User login
Hair follicle miniaturization common in persistent chemo-induced alopecia, case series suggests
and treatment with minoxidil (sometimes with antiandrogen therapy) was associated with improved hair density, according to a recently published retrospective case series.
“An improvement in hair density was observed in most of the patients treated with topical minoxidil or LDOM [low-dose oral minoxidil], with a more favorable outcome seen with LDOM with or without antiandrogens,” reported Bevin Bhoyrul, MBBS, of Sinclair Dermatology in Melbourne and coauthors from the United Kingdom and Germany.
The findings, published in JAMA Dermatology, suggest that pCIA “may be at least partly reversible,” they wrote.
The investigators analyzed the clinicopathologic characteristics of pCIA in 100 patients presenting to the hair clinics, as well as the results of trichoscopy performed in 90 of the patients and biopsies in 18. The researchers also assessed the effectiveness of treatment in 49 of these patients who met their criteria of completing at least 6 months of therapy with minoxidil.
Almost all patients in their series – 92% – were treated with taxanes and had more severe alopecia than those who weren’t exposed to taxanes (a median Sinclair scale grade of 4 vs. 2). Defined as absent or incomplete hair regrowth 6 months or more after completion of chemotherapy, pCIA has been increasingly reported in the literature, the authors note.
Of the 100 patients, all but one of whom were women, 39 had globally-reduced hair density that also involved the occipital area (diffuse alopecia), and 55 patients had thinning of the centroparietal scalp hair in a female pattern hair loss (FPHL) distribution. Patients presented between November 2011 and February 2020 and had a mean age of 54. The Sinclair scale, which grades from 1 to 5, was used to assess the severity of hair loss in these patients.
Five female patients had bitemporal recession or balding of the crown in a male pattern hair loss (MPHL) distribution, and the one male patient had extensive baldness resembling Hamilton-Norwood type VII.
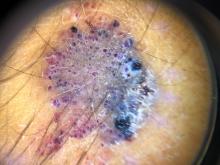
The vast majority of patients who had trichoscopy performed – 88% – had trichoscopic features that were “indistinguishable from those of androgenetic alopecia,” most commonly hair shaft diameter variability, increased vellus hairs, and predominant single-hair follicular units, the authors reported.
Of the 18 patients who had biopsies, 14 had androgenetic alopecia-like features with decreased terminal hairs, increased vellus hairs, and fibrous streamers. The reduced terminal-to-vellus ratio characterizes hair follicle miniaturization, a hallmark of androgenetic alopecia, they said. (Two patients had cicatricial alopecia, and two had features of both.)
“The predominant phenotypes of pCIA show prominent vellus hairs both clinically and histologically, suggesting that terminal hair follicles undergo miniaturization,” Dr. Bhoyrul and coauthors wrote. Among the 49 patients who completed 6 months or more of treatment, the median Sinclair grade improved from 4 to 3 in 21 patients who received topical minoxidil for a median duration of 17 months; from 4 to 2.5 in 18 patients who received LDOM for a median duration of 29 months; and from 5 to 3 in 10 patients who received LDOM combined with an antiandrogen, such as spironolactone, for a median of 33 months.
Almost three-quarters of the patients in the series received adjuvant hormone therapy, which is independently associated with hair loss, the authors noted. However, there was no statistically significant difference in the pattern or severity of alopecia between patients who were treated with endocrine therapy and those who weren’t.
Asked to comment on the study and on the care of patients with pCIA, Maria K. Hordinsky, MD, professor and chair of dermatology at the University of Minnesota, Minneapolis, and an expert in hair diseases, said the case series points to the value of biopsies in patients with pCIA.
“Some patients really do have a loss of hair follicles,” she said. “But if you do a biopsy and see this miniaturization of the hair follicles, then we have tools to stimulate the hair follicles to become more normal. ... These patients can be successfully treated.”
For patients who do not want to do a biopsy, a therapeutic trial is acceptable. “But knowing helps set expectations for people,” she said. “If the follicles are really small, it will take months [of therapy].”
In addition to topical minoxidil, which she said “is always a good tool,” and LDOM, which is “becoming very popular,” Dr. Hordinsky has used low-level laser light successfully. She cautioned against the use of spironolactone and other hair-growth promoting therapies with potentially significant hormonal impacts unless there is discussion between the dermatologist, oncologist, and patient.
The authors of the case series called in their conclusion for wider use of hair-protective strategies such as scalp hypothermia. But Dr. Hordinsky said that, in the United States, there are divergent opinions among oncologists and among cancer centers on the use of scalp cooling and whether or not it might lessen response to chemotherapy.
More research is needed, she noted, on chemotherapy-induced hair loss in patients of different races and ethnicities. Of the 100 patients in the case series, 91 were European; others were Afro Caribbean, Middle Eastern, and South Asian.
Dr. Bhoyrul is supported by the Geoffrey Dowling Fellowship from the British Association of Dermatologists. One coauthor disclosed serving as a principal investigator and/or scientific board member for various pharmaceutical companies, outside of the submitted study. There were no other disclosures reported. Dr. Hordinsky, the immediate past president of the American Hair Research Society and a section editor for hair diseases in UpToDate, had no relevant disclosures.
and treatment with minoxidil (sometimes with antiandrogen therapy) was associated with improved hair density, according to a recently published retrospective case series.
“An improvement in hair density was observed in most of the patients treated with topical minoxidil or LDOM [low-dose oral minoxidil], with a more favorable outcome seen with LDOM with or without antiandrogens,” reported Bevin Bhoyrul, MBBS, of Sinclair Dermatology in Melbourne and coauthors from the United Kingdom and Germany.
The findings, published in JAMA Dermatology, suggest that pCIA “may be at least partly reversible,” they wrote.
The investigators analyzed the clinicopathologic characteristics of pCIA in 100 patients presenting to the hair clinics, as well as the results of trichoscopy performed in 90 of the patients and biopsies in 18. The researchers also assessed the effectiveness of treatment in 49 of these patients who met their criteria of completing at least 6 months of therapy with minoxidil.
Almost all patients in their series – 92% – were treated with taxanes and had more severe alopecia than those who weren’t exposed to taxanes (a median Sinclair scale grade of 4 vs. 2). Defined as absent or incomplete hair regrowth 6 months or more after completion of chemotherapy, pCIA has been increasingly reported in the literature, the authors note.
Of the 100 patients, all but one of whom were women, 39 had globally-reduced hair density that also involved the occipital area (diffuse alopecia), and 55 patients had thinning of the centroparietal scalp hair in a female pattern hair loss (FPHL) distribution. Patients presented between November 2011 and February 2020 and had a mean age of 54. The Sinclair scale, which grades from 1 to 5, was used to assess the severity of hair loss in these patients.
Five female patients had bitemporal recession or balding of the crown in a male pattern hair loss (MPHL) distribution, and the one male patient had extensive baldness resembling Hamilton-Norwood type VII.
The vast majority of patients who had trichoscopy performed – 88% – had trichoscopic features that were “indistinguishable from those of androgenetic alopecia,” most commonly hair shaft diameter variability, increased vellus hairs, and predominant single-hair follicular units, the authors reported.
Of the 18 patients who had biopsies, 14 had androgenetic alopecia-like features with decreased terminal hairs, increased vellus hairs, and fibrous streamers. The reduced terminal-to-vellus ratio characterizes hair follicle miniaturization, a hallmark of androgenetic alopecia, they said. (Two patients had cicatricial alopecia, and two had features of both.)
“The predominant phenotypes of pCIA show prominent vellus hairs both clinically and histologically, suggesting that terminal hair follicles undergo miniaturization,” Dr. Bhoyrul and coauthors wrote. Among the 49 patients who completed 6 months or more of treatment, the median Sinclair grade improved from 4 to 3 in 21 patients who received topical minoxidil for a median duration of 17 months; from 4 to 2.5 in 18 patients who received LDOM for a median duration of 29 months; and from 5 to 3 in 10 patients who received LDOM combined with an antiandrogen, such as spironolactone, for a median of 33 months.
Almost three-quarters of the patients in the series received adjuvant hormone therapy, which is independently associated with hair loss, the authors noted. However, there was no statistically significant difference in the pattern or severity of alopecia between patients who were treated with endocrine therapy and those who weren’t.
Asked to comment on the study and on the care of patients with pCIA, Maria K. Hordinsky, MD, professor and chair of dermatology at the University of Minnesota, Minneapolis, and an expert in hair diseases, said the case series points to the value of biopsies in patients with pCIA.
“Some patients really do have a loss of hair follicles,” she said. “But if you do a biopsy and see this miniaturization of the hair follicles, then we have tools to stimulate the hair follicles to become more normal. ... These patients can be successfully treated.”
For patients who do not want to do a biopsy, a therapeutic trial is acceptable. “But knowing helps set expectations for people,” she said. “If the follicles are really small, it will take months [of therapy].”
In addition to topical minoxidil, which she said “is always a good tool,” and LDOM, which is “becoming very popular,” Dr. Hordinsky has used low-level laser light successfully. She cautioned against the use of spironolactone and other hair-growth promoting therapies with potentially significant hormonal impacts unless there is discussion between the dermatologist, oncologist, and patient.
The authors of the case series called in their conclusion for wider use of hair-protective strategies such as scalp hypothermia. But Dr. Hordinsky said that, in the United States, there are divergent opinions among oncologists and among cancer centers on the use of scalp cooling and whether or not it might lessen response to chemotherapy.
More research is needed, she noted, on chemotherapy-induced hair loss in patients of different races and ethnicities. Of the 100 patients in the case series, 91 were European; others were Afro Caribbean, Middle Eastern, and South Asian.
Dr. Bhoyrul is supported by the Geoffrey Dowling Fellowship from the British Association of Dermatologists. One coauthor disclosed serving as a principal investigator and/or scientific board member for various pharmaceutical companies, outside of the submitted study. There were no other disclosures reported. Dr. Hordinsky, the immediate past president of the American Hair Research Society and a section editor for hair diseases in UpToDate, had no relevant disclosures.
and treatment with minoxidil (sometimes with antiandrogen therapy) was associated with improved hair density, according to a recently published retrospective case series.
“An improvement in hair density was observed in most of the patients treated with topical minoxidil or LDOM [low-dose oral minoxidil], with a more favorable outcome seen with LDOM with or without antiandrogens,” reported Bevin Bhoyrul, MBBS, of Sinclair Dermatology in Melbourne and coauthors from the United Kingdom and Germany.
The findings, published in JAMA Dermatology, suggest that pCIA “may be at least partly reversible,” they wrote.
The investigators analyzed the clinicopathologic characteristics of pCIA in 100 patients presenting to the hair clinics, as well as the results of trichoscopy performed in 90 of the patients and biopsies in 18. The researchers also assessed the effectiveness of treatment in 49 of these patients who met their criteria of completing at least 6 months of therapy with minoxidil.
Almost all patients in their series – 92% – were treated with taxanes and had more severe alopecia than those who weren’t exposed to taxanes (a median Sinclair scale grade of 4 vs. 2). Defined as absent or incomplete hair regrowth 6 months or more after completion of chemotherapy, pCIA has been increasingly reported in the literature, the authors note.
Of the 100 patients, all but one of whom were women, 39 had globally-reduced hair density that also involved the occipital area (diffuse alopecia), and 55 patients had thinning of the centroparietal scalp hair in a female pattern hair loss (FPHL) distribution. Patients presented between November 2011 and February 2020 and had a mean age of 54. The Sinclair scale, which grades from 1 to 5, was used to assess the severity of hair loss in these patients.
Five female patients had bitemporal recession or balding of the crown in a male pattern hair loss (MPHL) distribution, and the one male patient had extensive baldness resembling Hamilton-Norwood type VII.
The vast majority of patients who had trichoscopy performed – 88% – had trichoscopic features that were “indistinguishable from those of androgenetic alopecia,” most commonly hair shaft diameter variability, increased vellus hairs, and predominant single-hair follicular units, the authors reported.
Of the 18 patients who had biopsies, 14 had androgenetic alopecia-like features with decreased terminal hairs, increased vellus hairs, and fibrous streamers. The reduced terminal-to-vellus ratio characterizes hair follicle miniaturization, a hallmark of androgenetic alopecia, they said. (Two patients had cicatricial alopecia, and two had features of both.)
“The predominant phenotypes of pCIA show prominent vellus hairs both clinically and histologically, suggesting that terminal hair follicles undergo miniaturization,” Dr. Bhoyrul and coauthors wrote. Among the 49 patients who completed 6 months or more of treatment, the median Sinclair grade improved from 4 to 3 in 21 patients who received topical minoxidil for a median duration of 17 months; from 4 to 2.5 in 18 patients who received LDOM for a median duration of 29 months; and from 5 to 3 in 10 patients who received LDOM combined with an antiandrogen, such as spironolactone, for a median of 33 months.
Almost three-quarters of the patients in the series received adjuvant hormone therapy, which is independently associated with hair loss, the authors noted. However, there was no statistically significant difference in the pattern or severity of alopecia between patients who were treated with endocrine therapy and those who weren’t.
Asked to comment on the study and on the care of patients with pCIA, Maria K. Hordinsky, MD, professor and chair of dermatology at the University of Minnesota, Minneapolis, and an expert in hair diseases, said the case series points to the value of biopsies in patients with pCIA.
“Some patients really do have a loss of hair follicles,” she said. “But if you do a biopsy and see this miniaturization of the hair follicles, then we have tools to stimulate the hair follicles to become more normal. ... These patients can be successfully treated.”
For patients who do not want to do a biopsy, a therapeutic trial is acceptable. “But knowing helps set expectations for people,” she said. “If the follicles are really small, it will take months [of therapy].”
In addition to topical minoxidil, which she said “is always a good tool,” and LDOM, which is “becoming very popular,” Dr. Hordinsky has used low-level laser light successfully. She cautioned against the use of spironolactone and other hair-growth promoting therapies with potentially significant hormonal impacts unless there is discussion between the dermatologist, oncologist, and patient.
The authors of the case series called in their conclusion for wider use of hair-protective strategies such as scalp hypothermia. But Dr. Hordinsky said that, in the United States, there are divergent opinions among oncologists and among cancer centers on the use of scalp cooling and whether or not it might lessen response to chemotherapy.
More research is needed, she noted, on chemotherapy-induced hair loss in patients of different races and ethnicities. Of the 100 patients in the case series, 91 were European; others were Afro Caribbean, Middle Eastern, and South Asian.
Dr. Bhoyrul is supported by the Geoffrey Dowling Fellowship from the British Association of Dermatologists. One coauthor disclosed serving as a principal investigator and/or scientific board member for various pharmaceutical companies, outside of the submitted study. There were no other disclosures reported. Dr. Hordinsky, the immediate past president of the American Hair Research Society and a section editor for hair diseases in UpToDate, had no relevant disclosures.
FROM JAMA DERMATOLOGY
Evaluations of novel approaches to treating NF-1 tumors are underway
In the clinical experience of R. Rox Anderson, MD, currently available treatment options for benign tumors caused by neurofibromatosis type 1 (NF-1) are not acceptable.
“Simply removing the tumors with surgery is not the answer,” Dr. Anderson, a dermatologist who is the director of the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston, said during a virtual course on laser and aesthetic skin therapy. “We need a way to inhibit the cutaneous neurofibromatosis early in life and prevent disfigurement that occurs when kids become adults.
