User login
Accused: Doc increases patient’s penis size with improper fillers; more
, as reported in NJ.com.
The physician, Muhammad A. Mirza, MD, is a board-certified internal medicine doctor and owner of Mirza Aesthetics, which has its main New Jersey office in Cedar Grove, a township in Essex County. The practice also leases space in New York, Pennsylvania, and Connecticut, where at press time Dr. Mirza was still licensed to practice medicine.
The acting New Jersey attorney general said that Dr. Mirza had deviated from the accepted standards of medical care in at least four key areas: he practiced in ways that put his patients in bodily danger; he lacked the formal training in and an adequate knowledge of aesthetic medicine; he practiced in office settings that inspectors found to be subpar; and he failed to safely store medical supplies or maintain proper medical records.
In one instance singled out by the attorney general’s office, Dr. Mirza used an injectable dermal filler to enhance a patient’s penis. As a result of that nonsurgical procedure, the patient needed to be rushed to a nearby hospital, where he underwent two emergency surgical interventions. Contacted by the emergency department doctor, Dr. Mirza allegedly failed to disclose the name of the filler he used, thereby complicating the patient’s recovery, according to the board complaint.
Dr. Mirza’s other alleged breaches of professional conduct include the following:
- Failure to wear a mask or surgical gloves during procedures
- Failure to keep electronic medical records of any kind
- Improper, off-label use of an injectable dermal filler in proximity to patients’ eyes
- Improper, off-label use of an injectable dermal filler for breast enhancement
- Use of a certain injectable dermal filler without first testing for skin allergies
In addition, site inspections of Dr. Mirza’s offices turned up substandard conditions. On April 23, 2021, in response to numerous patient complaints, the Enforcement Bureau of the Division of Consumer Affairs inspected Dr. Mirza’s Summit, N.J. office, one of several in the state.
Among other things, the inspection uncovered the following:
- The medical office was one large room. A curtain separated the reception area and the examination/treatment area, which consisted of only chairs and a fold-away table.
- “Duffle bags” were used to store injectable fillers. No medical storage refrigerators were observed.
- COVID-19 protocols were not followed. Inspectors could identify no barrier between receptionist and patients, no posted mask mandate, no social distancing policy, and no COVID-19 screening measures.
In addition to temporarily suspending Dr. Mirza’s license, the medical board has prohibited him from treating New Jersey patients in any of the out-of-state locations where he’s licensed to practice medicine.
Prosecutors have urged other patients who believe they’ve been injured by Mirza Aesthetics to file a complaint with the State Division of Consumer Affairs.
Dr. Mirza has agreed to the temporary suspension of his medical license, pending a hearing before an administrative law judge. In addition to facing civil penalties for each of the counts against him, he could be held responsible for paying investigative costs, attorney fees, trial costs, and other costs.
Doctor’s failure to diagnose results in mega award
In what is believed to be a record verdict in a wrongful death suit in Volusia County, Fla., a jury awarded $6.46 million to the family of a woman who died from an undiagnosed heart infection after being transferred from a local hospital, according to a report in The Daytona Beach News-Journal, among other news outlets.
In March 2016, Laura Staib went to what was then Florida Hospital DeLand — now AdventHealth DeLand — complaining of a variety of symptoms. There, she was examined by a doctor who was a member of a nearby cardiology group. His diagnosis: congestive heart failure, pneumonia, and sepsis. Transferred to a long-term care facility, Ms. Staib died 4 days later.
In their complaint against the cardiologist and his cardiology group, family members alleged that the doctor failed to identify Ms. Staib’s main problem: viral myocarditis.
“This was primarily a heart failure problem and a heart infection that was probably causing some problems in the lungs,” said the attorney representing the family. “A virus was attacking her heart, and they missed it,” he said. Claims against the hospital and other doctors were eventually resolved and dismissed.
The jury’s verdict will be appealed, said the attorney representing the cardiologist.
He argues that his client “did not cause that woman’s death. She died of an overwhelming lung infection...acute respiratory distress syndrome, caused by an overwhelming pneumonia that got worse after she was transferred to a facility where [my client] doesn’t practice.”
The bulk of the award will be in compensation for family members’ future pain and suffering and for other noneconomic damages.
Botched outpatient procedure leaves woman disfigured
In early September, a patient was allegedly administered the wrong drug during an outpatient procedure on her hand. She sued the Austin, Tex., hospital and surgical center where that procedure was performed, according to a story in Law/Street.
On January 9, 2020, Jessica Arguello went to HCA Healthcare’s South Austin Surgery Center to undergo a right-hand first metacarpophalangeal arthrodesis (fusion) and neuroma excision. In her suit against the hospital, Ms. Arguello claims that while her surgeon was preparing to close the incision after having irrigated the site, he called for a syringe containing an anesthetic. He was instead handed a syringe that contained formalin, the chemical used to preserve specimens for later review.
The mistake, Ms. Arguello claims, caused her to suffer massive chemical burns and necrosis of her flesh, which required four additional surgeries. In the end, she says, her right hand is disfigured and has limited mobility.
She adds that her injuries were preventable. Standard surgical procedure typically forbids chemicals such as formalin to be included among items on the prep tray. In addition to other compensation, she seeks damages for past and future medical expenses and past and future pain and suffering.
At press time, the defendants had not responded to Ms. Arguello’s complaint.
A version of this article first appeared on Medscape.com.
, as reported in NJ.com.
The physician, Muhammad A. Mirza, MD, is a board-certified internal medicine doctor and owner of Mirza Aesthetics, which has its main New Jersey office in Cedar Grove, a township in Essex County. The practice also leases space in New York, Pennsylvania, and Connecticut, where at press time Dr. Mirza was still licensed to practice medicine.
The acting New Jersey attorney general said that Dr. Mirza had deviated from the accepted standards of medical care in at least four key areas: he practiced in ways that put his patients in bodily danger; he lacked the formal training in and an adequate knowledge of aesthetic medicine; he practiced in office settings that inspectors found to be subpar; and he failed to safely store medical supplies or maintain proper medical records.
In one instance singled out by the attorney general’s office, Dr. Mirza used an injectable dermal filler to enhance a patient’s penis. As a result of that nonsurgical procedure, the patient needed to be rushed to a nearby hospital, where he underwent two emergency surgical interventions. Contacted by the emergency department doctor, Dr. Mirza allegedly failed to disclose the name of the filler he used, thereby complicating the patient’s recovery, according to the board complaint.
Dr. Mirza’s other alleged breaches of professional conduct include the following:
- Failure to wear a mask or surgical gloves during procedures
- Failure to keep electronic medical records of any kind
- Improper, off-label use of an injectable dermal filler in proximity to patients’ eyes
- Improper, off-label use of an injectable dermal filler for breast enhancement
- Use of a certain injectable dermal filler without first testing for skin allergies
In addition, site inspections of Dr. Mirza’s offices turned up substandard conditions. On April 23, 2021, in response to numerous patient complaints, the Enforcement Bureau of the Division of Consumer Affairs inspected Dr. Mirza’s Summit, N.J. office, one of several in the state.
Among other things, the inspection uncovered the following:
- The medical office was one large room. A curtain separated the reception area and the examination/treatment area, which consisted of only chairs and a fold-away table.
- “Duffle bags” were used to store injectable fillers. No medical storage refrigerators were observed.
- COVID-19 protocols were not followed. Inspectors could identify no barrier between receptionist and patients, no posted mask mandate, no social distancing policy, and no COVID-19 screening measures.
In addition to temporarily suspending Dr. Mirza’s license, the medical board has prohibited him from treating New Jersey patients in any of the out-of-state locations where he’s licensed to practice medicine.
Prosecutors have urged other patients who believe they’ve been injured by Mirza Aesthetics to file a complaint with the State Division of Consumer Affairs.
Dr. Mirza has agreed to the temporary suspension of his medical license, pending a hearing before an administrative law judge. In addition to facing civil penalties for each of the counts against him, he could be held responsible for paying investigative costs, attorney fees, trial costs, and other costs.
Doctor’s failure to diagnose results in mega award
In what is believed to be a record verdict in a wrongful death suit in Volusia County, Fla., a jury awarded $6.46 million to the family of a woman who died from an undiagnosed heart infection after being transferred from a local hospital, according to a report in The Daytona Beach News-Journal, among other news outlets.
In March 2016, Laura Staib went to what was then Florida Hospital DeLand — now AdventHealth DeLand — complaining of a variety of symptoms. There, she was examined by a doctor who was a member of a nearby cardiology group. His diagnosis: congestive heart failure, pneumonia, and sepsis. Transferred to a long-term care facility, Ms. Staib died 4 days later.
In their complaint against the cardiologist and his cardiology group, family members alleged that the doctor failed to identify Ms. Staib’s main problem: viral myocarditis.
“This was primarily a heart failure problem and a heart infection that was probably causing some problems in the lungs,” said the attorney representing the family. “A virus was attacking her heart, and they missed it,” he said. Claims against the hospital and other doctors were eventually resolved and dismissed.
The jury’s verdict will be appealed, said the attorney representing the cardiologist.
He argues that his client “did not cause that woman’s death. She died of an overwhelming lung infection...acute respiratory distress syndrome, caused by an overwhelming pneumonia that got worse after she was transferred to a facility where [my client] doesn’t practice.”
The bulk of the award will be in compensation for family members’ future pain and suffering and for other noneconomic damages.
Botched outpatient procedure leaves woman disfigured
In early September, a patient was allegedly administered the wrong drug during an outpatient procedure on her hand. She sued the Austin, Tex., hospital and surgical center where that procedure was performed, according to a story in Law/Street.
On January 9, 2020, Jessica Arguello went to HCA Healthcare’s South Austin Surgery Center to undergo a right-hand first metacarpophalangeal arthrodesis (fusion) and neuroma excision. In her suit against the hospital, Ms. Arguello claims that while her surgeon was preparing to close the incision after having irrigated the site, he called for a syringe containing an anesthetic. He was instead handed a syringe that contained formalin, the chemical used to preserve specimens for later review.
The mistake, Ms. Arguello claims, caused her to suffer massive chemical burns and necrosis of her flesh, which required four additional surgeries. In the end, she says, her right hand is disfigured and has limited mobility.
She adds that her injuries were preventable. Standard surgical procedure typically forbids chemicals such as formalin to be included among items on the prep tray. In addition to other compensation, she seeks damages for past and future medical expenses and past and future pain and suffering.
At press time, the defendants had not responded to Ms. Arguello’s complaint.
A version of this article first appeared on Medscape.com.
, as reported in NJ.com.
The physician, Muhammad A. Mirza, MD, is a board-certified internal medicine doctor and owner of Mirza Aesthetics, which has its main New Jersey office in Cedar Grove, a township in Essex County. The practice also leases space in New York, Pennsylvania, and Connecticut, where at press time Dr. Mirza was still licensed to practice medicine.
The acting New Jersey attorney general said that Dr. Mirza had deviated from the accepted standards of medical care in at least four key areas: he practiced in ways that put his patients in bodily danger; he lacked the formal training in and an adequate knowledge of aesthetic medicine; he practiced in office settings that inspectors found to be subpar; and he failed to safely store medical supplies or maintain proper medical records.
In one instance singled out by the attorney general’s office, Dr. Mirza used an injectable dermal filler to enhance a patient’s penis. As a result of that nonsurgical procedure, the patient needed to be rushed to a nearby hospital, where he underwent two emergency surgical interventions. Contacted by the emergency department doctor, Dr. Mirza allegedly failed to disclose the name of the filler he used, thereby complicating the patient’s recovery, according to the board complaint.
Dr. Mirza’s other alleged breaches of professional conduct include the following:
- Failure to wear a mask or surgical gloves during procedures
- Failure to keep electronic medical records of any kind
- Improper, off-label use of an injectable dermal filler in proximity to patients’ eyes
- Improper, off-label use of an injectable dermal filler for breast enhancement
- Use of a certain injectable dermal filler without first testing for skin allergies
In addition, site inspections of Dr. Mirza’s offices turned up substandard conditions. On April 23, 2021, in response to numerous patient complaints, the Enforcement Bureau of the Division of Consumer Affairs inspected Dr. Mirza’s Summit, N.J. office, one of several in the state.
Among other things, the inspection uncovered the following:
- The medical office was one large room. A curtain separated the reception area and the examination/treatment area, which consisted of only chairs and a fold-away table.
- “Duffle bags” were used to store injectable fillers. No medical storage refrigerators were observed.
- COVID-19 protocols were not followed. Inspectors could identify no barrier between receptionist and patients, no posted mask mandate, no social distancing policy, and no COVID-19 screening measures.
In addition to temporarily suspending Dr. Mirza’s license, the medical board has prohibited him from treating New Jersey patients in any of the out-of-state locations where he’s licensed to practice medicine.
Prosecutors have urged other patients who believe they’ve been injured by Mirza Aesthetics to file a complaint with the State Division of Consumer Affairs.
Dr. Mirza has agreed to the temporary suspension of his medical license, pending a hearing before an administrative law judge. In addition to facing civil penalties for each of the counts against him, he could be held responsible for paying investigative costs, attorney fees, trial costs, and other costs.
Doctor’s failure to diagnose results in mega award
In what is believed to be a record verdict in a wrongful death suit in Volusia County, Fla., a jury awarded $6.46 million to the family of a woman who died from an undiagnosed heart infection after being transferred from a local hospital, according to a report in The Daytona Beach News-Journal, among other news outlets.
In March 2016, Laura Staib went to what was then Florida Hospital DeLand — now AdventHealth DeLand — complaining of a variety of symptoms. There, she was examined by a doctor who was a member of a nearby cardiology group. His diagnosis: congestive heart failure, pneumonia, and sepsis. Transferred to a long-term care facility, Ms. Staib died 4 days later.
In their complaint against the cardiologist and his cardiology group, family members alleged that the doctor failed to identify Ms. Staib’s main problem: viral myocarditis.
“This was primarily a heart failure problem and a heart infection that was probably causing some problems in the lungs,” said the attorney representing the family. “A virus was attacking her heart, and they missed it,” he said. Claims against the hospital and other doctors were eventually resolved and dismissed.
The jury’s verdict will be appealed, said the attorney representing the cardiologist.
He argues that his client “did not cause that woman’s death. She died of an overwhelming lung infection...acute respiratory distress syndrome, caused by an overwhelming pneumonia that got worse after she was transferred to a facility where [my client] doesn’t practice.”
The bulk of the award will be in compensation for family members’ future pain and suffering and for other noneconomic damages.
Botched outpatient procedure leaves woman disfigured
In early September, a patient was allegedly administered the wrong drug during an outpatient procedure on her hand. She sued the Austin, Tex., hospital and surgical center where that procedure was performed, according to a story in Law/Street.
On January 9, 2020, Jessica Arguello went to HCA Healthcare’s South Austin Surgery Center to undergo a right-hand first metacarpophalangeal arthrodesis (fusion) and neuroma excision. In her suit against the hospital, Ms. Arguello claims that while her surgeon was preparing to close the incision after having irrigated the site, he called for a syringe containing an anesthetic. He was instead handed a syringe that contained formalin, the chemical used to preserve specimens for later review.
The mistake, Ms. Arguello claims, caused her to suffer massive chemical burns and necrosis of her flesh, which required four additional surgeries. In the end, she says, her right hand is disfigured and has limited mobility.
She adds that her injuries were preventable. Standard surgical procedure typically forbids chemicals such as formalin to be included among items on the prep tray. In addition to other compensation, she seeks damages for past and future medical expenses and past and future pain and suffering.
At press time, the defendants had not responded to Ms. Arguello’s complaint.
A version of this article first appeared on Medscape.com.
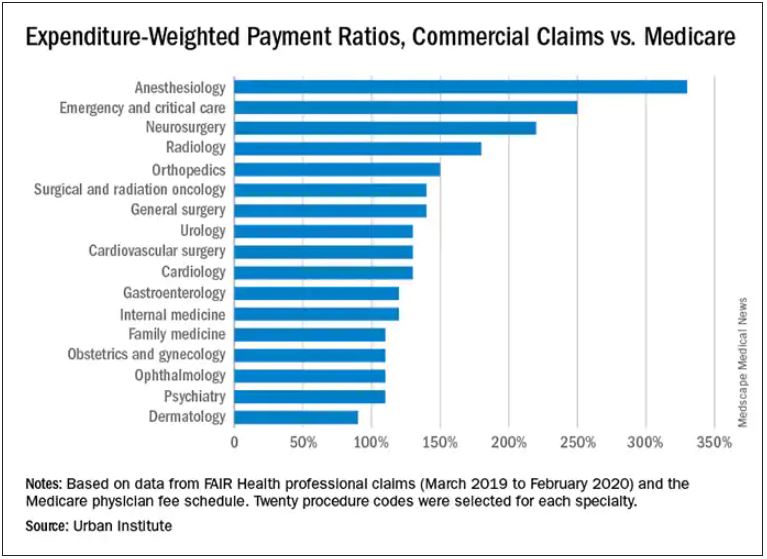
Which specialties get the biggest markups over Medicare rates?
Anesthesiologists charge private insurers more than 300% above Medicare rates, a markup that is higher than that of 16 other specialties, according to a study released by the Urban Institute.
The Washington-based nonprofit institute found that the lowest markups were in psychiatry, ophthalmology, ob.gyn., family medicine, gastroenterology, and internal medicine, at 110%-120% of Medicare rates. .
In the middle are cardiology and cardiovascular surgery (130%), urology (130%), general surgery, surgical and radiation oncology (all at 140%), and orthopedics (150%).
At the top end were radiology (180%), neurosurgery (220%), emergency and critical care (250%), and anesthesiology (330%).
The wide variation in payments could be cited in support of the idea of applying Medicare rates across all physician specialties, say the study authors. Although lowering practitioner payments might lead to savings, it “will also create more pushback from providers, especially if these rates are introduced in the employer market,” write researchers Stacey McMorrow, PhD, Robert A. Berenson, MD, and John Holahan, PhD.
