User login
Updated materials and mentoring can boost diversity in dermatology
LAS VEGAS – in the specialty.
The growing ethnic minority population in the United States “underscores the need for medical education to ensure dermatologists are prepared to provide quality care for patients of diverse racial and ethnic backgrounds,” said Dr. Taylor, the Bernett L. Johnson Jr., MD, Professor, and vice chair for diversity, equity, and inclusion in the department of dermatology at the University of Pennsylvania.
Improving education includes diversifying resource material, she said. A recent study in the Journal of the American Academy of Dermatology showed the representation of skin tones on Google searches for skin conditions was mostly light skin (91.7%), although non-Hispanic Whites account for less than two-thirds (approximately 60%) of the U.S. population, she said. Many people with darker skin tones “are not finding people who look like themselves” when they search skin conditions online, she noted.
The lack of diversity in images occurs not only on Google, “but in our textbooks, which are the foundational resources for our students,” said Nada M. Elbuluk, MD, founder and director of the Skin of Color and Pigmentary Disorders Program at the University of Southern California, Los Angeles. She also established the Dermatology Diversity and Inclusion Program at USC.
The underrepresentation of teaching images, combined with the lack of data on epidemiology and treatment, can translate to poorer quality of care for skin of color patients and contribute to more misdiagnoses in these populations, Dr. Elbuluk emphasized.
Cultural competency and workforce diversity are ongoing issues in dermatology, added Valerie D. Callender, MD, professor of dermatology at Howard University, Washington, and medical director of the Callender Dermatology & Cosmetic Center in Glenn Dale, Md.
“We know that patients of color seek physicians of color,” she said. “We need to target our residents’ interest in dermatology,” and all physicians need to be comfortable with treating patients of all races, she added.
Although more than 13% of Americans are Black, only 3% of dermatologists in the United States are Black, Dr. Callender noted. Similarly, 4.2% of dermatologists in the United States are Hispanic or Latino, but these groups make up more than 18% of the general U.S. population, according to a recent study, she said.
Cheryl M. Burgess, MD, founder and medical director of the Center for Dermatology and Dermatologic Surgery in Washington, presented a roadmap of strategies for improving diversity in dermatology, starting with increasing STEM education at the high school and college levels among all populations and increasing the pipeline of underrepresented students to medical schools.
Then, faculty should work to increase interest in dermatology among underrepresented medical students and increase the numbers of underrepresented medical students in dermatology residency programs, said Dr. Burgess, assistant clinical professor of dermatology at Georgetown University and George Washington University, Washington.
“The more diversity we have in our specialty, the more we learn from each other,” and increased diversity can promote new research questions, said Andrew F. Alexis, MD, vice chair for diversity and inclusion in the department of dermatology and professor of clinical dermatology at Weill Cornell Medicine, New York.
Increasing the diversity of populations in clinical trials is another important strategy to improve diversity in dermatology, he emphasized.
Mentoring is an excellent way to help underrepresented students develop and pursue a career in dermatology, the panelists agreed. Time is precious for everyone, so don’t hesitate to use Zoom and other technology to help connect with mentees, Dr. Burgess advised.
Dr. Taylor added that mentoring doesn’t have to be a huge time commitment, it can be as simple as volunteering once a year at a school career forum. “It is so gratifying to have these young people looking up to you,” she said.
The panelists disclosed relationships with multiple companies, but none were relevant to this panel discussion. MedscapeLive and this news organization are owned by the same parent company.
LAS VEGAS – in the specialty.
The growing ethnic minority population in the United States “underscores the need for medical education to ensure dermatologists are prepared to provide quality care for patients of diverse racial and ethnic backgrounds,” said Dr. Taylor, the Bernett L. Johnson Jr., MD, Professor, and vice chair for diversity, equity, and inclusion in the department of dermatology at the University of Pennsylvania.
Improving education includes diversifying resource material, she said. A recent study in the Journal of the American Academy of Dermatology showed the representation of skin tones on Google searches for skin conditions was mostly light skin (91.7%), although non-Hispanic Whites account for less than two-thirds (approximately 60%) of the U.S. population, she said. Many people with darker skin tones “are not finding people who look like themselves” when they search skin conditions online, she noted.
The lack of diversity in images occurs not only on Google, “but in our textbooks, which are the foundational resources for our students,” said Nada M. Elbuluk, MD, founder and director of the Skin of Color and Pigmentary Disorders Program at the University of Southern California, Los Angeles. She also established the Dermatology Diversity and Inclusion Program at USC.
The underrepresentation of teaching images, combined with the lack of data on epidemiology and treatment, can translate to poorer quality of care for skin of color patients and contribute to more misdiagnoses in these populations, Dr. Elbuluk emphasized.
Cultural competency and workforce diversity are ongoing issues in dermatology, added Valerie D. Callender, MD, professor of dermatology at Howard University, Washington, and medical director of the Callender Dermatology & Cosmetic Center in Glenn Dale, Md.
“We know that patients of color seek physicians of color,” she said. “We need to target our residents’ interest in dermatology,” and all physicians need to be comfortable with treating patients of all races, she added.
Although more than 13% of Americans are Black, only 3% of dermatologists in the United States are Black, Dr. Callender noted. Similarly, 4.2% of dermatologists in the United States are Hispanic or Latino, but these groups make up more than 18% of the general U.S. population, according to a recent study, she said.
Cheryl M. Burgess, MD, founder and medical director of the Center for Dermatology and Dermatologic Surgery in Washington, presented a roadmap of strategies for improving diversity in dermatology, starting with increasing STEM education at the high school and college levels among all populations and increasing the pipeline of underrepresented students to medical schools.
Then, faculty should work to increase interest in dermatology among underrepresented medical students and increase the numbers of underrepresented medical students in dermatology residency programs, said Dr. Burgess, assistant clinical professor of dermatology at Georgetown University and George Washington University, Washington.
“The more diversity we have in our specialty, the more we learn from each other,” and increased diversity can promote new research questions, said Andrew F. Alexis, MD, vice chair for diversity and inclusion in the department of dermatology and professor of clinical dermatology at Weill Cornell Medicine, New York.
Increasing the diversity of populations in clinical trials is another important strategy to improve diversity in dermatology, he emphasized.
Mentoring is an excellent way to help underrepresented students develop and pursue a career in dermatology, the panelists agreed. Time is precious for everyone, so don’t hesitate to use Zoom and other technology to help connect with mentees, Dr. Burgess advised.
Dr. Taylor added that mentoring doesn’t have to be a huge time commitment, it can be as simple as volunteering once a year at a school career forum. “It is so gratifying to have these young people looking up to you,” she said.
The panelists disclosed relationships with multiple companies, but none were relevant to this panel discussion. MedscapeLive and this news organization are owned by the same parent company.
LAS VEGAS – in the specialty.
The growing ethnic minority population in the United States “underscores the need for medical education to ensure dermatologists are prepared to provide quality care for patients of diverse racial and ethnic backgrounds,” said Dr. Taylor, the Bernett L. Johnson Jr., MD, Professor, and vice chair for diversity, equity, and inclusion in the department of dermatology at the University of Pennsylvania.
Improving education includes diversifying resource material, she said. A recent study in the Journal of the American Academy of Dermatology showed the representation of skin tones on Google searches for skin conditions was mostly light skin (91.7%), although non-Hispanic Whites account for less than two-thirds (approximately 60%) of the U.S. population, she said. Many people with darker skin tones “are not finding people who look like themselves” when they search skin conditions online, she noted.
The lack of diversity in images occurs not only on Google, “but in our textbooks, which are the foundational resources for our students,” said Nada M. Elbuluk, MD, founder and director of the Skin of Color and Pigmentary Disorders Program at the University of Southern California, Los Angeles. She also established the Dermatology Diversity and Inclusion Program at USC.
The underrepresentation of teaching images, combined with the lack of data on epidemiology and treatment, can translate to poorer quality of care for skin of color patients and contribute to more misdiagnoses in these populations, Dr. Elbuluk emphasized.
Cultural competency and workforce diversity are ongoing issues in dermatology, added Valerie D. Callender, MD, professor of dermatology at Howard University, Washington, and medical director of the Callender Dermatology & Cosmetic Center in Glenn Dale, Md.
“We know that patients of color seek physicians of color,” she said. “We need to target our residents’ interest in dermatology,” and all physicians need to be comfortable with treating patients of all races, she added.
Although more than 13% of Americans are Black, only 3% of dermatologists in the United States are Black, Dr. Callender noted. Similarly, 4.2% of dermatologists in the United States are Hispanic or Latino, but these groups make up more than 18% of the general U.S. population, according to a recent study, she said.
Cheryl M. Burgess, MD, founder and medical director of the Center for Dermatology and Dermatologic Surgery in Washington, presented a roadmap of strategies for improving diversity in dermatology, starting with increasing STEM education at the high school and college levels among all populations and increasing the pipeline of underrepresented students to medical schools.
Then, faculty should work to increase interest in dermatology among underrepresented medical students and increase the numbers of underrepresented medical students in dermatology residency programs, said Dr. Burgess, assistant clinical professor of dermatology at Georgetown University and George Washington University, Washington.
“The more diversity we have in our specialty, the more we learn from each other,” and increased diversity can promote new research questions, said Andrew F. Alexis, MD, vice chair for diversity and inclusion in the department of dermatology and professor of clinical dermatology at Weill Cornell Medicine, New York.
Increasing the diversity of populations in clinical trials is another important strategy to improve diversity in dermatology, he emphasized.
Mentoring is an excellent way to help underrepresented students develop and pursue a career in dermatology, the panelists agreed. Time is precious for everyone, so don’t hesitate to use Zoom and other technology to help connect with mentees, Dr. Burgess advised.
Dr. Taylor added that mentoring doesn’t have to be a huge time commitment, it can be as simple as volunteering once a year at a school career forum. “It is so gratifying to have these young people looking up to you,” she said.
The panelists disclosed relationships with multiple companies, but none were relevant to this panel discussion. MedscapeLive and this news organization are owned by the same parent company.
AT INNOVATIONS IN DERMATOLOGY
Significant racial disparities persist in status epilepticus
NASHVILLE, Tenn. – Investigators found that among Black patients with status epilepticus, the hospitalization rate was twice that of their White counterparts. Other findings reveal age and income disparities.
“The results suggest that racial minorities, those with a lower income, and the elderly are an appropriate target to improve health outcomes and reduce health inequality,” said Gabriela Tantillo Sepúlveda, MD, assistant professor of neurology, Baylor College of Medicine, Houston.
The findings were presented at the annual meeting of the American Epilepsy Society.
An examination of outcomes
Status epilepticus is associated with high rates of morbidity and mortality. Disparities in epilepsy care have previously been described, but little attention has been paid to the contribution of disparities to status epilepticus care and associated outcomes.
Researchers used 2010-2019 data from the Nationwide Inpatient Sample, a database covering a cross-section of hospitalizations in 48 states and the District of Columbia. From relevant diagnostic codes, they calculated status epilepticus prevalence as the rate per 10,000 hospitalizations and stratified this by demographics.
Over the study period, investigators identified 486,861 status epilepticus hospitalizations, most (71.3%) at urban teaching hospitals.
Status epilepticus prevalence was highest for non-Hispanic Black patients, at 27.3, followed by non-Hispanic others, at 16.1, Hispanic patients, at 15.8, and non-Hispanic-White patients, at 13.7 (P < .01).
The finding that Black patients had double the rate as White patients was “definitely surprising,” said Dr. Tantillo Sepúlveda.
Research over the past 20 years revealed similar disparities related to status epilepticus, “so it’s upsetting that these disparities have persisted. Unfortunately, we still have a lot of work to do to reduce health inequalities,” she said.
The investigators found that the prevalence of status epilepticus was higher in the lowest-income quartile, compared with the highest (18.7 vs. 14; P < .01).
Need for physician advocacy
Unlike previous studies, this research assessed various interventions in different age groups and showed that the likelihood of intubation, tracheostomy, gastrostomy, and in-hospital mortality increased with age.
For example, compared with the reference group (patients aged 18-39 years), the odds of intubation were 1.22 (95% confidence interval, 1.16-1.27) for those aged 40-59 years and 1.48 (95% CI, 1.42-1.54) for those aged 60-79. Those aged 80 and older were most likely to be intubated, at an odds ratio of 1.5 (95% CI, 1.43-1.58).
Elderly patients were most likely to undergo tracheostomy (OR, 2.0; 95% CI, 1.75-2.27), gastrostomy (OR, 3.37; 95% CI, 2.97-3.83), and to experience in-hospital mortality (OR, 6.51; 95% CI, 5.95-7.13), compared with the youngest patients.
These intervention rates also varied by racial/ethnic groups. Minority populations, particularly Black people, had higher odds of tracheostomy and gastrostomy, compared with non-Hispanic White persons.
The odds of undergoing electroencephalography monitoring progressively rose as income level increased (OR, 1.47; 95% CI, 1.34-1.62) for the highest income quartile versus the lowest quartile. The odds of undergoing EEG monitoring were also higher at urban teaching hospitals than at rural hospitals.
Tackling these disparities in this patient population include increasing resources, personnel, and health education aimed at minorities, low-income patients, and the elderly, said Dr. Tantillo Sepúlveda. She added that more research is needed “to determine the most effective ways of accomplishing this goal.”
The medical community can help reduce disparities, said Dr. Tantillo Sepúlveda, by working to improve health literacy, to reduce stigma associated with seizures, and to increase awareness of seizure risk factors.
They can also work to expand access to outpatient neurology clinics, epilepsy monitoring units, and epilepsy surgery. “Ethnic and racial minorities are less likely to receive epilepsy surgery for temporal lobe epilepsy, which has been shown to improve quality of life and reduce seizure burden,” Dr. Tantillo Sepúlveda noted.
Across-the-board problem
Commenting on the research, Daniel Lowenstein, MD, professor of neurology, University of California, San Francisco, said the findings aren’t at all surprising. “It’s yet another piece of evidence on what has now become a rather voluminous literature that documents the very significant disparities that exist in our health care system,” said Dr. Lowenstein. “There’s just a huge literature on ‘name your disease and you’ll see the disparities.’ ”
Disparities exist, for example, in diagnosing breast cancer and prostate cancer, in the treatment of stroke and in related outcomes, and there is a well-documented “big disparity” in the approach to pain control among patients presenting at the emergency department, said Dr. Lowenstein.
However, he doesn’t know how disparities in epilepsy and specifically in status epilepticus, compared with disparities regarding other diseases and disorders. He noted that in the case of epilepsy, the situation is likely exacerbated by the stigma associated with that disease.
Dr. Lowenstein agreed that clinicians should play a role in reversing disparities. “We as physicians have a responsibility to be a voice for change in our health care system.”
The study was supported by the Center of Excellence for health equity, training, and research at the Baylor College of Medicine. Dr. Tantillo Sepúlveda and Dr. Lowenstein report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NASHVILLE, Tenn. – Investigators found that among Black patients with status epilepticus, the hospitalization rate was twice that of their White counterparts. Other findings reveal age and income disparities.
“The results suggest that racial minorities, those with a lower income, and the elderly are an appropriate target to improve health outcomes and reduce health inequality,” said Gabriela Tantillo Sepúlveda, MD, assistant professor of neurology, Baylor College of Medicine, Houston.
The findings were presented at the annual meeting of the American Epilepsy Society.
An examination of outcomes
Status epilepticus is associated with high rates of morbidity and mortality. Disparities in epilepsy care have previously been described, but little attention has been paid to the contribution of disparities to status epilepticus care and associated outcomes.
Researchers used 2010-2019 data from the Nationwide Inpatient Sample, a database covering a cross-section of hospitalizations in 48 states and the District of Columbia. From relevant diagnostic codes, they calculated status epilepticus prevalence as the rate per 10,000 hospitalizations and stratified this by demographics.
Over the study period, investigators identified 486,861 status epilepticus hospitalizations, most (71.3%) at urban teaching hospitals.
Status epilepticus prevalence was highest for non-Hispanic Black patients, at 27.3, followed by non-Hispanic others, at 16.1, Hispanic patients, at 15.8, and non-Hispanic-White patients, at 13.7 (P < .01).
The finding that Black patients had double the rate as White patients was “definitely surprising,” said Dr. Tantillo Sepúlveda.
Research over the past 20 years revealed similar disparities related to status epilepticus, “so it’s upsetting that these disparities have persisted. Unfortunately, we still have a lot of work to do to reduce health inequalities,” she said.
The investigators found that the prevalence of status epilepticus was higher in the lowest-income quartile, compared with the highest (18.7 vs. 14; P < .01).
Need for physician advocacy
Unlike previous studies, this research assessed various interventions in different age groups and showed that the likelihood of intubation, tracheostomy, gastrostomy, and in-hospital mortality increased with age.
For example, compared with the reference group (patients aged 18-39 years), the odds of intubation were 1.22 (95% confidence interval, 1.16-1.27) for those aged 40-59 years and 1.48 (95% CI, 1.42-1.54) for those aged 60-79. Those aged 80 and older were most likely to be intubated, at an odds ratio of 1.5 (95% CI, 1.43-1.58).
Elderly patients were most likely to undergo tracheostomy (OR, 2.0; 95% CI, 1.75-2.27), gastrostomy (OR, 3.37; 95% CI, 2.97-3.83), and to experience in-hospital mortality (OR, 6.51; 95% CI, 5.95-7.13), compared with the youngest patients.
These intervention rates also varied by racial/ethnic groups. Minority populations, particularly Black people, had higher odds of tracheostomy and gastrostomy, compared with non-Hispanic White persons.
The odds of undergoing electroencephalography monitoring progressively rose as income level increased (OR, 1.47; 95% CI, 1.34-1.62) for the highest income quartile versus the lowest quartile. The odds of undergoing EEG monitoring were also higher at urban teaching hospitals than at rural hospitals.
Tackling these disparities in this patient population include increasing resources, personnel, and health education aimed at minorities, low-income patients, and the elderly, said Dr. Tantillo Sepúlveda. She added that more research is needed “to determine the most effective ways of accomplishing this goal.”
The medical community can help reduce disparities, said Dr. Tantillo Sepúlveda, by working to improve health literacy, to reduce stigma associated with seizures, and to increase awareness of seizure risk factors.
They can also work to expand access to outpatient neurology clinics, epilepsy monitoring units, and epilepsy surgery. “Ethnic and racial minorities are less likely to receive epilepsy surgery for temporal lobe epilepsy, which has been shown to improve quality of life and reduce seizure burden,” Dr. Tantillo Sepúlveda noted.
Across-the-board problem
Commenting on the research, Daniel Lowenstein, MD, professor of neurology, University of California, San Francisco, said the findings aren’t at all surprising. “It’s yet another piece of evidence on what has now become a rather voluminous literature that documents the very significant disparities that exist in our health care system,” said Dr. Lowenstein. “There’s just a huge literature on ‘name your disease and you’ll see the disparities.’ ”
Disparities exist, for example, in diagnosing breast cancer and prostate cancer, in the treatment of stroke and in related outcomes, and there is a well-documented “big disparity” in the approach to pain control among patients presenting at the emergency department, said Dr. Lowenstein.
However, he doesn’t know how disparities in epilepsy and specifically in status epilepticus, compared with disparities regarding other diseases and disorders. He noted that in the case of epilepsy, the situation is likely exacerbated by the stigma associated with that disease.
Dr. Lowenstein agreed that clinicians should play a role in reversing disparities. “We as physicians have a responsibility to be a voice for change in our health care system.”
The study was supported by the Center of Excellence for health equity, training, and research at the Baylor College of Medicine. Dr. Tantillo Sepúlveda and Dr. Lowenstein report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NASHVILLE, Tenn. – Investigators found that among Black patients with status epilepticus, the hospitalization rate was twice that of their White counterparts. Other findings reveal age and income disparities.
“The results suggest that racial minorities, those with a lower income, and the elderly are an appropriate target to improve health outcomes and reduce health inequality,” said Gabriela Tantillo Sepúlveda, MD, assistant professor of neurology, Baylor College of Medicine, Houston.
The findings were presented at the annual meeting of the American Epilepsy Society.
An examination of outcomes
Status epilepticus is associated with high rates of morbidity and mortality. Disparities in epilepsy care have previously been described, but little attention has been paid to the contribution of disparities to status epilepticus care and associated outcomes.
Researchers used 2010-2019 data from the Nationwide Inpatient Sample, a database covering a cross-section of hospitalizations in 48 states and the District of Columbia. From relevant diagnostic codes, they calculated status epilepticus prevalence as the rate per 10,000 hospitalizations and stratified this by demographics.
Over the study period, investigators identified 486,861 status epilepticus hospitalizations, most (71.3%) at urban teaching hospitals.
Status epilepticus prevalence was highest for non-Hispanic Black patients, at 27.3, followed by non-Hispanic others, at 16.1, Hispanic patients, at 15.8, and non-Hispanic-White patients, at 13.7 (P < .01).
The finding that Black patients had double the rate as White patients was “definitely surprising,” said Dr. Tantillo Sepúlveda.
Research over the past 20 years revealed similar disparities related to status epilepticus, “so it’s upsetting that these disparities have persisted. Unfortunately, we still have a lot of work to do to reduce health inequalities,” she said.
The investigators found that the prevalence of status epilepticus was higher in the lowest-income quartile, compared with the highest (18.7 vs. 14; P < .01).
Need for physician advocacy
Unlike previous studies, this research assessed various interventions in different age groups and showed that the likelihood of intubation, tracheostomy, gastrostomy, and in-hospital mortality increased with age.
For example, compared with the reference group (patients aged 18-39 years), the odds of intubation were 1.22 (95% confidence interval, 1.16-1.27) for those aged 40-59 years and 1.48 (95% CI, 1.42-1.54) for those aged 60-79. Those aged 80 and older were most likely to be intubated, at an odds ratio of 1.5 (95% CI, 1.43-1.58).
Elderly patients were most likely to undergo tracheostomy (OR, 2.0; 95% CI, 1.75-2.27), gastrostomy (OR, 3.37; 95% CI, 2.97-3.83), and to experience in-hospital mortality (OR, 6.51; 95% CI, 5.95-7.13), compared with the youngest patients.
These intervention rates also varied by racial/ethnic groups. Minority populations, particularly Black people, had higher odds of tracheostomy and gastrostomy, compared with non-Hispanic White persons.
The odds of undergoing electroencephalography monitoring progressively rose as income level increased (OR, 1.47; 95% CI, 1.34-1.62) for the highest income quartile versus the lowest quartile. The odds of undergoing EEG monitoring were also higher at urban teaching hospitals than at rural hospitals.
Tackling these disparities in this patient population include increasing resources, personnel, and health education aimed at minorities, low-income patients, and the elderly, said Dr. Tantillo Sepúlveda. She added that more research is needed “to determine the most effective ways of accomplishing this goal.”
The medical community can help reduce disparities, said Dr. Tantillo Sepúlveda, by working to improve health literacy, to reduce stigma associated with seizures, and to increase awareness of seizure risk factors.
