User login
50 years of growth: More dermatologists, more demand
A dive into the dermatology data pool reveals a great deal of change in the 50 years that Dermatology News and Skin & Allergy News have been covering the specialty.
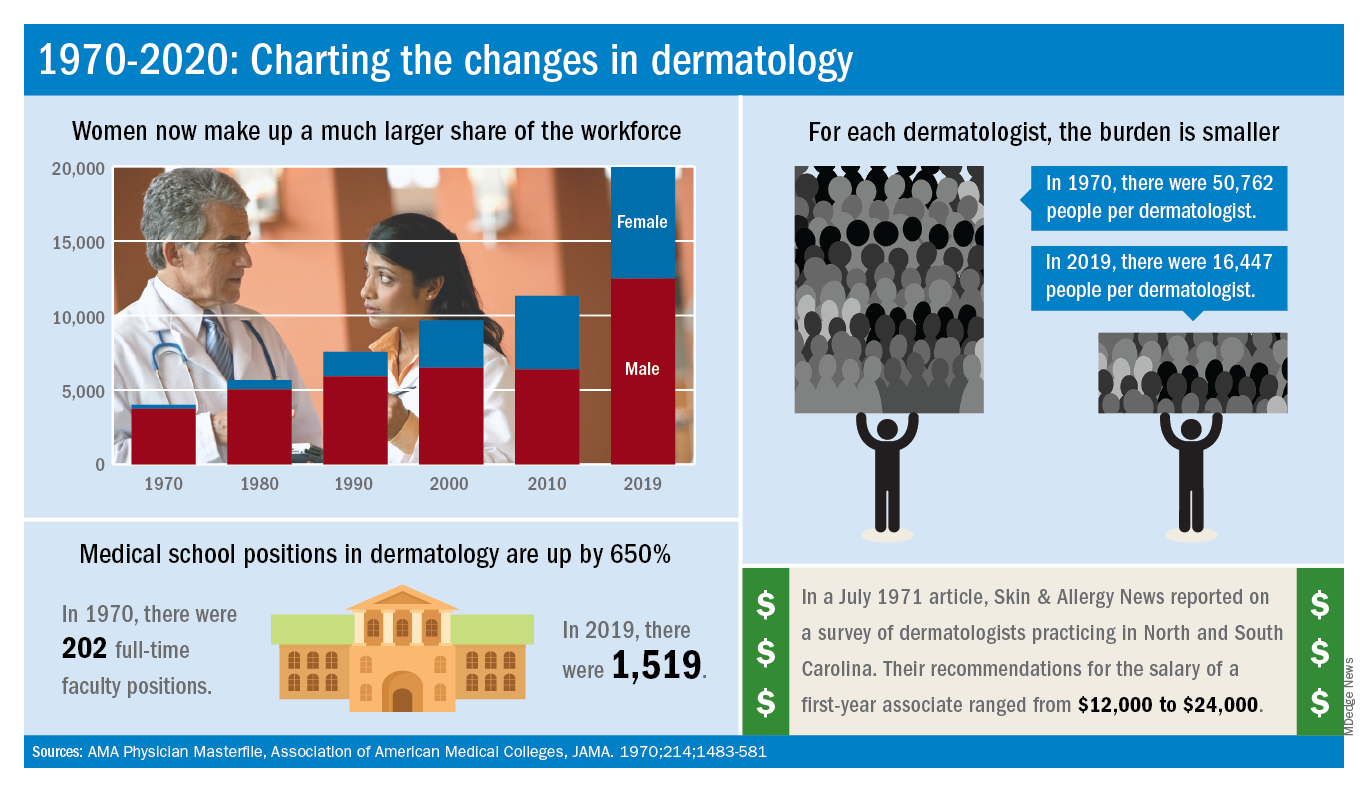
For one thing, there are a lot more dermatologists now. The American Academy of Dermatology puts its 2020 membership at a somewhat lower 18,898, noting that not all dermatologists are AAD members.
Much of that 50-year increase comes from the larger proportion of women entering the specialty. In 1970, only 7% of dermatologists were women, but by 2019 they represented over 37% of the dermatology workforce, according to the AMA numbers. The AAD, however, reports more women than the AMA (8,940 vs. 7,482), so the proportion of female academy members in 2020 is about 47%.
The population of dermatologists has increased faster than the general population since 1970, leading to a rising density of providers. A report from 1973 put the national figure at 1.7 dermatologists per 100,000 population in 1970, and two more recent studies in JAMA Dermatology reported density levels of 3.65 per 100,000 in 2013 and 3.36 per 100,000 in 2016.
In that 1973 report, the authors said that there was “no evidence to suggest that there will not be sufficient dermatologists in the future, if training centers are maintained and adequately financed,” noting that “the current rate of filling of dermatologic residency positions should not diminish and may continue to increase.”
In 2017, the conclusion was quite different: “Dermatologists alone have been unable to meet increasing patient demand for dermatologic services. The number of dermatology residency training positions has been relatively stagnant, suggesting that the current supply of dermatologists in training will be insufficient to fully meet growing future demand.”
The current state of strong demand for dermatologists does come with some benefits. In a 2019 survey by physician recruitment firm Merritt Hawkins, dermatologists had the 6th-highest starting salary at $420,000 a year. An article in the July 1971 issue of Skin & Allergy News offered a somewhat different perspective on compensation for first-year dermatologists: Recommendations offered by those already in practice ranged from $12,000 to $24,000.
Those first-year physicians are coming from residencies that, not too surprisingly, are now producing more new dermatologists than they did in 1970, although perhaps not as many more as might be expected.
There were an estimated 250 individuals completing dermatology residencies annually in 1976 (J Am Acad Dermatol. 1981;4[3]:344-5), which suggests a total of approximately 750 active residents at a time when there were about 5,000 practicing dermatologists in the country.
For the 2018-2019 academic year, there were 1,439 active residents in U.S. training programs, according to the Association of American Medical Colleges, so there were twice the number of residents but four times as many dermatologists in practice, compared with 1976.
The next link in the dermatology supply chain would be the medical schools, and there the numbers of full-time faculty have more than kept up. For the 1969-1970 academic year, there were 202 full-time positions in dermatology (JAMA. 1970;214:1483-581). By 2019, the number had risen to 1,519, according to the Association of American Medical Colleges.
A dive into the dermatology data pool reveals a great deal of change in the 50 years that Dermatology News and Skin & Allergy News have been covering the specialty.
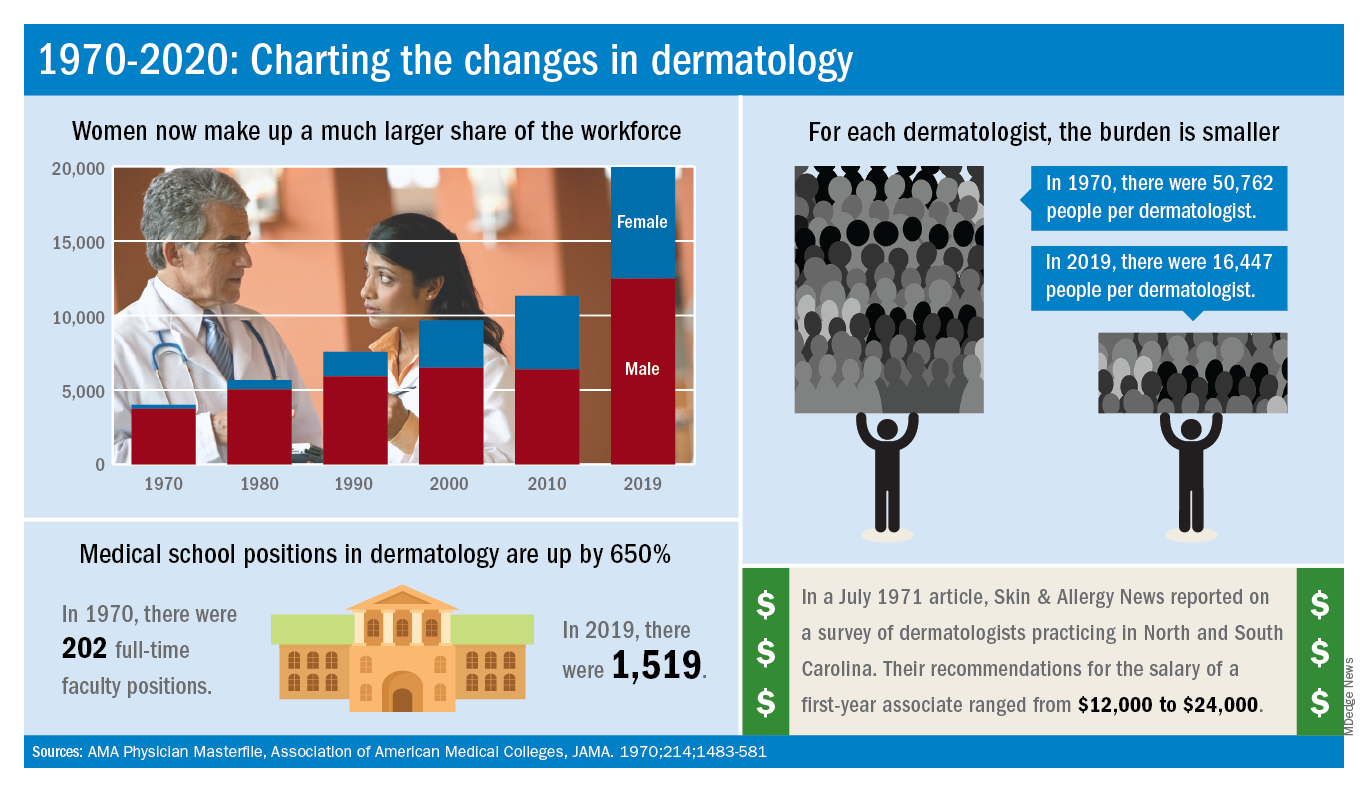
For one thing, there are a lot more dermatologists now. The American Academy of Dermatology puts its 2020 membership at a somewhat lower 18,898, noting that not all dermatologists are AAD members.
Much of that 50-year increase comes from the larger proportion of women entering the specialty. In 1970, only 7% of dermatologists were women, but by 2019 they represented over 37% of the dermatology workforce, according to the AMA numbers. The AAD, however, reports more women than the AMA (8,940 vs. 7,482), so the proportion of female academy members in 2020 is about 47%.
The population of dermatologists has increased faster than the general population since 1970, leading to a rising density of providers. A report from 1973 put the national figure at 1.7 dermatologists per 100,000 population in 1970, and two more recent studies in JAMA Dermatology reported density levels of 3.65 per 100,000 in 2013 and 3.36 per 100,000 in 2016.
In that 1973 report, the authors said that there was “no evidence to suggest that there will not be sufficient dermatologists in the future, if training centers are maintained and adequately financed,” noting that “the current rate of filling of dermatologic residency positions should not diminish and may continue to increase.”
In 2017, the conclusion was quite different: “Dermatologists alone have been unable to meet increasing patient demand for dermatologic services. The number of dermatology residency training positions has been relatively stagnant, suggesting that the current supply of dermatologists in training will be insufficient to fully meet growing future demand.”
The current state of strong demand for dermatologists does come with some benefits. In a 2019 survey by physician recruitment firm Merritt Hawkins, dermatologists had the 6th-highest starting salary at $420,000 a year. An article in the July 1971 issue of Skin & Allergy News offered a somewhat different perspective on compensation for first-year dermatologists: Recommendations offered by those already in practice ranged from $12,000 to $24,000.
Those first-year physicians are coming from residencies that, not too surprisingly, are now producing more new dermatologists than they did in 1970, although perhaps not as many more as might be expected.
There were an estimated 250 individuals completing dermatology residencies annually in 1976 (J Am Acad Dermatol. 1981;4[3]:344-5), which suggests a total of approximately 750 active residents at a time when there were about 5,000 practicing dermatologists in the country.
For the 2018-2019 academic year, there were 1,439 active residents in U.S. training programs, according to the Association of American Medical Colleges, so there were twice the number of residents but four times as many dermatologists in practice, compared with 1976.
The next link in the dermatology supply chain would be the medical schools, and there the numbers of full-time faculty have more than kept up. For the 1969-1970 academic year, there were 202 full-time positions in dermatology (JAMA. 1970;214:1483-581). By 2019, the number had risen to 1,519, according to the Association of American Medical Colleges.
A dive into the dermatology data pool reveals a great deal of change in the 50 years that Dermatology News and Skin & Allergy News have been covering the specialty.
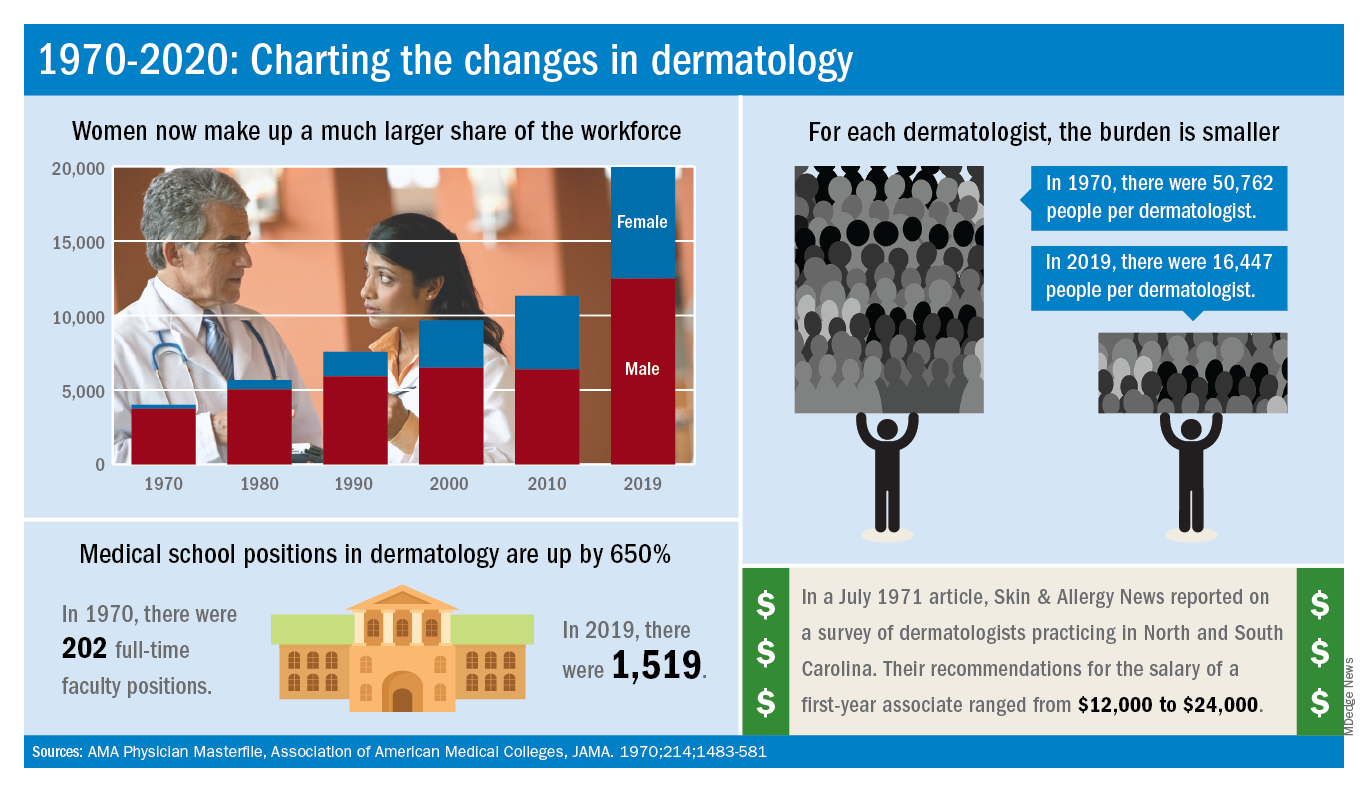
For one thing, there are a lot more dermatologists now. The American Academy of Dermatology puts its 2020 membership at a somewhat lower 18,898, noting that not all dermatologists are AAD members.
Much of that 50-year increase comes from the larger proportion of women entering the specialty. In 1970, only 7% of dermatologists were women, but by 2019 they represented over 37% of the dermatology workforce, according to the AMA numbers. The AAD, however, reports more women than the AMA (8,940 vs. 7,482), so the proportion of female academy members in 2020 is about 47%.
The population of dermatologists has increased faster than the general population since 1970, leading to a rising density of providers. A report from 1973 put the national figure at 1.7 dermatologists per 100,000 population in 1970, and two more recent studies in JAMA Dermatology reported density levels of 3.65 per 100,000 in 2013 and 3.36 per 100,000 in 2016.
In that 1973 report, the authors said that there was “no evidence to suggest that there will not be sufficient dermatologists in the future, if training centers are maintained and adequately financed,” noting that “the current rate of filling of dermatologic residency positions should not diminish and may continue to increase.”
In 2017, the conclusion was quite different: “Dermatologists alone have been unable to meet increasing patient demand for dermatologic services. The number of dermatology residency training positions has been relatively stagnant, suggesting that the current supply of dermatologists in training will be insufficient to fully meet growing future demand.”
The current state of strong demand for dermatologists does come with some benefits. In a 2019 survey by physician recruitment firm Merritt Hawkins, dermatologists had the 6th-highest starting salary at $420,000 a year. An article in the July 1971 issue of Skin & Allergy News offered a somewhat different perspective on compensation for first-year dermatologists: Recommendations offered by those already in practice ranged from $12,000 to $24,000.
Those first-year physicians are coming from residencies that, not too surprisingly, are now producing more new dermatologists than they did in 1970, although perhaps not as many more as might be expected.