It is not known whether lowering commercial payment rates might decrease patient access, they write.
The authors also note that specialties in which the potential for a fee reduction was greatest were also the specialties for which baseline compensation was highest – from $350,000 annually for emergency physicians to $800,000 a year for neurosurgeons. Annual compensation for ob.gyns., dermatologists, and opthalmologists is about $350,000 a year, which suggests that “these specialties are similarly well compensated by both Medicare and commercial insurers,” the authors write.
The investigators assessed the top 20 procedure codes by expenditure in each of 17 physician specialties. They estimated the commercial-to-Medicare payment ratio for each service and constructed weighted averages across services for each specialty at the national level and for 12 states for which data for all the specialties and services were available.
The researchers analyzed claims from the FAIR Health database between March 2019 and March 2020. That database represents 60 insurers covering 150 million people.
Pediatric and geriatric specialties, nonphysician practitioners, out-of-network clinicians, and ambulatory surgery center claims were excluded. Codes with modifiers, J codes, and clinical laboratory services were also not included.
The charges used in the study were not the actual contracted rates. The authors instead used “imputed allowed amounts” for each claim line. That method was used to protect the confidentiality of the negotiated rates.
With regard to all specialties, the lowest compensated services were procedures, evaluation and management, and tests, which received 140%-150% of the Medicare rate. Treatments and imaging were marked up 160%. Anesthesia was reimbursed at a rate 330% higher than the rate Medicare would pay.
The authors also assessed geographic variation for the 12 states for which they had data.
Similar to findings in other studies, the researchers found that the markup was lowest in Pennsylvania (120%) and highest in Wisconsin (260%). The U.S. average was 160%. California and Missouri were at 150%; Michigan was right at the average.
For physicians in Illinois, Louisiana, Colorado, Texas, and New York, markups were 170%-180% over the Medicare rate. Markups for clinicians in New Jersey (190%) and Arizona (200%) were closest to the Wisconsin rate.
The authors note some study limitations, including the fact that they excluded out-of-network practitioners, “and such payments may disproportionately affect certain specialties.”
A version of this article first appeared on Medscape.com.
Anesthesiologists charge private insurers more than 300% above Medicare rates, a markup that is higher than that of 16 other specialties, according to a study released by the Urban Institute.
The Washington-based nonprofit institute found that the lowest markups were in psychiatry, ophthalmology, ob.gyn., family medicine, gastroenterology, and internal medicine, at 110%-120% of Medicare rates. .
In the middle are cardiology and cardiovascular surgery (130%), urology (130%), general surgery, surgical and radiation oncology (all at 140%), and orthopedics (150%).
At the top end were radiology (180%), neurosurgery (220%), emergency and critical care (250%), and anesthesiology (330%).
The wide variation in payments could be cited in support of the idea of applying Medicare rates across all physician specialties, say the study authors. Although lowering practitioner payments might lead to savings, it “will also create more pushback from providers, especially if these rates are introduced in the employer market,” write researchers Stacey McMorrow, PhD, Robert A. Berenson, MD, and John Holahan, PhD.
It is not known whether lowering commercial payment rates might decrease patient access, they write.
The authors also note that specialties in which the potential for a fee reduction was greatest were also the specialties for which baseline compensation was highest – from $350,000 annually for emergency physicians to $800,000 a year for neurosurgeons. Annual compensation for ob.gyns., dermatologists, and opthalmologists is about $350,000 a year, which suggests that “these specialties are similarly well compensated by both Medicare and commercial insurers,” the authors write.
The investigators assessed the top 20 procedure codes by expenditure in each of 17 physician specialties. They estimated the commercial-to-Medicare payment ratio for each service and constructed weighted averages across services for each specialty at the national level and for 12 states for which data for all the specialties and services were available.
The researchers analyzed claims from the FAIR Health database between March 2019 and March 2020. That database represents 60 insurers covering 150 million people.
Pediatric and geriatric specialties, nonphysician practitioners, out-of-network clinicians, and ambulatory surgery center claims were excluded. Codes with modifiers, J codes, and clinical laboratory services were also not included.
The charges used in the study were not the actual contracted rates. The authors instead used “imputed allowed amounts” for each claim line. That method was used to protect the confidentiality of the negotiated rates.
With regard to all specialties, the lowest compensated services were procedures, evaluation and management, and tests, which received 140%-150% of the Medicare rate. Treatments and imaging were marked up 160%. Anesthesia was reimbursed at a rate 330% higher than the rate Medicare would pay.
The authors also assessed geographic variation for the 12 states for which they had data.
Similar to findings in other studies, the researchers found that the markup was lowest in Pennsylvania (120%) and highest in Wisconsin (260%). The U.S. average was 160%. California and Missouri were at 150%; Michigan was right at the average.
For physicians in Illinois, Louisiana, Colorado, Texas, and New York, markups were 170%-180% over the Medicare rate. Markups for clinicians in New Jersey (190%) and Arizona (200%) were closest to the Wisconsin rate.
The authors note some study limitations, including the fact that they excluded out-of-network practitioners, “and such payments may disproportionately affect certain specialties.”
A version of this article first appeared on Medscape.com.
Anesthesiologists charge private insurers more than 300% above Medicare rates, a markup that is higher than that of 16 other specialties, according to a study released by the Urban Institute.
The Washington-based nonprofit institute found that the lowest markups were in psychiatry, ophthalmology, ob.gyn., family medicine, gastroenterology, and internal medicine, at 110%-120% of Medicare rates. .
In the middle are cardiology and cardiovascular surgery (130%), urology (130%), general surgery, surgical and radiation oncology (all at 140%), and orthopedics (150%).
At the top end were radiology (180%), neurosurgery (220%), emergency and critical care (250%), and anesthesiology (330%).
The wide variation in payments could be cited in support of the idea of applying Medicare rates across all physician specialties, say the study authors. Although lowering practitioner payments might lead to savings, it “will also create more pushback from providers, especially if these rates are introduced in the employer market,” write researchers Stacey McMorrow, PhD, Robert A. Berenson, MD, and John Holahan, PhD.
It is not known whether lowering commercial payment rates might decrease patient access, they write.
The authors also note that specialties in which the potential for a fee reduction was greatest were also the specialties for which baseline compensation was highest – from $350,000 annually for emergency physicians to $800,000 a year for neurosurgeons. Annual compensation for ob.gyns., dermatologists, and opthalmologists is about $350,000 a year, which suggests that “these specialties are similarly well compensated by both Medicare and commercial insurers,” the authors write.
The investigators assessed the top 20 procedure codes by expenditure in each of 17 physician specialties. They estimated the commercial-to-Medicare payment ratio for each service and constructed weighted averages across services for each specialty at the national level and for 12 states for which data for all the specialties and services were available.
The researchers analyzed claims from the FAIR Health database between March 2019 and March 2020. That database represents 60 insurers covering 150 million people.
Pediatric and geriatric specialties, nonphysician practitioners, out-of-network clinicians, and ambulatory surgery center claims were excluded. Codes with modifiers, J codes, and clinical laboratory services were also not included.
The charges used in the study were not the actual contracted rates. The authors instead used “imputed allowed amounts” for each claim line. That method was used to protect the confidentiality of the negotiated rates.
With regard to all specialties, the lowest compensated services were procedures, evaluation and management, and tests, which received 140%-150% of the Medicare rate. Treatments and imaging were marked up 160%. Anesthesia was reimbursed at a rate 330% higher than the rate Medicare would pay.
The authors also assessed geographic variation for the 12 states for which they had data.
Similar to findings in other studies, the researchers found that the markup was lowest in Pennsylvania (120%) and highest in Wisconsin (260%). The U.S. average was 160%. California and Missouri were at 150%; Michigan was right at the average.
For physicians in Illinois, Louisiana, Colorado, Texas, and New York, markups were 170%-180% over the Medicare rate. Markups for clinicians in New Jersey (190%) and Arizona (200%) were closest to the Wisconsin rate.
The authors note some study limitations, including the fact that they excluded out-of-network practitioners, “and such payments may disproportionately affect certain specialties.”
A version of this article first appeared on Medscape.com.
Risk-based antenatal type-and-screen blood testing safe and economical
Implementing a selective type-and-screen blood testing policy in the labor and delivery unit was associated with projected annual savings of close to $200,000, a large single-center study found. Furthermore, there was no evidence of increased maternal morbidity in the university-based facility performing more than 4,400 deliveries per year, according to Ashley E. Benson, MD, MA, of the department of obstetrics and gynecology at the University of Utah, Salt Lake City, and colleagues.
The study, published in Obstetrics & Gynecology, evaluated patient safety, resource utilization, and transfusion-related costs after a policy change from universal type and screen to selective, risk-based type and screen on admission to labor and delivery.
“There had been some national interest in moving toward decreased resource utilization, and findings that universal screening was not cost effective,” Dr. Benson, who has since relocated to Oregon Health & Science University, Portland, said in an interview. An earlier cost-effective modeling study at her center had suggested that universal test and screen was not cost effective and likely not safer either. “So based on that data we felt an implementation study was warranted.”
The switch to a selective policy was made in 2018, after which her group compared outcomes from October 2017 to September 2019, looking those both 1 year preimplementation and 1 year post implementation.
One year post implementation, the following outcomes emerged, compared with preimplementation:
- Overall projected saving of $181,000 a year in the maternity unit
- Lower mean monthly type- and screen-related costs, such as those for ABO typing, antibody screen, and antibody workup. cross-matches, hold clots, and transfused products: $9,753 vs. $20,676 in the preimplementation year (P < .001)
- A lower mean monthly cost of total transfusion preparedness: $25,090 vs. $39,211 (P < .001)
- No differences in emergency-release transfusion events (four vs. three, P = .99),the study’s primary safety outcome
- Fewer emergency-release red blood cell units transfused (9 vs. 24, P = .002) and O-negative RBC units transfused (8 vs. 18, P = .016)
- No differences in hysterectomies (0.05% vs. 0.1%, P = .44) and ICU admissions (0.45% vs. 0.51%, P = .43)
“In a year of selective type and screen, we saw a 51% reduction in costs related to type and screen, and a 38% reduction in overall transfusion-related costs,” the authors wrote. “This study supports other literature suggesting that more judicious use of type and screen may be safe and cost effective.”
Dr. Benson said the results were positively received when presented a meeting 2 years ago but the published version has yet to prompt feedback.
The study
Antepartum patients underwent transfusion preparedness tests according to the center’s standard antenatal admission order sets and were risk stratified in alignment with California Maternal Quality Care Collaborative recommendations. The mean maternal age of patients in both time periods was similar at just over 29 years and the mean gestational age at delivery was just under 38 weeks.
Under the new policy, a “hold clot” is obtained for women stratified as low or medium risk on admission. In this instance, a tube of patient blood is held in the blood bank but processed only if needed, as in the event of active hemorrhage or an order for transfusion. A blood cross-match is obtained on all women stratified as high risk or having a prior positive antibody screen.
Relevant costs were the direct costs of transfusion-related testing in the labor and delivery unit from a health system perspective.
Obstetric hemorrhage is the leading cause of maternal death worldwide, the authors pointed out. While transfusion in obstetric patients occurs in only 1% or 2% of all deliveries it is nevertheless difficult to predict which patients will need transfusion, with only 2%-8% of those stratified as high risk ultimately requiring transfusion. Although obstetric hemorrhage safety bundles recommend risk stratification on admission to labor and delivery with selective type and screen for higher-risk individuals, for safety and simplicity’s sake, many labor and delivery units perform universal type and screen.
The authors cautioned that these results occurred in an academic tertiary care center with systems fine-tuned to deal with active hemorrhage and deliver timely transfusable blood. “At the moment we don’t have enough data to say whether the selective approach would be safe in hospitals with more limited blood bank capacity and access and fewer transfusion specialists in a setting optimized to respond to emergent needs, Dr. Benson said.
Katayoun F. M. Fomani, MD, a transfusion medicine specialist and medical director of blood bank and transfusion services at Long Island Jewish Medical Center, New York, agreed. “This approach only works in a controlled environment such as in this study where eligible women were assessed antenatally at the same center, but it would not work at every institution,” she said in an interview. “In addition, all patients were assessed according to the California Collaborative guideline, which itself increases the safety level but is not followed everywhere.”
The obstetric division at her hospital in New York adheres to the universal type and screen. “We have patients coming in from outside whose antenatal testing was not done at our hospital,” she said. “For this selective approach to work you need a controlled population and the electronic resources and personnel to follow each patient carefully.”
The authors indicated no specific funding for this study and disclosed no potential conflicts of interest. Dr. Fomani had no potential competing interests to declare.
Implementing a selective type-and-screen blood testing policy in the labor and delivery unit was associated with projected annual savings of close to $200,000, a large single-center study found. Furthermore, there was no evidence of increased maternal morbidity in the university-based facility performing more than 4,400 deliveries per year, according to Ashley E. Benson, MD, MA, of the department of obstetrics and gynecology at the University of Utah, Salt Lake City, and colleagues.
The study, published in Obstetrics & Gynecology, evaluated patient safety, resource utilization, and transfusion-related costs after a policy change from universal type and screen to selective, risk-based type and screen on admission to labor and delivery.
“There had been some national interest in moving toward decreased resource utilization, and findings that universal screening was not cost effective,” Dr. Benson, who has since relocated to Oregon Health & Science University, Portland, said in an interview. An earlier cost-effective modeling study at her center had suggested that universal test and screen was not cost effective and likely not safer either. “So based on that data we felt an implementation study was warranted.”
The switch to a selective policy was made in 2018, after which her group compared outcomes from October 2017 to September 2019, looking those both 1 year preimplementation and 1 year post implementation.
One year post implementation, the following outcomes emerged, compared with preimplementation:
- Overall projected saving of $181,000 a year in the maternity unit
- Lower mean monthly type- and screen-related costs, such as those for ABO typing, antibody screen, and antibody workup. cross-matches, hold clots, and transfused products: $9,753 vs. $20,676 in the preimplementation year (P < .001)
- A lower mean monthly cost of total transfusion preparedness: $25,090 vs. $39,211 (P < .001)
- No differences in emergency-release transfusion events (four vs. three, P = .99),the study’s primary safety outcome
- Fewer emergency-release red blood cell units transfused (9 vs. 24, P = .002) and O-negative RBC units transfused (8 vs. 18, P = .016)
- No differences in hysterectomies (0.05% vs. 0.1%, P = .44) and ICU admissions (0.45% vs. 0.51%, P = .43)
“In a year of selective type and screen, we saw a 51% reduction in costs related to type and screen, and a 38% reduction in overall transfusion-related costs,” the authors wrote. “This study supports other literature suggesting that more judicious use of type and screen may be safe and cost effective.”
Dr. Benson said the results were positively received when presented a meeting 2 years ago but the published version has yet to prompt feedback.
The study
Antepartum patients underwent transfusion preparedness tests according to the center’s standard antenatal admission order sets and were risk stratified in alignment with California Maternal Quality Care Collaborative recommendations. The mean maternal age of patients in both time periods was similar at just over 29 years and the mean gestational age at delivery was just under 38 weeks.
Under the new policy, a “hold clot” is obtained for women stratified as low or medium risk on admission. In this instance, a tube of patient blood is held in the blood bank but processed only if needed, as in the event of active hemorrhage or an order for transfusion. A blood cross-match is obtained on all women stratified as high risk or having a prior positive antibody screen.
Relevant costs were the direct costs of transfusion-related testing in the labor and delivery unit from a health system perspective.
Obstetric hemorrhage is the leading cause of maternal death worldwide, the authors pointed out. While transfusion in obstetric patients occurs in only 1% or 2% of all deliveries it is nevertheless difficult to predict which patients will need transfusion, with only 2%-8% of those stratified as high risk ultimately requiring transfusion. Although obstetric hemorrhage safety bundles recommend risk stratification on admission to labor and delivery with selective type and screen for higher-risk individuals, for safety and simplicity’s sake, many labor and delivery units perform universal type and screen.
The authors cautioned that these results occurred in an academic tertiary care center with systems fine-tuned to deal with active hemorrhage and deliver timely transfusable blood. “At the moment we don’t have enough data to say whether the selective approach would be safe in hospitals with more limited blood bank capacity and access and fewer transfusion specialists in a setting optimized to respond to emergent needs, Dr. Benson said.
Katayoun F. M. Fomani, MD, a transfusion medicine specialist and medical director of blood bank and transfusion services at Long Island Jewish Medical Center, New York, agreed. “This approach only works in a controlled environment such as in this study where eligible women were assessed antenatally at the same center, but it would not work at every institution,” she said in an interview. “In addition, all patients were assessed according to the California Collaborative guideline, which itself increases the safety level but is not followed everywhere.”
The obstetric division at her hospital in New York adheres to the universal type and screen. “We have patients coming in from outside whose antenatal testing was not done at our hospital,” she said. “For this selective approach to work you need a controlled population and the electronic resources and personnel to follow each patient carefully.”
The authors indicated no specific funding for this study and disclosed no potential conflicts of interest. Dr. Fomani had no potential competing interests to declare.
Implementing a selective type-and-screen blood testing policy in the labor and delivery unit was associated with projected annual savings of close to $200,000, a large single-center study found. Furthermore, there was no evidence of increased maternal morbidity in the university-based facility performing more than 4,400 deliveries per year, according to Ashley E. Benson, MD, MA, of the department of obstetrics and gynecology at the University of Utah, Salt Lake City, and colleagues.
The study, published in Obstetrics & Gynecology, evaluated patient safety, resource utilization, and transfusion-related costs after a policy change from universal type and screen to selective, risk-based type and screen on admission to labor and delivery.
“There had been some national interest in moving toward decreased resource utilization, and findings that universal screening was not cost effective,” Dr. Benson, who has since relocated to Oregon Health & Science University, Portland, said in an interview. An earlier cost-effective modeling study at her center had suggested that universal test and screen was not cost effective and likely not safer either. “So based on that data we felt an implementation study was warranted.”