They can also work to expand access to outpatient neurology clinics, epilepsy monitoring units, and epilepsy surgery. “Ethnic and racial minorities are less likely to receive epilepsy surgery for temporal lobe epilepsy, which has been shown to improve quality of life and reduce seizure burden,” Dr. Tantillo Sepúlveda noted.
Across-the-board problem
Commenting on the research, Daniel Lowenstein, MD, professor of neurology, University of California, San Francisco, said the findings aren’t at all surprising. “It’s yet another piece of evidence on what has now become a rather voluminous literature that documents the very significant disparities that exist in our health care system,” said Dr. Lowenstein. “There’s just a huge literature on ‘name your disease and you’ll see the disparities.’ ”
Disparities exist, for example, in diagnosing breast cancer and prostate cancer, in the treatment of stroke and in related outcomes, and there is a well-documented “big disparity” in the approach to pain control among patients presenting at the emergency department, said Dr. Lowenstein.
However, he doesn’t know how disparities in epilepsy and specifically in status epilepticus, compared with disparities regarding other diseases and disorders. He noted that in the case of epilepsy, the situation is likely exacerbated by the stigma associated with that disease.
Dr. Lowenstein agreed that clinicians should play a role in reversing disparities. “We as physicians have a responsibility to be a voice for change in our health care system.”
The study was supported by the Center of Excellence for health equity, training, and research at the Baylor College of Medicine. Dr. Tantillo Sepúlveda and Dr. Lowenstein report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT AES 2022
Erythrasma
THE COMPARISON
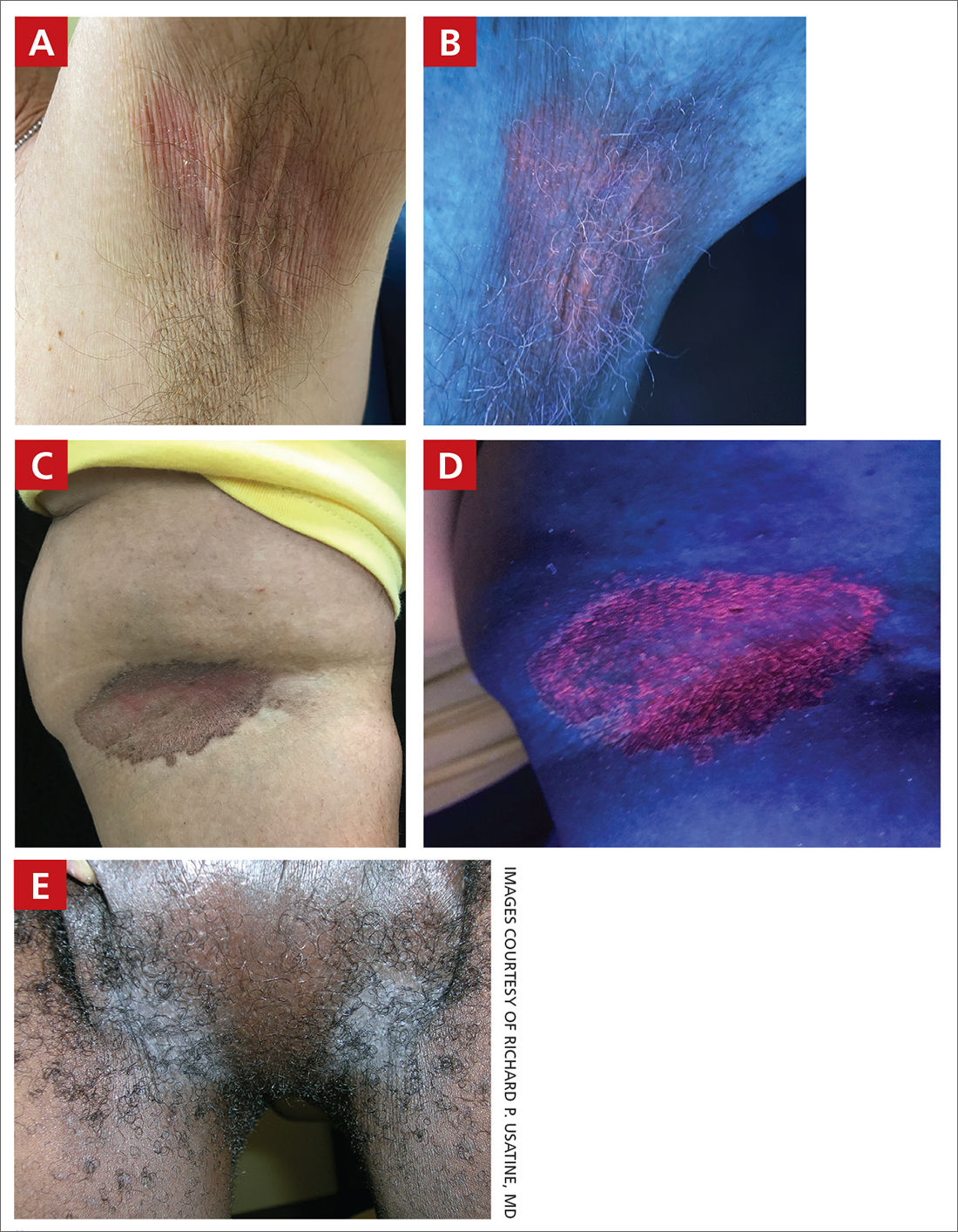
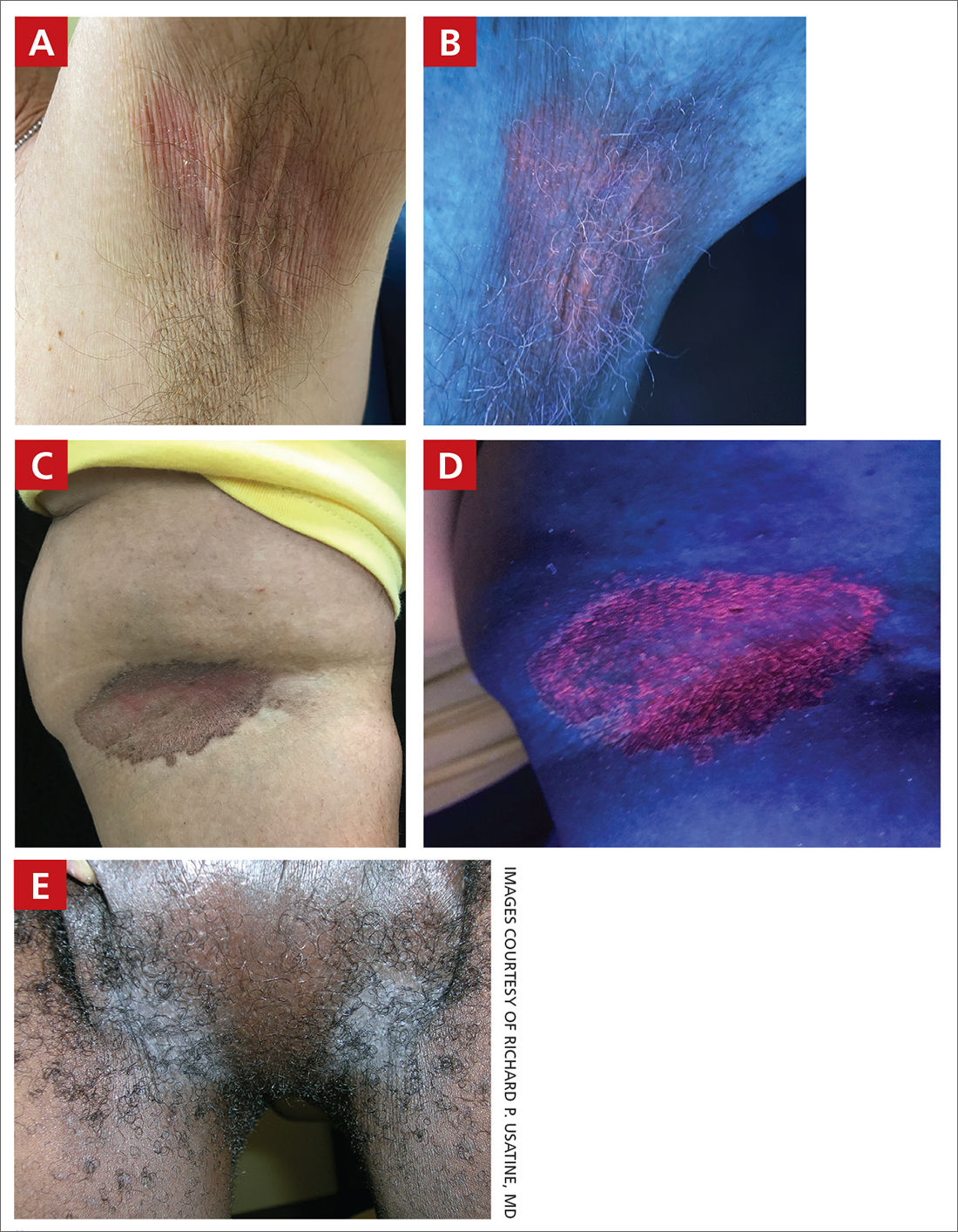
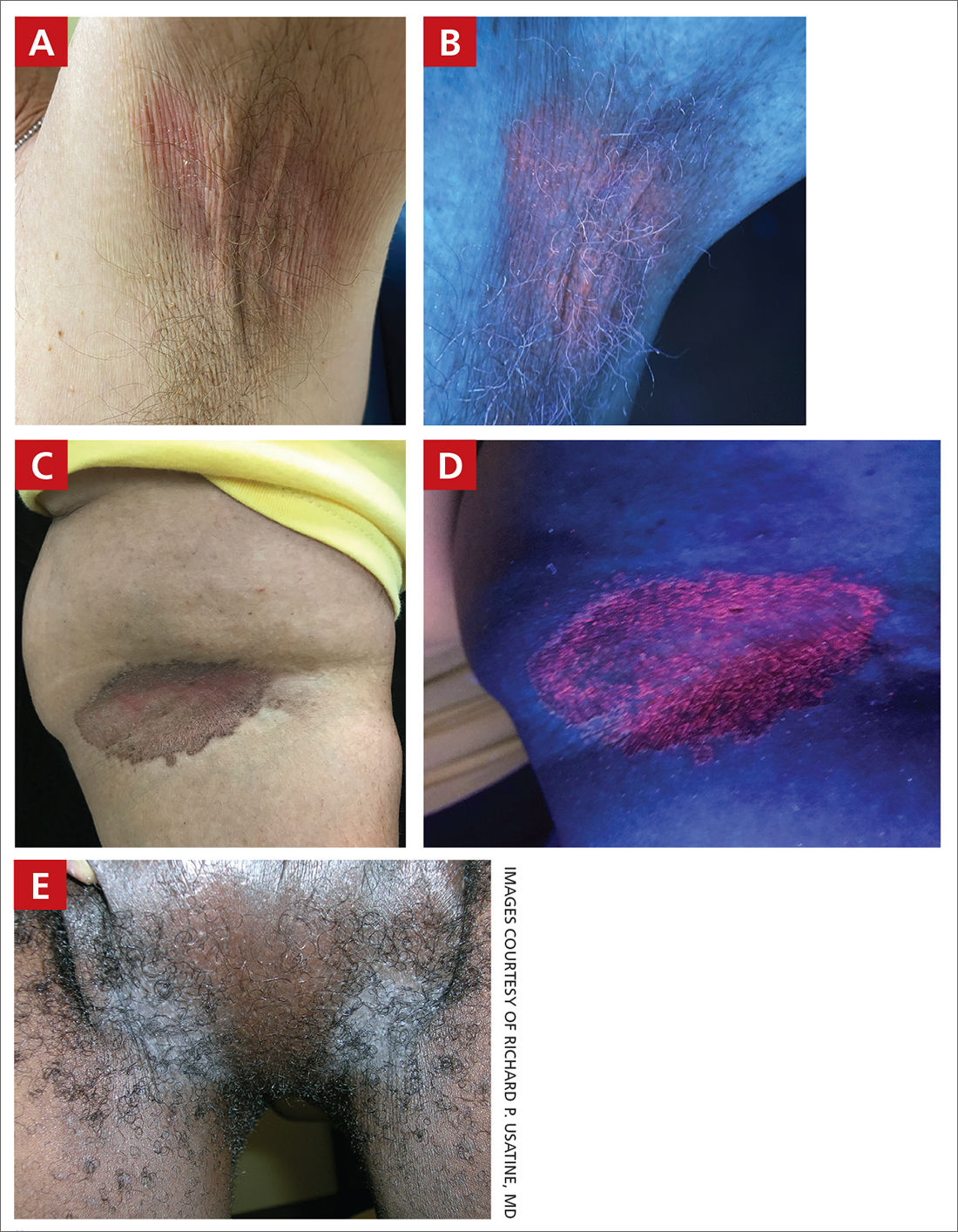
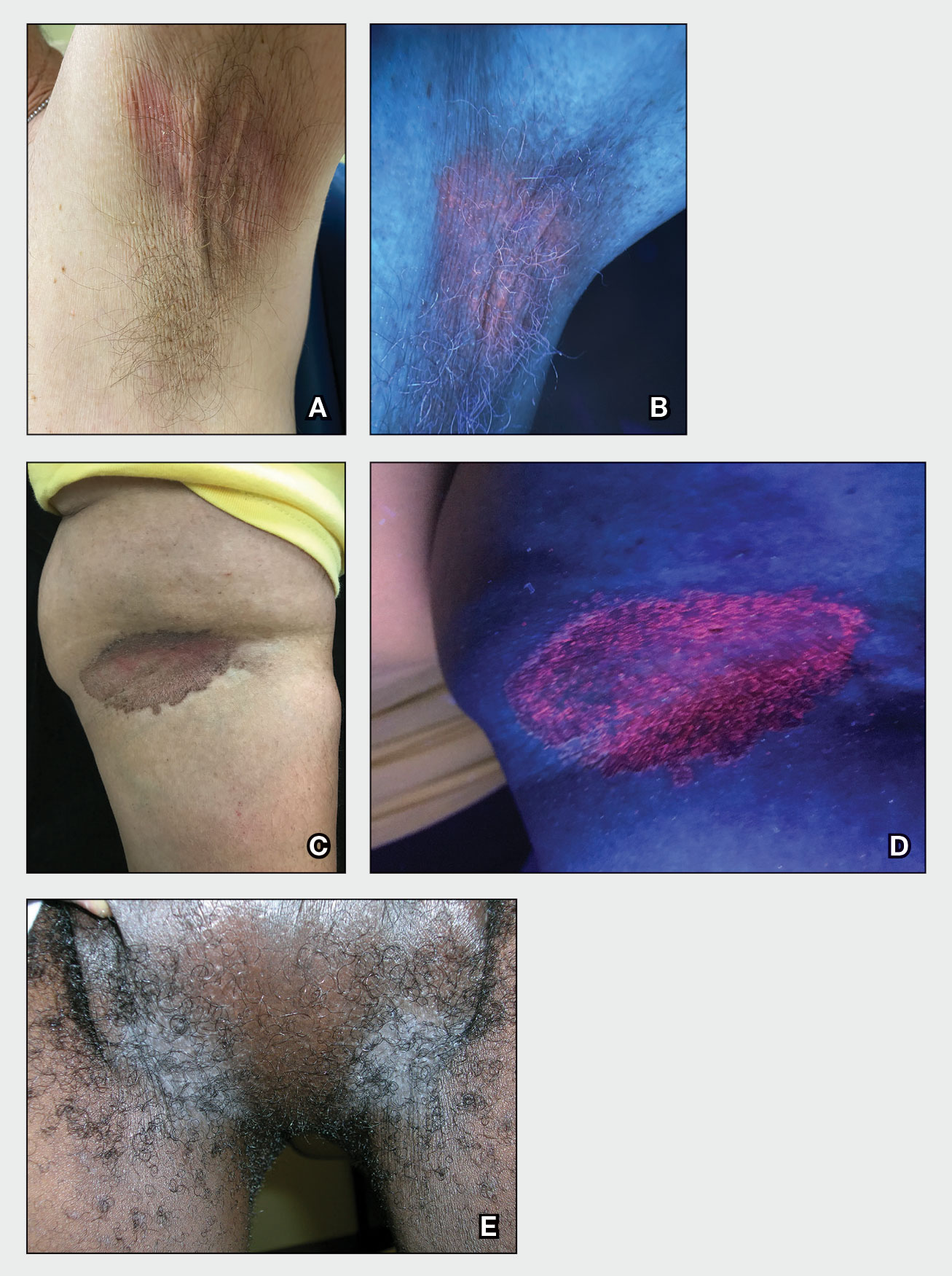
A and B Axilla of a 65-year-old White man with erythrasma showing a well-demarcated erythematous plaque with fine scale (A). Wood-lamp examination of the area showed characteristic bright coral red fluorescence (B).
C and D A well-demarcated, red-brown plaque with fine scale in the antecubital fossa of an obese Hispanic woman (C). Wood-lamp examination revealed bright coral red fluorescence (D).
E Hypopigmented patches (with pruritus) in the groin of a Black man. He also had erythrasma between the toes.
Erythrasma is a skin condition caused by acute or chronic infection of the outermost layer of the epidermis (stratum corneum) with Corynebacterium minutissimum. It has a predilection for intertriginous regions such as the axillae, groin, and interdigital spaces of the toes. It can be associated with pruritus or can be asymptomatic.
Epidemiology
Erythrasma typically affects adults, with greater prevalence among those residing in shared living facilities, such as dormitories or nursing homes, or in humid climates.1 It is a common disorder with an estimated prevalence of 17.6% of bacterial skin infections in elderly patients and 44% of diabetic interdigital toe space infections.2,3
Key clinical features
Erythrasma can manifest as red-brown hyperpigmented plaques with fine scale and little central clearing (FIGURES A and C) or as a hypopigmented patch (FIGURE E) with a sharply marginated, hyperpigmented border in patients with skin of color. In the interdigital toe spaces, the skin often is white and macerated. These findings may appear in patients of all skin tones.
Worth noting
- C minutissimum produces coproporphyrin III, which glows fluorescent red under Wood-lamp examination (FIGURES B and D). A recent shower or bath may remove the fluorescent coproporphyrins and cause a false-negative result. The interdigital space between the fourth and fifth toes is a common location for C minutissimum; thus clinicians should consider examining these areas with a Wood lamp.
- Associated risk factors include obesity, immunosuppression, diabetes mellitus, and excessive sweating.1
- The differential diagnosis includes intertrigo, inverse psoriasis, confluent and reticulated papillomatosis (Gougerot-Carteaud syndrome), acanthosis nigricans, seborrheic dermatitis, and tinea pedis when present in the interdigital toe spaces. Plaques occurring in circular patterns may be mistaken for tinea corporis or pityriasis rotunda.
- There is a high prevalence of erythrasma in patients with inverse psoriasis, and it may exacerbate psoriatic plaques.4
- Treatment options include application of topical clindamycin or erythromycin to the affected area.1 Some patients have responded to topical mupiricin.2 For larger areas, a 1-g dose of clarithromycin5 or a 14-day course of erythromycin may be appropriate.1 Avoid prescribing clarithromycin to patients with preexisting heart disease due to its increased risk for cardiac events or death; consider other agents.
Health disparity highlight
Obesity, most prevalent in non-Hispanic Black adults (49.9%) and Hispanic adults (45.6%) followed by non-Hispanic White adults (41.4%),6 may cause velvety dark plaques on the neck called acanthosis nigricans. However, acute or chronic erythrasma also may cause hyperpigmentation of the body folds. Although the pathology of erythrasma is due to bacterial infection of the superficial layer of the stratum corneum, acanthosis nigricans is due to fibroblast proliferation and stimulation of epidermal keratinocytes, likely from increased growth factors and insulinlike growth factor.7 If erythrasma is mistaken for acanthosis nigricans, the patient may be counseled inappropriately that the hyperpigmentation is something not easily resolved and subsequently left with an active treatable condition that adversely affects their quality of life.
1. Groves JB, Nassereddin A, Freeman AM. Erythrasma. In: StatPearls. StatPearls Publishing; August 11, 2021. Accessed November 17, 2022. https://www.ncbi.nlm.nih.gov/books/NBK513352/
2. Forouzan P, Cohen PR. Erythrasma revisited: diagnosis, differential diagnoses, and comprehensive review of treatment. Cureus. 2020;12:E10733. doi:10.7759/cureus.10733
3. Polat M, I˙lhan MN. Dermatological complaints of the elderly attending a dermatology outpatient clinic in Turkey: a prospective study over a one-year period. Acta Dermatovenerol Croat. 2015;23:277-281.
4. Janeczek M, Kozel Z, Bhasin R, et al. High prevalence of erythrasma in patients with inverse psoriasis: a cross-sectional study. J Clin Aesthet Dermatol. 2020;13:12-14.
5. Khan MJ. Interdigital pedal erythrasma treated with one-time dose of oral clarithromycin 1 g: two case reports. Clin Case Rep. 2020;8:672-674. doi:10.1002/ccr3.2712
6. Stierman B, Afful J, Carroll M, et al. National Health and Nutrition Examination Survey 2017–March 2020 Prepandemic Data Files Development of Files and Prevalence Estimates for Selected Health Outcomes. National Health Statistics Reports. Published June 14, 2021. Accessed November 17, 2022. https://stacks.cdc.gov/view/cdc/106273
7. Brady MF, Rawla P. Acanthosis nigricans. In: StatPearls. Stat- Pearls Publishing; 2022. Updated October 9, 2022. Accessed November 30, 2022. https://www.ncbi.nlm.nih.gov/books/NBK431057
THE COMPARISON
A and B Axilla of a 65-year-old White man with erythrasma showing a well-demarcated erythematous plaque with fine scale (A). Wood-lamp examination of the area showed characteristic bright coral red fluorescence (B).
C and D A well-demarcated, red-brown plaque with fine scale in the antecubital fossa of an obese Hispanic woman (C). Wood-lamp examination revealed bright coral red fluorescence (D).
E Hypopigmented patches (with pruritus) in the groin of a Black man. He also had erythrasma between the toes.
Erythrasma is a skin condition caused by acute or chronic infection of the outermost layer of the epidermis (stratum corneum) with Corynebacterium minutissimum. It has a predilection for intertriginous regions such as the axillae, groin, and interdigital spaces of the toes. It can be associated with pruritus or can be asymptomatic.
Epidemiology
Erythrasma typically affects adults, with greater prevalence among those residing in shared living facilities, such as dormitories or nursing homes, or in humid climates.1 It is a common disorder with an estimated prevalence of 17.6% of bacterial skin infections in elderly patients and 44% of diabetic interdigital toe space infections.2,3
Key clinical features
Erythrasma can manifest as red-brown hyperpigmented plaques with fine scale and little central clearing (FIGURES A and C) or as a hypopigmented patch (FIGURE E) with a sharply marginated, hyperpigmented border in patients with skin of color. In the interdigital toe spaces, the skin often is white and macerated. These findings may appear in patients of all skin tones.