There were an estimated 250 individuals completing dermatology residencies annually in 1976 (J Am Acad Dermatol. 1981;4[3]:344-5), which suggests a total of approximately 750 active residents at a time when there were about 5,000 practicing dermatologists in the country.
For the 2018-2019 academic year, there were 1,439 active residents in U.S. training programs, according to the Association of American Medical Colleges, so there were twice the number of residents but four times as many dermatologists in practice, compared with 1976.
The next link in the dermatology supply chain would be the medical schools, and there the numbers of full-time faculty have more than kept up. For the 1969-1970 academic year, there were 202 full-time positions in dermatology (JAMA. 1970;214:1483-581). By 2019, the number had risen to 1,519, according to the Association of American Medical Colleges.
Oncologists are average in terms of happiness, survey suggests
When it comes to physician happiness both in and outside the workplace, oncologists are about average, according to Medscape’s 2020 Lifestyle, Happiness, and Burnout Report.

Oncologists landed in the middle of the pack among all physicians surveyed for happiness. Rheumatologists were most likely to report being very or extremely happy outside of work (60%) and neurologists were least likely to do so (44%), but about half of oncologists (51%) reported being very/extremely happy outside of work. For happiness at work, dermatologists topped the list (41%), neurologists came in last (18%), and oncologists remained in the middle (29%).
Oncologists were average when it came to burnout as well, matching the rate of overall physicians. Specifically, 32% of oncologists were burned out, 4% were depressed, and 9% were both burned out and depressed.
The most commonly reported factors contributing to burnout among oncologists were an overabundance of bureaucratic tasks (74%), spending too many hours at work (42%), and a lack of respect from colleagues in the workplace (36%).
Exercise was the most commonly reported way oncologists dealt with burnout (51%), followed by talking with family and friends (49%), and isolating themselves from others (38%). In addition, 57% of oncologists took 3-4 weeks’ vacation, compared with 44% of physicians overall; 29% of oncologists took less than 3 weeks’ vacation.
About 18% of oncologists said they had contemplated suicide, and 1% said they’d attempted it; 72% said they’d never had thoughts of suicide. Just under one-quarter of oncologists said they were currently seeking professional help or were planning to seek help for symptoms of depression and/or burnout.
“The survey results are concerning on several levels,” Maurie Markman, MD, of Cancer Treatment Centers of America, Philadelphia, said in an interview.
“First, the data suggest a considerable number of oncologists are simply burned out from the day-to-day bureaucracy (paperwork, etc.) of medical practice, which has absolutely nothing to do with the actual care delivered. This likely impacts the willingness to continue in this role. Second, one must be concerned for the future recruitment of physicians to become clinical oncologists. And finally, one must wonder about the impact of these concerning figures on the quality of care being provided to cancer patients.”
This survey was conducted from June 25 to Sept. 19, 2019, and involved 15,181 physicians. Oncologists made up 1% of the survey pool.
When it comes to physician happiness both in and outside the workplace, oncologists are about average, according to Medscape’s 2020 Lifestyle, Happiness, and Burnout Report.

Oncologists landed in the middle of the pack among all physicians surveyed for happiness. Rheumatologists were most likely to report being very or extremely happy outside of work (60%) and neurologists were least likely to do so (44%), but about half of oncologists (51%) reported being very/extremely happy outside of work. For happiness at work, dermatologists topped the list (41%), neurologists came in last (18%), and oncologists remained in the middle (29%).
Oncologists were average when it came to burnout as well, matching the rate of overall physicians. Specifically, 32% of oncologists were burned out, 4% were depressed, and 9% were both burned out and depressed.
The most commonly reported factors contributing to burnout among oncologists were an overabundance of bureaucratic tasks (74%), spending too many hours at work (42%), and a lack of respect from colleagues in the workplace (36%).
Exercise was the most commonly reported way oncologists dealt with burnout (51%), followed by talking with family and friends (49%), and isolating themselves from others (38%). In addition, 57% of oncologists took 3-4 weeks’ vacation, compared with 44% of physicians overall; 29% of oncologists took less than 3 weeks’ vacation.
About 18% of oncologists said they had contemplated suicide, and 1% said they’d attempted it; 72% said they’d never had thoughts of suicide. Just under one-quarter of oncologists said they were currently seeking professional help or were planning to seek help for symptoms of depression and/or burnout.
“The survey results are concerning on several levels,” Maurie Markman, MD, of Cancer Treatment Centers of America, Philadelphia, said in an interview.
“First, the data suggest a considerable number of oncologists are simply burned out from the day-to-day bureaucracy (paperwork, etc.) of medical practice, which has absolutely nothing to do with the actual care delivered. This likely impacts the willingness to continue in this role. Second, one must be concerned for the future recruitment of physicians to become clinical oncologists. And finally, one must wonder about the impact of these concerning figures on the quality of care being provided to cancer patients.”
This survey was conducted from June 25 to Sept. 19, 2019, and involved 15,181 physicians. Oncologists made up 1% of the survey pool.
When it comes to physician happiness both in and outside the workplace, oncologists are about average, according to Medscape’s 2020 Lifestyle, Happiness, and Burnout Report.

Oncologists landed in the middle of the pack among all physicians surveyed for happiness. Rheumatologists were most likely to report being very or extremely happy outside of work (60%) and neurologists were least likely to do so (44%), but about half of oncologists (51%) reported being very/extremely happy outside of work. For happiness at work, dermatologists topped the list (41%), neurologists came in last (18%), and oncologists remained in the middle (29%).
Oncologists were average when it came to burnout as well, matching the rate of overall physicians. Specifically, 32% of oncologists were burned out, 4% were depressed, and 9% were both burned out and depressed.
The most commonly reported factors contributing to burnout among oncologists were an overabundance of bureaucratic tasks (74%), spending too many hours at work (42%), and a lack of respect from colleagues in the workplace (36%).
Exercise was the most commonly reported way oncologists dealt with burnout (51%), followed by talking with family and friends (49%), and isolating themselves from others (38%). In addition, 57% of oncologists took 3-4 weeks’ vacation, compared with 44% of physicians overall; 29% of oncologists took less than 3 weeks’ vacation.
About 18% of oncologists said they had contemplated suicide, and 1% said they’d attempted it; 72% said they’d never had thoughts of suicide. Just under one-quarter of oncologists said they were currently seeking professional help or were planning to seek help for symptoms of depression and/or burnout.
“The survey results are concerning on several levels,” Maurie Markman, MD, of Cancer Treatment Centers of America, Philadelphia, said in an interview.
“First, the data suggest a considerable number of oncologists are simply burned out from the day-to-day bureaucracy (paperwork, etc.) of medical practice, which has absolutely nothing to do with the actual care delivered. This likely impacts the willingness to continue in this role. Second, one must be concerned for the future recruitment of physicians to become clinical oncologists. And finally, one must wonder about the impact of these concerning figures on the quality of care being provided to cancer patients.”
This survey was conducted from June 25 to Sept. 19, 2019, and involved 15,181 physicians. Oncologists made up 1% of the survey pool.
Cardiologists’ happiness average both in and outside the office
Compared with their colleagues, cardiologists are in the middle when it comes to happiness both in and outside the workplace, according to Medscape’s 2020 Lifestyle, Happiness, and Burnout Report.

About 28% of cardiologists reported that they were very happy in the workplace, according to the Medscape report, with dermatologists taking the top spot at 41%; 51% of cardiologists said that they were very happy outside of work, 9 percentage points behind rheumatologists at 60%.
The burnout rate for cardiologists was 29%, well below the 41% average for all physicians. About 15% of cardiologists reported that they were both burned out and depressed. An overabundance of bureaucratic tasks was the most commonly reported contributing factor to burnout at 64%, followed by spending too many hours at work at 39% and increased usage of EHRs at 33%.
Cardiologists most commonly dealt with burnout by exercising (45%), talking with friends/family (43%), and isolating themselves from others (42%). In addition, 47% of cardiologists reported taking 3-4 weeks of vacation, slightly more than the 44% average for all physicians; only 29% said they had taken less than 3 weeks’ vacation.
About 10% of cardiologists said that they’d contemplated suicide and 1% reported that they’d attempted it; 83% reported that they’d never thought about suicide. Only 10% of cardiologists reported that they were either currently seeking help or were planning to seek professional help for symptoms of burnout and/or depression, while 76% said they had no plans to consult help and had not done so in the past.
The Medscape survey was conducted from June 25 to Sept. 19, 2019, and involved 15,181 physicians.
Compared with their colleagues, cardiologists are in the middle when it comes to happiness both in and outside the workplace, according to Medscape’s 2020 Lifestyle, Happiness, and Burnout Report.

About 28% of cardiologists reported that they were very happy in the workplace, according to the Medscape report, with dermatologists taking the top spot at 41%; 51% of cardiologists said that they were very happy outside of work, 9 percentage points behind rheumatologists at 60%.
The burnout rate for cardiologists was 29%, well below the 41% average for all physicians. About 15% of cardiologists reported that they were both burned out and depressed. An overabundance of bureaucratic tasks was the most commonly reported contributing factor to burnout at 64%, followed by spending too many hours at work at 39% and increased usage of EHRs at 33%.
Cardiologists most commonly dealt with burnout by exercising (45%), talking with friends/family (43%), and isolating themselves from others (42%). In addition, 47% of cardiologists reported taking 3-4 weeks of vacation, slightly more than the 44% average for all physicians; only 29% said they had taken less than 3 weeks’ vacation.
About 10% of cardiologists said that they’d contemplated suicide and 1% reported that they’d attempted it; 83% reported that they’d never thought about suicide. Only 10% of cardiologists reported that they were either currently seeking help or were planning to seek professional help for symptoms of burnout and/or depression, while 76% said they had no plans to consult help and had not done so in the past.
The Medscape survey was conducted from June 25 to Sept. 19, 2019, and involved 15,181 physicians.
Compared with their colleagues, cardiologists are in the middle when it comes to happiness both in and outside the workplace, according to Medscape’s 2020 Lifestyle, Happiness, and Burnout Report.

About 28% of cardiologists reported that they were very happy in the workplace, according to the Medscape report, with dermatologists taking the top spot at 41%; 51% of cardiologists said that they were very happy outside of work, 9 percentage points behind rheumatologists at 60%.
The burnout rate for cardiologists was 29%, well below the 41% average for all physicians. About 15% of cardiologists reported that they were both burned out and depressed. An overabundance of bureaucratic tasks was the most commonly reported contributing factor to burnout at 64%, followed by spending too many hours at work at 39% and increased usage of EHRs at 33%.
Cardiologists most commonly dealt with burnout by exercising (45%), talking with friends/family (43%), and isolating themselves from others (42%). In addition, 47% of cardiologists reported taking 3-4 weeks of vacation, slightly more than the 44% average for all physicians; only 29% said they had taken less than 3 weeks’ vacation.
About 10% of cardiologists said that they’d contemplated suicide and 1% reported that they’d attempted it; 83% reported that they’d never thought about suicide. Only 10% of cardiologists reported that they were either currently seeking help or were planning to seek professional help for symptoms of burnout and/or depression, while 76% said they had no plans to consult help and had not done so in the past.
The Medscape survey was conducted from June 25 to Sept. 19, 2019, and involved 15,181 physicians.
An epidemic of fear and misinformation
As I write this, the 2019 novel coronavirus* continues to spread, exceeding 59,000 cases and 1,300 deaths worldwide. With it spreads fear. In the modern world of social media, misinformation spreads even faster than disease.
The news about a novel and deadly illness crowds out more substantial worries. Humans are not particularly good at assessing risk or responding rationally and consistently to it. Risk is hard to fully define. If you look up “risk” in Merriam Webster’s online dictionary, you get the simple definition of “possibility of loss or injury; peril.” If you look up risk in Wikipedia, you get 12 pages of explanation and 8 more pages of links and references.
People handle risk differently. Some people are more risk adverse than others. Some get a pleasurable thrill from risk, whether a slot machine or a parachute jump. Most people really don’t comprehend small probabilities, with tens of billions of dollars spent annually on U.S. lotteries.
Because 98% of people who get COVID-19 are recovering, this is not an extinction-level event or the zombie apocalypse. It is a major health hazard, and one where morbidity and mortality might be assuaged by an early and effective public health response, including the population’s adoption of good habits such as hand washing, cough etiquette, and staying home when ill.
Three key factors may help reduce the fear factor.
One key factor is accurate communication of health information to the public. This has been severely harmed in the last few years by the promotion of gossip on social media, such as Facebook, within newsfeeds without any vetting, along with a smaller component of deliberate misinformation from untraceable sources. Compare this situation with the decision in May 1988 when Surgeon General C. Everett Koop chose to snail mail a brochure on AIDS to every household in America. It was unprecedented. One element of this communication is the public’s belief that government and health care officials will responsibly and timely convey the information. There are accusations that the Chinese government initially impeded early warnings about COVID-19. Dr. Koop, to his great credit and lifesaving leadership, overcame queasiness within the Reagan administration about issues of morality and taste in discussing some of the HIV information. Alas, no similar leadership occurred in the decade of the 2010s when deaths from the opioid epidemic in the United States skyrocketed to claim more lives annually than car accidents or suicide.
A second factor is the credibility of the scientists. Antivaxxers, climate change deniers, and mercenary scientists have severely damaged that credibility of science, compared with the trust in scientists 50 years ago during the Apollo moon shot.
A third factor is perspective. Poor journalism and clickbait can focus excessively on the rare events as news. Airline crashes make the front page while fatal car accidents, claiming a hundred times more lives annually, don’t even merit a story in local media. Someone wins the lottery weekly but few pay attention to those suffering from gambling debts.
Influenza is killing many times more people than the 2019 novel coronavirus, but the news is focused on cruise ships. In the United States, influenza annually will strike tens of millions, with about 10 per 1,000 hospitalized and 0.5 per 1,000 dying. The novel coronavirus is more lethal. SARS (a coronavirus epidemic in 2003) had 8,000 cases with a mortality rate of 96 per 1,000 while the novel 2019 strain so far is killing about 20 per 1,000. That value may be an overestimate, because there may be a significant fraction of COVID-19 patients with symptoms mild enough that they do not seek medical care and do not get tested and counted.
For perspective, in 1952 the United States reported 50,000 cases of polio (meningitis or paralytic) annually with 3,000 deaths. As many as 95% of cases of poliovirus infection have no or mild symptoms and would not have been reported, so the case fatality rate estimate is skewed. In the 1950s, the United States averaged about 500,000 cases of measles per year, with about 500 deaths annually for a case fatality rate of about 1 per 1,000 in a population that was well nourished with good medical care. In malnourished children without access to modern health care, the case fatality rate can be as high as 100 per 1,000, which is why globally measles killed 142,000 people in 2018, a substantial improvement from 536,000 deaths globally in 2000, but still a leading killer of children worldwide. Vaccines had reduced the annual death toll of polio and measles in the U.S. to zero.
In comparison, in this country the annual incidences are about 70,000 overdose deaths, 50,000 suicides, and 40,000 traffic deaths.
Reassurance is the most common product sold by pediatricians. We look for low-probability, high-impact bad things. Usually we don’t find them and can reassure parents that the child will be okay. Sometimes we spot a higher-risk situation and intervene. My job is to worry professionally so that parents can worry less.
COVID-19 worries me, but irrational people worry me more. The real enemies are fear, disinformation, discrimination, and economic warfare.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@mdedge.com.
*This article was updated 2/21/2020.
As I write this, the 2019 novel coronavirus* continues to spread, exceeding 59,000 cases and 1,300 deaths worldwide. With it spreads fear. In the modern world of social media, misinformation spreads even faster than disease.
The news about a novel and deadly illness crowds out more substantial worries. Humans are not particularly good at assessing risk or responding rationally and consistently to it. Risk is hard to fully define. If you look up “risk” in Merriam Webster’s online dictionary, you get the simple definition of “possibility of loss or injury; peril.” If you look up risk in Wikipedia, you get 12 pages of explanation and 8 more pages of links and references.
People handle risk differently. Some people are more risk adverse than others. Some get a pleasurable thrill from risk, whether a slot machine or a parachute jump. Most people really don’t comprehend small probabilities, with tens of billions of dollars spent annually on U.S. lotteries.
Because 98% of people who get COVID-19 are recovering, this is not an extinction-level event or the zombie apocalypse. It is a major health hazard, and one where morbidity and mortality might be assuaged by an early and effective public health response, including the population’s adoption of good habits such as hand washing, cough etiquette, and staying home when ill.
Three key factors may help reduce the fear factor.
One key factor is accurate communication of health information to the public. This has been severely harmed in the last few years by the promotion of gossip on social media, such as Facebook, within newsfeeds without any vetting, along with a smaller component of deliberate misinformation from untraceable sources. Compare this situation with the decision in May 1988 when Surgeon General C. Everett Koop chose to snail mail a brochure on AIDS to every household in America. It was unprecedented. One element of this communication is the public’s belief that government and health care officials will responsibly and timely convey the information. There are accusations that the Chinese government initially impeded early warnings about COVID-19. Dr. Koop, to his great credit and lifesaving leadership, overcame queasiness within the Reagan administration about issues of morality and taste in discussing some of the HIV information. Alas, no similar leadership occurred in the decade of the 2010s when deaths from the opioid epidemic in the United States skyrocketed to claim more lives annually than car accidents or suicide.
A second factor is the credibility of the scientists. Antivaxxers, climate change deniers, and mercenary scientists have severely damaged that credibility of science, compared with the trust in scientists 50 years ago during the Apollo moon shot.
A third factor is perspective. Poor journalism and clickbait can focus excessively on the rare events as news. Airline crashes make the front page while fatal car accidents, claiming a hundred times more lives annually, don’t even merit a story in local media. Someone wins the lottery weekly but few pay attention to those suffering from gambling debts.