The switch to a selective policy was made in 2018, after which her group compared outcomes from October 2017 to September 2019, looking those both 1 year preimplementation and 1 year post implementation.
One year post implementation, the following outcomes emerged, compared with preimplementation:
- Overall projected saving of $181,000 a year in the maternity unit
- Lower mean monthly type- and screen-related costs, such as those for ABO typing, antibody screen, and antibody workup. cross-matches, hold clots, and transfused products: $9,753 vs. $20,676 in the preimplementation year (P < .001)
- A lower mean monthly cost of total transfusion preparedness: $25,090 vs. $39,211 (P < .001)
- No differences in emergency-release transfusion events (four vs. three, P = .99),the study’s primary safety outcome
- Fewer emergency-release red blood cell units transfused (9 vs. 24, P = .002) and O-negative RBC units transfused (8 vs. 18, P = .016)
- No differences in hysterectomies (0.05% vs. 0.1%, P = .44) and ICU admissions (0.45% vs. 0.51%, P = .43)
“In a year of selective type and screen, we saw a 51% reduction in costs related to type and screen, and a 38% reduction in overall transfusion-related costs,” the authors wrote. “This study supports other literature suggesting that more judicious use of type and screen may be safe and cost effective.”
Dr. Benson said the results were positively received when presented a meeting 2 years ago but the published version has yet to prompt feedback.
The study
Antepartum patients underwent transfusion preparedness tests according to the center’s standard antenatal admission order sets and were risk stratified in alignment with California Maternal Quality Care Collaborative recommendations. The mean maternal age of patients in both time periods was similar at just over 29 years and the mean gestational age at delivery was just under 38 weeks.
Under the new policy, a “hold clot” is obtained for women stratified as low or medium risk on admission. In this instance, a tube of patient blood is held in the blood bank but processed only if needed, as in the event of active hemorrhage or an order for transfusion. A blood cross-match is obtained on all women stratified as high risk or having a prior positive antibody screen.
Relevant costs were the direct costs of transfusion-related testing in the labor and delivery unit from a health system perspective.
Obstetric hemorrhage is the leading cause of maternal death worldwide, the authors pointed out. While transfusion in obstetric patients occurs in only 1% or 2% of all deliveries it is nevertheless difficult to predict which patients will need transfusion, with only 2%-8% of those stratified as high risk ultimately requiring transfusion. Although obstetric hemorrhage safety bundles recommend risk stratification on admission to labor and delivery with selective type and screen for higher-risk individuals, for safety and simplicity’s sake, many labor and delivery units perform universal type and screen.
The authors cautioned that these results occurred in an academic tertiary care center with systems fine-tuned to deal with active hemorrhage and deliver timely transfusable blood. “At the moment we don’t have enough data to say whether the selective approach would be safe in hospitals with more limited blood bank capacity and access and fewer transfusion specialists in a setting optimized to respond to emergent needs, Dr. Benson said.
Katayoun F. M. Fomani, MD, a transfusion medicine specialist and medical director of blood bank and transfusion services at Long Island Jewish Medical Center, New York, agreed. “This approach only works in a controlled environment such as in this study where eligible women were assessed antenatally at the same center, but it would not work at every institution,” she said in an interview. “In addition, all patients were assessed according to the California Collaborative guideline, which itself increases the safety level but is not followed everywhere.”
The obstetric division at her hospital in New York adheres to the universal type and screen. “We have patients coming in from outside whose antenatal testing was not done at our hospital,” she said. “For this selective approach to work you need a controlled population and the electronic resources and personnel to follow each patient carefully.”
The authors indicated no specific funding for this study and disclosed no potential conflicts of interest. Dr. Fomani had no potential competing interests to declare.
FROM OBSTETRICS & GYNECOLOGY
The missing puzzle piece
Mrs. Stevens died last week. She was 87.
That’s nothing new. The nature of medicine is such that you’ll see patients pass on.
But Mrs. Stevens bothers me, because even to the end I’m not sure I ever had an answer.
Her case began with somewhat nebulous, but clearly neurological, symptoms. An initial workup was normal, as was the secondary one.
The third stage of increasingly esoteric tests turned up some clues as to what was going wrong, even as she continued to dwindle. I could at least start working on a differential, even if none of it was good.
I met with her and her husband, and they wanted an answer, good or bad.
I pulled some strings at a local tertiary subspecialty center and got her in. They agreed with my suspicions, though also couldn’t find something definitive. They even repeated the tests, and came to the same conclusions – narrowed down to a few things, but no smoking gun.
Throughout all of this Mrs. Stevens kept spiraling down. After a few hospital admissions and even a biopsy of an abdominal mass we thought would give us the answer, we still didn’t solve the puzzle.
At some point she and her husband grew tired of looking and accepted that it wouldn’t change anything. Her internist called hospice in. They kept her comfortable for her last few weeks.
They didn’t want an autopsy, so the secret stayed with her.
Looking back, I agree with their decision to stop the workup. When looking further won’t change anything, why bother?
But, as a doctor, it’s frustrating. There’s a degree of intellectual curiosity that drives us. We want answers. We want to solve puzzles.
And sometimes we never get that final piece. Even if it’s the right decision for the patient, at the end of the day it’s still an unsolved crime to us. A reminder that,
We probably never will.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Mrs. Stevens died last week. She was 87.
That’s nothing new. The nature of medicine is such that you’ll see patients pass on.
But Mrs. Stevens bothers me, because even to the end I’m not sure I ever had an answer.
Her case began with somewhat nebulous, but clearly neurological, symptoms. An initial workup was normal, as was the secondary one.
The third stage of increasingly esoteric tests turned up some clues as to what was going wrong, even as she continued to dwindle. I could at least start working on a differential, even if none of it was good.
I met with her and her husband, and they wanted an answer, good or bad.
I pulled some strings at a local tertiary subspecialty center and got her in. They agreed with my suspicions, though also couldn’t find something definitive. They even repeated the tests, and came to the same conclusions – narrowed down to a few things, but no smoking gun.
Throughout all of this Mrs. Stevens kept spiraling down. After a few hospital admissions and even a biopsy of an abdominal mass we thought would give us the answer, we still didn’t solve the puzzle.
At some point she and her husband grew tired of looking and accepted that it wouldn’t change anything. Her internist called hospice in. They kept her comfortable for her last few weeks.
They didn’t want an autopsy, so the secret stayed with her.
Looking back, I agree with their decision to stop the workup. When looking further won’t change anything, why bother?
But, as a doctor, it’s frustrating. There’s a degree of intellectual curiosity that drives us. We want answers. We want to solve puzzles.
And sometimes we never get that final piece. Even if it’s the right decision for the patient, at the end of the day it’s still an unsolved crime to us. A reminder that,
We probably never will.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Mrs. Stevens died last week. She was 87.
That’s nothing new. The nature of medicine is such that you’ll see patients pass on.
But Mrs. Stevens bothers me, because even to the end I’m not sure I ever had an answer.
Her case began with somewhat nebulous, but clearly neurological, symptoms. An initial workup was normal, as was the secondary one.
The third stage of increasingly esoteric tests turned up some clues as to what was going wrong, even as she continued to dwindle. I could at least start working on a differential, even if none of it was good.
I met with her and her husband, and they wanted an answer, good or bad.
I pulled some strings at a local tertiary subspecialty center and got her in. They agreed with my suspicions, though also couldn’t find something definitive. They even repeated the tests, and came to the same conclusions – narrowed down to a few things, but no smoking gun.
Throughout all of this Mrs. Stevens kept spiraling down. After a few hospital admissions and even a biopsy of an abdominal mass we thought would give us the answer, we still didn’t solve the puzzle.
At some point she and her husband grew tired of looking and accepted that it wouldn’t change anything. Her internist called hospice in. They kept her comfortable for her last few weeks.
They didn’t want an autopsy, so the secret stayed with her.
Looking back, I agree with their decision to stop the workup. When looking further won’t change anything, why bother?
But, as a doctor, it’s frustrating. There’s a degree of intellectual curiosity that drives us. We want answers. We want to solve puzzles.
And sometimes we never get that final piece. Even if it’s the right decision for the patient, at the end of the day it’s still an unsolved crime to us. A reminder that,
We probably never will.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Pandemic exacerbates primary care practices’ financial struggles
according to experts and the results of recent surveys by the Primary Care Collaborative (PCC).
Fewer than 30% (26.4%) of primary care clinicians report that their practices are financially healthy, according to the latest results from a periodic survey by the PCC. An earlier survey by the PCC suggests clinicians’ confidence in the financial viability of their practices has significantly declined since last year, when compared with the new survey’s results. When the older survey was taken between Sept. 4 and Sept. 8 of 2020, only 35% of primary care clinicians said that revenue and pay were significantly lower than they were before the pandemic.
Submissions to the new PCC survey were collected between Aug. 13 and Aug. 17 of 2021 and included 1,263 respondents from 49 states, the District of Columbia, and two territories. The PCC and the Larry A. Green Center have been regularly surveying primary care clinicians to better understand the impact of COVID-19 throughout the pandemic.
PCC President and CEO Ann Greiner said in an interview that the drop over a year follows a trend.
Though primary care faced struggles before the pandemic, the COVID-19 effect has been striking and cumulative, she noted.
“[Primary care practices] were healthier prepandemic,” said Ms. Greiner. “The precipitous drop in revenue when stay-at-home orders went into effect had a very big effect though pay structure and lack of investment in primary care was a problem long before COVID-19.”
COVID-19 has exacerbated all that ails primary care, and has increased fears of viability of primary care offices, she said.
Ms. Greiner pointed to a report from Health Affairs, that projected in 2020 that primary care would lose $65,000 in revenue per full-time physician by the end of the year for a total shortfall of $15 billion, following steep drops in office visits and fees for services from March to May, 2020.
In July of this year, she said, PCC’s survey found that, “Four in 10 clinicians worry that primary care will be gone in 5 years and one-fifth of respondents expect to leave the profession within the next three.”
The July PCC survey also showed that 13% of primary care clinicians said they have discussed selling their practice and cite high-level burnout/exhaustion as a main challenge for the next 6 months.
Robert L. Phillips, MD, a Virginia-based physician who oversees research for the American Board of Family Medicine, said, “Practices in our national primary care practice registry (PRIME) saw visit volumes drop 40% in the 2-3 months around the start of the pandemic and had not seen them return to normal as of June of this year. This means most remain financially underwater.”
End to paycheck protection hurt practices
Conrad L. Flick, MD, managing partner of Family Medical Associates in Raleigh, N.C., said the end of the federal Paycheck Protection Program (PPP) at the end of 2020 caused further distress to primary care and could also help explain the drop in healthy practices that PCC’s survey from last year suggested.
“Many of us who struggled financially as the pandemic hit last year were really worried. PPP certainly shored that up for a lot of us. But now it’s no longer here,” he said.
Dr. Flick said his 10-clinician independent practice is financially sound and he credits that to having the PPP loan, shared savings from an accountable care organization, and holding some profit over from last year to this year.
His practice had to cut two nurse practitioners this year when volume did not return to prepandemic levels.
“The PPP loan let us keep [those NPs] employed through spring, but we were hoping the volume would come back. Come spring this year the volume hasn’t come back, and we couldn’t afford to keep the office at full staff,” he said.
The way primary care physicians are paid is what makes them so vulnerable in a pandemic, he explained.
“Our revenue is purely based on how many people I can get through my office at a given period of time. We don’t have ways to generate revenue and build a cushion.”
Family physician L. Allen Dobson, MD, said the survey results may have become even more grim in the last year, because primary care practices, especially small practices, have not recovered from the 2020 losses and effects have snowballed.
Even though primary care offices have largely reopened and many patients have returned to in-person visits, he said, physicians are dealing with uncertainties of COVID-19 surges and variants and are having trouble recruiting and maintaining staff.
Revenue that should have come to primary care practices in testing and distributing vaccines instead went elsewhere to larger vaccination sites and retail clinics, noted Dr. Dobson, who is chair of the board of managers of Community Care Physicians Network in Mount Pleasant, N.C., which provides assistance with administrative tasks to small and solo primary care practices.
COVID-19 brought ‘accelerated change’
COVID-19 brought “an accelerated change,” in decreasing revenue, Dr. Dobson said.
Small primary care practices have followed the rules of changing to electronic health records, getting patient-centered medical home certification, and documenting quality improvement measures, but they have not reaped the financial benefits from these changes, he explained.
A report commissioned by the Physician Advocacy Institute found that the pandemic accelerated a long national trend of hospitals and corporate entities acquiring physician practices and employing physicians.
From January 2019 to January 2021, these entities acquired 20,900 additional physician practices and 48,000 additional physicians left independent practice for employment by hospital systems or other corporate entities.
Further straining practices is a thinning workforce, with 21% or respondents to the most recent PCC survey having said they were unable to hire clinicians for open positions and 54% saying they are unable to hire staff for open positions.
One respondent to the PCC survey from Utah said, “We need more support. It’s a moral injury to have our pay cut and be severely understaffed. Most of the burden of educating patients and getting them vaccinated has fallen to primary care and we are already overwhelmed with taking care of patients with worsening mental and physical health.”
According to Bruce Landon, MD, MBA, professor of health care policy at the Harvard Medical School’s Center for Primary Care, Boston, another source of financial strain for primary care practices is that they are having difficulty attracting doctors, nurses, and administrators.
These practices often need to increase pay for those positions to recruit people, and they are leaving many positions unfilled, Dr. Landon explained.
Plus, COVID-19 introduced costs for personal protective equipment (PPE) and cleaning products, and those expenses generally have not been reimbursed, Dr. Landon said.
Uncertainty around telemedicine
A new risk for primary care is a decline in telemedicine payments at a time when practices are still relying on telemedicine for revenue.
In the most recent PCC report, 40% of clinicians said they use telemedicine for at least a fifth of all office visits.
Even though most practices have reopened there’s still a fair amount of telemedicine and that will continue, Dr. Landon said in an interview.
In March of 2020, the Centers for Medicare & Medicaid Services lifted restrictions and that helped physicians with getting reimbursed for the services as they would office visits. But some commercial payers are starting to back off full payment for telemedicine, Dr. Landon noted.
“At some point the feds will probably start to do that with Medicare. I think that’s a mistake. [Telemedicine] has been one of the silver linings of this cloud of the pandemic,” he said.
If prepandemic payment regulations are restored, 41% of clinicians said, in the most recent PCC survey, that they worry their practices will no longer be able to support telemedicine.
Possible safety nets
Dr. Landon said that one thing that’s also clear is that some form of primary care capitation payment is necessary, at least for some of the work in primary care.
The practices that had capitation as part of payment were the ones who were most easily able to handle the pandemic because they didn’t see the immediate drop in revenue that fee-for-service practices saw, he noted.
“If we have a next pandemic, having a steady revenue stream to support primary care is really important and having a different way to pay for primary care is probably the best way to do that,” he said. “These longer-term strategies are going to be really crucial if we want to have a primary care system 10 years from now.”
Ms. Greiner, Dr. Flick, Dr. Phillips, Dr. Dobson, and Dr. Landon report no relevant financial relationships.
according to experts and the results of recent surveys by the Primary Care Collaborative (PCC).
Fewer than 30% (26.4%) of primary care clinicians report that their practices are financially healthy, according to the latest results from a periodic survey by the PCC. An earlier survey by the PCC suggests clinicians’ confidence in the financial viability of their practices has significantly declined since last year, when compared with the new survey’s results. When the older survey was taken between Sept. 4 and Sept. 8 of 2020, only 35% of primary care clinicians said that revenue and pay were significantly lower than they were before the pandemic.
Submissions to the new PCC survey were collected between Aug. 13 and Aug. 17 of 2021 and included 1,263 respondents from 49 states, the District of Columbia, and two territories. The PCC and the Larry A. Green Center have been regularly surveying primary care clinicians to better understand the impact of COVID-19 throughout the pandemic.
PCC President and CEO Ann Greiner said in an interview that the drop over a year follows a trend.
Though primary care faced struggles before the pandemic, the COVID-19 effect has been striking and cumulative, she noted.
“[Primary care practices] were healthier prepandemic,” said Ms. Greiner. “The precipitous drop in revenue when stay-at-home orders went into effect had a very big effect though pay structure and lack of investment in primary care was a problem long before COVID-19.”
COVID-19 has exacerbated all that ails primary care, and has increased fears of viability of primary care offices, she said.
Ms. Greiner pointed to a report from Health Affairs, that projected in 2020 that primary care would lose $65,000 in revenue per full-time physician by the end of the year for a total shortfall of $15 billion, following steep drops in office visits and fees for services from March to May, 2020.
In July of this year, she said, PCC’s survey found that, “Four in 10 clinicians worry that primary care will be gone in 5 years and one-fifth of respondents expect to leave the profession within the next three.”
The July PCC survey also showed that 13% of primary care clinicians said they have discussed selling their practice and cite high-level burnout/exhaustion as a main challenge for the next 6 months.
Robert L. Phillips, MD, a Virginia-based physician who oversees research for the American Board of Family Medicine, said, “Practices in our national primary care practice registry (PRIME) saw visit volumes drop 40% in the 2-3 months around the start of the pandemic and had not seen them return to normal as of June of this year. This means most remain financially underwater.”
End to paycheck protection hurt practices
Conrad L. Flick, MD, managing partner of Family Medical Associates in Raleigh, N.C., said the end of the federal Paycheck Protection Program (PPP) at the end of 2020 caused further distress to primary care and could also help explain the drop in healthy practices that PCC’s survey from last year suggested.
“Many of us who struggled financially as the pandemic hit last year were really worried. PPP certainly shored that up for a lot of us. But now it’s no longer here,” he said.
Dr. Flick said his 10-clinician independent practice is financially sound and he credits that to having the PPP loan, shared savings from an accountable care organization, and holding some profit over from last year to this year.
His practice had to cut two nurse practitioners this year when volume did not return to prepandemic levels.
