User login
Click for Credit: Endometriosis surgery benefits; diabetes & aging; more
Here are 5 articles from the March issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Endometriosis surgery: Women can expect years-long benefits
To take the posttest, go to: https://bit.ly/2Ez8mdu
Expires January 3, 2019
2. Cerebral small vessel disease progression linked to MCI in hypertensive patients
To take the posttest, go to: https://bit.ly/2ExDV7o
Expires January 4, 2019
3. Adult atopic dermatitis is fraught with dermatologic comorbidities
To take the posttest, go to: https://bit.ly/2Vl7E9a
Expires January 11, 2019
4. Antidepressants tied to greater hip fracture incidence in older adults
To take the posttest, go to: https://bit.ly/2GRfMeH
Expires January 4, 2019
5. Researchers exploring ways to mitigate aging’s impact on diabetes
To take the posttest, go to: https://bit.ly/2tFxF7v
Expires January 8, 2019
Here are 5 articles from the March issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Endometriosis surgery: Women can expect years-long benefits
To take the posttest, go to: https://bit.ly/2Ez8mdu
Expires January 3, 2019
2. Cerebral small vessel disease progression linked to MCI in hypertensive patients
To take the posttest, go to: https://bit.ly/2ExDV7o
Expires January 4, 2019
3. Adult atopic dermatitis is fraught with dermatologic comorbidities
To take the posttest, go to: https://bit.ly/2Vl7E9a
Expires January 11, 2019
4. Antidepressants tied to greater hip fracture incidence in older adults
To take the posttest, go to: https://bit.ly/2GRfMeH
Expires January 4, 2019
5. Researchers exploring ways to mitigate aging’s impact on diabetes
To take the posttest, go to: https://bit.ly/2tFxF7v
Expires January 8, 2019
Here are 5 articles from the March issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Endometriosis surgery: Women can expect years-long benefits
To take the posttest, go to: https://bit.ly/2Ez8mdu
Expires January 3, 2019
2. Cerebral small vessel disease progression linked to MCI in hypertensive patients
To take the posttest, go to: https://bit.ly/2ExDV7o
Expires January 4, 2019
3. Adult atopic dermatitis is fraught with dermatologic comorbidities
To take the posttest, go to: https://bit.ly/2Vl7E9a
Expires January 11, 2019
4. Antidepressants tied to greater hip fracture incidence in older adults
To take the posttest, go to: https://bit.ly/2GRfMeH
Expires January 4, 2019
5. Researchers exploring ways to mitigate aging’s impact on diabetes
To take the posttest, go to: https://bit.ly/2tFxF7v
Expires January 8, 2019
Myeloma therapies raise cardiovascular risks
WASHINGTON – Proteasome inhibitors are essential components of therapeutic regimens for multiple myeloma, but at least one member of this class of life-extending agents, carfilzomib (Kyprolis), is also associated with a significant increase in risk of heart failure, cautioned a specialist in plasma cell disorders.
In addition, immunomodulating agents such as lenalidomide (Revlimid) and pomalidomide (Pomalyst) are associated with increased risk for thromboembolic events, said R. Frank Cornell, MD, clinical director of plasma cell disorders at Vanderbilt University Medical Center in Nashville, Tenn.
In an ongoing, prospective study comparing rates of cardiac adverse events in patients receiving carfilzomib or another proteasome inhibitor, bortezomib (Velcade), Dr. Cornell and his colleagues found that while there were no significant differences in progression-free survival (PFS) or overall survival (OS) between the treatments, “patients who experienced a cardiovascular event had significantly worse progression-free and overall survival compared to those that did not have a cardiovascular event,” he said at the American College of Cardiology’s Advancing the Cardiovascular Care of the Oncology Patient meeting.
The Prospective Observation of Cardiac Safety With Proteasome Inhibition (PROTECT) trial, scheduled for completion in August 2019, enrolled 95 patients with relapsed multiple myeloma and randomly assigned them on a 2:1 basis to receive carfilzomib or bortezomib.
The investigators found that cardiovascular adverse events occurred in 33 of the 65 patients (51%) randomized to carfilzomib, compared with 5 of 30 patients (17%) assigned to bortezomib.
The events included grade 1 or 2 heart failure (HF) in 12 patients on carfilzomib vs. 2 on bortezomib, and grade 3 or 4 HF in 11 vs. 1, respectively. Hypertension was significantly more frequent among patients on carfilzomib, and one patient on carfilzomib died from the acute coronary syndrome 24 hours after receiving carfilzomib in the second week of treatment.
The investigators found that both B-type natriuretic peptide (BNP) and N-terminal pro b-type natriuretic peptide (NT-proBNP) were highly predictive of cardiovascular adverse events. Patients on carfilzomib who had levels of the markers above normal at baseline had an odds ratio (OR) for cardiovascular events of 7.39 (P less than .0001), and those with BNP or NT-proBNP increases at week 2 or 3 during cycle 1 had an OR for a cardiovascular adverse event of 63.5 (P less than .001).
In multivariate analysis, the risk for cardiovascular events for patients treated with carfilzomib was significantly lower for patients with one or no traditional cardiovascular risk factors, compared with patients with two or more.
“Prospective monitoring with natriuretic peptides should be considered, particularly early in treatment,” Dr. Cornell said.
IMiDs and thromboembolism
In early clinical trials of immunomodulators (IMiDs) for multiple myeloma, investigators saw that the incidence of thromboembolic events was lower among patients who received thromboprophylaxis than among those who did not, Dr. Cornell noted.
“From this, certain guidelines have been developed such that all patients considered to be at risk should at least receive an aspirin, 81-325 mg, and patients at higher risk for thromboembolism should receive low-molecular-weight heparin or therapeutic-dose warfarin,” he said.
There is little guidance, however, about the use of direct oral anticoagulants in this population, he added, a fact that prompted him and his colleagues in oncology and cardiology to perform a pilot study of apixaban (Eliquis) for primary prevention of venous thromboembolism (VTE) in patients with multiple myeloma who were receiving immunodulatory drugs.
Results of the pilot study, reported in a poster session at the 2018 annual meeting of the American Society of Hematology, showed that among 50 patients who received apixaban 2.5 mg twice daily for 6 months during IMiD therapy, there were no VTEs, stroke, or myocardial infarction, and no episodes of major bleeding. There were just three nonmajor bleeding events, and one early withdrawal from apixaban due to an allergic reaction manifesting as generalized edema.
“Further study is needed to validate this as a potential primary prophylaxis in patients receiving IMiDs for multiple myeloma,” Dr. Cornell said.
He reported having no financial disclosures. Millennium Pharmaceuticals is a sponsor of the PROTECT trial.
WASHINGTON – Proteasome inhibitors are essential components of therapeutic regimens for multiple myeloma, but at least one member of this class of life-extending agents, carfilzomib (Kyprolis), is also associated with a significant increase in risk of heart failure, cautioned a specialist in plasma cell disorders.
In addition, immunomodulating agents such as lenalidomide (Revlimid) and pomalidomide (Pomalyst) are associated with increased risk for thromboembolic events, said R. Frank Cornell, MD, clinical director of plasma cell disorders at Vanderbilt University Medical Center in Nashville, Tenn.
In an ongoing, prospective study comparing rates of cardiac adverse events in patients receiving carfilzomib or another proteasome inhibitor, bortezomib (Velcade), Dr. Cornell and his colleagues found that while there were no significant differences in progression-free survival (PFS) or overall survival (OS) between the treatments, “patients who experienced a cardiovascular event had significantly worse progression-free and overall survival compared to those that did not have a cardiovascular event,” he said at the American College of Cardiology’s Advancing the Cardiovascular Care of the Oncology Patient meeting.
The Prospective Observation of Cardiac Safety With Proteasome Inhibition (PROTECT) trial, scheduled for completion in August 2019, enrolled 95 patients with relapsed multiple myeloma and randomly assigned them on a 2:1 basis to receive carfilzomib or bortezomib.
The investigators found that cardiovascular adverse events occurred in 33 of the 65 patients (51%) randomized to carfilzomib, compared with 5 of 30 patients (17%) assigned to bortezomib.
The events included grade 1 or 2 heart failure (HF) in 12 patients on carfilzomib vs. 2 on bortezomib, and grade 3 or 4 HF in 11 vs. 1, respectively. Hypertension was significantly more frequent among patients on carfilzomib, and one patient on carfilzomib died from the acute coronary syndrome 24 hours after receiving carfilzomib in the second week of treatment.
The investigators found that both B-type natriuretic peptide (BNP) and N-terminal pro b-type natriuretic peptide (NT-proBNP) were highly predictive of cardiovascular adverse events. Patients on carfilzomib who had levels of the markers above normal at baseline had an odds ratio (OR) for cardiovascular events of 7.39 (P less than .0001), and those with BNP or NT-proBNP increases at week 2 or 3 during cycle 1 had an OR for a cardiovascular adverse event of 63.5 (P less than .001).
In multivariate analysis, the risk for cardiovascular events for patients treated with carfilzomib was significantly lower for patients with one or no traditional cardiovascular risk factors, compared with patients with two or more.
“Prospective monitoring with natriuretic peptides should be considered, particularly early in treatment,” Dr. Cornell said.
IMiDs and thromboembolism
In early clinical trials of immunomodulators (IMiDs) for multiple myeloma, investigators saw that the incidence of thromboembolic events was lower among patients who received thromboprophylaxis than among those who did not, Dr. Cornell noted.
“From this, certain guidelines have been developed such that all patients considered to be at risk should at least receive an aspirin, 81-325 mg, and patients at higher risk for thromboembolism should receive low-molecular-weight heparin or therapeutic-dose warfarin,” he said.
There is little guidance, however, about the use of direct oral anticoagulants in this population, he added, a fact that prompted him and his colleagues in oncology and cardiology to perform a pilot study of apixaban (Eliquis) for primary prevention of venous thromboembolism (VTE) in patients with multiple myeloma who were receiving immunodulatory drugs.
Results of the pilot study, reported in a poster session at the 2018 annual meeting of the American Society of Hematology, showed that among 50 patients who received apixaban 2.5 mg twice daily for 6 months during IMiD therapy, there were no VTEs, stroke, or myocardial infarction, and no episodes of major bleeding. There were just three nonmajor bleeding events, and one early withdrawal from apixaban due to an allergic reaction manifesting as generalized edema.
“Further study is needed to validate this as a potential primary prophylaxis in patients receiving IMiDs for multiple myeloma,” Dr. Cornell said.
He reported having no financial disclosures. Millennium Pharmaceuticals is a sponsor of the PROTECT trial.
WASHINGTON – Proteasome inhibitors are essential components of therapeutic regimens for multiple myeloma, but at least one member of this class of life-extending agents, carfilzomib (Kyprolis), is also associated with a significant increase in risk of heart failure, cautioned a specialist in plasma cell disorders.
In addition, immunomodulating agents such as lenalidomide (Revlimid) and pomalidomide (Pomalyst) are associated with increased risk for thromboembolic events, said R. Frank Cornell, MD, clinical director of plasma cell disorders at Vanderbilt University Medical Center in Nashville, Tenn.
In an ongoing, prospective study comparing rates of cardiac adverse events in patients receiving carfilzomib or another proteasome inhibitor, bortezomib (Velcade), Dr. Cornell and his colleagues found that while there were no significant differences in progression-free survival (PFS) or overall survival (OS) between the treatments, “patients who experienced a cardiovascular event had significantly worse progression-free and overall survival compared to those that did not have a cardiovascular event,” he said at the American College of Cardiology’s Advancing the Cardiovascular Care of the Oncology Patient meeting.
The Prospective Observation of Cardiac Safety With Proteasome Inhibition (PROTECT) trial, scheduled for completion in August 2019, enrolled 95 patients with relapsed multiple myeloma and randomly assigned them on a 2:1 basis to receive carfilzomib or bortezomib.
The investigators found that cardiovascular adverse events occurred in 33 of the 65 patients (51%) randomized to carfilzomib, compared with 5 of 30 patients (17%) assigned to bortezomib.
The events included grade 1 or 2 heart failure (HF) in 12 patients on carfilzomib vs. 2 on bortezomib, and grade 3 or 4 HF in 11 vs. 1, respectively. Hypertension was significantly more frequent among patients on carfilzomib, and one patient on carfilzomib died from the acute coronary syndrome 24 hours after receiving carfilzomib in the second week of treatment.
The investigators found that both B-type natriuretic peptide (BNP) and N-terminal pro b-type natriuretic peptide (NT-proBNP) were highly predictive of cardiovascular adverse events. Patients on carfilzomib who had levels of the markers above normal at baseline had an odds ratio (OR) for cardiovascular events of 7.39 (P less than .0001), and those with BNP or NT-proBNP increases at week 2 or 3 during cycle 1 had an OR for a cardiovascular adverse event of 63.5 (P less than .001).
In multivariate analysis, the risk for cardiovascular events for patients treated with carfilzomib was significantly lower for patients with one or no traditional cardiovascular risk factors, compared with patients with two or more.
“Prospective monitoring with natriuretic peptides should be considered, particularly early in treatment,” Dr. Cornell said.
IMiDs and thromboembolism
In early clinical trials of immunomodulators (IMiDs) for multiple myeloma, investigators saw that the incidence of thromboembolic events was lower among patients who received thromboprophylaxis than among those who did not, Dr. Cornell noted.
“From this, certain guidelines have been developed such that all patients considered to be at risk should at least receive an aspirin, 81-325 mg, and patients at higher risk for thromboembolism should receive low-molecular-weight heparin or therapeutic-dose warfarin,” he said.
There is little guidance, however, about the use of direct oral anticoagulants in this population, he added, a fact that prompted him and his colleagues in oncology and cardiology to perform a pilot study of apixaban (Eliquis) for primary prevention of venous thromboembolism (VTE) in patients with multiple myeloma who were receiving immunodulatory drugs.
Results of the pilot study, reported in a poster session at the 2018 annual meeting of the American Society of Hematology, showed that among 50 patients who received apixaban 2.5 mg twice daily for 6 months during IMiD therapy, there were no VTEs, stroke, or myocardial infarction, and no episodes of major bleeding. There were just three nonmajor bleeding events, and one early withdrawal from apixaban due to an allergic reaction manifesting as generalized edema.
“Further study is needed to validate this as a potential primary prophylaxis in patients receiving IMiDs for multiple myeloma,” Dr. Cornell said.
He reported having no financial disclosures. Millennium Pharmaceuticals is a sponsor of the PROTECT trial.
REPORTING FROM ACC CARDIO-ONCOLOGY
Does early repolarization on ECG increase the risk of cardiac death in healthy people?
No. The early repolarization pattern on electrocardiography (ECG) in asymptomatic patients is nearly always a benign incidental finding. However, in a patient with a history of idiopathic ventricular fibrillation or a family history of sudden cardiac death, the finding warrants further evaluation.
DEFINING EARLY REPOLARIZATION
The early repolarization pattern may mimic patterns seen in myocardial infarction, pericarditis, ventricular aneurysm, hyperkalemia, and hypothermia,1,3 and misinterpreting the pattern can lead to unnecessary laboratory testing, imaging, medication use, and hospital admissions. On the other hand, misinterpreting it as benign in the presence of certain features of the history or clinical presentation can delay the diagnosis and treatment of a potentially critical condition.
PREVALENCE AND MECHANISMS
The prevalence of the early repolarization pattern in the general population ranges from 5% to 15%; the wide range reflects differences in the definition, as well as variability in the pattern of early repolarization over time.4
The early repolarization pattern is more commonly seen in African American men and in young, physically active individuals.3 In one study, it was observed in 15% of cases of idiopathic ventricular fibrillation and sudden cardiac death, especially in people ages 35 to 45.4 While there is evidence of a heritable basis in the general population, a family history of early repolarization is not known to increase the risk of sudden cardiac death.
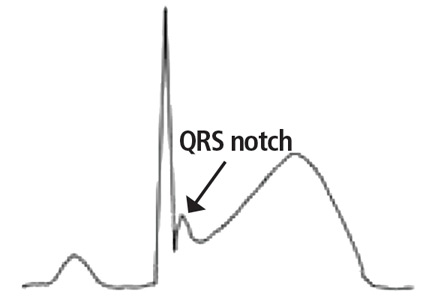
A proposed mechanism for the early repolarization pattern is an imbalance in the ion channel system, resulting in variable refractoriness of multiple myocardial regions and varying excitability in the myocardium. This can produce a voltage gradient between myocardial regions, which is believed to cause the major hallmarks of the early repolarization pattern, ie, ST-segment elevation and QRS notching or slurring.3
MANAGEMENT
The early repolarization pattern is nearly always a benign incidental finding on ECG, with no specific signs or symptoms attributed to it. High-risk features on ECG are associated with a modest increase in absolute risk of sudden cardiac death and warrant clinical correlation.
In the absence of syncope or family history of sudden cardiac death, early repolarization does not merit further workup.2
In patients with a history of unexplained syncope and a family history of sudden cardiac death, early repolarization should be considered in overall risk stratification.1 Early repolarization in a patient with previous idiopathic ventricular fibrillation warrants referral for electrophysiologic study and, if indicated, insertion of an implantable cardiac defibrillator for secondary prevention.5
- Patton KK, Ellinor PT, Ezekowitz M, et al; American Heart Association Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology and Council on Functional Genomics and Translational Biology. Electrocardiographic early repolarization: a scientific statement from the American Heart Association. Circulation 2016; 133(15):1520–1529. doi:10.1161/CIR.0000000000000388
- Macfarlane PW, Antzelevitch C, Haissaguerre M, et al. The early repolarization pattern: a consensus paper. J Am Coll Cardiol 2015; 66(4):470–477. doi:10.1016/j.jacc.2015.05.033
- Benito B, Guasch E, Rivard L, Nattel S. Clinical and mechanistic issues in early repolarization of normal variants and lethal arrhythmia syndromes. J Am Coll Cardiol 2010; 56(15):1177–1186. doi:10.1016/j.jacc.2010.05.037
- Maury P, Rollin A. Prevalence of early repolarisation/J wave patterns in the normal population. J Electrocardiol 2013; 46(5):411–416. doi:10.1016/j.jelectrocard.2013.06.014
- Mahida S, Sacher F, Berte B, et al. Evaluation of patients with early repolarization syndrome. J Atr Fibrillation 2014; 7(3):1083. doi:10.4022/jafib.1083
No. The early repolarization pattern on electrocardiography (ECG) in asymptomatic patients is nearly always a benign incidental finding. However, in a patient with a history of idiopathic ventricular fibrillation or a family history of sudden cardiac death, the finding warrants further evaluation.
