User login
Although inconclusive, CV safety study of cancer therapy attracts attention
The first global trial to compare the cardiovascular (CV) safety of two therapies for prostate cancer proved inconclusive because of inadequate enrollment and events, but the study is a harbinger of growth in the emerging specialty of cardio-oncology, according to experts.
“Many new cancer agents have extended patient survival, yet some of these agents have significant potential cardiovascular toxicity,” said Renato D. Lopes, MD, in presenting a study at the annual congress of the European Society of Cardiology.
In the context of improving survival in patients with or at risk for both cancer and cardiovascular disease, he suggested that the prostate cancer study he led could be “a model for interdisciplinary collaboration” needed to address the relative and sometimes competing risks of these disease states.
This point was seconded by several pioneers in cardio-oncology who participated in the discussion of the results of the trial, called PRONOUNCE.
“We know many drugs in oncology increase cardiovascular risk, so these are the types of trials we need,” according Thomas M. Suter, MD, who leads the cardio-oncology service at the University Hospital, Berne, Switzerland. He was the ESC-invited discussant for PRONOUNCE.
More than 100 centers in 12 countries involved
In PRONOUNCE, 545 patients with prostate cancer and established atherosclerotic cardiovascular disease were randomized to degarelix, a gonadotropin-releasing hormone antagonist, or leuprolide, a GnRH agonist. The patients were enrolled at 113 participating centers in 12 countries. All of the patients had an indication for an androgen-deprivation therapy (ADT).
In numerous previous studies, “ADT has been associated with higher CV morbidity and mortality, particularly in men with preexisting CV disease,” explained Dr. Lopes, but the relative cardiovascular safety of GnRH agonists relative to GnRH antagonists has been “controversial.”
The PRONOUNCE study was designed to resolve this issue, but the study was terminated early because of slow enrollment (not related to the COVID-19 pandemic). The planned enrollment was 900 patients.
In addition, the rate of major adverse cardiovascular events (MACE), defined as myocardial infarction, stroke, or death, was lower over the course of follow-up than anticipated in the study design.
No significant difference on primary endpoint
At the end of 12 months, MACE occurred in 11 (4.1%) of patients randomized to leuprolide and 15 (5.5%) of those randomized to degarelix. The greater hazard ratio for MACE in the degarelix group did not approach statistical significance (hazard ratio, 1.28; P = .53).
As a result, the question of the relative CV safety of these drugs “remains unresolved,” according to Dr. Lopes, professor of medicine at Duke University Medical Center, Durham, N.C.
This does not diminish the need to answer this question. In the addition to the fact that cancer is a malignancy primarily of advancing age when CV disease is prevalent – the mean age in this study was 73 years and 44% were over age 75 – it is often an indolent disease with long periods of survival, according to Dr. Lopes. About half of prostate cancer patients have concomitant CV disease, and about half will receive ADT at some point in their treatment.
In patients receiving ADT, leuprolide is far more commonly used than GnRH antagonists, which are offered in only about 4% of patients, according to data cited by Dr. Lopes. The underlying hypothesis of this study was that leuprolide is associated with greater CV risk, which might have been relevant to a risk-benefit calculation, if the hypothesis had been confirmed.
Cancer drugs can increase CV risk
Based on experimental data, “there is concern the leuprolide is involved in plaque destabilization,” said Dr. Lopes, but he noted that ADTs in general are associated with adverse metabolic changes, including increases in LDL cholesterol, insulin resistance, and body fat, all of which could be relevant to CV risk.
It is the improving rates of survival for prostate cancer as well for other types of cancer that have increased attention to the potential for cancer drugs to increase CV risk, another major cause of early mortality. For these competing risks, objective data are needed to evaluate a relative risk-to-benefit ratio for treatment choices.
This dilemma led the ESC to recently establish its Council on Cardio-Oncology, and many centers around the world are also creating interdisciplinary groups to guide treatment choices for patients with both diseases.
“You will certainly get a lot of referrals,” said Rudolf de Boer, MD, professor of translational cardiology, University Medical Center, Groningen, Netherlands. Basing his remark on his own experience starting a cardio-oncology clinic at his institution, he called this work challenging and agreed that the need for objective data is urgent.
“We need data to provide common ground on which to judge relative risks,” Dr. de Boer said. He also praised the PRONOUNCE investigators for their efforts even if the data failed to answer the question posed.
The PRONOUNCE results were published online in Circulation at the time of Dr. Lopes’s presentation.
The study received funding from Ferring Pharmaceuticals. Dr. Lopes reports financial relationships with Bristol-Myers Squibb, GlaxoSmithKline, Medtronic, Pfizer, and Sanofi. Dr. Suter reports financial relationships with Boehringer Ingelheim, GlaxoSmithKline, and Roche. Dr. de Boer reports financial relationships with AstraZeneca, Abbott, Bristol-Myers Squibb, Novartis, Novo Nordisk, and Roche.
The first global trial to compare the cardiovascular (CV) safety of two therapies for prostate cancer proved inconclusive because of inadequate enrollment and events, but the study is a harbinger of growth in the emerging specialty of cardio-oncology, according to experts.
“Many new cancer agents have extended patient survival, yet some of these agents have significant potential cardiovascular toxicity,” said Renato D. Lopes, MD, in presenting a study at the annual congress of the European Society of Cardiology.
In the context of improving survival in patients with or at risk for both cancer and cardiovascular disease, he suggested that the prostate cancer study he led could be “a model for interdisciplinary collaboration” needed to address the relative and sometimes competing risks of these disease states.
This point was seconded by several pioneers in cardio-oncology who participated in the discussion of the results of the trial, called PRONOUNCE.
“We know many drugs in oncology increase cardiovascular risk, so these are the types of trials we need,” according Thomas M. Suter, MD, who leads the cardio-oncology service at the University Hospital, Berne, Switzerland. He was the ESC-invited discussant for PRONOUNCE.
More than 100 centers in 12 countries involved
In PRONOUNCE, 545 patients with prostate cancer and established atherosclerotic cardiovascular disease were randomized to degarelix, a gonadotropin-releasing hormone antagonist, or leuprolide, a GnRH agonist. The patients were enrolled at 113 participating centers in 12 countries. All of the patients had an indication for an androgen-deprivation therapy (ADT).
In numerous previous studies, “ADT has been associated with higher CV morbidity and mortality, particularly in men with preexisting CV disease,” explained Dr. Lopes, but the relative cardiovascular safety of GnRH agonists relative to GnRH antagonists has been “controversial.”
The PRONOUNCE study was designed to resolve this issue, but the study was terminated early because of slow enrollment (not related to the COVID-19 pandemic). The planned enrollment was 900 patients.
In addition, the rate of major adverse cardiovascular events (MACE), defined as myocardial infarction, stroke, or death, was lower over the course of follow-up than anticipated in the study design.
No significant difference on primary endpoint
At the end of 12 months, MACE occurred in 11 (4.1%) of patients randomized to leuprolide and 15 (5.5%) of those randomized to degarelix. The greater hazard ratio for MACE in the degarelix group did not approach statistical significance (hazard ratio, 1.28; P = .53).
As a result, the question of the relative CV safety of these drugs “remains unresolved,” according to Dr. Lopes, professor of medicine at Duke University Medical Center, Durham, N.C.
This does not diminish the need to answer this question. In the addition to the fact that cancer is a malignancy primarily of advancing age when CV disease is prevalent – the mean age in this study was 73 years and 44% were over age 75 – it is often an indolent disease with long periods of survival, according to Dr. Lopes. About half of prostate cancer patients have concomitant CV disease, and about half will receive ADT at some point in their treatment.
In patients receiving ADT, leuprolide is far more commonly used than GnRH antagonists, which are offered in only about 4% of patients, according to data cited by Dr. Lopes. The underlying hypothesis of this study was that leuprolide is associated with greater CV risk, which might have been relevant to a risk-benefit calculation, if the hypothesis had been confirmed.
Cancer drugs can increase CV risk
Based on experimental data, “there is concern the leuprolide is involved in plaque destabilization,” said Dr. Lopes, but he noted that ADTs in general are associated with adverse metabolic changes, including increases in LDL cholesterol, insulin resistance, and body fat, all of which could be relevant to CV risk.
It is the improving rates of survival for prostate cancer as well for other types of cancer that have increased attention to the potential for cancer drugs to increase CV risk, another major cause of early mortality. For these competing risks, objective data are needed to evaluate a relative risk-to-benefit ratio for treatment choices.
This dilemma led the ESC to recently establish its Council on Cardio-Oncology, and many centers around the world are also creating interdisciplinary groups to guide treatment choices for patients with both diseases.
“You will certainly get a lot of referrals,” said Rudolf de Boer, MD, professor of translational cardiology, University Medical Center, Groningen, Netherlands. Basing his remark on his own experience starting a cardio-oncology clinic at his institution, he called this work challenging and agreed that the need for objective data is urgent.
“We need data to provide common ground on which to judge relative risks,” Dr. de Boer said. He also praised the PRONOUNCE investigators for their efforts even if the data failed to answer the question posed.
The PRONOUNCE results were published online in Circulation at the time of Dr. Lopes’s presentation.
The study received funding from Ferring Pharmaceuticals. Dr. Lopes reports financial relationships with Bristol-Myers Squibb, GlaxoSmithKline, Medtronic, Pfizer, and Sanofi. Dr. Suter reports financial relationships with Boehringer Ingelheim, GlaxoSmithKline, and Roche. Dr. de Boer reports financial relationships with AstraZeneca, Abbott, Bristol-Myers Squibb, Novartis, Novo Nordisk, and Roche.
The first global trial to compare the cardiovascular (CV) safety of two therapies for prostate cancer proved inconclusive because of inadequate enrollment and events, but the study is a harbinger of growth in the emerging specialty of cardio-oncology, according to experts.
“Many new cancer agents have extended patient survival, yet some of these agents have significant potential cardiovascular toxicity,” said Renato D. Lopes, MD, in presenting a study at the annual congress of the European Society of Cardiology.
In the context of improving survival in patients with or at risk for both cancer and cardiovascular disease, he suggested that the prostate cancer study he led could be “a model for interdisciplinary collaboration” needed to address the relative and sometimes competing risks of these disease states.
This point was seconded by several pioneers in cardio-oncology who participated in the discussion of the results of the trial, called PRONOUNCE.
“We know many drugs in oncology increase cardiovascular risk, so these are the types of trials we need,” according Thomas M. Suter, MD, who leads the cardio-oncology service at the University Hospital, Berne, Switzerland. He was the ESC-invited discussant for PRONOUNCE.
More than 100 centers in 12 countries involved
In PRONOUNCE, 545 patients with prostate cancer and established atherosclerotic cardiovascular disease were randomized to degarelix, a gonadotropin-releasing hormone antagonist, or leuprolide, a GnRH agonist. The patients were enrolled at 113 participating centers in 12 countries. All of the patients had an indication for an androgen-deprivation therapy (ADT).
In numerous previous studies, “ADT has been associated with higher CV morbidity and mortality, particularly in men with preexisting CV disease,” explained Dr. Lopes, but the relative cardiovascular safety of GnRH agonists relative to GnRH antagonists has been “controversial.”
The PRONOUNCE study was designed to resolve this issue, but the study was terminated early because of slow enrollment (not related to the COVID-19 pandemic). The planned enrollment was 900 patients.
In addition, the rate of major adverse cardiovascular events (MACE), defined as myocardial infarction, stroke, or death, was lower over the course of follow-up than anticipated in the study design.
No significant difference on primary endpoint
At the end of 12 months, MACE occurred in 11 (4.1%) of patients randomized to leuprolide and 15 (5.5%) of those randomized to degarelix. The greater hazard ratio for MACE in the degarelix group did not approach statistical significance (hazard ratio, 1.28; P = .53).
As a result, the question of the relative CV safety of these drugs “remains unresolved,” according to Dr. Lopes, professor of medicine at Duke University Medical Center, Durham, N.C.
This does not diminish the need to answer this question. In the addition to the fact that cancer is a malignancy primarily of advancing age when CV disease is prevalent – the mean age in this study was 73 years and 44% were over age 75 – it is often an indolent disease with long periods of survival, according to Dr. Lopes. About half of prostate cancer patients have concomitant CV disease, and about half will receive ADT at some point in their treatment.
In patients receiving ADT, leuprolide is far more commonly used than GnRH antagonists, which are offered in only about 4% of patients, according to data cited by Dr. Lopes. The underlying hypothesis of this study was that leuprolide is associated with greater CV risk, which might have been relevant to a risk-benefit calculation, if the hypothesis had been confirmed.
Cancer drugs can increase CV risk
Based on experimental data, “there is concern the leuprolide is involved in plaque destabilization,” said Dr. Lopes, but he noted that ADTs in general are associated with adverse metabolic changes, including increases in LDL cholesterol, insulin resistance, and body fat, all of which could be relevant to CV risk.
It is the improving rates of survival for prostate cancer as well for other types of cancer that have increased attention to the potential for cancer drugs to increase CV risk, another major cause of early mortality. For these competing risks, objective data are needed to evaluate a relative risk-to-benefit ratio for treatment choices.
This dilemma led the ESC to recently establish its Council on Cardio-Oncology, and many centers around the world are also creating interdisciplinary groups to guide treatment choices for patients with both diseases.
“You will certainly get a lot of referrals,” said Rudolf de Boer, MD, professor of translational cardiology, University Medical Center, Groningen, Netherlands. Basing his remark on his own experience starting a cardio-oncology clinic at his institution, he called this work challenging and agreed that the need for objective data is urgent.
“We need data to provide common ground on which to judge relative risks,” Dr. de Boer said. He also praised the PRONOUNCE investigators for their efforts even if the data failed to answer the question posed.
The PRONOUNCE results were published online in Circulation at the time of Dr. Lopes’s presentation.
The study received funding from Ferring Pharmaceuticals. Dr. Lopes reports financial relationships with Bristol-Myers Squibb, GlaxoSmithKline, Medtronic, Pfizer, and Sanofi. Dr. Suter reports financial relationships with Boehringer Ingelheim, GlaxoSmithKline, and Roche. Dr. de Boer reports financial relationships with AstraZeneca, Abbott, Bristol-Myers Squibb, Novartis, Novo Nordisk, and Roche.
FROM ESC 2021
Possible obesity effect detected in cancer death rates
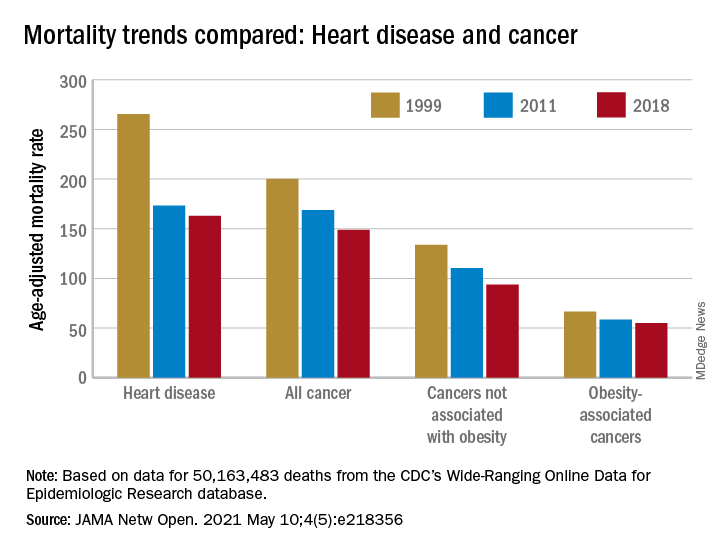
“By integrating 20 years of cancer mortality data, we demonstrated that trends in obesity-associated cancer mortality showed signs of recent deceleration, consistent with recent findings for heart disease mortality,” Christy L. Avery, PhD, and associates wrote in JAMA Network Open.
