User login
Cardiovascular societies less apt to recognize women, minorities
Major cardiovascular societies are more apt to give out awards to men and White individuals than to women and minorities, according to a look at 2 decades’ worth of data.
“Women received significantly fewer awards than men in all societies, countries, and award categories,” author Martha Gulati, MD, director of preventive cardiology at Smidt Heart Institute at Cedars-Sinai, Los Angeles, said in a news release. “This bias may be responsible for preventing underrepresented groups from ascending the academic ladder and receiving senior awards like lifetime achievement awards.”
The study was published online in the Journal of the American College of Cardiology.
A slow climb
The findings are based on a review of honors given from 2000 to 2021 by the ACC, the American Heart Association, the American Society of Echocardiography, the Society for Cardiovascular Angiography and Interventions, the Heart Rhythm Society, the European Society of Cardiology, and the Canadian Cardiovascular Society.
Among the 173 unique awards, 94 were given by the AHA, 27 by the HRS, 17 by the ACC, 16 by the CCS, 8 by the ASE, 7 by the ESC, and 4 by the SCAI. There were 3,044 recipients of these awards, including 2,830 unique awardees.
The vast majority of the awardees were White (75.2%), with Asian, Hispanic/Latino, and Black awardees representing just 18.9%, 4.5%, and 1.4% of the total awardees, respectively.
In a gender analysis, the researchers looked at 169 awards after excluding female-specific awards. These 169 awards were distributed to 2,995 recipients. More than three-quarters of these awardees (76.2%) were men, with women making up less than one-quarter (23.8%).
Encouragingly, there was an increasing trend in recognition of women over time, with 7.7% of female awardees in 2000 and climbing to 31.2% in 2021 (average annual percentage change, 6.6%; P < .05).
The distribution of awards also became more racially/ethnically diverse over time; in 2000, 92.3% of awardees were White versus 62.8% in 2021 (AAPC, –1.4%; P < .001).
There was also a significant increase in Asian (AAPC, 5.7%; P < .001), Hispanic/Latino (AAPC, 4.8%; P = .040), and Black (AAPC, 7.8%; P < .05) honorees.
Core influencers
By award type, women received fewer leadership awards than men, “which can be attributed to fewer leadership opportunities for women and a lack of acknowledgment of leadership responsibilities fulfilled by women,” the researchers said.
Award recipients with a PhD degree were nearly gender balanced (48.2% women), whereas men formed an overwhelming majority of awardees with an MD (84.7%).
Awards with male eponyms had fewer women recipients than did noneponymous awards (20.9% vs. 23.2%; P < .01).
“Male-eponymous awards can deter women applicants and give a subtle hint to selection committees to favor men as winners, creating an implicit bias,” the researchers said.
“Given the increased emphasis on redesigning cardiovascular health care delivery by incorporating the tenets of diversity, equity, and inclusion (DEI), cardiovascular societies have a significant role as core influencers,” Dr. Gulati and colleagues wrote.
They said that equitable award distribution can be a “key strategy to celebrate women and diverse members of the cardiovascular workforce and promulgate DEI.”
“Recognition of their contributions is pivotal to enhancing their self-perception. In addition to boosting confidence, receiving an award can also catalyze their career trajectory,” the authors added.
The study had no specific funding. The authors have declared no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Major cardiovascular societies are more apt to give out awards to men and White individuals than to women and minorities, according to a look at 2 decades’ worth of data.
“Women received significantly fewer awards than men in all societies, countries, and award categories,” author Martha Gulati, MD, director of preventive cardiology at Smidt Heart Institute at Cedars-Sinai, Los Angeles, said in a news release. “This bias may be responsible for preventing underrepresented groups from ascending the academic ladder and receiving senior awards like lifetime achievement awards.”
The study was published online in the Journal of the American College of Cardiology.
A slow climb
The findings are based on a review of honors given from 2000 to 2021 by the ACC, the American Heart Association, the American Society of Echocardiography, the Society for Cardiovascular Angiography and Interventions, the Heart Rhythm Society, the European Society of Cardiology, and the Canadian Cardiovascular Society.
Among the 173 unique awards, 94 were given by the AHA, 27 by the HRS, 17 by the ACC, 16 by the CCS, 8 by the ASE, 7 by the ESC, and 4 by the SCAI. There were 3,044 recipients of these awards, including 2,830 unique awardees.
The vast majority of the awardees were White (75.2%), with Asian, Hispanic/Latino, and Black awardees representing just 18.9%, 4.5%, and 1.4% of the total awardees, respectively.
In a gender analysis, the researchers looked at 169 awards after excluding female-specific awards. These 169 awards were distributed to 2,995 recipients. More than three-quarters of these awardees (76.2%) were men, with women making up less than one-quarter (23.8%).
Encouragingly, there was an increasing trend in recognition of women over time, with 7.7% of female awardees in 2000 and climbing to 31.2% in 2021 (average annual percentage change, 6.6%; P < .05).
The distribution of awards also became more racially/ethnically diverse over time; in 2000, 92.3% of awardees were White versus 62.8% in 2021 (AAPC, –1.4%; P < .001).
There was also a significant increase in Asian (AAPC, 5.7%; P < .001), Hispanic/Latino (AAPC, 4.8%; P = .040), and Black (AAPC, 7.8%; P < .05) honorees.
Core influencers
By award type, women received fewer leadership awards than men, “which can be attributed to fewer leadership opportunities for women and a lack of acknowledgment of leadership responsibilities fulfilled by women,” the researchers said.
Award recipients with a PhD degree were nearly gender balanced (48.2% women), whereas men formed an overwhelming majority of awardees with an MD (84.7%).
Awards with male eponyms had fewer women recipients than did noneponymous awards (20.9% vs. 23.2%; P < .01).
“Male-eponymous awards can deter women applicants and give a subtle hint to selection committees to favor men as winners, creating an implicit bias,” the researchers said.
“Given the increased emphasis on redesigning cardiovascular health care delivery by incorporating the tenets of diversity, equity, and inclusion (DEI), cardiovascular societies have a significant role as core influencers,” Dr. Gulati and colleagues wrote.
They said that equitable award distribution can be a “key strategy to celebrate women and diverse members of the cardiovascular workforce and promulgate DEI.”
“Recognition of their contributions is pivotal to enhancing their self-perception. In addition to boosting confidence, receiving an award can also catalyze their career trajectory,” the authors added.
The study had no specific funding. The authors have declared no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Major cardiovascular societies are more apt to give out awards to men and White individuals than to women and minorities, according to a look at 2 decades’ worth of data.
“Women received significantly fewer awards than men in all societies, countries, and award categories,” author Martha Gulati, MD, director of preventive cardiology at Smidt Heart Institute at Cedars-Sinai, Los Angeles, said in a news release. “This bias may be responsible for preventing underrepresented groups from ascending the academic ladder and receiving senior awards like lifetime achievement awards.”
The study was published online in the Journal of the American College of Cardiology.
A slow climb
The findings are based on a review of honors given from 2000 to 2021 by the ACC, the American Heart Association, the American Society of Echocardiography, the Society for Cardiovascular Angiography and Interventions, the Heart Rhythm Society, the European Society of Cardiology, and the Canadian Cardiovascular Society.
Among the 173 unique awards, 94 were given by the AHA, 27 by the HRS, 17 by the ACC, 16 by the CCS, 8 by the ASE, 7 by the ESC, and 4 by the SCAI. There were 3,044 recipients of these awards, including 2,830 unique awardees.
The vast majority of the awardees were White (75.2%), with Asian, Hispanic/Latino, and Black awardees representing just 18.9%, 4.5%, and 1.4% of the total awardees, respectively.
In a gender analysis, the researchers looked at 169 awards after excluding female-specific awards. These 169 awards were distributed to 2,995 recipients. More than three-quarters of these awardees (76.2%) were men, with women making up less than one-quarter (23.8%).
Encouragingly, there was an increasing trend in recognition of women over time, with 7.7% of female awardees in 2000 and climbing to 31.2% in 2021 (average annual percentage change, 6.6%; P < .05).
The distribution of awards also became more racially/ethnically diverse over time; in 2000, 92.3% of awardees were White versus 62.8% in 2021 (AAPC, –1.4%; P < .001).
There was also a significant increase in Asian (AAPC, 5.7%; P < .001), Hispanic/Latino (AAPC, 4.8%; P = .040), and Black (AAPC, 7.8%; P < .05) honorees.
Core influencers
By award type, women received fewer leadership awards than men, “which can be attributed to fewer leadership opportunities for women and a lack of acknowledgment of leadership responsibilities fulfilled by women,” the researchers said.
Award recipients with a PhD degree were nearly gender balanced (48.2% women), whereas men formed an overwhelming majority of awardees with an MD (84.7%).
Awards with male eponyms had fewer women recipients than did noneponymous awards (20.9% vs. 23.2%; P < .01).
“Male-eponymous awards can deter women applicants and give a subtle hint to selection committees to favor men as winners, creating an implicit bias,” the researchers said.
“Given the increased emphasis on redesigning cardiovascular health care delivery by incorporating the tenets of diversity, equity, and inclusion (DEI), cardiovascular societies have a significant role as core influencers,” Dr. Gulati and colleagues wrote.
They said that equitable award distribution can be a “key strategy to celebrate women and diverse members of the cardiovascular workforce and promulgate DEI.”
“Recognition of their contributions is pivotal to enhancing their self-perception. In addition to boosting confidence, receiving an award can also catalyze their career trajectory,” the authors added.
The study had no specific funding. The authors have declared no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Consider gaps in access and knowledge in diagnosis and treatment in skin of color
LAS VEGAS – and patients, Susan C. Taylor, MD, said in a presentation at MedscapeLive’s annual Las Vegas Dermatology Seminar.
Additionally, some disparities occur because of gaps in access to health care, said Dr. Taylor, vice chair, diversity, equity and inclusion, in the department of dermatology at the University of Pennsylvania, Philadelphia, who moderated an expert panel discussion of treatment tips for several common dermatologic conditions in skin of color patients.
Atopic dermatitis angles
Atopic dermatitis (AD) is the fourth most common dermatologic complaint in Black patients, based on data from the United States National Ambulatory Medical Care Survey. Also, data from the National Health and Nutrition Examination Survey show that Black children are nearly twice as likely as White children to develop AD after controlling for socioeconomic factors, Dr. Taylor said.
When Black patients present with AD, “you may not see the erythema,” said Valerie D. Callender, MD, of Howard University, Washington, who presented on AD. Instead, “you may see more follicular and papular presentations.” Erythema and erythroderma can present as shades of violet, gray, or dark brown in patients with rich skin tones, added Dr. Callender, who practices in Glenn Dale, Md.
Consequently, disease severity can be misinterpreted, she said, noting that data suggest that scoring systems such as the Eczema Area and Severity Index and Scoring Atopic Dermatitis underestimate AD severity in dark skin.
As for treatment, skin of color patients with AD are often as bothered by postinflammatory hyperpigmentation (PIH) as by active lesions, so treatment should take these concerns into account, Dr. Callender said. Studies evaluating the effectiveness of AD treatments in diverse populations are limited by lack of representation of racial groups in clinical trials and lack of subset analyses by race.
Acne awareness
An important consideration of acne in skin of color patients is that the acne “might not be red, it might just be darker,” said Andrew F. Alexis, MD, vice-chair for diversity and inclusion in the department of dermatology, and professor of clinical dermatology at Weill Cornell Medicine, New York. A study published in JAMA Dermatology of nearly 30,000 patients with acne from 2007 to 2017 found that non-Hispanic Black patients were more likely than non-Hispanic White patients to see a dermatologist for acne, but Black patients received fewer prescriptions for acne medications than White patients.
The study also showed that Black patients who received prescriptions for acne were more likely to receive topical retinoids and topical antibiotics, and less likely to receive oral antibiotics, spironolactone, or isotretinoin, compared with White patients. Similarly, Asian patients were more likely to receive topical antibiotics and less likely to receive oral antibiotics, compared with White patients.
Other panelists shared some of their best practices for acne in patients with skin of color, including treatment with topical retinoids (for inflammation) and spironolactone, and therapies that address both inflammation and pigmentation, such as salicylic acid and azelaic acid. Dr. Callender also advised asking patients about makeup, as they may not know that many types of makeup used to cover acne are in fact comedogenic.
Melanoma misconceptions
One of the most common misperceptions about melanoma among skin of color patients is that they don’t think they can get it, Dr. Taylor said. Many health care providers don’t think about melanoma in skin of color patients because of the dramatically lower incidence in this population, but as a result, cases may go undiagnosed, and as studies have shown, the mortality rate from melanoma is higher in Black patients.
Consider the palms, soles, nails, and web spaces as possible melanoma sites, Dr. Taylor added.
Educating skin of color patients about melanoma is important, although the incidence is 20 to 30 times lower than in non-Hispanic Whites, said Nada Elbuluk, MD, the founder and director of the University of Southern California Skin of Color Center and Pigmentary Disorders Clinic, Los Angeles. A 2020 editorial published in Cancer Cytopathology pointed out that 1 in 3 Black men or women with a melanoma diagnosis in the United States dies of the disease, compared with 1 in 7 non-Hispanic White men and 1 in 11 non-Hispanic White women with melanoma.
Don’t skip the total body skin exam in these patients, Dr. Elbuluk emphasized. Many patients will only partially undress, and areas such as toes can be missed.
Rosacea review
For patients with skin of color, clinicians need to look for different signs of rosacea than those typically seen in White patients, Dr. Elbuluk said. “The most common presentation of rosacea in skin of color is papulopustular,” and the granulomatous variant.