DEFINING EARLY REPOLARIZATION
The early repolarization pattern may mimic patterns seen in myocardial infarction, pericarditis, ventricular aneurysm, hyperkalemia, and hypothermia,1,3 and misinterpreting the pattern can lead to unnecessary laboratory testing, imaging, medication use, and hospital admissions. On the other hand, misinterpreting it as benign in the presence of certain features of the history or clinical presentation can delay the diagnosis and treatment of a potentially critical condition.
PREVALENCE AND MECHANISMS
The prevalence of the early repolarization pattern in the general population ranges from 5% to 15%; the wide range reflects differences in the definition, as well as variability in the pattern of early repolarization over time.4
The early repolarization pattern is more commonly seen in African American men and in young, physically active individuals.3 In one study, it was observed in 15% of cases of idiopathic ventricular fibrillation and sudden cardiac death, especially in people ages 35 to 45.4 While there is evidence of a heritable basis in the general population, a family history of early repolarization is not known to increase the risk of sudden cardiac death.
A proposed mechanism for the early repolarization pattern is an imbalance in the ion channel system, resulting in variable refractoriness of multiple myocardial regions and varying excitability in the myocardium. This can produce a voltage gradient between myocardial regions, which is believed to cause the major hallmarks of the early repolarization pattern, ie, ST-segment elevation and QRS notching or slurring.3
MANAGEMENT
The early repolarization pattern is nearly always a benign incidental finding on ECG, with no specific signs or symptoms attributed to it. High-risk features on ECG are associated with a modest increase in absolute risk of sudden cardiac death and warrant clinical correlation.
In the absence of syncope or family history of sudden cardiac death, early repolarization does not merit further workup.2
In patients with a history of unexplained syncope and a family history of sudden cardiac death, early repolarization should be considered in overall risk stratification.1 Early repolarization in a patient with previous idiopathic ventricular fibrillation warrants referral for electrophysiologic study and, if indicated, insertion of an implantable cardiac defibrillator for secondary prevention.5
No. The early repolarization pattern on electrocardiography (ECG) in asymptomatic patients is nearly always a benign incidental finding. However, in a patient with a history of idiopathic ventricular fibrillation or a family history of sudden cardiac death, the finding warrants further evaluation.
DEFINING EARLY REPOLARIZATION
The early repolarization pattern may mimic patterns seen in myocardial infarction, pericarditis, ventricular aneurysm, hyperkalemia, and hypothermia,1,3 and misinterpreting the pattern can lead to unnecessary laboratory testing, imaging, medication use, and hospital admissions. On the other hand, misinterpreting it as benign in the presence of certain features of the history or clinical presentation can delay the diagnosis and treatment of a potentially critical condition.
PREVALENCE AND MECHANISMS
The prevalence of the early repolarization pattern in the general population ranges from 5% to 15%; the wide range reflects differences in the definition, as well as variability in the pattern of early repolarization over time.4
The early repolarization pattern is more commonly seen in African American men and in young, physically active individuals.3 In one study, it was observed in 15% of cases of idiopathic ventricular fibrillation and sudden cardiac death, especially in people ages 35 to 45.4 While there is evidence of a heritable basis in the general population, a family history of early repolarization is not known to increase the risk of sudden cardiac death.
A proposed mechanism for the early repolarization pattern is an imbalance in the ion channel system, resulting in variable refractoriness of multiple myocardial regions and varying excitability in the myocardium. This can produce a voltage gradient between myocardial regions, which is believed to cause the major hallmarks of the early repolarization pattern, ie, ST-segment elevation and QRS notching or slurring.3
MANAGEMENT
The early repolarization pattern is nearly always a benign incidental finding on ECG, with no specific signs or symptoms attributed to it. High-risk features on ECG are associated with a modest increase in absolute risk of sudden cardiac death and warrant clinical correlation.
In the absence of syncope or family history of sudden cardiac death, early repolarization does not merit further workup.2
In patients with a history of unexplained syncope and a family history of sudden cardiac death, early repolarization should be considered in overall risk stratification.1 Early repolarization in a patient with previous idiopathic ventricular fibrillation warrants referral for electrophysiologic study and, if indicated, insertion of an implantable cardiac defibrillator for secondary prevention.5
- Patton KK, Ellinor PT, Ezekowitz M, et al; American Heart Association Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology and Council on Functional Genomics and Translational Biology. Electrocardiographic early repolarization: a scientific statement from the American Heart Association. Circulation 2016; 133(15):1520–1529. doi:10.1161/CIR.0000000000000388
- Macfarlane PW, Antzelevitch C, Haissaguerre M, et al. The early repolarization pattern: a consensus paper. J Am Coll Cardiol 2015; 66(4):470–477. doi:10.1016/j.jacc.2015.05.033
- Benito B, Guasch E, Rivard L, Nattel S. Clinical and mechanistic issues in early repolarization of normal variants and lethal arrhythmia syndromes. J Am Coll Cardiol 2010; 56(15):1177–1186. doi:10.1016/j.jacc.2010.05.037
- Maury P, Rollin A. Prevalence of early repolarisation/J wave patterns in the normal population. J Electrocardiol 2013; 46(5):411–416. doi:10.1016/j.jelectrocard.2013.06.014
- Mahida S, Sacher F, Berte B, et al. Evaluation of patients with early repolarization syndrome. J Atr Fibrillation 2014; 7(3):1083. doi:10.4022/jafib.1083
- Patton KK, Ellinor PT, Ezekowitz M, et al; American Heart Association Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology and Council on Functional Genomics and Translational Biology. Electrocardiographic early repolarization: a scientific statement from the American Heart Association. Circulation 2016; 133(15):1520–1529. doi:10.1161/CIR.0000000000000388
- Macfarlane PW, Antzelevitch C, Haissaguerre M, et al. The early repolarization pattern: a consensus paper. J Am Coll Cardiol 2015; 66(4):470–477. doi:10.1016/j.jacc.2015.05.033
- Benito B, Guasch E, Rivard L, Nattel S. Clinical and mechanistic issues in early repolarization of normal variants and lethal arrhythmia syndromes. J Am Coll Cardiol 2010; 56(15):1177–1186. doi:10.1016/j.jacc.2010.05.037
- Maury P, Rollin A. Prevalence of early repolarisation/J wave patterns in the normal population. J Electrocardiol 2013; 46(5):411–416. doi:10.1016/j.jelectrocard.2013.06.014
- Mahida S, Sacher F, Berte B, et al. Evaluation of patients with early repolarization syndrome. J Atr Fibrillation 2014; 7(3):1083. doi:10.4022/jafib.1083
A paraneoplastic potassium and acid-base disturbance
NOTE: The scenario presented here is partly based on cases reported elsewhere by Martínez-Valles et al1 and Fernández-Rodríguez et al.2
A 55-year-old man is admitted to the hospital with generalized malaise, paresthesias, and severe hypertension. He says he had experienced agitation along with weakness on exertion 24 hours before presentation to the emergency department, with subsequent onset of paresthesias in his lower extremities and perioral area.
He is already known to have mild chronic obstructive pulmonary disease, with a ratio of forced expiratory volume in 1 second (FEV1)to forced vital capacity (FVC) of less than 70% and an FEV1 85% of predicted. In addition, he was recently diagnosed with diabetes, resistant hypertension requiring maximum doses of 3 agents (a calcium channel blocker, an angiotensin-converting enzyme inhibitor, and a loop diuretic), and hyperlipidemia.
He is a current smoker with a 30-pack-year smoking history. He does not use alcohol. His family history is noncontributory.
ASSESSING ACID-BASE DISORDERS
1. What type of acid-base disorder does this patient have?
- Metabolic acidosis
- Respiratory acidosis
- Metabolic alkalosis
- Respiratory alkalosis
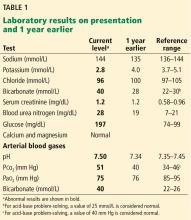
The patient has metabolic alkalosis.
A 5-step approach
1. Acidosis or alkalosis? The patient’s arterial pH is 7.5, which is alkalemic because it is higher than 7.44.
2. Metabolic or respiratory? The primary process in our patient is overwhelmingly metabolic, as his partial pressure of carbon dioxide (Pco2) is slightly elevated, a direction that would cause acidosis, not alkalosis.
3. The anion gap (the serum sodium concentration minus the sum of the chloride and bicarbonate concentrations) is normal at 8 mmol/L (DRG:HYBRiD-XL Immunoassay and Clinical Chemistry Analyzer, reference range 8–16).
4. Is the disturbance compensated? We have determined that this patient has a metabolic alkalemia; the question now is whether there is any compensation for the primary disturbance.
In metabolic alkalosis, the Pco2 may increase by approximately 0.6 mm Hg (range 0.5–0.8) above the nominal normal level of 40 mm Hg for each 1-mmol/L increase in bicarbonate above the nominal normal level of 25 mmol/L.4 If the patient requires oxygen, the calculation may be unreliable, however, as hypoxemia may have an overriding influence on respiratory drive.
Patients with chronically high Pco2 levels such as those with chronic obstructive pulmonary disease can become accustomed to high carbon dioxide levels and lose their hyper-
capnic respiratory drive. Giving oxygen supplementation is thought to decrease respiratory drive in these patients, so that they will breathe slower and retain more carbon dioxide. There is some degree of respiratory compensation for metabolic alkalosis that occurs by breathing less, though it is limited overall—even in very alkalotic patients, breathing less results in CO2 retention, which, by displacing O2 molecules in the alveoli, will in turn result in hypoxia. The brain then senses the hypoxia and makes one breathe faster, thereby limiting this compensation.
This patient’s serum bicarbonate level is 40 mmol/L, or 15 mmol/L higher than the nominal normal level. If he is compensating, his Pco2 should be 40 + (15 × 0.6) = 49 mm Hg, and in fact it is 51 mm Hg, which is within the normal range of expected compensation (47.5–52 mm Hg). Therefore, yes, he is compensating for the primary disturbance.
5. In metabolic acidosis, is there a delta gap? As our patient has metabolic alkalosis, not acidosis, this question does not apply in this case.
WHICH TEST TO FIND THE CAUSE?
2. Which is the best test to order next to determine the cause of this patient’s hypokalemic metabolic alkalosis?
- Serum magnesium level
- Spot urine chloride
- Renal ultrasonography
- 24-hour urine collection for sodium, potassium, and chloride
The patient’s loop diuretic is withheld for 12 hours and a spot urine chloride is obtained, which is reported as 44 mmol/L. This high value suggests that a volume-independent hypokalemic metabolic alkalosis is present with potassium depletion.
As for the other answer choices:
Serum magnesium. Though hypomagnesemia can cause hypokalemia due to lack of inhibition of renal outer medullary potassium channels and subsequent increased excretion of potassium in the apical tubular membrane, it is not independently associated with acid-base disturbances.5
Renal ultrasonography gives information about structural kidney disease but is of limited utility in identifying the cause of hypokalemic metabolic alkalosis.
A 24-hour urine collection is unnecessary in this setting and would ultimately result in delay in diagnosis, as spot urine chloride is a more efficient means of rapidly distinguishing volume-responsive vs volume-independent causes of hypokalemic metabolic alkalosis.6
IS HIS HYPERTENSION SECONDARY? IF SO, WHAT IS THE CAUSE?
Several features of this case suggest that the patient’s hypertension is secondary rather than primary. It is of recent onset. The patient’s family history is noncontributory, and his hypertension is resistant to the use of maximum doses of 3 antihypertensive agents.
3. Which of the following causes of secondary hypertension is not commonly associated with hypokalemia and metabolic alkalosis?
- Hyperaldosteronism
- Liddle syndrome
- Cushing syndrome
- Renal parenchymal disease
- Chronic licorice ingestion
Renal parenchymal disease is a cause of resistant hypertension, but it is not characterized by metabolic alkalosis, hypokalemia, and elevated urine chloride,7 while the others listed here—hyperaldosteronism, Liddle syndrome, Cushing syndrome, and chronic licorice ingestion—are. Other common causes of resistant hypertension without these metabolic abnormalities include obstructive sleep apnea, alcohol abuse, and nonadherence to treatment.
While treatment of hypertension with loop diuretics can result in hypokalemia and metabolic alkalosis due to the effect of these drugs on potassium reabsorption in the loop of Henle, the patient’s hypokalemia persisted after this agent was withdrawn.8
Causes of hypokalemic metabolic alkalosis with and without hypertension are further delineated in Figure 1.
Additional diagnostic testing: Plasma renin and plasma aldosterone
At this juncture, the differential diagnosis for this patient’s potassium depletion, metabolic alkalosis, high urine chloride, and hypertension has been narrowed to primary or secondary hyperaldosteronism, surreptitious mineralocorticoid ingestion, Cushing syndrome, licorice ingestion, Liddle syndrome, or one of the 3 hydroxylase deficiencies (11-, 17-, and 21-) (Figure 1).
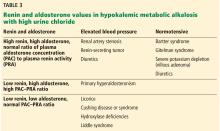
Although clues in the history, physical examination, and imaging may suggest a specific cause of his abnormal laboratory values, the next step in the diagnostic workup is to measure the plasma renin and aldosterone levels (Table 3).
HYPERALDOSTERONISM
4. Hyperaldosteronism is associated with which of the following patterns of renin and aldosterone values?
- High renin, high aldosterone, normal ratio of plasma aldosterone concentration (PAC) to plasma renin activity (PRA)
- Low renin, low aldosterone, normal PAC–PRA ratio
- Low renin, high aldosterone, high PAC–PRA ratio
- High renin, low aldosterone, low PAC–PRA ratio
The pattern of low renin, high aldosterone, and high PAC–PRA ratio is associated with hyperaldosteronism.
Primary hyperaldosteronism
Primary hyperaldosteronism is one of the most common causes of resistant hypertension and is underappreciated, being diagnosed in up to 20% of patients referred to hypertension specialty clinics.7 Potassium levels may be normal, likely contributing to its lack of recognition in this target population.
Primary hyperaldosteronism should be suspected in patients who have a plasma aldosterone PAC–PRA ratio greater than 20 with elevated plasma aldosterone concentrations
(> 15 ng/dL).
Persistently elevated aldosterone levels in the setting of elevated plasma volume is proof that aldosterone secretion is independent of the renin-angiotensin-aldosterone axis, and therefore is autonomous (secondary to adrenal tumor or hyperplasia). Further testing in the form of oral salt loading, saline infusion, or fludrocortisone (a sodium-retaining steroid) administration is thus required to confirm inappropriate, autonomous aldosterone secretion.9
After establishing the diagnosis of primary hyperaldosteronism, one should determine the subtype (ie, due to an adrenal carcinoma, unilateral hypersecreting adenoma, or unilateral or bilateral hyperplasia). Further testing includes adrenal computed tomography (CT) to rule out adrenal carcinomas, which are suspected with adenomas larger than 4 cm. Though part of the diagnostic workup, CT as a means of confirmational testing alone does not preclude the possibility of bilateral adrenal hyperplasia in some patients, even in the presence of an adrenal adenoma. For this reason, adrenal venous sampling is required to definitively determine whether the condition is due to a hypersecreting adrenal adenoma or unilateral or bilateral hyperplasia.9,10
Treatment of primary hyperaldosteronism depends on the subtype of the disease and involves salt restriction in addition to an aldosterone antagonist (spironolactone or eplerenone in the case of bilateral disease) or surgery (unilateral disease).9,11,12
Secondary hyperaldosteronism
Secondary hyperaldosteronism should be suspected when plasma renin and aldosterone levels are both elevated with a PAC–PRA ratio less than 10.
This pattern is most commonly seen with diuretic use but can also be a consequence of renal artery stenosis or, rarely, a renin-secreting tumor.13 Renal artery stenosis is a common finding in patients with hypertension undergoing cardiac catheterization, which is not surprising as more than 90% of such stenoses are atherosclerotic.7 Renin-secreting tumors are exceedingly rare, with fewer than 100 cases reported in the literature, and are more common in younger individuals.13
Our patient has low-normal aldosterone and plasma renin
On further testing, this patient’s plasma aldosterone level is 2.55 ng/dL (normal < 15 ng/dL), his plasma renin activity is 0.53 ng/mL/hour (normal 0.2–2.8 ng/mL/hour), and his PAC–PRA ratio is therefore 4.81.
The categories discussed thus far have included primary and secondary hyperaldosteronism, which typically do not present with low to normal levels of both renin and aldosterone. Surreptitious mineralocorticoid use could present in this manner, but is unlikely in this patient, whose medications do not include fludrocortisone.
The low-normal values thus lead to consideration of a third category: apparent mineralocorticoid excess. Diseases in this category such as Cushing disease or adrenocorticotropic hormone (ACTH) excess are characterized by increases in corticosteroids so that the potassium depletion, metabolic alkalosis, and hypertension are not a consequence of renin and aldosterone but rather the excess corticosteroids.14
Causes of apparent mineralocorticoid excess
There are several possible causes of mineralocorticoid excess associated with hypertension and hypokalemic metabolic alkalosis not due to renin and aldosterone.