“Kids with NF-1 are born looking normal,” he said. “They have café au lait macules and Lisch nodules in their eye, but they’re normal-looking kids. By early adulthood, many will grow hundreds of tumors that are disfiguring.”
In patients with NF-1, surgical excision works for cutaneous tumors but is expensive and not widely available, and is usually not covered by health insurance. “Plus, you have these adults who have already been through a lot of trauma, with the disfigurement in their lives, who have to be put under general anesthesia to remove a large number of tumors,” Dr. Anderson said at the meeting, which was named What’s the Truth and was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. Cryotherapy is a minimally invasive way to treat cutaneous neurofibroma tumors, “but this destroys the overlying skin, so you get unwanted destruction,” he said. “I like the idea of selecting heating, but we don’t know yet by what method.”
Dr. Anderson and his colleagues just launched a comparative clinical They plan to perform one or more treatment methods per patient in a single treatment session, then follow up at least 6 months later. Baseline and untreated cutaneous NF lesions will serve as controls. The researchers plan to conduct three-dimensional imaging, clinical assessments, and evaluate pain and other subjective measures.
Use of deoxycholate in a pilot trial was well tolerated and induced tumor regression in adults with cutaneous NF, he said.
Dr. Anderson noted that other researchers are studying the potential role of topical or local mitogen-activated protein kinase (MEK) inhibitors for these tumors. “Systemic MEK inhibitors are effective for plexiform neuromas, but cause significant cutaneous side effects,” he said. A “soft” MEK inhibitor, NFX-179 is rapidly metabolized such that high drug levels are achieved in skin without systemic drug levels. However, Dr. Anderson said that it remains unclear if this approach will prevent cutaneous NF tumors from forming, arrest their growth, or induce their regression.
Dr. Anderson reported having received research funding and/or consulting fees from numerous device and pharmaceutical companies.
Commentary by Lawrence F. Eichenfield, MD
Neurofibromatosis type 1 (NF1) is a common genodermatosis, associated with the development of neurofibromas derived from nerves, soft tissue, and skin. Cutaneous NFs often develop in later childhood onward and may be deforming, associated with pruritus, pain, and significant effect on quality of life. Dr. Anderson is a world leader in laser treatment, having developed the theories behind laser development for medical usage, as well as the laser technology used for vascular birthmarks and hair removal, laser and cooling techniques targeting fat, and “fractionating” laser energy, which has revolutionized scar management. We look forward to his group’s insights into better management of NF1 lesions!
Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children's Hospital-San Diego. He is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego. He disclosed that he has served as an investigator and/or consultant to AbbVie, Lilly, Pfizer, Regeneron, Sanofi-Genzyme, and Verrica.
A version of this article first appeared on Medscape.com.
This article was updated 6/18/22.
In the clinical experience of R. Rox Anderson, MD, currently available treatment options for benign tumors caused by neurofibromatosis type 1 (NF-1) are not acceptable.
“Simply removing the tumors with surgery is not the answer,” Dr. Anderson, a dermatologist who is the director of the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston, said during a virtual course on laser and aesthetic skin therapy. “We need a way to inhibit the cutaneous neurofibromatosis early in life and prevent disfigurement that occurs when kids become adults.
“Kids with NF-1 are born looking normal,” he said. “They have café au lait macules and Lisch nodules in their eye, but they’re normal-looking kids. By early adulthood, many will grow hundreds of tumors that are disfiguring.”
In patients with NF-1, surgical excision works for cutaneous tumors but is expensive and not widely available, and is usually not covered by health insurance. “Plus, you have these adults who have already been through a lot of trauma, with the disfigurement in their lives, who have to be put under general anesthesia to remove a large number of tumors,” Dr. Anderson said at the meeting, which was named What’s the Truth and was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. Cryotherapy is a minimally invasive way to treat cutaneous neurofibroma tumors, “but this destroys the overlying skin, so you get unwanted destruction,” he said. “I like the idea of selecting heating, but we don’t know yet by what method.”
Dr. Anderson and his colleagues just launched a comparative clinical They plan to perform one or more treatment methods per patient in a single treatment session, then follow up at least 6 months later. Baseline and untreated cutaneous NF lesions will serve as controls. The researchers plan to conduct three-dimensional imaging, clinical assessments, and evaluate pain and other subjective measures.
Use of deoxycholate in a pilot trial was well tolerated and induced tumor regression in adults with cutaneous NF, he said.
Dr. Anderson noted that other researchers are studying the potential role of topical or local mitogen-activated protein kinase (MEK) inhibitors for these tumors. “Systemic MEK inhibitors are effective for plexiform neuromas, but cause significant cutaneous side effects,” he said. A “soft” MEK inhibitor, NFX-179 is rapidly metabolized such that high drug levels are achieved in skin without systemic drug levels. However, Dr. Anderson said that it remains unclear if this approach will prevent cutaneous NF tumors from forming, arrest their growth, or induce their regression.
Dr. Anderson reported having received research funding and/or consulting fees from numerous device and pharmaceutical companies.
Commentary by Lawrence F. Eichenfield, MD
Neurofibromatosis type 1 (NF1) is a common genodermatosis, associated with the development of neurofibromas derived from nerves, soft tissue, and skin. Cutaneous NFs often develop in later childhood onward and may be deforming, associated with pruritus, pain, and significant effect on quality of life. Dr. Anderson is a world leader in laser treatment, having developed the theories behind laser development for medical usage, as well as the laser technology used for vascular birthmarks and hair removal, laser and cooling techniques targeting fat, and “fractionating” laser energy, which has revolutionized scar management. We look forward to his group’s insights into better management of NF1 lesions!
Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children's Hospital-San Diego. He is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego. He disclosed that he has served as an investigator and/or consultant to AbbVie, Lilly, Pfizer, Regeneron, Sanofi-Genzyme, and Verrica.
A version of this article first appeared on Medscape.com.
This article was updated 6/18/22.
In the clinical experience of R. Rox Anderson, MD, currently available treatment options for benign tumors caused by neurofibromatosis type 1 (NF-1) are not acceptable.
“Simply removing the tumors with surgery is not the answer,” Dr. Anderson, a dermatologist who is the director of the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston, said during a virtual course on laser and aesthetic skin therapy. “We need a way to inhibit the cutaneous neurofibromatosis early in life and prevent disfigurement that occurs when kids become adults.
“Kids with NF-1 are born looking normal,” he said. “They have café au lait macules and Lisch nodules in their eye, but they’re normal-looking kids. By early adulthood, many will grow hundreds of tumors that are disfiguring.”
In patients with NF-1, surgical excision works for cutaneous tumors but is expensive and not widely available, and is usually not covered by health insurance. “Plus, you have these adults who have already been through a lot of trauma, with the disfigurement in their lives, who have to be put under general anesthesia to remove a large number of tumors,” Dr. Anderson said at the meeting, which was named What’s the Truth and was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. Cryotherapy is a minimally invasive way to treat cutaneous neurofibroma tumors, “but this destroys the overlying skin, so you get unwanted destruction,” he said. “I like the idea of selecting heating, but we don’t know yet by what method.”
Dr. Anderson and his colleagues just launched a comparative clinical They plan to perform one or more treatment methods per patient in a single treatment session, then follow up at least 6 months later. Baseline and untreated cutaneous NF lesions will serve as controls. The researchers plan to conduct three-dimensional imaging, clinical assessments, and evaluate pain and other subjective measures.
Use of deoxycholate in a pilot trial was well tolerated and induced tumor regression in adults with cutaneous NF, he said.
Dr. Anderson noted that other researchers are studying the potential role of topical or local mitogen-activated protein kinase (MEK) inhibitors for these tumors. “Systemic MEK inhibitors are effective for plexiform neuromas, but cause significant cutaneous side effects,” he said. A “soft” MEK inhibitor, NFX-179 is rapidly metabolized such that high drug levels are achieved in skin without systemic drug levels. However, Dr. Anderson said that it remains unclear if this approach will prevent cutaneous NF tumors from forming, arrest their growth, or induce their regression.
Dr. Anderson reported having received research funding and/or consulting fees from numerous device and pharmaceutical companies.
Commentary by Lawrence F. Eichenfield, MD
Neurofibromatosis type 1 (NF1) is a common genodermatosis, associated with the development of neurofibromas derived from nerves, soft tissue, and skin. Cutaneous NFs often develop in later childhood onward and may be deforming, associated with pruritus, pain, and significant effect on quality of life. Dr. Anderson is a world leader in laser treatment, having developed the theories behind laser development for medical usage, as well as the laser technology used for vascular birthmarks and hair removal, laser and cooling techniques targeting fat, and “fractionating” laser energy, which has revolutionized scar management. We look forward to his group’s insights into better management of NF1 lesions!
Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children's Hospital-San Diego. He is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego. He disclosed that he has served as an investigator and/or consultant to AbbVie, Lilly, Pfizer, Regeneron, Sanofi-Genzyme, and Verrica.
A version of this article first appeared on Medscape.com.
This article was updated 6/18/22.
FROM A LASER & AESTHETIC SKIN THERAPY COURSE
Sunscreen, other sun-protective habits not linked with poorer bone health, fractures
Using , according to a new study that included more than 3,000 men and women.
“We have objective data for the first time, and in a large-scale representative population of the U.S. adults, to indicate sun protection is not associated with negative bone-related outcomes,” said study lead author Mohsen Afarideh, MD, MPH, a postdoctoral research fellow at the autoimmune skin diseases unit at the University of Pennsylvania, Philadelphia.
The study, published online in JAMA Dermatology, goes a step further than previous research by others that has found sunscreen use does not compromise vitamin D synthesis and has little effect on circulating 25-hydroxyvitamin D levels.
In the new study, researchers looked at three sun-protective behaviors – sunscreen use, staying in the shade, wearing long sleeves – and their effects on bone mineral density and the risk of fractures.
While the effects of sun-protective habits on blood levels of vitamin D and BMD scores are important, ‘’what we are more interested to know is if the sun-protective behaviors actually cause or increase the risk of fracture,” Dr. Afarideh said in an interview. “The answer to that is a firm ‘No.’ These data are very reassuring and will help clinicians to keep recommending sun protection to the public.”
Study details
Dr. Afarideh and his colleagues from the Mayo Clinic in Rochester, Minn., looked at data from the National Health and Nutrition Examination Survey (NHANES) from 2017 to 2018, obtaining final information on 3,403 men and women, ages 20-59, who completed a dermatology questionnaire The men and women reported on the three sun-protective habits, and noted whether they followed these practices always or most of the time, sometimes, or never or rarely.
The frequency of the three behaviors was not widespread. Frequent staying in the shade was reported by 31.6% of the sample, wearing long sleeves by 11.8%, and sunscreen use by 26.1%.
The researchers also had data on the participants’ bone mineral density (BMD) scores along with dietary information such as milk consumption, vitamin D supplement use, taking steroid drugs, and exercise activity.
“Moderate sunscreen use was linked with a slightly lower lumbar BMD score,” Dr. Afarideh said, which was “the only significant association that could be interpreted as concerning.” And this was more likely to be seen in older respondents, he said.
However, otherwise they found the practice of the three behaviors was not associated with lower total or site-specific BMD z scores, nor was it linked with an increased risk of osteoporotic fractures. (The BMD z score compares an individual’s bone density to the average bone density of someone their same age and gender.)
The focus on fracture risk is the more important outcome, Dr. Afarideh said. And they found no increased risk overall of osteoporotic fractures in those who practiced sun-protective behaviors.
Moderate to frequent staying in the shade was actually linked with a reduced prevalence of spine fractures in the multivariate model (odds ratio, 0.19; 95% confidence interval, 0.04-0.86, P = .02). The researchers say that may be attributable to these respondents also being careful in other areas of life, such as avoiding falls and not participating in high-risk activities that would increase the chance of fractures. “However, this is just an assumption,” Dr. Afarideh said.
Expert perspectives
Other dermatologists not involved in the new research said the study results provide some “real-world” information that’s valuable for clinicians to share with patients.
“I think this is an important study on multiple levels,” said Henry W. Lim, MD, a former president of the American Academy of Dermatology who is a member of the department of dermatology and senior vice president of academic affairs at Henry Ford Health System, Detroit. “It is a well-done study, involving a large number. It is a real-life situation, asking people their photo protective behaviors and then looking at their bone mineral density.” The bottom line, he said: “Bone health is not affected by photo protection habits in real life.”
The findings are important but not surprising, said Antony R. Young, PhD, emeritus professor of experimental photobiology at St. John’s Institute of Dermatology, King’s College, London, who has researched sunscreens and vitamin D status. “My study showed that correct sunscreen use, albeit with a relatively low SPF of 15, did prevent sunburn in a high UVR [ultraviolet radiation] environment but did allow very good vitamin D synthesis. I think this is because the necessary dose of UVB is very low.”
Michele Green, MD, a New York dermatologist and clinical staff member at Lenox Hill Hospital there, said she often hears concerns about bone health from patients. “Every week, patients ask, ‘Why would I wear sunblock? Don’t I need sun for bone health? Don’t I need it for vitamin D?’’’
Now, she said, ‘’Dermatologists can point to the study and say ‘Don’t worry.’ It clarifies that using sunscreen won’t cause you to have osteoporosis.’’
Dr. Afarideh, who was a postdoctoral research fellow at the Mayo Clinic, and his coauthors, Megha M. Tollefson, MD, and Julio C. Sartori-Valinotti, of the Mayo Clinic, and Dr. Green had no disclosures. Dr. Lim and Dr. Young consult for the sunscreen industry.
Using , according to a new study that included more than 3,000 men and women.
“We have objective data for the first time, and in a large-scale representative population of the U.S. adults, to indicate sun protection is not associated with negative bone-related outcomes,” said study lead author Mohsen Afarideh, MD, MPH, a postdoctoral research fellow at the autoimmune skin diseases unit at the University of Pennsylvania, Philadelphia.
The study, published online in JAMA Dermatology, goes a step further than previous research by others that has found sunscreen use does not compromise vitamin D synthesis and has little effect on circulating 25-hydroxyvitamin D levels.
In the new study, researchers looked at three sun-protective behaviors – sunscreen use, staying in the shade, wearing long sleeves – and their effects on bone mineral density and the risk of fractures.
While the effects of sun-protective habits on blood levels of vitamin D and BMD scores are important, ‘’what we are more interested to know is if the sun-protective behaviors actually cause or increase the risk of fracture,” Dr. Afarideh said in an interview. “The answer to that is a firm ‘No.’ These data are very reassuring and will help clinicians to keep recommending sun protection to the public.”
Study details
Dr. Afarideh and his colleagues from the Mayo Clinic in Rochester, Minn., looked at data from the National Health and Nutrition Examination Survey (NHANES) from 2017 to 2018, obtaining final information on 3,403 men and women, ages 20-59, who completed a dermatology questionnaire The men and women reported on the three sun-protective habits, and noted whether they followed these practices always or most of the time, sometimes, or never or rarely.
The frequency of the three behaviors was not widespread. Frequent staying in the shade was reported by 31.6% of the sample, wearing long sleeves by 11.8%, and sunscreen use by 26.1%.
The researchers also had data on the participants’ bone mineral density (BMD) scores along with dietary information such as milk consumption, vitamin D supplement use, taking steroid drugs, and exercise activity.
“Moderate sunscreen use was linked with a slightly lower lumbar BMD score,” Dr. Afarideh said, which was “the only significant association that could be interpreted as concerning.” And this was more likely to be seen in older respondents, he said.
