr. Asthana.
Possible mechanisms for the effects on appetite may be that cannabinoids increase levels of the hormone ghrelin, which is also known as the “hunger hormone,” and decrease leptin levels, a hormone that inhibits hunger. Dr. Asthana noted that, in these studies, the dose of THC was low and that overall, cannabinoids appeared to be safe.
“We found that, at least in these small-scale studies, cannabinoid analogues are well tolerated,” possibly because of the relatively low doses of THC, said Dr. Asthana. “They generally don’t seem to have a ton of side effects; they may make people a little sleepy, which is actually good, because these patents also have a lot of trouble sleeping.”
He noted that more recent research suggests cannabidiol oil may reduce agitation by up to 40%.
“Now that cannabis is losing a lot of its stigma, both culturally and in the scientific community, you’re seeing a lot of grant applications for clinical trials,” said Dr. Asthana. “I’m excited to see what we find in the next 5-10 years.”
In a comment, Kirsten Wilkins, MD, associate professor of psychiatry, Yale University, New Haven, Conn., who is also a geriatric psychiatrist at the Veterans Affairs Connecticut Health Care System, welcomed the new research in this area.
“With limited safe and effective treatments for food refusal and neuropsychiatric symptoms of dementia, Dr. Asthana and Dr. Sewell highlight the growing body of literature suggesting cannabinoids may be a novel treatment option,” she said.
A version of this article first appeared on Medscape.com.
For patients with dementia, cannabinoids may be a promising intervention for treating neuropsychiatric symptoms (NPS) and the refusing of food, new research suggests.
Results of a systematic literature review, presented at the 2021 meeting of the American Association for Geriatric Psychiatry, showed that cannabinoids were associated with reduced agitation, longer sleep, and lower NPS. They were also linked to increased meal consumption and weight gain.
Refusing food is a common problem for patients with dementia, often resulting in worsening sleep, agitation, and mood, study investigator Niraj Asthana, MD, a second-year resident in the department of psychiatry, University of California, San Diego, said in an interview. Dr. Asthana noted that certain cannabinoid analogues are now used to stimulate appetite for patients undergoing chemotherapy.
Filling a treatment gap
After years of legal and other problems affecting cannabinoid research, there is renewed interest in investigating its use for patients with dementia. Early evidence suggests that cannabinoids may also be beneficial for pain, sleep, and aggression.
The researchers noted that cannabinoids may be especially valuable in areas where there are currently limited therapies, including food refusal and NPS.
“Unfortunately, there are limited treatments available for food refusal, so we’re left with appetite stimulants and electroconvulsive therapy, and although atypical antipsychotics are commonly used to treat NPS, they’re associated with an increased risk of serious adverse events and mortality in older patients,” said Dr. Asthana.
Dr. Asthana and colleague Dan Sewell, MD, carried out a systematic literature review of relevant studies of the use of cannabinoids for dementia patients.
“We found there are lot of studies, but they’re small scale; I’d say the largest was probably about 50 patients, with most studies having 10-50 patients,” said Dr. Asthana. In part, this may be because, until very recently, research on cannabinoids was controversial.
To review the current literature on the potential applications of cannabinoids in the treatment of food refusal and NPS in dementia patients, the researchers conducted a literature review.
They identified 23 relevant studies of the use of synthetic cannabinoids, including dronabinol and nabilone, for dementia patients. These products contain tetrahydrocannabinol (THC), the main psychoactive compound in cannabis.
More research coming
Several studies showed that cannabinoid use was associated with reduced nighttime motor activity, improved sleep duration, reduced agitation, and lower Neuropsychiatric Inventory scores.
One crossover placebo-controlled trial showed an overall increase in body weight among dementia patients who took dronabinol.
This suggests there might be something to the “colloquial cultural association between cannabinoids and the munchies,” said Dr. Asthana.
Possible mechanisms for the effects on appetite may be that cannabinoids increase levels of the hormone ghrelin, which is also known as the “hunger hormone,” and decrease leptin levels, a hormone that inhibits hunger. Dr. Asthana noted that, in these studies, the dose of THC was low and that overall, cannabinoids appeared to be safe.
“We found that, at least in these small-scale studies, cannabinoid analogues are well tolerated,” possibly because of the relatively low doses of THC, said Dr. Asthana. “They generally don’t seem to have a ton of side effects; they may make people a little sleepy, which is actually good, because these patents also have a lot of trouble sleeping.”
He noted that more recent research suggests cannabidiol oil may reduce agitation by up to 40%.
“Now that cannabis is losing a lot of its stigma, both culturally and in the scientific community, you’re seeing a lot of grant applications for clinical trials,” said Dr. Asthana. “I’m excited to see what we find in the next 5-10 years.”
In a comment, Kirsten Wilkins, MD, associate professor of psychiatry, Yale University, New Haven, Conn., who is also a geriatric psychiatrist at the Veterans Affairs Connecticut Health Care System, welcomed the new research in this area.
“With limited safe and effective treatments for food refusal and neuropsychiatric symptoms of dementia, Dr. Asthana and Dr. Sewell highlight the growing body of literature suggesting cannabinoids may be a novel treatment option,” she said.
A version of this article first appeared on Medscape.com.
For patients with dementia, cannabinoids may be a promising intervention for treating neuropsychiatric symptoms (NPS) and the refusing of food, new research suggests.
Results of a systematic literature review, presented at the 2021 meeting of the American Association for Geriatric Psychiatry, showed that cannabinoids were associated with reduced agitation, longer sleep, and lower NPS. They were also linked to increased meal consumption and weight gain.
Refusing food is a common problem for patients with dementia, often resulting in worsening sleep, agitation, and mood, study investigator Niraj Asthana, MD, a second-year resident in the department of psychiatry, University of California, San Diego, said in an interview. Dr. Asthana noted that certain cannabinoid analogues are now used to stimulate appetite for patients undergoing chemotherapy.
Filling a treatment gap
After years of legal and other problems affecting cannabinoid research, there is renewed interest in investigating its use for patients with dementia. Early evidence suggests that cannabinoids may also be beneficial for pain, sleep, and aggression.
The researchers noted that cannabinoids may be especially valuable in areas where there are currently limited therapies, including food refusal and NPS.
“Unfortunately, there are limited treatments available for food refusal, so we’re left with appetite stimulants and electroconvulsive therapy, and although atypical antipsychotics are commonly used to treat NPS, they’re associated with an increased risk of serious adverse events and mortality in older patients,” said Dr. Asthana.
Dr. Asthana and colleague Dan Sewell, MD, carried out a systematic literature review of relevant studies of the use of cannabinoids for dementia patients.
“We found there are lot of studies, but they’re small scale; I’d say the largest was probably about 50 patients, with most studies having 10-50 patients,” said Dr. Asthana. In part, this may be because, until very recently, research on cannabinoids was controversial.
To review the current literature on the potential applications of cannabinoids in the treatment of food refusal and NPS in dementia patients, the researchers conducted a literature review.
They identified 23 relevant studies of the use of synthetic cannabinoids, including dronabinol and nabilone, for dementia patients. These products contain tetrahydrocannabinol (THC), the main psychoactive compound in cannabis.
More research coming
Several studies showed that cannabinoid use was associated with reduced nighttime motor activity, improved sleep duration, reduced agitation, and lower Neuropsychiatric Inventory scores.
One crossover placebo-controlled trial showed an overall increase in body weight among dementia patients who took dronabinol.
This suggests there might be something to the “colloquial cultural association between cannabinoids and the munchies,” said Dr. Asthana.
Possible mechanisms for the effects on appetite may be that cannabinoids increase levels of the hormone ghrelin, which is also known as the “hunger hormone,” and decrease leptin levels, a hormone that inhibits hunger. Dr. Asthana noted that, in these studies, the dose of THC was low and that overall, cannabinoids appeared to be safe.
“We found that, at least in these small-scale studies, cannabinoid analogues are well tolerated,” possibly because of the relatively low doses of THC, said Dr. Asthana. “They generally don’t seem to have a ton of side effects; they may make people a little sleepy, which is actually good, because these patents also have a lot of trouble sleeping.”
He noted that more recent research suggests cannabidiol oil may reduce agitation by up to 40%.
“Now that cannabis is losing a lot of its stigma, both culturally and in the scientific community, you’re seeing a lot of grant applications for clinical trials,” said Dr. Asthana. “I’m excited to see what we find in the next 5-10 years.”
In a comment, Kirsten Wilkins, MD, associate professor of psychiatry, Yale University, New Haven, Conn., who is also a geriatric psychiatrist at the Veterans Affairs Connecticut Health Care System, welcomed the new research in this area.
“With limited safe and effective treatments for food refusal and neuropsychiatric symptoms of dementia, Dr. Asthana and Dr. Sewell highlight the growing body of literature suggesting cannabinoids may be a novel treatment option,” she said.
A version of this article first appeared on Medscape.com.
Melatonin not recommended for early-stage NSCLC
There was a hint of benefit with melatonin among patients with stage III/IV NSCLC. These patients had a hazard reduction of 25% in 5-year DFS. However, the median DFS for patients with advanced disease was the same whether they received melatonin or placebo – 18 months.
In the overall study population, melatonin had no beneficial effects on quality of life, sleep, anxiety, depression, pain, or fatigue, and it did not reduce adverse events from chemotherapy or radiation.
These results were reported in EClinicalMedicine.
“In light of the results, we do not recommend the inclusion of adjuvant melatonin for patients with early-stage NSCLC. Evidence suggests there may be a benefit for those with late-stage disease,” the authors wrote. “However, because of the mixed findings observed, we recommend a follow-up randomized, controlled trial involving a larger population focusing on later-stage resected lung cancer to clarify these results.”
“I would very much like to pursue another controlled study of melatonin specifically in a group of late-stage lung cancer and possibly in other more advanced cancer types,” said lead author Dugald Seely, ND, of the Canadian College of Naturopathic Medicine in Toronto.
Study rationale and design
Melatonin has shown promise for treating patients with lung cancer, Dr. Seely and colleagues noted. Melatonin is often recommended by naturopathic doctors following lung cancer surgery, but until now there was no high-level evidence regarding the practice.
For their study, Dr. Seely and colleagues evaluated 709 patients who had undergone NSCLC resection. The patients were randomized to receive placebo (n = 353) or melatonin (n = 356) 1 hour before bedtime for 1 year. A 20-mg melatonin dose was used, which is common in clinical practice and research.
The study arms were well matched, with no “clinically meaningful” differences in demographics, surgery type, cancer type, stage of cancer, or preoperative comorbidities, according to the researchers.
The mean age in both treatment arms was 67 years. Overall, 134 participants received adjuvant chemotherapy (66 melatonin, 68 placebo), and 43 had adjuvant radiation (22 melatonin, 21 placebo).
Results
For 2-year DFS, melatonin showed an adjusted relative risk of 1.01 (95% confidence interval, 0.83-1.22; P = .94) versus placebo. The adjusted relative risk in the per-protocol analysis was 1.12 (95% CI, 0.96-1.32; P = .14.)
At 5 years, the median DFS was not reached in either treatment arm. Melatonin showed a hazard ratio of 0.97 (95% CI, 0.86-1.09; P = .84) for 5-year DFS.
Among patients with stage I-II NSCLC, the median DFS was not reached at 5 years in either treatment arm. Among patients with stage III-IV NSCLC, the median DFS was 18 months in both arms.
Melatonin showed a hazard ratio of 0.97 (95% CI, 0.85-1.11; P = .66) in patients with early-stage NSCLC and a hazard reduction of 25% (HR, 0.75; 95% CI, 0.61-0.92; P = .005) in patients with late-stage NSCLC.
For the entire cohort, there were no significant differences between treatment arms in the number, severity, or seriousness of adverse events. Likewise, there were no significant differences between the treatment arms with regard to fatigue, quality of life, or sleep at 1 or 2 years.
Dr. Seely said the most surprising thing about this study was that melatonin didn’t help with sleep.
“Since initiation of the trial, my thinking on the right dose of melatonin to support sleep has changed. Clinically, I see extended-release and, indeed, lower doses to be more effective than 20 mg nightly,” he noted.
Dr. Seely and colleagues also assessed proposed mechanisms for melatonin’s possible benefit in NSCLC but found no effect on natural killer cell cytotoxicity or phenotype and no effect on blood levels of inflammatory cytokines in a substudy of 92 patients.
This research was funded by the Lotte and John Hecht Memorial Foundation and the Gateway for Cancer Research Foundation. The researchers had no relevant disclosures.
There was a hint of benefit with melatonin among patients with stage III/IV NSCLC. These patients had a hazard reduction of 25% in 5-year DFS. However, the median DFS for patients with advanced disease was the same whether they received melatonin or placebo – 18 months.
In the overall study population, melatonin had no beneficial effects on quality of life, sleep, anxiety, depression, pain, or fatigue, and it did not reduce adverse events from chemotherapy or radiation.
These results were reported in EClinicalMedicine.
“In light of the results, we do not recommend the inclusion of adjuvant melatonin for patients with early-stage NSCLC. Evidence suggests there may be a benefit for those with late-stage disease,” the authors wrote. “However, because of the mixed findings observed, we recommend a follow-up randomized, controlled trial involving a larger population focusing on later-stage resected lung cancer to clarify these results.”
“I would very much like to pursue another controlled study of melatonin specifically in a group of late-stage lung cancer and possibly in other more advanced cancer types,” said lead author Dugald Seely, ND, of the Canadian College of Naturopathic Medicine in Toronto.
Study rationale and design
Melatonin has shown promise for treating patients with lung cancer, Dr. Seely and colleagues noted. Melatonin is often recommended by naturopathic doctors following lung cancer surgery, but until now there was no high-level evidence regarding the practice.
For their study, Dr. Seely and colleagues evaluated 709 patients who had undergone NSCLC resection. The patients were randomized to receive placebo (n = 353) or melatonin (n = 356) 1 hour before bedtime for 1 year. A 20-mg melatonin dose was used, which is common in clinical practice and research.