Influenza is killing many times more people than the 2019 novel coronavirus, but the news is focused on cruise ships. In the United States, influenza annually will strike tens of millions, with about 10 per 1,000 hospitalized and 0.5 per 1,000 dying. The novel coronavirus is more lethal. SARS (a coronavirus epidemic in 2003) had 8,000 cases with a mortality rate of 96 per 1,000 while the novel 2019 strain so far is killing about 20 per 1,000. That value may be an overestimate, because there may be a significant fraction of COVID-19 patients with symptoms mild enough that they do not seek medical care and do not get tested and counted.
For perspective, in 1952 the United States reported 50,000 cases of polio (meningitis or paralytic) annually with 3,000 deaths. As many as 95% of cases of poliovirus infection have no or mild symptoms and would not have been reported, so the case fatality rate estimate is skewed. In the 1950s, the United States averaged about 500,000 cases of measles per year, with about 500 deaths annually for a case fatality rate of about 1 per 1,000 in a population that was well nourished with good medical care. In malnourished children without access to modern health care, the case fatality rate can be as high as 100 per 1,000, which is why globally measles killed 142,000 people in 2018, a substantial improvement from 536,000 deaths globally in 2000, but still a leading killer of children worldwide. Vaccines had reduced the annual death toll of polio and measles in the U.S. to zero.
In comparison, in this country the annual incidences are about 70,000 overdose deaths, 50,000 suicides, and 40,000 traffic deaths.
Reassurance is the most common product sold by pediatricians. We look for low-probability, high-impact bad things. Usually we don’t find them and can reassure parents that the child will be okay. Sometimes we spot a higher-risk situation and intervene. My job is to worry professionally so that parents can worry less.
COVID-19 worries me, but irrational people worry me more. The real enemies are fear, disinformation, discrimination, and economic warfare.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@mdedge.com.
*This article was updated 2/21/2020.
As I write this, the 2019 novel coronavirus* continues to spread, exceeding 59,000 cases and 1,300 deaths worldwide. With it spreads fear. In the modern world of social media, misinformation spreads even faster than disease.
The news about a novel and deadly illness crowds out more substantial worries. Humans are not particularly good at assessing risk or responding rationally and consistently to it. Risk is hard to fully define. If you look up “risk” in Merriam Webster’s online dictionary, you get the simple definition of “possibility of loss or injury; peril.” If you look up risk in Wikipedia, you get 12 pages of explanation and 8 more pages of links and references.
People handle risk differently. Some people are more risk adverse than others. Some get a pleasurable thrill from risk, whether a slot machine or a parachute jump. Most people really don’t comprehend small probabilities, with tens of billions of dollars spent annually on U.S. lotteries.
Because 98% of people who get COVID-19 are recovering, this is not an extinction-level event or the zombie apocalypse. It is a major health hazard, and one where morbidity and mortality might be assuaged by an early and effective public health response, including the population’s adoption of good habits such as hand washing, cough etiquette, and staying home when ill.
Three key factors may help reduce the fear factor.
One key factor is accurate communication of health information to the public. This has been severely harmed in the last few years by the promotion of gossip on social media, such as Facebook, within newsfeeds without any vetting, along with a smaller component of deliberate misinformation from untraceable sources. Compare this situation with the decision in May 1988 when Surgeon General C. Everett Koop chose to snail mail a brochure on AIDS to every household in America. It was unprecedented. One element of this communication is the public’s belief that government and health care officials will responsibly and timely convey the information. There are accusations that the Chinese government initially impeded early warnings about COVID-19. Dr. Koop, to his great credit and lifesaving leadership, overcame queasiness within the Reagan administration about issues of morality and taste in discussing some of the HIV information. Alas, no similar leadership occurred in the decade of the 2010s when deaths from the opioid epidemic in the United States skyrocketed to claim more lives annually than car accidents or suicide.
A second factor is the credibility of the scientists. Antivaxxers, climate change deniers, and mercenary scientists have severely damaged that credibility of science, compared with the trust in scientists 50 years ago during the Apollo moon shot.
A third factor is perspective. Poor journalism and clickbait can focus excessively on the rare events as news. Airline crashes make the front page while fatal car accidents, claiming a hundred times more lives annually, don’t even merit a story in local media. Someone wins the lottery weekly but few pay attention to those suffering from gambling debts.
Influenza is killing many times more people than the 2019 novel coronavirus, but the news is focused on cruise ships. In the United States, influenza annually will strike tens of millions, with about 10 per 1,000 hospitalized and 0.5 per 1,000 dying. The novel coronavirus is more lethal. SARS (a coronavirus epidemic in 2003) had 8,000 cases with a mortality rate of 96 per 1,000 while the novel 2019 strain so far is killing about 20 per 1,000. That value may be an overestimate, because there may be a significant fraction of COVID-19 patients with symptoms mild enough that they do not seek medical care and do not get tested and counted.
For perspective, in 1952 the United States reported 50,000 cases of polio (meningitis or paralytic) annually with 3,000 deaths. As many as 95% of cases of poliovirus infection have no or mild symptoms and would not have been reported, so the case fatality rate estimate is skewed. In the 1950s, the United States averaged about 500,000 cases of measles per year, with about 500 deaths annually for a case fatality rate of about 1 per 1,000 in a population that was well nourished with good medical care. In malnourished children without access to modern health care, the case fatality rate can be as high as 100 per 1,000, which is why globally measles killed 142,000 people in 2018, a substantial improvement from 536,000 deaths globally in 2000, but still a leading killer of children worldwide. Vaccines had reduced the annual death toll of polio and measles in the U.S. to zero.
In comparison, in this country the annual incidences are about 70,000 overdose deaths, 50,000 suicides, and 40,000 traffic deaths.
Reassurance is the most common product sold by pediatricians. We look for low-probability, high-impact bad things. Usually we don’t find them and can reassure parents that the child will be okay. Sometimes we spot a higher-risk situation and intervene. My job is to worry professionally so that parents can worry less.
COVID-19 worries me, but irrational people worry me more. The real enemies are fear, disinformation, discrimination, and economic warfare.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@mdedge.com.
*This article was updated 2/21/2020.
Burnout rate lower among psychiatrists than physicians overall
Psychiatrists do better compared with those in most specialties in finding happiness at work, according to Medscape’s 2020 Lifestyle, Happiness, and Burnout Report.

About 32% of psychiatrists reported being happy at work, according to the Medscape survey, though they lagged well behind dermatologists, who were the most satisfied with their work lives. In terms of happiness outside the office, psychiatrists were in the middle of the pack with 51% reporting that they were happy.
Somewhat fewer psychiatrists reported being burned out, compared with physicians overall, at 37% versus 41%. The biggest contributing factors to psychiatrist burnout were an overabundance of bureaucratic tasks (63%), increased time devoted to EHRs (34%), and a lack of respect from colleagues in the workplace (32%).
Psychiatrists most commonly dealt with burnout by isolating themselves from others (57%), sleeping (43%), and talking with family/friends (42%). Just under half of psychiatrists took 3-4 weeks’ vacation, compared with 44% of all physicians, and 33% took less than 3 weeks’ vacation.
and 1% reported that they had attempted suicide. About 45% said that they were currently seeking professional help, planning to seek help, or had used help in the past to deal with burnout or depression; 48% said that they were not planning to seek help and had not done so in the past.
In an interview, Carol A. Bernstein, MD, said it is challenging to find the meaning in these survey results.
“The challenge with surveys that measure burnout is that the drivers may be somewhat different in different specialties. I am less interested in looking at ‘who has it worse’ than I am at trying to address those systemic factors that are important for all physicians, regardless of specialty,” said Dr. Bernstein of Montefiore Medical Center/Albert Einstein College of Medicine, New York.
“The survey noted some of these factors: the increased burden of regulation and bureaucratic tasks, an EHR that was designed for billing and scheduling – not for taking care of patients – and challenges of professionalism in the workplace. These are issues that we must address for the benefit of all health care providers and patients.”
Dr. Bernstein, a past president of the American Psychiatric Association, is vice chair for faculty development and well-being at Montefiore/Albert Einstein. She is a professor in the departments of psychiatry and behavioral sciences, and obstetrics/gynecology & women’s health.
The Medscape survey was conducted from June 25 to Sept. 19, 2019, and involved 15,181 physicians.
Psychiatrists do better compared with those in most specialties in finding happiness at work, according to Medscape’s 2020 Lifestyle, Happiness, and Burnout Report.

About 32% of psychiatrists reported being happy at work, according to the Medscape survey, though they lagged well behind dermatologists, who were the most satisfied with their work lives. In terms of happiness outside the office, psychiatrists were in the middle of the pack with 51% reporting that they were happy.
Somewhat fewer psychiatrists reported being burned out, compared with physicians overall, at 37% versus 41%. The biggest contributing factors to psychiatrist burnout were an overabundance of bureaucratic tasks (63%), increased time devoted to EHRs (34%), and a lack of respect from colleagues in the workplace (32%).
Psychiatrists most commonly dealt with burnout by isolating themselves from others (57%), sleeping (43%), and talking with family/friends (42%). Just under half of psychiatrists took 3-4 weeks’ vacation, compared with 44% of all physicians, and 33% took less than 3 weeks’ vacation.
and 1% reported that they had attempted suicide. About 45% said that they were currently seeking professional help, planning to seek help, or had used help in the past to deal with burnout or depression; 48% said that they were not planning to seek help and had not done so in the past.
In an interview, Carol A. Bernstein, MD, said it is challenging to find the meaning in these survey results.
“The challenge with surveys that measure burnout is that the drivers may be somewhat different in different specialties. I am less interested in looking at ‘who has it worse’ than I am at trying to address those systemic factors that are important for all physicians, regardless of specialty,” said Dr. Bernstein of Montefiore Medical Center/Albert Einstein College of Medicine, New York.
“The survey noted some of these factors: the increased burden of regulation and bureaucratic tasks, an EHR that was designed for billing and scheduling – not for taking care of patients – and challenges of professionalism in the workplace. These are issues that we must address for the benefit of all health care providers and patients.”
Dr. Bernstein, a past president of the American Psychiatric Association, is vice chair for faculty development and well-being at Montefiore/Albert Einstein. She is a professor in the departments of psychiatry and behavioral sciences, and obstetrics/gynecology & women’s health.
The Medscape survey was conducted from June 25 to Sept. 19, 2019, and involved 15,181 physicians.
Psychiatrists do better compared with those in most specialties in finding happiness at work, according to Medscape’s 2020 Lifestyle, Happiness, and Burnout Report.

About 32% of psychiatrists reported being happy at work, according to the Medscape survey, though they lagged well behind dermatologists, who were the most satisfied with their work lives. In terms of happiness outside the office, psychiatrists were in the middle of the pack with 51% reporting that they were happy.
Somewhat fewer psychiatrists reported being burned out, compared with physicians overall, at 37% versus 41%. The biggest contributing factors to psychiatrist burnout were an overabundance of bureaucratic tasks (63%), increased time devoted to EHRs (34%), and a lack of respect from colleagues in the workplace (32%).
Psychiatrists most commonly dealt with burnout by isolating themselves from others (57%), sleeping (43%), and talking with family/friends (42%). Just under half of psychiatrists took 3-4 weeks’ vacation, compared with 44% of all physicians, and 33% took less than 3 weeks’ vacation.
and 1% reported that they had attempted suicide. About 45% said that they were currently seeking professional help, planning to seek help, or had used help in the past to deal with burnout or depression; 48% said that they were not planning to seek help and had not done so in the past.
In an interview, Carol A. Bernstein, MD, said it is challenging to find the meaning in these survey results.
“The challenge with surveys that measure burnout is that the drivers may be somewhat different in different specialties. I am less interested in looking at ‘who has it worse’ than I am at trying to address those systemic factors that are important for all physicians, regardless of specialty,” said Dr. Bernstein of Montefiore Medical Center/Albert Einstein College of Medicine, New York.
“The survey noted some of these factors: the increased burden of regulation and bureaucratic tasks, an EHR that was designed for billing and scheduling – not for taking care of patients – and challenges of professionalism in the workplace. These are issues that we must address for the benefit of all health care providers and patients.”
Dr. Bernstein, a past president of the American Psychiatric Association, is vice chair for faculty development and well-being at Montefiore/Albert Einstein. She is a professor in the departments of psychiatry and behavioral sciences, and obstetrics/gynecology & women’s health.
The Medscape survey was conducted from June 25 to Sept. 19, 2019, and involved 15,181 physicians.
An unusual ‘retirement’ option
Whether “retirement” is withdrawing from one’s occupation or from an active working life, it is of utmost importance to not let one’s mind degenerate. Some individuals move on to gathering new intellectual skills by attending new educational courses or meetings, some travel, some become semiprofessional golfers or fishermen, and some find other forms of personal extension. I now serve to develop cost-saving medical programs for county jails in the state of Texas while attempting to improve the overall quality of inmate care.
Initially I was a pediatrician in Houston with special training in allergy and immunology, but because of a medical problem I was forced to abandon my first love – primary pediatrics. My move to a small town at the age of 40 required me to reevaluate my professional life, and I opted to provide care only in my allergy and immunology specialty.
However, living in a small town is different from life in a metropolis, and it was not uncommon for doctors to be asked to assist the community. A number of years ago, our county judge asked if I would help evaluate why our county jail was spending so much money. After several attempts to refuse, I eventually did evaluate the program there, and was flabbergasted by how much money was being wasted. I made some rather simple suggestions as how to correct the problem, but when no primary care doctor stepped forward to implement the changes and run the jail medical program, I became its medical director. When we saved $120,000 the first year, even I was astounded.
While I continued to run my private practice, I did accept other small community’s offers to look into their county jails’ programs. I found that their problems in cost control and quality of health care mirrored those I found in the first jail, and they were easily solvable if the county judge and the local sheriff wanted solutions. I also found that politics makes strange bedfellows, as the saying goes, and often the obvious changes were met with obstruction in one form or another. Nonetheless, I found that I could serve these communities in addition to my individual patients. When it was time for retirement, I continued to have a real desire to make the towns around which I lived and my own community more livable. So
In most things, I found that the same business philosophy and personal medical approach I learned in my pediatrics training and as a private practitioner applied to the jail system. Let me mention some specifics. Using generic medicines was less expensive than using brand names. The diagnoses which patients claimed when they entered jail might or might not be correct, so reevaluating the diagnosis and treatment was appropriate as soon as possible. Hospital and ED visits should be limited to patients’ medically requiring them rather than using the ED as a screening tool.
But I did come to understand that medical care in the county jail is different from medical care outside an incarcerated facility in that sometimes the prisoners had their own reasons for seeking medical care. This was complicated by the fact that often there were critically ill patients presenting to county jails. So carefully established criteria and protocols were an absolute necessity to save lives.
Let me expand on the topic of seeking medical care by the inmate-patients. A relatively small number of these individuals required immediate emergency treatment, without which they could not do well: The diabetic who was not taking his insulin, the out-of-control paranoid schizophrenic who decided he was cured and therefore was unattended, the alcoholic or drug addict who would develop delirium tremens if medications were stopped abruptly. These people had to be identified as quickly as possible and correctly treated. Confounding the problem was the fact that many, and I repeat many, individuals try to use the medical route to manipulate their incarceration environment. I called this the B problem: beds, blankets, barter, buzz, better food, and be out of here. They might claim an illness existed, and often they might believe it did.
A related situation might exist when individuals would demand psychiatric and pain medications, often in large quantities, when they in fact had not taken them for some time in the outside world. Often these patients were addicts, and of course this could create an entire other relationship with the medical team. A third example would be the claim of hypoglycemia so that the prisoner would receive more frequent meals.
One might think that as a pediatrician I was ill prepared to treat adults, and in fact, there was much review of the general medical care needed when I began this program. However, the internists and family physicians in town were glad to assist me whenever I encountered a difficult patient. When hospitalizations were required, the inpatient always was covered by one of the internists on hospital staff. Quite frankly, the doctors seemed pleased to not be dealing with this group of individuals as much as they had in the past.
On a slightly different note, skills honed during my pediatric career were extremely valuable. Children, particularly young children, do not verbally communicate with their parents or their doctor particularly well, so pediatricians are well trained in the skill of observation. The patient who claims a guard hurt his shoulder so badly during an altercation that he cannot move it is found out when he easily whips his arms over his head when asked to remove his shirt. It is not uncommon for an individual to demand antidepressant medications from the medical staff, but when evaluated more thoroughly and for a longer period of time, the patient ends up laughing, even denying any suicidal ideation or any other sign of depression. One also deals with a lot of adolescent behavior from the inmates, such as the individuals who say that unless they don’t get their way (more food) they are not going to take their medications and thus get sicker. That’s Adolescent Medicine 101.
Some of the modalities I utilized in modifying the jail programs will be familiar to every practicing pediatrician. I educate; I teach; I train. Parents of my asthmatic patients had to know what medications to keep handy and when to use them. It is pretty easy to see how that relates to jail medicine. Many patients come into jail with inhalers and with a diagnosis of asthma. Some have the condition, and some do not. By training jail and medical staff how to observe breathing patterns and by performing pulse oximetry, we eliminated a large number of unnecessary ED visits, and we often made the diagnosis of hyperventilation syndrome rather than misdiagnosed asthma.
Jail medicine is a large part of the cost of housing inmates. I did consultation work for a large urban jail, and we saved over $7 million in 1 year. In a medium-sized jail, the cost-savings after a 4-month consultation was over $300,000. This is a lot of money to me, and I suspect is to you, too. Just as in our general communities, we have enough resources to provide medical care and to provide a high level of care for all. However, we cannot waste money by providing inappropriate care or overtesting or overtreating. The medical care must be what treats the disease the patient actually has ... nothing more and nothing less!