However, otherwise they found the practice of the three behaviors was not associated with lower total or site-specific BMD z scores, nor was it linked with an increased risk of osteoporotic fractures. (The BMD z score compares an individual’s bone density to the average bone density of someone their same age and gender.)
The focus on fracture risk is the more important outcome, Dr. Afarideh said. And they found no increased risk overall of osteoporotic fractures in those who practiced sun-protective behaviors.
Moderate to frequent staying in the shade was actually linked with a reduced prevalence of spine fractures in the multivariate model (odds ratio, 0.19; 95% confidence interval, 0.04-0.86, P = .02). The researchers say that may be attributable to these respondents also being careful in other areas of life, such as avoiding falls and not participating in high-risk activities that would increase the chance of fractures. “However, this is just an assumption,” Dr. Afarideh said.
Expert perspectives
Other dermatologists not involved in the new research said the study results provide some “real-world” information that’s valuable for clinicians to share with patients.
“I think this is an important study on multiple levels,” said Henry W. Lim, MD, a former president of the American Academy of Dermatology who is a member of the department of dermatology and senior vice president of academic affairs at Henry Ford Health System, Detroit. “It is a well-done study, involving a large number. It is a real-life situation, asking people their photo protective behaviors and then looking at their bone mineral density.” The bottom line, he said: “Bone health is not affected by photo protection habits in real life.”
The findings are important but not surprising, said Antony R. Young, PhD, emeritus professor of experimental photobiology at St. John’s Institute of Dermatology, King’s College, London, who has researched sunscreens and vitamin D status. “My study showed that correct sunscreen use, albeit with a relatively low SPF of 15, did prevent sunburn in a high UVR [ultraviolet radiation] environment but did allow very good vitamin D synthesis. I think this is because the necessary dose of UVB is very low.”
Michele Green, MD, a New York dermatologist and clinical staff member at Lenox Hill Hospital there, said she often hears concerns about bone health from patients. “Every week, patients ask, ‘Why would I wear sunblock? Don’t I need sun for bone health? Don’t I need it for vitamin D?’’’
Now, she said, ‘’Dermatologists can point to the study and say ‘Don’t worry.’ It clarifies that using sunscreen won’t cause you to have osteoporosis.’’
Dr. Afarideh, who was a postdoctoral research fellow at the Mayo Clinic, and his coauthors, Megha M. Tollefson, MD, and Julio C. Sartori-Valinotti, of the Mayo Clinic, and Dr. Green had no disclosures. Dr. Lim and Dr. Young consult for the sunscreen industry.
Using , according to a new study that included more than 3,000 men and women.
“We have objective data for the first time, and in a large-scale representative population of the U.S. adults, to indicate sun protection is not associated with negative bone-related outcomes,” said study lead author Mohsen Afarideh, MD, MPH, a postdoctoral research fellow at the autoimmune skin diseases unit at the University of Pennsylvania, Philadelphia.
The study, published online in JAMA Dermatology, goes a step further than previous research by others that has found sunscreen use does not compromise vitamin D synthesis and has little effect on circulating 25-hydroxyvitamin D levels.
In the new study, researchers looked at three sun-protective behaviors – sunscreen use, staying in the shade, wearing long sleeves – and their effects on bone mineral density and the risk of fractures.
While the effects of sun-protective habits on blood levels of vitamin D and BMD scores are important, ‘’what we are more interested to know is if the sun-protective behaviors actually cause or increase the risk of fracture,” Dr. Afarideh said in an interview. “The answer to that is a firm ‘No.’ These data are very reassuring and will help clinicians to keep recommending sun protection to the public.”
Study details
Dr. Afarideh and his colleagues from the Mayo Clinic in Rochester, Minn., looked at data from the National Health and Nutrition Examination Survey (NHANES) from 2017 to 2018, obtaining final information on 3,403 men and women, ages 20-59, who completed a dermatology questionnaire The men and women reported on the three sun-protective habits, and noted whether they followed these practices always or most of the time, sometimes, or never or rarely.
The frequency of the three behaviors was not widespread. Frequent staying in the shade was reported by 31.6% of the sample, wearing long sleeves by 11.8%, and sunscreen use by 26.1%.
The researchers also had data on the participants’ bone mineral density (BMD) scores along with dietary information such as milk consumption, vitamin D supplement use, taking steroid drugs, and exercise activity.
“Moderate sunscreen use was linked with a slightly lower lumbar BMD score,” Dr. Afarideh said, which was “the only significant association that could be interpreted as concerning.” And this was more likely to be seen in older respondents, he said.
However, otherwise they found the practice of the three behaviors was not associated with lower total or site-specific BMD z scores, nor was it linked with an increased risk of osteoporotic fractures. (The BMD z score compares an individual’s bone density to the average bone density of someone their same age and gender.)
The focus on fracture risk is the more important outcome, Dr. Afarideh said. And they found no increased risk overall of osteoporotic fractures in those who practiced sun-protective behaviors.
Moderate to frequent staying in the shade was actually linked with a reduced prevalence of spine fractures in the multivariate model (odds ratio, 0.19; 95% confidence interval, 0.04-0.86, P = .02). The researchers say that may be attributable to these respondents also being careful in other areas of life, such as avoiding falls and not participating in high-risk activities that would increase the chance of fractures. “However, this is just an assumption,” Dr. Afarideh said.
Expert perspectives
Other dermatologists not involved in the new research said the study results provide some “real-world” information that’s valuable for clinicians to share with patients.
“I think this is an important study on multiple levels,” said Henry W. Lim, MD, a former president of the American Academy of Dermatology who is a member of the department of dermatology and senior vice president of academic affairs at Henry Ford Health System, Detroit. “It is a well-done study, involving a large number. It is a real-life situation, asking people their photo protective behaviors and then looking at their bone mineral density.” The bottom line, he said: “Bone health is not affected by photo protection habits in real life.”
The findings are important but not surprising, said Antony R. Young, PhD, emeritus professor of experimental photobiology at St. John’s Institute of Dermatology, King’s College, London, who has researched sunscreens and vitamin D status. “My study showed that correct sunscreen use, albeit with a relatively low SPF of 15, did prevent sunburn in a high UVR [ultraviolet radiation] environment but did allow very good vitamin D synthesis. I think this is because the necessary dose of UVB is very low.”
Michele Green, MD, a New York dermatologist and clinical staff member at Lenox Hill Hospital there, said she often hears concerns about bone health from patients. “Every week, patients ask, ‘Why would I wear sunblock? Don’t I need sun for bone health? Don’t I need it for vitamin D?’’’
Now, she said, ‘’Dermatologists can point to the study and say ‘Don’t worry.’ It clarifies that using sunscreen won’t cause you to have osteoporosis.’’
Dr. Afarideh, who was a postdoctoral research fellow at the Mayo Clinic, and his coauthors, Megha M. Tollefson, MD, and Julio C. Sartori-Valinotti, of the Mayo Clinic, and Dr. Green had no disclosures. Dr. Lim and Dr. Young consult for the sunscreen industry.
FROM JAMA DERMATOLOGY
One of the keys to success on social media? Entertain and educate the public
Social media isn’t everyone’s cup of tea, but
“I admit that I’m somewhat obsessed with it. I kind of blame it on my work as a dermatologist, that I’m trying to grow my social media as well. It’s interesting to me, fascinating, and I want to understand it more. I think that’s the mindset you need to approach it with.”
Perhaps no other public figure in dermatology has enjoyed success in social media more than Dr. Lee, a board-certified dermatologist who practices in Upland, Calif. In the fall of 2014, she started using Instagram to provide followers a glimpse into her life as a dermatologist, everything from Mohs surgery and Botox to keloid removals and ear lobe repair surgeries. From this she formed her alter ego, “Dr. Pimple Popper,” and became a YouTube sensation, building 7.1 million subscribers over the course of a few years, amounting to 4.5 billion lifetime views. She also grew 12 million followers on TikTok, 4.4 million followers on Instagram, 3 million on Facebook, and more than 139,000 on Twitter. About 80% of her followers are women who range between 18 and 40 years of age.
During the meeting she offered five social media marketing tips for busy clinicians:
You have to ‘play’ to ‘win.’ Active participation in social media is required to develop followers. “You cannot delegate this content,” Dr. Lee said. “You can hire people to help you or leave the task to a social media-savvy medical assistant in your office, but the content should be your responsibility ultimately, because you are the physician,” she added. Not everyone chooses to participate in social media, but it’s also something not to shy away from out of intimidation. “There is some talent associated with it, but it takes a lot of persistence as well,” she said.
Patients come first. Protect them at all costs. Dr. Lee rarely posts the faces of patients she cares for unless they grant consent in advance. “I try to show the work that I do and the beauty of dermatology,” she said during the meeting, which was named “Laser & Aesthetic Skin Therapy: What’s the Truth?” and was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. She added that taking part in social media can help you improve communication skills by engaging with followers who like, share, or respond to the material posted. “When you look back at your posts objectively, you learn about yourself and how you relate to your patients,” she said. “It helps to hone my bedside manner and my skills as a dermatologist.”
Show that you are human. Many dermatologists and other “skin influencers” have established their presence on the Internet and may be direct competitors for patients, but that doesn’t mean you can’t establish your own identity. One way to stand out is by posting content related to your authentic self, such as a photo or video that shows you engaged in a hobby, dining at a favorite restaurant, or visiting a beloved vacation spot. “Your followers don’t want a robot, someone who thinks they’re amazing and can do everything,” said Dr. Lee, who stars in her own TV reality show on TLC. “Show that you have a funny side. You want them to fall in love with you and see a little bit of your world, whatever it might be. Charm the socks off of them.”
Entertain first, educate a close second. The main way you’re going to get people to follow and watch you is to provide some entertainment, “not at the expense of a patient or your practice, though,” she said. “Then you’re going to educate people. We dermatologists have something to teach the world because we are experts on skin, hair, and nails. You want to impart this knowledge in a way that captivates people.” It’s like the sense of accomplishment that comes from learning something new after reading a book or watching a movie, she explained. “You feel good about it, and you can take that knowledge with you somewhere else. I love it when kids come up to me and tell me they know what a lipoma is, what a cyst is, and what psoriasis is because they’ve seen my show, or because they follow me on social media. It’s wonderful because I can see that I’ve educated them.”
Be kind and don’t activate the trolls. Dr. Lee allows positivity and kindness to rule the day on her social media content. “This is what I try to relay to followers, but I also do not engage with the negativity,” she said. “Every now and then, there will be someone who tries to insult what you do or who insults you personally. If you engage with them, it almost invites them to do it more. It almost gives them the ability to fight with you. Try to stay above that; just put out goodness and kindness.”
Several years ago, YouTube and Instagram temporarily shut down Dr. Lee’s accounts because she posted graphic images of skin lesions and procedures – a practice that wasn’t so commonplace at the time. “Don’t just post a graphic image just to be graphic,” she advised. “Make sure it has an educational message associated with it. That will help to validate your content. Posting a warning sign that some images may be graphic could help, too.”
Dr. Lee reported having no relevant financial disclosures.
Social media isn’t everyone’s cup of tea, but
“I admit that I’m somewhat obsessed with it. I kind of blame it on my work as a dermatologist, that I’m trying to grow my social media as well. It’s interesting to me, fascinating, and I want to understand it more. I think that’s the mindset you need to approach it with.”
Perhaps no other public figure in dermatology has enjoyed success in social media more than Dr. Lee, a board-certified dermatologist who practices in Upland, Calif. In the fall of 2014, she started using Instagram to provide followers a glimpse into her life as a dermatologist, everything from Mohs surgery and Botox to keloid removals and ear lobe repair surgeries. From this she formed her alter ego, “Dr. Pimple Popper,” and became a YouTube sensation, building 7.1 million subscribers over the course of a few years, amounting to 4.5 billion lifetime views. She also grew 12 million followers on TikTok, 4.4 million followers on Instagram, 3 million on Facebook, and more than 139,000 on Twitter. About 80% of her followers are women who range between 18 and 40 years of age.
During the meeting she offered five social media marketing tips for busy clinicians:
You have to ‘play’ to ‘win.’ Active participation in social media is required to develop followers. “You cannot delegate this content,” Dr. Lee said. “You can hire people to help you or leave the task to a social media-savvy medical assistant in your office, but the content should be your responsibility ultimately, because you are the physician,” she added. Not everyone chooses to participate in social media, but it’s also something not to shy away from out of intimidation. “There is some talent associated with it, but it takes a lot of persistence as well,” she said.
Patients come first. Protect them at all costs. Dr. Lee rarely posts the faces of patients she cares for unless they grant consent in advance. “I try to show the work that I do and the beauty of dermatology,” she said during the meeting, which was named “Laser & Aesthetic Skin Therapy: What’s the Truth?” and was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. She added that taking part in social media can help you improve communication skills by engaging with followers who like, share, or respond to the material posted. “When you look back at your posts objectively, you learn about yourself and how you relate to your patients,” she said. “It helps to hone my bedside manner and my skills as a dermatologist.”
Show that you are human. Many dermatologists and other “skin influencers” have established their presence on the Internet and may be direct competitors for patients, but that doesn’t mean you can’t establish your own identity. One way to stand out is by posting content related to your authentic self, such as a photo or video that shows you engaged in a hobby, dining at a favorite restaurant, or visiting a beloved vacation spot. “Your followers don’t want a robot, someone who thinks they’re amazing and can do everything,” said Dr. Lee, who stars in her own TV reality show on TLC. “Show that you have a funny side. You want them to fall in love with you and see a little bit of your world, whatever it might be. Charm the socks off of them.”
Entertain first, educate a close second. The main way you’re going to get people to follow and watch you is to provide some entertainment, “not at the expense of a patient or your practice, though,” she said. “Then you’re going to educate people. We dermatologists have something to teach the world because we are experts on skin, hair, and nails. You want to impart this knowledge in a way that captivates people.” It’s like the sense of accomplishment that comes from learning something new after reading a book or watching a movie, she explained. “You feel good about it, and you can take that knowledge with you somewhere else. I love it when kids come up to me and tell me they know what a lipoma is, what a cyst is, and what psoriasis is because they’ve seen my show, or because they follow me on social media. It’s wonderful because I can see that I’ve educated them.”
Be kind and don’t activate the trolls. Dr. Lee allows positivity and kindness to rule the day on her social media content. “This is what I try to relay to followers, but I also do not engage with the negativity,” she said. “Every now and then, there will be someone who tries to insult what you do or who insults you personally. If you engage with them, it almost invites them to do it more. It almost gives them the ability to fight with you. Try to stay above that; just put out goodness and kindness.”
Several years ago, YouTube and Instagram temporarily shut down Dr. Lee’s accounts because she posted graphic images of skin lesions and procedures – a practice that wasn’t so commonplace at the time. “Don’t just post a graphic image just to be graphic,” she advised. “Make sure it has an educational message associated with it. That will help to validate your content. Posting a warning sign that some images may be graphic could help, too.”
Dr. Lee reported having no relevant financial disclosures.
Social media isn’t everyone’s cup of tea, but
“I admit that I’m somewhat obsessed with it. I kind of blame it on my work as a dermatologist, that I’m trying to grow my social media as well. It’s interesting to me, fascinating, and I want to understand it more. I think that’s the mindset you need to approach it with.”