Worth noting
- C minutissimum produces coproporphyrin III, which glows fluorescent red under Wood-lamp examination (FIGURES B and D). A recent shower or bath may remove the fluorescent coproporphyrins and cause a false-negative result. The interdigital space between the fourth and fifth toes is a common location for C minutissimum; thus clinicians should consider examining these areas with a Wood lamp.
- Associated risk factors include obesity, immunosuppression, diabetes mellitus, and excessive sweating.1
- The differential diagnosis includes intertrigo, inverse psoriasis, confluent and reticulated papillomatosis (Gougerot-Carteaud syndrome), acanthosis nigricans, seborrheic dermatitis, and tinea pedis when present in the interdigital toe spaces. Plaques occurring in circular patterns may be mistaken for tinea corporis or pityriasis rotunda.
- There is a high prevalence of erythrasma in patients with inverse psoriasis, and it may exacerbate psoriatic plaques.4
- Treatment options include application of topical clindamycin or erythromycin to the affected area.1 Some patients have responded to topical mupiricin.2 For larger areas, a 1-g dose of clarithromycin5 or a 14-day course of erythromycin may be appropriate.1 Avoid prescribing clarithromycin to patients with preexisting heart disease due to its increased risk for cardiac events or death; consider other agents.
Health disparity highlight
Obesity, most prevalent in non-Hispanic Black adults (49.9%) and Hispanic adults (45.6%) followed by non-Hispanic White adults (41.4%),6 may cause velvety dark plaques on the neck called acanthosis nigricans. However, acute or chronic erythrasma also may cause hyperpigmentation of the body folds. Although the pathology of erythrasma is due to bacterial infection of the superficial layer of the stratum corneum, acanthosis nigricans is due to fibroblast proliferation and stimulation of epidermal keratinocytes, likely from increased growth factors and insulinlike growth factor.7 If erythrasma is mistaken for acanthosis nigricans, the patient may be counseled inappropriately that the hyperpigmentation is something not easily resolved and subsequently left with an active treatable condition that adversely affects their quality of life.
THE COMPARISON
A and B Axilla of a 65-year-old White man with erythrasma showing a well-demarcated erythematous plaque with fine scale (A). Wood-lamp examination of the area showed characteristic bright coral red fluorescence (B).
C and D A well-demarcated, red-brown plaque with fine scale in the antecubital fossa of an obese Hispanic woman (C). Wood-lamp examination revealed bright coral red fluorescence (D).
E Hypopigmented patches (with pruritus) in the groin of a Black man. He also had erythrasma between the toes.
Erythrasma is a skin condition caused by acute or chronic infection of the outermost layer of the epidermis (stratum corneum) with Corynebacterium minutissimum. It has a predilection for intertriginous regions such as the axillae, groin, and interdigital spaces of the toes. It can be associated with pruritus or can be asymptomatic.
Epidemiology
Erythrasma typically affects adults, with greater prevalence among those residing in shared living facilities, such as dormitories or nursing homes, or in humid climates.1 It is a common disorder with an estimated prevalence of 17.6% of bacterial skin infections in elderly patients and 44% of diabetic interdigital toe space infections.2,3
Key clinical features
Erythrasma can manifest as red-brown hyperpigmented plaques with fine scale and little central clearing (FIGURES A and C) or as a hypopigmented patch (FIGURE E) with a sharply marginated, hyperpigmented border in patients with skin of color. In the interdigital toe spaces, the skin often is white and macerated. These findings may appear in patients of all skin tones.
Worth noting
- C minutissimum produces coproporphyrin III, which glows fluorescent red under Wood-lamp examination (FIGURES B and D). A recent shower or bath may remove the fluorescent coproporphyrins and cause a false-negative result. The interdigital space between the fourth and fifth toes is a common location for C minutissimum; thus clinicians should consider examining these areas with a Wood lamp.
- Associated risk factors include obesity, immunosuppression, diabetes mellitus, and excessive sweating.1
- The differential diagnosis includes intertrigo, inverse psoriasis, confluent and reticulated papillomatosis (Gougerot-Carteaud syndrome), acanthosis nigricans, seborrheic dermatitis, and tinea pedis when present in the interdigital toe spaces. Plaques occurring in circular patterns may be mistaken for tinea corporis or pityriasis rotunda.
- There is a high prevalence of erythrasma in patients with inverse psoriasis, and it may exacerbate psoriatic plaques.4
- Treatment options include application of topical clindamycin or erythromycin to the affected area.1 Some patients have responded to topical mupiricin.2 For larger areas, a 1-g dose of clarithromycin5 or a 14-day course of erythromycin may be appropriate.1 Avoid prescribing clarithromycin to patients with preexisting heart disease due to its increased risk for cardiac events or death; consider other agents.
Health disparity highlight
Obesity, most prevalent in non-Hispanic Black adults (49.9%) and Hispanic adults (45.6%) followed by non-Hispanic White adults (41.4%),6 may cause velvety dark plaques on the neck called acanthosis nigricans. However, acute or chronic erythrasma also may cause hyperpigmentation of the body folds. Although the pathology of erythrasma is due to bacterial infection of the superficial layer of the stratum corneum, acanthosis nigricans is due to fibroblast proliferation and stimulation of epidermal keratinocytes, likely from increased growth factors and insulinlike growth factor.7 If erythrasma is mistaken for acanthosis nigricans, the patient may be counseled inappropriately that the hyperpigmentation is something not easily resolved and subsequently left with an active treatable condition that adversely affects their quality of life.
1. Groves JB, Nassereddin A, Freeman AM. Erythrasma. In: StatPearls. StatPearls Publishing; August 11, 2021. Accessed November 17, 2022. https://www.ncbi.nlm.nih.gov/books/NBK513352/
2. Forouzan P, Cohen PR. Erythrasma revisited: diagnosis, differential diagnoses, and comprehensive review of treatment. Cureus. 2020;12:E10733. doi:10.7759/cureus.10733
3. Polat M, I˙lhan MN. Dermatological complaints of the elderly attending a dermatology outpatient clinic in Turkey: a prospective study over a one-year period. Acta Dermatovenerol Croat. 2015;23:277-281.
4. Janeczek M, Kozel Z, Bhasin R, et al. High prevalence of erythrasma in patients with inverse psoriasis: a cross-sectional study. J Clin Aesthet Dermatol. 2020;13:12-14.
5. Khan MJ. Interdigital pedal erythrasma treated with one-time dose of oral clarithromycin 1 g: two case reports. Clin Case Rep. 2020;8:672-674. doi:10.1002/ccr3.2712
6. Stierman B, Afful J, Carroll M, et al. National Health and Nutrition Examination Survey 2017–March 2020 Prepandemic Data Files Development of Files and Prevalence Estimates for Selected Health Outcomes. National Health Statistics Reports. Published June 14, 2021. Accessed November 17, 2022. https://stacks.cdc.gov/view/cdc/106273
7. Brady MF, Rawla P. Acanthosis nigricans. In: StatPearls. Stat- Pearls Publishing; 2022. Updated October 9, 2022. Accessed November 30, 2022. https://www.ncbi.nlm.nih.gov/books/NBK431057
1. Groves JB, Nassereddin A, Freeman AM. Erythrasma. In: StatPearls. StatPearls Publishing; August 11, 2021. Accessed November 17, 2022. https://www.ncbi.nlm.nih.gov/books/NBK513352/
2. Forouzan P, Cohen PR. Erythrasma revisited: diagnosis, differential diagnoses, and comprehensive review of treatment. Cureus. 2020;12:E10733. doi:10.7759/cureus.10733
3. Polat M, I˙lhan MN. Dermatological complaints of the elderly attending a dermatology outpatient clinic in Turkey: a prospective study over a one-year period. Acta Dermatovenerol Croat. 2015;23:277-281.
4. Janeczek M, Kozel Z, Bhasin R, et al. High prevalence of erythrasma in patients with inverse psoriasis: a cross-sectional study. J Clin Aesthet Dermatol. 2020;13:12-14.
5. Khan MJ. Interdigital pedal erythrasma treated with one-time dose of oral clarithromycin 1 g: two case reports. Clin Case Rep. 2020;8:672-674. doi:10.1002/ccr3.2712
6. Stierman B, Afful J, Carroll M, et al. National Health and Nutrition Examination Survey 2017–March 2020 Prepandemic Data Files Development of Files and Prevalence Estimates for Selected Health Outcomes. National Health Statistics Reports. Published June 14, 2021. Accessed November 17, 2022. https://stacks.cdc.gov/view/cdc/106273
7. Brady MF, Rawla P. Acanthosis nigricans. In: StatPearls. Stat- Pearls Publishing; 2022. Updated October 9, 2022. Accessed November 30, 2022. https://www.ncbi.nlm.nih.gov/books/NBK431057
Poorly matched stem cell transplants linked to ancestry
There is “an intersectionality between ancestry and socioeconomic status and an association with donor type, with the most vulnerable patients” – those of non-European ancestry with low socioeconomic status (SES), especially people of African ancestry – “receiving the most complex [i.e., human leukocyte antigen (HLA)–disparate] transplants,” said lead investigator Warren Fingrut, MD, a research fellow in the Adult Bone Marrow Transplantation Service at Memorial Sloan Kettering Cancer Center, New York.
“Successful extension of transplant access to minority patients will be contingent on addressing [their] financial hardship,” said Dr. Fingrut, who presented the findings at the meeting.
To better channel support services and ensure that resources are available, he also noted that centers will have to do a better job of identifying patients with financial struggles.
“Household income data is not collected at our center, and neither is it collected at most centers,” hence assessments of SES are based on imperfect surrogates, such as neighborhood poverty by zip code. “Interventions to advance equity will require better SES classifications or detailed recording of household income,” Dr. Fingrut said.
Overall, the study highlights “inequities in the delivery of stem cell transplants,” pointing to opportunities “to improve access to this potentially curative treatment,” said hematologist/oncologist Chancellor Donald, MD, of Tulane University, New Orleans, who moderated the study presentation.
Dr. Donald said that the new research shows “how interactions between racial backgrounds and socioeconomic status relate to the type of allogenic stem cell transplant patients receive.” The team “identified that [people] of non-European ancestry and especially those of low SES, are more likely to receive the most specialized type of allogeneic stem cell transplantation, which notably require the highest level of care,” Dr. Donald said.
The investigators reviewed 372 consecutive adults transplanted at MSKCC from March 2020 to February 2022, mostly for myeloid malignancies.
Thirty-one percent of patients had non-European ancestry, including 11% of African, 9% of Asian, and 8% of White Hispanic descent.
With no information about household income, the team used neighborhood poverty (which affected 5% of patients); Medicaid as the primary insurance (6% of patients), and financial support for living and medical expenses (19%) as surrogates of lower SES. Classification depended largely on what criteria were used, with only 20 patients meeting two criteria and only one patient meeting all three.
Overall, more than half (58%) of non-European ancestry patients received HLA-disparate grafts, compared with 24% of people with European ancestry, including 48% of White Hispanic patients, 58% of Asian patients, and 78% of patients of African decent.
Markers of lower SES were more common among non-European patients. For instance, among people of European ancestry, 4% were on Medicaid and 15% were on financial aid, versus 10% on Medicaid and 29% on financial support among people of other ancestries. Medicaid use (12.5%) and financial aid (42.5%) were highest among patients of African descent.
Among patients who received HLA-disparate grafts, patients of non-European descent were three times more likely to be on Medicaid (12% versus 4%) and more than twice as likely to be on financial support (33% versus 15%).
People of African ancestry who received HLA-disparate grafts had the highest proportions of Medicaid reliance (16%) and financial support (45%).
There is “an intersectionality between ancestry and socioeconomic status and an association with donor type, with the most vulnerable patients” – those of non-European ancestry with low socioeconomic status (SES), especially people of African ancestry – “receiving the most complex [i.e., human leukocyte antigen (HLA)–disparate] transplants,” said lead investigator Warren Fingrut, MD, a research fellow in the Adult Bone Marrow Transplantation Service at Memorial Sloan Kettering Cancer Center, New York.
“Successful extension of transplant access to minority patients will be contingent on addressing [their] financial hardship,” said Dr. Fingrut, who presented the findings at the meeting.
To better channel support services and ensure that resources are available, he also noted that centers will have to do a better job of identifying patients with financial struggles.
“Household income data is not collected at our center, and neither is it collected at most centers,” hence assessments of SES are based on imperfect surrogates, such as neighborhood poverty by zip code. “Interventions to advance equity will require better SES classifications or detailed recording of household income,” Dr. Fingrut said.
Overall, the study highlights “inequities in the delivery of stem cell transplants,” pointing to opportunities “to improve access to this potentially curative treatment,” said hematologist/oncologist Chancellor Donald, MD, of Tulane University, New Orleans, who moderated the study presentation.
Dr. Donald said that the new research shows “how interactions between racial backgrounds and socioeconomic status relate to the type of allogenic stem cell transplant patients receive.” The team “identified that [people] of non-European ancestry and especially those of low SES, are more likely to receive the most specialized type of allogeneic stem cell transplantation, which notably require the highest level of care,” Dr. Donald said.
The investigators reviewed 372 consecutive adults transplanted at MSKCC from March 2020 to February 2022, mostly for myeloid malignancies.
Thirty-one percent of patients had non-European ancestry, including 11% of African, 9% of Asian, and 8% of White Hispanic descent.
With no information about household income, the team used neighborhood poverty (which affected 5% of patients); Medicaid as the primary insurance (6% of patients), and financial support for living and medical expenses (19%) as surrogates of lower SES. Classification depended largely on what criteria were used, with only 20 patients meeting two criteria and only one patient meeting all three.
Overall, more than half (58%) of non-European ancestry patients received HLA-disparate grafts, compared with 24% of people with European ancestry, including 48% of White Hispanic patients, 58% of Asian patients, and 78% of patients of African decent.
Markers of lower SES were more common among non-European patients. For instance, among people of European ancestry, 4% were on Medicaid and 15% were on financial aid, versus 10% on Medicaid and 29% on financial support among people of other ancestries. Medicaid use (12.5%) and financial aid (42.5%) were highest among patients of African descent.
Among patients who received HLA-disparate grafts, patients of non-European descent were three times more likely to be on Medicaid (12% versus 4%) and more than twice as likely to be on financial support (33% versus 15%).
People of African ancestry who received HLA-disparate grafts had the highest proportions of Medicaid reliance (16%) and financial support (45%).
There is “an intersectionality between ancestry and socioeconomic status and an association with donor type, with the most vulnerable patients” – those of non-European ancestry with low socioeconomic status (SES), especially people of African ancestry – “receiving the most complex [i.e., human leukocyte antigen (HLA)–disparate] transplants,” said lead investigator Warren Fingrut, MD, a research fellow in the Adult Bone Marrow Transplantation Service at Memorial Sloan Kettering Cancer Center, New York.
“Successful extension of transplant access to minority patients will be contingent on addressing [their] financial hardship,” said Dr. Fingrut, who presented the findings at the meeting.
To better channel support services and ensure that resources are available, he also noted that centers will have to do a better job of identifying patients with financial struggles.
“Household income data is not collected at our center, and neither is it collected at most centers,” hence assessments of SES are based on imperfect surrogates, such as neighborhood poverty by zip code. “Interventions to advance equity will require better SES classifications or detailed recording of household income,” Dr. Fingrut said.
Overall, the study highlights “inequities in the delivery of stem cell transplants,” pointing to opportunities “to improve access to this potentially curative treatment,” said hematologist/oncologist Chancellor Donald, MD, of Tulane University, New Orleans, who moderated the study presentation.
Dr. Donald said that the new research shows “how interactions between racial backgrounds and socioeconomic status relate to the type of allogenic stem cell transplant patients receive.” The team “identified that [people] of non-European ancestry and especially those of low SES, are more likely to receive the most specialized type of allogeneic stem cell transplantation, which notably require the highest level of care,” Dr. Donald said.
The investigators reviewed 372 consecutive adults transplanted at MSKCC from March 2020 to February 2022, mostly for myeloid malignancies.
Thirty-one percent of patients had non-European ancestry, including 11% of African, 9% of Asian, and 8% of White Hispanic descent.
With no information about household income, the team used neighborhood poverty (which affected 5% of patients); Medicaid as the primary insurance (6% of patients), and financial support for living and medical expenses (19%) as surrogates of lower SES. Classification depended largely on what criteria were used, with only 20 patients meeting two criteria and only one patient meeting all three.
Overall, more than half (58%) of non-European ancestry patients received HLA-disparate grafts, compared with 24% of people with European ancestry, including 48% of White Hispanic patients, 58% of Asian patients, and 78% of patients of African decent.
Markers of lower SES were more common among non-European patients. For instance, among people of European ancestry, 4% were on Medicaid and 15% were on financial aid, versus 10% on Medicaid and 29% on financial support among people of other ancestries. Medicaid use (12.5%) and financial aid (42.5%) were highest among patients of African descent.
Among patients who received HLA-disparate grafts, patients of non-European descent were three times more likely to be on Medicaid (12% versus 4%) and more than twice as likely to be on financial support (33% versus 15%).
People of African ancestry who received HLA-disparate grafts had the highest proportions of Medicaid reliance (16%) and financial support (45%).
FROM ASH 2022
Study eyes sunscreens marketed to individuals with skin of color
, and more than 40% contain a UV blocker that may create a white cast.
Those are among the findings from a study by Michelle Xiong, a medical student at Brown University, Providence, R.I., and Erin M. Warshaw, MD, of the department of dermatology at Park Nicollet/Health Partners Health Services, Minneapolis, which was published online in the Journal of the American Academy of Dermatology.
“There is increasing awareness of the negative effects of ultraviolet (UV) light in individuals with skin of color (SOC), especially in regards to pigmentation disorders induced and/or exacerbated by UV exposure,” the authors wrote. “As a result, there has been a surge in sunscreens marketed to this population. We aimed to characterize cost, marketing claims, and potential allergenic ingredients in sunscreens marketed to individuals with SOC.”
Between December 2021 and October 2022, the researchers used the following search terms on Google: “sunscreen” plus “skin of 36 color,” “dark skin,” “brown skin,” “LatinX skin,” and/or “Black skin.” They extracted price, marketing claims, and ingredients from manufacturers’ websites and used 90 allergens contained in the American Contact Dermatitis Society 2020 Core series to identify potential allergens. Next, they combined cross-reactors/synonyms into allergen categories based on ACDS Contact Allergen Management Plan (CAMP) cross-reactor classification. If multiple ingredients in a sunscreen were represented by a single allergen category, it was counted only once. A similar approach was utilized for marketing categories.
A total of 12 sunscreens were included in the analysis: Absolute Joi, Black Girl Sunscreen, Black Girl Sunscreen Make It Matte, Bolden SPF Brightening Moisturizer, Eleven on the Defense Unrivaled Sun Serum, Kinlo Golden Rays Sunscreen, Live Tinted Hueguard 3-in-1 Mineral Sunscreen, Mele Dew The Most Sheer Moisturizer SPF30 Broad Spectrum Sunscreen, Mele No Shade Sunscreen Oil, Specific Beauty Active Radiance Day Moi, Unsun Mineral Sunscreen, and Urban Skin Rx Complexion Protection. Their average cost was $19.30 per ounce (range, $6.33-$50.00) and common marketing claims for these products were “no white cast” (91.7%), being free of an ingredient (83.3%), and “moisturizing” (75%).
Of the 12 sunscreens, 7 (58.3%) contained a chemical sunscreen agent, 5 (41.7%) contained a physical UV blocker, and all contained at least one allergen. The average number of allergens per product was 4.7, most commonly fragrance/botanicals (83.3%), tocopherol (83.3%), sodium benzoates/derivatives (58.3%), and sorbitan sesquiolate/derivatives (58.3%).
“Average cost of sunscreens marketed to individuals with SOC was $19.30/oz, much higher than the median price of $3.32/oz reported in a separate study of 65 popular sunscreens,” the study authors wrote. “As many of the sunscreens in our study were sold by smaller businesses, higher prices may be due to higher production costs or a perceived smaller market.”
The authors expressed surprise that five sunscreens marketed to individuals with SOC contained a physical UV blocker which may create a white cast. They contacted the manufacturers of these five sunscreens and confirmed that three used micronized formulations. “While ingested/inhaled nanoparticles of titanium dioxide may cause tissue effects, most studies of topical products show excellent safety,” they wrote.
They also noted that the average of 4.7 allergens per product observed in the analysis was similar to the average of 4.9 seen in a separate study of 52 popular sunscreens. “However, that study only included 34 allergens while this study evaluated 90 allergens,” the authors wrote. “Consumers and providers should be aware sunscreens marketed to individuals with SOC may cause allergic contact dermatitis,” they commented.
“It is interesting to see how costly these products are now compared to store bought and general commercially available sunscreens several years ago,” said Lawrence J. Green, clinical professor of dermatology at George Washington University, Washington, who was asked to comment on the study. “However, to me that is not surprising as products marketed and targeted to specific populations are often priced at a premium. It wasn’t clear to me how many of these specialized online SOC sunscreens are tinted. I wish the authors had compared the cost of tinted sunscreens in general to nontinted sunscreens because tinted ones are more useful for SOC, because when rubbed in, they can readily match SOC and can also offer protection in the visible light spectrum.”
The authors reported having no financial disclosures; the study had no funding source. Dr. Green disclosed that he is a speaker, consultant, or investigator for many pharmaceutical companies.
, and more than 40% contain a UV blocker that may create a white cast.
Those are among the findings from a study by Michelle Xiong, a medical student at Brown University, Providence, R.I., and Erin M. Warshaw, MD, of the department of dermatology at Park Nicollet/Health Partners Health Services, Minneapolis, which was published online in the Journal of the American Academy of Dermatology.
“There is increasing awareness of the negative effects of ultraviolet (UV) light in individuals with skin of color (SOC), especially in regards to pigmentation disorders induced and/or exacerbated by UV exposure,” the authors wrote. “As a result, there has been a surge in sunscreens marketed to this population. We aimed to characterize cost, marketing claims, and potential allergenic ingredients in sunscreens marketed to individuals with SOC.”
Between December 2021 and October 2022, the researchers used the following search terms on Google: “sunscreen” plus “skin of 36 color,” “dark skin,” “brown skin,” “LatinX skin,” and/or “Black skin.” They extracted price, marketing claims, and ingredients from manufacturers’ websites and used 90 allergens contained in the American Contact Dermatitis Society 2020 Core series to identify potential allergens. Next, they combined cross-reactors/synonyms into allergen categories based on ACDS Contact Allergen Management Plan (CAMP) cross-reactor classification. If multiple ingredients in a sunscreen were represented by a single allergen category, it was counted only once. A similar approach was utilized for marketing categories.