“These patients will often give you a history of sensitivity to products,” Dr. Elbuluk noted. They may not always have the flushing, but they may report warmth or itching, in addition to product sensitivity.
When considering rosacea in skin of color patients, be sure to have good lighting for close examination, as skin thickening is another subtle sign of rosacea in these patients, she said. Skin thickening “is a very early sign that will present in skin of color with no erythema, so keep that in mind.”
Stinging and burning sensations may be reported by skin of color patients with rosacea. Use patient history to confirm the diagnosis of rosacea, which is often delayed in skin of color patients because of a low index of suspicion, she said.
Psoriasis pointers
Psoriasis in skin of color patients used to be considered rare, “but that is far from true,” Dr. Alexis said. In fact, many cases of psoriasis are undiagnosed or the diagnosis is delayed in these patients.
The panelists noted that current guidelines for psoriasis treatment are based on clinical trials composed mainly of White patients, and do not contain specific recommendations for skin of color patients.
Notably, the morphology, location, and color of psoriasis lesions may be different for patients with darker skin, such as thicker plaques and more scaling over larger areas, they said. Also, skin of color patients may experience long-lasting dyspigmentation from psoriasis lesions that have resolved.
When developing a strategy for psoriasis in skin of color patients, consider not only disease severity, but also comorbidities and medications, response (if any) to prior therapies, patient preferences, and quality of life, the panelists said.
Dr. Callender, Dr. Elbuluk, Dr. Taylor, and Dr. Alexis reported conflicts of interest from numerous sources in industry. MedscapeLive and this news organization are owned by the same parent company.
LAS VEGAS – and patients, Susan C. Taylor, MD, said in a presentation at MedscapeLive’s annual Las Vegas Dermatology Seminar.
Additionally, some disparities occur because of gaps in access to health care, said Dr. Taylor, vice chair, diversity, equity and inclusion, in the department of dermatology at the University of Pennsylvania, Philadelphia, who moderated an expert panel discussion of treatment tips for several common dermatologic conditions in skin of color patients.
Atopic dermatitis angles
Atopic dermatitis (AD) is the fourth most common dermatologic complaint in Black patients, based on data from the United States National Ambulatory Medical Care Survey. Also, data from the National Health and Nutrition Examination Survey show that Black children are nearly twice as likely as White children to develop AD after controlling for socioeconomic factors, Dr. Taylor said.
When Black patients present with AD, “you may not see the erythema,” said Valerie D. Callender, MD, of Howard University, Washington, who presented on AD. Instead, “you may see more follicular and papular presentations.” Erythema and erythroderma can present as shades of violet, gray, or dark brown in patients with rich skin tones, added Dr. Callender, who practices in Glenn Dale, Md.
Consequently, disease severity can be misinterpreted, she said, noting that data suggest that scoring systems such as the Eczema Area and Severity Index and Scoring Atopic Dermatitis underestimate AD severity in dark skin.
As for treatment, skin of color patients with AD are often as bothered by postinflammatory hyperpigmentation (PIH) as by active lesions, so treatment should take these concerns into account, Dr. Callender said. Studies evaluating the effectiveness of AD treatments in diverse populations are limited by lack of representation of racial groups in clinical trials and lack of subset analyses by race.
Acne awareness
An important consideration of acne in skin of color patients is that the acne “might not be red, it might just be darker,” said Andrew F. Alexis, MD, vice-chair for diversity and inclusion in the department of dermatology, and professor of clinical dermatology at Weill Cornell Medicine, New York. A study published in JAMA Dermatology of nearly 30,000 patients with acne from 2007 to 2017 found that non-Hispanic Black patients were more likely than non-Hispanic White patients to see a dermatologist for acne, but Black patients received fewer prescriptions for acne medications than White patients.
The study also showed that Black patients who received prescriptions for acne were more likely to receive topical retinoids and topical antibiotics, and less likely to receive oral antibiotics, spironolactone, or isotretinoin, compared with White patients. Similarly, Asian patients were more likely to receive topical antibiotics and less likely to receive oral antibiotics, compared with White patients.
Other panelists shared some of their best practices for acne in patients with skin of color, including treatment with topical retinoids (for inflammation) and spironolactone, and therapies that address both inflammation and pigmentation, such as salicylic acid and azelaic acid. Dr. Callender also advised asking patients about makeup, as they may not know that many types of makeup used to cover acne are in fact comedogenic.
Melanoma misconceptions
One of the most common misperceptions about melanoma among skin of color patients is that they don’t think they can get it, Dr. Taylor said. Many health care providers don’t think about melanoma in skin of color patients because of the dramatically lower incidence in this population, but as a result, cases may go undiagnosed, and as studies have shown, the mortality rate from melanoma is higher in Black patients.
Consider the palms, soles, nails, and web spaces as possible melanoma sites, Dr. Taylor added.
Educating skin of color patients about melanoma is important, although the incidence is 20 to 30 times lower than in non-Hispanic Whites, said Nada Elbuluk, MD, the founder and director of the University of Southern California Skin of Color Center and Pigmentary Disorders Clinic, Los Angeles. A 2020 editorial published in Cancer Cytopathology pointed out that 1 in 3 Black men or women with a melanoma diagnosis in the United States dies of the disease, compared with 1 in 7 non-Hispanic White men and 1 in 11 non-Hispanic White women with melanoma.
Don’t skip the total body skin exam in these patients, Dr. Elbuluk emphasized. Many patients will only partially undress, and areas such as toes can be missed.
Rosacea review
For patients with skin of color, clinicians need to look for different signs of rosacea than those typically seen in White patients, Dr. Elbuluk said. “The most common presentation of rosacea in skin of color is papulopustular,” and the granulomatous variant.
“These patients will often give you a history of sensitivity to products,” Dr. Elbuluk noted. They may not always have the flushing, but they may report warmth or itching, in addition to product sensitivity.
When considering rosacea in skin of color patients, be sure to have good lighting for close examination, as skin thickening is another subtle sign of rosacea in these patients, she said. Skin thickening “is a very early sign that will present in skin of color with no erythema, so keep that in mind.”
Stinging and burning sensations may be reported by skin of color patients with rosacea. Use patient history to confirm the diagnosis of rosacea, which is often delayed in skin of color patients because of a low index of suspicion, she said.
Psoriasis pointers
Psoriasis in skin of color patients used to be considered rare, “but that is far from true,” Dr. Alexis said. In fact, many cases of psoriasis are undiagnosed or the diagnosis is delayed in these patients.
The panelists noted that current guidelines for psoriasis treatment are based on clinical trials composed mainly of White patients, and do not contain specific recommendations for skin of color patients.
Notably, the morphology, location, and color of psoriasis lesions may be different for patients with darker skin, such as thicker plaques and more scaling over larger areas, they said. Also, skin of color patients may experience long-lasting dyspigmentation from psoriasis lesions that have resolved.
When developing a strategy for psoriasis in skin of color patients, consider not only disease severity, but also comorbidities and medications, response (if any) to prior therapies, patient preferences, and quality of life, the panelists said.
Dr. Callender, Dr. Elbuluk, Dr. Taylor, and Dr. Alexis reported conflicts of interest from numerous sources in industry. MedscapeLive and this news organization are owned by the same parent company.
LAS VEGAS – and patients, Susan C. Taylor, MD, said in a presentation at MedscapeLive’s annual Las Vegas Dermatology Seminar.
Additionally, some disparities occur because of gaps in access to health care, said Dr. Taylor, vice chair, diversity, equity and inclusion, in the department of dermatology at the University of Pennsylvania, Philadelphia, who moderated an expert panel discussion of treatment tips for several common dermatologic conditions in skin of color patients.
Atopic dermatitis angles
Atopic dermatitis (AD) is the fourth most common dermatologic complaint in Black patients, based on data from the United States National Ambulatory Medical Care Survey. Also, data from the National Health and Nutrition Examination Survey show that Black children are nearly twice as likely as White children to develop AD after controlling for socioeconomic factors, Dr. Taylor said.
When Black patients present with AD, “you may not see the erythema,” said Valerie D. Callender, MD, of Howard University, Washington, who presented on AD. Instead, “you may see more follicular and papular presentations.” Erythema and erythroderma can present as shades of violet, gray, or dark brown in patients with rich skin tones, added Dr. Callender, who practices in Glenn Dale, Md.
Consequently, disease severity can be misinterpreted, she said, noting that data suggest that scoring systems such as the Eczema Area and Severity Index and Scoring Atopic Dermatitis underestimate AD severity in dark skin.
As for treatment, skin of color patients with AD are often as bothered by postinflammatory hyperpigmentation (PIH) as by active lesions, so treatment should take these concerns into account, Dr. Callender said. Studies evaluating the effectiveness of AD treatments in diverse populations are limited by lack of representation of racial groups in clinical trials and lack of subset analyses by race.
Acne awareness
An important consideration of acne in skin of color patients is that the acne “might not be red, it might just be darker,” said Andrew F. Alexis, MD, vice-chair for diversity and inclusion in the department of dermatology, and professor of clinical dermatology at Weill Cornell Medicine, New York. A study published in JAMA Dermatology of nearly 30,000 patients with acne from 2007 to 2017 found that non-Hispanic Black patients were more likely than non-Hispanic White patients to see a dermatologist for acne, but Black patients received fewer prescriptions for acne medications than White patients.
The study also showed that Black patients who received prescriptions for acne were more likely to receive topical retinoids and topical antibiotics, and less likely to receive oral antibiotics, spironolactone, or isotretinoin, compared with White patients. Similarly, Asian patients were more likely to receive topical antibiotics and less likely to receive oral antibiotics, compared with White patients.
Other panelists shared some of their best practices for acne in patients with skin of color, including treatment with topical retinoids (for inflammation) and spironolactone, and therapies that address both inflammation and pigmentation, such as salicylic acid and azelaic acid. Dr. Callender also advised asking patients about makeup, as they may not know that many types of makeup used to cover acne are in fact comedogenic.
Melanoma misconceptions
One of the most common misperceptions about melanoma among skin of color patients is that they don’t think they can get it, Dr. Taylor said. Many health care providers don’t think about melanoma in skin of color patients because of the dramatically lower incidence in this population, but as a result, cases may go undiagnosed, and as studies have shown, the mortality rate from melanoma is higher in Black patients.
Consider the palms, soles, nails, and web spaces as possible melanoma sites, Dr. Taylor added.
Educating skin of color patients about melanoma is important, although the incidence is 20 to 30 times lower than in non-Hispanic Whites, said Nada Elbuluk, MD, the founder and director of the University of Southern California Skin of Color Center and Pigmentary Disorders Clinic, Los Angeles. A 2020 editorial published in Cancer Cytopathology pointed out that 1 in 3 Black men or women with a melanoma diagnosis in the United States dies of the disease, compared with 1 in 7 non-Hispanic White men and 1 in 11 non-Hispanic White women with melanoma.
Don’t skip the total body skin exam in these patients, Dr. Elbuluk emphasized. Many patients will only partially undress, and areas such as toes can be missed.
Rosacea review
For patients with skin of color, clinicians need to look for different signs of rosacea than those typically seen in White patients, Dr. Elbuluk said. “The most common presentation of rosacea in skin of color is papulopustular,” and the granulomatous variant.
“These patients will often give you a history of sensitivity to products,” Dr. Elbuluk noted. They may not always have the flushing, but they may report warmth or itching, in addition to product sensitivity.
When considering rosacea in skin of color patients, be sure to have good lighting for close examination, as skin thickening is another subtle sign of rosacea in these patients, she said. Skin thickening “is a very early sign that will present in skin of color with no erythema, so keep that in mind.”
Stinging and burning sensations may be reported by skin of color patients with rosacea. Use patient history to confirm the diagnosis of rosacea, which is often delayed in skin of color patients because of a low index of suspicion, she said.
Psoriasis pointers
Psoriasis in skin of color patients used to be considered rare, “but that is far from true,” Dr. Alexis said. In fact, many cases of psoriasis are undiagnosed or the diagnosis is delayed in these patients.
The panelists noted that current guidelines for psoriasis treatment are based on clinical trials composed mainly of White patients, and do not contain specific recommendations for skin of color patients.
Notably, the morphology, location, and color of psoriasis lesions may be different for patients with darker skin, such as thicker plaques and more scaling over larger areas, they said. Also, skin of color patients may experience long-lasting dyspigmentation from psoriasis lesions that have resolved.
When developing a strategy for psoriasis in skin of color patients, consider not only disease severity, but also comorbidities and medications, response (if any) to prior therapies, patient preferences, and quality of life, the panelists said.
Dr. Callender, Dr. Elbuluk, Dr. Taylor, and Dr. Alexis reported conflicts of interest from numerous sources in industry. MedscapeLive and this news organization are owned by the same parent company.
AT INNOVATIONS IN DERMATOLOGY
Chronic stress, especially race related, may hasten cancer death
The American folk hero John Henry pitted his hammer against a mechanical steam drill, only to die of exhaustion after winning the battle. In the legend, John Henry was African American, and it’s a fitting metaphor, according to Justin Xavier Moore, PhD.
It’s a metaphor for accumulated stress over a lifetime, also known as allostatic load. Though it affects everyone, Black, Indigenous, and people of color experience it in excess. “It serves as a symbolism for the plight of African Americans within the United States, that regardless of all the triumph and trying to overcompensate and work just as hard as your counterpart, it oftentimes leads to this overtaxing or exhaustion because your competitor has an unfair advantage. You have Jim Crow laws in the South. We have the history of slavery. We have individuals of racial subgroups that are exposed daily to microaggressions, racial discrimination, stereotypes, redlining, all of these different issues that basically reduce to systemic racism,” said Dr. Moore, who is an assistant professor of medicine at the Medical College of Georgia, Augusta.
