User login
Mental health in America: ‘The kids are not alright’
A new report shines a light on the toll the pandemic and other stressors have taken on the mental health of U.S. children and adolescents over the last 6 years.
The report shows a dramatic increase in use of acute care services for depression, anxiety, and other mental health conditions, especially among teens and preteens.
The report – The Kids Are Not Alright: Pediatric Mental Health Care Utilization from 2016-2021 – is the work of researchers at the Clarify Health Institute, the research arm of Clarify Health.
The results are “deeply concerning” and should “spark a conversation” around the need to improve access, utilization, and quality of pediatric behavioral health services, Niall Brennan, chief analytics and privacy officer for the Clarify Health Institute, told this news organization.
‘Startling’ trends
Leveraging an observational, national sample of insurance claims from more than 20 million children aged 1-19 years annually, the researchers observed several disturbing trends in mental health care.
From 2016 to 2021, inpatient (IP) admissions rose 61% (from 30 to 48 visits annually per 1,000) and emergency department visits rose 20% (from 55 to 66 visits annually per 1,000).
Mental health IP admissions ranged from a low of 27% in the West North Central region to a high of 137% in the Middle Atlantic region.
There were substantial increases from 2016 to 2021 in mental health IP admissions among children of all age groups, but particularly among adolescents 12 to 15 years old, increasing 84% among girls and 83% among boys in this age group.
There was also a sharp increase in mental health ED visits among girls and boys aged 12-15 years, increasing 20% overall during the study period.
Mental health IP use grew faster from 2016 to 2021 among children with commercial insurance than among those with Medicaid (103% vs. 40%).
In contrast, mental health–specific ED visits declined 10% among children with commercial insurance and increased by 20% among those with Medicaid.
ED utilization rates in 2021 were nearly twice as high in the Medicaid population, compared with those for children with commercial insurance.
These are “startling” increases, Mr. Brennan said in an interview.
These trends “reinforce health care leaders’ responsibility to address children’s mental health, especially when considering that half of all mental health conditions onset during adolescence and carry into adulthood,” Jean Drouin, MD, Clarify Health’s chief executive office and cofounder, adds in a news release.
“With a growing consensus that mental, behavioral, and physical health intersect, this research report aims to spark a conversation about the overall wellbeing of America’s next generation,” Dr. Drouin says.
Concern for the future
Commenting on the new report, Anish Dube, MD, chair of the American Psychiatric Association’s Council on Children, Adolescents, and their Families, said the findings are “concerning, though unsurprising.”
“They confirm what those of us in clinical practice have experienced in the last several years. The need for mental health services continues to rise every year, while access to adequate help remains lacking,” Dr. Dube said.
“With the recent COVID-19 pandemic, concerns about the effects of climate change, global political uncertainty, and a rapidly changing employment landscape, young people in particular are vulnerable to worries about their future and feelings of helplessness and hopelessness,” he added.
Dr. Dube said there is no one right solution, and addressing this problem must consider individual and local factors.
However, some of the broader interventions needed to tackle the problem include increasing access to care by enforcing mental health parity and increasing the number of trained and qualified mental health professionals, such as child and adolescent psychiatrists, who can assess and treat these conditions in young people before they become major crises and lead to acute interventions like inpatient hospitalization.
“Public health interventions aimed at schools and families in raising awareness of mental health and well-being, and simple, cost-effective interventions to practice mental wellness will also help reduce the burden of mental illness in young people,” Dr. Dube added.
“The APA continues to fight for mental health parity enforcement and for meaningful access to mental health care for children, adolescents, and their families,” Dr. Dube said.
This research was conducted by the Clarify Health Institute. Mr. Brennan and Dr. Dube report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new report shines a light on the toll the pandemic and other stressors have taken on the mental health of U.S. children and adolescents over the last 6 years.
The report shows a dramatic increase in use of acute care services for depression, anxiety, and other mental health conditions, especially among teens and preteens.
The report – The Kids Are Not Alright: Pediatric Mental Health Care Utilization from 2016-2021 – is the work of researchers at the Clarify Health Institute, the research arm of Clarify Health.
The results are “deeply concerning” and should “spark a conversation” around the need to improve access, utilization, and quality of pediatric behavioral health services, Niall Brennan, chief analytics and privacy officer for the Clarify Health Institute, told this news organization.
‘Startling’ trends
Leveraging an observational, national sample of insurance claims from more than 20 million children aged 1-19 years annually, the researchers observed several disturbing trends in mental health care.
From 2016 to 2021, inpatient (IP) admissions rose 61% (from 30 to 48 visits annually per 1,000) and emergency department visits rose 20% (from 55 to 66 visits annually per 1,000).
Mental health IP admissions ranged from a low of 27% in the West North Central region to a high of 137% in the Middle Atlantic region.
There were substantial increases from 2016 to 2021 in mental health IP admissions among children of all age groups, but particularly among adolescents 12 to 15 years old, increasing 84% among girls and 83% among boys in this age group.
There was also a sharp increase in mental health ED visits among girls and boys aged 12-15 years, increasing 20% overall during the study period.
Mental health IP use grew faster from 2016 to 2021 among children with commercial insurance than among those with Medicaid (103% vs. 40%).
In contrast, mental health–specific ED visits declined 10% among children with commercial insurance and increased by 20% among those with Medicaid.
ED utilization rates in 2021 were nearly twice as high in the Medicaid population, compared with those for children with commercial insurance.
These are “startling” increases, Mr. Brennan said in an interview.
These trends “reinforce health care leaders’ responsibility to address children’s mental health, especially when considering that half of all mental health conditions onset during adolescence and carry into adulthood,” Jean Drouin, MD, Clarify Health’s chief executive office and cofounder, adds in a news release.
“With a growing consensus that mental, behavioral, and physical health intersect, this research report aims to spark a conversation about the overall wellbeing of America’s next generation,” Dr. Drouin says.
Concern for the future
Commenting on the new report, Anish Dube, MD, chair of the American Psychiatric Association’s Council on Children, Adolescents, and their Families, said the findings are “concerning, though unsurprising.”
“They confirm what those of us in clinical practice have experienced in the last several years. The need for mental health services continues to rise every year, while access to adequate help remains lacking,” Dr. Dube said.
“With the recent COVID-19 pandemic, concerns about the effects of climate change, global political uncertainty, and a rapidly changing employment landscape, young people in particular are vulnerable to worries about their future and feelings of helplessness and hopelessness,” he added.
Dr. Dube said there is no one right solution, and addressing this problem must consider individual and local factors.
However, some of the broader interventions needed to tackle the problem include increasing access to care by enforcing mental health parity and increasing the number of trained and qualified mental health professionals, such as child and adolescent psychiatrists, who can assess and treat these conditions in young people before they become major crises and lead to acute interventions like inpatient hospitalization.
“Public health interventions aimed at schools and families in raising awareness of mental health and well-being, and simple, cost-effective interventions to practice mental wellness will also help reduce the burden of mental illness in young people,” Dr. Dube added.
“The APA continues to fight for mental health parity enforcement and for meaningful access to mental health care for children, adolescents, and their families,” Dr. Dube said.
This research was conducted by the Clarify Health Institute. Mr. Brennan and Dr. Dube report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new report shines a light on the toll the pandemic and other stressors have taken on the mental health of U.S. children and adolescents over the last 6 years.
The report shows a dramatic increase in use of acute care services for depression, anxiety, and other mental health conditions, especially among teens and preteens.
The report – The Kids Are Not Alright: Pediatric Mental Health Care Utilization from 2016-2021 – is the work of researchers at the Clarify Health Institute, the research arm of Clarify Health.
The results are “deeply concerning” and should “spark a conversation” around the need to improve access, utilization, and quality of pediatric behavioral health services, Niall Brennan, chief analytics and privacy officer for the Clarify Health Institute, told this news organization.
‘Startling’ trends
Leveraging an observational, national sample of insurance claims from more than 20 million children aged 1-19 years annually, the researchers observed several disturbing trends in mental health care.
From 2016 to 2021, inpatient (IP) admissions rose 61% (from 30 to 48 visits annually per 1,000) and emergency department visits rose 20% (from 55 to 66 visits annually per 1,000).
Mental health IP admissions ranged from a low of 27% in the West North Central region to a high of 137% in the Middle Atlantic region.
There were substantial increases from 2016 to 2021 in mental health IP admissions among children of all age groups, but particularly among adolescents 12 to 15 years old, increasing 84% among girls and 83% among boys in this age group.
There was also a sharp increase in mental health ED visits among girls and boys aged 12-15 years, increasing 20% overall during the study period.
Mental health IP use grew faster from 2016 to 2021 among children with commercial insurance than among those with Medicaid (103% vs. 40%).
In contrast, mental health–specific ED visits declined 10% among children with commercial insurance and increased by 20% among those with Medicaid.
ED utilization rates in 2021 were nearly twice as high in the Medicaid population, compared with those for children with commercial insurance.
These are “startling” increases, Mr. Brennan said in an interview.
These trends “reinforce health care leaders’ responsibility to address children’s mental health, especially when considering that half of all mental health conditions onset during adolescence and carry into adulthood,” Jean Drouin, MD, Clarify Health’s chief executive office and cofounder, adds in a news release.
“With a growing consensus that mental, behavioral, and physical health intersect, this research report aims to spark a conversation about the overall wellbeing of America’s next generation,” Dr. Drouin says.
Concern for the future
Commenting on the new report, Anish Dube, MD, chair of the American Psychiatric Association’s Council on Children, Adolescents, and their Families, said the findings are “concerning, though unsurprising.”
“They confirm what those of us in clinical practice have experienced in the last several years. The need for mental health services continues to rise every year, while access to adequate help remains lacking,” Dr. Dube said.
“With the recent COVID-19 pandemic, concerns about the effects of climate change, global political uncertainty, and a rapidly changing employment landscape, young people in particular are vulnerable to worries about their future and feelings of helplessness and hopelessness,” he added.
Dr. Dube said there is no one right solution, and addressing this problem must consider individual and local factors.
However, some of the broader interventions needed to tackle the problem include increasing access to care by enforcing mental health parity and increasing the number of trained and qualified mental health professionals, such as child and adolescent psychiatrists, who can assess and treat these conditions in young people before they become major crises and lead to acute interventions like inpatient hospitalization.
“Public health interventions aimed at schools and families in raising awareness of mental health and well-being, and simple, cost-effective interventions to practice mental wellness will also help reduce the burden of mental illness in young people,” Dr. Dube added.
“The APA continues to fight for mental health parity enforcement and for meaningful access to mental health care for children, adolescents, and their families,” Dr. Dube said.
This research was conducted by the Clarify Health Institute. Mr. Brennan and Dr. Dube report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
‘Dr. Caveman’ had a leg up on amputation
Monkey see, monkey do (advanced medical procedures)
We don’t tend to think too kindly of our prehistoric ancestors. We throw around the word “caveman” – hardly a term of endearment – and depictions of Paleolithic humans rarely flatter their subjects. In many ways, though, our conceptions are correct. Humans of the Stone Age lived short, often brutish lives, but civilization had to start somewhere, and our prehistoric ancestors were often far more capable than we give them credit for.
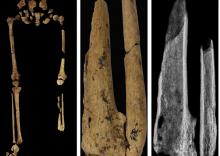
Case in point is a recent discovery from an archaeological dig in Borneo: A young adult who lived 31,000 years ago was discovered with the lower third of their left leg amputated. Save the clever retort about the person’s untimely death, because this individual did not die from the surgery. The amputation occurred when the individual was a child and the subject lived for several years after the operation.
Amputation is usually unnecessary given our current level of medical technology, but it’s actually quite an advanced procedure, and this example predates the previous first case of amputation by nearly 25,000 years. Not only did the surgeon need to cut at an appropriate place, they needed to understand blood loss, the risk of infection, and the need to preserve skin in order to seal the wound back up. That’s quite a lot for our Paleolithic doctor to know, and it’s even more impressive considering the, shall we say, limited tools they would have had available to perform the operation.
Rocks. They cut off the leg with a rock. And it worked.
This discovery also gives insight into the amputee’s society. Someone knew that amputation was the right move for this person, indicating that it had been done before. In addition, the individual would not have been able to spring back into action hunting mammoths right away, they would require care for the rest of their lives. And clearly the community provided, given the individual’s continued life post operation and their burial in a place of honor.
If only the American health care system was capable of such feats of compassion, but that would require the majority of politicians to be as clever as cavemen. We’re not hopeful on those odds.
The first step is admitting you have a crying baby. The second step is … a step
Knock, knock.
Who’s there?
Crying baby.
Crying baby who?
Crying baby who … umm … doesn’t have a punchline. Let’s try this again.
A priest, a rabbi, and a crying baby walk into a bar and … nope, that’s not going to work.
Why did the crying baby cross the road? Ugh, never mind.
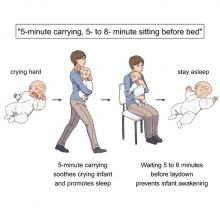
Clearly, crying babies are no laughing matter. What crying babies need is science. And the latest innovation – it’s fresh from a study conducted at the RIKEN Center for Brain Science in Saitama, Japan – in the science of crying babies is … walking. Researchers observed 21 unhappy infants and compared their responses to four strategies: being held by their walking mothers, held by their sitting mothers, lying in a motionless crib, or lying in a rocking cot.
The best strategy is for the mother – the experiment only involved mothers, but the results should apply to any caregiver – to pick up the crying baby, walk around for 5 minutes, sit for another 5-8 minutes, and then put the infant back to bed, the researchers said in a written statement.
The walking strategy, however, isn’t perfect. “Walking for 5 minutes promoted sleep, but only for crying infants. Surprisingly, this effect was absent when babies were already calm beforehand,” lead author Kumi O. Kuroda, MD, PhD, explained in a separate statement from the center.
It also doesn’t work on adults. We could not get a crying LOTME writer to fall asleep no matter how long his mother carried him around the office.
New way to detect Parkinson’s has already passed the sniff test
We humans aren’t generally known for our superpowers, but a woman from Scotland may just be the Smelling Superhero. Not only was she able to literally smell Parkinson’s disease (PD) on her husband 12 years before his diagnosis; she is also the reason that scientists have found a new way to test for PD.
Joy Milne, a retired nurse, told the BBC that her husband “had this musty rather unpleasant smell especially round his shoulders and the back of his neck and his skin had definitely changed.” She put two and two together after he had been diagnosed with PD and she came in contact with others with the same scent at a support group.
Researchers at the University of Manchester, working with Ms. Milne, have now created a skin test that uses mass spectroscopy to analyze a sample of the patient’s sebum in just 3 minutes and is 95% accurate. They tested 79 people with Parkinson’s and 71 without using this method and found “specific compounds unique to PD sebum samples when compared to healthy controls. Furthermore, we have identified two classes of lipids, namely, triacylglycerides and diglycerides, as components of human sebum that are significantly differentially expressed in PD,” they said in JACS Au.
This test could be available to general physicians within 2 years, which would provide new opportunities to the people who are waiting in line for neurologic consults. Ms. Milne’s husband passed away in 2015, but her courageous help and amazing nasal abilities may help millions down the line.
The power of flirting
It’s a common office stereotype: Women flirt with the boss to get ahead in the workplace, while men in power sexually harass women in subordinate positions. Nobody ever suspects the guys in the cubicles. A recent study takes a different look and paints a different picture.