A total of 12 sunscreens were included in the analysis: Absolute Joi, Black Girl Sunscreen, Black Girl Sunscreen Make It Matte, Bolden SPF Brightening Moisturizer, Eleven on the Defense Unrivaled Sun Serum, Kinlo Golden Rays Sunscreen, Live Tinted Hueguard 3-in-1 Mineral Sunscreen, Mele Dew The Most Sheer Moisturizer SPF30 Broad Spectrum Sunscreen, Mele No Shade Sunscreen Oil, Specific Beauty Active Radiance Day Moi, Unsun Mineral Sunscreen, and Urban Skin Rx Complexion Protection. Their average cost was $19.30 per ounce (range, $6.33-$50.00) and common marketing claims for these products were “no white cast” (91.7%), being free of an ingredient (83.3%), and “moisturizing” (75%).
Of the 12 sunscreens, 7 (58.3%) contained a chemical sunscreen agent, 5 (41.7%) contained a physical UV blocker, and all contained at least one allergen. The average number of allergens per product was 4.7, most commonly fragrance/botanicals (83.3%), tocopherol (83.3%), sodium benzoates/derivatives (58.3%), and sorbitan sesquiolate/derivatives (58.3%).
“Average cost of sunscreens marketed to individuals with SOC was $19.30/oz, much higher than the median price of $3.32/oz reported in a separate study of 65 popular sunscreens,” the study authors wrote. “As many of the sunscreens in our study were sold by smaller businesses, higher prices may be due to higher production costs or a perceived smaller market.”
The authors expressed surprise that five sunscreens marketed to individuals with SOC contained a physical UV blocker which may create a white cast. They contacted the manufacturers of these five sunscreens and confirmed that three used micronized formulations. “While ingested/inhaled nanoparticles of titanium dioxide may cause tissue effects, most studies of topical products show excellent safety,” they wrote.
They also noted that the average of 4.7 allergens per product observed in the analysis was similar to the average of 4.9 seen in a separate study of 52 popular sunscreens. “However, that study only included 34 allergens while this study evaluated 90 allergens,” the authors wrote. “Consumers and providers should be aware sunscreens marketed to individuals with SOC may cause allergic contact dermatitis,” they commented.
“It is interesting to see how costly these products are now compared to store bought and general commercially available sunscreens several years ago,” said Lawrence J. Green, clinical professor of dermatology at George Washington University, Washington, who was asked to comment on the study. “However, to me that is not surprising as products marketed and targeted to specific populations are often priced at a premium. It wasn’t clear to me how many of these specialized online SOC sunscreens are tinted. I wish the authors had compared the cost of tinted sunscreens in general to nontinted sunscreens because tinted ones are more useful for SOC, because when rubbed in, they can readily match SOC and can also offer protection in the visible light spectrum.”
The authors reported having no financial disclosures; the study had no funding source. Dr. Green disclosed that he is a speaker, consultant, or investigator for many pharmaceutical companies.
, and more than 40% contain a UV blocker that may create a white cast.
Those are among the findings from a study by Michelle Xiong, a medical student at Brown University, Providence, R.I., and Erin M. Warshaw, MD, of the department of dermatology at Park Nicollet/Health Partners Health Services, Minneapolis, which was published online in the Journal of the American Academy of Dermatology.
“There is increasing awareness of the negative effects of ultraviolet (UV) light in individuals with skin of color (SOC), especially in regards to pigmentation disorders induced and/or exacerbated by UV exposure,” the authors wrote. “As a result, there has been a surge in sunscreens marketed to this population. We aimed to characterize cost, marketing claims, and potential allergenic ingredients in sunscreens marketed to individuals with SOC.”
Between December 2021 and October 2022, the researchers used the following search terms on Google: “sunscreen” plus “skin of 36 color,” “dark skin,” “brown skin,” “LatinX skin,” and/or “Black skin.” They extracted price, marketing claims, and ingredients from manufacturers’ websites and used 90 allergens contained in the American Contact Dermatitis Society 2020 Core series to identify potential allergens. Next, they combined cross-reactors/synonyms into allergen categories based on ACDS Contact Allergen Management Plan (CAMP) cross-reactor classification. If multiple ingredients in a sunscreen were represented by a single allergen category, it was counted only once. A similar approach was utilized for marketing categories.
A total of 12 sunscreens were included in the analysis: Absolute Joi, Black Girl Sunscreen, Black Girl Sunscreen Make It Matte, Bolden SPF Brightening Moisturizer, Eleven on the Defense Unrivaled Sun Serum, Kinlo Golden Rays Sunscreen, Live Tinted Hueguard 3-in-1 Mineral Sunscreen, Mele Dew The Most Sheer Moisturizer SPF30 Broad Spectrum Sunscreen, Mele No Shade Sunscreen Oil, Specific Beauty Active Radiance Day Moi, Unsun Mineral Sunscreen, and Urban Skin Rx Complexion Protection. Their average cost was $19.30 per ounce (range, $6.33-$50.00) and common marketing claims for these products were “no white cast” (91.7%), being free of an ingredient (83.3%), and “moisturizing” (75%).
Of the 12 sunscreens, 7 (58.3%) contained a chemical sunscreen agent, 5 (41.7%) contained a physical UV blocker, and all contained at least one allergen. The average number of allergens per product was 4.7, most commonly fragrance/botanicals (83.3%), tocopherol (83.3%), sodium benzoates/derivatives (58.3%), and sorbitan sesquiolate/derivatives (58.3%).
“Average cost of sunscreens marketed to individuals with SOC was $19.30/oz, much higher than the median price of $3.32/oz reported in a separate study of 65 popular sunscreens,” the study authors wrote. “As many of the sunscreens in our study were sold by smaller businesses, higher prices may be due to higher production costs or a perceived smaller market.”
The authors expressed surprise that five sunscreens marketed to individuals with SOC contained a physical UV blocker which may create a white cast. They contacted the manufacturers of these five sunscreens and confirmed that three used micronized formulations. “While ingested/inhaled nanoparticles of titanium dioxide may cause tissue effects, most studies of topical products show excellent safety,” they wrote.
They also noted that the average of 4.7 allergens per product observed in the analysis was similar to the average of 4.9 seen in a separate study of 52 popular sunscreens. “However, that study only included 34 allergens while this study evaluated 90 allergens,” the authors wrote. “Consumers and providers should be aware sunscreens marketed to individuals with SOC may cause allergic contact dermatitis,” they commented.
“It is interesting to see how costly these products are now compared to store bought and general commercially available sunscreens several years ago,” said Lawrence J. Green, clinical professor of dermatology at George Washington University, Washington, who was asked to comment on the study. “However, to me that is not surprising as products marketed and targeted to specific populations are often priced at a premium. It wasn’t clear to me how many of these specialized online SOC sunscreens are tinted. I wish the authors had compared the cost of tinted sunscreens in general to nontinted sunscreens because tinted ones are more useful for SOC, because when rubbed in, they can readily match SOC and can also offer protection in the visible light spectrum.”
The authors reported having no financial disclosures; the study had no funding source. Dr. Green disclosed that he is a speaker, consultant, or investigator for many pharmaceutical companies.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Erythrasma
THE COMPARISON
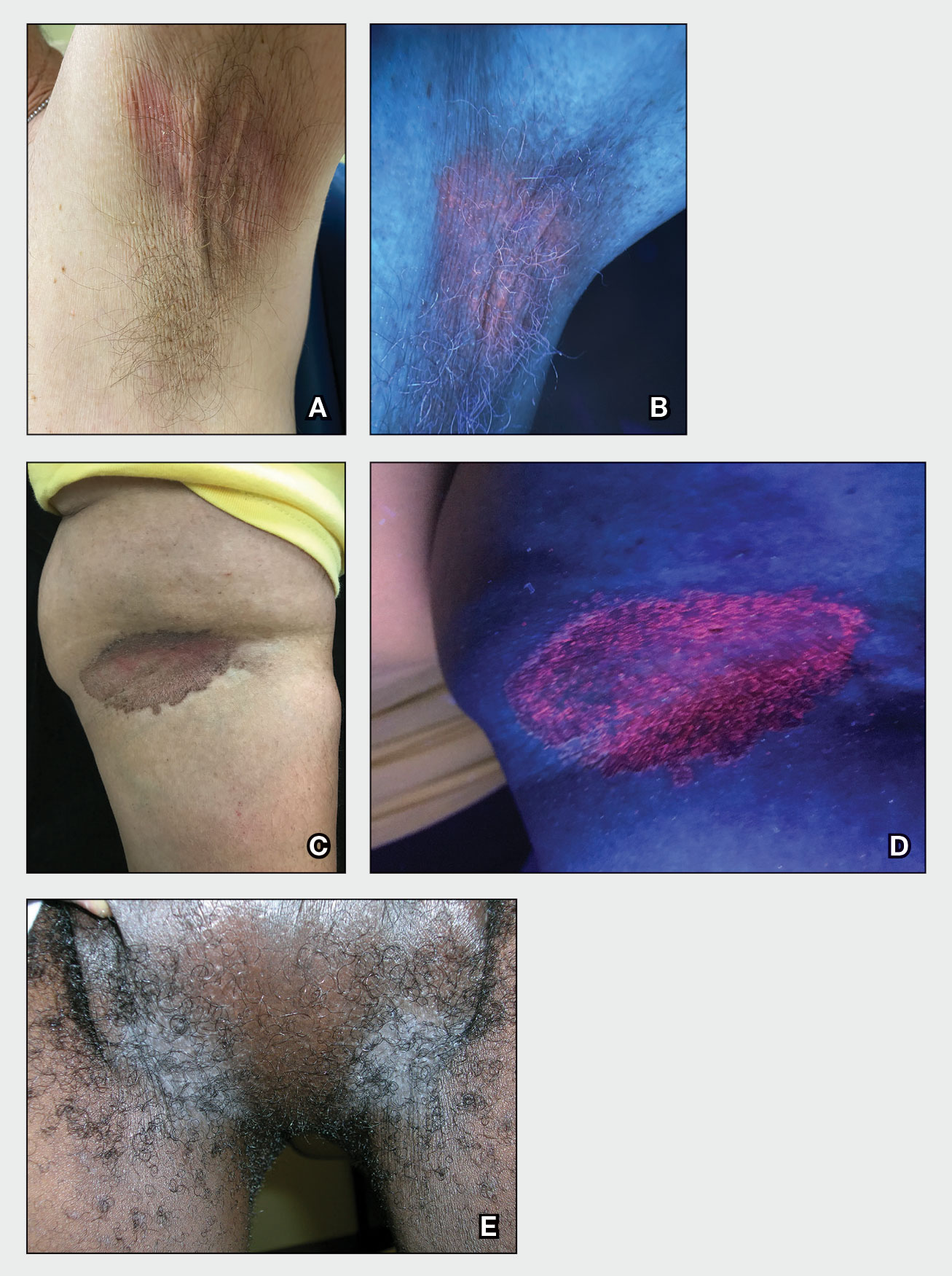
A and B Axilla of a 65-year-old White man with erythrasma showing a well-demarcated erythematous plaque with fine scale (A). Wood lamp examination of the area showed characteristic bright coral red fluorescence (B).
C and D A well-demarcated, red-brown plaque with fine scale in the antecubital fossa of an obese Hispanic woman (C). Wood lamp examination revealed bright coral red fluorescence (D).
E Hypopigmented patches in the groin with pruritus in a Black man. He also had erythrasma between the toes.
Erythrasma is a skin condition caused by acute or chronic infection of the outermost layer of the epidermis (stratum corneum) with Corynebacterium minutissimum. It has a predilection for intertriginous regions such as the axillae, groin, and interdigital spaces of the toes. It can be associated with pruritus or can be asymptomatic.
Epidemiology
Erythrasma typically affects adults, with greater prevalence among those residing in shared living facilities, such as dormitories or nursing homes, or in humid climates.1 It is a common disorder with an estimated prevalence of 17.6% of bacterial skin infections in elderly patients and 44% of diabetic interdigital toe space infections.2,3
Key clinical features
Erythrasma can manifest as red-brown hyperpigmented plaques with fine scale and little central clearing (Figures A and C) or as a hypopigmented patch (Figure E) with a sharply marginated, hyperpigmented border in patients with skin of color. In the interdigital toe spaces, the skin often is white and macerated. These findings may appear in patients of all skin tones.
Worth noting
• Corynebacterium minutissimum produces coproporphyrin III, which glows fluorescent red under Wood lamp examination (Figures B and D). A recent shower or bath may remove the fluorescent coproporphyrins and cause a false-negative result. The interdigital space between the fourth and fifth toes is a common location for C minutissimum; thus clinicians should consider examining these areas with a Wood lamp.
• Associated risk factors include obesity, immunosuppression, diabetes mellitus, and excessive sweating.1
• The differential diagnosis includes intertrigo, inverse psoriasis, confluent and reticulated papillomatosis (Gougerot-Carteaud syndrome), acanthosis nigricans, seborrheic dermatitis, and tinea pedis when present in the interdigital toe spaces. Plaques occurring in circular patterns may be mistaken for tinea corporis or pityriasis rotunda.
• There is a high prevalence of erythrasma in patients with inverse psoriasis, and it may exacerbate psoriatic plaques.4
• Treatment options include application of topical clindamycin or erythromycin to the affected area.1 Some patients have responded to topical mupiricin.2 For larger areas, a 1-g dose of clarithromycin5 or a 14-day course of erythromycin may be appropriate.1 Avoid prescribing clarithromycin to patients with preexisting heart disease due to its increased risk for cardiac events or death; consider other agents.
Health disparity highlight
Obesity, most prevalent in non-Hispanic Black adults (49.9%) and Hispanic adults (45.6%) followed by non- Hispanic White adults (41.4%),6 may cause velvety dark plaques on the neck called acanthosis nigricans. However, acute or chronic erythrasma also may cause hyperpigmentation of the body folds. Although the pathology of erythrasma is due to bacterial infection of the superficial layer of the stratum corneum, acanthosis nigricans is due to fibroblast proliferation and stimulation of epidermal keratinocytes likely from increased growth factors and insulinlike growth factor.7 If erythrasma is mistaken for acanthosis nigricans, the patient may be counseled inappropriately that the hyperpigmentation is something not easily resolved and subsequently left with an active treatable condition that adversely affects their quality of life.
- Groves JB, Nassereddin A, Freeman AM. Erythrasma. In: StatPearls. StatPearls Publishing; August 11, 2021. Accessed November 17, 2022. https://www.ncbi.nlm.nih.gov/books/NBK513352/
- Forouzan P, Cohen PR. Erythrasma revisited: diagnosis, differential diagnoses, and comprehensive review of treatment [published online September 30, 2020]. Cureus. 2020;12:E10733. doi:10.7759/cureus.10733
- Polat M, I˙lhan MN. Dermatological complaints of the elderly attending a dermatology outpatient clinic in Turkey: a prospective study over a one-year period. Acta Dermatovenerol Croat. 2015;23:277-281.
- Janeczek M, Kozel Z, Bhasin R, et al. High prevalence of erythrasma in patients with inverse psoriasis: a cross-sectional study. J Clin Aesthet Dermatol. 2020;13:12-14.
- Khan MJ. Interdigital pedal erythrasma treated with one-time dose of oral clarithromycin 1 g: two case reports [published online February 6, 2020]. Clin Case Rep. 2020;8:672-674. doi:10.1002/ccr3.2712
- Stierman B, Afful J, Carroll M, et al. National Health and Nutrition Examination Survey 2017–March 2020 Prepandemic Data Files Development of Files and Prevalence Estimates for Selected Health Outcomes. National Health Statistics Reports. Published June 14, 2021. Accessed November 17, 2022. https://stacks.cdc.gov/view/cdc/106273
- Brady MF, Rawla P. Acanthosis nigricans. In: StatPearls [Internet]. StatPearls Publishing; 2022. Updated October 9, 2022. Accessed November 30, 2022. https://www.ncbi.nlm.nih.gov/books/NBK431057
THE COMPARISON
A and B Axilla of a 65-year-old White man with erythrasma showing a well-demarcated erythematous plaque with fine scale (A). Wood lamp examination of the area showed characteristic bright coral red fluorescence (B).
C and D A well-demarcated, red-brown plaque with fine scale in the antecubital fossa of an obese Hispanic woman (C). Wood lamp examination revealed bright coral red fluorescence (D).
E Hypopigmented patches in the groin with pruritus in a Black man. He also had erythrasma between the toes.
Erythrasma is a skin condition caused by acute or chronic infection of the outermost layer of the epidermis (stratum corneum) with Corynebacterium minutissimum. It has a predilection for intertriginous regions such as the axillae, groin, and interdigital spaces of the toes. It can be associated with pruritus or can be asymptomatic.
Epidemiology
Erythrasma typically affects adults, with greater prevalence among those residing in shared living facilities, such as dormitories or nursing homes, or in humid climates.1 It is a common disorder with an estimated prevalence of 17.6% of bacterial skin infections in elderly patients and 44% of diabetic interdigital toe space infections.2,3
Key clinical features
Erythrasma can manifest as red-brown hyperpigmented plaques with fine scale and little central clearing (Figures A and C) or as a hypopigmented patch (Figure E) with a sharply marginated, hyperpigmented border in patients with skin of color. In the interdigital toe spaces, the skin often is white and macerated. These findings may appear in patients of all skin tones.
Worth noting
• Corynebacterium minutissimum produces coproporphyrin III, which glows fluorescent red under Wood lamp examination (Figures B and D). A recent shower or bath may remove the fluorescent coproporphyrins and cause a false-negative result. The interdigital space between the fourth and fifth toes is a common location for C minutissimum; thus clinicians should consider examining these areas with a Wood lamp.
• Associated risk factors include obesity, immunosuppression, diabetes mellitus, and excessive sweating.1
• The differential diagnosis includes intertrigo, inverse psoriasis, confluent and reticulated papillomatosis (Gougerot-Carteaud syndrome), acanthosis nigricans, seborrheic dermatitis, and tinea pedis when present in the interdigital toe spaces. Plaques occurring in circular patterns may be mistaken for tinea corporis or pityriasis rotunda.
• There is a high prevalence of erythrasma in patients with inverse psoriasis, and it may exacerbate psoriatic plaques.4
• Treatment options include application of topical clindamycin or erythromycin to the affected area.1 Some patients have responded to topical mupiricin.2 For larger areas, a 1-g dose of clarithromycin5 or a 14-day course of erythromycin may be appropriate.1 Avoid prescribing clarithromycin to patients with preexisting heart disease due to its increased risk for cardiac events or death; consider other agents.
Health disparity highlight
Obesity, most prevalent in non-Hispanic Black adults (49.9%) and Hispanic adults (45.6%) followed by non- Hispanic White adults (41.4%),6 may cause velvety dark plaques on the neck called acanthosis nigricans. However, acute or chronic erythrasma also may cause hyperpigmentation of the body folds. Although the pathology of erythrasma is due to bacterial infection of the superficial layer of the stratum corneum, acanthosis nigricans is due to fibroblast proliferation and stimulation of epidermal keratinocytes likely from increased growth factors and insulinlike growth factor.7 If erythrasma is mistaken for acanthosis nigricans, the patient may be counseled inappropriately that the hyperpigmentation is something not easily resolved and subsequently left with an active treatable condition that adversely affects their quality of life.
THE COMPARISON
A and B Axilla of a 65-year-old White man with erythrasma showing a well-demarcated erythematous plaque with fine scale (A). Wood lamp examination of the area showed characteristic bright coral red fluorescence (B).
C and D A well-demarcated, red-brown plaque with fine scale in the antecubital fossa of an obese Hispanic woman (C). Wood lamp examination revealed bright coral red fluorescence (D).
E Hypopigmented patches in the groin with pruritus in a Black man. He also had erythrasma between the toes.
Erythrasma is a skin condition caused by acute or chronic infection of the outermost layer of the epidermis (stratum corneum) with Corynebacterium minutissimum. It has a predilection for intertriginous regions such as the axillae, groin, and interdigital spaces of the toes. It can be associated with pruritus or can be asymptomatic.
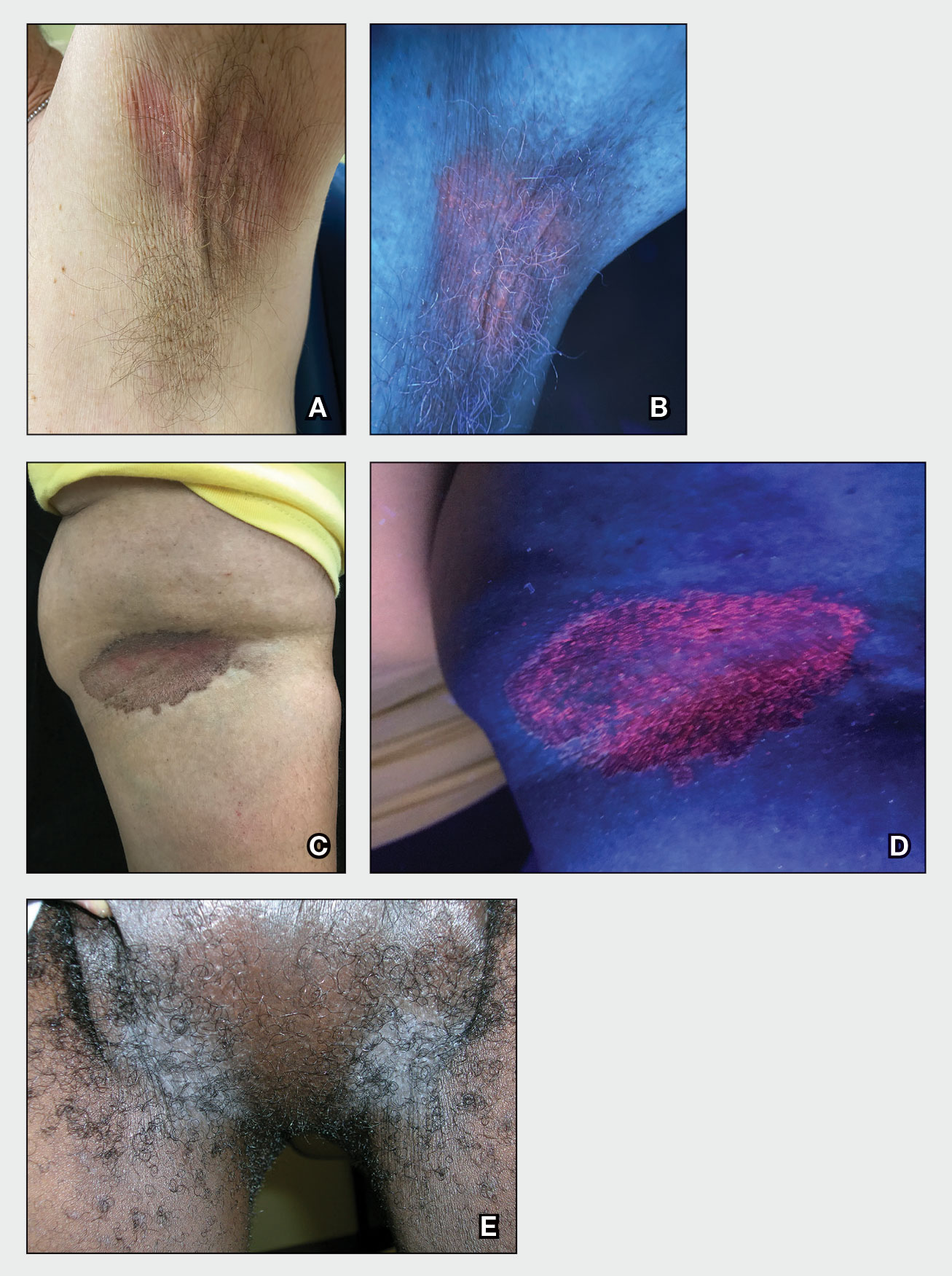
Epidemiology
Erythrasma typically affects adults, with greater prevalence among those residing in shared living facilities, such as dormitories or nursing homes, or in humid climates.1 It is a common disorder with an estimated prevalence of 17.6% of bacterial skin infections in elderly patients and 44% of diabetic interdigital toe space infections.2,3
Key clinical features
Erythrasma can manifest as red-brown hyperpigmented plaques with fine scale and little central clearing (Figures A and C) or as a hypopigmented patch (Figure E) with a sharply marginated, hyperpigmented border in patients with skin of color. In the interdigital toe spaces, the skin often is white and macerated. These findings may appear in patients of all skin tones.
