User login
For MD-IQ use only
A psychiatric patient confesses to murder: Now what?
NEW ORLEANS – The patient, a 60-year-old woman who’d just tried to kill herself by overdosing on gabapentin, felt the need to make a confession. As she told a resident psychiatrist late one night at a Philadelphia crisis response center, she’d just murdered two people and buried them in her backyard. More details kept coming, including who was dead and where their bodies were.
It didn’t take long for the attending physician’s phone to ring as the resident sought guidance. This wasn’t a typical “duty to warn” case since there was no one to warn of a threat of violence. But then what kind of case was it? As Meghan Musselman, MD, and colleagues noted in a report presented at the annual meeting of the American Psychiatric Association, the law and medical ethics didn’t present a clear-cut solution to whether the patient’s claim should be reported to the authorities.
“This was much more of a gray zone case than we typically see,” said Dr. Musselman, of the department of psychiatry at Temple University in Philadelphia, in an interview. “If someone is threatening to harm someone, most states have statutes about what to do in that situation. The same doesn’t really exist for when the crime has already happened.”
Even so, might the existing “duty to warn/protect” laws be helpful as a guide to what to do? Maybe, but it’s complicated. The laws, which address the waiving of therapist-patient confidentiality when violence is threatened, are widely variable. Some don’t specifically cover psychiatrists, according to the National Conference of State Legislatures. Some simply allow – but don’t require – certain mental-health professionals to take action regarding threats of violence without getting in trouble themselves.
There are no duty to warn/protect laws in Nevada, North Dakota, North Carolina, and Maine. Pennsylvania requires “mental-health professionals” to act when there’s a “clear and immediate danger to others or to society.”
In an interview, Columbia University, New York, psychiatrist and medical law/ethics specialist Paul S. Appelbaum, MD, said that “with the exception of situations like child abuse or elder abuse, for which psychiatrists are mandatory reporters, psychiatrists generally have the same responsibilities for reporting crimes as other citizens.”
He added that there is a crime in English common law known as “misprision” that refers to failing to report a felony. “A few states still have misprision statutes, but courts have tended to interpret them to require an affirmative act to conceal a crime, not just failure to report,” he said. “Unless the patient’s confession indicates a continuing threat to other people – e.g., a serial rapist or murderer – there is probably no obligation to report a previous crime.”
In this case, Dr. Musselman said, the physicians thought they might be able to waive confidentiality because it was possible that the alleged murder victims were still alive and in need of help.
However, the patient ultimately took the decision out of the hands of the psychiatrists and agreed to confess to the police. There’s a happy ending: The patient later recanted the story, Dr. Musselman said, and there was no follow-up by the authorities.
What should psychiatrists do in a similar situation? Besides the law, Dr. Musselman said, it’s important to consider medical ethics, confidentiality, and the greater good. “Doctors may have to ask themselves: Would I rather be sued because I’m breaking confidentiality or potentially play a part in someone’s suffering?”
She recommended reaching out to attorneys for legal guidance. “There’s a saying in forensic psychiatry by [Harvard University psychiatrist] Thomas Gutheil: Never worry alone.”
Dr. Applebaum agreed, and added: “Psychiatrists should consider the credibility of the patient’s confession: Could it represent a delusion? Is it being proffered as a way of manipulating the therapist? What is the extent to which, if valid, it indicates an ongoing threat to others? Is the patient is willing to contact the police and admit to the crime or authorize the psychiatrist to do so? Only in the case of a credible confession, an ongoing threat, and a patient unwilling to contact the police themselves should the psychiatrist seriously consider breaching confidentiality to report.”
No study funding or disclosures were reported.
NEW ORLEANS – The patient, a 60-year-old woman who’d just tried to kill herself by overdosing on gabapentin, felt the need to make a confession. As she told a resident psychiatrist late one night at a Philadelphia crisis response center, she’d just murdered two people and buried them in her backyard. More details kept coming, including who was dead and where their bodies were.
It didn’t take long for the attending physician’s phone to ring as the resident sought guidance. This wasn’t a typical “duty to warn” case since there was no one to warn of a threat of violence. But then what kind of case was it? As Meghan Musselman, MD, and colleagues noted in a report presented at the annual meeting of the American Psychiatric Association, the law and medical ethics didn’t present a clear-cut solution to whether the patient’s claim should be reported to the authorities.
“This was much more of a gray zone case than we typically see,” said Dr. Musselman, of the department of psychiatry at Temple University in Philadelphia, in an interview. “If someone is threatening to harm someone, most states have statutes about what to do in that situation. The same doesn’t really exist for when the crime has already happened.”
Even so, might the existing “duty to warn/protect” laws be helpful as a guide to what to do? Maybe, but it’s complicated. The laws, which address the waiving of therapist-patient confidentiality when violence is threatened, are widely variable. Some don’t specifically cover psychiatrists, according to the National Conference of State Legislatures. Some simply allow – but don’t require – certain mental-health professionals to take action regarding threats of violence without getting in trouble themselves.
There are no duty to warn/protect laws in Nevada, North Dakota, North Carolina, and Maine. Pennsylvania requires “mental-health professionals” to act when there’s a “clear and immediate danger to others or to society.”
In an interview, Columbia University, New York, psychiatrist and medical law/ethics specialist Paul S. Appelbaum, MD, said that “with the exception of situations like child abuse or elder abuse, for which psychiatrists are mandatory reporters, psychiatrists generally have the same responsibilities for reporting crimes as other citizens.”
He added that there is a crime in English common law known as “misprision” that refers to failing to report a felony. “A few states still have misprision statutes, but courts have tended to interpret them to require an affirmative act to conceal a crime, not just failure to report,” he said. “Unless the patient’s confession indicates a continuing threat to other people – e.g., a serial rapist or murderer – there is probably no obligation to report a previous crime.”
In this case, Dr. Musselman said, the physicians thought they might be able to waive confidentiality because it was possible that the alleged murder victims were still alive and in need of help.
However, the patient ultimately took the decision out of the hands of the psychiatrists and agreed to confess to the police. There’s a happy ending: The patient later recanted the story, Dr. Musselman said, and there was no follow-up by the authorities.
What should psychiatrists do in a similar situation? Besides the law, Dr. Musselman said, it’s important to consider medical ethics, confidentiality, and the greater good. “Doctors may have to ask themselves: Would I rather be sued because I’m breaking confidentiality or potentially play a part in someone’s suffering?”
She recommended reaching out to attorneys for legal guidance. “There’s a saying in forensic psychiatry by [Harvard University psychiatrist] Thomas Gutheil: Never worry alone.”
Dr. Applebaum agreed, and added: “Psychiatrists should consider the credibility of the patient’s confession: Could it represent a delusion? Is it being proffered as a way of manipulating the therapist? What is the extent to which, if valid, it indicates an ongoing threat to others? Is the patient is willing to contact the police and admit to the crime or authorize the psychiatrist to do so? Only in the case of a credible confession, an ongoing threat, and a patient unwilling to contact the police themselves should the psychiatrist seriously consider breaching confidentiality to report.”
No study funding or disclosures were reported.
NEW ORLEANS – The patient, a 60-year-old woman who’d just tried to kill herself by overdosing on gabapentin, felt the need to make a confession. As she told a resident psychiatrist late one night at a Philadelphia crisis response center, she’d just murdered two people and buried them in her backyard. More details kept coming, including who was dead and where their bodies were.
It didn’t take long for the attending physician’s phone to ring as the resident sought guidance. This wasn’t a typical “duty to warn” case since there was no one to warn of a threat of violence. But then what kind of case was it? As Meghan Musselman, MD, and colleagues noted in a report presented at the annual meeting of the American Psychiatric Association, the law and medical ethics didn’t present a clear-cut solution to whether the patient’s claim should be reported to the authorities.
“This was much more of a gray zone case than we typically see,” said Dr. Musselman, of the department of psychiatry at Temple University in Philadelphia, in an interview. “If someone is threatening to harm someone, most states have statutes about what to do in that situation. The same doesn’t really exist for when the crime has already happened.”
Even so, might the existing “duty to warn/protect” laws be helpful as a guide to what to do? Maybe, but it’s complicated. The laws, which address the waiving of therapist-patient confidentiality when violence is threatened, are widely variable. Some don’t specifically cover psychiatrists, according to the National Conference of State Legislatures. Some simply allow – but don’t require – certain mental-health professionals to take action regarding threats of violence without getting in trouble themselves.
There are no duty to warn/protect laws in Nevada, North Dakota, North Carolina, and Maine. Pennsylvania requires “mental-health professionals” to act when there’s a “clear and immediate danger to others or to society.”
In an interview, Columbia University, New York, psychiatrist and medical law/ethics specialist Paul S. Appelbaum, MD, said that “with the exception of situations like child abuse or elder abuse, for which psychiatrists are mandatory reporters, psychiatrists generally have the same responsibilities for reporting crimes as other citizens.”
He added that there is a crime in English common law known as “misprision” that refers to failing to report a felony. “A few states still have misprision statutes, but courts have tended to interpret them to require an affirmative act to conceal a crime, not just failure to report,” he said. “Unless the patient’s confession indicates a continuing threat to other people – e.g., a serial rapist or murderer – there is probably no obligation to report a previous crime.”
In this case, Dr. Musselman said, the physicians thought they might be able to waive confidentiality because it was possible that the alleged murder victims were still alive and in need of help.
However, the patient ultimately took the decision out of the hands of the psychiatrists and agreed to confess to the police. There’s a happy ending: The patient later recanted the story, Dr. Musselman said, and there was no follow-up by the authorities.
What should psychiatrists do in a similar situation? Besides the law, Dr. Musselman said, it’s important to consider medical ethics, confidentiality, and the greater good. “Doctors may have to ask themselves: Would I rather be sued because I’m breaking confidentiality or potentially play a part in someone’s suffering?”
She recommended reaching out to attorneys for legal guidance. “There’s a saying in forensic psychiatry by [Harvard University psychiatrist] Thomas Gutheil: Never worry alone.”
Dr. Applebaum agreed, and added: “Psychiatrists should consider the credibility of the patient’s confession: Could it represent a delusion? Is it being proffered as a way of manipulating the therapist? What is the extent to which, if valid, it indicates an ongoing threat to others? Is the patient is willing to contact the police and admit to the crime or authorize the psychiatrist to do so? Only in the case of a credible confession, an ongoing threat, and a patient unwilling to contact the police themselves should the psychiatrist seriously consider breaching confidentiality to report.”
No study funding or disclosures were reported.
AT APA 2022
Fever after a tropical trip: A guide to differential diagnosis
After 2 years of a pandemic in which traveling was barely possible, tropical diseases are becoming important once more. At a 2022 conference for internal medicine specialists, tropical medicine specialist Fritz Holst, MD, of the Center for Tropical and Travel Medicine in Marburg, Germany, explained what questions you should be asking travelers with a fever at your practice and how to proceed with a suspected case.
The following article is based on the lecture: “Differential Diagnosis of Fever After a Trip to the Tropics,” which Dr. Holst gave at the 128th conference of the German Society of Internal Medicine.
A meta-analysis of studies concerning the topic, “returnee travelers from the tropics with fever,” was published in 2020. According to the analysis, purely tropical infections make up a third (33%) of fever diagnoses worldwide following an exotic trip. Malaria accounts for a fifth (22%), 5% are dengue fever, and 2.2% are typhoid (enteric fever).
In 26% of the returnee travelers investigated, nontropical infections were the cause of the fever. Acute gastroenteritis was responsible for 14%, and respiratory infections were responsible for 13%. In 18% of the cases, the cause of the fever remained unclear.
In Germany, the number of malaria cases has increased, said Dr. Holst. In Hessen, for example, there was recently a malaria fatality. “What we should do has been forgotten again,” he warned. More attention should also be paid once more to prophylaxis.
How to proceed
Dr. Holst described the following steps for treating recently returned travelers who are sick:
- Severely ill or not: If there are signs of a severe disease, such as dyspnea, signs of bleeding, hypotension, or central nervous system symptoms, the patient should be referred to a clinic. A diagnosis should be made within 1 day and treatment should be started.
- Transmissible or dangerous disease: This question should be quickly clarified to protect health care personnel, especially those treating patients. By using a thorough medical history (discussed below), a range of diseases may be clarified.
- Disease outbreak in destination country: Find out about possible disease outbreaks in the country that the traveler visited.
- Malaria? Immediate diagnostics: Malaria should always be excluded in patients at the practice on the same day by using a thick blood smear, even if no fever is present. If this is not possible because of time constraints, the affected person should be transferred directly to the clinic.
- Fever independent of the travel? Exclude other causes of the fever (for example, endocarditis).
- Involve tropical medicine specialists in a timely manner.
Nine mandatory questions
Dr. Holst also listed nine questions that clinicians should ask this patient population.
Where were you exactly?
Depending on the regional prevalence of tropical diseases, certain pathogens can be excluded quickly. Approximately 35% of travelers returning from Africa have malaria, whereas typhoid is much rarer. In contrast, typhoid and dengue fever are much more widespread in Southeast Asia. In Latin America, this is the case for both dengue fever and leptospirosis.
When did you travel?
By using the incubation time of the pathogen in question, as well as the time of return journey, you can determine which diseases are possible and which are not. In one patient who visited the practice 4 weeks after his return, dengue or typhoid were excluded.
Where did you stay overnight?
Whether in an unhygienic bed or under the stars, the question regarding how and where travelers stayed overnight provides important evidence of the following nocturnal vectors:
- Sandflies: Leishmaniasis
- Kissing bugs: Chagas disease
- Fleas: Spotted fever, bubonic plague
- Mosquitoes: Malaria, dengue, filariasis
What did you eat?
Many infections can be attributed to careless eating. For example, when eating fish, crabs, crawfish, or frogs, especially if raw, liver fluke, lung fluke, or ciguatera should be considered. Mussel toxins have been found on the coast of Kenya and even in the south of France. In North African countries, you should be cautious when eating nonpasteurized milk products (for example, camel milk). They can transmit the pathogens for brucellosis and tuberculosis. In beef or pork that has not been cooked thoroughly, there is the risk of trichinosis or of a tapeworm. Even vegetarians need to be careful. Infections with the common liver fluke are possible after eating watercress.
What have you been doing?
You can only get some diseases through certain activities, said Dr. Holst. If long-distance travelers tell you about the following excursions, prick up your ears:
- Freshwater contact: Schistosomiasis, leptospirosis
- Caving: Histoplasmosis, rabies
- Excavations: Anthrax, coccidioidomycosis
- Camel tour: MERS coronavirus (Do not mount a sniffling camel!)
- Walking around barefoot: Strongyloides, hookworm
Was there contact with animals?
Because of the risk of rabies following contact with cats or biting apes, Dr. Holst advised long-distance travelers to get vaccinated.
Were there new sexual partners?
In the event of new sexual contacts, tests for hepatitis A, B, C, and HIV should be performed.
Are you undergoing medical treatment?
The patient may already be under medical supervision because of having a disease.
What prophylactic measures did you take before traveling?
To progress in the differential diagnosis, questions should also be asked regarding prophylactic measures. Vaccination against hepatitis A provides very efficient infection protection, whereas vaccines against typhoid offer a much lower level of protection.
Diagnostic tests
As long as there are no abnormalities, such as meningism or heart murmurs, further diagnostics include routine infectiologic laboratory investigations (C-reactive protein, blood count, etc), blood culture (aerobic, anaerobic), a urine dipstick test, and rapid tests for malaria and dengue.
To exclude malaria, a thick blood smear should always be performed on the same day, said Dr. Holst. “The rapid test is occasionally negative. But you often only detect tertian malaria in the thick blood smear. And you have to repeat the diagnostics the following day.” For this, it is important to know that a single test result does not exclude malaria right away. In contrast, detecting malaria antibodies is obsolete. Depending on the result, further tests include serologies, antigen investigations, and polymerase chain reaction.
Treat early
A complete set of results is not always available promptly. Experts recommend that, “if you already have a hunch, then start the therapy, even without a definite diagnosis.” This applies in particular for the suspected diagnoses in the following table.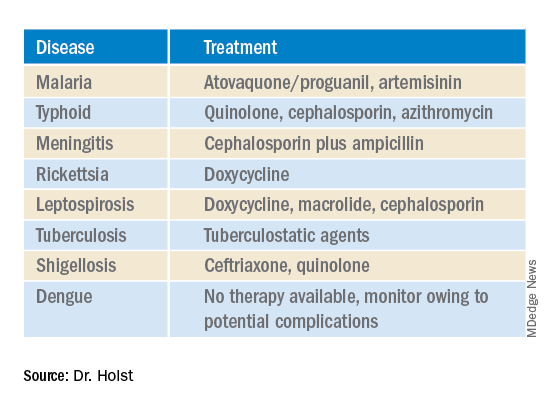
This article was translated from Coliquio. A version of this article appeared on Medscape.com.