The study arms were well matched, with no “clinically meaningful” differences in demographics, surgery type, cancer type, stage of cancer, or preoperative comorbidities, according to the researchers.
The mean age in both treatment arms was 67 years. Overall, 134 participants received adjuvant chemotherapy (66 melatonin, 68 placebo), and 43 had adjuvant radiation (22 melatonin, 21 placebo).
Results
For 2-year DFS, melatonin showed an adjusted relative risk of 1.01 (95% confidence interval, 0.83-1.22; P = .94) versus placebo. The adjusted relative risk in the per-protocol analysis was 1.12 (95% CI, 0.96-1.32; P = .14.)
At 5 years, the median DFS was not reached in either treatment arm. Melatonin showed a hazard ratio of 0.97 (95% CI, 0.86-1.09; P = .84) for 5-year DFS.
Among patients with stage I-II NSCLC, the median DFS was not reached at 5 years in either treatment arm. Among patients with stage III-IV NSCLC, the median DFS was 18 months in both arms.
Melatonin showed a hazard ratio of 0.97 (95% CI, 0.85-1.11; P = .66) in patients with early-stage NSCLC and a hazard reduction of 25% (HR, 0.75; 95% CI, 0.61-0.92; P = .005) in patients with late-stage NSCLC.
For the entire cohort, there were no significant differences between treatment arms in the number, severity, or seriousness of adverse events. Likewise, there were no significant differences between the treatment arms with regard to fatigue, quality of life, or sleep at 1 or 2 years.
Dr. Seely said the most surprising thing about this study was that melatonin didn’t help with sleep.
“Since initiation of the trial, my thinking on the right dose of melatonin to support sleep has changed. Clinically, I see extended-release and, indeed, lower doses to be more effective than 20 mg nightly,” he noted.
Dr. Seely and colleagues also assessed proposed mechanisms for melatonin’s possible benefit in NSCLC but found no effect on natural killer cell cytotoxicity or phenotype and no effect on blood levels of inflammatory cytokines in a substudy of 92 patients.
This research was funded by the Lotte and John Hecht Memorial Foundation and the Gateway for Cancer Research Foundation. The researchers had no relevant disclosures.
There was a hint of benefit with melatonin among patients with stage III/IV NSCLC. These patients had a hazard reduction of 25% in 5-year DFS. However, the median DFS for patients with advanced disease was the same whether they received melatonin or placebo – 18 months.
In the overall study population, melatonin had no beneficial effects on quality of life, sleep, anxiety, depression, pain, or fatigue, and it did not reduce adverse events from chemotherapy or radiation.
These results were reported in EClinicalMedicine.
“In light of the results, we do not recommend the inclusion of adjuvant melatonin for patients with early-stage NSCLC. Evidence suggests there may be a benefit for those with late-stage disease,” the authors wrote. “However, because of the mixed findings observed, we recommend a follow-up randomized, controlled trial involving a larger population focusing on later-stage resected lung cancer to clarify these results.”
“I would very much like to pursue another controlled study of melatonin specifically in a group of late-stage lung cancer and possibly in other more advanced cancer types,” said lead author Dugald Seely, ND, of the Canadian College of Naturopathic Medicine in Toronto.
Study rationale and design
Melatonin has shown promise for treating patients with lung cancer, Dr. Seely and colleagues noted. Melatonin is often recommended by naturopathic doctors following lung cancer surgery, but until now there was no high-level evidence regarding the practice.
For their study, Dr. Seely and colleagues evaluated 709 patients who had undergone NSCLC resection. The patients were randomized to receive placebo (n = 353) or melatonin (n = 356) 1 hour before bedtime for 1 year. A 20-mg melatonin dose was used, which is common in clinical practice and research.
The study arms were well matched, with no “clinically meaningful” differences in demographics, surgery type, cancer type, stage of cancer, or preoperative comorbidities, according to the researchers.
The mean age in both treatment arms was 67 years. Overall, 134 participants received adjuvant chemotherapy (66 melatonin, 68 placebo), and 43 had adjuvant radiation (22 melatonin, 21 placebo).
Results
For 2-year DFS, melatonin showed an adjusted relative risk of 1.01 (95% confidence interval, 0.83-1.22; P = .94) versus placebo. The adjusted relative risk in the per-protocol analysis was 1.12 (95% CI, 0.96-1.32; P = .14.)
At 5 years, the median DFS was not reached in either treatment arm. Melatonin showed a hazard ratio of 0.97 (95% CI, 0.86-1.09; P = .84) for 5-year DFS.
Among patients with stage I-II NSCLC, the median DFS was not reached at 5 years in either treatment arm. Among patients with stage III-IV NSCLC, the median DFS was 18 months in both arms.
Melatonin showed a hazard ratio of 0.97 (95% CI, 0.85-1.11; P = .66) in patients with early-stage NSCLC and a hazard reduction of 25% (HR, 0.75; 95% CI, 0.61-0.92; P = .005) in patients with late-stage NSCLC.
For the entire cohort, there were no significant differences between treatment arms in the number, severity, or seriousness of adverse events. Likewise, there were no significant differences between the treatment arms with regard to fatigue, quality of life, or sleep at 1 or 2 years.
Dr. Seely said the most surprising thing about this study was that melatonin didn’t help with sleep.
“Since initiation of the trial, my thinking on the right dose of melatonin to support sleep has changed. Clinically, I see extended-release and, indeed, lower doses to be more effective than 20 mg nightly,” he noted.
Dr. Seely and colleagues also assessed proposed mechanisms for melatonin’s possible benefit in NSCLC but found no effect on natural killer cell cytotoxicity or phenotype and no effect on blood levels of inflammatory cytokines in a substudy of 92 patients.
This research was funded by the Lotte and John Hecht Memorial Foundation and the Gateway for Cancer Research Foundation. The researchers had no relevant disclosures.
FROM ECLINICALMEDICINE
Blood pressure meds tied to increased schizophrenia risk
ACE inhibitors may be associated with an increased risk for schizophrenia and may affect psychiatric symptoms, new research suggests.
Investigators found individuals who carry a genetic variant associated with lower levels of the ACE gene and protein have increased liability to schizophrenia, suggesting that drugs that lower ACE levels or activity may do the same.
“Our findings warrant further investigation into the role of ACE in schizophrenia and closer monitoring by clinicians of individuals, especially those with schizophrenia, who may be on medication that lower ACE activity, such as ACE inhibitors,” Sonia Shah, PhD, Institute for Biomedical Sciences, University of Queensland, Brisbane, Australia, said in an interview.
The study was published online March 10, 2021, in JAMA Psychiatry.
Antihypertensives and mental illness
Hypertension is common in patients with psychiatric disorders and observational studies have reported associations between antihypertensive medication and these disorders, although the findings have been mixed.
Dr. Shah and colleagues estimated the potential of different antihypertensive drug classes on schizophrenia, bipolar disorder, and major depressive disorder.
In a two-sample Mendelian randomization study, they evaluated ties between a single-nucleotide variant and drug-target gene expression derived from expression quantitative trait loci data in blood (sample 1) and the SNV disease association from published case-control, genomewide association studies (sample 2).
The analyses included 40,675 patients with schizophrenia and 64,643 controls; 20,352 with bipolar disorder and 31,358 controls; and 135,458 with major depressive disorder and 344,901 controls.
The major finding was that a one standard deviation–lower expression of the ACE gene in blood was associated with lower systolic blood pressure of 4.0 mm Hg (95% confidence interval, 2.7-5.3), but also an increased risk of schizophrenia (odds ratio, 1.75; 95% CI, 1.28-2.38).
Could ACE inhibitors worsen symptoms or trigger episodes?
In their article, the researchers noted that, in most patients, onset of schizophrenia occurs in late adolescence or early adult life, ruling out ACE inhibitor treatment as a potential causal factor for most cases.
“However, if lower ACE levels play a causal role for schizophrenia risk, it would be reasonable to hypothesize that further lowering of ACE activity in existing patients could worsen symptoms or trigger a new episode,” they wrote.
Dr. Shah emphasized that evidence from genetic analyses alone is “not sufficient to justify changes in prescription guidelines.”
“Patients should not stop taking these medications if they are effective at controlling their blood pressure and they don’t suffer any adverse effects. But it would be reasonable to encourage greater pharmacovigilance,” she said in an interview.
“One way in which we are hoping to follow up these findings,” said Dr. Shah, “is to access electronic health record data for millions of individuals to investigate if there is evidence of increased rates of psychotic episodes in individuals who use ACE inhibitors, compared to other classes of blood pressure–lowering medication.”
Caution warranted
Reached for comment, Timothy Sullivan, MD, chair of psychiatry and behavioral sciences at Staten Island University Hospital in New York, noted that this is an “extremely complicated” study and urged caution in interpreting the results.
“Since most people develop schizophrenia earlier in life, before they usually develop problems with blood pressure, it’s not so much that these drugs might cause schizophrenia,” Dr. Sullivan said.
“But because of their effects on this particular gene, there’s a possibility that they might worsen symptoms or in somebody with borderline risk might cause them to develop symptoms later in life. This may apply to a relatively small number of people who develop symptoms of schizophrenia in their 40s and beyond,” he added.
That’s where “pharmacovigilance” comes into play, Dr. Sullivan said. “In other words, that they otherwise wouldn’t experience?”
Support for the study was provided by the National Health and Medical Research Council (Australia) and U.S. National Institute for Mental Health. Dr. Shah and Dr. Sullivan disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ACE inhibitors may be associated with an increased risk for schizophrenia and may affect psychiatric symptoms, new research suggests.
Investigators found individuals who carry a genetic variant associated with lower levels of the ACE gene and protein have increased liability to schizophrenia, suggesting that drugs that lower ACE levels or activity may do the same.
“Our findings warrant further investigation into the role of ACE in schizophrenia and closer monitoring by clinicians of individuals, especially those with schizophrenia, who may be on medication that lower ACE activity, such as ACE inhibitors,” Sonia Shah, PhD, Institute for Biomedical Sciences, University of Queensland, Brisbane, Australia, said in an interview.
The study was published online March 10, 2021, in JAMA Psychiatry.
Antihypertensives and mental illness
Hypertension is common in patients with psychiatric disorders and observational studies have reported associations between antihypertensive medication and these disorders, although the findings have been mixed.
Dr. Shah and colleagues estimated the potential of different antihypertensive drug classes on schizophrenia, bipolar disorder, and major depressive disorder.
In a two-sample Mendelian randomization study, they evaluated ties between a single-nucleotide variant and drug-target gene expression derived from expression quantitative trait loci data in blood (sample 1) and the SNV disease association from published case-control, genomewide association studies (sample 2).
The analyses included 40,675 patients with schizophrenia and 64,643 controls; 20,352 with bipolar disorder and 31,358 controls; and 135,458 with major depressive disorder and 344,901 controls.
The major finding was that a one standard deviation–lower expression of the ACE gene in blood was associated with lower systolic blood pressure of 4.0 mm Hg (95% confidence interval, 2.7-5.3), but also an increased risk of schizophrenia (odds ratio, 1.75; 95% CI, 1.28-2.38).
Could ACE inhibitors worsen symptoms or trigger episodes?
In their article, the researchers noted that, in most patients, onset of schizophrenia occurs in late adolescence or early adult life, ruling out ACE inhibitor treatment as a potential causal factor for most cases.
“However, if lower ACE levels play a causal role for schizophrenia risk, it would be reasonable to hypothesize that further lowering of ACE activity in existing patients could worsen symptoms or trigger a new episode,” they wrote.
Dr. Shah emphasized that evidence from genetic analyses alone is “not sufficient to justify changes in prescription guidelines.”
“Patients should not stop taking these medications if they are effective at controlling their blood pressure and they don’t suffer any adverse effects. But it would be reasonable to encourage greater pharmacovigilance,” she said in an interview.
“One way in which we are hoping to follow up these findings,” said Dr. Shah, “is to access electronic health record data for millions of individuals to investigate if there is evidence of increased rates of psychotic episodes in individuals who use ACE inhibitors, compared to other classes of blood pressure–lowering medication.”
Caution warranted
Reached for comment, Timothy Sullivan, MD, chair of psychiatry and behavioral sciences at Staten Island University Hospital in New York, noted that this is an “extremely complicated” study and urged caution in interpreting the results.
“Since most people develop schizophrenia earlier in life, before they usually develop problems with blood pressure, it’s not so much that these drugs might cause schizophrenia,” Dr. Sullivan said.
“But because of their effects on this particular gene, there’s a possibility that they might worsen symptoms or in somebody with borderline risk might cause them to develop symptoms later in life. This may apply to a relatively small number of people who develop symptoms of schizophrenia in their 40s and beyond,” he added.
That’s where “pharmacovigilance” comes into play, Dr. Sullivan said. “In other words, that they otherwise wouldn’t experience?”
Support for the study was provided by the National Health and Medical Research Council (Australia) and U.S. National Institute for Mental Health. Dr. Shah and Dr. Sullivan disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ACE inhibitors may be associated with an increased risk for schizophrenia and may affect psychiatric symptoms, new research suggests.
Investigators found individuals who carry a genetic variant associated with lower levels of the ACE gene and protein have increased liability to schizophrenia, suggesting that drugs that lower ACE levels or activity may do the same.
“Our findings warrant further investigation into the role of ACE in schizophrenia and closer monitoring by clinicians of individuals, especially those with schizophrenia, who may be on medication that lower ACE activity, such as ACE inhibitors,” Sonia Shah, PhD, Institute for Biomedical Sciences, University of Queensland, Brisbane, Australia, said in an interview.
The study was published online March 10, 2021, in JAMA Psychiatry.
Antihypertensives and mental illness
Hypertension is common in patients with psychiatric disorders and observational studies have reported associations between antihypertensive medication and these disorders, although the findings have been mixed.