Improvements in mortality related to heart disease slowed after 2011, a phenomenon that has been associated with rising obesity rates. The age-adjusted mortality rate (AAMR) declined at an average of 3.8 deaths per 100,000 persons from 1999 to 2011 but only 0.7 deaths per 100,000 from 2011 to 2018, based on data from the Centers for Disease Control and Prevention’s Wide-Ranging Online Data for Epidemiologic Research (WONDER).
To understand trends in cancer mortality and their possible connection with obesity, data for 1999-2018 from the WONDER database were divided into obesity-associated and non–obesity-associated categories and compared with heart disease mortality, they explained. The database included more than 50 million deaths that matched inclusion criteria.
The analysis showed there was difference between obesity-associated and non–obesity-associated cancers that was obscured when all cancer deaths were considered together. The average annual change in AAMR for obesity-associated cancers slowed from –1.19 deaths per 100,000 in 1999-2011 to –0.83 in 2011-2018, Dr. Avery and associates reported.
For non–obesity-associated cancers, the annual change in AAMR increased from –1.62 per 100,000 for 1999-2011 to –2.29 for 2011-2018, following the trend for all cancers: –1.48 per 100,000 during 1999-2011 and –1.77 in 2011-2018, they said.
“The largest mortality decreases were observed for melanoma of the skin and lung cancer, two cancers not associated with obesity. For obesity-associated cancers, stable or increasing mortality rates have been observed for liver and pancreatic cancer among both men and women as well as for uterine cancer among women,” the investigators wrote.
Demographically, however, the slowing improvement in mortality for obesity-associated cancers did not follow the trend for heart disease. The deceleration for cancer was more pronounced for women and for non-Hispanic Whites and not seen at all in non-Hispanic Asian/Pacific Islander individuals. “For heart disease, evidence of a deceleration was consistent across sex, race, and ethnicity,” they said.
There are “longstanding disparities in obesity” among various populations in the United States, and the recent trend of obesity occurring earlier in life may be having an effect. “Whether the findings of decelerating mortality rates potentially signal a changing profile of cancer and heart disease mortality as the consequences of the obesity epidemic are realized remains to be seen,” they concluded.
The investigators reported receiving grants from the National Institutes of Health during the conduct of the study, but no other disclosures were reported.
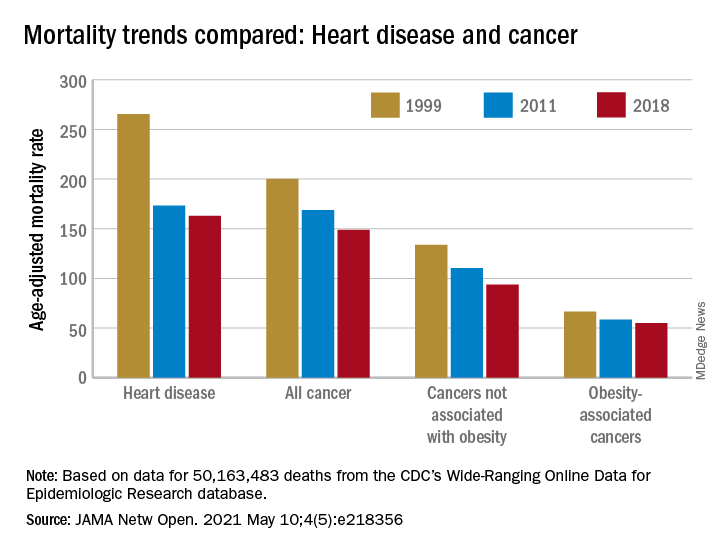
“By integrating 20 years of cancer mortality data, we demonstrated that trends in obesity-associated cancer mortality showed signs of recent deceleration, consistent with recent findings for heart disease mortality,” Christy L. Avery, PhD, and associates wrote in JAMA Network Open.
Improvements in mortality related to heart disease slowed after 2011, a phenomenon that has been associated with rising obesity rates. The age-adjusted mortality rate (AAMR) declined at an average of 3.8 deaths per 100,000 persons from 1999 to 2011 but only 0.7 deaths per 100,000 from 2011 to 2018, based on data from the Centers for Disease Control and Prevention’s Wide-Ranging Online Data for Epidemiologic Research (WONDER).
To understand trends in cancer mortality and their possible connection with obesity, data for 1999-2018 from the WONDER database were divided into obesity-associated and non–obesity-associated categories and compared with heart disease mortality, they explained. The database included more than 50 million deaths that matched inclusion criteria.
The analysis showed there was difference between obesity-associated and non–obesity-associated cancers that was obscured when all cancer deaths were considered together. The average annual change in AAMR for obesity-associated cancers slowed from –1.19 deaths per 100,000 in 1999-2011 to –0.83 in 2011-2018, Dr. Avery and associates reported.
For non–obesity-associated cancers, the annual change in AAMR increased from –1.62 per 100,000 for 1999-2011 to –2.29 for 2011-2018, following the trend for all cancers: –1.48 per 100,000 during 1999-2011 and –1.77 in 2011-2018, they said.
“The largest mortality decreases were observed for melanoma of the skin and lung cancer, two cancers not associated with obesity. For obesity-associated cancers, stable or increasing mortality rates have been observed for liver and pancreatic cancer among both men and women as well as for uterine cancer among women,” the investigators wrote.
Demographically, however, the slowing improvement in mortality for obesity-associated cancers did not follow the trend for heart disease. The deceleration for cancer was more pronounced for women and for non-Hispanic Whites and not seen at all in non-Hispanic Asian/Pacific Islander individuals. “For heart disease, evidence of a deceleration was consistent across sex, race, and ethnicity,” they said.
There are “longstanding disparities in obesity” among various populations in the United States, and the recent trend of obesity occurring earlier in life may be having an effect. “Whether the findings of decelerating mortality rates potentially signal a changing profile of cancer and heart disease mortality as the consequences of the obesity epidemic are realized remains to be seen,” they concluded.
The investigators reported receiving grants from the National Institutes of Health during the conduct of the study, but no other disclosures were reported.
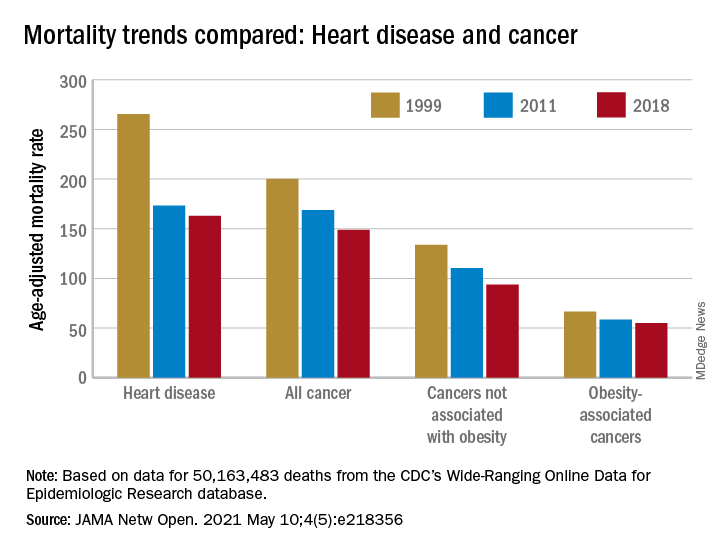
“By integrating 20 years of cancer mortality data, we demonstrated that trends in obesity-associated cancer mortality showed signs of recent deceleration, consistent with recent findings for heart disease mortality,” Christy L. Avery, PhD, and associates wrote in JAMA Network Open.
Improvements in mortality related to heart disease slowed after 2011, a phenomenon that has been associated with rising obesity rates. The age-adjusted mortality rate (AAMR) declined at an average of 3.8 deaths per 100,000 persons from 1999 to 2011 but only 0.7 deaths per 100,000 from 2011 to 2018, based on data from the Centers for Disease Control and Prevention’s Wide-Ranging Online Data for Epidemiologic Research (WONDER).
To understand trends in cancer mortality and their possible connection with obesity, data for 1999-2018 from the WONDER database were divided into obesity-associated and non–obesity-associated categories and compared with heart disease mortality, they explained. The database included more than 50 million deaths that matched inclusion criteria.
The analysis showed there was difference between obesity-associated and non–obesity-associated cancers that was obscured when all cancer deaths were considered together. The average annual change in AAMR for obesity-associated cancers slowed from –1.19 deaths per 100,000 in 1999-2011 to –0.83 in 2011-2018, Dr. Avery and associates reported.
For non–obesity-associated cancers, the annual change in AAMR increased from –1.62 per 100,000 for 1999-2011 to –2.29 for 2011-2018, following the trend for all cancers: –1.48 per 100,000 during 1999-2011 and –1.77 in 2011-2018, they said.
“The largest mortality decreases were observed for melanoma of the skin and lung cancer, two cancers not associated with obesity. For obesity-associated cancers, stable or increasing mortality rates have been observed for liver and pancreatic cancer among both men and women as well as for uterine cancer among women,” the investigators wrote.
Demographically, however, the slowing improvement in mortality for obesity-associated cancers did not follow the trend for heart disease. The deceleration for cancer was more pronounced for women and for non-Hispanic Whites and not seen at all in non-Hispanic Asian/Pacific Islander individuals. “For heart disease, evidence of a deceleration was consistent across sex, race, and ethnicity,” they said.
There are “longstanding disparities in obesity” among various populations in the United States, and the recent trend of obesity occurring earlier in life may be having an effect. “Whether the findings of decelerating mortality rates potentially signal a changing profile of cancer and heart disease mortality as the consequences of the obesity epidemic are realized remains to be seen,” they concluded.
The investigators reported receiving grants from the National Institutes of Health during the conduct of the study, but no other disclosures were reported.
FROM JAMA NETWORK OPEN
AHA statement flags CV risk of hormonal cancer therapies
Hormonal therapies for the treatment of hormone-dependent breast and prostate cancer could raise the risk for myocardial infarction and stroke, and patients need to be closely monitored to allow early detection and treatment of cardiovascular disease (CVD), the American Heart Association says in a new scientific statement.
“The statement provides data on the risks of each type of hormonal therapy so clinicians can use it as a guide to help manage cardiovascular risks during cancer treatment,” Tochi Okwuosa, DO, chair of the writing group, said in a news release.
“A team-based approach to patient care that includes the oncology team, cardiologist, primary care clinician, dietitian, endocrinologist, and other health care professionals as appropriate is needed to work with each patient to manage and reduce the increased risk of heart disease and strokes associated with hormonal therapy in breast and prostate cancer treatment,” said Dr. Okwuosa, director of cardio-oncology services, Rush University Medical Center, Chicago.
The scientific statement was published online April 26 in Circulation: Genomic and Precision Medicine.
Hormone-dependent cancers, such as prostate and breast cancer, are the most common noncutaneous cancers in the United States and around the world. As hormonal therapies have markedly improved survival in these patients, CVD has emerged as a leading cause illness and death.
The increased CVD burden might be explained by the increasing average age of cancer survivors, leading to higher rates of age-related CV risk factors and coronary artery disease.
The writing group reviewed existing evidence from observational studies and randomized controlled trials on the cardiovascular impact of anticancer hormonal therapies.
Among the key findings:
- In patients with breast cancer, has been shown to increase the risk for venous thromboembolic events, but to have somewhat protective to neutral effects on CVD risk burden and CVD events. Conversely, aromatase inhibitors have been shown to increase the risk for CVD risk factors and events, including MI and stroke.
- Androgen-deprivation therapy for prostate cancer appears to increase the risk for CV events, although gonadotrophin-releasing hormone (GnRH) antagonists are associated with a lower risk for CV events than are GnRH agonists. The oral antiandrogens appear to be associated with increased CVD risk as well, particularly when used for complete androgen blockade as combination GnRH/anti-androgen therapy.
- The duration of hormonal therapies has a significant impact on CVD risk; the longer patients receive hormonal therapy, the greater the risk. More research is needed to better define the risks associated with duration of treatment.
- The data are mixed on the impact of preexisting CV risk factors and CVD on CV events associated with hormonal therapy. Although the presence of baseline CV risk factors and CVD can increase CV events associated with aromatase inhibitors, it is not clear that tamoxifen does.
- Studies suggest that patients with prostate cancer and baseline CVD and CV risk factors have increased rates of CV events when treated with androgen-deprivation therapy.
- Although the prolonged use of some hormonal therapies worsens CV risk factors and , the effects of the duration of therapy on CV events are less clear.
The writing group noted that there are no definitive guidelines for the monitoring and management of hormonal therapy-related CVD risks.
The authors encourage clinicians to be alert for worsening CV problems in those with preexisting heart disease or risk factors, and to recognize that even patients without preexisting CV problems are at higher risk because of their exposure to hormonal therapies.
“For patients who have two or more cardiovascular risk factors, it is likely that referral to a cardiologist would be appropriate prior to beginning hormone treatment. For patients already receiving hormonal therapies, a discussion with the oncology team can help to determine if a cardiology referral is recommended,” Dr. Okwuosa said in the news release.
This scientific statement was prepared by the volunteer writing group on behalf of the AHA Cardio-Oncology Subcommittee of the Council on Clinical Cardiology and the Council on Genomic and Precision Medicine; the Council on Arteriosclerosis, Thrombosis, and Vascular Biology; and the Council on Cardiovascular Radiology and Intervention.
The research had no commercial funding. Dr. Okwuosa has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Hormonal therapies for the treatment of hormone-dependent breast and prostate cancer could raise the risk for myocardial infarction and stroke, and patients need to be closely monitored to allow early detection and treatment of cardiovascular disease (CVD), the American Heart Association says in a new scientific statement.
“The statement provides data on the risks of each type of hormonal therapy so clinicians can use it as a guide to help manage cardiovascular risks during cancer treatment,” Tochi Okwuosa, DO, chair of the writing group, said in a news release.
“A team-based approach to patient care that includes the oncology team, cardiologist, primary care clinician, dietitian, endocrinologist, and other health care professionals as appropriate is needed to work with each patient to manage and reduce the increased risk of heart disease and strokes associated with hormonal therapy in breast and prostate cancer treatment,” said Dr. Okwuosa, director of cardio-oncology services, Rush University Medical Center, Chicago.
The scientific statement was published online April 26 in Circulation: Genomic and Precision Medicine.
Hormone-dependent cancers, such as prostate and breast cancer, are the most common noncutaneous cancers in the United States and around the world. As hormonal therapies have markedly improved survival in these patients, CVD has emerged as a leading cause illness and death.
The increased CVD burden might be explained by the increasing average age of cancer survivors, leading to higher rates of age-related CV risk factors and coronary artery disease.
The writing group reviewed existing evidence from observational studies and randomized controlled trials on the cardiovascular impact of anticancer hormonal therapies.
