User login
Home visits: A practical approach
CASE
Mr. A is a 30-year-old man with neurofibromatosis and myelopathy with associated quadriplegia, complicated by dysphasia and chronic hypercapnic respiratory failure requiring a tracheostomy. He is cared for at home by his very competent mother but requires regular visits with his medical providers for assistance with his complex care needs. Due to logistical challenges, he had been receiving regular home visits even before the COVID-19 pandemic.
After estimating the risk of exposure to the patient, Mr. A’s family and his physician’s office staff scheduled a home visit. Before the appointment, the doctor conducted a virtual visit with the patient and family members to screen for COVID-19 infection, which proved negative. The doctor arranged a visit to coincide with Mr. A’s regular appointment with the home health nurse. He invited the patient’s social worker to attend, as well.
The providers donned masks, face shields, and gloves before entering the home. Mr. A’s temperature was checked and was normal. The team completed a physical exam, assessed the patient’s current needs, and refilled prescriptions. The doctor, nurse, and social worker met afterward in the family’s driveway to coordinate plans for the patient’s future care.
This encounter allowed a vulnerable patient with special needs to have access to care while reducing his risk of undesirable exposure. Also, his health care team’s provision of care in the home setting reduced Mr. A’s anxiety and that of his family members.
Home visits have long been an integral part of what it means to be a family physician. In 1930, roughly 40% of all patient-physician encounters in the United States occurred in patients’ homes. By 1980, this number had dropped to < 1%.1 Still, a 1994 survey of American doctors in 3 primary care specialties revealed that 63% of family physicians, more than the other 2 specialties, still made house calls.2 A 2016 analysis of Medicare claims data showed that between 2006 and 2011, only 5% of American doctors overall made house calls on Medicare recipients, but interestingly, the total number of home visits was increasing.3
This resurgence of interest in home health care is due in part to the increasing number of homebound patients in America, which exceeds the number of those in nursing homes.4 Further, a growing body of evidence indicates that home visits improve patient outcomes. And finally, many family physicians whose work lives have been centered around a busy office or hospital practice have found satisfaction in once again seeing patients in their own homes.
The COVID-19 pandemic has of course presented unique challenges—and opportunities, too—for home visits, which we discuss at the end of the article.
Why aren’t more of us making home visits?
For most of us, the decision not to make home visits is simply a matter of time and money. Although Medicare reimbursement for a home visit is typically about 150% that of a comparable office visit,5 it’s difficult, if not impossible, to make 2 home visits in the time you could see 3 patients in the office. So, economically it’s a net loss. Furthermore, we tend to feel less comfortable in our patients’ homes than in our offices. We have less control outside our own environment, and what happens away from our office is often less predictable—sometimes to the point that we may be concerned for our safety.
Continue to: So why make home visits at all?
So why make home visits at all?
First and foremost, home visits improve patient outcomes. This is most evident in our more vulnerable patients: newborns and the elderly, those who have been recently hospitalized, and those at risk because of their particular home situation. Multiple studies have shown that, for elders, home visits reduce functional decline, nursing home admissions, and mortality by around 25% to 33%.6-8 For those at risk of abuse, a recent systematic review showed that home visits reduce intimate partner violence and child abuse.9 Another systematic review demonstrated that patients with diabetes who received home visits vs usual care were more likely to show improvements in quality of life.10 These patients were also more likely to have lower HbA1c levels and lower systolic blood pressure readings.10 A few caveats apply to these studies:
- all of them targeted “vulnerable” patients
- most studies enlisted interdisciplinary teams and had regular team meetings
- most findings reached significance only after multiple home visits.
A further reason for choosing to become involved in home care is that it builds relationships, understanding, and empathy with our patients. “There is deep symbolism in the home visit.... It says, ‘I care enough about you to leave my power base … to come and see you on your own ground.’”11 And this benefit is 2-way; we also grow to understand and appreciate our patients better, especially if they are different from us culturally or socioeconomically.
Home visits allow the medical team to see challenges the patient has grown accustomed to, and perhaps ones that the patient has deemed too insignificant to mention. For the patient, home visits foster a strong sense of trust with the individual doctor and our health delivery network, and they decrease the need to seek emergency services. Finally, it has been demonstrated that provider satisfaction improves when home visits are incorporated into the work week.12
What is the role of community health workers in home-based care?
Community health workers (CHWs), defined as “frontline public health workers who are trusted members of and/or have an unusually close understanding of the community they serve,”13 can be an integral part of the home-based care team. Although CHWs have variable amounts of formal training, they have a unique perspective on local health beliefs and practices, which can assist the home-care team in providing culturally competent health care services and reduce health care costs.
In a study of children with asthma in Seattle, Washington, patients were randomized to a group that had 4 home visits by CHWs and a group that received usual care. The group that received home visits demonstrated more asthma symptom–free days, improved quality-of-life scores, and fewer urgent care visits.14 Furthermore, the intervention was estimated to save approximately $1300 per patient, resulting in a return on investment of 190%. Similarly, in a study comparing inappropriate emergency department (ED) visits between children who received CHW visits and those who did not, patients in the intervention group were significantly less likely to visit the ED for ambulatory complaints (18.2% vs 35.1%; P = .004).15
Continue to: What is the role of social workersin home-based care?
What is the role of social workersin home-based care?
Social workers can help meet the complex medical and biopsychosocial needs of the homebound population.16 A study by Cohen et al based in Israel concluded that homebound participants had a significantly higher risk for mortality, higher rates of depression, and difficulty completing instrumental activities of daily living when compared with their non-homebound counterparts.17
The Mount Sinai (New York) Visiting Doctors Program (MSVD) is a home-based care team that uses social workers to meet the needs of their complex patients.18 The social workers in the MSVD program provide direct counseling, make referrals to government and community resources, and monitor caregiver burden. Using a combination of measurement tools to assess caregiver burden, Ornstein et al demonstrated that the MSVD program led to a decrease in unmet needs and in caregiver burden.19,20 Caregiver burnout can be assessed using the Caregiver Burden Inventory, a validated 24-item questionnaire.21
What electronic tools are availableto monitor patients at home?
Although expensive in terms of both dollars and personnel time, telemonitoring allows home care providers to receive real-time, updated information regarding their patients.
Chronic obstructive pulmonary disease (COPD). One systematic review showed that although telemonitoring of patients with COPD improved quality of life and decreased COPD exacerbations, it did not reduce the risk of hospitalization and, therefore, did not reduce health care costs.22 Telemonitoring in COPD can include transmission of data about spirometry parameters, weight, temperature, blood pressure, sputum color, and 6-minute walk distance.23,24
Congestive heart failure (CHF). A 2010 Cochrane review found that telemonitoring of patients with CHF reduced all-cause mortality (risk ratio [RR] = 0.66; P < .0001).25 The Telemedical Interventional Management in Heart Failure II (TIM-HF2) trial,conducted from 2013 to 2017, compared usual care for CHF patients with care incorporating daily transmission of body weight, blood pressure, heart rate, electrocardiogram tracings, pulse oximetry, and self-rated health status.26 This study showed that the average number of days lost per year due to hospital admission was less in the telemonitoring group than in the usual care group (17.8 days vs. 24.2 days; P = .046). All-cause mortality was also reduced in the telemonitoring group (hazard ratio = 0.70; P = .028).
Continue to: What role do “home hospitals” play?
What role do “home hospitals” play?
Home hospitals provide acute or subacute treatment in a patient’s home for a condition that would normally require hospitalization.27 In a meta-analysis of 61 studies evaluating the effectiveness of home hospitals, this option was more likely to reduce mortality (odds ratio [OR] = 0.81; P = .008) and to reduce readmission rates (OR = 0.75; P = .02).28 In a study of 455 older adults, Leff et al found that hospital-at-home was associated with a shorter length of stay (3.2 vs. 4.9 days; P = .004) and that the mean cost was lower for hospital-at-home vs traditional hospital care.29
However, a 2016 Cochrane review of 16 randomized controlled trials comparing hospital-at-home with traditional hospital care showed that while care in a hospital-at-home may decrease formal costs, if costs for caregivers are taken into account, any difference in cost may disappear.30
Although the evidence for cost saving is variable, hospital-at-home admission has been shown to reduce the likelihood of living in a residential care facility at 6 months (RR = 0.35; P < .0001).30 Further, the same Cochrane review showed that admission avoidance may increase patient satisfaction with the care provided.30
Finally, a recent randomized trial in a Boston-area hospital system showed that patients cared for in hospital-at-home were significantly less likely to be readmitted within 30 days and that adjusted cost was about two-thirds the cost of traditional hospital care.31
What is the physician’s rolein home health care?
While home health care is a team effort, the physician has several crucial roles. First, he or she must make the determination that home care is appropriate and feasible for a particular patient. Appropriate, meaning there is evidence that this patient is likely to benefit from home care. Feasible, meaning there are resources available in the community and family to safely care for the patient at home. “Often a house call will serve as the first step in developing a home-based-management plan.”32
Continue to: Second, the physician serves...
Second, the physician serves an important role in directing and coordinating the team of professionals involved. This primarily means helping the team to communicate with one another. Before home visits begin, the physician’s office should reach out not only to the patient and family, but also to any other health care personnel involved in the patient’s home care. Otherwise, many of the health care providers involved will never have face-to-face interaction with the physician. Creation of the coordinated health team minimizes duplication and miscommunication; it also builds a valuable bond.
How does one go about making a home visit?
Scheduling. What often works best in a busy practice is to schedule home visits for the end of the workday or to devote an entire afternoon to making home visits to several patients in one locale. Also important is scheduling times, if possible, when important family members or other caregivers are at home or when other members of the home care team can accompany you.
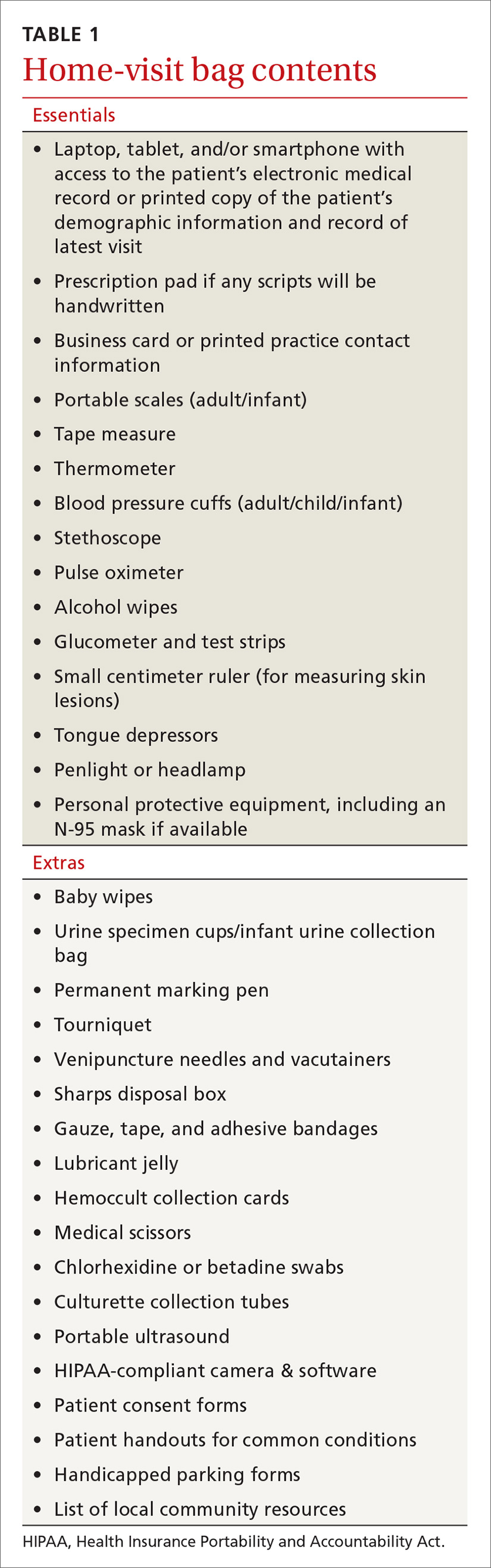
What to bring along. Carry a “home visit bag” that includes equipment you’re likely to need and that is not available away from your office. A minimally equipped visit bag would include different-sized blood pressure cuffs, a glucometer, a pulse oximeter, thermometers, and patient education materials. Other suggested contents are listed in TABLE 1.
Dos and don’ts. Take a few minutes when you first arrive to simply visit with the patient. Sit down and introduce yourself and any members of the home care team that the patient has not met. Take an interim history. While you’re doing this, be observant: Is the home neat or cluttered? Is the indoor temperature comfortable? Are there fall hazards? Is there a smell of cigarette smoke? Are there any indoor combustion sources (eg, wood stove or kerosene heater)? Ask questions such as: Who lives here with you? Can you show me where you keep your medicines? (If the patient keeps insulin or any other medicines in the refrigerator, ask to see it. Note any apparent food scarcity.)
During your exam, pay particular attention to whether vital signs are appreciably different than those measured in the office or hospital. Pay special attention to the patient’s functional abilities. “A subtle, but critical distinction between medical management in the home and medical management in the hospital, clinic, or office is the emphasis on the patient’s functional abilities, family assistance, and environmental factors.”33
Observe the patient’s use of any home technology, if possible; this can be as simple as home oxygenation or as complex as home hemodialysis. Assess for any apparent caregiver stress. Finally, don’t neglect to offer appropriate emotional and spiritual support to the patient and family and to schedule the next follow-up visit before you leave.
Continue to: Documentation and reimbursement.
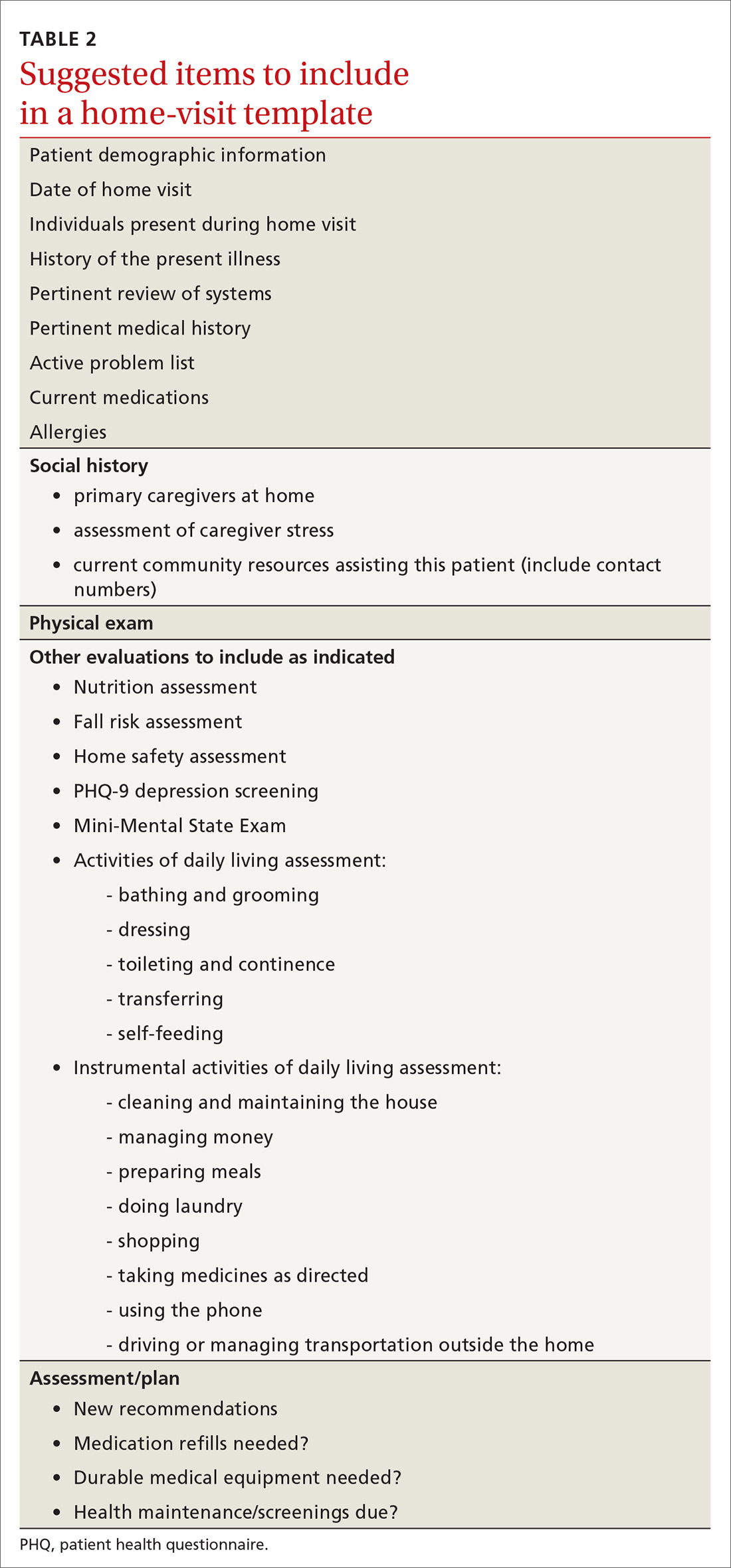
Documentation and reimbursement. While individual electronic medical records may require use of particular forms of documentation, using a home visit template when possible can be extremely helpful (TABLE 2). A template not only assures thoroughness and consistency (pharmacy, home health contacts, billing information) but also serves as a prompt to survey the patient and the caregivers about nonmedical, but essential, social and well-being services. The document should be as simple and user-friendly as possible.
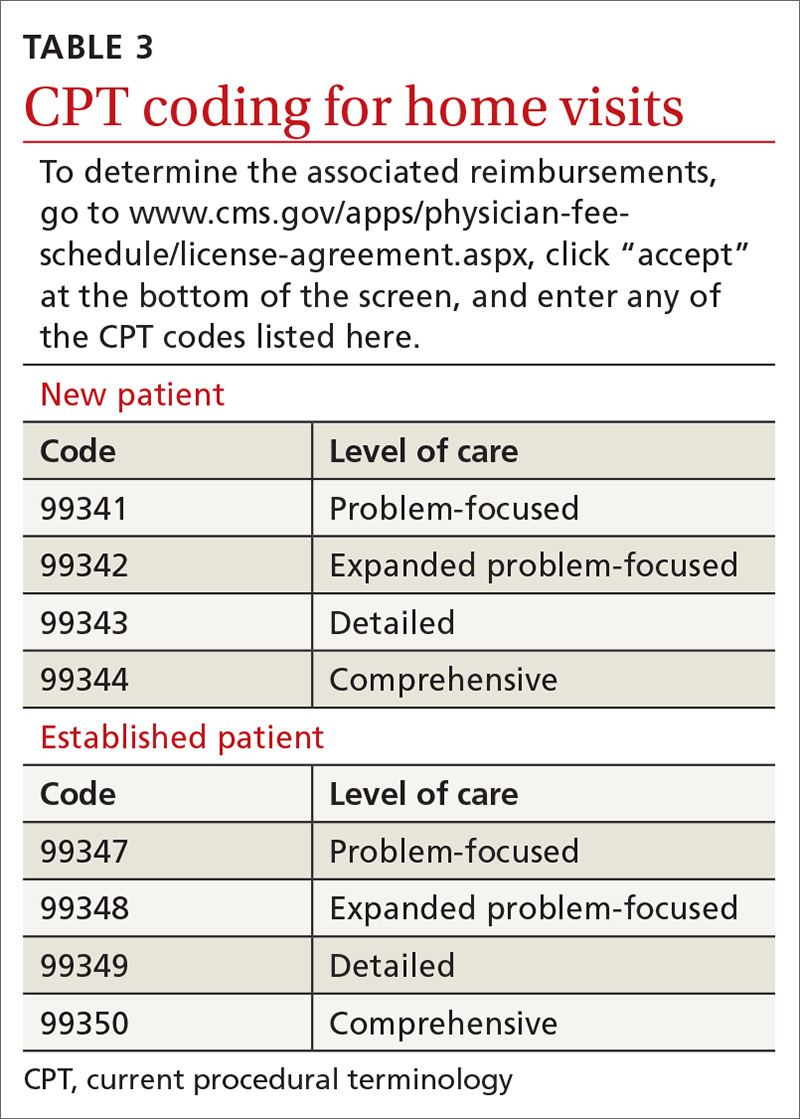
Not all assessments will be able to be done at each visit but seeing them listed in the template can be helpful. Billing follows the same principles as for office visits and has similar requirements for documentation. Codes for the most common types of home visits are listed in TABLE 3.
Where can I get help?
Graduates of family medicine residency programs are required to receive training in home visits by the Accreditation Council for Graduate Medical Education (ACGME). Current ACGME program requirements stipulate that “residents must demonstrate competence to independently diagnose, manage, and integrate the care of patients of all ages in various outpatient settings, including the FMP [family medicine practice] site and home environment,” and “residents must be primarily responsible for a panel of continuity patients, integrating each patient’s care across all settings, including the home ...” [emphasis added].34
For those already in practice, one of the hardest parts of doing home visits is feeling alone, especially if few other providers in your community engage in home care. As you run into questions and challenges with incorporating home care of patients into your practice, one excellent resource is the American Academy of Home Care Medicine (www.aahcm.org/). Founded in 1988 and headquartered in Chicago, it not only provides numerous helpful resources, but serves as a networking tool for physicians involved in home care.
This unprecedented pandemichas allowed home visits to shine
As depicted in our opening patient case, patients who have high-risk conditions and those who are older than 65 years of age may be cared for more appropriately in a home visit rather than having them come to the office. Home visits may also be a way for providers to “lay eyes” on patients who do not have technology available to participate in virtual visits.
Before performing a home visit, inquire as to whether the patient has symptoms of COVID-19. Adequate PPE should be donned at all times and social distancing should be practiced when appropriate. With adequate PPE, home visits may also allow providers to care for low-risk patients known to have COVID-19 and thereby minimize risks to staff and other patients in the office. JFP
CORRESPONDENCE
Curt Elliott, MD, Prisma Health USC Family Medicine Center, 3209 Colonial Drive, Columbia, SC 29203; curtis.elliott@uscmed.sc.edu.
1. Unwin BK, Tatum PE. House calls. Am Fam Physician. 2011;83:925-938.
3. Sairenji T, Jetty A, Peterson LE. Shifting patterns of physician home visits. J Prim Care Community Health. 2016;7:71-75.
4. Ornstein KA, Leff B, Covinsky K, et al. Epidemiology of the homebound population in the United States. JAMA Intern Med. 2015;175;1180-1186.
5. CMS. Current Procedural Terminology, Fourth Edition ("CPT®"). www.cms.gov/apps/physician-fee-schedule/license-agreement.aspx. Accessed November 30, 2020.
6. Elkan R, Kendrick D, Dewey M, et al. Effectiveness of home based support for older people: systematic review and meta-analysis. BMJ. 2001;323:719-725.
7. Stuck AE, Egger M, Hammer A, et al. Home visits to prevent nursing home admission and functional decline in elderly people: systematic review and meta-regression analysis. JAMA. 2002;287:1022-1028.
8. Stall N, Nowaczynski M, Sinha SK. Systematic review of outcomes from home-based primary care programs for homebound older adults. J Am Geriatr Soc. 2014;62:2243-2251.
9. Prosman GJ, Lo Fo Wong SH, van der Wouden JC, et al. Effectiveness of home visiting in reducing partner violence for families experiencing abuse: a systematic review. Fam Pract. 2015;32:247-256.
10. Han L, Ma Y, Wei S, et al. Are home visits an effective method for diabetes management? A quantitative systematic review and meta-analysis. J Diabetes Investig. 2017;8:701-708.
11. McWhinney IR. Fourth annual Nicholas J. Pisacano Lecture. The doctor, the patient, and the home: returning to our roots. J Am Board Fam Pract. 1997;10:430-435.
12. Kao H, Conant R, Soriano T, et al. The past, present, and future of house calls. Clin Geriatr Med. 2009;25:19-34.
13. American Public Health Association. Community health workers. www.apha.org/apha-communities/member-sections/community-health-workers. Accessed November 30, 2020.
14. Campbell JD, Brooks M, Hosokawa P, et al. Community health worker home visits for Medicaid-enrolled children with asthma: effects on asthma outcomes and costs. Am J Public Health. 2015;105:2366-2372.
15. Anugu M, Braksmajer A, Huang J, et al. Enriched medical home intervention using community health worker home visitation and ED use. Pediatrics. 2017;139:e20161849.
16. Reckrey JM, Gettenberg G, Ross H, et al. The critical role of social workers in home-based primary care. Soc Work in Health Care. 2014;53:330-343.
17. Cohen-Mansfield J, Shmotkin D, Hazan H. The effect of homebound status on older persons. J Am Geriatr Soc. 2010;58:2358-2362.
18. Mt. Sinai Visiting Doctors Program. www.mountsinai.org/care/primary-care/upper-east-side/visiting-doctors/about. Accessed November 30, 2020.
19. Ornstein K, Hernandez CR, DeCherrie LV, et al. The Mount Sinai (New York) Visiting Doctors Program: meeting the needs of the urban homebound population. Care Manag J. 2011;12:159-163.
20. Ornstein K, Smith K, Boal J. Understanding and improving the burden and unmet needs of informal caregivers of homebound patients enrolled in a home-based primary care program. J Appl Gerontol. 2009;28:482-503.
21. Novak M, Guest C. Application of a multidimensional caregiver burden inventory. Gerontologist. 1989;29:798-803.
22. Cruz J, Brooks D, Marques A. Home telemonitoring effectiveness in COPD: a systematic review. Int J Clin Pract. 2014;68:369-378.
23. Antoniades NC, Rochford PD, Pretto JJ, et al. Pilot study of remote telemonitoring in COPD. Telemed J E Health. 2012;18:634-640.
24. Koff PB, Jones RH, Cashman JM, et al. Proactive integrated care improves quality of life in patients with COPD. Eur Respir J. 2009;33:1031-1038.
25. Inglis SC, Clark RA, McAlister FA, et al. Which components of heart failure programmes are effective? A systematic review and meta-analysis of the outcomes of structured telephone support or telemonitoring as the primary component of chronic heart failure management in 8323 patients: abridged Cochrane review. Eur J Heart Fail. 2011;13:1028-1040.
26. Koehler F, Koehler K, Deckwart O, et al. Efficacy of telemedical interventional management in patients with heart failure (TIM-HF2): a randomised, controlled, parallel-group, unmasked trial. Lancet. 2018;392:1047-1057.
27. Ticona L, Schulman KA. Extreme home makeover–the role of intensive home health care. New Eng J Med. 2016;375:1707-1709.
28. Caplan GA. A meta-analysis of “hospital in the home.” Med J Aust. 2013;198:195-196.
29. Leff B, Burton L, Mader SL, et al. Hospital at home: feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med. 2005;143:798-808.
30. Shepperd S, Iliffe S, Doll HA, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev. 2016;9:CD007491.
31. Levine DM, Ouchi K, Blanchfield B, et al. Hospital-level care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020;172:77-85.
32. Cornwell T and Schwartzberg JG, eds. Medical Management of the Home Care Patient: Guidelines for Physicians. 4th ed. Chicago, IL: American Medical Association and American Academy of Home Care Physicians; 2012:p18.
33. Cornwell T and Schwartzberg JG, eds. Medical Management of the Home Care Patient: Guidelines for Physicians. 4th ed. Chicago, IL: American Medical Association and American Academy of Home Care Physicians; 2012:p19.
34. Accreditation Council for Graduate Medical Education. ACGME Program Requirements for Graduate Medical Education in Family Medicine. www.acgme.org/Portals/0/PFAssets/ProgramRequirements/120_FamilyMedicine_2020.pdf. (section IV.C.1.b). Accessed November 30, 2020.
CASE
Mr. A is a 30-year-old man with neurofibromatosis and myelopathy with associated quadriplegia, complicated by dysphasia and chronic hypercapnic respiratory failure requiring a tracheostomy. He is cared for at home by his very competent mother but requires regular visits with his medical providers for assistance with his complex care needs. Due to logistical challenges, he had been receiving regular home visits even before the COVID-19 pandemic.
After estimating the risk of exposure to the patient, Mr. A’s family and his physician’s office staff scheduled a home visit. Before the appointment, the doctor conducted a virtual visit with the patient and family members to screen for COVID-19 infection, which proved negative. The doctor arranged a visit to coincide with Mr. A’s regular appointment with the home health nurse. He invited the patient’s social worker to attend, as well.
The providers donned masks, face shields, and gloves before entering the home. Mr. A’s temperature was checked and was normal. The team completed a physical exam, assessed the patient’s current needs, and refilled prescriptions. The doctor, nurse, and social worker met afterward in the family’s driveway to coordinate plans for the patient’s future care.
This encounter allowed a vulnerable patient with special needs to have access to care while reducing his risk of undesirable exposure. Also, his health care team’s provision of care in the home setting reduced Mr. A’s anxiety and that of his family members.
Home visits have long been an integral part of what it means to be a family physician. In 1930, roughly 40% of all patient-physician encounters in the United States occurred in patients’ homes. By 1980, this number had dropped to < 1%.1 Still, a 1994 survey of American doctors in 3 primary care specialties revealed that 63% of family physicians, more than the other 2 specialties, still made house calls.2 A 2016 analysis of Medicare claims data showed that between 2006 and 2011, only 5% of American doctors overall made house calls on Medicare recipients, but interestingly, the total number of home visits was increasing.3
This resurgence of interest in home health care is due in part to the increasing number of homebound patients in America, which exceeds the number of those in nursing homes.4 Further, a growing body of evidence indicates that home visits improve patient outcomes. And finally, many family physicians whose work lives have been centered around a busy office or hospital practice have found satisfaction in once again seeing patients in their own homes.
The COVID-19 pandemic has of course presented unique challenges—and opportunities, too—for home visits, which we discuss at the end of the article.
Why aren’t more of us making home visits?
For most of us, the decision not to make home visits is simply a matter of time and money. Although Medicare reimbursement for a home visit is typically about 150% that of a comparable office visit,5 it’s difficult, if not impossible, to make 2 home visits in the time you could see 3 patients in the office. So, economically it’s a net loss. Furthermore, we tend to feel less comfortable in our patients’ homes than in our offices. We have less control outside our own environment, and what happens away from our office is often less predictable—sometimes to the point that we may be concerned for our safety.
Continue to: So why make home visits at all?
So why make home visits at all?
