User login
Without PrEP, a third of new HIV cases occur in MSM at low risk
Nearly one in three gay and bisexual men who were diagnosed with HIV at U.K. sexual health clinics didn’t meet the criteria for “high risk” that would signal to a clinician that they would be good candidates for pre-exposure prophylaxis (PrEP).
And that means that people who appear lower risk may still be good candidates for the HIV prevention pills, said Ann Sullivan, MD, consulting physician at Chelsea and Westminster Hospital, London.
“If people are coming forward for PrEP, they have self-identified that they need PrEP, [and] we should be allowing them to take PrEP,” said Dr. Sullivan at the 18th European AIDS Society Conference (EACS 2021). “We just need to trust patients. People know their risk, and we just have to accept that they know what they need best.”
And while this trial was made up of 95% gay and bisexual men, that ethos applies to every other group that could benefit from PrEP, including cisgender and transgender women and other gender-diverse people, Latinos, and Black Americans. In the United States, these groups make up nearly half of those who could benefit from PrEP under older guidelines but account for just 8% of people currently taking PrEP.
The finding also reinforces growing calls from health care providers to reduce gatekeeping around PrEP. For instance, there’s a move underway by the U.S. Centers for Disease Control and Prevention, where drafts of updated PrEP guidelines call for clinicians to talk to any sexually active teenager and adult about PrEP.
For the PrEP Impact trial, gay and bisexual men who received sexual health care at UK National Health Service sexual health clinics were invited to enroll in the study based on national PrEP guidelines. Those guidelines included being a cisgender man who had had sex with men not currently living with HIV and reporting condomless anal sex in the last 3 months; having a male partner whose HIV status they don’t know or who doesn’t have an undetectable viral load and with whom they’ve had condomless anal sex; or someone who doesn’t reach those criteria but whom the clinician thinks would be a good candidate.
Between Oct. 2017 and Feb. 2020, a total of 17,770 gay and bisexual men and 503 transgender or nonbinary people enrolled in the trial and were paired with 97,098 gay and bisexual men who didn’t use PrEP. (Data from the transgender participants were reported in a separate presentation.) The median age was 27 years, with 14.4% of the cisgender gay men between the ages of 16 and 24. Three out of four cis men were White, most lived in London, and more than half came from very-low-income neighborhoods.
Participants and controls were assessed for whether they were at particularly high risk for acquiring HIV, such as having used PrEP, having had two or more HIV tests, having had a rectal bacterial sexually transmitted infection (STI), or having had contact with someone with HIV or syphilis.
At the end of Feb. 2020, 24 cisgender men on PrEP had acquired HIV compared with 670 in the control group – an 87% reduction in HIV acquisition. Only one of those 24 cis men had lab-confirmed high adherence to PrEP. However, because the hair samples used to judge drug concentration weren’t long enough, Dr. Sullivan and colleagues were unable to assess whether the person really was fully adherent to treatment for the length of the trial.
But when they looked at the assessed behavior of people who acquired HIV, the two groups diverged. While a full 92% of people using PrEP had had STI diagnoses and other markers of increased risk, that was true for only 71% of people not taking PrEP. That meant, Dr. Sullivan said in an interview, that screening guidelines for PrEP were missing 29% of people with low assessed risk for HIV who nevertheless acquired the virus.
The findings led Antonio Urbina, MD, who both prescribes PrEP and manages Mount Sinai Medical Center’s PrEP program in New York, to the same conclusion that Dr. Sullivan and her team came to: that no screener is going to account for everything, and that there may be things that patients don’t want to tell their clinicians about their risk, either because of their own internalized stigma or their calculation that they aren’t comfortable enough with their providers to be honest.
“It reinforces to me that I need to ask more open-ended questions regarding risk and then just talk more about PrEP,” said Dr. Urbina, professor of medicine at Icahn School of Medicine. “Risk is dynamic and changes. And the great thing about PrEP is that if the risk goes up or down, if you have PrEP on board, you maintain this protection against HIV.”
An accompanying presentation on the transgender and nonbinary participants in the Impact Trial found that just one of 503 PrEP users acquired HIV. But here, too, there were people who could have benefited from PrEP but didn’t take it: Of the 477 trans and nonbinary participants who acted as controls, 97 were eligible by current guidelines but didn’t take PrEP. One in four of those declined the offer to take PrEP; the rest weren’t able to take it because they lived outside the treatment area. That, combined with a significantly lower likelihood that Black trans and nonbinary people took PrEP, indicated that work needs to be done to address the needs of people geographically and ethnically.
The data on gay men also raised the “who’s left out” issue for Gina Simoncini, MD, medical director for the Philadelphia AIDS Healthcare Foundation Healthcare Center. Dr. Simoncini previously taught attending physicians at Temple University how to prescribe PrEP and has done many grand rounds for primary care providers on how to manage PrEP.
“My biggest issue with this data is: What about the people who aren’t going to sexual health clinics?” she said. “What about the kid who’s 16 and maybe just barely putting his feet into the waters of sex and doesn’t feel quite comfortable going to a sexual health clinic? What about the trans Indian girl who can’t get to sexual health clinics because of family stigma and cultural stigma? The more we move toward primary care, the more people need to get on board with this.”
Dr. Sullivan reports no relevant financial relationships. Dr. Simoncini is an employee of AIDS Healthcare Foundation and has received advisory board fees from ViiV Healthcare. Dr. Urbina sits on the scientific advisory councils for Gilead Sciences, ViiV Healthcare, and Merck.
A version of this article first appeared on Medscape.com.
Nearly one in three gay and bisexual men who were diagnosed with HIV at U.K. sexual health clinics didn’t meet the criteria for “high risk” that would signal to a clinician that they would be good candidates for pre-exposure prophylaxis (PrEP).
And that means that people who appear lower risk may still be good candidates for the HIV prevention pills, said Ann Sullivan, MD, consulting physician at Chelsea and Westminster Hospital, London.
“If people are coming forward for PrEP, they have self-identified that they need PrEP, [and] we should be allowing them to take PrEP,” said Dr. Sullivan at the 18th European AIDS Society Conference (EACS 2021). “We just need to trust patients. People know their risk, and we just have to accept that they know what they need best.”
And while this trial was made up of 95% gay and bisexual men, that ethos applies to every other group that could benefit from PrEP, including cisgender and transgender women and other gender-diverse people, Latinos, and Black Americans. In the United States, these groups make up nearly half of those who could benefit from PrEP under older guidelines but account for just 8% of people currently taking PrEP.
The finding also reinforces growing calls from health care providers to reduce gatekeeping around PrEP. For instance, there’s a move underway by the U.S. Centers for Disease Control and Prevention, where drafts of updated PrEP guidelines call for clinicians to talk to any sexually active teenager and adult about PrEP.
For the PrEP Impact trial, gay and bisexual men who received sexual health care at UK National Health Service sexual health clinics were invited to enroll in the study based on national PrEP guidelines. Those guidelines included being a cisgender man who had had sex with men not currently living with HIV and reporting condomless anal sex in the last 3 months; having a male partner whose HIV status they don’t know or who doesn’t have an undetectable viral load and with whom they’ve had condomless anal sex; or someone who doesn’t reach those criteria but whom the clinician thinks would be a good candidate.
Between Oct. 2017 and Feb. 2020, a total of 17,770 gay and bisexual men and 503 transgender or nonbinary people enrolled in the trial and were paired with 97,098 gay and bisexual men who didn’t use PrEP. (Data from the transgender participants were reported in a separate presentation.) The median age was 27 years, with 14.4% of the cisgender gay men between the ages of 16 and 24. Three out of four cis men were White, most lived in London, and more than half came from very-low-income neighborhoods.
Participants and controls were assessed for whether they were at particularly high risk for acquiring HIV, such as having used PrEP, having had two or more HIV tests, having had a rectal bacterial sexually transmitted infection (STI), or having had contact with someone with HIV or syphilis.
At the end of Feb. 2020, 24 cisgender men on PrEP had acquired HIV compared with 670 in the control group – an 87% reduction in HIV acquisition. Only one of those 24 cis men had lab-confirmed high adherence to PrEP. However, because the hair samples used to judge drug concentration weren’t long enough, Dr. Sullivan and colleagues were unable to assess whether the person really was fully adherent to treatment for the length of the trial.
But when they looked at the assessed behavior of people who acquired HIV, the two groups diverged. While a full 92% of people using PrEP had had STI diagnoses and other markers of increased risk, that was true for only 71% of people not taking PrEP. That meant, Dr. Sullivan said in an interview, that screening guidelines for PrEP were missing 29% of people with low assessed risk for HIV who nevertheless acquired the virus.
The findings led Antonio Urbina, MD, who both prescribes PrEP and manages Mount Sinai Medical Center’s PrEP program in New York, to the same conclusion that Dr. Sullivan and her team came to: that no screener is going to account for everything, and that there may be things that patients don’t want to tell their clinicians about their risk, either because of their own internalized stigma or their calculation that they aren’t comfortable enough with their providers to be honest.
“It reinforces to me that I need to ask more open-ended questions regarding risk and then just talk more about PrEP,” said Dr. Urbina, professor of medicine at Icahn School of Medicine. “Risk is dynamic and changes. And the great thing about PrEP is that if the risk goes up or down, if you have PrEP on board, you maintain this protection against HIV.”
An accompanying presentation on the transgender and nonbinary participants in the Impact Trial found that just one of 503 PrEP users acquired HIV. But here, too, there were people who could have benefited from PrEP but didn’t take it: Of the 477 trans and nonbinary participants who acted as controls, 97 were eligible by current guidelines but didn’t take PrEP. One in four of those declined the offer to take PrEP; the rest weren’t able to take it because they lived outside the treatment area. That, combined with a significantly lower likelihood that Black trans and nonbinary people took PrEP, indicated that work needs to be done to address the needs of people geographically and ethnically.
The data on gay men also raised the “who’s left out” issue for Gina Simoncini, MD, medical director for the Philadelphia AIDS Healthcare Foundation Healthcare Center. Dr. Simoncini previously taught attending physicians at Temple University how to prescribe PrEP and has done many grand rounds for primary care providers on how to manage PrEP.
“My biggest issue with this data is: What about the people who aren’t going to sexual health clinics?” she said. “What about the kid who’s 16 and maybe just barely putting his feet into the waters of sex and doesn’t feel quite comfortable going to a sexual health clinic? What about the trans Indian girl who can’t get to sexual health clinics because of family stigma and cultural stigma? The more we move toward primary care, the more people need to get on board with this.”
Dr. Sullivan reports no relevant financial relationships. Dr. Simoncini is an employee of AIDS Healthcare Foundation and has received advisory board fees from ViiV Healthcare. Dr. Urbina sits on the scientific advisory councils for Gilead Sciences, ViiV Healthcare, and Merck.
A version of this article first appeared on Medscape.com.
Nearly one in three gay and bisexual men who were diagnosed with HIV at U.K. sexual health clinics didn’t meet the criteria for “high risk” that would signal to a clinician that they would be good candidates for pre-exposure prophylaxis (PrEP).
And that means that people who appear lower risk may still be good candidates for the HIV prevention pills, said Ann Sullivan, MD, consulting physician at Chelsea and Westminster Hospital, London.
“If people are coming forward for PrEP, they have self-identified that they need PrEP, [and] we should be allowing them to take PrEP,” said Dr. Sullivan at the 18th European AIDS Society Conference (EACS 2021). “We just need to trust patients. People know their risk, and we just have to accept that they know what they need best.”
And while this trial was made up of 95% gay and bisexual men, that ethos applies to every other group that could benefit from PrEP, including cisgender and transgender women and other gender-diverse people, Latinos, and Black Americans. In the United States, these groups make up nearly half of those who could benefit from PrEP under older guidelines but account for just 8% of people currently taking PrEP.
The finding also reinforces growing calls from health care providers to reduce gatekeeping around PrEP. For instance, there’s a move underway by the U.S. Centers for Disease Control and Prevention, where drafts of updated PrEP guidelines call for clinicians to talk to any sexually active teenager and adult about PrEP.
For the PrEP Impact trial, gay and bisexual men who received sexual health care at UK National Health Service sexual health clinics were invited to enroll in the study based on national PrEP guidelines. Those guidelines included being a cisgender man who had had sex with men not currently living with HIV and reporting condomless anal sex in the last 3 months; having a male partner whose HIV status they don’t know or who doesn’t have an undetectable viral load and with whom they’ve had condomless anal sex; or someone who doesn’t reach those criteria but whom the clinician thinks would be a good candidate.
Between Oct. 2017 and Feb. 2020, a total of 17,770 gay and bisexual men and 503 transgender or nonbinary people enrolled in the trial and were paired with 97,098 gay and bisexual men who didn’t use PrEP. (Data from the transgender participants were reported in a separate presentation.) The median age was 27 years, with 14.4% of the cisgender gay men between the ages of 16 and 24. Three out of four cis men were White, most lived in London, and more than half came from very-low-income neighborhoods.
Participants and controls were assessed for whether they were at particularly high risk for acquiring HIV, such as having used PrEP, having had two or more HIV tests, having had a rectal bacterial sexually transmitted infection (STI), or having had contact with someone with HIV or syphilis.
At the end of Feb. 2020, 24 cisgender men on PrEP had acquired HIV compared with 670 in the control group – an 87% reduction in HIV acquisition. Only one of those 24 cis men had lab-confirmed high adherence to PrEP. However, because the hair samples used to judge drug concentration weren’t long enough, Dr. Sullivan and colleagues were unable to assess whether the person really was fully adherent to treatment for the length of the trial.
But when they looked at the assessed behavior of people who acquired HIV, the two groups diverged. While a full 92% of people using PrEP had had STI diagnoses and other markers of increased risk, that was true for only 71% of people not taking PrEP. That meant, Dr. Sullivan said in an interview, that screening guidelines for PrEP were missing 29% of people with low assessed risk for HIV who nevertheless acquired the virus.
The findings led Antonio Urbina, MD, who both prescribes PrEP and manages Mount Sinai Medical Center’s PrEP program in New York, to the same conclusion that Dr. Sullivan and her team came to: that no screener is going to account for everything, and that there may be things that patients don’t want to tell their clinicians about their risk, either because of their own internalized stigma or their calculation that they aren’t comfortable enough with their providers to be honest.
“It reinforces to me that I need to ask more open-ended questions regarding risk and then just talk more about PrEP,” said Dr. Urbina, professor of medicine at Icahn School of Medicine. “Risk is dynamic and changes. And the great thing about PrEP is that if the risk goes up or down, if you have PrEP on board, you maintain this protection against HIV.”
An accompanying presentation on the transgender and nonbinary participants in the Impact Trial found that just one of 503 PrEP users acquired HIV. But here, too, there were people who could have benefited from PrEP but didn’t take it: Of the 477 trans and nonbinary participants who acted as controls, 97 were eligible by current guidelines but didn’t take PrEP. One in four of those declined the offer to take PrEP; the rest weren’t able to take it because they lived outside the treatment area. That, combined with a significantly lower likelihood that Black trans and nonbinary people took PrEP, indicated that work needs to be done to address the needs of people geographically and ethnically.
The data on gay men also raised the “who’s left out” issue for Gina Simoncini, MD, medical director for the Philadelphia AIDS Healthcare Foundation Healthcare Center. Dr. Simoncini previously taught attending physicians at Temple University how to prescribe PrEP and has done many grand rounds for primary care providers on how to manage PrEP.
“My biggest issue with this data is: What about the people who aren’t going to sexual health clinics?” she said. “What about the kid who’s 16 and maybe just barely putting his feet into the waters of sex and doesn’t feel quite comfortable going to a sexual health clinic? What about the trans Indian girl who can’t get to sexual health clinics because of family stigma and cultural stigma? The more we move toward primary care, the more people need to get on board with this.”
Dr. Sullivan reports no relevant financial relationships. Dr. Simoncini is an employee of AIDS Healthcare Foundation and has received advisory board fees from ViiV Healthcare. Dr. Urbina sits on the scientific advisory councils for Gilead Sciences, ViiV Healthcare, and Merck.
A version of this article first appeared on Medscape.com.
Long-acting HIV ART: Lessons from a year of Cabenuva
One year into offering the first long-acting injectable HIV treatment to his patients, Jonathan Angel, MD, head of the division of infectious diseases at the University of Ottawa, reported that 15 of the 21 of patients who started on the regimen are still taking it, all with viral suppression. Those who weren’t cited a combination of inconvenience, injection site pain, and “injection fatigue.”
These are just a few things HIV providers are learning as they begin what Chloe Orkin, MD, professor of HIV medicine at Queen Mary University of London, called a paradigm shift to long-acting treatment, which may soon include not just shots but rings, implants, and microarray patches.
“It’s a paradigm shift, and we are at the very beginning of this paradigm shift,” said Dr. Orkin, commenting during the discussion session of the European AIDS Clinical Society 2021 annual meeting. “We’re having to change our model, and it’s challenging.”
In the United States, the Food and Drug Administration approved the first long-acting injectable, a combination of cabotegravir and rilpivirine (CAB/RIL; Cabenuva, ViiV Healthcare) in January 2021. But it has been approved in Canada since March 2020 and available at Dr. Angel’s clinic since November 2020. It’s also available in Canada as an every-other-month shot. Injected into the buttocks, the shot was found to be noninferior to standard daily oral treatment in many studies, including the ATLAS, the ATLAS-2M – which tested the every-other-month approach – and FLAIR trials.
Dr. Angel’s clinic was part of all three of those trials, so his clinic has had 5 years’ experience preparing for the change in workflow and the new approach the shots require.
Of the 21 people Dr. Angel has treated, 11 were white Canadians, nine were Black African, and one was Indigenous Canadian, with women making up a third of the participants. Median age was 51 years, and all patients had had undetectable viral loads before beginning the regimen. (Studies of the drug’s effectiveness in people who struggle to take daily pills are still ongoing.)
Most of those 21 patients had had undetectable viral loads for more than 5 years, but a few had been undetectable for only 6 months before beginning the shots. Their immune systems were also healthy, with a median CD4 count of 618 cells/mcL. As in the clinical trials, none of the participants had experienced antiretroviral treatment failure. Because public health insurers in Canada have yet to approve the shots, Dr. Angel’s patients receiving Cabenuva also have private health insurance. Up to 90% of people in Canada receive pharmaceutical coverage through public insurance; therefore, the shot is not yet widely available.
Twenty patients switched from integrase-inhibitor regimens, and one had been receiving a nonnucleoside reverse transcriptase inhibitor–based regimen before starting Cabenuva.
And although the drug has not been approved for shot initiation this way, two patients requested – and Dr. Angel agreed – to start them on the shots without first doing a month of daily pills to check for safety.
“This is my conclusion from these data: the oral lead-in period is not necessary,” Dr. Angel said in his presentation at the meeting. “It can provide some comfort to either a physician or a patient, but it does not seem to be medically necessary.”
That approach is not without data to back it up. Research presented at HIV Glasgow 2020 showed that people who switched from daily oral dolutegravir/abacavir/lamivudine straight to the injections did so without problems.
At last clinic visit, 15 of those 21 were still receiving the shots. None have experienced treatment failure, and all were still virally suppressed. Four participants left the trials and one more person opted to return to daily pills, citing some level of what Dr. Angel called “injection fatigue.”
“Just as we use the term ‘pill fatigue’ for patients who are tired of taking pills, patients do get tired of coming in monthly for their visits and injections,” he said. They find the trip to the clinic for the intramuscular injections “inconvenient,” he said.
Unlike in the United States, where Cabenuva is approved for only monthly injections, Health Canada has already approved the shot for every-other-month injections, which Dr. Angel said may reduce the odds of injection fatigue.
Dr. Angel’s presentation drew comments, questions, and excitement from the crowd. Annemarie Wensing, MD, assistant professor of medicine at University Medical Center Utrecht (the Netherlands), asked whether dispensing with the oral lead-in period could mean that these shots could be useful for people going on longer trips, people having surgeries where they can’t swallow pills, or in other scenarios.
“These are not hypothetical conversations,” Dr. Angel said. “I’m having these conversations with patients now – temporary use, they travel for 3 months and come back, can they go from injectable to oral to injectable.”
For now, he said, the answer is, “We’ll figure it out.”
Meanwhile, there’s another big question when it comes to injectables, said Marta Vas ylyev, MD, from Lviv (Ukraine) Regional AIDS Center: When will they be available to the people who might benefit most from them – people in resource-limited settings, people who so far have struggled to remember to take their pills every day?
For now, Dr. Angel replied, injectables continue to be a treatment only for those who are already doing well while receiving HIV treatment: those with already suppressed viral load, who are good at taking daily pills, and who are being treated at well-resourced clinics.
“There are huge obstacles to overcome if this is ever to be available [in resource-limited settings], and way more obstacles than there are with any oral therapies,” he said. “There’s not been much discussion here about the necessity of cold-chain requirements of pharmacies either centrally or locally, [or] the requirements of additional nurses or health care staff to administer the medication. So you’re looking at a very resource-intensive therapy, which now is fairly restrictive [as to] who will have access to it.”
Dr. Angel reports serving on advisory boards for ViiV Healthcare and Gilead Sciences and has done contract research for ViiV Healthcare, Gilead, and Merck. Dr. Orkin has received research grants, fees as a consultant, travel sponsorship, and speaker fees from ViiV, Merck, and GlaxoSmithKline. Dr. Vasylyev reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
One year into offering the first long-acting injectable HIV treatment to his patients, Jonathan Angel, MD, head of the division of infectious diseases at the University of Ottawa, reported that 15 of the 21 of patients who started on the regimen are still taking it, all with viral suppression. Those who weren’t cited a combination of inconvenience, injection site pain, and “injection fatigue.”
These are just a few things HIV providers are learning as they begin what Chloe Orkin, MD, professor of HIV medicine at Queen Mary University of London, called a paradigm shift to long-acting treatment, which may soon include not just shots but rings, implants, and microarray patches.
“It’s a paradigm shift, and we are at the very beginning of this paradigm shift,” said Dr. Orkin, commenting during the discussion session of the European AIDS Clinical Society 2021 annual meeting. “We’re having to change our model, and it’s challenging.”
In the United States, the Food and Drug Administration approved the first long-acting injectable, a combination of cabotegravir and rilpivirine (CAB/RIL; Cabenuva, ViiV Healthcare) in January 2021. But it has been approved in Canada since March 2020 and available at Dr. Angel’s clinic since November 2020. It’s also available in Canada as an every-other-month shot. Injected into the buttocks, the shot was found to be noninferior to standard daily oral treatment in many studies, including the ATLAS, the ATLAS-2M – which tested the every-other-month approach – and FLAIR trials.
Dr. Angel’s clinic was part of all three of those trials, so his clinic has had 5 years’ experience preparing for the change in workflow and the new approach the shots require.
Of the 21 people Dr. Angel has treated, 11 were white Canadians, nine were Black African, and one was Indigenous Canadian, with women making up a third of the participants. Median age was 51 years, and all patients had had undetectable viral loads before beginning the regimen. (Studies of the drug’s effectiveness in people who struggle to take daily pills are still ongoing.)
Most of those 21 patients had had undetectable viral loads for more than 5 years, but a few had been undetectable for only 6 months before beginning the shots. Their immune systems were also healthy, with a median CD4 count of 618 cells/mcL. As in the clinical trials, none of the participants had experienced antiretroviral treatment failure. Because public health insurers in Canada have yet to approve the shots, Dr. Angel’s patients receiving Cabenuva also have private health insurance. Up to 90% of people in Canada receive pharmaceutical coverage through public insurance; therefore, the shot is not yet widely available.
Twenty patients switched from integrase-inhibitor regimens, and one had been receiving a nonnucleoside reverse transcriptase inhibitor–based regimen before starting Cabenuva.
And although the drug has not been approved for shot initiation this way, two patients requested – and Dr. Angel agreed – to start them on the shots without first doing a month of daily pills to check for safety.
“This is my conclusion from these data: the oral lead-in period is not necessary,” Dr. Angel said in his presentation at the meeting. “It can provide some comfort to either a physician or a patient, but it does not seem to be medically necessary.”
That approach is not without data to back it up. Research presented at HIV Glasgow 2020 showed that people who switched from daily oral dolutegravir/abacavir/lamivudine straight to the injections did so without problems.