The investigators conducted multiple online and lab experiments in how social sexual identity drives behavior in a workplace setting in relation to job placement. They found that it was most often men in lower-power positions who are insecure about their roles who initiate social sexual behavior, even though they know it’s offensive. Why? Power.
They randomly paired over 200 undergraduate students in a male/female fashion, placed them in subordinate and boss-like roles, and asked them to choose from a series of social sexual questions they wanted to ask their teammate. Male participants who were placed in subordinate positions to a female boss chose social sexual questions more often than did male bosses, female subordinates, and female bosses.
So what does this say about the threat of workplace harassment? The researchers found that men and women differ in their strategy for flirtation. For men, it’s a way to gain more power. But problems arise when they rationalize their behavior with a character trait like being a “big flirt.”
“When we take on that identity, it leads to certain behavioral patterns that reinforce the identity. And then, people use that identity as an excuse,” lead author Laura Kray of the University of California, Berkeley, said in a statement from the school.
The researchers make a point to note that the study isn’t about whether flirting is good or bad, nor are they suggesting that people in powerful positions don’t sexually harass underlings. It’s meant to provide insight to improve corporate sexual harassment training. A comment or conversation held in jest could potentially be a warning sign for future behavior.
Monkey see, monkey do (advanced medical procedures)
We don’t tend to think too kindly of our prehistoric ancestors. We throw around the word “caveman” – hardly a term of endearment – and depictions of Paleolithic humans rarely flatter their subjects. In many ways, though, our conceptions are correct. Humans of the Stone Age lived short, often brutish lives, but civilization had to start somewhere, and our prehistoric ancestors were often far more capable than we give them credit for.
Case in point is a recent discovery from an archaeological dig in Borneo: A young adult who lived 31,000 years ago was discovered with the lower third of their left leg amputated. Save the clever retort about the person’s untimely death, because this individual did not die from the surgery. The amputation occurred when the individual was a child and the subject lived for several years after the operation.
Amputation is usually unnecessary given our current level of medical technology, but it’s actually quite an advanced procedure, and this example predates the previous first case of amputation by nearly 25,000 years. Not only did the surgeon need to cut at an appropriate place, they needed to understand blood loss, the risk of infection, and the need to preserve skin in order to seal the wound back up. That’s quite a lot for our Paleolithic doctor to know, and it’s even more impressive considering the, shall we say, limited tools they would have had available to perform the operation.
Rocks. They cut off the leg with a rock. And it worked.
This discovery also gives insight into the amputee’s society. Someone knew that amputation was the right move for this person, indicating that it had been done before. In addition, the individual would not have been able to spring back into action hunting mammoths right away, they would require care for the rest of their lives. And clearly the community provided, given the individual’s continued life post operation and their burial in a place of honor.
If only the American health care system was capable of such feats of compassion, but that would require the majority of politicians to be as clever as cavemen. We’re not hopeful on those odds.
The first step is admitting you have a crying baby. The second step is … a step
Knock, knock.
Who’s there?
Crying baby.
Crying baby who?
Crying baby who … umm … doesn’t have a punchline. Let’s try this again.
A priest, a rabbi, and a crying baby walk into a bar and … nope, that’s not going to work.
Why did the crying baby cross the road? Ugh, never mind.
Clearly, crying babies are no laughing matter. What crying babies need is science. And the latest innovation – it’s fresh from a study conducted at the RIKEN Center for Brain Science in Saitama, Japan – in the science of crying babies is … walking. Researchers observed 21 unhappy infants and compared their responses to four strategies: being held by their walking mothers, held by their sitting mothers, lying in a motionless crib, or lying in a rocking cot.
The best strategy is for the mother – the experiment only involved mothers, but the results should apply to any caregiver – to pick up the crying baby, walk around for 5 minutes, sit for another 5-8 minutes, and then put the infant back to bed, the researchers said in a written statement.
The walking strategy, however, isn’t perfect. “Walking for 5 minutes promoted sleep, but only for crying infants. Surprisingly, this effect was absent when babies were already calm beforehand,” lead author Kumi O. Kuroda, MD, PhD, explained in a separate statement from the center.
It also doesn’t work on adults. We could not get a crying LOTME writer to fall asleep no matter how long his mother carried him around the office.
New way to detect Parkinson’s has already passed the sniff test
We humans aren’t generally known for our superpowers, but a woman from Scotland may just be the Smelling Superhero. Not only was she able to literally smell Parkinson’s disease (PD) on her husband 12 years before his diagnosis; she is also the reason that scientists have found a new way to test for PD.
Joy Milne, a retired nurse, told the BBC that her husband “had this musty rather unpleasant smell especially round his shoulders and the back of his neck and his skin had definitely changed.” She put two and two together after he had been diagnosed with PD and she came in contact with others with the same scent at a support group.
Researchers at the University of Manchester, working with Ms. Milne, have now created a skin test that uses mass spectroscopy to analyze a sample of the patient’s sebum in just 3 minutes and is 95% accurate. They tested 79 people with Parkinson’s and 71 without using this method and found “specific compounds unique to PD sebum samples when compared to healthy controls. Furthermore, we have identified two classes of lipids, namely, triacylglycerides and diglycerides, as components of human sebum that are significantly differentially expressed in PD,” they said in JACS Au.
This test could be available to general physicians within 2 years, which would provide new opportunities to the people who are waiting in line for neurologic consults. Ms. Milne’s husband passed away in 2015, but her courageous help and amazing nasal abilities may help millions down the line.
The power of flirting
It’s a common office stereotype: Women flirt with the boss to get ahead in the workplace, while men in power sexually harass women in subordinate positions. Nobody ever suspects the guys in the cubicles. A recent study takes a different look and paints a different picture.
The investigators conducted multiple online and lab experiments in how social sexual identity drives behavior in a workplace setting in relation to job placement. They found that it was most often men in lower-power positions who are insecure about their roles who initiate social sexual behavior, even though they know it’s offensive. Why? Power.
They randomly paired over 200 undergraduate students in a male/female fashion, placed them in subordinate and boss-like roles, and asked them to choose from a series of social sexual questions they wanted to ask their teammate. Male participants who were placed in subordinate positions to a female boss chose social sexual questions more often than did male bosses, female subordinates, and female bosses.
So what does this say about the threat of workplace harassment? The researchers found that men and women differ in their strategy for flirtation. For men, it’s a way to gain more power. But problems arise when they rationalize their behavior with a character trait like being a “big flirt.”
“When we take on that identity, it leads to certain behavioral patterns that reinforce the identity. And then, people use that identity as an excuse,” lead author Laura Kray of the University of California, Berkeley, said in a statement from the school.
The researchers make a point to note that the study isn’t about whether flirting is good or bad, nor are they suggesting that people in powerful positions don’t sexually harass underlings. It’s meant to provide insight to improve corporate sexual harassment training. A comment or conversation held in jest could potentially be a warning sign for future behavior.
Monkey see, monkey do (advanced medical procedures)
We don’t tend to think too kindly of our prehistoric ancestors. We throw around the word “caveman” – hardly a term of endearment – and depictions of Paleolithic humans rarely flatter their subjects. In many ways, though, our conceptions are correct. Humans of the Stone Age lived short, often brutish lives, but civilization had to start somewhere, and our prehistoric ancestors were often far more capable than we give them credit for.
Case in point is a recent discovery from an archaeological dig in Borneo: A young adult who lived 31,000 years ago was discovered with the lower third of their left leg amputated. Save the clever retort about the person’s untimely death, because this individual did not die from the surgery. The amputation occurred when the individual was a child and the subject lived for several years after the operation.
Amputation is usually unnecessary given our current level of medical technology, but it’s actually quite an advanced procedure, and this example predates the previous first case of amputation by nearly 25,000 years. Not only did the surgeon need to cut at an appropriate place, they needed to understand blood loss, the risk of infection, and the need to preserve skin in order to seal the wound back up. That’s quite a lot for our Paleolithic doctor to know, and it’s even more impressive considering the, shall we say, limited tools they would have had available to perform the operation.
Rocks. They cut off the leg with a rock. And it worked.
This discovery also gives insight into the amputee’s society. Someone knew that amputation was the right move for this person, indicating that it had been done before. In addition, the individual would not have been able to spring back into action hunting mammoths right away, they would require care for the rest of their lives. And clearly the community provided, given the individual’s continued life post operation and their burial in a place of honor.
If only the American health care system was capable of such feats of compassion, but that would require the majority of politicians to be as clever as cavemen. We’re not hopeful on those odds.
The first step is admitting you have a crying baby. The second step is … a step
Knock, knock.
Who’s there?
Crying baby.
Crying baby who?
Crying baby who … umm … doesn’t have a punchline. Let’s try this again.
A priest, a rabbi, and a crying baby walk into a bar and … nope, that’s not going to work.
Why did the crying baby cross the road? Ugh, never mind.
Clearly, crying babies are no laughing matter. What crying babies need is science. And the latest innovation – it’s fresh from a study conducted at the RIKEN Center for Brain Science in Saitama, Japan – in the science of crying babies is … walking. Researchers observed 21 unhappy infants and compared their responses to four strategies: being held by their walking mothers, held by their sitting mothers, lying in a motionless crib, or lying in a rocking cot.
The best strategy is for the mother – the experiment only involved mothers, but the results should apply to any caregiver – to pick up the crying baby, walk around for 5 minutes, sit for another 5-8 minutes, and then put the infant back to bed, the researchers said in a written statement.
The walking strategy, however, isn’t perfect. “Walking for 5 minutes promoted sleep, but only for crying infants. Surprisingly, this effect was absent when babies were already calm beforehand,” lead author Kumi O. Kuroda, MD, PhD, explained in a separate statement from the center.
It also doesn’t work on adults. We could not get a crying LOTME writer to fall asleep no matter how long his mother carried him around the office.
New way to detect Parkinson’s has already passed the sniff test
We humans aren’t generally known for our superpowers, but a woman from Scotland may just be the Smelling Superhero. Not only was she able to literally smell Parkinson’s disease (PD) on her husband 12 years before his diagnosis; she is also the reason that scientists have found a new way to test for PD.
Joy Milne, a retired nurse, told the BBC that her husband “had this musty rather unpleasant smell especially round his shoulders and the back of his neck and his skin had definitely changed.” She put two and two together after he had been diagnosed with PD and she came in contact with others with the same scent at a support group.
Researchers at the University of Manchester, working with Ms. Milne, have now created a skin test that uses mass spectroscopy to analyze a sample of the patient’s sebum in just 3 minutes and is 95% accurate. They tested 79 people with Parkinson’s and 71 without using this method and found “specific compounds unique to PD sebum samples when compared to healthy controls. Furthermore, we have identified two classes of lipids, namely, triacylglycerides and diglycerides, as components of human sebum that are significantly differentially expressed in PD,” they said in JACS Au.
This test could be available to general physicians within 2 years, which would provide new opportunities to the people who are waiting in line for neurologic consults. Ms. Milne’s husband passed away in 2015, but her courageous help and amazing nasal abilities may help millions down the line.
The power of flirting
It’s a common office stereotype: Women flirt with the boss to get ahead in the workplace, while men in power sexually harass women in subordinate positions. Nobody ever suspects the guys in the cubicles. A recent study takes a different look and paints a different picture.
The investigators conducted multiple online and lab experiments in how social sexual identity drives behavior in a workplace setting in relation to job placement. They found that it was most often men in lower-power positions who are insecure about their roles who initiate social sexual behavior, even though they know it’s offensive. Why? Power.
They randomly paired over 200 undergraduate students in a male/female fashion, placed them in subordinate and boss-like roles, and asked them to choose from a series of social sexual questions they wanted to ask their teammate. Male participants who were placed in subordinate positions to a female boss chose social sexual questions more often than did male bosses, female subordinates, and female bosses.
So what does this say about the threat of workplace harassment? The researchers found that men and women differ in their strategy for flirtation. For men, it’s a way to gain more power. But problems arise when they rationalize their behavior with a character trait like being a “big flirt.”
“When we take on that identity, it leads to certain behavioral patterns that reinforce the identity. And then, people use that identity as an excuse,” lead author Laura Kray of the University of California, Berkeley, said in a statement from the school.
The researchers make a point to note that the study isn’t about whether flirting is good or bad, nor are they suggesting that people in powerful positions don’t sexually harass underlings. It’s meant to provide insight to improve corporate sexual harassment training. A comment or conversation held in jest could potentially be a warning sign for future behavior.
Demystifying psychotherapy
Managing psychiatric illnesses is rapidly becoming routine practice for primary care pediatricians, whether screening for symptoms of anxiety and depression, starting medication, or providing psychoeducation to youth and parents. Pediatricians can provide strategies to address the impairments of sleep, energy, motivation and appetite that can accompany these illnesses. Psychotherapy, a relationship based on understanding and providing support, should be a core element of treatment for emotional disorders, but there is a great deal of uncertainty around what therapies are supported by evidence. This month, we offer a primer on the evidence-based psychotherapies for youth and we also recognize that research defining the effectiveness of psychotherapy is limited and complex.
Cognitive-behavioral psychotherapy (CBT)
Mention psychotherapy and most people think of a patient reclining on a couch free-associating about their childhood while a therapist sits behind them taking notes. This potent image stems from psychoanalytic psychotherapy, developed in the 19th century by Sigmund Freud, and was based on his theory that unconscious conflicts drove most of the puzzling behaviors and emotional distress associated with “neurosis.” Psychoanalysis became popular in 20th century America, even for use with children. Evidence is hard to develop since psychoanalytic therapy often lasts years, there are a limited number of patients, and the method is hard to standardize.
A focus on how to shape behaviors directly also emerged in the early 20th century (in the work of John Watson and Ivan Pavlov). Aaron Beck, MD, the father of CBT, observed in his psychoanalytic treatments that many patients appeared to be experiencing emotional distress around thoughts that were not unconscious. Instead, his patients were experiencing “automatic thoughts,” or rapid, often-distorted thoughts that have the force of truth in the thinker. These thoughts create emotional distress and behaviors that may reinforce the thoughts and emotional distress. For example, a depressed patient who is uncomfortable in social situations may think “nobody ever likes me.” This may cause them to appear uncomfortable or unfriendly in a new social situation and prevent them from making connections, perpetuating a cycle of isolation, insecurity, and loneliness. Identifying these automatic thoughts, and their connection to painful feelings and perpetuating behaviors is at the core of CBT.
In CBT the therapist is much more active than in psychoanalysis. They engage patients in identifying thought distortions together, challenging them on the truth of these thoughts and recognizing the connection to emotional distress. They also identify maladaptive behaviors and focus on strategies to build new more effective behavioral responses to thoughts, feelings, and situations. This is often done with gradual “exposures” to new behaviors, which are naturally reinforced by better outcomes or lowered distress. When performed with high fidelity, CBT is a very structured treatment that is closer to an emotionally supportive form of coaching and skill building. CBT is at the core of most evidence-based psychotherapies that have emerged in the past 60 years.
CBT is the first-line treatment for anxiety disorders in children, adolescents, and adults. A variant called “exposure and response prevention” is the first-line treatment for obsessive-compulsive disorder, and is predominantly behavioral. It is focused on preventing patients with anxiety disorders from engaging in the maladaptive behaviors that lower their anxiety in the short term but cause worsened anxiety and impairment over time (such as avoiding social situations when they are worried that others won’t like them).