After 2 years of a pandemic in which traveling was barely possible, tropical diseases are becoming important once more. At a 2022 conference for internal medicine specialists, tropical medicine specialist Fritz Holst, MD, of the Center for Tropical and Travel Medicine in Marburg, Germany, explained what questions you should be asking travelers with a fever at your practice and how to proceed with a suspected case.
The following article is based on the lecture: “Differential Diagnosis of Fever After a Trip to the Tropics,” which Dr. Holst gave at the 128th conference of the German Society of Internal Medicine.
A meta-analysis of studies concerning the topic, “returnee travelers from the tropics with fever,” was published in 2020. According to the analysis, purely tropical infections make up a third (33%) of fever diagnoses worldwide following an exotic trip. Malaria accounts for a fifth (22%), 5% are dengue fever, and 2.2% are typhoid (enteric fever).
In 26% of the returnee travelers investigated, nontropical infections were the cause of the fever. Acute gastroenteritis was responsible for 14%, and respiratory infections were responsible for 13%. In 18% of the cases, the cause of the fever remained unclear.
In Germany, the number of malaria cases has increased, said Dr. Holst. In Hessen, for example, there was recently a malaria fatality. “What we should do has been forgotten again,” he warned. More attention should also be paid once more to prophylaxis.
How to proceed
Dr. Holst described the following steps for treating recently returned travelers who are sick:
- Severely ill or not: If there are signs of a severe disease, such as dyspnea, signs of bleeding, hypotension, or central nervous system symptoms, the patient should be referred to a clinic. A diagnosis should be made within 1 day and treatment should be started.
- Transmissible or dangerous disease: This question should be quickly clarified to protect health care personnel, especially those treating patients. By using a thorough medical history (discussed below), a range of diseases may be clarified.
- Disease outbreak in destination country: Find out about possible disease outbreaks in the country that the traveler visited.
- Malaria? Immediate diagnostics: Malaria should always be excluded in patients at the practice on the same day by using a thick blood smear, even if no fever is present. If this is not possible because of time constraints, the affected person should be transferred directly to the clinic.
- Fever independent of the travel? Exclude other causes of the fever (for example, endocarditis).
- Involve tropical medicine specialists in a timely manner.
Nine mandatory questions
Dr. Holst also listed nine questions that clinicians should ask this patient population.
Where were you exactly?
Depending on the regional prevalence of tropical diseases, certain pathogens can be excluded quickly. Approximately 35% of travelers returning from Africa have malaria, whereas typhoid is much rarer. In contrast, typhoid and dengue fever are much more widespread in Southeast Asia. In Latin America, this is the case for both dengue fever and leptospirosis.
When did you travel?
By using the incubation time of the pathogen in question, as well as the time of return journey, you can determine which diseases are possible and which are not. In one patient who visited the practice 4 weeks after his return, dengue or typhoid were excluded.
Where did you stay overnight?
Whether in an unhygienic bed or under the stars, the question regarding how and where travelers stayed overnight provides important evidence of the following nocturnal vectors:
- Sandflies: Leishmaniasis
- Kissing bugs: Chagas disease
- Fleas: Spotted fever, bubonic plague
- Mosquitoes: Malaria, dengue, filariasis
What did you eat?
Many infections can be attributed to careless eating. For example, when eating fish, crabs, crawfish, or frogs, especially if raw, liver fluke, lung fluke, or ciguatera should be considered. Mussel toxins have been found on the coast of Kenya and even in the south of France. In North African countries, you should be cautious when eating nonpasteurized milk products (for example, camel milk). They can transmit the pathogens for brucellosis and tuberculosis. In beef or pork that has not been cooked thoroughly, there is the risk of trichinosis or of a tapeworm. Even vegetarians need to be careful. Infections with the common liver fluke are possible after eating watercress.
What have you been doing?
You can only get some diseases through certain activities, said Dr. Holst. If long-distance travelers tell you about the following excursions, prick up your ears:
- Freshwater contact: Schistosomiasis, leptospirosis
- Caving: Histoplasmosis, rabies
- Excavations: Anthrax, coccidioidomycosis
- Camel tour: MERS coronavirus (Do not mount a sniffling camel!)
- Walking around barefoot: Strongyloides, hookworm
Was there contact with animals?
Because of the risk of rabies following contact with cats or biting apes, Dr. Holst advised long-distance travelers to get vaccinated.
Were there new sexual partners?
In the event of new sexual contacts, tests for hepatitis A, B, C, and HIV should be performed.
Are you undergoing medical treatment?
The patient may already be under medical supervision because of having a disease.
What prophylactic measures did you take before traveling?
To progress in the differential diagnosis, questions should also be asked regarding prophylactic measures. Vaccination against hepatitis A provides very efficient infection protection, whereas vaccines against typhoid offer a much lower level of protection.
Diagnostic tests
As long as there are no abnormalities, such as meningism or heart murmurs, further diagnostics include routine infectiologic laboratory investigations (C-reactive protein, blood count, etc), blood culture (aerobic, anaerobic), a urine dipstick test, and rapid tests for malaria and dengue.
To exclude malaria, a thick blood smear should always be performed on the same day, said Dr. Holst. “The rapid test is occasionally negative. But you often only detect tertian malaria in the thick blood smear. And you have to repeat the diagnostics the following day.” For this, it is important to know that a single test result does not exclude malaria right away. In contrast, detecting malaria antibodies is obsolete. Depending on the result, further tests include serologies, antigen investigations, and polymerase chain reaction.
Treat early
A complete set of results is not always available promptly. Experts recommend that, “if you already have a hunch, then start the therapy, even without a definite diagnosis.” This applies in particular for the suspected diagnoses in the following table.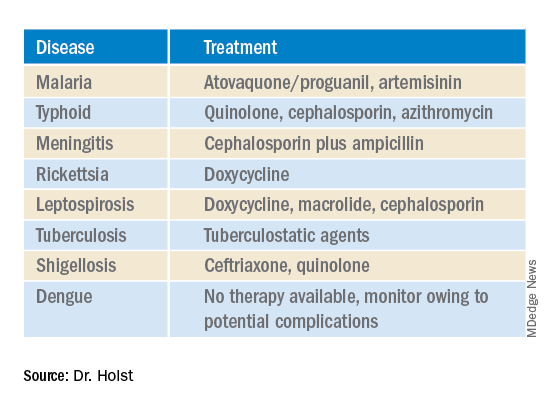
This article was translated from Coliquio. A version of this article appeared on Medscape.com.
After 2 years of a pandemic in which traveling was barely possible, tropical diseases are becoming important once more. At a 2022 conference for internal medicine specialists, tropical medicine specialist Fritz Holst, MD, of the Center for Tropical and Travel Medicine in Marburg, Germany, explained what questions you should be asking travelers with a fever at your practice and how to proceed with a suspected case.
The following article is based on the lecture: “Differential Diagnosis of Fever After a Trip to the Tropics,” which Dr. Holst gave at the 128th conference of the German Society of Internal Medicine.
A meta-analysis of studies concerning the topic, “returnee travelers from the tropics with fever,” was published in 2020. According to the analysis, purely tropical infections make up a third (33%) of fever diagnoses worldwide following an exotic trip. Malaria accounts for a fifth (22%), 5% are dengue fever, and 2.2% are typhoid (enteric fever).
In 26% of the returnee travelers investigated, nontropical infections were the cause of the fever. Acute gastroenteritis was responsible for 14%, and respiratory infections were responsible for 13%. In 18% of the cases, the cause of the fever remained unclear.
In Germany, the number of malaria cases has increased, said Dr. Holst. In Hessen, for example, there was recently a malaria fatality. “What we should do has been forgotten again,” he warned. More attention should also be paid once more to prophylaxis.
How to proceed
Dr. Holst described the following steps for treating recently returned travelers who are sick:
- Severely ill or not: If there are signs of a severe disease, such as dyspnea, signs of bleeding, hypotension, or central nervous system symptoms, the patient should be referred to a clinic. A diagnosis should be made within 1 day and treatment should be started.
- Transmissible or dangerous disease: This question should be quickly clarified to protect health care personnel, especially those treating patients. By using a thorough medical history (discussed below), a range of diseases may be clarified.
- Disease outbreak in destination country: Find out about possible disease outbreaks in the country that the traveler visited.
- Malaria? Immediate diagnostics: Malaria should always be excluded in patients at the practice on the same day by using a thick blood smear, even if no fever is present. If this is not possible because of time constraints, the affected person should be transferred directly to the clinic.
- Fever independent of the travel? Exclude other causes of the fever (for example, endocarditis).
- Involve tropical medicine specialists in a timely manner.
Nine mandatory questions
Dr. Holst also listed nine questions that clinicians should ask this patient population.
Where were you exactly?
Depending on the regional prevalence of tropical diseases, certain pathogens can be excluded quickly. Approximately 35% of travelers returning from Africa have malaria, whereas typhoid is much rarer. In contrast, typhoid and dengue fever are much more widespread in Southeast Asia. In Latin America, this is the case for both dengue fever and leptospirosis.
When did you travel?
By using the incubation time of the pathogen in question, as well as the time of return journey, you can determine which diseases are possible and which are not. In one patient who visited the practice 4 weeks after his return, dengue or typhoid were excluded.
Where did you stay overnight?
Whether in an unhygienic bed or under the stars, the question regarding how and where travelers stayed overnight provides important evidence of the following nocturnal vectors:
- Sandflies: Leishmaniasis
- Kissing bugs: Chagas disease
- Fleas: Spotted fever, bubonic plague
- Mosquitoes: Malaria, dengue, filariasis
What did you eat?
Many infections can be attributed to careless eating. For example, when eating fish, crabs, crawfish, or frogs, especially if raw, liver fluke, lung fluke, or ciguatera should be considered. Mussel toxins have been found on the coast of Kenya and even in the south of France. In North African countries, you should be cautious when eating nonpasteurized milk products (for example, camel milk). They can transmit the pathogens for brucellosis and tuberculosis. In beef or pork that has not been cooked thoroughly, there is the risk of trichinosis or of a tapeworm. Even vegetarians need to be careful. Infections with the common liver fluke are possible after eating watercress.
What have you been doing?
You can only get some diseases through certain activities, said Dr. Holst. If long-distance travelers tell you about the following excursions, prick up your ears:
- Freshwater contact: Schistosomiasis, leptospirosis
- Caving: Histoplasmosis, rabies
- Excavations: Anthrax, coccidioidomycosis
- Camel tour: MERS coronavirus (Do not mount a sniffling camel!)
- Walking around barefoot: Strongyloides, hookworm
Was there contact with animals?
Because of the risk of rabies following contact with cats or biting apes, Dr. Holst advised long-distance travelers to get vaccinated.
Were there new sexual partners?
In the event of new sexual contacts, tests for hepatitis A, B, C, and HIV should be performed.
Are you undergoing medical treatment?
The patient may already be under medical supervision because of having a disease.
What prophylactic measures did you take before traveling?
To progress in the differential diagnosis, questions should also be asked regarding prophylactic measures. Vaccination against hepatitis A provides very efficient infection protection, whereas vaccines against typhoid offer a much lower level of protection.
Diagnostic tests
As long as there are no abnormalities, such as meningism or heart murmurs, further diagnostics include routine infectiologic laboratory investigations (C-reactive protein, blood count, etc), blood culture (aerobic, anaerobic), a urine dipstick test, and rapid tests for malaria and dengue.
To exclude malaria, a thick blood smear should always be performed on the same day, said Dr. Holst. “The rapid test is occasionally negative. But you often only detect tertian malaria in the thick blood smear. And you have to repeat the diagnostics the following day.” For this, it is important to know that a single test result does not exclude malaria right away. In contrast, detecting malaria antibodies is obsolete. Depending on the result, further tests include serologies, antigen investigations, and polymerase chain reaction.
Treat early
A complete set of results is not always available promptly. Experts recommend that, “if you already have a hunch, then start the therapy, even without a definite diagnosis.” This applies in particular for the suspected diagnoses in the following table.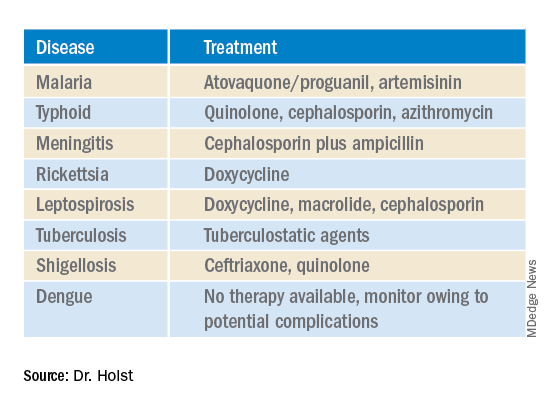
This article was translated from Coliquio. A version of this article appeared on Medscape.com.
Bacterial cocktail, spores counter recurrent C. diff
SAN DIEGO – A novel combination of eight human commensal bacteria has shown efficacy in preventing recurrent Clostridioides difficile infections in high-risk populations. The cocktail of bacterial strains (VE303), produced under tightly-controlled conditions, is delivered in powdered form over a period of 14 days.
The approach, sponsored by Vedanta Biosciences, is one of several efforts to use carefully defined microbial populations instead of fecal microbiota transplantation (FMT) to treat or prevent C. diff infections.
The key issue is that not all of the bacteria found in FMTs are needed to provide a therapeutic effect, according to Thomas Louie, MD, professor of medicine at the University of Calgary (Alta.). “You don’t need all the bugs. You don’t need raw [stool]. You can take only the good parts,” said Dr. Louie, who presented the results of the phase 2 study at the annual Digestive Disease Week® (DDW). In fact, FMT carries the risk of infection of pathogenic bacteria.
The strains found in VE303 were consistently identified in patients’ microbiota following successful FMTs, though they were absent before the transplant. Animal and human studies then showed that the microbes could repopulate microbiota.
Among 78 patients included in the efficacy analysis of the study, after 8 weeks, 13.8% of the VE303 group experienced a recurrent C. diff infection, versus 45.5% of the placebo group, amounting to more than an 80% reduction in risk (odds ratio, 0.192; P = .0077). Adverse events were mild and similar across both groups, with no treatment-related serious adverse events reported.
The same session included a post hoc analysis of a phase 3 study sponsored by Seres Therapeutics, which showed that the company’s oral product SER-109, composed of purified Firmicutes spores, reduced the risk of recurrent C. diff infection after 8 weeks compared to placebo (12.4% versus 39.8%; P < .001).
The new analysis examined short-, medium-, and branch-chained fatty acids in patient stools. After just 1 week of treatment, there was an increase in the short-chain fatty acid butyrate and medium-chain fatty acids valerate and hexanoate. They continued to be higher in weeks 2 and 8 in the treatment arm. The results suggest that increased fatty acid production might boost clinical outcomes, according to Kevin Litcofsky of Seres, who presented the results.
Both approaches have potential, according to Melinda Engevik, PhD, who comoderated the session where the study was presented. “I think that they’re both interesting ideas. The spores [from Seres], I think, are going to be better at passing through the stomach and a little bit more resistant, but then they have to germinate and engraft, whereas if you give the lyophilized bacteria [from Vedanta], you might lose some more, but they’re already primed and ready to go. So I think they’re both very different approaches, but the data from both seem to support that they worked and probably in different ways,” said Dr. Engevik, assistant professor at the Medical University of South Carolina, Charleston.
“Patients that have recurrent [C. diff], they are desperate to be able to break the cycle of recurrence. I think that they’ve shown a lot of safety with this, which is an issue for FMT. Both of the talks seemed like there is a path moving forward to help those patients. I was encouraged,” said Dr. Engevik.
Comoderator Anoop Kumar, PhD, assistant professor of gastroenterology and hepatology at University of Illinois, Chicago, agreed and noted the advantage of such treatments over FMT during the COVID-19 pandemic, which has disrupted FMT delivery.
Previous studies have looked at probiotics, but results so far have been mixed, said Dr. Engevik. She suspects these two approaches, containing more bacterial strains, are likely to have better success. “I think you really have to have a complex gut microbiota community, at least minimally complex, to be able to get the effects. I think it’s the wave of the future,” she said.
Dr. Engevik also suggested that the benefits might not stop at C. diff. She highlighted research in other gastrointestinal diseases such as inflammatory bowel disease, and even efforts underway to enhance responses to checkpoint inhibitors in the treatment of cancer. “Gut microbes are master regulators, so they have these wide-reaching effects. I think that a lot of human health will be started to be targeted by looking at the gut microbiota,” she said.
Dr. Louie also highlighted the potential for more applications. “C. diff is low-hanging fruit. I think these bugs will have some usefulness for [irritable bowel syndrome]. I’ve transplanted some patients with IBS and it seemed to work. I haven’t had time to design and do an IBS trial, but the future is these bugs.”
Dr. Louie also participated in the Seres study. He has been on the advisory board for Vedanta, Seres, Finch Therapeutics, and Artugen Therapeutics. Dr. Engevik and Dr. Kumar have no relevant financial disclosures.