Perhaps no other public figure in dermatology has enjoyed success in social media more than Dr. Lee, a board-certified dermatologist who practices in Upland, Calif. In the fall of 2014, she started using Instagram to provide followers a glimpse into her life as a dermatologist, everything from Mohs surgery and Botox to keloid removals and ear lobe repair surgeries. From this she formed her alter ego, “Dr. Pimple Popper,” and became a YouTube sensation, building 7.1 million subscribers over the course of a few years, amounting to 4.5 billion lifetime views. She also grew 12 million followers on TikTok, 4.4 million followers on Instagram, 3 million on Facebook, and more than 139,000 on Twitter. About 80% of her followers are women who range between 18 and 40 years of age.
During the meeting she offered five social media marketing tips for busy clinicians:
You have to ‘play’ to ‘win.’ Active participation in social media is required to develop followers. “You cannot delegate this content,” Dr. Lee said. “You can hire people to help you or leave the task to a social media-savvy medical assistant in your office, but the content should be your responsibility ultimately, because you are the physician,” she added. Not everyone chooses to participate in social media, but it’s also something not to shy away from out of intimidation. “There is some talent associated with it, but it takes a lot of persistence as well,” she said.
Patients come first. Protect them at all costs. Dr. Lee rarely posts the faces of patients she cares for unless they grant consent in advance. “I try to show the work that I do and the beauty of dermatology,” she said during the meeting, which was named “Laser & Aesthetic Skin Therapy: What’s the Truth?” and was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. She added that taking part in social media can help you improve communication skills by engaging with followers who like, share, or respond to the material posted. “When you look back at your posts objectively, you learn about yourself and how you relate to your patients,” she said. “It helps to hone my bedside manner and my skills as a dermatologist.”
Show that you are human. Many dermatologists and other “skin influencers” have established their presence on the Internet and may be direct competitors for patients, but that doesn’t mean you can’t establish your own identity. One way to stand out is by posting content related to your authentic self, such as a photo or video that shows you engaged in a hobby, dining at a favorite restaurant, or visiting a beloved vacation spot. “Your followers don’t want a robot, someone who thinks they’re amazing and can do everything,” said Dr. Lee, who stars in her own TV reality show on TLC. “Show that you have a funny side. You want them to fall in love with you and see a little bit of your world, whatever it might be. Charm the socks off of them.”
Entertain first, educate a close second. The main way you’re going to get people to follow and watch you is to provide some entertainment, “not at the expense of a patient or your practice, though,” she said. “Then you’re going to educate people. We dermatologists have something to teach the world because we are experts on skin, hair, and nails. You want to impart this knowledge in a way that captivates people.” It’s like the sense of accomplishment that comes from learning something new after reading a book or watching a movie, she explained. “You feel good about it, and you can take that knowledge with you somewhere else. I love it when kids come up to me and tell me they know what a lipoma is, what a cyst is, and what psoriasis is because they’ve seen my show, or because they follow me on social media. It’s wonderful because I can see that I’ve educated them.”
Be kind and don’t activate the trolls. Dr. Lee allows positivity and kindness to rule the day on her social media content. “This is what I try to relay to followers, but I also do not engage with the negativity,” she said. “Every now and then, there will be someone who tries to insult what you do or who insults you personally. If you engage with them, it almost invites them to do it more. It almost gives them the ability to fight with you. Try to stay above that; just put out goodness and kindness.”
Several years ago, YouTube and Instagram temporarily shut down Dr. Lee’s accounts because she posted graphic images of skin lesions and procedures – a practice that wasn’t so commonplace at the time. “Don’t just post a graphic image just to be graphic,” she advised. “Make sure it has an educational message associated with it. That will help to validate your content. Posting a warning sign that some images may be graphic could help, too.”
Dr. Lee reported having no relevant financial disclosures.
FROM A LASER & AESTHETIC SKIN THERAPY COURSE
‘Down to my last diaper’: The anxiety of parenting in poverty
For parents living in poverty, “diaper math” is a familiar and distressingly pressing daily calculation. Babies in the U.S. go through 6-10 disposable diapers a day, at an average cost of $70-$80 a month. Name-brand diapers with high-end absorption sell for as much as a half a dollar each, and can result in upwards of $120 a month in expenses.
One in every three American families cannot afford enough diapers to keep their infants and toddlers clean, dry, and healthy, according to the National Diaper Bank Network. For many parents, that leads to wrenching choices: diapers, food, or rent?
The COVID-19 pandemic has exacerbated the situation, both by expanding unemployment rolls and by causing supply chain disruptions that have triggered higher prices for a multitude of products, including diapers. Diaper banks – community-funded programs that offer free diapers to low-income families – distributed 86% more diapers on average in 2020 than in 2019, according to the National Diaper Bank Network. In some locations, distribution increased by as much as 800%.
Yet no federal program helps parents pay for this childhood essential. The government’s food assistance program does not cover diapers, nor do most state-level public aid programs.
California is the only state to directly fund diapers for families, but support is limited. CalWORKS, a financial assistance program for families with children, provides $30 per month to help families pay for diapers for children under age 3. Federal policy shifts also may be in the works: Democratic lawmakers are pushing to include $200 million for diaper distribution in the massive budget reconciliation package.
Without adequate resources, low-income parents are left scrambling for ways to get the most use out of each diaper. This stressful undertaking is the subject of a recent article in American Sociological Review by Jennifer Randles, PhD, professor of sociology at California State University–Fresno. In 2018, Randles conducted phone interviews with 70 mothers in California over nine months. She tried to recruit fathers as well, but only two men responded.
Dr. Randles spoke with KHN’s Jenny Gold about how the cost of diapers weighs on low-income moms, and the “inventive mothering” many low-income women adopt to shield their children from the harms of poverty. The conversation has been edited for length and clarity.
Q: How do diapers play into day-to-day anxieties for low-income mothers?
In my sample, half of the mothers told me that they worried more about diapers than they worried about food or housing.
I started to ask mothers, “Can you tell me how many diapers you have on hand right now?” Almost every one told me with exact specificity how many they had – 5 or 7 or 12. And they knew exactly how long that number of diapers would last, based on how often their children defecated and urinated, if their kid was sick, if they had a diaper rash at the time. So just all the emotional and cognitive labor that goes into keeping such careful track of diaper supplies.
They were worrying and figuring out, “OK, I’m down to almost my last diaper. What do I do now? Do I go find some cans [to sell]? Do I go sell some things in my house? Who in my social network might have some extra cash right now?” I talked to moms who sell blood plasma just to get their infants diapers.
Q: What coping strategies stood out to you?
Those of us who study diapers often call them diaper-stretching strategies. One was leaving on a diaper a little bit longer than someone might otherwise leave it on and letting it get completely full. Some mothers figured out if they bought a [more expensive] diaper that held more and leaked less, they could leave the diaper on longer.
They would also do things like letting the baby go diaperless, especially when they were at home and felt like they wouldn’t be judged for letting their baby go without a diaper. And they used every household good you can imagine to make makeshift diapers. Mothers are using cloth, sheets, and pillowcases. They’re using things that are disposable like paper towels with duct tape. They’re making diapers out their own period supplies or adult incontinence supplies when they can get a sample.
One of the questions I often get is, “Why don’t they just use cloth?” A lot of the mothers that I spoke with had tried cloth diapers and they found that they were very cost- and labor-prohibitive. If you pay for a full startup set of cloth diapers, you’re looking at anywhere from $500 to $1,000. And these moms never had that much money. Most of them didn’t have in-home washers and dryers. Some of them didn’t even have homes or consistent access to water, and it’s illegal in a lot of laundromats and public laundry facilities to wash your old diapers. So the same conditions that would prevent moms from being able to readily afford disposable diapers are the same conditions that keep them from being able to use cloth.
Q: You found that, for many women, the concept of being a good mother is wrapped up in diapering. Why is that?
Diapers and managing diapers was so fundamental to their identity as good moms. Most of the mothers in my sample went without their own food. They weren’t paying a cellphone bill or buying their own medicine or their own menstrual supplies, as a way of saving diaper money.
I talked to a lot of moms who said, when your baby is hungry, that’s horrible. Obviously, you do everything to prevent that. But there’s something about a diaper that covers this vulnerable part of a very young baby’s body, this very delicate skin. And being able to do something to meet this human need that we all have, and to maintain dignity and cleanliness.
A lot of the moms had been through the welfare system, and so they’re living in this constant fear [of losing their children]. This is especially true among mothers of color, who are much more likely to get wrapped up in the child welfare system. People can’t necessarily see when your baby’s hungry. But people can see a saggy diaper. That’s going to be one of the things that tags you as a bad mom.
Q: Was your work on diapers influenced by your experience as a parent?
When I was doing these interviews, my daughter was about 2 or 3. So still in diapers. When my daughter peed during a diaper change, I thought, “Oh, I can just toss that one. Here, let me get another clean one.” That’s a really easy choice. For me. That’s a crisis for the mothers I interviewed. Many of them told me they have an anxiety attack with every diaper change.
Q: Do you see a clear policy solution to diaper stress?
What’s kind of ironic is how much physical, emotional, and cognitive labor goes into managing something that society and lawmakers don’t even recognize. Diapers are still not really recognized as a basic need, as evidenced by the fact that they’re still taxed in 35 states.
I think what California is doing is an excellent start. And I think diaper banks are a fabulous type of community-based organization that are filling a huge need that is not being filled by safety net policies. So, public support for diaper banks.
The direct cash aid part of the social safety net has been all but dismantled in the last 25 years. California is pretty generous. But there are some states where just the cost of diapers alone would use almost half of the average state TANF [Temporary Assistance for Needy Families] benefit for a family of three. I think we really do have to address the fact that the value of cash aid buys so much less than it used to.
Q: Your body of work on marriage and families is fascinating and unusual. Is there a single animating question behind your research?
The common thread is: How do our safety net policies support low-income families’ parenting goals? And do they equalize the conditions of parenting? I think of it as a reproductive justice issue. The ability to have a child or to not have a child, and then to parent that child in conditions where the child’s basic needs are met.
We like to say that we’re child and family friendly. The diaper issue is just one of many, many issues where we don’t really put our money or our policies where our mouth is, in terms of supporting families and supporting children. I think my work is trying to get people to think more collectively about having a social responsibility to all families and to each other. No country, but especially the richest country on the planet, should have one in three very young children not having one of their basic needs met.
I interviewed one dad who was incarcerated because he wrote a bad check. And as he described it to me, he had a certain amount of money, and they needed both diapers and milk for the baby. And I’ll never forget, he said, “I didn’t make a good choice, but I made the right one.”
These are not fancy shoes. These are not name-brand clothes. This was a dad needing both milk and diapers. I don’t think it gets much more basic than that.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
For parents living in poverty, “diaper math” is a familiar and distressingly pressing daily calculation. Babies in the U.S. go through 6-10 disposable diapers a day, at an average cost of $70-$80 a month. Name-brand diapers with high-end absorption sell for as much as a half a dollar each, and can result in upwards of $120 a month in expenses.
One in every three American families cannot afford enough diapers to keep their infants and toddlers clean, dry, and healthy, according to the National Diaper Bank Network. For many parents, that leads to wrenching choices: diapers, food, or rent?
The COVID-19 pandemic has exacerbated the situation, both by expanding unemployment rolls and by causing supply chain disruptions that have triggered higher prices for a multitude of products, including diapers. Diaper banks – community-funded programs that offer free diapers to low-income families – distributed 86% more diapers on average in 2020 than in 2019, according to the National Diaper Bank Network. In some locations, distribution increased by as much as 800%.
Yet no federal program helps parents pay for this childhood essential. The government’s food assistance program does not cover diapers, nor do most state-level public aid programs.
California is the only state to directly fund diapers for families, but support is limited. CalWORKS, a financial assistance program for families with children, provides $30 per month to help families pay for diapers for children under age 3. Federal policy shifts also may be in the works: Democratic lawmakers are pushing to include $200 million for diaper distribution in the massive budget reconciliation package.
Without adequate resources, low-income parents are left scrambling for ways to get the most use out of each diaper. This stressful undertaking is the subject of a recent article in American Sociological Review by Jennifer Randles, PhD, professor of sociology at California State University–Fresno. In 2018, Randles conducted phone interviews with 70 mothers in California over nine months. She tried to recruit fathers as well, but only two men responded.
Dr. Randles spoke with KHN’s Jenny Gold about how the cost of diapers weighs on low-income moms, and the “inventive mothering” many low-income women adopt to shield their children from the harms of poverty. The conversation has been edited for length and clarity.
Q: How do diapers play into day-to-day anxieties for low-income mothers?
In my sample, half of the mothers told me that they worried more about diapers than they worried about food or housing.
I started to ask mothers, “Can you tell me how many diapers you have on hand right now?” Almost every one told me with exact specificity how many they had – 5 or 7 or 12. And they knew exactly how long that number of diapers would last, based on how often their children defecated and urinated, if their kid was sick, if they had a diaper rash at the time. So just all the emotional and cognitive labor that goes into keeping such careful track of diaper supplies.
They were worrying and figuring out, “OK, I’m down to almost my last diaper. What do I do now? Do I go find some cans [to sell]? Do I go sell some things in my house? Who in my social network might have some extra cash right now?” I talked to moms who sell blood plasma just to get their infants diapers.
Q: What coping strategies stood out to you?
Those of us who study diapers often call them diaper-stretching strategies. One was leaving on a diaper a little bit longer than someone might otherwise leave it on and letting it get completely full. Some mothers figured out if they bought a [more expensive] diaper that held more and leaked less, they could leave the diaper on longer.
They would also do things like letting the baby go diaperless, especially when they were at home and felt like they wouldn’t be judged for letting their baby go without a diaper. And they used every household good you can imagine to make makeshift diapers. Mothers are using cloth, sheets, and pillowcases. They’re using things that are disposable like paper towels with duct tape. They’re making diapers out their own period supplies or adult incontinence supplies when they can get a sample.
One of the questions I often get is, “Why don’t they just use cloth?” A lot of the mothers that I spoke with had tried cloth diapers and they found that they were very cost- and labor-prohibitive. If you pay for a full startup set of cloth diapers, you’re looking at anywhere from $500 to $1,000. And these moms never had that much money. Most of them didn’t have in-home washers and dryers. Some of them didn’t even have homes or consistent access to water, and it’s illegal in a lot of laundromats and public laundry facilities to wash your old diapers. So the same conditions that would prevent moms from being able to readily afford disposable diapers are the same conditions that keep them from being able to use cloth.
Q: You found that, for many women, the concept of being a good mother is wrapped up in diapering. Why is that?
Diapers and managing diapers was so fundamental to their identity as good moms. Most of the mothers in my sample went without their own food. They weren’t paying a cellphone bill or buying their own medicine or their own menstrual supplies, as a way of saving diaper money.
I talked to a lot of moms who said, when your baby is hungry, that’s horrible. Obviously, you do everything to prevent that. But there’s something about a diaper that covers this vulnerable part of a very young baby’s body, this very delicate skin. And being able to do something to meet this human need that we all have, and to maintain dignity and cleanliness.
A lot of the moms had been through the welfare system, and so they’re living in this constant fear [of losing their children]. This is especially true among mothers of color, who are much more likely to get wrapped up in the child welfare system. People can’t necessarily see when your baby’s hungry. But people can see a saggy diaper. That’s going to be one of the things that tags you as a bad mom.