Dr. Moore is also a coauthor of a new study published online in SSM–Population Health, which examined the association between increased allostatic load and cancer outcomes among participants in the National Health and Nutrition Examination Survey (NHANES) and the National Death Index. They found that both non-Hispanic Black and non-Hispanic White adults with high allostatic load had about a doubled risk of cancer death.
To determine allostatic load, the researchers looked at nine factors collected in NHANES: abnormal values of BMI, diastolic blood pressure, glycohemoglobin, systolic blood pressure, total cholesterol, serum triglycerides, serum albumin, serum creatinine, and C-reactive protein. “The fact that we’re looking at cardiovascular, metabolic and immune function, all in one gives us a better risk assessment for morbidity and mortality. Allostatic load has actually been associated with cardiovascular disease. I think we are one of the first studies to actually look at whether allostatic load is associated with cancer mortality,” said Dr. Moore.
Previous research coauthored by Dr. Moore showed 20-year old African Americans have an allostatic load comparable with that seen in 30-year-old non-Hispanic Whites. That can lead to a proinflammatory state that might be causing increased cancer risk. But stress isn’t a simple concept to pin down, Dr. Moore said. “One of the founding fathers of public health research and epidemiology, Paracelsus, [said] ‘the dose makes the poison.’ ”
In this case, it means that not all stress is bad. Exercise is good stress. “Your heart rate goes up, you compete, and then it comes back down. That’s healthy. But then there’s those stressful situations like dealing with a horrible job, and a boss that may just be overdemanding. Deadlines, and not having a work-life balance. Too much stress, in this case, can cause cancer death,” Dr. Moore said.
In the study, both non-Hispanic Black adults and non-Hispanic White adults heightened risk of cancer death when dealing with high allostatic load, even though the cause of stress may be different. “It’s almost like the cause of the stress does not matter as much. There are millions of Americans that live in environments that are not conducive to their health. The fact of the matter is that because of racial discrimination, because all these different biases, African Americans may have higher allostatic load, which they did on an average, but high allostatic load for even White people is associated with dying from cancer,” Dr. Moore said.
After adjustment, the (adjusted subdistributed hazard ratio, 1.14; 95% CI, 1.04-1.26). After stratification by age, high allostatic load was associated with an 80% increased risk of cancer death among adults (SHR, 1.80; 95% CI, 1.35-2.41). Non-Hispanic White adults had a 95% increased risk (SHR, 1.95; 95% CI, 1.22-3.12), non-Hispanic Black adults had a twofold increased risk (SHR, 1.06; 95% CI, 1.27-3.34), and Hispanic adults had a 36% increased risk.
Dr. Moore has no relevant financial disclosures.
The American folk hero John Henry pitted his hammer against a mechanical steam drill, only to die of exhaustion after winning the battle. In the legend, John Henry was African American, and it’s a fitting metaphor, according to Justin Xavier Moore, PhD.
It’s a metaphor for accumulated stress over a lifetime, also known as allostatic load. Though it affects everyone, Black, Indigenous, and people of color experience it in excess. “It serves as a symbolism for the plight of African Americans within the United States, that regardless of all the triumph and trying to overcompensate and work just as hard as your counterpart, it oftentimes leads to this overtaxing or exhaustion because your competitor has an unfair advantage. You have Jim Crow laws in the South. We have the history of slavery. We have individuals of racial subgroups that are exposed daily to microaggressions, racial discrimination, stereotypes, redlining, all of these different issues that basically reduce to systemic racism,” said Dr. Moore, who is an assistant professor of medicine at the Medical College of Georgia, Augusta.
Dr. Moore is also a coauthor of a new study published online in SSM–Population Health, which examined the association between increased allostatic load and cancer outcomes among participants in the National Health and Nutrition Examination Survey (NHANES) and the National Death Index. They found that both non-Hispanic Black and non-Hispanic White adults with high allostatic load had about a doubled risk of cancer death.
To determine allostatic load, the researchers looked at nine factors collected in NHANES: abnormal values of BMI, diastolic blood pressure, glycohemoglobin, systolic blood pressure, total cholesterol, serum triglycerides, serum albumin, serum creatinine, and C-reactive protein. “The fact that we’re looking at cardiovascular, metabolic and immune function, all in one gives us a better risk assessment for morbidity and mortality. Allostatic load has actually been associated with cardiovascular disease. I think we are one of the first studies to actually look at whether allostatic load is associated with cancer mortality,” said Dr. Moore.
Previous research coauthored by Dr. Moore showed 20-year old African Americans have an allostatic load comparable with that seen in 30-year-old non-Hispanic Whites. That can lead to a proinflammatory state that might be causing increased cancer risk. But stress isn’t a simple concept to pin down, Dr. Moore said. “One of the founding fathers of public health research and epidemiology, Paracelsus, [said] ‘the dose makes the poison.’ ”
In this case, it means that not all stress is bad. Exercise is good stress. “Your heart rate goes up, you compete, and then it comes back down. That’s healthy. But then there’s those stressful situations like dealing with a horrible job, and a boss that may just be overdemanding. Deadlines, and not having a work-life balance. Too much stress, in this case, can cause cancer death,” Dr. Moore said.
In the study, both non-Hispanic Black adults and non-Hispanic White adults heightened risk of cancer death when dealing with high allostatic load, even though the cause of stress may be different. “It’s almost like the cause of the stress does not matter as much. There are millions of Americans that live in environments that are not conducive to their health. The fact of the matter is that because of racial discrimination, because all these different biases, African Americans may have higher allostatic load, which they did on an average, but high allostatic load for even White people is associated with dying from cancer,” Dr. Moore said.
After adjustment, the (adjusted subdistributed hazard ratio, 1.14; 95% CI, 1.04-1.26). After stratification by age, high allostatic load was associated with an 80% increased risk of cancer death among adults (SHR, 1.80; 95% CI, 1.35-2.41). Non-Hispanic White adults had a 95% increased risk (SHR, 1.95; 95% CI, 1.22-3.12), non-Hispanic Black adults had a twofold increased risk (SHR, 1.06; 95% CI, 1.27-3.34), and Hispanic adults had a 36% increased risk.
Dr. Moore has no relevant financial disclosures.
The American folk hero John Henry pitted his hammer against a mechanical steam drill, only to die of exhaustion after winning the battle. In the legend, John Henry was African American, and it’s a fitting metaphor, according to Justin Xavier Moore, PhD.
It’s a metaphor for accumulated stress over a lifetime, also known as allostatic load. Though it affects everyone, Black, Indigenous, and people of color experience it in excess. “It serves as a symbolism for the plight of African Americans within the United States, that regardless of all the triumph and trying to overcompensate and work just as hard as your counterpart, it oftentimes leads to this overtaxing or exhaustion because your competitor has an unfair advantage. You have Jim Crow laws in the South. We have the history of slavery. We have individuals of racial subgroups that are exposed daily to microaggressions, racial discrimination, stereotypes, redlining, all of these different issues that basically reduce to systemic racism,” said Dr. Moore, who is an assistant professor of medicine at the Medical College of Georgia, Augusta.
Dr. Moore is also a coauthor of a new study published online in SSM–Population Health, which examined the association between increased allostatic load and cancer outcomes among participants in the National Health and Nutrition Examination Survey (NHANES) and the National Death Index. They found that both non-Hispanic Black and non-Hispanic White adults with high allostatic load had about a doubled risk of cancer death.
To determine allostatic load, the researchers looked at nine factors collected in NHANES: abnormal values of BMI, diastolic blood pressure, glycohemoglobin, systolic blood pressure, total cholesterol, serum triglycerides, serum albumin, serum creatinine, and C-reactive protein. “The fact that we’re looking at cardiovascular, metabolic and immune function, all in one gives us a better risk assessment for morbidity and mortality. Allostatic load has actually been associated with cardiovascular disease. I think we are one of the first studies to actually look at whether allostatic load is associated with cancer mortality,” said Dr. Moore.
Previous research coauthored by Dr. Moore showed 20-year old African Americans have an allostatic load comparable with that seen in 30-year-old non-Hispanic Whites. That can lead to a proinflammatory state that might be causing increased cancer risk. But stress isn’t a simple concept to pin down, Dr. Moore said. “One of the founding fathers of public health research and epidemiology, Paracelsus, [said] ‘the dose makes the poison.’ ”
In this case, it means that not all stress is bad. Exercise is good stress. “Your heart rate goes up, you compete, and then it comes back down. That’s healthy. But then there’s those stressful situations like dealing with a horrible job, and a boss that may just be overdemanding. Deadlines, and not having a work-life balance. Too much stress, in this case, can cause cancer death,” Dr. Moore said.
In the study, both non-Hispanic Black adults and non-Hispanic White adults heightened risk of cancer death when dealing with high allostatic load, even though the cause of stress may be different. “It’s almost like the cause of the stress does not matter as much. There are millions of Americans that live in environments that are not conducive to their health. The fact of the matter is that because of racial discrimination, because all these different biases, African Americans may have higher allostatic load, which they did on an average, but high allostatic load for even White people is associated with dying from cancer,” Dr. Moore said.
After adjustment, the (adjusted subdistributed hazard ratio, 1.14; 95% CI, 1.04-1.26). After stratification by age, high allostatic load was associated with an 80% increased risk of cancer death among adults (SHR, 1.80; 95% CI, 1.35-2.41). Non-Hispanic White adults had a 95% increased risk (SHR, 1.95; 95% CI, 1.22-3.12), non-Hispanic Black adults had a twofold increased risk (SHR, 1.06; 95% CI, 1.27-3.34), and Hispanic adults had a 36% increased risk.
Dr. Moore has no relevant financial disclosures.
FROM SSM–POPULATION HEALTH
Florida medical boards ban transgender care for minors
Florida’s two main medical bodies have voted to stop gender-affirming treatment of children, including the use of puberty blockers, cross-sex hormones, and surgery, other than in minors who are already receiving such care.
The move, which is unprecedented, makes Florida one of several U.S. states to restrict gender-affirming care for adolescents, but the first to do so via an administrative process, through the actions of its Board of Medicine and Board of Osteopathic Medicine.
“I appreciate the integrity of the Boards for ruling in the best interest of children in Florida despite facing tremendous pressure to permit these unproven and risky treatments,” Florida Surgeon General Joseph Ladapo, MD, PhD, said in a statement.
In a statement, The Endocrine Society criticizes the decision as “blatantly discriminatory” and not based on medical evidence.
During a meeting on Oct. 28 that involved testimonies from doctors, parents of transgender children, detransitioners, and patients, board members referred to similar changes in Europe, where some countries have pushed psychotherapy instead of surgery or hormone treatment.
Then, on Nov. 4, the boards each set slightly different instructions, with the Board of Osteopathic Medicine voting to restrict care for new patients but allowing an exception for children enrolled in clinical studies, which “must include long-term longitudinal assessments of the patients’ physiologic and psychologic outcomes,” according to the Florida Department of Health.
The Board of Medicine did not allow the latter.
The proposed rules are open to public comment before finalization.
Arkansas was the first state to enact such a ban on gender-affirming care, with Republican lawmakers in 2021 overriding GOP Gov. Asa Hutchinson’s veto of the legislation. Alabama Republicans in 2022 approved legislation to outlaw gender-affirming medications for transgender youths. Both laws have been paused amid unfolding legal battles, according to Associated Press.
Oklahoma Gov. Kevin Stitt, a Republican, signed a bill in October that bars federal funds earmarked for the University of Oklahoma Medical Center from being used for gender reassignment treatments for minors. Gov. Stitt also called for the legislature to ban some of those gender reassignment treatments statewide when it returns in February.
Top Tennessee Republicans also have vowed to push for strict antitransgender policies. The state already bans doctors from providing gender-confirming hormone treatment to prepubescent minors. To date, no one has legally challenged the law as medical experts maintain no doctor in Tennessee does so.
A version of this article first appeared on Medscape.com.
Florida’s two main medical bodies have voted to stop gender-affirming treatment of children, including the use of puberty blockers, cross-sex hormones, and surgery, other than in minors who are already receiving such care.
The move, which is unprecedented, makes Florida one of several U.S. states to restrict gender-affirming care for adolescents, but the first to do so via an administrative process, through the actions of its Board of Medicine and Board of Osteopathic Medicine.
“I appreciate the integrity of the Boards for ruling in the best interest of children in Florida despite facing tremendous pressure to permit these unproven and risky treatments,” Florida Surgeon General Joseph Ladapo, MD, PhD, said in a statement.
In a statement, The Endocrine Society criticizes the decision as “blatantly discriminatory” and not based on medical evidence.
During a meeting on Oct. 28 that involved testimonies from doctors, parents of transgender children, detransitioners, and patients, board members referred to similar changes in Europe, where some countries have pushed psychotherapy instead of surgery or hormone treatment.
Then, on Nov. 4, the boards each set slightly different instructions, with the Board of Osteopathic Medicine voting to restrict care for new patients but allowing an exception for children enrolled in clinical studies, which “must include long-term longitudinal assessments of the patients’ physiologic and psychologic outcomes,” according to the Florida Department of Health.
The Board of Medicine did not allow the latter.
The proposed rules are open to public comment before finalization.
Arkansas was the first state to enact such a ban on gender-affirming care, with Republican lawmakers in 2021 overriding GOP Gov. Asa Hutchinson’s veto of the legislation. Alabama Republicans in 2022 approved legislation to outlaw gender-affirming medications for transgender youths. Both laws have been paused amid unfolding legal battles, according to Associated Press.