Worth noting
• Corynebacterium minutissimum produces coproporphyrin III, which glows fluorescent red under Wood lamp examination (Figures B and D). A recent shower or bath may remove the fluorescent coproporphyrins and cause a false-negative result. The interdigital space between the fourth and fifth toes is a common location for C minutissimum; thus clinicians should consider examining these areas with a Wood lamp.
• Associated risk factors include obesity, immunosuppression, diabetes mellitus, and excessive sweating.1
• The differential diagnosis includes intertrigo, inverse psoriasis, confluent and reticulated papillomatosis (Gougerot-Carteaud syndrome), acanthosis nigricans, seborrheic dermatitis, and tinea pedis when present in the interdigital toe spaces. Plaques occurring in circular patterns may be mistaken for tinea corporis or pityriasis rotunda.
• There is a high prevalence of erythrasma in patients with inverse psoriasis, and it may exacerbate psoriatic plaques.4
• Treatment options include application of topical clindamycin or erythromycin to the affected area.1 Some patients have responded to topical mupiricin.2 For larger areas, a 1-g dose of clarithromycin5 or a 14-day course of erythromycin may be appropriate.1 Avoid prescribing clarithromycin to patients with preexisting heart disease due to its increased risk for cardiac events or death; consider other agents.
Health disparity highlight
Obesity, most prevalent in non-Hispanic Black adults (49.9%) and Hispanic adults (45.6%) followed by non- Hispanic White adults (41.4%),6 may cause velvety dark plaques on the neck called acanthosis nigricans. However, acute or chronic erythrasma also may cause hyperpigmentation of the body folds. Although the pathology of erythrasma is due to bacterial infection of the superficial layer of the stratum corneum, acanthosis nigricans is due to fibroblast proliferation and stimulation of epidermal keratinocytes likely from increased growth factors and insulinlike growth factor.7 If erythrasma is mistaken for acanthosis nigricans, the patient may be counseled inappropriately that the hyperpigmentation is something not easily resolved and subsequently left with an active treatable condition that adversely affects their quality of life.
- Groves JB, Nassereddin A, Freeman AM. Erythrasma. In: StatPearls. StatPearls Publishing; August 11, 2021. Accessed November 17, 2022. https://www.ncbi.nlm.nih.gov/books/NBK513352/
- Forouzan P, Cohen PR. Erythrasma revisited: diagnosis, differential diagnoses, and comprehensive review of treatment [published online September 30, 2020]. Cureus. 2020;12:E10733. doi:10.7759/cureus.10733
- Polat M, I˙lhan MN. Dermatological complaints of the elderly attending a dermatology outpatient clinic in Turkey: a prospective study over a one-year period. Acta Dermatovenerol Croat. 2015;23:277-281.
- Janeczek M, Kozel Z, Bhasin R, et al. High prevalence of erythrasma in patients with inverse psoriasis: a cross-sectional study. J Clin Aesthet Dermatol. 2020;13:12-14.
- Khan MJ. Interdigital pedal erythrasma treated with one-time dose of oral clarithromycin 1 g: two case reports [published online February 6, 2020]. Clin Case Rep. 2020;8:672-674. doi:10.1002/ccr3.2712
- Stierman B, Afful J, Carroll M, et al. National Health and Nutrition Examination Survey 2017–March 2020 Prepandemic Data Files Development of Files and Prevalence Estimates for Selected Health Outcomes. National Health Statistics Reports. Published June 14, 2021. Accessed November 17, 2022. https://stacks.cdc.gov/view/cdc/106273
- Brady MF, Rawla P. Acanthosis nigricans. In: StatPearls [Internet]. StatPearls Publishing; 2022. Updated October 9, 2022. Accessed November 30, 2022. https://www.ncbi.nlm.nih.gov/books/NBK431057
- Groves JB, Nassereddin A, Freeman AM. Erythrasma. In: StatPearls. StatPearls Publishing; August 11, 2021. Accessed November 17, 2022. https://www.ncbi.nlm.nih.gov/books/NBK513352/
- Forouzan P, Cohen PR. Erythrasma revisited: diagnosis, differential diagnoses, and comprehensive review of treatment [published online September 30, 2020]. Cureus. 2020;12:E10733. doi:10.7759/cureus.10733
- Polat M, I˙lhan MN. Dermatological complaints of the elderly attending a dermatology outpatient clinic in Turkey: a prospective study over a one-year period. Acta Dermatovenerol Croat. 2015;23:277-281.
- Janeczek M, Kozel Z, Bhasin R, et al. High prevalence of erythrasma in patients with inverse psoriasis: a cross-sectional study. J Clin Aesthet Dermatol. 2020;13:12-14.
- Khan MJ. Interdigital pedal erythrasma treated with one-time dose of oral clarithromycin 1 g: two case reports [published online February 6, 2020]. Clin Case Rep. 2020;8:672-674. doi:10.1002/ccr3.2712
- Stierman B, Afful J, Carroll M, et al. National Health and Nutrition Examination Survey 2017–March 2020 Prepandemic Data Files Development of Files and Prevalence Estimates for Selected Health Outcomes. National Health Statistics Reports. Published June 14, 2021. Accessed November 17, 2022. https://stacks.cdc.gov/view/cdc/106273
- Brady MF, Rawla P. Acanthosis nigricans. In: StatPearls [Internet]. StatPearls Publishing; 2022. Updated October 9, 2022. Accessed November 30, 2022. https://www.ncbi.nlm.nih.gov/books/NBK431057
Pregnancy not a barrier to interventional cardiology career
A new collaborative position paper on radiation exposure during pregnancy states that pregnant women can safely work in an ionizing radiation environment if exposure to the fetus does not exceed certain dose thresholds.
The position paper aims to “avoid discouraging” women from pursuing careers in interventional cardiology/electrophysiology (IC/EP) and to “dismantle” a barrier that says, “activity under x-rays, without any weighting, is incompatible with continuation of pregnancy,” lead author Stéphane Manzo-Silberman, MD, of AP-HP, Sorbonne Université, Paris, told this news organization.
“The main point of the statement is to show that it is possible and safe to maintain activity under radiation during pregnancy, [given] the data we have on the risk for the fetus at exposed doses, the regulations, and feedback from practice,” she said. “The data we currently have allowed us to be largely reassuring.”
The research showed that adverse effects on a fetus generally occur when radiation exposure is greater than 100 mGy. Most countries that permit pregnant women to work in IC/EP require that the cumulative dose during the pregnancy be less than 1 mSv. An exception is the United States, which permits a cumulative dose of less than 5 mSv.
The position paper, a collaboration among the European Association of Percutaneous Cardiovascular Interventions, the European Heart Rhythm Association, the European Association of Cardiovascular Imaging, the European Society of Cardiology Regulatory Affairs Committee, and Women as One, was published online in EuroIntervention.
The position paper covers regulations in various countries; fetal radiation doses that have been associated with ill effects, including abortion, malformations, and intelligence quotient reductions; the spontaneous probability of having a newborn with a congenital malformation or childhood cancer; and proposals to improve practice.
Highlights include the following:
- European, North American, Japanese, and Australian regulations permit pregnant women to work if closely monitored with an abdominal dosimeter; some countries, such as Austria, Hungary, Portugal, and Romania, do not allow women to work in IC/EP during pregnancy or breastfeeding.
- The maximum fetal dose exposure during pregnancy is 1 mSv in Europe, Australia, and Israel; 2 mSv in Japan; and 5 mSv in the United States.
- Doses associated with fetal harm are 100 times higher than those allowed during an interventional cardiologist’s entire pregnancy.
- There is a negligible risk increase in the spontaneous probability of a newborn having a congenital malformation or childhood cancer when the occupational exposure range of the mother respects a country’s limits.
- No studies have shown an increased risk of noncancerous adverse effects from prenatal radiation exposure less than 50 mSv.
To improve practice, the position paper suggests the following:
- Fluoroscopy operators must be guided by the “as low as reasonably achievable” principle: Obtaining optimal images must be balanced with procedure safety.
- Scatter radiation emitted from the patient is the main source of radiation exposure to the operator and personnel; reducing radiation to the patient will reduce exposure for staff.
- The three fundamentals of radiation safety for an operator are (1) time, (2) distance, and (3) shielding and dosimeter monitoring. Time refers to the amount of time the operator spends using the x-ray system; distance means maximizing distance from the x-ray source; and shielding includes personal, tableside, or external protection, with each form having a degree of lead equivalence defining its radiation protective effect.
- Changes in medical school curricula and creating a friendlier workplace environment for families and pregnant interventionists are among the strategies that will promote gender equity in the profession.
“Institutional radiation protection programs should be established to increase knowledge about radiation exposure and improve specific safety requirements for everyone. This would ensure safe exposure for all physicians, [including] during pregnancy,” Dr. Manzo-Silberman concluded.
Furthermore, she said, “As has already been demonstrated in the business world, improving representation and gender equity and diversity is key to improving results and efficiency. In the field of health, this translates into better care for our patients and better working conditions for health care professionals.”
No commercial funding was disclosed. Dr. Manzo-Silberman has received consulting fees from Bayer, Organon, and Exeltis; lecture fees from Bayer, BMS, Exeltis, and Organon; and has served on the adjudication board for a study for Biotronik.
A version of this article first appeared on Medscape.com.
A new collaborative position paper on radiation exposure during pregnancy states that pregnant women can safely work in an ionizing radiation environment if exposure to the fetus does not exceed certain dose thresholds.
The position paper aims to “avoid discouraging” women from pursuing careers in interventional cardiology/electrophysiology (IC/EP) and to “dismantle” a barrier that says, “activity under x-rays, without any weighting, is incompatible with continuation of pregnancy,” lead author Stéphane Manzo-Silberman, MD, of AP-HP, Sorbonne Université, Paris, told this news organization.
“The main point of the statement is to show that it is possible and safe to maintain activity under radiation during pregnancy, [given] the data we have on the risk for the fetus at exposed doses, the regulations, and feedback from practice,” she said. “The data we currently have allowed us to be largely reassuring.”
The research showed that adverse effects on a fetus generally occur when radiation exposure is greater than 100 mGy. Most countries that permit pregnant women to work in IC/EP require that the cumulative dose during the pregnancy be less than 1 mSv. An exception is the United States, which permits a cumulative dose of less than 5 mSv.
The position paper, a collaboration among the European Association of Percutaneous Cardiovascular Interventions, the European Heart Rhythm Association, the European Association of Cardiovascular Imaging, the European Society of Cardiology Regulatory Affairs Committee, and Women as One, was published online in EuroIntervention.
The position paper covers regulations in various countries; fetal radiation doses that have been associated with ill effects, including abortion, malformations, and intelligence quotient reductions; the spontaneous probability of having a newborn with a congenital malformation or childhood cancer; and proposals to improve practice.
Highlights include the following:
- European, North American, Japanese, and Australian regulations permit pregnant women to work if closely monitored with an abdominal dosimeter; some countries, such as Austria, Hungary, Portugal, and Romania, do not allow women to work in IC/EP during pregnancy or breastfeeding.
- The maximum fetal dose exposure during pregnancy is 1 mSv in Europe, Australia, and Israel; 2 mSv in Japan; and 5 mSv in the United States.
- Doses associated with fetal harm are 100 times higher than those allowed during an interventional cardiologist’s entire pregnancy.
- There is a negligible risk increase in the spontaneous probability of a newborn having a congenital malformation or childhood cancer when the occupational exposure range of the mother respects a country’s limits.
- No studies have shown an increased risk of noncancerous adverse effects from prenatal radiation exposure less than 50 mSv.
To improve practice, the position paper suggests the following:
- Fluoroscopy operators must be guided by the “as low as reasonably achievable” principle: Obtaining optimal images must be balanced with procedure safety.
- Scatter radiation emitted from the patient is the main source of radiation exposure to the operator and personnel; reducing radiation to the patient will reduce exposure for staff.
- The three fundamentals of radiation safety for an operator are (1) time, (2) distance, and (3) shielding and dosimeter monitoring. Time refers to the amount of time the operator spends using the x-ray system; distance means maximizing distance from the x-ray source; and shielding includes personal, tableside, or external protection, with each form having a degree of lead equivalence defining its radiation protective effect.
- Changes in medical school curricula and creating a friendlier workplace environment for families and pregnant interventionists are among the strategies that will promote gender equity in the profession.
“Institutional radiation protection programs should be established to increase knowledge about radiation exposure and improve specific safety requirements for everyone. This would ensure safe exposure for all physicians, [including] during pregnancy,” Dr. Manzo-Silberman concluded.
Furthermore, she said, “As has already been demonstrated in the business world, improving representation and gender equity and diversity is key to improving results and efficiency. In the field of health, this translates into better care for our patients and better working conditions for health care professionals.”
No commercial funding was disclosed. Dr. Manzo-Silberman has received consulting fees from Bayer, Organon, and Exeltis; lecture fees from Bayer, BMS, Exeltis, and Organon; and has served on the adjudication board for a study for Biotronik.
A version of this article first appeared on Medscape.com.
A new collaborative position paper on radiation exposure during pregnancy states that pregnant women can safely work in an ionizing radiation environment if exposure to the fetus does not exceed certain dose thresholds.
The position paper aims to “avoid discouraging” women from pursuing careers in interventional cardiology/electrophysiology (IC/EP) and to “dismantle” a barrier that says, “activity under x-rays, without any weighting, is incompatible with continuation of pregnancy,” lead author Stéphane Manzo-Silberman, MD, of AP-HP, Sorbonne Université, Paris, told this news organization.
“The main point of the statement is to show that it is possible and safe to maintain activity under radiation during pregnancy, [given] the data we have on the risk for the fetus at exposed doses, the regulations, and feedback from practice,” she said. “The data we currently have allowed us to be largely reassuring.”
The research showed that adverse effects on a fetus generally occur when radiation exposure is greater than 100 mGy. Most countries that permit pregnant women to work in IC/EP require that the cumulative dose during the pregnancy be less than 1 mSv. An exception is the United States, which permits a cumulative dose of less than 5 mSv.
The position paper, a collaboration among the European Association of Percutaneous Cardiovascular Interventions, the European Heart Rhythm Association, the European Association of Cardiovascular Imaging, the European Society of Cardiology Regulatory Affairs Committee, and Women as One, was published online in EuroIntervention.
The position paper covers regulations in various countries; fetal radiation doses that have been associated with ill effects, including abortion, malformations, and intelligence quotient reductions; the spontaneous probability of having a newborn with a congenital malformation or childhood cancer; and proposals to improve practice.
Highlights include the following:
- European, North American, Japanese, and Australian regulations permit pregnant women to work if closely monitored with an abdominal dosimeter; some countries, such as Austria, Hungary, Portugal, and Romania, do not allow women to work in IC/EP during pregnancy or breastfeeding.
- The maximum fetal dose exposure during pregnancy is 1 mSv in Europe, Australia, and Israel; 2 mSv in Japan; and 5 mSv in the United States.
- Doses associated with fetal harm are 100 times higher than those allowed during an interventional cardiologist’s entire pregnancy.
- There is a negligible risk increase in the spontaneous probability of a newborn having a congenital malformation or childhood cancer when the occupational exposure range of the mother respects a country’s limits.
- No studies have shown an increased risk of noncancerous adverse effects from prenatal radiation exposure less than 50 mSv.
To improve practice, the position paper suggests the following:
- Fluoroscopy operators must be guided by the “as low as reasonably achievable” principle: Obtaining optimal images must be balanced with procedure safety.
- Scatter radiation emitted from the patient is the main source of radiation exposure to the operator and personnel; reducing radiation to the patient will reduce exposure for staff.
- The three fundamentals of radiation safety for an operator are (1) time, (2) distance, and (3) shielding and dosimeter monitoring. Time refers to the amount of time the operator spends using the x-ray system; distance means maximizing distance from the x-ray source; and shielding includes personal, tableside, or external protection, with each form having a degree of lead equivalence defining its radiation protective effect.
- Changes in medical school curricula and creating a friendlier workplace environment for families and pregnant interventionists are among the strategies that will promote gender equity in the profession.
“Institutional radiation protection programs should be established to increase knowledge about radiation exposure and improve specific safety requirements for everyone. This would ensure safe exposure for all physicians, [including] during pregnancy,” Dr. Manzo-Silberman concluded.
Furthermore, she said, “As has already been demonstrated in the business world, improving representation and gender equity and diversity is key to improving results and efficiency. In the field of health, this translates into better care for our patients and better working conditions for health care professionals.”
No commercial funding was disclosed. Dr. Manzo-Silberman has received consulting fees from Bayer, Organon, and Exeltis; lecture fees from Bayer, BMS, Exeltis, and Organon; and has served on the adjudication board for a study for Biotronik.
A version of this article first appeared on Medscape.com.
FROM EUROINTERVENTION
Yellow Nodule on the Scalp
The Diagnosis: Solitary Sclerotic Fibroma
Based on the clinical and histologic findings, the patient was diagnosed with solitary sclerotic fibroma (SF). Sclerotic fibroma is a rare benign tumor that first was described in 1972 by Weary et al1 in the oral mucosa of a patient with Cowden syndrome, a genodermatosis associated with multiple benign and malignant tumors. Rapini and Golitz2 reported solitary SF in 11 otherwise-healthy individuals with no signs of multiple hamartoma syndrome. Solitary SF is a sporadic benign condition, whereas multiple lesions are suggestive of Cowden syndrome. Solitary SF most commonly appears as an asymptomatic white-yellow papule or nodule on the head or neck, though larger tumors have been reported on the trunk and extremities.3 Histologic features of solitary SF include a well-circumscribed dermal nodule composed of eosinophilic dense collagen bundles arranged in a plywoodlike pattern (Figure). Immunohistochemistry is positive for CD34 and vimentin but negative for S-100, epithelial membrane antigen, and neuron-specific enolase.4
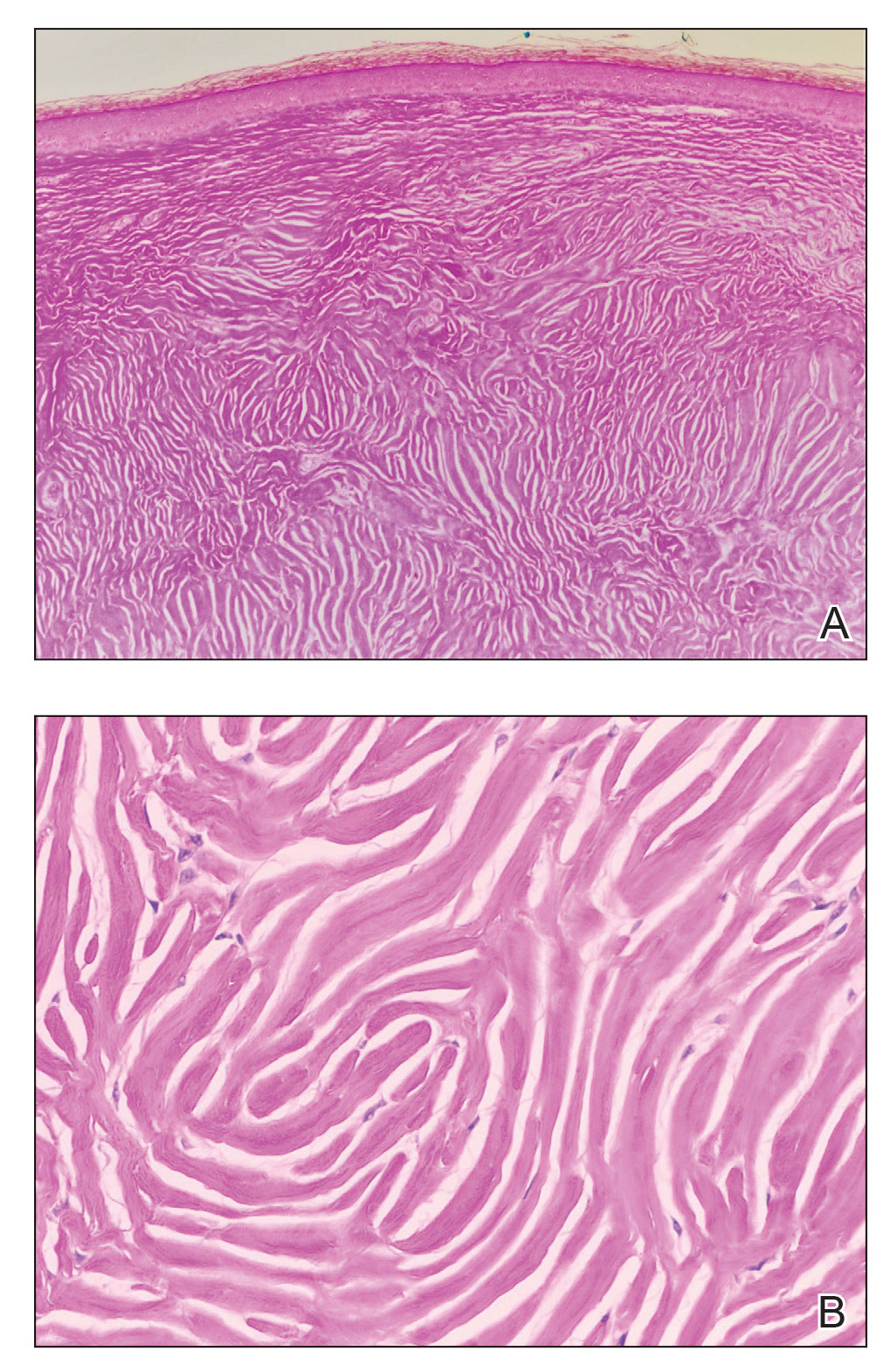
The differential diagnosis of solitary SF of the head and neck includes sebaceous adenoma, pilar cyst, nodular basal cell carcinoma, and giant molluscum contagiosum. Sebaceous adenomas usually are solitary yellow nodules less than 1 cm in diameter and located on the head and neck. They are the most common sebaceous neoplasm associated with Muir-Torre syndrome, an autosomal-dominant disorder characterized by sebaceous adenoma or carcinoma and colorectal cancer. Histopathology demonstrates well-circumscribed, round aggregations of mature lipid-filled sebocytes with a rim of basaloid germinative cells at the periphery. Pilar cysts typically are flesh-colored subcutaneous nodules on the scalp that are freely mobile over underlying tissue. Histopathology shows stratified squamous epithelium lining and trichilemmal keratinization. Nodular basal cell carcinoma has a pearly translucent appearance and arborizing telangiectases. Histopathology demonstrates nests of basaloid cells with palisading of the cells at the periphery. Giant solitary molluscum contagiosum is a dome-shaped, flesh-colored nodule with central umbilication. Histopathology reveals hyperplastic squamous epithelium with characteristic eosinophilic inclusion bodies above the basal layer.