Dr. Shah and colleagues estimated the potential of different antihypertensive drug classes on schizophrenia, bipolar disorder, and major depressive disorder.
In a two-sample Mendelian randomization study, they evaluated ties between a single-nucleotide variant and drug-target gene expression derived from expression quantitative trait loci data in blood (sample 1) and the SNV disease association from published case-control, genomewide association studies (sample 2).
The analyses included 40,675 patients with schizophrenia and 64,643 controls; 20,352 with bipolar disorder and 31,358 controls; and 135,458 with major depressive disorder and 344,901 controls.
The major finding was that a one standard deviation–lower expression of the ACE gene in blood was associated with lower systolic blood pressure of 4.0 mm Hg (95% confidence interval, 2.7-5.3), but also an increased risk of schizophrenia (odds ratio, 1.75; 95% CI, 1.28-2.38).
Could ACE inhibitors worsen symptoms or trigger episodes?
In their article, the researchers noted that, in most patients, onset of schizophrenia occurs in late adolescence or early adult life, ruling out ACE inhibitor treatment as a potential causal factor for most cases.
“However, if lower ACE levels play a causal role for schizophrenia risk, it would be reasonable to hypothesize that further lowering of ACE activity in existing patients could worsen symptoms or trigger a new episode,” they wrote.
Dr. Shah emphasized that evidence from genetic analyses alone is “not sufficient to justify changes in prescription guidelines.”
“Patients should not stop taking these medications if they are effective at controlling their blood pressure and they don’t suffer any adverse effects. But it would be reasonable to encourage greater pharmacovigilance,” she said in an interview.
“One way in which we are hoping to follow up these findings,” said Dr. Shah, “is to access electronic health record data for millions of individuals to investigate if there is evidence of increased rates of psychotic episodes in individuals who use ACE inhibitors, compared to other classes of blood pressure–lowering medication.”
Caution warranted
Reached for comment, Timothy Sullivan, MD, chair of psychiatry and behavioral sciences at Staten Island University Hospital in New York, noted that this is an “extremely complicated” study and urged caution in interpreting the results.
“Since most people develop schizophrenia earlier in life, before they usually develop problems with blood pressure, it’s not so much that these drugs might cause schizophrenia,” Dr. Sullivan said.
“But because of their effects on this particular gene, there’s a possibility that they might worsen symptoms or in somebody with borderline risk might cause them to develop symptoms later in life. This may apply to a relatively small number of people who develop symptoms of schizophrenia in their 40s and beyond,” he added.
That’s where “pharmacovigilance” comes into play, Dr. Sullivan said. “In other words, that they otherwise wouldn’t experience?”
Support for the study was provided by the National Health and Medical Research Council (Australia) and U.S. National Institute for Mental Health. Dr. Shah and Dr. Sullivan disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Diabetes prevention moves toward reality as studies published
Two newly published studies highlight recent success toward delaying the onset of type 1 diabetes in people at high risk and slowing progression in those with recent onset of the condition.
Both studies were initially presented in June 2020 at the annual scientific sessions of the American Diabetes Association and reported by this news organization at the time.
As yet, neither of the two strategies – preserving insulin-producing pancreatic beta-cell function soon after diagnosis or delaying type 1 diabetes onset in those at high risk – represent a cure or certain disease prevention.
However, both can potentially lead to better long-term glycemic control with less hypoglycemia and a lower risk for diabetes-related complications.
Combination treatment prolongs beta-cell function in new-onset disease
The first study, entitled, “Anti–interleukin-21 antibody and liraglutide for the preservation of beta-cell function in adults with recent-onset type 1 diabetes,” was published online March 1, 2021, in The Lancet Diabetes & Endocrinology by Matthias von Herrath, MD, of Novo Nordisk, Søborg, Denmark, and colleagues.
The randomized, placebo-controlled, double-blind, phase 2 combination treatment trial involved 308 individuals aged 18-45 years who had been diagnosed with type 1 diabetes in the previous 20 weeks and still had residual beta-cell function.
Patients were randomized with 77 per group to receive monoclonal anti-IL-21 plus liraglutide, anti-IL-21 alone, liraglutide alone, or placebo. The antibody was given intravenously every 6 weeks and liraglutide or matching placebo were self-administered by daily injections.
Compared with placebo (ratio to baseline, 0.61; 39% decrease), the decrease in mixed meal tolerance test stimulated C-peptide concentration from baseline to week 54 – the primary outcome – was significantly smaller with combination treatment (0.90, 10% decrease; estimated treatment ratio, 1.48; P = .0017), but not with anti-IL-21 alone (1.23; P = .093) or liraglutide alone (1.12; P = .38).
Despite greater insulin use in the placebo group, the decrease in hemoglobin A1c (a key secondary outcome) at week 54 was greater with all active treatments (–0.50 percentage points) than with placebo (–0.10 percentage points), although the differences versus placebo were not significant.
“The combination of anti-IL-21 and liraglutide could preserve beta-cell function in recently diagnosed type 1 diabetes,” the researchers said.
“These results suggest that this combination has the potential to offer a novel and valuable disease-modifying therapy for patients with recently diagnosed type 1 diabetes. However, the efficacy and safety need to be further investigated in a phase 3 program,” Dr. von Herrath and colleagues concluded.
Teplizumab: 3-year data continue to show benefit
The other study looked at delaying the onset of type 1 diabetes. Entitled, “Teplizumab improves and stabilizes beta cell function in antibody-positive high-risk individuals,” the article was published online March 3, 2021, in Science Translational Medicine by Emily K. Sims, MD, of the department of pediatrics, Indiana University, Indianapolis, and colleagues.
This trial of the anti-CD3 monoclonal antibody adds an additional year of follow-up to the “game-changer” 2-year data reported in 2019.
Among the 76 individuals aged 8-49 years who were positive for two or more type 1 diabetes–related autoantibodies, 50% of those randomized to a single 14-day infusion course of teplizumab remained diabetes free at a median follow-up of 923 days, compared with only 22% of those who received placebo infusions (hazard ratio, 0.457; P = .01).
The teplizumab group had a greater average C-peptide area under the curve, compared with placebo, reflecting improved beta-cell function (1.96 vs 1.68 pmol/mL; P = .006).
C-peptide levels declined over time in the placebo group but stabilized in those receiving teplizumab (P = .0015).
“It is very encouraging to see that a single course of teplizumab delayed insulin dependence in this high-risk population for approximately 3 years versus placebo,” said Frank Martin, PhD, JDRF director of research at Provention Bio, which is developing teplizumab.
“These exciting results have been made possible by the unwavering efforts of TrialNet and Provention Bio. Teplizumab, if approved by the FDA, could positively change the course of disease development for people at risk of developing T1D and their standard of care,” he concluded.
The teplizumab study was funded by TrialNet. Dr. von Herrath is an employee of Novo Nordisk, which funded the study involving its drug liraglutide. Dr. Sims reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Two newly published studies highlight recent success toward delaying the onset of type 1 diabetes in people at high risk and slowing progression in those with recent onset of the condition.
Both studies were initially presented in June 2020 at the annual scientific sessions of the American Diabetes Association and reported by this news organization at the time.
As yet, neither of the two strategies – preserving insulin-producing pancreatic beta-cell function soon after diagnosis or delaying type 1 diabetes onset in those at high risk – represent a cure or certain disease prevention.
However, both can potentially lead to better long-term glycemic control with less hypoglycemia and a lower risk for diabetes-related complications.
Combination treatment prolongs beta-cell function in new-onset disease
The first study, entitled, “Anti–interleukin-21 antibody and liraglutide for the preservation of beta-cell function in adults with recent-onset type 1 diabetes,” was published online March 1, 2021, in The Lancet Diabetes & Endocrinology by Matthias von Herrath, MD, of Novo Nordisk, Søborg, Denmark, and colleagues.
The randomized, placebo-controlled, double-blind, phase 2 combination treatment trial involved 308 individuals aged 18-45 years who had been diagnosed with type 1 diabetes in the previous 20 weeks and still had residual beta-cell function.
Patients were randomized with 77 per group to receive monoclonal anti-IL-21 plus liraglutide, anti-IL-21 alone, liraglutide alone, or placebo. The antibody was given intravenously every 6 weeks and liraglutide or matching placebo were self-administered by daily injections.
Compared with placebo (ratio to baseline, 0.61; 39% decrease), the decrease in mixed meal tolerance test stimulated C-peptide concentration from baseline to week 54 – the primary outcome – was significantly smaller with combination treatment (0.90, 10% decrease; estimated treatment ratio, 1.48; P = .0017), but not with anti-IL-21 alone (1.23; P = .093) or liraglutide alone (1.12; P = .38).
Despite greater insulin use in the placebo group, the decrease in hemoglobin A1c (a key secondary outcome) at week 54 was greater with all active treatments (–0.50 percentage points) than with placebo (–0.10 percentage points), although the differences versus placebo were not significant.
“The combination of anti-IL-21 and liraglutide could preserve beta-cell function in recently diagnosed type 1 diabetes,” the researchers said.
“These results suggest that this combination has the potential to offer a novel and valuable disease-modifying therapy for patients with recently diagnosed type 1 diabetes. However, the efficacy and safety need to be further investigated in a phase 3 program,” Dr. von Herrath and colleagues concluded.
Teplizumab: 3-year data continue to show benefit
The other study looked at delaying the onset of type 1 diabetes. Entitled, “Teplizumab improves and stabilizes beta cell function in antibody-positive high-risk individuals,” the article was published online March 3, 2021, in Science Translational Medicine by Emily K. Sims, MD, of the department of pediatrics, Indiana University, Indianapolis, and colleagues.
This trial of the anti-CD3 monoclonal antibody adds an additional year of follow-up to the “game-changer” 2-year data reported in 2019.
Among the 76 individuals aged 8-49 years who were positive for two or more type 1 diabetes–related autoantibodies, 50% of those randomized to a single 14-day infusion course of teplizumab remained diabetes free at a median follow-up of 923 days, compared with only 22% of those who received placebo infusions (hazard ratio, 0.457; P = .01).
The teplizumab group had a greater average C-peptide area under the curve, compared with placebo, reflecting improved beta-cell function (1.96 vs 1.68 pmol/mL; P = .006).
C-peptide levels declined over time in the placebo group but stabilized in those receiving teplizumab (P = .0015).
“It is very encouraging to see that a single course of teplizumab delayed insulin dependence in this high-risk population for approximately 3 years versus placebo,” said Frank Martin, PhD, JDRF director of research at Provention Bio, which is developing teplizumab.
“These exciting results have been made possible by the unwavering efforts of TrialNet and Provention Bio. Teplizumab, if approved by the FDA, could positively change the course of disease development for people at risk of developing T1D and their standard of care,” he concluded.
The teplizumab study was funded by TrialNet. Dr. von Herrath is an employee of Novo Nordisk, which funded the study involving its drug liraglutide. Dr. Sims reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Two newly published studies highlight recent success toward delaying the onset of type 1 diabetes in people at high risk and slowing progression in those with recent onset of the condition.
Both studies were initially presented in June 2020 at the annual scientific sessions of the American Diabetes Association and reported by this news organization at the time.
As yet, neither of the two strategies – preserving insulin-producing pancreatic beta-cell function soon after diagnosis or delaying type 1 diabetes onset in those at high risk – represent a cure or certain disease prevention.
However, both can potentially lead to better long-term glycemic control with less hypoglycemia and a lower risk for diabetes-related complications.
Combination treatment prolongs beta-cell function in new-onset disease
The first study, entitled, “Anti–interleukin-21 antibody and liraglutide for the preservation of beta-cell function in adults with recent-onset type 1 diabetes,” was published online March 1, 2021, in The Lancet Diabetes & Endocrinology by Matthias von Herrath, MD, of Novo Nordisk, Søborg, Denmark, and colleagues.
The randomized, placebo-controlled, double-blind, phase 2 combination treatment trial involved 308 individuals aged 18-45 years who had been diagnosed with type 1 diabetes in the previous 20 weeks and still had residual beta-cell function.
Patients were randomized with 77 per group to receive monoclonal anti-IL-21 plus liraglutide, anti-IL-21 alone, liraglutide alone, or placebo. The antibody was given intravenously every 6 weeks and liraglutide or matching placebo were self-administered by daily injections.
Compared with placebo (ratio to baseline, 0.61; 39% decrease), the decrease in mixed meal tolerance test stimulated C-peptide concentration from baseline to week 54 – the primary outcome – was significantly smaller with combination treatment (0.90, 10% decrease; estimated treatment ratio, 1.48; P = .0017), but not with anti-IL-21 alone (1.23; P = .093) or liraglutide alone (1.12; P = .38).
Despite greater insulin use in the placebo group, the decrease in hemoglobin A1c (a key secondary outcome) at week 54 was greater with all active treatments (–0.50 percentage points) than with placebo (–0.10 percentage points), although the differences versus placebo were not significant.
“The combination of anti-IL-21 and liraglutide could preserve beta-cell function in recently diagnosed type 1 diabetes,” the researchers said.
“These results suggest that this combination has the potential to offer a novel and valuable disease-modifying therapy for patients with recently diagnosed type 1 diabetes. However, the efficacy and safety need to be further investigated in a phase 3 program,” Dr. von Herrath and colleagues concluded.
Teplizumab: 3-year data continue to show benefit
The other study looked at delaying the onset of type 1 diabetes. Entitled, “Teplizumab improves and stabilizes beta cell function in antibody-positive high-risk individuals,” the article was published online March 3, 2021, in Science Translational Medicine by Emily K. Sims, MD, of the department of pediatrics, Indiana University, Indianapolis, and colleagues.
This trial of the anti-CD3 monoclonal antibody adds an additional year of follow-up to the “game-changer” 2-year data reported in 2019.
Among the 76 individuals aged 8-49 years who were positive for two or more type 1 diabetes–related autoantibodies, 50% of those randomized to a single 14-day infusion course of teplizumab remained diabetes free at a median follow-up of 923 days, compared with only 22% of those who received placebo infusions (hazard ratio, 0.457; P = .01).