Chronic licorice ingestion in high volumes is one such cause and is thought to result in inhibition of 11B-hydroxysteroid dehydrogenase or possibly cortisol oxidase by licorice’s active component, glycyrrhetinic acid. This inhibition results in an inability to convert cortisol to cortisone. The cortisol excess binds to mineralocorticoid receptors, and acting like aldosterone, results in hypertension and hypokalemic metabolic alkalosis as well as feedback inhibition of renin and aldosterone levels.15
Partial hydroxylase deficiencies, though rare, should also be considered as a cause of hypokalemic metabolic alkalosis, hypertension, and, potentially, hirsutism and clitoromegaly in women. They can be diagnosed with elevated levels of 17-ketosteroids and dehydroepiandrosterone sulfate, both of which, in excess, may act on aldosterone receptors in a manner similar to cortisol.16
Liddle syndrome, a rare autosomal dominant condition, may also present with suppressed levels of both renin and aldosterone. In contrast to the disorders of nonaldosterone mineralocorticoid excess, however, the sodium channel defect in Liddle syndrome is characterized by a primary increase in sodium reabsorption in the collecting tubule and potassium wasting. The resultant volume expansion leads to suppressed renin and aldosterone levels and hypertension with low potassium and elevated bicarbonate concentrations.17
Liddle syndrome is commonly diagnosed in childhood but may go unrecognized due to occasional absence of hypokalemia at presentation. Potassium-sparing diuretics such as amiloride or triamterene are the mainstays of treatment.18
Rates of cardiovascular and all-cause mortality are increased in patients with long-term hypercortisolism, even after plasma concentrations of cortisol are normalized.21
Figure 2 shows the cascade of the hypothalamic-pituitary-adrenal axis.
TESTING FOR HYPERCORTISOLISM IN OUR PATIENT
Given the patient’s clinical presentation and laboratory and imaging findings with normal plasma renin and aldosterone levels, a workup for suspected hypercortisolism is initiated.
Initial diagnostic testing for hypercortisolism depends on the degree of clinical suspicion. In those with low probability of the disease, testing should consist of 1 of the following, as a single negative test may be sufficient to rule out the disease:
- 24-hour urinary cortisol levels
- Overnight dexamethasone suppression testing
- Late-night salivary cortisol measurements.
In those with a high index of suspicion, 2 of the aforementioned tests should be performed, as 1 normal result may not be sufficient to exclude the diagnosis.22,23
A 24-hour urinary cortisol collection and overnight dexamethasone suppression test are obtained. His 24-hour urinary free cortisol level is elevated at 6,600 µg (normal 4–100), and suppression testing with 8 mg of dexamethasone (a form of “high-dose” testing)demonstrates only an 8% decline in serum cortisol levels. Cortisol should generally drop more than 90%.
Morning serum cortisol concentration is less than 5 µg/dL (140 nmol/L) in most patients with Cushing disease (ie, a pituitary tumor), and is usually undetectable in normal subjects. Only about 50% of neuroendocrine ACTH-secreting tumors will suppress with this test.
The patient’s clinical presentation, in conjunction with his diagnostic testing, are thus consistent with Cushing syndrome.
CUSHING SYNDROME
Cushing syndrome is most often exogenous or iatrogenic, ie, a result of supraphysiologic doses of glucocorticoids used to treat a variety of inflammatory, autoimmune, and neoplastic conditions.
Endogenous Cushing syndrome, on the other hand, is rare, with an estimated prevalence of 0.7 to 2.4 cases per million per year. ACTH-dependent causes account for 80% of endogenous Cushing syndrome cases, with ACTH-secreting pituitary adenomas (Cushing disease) accounting for 75% to 80% and ectopic ACTH secretion accounting for 15% to 20%. Less than 1% of cases are due to tumors that produce corticotropin-releasing hormone (CRH).
ACTH-independent Cushing syndrome is diagnosed in 20% of endogenous cases and is most commonly caused by a unilateral adrenal tumor. Rare causes of ACTH-independent disease include adrenal carcinoma, McCune-Albright syndrome, and adrenal hyperplasia.24
The patient’s ACTH is high
To determine whether this is an ACTH-dependent or independent process, the next step is to order an ACTH level. His ACTH level is high at 107 pg/mL (normal < 46 pg/mL), confirming the diagnosis of ACTH-dependent Cushing syndrome.
To find out if this ACTH-dependent process is due to a pituitary adenoma, magnetic resonance imaging (MRI) of the pituitary is obtained but is normal.
Large masses (> 6 mm) strongly suggest Cushing disease, but these tumors are often small and may be missed even with more advanced imaging techniques. Corticotropin-secreting adenomas arising from normal cells in the pituitary retain some sensitivity to glucocorticoid negative feedback and CRH stimulation, and thus high-dose dexamethasone suppression testing in conjunction with CRH stimulation testing can be used to differentiate Cushing disease from ectopic ACTH secretion.24,25 Both of these tests have poor diagnostic accuracy, however, and thus inferior petrosal sampling remains the gold standard for the diagnosis of Cushing disease.
ACTH-SECRETING TUMORS
5. Cushing syndrome due to ectopic ACTH secretion is most commonly attributed to which of the following tumors?
- Small-cell lung carcinoma
- Pancreatic carcinoma
- Medullary thyroid carcinoma
- Gastrinoma
Severe cases of Cushing syndrome are often attributable to ectopic ACTH secretion due to an underlying malignancy, most commonly small-cell lung carcinoma or neuroendocrine tumors of pulmonary origin. Other causes include pancreatic and thymic neuroendocrine tumors, gastrinomas, and medullary thyroid carcinoma.25,26
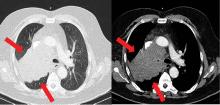
Because most ACTH-producing tumors are intrathoracic, initial imaging in cases of suspected ectopic ACTH secretion should focus on the chest, with CT the usual first choice. Octreotide scintigraphy can also be useful in localizing disease, as many neuroendocrine tumors express somatostatin receptors. Specialized positron-emission tomography scans may also be helpful in tumor identification.24
TREATMENT OF CUSHING SYNDROME DUE TO ECTOPIC ACTH SECRETION
6. Which of the following is most appropriate medical therapy for suppression of cortisol secretion in Cushing syndrome due to ectopic ACTH secretion?
- Spironolactone
- Dexamethasone
- Somatostatin
- Estrogen
- Ketoconazole
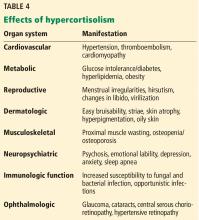
Hyperglycemia, hypokalemia, hypertension, psychiatric disturbances, venous thromboembolism, and systemic infections appear to be common in ectopic ACTH syndrome and often correlate with the degree of hypercortisolemia. Severe Cushing syndrome due to ectopic ACTH secretion is an emergency requiring prompt control of cortisol secretion.
First-line treatments include steroidogenesis inhibitors (ketoconazole, metyrapone, etomidate, mitotane) and glucocorticoid receptor antagonists (mifepristone). High-dose spironolactone and eplerenone can also be used to treat the hypertension and hypokalemia associated with mineralocorticoid receptor stimulation. Definitive treatment involves surgical resection, chemotherapy, or radiotherapy when applicable.24,25
After confirmation of the diagnosis, the patient is prescribed ketoconazole and spironolactone, with substantial improvement. He subsequently is started on combination chemotherapy and radiation therapy for his small-cell lung carcinoma.
DISCUSSION
The differential diagnosis for hypokalemia is broad and relies on information obtained during the history and physical examination, followed by interpretation of selected laboratory results. Myriad pathologies in diverse organ systems, eg, diarrhea, renal tubular acidosis, and adrenal disease, may be responsible for a low serum potassium. Further categorizing potassium depletion on the basis of an associated acid-base disturbance, such as metabolic alkalosis, allows one to use an algorithmic approach that can identify specific etiologies responsible for both the potassium and the acid-base disturbances.
Using the spot urine chloride in the setting of hypokalemic metabolic alkalosis with or without hypertension can narrow the differential diagnosis and allow additional clinical findings to guide clinical problem-solving and decision-making, even for conditions not commonly encountered in routine medical practice.
Obtaining renin and aldosterone measurements in patients with potassium depletion, metabolic alkalosis, high urine chloride excretion, and hypertension permits further categorization into 3 clinical groups: elevated aldosterone and renin (secondary hyperaldosteronism), elevated aldosterone and low renin (primary hyperaldosteronism), or apparent mineralocorticoid excess wherein neither renin nor aldosterone are responsible for the syndrome.
The patient in our case had apparent mineralocorticoid excess as a consequence of an ACTH-producing small-cell carcinoma.
- Martínez-Valles MA, Palafox-Cazarez A, Paredes-Avina JA. Severe hypokalemia, metabolic alkalosis and hypertension in a 54 year old male with ectopic ACTH syndrome: a case report. Cases J 2009; 2:6174. doi:10.4076/1757-1626-2-6174
- Fernández-Rodríguez E, Villar-Taibo R, Pinal-Osorio I, et al. Severe hypertension and hypokalemia as first clinical manifestations in ectopic Cushing’s syndrome. Arq Bras Endocrinol Metabol 2008; 52(6):1066–1070. pmid:18820819
- Mani S, Rutecki GW. A patient with altered mental status and an acid-base disturbance. Cleve Clin J Med 2017; 84(1):27–34. doi:10.3949/ccjm.84a.16042
- Adrogué HJ, Madias NE. Secondary responses to altered acid-base status: the rules of engagement. J Am Soc Nephrol 2010; 21(6):920–923. doi:10.1681/ASN.2009121211
- Huang CL, Kuo E. Mechanism of hypokalemia in magnesium deficiency. J Am Soc Nephrol 2007; 18(10):2649–2652. doi:10.1681/ASN.2007070792
- Rose BD. Metabolic alkalosis. In: Clinical Physiology of Acid-Base and Electrolyte Disorders. 4th ed. New York, NY: McGraw-Hill, Health Professions Division; 1994:515.
- Calhoun DA, Jones D, Textor S, et al; American Heart Association Professional Education Committee. Resistant hypertension: diagnosis, evaluation, and treatment: a scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Circulation 2008; 117(25):e510–e526. doi:10.1161/CIRCULATIONAHA.108.189141
- Koeppen BM, Stanton BA. Physiology of diuretic action. In: Renal Physiology. 5th ed. Philadelphia, PA: Elsevier Inc; 2013:167–178.
- Blumenfeld JD, Sealey JE, Schlussel Y, et al. Diagnosis and treatment of primary hyperaldosteronism. Ann Intern Med 1994; 121(11):877–885. pmid:7978702
- Kempers MJ, Lenders JW, van Outheusden L, et al. Systematic review: diagnostic procedures to differentiate unilateral from bilateral adrenal abnormality in primary aldosteronism. Ann Intern Med 2009; 151(5):329–337. pmid:19721021
- Karagiannis A, Tziomalos K, Papageorgiou A, et al. Spironolactone versus eplerenone for the treatment of idiopathic hyperaldosteronism. Expert Opin Pharmacother 2008; 9(4):509–515. doi:10.1517/14656566.9.4.509
- Sawka AM, Young WF, Thompson GB, et al. Primary aldosteronism: factors associated with normalization of blood pressure after surgery. Ann Intern Med 2001; 135(4):258–261. pmid:11511140
- Haab F, Duclos JM, Guyenne T, Plouin PF, Corvol P. Renin secreting tumors: diagnosis, conservative surgical approach and long-term results. J Urol 1995; 153(6):1781–1784. pmid:7752315
- Sabbadin C, Armanini D. Syndromes that mimic an excess of mineralocorticoids. High Blood Press Cardiovasc Prev 2016; 23(3):231–235. doi:10.1007/s40292-016-0160-5
- Apostolakos JM, Caines LC. Apparent mineralocorticoid excess syndrome: a case of resistant hypertension from licorice tea consumption. J Clin Hypertens (Greenwich) 2016; 18(10):991–993. doi:10.1111/jch.12841
- Glatt K, Garzon DL, Popovic J. Congenital adrenal hyperplasia due to 21-hydroxylase deficiency. J Spec Pediatr Nurs 2005; 10(3):104–114. doi:10.1111/j.1744-6155.2005.00022.x
- Findling JW, Raff H, Hansson JH, Lifton RP. Liddle’s syndrome: prospective genetic screening and suppressed aldosterone secretion in an extended kindred. J Clin Endocrinol Metab 1997; 82(4):1071–1074. doi:10.1210/jcem.82.4.3862
- Wang C, Chan TK, Yeung RT, Coghlan JP, Scoggins BA, Stockigt JR. The effect of triamterene and sodium intake on renin, aldosterone, and erythrocyte sodium transport in Liddle’s syndrome. J Clin Endocrinol Metab 1981; 52(5):1027–1032. doi:10.1210/jcem-52-5-1027
- Torpy DJ, Mullen N, Ilias I, Nieman LK. Association of hypertension and hypokalemia with Cushing’s syndrome caused by ectopic ACTH secretion: a series of 58 cases. Ann N Y Acad Sci 2002; 970:134–144. pmid:12381548
- Saruta T, Suzuki H, Handa M, Igarashi Y, Kondo K, Senba S. Multiple factors contribute to the pathogenesis of hypertension in Cushing’s syndrome. J Clin Endocrinol Metab 1986; 62(2):275–279. doi:10.1210/jcem-62-2-275
- Clayton RN, Jones PW, Reulen RC, et al. Mortality in patients with Cushing’s disease more than 10 years after remission: a multicentre, multinational, retrospective cohort study. Lancet Diabetes Endocrinol 2016; 4(7):569–576. doi:10.1016/S2213-8587(16)30005-5
- Baid SK, Rubino D, Sinaii N, Ramsey S, Frank A, Nieman LK. Specificity of screening tests for Cushing’s syndrome in an overweight and obese population. J Clin Endocrinol Metab 2009; 94(10):3857–3864. doi:10.1210/jc.2008-2766
- Nieman LK, Biller BM, Findling JW, et al. The diagnosis of Cushing’s syndrome: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2008; 93(5):1526–1540. doi:10.1210/jc.2008-0125
- Sharma ST, Nieman LK, Feelders RA. Cushing’s syndrome: epidemiology and developments in disease management. Clin Epidemiol 2015; 7:281–293. doi:10.2147/CLEP.S44336
- Tavares Bello C, van der Poest Clement E, Feelders R. Severe Cushing’s syndrome and bilateral pulmonary nodules: beyond ectopic ACTH. Endocrinol Diabetes Metab Case Rep 2017; pii:17–0100. doi:10.1530/EDM-17-0100
- Sathyakumar S, Paul TV, Asha HS, et al. Ectopic Cushing syndrome: a 10-year experience from a tertiary care center in southern India. Endocr Pract 2017; 23(8):907–914. doi:10.4158/EP161677.OR
NOTE: The scenario presented here is partly based on cases reported elsewhere by Martínez-Valles et al1 and Fernández-Rodríguez et al.2
A 55-year-old man is admitted to the hospital with generalized malaise, paresthesias, and severe hypertension. He says he had experienced agitation along with weakness on exertion 24 hours before presentation to the emergency department, with subsequent onset of paresthesias in his lower extremities and perioral area.
He is already known to have mild chronic obstructive pulmonary disease, with a ratio of forced expiratory volume in 1 second (FEV1)to forced vital capacity (FVC) of less than 70% and an FEV1 85% of predicted. In addition, he was recently diagnosed with diabetes, resistant hypertension requiring maximum doses of 3 agents (a calcium channel blocker, an angiotensin-converting enzyme inhibitor, and a loop diuretic), and hyperlipidemia.
He is a current smoker with a 30-pack-year smoking history. He does not use alcohol. His family history is noncontributory.
ASSESSING ACID-BASE DISORDERS
1. What type of acid-base disorder does this patient have?
- Metabolic acidosis
- Respiratory acidosis
- Metabolic alkalosis
- Respiratory alkalosis
The patient has metabolic alkalosis.
A 5-step approach
1. Acidosis or alkalosis? The patient’s arterial pH is 7.5, which is alkalemic because it is higher than 7.44.
2. Metabolic or respiratory? The primary process in our patient is overwhelmingly metabolic, as his partial pressure of carbon dioxide (Pco2) is slightly elevated, a direction that would cause acidosis, not alkalosis.
3. The anion gap (the serum sodium concentration minus the sum of the chloride and bicarbonate concentrations) is normal at 8 mmol/L (DRG:HYBRiD-XL Immunoassay and Clinical Chemistry Analyzer, reference range 8–16).
4. Is the disturbance compensated? We have determined that this patient has a metabolic alkalemia; the question now is whether there is any compensation for the primary disturbance.
In metabolic alkalosis, the Pco2 may increase by approximately 0.6 mm Hg (range 0.5–0.8) above the nominal normal level of 40 mm Hg for each 1-mmol/L increase in bicarbonate above the nominal normal level of 25 mmol/L.4 If the patient requires oxygen, the calculation may be unreliable, however, as hypoxemia may have an overriding influence on respiratory drive.
Patients with chronically high Pco2 levels such as those with chronic obstructive pulmonary disease can become accustomed to high carbon dioxide levels and lose their hyper-
capnic respiratory drive. Giving oxygen supplementation is thought to decrease respiratory drive in these patients, so that they will breathe slower and retain more carbon dioxide. There is some degree of respiratory compensation for metabolic alkalosis that occurs by breathing less, though it is limited overall—even in very alkalotic patients, breathing less results in CO2 retention, which, by displacing O2 molecules in the alveoli, will in turn result in hypoxia. The brain then senses the hypoxia and makes one breathe faster, thereby limiting this compensation.