“The PPP loan let us keep [those NPs] employed through spring, but we were hoping the volume would come back. Come spring this year the volume hasn’t come back, and we couldn’t afford to keep the office at full staff,” he said.
The way primary care physicians are paid is what makes them so vulnerable in a pandemic, he explained.
“Our revenue is purely based on how many people I can get through my office at a given period of time. We don’t have ways to generate revenue and build a cushion.”
Family physician L. Allen Dobson, MD, said the survey results may have become even more grim in the last year, because primary care practices, especially small practices, have not recovered from the 2020 losses and effects have snowballed.
Even though primary care offices have largely reopened and many patients have returned to in-person visits, he said, physicians are dealing with uncertainties of COVID-19 surges and variants and are having trouble recruiting and maintaining staff.
Revenue that should have come to primary care practices in testing and distributing vaccines instead went elsewhere to larger vaccination sites and retail clinics, noted Dr. Dobson, who is chair of the board of managers of Community Care Physicians Network in Mount Pleasant, N.C., which provides assistance with administrative tasks to small and solo primary care practices.
COVID-19 brought ‘accelerated change’
COVID-19 brought “an accelerated change,” in decreasing revenue, Dr. Dobson said.
Small primary care practices have followed the rules of changing to electronic health records, getting patient-centered medical home certification, and documenting quality improvement measures, but they have not reaped the financial benefits from these changes, he explained.
A report commissioned by the Physician Advocacy Institute found that the pandemic accelerated a long national trend of hospitals and corporate entities acquiring physician practices and employing physicians.
From January 2019 to January 2021, these entities acquired 20,900 additional physician practices and 48,000 additional physicians left independent practice for employment by hospital systems or other corporate entities.
Further straining practices is a thinning workforce, with 21% or respondents to the most recent PCC survey having said they were unable to hire clinicians for open positions and 54% saying they are unable to hire staff for open positions.
One respondent to the PCC survey from Utah said, “We need more support. It’s a moral injury to have our pay cut and be severely understaffed. Most of the burden of educating patients and getting them vaccinated has fallen to primary care and we are already overwhelmed with taking care of patients with worsening mental and physical health.”
According to Bruce Landon, MD, MBA, professor of health care policy at the Harvard Medical School’s Center for Primary Care, Boston, another source of financial strain for primary care practices is that they are having difficulty attracting doctors, nurses, and administrators.
These practices often need to increase pay for those positions to recruit people, and they are leaving many positions unfilled, Dr. Landon explained.
Plus, COVID-19 introduced costs for personal protective equipment (PPE) and cleaning products, and those expenses generally have not been reimbursed, Dr. Landon said.
Uncertainty around telemedicine
A new risk for primary care is a decline in telemedicine payments at a time when practices are still relying on telemedicine for revenue.
In the most recent PCC report, 40% of clinicians said they use telemedicine for at least a fifth of all office visits.
Even though most practices have reopened there’s still a fair amount of telemedicine and that will continue, Dr. Landon said in an interview.
In March of 2020, the Centers for Medicare & Medicaid Services lifted restrictions and that helped physicians with getting reimbursed for the services as they would office visits. But some commercial payers are starting to back off full payment for telemedicine, Dr. Landon noted.
“At some point the feds will probably start to do that with Medicare. I think that’s a mistake. [Telemedicine] has been one of the silver linings of this cloud of the pandemic,” he said.
If prepandemic payment regulations are restored, 41% of clinicians said, in the most recent PCC survey, that they worry their practices will no longer be able to support telemedicine.
Possible safety nets
Dr. Landon said that one thing that’s also clear is that some form of primary care capitation payment is necessary, at least for some of the work in primary care.
The practices that had capitation as part of payment were the ones who were most easily able to handle the pandemic because they didn’t see the immediate drop in revenue that fee-for-service practices saw, he noted.
“If we have a next pandemic, having a steady revenue stream to support primary care is really important and having a different way to pay for primary care is probably the best way to do that,” he said. “These longer-term strategies are going to be really crucial if we want to have a primary care system 10 years from now.”
Ms. Greiner, Dr. Flick, Dr. Phillips, Dr. Dobson, and Dr. Landon report no relevant financial relationships.
according to experts and the results of recent surveys by the Primary Care Collaborative (PCC).
Fewer than 30% (26.4%) of primary care clinicians report that their practices are financially healthy, according to the latest results from a periodic survey by the PCC. An earlier survey by the PCC suggests clinicians’ confidence in the financial viability of their practices has significantly declined since last year, when compared with the new survey’s results. When the older survey was taken between Sept. 4 and Sept. 8 of 2020, only 35% of primary care clinicians said that revenue and pay were significantly lower than they were before the pandemic.
Submissions to the new PCC survey were collected between Aug. 13 and Aug. 17 of 2021 and included 1,263 respondents from 49 states, the District of Columbia, and two territories. The PCC and the Larry A. Green Center have been regularly surveying primary care clinicians to better understand the impact of COVID-19 throughout the pandemic.
PCC President and CEO Ann Greiner said in an interview that the drop over a year follows a trend.
Though primary care faced struggles before the pandemic, the COVID-19 effect has been striking and cumulative, she noted.
“[Primary care practices] were healthier prepandemic,” said Ms. Greiner. “The precipitous drop in revenue when stay-at-home orders went into effect had a very big effect though pay structure and lack of investment in primary care was a problem long before COVID-19.”
COVID-19 has exacerbated all that ails primary care, and has increased fears of viability of primary care offices, she said.
Ms. Greiner pointed to a report from Health Affairs, that projected in 2020 that primary care would lose $65,000 in revenue per full-time physician by the end of the year for a total shortfall of $15 billion, following steep drops in office visits and fees for services from March to May, 2020.
In July of this year, she said, PCC’s survey found that, “Four in 10 clinicians worry that primary care will be gone in 5 years and one-fifth of respondents expect to leave the profession within the next three.”
The July PCC survey also showed that 13% of primary care clinicians said they have discussed selling their practice and cite high-level burnout/exhaustion as a main challenge for the next 6 months.
Robert L. Phillips, MD, a Virginia-based physician who oversees research for the American Board of Family Medicine, said, “Practices in our national primary care practice registry (PRIME) saw visit volumes drop 40% in the 2-3 months around the start of the pandemic and had not seen them return to normal as of June of this year. This means most remain financially underwater.”
End to paycheck protection hurt practices
Conrad L. Flick, MD, managing partner of Family Medical Associates in Raleigh, N.C., said the end of the federal Paycheck Protection Program (PPP) at the end of 2020 caused further distress to primary care and could also help explain the drop in healthy practices that PCC’s survey from last year suggested.
“Many of us who struggled financially as the pandemic hit last year were really worried. PPP certainly shored that up for a lot of us. But now it’s no longer here,” he said.
Dr. Flick said his 10-clinician independent practice is financially sound and he credits that to having the PPP loan, shared savings from an accountable care organization, and holding some profit over from last year to this year.
His practice had to cut two nurse practitioners this year when volume did not return to prepandemic levels.
“The PPP loan let us keep [those NPs] employed through spring, but we were hoping the volume would come back. Come spring this year the volume hasn’t come back, and we couldn’t afford to keep the office at full staff,” he said.
The way primary care physicians are paid is what makes them so vulnerable in a pandemic, he explained.
“Our revenue is purely based on how many people I can get through my office at a given period of time. We don’t have ways to generate revenue and build a cushion.”
Family physician L. Allen Dobson, MD, said the survey results may have become even more grim in the last year, because primary care practices, especially small practices, have not recovered from the 2020 losses and effects have snowballed.
Even though primary care offices have largely reopened and many patients have returned to in-person visits, he said, physicians are dealing with uncertainties of COVID-19 surges and variants and are having trouble recruiting and maintaining staff.
Revenue that should have come to primary care practices in testing and distributing vaccines instead went elsewhere to larger vaccination sites and retail clinics, noted Dr. Dobson, who is chair of the board of managers of Community Care Physicians Network in Mount Pleasant, N.C., which provides assistance with administrative tasks to small and solo primary care practices.
COVID-19 brought ‘accelerated change’
COVID-19 brought “an accelerated change,” in decreasing revenue, Dr. Dobson said.
Small primary care practices have followed the rules of changing to electronic health records, getting patient-centered medical home certification, and documenting quality improvement measures, but they have not reaped the financial benefits from these changes, he explained.
A report commissioned by the Physician Advocacy Institute found that the pandemic accelerated a long national trend of hospitals and corporate entities acquiring physician practices and employing physicians.
From January 2019 to January 2021, these entities acquired 20,900 additional physician practices and 48,000 additional physicians left independent practice for employment by hospital systems or other corporate entities.
Further straining practices is a thinning workforce, with 21% or respondents to the most recent PCC survey having said they were unable to hire clinicians for open positions and 54% saying they are unable to hire staff for open positions.
One respondent to the PCC survey from Utah said, “We need more support. It’s a moral injury to have our pay cut and be severely understaffed. Most of the burden of educating patients and getting them vaccinated has fallen to primary care and we are already overwhelmed with taking care of patients with worsening mental and physical health.”
According to Bruce Landon, MD, MBA, professor of health care policy at the Harvard Medical School’s Center for Primary Care, Boston, another source of financial strain for primary care practices is that they are having difficulty attracting doctors, nurses, and administrators.
These practices often need to increase pay for those positions to recruit people, and they are leaving many positions unfilled, Dr. Landon explained.
Plus, COVID-19 introduced costs for personal protective equipment (PPE) and cleaning products, and those expenses generally have not been reimbursed, Dr. Landon said.
Uncertainty around telemedicine
A new risk for primary care is a decline in telemedicine payments at a time when practices are still relying on telemedicine for revenue.
In the most recent PCC report, 40% of clinicians said they use telemedicine for at least a fifth of all office visits.
Even though most practices have reopened there’s still a fair amount of telemedicine and that will continue, Dr. Landon said in an interview.
In March of 2020, the Centers for Medicare & Medicaid Services lifted restrictions and that helped physicians with getting reimbursed for the services as they would office visits. But some commercial payers are starting to back off full payment for telemedicine, Dr. Landon noted.
“At some point the feds will probably start to do that with Medicare. I think that’s a mistake. [Telemedicine] has been one of the silver linings of this cloud of the pandemic,” he said.
If prepandemic payment regulations are restored, 41% of clinicians said, in the most recent PCC survey, that they worry their practices will no longer be able to support telemedicine.
Possible safety nets
Dr. Landon said that one thing that’s also clear is that some form of primary care capitation payment is necessary, at least for some of the work in primary care.
The practices that had capitation as part of payment were the ones who were most easily able to handle the pandemic because they didn’t see the immediate drop in revenue that fee-for-service practices saw, he noted.
“If we have a next pandemic, having a steady revenue stream to support primary care is really important and having a different way to pay for primary care is probably the best way to do that,” he said. “These longer-term strategies are going to be really crucial if we want to have a primary care system 10 years from now.”
Ms. Greiner, Dr. Flick, Dr. Phillips, Dr. Dobson, and Dr. Landon report no relevant financial relationships.
Identify patient and hospital factors to reduce maternal mortality
Maternal mortality is a public health crisis for all women, said Elizabeth A. Howell, MD, of the University of Pennsylvania, Philadelphia, in a presentation at the virtual Advancing NIH Research on the Health of Women conference sponsored by the National Institutes of Health.
The maternal mortality rate in the United States in 2018 was 17.4 maternal deaths per 100,000 live births, according to data from the Centers for Disease Control and Prevention, Dr. Howell said. Maternal mortality is defined as death during pregnancy or within 42 days of delivery; pregnancy-related mortality includes death during pregnancy or within 1 year of pregnancy, from pregnancy or as a result of any cause related to, or aggravated by, pregnancy, according to the CDC.
However, “Black women are two to three times more likely than White women to die from a pregnancy-related cause,” Dr. Howell said. These disparities are even more marked in some cities; data show that Black women in New York City are eight times more likely than White women to die from a pregnancy-related cause, she noted.
Pregnancy-related mortality persists regardless of education level, and remains significantly higher in Black women, compared with White women with at least a college degree, Dr. Howell added.
In her presentation, Dr. Howell reviewed some top causes of maternal mortality overall, and potential factors driving disparities. Data from the CDC show cardiomyopathy, cardiovascular conditions, and preeclampsia/eclampsia as the top three underlying causes of pregnancy-related deaths among non-Hispanic Black women, compared with mental health conditions, cardiovascular conditions, and hemorrhage in non-Hispanic White women, Dr. Howell said.
To help prevent maternal mortality across all populations, “It is important for us to think about the timing of deaths so we can better understand the causes,” said Dr. Howell.
CDC Vital Signs data show that approximately one-third of pregnancy-related deaths occur during pregnancy, but approximately 20% occur between 43 and 365 days postpartum, she said.
Although cardiovascular conditions top the list of clinical causes of pregnancy-related maternal mortality, maternal self-harm should not be discounted, and is likely underreported, Dr. Howell said. Data show that the peak incidence of maternal suicide occurs between 9 and 12 months’ postpartum, and risk factors include major depression, substance use disorder, and intimate partner violence, she noted.
Dr. Howell then shared the results of studies she conducted in 2020 and 2016 on racial disparities, hospital quality, and maternal mortality. One of her key findings in the 2020 study, presented at this year’s virtual meeting of the American College of Obstetricians and Gynecologists, showed that women delivering in the lowest-ranked hospitals had six times the rate of severe maternal morbidity, and an accompanying simulation/thought exercise showed that the hospital of delivery accounted for approximately half of the disparity in severe maternal morbidity between Black and White women. An earlier study she published in 2016 of between-hospital differences in New York City showed that Black and Latina women were significantly more likely than White women to deliver in hospitals with higher rates of severe maternal mortality.
These findings illustrate that “racial segregation in neighborhoods is also part of the story,” of maternal mortality, Dr. Howell said.
Dr. Howell outlined ways the health care community can reduce severe maternal morbidity and mortality for all women, including promoting contraception and preconception health, improving postpartum management, eliminating bias, and using patient navigators as needed to enhance communication among the care team,
“Think about ways to engage the community,” in support of women’s pregnancy health, Dr. Howell said. She also emphasized the need to enroll more pregnant women in clinical trials.
Don’t exclude pregnant women from trials
In a follow-up session, Cynthia Gyamfi-Bannerman, MD, of the University of California, San Diego, expanded on opportunities to include pregnant women in clinical research.
Clinical trials for pregnant people fall into two categories, she noted; those studying interventions to improve pregnancy outcomes and those studying interventions for common medical conditions that coexist with pregnancy. These trials are either initiated by the investigators, conducted under contract, or federally funded, Dr. Gyamfi-Bannerman said. Currently, the only obstetric clinical trials research network is the Maternal-Fetal Medicine Units Network, established in 1986 by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The MFMU has conducted significant and life-saving research, but “we need more networks to focus on researching pregnancy complications,” Dr. Gyamfi-Bannerman said. Once the infrastructure exists in multiple settings, the ability to conduct trials will improve, she said.
Dr. Gyamfi-Bannerman stressed the need to engage and involve community-based physicians in clinical trials; using those relationships to enroll a more diverse population for whom working with their local physician would be more feasible than traveling to a larger clinical trial center.
She also commented on the need to include pregnant women in nonobstetric clinical trials. The exclusion of pregnant women from COVID-19 vaccine trials left clinicians with no information for guiding pregnant patients, she said. “It is important to think about why we are excluding pregnant women,” she said.
Finally, Dr. Gyamfi-Bannerman recommended a national effort to coordinate and leverage EHR data, which could have an effect on reducing maternal morbidity by facilitating the study of nonobstetric interventions in pregnancy, such as behavior interventions and mental health care.
Dr. Howell and Dr. Gyamfi-Bannerman had no financial conflicts to disclose.
Maternal mortality is a public health crisis for all women, said Elizabeth A. Howell, MD, of the University of Pennsylvania, Philadelphia, in a presentation at the virtual Advancing NIH Research on the Health of Women conference sponsored by the National Institutes of Health.
The maternal mortality rate in the United States in 2018 was 17.4 maternal deaths per 100,000 live births, according to data from the Centers for Disease Control and Prevention, Dr. Howell said. Maternal mortality is defined as death during pregnancy or within 42 days of delivery; pregnancy-related mortality includes death during pregnancy or within 1 year of pregnancy, from pregnancy or as a result of any cause related to, or aggravated by, pregnancy, according to the CDC.
However, “Black women are two to three times more likely than White women to die from a pregnancy-related cause,” Dr. Howell said. These disparities are even more marked in some cities; data show that Black women in New York City are eight times more likely than White women to die from a pregnancy-related cause, she noted.
Pregnancy-related mortality persists regardless of education level, and remains significantly higher in Black women, compared with White women with at least a college degree, Dr. Howell added.
In her presentation, Dr. Howell reviewed some top causes of maternal mortality overall, and potential factors driving disparities. Data from the CDC show cardiomyopathy, cardiovascular conditions, and preeclampsia/eclampsia as the top three underlying causes of pregnancy-related deaths among non-Hispanic Black women, compared with mental health conditions, cardiovascular conditions, and hemorrhage in non-Hispanic White women, Dr. Howell said.
To help prevent maternal mortality across all populations, “It is important for us to think about the timing of deaths so we can better understand the causes,” said Dr. Howell.
CDC Vital Signs data show that approximately one-third of pregnancy-related deaths occur during pregnancy, but approximately 20% occur between 43 and 365 days postpartum, she said.
Although cardiovascular conditions top the list of clinical causes of pregnancy-related maternal mortality, maternal self-harm should not be discounted, and is likely underreported, Dr. Howell said. Data show that the peak incidence of maternal suicide occurs between 9 and 12 months’ postpartum, and risk factors include major depression, substance use disorder, and intimate partner violence, she noted.