The teplizumab group had a greater average C-peptide area under the curve, compared with placebo, reflecting improved beta-cell function (1.96 vs 1.68 pmol/mL; P = .006).
C-peptide levels declined over time in the placebo group but stabilized in those receiving teplizumab (P = .0015).
“It is very encouraging to see that a single course of teplizumab delayed insulin dependence in this high-risk population for approximately 3 years versus placebo,” said Frank Martin, PhD, JDRF director of research at Provention Bio, which is developing teplizumab.
“These exciting results have been made possible by the unwavering efforts of TrialNet and Provention Bio. Teplizumab, if approved by the FDA, could positively change the course of disease development for people at risk of developing T1D and their standard of care,” he concluded.
The teplizumab study was funded by TrialNet. Dr. von Herrath is an employee of Novo Nordisk, which funded the study involving its drug liraglutide. Dr. Sims reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
1 in 3 on levothyroxine take meds that interfere with thyroid tests
, potentially compromising treatment decisions, new research shows.
“We know from previous studies that thyroid hormone use is common in older adults and that there are a multitude of medications that can interfere with thyroid function tests in different ways,” senior author Maria Papaleontiou, MD, told Medscape Medical News.
“However, to our knowledge, the extent of concurrent use of thyroid hormone and interfering medications in older adults, age 65 years and older, has not been previously explored,” added Dr. Papaleontiou, of the Division of Metabolism, Endocrinology and Diabetes, Department of Internal Medicine, University of Michigan, Ann Arbor.
The findings were presented as a poster during virtual ENDO 2021, the Endocrine Society’s annual meeting.
Commenting on the study, Thanh Duc Hoang, DO, an endocrinologist with the Walter Reed National Military Medical Center, in Bethesda, Md., said: “It is important for clinicians to be aware of various interactions and interferences of medications affecting the accuracy of thyroid function tests.”
“If patients are not able to discontinue the medications shortly before the bloodwork, the clinicians may consider ordering different thyroid tests or assays that avoid the interferences,” he told Medscape Medical News.
32% of patients taking meds that could interfere with tests
In evaluating data on 538,137 patients treated with thyroid hormones from the Corporate Data Warehouse of the Veterans Health Administration, spanning 2004-2017, first author Rachel Beeson, MD, and colleagues with the University of Michigan found most patients in the study were men (96.5%), White (77.1%), and had two or more comorbidities (62.6%).
Of this total, 170,261 (31.6%) patients treated with thyroid hormones, over a median follow-up of 56 months, were taking at least one drug that could potentially interfere with thyroid function tests.
Among the drugs with potential thyroid test interference, about 28% of patients were taking prednisone or prednisolone, 8% were taking amiodarone, and 1.42% were taking phenytoin. Other reported drugs that could potentially interfere included carbamazepine (0.91%), phenobarbital (0.15%), lithium (0.40%), and tamoxifen (0.11%).
Multivariate analysis showed that characteristics associated with those most likely to have concurrent medication use included non-Whites (OR, 1.18 vs Whites), Hispanic ethnicity (OR 1.11 vs non-Hispanic), female sex (OR 1.12 vs males), and presence of comorbidities (eg, Charlson-Deyo comorbidity score ≥ 2, OR, 2.47 vs score of 0).
Meanwhile, older patients age 85 years and over had a lower likelihood of concurrent medications interfering with thyroid tests (OR, 0.47 vs age 65-74 years).
The findings are concerning given the wide use of levothyroxine to treat hypothyroidism, which is the most widely prescribed drug in the United States.
“Our findings not only highlight the complexity of thyroid hormone management in older adults in the context of polypharmacy and multimorbidity, but they also draw attention to vulnerable groups for this practice, which included female patients, non-Whites, patients of Hispanic ethnicity, and patients with comorbidities,” Dr. Papaleontiou said.
Nature of interference possibilities varies
Medications or supplements can interfere with thyroid function tests in a variety of ways, she explained. “Some medications could lead to a decrease in the absorption of levothyroxine, others may affect how well the pill dissolves.”
In addition, certain medications can affect the circulation of thyroid hormone in the blood and how it binds with proteins, or they can lead to decreasing thyroid hormone levels due to a variety of interactions.
And in contrast, “What is even more challenging is that some medications or supplements may appear to affect thyroid function based on lab tests when in reality they don’t actually affect thyroid function and may lead to dose adjustments unnecessarily,” Dr. Papaleontiou noted.
Recommendations to counter interference
Current recommendations to try to counter the effects of polypharmacy on thyroid treatment include advising patients to take thyroid hormones on an empty stomach at least 30-60 minutes prior to eating for optimal absorption.
If the patient is taking medications known to interfere with absorption of thyroid hormones, the recommendation is to space those out by at least 4 hours.
“The big challenge in older adults is that many of them do experience polypharmacy, being at risk for multiple drug-drug interactions,” Dr. Papaleontiou said.
“Physicians and patients should be vigilant and communicate closely every time there is initiation of a new medication or supplement to consider whether there may be interference.”
The authors have reported no relevant financial relationships. Dr. Hoang has reported being a speaker for Acella Pharmaceuticals.
A version of this article first appeared on Medscape.com.
, potentially compromising treatment decisions, new research shows.
“We know from previous studies that thyroid hormone use is common in older adults and that there are a multitude of medications that can interfere with thyroid function tests in different ways,” senior author Maria Papaleontiou, MD, told Medscape Medical News.
“However, to our knowledge, the extent of concurrent use of thyroid hormone and interfering medications in older adults, age 65 years and older, has not been previously explored,” added Dr. Papaleontiou, of the Division of Metabolism, Endocrinology and Diabetes, Department of Internal Medicine, University of Michigan, Ann Arbor.
The findings were presented as a poster during virtual ENDO 2021, the Endocrine Society’s annual meeting.
Commenting on the study, Thanh Duc Hoang, DO, an endocrinologist with the Walter Reed National Military Medical Center, in Bethesda, Md., said: “It is important for clinicians to be aware of various interactions and interferences of medications affecting the accuracy of thyroid function tests.”
“If patients are not able to discontinue the medications shortly before the bloodwork, the clinicians may consider ordering different thyroid tests or assays that avoid the interferences,” he told Medscape Medical News.
32% of patients taking meds that could interfere with tests
In evaluating data on 538,137 patients treated with thyroid hormones from the Corporate Data Warehouse of the Veterans Health Administration, spanning 2004-2017, first author Rachel Beeson, MD, and colleagues with the University of Michigan found most patients in the study were men (96.5%), White (77.1%), and had two or more comorbidities (62.6%).
Of this total, 170,261 (31.6%) patients treated with thyroid hormones, over a median follow-up of 56 months, were taking at least one drug that could potentially interfere with thyroid function tests.
Among the drugs with potential thyroid test interference, about 28% of patients were taking prednisone or prednisolone, 8% were taking amiodarone, and 1.42% were taking phenytoin. Other reported drugs that could potentially interfere included carbamazepine (0.91%), phenobarbital (0.15%), lithium (0.40%), and tamoxifen (0.11%).
Multivariate analysis showed that characteristics associated with those most likely to have concurrent medication use included non-Whites (OR, 1.18 vs Whites), Hispanic ethnicity (OR 1.11 vs non-Hispanic), female sex (OR 1.12 vs males), and presence of comorbidities (eg, Charlson-Deyo comorbidity score ≥ 2, OR, 2.47 vs score of 0).
Meanwhile, older patients age 85 years and over had a lower likelihood of concurrent medications interfering with thyroid tests (OR, 0.47 vs age 65-74 years).
The findings are concerning given the wide use of levothyroxine to treat hypothyroidism, which is the most widely prescribed drug in the United States.
“Our findings not only highlight the complexity of thyroid hormone management in older adults in the context of polypharmacy and multimorbidity, but they also draw attention to vulnerable groups for this practice, which included female patients, non-Whites, patients of Hispanic ethnicity, and patients with comorbidities,” Dr. Papaleontiou said.
Nature of interference possibilities varies
Medications or supplements can interfere with thyroid function tests in a variety of ways, she explained. “Some medications could lead to a decrease in the absorption of levothyroxine, others may affect how well the pill dissolves.”
In addition, certain medications can affect the circulation of thyroid hormone in the blood and how it binds with proteins, or they can lead to decreasing thyroid hormone levels due to a variety of interactions.
And in contrast, “What is even more challenging is that some medications or supplements may appear to affect thyroid function based on lab tests when in reality they don’t actually affect thyroid function and may lead to dose adjustments unnecessarily,” Dr. Papaleontiou noted.
Recommendations to counter interference
Current recommendations to try to counter the effects of polypharmacy on thyroid treatment include advising patients to take thyroid hormones on an empty stomach at least 30-60 minutes prior to eating for optimal absorption.
If the patient is taking medications known to interfere with absorption of thyroid hormones, the recommendation is to space those out by at least 4 hours.
“The big challenge in older adults is that many of them do experience polypharmacy, being at risk for multiple drug-drug interactions,” Dr. Papaleontiou said.
“Physicians and patients should be vigilant and communicate closely every time there is initiation of a new medication or supplement to consider whether there may be interference.”
The authors have reported no relevant financial relationships. Dr. Hoang has reported being a speaker for Acella Pharmaceuticals.
A version of this article first appeared on Medscape.com.
, potentially compromising treatment decisions, new research shows.
“We know from previous studies that thyroid hormone use is common in older adults and that there are a multitude of medications that can interfere with thyroid function tests in different ways,” senior author Maria Papaleontiou, MD, told Medscape Medical News.
“However, to our knowledge, the extent of concurrent use of thyroid hormone and interfering medications in older adults, age 65 years and older, has not been previously explored,” added Dr. Papaleontiou, of the Division of Metabolism, Endocrinology and Diabetes, Department of Internal Medicine, University of Michigan, Ann Arbor.
The findings were presented as a poster during virtual ENDO 2021, the Endocrine Society’s annual meeting.
Commenting on the study, Thanh Duc Hoang, DO, an endocrinologist with the Walter Reed National Military Medical Center, in Bethesda, Md., said: “It is important for clinicians to be aware of various interactions and interferences of medications affecting the accuracy of thyroid function tests.”
“If patients are not able to discontinue the medications shortly before the bloodwork, the clinicians may consider ordering different thyroid tests or assays that avoid the interferences,” he told Medscape Medical News.
32% of patients taking meds that could interfere with tests
In evaluating data on 538,137 patients treated with thyroid hormones from the Corporate Data Warehouse of the Veterans Health Administration, spanning 2004-2017, first author Rachel Beeson, MD, and colleagues with the University of Michigan found most patients in the study were men (96.5%), White (77.1%), and had two or more comorbidities (62.6%).
Of this total, 170,261 (31.6%) patients treated with thyroid hormones, over a median follow-up of 56 months, were taking at least one drug that could potentially interfere with thyroid function tests.
Among the drugs with potential thyroid test interference, about 28% of patients were taking prednisone or prednisolone, 8% were taking amiodarone, and 1.42% were taking phenytoin. Other reported drugs that could potentially interfere included carbamazepine (0.91%), phenobarbital (0.15%), lithium (0.40%), and tamoxifen (0.11%).
Multivariate analysis showed that characteristics associated with those most likely to have concurrent medication use included non-Whites (OR, 1.18 vs Whites), Hispanic ethnicity (OR 1.11 vs non-Hispanic), female sex (OR 1.12 vs males), and presence of comorbidities (eg, Charlson-Deyo comorbidity score ≥ 2, OR, 2.47 vs score of 0).
Meanwhile, older patients age 85 years and over had a lower likelihood of concurrent medications interfering with thyroid tests (OR, 0.47 vs age 65-74 years).
The findings are concerning given the wide use of levothyroxine to treat hypothyroidism, which is the most widely prescribed drug in the United States.
“Our findings not only highlight the complexity of thyroid hormone management in older adults in the context of polypharmacy and multimorbidity, but they also draw attention to vulnerable groups for this practice, which included female patients, non-Whites, patients of Hispanic ethnicity, and patients with comorbidities,” Dr. Papaleontiou said.
Nature of interference possibilities varies
Medications or supplements can interfere with thyroid function tests in a variety of ways, she explained. “Some medications could lead to a decrease in the absorption of levothyroxine, others may affect how well the pill dissolves.”
In addition, certain medications can affect the circulation of thyroid hormone in the blood and how it binds with proteins, or they can lead to decreasing thyroid hormone levels due to a variety of interactions.
And in contrast, “What is even more challenging is that some medications or supplements may appear to affect thyroid function based on lab tests when in reality they don’t actually affect thyroid function and may lead to dose adjustments unnecessarily,” Dr. Papaleontiou noted.
Recommendations to counter interference
Current recommendations to try to counter the effects of polypharmacy on thyroid treatment include advising patients to take thyroid hormones on an empty stomach at least 30-60 minutes prior to eating for optimal absorption.
If the patient is taking medications known to interfere with absorption of thyroid hormones, the recommendation is to space those out by at least 4 hours.
“The big challenge in older adults is that many of them do experience polypharmacy, being at risk for multiple drug-drug interactions,” Dr. Papaleontiou said.
“Physicians and patients should be vigilant and communicate closely every time there is initiation of a new medication or supplement to consider whether there may be interference.”
The authors have reported no relevant financial relationships. Dr. Hoang has reported being a speaker for Acella Pharmaceuticals.
A version of this article first appeared on Medscape.com.
Colchicine before PCI for acute MI fails to improve major outcomes
In a placebo-controlled randomized trial, a preprocedural dose of colchicine administered immediately before percutaneous coronary intervention (PCI) for an acute ST-segment elevated myocardial infarction (STEMI) did not reduce the no-reflow phenomenon or improve outcomes.