Solitary SF can be difficult to diagnose based solely on the clinical presentation; thus biopsy with histologic evaluation is recommended. If SF is confirmed, the clinician should inquire about a family history of Cowden syndrome and then perform a total-body skin examination to check for multiple SF and other clinical hamartomas of Cowden syndrome such as trichilemmomas, acral keratosis, and oral papillomas.
- Weary PE, Gorlin RJ, Gentry Jr WC, et al. Multiple hamartoma syndrome (Cowden’s disease). Arch Dermatol. 1972;106:682-690.
- Rapini RP, Golitz LE. Sclerotic fibromas of the skin. J Am Acad Dermatol. 1989;20(2 pt 1):266-271.
- Tosa M, Ansai S, Kuwahara H, et al. Two cases of sclerotic fibroma of the skin that mimicked keloids clinically. J Nippon Med Sch. 2018;85:283-286.
- High WA, Stewart D, Essary LR, et al. Sclerotic fibroma-like changes in various neoplastic and inflammatory skin lesions: is sclerotic fibroma a distinct entity? J Cutan Pathol. 2004;31:373-378.
The Diagnosis: Solitary Sclerotic Fibroma
Based on the clinical and histologic findings, the patient was diagnosed with solitary sclerotic fibroma (SF). Sclerotic fibroma is a rare benign tumor that first was described in 1972 by Weary et al1 in the oral mucosa of a patient with Cowden syndrome, a genodermatosis associated with multiple benign and malignant tumors. Rapini and Golitz2 reported solitary SF in 11 otherwise-healthy individuals with no signs of multiple hamartoma syndrome. Solitary SF is a sporadic benign condition, whereas multiple lesions are suggestive of Cowden syndrome. Solitary SF most commonly appears as an asymptomatic white-yellow papule or nodule on the head or neck, though larger tumors have been reported on the trunk and extremities.3 Histologic features of solitary SF include a well-circumscribed dermal nodule composed of eosinophilic dense collagen bundles arranged in a plywoodlike pattern (Figure). Immunohistochemistry is positive for CD34 and vimentin but negative for S-100, epithelial membrane antigen, and neuron-specific enolase.4
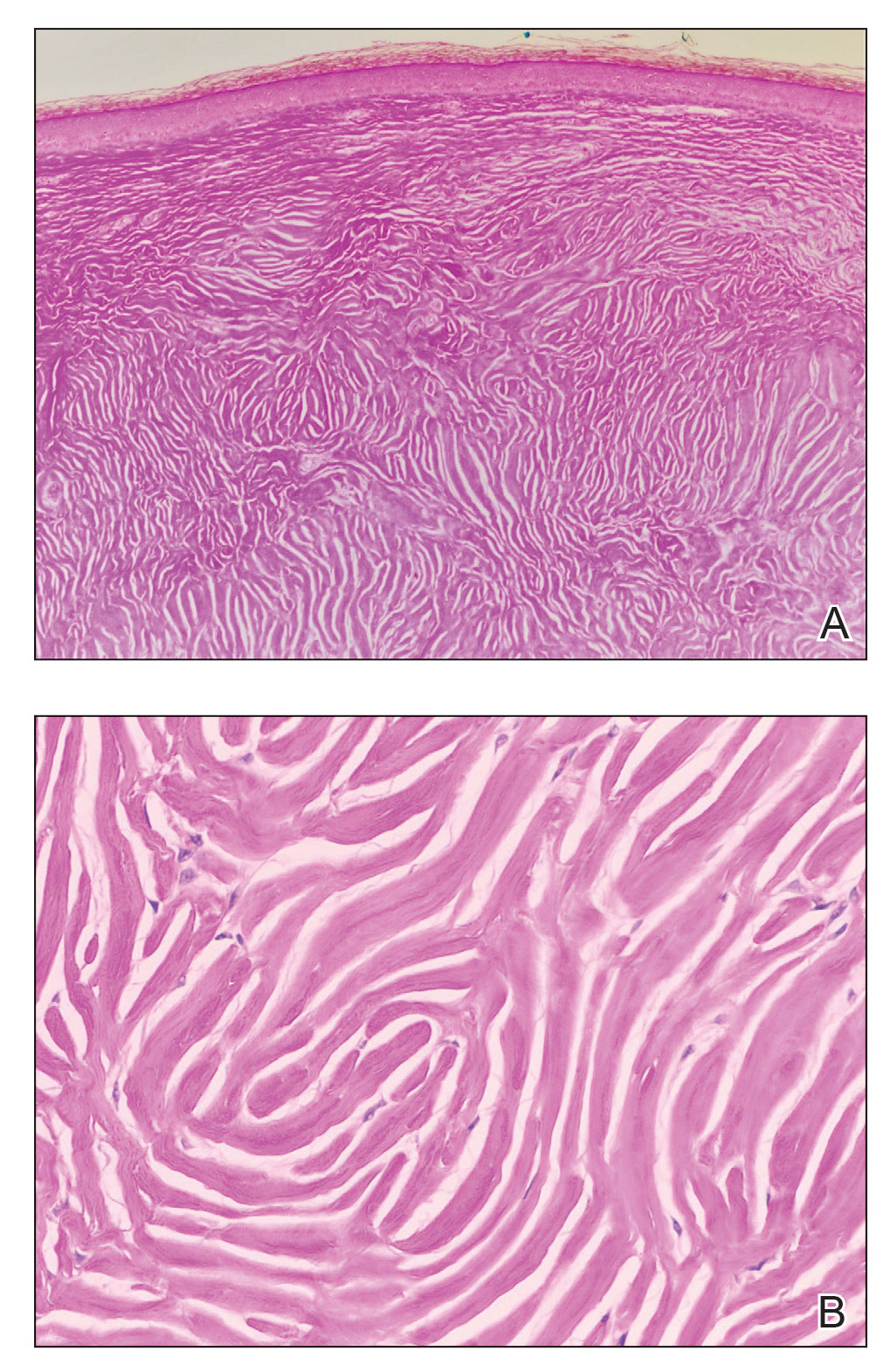
The differential diagnosis of solitary SF of the head and neck includes sebaceous adenoma, pilar cyst, nodular basal cell carcinoma, and giant molluscum contagiosum. Sebaceous adenomas usually are solitary yellow nodules less than 1 cm in diameter and located on the head and neck. They are the most common sebaceous neoplasm associated with Muir-Torre syndrome, an autosomal-dominant disorder characterized by sebaceous adenoma or carcinoma and colorectal cancer. Histopathology demonstrates well-circumscribed, round aggregations of mature lipid-filled sebocytes with a rim of basaloid germinative cells at the periphery. Pilar cysts typically are flesh-colored subcutaneous nodules on the scalp that are freely mobile over underlying tissue. Histopathology shows stratified squamous epithelium lining and trichilemmal keratinization. Nodular basal cell carcinoma has a pearly translucent appearance and arborizing telangiectases. Histopathology demonstrates nests of basaloid cells with palisading of the cells at the periphery. Giant solitary molluscum contagiosum is a dome-shaped, flesh-colored nodule with central umbilication. Histopathology reveals hyperplastic squamous epithelium with characteristic eosinophilic inclusion bodies above the basal layer.
Solitary SF can be difficult to diagnose based solely on the clinical presentation; thus biopsy with histologic evaluation is recommended. If SF is confirmed, the clinician should inquire about a family history of Cowden syndrome and then perform a total-body skin examination to check for multiple SF and other clinical hamartomas of Cowden syndrome such as trichilemmomas, acral keratosis, and oral papillomas.
The Diagnosis: Solitary Sclerotic Fibroma
Based on the clinical and histologic findings, the patient was diagnosed with solitary sclerotic fibroma (SF). Sclerotic fibroma is a rare benign tumor that first was described in 1972 by Weary et al1 in the oral mucosa of a patient with Cowden syndrome, a genodermatosis associated with multiple benign and malignant tumors. Rapini and Golitz2 reported solitary SF in 11 otherwise-healthy individuals with no signs of multiple hamartoma syndrome. Solitary SF is a sporadic benign condition, whereas multiple lesions are suggestive of Cowden syndrome. Solitary SF most commonly appears as an asymptomatic white-yellow papule or nodule on the head or neck, though larger tumors have been reported on the trunk and extremities.3 Histologic features of solitary SF include a well-circumscribed dermal nodule composed of eosinophilic dense collagen bundles arranged in a plywoodlike pattern (Figure). Immunohistochemistry is positive for CD34 and vimentin but negative for S-100, epithelial membrane antigen, and neuron-specific enolase.4
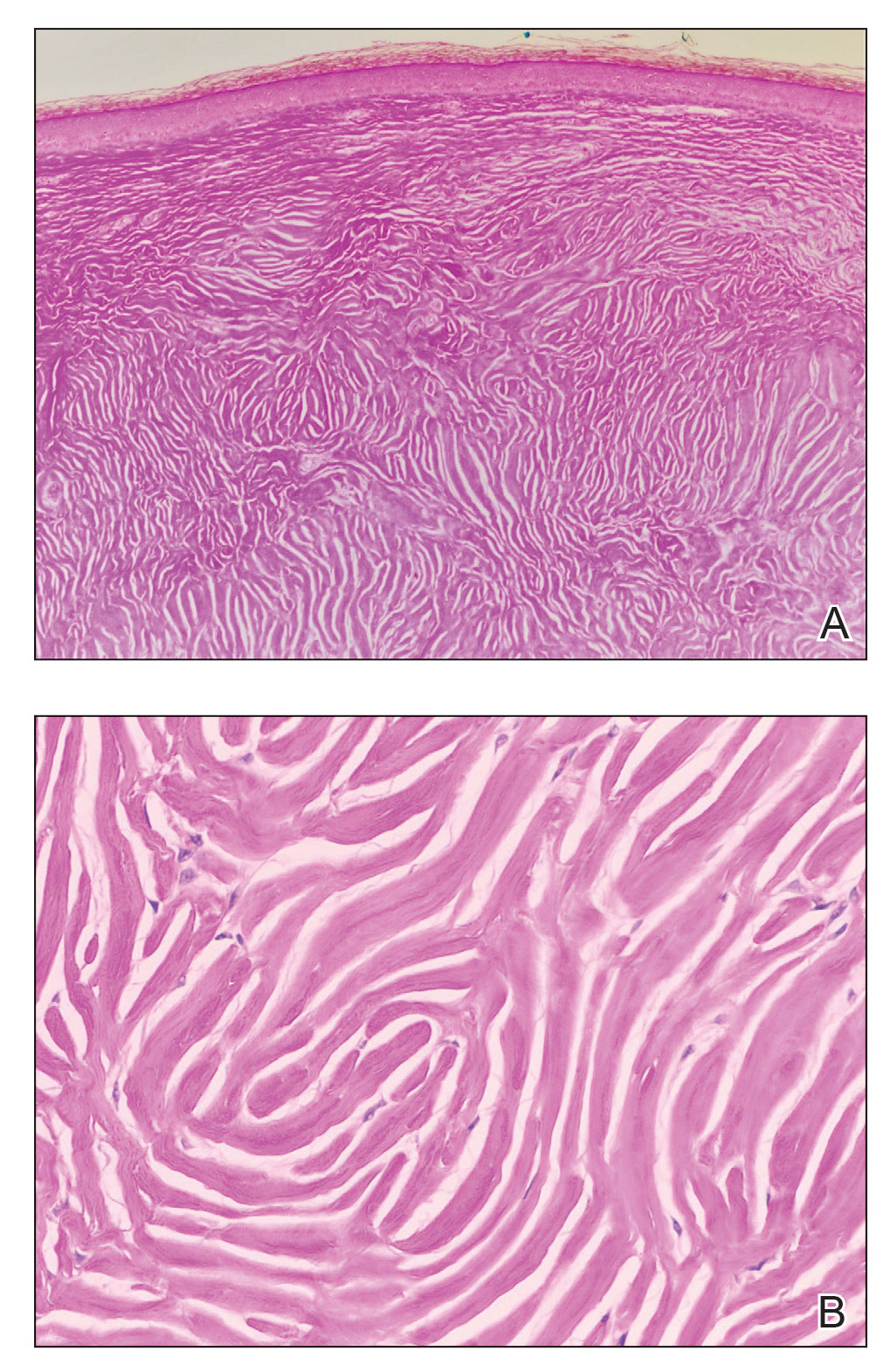
The differential diagnosis of solitary SF of the head and neck includes sebaceous adenoma, pilar cyst, nodular basal cell carcinoma, and giant molluscum contagiosum. Sebaceous adenomas usually are solitary yellow nodules less than 1 cm in diameter and located on the head and neck. They are the most common sebaceous neoplasm associated with Muir-Torre syndrome, an autosomal-dominant disorder characterized by sebaceous adenoma or carcinoma and colorectal cancer. Histopathology demonstrates well-circumscribed, round aggregations of mature lipid-filled sebocytes with a rim of basaloid germinative cells at the periphery. Pilar cysts typically are flesh-colored subcutaneous nodules on the scalp that are freely mobile over underlying tissue. Histopathology shows stratified squamous epithelium lining and trichilemmal keratinization. Nodular basal cell carcinoma has a pearly translucent appearance and arborizing telangiectases. Histopathology demonstrates nests of basaloid cells with palisading of the cells at the periphery. Giant solitary molluscum contagiosum is a dome-shaped, flesh-colored nodule with central umbilication. Histopathology reveals hyperplastic squamous epithelium with characteristic eosinophilic inclusion bodies above the basal layer.
Solitary SF can be difficult to diagnose based solely on the clinical presentation; thus biopsy with histologic evaluation is recommended. If SF is confirmed, the clinician should inquire about a family history of Cowden syndrome and then perform a total-body skin examination to check for multiple SF and other clinical hamartomas of Cowden syndrome such as trichilemmomas, acral keratosis, and oral papillomas.
- Weary PE, Gorlin RJ, Gentry Jr WC, et al. Multiple hamartoma syndrome (Cowden’s disease). Arch Dermatol. 1972;106:682-690.
- Rapini RP, Golitz LE. Sclerotic fibromas of the skin. J Am Acad Dermatol. 1989;20(2 pt 1):266-271.
- Tosa M, Ansai S, Kuwahara H, et al. Two cases of sclerotic fibroma of the skin that mimicked keloids clinically. J Nippon Med Sch. 2018;85:283-286.
- High WA, Stewart D, Essary LR, et al. Sclerotic fibroma-like changes in various neoplastic and inflammatory skin lesions: is sclerotic fibroma a distinct entity? J Cutan Pathol. 2004;31:373-378.
- Weary PE, Gorlin RJ, Gentry Jr WC, et al. Multiple hamartoma syndrome (Cowden’s disease). Arch Dermatol. 1972;106:682-690.
- Rapini RP, Golitz LE. Sclerotic fibromas of the skin. J Am Acad Dermatol. 1989;20(2 pt 1):266-271.
- Tosa M, Ansai S, Kuwahara H, et al. Two cases of sclerotic fibroma of the skin that mimicked keloids clinically. J Nippon Med Sch. 2018;85:283-286.
- High WA, Stewart D, Essary LR, et al. Sclerotic fibroma-like changes in various neoplastic and inflammatory skin lesions: is sclerotic fibroma a distinct entity? J Cutan Pathol. 2004;31:373-378.
A 45-year-old woman was referred to dermatology by a primary care physician for evaluation of a raised skin lesion on the scalp. She was otherwise healthy. The lesion had been present for many years but recently grew in size. The patient reported that the lesion was subject to recurrent physical trauma and she wanted it removed. Physical examination revealed a 6×6-mm, domeshaped, yellow nodule on the left inferior parietal scalp. There were no similar lesions located elsewhere on the body. A shave removal was performed and sent for histopathologic evaluation.

DEI advances in dermatology unremarkable to date, studies find
suggest.
To evaluate diversity and career goals of graduating allopathic medical students pursuing careers in dermatology, corresponding author Matthew Mansh, MD, of the department of dermatology at the University of Minnesota, Minneapolis, and colleagues drew from the 2016-2019 Association of American Medical Colleges Graduation Questionnaire for their study. The main outcome measures were the proportion of female students, students from racial and ethnic groups underrepresented in medicine (URM), and sexual minority (SM) students pursuing dermatology versus those pursuing other specialties, as well as the proportions and multivariable adjusted odds of intended career goals between students pursuing dermatology and those pursuing other specialties, and by sex, race, and ethnicity, and sexual orientation among students pursuing dermatology.
Of the 58,077 graduating students, 49% were women, 15% were URM, and 6% were SM. The researchers found that women pursuing dermatology were significantly less likely than women pursuing other specialties to identify as URM (11.6% vs. 17.2%; P < .001) or SM (1.9% vs. 5.7%; P < .001).
In multivariable-adjusted analyses of all students, those pursuing dermatology compared with other specialties had decreased odds of intending to care for underserved populations (18.3% vs. 34%; adjusted odd ratio, 0.40; P < .001), practice in underserved areas (12.7% vs. 25.9%; aOR, 0.40; P < .001), and practice public health (17% vs. 30.2%; aOR, 0.44; P < .001). The odds for pursuing research in their careers was greater among those pursuing dermatology (64.7% vs. 51.7%; aOR, 1.76; P < .001).
“Addressing health inequities and improving care for underserved patients is the responsibility of all dermatologists, and efforts are needed to increase diversity and interest in careers focused on underserved care among trainees in the dermatology workforce pipeline,” the authors concluded. They acknowledged certain limitations of the analysis, including lack of data delineating sex, sex assigned at birth, and gender identity, and lack of intersectional analyses between multiple minority identities and multiple career goals. “Importantly, diversity factors and their relationship to underserved care is likely multidimensional, and many students pursuing dermatology identified with multiple minority identities, highlighting the need for future studies focused on intersectionality,” they wrote.
Trends over 15 years
In a separate study, Jazzmin C. Williams, a medical student at the University of California, San Francisco, and coauthors drew from an Association of American Medical Colleges report of trainees’ and applicants’ self-reported race and ethnicity by specialty from 2005 to 2020 to evaluate diversity trends over the 15-year period. They found that Black and Latinx trainees were underrepresented in all specialties, but even more so in dermatology (mean annual rate ratios of 0.32 and 0.14, respectively), compared with those in primary care (mean annual RRs of 0.54 and 0.23) and those in specialty care (mean annual RRs of 0.39 and 0.18).
In other findings, the annual representation of Black trainees remained unchanged in dermatology between 2005 and 2020, but down-trended for primary (P < .001) and specialty care (P = .001). At the same time, representation of Latinx trainees remained unchanged in dermatology and specialty care but increased in primary care (P < .001). Finally, Black and Latinx race and ethnicity comprised a lower mean proportion of matriculating dermatology trainees (postgraduate year-2s) compared with annual dermatology applicants (4.01% vs. 5.97%, respectively, and 2.06% vs. 6.37% among Latinx; P < .001 for all associations).
“Much of these disparities can be attributed to the leaky pipeline – the disproportionate, stepwise reduction in racial and ethnic minority representation along the path to medicine,” the authors wrote. “This leaky pipeline is the direct result of structural racism, which includes, but is not limited to, historical and contemporary economic disinvestment from majority-minority schools, kindergarten through grade 12.” They concluded by stating that “dermatologists must intervene throughout the educational pipeline, including residency selection and mentorship, to effectively increase diversity.”
Solutions to address diversity
In an editorial accompanying the two studies published in the same issue of JAMA Dermatology, Ellen N. Pritchett, MD, MPH, of the department of dermatology at Howard University, Washington, and Andrew J. Park, MD, MBA, and Rebecca Vasquez, MD, of the department of dermatology at the University of Texas Southwestern Medical Center, Dallas, offered several solutions to address diversity in the dermatology work force. They include:
Go beyond individual bias in recruitment. “A residency selection framework that meaningfully incorporates diversity, equity, and inclusion (DEI) will require more than strategies that address individual bias,” they wrote. “Departmental recruitment committees must become familiar with systems that serve to perpetuate individual bias, like institutional racism or practices that disproportionately favor non-URM versus URM individuals.”
Challenge the myth of meritocracy. “The inaccurate notion of meritocracy – that success purely derives from individual effort has become the foundation of residency selection,” the authors wrote. “Unfortunately, this view ignores the inequitably distributed sociostructural resources that limit the rewards of individual effort.”
Avoid tokenism in retention strategies. Tokenism, which they defined as “a symbolic addition of members from a marginalized group to give the impression of social inclusiveness and diversity without meaningful incorporation of DEI in the policies, processes, and culture,” can lead to depression, burnout, and attrition, they wrote. They advise leaders of dermatology departments to “review their residency selection framework to ensure that it allows for meaningful representation, inclusion, and equity among trainees and faculty to better support URM individuals at all levels.”
Omar N. Qutub, MD, a Portland, Ore.–based dermatologist who was asked to comment on the studies, characterized the findings by Dr. Mansh and colleagues as sobering. “It appears that there is work to do as far as improving diversity in the dermatology workforce that will likely benefit greatly from an honest and steadfast approach to equitable application standards as well as mentorship during all stages of the application process,” such as medical school and residency, said Dr. Qutub, who is the director of equity, diversity, and inclusion of the ODAC Dermatology, Aesthetic & Surgical Conference. “With a focused attempt, we are likely to matriculate more racial minorities into our residency programs, maximizing patient outcomes.”
As for the study by Ms. Williams and colleagues, he told this news organization that efforts toward recruiting URM students as well as sexual minority students “is likely to not only improve health inequities in underserved areas, but will also enrich the specialty as a whole, allowing for better understanding of our diverse patient population and [for us to] to deliver quality care more readily for people and in areas where the focus has often been limited.”