If it sounds as if I am cynical about inmate patients, that is not true. However, I am realistic that no one wishes to be in jail. I realize that the medical route is just one that prisoners can and do use to modify their situation. I understand that the medical staff within a jail needs constant education and supervision at first, and with time they become more astute – just like a physician in this arena – at distinguishing the very serious from the mildly serious from malingering. In spite of this, we doctors also can be fooled. However, through constant vigilance and constant education we can get better.
Jail medicine is not for everyone in retirement. Heck, it is not for everyone ever. I found it interesting because it required me to match my diagnostic skills against the diseases and the psychodynamics of individuals who often – not always – made that diagnosis more difficult. Diagnosing illness and curing it – isn’t this why we all went into medicine?
Dr. Yoffe is a retired pediatrician specializing in allergy and immunology who resides in Brenham, Tex. Email him at pdnews@mdedge.com.
This article was updated 2/13/2020.
Whether “retirement” is withdrawing from one’s occupation or from an active working life, it is of utmost importance to not let one’s mind degenerate. Some individuals move on to gathering new intellectual skills by attending new educational courses or meetings, some travel, some become semiprofessional golfers or fishermen, and some find other forms of personal extension. I now serve to develop cost-saving medical programs for county jails in the state of Texas while attempting to improve the overall quality of inmate care.
Initially I was a pediatrician in Houston with special training in allergy and immunology, but because of a medical problem I was forced to abandon my first love – primary pediatrics. My move to a small town at the age of 40 required me to reevaluate my professional life, and I opted to provide care only in my allergy and immunology specialty.
However, living in a small town is different from life in a metropolis, and it was not uncommon for doctors to be asked to assist the community. A number of years ago, our county judge asked if I would help evaluate why our county jail was spending so much money. After several attempts to refuse, I eventually did evaluate the program there, and was flabbergasted by how much money was being wasted. I made some rather simple suggestions as how to correct the problem, but when no primary care doctor stepped forward to implement the changes and run the jail medical program, I became its medical director. When we saved $120,000 the first year, even I was astounded.
While I continued to run my private practice, I did accept other small community’s offers to look into their county jails’ programs. I found that their problems in cost control and quality of health care mirrored those I found in the first jail, and they were easily solvable if the county judge and the local sheriff wanted solutions. I also found that politics makes strange bedfellows, as the saying goes, and often the obvious changes were met with obstruction in one form or another. Nonetheless, I found that I could serve these communities in addition to my individual patients. When it was time for retirement, I continued to have a real desire to make the towns around which I lived and my own community more livable. So
In most things, I found that the same business philosophy and personal medical approach I learned in my pediatrics training and as a private practitioner applied to the jail system. Let me mention some specifics. Using generic medicines was less expensive than using brand names. The diagnoses which patients claimed when they entered jail might or might not be correct, so reevaluating the diagnosis and treatment was appropriate as soon as possible. Hospital and ED visits should be limited to patients’ medically requiring them rather than using the ED as a screening tool.
But I did come to understand that medical care in the county jail is different from medical care outside an incarcerated facility in that sometimes the prisoners had their own reasons for seeking medical care. This was complicated by the fact that often there were critically ill patients presenting to county jails. So carefully established criteria and protocols were an absolute necessity to save lives.
Let me expand on the topic of seeking medical care by the inmate-patients. A relatively small number of these individuals required immediate emergency treatment, without which they could not do well: The diabetic who was not taking his insulin, the out-of-control paranoid schizophrenic who decided he was cured and therefore was unattended, the alcoholic or drug addict who would develop delirium tremens if medications were stopped abruptly. These people had to be identified as quickly as possible and correctly treated. Confounding the problem was the fact that many, and I repeat many, individuals try to use the medical route to manipulate their incarceration environment. I called this the B problem: beds, blankets, barter, buzz, better food, and be out of here. They might claim an illness existed, and often they might believe it did.
A related situation might exist when individuals would demand psychiatric and pain medications, often in large quantities, when they in fact had not taken them for some time in the outside world. Often these patients were addicts, and of course this could create an entire other relationship with the medical team. A third example would be the claim of hypoglycemia so that the prisoner would receive more frequent meals.
One might think that as a pediatrician I was ill prepared to treat adults, and in fact, there was much review of the general medical care needed when I began this program. However, the internists and family physicians in town were glad to assist me whenever I encountered a difficult patient. When hospitalizations were required, the inpatient always was covered by one of the internists on hospital staff. Quite frankly, the doctors seemed pleased to not be dealing with this group of individuals as much as they had in the past.
On a slightly different note, skills honed during my pediatric career were extremely valuable. Children, particularly young children, do not verbally communicate with their parents or their doctor particularly well, so pediatricians are well trained in the skill of observation. The patient who claims a guard hurt his shoulder so badly during an altercation that he cannot move it is found out when he easily whips his arms over his head when asked to remove his shirt. It is not uncommon for an individual to demand antidepressant medications from the medical staff, but when evaluated more thoroughly and for a longer period of time, the patient ends up laughing, even denying any suicidal ideation or any other sign of depression. One also deals with a lot of adolescent behavior from the inmates, such as the individuals who say that unless they don’t get their way (more food) they are not going to take their medications and thus get sicker. That’s Adolescent Medicine 101.
Some of the modalities I utilized in modifying the jail programs will be familiar to every practicing pediatrician. I educate; I teach; I train. Parents of my asthmatic patients had to know what medications to keep handy and when to use them. It is pretty easy to see how that relates to jail medicine. Many patients come into jail with inhalers and with a diagnosis of asthma. Some have the condition, and some do not. By training jail and medical staff how to observe breathing patterns and by performing pulse oximetry, we eliminated a large number of unnecessary ED visits, and we often made the diagnosis of hyperventilation syndrome rather than misdiagnosed asthma.
Jail medicine is a large part of the cost of housing inmates. I did consultation work for a large urban jail, and we saved over $7 million in 1 year. In a medium-sized jail, the cost-savings after a 4-month consultation was over $300,000. This is a lot of money to me, and I suspect is to you, too. Just as in our general communities, we have enough resources to provide medical care and to provide a high level of care for all. However, we cannot waste money by providing inappropriate care or overtesting or overtreating. The medical care must be what treats the disease the patient actually has ... nothing more and nothing less!
If it sounds as if I am cynical about inmate patients, that is not true. However, I am realistic that no one wishes to be in jail. I realize that the medical route is just one that prisoners can and do use to modify their situation. I understand that the medical staff within a jail needs constant education and supervision at first, and with time they become more astute – just like a physician in this arena – at distinguishing the very serious from the mildly serious from malingering. In spite of this, we doctors also can be fooled. However, through constant vigilance and constant education we can get better.
Jail medicine is not for everyone in retirement. Heck, it is not for everyone ever. I found it interesting because it required me to match my diagnostic skills against the diseases and the psychodynamics of individuals who often – not always – made that diagnosis more difficult. Diagnosing illness and curing it – isn’t this why we all went into medicine?
Dr. Yoffe is a retired pediatrician specializing in allergy and immunology who resides in Brenham, Tex. Email him at pdnews@mdedge.com.
This article was updated 2/13/2020.
Whether “retirement” is withdrawing from one’s occupation or from an active working life, it is of utmost importance to not let one’s mind degenerate. Some individuals move on to gathering new intellectual skills by attending new educational courses or meetings, some travel, some become semiprofessional golfers or fishermen, and some find other forms of personal extension. I now serve to develop cost-saving medical programs for county jails in the state of Texas while attempting to improve the overall quality of inmate care.
Initially I was a pediatrician in Houston with special training in allergy and immunology, but because of a medical problem I was forced to abandon my first love – primary pediatrics. My move to a small town at the age of 40 required me to reevaluate my professional life, and I opted to provide care only in my allergy and immunology specialty.
However, living in a small town is different from life in a metropolis, and it was not uncommon for doctors to be asked to assist the community. A number of years ago, our county judge asked if I would help evaluate why our county jail was spending so much money. After several attempts to refuse, I eventually did evaluate the program there, and was flabbergasted by how much money was being wasted. I made some rather simple suggestions as how to correct the problem, but when no primary care doctor stepped forward to implement the changes and run the jail medical program, I became its medical director. When we saved $120,000 the first year, even I was astounded.
While I continued to run my private practice, I did accept other small community’s offers to look into their county jails’ programs. I found that their problems in cost control and quality of health care mirrored those I found in the first jail, and they were easily solvable if the county judge and the local sheriff wanted solutions. I also found that politics makes strange bedfellows, as the saying goes, and often the obvious changes were met with obstruction in one form or another. Nonetheless, I found that I could serve these communities in addition to my individual patients. When it was time for retirement, I continued to have a real desire to make the towns around which I lived and my own community more livable. So
In most things, I found that the same business philosophy and personal medical approach I learned in my pediatrics training and as a private practitioner applied to the jail system. Let me mention some specifics. Using generic medicines was less expensive than using brand names. The diagnoses which patients claimed when they entered jail might or might not be correct, so reevaluating the diagnosis and treatment was appropriate as soon as possible. Hospital and ED visits should be limited to patients’ medically requiring them rather than using the ED as a screening tool.
But I did come to understand that medical care in the county jail is different from medical care outside an incarcerated facility in that sometimes the prisoners had their own reasons for seeking medical care. This was complicated by the fact that often there were critically ill patients presenting to county jails. So carefully established criteria and protocols were an absolute necessity to save lives.
Let me expand on the topic of seeking medical care by the inmate-patients. A relatively small number of these individuals required immediate emergency treatment, without which they could not do well: The diabetic who was not taking his insulin, the out-of-control paranoid schizophrenic who decided he was cured and therefore was unattended, the alcoholic or drug addict who would develop delirium tremens if medications were stopped abruptly. These people had to be identified as quickly as possible and correctly treated. Confounding the problem was the fact that many, and I repeat many, individuals try to use the medical route to manipulate their incarceration environment. I called this the B problem: beds, blankets, barter, buzz, better food, and be out of here. They might claim an illness existed, and often they might believe it did.
A related situation might exist when individuals would demand psychiatric and pain medications, often in large quantities, when they in fact had not taken them for some time in the outside world. Often these patients were addicts, and of course this could create an entire other relationship with the medical team. A third example would be the claim of hypoglycemia so that the prisoner would receive more frequent meals.
One might think that as a pediatrician I was ill prepared to treat adults, and in fact, there was much review of the general medical care needed when I began this program. However, the internists and family physicians in town were glad to assist me whenever I encountered a difficult patient. When hospitalizations were required, the inpatient always was covered by one of the internists on hospital staff. Quite frankly, the doctors seemed pleased to not be dealing with this group of individuals as much as they had in the past.
On a slightly different note, skills honed during my pediatric career were extremely valuable. Children, particularly young children, do not verbally communicate with their parents or their doctor particularly well, so pediatricians are well trained in the skill of observation. The patient who claims a guard hurt his shoulder so badly during an altercation that he cannot move it is found out when he easily whips his arms over his head when asked to remove his shirt. It is not uncommon for an individual to demand antidepressant medications from the medical staff, but when evaluated more thoroughly and for a longer period of time, the patient ends up laughing, even denying any suicidal ideation or any other sign of depression. One also deals with a lot of adolescent behavior from the inmates, such as the individuals who say that unless they don’t get their way (more food) they are not going to take their medications and thus get sicker. That’s Adolescent Medicine 101.
Some of the modalities I utilized in modifying the jail programs will be familiar to every practicing pediatrician. I educate; I teach; I train. Parents of my asthmatic patients had to know what medications to keep handy and when to use them. It is pretty easy to see how that relates to jail medicine. Many patients come into jail with inhalers and with a diagnosis of asthma. Some have the condition, and some do not. By training jail and medical staff how to observe breathing patterns and by performing pulse oximetry, we eliminated a large number of unnecessary ED visits, and we often made the diagnosis of hyperventilation syndrome rather than misdiagnosed asthma.
Jail medicine is a large part of the cost of housing inmates. I did consultation work for a large urban jail, and we saved over $7 million in 1 year. In a medium-sized jail, the cost-savings after a 4-month consultation was over $300,000. This is a lot of money to me, and I suspect is to you, too. Just as in our general communities, we have enough resources to provide medical care and to provide a high level of care for all. However, we cannot waste money by providing inappropriate care or overtesting or overtreating. The medical care must be what treats the disease the patient actually has ... nothing more and nothing less!
If it sounds as if I am cynical about inmate patients, that is not true. However, I am realistic that no one wishes to be in jail. I realize that the medical route is just one that prisoners can and do use to modify their situation. I understand that the medical staff within a jail needs constant education and supervision at first, and with time they become more astute – just like a physician in this arena – at distinguishing the very serious from the mildly serious from malingering. In spite of this, we doctors also can be fooled. However, through constant vigilance and constant education we can get better.
Jail medicine is not for everyone in retirement. Heck, it is not for everyone ever. I found it interesting because it required me to match my diagnostic skills against the diseases and the psychodynamics of individuals who often – not always – made that diagnosis more difficult. Diagnosing illness and curing it – isn’t this why we all went into medicine?
Dr. Yoffe is a retired pediatrician specializing in allergy and immunology who resides in Brenham, Tex. Email him at pdnews@mdedge.com.
This article was updated 2/13/2020.
Pediatricians twice as happy outside work than at work
Pediatricians are twice as likely to be happy outside the office than they are at work, according to Medscape’s 2020 Lifestyle, Happiness, and Burnout Report.

About 29% of pediatricians reported being happy at work, with dermatologists taking the top spot at 41%. Pediatricians did much better when it came to finding happiness outside the office, with 57% reporting that they were very happy when away from work, according to the Medscape report.
The biggest contributing factors to burnout in pediatricians were an overabundance of bureaucratic tasks (59%), insufficient compensation/reimbursement (37%), and spending too many hours at work (34%).
Pediatricians most commonly dealt with burnout by talking with friends/family (54%), exercising (47%), and sleeping (41%). Just over half of pediatricians reported taking 3-4 weeks of vacation, compared with 44% of all physicians; 32% took less than 3 weeks’ vacation.
About 8% of pediatricians reported that they’d contemplated suicide, but 0% reported that they’d attempted it; 85% said that they’d never thought about it. Just under one-quarter of pediatricians said that were currently seeking or planning to seek professional help for depression and/or burnout; 55% said they were not seeking help and had never made use of it in the past.
The Medscape survey was conducted from June 25 to Sept. 19, 2019, and involved 15,181 physicians.
We all feel it. It is not surprising that only 29% of today's pediatricians report that they are "happy" at work and 30% report "burnout"!
This report serves to identify only some of the countless ways in which we are forced to compromise the 24-hour clock, leaving too little time for ourselves and families.
We spend too many hours at work, and other data show we are undercompensated for our efforts.
Today, electronically, most of us are reachable even when out of the office. It is difficult, if not impossible, to completely disconnect. The challenge to achieve the work/life balance we have all imagined is too great!
I try to carve out "forced escapes from reality" through novels, movies, and when possible, distant travel with my spouse. However, the bliss is too short lived. When I return to reality, some bliss fades as I jump back onto the "merry-go-round" for a few more turns.
Lillian M. Beard, MD, is a clinical professor of pediatrics at George Washington University, Washington. She is a Pediatric News Editorial Advisory Board member.
We all feel it. It is not surprising that only 29% of today's pediatricians report that they are "happy" at work and 30% report "burnout"!
This report serves to identify only some of the countless ways in which we are forced to compromise the 24-hour clock, leaving too little time for ourselves and families.
We spend too many hours at work, and other data show we are undercompensated for our efforts.
Today, electronically, most of us are reachable even when out of the office. It is difficult, if not impossible, to completely disconnect. The challenge to achieve the work/life balance we have all imagined is too great!
I try to carve out "forced escapes from reality" through novels, movies, and when possible, distant travel with my spouse. However, the bliss is too short lived. When I return to reality, some bliss fades as I jump back onto the "merry-go-round" for a few more turns.
Lillian M. Beard, MD, is a clinical professor of pediatrics at George Washington University, Washington. She is a Pediatric News Editorial Advisory Board member.
We all feel it. It is not surprising that only 29% of today's pediatricians report that they are "happy" at work and 30% report "burnout"!
This report serves to identify only some of the countless ways in which we are forced to compromise the 24-hour clock, leaving too little time for ourselves and families.
We spend too many hours at work, and other data show we are undercompensated for our efforts.
Today, electronically, most of us are reachable even when out of the office. It is difficult, if not impossible, to completely disconnect. The challenge to achieve the work/life balance we have all imagined is too great!
I try to carve out "forced escapes from reality" through novels, movies, and when possible, distant travel with my spouse. However, the bliss is too short lived. When I return to reality, some bliss fades as I jump back onto the "merry-go-round" for a few more turns.
Lillian M. Beard, MD, is a clinical professor of pediatrics at George Washington University, Washington. She is a Pediatric News Editorial Advisory Board member.
Pediatricians are twice as likely to be happy outside the office than they are at work, according to Medscape’s 2020 Lifestyle, Happiness, and Burnout Report.

About 29% of pediatricians reported being happy at work, with dermatologists taking the top spot at 41%. Pediatricians did much better when it came to finding happiness outside the office, with 57% reporting that they were very happy when away from work, according to the Medscape report.
The biggest contributing factors to burnout in pediatricians were an overabundance of bureaucratic tasks (59%), insufficient compensation/reimbursement (37%), and spending too many hours at work (34%).
Pediatricians most commonly dealt with burnout by talking with friends/family (54%), exercising (47%), and sleeping (41%). Just over half of pediatricians reported taking 3-4 weeks of vacation, compared with 44% of all physicians; 32% took less than 3 weeks’ vacation.