No-reflow, in which insufficient myocardial perfusion is present even though the coronary artery appears patent, was the primary outcome, and the proportion of patients experiencing this event was exactly the same (14.4%) in the colchicine and placebo groups, reported Yaser Jenab, MD, at CRT 2021 sponsored by MedStar Heart & Vascular Institute.
The hypothesis that colchicine would offer benefit in this setting was largely based on the Colchicine Cardiovascular Outcomes Trial (COLCOT). In that study, colchicine was associated with a 23% reduction in risk for major adverse cardiovascular events (MACE) relative to placebo when administered within 30 days after a myocardial infarction (hazard ratio, 0.77; P = .02).
The benefit in that trial was attributed to an anti-inflammatory effect, according to Dr. Jenab, associate professor of cardiology at Tehran (Iran) Heart Center. In particular as it relates to vascular disease, he cited experimental studies associating colchicine with a reduction in neutrophil activation and adherence to vascular endothelium.
The rationale for a preprocedural approach to colchicine was supplied by a subsequent time-to-treatment COLCOT analysis. In this study, MACE risk reduction for colchicine climbed to 48% (HR 0.52) for those treated within 3 days of the MI but largely disappeared (HR 0.96) if treatment was started at least 8 days post MI.
PodCAST-PCI trial
In the preprocedural study, called the PodCAST-PCI trial, 321 acute STEMI patients were randomized. Patients received a 1-mg dose of oral colchicine or placebo at the time PCI was scheduled. Another dose of colchicine (0.5 mg) or placebo was administered 1 hour after the procedure.
Of secondary outcomes, which included MACE at 1 month and 1 year, ST-segment resolution at 1 month, and change in inflammatory markers at 1 month, none were significant. Few even trended for significance.
For MACE, which included cardiac death, stroke, nonfatal MI, new hospitalization due to heart failure, or target vessel revascularization, the rates were lower in the colchicine group at 1 month (4.3% vs. 7.5%) and 1 year (9.3% vs. 11.2%), but neither approached significance.
For ST-segment resolution, the proportions were generally comparable among the colchicine and placebo groups, respectively, for the proportion below 50% (18.6% vs. 23.1%), between 50% and 70% (16.8% vs. 15.6%), and above 70% (64.6% vs. 61.3%).
The average troponin levels were nonsignificantly lower at 6 hours (1,847 vs. 2,883 ng/mL) in the colchicine group but higher at 48 hours (1,197 vs. 1,147 ng/mL). The average C-reactive protein (CRP) levels at 48 hours were nonsignificantly lower on colchicine (176.5 vs. 244.5 mg/L).
There were no significant differences in postprocedural perfusion, as measured with TIMI blood flow, or in the rate of stent thrombosis, which occurred in roughly 3% of each group of patients.
The small sample size was one limitation of this study, Dr. Jenab acknowledged. For this and other reasons, he cautioned that these data are not definitive and do not preclude a benefit on clinical outcomes in a study with a larger size, a different design, or different dosing.
Timing might be the issue
However, even if colchicine has a potential benefit in this setting, timing might be a major obstacle, according to Binata Shah, MD, associate director of research for the Cardiac Catheterization Laboratory at New York University.
“We have learned from our rheumatology colleagues that peak plasma levels of colchicine are not achieved for at least 1 hour after the full loading dose,” Dr. Shah said. “With us moving so quickly in a primary PCI setting, it is hard to imagine that colchicine would have had time to really kick in and exert its anti-inflammatory effect.”
Indeed, the problem might be worse than reaching the peak plasma level.
“Even though peak plasma levels occur as early as 1 hour after a full loading dose, we see that it takes about 24 hours to really see the effects translate downstream into more systemic inflammatory markers such as CRP and interleukin-6,” she added. If lowering these signals of inflammation is predictive of benefit, than this might be the biggest obstacle to benefit from colchicine in an urgent treatment setting.
Dr. Jenab and Dr. Shah reported no potential conflicts of interest.
In a placebo-controlled randomized trial, a preprocedural dose of colchicine administered immediately before percutaneous coronary intervention (PCI) for an acute ST-segment elevated myocardial infarction (STEMI) did not reduce the no-reflow phenomenon or improve outcomes.
No-reflow, in which insufficient myocardial perfusion is present even though the coronary artery appears patent, was the primary outcome, and the proportion of patients experiencing this event was exactly the same (14.4%) in the colchicine and placebo groups, reported Yaser Jenab, MD, at CRT 2021 sponsored by MedStar Heart & Vascular Institute.
The hypothesis that colchicine would offer benefit in this setting was largely based on the Colchicine Cardiovascular Outcomes Trial (COLCOT). In that study, colchicine was associated with a 23% reduction in risk for major adverse cardiovascular events (MACE) relative to placebo when administered within 30 days after a myocardial infarction (hazard ratio, 0.77; P = .02).
The benefit in that trial was attributed to an anti-inflammatory effect, according to Dr. Jenab, associate professor of cardiology at Tehran (Iran) Heart Center. In particular as it relates to vascular disease, he cited experimental studies associating colchicine with a reduction in neutrophil activation and adherence to vascular endothelium.
The rationale for a preprocedural approach to colchicine was supplied by a subsequent time-to-treatment COLCOT analysis. In this study, MACE risk reduction for colchicine climbed to 48% (HR 0.52) for those treated within 3 days of the MI but largely disappeared (HR 0.96) if treatment was started at least 8 days post MI.
PodCAST-PCI trial
In the preprocedural study, called the PodCAST-PCI trial, 321 acute STEMI patients were randomized. Patients received a 1-mg dose of oral colchicine or placebo at the time PCI was scheduled. Another dose of colchicine (0.5 mg) or placebo was administered 1 hour after the procedure.
Of secondary outcomes, which included MACE at 1 month and 1 year, ST-segment resolution at 1 month, and change in inflammatory markers at 1 month, none were significant. Few even trended for significance.
For MACE, which included cardiac death, stroke, nonfatal MI, new hospitalization due to heart failure, or target vessel revascularization, the rates were lower in the colchicine group at 1 month (4.3% vs. 7.5%) and 1 year (9.3% vs. 11.2%), but neither approached significance.
For ST-segment resolution, the proportions were generally comparable among the colchicine and placebo groups, respectively, for the proportion below 50% (18.6% vs. 23.1%), between 50% and 70% (16.8% vs. 15.6%), and above 70% (64.6% vs. 61.3%).
The average troponin levels were nonsignificantly lower at 6 hours (1,847 vs. 2,883 ng/mL) in the colchicine group but higher at 48 hours (1,197 vs. 1,147 ng/mL). The average C-reactive protein (CRP) levels at 48 hours were nonsignificantly lower on colchicine (176.5 vs. 244.5 mg/L).
There were no significant differences in postprocedural perfusion, as measured with TIMI blood flow, or in the rate of stent thrombosis, which occurred in roughly 3% of each group of patients.
The small sample size was one limitation of this study, Dr. Jenab acknowledged. For this and other reasons, he cautioned that these data are not definitive and do not preclude a benefit on clinical outcomes in a study with a larger size, a different design, or different dosing.
Timing might be the issue
However, even if colchicine has a potential benefit in this setting, timing might be a major obstacle, according to Binata Shah, MD, associate director of research for the Cardiac Catheterization Laboratory at New York University.
“We have learned from our rheumatology colleagues that peak plasma levels of colchicine are not achieved for at least 1 hour after the full loading dose,” Dr. Shah said. “With us moving so quickly in a primary PCI setting, it is hard to imagine that colchicine would have had time to really kick in and exert its anti-inflammatory effect.”
Indeed, the problem might be worse than reaching the peak plasma level.
“Even though peak plasma levels occur as early as 1 hour after a full loading dose, we see that it takes about 24 hours to really see the effects translate downstream into more systemic inflammatory markers such as CRP and interleukin-6,” she added. If lowering these signals of inflammation is predictive of benefit, than this might be the biggest obstacle to benefit from colchicine in an urgent treatment setting.
Dr. Jenab and Dr. Shah reported no potential conflicts of interest.
In a placebo-controlled randomized trial, a preprocedural dose of colchicine administered immediately before percutaneous coronary intervention (PCI) for an acute ST-segment elevated myocardial infarction (STEMI) did not reduce the no-reflow phenomenon or improve outcomes.
No-reflow, in which insufficient myocardial perfusion is present even though the coronary artery appears patent, was the primary outcome, and the proportion of patients experiencing this event was exactly the same (14.4%) in the colchicine and placebo groups, reported Yaser Jenab, MD, at CRT 2021 sponsored by MedStar Heart & Vascular Institute.
The hypothesis that colchicine would offer benefit in this setting was largely based on the Colchicine Cardiovascular Outcomes Trial (COLCOT). In that study, colchicine was associated with a 23% reduction in risk for major adverse cardiovascular events (MACE) relative to placebo when administered within 30 days after a myocardial infarction (hazard ratio, 0.77; P = .02).
The benefit in that trial was attributed to an anti-inflammatory effect, according to Dr. Jenab, associate professor of cardiology at Tehran (Iran) Heart Center. In particular as it relates to vascular disease, he cited experimental studies associating colchicine with a reduction in neutrophil activation and adherence to vascular endothelium.
The rationale for a preprocedural approach to colchicine was supplied by a subsequent time-to-treatment COLCOT analysis. In this study, MACE risk reduction for colchicine climbed to 48% (HR 0.52) for those treated within 3 days of the MI but largely disappeared (HR 0.96) if treatment was started at least 8 days post MI.
PodCAST-PCI trial
In the preprocedural study, called the PodCAST-PCI trial, 321 acute STEMI patients were randomized. Patients received a 1-mg dose of oral colchicine or placebo at the time PCI was scheduled. Another dose of colchicine (0.5 mg) or placebo was administered 1 hour after the procedure.
Of secondary outcomes, which included MACE at 1 month and 1 year, ST-segment resolution at 1 month, and change in inflammatory markers at 1 month, none were significant. Few even trended for significance.
For MACE, which included cardiac death, stroke, nonfatal MI, new hospitalization due to heart failure, or target vessel revascularization, the rates were lower in the colchicine group at 1 month (4.3% vs. 7.5%) and 1 year (9.3% vs. 11.2%), but neither approached significance.
For ST-segment resolution, the proportions were generally comparable among the colchicine and placebo groups, respectively, for the proportion below 50% (18.6% vs. 23.1%), between 50% and 70% (16.8% vs. 15.6%), and above 70% (64.6% vs. 61.3%).
The average troponin levels were nonsignificantly lower at 6 hours (1,847 vs. 2,883 ng/mL) in the colchicine group but higher at 48 hours (1,197 vs. 1,147 ng/mL). The average C-reactive protein (CRP) levels at 48 hours were nonsignificantly lower on colchicine (176.5 vs. 244.5 mg/L).
There were no significant differences in postprocedural perfusion, as measured with TIMI blood flow, or in the rate of stent thrombosis, which occurred in roughly 3% of each group of patients.
The small sample size was one limitation of this study, Dr. Jenab acknowledged. For this and other reasons, he cautioned that these data are not definitive and do not preclude a benefit on clinical outcomes in a study with a larger size, a different design, or different dosing.
Timing might be the issue
However, even if colchicine has a potential benefit in this setting, timing might be a major obstacle, according to Binata Shah, MD, associate director of research for the Cardiac Catheterization Laboratory at New York University.
“We have learned from our rheumatology colleagues that peak plasma levels of colchicine are not achieved for at least 1 hour after the full loading dose,” Dr. Shah said. “With us moving so quickly in a primary PCI setting, it is hard to imagine that colchicine would have had time to really kick in and exert its anti-inflammatory effect.”
Indeed, the problem might be worse than reaching the peak plasma level.
“Even though peak plasma levels occur as early as 1 hour after a full loading dose, we see that it takes about 24 hours to really see the effects translate downstream into more systemic inflammatory markers such as CRP and interleukin-6,” she added. If lowering these signals of inflammation is predictive of benefit, than this might be the biggest obstacle to benefit from colchicine in an urgent treatment setting.
Dr. Jenab and Dr. Shah reported no potential conflicts of interest.
FROM CRT 2021
High-dose chemo no better than standard dose for B-cell lymphoma
After 10 years of follow-up, event-free survival and overall survival were similar between conventional chemotherapy treated patients with aggressive B-cell lymphoma and those receiving high-dose chemotherapy followed by autologous hematopoietic stem-cell transplantation (HSCT), according to a report published online in the Lancet Hematology.
The open-label, randomized, phase 3 trial (NCT00129090) was conducted across 61 centers in Germany on patients aged 18-60 years who had newly diagnosed, high-risk, aggressive B-cell lymphoma, according to Fabian Frontzek, MD, of the University Hospital Münster (Germany) and colleagues.
Between March 2003 and April 2009, patients were randomly assigned to eight cycles of conventional chemotherapy (cyclophosphamide, doxorubicin, vincristine, etoposide, and prednisolone) plus rituximab (R-CHOEP-14) or four cycles of high-dose chemotherapy plus rituximab followed by autologous HSCT (R-MegaCHOEP). The intention-to-treat population comprised 130 patients in the R-CHOEP-14 group and 132 patients in the R-MegaCHOEP group. The median follow-up was 9.3 years.
Similar outcomes
The 10-year event-free survival was 51% in the R-MegaCHOEP group and 57% in the R-CHOEP-14 group, a nonsignificant difference (P = .23). Similarly, the 10-year progression-free survival was 59% in the
R-MegaCHOEP group and 60% (P = .64). The 10-year overall survival was 66% in the R-MegaCHOEP group and 72% in the R-CHOEP-14 group (P = .26). Among the 190 patients who had complete remission or unconfirmed complete remission, relapse occurred in 30 (16%); 17 (17%) of 100 patients in the R-CHOEP-14 group and 13 (14%) of 90 patients in the R-MegaCHOEP group.
In terms of secondary malignancies, 22 were reported in the intention-to-treat population; comprising 12 (9%) of 127 patients in the R-CHOEP-14 group and 10 (8%) of 126 patients in the R-MegaCHOEP group.