In an interview, Chesahna Kindred, MD, a Columbia, Md.–based dermatologist and immediate past chair of the National Medical Association dermatology section, pointed out that the number of Black physicians in the United States has increased by only 4% in the last 120 years. The study by Dr. Mansh and colleagues, she commented, “underscores what I’ve recognized in the last couple of years: Where are the Black male dermatologists? NMA Derm started recruiting this demographic aggressively about a year ago and started the Black Men in Derm events. Black male members of NMA Derm travel to the Student National Medical Association and NMA conference and hold a panel to expose Black male students into dermatology. This article provides the numbers needed to measure how successful this and other programs are to closing the equity gap.”
Ms. Williams reported having no financial disclosures. Dr. Mansh reported receiving grants from National Institute of Environmental Health Sciences outside the submitted work. Dr. Pritchett and colleagues reported having no relevant financial disclosures, as did Dr. Qutub and Dr. Kindred.
suggest.
To evaluate diversity and career goals of graduating allopathic medical students pursuing careers in dermatology, corresponding author Matthew Mansh, MD, of the department of dermatology at the University of Minnesota, Minneapolis, and colleagues drew from the 2016-2019 Association of American Medical Colleges Graduation Questionnaire for their study. The main outcome measures were the proportion of female students, students from racial and ethnic groups underrepresented in medicine (URM), and sexual minority (SM) students pursuing dermatology versus those pursuing other specialties, as well as the proportions and multivariable adjusted odds of intended career goals between students pursuing dermatology and those pursuing other specialties, and by sex, race, and ethnicity, and sexual orientation among students pursuing dermatology.
Of the 58,077 graduating students, 49% were women, 15% were URM, and 6% were SM. The researchers found that women pursuing dermatology were significantly less likely than women pursuing other specialties to identify as URM (11.6% vs. 17.2%; P < .001) or SM (1.9% vs. 5.7%; P < .001).
In multivariable-adjusted analyses of all students, those pursuing dermatology compared with other specialties had decreased odds of intending to care for underserved populations (18.3% vs. 34%; adjusted odd ratio, 0.40; P < .001), practice in underserved areas (12.7% vs. 25.9%; aOR, 0.40; P < .001), and practice public health (17% vs. 30.2%; aOR, 0.44; P < .001). The odds for pursuing research in their careers was greater among those pursuing dermatology (64.7% vs. 51.7%; aOR, 1.76; P < .001).
“Addressing health inequities and improving care for underserved patients is the responsibility of all dermatologists, and efforts are needed to increase diversity and interest in careers focused on underserved care among trainees in the dermatology workforce pipeline,” the authors concluded. They acknowledged certain limitations of the analysis, including lack of data delineating sex, sex assigned at birth, and gender identity, and lack of intersectional analyses between multiple minority identities and multiple career goals. “Importantly, diversity factors and their relationship to underserved care is likely multidimensional, and many students pursuing dermatology identified with multiple minority identities, highlighting the need for future studies focused on intersectionality,” they wrote.
Trends over 15 years
In a separate study, Jazzmin C. Williams, a medical student at the University of California, San Francisco, and coauthors drew from an Association of American Medical Colleges report of trainees’ and applicants’ self-reported race and ethnicity by specialty from 2005 to 2020 to evaluate diversity trends over the 15-year period. They found that Black and Latinx trainees were underrepresented in all specialties, but even more so in dermatology (mean annual rate ratios of 0.32 and 0.14, respectively), compared with those in primary care (mean annual RRs of 0.54 and 0.23) and those in specialty care (mean annual RRs of 0.39 and 0.18).
In other findings, the annual representation of Black trainees remained unchanged in dermatology between 2005 and 2020, but down-trended for primary (P < .001) and specialty care (P = .001). At the same time, representation of Latinx trainees remained unchanged in dermatology and specialty care but increased in primary care (P < .001). Finally, Black and Latinx race and ethnicity comprised a lower mean proportion of matriculating dermatology trainees (postgraduate year-2s) compared with annual dermatology applicants (4.01% vs. 5.97%, respectively, and 2.06% vs. 6.37% among Latinx; P < .001 for all associations).
“Much of these disparities can be attributed to the leaky pipeline – the disproportionate, stepwise reduction in racial and ethnic minority representation along the path to medicine,” the authors wrote. “This leaky pipeline is the direct result of structural racism, which includes, but is not limited to, historical and contemporary economic disinvestment from majority-minority schools, kindergarten through grade 12.” They concluded by stating that “dermatologists must intervene throughout the educational pipeline, including residency selection and mentorship, to effectively increase diversity.”
Solutions to address diversity
In an editorial accompanying the two studies published in the same issue of JAMA Dermatology, Ellen N. Pritchett, MD, MPH, of the department of dermatology at Howard University, Washington, and Andrew J. Park, MD, MBA, and Rebecca Vasquez, MD, of the department of dermatology at the University of Texas Southwestern Medical Center, Dallas, offered several solutions to address diversity in the dermatology work force. They include:
Go beyond individual bias in recruitment. “A residency selection framework that meaningfully incorporates diversity, equity, and inclusion (DEI) will require more than strategies that address individual bias,” they wrote. “Departmental recruitment committees must become familiar with systems that serve to perpetuate individual bias, like institutional racism or practices that disproportionately favor non-URM versus URM individuals.”
Challenge the myth of meritocracy. “The inaccurate notion of meritocracy – that success purely derives from individual effort has become the foundation of residency selection,” the authors wrote. “Unfortunately, this view ignores the inequitably distributed sociostructural resources that limit the rewards of individual effort.”
Avoid tokenism in retention strategies. Tokenism, which they defined as “a symbolic addition of members from a marginalized group to give the impression of social inclusiveness and diversity without meaningful incorporation of DEI in the policies, processes, and culture,” can lead to depression, burnout, and attrition, they wrote. They advise leaders of dermatology departments to “review their residency selection framework to ensure that it allows for meaningful representation, inclusion, and equity among trainees and faculty to better support URM individuals at all levels.”
Omar N. Qutub, MD, a Portland, Ore.–based dermatologist who was asked to comment on the studies, characterized the findings by Dr. Mansh and colleagues as sobering. “It appears that there is work to do as far as improving diversity in the dermatology workforce that will likely benefit greatly from an honest and steadfast approach to equitable application standards as well as mentorship during all stages of the application process,” such as medical school and residency, said Dr. Qutub, who is the director of equity, diversity, and inclusion of the ODAC Dermatology, Aesthetic & Surgical Conference. “With a focused attempt, we are likely to matriculate more racial minorities into our residency programs, maximizing patient outcomes.”
As for the study by Ms. Williams and colleagues, he told this news organization that efforts toward recruiting URM students as well as sexual minority students “is likely to not only improve health inequities in underserved areas, but will also enrich the specialty as a whole, allowing for better understanding of our diverse patient population and [for us to] to deliver quality care more readily for people and in areas where the focus has often been limited.”
In an interview, Chesahna Kindred, MD, a Columbia, Md.–based dermatologist and immediate past chair of the National Medical Association dermatology section, pointed out that the number of Black physicians in the United States has increased by only 4% in the last 120 years. The study by Dr. Mansh and colleagues, she commented, “underscores what I’ve recognized in the last couple of years: Where are the Black male dermatologists? NMA Derm started recruiting this demographic aggressively about a year ago and started the Black Men in Derm events. Black male members of NMA Derm travel to the Student National Medical Association and NMA conference and hold a panel to expose Black male students into dermatology. This article provides the numbers needed to measure how successful this and other programs are to closing the equity gap.”
Ms. Williams reported having no financial disclosures. Dr. Mansh reported receiving grants from National Institute of Environmental Health Sciences outside the submitted work. Dr. Pritchett and colleagues reported having no relevant financial disclosures, as did Dr. Qutub and Dr. Kindred.
suggest.
To evaluate diversity and career goals of graduating allopathic medical students pursuing careers in dermatology, corresponding author Matthew Mansh, MD, of the department of dermatology at the University of Minnesota, Minneapolis, and colleagues drew from the 2016-2019 Association of American Medical Colleges Graduation Questionnaire for their study. The main outcome measures were the proportion of female students, students from racial and ethnic groups underrepresented in medicine (URM), and sexual minority (SM) students pursuing dermatology versus those pursuing other specialties, as well as the proportions and multivariable adjusted odds of intended career goals between students pursuing dermatology and those pursuing other specialties, and by sex, race, and ethnicity, and sexual orientation among students pursuing dermatology.
Of the 58,077 graduating students, 49% were women, 15% were URM, and 6% were SM. The researchers found that women pursuing dermatology were significantly less likely than women pursuing other specialties to identify as URM (11.6% vs. 17.2%; P < .001) or SM (1.9% vs. 5.7%; P < .001).
In multivariable-adjusted analyses of all students, those pursuing dermatology compared with other specialties had decreased odds of intending to care for underserved populations (18.3% vs. 34%; adjusted odd ratio, 0.40; P < .001), practice in underserved areas (12.7% vs. 25.9%; aOR, 0.40; P < .001), and practice public health (17% vs. 30.2%; aOR, 0.44; P < .001). The odds for pursuing research in their careers was greater among those pursuing dermatology (64.7% vs. 51.7%; aOR, 1.76; P < .001).
“Addressing health inequities and improving care for underserved patients is the responsibility of all dermatologists, and efforts are needed to increase diversity and interest in careers focused on underserved care among trainees in the dermatology workforce pipeline,” the authors concluded. They acknowledged certain limitations of the analysis, including lack of data delineating sex, sex assigned at birth, and gender identity, and lack of intersectional analyses between multiple minority identities and multiple career goals. “Importantly, diversity factors and their relationship to underserved care is likely multidimensional, and many students pursuing dermatology identified with multiple minority identities, highlighting the need for future studies focused on intersectionality,” they wrote.
Trends over 15 years
In a separate study, Jazzmin C. Williams, a medical student at the University of California, San Francisco, and coauthors drew from an Association of American Medical Colleges report of trainees’ and applicants’ self-reported race and ethnicity by specialty from 2005 to 2020 to evaluate diversity trends over the 15-year period. They found that Black and Latinx trainees were underrepresented in all specialties, but even more so in dermatology (mean annual rate ratios of 0.32 and 0.14, respectively), compared with those in primary care (mean annual RRs of 0.54 and 0.23) and those in specialty care (mean annual RRs of 0.39 and 0.18).
In other findings, the annual representation of Black trainees remained unchanged in dermatology between 2005 and 2020, but down-trended for primary (P < .001) and specialty care (P = .001). At the same time, representation of Latinx trainees remained unchanged in dermatology and specialty care but increased in primary care (P < .001). Finally, Black and Latinx race and ethnicity comprised a lower mean proportion of matriculating dermatology trainees (postgraduate year-2s) compared with annual dermatology applicants (4.01% vs. 5.97%, respectively, and 2.06% vs. 6.37% among Latinx; P < .001 for all associations).
“Much of these disparities can be attributed to the leaky pipeline – the disproportionate, stepwise reduction in racial and ethnic minority representation along the path to medicine,” the authors wrote. “This leaky pipeline is the direct result of structural racism, which includes, but is not limited to, historical and contemporary economic disinvestment from majority-minority schools, kindergarten through grade 12.” They concluded by stating that “dermatologists must intervene throughout the educational pipeline, including residency selection and mentorship, to effectively increase diversity.”
Solutions to address diversity
In an editorial accompanying the two studies published in the same issue of JAMA Dermatology, Ellen N. Pritchett, MD, MPH, of the department of dermatology at Howard University, Washington, and Andrew J. Park, MD, MBA, and Rebecca Vasquez, MD, of the department of dermatology at the University of Texas Southwestern Medical Center, Dallas, offered several solutions to address diversity in the dermatology work force. They include:
Go beyond individual bias in recruitment. “A residency selection framework that meaningfully incorporates diversity, equity, and inclusion (DEI) will require more than strategies that address individual bias,” they wrote. “Departmental recruitment committees must become familiar with systems that serve to perpetuate individual bias, like institutional racism or practices that disproportionately favor non-URM versus URM individuals.”
Challenge the myth of meritocracy. “The inaccurate notion of meritocracy – that success purely derives from individual effort has become the foundation of residency selection,” the authors wrote. “Unfortunately, this view ignores the inequitably distributed sociostructural resources that limit the rewards of individual effort.”
Avoid tokenism in retention strategies. Tokenism, which they defined as “a symbolic addition of members from a marginalized group to give the impression of social inclusiveness and diversity without meaningful incorporation of DEI in the policies, processes, and culture,” can lead to depression, burnout, and attrition, they wrote. They advise leaders of dermatology departments to “review their residency selection framework to ensure that it allows for meaningful representation, inclusion, and equity among trainees and faculty to better support URM individuals at all levels.”
Omar N. Qutub, MD, a Portland, Ore.–based dermatologist who was asked to comment on the studies, characterized the findings by Dr. Mansh and colleagues as sobering. “It appears that there is work to do as far as improving diversity in the dermatology workforce that will likely benefit greatly from an honest and steadfast approach to equitable application standards as well as mentorship during all stages of the application process,” such as medical school and residency, said Dr. Qutub, who is the director of equity, diversity, and inclusion of the ODAC Dermatology, Aesthetic & Surgical Conference. “With a focused attempt, we are likely to matriculate more racial minorities into our residency programs, maximizing patient outcomes.”
As for the study by Ms. Williams and colleagues, he told this news organization that efforts toward recruiting URM students as well as sexual minority students “is likely to not only improve health inequities in underserved areas, but will also enrich the specialty as a whole, allowing for better understanding of our diverse patient population and [for us to] to deliver quality care more readily for people and in areas where the focus has often been limited.”
In an interview, Chesahna Kindred, MD, a Columbia, Md.–based dermatologist and immediate past chair of the National Medical Association dermatology section, pointed out that the number of Black physicians in the United States has increased by only 4% in the last 120 years. The study by Dr. Mansh and colleagues, she commented, “underscores what I’ve recognized in the last couple of years: Where are the Black male dermatologists? NMA Derm started recruiting this demographic aggressively about a year ago and started the Black Men in Derm events. Black male members of NMA Derm travel to the Student National Medical Association and NMA conference and hold a panel to expose Black male students into dermatology. This article provides the numbers needed to measure how successful this and other programs are to closing the equity gap.”
Ms. Williams reported having no financial disclosures. Dr. Mansh reported receiving grants from National Institute of Environmental Health Sciences outside the submitted work. Dr. Pritchett and colleagues reported having no relevant financial disclosures, as did Dr. Qutub and Dr. Kindred.
FROM JAMA DERMATOLOGY
Advancing health equity in neurology is essential to patient care
Black and Latinx older adults are up to three times as likely to develop Alzheimer’s disease than non-Latinx White adults and tend to experience onset at a younger age with more severe symptoms, according to Monica Rivera-Mindt, PhD, a professor of psychology at Fordham University and the Icahn School of Medicine at Mount Sinai, New York. Looking ahead, that means by 2030, nearly 40% of the 8.4 million Americans affected by Alzheimer’s disease will be Black and/or Latinx, she said. These facts were among the stark disparities in health care outcomes Dr. Rivera-Mindt discussed in her presentation on brain health equity at the 2022 annual meeting of the American Neurological Association.
Dr. Rivera-Mindt’s presentation opened the ANA’s plenary session on health disparities and inequities. The plenary, “Advancing Neurologic Equity: Challenges and Paths Forward,” did not simply enumerate racial and ethnic disparities that exist with various neurological conditions. Rather it went beyond the discussion of what disparities exist into understanding the roots of them as well as tips, tools, and resources that can aid clinicians in addressing or ameliorating them.
Roy Hamilton, MD, an associate professor of neurology and physical medicine and rehabilitation at the University of Pennsylvania, Philadelphia, said. “If clinicians are unaware of these disparities or don’t have any sense of how to start to address or think about them, then they’re really missing out on an important component of their education as persons who take care of patients with brain disorders.”
Dr. Hamilton, who organized the plenary, noted that awareness of these disparities is crucial to comprehensively caring for patients.
Missed opportunities
“We’re talking about disadvantages that are structural and large scale, but those disadvantages play themselves out in the individual encounter,” Dr. Hamilton said. “When physicians see patients, they have to treat the whole patient in front of them,” which means being aware of the risks and factors that could affect a patient’s clinical presentation. “Being aware of disparities has practical impacts on physician judgment,” he said.
For example, recent research in multiple sclerosis (MS) has highlighted how clinicians may be missing diagnosis of this condition in non-White populations because the condition has been regarded for so long as a “White person’s” disease, Dr. Hamilton said. In non-White patients exhibiting MS symptoms, then, clinicians may have been less likely to consider MS as a possibility, thereby delaying diagnosis and treatment.
Those patterns may partly explain why the mortality rate for MS is greater in Black patients, who also show more rapid neurodegeneration than White patients with MS, Lilyana Amezcua, MD, an associate professor of neurology at the University of Southern California, Los Angeles, reported in the plenary’s second presentation.
Transgender issues
The third session, presented by Nicole Rosendale, MD, an assistant professor of neurology at the University of California, San Francisco, and director of the San Francisco General Hospital neurology inpatient services, examined disparities in neurology within the LGBTQ+ community through representative case studies and then offered specific ways that neurologists could make their practices more inclusive and equitable for sexual and gender minorities.
Her first case study was a 52-year-old man who presented with new-onset seizures, right hemiparesis, and aphasia. A brain biopsy consistent with adenocarcinoma eventually led his physician to discover he had metastatic breast cancer. It turned out the man was transgender and, despite a family history of breast cancer, hadn’t been advised to get breast cancer screenings.
“Breast cancer was not initially on the differential as no one had identified that the patient was transmasculine,” Dr. Rosendale said. A major challenge to providing care to transgender patients is a dearth of data on risks and screening recommendations. Another barrier is low knowledge of LGBTQ+ health among neurologists, Dr. Rosendale said while sharing findings from her 2019 study on the topic and calling for more research in LGBTQ+ populations.
Dr. Rosendale’s second case study dealt with a nonbinary patient who suffered from debilitating headaches for decades, first because they lacked access to health insurance and then because negative experiences with providers dissuaded them from seeking care. In data from the Center for American Progress she shared, 8% of LGB respondents and 22% of transgender respondents said they had avoided or delayed care because of fear of discrimination or mistreatment.
“So it’s not only access but also what experiences people are having when they go in and whether they’re actually even getting access to care or being taken care of,” Dr. Rosendale said. Other findings from the CAP found that:
- 8% of LGB patients and 29% of transgender patients reported having a clinician refuse to see them.
- 6% of LGB patients and 12% of transgender patients reported that a clinician refused to give them health care.
- 9% of LGB patients and 21% of transgender patients experienced harsh or abusive language during a health care experience.
- 7% of LGB patients and nearly a third (29%) of transgender patients experienced unwanted physical contact, such as fondling or sexual assault.
Reducing the disparities
Adys Mendizabal, MD, an assistant professor of neurology at the Institute of Society and Genetics at the University of California, Los Angeles, who attended the presentation, was grateful to see how the various lectures enriched the discussion beyond stating the fact of racial/ethnic disparities and dug into the nuances on how to think about and address these disparities. She particularly appreciated discussion about the need to go out of the way to recruit diverse patient populations for clinical trials while also providing them care.
“It is definitely complicated, but it’s not impossible for an individual neurologist or an individual department to do something to reduce some of the disparities,” Dr. Mendizabal said. “It starts with just knowing that they exist and being aware of some of the things that may be impacting care for a particular patient.”
Tools to counter disparity
In the final presentation, Amy Kind, MD, PhD, the associate dean for social health sciences and programs at the University of Wisconsin–Madison, rounded out the discussion by exploring social determinants of health and their influence on outcomes.
“Social determinants impact brain health, and brain health is not distributed equally,” Dr. Kind told attendees. “We have known this for decades, yet disparities persist.”
Dr. Kind described the “exposome,” a “measure of all the exposures of an individual in a lifetime and how those exposures relate to health,” according to the CDC, and then introduced a tool clinicians can use to better understand social determinants of health in specific geographic areas. The Neighborhood Atlas, which Dr. Kind described in the New England Journal of Medicine in 2018, measures 17 social determinants across small population-sensitive areas and provides an area deprivation index. A high area deprivation index is linked to a range of negative outcomes, including reshopitalization, later diagnoses, less comprehensive diagnostic evaluation, increased risk of postsurgical complications, and decreased life expectancy.
“One of the things that really stood out to me about Dr. Kind’s discussion of the use of the area deprivation index was the fact that understanding and quantifying these kinds of risks and exposures is the vehicle for creating the kinds of social changes, including policy changes, that will actually lead to addressing and mitigating some of these lifelong risks and exposures,” Dr. Hamilton said. “It is implausible to think that a specific group of people would be genetically more susceptible to basically every disease that we know,” he added. “It makes much more sense to think that groups of individuals have been subjected systematically to conditions that impair health in a variety of ways.”
Not just race, ethnicity, sex, and gender
Following the four presentations from researchers in health inequities was an Emerging Scholar presentation in which Jay B. Lusk, an MD/MBA candidate at Duke University, Durham, N.C., shared new research findings on the role of neighborhood disadvantage in predicting mortality from coma, stroke, and other neurologic conditions. His findings revealed that living in a neighborhood with greater deprivation substantially increased risk of mortality even after accounting for individual wealth and demographics.
Maria Eugenia Diaz-Ortiz, PhD, of the department of neurology, University of Pennsylvania, Philadelphia, said she found the five presentations to be an excellent introduction to people like herself who are in the earlier stages of learning about health equity research.
“I think they introduced various important concepts and frameworks and provided tools for people who don’t know about them,” Dr. Diaz-Ortiz said. “Then they asked important questions and provided some solutions to them.”
Dr. Diaz-Ortiz also appreciated seemingly minor but actually important details in how the speakers presented themselves, such as Dr. Rivera-Mindt opening with a land acknowledgment and her disclosures of “positionality.” The former recognized the traditional Native American custodians of the land on which she lives and works, and the latter revealed details about her as an individual – such as being the Afro-Latinx daughter of immigrants yet being cisgender, able-bodied, and U.S.-born – that show where she falls on the axis of adversity and axis of privilege.
Implications for research
The biggest takeaway for Dr. Diaz-Ortiz, however, came from the first Q&A session when someone asked how to increase underrepresented populations in dementia research. Dr. Rivera-Mindt described her experience engaging these communities by employing “community-based participatory research practices, which involves making yourself a part of the community and making the community active participants in the research,” Dr. Diaz-Ortiz said. “It’s an evidence-based approach that has been shown to increase participation in research not only in her work but in the work of others.”
Preaching to the choir
Dr. Diaz-Ortiz was pleased overall with the plenary but disappointed in its placement at the end of the meeting, when attendance is always lower as attendees head home.
“The people who stayed were people who already know and recognize the value of health equity work, so I think that was a missed opportunity where the session could have been included on day one or two to boost attendance and also to educate like a broader group of neurologists,” Dr. Diaz-Ortiz said in an interview.