This patient’s serum bicarbonate level is 40 mmol/L, or 15 mmol/L higher than the nominal normal level. If he is compensating, his Pco2 should be 40 + (15 × 0.6) = 49 mm Hg, and in fact it is 51 mm Hg, which is within the normal range of expected compensation (47.5–52 mm Hg). Therefore, yes, he is compensating for the primary disturbance.
5. In metabolic acidosis, is there a delta gap? As our patient has metabolic alkalosis, not acidosis, this question does not apply in this case.
WHICH TEST TO FIND THE CAUSE?
2. Which is the best test to order next to determine the cause of this patient’s hypokalemic metabolic alkalosis?
- Serum magnesium level
- Spot urine chloride
- Renal ultrasonography
- 24-hour urine collection for sodium, potassium, and chloride
The patient’s loop diuretic is withheld for 12 hours and a spot urine chloride is obtained, which is reported as 44 mmol/L. This high value suggests that a volume-independent hypokalemic metabolic alkalosis is present with potassium depletion.
As for the other answer choices:
Serum magnesium. Though hypomagnesemia can cause hypokalemia due to lack of inhibition of renal outer medullary potassium channels and subsequent increased excretion of potassium in the apical tubular membrane, it is not independently associated with acid-base disturbances.5
Renal ultrasonography gives information about structural kidney disease but is of limited utility in identifying the cause of hypokalemic metabolic alkalosis.
A 24-hour urine collection is unnecessary in this setting and would ultimately result in delay in diagnosis, as spot urine chloride is a more efficient means of rapidly distinguishing volume-responsive vs volume-independent causes of hypokalemic metabolic alkalosis.6
IS HIS HYPERTENSION SECONDARY? IF SO, WHAT IS THE CAUSE?
Several features of this case suggest that the patient’s hypertension is secondary rather than primary. It is of recent onset. The patient’s family history is noncontributory, and his hypertension is resistant to the use of maximum doses of 3 antihypertensive agents.
3. Which of the following causes of secondary hypertension is not commonly associated with hypokalemia and metabolic alkalosis?
- Hyperaldosteronism
- Liddle syndrome
- Cushing syndrome
- Renal parenchymal disease
- Chronic licorice ingestion
Renal parenchymal disease is a cause of resistant hypertension, but it is not characterized by metabolic alkalosis, hypokalemia, and elevated urine chloride,7 while the others listed here—hyperaldosteronism, Liddle syndrome, Cushing syndrome, and chronic licorice ingestion—are. Other common causes of resistant hypertension without these metabolic abnormalities include obstructive sleep apnea, alcohol abuse, and nonadherence to treatment.
While treatment of hypertension with loop diuretics can result in hypokalemia and metabolic alkalosis due to the effect of these drugs on potassium reabsorption in the loop of Henle, the patient’s hypokalemia persisted after this agent was withdrawn.8
Causes of hypokalemic metabolic alkalosis with and without hypertension are further delineated in Figure 1.
Additional diagnostic testing: Plasma renin and plasma aldosterone
At this juncture, the differential diagnosis for this patient’s potassium depletion, metabolic alkalosis, high urine chloride, and hypertension has been narrowed to primary or secondary hyperaldosteronism, surreptitious mineralocorticoid ingestion, Cushing syndrome, licorice ingestion, Liddle syndrome, or one of the 3 hydroxylase deficiencies (11-, 17-, and 21-) (Figure 1).
Although clues in the history, physical examination, and imaging may suggest a specific cause of his abnormal laboratory values, the next step in the diagnostic workup is to measure the plasma renin and aldosterone levels (Table 3).
HYPERALDOSTERONISM
4. Hyperaldosteronism is associated with which of the following patterns of renin and aldosterone values?
- High renin, high aldosterone, normal ratio of plasma aldosterone concentration (PAC) to plasma renin activity (PRA)
- Low renin, low aldosterone, normal PAC–PRA ratio
- Low renin, high aldosterone, high PAC–PRA ratio
- High renin, low aldosterone, low PAC–PRA ratio
The pattern of low renin, high aldosterone, and high PAC–PRA ratio is associated with hyperaldosteronism.
Primary hyperaldosteronism
Primary hyperaldosteronism is one of the most common causes of resistant hypertension and is underappreciated, being diagnosed in up to 20% of patients referred to hypertension specialty clinics.7 Potassium levels may be normal, likely contributing to its lack of recognition in this target population.
Primary hyperaldosteronism should be suspected in patients who have a plasma aldosterone PAC–PRA ratio greater than 20 with elevated plasma aldosterone concentrations
(> 15 ng/dL).
Persistently elevated aldosterone levels in the setting of elevated plasma volume is proof that aldosterone secretion is independent of the renin-angiotensin-aldosterone axis, and therefore is autonomous (secondary to adrenal tumor or hyperplasia). Further testing in the form of oral salt loading, saline infusion, or fludrocortisone (a sodium-retaining steroid) administration is thus required to confirm inappropriate, autonomous aldosterone secretion.9
After establishing the diagnosis of primary hyperaldosteronism, one should determine the subtype (ie, due to an adrenal carcinoma, unilateral hypersecreting adenoma, or unilateral or bilateral hyperplasia). Further testing includes adrenal computed tomography (CT) to rule out adrenal carcinomas, which are suspected with adenomas larger than 4 cm. Though part of the diagnostic workup, CT as a means of confirmational testing alone does not preclude the possibility of bilateral adrenal hyperplasia in some patients, even in the presence of an adrenal adenoma. For this reason, adrenal venous sampling is required to definitively determine whether the condition is due to a hypersecreting adrenal adenoma or unilateral or bilateral hyperplasia.9,10
Treatment of primary hyperaldosteronism depends on the subtype of the disease and involves salt restriction in addition to an aldosterone antagonist (spironolactone or eplerenone in the case of bilateral disease) or surgery (unilateral disease).9,11,12
Secondary hyperaldosteronism
Secondary hyperaldosteronism should be suspected when plasma renin and aldosterone levels are both elevated with a PAC–PRA ratio less than 10.
This pattern is most commonly seen with diuretic use but can also be a consequence of renal artery stenosis or, rarely, a renin-secreting tumor.13 Renal artery stenosis is a common finding in patients with hypertension undergoing cardiac catheterization, which is not surprising as more than 90% of such stenoses are atherosclerotic.7 Renin-secreting tumors are exceedingly rare, with fewer than 100 cases reported in the literature, and are more common in younger individuals.13
Our patient has low-normal aldosterone and plasma renin
On further testing, this patient’s plasma aldosterone level is 2.55 ng/dL (normal < 15 ng/dL), his plasma renin activity is 0.53 ng/mL/hour (normal 0.2–2.8 ng/mL/hour), and his PAC–PRA ratio is therefore 4.81.
The categories discussed thus far have included primary and secondary hyperaldosteronism, which typically do not present with low to normal levels of both renin and aldosterone. Surreptitious mineralocorticoid use could present in this manner, but is unlikely in this patient, whose medications do not include fludrocortisone.
The low-normal values thus lead to consideration of a third category: apparent mineralocorticoid excess. Diseases in this category such as Cushing disease or adrenocorticotropic hormone (ACTH) excess are characterized by increases in corticosteroids so that the potassium depletion, metabolic alkalosis, and hypertension are not a consequence of renin and aldosterone but rather the excess corticosteroids.14
Causes of apparent mineralocorticoid excess
There are several possible causes of mineralocorticoid excess associated with hypertension and hypokalemic metabolic alkalosis not due to renin and aldosterone.
Chronic licorice ingestion in high volumes is one such cause and is thought to result in inhibition of 11B-hydroxysteroid dehydrogenase or possibly cortisol oxidase by licorice’s active component, glycyrrhetinic acid. This inhibition results in an inability to convert cortisol to cortisone. The cortisol excess binds to mineralocorticoid receptors, and acting like aldosterone, results in hypertension and hypokalemic metabolic alkalosis as well as feedback inhibition of renin and aldosterone levels.15
Partial hydroxylase deficiencies, though rare, should also be considered as a cause of hypokalemic metabolic alkalosis, hypertension, and, potentially, hirsutism and clitoromegaly in women. They can be diagnosed with elevated levels of 17-ketosteroids and dehydroepiandrosterone sulfate, both of which, in excess, may act on aldosterone receptors in a manner similar to cortisol.16
Liddle syndrome, a rare autosomal dominant condition, may also present with suppressed levels of both renin and aldosterone. In contrast to the disorders of nonaldosterone mineralocorticoid excess, however, the sodium channel defect in Liddle syndrome is characterized by a primary increase in sodium reabsorption in the collecting tubule and potassium wasting. The resultant volume expansion leads to suppressed renin and aldosterone levels and hypertension with low potassium and elevated bicarbonate concentrations.17
Liddle syndrome is commonly diagnosed in childhood but may go unrecognized due to occasional absence of hypokalemia at presentation. Potassium-sparing diuretics such as amiloride or triamterene are the mainstays of treatment.18
Rates of cardiovascular and all-cause mortality are increased in patients with long-term hypercortisolism, even after plasma concentrations of cortisol are normalized.21
Figure 2 shows the cascade of the hypothalamic-pituitary-adrenal axis.
TESTING FOR HYPERCORTISOLISM IN OUR PATIENT
Given the patient’s clinical presentation and laboratory and imaging findings with normal plasma renin and aldosterone levels, a workup for suspected hypercortisolism is initiated.
Initial diagnostic testing for hypercortisolism depends on the degree of clinical suspicion. In those with low probability of the disease, testing should consist of 1 of the following, as a single negative test may be sufficient to rule out the disease:
- 24-hour urinary cortisol levels
- Overnight dexamethasone suppression testing
- Late-night salivary cortisol measurements.
In those with a high index of suspicion, 2 of the aforementioned tests should be performed, as 1 normal result may not be sufficient to exclude the diagnosis.22,23
A 24-hour urinary cortisol collection and overnight dexamethasone suppression test are obtained. His 24-hour urinary free cortisol level is elevated at 6,600 µg (normal 4–100), and suppression testing with 8 mg of dexamethasone (a form of “high-dose” testing)demonstrates only an 8% decline in serum cortisol levels. Cortisol should generally drop more than 90%.
Morning serum cortisol concentration is less than 5 µg/dL (140 nmol/L) in most patients with Cushing disease (ie, a pituitary tumor), and is usually undetectable in normal subjects. Only about 50% of neuroendocrine ACTH-secreting tumors will suppress with this test.
The patient’s clinical presentation, in conjunction with his diagnostic testing, are thus consistent with Cushing syndrome.
CUSHING SYNDROME
Cushing syndrome is most often exogenous or iatrogenic, ie, a result of supraphysiologic doses of glucocorticoids used to treat a variety of inflammatory, autoimmune, and neoplastic conditions.
Endogenous Cushing syndrome, on the other hand, is rare, with an estimated prevalence of 0.7 to 2.4 cases per million per year. ACTH-dependent causes account for 80% of endogenous Cushing syndrome cases, with ACTH-secreting pituitary adenomas (Cushing disease) accounting for 75% to 80% and ectopic ACTH secretion accounting for 15% to 20%. Less than 1% of cases are due to tumors that produce corticotropin-releasing hormone (CRH).
ACTH-independent Cushing syndrome is diagnosed in 20% of endogenous cases and is most commonly caused by a unilateral adrenal tumor. Rare causes of ACTH-independent disease include adrenal carcinoma, McCune-Albright syndrome, and adrenal hyperplasia.24
The patient’s ACTH is high
To determine whether this is an ACTH-dependent or independent process, the next step is to order an ACTH level. His ACTH level is high at 107 pg/mL (normal < 46 pg/mL), confirming the diagnosis of ACTH-dependent Cushing syndrome.
To find out if this ACTH-dependent process is due to a pituitary adenoma, magnetic resonance imaging (MRI) of the pituitary is obtained but is normal.
Large masses (> 6 mm) strongly suggest Cushing disease, but these tumors are often small and may be missed even with more advanced imaging techniques. Corticotropin-secreting adenomas arising from normal cells in the pituitary retain some sensitivity to glucocorticoid negative feedback and CRH stimulation, and thus high-dose dexamethasone suppression testing in conjunction with CRH stimulation testing can be used to differentiate Cushing disease from ectopic ACTH secretion.24,25 Both of these tests have poor diagnostic accuracy, however, and thus inferior petrosal sampling remains the gold standard for the diagnosis of Cushing disease.
ACTH-SECRETING TUMORS
5. Cushing syndrome due to ectopic ACTH secretion is most commonly attributed to which of the following tumors?
- Small-cell lung carcinoma
- Pancreatic carcinoma
- Medullary thyroid carcinoma
- Gastrinoma
Severe cases of Cushing syndrome are often attributable to ectopic ACTH secretion due to an underlying malignancy, most commonly small-cell lung carcinoma or neuroendocrine tumors of pulmonary origin. Other causes include pancreatic and thymic neuroendocrine tumors, gastrinomas, and medullary thyroid carcinoma.25,26
Because most ACTH-producing tumors are intrathoracic, initial imaging in cases of suspected ectopic ACTH secretion should focus on the chest, with CT the usual first choice. Octreotide scintigraphy can also be useful in localizing disease, as many neuroendocrine tumors express somatostatin receptors. Specialized positron-emission tomography scans may also be helpful in tumor identification.24
TREATMENT OF CUSHING SYNDROME DUE TO ECTOPIC ACTH SECRETION
6. Which of the following is most appropriate medical therapy for suppression of cortisol secretion in Cushing syndrome due to ectopic ACTH secretion?
- Spironolactone
- Dexamethasone
- Somatostatin
- Estrogen
- Ketoconazole
Hyperglycemia, hypokalemia, hypertension, psychiatric disturbances, venous thromboembolism, and systemic infections appear to be common in ectopic ACTH syndrome and often correlate with the degree of hypercortisolemia. Severe Cushing syndrome due to ectopic ACTH secretion is an emergency requiring prompt control of cortisol secretion.
First-line treatments include steroidogenesis inhibitors (ketoconazole, metyrapone, etomidate, mitotane) and glucocorticoid receptor antagonists (mifepristone). High-dose spironolactone and eplerenone can also be used to treat the hypertension and hypokalemia associated with mineralocorticoid receptor stimulation. Definitive treatment involves surgical resection, chemotherapy, or radiotherapy when applicable.24,25
After confirmation of the diagnosis, the patient is prescribed ketoconazole and spironolactone, with substantial improvement. He subsequently is started on combination chemotherapy and radiation therapy for his small-cell lung carcinoma.
DISCUSSION
The differential diagnosis for hypokalemia is broad and relies on information obtained during the history and physical examination, followed by interpretation of selected laboratory results. Myriad pathologies in diverse organ systems, eg, diarrhea, renal tubular acidosis, and adrenal disease, may be responsible for a low serum potassium. Further categorizing potassium depletion on the basis of an associated acid-base disturbance, such as metabolic alkalosis, allows one to use an algorithmic approach that can identify specific etiologies responsible for both the potassium and the acid-base disturbances.
Using the spot urine chloride in the setting of hypokalemic metabolic alkalosis with or without hypertension can narrow the differential diagnosis and allow additional clinical findings to guide clinical problem-solving and decision-making, even for conditions not commonly encountered in routine medical practice.
Obtaining renin and aldosterone measurements in patients with potassium depletion, metabolic alkalosis, high urine chloride excretion, and hypertension permits further categorization into 3 clinical groups: elevated aldosterone and renin (secondary hyperaldosteronism), elevated aldosterone and low renin (primary hyperaldosteronism), or apparent mineralocorticoid excess wherein neither renin nor aldosterone are responsible for the syndrome.
The patient in our case had apparent mineralocorticoid excess as a consequence of an ACTH-producing small-cell carcinoma.
NOTE: The scenario presented here is partly based on cases reported elsewhere by Martínez-Valles et al1 and Fernández-Rodríguez et al.2
A 55-year-old man is admitted to the hospital with generalized malaise, paresthesias, and severe hypertension. He says he had experienced agitation along with weakness on exertion 24 hours before presentation to the emergency department, with subsequent onset of paresthesias in his lower extremities and perioral area.
He is already known to have mild chronic obstructive pulmonary disease, with a ratio of forced expiratory volume in 1 second (FEV1)to forced vital capacity (FVC) of less than 70% and an FEV1 85% of predicted. In addition, he was recently diagnosed with diabetes, resistant hypertension requiring maximum doses of 3 agents (a calcium channel blocker, an angiotensin-converting enzyme inhibitor, and a loop diuretic), and hyperlipidemia.
He is a current smoker with a 30-pack-year smoking history. He does not use alcohol. His family history is noncontributory.
ASSESSING ACID-BASE DISORDERS
1. What type of acid-base disorder does this patient have?
- Metabolic acidosis
- Respiratory acidosis
- Metabolic alkalosis
- Respiratory alkalosis
The patient has metabolic alkalosis.
A 5-step approach
1. Acidosis or alkalosis? The patient’s arterial pH is 7.5, which is alkalemic because it is higher than 7.44.
2. Metabolic or respiratory? The primary process in our patient is overwhelmingly metabolic, as his partial pressure of carbon dioxide (Pco2) is slightly elevated, a direction that would cause acidosis, not alkalosis.
3. The anion gap (the serum sodium concentration minus the sum of the chloride and bicarbonate concentrations) is normal at 8 mmol/L (DRG:HYBRiD-XL Immunoassay and Clinical Chemistry Analyzer, reference range 8–16).
4. Is the disturbance compensated? We have determined that this patient has a metabolic alkalemia; the question now is whether there is any compensation for the primary disturbance.