Patients who relapsed with aggressive histology and with CNS involvement in particular had worse outcomes and “represent a group with an unmet medical need, for which new molecular and cellular therapies should be studied,” the authors stated.
“This study shows that, in the rituximab era, high-dose therapy and autologous HSCT in first-line treatment does not improve long-term survival of younger high-risk patients with aggressive B-cell lymphoma. The R-CHOEP-14 regimen led to favorable outcomes, supporting its continued use in such patients,” the researchers concluded.
In an accompanying commentary, Gita Thanarajasingam, MD, of the Mayo Clinic, Rochester, Minn., and colleagues added that the issue of long-term outcomes is critical to evaluating these new regimens.
They applauded the inclusion of secondary malignancies in the long-term follow-up, but regretted the lack of the, admittedly resource-intensive, information on long-term nonneoplastic adverse events. They added that “the burden of late adverse events such as cardiotoxicity, cumulative neuropathy, delayed infections, or lasting cognitive effects, among others that might drive substantial morbidity, does matter to lymphoma survivors.”
They also commented on the importance of considering effects on fertility in these patients, noting that R-MegaCHOEP patients would be unable to conceive naturally, but that the effect of R-CHOEP-14 was less clear.
“We encourage ongoing emphasis on this type of longitudinal follow-up of secondary malignancies and other nonneoplastic late toxicities in phase 3 studies as well as in the real world in hematological malignancies, so that after prioritizing cure in the front-line setting, we do not neglect the life we have helped survivors achieve for years and decades to come,” they concluded.
The study was sponsored by the German High-Grade Non-Hodgkin’s Lymphoma Study Group. The authors reported grants, personal fees, and non-financial support from multiple pharmaceutical and biotechnology companies. Dr. Thanarajasingam and her colleagues reported that they had no competing interests.
After 10 years of follow-up, event-free survival and overall survival were similar between conventional chemotherapy treated patients with aggressive B-cell lymphoma and those receiving high-dose chemotherapy followed by autologous hematopoietic stem-cell transplantation (HSCT), according to a report published online in the Lancet Hematology.
The open-label, randomized, phase 3 trial (NCT00129090) was conducted across 61 centers in Germany on patients aged 18-60 years who had newly diagnosed, high-risk, aggressive B-cell lymphoma, according to Fabian Frontzek, MD, of the University Hospital Münster (Germany) and colleagues.
Between March 2003 and April 2009, patients were randomly assigned to eight cycles of conventional chemotherapy (cyclophosphamide, doxorubicin, vincristine, etoposide, and prednisolone) plus rituximab (R-CHOEP-14) or four cycles of high-dose chemotherapy plus rituximab followed by autologous HSCT (R-MegaCHOEP). The intention-to-treat population comprised 130 patients in the R-CHOEP-14 group and 132 patients in the R-MegaCHOEP group. The median follow-up was 9.3 years.
Similar outcomes
The 10-year event-free survival was 51% in the R-MegaCHOEP group and 57% in the R-CHOEP-14 group, a nonsignificant difference (P = .23). Similarly, the 10-year progression-free survival was 59% in the
R-MegaCHOEP group and 60% (P = .64). The 10-year overall survival was 66% in the R-MegaCHOEP group and 72% in the R-CHOEP-14 group (P = .26). Among the 190 patients who had complete remission or unconfirmed complete remission, relapse occurred in 30 (16%); 17 (17%) of 100 patients in the R-CHOEP-14 group and 13 (14%) of 90 patients in the R-MegaCHOEP group.
In terms of secondary malignancies, 22 were reported in the intention-to-treat population; comprising 12 (9%) of 127 patients in the R-CHOEP-14 group and 10 (8%) of 126 patients in the R-MegaCHOEP group.
Patients who relapsed with aggressive histology and with CNS involvement in particular had worse outcomes and “represent a group with an unmet medical need, for which new molecular and cellular therapies should be studied,” the authors stated.
“This study shows that, in the rituximab era, high-dose therapy and autologous HSCT in first-line treatment does not improve long-term survival of younger high-risk patients with aggressive B-cell lymphoma. The R-CHOEP-14 regimen led to favorable outcomes, supporting its continued use in such patients,” the researchers concluded.
In an accompanying commentary, Gita Thanarajasingam, MD, of the Mayo Clinic, Rochester, Minn., and colleagues added that the issue of long-term outcomes is critical to evaluating these new regimens.
They applauded the inclusion of secondary malignancies in the long-term follow-up, but regretted the lack of the, admittedly resource-intensive, information on long-term nonneoplastic adverse events. They added that “the burden of late adverse events such as cardiotoxicity, cumulative neuropathy, delayed infections, or lasting cognitive effects, among others that might drive substantial morbidity, does matter to lymphoma survivors.”
They also commented on the importance of considering effects on fertility in these patients, noting that R-MegaCHOEP patients would be unable to conceive naturally, but that the effect of R-CHOEP-14 was less clear.
“We encourage ongoing emphasis on this type of longitudinal follow-up of secondary malignancies and other nonneoplastic late toxicities in phase 3 studies as well as in the real world in hematological malignancies, so that after prioritizing cure in the front-line setting, we do not neglect the life we have helped survivors achieve for years and decades to come,” they concluded.
The study was sponsored by the German High-Grade Non-Hodgkin’s Lymphoma Study Group. The authors reported grants, personal fees, and non-financial support from multiple pharmaceutical and biotechnology companies. Dr. Thanarajasingam and her colleagues reported that they had no competing interests.
After 10 years of follow-up, event-free survival and overall survival were similar between conventional chemotherapy treated patients with aggressive B-cell lymphoma and those receiving high-dose chemotherapy followed by autologous hematopoietic stem-cell transplantation (HSCT), according to a report published online in the Lancet Hematology.
The open-label, randomized, phase 3 trial (NCT00129090) was conducted across 61 centers in Germany on patients aged 18-60 years who had newly diagnosed, high-risk, aggressive B-cell lymphoma, according to Fabian Frontzek, MD, of the University Hospital Münster (Germany) and colleagues.
Between March 2003 and April 2009, patients were randomly assigned to eight cycles of conventional chemotherapy (cyclophosphamide, doxorubicin, vincristine, etoposide, and prednisolone) plus rituximab (R-CHOEP-14) or four cycles of high-dose chemotherapy plus rituximab followed by autologous HSCT (R-MegaCHOEP). The intention-to-treat population comprised 130 patients in the R-CHOEP-14 group and 132 patients in the R-MegaCHOEP group. The median follow-up was 9.3 years.
Similar outcomes
The 10-year event-free survival was 51% in the R-MegaCHOEP group and 57% in the R-CHOEP-14 group, a nonsignificant difference (P = .23). Similarly, the 10-year progression-free survival was 59% in the
R-MegaCHOEP group and 60% (P = .64). The 10-year overall survival was 66% in the R-MegaCHOEP group and 72% in the R-CHOEP-14 group (P = .26). Among the 190 patients who had complete remission or unconfirmed complete remission, relapse occurred in 30 (16%); 17 (17%) of 100 patients in the R-CHOEP-14 group and 13 (14%) of 90 patients in the R-MegaCHOEP group.
In terms of secondary malignancies, 22 were reported in the intention-to-treat population; comprising 12 (9%) of 127 patients in the R-CHOEP-14 group and 10 (8%) of 126 patients in the R-MegaCHOEP group.
Patients who relapsed with aggressive histology and with CNS involvement in particular had worse outcomes and “represent a group with an unmet medical need, for which new molecular and cellular therapies should be studied,” the authors stated.
“This study shows that, in the rituximab era, high-dose therapy and autologous HSCT in first-line treatment does not improve long-term survival of younger high-risk patients with aggressive B-cell lymphoma. The R-CHOEP-14 regimen led to favorable outcomes, supporting its continued use in such patients,” the researchers concluded.
In an accompanying commentary, Gita Thanarajasingam, MD, of the Mayo Clinic, Rochester, Minn., and colleagues added that the issue of long-term outcomes is critical to evaluating these new regimens.
They applauded the inclusion of secondary malignancies in the long-term follow-up, but regretted the lack of the, admittedly resource-intensive, information on long-term nonneoplastic adverse events. They added that “the burden of late adverse events such as cardiotoxicity, cumulative neuropathy, delayed infections, or lasting cognitive effects, among others that might drive substantial morbidity, does matter to lymphoma survivors.”
They also commented on the importance of considering effects on fertility in these patients, noting that R-MegaCHOEP patients would be unable to conceive naturally, but that the effect of R-CHOEP-14 was less clear.
“We encourage ongoing emphasis on this type of longitudinal follow-up of secondary malignancies and other nonneoplastic late toxicities in phase 3 studies as well as in the real world in hematological malignancies, so that after prioritizing cure in the front-line setting, we do not neglect the life we have helped survivors achieve for years and decades to come,” they concluded.
The study was sponsored by the German High-Grade Non-Hodgkin’s Lymphoma Study Group. The authors reported grants, personal fees, and non-financial support from multiple pharmaceutical and biotechnology companies. Dr. Thanarajasingam and her colleagues reported that they had no competing interests.
FROM THE LANCET HEMATOLOGY
Neurologic drug prices jump 50% in five years
, new research shows. Results of the retrospective study also showed that most of the increased costs for these agents were due to rising costs for neuroimmunology drugs, mainly for those used to treat multiple sclerosis (MS).
“The same brand name medication in 2017 cost approximately 50% more than in 2013,” said Adam de Havenon, MD, assistant professor of neurology, University of Utah, Salt Lake City.
“An analogy would be if you bought an iPhone 5 in 2013 for $500, and then in 2017, you were asked to pay $750 for the exact same iPhone 5,” Dr. de Havenon added.
The study findings were published online March 10 in the journal Neurology.
$26 billion in payments
Both neurologists and patients are concerned about the high cost of prescription drugs for neurologic diseases, and Medicare Part D data indicate that these drugs are the most expensive component of neurologic care, the researchers noted. In addition, out-of-pocket costs have increased significantly for patients with neurologic disease such as Parkinson’s disease, epilepsy, and MS.
To understand trends in payments for neurologic drugs, Dr. de Havenon and colleagues analyzed Medicare Part D claims filed from 2013 to 2017. The payments include costs paid by Medicare, the patient, government subsidies, and other third-party payers.
In addition to examining more current Medicare Part D data than previous studies, the current analysis examined all medications prescribed by neurologists that consistently remained branded or generic during the 5-year study period, said Dr. de Havenon. This approach resulted in a large number of claims and a large total cost.
To calculate the percentage change in annual payment claims, the researchers used 2013 prices as a reference point. They identified drugs named in 2013 claims and classified them as generic, brand-name only, or brand-name with generic equivalent. Researchers also divided the drugs by neurologic subspecialty.
The analysis included 520 drugs, all of which were available in each year of the study period. Of these drugs, 322 were generic, 61 were brand-name only, and 137 were brand-name with a generic equivalent. There were 90.7 million total claims.
Results showed total payments amounted to $26.65 billion. Yearly total payments increased from $4.05 billion in 2013 to $6.09 billion in 2017, representing a 50.4% increase, even after adjusting for inflation. Total claims increased by 7.6% – from 17.1 million in 2013 to 18.4 million in 2017.
From 2013 to 2017, claim payments increased by 0.6% for generic drugs, 42.4% for brand-name only drugs, and 45% for brand-name drugs with generic equivalents. The proportion of claims increased from 81.9% to 88% for generic drugs and from 4.9% to 6.2% for brand-name only drugs.
However, the proportion of claims for brand-name drugs with generic equivalents decreased from 13.3% to 5.8%.
Treatment barrier
Neuroimmunologic drugs, most of which were prescribed for MS, had exceptional cost, the researchers noted. These drugs accounted for more than 50% of payments but only 4.3% of claims. Claim payment for these drugs increased by 46.9% during the study period, from $3,337 to $4,902.
When neuroimmunologic drugs were removed from the analysis there was still significant increase in claim payments for brand-name only drugs (50.4%) and brand-name drugs with generic equivalents (45.6%).
Although neuroimmunologic medicines, including monoclonal antibodies, are more expensive to produce, this factor alone does not explain their exceptional cost, said Dr. de Havenon. “The high cost of brand-name drugs in this speciality is likely because the market bears it,” he added. “In other words, MS is a disabling disease and the medications work, so historically the Centers for Medicare & Medicaid Services have been willing to tolerate the high cost of these primarily brand-name medications.”
Several countries have controlled drug costs by negotiating with pharmaceutical companies and through legislation, Dr. de Havenon noted.
“My intent with this article was to raise awareness on the topic, which I struggle with frequently as a clinician. I know I want my patients to have a medication, but the cost prevents it,” he said.
‘Unfettered’ price-setting
Commenting on the findings, Robert J. Fox, MD, vice chair for research at the Neurological Institute of the Cleveland Clinic, said the study “brings into clear light” what neurologists, particularly those who treat MS, have long suspected but did not really know. These neurologists “are typically distanced from the payment aspects of the medications they prescribe,” said Dr. Fox, who was not involved with the research.
Although a particular strength of the study was its comprehensiveness, the researchers excluded infusion claims – which account for a large portion of total patient care costs for many disorders, he noted.
Drugs for MS historically have been expensive, ostensibly because of their high cost of development. In addition, the large and continued price increase that occurs long after these drugs have been approved remains unexplained, said Dr. Fox.
He noted that the study findings might not directly affect clinical practice because neurologists will continue prescribing medications they think are best for their patients. “Instead, I think this is a lesson to lawmakers about the massive error in the Medicare Modernization Act of 2003, where the federal government was prohibited from negotiating drug prices. If the seller is unfettered in setting a price, then no one should be surprised when the price rises,” Dr. Fox said.
Because many new drugs and new generic formulations for treating MS have become available during the past year, “repeating these types of economic studies for the period 2020-2025 will help us understand if generic competition – as well as new laws if they are passed – alter price,” he concluded.