First and foremost, home visits improve patient outcomes. This is most evident in our more vulnerable patients: newborns and the elderly, those who have been recently hospitalized, and those at risk because of their particular home situation. Multiple studies have shown that, for elders, home visits reduce functional decline, nursing home admissions, and mortality by around 25% to 33%.6-8 For those at risk of abuse, a recent systematic review showed that home visits reduce intimate partner violence and child abuse.9 Another systematic review demonstrated that patients with diabetes who received home visits vs usual care were more likely to show improvements in quality of life.10 These patients were also more likely to have lower HbA1c levels and lower systolic blood pressure readings.10 A few caveats apply to these studies:
- all of them targeted “vulnerable” patients
- most studies enlisted interdisciplinary teams and had regular team meetings
- most findings reached significance only after multiple home visits.
A further reason for choosing to become involved in home care is that it builds relationships, understanding, and empathy with our patients. “There is deep symbolism in the home visit.... It says, ‘I care enough about you to leave my power base … to come and see you on your own ground.’”11 And this benefit is 2-way; we also grow to understand and appreciate our patients better, especially if they are different from us culturally or socioeconomically.
Home visits allow the medical team to see challenges the patient has grown accustomed to, and perhaps ones that the patient has deemed too insignificant to mention. For the patient, home visits foster a strong sense of trust with the individual doctor and our health delivery network, and they decrease the need to seek emergency services. Finally, it has been demonstrated that provider satisfaction improves when home visits are incorporated into the work week.12
What is the role of community health workers in home-based care?
Community health workers (CHWs), defined as “frontline public health workers who are trusted members of and/or have an unusually close understanding of the community they serve,”13 can be an integral part of the home-based care team. Although CHWs have variable amounts of formal training, they have a unique perspective on local health beliefs and practices, which can assist the home-care team in providing culturally competent health care services and reduce health care costs.
In a study of children with asthma in Seattle, Washington, patients were randomized to a group that had 4 home visits by CHWs and a group that received usual care. The group that received home visits demonstrated more asthma symptom–free days, improved quality-of-life scores, and fewer urgent care visits.14 Furthermore, the intervention was estimated to save approximately $1300 per patient, resulting in a return on investment of 190%. Similarly, in a study comparing inappropriate emergency department (ED) visits between children who received CHW visits and those who did not, patients in the intervention group were significantly less likely to visit the ED for ambulatory complaints (18.2% vs 35.1%; P = .004).15
Continue to: What is the role of social workersin home-based care?
What is the role of social workersin home-based care?
Social workers can help meet the complex medical and biopsychosocial needs of the homebound population.16 A study by Cohen et al based in Israel concluded that homebound participants had a significantly higher risk for mortality, higher rates of depression, and difficulty completing instrumental activities of daily living when compared with their non-homebound counterparts.17
The Mount Sinai (New York) Visiting Doctors Program (MSVD) is a home-based care team that uses social workers to meet the needs of their complex patients.18 The social workers in the MSVD program provide direct counseling, make referrals to government and community resources, and monitor caregiver burden. Using a combination of measurement tools to assess caregiver burden, Ornstein et al demonstrated that the MSVD program led to a decrease in unmet needs and in caregiver burden.19,20 Caregiver burnout can be assessed using the Caregiver Burden Inventory, a validated 24-item questionnaire.21
What electronic tools are availableto monitor patients at home?
Although expensive in terms of both dollars and personnel time, telemonitoring allows home care providers to receive real-time, updated information regarding their patients.
Chronic obstructive pulmonary disease (COPD). One systematic review showed that although telemonitoring of patients with COPD improved quality of life and decreased COPD exacerbations, it did not reduce the risk of hospitalization and, therefore, did not reduce health care costs.22 Telemonitoring in COPD can include transmission of data about spirometry parameters, weight, temperature, blood pressure, sputum color, and 6-minute walk distance.23,24
Congestive heart failure (CHF). A 2010 Cochrane review found that telemonitoring of patients with CHF reduced all-cause mortality (risk ratio [RR] = 0.66; P < .0001).25 The Telemedical Interventional Management in Heart Failure II (TIM-HF2) trial,conducted from 2013 to 2017, compared usual care for CHF patients with care incorporating daily transmission of body weight, blood pressure, heart rate, electrocardiogram tracings, pulse oximetry, and self-rated health status.26 This study showed that the average number of days lost per year due to hospital admission was less in the telemonitoring group than in the usual care group (17.8 days vs. 24.2 days; P = .046). All-cause mortality was also reduced in the telemonitoring group (hazard ratio = 0.70; P = .028).
Continue to: What role do “home hospitals” play?
What role do “home hospitals” play?
Home hospitals provide acute or subacute treatment in a patient’s home for a condition that would normally require hospitalization.27 In a meta-analysis of 61 studies evaluating the effectiveness of home hospitals, this option was more likely to reduce mortality (odds ratio [OR] = 0.81; P = .008) and to reduce readmission rates (OR = 0.75; P = .02).28 In a study of 455 older adults, Leff et al found that hospital-at-home was associated with a shorter length of stay (3.2 vs. 4.9 days; P = .004) and that the mean cost was lower for hospital-at-home vs traditional hospital care.29
However, a 2016 Cochrane review of 16 randomized controlled trials comparing hospital-at-home with traditional hospital care showed that while care in a hospital-at-home may decrease formal costs, if costs for caregivers are taken into account, any difference in cost may disappear.30
Although the evidence for cost saving is variable, hospital-at-home admission has been shown to reduce the likelihood of living in a residential care facility at 6 months (RR = 0.35; P < .0001).30 Further, the same Cochrane review showed that admission avoidance may increase patient satisfaction with the care provided.30
Finally, a recent randomized trial in a Boston-area hospital system showed that patients cared for in hospital-at-home were significantly less likely to be readmitted within 30 days and that adjusted cost was about two-thirds the cost of traditional hospital care.31
What is the physician’s rolein home health care?
While home health care is a team effort, the physician has several crucial roles. First, he or she must make the determination that home care is appropriate and feasible for a particular patient. Appropriate, meaning there is evidence that this patient is likely to benefit from home care. Feasible, meaning there are resources available in the community and family to safely care for the patient at home. “Often a house call will serve as the first step in developing a home-based-management plan.”32
Continue to: Second, the physician serves...
Second, the physician serves an important role in directing and coordinating the team of professionals involved. This primarily means helping the team to communicate with one another. Before home visits begin, the physician’s office should reach out not only to the patient and family, but also to any other health care personnel involved in the patient’s home care. Otherwise, many of the health care providers involved will never have face-to-face interaction with the physician. Creation of the coordinated health team minimizes duplication and miscommunication; it also builds a valuable bond.
How does one go about making a home visit?
Scheduling. What often works best in a busy practice is to schedule home visits for the end of the workday or to devote an entire afternoon to making home visits to several patients in one locale. Also important is scheduling times, if possible, when important family members or other caregivers are at home or when other members of the home care team can accompany you.
What to bring along. Carry a “home visit bag” that includes equipment you’re likely to need and that is not available away from your office. A minimally equipped visit bag would include different-sized blood pressure cuffs, a glucometer, a pulse oximeter, thermometers, and patient education materials. Other suggested contents are listed in TABLE 1.
Dos and don’ts. Take a few minutes when you first arrive to simply visit with the patient. Sit down and introduce yourself and any members of the home care team that the patient has not met. Take an interim history. While you’re doing this, be observant: Is the home neat or cluttered? Is the indoor temperature comfortable? Are there fall hazards? Is there a smell of cigarette smoke? Are there any indoor combustion sources (eg, wood stove or kerosene heater)? Ask questions such as: Who lives here with you? Can you show me where you keep your medicines? (If the patient keeps insulin or any other medicines in the refrigerator, ask to see it. Note any apparent food scarcity.)
During your exam, pay particular attention to whether vital signs are appreciably different than those measured in the office or hospital. Pay special attention to the patient’s functional abilities. “A subtle, but critical distinction between medical management in the home and medical management in the hospital, clinic, or office is the emphasis on the patient’s functional abilities, family assistance, and environmental factors.”33
Observe the patient’s use of any home technology, if possible; this can be as simple as home oxygenation or as complex as home hemodialysis. Assess for any apparent caregiver stress. Finally, don’t neglect to offer appropriate emotional and spiritual support to the patient and family and to schedule the next follow-up visit before you leave.
Continue to: Documentation and reimbursement.
Documentation and reimbursement. While individual electronic medical records may require use of particular forms of documentation, using a home visit template when possible can be extremely helpful (TABLE 2). A template not only assures thoroughness and consistency (pharmacy, home health contacts, billing information) but also serves as a prompt to survey the patient and the caregivers about nonmedical, but essential, social and well-being services. The document should be as simple and user-friendly as possible.
Not all assessments will be able to be done at each visit but seeing them listed in the template can be helpful. Billing follows the same principles as for office visits and has similar requirements for documentation. Codes for the most common types of home visits are listed in TABLE 3.
Where can I get help?
Graduates of family medicine residency programs are required to receive training in home visits by the Accreditation Council for Graduate Medical Education (ACGME). Current ACGME program requirements stipulate that “residents must demonstrate competence to independently diagnose, manage, and integrate the care of patients of all ages in various outpatient settings, including the FMP [family medicine practice] site and home environment,” and “residents must be primarily responsible for a panel of continuity patients, integrating each patient’s care across all settings, including the home ...” [emphasis added].34
For those already in practice, one of the hardest parts of doing home visits is feeling alone, especially if few other providers in your community engage in home care. As you run into questions and challenges with incorporating home care of patients into your practice, one excellent resource is the American Academy of Home Care Medicine (www.aahcm.org/). Founded in 1988 and headquartered in Chicago, it not only provides numerous helpful resources, but serves as a networking tool for physicians involved in home care.
This unprecedented pandemichas allowed home visits to shine
As depicted in our opening patient case, patients who have high-risk conditions and those who are older than 65 years of age may be cared for more appropriately in a home visit rather than having them come to the office. Home visits may also be a way for providers to “lay eyes” on patients who do not have technology available to participate in virtual visits.
Before performing a home visit, inquire as to whether the patient has symptoms of COVID-19. Adequate PPE should be donned at all times and social distancing should be practiced when appropriate. With adequate PPE, home visits may also allow providers to care for low-risk patients known to have COVID-19 and thereby minimize risks to staff and other patients in the office. JFP
CORRESPONDENCE
Curt Elliott, MD, Prisma Health USC Family Medicine Center, 3209 Colonial Drive, Columbia, SC 29203; curtis.elliott@uscmed.sc.edu.
CASE
Mr. A is a 30-year-old man with neurofibromatosis and myelopathy with associated quadriplegia, complicated by dysphasia and chronic hypercapnic respiratory failure requiring a tracheostomy. He is cared for at home by his very competent mother but requires regular visits with his medical providers for assistance with his complex care needs. Due to logistical challenges, he had been receiving regular home visits even before the COVID-19 pandemic.
After estimating the risk of exposure to the patient, Mr. A’s family and his physician’s office staff scheduled a home visit. Before the appointment, the doctor conducted a virtual visit with the patient and family members to screen for COVID-19 infection, which proved negative. The doctor arranged a visit to coincide with Mr. A’s regular appointment with the home health nurse. He invited the patient’s social worker to attend, as well.
The providers donned masks, face shields, and gloves before entering the home. Mr. A’s temperature was checked and was normal. The team completed a physical exam, assessed the patient’s current needs, and refilled prescriptions. The doctor, nurse, and social worker met afterward in the family’s driveway to coordinate plans for the patient’s future care.
This encounter allowed a vulnerable patient with special needs to have access to care while reducing his risk of undesirable exposure. Also, his health care team’s provision of care in the home setting reduced Mr. A’s anxiety and that of his family members.
Home visits have long been an integral part of what it means to be a family physician. In 1930, roughly 40% of all patient-physician encounters in the United States occurred in patients’ homes. By 1980, this number had dropped to < 1%.1 Still, a 1994 survey of American doctors in 3 primary care specialties revealed that 63% of family physicians, more than the other 2 specialties, still made house calls.2 A 2016 analysis of Medicare claims data showed that between 2006 and 2011, only 5% of American doctors overall made house calls on Medicare recipients, but interestingly, the total number of home visits was increasing.3
This resurgence of interest in home health care is due in part to the increasing number of homebound patients in America, which exceeds the number of those in nursing homes.4 Further, a growing body of evidence indicates that home visits improve patient outcomes. And finally, many family physicians whose work lives have been centered around a busy office or hospital practice have found satisfaction in once again seeing patients in their own homes.
The COVID-19 pandemic has of course presented unique challenges—and opportunities, too—for home visits, which we discuss at the end of the article.
Why aren’t more of us making home visits?
For most of us, the decision not to make home visits is simply a matter of time and money. Although Medicare reimbursement for a home visit is typically about 150% that of a comparable office visit,5 it’s difficult, if not impossible, to make 2 home visits in the time you could see 3 patients in the office. So, economically it’s a net loss. Furthermore, we tend to feel less comfortable in our patients’ homes than in our offices. We have less control outside our own environment, and what happens away from our office is often less predictable—sometimes to the point that we may be concerned for our safety.
Continue to: So why make home visits at all?
So why make home visits at all?
First and foremost, home visits improve patient outcomes. This is most evident in our more vulnerable patients: newborns and the elderly, those who have been recently hospitalized, and those at risk because of their particular home situation. Multiple studies have shown that, for elders, home visits reduce functional decline, nursing home admissions, and mortality by around 25% to 33%.6-8 For those at risk of abuse, a recent systematic review showed that home visits reduce intimate partner violence and child abuse.9 Another systematic review demonstrated that patients with diabetes who received home visits vs usual care were more likely to show improvements in quality of life.10 These patients were also more likely to have lower HbA1c levels and lower systolic blood pressure readings.10 A few caveats apply to these studies:
- all of them targeted “vulnerable” patients
- most studies enlisted interdisciplinary teams and had regular team meetings
- most findings reached significance only after multiple home visits.
A further reason for choosing to become involved in home care is that it builds relationships, understanding, and empathy with our patients. “There is deep symbolism in the home visit.... It says, ‘I care enough about you to leave my power base … to come and see you on your own ground.’”11 And this benefit is 2-way; we also grow to understand and appreciate our patients better, especially if they are different from us culturally or socioeconomically.
Home visits allow the medical team to see challenges the patient has grown accustomed to, and perhaps ones that the patient has deemed too insignificant to mention. For the patient, home visits foster a strong sense of trust with the individual doctor and our health delivery network, and they decrease the need to seek emergency services. Finally, it has been demonstrated that provider satisfaction improves when home visits are incorporated into the work week.12
What is the role of community health workers in home-based care?
Community health workers (CHWs), defined as “frontline public health workers who are trusted members of and/or have an unusually close understanding of the community they serve,”13 can be an integral part of the home-based care team. Although CHWs have variable amounts of formal training, they have a unique perspective on local health beliefs and practices, which can assist the home-care team in providing culturally competent health care services and reduce health care costs.
In a study of children with asthma in Seattle, Washington, patients were randomized to a group that had 4 home visits by CHWs and a group that received usual care. The group that received home visits demonstrated more asthma symptom–free days, improved quality-of-life scores, and fewer urgent care visits.14 Furthermore, the intervention was estimated to save approximately $1300 per patient, resulting in a return on investment of 190%. Similarly, in a study comparing inappropriate emergency department (ED) visits between children who received CHW visits and those who did not, patients in the intervention group were significantly less likely to visit the ED for ambulatory complaints (18.2% vs 35.1%; P = .004).15
Continue to: What is the role of social workersin home-based care?
What is the role of social workersin home-based care?
Social workers can help meet the complex medical and biopsychosocial needs of the homebound population.16 A study by Cohen et al based in Israel concluded that homebound participants had a significantly higher risk for mortality, higher rates of depression, and difficulty completing instrumental activities of daily living when compared with their non-homebound counterparts.17
The Mount Sinai (New York) Visiting Doctors Program (MSVD) is a home-based care team that uses social workers to meet the needs of their complex patients.18 The social workers in the MSVD program provide direct counseling, make referrals to government and community resources, and monitor caregiver burden. Using a combination of measurement tools to assess caregiver burden, Ornstein et al demonstrated that the MSVD program led to a decrease in unmet needs and in caregiver burden.19,20 Caregiver burnout can be assessed using the Caregiver Burden Inventory, a validated 24-item questionnaire.21
What electronic tools are availableto monitor patients at home?
Although expensive in terms of both dollars and personnel time, telemonitoring allows home care providers to receive real-time, updated information regarding their patients.
Chronic obstructive pulmonary disease (COPD). One systematic review showed that although telemonitoring of patients with COPD improved quality of life and decreased COPD exacerbations, it did not reduce the risk of hospitalization and, therefore, did not reduce health care costs.22 Telemonitoring in COPD can include transmission of data about spirometry parameters, weight, temperature, blood pressure, sputum color, and 6-minute walk distance.23,24
Congestive heart failure (CHF). A 2010 Cochrane review found that telemonitoring of patients with CHF reduced all-cause mortality (risk ratio [RR] = 0.66; P < .0001).25 The Telemedical Interventional Management in Heart Failure II (TIM-HF2) trial,conducted from 2013 to 2017, compared usual care for CHF patients with care incorporating daily transmission of body weight, blood pressure, heart rate, electrocardiogram tracings, pulse oximetry, and self-rated health status.26 This study showed that the average number of days lost per year due to hospital admission was less in the telemonitoring group than in the usual care group (17.8 days vs. 24.2 days; P = .046). All-cause mortality was also reduced in the telemonitoring group (hazard ratio = 0.70; P = .028).
Continue to: What role do “home hospitals” play?
What role do “home hospitals” play?
Home hospitals provide acute or subacute treatment in a patient’s home for a condition that would normally require hospitalization.27 In a meta-analysis of 61 studies evaluating the effectiveness of home hospitals, this option was more likely to reduce mortality (odds ratio [OR] = 0.81; P = .008) and to reduce readmission rates (OR = 0.75; P = .02).28 In a study of 455 older adults, Leff et al found that hospital-at-home was associated with a shorter length of stay (3.2 vs. 4.9 days; P = .004) and that the mean cost was lower for hospital-at-home vs traditional hospital care.29
However, a 2016 Cochrane review of 16 randomized controlled trials comparing hospital-at-home with traditional hospital care showed that while care in a hospital-at-home may decrease formal costs, if costs for caregivers are taken into account, any difference in cost may disappear.30
Although the evidence for cost saving is variable, hospital-at-home admission has been shown to reduce the likelihood of living in a residential care facility at 6 months (RR = 0.35; P < .0001).30 Further, the same Cochrane review showed that admission avoidance may increase patient satisfaction with the care provided.30
Finally, a recent randomized trial in a Boston-area hospital system showed that patients cared for in hospital-at-home were significantly less likely to be readmitted within 30 days and that adjusted cost was about two-thirds the cost of traditional hospital care.31
What is the physician’s rolein home health care?
While home health care is a team effort, the physician has several crucial roles. First, he or she must make the determination that home care is appropriate and feasible for a particular patient. Appropriate, meaning there is evidence that this patient is likely to benefit from home care. Feasible, meaning there are resources available in the community and family to safely care for the patient at home. “Often a house call will serve as the first step in developing a home-based-management plan.”32
Continue to: Second, the physician serves...
Second, the physician serves an important role in directing and coordinating the team of professionals involved. This primarily means helping the team to communicate with one another. Before home visits begin, the physician’s office should reach out not only to the patient and family, but also to any other health care personnel involved in the patient’s home care. Otherwise, many of the health care providers involved will never have face-to-face interaction with the physician. Creation of the coordinated health team minimizes duplication and miscommunication; it also builds a valuable bond.
How does one go about making a home visit?
Scheduling. What often works best in a busy practice is to schedule home visits for the end of the workday or to devote an entire afternoon to making home visits to several patients in one locale. Also important is scheduling times, if possible, when important family members or other caregivers are at home or when other members of the home care team can accompany you.
What to bring along. Carry a “home visit bag” that includes equipment you’re likely to need and that is not available away from your office. A minimally equipped visit bag would include different-sized blood pressure cuffs, a glucometer, a pulse oximeter, thermometers, and patient education materials. Other suggested contents are listed in TABLE 1.
Dos and don’ts. Take a few minutes when you first arrive to simply visit with the patient. Sit down and introduce yourself and any members of the home care team that the patient has not met. Take an interim history. While you’re doing this, be observant: Is the home neat or cluttered? Is the indoor temperature comfortable? Are there fall hazards? Is there a smell of cigarette smoke? Are there any indoor combustion sources (eg, wood stove or kerosene heater)? Ask questions such as: Who lives here with you? Can you show me where you keep your medicines? (If the patient keeps insulin or any other medicines in the refrigerator, ask to see it. Note any apparent food scarcity.)
During your exam, pay particular attention to whether vital signs are appreciably different than those measured in the office or hospital. Pay special attention to the patient’s functional abilities. “A subtle, but critical distinction between medical management in the home and medical management in the hospital, clinic, or office is the emphasis on the patient’s functional abilities, family assistance, and environmental factors.”33
Observe the patient’s use of any home technology, if possible; this can be as simple as home oxygenation or as complex as home hemodialysis. Assess for any apparent caregiver stress. Finally, don’t neglect to offer appropriate emotional and spiritual support to the patient and family and to schedule the next follow-up visit before you leave.
Continue to: Documentation and reimbursement.
Documentation and reimbursement. While individual electronic medical records may require use of particular forms of documentation, using a home visit template when possible can be extremely helpful (TABLE 2). A template not only assures thoroughness and consistency (pharmacy, home health contacts, billing information) but also serves as a prompt to survey the patient and the caregivers about nonmedical, but essential, social and well-being services. The document should be as simple and user-friendly as possible.
Not all assessments will be able to be done at each visit but seeing them listed in the template can be helpful. Billing follows the same principles as for office visits and has similar requirements for documentation. Codes for the most common types of home visits are listed in TABLE 3.
Where can I get help?
Graduates of family medicine residency programs are required to receive training in home visits by the Accreditation Council for Graduate Medical Education (ACGME). Current ACGME program requirements stipulate that “residents must demonstrate competence to independently diagnose, manage, and integrate the care of patients of all ages in various outpatient settings, including the FMP [family medicine practice] site and home environment,” and “residents must be primarily responsible for a panel of continuity patients, integrating each patient’s care across all settings, including the home ...” [emphasis added].34
For those already in practice, one of the hardest parts of doing home visits is feeling alone, especially if few other providers in your community engage in home care. As you run into questions and challenges with incorporating home care of patients into your practice, one excellent resource is the American Academy of Home Care Medicine (www.aahcm.org/). Founded in 1988 and headquartered in Chicago, it not only provides numerous helpful resources, but serves as a networking tool for physicians involved in home care.
This unprecedented pandemichas allowed home visits to shine
As depicted in our opening patient case, patients who have high-risk conditions and those who are older than 65 years of age may be cared for more appropriately in a home visit rather than having them come to the office. Home visits may also be a way for providers to “lay eyes” on patients who do not have technology available to participate in virtual visits.
Before performing a home visit, inquire as to whether the patient has symptoms of COVID-19. Adequate PPE should be donned at all times and social distancing should be practiced when appropriate. With adequate PPE, home visits may also allow providers to care for low-risk patients known to have COVID-19 and thereby minimize risks to staff and other patients in the office. JFP
CORRESPONDENCE
Curt Elliott, MD, Prisma Health USC Family Medicine Center, 3209 Colonial Drive, Columbia, SC 29203; curtis.elliott@uscmed.sc.edu.
1. Unwin BK, Tatum PE. House calls. Am Fam Physician. 2011;83:925-938.
3. Sairenji T, Jetty A, Peterson LE. Shifting patterns of physician home visits. J Prim Care Community Health. 2016;7:71-75.
4. Ornstein KA, Leff B, Covinsky K, et al. Epidemiology of the homebound population in the United States. JAMA Intern Med. 2015;175;1180-1186.
5. CMS. Current Procedural Terminology, Fourth Edition ("CPT®"). www.cms.gov/apps/physician-fee-schedule/license-agreement.aspx. Accessed November 30, 2020.
6. Elkan R, Kendrick D, Dewey M, et al. Effectiveness of home based support for older people: systematic review and meta-analysis. BMJ. 2001;323:719-725.
7. Stuck AE, Egger M, Hammer A, et al. Home visits to prevent nursing home admission and functional decline in elderly people: systematic review and meta-regression analysis. JAMA. 2002;287:1022-1028.
8. Stall N, Nowaczynski M, Sinha SK. Systematic review of outcomes from home-based primary care programs for homebound older adults. J Am Geriatr Soc. 2014;62:2243-2251.
9. Prosman GJ, Lo Fo Wong SH, van der Wouden JC, et al. Effectiveness of home visiting in reducing partner violence for families experiencing abuse: a systematic review. Fam Pract. 2015;32:247-256.
10. Han L, Ma Y, Wei S, et al. Are home visits an effective method for diabetes management? A quantitative systematic review and meta-analysis. J Diabetes Investig. 2017;8:701-708.
11. McWhinney IR. Fourth annual Nicholas J. Pisacano Lecture. The doctor, the patient, and the home: returning to our roots. J Am Board Fam Pract. 1997;10:430-435.
12. Kao H, Conant R, Soriano T, et al. The past, present, and future of house calls. Clin Geriatr Med. 2009;25:19-34.
13. American Public Health Association. Community health workers. www.apha.org/apha-communities/member-sections/community-health-workers. Accessed November 30, 2020.
14. Campbell JD, Brooks M, Hosokawa P, et al. Community health worker home visits for Medicaid-enrolled children with asthma: effects on asthma outcomes and costs. Am J Public Health. 2015;105:2366-2372.
15. Anugu M, Braksmajer A, Huang J, et al. Enriched medical home intervention using community health worker home visitation and ED use. Pediatrics. 2017;139:e20161849.
16. Reckrey JM, Gettenberg G, Ross H, et al. The critical role of social workers in home-based primary care. Soc Work in Health Care. 2014;53:330-343.
17. Cohen-Mansfield J, Shmotkin D, Hazan H. The effect of homebound status on older persons. J Am Geriatr Soc. 2010;58:2358-2362.
18. Mt. Sinai Visiting Doctors Program. www.mountsinai.org/care/primary-care/upper-east-side/visiting-doctors/about. Accessed November 30, 2020.
19. Ornstein K, Hernandez CR, DeCherrie LV, et al. The Mount Sinai (New York) Visiting Doctors Program: meeting the needs of the urban homebound population. Care Manag J. 2011;12:159-163.
20. Ornstein K, Smith K, Boal J. Understanding and improving the burden and unmet needs of informal caregivers of homebound patients enrolled in a home-based primary care program. J Appl Gerontol. 2009;28:482-503.
21. Novak M, Guest C. Application of a multidimensional caregiver burden inventory. Gerontologist. 1989;29:798-803.
22. Cruz J, Brooks D, Marques A. Home telemonitoring effectiveness in COPD: a systematic review. Int J Clin Pract. 2014;68:369-378.
23. Antoniades NC, Rochford PD, Pretto JJ, et al. Pilot study of remote telemonitoring in COPD. Telemed J E Health. 2012;18:634-640.
24. Koff PB, Jones RH, Cashman JM, et al. Proactive integrated care improves quality of life in patients with COPD. Eur Respir J. 2009;33:1031-1038.
25. Inglis SC, Clark RA, McAlister FA, et al. Which components of heart failure programmes are effective? A systematic review and meta-analysis of the outcomes of structured telephone support or telemonitoring as the primary component of chronic heart failure management in 8323 patients: abridged Cochrane review. Eur J Heart Fail. 2011;13:1028-1040.
26. Koehler F, Koehler K, Deckwart O, et al. Efficacy of telemedical interventional management in patients with heart failure (TIM-HF2): a randomised, controlled, parallel-group, unmasked trial. Lancet. 2018;392:1047-1057.
27. Ticona L, Schulman KA. Extreme home makeover–the role of intensive home health care. New Eng J Med. 2016;375:1707-1709.
28. Caplan GA. A meta-analysis of “hospital in the home.” Med J Aust. 2013;198:195-196.
29. Leff B, Burton L, Mader SL, et al. Hospital at home: feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med. 2005;143:798-808.
30. Shepperd S, Iliffe S, Doll HA, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev. 2016;9:CD007491.
31. Levine DM, Ouchi K, Blanchfield B, et al. Hospital-level care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020;172:77-85.
32. Cornwell T and Schwartzberg JG, eds. Medical Management of the Home Care Patient: Guidelines for Physicians. 4th ed. Chicago, IL: American Medical Association and American Academy of Home Care Physicians; 2012:p18.
33. Cornwell T and Schwartzberg JG, eds. Medical Management of the Home Care Patient: Guidelines for Physicians. 4th ed. Chicago, IL: American Medical Association and American Academy of Home Care Physicians; 2012:p19.
34. Accreditation Council for Graduate Medical Education. ACGME Program Requirements for Graduate Medical Education in Family Medicine. www.acgme.org/Portals/0/PFAssets/ProgramRequirements/120_FamilyMedicine_2020.pdf. (section IV.C.1.b). Accessed November 30, 2020.
1. Unwin BK, Tatum PE. House calls. Am Fam Physician. 2011;83:925-938.
3. Sairenji T, Jetty A, Peterson LE. Shifting patterns of physician home visits. J Prim Care Community Health. 2016;7:71-75.
4. Ornstein KA, Leff B, Covinsky K, et al. Epidemiology of the homebound population in the United States. JAMA Intern Med. 2015;175;1180-1186.
5. CMS. Current Procedural Terminology, Fourth Edition ("CPT®"). www.cms.gov/apps/physician-fee-schedule/license-agreement.aspx. Accessed November 30, 2020.
6. Elkan R, Kendrick D, Dewey M, et al. Effectiveness of home based support for older people: systematic review and meta-analysis. BMJ. 2001;323:719-725.
7. Stuck AE, Egger M, Hammer A, et al. Home visits to prevent nursing home admission and functional decline in elderly people: systematic review and meta-regression analysis. JAMA. 2002;287:1022-1028.
8. Stall N, Nowaczynski M, Sinha SK. Systematic review of outcomes from home-based primary care programs for homebound older adults. J Am Geriatr Soc. 2014;62:2243-2251.
9. Prosman GJ, Lo Fo Wong SH, van der Wouden JC, et al. Effectiveness of home visiting in reducing partner violence for families experiencing abuse: a systematic review. Fam Pract. 2015;32:247-256.