Among the key findings:
- In patients with breast cancer, has been shown to increase the risk for venous thromboembolic events, but to have somewhat protective to neutral effects on CVD risk burden and CVD events. Conversely, aromatase inhibitors have been shown to increase the risk for CVD risk factors and events, including MI and stroke.
- Androgen-deprivation therapy for prostate cancer appears to increase the risk for CV events, although gonadotrophin-releasing hormone (GnRH) antagonists are associated with a lower risk for CV events than are GnRH agonists. The oral antiandrogens appear to be associated with increased CVD risk as well, particularly when used for complete androgen blockade as combination GnRH/anti-androgen therapy.
- The duration of hormonal therapies has a significant impact on CVD risk; the longer patients receive hormonal therapy, the greater the risk. More research is needed to better define the risks associated with duration of treatment.
- The data are mixed on the impact of preexisting CV risk factors and CVD on CV events associated with hormonal therapy. Although the presence of baseline CV risk factors and CVD can increase CV events associated with aromatase inhibitors, it is not clear that tamoxifen does.
- Studies suggest that patients with prostate cancer and baseline CVD and CV risk factors have increased rates of CV events when treated with androgen-deprivation therapy.
- Although the prolonged use of some hormonal therapies worsens CV risk factors and , the effects of the duration of therapy on CV events are less clear.
The writing group noted that there are no definitive guidelines for the monitoring and management of hormonal therapy-related CVD risks.
The authors encourage clinicians to be alert for worsening CV problems in those with preexisting heart disease or risk factors, and to recognize that even patients without preexisting CV problems are at higher risk because of their exposure to hormonal therapies.
“For patients who have two or more cardiovascular risk factors, it is likely that referral to a cardiologist would be appropriate prior to beginning hormone treatment. For patients already receiving hormonal therapies, a discussion with the oncology team can help to determine if a cardiology referral is recommended,” Dr. Okwuosa said in the news release.
This scientific statement was prepared by the volunteer writing group on behalf of the AHA Cardio-Oncology Subcommittee of the Council on Clinical Cardiology and the Council on Genomic and Precision Medicine; the Council on Arteriosclerosis, Thrombosis, and Vascular Biology; and the Council on Cardiovascular Radiology and Intervention.
The research had no commercial funding. Dr. Okwuosa has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Hormonal therapies for the treatment of hormone-dependent breast and prostate cancer could raise the risk for myocardial infarction and stroke, and patients need to be closely monitored to allow early detection and treatment of cardiovascular disease (CVD), the American Heart Association says in a new scientific statement.
“The statement provides data on the risks of each type of hormonal therapy so clinicians can use it as a guide to help manage cardiovascular risks during cancer treatment,” Tochi Okwuosa, DO, chair of the writing group, said in a news release.
“A team-based approach to patient care that includes the oncology team, cardiologist, primary care clinician, dietitian, endocrinologist, and other health care professionals as appropriate is needed to work with each patient to manage and reduce the increased risk of heart disease and strokes associated with hormonal therapy in breast and prostate cancer treatment,” said Dr. Okwuosa, director of cardio-oncology services, Rush University Medical Center, Chicago.
The scientific statement was published online April 26 in Circulation: Genomic and Precision Medicine.
Hormone-dependent cancers, such as prostate and breast cancer, are the most common noncutaneous cancers in the United States and around the world. As hormonal therapies have markedly improved survival in these patients, CVD has emerged as a leading cause illness and death.
The increased CVD burden might be explained by the increasing average age of cancer survivors, leading to higher rates of age-related CV risk factors and coronary artery disease.
The writing group reviewed existing evidence from observational studies and randomized controlled trials on the cardiovascular impact of anticancer hormonal therapies.
Among the key findings:
- In patients with breast cancer, has been shown to increase the risk for venous thromboembolic events, but to have somewhat protective to neutral effects on CVD risk burden and CVD events. Conversely, aromatase inhibitors have been shown to increase the risk for CVD risk factors and events, including MI and stroke.
- Androgen-deprivation therapy for prostate cancer appears to increase the risk for CV events, although gonadotrophin-releasing hormone (GnRH) antagonists are associated with a lower risk for CV events than are GnRH agonists. The oral antiandrogens appear to be associated with increased CVD risk as well, particularly when used for complete androgen blockade as combination GnRH/anti-androgen therapy.
- The duration of hormonal therapies has a significant impact on CVD risk; the longer patients receive hormonal therapy, the greater the risk. More research is needed to better define the risks associated with duration of treatment.
- The data are mixed on the impact of preexisting CV risk factors and CVD on CV events associated with hormonal therapy. Although the presence of baseline CV risk factors and CVD can increase CV events associated with aromatase inhibitors, it is not clear that tamoxifen does.
- Studies suggest that patients with prostate cancer and baseline CVD and CV risk factors have increased rates of CV events when treated with androgen-deprivation therapy.
- Although the prolonged use of some hormonal therapies worsens CV risk factors and , the effects of the duration of therapy on CV events are less clear.
The writing group noted that there are no definitive guidelines for the monitoring and management of hormonal therapy-related CVD risks.
The authors encourage clinicians to be alert for worsening CV problems in those with preexisting heart disease or risk factors, and to recognize that even patients without preexisting CV problems are at higher risk because of their exposure to hormonal therapies.
“For patients who have two or more cardiovascular risk factors, it is likely that referral to a cardiologist would be appropriate prior to beginning hormone treatment. For patients already receiving hormonal therapies, a discussion with the oncology team can help to determine if a cardiology referral is recommended,” Dr. Okwuosa said in the news release.
This scientific statement was prepared by the volunteer writing group on behalf of the AHA Cardio-Oncology Subcommittee of the Council on Clinical Cardiology and the Council on Genomic and Precision Medicine; the Council on Arteriosclerosis, Thrombosis, and Vascular Biology; and the Council on Cardiovascular Radiology and Intervention.
The research had no commercial funding. Dr. Okwuosa has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ATA risk stratification for DTC performs well in real-world cohort
NEW ORLEANS – The 2015 American Thyroid Association risk stratification system for patients with differentiated thyroid cancer performed well in a real-world cohort with a high proportion of high-risk patients, according to a study presented at the annual meeting of the Endocrine Society.
“The 2015 ATA Risk Stratification System is an excellent predictor of both persisting disease and survival,” wrote Evert F.S. van Velsen, MD, and his colleagues at Erasmus Medical Center, Rotterdam, the Netherlands, in a poster accompanying the presentation.
Among a group of 236 patients with differentiated thyroid cancer (DTC), Dr. van Velsen and his coauthors looked at how the ATA high-risk criteria influenced patient response to therapy. By the end of the 14-year study period, initial gross extrathyroidal disease extension meant patients were much less likely to have an excellent response (odds ratio, 0.26; P less than .001), and much more likely to have persistent disease (OR, 2.57; P = .001).
Odds of having an excellent response were reduced by having high postoperative thyroglobulin levels (OR, 0.21; P less than .001), and persistent disease was more likely (OR, 2.39; P = .002).
Other high-risk criteria associated with significantly lower odds of excellent response included distant metastases (OR, 0.36), incomplete resection (OR, 0.51), and having follicular thyroid carcinoma (FTC) with extensive vascular invasion (OR, 0.27). All these risk factors also were associated with higher odds of persistent disease.
“Recurrence after no evidence of disease occurred in 14%” of the study population, said Dr. van Velsen and his coauthors, adding, “Clinicians should be aware of the relatively high recurrence risk, even after an excellent response to therapy.”
The study aimed to evaluate the 2015 ATA risk stratification system’s prognostic value in a population that included a relatively large proportion of high-risk DTC patients, to include many FTC patients. This work, they noted, augments previous assessments of the risk stratification system in lower-risk populations.
The authors noted that, in addition to predicting disease recurrence, the risk stratification system also worked as a predictor of disease-specific survival. Patients with structural incomplete response fared the worst, with a survival probability below 0.5 at 200 months on a Kaplan-Meier curve of disease-specific survival. Survival probability remained at 1.0 for patients with excellent response after first therapy and was intermediate for those with indeterminate response and biochemical incomplete response.
Overall mortality was higher in FTC patients. Over the study period, 31 of the 76 FTC patients (41%) died, compared with 39 of the PTC patients (24%; P = .010). In all, 28% of the FTC patients and 18% of the PTC patients died of thyroid cancer, but this difference didn’t reach statistical significance.
The retrospective study included adults with DTC meeting the 2015 ATA high-risk criteria who were diagnosed and/or treated at Erasmus Medical Center over a 13-year span ending in December 2015.
Overall, the investigators found 236 patients meeting inclusion criteria; 160 had papillary thyroid cancer (PTC), and the remaining 76 had FTC. The latter group were significantly older at baseline than PTC patients (64 versus 53 years), and were significantly less likely to undergo neck dissection (22% versus 55%).
In the full cohort, 96 patients (41%) had one high-risk factor, and an additional 74 (31%) had two risk factors. The remaining patients had three or more risk factors.
There was no between-group difference in the likelihood of receiving radioactive iodine treatment, but those with FTC had a lower cumulative radiation dose (195 versus 298 mCi; P less than .001).
More than half of patients (58%) had persistent disease after completing their first therapy. Of these, 51% had structural incomplete response and 7% had biochemical incomplete response. The response was indeterminate for about a quarter of the cohort, and the remaining 17% had an excellent initial response.
By the end of the study period, 55% of patients had persistent disease, and 51% had structural incomplete response (a more likely result for those with FTC than PTC). Just 4% had a biochemical incomplete response, and the response was indeterminate for 16%. Response was judged excellent for 29% of patients.
Dr. van Velsen and his coauthors reported that they had no relevant disclosures.
SOURCE: van Velsen EFS et al. ENDO 2019, Abstract MON-549.
NEW ORLEANS – The 2015 American Thyroid Association risk stratification system for patients with differentiated thyroid cancer performed well in a real-world cohort with a high proportion of high-risk patients, according to a study presented at the annual meeting of the Endocrine Society.
“The 2015 ATA Risk Stratification System is an excellent predictor of both persisting disease and survival,” wrote Evert F.S. van Velsen, MD, and his colleagues at Erasmus Medical Center, Rotterdam, the Netherlands, in a poster accompanying the presentation.
Among a group of 236 patients with differentiated thyroid cancer (DTC), Dr. van Velsen and his coauthors looked at how the ATA high-risk criteria influenced patient response to therapy. By the end of the 14-year study period, initial gross extrathyroidal disease extension meant patients were much less likely to have an excellent response (odds ratio, 0.26; P less than .001), and much more likely to have persistent disease (OR, 2.57; P = .001).
Odds of having an excellent response were reduced by having high postoperative thyroglobulin levels (OR, 0.21; P less than .001), and persistent disease was more likely (OR, 2.39; P = .002).
Other high-risk criteria associated with significantly lower odds of excellent response included distant metastases (OR, 0.36), incomplete resection (OR, 0.51), and having follicular thyroid carcinoma (FTC) with extensive vascular invasion (OR, 0.27). All these risk factors also were associated with higher odds of persistent disease.
“Recurrence after no evidence of disease occurred in 14%” of the study population, said Dr. van Velsen and his coauthors, adding, “Clinicians should be aware of the relatively high recurrence risk, even after an excellent response to therapy.”
The study aimed to evaluate the 2015 ATA risk stratification system’s prognostic value in a population that included a relatively large proportion of high-risk DTC patients, to include many FTC patients. This work, they noted, augments previous assessments of the risk stratification system in lower-risk populations.
The authors noted that, in addition to predicting disease recurrence, the risk stratification system also worked as a predictor of disease-specific survival. Patients with structural incomplete response fared the worst, with a survival probability below 0.5 at 200 months on a Kaplan-Meier curve of disease-specific survival. Survival probability remained at 1.0 for patients with excellent response after first therapy and was intermediate for those with indeterminate response and biochemical incomplete response.
Overall mortality was higher in FTC patients. Over the study period, 31 of the 76 FTC patients (41%) died, compared with 39 of the PTC patients (24%; P = .010). In all, 28% of the FTC patients and 18% of the PTC patients died of thyroid cancer, but this difference didn’t reach statistical significance.
The retrospective study included adults with DTC meeting the 2015 ATA high-risk criteria who were diagnosed and/or treated at Erasmus Medical Center over a 13-year span ending in December 2015.
Overall, the investigators found 236 patients meeting inclusion criteria; 160 had papillary thyroid cancer (PTC), and the remaining 76 had FTC. The latter group were significantly older at baseline than PTC patients (64 versus 53 years), and were significantly less likely to undergo neck dissection (22% versus 55%).
In the full cohort, 96 patients (41%) had one high-risk factor, and an additional 74 (31%) had two risk factors. The remaining patients had three or more risk factors.
There was no between-group difference in the likelihood of receiving radioactive iodine treatment, but those with FTC had a lower cumulative radiation dose (195 versus 298 mCi; P less than .001).
More than half of patients (58%) had persistent disease after completing their first therapy. Of these, 51% had structural incomplete response and 7% had biochemical incomplete response. The response was indeterminate for about a quarter of the cohort, and the remaining 17% had an excellent initial response.
By the end of the study period, 55% of patients had persistent disease, and 51% had structural incomplete response (a more likely result for those with FTC than PTC). Just 4% had a biochemical incomplete response, and the response was indeterminate for 16%. Response was judged excellent for 29% of patients.
Dr. van Velsen and his coauthors reported that they had no relevant disclosures.
SOURCE: van Velsen EFS et al. ENDO 2019, Abstract MON-549.
NEW ORLEANS – The 2015 American Thyroid Association risk stratification system for patients with differentiated thyroid cancer performed well in a real-world cohort with a high proportion of high-risk patients, according to a study presented at the annual meeting of the Endocrine Society.
“The 2015 ATA Risk Stratification System is an excellent predictor of both persisting disease and survival,” wrote Evert F.S. van Velsen, MD, and his colleagues at Erasmus Medical Center, Rotterdam, the Netherlands, in a poster accompanying the presentation.
Among a group of 236 patients with differentiated thyroid cancer (DTC), Dr. van Velsen and his coauthors looked at how the ATA high-risk criteria influenced patient response to therapy. By the end of the 14-year study period, initial gross extrathyroidal disease extension meant patients were much less likely to have an excellent response (odds ratio, 0.26; P less than .001), and much more likely to have persistent disease (OR, 2.57; P = .001).
Odds of having an excellent response were reduced by having high postoperative thyroglobulin levels (OR, 0.21; P less than .001), and persistent disease was more likely (OR, 2.39; P = .002).
Other high-risk criteria associated with significantly lower odds of excellent response included distant metastases (OR, 0.36), incomplete resection (OR, 0.51), and having follicular thyroid carcinoma (FTC) with extensive vascular invasion (OR, 0.27). All these risk factors also were associated with higher odds of persistent disease.
“Recurrence after no evidence of disease occurred in 14%” of the study population, said Dr. van Velsen and his coauthors, adding, “Clinicians should be aware of the relatively high recurrence risk, even after an excellent response to therapy.”
The study aimed to evaluate the 2015 ATA risk stratification system’s prognostic value in a population that included a relatively large proportion of high-risk DTC patients, to include many FTC patients. This work, they noted, augments previous assessments of the risk stratification system in lower-risk populations.