Dr. Howell then shared the results of studies she conducted in 2020 and 2016 on racial disparities, hospital quality, and maternal mortality. One of her key findings in the 2020 study, presented at this year’s virtual meeting of the American College of Obstetricians and Gynecologists, showed that women delivering in the lowest-ranked hospitals had six times the rate of severe maternal morbidity, and an accompanying simulation/thought exercise showed that the hospital of delivery accounted for approximately half of the disparity in severe maternal morbidity between Black and White women. An earlier study she published in 2016 of between-hospital differences in New York City showed that Black and Latina women were significantly more likely than White women to deliver in hospitals with higher rates of severe maternal mortality.
These findings illustrate that “racial segregation in neighborhoods is also part of the story,” of maternal mortality, Dr. Howell said.
Dr. Howell outlined ways the health care community can reduce severe maternal morbidity and mortality for all women, including promoting contraception and preconception health, improving postpartum management, eliminating bias, and using patient navigators as needed to enhance communication among the care team,
“Think about ways to engage the community,” in support of women’s pregnancy health, Dr. Howell said. She also emphasized the need to enroll more pregnant women in clinical trials.
Don’t exclude pregnant women from trials
In a follow-up session, Cynthia Gyamfi-Bannerman, MD, of the University of California, San Diego, expanded on opportunities to include pregnant women in clinical research.
Clinical trials for pregnant people fall into two categories, she noted; those studying interventions to improve pregnancy outcomes and those studying interventions for common medical conditions that coexist with pregnancy. These trials are either initiated by the investigators, conducted under contract, or federally funded, Dr. Gyamfi-Bannerman said. Currently, the only obstetric clinical trials research network is the Maternal-Fetal Medicine Units Network, established in 1986 by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The MFMU has conducted significant and life-saving research, but “we need more networks to focus on researching pregnancy complications,” Dr. Gyamfi-Bannerman said. Once the infrastructure exists in multiple settings, the ability to conduct trials will improve, she said.
Dr. Gyamfi-Bannerman stressed the need to engage and involve community-based physicians in clinical trials; using those relationships to enroll a more diverse population for whom working with their local physician would be more feasible than traveling to a larger clinical trial center.
She also commented on the need to include pregnant women in nonobstetric clinical trials. The exclusion of pregnant women from COVID-19 vaccine trials left clinicians with no information for guiding pregnant patients, she said. “It is important to think about why we are excluding pregnant women,” she said.
Finally, Dr. Gyamfi-Bannerman recommended a national effort to coordinate and leverage EHR data, which could have an effect on reducing maternal morbidity by facilitating the study of nonobstetric interventions in pregnancy, such as behavior interventions and mental health care.
Dr. Howell and Dr. Gyamfi-Bannerman had no financial conflicts to disclose.
Maternal mortality is a public health crisis for all women, said Elizabeth A. Howell, MD, of the University of Pennsylvania, Philadelphia, in a presentation at the virtual Advancing NIH Research on the Health of Women conference sponsored by the National Institutes of Health.
The maternal mortality rate in the United States in 2018 was 17.4 maternal deaths per 100,000 live births, according to data from the Centers for Disease Control and Prevention, Dr. Howell said. Maternal mortality is defined as death during pregnancy or within 42 days of delivery; pregnancy-related mortality includes death during pregnancy or within 1 year of pregnancy, from pregnancy or as a result of any cause related to, or aggravated by, pregnancy, according to the CDC.
However, “Black women are two to three times more likely than White women to die from a pregnancy-related cause,” Dr. Howell said. These disparities are even more marked in some cities; data show that Black women in New York City are eight times more likely than White women to die from a pregnancy-related cause, she noted.
Pregnancy-related mortality persists regardless of education level, and remains significantly higher in Black women, compared with White women with at least a college degree, Dr. Howell added.
In her presentation, Dr. Howell reviewed some top causes of maternal mortality overall, and potential factors driving disparities. Data from the CDC show cardiomyopathy, cardiovascular conditions, and preeclampsia/eclampsia as the top three underlying causes of pregnancy-related deaths among non-Hispanic Black women, compared with mental health conditions, cardiovascular conditions, and hemorrhage in non-Hispanic White women, Dr. Howell said.
To help prevent maternal mortality across all populations, “It is important for us to think about the timing of deaths so we can better understand the causes,” said Dr. Howell.
CDC Vital Signs data show that approximately one-third of pregnancy-related deaths occur during pregnancy, but approximately 20% occur between 43 and 365 days postpartum, she said.
Although cardiovascular conditions top the list of clinical causes of pregnancy-related maternal mortality, maternal self-harm should not be discounted, and is likely underreported, Dr. Howell said. Data show that the peak incidence of maternal suicide occurs between 9 and 12 months’ postpartum, and risk factors include major depression, substance use disorder, and intimate partner violence, she noted.
Dr. Howell then shared the results of studies she conducted in 2020 and 2016 on racial disparities, hospital quality, and maternal mortality. One of her key findings in the 2020 study, presented at this year’s virtual meeting of the American College of Obstetricians and Gynecologists, showed that women delivering in the lowest-ranked hospitals had six times the rate of severe maternal morbidity, and an accompanying simulation/thought exercise showed that the hospital of delivery accounted for approximately half of the disparity in severe maternal morbidity between Black and White women. An earlier study she published in 2016 of between-hospital differences in New York City showed that Black and Latina women were significantly more likely than White women to deliver in hospitals with higher rates of severe maternal mortality.
These findings illustrate that “racial segregation in neighborhoods is also part of the story,” of maternal mortality, Dr. Howell said.
Dr. Howell outlined ways the health care community can reduce severe maternal morbidity and mortality for all women, including promoting contraception and preconception health, improving postpartum management, eliminating bias, and using patient navigators as needed to enhance communication among the care team,
“Think about ways to engage the community,” in support of women’s pregnancy health, Dr. Howell said. She also emphasized the need to enroll more pregnant women in clinical trials.
Don’t exclude pregnant women from trials
In a follow-up session, Cynthia Gyamfi-Bannerman, MD, of the University of California, San Diego, expanded on opportunities to include pregnant women in clinical research.
Clinical trials for pregnant people fall into two categories, she noted; those studying interventions to improve pregnancy outcomes and those studying interventions for common medical conditions that coexist with pregnancy. These trials are either initiated by the investigators, conducted under contract, or federally funded, Dr. Gyamfi-Bannerman said. Currently, the only obstetric clinical trials research network is the Maternal-Fetal Medicine Units Network, established in 1986 by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The MFMU has conducted significant and life-saving research, but “we need more networks to focus on researching pregnancy complications,” Dr. Gyamfi-Bannerman said. Once the infrastructure exists in multiple settings, the ability to conduct trials will improve, she said.
Dr. Gyamfi-Bannerman stressed the need to engage and involve community-based physicians in clinical trials; using those relationships to enroll a more diverse population for whom working with their local physician would be more feasible than traveling to a larger clinical trial center.
She also commented on the need to include pregnant women in nonobstetric clinical trials. The exclusion of pregnant women from COVID-19 vaccine trials left clinicians with no information for guiding pregnant patients, she said. “It is important to think about why we are excluding pregnant women,” she said.
Finally, Dr. Gyamfi-Bannerman recommended a national effort to coordinate and leverage EHR data, which could have an effect on reducing maternal morbidity by facilitating the study of nonobstetric interventions in pregnancy, such as behavior interventions and mental health care.
Dr. Howell and Dr. Gyamfi-Bannerman had no financial conflicts to disclose.
FROM ADVANCING NIH RESEARCH ON THE HEALTH OF WOMEN
My experience as a family medicine resident in 2021
I did not get a medical school graduation; I was one of the many thousands of newly graduated students who simply left their 4th-year rotation sites one chilly day in March 2020 and just never went back. My medical school education didn’t end with me walking triumphantly across the stage – a first-generation college student finally achieving the greatest dream in her life. Instead, it ended with a Zoom “graduation” and a cross-country move from Georgia to Pennsylvania amidst the greatest pandemic in recent memory. To say my impostor syndrome was bad would be an understatement.
Residency in the COVID-19-era
The joy and the draw to family medicine for me has always been the broad scope of conditions that we see and treat. From day 1, however, much of my residency has been devoted to one very small subset of patients – those with COVID-19. At one point, our hospital was so strained that our family medicine program had to run a second inpatient service alongside our usual five-resident service team just to provide care to everybody. Patients were in the hallways. The ER was packed to the gills. We were sleepless, terrified, unvaccinated, and desperate to help our patients survive a disease that was incompletely understood, with very few tools in our toolbox to combat it.
I distinctly remember sitting in the workroom with a coresident of mine, our faces seemingly permanently lined from wearing N95s all shift, and saying to him, “I worry I will be a bad family medicine physician. I worry I haven’t seen enough, other than COVID.” It was midway through my intern year; the days were short, so I was driving to and from the hospital in chilly darkness. My patients, like many around the country, were doing poorly. Vaccines seemed like a promise too good to be true. Worst of all: Those of us who were interns, who had no triumphant podium moment to end our medical school education, were suffering with an intense sense of impostor syndrome which was strengthened by every “there is nothing else we can offer your loved one at this time,” conversation we had. My apprehension about not having seen a wider breadth of medicine during my training is a sentiment still widely shared by COVID-era residents.
Luckily, my coresident was supportive.
“We’re going to be great family medicine physicians,” he said. “We’re learning the hard stuff – the bread and butter of FM – up-front. You’ll see.”
In some ways, I think he was right. Clinical skills, empathy, humility, and forging strong relationships are at the center of every family medicine physician’s heart; my generation has had to learn these skills early and under pressure. Sometimes, there are no answers. Sometimes, the best thing a family doctor can do for a patient is to hear them, understand them, and hold their hand.
‘We watched Cinderella together’
Shortly after that conversation with my coresident, I had a particular case which moved me. This gentleman with intellectual disability and COVID had been declining steadily since his admission to the hospital. He was isolated from everybody he knew and loved, but it did not dampen his spirits. He was cheerful to every person who entered his room, clad in their shrouds of PPE, which more often than not felt more like mourning garb than protective wear. I remember very little about this patient’s clinical picture – the COVID, the superimposed pneumonia, the repeated intubations. What I do remember is he loved the Disney classic, Cinderella. I knew this because I developed a very close relationship with his family during the course of his hospitalization. Amidst the torrential onslaught of patients, I made sure to call families every day – not because I wanted to, but because my mentors and attendings and coresidents had all drilled into me from day 1 that we are family medicine, and a large part of our role is to advocate for our patients, and to communicate with their loved ones. So I called. I learned a lot about him; his likes, his dislikes, his close bond with his siblings, and of course his lifelong love for Cinderella. On the last week of my ICU rotation, my patient passed peacefully. His nurse and I were bedside. We held his hand. We told him his family loved him. We watched Cinderella together on an iPad encased in protective plastic.
My next rotation was an outpatient one and it looked more like the “bread and butter” of family medicine. But as I whisked in and out of patient rooms, attending to patients with diabetes, with depression, with pain, I could not stop thinking about my hospitalized patients who my coresidents had assumed care of. Each exam room I entered, I rather morbidly thought “this patient could be next on our hospital service.” Without realizing it, I made more of an effort to get to know each patient holistically. I learned who they were as people. I found myself writing small, medically low-yield details in the chart: “Margaret loves to sing in her church choir;” “Katherine is a self-published author.”
I learned from my attendings. As I sat at the precepting table with them, observing their conversations about patients, their collective decades of experience were apparent.
“I’ve been seeing this patient every few weeks since I was a resident,” said one of my attendings.
“I don’t even see my parents that often,” I thought.
The depth of her relationship with, understanding of, and compassion for this patient struck me deeply. This was why I went into family medicine. My attending knew her patients; they were not faceless unknowns in a hospital gown to her. She would have known to play Cinderella for them in the end.
This is a unique time for trainees. We have been challenged, terrified, overwhelmed, and heartbroken. But at no point have we been isolated. We’ve had the generations of doctors before us to lead the way, to teach us the “hard stuff.” We’ve had senior residents to lean on, who have taken us aside and told us, “I can do the goals-of-care talk today, you need a break.” While the plague seems to have passed over our hospital for now, it has left behind a class of family medicine residents who are proud to carry on our specialty’s long tradition of compassionate, empathetic, lifelong care. “We care for all life stages, from cradle to grave,” says every family medicine physician.
My class, for better or for worse, has cared more often for patients in the twilight of their lives, and while it has been hard, I believe it has made us all better doctors. Now, when I hold a newborn in my arms for a well-child check, I am exceptionally grateful – for the opportunities I have been given, for new beginnings amidst so much sadness, and for the great privilege of being a family medicine physician.
Dr. Persampiere is a 2nd-year resident in the family medicine residency program at Abington (Pa.) Jefferson Health. You can contact her directly at victoria.persampiere@jefferson.edu or via fpnews@mdedge.com.
I did not get a medical school graduation; I was one of the many thousands of newly graduated students who simply left their 4th-year rotation sites one chilly day in March 2020 and just never went back. My medical school education didn’t end with me walking triumphantly across the stage – a first-generation college student finally achieving the greatest dream in her life. Instead, it ended with a Zoom “graduation” and a cross-country move from Georgia to Pennsylvania amidst the greatest pandemic in recent memory. To say my impostor syndrome was bad would be an understatement.
Residency in the COVID-19-era
The joy and the draw to family medicine for me has always been the broad scope of conditions that we see and treat. From day 1, however, much of my residency has been devoted to one very small subset of patients – those with COVID-19. At one point, our hospital was so strained that our family medicine program had to run a second inpatient service alongside our usual five-resident service team just to provide care to everybody. Patients were in the hallways. The ER was packed to the gills. We were sleepless, terrified, unvaccinated, and desperate to help our patients survive a disease that was incompletely understood, with very few tools in our toolbox to combat it.
I distinctly remember sitting in the workroom with a coresident of mine, our faces seemingly permanently lined from wearing N95s all shift, and saying to him, “I worry I will be a bad family medicine physician. I worry I haven’t seen enough, other than COVID.” It was midway through my intern year; the days were short, so I was driving to and from the hospital in chilly darkness. My patients, like many around the country, were doing poorly. Vaccines seemed like a promise too good to be true. Worst of all: Those of us who were interns, who had no triumphant podium moment to end our medical school education, were suffering with an intense sense of impostor syndrome which was strengthened by every “there is nothing else we can offer your loved one at this time,” conversation we had. My apprehension about not having seen a wider breadth of medicine during my training is a sentiment still widely shared by COVID-era residents.
Luckily, my coresident was supportive.
“We’re going to be great family medicine physicians,” he said. “We’re learning the hard stuff – the bread and butter of FM – up-front. You’ll see.”
In some ways, I think he was right. Clinical skills, empathy, humility, and forging strong relationships are at the center of every family medicine physician’s heart; my generation has had to learn these skills early and under pressure. Sometimes, there are no answers. Sometimes, the best thing a family doctor can do for a patient is to hear them, understand them, and hold their hand.
‘We watched Cinderella together’
Shortly after that conversation with my coresident, I had a particular case which moved me. This gentleman with intellectual disability and COVID had been declining steadily since his admission to the hospital. He was isolated from everybody he knew and loved, but it did not dampen his spirits. He was cheerful to every person who entered his room, clad in their shrouds of PPE, which more often than not felt more like mourning garb than protective wear. I remember very little about this patient’s clinical picture – the COVID, the superimposed pneumonia, the repeated intubations. What I do remember is he loved the Disney classic, Cinderella. I knew this because I developed a very close relationship with his family during the course of his hospitalization. Amidst the torrential onslaught of patients, I made sure to call families every day – not because I wanted to, but because my mentors and attendings and coresidents had all drilled into me from day 1 that we are family medicine, and a large part of our role is to advocate for our patients, and to communicate with their loved ones. So I called. I learned a lot about him; his likes, his dislikes, his close bond with his siblings, and of course his lifelong love for Cinderella. On the last week of my ICU rotation, my patient passed peacefully. His nurse and I were bedside. We held his hand. We told him his family loved him. We watched Cinderella together on an iPad encased in protective plastic.
My next rotation was an outpatient one and it looked more like the “bread and butter” of family medicine. But as I whisked in and out of patient rooms, attending to patients with diabetes, with depression, with pain, I could not stop thinking about my hospitalized patients who my coresidents had assumed care of. Each exam room I entered, I rather morbidly thought “this patient could be next on our hospital service.” Without realizing it, I made more of an effort to get to know each patient holistically. I learned who they were as people. I found myself writing small, medically low-yield details in the chart: “Margaret loves to sing in her church choir;” “Katherine is a self-published author.”
I learned from my attendings. As I sat at the precepting table with them, observing their conversations about patients, their collective decades of experience were apparent.
“I’ve been seeing this patient every few weeks since I was a resident,” said one of my attendings.
“I don’t even see my parents that often,” I thought.
The depth of her relationship with, understanding of, and compassion for this patient struck me deeply. This was why I went into family medicine. My attending knew her patients; they were not faceless unknowns in a hospital gown to her. She would have known to play Cinderella for them in the end.
This is a unique time for trainees. We have been challenged, terrified, overwhelmed, and heartbroken. But at no point have we been isolated. We’ve had the generations of doctors before us to lead the way, to teach us the “hard stuff.” We’ve had senior residents to lean on, who have taken us aside and told us, “I can do the goals-of-care talk today, you need a break.” While the plague seems to have passed over our hospital for now, it has left behind a class of family medicine residents who are proud to carry on our specialty’s long tradition of compassionate, empathetic, lifelong care. “We care for all life stages, from cradle to grave,” says every family medicine physician.
My class, for better or for worse, has cared more often for patients in the twilight of their lives, and while it has been hard, I believe it has made us all better doctors. Now, when I hold a newborn in my arms for a well-child check, I am exceptionally grateful – for the opportunities I have been given, for new beginnings amidst so much sadness, and for the great privilege of being a family medicine physician.
Dr. Persampiere is a 2nd-year resident in the family medicine residency program at Abington (Pa.) Jefferson Health. You can contact her directly at victoria.persampiere@jefferson.edu or via fpnews@mdedge.com.