10. Han L, Ma Y, Wei S, et al. Are home visits an effective method for diabetes management? A quantitative systematic review and meta-analysis. J Diabetes Investig. 2017;8:701-708.
11. McWhinney IR. Fourth annual Nicholas J. Pisacano Lecture. The doctor, the patient, and the home: returning to our roots. J Am Board Fam Pract. 1997;10:430-435.
12. Kao H, Conant R, Soriano T, et al. The past, present, and future of house calls. Clin Geriatr Med. 2009;25:19-34.
13. American Public Health Association. Community health workers. www.apha.org/apha-communities/member-sections/community-health-workers. Accessed November 30, 2020.
14. Campbell JD, Brooks M, Hosokawa P, et al. Community health worker home visits for Medicaid-enrolled children with asthma: effects on asthma outcomes and costs. Am J Public Health. 2015;105:2366-2372.
15. Anugu M, Braksmajer A, Huang J, et al. Enriched medical home intervention using community health worker home visitation and ED use. Pediatrics. 2017;139:e20161849.
16. Reckrey JM, Gettenberg G, Ross H, et al. The critical role of social workers in home-based primary care. Soc Work in Health Care. 2014;53:330-343.
17. Cohen-Mansfield J, Shmotkin D, Hazan H. The effect of homebound status on older persons. J Am Geriatr Soc. 2010;58:2358-2362.
18. Mt. Sinai Visiting Doctors Program. www.mountsinai.org/care/primary-care/upper-east-side/visiting-doctors/about. Accessed November 30, 2020.
19. Ornstein K, Hernandez CR, DeCherrie LV, et al. The Mount Sinai (New York) Visiting Doctors Program: meeting the needs of the urban homebound population. Care Manag J. 2011;12:159-163.
20. Ornstein K, Smith K, Boal J. Understanding and improving the burden and unmet needs of informal caregivers of homebound patients enrolled in a home-based primary care program. J Appl Gerontol. 2009;28:482-503.
21. Novak M, Guest C. Application of a multidimensional caregiver burden inventory. Gerontologist. 1989;29:798-803.
22. Cruz J, Brooks D, Marques A. Home telemonitoring effectiveness in COPD: a systematic review. Int J Clin Pract. 2014;68:369-378.
23. Antoniades NC, Rochford PD, Pretto JJ, et al. Pilot study of remote telemonitoring in COPD. Telemed J E Health. 2012;18:634-640.
24. Koff PB, Jones RH, Cashman JM, et al. Proactive integrated care improves quality of life in patients with COPD. Eur Respir J. 2009;33:1031-1038.
25. Inglis SC, Clark RA, McAlister FA, et al. Which components of heart failure programmes are effective? A systematic review and meta-analysis of the outcomes of structured telephone support or telemonitoring as the primary component of chronic heart failure management in 8323 patients: abridged Cochrane review. Eur J Heart Fail. 2011;13:1028-1040.
26. Koehler F, Koehler K, Deckwart O, et al. Efficacy of telemedical interventional management in patients with heart failure (TIM-HF2): a randomised, controlled, parallel-group, unmasked trial. Lancet. 2018;392:1047-1057.
27. Ticona L, Schulman KA. Extreme home makeover–the role of intensive home health care. New Eng J Med. 2016;375:1707-1709.
28. Caplan GA. A meta-analysis of “hospital in the home.” Med J Aust. 2013;198:195-196.
29. Leff B, Burton L, Mader SL, et al. Hospital at home: feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med. 2005;143:798-808.
30. Shepperd S, Iliffe S, Doll HA, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev. 2016;9:CD007491.
31. Levine DM, Ouchi K, Blanchfield B, et al. Hospital-level care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020;172:77-85.
32. Cornwell T and Schwartzberg JG, eds. Medical Management of the Home Care Patient: Guidelines for Physicians. 4th ed. Chicago, IL: American Medical Association and American Academy of Home Care Physicians; 2012:p18.
33. Cornwell T and Schwartzberg JG, eds. Medical Management of the Home Care Patient: Guidelines for Physicians. 4th ed. Chicago, IL: American Medical Association and American Academy of Home Care Physicians; 2012:p19.
34. Accreditation Council for Graduate Medical Education. ACGME Program Requirements for Graduate Medical Education in Family Medicine. www.acgme.org/Portals/0/PFAssets/ProgramRequirements/120_FamilyMedicine_2020.pdf. (section IV.C.1.b). Accessed November 30, 2020.
PRACTICE RECOMMENDATIONS
❯ Consider incorporating home visits into the primary care of select vulnerable patients because doing so improves clinical outcomes, including mortality rates in neonates and elders. A
❯ Employ team-based home care and include community health workers, nurses, pharmacists, social workers, chaplains, and others. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Natural history of adrenal incidentalomas with and without mild autonomous cortisol excess
Background: Studies have suggested that adrenal incidentalomas may increase risk of cardiometabolic disease in patients. Guidelines for repeat imaging and hormonal assessment of adrenal incidentalomas are inconsistent because of inadequate studies.
Study design: Systematic review and meta-analysis.
Setting: MEDLINE, EMBASE, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, and Scopus were searched.
Synopsis: Of 1,139 studies screened; 32 met inclusion criteria: adult patients with adrenal adenoma who had 12 or more months of follow-up and outcomes of interest. Larger adrenal adenomas were less likely to have significant change in size on repeat imaging than did smaller tumors. There was no malignant transformation observed. Development of Cushing syndrome was seen in 6 of 2,745 patients. Cardiometabolic comorbid conditions were common in both MACE and NFAT patients with hypertension being the most frequently reported (64% and 58.2% respectively). Worsening of dyslipidemia was observed in both groups. Weight gain and the development of type 2 diabetes occurred more frequently in MACE than in NFAT patients (21.0% vs. 8.7%). In 1,356 patients, all-cause mortality was 11.2% (95% confidence interval, 9.5%-13.0%) for both groups over a mean follow-up of 56.3 months. Cardiovascular events accounted for 43.2% deaths. Limitations included the small number of patients in the studies assessed and the inconsistent definition of outcomes.
Bottom line: Patients with adrenal adenomas should be counseled on modifying cardiovascular risk factors whereas tumor growth, change in hormone production, and malignant transformation are less concerning based on the studies included.
Citation: Elhassan YS et al. Natural history of adrenal incidentalomas with and without mild autonomous cortisol excess: A systematic review and meta-analysis. Ann Intern Med. 2019 Jun 25;121:107-16.
Dr. Thompson is a hospitalist and assistant professor of medicine in the division of general internal medicine at Saint Louis University School of Medicine.
Background: Studies have suggested that adrenal incidentalomas may increase risk of cardiometabolic disease in patients. Guidelines for repeat imaging and hormonal assessment of adrenal incidentalomas are inconsistent because of inadequate studies.
Study design: Systematic review and meta-analysis.
Setting: MEDLINE, EMBASE, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, and Scopus were searched.
Synopsis: Of 1,139 studies screened; 32 met inclusion criteria: adult patients with adrenal adenoma who had 12 or more months of follow-up and outcomes of interest. Larger adrenal adenomas were less likely to have significant change in size on repeat imaging than did smaller tumors. There was no malignant transformation observed. Development of Cushing syndrome was seen in 6 of 2,745 patients. Cardiometabolic comorbid conditions were common in both MACE and NFAT patients with hypertension being the most frequently reported (64% and 58.2% respectively). Worsening of dyslipidemia was observed in both groups. Weight gain and the development of type 2 diabetes occurred more frequently in MACE than in NFAT patients (21.0% vs. 8.7%). In 1,356 patients, all-cause mortality was 11.2% (95% confidence interval, 9.5%-13.0%) for both groups over a mean follow-up of 56.3 months. Cardiovascular events accounted for 43.2% deaths. Limitations included the small number of patients in the studies assessed and the inconsistent definition of outcomes.
Bottom line: Patients with adrenal adenomas should be counseled on modifying cardiovascular risk factors whereas tumor growth, change in hormone production, and malignant transformation are less concerning based on the studies included.
Citation: Elhassan YS et al. Natural history of adrenal incidentalomas with and without mild autonomous cortisol excess: A systematic review and meta-analysis. Ann Intern Med. 2019 Jun 25;121:107-16.
Dr. Thompson is a hospitalist and assistant professor of medicine in the division of general internal medicine at Saint Louis University School of Medicine.
Background: Studies have suggested that adrenal incidentalomas may increase risk of cardiometabolic disease in patients. Guidelines for repeat imaging and hormonal assessment of adrenal incidentalomas are inconsistent because of inadequate studies.
Study design: Systematic review and meta-analysis.
Setting: MEDLINE, EMBASE, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, and Scopus were searched.
Synopsis: Of 1,139 studies screened; 32 met inclusion criteria: adult patients with adrenal adenoma who had 12 or more months of follow-up and outcomes of interest. Larger adrenal adenomas were less likely to have significant change in size on repeat imaging than did smaller tumors. There was no malignant transformation observed. Development of Cushing syndrome was seen in 6 of 2,745 patients. Cardiometabolic comorbid conditions were common in both MACE and NFAT patients with hypertension being the most frequently reported (64% and 58.2% respectively). Worsening of dyslipidemia was observed in both groups. Weight gain and the development of type 2 diabetes occurred more frequently in MACE than in NFAT patients (21.0% vs. 8.7%). In 1,356 patients, all-cause mortality was 11.2% (95% confidence interval, 9.5%-13.0%) for both groups over a mean follow-up of 56.3 months. Cardiovascular events accounted for 43.2% deaths. Limitations included the small number of patients in the studies assessed and the inconsistent definition of outcomes.
Bottom line: Patients with adrenal adenomas should be counseled on modifying cardiovascular risk factors whereas tumor growth, change in hormone production, and malignant transformation are less concerning based on the studies included.
Citation: Elhassan YS et al. Natural history of adrenal incidentalomas with and without mild autonomous cortisol excess: A systematic review and meta-analysis. Ann Intern Med. 2019 Jun 25;121:107-16.
Dr. Thompson is a hospitalist and assistant professor of medicine in the division of general internal medicine at Saint Louis University School of Medicine.
Fracking sites tied to increased heart failure hospitalizations
Living near hydraulic fracturing is associated with increased risk of hospitalization in people with heart failure (HF), a new study from Pennsylvania suggests.
The link was strongest among those with more severe heart failure but patients with either HF phenotype showed this association of increased risk with exposure to fracking activities, according to the investigators, led by Tara P. McAlexander, PhD, MPH, Drexel University Dornsife School of Public Health in Philadelphia.
“Our understanding has expanded well beyond the famous Harvard Six Cities study to know that it’s not just a short-term uptick in air pollution that›s going to send someone to the hospital a couple days later,” said Dr. McAlexander in an interview, referring to the study conducted from the mid-1970s through 1991. “We know that people who live in these environments and are exposed for long periods of time may have long-term detrimental effects.”
Although questions remain about specific mechanisms and how best to assess exposure, the evidence is mounting in a way that is consistent with the biologic hypotheses of how fracking would adversely affect health, Dr. McAlexander said. “We have many studies now on adverse pregnancy and birth outcomes, and that’s just the tip of the iceberg.”
Pennsylvania is a hot spot for fracking, also known as unconventional natural gas development (UNGD), with more than 12,000 wells drilled in the Marcellus shale since 2004. The shale extends from upstate New York in the north to northeastern Kentucky and Tennessee in the south and covers about 72,000 square miles. Last year, Pennsylvania pledged $3 million to study clusters of rare pediatric cancers and asthma near fracking operations. A recent grand jury report concluded government officials failed to protect residents from the health effects of fracking.
Fracking involves a cascade of activities that can trigger neural circuitry, sympathetic activation, and inflammation – all well-known pathways that potentiate heart failure, said Sanjay Rajagopalan, MD, who has researched the health effects of air pollution for two decades and was not involved with the study.
“If you think about it, it’s like environmental perturbation on steroids in some ways where they are pulling the trigger from a variety of different ways: noise, air pollution, social displacement, psychosocial impacts, economic disparities. So it’s not at all surprising that they saw an association,” said Dr. Rajagopalan, chief of cardiovascular medicine at University Hospitals Harrington Heart & Vascular Institute and director of the Case Western Cardiovascular Research Institute, both in Cleveland, Ohio.
As reported in the Journal of the American College of Cardiology, Dr. McAlexander and colleagues at Johns Hopkins University, Baltimore, used electronic health data from the Geisinger Health System to identify 9,054 patients with heart failure seen between 2008 and 2015. Of these, 5,839 patients had an incident HF hospitalization and 3,215 served as controls. Geisinger operates 13 hospitals and two research centers in 45 of Pennsylvania’s 67 counties, serving more than 3 million of the state’s residents.
Patients’ residential addresses were used to identify latitude and longitude coordinates that were matched with 9,669 UNGD wells in Pennsylvania and the location of major and minor roadways. The researchers also calculated a measure of community socioeconomic deprivation.
The adjusted odds of hospitalization were higher for patients in the highest quartile of exposure for three of the four UNGD phases: pad preparation (odds ratio, 1.70; 95% confidence interval, 1.35-2.13), stimulation or the actual fracking (OR, 1.80; 95% CI, 1.35-2.40), and production (OR, 1.62; 95% CI, 1.07-2.45).
Dr. McAlexander said she initially thought the lack of association with drilling (OR, 0.97; 95% CI, 0.75-1.27) was a mistake but noted that the drilling metric reflects a shorter time period than, for example, 30 days needed to clear the well pad and bring in the necessary equipment.
Stronger associations between pad preparation, fracking, and production are also consistent with the known increases in air pollution, traffic, and noise associated with these phases.
Individuals with more severe HF had greater odds of hospitalization, but the effect sizes were generally comparable between HF with preserved versus reduced ejection fraction. For those with the highest exposure to fracking, the odds ratios for hospitalization reached 2.25 (95% CI, 1.56-3.25) and 2.09 (95% CI, 1.44-3.03), respectively.
Notably, patients who could be phenotyped versus those who could not were more likely to die, to be hospitalized for HF, and to have a higher Charlson Comorbidity Index and other relevant diagnoses like myocardial infarction.
“Clinicians need to be increasingly aware that the environments their patients are in are a huge factor in their disease progression and outlook,” McAlexander said. “We know that UNGD, specifically now, is something that could be impacting a heart failure patient’s survival.”
She also suggested that the findings may also spur more advocacy work and “across-silo” collaboration between clinicians and environmental researchers.
Dr. Rajagopalan said there is increasing recognition that physicians need to be aware of environmental health links as extreme events like the California and Oregon wildfires and coastal flooding become increasingly common. “Unfortunately, unconventional is becoming the new convention.”
The problem for many physicians, however, is just having enough bandwidth to get through the day and get enough learning to keep above water, he said. Artificial intelligence could be used to seed electronic medical records with other personalized information from a bevy of sources including smartphones and the internet of things, but fundamental changes are also needed in the educational process to emphasize the environment.
“It’s going to take a huge societal shift in the way we view commodities, what we consider healthy, etc, but it can happen very quickly because all it takes is a crisis like COVID-19 to bring people to their knees and make them understand how this is going to take over our lives over the next decade,” Dr. Rajagopalan said.
The scientific community has been calling for “good” epidemiologic studies on the health effects of fracking since the early 2010s, Barrak Alahmad, MBChB, MPH, Harvard T.H. Chan School of Public Health, and Haitham Khraishah, MD, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, point out in an accompanying editorial.
The current study applied “extensive and rigorous methods” involving both the design and statistical approach, including use of a negative control analysis to assess for sources of spurious causal inference, several sensitivity analyses, and controlled for a wide range of covariates.
“Their results were consistent and robust across all these measures,” the editorialists wrote. “Most importantly, the effect size is probably too large to be explained away by an unmeasured confounder.”
Dr. Alahmad and Dr. Khraishah call for advancements in exposure assessment, citing a recent study reporting that ambient particle radioactivity near unconventional oil and gas sites could induce adverse health effects. Other unmet needs include a better understanding of racial disparities in the impacts of fracking and a fine-tuning of cause-specific cardiovascular morbidity and mortality.
The study was supported by training grants from the National Institute of Environmental Health Sciences to Dr. McAlexander and principal investigator Brian Schwartz, MD. The authors, Dr. Rajagopalan, Dr. Alahmad, and Dr. Khraishah have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Living near hydraulic fracturing is associated with increased risk of hospitalization in people with heart failure (HF), a new study from Pennsylvania suggests.
The link was strongest among those with more severe heart failure but patients with either HF phenotype showed this association of increased risk with exposure to fracking activities, according to the investigators, led by Tara P. McAlexander, PhD, MPH, Drexel University Dornsife School of Public Health in Philadelphia.
“Our understanding has expanded well beyond the famous Harvard Six Cities study to know that it’s not just a short-term uptick in air pollution that›s going to send someone to the hospital a couple days later,” said Dr. McAlexander in an interview, referring to the study conducted from the mid-1970s through 1991. “We know that people who live in these environments and are exposed for long periods of time may have long-term detrimental effects.”
Although questions remain about specific mechanisms and how best to assess exposure, the evidence is mounting in a way that is consistent with the biologic hypotheses of how fracking would adversely affect health, Dr. McAlexander said. “We have many studies now on adverse pregnancy and birth outcomes, and that’s just the tip of the iceberg.”
Pennsylvania is a hot spot for fracking, also known as unconventional natural gas development (UNGD), with more than 12,000 wells drilled in the Marcellus shale since 2004. The shale extends from upstate New York in the north to northeastern Kentucky and Tennessee in the south and covers about 72,000 square miles. Last year, Pennsylvania pledged $3 million to study clusters of rare pediatric cancers and asthma near fracking operations. A recent grand jury report concluded government officials failed to protect residents from the health effects of fracking.
Fracking involves a cascade of activities that can trigger neural circuitry, sympathetic activation, and inflammation – all well-known pathways that potentiate heart failure, said Sanjay Rajagopalan, MD, who has researched the health effects of air pollution for two decades and was not involved with the study.
“If you think about it, it’s like environmental perturbation on steroids in some ways where they are pulling the trigger from a variety of different ways: noise, air pollution, social displacement, psychosocial impacts, economic disparities. So it’s not at all surprising that they saw an association,” said Dr. Rajagopalan, chief of cardiovascular medicine at University Hospitals Harrington Heart & Vascular Institute and director of the Case Western Cardiovascular Research Institute, both in Cleveland, Ohio.
As reported in the Journal of the American College of Cardiology, Dr. McAlexander and colleagues at Johns Hopkins University, Baltimore, used electronic health data from the Geisinger Health System to identify 9,054 patients with heart failure seen between 2008 and 2015. Of these, 5,839 patients had an incident HF hospitalization and 3,215 served as controls. Geisinger operates 13 hospitals and two research centers in 45 of Pennsylvania’s 67 counties, serving more than 3 million of the state’s residents.
Patients’ residential addresses were used to identify latitude and longitude coordinates that were matched with 9,669 UNGD wells in Pennsylvania and the location of major and minor roadways. The researchers also calculated a measure of community socioeconomic deprivation.
The adjusted odds of hospitalization were higher for patients in the highest quartile of exposure for three of the four UNGD phases: pad preparation (odds ratio, 1.70; 95% confidence interval, 1.35-2.13), stimulation or the actual fracking (OR, 1.80; 95% CI, 1.35-2.40), and production (OR, 1.62; 95% CI, 1.07-2.45).
Dr. McAlexander said she initially thought the lack of association with drilling (OR, 0.97; 95% CI, 0.75-1.27) was a mistake but noted that the drilling metric reflects a shorter time period than, for example, 30 days needed to clear the well pad and bring in the necessary equipment.
Stronger associations between pad preparation, fracking, and production are also consistent with the known increases in air pollution, traffic, and noise associated with these phases.
Individuals with more severe HF had greater odds of hospitalization, but the effect sizes were generally comparable between HF with preserved versus reduced ejection fraction. For those with the highest exposure to fracking, the odds ratios for hospitalization reached 2.25 (95% CI, 1.56-3.25) and 2.09 (95% CI, 1.44-3.03), respectively.
Notably, patients who could be phenotyped versus those who could not were more likely to die, to be hospitalized for HF, and to have a higher Charlson Comorbidity Index and other relevant diagnoses like myocardial infarction.
“Clinicians need to be increasingly aware that the environments their patients are in are a huge factor in their disease progression and outlook,” McAlexander said. “We know that UNGD, specifically now, is something that could be impacting a heart failure patient’s survival.”
She also suggested that the findings may also spur more advocacy work and “across-silo” collaboration between clinicians and environmental researchers.
Dr. Rajagopalan said there is increasing recognition that physicians need to be aware of environmental health links as extreme events like the California and Oregon wildfires and coastal flooding become increasingly common. “Unfortunately, unconventional is becoming the new convention.”
The problem for many physicians, however, is just having enough bandwidth to get through the day and get enough learning to keep above water, he said. Artificial intelligence could be used to seed electronic medical records with other personalized information from a bevy of sources including smartphones and the internet of things, but fundamental changes are also needed in the educational process to emphasize the environment.
“It’s going to take a huge societal shift in the way we view commodities, what we consider healthy, etc, but it can happen very quickly because all it takes is a crisis like COVID-19 to bring people to their knees and make them understand how this is going to take over our lives over the next decade,” Dr. Rajagopalan said.
The scientific community has been calling for “good” epidemiologic studies on the health effects of fracking since the early 2010s, Barrak Alahmad, MBChB, MPH, Harvard T.H. Chan School of Public Health, and Haitham Khraishah, MD, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, point out in an accompanying editorial.
The current study applied “extensive and rigorous methods” involving both the design and statistical approach, including use of a negative control analysis to assess for sources of spurious causal inference, several sensitivity analyses, and controlled for a wide range of covariates.
“Their results were consistent and robust across all these measures,” the editorialists wrote. “Most importantly, the effect size is probably too large to be explained away by an unmeasured confounder.”
Dr. Alahmad and Dr. Khraishah call for advancements in exposure assessment, citing a recent study reporting that ambient particle radioactivity near unconventional oil and gas sites could induce adverse health effects. Other unmet needs include a better understanding of racial disparities in the impacts of fracking and a fine-tuning of cause-specific cardiovascular morbidity and mortality.
The study was supported by training grants from the National Institute of Environmental Health Sciences to Dr. McAlexander and principal investigator Brian Schwartz, MD. The authors, Dr. Rajagopalan, Dr. Alahmad, and Dr. Khraishah have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Living near hydraulic fracturing is associated with increased risk of hospitalization in people with heart failure (HF), a new study from Pennsylvania suggests.
The link was strongest among those with more severe heart failure but patients with either HF phenotype showed this association of increased risk with exposure to fracking activities, according to the investigators, led by Tara P. McAlexander, PhD, MPH, Drexel University Dornsife School of Public Health in Philadelphia.
“Our understanding has expanded well beyond the famous Harvard Six Cities study to know that it’s not just a short-term uptick in air pollution that›s going to send someone to the hospital a couple days later,” said Dr. McAlexander in an interview, referring to the study conducted from the mid-1970s through 1991. “We know that people who live in these environments and are exposed for long periods of time may have long-term detrimental effects.”
Although questions remain about specific mechanisms and how best to assess exposure, the evidence is mounting in a way that is consistent with the biologic hypotheses of how fracking would adversely affect health, Dr. McAlexander said. “We have many studies now on adverse pregnancy and birth outcomes, and that’s just the tip of the iceberg.”
Pennsylvania is a hot spot for fracking, also known as unconventional natural gas development (UNGD), with more than 12,000 wells drilled in the Marcellus shale since 2004. The shale extends from upstate New York in the north to northeastern Kentucky and Tennessee in the south and covers about 72,000 square miles. Last year, Pennsylvania pledged $3 million to study clusters of rare pediatric cancers and asthma near fracking operations. A recent grand jury report concluded government officials failed to protect residents from the health effects of fracking.
Fracking involves a cascade of activities that can trigger neural circuitry, sympathetic activation, and inflammation – all well-known pathways that potentiate heart failure, said Sanjay Rajagopalan, MD, who has researched the health effects of air pollution for two decades and was not involved with the study.
“If you think about it, it’s like environmental perturbation on steroids in some ways where they are pulling the trigger from a variety of different ways: noise, air pollution, social displacement, psychosocial impacts, economic disparities. So it’s not at all surprising that they saw an association,” said Dr. Rajagopalan, chief of cardiovascular medicine at University Hospitals Harrington Heart & Vascular Institute and director of the Case Western Cardiovascular Research Institute, both in Cleveland, Ohio.
As reported in the Journal of the American College of Cardiology, Dr. McAlexander and colleagues at Johns Hopkins University, Baltimore, used electronic health data from the Geisinger Health System to identify 9,054 patients with heart failure seen between 2008 and 2015. Of these, 5,839 patients had an incident HF hospitalization and 3,215 served as controls. Geisinger operates 13 hospitals and two research centers in 45 of Pennsylvania’s 67 counties, serving more than 3 million of the state’s residents.
Patients’ residential addresses were used to identify latitude and longitude coordinates that were matched with 9,669 UNGD wells in Pennsylvania and the location of major and minor roadways. The researchers also calculated a measure of community socioeconomic deprivation.
The adjusted odds of hospitalization were higher for patients in the highest quartile of exposure for three of the four UNGD phases: pad preparation (odds ratio, 1.70; 95% confidence interval, 1.35-2.13), stimulation or the actual fracking (OR, 1.80; 95% CI, 1.35-2.40), and production (OR, 1.62; 95% CI, 1.07-2.45).
Dr. McAlexander said she initially thought the lack of association with drilling (OR, 0.97; 95% CI, 0.75-1.27) was a mistake but noted that the drilling metric reflects a shorter time period than, for example, 30 days needed to clear the well pad and bring in the necessary equipment.
Stronger associations between pad preparation, fracking, and production are also consistent with the known increases in air pollution, traffic, and noise associated with these phases.
Individuals with more severe HF had greater odds of hospitalization, but the effect sizes were generally comparable between HF with preserved versus reduced ejection fraction. For those with the highest exposure to fracking, the odds ratios for hospitalization reached 2.25 (95% CI, 1.56-3.25) and 2.09 (95% CI, 1.44-3.03), respectively.
Notably, patients who could be phenotyped versus those who could not were more likely to die, to be hospitalized for HF, and to have a higher Charlson Comorbidity Index and other relevant diagnoses like myocardial infarction.
“Clinicians need to be increasingly aware that the environments their patients are in are a huge factor in their disease progression and outlook,” McAlexander said. “We know that UNGD, specifically now, is something that could be impacting a heart failure patient’s survival.”
She also suggested that the findings may also spur more advocacy work and “across-silo” collaboration between clinicians and environmental researchers.
Dr. Rajagopalan said there is increasing recognition that physicians need to be aware of environmental health links as extreme events like the California and Oregon wildfires and coastal flooding become increasingly common. “Unfortunately, unconventional is becoming the new convention.”
The problem for many physicians, however, is just having enough bandwidth to get through the day and get enough learning to keep above water, he said. Artificial intelligence could be used to seed electronic medical records with other personalized information from a bevy of sources including smartphones and the internet of things, but fundamental changes are also needed in the educational process to emphasize the environment.
“It’s going to take a huge societal shift in the way we view commodities, what we consider healthy, etc, but it can happen very quickly because all it takes is a crisis like COVID-19 to bring people to their knees and make them understand how this is going to take over our lives over the next decade,” Dr. Rajagopalan said.
The scientific community has been calling for “good” epidemiologic studies on the health effects of fracking since the early 2010s, Barrak Alahmad, MBChB, MPH, Harvard T.H. Chan School of Public Health, and Haitham Khraishah, MD, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, point out in an accompanying editorial.
The current study applied “extensive and rigorous methods” involving both the design and statistical approach, including use of a negative control analysis to assess for sources of spurious causal inference, several sensitivity analyses, and controlled for a wide range of covariates.
“Their results were consistent and robust across all these measures,” the editorialists wrote. “Most importantly, the effect size is probably too large to be explained away by an unmeasured confounder.”
Dr. Alahmad and Dr. Khraishah call for advancements in exposure assessment, citing a recent study reporting that ambient particle radioactivity near unconventional oil and gas sites could induce adverse health effects. Other unmet needs include a better understanding of racial disparities in the impacts of fracking and a fine-tuning of cause-specific cardiovascular morbidity and mortality.
The study was supported by training grants from the National Institute of Environmental Health Sciences to Dr. McAlexander and principal investigator Brian Schwartz, MD. The authors, Dr. Rajagopalan, Dr. Alahmad, and Dr. Khraishah have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Calcium burden drives CV risk whether coronary disease is obstructive or not
Coronary artery calcium (CAC) score as a measure of plaque burden more reliably predicts future cardiovascular (CV) risk in patients with suspected coronary disease (CAD) than whether or not the disease is obstructive, a large retrospective study suggests.
Indeed, CV risk went up in tandem with growing plaque burden regardless of whether there was obstructive disease in any coronary artery, defined as a 50% or greater stenosis by computed tomographic angiography (CTA).
The findings argue for plaque burden as measured by CAC score, rather than percent-stenosis severity, for guiding further treatment decisions in such patients, researchers say.
The research was based on more than 20,000 symptomatic patients referred to diagnostic CTA in the Western Denmark Heart Registry who were then followed for about 4 years for major CV events, including death, myocardial infarction, or stroke.
“What we show is that CAC is important for prognosis, and that patients with no stenosis have similar high risk as patients with stenosis when CAC burden is similar,” Martin Bødtker Mortensen, MD, PhD, Aarhus (Denmark) University Hospital, said in an interview.
The guidelines “distinguish between primary and secondary prevention patients” based on the presence or absence of obstructive CAD, he said, but “our results challenge this long-held approach. We show that patients with nonobstructive CAD carry similar risk as patients with obstructive CAD.”
In practice, risk tends to be greater in patients with obstructive compared with nonobstructive CAD. But the reason “is simply that they normally have higher atherosclerosis burden,” Dr. Mortensen said. “When you stratify based on atherosclerosis burden, then patients with obstructive and nonobstructive CAD have similar risk.”
The analysis was published online Dec. 7 in the Journal of the American College of Cardiology with Mortensen as lead author.
Until recently, it had long been believed that CV-event risk was driven by ischemia – but “ischemia is just a surrogate for the extent of atherosclerotic disease,” Armin Arbab Zadeh, MD, PhD, MPH, who is not connected with the current study, said in an interview.