Q: Was your work on diapers influenced by your experience as a parent?
When I was doing these interviews, my daughter was about 2 or 3. So still in diapers. When my daughter peed during a diaper change, I thought, “Oh, I can just toss that one. Here, let me get another clean one.” That’s a really easy choice. For me. That’s a crisis for the mothers I interviewed. Many of them told me they have an anxiety attack with every diaper change.
Q: Do you see a clear policy solution to diaper stress?
What’s kind of ironic is how much physical, emotional, and cognitive labor goes into managing something that society and lawmakers don’t even recognize. Diapers are still not really recognized as a basic need, as evidenced by the fact that they’re still taxed in 35 states.
I think what California is doing is an excellent start. And I think diaper banks are a fabulous type of community-based organization that are filling a huge need that is not being filled by safety net policies. So, public support for diaper banks.
The direct cash aid part of the social safety net has been all but dismantled in the last 25 years. California is pretty generous. But there are some states where just the cost of diapers alone would use almost half of the average state TANF [Temporary Assistance for Needy Families] benefit for a family of three. I think we really do have to address the fact that the value of cash aid buys so much less than it used to.
Q: Your body of work on marriage and families is fascinating and unusual. Is there a single animating question behind your research?
The common thread is: How do our safety net policies support low-income families’ parenting goals? And do they equalize the conditions of parenting? I think of it as a reproductive justice issue. The ability to have a child or to not have a child, and then to parent that child in conditions where the child’s basic needs are met.
We like to say that we’re child and family friendly. The diaper issue is just one of many, many issues where we don’t really put our money or our policies where our mouth is, in terms of supporting families and supporting children. I think my work is trying to get people to think more collectively about having a social responsibility to all families and to each other. No country, but especially the richest country on the planet, should have one in three very young children not having one of their basic needs met.
I interviewed one dad who was incarcerated because he wrote a bad check. And as he described it to me, he had a certain amount of money, and they needed both diapers and milk for the baby. And I’ll never forget, he said, “I didn’t make a good choice, but I made the right one.”
These are not fancy shoes. These are not name-brand clothes. This was a dad needing both milk and diapers. I don’t think it gets much more basic than that.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
For parents living in poverty, “diaper math” is a familiar and distressingly pressing daily calculation. Babies in the U.S. go through 6-10 disposable diapers a day, at an average cost of $70-$80 a month. Name-brand diapers with high-end absorption sell for as much as a half a dollar each, and can result in upwards of $120 a month in expenses.
One in every three American families cannot afford enough diapers to keep their infants and toddlers clean, dry, and healthy, according to the National Diaper Bank Network. For many parents, that leads to wrenching choices: diapers, food, or rent?
The COVID-19 pandemic has exacerbated the situation, both by expanding unemployment rolls and by causing supply chain disruptions that have triggered higher prices for a multitude of products, including diapers. Diaper banks – community-funded programs that offer free diapers to low-income families – distributed 86% more diapers on average in 2020 than in 2019, according to the National Diaper Bank Network. In some locations, distribution increased by as much as 800%.
Yet no federal program helps parents pay for this childhood essential. The government’s food assistance program does not cover diapers, nor do most state-level public aid programs.
California is the only state to directly fund diapers for families, but support is limited. CalWORKS, a financial assistance program for families with children, provides $30 per month to help families pay for diapers for children under age 3. Federal policy shifts also may be in the works: Democratic lawmakers are pushing to include $200 million for diaper distribution in the massive budget reconciliation package.
Without adequate resources, low-income parents are left scrambling for ways to get the most use out of each diaper. This stressful undertaking is the subject of a recent article in American Sociological Review by Jennifer Randles, PhD, professor of sociology at California State University–Fresno. In 2018, Randles conducted phone interviews with 70 mothers in California over nine months. She tried to recruit fathers as well, but only two men responded.
Dr. Randles spoke with KHN’s Jenny Gold about how the cost of diapers weighs on low-income moms, and the “inventive mothering” many low-income women adopt to shield their children from the harms of poverty. The conversation has been edited for length and clarity.
Q: How do diapers play into day-to-day anxieties for low-income mothers?
In my sample, half of the mothers told me that they worried more about diapers than they worried about food or housing.
I started to ask mothers, “Can you tell me how many diapers you have on hand right now?” Almost every one told me with exact specificity how many they had – 5 or 7 or 12. And they knew exactly how long that number of diapers would last, based on how often their children defecated and urinated, if their kid was sick, if they had a diaper rash at the time. So just all the emotional and cognitive labor that goes into keeping such careful track of diaper supplies.
They were worrying and figuring out, “OK, I’m down to almost my last diaper. What do I do now? Do I go find some cans [to sell]? Do I go sell some things in my house? Who in my social network might have some extra cash right now?” I talked to moms who sell blood plasma just to get their infants diapers.
Q: What coping strategies stood out to you?
Those of us who study diapers often call them diaper-stretching strategies. One was leaving on a diaper a little bit longer than someone might otherwise leave it on and letting it get completely full. Some mothers figured out if they bought a [more expensive] diaper that held more and leaked less, they could leave the diaper on longer.
They would also do things like letting the baby go diaperless, especially when they were at home and felt like they wouldn’t be judged for letting their baby go without a diaper. And they used every household good you can imagine to make makeshift diapers. Mothers are using cloth, sheets, and pillowcases. They’re using things that are disposable like paper towels with duct tape. They’re making diapers out their own period supplies or adult incontinence supplies when they can get a sample.
One of the questions I often get is, “Why don’t they just use cloth?” A lot of the mothers that I spoke with had tried cloth diapers and they found that they were very cost- and labor-prohibitive. If you pay for a full startup set of cloth diapers, you’re looking at anywhere from $500 to $1,000. And these moms never had that much money. Most of them didn’t have in-home washers and dryers. Some of them didn’t even have homes or consistent access to water, and it’s illegal in a lot of laundromats and public laundry facilities to wash your old diapers. So the same conditions that would prevent moms from being able to readily afford disposable diapers are the same conditions that keep them from being able to use cloth.
Q: You found that, for many women, the concept of being a good mother is wrapped up in diapering. Why is that?
Diapers and managing diapers was so fundamental to their identity as good moms. Most of the mothers in my sample went without their own food. They weren’t paying a cellphone bill or buying their own medicine or their own menstrual supplies, as a way of saving diaper money.
I talked to a lot of moms who said, when your baby is hungry, that’s horrible. Obviously, you do everything to prevent that. But there’s something about a diaper that covers this vulnerable part of a very young baby’s body, this very delicate skin. And being able to do something to meet this human need that we all have, and to maintain dignity and cleanliness.
A lot of the moms had been through the welfare system, and so they’re living in this constant fear [of losing their children]. This is especially true among mothers of color, who are much more likely to get wrapped up in the child welfare system. People can’t necessarily see when your baby’s hungry. But people can see a saggy diaper. That’s going to be one of the things that tags you as a bad mom.
Q: Was your work on diapers influenced by your experience as a parent?
When I was doing these interviews, my daughter was about 2 or 3. So still in diapers. When my daughter peed during a diaper change, I thought, “Oh, I can just toss that one. Here, let me get another clean one.” That’s a really easy choice. For me. That’s a crisis for the mothers I interviewed. Many of them told me they have an anxiety attack with every diaper change.
Q: Do you see a clear policy solution to diaper stress?
What’s kind of ironic is how much physical, emotional, and cognitive labor goes into managing something that society and lawmakers don’t even recognize. Diapers are still not really recognized as a basic need, as evidenced by the fact that they’re still taxed in 35 states.
I think what California is doing is an excellent start. And I think diaper banks are a fabulous type of community-based organization that are filling a huge need that is not being filled by safety net policies. So, public support for diaper banks.
The direct cash aid part of the social safety net has been all but dismantled in the last 25 years. California is pretty generous. But there are some states where just the cost of diapers alone would use almost half of the average state TANF [Temporary Assistance for Needy Families] benefit for a family of three. I think we really do have to address the fact that the value of cash aid buys so much less than it used to.
Q: Your body of work on marriage and families is fascinating and unusual. Is there a single animating question behind your research?
The common thread is: How do our safety net policies support low-income families’ parenting goals? And do they equalize the conditions of parenting? I think of it as a reproductive justice issue. The ability to have a child or to not have a child, and then to parent that child in conditions where the child’s basic needs are met.
We like to say that we’re child and family friendly. The diaper issue is just one of many, many issues where we don’t really put our money or our policies where our mouth is, in terms of supporting families and supporting children. I think my work is trying to get people to think more collectively about having a social responsibility to all families and to each other. No country, but especially the richest country on the planet, should have one in three very young children not having one of their basic needs met.
I interviewed one dad who was incarcerated because he wrote a bad check. And as he described it to me, he had a certain amount of money, and they needed both diapers and milk for the baby. And I’ll never forget, he said, “I didn’t make a good choice, but I made the right one.”
These are not fancy shoes. These are not name-brand clothes. This was a dad needing both milk and diapers. I don’t think it gets much more basic than that.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Rash in an immunocompromised patient
The patient’s history and presentation, as well as a positive varicella zoster virus (VZV) culture of vesicular fluid, led to a diagnosis of disseminated herpes zoster (DHZ). The patient’s laboratory studies were remarkable for mild lymphopenia, thrombocytopenia, and elevated liver function tests. Shave and punch biopsies of the lesion showed ballooning epithelial necrosis with multinucleated giant cells.
DHZ is characterized by more than 20 vesicles outside of a primary or adjacent dermatome and is caused by extensive reactivation of VZV. DHZ is most often encountered in immunocompromised patients.1 Untreated DHZ can lead to encephalitis, myelitis, nerve palsies, pneumonitis, hepatitis, and ocular complications.
Diagnosis is usually made clinically and confirmed by a polymerase chain reaction test, direct fluorescent antibody testing, or viral culture.2 In immunocompetent patients, uncomplicated DHZ is treated with oral acyclovir 800 mg 5 times daily, valacyclovir 1 g 3 times daily, or famciclovir 500 mg 3 times daily for 7 days. Hospital admission for intravenous acyclovir is recommended for immunocompromised patients, especially those with internal organ involvement, such as hepatitis or encephalitis.3
Early treatment is imperative to avoid life-threatening complications. Active herpes zoster lesions are infectious by contact with vesicular fluid until they dry and crust over. Patients should be instructed to avoid contact with susceptible people, including those who are immunocompromised, babies who have not received their varicella vaccine, and pregnant women. It is important to keep DHZ on the differential—especially in an immunosuppressed patient with a diffuse vesicular rash—as it can lead to significant morbidity and mortality.
Our patient was treated with oral valacyclovir 1 g tid for 10 days and he improved without developing systemic symptoms.
Image courtesy of Christen B. Samaan, MD. Text courtesy of Christen B. Samaan, MD, and Matthew F. Helm, MD, Department of Dermatology, and Nanjiba Nawaz, BA, Penn State College of Medicine, Hershey.
1. Bollea-Garlatti ML, Bollea-Garlatti LA, Vacas AS, et al. Clinical characteristics and outcomes in a population with disseminated herpes zoster: a retrospective cohort study. Actas Dermosifiliogr. 2017;108:145-152. doi: 10.1016/j.ad.2016.10.009
2. Chiriac A, Chiriac AE, Podoleanu C, et al. Disseminated cutaneous herpes zoster—a frequently misdiagnosed entity. Int Wound J. 2020;17:1089-1091. doi: 10.1111/iwj.13370
3. Lewis DJ, Schlichte MJ, Dao H Jr. Atypical disseminated herpes zoster: management guidelines in immunocompromised patients. Cutis. 2017;100:321;324;330.
The patient’s history and presentation, as well as a positive varicella zoster virus (VZV) culture of vesicular fluid, led to a diagnosis of disseminated herpes zoster (DHZ). The patient’s laboratory studies were remarkable for mild lymphopenia, thrombocytopenia, and elevated liver function tests. Shave and punch biopsies of the lesion showed ballooning epithelial necrosis with multinucleated giant cells.
DHZ is characterized by more than 20 vesicles outside of a primary or adjacent dermatome and is caused by extensive reactivation of VZV. DHZ is most often encountered in immunocompromised patients.1 Untreated DHZ can lead to encephalitis, myelitis, nerve palsies, pneumonitis, hepatitis, and ocular complications.
Diagnosis is usually made clinically and confirmed by a polymerase chain reaction test, direct fluorescent antibody testing, or viral culture.2 In immunocompetent patients, uncomplicated DHZ is treated with oral acyclovir 800 mg 5 times daily, valacyclovir 1 g 3 times daily, or famciclovir 500 mg 3 times daily for 7 days. Hospital admission for intravenous acyclovir is recommended for immunocompromised patients, especially those with internal organ involvement, such as hepatitis or encephalitis.3
Early treatment is imperative to avoid life-threatening complications. Active herpes zoster lesions are infectious by contact with vesicular fluid until they dry and crust over. Patients should be instructed to avoid contact with susceptible people, including those who are immunocompromised, babies who have not received their varicella vaccine, and pregnant women. It is important to keep DHZ on the differential—especially in an immunosuppressed patient with a diffuse vesicular rash—as it can lead to significant morbidity and mortality.
Our patient was treated with oral valacyclovir 1 g tid for 10 days and he improved without developing systemic symptoms.
Image courtesy of Christen B. Samaan, MD. Text courtesy of Christen B. Samaan, MD, and Matthew F. Helm, MD, Department of Dermatology, and Nanjiba Nawaz, BA, Penn State College of Medicine, Hershey.
The patient’s history and presentation, as well as a positive varicella zoster virus (VZV) culture of vesicular fluid, led to a diagnosis of disseminated herpes zoster (DHZ). The patient’s laboratory studies were remarkable for mild lymphopenia, thrombocytopenia, and elevated liver function tests. Shave and punch biopsies of the lesion showed ballooning epithelial necrosis with multinucleated giant cells.
DHZ is characterized by more than 20 vesicles outside of a primary or adjacent dermatome and is caused by extensive reactivation of VZV. DHZ is most often encountered in immunocompromised patients.1 Untreated DHZ can lead to encephalitis, myelitis, nerve palsies, pneumonitis, hepatitis, and ocular complications.
Diagnosis is usually made clinically and confirmed by a polymerase chain reaction test, direct fluorescent antibody testing, or viral culture.2 In immunocompetent patients, uncomplicated DHZ is treated with oral acyclovir 800 mg 5 times daily, valacyclovir 1 g 3 times daily, or famciclovir 500 mg 3 times daily for 7 days. Hospital admission for intravenous acyclovir is recommended for immunocompromised patients, especially those with internal organ involvement, such as hepatitis or encephalitis.3
Early treatment is imperative to avoid life-threatening complications. Active herpes zoster lesions are infectious by contact with vesicular fluid until they dry and crust over. Patients should be instructed to avoid contact with susceptible people, including those who are immunocompromised, babies who have not received their varicella vaccine, and pregnant women. It is important to keep DHZ on the differential—especially in an immunosuppressed patient with a diffuse vesicular rash—as it can lead to significant morbidity and mortality.
Our patient was treated with oral valacyclovir 1 g tid for 10 days and he improved without developing systemic symptoms.
Image courtesy of Christen B. Samaan, MD. Text courtesy of Christen B. Samaan, MD, and Matthew F. Helm, MD, Department of Dermatology, and Nanjiba Nawaz, BA, Penn State College of Medicine, Hershey.