CBT is also a first-line treatment for major depressive episodes in teenagers and adults, although those for whom the symptoms are severe often need medication to be able to fully participate in therapy. There are variants of CBT that have demonstrated efficacy in the treatment of posttraumatic stress disorder, bulimia, and even psychosis. It makes developmental sense that therapies with a problem-focused coaching approach might be more effective in children and adolescents than open-ended exploratory psychotherapies.
Traditional CBT was not very effective for patients with a variant of depression that is marked by stormy relationships, irritability, chronic suicidality, and impulsive attempts to regulate discomfort (including bingeing, purging, sexual acting-out, drug use, and self-injury or cutting), a symptom pattern called “borderline personality disorder.” These patients often ended up on multiple medications with only modest improvements in their function and well-being.
But in the 1990s, a research psychologist named Marsha Linnehan developed a modified version of CBT to use with these patients called dialectical-behavioral therapy (DBT). The “dialectic” emphasizes the role of two things being true at once, in this case the need for acceptance and change. DBT helps patients develop distress tolerance and emotional regulation skills alongside adaptive social and communication skills. DBT has demonstrated efficacy in the treatment of these patients as well as in the treatment of other disorders marked by poor distress tolerance and self-regulation (such as substance use disorders, binge-eating disorder, and PTSD).
DBT was adapted for use in adolescents given the prevalence of these problems in this age group, and it is the first-line treatment for adolescents with these specific mood and behavioral symptoms. High-fidelity DBT has an individual, group, and family component that are all essential for the treatment to be effective.
Instruction about the principles of CBT and DBT is a part of graduate school in psychology, but not every postgraduate training program includes thorough training in their practice. Completion of this specialized training leads to certification. It is very important that families understand that anyone may call themselves a psychotherapist. Those therapists who have master’s degrees (MSW, MFT, PCC, and others) may not have had exposure to these evidence-based treatments in their shorter graduate programs. Even doctoral-level training programs often do not include complete training in the high-fidelity delivery of these therapies.
It is critical that you help families be educated consumers and ask therapists if they have training and certification in the recommended therapy. The Psychology Today website has a therapist referral resource that includes this information. Training programs can provide access to therapists who are learning these therapies; with skilled supervision, they can provide excellent treatment.
We should note that there are several other evidence-based therapies, including family-based treatment for anorexia nervosa, motivational interviewing for substance use disorders, and interpersonal psychotherapy for depression associated with high family conflict in adolescents.
There is good evidence that the quality of the alliance between therapist and patient is a critical predictor of whether a therapy will be effective. It is appropriate for your patient to look for a therapist that they can trust and talk to and that their therapist be trained in the recommended psychotherapy. Otherwise, your patient is spending valuable time and money on an enterprise that may not be effective. This can leave them and their parents feeling discouraged or even hopeless about the prospects for recovery and promote an overreliance on medications. In addition to providing your patients with effective screening, initiating medication treatment, and psychoeducation, you can enhance their ability to find an optimal therapist to relieve their suffering.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at pdnews@mdedge.com.
Managing psychiatric illnesses is rapidly becoming routine practice for primary care pediatricians, whether screening for symptoms of anxiety and depression, starting medication, or providing psychoeducation to youth and parents. Pediatricians can provide strategies to address the impairments of sleep, energy, motivation and appetite that can accompany these illnesses. Psychotherapy, a relationship based on understanding and providing support, should be a core element of treatment for emotional disorders, but there is a great deal of uncertainty around what therapies are supported by evidence. This month, we offer a primer on the evidence-based psychotherapies for youth and we also recognize that research defining the effectiveness of psychotherapy is limited and complex.
Cognitive-behavioral psychotherapy (CBT)
Mention psychotherapy and most people think of a patient reclining on a couch free-associating about their childhood while a therapist sits behind them taking notes. This potent image stems from psychoanalytic psychotherapy, developed in the 19th century by Sigmund Freud, and was based on his theory that unconscious conflicts drove most of the puzzling behaviors and emotional distress associated with “neurosis.” Psychoanalysis became popular in 20th century America, even for use with children. Evidence is hard to develop since psychoanalytic therapy often lasts years, there are a limited number of patients, and the method is hard to standardize.
A focus on how to shape behaviors directly also emerged in the early 20th century (in the work of John Watson and Ivan Pavlov). Aaron Beck, MD, the father of CBT, observed in his psychoanalytic treatments that many patients appeared to be experiencing emotional distress around thoughts that were not unconscious. Instead, his patients were experiencing “automatic thoughts,” or rapid, often-distorted thoughts that have the force of truth in the thinker. These thoughts create emotional distress and behaviors that may reinforce the thoughts and emotional distress. For example, a depressed patient who is uncomfortable in social situations may think “nobody ever likes me.” This may cause them to appear uncomfortable or unfriendly in a new social situation and prevent them from making connections, perpetuating a cycle of isolation, insecurity, and loneliness. Identifying these automatic thoughts, and their connection to painful feelings and perpetuating behaviors is at the core of CBT.
In CBT the therapist is much more active than in psychoanalysis. They engage patients in identifying thought distortions together, challenging them on the truth of these thoughts and recognizing the connection to emotional distress. They also identify maladaptive behaviors and focus on strategies to build new more effective behavioral responses to thoughts, feelings, and situations. This is often done with gradual “exposures” to new behaviors, which are naturally reinforced by better outcomes or lowered distress. When performed with high fidelity, CBT is a very structured treatment that is closer to an emotionally supportive form of coaching and skill building. CBT is at the core of most evidence-based psychotherapies that have emerged in the past 60 years.
CBT is the first-line treatment for anxiety disorders in children, adolescents, and adults. A variant called “exposure and response prevention” is the first-line treatment for obsessive-compulsive disorder, and is predominantly behavioral. It is focused on preventing patients with anxiety disorders from engaging in the maladaptive behaviors that lower their anxiety in the short term but cause worsened anxiety and impairment over time (such as avoiding social situations when they are worried that others won’t like them).
CBT is also a first-line treatment for major depressive episodes in teenagers and adults, although those for whom the symptoms are severe often need medication to be able to fully participate in therapy. There are variants of CBT that have demonstrated efficacy in the treatment of posttraumatic stress disorder, bulimia, and even psychosis. It makes developmental sense that therapies with a problem-focused coaching approach might be more effective in children and adolescents than open-ended exploratory psychotherapies.
Traditional CBT was not very effective for patients with a variant of depression that is marked by stormy relationships, irritability, chronic suicidality, and impulsive attempts to regulate discomfort (including bingeing, purging, sexual acting-out, drug use, and self-injury or cutting), a symptom pattern called “borderline personality disorder.” These patients often ended up on multiple medications with only modest improvements in their function and well-being.
But in the 1990s, a research psychologist named Marsha Linnehan developed a modified version of CBT to use with these patients called dialectical-behavioral therapy (DBT). The “dialectic” emphasizes the role of two things being true at once, in this case the need for acceptance and change. DBT helps patients develop distress tolerance and emotional regulation skills alongside adaptive social and communication skills. DBT has demonstrated efficacy in the treatment of these patients as well as in the treatment of other disorders marked by poor distress tolerance and self-regulation (such as substance use disorders, binge-eating disorder, and PTSD).
DBT was adapted for use in adolescents given the prevalence of these problems in this age group, and it is the first-line treatment for adolescents with these specific mood and behavioral symptoms. High-fidelity DBT has an individual, group, and family component that are all essential for the treatment to be effective.
Instruction about the principles of CBT and DBT is a part of graduate school in psychology, but not every postgraduate training program includes thorough training in their practice. Completion of this specialized training leads to certification. It is very important that families understand that anyone may call themselves a psychotherapist. Those therapists who have master’s degrees (MSW, MFT, PCC, and others) may not have had exposure to these evidence-based treatments in their shorter graduate programs. Even doctoral-level training programs often do not include complete training in the high-fidelity delivery of these therapies.
It is critical that you help families be educated consumers and ask therapists if they have training and certification in the recommended therapy. The Psychology Today website has a therapist referral resource that includes this information. Training programs can provide access to therapists who are learning these therapies; with skilled supervision, they can provide excellent treatment.
We should note that there are several other evidence-based therapies, including family-based treatment for anorexia nervosa, motivational interviewing for substance use disorders, and interpersonal psychotherapy for depression associated with high family conflict in adolescents.
There is good evidence that the quality of the alliance between therapist and patient is a critical predictor of whether a therapy will be effective. It is appropriate for your patient to look for a therapist that they can trust and talk to and that their therapist be trained in the recommended psychotherapy. Otherwise, your patient is spending valuable time and money on an enterprise that may not be effective. This can leave them and their parents feeling discouraged or even hopeless about the prospects for recovery and promote an overreliance on medications. In addition to providing your patients with effective screening, initiating medication treatment, and psychoeducation, you can enhance their ability to find an optimal therapist to relieve their suffering.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at pdnews@mdedge.com.
Managing psychiatric illnesses is rapidly becoming routine practice for primary care pediatricians, whether screening for symptoms of anxiety and depression, starting medication, or providing psychoeducation to youth and parents. Pediatricians can provide strategies to address the impairments of sleep, energy, motivation and appetite that can accompany these illnesses. Psychotherapy, a relationship based on understanding and providing support, should be a core element of treatment for emotional disorders, but there is a great deal of uncertainty around what therapies are supported by evidence. This month, we offer a primer on the evidence-based psychotherapies for youth and we also recognize that research defining the effectiveness of psychotherapy is limited and complex.
Cognitive-behavioral psychotherapy (CBT)
Mention psychotherapy and most people think of a patient reclining on a couch free-associating about their childhood while a therapist sits behind them taking notes. This potent image stems from psychoanalytic psychotherapy, developed in the 19th century by Sigmund Freud, and was based on his theory that unconscious conflicts drove most of the puzzling behaviors and emotional distress associated with “neurosis.” Psychoanalysis became popular in 20th century America, even for use with children. Evidence is hard to develop since psychoanalytic therapy often lasts years, there are a limited number of patients, and the method is hard to standardize.
A focus on how to shape behaviors directly also emerged in the early 20th century (in the work of John Watson and Ivan Pavlov). Aaron Beck, MD, the father of CBT, observed in his psychoanalytic treatments that many patients appeared to be experiencing emotional distress around thoughts that were not unconscious. Instead, his patients were experiencing “automatic thoughts,” or rapid, often-distorted thoughts that have the force of truth in the thinker. These thoughts create emotional distress and behaviors that may reinforce the thoughts and emotional distress. For example, a depressed patient who is uncomfortable in social situations may think “nobody ever likes me.” This may cause them to appear uncomfortable or unfriendly in a new social situation and prevent them from making connections, perpetuating a cycle of isolation, insecurity, and loneliness. Identifying these automatic thoughts, and their connection to painful feelings and perpetuating behaviors is at the core of CBT.
In CBT the therapist is much more active than in psychoanalysis. They engage patients in identifying thought distortions together, challenging them on the truth of these thoughts and recognizing the connection to emotional distress. They also identify maladaptive behaviors and focus on strategies to build new more effective behavioral responses to thoughts, feelings, and situations. This is often done with gradual “exposures” to new behaviors, which are naturally reinforced by better outcomes or lowered distress. When performed with high fidelity, CBT is a very structured treatment that is closer to an emotionally supportive form of coaching and skill building. CBT is at the core of most evidence-based psychotherapies that have emerged in the past 60 years.
CBT is the first-line treatment for anxiety disorders in children, adolescents, and adults. A variant called “exposure and response prevention” is the first-line treatment for obsessive-compulsive disorder, and is predominantly behavioral. It is focused on preventing patients with anxiety disorders from engaging in the maladaptive behaviors that lower their anxiety in the short term but cause worsened anxiety and impairment over time (such as avoiding social situations when they are worried that others won’t like them).
CBT is also a first-line treatment for major depressive episodes in teenagers and adults, although those for whom the symptoms are severe often need medication to be able to fully participate in therapy. There are variants of CBT that have demonstrated efficacy in the treatment of posttraumatic stress disorder, bulimia, and even psychosis. It makes developmental sense that therapies with a problem-focused coaching approach might be more effective in children and adolescents than open-ended exploratory psychotherapies.
Traditional CBT was not very effective for patients with a variant of depression that is marked by stormy relationships, irritability, chronic suicidality, and impulsive attempts to regulate discomfort (including bingeing, purging, sexual acting-out, drug use, and self-injury or cutting), a symptom pattern called “borderline personality disorder.” These patients often ended up on multiple medications with only modest improvements in their function and well-being.
But in the 1990s, a research psychologist named Marsha Linnehan developed a modified version of CBT to use with these patients called dialectical-behavioral therapy (DBT). The “dialectic” emphasizes the role of two things being true at once, in this case the need for acceptance and change. DBT helps patients develop distress tolerance and emotional regulation skills alongside adaptive social and communication skills. DBT has demonstrated efficacy in the treatment of these patients as well as in the treatment of other disorders marked by poor distress tolerance and self-regulation (such as substance use disorders, binge-eating disorder, and PTSD).
DBT was adapted for use in adolescents given the prevalence of these problems in this age group, and it is the first-line treatment for adolescents with these specific mood and behavioral symptoms. High-fidelity DBT has an individual, group, and family component that are all essential for the treatment to be effective.
Instruction about the principles of CBT and DBT is a part of graduate school in psychology, but not every postgraduate training program includes thorough training in their practice. Completion of this specialized training leads to certification. It is very important that families understand that anyone may call themselves a psychotherapist. Those therapists who have master’s degrees (MSW, MFT, PCC, and others) may not have had exposure to these evidence-based treatments in their shorter graduate programs. Even doctoral-level training programs often do not include complete training in the high-fidelity delivery of these therapies.
It is critical that you help families be educated consumers and ask therapists if they have training and certification in the recommended therapy. The Psychology Today website has a therapist referral resource that includes this information. Training programs can provide access to therapists who are learning these therapies; with skilled supervision, they can provide excellent treatment.
We should note that there are several other evidence-based therapies, including family-based treatment for anorexia nervosa, motivational interviewing for substance use disorders, and interpersonal psychotherapy for depression associated with high family conflict in adolescents.
There is good evidence that the quality of the alliance between therapist and patient is a critical predictor of whether a therapy will be effective. It is appropriate for your patient to look for a therapist that they can trust and talk to and that their therapist be trained in the recommended psychotherapy. Otherwise, your patient is spending valuable time and money on an enterprise that may not be effective. This can leave them and their parents feeling discouraged or even hopeless about the prospects for recovery and promote an overreliance on medications. In addition to providing your patients with effective screening, initiating medication treatment, and psychoeducation, you can enhance their ability to find an optimal therapist to relieve their suffering.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at pdnews@mdedge.com.
Ages and Stages Questionnaire a first step to find developmental delays
The commonly used but sometimes debated Ages and Stages Questionnaire (ASQ), has modest utility for identifying developmental delays in young children, an Australian review and meta-analysis found.
On this easily administered parent-completed screening tool, scores of more than 2 standard deviations below the mean in more than one of five domains had moderate sensitivity and specificity to predict any delay, severe delay, motor delay, and cognitive delay, according to neonatologist Shripada Rao, PhD, a clinical associate professor in the neonatal intensive care unit at Perth Hospital and the University of Western Australia, also in Perth, and colleagues.
If a child of 12-60 months passes all ASQ domains, there is a moderate probability that child does not have severe developmental delay, the researchers concluded. If a child in that age range fails the motor or cognitive domain, there is a moderate probability that some motor or cognitive delay is present. The authors say the tool may work best as a screening test to identify children in need of more formal assessment.