About 8% of pediatricians reported that they’d contemplated suicide, but 0% reported that they’d attempted it; 85% said that they’d never thought about it. Just under one-quarter of pediatricians said that were currently seeking or planning to seek professional help for depression and/or burnout; 55% said they were not seeking help and had never made use of it in the past.
The Medscape survey was conducted from June 25 to Sept. 19, 2019, and involved 15,181 physicians.
Pediatricians are twice as likely to be happy outside the office than they are at work, according to Medscape’s 2020 Lifestyle, Happiness, and Burnout Report.

About 29% of pediatricians reported being happy at work, with dermatologists taking the top spot at 41%. Pediatricians did much better when it came to finding happiness outside the office, with 57% reporting that they were very happy when away from work, according to the Medscape report.
The biggest contributing factors to burnout in pediatricians were an overabundance of bureaucratic tasks (59%), insufficient compensation/reimbursement (37%), and spending too many hours at work (34%).
Pediatricians most commonly dealt with burnout by talking with friends/family (54%), exercising (47%), and sleeping (41%). Just over half of pediatricians reported taking 3-4 weeks of vacation, compared with 44% of all physicians; 32% took less than 3 weeks’ vacation.
About 8% of pediatricians reported that they’d contemplated suicide, but 0% reported that they’d attempted it; 85% said that they’d never thought about it. Just under one-quarter of pediatricians said that were currently seeking or planning to seek professional help for depression and/or burnout; 55% said they were not seeking help and had never made use of it in the past.
The Medscape survey was conducted from June 25 to Sept. 19, 2019, and involved 15,181 physicians.
Trump seeks to cut NIH, CDC budgets, some Medicare spending
The Trump administration on Feb. 10 argued for cutting spending for a federal agency at the forefront of the efforts to combat the coronavirus, while also seeking to slow spending in certain parts of the Medicare and Medicaid programs.
President Donald Trump presented his fiscal 2021 request to Congress for refilling the coffers of federal agencies. In any administration, an annual budget serves only as a political blueprint, as the White House document itself makes no changes in federal spending.
In Mr. Trump’s case, several of his requests for agencies within the Department of Health & Human Services run counter to recent budget trends. Republicans and Democrats in Congress have worked together in recent years to increase budgets for major federal health agencies.
But Mr. Trump asked Congress to cut annual budget authority for the National Institute of Allergy and Infectious Diseases by $430 million to $5.446 billion for fiscal 2021. In contrast, Congress has raised the annual budget for NIAID, a key agency in combating the coronavirus, from $5.545 billion in fiscal 2019 to $5.876 billion in fiscal 2020, which began in October, according to an HHS summary of Mr. Trump’s request.
For the Centers for Disease Control and Prevention, which is central to the battle against the coronavirus, Mr. Trump proposed a drop in discretionary funding to $5.627 billion. In contrast, Congress raised the CDC budget from $6.544 billion in fiscal 2019 to $6.917 in fiscal 2020.
Mr. Trump also wants to cut $559 million from the budget of the National Cancer Institute, dropping it to $5.881 billion in fiscal 2021. In contrast, Congress raised NCI’s budget from $6.121 billion in fiscal 2019 to $6.440 billion in fiscal 2020.
Mr. Trump requested a $2.6 billion reduction in the National Institutes of Health’s total discretionary budget, seeking to drop it to $37.70 billion. In contrast, Congress raised NIH’s budget from $37.887 in fiscal 2019 to $40.304 billion in fiscal 2020.
Mr. Trump’s budget proposal also includes an estimate of $152 billion in savings over a decade for Medicaid through the implementation of what the administration calls “community engagement” requirements.
The Trump administration has been at odds with Democrats for years about whether work requirements should be attached to Medicaid. “Well-designed community engagement incentives have great potential to improve health and well-being while empowering beneficiaries to rise out of poverty,” HHS said in a budget document.
Yet researchers last year reported that Arkansas’ attempt to attach work requirements to Medicaid caused almost 17,000 adults to lose this health care coverage within the first 6 months, and there was no significant difference in employment.
The researchers say this loss of coverage was partly a result of bureaucratic obstacles and confusion about the new rules. In June 2018, Arkansas became the first state to implement work requirements for Medicaid, Benjamin D. Sommers, MD, PhD, of the Harvard T.H. Chan School of Public Health, Boston, and colleagues wrote in the New England Journal of Medicine (2019 Sep 12;381[11]:1073-82).
Budget ‘would thwart’ progress
A few medical groups on Monday quickly criticized Mr. Trump’s proposals.
“In a time where our nation continues to face significant public health challenges — including 2019 novel coronavirus, climate change, gun violence, and costly chronic diseases such as heart disease and cancer – the administration should be investing more resources in better health, not cutting federal health budgets,” said Georges C. Benjamin, MD, executive director of the American Public Health Association, in a statement.
David J. Skorton, MD, chief executive and president of the Association of American Medical Colleges (AAMC) also urged increased investment in fighting disease.
“We must continue the bipartisan budget trajectory set forth by Congress over the last several years, not reverse course,” Dr. Skorton said in a statement.
Mr. Trump’s proposed cuts in medical research “would thwart scientific progress on strategies to prevent, diagnose, treat, and cure medical conditions that affect countless patients nationwide,” he said.
In total, the new 2021 appropriations for HHS would fall by $9.46 billion to $85.667 billion under Mr. Trump’s proposal. Appropriations, also called discretionary budget authority, represents the operating budgets for federal agencies. These are decided through annual spending bills.
Congress has separate sets of laws for handling payments the federal government makes through Medicare and Medicaid. These are known as mandatory spending.
‘Untenable cuts’
AAMC’s Dr. Skorton also objected to what he termed Mr. Trump’s bid “to reduce and consolidate Medicare, Medicaid, and children’s hospital graduate medical education into a single grant program.”
This would force teaching hospitals to absorb $52 billion in “untenable cuts,” he said.
“The proposal ignores the intent of the Medicare GME program, which is to ensure an adequate physician workforce to care for Medicare beneficiaries and support the critical patient care missions of America’s teaching hospitals,” Dr. Skorton said.
The budget also seeks cuts to Medicaid, which come in addition to the administration’s “recent proposals to scale back Medicaid coverage,” Dr. Skorton said.
“More than 26% of all Medicaid hospitalizations occur at AAMC-member teaching hospitals, even though these institutions represent only 5% of all hospitals,” Dr. Skorton said. “Each of the administration’s proposals on their own would be devastating for patients – and combined, they would be disastrous.”
Rick Pollack, the chief executive and president of the American Hospital Association, described Mr. Trump’s fiscal 2021 proposal as another bid to undermine medical care in the United States.
“Every year, we adapt to a constantly changing environment, but every year, the administration aims to gut our nation’s health care infrastructure,” Mr. Pollack said in a statement.
In it, he noted that about one in five people in America depend on Medicaid, with children accounting for a large proportion of those covered by the state-federal program.
“The budget’s proposal on Medicaid financing and service delivery would cut hundreds of billions of dollars from the Medicaid program annually,” Mr. Pollack said.
He also objected to “hundreds of billions of proposed reductions to Medicare” endorsed by Mr. Trump.
Medical malpractice overhaul
The Trump administration also offered many suggestions for changing federal laws to reduce health care spending. Among these was a proposed overhaul of the approach to medical malpractice cases.
The president’s budget proposal estimates $40 billion in savings over a decade from steps to limit medical liability, according to a report from the Office of Management and Budget (OMB).
“The current medical liability system does not work for patients or providers, nor does it promote high-quality, evidence-based care,” OMB said. “Providers practice with a threat of potentially frivolous lawsuits, and injured patients often do not receive just compensation for their injuries.”
Mr. Trump’s fiscal 2021 budget calls for a cap on noneconomic damage awards of $250,000, which would increase with inflation over time, and a 3-year statute of limitations. Under this plan, courts could also modify attorney’s fee arrangements. HHS could provide guidance to states on how to create expert panels and administrative health care tribunals to review medical liability.
These steps would lead to lower health care spending, with clinicians dropping “defensive medicine practices,” OMB said. That would benefit the Medicare and Medicaid programs as well as lowering costs of health insurance in general.
Mr. Trump’s fiscal 2021 budget also includes a series of proposals for Medicare that it estimates would, in aggregate, save $755.5 billion over a decade.
Site-neutral policy
A large chunk of the estimated Medicare savings in Mr. Trump’s fiscal 2021 health budget would come from lowering payments to hospitals for services provided in their outpatient and physician offices.
In the fiscal 2021 proposal, HHS noted that “Medicare generally pays on-campus hospital outpatient departments substantially more than physician offices for the same services.”
Mr. Trump’s budget proposal seeks a more expansive shift to what’s called a “site-neutral” payment for services delivered in hospital outpatient programs or physician offices. This would bring these payments more in line with those made to independent physician practices.
“This proposal would eliminate the often significant disparity between what Medicare pays in these different settings for the same services,” HHS said in the budget summary.
HHS estimated this change in policy would generate $117.2 billion in savings over a decade. Combined with saving from medical malpractice reforms, the Trump administration estimates these two moves combined could save about $164 billion over a decade.
The site-neutral policy has been a legal battleground, with hospital and physician groups winning a round last year.
Another Medicare proposal included in Mr. Trump’s fiscal 2021 budget homes in on this issue for cases where a hospital owns a physician office. Medicare now pays most off-campus hospital outpatient departments higher rates than the program’s physician fee schedule dictates for the same services.
Switching to a site-neutral policy for these hospital-owned physician offices would result in $47.2 billion in savings over a decade, HHS said in the budget document.
This article first appeared on Medscape.com.
The Trump administration on Feb. 10 argued for cutting spending for a federal agency at the forefront of the efforts to combat the coronavirus, while also seeking to slow spending in certain parts of the Medicare and Medicaid programs.
President Donald Trump presented his fiscal 2021 request to Congress for refilling the coffers of federal agencies. In any administration, an annual budget serves only as a political blueprint, as the White House document itself makes no changes in federal spending.
In Mr. Trump’s case, several of his requests for agencies within the Department of Health & Human Services run counter to recent budget trends. Republicans and Democrats in Congress have worked together in recent years to increase budgets for major federal health agencies.
But Mr. Trump asked Congress to cut annual budget authority for the National Institute of Allergy and Infectious Diseases by $430 million to $5.446 billion for fiscal 2021. In contrast, Congress has raised the annual budget for NIAID, a key agency in combating the coronavirus, from $5.545 billion in fiscal 2019 to $5.876 billion in fiscal 2020, which began in October, according to an HHS summary of Mr. Trump’s request.
For the Centers for Disease Control and Prevention, which is central to the battle against the coronavirus, Mr. Trump proposed a drop in discretionary funding to $5.627 billion. In contrast, Congress raised the CDC budget from $6.544 billion in fiscal 2019 to $6.917 in fiscal 2020.
Mr. Trump also wants to cut $559 million from the budget of the National Cancer Institute, dropping it to $5.881 billion in fiscal 2021. In contrast, Congress raised NCI’s budget from $6.121 billion in fiscal 2019 to $6.440 billion in fiscal 2020.
Mr. Trump requested a $2.6 billion reduction in the National Institutes of Health’s total discretionary budget, seeking to drop it to $37.70 billion. In contrast, Congress raised NIH’s budget from $37.887 in fiscal 2019 to $40.304 billion in fiscal 2020.
Mr. Trump’s budget proposal also includes an estimate of $152 billion in savings over a decade for Medicaid through the implementation of what the administration calls “community engagement” requirements.
The Trump administration has been at odds with Democrats for years about whether work requirements should be attached to Medicaid. “Well-designed community engagement incentives have great potential to improve health and well-being while empowering beneficiaries to rise out of poverty,” HHS said in a budget document.
Yet researchers last year reported that Arkansas’ attempt to attach work requirements to Medicaid caused almost 17,000 adults to lose this health care coverage within the first 6 months, and there was no significant difference in employment.
The researchers say this loss of coverage was partly a result of bureaucratic obstacles and confusion about the new rules. In June 2018, Arkansas became the first state to implement work requirements for Medicaid, Benjamin D. Sommers, MD, PhD, of the Harvard T.H. Chan School of Public Health, Boston, and colleagues wrote in the New England Journal of Medicine (2019 Sep 12;381[11]:1073-82).
Budget ‘would thwart’ progress
A few medical groups on Monday quickly criticized Mr. Trump’s proposals.
“In a time where our nation continues to face significant public health challenges — including 2019 novel coronavirus, climate change, gun violence, and costly chronic diseases such as heart disease and cancer – the administration should be investing more resources in better health, not cutting federal health budgets,” said Georges C. Benjamin, MD, executive director of the American Public Health Association, in a statement.
David J. Skorton, MD, chief executive and president of the Association of American Medical Colleges (AAMC) also urged increased investment in fighting disease.
“We must continue the bipartisan budget trajectory set forth by Congress over the last several years, not reverse course,” Dr. Skorton said in a statement.
Mr. Trump’s proposed cuts in medical research “would thwart scientific progress on strategies to prevent, diagnose, treat, and cure medical conditions that affect countless patients nationwide,” he said.
In total, the new 2021 appropriations for HHS would fall by $9.46 billion to $85.667 billion under Mr. Trump’s proposal. Appropriations, also called discretionary budget authority, represents the operating budgets for federal agencies. These are decided through annual spending bills.
Congress has separate sets of laws for handling payments the federal government makes through Medicare and Medicaid. These are known as mandatory spending.
‘Untenable cuts’
AAMC’s Dr. Skorton also objected to what he termed Mr. Trump’s bid “to reduce and consolidate Medicare, Medicaid, and children’s hospital graduate medical education into a single grant program.”
This would force teaching hospitals to absorb $52 billion in “untenable cuts,” he said.
“The proposal ignores the intent of the Medicare GME program, which is to ensure an adequate physician workforce to care for Medicare beneficiaries and support the critical patient care missions of America’s teaching hospitals,” Dr. Skorton said.
The budget also seeks cuts to Medicaid, which come in addition to the administration’s “recent proposals to scale back Medicaid coverage,” Dr. Skorton said.
“More than 26% of all Medicaid hospitalizations occur at AAMC-member teaching hospitals, even though these institutions represent only 5% of all hospitals,” Dr. Skorton said. “Each of the administration’s proposals on their own would be devastating for patients – and combined, they would be disastrous.”
Rick Pollack, the chief executive and president of the American Hospital Association, described Mr. Trump’s fiscal 2021 proposal as another bid to undermine medical care in the United States.
“Every year, we adapt to a constantly changing environment, but every year, the administration aims to gut our nation’s health care infrastructure,” Mr. Pollack said in a statement.
In it, he noted that about one in five people in America depend on Medicaid, with children accounting for a large proportion of those covered by the state-federal program.
“The budget’s proposal on Medicaid financing and service delivery would cut hundreds of billions of dollars from the Medicaid program annually,” Mr. Pollack said.
He also objected to “hundreds of billions of proposed reductions to Medicare” endorsed by Mr. Trump.
Medical malpractice overhaul
The Trump administration also offered many suggestions for changing federal laws to reduce health care spending. Among these was a proposed overhaul of the approach to medical malpractice cases.
The president’s budget proposal estimates $40 billion in savings over a decade from steps to limit medical liability, according to a report from the Office of Management and Budget (OMB).
“The current medical liability system does not work for patients or providers, nor does it promote high-quality, evidence-based care,” OMB said. “Providers practice with a threat of potentially frivolous lawsuits, and injured patients often do not receive just compensation for their injuries.”
Mr. Trump’s fiscal 2021 budget calls for a cap on noneconomic damage awards of $250,000, which would increase with inflation over time, and a 3-year statute of limitations. Under this plan, courts could also modify attorney’s fee arrangements. HHS could provide guidance to states on how to create expert panels and administrative health care tribunals to review medical liability.
These steps would lead to lower health care spending, with clinicians dropping “defensive medicine practices,” OMB said. That would benefit the Medicare and Medicaid programs as well as lowering costs of health insurance in general.
Mr. Trump’s fiscal 2021 budget also includes a series of proposals for Medicare that it estimates would, in aggregate, save $755.5 billion over a decade.
Site-neutral policy
A large chunk of the estimated Medicare savings in Mr. Trump’s fiscal 2021 health budget would come from lowering payments to hospitals for services provided in their outpatient and physician offices.
In the fiscal 2021 proposal, HHS noted that “Medicare generally pays on-campus hospital outpatient departments substantially more than physician offices for the same services.”
Mr. Trump’s budget proposal seeks a more expansive shift to what’s called a “site-neutral” payment for services delivered in hospital outpatient programs or physician offices. This would bring these payments more in line with those made to independent physician practices.
“This proposal would eliminate the often significant disparity between what Medicare pays in these different settings for the same services,” HHS said in the budget summary.
HHS estimated this change in policy would generate $117.2 billion in savings over a decade. Combined with saving from medical malpractice reforms, the Trump administration estimates these two moves combined could save about $164 billion over a decade.
The site-neutral policy has been a legal battleground, with hospital and physician groups winning a round last year.
Another Medicare proposal included in Mr. Trump’s fiscal 2021 budget homes in on this issue for cases where a hospital owns a physician office. Medicare now pays most off-campus hospital outpatient departments higher rates than the program’s physician fee schedule dictates for the same services.
Switching to a site-neutral policy for these hospital-owned physician offices would result in $47.2 billion in savings over a decade, HHS said in the budget document.
This article first appeared on Medscape.com.
The Trump administration on Feb. 10 argued for cutting spending for a federal agency at the forefront of the efforts to combat the coronavirus, while also seeking to slow spending in certain parts of the Medicare and Medicaid programs.