SAN DIEGO – A novel combination of eight human commensal bacteria has shown efficacy in preventing recurrent Clostridioides difficile infections in high-risk populations. The cocktail of bacterial strains (VE303), produced under tightly-controlled conditions, is delivered in powdered form over a period of 14 days.
The approach, sponsored by Vedanta Biosciences, is one of several efforts to use carefully defined microbial populations instead of fecal microbiota transplantation (FMT) to treat or prevent C. diff infections.
The key issue is that not all of the bacteria found in FMTs are needed to provide a therapeutic effect, according to Thomas Louie, MD, professor of medicine at the University of Calgary (Alta.). “You don’t need all the bugs. You don’t need raw [stool]. You can take only the good parts,” said Dr. Louie, who presented the results of the phase 2 study at the annual Digestive Disease Week® (DDW). In fact, FMT carries the risk of infection of pathogenic bacteria.
The strains found in VE303 were consistently identified in patients’ microbiota following successful FMTs, though they were absent before the transplant. Animal and human studies then showed that the microbes could repopulate microbiota.
Among 78 patients included in the efficacy analysis of the study, after 8 weeks, 13.8% of the VE303 group experienced a recurrent C. diff infection, versus 45.5% of the placebo group, amounting to more than an 80% reduction in risk (odds ratio, 0.192; P = .0077). Adverse events were mild and similar across both groups, with no treatment-related serious adverse events reported.
The same session included a post hoc analysis of a phase 3 study sponsored by Seres Therapeutics, which showed that the company’s oral product SER-109, composed of purified Firmicutes spores, reduced the risk of recurrent C. diff infection after 8 weeks compared to placebo (12.4% versus 39.8%; P < .001).
The new analysis examined short-, medium-, and branch-chained fatty acids in patient stools. After just 1 week of treatment, there was an increase in the short-chain fatty acid butyrate and medium-chain fatty acids valerate and hexanoate. They continued to be higher in weeks 2 and 8 in the treatment arm. The results suggest that increased fatty acid production might boost clinical outcomes, according to Kevin Litcofsky of Seres, who presented the results.
Both approaches have potential, according to Melinda Engevik, PhD, who comoderated the session where the study was presented. “I think that they’re both interesting ideas. The spores [from Seres], I think, are going to be better at passing through the stomach and a little bit more resistant, but then they have to germinate and engraft, whereas if you give the lyophilized bacteria [from Vedanta], you might lose some more, but they’re already primed and ready to go. So I think they’re both very different approaches, but the data from both seem to support that they worked and probably in different ways,” said Dr. Engevik, assistant professor at the Medical University of South Carolina, Charleston.
“Patients that have recurrent [C. diff], they are desperate to be able to break the cycle of recurrence. I think that they’ve shown a lot of safety with this, which is an issue for FMT. Both of the talks seemed like there is a path moving forward to help those patients. I was encouraged,” said Dr. Engevik.
Comoderator Anoop Kumar, PhD, assistant professor of gastroenterology and hepatology at University of Illinois, Chicago, agreed and noted the advantage of such treatments over FMT during the COVID-19 pandemic, which has disrupted FMT delivery.
Previous studies have looked at probiotics, but results so far have been mixed, said Dr. Engevik. She suspects these two approaches, containing more bacterial strains, are likely to have better success. “I think you really have to have a complex gut microbiota community, at least minimally complex, to be able to get the effects. I think it’s the wave of the future,” she said.
Dr. Engevik also suggested that the benefits might not stop at C. diff. She highlighted research in other gastrointestinal diseases such as inflammatory bowel disease, and even efforts underway to enhance responses to checkpoint inhibitors in the treatment of cancer. “Gut microbes are master regulators, so they have these wide-reaching effects. I think that a lot of human health will be started to be targeted by looking at the gut microbiota,” she said.
Dr. Louie also highlighted the potential for more applications. “C. diff is low-hanging fruit. I think these bugs will have some usefulness for [irritable bowel syndrome]. I’ve transplanted some patients with IBS and it seemed to work. I haven’t had time to design and do an IBS trial, but the future is these bugs.”
Dr. Louie also participated in the Seres study. He has been on the advisory board for Vedanta, Seres, Finch Therapeutics, and Artugen Therapeutics. Dr. Engevik and Dr. Kumar have no relevant financial disclosures.
SAN DIEGO – A novel combination of eight human commensal bacteria has shown efficacy in preventing recurrent Clostridioides difficile infections in high-risk populations. The cocktail of bacterial strains (VE303), produced under tightly-controlled conditions, is delivered in powdered form over a period of 14 days.
The approach, sponsored by Vedanta Biosciences, is one of several efforts to use carefully defined microbial populations instead of fecal microbiota transplantation (FMT) to treat or prevent C. diff infections.
The key issue is that not all of the bacteria found in FMTs are needed to provide a therapeutic effect, according to Thomas Louie, MD, professor of medicine at the University of Calgary (Alta.). “You don’t need all the bugs. You don’t need raw [stool]. You can take only the good parts,” said Dr. Louie, who presented the results of the phase 2 study at the annual Digestive Disease Week® (DDW). In fact, FMT carries the risk of infection of pathogenic bacteria.
The strains found in VE303 were consistently identified in patients’ microbiota following successful FMTs, though they were absent before the transplant. Animal and human studies then showed that the microbes could repopulate microbiota.
Among 78 patients included in the efficacy analysis of the study, after 8 weeks, 13.8% of the VE303 group experienced a recurrent C. diff infection, versus 45.5% of the placebo group, amounting to more than an 80% reduction in risk (odds ratio, 0.192; P = .0077). Adverse events were mild and similar across both groups, with no treatment-related serious adverse events reported.
The same session included a post hoc analysis of a phase 3 study sponsored by Seres Therapeutics, which showed that the company’s oral product SER-109, composed of purified Firmicutes spores, reduced the risk of recurrent C. diff infection after 8 weeks compared to placebo (12.4% versus 39.8%; P < .001).
The new analysis examined short-, medium-, and branch-chained fatty acids in patient stools. After just 1 week of treatment, there was an increase in the short-chain fatty acid butyrate and medium-chain fatty acids valerate and hexanoate. They continued to be higher in weeks 2 and 8 in the treatment arm. The results suggest that increased fatty acid production might boost clinical outcomes, according to Kevin Litcofsky of Seres, who presented the results.
Both approaches have potential, according to Melinda Engevik, PhD, who comoderated the session where the study was presented. “I think that they’re both interesting ideas. The spores [from Seres], I think, are going to be better at passing through the stomach and a little bit more resistant, but then they have to germinate and engraft, whereas if you give the lyophilized bacteria [from Vedanta], you might lose some more, but they’re already primed and ready to go. So I think they’re both very different approaches, but the data from both seem to support that they worked and probably in different ways,” said Dr. Engevik, assistant professor at the Medical University of South Carolina, Charleston.
“Patients that have recurrent [C. diff], they are desperate to be able to break the cycle of recurrence. I think that they’ve shown a lot of safety with this, which is an issue for FMT. Both of the talks seemed like there is a path moving forward to help those patients. I was encouraged,” said Dr. Engevik.
Comoderator Anoop Kumar, PhD, assistant professor of gastroenterology and hepatology at University of Illinois, Chicago, agreed and noted the advantage of such treatments over FMT during the COVID-19 pandemic, which has disrupted FMT delivery.
Previous studies have looked at probiotics, but results so far have been mixed, said Dr. Engevik. She suspects these two approaches, containing more bacterial strains, are likely to have better success. “I think you really have to have a complex gut microbiota community, at least minimally complex, to be able to get the effects. I think it’s the wave of the future,” she said.
Dr. Engevik also suggested that the benefits might not stop at C. diff. She highlighted research in other gastrointestinal diseases such as inflammatory bowel disease, and even efforts underway to enhance responses to checkpoint inhibitors in the treatment of cancer. “Gut microbes are master regulators, so they have these wide-reaching effects. I think that a lot of human health will be started to be targeted by looking at the gut microbiota,” she said.
Dr. Louie also highlighted the potential for more applications. “C. diff is low-hanging fruit. I think these bugs will have some usefulness for [irritable bowel syndrome]. I’ve transplanted some patients with IBS and it seemed to work. I haven’t had time to design and do an IBS trial, but the future is these bugs.”
Dr. Louie also participated in the Seres study. He has been on the advisory board for Vedanta, Seres, Finch Therapeutics, and Artugen Therapeutics. Dr. Engevik and Dr. Kumar have no relevant financial disclosures.
AT DDW 2022
Treatment for alcohol abuse reduces hepatitis readmission
SAN DIEGO – Treating people with alcoholic hepatitis for alcohol abuse may reduce their risk of hospital readmission, researchers reported.
In a retrospective analysis of nationwide data, 7.83% of those patients who received psychotherapy, counseling, or drug treatment for alcohol abuse were readmitted within 30 days, versus 11.67% of those who did not receive these kinds of treatment.
The finding lends support to the argument that hospitals should invest more in the treatments, despite the complexities involved.
“It takes a multidisciplinary approach, starting from the physician or the health care provider along with the pharmacists, the behavioral health specialists, or a psychiatrist or psychologist, along with case management as well,” said Harleen Chela, MD, a third-year resident at the University of Missouri in Columbia. She presented the findings at the annual Digestive Disease Week® (DDW).
The researchers started with the premise that patients with alcoholic hepatitis can prevent the condition from worsening by abstaining from alcohol. To see whether interventions aimed at encouraging that abstention could prevent readmissions, Dr. Chela and colleagues analyzed data on readmissions for the first 11 months of the year 2018.
They included patients who were at least 18 years of age and who had a nonelective admission with a principal diagnosis of alcohol abuse.
Using procedure codes, they compared those patients given psychotherapy (including cognitive behavioral therapy), formal inpatient counseling, and drug treatment for alcohol abuse to those who didn’t. Then they counted how many patients were readmitted within 30 days.
They found records of 45,617 patients admitted for alcoholic hepatitis of whom 1,552 received treatment for alcohol abuse and 44,065 did not.
They did not find any significant difference between the two groups in demographics, income, or insurance status.
Adjusting for such factors, the researchers found that people who received alcohol abuse treatment were 64% as likely to be readmitted as were those who did not (hazard ratio, 0.64; 95% confidence interval, 0.46-0.91; P = 0.01).
If alcohol abuse treatment is so effective, why isn’t it routine? “It’s not always feasible to implement this, on the inpatient side, because it takes more than a day or two just to get some of these things put in place,” Dr. Chela told this news organization.
They did find that people were more likely to get treatment for alcohol abuse if they were admitted to a hospital in a big city rather than a small town and if their hospital was owned by private investors rather than by a not-for-profit organization or the government.
“Larger hospitals and private sector institutions have more access to resources and money to have those kinds of systems in place for the patients,” said Dr. Chela.
She became interested in the issue at her hospital when she noticed that patients with alcoholic hepatitis were not getting behavioral counseling. “The inpatient load in the behavioral health side is so much that they don’t have time for these kinds of consults,” she said. “That’s one of the challenges: A shortage of behavioral specialists like psychiatrists.”
And hospitals tend to focus on treating conditions that threaten their patients’ lives in the short term. “Someone who has a heart attack or a gastrointestinal bleed – there’s more focus on resources for those kinds of patients,” she said.
Virginia Commonwealth University in Richmond provides alcohol abuse treatment to patients with alcoholic hepatitis partly using telehealth, said Richard Sterling, MD, MSc, chief of hepatology, who was not involved in the study. “For people who live too far away, don’t have transportation, or have other health disparities, we now have technology and mechanisms to keep them engaged in care,” he told this news organization. “We’re doing a lot of Zoom visits.”
Dr. Chela and colleagues also found that those who got alcohol abuse treatment were less likely to be discharged to a skilled nursing facility or to home health. The data couldn’t give the researchers a definitive reason for this, but Dr. Chela speculated that the patients who received treatment for alcohol abuse stayed longer in the hospital and may have been in better shape when they were discharged.
The U.S. health care system doesn’t necessarily provide incentives to keep patients healthy, Dr. Sterling said. “Hospital systems make money off of filling beds, and providing a lot of inpatient care and hospital days,” he said. “That may be not necessarily congruent with a health system that is supposed to provide health for these covered lives.”
Neither Dr. Chela nor Dr. Sterling reported any relevant financial relationships.
SAN DIEGO – Treating people with alcoholic hepatitis for alcohol abuse may reduce their risk of hospital readmission, researchers reported.
In a retrospective analysis of nationwide data, 7.83% of those patients who received psychotherapy, counseling, or drug treatment for alcohol abuse were readmitted within 30 days, versus 11.67% of those who did not receive these kinds of treatment.
The finding lends support to the argument that hospitals should invest more in the treatments, despite the complexities involved.
“It takes a multidisciplinary approach, starting from the physician or the health care provider along with the pharmacists, the behavioral health specialists, or a psychiatrist or psychologist, along with case management as well,” said Harleen Chela, MD, a third-year resident at the University of Missouri in Columbia. She presented the findings at the annual Digestive Disease Week® (DDW).
The researchers started with the premise that patients with alcoholic hepatitis can prevent the condition from worsening by abstaining from alcohol. To see whether interventions aimed at encouraging that abstention could prevent readmissions, Dr. Chela and colleagues analyzed data on readmissions for the first 11 months of the year 2018.
They included patients who were at least 18 years of age and who had a nonelective admission with a principal diagnosis of alcohol abuse.
Using procedure codes, they compared those patients given psychotherapy (including cognitive behavioral therapy), formal inpatient counseling, and drug treatment for alcohol abuse to those who didn’t. Then they counted how many patients were readmitted within 30 days.
They found records of 45,617 patients admitted for alcoholic hepatitis of whom 1,552 received treatment for alcohol abuse and 44,065 did not.
They did not find any significant difference between the two groups in demographics, income, or insurance status.
Adjusting for such factors, the researchers found that people who received alcohol abuse treatment were 64% as likely to be readmitted as were those who did not (hazard ratio, 0.64; 95% confidence interval, 0.46-0.91; P = 0.01).
If alcohol abuse treatment is so effective, why isn’t it routine? “It’s not always feasible to implement this, on the inpatient side, because it takes more than a day or two just to get some of these things put in place,” Dr. Chela told this news organization.
They did find that people were more likely to get treatment for alcohol abuse if they were admitted to a hospital in a big city rather than a small town and if their hospital was owned by private investors rather than by a not-for-profit organization or the government.
“Larger hospitals and private sector institutions have more access to resources and money to have those kinds of systems in place for the patients,” said Dr. Chela.
She became interested in the issue at her hospital when she noticed that patients with alcoholic hepatitis were not getting behavioral counseling. “The inpatient load in the behavioral health side is so much that they don’t have time for these kinds of consults,” she said. “That’s one of the challenges: A shortage of behavioral specialists like psychiatrists.”
And hospitals tend to focus on treating conditions that threaten their patients’ lives in the short term. “Someone who has a heart attack or a gastrointestinal bleed – there’s more focus on resources for those kinds of patients,” she said.
Virginia Commonwealth University in Richmond provides alcohol abuse treatment to patients with alcoholic hepatitis partly using telehealth, said Richard Sterling, MD, MSc, chief of hepatology, who was not involved in the study. “For people who live too far away, don’t have transportation, or have other health disparities, we now have technology and mechanisms to keep them engaged in care,” he told this news organization. “We’re doing a lot of Zoom visits.”
Dr. Chela and colleagues also found that those who got alcohol abuse treatment were less likely to be discharged to a skilled nursing facility or to home health. The data couldn’t give the researchers a definitive reason for this, but Dr. Chela speculated that the patients who received treatment for alcohol abuse stayed longer in the hospital and may have been in better shape when they were discharged.
The U.S. health care system doesn’t necessarily provide incentives to keep patients healthy, Dr. Sterling said. “Hospital systems make money off of filling beds, and providing a lot of inpatient care and hospital days,” he said. “That may be not necessarily congruent with a health system that is supposed to provide health for these covered lives.”
Neither Dr. Chela nor Dr. Sterling reported any relevant financial relationships.
SAN DIEGO – Treating people with alcoholic hepatitis for alcohol abuse may reduce their risk of hospital readmission, researchers reported.
In a retrospective analysis of nationwide data, 7.83% of those patients who received psychotherapy, counseling, or drug treatment for alcohol abuse were readmitted within 30 days, versus 11.67% of those who did not receive these kinds of treatment.
The finding lends support to the argument that hospitals should invest more in the treatments, despite the complexities involved.
“It takes a multidisciplinary approach, starting from the physician or the health care provider along with the pharmacists, the behavioral health specialists, or a psychiatrist or psychologist, along with case management as well,” said Harleen Chela, MD, a third-year resident at the University of Missouri in Columbia. She presented the findings at the annual Digestive Disease Week® (DDW).
The researchers started with the premise that patients with alcoholic hepatitis can prevent the condition from worsening by abstaining from alcohol. To see whether interventions aimed at encouraging that abstention could prevent readmissions, Dr. Chela and colleagues analyzed data on readmissions for the first 11 months of the year 2018.