“Our meta-analysis found that ASQ was somewhat more predictive in older children (older than 24 months), compared with younger age groups of 12-24 months,” Dr. Rao said in an interview. “However, the sample size for these comparisons was too small to reach definite conclusions, and we have called for future studies to evaluate ASQ separately for different age groups.”
Early identification of developmental delay in children is essential to enable timely intervention,” Dr. Rao and associates wrote in JAMA Pediatrics.
While formal assessments such as the Bayley Scales of Infant and Toddler Development are the gold standard, they are time-consuming and expensive, need the physical attendance of both the child and caregivers, and “thus may not be feasible in resource-limited settings or in pandemic conditions.”
According to Barbara J. Howard, MD, commenting on a recent update to the Center for Disease Control and Prevention’s developmental milestones guide, Learn the Signs. Act Early, fewer than 25% of children with delays or disabilities receive intervention before age 3 and most with emotional, behavioral, and developmental condition, other than autism spectrum disorder receive no intervention before age 5.
The ASQ
As an accessible alternative, the ASQ consists of questions on communication (language), gross-motor, fine-motor, problem-solving (cognitive), and personal-adaptive skills. The survey requires only 10-15 minutes, is relatively inexpensive, and also establishes a sense of parental involvement, the authors noted.
“Based on the generally accepted interpretation of LR [likelihood ratio] values, if a child passes ASQ-2SD, there is a moderate probability that the child does not have severe delay,” the investigators concluded.
The analysis
The final meta-analysis reviewed 36 eligible ASQ studies published from 1997 to 2022. Looking at the four indicators of pooled sensitivity, specificity, and positive and negative likelihood ratios, the following respective predictive values emerged for scores of more than 2 SDs below the mean across several domains: sensitivity of 0.77 (95% confidence interval, 0.64-0.86), specificity of 0.81 (95% CI 0.75-0.86), positive likelihood ratio of 4.10 (95% CI 3.17-5.30), and a negative likelihood ratio of 0.28 (95% CI, 0.18-0.44)
They cautioned, however, that the certainty of evidence from the reviewed studies was low or very low and given the small sample sizes for comparing domains, clinicians should be circumspect in interpreting the results.
An initial step
Commenting on the paper but not involved in it, David G. Fagan, MD, vice chairman of pediatric ambulatory administration in the department of pediatrics at Cohen Children’s Medical Center, New York, agreed that screening tools such as the ASQ have a place in clinical practice. “However, the purpose of a screening tool is not to make the diagnosis but to identify children at risk for developmental delays,” he said in an interview. “The meta-analysis highlights the fact that no screening is 100% accurate and that results need to be interpreted in context.
“Before screening tools were widely used, pediatricians trusted their gut,” Dr. Fagan continued. “‘I know it when I see it,’ which obviously resulted in tremendous variability based on experience.”
He added that, even if a child passes this validated questionnaire, any concern on the part of a parent or pediatrician about developmental delay should be addressed with further assessment.
The future
According to Dr. Rao, clinicians should continue to screen for developmental delays in young children using the ASQ. “Given the long wait times to see a developmental pediatrician or a clinical psychologist, a screening tool such as ASQ will enable appropriate triaging.”
Going forward, however, studies should evaluate this questionnaire separately for different age groups such as less than 12 months, 12-23 months, and at least 24 months. They should also be prospective in design and entail a low risk of bias, as well as report raw numbers for true and false positives and negatives. “Even if they use their own cutoff ASQ scores, they should also give results for the conventional cutoff scores to enable comparison with other studies,” the authors wrote.
The authors disclosed no specific funding for this study and no competing interests. Dr. Fagan disclosed no competing interests with regard to his comments.
The commonly used but sometimes debated Ages and Stages Questionnaire (ASQ), has modest utility for identifying developmental delays in young children, an Australian review and meta-analysis found.
On this easily administered parent-completed screening tool, scores of more than 2 standard deviations below the mean in more than one of five domains had moderate sensitivity and specificity to predict any delay, severe delay, motor delay, and cognitive delay, according to neonatologist Shripada Rao, PhD, a clinical associate professor in the neonatal intensive care unit at Perth Hospital and the University of Western Australia, also in Perth, and colleagues.
If a child of 12-60 months passes all ASQ domains, there is a moderate probability that child does not have severe developmental delay, the researchers concluded. If a child in that age range fails the motor or cognitive domain, there is a moderate probability that some motor or cognitive delay is present. The authors say the tool may work best as a screening test to identify children in need of more formal assessment.
“Our meta-analysis found that ASQ was somewhat more predictive in older children (older than 24 months), compared with younger age groups of 12-24 months,” Dr. Rao said in an interview. “However, the sample size for these comparisons was too small to reach definite conclusions, and we have called for future studies to evaluate ASQ separately for different age groups.”
Early identification of developmental delay in children is essential to enable timely intervention,” Dr. Rao and associates wrote in JAMA Pediatrics.
While formal assessments such as the Bayley Scales of Infant and Toddler Development are the gold standard, they are time-consuming and expensive, need the physical attendance of both the child and caregivers, and “thus may not be feasible in resource-limited settings or in pandemic conditions.”
According to Barbara J. Howard, MD, commenting on a recent update to the Center for Disease Control and Prevention’s developmental milestones guide, Learn the Signs. Act Early, fewer than 25% of children with delays or disabilities receive intervention before age 3 and most with emotional, behavioral, and developmental condition, other than autism spectrum disorder receive no intervention before age 5.
The ASQ
As an accessible alternative, the ASQ consists of questions on communication (language), gross-motor, fine-motor, problem-solving (cognitive), and personal-adaptive skills. The survey requires only 10-15 minutes, is relatively inexpensive, and also establishes a sense of parental involvement, the authors noted.
“Based on the generally accepted interpretation of LR [likelihood ratio] values, if a child passes ASQ-2SD, there is a moderate probability that the child does not have severe delay,” the investigators concluded.
The analysis
The final meta-analysis reviewed 36 eligible ASQ studies published from 1997 to 2022. Looking at the four indicators of pooled sensitivity, specificity, and positive and negative likelihood ratios, the following respective predictive values emerged for scores of more than 2 SDs below the mean across several domains: sensitivity of 0.77 (95% confidence interval, 0.64-0.86), specificity of 0.81 (95% CI 0.75-0.86), positive likelihood ratio of 4.10 (95% CI 3.17-5.30), and a negative likelihood ratio of 0.28 (95% CI, 0.18-0.44)
They cautioned, however, that the certainty of evidence from the reviewed studies was low or very low and given the small sample sizes for comparing domains, clinicians should be circumspect in interpreting the results.
An initial step
Commenting on the paper but not involved in it, David G. Fagan, MD, vice chairman of pediatric ambulatory administration in the department of pediatrics at Cohen Children’s Medical Center, New York, agreed that screening tools such as the ASQ have a place in clinical practice. “However, the purpose of a screening tool is not to make the diagnosis but to identify children at risk for developmental delays,” he said in an interview. “The meta-analysis highlights the fact that no screening is 100% accurate and that results need to be interpreted in context.
“Before screening tools were widely used, pediatricians trusted their gut,” Dr. Fagan continued. “‘I know it when I see it,’ which obviously resulted in tremendous variability based on experience.”
He added that, even if a child passes this validated questionnaire, any concern on the part of a parent or pediatrician about developmental delay should be addressed with further assessment.
The future
According to Dr. Rao, clinicians should continue to screen for developmental delays in young children using the ASQ. “Given the long wait times to see a developmental pediatrician or a clinical psychologist, a screening tool such as ASQ will enable appropriate triaging.”
Going forward, however, studies should evaluate this questionnaire separately for different age groups such as less than 12 months, 12-23 months, and at least 24 months. They should also be prospective in design and entail a low risk of bias, as well as report raw numbers for true and false positives and negatives. “Even if they use their own cutoff ASQ scores, they should also give results for the conventional cutoff scores to enable comparison with other studies,” the authors wrote.
The authors disclosed no specific funding for this study and no competing interests. Dr. Fagan disclosed no competing interests with regard to his comments.
The commonly used but sometimes debated Ages and Stages Questionnaire (ASQ), has modest utility for identifying developmental delays in young children, an Australian review and meta-analysis found.
On this easily administered parent-completed screening tool, scores of more than 2 standard deviations below the mean in more than one of five domains had moderate sensitivity and specificity to predict any delay, severe delay, motor delay, and cognitive delay, according to neonatologist Shripada Rao, PhD, a clinical associate professor in the neonatal intensive care unit at Perth Hospital and the University of Western Australia, also in Perth, and colleagues.
If a child of 12-60 months passes all ASQ domains, there is a moderate probability that child does not have severe developmental delay, the researchers concluded. If a child in that age range fails the motor or cognitive domain, there is a moderate probability that some motor or cognitive delay is present. The authors say the tool may work best as a screening test to identify children in need of more formal assessment.
“Our meta-analysis found that ASQ was somewhat more predictive in older children (older than 24 months), compared with younger age groups of 12-24 months,” Dr. Rao said in an interview. “However, the sample size for these comparisons was too small to reach definite conclusions, and we have called for future studies to evaluate ASQ separately for different age groups.”
Early identification of developmental delay in children is essential to enable timely intervention,” Dr. Rao and associates wrote in JAMA Pediatrics.
While formal assessments such as the Bayley Scales of Infant and Toddler Development are the gold standard, they are time-consuming and expensive, need the physical attendance of both the child and caregivers, and “thus may not be feasible in resource-limited settings or in pandemic conditions.”
According to Barbara J. Howard, MD, commenting on a recent update to the Center for Disease Control and Prevention’s developmental milestones guide, Learn the Signs. Act Early, fewer than 25% of children with delays or disabilities receive intervention before age 3 and most with emotional, behavioral, and developmental condition, other than autism spectrum disorder receive no intervention before age 5.
The ASQ
As an accessible alternative, the ASQ consists of questions on communication (language), gross-motor, fine-motor, problem-solving (cognitive), and personal-adaptive skills. The survey requires only 10-15 minutes, is relatively inexpensive, and also establishes a sense of parental involvement, the authors noted.
“Based on the generally accepted interpretation of LR [likelihood ratio] values, if a child passes ASQ-2SD, there is a moderate probability that the child does not have severe delay,” the investigators concluded.
The analysis
The final meta-analysis reviewed 36 eligible ASQ studies published from 1997 to 2022. Looking at the four indicators of pooled sensitivity, specificity, and positive and negative likelihood ratios, the following respective predictive values emerged for scores of more than 2 SDs below the mean across several domains: sensitivity of 0.77 (95% confidence interval, 0.64-0.86), specificity of 0.81 (95% CI 0.75-0.86), positive likelihood ratio of 4.10 (95% CI 3.17-5.30), and a negative likelihood ratio of 0.28 (95% CI, 0.18-0.44)
They cautioned, however, that the certainty of evidence from the reviewed studies was low or very low and given the small sample sizes for comparing domains, clinicians should be circumspect in interpreting the results.
An initial step
Commenting on the paper but not involved in it, David G. Fagan, MD, vice chairman of pediatric ambulatory administration in the department of pediatrics at Cohen Children’s Medical Center, New York, agreed that screening tools such as the ASQ have a place in clinical practice. “However, the purpose of a screening tool is not to make the diagnosis but to identify children at risk for developmental delays,” he said in an interview. “The meta-analysis highlights the fact that no screening is 100% accurate and that results need to be interpreted in context.
“Before screening tools were widely used, pediatricians trusted their gut,” Dr. Fagan continued. “‘I know it when I see it,’ which obviously resulted in tremendous variability based on experience.”
He added that, even if a child passes this validated questionnaire, any concern on the part of a parent or pediatrician about developmental delay should be addressed with further assessment.
The future
According to Dr. Rao, clinicians should continue to screen for developmental delays in young children using the ASQ. “Given the long wait times to see a developmental pediatrician or a clinical psychologist, a screening tool such as ASQ will enable appropriate triaging.”
Going forward, however, studies should evaluate this questionnaire separately for different age groups such as less than 12 months, 12-23 months, and at least 24 months. They should also be prospective in design and entail a low risk of bias, as well as report raw numbers for true and false positives and negatives. “Even if they use their own cutoff ASQ scores, they should also give results for the conventional cutoff scores to enable comparison with other studies,” the authors wrote.
The authors disclosed no specific funding for this study and no competing interests. Dr. Fagan disclosed no competing interests with regard to his comments.
FROM JAMA PEDIATRICS
Polycyclic Scaly Eruption
The Diagnosis: Netherton Syndrome
A punch biopsy from the right lower back supported the clinical diagnosis of ichthyosis linearis circumflexa. The patient underwent genetic testing and was found to have a heterozygous mutation in the serine protease inhibitor Kazal type 5 gene, SPINK5, that was consistent with a diagnosis of Netherton syndrome.
Netherton syndrome is an autosomal-recessive genodermatosis characterized by a triad of congenital ichthyosis, hair shaft abnormalities, and atopic diatheses.1,2 It affects approximately 1 in 200,000 live births2,3; however, it is considered by many to be underdiagnosed due to the variability in the clinical appearance. Therefore, the incidence of Netherton syndrome may actually be closer 1 in 50,000 live births.1 The manifestations of the disease are caused by a germline mutation in the SPINK5 gene, which encodes the serine protease inhibitor LEKTI.1,2 Dysfunctional LEKTI results in increased proteolytic activity of the lipid-processing enzymes in the stratum corneum, resulting in a disruption in the lipid bilayer.1 Dysfunctional LEKTI also results in a loss of the antiinflammatory and antimicrobial function of the stratum corneum. Clinical features of Netherton syndrome usually present at birth or shortly thereafter.1 Congenital ichthyosiform erythroderma, or the continuous peeling of the skin, is a common presentation seen at birth and in the neonatal period.2 As the patient ages, the dermatologic manifestations evolve into serpiginous and circinate, erythematous plaques with a characteristic peripheral, double-edged scaling.1,2 This distinctive finding is termed ichthyosis linearis circumflexa and is pathognomonic for the syndrome.2 Lesions often affect the trunk and extremities and demonstrate an undulating course.1 Because eczematous and lichenified plaques in flexural areas as well as pruritus are common clinical features, this disease often is misdiagnosed as atopic dermatitis,1,3 as was the case in our patient.