The finding that CV risk climbs with growing coronary plaque burden “essentially confirms” other recent studies, but with “added value in showing how well the calcium scores, compared to obstructive disease, track with risk. So it’s definitely a nice extension of the evidence,” said Dr. Zadeh, director of cardiac CT at Johns Hopkins University, Baltimore.
“This study clearly shows that there is no ischemia ‘threshold,’ that the risk starts from mild and goes up with the burden of atherosclerotic disease. We were essentially taught wrong for decades.”
Dr. Mortensen said that the new results “are in line with previous studies showing that atherosclerosis burden is very important for risk.” They also help explain why revascularization of patients with stable angina failed to cut the risk of MI or death in trials like COURAGE, FAME-2, and ISCHEMIA. It’s because “stenosis per se explains little of the risk compared to atherosclerosis burden.”
In the current analysis, for example, about 65% of events were in patients who did not show obstructive CAD at CTA. Its 23,759 patients with symptoms suggestive of CAD were referred for CTA from 2008 through 2017; 5,043 (21.2%) were found to have obstructive disease and 18,716 (78.8%) either had no CAD or nonobstructive disease.
About 4.4% of patients experienced a first major CV event over a median follow-up of 4.3 years. Only events occurring later than 90 days after CTA were counted in an effort to exclude any directly related to revascularization, Dr. Mortensen noted.
The risk of events went up proportionally with both CAC score and the number of coronaries with obstructive disease.
The number of major CV events per 1,000 person-years was 6.2 for patients with a CAC score of 0, of whom 87% had no CAD by CTA, 7% had nonobstructive CAD, and 6% had obstructive CAD.
The corresponding rate was 17.5 among patients with a CAC score >100-399 for a hazard ratio (HR) of 1.7 (95% confidence interval [CI] 1.4-2.1) vs. a CAC score of 0.
And it was 42.3 per 1,000 patient-years among patients with CAC score >1000, HR 3.4 (95% CI, 2.5-4.6) vs. a CAC score of 0. Among those with the highest-tier CAC score, none were without CAD by CTA, 17% had nonobstructive disease, and 83% had obstructive CAD.
The major CV event rate rose similarly by number of coronaries with obstructive disease. It was 6.1 per 1,000 person-years in patients with no CAD. But it was 12.3 in those with nonobstructive disease, HR 1.3 (95% CI 1.1-1.6), up to 34.7 in those with triple-vessel obstructive disease, HR 2.9 (95% CI 2.2-3.9), vs. no CAD.
However, in an analysis with stratification by CAC score tier (0, 1-99, 100-399, 400-1,000, and >1,000), obstructive CAD was not associated with increased major CV-event risk in any stratum. The findings were similar in each subgroup with 1-vessel, 2-vessel, or 3-vessel CAD when stratified by CAC score.
Nor did major CV event risk track with obstructive CAD in analyses by age or after excluding all patients who underwent coronary revascularization within 90 days of CTA, the group reported.
“I believe these results support the use of CTA as a first-line test in patients with symptoms suggestive of CAD, as it provides valuable information for both diagnosis and prognosis in symptomatic patients,” Dr. Mortensen said. Those found to have a higher burden of atherosclerosis, he added, should receive aggressive preventive therapy regardless of whether or not they have obstructive disease.
The evidence from this study and others “supports a CTA-based approach” in such patients, Dr. Zadeh said. “And I would go further to say that a stress test is really inadequate,” in that it “detects the disease at such a late stage, you’re missing the opportunity to identify these patients who have atherosclerotic disease while you can do something about it.”
Its continued use as a first-line test, Dr. Zadeh said, “is essentially, in my mind, dismissing the evidence.”
An accompanying editorial Todd C. Villines, MD, and Patricia Rodriguez Lozano, MD, of the University of Virginia, Charlottesville agreed that “it is time that the traditional definitions of primary and secondary prevention evolve to incorporate CAC and CTA measures of patient risk based on coronary artery plaque burden.”
But they pointed out some limitations of the current study.
“The authors compared CAC with ≥50% stenosis, not CAC to comprehensive, contemporary coronary CTA,” and so “did not assess numerous other well-validated measures of coronary plaque burden that are routinely obtained from coronary CTA that typically improve the prognostic accuracy of coronary CTA beyond stenosis alone.” Also not performed was “plaque quantification on coronary CTA, an emerging field of study.”
The editorialists noted that noncontrast CT as used in the study for CAC scoring “is generally not recommended as a standalone test in symptomatic patients. Most studies have shown that coronary CTA, a test that accurately detects stenosis and identifies all types of coronary atherosclerosis (calcified and noncalcified), has significantly higher diagnostic and prognostic accuracy than CAC when performed in symptomatic patients without known coronary artery disease.”
Dr. Mortensen has disclosed no relevant financial relationships. Disclosures for the other authors are in the report. Dr. Villines and Dr. Rodriguez Lozano have disclosed no relevant financial relationships. Dr. Zadeh disclosed receiving grant support from Canon Medical Systems.
A version of this article originally appeared on Medscape.com.
Coronary artery calcium (CAC) score as a measure of plaque burden more reliably predicts future cardiovascular (CV) risk in patients with suspected coronary disease (CAD) than whether or not the disease is obstructive, a large retrospective study suggests.
Indeed, CV risk went up in tandem with growing plaque burden regardless of whether there was obstructive disease in any coronary artery, defined as a 50% or greater stenosis by computed tomographic angiography (CTA).
The findings argue for plaque burden as measured by CAC score, rather than percent-stenosis severity, for guiding further treatment decisions in such patients, researchers say.
The research was based on more than 20,000 symptomatic patients referred to diagnostic CTA in the Western Denmark Heart Registry who were then followed for about 4 years for major CV events, including death, myocardial infarction, or stroke.
“What we show is that CAC is important for prognosis, and that patients with no stenosis have similar high risk as patients with stenosis when CAC burden is similar,” Martin Bødtker Mortensen, MD, PhD, Aarhus (Denmark) University Hospital, said in an interview.
The guidelines “distinguish between primary and secondary prevention patients” based on the presence or absence of obstructive CAD, he said, but “our results challenge this long-held approach. We show that patients with nonobstructive CAD carry similar risk as patients with obstructive CAD.”
In practice, risk tends to be greater in patients with obstructive compared with nonobstructive CAD. But the reason “is simply that they normally have higher atherosclerosis burden,” Dr. Mortensen said. “When you stratify based on atherosclerosis burden, then patients with obstructive and nonobstructive CAD have similar risk.”
The analysis was published online Dec. 7 in the Journal of the American College of Cardiology with Mortensen as lead author.
Until recently, it had long been believed that CV-event risk was driven by ischemia – but “ischemia is just a surrogate for the extent of atherosclerotic disease,” Armin Arbab Zadeh, MD, PhD, MPH, who is not connected with the current study, said in an interview.
The finding that CV risk climbs with growing coronary plaque burden “essentially confirms” other recent studies, but with “added value in showing how well the calcium scores, compared to obstructive disease, track with risk. So it’s definitely a nice extension of the evidence,” said Dr. Zadeh, director of cardiac CT at Johns Hopkins University, Baltimore.
“This study clearly shows that there is no ischemia ‘threshold,’ that the risk starts from mild and goes up with the burden of atherosclerotic disease. We were essentially taught wrong for decades.”
Dr. Mortensen said that the new results “are in line with previous studies showing that atherosclerosis burden is very important for risk.” They also help explain why revascularization of patients with stable angina failed to cut the risk of MI or death in trials like COURAGE, FAME-2, and ISCHEMIA. It’s because “stenosis per se explains little of the risk compared to atherosclerosis burden.”
In the current analysis, for example, about 65% of events were in patients who did not show obstructive CAD at CTA. Its 23,759 patients with symptoms suggestive of CAD were referred for CTA from 2008 through 2017; 5,043 (21.2%) were found to have obstructive disease and 18,716 (78.8%) either had no CAD or nonobstructive disease.
About 4.4% of patients experienced a first major CV event over a median follow-up of 4.3 years. Only events occurring later than 90 days after CTA were counted in an effort to exclude any directly related to revascularization, Dr. Mortensen noted.
The risk of events went up proportionally with both CAC score and the number of coronaries with obstructive disease.
The number of major CV events per 1,000 person-years was 6.2 for patients with a CAC score of 0, of whom 87% had no CAD by CTA, 7% had nonobstructive CAD, and 6% had obstructive CAD.
The corresponding rate was 17.5 among patients with a CAC score >100-399 for a hazard ratio (HR) of 1.7 (95% confidence interval [CI] 1.4-2.1) vs. a CAC score of 0.
And it was 42.3 per 1,000 patient-years among patients with CAC score >1000, HR 3.4 (95% CI, 2.5-4.6) vs. a CAC score of 0. Among those with the highest-tier CAC score, none were without CAD by CTA, 17% had nonobstructive disease, and 83% had obstructive CAD.
The major CV event rate rose similarly by number of coronaries with obstructive disease. It was 6.1 per 1,000 person-years in patients with no CAD. But it was 12.3 in those with nonobstructive disease, HR 1.3 (95% CI 1.1-1.6), up to 34.7 in those with triple-vessel obstructive disease, HR 2.9 (95% CI 2.2-3.9), vs. no CAD.
However, in an analysis with stratification by CAC score tier (0, 1-99, 100-399, 400-1,000, and >1,000), obstructive CAD was not associated with increased major CV-event risk in any stratum. The findings were similar in each subgroup with 1-vessel, 2-vessel, or 3-vessel CAD when stratified by CAC score.
Nor did major CV event risk track with obstructive CAD in analyses by age or after excluding all patients who underwent coronary revascularization within 90 days of CTA, the group reported.
“I believe these results support the use of CTA as a first-line test in patients with symptoms suggestive of CAD, as it provides valuable information for both diagnosis and prognosis in symptomatic patients,” Dr. Mortensen said. Those found to have a higher burden of atherosclerosis, he added, should receive aggressive preventive therapy regardless of whether or not they have obstructive disease.
The evidence from this study and others “supports a CTA-based approach” in such patients, Dr. Zadeh said. “And I would go further to say that a stress test is really inadequate,” in that it “detects the disease at such a late stage, you’re missing the opportunity to identify these patients who have atherosclerotic disease while you can do something about it.”
Its continued use as a first-line test, Dr. Zadeh said, “is essentially, in my mind, dismissing the evidence.”
An accompanying editorial Todd C. Villines, MD, and Patricia Rodriguez Lozano, MD, of the University of Virginia, Charlottesville agreed that “it is time that the traditional definitions of primary and secondary prevention evolve to incorporate CAC and CTA measures of patient risk based on coronary artery plaque burden.”
But they pointed out some limitations of the current study.
“The authors compared CAC with ≥50% stenosis, not CAC to comprehensive, contemporary coronary CTA,” and so “did not assess numerous other well-validated measures of coronary plaque burden that are routinely obtained from coronary CTA that typically improve the prognostic accuracy of coronary CTA beyond stenosis alone.” Also not performed was “plaque quantification on coronary CTA, an emerging field of study.”
The editorialists noted that noncontrast CT as used in the study for CAC scoring “is generally not recommended as a standalone test in symptomatic patients. Most studies have shown that coronary CTA, a test that accurately detects stenosis and identifies all types of coronary atherosclerosis (calcified and noncalcified), has significantly higher diagnostic and prognostic accuracy than CAC when performed in symptomatic patients without known coronary artery disease.”
Dr. Mortensen has disclosed no relevant financial relationships. Disclosures for the other authors are in the report. Dr. Villines and Dr. Rodriguez Lozano have disclosed no relevant financial relationships. Dr. Zadeh disclosed receiving grant support from Canon Medical Systems.
A version of this article originally appeared on Medscape.com.
Coronary artery calcium (CAC) score as a measure of plaque burden more reliably predicts future cardiovascular (CV) risk in patients with suspected coronary disease (CAD) than whether or not the disease is obstructive, a large retrospective study suggests.
Indeed, CV risk went up in tandem with growing plaque burden regardless of whether there was obstructive disease in any coronary artery, defined as a 50% or greater stenosis by computed tomographic angiography (CTA).
The findings argue for plaque burden as measured by CAC score, rather than percent-stenosis severity, for guiding further treatment decisions in such patients, researchers say.
The research was based on more than 20,000 symptomatic patients referred to diagnostic CTA in the Western Denmark Heart Registry who were then followed for about 4 years for major CV events, including death, myocardial infarction, or stroke.
“What we show is that CAC is important for prognosis, and that patients with no stenosis have similar high risk as patients with stenosis when CAC burden is similar,” Martin Bødtker Mortensen, MD, PhD, Aarhus (Denmark) University Hospital, said in an interview.
The guidelines “distinguish between primary and secondary prevention patients” based on the presence or absence of obstructive CAD, he said, but “our results challenge this long-held approach. We show that patients with nonobstructive CAD carry similar risk as patients with obstructive CAD.”
In practice, risk tends to be greater in patients with obstructive compared with nonobstructive CAD. But the reason “is simply that they normally have higher atherosclerosis burden,” Dr. Mortensen said. “When you stratify based on atherosclerosis burden, then patients with obstructive and nonobstructive CAD have similar risk.”
The analysis was published online Dec. 7 in the Journal of the American College of Cardiology with Mortensen as lead author.
Until recently, it had long been believed that CV-event risk was driven by ischemia – but “ischemia is just a surrogate for the extent of atherosclerotic disease,” Armin Arbab Zadeh, MD, PhD, MPH, who is not connected with the current study, said in an interview.
The finding that CV risk climbs with growing coronary plaque burden “essentially confirms” other recent studies, but with “added value in showing how well the calcium scores, compared to obstructive disease, track with risk. So it’s definitely a nice extension of the evidence,” said Dr. Zadeh, director of cardiac CT at Johns Hopkins University, Baltimore.
“This study clearly shows that there is no ischemia ‘threshold,’ that the risk starts from mild and goes up with the burden of atherosclerotic disease. We were essentially taught wrong for decades.”
Dr. Mortensen said that the new results “are in line with previous studies showing that atherosclerosis burden is very important for risk.” They also help explain why revascularization of patients with stable angina failed to cut the risk of MI or death in trials like COURAGE, FAME-2, and ISCHEMIA. It’s because “stenosis per se explains little of the risk compared to atherosclerosis burden.”
In the current analysis, for example, about 65% of events were in patients who did not show obstructive CAD at CTA. Its 23,759 patients with symptoms suggestive of CAD were referred for CTA from 2008 through 2017; 5,043 (21.2%) were found to have obstructive disease and 18,716 (78.8%) either had no CAD or nonobstructive disease.
About 4.4% of patients experienced a first major CV event over a median follow-up of 4.3 years. Only events occurring later than 90 days after CTA were counted in an effort to exclude any directly related to revascularization, Dr. Mortensen noted.
The risk of events went up proportionally with both CAC score and the number of coronaries with obstructive disease.
The number of major CV events per 1,000 person-years was 6.2 for patients with a CAC score of 0, of whom 87% had no CAD by CTA, 7% had nonobstructive CAD, and 6% had obstructive CAD.
The corresponding rate was 17.5 among patients with a CAC score >100-399 for a hazard ratio (HR) of 1.7 (95% confidence interval [CI] 1.4-2.1) vs. a CAC score of 0.
And it was 42.3 per 1,000 patient-years among patients with CAC score >1000, HR 3.4 (95% CI, 2.5-4.6) vs. a CAC score of 0. Among those with the highest-tier CAC score, none were without CAD by CTA, 17% had nonobstructive disease, and 83% had obstructive CAD.
The major CV event rate rose similarly by number of coronaries with obstructive disease. It was 6.1 per 1,000 person-years in patients with no CAD. But it was 12.3 in those with nonobstructive disease, HR 1.3 (95% CI 1.1-1.6), up to 34.7 in those with triple-vessel obstructive disease, HR 2.9 (95% CI 2.2-3.9), vs. no CAD.
However, in an analysis with stratification by CAC score tier (0, 1-99, 100-399, 400-1,000, and >1,000), obstructive CAD was not associated with increased major CV-event risk in any stratum. The findings were similar in each subgroup with 1-vessel, 2-vessel, or 3-vessel CAD when stratified by CAC score.
Nor did major CV event risk track with obstructive CAD in analyses by age or after excluding all patients who underwent coronary revascularization within 90 days of CTA, the group reported.
“I believe these results support the use of CTA as a first-line test in patients with symptoms suggestive of CAD, as it provides valuable information for both diagnosis and prognosis in symptomatic patients,” Dr. Mortensen said. Those found to have a higher burden of atherosclerosis, he added, should receive aggressive preventive therapy regardless of whether or not they have obstructive disease.
The evidence from this study and others “supports a CTA-based approach” in such patients, Dr. Zadeh said. “And I would go further to say that a stress test is really inadequate,” in that it “detects the disease at such a late stage, you’re missing the opportunity to identify these patients who have atherosclerotic disease while you can do something about it.”
Its continued use as a first-line test, Dr. Zadeh said, “is essentially, in my mind, dismissing the evidence.”
An accompanying editorial Todd C. Villines, MD, and Patricia Rodriguez Lozano, MD, of the University of Virginia, Charlottesville agreed that “it is time that the traditional definitions of primary and secondary prevention evolve to incorporate CAC and CTA measures of patient risk based on coronary artery plaque burden.”
But they pointed out some limitations of the current study.
“The authors compared CAC with ≥50% stenosis, not CAC to comprehensive, contemporary coronary CTA,” and so “did not assess numerous other well-validated measures of coronary plaque burden that are routinely obtained from coronary CTA that typically improve the prognostic accuracy of coronary CTA beyond stenosis alone.” Also not performed was “plaque quantification on coronary CTA, an emerging field of study.”
The editorialists noted that noncontrast CT as used in the study for CAC scoring “is generally not recommended as a standalone test in symptomatic patients. Most studies have shown that coronary CTA, a test that accurately detects stenosis and identifies all types of coronary atherosclerosis (calcified and noncalcified), has significantly higher diagnostic and prognostic accuracy than CAC when performed in symptomatic patients without known coronary artery disease.”
Dr. Mortensen has disclosed no relevant financial relationships. Disclosures for the other authors are in the report. Dr. Villines and Dr. Rodriguez Lozano have disclosed no relevant financial relationships. Dr. Zadeh disclosed receiving grant support from Canon Medical Systems.
A version of this article originally appeared on Medscape.com.
COVID-19 and risk of clotting: ‘Be proactive about prevention’
The risk of arterial and venous thrombosis in patients with COVID-19 has been a major issue throughout the pandemic, and how best to manage this risk is the subject of a new review article.
The article, by Gregory Dr. Piazza, MD, and David A. Morrow, MD, Brigham and Women’s Hospital, Boston, was published online in JAMA on Nov. 23.
“Basically we’re saying: ‘Be proactive about prevention,’” Dr. Piazza told this news organization.
There is growing recognition among those on the frontline that there is an increased risk of thrombosis in COVID-19 patients, Dr. Piazza said. The risk is highest in patients in the intensive care unit, but the risk is also increased in patients hospitalized with COVID-19, even those not in ICU.
“We don’t really know what the risk is in nonhospitalized COVID-19 patients, but we think it’s much lower than in those who are hospitalized,” he said. “We are waiting for data on the optimal way of managing this increased risk of thrombosis in COVID patients, but for the time being, we believe a systematic way of addressing this risk is best, with every patient hospitalized with COVID-19 receiving some type of thromboprophylaxis. This would mainly be with anticoagulation, but in patients in whom anticoagulation is contraindicated, then mechanical methods could be used, such as pneumatic compression boots or compression stockings.”
The authors report thrombotic complication rates of 2.6% in noncritically ill hospitalized patients with COVID-19 and 35.3% in critically ill patients from a recent U.S. registry study.
Autopsy findings of microthrombi in multiple organ systems, including the lungs, heart, and kidneys, suggest that thrombosis may contribute to multisystem organ dysfunction in severe COVID-19, they note. Although the pathophysiology is not fully defined, prothrombotic abnormalities have been identified in patients with COVID-19, including elevated levels of D-dimer, fibrinogen, and factor VIII, they add.
“There are several major questions about which COVID-19 patients to treat with thromboprophylaxis, how to treat them in term of levels of anticoagulation, and there are many ongoing clinical trials to try and answer these questions,” Dr. Piazza commented. “We need results from these randomized trials to provide a better compass for COVID-19 patients at risk of clotting.”
At present, clinicians can follow two different sets of guidelines on the issue, one from the American College of Chest Physicians and the other from the International Society on Thrombosis and Hemostasis, the authors note.
“The ACCP guidelines are very conservative and basically follow the evidence base for medical patients, while the ISTH guidelines are more aggressive and recommend increased levels of anticoagulation in both ICU and hospitalized non-ICU patients and also extend prophylaxis after discharge,” Dr. Piazza said.
“There is quite a difference between the two sets of guidelines, which can be a point of confusion,” he added.
Dr. Piazza notes that at his center every hospitalized COVID patient who does not have a contraindication to anticoagulation receives a standard prophylactic dose of a once-daily low-molecular-weight heparin (for example, enoxaparin 40 mg). A once-daily product is used to minimize infection risk to staff.
While all COVID patients in the ICU should automatically receive some anticoagulation, the optimal dose is an area of active investigation, he explained. “There were several early reports of ICU patients developing blood clots despite receiving standard thromboprophylaxis so perhaps we need to use higher doses. There are trials underway looking at this, and we would advise enrolling patients into these trials.”
If patients can’t be enrolled into trials, and clinicians feel higher anticoagulation levels are needed, Dr. Piazza advises following the ISTH guidance, which allows an intermediate dose of low-molecular-weight heparin (up to 1 mg/kg enoxaparin).
“Some experts are suggesting even higher doses may be needed in some ICU patients, such as the full therapeutic dose, but I worry about the risk of bleeding with such a strategy,” he said.
Dr. Piazza says they do not routinely give anticoagulation after discharge, but if this is desired then patients could be switched to an oral agent, and some of the direct-acting oral anticoagulants are approved for prophylactic use in medically ill patients.
Dr. Piazza points out that whether thromboprophylaxis should be used for nonhospitalized COVID patients who have risk factors for clotting such as a prior history of thrombosis or obesity is a pressing question, and he encourages clinicians to enroll these patients in clinical trials evaluating this issue, such as the PREVENT-HD trial.
“If they can’t enroll patents in a trial, then they have to make a decision whether the patient is high-enough risk to justify off-label use of anticoagulant. There is a case to be made for this, but there is no evidence for or against such action at present,” he noted.
At this time, neither the ISTH nor ACCP recommend measuring D-dimer to screen for venous thromboembolism or to determine intensity of prophylaxis or treatment, the authors note.
“Ongoing investigation will determine optimal preventive regimens in COVID-19 in the intensive care unit, at hospital discharge, and in nonhospitalized patients at high risk for thrombosis,” they conclude.
Dr. Piazza reported grants from Bayer, Bristol Myers Squibb, Boston Scientific, Janssen, and Portola, and personal fees from Agile, Amgen, Pfizer, and the Prairie Education and Research Cooperative outside the submitted work. Dr. Morrow reported grants from Abbott Laboratories, Amgen, Anthos Therapeutics, Esai, GlaxoSmithKline, Takeda, and The Medicines Company; grants and personal fees from AstraZeneca, Merck, Novartis, and Roche Diagnostics; and personal fees from Bayer Pharma and InCarda outside the submitted work.
A version of this article originally appeared on Medscape.com.
The risk of arterial and venous thrombosis in patients with COVID-19 has been a major issue throughout the pandemic, and how best to manage this risk is the subject of a new review article.
The article, by Gregory Dr. Piazza, MD, and David A. Morrow, MD, Brigham and Women’s Hospital, Boston, was published online in JAMA on Nov. 23.
“Basically we’re saying: ‘Be proactive about prevention,’” Dr. Piazza told this news organization.
There is growing recognition among those on the frontline that there is an increased risk of thrombosis in COVID-19 patients, Dr. Piazza said. The risk is highest in patients in the intensive care unit, but the risk is also increased in patients hospitalized with COVID-19, even those not in ICU.
“We don’t really know what the risk is in nonhospitalized COVID-19 patients, but we think it’s much lower than in those who are hospitalized,” he said. “We are waiting for data on the optimal way of managing this increased risk of thrombosis in COVID patients, but for the time being, we believe a systematic way of addressing this risk is best, with every patient hospitalized with COVID-19 receiving some type of thromboprophylaxis. This would mainly be with anticoagulation, but in patients in whom anticoagulation is contraindicated, then mechanical methods could be used, such as pneumatic compression boots or compression stockings.”
The authors report thrombotic complication rates of 2.6% in noncritically ill hospitalized patients with COVID-19 and 35.3% in critically ill patients from a recent U.S. registry study.
Autopsy findings of microthrombi in multiple organ systems, including the lungs, heart, and kidneys, suggest that thrombosis may contribute to multisystem organ dysfunction in severe COVID-19, they note. Although the pathophysiology is not fully defined, prothrombotic abnormalities have been identified in patients with COVID-19, including elevated levels of D-dimer, fibrinogen, and factor VIII, they add.
“There are several major questions about which COVID-19 patients to treat with thromboprophylaxis, how to treat them in term of levels of anticoagulation, and there are many ongoing clinical trials to try and answer these questions,” Dr. Piazza commented. “We need results from these randomized trials to provide a better compass for COVID-19 patients at risk of clotting.”
At present, clinicians can follow two different sets of guidelines on the issue, one from the American College of Chest Physicians and the other from the International Society on Thrombosis and Hemostasis, the authors note.
“The ACCP guidelines are very conservative and basically follow the evidence base for medical patients, while the ISTH guidelines are more aggressive and recommend increased levels of anticoagulation in both ICU and hospitalized non-ICU patients and also extend prophylaxis after discharge,” Dr. Piazza said.
“There is quite a difference between the two sets of guidelines, which can be a point of confusion,” he added.
Dr. Piazza notes that at his center every hospitalized COVID patient who does not have a contraindication to anticoagulation receives a standard prophylactic dose of a once-daily low-molecular-weight heparin (for example, enoxaparin 40 mg). A once-daily product is used to minimize infection risk to staff.
While all COVID patients in the ICU should automatically receive some anticoagulation, the optimal dose is an area of active investigation, he explained. “There were several early reports of ICU patients developing blood clots despite receiving standard thromboprophylaxis so perhaps we need to use higher doses. There are trials underway looking at this, and we would advise enrolling patients into these trials.”
If patients can’t be enrolled into trials, and clinicians feel higher anticoagulation levels are needed, Dr. Piazza advises following the ISTH guidance, which allows an intermediate dose of low-molecular-weight heparin (up to 1 mg/kg enoxaparin).
“Some experts are suggesting even higher doses may be needed in some ICU patients, such as the full therapeutic dose, but I worry about the risk of bleeding with such a strategy,” he said.
Dr. Piazza says they do not routinely give anticoagulation after discharge, but if this is desired then patients could be switched to an oral agent, and some of the direct-acting oral anticoagulants are approved for prophylactic use in medically ill patients.
Dr. Piazza points out that whether thromboprophylaxis should be used for nonhospitalized COVID patients who have risk factors for clotting such as a prior history of thrombosis or obesity is a pressing question, and he encourages clinicians to enroll these patients in clinical trials evaluating this issue, such as the PREVENT-HD trial.
“If they can’t enroll patents in a trial, then they have to make a decision whether the patient is high-enough risk to justify off-label use of anticoagulant. There is a case to be made for this, but there is no evidence for or against such action at present,” he noted.
At this time, neither the ISTH nor ACCP recommend measuring D-dimer to screen for venous thromboembolism or to determine intensity of prophylaxis or treatment, the authors note.
“Ongoing investigation will determine optimal preventive regimens in COVID-19 in the intensive care unit, at hospital discharge, and in nonhospitalized patients at high risk for thrombosis,” they conclude.
Dr. Piazza reported grants from Bayer, Bristol Myers Squibb, Boston Scientific, Janssen, and Portola, and personal fees from Agile, Amgen, Pfizer, and the Prairie Education and Research Cooperative outside the submitted work. Dr. Morrow reported grants from Abbott Laboratories, Amgen, Anthos Therapeutics, Esai, GlaxoSmithKline, Takeda, and The Medicines Company; grants and personal fees from AstraZeneca, Merck, Novartis, and Roche Diagnostics; and personal fees from Bayer Pharma and InCarda outside the submitted work.
A version of this article originally appeared on Medscape.com.
The risk of arterial and venous thrombosis in patients with COVID-19 has been a major issue throughout the pandemic, and how best to manage this risk is the subject of a new review article.
The article, by Gregory Dr. Piazza, MD, and David A. Morrow, MD, Brigham and Women’s Hospital, Boston, was published online in JAMA on Nov. 23.
“Basically we’re saying: ‘Be proactive about prevention,’” Dr. Piazza told this news organization.
There is growing recognition among those on the frontline that there is an increased risk of thrombosis in COVID-19 patients, Dr. Piazza said. The risk is highest in patients in the intensive care unit, but the risk is also increased in patients hospitalized with COVID-19, even those not in ICU.
“We don’t really know what the risk is in nonhospitalized COVID-19 patients, but we think it’s much lower than in those who are hospitalized,” he said. “We are waiting for data on the optimal way of managing this increased risk of thrombosis in COVID patients, but for the time being, we believe a systematic way of addressing this risk is best, with every patient hospitalized with COVID-19 receiving some type of thromboprophylaxis. This would mainly be with anticoagulation, but in patients in whom anticoagulation is contraindicated, then mechanical methods could be used, such as pneumatic compression boots or compression stockings.”
The authors report thrombotic complication rates of 2.6% in noncritically ill hospitalized patients with COVID-19 and 35.3% in critically ill patients from a recent U.S. registry study.
Autopsy findings of microthrombi in multiple organ systems, including the lungs, heart, and kidneys, suggest that thrombosis may contribute to multisystem organ dysfunction in severe COVID-19, they note. Although the pathophysiology is not fully defined, prothrombotic abnormalities have been identified in patients with COVID-19, including elevated levels of D-dimer, fibrinogen, and factor VIII, they add.
“There are several major questions about which COVID-19 patients to treat with thromboprophylaxis, how to treat them in term of levels of anticoagulation, and there are many ongoing clinical trials to try and answer these questions,” Dr. Piazza commented. “We need results from these randomized trials to provide a better compass for COVID-19 patients at risk of clotting.”
At present, clinicians can follow two different sets of guidelines on the issue, one from the American College of Chest Physicians and the other from the International Society on Thrombosis and Hemostasis, the authors note.