They included patients who were at least 18 years of age and who had a nonelective admission with a principal diagnosis of alcohol abuse.
Using procedure codes, they compared those patients given psychotherapy (including cognitive behavioral therapy), formal inpatient counseling, and drug treatment for alcohol abuse to those who didn’t. Then they counted how many patients were readmitted within 30 days.
They found records of 45,617 patients admitted for alcoholic hepatitis of whom 1,552 received treatment for alcohol abuse and 44,065 did not.
They did not find any significant difference between the two groups in demographics, income, or insurance status.
Adjusting for such factors, the researchers found that people who received alcohol abuse treatment were 64% as likely to be readmitted as were those who did not (hazard ratio, 0.64; 95% confidence interval, 0.46-0.91; P = 0.01).
If alcohol abuse treatment is so effective, why isn’t it routine? “It’s not always feasible to implement this, on the inpatient side, because it takes more than a day or two just to get some of these things put in place,” Dr. Chela told this news organization.
They did find that people were more likely to get treatment for alcohol abuse if they were admitted to a hospital in a big city rather than a small town and if their hospital was owned by private investors rather than by a not-for-profit organization or the government.
“Larger hospitals and private sector institutions have more access to resources and money to have those kinds of systems in place for the patients,” said Dr. Chela.
She became interested in the issue at her hospital when she noticed that patients with alcoholic hepatitis were not getting behavioral counseling. “The inpatient load in the behavioral health side is so much that they don’t have time for these kinds of consults,” she said. “That’s one of the challenges: A shortage of behavioral specialists like psychiatrists.”
And hospitals tend to focus on treating conditions that threaten their patients’ lives in the short term. “Someone who has a heart attack or a gastrointestinal bleed – there’s more focus on resources for those kinds of patients,” she said.
Virginia Commonwealth University in Richmond provides alcohol abuse treatment to patients with alcoholic hepatitis partly using telehealth, said Richard Sterling, MD, MSc, chief of hepatology, who was not involved in the study. “For people who live too far away, don’t have transportation, or have other health disparities, we now have technology and mechanisms to keep them engaged in care,” he told this news organization. “We’re doing a lot of Zoom visits.”
Dr. Chela and colleagues also found that those who got alcohol abuse treatment were less likely to be discharged to a skilled nursing facility or to home health. The data couldn’t give the researchers a definitive reason for this, but Dr. Chela speculated that the patients who received treatment for alcohol abuse stayed longer in the hospital and may have been in better shape when they were discharged.
The U.S. health care system doesn’t necessarily provide incentives to keep patients healthy, Dr. Sterling said. “Hospital systems make money off of filling beds, and providing a lot of inpatient care and hospital days,” he said. “That may be not necessarily congruent with a health system that is supposed to provide health for these covered lives.”
Neither Dr. Chela nor Dr. Sterling reported any relevant financial relationships.
AT DDW 2022
Climate change, medical education, and dermatology
The recent article on including the impact of climate on health in medical education programs shines an important light on the challenge – and urgent need – of integrating climate change training into medical education. These nascent efforts are just getting underway across the country, with some programs – notably Harvard’s C-CHANGE (Center for Climate, Health, and the Global Environment) program, mentioned in the article, and others, such as the University of Colorado’s Climate Medicine diploma course – leading the way. A number of publications, such as the editorial titled “A planetary health curriculum for medicine” published in 2021 in the BMJ, offer a roadmap to do so.
Medical schools, residency programs, and other medical specialty programs – including those for advanced practice providers, dentists, nurses, and more – should be incorporating climate change and its myriad of health impacts into their training pathways. The medical student group, Medical Students for a Sustainable Future, has put forth a planetary health report card that evaluates training programs on the strength of their focus on the intersections between climate and health.
While the article did not specifically focus on dermatology, these impacts are true in our field as well. The article notes that “at least one medical journal has recently ramped up its efforts to educate physicians on the links between health issues and climate change.” Notably in dermatology, the International Journal of Women’s Dermatology devoted an entire 124-page themed issue to climate change and dermatology in January, 2021, while JAMA Dermatology editor Kanade Shinkai, MD, PhD, called out climate change as one of the journal’s priorities in her annual editorial, stating, “Another priority for the journal is to better understand the effect of climate change on human health, specifically skin disease.”
The impacts of climate change in dermatology range from heat-related illness (a major cause of climate-associated mortality, with the skin serving as an essential thermoregulatory organ) to changing patterns of vector-borne illnesses to pollution and wildfire smoke flaring inflammatory skin diseases, to an increase in skin cancer, and more. While incorporation of health issues relating to climate change is important at a medical school level, it is also critical at the residency training – and board exam/certification – level as well.
Beyond the importance of building climate education into undergraduate and graduate medical education, it is also important that practicing physicians, post-residency training, remain up to date and keep abreast of changing patterns of disease in our rapidly changing climate. Lyme disease now occurs in Canada – and both earlier and later in the year even in places that are geographically used to seeing it. Early recognition is essential, but unprepared physicians may miss the early erythema migrans rash, and patients may suffer more severe sequelae as a result.
Finally, it’s important that medical organizations are aware of not just the health implications of climate change, but also potential policy impacts. Health care is a major emitter of CO2, and assistant secretary for health for the U.S. Department of Health and Human Services, Admiral Rachel L. Levine, MD, with the National Academy of Medicine, has appropriately pledged to reduce health care carbon emissions as part of the necessary steps that we must all take to avert the worst impacts of a warming world. The field of medicine and individual providers should educate themselves and actively work toward sustainability in health care, to improve the health of their patients, populations, and future generations.
Dr. Rosenbach is associate professor of dermatology and medicine at the University of Pennsylvania, Philadelphia, and is the founder and cochair of the American Academy of Dermatology Expert Resource Group for Climate Change and Environmental Issues. Dr. Rosenbach is speaking on behalf of himself and not the AAD.
The recent article on including the impact of climate on health in medical education programs shines an important light on the challenge – and urgent need – of integrating climate change training into medical education. These nascent efforts are just getting underway across the country, with some programs – notably Harvard’s C-CHANGE (Center for Climate, Health, and the Global Environment) program, mentioned in the article, and others, such as the University of Colorado’s Climate Medicine diploma course – leading the way. A number of publications, such as the editorial titled “A planetary health curriculum for medicine” published in 2021 in the BMJ, offer a roadmap to do so.
Medical schools, residency programs, and other medical specialty programs – including those for advanced practice providers, dentists, nurses, and more – should be incorporating climate change and its myriad of health impacts into their training pathways. The medical student group, Medical Students for a Sustainable Future, has put forth a planetary health report card that evaluates training programs on the strength of their focus on the intersections between climate and health.
While the article did not specifically focus on dermatology, these impacts are true in our field as well. The article notes that “at least one medical journal has recently ramped up its efforts to educate physicians on the links between health issues and climate change.” Notably in dermatology, the International Journal of Women’s Dermatology devoted an entire 124-page themed issue to climate change and dermatology in January, 2021, while JAMA Dermatology editor Kanade Shinkai, MD, PhD, called out climate change as one of the journal’s priorities in her annual editorial, stating, “Another priority for the journal is to better understand the effect of climate change on human health, specifically skin disease.”
The impacts of climate change in dermatology range from heat-related illness (a major cause of climate-associated mortality, with the skin serving as an essential thermoregulatory organ) to changing patterns of vector-borne illnesses to pollution and wildfire smoke flaring inflammatory skin diseases, to an increase in skin cancer, and more. While incorporation of health issues relating to climate change is important at a medical school level, it is also critical at the residency training – and board exam/certification – level as well.
Beyond the importance of building climate education into undergraduate and graduate medical education, it is also important that practicing physicians, post-residency training, remain up to date and keep abreast of changing patterns of disease in our rapidly changing climate. Lyme disease now occurs in Canada – and both earlier and later in the year even in places that are geographically used to seeing it. Early recognition is essential, but unprepared physicians may miss the early erythema migrans rash, and patients may suffer more severe sequelae as a result.
Finally, it’s important that medical organizations are aware of not just the health implications of climate change, but also potential policy impacts. Health care is a major emitter of CO2, and assistant secretary for health for the U.S. Department of Health and Human Services, Admiral Rachel L. Levine, MD, with the National Academy of Medicine, has appropriately pledged to reduce health care carbon emissions as part of the necessary steps that we must all take to avert the worst impacts of a warming world. The field of medicine and individual providers should educate themselves and actively work toward sustainability in health care, to improve the health of their patients, populations, and future generations.
Dr. Rosenbach is associate professor of dermatology and medicine at the University of Pennsylvania, Philadelphia, and is the founder and cochair of the American Academy of Dermatology Expert Resource Group for Climate Change and Environmental Issues. Dr. Rosenbach is speaking on behalf of himself and not the AAD.
The recent article on including the impact of climate on health in medical education programs shines an important light on the challenge – and urgent need – of integrating climate change training into medical education. These nascent efforts are just getting underway across the country, with some programs – notably Harvard’s C-CHANGE (Center for Climate, Health, and the Global Environment) program, mentioned in the article, and others, such as the University of Colorado’s Climate Medicine diploma course – leading the way. A number of publications, such as the editorial titled “A planetary health curriculum for medicine” published in 2021 in the BMJ, offer a roadmap to do so.
Medical schools, residency programs, and other medical specialty programs – including those for advanced practice providers, dentists, nurses, and more – should be incorporating climate change and its myriad of health impacts into their training pathways. The medical student group, Medical Students for a Sustainable Future, has put forth a planetary health report card that evaluates training programs on the strength of their focus on the intersections between climate and health.
While the article did not specifically focus on dermatology, these impacts are true in our field as well. The article notes that “at least one medical journal has recently ramped up its efforts to educate physicians on the links between health issues and climate change.” Notably in dermatology, the International Journal of Women’s Dermatology devoted an entire 124-page themed issue to climate change and dermatology in January, 2021, while JAMA Dermatology editor Kanade Shinkai, MD, PhD, called out climate change as one of the journal’s priorities in her annual editorial, stating, “Another priority for the journal is to better understand the effect of climate change on human health, specifically skin disease.”
The impacts of climate change in dermatology range from heat-related illness (a major cause of climate-associated mortality, with the skin serving as an essential thermoregulatory organ) to changing patterns of vector-borne illnesses to pollution and wildfire smoke flaring inflammatory skin diseases, to an increase in skin cancer, and more. While incorporation of health issues relating to climate change is important at a medical school level, it is also critical at the residency training – and board exam/certification – level as well.
Beyond the importance of building climate education into undergraduate and graduate medical education, it is also important that practicing physicians, post-residency training, remain up to date and keep abreast of changing patterns of disease in our rapidly changing climate. Lyme disease now occurs in Canada – and both earlier and later in the year even in places that are geographically used to seeing it. Early recognition is essential, but unprepared physicians may miss the early erythema migrans rash, and patients may suffer more severe sequelae as a result.
Finally, it’s important that medical organizations are aware of not just the health implications of climate change, but also potential policy impacts. Health care is a major emitter of CO2, and assistant secretary for health for the U.S. Department of Health and Human Services, Admiral Rachel L. Levine, MD, with the National Academy of Medicine, has appropriately pledged to reduce health care carbon emissions as part of the necessary steps that we must all take to avert the worst impacts of a warming world. The field of medicine and individual providers should educate themselves and actively work toward sustainability in health care, to improve the health of their patients, populations, and future generations.
Dr. Rosenbach is associate professor of dermatology and medicine at the University of Pennsylvania, Philadelphia, and is the founder and cochair of the American Academy of Dermatology Expert Resource Group for Climate Change and Environmental Issues. Dr. Rosenbach is speaking on behalf of himself and not the AAD.
AUA 2022: A report from the trenches
The annual meeting of the American Urological Association took place recently at the Ernest N. Morial Convention Center in New Orleans. Hundreds of talks and abstracts were presented over the 4 days in New Orleans; below is a summary of what I found to be the key scientific highlights.
1. Updates to the AUA’s guidelines for management of localized kidney cancer
The AUA’s recommendations for the treatment of localized kidney cancer have changed dramatically over the past few decades. Gone are the days of simply removing the entire kidney every time a mass is found. Today, a partial nephrectomy is preferred in most situations.
Our understanding that the prevalence of familial kidney cancer is much higher than previously thought has led to a change in the guidelines regarding which patients should receive genetic counseling. For the first time, the guidelines include the use of adjuvant medical treatment, such as pembrolizumab. A 2021 study in the New England Journal of Medicine showed a survival benefit for patients with high-risk disease who receive such therapies, so it›s not surprising that such treatments are now recommended.
The development of new second- and third-generation gadolinium contrast agents that spare the kidneys has dramatically increased the role for MRIs for patients with severe or even end-stage renal disease. As a result, the guidelines were updated to recommend the use of these agents. The role of a renal biopsy, which has always been limited, given the ability of cross-sectional imaging to diagnosis this disease, has further been constrained and should now be performed only when the results would clearly change a clinical decision, such as whether or not the lesion in question is a metastasis.
2. New and better ureteroscope technology
No one likes kidney stones, not the patient who deals with the incredible pain, nor the surgeon who has to remove them, given that these cases often present in the wee hours of the morning. The preferred surgical approach has changed dramatically over the past decade, moving away from extracorporeal shockwave lithotripsy toward flexible ureteroscope-based technology, which has a higher clearance rate and is more widely and more immediately available. Flexible ureteroscopy has been held back by technological barriers, including limited scope deflection and low laser power. The exceptionally high cost of repair and the tendency of the instruments to break haven’t helped, either. Although single-use ureteroscopes have been available for some time, it wasn’t until the recently introduced second-generation scopes became widely available that they have become popular. These new scopes have small external diameters, great optics, and can easily be used. Newer high-powered lasers and the change from holmium:YAG-based lasers to thulium technology is greatly increasing the size of stones that can be safely addressed ureteroscopically. The cost analysis of single-use technology versus reusable scopes tends to be site dependent but can be appealing in certain situations. Also, on the technology forefront, a new robotically assisted ureteroscope is being introduced that offers the chance for improved intrapelvic mobility and better ergonomics for the surgeon.
3. New options for the treatment of clinically localized prostate cancer
Since the guidelines were last updated in 2017, the definitive management of localized prostate cancer has changed dramatically. Although radical prostatectomy and radiotherapy remain the preferred options for men who choose treatment for their disease, the updated guidelines state that active surveillance is now the preferred approach for men with low-risk cancers.
Although the preferred surveillance protocol is still being debated, the consensus is that almost all men with low-risk disease can be safely monitored for some period. The imaging technology available to monitor patients is also radically changing with the rollout of prostate-specific membrane antigen–based PET technology. The increased sensitivity and specificity of this modality opens the door not only for better up-front staging of newly diagnosed patients with prostate cancer but also may allow clinicians to earlier identify and treat men with metastatic disease. The guidelines for the first time address the use of genetic markers to individualize treatment of men with advanced or metastatic prostate cancer. Exactly which treatments these patients need is still being debated, but the ability to use patient-specific genetic mutation information to customize treatment is potentially groundbreaking.
4. New treatment options for patients with high-grade non–muscle-invasive bladder cancer (NMIBC) refractory to bacille Calmette-Guérin (BCG) therapy
Patients with NMIBC who do not respond to BCG therapy are in a tough position. Cystectomy remains the preferred option as a second-line strategy, but the procedure has a complication rate approaching 30%. Further, many patients are not willing to have their bladder removed because of the life-altering changes that go along with having an urostomy or a neobladder. While intravesical treatments such as valrubicin, docetaxel, or gemcitabine have been available for many years, the success rates of those options are limited. The Food and Drug Administration recently approved the use of the immunotherapy-based treatment pembrolizumab. While none of these options is perfect, the fact that we now have at least some alternatives is a huge step in the right direction.
5. It’s all about the patient: Involving patients in designing the health care delivery system
Although it seems like an obvious concept, patients themselves have traditionally not been involved in designing the health care delivery system on which they rely. Research presented at the AUA shows that many health care outcomes improve when patients are actively involved in the process. For example, Angela Smith, MD, of the University of North Carolina at Chapel Hill, presented a study showing that including patients in the identification of possible research topics helps them feel engaged and more likely to participate in studies. Patients who are involved in advisory councils at the local hospital level are more likely to report having received high-quality care. And surveying patients on the goals of national health care policy helps them feel that the outcomes are more equitable.
As a small-town urologist who spends his days in the trenches of urology, I think the next time my group considers participating in new cancer research, I may talk to the local cancer support group first. If Dr. Smith’s data are correct, not only would our patients be better served, but we would also have an easier time filling the trial!
The 2023 AUA conference is going to be held in Chicago next spring. I hope to see you there!
A version of this article first appeared on Medscape.com.
The annual meeting of the American Urological Association took place recently at the Ernest N. Morial Convention Center in New Orleans. Hundreds of talks and abstracts were presented over the 4 days in New Orleans; below is a summary of what I found to be the key scientific highlights.