Patients with Netherton syndrome can present with various hair abnormalities. Trichorrhexis invaginata, known as bamboo hair, is the intussusception of the hair shaft and is characteristic of the disease.3 It develops from a reduced number of disulfide bonds, which results in cortical softening.1 Trichorrhexis invaginata may not be present at birth and often improves with age.1,3 Other hair shaft abnormalities such as pili torti, trichorrhexis nodosa, and helical hair also may be observed in Netherton syndrome.1 Extracutaneous manifestations also are typical. There is immune dysregulation of memory B cells and natural killer cells, which manifests as frequent respiratory and skin infections as well as sepsis.1,2 Patients also may have increased levels of serum IgE and eosinophilia resulting in atopy and allergic reactions to various triggers such as foods.1 The neonatal period also may be complicated by dehydration, electrolyte imbalances, inability to regulate body temperature, and failure to thrive.1,3
When there is an extensive disruption of the skin barrier during the neonatal period, there may be severe electrolyte imbalances and thermoregulatory challenges necessitating treatment in the neonatal intensive care unit. Cutaneous disease can be treated with topical therapies with variable success.1 Topical therapies for symptom management include emollients, corticosteroids, calcineurin inhibitors, calcipotriene, and retinoids; however, utmost caution must be employed with these therapies due to the increased risk for systemic absorption resulting from the disturbance of the skin barrier. When therapy with topical tacrolimus is implemented, monitoring of serum drug levels is required.1 Pruritus may be treated symptomatically with oral antihistamines. Intravenous immunoglobulin has been shown to decrease the frequency of infections and improve skin inflammation. Systemic retinoids have unpredictable effects and result in improvement of disease in some patients but exacerbation in others. Phototherapy with narrowband UVB, psoralen plus UVA, UVA1, and balneophototherapy also are effective treatments for cutaneous disease.1 Dupilumab has been shown to decrease pruritus, improve hair abnormalities, and improve skin disease, thereby demonstrating its effectiveness in treating the atopy and ichthyosis in Netherton syndrome.4
The differential diagnosis includes other figurate erythemas including erythema marginatum and erythrokeratodermia variabilis. Erythema marginatum is a cutaneous manifestation of acute rheumatic fever and is characterized by migratory polycyclic erythematous plaques without overlying scale, usually on the trunk and proximal extremities.5 Erythrokeratodermia variabilis is caused by heterozygous mutations in gap junction protein beta 3, GJB3, and gap junction protein beta 4, GJB4, and is characterized by transient geographic and erythematous patches and stable scaly plaques; however, double-edged scaling is not a feature.1 Acrodermatitis enteropathica is an autosomal-recessive disorder caused by mutations in the zinc transporter SLC39A4. Cutaneous manifestations occur after weaning from breast milk and are characterized by erythematous plaques with erosions, vesicles, and scaling, which characteristically occur in the perioral and perianal locations.6 Neonatal lupus is a form of subacute cutaneous lupus erythematosus. Typical skin lesions are erythematous annular plaques with overlying scaling, which may be present at birth and have a predilection for the face and other sun-exposed areas. Lesions generally resolve after clearance of the pathogenic maternal antibodies.7
- Richard G, Ringpfeil F. Ichthyoses, erythrokeratodermas, and related disorders. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2018:888-923.
- Garza JI, Herz-Ruelas ME, Guerrero-González GA, et al. Netherton syndrome: a diagnostic and therapeutic challenge. J Am Acad Dermatol. 2016;74(suppl 1):AB129.
- Heymann W. Appending the appendages: new perspectives on Netherton syndrome and green nail syndrome. J Am Acad Dermatol. 2020;83:735-736.
- Murase C, Takeichi T, Taki T, et al. Successful dupilumab treatment for ichthyotic and atopic features of Netherton syndrome. J Dermatol Sci. 2021;102:126-129.
- España A. Figurate erythemas. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2018:320-331.
- Noguera-Morel L, McLeish Schaefer S, Hivnor C. Nutritional diseases. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2018:793-809.
- Lee L, Werth V. Lupus erythematosus. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2018:662-680.
The Diagnosis: Netherton Syndrome
A punch biopsy from the right lower back supported the clinical diagnosis of ichthyosis linearis circumflexa. The patient underwent genetic testing and was found to have a heterozygous mutation in the serine protease inhibitor Kazal type 5 gene, SPINK5, that was consistent with a diagnosis of Netherton syndrome.
Netherton syndrome is an autosomal-recessive genodermatosis characterized by a triad of congenital ichthyosis, hair shaft abnormalities, and atopic diatheses.1,2 It affects approximately 1 in 200,000 live births2,3; however, it is considered by many to be underdiagnosed due to the variability in the clinical appearance. Therefore, the incidence of Netherton syndrome may actually be closer 1 in 50,000 live births.1 The manifestations of the disease are caused by a germline mutation in the SPINK5 gene, which encodes the serine protease inhibitor LEKTI.1,2 Dysfunctional LEKTI results in increased proteolytic activity of the lipid-processing enzymes in the stratum corneum, resulting in a disruption in the lipid bilayer.1 Dysfunctional LEKTI also results in a loss of the antiinflammatory and antimicrobial function of the stratum corneum. Clinical features of Netherton syndrome usually present at birth or shortly thereafter.1 Congenital ichthyosiform erythroderma, or the continuous peeling of the skin, is a common presentation seen at birth and in the neonatal period.2 As the patient ages, the dermatologic manifestations evolve into serpiginous and circinate, erythematous plaques with a characteristic peripheral, double-edged scaling.1,2 This distinctive finding is termed ichthyosis linearis circumflexa and is pathognomonic for the syndrome.2 Lesions often affect the trunk and extremities and demonstrate an undulating course.1 Because eczematous and lichenified plaques in flexural areas as well as pruritus are common clinical features, this disease often is misdiagnosed as atopic dermatitis,1,3 as was the case in our patient.
Patients with Netherton syndrome can present with various hair abnormalities. Trichorrhexis invaginata, known as bamboo hair, is the intussusception of the hair shaft and is characteristic of the disease.3 It develops from a reduced number of disulfide bonds, which results in cortical softening.1 Trichorrhexis invaginata may not be present at birth and often improves with age.1,3 Other hair shaft abnormalities such as pili torti, trichorrhexis nodosa, and helical hair also may be observed in Netherton syndrome.1 Extracutaneous manifestations also are typical. There is immune dysregulation of memory B cells and natural killer cells, which manifests as frequent respiratory and skin infections as well as sepsis.1,2 Patients also may have increased levels of serum IgE and eosinophilia resulting in atopy and allergic reactions to various triggers such as foods.1 The neonatal period also may be complicated by dehydration, electrolyte imbalances, inability to regulate body temperature, and failure to thrive.1,3
When there is an extensive disruption of the skin barrier during the neonatal period, there may be severe electrolyte imbalances and thermoregulatory challenges necessitating treatment in the neonatal intensive care unit. Cutaneous disease can be treated with topical therapies with variable success.1 Topical therapies for symptom management include emollients, corticosteroids, calcineurin inhibitors, calcipotriene, and retinoids; however, utmost caution must be employed with these therapies due to the increased risk for systemic absorption resulting from the disturbance of the skin barrier. When therapy with topical tacrolimus is implemented, monitoring of serum drug levels is required.1 Pruritus may be treated symptomatically with oral antihistamines. Intravenous immunoglobulin has been shown to decrease the frequency of infections and improve skin inflammation. Systemic retinoids have unpredictable effects and result in improvement of disease in some patients but exacerbation in others. Phototherapy with narrowband UVB, psoralen plus UVA, UVA1, and balneophototherapy also are effective treatments for cutaneous disease.1 Dupilumab has been shown to decrease pruritus, improve hair abnormalities, and improve skin disease, thereby demonstrating its effectiveness in treating the atopy and ichthyosis in Netherton syndrome.4
The differential diagnosis includes other figurate erythemas including erythema marginatum and erythrokeratodermia variabilis. Erythema marginatum is a cutaneous manifestation of acute rheumatic fever and is characterized by migratory polycyclic erythematous plaques without overlying scale, usually on the trunk and proximal extremities.5 Erythrokeratodermia variabilis is caused by heterozygous mutations in gap junction protein beta 3, GJB3, and gap junction protein beta 4, GJB4, and is characterized by transient geographic and erythematous patches and stable scaly plaques; however, double-edged scaling is not a feature.1 Acrodermatitis enteropathica is an autosomal-recessive disorder caused by mutations in the zinc transporter SLC39A4. Cutaneous manifestations occur after weaning from breast milk and are characterized by erythematous plaques with erosions, vesicles, and scaling, which characteristically occur in the perioral and perianal locations.6 Neonatal lupus is a form of subacute cutaneous lupus erythematosus. Typical skin lesions are erythematous annular plaques with overlying scaling, which may be present at birth and have a predilection for the face and other sun-exposed areas. Lesions generally resolve after clearance of the pathogenic maternal antibodies.7
The Diagnosis: Netherton Syndrome
A punch biopsy from the right lower back supported the clinical diagnosis of ichthyosis linearis circumflexa. The patient underwent genetic testing and was found to have a heterozygous mutation in the serine protease inhibitor Kazal type 5 gene, SPINK5, that was consistent with a diagnosis of Netherton syndrome.
Netherton syndrome is an autosomal-recessive genodermatosis characterized by a triad of congenital ichthyosis, hair shaft abnormalities, and atopic diatheses.1,2 It affects approximately 1 in 200,000 live births2,3; however, it is considered by many to be underdiagnosed due to the variability in the clinical appearance. Therefore, the incidence of Netherton syndrome may actually be closer 1 in 50,000 live births.1 The manifestations of the disease are caused by a germline mutation in the SPINK5 gene, which encodes the serine protease inhibitor LEKTI.1,2 Dysfunctional LEKTI results in increased proteolytic activity of the lipid-processing enzymes in the stratum corneum, resulting in a disruption in the lipid bilayer.1 Dysfunctional LEKTI also results in a loss of the antiinflammatory and antimicrobial function of the stratum corneum. Clinical features of Netherton syndrome usually present at birth or shortly thereafter.1 Congenital ichthyosiform erythroderma, or the continuous peeling of the skin, is a common presentation seen at birth and in the neonatal period.2 As the patient ages, the dermatologic manifestations evolve into serpiginous and circinate, erythematous plaques with a characteristic peripheral, double-edged scaling.1,2 This distinctive finding is termed ichthyosis linearis circumflexa and is pathognomonic for the syndrome.2 Lesions often affect the trunk and extremities and demonstrate an undulating course.1 Because eczematous and lichenified plaques in flexural areas as well as pruritus are common clinical features, this disease often is misdiagnosed as atopic dermatitis,1,3 as was the case in our patient.
Patients with Netherton syndrome can present with various hair abnormalities. Trichorrhexis invaginata, known as bamboo hair, is the intussusception of the hair shaft and is characteristic of the disease.3 It develops from a reduced number of disulfide bonds, which results in cortical softening.1 Trichorrhexis invaginata may not be present at birth and often improves with age.1,3 Other hair shaft abnormalities such as pili torti, trichorrhexis nodosa, and helical hair also may be observed in Netherton syndrome.1 Extracutaneous manifestations also are typical. There is immune dysregulation of memory B cells and natural killer cells, which manifests as frequent respiratory and skin infections as well as sepsis.1,2 Patients also may have increased levels of serum IgE and eosinophilia resulting in atopy and allergic reactions to various triggers such as foods.1 The neonatal period also may be complicated by dehydration, electrolyte imbalances, inability to regulate body temperature, and failure to thrive.1,3
When there is an extensive disruption of the skin barrier during the neonatal period, there may be severe electrolyte imbalances and thermoregulatory challenges necessitating treatment in the neonatal intensive care unit. Cutaneous disease can be treated with topical therapies with variable success.1 Topical therapies for symptom management include emollients, corticosteroids, calcineurin inhibitors, calcipotriene, and retinoids; however, utmost caution must be employed with these therapies due to the increased risk for systemic absorption resulting from the disturbance of the skin barrier. When therapy with topical tacrolimus is implemented, monitoring of serum drug levels is required.1 Pruritus may be treated symptomatically with oral antihistamines. Intravenous immunoglobulin has been shown to decrease the frequency of infections and improve skin inflammation. Systemic retinoids have unpredictable effects and result in improvement of disease in some patients but exacerbation in others. Phototherapy with narrowband UVB, psoralen plus UVA, UVA1, and balneophototherapy also are effective treatments for cutaneous disease.1 Dupilumab has been shown to decrease pruritus, improve hair abnormalities, and improve skin disease, thereby demonstrating its effectiveness in treating the atopy and ichthyosis in Netherton syndrome.4
The differential diagnosis includes other figurate erythemas including erythema marginatum and erythrokeratodermia variabilis. Erythema marginatum is a cutaneous manifestation of acute rheumatic fever and is characterized by migratory polycyclic erythematous plaques without overlying scale, usually on the trunk and proximal extremities.5 Erythrokeratodermia variabilis is caused by heterozygous mutations in gap junction protein beta 3, GJB3, and gap junction protein beta 4, GJB4, and is characterized by transient geographic and erythematous patches and stable scaly plaques; however, double-edged scaling is not a feature.1 Acrodermatitis enteropathica is an autosomal-recessive disorder caused by mutations in the zinc transporter SLC39A4. Cutaneous manifestations occur after weaning from breast milk and are characterized by erythematous plaques with erosions, vesicles, and scaling, which characteristically occur in the perioral and perianal locations.6 Neonatal lupus is a form of subacute cutaneous lupus erythematosus. Typical skin lesions are erythematous annular plaques with overlying scaling, which may be present at birth and have a predilection for the face and other sun-exposed areas. Lesions generally resolve after clearance of the pathogenic maternal antibodies.7
- Richard G, Ringpfeil F. Ichthyoses, erythrokeratodermas, and related disorders. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2018:888-923.
- Garza JI, Herz-Ruelas ME, Guerrero-González GA, et al. Netherton syndrome: a diagnostic and therapeutic challenge. J Am Acad Dermatol. 2016;74(suppl 1):AB129.
- Heymann W. Appending the appendages: new perspectives on Netherton syndrome and green nail syndrome. J Am Acad Dermatol. 2020;83:735-736.
- Murase C, Takeichi T, Taki T, et al. Successful dupilumab treatment for ichthyotic and atopic features of Netherton syndrome. J Dermatol Sci. 2021;102:126-129.
- España A. Figurate erythemas. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2018:320-331.
- Noguera-Morel L, McLeish Schaefer S, Hivnor C. Nutritional diseases. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2018:793-809.
- Lee L, Werth V. Lupus erythematosus. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2018:662-680.
- Richard G, Ringpfeil F. Ichthyoses, erythrokeratodermas, and related disorders. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2018:888-923.
- Garza JI, Herz-Ruelas ME, Guerrero-González GA, et al. Netherton syndrome: a diagnostic and therapeutic challenge. J Am Acad Dermatol. 2016;74(suppl 1):AB129.
- Heymann W. Appending the appendages: new perspectives on Netherton syndrome and green nail syndrome. J Am Acad Dermatol. 2020;83:735-736.
- Murase C, Takeichi T, Taki T, et al. Successful dupilumab treatment for ichthyotic and atopic features of Netherton syndrome. J Dermatol Sci. 2021;102:126-129.
- España A. Figurate erythemas. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2018:320-331.
- Noguera-Morel L, McLeish Schaefer S, Hivnor C. Nutritional diseases. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2018:793-809.
- Lee L, Werth V. Lupus erythematosus. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2018:662-680.
A 9-year-old boy presented to the dermatology clinic with a scaly eruption distributed throughout the body that had been present since birth. He had been diagnosed with atopic dermatitis by multiple dermatologists prior to the current presentation and had been treated with various topical steroids with minimal improvement. He had no family history of similar eruptions and no personal history of asthma or allergies. Physical examination revealed erythematous, serpiginous, polycyclic plaques with peripheral, double-edged scaling. Decreased hair density of the lateral eyebrows also was observed.

Ketamine promising for rare condition linked to autism
Also known as Helsmoortel–Van Der Aa syndrome, ADNP syndrome is caused by mutations in the ADNP gene. Studies in animal models suggest that low-dose ketamine increases expression of ADNP and is neuroprotective.
Intrigued by the preclinical evidence, Alexander Kolevzon, MD, clinical director of the Seaver Autism Center at Mount Sinai, New York, and colleagues treated 10 children with ADNP syndrome with a single low dose of ketamine (0.5mg/kg) infused intravenously over 40 minutes. The children ranged in ages 6-12 years.