I did not get a medical school graduation; I was one of the many thousands of newly graduated students who simply left their 4th-year rotation sites one chilly day in March 2020 and just never went back. My medical school education didn’t end with me walking triumphantly across the stage – a first-generation college student finally achieving the greatest dream in her life. Instead, it ended with a Zoom “graduation” and a cross-country move from Georgia to Pennsylvania amidst the greatest pandemic in recent memory. To say my impostor syndrome was bad would be an understatement.
Residency in the COVID-19-era
The joy and the draw to family medicine for me has always been the broad scope of conditions that we see and treat. From day 1, however, much of my residency has been devoted to one very small subset of patients – those with COVID-19. At one point, our hospital was so strained that our family medicine program had to run a second inpatient service alongside our usual five-resident service team just to provide care to everybody. Patients were in the hallways. The ER was packed to the gills. We were sleepless, terrified, unvaccinated, and desperate to help our patients survive a disease that was incompletely understood, with very few tools in our toolbox to combat it.
I distinctly remember sitting in the workroom with a coresident of mine, our faces seemingly permanently lined from wearing N95s all shift, and saying to him, “I worry I will be a bad family medicine physician. I worry I haven’t seen enough, other than COVID.” It was midway through my intern year; the days were short, so I was driving to and from the hospital in chilly darkness. My patients, like many around the country, were doing poorly. Vaccines seemed like a promise too good to be true. Worst of all: Those of us who were interns, who had no triumphant podium moment to end our medical school education, were suffering with an intense sense of impostor syndrome which was strengthened by every “there is nothing else we can offer your loved one at this time,” conversation we had. My apprehension about not having seen a wider breadth of medicine during my training is a sentiment still widely shared by COVID-era residents.
Luckily, my coresident was supportive.
“We’re going to be great family medicine physicians,” he said. “We’re learning the hard stuff – the bread and butter of FM – up-front. You’ll see.”
In some ways, I think he was right. Clinical skills, empathy, humility, and forging strong relationships are at the center of every family medicine physician’s heart; my generation has had to learn these skills early and under pressure. Sometimes, there are no answers. Sometimes, the best thing a family doctor can do for a patient is to hear them, understand them, and hold their hand.
‘We watched Cinderella together’
Shortly after that conversation with my coresident, I had a particular case which moved me. This gentleman with intellectual disability and COVID had been declining steadily since his admission to the hospital. He was isolated from everybody he knew and loved, but it did not dampen his spirits. He was cheerful to every person who entered his room, clad in their shrouds of PPE, which more often than not felt more like mourning garb than protective wear. I remember very little about this patient’s clinical picture – the COVID, the superimposed pneumonia, the repeated intubations. What I do remember is he loved the Disney classic, Cinderella. I knew this because I developed a very close relationship with his family during the course of his hospitalization. Amidst the torrential onslaught of patients, I made sure to call families every day – not because I wanted to, but because my mentors and attendings and coresidents had all drilled into me from day 1 that we are family medicine, and a large part of our role is to advocate for our patients, and to communicate with their loved ones. So I called. I learned a lot about him; his likes, his dislikes, his close bond with his siblings, and of course his lifelong love for Cinderella. On the last week of my ICU rotation, my patient passed peacefully. His nurse and I were bedside. We held his hand. We told him his family loved him. We watched Cinderella together on an iPad encased in protective plastic.
My next rotation was an outpatient one and it looked more like the “bread and butter” of family medicine. But as I whisked in and out of patient rooms, attending to patients with diabetes, with depression, with pain, I could not stop thinking about my hospitalized patients who my coresidents had assumed care of. Each exam room I entered, I rather morbidly thought “this patient could be next on our hospital service.” Without realizing it, I made more of an effort to get to know each patient holistically. I learned who they were as people. I found myself writing small, medically low-yield details in the chart: “Margaret loves to sing in her church choir;” “Katherine is a self-published author.”
I learned from my attendings. As I sat at the precepting table with them, observing their conversations about patients, their collective decades of experience were apparent.
“I’ve been seeing this patient every few weeks since I was a resident,” said one of my attendings.
“I don’t even see my parents that often,” I thought.
The depth of her relationship with, understanding of, and compassion for this patient struck me deeply. This was why I went into family medicine. My attending knew her patients; they were not faceless unknowns in a hospital gown to her. She would have known to play Cinderella for them in the end.
This is a unique time for trainees. We have been challenged, terrified, overwhelmed, and heartbroken. But at no point have we been isolated. We’ve had the generations of doctors before us to lead the way, to teach us the “hard stuff.” We’ve had senior residents to lean on, who have taken us aside and told us, “I can do the goals-of-care talk today, you need a break.” While the plague seems to have passed over our hospital for now, it has left behind a class of family medicine residents who are proud to carry on our specialty’s long tradition of compassionate, empathetic, lifelong care. “We care for all life stages, from cradle to grave,” says every family medicine physician.
My class, for better or for worse, has cared more often for patients in the twilight of their lives, and while it has been hard, I believe it has made us all better doctors. Now, when I hold a newborn in my arms for a well-child check, I am exceptionally grateful – for the opportunities I have been given, for new beginnings amidst so much sadness, and for the great privilege of being a family medicine physician.
Dr. Persampiere is a 2nd-year resident in the family medicine residency program at Abington (Pa.) Jefferson Health. You can contact her directly at victoria.persampiere@jefferson.edu or via fpnews@mdedge.com.
Social determinants of health may drive CVD risk in Black Americans
Investigators analyzed 20 years of data on over 50,500 U.S. adults drawn from the National Health and Nutrition Examination Surveys (NHANES) and found that, in the overall population, body mass index and hemoglobin A1c were significantly increased between 1999 and 2018, while serum total cholesterol and cigarette smoking were significantly decreased. Mean systolic blood pressure decreased between 1999 and 2010, but then increased after 2010.
The mean age- and sex-adjusted estimated 10-year risk for atherosclerotic cardiovascular disease (ASCVD) was consistently higher in Black participants vs. White participants, but the difference was attenuated after further adjusting for education, income, home ownership, employment, health insurance, and access to health care.
“These findings are helpful to guide the development of national public health policies for targeted interventions aimed at eliminating health disparities,” Jiang He, MD, PhD, Joseph S. Copes Chair and professor of epidemiology, Tulane University School of Public Health and Tropical Medicine, New Orleans, said in an interview.
“Interventions on social determinants of cardiovascular health should be tested in rigorous designed intervention trials,” said Dr. He, director of the Tulane University Translational Science Institute.
The study was published online Oct. 5 in JAMA.
‘Flattened’ CVD mortality?
Recent data show that the CVD mortality rate flattened, while the total number of cardiovascular deaths increased in the U.S. general population from 2010 to 2018, “but the reasons for this deceleration in the decline of CVD mortality are not entirely understood,” Dr. He said.
Moreover, “racial and ethnic differences in CVD mortality persist in the U.S. general population [but] the secular trends of cardiovascular risk factors among U.S. subpopulations with various racial and ethnic backgrounds and socioeconomic status are [also] not well understood,” he added. The effects of social determinants of health, such as education, income, home ownership, employment, health insurance, and access to health care on racial/ethnic differences in CVD risk, “are not well documented.”
To investigate these questions, the researchers drew on data from NHANES, a series of cross-sectional surveys in nationally representative samples of the U.S. population aged 20 years and older. The surveys are conducted in 2-year cycles and include data from 10 cycles conducted from 1999-2000 to 2017-2018 (n = 50,571, mean age 49.0-51.8 years; 48.2%-51.3% female).
Every 2 years, participants provided sociodemographic information, including age, race/ethnicity, sex, education, income, employment, housing, health insurance, and access to health care, as well as medical history and medication use. They underwent a physical examination that included weight and height, blood pressure, lipid levels, plasma glucose, and hemoglobin A1c.
Social determinants of health
Between 1999-2000 and 2017-2018, age- and sex-adjusted mean BMI and hemoglobin A1c increased, while mean serum total cholesterol and prevalence of smoking decreased (all P < .001).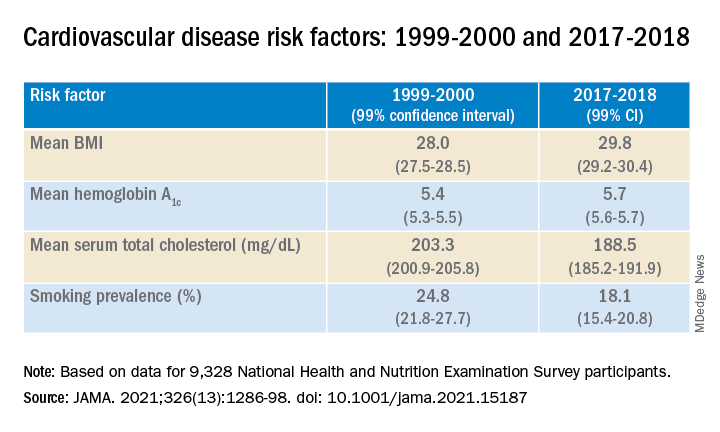
Age- and sex-adjusted 10-year atherosclerotic cardiovascular disease (ASCVD) risk decreased from 7.6% (6.9%-8.2%) in 1999-2000 to 6.5% (6.1%-6.8%) in 2011-2012, with no significant changes thereafter.
When the researchers looked at specific racial and ethnic groups, they found that age- and sex-adjusted BMI, systolic BP, and hemoglobin A1c were “consistently higher” in non-Hispanic Black participants compared with non-Hispanic White participants, but total cholesterol was lower (all P < .001).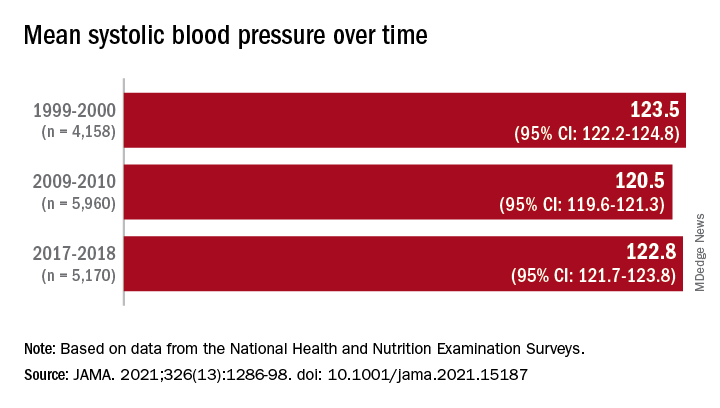
Participants with at least a college education or high family income had “consistently lower levels” of cardiovascular risk factors. And although the mean age- and sex-adjusted 10-year risk for ASCVD was significantly higher in non-Hispanic Black vs. non-Hispanic White participants (difference, 1.4% [1.0%-1.7%] in 1999-2008 and 2.0% [1.7%-2.4%] in 2009-2018), the difference was attenuated (by –0.3% in 1999-2008 and 0.7% in 2009-2018) after the researchers further adjusted for education, income, home ownership, employment, health insurance, and access to health care.
The differences in cardiovascular risk factors between Black and White participants “may have been moderated by social determinants of health,” the authors noted.
Provide appropriate education
Commenting on the study in an interview, Mary Ann McLaughlin, MD, MPH, associate professor of medicine, cardiology, Icahn School of Medicine at Mount Sinai, New York, pointed out that two important cardiovascular risk factors associated with being overweight – hypertension and diabetes – remained higher in the Black population compared with the White population in this analysis.
“Physicians and health care systems should provide appropriate education and resources regarding risk factor modification regarding diet, exercise, and blood pressure control,” advised Dr. McLaughlin, who was not involved with the study.
“Importantly, smoking rates and cholesterol levels are lower in the Black population, compared to the White population, when adjusted for many important socioeconomic factors,” she pointed out.
Dr. McLaughlin added that other “important social determinants of health, such as neighborhood and access to healthy food, were not measured and should be addressed by physicians when optimizing cardiovascular risk.”
The research reported in this publication was supported by the National Heart, Lung, and Blood Institute and by the National Institute of General Medical Sciences. One of the researchers, Joshua D. Bundy, PhD, was supported by a grant from the National Institutes of Health/Eunice Kennedy Shriver National Institute of Child Health and Human Development. Dr. He and the other coauthors and Dr. McLaughlin reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators analyzed 20 years of data on over 50,500 U.S. adults drawn from the National Health and Nutrition Examination Surveys (NHANES) and found that, in the overall population, body mass index and hemoglobin A1c were significantly increased between 1999 and 2018, while serum total cholesterol and cigarette smoking were significantly decreased. Mean systolic blood pressure decreased between 1999 and 2010, but then increased after 2010.
The mean age- and sex-adjusted estimated 10-year risk for atherosclerotic cardiovascular disease (ASCVD) was consistently higher in Black participants vs. White participants, but the difference was attenuated after further adjusting for education, income, home ownership, employment, health insurance, and access to health care.
“These findings are helpful to guide the development of national public health policies for targeted interventions aimed at eliminating health disparities,” Jiang He, MD, PhD, Joseph S. Copes Chair and professor of epidemiology, Tulane University School of Public Health and Tropical Medicine, New Orleans, said in an interview.
“Interventions on social determinants of cardiovascular health should be tested in rigorous designed intervention trials,” said Dr. He, director of the Tulane University Translational Science Institute.
The study was published online Oct. 5 in JAMA.
‘Flattened’ CVD mortality?
Recent data show that the CVD mortality rate flattened, while the total number of cardiovascular deaths increased in the U.S. general population from 2010 to 2018, “but the reasons for this deceleration in the decline of CVD mortality are not entirely understood,” Dr. He said.
Moreover, “racial and ethnic differences in CVD mortality persist in the U.S. general population [but] the secular trends of cardiovascular risk factors among U.S. subpopulations with various racial and ethnic backgrounds and socioeconomic status are [also] not well understood,” he added. The effects of social determinants of health, such as education, income, home ownership, employment, health insurance, and access to health care on racial/ethnic differences in CVD risk, “are not well documented.”
To investigate these questions, the researchers drew on data from NHANES, a series of cross-sectional surveys in nationally representative samples of the U.S. population aged 20 years and older. The surveys are conducted in 2-year cycles and include data from 10 cycles conducted from 1999-2000 to 2017-2018 (n = 50,571, mean age 49.0-51.8 years; 48.2%-51.3% female).
Every 2 years, participants provided sociodemographic information, including age, race/ethnicity, sex, education, income, employment, housing, health insurance, and access to health care, as well as medical history and medication use. They underwent a physical examination that included weight and height, blood pressure, lipid levels, plasma glucose, and hemoglobin A1c.
Social determinants of health
Between 1999-2000 and 2017-2018, age- and sex-adjusted mean BMI and hemoglobin A1c increased, while mean serum total cholesterol and prevalence of smoking decreased (all P < .001).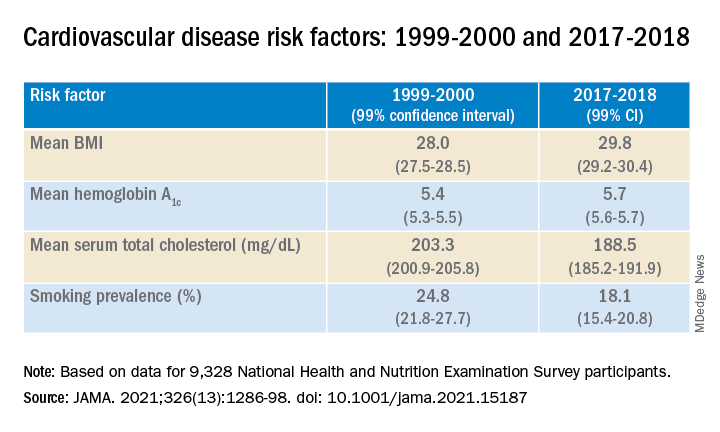
Age- and sex-adjusted 10-year atherosclerotic cardiovascular disease (ASCVD) risk decreased from 7.6% (6.9%-8.2%) in 1999-2000 to 6.5% (6.1%-6.8%) in 2011-2012, with no significant changes thereafter.
When the researchers looked at specific racial and ethnic groups, they found that age- and sex-adjusted BMI, systolic BP, and hemoglobin A1c were “consistently higher” in non-Hispanic Black participants compared with non-Hispanic White participants, but total cholesterol was lower (all P < .001).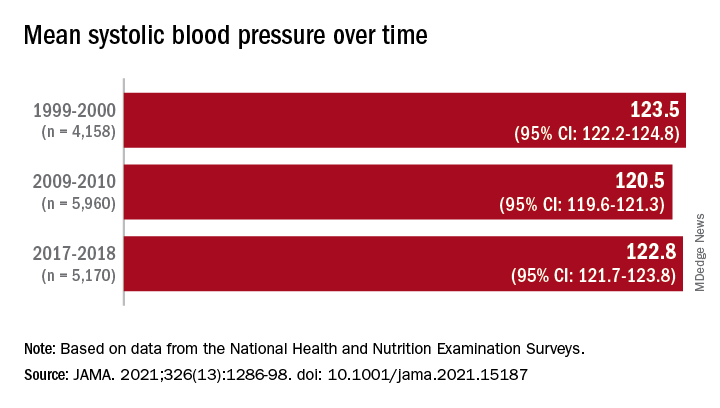
Participants with at least a college education or high family income had “consistently lower levels” of cardiovascular risk factors. And although the mean age- and sex-adjusted 10-year risk for ASCVD was significantly higher in non-Hispanic Black vs. non-Hispanic White participants (difference, 1.4% [1.0%-1.7%] in 1999-2008 and 2.0% [1.7%-2.4%] in 2009-2018), the difference was attenuated (by –0.3% in 1999-2008 and 0.7% in 2009-2018) after the researchers further adjusted for education, income, home ownership, employment, health insurance, and access to health care.
The differences in cardiovascular risk factors between Black and White participants “may have been moderated by social determinants of health,” the authors noted.