1. Updates to the AUA’s guidelines for management of localized kidney cancer
The AUA’s recommendations for the treatment of localized kidney cancer have changed dramatically over the past few decades. Gone are the days of simply removing the entire kidney every time a mass is found. Today, a partial nephrectomy is preferred in most situations.
Our understanding that the prevalence of familial kidney cancer is much higher than previously thought has led to a change in the guidelines regarding which patients should receive genetic counseling. For the first time, the guidelines include the use of adjuvant medical treatment, such as pembrolizumab. A 2021 study in the New England Journal of Medicine showed a survival benefit for patients with high-risk disease who receive such therapies, so it›s not surprising that such treatments are now recommended.
The development of new second- and third-generation gadolinium contrast agents that spare the kidneys has dramatically increased the role for MRIs for patients with severe or even end-stage renal disease. As a result, the guidelines were updated to recommend the use of these agents. The role of a renal biopsy, which has always been limited, given the ability of cross-sectional imaging to diagnosis this disease, has further been constrained and should now be performed only when the results would clearly change a clinical decision, such as whether or not the lesion in question is a metastasis.
2. New and better ureteroscope technology
No one likes kidney stones, not the patient who deals with the incredible pain, nor the surgeon who has to remove them, given that these cases often present in the wee hours of the morning. The preferred surgical approach has changed dramatically over the past decade, moving away from extracorporeal shockwave lithotripsy toward flexible ureteroscope-based technology, which has a higher clearance rate and is more widely and more immediately available. Flexible ureteroscopy has been held back by technological barriers, including limited scope deflection and low laser power. The exceptionally high cost of repair and the tendency of the instruments to break haven’t helped, either. Although single-use ureteroscopes have been available for some time, it wasn’t until the recently introduced second-generation scopes became widely available that they have become popular. These new scopes have small external diameters, great optics, and can easily be used. Newer high-powered lasers and the change from holmium:YAG-based lasers to thulium technology is greatly increasing the size of stones that can be safely addressed ureteroscopically. The cost analysis of single-use technology versus reusable scopes tends to be site dependent but can be appealing in certain situations. Also, on the technology forefront, a new robotically assisted ureteroscope is being introduced that offers the chance for improved intrapelvic mobility and better ergonomics for the surgeon.
3. New options for the treatment of clinically localized prostate cancer
Since the guidelines were last updated in 2017, the definitive management of localized prostate cancer has changed dramatically. Although radical prostatectomy and radiotherapy remain the preferred options for men who choose treatment for their disease, the updated guidelines state that active surveillance is now the preferred approach for men with low-risk cancers.
Although the preferred surveillance protocol is still being debated, the consensus is that almost all men with low-risk disease can be safely monitored for some period. The imaging technology available to monitor patients is also radically changing with the rollout of prostate-specific membrane antigen–based PET technology. The increased sensitivity and specificity of this modality opens the door not only for better up-front staging of newly diagnosed patients with prostate cancer but also may allow clinicians to earlier identify and treat men with metastatic disease. The guidelines for the first time address the use of genetic markers to individualize treatment of men with advanced or metastatic prostate cancer. Exactly which treatments these patients need is still being debated, but the ability to use patient-specific genetic mutation information to customize treatment is potentially groundbreaking.
4. New treatment options for patients with high-grade non–muscle-invasive bladder cancer (NMIBC) refractory to bacille Calmette-Guérin (BCG) therapy
Patients with NMIBC who do not respond to BCG therapy are in a tough position. Cystectomy remains the preferred option as a second-line strategy, but the procedure has a complication rate approaching 30%. Further, many patients are not willing to have their bladder removed because of the life-altering changes that go along with having an urostomy or a neobladder. While intravesical treatments such as valrubicin, docetaxel, or gemcitabine have been available for many years, the success rates of those options are limited. The Food and Drug Administration recently approved the use of the immunotherapy-based treatment pembrolizumab. While none of these options is perfect, the fact that we now have at least some alternatives is a huge step in the right direction.
5. It’s all about the patient: Involving patients in designing the health care delivery system
Although it seems like an obvious concept, patients themselves have traditionally not been involved in designing the health care delivery system on which they rely. Research presented at the AUA shows that many health care outcomes improve when patients are actively involved in the process. For example, Angela Smith, MD, of the University of North Carolina at Chapel Hill, presented a study showing that including patients in the identification of possible research topics helps them feel engaged and more likely to participate in studies. Patients who are involved in advisory councils at the local hospital level are more likely to report having received high-quality care. And surveying patients on the goals of national health care policy helps them feel that the outcomes are more equitable.
As a small-town urologist who spends his days in the trenches of urology, I think the next time my group considers participating in new cancer research, I may talk to the local cancer support group first. If Dr. Smith’s data are correct, not only would our patients be better served, but we would also have an easier time filling the trial!
The 2023 AUA conference is going to be held in Chicago next spring. I hope to see you there!
A version of this article first appeared on Medscape.com.
The annual meeting of the American Urological Association took place recently at the Ernest N. Morial Convention Center in New Orleans. Hundreds of talks and abstracts were presented over the 4 days in New Orleans; below is a summary of what I found to be the key scientific highlights.
1. Updates to the AUA’s guidelines for management of localized kidney cancer
The AUA’s recommendations for the treatment of localized kidney cancer have changed dramatically over the past few decades. Gone are the days of simply removing the entire kidney every time a mass is found. Today, a partial nephrectomy is preferred in most situations.
Our understanding that the prevalence of familial kidney cancer is much higher than previously thought has led to a change in the guidelines regarding which patients should receive genetic counseling. For the first time, the guidelines include the use of adjuvant medical treatment, such as pembrolizumab. A 2021 study in the New England Journal of Medicine showed a survival benefit for patients with high-risk disease who receive such therapies, so it›s not surprising that such treatments are now recommended.
The development of new second- and third-generation gadolinium contrast agents that spare the kidneys has dramatically increased the role for MRIs for patients with severe or even end-stage renal disease. As a result, the guidelines were updated to recommend the use of these agents. The role of a renal biopsy, which has always been limited, given the ability of cross-sectional imaging to diagnosis this disease, has further been constrained and should now be performed only when the results would clearly change a clinical decision, such as whether or not the lesion in question is a metastasis.
2. New and better ureteroscope technology
No one likes kidney stones, not the patient who deals with the incredible pain, nor the surgeon who has to remove them, given that these cases often present in the wee hours of the morning. The preferred surgical approach has changed dramatically over the past decade, moving away from extracorporeal shockwave lithotripsy toward flexible ureteroscope-based technology, which has a higher clearance rate and is more widely and more immediately available. Flexible ureteroscopy has been held back by technological barriers, including limited scope deflection and low laser power. The exceptionally high cost of repair and the tendency of the instruments to break haven’t helped, either. Although single-use ureteroscopes have been available for some time, it wasn’t until the recently introduced second-generation scopes became widely available that they have become popular. These new scopes have small external diameters, great optics, and can easily be used. Newer high-powered lasers and the change from holmium:YAG-based lasers to thulium technology is greatly increasing the size of stones that can be safely addressed ureteroscopically. The cost analysis of single-use technology versus reusable scopes tends to be site dependent but can be appealing in certain situations. Also, on the technology forefront, a new robotically assisted ureteroscope is being introduced that offers the chance for improved intrapelvic mobility and better ergonomics for the surgeon.
3. New options for the treatment of clinically localized prostate cancer
Since the guidelines were last updated in 2017, the definitive management of localized prostate cancer has changed dramatically. Although radical prostatectomy and radiotherapy remain the preferred options for men who choose treatment for their disease, the updated guidelines state that active surveillance is now the preferred approach for men with low-risk cancers.
Although the preferred surveillance protocol is still being debated, the consensus is that almost all men with low-risk disease can be safely monitored for some period. The imaging technology available to monitor patients is also radically changing with the rollout of prostate-specific membrane antigen–based PET technology. The increased sensitivity and specificity of this modality opens the door not only for better up-front staging of newly diagnosed patients with prostate cancer but also may allow clinicians to earlier identify and treat men with metastatic disease. The guidelines for the first time address the use of genetic markers to individualize treatment of men with advanced or metastatic prostate cancer. Exactly which treatments these patients need is still being debated, but the ability to use patient-specific genetic mutation information to customize treatment is potentially groundbreaking.
4. New treatment options for patients with high-grade non–muscle-invasive bladder cancer (NMIBC) refractory to bacille Calmette-Guérin (BCG) therapy
Patients with NMIBC who do not respond to BCG therapy are in a tough position. Cystectomy remains the preferred option as a second-line strategy, but the procedure has a complication rate approaching 30%. Further, many patients are not willing to have their bladder removed because of the life-altering changes that go along with having an urostomy or a neobladder. While intravesical treatments such as valrubicin, docetaxel, or gemcitabine have been available for many years, the success rates of those options are limited. The Food and Drug Administration recently approved the use of the immunotherapy-based treatment pembrolizumab. While none of these options is perfect, the fact that we now have at least some alternatives is a huge step in the right direction.
5. It’s all about the patient: Involving patients in designing the health care delivery system
Although it seems like an obvious concept, patients themselves have traditionally not been involved in designing the health care delivery system on which they rely. Research presented at the AUA shows that many health care outcomes improve when patients are actively involved in the process. For example, Angela Smith, MD, of the University of North Carolina at Chapel Hill, presented a study showing that including patients in the identification of possible research topics helps them feel engaged and more likely to participate in studies. Patients who are involved in advisory councils at the local hospital level are more likely to report having received high-quality care. And surveying patients on the goals of national health care policy helps them feel that the outcomes are more equitable.
As a small-town urologist who spends his days in the trenches of urology, I think the next time my group considers participating in new cancer research, I may talk to the local cancer support group first. If Dr. Smith’s data are correct, not only would our patients be better served, but we would also have an easier time filling the trial!
The 2023 AUA conference is going to be held in Chicago next spring. I hope to see you there!
A version of this article first appeared on Medscape.com.
FROM AUA 2022
Productively working together
Recently, some liberal colleagues urged a boycott of a conference in Orlando, Fla., because of various actions by its Republican state governor. At the same time, conservative colleagues advocated the boycott because business actions of Disney have become too leftist. Concerns about spreading COVID-19 at the national gathering have become small, compared with the desire to virtue-signal political viewpoints.
The 1960s in the United States were a time of social upheaval and polarization with many similarities to modern America. One difference is that, after a few years of social revolution, society emphasized bridging the differences. Politicians talked about reaching across the aisle. Religious groups sought ecumenical and interfaith ventures. Business and educational institutions promoted equal opportunity programs. The emphasis was finding common ground.
A half century later, the polarized work environment of medical organizations in 2022 has led to emphasis on cancel culture, litmus tests, and finding reasons not to work with others and to silence dissent. A professional working in a polarized environment faces frequent challenges that pit ethical and political principles against the pragmatic need to set and accomplish team goals that productively care for patients and support staff. One of the worst things societies can do for children’s health is to perpetuate the paralyzing divisiveness of modern politics.
As Justice Stephen Breyer nears retirement from the Supreme Court, I reflect back to 1994 when, on the day of his nomination to the court by President Clinton, Justice Breyer at a press conference said, “What [the law is] supposed to do seen as a whole is allow all people, all people, to live together in a society where they have so many different views, so many different needs, but to live together in a way that is more harmonious, that is better so that they can work productively together.”
I generally reject secondary boycotts and the hatred they spew. True inclusivity does not divide. True inclusivity is very messy. It rejects tyrants who insist on litmus tests to prove wokeness. Every red state has Democrats and every blue state has Republicans. If you are dedicated to loving your neighbor, I think it is necessary professionally to focus on who you will work with to improve the world. If woke extremism says you can only work with someone who echoes the same end of the blue or red political spectrum as yourself, that is not loving, not inclusive, and not productive.
My advice is to focus on the values, goals, and pathways you share with colleagues rather than using political or social differences to prejudice you against working with someone toward a common goal. The old adage is that politics makes strange bedfellows. People with diverse, divergent, and even opposed life views can work together to build schools and roads that benefit the community, contrary to the polarized examples that have flooded Washington, D.C., for the past 2 decades. (Generation Z: Take this as testimony from a Boomer who saw how politics used to work, especially in small towns.)
My other advice is to believe in free speech, but it requires a long civics lesson to understand what that means. Facebook promulgating unvetted posts as news feeds is not free speech. Facebook creating profiles so the app creates tailored echo chambers of misinformation is not free speech. President Obama ignoring the problem for 8 years as the iPhone became ubiquitous did not help. President Trump’s outreach to the masses via Twitter did not model responsible free speech. Surreptitiously promoting certain political viewpoints in math textbooks is not responsible behavior and has generated mistrust and the replacement of boards of education. Elon Musk wanting to buy Twitter is an unknown.
I won’t attempt to offer any pearls of wisdom on free speech in this column. It is a complex subject. I will suggest that doing a better job with free speech will save far more lives than eliminating crib bumpers.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@mdedge.com.
Recently, some liberal colleagues urged a boycott of a conference in Orlando, Fla., because of various actions by its Republican state governor. At the same time, conservative colleagues advocated the boycott because business actions of Disney have become too leftist. Concerns about spreading COVID-19 at the national gathering have become small, compared with the desire to virtue-signal political viewpoints.
The 1960s in the United States were a time of social upheaval and polarization with many similarities to modern America. One difference is that, after a few years of social revolution, society emphasized bridging the differences. Politicians talked about reaching across the aisle. Religious groups sought ecumenical and interfaith ventures. Business and educational institutions promoted equal opportunity programs. The emphasis was finding common ground.
A half century later, the polarized work environment of medical organizations in 2022 has led to emphasis on cancel culture, litmus tests, and finding reasons not to work with others and to silence dissent. A professional working in a polarized environment faces frequent challenges that pit ethical and political principles against the pragmatic need to set and accomplish team goals that productively care for patients and support staff. One of the worst things societies can do for children’s health is to perpetuate the paralyzing divisiveness of modern politics.
As Justice Stephen Breyer nears retirement from the Supreme Court, I reflect back to 1994 when, on the day of his nomination to the court by President Clinton, Justice Breyer at a press conference said, “What [the law is] supposed to do seen as a whole is allow all people, all people, to live together in a society where they have so many different views, so many different needs, but to live together in a way that is more harmonious, that is better so that they can work productively together.”
I generally reject secondary boycotts and the hatred they spew. True inclusivity does not divide. True inclusivity is very messy. It rejects tyrants who insist on litmus tests to prove wokeness. Every red state has Democrats and every blue state has Republicans. If you are dedicated to loving your neighbor, I think it is necessary professionally to focus on who you will work with to improve the world. If woke extremism says you can only work with someone who echoes the same end of the blue or red political spectrum as yourself, that is not loving, not inclusive, and not productive.
My advice is to focus on the values, goals, and pathways you share with colleagues rather than using political or social differences to prejudice you against working with someone toward a common goal. The old adage is that politics makes strange bedfellows. People with diverse, divergent, and even opposed life views can work together to build schools and roads that benefit the community, contrary to the polarized examples that have flooded Washington, D.C., for the past 2 decades. (Generation Z: Take this as testimony from a Boomer who saw how politics used to work, especially in small towns.)
My other advice is to believe in free speech, but it requires a long civics lesson to understand what that means. Facebook promulgating unvetted posts as news feeds is not free speech. Facebook creating profiles so the app creates tailored echo chambers of misinformation is not free speech. President Obama ignoring the problem for 8 years as the iPhone became ubiquitous did not help. President Trump’s outreach to the masses via Twitter did not model responsible free speech. Surreptitiously promoting certain political viewpoints in math textbooks is not responsible behavior and has generated mistrust and the replacement of boards of education. Elon Musk wanting to buy Twitter is an unknown.
I won’t attempt to offer any pearls of wisdom on free speech in this column. It is a complex subject. I will suggest that doing a better job with free speech will save far more lives than eliminating crib bumpers.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@mdedge.com.
Recently, some liberal colleagues urged a boycott of a conference in Orlando, Fla., because of various actions by its Republican state governor. At the same time, conservative colleagues advocated the boycott because business actions of Disney have become too leftist. Concerns about spreading COVID-19 at the national gathering have become small, compared with the desire to virtue-signal political viewpoints.
The 1960s in the United States were a time of social upheaval and polarization with many similarities to modern America. One difference is that, after a few years of social revolution, society emphasized bridging the differences. Politicians talked about reaching across the aisle. Religious groups sought ecumenical and interfaith ventures. Business and educational institutions promoted equal opportunity programs. The emphasis was finding common ground.
A half century later, the polarized work environment of medical organizations in 2022 has led to emphasis on cancel culture, litmus tests, and finding reasons not to work with others and to silence dissent. A professional working in a polarized environment faces frequent challenges that pit ethical and political principles against the pragmatic need to set and accomplish team goals that productively care for patients and support staff. One of the worst things societies can do for children’s health is to perpetuate the paralyzing divisiveness of modern politics.