Using parent-report instruments to assess treatment effects, ketamine was associated with “nominally significant” improvement in a variety of domains, including social behavior, attention-deficit and hyperactivity, restricted and repetitive behaviors, and sensory sensitivities.
Parent reports of improvement in these domains aligned with clinician-rated assessments based on the Clinical Global Impressions–Improvement scale.
The results also highlight the potential utility of electrophysiological measurement of auditory steady-state response and eye-tracking to track change with ketamine treatment, the researchers say.
The study was published online in Human Genetics and Genomic (HGG) Advances.
Hypothesis-generating
Ketamine was generally well tolerated. There were no clinically significant abnormalities in laboratory or cardiac monitoring, and there were no serious adverse events (AEs).
Treatment emergent AEs were all mild to moderate and no child required any interventions.
The most common AEs were elation/silliness in five children (50%), all of whom had a history of similar symptoms. Drowsiness and fatigue occurred in four children (40%) and two of them had a history of drowsiness. Aggression was likewise relatively common, reported in four children (40%), all of whom had aggression at baseline.
Decreased appetite emerged as a new AE in three children (30%), increased anxiety occurred in three children (30%), and irritability, nausea/vomiting, and restlessness each occurred in two children (20%).
The researchers caution that the findings are intended to be “hypothesis generating.”
“We are encouraged by these findings, which provide preliminary support for ketamine to help reduce negative effects of this devastating syndrome,” Dr. Kolevzon said in a news release from Mount Sinai.
Ketamine might help ease symptoms of ADNP syndrome “by increasing expression of the ADNP gene or by promoting synaptic plasticity through glutamatergic pathways,” Dr. Kolevzon told this news organization.
The next step, he said, is to get “a larger, placebo-controlled study approved for funding using repeated dosing over a longer duration of time. We are working with the FDA to get the design approved for an investigational new drug application.”
Support for the study was provided by the ADNP Kids Foundation and the Foundation for Mood Disorders. Support for mediKanren was provided by the National Center for Advancing Translational Sciences, and National Institutes of Health through the Biomedical Data Translator Program. Dr. Kolevzon is on the scientific advisory board of Ovid Therapeutics, Ritrova Therapeutics, and Jaguar Therapeutics and consults to Acadia, Alkermes, GW Pharmaceuticals, Neuren Pharmaceuticals, Clinilabs Drug Development Corporation, and Scioto Biosciences.
A version of this article first appeared on Medscape.com.
Also known as Helsmoortel–Van Der Aa syndrome, ADNP syndrome is caused by mutations in the ADNP gene. Studies in animal models suggest that low-dose ketamine increases expression of ADNP and is neuroprotective.
Intrigued by the preclinical evidence, Alexander Kolevzon, MD, clinical director of the Seaver Autism Center at Mount Sinai, New York, and colleagues treated 10 children with ADNP syndrome with a single low dose of ketamine (0.5mg/kg) infused intravenously over 40 minutes. The children ranged in ages 6-12 years.
Using parent-report instruments to assess treatment effects, ketamine was associated with “nominally significant” improvement in a variety of domains, including social behavior, attention-deficit and hyperactivity, restricted and repetitive behaviors, and sensory sensitivities.
Parent reports of improvement in these domains aligned with clinician-rated assessments based on the Clinical Global Impressions–Improvement scale.
The results also highlight the potential utility of electrophysiological measurement of auditory steady-state response and eye-tracking to track change with ketamine treatment, the researchers say.
The study was published online in Human Genetics and Genomic (HGG) Advances.
Hypothesis-generating
Ketamine was generally well tolerated. There were no clinically significant abnormalities in laboratory or cardiac monitoring, and there were no serious adverse events (AEs).
Treatment emergent AEs were all mild to moderate and no child required any interventions.
The most common AEs were elation/silliness in five children (50%), all of whom had a history of similar symptoms. Drowsiness and fatigue occurred in four children (40%) and two of them had a history of drowsiness. Aggression was likewise relatively common, reported in four children (40%), all of whom had aggression at baseline.
Decreased appetite emerged as a new AE in three children (30%), increased anxiety occurred in three children (30%), and irritability, nausea/vomiting, and restlessness each occurred in two children (20%).
The researchers caution that the findings are intended to be “hypothesis generating.”
“We are encouraged by these findings, which provide preliminary support for ketamine to help reduce negative effects of this devastating syndrome,” Dr. Kolevzon said in a news release from Mount Sinai.
Ketamine might help ease symptoms of ADNP syndrome “by increasing expression of the ADNP gene or by promoting synaptic plasticity through glutamatergic pathways,” Dr. Kolevzon told this news organization.
The next step, he said, is to get “a larger, placebo-controlled study approved for funding using repeated dosing over a longer duration of time. We are working with the FDA to get the design approved for an investigational new drug application.”
Support for the study was provided by the ADNP Kids Foundation and the Foundation for Mood Disorders. Support for mediKanren was provided by the National Center for Advancing Translational Sciences, and National Institutes of Health through the Biomedical Data Translator Program. Dr. Kolevzon is on the scientific advisory board of Ovid Therapeutics, Ritrova Therapeutics, and Jaguar Therapeutics and consults to Acadia, Alkermes, GW Pharmaceuticals, Neuren Pharmaceuticals, Clinilabs Drug Development Corporation, and Scioto Biosciences.
A version of this article first appeared on Medscape.com.
Also known as Helsmoortel–Van Der Aa syndrome, ADNP syndrome is caused by mutations in the ADNP gene. Studies in animal models suggest that low-dose ketamine increases expression of ADNP and is neuroprotective.
Intrigued by the preclinical evidence, Alexander Kolevzon, MD, clinical director of the Seaver Autism Center at Mount Sinai, New York, and colleagues treated 10 children with ADNP syndrome with a single low dose of ketamine (0.5mg/kg) infused intravenously over 40 minutes. The children ranged in ages 6-12 years.
Using parent-report instruments to assess treatment effects, ketamine was associated with “nominally significant” improvement in a variety of domains, including social behavior, attention-deficit and hyperactivity, restricted and repetitive behaviors, and sensory sensitivities.
Parent reports of improvement in these domains aligned with clinician-rated assessments based on the Clinical Global Impressions–Improvement scale.
The results also highlight the potential utility of electrophysiological measurement of auditory steady-state response and eye-tracking to track change with ketamine treatment, the researchers say.
The study was published online in Human Genetics and Genomic (HGG) Advances.
Hypothesis-generating
Ketamine was generally well tolerated. There were no clinically significant abnormalities in laboratory or cardiac monitoring, and there were no serious adverse events (AEs).
Treatment emergent AEs were all mild to moderate and no child required any interventions.
The most common AEs were elation/silliness in five children (50%), all of whom had a history of similar symptoms. Drowsiness and fatigue occurred in four children (40%) and two of them had a history of drowsiness. Aggression was likewise relatively common, reported in four children (40%), all of whom had aggression at baseline.
Decreased appetite emerged as a new AE in three children (30%), increased anxiety occurred in three children (30%), and irritability, nausea/vomiting, and restlessness each occurred in two children (20%).
The researchers caution that the findings are intended to be “hypothesis generating.”
“We are encouraged by these findings, which provide preliminary support for ketamine to help reduce negative effects of this devastating syndrome,” Dr. Kolevzon said in a news release from Mount Sinai.
Ketamine might help ease symptoms of ADNP syndrome “by increasing expression of the ADNP gene or by promoting synaptic plasticity through glutamatergic pathways,” Dr. Kolevzon told this news organization.
The next step, he said, is to get “a larger, placebo-controlled study approved for funding using repeated dosing over a longer duration of time. We are working with the FDA to get the design approved for an investigational new drug application.”
Support for the study was provided by the ADNP Kids Foundation and the Foundation for Mood Disorders. Support for mediKanren was provided by the National Center for Advancing Translational Sciences, and National Institutes of Health through the Biomedical Data Translator Program. Dr. Kolevzon is on the scientific advisory board of Ovid Therapeutics, Ritrova Therapeutics, and Jaguar Therapeutics and consults to Acadia, Alkermes, GW Pharmaceuticals, Neuren Pharmaceuticals, Clinilabs Drug Development Corporation, and Scioto Biosciences.
A version of this article first appeared on Medscape.com.
From Human Genetics and Genomic Advances
Children and COVID: New cases took a downturn in September
After 2 weeks of increases in the number of new COVID-19 cases in children – a trend that just happened to coincide with the start of a new school year – there were fewer cases reported during the first full week of September, according to the American Academy of Pediatrics and the Children’s Hospital Association.
, the AAP and CHA said in their weekly COVID-19 report, noting also that seven states and the District of Columbia no longer update their online dashboards while others publish new data less often than every week.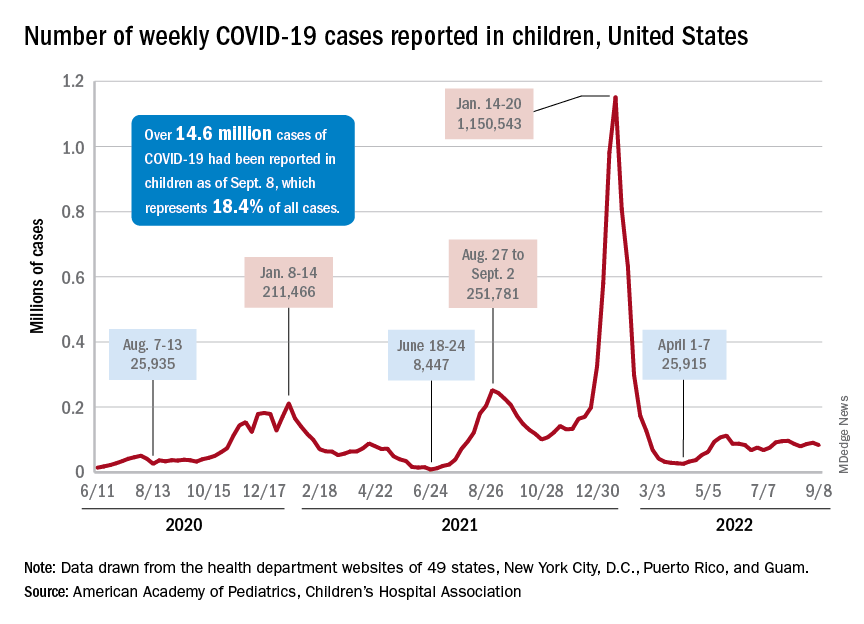
The drop in new cases was accompanied by declines in emergency department visits and hospital admissions, both of which had shown some signs of resurgence in mid- to late August. The brief rise in ED visits seemed to be age-related, occurring in those aged 12 years and older but not in younger children, whose ED visit rate fell steadily through August. Through the first week of September, however, 7-day averages were down for both those aged 12-15 and for 16- to 17-year-olds, the Centers for Disease Control and Prevention reported.
The rate of new hospital admissions of children with confirmed COVID-19, available only for ages 0-17 years, has declined every day since Aug. 28, when it reached 0.44 per 100,000 population after a week of climbing, the CDC said on its COVID Data Tracker.
Cumulatively, about 156,000 children were hospitalized with COVID from Aug. 1, 2020 to Sept. 10, 2022, according to the CDC, which puts the total number of pediatric cases at just over 15 million and deaths at 1,778. Those last two figures represent 17.4% and about 0.4% of all U.S. cases and deaths. The AAP and CHA estimate that about 14.6 million child cases have been reported so far, which is 18.4% of cases in all ages.
Vaccinations are slowly adding up
On the prevention side of the health care system’s response to COVID, the CDC’s cumulative numbers looked like this as of Sept. 6:
- 1.1 million children under age 5 (about 5.8% of the age group) had received at least one dose of vaccine, and 280,000 (1.4%) were fully vaccinated.
- Almost 11 million (38.2%) children aged 5-11 had gotten one dose, and 8.9 million (31.1%) were fully vaccinated.
- 17.9 million (70.8%) children aged 12-17 had received at least one dose, and 15.3 million (60.5%) were fully vaccinated.
Over the 14 days ending Sept. 7, children aged 2-4 years made up the largest group (21.4%) of Americans getting their first vaccine doses, while those aged 5-11 years were the third largest age group at 16.7% of all vaccinees (25- to 49-year-olds were second). The situation was reversed for vaccine completion over the last 2 weeks: Those aged 5-11 were first at 24.7%, and the 2- to 4-year-olds were third at 16.7% (those aged 25-49 were second again), according to the COVID Data Tracker.
After 2 weeks of increases in the number of new COVID-19 cases in children – a trend that just happened to coincide with the start of a new school year – there were fewer cases reported during the first full week of September, according to the American Academy of Pediatrics and the Children’s Hospital Association.
, the AAP and CHA said in their weekly COVID-19 report, noting also that seven states and the District of Columbia no longer update their online dashboards while others publish new data less often than every week.
The drop in new cases was accompanied by declines in emergency department visits and hospital admissions, both of which had shown some signs of resurgence in mid- to late August. The brief rise in ED visits seemed to be age-related, occurring in those aged 12 years and older but not in younger children, whose ED visit rate fell steadily through August. Through the first week of September, however, 7-day averages were down for both those aged 12-15 and for 16- to 17-year-olds, the Centers for Disease Control and Prevention reported.
The rate of new hospital admissions of children with confirmed COVID-19, available only for ages 0-17 years, has declined every day since Aug. 28, when it reached 0.44 per 100,000 population after a week of climbing, the CDC said on its COVID Data Tracker.
Cumulatively, about 156,000 children were hospitalized with COVID from Aug. 1, 2020 to Sept. 10, 2022, according to the CDC, which puts the total number of pediatric cases at just over 15 million and deaths at 1,778. Those last two figures represent 17.4% and about 0.4% of all U.S. cases and deaths. The AAP and CHA estimate that about 14.6 million child cases have been reported so far, which is 18.4% of cases in all ages.
Vaccinations are slowly adding up
On the prevention side of the health care system’s response to COVID, the CDC’s cumulative numbers looked like this as of Sept. 6:
- 1.1 million children under age 5 (about 5.8% of the age group) had received at least one dose of vaccine, and 280,000 (1.4%) were fully vaccinated.
- Almost 11 million (38.2%) children aged 5-11 had gotten one dose, and 8.9 million (31.1%) were fully vaccinated.
- 17.9 million (70.8%) children aged 12-17 had received at least one dose, and 15.3 million (60.5%) were fully vaccinated.
Over the 14 days ending Sept. 7, children aged 2-4 years made up the largest group (21.4%) of Americans getting their first vaccine doses, while those aged 5-11 years were the third largest age group at 16.7% of all vaccinees (25- to 49-year-olds were second). The situation was reversed for vaccine completion over the last 2 weeks: Those aged 5-11 were first at 24.7%, and the 2- to 4-year-olds were third at 16.7% (those aged 25-49 were second again), according to the COVID Data Tracker.
After 2 weeks of increases in the number of new COVID-19 cases in children – a trend that just happened to coincide with the start of a new school year – there were fewer cases reported during the first full week of September, according to the American Academy of Pediatrics and the Children’s Hospital Association.