Provide appropriate education
Commenting on the study in an interview, Mary Ann McLaughlin, MD, MPH, associate professor of medicine, cardiology, Icahn School of Medicine at Mount Sinai, New York, pointed out that two important cardiovascular risk factors associated with being overweight – hypertension and diabetes – remained higher in the Black population compared with the White population in this analysis.
“Physicians and health care systems should provide appropriate education and resources regarding risk factor modification regarding diet, exercise, and blood pressure control,” advised Dr. McLaughlin, who was not involved with the study.
“Importantly, smoking rates and cholesterol levels are lower in the Black population, compared to the White population, when adjusted for many important socioeconomic factors,” she pointed out.
Dr. McLaughlin added that other “important social determinants of health, such as neighborhood and access to healthy food, were not measured and should be addressed by physicians when optimizing cardiovascular risk.”
The research reported in this publication was supported by the National Heart, Lung, and Blood Institute and by the National Institute of General Medical Sciences. One of the researchers, Joshua D. Bundy, PhD, was supported by a grant from the National Institutes of Health/Eunice Kennedy Shriver National Institute of Child Health and Human Development. Dr. He and the other coauthors and Dr. McLaughlin reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators analyzed 20 years of data on over 50,500 U.S. adults drawn from the National Health and Nutrition Examination Surveys (NHANES) and found that, in the overall population, body mass index and hemoglobin A1c were significantly increased between 1999 and 2018, while serum total cholesterol and cigarette smoking were significantly decreased. Mean systolic blood pressure decreased between 1999 and 2010, but then increased after 2010.
The mean age- and sex-adjusted estimated 10-year risk for atherosclerotic cardiovascular disease (ASCVD) was consistently higher in Black participants vs. White participants, but the difference was attenuated after further adjusting for education, income, home ownership, employment, health insurance, and access to health care.
“These findings are helpful to guide the development of national public health policies for targeted interventions aimed at eliminating health disparities,” Jiang He, MD, PhD, Joseph S. Copes Chair and professor of epidemiology, Tulane University School of Public Health and Tropical Medicine, New Orleans, said in an interview.
“Interventions on social determinants of cardiovascular health should be tested in rigorous designed intervention trials,” said Dr. He, director of the Tulane University Translational Science Institute.
The study was published online Oct. 5 in JAMA.
‘Flattened’ CVD mortality?
Recent data show that the CVD mortality rate flattened, while the total number of cardiovascular deaths increased in the U.S. general population from 2010 to 2018, “but the reasons for this deceleration in the decline of CVD mortality are not entirely understood,” Dr. He said.
Moreover, “racial and ethnic differences in CVD mortality persist in the U.S. general population [but] the secular trends of cardiovascular risk factors among U.S. subpopulations with various racial and ethnic backgrounds and socioeconomic status are [also] not well understood,” he added. The effects of social determinants of health, such as education, income, home ownership, employment, health insurance, and access to health care on racial/ethnic differences in CVD risk, “are not well documented.”
To investigate these questions, the researchers drew on data from NHANES, a series of cross-sectional surveys in nationally representative samples of the U.S. population aged 20 years and older. The surveys are conducted in 2-year cycles and include data from 10 cycles conducted from 1999-2000 to 2017-2018 (n = 50,571, mean age 49.0-51.8 years; 48.2%-51.3% female).
Every 2 years, participants provided sociodemographic information, including age, race/ethnicity, sex, education, income, employment, housing, health insurance, and access to health care, as well as medical history and medication use. They underwent a physical examination that included weight and height, blood pressure, lipid levels, plasma glucose, and hemoglobin A1c.
Social determinants of health
Between 1999-2000 and 2017-2018, age- and sex-adjusted mean BMI and hemoglobin A1c increased, while mean serum total cholesterol and prevalence of smoking decreased (all P < .001).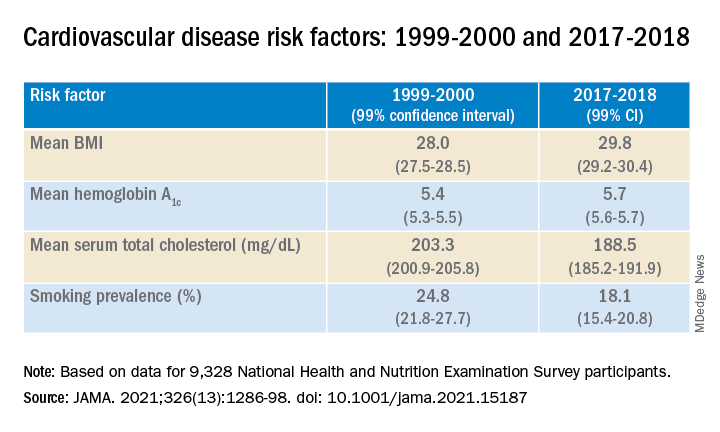
Age- and sex-adjusted 10-year atherosclerotic cardiovascular disease (ASCVD) risk decreased from 7.6% (6.9%-8.2%) in 1999-2000 to 6.5% (6.1%-6.8%) in 2011-2012, with no significant changes thereafter.
When the researchers looked at specific racial and ethnic groups, they found that age- and sex-adjusted BMI, systolic BP, and hemoglobin A1c were “consistently higher” in non-Hispanic Black participants compared with non-Hispanic White participants, but total cholesterol was lower (all P < .001).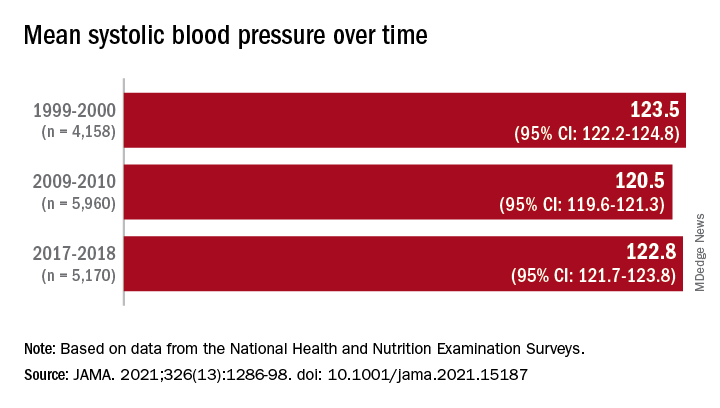
Participants with at least a college education or high family income had “consistently lower levels” of cardiovascular risk factors. And although the mean age- and sex-adjusted 10-year risk for ASCVD was significantly higher in non-Hispanic Black vs. non-Hispanic White participants (difference, 1.4% [1.0%-1.7%] in 1999-2008 and 2.0% [1.7%-2.4%] in 2009-2018), the difference was attenuated (by –0.3% in 1999-2008 and 0.7% in 2009-2018) after the researchers further adjusted for education, income, home ownership, employment, health insurance, and access to health care.
The differences in cardiovascular risk factors between Black and White participants “may have been moderated by social determinants of health,” the authors noted.
Provide appropriate education
Commenting on the study in an interview, Mary Ann McLaughlin, MD, MPH, associate professor of medicine, cardiology, Icahn School of Medicine at Mount Sinai, New York, pointed out that two important cardiovascular risk factors associated with being overweight – hypertension and diabetes – remained higher in the Black population compared with the White population in this analysis.
“Physicians and health care systems should provide appropriate education and resources regarding risk factor modification regarding diet, exercise, and blood pressure control,” advised Dr. McLaughlin, who was not involved with the study.
“Importantly, smoking rates and cholesterol levels are lower in the Black population, compared to the White population, when adjusted for many important socioeconomic factors,” she pointed out.
Dr. McLaughlin added that other “important social determinants of health, such as neighborhood and access to healthy food, were not measured and should be addressed by physicians when optimizing cardiovascular risk.”
The research reported in this publication was supported by the National Heart, Lung, and Blood Institute and by the National Institute of General Medical Sciences. One of the researchers, Joshua D. Bundy, PhD, was supported by a grant from the National Institutes of Health/Eunice Kennedy Shriver National Institute of Child Health and Human Development. Dr. He and the other coauthors and Dr. McLaughlin reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
How the pandemic prompted one clinic to embrace digital innovation
When the .
“Before COVID, we had zero use of teledermatology,” Dr. Afanasiev, a dermatologist at the practice, said during the annual meeting of the Pacific Dermatologic Association. “We didn’t do photography other than the required pre-biopsy photographs, and minimal evaluation of home photos, in response to the patients who say, ‘Wait, doc. Let me pull out my phone and show my photographs.”
During the very first days of the pandemic, in order to accommodate urgent patient requests, she and her colleagues used cloud services for patients to submit photos for concerning skin conditions or lesions, which were then discussed over commonly available video platforms. But they quickly realized that this would not work long-term so within two months, they created an electronic health record–integrated workflow that they are still using, she said.
Here’s how it works. If the patient request is deemed nonacute or does not require a full-body skin exam, the scheduling team offers that patient a store-and-video evaluation (SAVe) or an in-person visit. If a SAVe visit is requested, the patient is required to submit a photograph of his or her condition, then a medical assistant checks for the presence and quality of up to nine patient-submitted photos and contacts the patient if additional photos are required.
Immediately before the encounter, a medical assistant calls the patient to ensure video connectivity and performs a brief intake history. The patient and physician then connect via a video-capable platform – most commonly Vidyo, which is integrated with EPIC. After the visit, the provider notifies the scheduling team if any additional in-person or virtual follow up is required.
In a half day of practice, Dr. Afanasiev sees about 20 patients via video visits scheduled every 15 minutes. On a recent day, 55% of visits were related to acne and 10% were related to a mole check, which usually resulted in recommendation for biopsy. Most (70%) were existing patients, while 30% were new.
“There is no store-and-forward option at this time, meaning that patients can’t just submit a photo without a visit,” she said. “In addition, part of our consent is, if you don’t show up to your scheduled video visit, your photos will not be reviewed. The photos are linked to the video visit and uploaded to the patient’s chart. The rooming workflow is very similar to in clinic, except you’re at home and the medical assistant is remote.”
In an article recently published in the Journal of the American Academy of Dermatology, Dr. Afanasiev and her colleagues described their experience with this photo plus video teledermatology – SAVe – workflow between March 16, 2020, and Aug. 31, 2020. The researchers analyzed 74,411 dermatology cases encountered by 89 providers who cared for 46,024 patients during that time frame. Most of the encounters (79%) were in-person, while the remaining 21% were digital in nature – SAVe in 89% of cases, followed by telephone/message encounters.
At the initial peak of the COVID-19 pandemic in April 2020, SAVe encounters increased to 72% of all encounters from 0% prior to March 16, 2020, and were sustained at 12% when the clinic reopened in the summer of 2020. Over the study period, the clinic’s incorporation of SAVe increased care access to patients located in 731 unique ZIP codes in and near California. “We also have been able to retain many patients within our system,” Dr. Afanasiev said. “We have a large proportion of patients that require 2-3 hours of travel time to get to our clinic, so virtual visits allowed for increased rural access. It also allowed for flexibility for patients and providers.”
The new workflow also led to faster access to care. The time from referral to an in-person evaluation fell from an average of 56 days in 2019 to average of 27 days in 2020, while the wait time for a virtual visit was just 14 days in 2020. “We were able to see a diverse number of diagnostic categories with both in-person and virtual care, most commonly rashes, acne, dermal growths, and pigmentary disorders,” she said.
For clinicians interested in incorporating a SAVe-like system into their workflow, Dr. Afanasiev advises them to think seriously about consent. “You want to make sure patients understand what they’re getting themselves into,” she said. “You want to make sure they know that some diagnoses cannot be adequately addressed by teledermatology.” Photo quality is also important, she said. “Video quality is not good enough for most of our diagnoses, so photos are an important part of this evaluation. In this day and age, patients are actually pretty good photographers most of the time.”
She urges practices to carefully think about how they allow patients to submit photos, especially if photographs are not attached to a billable visit.
In her opinion, a good teledermatology platform should have trained support staff with the ability for patients to send photos prior to their visit, and should be safe, secure, and HIPAA compliant. It should also be app and browser compatible and have high resolution and low downtime.
“Into the future, I think it’s important to maintain teledermatology within our clinical practice, especially for remote monitoring of chronic skin diseases,” Dr. Afanasiev said. “Oftentimes we schedule 3- or 6-month follow-ups but often those do not correspond to the patients’ disease flare. They may have had an eczema or psoriatic flare 3 weeks prior, but we see them in clinic with clear skin, which makes it hard to judge how to tailor our treatment. It will also be important for us to understand the safety and security and legal implications of these new practice styles.”
She also referred to technological advances, which she said “will dovetail well with teledermatology, including robust at-home and commercial 3D virtual capture technology, machine learning algorithms for improved photos, and virtual biopsy technology.”
Dr. Afanasiev is a member of the American Academy of Dermatology Teledermatology Task Force. She had no relevant disclosures.
When the .
“Before COVID, we had zero use of teledermatology,” Dr. Afanasiev, a dermatologist at the practice, said during the annual meeting of the Pacific Dermatologic Association. “We didn’t do photography other than the required pre-biopsy photographs, and minimal evaluation of home photos, in response to the patients who say, ‘Wait, doc. Let me pull out my phone and show my photographs.”
During the very first days of the pandemic, in order to accommodate urgent patient requests, she and her colleagues used cloud services for patients to submit photos for concerning skin conditions or lesions, which were then discussed over commonly available video platforms. But they quickly realized that this would not work long-term so within two months, they created an electronic health record–integrated workflow that they are still using, she said.
Here’s how it works. If the patient request is deemed nonacute or does not require a full-body skin exam, the scheduling team offers that patient a store-and-video evaluation (SAVe) or an in-person visit. If a SAVe visit is requested, the patient is required to submit a photograph of his or her condition, then a medical assistant checks for the presence and quality of up to nine patient-submitted photos and contacts the patient if additional photos are required.
Immediately before the encounter, a medical assistant calls the patient to ensure video connectivity and performs a brief intake history. The patient and physician then connect via a video-capable platform – most commonly Vidyo, which is integrated with EPIC. After the visit, the provider notifies the scheduling team if any additional in-person or virtual follow up is required.
In a half day of practice, Dr. Afanasiev sees about 20 patients via video visits scheduled every 15 minutes. On a recent day, 55% of visits were related to acne and 10% were related to a mole check, which usually resulted in recommendation for biopsy. Most (70%) were existing patients, while 30% were new.
“There is no store-and-forward option at this time, meaning that patients can’t just submit a photo without a visit,” she said. “In addition, part of our consent is, if you don’t show up to your scheduled video visit, your photos will not be reviewed. The photos are linked to the video visit and uploaded to the patient’s chart. The rooming workflow is very similar to in clinic, except you’re at home and the medical assistant is remote.”
In an article recently published in the Journal of the American Academy of Dermatology, Dr. Afanasiev and her colleagues described their experience with this photo plus video teledermatology – SAVe – workflow between March 16, 2020, and Aug. 31, 2020. The researchers analyzed 74,411 dermatology cases encountered by 89 providers who cared for 46,024 patients during that time frame. Most of the encounters (79%) were in-person, while the remaining 21% were digital in nature – SAVe in 89% of cases, followed by telephone/message encounters.
At the initial peak of the COVID-19 pandemic in April 2020, SAVe encounters increased to 72% of all encounters from 0% prior to March 16, 2020, and were sustained at 12% when the clinic reopened in the summer of 2020. Over the study period, the clinic’s incorporation of SAVe increased care access to patients located in 731 unique ZIP codes in and near California. “We also have been able to retain many patients within our system,” Dr. Afanasiev said. “We have a large proportion of patients that require 2-3 hours of travel time to get to our clinic, so virtual visits allowed for increased rural access. It also allowed for flexibility for patients and providers.”
The new workflow also led to faster access to care. The time from referral to an in-person evaluation fell from an average of 56 days in 2019 to average of 27 days in 2020, while the wait time for a virtual visit was just 14 days in 2020. “We were able to see a diverse number of diagnostic categories with both in-person and virtual care, most commonly rashes, acne, dermal growths, and pigmentary disorders,” she said.
For clinicians interested in incorporating a SAVe-like system into their workflow, Dr. Afanasiev advises them to think seriously about consent. “You want to make sure patients understand what they’re getting themselves into,” she said. “You want to make sure they know that some diagnoses cannot be adequately addressed by teledermatology.” Photo quality is also important, she said. “Video quality is not good enough for most of our diagnoses, so photos are an important part of this evaluation. In this day and age, patients are actually pretty good photographers most of the time.”
She urges practices to carefully think about how they allow patients to submit photos, especially if photographs are not attached to a billable visit.
In her opinion, a good teledermatology platform should have trained support staff with the ability for patients to send photos prior to their visit, and should be safe, secure, and HIPAA compliant. It should also be app and browser compatible and have high resolution and low downtime.
“Into the future, I think it’s important to maintain teledermatology within our clinical practice, especially for remote monitoring of chronic skin diseases,” Dr. Afanasiev said. “Oftentimes we schedule 3- or 6-month follow-ups but often those do not correspond to the patients’ disease flare. They may have had an eczema or psoriatic flare 3 weeks prior, but we see them in clinic with clear skin, which makes it hard to judge how to tailor our treatment. It will also be important for us to understand the safety and security and legal implications of these new practice styles.”
She also referred to technological advances, which she said “will dovetail well with teledermatology, including robust at-home and commercial 3D virtual capture technology, machine learning algorithms for improved photos, and virtual biopsy technology.”
Dr. Afanasiev is a member of the American Academy of Dermatology Teledermatology Task Force. She had no relevant disclosures.
When the .
“Before COVID, we had zero use of teledermatology,” Dr. Afanasiev, a dermatologist at the practice, said during the annual meeting of the Pacific Dermatologic Association. “We didn’t do photography other than the required pre-biopsy photographs, and minimal evaluation of home photos, in response to the patients who say, ‘Wait, doc. Let me pull out my phone and show my photographs.”
During the very first days of the pandemic, in order to accommodate urgent patient requests, she and her colleagues used cloud services for patients to submit photos for concerning skin conditions or lesions, which were then discussed over commonly available video platforms. But they quickly realized that this would not work long-term so within two months, they created an electronic health record–integrated workflow that they are still using, she said.