President Donald Trump presented his fiscal 2021 request to Congress for refilling the coffers of federal agencies. In any administration, an annual budget serves only as a political blueprint, as the White House document itself makes no changes in federal spending.
In Mr. Trump’s case, several of his requests for agencies within the Department of Health & Human Services run counter to recent budget trends. Republicans and Democrats in Congress have worked together in recent years to increase budgets for major federal health agencies.
But Mr. Trump asked Congress to cut annual budget authority for the National Institute of Allergy and Infectious Diseases by $430 million to $5.446 billion for fiscal 2021. In contrast, Congress has raised the annual budget for NIAID, a key agency in combating the coronavirus, from $5.545 billion in fiscal 2019 to $5.876 billion in fiscal 2020, which began in October, according to an HHS summary of Mr. Trump’s request.
For the Centers for Disease Control and Prevention, which is central to the battle against the coronavirus, Mr. Trump proposed a drop in discretionary funding to $5.627 billion. In contrast, Congress raised the CDC budget from $6.544 billion in fiscal 2019 to $6.917 in fiscal 2020.
Mr. Trump also wants to cut $559 million from the budget of the National Cancer Institute, dropping it to $5.881 billion in fiscal 2021. In contrast, Congress raised NCI’s budget from $6.121 billion in fiscal 2019 to $6.440 billion in fiscal 2020.
Mr. Trump requested a $2.6 billion reduction in the National Institutes of Health’s total discretionary budget, seeking to drop it to $37.70 billion. In contrast, Congress raised NIH’s budget from $37.887 in fiscal 2019 to $40.304 billion in fiscal 2020.
Mr. Trump’s budget proposal also includes an estimate of $152 billion in savings over a decade for Medicaid through the implementation of what the administration calls “community engagement” requirements.
The Trump administration has been at odds with Democrats for years about whether work requirements should be attached to Medicaid. “Well-designed community engagement incentives have great potential to improve health and well-being while empowering beneficiaries to rise out of poverty,” HHS said in a budget document.
Yet researchers last year reported that Arkansas’ attempt to attach work requirements to Medicaid caused almost 17,000 adults to lose this health care coverage within the first 6 months, and there was no significant difference in employment.
The researchers say this loss of coverage was partly a result of bureaucratic obstacles and confusion about the new rules. In June 2018, Arkansas became the first state to implement work requirements for Medicaid, Benjamin D. Sommers, MD, PhD, of the Harvard T.H. Chan School of Public Health, Boston, and colleagues wrote in the New England Journal of Medicine (2019 Sep 12;381[11]:1073-82).
Budget ‘would thwart’ progress
A few medical groups on Monday quickly criticized Mr. Trump’s proposals.
“In a time where our nation continues to face significant public health challenges — including 2019 novel coronavirus, climate change, gun violence, and costly chronic diseases such as heart disease and cancer – the administration should be investing more resources in better health, not cutting federal health budgets,” said Georges C. Benjamin, MD, executive director of the American Public Health Association, in a statement.
David J. Skorton, MD, chief executive and president of the Association of American Medical Colleges (AAMC) also urged increased investment in fighting disease.
“We must continue the bipartisan budget trajectory set forth by Congress over the last several years, not reverse course,” Dr. Skorton said in a statement.
Mr. Trump’s proposed cuts in medical research “would thwart scientific progress on strategies to prevent, diagnose, treat, and cure medical conditions that affect countless patients nationwide,” he said.
In total, the new 2021 appropriations for HHS would fall by $9.46 billion to $85.667 billion under Mr. Trump’s proposal. Appropriations, also called discretionary budget authority, represents the operating budgets for federal agencies. These are decided through annual spending bills.
Congress has separate sets of laws for handling payments the federal government makes through Medicare and Medicaid. These are known as mandatory spending.
‘Untenable cuts’
AAMC’s Dr. Skorton also objected to what he termed Mr. Trump’s bid “to reduce and consolidate Medicare, Medicaid, and children’s hospital graduate medical education into a single grant program.”
This would force teaching hospitals to absorb $52 billion in “untenable cuts,” he said.
“The proposal ignores the intent of the Medicare GME program, which is to ensure an adequate physician workforce to care for Medicare beneficiaries and support the critical patient care missions of America’s teaching hospitals,” Dr. Skorton said.
The budget also seeks cuts to Medicaid, which come in addition to the administration’s “recent proposals to scale back Medicaid coverage,” Dr. Skorton said.
“More than 26% of all Medicaid hospitalizations occur at AAMC-member teaching hospitals, even though these institutions represent only 5% of all hospitals,” Dr. Skorton said. “Each of the administration’s proposals on their own would be devastating for patients – and combined, they would be disastrous.”
Rick Pollack, the chief executive and president of the American Hospital Association, described Mr. Trump’s fiscal 2021 proposal as another bid to undermine medical care in the United States.
“Every year, we adapt to a constantly changing environment, but every year, the administration aims to gut our nation’s health care infrastructure,” Mr. Pollack said in a statement.
In it, he noted that about one in five people in America depend on Medicaid, with children accounting for a large proportion of those covered by the state-federal program.
“The budget’s proposal on Medicaid financing and service delivery would cut hundreds of billions of dollars from the Medicaid program annually,” Mr. Pollack said.
He also objected to “hundreds of billions of proposed reductions to Medicare” endorsed by Mr. Trump.
Medical malpractice overhaul
The Trump administration also offered many suggestions for changing federal laws to reduce health care spending. Among these was a proposed overhaul of the approach to medical malpractice cases.
The president’s budget proposal estimates $40 billion in savings over a decade from steps to limit medical liability, according to a report from the Office of Management and Budget (OMB).
“The current medical liability system does not work for patients or providers, nor does it promote high-quality, evidence-based care,” OMB said. “Providers practice with a threat of potentially frivolous lawsuits, and injured patients often do not receive just compensation for their injuries.”
Mr. Trump’s fiscal 2021 budget calls for a cap on noneconomic damage awards of $250,000, which would increase with inflation over time, and a 3-year statute of limitations. Under this plan, courts could also modify attorney’s fee arrangements. HHS could provide guidance to states on how to create expert panels and administrative health care tribunals to review medical liability.
These steps would lead to lower health care spending, with clinicians dropping “defensive medicine practices,” OMB said. That would benefit the Medicare and Medicaid programs as well as lowering costs of health insurance in general.
Mr. Trump’s fiscal 2021 budget also includes a series of proposals for Medicare that it estimates would, in aggregate, save $755.5 billion over a decade.
Site-neutral policy
A large chunk of the estimated Medicare savings in Mr. Trump’s fiscal 2021 health budget would come from lowering payments to hospitals for services provided in their outpatient and physician offices.
In the fiscal 2021 proposal, HHS noted that “Medicare generally pays on-campus hospital outpatient departments substantially more than physician offices for the same services.”
Mr. Trump’s budget proposal seeks a more expansive shift to what’s called a “site-neutral” payment for services delivered in hospital outpatient programs or physician offices. This would bring these payments more in line with those made to independent physician practices.
“This proposal would eliminate the often significant disparity between what Medicare pays in these different settings for the same services,” HHS said in the budget summary.
HHS estimated this change in policy would generate $117.2 billion in savings over a decade. Combined with saving from medical malpractice reforms, the Trump administration estimates these two moves combined could save about $164 billion over a decade.
The site-neutral policy has been a legal battleground, with hospital and physician groups winning a round last year.
Another Medicare proposal included in Mr. Trump’s fiscal 2021 budget homes in on this issue for cases where a hospital owns a physician office. Medicare now pays most off-campus hospital outpatient departments higher rates than the program’s physician fee schedule dictates for the same services.
Switching to a site-neutral policy for these hospital-owned physician offices would result in $47.2 billion in savings over a decade, HHS said in the budget document.
This article first appeared on Medscape.com.
Be alert for embezzlement
With myriad complex, high-tech problems facing private practice in this modern era, I am periodically reminded by long-time readers to revisit some of the low-tech issues that will always require our attention.
Few are lower tech (in most cases) and more easily overlooked than theft from within. Embezzlement remains far more common in medical offices than generally assumed – and it often occurs in full view of physicians who think everything is fine. Most embezzlers are not skillful or discreet; their transgressions may go undetected for years, simply because no one suspects it is happening.
Detecting fraud is an inexact science. There is no textbook approach that one can follow, but a few simple measures will prevent or expose the most common forms:
- Make it more difficult. Theft and embezzlement are usually products of opportunity, so minimize those opportunities. No one person should be in charge of the entire bookkeeping process: The person who enters charges should be different from the one who enters payments. The one who writes checks or makes electronic fund transfers should not balance the books, and so on. Internal audits should be done on a regular basis, and all employees should know that. Your accountant can help.
- Reconcile cash receipts daily. Embezzlement does not require sophisticated technology; the most common form is simply taking cash out of the till. In a typical scenario, a patient pays a copay of $15 in cash; the receptionist records the payment as $5, and pockets the rest. Make sure a receipt is generated for every cash transaction, and that someone other than the person accepting cash reconciles the charges, receipts, and cash totals daily.
- Inventory your stock. Cash isn’t the only susceptible commodity. If you sell cosmetics or other products, inventory your stock frequently. And office personnel are not the only potential thieves: Last year, a locum tenens physician down the street conspired with a receptionist to take cash transactions for cosmetic neurotoxins and fillers “off the books” and split the spoils. That office was being ripped off twice; first for the neurotoxin and filler materials themselves, and then for the cash proceeds.
- Separate all accounting duties. Another popular ploy is false invoicing for imaginary supplies. A friend’s experience provides a good example (retold with his permission): His bookkeeper wrote sizable checks to herself, disguising them in the ledger as payments to vendors commonly used by his practice. Since the same employee also balanced the checkbook, she got away with it for years. “It wasn’t at all clever,” he told me, “and I’m embarrassed to admit that it happened to me.” Once again, separation of duties is the key to prevention. One employee should enter invoices into the data system, another should issue the check or make the electronic transfer, and a third should match invoices to goods and services received.
- Verify expense reports. False expense reporting is a subset of the fake invoice scam. When an employee asks for reimbursement of expenses, make sure those expenses are real.
- Consider computer safeguards. Computers facilitate a lot of financial chores, but they also consolidate financial data in one place, where it is potentially accessible to anybody, anywhere. Your computer vendor should be aware of this, and there should be safeguards built into your system. Ask about them. If they aren’t there, ask why.
- Hire honest employees. All applicants look great on paper, so check their references; and with their permission, you can run background checks for a few dollars on any of several public information web sites. My columns on hiring are available on the MDedge Dermatology website.
- Look for “red flags.” Examples include employees who refuse to take vacations, because someone else will have do their work or who insist on posting expenses that are a coworker’s responsibility, “just to be nice.” Anyone obviously living beyond his or her means merits suspicion as well.
- Consider bonding your employees. Dishonesty bonds are relatively inexpensive, and provide assurance of some measure of recovery if your safeguards fail. Also, just knowing that your staff is bonded will scare off most dishonest applicants. One effective screen is a question on your employment application: “Would you object to being bonded?”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
With myriad complex, high-tech problems facing private practice in this modern era, I am periodically reminded by long-time readers to revisit some of the low-tech issues that will always require our attention.
Few are lower tech (in most cases) and more easily overlooked than theft from within. Embezzlement remains far more common in medical offices than generally assumed – and it often occurs in full view of physicians who think everything is fine. Most embezzlers are not skillful or discreet; their transgressions may go undetected for years, simply because no one suspects it is happening.
Detecting fraud is an inexact science. There is no textbook approach that one can follow, but a few simple measures will prevent or expose the most common forms:
- Make it more difficult. Theft and embezzlement are usually products of opportunity, so minimize those opportunities. No one person should be in charge of the entire bookkeeping process: The person who enters charges should be different from the one who enters payments. The one who writes checks or makes electronic fund transfers should not balance the books, and so on. Internal audits should be done on a regular basis, and all employees should know that. Your accountant can help.
- Reconcile cash receipts daily. Embezzlement does not require sophisticated technology; the most common form is simply taking cash out of the till. In a typical scenario, a patient pays a copay of $15 in cash; the receptionist records the payment as $5, and pockets the rest. Make sure a receipt is generated for every cash transaction, and that someone other than the person accepting cash reconciles the charges, receipts, and cash totals daily.
- Inventory your stock. Cash isn’t the only susceptible commodity. If you sell cosmetics or other products, inventory your stock frequently. And office personnel are not the only potential thieves: Last year, a locum tenens physician down the street conspired with a receptionist to take cash transactions for cosmetic neurotoxins and fillers “off the books” and split the spoils. That office was being ripped off twice; first for the neurotoxin and filler materials themselves, and then for the cash proceeds.
- Separate all accounting duties. Another popular ploy is false invoicing for imaginary supplies. A friend’s experience provides a good example (retold with his permission): His bookkeeper wrote sizable checks to herself, disguising them in the ledger as payments to vendors commonly used by his practice. Since the same employee also balanced the checkbook, she got away with it for years. “It wasn’t at all clever,” he told me, “and I’m embarrassed to admit that it happened to me.” Once again, separation of duties is the key to prevention. One employee should enter invoices into the data system, another should issue the check or make the electronic transfer, and a third should match invoices to goods and services received.
- Verify expense reports. False expense reporting is a subset of the fake invoice scam. When an employee asks for reimbursement of expenses, make sure those expenses are real.
- Consider computer safeguards. Computers facilitate a lot of financial chores, but they also consolidate financial data in one place, where it is potentially accessible to anybody, anywhere. Your computer vendor should be aware of this, and there should be safeguards built into your system. Ask about them. If they aren’t there, ask why.
- Hire honest employees. All applicants look great on paper, so check their references; and with their permission, you can run background checks for a few dollars on any of several public information web sites. My columns on hiring are available on the MDedge Dermatology website.
- Look for “red flags.” Examples include employees who refuse to take vacations, because someone else will have do their work or who insist on posting expenses that are a coworker’s responsibility, “just to be nice.” Anyone obviously living beyond his or her means merits suspicion as well.
- Consider bonding your employees. Dishonesty bonds are relatively inexpensive, and provide assurance of some measure of recovery if your safeguards fail. Also, just knowing that your staff is bonded will scare off most dishonest applicants. One effective screen is a question on your employment application: “Would you object to being bonded?”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
With myriad complex, high-tech problems facing private practice in this modern era, I am periodically reminded by long-time readers to revisit some of the low-tech issues that will always require our attention.
Few are lower tech (in most cases) and more easily overlooked than theft from within. Embezzlement remains far more common in medical offices than generally assumed – and it often occurs in full view of physicians who think everything is fine. Most embezzlers are not skillful or discreet; their transgressions may go undetected for years, simply because no one suspects it is happening.
Detecting fraud is an inexact science. There is no textbook approach that one can follow, but a few simple measures will prevent or expose the most common forms:
- Make it more difficult. Theft and embezzlement are usually products of opportunity, so minimize those opportunities. No one person should be in charge of the entire bookkeeping process: The person who enters charges should be different from the one who enters payments. The one who writes checks or makes electronic fund transfers should not balance the books, and so on. Internal audits should be done on a regular basis, and all employees should know that. Your accountant can help.
- Reconcile cash receipts daily. Embezzlement does not require sophisticated technology; the most common form is simply taking cash out of the till. In a typical scenario, a patient pays a copay of $15 in cash; the receptionist records the payment as $5, and pockets the rest. Make sure a receipt is generated for every cash transaction, and that someone other than the person accepting cash reconciles the charges, receipts, and cash totals daily.
- Inventory your stock. Cash isn’t the only susceptible commodity. If you sell cosmetics or other products, inventory your stock frequently. And office personnel are not the only potential thieves: Last year, a locum tenens physician down the street conspired with a receptionist to take cash transactions for cosmetic neurotoxins and fillers “off the books” and split the spoils. That office was being ripped off twice; first for the neurotoxin and filler materials themselves, and then for the cash proceeds.
- Separate all accounting duties. Another popular ploy is false invoicing for imaginary supplies. A friend’s experience provides a good example (retold with his permission): His bookkeeper wrote sizable checks to herself, disguising them in the ledger as payments to vendors commonly used by his practice. Since the same employee also balanced the checkbook, she got away with it for years. “It wasn’t at all clever,” he told me, “and I’m embarrassed to admit that it happened to me.” Once again, separation of duties is the key to prevention. One employee should enter invoices into the data system, another should issue the check or make the electronic transfer, and a third should match invoices to goods and services received.
- Verify expense reports. False expense reporting is a subset of the fake invoice scam. When an employee asks for reimbursement of expenses, make sure those expenses are real.
- Consider computer safeguards. Computers facilitate a lot of financial chores, but they also consolidate financial data in one place, where it is potentially accessible to anybody, anywhere. Your computer vendor should be aware of this, and there should be safeguards built into your system. Ask about them. If they aren’t there, ask why.
- Hire honest employees. All applicants look great on paper, so check their references; and with their permission, you can run background checks for a few dollars on any of several public information web sites. My columns on hiring are available on the MDedge Dermatology website.
- Look for “red flags.” Examples include employees who refuse to take vacations, because someone else will have do their work or who insist on posting expenses that are a coworker’s responsibility, “just to be nice.” Anyone obviously living beyond his or her means merits suspicion as well.
- Consider bonding your employees. Dishonesty bonds are relatively inexpensive, and provide assurance of some measure of recovery if your safeguards fail. Also, just knowing that your staff is bonded will scare off most dishonest applicants. One effective screen is a question on your employment application: “Would you object to being bonded?”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at dermnews@mdedge.com.
What you absolutely need to know about tail coverage
A 28-year-old pediatrician working in a large group practice in California found a new job in Pennsylvania. The job would allow her to live with her husband, who was a nonphysician.