, the AAP and CHA said in their weekly COVID-19 report, noting also that seven states and the District of Columbia no longer update their online dashboards while others publish new data less often than every week.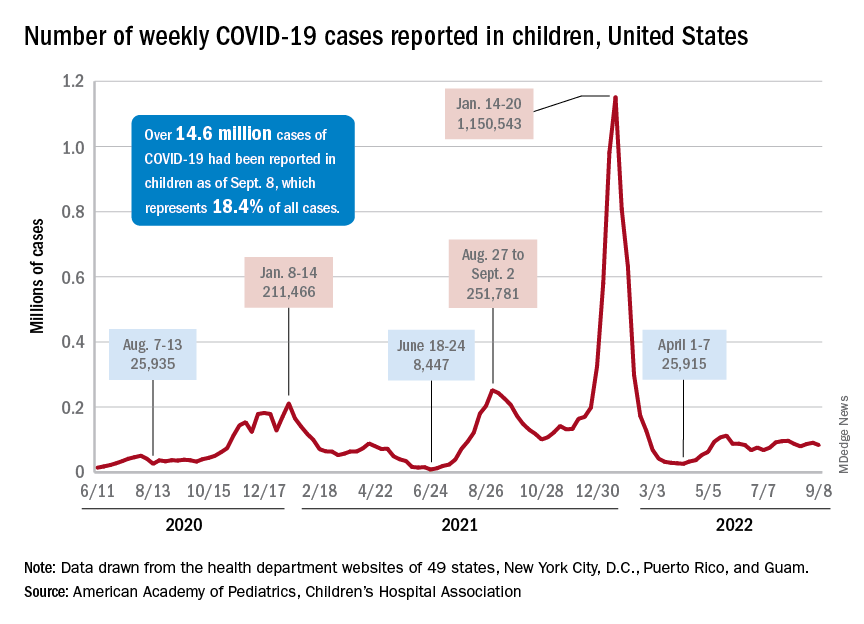
The drop in new cases was accompanied by declines in emergency department visits and hospital admissions, both of which had shown some signs of resurgence in mid- to late August. The brief rise in ED visits seemed to be age-related, occurring in those aged 12 years and older but not in younger children, whose ED visit rate fell steadily through August. Through the first week of September, however, 7-day averages were down for both those aged 12-15 and for 16- to 17-year-olds, the Centers for Disease Control and Prevention reported.
The rate of new hospital admissions of children with confirmed COVID-19, available only for ages 0-17 years, has declined every day since Aug. 28, when it reached 0.44 per 100,000 population after a week of climbing, the CDC said on its COVID Data Tracker.
Cumulatively, about 156,000 children were hospitalized with COVID from Aug. 1, 2020 to Sept. 10, 2022, according to the CDC, which puts the total number of pediatric cases at just over 15 million and deaths at 1,778. Those last two figures represent 17.4% and about 0.4% of all U.S. cases and deaths. The AAP and CHA estimate that about 14.6 million child cases have been reported so far, which is 18.4% of cases in all ages.
Vaccinations are slowly adding up
On the prevention side of the health care system’s response to COVID, the CDC’s cumulative numbers looked like this as of Sept. 6:
- 1.1 million children under age 5 (about 5.8% of the age group) had received at least one dose of vaccine, and 280,000 (1.4%) were fully vaccinated.
- Almost 11 million (38.2%) children aged 5-11 had gotten one dose, and 8.9 million (31.1%) were fully vaccinated.
- 17.9 million (70.8%) children aged 12-17 had received at least one dose, and 15.3 million (60.5%) were fully vaccinated.
Over the 14 days ending Sept. 7, children aged 2-4 years made up the largest group (21.4%) of Americans getting their first vaccine doses, while those aged 5-11 years were the third largest age group at 16.7% of all vaccinees (25- to 49-year-olds were second). The situation was reversed for vaccine completion over the last 2 weeks: Those aged 5-11 were first at 24.7%, and the 2- to 4-year-olds were third at 16.7% (those aged 25-49 were second again), according to the COVID Data Tracker.
CDC warns of enterovirus strain linked to polio-like condition
, according to a Health Network Alert advisory by the Centers for Disease Control and Prevention.
In August, health care providers and hospitals notified the CDC of an increase in severe respiratory illness in children who also tested positive for rhinovirus (RV) or enterovirus (EV). Additional testing revealed that some children were positive for EV-D68, which primarily causes acute respiratory illness. However, the virus has been associated with acute flaccid myelitis (AFM), a rare neurologic condition involving muscle weakness.
Also, in July and August 2022, surveillance networks reported an increase in EV-D68 activity compared with the same months in 2019, 2020, and 2021, the agency said in the alert. As of Aug. 30, the CDC has not received any reports of AFM beginning this year; however, spikes in EV-D68 typically come before cases of AFM, they said.
“Something we are always on the lookout for in the late summer and fall is AFM cases,” said Rick Malley, MD, of the division of infectious disease at Boston Children’s Hospital, in an interview with this news organization. “Unfortunately, we kind of expect them during enterovirus season,” he said. That season is thought to peak in the late summer and early fall.
Since the CDC began tracking AFM in August 2014, there have been 692 confirmed cases in the United States. AFM cases spiked in 2014, 2016, and 2018, mostly in young children. In 2021, there were 28 confirmed cases across 15 states. The CDC did not specify the age of those cases, but in 2018 – when EV-D68 most recently circulated at high levels – the median age of children who visited the emergency department or were hospitalized for EV-D68–associated respiratory illness was 3 years.
“[AFM] can be very severe and it can be very scary for the parents of children who have it,” Dr. Malley said, “but given the prevalence of enteroviruses in the community, you have to conclude it’s a relatively rare event in susceptible individuals. Why some get it and others don’t is unfortunately unclear at this moment.”
The CDC recommends that providers consider EV-D68 as a possible cause for acute, severe respiratory illness in children. If the cause of a respiratory illness in a severely ill patient is not clear, health professionals should test for RVs and EVs, if this is not already part of a typical diagnostic workflow, the agency said. Currently, there are no vaccines or specific treatments for RV or EV, and the CDC recommends supportive clinical management.
The advisory also urged providers to “strongly consider AFM in patients with acute flaccid limb weakness, especially after respiratory illness or fever, and between the months of August and November 2022.”
For any patient presenting with possible AFM, clinicians should collect samples from multiple sources, including cerebrospinal fluid, serum, stool, and a nasopharyngeal or oropharyngeal swab. Samples should be taken “as early as possible and preferably on the day of onset of limb weakness,” the alert said. There is currently no specific medicine for AFM, the agency said, though recommended interventions may vary for each patient.
A version of this article first appeared on Medscape.com.
, according to a Health Network Alert advisory by the Centers for Disease Control and Prevention.
In August, health care providers and hospitals notified the CDC of an increase in severe respiratory illness in children who also tested positive for rhinovirus (RV) or enterovirus (EV). Additional testing revealed that some children were positive for EV-D68, which primarily causes acute respiratory illness. However, the virus has been associated with acute flaccid myelitis (AFM), a rare neurologic condition involving muscle weakness.
Also, in July and August 2022, surveillance networks reported an increase in EV-D68 activity compared with the same months in 2019, 2020, and 2021, the agency said in the alert. As of Aug. 30, the CDC has not received any reports of AFM beginning this year; however, spikes in EV-D68 typically come before cases of AFM, they said.
“Something we are always on the lookout for in the late summer and fall is AFM cases,” said Rick Malley, MD, of the division of infectious disease at Boston Children’s Hospital, in an interview with this news organization. “Unfortunately, we kind of expect them during enterovirus season,” he said. That season is thought to peak in the late summer and early fall.
Since the CDC began tracking AFM in August 2014, there have been 692 confirmed cases in the United States. AFM cases spiked in 2014, 2016, and 2018, mostly in young children. In 2021, there were 28 confirmed cases across 15 states. The CDC did not specify the age of those cases, but in 2018 – when EV-D68 most recently circulated at high levels – the median age of children who visited the emergency department or were hospitalized for EV-D68–associated respiratory illness was 3 years.
“[AFM] can be very severe and it can be very scary for the parents of children who have it,” Dr. Malley said, “but given the prevalence of enteroviruses in the community, you have to conclude it’s a relatively rare event in susceptible individuals. Why some get it and others don’t is unfortunately unclear at this moment.”
The CDC recommends that providers consider EV-D68 as a possible cause for acute, severe respiratory illness in children. If the cause of a respiratory illness in a severely ill patient is not clear, health professionals should test for RVs and EVs, if this is not already part of a typical diagnostic workflow, the agency said. Currently, there are no vaccines or specific treatments for RV or EV, and the CDC recommends supportive clinical management.
The advisory also urged providers to “strongly consider AFM in patients with acute flaccid limb weakness, especially after respiratory illness or fever, and between the months of August and November 2022.”
For any patient presenting with possible AFM, clinicians should collect samples from multiple sources, including cerebrospinal fluid, serum, stool, and a nasopharyngeal or oropharyngeal swab. Samples should be taken “as early as possible and preferably on the day of onset of limb weakness,” the alert said. There is currently no specific medicine for AFM, the agency said, though recommended interventions may vary for each patient.
A version of this article first appeared on Medscape.com.
, according to a Health Network Alert advisory by the Centers for Disease Control and Prevention.
In August, health care providers and hospitals notified the CDC of an increase in severe respiratory illness in children who also tested positive for rhinovirus (RV) or enterovirus (EV). Additional testing revealed that some children were positive for EV-D68, which primarily causes acute respiratory illness. However, the virus has been associated with acute flaccid myelitis (AFM), a rare neurologic condition involving muscle weakness.
Also, in July and August 2022, surveillance networks reported an increase in EV-D68 activity compared with the same months in 2019, 2020, and 2021, the agency said in the alert. As of Aug. 30, the CDC has not received any reports of AFM beginning this year; however, spikes in EV-D68 typically come before cases of AFM, they said.
“Something we are always on the lookout for in the late summer and fall is AFM cases,” said Rick Malley, MD, of the division of infectious disease at Boston Children’s Hospital, in an interview with this news organization. “Unfortunately, we kind of expect them during enterovirus season,” he said. That season is thought to peak in the late summer and early fall.
Since the CDC began tracking AFM in August 2014, there have been 692 confirmed cases in the United States. AFM cases spiked in 2014, 2016, and 2018, mostly in young children. In 2021, there were 28 confirmed cases across 15 states. The CDC did not specify the age of those cases, but in 2018 – when EV-D68 most recently circulated at high levels – the median age of children who visited the emergency department or were hospitalized for EV-D68–associated respiratory illness was 3 years.
“[AFM] can be very severe and it can be very scary for the parents of children who have it,” Dr. Malley said, “but given the prevalence of enteroviruses in the community, you have to conclude it’s a relatively rare event in susceptible individuals. Why some get it and others don’t is unfortunately unclear at this moment.”
The CDC recommends that providers consider EV-D68 as a possible cause for acute, severe respiratory illness in children. If the cause of a respiratory illness in a severely ill patient is not clear, health professionals should test for RVs and EVs, if this is not already part of a typical diagnostic workflow, the agency said. Currently, there are no vaccines or specific treatments for RV or EV, and the CDC recommends supportive clinical management.
The advisory also urged providers to “strongly consider AFM in patients with acute flaccid limb weakness, especially after respiratory illness or fever, and between the months of August and November 2022.”
For any patient presenting with possible AFM, clinicians should collect samples from multiple sources, including cerebrospinal fluid, serum, stool, and a nasopharyngeal or oropharyngeal swab. Samples should be taken “as early as possible and preferably on the day of onset of limb weakness,” the alert said. There is currently no specific medicine for AFM, the agency said, though recommended interventions may vary for each patient.
A version of this article first appeared on Medscape.com.
Weight gain during pregnancy may play role in child ADHD risk
Obesity in women of reproductive age has emerged as one of the main risk factors associated with neonatal complications and long-term neuropsychiatric consequences in offspring, including attention-deficit/hyperactivity disorder.
Research has also linked pregestational diabetes and gestational diabetes mellitus (GDM) to an increased risk for ADHD in offspring. Now, an observational study of 1,036 singleton births at one hospital between 1998 and 2008 suggests that in the presence of GDM, maternal obesity combined with excessive weight gain during pregnancy may be jointly associated with increased risk of offspring ADHD. The median follow-up was 17.7 years.
Maternal obesity was independently associated with ADHD (adjusted hazard ratio, 1.66; 95% confidence interval: 1.07-2.60), but excessive weight gain during pregnancy and maternal overweight were not, reported Verónica Perea, MD, PhD, of the Hospital Universitari Mútua de Terrassa, Barcelona, and colleagues in the Journal of Clinical Endocrinology & Metabolism.
However, in women with pregestation obesity who gained more weight than recommended by the National Academy of Medicine (NAM), the risk of offspring ADHD was higher, compared with women of normal weight whose pregnancy weight stayed within NAM guidelines (adjusted hazard ratio, 2.13; 95% confidence interval: 1.14-4.01).
“The results of this study suggest that the negative repercussions of excessive weight gain on children within the setting of a high-risk population with GDM and obesity were not only observed during the prenatal period but also years later with a development of ADHD,” the researchers wrote.
The study also showed that when maternal weight gain did not exceed NAM guidelines, maternal obesity was no longer independently associated with ADHD in offspring (aHR, 1.36; 95% CI: 0.78-2.36). This finding conflicts with earlier studies focusing primarily on the role of pregestational maternal weight, the researchers said. A 2018 nationwide Finnish cohort study in newborns showed an increased long-term risk of ADHD in those born to women with GDM, compared with the nondiabetic population. This long-term risk of ADHD increased in the presence of pregestational obesity (HR, 1.64).
Similarly, evidence from systematic reviews and meta-analyses has demonstrated that antenatal lifestyle interventions to prevent excessive weight gain during pregnancy were associated with a reduction in adverse pregnancy outcomes. However, evidence on offspring mental health was lacking, especially in high-risk pregnancies with gestational diabetes, the study authors said.
Although causal inferences can’t be drawn from the current observational study, “it seems that the higher risk [of ADHD] observed would be explained by the role of gestational weight gain during the antenatal period,” Dr. Perea said in an interview. Importantly, the study highlights a window of opportunity for promoting healthy weight gain during pregnancy, Dr. Perea said. ”This should be a priority in the current management of gestation.”
Fatima Cody Stanford, MD, MPH, an associate professor of medicine and pediatrics at Harvard Medical School, Boston, agreed. “I think one of the key issues is that there’s very little attention paid to how weight gain is regulated during pregnancy,” she said in an interview. On many other points, however, Dr. Stanford, who is a specialist in obesity medicine at Massachusetts General Hospital Weight Center, did not agree.
The association between ADHD and obesity has already been well established by a 2019 meta-analysis and systematic review of studies over the last 10 years, she emphasized. “These studies were able to show a much stronger association between maternal obesity and ADHD in offspring because they were powered to detect differences.”
The current study does not say “anything new or novel,” Dr. Stanford added. “Maternal obesity and the association with an increased risk of ADHD in offspring is the main issue. I don’t think there was any appreciable increase when weight gain during pregnancy was factored in. It’s mild at best.”
Eran Bornstein, MD, vice-chair of obstetrics and gynecology at Lenox Hill Hospital, New York, expressed a similar point of view. Although the study findings “add to the current literature,” they should be interpreted “cautiously,” Dr. Bornstein said in an interview.
The size of the effect on ADHD risk attributable to maternal weight gain during pregnancy “was not clear,” he said. “Cohort studies of this sort are excellent for finding associations which help us generate the hypothesis, but this doesn’t demonstrate a cause and effect or a magnitude for this effect.”