1. Bollea-Garlatti ML, Bollea-Garlatti LA, Vacas AS, et al. Clinical characteristics and outcomes in a population with disseminated herpes zoster: a retrospective cohort study. Actas Dermosifiliogr. 2017;108:145-152. doi: 10.1016/j.ad.2016.10.009
2. Chiriac A, Chiriac AE, Podoleanu C, et al. Disseminated cutaneous herpes zoster—a frequently misdiagnosed entity. Int Wound J. 2020;17:1089-1091. doi: 10.1111/iwj.13370
3. Lewis DJ, Schlichte MJ, Dao H Jr. Atypical disseminated herpes zoster: management guidelines in immunocompromised patients. Cutis. 2017;100:321;324;330.
1. Bollea-Garlatti ML, Bollea-Garlatti LA, Vacas AS, et al. Clinical characteristics and outcomes in a population with disseminated herpes zoster: a retrospective cohort study. Actas Dermosifiliogr. 2017;108:145-152. doi: 10.1016/j.ad.2016.10.009
2. Chiriac A, Chiriac AE, Podoleanu C, et al. Disseminated cutaneous herpes zoster—a frequently misdiagnosed entity. Int Wound J. 2020;17:1089-1091. doi: 10.1111/iwj.13370
3. Lewis DJ, Schlichte MJ, Dao H Jr. Atypical disseminated herpes zoster: management guidelines in immunocompromised patients. Cutis. 2017;100:321;324;330.
Better COVID-19 outcomes confirmed in TNF inhibitor users
Among patients with immune-mediated inflammatory diseases (IMIDs) who get COVID-19, the risk for hospitalization and death is lower if they are receiving tumor necrosis factor (TNF) inhibitor monotherapy, compared with receiving most other common drugs for these conditions, with or without TNF inhibitors, according to a study published in JAMA Network Open The only combination not associated with an increased risk for hospitalization or death was TNF inhibitor therapy with methotrexate.
“These findings support the continued use of TNF inhibitor monotherapy during the pandemic and warrant further research investigating the association of other biologic therapies with COVID-19 outcomes,” write Zara Izadi, MPharm, of the University of California, San Francisco, and her colleagues. “Treatment with TNF inhibitor combination therapy was associated with a more favorable safety profile when methotrexate rather than azathioprine/6-mercaptopurine was used, suggesting that clinicians would benefit from weighing the risks versus benefits of deescalating treatment or changing medications when a patient is receiving concomitant TNF inhibitors and azathioprine/6-mercaptopurine,” they write.
Findings mirror those seen in other settings
These findings are in line with what has been found in other settings, according to Joel M. Gelfand, MD, director of the psoriasis and phototherapy treatment center, vice chair of clinical research, and medical director of the dermatology clinical studies unit at the University of Pennsylvania, Philadelphia.
“In the beginning of the pandemic, there was concern about use of immune-modulating treatments, and many patients self-discontinued treatments like TNF inhibitors,” Dr. Gelfand, who was not involved in the study, told this news organization. “This has ultimately proved unnecessary and unfortunately resulted in harm to many patients due to flaring of their underlying disease.”
Dr. Gelfand emphasized the importance of vaccinating patients against COVID-19 as soon as possible and of getting a third dose for those who are already fully vaccinated with the Pfizer or Moderna shots, as recommended by the Centers for Disease Control and Prevention.
“I typically recommend this third dose be taken 6 months after the second dose,” Dr. Gelfand said. “The good news is that TNF inhibitors do not seem to meaningfully impact response to mRNA vaccines.”
Study details
The researchers analyzed data from three international registries of adults with rheumatic diseases, inflammatory bowel disease, and psoriasis who had COVID-19 between March 12, 2020, and Feb. 1, 2021. The registries included the Secure Epidemiology of Coronavirus Under Research Exclusion for Inflammatory Bowel Disease (SECURE-IBD) registry, the Psoriasis Patient Registry for Outcomes, Therapy and Epidemiology of COVID-19 Infection (PsoProtect), and the physician-reported registry from the Global Rheumatology Alliance (GRA).
The population included 6,077 patients from 74 countries. About half of the cohort (52.9%) were from Europe; more than half were women (58.6%). The average age was 48 years. A little over one-third of the patients (35.3%) had rheumatoid arthritis, 25.3% had Crohn’s disease, 12.5% had ulcerative colitis, 10.3% had spondyloarthritis, and 9.3% had psoriatic arthritis. Smaller percentages had psoriasis (4.9%), another type of arthritis or multiple types (1.7%), or another inflammatory bowel disease (0.6%).
One in five patients (21.3%) were hospitalized, and 3.1% died. The researchers compared outcomes for those who were receiving TNF inhibitor therapy alone to outcomes for those who were taking azathioprine/6-mercaptopurine therapy (alone or with a TNF inhibitor), methotrexate (alone or with a TNF inhibitor), and Janus kinase (JAK) inhibitors. They adjusted their analysis to account for active disease and common comorbidities, as well as geography and the period during the pandemic in which the person was admitted, because treatment regimens and hospitalization indications have varied over time.
All of the therapies except the combination of TNF inhibitors and methotrexate were associated with higher odds of hospitalization and death than TNF inhibitor monotherapy.
The researchers explored several possible explanations for the findings, including the possibility that high serum TNF concentrations may have been associated with more organ damage at the time of COVID-19 admission, owing to interaction with SARS-CoV-2–associated hyperinflammation.
“Therefore, blocking TNF could inhibit this detrimental immune response,” the authors write. “Multiple case series reporting favorable outcomes among patients receiving TNF inhibitor therapy support this assertion.”
Another possibility relates to the effects of taking non–TNF inhibitor medications for immunosuppression. The authors note that thiopurine medications are linked to a greater risk for opportunistic viral infections and that JAK inhibitors may reduce the body’s ability to clear the virus because of its suppression of innate immune response.
The authors also postulate that methotrexate may lower the likelihood of cytokine storm linked to COVID-19, even though methotrexate monotherapy was associated with poorer outcomes. “This association could mean that TNF inhibitor therapy is exerting a protective benefit or that methotrexate therapy is exerting a harmful consequence,” the authors write.
Caution needed in interpreting uncontrolled, registry-based data
The findings were not surprising to Stephen B. Hanauer, MD, medical director of the Digestive Health Center at Northwestern University, Chicago, who was not involved in the research.
“We’ve been monitoring IBD [inflammatory bowel disease] patients through the Secure registry similar to the rheumatologic and dermatologic societies and have not identified a signal of harm from any international groups,” Dr. Hanauer told this news organization. He noted that these registries also have not shown an increased risk for COVID-19 complications among patients receiving TNF inhibitors, antiadhesion therapies, or anti–IL12/23 inhibitors, compared with the general population not taking these therapies.
The study’s size and the diversity of patients strengthen its findings. However, the registries’ use of convenience sampling increases the potential for reporting bias, although the results remained similar after a sensitivity analysis. The study also lacked a control group, and the registries did not collect data uniformly.
“These are databases that rely on reporting from investigators and are not comprehensive prospective studies,” Dr. Hanauer noted as another study limitation.
Dr. Gelfand similarly advised caution in interpreting these findings, inasmuch as the study is a “collection of spontaneous reports” that should be viewed as hypothesis-generating rather than testing.
“Fortunately, more rigorous studies have been conducted, typically in large medical record systems, and have confirmed the hypothesis that TNF inhibitors are associated with a lower risk of poor COVID-19 outcomes, compared to other treatments,” Dr. Gelfand said.
Previous smaller studies similarly found better outcomes among patients taking TNF inhibitors, compared with other therapies, but their participants were predominantly from North America and Europe, noted Licio A. Velloso, MD, PhD, of the University of Campinas, in São Paulo, in an accompanying commentary.
On the basis of the findings of this study, “which included a much larger sample comprising distinct diseases and patients with a multitude of genetic backgrounds, the evidence in favor of the continued use of TNF inhibitor monotherapy for patients with IMIDs during the COVID-19 pandemic has become more substantial,” Dr. Velloso writes. “The finding that maintenance of TNF inhibitor monotherapy is associated with reductions in the risk of severe COVID-19 among patients with IMIDs offers new perspective that may guide health care professionals in the difficult decisions regarding therapeutic approaches among this specific group of patients.”
The research was funded by the American College of Rheumatology, the European Alliance of Associations for Rheumatology, the United Kingdom’s National Institute for Health Research Biomedical Research Center, and the Psoriasis Association. Many authors reported receiving grants and/or personal fees from a variety of pharmaceutical companies. Dr. Velloso has disclosed no relevant financial relationships. Dr. Hanauer has served as a consultant to companies that market TNF inhibitors. Dr. Gelfand has consulted for and received research grants from companies that market TNF inhibitors.
A version of this article first appeared on Medscape.com.
Among patients with immune-mediated inflammatory diseases (IMIDs) who get COVID-19, the risk for hospitalization and death is lower if they are receiving tumor necrosis factor (TNF) inhibitor monotherapy, compared with receiving most other common drugs for these conditions, with or without TNF inhibitors, according to a study published in JAMA Network Open The only combination not associated with an increased risk for hospitalization or death was TNF inhibitor therapy with methotrexate.
“These findings support the continued use of TNF inhibitor monotherapy during the pandemic and warrant further research investigating the association of other biologic therapies with COVID-19 outcomes,” write Zara Izadi, MPharm, of the University of California, San Francisco, and her colleagues. “Treatment with TNF inhibitor combination therapy was associated with a more favorable safety profile when methotrexate rather than azathioprine/6-mercaptopurine was used, suggesting that clinicians would benefit from weighing the risks versus benefits of deescalating treatment or changing medications when a patient is receiving concomitant TNF inhibitors and azathioprine/6-mercaptopurine,” they write.
Findings mirror those seen in other settings
These findings are in line with what has been found in other settings, according to Joel M. Gelfand, MD, director of the psoriasis and phototherapy treatment center, vice chair of clinical research, and medical director of the dermatology clinical studies unit at the University of Pennsylvania, Philadelphia.
“In the beginning of the pandemic, there was concern about use of immune-modulating treatments, and many patients self-discontinued treatments like TNF inhibitors,” Dr. Gelfand, who was not involved in the study, told this news organization. “This has ultimately proved unnecessary and unfortunately resulted in harm to many patients due to flaring of their underlying disease.”
Dr. Gelfand emphasized the importance of vaccinating patients against COVID-19 as soon as possible and of getting a third dose for those who are already fully vaccinated with the Pfizer or Moderna shots, as recommended by the Centers for Disease Control and Prevention.
“I typically recommend this third dose be taken 6 months after the second dose,” Dr. Gelfand said. “The good news is that TNF inhibitors do not seem to meaningfully impact response to mRNA vaccines.”
Study details
The researchers analyzed data from three international registries of adults with rheumatic diseases, inflammatory bowel disease, and psoriasis who had COVID-19 between March 12, 2020, and Feb. 1, 2021. The registries included the Secure Epidemiology of Coronavirus Under Research Exclusion for Inflammatory Bowel Disease (SECURE-IBD) registry, the Psoriasis Patient Registry for Outcomes, Therapy and Epidemiology of COVID-19 Infection (PsoProtect), and the physician-reported registry from the Global Rheumatology Alliance (GRA).
The population included 6,077 patients from 74 countries. About half of the cohort (52.9%) were from Europe; more than half were women (58.6%). The average age was 48 years. A little over one-third of the patients (35.3%) had rheumatoid arthritis, 25.3% had Crohn’s disease, 12.5% had ulcerative colitis, 10.3% had spondyloarthritis, and 9.3% had psoriatic arthritis. Smaller percentages had psoriasis (4.9%), another type of arthritis or multiple types (1.7%), or another inflammatory bowel disease (0.6%).
One in five patients (21.3%) were hospitalized, and 3.1% died. The researchers compared outcomes for those who were receiving TNF inhibitor therapy alone to outcomes for those who were taking azathioprine/6-mercaptopurine therapy (alone or with a TNF inhibitor), methotrexate (alone or with a TNF inhibitor), and Janus kinase (JAK) inhibitors. They adjusted their analysis to account for active disease and common comorbidities, as well as geography and the period during the pandemic in which the person was admitted, because treatment regimens and hospitalization indications have varied over time.
All of the therapies except the combination of TNF inhibitors and methotrexate were associated with higher odds of hospitalization and death than TNF inhibitor monotherapy.
The researchers explored several possible explanations for the findings, including the possibility that high serum TNF concentrations may have been associated with more organ damage at the time of COVID-19 admission, owing to interaction with SARS-CoV-2–associated hyperinflammation.
“Therefore, blocking TNF could inhibit this detrimental immune response,” the authors write. “Multiple case series reporting favorable outcomes among patients receiving TNF inhibitor therapy support this assertion.”
Another possibility relates to the effects of taking non–TNF inhibitor medications for immunosuppression. The authors note that thiopurine medications are linked to a greater risk for opportunistic viral infections and that JAK inhibitors may reduce the body’s ability to clear the virus because of its suppression of innate immune response.
The authors also postulate that methotrexate may lower the likelihood of cytokine storm linked to COVID-19, even though methotrexate monotherapy was associated with poorer outcomes. “This association could mean that TNF inhibitor therapy is exerting a protective benefit or that methotrexate therapy is exerting a harmful consequence,” the authors write.
Caution needed in interpreting uncontrolled, registry-based data
The findings were not surprising to Stephen B. Hanauer, MD, medical director of the Digestive Health Center at Northwestern University, Chicago, who was not involved in the research.
“We’ve been monitoring IBD [inflammatory bowel disease] patients through the Secure registry similar to the rheumatologic and dermatologic societies and have not identified a signal of harm from any international groups,” Dr. Hanauer told this news organization. He noted that these registries also have not shown an increased risk for COVID-19 complications among patients receiving TNF inhibitors, antiadhesion therapies, or anti–IL12/23 inhibitors, compared with the general population not taking these therapies.
The study’s size and the diversity of patients strengthen its findings. However, the registries’ use of convenience sampling increases the potential for reporting bias, although the results remained similar after a sensitivity analysis. The study also lacked a control group, and the registries did not collect data uniformly.
“These are databases that rely on reporting from investigators and are not comprehensive prospective studies,” Dr. Hanauer noted as another study limitation.
Dr. Gelfand similarly advised caution in interpreting these findings, inasmuch as the study is a “collection of spontaneous reports” that should be viewed as hypothesis-generating rather than testing.
“Fortunately, more rigorous studies have been conducted, typically in large medical record systems, and have confirmed the hypothesis that TNF inhibitors are associated with a lower risk of poor COVID-19 outcomes, compared to other treatments,” Dr. Gelfand said.
Previous smaller studies similarly found better outcomes among patients taking TNF inhibitors, compared with other therapies, but their participants were predominantly from North America and Europe, noted Licio A. Velloso, MD, PhD, of the University of Campinas, in São Paulo, in an accompanying commentary.
On the basis of the findings of this study, “which included a much larger sample comprising distinct diseases and patients with a multitude of genetic backgrounds, the evidence in favor of the continued use of TNF inhibitor monotherapy for patients with IMIDs during the COVID-19 pandemic has become more substantial,” Dr. Velloso writes. “The finding that maintenance of TNF inhibitor monotherapy is associated with reductions in the risk of severe COVID-19 among patients with IMIDs offers new perspective that may guide health care professionals in the difficult decisions regarding therapeutic approaches among this specific group of patients.”