The authors noted that, in addition to predicting disease recurrence, the risk stratification system also worked as a predictor of disease-specific survival. Patients with structural incomplete response fared the worst, with a survival probability below 0.5 at 200 months on a Kaplan-Meier curve of disease-specific survival. Survival probability remained at 1.0 for patients with excellent response after first therapy and was intermediate for those with indeterminate response and biochemical incomplete response.
Overall mortality was higher in FTC patients. Over the study period, 31 of the 76 FTC patients (41%) died, compared with 39 of the PTC patients (24%; P = .010). In all, 28% of the FTC patients and 18% of the PTC patients died of thyroid cancer, but this difference didn’t reach statistical significance.
The retrospective study included adults with DTC meeting the 2015 ATA high-risk criteria who were diagnosed and/or treated at Erasmus Medical Center over a 13-year span ending in December 2015.
Overall, the investigators found 236 patients meeting inclusion criteria; 160 had papillary thyroid cancer (PTC), and the remaining 76 had FTC. The latter group were significantly older at baseline than PTC patients (64 versus 53 years), and were significantly less likely to undergo neck dissection (22% versus 55%).
In the full cohort, 96 patients (41%) had one high-risk factor, and an additional 74 (31%) had two risk factors. The remaining patients had three or more risk factors.
There was no between-group difference in the likelihood of receiving radioactive iodine treatment, but those with FTC had a lower cumulative radiation dose (195 versus 298 mCi; P less than .001).
More than half of patients (58%) had persistent disease after completing their first therapy. Of these, 51% had structural incomplete response and 7% had biochemical incomplete response. The response was indeterminate for about a quarter of the cohort, and the remaining 17% had an excellent initial response.
By the end of the study period, 55% of patients had persistent disease, and 51% had structural incomplete response (a more likely result for those with FTC than PTC). Just 4% had a biochemical incomplete response, and the response was indeterminate for 16%. Response was judged excellent for 29% of patients.
Dr. van Velsen and his coauthors reported that they had no relevant disclosures.
SOURCE: van Velsen EFS et al. ENDO 2019, Abstract MON-549.
REPORTING FROM ENDO 2019
Key clinical point: in a cohort of high-risk patients.
Major finding: Gross extrathyroidal disease extension and high postoperative thyroglobulin levels predicted poor response (OR for excellent response, 0.26 and 0.21, respectively).
Study details: Retrospective single-center study of 236 patients with DTC meeting American Thyroid Association criteria for high risk.
Disclosures: The authors reported no external sources of funding and that they had no conflicts of interest.
Source: van Velsen EFS et al. ENDO 2019, Abstract MON-549.
PCOS linked to increased cancer risk in premenopausal women
based on an analysis of nearly 3.5 million women in a large Swedish database.
Women with PCOS had a sixfold increased risk of endometrial cancer, a tripling of endocrine gland cancers, and more than a doubling in the risk of ovarian and pancreatic cancers. Once women reached menopausal status, however, their cancer risk was comparable to that of women without a history of PCOS.
“Several carcinogenic processes are associated with PCOS, including dyslipidemia, hyperinsulinemia, and chronic inflammation,” wrote Weimin Ye, MD, PhD, of the Karolinska Institutet, Stockholm, and his colleagues. “Our study indicates that cancer may need to be added to the spectrum of long-term health consequences of PCOS and warrants increased surveillance among those patients.”
The research letter was published online in JAMA Oncology.
The team examined the relationship between PCOS and primary cancers in about 3.5 million women over a span of up to 24 years (1985-2009), although the mean follow-up time was not mentioned. To examine the potential impact of menopause, they conducted separate multivariate logistic regression analyses for those younger than 51 years, and those aged 51 years or older. The analyses controlled for use of some medications (metformin, oral contraceptives, and hormone therapy); as well as educational level (a proxy for socioeconomic status); smoking; parity (a proxy for fertility); parental cancers; and diabetes.
Overall, 14,764 women had been diagnosed with PCOS; they were a mean of 28 years at baseline and 182 developed a primary cancer 1 year or more after PCOS diagnosis.
These women had a 15% overall increased risk of cancer, compared with women without PCOS.
The risks for specific cancers also were increased, compared with women without PCOS, including endometrial (hazard ratio, 2.62), ovarian (HR, 2.16), endocrine (HR, 1.92), pancreatic (HR, 3.4), kidney (HR, 3.0), and skeletal and hematopoietic (HR, 1.69) cancers.
The risks were associated with younger age, however. In the group under age 51 years, the overall risk was 22% higher. The increased risk of specific cancers were endometrial (HR, 6.45), ovarian (HR, 2.55), pancreatic (HR, 6.68), kidney (HR, 4.57), and endocrine (not thyroid) gland (HR, 2.9) cancers.
The authors had no relevant financial disclosures.
SOURCE: Yin W et al. JAMA Oncol. 2018 Nov 29. doi:10.1001/jamaoncol.2018.5188.
based on an analysis of nearly 3.5 million women in a large Swedish database.
Women with PCOS had a sixfold increased risk of endometrial cancer, a tripling of endocrine gland cancers, and more than a doubling in the risk of ovarian and pancreatic cancers. Once women reached menopausal status, however, their cancer risk was comparable to that of women without a history of PCOS.
“Several carcinogenic processes are associated with PCOS, including dyslipidemia, hyperinsulinemia, and chronic inflammation,” wrote Weimin Ye, MD, PhD, of the Karolinska Institutet, Stockholm, and his colleagues. “Our study indicates that cancer may need to be added to the spectrum of long-term health consequences of PCOS and warrants increased surveillance among those patients.”
The research letter was published online in JAMA Oncology.
The team examined the relationship between PCOS and primary cancers in about 3.5 million women over a span of up to 24 years (1985-2009), although the mean follow-up time was not mentioned. To examine the potential impact of menopause, they conducted separate multivariate logistic regression analyses for those younger than 51 years, and those aged 51 years or older. The analyses controlled for use of some medications (metformin, oral contraceptives, and hormone therapy); as well as educational level (a proxy for socioeconomic status); smoking; parity (a proxy for fertility); parental cancers; and diabetes.
Overall, 14,764 women had been diagnosed with PCOS; they were a mean of 28 years at baseline and 182 developed a primary cancer 1 year or more after PCOS diagnosis.
These women had a 15% overall increased risk of cancer, compared with women without PCOS.
The risks for specific cancers also were increased, compared with women without PCOS, including endometrial (hazard ratio, 2.62), ovarian (HR, 2.16), endocrine (HR, 1.92), pancreatic (HR, 3.4), kidney (HR, 3.0), and skeletal and hematopoietic (HR, 1.69) cancers.
The risks were associated with younger age, however. In the group under age 51 years, the overall risk was 22% higher. The increased risk of specific cancers were endometrial (HR, 6.45), ovarian (HR, 2.55), pancreatic (HR, 6.68), kidney (HR, 4.57), and endocrine (not thyroid) gland (HR, 2.9) cancers.
The authors had no relevant financial disclosures.
SOURCE: Yin W et al. JAMA Oncol. 2018 Nov 29. doi:10.1001/jamaoncol.2018.5188.
based on an analysis of nearly 3.5 million women in a large Swedish database.
Women with PCOS had a sixfold increased risk of endometrial cancer, a tripling of endocrine gland cancers, and more than a doubling in the risk of ovarian and pancreatic cancers. Once women reached menopausal status, however, their cancer risk was comparable to that of women without a history of PCOS.
“Several carcinogenic processes are associated with PCOS, including dyslipidemia, hyperinsulinemia, and chronic inflammation,” wrote Weimin Ye, MD, PhD, of the Karolinska Institutet, Stockholm, and his colleagues. “Our study indicates that cancer may need to be added to the spectrum of long-term health consequences of PCOS and warrants increased surveillance among those patients.”
The research letter was published online in JAMA Oncology.
The team examined the relationship between PCOS and primary cancers in about 3.5 million women over a span of up to 24 years (1985-2009), although the mean follow-up time was not mentioned. To examine the potential impact of menopause, they conducted separate multivariate logistic regression analyses for those younger than 51 years, and those aged 51 years or older. The analyses controlled for use of some medications (metformin, oral contraceptives, and hormone therapy); as well as educational level (a proxy for socioeconomic status); smoking; parity (a proxy for fertility); parental cancers; and diabetes.
Overall, 14,764 women had been diagnosed with PCOS; they were a mean of 28 years at baseline and 182 developed a primary cancer 1 year or more after PCOS diagnosis.
These women had a 15% overall increased risk of cancer, compared with women without PCOS.
The risks for specific cancers also were increased, compared with women without PCOS, including endometrial (hazard ratio, 2.62), ovarian (HR, 2.16), endocrine (HR, 1.92), pancreatic (HR, 3.4), kidney (HR, 3.0), and skeletal and hematopoietic (HR, 1.69) cancers.
The risks were associated with younger age, however. In the group under age 51 years, the overall risk was 22% higher. The increased risk of specific cancers were endometrial (HR, 6.45), ovarian (HR, 2.55), pancreatic (HR, 6.68), kidney (HR, 4.57), and endocrine (not thyroid) gland (HR, 2.9) cancers.
The authors had no relevant financial disclosures.
SOURCE: Yin W et al. JAMA Oncol. 2018 Nov 29. doi:10.1001/jamaoncol.2018.5188.
FROM JAMA ONCOLOGY
Key clinical point: Polycystic ovarian syndrome may be associated with increased cancer risks among younger women.
Major finding: Among premenopausal women, there was a sixfold increased risk of endometrial cancer, a tripling of endocrine gland cancers, and a more than doubling in the risk of ovarian and pancreatic cancers
Study details: The study examined risks in 3.5 million women with up to 24 years of follow-up.
Disclosures: The study authors had no financial disclosures.
Source: Yin W et al. JAMA Oncol. 2018 Nov 29. doi:10.1001/jamaoncol.2018.5188.
CTCs linked to late recurrence in HER2–, HR+ breast cancer
Circulating tumor cells could be used to stratify patients with hormone receptor (HR)–positive, HER2-negative breast cancer for late recurrence risk, results of a secondary analysis of a randomized clinical trial suggest.
Risk of late clinical recurrence was about 13-fold higher among HR-positive patients with a positive circulating tumor cell (CTC) assay result, according to results of the study, published in JAMA Oncology.
“This prospectively conducted study offers a high level of evidence supporting the association between a positive CTC assay result and risk of clinical recurrence,” said Joseph A. Sparano, MD, of Albert Einstein College of Medicine, New York, and his coauthors.
The present study is the first to show that this CTC assay may play a role in determining late clinical recurrence after local and systemic adjuvant therapy, according to the investigators.
The study is a secondary analysis of E5103, a phase 3 trial of adjuvant doxorubicin and cyclophosphamide followed by paclitaxel with bevacizumab in patients with HER2-negative stage II-III breast cancer. Investigators included a total of 547 patients who had no clinical evidence of recurrence between 4.5 and 7.5 years of registration in that trial.
Positive CTC assay results occurred in 26 of those patients (4.8%), they found.
At a median follow-up of 2.6 years, 24 patients had a clinical recurrence, including 23 HR-positive patients and just 1 HR-negative patient. Accordingly, the investigators focused most of their further analysis on the HR-positive subset.
A total of 7 of 23 patients with HR-positive disease (30.4%) had a positive CTC assay result.
A positive CTC result in HR-positive patients was associated with a 13.1-fold increased risk of recurrence, multivariate analysis showed.
Higher CTC burden appeared to be associated with a numerically higher recurrence risk in HR-positive patients, the investigators found. They saw recurrences in 16 of 335 patients with a CTC count of 0 cells per 7.5 mL blood (4.8%), compared with 2 of 12 patients with 1 cell per 7.5 mL blood (16.7%), and 5 of 6 patients with 2 or more cells per 7.5 mL (83.3%).
Taken together, these results provided proof of concept to support additional investigations of the CTC assay and other blood-based biomarker tests in the setting of late clinical recurrence in HR-positive patients, the researchers said.
They acknowledged several limitations of this study: It was small, it had relatively short follow-up, and it did not evaluate the CTC assay in the context of other assays.
“Notwithstanding proof of concept, further evaluation is required to confirm the clinical validity and determine the clinical utility of performing the CTC assay in this context,” Dr. Sparano and his coauthors wrote.
Late recurrences, or those that occur more than 5 years after diagnosis, account for about half of all recurrences among HR-positive receptive breast cancers, Dr. Sparano and his colleagues said.
The researchers had no conflicts of interest to report. The study was supported by grants from the National Cancer Institute, National Institutes of Health, Breast Cancer Research Foundation, and Susan G. Komen Foundation.
SOURCE: Sparano J et al. JAMA Oncol. 2018 Jul 26. doi: 10.1001/jamaoncol.2018.2574.
Circulating tumor cells could be used to stratify patients with hormone receptor (HR)–positive, HER2-negative breast cancer for late recurrence risk, results of a secondary analysis of a randomized clinical trial suggest.
Risk of late clinical recurrence was about 13-fold higher among HR-positive patients with a positive circulating tumor cell (CTC) assay result, according to results of the study, published in JAMA Oncology.
“This prospectively conducted study offers a high level of evidence supporting the association between a positive CTC assay result and risk of clinical recurrence,” said Joseph A. Sparano, MD, of Albert Einstein College of Medicine, New York, and his coauthors.
The present study is the first to show that this CTC assay may play a role in determining late clinical recurrence after local and systemic adjuvant therapy, according to the investigators.
The study is a secondary analysis of E5103, a phase 3 trial of adjuvant doxorubicin and cyclophosphamide followed by paclitaxel with bevacizumab in patients with HER2-negative stage II-III breast cancer. Investigators included a total of 547 patients who had no clinical evidence of recurrence between 4.5 and 7.5 years of registration in that trial.
Positive CTC assay results occurred in 26 of those patients (4.8%), they found.
At a median follow-up of 2.6 years, 24 patients had a clinical recurrence, including 23 HR-positive patients and just 1 HR-negative patient. Accordingly, the investigators focused most of their further analysis on the HR-positive subset.
A total of 7 of 23 patients with HR-positive disease (30.4%) had a positive CTC assay result.
A positive CTC result in HR-positive patients was associated with a 13.1-fold increased risk of recurrence, multivariate analysis showed.
Higher CTC burden appeared to be associated with a numerically higher recurrence risk in HR-positive patients, the investigators found. They saw recurrences in 16 of 335 patients with a CTC count of 0 cells per 7.5 mL blood (4.8%), compared with 2 of 12 patients with 1 cell per 7.5 mL blood (16.7%), and 5 of 6 patients with 2 or more cells per 7.5 mL (83.3%).
Taken together, these results provided proof of concept to support additional investigations of the CTC assay and other blood-based biomarker tests in the setting of late clinical recurrence in HR-positive patients, the researchers said.
They acknowledged several limitations of this study: It was small, it had relatively short follow-up, and it did not evaluate the CTC assay in the context of other assays.
“Notwithstanding proof of concept, further evaluation is required to confirm the clinical validity and determine the clinical utility of performing the CTC assay in this context,” Dr. Sparano and his coauthors wrote.
Late recurrences, or those that occur more than 5 years after diagnosis, account for about half of all recurrences among HR-positive receptive breast cancers, Dr. Sparano and his colleagues said.
The researchers had no conflicts of interest to report. The study was supported by grants from the National Cancer Institute, National Institutes of Health, Breast Cancer Research Foundation, and Susan G. Komen Foundation.