As Justice Stephen Breyer nears retirement from the Supreme Court, I reflect back to 1994 when, on the day of his nomination to the court by President Clinton, Justice Breyer at a press conference said, “What [the law is] supposed to do seen as a whole is allow all people, all people, to live together in a society where they have so many different views, so many different needs, but to live together in a way that is more harmonious, that is better so that they can work productively together.”
I generally reject secondary boycotts and the hatred they spew. True inclusivity does not divide. True inclusivity is very messy. It rejects tyrants who insist on litmus tests to prove wokeness. Every red state has Democrats and every blue state has Republicans. If you are dedicated to loving your neighbor, I think it is necessary professionally to focus on who you will work with to improve the world. If woke extremism says you can only work with someone who echoes the same end of the blue or red political spectrum as yourself, that is not loving, not inclusive, and not productive.
My advice is to focus on the values, goals, and pathways you share with colleagues rather than using political or social differences to prejudice you against working with someone toward a common goal. The old adage is that politics makes strange bedfellows. People with diverse, divergent, and even opposed life views can work together to build schools and roads that benefit the community, contrary to the polarized examples that have flooded Washington, D.C., for the past 2 decades. (Generation Z: Take this as testimony from a Boomer who saw how politics used to work, especially in small towns.)
My other advice is to believe in free speech, but it requires a long civics lesson to understand what that means. Facebook promulgating unvetted posts as news feeds is not free speech. Facebook creating profiles so the app creates tailored echo chambers of misinformation is not free speech. President Obama ignoring the problem for 8 years as the iPhone became ubiquitous did not help. President Trump’s outreach to the masses via Twitter did not model responsible free speech. Surreptitiously promoting certain political viewpoints in math textbooks is not responsible behavior and has generated mistrust and the replacement of boards of education. Elon Musk wanting to buy Twitter is an unknown.
I won’t attempt to offer any pearls of wisdom on free speech in this column. It is a complex subject. I will suggest that doing a better job with free speech will save far more lives than eliminating crib bumpers.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at pdnews@mdedge.com.
Up in smoke: Cannabis-related ED visits increased 18-fold for older Californians
Researchers in California found an 18-fold increase in the rate of cannabis-related trips to the ED visits among adults over age 65 in the state from 2005 to 2019.
Addressing potential harms of cannabis use among older adults, who face heightened risk for adverse reactions to the substance, “is urgently required,” the researchers reported at the annual meeting of the American Geriatrics Society.
The researchers advised doctors to discuss cannabis use with older patients and screen older adults for cannabis use. Those living with multiple chronic conditions and taking multiple medications are especially likely to be at risk for harm, coinvestigator Benjamin Han, MD, MPH, a geriatrician at the University of California, San Diego, said in an interview.
Dr. Han added that “very little” is understood about the risks and benefits of cannabis use in the elderly, and more studies are needed “so that clinicians can have data-informed discussions with their patients.”
California legalized medical marijuana in 1996 and recreational marijuana in 2016.
The researchers used diagnostic code data from California’s nonmilitary acute care hospitals, collected by the state’s Department of Healthcare Access and Information, to calculate annual rates of cannabis-related visits per 10,000 ED visits.
ED trips up sharply among older adults
Rates of cannabis-related visits increased significantly for all older adult age ranges (P < .001), according to the researchers. Among those aged 65-74 years, the rate increased about 15-fold, from 44.9 per 10,000 visits in 2005 to 714.5 per 100,000 in 2019; for ages 75-84, the rate increased about 22-fold, from 8.4 to 193.9 per 10,000; and for those 85 and older the rate jumped nearly 18-fold, from 2.1 to 39.2 per 10,000.
The greatest increase occurred in visits categorized in diagnostic codes as cannabis abuse and unspecified use. Cannabis dependence and cannabis poisoning accounted for only a small fraction of cases, the investigators found.
The researchers did not have data on specific reasons for a visit, or whether patients had smoked or ingested marijuana products. They also could not discern whether patients had used delta-9-tetrahydrocannabinol, which has psychoactive properties, or cannabidiol, which typically does not have the same mind-altering effects.
Dr. Han said the data may not present a full picture of marijuana-related ED visits. “It is important to recognize that older adults have lived through the very putative language around drug use – including cannabis – as part of the racist war on drugs,” which could lead them to omit having used drugs during the intake process.
A 2017 study linked cannabis use among older adults with more injuries, which in turn led to greater emergency department use. Brian Kaskie, PhD, associate professor in health management and policy at the University of Iowa, Iowa City, said in an interview that the new findings show a state-specific, but alarming trend, and that more research is needed.
“Were these first-time users who were not familiar with anxiety-inducing aspects of cannabis use and took high potency products? Did they complete any education about how to use cannabis?” said Dr. Kaskie, who was not involved in the new study. “Were the ER visits for relatively benign, nonemergent reasons or were these ... visits an outcome of a tragic, harmful event like a car accident or overdose?”
Dr. Han and Dr. Kaskie disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Researchers in California found an 18-fold increase in the rate of cannabis-related trips to the ED visits among adults over age 65 in the state from 2005 to 2019.
Addressing potential harms of cannabis use among older adults, who face heightened risk for adverse reactions to the substance, “is urgently required,” the researchers reported at the annual meeting of the American Geriatrics Society.
The researchers advised doctors to discuss cannabis use with older patients and screen older adults for cannabis use. Those living with multiple chronic conditions and taking multiple medications are especially likely to be at risk for harm, coinvestigator Benjamin Han, MD, MPH, a geriatrician at the University of California, San Diego, said in an interview.
Dr. Han added that “very little” is understood about the risks and benefits of cannabis use in the elderly, and more studies are needed “so that clinicians can have data-informed discussions with their patients.”
California legalized medical marijuana in 1996 and recreational marijuana in 2016.
The researchers used diagnostic code data from California’s nonmilitary acute care hospitals, collected by the state’s Department of Healthcare Access and Information, to calculate annual rates of cannabis-related visits per 10,000 ED visits.
ED trips up sharply among older adults
Rates of cannabis-related visits increased significantly for all older adult age ranges (P < .001), according to the researchers. Among those aged 65-74 years, the rate increased about 15-fold, from 44.9 per 10,000 visits in 2005 to 714.5 per 100,000 in 2019; for ages 75-84, the rate increased about 22-fold, from 8.4 to 193.9 per 10,000; and for those 85 and older the rate jumped nearly 18-fold, from 2.1 to 39.2 per 10,000.
The greatest increase occurred in visits categorized in diagnostic codes as cannabis abuse and unspecified use. Cannabis dependence and cannabis poisoning accounted for only a small fraction of cases, the investigators found.
The researchers did not have data on specific reasons for a visit, or whether patients had smoked or ingested marijuana products. They also could not discern whether patients had used delta-9-tetrahydrocannabinol, which has psychoactive properties, or cannabidiol, which typically does not have the same mind-altering effects.
Dr. Han said the data may not present a full picture of marijuana-related ED visits. “It is important to recognize that older adults have lived through the very putative language around drug use – including cannabis – as part of the racist war on drugs,” which could lead them to omit having used drugs during the intake process.
A 2017 study linked cannabis use among older adults with more injuries, which in turn led to greater emergency department use. Brian Kaskie, PhD, associate professor in health management and policy at the University of Iowa, Iowa City, said in an interview that the new findings show a state-specific, but alarming trend, and that more research is needed.
“Were these first-time users who were not familiar with anxiety-inducing aspects of cannabis use and took high potency products? Did they complete any education about how to use cannabis?” said Dr. Kaskie, who was not involved in the new study. “Were the ER visits for relatively benign, nonemergent reasons or were these ... visits an outcome of a tragic, harmful event like a car accident or overdose?”
Dr. Han and Dr. Kaskie disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Researchers in California found an 18-fold increase in the rate of cannabis-related trips to the ED visits among adults over age 65 in the state from 2005 to 2019.
Addressing potential harms of cannabis use among older adults, who face heightened risk for adverse reactions to the substance, “is urgently required,” the researchers reported at the annual meeting of the American Geriatrics Society.
The researchers advised doctors to discuss cannabis use with older patients and screen older adults for cannabis use. Those living with multiple chronic conditions and taking multiple medications are especially likely to be at risk for harm, coinvestigator Benjamin Han, MD, MPH, a geriatrician at the University of California, San Diego, said in an interview.
Dr. Han added that “very little” is understood about the risks and benefits of cannabis use in the elderly, and more studies are needed “so that clinicians can have data-informed discussions with their patients.”
California legalized medical marijuana in 1996 and recreational marijuana in 2016.
The researchers used diagnostic code data from California’s nonmilitary acute care hospitals, collected by the state’s Department of Healthcare Access and Information, to calculate annual rates of cannabis-related visits per 10,000 ED visits.
ED trips up sharply among older adults
Rates of cannabis-related visits increased significantly for all older adult age ranges (P < .001), according to the researchers. Among those aged 65-74 years, the rate increased about 15-fold, from 44.9 per 10,000 visits in 2005 to 714.5 per 100,000 in 2019; for ages 75-84, the rate increased about 22-fold, from 8.4 to 193.9 per 10,000; and for those 85 and older the rate jumped nearly 18-fold, from 2.1 to 39.2 per 10,000.
The greatest increase occurred in visits categorized in diagnostic codes as cannabis abuse and unspecified use. Cannabis dependence and cannabis poisoning accounted for only a small fraction of cases, the investigators found.
The researchers did not have data on specific reasons for a visit, or whether patients had smoked or ingested marijuana products. They also could not discern whether patients had used delta-9-tetrahydrocannabinol, which has psychoactive properties, or cannabidiol, which typically does not have the same mind-altering effects.
Dr. Han said the data may not present a full picture of marijuana-related ED visits. “It is important to recognize that older adults have lived through the very putative language around drug use – including cannabis – as part of the racist war on drugs,” which could lead them to omit having used drugs during the intake process.
A 2017 study linked cannabis use among older adults with more injuries, which in turn led to greater emergency department use. Brian Kaskie, PhD, associate professor in health management and policy at the University of Iowa, Iowa City, said in an interview that the new findings show a state-specific, but alarming trend, and that more research is needed.
“Were these first-time users who were not familiar with anxiety-inducing aspects of cannabis use and took high potency products? Did they complete any education about how to use cannabis?” said Dr. Kaskie, who was not involved in the new study. “Were the ER visits for relatively benign, nonemergent reasons or were these ... visits an outcome of a tragic, harmful event like a car accident or overdose?”
Dr. Han and Dr. Kaskie disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AGS 2022
Common brain parasite linked to attractiveness, new study
That Toxoplasma gondii looks good on you
Parasite and attractiveness don’t usually go together, but it appears that nobody told Toxoplasma gondii. The world’s most successful parasite affects 30%-50% of the world’s population, and it’s mainly thought to go after the brain in humans, possibly changing behavior and leading to neurological disorders and mental illness.
Now, are you ready to be super confused? According to a recent study, those affected with T. gondii were seen as more attractive and healthy looking, compared with noninfected people. It doesn’t make much sense to us, but it could be an evolutionary thing: The more attractive the parasite makes a person or animal, the more likely it is to spread.
“Some sexually transmitted parasites, such as T. gondii, may produce changes in the appearance and behavior of the human host, either as a by-product of the infection or as the result of the manipulation of the parasite to increase its spread to new hosts,” Javier Borráz-León, PhD, of the University of Turku (Finland), and associates wrote in PeerJ.
Previous research has suggested that men with more testosterone are more likely to become infected because of their behavior with the extra hormones. It’s also been noted that the parasite may manipulate hormones for its own gain, but that’s not proven. Infected women were found to have a lower BMI, more confidence in their appearance, and more partners. Dr. Borráz-León and associates also found that “Toxoplasma-infected subjects had significantly lower facial fluctuating asymmetry than the noninfected people,” ScienceAlert said.
We usually perceive parasites as a bad thing, but honestly this one isn’t sounding too bad. It seems to help with some confidence boosters, and who doesn’t want that? We’re thinking that T. gondii could be the Next Big Thing. All it needs is some marketing and … what if it was covered with nonpareils?
Give it to me straight, Doc. Don’t sugar coat it.
Okay, so he’s not a doctor – not a medical doctor, anyway – but that’s exactly what he did. William H. Grover, PhD, has sugar coated drugs in the name of fraud prevention. We will explain.
The sugar coating comes in the form of nonpareils, the tiny and colorful round sprinkles often found covering small discs of chocolate. Dr. Grover, a bioengineering professor at the University of California, Riverside, who has been working on ways to ensure the authenticity of pharmaceuticals, “started wondering how many different patterns of colored nonpareils were possible on these candies,” he said in a statement from the university.
With just eight colors and an average of 92 individual nonpareils on each candy, the combinations, he found out, are almost endless. Could the same thing be done with a pill? Could the nonpareils be applied as a coating to a pill, giving it a unique pattern that could be stored by the manufacturer and used later as identification?
After much time and effort involving edible cake-decorating glue, Tylenol capsules, smartphones, and computer simulations, he produced CandyCode, an algorithm that converts a photo of a nonpareil-covered pill “into a set of text strings suitable for storing in a computer database and querying by consumers,” the statement explained.
Dr. Grover also mentioned a side benefit: “Anecdotally, I found that CandyCoded caplets were more pleasant to swallow than plain caplets, confirming Mary Poppins’ classic observation about the relationship between sugar and medicine.”
First of all, we can’t believe we just used a Mary Poppins reference. Not exactly what you’d call MDedgey, is it? Second of all, what about the children? We’re talking about drugs that, literally, have been turned into candy. Are the kids going to love them, too? Sounds more like a job for Mr. Yuk.
So you want to be a superhero?
Be honest, who didn’t want to be a superhero when they were a kid? There’s a reason every other movie released in the past decade has been a superhero movie. That’s how we’ve ended up with the millionth Batman reboot and Marvel scraping the bottom of the C-list hero barrel. (Seriously, who’d actually heard of Moon Knight before now?)
Point is, we all like to fantasize, and now a meta-analysis from researchers in Germany and the United States has given us all a reason to strike those dashing superhero poses. Through evaluation of 130 studies and over 10,000 people, the researchers found that power posing (and perfect posture) was strongly associated with increased confidence and self-worth. It was also associated with improved behavior, though the connection was less strong.
Sadly though, the research found no connection with power posing and changes in testosterone or cortisol levels. Standing like a superhero may make you feel good, but it won’t give your body any cool powers or superhuman abilities. But don’t despair, because we’re not finished yet. In fact, it may be the biggest news we’ve ever reported for LOTME: A group of scientists from the University of Kentucky has assembled the full genome of a salamander.
Wait, we have more! Beyond having a genome ten times bigger than a human, this salamander, the axolotl from Mexico, is the model of natural regeneration. Name a body part, and the axolotl can grow it back. It can even regenerate portions of its brain. And now that we have access to the complete genome, it’s possible that one day we could use the axolotl’s regeneration for ourselves. Growing back limbs, regenerating spinal cords, the sky’s the limit. And if Wolverine and Deadpool are anything to go by, it’s all you need to get that superhero career off the ground. Salamander powers may not have the cachet of a radioactive spider, but we’ll take what we can get.
Post your way to financial hardship
After you pump your gas at the gas station, how do you pay? At the pump or inside? How frequently do you post to your social media pages? What kind of content are you posting?
That kind of nontraditional credit data hasn’t been considered by lenders and credit agencies, but that is changing. The reasoning? It’s opening more opportunities for those without much credit history. But according to a paper published by Janine S. Hiller of Virginia Tech and Lindsay Sain Jones, a financial regulation researcher at the University of Georgia, this just opens a can of worms.
Why is this so dangerous? Well, alternative credit scoring isn’t covered by the Fair Credit Reporting Act or Equal Opportunity Act, so the consumer doesn’t have the ability to dispute any data the credit agencies or lenders receive. Then there’s the “credit boost,” which some companies offer to gain access to the consumer’s data. Often there are no limitations on how long it’s kept. That purchase you made 2 years ago can come back to haunt you.
It also creates a cause for the possibility of discrimination based on “lifestyle-related data points,” which some lenders use to determine creditworthiness: zip code, age, gender, race, socioeconomic status. Even where the consumer went to college is a factor taken under consideration.
“There are all kinds of factors that can be correlated with creditworthiness, but that doesn’t mean they should be used,” Ms. Jones said in the EurekAlert statement.
Let’s say someone applies for a loan needed for a medical procedure. They could be denied because the lender or a credit-reporting agency didn’t like the data they received (most times without the consumer’s consent). Talk about a broken system.
That Toxoplasma gondii looks good on you
Parasite and attractiveness don’t usually go together, but it appears that nobody told Toxoplasma gondii. The world’s most successful parasite affects 30%-50% of the world’s population, and it’s mainly thought to go after the brain in humans, possibly changing behavior and leading to neurological disorders and mental illness.
Now, are you ready to be super confused? According to a recent study, those affected with T. gondii were seen as more attractive and healthy looking, compared with noninfected people. It doesn’t make much sense to us, but it could be an evolutionary thing: The more attractive the parasite makes a person or animal, the more likely it is to spread.