At last clinic visit, 15 of those 21 were still receiving the shots. None have experienced treatment failure, and all were still virally suppressed. Four participants left the trials and one more person opted to return to daily pills, citing some level of what Dr. Angel called “injection fatigue.”
“Just as we use the term ‘pill fatigue’ for patients who are tired of taking pills, patients do get tired of coming in monthly for their visits and injections,” he said. They find the trip to the clinic for the intramuscular injections “inconvenient,” he said.
Unlike in the United States, where Cabenuva is approved for only monthly injections, Health Canada has already approved the shot for every-other-month injections, which Dr. Angel said may reduce the odds of injection fatigue.
Dr. Angel’s presentation drew comments, questions, and excitement from the crowd. Annemarie Wensing, MD, assistant professor of medicine at University Medical Center Utrecht (the Netherlands), asked whether dispensing with the oral lead-in period could mean that these shots could be useful for people going on longer trips, people having surgeries where they can’t swallow pills, or in other scenarios.
“These are not hypothetical conversations,” Dr. Angel said. “I’m having these conversations with patients now – temporary use, they travel for 3 months and come back, can they go from injectable to oral to injectable.”
For now, he said, the answer is, “We’ll figure it out.”
Meanwhile, there’s another big question when it comes to injectables, said Marta Vas ylyev, MD, from Lviv (Ukraine) Regional AIDS Center: When will they be available to the people who might benefit most from them – people in resource-limited settings, people who so far have struggled to remember to take their pills every day?
For now, Dr. Angel replied, injectables continue to be a treatment only for those who are already doing well while receiving HIV treatment: those with already suppressed viral load, who are good at taking daily pills, and who are being treated at well-resourced clinics.
“There are huge obstacles to overcome if this is ever to be available [in resource-limited settings], and way more obstacles than there are with any oral therapies,” he said. “There’s not been much discussion here about the necessity of cold-chain requirements of pharmacies either centrally or locally, [or] the requirements of additional nurses or health care staff to administer the medication. So you’re looking at a very resource-intensive therapy, which now is fairly restrictive [as to] who will have access to it.”
Dr. Angel reports serving on advisory boards for ViiV Healthcare and Gilead Sciences and has done contract research for ViiV Healthcare, Gilead, and Merck. Dr. Orkin has received research grants, fees as a consultant, travel sponsorship, and speaker fees from ViiV, Merck, and GlaxoSmithKline. Dr. Vasylyev reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
One year into offering the first long-acting injectable HIV treatment to his patients, Jonathan Angel, MD, head of the division of infectious diseases at the University of Ottawa, reported that 15 of the 21 of patients who started on the regimen are still taking it, all with viral suppression. Those who weren’t cited a combination of inconvenience, injection site pain, and “injection fatigue.”
These are just a few things HIV providers are learning as they begin what Chloe Orkin, MD, professor of HIV medicine at Queen Mary University of London, called a paradigm shift to long-acting treatment, which may soon include not just shots but rings, implants, and microarray patches.
“It’s a paradigm shift, and we are at the very beginning of this paradigm shift,” said Dr. Orkin, commenting during the discussion session of the European AIDS Clinical Society 2021 annual meeting. “We’re having to change our model, and it’s challenging.”
In the United States, the Food and Drug Administration approved the first long-acting injectable, a combination of cabotegravir and rilpivirine (CAB/RIL; Cabenuva, ViiV Healthcare) in January 2021. But it has been approved in Canada since March 2020 and available at Dr. Angel’s clinic since November 2020. It’s also available in Canada as an every-other-month shot. Injected into the buttocks, the shot was found to be noninferior to standard daily oral treatment in many studies, including the ATLAS, the ATLAS-2M – which tested the every-other-month approach – and FLAIR trials.
Dr. Angel’s clinic was part of all three of those trials, so his clinic has had 5 years’ experience preparing for the change in workflow and the new approach the shots require.
Of the 21 people Dr. Angel has treated, 11 were white Canadians, nine were Black African, and one was Indigenous Canadian, with women making up a third of the participants. Median age was 51 years, and all patients had had undetectable viral loads before beginning the regimen. (Studies of the drug’s effectiveness in people who struggle to take daily pills are still ongoing.)
Most of those 21 patients had had undetectable viral loads for more than 5 years, but a few had been undetectable for only 6 months before beginning the shots. Their immune systems were also healthy, with a median CD4 count of 618 cells/mcL. As in the clinical trials, none of the participants had experienced antiretroviral treatment failure. Because public health insurers in Canada have yet to approve the shots, Dr. Angel’s patients receiving Cabenuva also have private health insurance. Up to 90% of people in Canada receive pharmaceutical coverage through public insurance; therefore, the shot is not yet widely available.
Twenty patients switched from integrase-inhibitor regimens, and one had been receiving a nonnucleoside reverse transcriptase inhibitor–based regimen before starting Cabenuva.
And although the drug has not been approved for shot initiation this way, two patients requested – and Dr. Angel agreed – to start them on the shots without first doing a month of daily pills to check for safety.
“This is my conclusion from these data: the oral lead-in period is not necessary,” Dr. Angel said in his presentation at the meeting. “It can provide some comfort to either a physician or a patient, but it does not seem to be medically necessary.”
That approach is not without data to back it up. Research presented at HIV Glasgow 2020 showed that people who switched from daily oral dolutegravir/abacavir/lamivudine straight to the injections did so without problems.
At last clinic visit, 15 of those 21 were still receiving the shots. None have experienced treatment failure, and all were still virally suppressed. Four participants left the trials and one more person opted to return to daily pills, citing some level of what Dr. Angel called “injection fatigue.”
“Just as we use the term ‘pill fatigue’ for patients who are tired of taking pills, patients do get tired of coming in monthly for their visits and injections,” he said. They find the trip to the clinic for the intramuscular injections “inconvenient,” he said.
Unlike in the United States, where Cabenuva is approved for only monthly injections, Health Canada has already approved the shot for every-other-month injections, which Dr. Angel said may reduce the odds of injection fatigue.
Dr. Angel’s presentation drew comments, questions, and excitement from the crowd. Annemarie Wensing, MD, assistant professor of medicine at University Medical Center Utrecht (the Netherlands), asked whether dispensing with the oral lead-in period could mean that these shots could be useful for people going on longer trips, people having surgeries where they can’t swallow pills, or in other scenarios.
“These are not hypothetical conversations,” Dr. Angel said. “I’m having these conversations with patients now – temporary use, they travel for 3 months and come back, can they go from injectable to oral to injectable.”
For now, he said, the answer is, “We’ll figure it out.”
Meanwhile, there’s another big question when it comes to injectables, said Marta Vas ylyev, MD, from Lviv (Ukraine) Regional AIDS Center: When will they be available to the people who might benefit most from them – people in resource-limited settings, people who so far have struggled to remember to take their pills every day?
For now, Dr. Angel replied, injectables continue to be a treatment only for those who are already doing well while receiving HIV treatment: those with already suppressed viral load, who are good at taking daily pills, and who are being treated at well-resourced clinics.
“There are huge obstacles to overcome if this is ever to be available [in resource-limited settings], and way more obstacles than there are with any oral therapies,” he said. “There’s not been much discussion here about the necessity of cold-chain requirements of pharmacies either centrally or locally, [or] the requirements of additional nurses or health care staff to administer the medication. So you’re looking at a very resource-intensive therapy, which now is fairly restrictive [as to] who will have access to it.”
Dr. Angel reports serving on advisory boards for ViiV Healthcare and Gilead Sciences and has done contract research for ViiV Healthcare, Gilead, and Merck. Dr. Orkin has received research grants, fees as a consultant, travel sponsorship, and speaker fees from ViiV, Merck, and GlaxoSmithKline. Dr. Vasylyev reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Clinicians may overprescribe clarithromycin for H. pylori
Clinicians are prescribing clarithromycin at high rates for Helicobacter pylori infections, despite increasing resistance to this antibiotic, researchers say.
In an analysis of 1 million U.S. prescriptions for H. pylori infections, 80% contained clarithromycin, said Carol Rockett, PharmD, associate vice president of RedHill Biopharma in Raleigh, N.C.
Dr. Rockett presented the findings at the annual meeting of the American College of Gastroenterology.
“Multiple talks [at the meeting] have suggested that the use of clarithromycin in H. pylori is obsolete,” she told this news organization. “Clarithromycin is particularly ineffective in people with a genetic variant that causes rapid metabolism.”
According to the 2017 ACG clinical guideline for treating H. pylori, patients diagnosed with this infection should be asked about their previous antibiotic exposure prior to treatment.
Additionally, clinicians should prescribe clarithromycin triple therapy with a proton pump inhibitor (PPI) and amoxicillin or metronidazole as a first-line treatment only in “regions where H. pylori clarithromycin resistance is known to be less than 15%” and in patients with no previous history of macrolide exposure.
The guideline puts bismuth quadruple therapy, consisting of a PPI, bismuth, tetracycline, and a nitroimidazole, at the top of its list of six alternative first-line therapies. However, three of the six alternatives include clarithromycin.
ERADICATE Hp and ERADICATE Hp2
To understand how U.S. physicians are treating patients with H. pylori, Dr. Rockett’s colleagues analyzed data from two phase 3 clinical trials of RedHill’s RHB-105 (Talicia): ERADICATE Hp and ERADICATE Hp2.
RHB-105 is an all-in‐one combination of omeprazole (40 mg), amoxicillin (1,000 mg), and rifabutin (50 mg) that the Food and Drug Administration approved for treatment of H pylori in 2019.
The researchers followed 38 subjects from ERADICATE Hp who remained positive for H. pylori after the study’s completion. A total of 33 had received a placebo in that trial, while the other 5 had received RHB-105.
The researchers obtained data on 31 of these patients. The overall cure rate was 61.3%. Of the 31 patients, 27 received a regimen including clarithromycin. Their cure rate was 59.3%.
Turning to ERADICATE Hp2, the researchers obtained data on 94 patients whose H. pylori infections persisted after the trial. Of those, 67 had received an active comparator (amoxicillin 250 mg and omeprazole 10 mg) and 27 had received RHB-105.
The overall cure rate was 56.2%. For the 48 subjects who received therapies including clarithromycin, the cure rate was 60.4%. For the 22 subjects who received a bismuth-based quadruple regimen, the cure rate was 45.4%.
In another analysis, the researchers crunched 12 months of numbers from IQVIA PharMetrics Plus medical and prescription claim database of over 1 million prescriptions for H. pylori. They found that 80% of the prescriptions made by gastroenterologists were for regimens containing clarithromycin. That proportion increased to 84% for physician assistants and internists, 85% for nurse practitioners, 86% for family practitioners, and 89% for general practitioners.
Finally, the researchers also analyzed patients for CYP2C19 gene status. They tested 65 subjects who received RHB-105 in ERADICATE Hp and all 445 subjects in ERADICATE Hp2. They found that 58.5% in ERADICATE Hp and 48.6% in ERADICATE Hp2 were normal metabolizers.
In 20 normal metabolizers who received clarithromycin, the drug eradicated the infection in 16 (80%). Out of 11 rapid metabolizers, clarithromycin eradicated the bacterium in 2 (18.2%). The difference was statistically significant (P = .0017).
“With clarithromycin, you can see that the efficacy is reduced in those patients who are rapid metabolizers,” Dr. Rockett said. “We didn’t see that with rifabutin [one of the drugs in RHB-105].”
Jared Magee, DO, MPH, a gastroenterology fellow at the Walter Reed National Military Medical Center in Bethesda, Md., said in treating H. pylori infections, he checks the patients’ medical records to see what antibiotics they have received in the past and generally begins treatment with the bismuth quadruple therapy.
“There is education needed to get the data out there that clarithromycin-based therapies may not be the right choice for patients,” he said. “There is a subset who will do well with it, but I think where we’re at now, with the frequency of macrolide prescriptions for other conditions, that clarithromycin is going to be a difficult therapy for a lot of people.”
Clinicians who are not gastroenterologists may not be aware of the guideline promulgated by the ACG, he pointed out.
Dr. Rockett is an employee of RedHill Biopharma. Dr. Magee has disclosed no relevant financial relationships. The study was funded by RedHill Biopharma.
A version of this article first appeared on Medscape.com.
Clinicians are prescribing clarithromycin at high rates for Helicobacter pylori infections, despite increasing resistance to this antibiotic, researchers say.
In an analysis of 1 million U.S. prescriptions for H. pylori infections, 80% contained clarithromycin, said Carol Rockett, PharmD, associate vice president of RedHill Biopharma in Raleigh, N.C.
Dr. Rockett presented the findings at the annual meeting of the American College of Gastroenterology.
“Multiple talks [at the meeting] have suggested that the use of clarithromycin in H. pylori is obsolete,” she told this news organization. “Clarithromycin is particularly ineffective in people with a genetic variant that causes rapid metabolism.”
According to the 2017 ACG clinical guideline for treating H. pylori, patients diagnosed with this infection should be asked about their previous antibiotic exposure prior to treatment.
Additionally, clinicians should prescribe clarithromycin triple therapy with a proton pump inhibitor (PPI) and amoxicillin or metronidazole as a first-line treatment only in “regions where H. pylori clarithromycin resistance is known to be less than 15%” and in patients with no previous history of macrolide exposure.
The guideline puts bismuth quadruple therapy, consisting of a PPI, bismuth, tetracycline, and a nitroimidazole, at the top of its list of six alternative first-line therapies. However, three of the six alternatives include clarithromycin.
ERADICATE Hp and ERADICATE Hp2
To understand how U.S. physicians are treating patients with H. pylori, Dr. Rockett’s colleagues analyzed data from two phase 3 clinical trials of RedHill’s RHB-105 (Talicia): ERADICATE Hp and ERADICATE Hp2.
RHB-105 is an all-in‐one combination of omeprazole (40 mg), amoxicillin (1,000 mg), and rifabutin (50 mg) that the Food and Drug Administration approved for treatment of H pylori in 2019.
The researchers followed 38 subjects from ERADICATE Hp who remained positive for H. pylori after the study’s completion. A total of 33 had received a placebo in that trial, while the other 5 had received RHB-105.
The researchers obtained data on 31 of these patients. The overall cure rate was 61.3%. Of the 31 patients, 27 received a regimen including clarithromycin. Their cure rate was 59.3%.
Turning to ERADICATE Hp2, the researchers obtained data on 94 patients whose H. pylori infections persisted after the trial. Of those, 67 had received an active comparator (amoxicillin 250 mg and omeprazole 10 mg) and 27 had received RHB-105.
The overall cure rate was 56.2%. For the 48 subjects who received therapies including clarithromycin, the cure rate was 60.4%. For the 22 subjects who received a bismuth-based quadruple regimen, the cure rate was 45.4%.
In another analysis, the researchers crunched 12 months of numbers from IQVIA PharMetrics Plus medical and prescription claim database of over 1 million prescriptions for H. pylori. They found that 80% of the prescriptions made by gastroenterologists were for regimens containing clarithromycin. That proportion increased to 84% for physician assistants and internists, 85% for nurse practitioners, 86% for family practitioners, and 89% for general practitioners.
Finally, the researchers also analyzed patients for CYP2C19 gene status. They tested 65 subjects who received RHB-105 in ERADICATE Hp and all 445 subjects in ERADICATE Hp2. They found that 58.5% in ERADICATE Hp and 48.6% in ERADICATE Hp2 were normal metabolizers.
In 20 normal metabolizers who received clarithromycin, the drug eradicated the infection in 16 (80%). Out of 11 rapid metabolizers, clarithromycin eradicated the bacterium in 2 (18.2%). The difference was statistically significant (P = .0017).
“With clarithromycin, you can see that the efficacy is reduced in those patients who are rapid metabolizers,” Dr. Rockett said. “We didn’t see that with rifabutin [one of the drugs in RHB-105].”
Jared Magee, DO, MPH, a gastroenterology fellow at the Walter Reed National Military Medical Center in Bethesda, Md., said in treating H. pylori infections, he checks the patients’ medical records to see what antibiotics they have received in the past and generally begins treatment with the bismuth quadruple therapy.
“There is education needed to get the data out there that clarithromycin-based therapies may not be the right choice for patients,” he said. “There is a subset who will do well with it, but I think where we’re at now, with the frequency of macrolide prescriptions for other conditions, that clarithromycin is going to be a difficult therapy for a lot of people.”
Clinicians who are not gastroenterologists may not be aware of the guideline promulgated by the ACG, he pointed out.
Dr. Rockett is an employee of RedHill Biopharma. Dr. Magee has disclosed no relevant financial relationships. The study was funded by RedHill Biopharma.
A version of this article first appeared on Medscape.com.
Clinicians are prescribing clarithromycin at high rates for Helicobacter pylori infections, despite increasing resistance to this antibiotic, researchers say.
In an analysis of 1 million U.S. prescriptions for H. pylori infections, 80% contained clarithromycin, said Carol Rockett, PharmD, associate vice president of RedHill Biopharma in Raleigh, N.C.
Dr. Rockett presented the findings at the annual meeting of the American College of Gastroenterology.
“Multiple talks [at the meeting] have suggested that the use of clarithromycin in H. pylori is obsolete,” she told this news organization. “Clarithromycin is particularly ineffective in people with a genetic variant that causes rapid metabolism.”
According to the 2017 ACG clinical guideline for treating H. pylori, patients diagnosed with this infection should be asked about their previous antibiotic exposure prior to treatment.
Additionally, clinicians should prescribe clarithromycin triple therapy with a proton pump inhibitor (PPI) and amoxicillin or metronidazole as a first-line treatment only in “regions where H. pylori clarithromycin resistance is known to be less than 15%” and in patients with no previous history of macrolide exposure.
The guideline puts bismuth quadruple therapy, consisting of a PPI, bismuth, tetracycline, and a nitroimidazole, at the top of its list of six alternative first-line therapies. However, three of the six alternatives include clarithromycin.
ERADICATE Hp and ERADICATE Hp2
To understand how U.S. physicians are treating patients with H. pylori, Dr. Rockett’s colleagues analyzed data from two phase 3 clinical trials of RedHill’s RHB-105 (Talicia): ERADICATE Hp and ERADICATE Hp2.
RHB-105 is an all-in‐one combination of omeprazole (40 mg), amoxicillin (1,000 mg), and rifabutin (50 mg) that the Food and Drug Administration approved for treatment of H pylori in 2019.
The researchers followed 38 subjects from ERADICATE Hp who remained positive for H. pylori after the study’s completion. A total of 33 had received a placebo in that trial, while the other 5 had received RHB-105.
The researchers obtained data on 31 of these patients. The overall cure rate was 61.3%. Of the 31 patients, 27 received a regimen including clarithromycin. Their cure rate was 59.3%.
Turning to ERADICATE Hp2, the researchers obtained data on 94 patients whose H. pylori infections persisted after the trial. Of those, 67 had received an active comparator (amoxicillin 250 mg and omeprazole 10 mg) and 27 had received RHB-105.
The overall cure rate was 56.2%. For the 48 subjects who received therapies including clarithromycin, the cure rate was 60.4%. For the 22 subjects who received a bismuth-based quadruple regimen, the cure rate was 45.4%.
In another analysis, the researchers crunched 12 months of numbers from IQVIA PharMetrics Plus medical and prescription claim database of over 1 million prescriptions for H. pylori. They found that 80% of the prescriptions made by gastroenterologists were for regimens containing clarithromycin. That proportion increased to 84% for physician assistants and internists, 85% for nurse practitioners, 86% for family practitioners, and 89% for general practitioners.
Finally, the researchers also analyzed patients for CYP2C19 gene status. They tested 65 subjects who received RHB-105 in ERADICATE Hp and all 445 subjects in ERADICATE Hp2. They found that 58.5% in ERADICATE Hp and 48.6% in ERADICATE Hp2 were normal metabolizers.
In 20 normal metabolizers who received clarithromycin, the drug eradicated the infection in 16 (80%). Out of 11 rapid metabolizers, clarithromycin eradicated the bacterium in 2 (18.2%). The difference was statistically significant (P = .0017).
“With clarithromycin, you can see that the efficacy is reduced in those patients who are rapid metabolizers,” Dr. Rockett said. “We didn’t see that with rifabutin [one of the drugs in RHB-105].”
Jared Magee, DO, MPH, a gastroenterology fellow at the Walter Reed National Military Medical Center in Bethesda, Md., said in treating H. pylori infections, he checks the patients’ medical records to see what antibiotics they have received in the past and generally begins treatment with the bismuth quadruple therapy.
“There is education needed to get the data out there that clarithromycin-based therapies may not be the right choice for patients,” he said. “There is a subset who will do well with it, but I think where we’re at now, with the frequency of macrolide prescriptions for other conditions, that clarithromycin is going to be a difficult therapy for a lot of people.”
Clinicians who are not gastroenterologists may not be aware of the guideline promulgated by the ACG, he pointed out.
Dr. Rockett is an employee of RedHill Biopharma. Dr. Magee has disclosed no relevant financial relationships. The study was funded by RedHill Biopharma.
A version of this article first appeared on Medscape.com.
Antidepressant may cut COVID-19–related hospitalization, mortality: TOGETHER
The antidepressant fluvoxamine (Luvox) may prevent hospitalization and death in outpatients with COVID-19, new research suggests.
Results from the placebo-controlled, multisite, phase 3 TOGETHER trial showed that in COVID-19 outpatients at high risk for complications, hospitalizations were cut by 66% and deaths were reduced by 91% in those who tolerated fluvoxamine.
“Our trial has found that fluvoxamine, an inexpensive existing drug, reduces the need for advanced disease care in this high-risk population,” wrote the investigators, led by Gilmar Reis, MD, PhD, research division, Cardresearch, Belo Horizonte, Brazil.
The findings were published online Oct. 27 in The Lancet Global Health.
Alternative mechanisms
Fluvoxamine, a selective serotonin reuptake inhibitor (SSRI), is an antidepressant commonly prescribed for obsessive-compulsive disorder.
Besides its known effects on serotonin, the drug acts in other molecular pathways to dampen the production of inflammatory cytokines. Those alternative mechanisms are the ones believed to help patients with COVID-19, said coinvestigator Angela Reiersen, MD, child psychiatrist at Washington University, St. Louis.
Based on cell culture and mouse studies showing effects of the molecule’s binding to the sigma-1 receptor in the endoplasmic reticulum, Dr. Reiersen came up with the idea of testing if fluvoxamine could keep COVID-19 from progressing in newly infected patients.
Dr. Reiersen and psychiatrist Eric Lenze, MD, also from Washington University, led the phase 2 trial that initially suggested fluvoxamine’s promise as an outpatient medication. They are coinvestigators on the new phase 3 adaptive platform trial called TOGETHER, which was conducted by an international team of investigators in Brazil, Canada, and the United States.
For this latest study, researchers at McMaster University, Hamilton, Ont., partnered with the research clinic Cardresearch in Brazil to recruit unvaccinated, high-risk adults within 7 days of developing flu-like symptoms from COVID-19. They analyzed 1,497 newly symptomatic COVID-19 patients at 11 clinical sites in Brazil.
Patients entered the trial between January and August 2021 and were assigned to receive 100 mg fluvoxamine or placebo pills twice a day for 10 days. Investigators monitored participants through 28 days post treatment, noting whether complications developed requiring hospitalization or more than 6 hours of emergency care.
In the placebo group, 119 of 756 patients (15.7%) worsened to this extent. In comparison, 79 of 741 (10.7%) fluvoxamine-treated patients met these primary criteria. This represented a 32% reduction in hospitalizations and emergency visits.
Additional analysis requested
As Lancet Global Health reviewed these findings from the submitted manuscript, journal reviewers requested an additional “pre-protocol analysis” that was not specified in the trial’s original protocol. The request was to examine the subgroup of patients with good adherence (74% of treated group, 82% of placebo group).
Among these three quarters of patients who took at least 80% of their doses, benefits were better.
Fluvoxamine cut serious complications in this group by 66% and reduced mortality by 91%. In the placebo group, 12 people died compared with one who received the study drug.
from complications of the infection.
However, clinicians should note that the drug can cause side effects such as nausea, dizziness, and insomnia, she added. In addition, because it prevents the body from metabolizing caffeine, patients should limit their daily intake to half of a small cup of coffee or one can of soda or one tea while taking the drug.