The study was funded by the American Academy of Neurology, which publishes Neurology. Dr. de Havenon has received clinical research funding from AMAG Pharmaceuticals and Regeneron Pharmaceuticals. Dr. Fox receives consulting fees from many pharmaceutical companies involved in the development of therapies for MS.
A version of this article first appeared on Medscape.com.
, new research shows. Results of the retrospective study also showed that most of the increased costs for these agents were due to rising costs for neuroimmunology drugs, mainly for those used to treat multiple sclerosis (MS).
“The same brand name medication in 2017 cost approximately 50% more than in 2013,” said Adam de Havenon, MD, assistant professor of neurology, University of Utah, Salt Lake City.
“An analogy would be if you bought an iPhone 5 in 2013 for $500, and then in 2017, you were asked to pay $750 for the exact same iPhone 5,” Dr. de Havenon added.
The study findings were published online March 10 in the journal Neurology.
$26 billion in payments
Both neurologists and patients are concerned about the high cost of prescription drugs for neurologic diseases, and Medicare Part D data indicate that these drugs are the most expensive component of neurologic care, the researchers noted. In addition, out-of-pocket costs have increased significantly for patients with neurologic disease such as Parkinson’s disease, epilepsy, and MS.
To understand trends in payments for neurologic drugs, Dr. de Havenon and colleagues analyzed Medicare Part D claims filed from 2013 to 2017. The payments include costs paid by Medicare, the patient, government subsidies, and other third-party payers.
In addition to examining more current Medicare Part D data than previous studies, the current analysis examined all medications prescribed by neurologists that consistently remained branded or generic during the 5-year study period, said Dr. de Havenon. This approach resulted in a large number of claims and a large total cost.
To calculate the percentage change in annual payment claims, the researchers used 2013 prices as a reference point. They identified drugs named in 2013 claims and classified them as generic, brand-name only, or brand-name with generic equivalent. Researchers also divided the drugs by neurologic subspecialty.
The analysis included 520 drugs, all of which were available in each year of the study period. Of these drugs, 322 were generic, 61 were brand-name only, and 137 were brand-name with a generic equivalent. There were 90.7 million total claims.
Results showed total payments amounted to $26.65 billion. Yearly total payments increased from $4.05 billion in 2013 to $6.09 billion in 2017, representing a 50.4% increase, even after adjusting for inflation. Total claims increased by 7.6% – from 17.1 million in 2013 to 18.4 million in 2017.
From 2013 to 2017, claim payments increased by 0.6% for generic drugs, 42.4% for brand-name only drugs, and 45% for brand-name drugs with generic equivalents. The proportion of claims increased from 81.9% to 88% for generic drugs and from 4.9% to 6.2% for brand-name only drugs.
However, the proportion of claims for brand-name drugs with generic equivalents decreased from 13.3% to 5.8%.
Treatment barrier
Neuroimmunologic drugs, most of which were prescribed for MS, had exceptional cost, the researchers noted. These drugs accounted for more than 50% of payments but only 4.3% of claims. Claim payment for these drugs increased by 46.9% during the study period, from $3,337 to $4,902.
When neuroimmunologic drugs were removed from the analysis there was still significant increase in claim payments for brand-name only drugs (50.4%) and brand-name drugs with generic equivalents (45.6%).
Although neuroimmunologic medicines, including monoclonal antibodies, are more expensive to produce, this factor alone does not explain their exceptional cost, said Dr. de Havenon. “The high cost of brand-name drugs in this speciality is likely because the market bears it,” he added. “In other words, MS is a disabling disease and the medications work, so historically the Centers for Medicare & Medicaid Services have been willing to tolerate the high cost of these primarily brand-name medications.”
Several countries have controlled drug costs by negotiating with pharmaceutical companies and through legislation, Dr. de Havenon noted.
“My intent with this article was to raise awareness on the topic, which I struggle with frequently as a clinician. I know I want my patients to have a medication, but the cost prevents it,” he said.
‘Unfettered’ price-setting
Commenting on the findings, Robert J. Fox, MD, vice chair for research at the Neurological Institute of the Cleveland Clinic, said the study “brings into clear light” what neurologists, particularly those who treat MS, have long suspected but did not really know. These neurologists “are typically distanced from the payment aspects of the medications they prescribe,” said Dr. Fox, who was not involved with the research.
Although a particular strength of the study was its comprehensiveness, the researchers excluded infusion claims – which account for a large portion of total patient care costs for many disorders, he noted.
Drugs for MS historically have been expensive, ostensibly because of their high cost of development. In addition, the large and continued price increase that occurs long after these drugs have been approved remains unexplained, said Dr. Fox.
He noted that the study findings might not directly affect clinical practice because neurologists will continue prescribing medications they think are best for their patients. “Instead, I think this is a lesson to lawmakers about the massive error in the Medicare Modernization Act of 2003, where the federal government was prohibited from negotiating drug prices. If the seller is unfettered in setting a price, then no one should be surprised when the price rises,” Dr. Fox said.
Because many new drugs and new generic formulations for treating MS have become available during the past year, “repeating these types of economic studies for the period 2020-2025 will help us understand if generic competition – as well as new laws if they are passed – alter price,” he concluded.
The study was funded by the American Academy of Neurology, which publishes Neurology. Dr. de Havenon has received clinical research funding from AMAG Pharmaceuticals and Regeneron Pharmaceuticals. Dr. Fox receives consulting fees from many pharmaceutical companies involved in the development of therapies for MS.
A version of this article first appeared on Medscape.com.
, new research shows. Results of the retrospective study also showed that most of the increased costs for these agents were due to rising costs for neuroimmunology drugs, mainly for those used to treat multiple sclerosis (MS).
“The same brand name medication in 2017 cost approximately 50% more than in 2013,” said Adam de Havenon, MD, assistant professor of neurology, University of Utah, Salt Lake City.
“An analogy would be if you bought an iPhone 5 in 2013 for $500, and then in 2017, you were asked to pay $750 for the exact same iPhone 5,” Dr. de Havenon added.
The study findings were published online March 10 in the journal Neurology.
$26 billion in payments
Both neurologists and patients are concerned about the high cost of prescription drugs for neurologic diseases, and Medicare Part D data indicate that these drugs are the most expensive component of neurologic care, the researchers noted. In addition, out-of-pocket costs have increased significantly for patients with neurologic disease such as Parkinson’s disease, epilepsy, and MS.
To understand trends in payments for neurologic drugs, Dr. de Havenon and colleagues analyzed Medicare Part D claims filed from 2013 to 2017. The payments include costs paid by Medicare, the patient, government subsidies, and other third-party payers.
In addition to examining more current Medicare Part D data than previous studies, the current analysis examined all medications prescribed by neurologists that consistently remained branded or generic during the 5-year study period, said Dr. de Havenon. This approach resulted in a large number of claims and a large total cost.
To calculate the percentage change in annual payment claims, the researchers used 2013 prices as a reference point. They identified drugs named in 2013 claims and classified them as generic, brand-name only, or brand-name with generic equivalent. Researchers also divided the drugs by neurologic subspecialty.
The analysis included 520 drugs, all of which were available in each year of the study period. Of these drugs, 322 were generic, 61 were brand-name only, and 137 were brand-name with a generic equivalent. There were 90.7 million total claims.
Results showed total payments amounted to $26.65 billion. Yearly total payments increased from $4.05 billion in 2013 to $6.09 billion in 2017, representing a 50.4% increase, even after adjusting for inflation. Total claims increased by 7.6% – from 17.1 million in 2013 to 18.4 million in 2017.
From 2013 to 2017, claim payments increased by 0.6% for generic drugs, 42.4% for brand-name only drugs, and 45% for brand-name drugs with generic equivalents. The proportion of claims increased from 81.9% to 88% for generic drugs and from 4.9% to 6.2% for brand-name only drugs.
However, the proportion of claims for brand-name drugs with generic equivalents decreased from 13.3% to 5.8%.
Treatment barrier
Neuroimmunologic drugs, most of which were prescribed for MS, had exceptional cost, the researchers noted. These drugs accounted for more than 50% of payments but only 4.3% of claims. Claim payment for these drugs increased by 46.9% during the study period, from $3,337 to $4,902.
When neuroimmunologic drugs were removed from the analysis there was still significant increase in claim payments for brand-name only drugs (50.4%) and brand-name drugs with generic equivalents (45.6%).
Although neuroimmunologic medicines, including monoclonal antibodies, are more expensive to produce, this factor alone does not explain their exceptional cost, said Dr. de Havenon. “The high cost of brand-name drugs in this speciality is likely because the market bears it,” he added. “In other words, MS is a disabling disease and the medications work, so historically the Centers for Medicare & Medicaid Services have been willing to tolerate the high cost of these primarily brand-name medications.”
Several countries have controlled drug costs by negotiating with pharmaceutical companies and through legislation, Dr. de Havenon noted.
“My intent with this article was to raise awareness on the topic, which I struggle with frequently as a clinician. I know I want my patients to have a medication, but the cost prevents it,” he said.
‘Unfettered’ price-setting
Commenting on the findings, Robert J. Fox, MD, vice chair for research at the Neurological Institute of the Cleveland Clinic, said the study “brings into clear light” what neurologists, particularly those who treat MS, have long suspected but did not really know. These neurologists “are typically distanced from the payment aspects of the medications they prescribe,” said Dr. Fox, who was not involved with the research.
Although a particular strength of the study was its comprehensiveness, the researchers excluded infusion claims – which account for a large portion of total patient care costs for many disorders, he noted.
Drugs for MS historically have been expensive, ostensibly because of their high cost of development. In addition, the large and continued price increase that occurs long after these drugs have been approved remains unexplained, said Dr. Fox.
He noted that the study findings might not directly affect clinical practice because neurologists will continue prescribing medications they think are best for their patients. “Instead, I think this is a lesson to lawmakers about the massive error in the Medicare Modernization Act of 2003, where the federal government was prohibited from negotiating drug prices. If the seller is unfettered in setting a price, then no one should be surprised when the price rises,” Dr. Fox said.
Because many new drugs and new generic formulations for treating MS have become available during the past year, “repeating these types of economic studies for the period 2020-2025 will help us understand if generic competition – as well as new laws if they are passed – alter price,” he concluded.
The study was funded by the American Academy of Neurology, which publishes Neurology. Dr. de Havenon has received clinical research funding from AMAG Pharmaceuticals and Regeneron Pharmaceuticals. Dr. Fox receives consulting fees from many pharmaceutical companies involved in the development of therapies for MS.
A version of this article first appeared on Medscape.com.
FROM NEUROLOGY
Novel Alzheimer’s drug slows cognitive decline in phase 2 trial
Results from the TRAILBLAZER-ALZ trial were presented at the 2021 International Conference on Alzheimer’s and Parkinson’s Diseases (AD/PD) and were simultaneously published online March 13 in the New England Journal of Medicine.
As previously reported by Medscape Medical News, topline results showed that donanemab slowed cognitive decline by 32% on the Integrated AD Rating Scale (iADRS) from baseline to 76 weeks relative to placebo.
The newly released detailed findings showed that “the use of donanemab resulted in a better composite score for cognition and for the ability to perform activities of daily living than placebo at 76 weeks, although results for secondary outcomes were mixed,” the investigators, with first author Mark A. Mintun, MD, an employee of Eli Lilly, reported.
Results revealed improvement in scores on the Clinical Dementia Rating Scale-Sum of Boxes (CDR-SB) and the 13-item cognitive subscale of the AD Assessment Scale (ADAS-Cog13), but the differences between the two treatment groups were not significant. In addition, score changes on the AD Cooperative Study–Instrumental Activities of Daily Inventory (ADCS-iADL) and the Mini-Mental State Examination (MMSE) were not “substantial.”
However, the donanemab group did show an 85-centiloid greater reduction in amyloid plaque level at 76 weeks, as shown on PET, compared with the placebo group.
Proof of concept?
The humanized antibody donanemab, which was previously known as LY3002813, targets a modified form of deposited amyloid-beta (A-beta) peptide called N3pG.
The randomized, placebo-controlled, double-blind TRAILBLAZER-ALZ trial, which was described as a “phase 2 proof of concept trial” in the AD/PD program, was conducted at 56 sites in the United States and Canada and included 257 patients between the ages of 60 and 85 years (52% were women). PET confirmed tau and amyloid deposition in all participants.
The active treatment group (n = 131) was randomly assigned to receive donanemab 700 mg for three doses; after that, treatment was bumped up to 1,400 mg. Both the donanemab and placebo groups (n = 126) received treatment intravenously every 4 weeks for up to 72 weeks.
Participants also underwent F-florbetapir and F-flortaucipir PET scans at various timepoints and completed a slew of cognitive tests.
The study’s primary outcome measure was change between baseline and 76 weeks post treatment on composite score for cognition, as measured by the iADRS. The iADRS combines the ADAS-Cog13 and the ADCS-iADL.
This measure ranges from 0 to 144, with lower scores associated with greater cognitive impairment. Both treatment groups had an iADRS score of 106 at baseline.
More research needed
Results showed that the score change from baseline on the iADRS was –6.86 for the active treatment group vs –10.06 for the placebo group (group difference, 3.2; 95% confidence interval [CI], 0.12-6.27; P = .04). Although significant, “the trial was powered to show a 6-point difference,” which was not met, the investigators note.
Differences in score changes from baseline to 76 weeks for the treatment vs. placebo groups on the following secondary outcome measures were:
- CDR-SB: –0.36 (95% CI, –0.83 to –0.12).
- ADAS-Cog13: –1.86 (95% CI, –3.63 to –0.09).
- ADCS-iADL: 1.21 (95% CI, –0.77 to 3.2).
- MMSE: 0.64 (95% CI, –0.4 to 1.67).
The CDR-SB was designated as the first secondary outcome, and because it did not show a significant between-group difference, “the hierarchy failed and no definite conclusions can be drawn from data regarding the differences between groups in the change in the ADAS-Cog13,” the investigators wrote.