SOURCE: Sparano J et al. JAMA Oncol. 2018 Jul 26. doi: 10.1001/jamaoncol.2018.2574.
Circulating tumor cells could be used to stratify patients with hormone receptor (HR)–positive, HER2-negative breast cancer for late recurrence risk, results of a secondary analysis of a randomized clinical trial suggest.
Risk of late clinical recurrence was about 13-fold higher among HR-positive patients with a positive circulating tumor cell (CTC) assay result, according to results of the study, published in JAMA Oncology.
“This prospectively conducted study offers a high level of evidence supporting the association between a positive CTC assay result and risk of clinical recurrence,” said Joseph A. Sparano, MD, of Albert Einstein College of Medicine, New York, and his coauthors.
The present study is the first to show that this CTC assay may play a role in determining late clinical recurrence after local and systemic adjuvant therapy, according to the investigators.
The study is a secondary analysis of E5103, a phase 3 trial of adjuvant doxorubicin and cyclophosphamide followed by paclitaxel with bevacizumab in patients with HER2-negative stage II-III breast cancer. Investigators included a total of 547 patients who had no clinical evidence of recurrence between 4.5 and 7.5 years of registration in that trial.
Positive CTC assay results occurred in 26 of those patients (4.8%), they found.
At a median follow-up of 2.6 years, 24 patients had a clinical recurrence, including 23 HR-positive patients and just 1 HR-negative patient. Accordingly, the investigators focused most of their further analysis on the HR-positive subset.
A total of 7 of 23 patients with HR-positive disease (30.4%) had a positive CTC assay result.
A positive CTC result in HR-positive patients was associated with a 13.1-fold increased risk of recurrence, multivariate analysis showed.
Higher CTC burden appeared to be associated with a numerically higher recurrence risk in HR-positive patients, the investigators found. They saw recurrences in 16 of 335 patients with a CTC count of 0 cells per 7.5 mL blood (4.8%), compared with 2 of 12 patients with 1 cell per 7.5 mL blood (16.7%), and 5 of 6 patients with 2 or more cells per 7.5 mL (83.3%).
Taken together, these results provided proof of concept to support additional investigations of the CTC assay and other blood-based biomarker tests in the setting of late clinical recurrence in HR-positive patients, the researchers said.
They acknowledged several limitations of this study: It was small, it had relatively short follow-up, and it did not evaluate the CTC assay in the context of other assays.
“Notwithstanding proof of concept, further evaluation is required to confirm the clinical validity and determine the clinical utility of performing the CTC assay in this context,” Dr. Sparano and his coauthors wrote.
Late recurrences, or those that occur more than 5 years after diagnosis, account for about half of all recurrences among HR-positive receptive breast cancers, Dr. Sparano and his colleagues said.
The researchers had no conflicts of interest to report. The study was supported by grants from the National Cancer Institute, National Institutes of Health, Breast Cancer Research Foundation, and Susan G. Komen Foundation.
SOURCE: Sparano J et al. JAMA Oncol. 2018 Jul 26. doi: 10.1001/jamaoncol.2018.2574.
FROM JAMA ONCOLOGY
Key clinical point: Circulating tumor cells (CTC) may help to evaluate late recurrence risk in patients with HER2-negative breast cancer.
Major finding: A positive CTC result was associated with a 13.1-fold increased risk of recurrence in hormone receptor–positive patients.
Study details: Secondary analysis of a randomized clinical trial including 547 patients with HER2-negative stage II-III breast cancer.
Disclosures: The study was supported by grants from the National Cancer Institute, National Institutes of Health, Breast Cancer Research Foundation, and Susan G. Komen Foundation. The authors reported no conflicts of interest.
Source: Sparano J et al. JAMA Oncol. 2018 Jul 26. doi: 10.1001/jamaoncol.2018.2574.
U.S. pancreatic insufficiency patients often get inadequate enzyme replacement
WASHINGTON – according to a recent analysis of insurance claims data from more than 48 million Americans.
Amid concerns that some people with nonspecific symptoms are overdiagnosed with exocrine pancreatic insufficiency (EPI) and hence getting unneeded treatment with pancreatic enzyme replacement therapy (PERT), it seems like substantial numbers of patients with legitimate pancreatic morbidity are often missed and are going untreated, Chris E. Forsmark, MD, said at the annual Digestive Disease Week®. This includes patients with chronic pancreatitis, pancreatic cancer, and patients who underwent pancreatic resection surgery.
Dr. Forsmark cited still-unpublished evidence that he has reported at meetings during the past year. At DDW 2017 he and his associates reported findings from an analysis of health insurance claims data collected in the PharMetrics database for more than 48 million Americans during 2006-2013, which included 37,061 insured adults diagnosed with chronic pancreatitis. Analysis of these data showed that just 7% had ever undergone testing for EPI and 30% had received a prescription for PERT, of which only 31% received an appropriate dosage (Gastroenterology. 2017 Apr;152[5, suppl 1]:S677). In other words, a scant 9% of insured U.S. adults with chronic pancreatitis during the studied period had received a minimally effective dosage of PERT.
Dr. Forsmark and his associates ran a second analysis using the same 2006-2013 insurance database, but this time looked at 32,461 insured American adults diagnosed with pancreatic cancer and reported similar findings: Fewer than 2% of patients underwent testing for EPI, 22% were prescribed PERT, and of these, 22% of patients per quarter received a minimally effective dosage of PERT, meaning that, overall, only 6% of pancreatic cancer patients received treatment that could be expected to resolve their presumed enzyme deficiency. Dr. Forsmark and his associates presented this report at the annual meeting of the American Pancreatic Association in San Diego in November 2017 (Pancreas. 2017 Nov/Dec;46[10]:1386-1448).
An irony is that PERT underuse comes at a time when some Internet sites promote PERT as a treatment for patients with nonspecific symptoms of EPI such as bloating, dyspepsia, and loose stools, Dr. Forsmark noted. “There is a possibility that patients with nonspecific gastrointestinal symptoms may request or receive PERT. Some patients may receive PERT who do not have EPI.” In 2015, clinicians had written roughly 746,000 prescriptions for PERT to U.S. patients, with the number of prescriptions steadily increasing during 2010-2015. Five different formulations for PERT are currently on the U.S. market, and a typical course of treatment costs about $1,500-$2,000 per month, he added.
Dr. Forsmark had no disclosures to report.
WASHINGTON – according to a recent analysis of insurance claims data from more than 48 million Americans.
Amid concerns that some people with nonspecific symptoms are overdiagnosed with exocrine pancreatic insufficiency (EPI) and hence getting unneeded treatment with pancreatic enzyme replacement therapy (PERT), it seems like substantial numbers of patients with legitimate pancreatic morbidity are often missed and are going untreated, Chris E. Forsmark, MD, said at the annual Digestive Disease Week®. This includes patients with chronic pancreatitis, pancreatic cancer, and patients who underwent pancreatic resection surgery.
Dr. Forsmark cited still-unpublished evidence that he has reported at meetings during the past year. At DDW 2017 he and his associates reported findings from an analysis of health insurance claims data collected in the PharMetrics database for more than 48 million Americans during 2006-2013, which included 37,061 insured adults diagnosed with chronic pancreatitis. Analysis of these data showed that just 7% had ever undergone testing for EPI and 30% had received a prescription for PERT, of which only 31% received an appropriate dosage (Gastroenterology. 2017 Apr;152[5, suppl 1]:S677). In other words, a scant 9% of insured U.S. adults with chronic pancreatitis during the studied period had received a minimally effective dosage of PERT.
Dr. Forsmark and his associates ran a second analysis using the same 2006-2013 insurance database, but this time looked at 32,461 insured American adults diagnosed with pancreatic cancer and reported similar findings: Fewer than 2% of patients underwent testing for EPI, 22% were prescribed PERT, and of these, 22% of patients per quarter received a minimally effective dosage of PERT, meaning that, overall, only 6% of pancreatic cancer patients received treatment that could be expected to resolve their presumed enzyme deficiency. Dr. Forsmark and his associates presented this report at the annual meeting of the American Pancreatic Association in San Diego in November 2017 (Pancreas. 2017 Nov/Dec;46[10]:1386-1448).
An irony is that PERT underuse comes at a time when some Internet sites promote PERT as a treatment for patients with nonspecific symptoms of EPI such as bloating, dyspepsia, and loose stools, Dr. Forsmark noted. “There is a possibility that patients with nonspecific gastrointestinal symptoms may request or receive PERT. Some patients may receive PERT who do not have EPI.” In 2015, clinicians had written roughly 746,000 prescriptions for PERT to U.S. patients, with the number of prescriptions steadily increasing during 2010-2015. Five different formulations for PERT are currently on the U.S. market, and a typical course of treatment costs about $1,500-$2,000 per month, he added.
Dr. Forsmark had no disclosures to report.
WASHINGTON – according to a recent analysis of insurance claims data from more than 48 million Americans.
Amid concerns that some people with nonspecific symptoms are overdiagnosed with exocrine pancreatic insufficiency (EPI) and hence getting unneeded treatment with pancreatic enzyme replacement therapy (PERT), it seems like substantial numbers of patients with legitimate pancreatic morbidity are often missed and are going untreated, Chris E. Forsmark, MD, said at the annual Digestive Disease Week®. This includes patients with chronic pancreatitis, pancreatic cancer, and patients who underwent pancreatic resection surgery.
Dr. Forsmark cited still-unpublished evidence that he has reported at meetings during the past year. At DDW 2017 he and his associates reported findings from an analysis of health insurance claims data collected in the PharMetrics database for more than 48 million Americans during 2006-2013, which included 37,061 insured adults diagnosed with chronic pancreatitis. Analysis of these data showed that just 7% had ever undergone testing for EPI and 30% had received a prescription for PERT, of which only 31% received an appropriate dosage (Gastroenterology. 2017 Apr;152[5, suppl 1]:S677). In other words, a scant 9% of insured U.S. adults with chronic pancreatitis during the studied period had received a minimally effective dosage of PERT.
Dr. Forsmark and his associates ran a second analysis using the same 2006-2013 insurance database, but this time looked at 32,461 insured American adults diagnosed with pancreatic cancer and reported similar findings: Fewer than 2% of patients underwent testing for EPI, 22% were prescribed PERT, and of these, 22% of patients per quarter received a minimally effective dosage of PERT, meaning that, overall, only 6% of pancreatic cancer patients received treatment that could be expected to resolve their presumed enzyme deficiency. Dr. Forsmark and his associates presented this report at the annual meeting of the American Pancreatic Association in San Diego in November 2017 (Pancreas. 2017 Nov/Dec;46[10]:1386-1448).
An irony is that PERT underuse comes at a time when some Internet sites promote PERT as a treatment for patients with nonspecific symptoms of EPI such as bloating, dyspepsia, and loose stools, Dr. Forsmark noted. “There is a possibility that patients with nonspecific gastrointestinal symptoms may request or receive PERT. Some patients may receive PERT who do not have EPI.” In 2015, clinicians had written roughly 746,000 prescriptions for PERT to U.S. patients, with the number of prescriptions steadily increasing during 2010-2015. Five different formulations for PERT are currently on the U.S. market, and a typical course of treatment costs about $1,500-$2,000 per month, he added.
Dr. Forsmark had no disclosures to report.
REPORTING FROM DDW 2018
Key clinical point: U.S. patients with presumed exocrine pancreatic insufficiency often appear undertreated.
Major finding: During 2006-2013, only 9% of U.S. adults with chronic pancreatitis and 6% with pancreatic cancer received adequate enzyme replacement.
Study details: A review of diagnosis and claims data from 48.67 million insured U.S. adults during 2006-2013.
Disclosures: Dr. Forsmark had no disclosures to report.
Pancreatic cancer has a pancreatopathy distinct from type 2 diabetes
WASHINGTON –
“The endocrinopathies associated with type 2 diabetes mellitus and pancreatic cancer are distinct, the former represented by an increase in glucagon and the latter characterized by a reduction in islet size,” said Sajan Nagpal, MD, of the Mayo Clinic in Rochester, Minn., at Digestive Disease Week 2018®. “These data lend insight to a unique pathophysiology of diabetes that results from pancreatic cancer.”
Prior to presenting his results, Dr. Nagpal pointed out an interesting relationship between pancreatic cancer and diabetes.
“Pancreatic cancer and diabetes have a very unique, two-way relationship. While long-standing diabetes [LSDM] increases the risk of developing pancreatic cancer by 1.5-2 times over a person’s lifetime, pancreatic cancer itself causes a paraneoplastic form of diabetes. A person with a new diagnosis of diabetes mellitus has a five to eight times increased risk of being diagnosed with pancreatic cancer as compared to the general population within 3 years.“
This form of diabetes is referred to as pancreatic cancer–induced new onset diabetes (PC-NOD).
Dr. Nagpal and his team conducted a study that included 46 patients: 16 patients with pancreatic cancer (5 with LSDM, 5 NOD, and 6 without diabetes mellitus), 15 patients with T2DM (9 LSDM, 6 NOD), and 15 controls matched for age and body mass index. NOD was defined as a diabetes mellitus diagnosis less than 3 years from the date of autopsy or pancreatic cancer diagnosis. All pancreatic specimens were resected from pancreatic cancer patients or obtained as autopsy specimens. Researchers performed islet morphometric studies utilizing immunofluorescence analysis with specific insulin and glucagon antibodies.
The results of the study showed that patients with pancreatic cancer had islet sizes that were about a third smaller than those in the patients with T2DM and the healthy controls (P = .005). This held true for both LSDM and NOD pancreatic cancer patients, compared with the T2DM and healthy control groups. Researchers also found that insulin to glucagon (I:G) ratios were preserved in pancreatic cancer patients, whereas they were lower in patients with T2DM because of a higher percentage of glucagon in the islets (P = .08). Additionally, islet amyloid was much higher in T2DM patients (66.7%) versus patients with diabetes associated with pancreatic cancer (55.6%) and healthy controls (13.3%; P = .01).
There were several limitations to this study, including the small number of patients in each group and how pancreatic islet characteristics can vary based on their location. Finally, ductal obstruction can cause changes to islet morphology.
Along with the pathological changes found by Dr. Nagpal and his research team, PC-NOD and T2DM also have unique clinical profiles. As patients with pancreatic cancer approach their diagnosis, they begin to lose weight. This begins about 1 year before the patient’s diagnosis of pancreatic cancer. Conversely, these patients have worsening fasting glucose levels despite the fact that they are losing weight. The paradoxical relationship between weight loss and hyperglycemia are what distinguishes PC-NOD from T2DM, according to Dr. Nagpal. In patients with PC-NOD, worsening hyperglycemia happens over a periods of months, compared with the gradual increase over the course of years seen in T2DM.
The differences between these diseases may be caused by differences in their pancreatopathy.
When discussing the pancreatopathy associated with T2DM, Dr. Nagpal pointed out that there is a decrease in the I:G ratio, compared with those seen in patients without diabetes. The prevailing theory is that this decrease in the I:G ratio is caused by beta-cell apoptosis and transdifferentiation to alpha-cells. T2DM patients also have increased amyloid deposits, the result of increased islet amyloid polypeptide.
”Pancreatic cancer provides subtle metabolic clues, such as worsening glucose tolerance and weight loss, that can serve as potential targets for its early detection.”
According to Dr. Nagpal, more research is needed on pathogenesis of PC-NOD. Identification of biomarkers for screening may be possible in patients with new onset diabetes.