Oklahoma Gov. Kevin Stitt, a Republican, signed a bill in October that bars federal funds earmarked for the University of Oklahoma Medical Center from being used for gender reassignment treatments for minors. Gov. Stitt also called for the legislature to ban some of those gender reassignment treatments statewide when it returns in February.
Top Tennessee Republicans also have vowed to push for strict antitransgender policies. The state already bans doctors from providing gender-confirming hormone treatment to prepubescent minors. To date, no one has legally challenged the law as medical experts maintain no doctor in Tennessee does so.
A version of this article first appeared on Medscape.com.
Florida’s two main medical bodies have voted to stop gender-affirming treatment of children, including the use of puberty blockers, cross-sex hormones, and surgery, other than in minors who are already receiving such care.
The move, which is unprecedented, makes Florida one of several U.S. states to restrict gender-affirming care for adolescents, but the first to do so via an administrative process, through the actions of its Board of Medicine and Board of Osteopathic Medicine.
“I appreciate the integrity of the Boards for ruling in the best interest of children in Florida despite facing tremendous pressure to permit these unproven and risky treatments,” Florida Surgeon General Joseph Ladapo, MD, PhD, said in a statement.
In a statement, The Endocrine Society criticizes the decision as “blatantly discriminatory” and not based on medical evidence.
During a meeting on Oct. 28 that involved testimonies from doctors, parents of transgender children, detransitioners, and patients, board members referred to similar changes in Europe, where some countries have pushed psychotherapy instead of surgery or hormone treatment.
Then, on Nov. 4, the boards each set slightly different instructions, with the Board of Osteopathic Medicine voting to restrict care for new patients but allowing an exception for children enrolled in clinical studies, which “must include long-term longitudinal assessments of the patients’ physiologic and psychologic outcomes,” according to the Florida Department of Health.
The Board of Medicine did not allow the latter.
The proposed rules are open to public comment before finalization.
Arkansas was the first state to enact such a ban on gender-affirming care, with Republican lawmakers in 2021 overriding GOP Gov. Asa Hutchinson’s veto of the legislation. Alabama Republicans in 2022 approved legislation to outlaw gender-affirming medications for transgender youths. Both laws have been paused amid unfolding legal battles, according to Associated Press.
Oklahoma Gov. Kevin Stitt, a Republican, signed a bill in October that bars federal funds earmarked for the University of Oklahoma Medical Center from being used for gender reassignment treatments for minors. Gov. Stitt also called for the legislature to ban some of those gender reassignment treatments statewide when it returns in February.
Top Tennessee Republicans also have vowed to push for strict antitransgender policies. The state already bans doctors from providing gender-confirming hormone treatment to prepubescent minors. To date, no one has legally challenged the law as medical experts maintain no doctor in Tennessee does so.
A version of this article first appeared on Medscape.com.
Physicians react: Climate change and other social issues
Around half of them rated climate change among their five most important issues. Slightly lower percentages of doctors prioritized domestic violence and immigration/refugee policies that highly, and about 40% did so regarding reproductive rights in the United States.
Survey responses and comments left on the Physicians’ Views on Today’s Divisive Social Issues 2022 report provide insights into doctors’ attitudes and thinking about these four social challenges.
Relevance of climate change to health care
In the Medscape report, 61% of physicians described themselves as “very concerned” or “concerned” about climate change, and about 7 in 10 agreed with the statement that it should be a top worldwide priority. “Climate change is the most pressing issue of this century,” a psychiatrist respondent wrote.
What about direct effects on patients’ health? An internist worried that rising temperatures will cause “pathogens to spread and infect disadvantaged people who do not have health access and have immunocompromised conditions.” A family medicine physician predicted “more weather disasters, more asthma, more hormonal changes, and more obesity.”
However, physician viewpoints ran the gamut with an issue that has become politically and emotionally charged. Descriptions such as “overblown,” “hysteria,” “hoax,” and “farce” were used. “Climate change is a natural phenomenon under God’s purview,” an emergency medicine physician said.
And there was some middle-ground thinking. “It’s overstated but quite real,” a pediatrician respondent wrote. Added an ophthalmologist: “It has gone on for ages. We must work to decrease man-made conditions that affect climate change, but it must be done in an intelligent fashion.”
Domestic violence: What physicians can do
About 7 in 10 physicians surveyed by Medscape said they don’t think the United States is adequately tackling domestic violence. “It is underrecognized and ignored,” a psychiatrist respondent argued. The problem is “rampant and unacceptable, pushed into a closet and normalized, with associated shame,” an emergency medicine doctor wrote.
Many respondents noted that physicians are under a mandate to report abuse of or a suspicious injury to a patient. Some shared anecdotes about how they reported action they had taken when they suspected it. “I’ve told patients who may be in dangerous situations that I’m a safe person and provide a safe space,” a radiologist added. An internist said, “I’ve recently started to ask about safety at home during triage on every patient.”
Other doctors bemoaned a lack of adequate education on detecting and managing domestic violence and abuse. “Domestic violence is often not recognized by health care providers,” a psychiatrist respondent observed.
Expanding legal immigration
In the Medscape report, 34% of physicians felt U.S. immigration/refugee policies need to be tougher, while 28% said they are too restrictive, and about a fifth saw them as appropriate.
“As an immigrant, I can tell you that the system is flawed and needs a complete overhaul, which will take a bipartisan effort,” an endocrinologist respondent wrote.
A number of respondents argued that it’s critical to simplify the process of obtaining U.S. citizenship so that fewer will feel forced to enter the country illegally. “For a country that relies very heavily on immigrants to sustain our health care system, we behave like idiots in denying safe harbor,” a nephrologist asserted.
A neurologist concurred. “Legal immigration needs to be encouraged. It should be easier to exchange visitor or student visa to immigrant visa in order to retain talent in the health care and technology fields, which would alleviate the shortage of workers in health care.”
Reproductive rights: No easy answers
Medscape’s survey was conducted before the U.S. Supreme Court in June reversed Roe v. Wade. In the report, 71% of physicians described themselves as very to somewhat concerned about women’s reproductive rights, but their viewpoints became nuanced after that. “There is a big disparity among physicians on this topic,” an oncologist respondent wrote.
At one end of the spectrum, 3% of doctors felt that abortions should never be permitted. “The human baby in the womb is an independent person with the right to life,” a pathologist said. At the other end, nearly one-fourth of physicians believed abortion should be accessible under all circumstances, regardless of trimester or reason. “I am just here to support the woman and make her decision a reality,” an internist said.
While saying an abortion should be granted after “fetal viability” only “in extenuating circumstances,” an ob.gyn. respondent said she is “extremely concerned” about attacks on abortion rights. “Some of us are old enough to remember women coming to the ER in extremis after illegal procedures, prior to Roe v. Wade.”
A version of this article first appeared on Medscape.com.
Around half of them rated climate change among their five most important issues. Slightly lower percentages of doctors prioritized domestic violence and immigration/refugee policies that highly, and about 40% did so regarding reproductive rights in the United States.
Survey responses and comments left on the Physicians’ Views on Today’s Divisive Social Issues 2022 report provide insights into doctors’ attitudes and thinking about these four social challenges.
Relevance of climate change to health care
In the Medscape report, 61% of physicians described themselves as “very concerned” or “concerned” about climate change, and about 7 in 10 agreed with the statement that it should be a top worldwide priority. “Climate change is the most pressing issue of this century,” a psychiatrist respondent wrote.
What about direct effects on patients’ health? An internist worried that rising temperatures will cause “pathogens to spread and infect disadvantaged people who do not have health access and have immunocompromised conditions.” A family medicine physician predicted “more weather disasters, more asthma, more hormonal changes, and more obesity.”
However, physician viewpoints ran the gamut with an issue that has become politically and emotionally charged. Descriptions such as “overblown,” “hysteria,” “hoax,” and “farce” were used. “Climate change is a natural phenomenon under God’s purview,” an emergency medicine physician said.
And there was some middle-ground thinking. “It’s overstated but quite real,” a pediatrician respondent wrote. Added an ophthalmologist: “It has gone on for ages. We must work to decrease man-made conditions that affect climate change, but it must be done in an intelligent fashion.”
Domestic violence: What physicians can do
About 7 in 10 physicians surveyed by Medscape said they don’t think the United States is adequately tackling domestic violence. “It is underrecognized and ignored,” a psychiatrist respondent argued. The problem is “rampant and unacceptable, pushed into a closet and normalized, with associated shame,” an emergency medicine doctor wrote.
Many respondents noted that physicians are under a mandate to report abuse of or a suspicious injury to a patient. Some shared anecdotes about how they reported action they had taken when they suspected it. “I’ve told patients who may be in dangerous situations that I’m a safe person and provide a safe space,” a radiologist added. An internist said, “I’ve recently started to ask about safety at home during triage on every patient.”
Other doctors bemoaned a lack of adequate education on detecting and managing domestic violence and abuse. “Domestic violence is often not recognized by health care providers,” a psychiatrist respondent observed.
Expanding legal immigration
In the Medscape report, 34% of physicians felt U.S. immigration/refugee policies need to be tougher, while 28% said they are too restrictive, and about a fifth saw them as appropriate.
“As an immigrant, I can tell you that the system is flawed and needs a complete overhaul, which will take a bipartisan effort,” an endocrinologist respondent wrote.
A number of respondents argued that it’s critical to simplify the process of obtaining U.S. citizenship so that fewer will feel forced to enter the country illegally. “For a country that relies very heavily on immigrants to sustain our health care system, we behave like idiots in denying safe harbor,” a nephrologist asserted.
A neurologist concurred. “Legal immigration needs to be encouraged. It should be easier to exchange visitor or student visa to immigrant visa in order to retain talent in the health care and technology fields, which would alleviate the shortage of workers in health care.”
Reproductive rights: No easy answers
Medscape’s survey was conducted before the U.S. Supreme Court in June reversed Roe v. Wade. In the report, 71% of physicians described themselves as very to somewhat concerned about women’s reproductive rights, but their viewpoints became nuanced after that. “There is a big disparity among physicians on this topic,” an oncologist respondent wrote.
At one end of the spectrum, 3% of doctors felt that abortions should never be permitted. “The human baby in the womb is an independent person with the right to life,” a pathologist said. At the other end, nearly one-fourth of physicians believed abortion should be accessible under all circumstances, regardless of trimester or reason. “I am just here to support the woman and make her decision a reality,” an internist said.
While saying an abortion should be granted after “fetal viability” only “in extenuating circumstances,” an ob.gyn. respondent said she is “extremely concerned” about attacks on abortion rights. “Some of us are old enough to remember women coming to the ER in extremis after illegal procedures, prior to Roe v. Wade.”
A version of this article first appeared on Medscape.com.
Around half of them rated climate change among their five most important issues. Slightly lower percentages of doctors prioritized domestic violence and immigration/refugee policies that highly, and about 40% did so regarding reproductive rights in the United States.
Survey responses and comments left on the Physicians’ Views on Today’s Divisive Social Issues 2022 report provide insights into doctors’ attitudes and thinking about these four social challenges.
Relevance of climate change to health care
In the Medscape report, 61% of physicians described themselves as “very concerned” or “concerned” about climate change, and about 7 in 10 agreed with the statement that it should be a top worldwide priority. “Climate change is the most pressing issue of this century,” a psychiatrist respondent wrote.
What about direct effects on patients’ health? An internist worried that rising temperatures will cause “pathogens to spread and infect disadvantaged people who do not have health access and have immunocompromised conditions.” A family medicine physician predicted “more weather disasters, more asthma, more hormonal changes, and more obesity.”
However, physician viewpoints ran the gamut with an issue that has become politically and emotionally charged. Descriptions such as “overblown,” “hysteria,” “hoax,” and “farce” were used. “Climate change is a natural phenomenon under God’s purview,” an emergency medicine physician said.
And there was some middle-ground thinking. “It’s overstated but quite real,” a pediatrician respondent wrote. Added an ophthalmologist: “It has gone on for ages. We must work to decrease man-made conditions that affect climate change, but it must be done in an intelligent fashion.”
Domestic violence: What physicians can do
About 7 in 10 physicians surveyed by Medscape said they don’t think the United States is adequately tackling domestic violence. “It is underrecognized and ignored,” a psychiatrist respondent argued. The problem is “rampant and unacceptable, pushed into a closet and normalized, with associated shame,” an emergency medicine doctor wrote.
Many respondents noted that physicians are under a mandate to report abuse of or a suspicious injury to a patient. Some shared anecdotes about how they reported action they had taken when they suspected it. “I’ve told patients who may be in dangerous situations that I’m a safe person and provide a safe space,” a radiologist added. An internist said, “I’ve recently started to ask about safety at home during triage on every patient.”
Other doctors bemoaned a lack of adequate education on detecting and managing domestic violence and abuse. “Domestic violence is often not recognized by health care providers,” a psychiatrist respondent observed.
Expanding legal immigration
In the Medscape report, 34% of physicians felt U.S. immigration/refugee policies need to be tougher, while 28% said they are too restrictive, and about a fifth saw them as appropriate.
“As an immigrant, I can tell you that the system is flawed and needs a complete overhaul, which will take a bipartisan effort,” an endocrinologist respondent wrote.
A number of respondents argued that it’s critical to simplify the process of obtaining U.S. citizenship so that fewer will feel forced to enter the country illegally. “For a country that relies very heavily on immigrants to sustain our health care system, we behave like idiots in denying safe harbor,” a nephrologist asserted.
A neurologist concurred. “Legal immigration needs to be encouraged. It should be easier to exchange visitor or student visa to immigrant visa in order to retain talent in the health care and technology fields, which would alleviate the shortage of workers in health care.”