In metabolic alkalosis, the Pco2 may increase by approximately 0.6 mm Hg (range 0.5–0.8) above the nominal normal level of 40 mm Hg for each 1-mmol/L increase in bicarbonate above the nominal normal level of 25 mmol/L.4 If the patient requires oxygen, the calculation may be unreliable, however, as hypoxemia may have an overriding influence on respiratory drive.
Patients with chronically high Pco2 levels such as those with chronic obstructive pulmonary disease can become accustomed to high carbon dioxide levels and lose their hyper-
capnic respiratory drive. Giving oxygen supplementation is thought to decrease respiratory drive in these patients, so that they will breathe slower and retain more carbon dioxide. There is some degree of respiratory compensation for metabolic alkalosis that occurs by breathing less, though it is limited overall—even in very alkalotic patients, breathing less results in CO2 retention, which, by displacing O2 molecules in the alveoli, will in turn result in hypoxia. The brain then senses the hypoxia and makes one breathe faster, thereby limiting this compensation.
This patient’s serum bicarbonate level is 40 mmol/L, or 15 mmol/L higher than the nominal normal level. If he is compensating, his Pco2 should be 40 + (15 × 0.6) = 49 mm Hg, and in fact it is 51 mm Hg, which is within the normal range of expected compensation (47.5–52 mm Hg). Therefore, yes, he is compensating for the primary disturbance.
5. In metabolic acidosis, is there a delta gap? As our patient has metabolic alkalosis, not acidosis, this question does not apply in this case.
WHICH TEST TO FIND THE CAUSE?
2. Which is the best test to order next to determine the cause of this patient’s hypokalemic metabolic alkalosis?
- Serum magnesium level
- Spot urine chloride
- Renal ultrasonography
- 24-hour urine collection for sodium, potassium, and chloride
The patient’s loop diuretic is withheld for 12 hours and a spot urine chloride is obtained, which is reported as 44 mmol/L. This high value suggests that a volume-independent hypokalemic metabolic alkalosis is present with potassium depletion.
As for the other answer choices:
Serum magnesium. Though hypomagnesemia can cause hypokalemia due to lack of inhibition of renal outer medullary potassium channels and subsequent increased excretion of potassium in the apical tubular membrane, it is not independently associated with acid-base disturbances.5
Renal ultrasonography gives information about structural kidney disease but is of limited utility in identifying the cause of hypokalemic metabolic alkalosis.
A 24-hour urine collection is unnecessary in this setting and would ultimately result in delay in diagnosis, as spot urine chloride is a more efficient means of rapidly distinguishing volume-responsive vs volume-independent causes of hypokalemic metabolic alkalosis.6
IS HIS HYPERTENSION SECONDARY? IF SO, WHAT IS THE CAUSE?
Several features of this case suggest that the patient’s hypertension is secondary rather than primary. It is of recent onset. The patient’s family history is noncontributory, and his hypertension is resistant to the use of maximum doses of 3 antihypertensive agents.
3. Which of the following causes of secondary hypertension is not commonly associated with hypokalemia and metabolic alkalosis?
- Hyperaldosteronism
- Liddle syndrome
- Cushing syndrome
- Renal parenchymal disease
- Chronic licorice ingestion
Renal parenchymal disease is a cause of resistant hypertension, but it is not characterized by metabolic alkalosis, hypokalemia, and elevated urine chloride,7 while the others listed here—hyperaldosteronism, Liddle syndrome, Cushing syndrome, and chronic licorice ingestion—are. Other common causes of resistant hypertension without these metabolic abnormalities include obstructive sleep apnea, alcohol abuse, and nonadherence to treatment.
While treatment of hypertension with loop diuretics can result in hypokalemia and metabolic alkalosis due to the effect of these drugs on potassium reabsorption in the loop of Henle, the patient’s hypokalemia persisted after this agent was withdrawn.8
Causes of hypokalemic metabolic alkalosis with and without hypertension are further delineated in Figure 1.
Additional diagnostic testing: Plasma renin and plasma aldosterone
At this juncture, the differential diagnosis for this patient’s potassium depletion, metabolic alkalosis, high urine chloride, and hypertension has been narrowed to primary or secondary hyperaldosteronism, surreptitious mineralocorticoid ingestion, Cushing syndrome, licorice ingestion, Liddle syndrome, or one of the 3 hydroxylase deficiencies (11-, 17-, and 21-) (Figure 1).
Although clues in the history, physical examination, and imaging may suggest a specific cause of his abnormal laboratory values, the next step in the diagnostic workup is to measure the plasma renin and aldosterone levels (Table 3).
HYPERALDOSTERONISM
4. Hyperaldosteronism is associated with which of the following patterns of renin and aldosterone values?
- High renin, high aldosterone, normal ratio of plasma aldosterone concentration (PAC) to plasma renin activity (PRA)
- Low renin, low aldosterone, normal PAC–PRA ratio
- Low renin, high aldosterone, high PAC–PRA ratio
- High renin, low aldosterone, low PAC–PRA ratio
The pattern of low renin, high aldosterone, and high PAC–PRA ratio is associated with hyperaldosteronism.
Primary hyperaldosteronism
Primary hyperaldosteronism is one of the most common causes of resistant hypertension and is underappreciated, being diagnosed in up to 20% of patients referred to hypertension specialty clinics.7 Potassium levels may be normal, likely contributing to its lack of recognition in this target population.
Primary hyperaldosteronism should be suspected in patients who have a plasma aldosterone PAC–PRA ratio greater than 20 with elevated plasma aldosterone concentrations
(> 15 ng/dL).
Persistently elevated aldosterone levels in the setting of elevated plasma volume is proof that aldosterone secretion is independent of the renin-angiotensin-aldosterone axis, and therefore is autonomous (secondary to adrenal tumor or hyperplasia). Further testing in the form of oral salt loading, saline infusion, or fludrocortisone (a sodium-retaining steroid) administration is thus required to confirm inappropriate, autonomous aldosterone secretion.9
After establishing the diagnosis of primary hyperaldosteronism, one should determine the subtype (ie, due to an adrenal carcinoma, unilateral hypersecreting adenoma, or unilateral or bilateral hyperplasia). Further testing includes adrenal computed tomography (CT) to rule out adrenal carcinomas, which are suspected with adenomas larger than 4 cm. Though part of the diagnostic workup, CT as a means of confirmational testing alone does not preclude the possibility of bilateral adrenal hyperplasia in some patients, even in the presence of an adrenal adenoma. For this reason, adrenal venous sampling is required to definitively determine whether the condition is due to a hypersecreting adrenal adenoma or unilateral or bilateral hyperplasia.9,10
Treatment of primary hyperaldosteronism depends on the subtype of the disease and involves salt restriction in addition to an aldosterone antagonist (spironolactone or eplerenone in the case of bilateral disease) or surgery (unilateral disease).9,11,12
Secondary hyperaldosteronism
Secondary hyperaldosteronism should be suspected when plasma renin and aldosterone levels are both elevated with a PAC–PRA ratio less than 10.
This pattern is most commonly seen with diuretic use but can also be a consequence of renal artery stenosis or, rarely, a renin-secreting tumor.13 Renal artery stenosis is a common finding in patients with hypertension undergoing cardiac catheterization, which is not surprising as more than 90% of such stenoses are atherosclerotic.7 Renin-secreting tumors are exceedingly rare, with fewer than 100 cases reported in the literature, and are more common in younger individuals.13
Our patient has low-normal aldosterone and plasma renin
On further testing, this patient’s plasma aldosterone level is 2.55 ng/dL (normal < 15 ng/dL), his plasma renin activity is 0.53 ng/mL/hour (normal 0.2–2.8 ng/mL/hour), and his PAC–PRA ratio is therefore 4.81.
The categories discussed thus far have included primary and secondary hyperaldosteronism, which typically do not present with low to normal levels of both renin and aldosterone. Surreptitious mineralocorticoid use could present in this manner, but is unlikely in this patient, whose medications do not include fludrocortisone.
The low-normal values thus lead to consideration of a third category: apparent mineralocorticoid excess. Diseases in this category such as Cushing disease or adrenocorticotropic hormone (ACTH) excess are characterized by increases in corticosteroids so that the potassium depletion, metabolic alkalosis, and hypertension are not a consequence of renin and aldosterone but rather the excess corticosteroids.14
Causes of apparent mineralocorticoid excess
There are several possible causes of mineralocorticoid excess associated with hypertension and hypokalemic metabolic alkalosis not due to renin and aldosterone.
Chronic licorice ingestion in high volumes is one such cause and is thought to result in inhibition of 11B-hydroxysteroid dehydrogenase or possibly cortisol oxidase by licorice’s active component, glycyrrhetinic acid. This inhibition results in an inability to convert cortisol to cortisone. The cortisol excess binds to mineralocorticoid receptors, and acting like aldosterone, results in hypertension and hypokalemic metabolic alkalosis as well as feedback inhibition of renin and aldosterone levels.15
Partial hydroxylase deficiencies, though rare, should also be considered as a cause of hypokalemic metabolic alkalosis, hypertension, and, potentially, hirsutism and clitoromegaly in women. They can be diagnosed with elevated levels of 17-ketosteroids and dehydroepiandrosterone sulfate, both of which, in excess, may act on aldosterone receptors in a manner similar to cortisol.16
Liddle syndrome, a rare autosomal dominant condition, may also present with suppressed levels of both renin and aldosterone. In contrast to the disorders of nonaldosterone mineralocorticoid excess, however, the sodium channel defect in Liddle syndrome is characterized by a primary increase in sodium reabsorption in the collecting tubule and potassium wasting. The resultant volume expansion leads to suppressed renin and aldosterone levels and hypertension with low potassium and elevated bicarbonate concentrations.17
Liddle syndrome is commonly diagnosed in childhood but may go unrecognized due to occasional absence of hypokalemia at presentation. Potassium-sparing diuretics such as amiloride or triamterene are the mainstays of treatment.18
Rates of cardiovascular and all-cause mortality are increased in patients with long-term hypercortisolism, even after plasma concentrations of cortisol are normalized.21
Figure 2 shows the cascade of the hypothalamic-pituitary-adrenal axis.
TESTING FOR HYPERCORTISOLISM IN OUR PATIENT
Given the patient’s clinical presentation and laboratory and imaging findings with normal plasma renin and aldosterone levels, a workup for suspected hypercortisolism is initiated.
Initial diagnostic testing for hypercortisolism depends on the degree of clinical suspicion. In those with low probability of the disease, testing should consist of 1 of the following, as a single negative test may be sufficient to rule out the disease:
- 24-hour urinary cortisol levels
- Overnight dexamethasone suppression testing
- Late-night salivary cortisol measurements.
In those with a high index of suspicion, 2 of the aforementioned tests should be performed, as 1 normal result may not be sufficient to exclude the diagnosis.22,23
A 24-hour urinary cortisol collection and overnight dexamethasone suppression test are obtained. His 24-hour urinary free cortisol level is elevated at 6,600 µg (normal 4–100), and suppression testing with 8 mg of dexamethasone (a form of “high-dose” testing)demonstrates only an 8% decline in serum cortisol levels. Cortisol should generally drop more than 90%.
Morning serum cortisol concentration is less than 5 µg/dL (140 nmol/L) in most patients with Cushing disease (ie, a pituitary tumor), and is usually undetectable in normal subjects. Only about 50% of neuroendocrine ACTH-secreting tumors will suppress with this test.
The patient’s clinical presentation, in conjunction with his diagnostic testing, are thus consistent with Cushing syndrome.
CUSHING SYNDROME
Cushing syndrome is most often exogenous or iatrogenic, ie, a result of supraphysiologic doses of glucocorticoids used to treat a variety of inflammatory, autoimmune, and neoplastic conditions.
Endogenous Cushing syndrome, on the other hand, is rare, with an estimated prevalence of 0.7 to 2.4 cases per million per year. ACTH-dependent causes account for 80% of endogenous Cushing syndrome cases, with ACTH-secreting pituitary adenomas (Cushing disease) accounting for 75% to 80% and ectopic ACTH secretion accounting for 15% to 20%. Less than 1% of cases are due to tumors that produce corticotropin-releasing hormone (CRH).
ACTH-independent Cushing syndrome is diagnosed in 20% of endogenous cases and is most commonly caused by a unilateral adrenal tumor. Rare causes of ACTH-independent disease include adrenal carcinoma, McCune-Albright syndrome, and adrenal hyperplasia.24
The patient’s ACTH is high
To determine whether this is an ACTH-dependent or independent process, the next step is to order an ACTH level. His ACTH level is high at 107 pg/mL (normal < 46 pg/mL), confirming the diagnosis of ACTH-dependent Cushing syndrome.
To find out if this ACTH-dependent process is due to a pituitary adenoma, magnetic resonance imaging (MRI) of the pituitary is obtained but is normal.
Large masses (> 6 mm) strongly suggest Cushing disease, but these tumors are often small and may be missed even with more advanced imaging techniques. Corticotropin-secreting adenomas arising from normal cells in the pituitary retain some sensitivity to glucocorticoid negative feedback and CRH stimulation, and thus high-dose dexamethasone suppression testing in conjunction with CRH stimulation testing can be used to differentiate Cushing disease from ectopic ACTH secretion.24,25 Both of these tests have poor diagnostic accuracy, however, and thus inferior petrosal sampling remains the gold standard for the diagnosis of Cushing disease.
ACTH-SECRETING TUMORS
5. Cushing syndrome due to ectopic ACTH secretion is most commonly attributed to which of the following tumors?
- Small-cell lung carcinoma
- Pancreatic carcinoma
- Medullary thyroid carcinoma
- Gastrinoma
Severe cases of Cushing syndrome are often attributable to ectopic ACTH secretion due to an underlying malignancy, most commonly small-cell lung carcinoma or neuroendocrine tumors of pulmonary origin. Other causes include pancreatic and thymic neuroendocrine tumors, gastrinomas, and medullary thyroid carcinoma.25,26
Because most ACTH-producing tumors are intrathoracic, initial imaging in cases of suspected ectopic ACTH secretion should focus on the chest, with CT the usual first choice. Octreotide scintigraphy can also be useful in localizing disease, as many neuroendocrine tumors express somatostatin receptors. Specialized positron-emission tomography scans may also be helpful in tumor identification.24
TREATMENT OF CUSHING SYNDROME DUE TO ECTOPIC ACTH SECRETION
6. Which of the following is most appropriate medical therapy for suppression of cortisol secretion in Cushing syndrome due to ectopic ACTH secretion?
- Spironolactone
- Dexamethasone
- Somatostatin
- Estrogen
- Ketoconazole
Hyperglycemia, hypokalemia, hypertension, psychiatric disturbances, venous thromboembolism, and systemic infections appear to be common in ectopic ACTH syndrome and often correlate with the degree of hypercortisolemia. Severe Cushing syndrome due to ectopic ACTH secretion is an emergency requiring prompt control of cortisol secretion.
First-line treatments include steroidogenesis inhibitors (ketoconazole, metyrapone, etomidate, mitotane) and glucocorticoid receptor antagonists (mifepristone). High-dose spironolactone and eplerenone can also be used to treat the hypertension and hypokalemia associated with mineralocorticoid receptor stimulation. Definitive treatment involves surgical resection, chemotherapy, or radiotherapy when applicable.24,25
After confirmation of the diagnosis, the patient is prescribed ketoconazole and spironolactone, with substantial improvement. He subsequently is started on combination chemotherapy and radiation therapy for his small-cell lung carcinoma.
DISCUSSION
The differential diagnosis for hypokalemia is broad and relies on information obtained during the history and physical examination, followed by interpretation of selected laboratory results. Myriad pathologies in diverse organ systems, eg, diarrhea, renal tubular acidosis, and adrenal disease, may be responsible for a low serum potassium. Further categorizing potassium depletion on the basis of an associated acid-base disturbance, such as metabolic alkalosis, allows one to use an algorithmic approach that can identify specific etiologies responsible for both the potassium and the acid-base disturbances.
Using the spot urine chloride in the setting of hypokalemic metabolic alkalosis with or without hypertension can narrow the differential diagnosis and allow additional clinical findings to guide clinical problem-solving and decision-making, even for conditions not commonly encountered in routine medical practice.
Obtaining renin and aldosterone measurements in patients with potassium depletion, metabolic alkalosis, high urine chloride excretion, and hypertension permits further categorization into 3 clinical groups: elevated aldosterone and renin (secondary hyperaldosteronism), elevated aldosterone and low renin (primary hyperaldosteronism), or apparent mineralocorticoid excess wherein neither renin nor aldosterone are responsible for the syndrome.
The patient in our case had apparent mineralocorticoid excess as a consequence of an ACTH-producing small-cell carcinoma.
- Martínez-Valles MA, Palafox-Cazarez A, Paredes-Avina JA. Severe hypokalemia, metabolic alkalosis and hypertension in a 54 year old male with ectopic ACTH syndrome: a case report. Cases J 2009; 2:6174. doi:10.4076/1757-1626-2-6174
- Fernández-Rodríguez E, Villar-Taibo R, Pinal-Osorio I, et al. Severe hypertension and hypokalemia as first clinical manifestations in ectopic Cushing’s syndrome. Arq Bras Endocrinol Metabol 2008; 52(6):1066–1070. pmid:18820819
- Mani S, Rutecki GW. A patient with altered mental status and an acid-base disturbance. Cleve Clin J Med 2017; 84(1):27–34. doi:10.3949/ccjm.84a.16042
- Adrogué HJ, Madias NE. Secondary responses to altered acid-base status: the rules of engagement. J Am Soc Nephrol 2010; 21(6):920–923. doi:10.1681/ASN.2009121211
- Huang CL, Kuo E. Mechanism of hypokalemia in magnesium deficiency. J Am Soc Nephrol 2007; 18(10):2649–2652. doi:10.1681/ASN.2007070792
- Rose BD. Metabolic alkalosis. In: Clinical Physiology of Acid-Base and Electrolyte Disorders. 4th ed. New York, NY: McGraw-Hill, Health Professions Division; 1994:515.