Dr. Mendizabal felt similarly, appreciating the plenary but noting it was “definitely overdue” and that it should not be the last session. Instead, sessions on health equity should be as easy as possible to attend to bring in larger audiences. “Perhaps having that session on a Saturday or Sunday would have a higher likelihood of greater attendance than on a Tuesday,” she said. That said, Dr. Mendizabal also noticed that greater attention to health care disparities was woven into many other sessions throughout the conference, which is “the best way of addressing health equity instead of trying to just designate a session,” she said.
Dr. Mendizabal hopes that plenaries like this one and the weaving of health equity issues into presentations throughout neurology conferences continue.
“After the racial reckoning in 2020, there was a big impetus and a big wave of energy in addressing health disparities in the field, and I hope that that momentum is not starting to wane,” Dr. Mendizabal said. “It’s important because not talking about is not going to make this issue go away.”
Dr. Hamilton agreed that it is important that the conversation continue and that physicians recognize the importance of understanding health care disparities and determinants of health, regardless of where they fall on the political spectrum or whether they choose to get involved in policy or advocacy.
“Irrespective of whether you think race or ethnicity or socioeconomic status are political issues or not, it is the case that you’re obligated to have an objective understanding of the factors that contribute to your patient’s health and as points of intervention,” Dr. Hamilton said. “So even if you don’t want to sit down and jot off that email to your senator, you still have to take these factors into account when you’re treating the person who’s sitting right in front of you, and that’s not political. That’s the promise of being a physician.”
Dr. Amezcua has received personal compensation for consulting, speaking, or serving on steering committees or advisory boards for Biogen Idec, Novartis, Genentech, and EMD Serono, and she has received research support from Biogen Idec and Bristol Myers Squibb Foundation. Dr. Kind reported support from the Alzheimer’s Association. Dr. Diaz-Ortiz is coinventor of a provisional patent submitted by the University of Pennsylvania that relates to a potential therapeutic in Parkinson’s disease. Mr. Lusk reported fellowship support from American Heart Association and travel support from the American Neurological Association. No other speakers or sources had relevant disclosures.
Black and Latinx older adults are up to three times as likely to develop Alzheimer’s disease than non-Latinx White adults and tend to experience onset at a younger age with more severe symptoms, according to Monica Rivera-Mindt, PhD, a professor of psychology at Fordham University and the Icahn School of Medicine at Mount Sinai, New York. Looking ahead, that means by 2030, nearly 40% of the 8.4 million Americans affected by Alzheimer’s disease will be Black and/or Latinx, she said. These facts were among the stark disparities in health care outcomes Dr. Rivera-Mindt discussed in her presentation on brain health equity at the 2022 annual meeting of the American Neurological Association.
Dr. Rivera-Mindt’s presentation opened the ANA’s plenary session on health disparities and inequities. The plenary, “Advancing Neurologic Equity: Challenges and Paths Forward,” did not simply enumerate racial and ethnic disparities that exist with various neurological conditions. Rather it went beyond the discussion of what disparities exist into understanding the roots of them as well as tips, tools, and resources that can aid clinicians in addressing or ameliorating them.
Roy Hamilton, MD, an associate professor of neurology and physical medicine and rehabilitation at the University of Pennsylvania, Philadelphia, said. “If clinicians are unaware of these disparities or don’t have any sense of how to start to address or think about them, then they’re really missing out on an important component of their education as persons who take care of patients with brain disorders.”
Dr. Hamilton, who organized the plenary, noted that awareness of these disparities is crucial to comprehensively caring for patients.
Missed opportunities
“We’re talking about disadvantages that are structural and large scale, but those disadvantages play themselves out in the individual encounter,” Dr. Hamilton said. “When physicians see patients, they have to treat the whole patient in front of them,” which means being aware of the risks and factors that could affect a patient’s clinical presentation. “Being aware of disparities has practical impacts on physician judgment,” he said.
For example, recent research in multiple sclerosis (MS) has highlighted how clinicians may be missing diagnosis of this condition in non-White populations because the condition has been regarded for so long as a “White person’s” disease, Dr. Hamilton said. In non-White patients exhibiting MS symptoms, then, clinicians may have been less likely to consider MS as a possibility, thereby delaying diagnosis and treatment.
Those patterns may partly explain why the mortality rate for MS is greater in Black patients, who also show more rapid neurodegeneration than White patients with MS, Lilyana Amezcua, MD, an associate professor of neurology at the University of Southern California, Los Angeles, reported in the plenary’s second presentation.
Transgender issues
The third session, presented by Nicole Rosendale, MD, an assistant professor of neurology at the University of California, San Francisco, and director of the San Francisco General Hospital neurology inpatient services, examined disparities in neurology within the LGBTQ+ community through representative case studies and then offered specific ways that neurologists could make their practices more inclusive and equitable for sexual and gender minorities.
Her first case study was a 52-year-old man who presented with new-onset seizures, right hemiparesis, and aphasia. A brain biopsy consistent with adenocarcinoma eventually led his physician to discover he had metastatic breast cancer. It turned out the man was transgender and, despite a family history of breast cancer, hadn’t been advised to get breast cancer screenings.
“Breast cancer was not initially on the differential as no one had identified that the patient was transmasculine,” Dr. Rosendale said. A major challenge to providing care to transgender patients is a dearth of data on risks and screening recommendations. Another barrier is low knowledge of LGBTQ+ health among neurologists, Dr. Rosendale said while sharing findings from her 2019 study on the topic and calling for more research in LGBTQ+ populations.
Dr. Rosendale’s second case study dealt with a nonbinary patient who suffered from debilitating headaches for decades, first because they lacked access to health insurance and then because negative experiences with providers dissuaded them from seeking care. In data from the Center for American Progress she shared, 8% of LGB respondents and 22% of transgender respondents said they had avoided or delayed care because of fear of discrimination or mistreatment.
“So it’s not only access but also what experiences people are having when they go in and whether they’re actually even getting access to care or being taken care of,” Dr. Rosendale said. Other findings from the CAP found that:
- 8% of LGB patients and 29% of transgender patients reported having a clinician refuse to see them.
- 6% of LGB patients and 12% of transgender patients reported that a clinician refused to give them health care.
- 9% of LGB patients and 21% of transgender patients experienced harsh or abusive language during a health care experience.
- 7% of LGB patients and nearly a third (29%) of transgender patients experienced unwanted physical contact, such as fondling or sexual assault.
Reducing the disparities
Adys Mendizabal, MD, an assistant professor of neurology at the Institute of Society and Genetics at the University of California, Los Angeles, who attended the presentation, was grateful to see how the various lectures enriched the discussion beyond stating the fact of racial/ethnic disparities and dug into the nuances on how to think about and address these disparities. She particularly appreciated discussion about the need to go out of the way to recruit diverse patient populations for clinical trials while also providing them care.
“It is definitely complicated, but it’s not impossible for an individual neurologist or an individual department to do something to reduce some of the disparities,” Dr. Mendizabal said. “It starts with just knowing that they exist and being aware of some of the things that may be impacting care for a particular patient.”
Tools to counter disparity
In the final presentation, Amy Kind, MD, PhD, the associate dean for social health sciences and programs at the University of Wisconsin–Madison, rounded out the discussion by exploring social determinants of health and their influence on outcomes.
“Social determinants impact brain health, and brain health is not distributed equally,” Dr. Kind told attendees. “We have known this for decades, yet disparities persist.”
Dr. Kind described the “exposome,” a “measure of all the exposures of an individual in a lifetime and how those exposures relate to health,” according to the CDC, and then introduced a tool clinicians can use to better understand social determinants of health in specific geographic areas. The Neighborhood Atlas, which Dr. Kind described in the New England Journal of Medicine in 2018, measures 17 social determinants across small population-sensitive areas and provides an area deprivation index. A high area deprivation index is linked to a range of negative outcomes, including reshopitalization, later diagnoses, less comprehensive diagnostic evaluation, increased risk of postsurgical complications, and decreased life expectancy.
“One of the things that really stood out to me about Dr. Kind’s discussion of the use of the area deprivation index was the fact that understanding and quantifying these kinds of risks and exposures is the vehicle for creating the kinds of social changes, including policy changes, that will actually lead to addressing and mitigating some of these lifelong risks and exposures,” Dr. Hamilton said. “It is implausible to think that a specific group of people would be genetically more susceptible to basically every disease that we know,” he added. “It makes much more sense to think that groups of individuals have been subjected systematically to conditions that impair health in a variety of ways.”
Not just race, ethnicity, sex, and gender
Following the four presentations from researchers in health inequities was an Emerging Scholar presentation in which Jay B. Lusk, an MD/MBA candidate at Duke University, Durham, N.C., shared new research findings on the role of neighborhood disadvantage in predicting mortality from coma, stroke, and other neurologic conditions. His findings revealed that living in a neighborhood with greater deprivation substantially increased risk of mortality even after accounting for individual wealth and demographics.
Maria Eugenia Diaz-Ortiz, PhD, of the department of neurology, University of Pennsylvania, Philadelphia, said she found the five presentations to be an excellent introduction to people like herself who are in the earlier stages of learning about health equity research.
“I think they introduced various important concepts and frameworks and provided tools for people who don’t know about them,” Dr. Diaz-Ortiz said. “Then they asked important questions and provided some solutions to them.”
Dr. Diaz-Ortiz also appreciated seemingly minor but actually important details in how the speakers presented themselves, such as Dr. Rivera-Mindt opening with a land acknowledgment and her disclosures of “positionality.” The former recognized the traditional Native American custodians of the land on which she lives and works, and the latter revealed details about her as an individual – such as being the Afro-Latinx daughter of immigrants yet being cisgender, able-bodied, and U.S.-born – that show where she falls on the axis of adversity and axis of privilege.
Implications for research
The biggest takeaway for Dr. Diaz-Ortiz, however, came from the first Q&A session when someone asked how to increase underrepresented populations in dementia research. Dr. Rivera-Mindt described her experience engaging these communities by employing “community-based participatory research practices, which involves making yourself a part of the community and making the community active participants in the research,” Dr. Diaz-Ortiz said. “It’s an evidence-based approach that has been shown to increase participation in research not only in her work but in the work of others.”
Preaching to the choir
Dr. Diaz-Ortiz was pleased overall with the plenary but disappointed in its placement at the end of the meeting, when attendance is always lower as attendees head home.
“The people who stayed were people who already know and recognize the value of health equity work, so I think that was a missed opportunity where the session could have been included on day one or two to boost attendance and also to educate like a broader group of neurologists,” Dr. Diaz-Ortiz said in an interview.
Dr. Mendizabal felt similarly, appreciating the plenary but noting it was “definitely overdue” and that it should not be the last session. Instead, sessions on health equity should be as easy as possible to attend to bring in larger audiences. “Perhaps having that session on a Saturday or Sunday would have a higher likelihood of greater attendance than on a Tuesday,” she said. That said, Dr. Mendizabal also noticed that greater attention to health care disparities was woven into many other sessions throughout the conference, which is “the best way of addressing health equity instead of trying to just designate a session,” she said.
Dr. Mendizabal hopes that plenaries like this one and the weaving of health equity issues into presentations throughout neurology conferences continue.
“After the racial reckoning in 2020, there was a big impetus and a big wave of energy in addressing health disparities in the field, and I hope that that momentum is not starting to wane,” Dr. Mendizabal said. “It’s important because not talking about is not going to make this issue go away.”
Dr. Hamilton agreed that it is important that the conversation continue and that physicians recognize the importance of understanding health care disparities and determinants of health, regardless of where they fall on the political spectrum or whether they choose to get involved in policy or advocacy.
“Irrespective of whether you think race or ethnicity or socioeconomic status are political issues or not, it is the case that you’re obligated to have an objective understanding of the factors that contribute to your patient’s health and as points of intervention,” Dr. Hamilton said. “So even if you don’t want to sit down and jot off that email to your senator, you still have to take these factors into account when you’re treating the person who’s sitting right in front of you, and that’s not political. That’s the promise of being a physician.”
Dr. Amezcua has received personal compensation for consulting, speaking, or serving on steering committees or advisory boards for Biogen Idec, Novartis, Genentech, and EMD Serono, and she has received research support from Biogen Idec and Bristol Myers Squibb Foundation. Dr. Kind reported support from the Alzheimer’s Association. Dr. Diaz-Ortiz is coinventor of a provisional patent submitted by the University of Pennsylvania that relates to a potential therapeutic in Parkinson’s disease. Mr. Lusk reported fellowship support from American Heart Association and travel support from the American Neurological Association. No other speakers or sources had relevant disclosures.
Black and Latinx older adults are up to three times as likely to develop Alzheimer’s disease than non-Latinx White adults and tend to experience onset at a younger age with more severe symptoms, according to Monica Rivera-Mindt, PhD, a professor of psychology at Fordham University and the Icahn School of Medicine at Mount Sinai, New York. Looking ahead, that means by 2030, nearly 40% of the 8.4 million Americans affected by Alzheimer’s disease will be Black and/or Latinx, she said. These facts were among the stark disparities in health care outcomes Dr. Rivera-Mindt discussed in her presentation on brain health equity at the 2022 annual meeting of the American Neurological Association.
Dr. Rivera-Mindt’s presentation opened the ANA’s plenary session on health disparities and inequities. The plenary, “Advancing Neurologic Equity: Challenges and Paths Forward,” did not simply enumerate racial and ethnic disparities that exist with various neurological conditions. Rather it went beyond the discussion of what disparities exist into understanding the roots of them as well as tips, tools, and resources that can aid clinicians in addressing or ameliorating them.
Roy Hamilton, MD, an associate professor of neurology and physical medicine and rehabilitation at the University of Pennsylvania, Philadelphia, said. “If clinicians are unaware of these disparities or don’t have any sense of how to start to address or think about them, then they’re really missing out on an important component of their education as persons who take care of patients with brain disorders.”
Dr. Hamilton, who organized the plenary, noted that awareness of these disparities is crucial to comprehensively caring for patients.
Missed opportunities
“We’re talking about disadvantages that are structural and large scale, but those disadvantages play themselves out in the individual encounter,” Dr. Hamilton said. “When physicians see patients, they have to treat the whole patient in front of them,” which means being aware of the risks and factors that could affect a patient’s clinical presentation. “Being aware of disparities has practical impacts on physician judgment,” he said.
For example, recent research in multiple sclerosis (MS) has highlighted how clinicians may be missing diagnosis of this condition in non-White populations because the condition has been regarded for so long as a “White person’s” disease, Dr. Hamilton said. In non-White patients exhibiting MS symptoms, then, clinicians may have been less likely to consider MS as a possibility, thereby delaying diagnosis and treatment.
Those patterns may partly explain why the mortality rate for MS is greater in Black patients, who also show more rapid neurodegeneration than White patients with MS, Lilyana Amezcua, MD, an associate professor of neurology at the University of Southern California, Los Angeles, reported in the plenary’s second presentation.
Transgender issues
The third session, presented by Nicole Rosendale, MD, an assistant professor of neurology at the University of California, San Francisco, and director of the San Francisco General Hospital neurology inpatient services, examined disparities in neurology within the LGBTQ+ community through representative case studies and then offered specific ways that neurologists could make their practices more inclusive and equitable for sexual and gender minorities.
Her first case study was a 52-year-old man who presented with new-onset seizures, right hemiparesis, and aphasia. A brain biopsy consistent with adenocarcinoma eventually led his physician to discover he had metastatic breast cancer. It turned out the man was transgender and, despite a family history of breast cancer, hadn’t been advised to get breast cancer screenings.
“Breast cancer was not initially on the differential as no one had identified that the patient was transmasculine,” Dr. Rosendale said. A major challenge to providing care to transgender patients is a dearth of data on risks and screening recommendations. Another barrier is low knowledge of LGBTQ+ health among neurologists, Dr. Rosendale said while sharing findings from her 2019 study on the topic and calling for more research in LGBTQ+ populations.
Dr. Rosendale’s second case study dealt with a nonbinary patient who suffered from debilitating headaches for decades, first because they lacked access to health insurance and then because negative experiences with providers dissuaded them from seeking care. In data from the Center for American Progress she shared, 8% of LGB respondents and 22% of transgender respondents said they had avoided or delayed care because of fear of discrimination or mistreatment.
“So it’s not only access but also what experiences people are having when they go in and whether they’re actually even getting access to care or being taken care of,” Dr. Rosendale said. Other findings from the CAP found that:
- 8% of LGB patients and 29% of transgender patients reported having a clinician refuse to see them.
- 6% of LGB patients and 12% of transgender patients reported that a clinician refused to give them health care.
- 9% of LGB patients and 21% of transgender patients experienced harsh or abusive language during a health care experience.
- 7% of LGB patients and nearly a third (29%) of transgender patients experienced unwanted physical contact, such as fondling or sexual assault.
Reducing the disparities
Adys Mendizabal, MD, an assistant professor of neurology at the Institute of Society and Genetics at the University of California, Los Angeles, who attended the presentation, was grateful to see how the various lectures enriched the discussion beyond stating the fact of racial/ethnic disparities and dug into the nuances on how to think about and address these disparities. She particularly appreciated discussion about the need to go out of the way to recruit diverse patient populations for clinical trials while also providing them care.
“It is definitely complicated, but it’s not impossible for an individual neurologist or an individual department to do something to reduce some of the disparities,” Dr. Mendizabal said. “It starts with just knowing that they exist and being aware of some of the things that may be impacting care for a particular patient.”
Tools to counter disparity
In the final presentation, Amy Kind, MD, PhD, the associate dean for social health sciences and programs at the University of Wisconsin–Madison, rounded out the discussion by exploring social determinants of health and their influence on outcomes.
“Social determinants impact brain health, and brain health is not distributed equally,” Dr. Kind told attendees. “We have known this for decades, yet disparities persist.”
Dr. Kind described the “exposome,” a “measure of all the exposures of an individual in a lifetime and how those exposures relate to health,” according to the CDC, and then introduced a tool clinicians can use to better understand social determinants of health in specific geographic areas. The Neighborhood Atlas, which Dr. Kind described in the New England Journal of Medicine in 2018, measures 17 social determinants across small population-sensitive areas and provides an area deprivation index. A high area deprivation index is linked to a range of negative outcomes, including reshopitalization, later diagnoses, less comprehensive diagnostic evaluation, increased risk of postsurgical complications, and decreased life expectancy.
“One of the things that really stood out to me about Dr. Kind’s discussion of the use of the area deprivation index was the fact that understanding and quantifying these kinds of risks and exposures is the vehicle for creating the kinds of social changes, including policy changes, that will actually lead to addressing and mitigating some of these lifelong risks and exposures,” Dr. Hamilton said. “It is implausible to think that a specific group of people would be genetically more susceptible to basically every disease that we know,” he added. “It makes much more sense to think that groups of individuals have been subjected systematically to conditions that impair health in a variety of ways.”
Not just race, ethnicity, sex, and gender
Following the four presentations from researchers in health inequities was an Emerging Scholar presentation in which Jay B. Lusk, an MD/MBA candidate at Duke University, Durham, N.C., shared new research findings on the role of neighborhood disadvantage in predicting mortality from coma, stroke, and other neurologic conditions. His findings revealed that living in a neighborhood with greater deprivation substantially increased risk of mortality even after accounting for individual wealth and demographics.
Maria Eugenia Diaz-Ortiz, PhD, of the department of neurology, University of Pennsylvania, Philadelphia, said she found the five presentations to be an excellent introduction to people like herself who are in the earlier stages of learning about health equity research.
“I think they introduced various important concepts and frameworks and provided tools for people who don’t know about them,” Dr. Diaz-Ortiz said. “Then they asked important questions and provided some solutions to them.”
Dr. Diaz-Ortiz also appreciated seemingly minor but actually important details in how the speakers presented themselves, such as Dr. Rivera-Mindt opening with a land acknowledgment and her disclosures of “positionality.” The former recognized the traditional Native American custodians of the land on which she lives and works, and the latter revealed details about her as an individual – such as being the Afro-Latinx daughter of immigrants yet being cisgender, able-bodied, and U.S.-born – that show where she falls on the axis of adversity and axis of privilege.
Implications for research
The biggest takeaway for Dr. Diaz-Ortiz, however, came from the first Q&A session when someone asked how to increase underrepresented populations in dementia research. Dr. Rivera-Mindt described her experience engaging these communities by employing “community-based participatory research practices, which involves making yourself a part of the community and making the community active participants in the research,” Dr. Diaz-Ortiz said. “It’s an evidence-based approach that has been shown to increase participation in research not only in her work but in the work of others.”
Preaching to the choir
Dr. Diaz-Ortiz was pleased overall with the plenary but disappointed in its placement at the end of the meeting, when attendance is always lower as attendees head home.
“The people who stayed were people who already know and recognize the value of health equity work, so I think that was a missed opportunity where the session could have been included on day one or two to boost attendance and also to educate like a broader group of neurologists,” Dr. Diaz-Ortiz said in an interview.
Dr. Mendizabal felt similarly, appreciating the plenary but noting it was “definitely overdue” and that it should not be the last session. Instead, sessions on health equity should be as easy as possible to attend to bring in larger audiences. “Perhaps having that session on a Saturday or Sunday would have a higher likelihood of greater attendance than on a Tuesday,” she said. That said, Dr. Mendizabal also noticed that greater attention to health care disparities was woven into many other sessions throughout the conference, which is “the best way of addressing health equity instead of trying to just designate a session,” she said.
Dr. Mendizabal hopes that plenaries like this one and the weaving of health equity issues into presentations throughout neurology conferences continue.
“After the racial reckoning in 2020, there was a big impetus and a big wave of energy in addressing health disparities in the field, and I hope that that momentum is not starting to wane,” Dr. Mendizabal said. “It’s important because not talking about is not going to make this issue go away.”
Dr. Hamilton agreed that it is important that the conversation continue and that physicians recognize the importance of understanding health care disparities and determinants of health, regardless of where they fall on the political spectrum or whether they choose to get involved in policy or advocacy.
“Irrespective of whether you think race or ethnicity or socioeconomic status are political issues or not, it is the case that you’re obligated to have an objective understanding of the factors that contribute to your patient’s health and as points of intervention,” Dr. Hamilton said. “So even if you don’t want to sit down and jot off that email to your senator, you still have to take these factors into account when you’re treating the person who’s sitting right in front of you, and that’s not political. That’s the promise of being a physician.”
Dr. Amezcua has received personal compensation for consulting, speaking, or serving on steering committees or advisory boards for Biogen Idec, Novartis, Genentech, and EMD Serono, and she has received research support from Biogen Idec and Bristol Myers Squibb Foundation. Dr. Kind reported support from the Alzheimer’s Association. Dr. Diaz-Ortiz is coinventor of a provisional patent submitted by the University of Pennsylvania that relates to a potential therapeutic in Parkinson’s disease. Mr. Lusk reported fellowship support from American Heart Association and travel support from the American Neurological Association. No other speakers or sources had relevant disclosures.
FROM ANA 2022