“The ACCP guidelines are very conservative and basically follow the evidence base for medical patients, while the ISTH guidelines are more aggressive and recommend increased levels of anticoagulation in both ICU and hospitalized non-ICU patients and also extend prophylaxis after discharge,” Dr. Piazza said.
“There is quite a difference between the two sets of guidelines, which can be a point of confusion,” he added.
Dr. Piazza notes that at his center every hospitalized COVID patient who does not have a contraindication to anticoagulation receives a standard prophylactic dose of a once-daily low-molecular-weight heparin (for example, enoxaparin 40 mg). A once-daily product is used to minimize infection risk to staff.
While all COVID patients in the ICU should automatically receive some anticoagulation, the optimal dose is an area of active investigation, he explained. “There were several early reports of ICU patients developing blood clots despite receiving standard thromboprophylaxis so perhaps we need to use higher doses. There are trials underway looking at this, and we would advise enrolling patients into these trials.”
If patients can’t be enrolled into trials, and clinicians feel higher anticoagulation levels are needed, Dr. Piazza advises following the ISTH guidance, which allows an intermediate dose of low-molecular-weight heparin (up to 1 mg/kg enoxaparin).
“Some experts are suggesting even higher doses may be needed in some ICU patients, such as the full therapeutic dose, but I worry about the risk of bleeding with such a strategy,” he said.
Dr. Piazza says they do not routinely give anticoagulation after discharge, but if this is desired then patients could be switched to an oral agent, and some of the direct-acting oral anticoagulants are approved for prophylactic use in medically ill patients.
Dr. Piazza points out that whether thromboprophylaxis should be used for nonhospitalized COVID patients who have risk factors for clotting such as a prior history of thrombosis or obesity is a pressing question, and he encourages clinicians to enroll these patients in clinical trials evaluating this issue, such as the PREVENT-HD trial.
“If they can’t enroll patents in a trial, then they have to make a decision whether the patient is high-enough risk to justify off-label use of anticoagulant. There is a case to be made for this, but there is no evidence for or against such action at present,” he noted.
At this time, neither the ISTH nor ACCP recommend measuring D-dimer to screen for venous thromboembolism or to determine intensity of prophylaxis or treatment, the authors note.
“Ongoing investigation will determine optimal preventive regimens in COVID-19 in the intensive care unit, at hospital discharge, and in nonhospitalized patients at high risk for thrombosis,” they conclude.
Dr. Piazza reported grants from Bayer, Bristol Myers Squibb, Boston Scientific, Janssen, and Portola, and personal fees from Agile, Amgen, Pfizer, and the Prairie Education and Research Cooperative outside the submitted work. Dr. Morrow reported grants from Abbott Laboratories, Amgen, Anthos Therapeutics, Esai, GlaxoSmithKline, Takeda, and The Medicines Company; grants and personal fees from AstraZeneca, Merck, Novartis, and Roche Diagnostics; and personal fees from Bayer Pharma and InCarda outside the submitted work.
A version of this article originally appeared on Medscape.com.
COVID-19 fuels surge in overdose-related cardiac arrests
There has been a sharp increase in overdose-related cardiac arrests in the United States during the COVID-19 pandemic, a new analysis shows.
Overall rates in 2020 were elevated above the baseline from 2018 and 2019 by about 50%, the data show.
and efforts to combat the COVID-19 pandemic have not been effective at reducing overdoses,” Joseph Friedman, MPH, MD/PhD student, medical scientist training program, University of California, Los Angeles, said in an interview.
“We need to invest heavily in substance use treatment, harm reduction, and the structural drivers of overdose as core elements of the COVID-19 response,” said Mr. Friedman, who coauthored the study with UCLA colleague David Schriger, MD, MPH, and Leo Beletsky, JD, MPH, Northeastern University, Boston.
The study was published as a research letter Dec. 3 in JAMA Psychiatry.
Social isolation a key driver
Emergency medical services (EMS) data are available in near real time, providing a novel source of up-to-date information to monitor epidemiological shifts during the COVID-19 pandemic.
For the study, the researchers leveraged data from the National EMS Information System, a large registry of more than 10,000 EMS agencies in 47 states that represent over 80% of all EMS calls nationally in 2020. They used the data to track shifts in overdose-related cardiac arrests observed by EMS.
They found clear evidence of a large-scale uptick in overdose-related deaths during the COVID-19 pandemic.
The overall rate of overdose-related cardiac arrests in 2020 was about 50% higher than trends observed during 2018 and 2019, including a maximum peak of 123% above baseline reached in early May.
All overdose-related incidents (fatal and nonfatal) were elevated in 2020, by about 17% above baseline. However, there were larger increases in fatal overdose-related incidents, compared to all incidents, which may suggest a rising case fatality rate, the authors noted.
The observed trends line up in time with reductions in mobility (a metric of social interaction), as measured using cell phone data, they wrote.
“Many of the trends predicted by experts at the beginning of the pandemic could cause these shifts. Increases in social isolation likely play an important role, as people using [drugs] alone are less likely to receive help when they need it. Also shifts in the drug supply, and reduced access to healthcare and treatment,” said Mr. Friedman.
“We need to undertake short- and long-term strategies to combat the rising tide of overdose mortality in the United States,” he added.
In the short term, Mr. Friedman suggested reducing financial and logistical barriers for accessing a safe opioid supply. Such measures include allowing pharmacies to dispense methadone, allowing all physicians to prescribe buprenorphine without a special waiver, and releasing emergency funds to make these medications universally affordable.
“In the longer term, we should acknowledge that overdose is a symptom of structural problems in the U.S. We need to invest in making employment, housing, education, and health care accessible to all to address the upstream drivers of overdose,” he added.
The study had no commercial funding. The authors disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
There has been a sharp increase in overdose-related cardiac arrests in the United States during the COVID-19 pandemic, a new analysis shows.
Overall rates in 2020 were elevated above the baseline from 2018 and 2019 by about 50%, the data show.
and efforts to combat the COVID-19 pandemic have not been effective at reducing overdoses,” Joseph Friedman, MPH, MD/PhD student, medical scientist training program, University of California, Los Angeles, said in an interview.
“We need to invest heavily in substance use treatment, harm reduction, and the structural drivers of overdose as core elements of the COVID-19 response,” said Mr. Friedman, who coauthored the study with UCLA colleague David Schriger, MD, MPH, and Leo Beletsky, JD, MPH, Northeastern University, Boston.
The study was published as a research letter Dec. 3 in JAMA Psychiatry.
Social isolation a key driver
Emergency medical services (EMS) data are available in near real time, providing a novel source of up-to-date information to monitor epidemiological shifts during the COVID-19 pandemic.
For the study, the researchers leveraged data from the National EMS Information System, a large registry of more than 10,000 EMS agencies in 47 states that represent over 80% of all EMS calls nationally in 2020. They used the data to track shifts in overdose-related cardiac arrests observed by EMS.
They found clear evidence of a large-scale uptick in overdose-related deaths during the COVID-19 pandemic.
The overall rate of overdose-related cardiac arrests in 2020 was about 50% higher than trends observed during 2018 and 2019, including a maximum peak of 123% above baseline reached in early May.
All overdose-related incidents (fatal and nonfatal) were elevated in 2020, by about 17% above baseline. However, there were larger increases in fatal overdose-related incidents, compared to all incidents, which may suggest a rising case fatality rate, the authors noted.
The observed trends line up in time with reductions in mobility (a metric of social interaction), as measured using cell phone data, they wrote.
“Many of the trends predicted by experts at the beginning of the pandemic could cause these shifts. Increases in social isolation likely play an important role, as people using [drugs] alone are less likely to receive help when they need it. Also shifts in the drug supply, and reduced access to healthcare and treatment,” said Mr. Friedman.
“We need to undertake short- and long-term strategies to combat the rising tide of overdose mortality in the United States,” he added.
In the short term, Mr. Friedman suggested reducing financial and logistical barriers for accessing a safe opioid supply. Such measures include allowing pharmacies to dispense methadone, allowing all physicians to prescribe buprenorphine without a special waiver, and releasing emergency funds to make these medications universally affordable.
“In the longer term, we should acknowledge that overdose is a symptom of structural problems in the U.S. We need to invest in making employment, housing, education, and health care accessible to all to address the upstream drivers of overdose,” he added.
The study had no commercial funding. The authors disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
There has been a sharp increase in overdose-related cardiac arrests in the United States during the COVID-19 pandemic, a new analysis shows.
Overall rates in 2020 were elevated above the baseline from 2018 and 2019 by about 50%, the data show.
and efforts to combat the COVID-19 pandemic have not been effective at reducing overdoses,” Joseph Friedman, MPH, MD/PhD student, medical scientist training program, University of California, Los Angeles, said in an interview.
“We need to invest heavily in substance use treatment, harm reduction, and the structural drivers of overdose as core elements of the COVID-19 response,” said Mr. Friedman, who coauthored the study with UCLA colleague David Schriger, MD, MPH, and Leo Beletsky, JD, MPH, Northeastern University, Boston.
The study was published as a research letter Dec. 3 in JAMA Psychiatry.
Social isolation a key driver
Emergency medical services (EMS) data are available in near real time, providing a novel source of up-to-date information to monitor epidemiological shifts during the COVID-19 pandemic.
For the study, the researchers leveraged data from the National EMS Information System, a large registry of more than 10,000 EMS agencies in 47 states that represent over 80% of all EMS calls nationally in 2020. They used the data to track shifts in overdose-related cardiac arrests observed by EMS.
They found clear evidence of a large-scale uptick in overdose-related deaths during the COVID-19 pandemic.
The overall rate of overdose-related cardiac arrests in 2020 was about 50% higher than trends observed during 2018 and 2019, including a maximum peak of 123% above baseline reached in early May.
All overdose-related incidents (fatal and nonfatal) were elevated in 2020, by about 17% above baseline. However, there were larger increases in fatal overdose-related incidents, compared to all incidents, which may suggest a rising case fatality rate, the authors noted.
The observed trends line up in time with reductions in mobility (a metric of social interaction), as measured using cell phone data, they wrote.
“Many of the trends predicted by experts at the beginning of the pandemic could cause these shifts. Increases in social isolation likely play an important role, as people using [drugs] alone are less likely to receive help when they need it. Also shifts in the drug supply, and reduced access to healthcare and treatment,” said Mr. Friedman.
“We need to undertake short- and long-term strategies to combat the rising tide of overdose mortality in the United States,” he added.
In the short term, Mr. Friedman suggested reducing financial and logistical barriers for accessing a safe opioid supply. Such measures include allowing pharmacies to dispense methadone, allowing all physicians to prescribe buprenorphine without a special waiver, and releasing emergency funds to make these medications universally affordable.
“In the longer term, we should acknowledge that overdose is a symptom of structural problems in the U.S. We need to invest in making employment, housing, education, and health care accessible to all to address the upstream drivers of overdose,” he added.
The study had no commercial funding. The authors disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Infant’s COVID-19–related myocardial injury reversed
Reports of signs of heart failure in adults with COVID-19 have been rare – just four such cases have been published since the outbreak started in China – and now a team of pediatric cardiologists in New York have reported a case of acute but reversible myocardial injury in an infant with COVID-19.
and right upper lobe atelectasis.
The 2-month-old infant went home after more than 2 weeks in the hospital with no apparent lingering cardiac effects of the illness and not needing any oral heart failure medications, Madhu Sharma, MD, of the Children’s Hospital and Montefiore in New York and colleagues reported in JACC Case Reports. With close follow-up, the child’s left ventricle size and systolic function have remained normal and mitral regurgitation resolved. The case report didn’t mention the infant’s gender.
But before the straightforward postdischarge course emerged, the infant was in a precarious state, and Dr. Sharma and her team were challenged to diagnose the underlying causes.
The child, who was born about 7 weeks premature, first came to the hospital having turned blue after choking on food. Nonrebreather mask ventilation was initiated in the ED, and an examination detected a holosystolic murmur. A test for COVID-19 was negative, but a later test was positive, and a chest x-ray exhibited cardiomegaly and signs of fluid and inflammation in the lungs.
An electrocardiogram detected sinus tachycardia, ST-segment depression and other anomalies in cardiac function. Further investigation with a transthoracic ECG showed severely depressed left ventricle systolic function with an ejection fraction of 30%, severe mitral regurgitation, and normal right ventricular systolic function.
Treatment included remdesivir and intravenous antibiotics. Through the hospital course, the patient was extubated to noninvasive ventilation, reintubated, put on intravenous steroid (methylprednisolone) and low-molecular-weight heparin, extubated, and tested throughout for cardiac function.
By day 14, left ventricle size and function normalized, and while the mitral regurgitation remained severe, it improved later without HF therapies. Left ventricle ejection fraction had recovered to 60%, and key cardiac biomarkers had normalized. On day 16, milrinone was discontinued, and the care team determined the patient no longer needed oral heart failure therapies.
“Most children with COVID-19 are either asymptomatic or have mild symptoms, but our case shows the potential for reversible myocardial injury in infants with COVID-19,” said Dr. Sharma. “Testing for COVID-19 in children presenting with signs and symptoms of heart failure is very important as we learn more about the impact of this virus.”
Dr. Sharma and coauthors have no relevant financial relationships to disclose.
SOURCE: Sharma M et al. JACC Case Rep. 2020. doi: 10.1016/j.jaccas.2020.09.031.
Reports of signs of heart failure in adults with COVID-19 have been rare – just four such cases have been published since the outbreak started in China – and now a team of pediatric cardiologists in New York have reported a case of acute but reversible myocardial injury in an infant with COVID-19.
and right upper lobe atelectasis.
The 2-month-old infant went home after more than 2 weeks in the hospital with no apparent lingering cardiac effects of the illness and not needing any oral heart failure medications, Madhu Sharma, MD, of the Children’s Hospital and Montefiore in New York and colleagues reported in JACC Case Reports. With close follow-up, the child’s left ventricle size and systolic function have remained normal and mitral regurgitation resolved. The case report didn’t mention the infant’s gender.
But before the straightforward postdischarge course emerged, the infant was in a precarious state, and Dr. Sharma and her team were challenged to diagnose the underlying causes.
The child, who was born about 7 weeks premature, first came to the hospital having turned blue after choking on food. Nonrebreather mask ventilation was initiated in the ED, and an examination detected a holosystolic murmur. A test for COVID-19 was negative, but a later test was positive, and a chest x-ray exhibited cardiomegaly and signs of fluid and inflammation in the lungs.
An electrocardiogram detected sinus tachycardia, ST-segment depression and other anomalies in cardiac function. Further investigation with a transthoracic ECG showed severely depressed left ventricle systolic function with an ejection fraction of 30%, severe mitral regurgitation, and normal right ventricular systolic function.
Treatment included remdesivir and intravenous antibiotics. Through the hospital course, the patient was extubated to noninvasive ventilation, reintubated, put on intravenous steroid (methylprednisolone) and low-molecular-weight heparin, extubated, and tested throughout for cardiac function.
By day 14, left ventricle size and function normalized, and while the mitral regurgitation remained severe, it improved later without HF therapies. Left ventricle ejection fraction had recovered to 60%, and key cardiac biomarkers had normalized. On day 16, milrinone was discontinued, and the care team determined the patient no longer needed oral heart failure therapies.
“Most children with COVID-19 are either asymptomatic or have mild symptoms, but our case shows the potential for reversible myocardial injury in infants with COVID-19,” said Dr. Sharma. “Testing for COVID-19 in children presenting with signs and symptoms of heart failure is very important as we learn more about the impact of this virus.”
Dr. Sharma and coauthors have no relevant financial relationships to disclose.
SOURCE: Sharma M et al. JACC Case Rep. 2020. doi: 10.1016/j.jaccas.2020.09.031.
Reports of signs of heart failure in adults with COVID-19 have been rare – just four such cases have been published since the outbreak started in China – and now a team of pediatric cardiologists in New York have reported a case of acute but reversible myocardial injury in an infant with COVID-19.
and right upper lobe atelectasis.
The 2-month-old infant went home after more than 2 weeks in the hospital with no apparent lingering cardiac effects of the illness and not needing any oral heart failure medications, Madhu Sharma, MD, of the Children’s Hospital and Montefiore in New York and colleagues reported in JACC Case Reports. With close follow-up, the child’s left ventricle size and systolic function have remained normal and mitral regurgitation resolved. The case report didn’t mention the infant’s gender.
But before the straightforward postdischarge course emerged, the infant was in a precarious state, and Dr. Sharma and her team were challenged to diagnose the underlying causes.
The child, who was born about 7 weeks premature, first came to the hospital having turned blue after choking on food. Nonrebreather mask ventilation was initiated in the ED, and an examination detected a holosystolic murmur. A test for COVID-19 was negative, but a later test was positive, and a chest x-ray exhibited cardiomegaly and signs of fluid and inflammation in the lungs.
An electrocardiogram detected sinus tachycardia, ST-segment depression and other anomalies in cardiac function. Further investigation with a transthoracic ECG showed severely depressed left ventricle systolic function with an ejection fraction of 30%, severe mitral regurgitation, and normal right ventricular systolic function.
Treatment included remdesivir and intravenous antibiotics. Through the hospital course, the patient was extubated to noninvasive ventilation, reintubated, put on intravenous steroid (methylprednisolone) and low-molecular-weight heparin, extubated, and tested throughout for cardiac function.
By day 14, left ventricle size and function normalized, and while the mitral regurgitation remained severe, it improved later without HF therapies. Left ventricle ejection fraction had recovered to 60%, and key cardiac biomarkers had normalized. On day 16, milrinone was discontinued, and the care team determined the patient no longer needed oral heart failure therapies.
“Most children with COVID-19 are either asymptomatic or have mild symptoms, but our case shows the potential for reversible myocardial injury in infants with COVID-19,” said Dr. Sharma. “Testing for COVID-19 in children presenting with signs and symptoms of heart failure is very important as we learn more about the impact of this virus.”
Dr. Sharma and coauthors have no relevant financial relationships to disclose.
SOURCE: Sharma M et al. JACC Case Rep. 2020. doi: 10.1016/j.jaccas.2020.09.031.
FROM JACC CASE REPORTS
Key clinical point: Children presenting with COVID-19 should be tested for heart failure.
Major finding: A 2-month-old infant with COVID-19 had acute but reversible myocardial injury.
Study details: Single case report.
Disclosures: Dr. Sharma, MD, has no relevant financial relationships to disclose.
Source: Sharma M et al. JACC Case Rep. 2020. doi: 10.1016/j.jaccas.2020.09.031.
The Design and Implementation of a Heart Disease Reversal Program in the Veterans Health Administration: Before and During the COVID-19 Pandemic
While cardiovascular mortality rates have declined, heart disease continues to be the leading cause of death in the US, and the number of people with cardiovascular disease (CVD) is rising.1 CVD is more prevalent among military veterans than it is among nonveterans aged ≥ 25 years, and veteran status is associated with higher risk of incident heart disease after controlling for socioeconomic status, other medical diseases, depression, and lifestyle.2-4 Combat exposure, posttraumatic stress disorder (PTSD), and Purple Heart commendation are associated with higher rates of CVD, including adverse cardiovascular events.5-7 Many patients seeking care in the Veterans Health Administration (VHA), including those who undergo cardiac catheterization, meet the criteria for multimorbidity (defined as having ≥ 2 chronic diseases8), which is common among veterans.9,10 Multimorbidity presents a challenge for lifestyle intervention, as different diets may be prescribed to treat different conditions, such as Dietary Approaches to Stop Hypertension, and low-glycemic diet for diabetes mellitus (DM). Veterans with CVD are often clinically complex and may require more multifaceted secondary prevention programs.
During the coronavirus 2019 (COVID-19) pandemic, effective secondary prevention intervention is needed more than ever. Older age, CVD, and common comorbidities, including hypertension, DM, and obesity, place patients at the highest risk for severe COVID-19 infection.11 COVID-19 social distancing encourages vulnerable populations to stay home, which can make engaging in any levels of physical activity more challenging. The International Food Council found that 85% of adults have made a change to their food consumption pattern, including eating more, during the COVID-19 pandemic.12 Thus, secondary CVD prevention programs for veterans need to provide treatment that addresses these specific challenges and can be delivered via telehealth for continuity of care after disruption of traditional services.
Clinical practice guidelines for the treatment of patients with recent cardiovascular adverse events (AEs) include a referral to cardiac rehabilitation (CR).13 CR emphasizes exercise as the main intervention, along with coaching to promote multiple risk reduction. The most comprehensive CR program is intensive CR (ICR), including the Ornish ICR program.14 ICR includes 4 components: vegetarian diet, exercise, stress management (yoga, meditation), and group support. Ornish ICR has been shown to be efficacious in randomized controlled trials (RCTs).15-17 Three effectiveness studies, with 5,372 participants, demonstrated the real-world effectiveness of Ornish ICR in US hospitals.14,18,19 The program also was adapted successfully for the active-duty military and veteran population.20,21 Yet Ornish ICR is time intensive, and there are no certified VHA ICR Ornish sites. Furthermore, there is no formal strategy for targeting people with atherosclerotic CVD who no longer meet the criteria for CR or ICR. While Ornish ICR is highly effective for patients who are eligible and have access, a more effective and streamlined approach is needed for targeting many patients.
Nutrition may be the most powerful Ornish ICR component. The initial RCT conducted by Ornish and colleagues included only stress management training and a whole-food, plant-based (WFPB) diet, including grains, legumes, vegetables, fruits, nuts, and seeds. The trial found 91% of participants experienced reduced angina after only 24 days.15 The only single-component intervention study resulting in partial reversal of atherosclerosis was a WFPB diet-only study, which documented regression of atherosclerotic plaques after 5 years, using coronary angiography in 73% of participants, with arrested progression in the other 27%.22 Participants reported no cardiovascular AEs after 12 years.23 Furthermore, a number of other recent studies have demonstrated the benefits of WFPB diet-only interventions for type 2 DM (T2DM), hypertension, and obesity.24-27 The Heart Disease Reversal Program (HDRP) was developed to create an interdisciplinary lifestyle intervention that emphasized nutrition for a broad population of veterans with atherosclerotic CVD, of varying levels of functional ability, to promote comprehensive CVD risk reduction and bring heart disease reversal intervention into routine clinical practice.
Program Description
The Mental Health, Cardiology, and Nutrition and Food services all approved the launch of HDRP. We contacted veterans by mail, and 11% expressed interest (Figure). Among patients who received the initial mailed letter (prior to our accepting staff referrals), only 5% of patients who enrolled in HDRP reported previously being told about or prescribed a WFPB diet by any health care provider (HCP). Currently, patients are primarily referred to HDRP by Cardiology, Primary Care, and Mental Health services.
Design
HDRP is an adaptation of interdisciplinary lifestyle interventions that have resulted in regression of atherosclerotic blockages confirmed with invasive coronary angiography.15-17,22,28 HDRP currently is offered in a Behavioral Medicine Clinic at the Sacramento US Department of Veterans Affairs (VA) Medical Center (VAMC) in California. Program staff include a clinical health psychologist who organizes, coordinates, and act as the lead facilitator of the program; registered dietitians; clinical pharmacists; and a consulting physician. Patients engage in the 4-month core HDRP program in small cohorts (ie, 6-10 patients), and spouses/partners are highly encouraged to attend all sessions.
Components
Telephone screening. Patients are screened for the inclusion and exclusion criteria (Table 1). Patients engaging in a traditional CR program are included in the screening. Patients are informed that the program consists of lifestyle intervention, including emphasis on following a WFPB diet.
Health assessment. Once approved, all patients are instructed to complete baseline laboratory tests and questionnaires. Along with an electronic health record (EHR) review, a psychosocial assessment is completed by a licensed clinical health psychologist who assesses CVD history, eating behavior, exercise/physical activity, sleep, mental health, substance use, and social history, with the aim of enhancing our ability to help the patient to benefit from HDRP.29 The patient data are used to develop a case conceptualization (ie, integrated understanding of the particular patient’s psychiatric and medical diagnoses, behavioral patterns, social supports, lifestyle habits, strengths and weaknesses, and their interrelationships with each other and the patient’s environment), resulting in an individualized plan. Patients are encouraged to ask questions about the program, and those who are still interested are invited to attend a seminar. A request for medical clearance to participate in the program is initiated through the EHR or by patients scheduling an appointment with their HCP. All patients are medically cleared by their HCP for participation. Safe exercise recommendations also are provided and guide patient goals.
CVD risk profile. Patients complete psychosocial questionnaires and fasting laboratory tests to produce a tailored CVD risk profile. Laboratory tests include fasting lipid, fasting glucose, hemoglobin A1c (HbA1c) C-reactive protein, vitamin B12, and vitamin D. The same tests (excluding HbA1c) are completed 1 month later (after completing 4 group sessions) and again posttreatment (including HbA1c). Self-reported questionnaires are completed at the same time points, which include the Rate Your Plate dietary composition questionnaire, CHAMPS physical activity questionnaire for older adults, Beck Depression Inventory-II, and the Perceived Stress Scale.
Seminar. A 2-hour seminar provides patients and families with an opportunity to meet HDRP program staff, learn the background and rationale for chronic disease reversal, obtain a summary of the program, and hear a patient testimonial. Patients are asked to make a commitment, and the informed consent process includes all patients signing a behavioral contract.
Assessment and feedback. A licensed clinical health psychologist provides feedback to patients on their comprehensive CVD risk profile, using motivational interviewing.30,31 Smokers are encouraged to quit, and those interested are referred to their HCP and/or facility smoking cessation program.
Group sessions. Twelve weekly group sessions cover nutrition education and cooking, physical activity and exercise, stress management training, and medication reconciliation and adjustment. The nutrition component is the centerpiece of HDRP and is delivered by registered dietitians (Table 2). Patients are instructed to use the 3-week period between the HDRP seminar and the first core group session to try new recipes and prepare their kitchens, pantries, and mind-set to adopt the HDRP diet with 100% adherence. The WFPB diet used is consistent with the current guidelines of Caldwell Esselstyn, MD, and Dean Ornish, MD.32-34
A psychologist delivers the physical activity component. Patients are encouraged to meet the American Heart Association/American College of Cardiology recommendations for aerobic exercise (at least 150 minutes of moderate intensity physical activity per week) through a walking program.35 Patients with medical contraindications (eg, severe pain, mobility restrictions) are encouraged to follow the exercise/activity recommendations they had been given by their primary care provider (PCP), physical therapist, or other HCP.
A psychologist provides evidence-based cognitive behavioral stress management (CBSM) training, adapted from models developed for patients with stable ischemic heart disease, HIV/AIDS, and cancer.36-38 CBSM is a psychotherapy grounded in stress/coping theory and cognitive behavioral theory of psychopathology that integrates cognitive restructuring, coping skills training, communication/assertiveness training, anger management, and mindfulness/acceptance-based approaches. Additional emphasis is placed on assisting patients’ adjustment to the lifestyle challenges for following a plant-based diet, dealing with food cravings and emotional eating, and connecting lifestyle change to patients’ deepest values and goals.
A clinical pharmacist conducts a medication reconciliation for each patient at baseline. The pharmacist consults with each patient’s PCP, cardiologist, and HDRP consulting physician, as needed, to ensure safe adjustments to medications. Pharmacists also provide education on medications at group sessions.
After completion of the 12-week core program, graduates are encouraged to attend the monthly graduates’ group indefinitely, and as often as they desire to promote maintenance of the disease reversal lifestyle. Patients are encouraged to complete our recommended fasting laboratory work every 3 to 6 months to facilitate maintenance of treatment gains.
Program Evaluation
Patients frequently reported that the group format was vital to their success. Patients requested a cooking class, yet we lacked a full teaching kitchen. Integrating plant-based meal samples at every session and cooking videos helped. Patients reported that 100% adherence to the WFPB diet led to significant changes in their food preferences, including a loss of interest in meat.39 Patients encouraged us to keep the “disease reversal” language and focus. One veteran stated: “Disease reversal, that is the reason I called you when I got your letter.” Showing before and after images of coronary angiograms and cardiac positron emission tomography scans depicting regression of atherosclerotic plaque and restored myocardial perfusion were described as highly motivating and generated willingness to commit to a more aggressive lifestyle change.31
Patients routinely stated that they lacked understanding of their laboratory test results, which HDRP remedied. Some patients reported their adult children followed a plant-based diet, and our program resulted in a new commonality and source of bonding that was highly valued. Some patients reported that HDRP was helpful for controlling their COVID-19 anxiety and feeling in control of their health. Satisfaction surveys were completed by participants at the end of the core program, which demonstrated very high satisfaction with and acceptability of HDRP (Table 3).
The program also has received positive feedback from HCPs when we alert them to improvements in outcome measures for their patients. These HCPs expressed satisfaction with having a program to refer patients to that can help with chronic illness in more depth.
COVID-19 Response
Face-to-face group appointments were converted to videoconferencing as a result of the COVID-19 pandemic. While HDRP always promoted the use of technology and mHealth tools, the pandemic led us to develop novel technology-based interventions.40 One cohort transitioned from in-person to videoconferencing sessions, and 2 cohorts recently started this format and are ongoing. We have successfully used videoconferencing with Cisco Webex, the VA-approved backup platform, as we encountered technical barriers when using VA Video Connect. Program materials were shared electronically, and participants sent blood pressure/sugar logs by secure messaging. Guidance for online grocery shopping with home delivery was provided, and research on the benefits of the HDRP lifestyle on immune function was incorporated.
The stress management component incorporated coping with COVID-19, including normalizing common emotional difficulties with sheltering-in-place and quarantine, acknowledging and processing fear and anxiety related to being at very high risk for severe COVID-19. We presented heart disease reversal as an urgent and feasible goal during the pandemic both reducing risk of premature death and major adverse cardiovascular events in the long-term and also reducing personal risk of severe COVID complications. The new VA COVID Coach app was also presented as a resource. Reputable sources of COVID-19 and public health information were shared. Walking continued to be the primary recommended form of exercise, while indoor home exercise options were promoted during the periods of very poor air quality due to the widespread California fires and smoke.
Considering the research suggesting benefits of our intervention for treating T2DM,promoting sustained weight loss, and promoting comprehensive cardiometabolic risk reduction, we have begun accepting referrals for patients with any type of atherosclerotic CVD (eg, peripheral artery disease, carotid artery disease), patients with T2DM (without CVD), and patients with only a history of ischemic stroke or transient ischemic attack.24-27 Vascular surgery has become a new referral source, primarily for patients with peripheral and carotid artery diseases. Finally, we are leveraging videoconferencing and accepting referrals across the VA Northern California Health Care System (VANCHCS)catchment (from the California-Oregon state border to the San Francisco Bay Area). This also helps address a long-standing problem with reaching the many rural veterans who live far from a VA clinic. We successfully implemented a consult/referral process within the EHR that is available to providers across VANCHCS.