Previous research has shown that fluvoxamine affects the metabolism of some drugs, such as theophylline, clozapine, olanzapine, and tizanidine.
Despite huge challenges with studying generic drugs as early COVID-19 treatment, the TOGETHER trial shows it is possible to produce quality evidence during a pandemic on a shoestring budget, noted co-principal investigator Edward Mills, PhD, professor in the department of health research methods, evidence, and impact at McMaster University.
To screen more than 12,000 patients and enroll 4,000 to test nine interventions, “our total budget was less than $8 million,” Dr. Mills said. The trial was funded by Fast Grants and the Rainwater Charitable Foundation.
‘A $10 medicine’
Commenting on the findings, David Boulware, MD, MPH, an infectious disease physician-researcher at the University of Minnesota in Minneapolis, noted fluvoxamine is “a $10 medicine that’s available and has a very good safety record.”
By comparison, a 5-day course of Merck’s antiviral molnupiravir, another oral drug that the company says can cut hospitalizations in COVID-19 outpatients, costs $700. However, the data have not been peer reviewed – and molnupiravir is not currently available and has unknown long-term safety implications, Dr. Boulware said.
Pharmaceutical companies typically spend tens of thousands of dollars on a trial evaluating a single drug, he noted.
In addition, the National Institutes of Health’s ACTIV-6 study, a nationwide trial on the effect of fluvoxamine and other repurposed generic drugs on thousands of COVID-19 outpatients, is a $110 million effort, according to Dr. Boulware, who cochairs its steering committee.
ACTIV-6 is currently enrolling outpatients with COVID-19 to test a lower dose of fluvoxamine, at 50 mg twice daily instead of the 100-mg dose used in the TOGETHER trial, as well as ivermectin and inhaled fluticasone. The COVID-OUT trial is also recruiting newly diagnosed COVID-19 patients to test various combinations of fluvoxamine, ivermectin, and the diabetes drug metformin.
Unanswered safety, efficacy questions
In an accompanying editorial in The Lancet Global Health, Otavio Berwanger, MD, cardiologist and clinical trialist, Academic Research Organization, Hospital Israelita Albert Einstein, São Paulo, Brazil, commends the investigators for rapidly generating evidence during the COVID-19 pandemic.
However, despite the important findings, “some questions related to efficacy and safety of fluvoxamine for patients with COVID-19 remain open,” Dr. Berwanger wrote.
The effects of the drug on reducing both mortality and hospitalizations also “still need addressing,” he noted.
“In addition, it remains to be established whether fluvoxamine has an additive effect to other therapies such as monoclonal antibodies and budesonide, and what is the optimal fluvoxamine therapeutic scheme,” wrote Dr. Berwanger.
In an interview, he noted that 74% of the Brazil population have currently received at least one dose of a COVID-19 vaccine and 52% have received two doses. In addition, deaths have gone down from 4,000 per day during the March-April second wave to about 400 per day. “That is still unfortunate and far from ideal,” he said. In total, they have had about 600,000 deaths because of COVID-19.
Asked whether public health authorities are now recommending fluvoxamine as an early treatment for COVID-19 based on the TOGETHER trial data, Dr. Berwanger answered, “Not yet.
“I believe medical and scientific societies will need to critically appraise the manuscript in order to inform their decisions and recommendations. This interesting trial adds another important piece of information in this regard,” he said.
Dr. Reiersen and Dr. Lenze are inventors on a patent application related to methods for treating COVID-19, which was filed by Washington University. Dr. Mills reports no relevant financial relationships, as does Dr. Boulware – except that the TOGETHER trial funders are also funding the University of Minnesota COVID-OUT trial. Dr. Berwanger reports having received research grants outside of the submitted work that were paid to his institution by AstraZeneca, Bayer, Amgen, Servier, Novartis, Pfizer, and Boehringer Ingelheim.
A version of this article first appeared on Medscape.com.
The antidepressant fluvoxamine (Luvox) may prevent hospitalization and death in outpatients with COVID-19, new research suggests.
Results from the placebo-controlled, multisite, phase 3 TOGETHER trial showed that in COVID-19 outpatients at high risk for complications, hospitalizations were cut by 66% and deaths were reduced by 91% in those who tolerated fluvoxamine.
“Our trial has found that fluvoxamine, an inexpensive existing drug, reduces the need for advanced disease care in this high-risk population,” wrote the investigators, led by Gilmar Reis, MD, PhD, research division, Cardresearch, Belo Horizonte, Brazil.
The findings were published online Oct. 27 in The Lancet Global Health.
Alternative mechanisms
Fluvoxamine, a selective serotonin reuptake inhibitor (SSRI), is an antidepressant commonly prescribed for obsessive-compulsive disorder.
Besides its known effects on serotonin, the drug acts in other molecular pathways to dampen the production of inflammatory cytokines. Those alternative mechanisms are the ones believed to help patients with COVID-19, said coinvestigator Angela Reiersen, MD, child psychiatrist at Washington University, St. Louis.
Based on cell culture and mouse studies showing effects of the molecule’s binding to the sigma-1 receptor in the endoplasmic reticulum, Dr. Reiersen came up with the idea of testing if fluvoxamine could keep COVID-19 from progressing in newly infected patients.
Dr. Reiersen and psychiatrist Eric Lenze, MD, also from Washington University, led the phase 2 trial that initially suggested fluvoxamine’s promise as an outpatient medication. They are coinvestigators on the new phase 3 adaptive platform trial called TOGETHER, which was conducted by an international team of investigators in Brazil, Canada, and the United States.
For this latest study, researchers at McMaster University, Hamilton, Ont., partnered with the research clinic Cardresearch in Brazil to recruit unvaccinated, high-risk adults within 7 days of developing flu-like symptoms from COVID-19. They analyzed 1,497 newly symptomatic COVID-19 patients at 11 clinical sites in Brazil.
Patients entered the trial between January and August 2021 and were assigned to receive 100 mg fluvoxamine or placebo pills twice a day for 10 days. Investigators monitored participants through 28 days post treatment, noting whether complications developed requiring hospitalization or more than 6 hours of emergency care.
In the placebo group, 119 of 756 patients (15.7%) worsened to this extent. In comparison, 79 of 741 (10.7%) fluvoxamine-treated patients met these primary criteria. This represented a 32% reduction in hospitalizations and emergency visits.
Additional analysis requested
As Lancet Global Health reviewed these findings from the submitted manuscript, journal reviewers requested an additional “pre-protocol analysis” that was not specified in the trial’s original protocol. The request was to examine the subgroup of patients with good adherence (74% of treated group, 82% of placebo group).
Among these three quarters of patients who took at least 80% of their doses, benefits were better.
Fluvoxamine cut serious complications in this group by 66% and reduced mortality by 91%. In the placebo group, 12 people died compared with one who received the study drug.
from complications of the infection.
However, clinicians should note that the drug can cause side effects such as nausea, dizziness, and insomnia, she added. In addition, because it prevents the body from metabolizing caffeine, patients should limit their daily intake to half of a small cup of coffee or one can of soda or one tea while taking the drug.
Previous research has shown that fluvoxamine affects the metabolism of some drugs, such as theophylline, clozapine, olanzapine, and tizanidine.
Despite huge challenges with studying generic drugs as early COVID-19 treatment, the TOGETHER trial shows it is possible to produce quality evidence during a pandemic on a shoestring budget, noted co-principal investigator Edward Mills, PhD, professor in the department of health research methods, evidence, and impact at McMaster University.
To screen more than 12,000 patients and enroll 4,000 to test nine interventions, “our total budget was less than $8 million,” Dr. Mills said. The trial was funded by Fast Grants and the Rainwater Charitable Foundation.
‘A $10 medicine’
Commenting on the findings, David Boulware, MD, MPH, an infectious disease physician-researcher at the University of Minnesota in Minneapolis, noted fluvoxamine is “a $10 medicine that’s available and has a very good safety record.”
By comparison, a 5-day course of Merck’s antiviral molnupiravir, another oral drug that the company says can cut hospitalizations in COVID-19 outpatients, costs $700. However, the data have not been peer reviewed – and molnupiravir is not currently available and has unknown long-term safety implications, Dr. Boulware said.
Pharmaceutical companies typically spend tens of thousands of dollars on a trial evaluating a single drug, he noted.
In addition, the National Institutes of Health’s ACTIV-6 study, a nationwide trial on the effect of fluvoxamine and other repurposed generic drugs on thousands of COVID-19 outpatients, is a $110 million effort, according to Dr. Boulware, who cochairs its steering committee.
ACTIV-6 is currently enrolling outpatients with COVID-19 to test a lower dose of fluvoxamine, at 50 mg twice daily instead of the 100-mg dose used in the TOGETHER trial, as well as ivermectin and inhaled fluticasone. The COVID-OUT trial is also recruiting newly diagnosed COVID-19 patients to test various combinations of fluvoxamine, ivermectin, and the diabetes drug metformin.
Unanswered safety, efficacy questions
In an accompanying editorial in The Lancet Global Health, Otavio Berwanger, MD, cardiologist and clinical trialist, Academic Research Organization, Hospital Israelita Albert Einstein, São Paulo, Brazil, commends the investigators for rapidly generating evidence during the COVID-19 pandemic.
However, despite the important findings, “some questions related to efficacy and safety of fluvoxamine for patients with COVID-19 remain open,” Dr. Berwanger wrote.
The effects of the drug on reducing both mortality and hospitalizations also “still need addressing,” he noted.
“In addition, it remains to be established whether fluvoxamine has an additive effect to other therapies such as monoclonal antibodies and budesonide, and what is the optimal fluvoxamine therapeutic scheme,” wrote Dr. Berwanger.
In an interview, he noted that 74% of the Brazil population have currently received at least one dose of a COVID-19 vaccine and 52% have received two doses. In addition, deaths have gone down from 4,000 per day during the March-April second wave to about 400 per day. “That is still unfortunate and far from ideal,” he said. In total, they have had about 600,000 deaths because of COVID-19.
Asked whether public health authorities are now recommending fluvoxamine as an early treatment for COVID-19 based on the TOGETHER trial data, Dr. Berwanger answered, “Not yet.
“I believe medical and scientific societies will need to critically appraise the manuscript in order to inform their decisions and recommendations. This interesting trial adds another important piece of information in this regard,” he said.
Dr. Reiersen and Dr. Lenze are inventors on a patent application related to methods for treating COVID-19, which was filed by Washington University. Dr. Mills reports no relevant financial relationships, as does Dr. Boulware – except that the TOGETHER trial funders are also funding the University of Minnesota COVID-OUT trial. Dr. Berwanger reports having received research grants outside of the submitted work that were paid to his institution by AstraZeneca, Bayer, Amgen, Servier, Novartis, Pfizer, and Boehringer Ingelheim.
A version of this article first appeared on Medscape.com.
The antidepressant fluvoxamine (Luvox) may prevent hospitalization and death in outpatients with COVID-19, new research suggests.
Results from the placebo-controlled, multisite, phase 3 TOGETHER trial showed that in COVID-19 outpatients at high risk for complications, hospitalizations were cut by 66% and deaths were reduced by 91% in those who tolerated fluvoxamine.
“Our trial has found that fluvoxamine, an inexpensive existing drug, reduces the need for advanced disease care in this high-risk population,” wrote the investigators, led by Gilmar Reis, MD, PhD, research division, Cardresearch, Belo Horizonte, Brazil.
The findings were published online Oct. 27 in The Lancet Global Health.
Alternative mechanisms
Fluvoxamine, a selective serotonin reuptake inhibitor (SSRI), is an antidepressant commonly prescribed for obsessive-compulsive disorder.
Besides its known effects on serotonin, the drug acts in other molecular pathways to dampen the production of inflammatory cytokines. Those alternative mechanisms are the ones believed to help patients with COVID-19, said coinvestigator Angela Reiersen, MD, child psychiatrist at Washington University, St. Louis.
Based on cell culture and mouse studies showing effects of the molecule’s binding to the sigma-1 receptor in the endoplasmic reticulum, Dr. Reiersen came up with the idea of testing if fluvoxamine could keep COVID-19 from progressing in newly infected patients.
Dr. Reiersen and psychiatrist Eric Lenze, MD, also from Washington University, led the phase 2 trial that initially suggested fluvoxamine’s promise as an outpatient medication. They are coinvestigators on the new phase 3 adaptive platform trial called TOGETHER, which was conducted by an international team of investigators in Brazil, Canada, and the United States.
For this latest study, researchers at McMaster University, Hamilton, Ont., partnered with the research clinic Cardresearch in Brazil to recruit unvaccinated, high-risk adults within 7 days of developing flu-like symptoms from COVID-19. They analyzed 1,497 newly symptomatic COVID-19 patients at 11 clinical sites in Brazil.
Patients entered the trial between January and August 2021 and were assigned to receive 100 mg fluvoxamine or placebo pills twice a day for 10 days. Investigators monitored participants through 28 days post treatment, noting whether complications developed requiring hospitalization or more than 6 hours of emergency care.
In the placebo group, 119 of 756 patients (15.7%) worsened to this extent. In comparison, 79 of 741 (10.7%) fluvoxamine-treated patients met these primary criteria. This represented a 32% reduction in hospitalizations and emergency visits.
Additional analysis requested
As Lancet Global Health reviewed these findings from the submitted manuscript, journal reviewers requested an additional “pre-protocol analysis” that was not specified in the trial’s original protocol. The request was to examine the subgroup of patients with good adherence (74% of treated group, 82% of placebo group).
Among these three quarters of patients who took at least 80% of their doses, benefits were better.
Fluvoxamine cut serious complications in this group by 66% and reduced mortality by 91%. In the placebo group, 12 people died compared with one who received the study drug.
from complications of the infection.
However, clinicians should note that the drug can cause side effects such as nausea, dizziness, and insomnia, she added. In addition, because it prevents the body from metabolizing caffeine, patients should limit their daily intake to half of a small cup of coffee or one can of soda or one tea while taking the drug.
Previous research has shown that fluvoxamine affects the metabolism of some drugs, such as theophylline, clozapine, olanzapine, and tizanidine.
Despite huge challenges with studying generic drugs as early COVID-19 treatment, the TOGETHER trial shows it is possible to produce quality evidence during a pandemic on a shoestring budget, noted co-principal investigator Edward Mills, PhD, professor in the department of health research methods, evidence, and impact at McMaster University.
To screen more than 12,000 patients and enroll 4,000 to test nine interventions, “our total budget was less than $8 million,” Dr. Mills said. The trial was funded by Fast Grants and the Rainwater Charitable Foundation.
‘A $10 medicine’
Commenting on the findings, David Boulware, MD, MPH, an infectious disease physician-researcher at the University of Minnesota in Minneapolis, noted fluvoxamine is “a $10 medicine that’s available and has a very good safety record.”
By comparison, a 5-day course of Merck’s antiviral molnupiravir, another oral drug that the company says can cut hospitalizations in COVID-19 outpatients, costs $700. However, the data have not been peer reviewed – and molnupiravir is not currently available and has unknown long-term safety implications, Dr. Boulware said.
Pharmaceutical companies typically spend tens of thousands of dollars on a trial evaluating a single drug, he noted.
In addition, the National Institutes of Health’s ACTIV-6 study, a nationwide trial on the effect of fluvoxamine and other repurposed generic drugs on thousands of COVID-19 outpatients, is a $110 million effort, according to Dr. Boulware, who cochairs its steering committee.
ACTIV-6 is currently enrolling outpatients with COVID-19 to test a lower dose of fluvoxamine, at 50 mg twice daily instead of the 100-mg dose used in the TOGETHER trial, as well as ivermectin and inhaled fluticasone. The COVID-OUT trial is also recruiting newly diagnosed COVID-19 patients to test various combinations of fluvoxamine, ivermectin, and the diabetes drug metformin.
Unanswered safety, efficacy questions
In an accompanying editorial in The Lancet Global Health, Otavio Berwanger, MD, cardiologist and clinical trialist, Academic Research Organization, Hospital Israelita Albert Einstein, São Paulo, Brazil, commends the investigators for rapidly generating evidence during the COVID-19 pandemic.
However, despite the important findings, “some questions related to efficacy and safety of fluvoxamine for patients with COVID-19 remain open,” Dr. Berwanger wrote.
The effects of the drug on reducing both mortality and hospitalizations also “still need addressing,” he noted.
“In addition, it remains to be established whether fluvoxamine has an additive effect to other therapies such as monoclonal antibodies and budesonide, and what is the optimal fluvoxamine therapeutic scheme,” wrote Dr. Berwanger.
In an interview, he noted that 74% of the Brazil population have currently received at least one dose of a COVID-19 vaccine and 52% have received two doses. In addition, deaths have gone down from 4,000 per day during the March-April second wave to about 400 per day. “That is still unfortunate and far from ideal,” he said. In total, they have had about 600,000 deaths because of COVID-19.
Asked whether public health authorities are now recommending fluvoxamine as an early treatment for COVID-19 based on the TOGETHER trial data, Dr. Berwanger answered, “Not yet.
“I believe medical and scientific societies will need to critically appraise the manuscript in order to inform their decisions and recommendations. This interesting trial adds another important piece of information in this regard,” he said.
Dr. Reiersen and Dr. Lenze are inventors on a patent application related to methods for treating COVID-19, which was filed by Washington University. Dr. Mills reports no relevant financial relationships, as does Dr. Boulware – except that the TOGETHER trial funders are also funding the University of Minnesota COVID-OUT trial. Dr. Berwanger reports having received research grants outside of the submitted work that were paid to his institution by AstraZeneca, Bayer, Amgen, Servier, Novartis, Pfizer, and Boehringer Ingelheim.
A version of this article first appeared on Medscape.com.
CDC: Urgency remains to vaccinate children
The CDC is urging parents and guardians to vaccinate children ages 5-11 against COVID-19 once the shot is fully approved, despite questions from FDA advisers about the urgency given falling national case rates.
On Oct. 26, the FDA’s Vaccines and Related Biological Products Advisory Committee voted to recommend a 10-microgram shot for children. Though 17 of the 18 panelists voted in favor of it, some members said it was a hard decision and questioned the need for it now that cases and hospitalizations are down.
“There’s urgency because we’re seeing disease in children, we’ve seen deaths in children, we’ve seen long COVID,” CDC Director Rochelle Walensky, MD, said at a White House briefing on Oct. 27. “Certainly we’ve seen cases come down before, and the way to prevent surges again is to get more and more people vaccinated.”
CDC data presented at an Oct. 26 advisory committee meeting show that among children 5-11, COVID-19 was one of top 10 causes of death over last year, Dr. Walensky said. There have been more than 8,300 hospitalizations and 745 deaths in children under 18.
As of yesterday, the 7-day average of daily COVID-19 cases was 65,900, a 16% decrease from the prior week. Hospitalizations are down 54% from the week of Aug. 28, Dr. Walensky said.
“If the trends continue the way they are going, the emergency for children is not what we might think it would be. That was my concern,” James Hildreth, MD, president and CEO at Meharry Medical College in Nashville, said at the advisory committee meeting on Oct. 26.
But according to one CDC study, hospitalization rates for adolescents were 10 times higher in those who were unvaccinated. Another study found that COVID-related emergency room visits and hospital admissions among children were more than 3 times as high in states with the lowest vaccination rates.
“We are down from our peak in early September, and we are now heading in the right direction, but with cases still high, we must remain vigilant heading into the colder, drier winter months,” Dr. Walensky said, noting that the 7-day average of daily deaths still exceeds 1,000.
Meanwhile, the booster program is off to a “very strong start,” said White House COVID-19 Response Coordinator Jeff Zients.
In the 5 days since authorizations, about 15 million people have received an additional dose of the Pfizer, Moderna, and Johnson & Johnson vaccines.
A version of this article first appeared on WebMD.com.
The CDC is urging parents and guardians to vaccinate children ages 5-11 against COVID-19 once the shot is fully approved, despite questions from FDA advisers about the urgency given falling national case rates.
On Oct. 26, the FDA’s Vaccines and Related Biological Products Advisory Committee voted to recommend a 10-microgram shot for children. Though 17 of the 18 panelists voted in favor of it, some members said it was a hard decision and questioned the need for it now that cases and hospitalizations are down.
“There’s urgency because we’re seeing disease in children, we’ve seen deaths in children, we’ve seen long COVID,” CDC Director Rochelle Walensky, MD, said at a White House briefing on Oct. 27. “Certainly we’ve seen cases come down before, and the way to prevent surges again is to get more and more people vaccinated.”
CDC data presented at an Oct. 26 advisory committee meeting show that among children 5-11, COVID-19 was one of top 10 causes of death over last year, Dr. Walensky said. There have been more than 8,300 hospitalizations and 745 deaths in children under 18.
As of yesterday, the 7-day average of daily COVID-19 cases was 65,900, a 16% decrease from the prior week. Hospitalizations are down 54% from the week of Aug. 28, Dr. Walensky said.
“If the trends continue the way they are going, the emergency for children is not what we might think it would be. That was my concern,” James Hildreth, MD, president and CEO at Meharry Medical College in Nashville, said at the advisory committee meeting on Oct. 26.
But according to one CDC study, hospitalization rates for adolescents were 10 times higher in those who were unvaccinated. Another study found that COVID-related emergency room visits and hospital admissions among children were more than 3 times as high in states with the lowest vaccination rates.
“We are down from our peak in early September, and we are now heading in the right direction, but with cases still high, we must remain vigilant heading into the colder, drier winter months,” Dr. Walensky said, noting that the 7-day average of daily deaths still exceeds 1,000.
Meanwhile, the booster program is off to a “very strong start,” said White House COVID-19 Response Coordinator Jeff Zients.
In the 5 days since authorizations, about 15 million people have received an additional dose of the Pfizer, Moderna, and Johnson & Johnson vaccines.
A version of this article first appeared on WebMD.com.
The CDC is urging parents and guardians to vaccinate children ages 5-11 against COVID-19 once the shot is fully approved, despite questions from FDA advisers about the urgency given falling national case rates.
On Oct. 26, the FDA’s Vaccines and Related Biological Products Advisory Committee voted to recommend a 10-microgram shot for children. Though 17 of the 18 panelists voted in favor of it, some members said it was a hard decision and questioned the need for it now that cases and hospitalizations are down.
“There’s urgency because we’re seeing disease in children, we’ve seen deaths in children, we’ve seen long COVID,” CDC Director Rochelle Walensky, MD, said at a White House briefing on Oct. 27. “Certainly we’ve seen cases come down before, and the way to prevent surges again is to get more and more people vaccinated.”
CDC data presented at an Oct. 26 advisory committee meeting show that among children 5-11, COVID-19 was one of top 10 causes of death over last year, Dr. Walensky said. There have been more than 8,300 hospitalizations and 745 deaths in children under 18.
As of yesterday, the 7-day average of daily COVID-19 cases was 65,900, a 16% decrease from the prior week. Hospitalizations are down 54% from the week of Aug. 28, Dr. Walensky said.
“If the trends continue the way they are going, the emergency for children is not what we might think it would be. That was my concern,” James Hildreth, MD, president and CEO at Meharry Medical College in Nashville, said at the advisory committee meeting on Oct. 26.
But according to one CDC study, hospitalization rates for adolescents were 10 times higher in those who were unvaccinated. Another study found that COVID-related emergency room visits and hospital admissions among children were more than 3 times as high in states with the lowest vaccination rates.
“We are down from our peak in early September, and we are now heading in the right direction, but with cases still high, we must remain vigilant heading into the colder, drier winter months,” Dr. Walensky said, noting that the 7-day average of daily deaths still exceeds 1,000.
Meanwhile, the booster program is off to a “very strong start,” said White House COVID-19 Response Coordinator Jeff Zients.
In the 5 days since authorizations, about 15 million people have received an additional dose of the Pfizer, Moderna, and Johnson & Johnson vaccines.
A version of this article first appeared on WebMD.com.
Antibiotic and glucocorticoid use before cancer therapy could have detrimental effect on outcomes
“Our results confirm the detrimental impact on oncological outcomes of antibiotics and glucocorticoids at a dosage ≥10 mg/day when given within 1 month before or after ICI onset,” Marie Kostine, MD, of Bordeaux (France) University Hospital, and colleagues wrote in the European Journal of Cancer. “Moreover, we show that other comedications may significantly alter the antitumoral response of ICI, such as proton pump inhibitors, psychotropic drugs, morphine, aspirin, and insulin, whereas others seem to have no impact.”