Dr. Nagpal had no financial conflicts of interest to report.
SOURCE: Nagpal S et al. DDW 2018, Abstract 392.
WASHINGTON –
“The endocrinopathies associated with type 2 diabetes mellitus and pancreatic cancer are distinct, the former represented by an increase in glucagon and the latter characterized by a reduction in islet size,” said Sajan Nagpal, MD, of the Mayo Clinic in Rochester, Minn., at Digestive Disease Week 2018®. “These data lend insight to a unique pathophysiology of diabetes that results from pancreatic cancer.”
Prior to presenting his results, Dr. Nagpal pointed out an interesting relationship between pancreatic cancer and diabetes.
“Pancreatic cancer and diabetes have a very unique, two-way relationship. While long-standing diabetes [LSDM] increases the risk of developing pancreatic cancer by 1.5-2 times over a person’s lifetime, pancreatic cancer itself causes a paraneoplastic form of diabetes. A person with a new diagnosis of diabetes mellitus has a five to eight times increased risk of being diagnosed with pancreatic cancer as compared to the general population within 3 years.“
This form of diabetes is referred to as pancreatic cancer–induced new onset diabetes (PC-NOD).
Dr. Nagpal and his team conducted a study that included 46 patients: 16 patients with pancreatic cancer (5 with LSDM, 5 NOD, and 6 without diabetes mellitus), 15 patients with T2DM (9 LSDM, 6 NOD), and 15 controls matched for age and body mass index. NOD was defined as a diabetes mellitus diagnosis less than 3 years from the date of autopsy or pancreatic cancer diagnosis. All pancreatic specimens were resected from pancreatic cancer patients or obtained as autopsy specimens. Researchers performed islet morphometric studies utilizing immunofluorescence analysis with specific insulin and glucagon antibodies.
The results of the study showed that patients with pancreatic cancer had islet sizes that were about a third smaller than those in the patients with T2DM and the healthy controls (P = .005). This held true for both LSDM and NOD pancreatic cancer patients, compared with the T2DM and healthy control groups. Researchers also found that insulin to glucagon (I:G) ratios were preserved in pancreatic cancer patients, whereas they were lower in patients with T2DM because of a higher percentage of glucagon in the islets (P = .08). Additionally, islet amyloid was much higher in T2DM patients (66.7%) versus patients with diabetes associated with pancreatic cancer (55.6%) and healthy controls (13.3%; P = .01).
There were several limitations to this study, including the small number of patients in each group and how pancreatic islet characteristics can vary based on their location. Finally, ductal obstruction can cause changes to islet morphology.
Along with the pathological changes found by Dr. Nagpal and his research team, PC-NOD and T2DM also have unique clinical profiles. As patients with pancreatic cancer approach their diagnosis, they begin to lose weight. This begins about 1 year before the patient’s diagnosis of pancreatic cancer. Conversely, these patients have worsening fasting glucose levels despite the fact that they are losing weight. The paradoxical relationship between weight loss and hyperglycemia are what distinguishes PC-NOD from T2DM, according to Dr. Nagpal. In patients with PC-NOD, worsening hyperglycemia happens over a periods of months, compared with the gradual increase over the course of years seen in T2DM.
The differences between these diseases may be caused by differences in their pancreatopathy.
When discussing the pancreatopathy associated with T2DM, Dr. Nagpal pointed out that there is a decrease in the I:G ratio, compared with those seen in patients without diabetes. The prevailing theory is that this decrease in the I:G ratio is caused by beta-cell apoptosis and transdifferentiation to alpha-cells. T2DM patients also have increased amyloid deposits, the result of increased islet amyloid polypeptide.
”Pancreatic cancer provides subtle metabolic clues, such as worsening glucose tolerance and weight loss, that can serve as potential targets for its early detection.”
According to Dr. Nagpal, more research is needed on pathogenesis of PC-NOD. Identification of biomarkers for screening may be possible in patients with new onset diabetes.
Dr. Nagpal had no financial conflicts of interest to report.
SOURCE: Nagpal S et al. DDW 2018, Abstract 392.
WASHINGTON –
“The endocrinopathies associated with type 2 diabetes mellitus and pancreatic cancer are distinct, the former represented by an increase in glucagon and the latter characterized by a reduction in islet size,” said Sajan Nagpal, MD, of the Mayo Clinic in Rochester, Minn., at Digestive Disease Week 2018®. “These data lend insight to a unique pathophysiology of diabetes that results from pancreatic cancer.”
Prior to presenting his results, Dr. Nagpal pointed out an interesting relationship between pancreatic cancer and diabetes.
“Pancreatic cancer and diabetes have a very unique, two-way relationship. While long-standing diabetes [LSDM] increases the risk of developing pancreatic cancer by 1.5-2 times over a person’s lifetime, pancreatic cancer itself causes a paraneoplastic form of diabetes. A person with a new diagnosis of diabetes mellitus has a five to eight times increased risk of being diagnosed with pancreatic cancer as compared to the general population within 3 years.“
This form of diabetes is referred to as pancreatic cancer–induced new onset diabetes (PC-NOD).
Dr. Nagpal and his team conducted a study that included 46 patients: 16 patients with pancreatic cancer (5 with LSDM, 5 NOD, and 6 without diabetes mellitus), 15 patients with T2DM (9 LSDM, 6 NOD), and 15 controls matched for age and body mass index. NOD was defined as a diabetes mellitus diagnosis less than 3 years from the date of autopsy or pancreatic cancer diagnosis. All pancreatic specimens were resected from pancreatic cancer patients or obtained as autopsy specimens. Researchers performed islet morphometric studies utilizing immunofluorescence analysis with specific insulin and glucagon antibodies.
The results of the study showed that patients with pancreatic cancer had islet sizes that were about a third smaller than those in the patients with T2DM and the healthy controls (P = .005). This held true for both LSDM and NOD pancreatic cancer patients, compared with the T2DM and healthy control groups. Researchers also found that insulin to glucagon (I:G) ratios were preserved in pancreatic cancer patients, whereas they were lower in patients with T2DM because of a higher percentage of glucagon in the islets (P = .08). Additionally, islet amyloid was much higher in T2DM patients (66.7%) versus patients with diabetes associated with pancreatic cancer (55.6%) and healthy controls (13.3%; P = .01).
There were several limitations to this study, including the small number of patients in each group and how pancreatic islet characteristics can vary based on their location. Finally, ductal obstruction can cause changes to islet morphology.
Along with the pathological changes found by Dr. Nagpal and his research team, PC-NOD and T2DM also have unique clinical profiles. As patients with pancreatic cancer approach their diagnosis, they begin to lose weight. This begins about 1 year before the patient’s diagnosis of pancreatic cancer. Conversely, these patients have worsening fasting glucose levels despite the fact that they are losing weight. The paradoxical relationship between weight loss and hyperglycemia are what distinguishes PC-NOD from T2DM, according to Dr. Nagpal. In patients with PC-NOD, worsening hyperglycemia happens over a periods of months, compared with the gradual increase over the course of years seen in T2DM.
The differences between these diseases may be caused by differences in their pancreatopathy.
When discussing the pancreatopathy associated with T2DM, Dr. Nagpal pointed out that there is a decrease in the I:G ratio, compared with those seen in patients without diabetes. The prevailing theory is that this decrease in the I:G ratio is caused by beta-cell apoptosis and transdifferentiation to alpha-cells. T2DM patients also have increased amyloid deposits, the result of increased islet amyloid polypeptide.
”Pancreatic cancer provides subtle metabolic clues, such as worsening glucose tolerance and weight loss, that can serve as potential targets for its early detection.”
According to Dr. Nagpal, more research is needed on pathogenesis of PC-NOD. Identification of biomarkers for screening may be possible in patients with new onset diabetes.
Dr. Nagpal had no financial conflicts of interest to report.
SOURCE: Nagpal S et al. DDW 2018, Abstract 392.
REPORTING FROM DDW 2018
Key clinical point: Pancreatic cancer has a distinct endocrine pancreatopathy.
Major finding: Patients with pancreatic cancer had islet sizes that were about a third smaller than those in patients with type 2 diabetes and healthy controls (P = .005).
Study details: Small study analyzing the pathology of pancreatic cancer resections and autopsy specimens.
Disclosures: The authors of this study had no financial conflicts to disclose.
Source: Nagpal S et al. DDW 2018, Abstract 392.
Diabetes from checkpoint inhibitors probably means lifelong insulin
CHICAGO – , according to Priyanka Iyer, MD, an endocrinology fellow at MD Anderson Cancer Center, Houston.
“As long as we get glycemic control, they can continue,” she said at the annual meeting of the Endocrine Society.
Diabetes is a known side effect of immune checkpoint inhibitors (ICIs) but it’s rare, occurring in maybe 0.17% of patients, and its natural history and risk factors are unknown.
ICIs are fairly new agents, and as their use expands beyond clinical trials, “we anticipate seeing larger numbers of cases. Patients should be educated about the symptoms of uncontrolled blood sugars while on ICIs,” and endocrinologists “have to get involved and recognize this entity sooner,” Dr. Iyer said.
In short, her team found that ICI-mediated diabetes can occur in patients with or without preexisting diabetes, and that most patients have evidence of beta-cell failure, likely T-cell mediated destruction due to immune activation. In all but one case, patients remained on insulin at a median follow-up of 44 weeks, even after stopping ICIs. For most, ICI-mediated diabetes likely means lifelong insulin.
They were all on the programmed cell death protein (PD-1) inhibitors nivolumab (Opdivo) or pembrolizumab (Keytruda), or the PD-1 ligand (PD-L) inhibitor durvalumab (Imfinzi). The agents are used for a range of cancers, including renal cell, melanoma, and Hodgkin lymphoma. There were no diabetes cases in patients on single-agent ipilimumab (Yervoy) or tremelimumab, which target cytotoxic T-lymphocyte associated antigen-4 and are used for melanoma and mesothelioma.
Median time to diabetes presentation after the start of ICI treatment was 12.3 weeks but ranged from 1 to 67.2 weeks. Half of the cases presented in diabetic ketoacidosis (DKA). Patients had upward trending hyperglycemia and most had diabetes symptoms for a while before diagnosis. They presented with a blood glucose above 250 mg/dL, and more than half above 500 mg/dL. Median hemoglobin A1c at presentation was 8%, but ranged up to 12.5%.
Every patient required insulin, including the six that discontinued ICIs after developing diabetes. Diabetes resolved in just one patient at 10.2 months; she presented with DKA.
There were no obvious predisposing factors. None of the patients had histories of type 1 diabetes or other autoimmune disease. Five patients had well-controlled type 2 diabetes prior to ICI initiation; four had prediabetes. Some had family members with type 2 diabetes, but not type 1. Four had prior ICI exposure. Just three patients were on concomitant steroids.
A few patients also developed thyroid or pituitary dysfunction, which are more common side effects of ICIs.
The median age at diabetes presentation was 61 years and ranged from 32 to 82 years. The majority of patients were men, which reflects MD Anderson demographics, not a predisposing risk factor, Dr. Iyer said.
Melanoma was the most common cancer, followed by renal cell and prostate; patients had stage 2-4 disease. About half the subjects were on single agent anti-PD-1 treatment, about a third on anti-PD-1 combination treatment, and the rest on anti-PD-L1 combination therapy. C-peptide levels were below 0.9 ng/mL at diabetes diagnosis in most of the patients. Eleven of the 20 tested (55%) were positive for the pancreatic islet cell antibody GAD65.
The investigators had no disclosures. A funding source was not reported.
SOURCE: Iyer PC et al. Abstract OR05-5.
CHICAGO – , according to Priyanka Iyer, MD, an endocrinology fellow at MD Anderson Cancer Center, Houston.
“As long as we get glycemic control, they can continue,” she said at the annual meeting of the Endocrine Society.
Diabetes is a known side effect of immune checkpoint inhibitors (ICIs) but it’s rare, occurring in maybe 0.17% of patients, and its natural history and risk factors are unknown.
ICIs are fairly new agents, and as their use expands beyond clinical trials, “we anticipate seeing larger numbers of cases. Patients should be educated about the symptoms of uncontrolled blood sugars while on ICIs,” and endocrinologists “have to get involved and recognize this entity sooner,” Dr. Iyer said.
In short, her team found that ICI-mediated diabetes can occur in patients with or without preexisting diabetes, and that most patients have evidence of beta-cell failure, likely T-cell mediated destruction due to immune activation. In all but one case, patients remained on insulin at a median follow-up of 44 weeks, even after stopping ICIs. For most, ICI-mediated diabetes likely means lifelong insulin.
They were all on the programmed cell death protein (PD-1) inhibitors nivolumab (Opdivo) or pembrolizumab (Keytruda), or the PD-1 ligand (PD-L) inhibitor durvalumab (Imfinzi). The agents are used for a range of cancers, including renal cell, melanoma, and Hodgkin lymphoma. There were no diabetes cases in patients on single-agent ipilimumab (Yervoy) or tremelimumab, which target cytotoxic T-lymphocyte associated antigen-4 and are used for melanoma and mesothelioma.
Median time to diabetes presentation after the start of ICI treatment was 12.3 weeks but ranged from 1 to 67.2 weeks. Half of the cases presented in diabetic ketoacidosis (DKA). Patients had upward trending hyperglycemia and most had diabetes symptoms for a while before diagnosis. They presented with a blood glucose above 250 mg/dL, and more than half above 500 mg/dL. Median hemoglobin A1c at presentation was 8%, but ranged up to 12.5%.
Every patient required insulin, including the six that discontinued ICIs after developing diabetes. Diabetes resolved in just one patient at 10.2 months; she presented with DKA.
There were no obvious predisposing factors. None of the patients had histories of type 1 diabetes or other autoimmune disease. Five patients had well-controlled type 2 diabetes prior to ICI initiation; four had prediabetes. Some had family members with type 2 diabetes, but not type 1. Four had prior ICI exposure. Just three patients were on concomitant steroids.
A few patients also developed thyroid or pituitary dysfunction, which are more common side effects of ICIs.
The median age at diabetes presentation was 61 years and ranged from 32 to 82 years. The majority of patients were men, which reflects MD Anderson demographics, not a predisposing risk factor, Dr. Iyer said.
Melanoma was the most common cancer, followed by renal cell and prostate; patients had stage 2-4 disease. About half the subjects were on single agent anti-PD-1 treatment, about a third on anti-PD-1 combination treatment, and the rest on anti-PD-L1 combination therapy. C-peptide levels were below 0.9 ng/mL at diabetes diagnosis in most of the patients. Eleven of the 20 tested (55%) were positive for the pancreatic islet cell antibody GAD65.
The investigators had no disclosures. A funding source was not reported.
SOURCE: Iyer PC et al. Abstract OR05-5.
CHICAGO – , according to Priyanka Iyer, MD, an endocrinology fellow at MD Anderson Cancer Center, Houston.
“As long as we get glycemic control, they can continue,” she said at the annual meeting of the Endocrine Society.
Diabetes is a known side effect of immune checkpoint inhibitors (ICIs) but it’s rare, occurring in maybe 0.17% of patients, and its natural history and risk factors are unknown.
ICIs are fairly new agents, and as their use expands beyond clinical trials, “we anticipate seeing larger numbers of cases. Patients should be educated about the symptoms of uncontrolled blood sugars while on ICIs,” and endocrinologists “have to get involved and recognize this entity sooner,” Dr. Iyer said.