On her last day of work at the California job, the practice’s office manager asked her, “Do you know about the tail coverage?”
He explained that it is malpractice insurance for any cases filed against her after leaving the job. Without it, he said, she would not be covered for those claims.
The physician (who asked not to be identified) had very little savings and suddenly had to pay a five-figure bill for tail coverage. To provide the extra malpractice coverage, she and her husband had to use savings they’d set aside to buy a house.
Getting tail coverage, known formally as an extended reporting endorsement, often comes as a complete and costly surprise for new doctors, says Dennis Hursh, Esq, a health care attorney based in Middletown, Penn., who deals with physicians’ employment contracts.
“Having to pay for a tail can disrupt lives,” Hursh said. “A tail can cost about one third of a young doctor’s salary. If you don’t feel you can afford to pay that, you may be forced to stay with a job you don’t like.”
Most medical residents don’t think about tail coverage until they apply for their first job, but last year, residents at Hahnemann University Hospital in Philadelphia got a painful early lesson.
In the summer, the hospital went out of business because of financial problems. Hundreds of medical residents and fellows not only were forced to find new programs but also had to prepare to buy tail coverage for their training years at Hahnemann.
“All the guarantees have been yanked out from under us,” said Tom Sibert, MD, a former internal medicine resident at the hospital, who is now finishing his training in California. “Residents don’t have that kind of money.”
Hahnemann trainees have asked the judge in the bankruptcy proceedings to put them ahead of other creditors and to ensure their tail coverage is paid. As of early February, the issue had not been resolved.
Meanwhile, Sibert and many other former trainees were trying to get quotes for purchasing tail coverage. They have been shocked by the amounts they would have to pay.
How tail coverage works
Medical malpractice tail coverage protects from incidents that took place when doctors were at their previous jobs but that later resulted in malpractice claims after they had left that employer.
One type of malpractice insurance, an occurrence policy, does not need tail coverage. Occurrence policies cover any incident that occurred when the policy was in force, no matter when a claim was filed – even if it is filed many years after the claims-filing period of the policy ends.
However, most malpractice policies – as many as 85%, according to one estimate – are claims-made policies. Claims-made policies are more much common because they’re significantly less expensive than occurrence policies.
Under a claims-made policy, coverage for malpractice claims completely stops when the policy ends. It does not cover incidents that occurred when the policy was in force but for which the patients later filed claims, as the occurrence policy does. So a tail is needed to cover these claims.
Physicians in all stages of their career may need tail coverage when they leave a job, change malpractice carriers, or retire.
But young physicians often have greater problems with tail coverage, for several reasons. They tend to be employed, and as such, they cannot choose the coverage they want. As a result, they most likely get claims-made coverage. In addition, the job turnover tends to be higher for these doctors. When leaving a job, the tail comes into play. More than half of new physicians leave their first job within 5 years, and of those, more than half leave after only 1 or 2 years.
Young physicians have no experience with tails and may not even know what they are. “In training, malpractice coverage is not a problem because the program handles it,” Mr. Hursh said. Accreditation standards require that teaching hospitals buy coverage, including a tail when residents leave.
So when young physicians are offered their first job and are handed an employment contract to sign, they may not even look for tail coverage, says Mr. Hursh, who wrote The Final Hurdle, a Physician’s Guide to Negotiating a Fair Employment Agreement. Instead, “young physicians tend to focus on issues like salary, benefits, and signing bonuses,” he said.
Mr. Hursh says the tail is usually the most expensive potential cost in the contract.
There’s no easy way to get out of paying the tail coverage once it is enshrined in the contract. The full tail can cost five or even six figures, depending on the physicians’ specialty, the local malpractice premium, and the physician’s own claims history.
Can you negotiate your tail coverage?
Negotiating tail coverage in the employment contract involves some familiarity with medical malpractice insurance and a close reading of the contract. First, you have to determine that the employer is providing claims-made coverage, which would require a tail if you leave. Then you have to determine whether the employer will pay for the tail coverage.
Often, the contract does not even mention tail coverage. “It could merely state that the practice will be responsible for malpractice coverage while you are working there,” Mr. Hursh said. Although it never specifies the tail, this language indicates that you will be paying for it, he says.
Therefore, it’s wise to have a conversation with your prospective employer about the tail. “Some new doctors never ask the question ‘What happens if I leave? Do I get tail coverage?’ ” said Israel Teitelbaum, an attorney who is chairman of Contemporary Insurance Services, an insurance broker in Silver Spring, Md.
Talking about the tail, however, can be a touchy subject for many young doctors applying for their first job. The tail matters only if you leave the job, and you may not want to imply that you would ever want to leave. Too much money, however, is on the line for you not to ask, Mr. Teitelbaum said.
Even if the employer verbally agrees to pay for the tail coverage, experts advise that you try to get the employer’s commitment in writing and have it put it into the contract.
Getting the employer to cover the tail in the initial contract is crucial because once you have agreed to work there, “it’s much more difficult to get it changed,” Mr. Teitelbaum said. However, even if tail coverage is not in the first contract, you shouldn’t give up, he says. You should try again in the next contract a few years later.
“It’s never too late to bring it up,” Mr. Teitelbaum said. After a few years of employment, you have a track record at the job. “A doctor who is very desirable to the employer may be able to get tail coverage on contract renewal.”
Coverage: Large employers vs. small employers
Willingness to pay for an employee’s tail coverage varies depending on the size of the employer. Large employers – systems, hospitals, and large practices – are much more likely to cover the tail than small and medium-sized practices.
Large employers tend to pay for at least part of the tail because they realize that it is in their interest to do so. Since they have the deepest pockets, they’re often the first to be named in a lawsuit. They might have to pay the whole claim if the physician did not have tail coverage.
However, many large employers want to use tail coverage as a bargaining chip to make sure doctors stay for a while at least. One typical arrangement, Mr. Hursh says, is to pay only one-fifth of the tail if the physician leaves in the first year of employment and then to pay one fifth more in each succeeding year until year five, when the employer assumes the entire cost of the tail.
Smaller practices, on the other hand, are usually close-fisted about tail coverage. “They tend to view the tail as an unnecessary expense,” Mr. Hursh said. “They don’t want to pay for a doctor who is not generating revenue for them any more.”
Traditionally, when physicians become partners, practices are more generous and agree to pay their tails if they leave, Mr. Hursh says. But he thinks this is changing, too – recent partnership contracts he has reviewed did not provide for tail coverage.
Times you don’t need to pay for tail coverage
Even if you’re responsible for the tail coverage, your insurance arrangement may be such that you don’t have to pay for it, says Michelle Perron, a malpractice insurance broker in North Hampton, N.H.
For example, if the carrier at your new job is the same as the one at your old job, your coverage would continue with no break, and you would not need a tail, she says. Even if you move to another state, your old carrier might also sell policies there, and you would then likely have seamless coverage, Ms. Perron says. This would be handy if you could choose your new carrier.
Even when you change carriers, Ms. Perron says, the new one might agree to pick up the old carrier’s coverage in return for getting your business, assuming you are an independent physician buying your own coverage. The new carrier would issue prior acts coverage, also known as nose coverage.
Older doctors going into retirement also have a potential tail coverage problem, but their tail coverage premium is often waived, Ms. Perron says. The need for a tail has to do with claims arising post retirement, after your coverage has ended. Typically, if you have been with the carrier for at least 5 years and you are age 55 years or older, your carrier will waive the tail coverage premium, she says.
However, if the retired doctor starts practicing again, even part time, the carrier may want to take back the free tail, she says. Some retired doctors get around this by buying a lower-priced tail from another company, but the former carrier may still want its money back, Ms. Perron says.
Can you just go without tail coverage?
What happens if physicians with a tail commitment choose to wing it and not pay for the tail? If a claim was never made against them, they may believe that the expense is unnecessary. The situation, however, is not so simple.
Some states require having tail coverage. Malpractice coverage is required in seven states, and at least some of those states explicitly extend this requirement to tails. They are Colorado, Connecticut, Kansas, Massachusetts, New Jersey, Rhode Island, and Wisconsin. Eleven more states tie malpractice coverage, perhaps including tails, to some benefit for the doctor, such as tort reform. These states include Indiana, Nebraska, New Mexico, New York, and Pennsylvania.
Many hospitals require tail coverage for privileges, and some insurers do as well. In addition, Ms. Perron says a missing tail reduces your prospects when looking for a job. “For the employer, having to pay coverage for a new hire will cost more than starting fresh with someone else,” she said.
Still, it’s important to remember the risk of being sued. “If you don’t buy the tail coverage, you are at risk for a lawsuit for many years to come,” Mr. Teitelbaum said.
Doctors should consider their potential lifetime risk, not just their current risk. Although only 8% of doctors younger than age 40 have been sued for malpractice, that figure climbs to almost half by the time doctors reach age 55.
The risks are higher in some specialties. About 63% of general surgeons and ob.gyns. have been sued.
Many of these claims are without merit, and doctors pay only the legal expenses of defending the case. Some doctors may think they could risk frivolous suits and cover legal expenses out of pocket. An American Medical Association survey showed that 68% of closed claims against doctors were dropped, dismissed, or withdrawn. It said these claims cost an average of more than $30,000 to defend.
However, Mr. Teitelbaum puts the defense costs for so-called frivolous suits much higher than the AMA, at $250,000 or more. “Even if you’re sure you won’t have to pay a claim, you still have to defend yourself against frivolous suits,” he said. “You won’t recover those expenses.”
How to lower your tail coverage cost
Physicians typically have 60 days to buy tail coverage after their regular coverage has ended. Specialized brokers such as Mr. Teitelbaum and Ms. Perron help physicians look for the best tails to buy.
The cost of the tail depends on how long you’ve been at your job when you leave it, Ms. Perron says. If you leave in the first 1 or 2 years of the policy, she says, the tail price will be lower because the coverage period is shorter.
Usually the most expensive tail available is from the carrier that issued the original policy. Why is this? “Carriers rarely sell a tail that undercuts their retail price,” Mr. Teitelbaum said. “They don’t want to compete with themselves, and in fact doing so could pose regulatory problems for them.”
Instead of buying from their own carrier, doctors can purchase stand-alone tails from competitors, which Mr. Teitelbaum says are 10%-30% less expensive than the policy the original carrier issues. However, stand-alone tails are not always easy to find, especially for high-cost specialties such as neurosurgery and ob.gyn., he says.
Some physicians try to bring down the cost of the tail by limiting the duration of the tail. You can buy tails that only cover claims filed 1-5 years after the incident took place, rather than indefinitely. These limits mirror the typical statute of limitations – the time limit to file a claim in each state. This limit is as little as 2 years in some states, though it can be as long as 6 years in others.
However, some states make exceptions to the statute of limitations. The 2- to 6-year clock doesn’t start ticking until the mistake is discovered or, in the case of children, when they reach adulthood. “This means that with a limited tail, you always have risk,” Perron said.
And yet some doctors insist on these time-limited tails. “If a doctor opts for 3 years’ coverage, that’s better than no years,” Mr. Teitelbaum said. “But I would advise them to take at least 5 years because that gives you coverage for the basic statute of limitations in most states. Three-year tails do yield savings, but often they’re not enough to warrant the risk.”
Another way to reduce costs is to lower the coverage limits of the tail. The standard coverage limit is $1 million per case and $3 million per year, so doctors might be able to save money on the premium by buying limits of $200,000/$600,000. But Mr. Teitelbaum says most companies would refuse to sell a policy with a limit lower than that of the expiring policy.
Further ways to reduce the cost of the tail include buying tail coverage that doesn’t give the physician the right to approve a settlement or that doesn’t include legal fees in the coverage limits. But these options, too, raise the physician’s risks. Whichever option you choose, the important thing is to protect yourself against costly lawsuits.
This article first appeared on Medscape.com.
A 28-year-old pediatrician working in a large group practice in California found a new job in Pennsylvania. The job would allow her to live with her husband, who was a nonphysician.
On her last day of work at the California job, the practice’s office manager asked her, “Do you know about the tail coverage?”
He explained that it is malpractice insurance for any cases filed against her after leaving the job. Without it, he said, she would not be covered for those claims.
The physician (who asked not to be identified) had very little savings and suddenly had to pay a five-figure bill for tail coverage. To provide the extra malpractice coverage, she and her husband had to use savings they’d set aside to buy a house.
Getting tail coverage, known formally as an extended reporting endorsement, often comes as a complete and costly surprise for new doctors, says Dennis Hursh, Esq, a health care attorney based in Middletown, Penn., who deals with physicians’ employment contracts.
“Having to pay for a tail can disrupt lives,” Hursh said. “A tail can cost about one third of a young doctor’s salary. If you don’t feel you can afford to pay that, you may be forced to stay with a job you don’t like.”
Most medical residents don’t think about tail coverage until they apply for their first job, but last year, residents at Hahnemann University Hospital in Philadelphia got a painful early lesson.
In the summer, the hospital went out of business because of financial problems. Hundreds of medical residents and fellows not only were forced to find new programs but also had to prepare to buy tail coverage for their training years at Hahnemann.
“All the guarantees have been yanked out from under us,” said Tom Sibert, MD, a former internal medicine resident at the hospital, who is now finishing his training in California. “Residents don’t have that kind of money.”
Hahnemann trainees have asked the judge in the bankruptcy proceedings to put them ahead of other creditors and to ensure their tail coverage is paid. As of early February, the issue had not been resolved.
Meanwhile, Sibert and many other former trainees were trying to get quotes for purchasing tail coverage. They have been shocked by the amounts they would have to pay.
How tail coverage works
Medical malpractice tail coverage protects from incidents that took place when doctors were at their previous jobs but that later resulted in malpractice claims after they had left that employer.
One type of malpractice insurance, an occurrence policy, does not need tail coverage. Occurrence policies cover any incident that occurred when the policy was in force, no matter when a claim was filed – even if it is filed many years after the claims-filing period of the policy ends.
However, most malpractice policies – as many as 85%, according to one estimate – are claims-made policies. Claims-made policies are more much common because they’re significantly less expensive than occurrence policies.
Under a claims-made policy, coverage for malpractice claims completely stops when the policy ends. It does not cover incidents that occurred when the policy was in force but for which the patients later filed claims, as the occurrence policy does. So a tail is needed to cover these claims.
Physicians in all stages of their career may need tail coverage when they leave a job, change malpractice carriers, or retire.
But young physicians often have greater problems with tail coverage, for several reasons. They tend to be employed, and as such, they cannot choose the coverage they want. As a result, they most likely get claims-made coverage. In addition, the job turnover tends to be higher for these doctors. When leaving a job, the tail comes into play. More than half of new physicians leave their first job within 5 years, and of those, more than half leave after only 1 or 2 years.
Young physicians have no experience with tails and may not even know what they are. “In training, malpractice coverage is not a problem because the program handles it,” Mr. Hursh said. Accreditation standards require that teaching hospitals buy coverage, including a tail when residents leave.
So when young physicians are offered their first job and are handed an employment contract to sign, they may not even look for tail coverage, says Mr. Hursh, who wrote The Final Hurdle, a Physician’s Guide to Negotiating a Fair Employment Agreement. Instead, “young physicians tend to focus on issues like salary, benefits, and signing bonuses,” he said.
Mr. Hursh says the tail is usually the most expensive potential cost in the contract.
There’s no easy way to get out of paying the tail coverage once it is enshrined in the contract. The full tail can cost five or even six figures, depending on the physicians’ specialty, the local malpractice premium, and the physician’s own claims history.
Can you negotiate your tail coverage?
Negotiating tail coverage in the employment contract involves some familiarity with medical malpractice insurance and a close reading of the contract. First, you have to determine that the employer is providing claims-made coverage, which would require a tail if you leave. Then you have to determine whether the employer will pay for the tail coverage.
Often, the contract does not even mention tail coverage. “It could merely state that the practice will be responsible for malpractice coverage while you are working there,” Mr. Hursh said. Although it never specifies the tail, this language indicates that you will be paying for it, he says.
Therefore, it’s wise to have a conversation with your prospective employer about the tail. “Some new doctors never ask the question ‘What happens if I leave? Do I get tail coverage?’ ” said Israel Teitelbaum, an attorney who is chairman of Contemporary Insurance Services, an insurance broker in Silver Spring, Md.
Talking about the tail, however, can be a touchy subject for many young doctors applying for their first job. The tail matters only if you leave the job, and you may not want to imply that you would ever want to leave. Too much money, however, is on the line for you not to ask, Mr. Teitelbaum said.
Even if the employer verbally agrees to pay for the tail coverage, experts advise that you try to get the employer’s commitment in writing and have it put it into the contract.
Getting the employer to cover the tail in the initial contract is crucial because once you have agreed to work there, “it’s much more difficult to get it changed,” Mr. Teitelbaum said. However, even if tail coverage is not in the first contract, you shouldn’t give up, he says. You should try again in the next contract a few years later.
“It’s never too late to bring it up,” Mr. Teitelbaum said. After a few years of employment, you have a track record at the job. “A doctor who is very desirable to the employer may be able to get tail coverage on contract renewal.”
Coverage: Large employers vs. small employers
Willingness to pay for an employee’s tail coverage varies depending on the size of the employer. Large employers – systems, hospitals, and large practices – are much more likely to cover the tail than small and medium-sized practices.
Large employers tend to pay for at least part of the tail because they realize that it is in their interest to do so. Since they have the deepest pockets, they’re often the first to be named in a lawsuit. They might have to pay the whole claim if the physician did not have tail coverage.
However, many large employers want to use tail coverage as a bargaining chip to make sure doctors stay for a while at least. One typical arrangement, Mr. Hursh says, is to pay only one-fifth of the tail if the physician leaves in the first year of employment and then to pay one fifth more in each succeeding year until year five, when the employer assumes the entire cost of the tail.