“Some sexually transmitted parasites, such as T. gondii, may produce changes in the appearance and behavior of the human host, either as a by-product of the infection or as the result of the manipulation of the parasite to increase its spread to new hosts,” Javier Borráz-León, PhD, of the University of Turku (Finland), and associates wrote in PeerJ.
Previous research has suggested that men with more testosterone are more likely to become infected because of their behavior with the extra hormones. It’s also been noted that the parasite may manipulate hormones for its own gain, but that’s not proven. Infected women were found to have a lower BMI, more confidence in their appearance, and more partners. Dr. Borráz-León and associates also found that “Toxoplasma-infected subjects had significantly lower facial fluctuating asymmetry than the noninfected people,” ScienceAlert said.
We usually perceive parasites as a bad thing, but honestly this one isn’t sounding too bad. It seems to help with some confidence boosters, and who doesn’t want that? We’re thinking that T. gondii could be the Next Big Thing. All it needs is some marketing and … what if it was covered with nonpareils?
Give it to me straight, Doc. Don’t sugar coat it.
Okay, so he’s not a doctor – not a medical doctor, anyway – but that’s exactly what he did. William H. Grover, PhD, has sugar coated drugs in the name of fraud prevention. We will explain.
The sugar coating comes in the form of nonpareils, the tiny and colorful round sprinkles often found covering small discs of chocolate. Dr. Grover, a bioengineering professor at the University of California, Riverside, who has been working on ways to ensure the authenticity of pharmaceuticals, “started wondering how many different patterns of colored nonpareils were possible on these candies,” he said in a statement from the university.
With just eight colors and an average of 92 individual nonpareils on each candy, the combinations, he found out, are almost endless. Could the same thing be done with a pill? Could the nonpareils be applied as a coating to a pill, giving it a unique pattern that could be stored by the manufacturer and used later as identification?
After much time and effort involving edible cake-decorating glue, Tylenol capsules, smartphones, and computer simulations, he produced CandyCode, an algorithm that converts a photo of a nonpareil-covered pill “into a set of text strings suitable for storing in a computer database and querying by consumers,” the statement explained.
Dr. Grover also mentioned a side benefit: “Anecdotally, I found that CandyCoded caplets were more pleasant to swallow than plain caplets, confirming Mary Poppins’ classic observation about the relationship between sugar and medicine.”
First of all, we can’t believe we just used a Mary Poppins reference. Not exactly what you’d call MDedgey, is it? Second of all, what about the children? We’re talking about drugs that, literally, have been turned into candy. Are the kids going to love them, too? Sounds more like a job for Mr. Yuk.
So you want to be a superhero?
Be honest, who didn’t want to be a superhero when they were a kid? There’s a reason every other movie released in the past decade has been a superhero movie. That’s how we’ve ended up with the millionth Batman reboot and Marvel scraping the bottom of the C-list hero barrel. (Seriously, who’d actually heard of Moon Knight before now?)
Point is, we all like to fantasize, and now a meta-analysis from researchers in Germany and the United States has given us all a reason to strike those dashing superhero poses. Through evaluation of 130 studies and over 10,000 people, the researchers found that power posing (and perfect posture) was strongly associated with increased confidence and self-worth. It was also associated with improved behavior, though the connection was less strong.
Sadly though, the research found no connection with power posing and changes in testosterone or cortisol levels. Standing like a superhero may make you feel good, but it won’t give your body any cool powers or superhuman abilities. But don’t despair, because we’re not finished yet. In fact, it may be the biggest news we’ve ever reported for LOTME: A group of scientists from the University of Kentucky has assembled the full genome of a salamander.
Wait, we have more! Beyond having a genome ten times bigger than a human, this salamander, the axolotl from Mexico, is the model of natural regeneration. Name a body part, and the axolotl can grow it back. It can even regenerate portions of its brain. And now that we have access to the complete genome, it’s possible that one day we could use the axolotl’s regeneration for ourselves. Growing back limbs, regenerating spinal cords, the sky’s the limit. And if Wolverine and Deadpool are anything to go by, it’s all you need to get that superhero career off the ground. Salamander powers may not have the cachet of a radioactive spider, but we’ll take what we can get.
Post your way to financial hardship
After you pump your gas at the gas station, how do you pay? At the pump or inside? How frequently do you post to your social media pages? What kind of content are you posting?
That kind of nontraditional credit data hasn’t been considered by lenders and credit agencies, but that is changing. The reasoning? It’s opening more opportunities for those without much credit history. But according to a paper published by Janine S. Hiller of Virginia Tech and Lindsay Sain Jones, a financial regulation researcher at the University of Georgia, this just opens a can of worms.
Why is this so dangerous? Well, alternative credit scoring isn’t covered by the Fair Credit Reporting Act or Equal Opportunity Act, so the consumer doesn’t have the ability to dispute any data the credit agencies or lenders receive. Then there’s the “credit boost,” which some companies offer to gain access to the consumer’s data. Often there are no limitations on how long it’s kept. That purchase you made 2 years ago can come back to haunt you.
It also creates a cause for the possibility of discrimination based on “lifestyle-related data points,” which some lenders use to determine creditworthiness: zip code, age, gender, race, socioeconomic status. Even where the consumer went to college is a factor taken under consideration.
“There are all kinds of factors that can be correlated with creditworthiness, but that doesn’t mean they should be used,” Ms. Jones said in the EurekAlert statement.
Let’s say someone applies for a loan needed for a medical procedure. They could be denied because the lender or a credit-reporting agency didn’t like the data they received (most times without the consumer’s consent). Talk about a broken system.
That Toxoplasma gondii looks good on you
Parasite and attractiveness don’t usually go together, but it appears that nobody told Toxoplasma gondii. The world’s most successful parasite affects 30%-50% of the world’s population, and it’s mainly thought to go after the brain in humans, possibly changing behavior and leading to neurological disorders and mental illness.
Now, are you ready to be super confused? According to a recent study, those affected with T. gondii were seen as more attractive and healthy looking, compared with noninfected people. It doesn’t make much sense to us, but it could be an evolutionary thing: The more attractive the parasite makes a person or animal, the more likely it is to spread.
“Some sexually transmitted parasites, such as T. gondii, may produce changes in the appearance and behavior of the human host, either as a by-product of the infection or as the result of the manipulation of the parasite to increase its spread to new hosts,” Javier Borráz-León, PhD, of the University of Turku (Finland), and associates wrote in PeerJ.
Previous research has suggested that men with more testosterone are more likely to become infected because of their behavior with the extra hormones. It’s also been noted that the parasite may manipulate hormones for its own gain, but that’s not proven. Infected women were found to have a lower BMI, more confidence in their appearance, and more partners. Dr. Borráz-León and associates also found that “Toxoplasma-infected subjects had significantly lower facial fluctuating asymmetry than the noninfected people,” ScienceAlert said.
We usually perceive parasites as a bad thing, but honestly this one isn’t sounding too bad. It seems to help with some confidence boosters, and who doesn’t want that? We’re thinking that T. gondii could be the Next Big Thing. All it needs is some marketing and … what if it was covered with nonpareils?
Give it to me straight, Doc. Don’t sugar coat it.
Okay, so he’s not a doctor – not a medical doctor, anyway – but that’s exactly what he did. William H. Grover, PhD, has sugar coated drugs in the name of fraud prevention. We will explain.
The sugar coating comes in the form of nonpareils, the tiny and colorful round sprinkles often found covering small discs of chocolate. Dr. Grover, a bioengineering professor at the University of California, Riverside, who has been working on ways to ensure the authenticity of pharmaceuticals, “started wondering how many different patterns of colored nonpareils were possible on these candies,” he said in a statement from the university.
With just eight colors and an average of 92 individual nonpareils on each candy, the combinations, he found out, are almost endless. Could the same thing be done with a pill? Could the nonpareils be applied as a coating to a pill, giving it a unique pattern that could be stored by the manufacturer and used later as identification?
After much time and effort involving edible cake-decorating glue, Tylenol capsules, smartphones, and computer simulations, he produced CandyCode, an algorithm that converts a photo of a nonpareil-covered pill “into a set of text strings suitable for storing in a computer database and querying by consumers,” the statement explained.
Dr. Grover also mentioned a side benefit: “Anecdotally, I found that CandyCoded caplets were more pleasant to swallow than plain caplets, confirming Mary Poppins’ classic observation about the relationship between sugar and medicine.”
First of all, we can’t believe we just used a Mary Poppins reference. Not exactly what you’d call MDedgey, is it? Second of all, what about the children? We’re talking about drugs that, literally, have been turned into candy. Are the kids going to love them, too? Sounds more like a job for Mr. Yuk.
So you want to be a superhero?
Be honest, who didn’t want to be a superhero when they were a kid? There’s a reason every other movie released in the past decade has been a superhero movie. That’s how we’ve ended up with the millionth Batman reboot and Marvel scraping the bottom of the C-list hero barrel. (Seriously, who’d actually heard of Moon Knight before now?)
Point is, we all like to fantasize, and now a meta-analysis from researchers in Germany and the United States has given us all a reason to strike those dashing superhero poses. Through evaluation of 130 studies and over 10,000 people, the researchers found that power posing (and perfect posture) was strongly associated with increased confidence and self-worth. It was also associated with improved behavior, though the connection was less strong.
Sadly though, the research found no connection with power posing and changes in testosterone or cortisol levels. Standing like a superhero may make you feel good, but it won’t give your body any cool powers or superhuman abilities. But don’t despair, because we’re not finished yet. In fact, it may be the biggest news we’ve ever reported for LOTME: A group of scientists from the University of Kentucky has assembled the full genome of a salamander.
Wait, we have more! Beyond having a genome ten times bigger than a human, this salamander, the axolotl from Mexico, is the model of natural regeneration. Name a body part, and the axolotl can grow it back. It can even regenerate portions of its brain. And now that we have access to the complete genome, it’s possible that one day we could use the axolotl’s regeneration for ourselves. Growing back limbs, regenerating spinal cords, the sky’s the limit. And if Wolverine and Deadpool are anything to go by, it’s all you need to get that superhero career off the ground. Salamander powers may not have the cachet of a radioactive spider, but we’ll take what we can get.
Post your way to financial hardship
After you pump your gas at the gas station, how do you pay? At the pump or inside? How frequently do you post to your social media pages? What kind of content are you posting?
That kind of nontraditional credit data hasn’t been considered by lenders and credit agencies, but that is changing. The reasoning? It’s opening more opportunities for those without much credit history. But according to a paper published by Janine S. Hiller of Virginia Tech and Lindsay Sain Jones, a financial regulation researcher at the University of Georgia, this just opens a can of worms.
Why is this so dangerous? Well, alternative credit scoring isn’t covered by the Fair Credit Reporting Act or Equal Opportunity Act, so the consumer doesn’t have the ability to dispute any data the credit agencies or lenders receive. Then there’s the “credit boost,” which some companies offer to gain access to the consumer’s data. Often there are no limitations on how long it’s kept. That purchase you made 2 years ago can come back to haunt you.
It also creates a cause for the possibility of discrimination based on “lifestyle-related data points,” which some lenders use to determine creditworthiness: zip code, age, gender, race, socioeconomic status. Even where the consumer went to college is a factor taken under consideration.
“There are all kinds of factors that can be correlated with creditworthiness, but that doesn’t mean they should be used,” Ms. Jones said in the EurekAlert statement.
Let’s say someone applies for a loan needed for a medical procedure. They could be denied because the lender or a credit-reporting agency didn’t like the data they received (most times without the consumer’s consent). Talk about a broken system.
Is benzophenone safe in skin care? Part 1: Risks to humans
Benzophenones are a family of compounds that include dixoxybenzone, sulisobenzone, and benzophenone-3, or oxybenzone. These . Benzophenones (BPs) act as penetration enhancers, as they modify the structure of the skin and facilitate the absorption of other chemical ingredients into the body. The best known uses of these compounds are as perfume fixatives and sunscreen agents.
Sunscreens and benzophenones
BP-2, -3 and -4 are used as sunscreens but have many downsides. They are well known photoallergens, are toxic to aquatic animals (especially BP-3), and are found in urine. BP-2 has weak estrogenic effects, and some studies suggest that it decreases fertility in men. BP-4 can increase absorption of pesticides. BP-3 is banned in Hawaii because of the risk to coral and is the most worrisome.
In particular, BP-3 is known to protect skin and hair from UV radiation-induced harm.1 Unfortunately, BPs are also associated with photocontact allergies, hypersensitivity, hives, contact urticaria, anaphylaxis, hormone disruption, and DNA damage.2,3 BP-3 has also been implicated as an environmental contaminant. This column will focus on recent studies pertaining to effects on humans, primarily, and on the role of BPs in sunscreen agents.
Effects of BPs in animals
A recent study on the cytotoxicity of BP-3 against thymocytes in rats revealed that cell mortality increased significantly after 3 hours of exposure to 300 μM BP-3, but the membrane potential of thymocytes was unchanged by BP-3 exposure. In a concentration-dependent fashion, intracellular Zn2+ levels increased significantly after administration of at least 30 μM BP-3. The investigators concluded that the cytotoxicity engendered by BP-3 could be the result of oxidative stress linked to elevated intracellular Zn2+ levels.1
Effects of BPs in humans and systemic absorption
In multiple studies, exposure to BP-3, as well as to octinoxate, has been linked to endocrine and hormonal disruptions in humans and animals.4,5 Motivated by several notable observations (global increase in the use of sunscreens with UV filters; rapid rise in malignant melanoma, against which sunscreens should protect; increase in reported experimental findings of UV filters acting as endocrine disruptors), Krause et al. in 2012 reviewed animal and human data on the UV filters BP-3, 3-benzylidene camphor (3-BC), 3-(4-methyl-benzylidene) camphor (4-MBC), 2-ethylhexyl 4-methoxy cinnamate (OMC), homosalate (HMS), 2-ethylhexyl 4-dimethylaminobenzoate, and 4-aminobenzoic acid (PABA). Importantly, BP-3 was present in 96% of human urine samples in the United States, and various filters were found in 85% of the human breast milk samples in Switzerland.6
A 2019 analysis by Wang and Ganley reported that systemic absorption of the active sunscreen ingredient BP-3 can be substantial, justifying the assessment and understanding of systemic exposure to characterize the risks of long-term usage.7
Between January and February 2019, Matta et al. conducted a randomized clinical trial with 48 healthy participants to evaluate the systemic absorption and pharmacokinetics of six active ingredients in four sunscreen formulations, including avobenzone and BP-3. The researchers found that all ingredients were systemically absorbed, with plasma concentrations exceeding the Food and Drug Administration threshold for considering the waiving of further safety studies. They concluded that these results did not warrant discontinuing the use of the tested sunscreen ingredients.8 Yeager and Lim add that, while BP-3 has been incorporated into sunscreen formulations for sale in the United States since 1978, there have been no reports of adverse systemic reactions in human beings.3
However, topical reactions have elicited a different assessment. That is, in 2014, the American Contact Dermatitis Society labeled BPs the Contact Allergen of the Year, as they were identified as the most common source of photoallergic and contact allergic reactions of all UV filters.3,9
Risks of BPs in sunscreens and other skincare products
In 2015, Amar et al. investigated the photogenotoxicity and apoptotic effects in human keratinocytes (HaCaT cells) of BP-1, which is used as a UV blocker in sunscreens. They found that BP-1, when exposed to UV radiation, photosensitized cells and yielded intracellular reactive oxygen species. Significant reductions in cell viability were also seen with exposure to sunlight, UVA, and UVB. The researchers also confirmed genotoxic activity, with BP-1 augmenting lipid peroxidation and upregulating apoptotic proteins. They concluded that sunscreen users should be advised to avoid products that contain BP-1.10
In 2019, Amar et al. evaluated the effects of BPs on the differential expression of proteins in HaCaT cells exposed to UVA. Their findings indicated the expression of novel proteins that helped to initiate or promote apoptosis. They concluded that, because of the predilection to render such effects in human skin keratinocytes, consumers should avoid the use of sunscreens that contain BPs as UV blocking ingredients.11
Still widely used as an effective filter against UVA2 and UVB, BP-3 was believed to be present in two thirds of nonmineral sunscreens in the United States in 2018.3,12
Notably, BP-1 and BP-3 were found in small proportions (3.7% and 4.9%, respectively) among a total of 283 products culled from various stores in Lecce, Italy, in a survey of the potentially dangerous chemicals found in rinse-off, leave-on, and makeup products in 2019.13 The authors added that the International Agency for Research on Cancer, in 2010, classified BP as potentially carcinogenic to humans (2B group).13,14
Promising use of nanocapsules
The widespread concern about the phototoxicity of BP has prompted some interesting research into workarounds. Specifically, in 2019, Barbosa et al. reported on the creation of a new sunscreen formulation using polymeric nanocapsules loading BP-3. The nanocapsules are made of poly(ε-caprolactone) carrot oil and Pluronic F68 (nonionic surfactant used in suspension cultures), and the BP-3–loaded capsules were found to be noncytotoxic in L929 fibroblast cell lines with a sun protection factor of 8.64. The researchers concluded that this promising nanocapsule may be an effective and safe way to use lipophilic sunscreen ingredients such as BP-3.15
Conclusion
The body of evidence is weighted against the use of BPs. Luckily, we have safe sunscreen choices that allow us to protect our skin without using these compounds.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks and a New York Times Best Sellers book for consumers. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Revance, Evolus, and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., a company that independently tests skin care products and makes recommendations to physicians on which skin care technologies are best. Write to her at dermnews@mdedge.com.