In short, her team found that ICI-mediated diabetes can occur in patients with or without preexisting diabetes, and that most patients have evidence of beta-cell failure, likely T-cell mediated destruction due to immune activation. In all but one case, patients remained on insulin at a median follow-up of 44 weeks, even after stopping ICIs. For most, ICI-mediated diabetes likely means lifelong insulin.
They were all on the programmed cell death protein (PD-1) inhibitors nivolumab (Opdivo) or pembrolizumab (Keytruda), or the PD-1 ligand (PD-L) inhibitor durvalumab (Imfinzi). The agents are used for a range of cancers, including renal cell, melanoma, and Hodgkin lymphoma. There were no diabetes cases in patients on single-agent ipilimumab (Yervoy) or tremelimumab, which target cytotoxic T-lymphocyte associated antigen-4 and are used for melanoma and mesothelioma.
Median time to diabetes presentation after the start of ICI treatment was 12.3 weeks but ranged from 1 to 67.2 weeks. Half of the cases presented in diabetic ketoacidosis (DKA). Patients had upward trending hyperglycemia and most had diabetes symptoms for a while before diagnosis. They presented with a blood glucose above 250 mg/dL, and more than half above 500 mg/dL. Median hemoglobin A1c at presentation was 8%, but ranged up to 12.5%.
Every patient required insulin, including the six that discontinued ICIs after developing diabetes. Diabetes resolved in just one patient at 10.2 months; she presented with DKA.
There were no obvious predisposing factors. None of the patients had histories of type 1 diabetes or other autoimmune disease. Five patients had well-controlled type 2 diabetes prior to ICI initiation; four had prediabetes. Some had family members with type 2 diabetes, but not type 1. Four had prior ICI exposure. Just three patients were on concomitant steroids.
A few patients also developed thyroid or pituitary dysfunction, which are more common side effects of ICIs.
The median age at diabetes presentation was 61 years and ranged from 32 to 82 years. The majority of patients were men, which reflects MD Anderson demographics, not a predisposing risk factor, Dr. Iyer said.
Melanoma was the most common cancer, followed by renal cell and prostate; patients had stage 2-4 disease. About half the subjects were on single agent anti-PD-1 treatment, about a third on anti-PD-1 combination treatment, and the rest on anti-PD-L1 combination therapy. C-peptide levels were below 0.9 ng/mL at diabetes diagnosis in most of the patients. Eleven of the 20 tested (55%) were positive for the pancreatic islet cell antibody GAD65.
The investigators had no disclosures. A funding source was not reported.
SOURCE: Iyer PC et al. Abstract OR05-5.
REPORTING FROM ENDO 2018
Key clinical point: Be on the lookout for new-onset diabetes when patients start immune checkpoint inhibitors.
Major finding: In all but one case, patients remained on insulin at a median follow-up of 44 weeks, even after stopping ICIs.
Study details: Review of 24 cases.
Disclosures: The investigators had no disclosures. A funding source was not reported.
Source: Iyer PC et al. Abstract OR05-5.
New and improved classifiers may sharpen thyroid nodule diagnosis
VICTORIA, B.C. – Several new and improved molecular classifiers show good performance for preoperatively assessing the nature of thyroid nodules, including histologic subsets that continue to pose diagnostic challenges, according to a trio of studies reported at the annual meeting of the American Thyroid Association.
ThyroSeq v3 classifier
In a prospective, blinded, multi-institutional study, investigators validated the ThyroSeq v3 genomic classifier, which uses next-generation sequencing to test for mutations, fusions, gene expression alterations, and copy number variations in 112 genes.
The validation cohort consisted of 234 patients from 10 centers who had thyroid nodules with Bethesda III to V cytology and known surgical outcome, with central pathology review, and successful molecular testing. In total, they had 257 fine needle aspiration samples.
Of the 247 samples from nodules having Bethesda III or IV cytology – those of greatest interest – 28% were cancer or noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP), reported senior author Yuri Nikiforov, MD, PhD, professor of pathology and director of the division of molecular & genomic pathology at the University of Pittsburgh Medical Center. “Both cancer and NIFTP are surgical diseases, so we felt they belong in one group,” he noted.
Among the Bethesda III or IV samples, ThyroSeq v3 had a sensitivity of 94%, a specificity of 82%, a positive predictive value of 66%, and a negative predictive value of 97%. Additional analyses showed that the test would still have a negative predictive value of 95% or better up to a cancer/NIFTP prevalence of 44%.
All five false-negative cases in the entire study cohort were intrathyroidal nodules of low stage and without aggressive histology.
Of the 33 false-positive cases, 68% were diagnosed on pathology as Hurthle cell or follicular adenomas, 10% were initially diagnosed by local pathologists as cancer or NIFTP, and 94% harbored clonal oncogenic molecular alterations.
“So, these are not actually hyperplasia; these are true tumors. Probably at least some of them would have the potential to progress,” said Dr. Nikiforov. “I believe that this so-called false-positive rate may not be really false positive. This is a rate of detection of precancerous tumors, not hyperplasia, that still may require surgical excision.”
In this study, “we found very high sensitivity and negative predictive value of ThyroSeq v3, with robust negative predictive value in populations with different disease prevalence,” he concluded. “Robust performance was achieved in many thyroid cancer types, including Hurthle cell cancer.”
All study patients underwent surgery, so it is not clear how the classifier would perform in the context of surveillance, he acknowledged. But the 97% negative predictive value gives confidence for patients having a negative result.
“Those patients very likely can be observed – not necessarily dismissed from medical surveillance, but observed – and could probably avoid surgery,” he said. “If patients have a positive test, it will depend on the type of mutation, because some of them confer a high risk and others confer low risk. So, there may be a spectrum of management based on combination of clinical parameters and molecular testing. But those are more likely to be surgical candidates.”
“This is a study that is desperately needed in this field,” session attendee Bryan McIver, MD, PhD, an endocrinologist and deputy physician-in-chief at the Moffitt Cancer Center in Tampa, said in an interview. “These are very challenging studies to do, because the marketing of these molecular tests has run ahead of a lot of the clinical studies.
“It’s very hard in the United States, at least, to find patients who are truly naive to molecular testing whom you can take to the operating room,” he explained. “And if you can’t take patients with a negative molecular test to the operating room, then you can’t actually calculate the true sensitivity and specificity of the test, and the whole evaluation of the test starts to become skewed.”
According to Dr. McIver, this study is noteworthy in that it largely fulfills four key criteria: There were no post hoc sample exclusions after unblinding of data, both pathology evaluation and decision to operate were blinded to classifier results, and patients were generally unselected, with little to no prior molecular testing.
“So, we actually have a proper high-quality validation study now available for this new test, the ThyroSeq v3,” he noted. “That sets the bar where it needed to be set a long time ago, and I can’t begin to tell you how excited I am to finally have a test that passed that bar. The fact that it shows a negative predictive value of 97% in this clinical study and a positive predictive value in the mid-60% range means that there is a potential for a clinical utility there that is backed by solid science. In this field, that’s almost unique.”
Afirma GSC with Hurthle classifiers
In a second study, investigators led by Quan-Yang Duh, MD, professor of surgery, division of general surgery, and chief, section of endocrine surgery, University of California, San Francisco, developed and validated a pair of classifiers to enhance performance of the Afirma platform among Hurthle cell specimens.
“The Hurthle cell lesions tend to give us trouble,” Dr. Duh said. On molecular analysis, those that are malignant seldom harbor mutations that would aid diagnosis, whereas those that are benign are usually classified as suspicious by the original Afirma Gene Expression Classifier (GEC).
“The specific group that is causing trouble are those that are Hurthle cell but not neoplasm, because they are the ones that give you the false positives,” Dr. Duh said. Therefore, it makes sense to stratify lesions on both of these factors, and then subject that specific subset to a more stringent threshold.
The investigators developed two classifiers that work with the Afirma core Genomic Sequencing Classifier (GSC), which uses RNA sequencing and machine learning algorithms.
The first classifier uses differential expression of 1,408 genes to determine whether a sample contains Hurthle cells. The second classifier, applied only to lesions containing Hurthle cells, uses differential expression of 2,041 genes and assesses loss of heterozygosity – which is prevalent in Hurthle cell neoplasms – to determine whether a Hurthle cell lesion is a neoplasm.
The ensemble model then makes a final classification, using a higher threshold for suspicious lesions determined to be Hurthle cell but not neoplasm, and a normal threshold for all the rest.
The investigators validated the Afirma GSC with the two classifiers in blinded fashion using 186 thyroid lesion samples having Bethesda III or IV cytology that had been part of the overall multicenter validation of the original Afirma GEC (N Engl J Med. 2012 Aug 23;367[8]:705-15).
Among the 26 Hurthle cell lesions, specificity for identifying benign lesions improved from 11.8% with the original Afirma GEC to 58.8% with the Afirma GSC and new classifiers. That was an absolute gain of 47% (P = .012), Dr. Duh reported. Sensitivity for identifying cancer was 88.9%.
There were also smaller absolute gains in specificity of 18% among all lesions in the cohort (P = .0028) and 14% among non-Hurthle lesions (P = .028).
“The new GSC test has significantly improved specificity in the patients with Bethesda III and IV specimens with Hurthle cells, and this may reduce unnecessary diagnostic surgery,” said Dr. Duh. “Basically, there are fewer false positives and more patients who can be called benign in the Hurthle cell group who would not need an operation.”
Further validation is needed, he acknowledged. “For a while, I wouldn’t send my Hurthle cell aspirate patients for Afirma, because I knew it was going to come back suspicious. I think I will start to do it now, but we need to see what the answers look like” with additional validation.
Afirma GSC with medullary thyroid cancer classifier
In a third study, investigators developed and validated a classifier for medullary thyroid cancer to be used with the Afirma GSC. They were led by Gregory Randolph, MD, professor of otolaryngology and the Claire and John Bertucci Endowed Chair in Thyroid Surgical Oncology at Harvard Medical School, and division chief of the general and thyroid/parathyroid endocrine surgical divisions at the Massachusetts Eye and Ear Infirmary, Boston.
Better preoperative identification of this cancer is key for several reasons, he maintained.
Establishing the diagnosis from needle biopsy is challenging, because some features overlap with those of other thyroid lesions, according to Dr. Randolph. In about a third of patients with medullary thyroid cancer brought to the operating room, the diagnosis is unknown at the time, and that often results in inadequate initial surgery.
The investigators developed a medullary thyroid cancer classifier cassette that assesses differential expression of 108 genes. They then performed blinded, independent validation in a cohort of 211 fine-needle aspiration samples from thyroid nodules: 21 medullary thyroid cancers and 190 other benign and malignant neoplasms.
Results showed that the Afirma GSC with the medullary thyroid cancer classifier had sensitivity of 100% and specificity of 100%, reported Dr. Randolph.
“The Afirma GSC medullary thyroid cancer testing cassette, within the larger GSC system, uses RNA sequencing and advanced machine learning to improve the diagnostic detection of medullary thyroid cancer, which currently misses approximately a third of medullary thyroid cancer patients,” he said.
Session attendees wondered which patients are appropriate candidates and how much the test will cost.
“We have to have a discussion about that, because the missed medullaries are, frankly, widely distributed – they can be in any of the Bethesda categories, basically,” Dr. Randolph said. “So, there are cytopathologic mistakes made uniformly, including in the suspicious and frankly malignant Bethesda categories. In terms of cost, this is embedded in the GSC classifier; so, if you order that test, you will obtain this medullary cassette.”
Actual sensitivity of the classifier may ultimately be less than 100% with use in larger samples, he acknowledged. “I think a greater number of validation tests is absolutely in order. I imagine this classifier may not be perfect, but it is way better than the third we miss with just cytopathology.”
Dr. Nikiforov disclosed that he is owner of an IP for ThyroSeq, and that his laboratory has a contract to offer the test commercially. Dr. Duh disclosed that he had no relevant conflicts of interest. Dr. Randolph disclosed that he had no relevant conflicts of interest.
VICTORIA, B.C. – Several new and improved molecular classifiers show good performance for preoperatively assessing the nature of thyroid nodules, including histologic subsets that continue to pose diagnostic challenges, according to a trio of studies reported at the annual meeting of the American Thyroid Association.
ThyroSeq v3 classifier
In a prospective, blinded, multi-institutional study, investigators validated the ThyroSeq v3 genomic classifier, which uses next-generation sequencing to test for mutations, fusions, gene expression alterations, and copy number variations in 112 genes.
The validation cohort consisted of 234 patients from 10 centers who had thyroid nodules with Bethesda III to V cytology and known surgical outcome, with central pathology review, and successful molecular testing. In total, they had 257 fine needle aspiration samples.
Of the 247 samples from nodules having Bethesda III or IV cytology – those of greatest interest – 28% were cancer or noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP), reported senior author Yuri Nikiforov, MD, PhD, professor of pathology and director of the division of molecular & genomic pathology at the University of Pittsburgh Medical Center. “Both cancer and NIFTP are surgical diseases, so we felt they belong in one group,” he noted.
Among the Bethesda III or IV samples, ThyroSeq v3 had a sensitivity of 94%, a specificity of 82%, a positive predictive value of 66%, and a negative predictive value of 97%. Additional analyses showed that the test would still have a negative predictive value of 95% or better up to a cancer/NIFTP prevalence of 44%.
All five false-negative cases in the entire study cohort were intrathyroidal nodules of low stage and without aggressive histology.
Of the 33 false-positive cases, 68% were diagnosed on pathology as Hurthle cell or follicular adenomas, 10% were initially diagnosed by local pathologists as cancer or NIFTP, and 94% harbored clonal oncogenic molecular alterations.
“So, these are not actually hyperplasia; these are true tumors. Probably at least some of them would have the potential to progress,” said Dr. Nikiforov. “I believe that this so-called false-positive rate may not be really false positive. This is a rate of detection of precancerous tumors, not hyperplasia, that still may require surgical excision.”
In this study, “we found very high sensitivity and negative predictive value of ThyroSeq v3, with robust negative predictive value in populations with different disease prevalence,” he concluded. “Robust performance was achieved in many thyroid cancer types, including Hurthle cell cancer.”
All study patients underwent surgery, so it is not clear how the classifier would perform in the context of surveillance, he acknowledged. But the 97% negative predictive value gives confidence for patients having a negative result.
“Those patients very likely can be observed – not necessarily dismissed from medical surveillance, but observed – and could probably avoid surgery,” he said. “If patients have a positive test, it will depend on the type of mutation, because some of them confer a high risk and others confer low risk. So, there may be a spectrum of management based on combination of clinical parameters and molecular testing. But those are more likely to be surgical candidates.”
“This is a study that is desperately needed in this field,” session attendee Bryan McIver, MD, PhD, an endocrinologist and deputy physician-in-chief at the Moffitt Cancer Center in Tampa, said in an interview. “These are very challenging studies to do, because the marketing of these molecular tests has run ahead of a lot of the clinical studies.
“It’s very hard in the United States, at least, to find patients who are truly naive to molecular testing whom you can take to the operating room,” he explained. “And if you can’t take patients with a negative molecular test to the operating room, then you can’t actually calculate the true sensitivity and specificity of the test, and the whole evaluation of the test starts to become skewed.”