Reproductive rights: No easy answers
Medscape’s survey was conducted before the U.S. Supreme Court in June reversed Roe v. Wade. In the report, 71% of physicians described themselves as very to somewhat concerned about women’s reproductive rights, but their viewpoints became nuanced after that. “There is a big disparity among physicians on this topic,” an oncologist respondent wrote.
At one end of the spectrum, 3% of doctors felt that abortions should never be permitted. “The human baby in the womb is an independent person with the right to life,” a pathologist said. At the other end, nearly one-fourth of physicians believed abortion should be accessible under all circumstances, regardless of trimester or reason. “I am just here to support the woman and make her decision a reality,” an internist said.
While saying an abortion should be granted after “fetal viability” only “in extenuating circumstances,” an ob.gyn. respondent said she is “extremely concerned” about attacks on abortion rights. “Some of us are old enough to remember women coming to the ER in extremis after illegal procedures, prior to Roe v. Wade.”
A version of this article first appeared on Medscape.com.
DTC telemedicine expands access to gender-affirming therapy
Direct-to-consumer telemedicine services that provide gender-affirming hormone therapy appear to follow evidence-based guidelines and charge about the same as brick-and-mortar medical centers, according to researchers who reviewed the platforms’ websites.
The findings suggest that virtual care “may be a good option” for transgender, nonbinary, and intersex people, who often report difficulty finding physicians they trust, Erin Jesse, MD, a fifth-year urology resident at University Hospitals Cleveland Medical Center, who is the first author of the study, told this news organization.
Dr. Jesse’s group presented their findings at a joint scientific meeting of the Sexual Medicine Society of North America and the International Society for Sexual Medicine in Miami. The results have not been published in a peer-reviewed journal.
New direct-to-consumer telemedicine companies have emerged with gender-diverse staff and services tailored to the needs of these individuals. They offer “a more inclusive feel” than might be encountered at a physician’s office, Dr. Jesse said.
Confirming that these companies adhere to standards of care and cost-effectiveness “is especially important considering the reduced access to care and potentially increased vulnerability of the gender-diverse population,” she and her colleagues wrote.
From a Google search in March, the team identified six U.S.-based platforms that offer gender-affirming medical therapy: FOLX, True U Clinic, QueerDoc, Queer Med, TransClinique, and Plume.
From information posted on the companies’ websites, the researchers determined that all aligned with the World Professional Association for Transgender Health’s Standards of Care in two areas: use of an informed consent model to ensure that patients have sufficient information and understanding to decide on their own treatment and endorsement of frequent laboratory monitoring of hormone levels in early stages of treatment.
The team also compared the costs listed on the websites for the first year of therapy to the costs of similar care at a tertiary center, as determined using University Hospitals Cleveland Medical Center’s online estimator.
The platforms offered various pricing models, including fee-for-service and monthly membership plans ranging from $59 to $139. For individuals without insurance, estimates ranged from $1,022 to $1,428 for oral estradiol and from $1,184 to $1,668 for intramuscular testosterone from the online companies, compared with $1,184 and $1,216, respectively, at the tertiary center.
Although some platforms accept insurance, the researchers were not able to evaluate the cost of using private insurance or Medicaid, Dr. Jesse said. She noted that transgender individuals are more likely to lack insurance than are cisgender patients.
The team also assessed the scope of services. All companies offered legal help with changes to names and gender markers, such as “M” and “F.” Three or more companies offered preexposure prophylaxis to prevent HIV infection, treatment for erectile dysfunction, referrals for surgery, and medical letters of support for surgery.
Two offered puberty blockers, although the researchers were unable to determine the risk of adolescents obtaining treatment without proper assessments, because details of those services are not disclosed on websites, Dr. Jesse said.
An avenue of further research would be to interview patients to learn how platforms operate in practice and whether patients are properly assessed before treatment. “Those sorts of questions we can’t answer just by looking at the websites,” she said.
However, Charlotte Hoffman, JD, senior policy counsel for the National Center for Transgender Equality, an advocacy group, said she does not harbor concerns about patients being treated inappropriately simply because care is virtual. All clinicians who provide gender-affirming care face potential repercussions, such as malpractice lawsuits or state disciplinary action, if they veer from treatment guidelines, she said.
“I don’t necessarily take the premise that telehealth is inherently worse than in-person care as a given,” Ms. Hoffman said.
During the COVID-19 pandemic, Ms. Hoffman added, direct-to-consumer telemedicine has expanded access for individuals in rural areas, people with disabilities, and those who live in places where in-person providers of transgender care face public hostility, although individuals without the resources to pay may still be left out.
What might happen to that access if telemedicine restrictions that were loosened during the pandemic are reinstated is unclear, she said.
The researchers and Ms. Hoffman have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Direct-to-consumer telemedicine services that provide gender-affirming hormone therapy appear to follow evidence-based guidelines and charge about the same as brick-and-mortar medical centers, according to researchers who reviewed the platforms’ websites.
The findings suggest that virtual care “may be a good option” for transgender, nonbinary, and intersex people, who often report difficulty finding physicians they trust, Erin Jesse, MD, a fifth-year urology resident at University Hospitals Cleveland Medical Center, who is the first author of the study, told this news organization.
Dr. Jesse’s group presented their findings at a joint scientific meeting of the Sexual Medicine Society of North America and the International Society for Sexual Medicine in Miami. The results have not been published in a peer-reviewed journal.
New direct-to-consumer telemedicine companies have emerged with gender-diverse staff and services tailored to the needs of these individuals. They offer “a more inclusive feel” than might be encountered at a physician’s office, Dr. Jesse said.
Confirming that these companies adhere to standards of care and cost-effectiveness “is especially important considering the reduced access to care and potentially increased vulnerability of the gender-diverse population,” she and her colleagues wrote.
From a Google search in March, the team identified six U.S.-based platforms that offer gender-affirming medical therapy: FOLX, True U Clinic, QueerDoc, Queer Med, TransClinique, and Plume.
From information posted on the companies’ websites, the researchers determined that all aligned with the World Professional Association for Transgender Health’s Standards of Care in two areas: use of an informed consent model to ensure that patients have sufficient information and understanding to decide on their own treatment and endorsement of frequent laboratory monitoring of hormone levels in early stages of treatment.
The team also compared the costs listed on the websites for the first year of therapy to the costs of similar care at a tertiary center, as determined using University Hospitals Cleveland Medical Center’s online estimator.
The platforms offered various pricing models, including fee-for-service and monthly membership plans ranging from $59 to $139. For individuals without insurance, estimates ranged from $1,022 to $1,428 for oral estradiol and from $1,184 to $1,668 for intramuscular testosterone from the online companies, compared with $1,184 and $1,216, respectively, at the tertiary center.
Although some platforms accept insurance, the researchers were not able to evaluate the cost of using private insurance or Medicaid, Dr. Jesse said. She noted that transgender individuals are more likely to lack insurance than are cisgender patients.
The team also assessed the scope of services. All companies offered legal help with changes to names and gender markers, such as “M” and “F.” Three or more companies offered preexposure prophylaxis to prevent HIV infection, treatment for erectile dysfunction, referrals for surgery, and medical letters of support for surgery.
Two offered puberty blockers, although the researchers were unable to determine the risk of adolescents obtaining treatment without proper assessments, because details of those services are not disclosed on websites, Dr. Jesse said.
An avenue of further research would be to interview patients to learn how platforms operate in practice and whether patients are properly assessed before treatment. “Those sorts of questions we can’t answer just by looking at the websites,” she said.
However, Charlotte Hoffman, JD, senior policy counsel for the National Center for Transgender Equality, an advocacy group, said she does not harbor concerns about patients being treated inappropriately simply because care is virtual. All clinicians who provide gender-affirming care face potential repercussions, such as malpractice lawsuits or state disciplinary action, if they veer from treatment guidelines, she said.
“I don’t necessarily take the premise that telehealth is inherently worse than in-person care as a given,” Ms. Hoffman said.
During the COVID-19 pandemic, Ms. Hoffman added, direct-to-consumer telemedicine has expanded access for individuals in rural areas, people with disabilities, and those who live in places where in-person providers of transgender care face public hostility, although individuals without the resources to pay may still be left out.
What might happen to that access if telemedicine restrictions that were loosened during the pandemic are reinstated is unclear, she said.
The researchers and Ms. Hoffman have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Direct-to-consumer telemedicine services that provide gender-affirming hormone therapy appear to follow evidence-based guidelines and charge about the same as brick-and-mortar medical centers, according to researchers who reviewed the platforms’ websites.
The findings suggest that virtual care “may be a good option” for transgender, nonbinary, and intersex people, who often report difficulty finding physicians they trust, Erin Jesse, MD, a fifth-year urology resident at University Hospitals Cleveland Medical Center, who is the first author of the study, told this news organization.
Dr. Jesse’s group presented their findings at a joint scientific meeting of the Sexual Medicine Society of North America and the International Society for Sexual Medicine in Miami. The results have not been published in a peer-reviewed journal.
New direct-to-consumer telemedicine companies have emerged with gender-diverse staff and services tailored to the needs of these individuals. They offer “a more inclusive feel” than might be encountered at a physician’s office, Dr. Jesse said.
Confirming that these companies adhere to standards of care and cost-effectiveness “is especially important considering the reduced access to care and potentially increased vulnerability of the gender-diverse population,” she and her colleagues wrote.
From a Google search in March, the team identified six U.S.-based platforms that offer gender-affirming medical therapy: FOLX, True U Clinic, QueerDoc, Queer Med, TransClinique, and Plume.
From information posted on the companies’ websites, the researchers determined that all aligned with the World Professional Association for Transgender Health’s Standards of Care in two areas: use of an informed consent model to ensure that patients have sufficient information and understanding to decide on their own treatment and endorsement of frequent laboratory monitoring of hormone levels in early stages of treatment.
The team also compared the costs listed on the websites for the first year of therapy to the costs of similar care at a tertiary center, as determined using University Hospitals Cleveland Medical Center’s online estimator.
The platforms offered various pricing models, including fee-for-service and monthly membership plans ranging from $59 to $139. For individuals without insurance, estimates ranged from $1,022 to $1,428 for oral estradiol and from $1,184 to $1,668 for intramuscular testosterone from the online companies, compared with $1,184 and $1,216, respectively, at the tertiary center.
Although some platforms accept insurance, the researchers were not able to evaluate the cost of using private insurance or Medicaid, Dr. Jesse said. She noted that transgender individuals are more likely to lack insurance than are cisgender patients.
The team also assessed the scope of services. All companies offered legal help with changes to names and gender markers, such as “M” and “F.” Three or more companies offered preexposure prophylaxis to prevent HIV infection, treatment for erectile dysfunction, referrals for surgery, and medical letters of support for surgery.
Two offered puberty blockers, although the researchers were unable to determine the risk of adolescents obtaining treatment without proper assessments, because details of those services are not disclosed on websites, Dr. Jesse said.
An avenue of further research would be to interview patients to learn how platforms operate in practice and whether patients are properly assessed before treatment. “Those sorts of questions we can’t answer just by looking at the websites,” she said.
However, Charlotte Hoffman, JD, senior policy counsel for the National Center for Transgender Equality, an advocacy group, said she does not harbor concerns about patients being treated inappropriately simply because care is virtual. All clinicians who provide gender-affirming care face potential repercussions, such as malpractice lawsuits or state disciplinary action, if they veer from treatment guidelines, she said.
“I don’t necessarily take the premise that telehealth is inherently worse than in-person care as a given,” Ms. Hoffman said.
During the COVID-19 pandemic, Ms. Hoffman added, direct-to-consumer telemedicine has expanded access for individuals in rural areas, people with disabilities, and those who live in places where in-person providers of transgender care face public hostility, although individuals without the resources to pay may still be left out.
What might happen to that access if telemedicine restrictions that were loosened during the pandemic are reinstated is unclear, she said.
The researchers and Ms. Hoffman have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Academic dermatology: Gender diversity advances as some gaps persist
, according to a recent cross-sectional study.
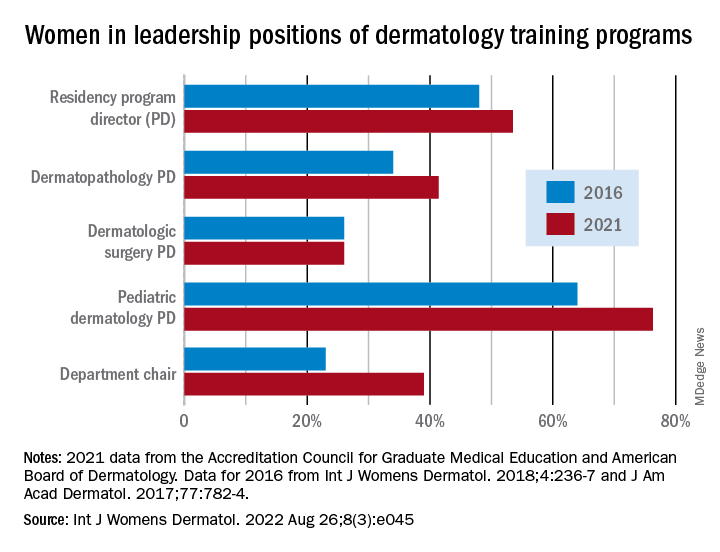
Although women made up more than half of the dermatology residency program directors (53.5%), associate directors (62.6%), and assistant directors (58.3%) in 2021, those numbers fall short of women’s majority (65% in 2018) among the trainees themselves, Yasmine Abushukur of Oakland University in Rochester, Mich., and associates said in a research letter.