Discussion
The efficacy and effectiveness of reversal programs are well established in intensive programs (eg, ICR), yet such programs have yet to be streamlined and disseminated broadly into routine clinical care. HDRP has endeavored to address this by emphasizing nutrition relative to other program components. We have learned that the words “disease reversal” are very often the reason patients initially reach out or accept referral to our program.
Consistent with past research on plant-based nutrition interventions, the group format was indispensable.41 Individual sessions with a clinical health psychologist enabled tailored feedback and education on how behavior changes could impact laboratory results and how certain psychosocial factors could support success. Participants reported that seeing significantly favorable laboratory results was highly motivating and confirmed the power of their lifestyle changes. Furthermore, a psychosocial health assessment with individual sessions promoted a tailored treatment plan with targeted clinical interventions, such as behavioral health education, motivational interviewing, and advanced methods, including cognitive behavioral therapy and techniques drawn from dialectical behavior therapy and acceptance and commitment therapy.
Veterans with multimorbidity face the difficult task of learning and maintaining a complex disease self-management program and implementing a lifestyle approach that is feasible, effective, promotes weight loss, and treats multiple conditions. HDRP is a model approach for this population, as demonstrated by a recent case report of a 65-year-old male veteran with atherosclerotic CVD, T2DM, hypertension, and myasthenia gravis who had 2 heart attacks within 2 months.42 His neurologic disease precluded significant physical activity. Although he achieved some initial weight loss through lifestyle changes, he continued to have daily angina despite optimal and aggressive cardiology management. After enrolling in HDRP and adopting the WFPB diet, the patient reported almost complete resolution of angina within 1 month, similar to that found in other studies.15
The literature suggests that concern over the acceptability of plant-based diets and patients’ ability to adhere to them long-term may be misplaced. A review paper on dietary interventions lasting > 1 year found that 51 to 61% of vegetarian and vegan study participants had maintained dietary adherence, while 20 to 55% of omnivorous diet intervention participants adhered to their study diets.43 Remarkably, there were no statistically significant differences in the acceptability of the vegan, vegetarian, or omnivorous diets in the studies reviewed.43 Recent dietary research also suggests that providing patients with higher goals (eg, adopting a vegan diet instead of only moderate dietary changes) results in greater weight loss and maintenance.26 HDRP provides training on consumption of whole plant foods, which may offer patients a unique advantage for maximizing results and higher adherence over time.
Limitations
Hands-on cooking instruction was not provided at our VAMC. The total time of the intervention was significantly less in HDRP (25 hours) than it was for the Ornish ICR program (72 hours), which may hinder long-term adherence. Without an exercise facility, we were not able to provide more detailed exercise instruction and supervised exercise.
Program Improvements Planned
There are a number of improvements that are planned for HDRP. First, the program anticipates requesting medical clearance at the telephone screening stage for self-referred patients. Second,
Conclusions
Although our patient population was self-selected for participation, early program evaluation demonstrates high acceptability. Very few patients had ever been told about a heart disease reversing lifestyle, and we found direct-to-patient clinical outreach an effective method for launching a disease reversal program (optimally timed with HCP presentations). Furthermore, the program is adaptable to current restrictions on in-person appointments due to the COVID-19 pandemic, and much more convenient for rural veterans who live far from any VA clinic. Being able to offer sustainable health care for individuals during unexpected public health crises is critically important. Additionally, treating veterans who are most vulnerable to pandemic illness due to existing medical conditions, such as CVD, should be a high priority. Last, HDRP also may represent a novel integrated treatment for COVID-19 anxiety and secondary CVD prevention, as lifestyle habits are optimized to improve chronic diseases that elevate risk for severe COVID-19 infection and mortality, as well as including coping strategies consistent with evidence-based psychotherapies for anxiety disorders.44
We believe that beyond the clinical benefits to patients, there is significant value and benefit added to the health care system by offering an intervention within the “disease reversal” paradigm. Efforts of the health care team to reverse a disease can be considered the highest aim of medicine and health care.45
Acknowledgments
This work was supported by the US Department of Veterans Affairs. We give special thanks to David M. Gellerman, MD, PhD, and David W. Schafer, PsyD, for providing Mental Health Service support for initiating the Heart Disease Reversal Program, and to Joseph Giorgio, PsyD (Program Manager, Integrated Care Program) for sustaining it. We thank Amogh Bhat, MD, Chief of Cardiology, for his continued support and partnership with the Cardiology Department. We express thanks to Stephanie Mohney, RDN (Chief, Nutrition and Food Service), Amy Klotz, RDN (Supervisory Dietician), Sian M. Carr-Lopez, PharmD (Associate Chief of Pharmacy, Primary Care), and Michelle Rand, PharmD, CACP (Anticoagulation Clinical Pharmacist-Supervisor) for their staff support of this interdisciplinary program. We thank the patients and their families for their participation in the program and commitment to the lifestyle changes. We also thank the following individuals for their contributions to this program: Lisa Wagaman, RDN, Karen Soong, PharmD, Sara S. Ali, PharmD, Suzan Hua, PharmD, and Stephen Cooperman.
1. Benjamin EJ, Virani SS, Callaway CW, et al. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association [published correction appears in Circulation. 2018 Mar 20;137(12 ): e493]. Circulation. 2018;137(12):e67-e492. doi:10.1161/CIR.0000000000000558
2. Hinojosa R. Cardiovascular disease among United States military veterans: evidence of a waning healthy soldier effect using the National Health Interview Survey. Chronic Illn. 2020;16(1):55-68. doi:10.1177/1742395318785237.
3. Hinojosa R. Sex, age, race/ethnicity, veteran status, and the likelihood of reporting cardiovascular conditions in the National Health Interview Survey. J Cardiovasc Nurs. 2019;34(3):215-221. doi:10.1097/JCN.0000000000000561 4. Assari S. Veterans and risk of heart disease in the United States: a cohort with 20 years of follow up. Int J Prev Med. 2014;5(6):703-709.
5. Thomas MM, Harpaz-Rotem I, Tsai J, Southwick SM, Pietrzak RH. Mental and physical health conditions in US combat veterans: results from the National Health and Resilience in Veterans Study. Prim Care Companion CNS Disord. 2017;19(3):10.4088/PCC.17m02118. Published 2017 Jun 22. doi:10.4088/PCC.17m02118
6. Bukhbinder AS, Wang AC, Qureshi SU, et al. Increased vascular pathology in older veterans with a purple heart commendation or chronic post-traumatic stress disorder. J Geriatr Psychiatry Neurol. 2020;33(4):195-206. doi:10.1177/0891988719868308
7. Edmondson D, von Känel R. Post-traumatic stress disorder and cardiovascular disease. Lancet Psychiatry. 2017;4(4):320-329. doi:10.1016/S2215-0366(16)30377-7
8. Forman DE, Maurer MS, Boyd C, et a;. Multimorbidity in older adults with cardiovascular disease. J Am Coll Cardiol. 2018;71(19):2149-2161. doi:10.1016/j.jacc.2018.03.022
9. Agha Z, Lofgren RP, VanRuiswyk JV, Layde PM. Are patients at Veterans Affairs medical centers sicker? A comparative analysis of health status and medical resource use. Arch Intern Med. 2000;160(21):3252-3257. doi:10.1001/archinte.160.21.3252
10. Maddox TM, Plomondon ME, Petrich M, et al. A national clinical quality program for Veterans Affairs catheterization laboratories (from the Veterans Affairs clinical assessment, reporting, and tracking program). Am J Cardiol. 2014;114(11):1750-1757. doi:10.1016/j.amjcard.2014.08.045
11. Centers for Disease Control and Prevention. Coronavirus 2019 (COVID-19):people at increased risk and other people who need to take extra precautions. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/index.html. Updated September 11, 2020. Accessed November 12, 2020.
12. International Food Information Council. 2020 food and health survey. https://foodinsight.org/2020-food-and-health-survey. Updated June 9, 2020. Accessed November 12, 2020.
13. American Association of Cardiovascular and Pulmonary Rehabilitation. Guidelines for Cardiac Rehabilitation and Secondary Prevention Programs. 5th ed. Champaign, IL: Human Kinetics; 2013.
14. Silberman A, Banthia R, Estay IS, et al. The effectiveness and efficacy of an intensive cardiac rehabilitation program in 24 sites. Am J Health Promot. 2010;24(4):260-266. doi:10.4278/ajhp.24.4.arb
15. Ornish D, Scherwitz LW, Doody RS, et al. Effects of stress management training and dietary changes in treating ischemic heart disease. JAMA. 1983;249(1):54-59.
16. Ornish D, Brown SE, Scherwitz LW, et al. Can lifestyle changes reverse coronary heart disease? The Lifestyle Heart Trial. Lancet. 1990;336(8708):129-133. doi:10.1016/0140-6736(90)91656-u.
17. Ornish D, Scherwitz LW, Billings JH, et al. Intensive lifestyle changes for reversal of coronary heart disease [published correction appears in JAMA 1999 Apr 21;281(15):1380]. JAMA. 1998;280(23):2001-2007. doi:10.1001/jama.280.23.2001
18. Frattaroli J, Weidner G, Merritt-Worden TA, Frenda S, Ornish D. Angina pectoris and atherosclerotic risk factors in the multisite cardiac lifestyle intervention program. Am J Cardiol. 2008;101(7):911-918. doi:10.1016/j.amjcard.2007.11.039
19. Koertge J, Weidner G, Elliott-Eller M, et al. Improvement in medical risk factors and quality of life in women and men with coronary artery disease in the Multicenter Lifestyle Demonstration Project. Am J Cardiol. 2003;91(11):1316-1322. doi:10.1016/s0002-9149(03)00320-5
20. Marshall DA, Walizer EM, Vernalis MN. Achievement of heart health characteristics through participation in an intensive lifestyle change program (Coronary Artery Disease Reversal Study). J Cardiopulm Rehabil Prev. 2009;29(2):84-96. doi:10.1097/HCR.0b013e31819a00b2
21. Marshall D, Elaine W, Vernalis M. The effect of a one-year lifestyle intervention program on carotid intima media thickness. Mil Med. 2011;176(7):798-804. doi:10.7205/milmed-d-10-00447
22. Esselstyn CB Jr, Ellis SG, Medendorp SV, Crowe TD. A strategy to arrest and reverse coronary artery disease: a 5-year longitudinal study of a single physician’s practice. J Fam Pract. 1995;41(6):560-568.
23. Esselstyn CB Jr. Updating a 12-year experience with arrest and reversal therapy for coronary heart disease (an overdue requiem for palliative cardiology). Am J Cardiol. 1999;84(3):339-A8. doi:10.1016/s0002-9149(99)00290-8
24. Barnard ND, Cohen J, Jenkins DJ, et al. A low-fat vegan diet improves glycemic control and cardiovascular risk factors in a randomized clinical trial in individuals with type 2 diabetes. Diabetes Care. 2006;29(8):1777-1783. doi:10.2337/dc06-0606
25. McDougall J, Thomas LE, McDougall C, et al. Effects of 7 days on an ad libitum low-fat vegan diet: the McDougall Program cohort [published correction appears in Nutr J. 2017 Feb 10;16(1):12]. Nutr J. 2014;13:99. Published 2014 Oct 14. doi:10.1186/1475-2891-13-99
26. Turner-McGrievy GM, Davidson CR, Wingard EE, Wilcox S, Frongillo EA. Comparative effectiveness of plant-based diets for weight loss: a randomized controlled trial of five different diets. Nutrition. 2015;31(2):350-358. doi:10.1016/j.nut.2014.09.002
27. Wright N, Wilson L, Smith M, Duncan B, McHugh P. The BROAD study: a randomised controlled trial using a whole food plant-based diet in the community for obesity, ischaemic heart disease or diabetes. Nutr Diabetes. 2017;7(3):e256. Published 2017 Mar 20. doi:10.1038/nutd.2017.3

28. Schaefer S, Hussein H, Gershony GR, Rutledge JC, Kappagoda CT. Regression of severe atherosclerotic plaque in patients with mild elevation of LDL cholesterol. J Investig Med. 1997;45(9):536-541.
29. Kitazono R. Know thy patient: Enhancing lifestyle interventions with psychological assessment. Int J Dis Rev Prev. 2020;2(1):76-81.
30. Miller WR, Rollnick S. Motivational Interviewing: Helping People Change. 3rd ed. New York, NY: Guilford Press; 2013.
31. Mascola AJ, Yiaslas TA, Meir RL, et al. Framing physical activity as a distinct and uniquely valuable behavior independent of weight management: A pilot randomized controlled trial for overweight and obese sedentary persons. Eat Weight Disord. 2009;14(2-3):e148-e152. doi:10.1007/BF03327814
32. Esselstyn AC, Esselstyn J. The Prevent and Reverse Heart Disease Cookbook: Over 125 Delicious, Life-Changing, Plant-Based Recipes. New York, NY: Avery; 2014.
33. Esselstyn CB Jr, Gendy G, Doyle J, Golubic M, Roizen MF. A way to reverse CAD? J Fam Pract. 2014;63(7):356-364.
34. Ornish D, Ornish A. Undo It! How Simple Lifestyle Changes Can Reverse Most Chronic Diseases. New York, NY: Ballantine Books; 2019.
35. Smith SC Jr, Benjamin EJ, Bonow RO, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association [published correction appears in J Am Coll Cardiol. 2015 Apr 14;65(14):1495. Dosage error in article text.]. J Am Coll Cardiol. 2011;58(23):2432-2446. doi:10.1016/j.jacc.2011.10.824
36. Blumenthal JA, Babyak M, Wei J, et al. Usefulness of psychosocial treatment of mental stress-induced myocardial ischemia in men. Am J Cardiol. 2002;89(2):164-168. doi:10.1016/s0002-9149(01)02194-4
37. Antoni MH. Stress management effects on psychological, endocrinological, and immune functioning in men with HIV infection: empirical support for a psychoneuroimmunological model. Stress. 2003;6(3):173-188. doi:10.1080/1025389031000156727
38. Penedo FJ, Molton I, Dahn JR, et al. A randomized clinical trial of group-based cognitive-behavioral stress management in localized prostate cancer: development of stress management skills improves quality of life and benefit finding. Ann Behav Med. 2006;31(3):261-270. doi:10.1207/s15324796abm3103_8
39. Yiaslas TA. “Look doctor, I’m a carnivore.” Int J Dis Rev Prev. 2020;2(2):35-39.
40. Khaylis A, Yiaslas T, Bergstrom J, Gore-Felton C. A review of efficacious technology-based weight-loss interventions: five key components. Telemed J E Health. 2010;16(9):931-938. doi:10.1089/tmj.2010.0065
41. Barnard ND, Sherwitz L, Ornish D. Adherence and acceptability of a low-fat, vegetarian diet among patients with cardiac disease. J Cardiopulm Rehabil. 1992;12(6):423-431.
42. Yiaslas TA, Taylor J, Embree J, Schaefer S. Elimination of angina, comprehensive cardio-metabolic risk reduction, and 50-pound weight loss in a US Navy veteran with myasthenia gravis. Int J Dis Rev Prev. 2019;1(1):77-83.
43. Berkow SE, Barnard N, Eckart J, Katcher H. Four therapeutic diets: adherence and acceptability. Can J Diet Pract Res. 2010;71(4):199-204. doi:10.3148/71.4.2010.199
44. Carpenter JK, Andrews LA, Witcraft SM, Powers MB, Smits JAJ, Hofmann SG. Cognitive behavioral therapy for anxiety and related disorders: A meta-analysis of randomized placebo-controlled trials. Depress Anxiety. 2018;35(6):502-514. doi:10.1002/da.22728
45. Yiaslas TA. The pursuit of arete in medicine and health care. Int J Dis Rev Prev. 2019;1(2):53-56.
While cardiovascular mortality rates have declined, heart disease continues to be the leading cause of death in the US, and the number of people with cardiovascular disease (CVD) is rising.1 CVD is more prevalent among military veterans than it is among nonveterans aged ≥ 25 years, and veteran status is associated with higher risk of incident heart disease after controlling for socioeconomic status, other medical diseases, depression, and lifestyle.2-4 Combat exposure, posttraumatic stress disorder (PTSD), and Purple Heart commendation are associated with higher rates of CVD, including adverse cardiovascular events.5-7 Many patients seeking care in the Veterans Health Administration (VHA), including those who undergo cardiac catheterization, meet the criteria for multimorbidity (defined as having ≥ 2 chronic diseases8), which is common among veterans.9,10 Multimorbidity presents a challenge for lifestyle intervention, as different diets may be prescribed to treat different conditions, such as Dietary Approaches to Stop Hypertension, and low-glycemic diet for diabetes mellitus (DM). Veterans with CVD are often clinically complex and may require more multifaceted secondary prevention programs.
During the coronavirus 2019 (COVID-19) pandemic, effective secondary prevention intervention is needed more than ever. Older age, CVD, and common comorbidities, including hypertension, DM, and obesity, place patients at the highest risk for severe COVID-19 infection.11 COVID-19 social distancing encourages vulnerable populations to stay home, which can make engaging in any levels of physical activity more challenging. The International Food Council found that 85% of adults have made a change to their food consumption pattern, including eating more, during the COVID-19 pandemic.12 Thus, secondary CVD prevention programs for veterans need to provide treatment that addresses these specific challenges and can be delivered via telehealth for continuity of care after disruption of traditional services.
Clinical practice guidelines for the treatment of patients with recent cardiovascular adverse events (AEs) include a referral to cardiac rehabilitation (CR).13 CR emphasizes exercise as the main intervention, along with coaching to promote multiple risk reduction. The most comprehensive CR program is intensive CR (ICR), including the Ornish ICR program.14 ICR includes 4 components: vegetarian diet, exercise, stress management (yoga, meditation), and group support. Ornish ICR has been shown to be efficacious in randomized controlled trials (RCTs).15-17 Three effectiveness studies, with 5,372 participants, demonstrated the real-world effectiveness of Ornish ICR in US hospitals.14,18,19 The program also was adapted successfully for the active-duty military and veteran population.20,21 Yet Ornish ICR is time intensive, and there are no certified VHA ICR Ornish sites. Furthermore, there is no formal strategy for targeting people with atherosclerotic CVD who no longer meet the criteria for CR or ICR. While Ornish ICR is highly effective for patients who are eligible and have access, a more effective and streamlined approach is needed for targeting many patients.
Nutrition may be the most powerful Ornish ICR component. The initial RCT conducted by Ornish and colleagues included only stress management training and a whole-food, plant-based (WFPB) diet, including grains, legumes, vegetables, fruits, nuts, and seeds. The trial found 91% of participants experienced reduced angina after only 24 days.15 The only single-component intervention study resulting in partial reversal of atherosclerosis was a WFPB diet-only study, which documented regression of atherosclerotic plaques after 5 years, using coronary angiography in 73% of participants, with arrested progression in the other 27%.22 Participants reported no cardiovascular AEs after 12 years.23 Furthermore, a number of other recent studies have demonstrated the benefits of WFPB diet-only interventions for type 2 DM (T2DM), hypertension, and obesity.24-27 The Heart Disease Reversal Program (HDRP) was developed to create an interdisciplinary lifestyle intervention that emphasized nutrition for a broad population of veterans with atherosclerotic CVD, of varying levels of functional ability, to promote comprehensive CVD risk reduction and bring heart disease reversal intervention into routine clinical practice.
Program Description
The Mental Health, Cardiology, and Nutrition and Food services all approved the launch of HDRP. We contacted veterans by mail, and 11% expressed interest (Figure). Among patients who received the initial mailed letter (prior to our accepting staff referrals), only 5% of patients who enrolled in HDRP reported previously being told about or prescribed a WFPB diet by any health care provider (HCP). Currently, patients are primarily referred to HDRP by Cardiology, Primary Care, and Mental Health services.
Design
HDRP is an adaptation of interdisciplinary lifestyle interventions that have resulted in regression of atherosclerotic blockages confirmed with invasive coronary angiography.15-17,22,28 HDRP currently is offered in a Behavioral Medicine Clinic at the Sacramento US Department of Veterans Affairs (VA) Medical Center (VAMC) in California. Program staff include a clinical health psychologist who organizes, coordinates, and act as the lead facilitator of the program; registered dietitians; clinical pharmacists; and a consulting physician. Patients engage in the 4-month core HDRP program in small cohorts (ie, 6-10 patients), and spouses/partners are highly encouraged to attend all sessions.
Components
Telephone screening. Patients are screened for the inclusion and exclusion criteria (Table 1). Patients engaging in a traditional CR program are included in the screening. Patients are informed that the program consists of lifestyle intervention, including emphasis on following a WFPB diet.
Health assessment. Once approved, all patients are instructed to complete baseline laboratory tests and questionnaires. Along with an electronic health record (EHR) review, a psychosocial assessment is completed by a licensed clinical health psychologist who assesses CVD history, eating behavior, exercise/physical activity, sleep, mental health, substance use, and social history, with the aim of enhancing our ability to help the patient to benefit from HDRP.29 The patient data are used to develop a case conceptualization (ie, integrated understanding of the particular patient’s psychiatric and medical diagnoses, behavioral patterns, social supports, lifestyle habits, strengths and weaknesses, and their interrelationships with each other and the patient’s environment), resulting in an individualized plan. Patients are encouraged to ask questions about the program, and those who are still interested are invited to attend a seminar. A request for medical clearance to participate in the program is initiated through the EHR or by patients scheduling an appointment with their HCP. All patients are medically cleared by their HCP for participation. Safe exercise recommendations also are provided and guide patient goals.
CVD risk profile. Patients complete psychosocial questionnaires and fasting laboratory tests to produce a tailored CVD risk profile. Laboratory tests include fasting lipid, fasting glucose, hemoglobin A1c (HbA1c) C-reactive protein, vitamin B12, and vitamin D. The same tests (excluding HbA1c) are completed 1 month later (after completing 4 group sessions) and again posttreatment (including HbA1c). Self-reported questionnaires are completed at the same time points, which include the Rate Your Plate dietary composition questionnaire, CHAMPS physical activity questionnaire for older adults, Beck Depression Inventory-II, and the Perceived Stress Scale.
Seminar. A 2-hour seminar provides patients and families with an opportunity to meet HDRP program staff, learn the background and rationale for chronic disease reversal, obtain a summary of the program, and hear a patient testimonial. Patients are asked to make a commitment, and the informed consent process includes all patients signing a behavioral contract.
Assessment and feedback. A licensed clinical health psychologist provides feedback to patients on their comprehensive CVD risk profile, using motivational interviewing.30,31 Smokers are encouraged to quit, and those interested are referred to their HCP and/or facility smoking cessation program.
Group sessions. Twelve weekly group sessions cover nutrition education and cooking, physical activity and exercise, stress management training, and medication reconciliation and adjustment. The nutrition component is the centerpiece of HDRP and is delivered by registered dietitians (Table 2). Patients are instructed to use the 3-week period between the HDRP seminar and the first core group session to try new recipes and prepare their kitchens, pantries, and mind-set to adopt the HDRP diet with 100% adherence. The WFPB diet used is consistent with the current guidelines of Caldwell Esselstyn, MD, and Dean Ornish, MD.32-34
A psychologist delivers the physical activity component. Patients are encouraged to meet the American Heart Association/American College of Cardiology recommendations for aerobic exercise (at least 150 minutes of moderate intensity physical activity per week) through a walking program.35 Patients with medical contraindications (eg, severe pain, mobility restrictions) are encouraged to follow the exercise/activity recommendations they had been given by their primary care provider (PCP), physical therapist, or other HCP.
A psychologist provides evidence-based cognitive behavioral stress management (CBSM) training, adapted from models developed for patients with stable ischemic heart disease, HIV/AIDS, and cancer.36-38 CBSM is a psychotherapy grounded in stress/coping theory and cognitive behavioral theory of psychopathology that integrates cognitive restructuring, coping skills training, communication/assertiveness training, anger management, and mindfulness/acceptance-based approaches. Additional emphasis is placed on assisting patients’ adjustment to the lifestyle challenges for following a plant-based diet, dealing with food cravings and emotional eating, and connecting lifestyle change to patients’ deepest values and goals.
A clinical pharmacist conducts a medication reconciliation for each patient at baseline. The pharmacist consults with each patient’s PCP, cardiologist, and HDRP consulting physician, as needed, to ensure safe adjustments to medications. Pharmacists also provide education on medications at group sessions.
After completion of the 12-week core program, graduates are encouraged to attend the monthly graduates’ group indefinitely, and as often as they desire to promote maintenance of the disease reversal lifestyle. Patients are encouraged to complete our recommended fasting laboratory work every 3 to 6 months to facilitate maintenance of treatment gains.
Program Evaluation
Patients frequently reported that the group format was vital to their success. Patients requested a cooking class, yet we lacked a full teaching kitchen. Integrating plant-based meal samples at every session and cooking videos helped. Patients reported that 100% adherence to the WFPB diet led to significant changes in their food preferences, including a loss of interest in meat.39 Patients encouraged us to keep the “disease reversal” language and focus. One veteran stated: “Disease reversal, that is the reason I called you when I got your letter.” Showing before and after images of coronary angiograms and cardiac positron emission tomography scans depicting regression of atherosclerotic plaque and restored myocardial perfusion were described as highly motivating and generated willingness to commit to a more aggressive lifestyle change.31
Patients routinely stated that they lacked understanding of their laboratory test results, which HDRP remedied. Some patients reported their adult children followed a plant-based diet, and our program resulted in a new commonality and source of bonding that was highly valued. Some patients reported that HDRP was helpful for controlling their COVID-19 anxiety and feeling in control of their health. Satisfaction surveys were completed by participants at the end of the core program, which demonstrated very high satisfaction with and acceptability of HDRP (Table 3).
The program also has received positive feedback from HCPs when we alert them to improvements in outcome measures for their patients. These HCPs expressed satisfaction with having a program to refer patients to that can help with chronic illness in more depth.
COVID-19 Response
Face-to-face group appointments were converted to videoconferencing as a result of the COVID-19 pandemic. While HDRP always promoted the use of technology and mHealth tools, the pandemic led us to develop novel technology-based interventions.40 One cohort transitioned from in-person to videoconferencing sessions, and 2 cohorts recently started this format and are ongoing. We have successfully used videoconferencing with Cisco Webex, the VA-approved backup platform, as we encountered technical barriers when using VA Video Connect. Program materials were shared electronically, and participants sent blood pressure/sugar logs by secure messaging. Guidance for online grocery shopping with home delivery was provided, and research on the benefits of the HDRP lifestyle on immune function was incorporated.
The stress management component incorporated coping with COVID-19, including normalizing common emotional difficulties with sheltering-in-place and quarantine, acknowledging and processing fear and anxiety related to being at very high risk for severe COVID-19. We presented heart disease reversal as an urgent and feasible goal during the pandemic both reducing risk of premature death and major adverse cardiovascular events in the long-term and also reducing personal risk of severe COVID complications. The new VA COVID Coach app was also presented as a resource. Reputable sources of COVID-19 and public health information were shared. Walking continued to be the primary recommended form of exercise, while indoor home exercise options were promoted during the periods of very poor air quality due to the widespread California fires and smoke.
Considering the research suggesting benefits of our intervention for treating T2DM,promoting sustained weight loss, and promoting comprehensive cardiometabolic risk reduction, we have begun accepting referrals for patients with any type of atherosclerotic CVD (eg, peripheral artery disease, carotid artery disease), patients with T2DM (without CVD), and patients with only a history of ischemic stroke or transient ischemic attack.24-27 Vascular surgery has become a new referral source, primarily for patients with peripheral and carotid artery diseases. Finally, we are leveraging videoconferencing and accepting referrals across the VA Northern California Health Care System (VANCHCS)catchment (from the California-Oregon state border to the San Francisco Bay Area). This also helps address a long-standing problem with reaching the many rural veterans who live far from a VA clinic. We successfully implemented a consult/referral process within the EHR that is available to providers across VANCHCS.
Discussion
The efficacy and effectiveness of reversal programs are well established in intensive programs (eg, ICR), yet such programs have yet to be streamlined and disseminated broadly into routine clinical care. HDRP has endeavored to address this by emphasizing nutrition relative to other program components. We have learned that the words “disease reversal” are very often the reason patients initially reach out or accept referral to our program.
Consistent with past research on plant-based nutrition interventions, the group format was indispensable.41 Individual sessions with a clinical health psychologist enabled tailored feedback and education on how behavior changes could impact laboratory results and how certain psychosocial factors could support success. Participants reported that seeing significantly favorable laboratory results was highly motivating and confirmed the power of their lifestyle changes. Furthermore, a psychosocial health assessment with individual sessions promoted a tailored treatment plan with targeted clinical interventions, such as behavioral health education, motivational interviewing, and advanced methods, including cognitive behavioral therapy and techniques drawn from dialectical behavior therapy and acceptance and commitment therapy.
Veterans with multimorbidity face the difficult task of learning and maintaining a complex disease self-management program and implementing a lifestyle approach that is feasible, effective, promotes weight loss, and treats multiple conditions. HDRP is a model approach for this population, as demonstrated by a recent case report of a 65-year-old male veteran with atherosclerotic CVD, T2DM, hypertension, and myasthenia gravis who had 2 heart attacks within 2 months.42 His neurologic disease precluded significant physical activity. Although he achieved some initial weight loss through lifestyle changes, he continued to have daily angina despite optimal and aggressive cardiology management. After enrolling in HDRP and adopting the WFPB diet, the patient reported almost complete resolution of angina within 1 month, similar to that found in other studies.15
The literature suggests that concern over the acceptability of plant-based diets and patients’ ability to adhere to them long-term may be misplaced. A review paper on dietary interventions lasting > 1 year found that 51 to 61% of vegetarian and vegan study participants had maintained dietary adherence, while 20 to 55% of omnivorous diet intervention participants adhered to their study diets.43 Remarkably, there were no statistically significant differences in the acceptability of the vegan, vegetarian, or omnivorous diets in the studies reviewed.43 Recent dietary research also suggests that providing patients with higher goals (eg, adopting a vegan diet instead of only moderate dietary changes) results in greater weight loss and maintenance.26 HDRP provides training on consumption of whole plant foods, which may offer patients a unique advantage for maximizing results and higher adherence over time.