Smaller practices, on the other hand, are usually close-fisted about tail coverage. “They tend to view the tail as an unnecessary expense,” Mr. Hursh said. “They don’t want to pay for a doctor who is not generating revenue for them any more.”
Traditionally, when physicians become partners, practices are more generous and agree to pay their tails if they leave, Mr. Hursh says. But he thinks this is changing, too – recent partnership contracts he has reviewed did not provide for tail coverage.
Times you don’t need to pay for tail coverage
Even if you’re responsible for the tail coverage, your insurance arrangement may be such that you don’t have to pay for it, says Michelle Perron, a malpractice insurance broker in North Hampton, N.H.
For example, if the carrier at your new job is the same as the one at your old job, your coverage would continue with no break, and you would not need a tail, she says. Even if you move to another state, your old carrier might also sell policies there, and you would then likely have seamless coverage, Ms. Perron says. This would be handy if you could choose your new carrier.
Even when you change carriers, Ms. Perron says, the new one might agree to pick up the old carrier’s coverage in return for getting your business, assuming you are an independent physician buying your own coverage. The new carrier would issue prior acts coverage, also known as nose coverage.
Older doctors going into retirement also have a potential tail coverage problem, but their tail coverage premium is often waived, Ms. Perron says. The need for a tail has to do with claims arising post retirement, after your coverage has ended. Typically, if you have been with the carrier for at least 5 years and you are age 55 years or older, your carrier will waive the tail coverage premium, she says.
However, if the retired doctor starts practicing again, even part time, the carrier may want to take back the free tail, she says. Some retired doctors get around this by buying a lower-priced tail from another company, but the former carrier may still want its money back, Ms. Perron says.
Can you just go without tail coverage?
What happens if physicians with a tail commitment choose to wing it and not pay for the tail? If a claim was never made against them, they may believe that the expense is unnecessary. The situation, however, is not so simple.
Some states require having tail coverage. Malpractice coverage is required in seven states, and at least some of those states explicitly extend this requirement to tails. They are Colorado, Connecticut, Kansas, Massachusetts, New Jersey, Rhode Island, and Wisconsin. Eleven more states tie malpractice coverage, perhaps including tails, to some benefit for the doctor, such as tort reform. These states include Indiana, Nebraska, New Mexico, New York, and Pennsylvania.
Many hospitals require tail coverage for privileges, and some insurers do as well. In addition, Ms. Perron says a missing tail reduces your prospects when looking for a job. “For the employer, having to pay coverage for a new hire will cost more than starting fresh with someone else,” she said.
Still, it’s important to remember the risk of being sued. “If you don’t buy the tail coverage, you are at risk for a lawsuit for many years to come,” Mr. Teitelbaum said.
Doctors should consider their potential lifetime risk, not just their current risk. Although only 8% of doctors younger than age 40 have been sued for malpractice, that figure climbs to almost half by the time doctors reach age 55.
The risks are higher in some specialties. About 63% of general surgeons and ob.gyns. have been sued.
Many of these claims are without merit, and doctors pay only the legal expenses of defending the case. Some doctors may think they could risk frivolous suits and cover legal expenses out of pocket. An American Medical Association survey showed that 68% of closed claims against doctors were dropped, dismissed, or withdrawn. It said these claims cost an average of more than $30,000 to defend.
However, Mr. Teitelbaum puts the defense costs for so-called frivolous suits much higher than the AMA, at $250,000 or more. “Even if you’re sure you won’t have to pay a claim, you still have to defend yourself against frivolous suits,” he said. “You won’t recover those expenses.”
How to lower your tail coverage cost
Physicians typically have 60 days to buy tail coverage after their regular coverage has ended. Specialized brokers such as Mr. Teitelbaum and Ms. Perron help physicians look for the best tails to buy.
The cost of the tail depends on how long you’ve been at your job when you leave it, Ms. Perron says. If you leave in the first 1 or 2 years of the policy, she says, the tail price will be lower because the coverage period is shorter.
Usually the most expensive tail available is from the carrier that issued the original policy. Why is this? “Carriers rarely sell a tail that undercuts their retail price,” Mr. Teitelbaum said. “They don’t want to compete with themselves, and in fact doing so could pose regulatory problems for them.”
Instead of buying from their own carrier, doctors can purchase stand-alone tails from competitors, which Mr. Teitelbaum says are 10%-30% less expensive than the policy the original carrier issues. However, stand-alone tails are not always easy to find, especially for high-cost specialties such as neurosurgery and ob.gyn., he says.
Some physicians try to bring down the cost of the tail by limiting the duration of the tail. You can buy tails that only cover claims filed 1-5 years after the incident took place, rather than indefinitely. These limits mirror the typical statute of limitations – the time limit to file a claim in each state. This limit is as little as 2 years in some states, though it can be as long as 6 years in others.
However, some states make exceptions to the statute of limitations. The 2- to 6-year clock doesn’t start ticking until the mistake is discovered or, in the case of children, when they reach adulthood. “This means that with a limited tail, you always have risk,” Perron said.
And yet some doctors insist on these time-limited tails. “If a doctor opts for 3 years’ coverage, that’s better than no years,” Mr. Teitelbaum said. “But I would advise them to take at least 5 years because that gives you coverage for the basic statute of limitations in most states. Three-year tails do yield savings, but often they’re not enough to warrant the risk.”
Another way to reduce costs is to lower the coverage limits of the tail. The standard coverage limit is $1 million per case and $3 million per year, so doctors might be able to save money on the premium by buying limits of $200,000/$600,000. But Mr. Teitelbaum says most companies would refuse to sell a policy with a limit lower than that of the expiring policy.
Further ways to reduce the cost of the tail include buying tail coverage that doesn’t give the physician the right to approve a settlement or that doesn’t include legal fees in the coverage limits. But these options, too, raise the physician’s risks. Whichever option you choose, the important thing is to protect yourself against costly lawsuits.
This article first appeared on Medscape.com.
A 28-year-old pediatrician working in a large group practice in California found a new job in Pennsylvania. The job would allow her to live with her husband, who was a nonphysician.
On her last day of work at the California job, the practice’s office manager asked her, “Do you know about the tail coverage?”
He explained that it is malpractice insurance for any cases filed against her after leaving the job. Without it, he said, she would not be covered for those claims.
The physician (who asked not to be identified) had very little savings and suddenly had to pay a five-figure bill for tail coverage. To provide the extra malpractice coverage, she and her husband had to use savings they’d set aside to buy a house.
Getting tail coverage, known formally as an extended reporting endorsement, often comes as a complete and costly surprise for new doctors, says Dennis Hursh, Esq, a health care attorney based in Middletown, Penn., who deals with physicians’ employment contracts.
“Having to pay for a tail can disrupt lives,” Hursh said. “A tail can cost about one third of a young doctor’s salary. If you don’t feel you can afford to pay that, you may be forced to stay with a job you don’t like.”
Most medical residents don’t think about tail coverage until they apply for their first job, but last year, residents at Hahnemann University Hospital in Philadelphia got a painful early lesson.
In the summer, the hospital went out of business because of financial problems. Hundreds of medical residents and fellows not only were forced to find new programs but also had to prepare to buy tail coverage for their training years at Hahnemann.
“All the guarantees have been yanked out from under us,” said Tom Sibert, MD, a former internal medicine resident at the hospital, who is now finishing his training in California. “Residents don’t have that kind of money.”
Hahnemann trainees have asked the judge in the bankruptcy proceedings to put them ahead of other creditors and to ensure their tail coverage is paid. As of early February, the issue had not been resolved.
Meanwhile, Sibert and many other former trainees were trying to get quotes for purchasing tail coverage. They have been shocked by the amounts they would have to pay.
How tail coverage works
Medical malpractice tail coverage protects from incidents that took place when doctors were at their previous jobs but that later resulted in malpractice claims after they had left that employer.
One type of malpractice insurance, an occurrence policy, does not need tail coverage. Occurrence policies cover any incident that occurred when the policy was in force, no matter when a claim was filed – even if it is filed many years after the claims-filing period of the policy ends.
However, most malpractice policies – as many as 85%, according to one estimate – are claims-made policies. Claims-made policies are more much common because they’re significantly less expensive than occurrence policies.
Under a claims-made policy, coverage for malpractice claims completely stops when the policy ends. It does not cover incidents that occurred when the policy was in force but for which the patients later filed claims, as the occurrence policy does. So a tail is needed to cover these claims.
Physicians in all stages of their career may need tail coverage when they leave a job, change malpractice carriers, or retire.
But young physicians often have greater problems with tail coverage, for several reasons. They tend to be employed, and as such, they cannot choose the coverage they want. As a result, they most likely get claims-made coverage. In addition, the job turnover tends to be higher for these doctors. When leaving a job, the tail comes into play. More than half of new physicians leave their first job within 5 years, and of those, more than half leave after only 1 or 2 years.
Young physicians have no experience with tails and may not even know what they are. “In training, malpractice coverage is not a problem because the program handles it,” Mr. Hursh said. Accreditation standards require that teaching hospitals buy coverage, including a tail when residents leave.
So when young physicians are offered their first job and are handed an employment contract to sign, they may not even look for tail coverage, says Mr. Hursh, who wrote The Final Hurdle, a Physician’s Guide to Negotiating a Fair Employment Agreement. Instead, “young physicians tend to focus on issues like salary, benefits, and signing bonuses,” he said.
Mr. Hursh says the tail is usually the most expensive potential cost in the contract.
There’s no easy way to get out of paying the tail coverage once it is enshrined in the contract. The full tail can cost five or even six figures, depending on the physicians’ specialty, the local malpractice premium, and the physician’s own claims history.
Can you negotiate your tail coverage?
Negotiating tail coverage in the employment contract involves some familiarity with medical malpractice insurance and a close reading of the contract. First, you have to determine that the employer is providing claims-made coverage, which would require a tail if you leave. Then you have to determine whether the employer will pay for the tail coverage.
Often, the contract does not even mention tail coverage. “It could merely state that the practice will be responsible for malpractice coverage while you are working there,” Mr. Hursh said. Although it never specifies the tail, this language indicates that you will be paying for it, he says.
Therefore, it’s wise to have a conversation with your prospective employer about the tail. “Some new doctors never ask the question ‘What happens if I leave? Do I get tail coverage?’ ” said Israel Teitelbaum, an attorney who is chairman of Contemporary Insurance Services, an insurance broker in Silver Spring, Md.
Talking about the tail, however, can be a touchy subject for many young doctors applying for their first job. The tail matters only if you leave the job, and you may not want to imply that you would ever want to leave. Too much money, however, is on the line for you not to ask, Mr. Teitelbaum said.
Even if the employer verbally agrees to pay for the tail coverage, experts advise that you try to get the employer’s commitment in writing and have it put it into the contract.
Getting the employer to cover the tail in the initial contract is crucial because once you have agreed to work there, “it’s much more difficult to get it changed,” Mr. Teitelbaum said. However, even if tail coverage is not in the first contract, you shouldn’t give up, he says. You should try again in the next contract a few years later.
“It’s never too late to bring it up,” Mr. Teitelbaum said. After a few years of employment, you have a track record at the job. “A doctor who is very desirable to the employer may be able to get tail coverage on contract renewal.”
Coverage: Large employers vs. small employers
Willingness to pay for an employee’s tail coverage varies depending on the size of the employer. Large employers – systems, hospitals, and large practices – are much more likely to cover the tail than small and medium-sized practices.
Large employers tend to pay for at least part of the tail because they realize that it is in their interest to do so. Since they have the deepest pockets, they’re often the first to be named in a lawsuit. They might have to pay the whole claim if the physician did not have tail coverage.
However, many large employers want to use tail coverage as a bargaining chip to make sure doctors stay for a while at least. One typical arrangement, Mr. Hursh says, is to pay only one-fifth of the tail if the physician leaves in the first year of employment and then to pay one fifth more in each succeeding year until year five, when the employer assumes the entire cost of the tail.
Smaller practices, on the other hand, are usually close-fisted about tail coverage. “They tend to view the tail as an unnecessary expense,” Mr. Hursh said. “They don’t want to pay for a doctor who is not generating revenue for them any more.”
Traditionally, when physicians become partners, practices are more generous and agree to pay their tails if they leave, Mr. Hursh says. But he thinks this is changing, too – recent partnership contracts he has reviewed did not provide for tail coverage.
Times you don’t need to pay for tail coverage
Even if you’re responsible for the tail coverage, your insurance arrangement may be such that you don’t have to pay for it, says Michelle Perron, a malpractice insurance broker in North Hampton, N.H.
For example, if the carrier at your new job is the same as the one at your old job, your coverage would continue with no break, and you would not need a tail, she says. Even if you move to another state, your old carrier might also sell policies there, and you would then likely have seamless coverage, Ms. Perron says. This would be handy if you could choose your new carrier.
Even when you change carriers, Ms. Perron says, the new one might agree to pick up the old carrier’s coverage in return for getting your business, assuming you are an independent physician buying your own coverage. The new carrier would issue prior acts coverage, also known as nose coverage.
Older doctors going into retirement also have a potential tail coverage problem, but their tail coverage premium is often waived, Ms. Perron says. The need for a tail has to do with claims arising post retirement, after your coverage has ended. Typically, if you have been with the carrier for at least 5 years and you are age 55 years or older, your carrier will waive the tail coverage premium, she says.
However, if the retired doctor starts practicing again, even part time, the carrier may want to take back the free tail, she says. Some retired doctors get around this by buying a lower-priced tail from another company, but the former carrier may still want its money back, Ms. Perron says.
Can you just go without tail coverage?
What happens if physicians with a tail commitment choose to wing it and not pay for the tail? If a claim was never made against them, they may believe that the expense is unnecessary. The situation, however, is not so simple.
Some states require having tail coverage. Malpractice coverage is required in seven states, and at least some of those states explicitly extend this requirement to tails. They are Colorado, Connecticut, Kansas, Massachusetts, New Jersey, Rhode Island, and Wisconsin. Eleven more states tie malpractice coverage, perhaps including tails, to some benefit for the doctor, such as tort reform. These states include Indiana, Nebraska, New Mexico, New York, and Pennsylvania.
Many hospitals require tail coverage for privileges, and some insurers do as well. In addition, Ms. Perron says a missing tail reduces your prospects when looking for a job. “For the employer, having to pay coverage for a new hire will cost more than starting fresh with someone else,” she said.
Still, it’s important to remember the risk of being sued. “If you don’t buy the tail coverage, you are at risk for a lawsuit for many years to come,” Mr. Teitelbaum said.
Doctors should consider their potential lifetime risk, not just their current risk. Although only 8% of doctors younger than age 40 have been sued for malpractice, that figure climbs to almost half by the time doctors reach age 55.
The risks are higher in some specialties. About 63% of general surgeons and ob.gyns. have been sued.
Many of these claims are without merit, and doctors pay only the legal expenses of defending the case. Some doctors may think they could risk frivolous suits and cover legal expenses out of pocket. An American Medical Association survey showed that 68% of closed claims against doctors were dropped, dismissed, or withdrawn. It said these claims cost an average of more than $30,000 to defend.
However, Mr. Teitelbaum puts the defense costs for so-called frivolous suits much higher than the AMA, at $250,000 or more. “Even if you’re sure you won’t have to pay a claim, you still have to defend yourself against frivolous suits,” he said. “You won’t recover those expenses.”
How to lower your tail coverage cost
Physicians typically have 60 days to buy tail coverage after their regular coverage has ended. Specialized brokers such as Mr. Teitelbaum and Ms. Perron help physicians look for the best tails to buy.
The cost of the tail depends on how long you’ve been at your job when you leave it, Ms. Perron says. If you leave in the first 1 or 2 years of the policy, she says, the tail price will be lower because the coverage period is shorter.
Usually the most expensive tail available is from the carrier that issued the original policy. Why is this? “Carriers rarely sell a tail that undercuts their retail price,” Mr. Teitelbaum said. “They don’t want to compete with themselves, and in fact doing so could pose regulatory problems for them.”
Instead of buying from their own carrier, doctors can purchase stand-alone tails from competitors, which Mr. Teitelbaum says are 10%-30% less expensive than the policy the original carrier issues. However, stand-alone tails are not always easy to find, especially for high-cost specialties such as neurosurgery and ob.gyn., he says.
Some physicians try to bring down the cost of the tail by limiting the duration of the tail. You can buy tails that only cover claims filed 1-5 years after the incident took place, rather than indefinitely. These limits mirror the typical statute of limitations – the time limit to file a claim in each state. This limit is as little as 2 years in some states, though it can be as long as 6 years in others.
However, some states make exceptions to the statute of limitations. The 2- to 6-year clock doesn’t start ticking until the mistake is discovered or, in the case of children, when they reach adulthood. “This means that with a limited tail, you always have risk,” Perron said.
And yet some doctors insist on these time-limited tails. “If a doctor opts for 3 years’ coverage, that’s better than no years,” Mr. Teitelbaum said. “But I would advise them to take at least 5 years because that gives you coverage for the basic statute of limitations in most states. Three-year tails do yield savings, but often they’re not enough to warrant the risk.”
Another way to reduce costs is to lower the coverage limits of the tail. The standard coverage limit is $1 million per case and $3 million per year, so doctors might be able to save money on the premium by buying limits of $200,000/$600,000. But Mr. Teitelbaum says most companies would refuse to sell a policy with a limit lower than that of the expiring policy.
Further ways to reduce the cost of the tail include buying tail coverage that doesn’t give the physician the right to approve a settlement or that doesn’t include legal fees in the coverage limits. But these options, too, raise the physician’s risks. Whichever option you choose, the important thing is to protect yourself against costly lawsuits.
This article first appeared on Medscape.com.