Here’s how it works. If the patient request is deemed nonacute or does not require a full-body skin exam, the scheduling team offers that patient a store-and-video evaluation (SAVe) or an in-person visit. If a SAVe visit is requested, the patient is required to submit a photograph of his or her condition, then a medical assistant checks for the presence and quality of up to nine patient-submitted photos and contacts the patient if additional photos are required.
Immediately before the encounter, a medical assistant calls the patient to ensure video connectivity and performs a brief intake history. The patient and physician then connect via a video-capable platform – most commonly Vidyo, which is integrated with EPIC. After the visit, the provider notifies the scheduling team if any additional in-person or virtual follow up is required.
In a half day of practice, Dr. Afanasiev sees about 20 patients via video visits scheduled every 15 minutes. On a recent day, 55% of visits were related to acne and 10% were related to a mole check, which usually resulted in recommendation for biopsy. Most (70%) were existing patients, while 30% were new.
“There is no store-and-forward option at this time, meaning that patients can’t just submit a photo without a visit,” she said. “In addition, part of our consent is, if you don’t show up to your scheduled video visit, your photos will not be reviewed. The photos are linked to the video visit and uploaded to the patient’s chart. The rooming workflow is very similar to in clinic, except you’re at home and the medical assistant is remote.”
In an article recently published in the Journal of the American Academy of Dermatology, Dr. Afanasiev and her colleagues described their experience with this photo plus video teledermatology – SAVe – workflow between March 16, 2020, and Aug. 31, 2020. The researchers analyzed 74,411 dermatology cases encountered by 89 providers who cared for 46,024 patients during that time frame. Most of the encounters (79%) were in-person, while the remaining 21% were digital in nature – SAVe in 89% of cases, followed by telephone/message encounters.
At the initial peak of the COVID-19 pandemic in April 2020, SAVe encounters increased to 72% of all encounters from 0% prior to March 16, 2020, and were sustained at 12% when the clinic reopened in the summer of 2020. Over the study period, the clinic’s incorporation of SAVe increased care access to patients located in 731 unique ZIP codes in and near California. “We also have been able to retain many patients within our system,” Dr. Afanasiev said. “We have a large proportion of patients that require 2-3 hours of travel time to get to our clinic, so virtual visits allowed for increased rural access. It also allowed for flexibility for patients and providers.”
The new workflow also led to faster access to care. The time from referral to an in-person evaluation fell from an average of 56 days in 2019 to average of 27 days in 2020, while the wait time for a virtual visit was just 14 days in 2020. “We were able to see a diverse number of diagnostic categories with both in-person and virtual care, most commonly rashes, acne, dermal growths, and pigmentary disorders,” she said.
For clinicians interested in incorporating a SAVe-like system into their workflow, Dr. Afanasiev advises them to think seriously about consent. “You want to make sure patients understand what they’re getting themselves into,” she said. “You want to make sure they know that some diagnoses cannot be adequately addressed by teledermatology.” Photo quality is also important, she said. “Video quality is not good enough for most of our diagnoses, so photos are an important part of this evaluation. In this day and age, patients are actually pretty good photographers most of the time.”
She urges practices to carefully think about how they allow patients to submit photos, especially if photographs are not attached to a billable visit.
In her opinion, a good teledermatology platform should have trained support staff with the ability for patients to send photos prior to their visit, and should be safe, secure, and HIPAA compliant. It should also be app and browser compatible and have high resolution and low downtime.
“Into the future, I think it’s important to maintain teledermatology within our clinical practice, especially for remote monitoring of chronic skin diseases,” Dr. Afanasiev said. “Oftentimes we schedule 3- or 6-month follow-ups but often those do not correspond to the patients’ disease flare. They may have had an eczema or psoriatic flare 3 weeks prior, but we see them in clinic with clear skin, which makes it hard to judge how to tailor our treatment. It will also be important for us to understand the safety and security and legal implications of these new practice styles.”
She also referred to technological advances, which she said “will dovetail well with teledermatology, including robust at-home and commercial 3D virtual capture technology, machine learning algorithms for improved photos, and virtual biopsy technology.”
Dr. Afanasiev is a member of the American Academy of Dermatology Teledermatology Task Force. She had no relevant disclosures.
FROM PDA 2021
But I am the therapist!
Dr. Smith’s patient, Anna, was struggling. Her mother, with whom she lived, had died, her boyfriend had broken up with her, her teenagers were being difficult, and her anxiety about catching COVID left her isolated and lonely.
She was working in psychotherapy and a number of medications had been tried, but when Anna suggested that her children might be better off without her, Dr. Smith referred her to an inpatient unit at a local hospital for admission. He faxed over the clinical and demographic information that the hospital wanted, and he never heard a word from the inpatient unit until Anna texted him that she had been discharged. She noted that the hospitalization had been helpful.
“I have an appointment next week with a therapist,” Anna texted.
Dr. Smith was puzzled and he conveyed that in his response to her.
“They told me that you are the psychiatrist and I should see you once a month and that I need a therapist to see weekly.”
Dr. Smith remained puzzled. At times he had seen Anna weekly, and he always saw her for 50-minute (or longer) sessions, but he realized that the person in charge of discharge had decided that psychiatrists are not psychotherapists. As a psychiatrist who sees patients for psychotherapy, Dr. Smith was not in Anna’s health insurance plan, and perhaps the hospital discharged people to see in-network clinicians. Or perhaps they thought that if he were a better psychiatrist, his patient would not need an inpatient admission. All he could do was surmise, but clearly ; they had changed Anna’s treatment without the courtesy of a phone call.
“This happens to me all the time,” said Sally Waddington, MD, a psychiatrist in private practice in Laurel, Md. “Hospitals will tell my patients that psychiatrists are for medications and they need a separate therapist. It really undermines the treatment.”
Ramin Mojtabai, MD, PhD, MPH, is a psychiatrist at Johns Hopkins Hospital in Baltimore. He has done research on trends in psychotherapy among psychiatrists and in 2008 published a study which showed that only 10.8% of psychiatrists see all of their patients for psychotherapy. The same data, however, revealed that 59.4% – or a majority – of psychiatrists see at least some of their patients for psychotherapy.
“Unfortunately, our profession has been defined by the insurance industry for decades,” Dr. Mojtabai said in an interview, “so, I am not surprised that the patient was told to see a ‘proper’ psychotherapist.”
George Dawson, MD, spent 22 years as a psychiatrist on an inpatient unit in Minnesota. On his blog, “Real Psychiatry,” Dr. Dawson has a lengthy post dated Oct. 3, 2021, titled “The problem with inpatient units.” Dr. Dawson writes, “There is a lack of collaboration with outpatient staff: Good inpatient care proceeds from the assumption that the main focus of treatment is with the primary psychiatrist or treatment team. ... The only acceptable reasons are that the patient does not have outpatient care, the patient refuses to consent to the communication, or the outpatient physician or their proxy cannot be contacted with a good faith effort. Being on both ends of that call – a good faith effort to me means leaving a cell phone number with the message to ‘call me at any time.’ I have found that effort is required in an era of overproduction and no set times in the outpatient clinic for necessary phone calls.”
In an interview, Dr. Dawson commented on the predicament of Dr. Smith and Anna. “The inpatient staff seem to have a grandiose idea of where the care should be centered and that is with the outpatient doctor making the referral. Any plan not involving the referring doctor is not likely to be successful.”
Dr. Waddington talked about how she handles the situation when an inpatient unit refers her patients to a separate psychotherapist. “Usually, I discuss it with my patient. Sometimes they want a change and so I continue to see them for medications. Most of the time, they keep seeing me for therapy.” She went on to note, “I recently had a patient who was in the hospital and was referred to a trauma specialist for therapy. The referral was probably appropriate in her case; I just wish they had discussed this with me first.”
Dr. Smith calls himself “a dinosaur” – he likes treating patients with a combination of medications and psychotherapy and he does not enjoy seeing patients for brief visits for medication management. He was, however, concerned that Anna had been stretching out the time between sessions because of financial concerns, so he suggested she could meet with the therapist and see if she thought this might be helpful to her. If it was, he recommended she find a psychiatrist in her insurance network to prescribe her medications, with the hope that this would be a reasonable alternative to their current conundrum.
“I believe that many patients are best served by having their care come from a single psychiatrist and not treatment split between clinicians; however, I recognize that this is not always financially the best option. Anna might benefit from not having the financial stress of care from a psychiatrist where she is not reimbursed as well – if at all – by insurance. Still, I am annoyed; it feels like the inpatient team decided to write a new job description for me and to dictate through my patient how it is I should be practicing. And after they implied that I was not the best therapist for her, they hijacked her and sent her to someone who may well have much less experience than I do.”
In the clinical care of any patient, communication between the inpatient team and the outpatient physician is essential, and all too often, this doesn’t happen.
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2018). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore.
Dr. Smith’s patient, Anna, was struggling. Her mother, with whom she lived, had died, her boyfriend had broken up with her, her teenagers were being difficult, and her anxiety about catching COVID left her isolated and lonely.
She was working in psychotherapy and a number of medications had been tried, but when Anna suggested that her children might be better off without her, Dr. Smith referred her to an inpatient unit at a local hospital for admission. He faxed over the clinical and demographic information that the hospital wanted, and he never heard a word from the inpatient unit until Anna texted him that she had been discharged. She noted that the hospitalization had been helpful.
“I have an appointment next week with a therapist,” Anna texted.
Dr. Smith was puzzled and he conveyed that in his response to her.
“They told me that you are the psychiatrist and I should see you once a month and that I need a therapist to see weekly.”
Dr. Smith remained puzzled. At times he had seen Anna weekly, and he always saw her for 50-minute (or longer) sessions, but he realized that the person in charge of discharge had decided that psychiatrists are not psychotherapists. As a psychiatrist who sees patients for psychotherapy, Dr. Smith was not in Anna’s health insurance plan, and perhaps the hospital discharged people to see in-network clinicians. Or perhaps they thought that if he were a better psychiatrist, his patient would not need an inpatient admission. All he could do was surmise, but clearly ; they had changed Anna’s treatment without the courtesy of a phone call.
“This happens to me all the time,” said Sally Waddington, MD, a psychiatrist in private practice in Laurel, Md. “Hospitals will tell my patients that psychiatrists are for medications and they need a separate therapist. It really undermines the treatment.”
Ramin Mojtabai, MD, PhD, MPH, is a psychiatrist at Johns Hopkins Hospital in Baltimore. He has done research on trends in psychotherapy among psychiatrists and in 2008 published a study which showed that only 10.8% of psychiatrists see all of their patients for psychotherapy. The same data, however, revealed that 59.4% – or a majority – of psychiatrists see at least some of their patients for psychotherapy.
“Unfortunately, our profession has been defined by the insurance industry for decades,” Dr. Mojtabai said in an interview, “so, I am not surprised that the patient was told to see a ‘proper’ psychotherapist.”
George Dawson, MD, spent 22 years as a psychiatrist on an inpatient unit in Minnesota. On his blog, “Real Psychiatry,” Dr. Dawson has a lengthy post dated Oct. 3, 2021, titled “The problem with inpatient units.” Dr. Dawson writes, “There is a lack of collaboration with outpatient staff: Good inpatient care proceeds from the assumption that the main focus of treatment is with the primary psychiatrist or treatment team. ... The only acceptable reasons are that the patient does not have outpatient care, the patient refuses to consent to the communication, or the outpatient physician or their proxy cannot be contacted with a good faith effort. Being on both ends of that call – a good faith effort to me means leaving a cell phone number with the message to ‘call me at any time.’ I have found that effort is required in an era of overproduction and no set times in the outpatient clinic for necessary phone calls.”
In an interview, Dr. Dawson commented on the predicament of Dr. Smith and Anna. “The inpatient staff seem to have a grandiose idea of where the care should be centered and that is with the outpatient doctor making the referral. Any plan not involving the referring doctor is not likely to be successful.”
Dr. Waddington talked about how she handles the situation when an inpatient unit refers her patients to a separate psychotherapist. “Usually, I discuss it with my patient. Sometimes they want a change and so I continue to see them for medications. Most of the time, they keep seeing me for therapy.” She went on to note, “I recently had a patient who was in the hospital and was referred to a trauma specialist for therapy. The referral was probably appropriate in her case; I just wish they had discussed this with me first.”
Dr. Smith calls himself “a dinosaur” – he likes treating patients with a combination of medications and psychotherapy and he does not enjoy seeing patients for brief visits for medication management. He was, however, concerned that Anna had been stretching out the time between sessions because of financial concerns, so he suggested she could meet with the therapist and see if she thought this might be helpful to her. If it was, he recommended she find a psychiatrist in her insurance network to prescribe her medications, with the hope that this would be a reasonable alternative to their current conundrum.
“I believe that many patients are best served by having their care come from a single psychiatrist and not treatment split between clinicians; however, I recognize that this is not always financially the best option. Anna might benefit from not having the financial stress of care from a psychiatrist where she is not reimbursed as well – if at all – by insurance. Still, I am annoyed; it feels like the inpatient team decided to write a new job description for me and to dictate through my patient how it is I should be practicing. And after they implied that I was not the best therapist for her, they hijacked her and sent her to someone who may well have much less experience than I do.”
In the clinical care of any patient, communication between the inpatient team and the outpatient physician is essential, and all too often, this doesn’t happen.
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2018). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore.
Dr. Smith’s patient, Anna, was struggling. Her mother, with whom she lived, had died, her boyfriend had broken up with her, her teenagers were being difficult, and her anxiety about catching COVID left her isolated and lonely.
She was working in psychotherapy and a number of medications had been tried, but when Anna suggested that her children might be better off without her, Dr. Smith referred her to an inpatient unit at a local hospital for admission. He faxed over the clinical and demographic information that the hospital wanted, and he never heard a word from the inpatient unit until Anna texted him that she had been discharged. She noted that the hospitalization had been helpful.
“I have an appointment next week with a therapist,” Anna texted.
Dr. Smith was puzzled and he conveyed that in his response to her.
“They told me that you are the psychiatrist and I should see you once a month and that I need a therapist to see weekly.”
Dr. Smith remained puzzled. At times he had seen Anna weekly, and he always saw her for 50-minute (or longer) sessions, but he realized that the person in charge of discharge had decided that psychiatrists are not psychotherapists. As a psychiatrist who sees patients for psychotherapy, Dr. Smith was not in Anna’s health insurance plan, and perhaps the hospital discharged people to see in-network clinicians. Or perhaps they thought that if he were a better psychiatrist, his patient would not need an inpatient admission. All he could do was surmise, but clearly ; they had changed Anna’s treatment without the courtesy of a phone call.
“This happens to me all the time,” said Sally Waddington, MD, a psychiatrist in private practice in Laurel, Md. “Hospitals will tell my patients that psychiatrists are for medications and they need a separate therapist. It really undermines the treatment.”
Ramin Mojtabai, MD, PhD, MPH, is a psychiatrist at Johns Hopkins Hospital in Baltimore. He has done research on trends in psychotherapy among psychiatrists and in 2008 published a study which showed that only 10.8% of psychiatrists see all of their patients for psychotherapy. The same data, however, revealed that 59.4% – or a majority – of psychiatrists see at least some of their patients for psychotherapy.
“Unfortunately, our profession has been defined by the insurance industry for decades,” Dr. Mojtabai said in an interview, “so, I am not surprised that the patient was told to see a ‘proper’ psychotherapist.”
George Dawson, MD, spent 22 years as a psychiatrist on an inpatient unit in Minnesota. On his blog, “Real Psychiatry,” Dr. Dawson has a lengthy post dated Oct. 3, 2021, titled “The problem with inpatient units.” Dr. Dawson writes, “There is a lack of collaboration with outpatient staff: Good inpatient care proceeds from the assumption that the main focus of treatment is with the primary psychiatrist or treatment team. ... The only acceptable reasons are that the patient does not have outpatient care, the patient refuses to consent to the communication, or the outpatient physician or their proxy cannot be contacted with a good faith effort. Being on both ends of that call – a good faith effort to me means leaving a cell phone number with the message to ‘call me at any time.’ I have found that effort is required in an era of overproduction and no set times in the outpatient clinic for necessary phone calls.”
In an interview, Dr. Dawson commented on the predicament of Dr. Smith and Anna. “The inpatient staff seem to have a grandiose idea of where the care should be centered and that is with the outpatient doctor making the referral. Any plan not involving the referring doctor is not likely to be successful.”
Dr. Waddington talked about how she handles the situation when an inpatient unit refers her patients to a separate psychotherapist. “Usually, I discuss it with my patient. Sometimes they want a change and so I continue to see them for medications. Most of the time, they keep seeing me for therapy.” She went on to note, “I recently had a patient who was in the hospital and was referred to a trauma specialist for therapy. The referral was probably appropriate in her case; I just wish they had discussed this with me first.”
Dr. Smith calls himself “a dinosaur” – he likes treating patients with a combination of medications and psychotherapy and he does not enjoy seeing patients for brief visits for medication management. He was, however, concerned that Anna had been stretching out the time between sessions because of financial concerns, so he suggested she could meet with the therapist and see if she thought this might be helpful to her. If it was, he recommended she find a psychiatrist in her insurance network to prescribe her medications, with the hope that this would be a reasonable alternative to their current conundrum.
“I believe that many patients are best served by having their care come from a single psychiatrist and not treatment split between clinicians; however, I recognize that this is not always financially the best option. Anna might benefit from not having the financial stress of care from a psychiatrist where she is not reimbursed as well – if at all – by insurance. Still, I am annoyed; it feels like the inpatient team decided to write a new job description for me and to dictate through my patient how it is I should be practicing. And after they implied that I was not the best therapist for her, they hijacked her and sent her to someone who may well have much less experience than I do.”
In the clinical care of any patient, communication between the inpatient team and the outpatient physician is essential, and all too often, this doesn’t happen.
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2018). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore.