User login
Unnecessary pelvic exams, Pap tests common in young women
according to estimates from a study published online in JAMA Internal Medicine.
Approximately 2.6 million young women – about a quarter of those in this age group – reported receiving a pelvic exam in the previous year even though fewer than 10% were pregnant or receiving treatment for a sexually transmitted infection (STI) at the time.
Similarly, an estimated three in four Pap tests given to women aged 15-20 years likely were unnecessary. Based on Medicare payments for screening Pap tests and pelvic exams, the unnecessary procedures represented an estimated $123 million in a year.
“The American College of Obstetricians and Gynecologists recognizes that no evidence supports routine speculum examination or BPE in healthy, asymptomatic women younger than 21 years and recommends that these examinations be performed only when medically indicated,” said Jin Qin, ScD, of the Centers for Disease Control and Prevention and colleagues.
“Our results showed that, despite the recommendation, many young women without discernible medical indication received potentially unnecessary BPE or Pap tests, which may be a reflection of a long-standing clinical practice in the United States.”
These findings “demonstrate what happens to vulnerable populations (in this case, girls and young women) when clinicians do not keep up with or do not adhere to new guidelines,” Melissa A. Simon, MD, MPH, wrote in an invited commentary. She acknowledged the challenges of keeping up with new guidelines but noted the potential for harm from unnecessary screening. Dr. Simon is vice chair for clinical research in the department of obstetrics and gynecology at Northwestern University, Chicago.
The researchers analyzed responses from 3,410 young women aged 15-20 years in the National Survey of Family Growth (NSFG) during 2011-2017 and extrapolated the results to estimate nationwide statistics. The researchers found that 23% of young women – 2.6 million in the United States – had received a bimanual pelvic exam during the previous year.
“This analysis focused on the bimanual component of the pelvic examination because it is the most invasive of the pelvic examination components and less likely to be confused with a speculum examination for cervical cancer or STI screening,” the authors note.
More than half of these pelvic exams (54%) – an estimated 1.4 million exams – potentially were unnecessary. The authors classified these pelvic exams as potentially unnecessary if it was not indicated for pregnancy, intrauterine device (IUD) use, or STI treatment in the past 12 months or for another medical problem.
Among the respondents, 5% were pregnant, 22% had been tested for an STI, and 5% had been treated for an STI during the previous year. About a third of respondents (33%) had used at least one type of hormonal contraception besides an IUD in the past year, but only 2% had used an IUD.
Dr. Simon said that some have advocated for routine bimanual pelvic exams to prompt women to see their provider every year, but without evidence to support the practice.
“In fact, many women (younger and older) associate the bimanual pelvic and speculum examinations with fear, anxiety, embarrassment, discomfort, and pain,” Dr. Simon emphasized. “Girls and women with a history of sexual violence may be more vulnerable to these harms. In addition, adolescent girls may delay starting contraception use or obtaining screening for sexually transmitted infections because of fear of pelvic examination, which thus creates unnecessary barriers to obtaining important screening and family-planning methods.”
The researchers also found that 19% of young women, about 2.2 million, had received a Pap test in the previous year. The majority of these (72%) likely were unnecessary, they wrote, explaining that cervical cancer screening is not recommended for those younger than 21 years unless they are HIV positive and sexually active.
“Because HIV infection status is not available in the NSFG, we estimated prevalence of Pap tests performed as part of a routine examination and considered them potentially unnecessary,” the authors explained.
Young women were seven times more likely to have undergone a bimanual pelvic exam if they received a Pap test (adjusted prevalence ratio [aPR], 7.12). In fact, the authors reported that nearly all potentially unnecessary bimanual pelvic exams (98%) occurred during the same visit as a Pap test that was potentially unnecessary as well.
Young women also were more likely to receive a bimanual pelvic exam if they underwent STI testing or used any hormonal contraception besides an IUD (aPR, 1.6 and 1.31, respectively). Those with public insurance or no insurance were less likely to receive a pelvic exam compared with those who had private insurance, although no associations were found with race/ethnicity.
Young women were about four times more likely to have a Pap test if they had STI testing (aPR, 3.77). Odds of a Pap test also were greater among those aged 18-20 years (aPR, 1.54), those with a pregnancy (aPR, 2.31), those with an IUD (aPR, 1.54), and those using any non-IUD hormonal contraception (aPR, 1.75).
Staying up to date on current guidelines and consistently delivering evidence-based care according to those guidelines “is not easy,” Dr. Simon commented. It involves building and maintaining a trusting clinician-patient relationship that centers on shared decision making, keeping up with research, and “unlearn[ing] deeply ingrained practices,” which is difficult.
“Clinicians are not well instructed on how to pivot or unlearn a practice,” Dr. Simon continued. “The science of deimplementation, especially with respect to guideline-concordant care, is in its infancy.” She also noted the value of annual visits, even without routine pelvic exams.
“Rethinking the goals of the annual health examination for young women and learning to unlearn will not put anyone out of business,” Dr. Simon concluded. “Rather, change can increase patients’ connectivity, trust, and engagement with primary care clinicians and, most importantly, avoid harms, especially to those who are most vulnerable.”
No external funding was used. The study authors and Dr. Simon have disclosed no relevant financial relationships.
SOURCE: Qin J et al. JAMA Intern Med. 2019 Jan 6. doi: 10.1001/jamainternmed.2019.5727.
An earlier version of this story appeared on Medscape.com.
A call for shared decision making
The experts who wrote American College of Obstetricians and Gynecologists’ clinical guideline on the pelvic exam (Obstet Gynecol. 2018 Oct;132[4]:e174-80) reviewed available evidence and found insufficient evidence to support routine screening for asymptomatic nonpregnant women who have no increased risk for specific gynecologic conditions (e.g., history of gynecologic cancer). Hence, ACOG recommends routine screening based on a shared decision between the asymptomatic woman and her doctor keeping in mind her medical and family history and her preference. This decision should be made after reviewing the limitations of the exam with regard to insufficient evidence to support its accuracy in screening for ovarian cancer, bacterial vaginosis, trichomoniasis, and genital herpes, plus lack of evidence for other gynecologic conditions.
In addition, we physicians must educate women, especially vulnerable populations, that deferring a pelvic exam for asymptomatic women entails judicious care. Deferring an exam does not mean that we are withholding medical care. If she wants an exam, understanding its limitations, then this preference is an indication itself for the exam as stated in our guideline.
It is important to emphasize to patients that we are deferring Pap smears until age 21 years per ACOG and the American Society for Colposcopy and Cervical Pathology, and that there is no need for a pelvic exam for sexually transmitted infection screening per the Centers for Disease Control and Prevention. Likewise, there is no need for a pelvic exam prior initiation of contraception except for intrauterine device insertion also according to the CDC.
Catherine Cansino, MD, MPH , is associate clinical professor of obstetrics and gynecology at the University of California, Davis. She was asked to comment on the Qin et al. article. Dr. Cansino is a coauthor of the ACOG 2018 guideline on the utility of pelvic exam. She also is a member of the Ob.Gyn. News editorial advisory board. She reported no relevant financial disclosures.
A call for shared decision making
The experts who wrote American College of Obstetricians and Gynecologists’ clinical guideline on the pelvic exam (Obstet Gynecol. 2018 Oct;132[4]:e174-80) reviewed available evidence and found insufficient evidence to support routine screening for asymptomatic nonpregnant women who have no increased risk for specific gynecologic conditions (e.g., history of gynecologic cancer). Hence, ACOG recommends routine screening based on a shared decision between the asymptomatic woman and her doctor keeping in mind her medical and family history and her preference. This decision should be made after reviewing the limitations of the exam with regard to insufficient evidence to support its accuracy in screening for ovarian cancer, bacterial vaginosis, trichomoniasis, and genital herpes, plus lack of evidence for other gynecologic conditions.
In addition, we physicians must educate women, especially vulnerable populations, that deferring a pelvic exam for asymptomatic women entails judicious care. Deferring an exam does not mean that we are withholding medical care. If she wants an exam, understanding its limitations, then this preference is an indication itself for the exam as stated in our guideline.
It is important to emphasize to patients that we are deferring Pap smears until age 21 years per ACOG and the American Society for Colposcopy and Cervical Pathology, and that there is no need for a pelvic exam for sexually transmitted infection screening per the Centers for Disease Control and Prevention. Likewise, there is no need for a pelvic exam prior initiation of contraception except for intrauterine device insertion also according to the CDC.
Catherine Cansino, MD, MPH , is associate clinical professor of obstetrics and gynecology at the University of California, Davis. She was asked to comment on the Qin et al. article. Dr. Cansino is a coauthor of the ACOG 2018 guideline on the utility of pelvic exam. She also is a member of the Ob.Gyn. News editorial advisory board. She reported no relevant financial disclosures.
A call for shared decision making
The experts who wrote American College of Obstetricians and Gynecologists’ clinical guideline on the pelvic exam (Obstet Gynecol. 2018 Oct;132[4]:e174-80) reviewed available evidence and found insufficient evidence to support routine screening for asymptomatic nonpregnant women who have no increased risk for specific gynecologic conditions (e.g., history of gynecologic cancer). Hence, ACOG recommends routine screening based on a shared decision between the asymptomatic woman and her doctor keeping in mind her medical and family history and her preference. This decision should be made after reviewing the limitations of the exam with regard to insufficient evidence to support its accuracy in screening for ovarian cancer, bacterial vaginosis, trichomoniasis, and genital herpes, plus lack of evidence for other gynecologic conditions.
In addition, we physicians must educate women, especially vulnerable populations, that deferring a pelvic exam for asymptomatic women entails judicious care. Deferring an exam does not mean that we are withholding medical care. If she wants an exam, understanding its limitations, then this preference is an indication itself for the exam as stated in our guideline.
It is important to emphasize to patients that we are deferring Pap smears until age 21 years per ACOG and the American Society for Colposcopy and Cervical Pathology, and that there is no need for a pelvic exam for sexually transmitted infection screening per the Centers for Disease Control and Prevention. Likewise, there is no need for a pelvic exam prior initiation of contraception except for intrauterine device insertion also according to the CDC.
Catherine Cansino, MD, MPH , is associate clinical professor of obstetrics and gynecology at the University of California, Davis. She was asked to comment on the Qin et al. article. Dr. Cansino is a coauthor of the ACOG 2018 guideline on the utility of pelvic exam. She also is a member of the Ob.Gyn. News editorial advisory board. She reported no relevant financial disclosures.
according to estimates from a study published online in JAMA Internal Medicine.
Approximately 2.6 million young women – about a quarter of those in this age group – reported receiving a pelvic exam in the previous year even though fewer than 10% were pregnant or receiving treatment for a sexually transmitted infection (STI) at the time.
Similarly, an estimated three in four Pap tests given to women aged 15-20 years likely were unnecessary. Based on Medicare payments for screening Pap tests and pelvic exams, the unnecessary procedures represented an estimated $123 million in a year.
“The American College of Obstetricians and Gynecologists recognizes that no evidence supports routine speculum examination or BPE in healthy, asymptomatic women younger than 21 years and recommends that these examinations be performed only when medically indicated,” said Jin Qin, ScD, of the Centers for Disease Control and Prevention and colleagues.
“Our results showed that, despite the recommendation, many young women without discernible medical indication received potentially unnecessary BPE or Pap tests, which may be a reflection of a long-standing clinical practice in the United States.”
These findings “demonstrate what happens to vulnerable populations (in this case, girls and young women) when clinicians do not keep up with or do not adhere to new guidelines,” Melissa A. Simon, MD, MPH, wrote in an invited commentary. She acknowledged the challenges of keeping up with new guidelines but noted the potential for harm from unnecessary screening. Dr. Simon is vice chair for clinical research in the department of obstetrics and gynecology at Northwestern University, Chicago.
The researchers analyzed responses from 3,410 young women aged 15-20 years in the National Survey of Family Growth (NSFG) during 2011-2017 and extrapolated the results to estimate nationwide statistics. The researchers found that 23% of young women – 2.6 million in the United States – had received a bimanual pelvic exam during the previous year.
“This analysis focused on the bimanual component of the pelvic examination because it is the most invasive of the pelvic examination components and less likely to be confused with a speculum examination for cervical cancer or STI screening,” the authors note.
More than half of these pelvic exams (54%) – an estimated 1.4 million exams – potentially were unnecessary. The authors classified these pelvic exams as potentially unnecessary if it was not indicated for pregnancy, intrauterine device (IUD) use, or STI treatment in the past 12 months or for another medical problem.
Among the respondents, 5% were pregnant, 22% had been tested for an STI, and 5% had been treated for an STI during the previous year. About a third of respondents (33%) had used at least one type of hormonal contraception besides an IUD in the past year, but only 2% had used an IUD.
Dr. Simon said that some have advocated for routine bimanual pelvic exams to prompt women to see their provider every year, but without evidence to support the practice.
“In fact, many women (younger and older) associate the bimanual pelvic and speculum examinations with fear, anxiety, embarrassment, discomfort, and pain,” Dr. Simon emphasized. “Girls and women with a history of sexual violence may be more vulnerable to these harms. In addition, adolescent girls may delay starting contraception use or obtaining screening for sexually transmitted infections because of fear of pelvic examination, which thus creates unnecessary barriers to obtaining important screening and family-planning methods.”
The researchers also found that 19% of young women, about 2.2 million, had received a Pap test in the previous year. The majority of these (72%) likely were unnecessary, they wrote, explaining that cervical cancer screening is not recommended for those younger than 21 years unless they are HIV positive and sexually active.
“Because HIV infection status is not available in the NSFG, we estimated prevalence of Pap tests performed as part of a routine examination and considered them potentially unnecessary,” the authors explained.
Young women were seven times more likely to have undergone a bimanual pelvic exam if they received a Pap test (adjusted prevalence ratio [aPR], 7.12). In fact, the authors reported that nearly all potentially unnecessary bimanual pelvic exams (98%) occurred during the same visit as a Pap test that was potentially unnecessary as well.
Young women also were more likely to receive a bimanual pelvic exam if they underwent STI testing or used any hormonal contraception besides an IUD (aPR, 1.6 and 1.31, respectively). Those with public insurance or no insurance were less likely to receive a pelvic exam compared with those who had private insurance, although no associations were found with race/ethnicity.
Young women were about four times more likely to have a Pap test if they had STI testing (aPR, 3.77). Odds of a Pap test also were greater among those aged 18-20 years (aPR, 1.54), those with a pregnancy (aPR, 2.31), those with an IUD (aPR, 1.54), and those using any non-IUD hormonal contraception (aPR, 1.75).
Staying up to date on current guidelines and consistently delivering evidence-based care according to those guidelines “is not easy,” Dr. Simon commented. It involves building and maintaining a trusting clinician-patient relationship that centers on shared decision making, keeping up with research, and “unlearn[ing] deeply ingrained practices,” which is difficult.
“Clinicians are not well instructed on how to pivot or unlearn a practice,” Dr. Simon continued. “The science of deimplementation, especially with respect to guideline-concordant care, is in its infancy.” She also noted the value of annual visits, even without routine pelvic exams.
“Rethinking the goals of the annual health examination for young women and learning to unlearn will not put anyone out of business,” Dr. Simon concluded. “Rather, change can increase patients’ connectivity, trust, and engagement with primary care clinicians and, most importantly, avoid harms, especially to those who are most vulnerable.”
No external funding was used. The study authors and Dr. Simon have disclosed no relevant financial relationships.
SOURCE: Qin J et al. JAMA Intern Med. 2019 Jan 6. doi: 10.1001/jamainternmed.2019.5727.
An earlier version of this story appeared on Medscape.com.
according to estimates from a study published online in JAMA Internal Medicine.
Approximately 2.6 million young women – about a quarter of those in this age group – reported receiving a pelvic exam in the previous year even though fewer than 10% were pregnant or receiving treatment for a sexually transmitted infection (STI) at the time.
Similarly, an estimated three in four Pap tests given to women aged 15-20 years likely were unnecessary. Based on Medicare payments for screening Pap tests and pelvic exams, the unnecessary procedures represented an estimated $123 million in a year.
“The American College of Obstetricians and Gynecologists recognizes that no evidence supports routine speculum examination or BPE in healthy, asymptomatic women younger than 21 years and recommends that these examinations be performed only when medically indicated,” said Jin Qin, ScD, of the Centers for Disease Control and Prevention and colleagues.
“Our results showed that, despite the recommendation, many young women without discernible medical indication received potentially unnecessary BPE or Pap tests, which may be a reflection of a long-standing clinical practice in the United States.”
These findings “demonstrate what happens to vulnerable populations (in this case, girls and young women) when clinicians do not keep up with or do not adhere to new guidelines,” Melissa A. Simon, MD, MPH, wrote in an invited commentary. She acknowledged the challenges of keeping up with new guidelines but noted the potential for harm from unnecessary screening. Dr. Simon is vice chair for clinical research in the department of obstetrics and gynecology at Northwestern University, Chicago.
The researchers analyzed responses from 3,410 young women aged 15-20 years in the National Survey of Family Growth (NSFG) during 2011-2017 and extrapolated the results to estimate nationwide statistics. The researchers found that 23% of young women – 2.6 million in the United States – had received a bimanual pelvic exam during the previous year.
“This analysis focused on the bimanual component of the pelvic examination because it is the most invasive of the pelvic examination components and less likely to be confused with a speculum examination for cervical cancer or STI screening,” the authors note.
More than half of these pelvic exams (54%) – an estimated 1.4 million exams – potentially were unnecessary. The authors classified these pelvic exams as potentially unnecessary if it was not indicated for pregnancy, intrauterine device (IUD) use, or STI treatment in the past 12 months or for another medical problem.
Among the respondents, 5% were pregnant, 22% had been tested for an STI, and 5% had been treated for an STI during the previous year. About a third of respondents (33%) had used at least one type of hormonal contraception besides an IUD in the past year, but only 2% had used an IUD.
Dr. Simon said that some have advocated for routine bimanual pelvic exams to prompt women to see their provider every year, but without evidence to support the practice.
“In fact, many women (younger and older) associate the bimanual pelvic and speculum examinations with fear, anxiety, embarrassment, discomfort, and pain,” Dr. Simon emphasized. “Girls and women with a history of sexual violence may be more vulnerable to these harms. In addition, adolescent girls may delay starting contraception use or obtaining screening for sexually transmitted infections because of fear of pelvic examination, which thus creates unnecessary barriers to obtaining important screening and family-planning methods.”
The researchers also found that 19% of young women, about 2.2 million, had received a Pap test in the previous year. The majority of these (72%) likely were unnecessary, they wrote, explaining that cervical cancer screening is not recommended for those younger than 21 years unless they are HIV positive and sexually active.
“Because HIV infection status is not available in the NSFG, we estimated prevalence of Pap tests performed as part of a routine examination and considered them potentially unnecessary,” the authors explained.
Young women were seven times more likely to have undergone a bimanual pelvic exam if they received a Pap test (adjusted prevalence ratio [aPR], 7.12). In fact, the authors reported that nearly all potentially unnecessary bimanual pelvic exams (98%) occurred during the same visit as a Pap test that was potentially unnecessary as well.
Young women also were more likely to receive a bimanual pelvic exam if they underwent STI testing or used any hormonal contraception besides an IUD (aPR, 1.6 and 1.31, respectively). Those with public insurance or no insurance were less likely to receive a pelvic exam compared with those who had private insurance, although no associations were found with race/ethnicity.
Young women were about four times more likely to have a Pap test if they had STI testing (aPR, 3.77). Odds of a Pap test also were greater among those aged 18-20 years (aPR, 1.54), those with a pregnancy (aPR, 2.31), those with an IUD (aPR, 1.54), and those using any non-IUD hormonal contraception (aPR, 1.75).
Staying up to date on current guidelines and consistently delivering evidence-based care according to those guidelines “is not easy,” Dr. Simon commented. It involves building and maintaining a trusting clinician-patient relationship that centers on shared decision making, keeping up with research, and “unlearn[ing] deeply ingrained practices,” which is difficult.
“Clinicians are not well instructed on how to pivot or unlearn a practice,” Dr. Simon continued. “The science of deimplementation, especially with respect to guideline-concordant care, is in its infancy.” She also noted the value of annual visits, even without routine pelvic exams.
“Rethinking the goals of the annual health examination for young women and learning to unlearn will not put anyone out of business,” Dr. Simon concluded. “Rather, change can increase patients’ connectivity, trust, and engagement with primary care clinicians and, most importantly, avoid harms, especially to those who are most vulnerable.”
No external funding was used. The study authors and Dr. Simon have disclosed no relevant financial relationships.
SOURCE: Qin J et al. JAMA Intern Med. 2019 Jan 6. doi: 10.1001/jamainternmed.2019.5727.
An earlier version of this story appeared on Medscape.com.
Pediatricians take on more mental health care
Assessment and treatment of many of the more common behavioral disorders in childhood, such as ADHD and anxiety, should be considered within a pediatrician’s scope of practice, a stance made very clear by a recent policy statement published by the American Academy of Pediatrics entitled “Mental health competencies for pediatric practice.”1 These competencies include medication treatment. As stated in the article, “certain disorders (ADHD, common anxiety disorders, depression), if associated with no more than moderate impairment, are amenable to primary care medication management because there are indicated medications with a well-established safety profile.”
This shift to shared ownership when it comes to mental health care is likely coming from multiple sources, not the least of them being necessity and an acknowledgment that there simply aren’t enough psychiatrists to take over the mental health care of every youth with a diagnosable psychiatric disorder. While the number of child and adolescent psychiatrists remains relatively flat, the youth suicide rate is rising, as are the numbers presenting to emergency departments in crisis – all for reasons still to be fully understood. And these trends all are occurring as the medical community overall is appreciating more and more that good mental health is a cornerstone of all health.
The response from the pediatric community, whether it be because of personal conviction or simply a lack of options, largely has been to step up to the plate and take on these new responsibilities and challenges while trying to get up to speed with the latest information about mental health best practices. From my own experience doing evaluations and consultations from area primary care clinicians for over 15 years, the shift is noticeable. The typical patient now coming in has already seen a mental health counselor and tried at least one medication, while evaluations for diagnosis and treatment recommendations for things like uncomplicated and treatment-naive ADHD symptoms, for example, are becoming much more infrequent – although still far from extinct.
Nevertheless, there remain concerns about the extent of these new charges. Joe Nasca, MD, an experienced pediatrician who has been practicing in rural Vermont for decades, is worried that there is simply too much already for pediatricians to know and do to be able to add extensive mental health care. “There is so much to know in general peds [pediatrics] that I would guess a year or more of additional residency and experience would adequately prepare me to take this on,” he said in an interview. In comparing psychiatric care to other specialties, Dr. Nasca went on to say that, “I would not presume to treat chronic renal failure without the help of a nephrologist or a dilated aortic arch without a cardiologist.”
In a similar vein, however, it also is true that a significant percentage of children presenting to pediatricians for orthopedic problems, infections, asthma, and rashes are managed without referrals to specialists. The right balance, of course, will vary from clinician to clinician based on that pediatrician’s level of interest, experience, and available resources in the community. The AAP position papers don’t mandate or even encourage the notion that all pediatricians need to be at the same place when it comes to competency in assessment and treatment of mental health problems, although it is probably fair to say that there is a push for the pediatric community as a whole to raise the collective bar at least a notch or two.
In response, the mental health community has moved to support the primary care community in their expanded role. These efforts have taken many forms, most notably the model of integrated care, in which mental health clinicians of various types see patients in primary care offices rather than making patients come to them. There also are new consultation programs that provide easy access to a child psychiatrist or other mental health professional for case-related questions delivered by phone, email, or for single in-person consultations. Additional training and educational offerings also are now available for pediatricians either in training and for those already in practice. These initiatives are bolstered by research showing that, not only can good mental health care be delivered in pediatric settings, but there are cost savings that can be realized, particularly for nonpsychiatric medical care.2 Despite these promising leads, however, there will remain some for whom anything less than the increased availability of a psychiatrist to “take over” a patient’s mental health care will be seen as a falling short of the clinical need.
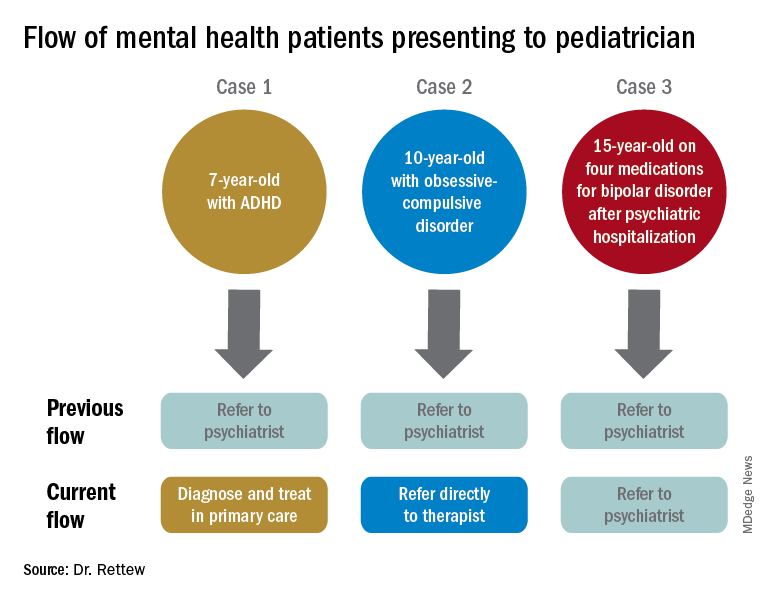
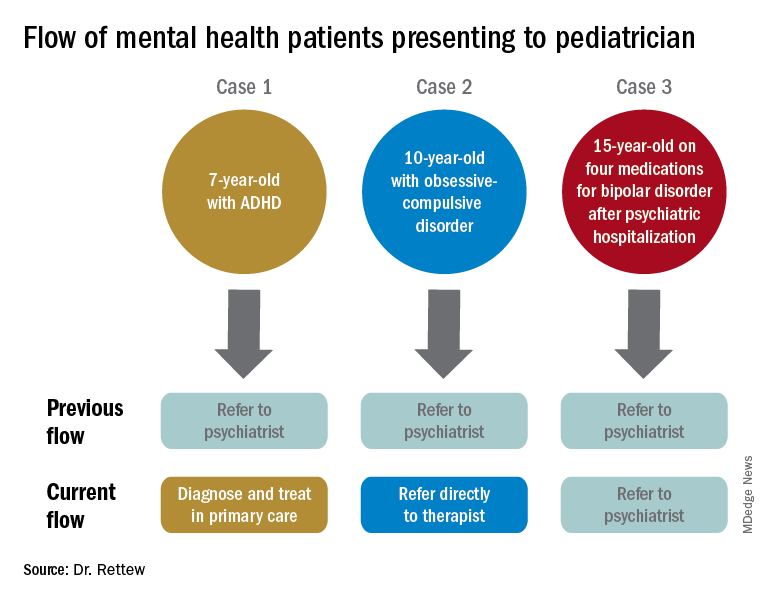
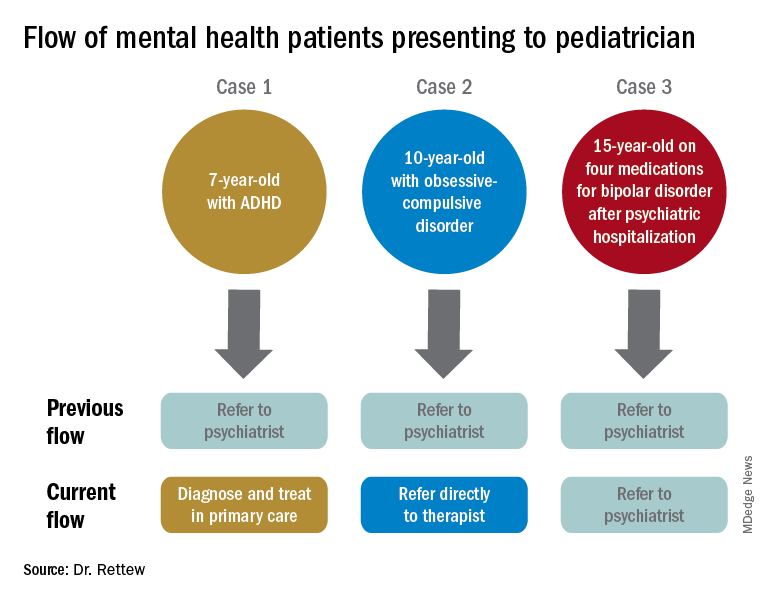
To illustrate how things have and continue to change, consider the following three common clinical scenarios that generally present to a pediatrician:
- New presentation of ADHD symptoms.
- Anxiety or obsessive-compulsive problems.
- Return of a patient who has been psychiatrically hospitalized and now is taking multiple medications.
In the past, all three cases often would have resulted in a referral to a psychiatrist. Today, however, it is quite likely that only one of these cases would be referred because ADHD could be well diagnosed and managed within the primary care setting, and problems like anxiety and obsessive-compulsive disorder are sent first not to a psychiatrist but to a non-MD psychotherapist.
Moving forward, today’s pediatricians are expected to do more for the mental health care of patients themselves instead of referring to a psychiatrist. Most already do, despite having had little in the way of formal training. As the evidence grows that the promotion of mental well-being can be a key to future overall health, as well as to the cost of future health care, there are many reasons to be optimistic that support for pediatricians and collaborative care models for clinicians trying to fulfill these new responsibilities will get only stronger.
References
1. Pediatrics. 2019 Nov;144(5). pii: e20192757.
2. Pediatrics. 2019 Jul;144(1). pii: e20183243.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Follow him on Twitter @PediPsych. Email him at pdnews@mdedge.com. Looking for more mental health training? Attend the 14th annual Child Psychiatry in Primary Care conference in Burlington on May 8, 2020 (http://www.med.uvm.edu/cme/conferences).
Assessment and treatment of many of the more common behavioral disorders in childhood, such as ADHD and anxiety, should be considered within a pediatrician’s scope of practice, a stance made very clear by a recent policy statement published by the American Academy of Pediatrics entitled “Mental health competencies for pediatric practice.”1 These competencies include medication treatment. As stated in the article, “certain disorders (ADHD, common anxiety disorders, depression), if associated with no more than moderate impairment, are amenable to primary care medication management because there are indicated medications with a well-established safety profile.”
This shift to shared ownership when it comes to mental health care is likely coming from multiple sources, not the least of them being necessity and an acknowledgment that there simply aren’t enough psychiatrists to take over the mental health care of every youth with a diagnosable psychiatric disorder. While the number of child and adolescent psychiatrists remains relatively flat, the youth suicide rate is rising, as are the numbers presenting to emergency departments in crisis – all for reasons still to be fully understood. And these trends all are occurring as the medical community overall is appreciating more and more that good mental health is a cornerstone of all health.
The response from the pediatric community, whether it be because of personal conviction or simply a lack of options, largely has been to step up to the plate and take on these new responsibilities and challenges while trying to get up to speed with the latest information about mental health best practices. From my own experience doing evaluations and consultations from area primary care clinicians for over 15 years, the shift is noticeable. The typical patient now coming in has already seen a mental health counselor and tried at least one medication, while evaluations for diagnosis and treatment recommendations for things like uncomplicated and treatment-naive ADHD symptoms, for example, are becoming much more infrequent – although still far from extinct.
Nevertheless, there remain concerns about the extent of these new charges. Joe Nasca, MD, an experienced pediatrician who has been practicing in rural Vermont for decades, is worried that there is simply too much already for pediatricians to know and do to be able to add extensive mental health care. “There is so much to know in general peds [pediatrics] that I would guess a year or more of additional residency and experience would adequately prepare me to take this on,” he said in an interview. In comparing psychiatric care to other specialties, Dr. Nasca went on to say that, “I would not presume to treat chronic renal failure without the help of a nephrologist or a dilated aortic arch without a cardiologist.”
In a similar vein, however, it also is true that a significant percentage of children presenting to pediatricians for orthopedic problems, infections, asthma, and rashes are managed without referrals to specialists. The right balance, of course, will vary from clinician to clinician based on that pediatrician’s level of interest, experience, and available resources in the community. The AAP position papers don’t mandate or even encourage the notion that all pediatricians need to be at the same place when it comes to competency in assessment and treatment of mental health problems, although it is probably fair to say that there is a push for the pediatric community as a whole to raise the collective bar at least a notch or two.
In response, the mental health community has moved to support the primary care community in their expanded role. These efforts have taken many forms, most notably the model of integrated care, in which mental health clinicians of various types see patients in primary care offices rather than making patients come to them. There also are new consultation programs that provide easy access to a child psychiatrist or other mental health professional for case-related questions delivered by phone, email, or for single in-person consultations. Additional training and educational offerings also are now available for pediatricians either in training and for those already in practice. These initiatives are bolstered by research showing that, not only can good mental health care be delivered in pediatric settings, but there are cost savings that can be realized, particularly for nonpsychiatric medical care.2 Despite these promising leads, however, there will remain some for whom anything less than the increased availability of a psychiatrist to “take over” a patient’s mental health care will be seen as a falling short of the clinical need.
To illustrate how things have and continue to change, consider the following three common clinical scenarios that generally present to a pediatrician:
- New presentation of ADHD symptoms.
- Anxiety or obsessive-compulsive problems.
- Return of a patient who has been psychiatrically hospitalized and now is taking multiple medications.
In the past, all three cases often would have resulted in a referral to a psychiatrist. Today, however, it is quite likely that only one of these cases would be referred because ADHD could be well diagnosed and managed within the primary care setting, and problems like anxiety and obsessive-compulsive disorder are sent first not to a psychiatrist but to a non-MD psychotherapist.
Moving forward, today’s pediatricians are expected to do more for the mental health care of patients themselves instead of referring to a psychiatrist. Most already do, despite having had little in the way of formal training. As the evidence grows that the promotion of mental well-being can be a key to future overall health, as well as to the cost of future health care, there are many reasons to be optimistic that support for pediatricians and collaborative care models for clinicians trying to fulfill these new responsibilities will get only stronger.
References
1. Pediatrics. 2019 Nov;144(5). pii: e20192757.
2. Pediatrics. 2019 Jul;144(1). pii: e20183243.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Follow him on Twitter @PediPsych. Email him at pdnews@mdedge.com. Looking for more mental health training? Attend the 14th annual Child Psychiatry in Primary Care conference in Burlington on May 8, 2020 (http://www.med.uvm.edu/cme/conferences).
Assessment and treatment of many of the more common behavioral disorders in childhood, such as ADHD and anxiety, should be considered within a pediatrician’s scope of practice, a stance made very clear by a recent policy statement published by the American Academy of Pediatrics entitled “Mental health competencies for pediatric practice.”1 These competencies include medication treatment. As stated in the article, “certain disorders (ADHD, common anxiety disorders, depression), if associated with no more than moderate impairment, are amenable to primary care medication management because there are indicated medications with a well-established safety profile.”
This shift to shared ownership when it comes to mental health care is likely coming from multiple sources, not the least of them being necessity and an acknowledgment that there simply aren’t enough psychiatrists to take over the mental health care of every youth with a diagnosable psychiatric disorder. While the number of child and adolescent psychiatrists remains relatively flat, the youth suicide rate is rising, as are the numbers presenting to emergency departments in crisis – all for reasons still to be fully understood. And these trends all are occurring as the medical community overall is appreciating more and more that good mental health is a cornerstone of all health.
The response from the pediatric community, whether it be because of personal conviction or simply a lack of options, largely has been to step up to the plate and take on these new responsibilities and challenges while trying to get up to speed with the latest information about mental health best practices. From my own experience doing evaluations and consultations from area primary care clinicians for over 15 years, the shift is noticeable. The typical patient now coming in has already seen a mental health counselor and tried at least one medication, while evaluations for diagnosis and treatment recommendations for things like uncomplicated and treatment-naive ADHD symptoms, for example, are becoming much more infrequent – although still far from extinct.
Nevertheless, there remain concerns about the extent of these new charges. Joe Nasca, MD, an experienced pediatrician who has been practicing in rural Vermont for decades, is worried that there is simply too much already for pediatricians to know and do to be able to add extensive mental health care. “There is so much to know in general peds [pediatrics] that I would guess a year or more of additional residency and experience would adequately prepare me to take this on,” he said in an interview. In comparing psychiatric care to other specialties, Dr. Nasca went on to say that, “I would not presume to treat chronic renal failure without the help of a nephrologist or a dilated aortic arch without a cardiologist.”
In a similar vein, however, it also is true that a significant percentage of children presenting to pediatricians for orthopedic problems, infections, asthma, and rashes are managed without referrals to specialists. The right balance, of course, will vary from clinician to clinician based on that pediatrician’s level of interest, experience, and available resources in the community. The AAP position papers don’t mandate or even encourage the notion that all pediatricians need to be at the same place when it comes to competency in assessment and treatment of mental health problems, although it is probably fair to say that there is a push for the pediatric community as a whole to raise the collective bar at least a notch or two.
In response, the mental health community has moved to support the primary care community in their expanded role. These efforts have taken many forms, most notably the model of integrated care, in which mental health clinicians of various types see patients in primary care offices rather than making patients come to them. There also are new consultation programs that provide easy access to a child psychiatrist or other mental health professional for case-related questions delivered by phone, email, or for single in-person consultations. Additional training and educational offerings also are now available for pediatricians either in training and for those already in practice. These initiatives are bolstered by research showing that, not only can good mental health care be delivered in pediatric settings, but there are cost savings that can be realized, particularly for nonpsychiatric medical care.2 Despite these promising leads, however, there will remain some for whom anything less than the increased availability of a psychiatrist to “take over” a patient’s mental health care will be seen as a falling short of the clinical need.
To illustrate how things have and continue to change, consider the following three common clinical scenarios that generally present to a pediatrician:
- New presentation of ADHD symptoms.
- Anxiety or obsessive-compulsive problems.
- Return of a patient who has been psychiatrically hospitalized and now is taking multiple medications.
In the past, all three cases often would have resulted in a referral to a psychiatrist. Today, however, it is quite likely that only one of these cases would be referred because ADHD could be well diagnosed and managed within the primary care setting, and problems like anxiety and obsessive-compulsive disorder are sent first not to a psychiatrist but to a non-MD psychotherapist.
Moving forward, today’s pediatricians are expected to do more for the mental health care of patients themselves instead of referring to a psychiatrist. Most already do, despite having had little in the way of formal training. As the evidence grows that the promotion of mental well-being can be a key to future overall health, as well as to the cost of future health care, there are many reasons to be optimistic that support for pediatricians and collaborative care models for clinicians trying to fulfill these new responsibilities will get only stronger.
References
1. Pediatrics. 2019 Nov;144(5). pii: e20192757.
2. Pediatrics. 2019 Jul;144(1). pii: e20183243.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Follow him on Twitter @PediPsych. Email him at pdnews@mdedge.com. Looking for more mental health training? Attend the 14th annual Child Psychiatry in Primary Care conference in Burlington on May 8, 2020 (http://www.med.uvm.edu/cme/conferences).
Standards for health claims in advertisements need to go up
Three months is how long I’ll leave a magazine out in my waiting room. When its lobby lifespan is up, I’ll usually recycle it, though sometimes will take it home to read myself when I have down time.
Leafing through an accumulated pile of them over the recent holiday break, I was struck by how many carry ads for questionable “cures”: magnetic bracelets for headaches, copper-based topical creams that claim to cure diabetic neuropathy. Another was from a company with something that looks like a standard tanning bed advertising that it has special lights to “alternatively treat cancer.”
How on Earth is this legal?
Seriously. Since college I’ve been through 4 years of medical school, another 5 combined of residency and fellowship, and now 21 years of frontline neurology experience. And if, after all that, I were to start marketing such horse hockey as a cure for anything (besides my wallet), I’d be hounded by the Food and Drug Administration and state board and probably driven out of practice.
Yet, people with no “real” (science-based) medical treatment experience are free to market this stuff to a public who, for the most part, don’t have the training, knowledge, or experience to know it’s a crock.
I’m sure some of the people selling this stuff really believe they’re helping. Admittedly, there are a lot of things we don’t know in medicine. But anything that’s making such claims should have real evidence – like a large double-blind, placebo-controlled trial – behind it. Not anecdotal reports, small uncontrolled trials, and patient testimonials. The placebo effect is remarkably strong.
There are also some selling this stuff who are less than scrupulous. They’ll claim to have good intentions, but are well aware they’re bilking people – often desperate – out of their savings. They’re no better than the doctors who make headlines for Medicare and insurance fraud by performing unnecessary surgeries and billing for medications that weren’t given.
Either way, the point is the same. Unproven treatments are just that – unproven – and shouldn’t be marketed as effective ones. If it works, let the evidence prove it. But if it doesn’t, no one should be promoting it to anyone, regardless of how long (and where) they went to school.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Three months is how long I’ll leave a magazine out in my waiting room. When its lobby lifespan is up, I’ll usually recycle it, though sometimes will take it home to read myself when I have down time.
Leafing through an accumulated pile of them over the recent holiday break, I was struck by how many carry ads for questionable “cures”: magnetic bracelets for headaches, copper-based topical creams that claim to cure diabetic neuropathy. Another was from a company with something that looks like a standard tanning bed advertising that it has special lights to “alternatively treat cancer.”
How on Earth is this legal?
Seriously. Since college I’ve been through 4 years of medical school, another 5 combined of residency and fellowship, and now 21 years of frontline neurology experience. And if, after all that, I were to start marketing such horse hockey as a cure for anything (besides my wallet), I’d be hounded by the Food and Drug Administration and state board and probably driven out of practice.
Yet, people with no “real” (science-based) medical treatment experience are free to market this stuff to a public who, for the most part, don’t have the training, knowledge, or experience to know it’s a crock.
I’m sure some of the people selling this stuff really believe they’re helping. Admittedly, there are a lot of things we don’t know in medicine. But anything that’s making such claims should have real evidence – like a large double-blind, placebo-controlled trial – behind it. Not anecdotal reports, small uncontrolled trials, and patient testimonials. The placebo effect is remarkably strong.
There are also some selling this stuff who are less than scrupulous. They’ll claim to have good intentions, but are well aware they’re bilking people – often desperate – out of their savings. They’re no better than the doctors who make headlines for Medicare and insurance fraud by performing unnecessary surgeries and billing for medications that weren’t given.
Either way, the point is the same. Unproven treatments are just that – unproven – and shouldn’t be marketed as effective ones. If it works, let the evidence prove it. But if it doesn’t, no one should be promoting it to anyone, regardless of how long (and where) they went to school.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Three months is how long I’ll leave a magazine out in my waiting room. When its lobby lifespan is up, I’ll usually recycle it, though sometimes will take it home to read myself when I have down time.
Leafing through an accumulated pile of them over the recent holiday break, I was struck by how many carry ads for questionable “cures”: magnetic bracelets for headaches, copper-based topical creams that claim to cure diabetic neuropathy. Another was from a company with something that looks like a standard tanning bed advertising that it has special lights to “alternatively treat cancer.”
How on Earth is this legal?
Seriously. Since college I’ve been through 4 years of medical school, another 5 combined of residency and fellowship, and now 21 years of frontline neurology experience. And if, after all that, I were to start marketing such horse hockey as a cure for anything (besides my wallet), I’d be hounded by the Food and Drug Administration and state board and probably driven out of practice.
Yet, people with no “real” (science-based) medical treatment experience are free to market this stuff to a public who, for the most part, don’t have the training, knowledge, or experience to know it’s a crock.
I’m sure some of the people selling this stuff really believe they’re helping. Admittedly, there are a lot of things we don’t know in medicine. But anything that’s making such claims should have real evidence – like a large double-blind, placebo-controlled trial – behind it. Not anecdotal reports, small uncontrolled trials, and patient testimonials. The placebo effect is remarkably strong.
There are also some selling this stuff who are less than scrupulous. They’ll claim to have good intentions, but are well aware they’re bilking people – often desperate – out of their savings. They’re no better than the doctors who make headlines for Medicare and insurance fraud by performing unnecessary surgeries and billing for medications that weren’t given.
Either way, the point is the same. Unproven treatments are just that – unproven – and shouldn’t be marketed as effective ones. If it works, let the evidence prove it. But if it doesn’t, no one should be promoting it to anyone, regardless of how long (and where) they went to school.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Letter to the Editor
Editor’s note: This is one of the many emails readers sent to Dermatology News in response to Dr. Alan Rockoff’s last “Under My Skin” column in the December issue.
Dr. Rockoff,
I was deeply heartbroken to read that this would be your last column in Dermatology News today. I am a medical dermatologist with 19 years of experience in a small town in North Carolina and have always looked forward to reading your columns. No matter what the topic for the article you chose, I would always glean something worthwhile from it, be it a poignant insight, a relevant practice tip on treatment or patient management, and nearly always a hearty laugh.
Being somewhat rural and without a lot of competition, my very busy practice consists mainly of salt of the earth patients needing straight dermatologic care, mostly skin cancer, psoriasis, acne, the general stuff. Your ability to capture the essence of what it is like to be one of us in the trenches, to expose and eloquently define the most common and frustrating issues we face, has been a source of pleasure for years. On more than one occasion, I put down the magazine and attempted to write a thank you letter for one article or another you wrote, to say that you are doing a great job and please continue to enlighten us with your insight and that your efforts are greatly valued. I am embarrassed to admit, I never could complete those emails, thinking “Why bother the man? He is clearly as busy as me, and why would he want to hear from me anyway?”
Well, at the risk of bothering you, sir, please do accept my apologies for not writing you before you retired your article, and please know that your articles have personally given me years of immense happiness. They will be sorely missed, and likely not ever replaced.
With gratitude,
Jeff Suchniak, MD
Rocky Mount, N.C.
Editor’s note: This is one of the many emails readers sent to Dermatology News in response to Dr. Alan Rockoff’s last “Under My Skin” column in the December issue.
Dr. Rockoff,
I was deeply heartbroken to read that this would be your last column in Dermatology News today. I am a medical dermatologist with 19 years of experience in a small town in North Carolina and have always looked forward to reading your columns. No matter what the topic for the article you chose, I would always glean something worthwhile from it, be it a poignant insight, a relevant practice tip on treatment or patient management, and nearly always a hearty laugh.
Being somewhat rural and without a lot of competition, my very busy practice consists mainly of salt of the earth patients needing straight dermatologic care, mostly skin cancer, psoriasis, acne, the general stuff. Your ability to capture the essence of what it is like to be one of us in the trenches, to expose and eloquently define the most common and frustrating issues we face, has been a source of pleasure for years. On more than one occasion, I put down the magazine and attempted to write a thank you letter for one article or another you wrote, to say that you are doing a great job and please continue to enlighten us with your insight and that your efforts are greatly valued. I am embarrassed to admit, I never could complete those emails, thinking “Why bother the man? He is clearly as busy as me, and why would he want to hear from me anyway?”
Well, at the risk of bothering you, sir, please do accept my apologies for not writing you before you retired your article, and please know that your articles have personally given me years of immense happiness. They will be sorely missed, and likely not ever replaced.
With gratitude,
Jeff Suchniak, MD
Rocky Mount, N.C.
Editor’s note: This is one of the many emails readers sent to Dermatology News in response to Dr. Alan Rockoff’s last “Under My Skin” column in the December issue.
Dr. Rockoff,
I was deeply heartbroken to read that this would be your last column in Dermatology News today. I am a medical dermatologist with 19 years of experience in a small town in North Carolina and have always looked forward to reading your columns. No matter what the topic for the article you chose, I would always glean something worthwhile from it, be it a poignant insight, a relevant practice tip on treatment or patient management, and nearly always a hearty laugh.
Being somewhat rural and without a lot of competition, my very busy practice consists mainly of salt of the earth patients needing straight dermatologic care, mostly skin cancer, psoriasis, acne, the general stuff. Your ability to capture the essence of what it is like to be one of us in the trenches, to expose and eloquently define the most common and frustrating issues we face, has been a source of pleasure for years. On more than one occasion, I put down the magazine and attempted to write a thank you letter for one article or another you wrote, to say that you are doing a great job and please continue to enlighten us with your insight and that your efforts are greatly valued. I am embarrassed to admit, I never could complete those emails, thinking “Why bother the man? He is clearly as busy as me, and why would he want to hear from me anyway?”
Well, at the risk of bothering you, sir, please do accept my apologies for not writing you before you retired your article, and please know that your articles have personally given me years of immense happiness. They will be sorely missed, and likely not ever replaced.
With gratitude,
Jeff Suchniak, MD
Rocky Mount, N.C.
Big practices outpace small ones in Medicare pay bonuses
More physician practices are earning positive payments under Medicare’s Merit-Based Incentive Payment System, but smaller practices won’t fare quite as well as larger ones in 2020.
Under the Quality Payment Program, 97% of MIPS-eligible clinicians are scheduled to receive an incentive payment this year, based on meeting performance criteria in 2018. That’s up five percentage points from the 2017 performance year, the Centers for Medicare & Medicaid Services reported Jan. 6. But 2% of clinicians will see a negative adjustment for not having met those criteria.
Among small practices, however, the rate of MIPS-eligible clinicians earning a positive payment adjustment in 2020 is about 84%. While lower than the overall rate, that’s still a 10 percentage point improvement from the previous performance year. But 13% of MIPS-eligible clinicians in small practices face a negative adjustment.
The bonus rate among rural practices mirrors the national rate, with more than 97% of rural practices eligible to receive a bonus in 2020. In 2019, 93% of MIPS-eligible clinicians in rural settings received a positive adjustment.
More small and rural practices will see positive payment adjustments in 2020, compared with 2019, CMS Administrator Seema Verma said. “This shows we are making strides toward making MIPS a practical program for every clinician, regardless of size.”
While most clinicians earned a positive adjustment, Ms. Verma acknowledged that the dollar value of the adjustment remains relatively small.
For clinicians who met the exceptional performance criteria for 2020 based on work in 2018, the maximum adjustment will be 1.68%. For those who failed to meet the exceptional performance threshold, the maximum positive adjustment will be 0.2%. The range of negative payment adjustments will be between –0.01% and –5%.
Those positive payment adjustments are modest in part because adjustments overall must be budget neutral, Ms. Verma explained. But CMS expects that to change in future years. As the program matures, increased performance thresholds will shrink distribution of positive payment adjustments for high-performing clinicians. That will lead to larger positive payment adjustments for those who do earn them.
More physician practices are earning positive payments under Medicare’s Merit-Based Incentive Payment System, but smaller practices won’t fare quite as well as larger ones in 2020.
Under the Quality Payment Program, 97% of MIPS-eligible clinicians are scheduled to receive an incentive payment this year, based on meeting performance criteria in 2018. That’s up five percentage points from the 2017 performance year, the Centers for Medicare & Medicaid Services reported Jan. 6. But 2% of clinicians will see a negative adjustment for not having met those criteria.
Among small practices, however, the rate of MIPS-eligible clinicians earning a positive payment adjustment in 2020 is about 84%. While lower than the overall rate, that’s still a 10 percentage point improvement from the previous performance year. But 13% of MIPS-eligible clinicians in small practices face a negative adjustment.
The bonus rate among rural practices mirrors the national rate, with more than 97% of rural practices eligible to receive a bonus in 2020. In 2019, 93% of MIPS-eligible clinicians in rural settings received a positive adjustment.
More small and rural practices will see positive payment adjustments in 2020, compared with 2019, CMS Administrator Seema Verma said. “This shows we are making strides toward making MIPS a practical program for every clinician, regardless of size.”
While most clinicians earned a positive adjustment, Ms. Verma acknowledged that the dollar value of the adjustment remains relatively small.
For clinicians who met the exceptional performance criteria for 2020 based on work in 2018, the maximum adjustment will be 1.68%. For those who failed to meet the exceptional performance threshold, the maximum positive adjustment will be 0.2%. The range of negative payment adjustments will be between –0.01% and –5%.
Those positive payment adjustments are modest in part because adjustments overall must be budget neutral, Ms. Verma explained. But CMS expects that to change in future years. As the program matures, increased performance thresholds will shrink distribution of positive payment adjustments for high-performing clinicians. That will lead to larger positive payment adjustments for those who do earn them.
More physician practices are earning positive payments under Medicare’s Merit-Based Incentive Payment System, but smaller practices won’t fare quite as well as larger ones in 2020.
Under the Quality Payment Program, 97% of MIPS-eligible clinicians are scheduled to receive an incentive payment this year, based on meeting performance criteria in 2018. That’s up five percentage points from the 2017 performance year, the Centers for Medicare & Medicaid Services reported Jan. 6. But 2% of clinicians will see a negative adjustment for not having met those criteria.
Among small practices, however, the rate of MIPS-eligible clinicians earning a positive payment adjustment in 2020 is about 84%. While lower than the overall rate, that’s still a 10 percentage point improvement from the previous performance year. But 13% of MIPS-eligible clinicians in small practices face a negative adjustment.
The bonus rate among rural practices mirrors the national rate, with more than 97% of rural practices eligible to receive a bonus in 2020. In 2019, 93% of MIPS-eligible clinicians in rural settings received a positive adjustment.
More small and rural practices will see positive payment adjustments in 2020, compared with 2019, CMS Administrator Seema Verma said. “This shows we are making strides toward making MIPS a practical program for every clinician, regardless of size.”
While most clinicians earned a positive adjustment, Ms. Verma acknowledged that the dollar value of the adjustment remains relatively small.
For clinicians who met the exceptional performance criteria for 2020 based on work in 2018, the maximum adjustment will be 1.68%. For those who failed to meet the exceptional performance threshold, the maximum positive adjustment will be 0.2%. The range of negative payment adjustments will be between –0.01% and –5%.
Those positive payment adjustments are modest in part because adjustments overall must be budget neutral, Ms. Verma explained. But CMS expects that to change in future years. As the program matures, increased performance thresholds will shrink distribution of positive payment adjustments for high-performing clinicians. That will lead to larger positive payment adjustments for those who do earn them.
Beware the dangers of nerve injury in vaginal surgery
LAS VEGAS – a pelvic surgeon urged colleagues.
“It’s a very high medical and legal risk. You have to think about the various nerves that can be influenced,” urogynecologist Mickey M. Karram, MD, said at the Pelvic Anatomy and Gynecologic Surgery Symposium.
Dr. Karram, director of urogynecology and reconstructive surgery at the Christ Hospital in Cincinnati and clinical professor of obstetrics and gynecology at the University of Cincinnati, offered these pearls:
- Understand the anatomy of nerves at risk. These include the ilioinguinal nerve, obturator neurovascular bundle, and pudendal nerve.
- Position the patient correctly. The buttocks should be at edge of table, Dr. Karram said, and there should be slight extension and lateral rotation of the thigh. Beware of compression of the lateral knee.
- Avoid compression from stirrups. If you still use candy-cane stirrups, he said, you can get compression along the lateral aspect of the knee. “You can [get] common perineal nerve injuries. You can also get femoral nerve injuries that are stretch injuries and over-extension injuries as well. Just be careful about this.” Dr. Karram said he prefers fin-type stirrups such as the Allen Yellofin brand. Also, he said, avoid compression injuries that result when there are too many people between the patient’s legs and someone leans on the thighs, he said.
- Free the retractor in abdominal procedures. “If you’re operating abdominally and use retractors, free the retractor at times,” he said. Otherwise, “you can get injuries to the genitofemoral nerve and the femoral nerve itself.”
- Beware buttock pain after sacrospinous fixation. “About 15%-20% of the time, you’ll get extreme buttock pain,” Dr. Karram said. “Assuming the buttock pain doesn’t radiate anywhere and doesn’t go down the leg, it’s definitely not a problem. If it goes down the leg, then you have to think about things like deligating pretty quickly.”
Dr. Karram disclosed consulting (Coloplast and Cynosure/Hologic) and speaker (Allergan, Astellas, Coloplast, and Cynosure/Hologic) relationships. He has royalties from Fidelis Medical and LumeNXT.
This meeting was jointly provided by Global Academy for Medical Education and the University of Cincinnati. Global Academy and this news organization are owned by the same company.
LAS VEGAS – a pelvic surgeon urged colleagues.
“It’s a very high medical and legal risk. You have to think about the various nerves that can be influenced,” urogynecologist Mickey M. Karram, MD, said at the Pelvic Anatomy and Gynecologic Surgery Symposium.
Dr. Karram, director of urogynecology and reconstructive surgery at the Christ Hospital in Cincinnati and clinical professor of obstetrics and gynecology at the University of Cincinnati, offered these pearls:
- Understand the anatomy of nerves at risk. These include the ilioinguinal nerve, obturator neurovascular bundle, and pudendal nerve.
- Position the patient correctly. The buttocks should be at edge of table, Dr. Karram said, and there should be slight extension and lateral rotation of the thigh. Beware of compression of the lateral knee.
- Avoid compression from stirrups. If you still use candy-cane stirrups, he said, you can get compression along the lateral aspect of the knee. “You can [get] common perineal nerve injuries. You can also get femoral nerve injuries that are stretch injuries and over-extension injuries as well. Just be careful about this.” Dr. Karram said he prefers fin-type stirrups such as the Allen Yellofin brand. Also, he said, avoid compression injuries that result when there are too many people between the patient’s legs and someone leans on the thighs, he said.
- Free the retractor in abdominal procedures. “If you’re operating abdominally and use retractors, free the retractor at times,” he said. Otherwise, “you can get injuries to the genitofemoral nerve and the femoral nerve itself.”
- Beware buttock pain after sacrospinous fixation. “About 15%-20% of the time, you’ll get extreme buttock pain,” Dr. Karram said. “Assuming the buttock pain doesn’t radiate anywhere and doesn’t go down the leg, it’s definitely not a problem. If it goes down the leg, then you have to think about things like deligating pretty quickly.”
Dr. Karram disclosed consulting (Coloplast and Cynosure/Hologic) and speaker (Allergan, Astellas, Coloplast, and Cynosure/Hologic) relationships. He has royalties from Fidelis Medical and LumeNXT.
This meeting was jointly provided by Global Academy for Medical Education and the University of Cincinnati. Global Academy and this news organization are owned by the same company.
LAS VEGAS – a pelvic surgeon urged colleagues.
“It’s a very high medical and legal risk. You have to think about the various nerves that can be influenced,” urogynecologist Mickey M. Karram, MD, said at the Pelvic Anatomy and Gynecologic Surgery Symposium.
Dr. Karram, director of urogynecology and reconstructive surgery at the Christ Hospital in Cincinnati and clinical professor of obstetrics and gynecology at the University of Cincinnati, offered these pearls:
- Understand the anatomy of nerves at risk. These include the ilioinguinal nerve, obturator neurovascular bundle, and pudendal nerve.
- Position the patient correctly. The buttocks should be at edge of table, Dr. Karram said, and there should be slight extension and lateral rotation of the thigh. Beware of compression of the lateral knee.
- Avoid compression from stirrups. If you still use candy-cane stirrups, he said, you can get compression along the lateral aspect of the knee. “You can [get] common perineal nerve injuries. You can also get femoral nerve injuries that are stretch injuries and over-extension injuries as well. Just be careful about this.” Dr. Karram said he prefers fin-type stirrups such as the Allen Yellofin brand. Also, he said, avoid compression injuries that result when there are too many people between the patient’s legs and someone leans on the thighs, he said.
- Free the retractor in abdominal procedures. “If you’re operating abdominally and use retractors, free the retractor at times,” he said. Otherwise, “you can get injuries to the genitofemoral nerve and the femoral nerve itself.”
- Beware buttock pain after sacrospinous fixation. “About 15%-20% of the time, you’ll get extreme buttock pain,” Dr. Karram said. “Assuming the buttock pain doesn’t radiate anywhere and doesn’t go down the leg, it’s definitely not a problem. If it goes down the leg, then you have to think about things like deligating pretty quickly.”
Dr. Karram disclosed consulting (Coloplast and Cynosure/Hologic) and speaker (Allergan, Astellas, Coloplast, and Cynosure/Hologic) relationships. He has royalties from Fidelis Medical and LumeNXT.
This meeting was jointly provided by Global Academy for Medical Education and the University of Cincinnati. Global Academy and this news organization are owned by the same company.
EXPERT ANALYSIS FROM PAGS 2019
Using Democratic Deliberation to Engage Veterans in Complex Policy Making for the Veterans Health Administration
Providing high-quality, patient-centered health care is a top priority for the US Department of Veterans Affairs (VA) Veteran Health Administration (VHA), whose core mission is to improve the health and well-being of US veterans. Thus, news of long wait times for medical appointments in the VHA sparked intense national attention and debate and led to changes in senior management and legislative action. 1 On August 8, 2014, President Bara c k Obama signed the Veterans Access, Choice, and Accountability Act of 2014, also known as the Choice Act, which provided an additional $16 billion in emergency spending over 3 years to improve veterans’ access to timely health care. 2 The Choice Act sought to develop an integrated health care network that allowed qualified VHA patients to receive specific health care services in their communities delivered by non-VHA health care providers (HCPs) but paid for by the VHA. The Choice Act also laid out explicit criteria for how to prioritize who would be eligible for VHA-purchased civilian care: (1) veterans who could not get timely appointments at a VHA medical facility within 30 days of referral; or (2) veterans who lived > 40 miles from the closest VHA medical facility.
VHA decision makers seeking to improve care delivery also need to weigh trade-offs between alternative approaches to providing rapid access. For instance, increasing access to non-VHA HCPs may not always decrease wait times and could result in loss of continuity, limited care coordination, limited ability to ensure and enforce high-quality standards at the VHA, and other challenges.3-6 Although the concerns and views of elected representatives, advocacy groups, and health system leaders are important, it is unknown whether these views and preferences align with those of veterans. Arguably, the range of views and concerns of informed veterans whose health is at stake should be particularly prominent in such policy decision making.
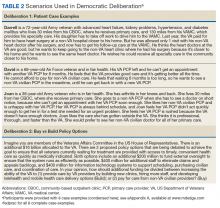
To identify the considerations that were most important to veterans regarding VHA policy around decreasing wait times, a study was designed to engage a group of veterans who were eligible for civilian care under the Choice Act. The study took place 1 year after the Choice Act was passed. Veterans were asked to focus on 2 related questions: First, how should funding be used for building VHA capacity (build) vs purchasing civilian care (buy)? Second, under what circumstances should civilian care be prioritized?
The aim of this paper is to describe democratic deliberation (DD), a specific method that engaged veteran patients in complex policy decisions around access to care. DD methods have been used increasingly in health care for developing policy guidance, setting priorities, providing advice on ethical dilemmas, weighing risk-benefit trade-offs, and determining decision-making authority.7-12 For example, DD helped guide national policy for mammography screening for breast cancer in New Zealand.13 The Agency for Healthcare Research and Quality has completed a systematic review and a large, randomized experiment on best practices for carrying out public deliberation.8,13,14 However, despite the potential value of this approach, there has been little use of deliberative methods within the VHA for the explicit purpose of informing veteran health care delivery.
This paper describes the experience engaging veterans by using DD methodology and informing VHA leadership about the results of those deliberations. The specific aims were to understand whether DD is an acceptable approach to use to engage patients in the medical services policy-making process within VHA and whether veterans are able to come to an informed consensus.
Methods
Engaging patients and incorporating their needs and concerns within the policy-making process may improve health system policies and make those policies more patient centered. Such engagement also could be a way to generate creative solutions. However, because health-system decisions often involve making difficult trade-offs, effectively obtaining patient population input on complex care delivery issues can be challenging.
Although surveys can provide intuitive, top-of-mind input from respondents, these opinions are generally not sufficient for resolving complex problems.15 Focus groups and interviews may produce results that are more in-depth than surveys, but these methods tend to elicit settled private preferences rather than opinions about what the community should do.16 DD, on the other hand, is designed to elicit deeply informed public opinions on complex, value-laden topics to develop recommendations and policies for a larger community.17 The goal is to find collective solutions to challenging social problems. DD achieves this by giving participants an opportunity to explore a topic in-depth, question experts, and engage peers in reason-based discussions.18,19 This method has its roots in political science and has been used over several decades to successfully inform policy making on a broad array of topics nationally and internationally—from health research ethics in the US to nuclear and energy policy in Japan.7,16,20,21 DD has been found to promote ownership of public programs and lend legitimacy to policy decisions, political institutions, and democracy itself.18
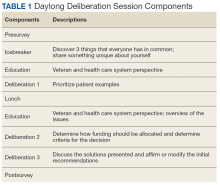
A single day (8 hours) DD session was convened, following a Citizens Jury model of deliberation, which brings veteran patients together to learn about a topic, ask questions of experts, deliberate with peers, and generate a “citizen’s report” that contains a set of recommendations (Table 1). An overview of the different models of DD and rationale for each can be found elsewhere.8,15
Recruitment Considerations
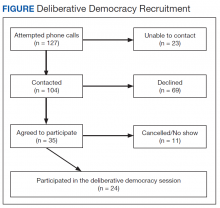
A purposively selected sample of civilian care-eligible veterans from a midwestern VHA health care system (1 medical center and 3 community-based outpatient clinics [CBOCs]) were invited to the DD session. The targeted number of participants was 30. Female veterans, who comprise only 7% of the local veteran population, were oversampled to account for their potentially different health care needs and to create balance between males and females in the session. Oversampling for other characteristics was not possible due to the relatively small sample size. Based on prior experience,7 it was assumed that 70% of willing participants would attend the session; therefore 34 veterans were invited and 24 attended. Each participant received a $200 incentive in appreciation for their substantial time commitment and to offset transportation costs.
Background Materials
A packet with educational materials (Flesch-Kincaid Grade Level of 10.5) was mailed to participants about 2 weeks before the DD session. Participants were asked to review prior to attending the session. These materials described the session (eg, purpose, organizers, importance) and provided factual information about the Choice Act (eg, eligibility, out-of-pocket costs, travel pay, prescription drug policies).
Session Overview
The session was structured to accomplish the following goals: (1) Elicit participants’ opinions about access to health care and reasons for those opinions; (2) Provide in-depth education about the Choice Act through presentations and discussions with topical experts; and (3) Elicit reasoning and recommendations on both the criteria by which participants prioritize candidates for civilian care and how participants would allocate additional funding to improve access (ie, by building VHA capacity to deliver more timely health care vs purchasing health care from civilian HCPs).
Participants were asked to fill out a survey on arrival in the morning and were assigned to 1 of 3 tables or small groups. Each table had a facilitator who had extensive experience in qualitative data collection methods and guided the dialogue using a scripted protocol that they helped develop and refine. The facilitation materials drew from and used previously published studies.22,23 Each facilitator audio recorded the sessions and took notes. Three experts presented during plenary education sessions. Presentations were designed to provide balanced factual information and included a veteran’s perspective. One presenter was a clinician on the project team, another was a local clinical leader responsible for making decisions about what services to provide via civilian care (buy) vs enhancing the local VHA health system’s ability to provide those services (build), and the third presenter was a veteran who was on the project team.
Education Session 1
The first plenary education session with expert presentations was conducted after each table completed an icebreaker exercise. The project team physician provided a brief history and description of the Choice Act to reinforce educational materials sent to participants prior to the session. The health system clinical leader described his decision process and principles and highlighted constraints placed on him by the Choice Act that were in place at the time of the DD session. He also described existing local and national programs to provide civilian care (eg, local fee-basis non-VHA care programs) and how these programs sought to achieve goals similar to the Choice Act. The veteran presenter focused on the importance of session participants providing candid insight and observations and emphasized that this session was a significant opportunity to “have their voices heard.”
Deliberation 1: What criteria should be used to prioritize patients for receiving civilian care paid for by the VHA? To elicit preferences on the central question of this deliberation, participants were presented with 8 real-world cases that were based on interviews conducted with Choice Act-eligible veterans (Table 2 and eAppendices A
Education Session 2
In the second plenary session, the project team physician provided information about health care access issues, both inside and outside of the VHA, particularly between urban and rural areas. He also discussed factors related to the insufficient capacity to meet growing demand that contributed to the VHA wait-time crisis. The veteran presenter shared reflections on health care access from a veteran’s perspective.
Deliberation 2: How should additional funding be divided between increasing the ability of the VHA to (1) provide care by VHA HCPs; and (2) pay for care from non-VHA civilian HCPs? Participants were presented the patient examples and Choice Act funding scenarios (the buy policy option) and contrasted that with a build policy option. Participants were explicitly encouraged to shift their perspectives from thinking about individual cases to considering policy-level decisions and the broader social good (Table 2).
Ensuring Robust Deliberations
If participants do not adequately grasp the complexities of the topic, a deliberation can fail. To facilitate nuanced reasoning, real-world concrete examples were developed as the starting point of each deliberation based on interviews with actual patients (deliberation 1) and actual policy proposals relevant to the funding allocation decisions within the Choice Act (deliberation 2).
A deliberation also can fail with self-silencing, where participants withhold opinions that differ from those articulated first or by more vocal members of the group.24 To combat self-silencing, highly experienced facilitators were used to ensure sharing from all participants and to support an open-minded, courteous, and reason-based environment for discourse. It was specified that the best solutions are achieved through reason-based and cordial disagreement and that success can be undermined when participants simply agree because it is easier or more comfortable.
A third way a deliberation can fail is if individuals do not adopt a group or system-level perspective. To counter this, facilitators reinforced at multiple points the importance of taking a broader social perspective rather than sharing only one’s personal preferences.
Finally, it is important to assess the quality of the deliberative process itself, to ensure that results are trustworthy.25 To assess the quality of the deliberative process, participants knowledge about key issues pre- and postdeliberation were assessed. Participants also were asked to rate the quality of the facilitators and how well they felt their voice was heard and respected, and facilitators made qualitative assessments about the extent to which participants were engaged in reason-based and collaborative discussion.
Data
Quantitative data were collected via pre- and postsession surveys. The surveys contained items related to knowledge about the Choice Act, expectations for the DD session, beliefs and opinions about the provision of health care for veterans, recommended funding allocations between build vs buy policy options, and general demographics. Qualitative data were collected through detailed notes taken by the 3 facilitators. Each table’s deliberations were audio recorded so that gaps in the notes could be filled.
The 3 facilitators, who were all experienced qualitative researchers, typed their written notes into a template immediately after the session. Two of the 3 facilitators led the analysis of the session notes. Findings within and across the 3 deliberation tables were developed using content and matrix analysis methods.26 Descriptive statistics were generated from survey responses and compared survey items pre- and postsession using paired t tests or χ2 tests for categorical responses.
Results
Thirty-three percent of individuals invited (n = 127) agreed to participate. Those who declined cited conflicts related to distance, transportation, work/school, medical appointments, family commitments, or were not interested. In all, 24 (69%) of the 35 veterans who accepted the invitation attended the deliberation session. Of the 11 who accepted but did not attend, 5 cancelled ahead of time because of conflicts (Figure). Most participants were male (70%), 48% were aged 61 to 75 years, 65% were white, 43% had some college education, 43% reported an annual income of between $25,000 and $40,000, and only 35% reported very good health (eAppendix D).
Deliberation 1
During the deliberation on the prioritization criteria, the concept of “condition severity” emerged as an important criterion for veterans. This criterion captured simultaneous consideration of both clinical necessity and burden on the veteran to obtain care. For example, participants felt that patients with a life-threatening illness should be prioritized for civilian care over patients who need preventative or primary care (clinical necessity) and that elderly patients with substantial difficulty traveling to VHA appointments should be prioritized over patients who can travel more easily (burden). The Choice Act regulations at the time of the DD session did not reflect this nuanced perspective, stipulating only that veterans must live > 40 miles from the nearest VHA medical facility.
One of the 3 groups did not prioritize the patient cases because some members felt that no veteran should be constrained from receiving civilian care if they desired it. Nonetheless, this group did agree with prioritizing the first 2 cases in Table 3. The other groups prioritized all 8 cases in generally similar ways.
Deliberation 2
No clear consensus emerged on the buy vs build question. A representative from each table presented their group’s positions, rationale, and recommendations after deliberations were completed. After hearing the range of positions, the groups then had another opportunity to deliberate based on what they heard from the other tables; no new recommendations or consensus emerged.
Participants who were in favor of allocating more funds toward the build policy offered a range of rationales, saying that it would (1) increase access for rural veterans by building CBOCs and deploying more mobile units that could bring outlets for health care closer to their home communities; (2) provide critical and unique medical expertise to address veteran-specific issues such as prosthetics, traumatic brain injury, posttraumatic stress disorder, spinal cord injury, and shrapnel wounds that are typically not available through civilian providers; (3) give VHA more oversight over the quality and cost of care, which is more challenging to do with civilian providers; and (4) Improve VHA infrastructure by, for example, upgrading technology and attracting the best clinicians and staff to support “our VHA.”
Participants who were in favor of allocating more funds toward the buy policy also offered a range of rationales, saying that it would (1) decrease patient burden by increasing access through community providers, decreasing wait time, and lessening personal cost and travel time; (2) allow more patients to receive civilian care, which was generally seen as beneficial by a few participants because of perceptions that the VHA provides lower quality care due to a shortage of VHA providers, run-down/older facilities, lack of technology, and poorer-quality VHA providers; and (3) provide an opportunity to divest of costly facilities and invest in other innovative approaches. Regarding this last reason, a few participants felt that the VHA is “gouged” when building medical centers that overrun budgets. They also were concerned that investing in facilities tied VHA to specific locations when current locations of veterans may change “25 years from now.”
Survey Results
Twenty-three of the 24 participants completed both pre- and postsession surveys. The majority of participants in the session felt people in the group respected their opinion (96%); felt that the facilitator did not try to influence the group with her own opinions (96%); indicated they understood the information enough to participate as much as they wanted (100%); and were hopeful that their reasoning and recommendations would help inform VHA policy makers (82%).
The surveys also provided an opportunity to examine the extent to which knowledge, attitudes, and opinions changed from before to after the deliberation. Even with the small sample, responses revealed a trend toward improved knowledge about key elements of the Choice Act and its goals. Further, there was a shift in some participants’ opinions about how patients should be prioritized to receive civilian care. For example, before the deliberation participants generally felt that all veterans should be able to receive civilian care, whereas postdeliberation this was not the case. Postdeliberation, most participants felt that primary care should not be a high priority for civilian care but continued to endorse prioritizing civilian care for specialty services like orthopedic or cardiology-related care. Finally, participants moved from more diverse recommendations regarding additional funds allocations, toward consensus after the deliberation around allocating funds to the build policy. Eight participants supported a build policy beforehand, whereas 16 supported this policy afterward.
Discussion
This study explored DD as a method for deeply engaging veterans in complex policy making to guide funding allocation and prioritization decisions related to the Choice Act, decisions that are still very relevant today within the context of the Mission Act and have substantial implications for how health care is delivered in the VHA. The Mission Act passed on June 6, 2018, with the goal of improving access to and the reliability of civilian or community care for eligible veterans.27 Decisions related to appropriating scarce funding to improve access to care is an emotional and value-laden topic that elicited strong and divergent opinions among the participants. Veterans were eager to have their voices heard and had strong expectations that VHA leadership would be briefed about their recommendations. The majority of participants were satisfied with the deliberation process, felt they understood the issues, and felt their opinions were respected. They expressed feelings of comradery and community throughout the process.
In this single deliberation session, the groups did not achieve a single, final consensus regarding how VHA funding should ultimately be allocated between buy and build policy options. Nonetheless, participants provided a rich array of recommendations and rationale for them. Session moderators observed rich, sophisticated, fair, and reason-based discussions on this complex topic. Participants left with a deeper knowledge and appreciation for the complex trade-offs and expressed strong rationales for both sides of the policy debate on build vs buy. In addition, the project yielded results of high interest to VHA policy makers.
This work was presented in multiple venues between 2015 to 2016, and to both local and national VHA leadership, including the local Executive Quality Leadership Boards, the VHA Central Office Committee on the Future State of VA Community Care, the VA Office of Patient Centered Care, and the National Veteran Experience Committee. Through these discussions and others, we saw great interest within the VHA system and high-level leaders to explore ways to include veterans’ voices in the policy-making process. This work was invaluable to our research team (eAppendix E
Many health system decisions regarding what care should be delivered (and how) involve making difficult, value-laden choices in the context of limited resources. DD methods can be used to target and obtain specific viewpoints from diverse populations, such as the informed perspectives of minority and underrepresented populations within the VHA.19 For example, female veterans were oversampled to ensure that the informed preferences of this population was obtained. Thus, DD methods could provide a valuable tool for health systems to elicit in-depth diverse patient input on high-profile policies that will have a substantial impact on the system’s patient population.
Limitations
One potential downside of DD is that, because of the resource-intensive nature of deliberation sessions, they are often conducted with relatively small groups.9 Viewpoints of those within these small samples who are willing to spend an entire day discussing a complex topic may not be representative of the larger patient community. However, the core goal of DD is diversity of opinions rather than representativeness.
A stratified random sampling strategy that oversampled for underrepresented and minority populations was used to help select a diverse group that represents the population on key characteristics and partially addresses concern about representativeness. Efforts to optimize participation rates, including providing monetary incentives, also are helpful and have led to high participation rates in past deliberations.7
Health system communication strategies that promote the importance of becoming involved in DD sessions also may be helpful in improving rates of recruitment. On particularly important topics where health system leaders feel a larger resource investment is justified, conducting larger scale deliberations with many small groups may obtain more generalizable evidence about what individual patients and groups of patients recommend.7 However, due to the inherent limitations of surveys and focus group approaches for obtaining informed views on complex topics, there are no clear systematic alternatives to the DD approach.
Conclusion
DD is an effective method to meaningfully engage patients in deep deliberations to guide complex policy making. Although design of deliberative sessions is resource-intensive, patient engagement efforts, such as those described in this paper, could be an important aspect of a well-functioning learning health system. Further research into alternative, streamlined methods that can also engage veterans more deeply is needed. DD also can be combined with other approaches to broaden and confirm findings, including focus groups, town hall meetings, or surveys.
Although this study did not provide consensus on how the VHA should allocate funds with respect to the Choice Act, it did provide insight into the importance and feasibility of engaging veterans in the policy-making process. As more policies aimed at improving veterans’ access to civilian care are created, such as the most recent Mission Act, policy makers should strongly consider using the DD method of obtaining informed veteran input into future policy decisions.
Acknowledgments
Funding was provided by the US Department of Veterans Affairs Office of Analytics and Business Intelligence (OABI) and the VA Quality Enhancement Research Initiative (QUERI). Dr. Caverly was supported in part by a VA Career Development Award (CDA 16-151). Dr. Krein is supported by a VA Health Services Research and Development Research Career Scientist Award (RCS 11-222). The authors thank the veterans who participated in this work. They also thank Caitlin Reardon and Natalya Wawrin for their assistance in organizing the deliberation session.
1. VA Office of the Inspector General. Veterans Health Administration. Interim report: review of patient wait times, scheduling practices, and alleged patient deaths at the Phoenix Health Care System. https://www.va.gov/oig/pubs/VAOIG-14-02603-178.pdf. Published May 28, 2014. Accessed December 9, 2019.
2. Veterans Access, Choice, and Accountability Act of 2014. 42 USC §1395 (2014).
3. Penn M, Bhatnagar S, Kuy S, et al. Comparison of wait times for new patients between the private sector and United States Department of Veterans Affairs medical centers. JAMA Netw Open. 2019;2(1):e187096.
4. Thorpe JM, Thorpe CT, Schleiden L, et al. Association between dual use of Department of Veterans Affairs and Medicare Part D drug benefits and potentially unsafe prescribing. JAMA Intern Med. 2019; July 22. [Epub ahead of print.]
5. Moyo P, Zhao X, Thorpe CT, et al. Dual receipt of prescription opioids from the Department of Veterans Affairs and Medicare Part D and prescription opioid overdose death among veterans: a nested case-control study. Ann Intern Med. 2019;170(7):433-442.
6. Meyer LJ, Clancy CM. Care fragmentation and prescription opioids. Ann Intern Med. 2019;170(7):497-498.
7. Damschroder LJ, Pritts JL, Neblo MA, Kalarickal RJ, Creswell JW, Hayward RA. Patients, privacy and trust: patients’ willingness to allow researchers to access their medical records. Soc Sci Med. 2007;64(1):223-235.
8. Street J, Duszynski K, Krawczyk S, Braunack-Mayer A. The use of citizens’ juries in health policy decision-making: a systematic review. Soc Sci Med. 2014;109:1-9.
9. Paul C, Nicholls R, Priest P, McGee R. Making policy decisions about population screening for breast cancer: the role of citizens’ deliberation. Health Policy. 2008;85(3):314-320.
10. Martin D, Abelson J, Singer P. Participation in health care priority-setting through the eyes of the participants. J Health Serv Res Pol. 2002;7(4):222-229.
11. Mort M, Finch T. Principles for telemedicine and telecare: the perspective of a citizens’ panel. J Telemed Telecare. 2005;11(suppl 1):66-68.
12. Kass N, Faden R, Fabi RE, et al. Alternative consent models for comparative effectiveness studies: views of patients from two institutions. AJOB Empir Bioeth. 2016;7(2):92-105.
13. Carman KL, Mallery C, Maurer M, et al. Effectiveness of public deliberation methods for gathering input on issues in healthcare: results from a randomized trial. Soc Sci Med. 2015;133:11-20.
14. Carman KL, Maurer M, Mangrum R, et al. Understanding an informed public’s views on the role of evidence in making health care decisions. Health Aff (Millwood). 2016;35(4):566-574.
15. Kim SYH, Wall IF, Stanczyk A, De Vries R. Assessing the public’s views in research ethics controversies: deliberative democracy and bioethics as natural allies, J Empir Res Hum Res Ethics. 2009;4(4):3-16.
16. Gastil J, Levine P, eds. The Deliberative Democracy Handbook: Strategies for Effective Civic Engagement in the Twenty-First Century. San Francisco, CA: Jossey-Bass; 2005.
17. Dryzek JS, Bächtiger A, Chambers S, et al. The crisis of democracy and the science of deliberation. Science. 2019;363(6432):1144-1146.
18. Blacksher E, Diebel A, Forest PG, Goold SD, Abelson J. What is public deliberation? Hastings Cent Rep. 2012;4(2):14-17.
19. Wang G, Gold M, Siegel J, et al. Deliberation: obtaining informed input from a diverse public. J Health Care Poor Underserved. 2015;26(1):223-242.
20. Simon RL, ed. The Blackwell Guide to Social and Political Philosophy. Malden, MA: Wiley-Blackwell; 2002.
21. Stanford University, Center for Deliberative Democracy. Deliberative polling on energy and environmental policy options in Japan. https://cdd.stanford.edu/2012/deliberative-polling-on-energy-and-environmental-policy-options-in-japan. Published August 12, 2012. Accessed December 9, 2019.
22. Damschroder LJ, Pritts JL, Neblo MA, Kalarickal RJ, Creswell JW, Hayward RA. Patients, privacy and trust: patients’ willingness to allow researchers to access their medical records. Soc Sci Med. 2007;64(1):223-235.
23. Carman KL, Maurer M, Mallery C, et al. Community forum deliberative methods demonstration: evaluating effectiveness and eliciting public views on use of evidence. Final report. https://effectivehealthcare.ahrq.gov/sites/default/files/pdf/deliberative-methods_research-2013-1.pdf. Published November 2014. Accessed December 9, 2019.
24. Sunstein CR, Hastie R. Wiser: Getting Beyond Groupthink to Make Groups Smarter. Boston, MA: Harvard Business Review Press; 2014.
25. Damschroder LJ, Kim SY. Assessing the quality of democratic deliberation: a case study of public deliberation on the ethics of surrogate consent for research. Soc Sci Med. 2010;70(12):1896-1903.
26. Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. 2nd ed. Thousand Oaks: SAGE Publications, Inc; 1994.
27. US Department of Veterans Affairs. Veteran community care – general information. https://www.va.gov/COMMUNITYCARE/docs/pubfiles/factsheets/VHA-FS_MISSION-Act.pdf. Published September 9 2019. Accessed December 9, 2019.
Providing high-quality, patient-centered health care is a top priority for the US Department of Veterans Affairs (VA) Veteran Health Administration (VHA), whose core mission is to improve the health and well-being of US veterans. Thus, news of long wait times for medical appointments in the VHA sparked intense national attention and debate and led to changes in senior management and legislative action. 1 On August 8, 2014, President Bara c k Obama signed the Veterans Access, Choice, and Accountability Act of 2014, also known as the Choice Act, which provided an additional $16 billion in emergency spending over 3 years to improve veterans’ access to timely health care. 2 The Choice Act sought to develop an integrated health care network that allowed qualified VHA patients to receive specific health care services in their communities delivered by non-VHA health care providers (HCPs) but paid for by the VHA. The Choice Act also laid out explicit criteria for how to prioritize who would be eligible for VHA-purchased civilian care: (1) veterans who could not get timely appointments at a VHA medical facility within 30 days of referral; or (2) veterans who lived > 40 miles from the closest VHA medical facility.
VHA decision makers seeking to improve care delivery also need to weigh trade-offs between alternative approaches to providing rapid access. For instance, increasing access to non-VHA HCPs may not always decrease wait times and could result in loss of continuity, limited care coordination, limited ability to ensure and enforce high-quality standards at the VHA, and other challenges.3-6 Although the concerns and views of elected representatives, advocacy groups, and health system leaders are important, it is unknown whether these views and preferences align with those of veterans. Arguably, the range of views and concerns of informed veterans whose health is at stake should be particularly prominent in such policy decision making.
To identify the considerations that were most important to veterans regarding VHA policy around decreasing wait times, a study was designed to engage a group of veterans who were eligible for civilian care under the Choice Act. The study took place 1 year after the Choice Act was passed. Veterans were asked to focus on 2 related questions: First, how should funding be used for building VHA capacity (build) vs purchasing civilian care (buy)? Second, under what circumstances should civilian care be prioritized?
The aim of this paper is to describe democratic deliberation (DD), a specific method that engaged veteran patients in complex policy decisions around access to care. DD methods have been used increasingly in health care for developing policy guidance, setting priorities, providing advice on ethical dilemmas, weighing risk-benefit trade-offs, and determining decision-making authority.7-12 For example, DD helped guide national policy for mammography screening for breast cancer in New Zealand.13 The Agency for Healthcare Research and Quality has completed a systematic review and a large, randomized experiment on best practices for carrying out public deliberation.8,13,14 However, despite the potential value of this approach, there has been little use of deliberative methods within the VHA for the explicit purpose of informing veteran health care delivery.
This paper describes the experience engaging veterans by using DD methodology and informing VHA leadership about the results of those deliberations. The specific aims were to understand whether DD is an acceptable approach to use to engage patients in the medical services policy-making process within VHA and whether veterans are able to come to an informed consensus.
Methods
Engaging patients and incorporating their needs and concerns within the policy-making process may improve health system policies and make those policies more patient centered. Such engagement also could be a way to generate creative solutions. However, because health-system decisions often involve making difficult trade-offs, effectively obtaining patient population input on complex care delivery issues can be challenging.
Although surveys can provide intuitive, top-of-mind input from respondents, these opinions are generally not sufficient for resolving complex problems.15 Focus groups and interviews may produce results that are more in-depth than surveys, but these methods tend to elicit settled private preferences rather than opinions about what the community should do.16 DD, on the other hand, is designed to elicit deeply informed public opinions on complex, value-laden topics to develop recommendations and policies for a larger community.17 The goal is to find collective solutions to challenging social problems. DD achieves this by giving participants an opportunity to explore a topic in-depth, question experts, and engage peers in reason-based discussions.18,19 This method has its roots in political science and has been used over several decades to successfully inform policy making on a broad array of topics nationally and internationally—from health research ethics in the US to nuclear and energy policy in Japan.7,16,20,21 DD has been found to promote ownership of public programs and lend legitimacy to policy decisions, political institutions, and democracy itself.18
A single day (8 hours) DD session was convened, following a Citizens Jury model of deliberation, which brings veteran patients together to learn about a topic, ask questions of experts, deliberate with peers, and generate a “citizen’s report” that contains a set of recommendations (Table 1). An overview of the different models of DD and rationale for each can be found elsewhere.8,15
Recruitment Considerations
A purposively selected sample of civilian care-eligible veterans from a midwestern VHA health care system (1 medical center and 3 community-based outpatient clinics [CBOCs]) were invited to the DD session. The targeted number of participants was 30. Female veterans, who comprise only 7% of the local veteran population, were oversampled to account for their potentially different health care needs and to create balance between males and females in the session. Oversampling for other characteristics was not possible due to the relatively small sample size. Based on prior experience,7 it was assumed that 70% of willing participants would attend the session; therefore 34 veterans were invited and 24 attended. Each participant received a $200 incentive in appreciation for their substantial time commitment and to offset transportation costs.
Background Materials
A packet with educational materials (Flesch-Kincaid Grade Level of 10.5) was mailed to participants about 2 weeks before the DD session. Participants were asked to review prior to attending the session. These materials described the session (eg, purpose, organizers, importance) and provided factual information about the Choice Act (eg, eligibility, out-of-pocket costs, travel pay, prescription drug policies).
Session Overview
The session was structured to accomplish the following goals: (1) Elicit participants’ opinions about access to health care and reasons for those opinions; (2) Provide in-depth education about the Choice Act through presentations and discussions with topical experts; and (3) Elicit reasoning and recommendations on both the criteria by which participants prioritize candidates for civilian care and how participants would allocate additional funding to improve access (ie, by building VHA capacity to deliver more timely health care vs purchasing health care from civilian HCPs).
Participants were asked to fill out a survey on arrival in the morning and were assigned to 1 of 3 tables or small groups. Each table had a facilitator who had extensive experience in qualitative data collection methods and guided the dialogue using a scripted protocol that they helped develop and refine. The facilitation materials drew from and used previously published studies.22,23 Each facilitator audio recorded the sessions and took notes. Three experts presented during plenary education sessions. Presentations were designed to provide balanced factual information and included a veteran’s perspective. One presenter was a clinician on the project team, another was a local clinical leader responsible for making decisions about what services to provide via civilian care (buy) vs enhancing the local VHA health system’s ability to provide those services (build), and the third presenter was a veteran who was on the project team.
Education Session 1
The first plenary education session with expert presentations was conducted after each table completed an icebreaker exercise. The project team physician provided a brief history and description of the Choice Act to reinforce educational materials sent to participants prior to the session. The health system clinical leader described his decision process and principles and highlighted constraints placed on him by the Choice Act that were in place at the time of the DD session. He also described existing local and national programs to provide civilian care (eg, local fee-basis non-VHA care programs) and how these programs sought to achieve goals similar to the Choice Act. The veteran presenter focused on the importance of session participants providing candid insight and observations and emphasized that this session was a significant opportunity to “have their voices heard.”
Deliberation 1: What criteria should be used to prioritize patients for receiving civilian care paid for by the VHA? To elicit preferences on the central question of this deliberation, participants were presented with 8 real-world cases that were based on interviews conducted with Choice Act-eligible veterans (Table 2 and eAppendices A
Education Session 2
In the second plenary session, the project team physician provided information about health care access issues, both inside and outside of the VHA, particularly between urban and rural areas. He also discussed factors related to the insufficient capacity to meet growing demand that contributed to the VHA wait-time crisis. The veteran presenter shared reflections on health care access from a veteran’s perspective.
Deliberation 2: How should additional funding be divided between increasing the ability of the VHA to (1) provide care by VHA HCPs; and (2) pay for care from non-VHA civilian HCPs? Participants were presented the patient examples and Choice Act funding scenarios (the buy policy option) and contrasted that with a build policy option. Participants were explicitly encouraged to shift their perspectives from thinking about individual cases to considering policy-level decisions and the broader social good (Table 2).
Ensuring Robust Deliberations
If participants do not adequately grasp the complexities of the topic, a deliberation can fail. To facilitate nuanced reasoning, real-world concrete examples were developed as the starting point of each deliberation based on interviews with actual patients (deliberation 1) and actual policy proposals relevant to the funding allocation decisions within the Choice Act (deliberation 2).
A deliberation also can fail with self-silencing, where participants withhold opinions that differ from those articulated first or by more vocal members of the group.24 To combat self-silencing, highly experienced facilitators were used to ensure sharing from all participants and to support an open-minded, courteous, and reason-based environment for discourse. It was specified that the best solutions are achieved through reason-based and cordial disagreement and that success can be undermined when participants simply agree because it is easier or more comfortable.
A third way a deliberation can fail is if individuals do not adopt a group or system-level perspective. To counter this, facilitators reinforced at multiple points the importance of taking a broader social perspective rather than sharing only one’s personal preferences.
Finally, it is important to assess the quality of the deliberative process itself, to ensure that results are trustworthy.25 To assess the quality of the deliberative process, participants knowledge about key issues pre- and postdeliberation were assessed. Participants also were asked to rate the quality of the facilitators and how well they felt their voice was heard and respected, and facilitators made qualitative assessments about the extent to which participants were engaged in reason-based and collaborative discussion.
Data
Quantitative data were collected via pre- and postsession surveys. The surveys contained items related to knowledge about the Choice Act, expectations for the DD session, beliefs and opinions about the provision of health care for veterans, recommended funding allocations between build vs buy policy options, and general demographics. Qualitative data were collected through detailed notes taken by the 3 facilitators. Each table’s deliberations were audio recorded so that gaps in the notes could be filled.
The 3 facilitators, who were all experienced qualitative researchers, typed their written notes into a template immediately after the session. Two of the 3 facilitators led the analysis of the session notes. Findings within and across the 3 deliberation tables were developed using content and matrix analysis methods.26 Descriptive statistics were generated from survey responses and compared survey items pre- and postsession using paired t tests or χ2 tests for categorical responses.
Results
Thirty-three percent of individuals invited (n = 127) agreed to participate. Those who declined cited conflicts related to distance, transportation, work/school, medical appointments, family commitments, or were not interested. In all, 24 (69%) of the 35 veterans who accepted the invitation attended the deliberation session. Of the 11 who accepted but did not attend, 5 cancelled ahead of time because of conflicts (Figure). Most participants were male (70%), 48% were aged 61 to 75 years, 65% were white, 43% had some college education, 43% reported an annual income of between $25,000 and $40,000, and only 35% reported very good health (eAppendix D).
Deliberation 1
During the deliberation on the prioritization criteria, the concept of “condition severity” emerged as an important criterion for veterans. This criterion captured simultaneous consideration of both clinical necessity and burden on the veteran to obtain care. For example, participants felt that patients with a life-threatening illness should be prioritized for civilian care over patients who need preventative or primary care (clinical necessity) and that elderly patients with substantial difficulty traveling to VHA appointments should be prioritized over patients who can travel more easily (burden). The Choice Act regulations at the time of the DD session did not reflect this nuanced perspective, stipulating only that veterans must live > 40 miles from the nearest VHA medical facility.
One of the 3 groups did not prioritize the patient cases because some members felt that no veteran should be constrained from receiving civilian care if they desired it. Nonetheless, this group did agree with prioritizing the first 2 cases in Table 3. The other groups prioritized all 8 cases in generally similar ways.
Deliberation 2
No clear consensus emerged on the buy vs build question. A representative from each table presented their group’s positions, rationale, and recommendations after deliberations were completed. After hearing the range of positions, the groups then had another opportunity to deliberate based on what they heard from the other tables; no new recommendations or consensus emerged.
Participants who were in favor of allocating more funds toward the build policy offered a range of rationales, saying that it would (1) increase access for rural veterans by building CBOCs and deploying more mobile units that could bring outlets for health care closer to their home communities; (2) provide critical and unique medical expertise to address veteran-specific issues such as prosthetics, traumatic brain injury, posttraumatic stress disorder, spinal cord injury, and shrapnel wounds that are typically not available through civilian providers; (3) give VHA more oversight over the quality and cost of care, which is more challenging to do with civilian providers; and (4) Improve VHA infrastructure by, for example, upgrading technology and attracting the best clinicians and staff to support “our VHA.”
Participants who were in favor of allocating more funds toward the buy policy also offered a range of rationales, saying that it would (1) decrease patient burden by increasing access through community providers, decreasing wait time, and lessening personal cost and travel time; (2) allow more patients to receive civilian care, which was generally seen as beneficial by a few participants because of perceptions that the VHA provides lower quality care due to a shortage of VHA providers, run-down/older facilities, lack of technology, and poorer-quality VHA providers; and (3) provide an opportunity to divest of costly facilities and invest in other innovative approaches. Regarding this last reason, a few participants felt that the VHA is “gouged” when building medical centers that overrun budgets. They also were concerned that investing in facilities tied VHA to specific locations when current locations of veterans may change “25 years from now.”
Survey Results
Twenty-three of the 24 participants completed both pre- and postsession surveys. The majority of participants in the session felt people in the group respected their opinion (96%); felt that the facilitator did not try to influence the group with her own opinions (96%); indicated they understood the information enough to participate as much as they wanted (100%); and were hopeful that their reasoning and recommendations would help inform VHA policy makers (82%).
The surveys also provided an opportunity to examine the extent to which knowledge, attitudes, and opinions changed from before to after the deliberation. Even with the small sample, responses revealed a trend toward improved knowledge about key elements of the Choice Act and its goals. Further, there was a shift in some participants’ opinions about how patients should be prioritized to receive civilian care. For example, before the deliberation participants generally felt that all veterans should be able to receive civilian care, whereas postdeliberation this was not the case. Postdeliberation, most participants felt that primary care should not be a high priority for civilian care but continued to endorse prioritizing civilian care for specialty services like orthopedic or cardiology-related care. Finally, participants moved from more diverse recommendations regarding additional funds allocations, toward consensus after the deliberation around allocating funds to the build policy. Eight participants supported a build policy beforehand, whereas 16 supported this policy afterward.
Discussion
This study explored DD as a method for deeply engaging veterans in complex policy making to guide funding allocation and prioritization decisions related to the Choice Act, decisions that are still very relevant today within the context of the Mission Act and have substantial implications for how health care is delivered in the VHA. The Mission Act passed on June 6, 2018, with the goal of improving access to and the reliability of civilian or community care for eligible veterans.27 Decisions related to appropriating scarce funding to improve access to care is an emotional and value-laden topic that elicited strong and divergent opinions among the participants. Veterans were eager to have their voices heard and had strong expectations that VHA leadership would be briefed about their recommendations. The majority of participants were satisfied with the deliberation process, felt they understood the issues, and felt their opinions were respected. They expressed feelings of comradery and community throughout the process.
In this single deliberation session, the groups did not achieve a single, final consensus regarding how VHA funding should ultimately be allocated between buy and build policy options. Nonetheless, participants provided a rich array of recommendations and rationale for them. Session moderators observed rich, sophisticated, fair, and reason-based discussions on this complex topic. Participants left with a deeper knowledge and appreciation for the complex trade-offs and expressed strong rationales for both sides of the policy debate on build vs buy. In addition, the project yielded results of high interest to VHA policy makers.
This work was presented in multiple venues between 2015 to 2016, and to both local and national VHA leadership, including the local Executive Quality Leadership Boards, the VHA Central Office Committee on the Future State of VA Community Care, the VA Office of Patient Centered Care, and the National Veteran Experience Committee. Through these discussions and others, we saw great interest within the VHA system and high-level leaders to explore ways to include veterans’ voices in the policy-making process. This work was invaluable to our research team (eAppendix E
Many health system decisions regarding what care should be delivered (and how) involve making difficult, value-laden choices in the context of limited resources. DD methods can be used to target and obtain specific viewpoints from diverse populations, such as the informed perspectives of minority and underrepresented populations within the VHA.19 For example, female veterans were oversampled to ensure that the informed preferences of this population was obtained. Thus, DD methods could provide a valuable tool for health systems to elicit in-depth diverse patient input on high-profile policies that will have a substantial impact on the system’s patient population.
Limitations
One potential downside of DD is that, because of the resource-intensive nature of deliberation sessions, they are often conducted with relatively small groups.9 Viewpoints of those within these small samples who are willing to spend an entire day discussing a complex topic may not be representative of the larger patient community. However, the core goal of DD is diversity of opinions rather than representativeness.
A stratified random sampling strategy that oversampled for underrepresented and minority populations was used to help select a diverse group that represents the population on key characteristics and partially addresses concern about representativeness. Efforts to optimize participation rates, including providing monetary incentives, also are helpful and have led to high participation rates in past deliberations.7
Health system communication strategies that promote the importance of becoming involved in DD sessions also may be helpful in improving rates of recruitment. On particularly important topics where health system leaders feel a larger resource investment is justified, conducting larger scale deliberations with many small groups may obtain more generalizable evidence about what individual patients and groups of patients recommend.7 However, due to the inherent limitations of surveys and focus group approaches for obtaining informed views on complex topics, there are no clear systematic alternatives to the DD approach.
Conclusion
DD is an effective method to meaningfully engage patients in deep deliberations to guide complex policy making. Although design of deliberative sessions is resource-intensive, patient engagement efforts, such as those described in this paper, could be an important aspect of a well-functioning learning health system. Further research into alternative, streamlined methods that can also engage veterans more deeply is needed. DD also can be combined with other approaches to broaden and confirm findings, including focus groups, town hall meetings, or surveys.
Although this study did not provide consensus on how the VHA should allocate funds with respect to the Choice Act, it did provide insight into the importance and feasibility of engaging veterans in the policy-making process. As more policies aimed at improving veterans’ access to civilian care are created, such as the most recent Mission Act, policy makers should strongly consider using the DD method of obtaining informed veteran input into future policy decisions.
Acknowledgments
Funding was provided by the US Department of Veterans Affairs Office of Analytics and Business Intelligence (OABI) and the VA Quality Enhancement Research Initiative (QUERI). Dr. Caverly was supported in part by a VA Career Development Award (CDA 16-151). Dr. Krein is supported by a VA Health Services Research and Development Research Career Scientist Award (RCS 11-222). The authors thank the veterans who participated in this work. They also thank Caitlin Reardon and Natalya Wawrin for their assistance in organizing the deliberation session.
Providing high-quality, patient-centered health care is a top priority for the US Department of Veterans Affairs (VA) Veteran Health Administration (VHA), whose core mission is to improve the health and well-being of US veterans. Thus, news of long wait times for medical appointments in the VHA sparked intense national attention and debate and led to changes in senior management and legislative action. 1 On August 8, 2014, President Bara c k Obama signed the Veterans Access, Choice, and Accountability Act of 2014, also known as the Choice Act, which provided an additional $16 billion in emergency spending over 3 years to improve veterans’ access to timely health care. 2 The Choice Act sought to develop an integrated health care network that allowed qualified VHA patients to receive specific health care services in their communities delivered by non-VHA health care providers (HCPs) but paid for by the VHA. The Choice Act also laid out explicit criteria for how to prioritize who would be eligible for VHA-purchased civilian care: (1) veterans who could not get timely appointments at a VHA medical facility within 30 days of referral; or (2) veterans who lived > 40 miles from the closest VHA medical facility.
VHA decision makers seeking to improve care delivery also need to weigh trade-offs between alternative approaches to providing rapid access. For instance, increasing access to non-VHA HCPs may not always decrease wait times and could result in loss of continuity, limited care coordination, limited ability to ensure and enforce high-quality standards at the VHA, and other challenges.3-6 Although the concerns and views of elected representatives, advocacy groups, and health system leaders are important, it is unknown whether these views and preferences align with those of veterans. Arguably, the range of views and concerns of informed veterans whose health is at stake should be particularly prominent in such policy decision making.
To identify the considerations that were most important to veterans regarding VHA policy around decreasing wait times, a study was designed to engage a group of veterans who were eligible for civilian care under the Choice Act. The study took place 1 year after the Choice Act was passed. Veterans were asked to focus on 2 related questions: First, how should funding be used for building VHA capacity (build) vs purchasing civilian care (buy)? Second, under what circumstances should civilian care be prioritized?
The aim of this paper is to describe democratic deliberation (DD), a specific method that engaged veteran patients in complex policy decisions around access to care. DD methods have been used increasingly in health care for developing policy guidance, setting priorities, providing advice on ethical dilemmas, weighing risk-benefit trade-offs, and determining decision-making authority.7-12 For example, DD helped guide national policy for mammography screening for breast cancer in New Zealand.13 The Agency for Healthcare Research and Quality has completed a systematic review and a large, randomized experiment on best practices for carrying out public deliberation.8,13,14 However, despite the potential value of this approach, there has been little use of deliberative methods within the VHA for the explicit purpose of informing veteran health care delivery.
This paper describes the experience engaging veterans by using DD methodology and informing VHA leadership about the results of those deliberations. The specific aims were to understand whether DD is an acceptable approach to use to engage patients in the medical services policy-making process within VHA and whether veterans are able to come to an informed consensus.
Methods
Engaging patients and incorporating their needs and concerns within the policy-making process may improve health system policies and make those policies more patient centered. Such engagement also could be a way to generate creative solutions. However, because health-system decisions often involve making difficult trade-offs, effectively obtaining patient population input on complex care delivery issues can be challenging.
Although surveys can provide intuitive, top-of-mind input from respondents, these opinions are generally not sufficient for resolving complex problems.15 Focus groups and interviews may produce results that are more in-depth than surveys, but these methods tend to elicit settled private preferences rather than opinions about what the community should do.16 DD, on the other hand, is designed to elicit deeply informed public opinions on complex, value-laden topics to develop recommendations and policies for a larger community.17 The goal is to find collective solutions to challenging social problems. DD achieves this by giving participants an opportunity to explore a topic in-depth, question experts, and engage peers in reason-based discussions.18,19 This method has its roots in political science and has been used over several decades to successfully inform policy making on a broad array of topics nationally and internationally—from health research ethics in the US to nuclear and energy policy in Japan.7,16,20,21 DD has been found to promote ownership of public programs and lend legitimacy to policy decisions, political institutions, and democracy itself.18
A single day (8 hours) DD session was convened, following a Citizens Jury model of deliberation, which brings veteran patients together to learn about a topic, ask questions of experts, deliberate with peers, and generate a “citizen’s report” that contains a set of recommendations (Table 1). An overview of the different models of DD and rationale for each can be found elsewhere.8,15
Recruitment Considerations
A purposively selected sample of civilian care-eligible veterans from a midwestern VHA health care system (1 medical center and 3 community-based outpatient clinics [CBOCs]) were invited to the DD session. The targeted number of participants was 30. Female veterans, who comprise only 7% of the local veteran population, were oversampled to account for their potentially different health care needs and to create balance between males and females in the session. Oversampling for other characteristics was not possible due to the relatively small sample size. Based on prior experience,7 it was assumed that 70% of willing participants would attend the session; therefore 34 veterans were invited and 24 attended. Each participant received a $200 incentive in appreciation for their substantial time commitment and to offset transportation costs.
Background Materials
A packet with educational materials (Flesch-Kincaid Grade Level of 10.5) was mailed to participants about 2 weeks before the DD session. Participants were asked to review prior to attending the session. These materials described the session (eg, purpose, organizers, importance) and provided factual information about the Choice Act (eg, eligibility, out-of-pocket costs, travel pay, prescription drug policies).
Session Overview
The session was structured to accomplish the following goals: (1) Elicit participants’ opinions about access to health care and reasons for those opinions; (2) Provide in-depth education about the Choice Act through presentations and discussions with topical experts; and (3) Elicit reasoning and recommendations on both the criteria by which participants prioritize candidates for civilian care and how participants would allocate additional funding to improve access (ie, by building VHA capacity to deliver more timely health care vs purchasing health care from civilian HCPs).
Participants were asked to fill out a survey on arrival in the morning and were assigned to 1 of 3 tables or small groups. Each table had a facilitator who had extensive experience in qualitative data collection methods and guided the dialogue using a scripted protocol that they helped develop and refine. The facilitation materials drew from and used previously published studies.22,23 Each facilitator audio recorded the sessions and took notes. Three experts presented during plenary education sessions. Presentations were designed to provide balanced factual information and included a veteran’s perspective. One presenter was a clinician on the project team, another was a local clinical leader responsible for making decisions about what services to provide via civilian care (buy) vs enhancing the local VHA health system’s ability to provide those services (build), and the third presenter was a veteran who was on the project team.
Education Session 1
The first plenary education session with expert presentations was conducted after each table completed an icebreaker exercise. The project team physician provided a brief history and description of the Choice Act to reinforce educational materials sent to participants prior to the session. The health system clinical leader described his decision process and principles and highlighted constraints placed on him by the Choice Act that were in place at the time of the DD session. He also described existing local and national programs to provide civilian care (eg, local fee-basis non-VHA care programs) and how these programs sought to achieve goals similar to the Choice Act. The veteran presenter focused on the importance of session participants providing candid insight and observations and emphasized that this session was a significant opportunity to “have their voices heard.”
Deliberation 1: What criteria should be used to prioritize patients for receiving civilian care paid for by the VHA? To elicit preferences on the central question of this deliberation, participants were presented with 8 real-world cases that were based on interviews conducted with Choice Act-eligible veterans (Table 2 and eAppendices A
Education Session 2
In the second plenary session, the project team physician provided information about health care access issues, both inside and outside of the VHA, particularly between urban and rural areas. He also discussed factors related to the insufficient capacity to meet growing demand that contributed to the VHA wait-time crisis. The veteran presenter shared reflections on health care access from a veteran’s perspective.
Deliberation 2: How should additional funding be divided between increasing the ability of the VHA to (1) provide care by VHA HCPs; and (2) pay for care from non-VHA civilian HCPs? Participants were presented the patient examples and Choice Act funding scenarios (the buy policy option) and contrasted that with a build policy option. Participants were explicitly encouraged to shift their perspectives from thinking about individual cases to considering policy-level decisions and the broader social good (Table 2).
Ensuring Robust Deliberations
If participants do not adequately grasp the complexities of the topic, a deliberation can fail. To facilitate nuanced reasoning, real-world concrete examples were developed as the starting point of each deliberation based on interviews with actual patients (deliberation 1) and actual policy proposals relevant to the funding allocation decisions within the Choice Act (deliberation 2).
A deliberation also can fail with self-silencing, where participants withhold opinions that differ from those articulated first or by more vocal members of the group.24 To combat self-silencing, highly experienced facilitators were used to ensure sharing from all participants and to support an open-minded, courteous, and reason-based environment for discourse. It was specified that the best solutions are achieved through reason-based and cordial disagreement and that success can be undermined when participants simply agree because it is easier or more comfortable.
A third way a deliberation can fail is if individuals do not adopt a group or system-level perspective. To counter this, facilitators reinforced at multiple points the importance of taking a broader social perspective rather than sharing only one’s personal preferences.
Finally, it is important to assess the quality of the deliberative process itself, to ensure that results are trustworthy.25 To assess the quality of the deliberative process, participants knowledge about key issues pre- and postdeliberation were assessed. Participants also were asked to rate the quality of the facilitators and how well they felt their voice was heard and respected, and facilitators made qualitative assessments about the extent to which participants were engaged in reason-based and collaborative discussion.
Data
Quantitative data were collected via pre- and postsession surveys. The surveys contained items related to knowledge about the Choice Act, expectations for the DD session, beliefs and opinions about the provision of health care for veterans, recommended funding allocations between build vs buy policy options, and general demographics. Qualitative data were collected through detailed notes taken by the 3 facilitators. Each table’s deliberations were audio recorded so that gaps in the notes could be filled.
The 3 facilitators, who were all experienced qualitative researchers, typed their written notes into a template immediately after the session. Two of the 3 facilitators led the analysis of the session notes. Findings within and across the 3 deliberation tables were developed using content and matrix analysis methods.26 Descriptive statistics were generated from survey responses and compared survey items pre- and postsession using paired t tests or χ2 tests for categorical responses.
Results
Thirty-three percent of individuals invited (n = 127) agreed to participate. Those who declined cited conflicts related to distance, transportation, work/school, medical appointments, family commitments, or were not interested. In all, 24 (69%) of the 35 veterans who accepted the invitation attended the deliberation session. Of the 11 who accepted but did not attend, 5 cancelled ahead of time because of conflicts (Figure). Most participants were male (70%), 48% were aged 61 to 75 years, 65% were white, 43% had some college education, 43% reported an annual income of between $25,000 and $40,000, and only 35% reported very good health (eAppendix D).
Deliberation 1
During the deliberation on the prioritization criteria, the concept of “condition severity” emerged as an important criterion for veterans. This criterion captured simultaneous consideration of both clinical necessity and burden on the veteran to obtain care. For example, participants felt that patients with a life-threatening illness should be prioritized for civilian care over patients who need preventative or primary care (clinical necessity) and that elderly patients with substantial difficulty traveling to VHA appointments should be prioritized over patients who can travel more easily (burden). The Choice Act regulations at the time of the DD session did not reflect this nuanced perspective, stipulating only that veterans must live > 40 miles from the nearest VHA medical facility.
One of the 3 groups did not prioritize the patient cases because some members felt that no veteran should be constrained from receiving civilian care if they desired it. Nonetheless, this group did agree with prioritizing the first 2 cases in Table 3. The other groups prioritized all 8 cases in generally similar ways.
Deliberation 2
No clear consensus emerged on the buy vs build question. A representative from each table presented their group’s positions, rationale, and recommendations after deliberations were completed. After hearing the range of positions, the groups then had another opportunity to deliberate based on what they heard from the other tables; no new recommendations or consensus emerged.
Participants who were in favor of allocating more funds toward the build policy offered a range of rationales, saying that it would (1) increase access for rural veterans by building CBOCs and deploying more mobile units that could bring outlets for health care closer to their home communities; (2) provide critical and unique medical expertise to address veteran-specific issues such as prosthetics, traumatic brain injury, posttraumatic stress disorder, spinal cord injury, and shrapnel wounds that are typically not available through civilian providers; (3) give VHA more oversight over the quality and cost of care, which is more challenging to do with civilian providers; and (4) Improve VHA infrastructure by, for example, upgrading technology and attracting the best clinicians and staff to support “our VHA.”
Participants who were in favor of allocating more funds toward the buy policy also offered a range of rationales, saying that it would (1) decrease patient burden by increasing access through community providers, decreasing wait time, and lessening personal cost and travel time; (2) allow more patients to receive civilian care, which was generally seen as beneficial by a few participants because of perceptions that the VHA provides lower quality care due to a shortage of VHA providers, run-down/older facilities, lack of technology, and poorer-quality VHA providers; and (3) provide an opportunity to divest of costly facilities and invest in other innovative approaches. Regarding this last reason, a few participants felt that the VHA is “gouged” when building medical centers that overrun budgets. They also were concerned that investing in facilities tied VHA to specific locations when current locations of veterans may change “25 years from now.”
Survey Results
Twenty-three of the 24 participants completed both pre- and postsession surveys. The majority of participants in the session felt people in the group respected their opinion (96%); felt that the facilitator did not try to influence the group with her own opinions (96%); indicated they understood the information enough to participate as much as they wanted (100%); and were hopeful that their reasoning and recommendations would help inform VHA policy makers (82%).
The surveys also provided an opportunity to examine the extent to which knowledge, attitudes, and opinions changed from before to after the deliberation. Even with the small sample, responses revealed a trend toward improved knowledge about key elements of the Choice Act and its goals. Further, there was a shift in some participants’ opinions about how patients should be prioritized to receive civilian care. For example, before the deliberation participants generally felt that all veterans should be able to receive civilian care, whereas postdeliberation this was not the case. Postdeliberation, most participants felt that primary care should not be a high priority for civilian care but continued to endorse prioritizing civilian care for specialty services like orthopedic or cardiology-related care. Finally, participants moved from more diverse recommendations regarding additional funds allocations, toward consensus after the deliberation around allocating funds to the build policy. Eight participants supported a build policy beforehand, whereas 16 supported this policy afterward.
Discussion
This study explored DD as a method for deeply engaging veterans in complex policy making to guide funding allocation and prioritization decisions related to the Choice Act, decisions that are still very relevant today within the context of the Mission Act and have substantial implications for how health care is delivered in the VHA. The Mission Act passed on June 6, 2018, with the goal of improving access to and the reliability of civilian or community care for eligible veterans.27 Decisions related to appropriating scarce funding to improve access to care is an emotional and value-laden topic that elicited strong and divergent opinions among the participants. Veterans were eager to have their voices heard and had strong expectations that VHA leadership would be briefed about their recommendations. The majority of participants were satisfied with the deliberation process, felt they understood the issues, and felt their opinions were respected. They expressed feelings of comradery and community throughout the process.
In this single deliberation session, the groups did not achieve a single, final consensus regarding how VHA funding should ultimately be allocated between buy and build policy options. Nonetheless, participants provided a rich array of recommendations and rationale for them. Session moderators observed rich, sophisticated, fair, and reason-based discussions on this complex topic. Participants left with a deeper knowledge and appreciation for the complex trade-offs and expressed strong rationales for both sides of the policy debate on build vs buy. In addition, the project yielded results of high interest to VHA policy makers.
This work was presented in multiple venues between 2015 to 2016, and to both local and national VHA leadership, including the local Executive Quality Leadership Boards, the VHA Central Office Committee on the Future State of VA Community Care, the VA Office of Patient Centered Care, and the National Veteran Experience Committee. Through these discussions and others, we saw great interest within the VHA system and high-level leaders to explore ways to include veterans’ voices in the policy-making process. This work was invaluable to our research team (eAppendix E
Many health system decisions regarding what care should be delivered (and how) involve making difficult, value-laden choices in the context of limited resources. DD methods can be used to target and obtain specific viewpoints from diverse populations, such as the informed perspectives of minority and underrepresented populations within the VHA.19 For example, female veterans were oversampled to ensure that the informed preferences of this population was obtained. Thus, DD methods could provide a valuable tool for health systems to elicit in-depth diverse patient input on high-profile policies that will have a substantial impact on the system’s patient population.
Limitations
One potential downside of DD is that, because of the resource-intensive nature of deliberation sessions, they are often conducted with relatively small groups.9 Viewpoints of those within these small samples who are willing to spend an entire day discussing a complex topic may not be representative of the larger patient community. However, the core goal of DD is diversity of opinions rather than representativeness.
A stratified random sampling strategy that oversampled for underrepresented and minority populations was used to help select a diverse group that represents the population on key characteristics and partially addresses concern about representativeness. Efforts to optimize participation rates, including providing monetary incentives, also are helpful and have led to high participation rates in past deliberations.7
Health system communication strategies that promote the importance of becoming involved in DD sessions also may be helpful in improving rates of recruitment. On particularly important topics where health system leaders feel a larger resource investment is justified, conducting larger scale deliberations with many small groups may obtain more generalizable evidence about what individual patients and groups of patients recommend.7 However, due to the inherent limitations of surveys and focus group approaches for obtaining informed views on complex topics, there are no clear systematic alternatives to the DD approach.
Conclusion
DD is an effective method to meaningfully engage patients in deep deliberations to guide complex policy making. Although design of deliberative sessions is resource-intensive, patient engagement efforts, such as those described in this paper, could be an important aspect of a well-functioning learning health system. Further research into alternative, streamlined methods that can also engage veterans more deeply is needed. DD also can be combined with other approaches to broaden and confirm findings, including focus groups, town hall meetings, or surveys.
Although this study did not provide consensus on how the VHA should allocate funds with respect to the Choice Act, it did provide insight into the importance and feasibility of engaging veterans in the policy-making process. As more policies aimed at improving veterans’ access to civilian care are created, such as the most recent Mission Act, policy makers should strongly consider using the DD method of obtaining informed veteran input into future policy decisions.
Acknowledgments
Funding was provided by the US Department of Veterans Affairs Office of Analytics and Business Intelligence (OABI) and the VA Quality Enhancement Research Initiative (QUERI). Dr. Caverly was supported in part by a VA Career Development Award (CDA 16-151). Dr. Krein is supported by a VA Health Services Research and Development Research Career Scientist Award (RCS 11-222). The authors thank the veterans who participated in this work. They also thank Caitlin Reardon and Natalya Wawrin for their assistance in organizing the deliberation session.
1. VA Office of the Inspector General. Veterans Health Administration. Interim report: review of patient wait times, scheduling practices, and alleged patient deaths at the Phoenix Health Care System. https://www.va.gov/oig/pubs/VAOIG-14-02603-178.pdf. Published May 28, 2014. Accessed December 9, 2019.
2. Veterans Access, Choice, and Accountability Act of 2014. 42 USC §1395 (2014).
3. Penn M, Bhatnagar S, Kuy S, et al. Comparison of wait times for new patients between the private sector and United States Department of Veterans Affairs medical centers. JAMA Netw Open. 2019;2(1):e187096.
4. Thorpe JM, Thorpe CT, Schleiden L, et al. Association between dual use of Department of Veterans Affairs and Medicare Part D drug benefits and potentially unsafe prescribing. JAMA Intern Med. 2019; July 22. [Epub ahead of print.]
5. Moyo P, Zhao X, Thorpe CT, et al. Dual receipt of prescription opioids from the Department of Veterans Affairs and Medicare Part D and prescription opioid overdose death among veterans: a nested case-control study. Ann Intern Med. 2019;170(7):433-442.
6. Meyer LJ, Clancy CM. Care fragmentation and prescription opioids. Ann Intern Med. 2019;170(7):497-498.
7. Damschroder LJ, Pritts JL, Neblo MA, Kalarickal RJ, Creswell JW, Hayward RA. Patients, privacy and trust: patients’ willingness to allow researchers to access their medical records. Soc Sci Med. 2007;64(1):223-235.
8. Street J, Duszynski K, Krawczyk S, Braunack-Mayer A. The use of citizens’ juries in health policy decision-making: a systematic review. Soc Sci Med. 2014;109:1-9.
9. Paul C, Nicholls R, Priest P, McGee R. Making policy decisions about population screening for breast cancer: the role of citizens’ deliberation. Health Policy. 2008;85(3):314-320.
10. Martin D, Abelson J, Singer P. Participation in health care priority-setting through the eyes of the participants. J Health Serv Res Pol. 2002;7(4):222-229.
11. Mort M, Finch T. Principles for telemedicine and telecare: the perspective of a citizens’ panel. J Telemed Telecare. 2005;11(suppl 1):66-68.
12. Kass N, Faden R, Fabi RE, et al. Alternative consent models for comparative effectiveness studies: views of patients from two institutions. AJOB Empir Bioeth. 2016;7(2):92-105.
13. Carman KL, Mallery C, Maurer M, et al. Effectiveness of public deliberation methods for gathering input on issues in healthcare: results from a randomized trial. Soc Sci Med. 2015;133:11-20.
14. Carman KL, Maurer M, Mangrum R, et al. Understanding an informed public’s views on the role of evidence in making health care decisions. Health Aff (Millwood). 2016;35(4):566-574.
15. Kim SYH, Wall IF, Stanczyk A, De Vries R. Assessing the public’s views in research ethics controversies: deliberative democracy and bioethics as natural allies, J Empir Res Hum Res Ethics. 2009;4(4):3-16.
16. Gastil J, Levine P, eds. The Deliberative Democracy Handbook: Strategies for Effective Civic Engagement in the Twenty-First Century. San Francisco, CA: Jossey-Bass; 2005.
17. Dryzek JS, Bächtiger A, Chambers S, et al. The crisis of democracy and the science of deliberation. Science. 2019;363(6432):1144-1146.
18. Blacksher E, Diebel A, Forest PG, Goold SD, Abelson J. What is public deliberation? Hastings Cent Rep. 2012;4(2):14-17.
19. Wang G, Gold M, Siegel J, et al. Deliberation: obtaining informed input from a diverse public. J Health Care Poor Underserved. 2015;26(1):223-242.
20. Simon RL, ed. The Blackwell Guide to Social and Political Philosophy. Malden, MA: Wiley-Blackwell; 2002.
21. Stanford University, Center for Deliberative Democracy. Deliberative polling on energy and environmental policy options in Japan. https://cdd.stanford.edu/2012/deliberative-polling-on-energy-and-environmental-policy-options-in-japan. Published August 12, 2012. Accessed December 9, 2019.
22. Damschroder LJ, Pritts JL, Neblo MA, Kalarickal RJ, Creswell JW, Hayward RA. Patients, privacy and trust: patients’ willingness to allow researchers to access their medical records. Soc Sci Med. 2007;64(1):223-235.
23. Carman KL, Maurer M, Mallery C, et al. Community forum deliberative methods demonstration: evaluating effectiveness and eliciting public views on use of evidence. Final report. https://effectivehealthcare.ahrq.gov/sites/default/files/pdf/deliberative-methods_research-2013-1.pdf. Published November 2014. Accessed December 9, 2019.
24. Sunstein CR, Hastie R. Wiser: Getting Beyond Groupthink to Make Groups Smarter. Boston, MA: Harvard Business Review Press; 2014.
25. Damschroder LJ, Kim SY. Assessing the quality of democratic deliberation: a case study of public deliberation on the ethics of surrogate consent for research. Soc Sci Med. 2010;70(12):1896-1903.
26. Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. 2nd ed. Thousand Oaks: SAGE Publications, Inc; 1994.
27. US Department of Veterans Affairs. Veteran community care – general information. https://www.va.gov/COMMUNITYCARE/docs/pubfiles/factsheets/VHA-FS_MISSION-Act.pdf. Published September 9 2019. Accessed December 9, 2019.
1. VA Office of the Inspector General. Veterans Health Administration. Interim report: review of patient wait times, scheduling practices, and alleged patient deaths at the Phoenix Health Care System. https://www.va.gov/oig/pubs/VAOIG-14-02603-178.pdf. Published May 28, 2014. Accessed December 9, 2019.
2. Veterans Access, Choice, and Accountability Act of 2014. 42 USC §1395 (2014).
3. Penn M, Bhatnagar S, Kuy S, et al. Comparison of wait times for new patients between the private sector and United States Department of Veterans Affairs medical centers. JAMA Netw Open. 2019;2(1):e187096.
4. Thorpe JM, Thorpe CT, Schleiden L, et al. Association between dual use of Department of Veterans Affairs and Medicare Part D drug benefits and potentially unsafe prescribing. JAMA Intern Med. 2019; July 22. [Epub ahead of print.]
5. Moyo P, Zhao X, Thorpe CT, et al. Dual receipt of prescription opioids from the Department of Veterans Affairs and Medicare Part D and prescription opioid overdose death among veterans: a nested case-control study. Ann Intern Med. 2019;170(7):433-442.
6. Meyer LJ, Clancy CM. Care fragmentation and prescription opioids. Ann Intern Med. 2019;170(7):497-498.
7. Damschroder LJ, Pritts JL, Neblo MA, Kalarickal RJ, Creswell JW, Hayward RA. Patients, privacy and trust: patients’ willingness to allow researchers to access their medical records. Soc Sci Med. 2007;64(1):223-235.
8. Street J, Duszynski K, Krawczyk S, Braunack-Mayer A. The use of citizens’ juries in health policy decision-making: a systematic review. Soc Sci Med. 2014;109:1-9.
9. Paul C, Nicholls R, Priest P, McGee R. Making policy decisions about population screening for breast cancer: the role of citizens’ deliberation. Health Policy. 2008;85(3):314-320.
10. Martin D, Abelson J, Singer P. Participation in health care priority-setting through the eyes of the participants. J Health Serv Res Pol. 2002;7(4):222-229.
11. Mort M, Finch T. Principles for telemedicine and telecare: the perspective of a citizens’ panel. J Telemed Telecare. 2005;11(suppl 1):66-68.
12. Kass N, Faden R, Fabi RE, et al. Alternative consent models for comparative effectiveness studies: views of patients from two institutions. AJOB Empir Bioeth. 2016;7(2):92-105.
13. Carman KL, Mallery C, Maurer M, et al. Effectiveness of public deliberation methods for gathering input on issues in healthcare: results from a randomized trial. Soc Sci Med. 2015;133:11-20.
14. Carman KL, Maurer M, Mangrum R, et al. Understanding an informed public’s views on the role of evidence in making health care decisions. Health Aff (Millwood). 2016;35(4):566-574.
15. Kim SYH, Wall IF, Stanczyk A, De Vries R. Assessing the public’s views in research ethics controversies: deliberative democracy and bioethics as natural allies, J Empir Res Hum Res Ethics. 2009;4(4):3-16.
16. Gastil J, Levine P, eds. The Deliberative Democracy Handbook: Strategies for Effective Civic Engagement in the Twenty-First Century. San Francisco, CA: Jossey-Bass; 2005.
17. Dryzek JS, Bächtiger A, Chambers S, et al. The crisis of democracy and the science of deliberation. Science. 2019;363(6432):1144-1146.
18. Blacksher E, Diebel A, Forest PG, Goold SD, Abelson J. What is public deliberation? Hastings Cent Rep. 2012;4(2):14-17.
19. Wang G, Gold M, Siegel J, et al. Deliberation: obtaining informed input from a diverse public. J Health Care Poor Underserved. 2015;26(1):223-242.
20. Simon RL, ed. The Blackwell Guide to Social and Political Philosophy. Malden, MA: Wiley-Blackwell; 2002.
21. Stanford University, Center for Deliberative Democracy. Deliberative polling on energy and environmental policy options in Japan. https://cdd.stanford.edu/2012/deliberative-polling-on-energy-and-environmental-policy-options-in-japan. Published August 12, 2012. Accessed December 9, 2019.
22. Damschroder LJ, Pritts JL, Neblo MA, Kalarickal RJ, Creswell JW, Hayward RA. Patients, privacy and trust: patients’ willingness to allow researchers to access their medical records. Soc Sci Med. 2007;64(1):223-235.
23. Carman KL, Maurer M, Mallery C, et al. Community forum deliberative methods demonstration: evaluating effectiveness and eliciting public views on use of evidence. Final report. https://effectivehealthcare.ahrq.gov/sites/default/files/pdf/deliberative-methods_research-2013-1.pdf. Published November 2014. Accessed December 9, 2019.
24. Sunstein CR, Hastie R. Wiser: Getting Beyond Groupthink to Make Groups Smarter. Boston, MA: Harvard Business Review Press; 2014.
25. Damschroder LJ, Kim SY. Assessing the quality of democratic deliberation: a case study of public deliberation on the ethics of surrogate consent for research. Soc Sci Med. 2010;70(12):1896-1903.
26. Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. 2nd ed. Thousand Oaks: SAGE Publications, Inc; 1994.
27. US Department of Veterans Affairs. Veteran community care – general information. https://www.va.gov/COMMUNITYCARE/docs/pubfiles/factsheets/VHA-FS_MISSION-Act.pdf. Published September 9 2019. Accessed December 9, 2019.
Armed conflict disproportionately affects children
I was asked recently about the trauma of 9/11 by a teen patient who was too young to remember the terrorist attacks. I was surprised that even today I become teary eyed thinking about it. My son was in his first week of college at Georgetown, and in the early confusion about what was going on I was panicked at reports of bombings in Washington. Fortunately, for me and my family at least, none of us were physically harmed. But the mental trauma still is with us. It was a momentary panic for me, but it’s not so fleeting for many families around the world today.
I can’t imagine what it is like today to be a parent in an armed conflict zone, or even in an area with very high levels of criminal violence. At a meeting of the International Society for Social Pediatrics (ISSOP), I learned that an estimated 1.5 billion residents of Earth, or about one in five inhabitants, lived in war zones or in areas of tremendous violence, according to the World Bank’s 2011 World Development Report. And I learned that children are disproportionately affected – physically, mentally, and developmentally – from Stella Tsitoura, MD, of the Network for Children’s Rights, Athens, and others at the ISSOP meeting in Beirut, Lebanon, where pediatricians from around the world gathered in Oct. 2019 to consider what we as a profession should be doing in the context of armed conflict’s impact on so many children. The meeting was held in the Middle East because it is an especially hot conflict area, but children in South Asia, central Africa, South America, Central America, even rough inner-city areas in the United States are also affected.
Child soldiers in some parts of the world particularly are affected, sometimes being forced to commit violence on neighbors and kin. One country that I worked in years ago, Yemen, is a horrifying example of the complex impact of war on children and families. In 2017, over 2,100 children had been recruited as soldiers during the 3-year conflict in Yemen, a UNICEF representative reported. The death toll in Yemen was over 17,500 by Nov. 2018, according to a Human Rights Watch report.
Samuel Perlo-Freeman, PhD, an expert on the economics of arms trade, noted at the ISSOP meeting that two-thirds of civilian casualties in Yemen are caused by Coalition air strikes, whose members include Bahrain, Egypt, Jordan, Kuwait, Saudi Arabia, Sudan, and United Arab Emirates. He also said rebel groups in Yemen and elsewhere acquire their arms by capture, by smuggling, or through the aid of foreign backers. Six countries – the United States, Russia, and several western European countries – account for the majority of war tools used in armed conflict zones. In June 2019, courts in Great Britain ruled that British arms sales to the parties involved in Yemen were illegal without an assessment as to whether any violation of internal humanitarian law had taken place.
Many of us feel impotent when facing the magnitude of this problem, and the lives of despair that affected children lead are sometimes too heart breaking to dwell on. ISSOP, the American Academy of Pediatrics, and the International Pediatric Association (IPA) are teaching us differently: Standing up for the human rights of children living in areas of conflict or refugees from those areas is our responsibility, both as individuals and as members of our pediatric associations. At a basic level we need to witness – we need to share what we see with our patients who have immigrated legally or illegally in our practices, our hospitals, and our communities. It’s important to be knowledgeable of current standards of clinical care outlined by both ISSOP and the AAP to ensure our patients affected by conflict and violence get appropriate treatment.
Some of the most lasting health impacts for children in conflict are their mental health needs; the World Health Organization prevalence estimates of mental disorders in conflict settings is 22%, according to a 2019 report in the Lancet (2019 Jun;394[10194]:240-8). Not only do mental health conditions last throughout a lifetime, the impact of war can affect generations through epigenetic forces.
Arms manufacturers should be held accountable as the courts are doing in Great Britain. Too often American-made armaments are falling into the wrong hands. More can be done to limit the sale of weapons that go into conflict zones. Chemical weapons, cluster bombs, and biologic weapons are banned by international agreement; shouldn’t we do the same with nuclear weapons?
Some pediatric health care facilities are impacted by the needs of traumatized children more than others. Countries at the front line of conflict – like Lebanon, Jordon, Turkey, Greece, Italy, and Mexico – should be supported in their efforts on behalf of child refugees. We need to share the burden and support entities such as Doctors Without Borders, Save the Children, and the Red Cross/Crescent as they present themselves in crisis zones. We recognize that the fundamental human rights of children are being ignored by warring parties. especially Goal 16, which asks the world community to make real progress in promoting peace and justice by 2030. Pediatricians may not be experts in armed conflict, but we are experts in what warfare does to the health and well-being of young children. It’s time to speak out and act.
I was asked recently about the trauma of 9/11 by a teen patient who was too young to remember the terrorist attacks. I was surprised that even today I become teary eyed thinking about it. My son was in his first week of college at Georgetown, and in the early confusion about what was going on I was panicked at reports of bombings in Washington. Fortunately, for me and my family at least, none of us were physically harmed. But the mental trauma still is with us. It was a momentary panic for me, but it’s not so fleeting for many families around the world today.
I can’t imagine what it is like today to be a parent in an armed conflict zone, or even in an area with very high levels of criminal violence. At a meeting of the International Society for Social Pediatrics (ISSOP), I learned that an estimated 1.5 billion residents of Earth, or about one in five inhabitants, lived in war zones or in areas of tremendous violence, according to the World Bank’s 2011 World Development Report. And I learned that children are disproportionately affected – physically, mentally, and developmentally – from Stella Tsitoura, MD, of the Network for Children’s Rights, Athens, and others at the ISSOP meeting in Beirut, Lebanon, where pediatricians from around the world gathered in Oct. 2019 to consider what we as a profession should be doing in the context of armed conflict’s impact on so many children. The meeting was held in the Middle East because it is an especially hot conflict area, but children in South Asia, central Africa, South America, Central America, even rough inner-city areas in the United States are also affected.
Child soldiers in some parts of the world particularly are affected, sometimes being forced to commit violence on neighbors and kin. One country that I worked in years ago, Yemen, is a horrifying example of the complex impact of war on children and families. In 2017, over 2,100 children had been recruited as soldiers during the 3-year conflict in Yemen, a UNICEF representative reported. The death toll in Yemen was over 17,500 by Nov. 2018, according to a Human Rights Watch report.
Samuel Perlo-Freeman, PhD, an expert on the economics of arms trade, noted at the ISSOP meeting that two-thirds of civilian casualties in Yemen are caused by Coalition air strikes, whose members include Bahrain, Egypt, Jordan, Kuwait, Saudi Arabia, Sudan, and United Arab Emirates. He also said rebel groups in Yemen and elsewhere acquire their arms by capture, by smuggling, or through the aid of foreign backers. Six countries – the United States, Russia, and several western European countries – account for the majority of war tools used in armed conflict zones. In June 2019, courts in Great Britain ruled that British arms sales to the parties involved in Yemen were illegal without an assessment as to whether any violation of internal humanitarian law had taken place.
Many of us feel impotent when facing the magnitude of this problem, and the lives of despair that affected children lead are sometimes too heart breaking to dwell on. ISSOP, the American Academy of Pediatrics, and the International Pediatric Association (IPA) are teaching us differently: Standing up for the human rights of children living in areas of conflict or refugees from those areas is our responsibility, both as individuals and as members of our pediatric associations. At a basic level we need to witness – we need to share what we see with our patients who have immigrated legally or illegally in our practices, our hospitals, and our communities. It’s important to be knowledgeable of current standards of clinical care outlined by both ISSOP and the AAP to ensure our patients affected by conflict and violence get appropriate treatment.
Some of the most lasting health impacts for children in conflict are their mental health needs; the World Health Organization prevalence estimates of mental disorders in conflict settings is 22%, according to a 2019 report in the Lancet (2019 Jun;394[10194]:240-8). Not only do mental health conditions last throughout a lifetime, the impact of war can affect generations through epigenetic forces.
Arms manufacturers should be held accountable as the courts are doing in Great Britain. Too often American-made armaments are falling into the wrong hands. More can be done to limit the sale of weapons that go into conflict zones. Chemical weapons, cluster bombs, and biologic weapons are banned by international agreement; shouldn’t we do the same with nuclear weapons?
Some pediatric health care facilities are impacted by the needs of traumatized children more than others. Countries at the front line of conflict – like Lebanon, Jordon, Turkey, Greece, Italy, and Mexico – should be supported in their efforts on behalf of child refugees. We need to share the burden and support entities such as Doctors Without Borders, Save the Children, and the Red Cross/Crescent as they present themselves in crisis zones. We recognize that the fundamental human rights of children are being ignored by warring parties. especially Goal 16, which asks the world community to make real progress in promoting peace and justice by 2030. Pediatricians may not be experts in armed conflict, but we are experts in what warfare does to the health and well-being of young children. It’s time to speak out and act.
I was asked recently about the trauma of 9/11 by a teen patient who was too young to remember the terrorist attacks. I was surprised that even today I become teary eyed thinking about it. My son was in his first week of college at Georgetown, and in the early confusion about what was going on I was panicked at reports of bombings in Washington. Fortunately, for me and my family at least, none of us were physically harmed. But the mental trauma still is with us. It was a momentary panic for me, but it’s not so fleeting for many families around the world today.
I can’t imagine what it is like today to be a parent in an armed conflict zone, or even in an area with very high levels of criminal violence. At a meeting of the International Society for Social Pediatrics (ISSOP), I learned that an estimated 1.5 billion residents of Earth, or about one in five inhabitants, lived in war zones or in areas of tremendous violence, according to the World Bank’s 2011 World Development Report. And I learned that children are disproportionately affected – physically, mentally, and developmentally – from Stella Tsitoura, MD, of the Network for Children’s Rights, Athens, and others at the ISSOP meeting in Beirut, Lebanon, where pediatricians from around the world gathered in Oct. 2019 to consider what we as a profession should be doing in the context of armed conflict’s impact on so many children. The meeting was held in the Middle East because it is an especially hot conflict area, but children in South Asia, central Africa, South America, Central America, even rough inner-city areas in the United States are also affected.
Child soldiers in some parts of the world particularly are affected, sometimes being forced to commit violence on neighbors and kin. One country that I worked in years ago, Yemen, is a horrifying example of the complex impact of war on children and families. In 2017, over 2,100 children had been recruited as soldiers during the 3-year conflict in Yemen, a UNICEF representative reported. The death toll in Yemen was over 17,500 by Nov. 2018, according to a Human Rights Watch report.