The research was funded by the American College of Rheumatology, the European Alliance of Associations for Rheumatology, the United Kingdom’s National Institute for Health Research Biomedical Research Center, and the Psoriasis Association. Many authors reported receiving grants and/or personal fees from a variety of pharmaceutical companies. Dr. Velloso has disclosed no relevant financial relationships. Dr. Hanauer has served as a consultant to companies that market TNF inhibitors. Dr. Gelfand has consulted for and received research grants from companies that market TNF inhibitors.
A version of this article first appeared on Medscape.com.
Among patients with immune-mediated inflammatory diseases (IMIDs) who get COVID-19, the risk for hospitalization and death is lower if they are receiving tumor necrosis factor (TNF) inhibitor monotherapy, compared with receiving most other common drugs for these conditions, with or without TNF inhibitors, according to a study published in JAMA Network Open The only combination not associated with an increased risk for hospitalization or death was TNF inhibitor therapy with methotrexate.
“These findings support the continued use of TNF inhibitor monotherapy during the pandemic and warrant further research investigating the association of other biologic therapies with COVID-19 outcomes,” write Zara Izadi, MPharm, of the University of California, San Francisco, and her colleagues. “Treatment with TNF inhibitor combination therapy was associated with a more favorable safety profile when methotrexate rather than azathioprine/6-mercaptopurine was used, suggesting that clinicians would benefit from weighing the risks versus benefits of deescalating treatment or changing medications when a patient is receiving concomitant TNF inhibitors and azathioprine/6-mercaptopurine,” they write.
Findings mirror those seen in other settings
These findings are in line with what has been found in other settings, according to Joel M. Gelfand, MD, director of the psoriasis and phototherapy treatment center, vice chair of clinical research, and medical director of the dermatology clinical studies unit at the University of Pennsylvania, Philadelphia.
“In the beginning of the pandemic, there was concern about use of immune-modulating treatments, and many patients self-discontinued treatments like TNF inhibitors,” Dr. Gelfand, who was not involved in the study, told this news organization. “This has ultimately proved unnecessary and unfortunately resulted in harm to many patients due to flaring of their underlying disease.”
Dr. Gelfand emphasized the importance of vaccinating patients against COVID-19 as soon as possible and of getting a third dose for those who are already fully vaccinated with the Pfizer or Moderna shots, as recommended by the Centers for Disease Control and Prevention.
“I typically recommend this third dose be taken 6 months after the second dose,” Dr. Gelfand said. “The good news is that TNF inhibitors do not seem to meaningfully impact response to mRNA vaccines.”
Study details
The researchers analyzed data from three international registries of adults with rheumatic diseases, inflammatory bowel disease, and psoriasis who had COVID-19 between March 12, 2020, and Feb. 1, 2021. The registries included the Secure Epidemiology of Coronavirus Under Research Exclusion for Inflammatory Bowel Disease (SECURE-IBD) registry, the Psoriasis Patient Registry for Outcomes, Therapy and Epidemiology of COVID-19 Infection (PsoProtect), and the physician-reported registry from the Global Rheumatology Alliance (GRA).
The population included 6,077 patients from 74 countries. About half of the cohort (52.9%) were from Europe; more than half were women (58.6%). The average age was 48 years. A little over one-third of the patients (35.3%) had rheumatoid arthritis, 25.3% had Crohn’s disease, 12.5% had ulcerative colitis, 10.3% had spondyloarthritis, and 9.3% had psoriatic arthritis. Smaller percentages had psoriasis (4.9%), another type of arthritis or multiple types (1.7%), or another inflammatory bowel disease (0.6%).
One in five patients (21.3%) were hospitalized, and 3.1% died. The researchers compared outcomes for those who were receiving TNF inhibitor therapy alone to outcomes for those who were taking azathioprine/6-mercaptopurine therapy (alone or with a TNF inhibitor), methotrexate (alone or with a TNF inhibitor), and Janus kinase (JAK) inhibitors. They adjusted their analysis to account for active disease and common comorbidities, as well as geography and the period during the pandemic in which the person was admitted, because treatment regimens and hospitalization indications have varied over time.
All of the therapies except the combination of TNF inhibitors and methotrexate were associated with higher odds of hospitalization and death than TNF inhibitor monotherapy.
The researchers explored several possible explanations for the findings, including the possibility that high serum TNF concentrations may have been associated with more organ damage at the time of COVID-19 admission, owing to interaction with SARS-CoV-2–associated hyperinflammation.
“Therefore, blocking TNF could inhibit this detrimental immune response,” the authors write. “Multiple case series reporting favorable outcomes among patients receiving TNF inhibitor therapy support this assertion.”
Another possibility relates to the effects of taking non–TNF inhibitor medications for immunosuppression. The authors note that thiopurine medications are linked to a greater risk for opportunistic viral infections and that JAK inhibitors may reduce the body’s ability to clear the virus because of its suppression of innate immune response.
The authors also postulate that methotrexate may lower the likelihood of cytokine storm linked to COVID-19, even though methotrexate monotherapy was associated with poorer outcomes. “This association could mean that TNF inhibitor therapy is exerting a protective benefit or that methotrexate therapy is exerting a harmful consequence,” the authors write.
Caution needed in interpreting uncontrolled, registry-based data
The findings were not surprising to Stephen B. Hanauer, MD, medical director of the Digestive Health Center at Northwestern University, Chicago, who was not involved in the research.
“We’ve been monitoring IBD [inflammatory bowel disease] patients through the Secure registry similar to the rheumatologic and dermatologic societies and have not identified a signal of harm from any international groups,” Dr. Hanauer told this news organization. He noted that these registries also have not shown an increased risk for COVID-19 complications among patients receiving TNF inhibitors, antiadhesion therapies, or anti–IL12/23 inhibitors, compared with the general population not taking these therapies.
The study’s size and the diversity of patients strengthen its findings. However, the registries’ use of convenience sampling increases the potential for reporting bias, although the results remained similar after a sensitivity analysis. The study also lacked a control group, and the registries did not collect data uniformly.
“These are databases that rely on reporting from investigators and are not comprehensive prospective studies,” Dr. Hanauer noted as another study limitation.
Dr. Gelfand similarly advised caution in interpreting these findings, inasmuch as the study is a “collection of spontaneous reports” that should be viewed as hypothesis-generating rather than testing.
“Fortunately, more rigorous studies have been conducted, typically in large medical record systems, and have confirmed the hypothesis that TNF inhibitors are associated with a lower risk of poor COVID-19 outcomes, compared to other treatments,” Dr. Gelfand said.
Previous smaller studies similarly found better outcomes among patients taking TNF inhibitors, compared with other therapies, but their participants were predominantly from North America and Europe, noted Licio A. Velloso, MD, PhD, of the University of Campinas, in São Paulo, in an accompanying commentary.
On the basis of the findings of this study, “which included a much larger sample comprising distinct diseases and patients with a multitude of genetic backgrounds, the evidence in favor of the continued use of TNF inhibitor monotherapy for patients with IMIDs during the COVID-19 pandemic has become more substantial,” Dr. Velloso writes. “The finding that maintenance of TNF inhibitor monotherapy is associated with reductions in the risk of severe COVID-19 among patients with IMIDs offers new perspective that may guide health care professionals in the difficult decisions regarding therapeutic approaches among this specific group of patients.”
The research was funded by the American College of Rheumatology, the European Alliance of Associations for Rheumatology, the United Kingdom’s National Institute for Health Research Biomedical Research Center, and the Psoriasis Association. Many authors reported receiving grants and/or personal fees from a variety of pharmaceutical companies. Dr. Velloso has disclosed no relevant financial relationships. Dr. Hanauer has served as a consultant to companies that market TNF inhibitors. Dr. Gelfand has consulted for and received research grants from companies that market TNF inhibitors.
A version of this article first appeared on Medscape.com.
A 70-year-old man presents with firm papules on his hand and fingers
, although women are more often affected than men. GA most commonly appears in the first 3 decades of life. Although the etiology is not known, GA may represent a delayed hypersensitivity reaction. A link between GA and diabetes mellitus, autoimmune thyroiditis, dyslipidemia, and rarely, malignancy may exist.
GA is most commonly localized, presenting as an asymptomatic, erythematous, annular plaque with a firm border and central clearing localized to the wrists, ankles, and dorsal hands or feet. This form is the type most often seen in children. Generalized GA is far less common and presents later in life as multiple asymptomatic or pruritic papules and plaques on the trunk and extremities. Less common variants include subcutaneous GA, patch GA, atypical GA, and perforating GA. Perforating GA occurs on the dorsal hands and presents as (umbilicated) papules, and seems consistent with this patient’s clinical presentation. Histologically, transepidermal elimination of collagen is typically seen in perforating GA.1
Histology in this patient’s biopsy revealed a granulomatous dermatitis consistent with granuloma annulare. A palisaded arrangement of histiocytic cells surrounding altered collagen with increased dermal mucin was seen. There was associated perivascular mononuclear inflammatory infiltrates. The overlying epidermis was unremarkable.
Granuloma annulare often spontaneously resolves without sequelae. In some cases, atrophy may result. Lesions may also recur. Localized GA is often treated with high-potency topical corticosteroids or intralesional corticosteroids. For generalized GA, topical or intralesional corticosteroids may be used for select lesions. Topical calcineurin inhibitors, light therapy, cryotherapy, imiquimod, hydroxychloroquine, isotretinoin, and dapsone have also been reported in the literature as possible treatments.
This case and photo were provided by Dr. Berke, of Three Rivers Dermatology, Pittsburgh, and Dr. Bilu Martin.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
1 Alves J, Barreiros H, Bartolo E. Healthcare (Basel). 2014 Sep 4;2(3):338-45.
2. Bolognia J et al. Dermatology (St. Louis: Mosby/Elsevier, 2008).
3. “Andrews’ Diseases of the Skin,” 13th ed. James W et al. Philadelphia: Saunders Elsevier, 2006.
, although women are more often affected than men. GA most commonly appears in the first 3 decades of life. Although the etiology is not known, GA may represent a delayed hypersensitivity reaction. A link between GA and diabetes mellitus, autoimmune thyroiditis, dyslipidemia, and rarely, malignancy may exist.
GA is most commonly localized, presenting as an asymptomatic, erythematous, annular plaque with a firm border and central clearing localized to the wrists, ankles, and dorsal hands or feet. This form is the type most often seen in children. Generalized GA is far less common and presents later in life as multiple asymptomatic or pruritic papules and plaques on the trunk and extremities. Less common variants include subcutaneous GA, patch GA, atypical GA, and perforating GA. Perforating GA occurs on the dorsal hands and presents as (umbilicated) papules, and seems consistent with this patient’s clinical presentation. Histologically, transepidermal elimination of collagen is typically seen in perforating GA.1
Histology in this patient’s biopsy revealed a granulomatous dermatitis consistent with granuloma annulare. A palisaded arrangement of histiocytic cells surrounding altered collagen with increased dermal mucin was seen. There was associated perivascular mononuclear inflammatory infiltrates. The overlying epidermis was unremarkable.
Granuloma annulare often spontaneously resolves without sequelae. In some cases, atrophy may result. Lesions may also recur. Localized GA is often treated with high-potency topical corticosteroids or intralesional corticosteroids. For generalized GA, topical or intralesional corticosteroids may be used for select lesions. Topical calcineurin inhibitors, light therapy, cryotherapy, imiquimod, hydroxychloroquine, isotretinoin, and dapsone have also been reported in the literature as possible treatments.
This case and photo were provided by Dr. Berke, of Three Rivers Dermatology, Pittsburgh, and Dr. Bilu Martin.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
1 Alves J, Barreiros H, Bartolo E. Healthcare (Basel). 2014 Sep 4;2(3):338-45.
2. Bolognia J et al. Dermatology (St. Louis: Mosby/Elsevier, 2008).
3. “Andrews’ Diseases of the Skin,” 13th ed. James W et al. Philadelphia: Saunders Elsevier, 2006.
, although women are more often affected than men. GA most commonly appears in the first 3 decades of life. Although the etiology is not known, GA may represent a delayed hypersensitivity reaction. A link between GA and diabetes mellitus, autoimmune thyroiditis, dyslipidemia, and rarely, malignancy may exist.
GA is most commonly localized, presenting as an asymptomatic, erythematous, annular plaque with a firm border and central clearing localized to the wrists, ankles, and dorsal hands or feet. This form is the type most often seen in children. Generalized GA is far less common and presents later in life as multiple asymptomatic or pruritic papules and plaques on the trunk and extremities. Less common variants include subcutaneous GA, patch GA, atypical GA, and perforating GA. Perforating GA occurs on the dorsal hands and presents as (umbilicated) papules, and seems consistent with this patient’s clinical presentation. Histologically, transepidermal elimination of collagen is typically seen in perforating GA.1
Histology in this patient’s biopsy revealed a granulomatous dermatitis consistent with granuloma annulare. A palisaded arrangement of histiocytic cells surrounding altered collagen with increased dermal mucin was seen. There was associated perivascular mononuclear inflammatory infiltrates. The overlying epidermis was unremarkable.
Granuloma annulare often spontaneously resolves without sequelae. In some cases, atrophy may result. Lesions may also recur. Localized GA is often treated with high-potency topical corticosteroids or intralesional corticosteroids. For generalized GA, topical or intralesional corticosteroids may be used for select lesions. Topical calcineurin inhibitors, light therapy, cryotherapy, imiquimod, hydroxychloroquine, isotretinoin, and dapsone have also been reported in the literature as possible treatments.
This case and photo were provided by Dr. Berke, of Three Rivers Dermatology, Pittsburgh, and Dr. Bilu Martin.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
1 Alves J, Barreiros H, Bartolo E. Healthcare (Basel). 2014 Sep 4;2(3):338-45.
2. Bolognia J et al. Dermatology (St. Louis: Mosby/Elsevier, 2008).
3. “Andrews’ Diseases of the Skin,” 13th ed. James W et al. Philadelphia: Saunders Elsevier, 2006.
Yellow pruritic eruption


This pruritic, eruption with yellowing atrophy and telangiectasias on the lower extremities is a classic presentation for necrobiosis lipoidica (NL).
NL is a chronic granulomatous disorder with a predilection for the lower extremities. Patients with NL present with progressive, yellow-brown atrophic plaques on the pretibial aspect of the legs. The plaques have underlying telangiectasias, revealed by the atrophy, and may ulcerate. While these lesions are primarily asymptomatic, associated symptoms may include pruritus, pain, or altered sensation on the affected skin. The classic pathology of NL is notable for altered collagen bundles layered with palisading granulomas extending deep into the dermis. Other notable findings may include mixed inflammatory cells, multinucleated giant cells, and plasma cells; mucin is notably absent.
There is an established relationship between NL and diabetes. When these 2 entities are present, the skin eruption may be referred to as “necrobiosis lipoidica diabeticorum” or “NLD.” Only a small percentage of patients with diabetes will develop NL. Furthermore, there is growing evidence to suggest that NL may be associated with other comorbidities, such as obesity, hypertension, dyslipidemia, and thyroid disease.1 Additionally, squamous cell carcinoma has been reported as arising within skin affected by NL.2
The etiology of NL is not completely understood. Current theories suggest that blood vessel inflammation related to autoimmune factors may be at work.2 The differential diagnosis of NL includes granuloma annulare, pretibial myxedema, stasis dermatitis, panniculitis, morphea, and lichen sclerosis.