Advancements were “made in gender diversity within academic dermatology from 2016 to 2021, [but] women remain underrepresented, particularly in leadership of dermatopathology and dermatologic surgery fellowships,” the investigators wrote.
Data gathered from 142 dermatology residency programs accredited by the Accreditation Council for Graduate Medical Education show that progress has been made since 2016, at least among program directors (PDs), of whom 48% were women, according to a previous study. Data on associate and assistant PDs from 2016 were not available to Ms. Abushukur and associates.
At the fellowship program level, women made gains as PDs in dermatopathology (34% in 2016 and 41% in 2021) and pediatric dermatology (64% in 2016 and 76% in 2021), but not in dermatologic surgery, where the proportion held at 26% over the study period. “This disparity is reflective of the general trend in surgery and pathology leadership nationally,” the researchers noted.
Taking a couple of steps up the ladder of authority shows that 39% of dermatology chairs were women in 2021, compared with 23% in 2016. A study published in 2016 demonstrated decreased diversity among academic faculty members as faculty rank increased, and “our data mirror this sentiment by demonstrating a majority of women in assistant and associate PD positions, with a minority of women chairs,” they wrote.
The investigators said that they had no conflicts of interest and no outside funding. Ms. Abushukur’s coauthors were from the departments of dermatology at the Henry Ford Health System, Detroit, and Wayne State University, Dearborn, Mich.
, according to a recent cross-sectional study.
Although women made up more than half of the dermatology residency program directors (53.5%), associate directors (62.6%), and assistant directors (58.3%) in 2021, those numbers fall short of women’s majority (65% in 2018) among the trainees themselves, Yasmine Abushukur of Oakland University in Rochester, Mich., and associates said in a research letter.
Advancements were “made in gender diversity within academic dermatology from 2016 to 2021, [but] women remain underrepresented, particularly in leadership of dermatopathology and dermatologic surgery fellowships,” the investigators wrote.
Data gathered from 142 dermatology residency programs accredited by the Accreditation Council for Graduate Medical Education show that progress has been made since 2016, at least among program directors (PDs), of whom 48% were women, according to a previous study. Data on associate and assistant PDs from 2016 were not available to Ms. Abushukur and associates.
At the fellowship program level, women made gains as PDs in dermatopathology (34% in 2016 and 41% in 2021) and pediatric dermatology (64% in 2016 and 76% in 2021), but not in dermatologic surgery, where the proportion held at 26% over the study period. “This disparity is reflective of the general trend in surgery and pathology leadership nationally,” the researchers noted.
Taking a couple of steps up the ladder of authority shows that 39% of dermatology chairs were women in 2021, compared with 23% in 2016. A study published in 2016 demonstrated decreased diversity among academic faculty members as faculty rank increased, and “our data mirror this sentiment by demonstrating a majority of women in assistant and associate PD positions, with a minority of women chairs,” they wrote.
The investigators said that they had no conflicts of interest and no outside funding. Ms. Abushukur’s coauthors were from the departments of dermatology at the Henry Ford Health System, Detroit, and Wayne State University, Dearborn, Mich.
, according to a recent cross-sectional study.
Although women made up more than half of the dermatology residency program directors (53.5%), associate directors (62.6%), and assistant directors (58.3%) in 2021, those numbers fall short of women’s majority (65% in 2018) among the trainees themselves, Yasmine Abushukur of Oakland University in Rochester, Mich., and associates said in a research letter.
Advancements were “made in gender diversity within academic dermatology from 2016 to 2021, [but] women remain underrepresented, particularly in leadership of dermatopathology and dermatologic surgery fellowships,” the investigators wrote.
Data gathered from 142 dermatology residency programs accredited by the Accreditation Council for Graduate Medical Education show that progress has been made since 2016, at least among program directors (PDs), of whom 48% were women, according to a previous study. Data on associate and assistant PDs from 2016 were not available to Ms. Abushukur and associates.
At the fellowship program level, women made gains as PDs in dermatopathology (34% in 2016 and 41% in 2021) and pediatric dermatology (64% in 2016 and 76% in 2021), but not in dermatologic surgery, where the proportion held at 26% over the study period. “This disparity is reflective of the general trend in surgery and pathology leadership nationally,” the researchers noted.
Taking a couple of steps up the ladder of authority shows that 39% of dermatology chairs were women in 2021, compared with 23% in 2016. A study published in 2016 demonstrated decreased diversity among academic faculty members as faculty rank increased, and “our data mirror this sentiment by demonstrating a majority of women in assistant and associate PD positions, with a minority of women chairs,” they wrote.
The investigators said that they had no conflicts of interest and no outside funding. Ms. Abushukur’s coauthors were from the departments of dermatology at the Henry Ford Health System, Detroit, and Wayne State University, Dearborn, Mich.
FROM INTERNATIONAL JOURNAL OF WOMEN’S DERMATOLOGY
Black Veterans Less Likely to Get COVID-Specific Treatments at VAMCs
Black veterans hospitalized with COVID-19 were less likely to be treated with evidence-based treatments, in a study conducted in 130 US Department of Veterans Affairs (VA) medical centers between March 1, 2020, and February 28, 2022.
The study involved 12,135 Black veterans and 40,717 White veterans. Most patients hospitalized during period 1 (March-September 2020) were Black veterans and the proportion of White patients increased over time. The latter 3 periods, which included the Delta- and Omicron-predominant periods, saw the most admissions.
Controlling for the site of treatment, Black patients were equally likely to be admitted to the intensive care unit (40% vs 43%). However, they were less likely to receive steroids, remdesivir, or immunomodulatory drugs.
The researchers say their data confirm other findings from 41 US health care systems participating in the National Patient-Centered Clinical Research Network (PCORNet), which found lower use of monoclonal antibody treatment for COVID infection for patients who identified as Asian, Black, Hispanic, American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, or multiple races.
The researchers did not observe consistent differences in clinical outcomes between Black and White patients. After adjusting for demographics, chronic health conditions, severity of acute illness, and receipt of COVID-19–specific treatments, there was no association of Black race with hospital mortality or 30-day readmission. Black and White patients had a similar burden of preexisting health conditions. Of 38,782 patients discharged, 14% were readmitted within 30 days; the median time to readmission for both groups was 9 days.
Differences in care were partially explained by within- and between-hospital differences, the researchers say. They also cite research that demonstrated a poorer quality of care for hospitals with higher monthly COVID-19 discharges and hospital size.
The study results contradict the assumptions that differences in inpatient treatment by race and ethnicity may be due to differences in clinical indications for medication use based on age and comorbidities, such as chronic kidney or liver disease, the researchers say. For one thing, the VA issued a systemwide COVID-19 response plan that included specific treatment guidelines and distribution plans. But they also point to recent reports that have suggested that occult hypoxemia not detected by pulse oximetry occurs “far more often in Black patients than White patients,” which could result in delayed or missed opportunities to treat patients with COVID-19.
Black veterans hospitalized with COVID-19 were less likely to be treated with evidence-based treatments, in a study conducted in 130 US Department of Veterans Affairs (VA) medical centers between March 1, 2020, and February 28, 2022.
The study involved 12,135 Black veterans and 40,717 White veterans. Most patients hospitalized during period 1 (March-September 2020) were Black veterans and the proportion of White patients increased over time. The latter 3 periods, which included the Delta- and Omicron-predominant periods, saw the most admissions.
Controlling for the site of treatment, Black patients were equally likely to be admitted to the intensive care unit (40% vs 43%). However, they were less likely to receive steroids, remdesivir, or immunomodulatory drugs.
The researchers say their data confirm other findings from 41 US health care systems participating in the National Patient-Centered Clinical Research Network (PCORNet), which found lower use of monoclonal antibody treatment for COVID infection for patients who identified as Asian, Black, Hispanic, American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, or multiple races.
The researchers did not observe consistent differences in clinical outcomes between Black and White patients. After adjusting for demographics, chronic health conditions, severity of acute illness, and receipt of COVID-19–specific treatments, there was no association of Black race with hospital mortality or 30-day readmission. Black and White patients had a similar burden of preexisting health conditions. Of 38,782 patients discharged, 14% were readmitted within 30 days; the median time to readmission for both groups was 9 days.
Differences in care were partially explained by within- and between-hospital differences, the researchers say. They also cite research that demonstrated a poorer quality of care for hospitals with higher monthly COVID-19 discharges and hospital size.
The study results contradict the assumptions that differences in inpatient treatment by race and ethnicity may be due to differences in clinical indications for medication use based on age and comorbidities, such as chronic kidney or liver disease, the researchers say. For one thing, the VA issued a systemwide COVID-19 response plan that included specific treatment guidelines and distribution plans. But they also point to recent reports that have suggested that occult hypoxemia not detected by pulse oximetry occurs “far more often in Black patients than White patients,” which could result in delayed or missed opportunities to treat patients with COVID-19.
Black veterans hospitalized with COVID-19 were less likely to be treated with evidence-based treatments, in a study conducted in 130 US Department of Veterans Affairs (VA) medical centers between March 1, 2020, and February 28, 2022.
The study involved 12,135 Black veterans and 40,717 White veterans. Most patients hospitalized during period 1 (March-September 2020) were Black veterans and the proportion of White patients increased over time. The latter 3 periods, which included the Delta- and Omicron-predominant periods, saw the most admissions.
Controlling for the site of treatment, Black patients were equally likely to be admitted to the intensive care unit (40% vs 43%). However, they were less likely to receive steroids, remdesivir, or immunomodulatory drugs.
The researchers say their data confirm other findings from 41 US health care systems participating in the National Patient-Centered Clinical Research Network (PCORNet), which found lower use of monoclonal antibody treatment for COVID infection for patients who identified as Asian, Black, Hispanic, American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, or multiple races.
The researchers did not observe consistent differences in clinical outcomes between Black and White patients. After adjusting for demographics, chronic health conditions, severity of acute illness, and receipt of COVID-19–specific treatments, there was no association of Black race with hospital mortality or 30-day readmission. Black and White patients had a similar burden of preexisting health conditions. Of 38,782 patients discharged, 14% were readmitted within 30 days; the median time to readmission for both groups was 9 days.
Differences in care were partially explained by within- and between-hospital differences, the researchers say. They also cite research that demonstrated a poorer quality of care for hospitals with higher monthly COVID-19 discharges and hospital size.
The study results contradict the assumptions that differences in inpatient treatment by race and ethnicity may be due to differences in clinical indications for medication use based on age and comorbidities, such as chronic kidney or liver disease, the researchers say. For one thing, the VA issued a systemwide COVID-19 response plan that included specific treatment guidelines and distribution plans. But they also point to recent reports that have suggested that occult hypoxemia not detected by pulse oximetry occurs “far more often in Black patients than White patients,” which could result in delayed or missed opportunities to treat patients with COVID-19.
Race and gender: Tailoring treatment for sleep disorders is preferred and better
While trials of various interventions for obstructive sleep apnea and insomnia were effective, there was a strong suggestion that tailoring them according to the race/gender of the target populations strengthens engagement and improvements, according to a presentation by Dayna A. Johnson, PhD, MPH, at the annual meeting of the American College of Chest Physicians (CHEST).
Dr. Johnson, assistant professor at Emory University in Atlanta, stated that determinants of sleep disparities are multifactorial across the lifespan, from in utero to aging, but it was also important to focus on social determinants of poor sleep.
The complexity of factors, she said, calls for multilevel interventions beyond screening and treatment. In addition, neighborhood factors including safety, noise and light pollution, ventilation, and thermal comfort come into play.
Dr. Johnson cited the example of parents who work multiple jobs to provide for their families: “Minimum wage is not a livable wage, and parents may not be available to ensure that children have consistent bedtimes.” Interventions, she added, may have to be at the neighborhood level, including placing sleep specialists in the local neighborhood “where the need is.” Cleaning up a neighborhood reduces crime and overall health, while light shielding in public housing can lower light pollution.
Observing that African Americans have higher rates of obstructive sleep apnea, Dr. Johnson and colleagues designed a screening tool specifically for African Americans with five prediction models with increasing levels of factor measurements (from 4 to 10). The prediction accuracy across the models ascended in lockstep with the number of measures from 74.0% to 76.1%, with the simplest model including only age, body mass index, male sex, and snoring. The latter model added witnessed apneas, high depressive symptoms, two measures of waist and neck size, and sleepiness. Dr. Johnson pointed out that accuracy for well-established predictive models is notably lower: STOP-Bang score ranges from 56% to 66%; NoSAS ranges from 58% to 66% and the HCHS prediction model accuracy is 70%. Dr. Johnson said that a Latino model they developed was more accurate than the traditional models, but not as accurate as their model for African Americans.
Turning to specific interventions, and underscoring higher levels of stress and anxiety among African American and Hispanic populations, Dr. Johnson cited MINDS (Mindfulness Intervention to Improve Sleep and Reduce Diabetes Risk Among a Diverse Sample in Atlanta), her study at Emory University of mindfulness meditation. Although prior studies have confirmed sleep benefits of mindfulness meditation, studies tailored for African American or Hispanic populations have been lacking.
The MINDS pilot study investigators enrolled 17 individuals (mostly women, with a mixture of racial and ethnic groups comprising Black, White, Asian and Hispanic patients) with poor sleep quality as measured by the Pittsburgh Sleep Quality Index (PSQI). Most patients, Dr. Johnson said, were overweight. Because of COVID restrictions on clinic visits, the diabetes portion of the study was dropped. All participants received at least 3 days of instruction on mindfulness meditation, on dealing with stress and anxiety, and on optimum sleep health practices. While PSQI scores higher than 5 are considered to indicate poor sleep quality, the mean PSQI score at study outset in MINDS was 9.2, she stated.