Limitations
Hands-on cooking instruction was not provided at our VAMC. The total time of the intervention was significantly less in HDRP (25 hours) than it was for the Ornish ICR program (72 hours), which may hinder long-term adherence. Without an exercise facility, we were not able to provide more detailed exercise instruction and supervised exercise.
Program Improvements Planned
There are a number of improvements that are planned for HDRP. First, the program anticipates requesting medical clearance at the telephone screening stage for self-referred patients. Second,
Conclusions
Although our patient population was self-selected for participation, early program evaluation demonstrates high acceptability. Very few patients had ever been told about a heart disease reversing lifestyle, and we found direct-to-patient clinical outreach an effective method for launching a disease reversal program (optimally timed with HCP presentations). Furthermore, the program is adaptable to current restrictions on in-person appointments due to the COVID-19 pandemic, and much more convenient for rural veterans who live far from any VA clinic. Being able to offer sustainable health care for individuals during unexpected public health crises is critically important. Additionally, treating veterans who are most vulnerable to pandemic illness due to existing medical conditions, such as CVD, should be a high priority. Last, HDRP also may represent a novel integrated treatment for COVID-19 anxiety and secondary CVD prevention, as lifestyle habits are optimized to improve chronic diseases that elevate risk for severe COVID-19 infection and mortality, as well as including coping strategies consistent with evidence-based psychotherapies for anxiety disorders.44
We believe that beyond the clinical benefits to patients, there is significant value and benefit added to the health care system by offering an intervention within the “disease reversal” paradigm. Efforts of the health care team to reverse a disease can be considered the highest aim of medicine and health care.45
Acknowledgments
This work was supported by the US Department of Veterans Affairs. We give special thanks to David M. Gellerman, MD, PhD, and David W. Schafer, PsyD, for providing Mental Health Service support for initiating the Heart Disease Reversal Program, and to Joseph Giorgio, PsyD (Program Manager, Integrated Care Program) for sustaining it. We thank Amogh Bhat, MD, Chief of Cardiology, for his continued support and partnership with the Cardiology Department. We express thanks to Stephanie Mohney, RDN (Chief, Nutrition and Food Service), Amy Klotz, RDN (Supervisory Dietician), Sian M. Carr-Lopez, PharmD (Associate Chief of Pharmacy, Primary Care), and Michelle Rand, PharmD, CACP (Anticoagulation Clinical Pharmacist-Supervisor) for their staff support of this interdisciplinary program. We thank the patients and their families for their participation in the program and commitment to the lifestyle changes. We also thank the following individuals for their contributions to this program: Lisa Wagaman, RDN, Karen Soong, PharmD, Sara S. Ali, PharmD, Suzan Hua, PharmD, and Stephen Cooperman.
While cardiovascular mortality rates have declined, heart disease continues to be the leading cause of death in the US, and the number of people with cardiovascular disease (CVD) is rising.1 CVD is more prevalent among military veterans than it is among nonveterans aged ≥ 25 years, and veteran status is associated with higher risk of incident heart disease after controlling for socioeconomic status, other medical diseases, depression, and lifestyle.2-4 Combat exposure, posttraumatic stress disorder (PTSD), and Purple Heart commendation are associated with higher rates of CVD, including adverse cardiovascular events.5-7 Many patients seeking care in the Veterans Health Administration (VHA), including those who undergo cardiac catheterization, meet the criteria for multimorbidity (defined as having ≥ 2 chronic diseases8), which is common among veterans.9,10 Multimorbidity presents a challenge for lifestyle intervention, as different diets may be prescribed to treat different conditions, such as Dietary Approaches to Stop Hypertension, and low-glycemic diet for diabetes mellitus (DM). Veterans with CVD are often clinically complex and may require more multifaceted secondary prevention programs.
During the coronavirus 2019 (COVID-19) pandemic, effective secondary prevention intervention is needed more than ever. Older age, CVD, and common comorbidities, including hypertension, DM, and obesity, place patients at the highest risk for severe COVID-19 infection.11 COVID-19 social distancing encourages vulnerable populations to stay home, which can make engaging in any levels of physical activity more challenging. The International Food Council found that 85% of adults have made a change to their food consumption pattern, including eating more, during the COVID-19 pandemic.12 Thus, secondary CVD prevention programs for veterans need to provide treatment that addresses these specific challenges and can be delivered via telehealth for continuity of care after disruption of traditional services.
Clinical practice guidelines for the treatment of patients with recent cardiovascular adverse events (AEs) include a referral to cardiac rehabilitation (CR).13 CR emphasizes exercise as the main intervention, along with coaching to promote multiple risk reduction. The most comprehensive CR program is intensive CR (ICR), including the Ornish ICR program.14 ICR includes 4 components: vegetarian diet, exercise, stress management (yoga, meditation), and group support. Ornish ICR has been shown to be efficacious in randomized controlled trials (RCTs).15-17 Three effectiveness studies, with 5,372 participants, demonstrated the real-world effectiveness of Ornish ICR in US hospitals.14,18,19 The program also was adapted successfully for the active-duty military and veteran population.20,21 Yet Ornish ICR is time intensive, and there are no certified VHA ICR Ornish sites. Furthermore, there is no formal strategy for targeting people with atherosclerotic CVD who no longer meet the criteria for CR or ICR. While Ornish ICR is highly effective for patients who are eligible and have access, a more effective and streamlined approach is needed for targeting many patients.
Nutrition may be the most powerful Ornish ICR component. The initial RCT conducted by Ornish and colleagues included only stress management training and a whole-food, plant-based (WFPB) diet, including grains, legumes, vegetables, fruits, nuts, and seeds. The trial found 91% of participants experienced reduced angina after only 24 days.15 The only single-component intervention study resulting in partial reversal of atherosclerosis was a WFPB diet-only study, which documented regression of atherosclerotic plaques after 5 years, using coronary angiography in 73% of participants, with arrested progression in the other 27%.22 Participants reported no cardiovascular AEs after 12 years.23 Furthermore, a number of other recent studies have demonstrated the benefits of WFPB diet-only interventions for type 2 DM (T2DM), hypertension, and obesity.24-27 The Heart Disease Reversal Program (HDRP) was developed to create an interdisciplinary lifestyle intervention that emphasized nutrition for a broad population of veterans with atherosclerotic CVD, of varying levels of functional ability, to promote comprehensive CVD risk reduction and bring heart disease reversal intervention into routine clinical practice.
Program Description
The Mental Health, Cardiology, and Nutrition and Food services all approved the launch of HDRP. We contacted veterans by mail, and 11% expressed interest (Figure). Among patients who received the initial mailed letter (prior to our accepting staff referrals), only 5% of patients who enrolled in HDRP reported previously being told about or prescribed a WFPB diet by any health care provider (HCP). Currently, patients are primarily referred to HDRP by Cardiology, Primary Care, and Mental Health services.
Design
HDRP is an adaptation of interdisciplinary lifestyle interventions that have resulted in regression of atherosclerotic blockages confirmed with invasive coronary angiography.15-17,22,28 HDRP currently is offered in a Behavioral Medicine Clinic at the Sacramento US Department of Veterans Affairs (VA) Medical Center (VAMC) in California. Program staff include a clinical health psychologist who organizes, coordinates, and act as the lead facilitator of the program; registered dietitians; clinical pharmacists; and a consulting physician. Patients engage in the 4-month core HDRP program in small cohorts (ie, 6-10 patients), and spouses/partners are highly encouraged to attend all sessions.
Components
Telephone screening. Patients are screened for the inclusion and exclusion criteria (Table 1). Patients engaging in a traditional CR program are included in the screening. Patients are informed that the program consists of lifestyle intervention, including emphasis on following a WFPB diet.
Health assessment. Once approved, all patients are instructed to complete baseline laboratory tests and questionnaires. Along with an electronic health record (EHR) review, a psychosocial assessment is completed by a licensed clinical health psychologist who assesses CVD history, eating behavior, exercise/physical activity, sleep, mental health, substance use, and social history, with the aim of enhancing our ability to help the patient to benefit from HDRP.29 The patient data are used to develop a case conceptualization (ie, integrated understanding of the particular patient’s psychiatric and medical diagnoses, behavioral patterns, social supports, lifestyle habits, strengths and weaknesses, and their interrelationships with each other and the patient’s environment), resulting in an individualized plan. Patients are encouraged to ask questions about the program, and those who are still interested are invited to attend a seminar. A request for medical clearance to participate in the program is initiated through the EHR or by patients scheduling an appointment with their HCP. All patients are medically cleared by their HCP for participation. Safe exercise recommendations also are provided and guide patient goals.
CVD risk profile. Patients complete psychosocial questionnaires and fasting laboratory tests to produce a tailored CVD risk profile. Laboratory tests include fasting lipid, fasting glucose, hemoglobin A1c (HbA1c) C-reactive protein, vitamin B12, and vitamin D. The same tests (excluding HbA1c) are completed 1 month later (after completing 4 group sessions) and again posttreatment (including HbA1c). Self-reported questionnaires are completed at the same time points, which include the Rate Your Plate dietary composition questionnaire, CHAMPS physical activity questionnaire for older adults, Beck Depression Inventory-II, and the Perceived Stress Scale.
Seminar. A 2-hour seminar provides patients and families with an opportunity to meet HDRP program staff, learn the background and rationale for chronic disease reversal, obtain a summary of the program, and hear a patient testimonial. Patients are asked to make a commitment, and the informed consent process includes all patients signing a behavioral contract.
Assessment and feedback. A licensed clinical health psychologist provides feedback to patients on their comprehensive CVD risk profile, using motivational interviewing.30,31 Smokers are encouraged to quit, and those interested are referred to their HCP and/or facility smoking cessation program.
Group sessions. Twelve weekly group sessions cover nutrition education and cooking, physical activity and exercise, stress management training, and medication reconciliation and adjustment. The nutrition component is the centerpiece of HDRP and is delivered by registered dietitians (Table 2). Patients are instructed to use the 3-week period between the HDRP seminar and the first core group session to try new recipes and prepare their kitchens, pantries, and mind-set to adopt the HDRP diet with 100% adherence. The WFPB diet used is consistent with the current guidelines of Caldwell Esselstyn, MD, and Dean Ornish, MD.32-34
A psychologist delivers the physical activity component. Patients are encouraged to meet the American Heart Association/American College of Cardiology recommendations for aerobic exercise (at least 150 minutes of moderate intensity physical activity per week) through a walking program.35 Patients with medical contraindications (eg, severe pain, mobility restrictions) are encouraged to follow the exercise/activity recommendations they had been given by their primary care provider (PCP), physical therapist, or other HCP.
A psychologist provides evidence-based cognitive behavioral stress management (CBSM) training, adapted from models developed for patients with stable ischemic heart disease, HIV/AIDS, and cancer.36-38 CBSM is a psychotherapy grounded in stress/coping theory and cognitive behavioral theory of psychopathology that integrates cognitive restructuring, coping skills training, communication/assertiveness training, anger management, and mindfulness/acceptance-based approaches. Additional emphasis is placed on assisting patients’ adjustment to the lifestyle challenges for following a plant-based diet, dealing with food cravings and emotional eating, and connecting lifestyle change to patients’ deepest values and goals.
A clinical pharmacist conducts a medication reconciliation for each patient at baseline. The pharmacist consults with each patient’s PCP, cardiologist, and HDRP consulting physician, as needed, to ensure safe adjustments to medications. Pharmacists also provide education on medications at group sessions.
After completion of the 12-week core program, graduates are encouraged to attend the monthly graduates’ group indefinitely, and as often as they desire to promote maintenance of the disease reversal lifestyle. Patients are encouraged to complete our recommended fasting laboratory work every 3 to 6 months to facilitate maintenance of treatment gains.
Program Evaluation
Patients frequently reported that the group format was vital to their success. Patients requested a cooking class, yet we lacked a full teaching kitchen. Integrating plant-based meal samples at every session and cooking videos helped. Patients reported that 100% adherence to the WFPB diet led to significant changes in their food preferences, including a loss of interest in meat.39 Patients encouraged us to keep the “disease reversal” language and focus. One veteran stated: “Disease reversal, that is the reason I called you when I got your letter.” Showing before and after images of coronary angiograms and cardiac positron emission tomography scans depicting regression of atherosclerotic plaque and restored myocardial perfusion were described as highly motivating and generated willingness to commit to a more aggressive lifestyle change.31
Patients routinely stated that they lacked understanding of their laboratory test results, which HDRP remedied. Some patients reported their adult children followed a plant-based diet, and our program resulted in a new commonality and source of bonding that was highly valued. Some patients reported that HDRP was helpful for controlling their COVID-19 anxiety and feeling in control of their health. Satisfaction surveys were completed by participants at the end of the core program, which demonstrated very high satisfaction with and acceptability of HDRP (Table 3).
The program also has received positive feedback from HCPs when we alert them to improvements in outcome measures for their patients. These HCPs expressed satisfaction with having a program to refer patients to that can help with chronic illness in more depth.
COVID-19 Response
Face-to-face group appointments were converted to videoconferencing as a result of the COVID-19 pandemic. While HDRP always promoted the use of technology and mHealth tools, the pandemic led us to develop novel technology-based interventions.40 One cohort transitioned from in-person to videoconferencing sessions, and 2 cohorts recently started this format and are ongoing. We have successfully used videoconferencing with Cisco Webex, the VA-approved backup platform, as we encountered technical barriers when using VA Video Connect. Program materials were shared electronically, and participants sent blood pressure/sugar logs by secure messaging. Guidance for online grocery shopping with home delivery was provided, and research on the benefits of the HDRP lifestyle on immune function was incorporated.
The stress management component incorporated coping with COVID-19, including normalizing common emotional difficulties with sheltering-in-place and quarantine, acknowledging and processing fear and anxiety related to being at very high risk for severe COVID-19. We presented heart disease reversal as an urgent and feasible goal during the pandemic both reducing risk of premature death and major adverse cardiovascular events in the long-term and also reducing personal risk of severe COVID complications. The new VA COVID Coach app was also presented as a resource. Reputable sources of COVID-19 and public health information were shared. Walking continued to be the primary recommended form of exercise, while indoor home exercise options were promoted during the periods of very poor air quality due to the widespread California fires and smoke.
Considering the research suggesting benefits of our intervention for treating T2DM,promoting sustained weight loss, and promoting comprehensive cardiometabolic risk reduction, we have begun accepting referrals for patients with any type of atherosclerotic CVD (eg, peripheral artery disease, carotid artery disease), patients with T2DM (without CVD), and patients with only a history of ischemic stroke or transient ischemic attack.24-27 Vascular surgery has become a new referral source, primarily for patients with peripheral and carotid artery diseases. Finally, we are leveraging videoconferencing and accepting referrals across the VA Northern California Health Care System (VANCHCS)catchment (from the California-Oregon state border to the San Francisco Bay Area). This also helps address a long-standing problem with reaching the many rural veterans who live far from a VA clinic. We successfully implemented a consult/referral process within the EHR that is available to providers across VANCHCS.
Discussion
The efficacy and effectiveness of reversal programs are well established in intensive programs (eg, ICR), yet such programs have yet to be streamlined and disseminated broadly into routine clinical care. HDRP has endeavored to address this by emphasizing nutrition relative to other program components. We have learned that the words “disease reversal” are very often the reason patients initially reach out or accept referral to our program.
Consistent with past research on plant-based nutrition interventions, the group format was indispensable.41 Individual sessions with a clinical health psychologist enabled tailored feedback and education on how behavior changes could impact laboratory results and how certain psychosocial factors could support success. Participants reported that seeing significantly favorable laboratory results was highly motivating and confirmed the power of their lifestyle changes. Furthermore, a psychosocial health assessment with individual sessions promoted a tailored treatment plan with targeted clinical interventions, such as behavioral health education, motivational interviewing, and advanced methods, including cognitive behavioral therapy and techniques drawn from dialectical behavior therapy and acceptance and commitment therapy.
Veterans with multimorbidity face the difficult task of learning and maintaining a complex disease self-management program and implementing a lifestyle approach that is feasible, effective, promotes weight loss, and treats multiple conditions. HDRP is a model approach for this population, as demonstrated by a recent case report of a 65-year-old male veteran with atherosclerotic CVD, T2DM, hypertension, and myasthenia gravis who had 2 heart attacks within 2 months.42 His neurologic disease precluded significant physical activity. Although he achieved some initial weight loss through lifestyle changes, he continued to have daily angina despite optimal and aggressive cardiology management. After enrolling in HDRP and adopting the WFPB diet, the patient reported almost complete resolution of angina within 1 month, similar to that found in other studies.15
The literature suggests that concern over the acceptability of plant-based diets and patients’ ability to adhere to them long-term may be misplaced. A review paper on dietary interventions lasting > 1 year found that 51 to 61% of vegetarian and vegan study participants had maintained dietary adherence, while 20 to 55% of omnivorous diet intervention participants adhered to their study diets.43 Remarkably, there were no statistically significant differences in the acceptability of the vegan, vegetarian, or omnivorous diets in the studies reviewed.43 Recent dietary research also suggests that providing patients with higher goals (eg, adopting a vegan diet instead of only moderate dietary changes) results in greater weight loss and maintenance.26 HDRP provides training on consumption of whole plant foods, which may offer patients a unique advantage for maximizing results and higher adherence over time.
Limitations
Hands-on cooking instruction was not provided at our VAMC. The total time of the intervention was significantly less in HDRP (25 hours) than it was for the Ornish ICR program (72 hours), which may hinder long-term adherence. Without an exercise facility, we were not able to provide more detailed exercise instruction and supervised exercise.
Program Improvements Planned
There are a number of improvements that are planned for HDRP. First, the program anticipates requesting medical clearance at the telephone screening stage for self-referred patients. Second,
Conclusions
Although our patient population was self-selected for participation, early program evaluation demonstrates high acceptability. Very few patients had ever been told about a heart disease reversing lifestyle, and we found direct-to-patient clinical outreach an effective method for launching a disease reversal program (optimally timed with HCP presentations). Furthermore, the program is adaptable to current restrictions on in-person appointments due to the COVID-19 pandemic, and much more convenient for rural veterans who live far from any VA clinic. Being able to offer sustainable health care for individuals during unexpected public health crises is critically important. Additionally, treating veterans who are most vulnerable to pandemic illness due to existing medical conditions, such as CVD, should be a high priority. Last, HDRP also may represent a novel integrated treatment for COVID-19 anxiety and secondary CVD prevention, as lifestyle habits are optimized to improve chronic diseases that elevate risk for severe COVID-19 infection and mortality, as well as including coping strategies consistent with evidence-based psychotherapies for anxiety disorders.44
We believe that beyond the clinical benefits to patients, there is significant value and benefit added to the health care system by offering an intervention within the “disease reversal” paradigm. Efforts of the health care team to reverse a disease can be considered the highest aim of medicine and health care.45
Acknowledgments
This work was supported by the US Department of Veterans Affairs. We give special thanks to David M. Gellerman, MD, PhD, and David W. Schafer, PsyD, for providing Mental Health Service support for initiating the Heart Disease Reversal Program, and to Joseph Giorgio, PsyD (Program Manager, Integrated Care Program) for sustaining it. We thank Amogh Bhat, MD, Chief of Cardiology, for his continued support and partnership with the Cardiology Department. We express thanks to Stephanie Mohney, RDN (Chief, Nutrition and Food Service), Amy Klotz, RDN (Supervisory Dietician), Sian M. Carr-Lopez, PharmD (Associate Chief of Pharmacy, Primary Care), and Michelle Rand, PharmD, CACP (Anticoagulation Clinical Pharmacist-Supervisor) for their staff support of this interdisciplinary program. We thank the patients and their families for their participation in the program and commitment to the lifestyle changes. We also thank the following individuals for their contributions to this program: Lisa Wagaman, RDN, Karen Soong, PharmD, Sara S. Ali, PharmD, Suzan Hua, PharmD, and Stephen Cooperman.
1. Benjamin EJ, Virani SS, Callaway CW, et al. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association [published correction appears in Circulation. 2018 Mar 20;137(12 ): e493]. Circulation. 2018;137(12):e67-e492. doi:10.1161/CIR.0000000000000558
2. Hinojosa R. Cardiovascular disease among United States military veterans: evidence of a waning healthy soldier effect using the National Health Interview Survey. Chronic Illn. 2020;16(1):55-68. doi:10.1177/1742395318785237.
3. Hinojosa R. Sex, age, race/ethnicity, veteran status, and the likelihood of reporting cardiovascular conditions in the National Health Interview Survey. J Cardiovasc Nurs. 2019;34(3):215-221. doi:10.1097/JCN.0000000000000561 4. Assari S. Veterans and risk of heart disease in the United States: a cohort with 20 years of follow up. Int J Prev Med. 2014;5(6):703-709.
5. Thomas MM, Harpaz-Rotem I, Tsai J, Southwick SM, Pietrzak RH. Mental and physical health conditions in US combat veterans: results from the National Health and Resilience in Veterans Study. Prim Care Companion CNS Disord. 2017;19(3):10.4088/PCC.17m02118. Published 2017 Jun 22. doi:10.4088/PCC.17m02118
6. Bukhbinder AS, Wang AC, Qureshi SU, et al. Increased vascular pathology in older veterans with a purple heart commendation or chronic post-traumatic stress disorder. J Geriatr Psychiatry Neurol. 2020;33(4):195-206. doi:10.1177/0891988719868308
7. Edmondson D, von Känel R. Post-traumatic stress disorder and cardiovascular disease. Lancet Psychiatry. 2017;4(4):320-329. doi:10.1016/S2215-0366(16)30377-7
8. Forman DE, Maurer MS, Boyd C, et a;. Multimorbidity in older adults with cardiovascular disease. J Am Coll Cardiol. 2018;71(19):2149-2161. doi:10.1016/j.jacc.2018.03.022
9. Agha Z, Lofgren RP, VanRuiswyk JV, Layde PM. Are patients at Veterans Affairs medical centers sicker? A comparative analysis of health status and medical resource use. Arch Intern Med. 2000;160(21):3252-3257. doi:10.1001/archinte.160.21.3252
10. Maddox TM, Plomondon ME, Petrich M, et al. A national clinical quality program for Veterans Affairs catheterization laboratories (from the Veterans Affairs clinical assessment, reporting, and tracking program). Am J Cardiol. 2014;114(11):1750-1757. doi:10.1016/j.amjcard.2014.08.045
11. Centers for Disease Control and Prevention. Coronavirus 2019 (COVID-19):people at increased risk and other people who need to take extra precautions. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/index.html. Updated September 11, 2020. Accessed November 12, 2020.
12. International Food Information Council. 2020 food and health survey. https://foodinsight.org/2020-food-and-health-survey. Updated June 9, 2020. Accessed November 12, 2020.
13. American Association of Cardiovascular and Pulmonary Rehabilitation. Guidelines for Cardiac Rehabilitation and Secondary Prevention Programs. 5th ed. Champaign, IL: Human Kinetics; 2013.
14. Silberman A, Banthia R, Estay IS, et al. The effectiveness and efficacy of an intensive cardiac rehabilitation program in 24 sites. Am J Health Promot. 2010;24(4):260-266. doi:10.4278/ajhp.24.4.arb
15. Ornish D, Scherwitz LW, Doody RS, et al. Effects of stress management training and dietary changes in treating ischemic heart disease. JAMA. 1983;249(1):54-59.
16. Ornish D, Brown SE, Scherwitz LW, et al. Can lifestyle changes reverse coronary heart disease? The Lifestyle Heart Trial. Lancet. 1990;336(8708):129-133. doi:10.1016/0140-6736(90)91656-u.
17. Ornish D, Scherwitz LW, Billings JH, et al. Intensive lifestyle changes for reversal of coronary heart disease [published correction appears in JAMA 1999 Apr 21;281(15):1380]. JAMA. 1998;280(23):2001-2007. doi:10.1001/jama.280.23.2001
18. Frattaroli J, Weidner G, Merritt-Worden TA, Frenda S, Ornish D. Angina pectoris and atherosclerotic risk factors in the multisite cardiac lifestyle intervention program. Am J Cardiol. 2008;101(7):911-918. doi:10.1016/j.amjcard.2007.11.039
19. Koertge J, Weidner G, Elliott-Eller M, et al. Improvement in medical risk factors and quality of life in women and men with coronary artery disease in the Multicenter Lifestyle Demonstration Project. Am J Cardiol. 2003;91(11):1316-1322. doi:10.1016/s0002-9149(03)00320-5
20. Marshall DA, Walizer EM, Vernalis MN. Achievement of heart health characteristics through participation in an intensive lifestyle change program (Coronary Artery Disease Reversal Study). J Cardiopulm Rehabil Prev. 2009;29(2):84-96. doi:10.1097/HCR.0b013e31819a00b2
21. Marshall D, Elaine W, Vernalis M. The effect of a one-year lifestyle intervention program on carotid intima media thickness. Mil Med. 2011;176(7):798-804. doi:10.7205/milmed-d-10-00447
22. Esselstyn CB Jr, Ellis SG, Medendorp SV, Crowe TD. A strategy to arrest and reverse coronary artery disease: a 5-year longitudinal study of a single physician’s practice. J Fam Pract. 1995;41(6):560-568.
23. Esselstyn CB Jr. Updating a 12-year experience with arrest and reversal therapy for coronary heart disease (an overdue requiem for palliative cardiology). Am J Cardiol. 1999;84(3):339-A8. doi:10.1016/s0002-9149(99)00290-8
24. Barnard ND, Cohen J, Jenkins DJ, et al. A low-fat vegan diet improves glycemic control and cardiovascular risk factors in a randomized clinical trial in individuals with type 2 diabetes. Diabetes Care. 2006;29(8):1777-1783. doi:10.2337/dc06-0606
25. McDougall J, Thomas LE, McDougall C, et al. Effects of 7 days on an ad libitum low-fat vegan diet: the McDougall Program cohort [published correction appears in Nutr J. 2017 Feb 10;16(1):12]. Nutr J. 2014;13:99. Published 2014 Oct 14. doi:10.1186/1475-2891-13-99
26. Turner-McGrievy GM, Davidson CR, Wingard EE, Wilcox S, Frongillo EA. Comparative effectiveness of plant-based diets for weight loss: a randomized controlled trial of five different diets. Nutrition. 2015;31(2):350-358. doi:10.1016/j.nut.2014.09.002
27. Wright N, Wilson L, Smith M, Duncan B, McHugh P. The BROAD study: a randomised controlled trial using a whole food plant-based diet in the community for obesity, ischaemic heart disease or diabetes. Nutr Diabetes. 2017;7(3):e256. Published 2017 Mar 20. doi:10.1038/nutd.2017.3

28. Schaefer S, Hussein H, Gershony GR, Rutledge JC, Kappagoda CT. Regression of severe atherosclerotic plaque in patients with mild elevation of LDL cholesterol. J Investig Med. 1997;45(9):536-541.
29. Kitazono R. Know thy patient: Enhancing lifestyle interventions with psychological assessment. Int J Dis Rev Prev. 2020;2(1):76-81.
30. Miller WR, Rollnick S. Motivational Interviewing: Helping People Change. 3rd ed. New York, NY: Guilford Press; 2013.
31. Mascola AJ, Yiaslas TA, Meir RL, et al. Framing physical activity as a distinct and uniquely valuable behavior independent of weight management: A pilot randomized controlled trial for overweight and obese sedentary persons. Eat Weight Disord. 2009;14(2-3):e148-e152. doi:10.1007/BF03327814
32. Esselstyn AC, Esselstyn J. The Prevent and Reverse Heart Disease Cookbook: Over 125 Delicious, Life-Changing, Plant-Based Recipes. New York, NY: Avery; 2014.
33. Esselstyn CB Jr, Gendy G, Doyle J, Golubic M, Roizen MF. A way to reverse CAD? J Fam Pract. 2014;63(7):356-364.
34. Ornish D, Ornish A. Undo It! How Simple Lifestyle Changes Can Reverse Most Chronic Diseases. New York, NY: Ballantine Books; 2019.
35. Smith SC Jr, Benjamin EJ, Bonow RO, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association [published correction appears in J Am Coll Cardiol. 2015 Apr 14;65(14):1495. Dosage error in article text.]. J Am Coll Cardiol. 2011;58(23):2432-2446. doi:10.1016/j.jacc.2011.10.824
36. Blumenthal JA, Babyak M, Wei J, et al. Usefulness of psychosocial treatment of mental stress-induced myocardial ischemia in men. Am J Cardiol. 2002;89(2):164-168. doi:10.1016/s0002-9149(01)02194-4
37. Antoni MH. Stress management effects on psychological, endocrinological, and immune functioning in men with HIV infection: empirical support for a psychoneuroimmunological model. Stress. 2003;6(3):173-188. doi:10.1080/1025389031000156727
38. Penedo FJ, Molton I, Dahn JR, et al. A randomized clinical trial of group-based cognitive-behavioral stress management in localized prostate cancer: development of stress management skills improves quality of life and benefit finding. Ann Behav Med. 2006;31(3):261-270. doi:10.1207/s15324796abm3103_8
39. Yiaslas TA. “Look doctor, I’m a carnivore.” Int J Dis Rev Prev. 2020;2(2):35-39.
40. Khaylis A, Yiaslas T, Bergstrom J, Gore-Felton C. A review of efficacious technology-based weight-loss interventions: five key components. Telemed J E Health. 2010;16(9):931-938. doi:10.1089/tmj.2010.0065
41. Barnard ND, Sherwitz L, Ornish D. Adherence and acceptability of a low-fat, vegetarian diet among patients with cardiac disease. J Cardiopulm Rehabil. 1992;12(6):423-431.
42. Yiaslas TA, Taylor J, Embree J, Schaefer S. Elimination of angina, comprehensive cardio-metabolic risk reduction, and 50-pound weight loss in a US Navy veteran with myasthenia gravis. Int J Dis Rev Prev. 2019;1(1):77-83.
43. Berkow SE, Barnard N, Eckart J, Katcher H. Four therapeutic diets: adherence and acceptability. Can J Diet Pract Res. 2010;71(4):199-204. doi:10.3148/71.4.2010.199
44. Carpenter JK, Andrews LA, Witcraft SM, Powers MB, Smits JAJ, Hofmann SG. Cognitive behavioral therapy for anxiety and related disorders: A meta-analysis of randomized placebo-controlled trials. Depress Anxiety. 2018;35(6):502-514. doi:10.1002/da.22728
45. Yiaslas TA. The pursuit of arete in medicine and health care. Int J Dis Rev Prev. 2019;1(2):53-56.
1. Benjamin EJ, Virani SS, Callaway CW, et al. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association [published correction appears in Circulation. 2018 Mar 20;137(12 ): e493]. Circulation. 2018;137(12):e67-e492. doi:10.1161/CIR.0000000000000558
2. Hinojosa R. Cardiovascular disease among United States military veterans: evidence of a waning healthy soldier effect using the National Health Interview Survey. Chronic Illn. 2020;16(1):55-68. doi:10.1177/1742395318785237.