NL can be refractory to therapy. Paramount to management is the avoidance of trauma to the affected skin. Topical therapies include corticosteroids, tretinoin, and tacrolimus. Systemic immunomodulation with infliximab, etanercept, thalidomide, and cyclosporine has also been trialed. There is evidence for the utility of pentoxifylline (400 mg po tid), a xanthine derivative often used for peripheral artery disease, to reverse ulceration that can arise in NL.
The patient in this case opted for topical therapy with clobetasol 0.05% ointment and tacrolimus 0.1% ointment. She was subsequently lost to follow-up.
Image courtesy of Cyrelle Fermin, MD, Department of Dermatology, University of New Mexico School of Medicine, Albuquerque. Text courtesy of Cyrelle Fermin, MD, and Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
1. Hashemi DA, Brown-Joel ZO, Tkachenko E, et al. Clinical features and comorbidities of patients with necrobiosis lipoidica with or without diabetes. JAMA Dermatol. 2019;155:455-459. doi: 10.1001/jamadermatol.2018.5635
2. Sibbald C, Reid S, Alavi A. Necrobiosis lipoidica. Dermatol Clin. 2015;33:343-360. doi: 10.1016/j.det.2015.03.003


This pruritic, eruption with yellowing atrophy and telangiectasias on the lower extremities is a classic presentation for necrobiosis lipoidica (NL).
NL is a chronic granulomatous disorder with a predilection for the lower extremities. Patients with NL present with progressive, yellow-brown atrophic plaques on the pretibial aspect of the legs. The plaques have underlying telangiectasias, revealed by the atrophy, and may ulcerate. While these lesions are primarily asymptomatic, associated symptoms may include pruritus, pain, or altered sensation on the affected skin. The classic pathology of NL is notable for altered collagen bundles layered with palisading granulomas extending deep into the dermis. Other notable findings may include mixed inflammatory cells, multinucleated giant cells, and plasma cells; mucin is notably absent.
There is an established relationship between NL and diabetes. When these 2 entities are present, the skin eruption may be referred to as “necrobiosis lipoidica diabeticorum” or “NLD.” Only a small percentage of patients with diabetes will develop NL. Furthermore, there is growing evidence to suggest that NL may be associated with other comorbidities, such as obesity, hypertension, dyslipidemia, and thyroid disease.1 Additionally, squamous cell carcinoma has been reported as arising within skin affected by NL.2
The etiology of NL is not completely understood. Current theories suggest that blood vessel inflammation related to autoimmune factors may be at work.2 The differential diagnosis of NL includes granuloma annulare, pretibial myxedema, stasis dermatitis, panniculitis, morphea, and lichen sclerosis.
NL can be refractory to therapy. Paramount to management is the avoidance of trauma to the affected skin. Topical therapies include corticosteroids, tretinoin, and tacrolimus. Systemic immunomodulation with infliximab, etanercept, thalidomide, and cyclosporine has also been trialed. There is evidence for the utility of pentoxifylline (400 mg po tid), a xanthine derivative often used for peripheral artery disease, to reverse ulceration that can arise in NL.
The patient in this case opted for topical therapy with clobetasol 0.05% ointment and tacrolimus 0.1% ointment. She was subsequently lost to follow-up.
Image courtesy of Cyrelle Fermin, MD, Department of Dermatology, University of New Mexico School of Medicine, Albuquerque. Text courtesy of Cyrelle Fermin, MD, and Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.


This pruritic, eruption with yellowing atrophy and telangiectasias on the lower extremities is a classic presentation for necrobiosis lipoidica (NL).
NL is a chronic granulomatous disorder with a predilection for the lower extremities. Patients with NL present with progressive, yellow-brown atrophic plaques on the pretibial aspect of the legs. The plaques have underlying telangiectasias, revealed by the atrophy, and may ulcerate. While these lesions are primarily asymptomatic, associated symptoms may include pruritus, pain, or altered sensation on the affected skin. The classic pathology of NL is notable for altered collagen bundles layered with palisading granulomas extending deep into the dermis. Other notable findings may include mixed inflammatory cells, multinucleated giant cells, and plasma cells; mucin is notably absent.
There is an established relationship between NL and diabetes. When these 2 entities are present, the skin eruption may be referred to as “necrobiosis lipoidica diabeticorum” or “NLD.” Only a small percentage of patients with diabetes will develop NL. Furthermore, there is growing evidence to suggest that NL may be associated with other comorbidities, such as obesity, hypertension, dyslipidemia, and thyroid disease.1 Additionally, squamous cell carcinoma has been reported as arising within skin affected by NL.2
The etiology of NL is not completely understood. Current theories suggest that blood vessel inflammation related to autoimmune factors may be at work.2 The differential diagnosis of NL includes granuloma annulare, pretibial myxedema, stasis dermatitis, panniculitis, morphea, and lichen sclerosis.
NL can be refractory to therapy. Paramount to management is the avoidance of trauma to the affected skin. Topical therapies include corticosteroids, tretinoin, and tacrolimus. Systemic immunomodulation with infliximab, etanercept, thalidomide, and cyclosporine has also been trialed. There is evidence for the utility of pentoxifylline (400 mg po tid), a xanthine derivative often used for peripheral artery disease, to reverse ulceration that can arise in NL.
The patient in this case opted for topical therapy with clobetasol 0.05% ointment and tacrolimus 0.1% ointment. She was subsequently lost to follow-up.
Image courtesy of Cyrelle Fermin, MD, Department of Dermatology, University of New Mexico School of Medicine, Albuquerque. Text courtesy of Cyrelle Fermin, MD, and Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
1. Hashemi DA, Brown-Joel ZO, Tkachenko E, et al. Clinical features and comorbidities of patients with necrobiosis lipoidica with or without diabetes. JAMA Dermatol. 2019;155:455-459. doi: 10.1001/jamadermatol.2018.5635
2. Sibbald C, Reid S, Alavi A. Necrobiosis lipoidica. Dermatol Clin. 2015;33:343-360. doi: 10.1016/j.det.2015.03.003
1. Hashemi DA, Brown-Joel ZO, Tkachenko E, et al. Clinical features and comorbidities of patients with necrobiosis lipoidica with or without diabetes. JAMA Dermatol. 2019;155:455-459. doi: 10.1001/jamadermatol.2018.5635
2. Sibbald C, Reid S, Alavi A. Necrobiosis lipoidica. Dermatol Clin. 2015;33:343-360. doi: 10.1016/j.det.2015.03.003
Teen boy’s knee lesion has changed
A biopsy of the lesion was performed which showed an increased number of eccrine glands and blood vessels within the dermis. Some areas showed an increase in adipocytes and smooth muscle bundles. The changes were consistent with eccrine angiomatous hamartoma (EAH).
The boy was referred to vascular laser therapy for treatment of the lesion.
EAH is a rare benign vascular growth characterized by an increased number of mature eccrine glands and blood vessels in the dermis and subcutis. The lesions are mostly present on the extremities, but cases of diffuse congenital lesions and lesions on the face and trunk have also been described. The lesions can be seen at birth or during the first years of life in about half of the cases, and the others tend to occur later in puberty and rarely in adulthood.1
Clinically, EAH lesions present as red, yellow to brown papules and plaques. Different dermoscopic patterns have been described which include the popcorn pattern that presents as yellow, confluent nodules with popcornlike shapes over a background of erythema, and linear arborizing vessels. The spitzoid pattern are brown globules on a background of erythema and pseudoreticular pigmentation around the globules. The verrucous hemangiomalike pattern has a bluish-white hue, reddish-blue or bluish lacunae, as seen in our patient.2-4
Most of the lesions are asymptomatic, but in some patients, they can be associated with pain, hyperhidrosis, and sometimes bleeding. Hyperhidrosis has been reported early in the presentation or during puberty or pregnancy. Our patient had started on amphetamines when hyperhidrosis occurred. Hyperhidrosis is a knowns side effect of this type of medication and may have had a role in the increased sweating noted on the hamartoma.
EAH can clinically look like verrucous hemangiomas, angiokeratomas, and vascular malformations, and histopathology may be needed to differentiate between them. Eccrine nevi and EAH can be similar. Hyperhidrosis is an early and predominant component of eccrine nevi, compared with one-third of EAH.
The exact etiology of this lesion is not known. It is thought to be caused by an abnormal differentiation of the epithelium, adnexal structure, and the mesenchyme during organogenesis.3 No other associated conditions have been described with EAH.
EAH are benign lesions that rarely require treatment. If the lesions are symptomatic or because of cosmetic reasons, they can be removed surgically. There are some reports of successful treatment with pulse dual-wavelength sequential 595- and 1064-nm lasers.5 Botulinum toxin has also been used in cases of symptomatic hyperhidrosis.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. She has no conflicts. Email her at pdnews@mdedge.com.
References
1. Smith SD et al. Pediatr Dermatol. 2019 Nov;36(6):909-12.
2. Patterson AT et al. Am J Dermatopathol. 2016;38:413-7.
3. Garcıa-Garcıa SC et al. JAAD Case Rep. 2018;4(2):165-7.
4. Awatef Kelati et al. JAAD Case Rep. 2018;4(8)835-6.
5. Felgueiras J et al. Dermatol Surg. 2015 Mar;41(3):428-30.
A biopsy of the lesion was performed which showed an increased number of eccrine glands and blood vessels within the dermis. Some areas showed an increase in adipocytes and smooth muscle bundles. The changes were consistent with eccrine angiomatous hamartoma (EAH).
The boy was referred to vascular laser therapy for treatment of the lesion.
EAH is a rare benign vascular growth characterized by an increased number of mature eccrine glands and blood vessels in the dermis and subcutis. The lesions are mostly present on the extremities, but cases of diffuse congenital lesions and lesions on the face and trunk have also been described. The lesions can be seen at birth or during the first years of life in about half of the cases, and the others tend to occur later in puberty and rarely in adulthood.1
Clinically, EAH lesions present as red, yellow to brown papules and plaques. Different dermoscopic patterns have been described which include the popcorn pattern that presents as yellow, confluent nodules with popcornlike shapes over a background of erythema, and linear arborizing vessels. The spitzoid pattern are brown globules on a background of erythema and pseudoreticular pigmentation around the globules. The verrucous hemangiomalike pattern has a bluish-white hue, reddish-blue or bluish lacunae, as seen in our patient.2-4
Most of the lesions are asymptomatic, but in some patients, they can be associated with pain, hyperhidrosis, and sometimes bleeding. Hyperhidrosis has been reported early in the presentation or during puberty or pregnancy. Our patient had started on amphetamines when hyperhidrosis occurred. Hyperhidrosis is a knowns side effect of this type of medication and may have had a role in the increased sweating noted on the hamartoma.
EAH can clinically look like verrucous hemangiomas, angiokeratomas, and vascular malformations, and histopathology may be needed to differentiate between them. Eccrine nevi and EAH can be similar. Hyperhidrosis is an early and predominant component of eccrine nevi, compared with one-third of EAH.
The exact etiology of this lesion is not known. It is thought to be caused by an abnormal differentiation of the epithelium, adnexal structure, and the mesenchyme during organogenesis.3 No other associated conditions have been described with EAH.
EAH are benign lesions that rarely require treatment. If the lesions are symptomatic or because of cosmetic reasons, they can be removed surgically. There are some reports of successful treatment with pulse dual-wavelength sequential 595- and 1064-nm lasers.5 Botulinum toxin has also been used in cases of symptomatic hyperhidrosis.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. She has no conflicts. Email her at pdnews@mdedge.com.
References
1. Smith SD et al. Pediatr Dermatol. 2019 Nov;36(6):909-12.
2. Patterson AT et al. Am J Dermatopathol. 2016;38:413-7.
3. Garcıa-Garcıa SC et al. JAAD Case Rep. 2018;4(2):165-7.
4. Awatef Kelati et al. JAAD Case Rep. 2018;4(8)835-6.
5. Felgueiras J et al. Dermatol Surg. 2015 Mar;41(3):428-30.
A biopsy of the lesion was performed which showed an increased number of eccrine glands and blood vessels within the dermis. Some areas showed an increase in adipocytes and smooth muscle bundles. The changes were consistent with eccrine angiomatous hamartoma (EAH).
The boy was referred to vascular laser therapy for treatment of the lesion.
EAH is a rare benign vascular growth characterized by an increased number of mature eccrine glands and blood vessels in the dermis and subcutis. The lesions are mostly present on the extremities, but cases of diffuse congenital lesions and lesions on the face and trunk have also been described. The lesions can be seen at birth or during the first years of life in about half of the cases, and the others tend to occur later in puberty and rarely in adulthood.1
Clinically, EAH lesions present as red, yellow to brown papules and plaques. Different dermoscopic patterns have been described which include the popcorn pattern that presents as yellow, confluent nodules with popcornlike shapes over a background of erythema, and linear arborizing vessels. The spitzoid pattern are brown globules on a background of erythema and pseudoreticular pigmentation around the globules. The verrucous hemangiomalike pattern has a bluish-white hue, reddish-blue or bluish lacunae, as seen in our patient.2-4
Most of the lesions are asymptomatic, but in some patients, they can be associated with pain, hyperhidrosis, and sometimes bleeding. Hyperhidrosis has been reported early in the presentation or during puberty or pregnancy. Our patient had started on amphetamines when hyperhidrosis occurred. Hyperhidrosis is a knowns side effect of this type of medication and may have had a role in the increased sweating noted on the hamartoma.
EAH can clinically look like verrucous hemangiomas, angiokeratomas, and vascular malformations, and histopathology may be needed to differentiate between them. Eccrine nevi and EAH can be similar. Hyperhidrosis is an early and predominant component of eccrine nevi, compared with one-third of EAH.
The exact etiology of this lesion is not known. It is thought to be caused by an abnormal differentiation of the epithelium, adnexal structure, and the mesenchyme during organogenesis.3 No other associated conditions have been described with EAH.
EAH are benign lesions that rarely require treatment. If the lesions are symptomatic or because of cosmetic reasons, they can be removed surgically. There are some reports of successful treatment with pulse dual-wavelength sequential 595- and 1064-nm lasers.5 Botulinum toxin has also been used in cases of symptomatic hyperhidrosis.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. She has no conflicts. Email her at pdnews@mdedge.com.
References
1. Smith SD et al. Pediatr Dermatol. 2019 Nov;36(6):909-12.
2. Patterson AT et al. Am J Dermatopathol. 2016;38:413-7.
3. Garcıa-Garcıa SC et al. JAAD Case Rep. 2018;4(2):165-7.
4. Awatef Kelati et al. JAAD Case Rep. 2018;4(8)835-6.
5. Felgueiras J et al. Dermatol Surg. 2015 Mar;41(3):428-30.
A 14-year-old male was referred to our pediatric dermatology clinic for evaluation of a lesion on the left knee that appeared at 1 year of age. The lesion has been growing with him and was not symptomatic until 6 months prior to the consultation, when it started bleeding and feeling wet.
He has a history of attention-deficit/hyperactivity disorder managed with dextroamphetamine-amphetamine. The changes noted on the knee lesion seem to occur at the same time that his ADHD medication was started.
On physical exam he had a violaceous circular plaque on the left knee.
On dermoscopy the lesion showed multiple dilated red and violaceous lacunae and whitish blue hue.