- Calhoun DA, Jones D, Textor S, et al; American Heart Association Professional Education Committee. Resistant hypertension: diagnosis, evaluation, and treatment: a scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Circulation 2008; 117(25):e510–e526. doi:10.1161/CIRCULATIONAHA.108.189141
- Koeppen BM, Stanton BA. Physiology of diuretic action. In: Renal Physiology. 5th ed. Philadelphia, PA: Elsevier Inc; 2013:167–178.
- Blumenfeld JD, Sealey JE, Schlussel Y, et al. Diagnosis and treatment of primary hyperaldosteronism. Ann Intern Med 1994; 121(11):877–885. pmid:7978702
- Kempers MJ, Lenders JW, van Outheusden L, et al. Systematic review: diagnostic procedures to differentiate unilateral from bilateral adrenal abnormality in primary aldosteronism. Ann Intern Med 2009; 151(5):329–337. pmid:19721021
- Karagiannis A, Tziomalos K, Papageorgiou A, et al. Spironolactone versus eplerenone for the treatment of idiopathic hyperaldosteronism. Expert Opin Pharmacother 2008; 9(4):509–515. doi:10.1517/14656566.9.4.509
- Sawka AM, Young WF, Thompson GB, et al. Primary aldosteronism: factors associated with normalization of blood pressure after surgery. Ann Intern Med 2001; 135(4):258–261. pmid:11511140
- Haab F, Duclos JM, Guyenne T, Plouin PF, Corvol P. Renin secreting tumors: diagnosis, conservative surgical approach and long-term results. J Urol 1995; 153(6):1781–1784. pmid:7752315
- Sabbadin C, Armanini D. Syndromes that mimic an excess of mineralocorticoids. High Blood Press Cardiovasc Prev 2016; 23(3):231–235. doi:10.1007/s40292-016-0160-5
- Apostolakos JM, Caines LC. Apparent mineralocorticoid excess syndrome: a case of resistant hypertension from licorice tea consumption. J Clin Hypertens (Greenwich) 2016; 18(10):991–993. doi:10.1111/jch.12841
- Glatt K, Garzon DL, Popovic J. Congenital adrenal hyperplasia due to 21-hydroxylase deficiency. J Spec Pediatr Nurs 2005; 10(3):104–114. doi:10.1111/j.1744-6155.2005.00022.x
- Findling JW, Raff H, Hansson JH, Lifton RP. Liddle’s syndrome: prospective genetic screening and suppressed aldosterone secretion in an extended kindred. J Clin Endocrinol Metab 1997; 82(4):1071–1074. doi:10.1210/jcem.82.4.3862
- Wang C, Chan TK, Yeung RT, Coghlan JP, Scoggins BA, Stockigt JR. The effect of triamterene and sodium intake on renin, aldosterone, and erythrocyte sodium transport in Liddle’s syndrome. J Clin Endocrinol Metab 1981; 52(5):1027–1032. doi:10.1210/jcem-52-5-1027
- Torpy DJ, Mullen N, Ilias I, Nieman LK. Association of hypertension and hypokalemia with Cushing’s syndrome caused by ectopic ACTH secretion: a series of 58 cases. Ann N Y Acad Sci 2002; 970:134–144. pmid:12381548
- Saruta T, Suzuki H, Handa M, Igarashi Y, Kondo K, Senba S. Multiple factors contribute to the pathogenesis of hypertension in Cushing’s syndrome. J Clin Endocrinol Metab 1986; 62(2):275–279. doi:10.1210/jcem-62-2-275
- Clayton RN, Jones PW, Reulen RC, et al. Mortality in patients with Cushing’s disease more than 10 years after remission: a multicentre, multinational, retrospective cohort study. Lancet Diabetes Endocrinol 2016; 4(7):569–576. doi:10.1016/S2213-8587(16)30005-5
- Baid SK, Rubino D, Sinaii N, Ramsey S, Frank A, Nieman LK. Specificity of screening tests for Cushing’s syndrome in an overweight and obese population. J Clin Endocrinol Metab 2009; 94(10):3857–3864. doi:10.1210/jc.2008-2766
- Nieman LK, Biller BM, Findling JW, et al. The diagnosis of Cushing’s syndrome: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2008; 93(5):1526–1540. doi:10.1210/jc.2008-0125
- Sharma ST, Nieman LK, Feelders RA. Cushing’s syndrome: epidemiology and developments in disease management. Clin Epidemiol 2015; 7:281–293. doi:10.2147/CLEP.S44336
- Tavares Bello C, van der Poest Clement E, Feelders R. Severe Cushing’s syndrome and bilateral pulmonary nodules: beyond ectopic ACTH. Endocrinol Diabetes Metab Case Rep 2017; pii:17–0100. doi:10.1530/EDM-17-0100
- Sathyakumar S, Paul TV, Asha HS, et al. Ectopic Cushing syndrome: a 10-year experience from a tertiary care center in southern India. Endocr Pract 2017; 23(8):907–914. doi:10.4158/EP161677.OR
- Martínez-Valles MA, Palafox-Cazarez A, Paredes-Avina JA. Severe hypokalemia, metabolic alkalosis and hypertension in a 54 year old male with ectopic ACTH syndrome: a case report. Cases J 2009; 2:6174. doi:10.4076/1757-1626-2-6174
- Fernández-Rodríguez E, Villar-Taibo R, Pinal-Osorio I, et al. Severe hypertension and hypokalemia as first clinical manifestations in ectopic Cushing’s syndrome. Arq Bras Endocrinol Metabol 2008; 52(6):1066–1070. pmid:18820819
- Mani S, Rutecki GW. A patient with altered mental status and an acid-base disturbance. Cleve Clin J Med 2017; 84(1):27–34. doi:10.3949/ccjm.84a.16042
- Adrogué HJ, Madias NE. Secondary responses to altered acid-base status: the rules of engagement. J Am Soc Nephrol 2010; 21(6):920–923. doi:10.1681/ASN.2009121211
- Huang CL, Kuo E. Mechanism of hypokalemia in magnesium deficiency. J Am Soc Nephrol 2007; 18(10):2649–2652. doi:10.1681/ASN.2007070792
- Rose BD. Metabolic alkalosis. In: Clinical Physiology of Acid-Base and Electrolyte Disorders. 4th ed. New York, NY: McGraw-Hill, Health Professions Division; 1994:515.
- Calhoun DA, Jones D, Textor S, et al; American Heart Association Professional Education Committee. Resistant hypertension: diagnosis, evaluation, and treatment: a scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Circulation 2008; 117(25):e510–e526. doi:10.1161/CIRCULATIONAHA.108.189141
- Koeppen BM, Stanton BA. Physiology of diuretic action. In: Renal Physiology. 5th ed. Philadelphia, PA: Elsevier Inc; 2013:167–178.
- Blumenfeld JD, Sealey JE, Schlussel Y, et al. Diagnosis and treatment of primary hyperaldosteronism. Ann Intern Med 1994; 121(11):877–885. pmid:7978702
- Kempers MJ, Lenders JW, van Outheusden L, et al. Systematic review: diagnostic procedures to differentiate unilateral from bilateral adrenal abnormality in primary aldosteronism. Ann Intern Med 2009; 151(5):329–337. pmid:19721021
- Karagiannis A, Tziomalos K, Papageorgiou A, et al. Spironolactone versus eplerenone for the treatment of idiopathic hyperaldosteronism. Expert Opin Pharmacother 2008; 9(4):509–515. doi:10.1517/14656566.9.4.509
- Sawka AM, Young WF, Thompson GB, et al. Primary aldosteronism: factors associated with normalization of blood pressure after surgery. Ann Intern Med 2001; 135(4):258–261. pmid:11511140
- Haab F, Duclos JM, Guyenne T, Plouin PF, Corvol P. Renin secreting tumors: diagnosis, conservative surgical approach and long-term results. J Urol 1995; 153(6):1781–1784. pmid:7752315
- Sabbadin C, Armanini D. Syndromes that mimic an excess of mineralocorticoids. High Blood Press Cardiovasc Prev 2016; 23(3):231–235. doi:10.1007/s40292-016-0160-5
- Apostolakos JM, Caines LC. Apparent mineralocorticoid excess syndrome: a case of resistant hypertension from licorice tea consumption. J Clin Hypertens (Greenwich) 2016; 18(10):991–993. doi:10.1111/jch.12841
- Glatt K, Garzon DL, Popovic J. Congenital adrenal hyperplasia due to 21-hydroxylase deficiency. J Spec Pediatr Nurs 2005; 10(3):104–114. doi:10.1111/j.1744-6155.2005.00022.x
- Findling JW, Raff H, Hansson JH, Lifton RP. Liddle’s syndrome: prospective genetic screening and suppressed aldosterone secretion in an extended kindred. J Clin Endocrinol Metab 1997; 82(4):1071–1074. doi:10.1210/jcem.82.4.3862
- Wang C, Chan TK, Yeung RT, Coghlan JP, Scoggins BA, Stockigt JR. The effect of triamterene and sodium intake on renin, aldosterone, and erythrocyte sodium transport in Liddle’s syndrome. J Clin Endocrinol Metab 1981; 52(5):1027–1032. doi:10.1210/jcem-52-5-1027
- Torpy DJ, Mullen N, Ilias I, Nieman LK. Association of hypertension and hypokalemia with Cushing’s syndrome caused by ectopic ACTH secretion: a series of 58 cases. Ann N Y Acad Sci 2002; 970:134–144. pmid:12381548
- Saruta T, Suzuki H, Handa M, Igarashi Y, Kondo K, Senba S. Multiple factors contribute to the pathogenesis of hypertension in Cushing’s syndrome. J Clin Endocrinol Metab 1986; 62(2):275–279. doi:10.1210/jcem-62-2-275
- Clayton RN, Jones PW, Reulen RC, et al. Mortality in patients with Cushing’s disease more than 10 years after remission: a multicentre, multinational, retrospective cohort study. Lancet Diabetes Endocrinol 2016; 4(7):569–576. doi:10.1016/S2213-8587(16)30005-5
- Baid SK, Rubino D, Sinaii N, Ramsey S, Frank A, Nieman LK. Specificity of screening tests for Cushing’s syndrome in an overweight and obese population. J Clin Endocrinol Metab 2009; 94(10):3857–3864. doi:10.1210/jc.2008-2766
- Nieman LK, Biller BM, Findling JW, et al. The diagnosis of Cushing’s syndrome: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2008; 93(5):1526–1540. doi:10.1210/jc.2008-0125
- Sharma ST, Nieman LK, Feelders RA. Cushing’s syndrome: epidemiology and developments in disease management. Clin Epidemiol 2015; 7:281–293. doi:10.2147/CLEP.S44336
- Tavares Bello C, van der Poest Clement E, Feelders R. Severe Cushing’s syndrome and bilateral pulmonary nodules: beyond ectopic ACTH. Endocrinol Diabetes Metab Case Rep 2017; pii:17–0100. doi:10.1530/EDM-17-0100
- Sathyakumar S, Paul TV, Asha HS, et al. Ectopic Cushing syndrome: a 10-year experience from a tertiary care center in southern India. Endocr Pract 2017; 23(8):907–914. doi:10.4158/EP161677.OR
Correction: Hypertension guidelines
In Aleyadeh W, Hutt-Centeno E, Ahmed HM, Shah NP. Hypertension guidelines: treat patients, not numbers. Cleve Clin J Med 2019; 86(1):47–56. doi:10.3949/ccjm.86a.18027, on page 50, the following statement was incorrect: “In 2017, the American College of Physicians (ACP) and the American Academy of Family Physicians (AAFP) recommended a relaxed systolic blood pressure target, ie, below 150 mm Hg, for adults over age 60, but a tighter goal of less than 130 mm Hg for the same age group if they have transient ischemic attack, stroke, or high cardiovascular risk.9” In fact, the ACP and AAFP recommended a tighter goal of less than 140 mm Hg for this higher-risk group. This has been corrected online.
In Aleyadeh W, Hutt-Centeno E, Ahmed HM, Shah NP. Hypertension guidelines: treat patients, not numbers. Cleve Clin J Med 2019; 86(1):47–56. doi:10.3949/ccjm.86a.18027, on page 50, the following statement was incorrect: “In 2017, the American College of Physicians (ACP) and the American Academy of Family Physicians (AAFP) recommended a relaxed systolic blood pressure target, ie, below 150 mm Hg, for adults over age 60, but a tighter goal of less than 130 mm Hg for the same age group if they have transient ischemic attack, stroke, or high cardiovascular risk.9” In fact, the ACP and AAFP recommended a tighter goal of less than 140 mm Hg for this higher-risk group. This has been corrected online.
In Aleyadeh W, Hutt-Centeno E, Ahmed HM, Shah NP. Hypertension guidelines: treat patients, not numbers. Cleve Clin J Med 2019; 86(1):47–56. doi:10.3949/ccjm.86a.18027, on page 50, the following statement was incorrect: “In 2017, the American College of Physicians (ACP) and the American Academy of Family Physicians (AAFP) recommended a relaxed systolic blood pressure target, ie, below 150 mm Hg, for adults over age 60, but a tighter goal of less than 130 mm Hg for the same age group if they have transient ischemic attack, stroke, or high cardiovascular risk.9” In fact, the ACP and AAFP recommended a tighter goal of less than 140 mm Hg for this higher-risk group. This has been corrected online.
AHA drills into CV risk factors in children
the FDA says a popular gout drug raises cardiovascular risk, an AHA statement targets CV risk factors in children, and a class action suit against the American Board of Internal Medicine over MOC gets financial support from doctors.
the FDA says a popular gout drug raises cardiovascular risk, an AHA statement targets CV risk factors in children, and a class action suit against the American Board of Internal Medicine over MOC gets financial support from doctors.
the FDA says a popular gout drug raises cardiovascular risk, an AHA statement targets CV risk factors in children, and a class action suit against the American Board of Internal Medicine over MOC gets financial support from doctors.
ICU admissions raise chronic condition risk
SAN DIEGO – The research showed rising likelihood of conditions such as depression, diabetes, and heart disease.
By merging two existing databases, the researchers were able to capture a more comprehensive picture of post-ICU patients. “We were able to include almost the entire country,” Ilse van Beusekom, a PhD candidate in health sciences at the University of Amsterdam and data manager at the National Intensive Care Evaluation (NICE) foundation, said in an interview.
Ms. van Beusekom presented the study at the Critical Care Congress sponsored by the Society of Critical Care Medicine. The study was simultaneously published in Critical Care Medicine.
The work compared 56,760 ICU survivors from 81 facilities across the Netherlands to 75,232 age-, sex-, and socioeconomic status–matched controls. The mean age was 65 years and 60% of the population was male. “The types of chronic conditions are the same, only the prevalences are different,” said Ms. van Beusekom.
The researchers compared chronic conditions in the year before ICU admission and the year after, based on data pulled from the NICE national quality database, which includes data describing the first 24 hours of ICU admission, and the Vektis insurance claims database, which includes information on medical treatment. Before ICU admission, 45% of the ICU population was free of chronic conditions, as were 62% of controls. One chronic condition was present in 36% of ICU patients, versus 29% of controls, and two or more conditions were present in 19% versus 9% of controls.
The ICU population was more likely to have high cholesterol (16% vs. 14%), heart disease (14% vs. 6%), chronic obstructive pulmonary disease (8% vs. 3%), type II diabetes (8% vs. 6%), type I diabetes (6% vs. 3%), and depression (6% vs. 4%).
The ICU population also was at greater risk of developing one or more new chronic conditions during the year following their stay. The risk was three- to fourfold higher throughout age ranges.
The study suggests the need for greater follow-up after an ICU admission in order to help patients cope with lingering problems. Ms. van Beusekom noted that there are follow-up programs in the Netherlands for several patient groups, but none for ICU survivors. One possibility would be to have the patient return to the ICU 3 months or so after release to discuss their diagnosis, treatment, and any lingering concerns. “A lot of people don’t know that their complaints are linked with the ICU visit,” said Ms. van Beusekom.
Timothy G. Buchman, MD, professor of surgery at Emory University, Atlanta, who moderated the session, wondered why the ICU seems to be an inflection point for developing new chronic conditions. Could it simply be because patients are sicker to begin with and have reached an inflection point of their illness, or could the treatments in ICU be contributing to or exposing those conditions? Ms. van Beusekom believed it was likely a combination of factors, and she referred to data she had not presented showing that even control patients who had been to the hospital (though not the ICU) during the study period were at lower risk of new chronic conditions than ICU patients.
Ms. van Beusekom’s group plans to investigate ICU-related variables that might be associated with risk of chronic conditions.
The study was not funded. Ms. van Beusekom had no relevant disclosures.
SOURCE: van Beusekom I et al. CCC48, Abstract Crit Care Med. 2019;47:324-30.
SAN DIEGO – The research showed rising likelihood of conditions such as depression, diabetes, and heart disease.
By merging two existing databases, the researchers were able to capture a more comprehensive picture of post-ICU patients. “We were able to include almost the entire country,” Ilse van Beusekom, a PhD candidate in health sciences at the University of Amsterdam and data manager at the National Intensive Care Evaluation (NICE) foundation, said in an interview.
Ms. van Beusekom presented the study at the Critical Care Congress sponsored by the Society of Critical Care Medicine. The study was simultaneously published in Critical Care Medicine.
The work compared 56,760 ICU survivors from 81 facilities across the Netherlands to 75,232 age-, sex-, and socioeconomic status–matched controls. The mean age was 65 years and 60% of the population was male. “The types of chronic conditions are the same, only the prevalences are different,” said Ms. van Beusekom.