While immune checkpoint inhibitors are transforming the treatment of advanced cancers, gut microbiota composition is an important determinant of response to ICIs. Antibiotic treatments are known to alter the gut microbiota. Other drugs, such as proton pump inhibitors, antidiabetic agents, aspirin, NSAIDs, glucocorticoids, immunomodulators, psychotropic drugs, and analgesics, have been associated with changes in microbiome composition. Since many patients with advanced cancer are exposed to such drugs, this study looked at the possible influence of these comedications on the antitumor effect and safety of ICIs.
The observational study included 635 patients with advanced cancer treated with ICIs between May 2015 and September 2017. Comedications given within 1 month before or 1 month after the first administration of an ICI were reviewed from medical records. Psychotropic drugs, proton pump inhibitors, ACE inhibitors and/or angiotensin II receptor blockers (ARBs), glucocorticoids, antibiotics, statins, and morphine were the most prescribed comedications.
Baseline use of antibiotics, glucocorticoids greater than 10 mg/day, proton pump inhibitors, psychotropic drugs, morphine, and insulin was associated with decreased overall survival and tumor response. However, the coadministration of statins, ACE inhibitors and/or ARBs, NSAIDs, aspirin, and oral diabetes drugs did not impact patient outcomes. Additionally, treatments that altered the response to ICIs were associated with a decreased incidence of immune-related adverse events.
“These results suggest some practical advice in a patient candidate to ICIs,” the authors wrote. “First, antibiotic treatment should be limited to documented infections,” and “withdrawal of proton pump inhibitors and psychotropic drugs should be considered.
“Regarding baseline glucocorticoids use, the cutoff of 10 mg/day should be respected, considering the deleterious effect of higher dosage. Moreover, because of the lack of impact of inhaled or topical glucocorticoids, local routes should be preferred,” the authors wrote. “Conversely, our study brings reassuring data regarding the use of glucocorticoids for the management of immune-related adverse events, which did not alter ICI efficacy, confirming previous reports.”
The authors noted that the observational nature of the study does not allow any causal conclusion, adding that it remains unknown whether the effect of comedications “on cancer outcomes is thoroughly mediated by changes in microbiota or other immunomodulatory properties.”
Along with the retrospective design, study limitations included reporting bias and missing data on baseline comedications, specific prognostic factors and cancer outcomes.
The authors noted no conflicts of interest.
“Our results confirm the detrimental impact on oncological outcomes of antibiotics and glucocorticoids at a dosage ≥10 mg/day when given within 1 month before or after ICI onset,” Marie Kostine, MD, of Bordeaux (France) University Hospital, and colleagues wrote in the European Journal of Cancer. “Moreover, we show that other comedications may significantly alter the antitumoral response of ICI, such as proton pump inhibitors, psychotropic drugs, morphine, aspirin, and insulin, whereas others seem to have no impact.”
While immune checkpoint inhibitors are transforming the treatment of advanced cancers, gut microbiota composition is an important determinant of response to ICIs. Antibiotic treatments are known to alter the gut microbiota. Other drugs, such as proton pump inhibitors, antidiabetic agents, aspirin, NSAIDs, glucocorticoids, immunomodulators, psychotropic drugs, and analgesics, have been associated with changes in microbiome composition. Since many patients with advanced cancer are exposed to such drugs, this study looked at the possible influence of these comedications on the antitumor effect and safety of ICIs.
The observational study included 635 patients with advanced cancer treated with ICIs between May 2015 and September 2017. Comedications given within 1 month before or 1 month after the first administration of an ICI were reviewed from medical records. Psychotropic drugs, proton pump inhibitors, ACE inhibitors and/or angiotensin II receptor blockers (ARBs), glucocorticoids, antibiotics, statins, and morphine were the most prescribed comedications.
Baseline use of antibiotics, glucocorticoids greater than 10 mg/day, proton pump inhibitors, psychotropic drugs, morphine, and insulin was associated with decreased overall survival and tumor response. However, the coadministration of statins, ACE inhibitors and/or ARBs, NSAIDs, aspirin, and oral diabetes drugs did not impact patient outcomes. Additionally, treatments that altered the response to ICIs were associated with a decreased incidence of immune-related adverse events.
“These results suggest some practical advice in a patient candidate to ICIs,” the authors wrote. “First, antibiotic treatment should be limited to documented infections,” and “withdrawal of proton pump inhibitors and psychotropic drugs should be considered.
“Regarding baseline glucocorticoids use, the cutoff of 10 mg/day should be respected, considering the deleterious effect of higher dosage. Moreover, because of the lack of impact of inhaled or topical glucocorticoids, local routes should be preferred,” the authors wrote. “Conversely, our study brings reassuring data regarding the use of glucocorticoids for the management of immune-related adverse events, which did not alter ICI efficacy, confirming previous reports.”
The authors noted that the observational nature of the study does not allow any causal conclusion, adding that it remains unknown whether the effect of comedications “on cancer outcomes is thoroughly mediated by changes in microbiota or other immunomodulatory properties.”
Along with the retrospective design, study limitations included reporting bias and missing data on baseline comedications, specific prognostic factors and cancer outcomes.
The authors noted no conflicts of interest.
“Our results confirm the detrimental impact on oncological outcomes of antibiotics and glucocorticoids at a dosage ≥10 mg/day when given within 1 month before or after ICI onset,” Marie Kostine, MD, of Bordeaux (France) University Hospital, and colleagues wrote in the European Journal of Cancer. “Moreover, we show that other comedications may significantly alter the antitumoral response of ICI, such as proton pump inhibitors, psychotropic drugs, morphine, aspirin, and insulin, whereas others seem to have no impact.”
While immune checkpoint inhibitors are transforming the treatment of advanced cancers, gut microbiota composition is an important determinant of response to ICIs. Antibiotic treatments are known to alter the gut microbiota. Other drugs, such as proton pump inhibitors, antidiabetic agents, aspirin, NSAIDs, glucocorticoids, immunomodulators, psychotropic drugs, and analgesics, have been associated with changes in microbiome composition. Since many patients with advanced cancer are exposed to such drugs, this study looked at the possible influence of these comedications on the antitumor effect and safety of ICIs.
The observational study included 635 patients with advanced cancer treated with ICIs between May 2015 and September 2017. Comedications given within 1 month before or 1 month after the first administration of an ICI were reviewed from medical records. Psychotropic drugs, proton pump inhibitors, ACE inhibitors and/or angiotensin II receptor blockers (ARBs), glucocorticoids, antibiotics, statins, and morphine were the most prescribed comedications.
Baseline use of antibiotics, glucocorticoids greater than 10 mg/day, proton pump inhibitors, psychotropic drugs, morphine, and insulin was associated with decreased overall survival and tumor response. However, the coadministration of statins, ACE inhibitors and/or ARBs, NSAIDs, aspirin, and oral diabetes drugs did not impact patient outcomes. Additionally, treatments that altered the response to ICIs were associated with a decreased incidence of immune-related adverse events.
“These results suggest some practical advice in a patient candidate to ICIs,” the authors wrote. “First, antibiotic treatment should be limited to documented infections,” and “withdrawal of proton pump inhibitors and psychotropic drugs should be considered.
“Regarding baseline glucocorticoids use, the cutoff of 10 mg/day should be respected, considering the deleterious effect of higher dosage. Moreover, because of the lack of impact of inhaled or topical glucocorticoids, local routes should be preferred,” the authors wrote. “Conversely, our study brings reassuring data regarding the use of glucocorticoids for the management of immune-related adverse events, which did not alter ICI efficacy, confirming previous reports.”
The authors noted that the observational nature of the study does not allow any causal conclusion, adding that it remains unknown whether the effect of comedications “on cancer outcomes is thoroughly mediated by changes in microbiota or other immunomodulatory properties.”
Along with the retrospective design, study limitations included reporting bias and missing data on baseline comedications, specific prognostic factors and cancer outcomes.
The authors noted no conflicts of interest.
FROM THE EUROPEAN JOURNAL OF CANCER
ANCHOR study findings may usher in new care standards for anal cancer in HIV-infected patients
Can treatment or removal of high-grade squamous intraepithelial lesions (HSIL) reduce the likelihood of developing anal cancer in people living with HIV (PLHIV)?
“In theory, looking for and treating high-grade disease (like we know works in the cervix) is a potential way to prevent anal cancer in high-risk individuals,” Joel Palefsky, MD, lead investigator of the Anal Cancer/HSIL Outcomes Research (ANCHOR) study and founder/director of the University of California, San Francisco’s Anal Neoplasia Clinic, told this news organization. “But we’ve never had any direct evidence that it worked,” he said.
Initial findings from ANCHOR – the first randomized trial to demonstrate that anal cancer can be prevented in high-risk, HIV-infected patients – promise to change that paradigm and may even portend a new standard of care.
Undoubtedly, this is welcome news for the HIV community, who are not only at increased risk for anal HSIL overall, but among whom anal cancer cases have been rising over the past decade. This is especially true for women who are expected to bear a large portion of overall burden of human papillomavirus (HPV)–associated anal squamous cell carcinoma over the next 10 to 20 years.
In the study, 4,446 PLHIV ages 35 and older with precursor anal HSIL were randomly assigned to topical (imiquimod intra-anally, perianally, or both, or fluorouracil) or ablative (infrared coagulation, hyfrecation/electrocautery) treatment, or active surveillance, and followed every 6 months for 5 years. The study population was broadly representative, including men who have sex with men (MSM), women, transgender people, and historically underrepresented minorities, a factor that reinforces the study’s importance in this specific population.
Because the primary endpoint was reached (that is, to determine if HSIL treatment and removal effectively reduces anal cancer incidence in HIV-infected men and women), the Data Safety Board halted accrual and recommended that participants in the surveillance group be offered treatment moving forward. While the investigators are currently working on publication of the results, the study is ongoing.
Still, the ANCHOR study, which is one of the largest malignancy screening studies conducted in PLHIV, has also highlighted significant challenges in how anal cancer is approached in general.
“Anal cancer has many similarities to cervical cancer, where screening for precancerous lesions and treatment have been shown to substantially reduce morbidity and mortality,” said Joseph Sparano, MD, a medical oncologist specializing in HIV and breast cancer at Icahn School of Medicine at Mount Sinai, New York. Dr. Sparano is chair and principal investigator of the AIDS Malignancy Consortium but was not involved in the ANCHOR study.
But, he explained in an interview, “it’s much more difficult and technically challenging to screen for and evaluate the anal canal histology,” noting that
Availability and access to high-resolution anoscopy is limited, said Robert Yarchoan, MD, chief of the HIV and AIDS Malignancy Branch at the National Cancer Institute’s Clinical Cancer Research Division and director of the Office of HIV and AIDS Malignancy (which, incidentally, cosponsored ANCHOR).
“There are relatively few people that do this at this time,” he added in an interview, pointing out that among those who do, most are obstetricians/gynecologists.
A bit of digging into ANCHOR’s backstory revealed that this was a point of contention at the study’s onset. While physicians participating in the study received extensive training in high-resolution anoscopy, ob/gyns were the fastest to achieve competency and/or had the most prior experience, namely because of their experience in cervical cancer screening in women.
But initial objections by the American Board of Obstetricians and Gynecologists (which at the time, insisted that its members only treat women and threatened to remove their certification if they participated in the research), almost threw a wrench into the study’s start, according to a report in The New York Times. While rational minds prevailed and the board reversed its earlier statements, lack of ample training in the procedure may signal future barriers to treatment.
Another challenge lies in how study findings might be applicable to other groups outside of the HIV/AIDS population, such as people with other forms of immunosuppression who have HSIL, or even healthy women or men who are at risk as a result of penetrative/nonpenetrative sexual or nonsexual (for example, vaginal discharge to the anus) contact.
Although he was unable to share specifics at this time, Dr. Palefsky said that when they designed the ANCHOR study, they were aware that “merely showing efficacy wouldn’t necessarily be sufficient for establishing a standard of care, where[as] other pieces of information undoubtedly would be considered by entities that make guidelines” (for example, an examination of adverse events, risks/benefits, and factors that influence quality of life).
“With that in mind, we are doing a quality-of-life study and, in fact, have [collaborated on], developed, and validated what I think is the first anal disease-specific, quality of life instrument,” Dr. Palefsky said. “The work is still ongoing because we did not complete enrollment in the study, but we are continuing it as part of the follow up.”
Study investigators have also collected samples for a biorepository of specimens that will hopefully facilitate a better understanding of the molecular events driving progression from precancer to cancer. “A lot of people with HIV have these high-grade lesions,” Dr. Palefsky said. “If we were able to identify who’s at highest risk of all of them, that would be very important, because we prefer not to treat everybody with high-grade disease,” he noted, adding that the “underlying hope is that the biomarkers we find in the setting will also be relevant for other HPV-related cancers,” especially in women.
Dr. Yarchoan concurred. “One of the challenges is going to be to digest this information and see how to use it to potentially address the growing problem of females with HIV,” he said.
Dr. Palefsky, Dr. Sparano, and Dr. Yarchoan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Can treatment or removal of high-grade squamous intraepithelial lesions (HSIL) reduce the likelihood of developing anal cancer in people living with HIV (PLHIV)?
“In theory, looking for and treating high-grade disease (like we know works in the cervix) is a potential way to prevent anal cancer in high-risk individuals,” Joel Palefsky, MD, lead investigator of the Anal Cancer/HSIL Outcomes Research (ANCHOR) study and founder/director of the University of California, San Francisco’s Anal Neoplasia Clinic, told this news organization. “But we’ve never had any direct evidence that it worked,” he said.
Initial findings from ANCHOR – the first randomized trial to demonstrate that anal cancer can be prevented in high-risk, HIV-infected patients – promise to change that paradigm and may even portend a new standard of care.
Undoubtedly, this is welcome news for the HIV community, who are not only at increased risk for anal HSIL overall, but among whom anal cancer cases have been rising over the past decade. This is especially true for women who are expected to bear a large portion of overall burden of human papillomavirus (HPV)–associated anal squamous cell carcinoma over the next 10 to 20 years.
In the study, 4,446 PLHIV ages 35 and older with precursor anal HSIL were randomly assigned to topical (imiquimod intra-anally, perianally, or both, or fluorouracil) or ablative (infrared coagulation, hyfrecation/electrocautery) treatment, or active surveillance, and followed every 6 months for 5 years. The study population was broadly representative, including men who have sex with men (MSM), women, transgender people, and historically underrepresented minorities, a factor that reinforces the study’s importance in this specific population.
Because the primary endpoint was reached (that is, to determine if HSIL treatment and removal effectively reduces anal cancer incidence in HIV-infected men and women), the Data Safety Board halted accrual and recommended that participants in the surveillance group be offered treatment moving forward. While the investigators are currently working on publication of the results, the study is ongoing.
Still, the ANCHOR study, which is one of the largest malignancy screening studies conducted in PLHIV, has also highlighted significant challenges in how anal cancer is approached in general.
“Anal cancer has many similarities to cervical cancer, where screening for precancerous lesions and treatment have been shown to substantially reduce morbidity and mortality,” said Joseph Sparano, MD, a medical oncologist specializing in HIV and breast cancer at Icahn School of Medicine at Mount Sinai, New York. Dr. Sparano is chair and principal investigator of the AIDS Malignancy Consortium but was not involved in the ANCHOR study.
But, he explained in an interview, “it’s much more difficult and technically challenging to screen for and evaluate the anal canal histology,” noting that
Availability and access to high-resolution anoscopy is limited, said Robert Yarchoan, MD, chief of the HIV and AIDS Malignancy Branch at the National Cancer Institute’s Clinical Cancer Research Division and director of the Office of HIV and AIDS Malignancy (which, incidentally, cosponsored ANCHOR).
“There are relatively few people that do this at this time,” he added in an interview, pointing out that among those who do, most are obstetricians/gynecologists.
A bit of digging into ANCHOR’s backstory revealed that this was a point of contention at the study’s onset. While physicians participating in the study received extensive training in high-resolution anoscopy, ob/gyns were the fastest to achieve competency and/or had the most prior experience, namely because of their experience in cervical cancer screening in women.
But initial objections by the American Board of Obstetricians and Gynecologists (which at the time, insisted that its members only treat women and threatened to remove their certification if they participated in the research), almost threw a wrench into the study’s start, according to a report in The New York Times. While rational minds prevailed and the board reversed its earlier statements, lack of ample training in the procedure may signal future barriers to treatment.
Another challenge lies in how study findings might be applicable to other groups outside of the HIV/AIDS population, such as people with other forms of immunosuppression who have HSIL, or even healthy women or men who are at risk as a result of penetrative/nonpenetrative sexual or nonsexual (for example, vaginal discharge to the anus) contact.
Although he was unable to share specifics at this time, Dr. Palefsky said that when they designed the ANCHOR study, they were aware that “merely showing efficacy wouldn’t necessarily be sufficient for establishing a standard of care, where[as] other pieces of information undoubtedly would be considered by entities that make guidelines” (for example, an examination of adverse events, risks/benefits, and factors that influence quality of life).
“With that in mind, we are doing a quality-of-life study and, in fact, have [collaborated on], developed, and validated what I think is the first anal disease-specific, quality of life instrument,” Dr. Palefsky said. “The work is still ongoing because we did not complete enrollment in the study, but we are continuing it as part of the follow up.”
Study investigators have also collected samples for a biorepository of specimens that will hopefully facilitate a better understanding of the molecular events driving progression from precancer to cancer. “A lot of people with HIV have these high-grade lesions,” Dr. Palefsky said. “If we were able to identify who’s at highest risk of all of them, that would be very important, because we prefer not to treat everybody with high-grade disease,” he noted, adding that the “underlying hope is that the biomarkers we find in the setting will also be relevant for other HPV-related cancers,” especially in women.
Dr. Yarchoan concurred. “One of the challenges is going to be to digest this information and see how to use it to potentially address the growing problem of females with HIV,” he said.
Dr. Palefsky, Dr. Sparano, and Dr. Yarchoan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Can treatment or removal of high-grade squamous intraepithelial lesions (HSIL) reduce the likelihood of developing anal cancer in people living with HIV (PLHIV)?
“In theory, looking for and treating high-grade disease (like we know works in the cervix) is a potential way to prevent anal cancer in high-risk individuals,” Joel Palefsky, MD, lead investigator of the Anal Cancer/HSIL Outcomes Research (ANCHOR) study and founder/director of the University of California, San Francisco’s Anal Neoplasia Clinic, told this news organization. “But we’ve never had any direct evidence that it worked,” he said.
Initial findings from ANCHOR – the first randomized trial to demonstrate that anal cancer can be prevented in high-risk, HIV-infected patients – promise to change that paradigm and may even portend a new standard of care.
Undoubtedly, this is welcome news for the HIV community, who are not only at increased risk for anal HSIL overall, but among whom anal cancer cases have been rising over the past decade. This is especially true for women who are expected to bear a large portion of overall burden of human papillomavirus (HPV)–associated anal squamous cell carcinoma over the next 10 to 20 years.
In the study, 4,446 PLHIV ages 35 and older with precursor anal HSIL were randomly assigned to topical (imiquimod intra-anally, perianally, or both, or fluorouracil) or ablative (infrared coagulation, hyfrecation/electrocautery) treatment, or active surveillance, and followed every 6 months for 5 years. The study population was broadly representative, including men who have sex with men (MSM), women, transgender people, and historically underrepresented minorities, a factor that reinforces the study’s importance in this specific population.
Because the primary endpoint was reached (that is, to determine if HSIL treatment and removal effectively reduces anal cancer incidence in HIV-infected men and women), the Data Safety Board halted accrual and recommended that participants in the surveillance group be offered treatment moving forward. While the investigators are currently working on publication of the results, the study is ongoing.
Still, the ANCHOR study, which is one of the largest malignancy screening studies conducted in PLHIV, has also highlighted significant challenges in how anal cancer is approached in general.
“Anal cancer has many similarities to cervical cancer, where screening for precancerous lesions and treatment have been shown to substantially reduce morbidity and mortality,” said Joseph Sparano, MD, a medical oncologist specializing in HIV and breast cancer at Icahn School of Medicine at Mount Sinai, New York. Dr. Sparano is chair and principal investigator of the AIDS Malignancy Consortium but was not involved in the ANCHOR study.
But, he explained in an interview, “it’s much more difficult and technically challenging to screen for and evaluate the anal canal histology,” noting that
Availability and access to high-resolution anoscopy is limited, said Robert Yarchoan, MD, chief of the HIV and AIDS Malignancy Branch at the National Cancer Institute’s Clinical Cancer Research Division and director of the Office of HIV and AIDS Malignancy (which, incidentally, cosponsored ANCHOR).
“There are relatively few people that do this at this time,” he added in an interview, pointing out that among those who do, most are obstetricians/gynecologists.
A bit of digging into ANCHOR’s backstory revealed that this was a point of contention at the study’s onset. While physicians participating in the study received extensive training in high-resolution anoscopy, ob/gyns were the fastest to achieve competency and/or had the most prior experience, namely because of their experience in cervical cancer screening in women.
But initial objections by the American Board of Obstetricians and Gynecologists (which at the time, insisted that its members only treat women and threatened to remove their certification if they participated in the research), almost threw a wrench into the study’s start, according to a report in The New York Times. While rational minds prevailed and the board reversed its earlier statements, lack of ample training in the procedure may signal future barriers to treatment.
Another challenge lies in how study findings might be applicable to other groups outside of the HIV/AIDS population, such as people with other forms of immunosuppression who have HSIL, or even healthy women or men who are at risk as a result of penetrative/nonpenetrative sexual or nonsexual (for example, vaginal discharge to the anus) contact.
Although he was unable to share specifics at this time, Dr. Palefsky said that when they designed the ANCHOR study, they were aware that “merely showing efficacy wouldn’t necessarily be sufficient for establishing a standard of care, where[as] other pieces of information undoubtedly would be considered by entities that make guidelines” (for example, an examination of adverse events, risks/benefits, and factors that influence quality of life).
“With that in mind, we are doing a quality-of-life study and, in fact, have [collaborated on], developed, and validated what I think is the first anal disease-specific, quality of life instrument,” Dr. Palefsky said. “The work is still ongoing because we did not complete enrollment in the study, but we are continuing it as part of the follow up.”
Study investigators have also collected samples for a biorepository of specimens that will hopefully facilitate a better understanding of the molecular events driving progression from precancer to cancer. “A lot of people with HIV have these high-grade lesions,” Dr. Palefsky said. “If we were able to identify who’s at highest risk of all of them, that would be very important, because we prefer not to treat everybody with high-grade disease,” he noted, adding that the “underlying hope is that the biomarkers we find in the setting will also be relevant for other HPV-related cancers,” especially in women.
Dr. Yarchoan concurred. “One of the challenges is going to be to digest this information and see how to use it to potentially address the growing problem of females with HIV,” he said.
Dr. Palefsky, Dr. Sparano, and Dr. Yarchoan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Rash in an immunocompromised patient
The patient’s history and presentation, as well as a positive varicella zoster virus (VZV) culture of vesicular fluid, led to a diagnosis of disseminated herpes zoster (DHZ). The patient’s laboratory studies were remarkable for mild lymphopenia, thrombocytopenia, and elevated liver function tests. Shave and punch biopsies of the lesion showed ballooning epithelial necrosis with multinucleated giant cells.
DHZ is characterized by more than 20 vesicles outside of a primary or adjacent dermatome and is caused by extensive reactivation of VZV. DHZ is most often encountered in immunocompromised patients.1 Untreated DHZ can lead to encephalitis, myelitis, nerve palsies, pneumonitis, hepatitis, and ocular complications.
Diagnosis is usually made clinically and confirmed by a polymerase chain reaction test, direct fluorescent antibody testing, or viral culture.2 In immunocompetent patients, uncomplicated DHZ is treated with oral acyclovir 800 mg 5 times daily, valacyclovir 1 g 3 times daily, or famciclovir 500 mg 3 times daily for 7 days. Hospital admission for intravenous acyclovir is recommended for immunocompromised patients, especially those with internal organ involvement, such as hepatitis or encephalitis.3
Early treatment is imperative to avoid life-threatening complications. Active herpes zoster lesions are infectious by contact with vesicular fluid until they dry and crust over. Patients should be instructed to avoid contact with susceptible people, including those who are immunocompromised, babies who have not received their varicella vaccine, and pregnant women. It is important to keep DHZ on the differential—especially in an immunosuppressed patient with a diffuse vesicular rash—as it can lead to significant morbidity and mortality.