According to Dr. McIver, this study is noteworthy in that it largely fulfills four key criteria: There were no post hoc sample exclusions after unblinding of data, both pathology evaluation and decision to operate were blinded to classifier results, and patients were generally unselected, with little to no prior molecular testing.
“So, we actually have a proper high-quality validation study now available for this new test, the ThyroSeq v3,” he noted. “That sets the bar where it needed to be set a long time ago, and I can’t begin to tell you how excited I am to finally have a test that passed that bar. The fact that it shows a negative predictive value of 97% in this clinical study and a positive predictive value in the mid-60% range means that there is a potential for a clinical utility there that is backed by solid science. In this field, that’s almost unique.”
Afirma GSC with Hurthle classifiers
In a second study, investigators led by Quan-Yang Duh, MD, professor of surgery, division of general surgery, and chief, section of endocrine surgery, University of California, San Francisco, developed and validated a pair of classifiers to enhance performance of the Afirma platform among Hurthle cell specimens.
“The Hurthle cell lesions tend to give us trouble,” Dr. Duh said. On molecular analysis, those that are malignant seldom harbor mutations that would aid diagnosis, whereas those that are benign are usually classified as suspicious by the original Afirma Gene Expression Classifier (GEC).
“The specific group that is causing trouble are those that are Hurthle cell but not neoplasm, because they are the ones that give you the false positives,” Dr. Duh said. Therefore, it makes sense to stratify lesions on both of these factors, and then subject that specific subset to a more stringent threshold.
The investigators developed two classifiers that work with the Afirma core Genomic Sequencing Classifier (GSC), which uses RNA sequencing and machine learning algorithms.
The first classifier uses differential expression of 1,408 genes to determine whether a sample contains Hurthle cells. The second classifier, applied only to lesions containing Hurthle cells, uses differential expression of 2,041 genes and assesses loss of heterozygosity – which is prevalent in Hurthle cell neoplasms – to determine whether a Hurthle cell lesion is a neoplasm.
The ensemble model then makes a final classification, using a higher threshold for suspicious lesions determined to be Hurthle cell but not neoplasm, and a normal threshold for all the rest.
The investigators validated the Afirma GSC with the two classifiers in blinded fashion using 186 thyroid lesion samples having Bethesda III or IV cytology that had been part of the overall multicenter validation of the original Afirma GEC (N Engl J Med. 2012 Aug 23;367[8]:705-15).
Among the 26 Hurthle cell lesions, specificity for identifying benign lesions improved from 11.8% with the original Afirma GEC to 58.8% with the Afirma GSC and new classifiers. That was an absolute gain of 47% (P = .012), Dr. Duh reported. Sensitivity for identifying cancer was 88.9%.
There were also smaller absolute gains in specificity of 18% among all lesions in the cohort (P = .0028) and 14% among non-Hurthle lesions (P = .028).
“The new GSC test has significantly improved specificity in the patients with Bethesda III and IV specimens with Hurthle cells, and this may reduce unnecessary diagnostic surgery,” said Dr. Duh. “Basically, there are fewer false positives and more patients who can be called benign in the Hurthle cell group who would not need an operation.”
Further validation is needed, he acknowledged. “For a while, I wouldn’t send my Hurthle cell aspirate patients for Afirma, because I knew it was going to come back suspicious. I think I will start to do it now, but we need to see what the answers look like” with additional validation.
Afirma GSC with medullary thyroid cancer classifier
In a third study, investigators developed and validated a classifier for medullary thyroid cancer to be used with the Afirma GSC. They were led by Gregory Randolph, MD, professor of otolaryngology and the Claire and John Bertucci Endowed Chair in Thyroid Surgical Oncology at Harvard Medical School, and division chief of the general and thyroid/parathyroid endocrine surgical divisions at the Massachusetts Eye and Ear Infirmary, Boston.
Better preoperative identification of this cancer is key for several reasons, he maintained.
Establishing the diagnosis from needle biopsy is challenging, because some features overlap with those of other thyroid lesions, according to Dr. Randolph. In about a third of patients with medullary thyroid cancer brought to the operating room, the diagnosis is unknown at the time, and that often results in inadequate initial surgery.
The investigators developed a medullary thyroid cancer classifier cassette that assesses differential expression of 108 genes. They then performed blinded, independent validation in a cohort of 211 fine-needle aspiration samples from thyroid nodules: 21 medullary thyroid cancers and 190 other benign and malignant neoplasms.
Results showed that the Afirma GSC with the medullary thyroid cancer classifier had sensitivity of 100% and specificity of 100%, reported Dr. Randolph.
“The Afirma GSC medullary thyroid cancer testing cassette, within the larger GSC system, uses RNA sequencing and advanced machine learning to improve the diagnostic detection of medullary thyroid cancer, which currently misses approximately a third of medullary thyroid cancer patients,” he said.
Session attendees wondered which patients are appropriate candidates and how much the test will cost.
“We have to have a discussion about that, because the missed medullaries are, frankly, widely distributed – they can be in any of the Bethesda categories, basically,” Dr. Randolph said. “So, there are cytopathologic mistakes made uniformly, including in the suspicious and frankly malignant Bethesda categories. In terms of cost, this is embedded in the GSC classifier; so, if you order that test, you will obtain this medullary cassette.”
Actual sensitivity of the classifier may ultimately be less than 100% with use in larger samples, he acknowledged. “I think a greater number of validation tests is absolutely in order. I imagine this classifier may not be perfect, but it is way better than the third we miss with just cytopathology.”
Dr. Nikiforov disclosed that he is owner of an IP for ThyroSeq, and that his laboratory has a contract to offer the test commercially. Dr. Duh disclosed that he had no relevant conflicts of interest. Dr. Randolph disclosed that he had no relevant conflicts of interest.
VICTORIA, B.C. – Several new and improved molecular classifiers show good performance for preoperatively assessing the nature of thyroid nodules, including histologic subsets that continue to pose diagnostic challenges, according to a trio of studies reported at the annual meeting of the American Thyroid Association.
ThyroSeq v3 classifier
In a prospective, blinded, multi-institutional study, investigators validated the ThyroSeq v3 genomic classifier, which uses next-generation sequencing to test for mutations, fusions, gene expression alterations, and copy number variations in 112 genes.
The validation cohort consisted of 234 patients from 10 centers who had thyroid nodules with Bethesda III to V cytology and known surgical outcome, with central pathology review, and successful molecular testing. In total, they had 257 fine needle aspiration samples.
Of the 247 samples from nodules having Bethesda III or IV cytology – those of greatest interest – 28% were cancer or noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP), reported senior author Yuri Nikiforov, MD, PhD, professor of pathology and director of the division of molecular & genomic pathology at the University of Pittsburgh Medical Center. “Both cancer and NIFTP are surgical diseases, so we felt they belong in one group,” he noted.
Among the Bethesda III or IV samples, ThyroSeq v3 had a sensitivity of 94%, a specificity of 82%, a positive predictive value of 66%, and a negative predictive value of 97%. Additional analyses showed that the test would still have a negative predictive value of 95% or better up to a cancer/NIFTP prevalence of 44%.
All five false-negative cases in the entire study cohort were intrathyroidal nodules of low stage and without aggressive histology.
Of the 33 false-positive cases, 68% were diagnosed on pathology as Hurthle cell or follicular adenomas, 10% were initially diagnosed by local pathologists as cancer or NIFTP, and 94% harbored clonal oncogenic molecular alterations.
“So, these are not actually hyperplasia; these are true tumors. Probably at least some of them would have the potential to progress,” said Dr. Nikiforov. “I believe that this so-called false-positive rate may not be really false positive. This is a rate of detection of precancerous tumors, not hyperplasia, that still may require surgical excision.”
In this study, “we found very high sensitivity and negative predictive value of ThyroSeq v3, with robust negative predictive value in populations with different disease prevalence,” he concluded. “Robust performance was achieved in many thyroid cancer types, including Hurthle cell cancer.”
All study patients underwent surgery, so it is not clear how the classifier would perform in the context of surveillance, he acknowledged. But the 97% negative predictive value gives confidence for patients having a negative result.
“Those patients very likely can be observed – not necessarily dismissed from medical surveillance, but observed – and could probably avoid surgery,” he said. “If patients have a positive test, it will depend on the type of mutation, because some of them confer a high risk and others confer low risk. So, there may be a spectrum of management based on combination of clinical parameters and molecular testing. But those are more likely to be surgical candidates.”
“This is a study that is desperately needed in this field,” session attendee Bryan McIver, MD, PhD, an endocrinologist and deputy physician-in-chief at the Moffitt Cancer Center in Tampa, said in an interview. “These are very challenging studies to do, because the marketing of these molecular tests has run ahead of a lot of the clinical studies.
“It’s very hard in the United States, at least, to find patients who are truly naive to molecular testing whom you can take to the operating room,” he explained. “And if you can’t take patients with a negative molecular test to the operating room, then you can’t actually calculate the true sensitivity and specificity of the test, and the whole evaluation of the test starts to become skewed.”
According to Dr. McIver, this study is noteworthy in that it largely fulfills four key criteria: There were no post hoc sample exclusions after unblinding of data, both pathology evaluation and decision to operate were blinded to classifier results, and patients were generally unselected, with little to no prior molecular testing.
“So, we actually have a proper high-quality validation study now available for this new test, the ThyroSeq v3,” he noted. “That sets the bar where it needed to be set a long time ago, and I can’t begin to tell you how excited I am to finally have a test that passed that bar. The fact that it shows a negative predictive value of 97% in this clinical study and a positive predictive value in the mid-60% range means that there is a potential for a clinical utility there that is backed by solid science. In this field, that’s almost unique.”
Afirma GSC with Hurthle classifiers
In a second study, investigators led by Quan-Yang Duh, MD, professor of surgery, division of general surgery, and chief, section of endocrine surgery, University of California, San Francisco, developed and validated a pair of classifiers to enhance performance of the Afirma platform among Hurthle cell specimens.
“The Hurthle cell lesions tend to give us trouble,” Dr. Duh said. On molecular analysis, those that are malignant seldom harbor mutations that would aid diagnosis, whereas those that are benign are usually classified as suspicious by the original Afirma Gene Expression Classifier (GEC).
“The specific group that is causing trouble are those that are Hurthle cell but not neoplasm, because they are the ones that give you the false positives,” Dr. Duh said. Therefore, it makes sense to stratify lesions on both of these factors, and then subject that specific subset to a more stringent threshold.
The investigators developed two classifiers that work with the Afirma core Genomic Sequencing Classifier (GSC), which uses RNA sequencing and machine learning algorithms.
The first classifier uses differential expression of 1,408 genes to determine whether a sample contains Hurthle cells. The second classifier, applied only to lesions containing Hurthle cells, uses differential expression of 2,041 genes and assesses loss of heterozygosity – which is prevalent in Hurthle cell neoplasms – to determine whether a Hurthle cell lesion is a neoplasm.
The ensemble model then makes a final classification, using a higher threshold for suspicious lesions determined to be Hurthle cell but not neoplasm, and a normal threshold for all the rest.
The investigators validated the Afirma GSC with the two classifiers in blinded fashion using 186 thyroid lesion samples having Bethesda III or IV cytology that had been part of the overall multicenter validation of the original Afirma GEC (N Engl J Med. 2012 Aug 23;367[8]:705-15).
Among the 26 Hurthle cell lesions, specificity for identifying benign lesions improved from 11.8% with the original Afirma GEC to 58.8% with the Afirma GSC and new classifiers. That was an absolute gain of 47% (P = .012), Dr. Duh reported. Sensitivity for identifying cancer was 88.9%.
There were also smaller absolute gains in specificity of 18% among all lesions in the cohort (P = .0028) and 14% among non-Hurthle lesions (P = .028).
“The new GSC test has significantly improved specificity in the patients with Bethesda III and IV specimens with Hurthle cells, and this may reduce unnecessary diagnostic surgery,” said Dr. Duh. “Basically, there are fewer false positives and more patients who can be called benign in the Hurthle cell group who would not need an operation.”
Further validation is needed, he acknowledged. “For a while, I wouldn’t send my Hurthle cell aspirate patients for Afirma, because I knew it was going to come back suspicious. I think I will start to do it now, but we need to see what the answers look like” with additional validation.
Afirma GSC with medullary thyroid cancer classifier
In a third study, investigators developed and validated a classifier for medullary thyroid cancer to be used with the Afirma GSC. They were led by Gregory Randolph, MD, professor of otolaryngology and the Claire and John Bertucci Endowed Chair in Thyroid Surgical Oncology at Harvard Medical School, and division chief of the general and thyroid/parathyroid endocrine surgical divisions at the Massachusetts Eye and Ear Infirmary, Boston.
Better preoperative identification of this cancer is key for several reasons, he maintained.
Establishing the diagnosis from needle biopsy is challenging, because some features overlap with those of other thyroid lesions, according to Dr. Randolph. In about a third of patients with medullary thyroid cancer brought to the operating room, the diagnosis is unknown at the time, and that often results in inadequate initial surgery.
The investigators developed a medullary thyroid cancer classifier cassette that assesses differential expression of 108 genes. They then performed blinded, independent validation in a cohort of 211 fine-needle aspiration samples from thyroid nodules: 21 medullary thyroid cancers and 190 other benign and malignant neoplasms.
Results showed that the Afirma GSC with the medullary thyroid cancer classifier had sensitivity of 100% and specificity of 100%, reported Dr. Randolph.
“The Afirma GSC medullary thyroid cancer testing cassette, within the larger GSC system, uses RNA sequencing and advanced machine learning to improve the diagnostic detection of medullary thyroid cancer, which currently misses approximately a third of medullary thyroid cancer patients,” he said.
Session attendees wondered which patients are appropriate candidates and how much the test will cost.
“We have to have a discussion about that, because the missed medullaries are, frankly, widely distributed – they can be in any of the Bethesda categories, basically,” Dr. Randolph said. “So, there are cytopathologic mistakes made uniformly, including in the suspicious and frankly malignant Bethesda categories. In terms of cost, this is embedded in the GSC classifier; so, if you order that test, you will obtain this medullary cassette.”
Actual sensitivity of the classifier may ultimately be less than 100% with use in larger samples, he acknowledged. “I think a greater number of validation tests is absolutely in order. I imagine this classifier may not be perfect, but it is way better than the third we miss with just cytopathology.”
Dr. Nikiforov disclosed that he is owner of an IP for ThyroSeq, and that his laboratory has a contract to offer the test commercially. Dr. Duh disclosed that he had no relevant conflicts of interest. Dr. Randolph disclosed that he had no relevant conflicts of interest.
AT ATA 2017
Key clinical point:
Major finding: ThyroSeq v3 had a negative predictive value of 97%. Specificity was an absolute 47% greater for Afirma GSC with Hurthle-specific classifiers than for Afirma GEC. The Afirma GSC with a medullary thyroid cancer classifier had 100% sensitivity and specificity.
Data source: Validation studies of the ThyroSeq v3 classifier (257 samples), the Afirma GSC with Hurthle-specific classifiers (186 samples), and the Afirma GSC with a medullary thyroid cancer classifier (211 samples).
Disclosures: Dr. Nikiforov disclosed that he is owner of an IP for ThyroSeq, and that his laboratory has a contract to offer the test commercially. Dr. Duh disclosed that he had no relevant conflicts of interest. Dr. Randolph disclosed that he had no relevant conflicts of interest.