Samuel Perlo-Freeman, PhD, an expert on the economics of arms trade, noted at the ISSOP meeting that two-thirds of civilian casualties in Yemen are caused by Coalition air strikes, whose members include Bahrain, Egypt, Jordan, Kuwait, Saudi Arabia, Sudan, and United Arab Emirates. He also said rebel groups in Yemen and elsewhere acquire their arms by capture, by smuggling, or through the aid of foreign backers. Six countries – the United States, Russia, and several western European countries – account for the majority of war tools used in armed conflict zones. In June 2019, courts in Great Britain ruled that British arms sales to the parties involved in Yemen were illegal without an assessment as to whether any violation of internal humanitarian law had taken place.
Many of us feel impotent when facing the magnitude of this problem, and the lives of despair that affected children lead are sometimes too heart breaking to dwell on. ISSOP, the American Academy of Pediatrics, and the International Pediatric Association (IPA) are teaching us differently: Standing up for the human rights of children living in areas of conflict or refugees from those areas is our responsibility, both as individuals and as members of our pediatric associations. At a basic level we need to witness – we need to share what we see with our patients who have immigrated legally or illegally in our practices, our hospitals, and our communities. It’s important to be knowledgeable of current standards of clinical care outlined by both ISSOP and the AAP to ensure our patients affected by conflict and violence get appropriate treatment.
Some of the most lasting health impacts for children in conflict are their mental health needs; the World Health Organization prevalence estimates of mental disorders in conflict settings is 22%, according to a 2019 report in the Lancet (2019 Jun;394[10194]:240-8). Not only do mental health conditions last throughout a lifetime, the impact of war can affect generations through epigenetic forces.
Arms manufacturers should be held accountable as the courts are doing in Great Britain. Too often American-made armaments are falling into the wrong hands. More can be done to limit the sale of weapons that go into conflict zones. Chemical weapons, cluster bombs, and biologic weapons are banned by international agreement; shouldn’t we do the same with nuclear weapons?
Some pediatric health care facilities are impacted by the needs of traumatized children more than others. Countries at the front line of conflict – like Lebanon, Jordon, Turkey, Greece, Italy, and Mexico – should be supported in their efforts on behalf of child refugees. We need to share the burden and support entities such as Doctors Without Borders, Save the Children, and the Red Cross/Crescent as they present themselves in crisis zones. We recognize that the fundamental human rights of children are being ignored by warring parties. especially Goal 16, which asks the world community to make real progress in promoting peace and justice by 2030. Pediatricians may not be experts in armed conflict, but we are experts in what warfare does to the health and well-being of young children. It’s time to speak out and act.
Patient poaching: High on practices’ dirty tricks list
Years ago, I wrote about patient poaching – the practice of stealing another practice’s patients without the patient or other physician realizing what’s going on.
This is high on the dirty tricks list of some practices. It’s certainly not illegal, but seems pretty unethical. Fortunately, it’s infrequent (at least where I work), but still occurs.
Recently, I encountered a particularly egregious example.
One of my patients, a nice lady in her 70s, had a syncopal event and landed in a hospital I don’t cover. A neurologist who saw her there did a brain MRI and head/neck MR angiogram, which were fine. A cardiology evaluation was also fine, so she was sent home. The neurologist there told her to follow-up with him at his office.
As my nurse says, “some people just do whatever they’re told, they don’t want to make a doctor angry.” So my patient did, and at the other doctor’s office had a four-limb electromyogram test and nerve conduction study, carotid Dopplers, transcranial Dopplers, and an EEG. He also made changes in her medications.
The first time I found out about it was when the patient scheduled an unrelated procedure, and I got a clearance request to take her off a medication in advance of it. Since I hadn’t started her on the medication (or was even aware she was on it) I refused, saying they’d have to contact the physician who prescribed it.
This got back to the patient, who was under the impression I’d been aware of all this the whole time, and she called the other neurologist to have his records sent to me.
When I got them, I was surprised to find he’d documented that I’d asked him to assume her outpatient care and do these studies for me. I have no recollection of such a conversation, and I would not have agreed to such a thing unless the patient had informed me she was transferring care to him (in which case it’s no longer my concern). Unless I was in a coma at the time this conversation occurred, I’m pretty sure it didn’t happen.
Basically, what the other doctor did was perform a walletectomy (or, in this case insurance-ectomy) on the patient under the guise (to her) that he was doing this as a favor to me.
How do you look yourself in mirror each day when you do stuff like this? Apparently, it’s easier for some doctors than it is for me.
I’ll do my best to keep it that way, too. I can’t change others, but I can do my best to take the high road.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Years ago, I wrote about patient poaching – the practice of stealing another practice’s patients without the patient or other physician realizing what’s going on.
This is high on the dirty tricks list of some practices. It’s certainly not illegal, but seems pretty unethical. Fortunately, it’s infrequent (at least where I work), but still occurs.
Recently, I encountered a particularly egregious example.
One of my patients, a nice lady in her 70s, had a syncopal event and landed in a hospital I don’t cover. A neurologist who saw her there did a brain MRI and head/neck MR angiogram, which were fine. A cardiology evaluation was also fine, so she was sent home. The neurologist there told her to follow-up with him at his office.
As my nurse says, “some people just do whatever they’re told, they don’t want to make a doctor angry.” So my patient did, and at the other doctor’s office had a four-limb electromyogram test and nerve conduction study, carotid Dopplers, transcranial Dopplers, and an EEG. He also made changes in her medications.
The first time I found out about it was when the patient scheduled an unrelated procedure, and I got a clearance request to take her off a medication in advance of it. Since I hadn’t started her on the medication (or was even aware she was on it) I refused, saying they’d have to contact the physician who prescribed it.
This got back to the patient, who was under the impression I’d been aware of all this the whole time, and she called the other neurologist to have his records sent to me.
When I got them, I was surprised to find he’d documented that I’d asked him to assume her outpatient care and do these studies for me. I have no recollection of such a conversation, and I would not have agreed to such a thing unless the patient had informed me she was transferring care to him (in which case it’s no longer my concern). Unless I was in a coma at the time this conversation occurred, I’m pretty sure it didn’t happen.
Basically, what the other doctor did was perform a walletectomy (or, in this case insurance-ectomy) on the patient under the guise (to her) that he was doing this as a favor to me.
How do you look yourself in mirror each day when you do stuff like this? Apparently, it’s easier for some doctors than it is for me.
I’ll do my best to keep it that way, too. I can’t change others, but I can do my best to take the high road.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Years ago, I wrote about patient poaching – the practice of stealing another practice’s patients without the patient or other physician realizing what’s going on.
This is high on the dirty tricks list of some practices. It’s certainly not illegal, but seems pretty unethical. Fortunately, it’s infrequent (at least where I work), but still occurs.
Recently, I encountered a particularly egregious example.
One of my patients, a nice lady in her 70s, had a syncopal event and landed in a hospital I don’t cover. A neurologist who saw her there did a brain MRI and head/neck MR angiogram, which were fine. A cardiology evaluation was also fine, so she was sent home. The neurologist there told her to follow-up with him at his office.
As my nurse says, “some people just do whatever they’re told, they don’t want to make a doctor angry.” So my patient did, and at the other doctor’s office had a four-limb electromyogram test and nerve conduction study, carotid Dopplers, transcranial Dopplers, and an EEG. He also made changes in her medications.
The first time I found out about it was when the patient scheduled an unrelated procedure, and I got a clearance request to take her off a medication in advance of it. Since I hadn’t started her on the medication (or was even aware she was on it) I refused, saying they’d have to contact the physician who prescribed it.
This got back to the patient, who was under the impression I’d been aware of all this the whole time, and she called the other neurologist to have his records sent to me.
When I got them, I was surprised to find he’d documented that I’d asked him to assume her outpatient care and do these studies for me. I have no recollection of such a conversation, and I would not have agreed to such a thing unless the patient had informed me she was transferring care to him (in which case it’s no longer my concern). Unless I was in a coma at the time this conversation occurred, I’m pretty sure it didn’t happen.
Basically, what the other doctor did was perform a walletectomy (or, in this case insurance-ectomy) on the patient under the guise (to her) that he was doing this as a favor to me.
How do you look yourself in mirror each day when you do stuff like this? Apparently, it’s easier for some doctors than it is for me.
I’ll do my best to keep it that way, too. I can’t change others, but I can do my best to take the high road.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
FDA targets flavored cartridge-based e-cigarettes, but says it is not a ‘ban’
but states it is not a “ban.”
On Jan. 2, the agency issued enforcement guidance alerting companies that manufacture, distribute, and sell unauthorized flavored cartridge-based e-cigarettes within the next 30 days will risk FDA enforcement action.
FDA has had the authority to require premarket authorization of all e-cigarettes and other electronic nicotine delivery systems (ENDS) since August 2016, but thus far has exercised enforcement discretion regarding the need for premarket authorization for these types of products.
“By prioritizing enforcement against the products that are most widely used by children, our action today seeks to strike the right public health balance by maintaining e-cigarettes as a potential off-ramp for adults using combustible tobacco while ensuring these products don’t provide an on-ramp to nicotine addiction for our youth,” Department of Health & Human Services Secretary Alex Azar said in a statement.
The action comes in the wake of more than 2,500 vaping-related injuries being reported, including more than 50 deaths associated with vaping reported by the Centers for Disease Control and Prevention (although many are related to the use of tetrahydrocannabinol [THC] within vaping products) and a continued rise in youth use of e-cigarettes noted in government surveys.
The agency noted in a Jan. 2 statement announcing the enforcement action that, to date, no ENDS products have received a premarket authorization, “meaning that all ENDS products currently on the market are considered illegally marketed and are subject to enforcement, at any time, in the FDA’s discretion.”
FDA said it is prioritizing enforcement in 30 days against:
- Any flavored, cartridge-based ENDS product, other than those with a tobacco or menthol flavoring.
- All other ENDS products for which manufacturers are failing to take adequate measures to prevent access by minors.
- Any ENDS product that is targeted to minors or is likely to promote use by minors.
In the last category, this might include labeling or advertising resembling “kid-friendly food and drinks such as juice boxes or kid-friendly cereal; products marketed directly to minors by promoting ease of concealing the product or disguising it as another product; and products marketed with characters designed to appeal to youth,” according to the FDA statement.
As of May 12, FDA also will prioritize enforcement against any ENDS product for which the manufacturer has not submitted a premarket application. The agency will continue to exercise enforcement discretion for up to 1 year on these products if an application has been submitted, pending the review of that application.
“By not prioritizing enforcement against other flavored ENDS products in the same way as flavored cartridge-based ENDS products, the FDA has attempted to balance the public health concerns related to youth use of ENDS products with consideration regarding addicted adult cigarette smokers who may try to use ENDS products to transition away from combustible tobacco products,” the agency stated, adding that cartridge-based ENDS products are most commonly used among youth.
The FDA statement noted that the enforcement priorities outlined in the guidance document were not a “ban” on flavored or cartridge-based ENDS, noting the agency “has already accepted and begun review of several premarket applications for flavored ENDS products through the pathway that Congress established in the Tobacco Control Act. ... If a company can demonstrate to the FDA that a specific product meets the applicable standard set forth by Congress, including considering how the marketing of the product may affect youth initiation and use, then the FDA could authorize that product for sale.”
“Coupled with the recently signed legislation increasing the minimum age of sale of tobacco to 21, we believe this policy balances the urgency with which we must address the public health threat of youth use of e-cigarette products with the potential role that e-cigarettes may play in helping adult smokers transition completely away from combustible tobacco to a potentially less risky form of nicotine delivery,” FDA Commissioner Stephen Hahn, MD, said in a statement. “While we expect that responsible members of industry will comply with premarket requirements, we’re ready to take action against any unauthorized e-cigarette products as outlined in our priorities. We’ll also closely monitor the use rates of all e-cigarette products and take additional steps to address youth use as necessary.”
The American Medical Association criticized the action as not going far enough, even though it was a step in the right direction.
“The AMA is disappointed that menthol flavors, one of the most popular, will still be allowed, and that flavored e-liquids will remain on the market, leaving young people with easy access to alternative flavored e-cigarette products,” AMA President Patrice A. Harris, MD, said in a statement. “If we are serious about tackling this epidemic and keeping these harmful products out of the hands of young people, a total ban on all flavored e-cigarettes, in all forms and at all locations, is prudent and urgently needed. We are pleased the administration committed today to closely monitoring the situation and trends in e-cigarette use among young people, and to taking further action if needed.”
but states it is not a “ban.”
On Jan. 2, the agency issued enforcement guidance alerting companies that manufacture, distribute, and sell unauthorized flavored cartridge-based e-cigarettes within the next 30 days will risk FDA enforcement action.
FDA has had the authority to require premarket authorization of all e-cigarettes and other electronic nicotine delivery systems (ENDS) since August 2016, but thus far has exercised enforcement discretion regarding the need for premarket authorization for these types of products.
“By prioritizing enforcement against the products that are most widely used by children, our action today seeks to strike the right public health balance by maintaining e-cigarettes as a potential off-ramp for adults using combustible tobacco while ensuring these products don’t provide an on-ramp to nicotine addiction for our youth,” Department of Health & Human Services Secretary Alex Azar said in a statement.
The action comes in the wake of more than 2,500 vaping-related injuries being reported, including more than 50 deaths associated with vaping reported by the Centers for Disease Control and Prevention (although many are related to the use of tetrahydrocannabinol [THC] within vaping products) and a continued rise in youth use of e-cigarettes noted in government surveys.
The agency noted in a Jan. 2 statement announcing the enforcement action that, to date, no ENDS products have received a premarket authorization, “meaning that all ENDS products currently on the market are considered illegally marketed and are subject to enforcement, at any time, in the FDA’s discretion.”
FDA said it is prioritizing enforcement in 30 days against:
- Any flavored, cartridge-based ENDS product, other than those with a tobacco or menthol flavoring.
- All other ENDS products for which manufacturers are failing to take adequate measures to prevent access by minors.
- Any ENDS product that is targeted to minors or is likely to promote use by minors.
In the last category, this might include labeling or advertising resembling “kid-friendly food and drinks such as juice boxes or kid-friendly cereal; products marketed directly to minors by promoting ease of concealing the product or disguising it as another product; and products marketed with characters designed to appeal to youth,” according to the FDA statement.
As of May 12, FDA also will prioritize enforcement against any ENDS product for which the manufacturer has not submitted a premarket application. The agency will continue to exercise enforcement discretion for up to 1 year on these products if an application has been submitted, pending the review of that application.
“By not prioritizing enforcement against other flavored ENDS products in the same way as flavored cartridge-based ENDS products, the FDA has attempted to balance the public health concerns related to youth use of ENDS products with consideration regarding addicted adult cigarette smokers who may try to use ENDS products to transition away from combustible tobacco products,” the agency stated, adding that cartridge-based ENDS products are most commonly used among youth.
The FDA statement noted that the enforcement priorities outlined in the guidance document were not a “ban” on flavored or cartridge-based ENDS, noting the agency “has already accepted and begun review of several premarket applications for flavored ENDS products through the pathway that Congress established in the Tobacco Control Act. ... If a company can demonstrate to the FDA that a specific product meets the applicable standard set forth by Congress, including considering how the marketing of the product may affect youth initiation and use, then the FDA could authorize that product for sale.”
“Coupled with the recently signed legislation increasing the minimum age of sale of tobacco to 21, we believe this policy balances the urgency with which we must address the public health threat of youth use of e-cigarette products with the potential role that e-cigarettes may play in helping adult smokers transition completely away from combustible tobacco to a potentially less risky form of nicotine delivery,” FDA Commissioner Stephen Hahn, MD, said in a statement. “While we expect that responsible members of industry will comply with premarket requirements, we’re ready to take action against any unauthorized e-cigarette products as outlined in our priorities. We’ll also closely monitor the use rates of all e-cigarette products and take additional steps to address youth use as necessary.”
The American Medical Association criticized the action as not going far enough, even though it was a step in the right direction.
“The AMA is disappointed that menthol flavors, one of the most popular, will still be allowed, and that flavored e-liquids will remain on the market, leaving young people with easy access to alternative flavored e-cigarette products,” AMA President Patrice A. Harris, MD, said in a statement. “If we are serious about tackling this epidemic and keeping these harmful products out of the hands of young people, a total ban on all flavored e-cigarettes, in all forms and at all locations, is prudent and urgently needed. We are pleased the administration committed today to closely monitoring the situation and trends in e-cigarette use among young people, and to taking further action if needed.”
but states it is not a “ban.”
On Jan. 2, the agency issued enforcement guidance alerting companies that manufacture, distribute, and sell unauthorized flavored cartridge-based e-cigarettes within the next 30 days will risk FDA enforcement action.
FDA has had the authority to require premarket authorization of all e-cigarettes and other electronic nicotine delivery systems (ENDS) since August 2016, but thus far has exercised enforcement discretion regarding the need for premarket authorization for these types of products.
“By prioritizing enforcement against the products that are most widely used by children, our action today seeks to strike the right public health balance by maintaining e-cigarettes as a potential off-ramp for adults using combustible tobacco while ensuring these products don’t provide an on-ramp to nicotine addiction for our youth,” Department of Health & Human Services Secretary Alex Azar said in a statement.
The action comes in the wake of more than 2,500 vaping-related injuries being reported, including more than 50 deaths associated with vaping reported by the Centers for Disease Control and Prevention (although many are related to the use of tetrahydrocannabinol [THC] within vaping products) and a continued rise in youth use of e-cigarettes noted in government surveys.
The agency noted in a Jan. 2 statement announcing the enforcement action that, to date, no ENDS products have received a premarket authorization, “meaning that all ENDS products currently on the market are considered illegally marketed and are subject to enforcement, at any time, in the FDA’s discretion.”
FDA said it is prioritizing enforcement in 30 days against:
- Any flavored, cartridge-based ENDS product, other than those with a tobacco or menthol flavoring.
- All other ENDS products for which manufacturers are failing to take adequate measures to prevent access by minors.
- Any ENDS product that is targeted to minors or is likely to promote use by minors.
In the last category, this might include labeling or advertising resembling “kid-friendly food and drinks such as juice boxes or kid-friendly cereal; products marketed directly to minors by promoting ease of concealing the product or disguising it as another product; and products marketed with characters designed to appeal to youth,” according to the FDA statement.
As of May 12, FDA also will prioritize enforcement against any ENDS product for which the manufacturer has not submitted a premarket application. The agency will continue to exercise enforcement discretion for up to 1 year on these products if an application has been submitted, pending the review of that application.
“By not prioritizing enforcement against other flavored ENDS products in the same way as flavored cartridge-based ENDS products, the FDA has attempted to balance the public health concerns related to youth use of ENDS products with consideration regarding addicted adult cigarette smokers who may try to use ENDS products to transition away from combustible tobacco products,” the agency stated, adding that cartridge-based ENDS products are most commonly used among youth.
The FDA statement noted that the enforcement priorities outlined in the guidance document were not a “ban” on flavored or cartridge-based ENDS, noting the agency “has already accepted and begun review of several premarket applications for flavored ENDS products through the pathway that Congress established in the Tobacco Control Act. ... If a company can demonstrate to the FDA that a specific product meets the applicable standard set forth by Congress, including considering how the marketing of the product may affect youth initiation and use, then the FDA could authorize that product for sale.”
“Coupled with the recently signed legislation increasing the minimum age of sale of tobacco to 21, we believe this policy balances the urgency with which we must address the public health threat of youth use of e-cigarette products with the potential role that e-cigarettes may play in helping adult smokers transition completely away from combustible tobacco to a potentially less risky form of nicotine delivery,” FDA Commissioner Stephen Hahn, MD, said in a statement. “While we expect that responsible members of industry will comply with premarket requirements, we’re ready to take action against any unauthorized e-cigarette products as outlined in our priorities. We’ll also closely monitor the use rates of all e-cigarette products and take additional steps to address youth use as necessary.”
The American Medical Association criticized the action as not going far enough, even though it was a step in the right direction.
“The AMA is disappointed that menthol flavors, one of the most popular, will still be allowed, and that flavored e-liquids will remain on the market, leaving young people with easy access to alternative flavored e-cigarette products,” AMA President Patrice A. Harris, MD, said in a statement. “If we are serious about tackling this epidemic and keeping these harmful products out of the hands of young people, a total ban on all flavored e-cigarettes, in all forms and at all locations, is prudent and urgently needed. We are pleased the administration committed today to closely monitoring the situation and trends in e-cigarette use among young people, and to taking further action if needed.”