Our patient was treated with oral valacyclovir 1 g tid for 10 days and he improved without developing systemic symptoms.
Image courtesy of Christen B. Samaan, MD. Text courtesy of Christen B. Samaan, MD, and Matthew F. Helm, MD, Department of Dermatology, and Nanjiba Nawaz, BA, Penn State College of Medicine, Hershey.
1. Bollea-Garlatti ML, Bollea-Garlatti LA, Vacas AS, et al. Clinical characteristics and outcomes in a population with disseminated herpes zoster: a retrospective cohort study. Actas Dermosifiliogr. 2017;108:145-152. doi: 10.1016/j.ad.2016.10.009
2. Chiriac A, Chiriac AE, Podoleanu C, et al. Disseminated cutaneous herpes zoster—a frequently misdiagnosed entity. Int Wound J. 2020;17:1089-1091. doi: 10.1111/iwj.13370
3. Lewis DJ, Schlichte MJ, Dao H Jr. Atypical disseminated herpes zoster: management guidelines in immunocompromised patients. Cutis. 2017;100:321;324;330.
The patient’s history and presentation, as well as a positive varicella zoster virus (VZV) culture of vesicular fluid, led to a diagnosis of disseminated herpes zoster (DHZ). The patient’s laboratory studies were remarkable for mild lymphopenia, thrombocytopenia, and elevated liver function tests. Shave and punch biopsies of the lesion showed ballooning epithelial necrosis with multinucleated giant cells.
DHZ is characterized by more than 20 vesicles outside of a primary or adjacent dermatome and is caused by extensive reactivation of VZV. DHZ is most often encountered in immunocompromised patients.1 Untreated DHZ can lead to encephalitis, myelitis, nerve palsies, pneumonitis, hepatitis, and ocular complications.
Diagnosis is usually made clinically and confirmed by a polymerase chain reaction test, direct fluorescent antibody testing, or viral culture.2 In immunocompetent patients, uncomplicated DHZ is treated with oral acyclovir 800 mg 5 times daily, valacyclovir 1 g 3 times daily, or famciclovir 500 mg 3 times daily for 7 days. Hospital admission for intravenous acyclovir is recommended for immunocompromised patients, especially those with internal organ involvement, such as hepatitis or encephalitis.3
Early treatment is imperative to avoid life-threatening complications. Active herpes zoster lesions are infectious by contact with vesicular fluid until they dry and crust over. Patients should be instructed to avoid contact with susceptible people, including those who are immunocompromised, babies who have not received their varicella vaccine, and pregnant women. It is important to keep DHZ on the differential—especially in an immunosuppressed patient with a diffuse vesicular rash—as it can lead to significant morbidity and mortality.
Our patient was treated with oral valacyclovir 1 g tid for 10 days and he improved without developing systemic symptoms.
Image courtesy of Christen B. Samaan, MD. Text courtesy of Christen B. Samaan, MD, and Matthew F. Helm, MD, Department of Dermatology, and Nanjiba Nawaz, BA, Penn State College of Medicine, Hershey.
The patient’s history and presentation, as well as a positive varicella zoster virus (VZV) culture of vesicular fluid, led to a diagnosis of disseminated herpes zoster (DHZ). The patient’s laboratory studies were remarkable for mild lymphopenia, thrombocytopenia, and elevated liver function tests. Shave and punch biopsies of the lesion showed ballooning epithelial necrosis with multinucleated giant cells.
DHZ is characterized by more than 20 vesicles outside of a primary or adjacent dermatome and is caused by extensive reactivation of VZV. DHZ is most often encountered in immunocompromised patients.1 Untreated DHZ can lead to encephalitis, myelitis, nerve palsies, pneumonitis, hepatitis, and ocular complications.
Diagnosis is usually made clinically and confirmed by a polymerase chain reaction test, direct fluorescent antibody testing, or viral culture.2 In immunocompetent patients, uncomplicated DHZ is treated with oral acyclovir 800 mg 5 times daily, valacyclovir 1 g 3 times daily, or famciclovir 500 mg 3 times daily for 7 days. Hospital admission for intravenous acyclovir is recommended for immunocompromised patients, especially those with internal organ involvement, such as hepatitis or encephalitis.3
Early treatment is imperative to avoid life-threatening complications. Active herpes zoster lesions are infectious by contact with vesicular fluid until they dry and crust over. Patients should be instructed to avoid contact with susceptible people, including those who are immunocompromised, babies who have not received their varicella vaccine, and pregnant women. It is important to keep DHZ on the differential—especially in an immunosuppressed patient with a diffuse vesicular rash—as it can lead to significant morbidity and mortality.
Our patient was treated with oral valacyclovir 1 g tid for 10 days and he improved without developing systemic symptoms.
Image courtesy of Christen B. Samaan, MD. Text courtesy of Christen B. Samaan, MD, and Matthew F. Helm, MD, Department of Dermatology, and Nanjiba Nawaz, BA, Penn State College of Medicine, Hershey.
1. Bollea-Garlatti ML, Bollea-Garlatti LA, Vacas AS, et al. Clinical characteristics and outcomes in a population with disseminated herpes zoster: a retrospective cohort study. Actas Dermosifiliogr. 2017;108:145-152. doi: 10.1016/j.ad.2016.10.009
2. Chiriac A, Chiriac AE, Podoleanu C, et al. Disseminated cutaneous herpes zoster—a frequently misdiagnosed entity. Int Wound J. 2020;17:1089-1091. doi: 10.1111/iwj.13370
3. Lewis DJ, Schlichte MJ, Dao H Jr. Atypical disseminated herpes zoster: management guidelines in immunocompromised patients. Cutis. 2017;100:321;324;330.
1. Bollea-Garlatti ML, Bollea-Garlatti LA, Vacas AS, et al. Clinical characteristics and outcomes in a population with disseminated herpes zoster: a retrospective cohort study. Actas Dermosifiliogr. 2017;108:145-152. doi: 10.1016/j.ad.2016.10.009
2. Chiriac A, Chiriac AE, Podoleanu C, et al. Disseminated cutaneous herpes zoster—a frequently misdiagnosed entity. Int Wound J. 2020;17:1089-1091. doi: 10.1111/iwj.13370
3. Lewis DJ, Schlichte MJ, Dao H Jr. Atypical disseminated herpes zoster: management guidelines in immunocompromised patients. Cutis. 2017;100:321;324;330.
Opioid-induced adrenal insufficiency for the hospitalist
Consider OIAI, even among patients with common infections
Case
A 60-year-old woman with metastatic breast cancer using morphine extended release 30 mg twice daily and as-needed oxycodone for cancer-related pain presents with fever, dyspnea, and productive cough for 2 days. She also notes several weeks of fatigue, nausea, weight loss, and orthostatic lightheadedness. She is found to have pneumonia and is admitted for intravenous antibiotics. She remains borderline hypotensive after intravenous fluids and the hospitalist suspects opioid-induced adrenal insufficiency (OIAI).
How is OIAI diagnosed and managed?
Brief overview of issue
In the United States, 5.4% of the population is currently using long-term opioids.1 Patients using high doses of opioids for greater than 3 months are 40%-50% more likely to be hospitalized than those on a lower dose or no opioids.2 Hospitalists frequently encounter common opioid side effects such as constipation, nausea, and drowsiness, but may be less familiar with their effects on the endocrine system. Chronic, high-dose opioids can suppress the hypothalamic-pituitary-adrenal (HPA) axis and cause secondary, or central, adrenal insufficiency (AI).1
Recognition of OIAI is critical given the current opioid epidemic and life-threatening consequences of AI in systemically ill patients. While high-dose opioids may acutely suppress the HPA axis,3 OIAI is more commonly associated with long-term opioid use.4 The prevalence of OIAI among patients receiving long-term opioids ranges from 8.3% to 29%. This range reflects variations in opioid dose, duration of use, and different methods of assessing the HPA axis.1,4 When screening for HPA axis suppression in subjects taking chronic opioids, Lamprecht and colleagues found a prevalence of 22.5%.5 In comparison, Gibb and colleagues found the prevalence of secondary AI to be 8.3% in patients enrolled in a chronic pain clinic.6 Despite the high prevalence on biochemical screening, the clinical significance of OIAI is less clear. Clinical AI and adrenal crisis among patients on opioids are less frequent and mostly limited to case reports.7,8 In one retrospective cohort, one in 40 patients with OIAI presented with adrenal crisis during a hospitalization for viral gastroenteritis.9
With this prevalence, one would expect to diagnose OIAI more commonly in hospitalized patients. A concerning possibility is that this diagnosis is underrecognized because of either a lack of knowledge of the disease or the clinical overlap between the nonspecific symptoms of AI and other diagnoses. In patients reporting symptoms suggestive of OIAI, the diagnosis was delayed by a median of 12 months.9 The challenge for the hospitalist is to consider OIAI, even among patients with common infections such as pneumonia, viral gastroenteritis, or endocarditis who present with these nonspecific symptoms, while also avoiding unnecessary testing and treatment with glucocorticoids.
Overview of the data
Opiates and opioids exert their physiologic effect through activation of the mu, kappa, and delta receptors. These receptors are located throughout the body, including the hypothalamus and pituitary gland.4 Activation of these receptors results in tonic inhibition of the HPA axis and results in central AI.4 Central AI is characterized by a low a.m. cortisol, low adrenocorticotropic hormone (ACTH), and low dehydroepiandrosterone sulfate (DHEAS) levels.1,4 The low ACTH is indicative of central etiology. This effect of opioids is likely dose dependent with patients using more than 60 morphine-equivalent daily dose at greater risk.1,5
Unexplained or unresolved fatigue, musculoskeletal pain, nausea, vomiting, anorexia, abdominal pain, and orthostatic hypotension in a patient on chronic opioids should prompt consideration of OIAI.9 Once suspected, an 8 a.m. cortisol, ACTH level, and DHEAS level should be ordered. Because of the diurnal variation of cortisol levels, 8 a.m. values are best validated for diagnosis.10 While cutoffs differ, an 8 a.m. cortisol less than 5 mcg/dL combined with ACTH less than 10 pmol/L, and DHEAS less than 50 mcg/dL are highly suggestive of OIAI. Low or indeterminate baseline a.m. cortisol levels warrant confirmatory testing.4,10 While the insulin tolerance test is considered the gold standard, the high dose (250 mcg) cosyntropin stimulation test (CST) is the more commonly used test to diagnose and confirm AI. A CST peak response greater than 18-20 mcg/dL suggests an intact HPA axis (see Figure 1).10 This testing will diagnose central AI, but is not specific for OIAI. Other causes of central AI such as exogenous steroid use, pituitary pathology, and head trauma should be considered before attributing AI to opioids (see Table 1).4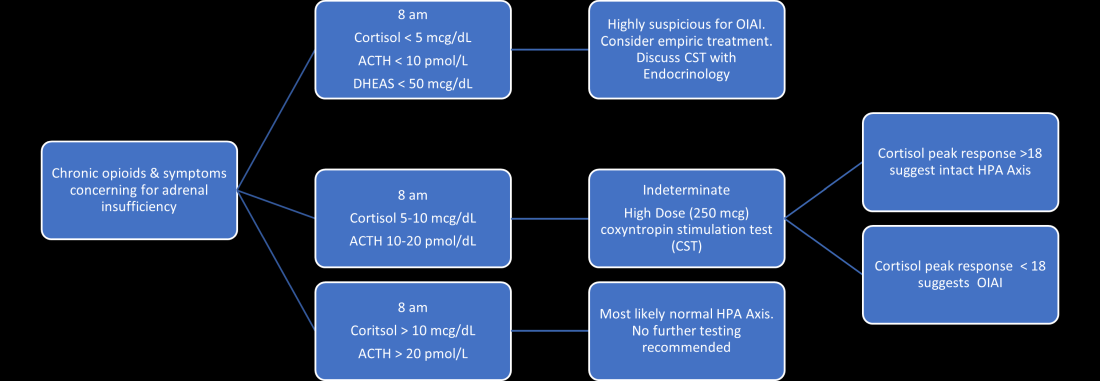
The abnormal CST in central AI is from chronic ACTH deficiency and lack of adrenal stimulation resulting in adrenal atrophy. Adrenal atrophy leaves the adrenal glands incapable of responding to exogenous ACTH. This process takes several weeks; therefore, those with ACTH suppression caused by recent high-dose opioid use or subacute pituitary injury may have an indeterminate or normal cortisol response to high-dose exogenous ACTH.4 Even in the setting of a normal CST, there may remain uncertainty in the diagnosis of OIAI. When evaluating for central AI, the sensitivity and negative likelihood ratio of the CST are only 0.64 and 0.39, respectively.4 In the same cohort of 40 patients with OIAI, 11 patients had a normal CST.9 The low-dose (1 mcg) CST may increase the sensitivity, but the use of this test is limited because of technical challenges.1 Endocrinology consultation can assist when the initial diagnostic and clinical presentation is unclear.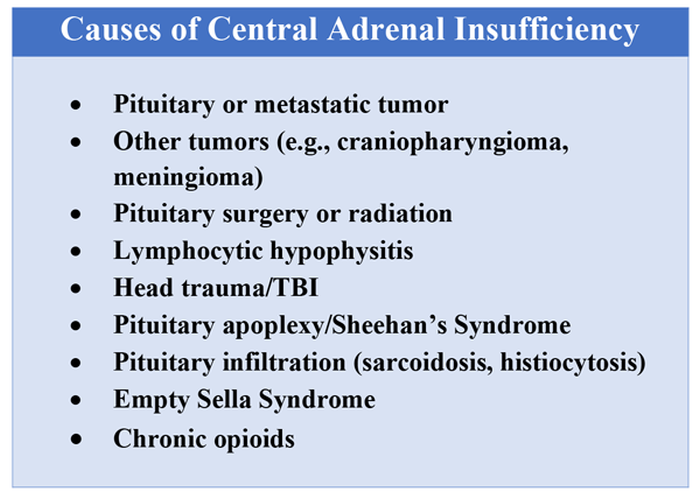
To manage a patient on opioid therapy who has laboratory data consistent with central AI, the clinician must weigh the severity of symptoms, probability of opioid weaning, and risks associated with glucocorticoid treatment. Patients presenting with acute adrenal crisis, hypotension, or critical illness should be managed with intravenous steroid replacement per existing guideline recommendations.10,11
Patients with mild symptoms of nausea, vomiting, or orthostatic symptoms that resolve with treatment of their admitting diagnosis but who have evidence of an abnormal HPA axis should be considered for weaning opioid therapy. Evidence suggests that OIAI is reversible with reduction and cessation of chronic opioid use.4,9 These patients may not need chronic steroid replacement; however, they should receive education on the symptoms of AI and potentially rescue steroids for home use in the setting of severe illness. Patients with OIAI admitted for surgical procedures should be managed in accordance with existing guidelines for perioperative stress dosing of glucocorticoids for AI.
Those with persisting symptoms of OIAI and an abnormal HPA axis require endocrinology consultation and glucocorticoid replacement. There is limited evidence that suggests low dose steroid replacement in patients with OIAI can improve subjective perception of bodily pain, activity level, and mood in chronic opioid users.9 Li and colleagues found that 16 of 23 patients experienced improvement of symptoms on glucocorticoids, and 15 were able to discontinue opioids completely.9 The authors speculated that the improvement in fatigue and musculoskeletal pain after steroid replacement is what allowed for successful opioid weaning. Seven of 10 of these patients with available follow-up had recovery of the HPA axis during the follow-up period.9 In central AI, doses as low as 10-20 mg/day of hydrocortisone have been used.10,11 Hospitalists should educate patients on recognizing symptoms of AI, as this low dose may not be sufficient to prevent adrenal crisis.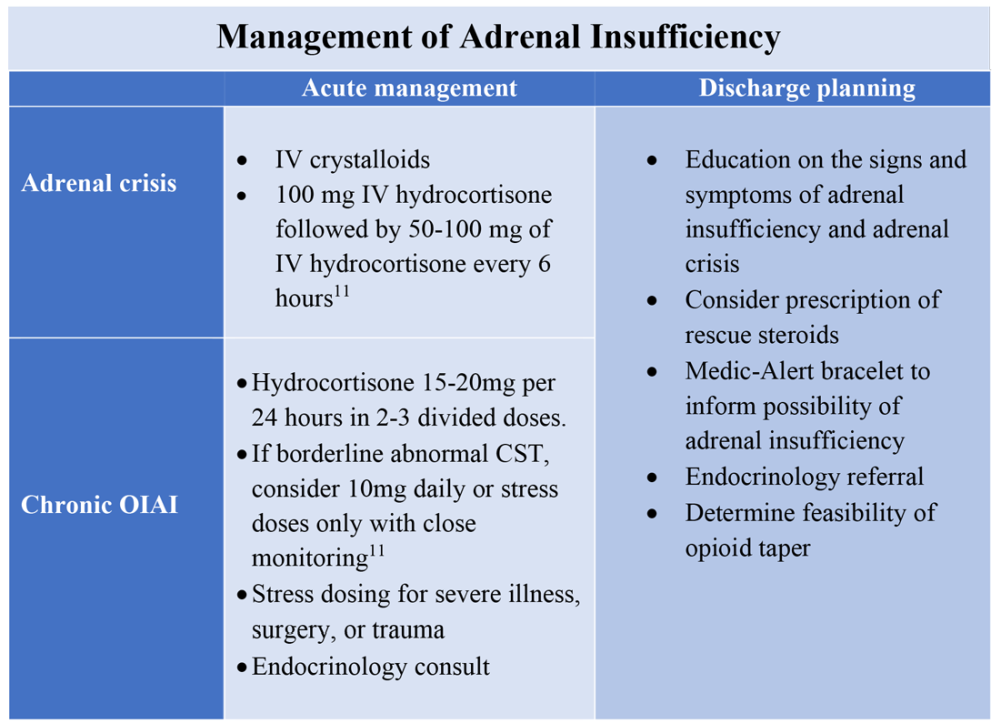
All patients with evidence of abnormalities in the HPA axis should receive a Medic-Alert bracelet to inform other providers of the possibility of adrenal crisis should a major trauma or critical illness render them unconscious.4,10 Since OIAI is a form of central AI, mineralocorticoid replacement is not generally necessary.11 Endocrinology follow-up can help wean steroids as the HPA axis recovers after weaning opioid therapy. Recognizing and diagnosing OIAI can identify patients with untreated symptoms who are at risk for adrenal crisis, improve communication with patients on benefits of weaning opioids, and provide valuable patient education and safe transition of care.
Application of the data to the original case
To make the diagnosis of OIAI, 8 a.m. cortisol, ACTH, and DHEAS should be obtained. Her cortisol was less than 5 mcg/dL, ACTH was 6 pmol/L and DHEAS was 30 mcg/dL. A high dose CST was performed with 30-minute and 60-minute cortisol values of 6 mcg/dL and 9 mcg/dL, respectively. The abnormal CST and low ACTH indicate central AI. She should undergo testing for other etiologies of central AI, such as a brain MRI and pituitary hormone testing, before confirming the diagnosis of OIAI.
The insufficient adrenal response to ACTH in the setting of infection and hypotension should prompt glucocorticoid replacement. Tapering opioids could result in recovery of the HPA axis, though may not be realistic in this patient with chronic cancer-related pain. If the patient is at high risk for adverse effects of glucocorticoids, repeat testing of the HPA axis in the outpatient setting can assess if the patient truly needs steroid replacement daily rather than only during physiologic stress. The patient should be given a Medic-Alert bracelet and instructions on symptoms of AI and stress dosing upon discharge.
Bottom line
OIAI is underrecognized because of central adrenal insufficiency. Knowing its clinical characteristics, diagnostic pathways, and treatment options aids in recognition and management.
Dr. Cunningham, Dr. Munoa, and Dr. Indovina are based in the division of hospital medicine at Denver Health and Hospital Authority.
References
1. Donegan D. Opioid induced adrenal insufficiency: What is new? Curr Opin Endocrinol Diabetes Obes. 2019 Jun;26(3):133-8. doi: 10.1097/MED.0000000000000474.
2. Liang Y and Turner BJ. Opioid risk measure for hospitalization. J Hosp Med. 2015 July;10(7):425-31. doi: 10.1002/jhm.2350.
3. Policola C et al. Adrenal insufficiency in acute oral opiate therapy. Endocrinol Diabetes Metab Case Rep. 2014;2014:130071. doi: 10.1530/EDM-13-0071.
4. Donegan D and Bancos I. Opioid-induced adrenal insufficiency. Mayo Clin Proc. 2018 July;93(7):937-44. doi: 10.1016/j.mayocp.2018.04.010.
5. Lamprecht A et al. Secondary adrenal insufficiency and pituitary dysfunction in oral/transdermal opioid users with non-cancer pain. Eur J Endocrinol. 2018 Dec 1;179(6):353-62. doi: 10.1530/EJE-18-0530.
6. Gibb FW et al. Adrenal insufficiency in patients on long-term opioid analgesia. Clin Endocrinol (Oxf). 2016 June;85(6):831-5. doi:10.1111/cen.13125.
7. Abs R et al. Endocrine consequences of long-term intrathecal administration of opioids. J Clin Endocrinol Metab. 2000 June;85(6):2215-22. doi: 10.1210/jcem.85.6.6615.
8. Tabet EJ et al. Opioid-induced hypoadrenalism resulting in fasting hypoglycaemia. BMJ Case Rep. 2019 Dec 11;12(12):e230551. doi: 10.1136/bcr-2019-230551.
9. Li T et al. Clinical presentation and outcomes of opioid induced adrenal insufficiency. Endocr Pract. 2020 Nov;26(11):1291-1297. doi: 10.4158/EP-2020-0297.
10. Grossman AB. Clinical Review: The diagnosis and management of central hypoadrenalism. J Clin Endocrinol Metab. 2010 Nov;95(11):4855-63. doi: 10.1210/jc.2010-0982.
11. Charmandari E et al. Adrenal insufficiency. Lancet. 2014 June 21;383(9935):2152-67. doi: 10.1016/S0140-6736(13)61684-0.
Key points
- Opioids can cause central adrenal insufficiency because of tonic suppression of the HPA axis. This effect is likely dose dependent, and reversible upon tapering or withdrawal of opioids.
- The prevalence of biochemical OIAI in chronic opioid users of 8%-29% clinical AI is less frequent but may be underrecognized in hospitalized patients leading to delayed diagnosis.
- Diagnosis of central adrenal insufficiency is based upon low 8 a.m. cortisol and ACTH levels and/or an abnormal CST. OIAI is the likely etiology in patients on chronic opioids for whom other causes of central adrenal insufficiency have been ruled out.
- Management with glucocorticoid replacement is variable depending on clinical presentation, severity of HPA axis suppression, and ability to wean opioid therapy. Patient education regarding symptoms of AI and stress dosing is essential.
Additional reading
Grossman AB. Clinical Review: The diagnosis and management of central hypoadrenalism. J Clin Endocrinol Metab. 2010 Nov;95(11):4855-63. doi: 10.1210/jc.2010-0982.
Donegan D and Bancos I. Opioid-induced adrenal insufficiency. Mayo Clin Proc. 2018 July;93(7):937-44. doi: 10.1016/j.mayocp.2018.04.010.
Li T et al. Clinical presentation and outcomes of opioid induced adrenal insufficiency. Endocr Pract. 2020 Nov;26(11):1291-7. doi: 10.4158/EP-2020-0297.
Quiz
A 55-year-old man with chronic back pain, for which he takes a total of 90 mg of oral morphine daily, is admitted for pyelonephritis with fever, nausea, vomiting, dysuria, and abdominal pain. He is febrile and tachycardic on presentation, but his vitals quickly normalize after hydration and antibiotics. About 48 hours into his hospitalization his fevers, dysuria, and abdominal pain have resolved, but he has persistent nausea and headaches. On further questioning, he also reports weight loss and fatigue over the past 3 weeks. He is found to have a morning cortisol level less than 5 mcg/dL, as well as low levels of ACTH and DHEAS. OIAI is suspected.