After 30 days of the intervention, stress (on a perceived stress scale) was improved, as were PSQI scores and actigraphy measures of sleep duration, efficiency and wakefulness after sleep onset, Dr. Johnson reported. “Participants found the mindfulness app to be acceptable and appropriate, and to reduce time to falling asleep,” Dr. Johnson said.
Qualitative data gathered post intervention from four focus groups (two to six participants in each; 1-1.5 hours in length), revealed general acceptability of the MINDS app. It showed also that among those with 50% or more adherence to the intervention, time to falling asleep was reduced, as were sleep awakenings at night. The most striking finding, Dr. Johnson said, was that individuals from among racial/ethnic minorities expressed appreciation of the diversity of the meditation instructors, and said that they preferred instruction from a person of their own race and sex. Findings would be even more striking with a larger sample size, Dr. Johnson speculated.
Citing TASHE (Tailored Approach to Sleep Health Education), a further observational study on obstructive sleep apnea knowledge conducted at New York University, Dr. Johnson addressed the fact that current messages are not tailored to race/ethnic minorities with low-to-moderate symptom knowledge. Also, a 3-arm randomized clinical trial of Internet-delivered treatment (Sleep Healthy or SHUTI) with a version revised for Black women (SHUTI-BWHS) showed findings similar to those of other studies cited and suggested: “Tailoring may be necessary to increase uptake and sustainability and to improve sleep among racial/ethnic minorities.”
Dr. Johnson noted, in closing, that Black/African American individuals have higher risk for obstructive sleep apnea than that of their White counterparts and lower rates of screening for treatment.
Dr. Johnson’s research was funded by the National Institutes of Health; National Heart, Lung, and Blood Institute; Woodruff Health Sciences Center; Synergy Award; Rollins School of Public Health Dean’s Pilot and Innovation Award; and Georgia Center for Diabetes Translation Research Pilot and Feasibility award program. She reported no relevant conflicts.
While trials of various interventions for obstructive sleep apnea and insomnia were effective, there was a strong suggestion that tailoring them according to the race/gender of the target populations strengthens engagement and improvements, according to a presentation by Dayna A. Johnson, PhD, MPH, at the annual meeting of the American College of Chest Physicians (CHEST).
Dr. Johnson, assistant professor at Emory University in Atlanta, stated that determinants of sleep disparities are multifactorial across the lifespan, from in utero to aging, but it was also important to focus on social determinants of poor sleep.
The complexity of factors, she said, calls for multilevel interventions beyond screening and treatment. In addition, neighborhood factors including safety, noise and light pollution, ventilation, and thermal comfort come into play.
Dr. Johnson cited the example of parents who work multiple jobs to provide for their families: “Minimum wage is not a livable wage, and parents may not be available to ensure that children have consistent bedtimes.” Interventions, she added, may have to be at the neighborhood level, including placing sleep specialists in the local neighborhood “where the need is.” Cleaning up a neighborhood reduces crime and overall health, while light shielding in public housing can lower light pollution.
Observing that African Americans have higher rates of obstructive sleep apnea, Dr. Johnson and colleagues designed a screening tool specifically for African Americans with five prediction models with increasing levels of factor measurements (from 4 to 10). The prediction accuracy across the models ascended in lockstep with the number of measures from 74.0% to 76.1%, with the simplest model including only age, body mass index, male sex, and snoring. The latter model added witnessed apneas, high depressive symptoms, two measures of waist and neck size, and sleepiness. Dr. Johnson pointed out that accuracy for well-established predictive models is notably lower: STOP-Bang score ranges from 56% to 66%; NoSAS ranges from 58% to 66% and the HCHS prediction model accuracy is 70%. Dr. Johnson said that a Latino model they developed was more accurate than the traditional models, but not as accurate as their model for African Americans.
Turning to specific interventions, and underscoring higher levels of stress and anxiety among African American and Hispanic populations, Dr. Johnson cited MINDS (Mindfulness Intervention to Improve Sleep and Reduce Diabetes Risk Among a Diverse Sample in Atlanta), her study at Emory University of mindfulness meditation. Although prior studies have confirmed sleep benefits of mindfulness meditation, studies tailored for African American or Hispanic populations have been lacking.
The MINDS pilot study investigators enrolled 17 individuals (mostly women, with a mixture of racial and ethnic groups comprising Black, White, Asian and Hispanic patients) with poor sleep quality as measured by the Pittsburgh Sleep Quality Index (PSQI). Most patients, Dr. Johnson said, were overweight. Because of COVID restrictions on clinic visits, the diabetes portion of the study was dropped. All participants received at least 3 days of instruction on mindfulness meditation, on dealing with stress and anxiety, and on optimum sleep health practices. While PSQI scores higher than 5 are considered to indicate poor sleep quality, the mean PSQI score at study outset in MINDS was 9.2, she stated.
After 30 days of the intervention, stress (on a perceived stress scale) was improved, as were PSQI scores and actigraphy measures of sleep duration, efficiency and wakefulness after sleep onset, Dr. Johnson reported. “Participants found the mindfulness app to be acceptable and appropriate, and to reduce time to falling asleep,” Dr. Johnson said.
Qualitative data gathered post intervention from four focus groups (two to six participants in each; 1-1.5 hours in length), revealed general acceptability of the MINDS app. It showed also that among those with 50% or more adherence to the intervention, time to falling asleep was reduced, as were sleep awakenings at night. The most striking finding, Dr. Johnson said, was that individuals from among racial/ethnic minorities expressed appreciation of the diversity of the meditation instructors, and said that they preferred instruction from a person of their own race and sex. Findings would be even more striking with a larger sample size, Dr. Johnson speculated.
Citing TASHE (Tailored Approach to Sleep Health Education), a further observational study on obstructive sleep apnea knowledge conducted at New York University, Dr. Johnson addressed the fact that current messages are not tailored to race/ethnic minorities with low-to-moderate symptom knowledge. Also, a 3-arm randomized clinical trial of Internet-delivered treatment (Sleep Healthy or SHUTI) with a version revised for Black women (SHUTI-BWHS) showed findings similar to those of other studies cited and suggested: “Tailoring may be necessary to increase uptake and sustainability and to improve sleep among racial/ethnic minorities.”
Dr. Johnson noted, in closing, that Black/African American individuals have higher risk for obstructive sleep apnea than that of their White counterparts and lower rates of screening for treatment.
Dr. Johnson’s research was funded by the National Institutes of Health; National Heart, Lung, and Blood Institute; Woodruff Health Sciences Center; Synergy Award; Rollins School of Public Health Dean’s Pilot and Innovation Award; and Georgia Center for Diabetes Translation Research Pilot and Feasibility award program. She reported no relevant conflicts.
While trials of various interventions for obstructive sleep apnea and insomnia were effective, there was a strong suggestion that tailoring them according to the race/gender of the target populations strengthens engagement and improvements, according to a presentation by Dayna A. Johnson, PhD, MPH, at the annual meeting of the American College of Chest Physicians (CHEST).
Dr. Johnson, assistant professor at Emory University in Atlanta, stated that determinants of sleep disparities are multifactorial across the lifespan, from in utero to aging, but it was also important to focus on social determinants of poor sleep.
The complexity of factors, she said, calls for multilevel interventions beyond screening and treatment. In addition, neighborhood factors including safety, noise and light pollution, ventilation, and thermal comfort come into play.
Dr. Johnson cited the example of parents who work multiple jobs to provide for their families: “Minimum wage is not a livable wage, and parents may not be available to ensure that children have consistent bedtimes.” Interventions, she added, may have to be at the neighborhood level, including placing sleep specialists in the local neighborhood “where the need is.” Cleaning up a neighborhood reduces crime and overall health, while light shielding in public housing can lower light pollution.
Observing that African Americans have higher rates of obstructive sleep apnea, Dr. Johnson and colleagues designed a screening tool specifically for African Americans with five prediction models with increasing levels of factor measurements (from 4 to 10). The prediction accuracy across the models ascended in lockstep with the number of measures from 74.0% to 76.1%, with the simplest model including only age, body mass index, male sex, and snoring. The latter model added witnessed apneas, high depressive symptoms, two measures of waist and neck size, and sleepiness. Dr. Johnson pointed out that accuracy for well-established predictive models is notably lower: STOP-Bang score ranges from 56% to 66%; NoSAS ranges from 58% to 66% and the HCHS prediction model accuracy is 70%. Dr. Johnson said that a Latino model they developed was more accurate than the traditional models, but not as accurate as their model for African Americans.
Turning to specific interventions, and underscoring higher levels of stress and anxiety among African American and Hispanic populations, Dr. Johnson cited MINDS (Mindfulness Intervention to Improve Sleep and Reduce Diabetes Risk Among a Diverse Sample in Atlanta), her study at Emory University of mindfulness meditation. Although prior studies have confirmed sleep benefits of mindfulness meditation, studies tailored for African American or Hispanic populations have been lacking.
The MINDS pilot study investigators enrolled 17 individuals (mostly women, with a mixture of racial and ethnic groups comprising Black, White, Asian and Hispanic patients) with poor sleep quality as measured by the Pittsburgh Sleep Quality Index (PSQI). Most patients, Dr. Johnson said, were overweight. Because of COVID restrictions on clinic visits, the diabetes portion of the study was dropped. All participants received at least 3 days of instruction on mindfulness meditation, on dealing with stress and anxiety, and on optimum sleep health practices. While PSQI scores higher than 5 are considered to indicate poor sleep quality, the mean PSQI score at study outset in MINDS was 9.2, she stated.
After 30 days of the intervention, stress (on a perceived stress scale) was improved, as were PSQI scores and actigraphy measures of sleep duration, efficiency and wakefulness after sleep onset, Dr. Johnson reported. “Participants found the mindfulness app to be acceptable and appropriate, and to reduce time to falling asleep,” Dr. Johnson said.
Qualitative data gathered post intervention from four focus groups (two to six participants in each; 1-1.5 hours in length), revealed general acceptability of the MINDS app. It showed also that among those with 50% or more adherence to the intervention, time to falling asleep was reduced, as were sleep awakenings at night. The most striking finding, Dr. Johnson said, was that individuals from among racial/ethnic minorities expressed appreciation of the diversity of the meditation instructors, and said that they preferred instruction from a person of their own race and sex. Findings would be even more striking with a larger sample size, Dr. Johnson speculated.
Citing TASHE (Tailored Approach to Sleep Health Education), a further observational study on obstructive sleep apnea knowledge conducted at New York University, Dr. Johnson addressed the fact that current messages are not tailored to race/ethnic minorities with low-to-moderate symptom knowledge. Also, a 3-arm randomized clinical trial of Internet-delivered treatment (Sleep Healthy or SHUTI) with a version revised for Black women (SHUTI-BWHS) showed findings similar to those of other studies cited and suggested: “Tailoring may be necessary to increase uptake and sustainability and to improve sleep among racial/ethnic minorities.”
Dr. Johnson noted, in closing, that Black/African American individuals have higher risk for obstructive sleep apnea than that of their White counterparts and lower rates of screening for treatment.
Dr. Johnson’s research was funded by the National Institutes of Health; National Heart, Lung, and Blood Institute; Woodruff Health Sciences Center; Synergy Award; Rollins School of Public Health Dean’s Pilot and Innovation Award; and Georgia Center for Diabetes Translation Research Pilot and Feasibility award program. She reported no relevant conflicts.
FROM CHEST 2022
Higher rates of PTSD, BPD in transgender vs. cisgender psych patients
Although mood disorders, depression, and anxiety were the most common diagnoses in both TGD and cisgender patients, “when we compared the diagnostic profiles [of TGD patients] to those of cisgender patients, we found an increased prevalence of PTSD and BPD,” study investigator Mark Zimmerman, MD, professor of psychiatry and human behavior, Brown University, Providence, R.I., told this news organization.
“What we concluded is that psychiatric programs that wish to treat TGD patients should either have or should develop expertise in treating PTSD and BPD, not just mood and anxiety disorders,” Dr. Zimmerman said.
The study was published online September 26 in the Journal of Clinical Psychiatry.
‘Piecemeal literature’
TGD individuals “experience high rates of various forms of psychopathology in general and when compared with cisgender persons,” the investigators note.
They point out that most empirical evidence has relied upon the use of brief, unstructured psychodiagnostic assessment measures and assessment of a “limited constellation of psychiatric symptoms domains,” resulting in a “piecemeal literature wherein each piece of research documents elevations in one – or a few – diagnostic domains.”
Studies pointing to broader psychosocial health variables have often relied upon self-reported measures. In addition, in studies that utilized a structured interview approach, none “used a formal interview procedure to assess psychiatric diagnoses” and most focused only on a “limited number of psychiatric conditions based on self-reports of past diagnosis.”
The goal of the current study was to use semistructured interviews administered by professionals to compare the diagnostic profiles of a samples of TGD and cisgender patients who presented for treatment at a single naturalistic, clinically acute setting – a partial hospital program.
Dr. Zimmerman said that there was an additional motive for conducting the study. “There has been discussion in the field as to whether or not transgender or gender-diverse individuals all have borderline personality disorder, but that hasn’t been our clinical impression.”
Rather, Dr. Zimmerman and colleagues believe TGD people “may have had more difficult childhoods and more difficult adjustments in society because of societal attitudes and have to deal with that stress, whether it be microaggressions or overt bullying and aggression.” The study was designed to investigate this issue.
In addition, studies conducted in primary care programs in individuals seeking gender-affirming surgery have “reported a limited number of psychiatric diagnoses, but we were wondering whether, amongst psychiatric patients specifically, there were differences in diagnostic profiles between transgender and gender-diverse patients and cisgender patients. If so, what might the implications be for providing care for this population?”