The researchers compared chronic conditions in the year before ICU admission and the year after, based on data pulled from the NICE national quality database, which includes data describing the first 24 hours of ICU admission, and the Vektis insurance claims database, which includes information on medical treatment. Before ICU admission, 45% of the ICU population was free of chronic conditions, as were 62% of controls. One chronic condition was present in 36% of ICU patients, versus 29% of controls, and two or more conditions were present in 19% versus 9% of controls.
The ICU population was more likely to have high cholesterol (16% vs. 14%), heart disease (14% vs. 6%), chronic obstructive pulmonary disease (8% vs. 3%), type II diabetes (8% vs. 6%), type I diabetes (6% vs. 3%), and depression (6% vs. 4%).
The ICU population also was at greater risk of developing one or more new chronic conditions during the year following their stay. The risk was three- to fourfold higher throughout age ranges.
The study suggests the need for greater follow-up after an ICU admission in order to help patients cope with lingering problems. Ms. van Beusekom noted that there are follow-up programs in the Netherlands for several patient groups, but none for ICU survivors. One possibility would be to have the patient return to the ICU 3 months or so after release to discuss their diagnosis, treatment, and any lingering concerns. “A lot of people don’t know that their complaints are linked with the ICU visit,” said Ms. van Beusekom.
Timothy G. Buchman, MD, professor of surgery at Emory University, Atlanta, who moderated the session, wondered why the ICU seems to be an inflection point for developing new chronic conditions. Could it simply be because patients are sicker to begin with and have reached an inflection point of their illness, or could the treatments in ICU be contributing to or exposing those conditions? Ms. van Beusekom believed it was likely a combination of factors, and she referred to data she had not presented showing that even control patients who had been to the hospital (though not the ICU) during the study period were at lower risk of new chronic conditions than ICU patients.
Ms. van Beusekom’s group plans to investigate ICU-related variables that might be associated with risk of chronic conditions.
The study was not funded. Ms. van Beusekom had no relevant disclosures.
SOURCE: van Beusekom I et al. CCC48, Abstract Crit Care Med. 2019;47:324-30.
SAN DIEGO – The research showed rising likelihood of conditions such as depression, diabetes, and heart disease.
By merging two existing databases, the researchers were able to capture a more comprehensive picture of post-ICU patients. “We were able to include almost the entire country,” Ilse van Beusekom, a PhD candidate in health sciences at the University of Amsterdam and data manager at the National Intensive Care Evaluation (NICE) foundation, said in an interview.
Ms. van Beusekom presented the study at the Critical Care Congress sponsored by the Society of Critical Care Medicine. The study was simultaneously published in Critical Care Medicine.
The work compared 56,760 ICU survivors from 81 facilities across the Netherlands to 75,232 age-, sex-, and socioeconomic status–matched controls. The mean age was 65 years and 60% of the population was male. “The types of chronic conditions are the same, only the prevalences are different,” said Ms. van Beusekom.
The researchers compared chronic conditions in the year before ICU admission and the year after, based on data pulled from the NICE national quality database, which includes data describing the first 24 hours of ICU admission, and the Vektis insurance claims database, which includes information on medical treatment. Before ICU admission, 45% of the ICU population was free of chronic conditions, as were 62% of controls. One chronic condition was present in 36% of ICU patients, versus 29% of controls, and two or more conditions were present in 19% versus 9% of controls.
The ICU population was more likely to have high cholesterol (16% vs. 14%), heart disease (14% vs. 6%), chronic obstructive pulmonary disease (8% vs. 3%), type II diabetes (8% vs. 6%), type I diabetes (6% vs. 3%), and depression (6% vs. 4%).
The ICU population also was at greater risk of developing one or more new chronic conditions during the year following their stay. The risk was three- to fourfold higher throughout age ranges.
The study suggests the need for greater follow-up after an ICU admission in order to help patients cope with lingering problems. Ms. van Beusekom noted that there are follow-up programs in the Netherlands for several patient groups, but none for ICU survivors. One possibility would be to have the patient return to the ICU 3 months or so after release to discuss their diagnosis, treatment, and any lingering concerns. “A lot of people don’t know that their complaints are linked with the ICU visit,” said Ms. van Beusekom.
Timothy G. Buchman, MD, professor of surgery at Emory University, Atlanta, who moderated the session, wondered why the ICU seems to be an inflection point for developing new chronic conditions. Could it simply be because patients are sicker to begin with and have reached an inflection point of their illness, or could the treatments in ICU be contributing to or exposing those conditions? Ms. van Beusekom believed it was likely a combination of factors, and she referred to data she had not presented showing that even control patients who had been to the hospital (though not the ICU) during the study period were at lower risk of new chronic conditions than ICU patients.
Ms. van Beusekom’s group plans to investigate ICU-related variables that might be associated with risk of chronic conditions.
The study was not funded. Ms. van Beusekom had no relevant disclosures.
SOURCE: van Beusekom I et al. CCC48, Abstract Crit Care Med. 2019;47:324-30.
REPORTING FROM CCC48
Much still unknown about inflammation’s role in RA patients’ CVD risk
A variety of trials, some recent and some a decade old, have highlighted the role of inflammation on cardiovascular disease risk in both patients with and without rheumatoid arthritis, spurring greater interest in alleviating inflammation across a wide range of patients, Jon T. Giles, MD, said at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
However, questions remain about the unique contributions of inflammation to CVD risk in RA patients and the effect of RA treatments on that risk, which future studies hope to answer.
Hints of inflammation’s effects in non-RA patients
The JUPITER trial published more than a decade ago, for example, tested the effects of statins in nearly 18,000 older adults without rheumatoid arthritis (RA) who had elevated levels of inflammation, defined as a C-reactive protein (CRP) level of greater than 2 mg/L and low-density lipoprotein (LDL) cholesterol less than 130 mg/dL. Such patients would otherwise be considered low risk and not eligible for statin therapy, said Dr. Giles, a rheumatologist, epidemiologist, and clinical researcher in the division of rheumatology at Columbia University, New York.
A marked decrease in the incidence of cardiovascular disease (CVD) events was seen in those treated with statins, compared with those who received placebo, and all patient subgroups benefited; the number needed to treat to prevent one event was 32 at 5 years (N Engl J Med. 2008;359:2195-207).
The trial was remarkable in that it was stopped early for efficacy, he noted.
“So the question is: Should we be thinking about systemic inflammation as the real target here? And should RA patients who have elevated persistent levels of CRP really be the people that we’re thinking about?” he asked. “Obviously this needs to be tested; we don’t know.”
The more recent CANTOS trial looking at secondary CVD prevention in more than 10,000 non-RA patients with a prior myocardial infarction also highlighted the role of inflammation and provided “some support that decreasing inflammatory cytokines may be important for reducing [CVD] events,” he said (N Engl J Med. 2017;377:1119-31).
Participants were treated with the interleukin-1 inhibitor canakinumab (Ilaris) or placebo, and canakinumab was associated with about a 15% reduction in CVD events, providing “more proof of concept to look at the inflammatory innate immune contribution to CVD risk,” Dr. Giles said.
Treated patients had more infections, but they also had less gout, less arthritis, and less cancer than did those who received placebo, he noted.
Effect of RA treatments on CVD risk
The effects of existing treatments for RA also highlight the importance of inflammation in CVD risk in RA patients, he said, noting that data support a role for immunomodulators for risk reduction.
“There’s a lot of observational epidemiology in this space – mostly for methotrexate and [tumor necrosis factor (TNF)] inhibitors,” he said.
One analysis showed that across 8 cohort studies involving methotrexate, the disease-modifying antirheumatic agent reduced the risk of CVD events by 28%, and that across 16 cohort studies, TNF inhibitors reduced the risk by 30% (Ann Rheum Dis. 2015 Mar;74[3]:480-9).
All of the methotrexate studies showed a reduction, and almost all of the TNF inhibitor trials showed a reduction, Dr. Giles noted.
With respect to other non-TNF biologics, claims data suggest that abatacept (Orencia) is similar to the TNF inhibitor etanercept (Enbrel) with respect to CVD risk, and in a head-to-head, randomized clinical trial of more than 3,000 RA patients presented as a late-breaking abstract at the ACR annual meeting in 2016, Dr. Giles and his colleagues found similar cardiovascular safety between the anti-IL-6 receptor blocker tocilizumab (Actemra) and etanercept.
“I think we’ll know more about this in the near future,” he said.
As for the mechanisms of these agents, early data and animal models suggest that abatacept may play “a special role” in atherosclerosis reduction related to its effects on T cell CTLA-4 over-expression, and methotrexate also seems to have a number of “potential mechanistic benefits” that render it atheroprotective, he said.
The disappointing findings from the recently reported CIRT trial, which showed no benefit of methotrexate for secondary CVD prevention in non-RA patients (N Engl J Med. 2019;380:752-62), has dampened enthusiasm regarding methotrexate’s role here, but it is important to note that patients enrolled in CIRT, unlike those in JUPITER and CANTOS, were not enrolled based on elevated levels of CRP, Dr. Giles said.
Various studies of TNF inhibitors have shown atheroprotective effects through reductions in macrophage-derived inflammatory cytokines, downregulation of adhesion molecules on endothelial cells, improving the function of high-density lipoprotein, stabilizing atherosclerotic plaque remodeling, and reducing procoagulant states.
The TARGET trial
In a recent study of 17 patients with RA, Dr. Giles and his colleagues showed that TNF inhibitor therapy with either adalimumab (Humira) or etanercept significantly reduced aortic inflammation as measured by baseline and 8-week fluorodeoxyglucose (FDG) PET-CT.
“Is this proof that this helps? It’s not proof; there’s no control group, we don’t know that this is not the natural progression of vascular inflammation in these patients,” he said.
However, the findings were suggestive enough to prompt the launch of the TARGET trial, which is now enrolling patients at centers in the United States and Canada, Dr. Giles said.
The TARGET trial is a project involving his team at Columbia University along with researchers from Brigham and Women’s Hospital, Boston. They plan to enroll 200 RA patients without CVD who have an inadequate response to methotrexate. Participants will be randomized to receive an added TNF inhibitor or added triple therapy, and the primary outcome will be changes in inflammation in the aortic and carotid arteries on FDG PET-CT at 6 months versus baseline.
“So stay tuned and hopefully we’ll have some good information about the effect of two different types of treatments for rheumatoid arthritis on vascular inflammation,” Dr. Giles said.
A final question he addressed is whether the RA-CVD risk link is really a problem that has already been solved – one that “we’re just learning about after the fact.”
“The answer is partially yes and partially no,” he said.
The most up-to-date estimate of whether RA patients have a problem with CVD comes from a Swedish population-based study of more than 15,700 RA patients and nearly 70,900 comparators, which was published in 2018 and showed across-the-board declines in CVD rates over time.
RA and non-RA patients experienced an overall 40% reduction in acute coronary syndromes between 1997 and 2014, but the relative difference in event rates between the groups persisted (Ann Rheum Dis. 2017;76:1642-7).
“There is still a gap ... so we haven’t answered this question yet,” he said, adding that “the rates have been reduced, but we want those rates to be equal or maybe even less.
“Why can’t RA patients have less cardiovascular disease if we’re using drugs that are so effective for treating the inflammatory component of atherogenesis?” he asked.
The authors of the study noted that most RA patients in Sweden are in low disease activity by 3-6 months, so they were “a little confounded by why there is no equalization of these rates as of yet,” he said.
“I think we still have more to learn about this problem, and it is still a problem in our patients,” Dr. Giles said.
Dr. Giles is a consultant for Genentech, Lilly, Horizon, Bristol-Myers Squibb, and UCB, and he has received grant support from Pfizer.
A variety of trials, some recent and some a decade old, have highlighted the role of inflammation on cardiovascular disease risk in both patients with and without rheumatoid arthritis, spurring greater interest in alleviating inflammation across a wide range of patients, Jon T. Giles, MD, said at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
However, questions remain about the unique contributions of inflammation to CVD risk in RA patients and the effect of RA treatments on that risk, which future studies hope to answer.
Hints of inflammation’s effects in non-RA patients
The JUPITER trial published more than a decade ago, for example, tested the effects of statins in nearly 18,000 older adults without rheumatoid arthritis (RA) who had elevated levels of inflammation, defined as a C-reactive protein (CRP) level of greater than 2 mg/L and low-density lipoprotein (LDL) cholesterol less than 130 mg/dL. Such patients would otherwise be considered low risk and not eligible for statin therapy, said Dr. Giles, a rheumatologist, epidemiologist, and clinical researcher in the division of rheumatology at Columbia University, New York.
A marked decrease in the incidence of cardiovascular disease (CVD) events was seen in those treated with statins, compared with those who received placebo, and all patient subgroups benefited; the number needed to treat to prevent one event was 32 at 5 years (N Engl J Med. 2008;359:2195-207).
The trial was remarkable in that it was stopped early for efficacy, he noted.
“So the question is: Should we be thinking about systemic inflammation as the real target here? And should RA patients who have elevated persistent levels of CRP really be the people that we’re thinking about?” he asked. “Obviously this needs to be tested; we don’t know.”
The more recent CANTOS trial looking at secondary CVD prevention in more than 10,000 non-RA patients with a prior myocardial infarction also highlighted the role of inflammation and provided “some support that decreasing inflammatory cytokines may be important for reducing [CVD] events,” he said (N Engl J Med. 2017;377:1119-31).
Participants were treated with the interleukin-1 inhibitor canakinumab (Ilaris) or placebo, and canakinumab was associated with about a 15% reduction in CVD events, providing “more proof of concept to look at the inflammatory innate immune contribution to CVD risk,” Dr. Giles said.
Treated patients had more infections, but they also had less gout, less arthritis, and less cancer than did those who received placebo, he noted.
Effect of RA treatments on CVD risk
The effects of existing treatments for RA also highlight the importance of inflammation in CVD risk in RA patients, he said, noting that data support a role for immunomodulators for risk reduction.
“There’s a lot of observational epidemiology in this space – mostly for methotrexate and [tumor necrosis factor (TNF)] inhibitors,” he said.
One analysis showed that across 8 cohort studies involving methotrexate, the disease-modifying antirheumatic agent reduced the risk of CVD events by 28%, and that across 16 cohort studies, TNF inhibitors reduced the risk by 30% (Ann Rheum Dis. 2015 Mar;74[3]:480-9).
All of the methotrexate studies showed a reduction, and almost all of the TNF inhibitor trials showed a reduction, Dr. Giles noted.
With respect to other non-TNF biologics, claims data suggest that abatacept (Orencia) is similar to the TNF inhibitor etanercept (Enbrel) with respect to CVD risk, and in a head-to-head, randomized clinical trial of more than 3,000 RA patients presented as a late-breaking abstract at the ACR annual meeting in 2016, Dr. Giles and his colleagues found similar cardiovascular safety between the anti-IL-6 receptor blocker tocilizumab (Actemra) and etanercept.
“I think we’ll know more about this in the near future,” he said.
As for the mechanisms of these agents, early data and animal models suggest that abatacept may play “a special role” in atherosclerosis reduction related to its effects on T cell CTLA-4 over-expression, and methotrexate also seems to have a number of “potential mechanistic benefits” that render it atheroprotective, he said.
The disappointing findings from the recently reported CIRT trial, which showed no benefit of methotrexate for secondary CVD prevention in non-RA patients (N Engl J Med. 2019;380:752-62), has dampened enthusiasm regarding methotrexate’s role here, but it is important to note that patients enrolled in CIRT, unlike those in JUPITER and CANTOS, were not enrolled based on elevated levels of CRP, Dr. Giles said.
Various studies of TNF inhibitors have shown atheroprotective effects through reductions in macrophage-derived inflammatory cytokines, downregulation of adhesion molecules on endothelial cells, improving the function of high-density lipoprotein, stabilizing atherosclerotic plaque remodeling, and reducing procoagulant states.
The TARGET trial
In a recent study of 17 patients with RA, Dr. Giles and his colleagues showed that TNF inhibitor therapy with either adalimumab (Humira) or etanercept significantly reduced aortic inflammation as measured by baseline and 8-week fluorodeoxyglucose (FDG) PET-CT.
“Is this proof that this helps? It’s not proof; there’s no control group, we don’t know that this is not the natural progression of vascular inflammation in these patients,” he said.
However, the findings were suggestive enough to prompt the launch of the TARGET trial, which is now enrolling patients at centers in the United States and Canada, Dr. Giles said.
The TARGET trial is a project involving his team at Columbia University along with researchers from Brigham and Women’s Hospital, Boston. They plan to enroll 200 RA patients without CVD who have an inadequate response to methotrexate. Participants will be randomized to receive an added TNF inhibitor or added triple therapy, and the primary outcome will be changes in inflammation in the aortic and carotid arteries on FDG PET-CT at 6 months versus baseline.
“So stay tuned and hopefully we’ll have some good information about the effect of two different types of treatments for rheumatoid arthritis on vascular inflammation,” Dr. Giles said.
A final question he addressed is whether the RA-CVD risk link is really a problem that has already been solved – one that “we’re just learning about after the fact.”
“The answer is partially yes and partially no,” he said.
The most up-to-date estimate of whether RA patients have a problem with CVD comes from a Swedish population-based study of more than 15,700 RA patients and nearly 70,900 comparators, which was published in 2018 and showed across-the-board declines in CVD rates over time.
RA and non-RA patients experienced an overall 40% reduction in acute coronary syndromes between 1997 and 2014, but the relative difference in event rates between the groups persisted (Ann Rheum Dis. 2017;76:1642-7).
“There is still a gap ... so we haven’t answered this question yet,” he said, adding that “the rates have been reduced, but we want those rates to be equal or maybe even less.
“Why can’t RA patients have less cardiovascular disease if we’re using drugs that are so effective for treating the inflammatory component of atherogenesis?” he asked.