Which of the following is true about management?
A. Glucocorticoid replacement therapy with oral hydrocortisone should be considered to improve his symptoms.
B. Tapering off opioids is unlikely to resolve his adrenal insufficiency.
C. Stress dose steroids should be started immediately with high-dose intravenous hydrocortisone.
D. Given high clinical suspicion for OIAI, further testing for other etiologies of central adrenal insufficiency is not recommended.
Explanation of correct answer
The correct answer is A. This patient’s ongoing nonspecific symptoms that have persisted despite treatment of his acute pyelonephritis are likely caused by adrenal insufficiency. In a symptomatic patient with OIAI, treatment with oral hydrocortisone should be considered to control symptoms and facilitate tapering opioids. Tapering and stopping opioids often leads to recovery of the HPA axis and resolution of the OIAI. Tapering opioids should be considered a mainstay of therapy for OIAI when clinically appropriate, as in this patient with chronic benign pain. Stress dose steroids are not indicated in the absence of critical illness, adrenal crisis, or major surgery. OIAI is a diagnosis of exclusion, and patients should undergo workup for other causes of secondary adrenal insufficiency.
Consider OIAI, even among patients with common infections
Consider OIAI, even among patients with common infections
Case
A 60-year-old woman with metastatic breast cancer using morphine extended release 30 mg twice daily and as-needed oxycodone for cancer-related pain presents with fever, dyspnea, and productive cough for 2 days. She also notes several weeks of fatigue, nausea, weight loss, and orthostatic lightheadedness. She is found to have pneumonia and is admitted for intravenous antibiotics. She remains borderline hypotensive after intravenous fluids and the hospitalist suspects opioid-induced adrenal insufficiency (OIAI).
How is OIAI diagnosed and managed?
Brief overview of issue
In the United States, 5.4% of the population is currently using long-term opioids.1 Patients using high doses of opioids for greater than 3 months are 40%-50% more likely to be hospitalized than those on a lower dose or no opioids.2 Hospitalists frequently encounter common opioid side effects such as constipation, nausea, and drowsiness, but may be less familiar with their effects on the endocrine system. Chronic, high-dose opioids can suppress the hypothalamic-pituitary-adrenal (HPA) axis and cause secondary, or central, adrenal insufficiency (AI).1
Recognition of OIAI is critical given the current opioid epidemic and life-threatening consequences of AI in systemically ill patients. While high-dose opioids may acutely suppress the HPA axis,3 OIAI is more commonly associated with long-term opioid use.4 The prevalence of OIAI among patients receiving long-term opioids ranges from 8.3% to 29%. This range reflects variations in opioid dose, duration of use, and different methods of assessing the HPA axis.1,4 When screening for HPA axis suppression in subjects taking chronic opioids, Lamprecht and colleagues found a prevalence of 22.5%.5 In comparison, Gibb and colleagues found the prevalence of secondary AI to be 8.3% in patients enrolled in a chronic pain clinic.6 Despite the high prevalence on biochemical screening, the clinical significance of OIAI is less clear. Clinical AI and adrenal crisis among patients on opioids are less frequent and mostly limited to case reports.7,8 In one retrospective cohort, one in 40 patients with OIAI presented with adrenal crisis during a hospitalization for viral gastroenteritis.9
With this prevalence, one would expect to diagnose OIAI more commonly in hospitalized patients. A concerning possibility is that this diagnosis is underrecognized because of either a lack of knowledge of the disease or the clinical overlap between the nonspecific symptoms of AI and other diagnoses. In patients reporting symptoms suggestive of OIAI, the diagnosis was delayed by a median of 12 months.9 The challenge for the hospitalist is to consider OIAI, even among patients with common infections such as pneumonia, viral gastroenteritis, or endocarditis who present with these nonspecific symptoms, while also avoiding unnecessary testing and treatment with glucocorticoids.
Overview of the data
Opiates and opioids exert their physiologic effect through activation of the mu, kappa, and delta receptors. These receptors are located throughout the body, including the hypothalamus and pituitary gland.4 Activation of these receptors results in tonic inhibition of the HPA axis and results in central AI.4 Central AI is characterized by a low a.m. cortisol, low adrenocorticotropic hormone (ACTH), and low dehydroepiandrosterone sulfate (DHEAS) levels.1,4 The low ACTH is indicative of central etiology. This effect of opioids is likely dose dependent with patients using more than 60 morphine-equivalent daily dose at greater risk.1,5
Unexplained or unresolved fatigue, musculoskeletal pain, nausea, vomiting, anorexia, abdominal pain, and orthostatic hypotension in a patient on chronic opioids should prompt consideration of OIAI.9 Once suspected, an 8 a.m. cortisol, ACTH level, and DHEAS level should be ordered. Because of the diurnal variation of cortisol levels, 8 a.m. values are best validated for diagnosis.10 While cutoffs differ, an 8 a.m. cortisol less than 5 mcg/dL combined with ACTH less than 10 pmol/L, and DHEAS less than 50 mcg/dL are highly suggestive of OIAI. Low or indeterminate baseline a.m. cortisol levels warrant confirmatory testing.4,10 While the insulin tolerance test is considered the gold standard, the high dose (250 mcg) cosyntropin stimulation test (CST) is the more commonly used test to diagnose and confirm AI. A CST peak response greater than 18-20 mcg/dL suggests an intact HPA axis (see Figure 1).10 This testing will diagnose central AI, but is not specific for OIAI. Other causes of central AI such as exogenous steroid use, pituitary pathology, and head trauma should be considered before attributing AI to opioids (see Table 1).4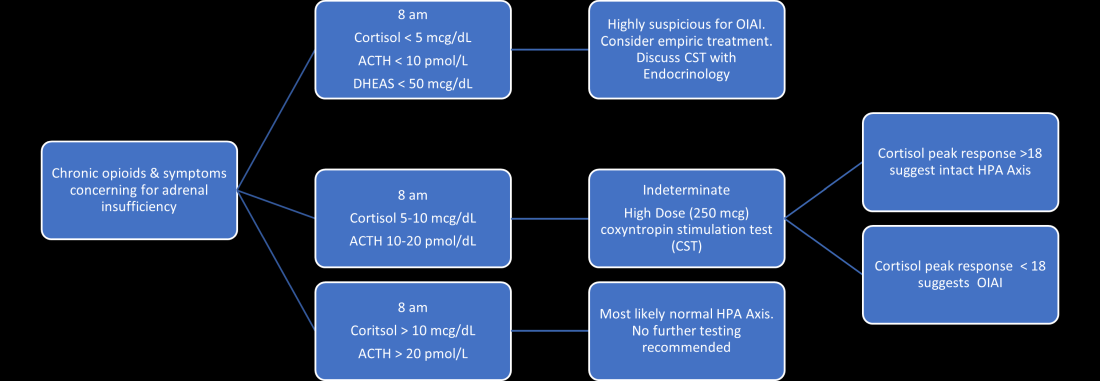
The abnormal CST in central AI is from chronic ACTH deficiency and lack of adrenal stimulation resulting in adrenal atrophy. Adrenal atrophy leaves the adrenal glands incapable of responding to exogenous ACTH. This process takes several weeks; therefore, those with ACTH suppression caused by recent high-dose opioid use or subacute pituitary injury may have an indeterminate or normal cortisol response to high-dose exogenous ACTH.4 Even in the setting of a normal CST, there may remain uncertainty in the diagnosis of OIAI. When evaluating for central AI, the sensitivity and negative likelihood ratio of the CST are only 0.64 and 0.39, respectively.4 In the same cohort of 40 patients with OIAI, 11 patients had a normal CST.9 The low-dose (1 mcg) CST may increase the sensitivity, but the use of this test is limited because of technical challenges.1 Endocrinology consultation can assist when the initial diagnostic and clinical presentation is unclear.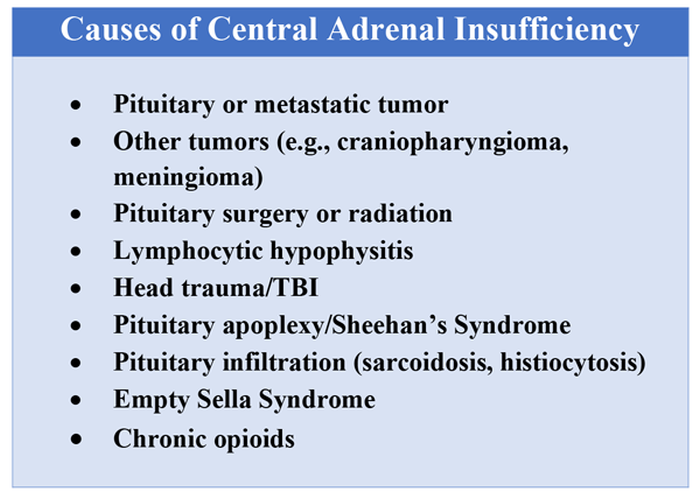
To manage a patient on opioid therapy who has laboratory data consistent with central AI, the clinician must weigh the severity of symptoms, probability of opioid weaning, and risks associated with glucocorticoid treatment. Patients presenting with acute adrenal crisis, hypotension, or critical illness should be managed with intravenous steroid replacement per existing guideline recommendations.10,11
Patients with mild symptoms of nausea, vomiting, or orthostatic symptoms that resolve with treatment of their admitting diagnosis but who have evidence of an abnormal HPA axis should be considered for weaning opioid therapy. Evidence suggests that OIAI is reversible with reduction and cessation of chronic opioid use.4,9 These patients may not need chronic steroid replacement; however, they should receive education on the symptoms of AI and potentially rescue steroids for home use in the setting of severe illness. Patients with OIAI admitted for surgical procedures should be managed in accordance with existing guidelines for perioperative stress dosing of glucocorticoids for AI.
Those with persisting symptoms of OIAI and an abnormal HPA axis require endocrinology consultation and glucocorticoid replacement. There is limited evidence that suggests low dose steroid replacement in patients with OIAI can improve subjective perception of bodily pain, activity level, and mood in chronic opioid users.9 Li and colleagues found that 16 of 23 patients experienced improvement of symptoms on glucocorticoids, and 15 were able to discontinue opioids completely.9 The authors speculated that the improvement in fatigue and musculoskeletal pain after steroid replacement is what allowed for successful opioid weaning. Seven of 10 of these patients with available follow-up had recovery of the HPA axis during the follow-up period.9 In central AI, doses as low as 10-20 mg/day of hydrocortisone have been used.10,11 Hospitalists should educate patients on recognizing symptoms of AI, as this low dose may not be sufficient to prevent adrenal crisis.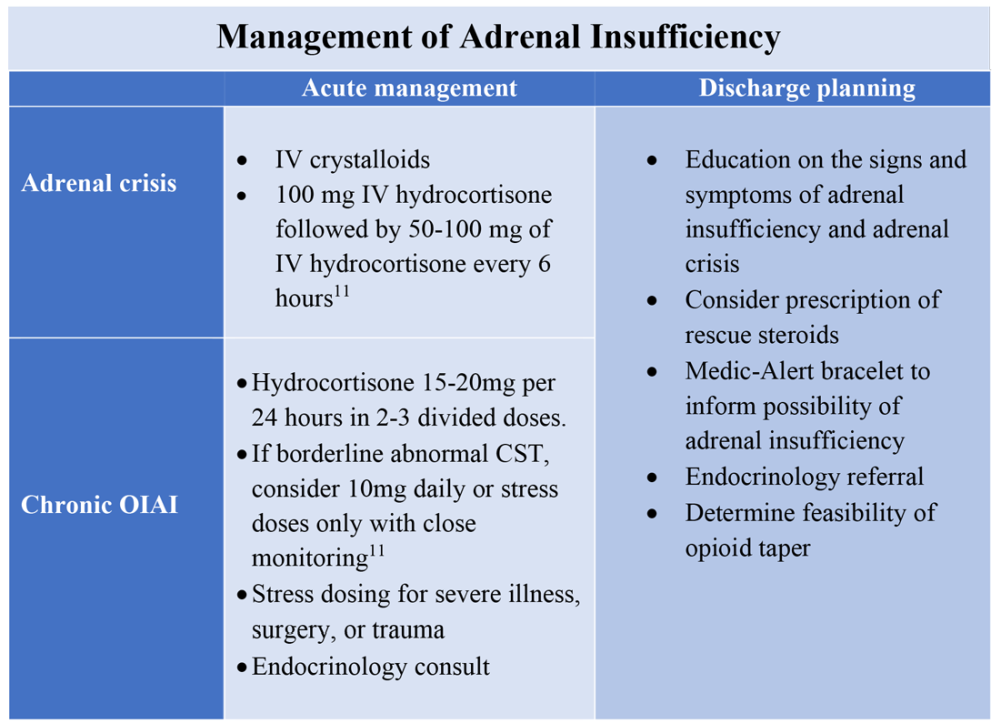
All patients with evidence of abnormalities in the HPA axis should receive a Medic-Alert bracelet to inform other providers of the possibility of adrenal crisis should a major trauma or critical illness render them unconscious.4,10 Since OIAI is a form of central AI, mineralocorticoid replacement is not generally necessary.11 Endocrinology follow-up can help wean steroids as the HPA axis recovers after weaning opioid therapy. Recognizing and diagnosing OIAI can identify patients with untreated symptoms who are at risk for adrenal crisis, improve communication with patients on benefits of weaning opioids, and provide valuable patient education and safe transition of care.
Application of the data to the original case
To make the diagnosis of OIAI, 8 a.m. cortisol, ACTH, and DHEAS should be obtained. Her cortisol was less than 5 mcg/dL, ACTH was 6 pmol/L and DHEAS was 30 mcg/dL. A high dose CST was performed with 30-minute and 60-minute cortisol values of 6 mcg/dL and 9 mcg/dL, respectively. The abnormal CST and low ACTH indicate central AI. She should undergo testing for other etiologies of central AI, such as a brain MRI and pituitary hormone testing, before confirming the diagnosis of OIAI.
The insufficient adrenal response to ACTH in the setting of infection and hypotension should prompt glucocorticoid replacement. Tapering opioids could result in recovery of the HPA axis, though may not be realistic in this patient with chronic cancer-related pain. If the patient is at high risk for adverse effects of glucocorticoids, repeat testing of the HPA axis in the outpatient setting can assess if the patient truly needs steroid replacement daily rather than only during physiologic stress. The patient should be given a Medic-Alert bracelet and instructions on symptoms of AI and stress dosing upon discharge.
Bottom line
OIAI is underrecognized because of central adrenal insufficiency. Knowing its clinical characteristics, diagnostic pathways, and treatment options aids in recognition and management.
Dr. Cunningham, Dr. Munoa, and Dr. Indovina are based in the division of hospital medicine at Denver Health and Hospital Authority.
References
1. Donegan D. Opioid induced adrenal insufficiency: What is new? Curr Opin Endocrinol Diabetes Obes. 2019 Jun;26(3):133-8. doi: 10.1097/MED.0000000000000474.
2. Liang Y and Turner BJ. Opioid risk measure for hospitalization. J Hosp Med. 2015 July;10(7):425-31. doi: 10.1002/jhm.2350.
3. Policola C et al. Adrenal insufficiency in acute oral opiate therapy. Endocrinol Diabetes Metab Case Rep. 2014;2014:130071. doi: 10.1530/EDM-13-0071.
4. Donegan D and Bancos I. Opioid-induced adrenal insufficiency. Mayo Clin Proc. 2018 July;93(7):937-44. doi: 10.1016/j.mayocp.2018.04.010.
5. Lamprecht A et al. Secondary adrenal insufficiency and pituitary dysfunction in oral/transdermal opioid users with non-cancer pain. Eur J Endocrinol. 2018 Dec 1;179(6):353-62. doi: 10.1530/EJE-18-0530.
6. Gibb FW et al. Adrenal insufficiency in patients on long-term opioid analgesia. Clin Endocrinol (Oxf). 2016 June;85(6):831-5. doi:10.1111/cen.13125.
7. Abs R et al. Endocrine consequences of long-term intrathecal administration of opioids. J Clin Endocrinol Metab. 2000 June;85(6):2215-22. doi: 10.1210/jcem.85.6.6615.
8. Tabet EJ et al. Opioid-induced hypoadrenalism resulting in fasting hypoglycaemia. BMJ Case Rep. 2019 Dec 11;12(12):e230551. doi: 10.1136/bcr-2019-230551.
9. Li T et al. Clinical presentation and outcomes of opioid induced adrenal insufficiency. Endocr Pract. 2020 Nov;26(11):1291-1297. doi: 10.4158/EP-2020-0297.
10. Grossman AB. Clinical Review: The diagnosis and management of central hypoadrenalism. J Clin Endocrinol Metab. 2010 Nov;95(11):4855-63. doi: 10.1210/jc.2010-0982.
11. Charmandari E et al. Adrenal insufficiency. Lancet. 2014 June 21;383(9935):2152-67. doi: 10.1016/S0140-6736(13)61684-0.
Key points
- Opioids can cause central adrenal insufficiency because of tonic suppression of the HPA axis. This effect is likely dose dependent, and reversible upon tapering or withdrawal of opioids.
- The prevalence of biochemical OIAI in chronic opioid users of 8%-29% clinical AI is less frequent but may be underrecognized in hospitalized patients leading to delayed diagnosis.
- Diagnosis of central adrenal insufficiency is based upon low 8 a.m. cortisol and ACTH levels and/or an abnormal CST. OIAI is the likely etiology in patients on chronic opioids for whom other causes of central adrenal insufficiency have been ruled out.
- Management with glucocorticoid replacement is variable depending on clinical presentation, severity of HPA axis suppression, and ability to wean opioid therapy. Patient education regarding symptoms of AI and stress dosing is essential.
Additional reading
Grossman AB. Clinical Review: The diagnosis and management of central hypoadrenalism. J Clin Endocrinol Metab. 2010 Nov;95(11):4855-63. doi: 10.1210/jc.2010-0982.
Donegan D and Bancos I. Opioid-induced adrenal insufficiency. Mayo Clin Proc. 2018 July;93(7):937-44. doi: 10.1016/j.mayocp.2018.04.010.
Li T et al. Clinical presentation and outcomes of opioid induced adrenal insufficiency. Endocr Pract. 2020 Nov;26(11):1291-7. doi: 10.4158/EP-2020-0297.
Quiz
A 55-year-old man with chronic back pain, for which he takes a total of 90 mg of oral morphine daily, is admitted for pyelonephritis with fever, nausea, vomiting, dysuria, and abdominal pain. He is febrile and tachycardic on presentation, but his vitals quickly normalize after hydration and antibiotics. About 48 hours into his hospitalization his fevers, dysuria, and abdominal pain have resolved, but he has persistent nausea and headaches. On further questioning, he also reports weight loss and fatigue over the past 3 weeks. He is found to have a morning cortisol level less than 5 mcg/dL, as well as low levels of ACTH and DHEAS. OIAI is suspected.
Which of the following is true about management?
A. Glucocorticoid replacement therapy with oral hydrocortisone should be considered to improve his symptoms.
B. Tapering off opioids is unlikely to resolve his adrenal insufficiency.
C. Stress dose steroids should be started immediately with high-dose intravenous hydrocortisone.
D. Given high clinical suspicion for OIAI, further testing for other etiologies of central adrenal insufficiency is not recommended.
Explanation of correct answer
The correct answer is A. This patient’s ongoing nonspecific symptoms that have persisted despite treatment of his acute pyelonephritis are likely caused by adrenal insufficiency. In a symptomatic patient with OIAI, treatment with oral hydrocortisone should be considered to control symptoms and facilitate tapering opioids. Tapering and stopping opioids often leads to recovery of the HPA axis and resolution of the OIAI. Tapering opioids should be considered a mainstay of therapy for OIAI when clinically appropriate, as in this patient with chronic benign pain. Stress dose steroids are not indicated in the absence of critical illness, adrenal crisis, or major surgery. OIAI is a diagnosis of exclusion, and patients should undergo workup for other causes of secondary adrenal insufficiency.
Case
A 60-year-old woman with metastatic breast cancer using morphine extended release 30 mg twice daily and as-needed oxycodone for cancer-related pain presents with fever, dyspnea, and productive cough for 2 days. She also notes several weeks of fatigue, nausea, weight loss, and orthostatic lightheadedness. She is found to have pneumonia and is admitted for intravenous antibiotics. She remains borderline hypotensive after intravenous fluids and the hospitalist suspects opioid-induced adrenal insufficiency (OIAI).
How is OIAI diagnosed and managed?
Brief overview of issue
In the United States, 5.4% of the population is currently using long-term opioids.1 Patients using high doses of opioids for greater than 3 months are 40%-50% more likely to be hospitalized than those on a lower dose or no opioids.2 Hospitalists frequently encounter common opioid side effects such as constipation, nausea, and drowsiness, but may be less familiar with their effects on the endocrine system. Chronic, high-dose opioids can suppress the hypothalamic-pituitary-adrenal (HPA) axis and cause secondary, or central, adrenal insufficiency (AI).1
Recognition of OIAI is critical given the current opioid epidemic and life-threatening consequences of AI in systemically ill patients. While high-dose opioids may acutely suppress the HPA axis,3 OIAI is more commonly associated with long-term opioid use.4 The prevalence of OIAI among patients receiving long-term opioids ranges from 8.3% to 29%. This range reflects variations in opioid dose, duration of use, and different methods of assessing the HPA axis.1,4 When screening for HPA axis suppression in subjects taking chronic opioids, Lamprecht and colleagues found a prevalence of 22.5%.5 In comparison, Gibb and colleagues found the prevalence of secondary AI to be 8.3% in patients enrolled in a chronic pain clinic.6 Despite the high prevalence on biochemical screening, the clinical significance of OIAI is less clear. Clinical AI and adrenal crisis among patients on opioids are less frequent and mostly limited to case reports.7,8 In one retrospective cohort, one in 40 patients with OIAI presented with adrenal crisis during a hospitalization for viral gastroenteritis.9
With this prevalence, one would expect to diagnose OIAI more commonly in hospitalized patients. A concerning possibility is that this diagnosis is underrecognized because of either a lack of knowledge of the disease or the clinical overlap between the nonspecific symptoms of AI and other diagnoses. In patients reporting symptoms suggestive of OIAI, the diagnosis was delayed by a median of 12 months.9 The challenge for the hospitalist is to consider OIAI, even among patients with common infections such as pneumonia, viral gastroenteritis, or endocarditis who present with these nonspecific symptoms, while also avoiding unnecessary testing and treatment with glucocorticoids.
Overview of the data
Opiates and opioids exert their physiologic effect through activation of the mu, kappa, and delta receptors. These receptors are located throughout the body, including the hypothalamus and pituitary gland.4 Activation of these receptors results in tonic inhibition of the HPA axis and results in central AI.4 Central AI is characterized by a low a.m. cortisol, low adrenocorticotropic hormone (ACTH), and low dehydroepiandrosterone sulfate (DHEAS) levels.1,4 The low ACTH is indicative of central etiology. This effect of opioids is likely dose dependent with patients using more than 60 morphine-equivalent daily dose at greater risk.1,5
Unexplained or unresolved fatigue, musculoskeletal pain, nausea, vomiting, anorexia, abdominal pain, and orthostatic hypotension in a patient on chronic opioids should prompt consideration of OIAI.9 Once suspected, an 8 a.m. cortisol, ACTH level, and DHEAS level should be ordered. Because of the diurnal variation of cortisol levels, 8 a.m. values are best validated for diagnosis.10 While cutoffs differ, an 8 a.m. cortisol less than 5 mcg/dL combined with ACTH less than 10 pmol/L, and DHEAS less than 50 mcg/dL are highly suggestive of OIAI. Low or indeterminate baseline a.m. cortisol levels warrant confirmatory testing.4,10 While the insulin tolerance test is considered the gold standard, the high dose (250 mcg) cosyntropin stimulation test (CST) is the more commonly used test to diagnose and confirm AI. A CST peak response greater than 18-20 mcg/dL suggests an intact HPA axis (see Figure 1).10 This testing will diagnose central AI, but is not specific for OIAI. Other causes of central AI such as exogenous steroid use, pituitary pathology, and head trauma should be considered before attributing AI to opioids (see Table 1).4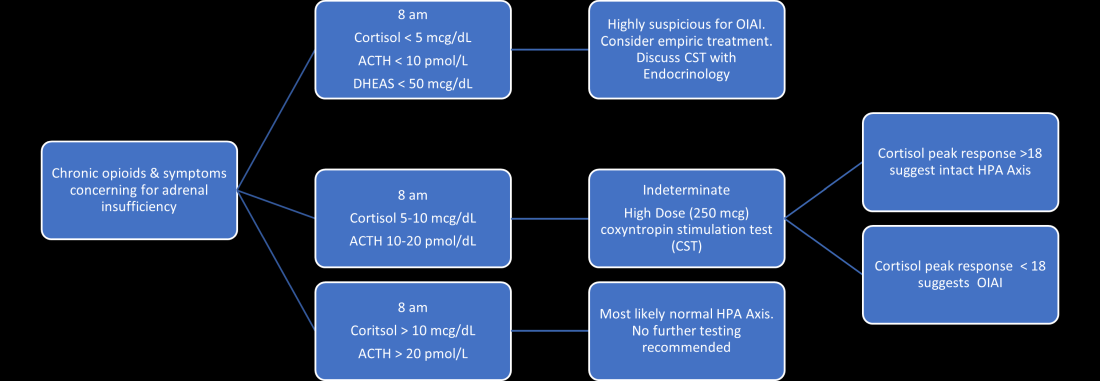
The abnormal CST in central AI is from chronic ACTH deficiency and lack of adrenal stimulation resulting in adrenal atrophy. Adrenal atrophy leaves the adrenal glands incapable of responding to exogenous ACTH. This process takes several weeks; therefore, those with ACTH suppression caused by recent high-dose opioid use or subacute pituitary injury may have an indeterminate or normal cortisol response to high-dose exogenous ACTH.4 Even in the setting of a normal CST, there may remain uncertainty in the diagnosis of OIAI. When evaluating for central AI, the sensitivity and negative likelihood ratio of the CST are only 0.64 and 0.39, respectively.4 In the same cohort of 40 patients with OIAI, 11 patients had a normal CST.9 The low-dose (1 mcg) CST may increase the sensitivity, but the use of this test is limited because of technical challenges.1 Endocrinology consultation can assist when the initial diagnostic and clinical presentation is unclear.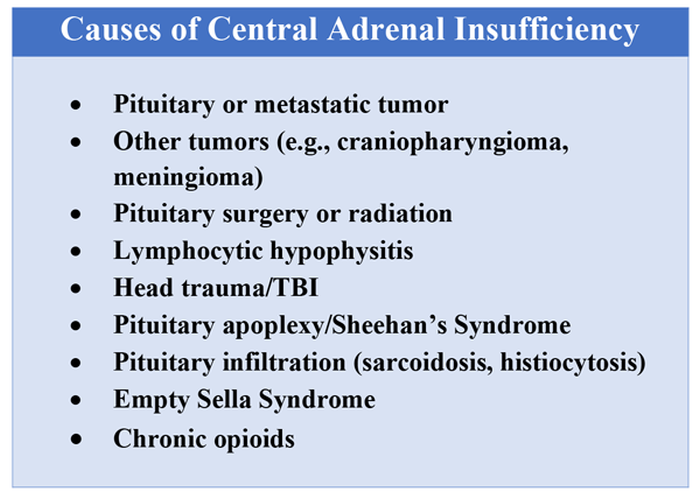
To manage a patient on opioid therapy who has laboratory data consistent with central AI, the clinician must weigh the severity of symptoms, probability of opioid weaning, and risks associated with glucocorticoid treatment. Patients presenting with acute adrenal crisis, hypotension, or critical illness should be managed with intravenous steroid replacement per existing guideline recommendations.10,11
Patients with mild symptoms of nausea, vomiting, or orthostatic symptoms that resolve with treatment of their admitting diagnosis but who have evidence of an abnormal HPA axis should be considered for weaning opioid therapy. Evidence suggests that OIAI is reversible with reduction and cessation of chronic opioid use.4,9 These patients may not need chronic steroid replacement; however, they should receive education on the symptoms of AI and potentially rescue steroids for home use in the setting of severe illness. Patients with OIAI admitted for surgical procedures should be managed in accordance with existing guidelines for perioperative stress dosing of glucocorticoids for AI.
Those with persisting symptoms of OIAI and an abnormal HPA axis require endocrinology consultation and glucocorticoid replacement. There is limited evidence that suggests low dose steroid replacement in patients with OIAI can improve subjective perception of bodily pain, activity level, and mood in chronic opioid users.9 Li and colleagues found that 16 of 23 patients experienced improvement of symptoms on glucocorticoids, and 15 were able to discontinue opioids completely.9 The authors speculated that the improvement in fatigue and musculoskeletal pain after steroid replacement is what allowed for successful opioid weaning. Seven of 10 of these patients with available follow-up had recovery of the HPA axis during the follow-up period.9 In central AI, doses as low as 10-20 mg/day of hydrocortisone have been used.10,11 Hospitalists should educate patients on recognizing symptoms of AI, as this low dose may not be sufficient to prevent adrenal crisis.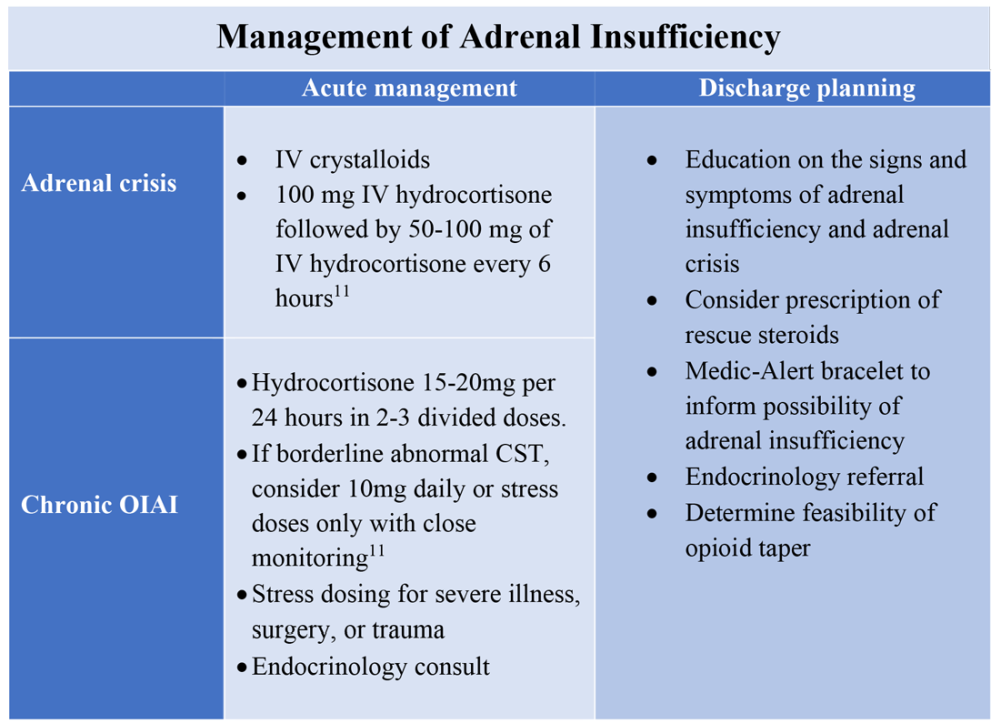
All patients with evidence of abnormalities in the HPA axis should receive a Medic-Alert bracelet to inform other providers of the possibility of adrenal crisis should a major trauma or critical illness render them unconscious.4,10 Since OIAI is a form of central AI, mineralocorticoid replacement is not generally necessary.11 Endocrinology follow-up can help wean steroids as the HPA axis recovers after weaning opioid therapy. Recognizing and diagnosing OIAI can identify patients with untreated symptoms who are at risk for adrenal crisis, improve communication with patients on benefits of weaning opioids, and provide valuable patient education and safe transition of care.
Application of the data to the original case
To make the diagnosis of OIAI, 8 a.m. cortisol, ACTH, and DHEAS should be obtained. Her cortisol was less than 5 mcg/dL, ACTH was 6 pmol/L and DHEAS was 30 mcg/dL. A high dose CST was performed with 30-minute and 60-minute cortisol values of 6 mcg/dL and 9 mcg/dL, respectively. The abnormal CST and low ACTH indicate central AI. She should undergo testing for other etiologies of central AI, such as a brain MRI and pituitary hormone testing, before confirming the diagnosis of OIAI.
The insufficient adrenal response to ACTH in the setting of infection and hypotension should prompt glucocorticoid replacement. Tapering opioids could result in recovery of the HPA axis, though may not be realistic in this patient with chronic cancer-related pain. If the patient is at high risk for adverse effects of glucocorticoids, repeat testing of the HPA axis in the outpatient setting can assess if the patient truly needs steroid replacement daily rather than only during physiologic stress. The patient should be given a Medic-Alert bracelet and instructions on symptoms of AI and stress dosing upon discharge.
Bottom line
OIAI is underrecognized because of central adrenal insufficiency. Knowing its clinical characteristics, diagnostic pathways, and treatment options aids in recognition and management.
Dr. Cunningham, Dr. Munoa, and Dr. Indovina are based in the division of hospital medicine at Denver Health and Hospital Authority.
References
1. Donegan D. Opioid induced adrenal insufficiency: What is new? Curr Opin Endocrinol Diabetes Obes. 2019 Jun;26(3):133-8. doi: 10.1097/MED.0000000000000474.
2. Liang Y and Turner BJ. Opioid risk measure for hospitalization. J Hosp Med. 2015 July;10(7):425-31. doi: 10.1002/jhm.2350.
3. Policola C et al. Adrenal insufficiency in acute oral opiate therapy. Endocrinol Diabetes Metab Case Rep. 2014;2014:130071. doi: 10.1530/EDM-13-0071.
4. Donegan D and Bancos I. Opioid-induced adrenal insufficiency. Mayo Clin Proc. 2018 July;93(7):937-44. doi: 10.1016/j.mayocp.2018.04.010.
5. Lamprecht A et al. Secondary adrenal insufficiency and pituitary dysfunction in oral/transdermal opioid users with non-cancer pain. Eur J Endocrinol. 2018 Dec 1;179(6):353-62. doi: 10.1530/EJE-18-0530.
6. Gibb FW et al. Adrenal insufficiency in patients on long-term opioid analgesia. Clin Endocrinol (Oxf). 2016 June;85(6):831-5. doi:10.1111/cen.13125.
7. Abs R et al. Endocrine consequences of long-term intrathecal administration of opioids. J Clin Endocrinol Metab. 2000 June;85(6):2215-22. doi: 10.1210/jcem.85.6.6615.
8. Tabet EJ et al. Opioid-induced hypoadrenalism resulting in fasting hypoglycaemia. BMJ Case Rep. 2019 Dec 11;12(12):e230551. doi: 10.1136/bcr-2019-230551.
9. Li T et al. Clinical presentation and outcomes of opioid induced adrenal insufficiency. Endocr Pract. 2020 Nov;26(11):1291-1297. doi: 10.4158/EP-2020-0297.
10. Grossman AB. Clinical Review: The diagnosis and management of central hypoadrenalism. J Clin Endocrinol Metab. 2010 Nov;95(11):4855-63. doi: 10.1210/jc.2010-0982.
11. Charmandari E et al. Adrenal insufficiency. Lancet. 2014 June 21;383(9935):2152-67. doi: 10.1016/S0140-6736(13)61684-0.
Key points
- Opioids can cause central adrenal insufficiency because of tonic suppression of the HPA axis. This effect is likely dose dependent, and reversible upon tapering or withdrawal of opioids.
- The prevalence of biochemical OIAI in chronic opioid users of 8%-29% clinical AI is less frequent but may be underrecognized in hospitalized patients leading to delayed diagnosis.
- Diagnosis of central adrenal insufficiency is based upon low 8 a.m. cortisol and ACTH levels and/or an abnormal CST. OIAI is the likely etiology in patients on chronic opioids for whom other causes of central adrenal insufficiency have been ruled out.
- Management with glucocorticoid replacement is variable depending on clinical presentation, severity of HPA axis suppression, and ability to wean opioid therapy. Patient education regarding symptoms of AI and stress dosing is essential.
Additional reading
Grossman AB. Clinical Review: The diagnosis and management of central hypoadrenalism. J Clin Endocrinol Metab. 2010 Nov;95(11):4855-63. doi: 10.1210/jc.2010-0982.
Donegan D and Bancos I. Opioid-induced adrenal insufficiency. Mayo Clin Proc. 2018 July;93(7):937-44. doi: 10.1016/j.mayocp.2018.04.010.
Li T et al. Clinical presentation and outcomes of opioid induced adrenal insufficiency. Endocr Pract. 2020 Nov;26(11):1291-7. doi: 10.4158/EP-2020-0297.
Quiz
A 55-year-old man with chronic back pain, for which he takes a total of 90 mg of oral morphine daily, is admitted for pyelonephritis with fever, nausea, vomiting, dysuria, and abdominal pain. He is febrile and tachycardic on presentation, but his vitals quickly normalize after hydration and antibiotics. About 48 hours into his hospitalization his fevers, dysuria, and abdominal pain have resolved, but he has persistent nausea and headaches. On further questioning, he also reports weight loss and fatigue over the past 3 weeks. He is found to have a morning cortisol level less than 5 mcg/dL, as well as low levels of ACTH and DHEAS. OIAI is suspected.
Which of the following is true about management?
A. Glucocorticoid replacement therapy with oral hydrocortisone should be considered to improve his symptoms.
B. Tapering off opioids is unlikely to resolve his adrenal insufficiency.
C. Stress dose steroids should be started immediately with high-dose intravenous hydrocortisone.
D. Given high clinical suspicion for OIAI, further testing for other etiologies of central adrenal insufficiency is not recommended.
Explanation of correct answer
The correct answer is A. This patient’s ongoing nonspecific symptoms that have persisted despite treatment of his acute pyelonephritis are likely caused by adrenal insufficiency. In a symptomatic patient with OIAI, treatment with oral hydrocortisone should be considered to control symptoms and facilitate tapering opioids. Tapering and stopping opioids often leads to recovery of the HPA axis and resolution of the OIAI. Tapering opioids should be considered a mainstay of therapy for OIAI when clinically appropriate, as in this patient with chronic benign pain. Stress dose steroids are not indicated in the absence of critical illness, adrenal crisis, or major surgery. OIAI is a diagnosis of exclusion, and patients should undergo workup for other causes of secondary adrenal insufficiency.
Judge dismisses Lyme disease lawsuit against IDSA, doctors, but the ordeal has left its scars
Years ago, when rheumatologist Leonard Sigal, MD, was undertaking research on Lyme disease and treating patients with the condition at the Robert Wood Johnson Medical School, New Brunswick, N.J., a regular stream of abuse and threats became the usual background noise of his work. He didn’t get used to it, but it never stopped.
“I was accused of incredibly heinous crimes,” Dr. Sigal said in an interview. “I was accused of lying, cheating, of doing things to make money that were against the public interest and against the interest of patients in general.”
It’s an experience many doctors who treat Lyme disease have endured, so much so that some infectious disease doctors aren’t comfortable treating patients with Lyme disease, according to Timothy Flanigan, MD, a professor of infectious disease at Brown University, Providence, R.I.
But it wasn’t until Dr. Sigal left academia in 2003 that he realized the toll all that background abuse had been taking on him.
“It was a breath of fresh air,” he said. “I didn’t have to go into clinic and argue with people. I didn’t have to read articles in the newspaper that made no sense whatsoever. I didn’t have to hear through second and third parties how such and such was saying horrible things about me. I didn’t have to fight anymore. When I was in industry and working on stuff that had nothing to do with Lyme disease, I realized what a relief it was not to have that burden.”
So the last thing Dr. Sigal expected after all these years was to find himself named in a lawsuit alleging that he was part of a conspiracy to deny patients of what they claimed was appropriate treatment for Lyme disease. Yet, that’s exactly what happened in November 2017, when a group of 24 patients with Lyme disease, led by Texas resident Lisa Torrey, filed a lawsuit against the Infectious Diseases Society of America, eight insurance companies, and 7 of the doctors involved in producing the IDSA guidelines on Lyme disease diagnosis and management. Dr. Sigal himself had not even participated in writing the guidelines. He simply reviewed them, made a few grammatical suggestions, and said they looked good. Over the next 4 years, however, he and his fellow defendants rode an emotional roller coaster of seemingly endless motions, amendments, and other legal developments, waiting to find out whether they would owe millions of dollars for simply summarizing – or just reviewing – the available medical literature on Lyme disease.
“There were times I was on the verge of real anger. I was frustrated. There were times I was frightened, and, occasionally, I would just think of it as being silly. But when I thought of it as being silly, I had to remember I was being sued in Texas, because who knows what’s going to happen,” Dr. Sigal said. “It’s not as though I was being sued in a jurisdiction where anybody knew about Lyme disease. There are examples of physicians who are convicted of doing things they didn’t do because they were sued in the wrong jurisdiction.”
Several individuals who spoke with this news organization on condition of anonymity said that the district court where the suit was filed is notorious for being especially friendly to plaintiffs. But in legal rulings issued on Sept. 1 and Sept. 20, 2021, a federal judge in Texas dismissed all the patient group’s claims. The plaintiffs filed an appeal on Oct. 19. It’s unclear whether that has any reasonable chance of success.
“One of the things this court case does is validate the fact that our [guidelines] process is a legitimate process and there isn’t outside influence from insurance companies or pharma firms,” Daniel McQuillen, MD, president of IDSA, said in an interview. “We don’t really want anything other than to be vindicated, which we were, 100%.”
But that vindication came with a cost, both emotional and financial. Although IDSA’s insurance covered many of its legal costs, “it’s not a trivial expense,” Dr. McQuillen said. “We’re left with a baseless lawsuit with no facts that went on for 4 years, and our [medical] society basically bore all that expense, which isn’t really particularly fair.”
‘Preposterous’ accusations
The lawsuit alleged that the IDSA, the seven named physicians, and the insurance companies had “engaged in a decades-long conspiracy to deny the existence and prevent treatment of chronic Lyme disease.” The patient group claimed that the doctors knew that many patients with Lyme disease do not respond to short-term antibiotic treatment and instead need “long-term antibiotic treatment until the symptoms are resolved,” an assertion not supported by the scientific evidence.
What many patients call “chronic Lyme disease” is termed posttreatment Lyme disease syndrome (PTDLS), a constellation of symptoms that include pain, fatigue, and cognitive difficulties that some people experience after a 2- to 4-week course of antibiotics for Lyme disease. It took years of patient advocacy before the Centers for Disease Control and Prevention recognized PTLDS as a condition, but awareness of it has been increasing, said Dr. Flanigan, who was not involved in the lawsuit but treats patients with Lyme disease and PTLDS.
“Long haulers and sequelae of COVID have really opened the eyes of many practitioners that these long-term inflammatory conditions are real and very challenging to treat, and we need to work with patients to help them improve their health,” Dr. Flanigan said. “It’s a sad commentary on our society that the difficulty in treating patients with posttreatment Lyme disease syndrome, or what is commonly referred to by patients as chronic Lyme, ends up in a lawsuit in court.” He said he’s glad the lawsuit was dismissed but added that “there’s a crying need for additional high-quality, evidence-based research to help patients who are suffering from posttreatment Lyme disease syndrome.”
Patients fought for broader recognition of their condition, and some of them organized. They came up with their own ideas of what was causing their symptoms to persist. One that especially took hold was that infection from Borrelia burgdorferi, the bacteria that causes Lyme disease, persists after initial antibiotic treatment, causing so-called chronic Lyme disease. The cause of PTLDS is still under investigation, and the evidence does not support the idea of a persistent bacterial infection. Multiple studies from the National Institutes of Health have shown that long-term use of antibiotics does not benefit patients who continue to experience symptoms after initial treatment. Several studies have shown that severe adverse effects can result from extended intravenous antibiotic treatment, including death.
Nevertheless, the plaintiffs in the lawsuit argued that the insurance companies “enlisted the help of doctors who were researching Lyme disease – the IDSA panelists – and paid them large fees to develop arbitrary guidelines for testing Lyme disease,” thereby enabling the insurance companies to deny coverage for long-term antibiotic treatment to patients.
“The assertions were just preposterous,” Dr. McQuillen said.
In addition to the conspiracy charge, the plaintiffs brought additional accusations to the lawsuit over the years, including racketeering and claims that the guidelines contain false representations regarding Lyme disease testing and treatment. The plaintiffs claimed that the guidelines didn’t acknowledge that treatment can fail and included false information about how to test for Lyme disease. In reality, however, the guidelines do acknowledge that not all patients respond to the recommended 2- to 4-week course of antibiotics and that some diagnoses should be made clinically rather than on the basis of testing.
Regardless, guidelines are not stipulations. They’re a summation of the medical and scientific findings on Lyme disease based on careful review of hundreds of studies.
“They make really clear that adherence to the guidelines [is] voluntary. They aren’t a standard of care from which deviation of care is a problem,” Dr. McQuillen said. “You take those guidelines and apply it to the patient in front of you, and you see what fits best for that patient, because not every patient is going to fit into guidelines.”
Further, the authors said that IDSA vets their recommendations for any potential conflicts of interest in accordance with the organization’s guidelines practices.
“The point of the guidelines is to have people on the committee who don’t care what the guidelines are as long as we have good patient care,” Dr. McQuillen said.
Choosing to fight
Malpractice insurance does not cover this kind of lawsuit, because the doctors named in it did not personally treat any of the patients who filed it. Thus, the doctors were at risk of losing thousands, or millions, of dollars in legal fees, even if they ultimately prevail. Several of the physicians’ academic and health care institutions stepped in to cover some fees, and IDSA covered the rest in a joint defense.
“The IDSA provided me a lawyer at no cost to me, and I felt protected by them,” Dr. Sigal said. “They took care of me and made sure I was safe, and I am grateful to them for that.”
Dr. McQuillen said the expenses exceeded what the organization’s umbrella insurance covered. The physicians had invested their time and effort into the guidelines without any financial compensation.
“They’ve basically put a lot of sweat equity into producing guidelines” that follow the organization’s practices and ethics, Dr. McQuillen said. “To leave them out on an island by themselves is just not the right thing to do. We wouldn’t do that for any of our members who did something on behalf of our society.”
IDSA could have chosen to settle the lawsuit, as the insurance companies did.
“None of us on the board felt that was the right thing to do, because we believe in the process, and the science is right, and you shouldn’t be able to try to change that by having a lawsuit that’s baseless,” Dr. McQuillen said.
Several of the doctors named in the suit spoke with this news organization off the record about the exhaustion, frustration, and general suffering the suit has caused them over the past several years, including ongoing harassment that targeted their families and often became quite personal. But none expressed any wish that IDSA had chosen the faster, cheaper, easier route of settling.
“I love the organization for having done this rather than caving and paying,” Dr. Sigal said. “They showed real moral character, real integrity in fighting this suit, because they had done nothing wrong.”
Fighting the suit was about more than standing by the science, though. It’s essential to ensure physicians continue to conduct research and write clinical guidelines, even about ambiguous or controversial topics, said Raymond J. Dattwyler, MD, a professor of microbiology, immunology, and medicine at New York Medical College, Valhalla, who wrote the treatment part of the guidelines and was named in the suit.
“I was really surprised that someone would sue for scientific guidelines, because guidelines are common across medicine, and they’re just a roadmap to help practicing physicians understand how to handle evaluation or treatment of any number of particular problems,” Dr. Dattwyler said in an interview. But he wasn’t surprised that IDSA chose to fight the accusations, “because the principle involved is so compelling. It’s really standing up for all medical societies, and it’s very important to have guidelines. For the health and welfare of the American public, you need to have good information readily available to the practicing physicians.”
If the patient group had won in a settlement, it could potentially have led to less rigorous guidelines from other medical organizations, which would have had an adverse effect on public health, Dr. Dattwyler said. Such a chilling effect could reverberate far beyond the management of Lyme disease.
“One of the problems with our legal system is anybody can sue anybody, but it costs so much to defend yourself,” Dr. Dattwyler said. “This lawsuit costs millions, so that’s chilling. That’s going to inhibit guidelines, and it’s not only guidelines for infectious disease but it’s guidelines for cancer, guidelines for allergic diseases, guidelines for any number of things.”