References
1. Utsunomiya H et al. Chem Biol Interact. 2019 Jan 25;298:52-6.
2. Schneider SL and Lim HW. J Am Acad Dermatol. 2019 Jan;80(1):266-71.
3. Yeager DG and Lim HW. Dermatol Clin. 2019 Apr;37(2):149-57.
4. Ramos S et al. Sci Total Environ. 2015 Sep 1;526:278-311.
5. Siller A et al. Plast Surg Nur. 2019 Oct/Dec;39(4):157-60.
6. Krause M et al. Int J Androl. 2012 Jun;35(3):424-36.
7. Wang J and Ganley CJ. Clin Pharmacol Ther. 2019 Jan;105(1):161-7.
8. Matta MK et al. JAMA. 2020 Jan 21;323(3):256-67.
9. Warshaw EM et al. Dermatitis. 2013 Jul-Aug;24(4):176-82.
10. Amar SK et al. Toxicol Lett. 2015 Dec 15;239(3):182-93.
11. Amar SK et al. Toxicol Ind Health. 2019 Jul;35(7):457-65.
12. EWG. The trouble with ingredients in sunscreens. Accessed on 4 April 2020.
13. Panico A et al. J Prev Med Hyg. 2019 Mar 29;60(1):E50-7.
14. International Agency for Research on Cancer (IARC). Benzophenone. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. WHO, IARC Press, Lyon, France. 2010;101:285-304.
15. Barbosa TC et al. Toxics. 2019 Sep 22;7(4):51.
Benzophenones are a family of compounds that include dixoxybenzone, sulisobenzone, and benzophenone-3, or oxybenzone. These . Benzophenones (BPs) act as penetration enhancers, as they modify the structure of the skin and facilitate the absorption of other chemical ingredients into the body. The best known uses of these compounds are as perfume fixatives and sunscreen agents.
Sunscreens and benzophenones
BP-2, -3 and -4 are used as sunscreens but have many downsides. They are well known photoallergens, are toxic to aquatic animals (especially BP-3), and are found in urine. BP-2 has weak estrogenic effects, and some studies suggest that it decreases fertility in men. BP-4 can increase absorption of pesticides. BP-3 is banned in Hawaii because of the risk to coral and is the most worrisome.
In particular, BP-3 is known to protect skin and hair from UV radiation-induced harm.1 Unfortunately, BPs are also associated with photocontact allergies, hypersensitivity, hives, contact urticaria, anaphylaxis, hormone disruption, and DNA damage.2,3 BP-3 has also been implicated as an environmental contaminant. This column will focus on recent studies pertaining to effects on humans, primarily, and on the role of BPs in sunscreen agents.
Effects of BPs in animals
A recent study on the cytotoxicity of BP-3 against thymocytes in rats revealed that cell mortality increased significantly after 3 hours of exposure to 300 μM BP-3, but the membrane potential of thymocytes was unchanged by BP-3 exposure. In a concentration-dependent fashion, intracellular Zn2+ levels increased significantly after administration of at least 30 μM BP-3. The investigators concluded that the cytotoxicity engendered by BP-3 could be the result of oxidative stress linked to elevated intracellular Zn2+ levels.1
Effects of BPs in humans and systemic absorption
In multiple studies, exposure to BP-3, as well as to octinoxate, has been linked to endocrine and hormonal disruptions in humans and animals.4,5 Motivated by several notable observations (global increase in the use of sunscreens with UV filters; rapid rise in malignant melanoma, against which sunscreens should protect; increase in reported experimental findings of UV filters acting as endocrine disruptors), Krause et al. in 2012 reviewed animal and human data on the UV filters BP-3, 3-benzylidene camphor (3-BC), 3-(4-methyl-benzylidene) camphor (4-MBC), 2-ethylhexyl 4-methoxy cinnamate (OMC), homosalate (HMS), 2-ethylhexyl 4-dimethylaminobenzoate, and 4-aminobenzoic acid (PABA). Importantly, BP-3 was present in 96% of human urine samples in the United States, and various filters were found in 85% of the human breast milk samples in Switzerland.6
A 2019 analysis by Wang and Ganley reported that systemic absorption of the active sunscreen ingredient BP-3 can be substantial, justifying the assessment and understanding of systemic exposure to characterize the risks of long-term usage.7
Between January and February 2019, Matta et al. conducted a randomized clinical trial with 48 healthy participants to evaluate the systemic absorption and pharmacokinetics of six active ingredients in four sunscreen formulations, including avobenzone and BP-3. The researchers found that all ingredients were systemically absorbed, with plasma concentrations exceeding the Food and Drug Administration threshold for considering the waiving of further safety studies. They concluded that these results did not warrant discontinuing the use of the tested sunscreen ingredients.8 Yeager and Lim add that, while BP-3 has been incorporated into sunscreen formulations for sale in the United States since 1978, there have been no reports of adverse systemic reactions in human beings.3
However, topical reactions have elicited a different assessment. That is, in 2014, the American Contact Dermatitis Society labeled BPs the Contact Allergen of the Year, as they were identified as the most common source of photoallergic and contact allergic reactions of all UV filters.3,9
Risks of BPs in sunscreens and other skincare products
In 2015, Amar et al. investigated the photogenotoxicity and apoptotic effects in human keratinocytes (HaCaT cells) of BP-1, which is used as a UV blocker in sunscreens. They found that BP-1, when exposed to UV radiation, photosensitized cells and yielded intracellular reactive oxygen species. Significant reductions in cell viability were also seen with exposure to sunlight, UVA, and UVB. The researchers also confirmed genotoxic activity, with BP-1 augmenting lipid peroxidation and upregulating apoptotic proteins. They concluded that sunscreen users should be advised to avoid products that contain BP-1.10
In 2019, Amar et al. evaluated the effects of BPs on the differential expression of proteins in HaCaT cells exposed to UVA. Their findings indicated the expression of novel proteins that helped to initiate or promote apoptosis. They concluded that, because of the predilection to render such effects in human skin keratinocytes, consumers should avoid the use of sunscreens that contain BPs as UV blocking ingredients.11
Still widely used as an effective filter against UVA2 and UVB, BP-3 was believed to be present in two thirds of nonmineral sunscreens in the United States in 2018.3,12
Notably, BP-1 and BP-3 were found in small proportions (3.7% and 4.9%, respectively) among a total of 283 products culled from various stores in Lecce, Italy, in a survey of the potentially dangerous chemicals found in rinse-off, leave-on, and makeup products in 2019.13 The authors added that the International Agency for Research on Cancer, in 2010, classified BP as potentially carcinogenic to humans (2B group).13,14
Promising use of nanocapsules
The widespread concern about the phototoxicity of BP has prompted some interesting research into workarounds. Specifically, in 2019, Barbosa et al. reported on the creation of a new sunscreen formulation using polymeric nanocapsules loading BP-3. The nanocapsules are made of poly(ε-caprolactone) carrot oil and Pluronic F68 (nonionic surfactant used in suspension cultures), and the BP-3–loaded capsules were found to be noncytotoxic in L929 fibroblast cell lines with a sun protection factor of 8.64. The researchers concluded that this promising nanocapsule may be an effective and safe way to use lipophilic sunscreen ingredients such as BP-3.15
Conclusion
The body of evidence is weighted against the use of BPs. Luckily, we have safe sunscreen choices that allow us to protect our skin without using these compounds.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks and a New York Times Best Sellers book for consumers. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Revance, Evolus, and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., a company that independently tests skin care products and makes recommendations to physicians on which skin care technologies are best. Write to her at dermnews@mdedge.com.
References
1. Utsunomiya H et al. Chem Biol Interact. 2019 Jan 25;298:52-6.
2. Schneider SL and Lim HW. J Am Acad Dermatol. 2019 Jan;80(1):266-71.
3. Yeager DG and Lim HW. Dermatol Clin. 2019 Apr;37(2):149-57.
4. Ramos S et al. Sci Total Environ. 2015 Sep 1;526:278-311.
5. Siller A et al. Plast Surg Nur. 2019 Oct/Dec;39(4):157-60.
6. Krause M et al. Int J Androl. 2012 Jun;35(3):424-36.
7. Wang J and Ganley CJ. Clin Pharmacol Ther. 2019 Jan;105(1):161-7.
8. Matta MK et al. JAMA. 2020 Jan 21;323(3):256-67.
9. Warshaw EM et al. Dermatitis. 2013 Jul-Aug;24(4):176-82.
10. Amar SK et al. Toxicol Lett. 2015 Dec 15;239(3):182-93.
11. Amar SK et al. Toxicol Ind Health. 2019 Jul;35(7):457-65.
12. EWG. The trouble with ingredients in sunscreens. Accessed on 4 April 2020.
13. Panico A et al. J Prev Med Hyg. 2019 Mar 29;60(1):E50-7.
14. International Agency for Research on Cancer (IARC). Benzophenone. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. WHO, IARC Press, Lyon, France. 2010;101:285-304.
15. Barbosa TC et al. Toxics. 2019 Sep 22;7(4):51.
Benzophenones are a family of compounds that include dixoxybenzone, sulisobenzone, and benzophenone-3, or oxybenzone. These . Benzophenones (BPs) act as penetration enhancers, as they modify the structure of the skin and facilitate the absorption of other chemical ingredients into the body. The best known uses of these compounds are as perfume fixatives and sunscreen agents.
Sunscreens and benzophenones
BP-2, -3 and -4 are used as sunscreens but have many downsides. They are well known photoallergens, are toxic to aquatic animals (especially BP-3), and are found in urine. BP-2 has weak estrogenic effects, and some studies suggest that it decreases fertility in men. BP-4 can increase absorption of pesticides. BP-3 is banned in Hawaii because of the risk to coral and is the most worrisome.
In particular, BP-3 is known to protect skin and hair from UV radiation-induced harm.1 Unfortunately, BPs are also associated with photocontact allergies, hypersensitivity, hives, contact urticaria, anaphylaxis, hormone disruption, and DNA damage.2,3 BP-3 has also been implicated as an environmental contaminant. This column will focus on recent studies pertaining to effects on humans, primarily, and on the role of BPs in sunscreen agents.
Effects of BPs in animals
A recent study on the cytotoxicity of BP-3 against thymocytes in rats revealed that cell mortality increased significantly after 3 hours of exposure to 300 μM BP-3, but the membrane potential of thymocytes was unchanged by BP-3 exposure. In a concentration-dependent fashion, intracellular Zn2+ levels increased significantly after administration of at least 30 μM BP-3. The investigators concluded that the cytotoxicity engendered by BP-3 could be the result of oxidative stress linked to elevated intracellular Zn2+ levels.1
Effects of BPs in humans and systemic absorption
In multiple studies, exposure to BP-3, as well as to octinoxate, has been linked to endocrine and hormonal disruptions in humans and animals.4,5 Motivated by several notable observations (global increase in the use of sunscreens with UV filters; rapid rise in malignant melanoma, against which sunscreens should protect; increase in reported experimental findings of UV filters acting as endocrine disruptors), Krause et al. in 2012 reviewed animal and human data on the UV filters BP-3, 3-benzylidene camphor (3-BC), 3-(4-methyl-benzylidene) camphor (4-MBC), 2-ethylhexyl 4-methoxy cinnamate (OMC), homosalate (HMS), 2-ethylhexyl 4-dimethylaminobenzoate, and 4-aminobenzoic acid (PABA). Importantly, BP-3 was present in 96% of human urine samples in the United States, and various filters were found in 85% of the human breast milk samples in Switzerland.6
A 2019 analysis by Wang and Ganley reported that systemic absorption of the active sunscreen ingredient BP-3 can be substantial, justifying the assessment and understanding of systemic exposure to characterize the risks of long-term usage.7
Between January and February 2019, Matta et al. conducted a randomized clinical trial with 48 healthy participants to evaluate the systemic absorption and pharmacokinetics of six active ingredients in four sunscreen formulations, including avobenzone and BP-3. The researchers found that all ingredients were systemically absorbed, with plasma concentrations exceeding the Food and Drug Administration threshold for considering the waiving of further safety studies. They concluded that these results did not warrant discontinuing the use of the tested sunscreen ingredients.8 Yeager and Lim add that, while BP-3 has been incorporated into sunscreen formulations for sale in the United States since 1978, there have been no reports of adverse systemic reactions in human beings.3
However, topical reactions have elicited a different assessment. That is, in 2014, the American Contact Dermatitis Society labeled BPs the Contact Allergen of the Year, as they were identified as the most common source of photoallergic and contact allergic reactions of all UV filters.3,9
Risks of BPs in sunscreens and other skincare products
In 2015, Amar et al. investigated the photogenotoxicity and apoptotic effects in human keratinocytes (HaCaT cells) of BP-1, which is used as a UV blocker in sunscreens. They found that BP-1, when exposed to UV radiation, photosensitized cells and yielded intracellular reactive oxygen species. Significant reductions in cell viability were also seen with exposure to sunlight, UVA, and UVB. The researchers also confirmed genotoxic activity, with BP-1 augmenting lipid peroxidation and upregulating apoptotic proteins. They concluded that sunscreen users should be advised to avoid products that contain BP-1.10
In 2019, Amar et al. evaluated the effects of BPs on the differential expression of proteins in HaCaT cells exposed to UVA. Their findings indicated the expression of novel proteins that helped to initiate or promote apoptosis. They concluded that, because of the predilection to render such effects in human skin keratinocytes, consumers should avoid the use of sunscreens that contain BPs as UV blocking ingredients.11
Still widely used as an effective filter against UVA2 and UVB, BP-3 was believed to be present in two thirds of nonmineral sunscreens in the United States in 2018.3,12
Notably, BP-1 and BP-3 were found in small proportions (3.7% and 4.9%, respectively) among a total of 283 products culled from various stores in Lecce, Italy, in a survey of the potentially dangerous chemicals found in rinse-off, leave-on, and makeup products in 2019.13 The authors added that the International Agency for Research on Cancer, in 2010, classified BP as potentially carcinogenic to humans (2B group).13,14
Promising use of nanocapsules
The widespread concern about the phototoxicity of BP has prompted some interesting research into workarounds. Specifically, in 2019, Barbosa et al. reported on the creation of a new sunscreen formulation using polymeric nanocapsules loading BP-3. The nanocapsules are made of poly(ε-caprolactone) carrot oil and Pluronic F68 (nonionic surfactant used in suspension cultures), and the BP-3–loaded capsules were found to be noncytotoxic in L929 fibroblast cell lines with a sun protection factor of 8.64. The researchers concluded that this promising nanocapsule may be an effective and safe way to use lipophilic sunscreen ingredients such as BP-3.15
Conclusion
The body of evidence is weighted against the use of BPs. Luckily, we have safe sunscreen choices that allow us to protect our skin without using these compounds.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann has written two textbooks and a New York Times Best Sellers book for consumers. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Revance, Evolus, and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., a company that independently tests skin care products and makes recommendations to physicians on which skin care technologies are best. Write to her at dermnews@mdedge.com.
References
1. Utsunomiya H et al. Chem Biol Interact. 2019 Jan 25;298:52-6.
2. Schneider SL and Lim HW. J Am Acad Dermatol. 2019 Jan;80(1):266-71.
3. Yeager DG and Lim HW. Dermatol Clin. 2019 Apr;37(2):149-57.
4. Ramos S et al. Sci Total Environ. 2015 Sep 1;526:278-311.
5. Siller A et al. Plast Surg Nur. 2019 Oct/Dec;39(4):157-60.
6. Krause M et al. Int J Androl. 2012 Jun;35(3):424-36.
7. Wang J and Ganley CJ. Clin Pharmacol Ther. 2019 Jan;105(1):161-7.
8. Matta MK et al. JAMA. 2020 Jan 21;323(3):256-67.
9. Warshaw EM et al. Dermatitis. 2013 Jul-Aug;24(4):176-82.
10. Amar SK et al. Toxicol Lett. 2015 Dec 15;239(3):182-93.
11. Amar SK et al. Toxicol Ind Health. 2019 Jul;35(7):457-65.
12. EWG. The trouble with ingredients in sunscreens. Accessed on 4 April 2020.
13. Panico A et al. J Prev Med Hyg. 2019 Mar 29;60(1):E50-7.
14. International Agency for Research on Cancer (IARC). Benzophenone. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. WHO, IARC Press, Lyon, France. 2010;101:285-304.
15. Barbosa TC et al. Toxics. 2019 Sep 22;7(4):51.