Physicians should follow cumulative data suggesting that maternal obesity is associated with a number of pregnancy complications and neonatal outcomes in women with and without diabetes, Dr. Bornstein suggested. “Optimizing maternal weight prior to pregnancy and adhering to recommendations regarding weight gain has the potential to improve some of these outcomes.”
Treating obesity prior to conception mitigates GDM risk, agreed Dr. Stanford. “The issue,” she explained, “is that all of the drugs approved for the treatment of obesity are contraindicated in pregnancy and lifestyle modification fails in 96% of cases, even when there is no pregnancy.” Drugs such as metformin are being used off-label to treat obesity and to safely manage gestational weight gain, she said. “Those of us who practice obesity medicine know that metformin can be safely used throughout pregnancy with no harm to the fetus.”
This study was partially funded by Fundació Docència i Recerca MútuaTerrassa. Dr. Perea and study coauthors reporting have no conflicts of interest. Dr. Stanford disclosed relationships with Novo Nordisk, Eli Lilly, Boehringer Ingelheim, Gelesis, Pfizer, Currax, and Rhythm. Dr. Bornstein reported having no conflicts of interest.
This story was updated on 11/7/2022.
Obesity in women of reproductive age has emerged as one of the main risk factors associated with neonatal complications and long-term neuropsychiatric consequences in offspring, including attention-deficit/hyperactivity disorder.
Research has also linked pregestational diabetes and gestational diabetes mellitus (GDM) to an increased risk for ADHD in offspring. Now, an observational study of 1,036 singleton births at one hospital between 1998 and 2008 suggests that in the presence of GDM, maternal obesity combined with excessive weight gain during pregnancy may be jointly associated with increased risk of offspring ADHD. The median follow-up was 17.7 years.
Maternal obesity was independently associated with ADHD (adjusted hazard ratio, 1.66; 95% confidence interval: 1.07-2.60), but excessive weight gain during pregnancy and maternal overweight were not, reported Verónica Perea, MD, PhD, of the Hospital Universitari Mútua de Terrassa, Barcelona, and colleagues in the Journal of Clinical Endocrinology & Metabolism.
However, in women with pregestation obesity who gained more weight than recommended by the National Academy of Medicine (NAM), the risk of offspring ADHD was higher, compared with women of normal weight whose pregnancy weight stayed within NAM guidelines (adjusted hazard ratio, 2.13; 95% confidence interval: 1.14-4.01).
“The results of this study suggest that the negative repercussions of excessive weight gain on children within the setting of a high-risk population with GDM and obesity were not only observed during the prenatal period but also years later with a development of ADHD,” the researchers wrote.
The study also showed that when maternal weight gain did not exceed NAM guidelines, maternal obesity was no longer independently associated with ADHD in offspring (aHR, 1.36; 95% CI: 0.78-2.36). This finding conflicts with earlier studies focusing primarily on the role of pregestational maternal weight, the researchers said. A 2018 nationwide Finnish cohort study in newborns showed an increased long-term risk of ADHD in those born to women with GDM, compared with the nondiabetic population. This long-term risk of ADHD increased in the presence of pregestational obesity (HR, 1.64).
Similarly, evidence from systematic reviews and meta-analyses has demonstrated that antenatal lifestyle interventions to prevent excessive weight gain during pregnancy were associated with a reduction in adverse pregnancy outcomes. However, evidence on offspring mental health was lacking, especially in high-risk pregnancies with gestational diabetes, the study authors said.
Although causal inferences can’t be drawn from the current observational study, “it seems that the higher risk [of ADHD] observed would be explained by the role of gestational weight gain during the antenatal period,” Dr. Perea said in an interview. Importantly, the study highlights a window of opportunity for promoting healthy weight gain during pregnancy, Dr. Perea said. ”This should be a priority in the current management of gestation.”
Fatima Cody Stanford, MD, MPH, an associate professor of medicine and pediatrics at Harvard Medical School, Boston, agreed. “I think one of the key issues is that there’s very little attention paid to how weight gain is regulated during pregnancy,” she said in an interview. On many other points, however, Dr. Stanford, who is a specialist in obesity medicine at Massachusetts General Hospital Weight Center, did not agree.
The association between ADHD and obesity has already been well established by a 2019 meta-analysis and systematic review of studies over the last 10 years, she emphasized. “These studies were able to show a much stronger association between maternal obesity and ADHD in offspring because they were powered to detect differences.”
The current study does not say “anything new or novel,” Dr. Stanford added. “Maternal obesity and the association with an increased risk of ADHD in offspring is the main issue. I don’t think there was any appreciable increase when weight gain during pregnancy was factored in. It’s mild at best.”
Eran Bornstein, MD, vice-chair of obstetrics and gynecology at Lenox Hill Hospital, New York, expressed a similar point of view. Although the study findings “add to the current literature,” they should be interpreted “cautiously,” Dr. Bornstein said in an interview.
The size of the effect on ADHD risk attributable to maternal weight gain during pregnancy “was not clear,” he said. “Cohort studies of this sort are excellent for finding associations which help us generate the hypothesis, but this doesn’t demonstrate a cause and effect or a magnitude for this effect.”
Physicians should follow cumulative data suggesting that maternal obesity is associated with a number of pregnancy complications and neonatal outcomes in women with and without diabetes, Dr. Bornstein suggested. “Optimizing maternal weight prior to pregnancy and adhering to recommendations regarding weight gain has the potential to improve some of these outcomes.”
Treating obesity prior to conception mitigates GDM risk, agreed Dr. Stanford. “The issue,” she explained, “is that all of the drugs approved for the treatment of obesity are contraindicated in pregnancy and lifestyle modification fails in 96% of cases, even when there is no pregnancy.” Drugs such as metformin are being used off-label to treat obesity and to safely manage gestational weight gain, she said. “Those of us who practice obesity medicine know that metformin can be safely used throughout pregnancy with no harm to the fetus.”
This study was partially funded by Fundació Docència i Recerca MútuaTerrassa. Dr. Perea and study coauthors reporting have no conflicts of interest. Dr. Stanford disclosed relationships with Novo Nordisk, Eli Lilly, Boehringer Ingelheim, Gelesis, Pfizer, Currax, and Rhythm. Dr. Bornstein reported having no conflicts of interest.
This story was updated on 11/7/2022.
Obesity in women of reproductive age has emerged as one of the main risk factors associated with neonatal complications and long-term neuropsychiatric consequences in offspring, including attention-deficit/hyperactivity disorder.
Research has also linked pregestational diabetes and gestational diabetes mellitus (GDM) to an increased risk for ADHD in offspring. Now, an observational study of 1,036 singleton births at one hospital between 1998 and 2008 suggests that in the presence of GDM, maternal obesity combined with excessive weight gain during pregnancy may be jointly associated with increased risk of offspring ADHD. The median follow-up was 17.7 years.
Maternal obesity was independently associated with ADHD (adjusted hazard ratio, 1.66; 95% confidence interval: 1.07-2.60), but excessive weight gain during pregnancy and maternal overweight were not, reported Verónica Perea, MD, PhD, of the Hospital Universitari Mútua de Terrassa, Barcelona, and colleagues in the Journal of Clinical Endocrinology & Metabolism.
However, in women with pregestation obesity who gained more weight than recommended by the National Academy of Medicine (NAM), the risk of offspring ADHD was higher, compared with women of normal weight whose pregnancy weight stayed within NAM guidelines (adjusted hazard ratio, 2.13; 95% confidence interval: 1.14-4.01).
“The results of this study suggest that the negative repercussions of excessive weight gain on children within the setting of a high-risk population with GDM and obesity were not only observed during the prenatal period but also years later with a development of ADHD,” the researchers wrote.
The study also showed that when maternal weight gain did not exceed NAM guidelines, maternal obesity was no longer independently associated with ADHD in offspring (aHR, 1.36; 95% CI: 0.78-2.36). This finding conflicts with earlier studies focusing primarily on the role of pregestational maternal weight, the researchers said. A 2018 nationwide Finnish cohort study in newborns showed an increased long-term risk of ADHD in those born to women with GDM, compared with the nondiabetic population. This long-term risk of ADHD increased in the presence of pregestational obesity (HR, 1.64).
Similarly, evidence from systematic reviews and meta-analyses has demonstrated that antenatal lifestyle interventions to prevent excessive weight gain during pregnancy were associated with a reduction in adverse pregnancy outcomes. However, evidence on offspring mental health was lacking, especially in high-risk pregnancies with gestational diabetes, the study authors said.
Although causal inferences can’t be drawn from the current observational study, “it seems that the higher risk [of ADHD] observed would be explained by the role of gestational weight gain during the antenatal period,” Dr. Perea said in an interview. Importantly, the study highlights a window of opportunity for promoting healthy weight gain during pregnancy, Dr. Perea said. ”This should be a priority in the current management of gestation.”
Fatima Cody Stanford, MD, MPH, an associate professor of medicine and pediatrics at Harvard Medical School, Boston, agreed. “I think one of the key issues is that there’s very little attention paid to how weight gain is regulated during pregnancy,” she said in an interview. On many other points, however, Dr. Stanford, who is a specialist in obesity medicine at Massachusetts General Hospital Weight Center, did not agree.
The association between ADHD and obesity has already been well established by a 2019 meta-analysis and systematic review of studies over the last 10 years, she emphasized. “These studies were able to show a much stronger association between maternal obesity and ADHD in offspring because they were powered to detect differences.”
The current study does not say “anything new or novel,” Dr. Stanford added. “Maternal obesity and the association with an increased risk of ADHD in offspring is the main issue. I don’t think there was any appreciable increase when weight gain during pregnancy was factored in. It’s mild at best.”
Eran Bornstein, MD, vice-chair of obstetrics and gynecology at Lenox Hill Hospital, New York, expressed a similar point of view. Although the study findings “add to the current literature,” they should be interpreted “cautiously,” Dr. Bornstein said in an interview.
The size of the effect on ADHD risk attributable to maternal weight gain during pregnancy “was not clear,” he said. “Cohort studies of this sort are excellent for finding associations which help us generate the hypothesis, but this doesn’t demonstrate a cause and effect or a magnitude for this effect.”
Physicians should follow cumulative data suggesting that maternal obesity is associated with a number of pregnancy complications and neonatal outcomes in women with and without diabetes, Dr. Bornstein suggested. “Optimizing maternal weight prior to pregnancy and adhering to recommendations regarding weight gain has the potential to improve some of these outcomes.”
Treating obesity prior to conception mitigates GDM risk, agreed Dr. Stanford. “The issue,” she explained, “is that all of the drugs approved for the treatment of obesity are contraindicated in pregnancy and lifestyle modification fails in 96% of cases, even when there is no pregnancy.” Drugs such as metformin are being used off-label to treat obesity and to safely manage gestational weight gain, she said. “Those of us who practice obesity medicine know that metformin can be safely used throughout pregnancy with no harm to the fetus.”
This study was partially funded by Fundació Docència i Recerca MútuaTerrassa. Dr. Perea and study coauthors reporting have no conflicts of interest. Dr. Stanford disclosed relationships with Novo Nordisk, Eli Lilly, Boehringer Ingelheim, Gelesis, Pfizer, Currax, and Rhythm. Dr. Bornstein reported having no conflicts of interest.
This story was updated on 11/7/2022.
The Journal of Clinical Endocrinology & Metabolism
N.Y. governor declares state disaster emergency to boost polio vaccination
New York Governor Kathy Hochul declared a state disaster emergency on Sept. 9 after the polio virus has been detected in another county. The order allows EMS workers, midwives, and pharmacists to administer the vaccine and permits physicians and nurse practitioners to issue standing orders for polio vaccines.
“On polio, we simply cannot roll the dice,” New York State Health Commissioner Dr. Mary T. Bassett said in a news release. “If you or your child are unvaccinated or not up to date with vaccinations, the risk of paralytic disease is real. I urge New Yorkers to not accept any risk at all.”
In July, an unvaccinated adult man in Rockland County, which is north of New York City, was diagnosed with polio virus. It was the first confirmed case of the virus in the United States since 2013.
New York state health officials have not announced any additional polio cases. Since as early as April, polio has also been detected in wastewater samples in New York City and in Rockland, Orange, and Sullivan counties. In August, the virus was detected in wastewater from Nassau County on Long Island.
New York’s statewide polio vaccination rate is 79%, and the New York State Department of Health is aiming for a rate over 90%, the announcement said. In some counties, vaccination rates are far below the state average, including Rockland County (60%), Orange County (59%), and Sullivan County (62%). Nassau County’s polio vaccination rate is similar to the state average.
“Polio immunization is safe and effective – protecting nearly all people against disease who receive the recommended doses,” Dr. Basset said; “Do not wait to vaccinate.”
A version of this article first appeared on Medscape.com.
New York Governor Kathy Hochul declared a state disaster emergency on Sept. 9 after the polio virus has been detected in another county. The order allows EMS workers, midwives, and pharmacists to administer the vaccine and permits physicians and nurse practitioners to issue standing orders for polio vaccines.
“On polio, we simply cannot roll the dice,” New York State Health Commissioner Dr. Mary T. Bassett said in a news release. “If you or your child are unvaccinated or not up to date with vaccinations, the risk of paralytic disease is real. I urge New Yorkers to not accept any risk at all.”
In July, an unvaccinated adult man in Rockland County, which is north of New York City, was diagnosed with polio virus. It was the first confirmed case of the virus in the United States since 2013.
New York state health officials have not announced any additional polio cases. Since as early as April, polio has also been detected in wastewater samples in New York City and in Rockland, Orange, and Sullivan counties. In August, the virus was detected in wastewater from Nassau County on Long Island.
New York’s statewide polio vaccination rate is 79%, and the New York State Department of Health is aiming for a rate over 90%, the announcement said. In some counties, vaccination rates are far below the state average, including Rockland County (60%), Orange County (59%), and Sullivan County (62%). Nassau County’s polio vaccination rate is similar to the state average.
“Polio immunization is safe and effective – protecting nearly all people against disease who receive the recommended doses,” Dr. Basset said; “Do not wait to vaccinate.”
A version of this article first appeared on Medscape.com.
New York Governor Kathy Hochul declared a state disaster emergency on Sept. 9 after the polio virus has been detected in another county. The order allows EMS workers, midwives, and pharmacists to administer the vaccine and permits physicians and nurse practitioners to issue standing orders for polio vaccines.
“On polio, we simply cannot roll the dice,” New York State Health Commissioner Dr. Mary T. Bassett said in a news release. “If you or your child are unvaccinated or not up to date with vaccinations, the risk of paralytic disease is real. I urge New Yorkers to not accept any risk at all.”
In July, an unvaccinated adult man in Rockland County, which is north of New York City, was diagnosed with polio virus. It was the first confirmed case of the virus in the United States since 2013.
New York state health officials have not announced any additional polio cases. Since as early as April, polio has also been detected in wastewater samples in New York City and in Rockland, Orange, and Sullivan counties. In August, the virus was detected in wastewater from Nassau County on Long Island.
New York’s statewide polio vaccination rate is 79%, and the New York State Department of Health is aiming for a rate over 90%, the announcement said. In some counties, vaccination rates are far below the state average, including Rockland County (60%), Orange County (59%), and Sullivan County (62%). Nassau County’s polio vaccination rate is similar to the state average.
“Polio immunization is safe and effective – protecting nearly all people against disease who receive the recommended doses,” Dr. Basset said; “Do not wait to vaccinate.”
A version of this article first appeared on Medscape.com.