To an extent, the threats and harassment that patient groups have directed toward different doctors have already had a chilling effect.
“For the people who gave of their time in good faith to generate these guidelines to get harassed everywhere, all the time, sometimes at home, sometimes at their place of work, it’s just unfair,” Dr. McQuillen said. “It also might discourage people from working in research to try to figure out better diagnostics or get a vaccine that actually works. Even if you really find it incredibly interesting, if laying over you is the threat that someone is going to sue you baselessly, and you’re going to have to put the time and effort into defending that, not to mention the money, I can’t see how that would be considered a positive that would encourage you to do it. In some ways, attacking people that are trying to help may drive them away from trying to help.
“At the same time, professional disagreements among practitioners – including a small minority who do treat patients with lengthy courses of antibiotics – can ultimately harm patient care, Dr. Flanigan said.
“There’s a lot of energy being expended fighting among different care providers, and often the individual needs of the patients seem to be not addressed,” Dr. Flanigan said. “The discord between different approaches often seems more important than spending time with the individual patient and trying to find a tailored approach to treatment which can benefit the patient best.”
At the same time, Dr. Sigal said he believes most of the clinicians who use non–evidence-based treatments for their patients do so because they genuinely believe it’s the right thing to do.
“I think they’re motivated by the same concerns that I have, and that is, I need to do what’s best for my patient,” Dr. Sigal said. Ultimately, the evidence should lead the way. “The only arbiter we possibly have in deciding these things is the medical scientific literature,” he added, “and if you can’t subscribe to that, then this way lies madness.”
A version of this article first appeared on Medscape.com.
Years ago, when rheumatologist Leonard Sigal, MD, was undertaking research on Lyme disease and treating patients with the condition at the Robert Wood Johnson Medical School, New Brunswick, N.J., a regular stream of abuse and threats became the usual background noise of his work. He didn’t get used to it, but it never stopped.
“I was accused of incredibly heinous crimes,” Dr. Sigal said in an interview. “I was accused of lying, cheating, of doing things to make money that were against the public interest and against the interest of patients in general.”
It’s an experience many doctors who treat Lyme disease have endured, so much so that some infectious disease doctors aren’t comfortable treating patients with Lyme disease, according to Timothy Flanigan, MD, a professor of infectious disease at Brown University, Providence, R.I.
But it wasn’t until Dr. Sigal left academia in 2003 that he realized the toll all that background abuse had been taking on him.
“It was a breath of fresh air,” he said. “I didn’t have to go into clinic and argue with people. I didn’t have to read articles in the newspaper that made no sense whatsoever. I didn’t have to hear through second and third parties how such and such was saying horrible things about me. I didn’t have to fight anymore. When I was in industry and working on stuff that had nothing to do with Lyme disease, I realized what a relief it was not to have that burden.”
So the last thing Dr. Sigal expected after all these years was to find himself named in a lawsuit alleging that he was part of a conspiracy to deny patients of what they claimed was appropriate treatment for Lyme disease. Yet, that’s exactly what happened in November 2017, when a group of 24 patients with Lyme disease, led by Texas resident Lisa Torrey, filed a lawsuit against the Infectious Diseases Society of America, eight insurance companies, and 7 of the doctors involved in producing the IDSA guidelines on Lyme disease diagnosis and management. Dr. Sigal himself had not even participated in writing the guidelines. He simply reviewed them, made a few grammatical suggestions, and said they looked good. Over the next 4 years, however, he and his fellow defendants rode an emotional roller coaster of seemingly endless motions, amendments, and other legal developments, waiting to find out whether they would owe millions of dollars for simply summarizing – or just reviewing – the available medical literature on Lyme disease.
“There were times I was on the verge of real anger. I was frustrated. There were times I was frightened, and, occasionally, I would just think of it as being silly. But when I thought of it as being silly, I had to remember I was being sued in Texas, because who knows what’s going to happen,” Dr. Sigal said. “It’s not as though I was being sued in a jurisdiction where anybody knew about Lyme disease. There are examples of physicians who are convicted of doing things they didn’t do because they were sued in the wrong jurisdiction.”
Several individuals who spoke with this news organization on condition of anonymity said that the district court where the suit was filed is notorious for being especially friendly to plaintiffs. But in legal rulings issued on Sept. 1 and Sept. 20, 2021, a federal judge in Texas dismissed all the patient group’s claims. The plaintiffs filed an appeal on Oct. 19. It’s unclear whether that has any reasonable chance of success.
“One of the things this court case does is validate the fact that our [guidelines] process is a legitimate process and there isn’t outside influence from insurance companies or pharma firms,” Daniel McQuillen, MD, president of IDSA, said in an interview. “We don’t really want anything other than to be vindicated, which we were, 100%.”
But that vindication came with a cost, both emotional and financial. Although IDSA’s insurance covered many of its legal costs, “it’s not a trivial expense,” Dr. McQuillen said. “We’re left with a baseless lawsuit with no facts that went on for 4 years, and our [medical] society basically bore all that expense, which isn’t really particularly fair.”
‘Preposterous’ accusations
The lawsuit alleged that the IDSA, the seven named physicians, and the insurance companies had “engaged in a decades-long conspiracy to deny the existence and prevent treatment of chronic Lyme disease.” The patient group claimed that the doctors knew that many patients with Lyme disease do not respond to short-term antibiotic treatment and instead need “long-term antibiotic treatment until the symptoms are resolved,” an assertion not supported by the scientific evidence.
What many patients call “chronic Lyme disease” is termed posttreatment Lyme disease syndrome (PTDLS), a constellation of symptoms that include pain, fatigue, and cognitive difficulties that some people experience after a 2- to 4-week course of antibiotics for Lyme disease. It took years of patient advocacy before the Centers for Disease Control and Prevention recognized PTLDS as a condition, but awareness of it has been increasing, said Dr. Flanigan, who was not involved in the lawsuit but treats patients with Lyme disease and PTLDS.
“Long haulers and sequelae of COVID have really opened the eyes of many practitioners that these long-term inflammatory conditions are real and very challenging to treat, and we need to work with patients to help them improve their health,” Dr. Flanigan said. “It’s a sad commentary on our society that the difficulty in treating patients with posttreatment Lyme disease syndrome, or what is commonly referred to by patients as chronic Lyme, ends up in a lawsuit in court.” He said he’s glad the lawsuit was dismissed but added that “there’s a crying need for additional high-quality, evidence-based research to help patients who are suffering from posttreatment Lyme disease syndrome.”
Patients fought for broader recognition of their condition, and some of them organized. They came up with their own ideas of what was causing their symptoms to persist. One that especially took hold was that infection from Borrelia burgdorferi, the bacteria that causes Lyme disease, persists after initial antibiotic treatment, causing so-called chronic Lyme disease. The cause of PTLDS is still under investigation, and the evidence does not support the idea of a persistent bacterial infection. Multiple studies from the National Institutes of Health have shown that long-term use of antibiotics does not benefit patients who continue to experience symptoms after initial treatment. Several studies have shown that severe adverse effects can result from extended intravenous antibiotic treatment, including death.
Nevertheless, the plaintiffs in the lawsuit argued that the insurance companies “enlisted the help of doctors who were researching Lyme disease – the IDSA panelists – and paid them large fees to develop arbitrary guidelines for testing Lyme disease,” thereby enabling the insurance companies to deny coverage for long-term antibiotic treatment to patients.
“The assertions were just preposterous,” Dr. McQuillen said.
In addition to the conspiracy charge, the plaintiffs brought additional accusations to the lawsuit over the years, including racketeering and claims that the guidelines contain false representations regarding Lyme disease testing and treatment. The plaintiffs claimed that the guidelines didn’t acknowledge that treatment can fail and included false information about how to test for Lyme disease. In reality, however, the guidelines do acknowledge that not all patients respond to the recommended 2- to 4-week course of antibiotics and that some diagnoses should be made clinically rather than on the basis of testing.
Regardless, guidelines are not stipulations. They’re a summation of the medical and scientific findings on Lyme disease based on careful review of hundreds of studies.
“They make really clear that adherence to the guidelines [is] voluntary. They aren’t a standard of care from which deviation of care is a problem,” Dr. McQuillen said. “You take those guidelines and apply it to the patient in front of you, and you see what fits best for that patient, because not every patient is going to fit into guidelines.”
Further, the authors said that IDSA vets their recommendations for any potential conflicts of interest in accordance with the organization’s guidelines practices.
“The point of the guidelines is to have people on the committee who don’t care what the guidelines are as long as we have good patient care,” Dr. McQuillen said.
Choosing to fight
Malpractice insurance does not cover this kind of lawsuit, because the doctors named in it did not personally treat any of the patients who filed it. Thus, the doctors were at risk of losing thousands, or millions, of dollars in legal fees, even if they ultimately prevail. Several of the physicians’ academic and health care institutions stepped in to cover some fees, and IDSA covered the rest in a joint defense.
“The IDSA provided me a lawyer at no cost to me, and I felt protected by them,” Dr. Sigal said. “They took care of me and made sure I was safe, and I am grateful to them for that.”
Dr. McQuillen said the expenses exceeded what the organization’s umbrella insurance covered. The physicians had invested their time and effort into the guidelines without any financial compensation.
“They’ve basically put a lot of sweat equity into producing guidelines” that follow the organization’s practices and ethics, Dr. McQuillen said. “To leave them out on an island by themselves is just not the right thing to do. We wouldn’t do that for any of our members who did something on behalf of our society.”
IDSA could have chosen to settle the lawsuit, as the insurance companies did.
“None of us on the board felt that was the right thing to do, because we believe in the process, and the science is right, and you shouldn’t be able to try to change that by having a lawsuit that’s baseless,” Dr. McQuillen said.
Several of the doctors named in the suit spoke with this news organization off the record about the exhaustion, frustration, and general suffering the suit has caused them over the past several years, including ongoing harassment that targeted their families and often became quite personal. But none expressed any wish that IDSA had chosen the faster, cheaper, easier route of settling.
“I love the organization for having done this rather than caving and paying,” Dr. Sigal said. “They showed real moral character, real integrity in fighting this suit, because they had done nothing wrong.”
Fighting the suit was about more than standing by the science, though. It’s essential to ensure physicians continue to conduct research and write clinical guidelines, even about ambiguous or controversial topics, said Raymond J. Dattwyler, MD, a professor of microbiology, immunology, and medicine at New York Medical College, Valhalla, who wrote the treatment part of the guidelines and was named in the suit.
“I was really surprised that someone would sue for scientific guidelines, because guidelines are common across medicine, and they’re just a roadmap to help practicing physicians understand how to handle evaluation or treatment of any number of particular problems,” Dr. Dattwyler said in an interview. But he wasn’t surprised that IDSA chose to fight the accusations, “because the principle involved is so compelling. It’s really standing up for all medical societies, and it’s very important to have guidelines. For the health and welfare of the American public, you need to have good information readily available to the practicing physicians.”
If the patient group had won in a settlement, it could potentially have led to less rigorous guidelines from other medical organizations, which would have had an adverse effect on public health, Dr. Dattwyler said. Such a chilling effect could reverberate far beyond the management of Lyme disease.
“One of the problems with our legal system is anybody can sue anybody, but it costs so much to defend yourself,” Dr. Dattwyler said. “This lawsuit costs millions, so that’s chilling. That’s going to inhibit guidelines, and it’s not only guidelines for infectious disease but it’s guidelines for cancer, guidelines for allergic diseases, guidelines for any number of things.”
To an extent, the threats and harassment that patient groups have directed toward different doctors have already had a chilling effect.
“For the people who gave of their time in good faith to generate these guidelines to get harassed everywhere, all the time, sometimes at home, sometimes at their place of work, it’s just unfair,” Dr. McQuillen said. “It also might discourage people from working in research to try to figure out better diagnostics or get a vaccine that actually works. Even if you really find it incredibly interesting, if laying over you is the threat that someone is going to sue you baselessly, and you’re going to have to put the time and effort into defending that, not to mention the money, I can’t see how that would be considered a positive that would encourage you to do it. In some ways, attacking people that are trying to help may drive them away from trying to help.
“At the same time, professional disagreements among practitioners – including a small minority who do treat patients with lengthy courses of antibiotics – can ultimately harm patient care, Dr. Flanigan said.
“There’s a lot of energy being expended fighting among different care providers, and often the individual needs of the patients seem to be not addressed,” Dr. Flanigan said. “The discord between different approaches often seems more important than spending time with the individual patient and trying to find a tailored approach to treatment which can benefit the patient best.”
At the same time, Dr. Sigal said he believes most of the clinicians who use non–evidence-based treatments for their patients do so because they genuinely believe it’s the right thing to do.
“I think they’re motivated by the same concerns that I have, and that is, I need to do what’s best for my patient,” Dr. Sigal said. Ultimately, the evidence should lead the way. “The only arbiter we possibly have in deciding these things is the medical scientific literature,” he added, “and if you can’t subscribe to that, then this way lies madness.”
A version of this article first appeared on Medscape.com.
Years ago, when rheumatologist Leonard Sigal, MD, was undertaking research on Lyme disease and treating patients with the condition at the Robert Wood Johnson Medical School, New Brunswick, N.J., a regular stream of abuse and threats became the usual background noise of his work. He didn’t get used to it, but it never stopped.
“I was accused of incredibly heinous crimes,” Dr. Sigal said in an interview. “I was accused of lying, cheating, of doing things to make money that were against the public interest and against the interest of patients in general.”
It’s an experience many doctors who treat Lyme disease have endured, so much so that some infectious disease doctors aren’t comfortable treating patients with Lyme disease, according to Timothy Flanigan, MD, a professor of infectious disease at Brown University, Providence, R.I.
But it wasn’t until Dr. Sigal left academia in 2003 that he realized the toll all that background abuse had been taking on him.
“It was a breath of fresh air,” he said. “I didn’t have to go into clinic and argue with people. I didn’t have to read articles in the newspaper that made no sense whatsoever. I didn’t have to hear through second and third parties how such and such was saying horrible things about me. I didn’t have to fight anymore. When I was in industry and working on stuff that had nothing to do with Lyme disease, I realized what a relief it was not to have that burden.”
So the last thing Dr. Sigal expected after all these years was to find himself named in a lawsuit alleging that he was part of a conspiracy to deny patients of what they claimed was appropriate treatment for Lyme disease. Yet, that’s exactly what happened in November 2017, when a group of 24 patients with Lyme disease, led by Texas resident Lisa Torrey, filed a lawsuit against the Infectious Diseases Society of America, eight insurance companies, and 7 of the doctors involved in producing the IDSA guidelines on Lyme disease diagnosis and management. Dr. Sigal himself had not even participated in writing the guidelines. He simply reviewed them, made a few grammatical suggestions, and said they looked good. Over the next 4 years, however, he and his fellow defendants rode an emotional roller coaster of seemingly endless motions, amendments, and other legal developments, waiting to find out whether they would owe millions of dollars for simply summarizing – or just reviewing – the available medical literature on Lyme disease.
“There were times I was on the verge of real anger. I was frustrated. There were times I was frightened, and, occasionally, I would just think of it as being silly. But when I thought of it as being silly, I had to remember I was being sued in Texas, because who knows what’s going to happen,” Dr. Sigal said. “It’s not as though I was being sued in a jurisdiction where anybody knew about Lyme disease. There are examples of physicians who are convicted of doing things they didn’t do because they were sued in the wrong jurisdiction.”
Several individuals who spoke with this news organization on condition of anonymity said that the district court where the suit was filed is notorious for being especially friendly to plaintiffs. But in legal rulings issued on Sept. 1 and Sept. 20, 2021, a federal judge in Texas dismissed all the patient group’s claims. The plaintiffs filed an appeal on Oct. 19. It’s unclear whether that has any reasonable chance of success.
“One of the things this court case does is validate the fact that our [guidelines] process is a legitimate process and there isn’t outside influence from insurance companies or pharma firms,” Daniel McQuillen, MD, president of IDSA, said in an interview. “We don’t really want anything other than to be vindicated, which we were, 100%.”
But that vindication came with a cost, both emotional and financial. Although IDSA’s insurance covered many of its legal costs, “it’s not a trivial expense,” Dr. McQuillen said. “We’re left with a baseless lawsuit with no facts that went on for 4 years, and our [medical] society basically bore all that expense, which isn’t really particularly fair.”
‘Preposterous’ accusations
The lawsuit alleged that the IDSA, the seven named physicians, and the insurance companies had “engaged in a decades-long conspiracy to deny the existence and prevent treatment of chronic Lyme disease.” The patient group claimed that the doctors knew that many patients with Lyme disease do not respond to short-term antibiotic treatment and instead need “long-term antibiotic treatment until the symptoms are resolved,” an assertion not supported by the scientific evidence.
What many patients call “chronic Lyme disease” is termed posttreatment Lyme disease syndrome (PTDLS), a constellation of symptoms that include pain, fatigue, and cognitive difficulties that some people experience after a 2- to 4-week course of antibiotics for Lyme disease. It took years of patient advocacy before the Centers for Disease Control and Prevention recognized PTLDS as a condition, but awareness of it has been increasing, said Dr. Flanigan, who was not involved in the lawsuit but treats patients with Lyme disease and PTLDS.
“Long haulers and sequelae of COVID have really opened the eyes of many practitioners that these long-term inflammatory conditions are real and very challenging to treat, and we need to work with patients to help them improve their health,” Dr. Flanigan said. “It’s a sad commentary on our society that the difficulty in treating patients with posttreatment Lyme disease syndrome, or what is commonly referred to by patients as chronic Lyme, ends up in a lawsuit in court.” He said he’s glad the lawsuit was dismissed but added that “there’s a crying need for additional high-quality, evidence-based research to help patients who are suffering from posttreatment Lyme disease syndrome.”
Patients fought for broader recognition of their condition, and some of them organized. They came up with their own ideas of what was causing their symptoms to persist. One that especially took hold was that infection from Borrelia burgdorferi, the bacteria that causes Lyme disease, persists after initial antibiotic treatment, causing so-called chronic Lyme disease. The cause of PTLDS is still under investigation, and the evidence does not support the idea of a persistent bacterial infection. Multiple studies from the National Institutes of Health have shown that long-term use of antibiotics does not benefit patients who continue to experience symptoms after initial treatment. Several studies have shown that severe adverse effects can result from extended intravenous antibiotic treatment, including death.
Nevertheless, the plaintiffs in the lawsuit argued that the insurance companies “enlisted the help of doctors who were researching Lyme disease – the IDSA panelists – and paid them large fees to develop arbitrary guidelines for testing Lyme disease,” thereby enabling the insurance companies to deny coverage for long-term antibiotic treatment to patients.
“The assertions were just preposterous,” Dr. McQuillen said.
In addition to the conspiracy charge, the plaintiffs brought additional accusations to the lawsuit over the years, including racketeering and claims that the guidelines contain false representations regarding Lyme disease testing and treatment. The plaintiffs claimed that the guidelines didn’t acknowledge that treatment can fail and included false information about how to test for Lyme disease. In reality, however, the guidelines do acknowledge that not all patients respond to the recommended 2- to 4-week course of antibiotics and that some diagnoses should be made clinically rather than on the basis of testing.
Regardless, guidelines are not stipulations. They’re a summation of the medical and scientific findings on Lyme disease based on careful review of hundreds of studies.
“They make really clear that adherence to the guidelines [is] voluntary. They aren’t a standard of care from which deviation of care is a problem,” Dr. McQuillen said. “You take those guidelines and apply it to the patient in front of you, and you see what fits best for that patient, because not every patient is going to fit into guidelines.”
Further, the authors said that IDSA vets their recommendations for any potential conflicts of interest in accordance with the organization’s guidelines practices.
“The point of the guidelines is to have people on the committee who don’t care what the guidelines are as long as we have good patient care,” Dr. McQuillen said.
Choosing to fight
Malpractice insurance does not cover this kind of lawsuit, because the doctors named in it did not personally treat any of the patients who filed it. Thus, the doctors were at risk of losing thousands, or millions, of dollars in legal fees, even if they ultimately prevail. Several of the physicians’ academic and health care institutions stepped in to cover some fees, and IDSA covered the rest in a joint defense.
“The IDSA provided me a lawyer at no cost to me, and I felt protected by them,” Dr. Sigal said. “They took care of me and made sure I was safe, and I am grateful to them for that.”
Dr. McQuillen said the expenses exceeded what the organization’s umbrella insurance covered. The physicians had invested their time and effort into the guidelines without any financial compensation.
“They’ve basically put a lot of sweat equity into producing guidelines” that follow the organization’s practices and ethics, Dr. McQuillen said. “To leave them out on an island by themselves is just not the right thing to do. We wouldn’t do that for any of our members who did something on behalf of our society.”
IDSA could have chosen to settle the lawsuit, as the insurance companies did.
“None of us on the board felt that was the right thing to do, because we believe in the process, and the science is right, and you shouldn’t be able to try to change that by having a lawsuit that’s baseless,” Dr. McQuillen said.
Several of the doctors named in the suit spoke with this news organization off the record about the exhaustion, frustration, and general suffering the suit has caused them over the past several years, including ongoing harassment that targeted their families and often became quite personal. But none expressed any wish that IDSA had chosen the faster, cheaper, easier route of settling.
“I love the organization for having done this rather than caving and paying,” Dr. Sigal said. “They showed real moral character, real integrity in fighting this suit, because they had done nothing wrong.”
Fighting the suit was about more than standing by the science, though. It’s essential to ensure physicians continue to conduct research and write clinical guidelines, even about ambiguous or controversial topics, said Raymond J. Dattwyler, MD, a professor of microbiology, immunology, and medicine at New York Medical College, Valhalla, who wrote the treatment part of the guidelines and was named in the suit.
“I was really surprised that someone would sue for scientific guidelines, because guidelines are common across medicine, and they’re just a roadmap to help practicing physicians understand how to handle evaluation or treatment of any number of particular problems,” Dr. Dattwyler said in an interview. But he wasn’t surprised that IDSA chose to fight the accusations, “because the principle involved is so compelling. It’s really standing up for all medical societies, and it’s very important to have guidelines. For the health and welfare of the American public, you need to have good information readily available to the practicing physicians.”
If the patient group had won in a settlement, it could potentially have led to less rigorous guidelines from other medical organizations, which would have had an adverse effect on public health, Dr. Dattwyler said. Such a chilling effect could reverberate far beyond the management of Lyme disease.
“One of the problems with our legal system is anybody can sue anybody, but it costs so much to defend yourself,” Dr. Dattwyler said. “This lawsuit costs millions, so that’s chilling. That’s going to inhibit guidelines, and it’s not only guidelines for infectious disease but it’s guidelines for cancer, guidelines for allergic diseases, guidelines for any number of things.”
To an extent, the threats and harassment that patient groups have directed toward different doctors have already had a chilling effect.
“For the people who gave of their time in good faith to generate these guidelines to get harassed everywhere, all the time, sometimes at home, sometimes at their place of work, it’s just unfair,” Dr. McQuillen said. “It also might discourage people from working in research to try to figure out better diagnostics or get a vaccine that actually works. Even if you really find it incredibly interesting, if laying over you is the threat that someone is going to sue you baselessly, and you’re going to have to put the time and effort into defending that, not to mention the money, I can’t see how that would be considered a positive that would encourage you to do it. In some ways, attacking people that are trying to help may drive them away from trying to help.
“At the same time, professional disagreements among practitioners – including a small minority who do treat patients with lengthy courses of antibiotics – can ultimately harm patient care, Dr. Flanigan said.
“There’s a lot of energy being expended fighting among different care providers, and often the individual needs of the patients seem to be not addressed,” Dr. Flanigan said. “The discord between different approaches often seems more important than spending time with the individual patient and trying to find a tailored approach to treatment which can benefit the patient best.”
At the same time, Dr. Sigal said he believes most of the clinicians who use non–evidence-based treatments for their patients do so because they genuinely believe it’s the right thing to do.
“I think they’re motivated by the same concerns that I have, and that is, I need to do what’s best for my patient,” Dr. Sigal said. Ultimately, the evidence should lead the way. “The only arbiter we possibly have in deciding these things is the medical scientific literature,” he added, “and if you can’t subscribe to that, then this way lies madness.”
A version of this article first appeared on Medscape.com.