TGD not synonymous with borderline
To investigate, the researchers administered semistructured diagnostic interviews for DSM-IV disorders to 2,212 psychiatric patients (66% cisgender women, 30.8% cisgender men, 3.1% TGD; mean [standard deviation] age 36.7 [14.4] years) presenting to the Rhode Island Hospital Department of Psychiatry Partial Hospital Program between April 2014 and January 2021.
Patients also completed a demographic questionnaire including their assigned sex at birth and their current gender identity.
Most patients (44.9%) were single, followed by 23.5% who were married, 14.1% living in a relationship as if married, 12.0% divorced, 3.6% separated, and 1.9% widowed.
Almost three-quarters of participants (73.2%) identified as White, followed by Hispanic (10.7%), Black (6.7%), “other” or a combination of racial/ethnic backgrounds (6.6%), and Asian (2.7%).
There were no differences between cisgender and TGD groups in terms of race or education, but the TGD patients were significantly younger compared with their cisgender counterparts and were significantly more likely to have never been married.
The average number of psychiatric diagnoses in the sample was 3.05 (± 1.73), with TGD patients having a larger number of psychiatric diagnoses than did their cisgender peers (an average of 3.54 ± 1.88 vs. 3.04 ± 1.72, respectively; t = 2.37; P = .02).
Major depressive disorder (MDD) and generalized anxiety disorder (GAD) were the most common disorders among both cisgender and TGD patients. However, after controlling for age, the researchers found that TGD patients were significantly more likely than were the cisgender patients to be diagnosed with PTSD and BPD (P < .05 for both).
“Of note, only about one-third of the TGD individuals were diagnosed with BPD, so it is important to realize that transgender or gender-diverse identity is not synonymous with BPD, as some have suggested,” noted Dr. Zimmerman, who is also the director of the outpatient division at the Partial Hospital Program, Rhode Island Hospital.
A representative sample?
Commenting on the study, Jack Drescher, MD, distinguished life fellow of the American Psychiatric Association and clinical professor of psychiatry, Columbia University, New York, called the findings “interesting” but noted that a limitation of the study is that it included “a patient population with likely more severe psychiatric illness, since they were all day hospital patients.”
The question is whether similar findings would be obtained in a less severely ill population, said Dr. Drescher, who is also a senior consulting analyst for sexuality and gender at Columbia University and was not involved with the study. “The patients in the study may not be representative of the general population, either cisgender or transgender.”
Dr. Drescher was “not surprised” by the finding regarding PTSD because the finding “is consistent with our understanding of the kinds of traumas that transgender people go through in day-to-day life.”
He noted that some people misunderstand the diagnostic criterion in BPD of identity confusion and think that because people with gender dysphoria may be confused about their identity, it means that all people who are transgender have borderline personality disorder, “but that’s not true.”
Dr. Zimmerman agreed. “The vast majority of individuals with BPD do not have a transgender or gender-diverse identity, and TGD should not be equated with BPD,” he said.
No source of study funding was disclosed. Dr. Zimmerman and coauthors and Dr. Drescher report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Although mood disorders, depression, and anxiety were the most common diagnoses in both TGD and cisgender patients, “when we compared the diagnostic profiles [of TGD patients] to those of cisgender patients, we found an increased prevalence of PTSD and BPD,” study investigator Mark Zimmerman, MD, professor of psychiatry and human behavior, Brown University, Providence, R.I., told this news organization.
“What we concluded is that psychiatric programs that wish to treat TGD patients should either have or should develop expertise in treating PTSD and BPD, not just mood and anxiety disorders,” Dr. Zimmerman said.
The study was published online September 26 in the Journal of Clinical Psychiatry.
‘Piecemeal literature’
TGD individuals “experience high rates of various forms of psychopathology in general and when compared with cisgender persons,” the investigators note.
They point out that most empirical evidence has relied upon the use of brief, unstructured psychodiagnostic assessment measures and assessment of a “limited constellation of psychiatric symptoms domains,” resulting in a “piecemeal literature wherein each piece of research documents elevations in one – or a few – diagnostic domains.”
Studies pointing to broader psychosocial health variables have often relied upon self-reported measures. In addition, in studies that utilized a structured interview approach, none “used a formal interview procedure to assess psychiatric diagnoses” and most focused only on a “limited number of psychiatric conditions based on self-reports of past diagnosis.”
The goal of the current study was to use semistructured interviews administered by professionals to compare the diagnostic profiles of a samples of TGD and cisgender patients who presented for treatment at a single naturalistic, clinically acute setting – a partial hospital program.
Dr. Zimmerman said that there was an additional motive for conducting the study. “There has been discussion in the field as to whether or not transgender or gender-diverse individuals all have borderline personality disorder, but that hasn’t been our clinical impression.”
Rather, Dr. Zimmerman and colleagues believe TGD people “may have had more difficult childhoods and more difficult adjustments in society because of societal attitudes and have to deal with that stress, whether it be microaggressions or overt bullying and aggression.” The study was designed to investigate this issue.
In addition, studies conducted in primary care programs in individuals seeking gender-affirming surgery have “reported a limited number of psychiatric diagnoses, but we were wondering whether, amongst psychiatric patients specifically, there were differences in diagnostic profiles between transgender and gender-diverse patients and cisgender patients. If so, what might the implications be for providing care for this population?”
TGD not synonymous with borderline
To investigate, the researchers administered semistructured diagnostic interviews for DSM-IV disorders to 2,212 psychiatric patients (66% cisgender women, 30.8% cisgender men, 3.1% TGD; mean [standard deviation] age 36.7 [14.4] years) presenting to the Rhode Island Hospital Department of Psychiatry Partial Hospital Program between April 2014 and January 2021.
Patients also completed a demographic questionnaire including their assigned sex at birth and their current gender identity.
Most patients (44.9%) were single, followed by 23.5% who were married, 14.1% living in a relationship as if married, 12.0% divorced, 3.6% separated, and 1.9% widowed.
Almost three-quarters of participants (73.2%) identified as White, followed by Hispanic (10.7%), Black (6.7%), “other” or a combination of racial/ethnic backgrounds (6.6%), and Asian (2.7%).
There were no differences between cisgender and TGD groups in terms of race or education, but the TGD patients were significantly younger compared with their cisgender counterparts and were significantly more likely to have never been married.
The average number of psychiatric diagnoses in the sample was 3.05 (± 1.73), with TGD patients having a larger number of psychiatric diagnoses than did their cisgender peers (an average of 3.54 ± 1.88 vs. 3.04 ± 1.72, respectively; t = 2.37; P = .02).
Major depressive disorder (MDD) and generalized anxiety disorder (GAD) were the most common disorders among both cisgender and TGD patients. However, after controlling for age, the researchers found that TGD patients were significantly more likely than were the cisgender patients to be diagnosed with PTSD and BPD (P < .05 for both).
“Of note, only about one-third of the TGD individuals were diagnosed with BPD, so it is important to realize that transgender or gender-diverse identity is not synonymous with BPD, as some have suggested,” noted Dr. Zimmerman, who is also the director of the outpatient division at the Partial Hospital Program, Rhode Island Hospital.
A representative sample?
Commenting on the study, Jack Drescher, MD, distinguished life fellow of the American Psychiatric Association and clinical professor of psychiatry, Columbia University, New York, called the findings “interesting” but noted that a limitation of the study is that it included “a patient population with likely more severe psychiatric illness, since they were all day hospital patients.”
The question is whether similar findings would be obtained in a less severely ill population, said Dr. Drescher, who is also a senior consulting analyst for sexuality and gender at Columbia University and was not involved with the study. “The patients in the study may not be representative of the general population, either cisgender or transgender.”
Dr. Drescher was “not surprised” by the finding regarding PTSD because the finding “is consistent with our understanding of the kinds of traumas that transgender people go through in day-to-day life.”
He noted that some people misunderstand the diagnostic criterion in BPD of identity confusion and think that because people with gender dysphoria may be confused about their identity, it means that all people who are transgender have borderline personality disorder, “but that’s not true.”
Dr. Zimmerman agreed. “The vast majority of individuals with BPD do not have a transgender or gender-diverse identity, and TGD should not be equated with BPD,” he said.
No source of study funding was disclosed. Dr. Zimmerman and coauthors and Dr. Drescher report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Although mood disorders, depression, and anxiety were the most common diagnoses in both TGD and cisgender patients, “when we compared the diagnostic profiles [of TGD patients] to those of cisgender patients, we found an increased prevalence of PTSD and BPD,” study investigator Mark Zimmerman, MD, professor of psychiatry and human behavior, Brown University, Providence, R.I., told this news organization.
“What we concluded is that psychiatric programs that wish to treat TGD patients should either have or should develop expertise in treating PTSD and BPD, not just mood and anxiety disorders,” Dr. Zimmerman said.
The study was published online September 26 in the Journal of Clinical Psychiatry.
‘Piecemeal literature’
TGD individuals “experience high rates of various forms of psychopathology in general and when compared with cisgender persons,” the investigators note.
They point out that most empirical evidence has relied upon the use of brief, unstructured psychodiagnostic assessment measures and assessment of a “limited constellation of psychiatric symptoms domains,” resulting in a “piecemeal literature wherein each piece of research documents elevations in one – or a few – diagnostic domains.”
Studies pointing to broader psychosocial health variables have often relied upon self-reported measures. In addition, in studies that utilized a structured interview approach, none “used a formal interview procedure to assess psychiatric diagnoses” and most focused only on a “limited number of psychiatric conditions based on self-reports of past diagnosis.”
The goal of the current study was to use semistructured interviews administered by professionals to compare the diagnostic profiles of a samples of TGD and cisgender patients who presented for treatment at a single naturalistic, clinically acute setting – a partial hospital program.
Dr. Zimmerman said that there was an additional motive for conducting the study. “There has been discussion in the field as to whether or not transgender or gender-diverse individuals all have borderline personality disorder, but that hasn’t been our clinical impression.”
Rather, Dr. Zimmerman and colleagues believe TGD people “may have had more difficult childhoods and more difficult adjustments in society because of societal attitudes and have to deal with that stress, whether it be microaggressions or overt bullying and aggression.” The study was designed to investigate this issue.
In addition, studies conducted in primary care programs in individuals seeking gender-affirming surgery have “reported a limited number of psychiatric diagnoses, but we were wondering whether, amongst psychiatric patients specifically, there were differences in diagnostic profiles between transgender and gender-diverse patients and cisgender patients. If so, what might the implications be for providing care for this population?”
TGD not synonymous with borderline
To investigate, the researchers administered semistructured diagnostic interviews for DSM-IV disorders to 2,212 psychiatric patients (66% cisgender women, 30.8% cisgender men, 3.1% TGD; mean [standard deviation] age 36.7 [14.4] years) presenting to the Rhode Island Hospital Department of Psychiatry Partial Hospital Program between April 2014 and January 2021.
Patients also completed a demographic questionnaire including their assigned sex at birth and their current gender identity.
Most patients (44.9%) were single, followed by 23.5% who were married, 14.1% living in a relationship as if married, 12.0% divorced, 3.6% separated, and 1.9% widowed.
Almost three-quarters of participants (73.2%) identified as White, followed by Hispanic (10.7%), Black (6.7%), “other” or a combination of racial/ethnic backgrounds (6.6%), and Asian (2.7%).
There were no differences between cisgender and TGD groups in terms of race or education, but the TGD patients were significantly younger compared with their cisgender counterparts and were significantly more likely to have never been married.
The average number of psychiatric diagnoses in the sample was 3.05 (± 1.73), with TGD patients having a larger number of psychiatric diagnoses than did their cisgender peers (an average of 3.54 ± 1.88 vs. 3.04 ± 1.72, respectively; t = 2.37; P = .02).
Major depressive disorder (MDD) and generalized anxiety disorder (GAD) were the most common disorders among both cisgender and TGD patients. However, after controlling for age, the researchers found that TGD patients were significantly more likely than were the cisgender patients to be diagnosed with PTSD and BPD (P < .05 for both).
“Of note, only about one-third of the TGD individuals were diagnosed with BPD, so it is important to realize that transgender or gender-diverse identity is not synonymous with BPD, as some have suggested,” noted Dr. Zimmerman, who is also the director of the outpatient division at the Partial Hospital Program, Rhode Island Hospital.
A representative sample?
Commenting on the study, Jack Drescher, MD, distinguished life fellow of the American Psychiatric Association and clinical professor of psychiatry, Columbia University, New York, called the findings “interesting” but noted that a limitation of the study is that it included “a patient population with likely more severe psychiatric illness, since they were all day hospital patients.”
The question is whether similar findings would be obtained in a less severely ill population, said Dr. Drescher, who is also a senior consulting analyst for sexuality and gender at Columbia University and was not involved with the study. “The patients in the study may not be representative of the general population, either cisgender or transgender.”
Dr. Drescher was “not surprised” by the finding regarding PTSD because the finding “is consistent with our understanding of the kinds of traumas that transgender people go through in day-to-day life.”
He noted that some people misunderstand the diagnostic criterion in BPD of identity confusion and think that because people with gender dysphoria may be confused about their identity, it means that all people who are transgender have borderline personality disorder, “but that’s not true.”
Dr. Zimmerman agreed. “The vast majority of individuals with BPD do not have a transgender or gender-diverse identity, and TGD should not be equated with BPD,” he said.
No source of study funding was disclosed. Dr. Zimmerman and coauthors and Dr. Drescher report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JOURNAL OF CLINICAL PSYCHIATRY