3. Hinojosa R. Sex, age, race/ethnicity, veteran status, and the likelihood of reporting cardiovascular conditions in the National Health Interview Survey. J Cardiovasc Nurs. 2019;34(3):215-221. doi:10.1097/JCN.0000000000000561 4. Assari S. Veterans and risk of heart disease in the United States: a cohort with 20 years of follow up. Int J Prev Med. 2014;5(6):703-709.
5. Thomas MM, Harpaz-Rotem I, Tsai J, Southwick SM, Pietrzak RH. Mental and physical health conditions in US combat veterans: results from the National Health and Resilience in Veterans Study. Prim Care Companion CNS Disord. 2017;19(3):10.4088/PCC.17m02118. Published 2017 Jun 22. doi:10.4088/PCC.17m02118
6. Bukhbinder AS, Wang AC, Qureshi SU, et al. Increased vascular pathology in older veterans with a purple heart commendation or chronic post-traumatic stress disorder. J Geriatr Psychiatry Neurol. 2020;33(4):195-206. doi:10.1177/0891988719868308
7. Edmondson D, von Känel R. Post-traumatic stress disorder and cardiovascular disease. Lancet Psychiatry. 2017;4(4):320-329. doi:10.1016/S2215-0366(16)30377-7
8. Forman DE, Maurer MS, Boyd C, et a;. Multimorbidity in older adults with cardiovascular disease. J Am Coll Cardiol. 2018;71(19):2149-2161. doi:10.1016/j.jacc.2018.03.022
9. Agha Z, Lofgren RP, VanRuiswyk JV, Layde PM. Are patients at Veterans Affairs medical centers sicker? A comparative analysis of health status and medical resource use. Arch Intern Med. 2000;160(21):3252-3257. doi:10.1001/archinte.160.21.3252
10. Maddox TM, Plomondon ME, Petrich M, et al. A national clinical quality program for Veterans Affairs catheterization laboratories (from the Veterans Affairs clinical assessment, reporting, and tracking program). Am J Cardiol. 2014;114(11):1750-1757. doi:10.1016/j.amjcard.2014.08.045
11. Centers for Disease Control and Prevention. Coronavirus 2019 (COVID-19):people at increased risk and other people who need to take extra precautions. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/index.html. Updated September 11, 2020. Accessed November 12, 2020.
12. International Food Information Council. 2020 food and health survey. https://foodinsight.org/2020-food-and-health-survey. Updated June 9, 2020. Accessed November 12, 2020.
13. American Association of Cardiovascular and Pulmonary Rehabilitation. Guidelines for Cardiac Rehabilitation and Secondary Prevention Programs. 5th ed. Champaign, IL: Human Kinetics; 2013.
14. Silberman A, Banthia R, Estay IS, et al. The effectiveness and efficacy of an intensive cardiac rehabilitation program in 24 sites. Am J Health Promot. 2010;24(4):260-266. doi:10.4278/ajhp.24.4.arb
15. Ornish D, Scherwitz LW, Doody RS, et al. Effects of stress management training and dietary changes in treating ischemic heart disease. JAMA. 1983;249(1):54-59.
16. Ornish D, Brown SE, Scherwitz LW, et al. Can lifestyle changes reverse coronary heart disease? The Lifestyle Heart Trial. Lancet. 1990;336(8708):129-133. doi:10.1016/0140-6736(90)91656-u.
17. Ornish D, Scherwitz LW, Billings JH, et al. Intensive lifestyle changes for reversal of coronary heart disease [published correction appears in JAMA 1999 Apr 21;281(15):1380]. JAMA. 1998;280(23):2001-2007. doi:10.1001/jama.280.23.2001
18. Frattaroli J, Weidner G, Merritt-Worden TA, Frenda S, Ornish D. Angina pectoris and atherosclerotic risk factors in the multisite cardiac lifestyle intervention program. Am J Cardiol. 2008;101(7):911-918. doi:10.1016/j.amjcard.2007.11.039
19. Koertge J, Weidner G, Elliott-Eller M, et al. Improvement in medical risk factors and quality of life in women and men with coronary artery disease in the Multicenter Lifestyle Demonstration Project. Am J Cardiol. 2003;91(11):1316-1322. doi:10.1016/s0002-9149(03)00320-5
20. Marshall DA, Walizer EM, Vernalis MN. Achievement of heart health characteristics through participation in an intensive lifestyle change program (Coronary Artery Disease Reversal Study). J Cardiopulm Rehabil Prev. 2009;29(2):84-96. doi:10.1097/HCR.0b013e31819a00b2
21. Marshall D, Elaine W, Vernalis M. The effect of a one-year lifestyle intervention program on carotid intima media thickness. Mil Med. 2011;176(7):798-804. doi:10.7205/milmed-d-10-00447
22. Esselstyn CB Jr, Ellis SG, Medendorp SV, Crowe TD. A strategy to arrest and reverse coronary artery disease: a 5-year longitudinal study of a single physician’s practice. J Fam Pract. 1995;41(6):560-568.
23. Esselstyn CB Jr. Updating a 12-year experience with arrest and reversal therapy for coronary heart disease (an overdue requiem for palliative cardiology). Am J Cardiol. 1999;84(3):339-A8. doi:10.1016/s0002-9149(99)00290-8
24. Barnard ND, Cohen J, Jenkins DJ, et al. A low-fat vegan diet improves glycemic control and cardiovascular risk factors in a randomized clinical trial in individuals with type 2 diabetes. Diabetes Care. 2006;29(8):1777-1783. doi:10.2337/dc06-0606
25. McDougall J, Thomas LE, McDougall C, et al. Effects of 7 days on an ad libitum low-fat vegan diet: the McDougall Program cohort [published correction appears in Nutr J. 2017 Feb 10;16(1):12]. Nutr J. 2014;13:99. Published 2014 Oct 14. doi:10.1186/1475-2891-13-99
26. Turner-McGrievy GM, Davidson CR, Wingard EE, Wilcox S, Frongillo EA. Comparative effectiveness of plant-based diets for weight loss: a randomized controlled trial of five different diets. Nutrition. 2015;31(2):350-358. doi:10.1016/j.nut.2014.09.002
27. Wright N, Wilson L, Smith M, Duncan B, McHugh P. The BROAD study: a randomised controlled trial using a whole food plant-based diet in the community for obesity, ischaemic heart disease or diabetes. Nutr Diabetes. 2017;7(3):e256. Published 2017 Mar 20. doi:10.1038/nutd.2017.3

28. Schaefer S, Hussein H, Gershony GR, Rutledge JC, Kappagoda CT. Regression of severe atherosclerotic plaque in patients with mild elevation of LDL cholesterol. J Investig Med. 1997;45(9):536-541.
29. Kitazono R. Know thy patient: Enhancing lifestyle interventions with psychological assessment. Int J Dis Rev Prev. 2020;2(1):76-81.
30. Miller WR, Rollnick S. Motivational Interviewing: Helping People Change. 3rd ed. New York, NY: Guilford Press; 2013.
31. Mascola AJ, Yiaslas TA, Meir RL, et al. Framing physical activity as a distinct and uniquely valuable behavior independent of weight management: A pilot randomized controlled trial for overweight and obese sedentary persons. Eat Weight Disord. 2009;14(2-3):e148-e152. doi:10.1007/BF03327814
32. Esselstyn AC, Esselstyn J. The Prevent and Reverse Heart Disease Cookbook: Over 125 Delicious, Life-Changing, Plant-Based Recipes. New York, NY: Avery; 2014.
33. Esselstyn CB Jr, Gendy G, Doyle J, Golubic M, Roizen MF. A way to reverse CAD? J Fam Pract. 2014;63(7):356-364.
34. Ornish D, Ornish A. Undo It! How Simple Lifestyle Changes Can Reverse Most Chronic Diseases. New York, NY: Ballantine Books; 2019.
35. Smith SC Jr, Benjamin EJ, Bonow RO, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association [published correction appears in J Am Coll Cardiol. 2015 Apr 14;65(14):1495. Dosage error in article text.]. J Am Coll Cardiol. 2011;58(23):2432-2446. doi:10.1016/j.jacc.2011.10.824
36. Blumenthal JA, Babyak M, Wei J, et al. Usefulness of psychosocial treatment of mental stress-induced myocardial ischemia in men. Am J Cardiol. 2002;89(2):164-168. doi:10.1016/s0002-9149(01)02194-4
37. Antoni MH. Stress management effects on psychological, endocrinological, and immune functioning in men with HIV infection: empirical support for a psychoneuroimmunological model. Stress. 2003;6(3):173-188. doi:10.1080/1025389031000156727
38. Penedo FJ, Molton I, Dahn JR, et al. A randomized clinical trial of group-based cognitive-behavioral stress management in localized prostate cancer: development of stress management skills improves quality of life and benefit finding. Ann Behav Med. 2006;31(3):261-270. doi:10.1207/s15324796abm3103_8
39. Yiaslas TA. “Look doctor, I’m a carnivore.” Int J Dis Rev Prev. 2020;2(2):35-39.
40. Khaylis A, Yiaslas T, Bergstrom J, Gore-Felton C. A review of efficacious technology-based weight-loss interventions: five key components. Telemed J E Health. 2010;16(9):931-938. doi:10.1089/tmj.2010.0065
41. Barnard ND, Sherwitz L, Ornish D. Adherence and acceptability of a low-fat, vegetarian diet among patients with cardiac disease. J Cardiopulm Rehabil. 1992;12(6):423-431.
42. Yiaslas TA, Taylor J, Embree J, Schaefer S. Elimination of angina, comprehensive cardio-metabolic risk reduction, and 50-pound weight loss in a US Navy veteran with myasthenia gravis. Int J Dis Rev Prev. 2019;1(1):77-83.
43. Berkow SE, Barnard N, Eckart J, Katcher H. Four therapeutic diets: adherence and acceptability. Can J Diet Pract Res. 2010;71(4):199-204. doi:10.3148/71.4.2010.199
44. Carpenter JK, Andrews LA, Witcraft SM, Powers MB, Smits JAJ, Hofmann SG. Cognitive behavioral therapy for anxiety and related disorders: A meta-analysis of randomized placebo-controlled trials. Depress Anxiety. 2018;35(6):502-514. doi:10.1002/da.22728
45. Yiaslas TA. The pursuit of arete in medicine and health care. Int J Dis Rev Prev. 2019;1(2):53-56.
Risk associated with perioperative atrial fibrillation
Background: New-onset POAF occurs with 10% of noncardiac surgery and 15%-42% of cardiac surgery. POAF is believed to be self-limiting and most patients revert to sinus rhythm before hospital discharge. Previous studies on this topic are both limited and conflicting, but several suggest there is an association of stroke and mortality with POAF.
Study design: Systematic review and meta-analysis. Odds ratios with 95% confidence intervals were used for early outcomes and hazard ratios were used for long-term outcomes.
Setting: Prospective and retrospective cohort studies.
Synopsis: A total of 35 carefully selected studies were analyzed for a total of 2,458,010 patients. Outcomes of interest were early stroke or mortality within 30 days of surgery and long-term stroke or mortality after 30 days. The reference group was patients without POAF at baseline. Subgroup analysis included separating patients into cardiac surgery and noncardiac surgery.
New-onset POAF was associated with increased risk of early stroke (OR, 1.62; 95% CI, 1.47-1.80) and early mortality (OR, 1.44; 95% CI, 1.11-1.88). POAF also was associated with risk for long-term stroke (hazard ratio, 1.37; 95% CI, 1.07-1.77) and long-term mortality (HR, 1.37; 95% CI, 1.27-1.49). The risk of long-term stroke from new-onset POAF was highest among patients who received noncardiac surgery.
Despite identifying high-quality studies with thoughtful analysis, some data had the potential for publication bias. The representative sample did not report paroxysmal vs. persistent atrial fibrillation separately. Furthermore, the study had the potential to be confounded by detection bias of preexisting atrial fibrillation.
Bottom line: New-onset POAF is associated with early and long-term risk of stroke and mortality. Subsequent strategies to reduce this risk have yet to be determined.
Citation: Lin MH et al. Perioperative/postoperative atrial fibrillation and risk of subsequent stroke and/or mortality. Stroke. 2019 May;50:1364-71.
Dr. Mayer is a hospitalist and assistant professor of medicine at St. Louis University School of Medicine.
Background: New-onset POAF occurs with 10% of noncardiac surgery and 15%-42% of cardiac surgery. POAF is believed to be self-limiting and most patients revert to sinus rhythm before hospital discharge. Previous studies on this topic are both limited and conflicting, but several suggest there is an association of stroke and mortality with POAF.
Study design: Systematic review and meta-analysis. Odds ratios with 95% confidence intervals were used for early outcomes and hazard ratios were used for long-term outcomes.
Setting: Prospective and retrospective cohort studies.
Synopsis: A total of 35 carefully selected studies were analyzed for a total of 2,458,010 patients. Outcomes of interest were early stroke or mortality within 30 days of surgery and long-term stroke or mortality after 30 days. The reference group was patients without POAF at baseline. Subgroup analysis included separating patients into cardiac surgery and noncardiac surgery.
New-onset POAF was associated with increased risk of early stroke (OR, 1.62; 95% CI, 1.47-1.80) and early mortality (OR, 1.44; 95% CI, 1.11-1.88). POAF also was associated with risk for long-term stroke (hazard ratio, 1.37; 95% CI, 1.07-1.77) and long-term mortality (HR, 1.37; 95% CI, 1.27-1.49). The risk of long-term stroke from new-onset POAF was highest among patients who received noncardiac surgery.
Despite identifying high-quality studies with thoughtful analysis, some data had the potential for publication bias. The representative sample did not report paroxysmal vs. persistent atrial fibrillation separately. Furthermore, the study had the potential to be confounded by detection bias of preexisting atrial fibrillation.
Bottom line: New-onset POAF is associated with early and long-term risk of stroke and mortality. Subsequent strategies to reduce this risk have yet to be determined.
Citation: Lin MH et al. Perioperative/postoperative atrial fibrillation and risk of subsequent stroke and/or mortality. Stroke. 2019 May;50:1364-71.
Dr. Mayer is a hospitalist and assistant professor of medicine at St. Louis University School of Medicine.
Background: New-onset POAF occurs with 10% of noncardiac surgery and 15%-42% of cardiac surgery. POAF is believed to be self-limiting and most patients revert to sinus rhythm before hospital discharge. Previous studies on this topic are both limited and conflicting, but several suggest there is an association of stroke and mortality with POAF.
Study design: Systematic review and meta-analysis. Odds ratios with 95% confidence intervals were used for early outcomes and hazard ratios were used for long-term outcomes.
Setting: Prospective and retrospective cohort studies.
Synopsis: A total of 35 carefully selected studies were analyzed for a total of 2,458,010 patients. Outcomes of interest were early stroke or mortality within 30 days of surgery and long-term stroke or mortality after 30 days. The reference group was patients without POAF at baseline. Subgroup analysis included separating patients into cardiac surgery and noncardiac surgery.
New-onset POAF was associated with increased risk of early stroke (OR, 1.62; 95% CI, 1.47-1.80) and early mortality (OR, 1.44; 95% CI, 1.11-1.88). POAF also was associated with risk for long-term stroke (hazard ratio, 1.37; 95% CI, 1.07-1.77) and long-term mortality (HR, 1.37; 95% CI, 1.27-1.49). The risk of long-term stroke from new-onset POAF was highest among patients who received noncardiac surgery.
Despite identifying high-quality studies with thoughtful analysis, some data had the potential for publication bias. The representative sample did not report paroxysmal vs. persistent atrial fibrillation separately. Furthermore, the study had the potential to be confounded by detection bias of preexisting atrial fibrillation.
Bottom line: New-onset POAF is associated with early and long-term risk of stroke and mortality. Subsequent strategies to reduce this risk have yet to be determined.
Citation: Lin MH et al. Perioperative/postoperative atrial fibrillation and risk of subsequent stroke and/or mortality. Stroke. 2019 May;50:1364-71.
Dr. Mayer is a hospitalist and assistant professor of medicine at St. Louis University School of Medicine.
Colchicine a case study for what’s wrong with U.S. drug pricing
Public spending on colchicine has grown exponentially over the past decade despite generics suggesting an uphill slog for patients seeking access to long-term therapy for gout or cardiac conditions.
Medicaid spending on single-ingredient colchicine jumped 2,833%, from $1.1 million in 2008 to $32.2 million in 2017, new findings show. Medicaid expansion likely played a role in the increase, but 58% was due to price hikes alone.
The centuries-old drug sold for pennies in the United States before increasing 50-fold to about $5 per pill in 2009 after the first FDA-approved colchicine product, Colcrys, was granted 3 years’ market exclusivity for the treatment of acute gout based on a 1-week trial.
If prices had remained at pre-Colcrys levels, Medicaid spending in 2017 would have totaled just $2.1 million rather than $32.2 million according to the analysis, published online Nov. 30 in JAMA Internal Medicine (doi: 10.1001/jamainternmed.2020.5017).
The study was motivated by difficulties gout patients have in accessing colchicine, but also last year’s COLCOT trial, which reported fewer ischemic cardiovascular events in patients receiving colchicine after MI, observed Natalie McCormick, PhD, of Massachusetts General Hospital and Harvard Medical School, both in Boston.
“They were suggesting it could be a cost-effective way for secondary prevention and it is fairly inexpensive in most countries, but not the U.S.,” she said in an interview. “So there’s really a potential to increase public spending if more and more patients are then taking colchicine for prevention of cardiovascular events and the prices don’t change.”
The current pandemic could potentially further increase demand. Results initially slated for September are expected this month from the COLCORONA trial, which is testing whether the anti-inflammatory agent can prevent hospitalizations, lung complications, and death when given early in the course of COVID-19.
University of Oxford (England) researchers also announced last week that colchicine is being added to the massive RECOVERY trial, which is studying treatments for hospitalized COVID-19 patients.
Notably, the Canadian-based COLCOT trial did not use Colcrys, but rather a colchicine product that costs just $0.26 a pill in Canada, roughly the price of most generics available worldwide.
Authorized generics typically drive down drug prices when competing with independent generics, but this competition is missing in the United States, where Colcrys holds patents until 2029, Dr. McCormick and colleagues noted. More than a half-dozen independent generics have FDA approval to date, but only authorized generics with price points set by the brand-name companies are available to treat acute gout, pericarditis, and potentially millions with MI.
“One of the key takeaways is this difference between the brand names and the authorized generics and the independents,” she said. “The authorized [generics] have really not saved money. The list prices were just slightly lower and patients can also have more difficulty in getting those covered.”
For this analysis, the investigators used Medicaid and Medicare data to examine prices for all available forms of colchicine from 2008 to 2017, including unregulated/unapproved colchicine (2008-2010), generic combination probenecid-colchicine (2008-2017), Colcrys (2009-2017), brand-name single-ingredient colchicine Mitigare (approved in late 2014 but not marketed until 2015), and their authorized generics (2015-2017). Medicare trends from 2012 to 2017 were analyzed separately because pre-Colcrys Medicare data were not available.
Based on the results, combined spending on Medicare and Medicaid claims for single-ingredient colchicine exceeded $340 million in 2017.
Inflation- and rebate-adjusted Medicaid unit prices rose from $0.24 a pill in 2008, when unapproved formulations were still available, to $4.20 a pill in 2011 (Colcrys only), and peaked at $4.66 a pill in 2015 (Colcrys plus authorized generics).
Prescribing of lower-priced probenecid-colchicine ($0.66/pill in 2017) remained stable throughout. Medicaid rebate-adjusted prices in 2017 were $3.99/pill for all single-ingredient colchicine products, $5.13/pill for Colcrys, $4.49/pill for Mitigare, and $3.88/pill for authorized generics.
Medicare rebate-adjusted 2017 per-pill prices were $5.81 for all single-ingredient colchicine products, $6.78 for Colcrys, $5.68 for Mitigare, $5.16 for authorized generics, and $0.70 for probenecid-colchicine.
“Authorized generics have still driven high spending,” Dr. McCormick said. “We really need to encourage more competition in order to improve access.”
In an accompanying commentary, B. Joseph Guglielmo, PharmD, University of California, San Francisco, pointed out that the estimated median research and development cost to bring a drug to market is between $985 million and $1,335 million, which inevitably translates into a high selling price for the drug. Such investment and its resultant cost, however, should be associated with potential worth to society.
“Only a fraction of an investment was required for Colcrys, a product that has provided no increased value and an unnecessary, long-term cost burden to the health care system,” he wrote. “The current study findings illustrate that we can never allow such an egregious case to take place again.”
Dr. McCormick reported grants from Canadian Institutes of Health Research during the conduct of the study. Dr. Guglielmo reported having no relevant conflicts of interest.
This article first appeared on Medscape.com.
Public spending on colchicine has grown exponentially over the past decade despite generics suggesting an uphill slog for patients seeking access to long-term therapy for gout or cardiac conditions.
Medicaid spending on single-ingredient colchicine jumped 2,833%, from $1.1 million in 2008 to $32.2 million in 2017, new findings show. Medicaid expansion likely played a role in the increase, but 58% was due to price hikes alone.
The centuries-old drug sold for pennies in the United States before increasing 50-fold to about $5 per pill in 2009 after the first FDA-approved colchicine product, Colcrys, was granted 3 years’ market exclusivity for the treatment of acute gout based on a 1-week trial.
If prices had remained at pre-Colcrys levels, Medicaid spending in 2017 would have totaled just $2.1 million rather than $32.2 million according to the analysis, published online Nov. 30 in JAMA Internal Medicine (doi: 10.1001/jamainternmed.2020.5017).
The study was motivated by difficulties gout patients have in accessing colchicine, but also last year’s COLCOT trial, which reported fewer ischemic cardiovascular events in patients receiving colchicine after MI, observed Natalie McCormick, PhD, of Massachusetts General Hospital and Harvard Medical School, both in Boston.
“They were suggesting it could be a cost-effective way for secondary prevention and it is fairly inexpensive in most countries, but not the U.S.,” she said in an interview. “So there’s really a potential to increase public spending if more and more patients are then taking colchicine for prevention of cardiovascular events and the prices don’t change.”
The current pandemic could potentially further increase demand. Results initially slated for September are expected this month from the COLCORONA trial, which is testing whether the anti-inflammatory agent can prevent hospitalizations, lung complications, and death when given early in the course of COVID-19.
University of Oxford (England) researchers also announced last week that colchicine is being added to the massive RECOVERY trial, which is studying treatments for hospitalized COVID-19 patients.
Notably, the Canadian-based COLCOT trial did not use Colcrys, but rather a colchicine product that costs just $0.26 a pill in Canada, roughly the price of most generics available worldwide.
Authorized generics typically drive down drug prices when competing with independent generics, but this competition is missing in the United States, where Colcrys holds patents until 2029, Dr. McCormick and colleagues noted. More than a half-dozen independent generics have FDA approval to date, but only authorized generics with price points set by the brand-name companies are available to treat acute gout, pericarditis, and potentially millions with MI.
“One of the key takeaways is this difference between the brand names and the authorized generics and the independents,” she said. “The authorized [generics] have really not saved money. The list prices were just slightly lower and patients can also have more difficulty in getting those covered.”
For this analysis, the investigators used Medicaid and Medicare data to examine prices for all available forms of colchicine from 2008 to 2017, including unregulated/unapproved colchicine (2008-2010), generic combination probenecid-colchicine (2008-2017), Colcrys (2009-2017), brand-name single-ingredient colchicine Mitigare (approved in late 2014 but not marketed until 2015), and their authorized generics (2015-2017). Medicare trends from 2012 to 2017 were analyzed separately because pre-Colcrys Medicare data were not available.
Based on the results, combined spending on Medicare and Medicaid claims for single-ingredient colchicine exceeded $340 million in 2017.
Inflation- and rebate-adjusted Medicaid unit prices rose from $0.24 a pill in 2008, when unapproved formulations were still available, to $4.20 a pill in 2011 (Colcrys only), and peaked at $4.66 a pill in 2015 (Colcrys plus authorized generics).
Prescribing of lower-priced probenecid-colchicine ($0.66/pill in 2017) remained stable throughout. Medicaid rebate-adjusted prices in 2017 were $3.99/pill for all single-ingredient colchicine products, $5.13/pill for Colcrys, $4.49/pill for Mitigare, and $3.88/pill for authorized generics.
Medicare rebate-adjusted 2017 per-pill prices were $5.81 for all single-ingredient colchicine products, $6.78 for Colcrys, $5.68 for Mitigare, $5.16 for authorized generics, and $0.70 for probenecid-colchicine.
“Authorized generics have still driven high spending,” Dr. McCormick said. “We really need to encourage more competition in order to improve access.”
In an accompanying commentary, B. Joseph Guglielmo, PharmD, University of California, San Francisco, pointed out that the estimated median research and development cost to bring a drug to market is between $985 million and $1,335 million, which inevitably translates into a high selling price for the drug. Such investment and its resultant cost, however, should be associated with potential worth to society.
“Only a fraction of an investment was required for Colcrys, a product that has provided no increased value and an unnecessary, long-term cost burden to the health care system,” he wrote. “The current study findings illustrate that we can never allow such an egregious case to take place again.”
Dr. McCormick reported grants from Canadian Institutes of Health Research during the conduct of the study. Dr. Guglielmo reported having no relevant conflicts of interest.
This article first appeared on Medscape.com.
Public spending on colchicine has grown exponentially over the past decade despite generics suggesting an uphill slog for patients seeking access to long-term therapy for gout or cardiac conditions.
Medicaid spending on single-ingredient colchicine jumped 2,833%, from $1.1 million in 2008 to $32.2 million in 2017, new findings show. Medicaid expansion likely played a role in the increase, but 58% was due to price hikes alone.
The centuries-old drug sold for pennies in the United States before increasing 50-fold to about $5 per pill in 2009 after the first FDA-approved colchicine product, Colcrys, was granted 3 years’ market exclusivity for the treatment of acute gout based on a 1-week trial.
If prices had remained at pre-Colcrys levels, Medicaid spending in 2017 would have totaled just $2.1 million rather than $32.2 million according to the analysis, published online Nov. 30 in JAMA Internal Medicine (doi: 10.1001/jamainternmed.2020.5017).
The study was motivated by difficulties gout patients have in accessing colchicine, but also last year’s COLCOT trial, which reported fewer ischemic cardiovascular events in patients receiving colchicine after MI, observed Natalie McCormick, PhD, of Massachusetts General Hospital and Harvard Medical School, both in Boston.
“They were suggesting it could be a cost-effective way for secondary prevention and it is fairly inexpensive in most countries, but not the U.S.,” she said in an interview. “So there’s really a potential to increase public spending if more and more patients are then taking colchicine for prevention of cardiovascular events and the prices don’t change.”
The current pandemic could potentially further increase demand. Results initially slated for September are expected this month from the COLCORONA trial, which is testing whether the anti-inflammatory agent can prevent hospitalizations, lung complications, and death when given early in the course of COVID-19.
University of Oxford (England) researchers also announced last week that colchicine is being added to the massive RECOVERY trial, which is studying treatments for hospitalized COVID-19 patients.
Notably, the Canadian-based COLCOT trial did not use Colcrys, but rather a colchicine product that costs just $0.26 a pill in Canada, roughly the price of most generics available worldwide.
Authorized generics typically drive down drug prices when competing with independent generics, but this competition is missing in the United States, where Colcrys holds patents until 2029, Dr. McCormick and colleagues noted. More than a half-dozen independent generics have FDA approval to date, but only authorized generics with price points set by the brand-name companies are available to treat acute gout, pericarditis, and potentially millions with MI.
“One of the key takeaways is this difference between the brand names and the authorized generics and the independents,” she said. “The authorized [generics] have really not saved money. The list prices were just slightly lower and patients can also have more difficulty in getting those covered.”
For this analysis, the investigators used Medicaid and Medicare data to examine prices for all available forms of colchicine from 2008 to 2017, including unregulated/unapproved colchicine (2008-2010), generic combination probenecid-colchicine (2008-2017), Colcrys (2009-2017), brand-name single-ingredient colchicine Mitigare (approved in late 2014 but not marketed until 2015), and their authorized generics (2015-2017). Medicare trends from 2012 to 2017 were analyzed separately because pre-Colcrys Medicare data were not available.
Based on the results, combined spending on Medicare and Medicaid claims for single-ingredient colchicine exceeded $340 million in 2017.
Inflation- and rebate-adjusted Medicaid unit prices rose from $0.24 a pill in 2008, when unapproved formulations were still available, to $4.20 a pill in 2011 (Colcrys only), and peaked at $4.66 a pill in 2015 (Colcrys plus authorized generics).
Prescribing of lower-priced probenecid-colchicine ($0.66/pill in 2017) remained stable throughout. Medicaid rebate-adjusted prices in 2017 were $3.99/pill for all single-ingredient colchicine products, $5.13/pill for Colcrys, $4.49/pill for Mitigare, and $3.88/pill for authorized generics.
Medicare rebate-adjusted 2017 per-pill prices were $5.81 for all single-ingredient colchicine products, $6.78 for Colcrys, $5.68 for Mitigare, $5.16 for authorized generics, and $0.70 for probenecid-colchicine.
“Authorized generics have still driven high spending,” Dr. McCormick said. “We really need to encourage more competition in order to improve access.”
In an accompanying commentary, B. Joseph Guglielmo, PharmD, University of California, San Francisco, pointed out that the estimated median research and development cost to bring a drug to market is between $985 million and $1,335 million, which inevitably translates into a high selling price for the drug. Such investment and its resultant cost, however, should be associated with potential worth to society.
“Only a fraction of an investment was required for Colcrys, a product that has provided no increased value and an unnecessary, long-term cost burden to the health care system,” he wrote. “The current study findings illustrate that we can never allow such an egregious case to take place again.”
Dr. McCormick reported grants from Canadian Institutes of Health Research during the conduct of the study. Dr. Guglielmo reported having no relevant conflicts of interest.
This article first appeared on Medscape.com.