In addition, the differences in scores on the latter two secondary outcomes were not “substantial,” they reported.
However, at 76 weeks, the donanemab group showed a reduction of 84.13 centiloids in amyloid plaque level vs. an increase of 0.93 centiloids in the placebo group (between-group difference, 85.06 centiloids). At 24 weeks, the active-treatment group had a 67.83-centiloids greater reduction vs. the placebo group.
In addition, 40%, 59.8%, and 67.8% of the donanemab group achieved “amyloid-negative status” at 24, 52, and 76 weeks, respectively. Amyloid-negative status was defined as an amyloid plaque level of less than 24.1 centiloids.
Total incidence of death or serious adverse events did not differ significantly between the groups. However, the donanemab group had significantly more reports of ARIA-E compared with the placebo group (26.7% vs. 0.8%).
Overall, the researchers noted that more trials of longer duration with larger patient numbers are warranted “to further determine the efficacy and safety of donanemab” in AD.
Positive signal?
In a statement, Maria Carrillo, PhD, chief science officer for the Alzheimer’s Association, said the organization “is encouraged by this promising data.
“It is the first phase 2 Alzheimer’s trial to show positive results on a primary outcome measure related to memory and thinking,” Dr. Carrillo said. However, “more work needs to be done on this experimental drug therapy.”
Dr. Carrillo noted that because the trial was moderately sized and only 180 participants completed the study, “we look forward to the results of a second, larger phase 2 trial of this drug.”
Still, she added, there were several “novel and innovative aspects” in the way the study was conducted noting that it showcases the evolution of AD research.
“I’m hopeful for the future,” Dr. Carrillo said.
Also commenting on the results, Howard Fillit, MD, neuroscientist and founding executive director and chief science officer of the Alzheimer’s Drug Discovery Foundation, said the study showed “the pharmacology works” and that the drug did what it was supposed to do in terms of removing A-beta plaque.
“It also gave us a signal in a relatively small phase 2 study that there might be a modest cognitive benefit,” said Dr. Fillit, who was not involved with the research.
He noted that although the rate of decline slowing was statistically significant it remains to be seen whether this is clinically meaningful, particularly in light of the fact that the secondary outcome results were mixed.
“Basically, it was a positive study that probably needs to be followed by another, much larger study to get us to really see the benefit,” Dr. Fillit said.
Dr. Mintun is an employee of Eli Lilly, which funded the study. Dr. Carrillo and Dr. Fillit have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results from the TRAILBLAZER-ALZ trial were presented at the 2021 International Conference on Alzheimer’s and Parkinson’s Diseases (AD/PD) and were simultaneously published online March 13 in the New England Journal of Medicine.
As previously reported by Medscape Medical News, topline results showed that donanemab slowed cognitive decline by 32% on the Integrated AD Rating Scale (iADRS) from baseline to 76 weeks relative to placebo.
The newly released detailed findings showed that “the use of donanemab resulted in a better composite score for cognition and for the ability to perform activities of daily living than placebo at 76 weeks, although results for secondary outcomes were mixed,” the investigators, with first author Mark A. Mintun, MD, an employee of Eli Lilly, reported.
Results revealed improvement in scores on the Clinical Dementia Rating Scale-Sum of Boxes (CDR-SB) and the 13-item cognitive subscale of the AD Assessment Scale (ADAS-Cog13), but the differences between the two treatment groups were not significant. In addition, score changes on the AD Cooperative Study–Instrumental Activities of Daily Inventory (ADCS-iADL) and the Mini-Mental State Examination (MMSE) were not “substantial.”
However, the donanemab group did show an 85-centiloid greater reduction in amyloid plaque level at 76 weeks, as shown on PET, compared with the placebo group.
Proof of concept?
The humanized antibody donanemab, which was previously known as LY3002813, targets a modified form of deposited amyloid-beta (A-beta) peptide called N3pG.
The randomized, placebo-controlled, double-blind TRAILBLAZER-ALZ trial, which was described as a “phase 2 proof of concept trial” in the AD/PD program, was conducted at 56 sites in the United States and Canada and included 257 patients between the ages of 60 and 85 years (52% were women). PET confirmed tau and amyloid deposition in all participants.
The active treatment group (n = 131) was randomly assigned to receive donanemab 700 mg for three doses; after that, treatment was bumped up to 1,400 mg. Both the donanemab and placebo groups (n = 126) received treatment intravenously every 4 weeks for up to 72 weeks.
Participants also underwent F-florbetapir and F-flortaucipir PET scans at various timepoints and completed a slew of cognitive tests.
The study’s primary outcome measure was change between baseline and 76 weeks post treatment on composite score for cognition, as measured by the iADRS. The iADRS combines the ADAS-Cog13 and the ADCS-iADL.
This measure ranges from 0 to 144, with lower scores associated with greater cognitive impairment. Both treatment groups had an iADRS score of 106 at baseline.
More research needed
Results showed that the score change from baseline on the iADRS was –6.86 for the active treatment group vs –10.06 for the placebo group (group difference, 3.2; 95% confidence interval [CI], 0.12-6.27; P = .04). Although significant, “the trial was powered to show a 6-point difference,” which was not met, the investigators note.
Differences in score changes from baseline to 76 weeks for the treatment vs. placebo groups on the following secondary outcome measures were:
- CDR-SB: –0.36 (95% CI, –0.83 to –0.12).
- ADAS-Cog13: –1.86 (95% CI, –3.63 to –0.09).
- ADCS-iADL: 1.21 (95% CI, –0.77 to 3.2).
- MMSE: 0.64 (95% CI, –0.4 to 1.67).
The CDR-SB was designated as the first secondary outcome, and because it did not show a significant between-group difference, “the hierarchy failed and no definite conclusions can be drawn from data regarding the differences between groups in the change in the ADAS-Cog13,” the investigators wrote.
In addition, the differences in scores on the latter two secondary outcomes were not “substantial,” they reported.
However, at 76 weeks, the donanemab group showed a reduction of 84.13 centiloids in amyloid plaque level vs. an increase of 0.93 centiloids in the placebo group (between-group difference, 85.06 centiloids). At 24 weeks, the active-treatment group had a 67.83-centiloids greater reduction vs. the placebo group.
In addition, 40%, 59.8%, and 67.8% of the donanemab group achieved “amyloid-negative status” at 24, 52, and 76 weeks, respectively. Amyloid-negative status was defined as an amyloid plaque level of less than 24.1 centiloids.
Total incidence of death or serious adverse events did not differ significantly between the groups. However, the donanemab group had significantly more reports of ARIA-E compared with the placebo group (26.7% vs. 0.8%).
Overall, the researchers noted that more trials of longer duration with larger patient numbers are warranted “to further determine the efficacy and safety of donanemab” in AD.
Positive signal?
In a statement, Maria Carrillo, PhD, chief science officer for the Alzheimer’s Association, said the organization “is encouraged by this promising data.
“It is the first phase 2 Alzheimer’s trial to show positive results on a primary outcome measure related to memory and thinking,” Dr. Carrillo said. However, “more work needs to be done on this experimental drug therapy.”
Dr. Carrillo noted that because the trial was moderately sized and only 180 participants completed the study, “we look forward to the results of a second, larger phase 2 trial of this drug.”
Still, she added, there were several “novel and innovative aspects” in the way the study was conducted noting that it showcases the evolution of AD research.
“I’m hopeful for the future,” Dr. Carrillo said.
Also commenting on the results, Howard Fillit, MD, neuroscientist and founding executive director and chief science officer of the Alzheimer’s Drug Discovery Foundation, said the study showed “the pharmacology works” and that the drug did what it was supposed to do in terms of removing A-beta plaque.
“It also gave us a signal in a relatively small phase 2 study that there might be a modest cognitive benefit,” said Dr. Fillit, who was not involved with the research.
He noted that although the rate of decline slowing was statistically significant it remains to be seen whether this is clinically meaningful, particularly in light of the fact that the secondary outcome results were mixed.
“Basically, it was a positive study that probably needs to be followed by another, much larger study to get us to really see the benefit,” Dr. Fillit said.
Dr. Mintun is an employee of Eli Lilly, which funded the study. Dr. Carrillo and Dr. Fillit have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results from the TRAILBLAZER-ALZ trial were presented at the 2021 International Conference on Alzheimer’s and Parkinson’s Diseases (AD/PD) and were simultaneously published online March 13 in the New England Journal of Medicine.
As previously reported by Medscape Medical News, topline results showed that donanemab slowed cognitive decline by 32% on the Integrated AD Rating Scale (iADRS) from baseline to 76 weeks relative to placebo.
The newly released detailed findings showed that “the use of donanemab resulted in a better composite score for cognition and for the ability to perform activities of daily living than placebo at 76 weeks, although results for secondary outcomes were mixed,” the investigators, with first author Mark A. Mintun, MD, an employee of Eli Lilly, reported.
Results revealed improvement in scores on the Clinical Dementia Rating Scale-Sum of Boxes (CDR-SB) and the 13-item cognitive subscale of the AD Assessment Scale (ADAS-Cog13), but the differences between the two treatment groups were not significant. In addition, score changes on the AD Cooperative Study–Instrumental Activities of Daily Inventory (ADCS-iADL) and the Mini-Mental State Examination (MMSE) were not “substantial.”
However, the donanemab group did show an 85-centiloid greater reduction in amyloid plaque level at 76 weeks, as shown on PET, compared with the placebo group.
Proof of concept?
The humanized antibody donanemab, which was previously known as LY3002813, targets a modified form of deposited amyloid-beta (A-beta) peptide called N3pG.
The randomized, placebo-controlled, double-blind TRAILBLAZER-ALZ trial, which was described as a “phase 2 proof of concept trial” in the AD/PD program, was conducted at 56 sites in the United States and Canada and included 257 patients between the ages of 60 and 85 years (52% were women). PET confirmed tau and amyloid deposition in all participants.
The active treatment group (n = 131) was randomly assigned to receive donanemab 700 mg for three doses; after that, treatment was bumped up to 1,400 mg. Both the donanemab and placebo groups (n = 126) received treatment intravenously every 4 weeks for up to 72 weeks.
Participants also underwent F-florbetapir and F-flortaucipir PET scans at various timepoints and completed a slew of cognitive tests.
The study’s primary outcome measure was change between baseline and 76 weeks post treatment on composite score for cognition, as measured by the iADRS. The iADRS combines the ADAS-Cog13 and the ADCS-iADL.
This measure ranges from 0 to 144, with lower scores associated with greater cognitive impairment. Both treatment groups had an iADRS score of 106 at baseline.
More research needed
Results showed that the score change from baseline on the iADRS was –6.86 for the active treatment group vs –10.06 for the placebo group (group difference, 3.2; 95% confidence interval [CI], 0.12-6.27; P = .04). Although significant, “the trial was powered to show a 6-point difference,” which was not met, the investigators note.
Differences in score changes from baseline to 76 weeks for the treatment vs. placebo groups on the following secondary outcome measures were:
- CDR-SB: –0.36 (95% CI, –0.83 to –0.12).
- ADAS-Cog13: –1.86 (95% CI, –3.63 to –0.09).
- ADCS-iADL: 1.21 (95% CI, –0.77 to 3.2).
- MMSE: 0.64 (95% CI, –0.4 to 1.67).
The CDR-SB was designated as the first secondary outcome, and because it did not show a significant between-group difference, “the hierarchy failed and no definite conclusions can be drawn from data regarding the differences between groups in the change in the ADAS-Cog13,” the investigators wrote.
In addition, the differences in scores on the latter two secondary outcomes were not “substantial,” they reported.
However, at 76 weeks, the donanemab group showed a reduction of 84.13 centiloids in amyloid plaque level vs. an increase of 0.93 centiloids in the placebo group (between-group difference, 85.06 centiloids). At 24 weeks, the active-treatment group had a 67.83-centiloids greater reduction vs. the placebo group.
In addition, 40%, 59.8%, and 67.8% of the donanemab group achieved “amyloid-negative status” at 24, 52, and 76 weeks, respectively. Amyloid-negative status was defined as an amyloid plaque level of less than 24.1 centiloids.
Total incidence of death or serious adverse events did not differ significantly between the groups. However, the donanemab group had significantly more reports of ARIA-E compared with the placebo group (26.7% vs. 0.8%).
Overall, the researchers noted that more trials of longer duration with larger patient numbers are warranted “to further determine the efficacy and safety of donanemab” in AD.
Positive signal?
In a statement, Maria Carrillo, PhD, chief science officer for the Alzheimer’s Association, said the organization “is encouraged by this promising data.
“It is the first phase 2 Alzheimer’s trial to show positive results on a primary outcome measure related to memory and thinking,” Dr. Carrillo said. However, “more work needs to be done on this experimental drug therapy.”
Dr. Carrillo noted that because the trial was moderately sized and only 180 participants completed the study, “we look forward to the results of a second, larger phase 2 trial of this drug.”
Still, she added, there were several “novel and innovative aspects” in the way the study was conducted noting that it showcases the evolution of AD research.
“I’m hopeful for the future,” Dr. Carrillo said.
Also commenting on the results, Howard Fillit, MD, neuroscientist and founding executive director and chief science officer of the Alzheimer’s Drug Discovery Foundation, said the study showed “the pharmacology works” and that the drug did what it was supposed to do in terms of removing A-beta plaque.
“It also gave us a signal in a relatively small phase 2 study that there might be a modest cognitive benefit,” said Dr. Fillit, who was not involved with the research.
He noted that although the rate of decline slowing was statistically significant it remains to be seen whether this is clinically meaningful, particularly in light of the fact that the secondary outcome results were mixed.
“Basically, it was a positive study that probably needs to be followed by another, much larger study to get us to really see the benefit,” Dr. Fillit said.
Dr. Mintun is an employee of Eli Lilly, which funded the study. Dr. Carrillo and Dr. Fillit have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.