The authors of the study noted that most RA patients in Sweden are in low disease activity by 3-6 months, so they were “a little confounded by why there is no equalization of these rates as of yet,” he said.
“I think we still have more to learn about this problem, and it is still a problem in our patients,” Dr. Giles said.
Dr. Giles is a consultant for Genentech, Lilly, Horizon, Bristol-Myers Squibb, and UCB, and he has received grant support from Pfizer.
A variety of trials, some recent and some a decade old, have highlighted the role of inflammation on cardiovascular disease risk in both patients with and without rheumatoid arthritis, spurring greater interest in alleviating inflammation across a wide range of patients, Jon T. Giles, MD, said at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
However, questions remain about the unique contributions of inflammation to CVD risk in RA patients and the effect of RA treatments on that risk, which future studies hope to answer.
Hints of inflammation’s effects in non-RA patients
The JUPITER trial published more than a decade ago, for example, tested the effects of statins in nearly 18,000 older adults without rheumatoid arthritis (RA) who had elevated levels of inflammation, defined as a C-reactive protein (CRP) level of greater than 2 mg/L and low-density lipoprotein (LDL) cholesterol less than 130 mg/dL. Such patients would otherwise be considered low risk and not eligible for statin therapy, said Dr. Giles, a rheumatologist, epidemiologist, and clinical researcher in the division of rheumatology at Columbia University, New York.
A marked decrease in the incidence of cardiovascular disease (CVD) events was seen in those treated with statins, compared with those who received placebo, and all patient subgroups benefited; the number needed to treat to prevent one event was 32 at 5 years (N Engl J Med. 2008;359:2195-207).
The trial was remarkable in that it was stopped early for efficacy, he noted.
“So the question is: Should we be thinking about systemic inflammation as the real target here? And should RA patients who have elevated persistent levels of CRP really be the people that we’re thinking about?” he asked. “Obviously this needs to be tested; we don’t know.”
The more recent CANTOS trial looking at secondary CVD prevention in more than 10,000 non-RA patients with a prior myocardial infarction also highlighted the role of inflammation and provided “some support that decreasing inflammatory cytokines may be important for reducing [CVD] events,” he said (N Engl J Med. 2017;377:1119-31).
Participants were treated with the interleukin-1 inhibitor canakinumab (Ilaris) or placebo, and canakinumab was associated with about a 15% reduction in CVD events, providing “more proof of concept to look at the inflammatory innate immune contribution to CVD risk,” Dr. Giles said.
Treated patients had more infections, but they also had less gout, less arthritis, and less cancer than did those who received placebo, he noted.
Effect of RA treatments on CVD risk
The effects of existing treatments for RA also highlight the importance of inflammation in CVD risk in RA patients, he said, noting that data support a role for immunomodulators for risk reduction.
“There’s a lot of observational epidemiology in this space – mostly for methotrexate and [tumor necrosis factor (TNF)] inhibitors,” he said.
One analysis showed that across 8 cohort studies involving methotrexate, the disease-modifying antirheumatic agent reduced the risk of CVD events by 28%, and that across 16 cohort studies, TNF inhibitors reduced the risk by 30% (Ann Rheum Dis. 2015 Mar;74[3]:480-9).
All of the methotrexate studies showed a reduction, and almost all of the TNF inhibitor trials showed a reduction, Dr. Giles noted.
With respect to other non-TNF biologics, claims data suggest that abatacept (Orencia) is similar to the TNF inhibitor etanercept (Enbrel) with respect to CVD risk, and in a head-to-head, randomized clinical trial of more than 3,000 RA patients presented as a late-breaking abstract at the ACR annual meeting in 2016, Dr. Giles and his colleagues found similar cardiovascular safety between the anti-IL-6 receptor blocker tocilizumab (Actemra) and etanercept.
“I think we’ll know more about this in the near future,” he said.
As for the mechanisms of these agents, early data and animal models suggest that abatacept may play “a special role” in atherosclerosis reduction related to its effects on T cell CTLA-4 over-expression, and methotrexate also seems to have a number of “potential mechanistic benefits” that render it atheroprotective, he said.
The disappointing findings from the recently reported CIRT trial, which showed no benefit of methotrexate for secondary CVD prevention in non-RA patients (N Engl J Med. 2019;380:752-62), has dampened enthusiasm regarding methotrexate’s role here, but it is important to note that patients enrolled in CIRT, unlike those in JUPITER and CANTOS, were not enrolled based on elevated levels of CRP, Dr. Giles said.
Various studies of TNF inhibitors have shown atheroprotective effects through reductions in macrophage-derived inflammatory cytokines, downregulation of adhesion molecules on endothelial cells, improving the function of high-density lipoprotein, stabilizing atherosclerotic plaque remodeling, and reducing procoagulant states.
The TARGET trial
In a recent study of 17 patients with RA, Dr. Giles and his colleagues showed that TNF inhibitor therapy with either adalimumab (Humira) or etanercept significantly reduced aortic inflammation as measured by baseline and 8-week fluorodeoxyglucose (FDG) PET-CT.
“Is this proof that this helps? It’s not proof; there’s no control group, we don’t know that this is not the natural progression of vascular inflammation in these patients,” he said.
However, the findings were suggestive enough to prompt the launch of the TARGET trial, which is now enrolling patients at centers in the United States and Canada, Dr. Giles said.
The TARGET trial is a project involving his team at Columbia University along with researchers from Brigham and Women’s Hospital, Boston. They plan to enroll 200 RA patients without CVD who have an inadequate response to methotrexate. Participants will be randomized to receive an added TNF inhibitor or added triple therapy, and the primary outcome will be changes in inflammation in the aortic and carotid arteries on FDG PET-CT at 6 months versus baseline.
“So stay tuned and hopefully we’ll have some good information about the effect of two different types of treatments for rheumatoid arthritis on vascular inflammation,” Dr. Giles said.
A final question he addressed is whether the RA-CVD risk link is really a problem that has already been solved – one that “we’re just learning about after the fact.”
“The answer is partially yes and partially no,” he said.
The most up-to-date estimate of whether RA patients have a problem with CVD comes from a Swedish population-based study of more than 15,700 RA patients and nearly 70,900 comparators, which was published in 2018 and showed across-the-board declines in CVD rates over time.
RA and non-RA patients experienced an overall 40% reduction in acute coronary syndromes between 1997 and 2014, but the relative difference in event rates between the groups persisted (Ann Rheum Dis. 2017;76:1642-7).
“There is still a gap ... so we haven’t answered this question yet,” he said, adding that “the rates have been reduced, but we want those rates to be equal or maybe even less.
“Why can’t RA patients have less cardiovascular disease if we’re using drugs that are so effective for treating the inflammatory component of atherogenesis?” he asked.
The authors of the study noted that most RA patients in Sweden are in low disease activity by 3-6 months, so they were “a little confounded by why there is no equalization of these rates as of yet,” he said.
“I think we still have more to learn about this problem, and it is still a problem in our patients,” Dr. Giles said.
Dr. Giles is a consultant for Genentech, Lilly, Horizon, Bristol-Myers Squibb, and UCB, and he has received grant support from Pfizer.
EXPERT ANALYSIS FROM THE WINTER RHEUMATOLOGY SYMPOSIUM
Brilinta reduces MACE in THEMIS trial
The maker of ticagrelor has released top-line results from the phase 3 trial known as THEMIS.
AstraZeneca announced that THEMIS met its primary endpoint of reduction of major adverse cardiovascular events (MACE) among patients with coronary artery disease (CAD) and type 2 diabetes with no history of heart attack or stroke. (MACE is a composite of cardiovascular death, heart attack, and stroke.)
The trial (NCT01991795) explored these risks by comparing ticagrelor (Brilinta) plus aspirin versus aspirin alone. The oral, reversibly binding, direct-acting P2Y12 receptor antagonist is currently indicated for reducing MACE among patients with acute coronary syndrome or a history of MI. According to the press release, the multinational, randomized, double-blind trial is exploring the use of ticagrelor/aspirin among patients with CAD and type 2 diabetes because of this population’s high risk and the lack of treatment options.
Gabriel Steg, MD, THEMIS cochair and professor at Université Paris–Diderot, said in the release that “patients who have both stable coronary artery disease and diabetes are a sizable group which remains at particularly high risk of major adverse cardiac events. The optimal long-term antiplatelet therapy in that group is not fully established.” He added that the full results from the THEMIS trial will be presented later this year.
Ticagrelor comes with risks of significant and sometimes fatal bleeding; as such it is contraindicated for patients with pathological bleeding risk or history of intracranial hemorrhage. Its use is also discouraged among patients with severe hepatic impairment and in patients who are breastfeeding. Although usually self-limiting when related to ticagrelor use, dyspnea was reported in about 14% of patients taking the drug. Dyspnea and bleeding were among the most common adverse reactions seen with ticagrelor.
The maker of ticagrelor has released top-line results from the phase 3 trial known as THEMIS.
AstraZeneca announced that THEMIS met its primary endpoint of reduction of major adverse cardiovascular events (MACE) among patients with coronary artery disease (CAD) and type 2 diabetes with no history of heart attack or stroke. (MACE is a composite of cardiovascular death, heart attack, and stroke.)
The trial (NCT01991795) explored these risks by comparing ticagrelor (Brilinta) plus aspirin versus aspirin alone. The oral, reversibly binding, direct-acting P2Y12 receptor antagonist is currently indicated for reducing MACE among patients with acute coronary syndrome or a history of MI. According to the press release, the multinational, randomized, double-blind trial is exploring the use of ticagrelor/aspirin among patients with CAD and type 2 diabetes because of this population’s high risk and the lack of treatment options.
Gabriel Steg, MD, THEMIS cochair and professor at Université Paris–Diderot, said in the release that “patients who have both stable coronary artery disease and diabetes are a sizable group which remains at particularly high risk of major adverse cardiac events. The optimal long-term antiplatelet therapy in that group is not fully established.” He added that the full results from the THEMIS trial will be presented later this year.
Ticagrelor comes with risks of significant and sometimes fatal bleeding; as such it is contraindicated for patients with pathological bleeding risk or history of intracranial hemorrhage. Its use is also discouraged among patients with severe hepatic impairment and in patients who are breastfeeding. Although usually self-limiting when related to ticagrelor use, dyspnea was reported in about 14% of patients taking the drug. Dyspnea and bleeding were among the most common adverse reactions seen with ticagrelor.
The maker of ticagrelor has released top-line results from the phase 3 trial known as THEMIS.
AstraZeneca announced that THEMIS met its primary endpoint of reduction of major adverse cardiovascular events (MACE) among patients with coronary artery disease (CAD) and type 2 diabetes with no history of heart attack or stroke. (MACE is a composite of cardiovascular death, heart attack, and stroke.)
The trial (NCT01991795) explored these risks by comparing ticagrelor (Brilinta) plus aspirin versus aspirin alone. The oral, reversibly binding, direct-acting P2Y12 receptor antagonist is currently indicated for reducing MACE among patients with acute coronary syndrome or a history of MI. According to the press release, the multinational, randomized, double-blind trial is exploring the use of ticagrelor/aspirin among patients with CAD and type 2 diabetes because of this population’s high risk and the lack of treatment options.
Gabriel Steg, MD, THEMIS cochair and professor at Université Paris–Diderot, said in the release that “patients who have both stable coronary artery disease and diabetes are a sizable group which remains at particularly high risk of major adverse cardiac events. The optimal long-term antiplatelet therapy in that group is not fully established.” He added that the full results from the THEMIS trial will be presented later this year.
Ticagrelor comes with risks of significant and sometimes fatal bleeding; as such it is contraindicated for patients with pathological bleeding risk or history of intracranial hemorrhage. Its use is also discouraged among patients with severe hepatic impairment and in patients who are breastfeeding. Although usually self-limiting when related to ticagrelor use, dyspnea was reported in about 14% of patients taking the drug. Dyspnea and bleeding were among the most common adverse reactions seen with ticagrelor.
Heart failure outcomes are worse in select HIV-infected individuals
People living with HIV (PLHIV) who have a low CD4 count or detectable viral load (VL) have an increased 30-day heart failure (HF) readmission rate as well as increased cardiovascular and all-cause mortality, compared with uninfected controls, according to Raza M. Alvi, MD, of Massachusetts General Hospital and Harvard Medical School, Boston, and his colleagues.
Overall, the 30-day HF hospital readmission rate was higher among PLHIV versus non-HIV–infected individuals (49% vs. 32%, P less than .001), according to the results of their cohort study of 2,308 individuals admitted to the hospital with decompensated HF.
PLHIV and the non-HIV control groups were both followed over 2 years with a median follow-up period of 19 months, the authors wrote in the American Heart Journal. Demographic make-up of the two groups was similar; in particular, there was no difference in blood pressure and heart rate between the PLHIV and non-HIV controls, suggesting that adherence with HF medications may be similar between groups. The cohorts differed primarily in that pulmonary artery systolic pressure was significantly higher (45 vs. 40 mm Hg; P less than .001) in the HIV group, as was cocaine use (36% vs. 19%; P less than .001) and hepatitis C virus (HCV) infection (13% vs. 7%; P less than .001).
The differing results between the two cohorts were primarily caused by the fact that, for PLHIV with HF, CD4 count and VL were risk factors for adverse outcomes among patients with all types of HF. (30-day HF readmission, cardiovascular [CV] mortality, and all-cause mortality), compared with those with CD4 count greater than or equal to 200 cells/mm3. In addition, a low CD4 count/high VL independently related to an increased 30-day HF readmission rate even after the researchers controlled for major traditional and nontraditional HF risk factors.
“Rates of 30-day HF readmission, CV mortality, and all-cause mortality are worse among individuals with a low CD4 count or nonsuppressed viral load,” the researchers concluded.
The National Institutes of Health sponsored the study. The authors reported that they had no conflicts.
SOURCE: Alvi RM et al. Am Heart J. 2019 Apr;210:39-48.
People living with HIV (PLHIV) who have a low CD4 count or detectable viral load (VL) have an increased 30-day heart failure (HF) readmission rate as well as increased cardiovascular and all-cause mortality, compared with uninfected controls, according to Raza M. Alvi, MD, of Massachusetts General Hospital and Harvard Medical School, Boston, and his colleagues.
Overall, the 30-day HF hospital readmission rate was higher among PLHIV versus non-HIV–infected individuals (49% vs. 32%, P less than .001), according to the results of their cohort study of 2,308 individuals admitted to the hospital with decompensated HF.
PLHIV and the non-HIV control groups were both followed over 2 years with a median follow-up period of 19 months, the authors wrote in the American Heart Journal. Demographic make-up of the two groups was similar; in particular, there was no difference in blood pressure and heart rate between the PLHIV and non-HIV controls, suggesting that adherence with HF medications may be similar between groups. The cohorts differed primarily in that pulmonary artery systolic pressure was significantly higher (45 vs. 40 mm Hg; P less than .001) in the HIV group, as was cocaine use (36% vs. 19%; P less than .001) and hepatitis C virus (HCV) infection (13% vs. 7%; P less than .001).
The differing results between the two cohorts were primarily caused by the fact that, for PLHIV with HF, CD4 count and VL were risk factors for adverse outcomes among patients with all types of HF. (30-day HF readmission, cardiovascular [CV] mortality, and all-cause mortality), compared with those with CD4 count greater than or equal to 200 cells/mm3. In addition, a low CD4 count/high VL independently related to an increased 30-day HF readmission rate even after the researchers controlled for major traditional and nontraditional HF risk factors.
“Rates of 30-day HF readmission, CV mortality, and all-cause mortality are worse among individuals with a low CD4 count or nonsuppressed viral load,” the researchers concluded.
The National Institutes of Health sponsored the study. The authors reported that they had no conflicts.
SOURCE: Alvi RM et al. Am Heart J. 2019 Apr;210:39-48.
People living with HIV (PLHIV) who have a low CD4 count or detectable viral load (VL) have an increased 30-day heart failure (HF) readmission rate as well as increased cardiovascular and all-cause mortality, compared with uninfected controls, according to Raza M. Alvi, MD, of Massachusetts General Hospital and Harvard Medical School, Boston, and his colleagues.
Overall, the 30-day HF hospital readmission rate was higher among PLHIV versus non-HIV–infected individuals (49% vs. 32%, P less than .001), according to the results of their cohort study of 2,308 individuals admitted to the hospital with decompensated HF.
PLHIV and the non-HIV control groups were both followed over 2 years with a median follow-up period of 19 months, the authors wrote in the American Heart Journal. Demographic make-up of the two groups was similar; in particular, there was no difference in blood pressure and heart rate between the PLHIV and non-HIV controls, suggesting that adherence with HF medications may be similar between groups. The cohorts differed primarily in that pulmonary artery systolic pressure was significantly higher (45 vs. 40 mm Hg; P less than .001) in the HIV group, as was cocaine use (36% vs. 19%; P less than .001) and hepatitis C virus (HCV) infection (13% vs. 7%; P less than .001).
The differing results between the two cohorts were primarily caused by the fact that, for PLHIV with HF, CD4 count and VL were risk factors for adverse outcomes among patients with all types of HF. (30-day HF readmission, cardiovascular [CV] mortality, and all-cause mortality), compared with those with CD4 count greater than or equal to 200 cells/mm3. In addition, a low CD4 count/high VL independently related to an increased 30-day HF readmission rate even after the researchers controlled for major traditional and nontraditional HF risk factors.
“Rates of 30-day HF readmission, CV mortality, and all-cause mortality are worse among individuals with a low CD4 count or nonsuppressed viral load,” the researchers concluded.
The National Institutes of Health sponsored the study. The authors reported that they had no conflicts.
SOURCE: Alvi RM et al. Am Heart J. 2019 Apr;210:39-48.
FROM THE AMERICAN HEART JOURNAL